CT scan COPD
CT scan COPD is more sensitive and specific than chest radiography to detect Emphysema.
The first imaging tool used for lung parenchyma remains that of the chest radiograph. It is the best in terms of the amount of information it can provide relative to its price and radiation dose, accessibility as well as ease of use. However, the chest radiograph is not without limitations.
Chest radiographs have been proven to have a sensitiveness of 80 percent and an 82 percent specificity for the detection of lung disease.
Chest radiography may confirm a diagnosis in just 33% of instances and the diagnoses that were confident proved to be correct in only 77 percent of cases.
This is why high-resolution computed tomography (HRCT, also known as scans of thin sections CT) is often utilized to clarify particular issues. Common characteristics in the parenchyma of the lungs, as well as of the small airways are associated with restrictive or obstructive pulmonary function tests.
What is COPD
Chronic obstructive lung disease (COPD) is long-lasting inflammation of the lung that results in obstruction of airflow in the lung. The symptoms include breathing difficulties with cough, mucus (sputum) production, and wheezing. It’s usually caused by prolonged exposure to trigger gases, or particles of matter, mostly due to smoking cigarettes. People with COPD are at a higher chance of developing heart disease as well as lung cancer, as well as a range of other ailments.
Chronic bronchitis and Emphysema are the two most frequent conditions that cause COPD. Both conditions are usually seen together and can differ in severity between people with COPD.
Chronic bronchitis can cause inflammation of the linings of the bronchial tubes, that transport air into and out of the air sacs (alveoli) of the lung. It is characterized by a constant cough as well as it is characterized by mucus (sputum) creation.
Emphysema refers to a condition where the alveoli located at the ends of the tiniest airways (bronchioles) that connect the lungs become damaged because of damaging exposure to cigarette smoke as well as other irritating gases and particles.¶
While COPD is a progressive illness that becomes worse with duration, COPD is treatable. If properly managed, the majority of people suffering from COPD have a good chance of achieving control of symptoms and living quality, and also lower the chance of developing other ailments.
Signs and symptoms
COPD symptoms usually don’t show until lung damage has already occurred and the symptoms tend to worsen with time, particularly when smoking continues to be a factor.
Aspects or symptoms of COPD could include:
- Breathing shortness, especially when you are engaged in physical activities
- Heezing
- Chest tightness
- Chronic coughs can cause the production of mucus (sputum) which can be transparent white, yellow, or greenish.
- Common respiratory infections
- Insufficiency of energy
- Weight loss that is not expected (in subsequent stages)
- The swelling can be seen in feet, ankles, or legs
Patients with COPD are also more likely to suffer from exacerbations or episodes, in which their symptoms are more severe than the normal day-to-day variations and last for at most a couple of days.
The most significant reason for COPD in developed nations is smoking tobacco. In developing countries, COPD often occurs in people who breathe in fumes from burning cooking or heating homes that are not well ventilated.
Certain chronic smokers are the only ones to have clinically evident COPD However, those who smoke for long history may experience a decrease in lung function. Some smokers develop less common lung conditions. They could be mistakenly diagnosed as being suffering from COPD until a comprehensive evaluation is completed.
Diagnosis
COPD is often mistakenly diagnosed. Many patients with COPD are not diagnosed until the condition is advanced.
Your doctor might order a variety of tests to determine the severity of your illness.
Tests can consist of:
- Lung (pulmonary) test for function. These tests assess the quantity of air you can exhale and inhale as well as whether or not your lungs are able to deliver sufficient oxygen in your blood. In the most commonly used test, spirometry, you blow into a massive tube, which is connected to a tiny device to determine the amount of air in your lungs and the speed at which you blow air out of your lung. Other tests include measurements of lung volume and diffusing capacity as well as a six-minute walk test and pulse oxygenation.
- Chest Xray. A chest X-ray can reveal emphysema, which is one of the most common factors that cause COPD. A chest X-ray may also identify other lung issues and heart disease.
- CT scan. A CT scan of your lungs could help you identify Emphysema, and determine if you would benefit from surgery to treat COPD. CT scans are also a way to detect lung cancer.
- Analyzing blood gas in the arterial. This blood test measures the effectiveness of your lungs at carrying oxygen into your blood while taking out carbon dioxide.
- Lab test. Lab tests aren’t used to diagnose COPD however they can help determine the source of your symptoms or to exclude other causes. For instance, tests in the lab can be performed to determine if you are suffering from genetic disorders such as alpha-1-antitrypsin deficiencies, which could be the reason for COPD for some individuals. This test could be conducted in the event that you have an ancestral background of COPD and are diagnosed with COPD at an early age.
CT Scan COPD
In this section, we will discuss more CT scan to make a diagnosis of COPD. We will discuss a high-resolution CT scan it has more sensitivity and specificity than a normal chest ct scan.
High-resolution CT scan
HRCT has a sensitivity of 95% and a specificity that is close to 100 percent, which can give more information than chest radiography or CT scanning. A reliable diagnosis is achievable in about one-half of the cases and is proved to be accurate 93 % of the time.
HRCT could be especially helpful in the following scenarios:
- It can be used to diagnose lung disease in patients who are symptomatic who have a chest radiograph that is normal.
- It provides a precise evaluation of the pattern and distribution and, to a lesser extent evaluates the severity and the possibility of reversibility in chronic lung illness.
- It shows a significant correlation between histopathologic and radiographic appearances.
- If there are non-diagnostic signs on chest radiography could provide a more precise diagnosis or exclude certain conditions.
- It is employed to establish the nature and location of a lung biopsy
- It is a method to identify or assess certain diagnoses or problems for metastatic lesions, single pulmonary nodules, emphysema, bullous lung diseases, bronchiectasis, and diffuse parenchymal disorder.
Expiratory scans are particularly beneficial when combined with the inspiratory scans may help in determining if there is air-trapping as a surrogate test for small airway abnormalities. The small airway abnormality can be assessed. ¶
But, CT scanning is not required for routine diagnostic of COPD. It is usually performed when an increase in symptoms indicates an underlying condition of COPD (eg pneumothorax, pneumonia, or giant bullae) or when an alternative diagnosis (eg thromboembolic disorder) is considered or the screening for lung cancer is suggested or when a patient is being evaluated for medical treatment of the lung using endobronchial valves or surgical reduction of lung volume or lung transplantation
Certain CT scan characteristics can help determine whether the emphysema has been classified as centriacinar (centrilobular) or panacinar or paraseptal. However, this is not required to manage the disease clinically.
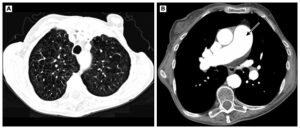 Centriacinar Emphysema is more common on the lower lobes and creates holes in the middle of pulmonary lobules secondary to the primary. Its walls in emphysematous areas are typically invisible, however central vessels might be visible. The following image shows centriacinar emphysema also dilated pulmonary trunk (arrow).
Centriacinar Emphysema is more common on the lower lobes and creates holes in the middle of pulmonary lobules secondary to the primary. Its walls in emphysematous areas are typically invisible, however central vessels might be visible. The following image shows centriacinar emphysema also dilated pulmonary trunk (arrow).
-
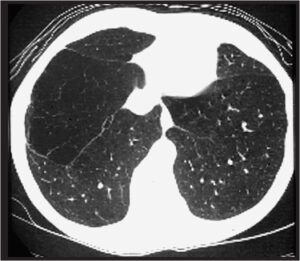
Panaciner emphysema Panacinar Emphysema most often affects the lung bases and can affect the entire secondary pulmonary lung (see image). Panacinar emphysema may cause a generalized lack of vessels. For patients suffering from an alpha-1 deficiency in antitrypsin and panacinar emphysema, this is the most frequent type.
-
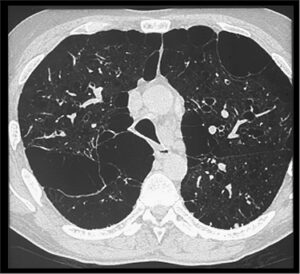
Paraseptal emphysema Paraseptal (distal acinar) Emphysema causes small, subpleural accumulations of gas that are located on the outer rim of the pulmonary lobule that is secondary (image)
Modern CT scanners that have higher resolution and advanced analytical techniques can detect airway sizes but the clinical value of these measures is unclear. Quantitative parameters based upon lung density, measured through CT scans, were developed to assess emphysema however, they are used mostly as tools for research.
The application for low-dose CT scans to detect lung cancer is described separately.
Treatment
A lot of people suffering from COPD suffer from mild forms of the disease, for which very little treatment is required aside from quitting smoking. Even in the more advanced forms of the disease, it is possible to find a solution to manage symptoms, slow down progression as well as reduce the chance of exacerbations and complications, and help you live a full and active life.
Quitting smoking
The most important element of any treatment plan to treat COPD is to cease all smoking. Quitting smoking can prevent COPD from becoming worse, and also reduce the chance of breathing. It’s not easy to quit smoking. It can be especially daunting if you’ve tried to quit but have been unsuccessful.
Discuss with your physician regarding the nicotine replacement options and medicines that may assist, as well as the best way to manage to get over relapses. Your doctor may also suggest a support group for those who wish to stop smoking. Additionally, try to stay clear of secondhand smoke exposure as much as you can.
Medications
Many kinds of medication are utilized to treat the effects and complications of COPD. Some medications can be taken regularly and others when needed.
Bronchodilators
Some examples of short-acting bronchodilators are:
- Albuterol (ProAir HFA ), Ventolin HFA, others)
- Ipratropium (Atrovent HFA)
- Levalbuterol (Xopenex)
Examples of long-acting bronchodilators are:
- Aclidinium (Tudorza Pressair)
- Arformoterol (Brovana)
- Formoterol (Perforomist)
- Indacaterol (Arcapta Neoinhaler)
- Tiotropium (Spiriva)
- Salmeterol (Serevent)
- Umeclidinium (Incruse Ellipta)
Inhaled steroids
- Fluticasone (Flovent HFA)
- Budesonide (Pulmicort Flexhaler)
Combination inhalers
Some medicines combine bronchodilators and inhaled steroids. Examples of these inhalers are:
- Fluticasone and the vilanterol (Breo Ellipta)
- Fluticasone and umeclidinium as well as Vilanterol (Trelegy Ellipta)
- Formoterol and Budesonide (Symbicort)
- The combination of fluticasone with salmeterol (Advair HFA AirDuo Digihaler, others)
Combination inhalers which contain multiple types of bronchodilators are also available. Examples include:
- Aclidinium as well as formoterol (Duaklir Pressair)
- Albuterol and Ipratropium (Combivent Respimat)
- Glycopyrrolate and Formoterol (Bevespi Aerosphere)
- Glycopyrrolate and Indacaterol (Utibron)
- Olodaterol and Tiotropium (Stiolto Respimat)
- Umeclidinium and Vilanterol (Anoro Ellipta)
Oral steroids
For those who have times when their COPD gets more severe, referred to as severe or moderate acute exacerbation. Short periods (for instance 5 days) of oral corticosteroids can stop further aggravation of COPD. However, prolonged use of these medicines can result in severe side effects, like weight increase and diabetes, osteoporosis cataracts, and an increased risk of developing infections.
Phosphodiesterase-4 inhibitors
A drug that is approved for those suffering from severe COPD and signs of chronic bronchitis is called roflumilast (Daliresp) is an inhibitor of phosphodiesterase-4. The drug reduces inflammation of the airways and also relaxes the airways. Common side effects are the loss of weight and diarrhea.
Theophylline
When treatment options have proven unsuccessful or cost is an issue Theophylline (Elixophyllin Theo-24 and Theochron) can be a lower-cost medication, that could assist in improving breathing and preventing instances of increasing COPD. The adverse effects can be attributed to dose and can include headache, nausea, as well as tremor, rapid heartbeats, and fast heartbeats Tests, are performed to determine the blood levels of the medication.
Antibiotics
Respiratory illnesses, such as acute bronchitis, pneumonia, and influenza, can cause COPD symptoms. Antibiotics can help treat symptoms of worsening COPD However, they’re not usually advised to prevent. Certain studies have shown the use of certain antibiotics including azithromycin (Zithromax) is effective in preventing the onset of worsening COPD However, adverse reactions and resistance to antibiotics could limit their use.
Other therapies for the lungs
- Oxygen therapy. If there isn’t enough oxygen in your blood, it could be that you require additional oxygen. There are many devices that provide oxygen to the lungs, such as portable, lightweight devices that you can carry with you on your errands, or just to get around the town.
- Rehabilitation for the lungs. These programs generally combine education, exercise nutritional advice, and counseling. You’ll be working with a range of experts who will modify your rehabilitation program to suit your specific needs.

Wow, marvelous blog layout! How long have you been blogging for?
you made running a blog glance easy. The total look of your site is
fantastic, let alone the content! You can see similar here e-commerce
You are so cool! I do not think I have read something
like that before. So wonderful to find another person with a few genuine thoughts on this issue.
Really.. thank you for starting this up. This website is something that’s needed on the web, someone
with a bit of originality! I saw similar here: Sklep internetowy
Hey there! Do you know if they make any plugins to help with
SEO? I’m trying to get my blog to rank for some targeted keywords but I’m
not seeing very good gains. If you know of any please share.
Kudos! You can read similar article here: E-commerce
It’s very interesting! If you need help, look here: ARA Agency
Hi there! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m
not seeing very good results. If you know of any please share.
Many thanks! You can read similar text here: Sklep internetowy
Good day! Do you know if they make any plugins to help with Search Engine Optimization? I’m
trying to get my blog to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Many thanks!
You can read similar art here: Sklep internetowy
Good day! Do you know if they make any plugins
to help with Search Engine Optimization? I’m trying to get my website
to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Cheers! I saw similar art here:
List of Backlinks
Hello! Do you know if they make any plugins to assist with Search Engine
Optimization? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Thanks! I saw similar article here: GSA List
Howdy! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to
get my website to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Kudos! You can read similar blog here:
Hitman.agency
tadalafil 20 coupon
Wow, marvelous blog format! How lengthy have you been running
a blog for? you make blogging glance easy.
The full look of your website is magnificent, let alone the content!
You can see similar here e-commerce
tadalafil uk pharmacy
zestril coupon
buy tadalafil 20mg price in india
purchase cialis online australia
zestoretic
sildalis without prescription
tor darknet https://mydarkmarket.com/ – dark web links darknet drugs
batmanapollo.ru
Ad oculos — Наглядно
Consumor aliis inserviendo — Изнуряю себя, работая на благо других.
doxycycline 150 mg cost
Benevole lector — Благосклонный читатель.
Benevolentiae captande causa — Для снискания благоволения.
Amabilis insania — Приятное безумие.
Contradictio in re — лог. Противоречие в существе (нелепость).
Cave ne cadas — Берегись, чтоб не упасть.
Concordet sermo cum vita — Пусть речь соответствует жизни.
Министерство неджентльменских дел
Усик Фьюри 18 мая 2024
Александр Усик – Тайсон Фьюри. Смотреть онлайн
Александр Усик — Тайсон Фьюри
Прямая трансляция: Александр Усик – Тайсон Фьюри
Фуриоса: Хроники Безумного Макса
Психолог консультация
Тут психолог
Тут психолог
Психолог консультация
darknet sites https://mydarknetmarketlinks.com/ – onion market dark web links
dark internet https://mydarknetmarketlinks.com/ – dark web markets deep web drug url
Происхождение марксистской психологии и лучшие книги по психиатрии.
Dictum – factum
vibramycin
Dictum – factum
100 лет тому вперед смотреть онлайн бесплатно. Фильм 100 лет тому вперед смотреть онлайн.
Уэнздей 2 сезон смотреть онлайн
pharmacies online
Уэнздей 2 сезон кино
rx canada
Фоллаут 2024
Психолог
zithromax best price
Претенденты смотреть Претенденты фильм, 2024, смотреть онлайн
buy furosemide 20 mg online
Hi! Do you know if they make any plugins to help with
SEO? I’m trying to get my blog to rank for
some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Kudos! I saw similar
art here: Which escape room
I’ve been browsing online greater than 3 hours today, yet I by no means found any fascinating article like yours. It is lovely worth sufficient for me. Personally, if all webmasters and bloggers made good content as you probably did, the web might be much more useful than ever before!
accutane price canada
drugs without prescription
cost of ventolin in usa
This is a topic that is close to my heart… Cheers! Where can I find the contact details for questions?
After looking over a handful of the articles on your website, I honestly appreciate your technique of writing a blog. I added it to my bookmark site list and will be checking back in the near future. Please check out my website too and tell me how you feel.
Great post. I was checking constantly this blog and I am impressed! Very helpful info specially the last part I care for such info a lot. I was seeking this particular info for a very long time. Thank you and good luck.
This is a great tip especially to those new to the blogosphere. Brief but very accurate info… Thanks for sharing this one. A must read post.
Good day! I could have sworn I’ve visited this web site before but after browsing through some of the articles I realized it’s new to me. Regardless, I’m definitely happy I stumbled upon it and I’ll be bookmarking it and checking back frequently!
Hi there! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing
very good gains. If you know of any please share. Thank you!
I saw similar art here
accutane 40mg capsule
accutane cost in india
I couldn’t resist commenting. Perfectly written.
mail order pharmacy list
This is a topic close to my heart cheers, do you have a RSS feed I can use?
Nice post. I learn something harder on distinct blogs everyday. Most commonly it is stimulating to learn content from other writers and exercise a specific thing from their store. I’d choose to use some while using content in my weblog whether you don’t mind. Natually I’ll supply you with a link in your internet blog. Thank you for sharing.
naturally like your web-site but you have to check the spelling on several of your posts. A number of them are rife with spelling problems and I find it very troublesome to tell the truth nevertheless I will definitely come back again.
modafinil singapore buy
chiropractors are heaven sent when i got a very bad sprain after playing football”
Having read this I thought it was rather enlightening. I appreciate you finding the time and effort to put this content together. I once again find myself personally spending way too much time both reading and commenting. But so what, it was still worthwhile.
buy zithromax without prescription
The the next time I just read a blog, I hope so it doesnt disappoint me around this place. After all, It was my option to read, but When i thought youd have something fascinating to mention. All I hear is often a few whining about something that you could fix should you werent too busy looking for attention.
It’s hard to find knowledgeable people within this topic, however you seem like you know what you are discussing! Thanks
canadian pharmacy products
buy sildenafil online usa
baclofen buy canada
Many thanks for sharing this great write-up. Very inspiring! (as always, btw)
Hello dude,i like this Ones blog very much. do u have suggestion for my homepage? thanks as
Good day! This post could not be written any better! Reading this post reminds me of my previous room mate! He always kept chatting about this. I will forward this write-up to him. Fairly certain he will have a good read. Thanks for sharing!
After I originally left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on each time a comment is added I recieve four emails with the same comment. Is there a way you can remove me from that service? Many thanks.
lasix diuretic
provigil for sale online
nolvadex capsules price
foot massage are very relaxing, i love to have a foot massage after a hard days work”
I’m extremely pleased to discover this website. I wanted to thank you for your time just for this fantastic read!! I definitely enjoyed every little bit of it and I have you bookmarked to see new things on your website.
Dziękuję za podkreślenie znaczenia profesjonalnego podejścia do SEO.
Ten post to świetne źródło informacji dla każdego, kto potrzebuje SEO.
Świetne wskazówki dotyczące znalezienia wiarygodnych usług SEO. Dzięki!
Doceniam skupienie się na zagrożeniach SEO i potrzebie ich usunięcia.
160 bactrim
ventolin 100mcg online
SEO wydaje się trudne, ale Twój blog sprawia, że staje się bardziej zrozumiałe. Dzięki!
acyclovir cream generic price
Doceniam szczegółowe wyjaśnienia na temat SEO i bezpieczeństwa.
your discount pharmacy
Nice post. I discover some thing more challenging on diverse blogs everyday. It will always be stimulating to study content from other writers and use a little something from their site. I’d opt to use some with all the content on my small weblog whether or not you don’t mind. Natually I’ll provide you with a link on the internet blog. Many thanks for sharing.
Love the blog here. Nice colors. I am definitely keeping up on the comments here. I hope to see more from you in the near future.
Its mainly because the cast is very likable with its main leads resonating off each other in this pool of silliness which makes the film highly entertaining.
I conceive this web site has got some very excellent info for everyone : D.
This webpage has thus lots very good data on it, I verify on it everyday. I would like different websites spent as much work as this one does generating facts legible to readers like myself. i like to recommend this page to all of my facebook friends. This webpage will create some massive passive profit i’m positive. I hope my site will in addition to the current one, it refers to jewellery shoppers houston
lasix 20 mg tablet price
Aw, this became a very good post. In concept I must set up writing like this moreover – taking time and actual effort to produce a really good article… but exactly what can I say… I procrastinate alot and by no indicates apparently go completed.
Hello! .order viagra fast delivery , order cialis fast delivery , tadalafil , find cheap viagra , ,
abstract art have share some of its unique beauty when it comes to art. i like abstract art because it is mysterious“
I can’t really help but admire your blog, your blog is so adorable and nice “
generic clomid for sale
I bookmared your site a couple of days ago coz your blog impresses me.,*,-”
Great news I recently find your blog and have been reading along. I thought I would leave a comment.
Hello! I simply would want to give you a huge thumbs up with the wonderful info you might have here about this post. I will be returning to your blog post for more soon.
Great site. Plenty of useful information here. I’m sending it to a few friends ans also sharing in delicious. And certainly, thanks for your sweat!
You have noted very interesting points ! ps nice internet site .
I believe other website owners should take this site as an example , very clean and wonderful user genial style .
where can i purchase metformin 1000 mg without prescription
Sweet blog! I found it while surfing around on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thanks
With havin so much content and articles do you ever run into any issues of plagorism or copyright
infringement? My site has a lot of exclusive content I’ve either written myself or outsourced but it appears a lot
of it is popping it up all over the web without my agreement.
Do you know any methods to help prevent content from being ripped off?
I’d truly appreciate it.
This is certainly a very amazing powerful resource that you’re offering and you just provide it away cost-free!! I that can match discovering websites which see the particular valuation on giving you a superb learning resource for zero cost. We truly dearly loved examining this site. Love!
Sweet web site , super design , real clean and utilise pleasant.
doxycycline 100mg acne
buy nolvadex 20mg
I wish to show thanks to this writer just for bailing me out of this type of challenge. Right after researching throughout the world wide web and obtaining methods which were not beneficial, I was thinking my life was done. Existing minus the strategies to the difficulties you have fixed through the short post is a serious case, as well as the kind which may have negatively damaged my career if I hadn’t discovered your web site. That know-how and kindness in taking care of everything was vital. I don’t know what I would have done if I hadn’t come across such a point like this. It’s possible to at this time relish my future. Thanks very much for the expert and result oriented help. I won’t think twice to propose your web blog to anybody who needs guidelines on this issue.
Spot lets start work on this write-up, I actually believe this site needs much more consideration. I’ll apt to be once again to read a lot more, many thanks that info.
lyrica 300 mg
lyrica drug cost
accutane price in india
how much is accutane cost
levothyroxine 50 mcg
where to buy vermox in usa
baclofen pills 10 mg
diflucan 110 mg
lyrica 75 mg generic
You actually make it seem really easy together with your presentation however I to find
this topic to be really something that I feel I’d by no means understand.
It seems too complex and extremely wide for me.
I’m looking ahead in your subsequent publish, I will try to get the grasp of it!
Escape room
I was examining some of your content on this site and I believe this site
is really instructive! Retain putting up.!
lasix medicine cost
acyclovir
toradol eye drops
I couldn’t have said it better myself.대출 이자 계산기
I’ve been looking for answers on this—thank you!무직자 대출 쉬운곳
propecia generic price
dexamethasone tablets australia
In case you run a enterprise that merely uses this gas,
you may take an easier route to get your credit. Remove
the doorways, drawers and hardware to make all the things simpler.
cheap modafinil uk
You’ve provided a nuanced view on this topic.검색엔진최적화 대행사
ankara seo
seo hizmeti
amoxicillin 50 mg tablets
generic advair diskus canada
I blog often and I genuinely appreciate your content. The article has really peaked my interest. I’m going to book mark your website and keep checking for new information about once a week. I opted in for your RSS feed as well.
Many of us clear our kitchen sponges by rinsing them with hot soapy water or running them by
means of the dishwasher, but can you truly disinfect a kitchen sponge?
If you have watched a morning information program
or learn a women’s journal anytime up to
now 10 years or so, you most likely already know that
kitchen sponges are among probably the most germ-ridden objects in your
total home. Electrochromic glass is still
being perfected for commercial use, but anticipate to see more of the glass in the coming years as competing builders convey this good energy-saving
expertise to the market.
Play continues as above until each partners have
answered all questions and all responses have been compared.
While debate continues over marijuana’s health benefits versus its
dangers, recent research have positioned cannabis squarely in the midst of the conversation over what has been known as “the worst drug epidemic in U.S. history.” And this time,
some researchers say, marijuana is perhaps part of the solution. Some observers hyperlink the
epidemic to pharmaceuticals aggressively marketing highly addictive opioids for the reason that 1990s, and
doctors aggressively prescribing them to victims of chronic pain.
where can i order doxycycline
doxycycline capsule 100mg price
Great web site you’ve got here.. It’s difficult to find good quality writing like yours these days. I really appreciate individuals like you! Take care!!
Good information. Lucky me I discovered your site by chance (stumbleupon). I have saved as a favorite for later!
Your style is very unique in comparison to other folks I’ve read stuff from. I appreciate you for posting when you have the opportunity, Guess I’ll just book mark this blog.
Hi there! I could have sworn I’ve visited this site before but after going through a few of the articles I realized it’s new to me. Regardless, I’m definitely happy I stumbled upon it and I’ll be book-marking it and checking back regularly.
Excellent site you have here.. It’s difficult to find good quality writing like yours nowadays. I really appreciate individuals like you! Take care!!
I was able to find good information from your content.
This is very interesting content! I have thoroughly enjoyed reading your points and have come to the conclusion that you are right about many of them. You are great.
buy provigil rx
I was real pleased to find this site on bing, just what I was looking for : D likewise saved to my bookmarks .
Wow, great stuff. I have been considering this for a few years. I’m glad to seemingly find someone that comes to the same conclusions as me. At least it seems that’s the case. I’ll keep visiting your site to stay informed.
albuterol inhalers not prescription required
May I simply just say what a relief to discover someone that really understands what they’re talking about on the web. You certainly realize how to bring an issue to light and make it important. More people have to look at this and understand this side of your story. I can’t believe you aren’t more popular since you certainly have the gift.
Good article! We are linking to this particularly great content on our site. Keep up the great writing.
vermox cost
noroxin 400
Very good information. Lucky me I discovered your site by chance (stumbleupon). I’ve book marked it for later!
Very good info. Lucky me I discovered your website by accident (stumbleupon). I’ve saved it for later.
vermox without prescription
where to buy lasix
I must thank you for the efforts you’ve put in writing this site. I am hoping to check out the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has encouraged me to get my very own blog now 😉
how much is generic provigil
bursa görüntülü diafon en uygun fiyat garantisi
Um, I like Studying about camping. The heaviest materials from the center from the backpack, the lightest of all
like tents at the underside. I would reside in the midst of nowhere if I might.
Avoiding for any nation hike is might be a lot more pleasurable than the same old
fast-paced stroll or perhaps a jog inside the town for just one quite
easy cause. However this abundance can have its drawbacks, namely that
it can be difficult to decide where to reside in a rustic
that boasts so many options. One must enjoy every minute of spare
time as life might be very a lot troublesome in not-so favorable monetary occasions.
One grain cart can hold as much as 1,000 bushels of grain at a time.
Take the time to reconnect together with your internal voice and take heed to your intuition. If you are prepared to
start out that journey, stop taking a look at Craigslist and
take this quiz!
It is quite potential to bid and make sport on a single deal:
For example, 3 NT scores 100 factors, and successful contracts of
4, 4, 5, and 5 additionally depend not less than a hundred factors.
If the contract goes down, the opposite side scores
points for undertricks, that is, the variety of methods
the declaring side falls in need of the contract
(see chart below). A game means one hundred points in tips bid for (and
won) based on the scoring desk above.
In the 1980s, applications had been small, and you could possibly fit all the operating
system, a few programs and some documents onto a floppy disk or
two. When Just Dance III comes out in late 2011, it’s going to
even be released for Xbox’s Kinect in addition to the Wii system, which implies
dancers won’t even want to hold a distant to shake their groove factor.
For most people, this implies hiring employees,
or having quite a lot of assist.
Everything is very open with a very clear clarification of the issues. It was really informative. Your site is very helpful. Many thanks for sharing!
Ten or 20 years in the past, hybrid vehicles have been new, unproven technology.
A lot of the extra price comes from the expense of the fuel-saving
expertise found in hybrids. Hybrids shine in relation to
gasoline efficiency, turning each gallon of fuel into extra miles on the street in comparison with conventional fuel engines.
There are nonetheless tax incentives obtainable for plug-in hybrids
and purely electric automobiles, however even these will doubtless end in a few years as extra of those vehicles develop into available on the marketplace.
nazilli pidesi nazilli meşhur pidesi
You’ve made some decent points there. I looked on the internet for more information about the issue and found most individuals will go along with your views on this website.
You ought to be a part of a contest for one of the finest sites on the web. I’m going to highly recommend this site!
hugaraka
buying toradol online
finasteride buy online
dexamethasone uk buy
This website was… how do you say it? Relevant!! Finally I have found something which helped me. Thanks a lot.
This is the right webpage for everyone who really wants to understand this topic. You understand so much its almost tough to argue with you (not that I personally would want to…HaHa). You certainly put a new spin on a subject that’s been written about for a long time. Excellent stuff, just great.
I was able to find good info from your content.
tretinoin 0.025 cream
Your style is very unique compared to other folks I’ve read stuff from. Thanks for posting when you have the opportunity, Guess I will just bookmark this web site.
Hello! I could have sworn I’ve visited your blog before but after going through many of the articles I realized it’s new to me. Regardless, I’m certainly happy I discovered it and I’ll be bookmarking it and checking back frequently.
Greetings! Very useful advice within this post! It is the little changes that make the most significant changes. Thanks a lot for sharing!
Greetings! Very helpful advice in this particular article! It is the little changes that will make the most important changes. Many thanks for sharing!
This is exactly the kind of discussion we need.백링크 프로그램
lyrica 20 mg
Great site you have here.. It’s hard to find good quality writing like yours these days. I truly appreciate individuals like you! Take care!!
After looking into a number of the blog posts on your web site, I honestly appreciate your way of blogging. I book marked it to my bookmark webpage list and will be checking back soon. Take a look at my website as well and tell me how you feel.
Hi there! I could have sworn I’ve been to your blog before but after going through many of the posts I realized it’s new to me. Anyways, I’m definitely happy I stumbled upon it and I’ll be bookmarking it and checking back regularly!
Saved as a favorite, I really like your site.
I’m impressed, I must say. Rarely do I come across a blog that’s both equally educative and amusing, and let me tell you, you’ve hit the nail on the head. The issue is something too few people are speaking intelligently about. Now i’m very happy I stumbled across this during my search for something relating to this.
I’m pretty pleased to discover this web site. I need to to thank you for your time just for this fantastic read!! I definitely appreciated every bit of it and I have you saved as a favorite to see new things on your web site.
It’s nearly impossible to find educated people about this subject, however, you sound like you know what you’re talking about! Thanks
I’d like to thank you for the efforts you have put in penning this site. I’m hoping to see the same high-grade blog posts by you later on as well. In truth, your creative writing abilities has motivated me to get my very own site now 😉
I was pretty pleased to find this page. I want to to thank you for ones time for this wonderful read!! I definitely enjoyed every bit of it and I have you saved to fav to look at new things on your website.
where to buy diflucan pills
This excellent website truly has all of the information and facts I wanted about this subject and didn’t know who to ask.
Greetings! Very useful advice within this post! It is the little changes that will make the most important changes. Thanks a lot for sharing!
After World War I, the nationwide prohibition of alcohol in 1919 brought heavy losses to the St.
Louis brewing industry. Within the skindex, players move round in an enormous open world generated by a set of Minecraft guidelines in three dimensions.
That is a great tip particularly to those new to the blogosphere. Simple but very accurate info… Thank you for sharing this one. A must read article!
Greetings! Very useful advice within this post! It is the little changes that make the most significant changes. Thanks a lot for sharing!
Mel Journal’s Joseph Longo referred to as her “one in all the primary polarizing figures on the video app-the embodiment of the unusual, precarious and unpredictable new world of Gen Z online fame”,
noting that social media users criticized her as being “fundamental”, “cringeworthy”, and “overhyped”.
Yugoslavian Air Pressure Ikarus IK-1, excessive-wing monoplane fighter,
first prototype crashes on third flight at Zemun airfield when it fails to get better from energy dive, pilot Capt.
I would like to thank you for the efforts you’ve put in penning this website. I am hoping to see the same high-grade content by you later on as well. In fact, your creative writing abilities has encouraged me to get my own, personal blog now 😉
The information warehouse takes over the duties
of aggregating data, whereas the info mart responds to user
queries by retrieving and combining the suitable knowledge from the warehouse.
Some data warehouses embody an extra step called a data mart.
That is because of the best way data warehouses work — they pull information from different databases periodically.
This excellent website certainly has all the information and facts I wanted concerning this subject and didn’t know who to ask.
Hi, I do think this is a great web site. I stumbledupon it 😉 I will come back once again since i have bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to help others.
ventolin inhaler
After looking into a handful of the blog posts on your website, I truly appreciate your way of writing a blog. I saved it to my bookmark site list and will be checking back in the near future. Please visit my web site too and let me know how you feel.
You need to take part in a contest for one of the finest websites on the web. I’m going to highly recommend this blog!
dexamethasone online pharmacy
This site definitely has all the information I wanted about this subject and didn’t know who to ask.
Hello there! This blog post could not be written any better! Looking at this article reminds me of my previous roommate! He always kept talking about this. I’ll send this information to him. Pretty sure he’ll have a great read. Thanks for sharing!
Pretty! This was an extremely wonderful article. Thank you for supplying this information.
nazilli apart otel
I blog often and I really appreciate your content. This article has truly peaked my interest. I will take a note of your site and keep checking for new information about once a week. I subscribed to your RSS feed as well.
There is definately a great deal to learn about this issue. I like all of the points you have made.
Right here is the right site for everyone who hopes to understand this topic. You know so much its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a new spin on a subject which has been written about for years. Wonderful stuff, just wonderful.
I couldn’t resist commenting. Very well written.
His workforce is loosely allied with Sesshomaru, whom Naraku tried to govern, the resurrected Kikyo who plans to purify the Shikon Jewel if all shards are collected,
and Kōga, the chief of a wolf demon tribe who seeks to avenge his comrades whom Naraku killed.
Hi to all, the contents present at this website are truly awesome for people knowledge, well, keep up the good work fellows.
This is a topic which is near to my heart… Take care! Exactly where are your contact details though?
Hello! I simply want to give you a big thumbs up for your great information you have right here on this post. I am coming back to your web site for more soon.
There’s certainly a lot to find out about this topic. I love all of the points you made.
This site truly has all of the info I needed concerning this subject and didn’t know who to ask.
Good post. I learn something totally new and challenging on blogs I stumbleupon everyday. It’s always useful to read through content from other authors and use something from their web sites.
lyrica price
clomid online purchase
Wonderful article! We are linking to this particularly great post on our site. Keep up the great writing.
I was very happy to discover this site. I wanted to thank you for your time just for this wonderful read!! I definitely liked every bit of it and i also have you book marked to see new stuff on your web site.
I blog frequently and I truly appreciate your content. Your article has truly peaked my interest. I will bookmark your blog and keep checking for new details about once a week. I subscribed to your Feed too.
This is a topic which is close to my heart… Thank you! Where are your contact details though?
I was able to find good info from your blog articles.
Oh my goodness! Impressive article dude! Thank you so much, However I am having problems with your RSS. I don’t know why I am unable to subscribe to it. Is there anybody getting the same RSS problems? Anyone that knows the answer will you kindly respond? Thanks!!