Overview
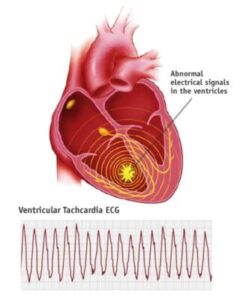
Ventricular tachycardia can be described as an abnormal heart rhythm (arrhythmia) that is caused by the abnormal electrical signals that occur in those lower heart chambers (ventricles). This condition can also be known as V-tach.
A healthy heart usually runs between 60 and 100 times per minute when in rest. In ventricular tachycardia, the heart beats faster than usual typically 100 or more beats per minute.
Rapid heartbeats can prevent the heart chambers from filling with blood. This means that your heart might not be able sufficient blood into your body or your lungs.
Ventricular Tachycardia could last just a few seconds or it could last more than. You might feel dizzy or exhausted or feel chest discomfort. Sometimes, ventricular tachycardia may make your heart stop (sudden heart attack) this is a serious medical emergency.
Symptoms
A brief episode of ventricular tachycardia does not cause symptoms for some individuals. You may also be suffering from:
- Dizziness
- Breathing shortness
- Lightheadedness
- You feel like your heart rate is racing (palpitations)
- The chest pain (angina)
More-serious and prolonged instances of ventricular tachycardia could be the cause of:
- The loss in consciousness, or fainting
- Cardiac arrest (sudden death)
When is the best time to seek medical help?
Numerous conditions can cause ventricular Tachycardia. It’s crucial to get an accurate, prompt diagnosis and the appropriate treatment. Consult your physician if you or your child have problems with your heartbeat. In some instances, urgent medical attention is required.
Take immediate care or call your urgent number for those who is experiencing these signs:
- The pain in the chest lasts longer than just a few minutes
- Trouble breathing
- Fainting
Causes
Ventricular Tachycardia is caused by a disturbance in regular electrical signals which regulate the heart’s pumping.
Numerous things can trigger or contribute to issues with the electrical circuits of the heart. This includes:
- Heart abnormalities that cause scarring of the heart tissues (sometimes called “structural heart disease”) The most frequent reason is a previous heart attack
- A lack of blood flow to the heart muscle as a result of coronary arterial disease
- Congenital heart conditions, including long QT syndrome
- The electrolytes must be balanced to ensure that they are conductors of electrical impulses
- Medication side effects
- The use of drugs like methamphetamine and cocaine
In some instances, the cause of the ventricular tachycardia cannot be identified (idiopathic ventricular Tachycardia).
The electrical system of the heart.
To better understand the root of heart rate problems or rhythm issues like tachycardia, it is helpful to understand how the electrical system of the heart functions.
The heart is comprised of four chambers: two chambers in the upper (atria) along with two lower chambers (ventricles). The heartbeat is controlled by a naturally-occurring pacemaker, called the sinus node. It lies in the atrium of your right. The sinus node creates electrical impulses, which normally begin every heartbeat.
Through the sinus node, electrical impulses flow across the atria and cause the muscles in the atrial region to tighten and to pump blood to smaller chambers in the heart (ventricles).
The electrical signals then land at a collection of cells known as an Atrioventricular (AV) node, which is generally the sole route for signals to go between the atria and the ventricles.
The AV Node slows down electrical signal before it is sent through the ventricles. This delay is just enough to allow ventricles to fill up with blood. When electrical signals reach the ventricles’ muscles they contract, prompting them to push blood to the lungs or the rest of the body.
If anything disturbs this intricate system, it could cause the heartbeat to be too quickly (tachycardia) or too slowly (bradycardia) or have irregular heartbeats.
Risk factors
Any illness that puts an undue strain on your heart or causes damage to the heart tissue could increase your chance of suffering from ventricular Tachycardia. Medical treatment or lifestyle changes could reduce the risk associated with the following risk factors:
- Heart disease
- Medication side effects
- Severe electrolyte imbalances
- Utilization of stimulant drugs, like methamphetamine and cocaine
If you’ve got a family background of ventricular tachycardia or any other irregular heartbeats, then you could be at a higher risk of Ventricular Tachycardia.
Complications
Complications of ventricular Tachycardia differ in severity and are based on the speed at which your heart beats as well as how long the rapid heartbeat continues, how frequently the tachycardia happens and the overall health of your heart. Some possible complications include:
- Consistent fainting or unconsciousness
- Heart failure
- Sudden death due to cardiac arrest
Ventricular fibrillation
A potentially dangerous condition associated with ventricular tachycardia can be ventricular fibrillation (V-fib). In vfib, the lower chambers of your heart contract very quickly and uncoordinatedly way.
The abnormal rhythm is seen typically in patients who suffer from heart disease or a previous heart attack. It could also be due to electrolyte issues (such as low or high potassium levels) or, more rarely the heart is otherwise healthy.
Ventricular fibrillation could also cause sudden cardiac arrest, which can cause death if not treated promptly.
Prevention
The most effective way to avoid ventricular tachycardia is by treating or eliminating risk factors that can cause heart disease. If you are already suffering from heart disease, you must follow your treatment regimen and lifestyle that is healthy for your heart.
Follow these steps:
- Get active and eat a wholesome food plan. Live a heart-healthy life by regularly exercising and eating a balanced low-fat, low-fat diet that’s abundant in vegetables, fruits along with whole-grains.
- Maintain an ideal weight. Being overweight increases your chance to develop heart problems.
- Maintain cholesterol levels and blood pressure in check. Make lifestyle changes and take prescribed medication to treat the problem of high blood pressure (hypertension) and high cholesterol.
- Manage the stress. Avoid unnecessary stress and learn strategies to deal with stress in a healthy manner.
- Do not use recreational drug. Don’t use stimulants like cocaine. Discuss with your physician the best program for you if you require assistance with stopping recreational drug use.
- Check-ups are scheduled for the day. Have regular physical examinations and report any signs or symptoms to your physician.
- Limit your consumption of alcohol. If you choose to consume alcohol, you should do it in moderate quantities. for healthy people, this is one drink per day for women from all age groups, those over 65, and as much as two drinks per day for those aged 65 or younger. For certain ailments, it’s suggested to avoid drinking alcohol completely. Consult your physician for advice specific to your situation.
- Limit the amount of caffeine. If you drink caffeinated drinks, drink it moderately (no greater than 1 or two drinks a day).
- Quit smoking. If you smoke and are unable to quit by yourself consult your physician about programs or strategies to aid you in breaking the smoking habit.
- Take your prescription medications with care. Some cold and cough medicines contain stimulants that can cause rapid heartbeats. Consult your physician about the drugs you should stay away from.
Diagnosis
A thorough physical examination along with medical history and testing is necessary to determine if you have the condition of ventricular tachycardia.
Your doctor will assess your symptoms, conduct an examination of your body and inquire about your lifestyle and medical background. In some instances, ventricular tachycardia could be an emergency medical situation that requires immediate evaluation and intervention.
There are a variety of tests that can be conducted to determine if you have the condition of Ventricular Tachycardia.
 Electrocardiogram (ECG also known as EKG) is the largest and most commonly used tool to detect the presence of tachycardia. The test is painless and the heart’s electrical activity by using tiny sensors (electrodes) that are attached to your chest and arms.
Electrocardiogram (ECG also known as EKG) is the largest and most commonly used tool to detect the presence of tachycardia. The test is painless and the heart’s electrical activity by using tiny sensors (electrodes) that are attached to your chest and arms.
An ECG test measures the strength and timing of electrical signals as they move throughout your heart. Your doctor can search for patterns in those signals and determine the type of tachycardia you suffer from and what issues in your heart might be contributing to rapid heart rate.
Your doctor may also suggest you carry the portable devices at home to get additional information regarding the heartbeat. These devices include:
- Holter monitor. It is portable and you can carry it around. The device can be carried in your pocket or put in your Belt or shoulder strap. It tracks the heart’s activity over the entire 24 hours that allows your doctor to take a longer examination of your heart’s rhythms. Your doctor is likely to request that you keep a journal for the same period of time. You’ll write down any symptoms you experience and note the time when they happen.
- Event monitor. This is a portable EKG. This device is designed to record your heart rate over the course of a few months. It is worn all day long, but it will record only at specific times for a short period of time at the same time. It is usually activated by pressing a button whenever you notice signs of a rapid heart rate. Some monitors, however, automatically detect abnormal heart rhythms and begin recording.
- Additional screens. Some personal devices like smartwatches can provide electrocardiogram monitoring. Discuss with your doctor whether this is an option for you.
- Transtelephonic Monitor. This device provides continuous monitoring of heartbeats however, it must be worn for a long time. It could or might not contain wires.
- A recorder that can be implanted. This is an implantable device with no wires, and it can be placed under your skin for as long as three years, to keep track of your heart’s rhythm.
Electrophysiological test
The doctor might recommend an electrophysiological test to confirm your diagnosis or to determine the source of the problem in your heart.
In this test, a physician introduces flexible, thin tubes (catheters) that are topped with electrodes in your arm, groin, or neck, and guides them through blood vessels to the various locations within your heart. Once they are in place, the electrodes are able to precisely track the electrical impulses that travel throughout each heartbeat and detect irregularities in your circuit.
Cardiac imaging
The doctor might take images from your heart, to see whether structural issues can affect blood flow, and are causing your ventricular Tachycardia.
Cardiac imaging tests to determine if a ventricular tachycardia is a present include:
- Echocardiogram. An echocardiogram creates an image of the heart with sound waves. It is able to identify areas of low circulation, heart valves, and muscles that aren’t working normally.
- Imaging with magnetic resonance (MRI). A cardiac MRI It can give still or moving images of the way blood is moving through the heart. It can also be used to detect any irregularities.
- Computerized Tomography (CT). CT scans are a combination of several X-rays to provide a better sectional view of the heart.
- Angiogram of your coronary. To study the circulation of blood through your blood vessels and the heart Your doctor might perform a coronary angiogram in order to detect obstructions or other abnormalities. The procedure uses a dye as well as special X-rays that show the insides of the coronary arteries.
- Chest Xray. This test is used to capture still images of your lungs and heart and detect whether your heart is larger.
A look inside the heart using MRI
Cardiac MRI offers images that are still or moving of the blood moving through the heart and detects any irregularities. It is commonly used to detect ventricular tachycardia.
Stress test
Your doctor may suggest the stress test to check the way your heart functions during your activity or when you are prescribed medication to make your heart run more quickly.
In an exercise stress test, the electrodes will be placed over your chest in order to check your heart’s activity while you exercise, typically using the treadmill. Other tests for heart function could be conducted in conjunction with the stress test.
Tilt table test
This test can be utilized to assist your doctor know how your tachycardia can contribute to fainting periods. With careful supervision, the patient will receive medicine that triggers a tachycardia event. You lay flat on a table and the table is tilted to the point that it appears as like you’re standing. The doctor will note the way that your nervous and heart react to these changes in posture.
Additional tests
Your doctor might order additional tests to determine if there is an underlying issue that is causing heart tachycardia ventricular and assess the health that your heart is in.
Treatment
MDtodate doctors provide specialized treatment to treat ventricular tachycardia with the most advanced treatments technologies.
The primary goals of ventricular Tachycardia treatment include:
- Restore a normal heart beat
- Manage the heart rate of your fast at the time it occurs.
- Avoid future episodes of tachycardia.
The type of treatment you are given is dependent on the cause of the arrhythmia as well as the nature or degree of your ventricular tachycardia.
The tachycardia in the ventricular region could disappear by itself in less than 30 minutes (nonsustained V-tach ) or last longer than thirty seconds (sustained V-tach or VT ). Sustained VT could disrupt the normal flow of blood and require immediate medical attention.
Treatment for ventricular tachycardia that is sustained
The condition is often referred to as sustained ventricular tachycardia and needs medical attention immediately in order to prevent cause sudden cardiac death.
Treatment involves restoring normal heart beat by sending the heart with a surge of electric current. the heart. This can be accomplished with an implantable defibrillator or through the treatment known as cardioversion.
Defibrillation is performed using the automated external defibrillator (AED) or by a passerby who is aware of the symptoms warnings of cardiac collapse.
Cardioversion can be performed in a hospital environment using the aid of a device that monitors your heart’s rhythm before and after shocks are given. In this method, medical experts shock your heart with paddles as well as the automated external defibrillator (AED) or patches placed on your chest.
You can also receive medication via mouth or intravenous (intravenously).
In preventing episodes of a rapid heart rate
Through treatment, it might be possible to stop or reduce the frequency of Ventricular Tachycardia.
- Catheter ablation. This technique is commonly utilized when a distinct electrical pathway is the cause of an increase in heart rate. In this process, the doctor inserts catheters into your heart via the veins that run through your arm, groin, or neck. The electrodes at the tips of the catheter could utilize extreme radiation or cold to destroy (ablate) the electrical pathway and block the electrical signal from being transmitted to it.
- Medicines. Anti-arrhythmic medications may slow the heart rate when they are used regularly. Other heart-related medicines, such as beta blockers, calcium channel blockers can be prescribed in conjunction with anti-arrhythmic medicines.
- Implantable cardioverter-defibrillator. If you’re at risk of having a life-threatening tachycardia episode, your doctor may recommend an implantable cardioverter-defibrillator (ICD). The device, which is sized like a pager, is surgically implanted inside your chest. The ICD device continuously monitors your heartbeat determines an increase of your heart rate and gives precisely calibrated electrical stimulation when needed to restore a healthy heart rhythm.
- Surgery. Surgery to open the heart may be required in certain cases to address a cause that contributes to ventricular Tachycardia (for example, in the event that there is blockage of the blood vessels). Tachycardia is also treated using a maze process. In this procedure, the surgeon makes tiny cuts in the heart tissue to create a pattern or maze made of the scar. Since scar tissue isn’t able to carry electricity through it, it causes interference with the stray electrical impulses which trigger a variety of tachycardia. Surgery is generally only needed when other treatments do not work, or if surgery is required to treat a heart problem.
Diagnose and treat any disease that is present
If a medical condition contributes to ventricular tachycardia like coronary artery disease, receiving treatment for the root issue can prevent or decrease the frequency of ventricular tachycardia events.
Follow-up on your treatment program is essential. It will help reduce your chance of developing the development of heart rhythm issues in the future. If your symptoms change or get worse or you develop new symptoms, tell your doctor immediately.
Support and Coping
When you’ve got a strategy that you have in place to handle the sudden occurrence of a rapid heartbeat, you might be more relaxed and feel more in control whenever one happens. Consult your physician about:
- How do you take your pulse and what’s the normal pulse rate for you
- When should you call your doctor?
- When should you seek emergency medical attention?

Hi there, just became aware of your blog through Google,
and found that it is truly informative. I am going to watch out for brussels.
I will appreciate if you continue this in future. A lot of people will be benefited
from your writing. Cheers! Najlepsze escape roomy
You have remarked very interesting points! ps decent internet site.!