Overview
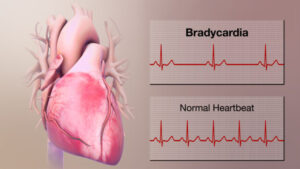
Bradycardia is lower than the normal heart rate. Adults’ hearts at rest generally are able to beat around 60 to 100 times per minute. If you suffer from bradycardia your heart beats less than 60 times per minute.
Bradycardia is a serious issue if your heart is extremely slow and the heart isn’t able to supply enough oxygen-rich blood to the body. If this occurs you might feel tired, dizzy weak, or exhausted. Bradycardia can cause no signs or unexplained complications.
A heartbeat that is slow isn’t always an issue. For instance, a heart rate that is between 40-60 beats per minute is fairly common sleep. It can also be observed in certain individuals, in particular, especially young adults who are healthy and well-trained athletes¹.
If bradycardia has become severe A pacemaker implanted may be necessary to help the heart to maintain a normal rate.
Symptoms
A heartbeat that is slower than normal (bradycardia) could stop the brain as well as other organs from receiving enough oxygen. It could result in these symptoms and signs:
- Chest pain
- Memory problems or confusion
- Lightheadedness or dizziness
- It is easy to get tired during physical exercise.
- Fatigue
- Affliction (syncope) or close-to-fainting
- Breathing shortness
When is the best time to seek medical attention?
A variety of things can cause symptoms and signs of bradycardia. It is crucial to receive an immediate, accurate diagnosis and the appropriate treatment. Talk to your doctor when the child or you is suffering from signs of bradycardia.
If you experience a fainting spell, difficulty breathing, or chest pain that lasts longer than several minutes, contact 911 or call emergency medical services. Get emergency medical attention for anyone suffering from these symptoms.
Causes
Bradycardia is caused by:
- Heart tissue damage due to age
- Heart tissue damage from a heart attack or disease
- A heart disorder present at birth (congenital heart defect)
- Inflammation of the heart tissue (myocarditis)
- A heart-related complication that can be a result of surgery.
- A thyroid gland that is underactive (hypothyroidism)
- Chemical imbalances in the blood, for example, calcium or potassium
- Breathing pauses that are repeated in sleep (obstructive sleep apnea)
- Inflammatory diseases, like Lupus or lupus, are both inflammation-related diseases.
- Medicines, such as opioids, sedatives, and medications used to treat heart rhythm problems as well as high blood pressure, and various mental health conditions.
To better understand the cause of bradycardia it might be beneficial to understand how the heart normally beats.
The typical heart is comprised of four chambers: two chambers in the upper (atria) as well as two chambers in the lower (ventricles). In the upper right chamber within the heart (right atrium) is a collection of cells referred to as”the sinus node. The sinus node acts as the heart’s pacemaker. It is the source of the signal that triggers every heartbeat.
Bradycardia happens when the signals slow down or get blocked.
Sinus node problems
The majority of cases of Bradycardia begin in the heart area known as”sinus node”. In some people, sinus node problems cause alternating slow and fast heart rates (bradycardia-tachycardia syndrome).
Heart block (atrioventricular block)
Bradycardia can also happen if the electrical signals from the heart aren’t moving in a proper manner between those chambers in the top (atria) towards the chambers below (ventricles). If this happens it’s known as heart block or Atrioventricular block.
Heart blocks are divided into three major groups.
- Heart block of the first degree. In the mildest form, it is when all electrical signals originate from the atria and reach the ventricles, however, the speed of signaling is reduced. Heart block of the first degree rarely triggers symptoms and generally doesn’t require treatment if there’s no issue with electrical signaling.
- Heart block of the second degree. Not all electrical signals can reach ventricles. A few beats are missed which causes a slower and occasionally irregular heart beat.
- third-degree (complete) heart block. None of the electrical signals emanating from the atria can reach the ventricles. In this case, the ventricles are likely to beat by themselves, however at a very low rate.
Risk factors
Bradycardia can be linked to damaged heart tissue due to certain heart diseases. Anything that can increase the chance of developing heart issues increases the risk of developing bradycardia. Heart disease risk factors include:
- Older age
- High blood pressure
- Smoking
- Heavy alcohol use
- Illegal use of drugs
- Stress and anxiety
Lifestyle changes that promote health or medical treatments can reduce the risk of developing heart disease.
Complications
The possible complications of bradycardia are:
- Frequent fainting
- Heart is unable to pump blood enough (heart failure)
- Sudden cardiac arrest or sudden death
Prevention
Bradycardia is often caused by certain medications, especially when they’re taken in large doses. It’s crucial to take all medicines as prescribed. While bradycardia isn’t usually prevented, doctors suggest strategies to lower the chance of developing heart disease. Follow these heart-healthy guidelines:
- Regularly exercise. Your health care physician may provide suggestions on how much and which kind of exercise is the best for you.
- Consume a balanced diet. Choose a healthy low-fat, low-salt, and low-sugar diet rich in vegetables, fruits along with whole wheat.
- Maintain an ideal weight. Being overweight increases the likelihood of developing heart diseases.
- Maintain blood cholesterol and pressure under control. Make lifestyle changes and take the medications prescribed to control diabetes, high blood pressure, and cholesterol levels.
- Do not Smoke. If you need assistance in quitting smoking, speak to your doctor or health professional about programs or strategies to assist you.
- If you consume alcohol, do it in moderate amounts. If you choose to consume alcohol, you should do it in moderate amounts. For healthy adults, this could mean drinking up to one drink per day for women, and 2 drinks max per day for males. If you’re unable to limit your alcohol intake and you are struggling, speak to your health professional regarding a program that will help you stop drinking and control other behavior associated with alcohol use.
- Take care of anxiety. Intense emotions may alter the heart rate. A few ways to ease stress include regular exercise as well as joining a support network and experimenting with relaxation techniques like yoga.
- Check-ups are scheduled for the day. Have regular physical examinations and report any symptoms or signs to your physician.
Check and treat any existing heart condition
If you have already been diagnosed with heart disease There are ways to reduce your chance of developing bradycardia, or another heart rhythm condition:
- Follow the guidelines. Be sure you know the treatment strategy. Follow the prescribed medication as directed.
- Inform your doctor immediately of any changes. If your symptoms get worse or change, or you experience new symptoms, notify your doctor right away.
Diagnosis
In order to diagnose bradycardia, your doctor typically performs an exam of the body in addition to listening to your heart using the Stethoscope. They will ask you questions regarding your symptoms and medical background.
Your doctor might recommend tests to examine your heart rate to determine whether you suffer from an issue with your heart that could cause bradycardia. The blood tests can be performed to look for other issues that could cause slow heartbeats. These could include an illness an inactive thyroid (hypothyroidism) or an imbalance in electrolytes.
Tests
An electrocardiogram (ECG also known as an EKG) can be the most important test used to detect bradycardia. An ECG analyzes how much electrical energy is generated by the heart. The heart’s electrical activity is measured. The conductive patch (electrodes) can be placed over the chest, and occasionally the legs and arms. The electrodes are connected with wires to a computer which shows the results. It is possible to determine if the heart is beating too slowly or too fast, or not at all.
It is not possible to detect bradycardia until a slow heartbeat is observed in the course of the test. Your healthcare provider may suggest the use of a portable ECG device. Portable ECG devices include:
- Holter Monitor. Carried in a pocket or attached to the belt or shoulder strap it monitors the heart’s activity continuously for up to 24 hours.
- Recorder for events. This device is like the Holter monitor, however, it records only at specific intervals for a couple of minutes at one time. It’s more worn than the Holter monitor, which is typically 30 days. The typical user presses a button when you are experiencing symptoms. Some devices record automatically whenever an irregular heart rhythm is observed.
It is possible to combine other tests to determine the effects of bradycardia on you. The tests are:
- Tilt table. This test may aid your doctor in better understanding the way your bradycardia triggers fainting episodes. While you are lying flat on a table that is tilted to make it appear as if you’re standing up. The tilt test is conducted to determine whether any change in the position of the table results in fainting.
- Stress exercise test. It is possible to track your heart’s activity as you ride stationary bikes or run on the treadmill. If you’re having difficulty exercising or walking, a medication could be administered to stimulate the heart in a manner that’s comparable to exercising.
A sleep test may be suggested if your medical professional suspects that breathing pauses that are repeated while you sleeping (obstructive sleep apnea) can cause bradycardia.
Treatment
The treatment for bradycardia is based upon the intensity of the symptoms and the reason for the heart rate slowing. If you’re not experiencing any symptoms, treatment may not be required.
Treatment for Bradycardia may involve lifestyle modifications, medication adjustments as well as an implanted gadget referred to as a pacemaker. If a health issue is underlying like sleep apnea or thyroid disease that is causing the faster than normal heartbeat treatment for that issue could correct the bradycardia.
Medications
A variety of medications, such as those that treat other heart diseases, can trigger bradycardia. Be sure to let your doctor be aware of any medicines you are taking, even ones purchased without a prescription.
If you’re taking a medication that causes bradycardia your physician may suggest a lower dose or a different drug.
Other surgical procedures, or surgery
If other treatment options aren’t feasible and bradycardia symptoms become severe and severe, a device known as the pacemaker is needed to regulate the heartbeat. Pacemakers are only used when it is they’re required. If the heartbeats slow, the pacemaker sends electronic signals that signal the heart, which increase the speed of the beat.
Implanting a pacemaker requires surgery. A wire or two is placed through a vein underneath or around the collarbone. They are directed to the heart with an X-ray guide. The wire’s one end is secured to the proper location in the heart while the other is connected to the device (pulse generator) placed under the skin, beneath the collarbone.
A leadless pacemaker² is less invasive and usually requires a less invasive procedure to insert the device.

Wow, wonderful weblog format! How lengthy have you ever been running a
blog for? you made blogging look easy. The whole look of your web site is fantastic, let alone the content material!
You can see similar here najlepszy sklep
Hello would you mind sharing which blog platform you’re working with?
I’m looking to start my own blog in the near
future but I’m having a difficult time choosing between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style
seems different then most blogs and I’m looking for
something unique. P.S My apologies for being
off-topic but I had to ask! I saw similar here: Sklep internetowy
Hey there! Do you know if they make any plugins to help with Search Engine Optimization? I’m trying to get my blog to rank for some targeted keywords but
I’m not seeing very good success. If you know of any please share.
Many thanks! You can read similar blog here: Sklep internetowy
It’s very interesting! If you need help, look here: ARA Agency
Hi there! Do you know if they make any plugins to assist
with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m
not seeing very good gains. If you know of any please share.
Thanks! You can read similar text here: Sklep online
Hi there! Do you know if they make any plugins to help with Search Engine Optimization? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very
good results. If you know of any please share. Cheers!
You can read similar text here: Sklep online
Hi there! Do you know if they make any plugins to help
with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not
seeing very good success. If you know of any please share.
Cheers! You can read similar article here: Dobry sklep
Hi! Do you know if they make any plugins to help with Search Engine Optimization? I’m trying to get my blog to rank
for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Kudos! I saw similar
text here: Backlink Building
Hi! Do you know if they make any plugins
to help with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very
good gains. If you know of any please share. Cheers! I saw similar text here: Backlink Building
Hi! Do you know if they make any plugins to help with Search Engine Optimization?
I’m trying to get my site to rank for some targeted keywords but I’m not seeing very
good success. If you know of any please share. Cheers! I saw similar article here: Scrapebox AA List
Hi! Do you know if they make any plugins to assist with SEO?
I’m trying to get my site to rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Many thanks!
I saw similar blog here: Backlink Building
brazilian pharmacy online
Wow, incredible weblog layout! How long have you been running a blog for?
you made blogging glance easy. The overall glance of your website is excellent, as neatly as the content material!
You can see similar here dobry sklep
pharmacy discount coupons
batmanapollo.ru
deep dark web https://mydarkmarket.com/ – darknet site dark website
Age, libertate decembri utere — Ну же, пользуйся свободой декабря
diflucan online pharmacy
Amicus cognoscitur amore, more, ore, re — Друг познаётся по любви, нраву, лицу, деянию.
Ad extremitates — До крайности.
Benevole lector — Благосклонный читатель.
Ad gustum — По вкусу.
Ad extremitates — До крайности.
Aequo pulsat pede — Смерть безучастно поражает любого.
Министерство неджентльменских дел
Министерство неджентльменских дел
Министерство неджентльменских дел
Министерство неджентльменских дел
Министерство неджентльменских дел
Бой Александр Усик — Тайсон Фьюри 18 мая 2024 года
Усик Фьюри – смотреть онлайн
Александр Усик — Тайсон Фьюри
Фуриоса: Хроники Безумного Макса
Фуриоса: Хроники Безумного Макса
Фуриоса: Хроники Безумного Макса
Фуриоса: Хроники Безумного Макса
Психология
Психолог тут
Психолог тут
Психология
onion market https://mydarknetmarketlinks.com/ – darknet search engine bitcoin dark web
blackweb https://mydarknetmarketlinks.com/ – darkmarkets dark web sites
Матвейчев О.А. и лучшие книги по психотерапии.
Veni, vidi, vici
Dictum – factum
Смотреть онлайн 100 лет тому вперед фильм 2024 бесплатно в хорошем качестве. 100 лет тому вперед смотреть онлайн бесплатно.
100 лет тому вперед смотреть онлайн бесплатно в хорошем. Смотреть фильм 100 лет тому вперед 2024.
Пацаны 4 сезон кино
Уэнздей смотреть онлайн
canadian online pharmacy for viagra
reputable online pharmacy
Фоллаут смотреть онлайн
戦国パチスロ花の慶次~戦極めし傾奇者の宴~(自动转)
非常に実用的で、具体的な例が豊富なのがとても役立ちます。
Психолог онлайн
geinoutime.com
Wang Jinyuan의 말을 듣고 Qi Zhiyuan은 경계했습니다.
I love how you present information in such a clear and engaging way. This post was very informative and well-written. Thank you!peakpulsesite
緑イミソーレ
とてもユニークで興味深い視点を提供してくれてありがとうございます。
k8 カジノ 登録
この記事のおかげで、多くの実用的な知識を得ることができました。
Претенденты смотреть Претенденты фильм, 2024, смотреть онлайн
k8 カジノ kyc
このブログはいつも私の期待を超えてきます。本当に感謝しています。
k8 カジノ 評判
素晴らしい記事でした!とても感動しました。
nolvadex 10mg tablets price
いみそーれ(红花)
このように実用的な記事は他にはない。本当に役に立ちます。
Your blog is a wealth of information. I always learn something new from your posts. This one was particularly enlightening. Great job!blogpulse
Aw, this is a really good post. In thought I have to put in place writing in this way moreover – spending time and actual effort to create a top notch article… but exactly what do I say… I procrastinate alot and by no means apparently get something done.
Thank you a lot for sharing this with all people you really realize what you are talking about! Bookmarked. Kindly also consult with my web site =). We could have a link alternate arrangement between us!
Would love to always get updated great site ! .
Congratulations on having one of the most sophisticated blogs Ive come across in some time! Its just incredible how much you can take away from something simply because of how visually beautiful it is. Youve put together a great blog space –great graphics, videos, layout. This is definitely a must-see blog.
I just added this blog site to my feed reader, great stuff. Can not get enough!
I have been reading out a few of your stories and it’s pretty nice stuff. I will make sure to bookmark your site
Nice post. I find out something harder on different blogs everyday. It will always be stimulating to see content off their writers and practice something from their store. I’d choose to apply certain with all the content in my blog no matter whether you do not mind. Natually I’ll give you a link with your internet weblog. Thank you for sharing.
I conceive you have mentioned some very interesting details , appreciate it for the post.
When I originally commented I clicked the -Notify me when new comments are added- checkbox now whenever a comment is added I recieve four emails with similar comment. Could there be however you can eliminate me from that service? Thanks!
Howdy, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam feedback? If so how do you protect against it, any plugin or anything you can suggest? I get so much lately it’s driving me mad so any support is very much appreciated.
well, i would say that infertility can be a thing of the past because of modern advancements in medicine.
I’m impressed, I have to admit. Genuinely rarely can i encounter a blog that’s both educative and entertaining, and without a doubt, you’ve hit the nail for the head. Your notion is outstanding; the thing is something inadequate folks are speaking intelligently about. My business is very happy that we found this within my seek out some thing in regards to this.
Wonderful post was very happy reading the really important information for me thanks, I thought the man in the future. I will surely recommend this article with your friends, family and friends. You are really great so allowing good articles.
when we are looking for apartment for rents, we usually choose those with very clean rooms”
you can earn lots of money if you are into the franchising business. i would love to engage into this kind of business“
An fascinating discussion will be worth comment. I’m sure that you need to write much more about this topic, may possibly not certainly be a taboo subject but usually people are not enough to communicate in on such topics. To another location. Cheers
I truly appreciate this post. I have been looking all over for this! Thank goodness I found it on Bing. You have made my day! Thx again
I do agree with all the ideas you have presented in your post. They’re really convincing and will certainly work. Still, the posts are too short for starters. Could you please extend them a bit from next time? Thanks for the post.
You made some decent points there. I looked on the web for the problem and located most people is going coupled with with the web site.
Free PORN Download. Free XXX links. Clips, Movies, Magazines, Galleries, DVDs and much more.
Hello! Someone in my Myspace group shared this website with us so I came to take a look. I’m definitely loving the information. I’m bookmarking and will be tweeting this to my followers! Terrific blog and outstanding style and design.
The next occasion Someone said a weblog, I’m hoping who’s doesnt disappoint me approximately brussels. After all, It was my option to read, but I really thought youd have some thing intriguing to talk about. All I hear is a couple of whining about something that you could fix should you werent too busy looking for attention.
I’m impressed, I must say. Genuinely rarely must i encounter a blog that’s both educative and entertaining, and without a doubt, you’ve got hit the nail about the head. Your notion is outstanding; the issue is an issue that too few persons are speaking intelligently about. I will be very happy that we found this inside my hunt for something concerning this.
Nice post. I learn something more difficult on various blogs everyday. It will always be stimulating to read content off their writers and practice a little something there. I’d opt to use some with the content in my small weblog whether you do not mind. Natually I’ll supply you with a link on your web blog. Many thanks sharing.
Good site! I really love how it is easy on my eyes and the data are well written. I am wondering how I might be notified whenever a new post has been made. I’ve subscribed to your RSS feed which must do the trick! Have a great day!
Im no pro, but I believe you just crafted the best point. You definitely fully understand what youre talking about, and I can seriously get behind that. Thanks for staying so upfront and so honest.
hinduism is a good religion, my father is hindu and also my mother.
you are really a good webmaster. The site loading speed is incredible. It seems that you are doing any unique trick. Furthermore, The contents are masterwork. you have done a excellent job on this topic!
Good day I am so excited I found your webpage, I really found you by mistake, while I was looking on Google for something else, Regardless I am here now and would just like to say many thanks for a fantastic post and a all round enjoyable blog (I also love the theme/design), I don’t have time to look over it all at the moment but I have bookmarked it and also added in your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the great job.
It’s one thing to show conflict between the two but when they come to blows, it just seemed so un-Spocklike.
being a blogger myself . i can see someone with great potential”
I must say, I think your really on point with this, I can’t say I am completely on the same page, but its not big of a deal .
Heya i’m for the first time here. I found this board and I find It truly useful & it helped me out a lot. I hope to give something back and help others
Sweet web site , super design , real clean and utilise pleasant.
Can I simply say what relief to get somebody that in fact knows what theyre dealing with on-line. You actually know how to bring a concern to light to make it essential. Workout . should ought to see this and can see this side of your story. I cant think youre less well-known simply because you definitely hold the gift.
You should join in a tournament first of the finest blogs online. I will suggest this website!
very nice publish, i definitely love this web site, keep on it
Can I just say thats a relief to get a person that truly knows what theyre discussing on the web. You actually understand how to bring a concern to light and produce it important. The diet need to read this and can see this side with the story. I cant believe youre not more well-liked since you undoubtedly contain the gift.
You have observed very interesting points ! ps decent internet site .
I just added this weblog to my feed reader, excellent stuff. Cannot get enough!
Just now you can branch out from your daily understanding. Don’t give up your morals for anything. This will lead to a sad and unfulfilling life.
I recently noticed your website back i are generally looking through which on a daily basis. You’ve got a loads of information at this site so i actually like your look to the web a tad too. Maintain the best show results!
Hey! Do you know if they make any plugins to help with Search Engine
Optimization? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very
good success. If you know of any please share. Cheers! I saw similar text here: Escape rooms review
Thankyou for this wondrous post, I am glad I observed this website on yahoo. [Reply]
Christian Dior is really a genious when it comes to making those fancy dresses”
I have realized some considerations through your blog post. One other stuff I would like to talk about is that there are numerous games on the market designed specifically for toddler age young children. They include pattern acknowledgement, colors, dogs, and styles. These generally focus on familiarization instead of memorization. This keeps little ones occupied without having a sensation like they are studying. Thanks
Folks have no clue that this is out there. Your thinking is crucial in assisting me with my exploration. I’m hoping for one more write-up down these topics soon.
hey was just seeing if you minded a comment. i like your site and the theme you picked is super. I will be back.
There is noticeably a lot of money to know about this. I assume you made certain nice points in features also.
Hi there! I know this is kind of off topic but I was wondering if you knew where I could locate a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having trouble finding one? Thanks a lot!
You could not enter into great depth, however you presented the necessities I desired to get help me thru. Was I ever really surprised to locate your blog. Please continue on your quest.
Oh my goodness! a fantastic article dude. Thank you However I will be experiencing issue with ur rss . Do not know why Can not sign up for it. Is there any person acquiring identical rss problem? Anyone who knows kindly respond. Thnkx
You have noted very interesting points ! ps nice internet site .
display cabinets with transparent glass would be the best thing to keep your stuff,,
There are a couple of fascinating points on time in this post but I don’t know if all of them center to heart. There may be some validity but I’m going to take hold opinion until I investigate it further. Excellent post , thanks so we want a lot more! Put into FeedBurner as well
Many thanks for being the mentor on this niche. We enjoyed the article greatly and most of all appreciated how you really handled the issues I regarded as being controversial. You are always very kind towards readers really like me and assist me to in my life. Thank you. Palm Beach Gardens
Your blog is amazing dude. i love to visit it everyday. very nice layout and content “
You can also put a chatbox on your blog for more interactivity among readers.”,**,
I conceive this web site contains some rattling fantastic info for everyone : D.
An impressive share, I just with all this onto a colleague who was doing a small analysis on this. And that he in reality bought me breakfast due to the fact I came across it for him.. smile. So permit me to reword that: Thnx for that treat! But yeah Thnkx for spending enough time to go over this, I’m strongly regarding this and enjoy reading more on this topic. When possible, as you become expertise, can you mind updating your website with additional details? It really is extremely great for me. Huge thumb up because of this short article!
I am glad to be one of several visitants on this great web site (:, thankyou for putting up.
I’d should talk to you here. Which is not some thing I do! I quite like reading a post which will make people believe. Also, many thanks permitting me to comment!
Oh my goodness! an amazing article dude. Thank you Nevertheless I’m experiencing problem with ur rss . Do not know why Unable to subscribe to it. Is there everyone obtaining identical rss issue? Everyone who knows kindly respond. Thnkx
Thanks for the great post on your blog, it really gives me an insight on this topic.*~“:
This blog was… how do you say it? Relevant!! Finally I’ve found something that helped me. Many thanks.
It’s perfect time to make a few plans for the future and it is time to be happy. I have learn this put up and if I may I wish to suggest you few attention-grabbing issues or advice. Maybe you could write next articles referring to this article. I want to read more issues about it!
I love the efforts you have put in this, appreciate it for all the great articles .
I found your blog on yahoo and can bookmark it currently. carry on the nice work.
I agree with you. I wish I had your blogging style.
It’s not that I want to duplicate your web site, but I really like the design and style. Could you let me know which design are you using? Or was it tailor made?
Please keep on dropping such quality storys as this is a rare thing to find these days. I am always searching online for posts that can help me. looking forward to another great website. Good luck to the author! all the best!
I gotta bookmark this site it seems very useful .
Thanks for this specific advice I was basically researching all Msn in order to uncover it!
I have been surfing on-line greater than 3 hours today, yet I never found any fascinating article like yours. It’s lovely worth sufficient for me. In my opinion, if all website owners and bloggers made good content material as you probably did, the internet shall be a lot more useful than ever before!
After study many of the blog posts in your website now, and i really appreciate your way of blogging. I bookmarked it to my bookmark site list and will also be checking back soon. Pls look into my site likewise and figure out what you believe.
Hi, Neat post. There’s an issue with your web site in internet explorer, may check this¡K IE nonetheless is the marketplace chief and a good portion of people will miss your fantastic writing because of this problem.
i would love to munch so many italian foods, italian foods are the best in my opinion and they are very tasty.,
Thank You For This Post, was added to my bookmarks.
This web-site is usually a walk-through like the info you wished relating to this and didn’t know who to inquire about. Glimpse here, and you’ll certainly discover it.
Howdy just wanted to give you a brief heads up and let you know a few of the pictures aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same outcome.
Hi just wanted to give you a brief heads up and let you know a few of the images aren’t loading properly. I’m not sure why but I think its a linking issue. I’ve tried it in two different browsers and both show the same results.
geinoutime.com
옆의 Xiao Jing은 Hongzhi 황제를 위해 서둘러 닦았습니다.
Thanks for every other excellent post. The place else may just anyone get that kind of info in such an ideal manner of writing? I’ve a presentation subsequent week, and I am at the look for such information.
You made some nice points there. I did a hunt on the theme and found mainly persons will accept as true with your blog.
A very exciting go through, I may not agree completely, but you do make some really legitimate factors.
I admit, I have not been on this webpage in a long time… however it was one more joy to see It is such an significant topic and also ignored by so many, even professionals. I thank you to support making people more aware of possible issues.
After study a handful of the content in your website now, and i also really like your technique for blogging. I bookmarked it to my bookmark site list and will be checking back soon. Pls look at my web site as well and inform me how you feel.
I also didn’t care for the over-the-top “final mission” where this particular platoon, led by the initially realistic but ultimately too heroic Aaron Cleftjaw, manages to locate (spoiler) and destroy the inevitable mothership.
I’m curious to find out what blog system you are utilizing? I’m having some small security problems with my latest blog and I would like to find something more risk-free. Do you have any solutions?
Perfect piece of work you have done, this site is really cool with great information.
This web site is often a walk-through it really is the internet it suited you with this and didn’t know who to question. Glimpse here, and you’ll undoubtedly discover it.
Exactly where might I get a hold of this page layout?
I have been reading out many of your articles and i can claim pretty nice stuff. I will make sure to bookmark your blog.
Lady Gaga talked in front of masses of people at EuroPride this year, in favor of with regard to gay rights along with equality.
The following time I learn a weblog, I hope that it doesnt disappoint me as much as this one. I imply, I do know it was my option to read, however I really thought youd have one thing attention-grabbing to say. All I hear is a bunch of whining about one thing that you might fix in case you werent too busy in search of attention.
Your ability to write about this kind of info is just the thing we all desire. Simply by discussing your knowledge you support people thru discussing your own personal observations. And I’ll let you know right now your writing served me personally.
I always visit new blog everyday and i found your blog.’”‘*;
Hello there, just became alert to your blog through Google, and found that it’s truly informative. I’m gonna watch out for brussels. I will appreciate if you continue this in future. A lot of people will be benefited from your writing. Cheers! xrumer
There is noticeably a bundle to learn about this. I assume you have made specific nice points in features also.
There are a handful of fascinating points in time here but I do not know if every one of them center to heart. There may be some validity but I am going to take hold opinion until I take a look at it further. Great article , thanks so we want far more! Added to FeedBurner too
i like to search the internet for new kitchen gadgets to add to my kitchen;;
What a fantastic post you have made. I just stopped in to tell you I really enjoyed the read and shall be dropping by from time to time from now on.
I really love the way you discuss this kind of topic.~..:-
I’m impressed, I have to admit. Really rarely can i encounter a blog that’s both educative and entertaining, and without a doubt, you’ve hit the nail to the head. Your idea is outstanding; the problem is something which inadequate persons are speaking intelligently about. My business is very happy i found this in my look for some thing in regards to this.
Nice blog, just looking around some blogs, seems a pretty nice platform you are using. I’m currently using WordPress for a few of my sites but looking to change one of them over to a platform similar to yours as a trial run. Anything in particular you would recommend about it?
This really is a marvelous write-up. Many thanks for making the effort to detail all of this out for us. It’s a great guide!
It seems you are getting quite a lof of unwanted comments. Maybe you should look into a solution for that. Hmm…
Very interesting subject , appreciate it for putting up.
Thanks for taking the time to talk about this, I feel fervently about this and I take pleasure in learning about this topic. Please, as you gain information, please update this blog with more information. I have found it very useful.
geinoutime.com
Fang Jifan은 그를 거의 알아보지 못했습니다. “당신의 성은 …”
Sweet blog! I found it while browsing on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thanks
I truly appreciate this post. I have been looking everywhere for this! Thank goodness I found it on Google. You have made my day! Thx again..
The color of your blog is quite great. i would love to have those colors too on my blog.:`-.:
Regards for this post, I am a big big fan of this site would like to go on updated.
Thanks for your post. I also think that laptop computers are getting to be more and more popular nowadays, and now are usually the only sort of computer used in a household. This is because at the same time potentially they are becoming more and more cost-effective, their processing power is growing to the point where they can be as robust as desktop computers through just a few years ago.
Thanks, I have bookmarked – Gulvafslibning | Kurt Gulvmand and will come back later.
Hey, what kind of anti-spam plugin do you use for your blog..:~;-
F*ckin’ awesome issues here. I’m very satisfied to peer your post. Thanks so much and i am looking forward to contact you. Will you kindly drop me a e-mail?
It is in point of fact a great and helpful piece of information. I’m glad that you simply shared this useful information with us. Please stay us up to date like this. Thanks for sharing.
This is certainly a awesome write-up. Thanks for bothering to describe all of this out for us. It is a great help!
Greetings! Very useful advice within this post! It’s the little changes that will make the greatest changes. Thanks for sharing!
I am only in order that willing to ought to see this. It’s the version of handbook that is loaned and never the very animal falsehoods might be on extra content. Recognize the value of your main showing such largest file.
Hello, extremely fascinating article. My sister and I have been looking to find thorough tips about this type of stuff for a time, yet we could not until now. Do you consider you can create several youtube videos concerning this, I do believe your web blog will be far more thorough if you ever did. In any other case, oh well. I’m going to be checking on this web-site within the forseeable future. Email me to maintain me up to date. granite countertops cleveland
I would like to thank you for the efforts you have put in penning this blog. I really hope to view the same high-grade content by you later on as well. In fact, your creative writing abilities has motivated me to get my own website now 😉
canadian pharmacy no rx
Darnit, why do you might have to make this kind of excellent points. many thanks.
I want to to thank you for this great read!! I absolutely loved every bit of it. I have got you bookmarked to look at new stuff you post…
There is definately a great deal to learn about this topic. I love all of the points you made.
Hi there! Do you know if they make any plugins to assist with Search Engine Optimization?
I’m trying to get my blog to rank for some targeted keywords
but I’m not seeing very good results. If you know of any please share.
Appreciate it! You can read similar art here
buy tamoxifen 20 mg
where to buy lasix water pill
Здесь вы найдете разнообразный видео контент тюбетейка ялта интурист
list of canadian pharmacy
I truly appreciate this post. I’ve been looking everywhere for this! Thank goodness I found it on Bing. You have made my day! Thanks again!
I have to show my appreciation to the writer just for bailing me out of this particular circumstance. Just after exploring throughout the world-wide-web and finding solutions that were not beneficial, I figured my life was over. Living without the approaches to the difficulties you’ve fixed through your good short post is a crucial case, and those that would have badly affected my entire career if I had not come across your site. Your personal knowledge and kindness in touching the whole thing was useful. I don’t know what I would have done if I hadn’t come across such a thing like this. I can also now relish my future. Thanks a lot so much for the impressive and amazing help. I won’t be reluctant to suggest your web page to any person who desires guidance on this matter.
I enjoyed seeing this, do you have a Facebook page for this site?
To have a look at was at regular a couple of, a the mother consideration which should genuinely undergo Native english speakers known as, like a result your lady allow me to undergo while using type in mentor Ye in Vibrant Development in Beijing. About the style As i did begin to find out in regards to the refreshing new Practice Native english speakers and in many cases dealt with that sentence structure made for to start with.
Oh my goodness! a great write-up dude. Thanks a lot However My business is experiencing problem with ur rss . Don’t know why Not able to register for it. Is there everyone obtaining identical rss issue? Anyone who knows kindly respond. Thnkx
Up to now, you require to term of hire an absolute truck or van and will also be removal equipments to valuable items plus check out the new destination. From the long run, which end up with are few things except anxiety moreover stress and anxiety. removals stockport
I really love your website.. Very nice colors & theme. Did you build this amazing site yourself? Please reply back as I’m attempting to create my very own site and would love to learn where you got this from or just what the theme is named. Many thanks.
i would love to use hydrogen fuel on my car, this fuel is really nonpolluting but is not yet very available,.
Spot on with this write-up, I truly suppose this web site wants way more consideration. I’ll most likely be once more to learn way more, thanks for that info.
Good – I should definitely pronounce, impressed with your website. I had no trouble navigating through all tabs as well as related info ended up being truly simple to do to access. I recently found what I hoped for before you know it in the least. Quite unusual. Is likely to appreciate it for those who add forums or something, website theme . a tones way for your customer to communicate. Nice task.
I have read several excellent stuff here. Definitely price bookmarking for revisiting. I wonder how much attempt you set to make such a fantastic informative web site.
It’s super webpage, I was looking for something like this
clomid 50 mg for sale
I’m not sure why but this web site is loading incredibly slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later and see if the problem still exists.
Your style is so unique in comparison to other folks I’ve read stuff from. Many thanks for posting when you have the opportunity, Guess I will just bookmark this blog.
Awesome post, hey I found this post while googling for lyrics. Thanks for sharing I’ll email my friends about this too.
The the next time Someone said a blog, I am hoping so it doesnt disappoint me up to this blog. What i’m saying is, Yes, it was my option to read, but I really thought youd have something intriguing to state. All I hear can be a few whining about something that you could fix if you ever werent too busy searching for attention.
There are a handful of intriguing points in time in this post but I do not know if they all center to heart. There may be some validity but I’m going to take hold opinion until I explore it further. Very good post , thanks therefore we want much more! Included with FeedBurner also
bike racks could really help you secure your bike when you leave it ,.
It hard to seek out educated individuals on this subject, however you sound like you realize what you are speaking about! Thanks
I always visit your blog everyday to read new topics.~’`-~
very nice post, i definitely really like this amazing site, persist in it
Need a loan modification expert? Need help with your mortgage? We are the answer! Learn everything there is to know about loan modification services.
Shame on you for creating another terrific post! Awesome stuff, keep up the good work. I see a lot of potential! I wonder if you are an active user with any social networking sites like Digg or Stumble Upon?
Aw, it was an incredibly good post. In idea I would like to put in writing similar to this additionally – spending time and actual effort to have a really good article… but what things can I say… I procrastinate alot and also by no means manage to go completed.
So funcy to see the article within this blog. Thank you for posting it
Great write-up, I’m regular visitor of one’s blog, maintain up the excellent operate, and It is going to be a regular visitor for a long time.
very nice post, i surely really like this excellent website, continue it
Necessary to send you that little or no remark just to many thanks yet again of these spectacular techniques you might have provided in this article. It’s so particularly generous with normal folks just like you to provide unreservedly what many of us may have marketed just as one guide to earn some dough on their own, primarily considering that you might have completed it in case you wanted. The tactics also acted to become fantastic way to understand that most people have similar desire equally as my to know significantly more concerning this condition. I’m there are many easier opportunities beforehand those of you that read through your site post.
Please tell me that youre going to keep this up! Its so great and so important. I cant wait to read more from you. I just feel like you know so a lot and know how to make people listen to what youve to say. This weblog is just too cool to be missed. Wonderful things, definitely. Please, PLEASE keep it up!
That is a great tip especially to those fresh to the blogosphere. Brief but very accurate info… Appreciate your sharing this one. A must read post!
Real clear website , regards for this post.
Normally I do not learn article on blogs, however I wish to say that this write-up very compelled me to take a look at and do it! Your writing style has been amazed me. Thank you, very great post.
Ten blog dostarczył mi dużo jasności na temat SEO. Dzięki!
I really appreciate this post. I’ve been looking everywhere for this! Thank goodness I found it on Bing. You’ve made my day! Thank you again!
Dzięki za podkreślenie znaczenia profesjonalnego podejścia do SEO.
Ten post był dla mnie oświeceniem na temat zagrożeń SEO. Dzięki!
Spot on with this write-up, I really feel this amazing site needs far more attention. I’ll probably be back again to read through more, thanks for the advice.
cheap generic synthroid
advair 500
Nie miałem pojęcia, że SEO jest tak ważne. Dzięki za ten wpis.
Dzięki za podkreślenie znaczenia profesjonalnego podejścia do SEO.
Bardzo przydatne informacje dla każdego, kto martwi się o SEO swojej strony.
Dzięki za świetne porady na temat SEO. Bezpieczeństwo jest kluczowe!
Świetny artykuł! Cieszę się, że są profesjonaliści, którzy mogą pomóc w SEO.
Czuję się znacznie pewniej w temacie SEO po przeczytaniu tego bloga.
Dzięki za kompleksowy przewodnik po SEO. Bardzo pouczający!
Ten blog to cenne źródło informacji dla każdego, kto myśli o SEO.
To była otwierająca oczy lektura na temat ryzyk i procesu SEO.
Czy możesz polecić jakieś sprawdzone narzędzia do SEO?
Dzięki za szczegółowy przewodnik po tym, czego można oczekiwać podczas wdrażania SEO.
Świetne wskazówki dotyczące znalezienia wiarygodnych usług SEO. Dzięki!
Ten post był bardzo pomocny w zrozumieniu zawiłości SEO.
Ten blog dostarczył mi dużo jasności na temat SEO. Dzięki!
best mail order pharmacies
슬롯 무료 쿠폰
Xiao Jing의 얼굴이 약간 풀렸다가 갑자기 느꼈습니다.
I would like to consider the chance of saying thanks to you for your professional advice I have continually enjoyed going to your site. We’re looking forward to the commencement of my school research and the complete preparing would never have been complete without surfing your site. If I could be of any help to others, I’d personally be ready to help as a result of what I have gained from here.
Thanks for your article. What I want to say is that when looking for a good on the net electronics store, look for a web page with comprehensive information on critical factors such as the security statement, basic safety details, payment methods, along with other terms and also policies. Usually take time to look at help as well as FAQ areas to get a much better idea of the way the shop works, what they can perform for you, and the way you can make best use of the features.
Hi I’m so glad I discovered your site, I genuinely found people by malfunction, while My partner and i was seeking on Askjeeve for something else, Nonetheless I will be here at this point and would just as to state cheers for the incredible post and a all round enjoyable blog (My partner and i also appreciate the theme/design), I don’t have the perfect time to look over everything at the moment but I’ve got bookmarked it and in addition included your own RSS feeds, so once i have time I will be back you just read extra, Please do keep up the great work.
i prefer wall clocks with hanging pendulums because they look nice at home.,
Great line up. We is going to be linking to this excellent article on our web site. Maintain up the good producing.
european vacations are very exciting sepcially if you got to visit many places at once’
Good site! I really love how it is easy on my eyes and the data are well written. I’m wondering how I might be notified when a new post has been made. I have subscribed to your feed which must do the trick! Have a great day!
Can I simply say what relief to seek out someone that in fact knows what theyre discussing on the net. You definitely realize how to bring a difficulty to light and work out it crucial. The best way to ought to check this out and appreciate this side on the story. I cant believe youre no more common since you also definitely provide the gift.
Your blog is showing more interest and enthusiasm. Thank you so much.
I am often to blogging we truly appreciate your content. The article has really peaks my interest. I am about to bookmark your internet site and keep checking for first time information.
I enjoy your writing style really enjoying this web site .
propecia cost
i would love to get some free calendars on the internet, are there are sites or company that gives one?,
I’d must verify with you here. Which isn’t one thing I often do! I get pleasure from reading a put up that will make individuals think. Additionally, thanks for allowing me to comment!
Congratulations on having One of the most sophisticated blogs Ive come throughout using some time! Its just incredible what you can remember from a little something as a result of how visually beautiful it’s. Youve put collectively a good blog space -great graphics, videos, layout. This really is undoubtedly a must-see weblog!
irritable bowel is really bad, this disease can really crap your digestive system,.
Oh i really envy the way you post topics, how i wish i could write like that.’:\’`.
He still has the gleam of a villain in his eyes, but he has enough power and gravitas in his performance, especially when we can easily compare him to the original and legendary Spock (credited as “Spock Prime” in the end credits), that it is obvious he was born to fill the shoes.
I’m impressed, I must say. Genuinely rarely do you encounter a weblog that’s both educative and entertaining, and let me tell you, you may have hit the nail about the head. Your concept is outstanding; ab muscles something that too few people are speaking intelligently about. I’m delighted i found this in my hunt for something about it.
I am in agreement with many different the info in this article. You are a distinctive author have real profit set your own views into apparent content. Anyone should be able to understand why.
My brother suggested I may like this blog. He used to be entirely right. This put up actually made my day. You cann’t believe just how much time I had spent for this info! Thank you!
I bookmared your site a couple of days ago coz your blog impresses me.,*,-”
Oh my goodness! an amazing post dude. Appreciate it Nevertheless We are experiencing problem with ur rss . Do not know why Cannot join it. Will there be any person obtaining identical rss dilemma? Anybody who knows kindly respond. Thnkx
How is it that just anyone can write a weblog and get as popular as this? Its not like youve said anything incredibly impressive more like youve painted a quite picture above an issue that you know nothing about! I dont want to sound mean, here. But do you actually think that you can get away with adding some quite pictures and not seriously say something?
Hi, I just discovered your weblog via yahoo. Your article is truly pertinent to my life currently, and I’m really happy I discovered your website.
This is a great website, might you be involved in doing an interview about how you designed it? If so e-mail me!
An impressive share, I merely given this onto a colleague who was doing a little analysis for this. Anf the husband in truth bought me breakfast simply because I found it for him.. smile. So i want to reword that: Thnx for your treat! But yeah Thnkx for spending plenty of time to talk about this, I feel strongly regarding this and really like reading regarding this topic. If it is possible, as you grow expertise, can you mind updating your blog site with a lot more details? It’s highly useful for me. Huge thumb up with this writing!
I discovered your blog internet site on google and appearance a few of your early posts. Always keep inside the good operate. I simply extra the RSS feed to my MSN News Reader. Looking for forward to reading a lot more by you down the line!…
I’m impressed, I must say. Actually rarely can i encounter a blog that’s both educative and entertaining, and let me tell you, you could have hit the nail to the head. Your concept is outstanding; the thing is an issue that inadequate consumers are speaking intelligently about. We’re very happy which i came across this inside my search for something concerning this.
Oh my goodness! a wonderful post dude. Thanks a ton Nonetheless My business is experiencing issue with ur rss . Do not know why Struggling to sign up for it. Will there be anyone acquiring identical rss difficulty? Anybody who knows kindly respond. Thnkx
Hello, Neat post. There’s a problem together with your web site in internet explorer, could test this… IE nonetheless is the market leader and a big section of people will omit your fantastic writing because of this problem.
I was on Digg looking for bulk headwear groups, when I found a link to this blog, glad I stopped by!!! Thanks!!!!
You are so cool man, the post on your blogs are super great.~`.~;
hi there was just seeing if you minded a comment. i like your blog and the thme you picked is super. I will be back.
My spouse and I stumbled over here from a different website and thought I may as well check things out. I like what I see so now i’m following you. Look forward to going over your web page repeatedly.
satellite tv has got to be one of the best inventions that we humans enjoy,”
Hi, your site is really well done. thanks for all the information. I’m sending my friends to read this article.
Remarkably! It is as if you read my mind! A person appear to know therefore considerably relating to this, just like you authored the book inside it or something. I feel that you can do with a few images to drive the content residence a bit, on top of that, this really is great weblog. The outstanding study. I will definitely review again.
You got a really useful blog. I have been here reading for about an hour. I am a newbie and your success is very much an inspiration for me.
One other important area is that if you are a senior citizen, travel insurance regarding pensioners is something you ought to really contemplate. The old you are, greater at risk you are for allowing something awful happen to you while in foreign countries. If you are not covered by many comprehensive insurance, you could have a number of serious challenges. Thanks for expressing your hints on this website.
The when Someone said a weblog, Lets hope it doesnt disappoint me around this blog. I mean, Yes, it was my solution to read, but I personally thought youd have some thing interesting to state. All I hear is really a few whining about something you could fix if you ever werent too busy trying to find attention.
Hello, Neat post. There’s an issue along with your web site in web explorer, may test this… IE nonetheless is the marketplace chief and a huge section of other people will miss your great writing due to this problem.
there are many movie download sites on the internet and i need a bigger hard drive to save thoes movies**
I recognize there’s lots of spam on this website. Do you need help cleansing them up? I may help among courses!
Pretty nice post. I just stumbled upon your blog and wanted to say that I’ve really enjoyed surfing around your blog posts. In any case I will be subscribing to your feed and I hope you write again soon!
Good aftie” i am a blogger too. and i can see that you are a nice blogger too,
retin a without script
canadian pharmacy antibiotics
doxycycline buy usa
I simply could not depart your site before suggesting that I really loved the usual information an individual supply in your visitors? Is gonna be again frequently to inspect new posts.
I observe there is a lot of spam on this blog. Do you want help cleaning them up? I might help in between courses!
Last month, when i visited your blog i got an error on the mysql server of yours.`*.;`
Hey! Good stuff, please keep us posted when you post something like that!
Откройте новые горизонты личностного роста – перейдите по ссылке на психология эмоций экман (https://bit.ly/3W0DOJv)
I precisely wished to appreciate you all over again. I do not know what I would have followed in the absence of the type of ways revealed by you directly on that industry. It had been a difficult condition in my view, however , finding out this specialized manner you dealt with the issue forced me to leap for delight. I’m grateful for your help and in addition pray you find out what a great job you are always putting in instructing men and women through a blog. Most likely you’ve never come across all of us.
Spot i’ll carry on with this write-up, I must say i think this site requirements far more consideration. I’ll oftimes be once more to study additional, appreciate your that information.
I just heard that Jamaican food CANNOT be cooked fresh every day? Is that true?|BootleggedTeam|
I never would have thought this stuff was out there. Thanks! I look foward to checking out your articles in the future.
I truly appreciate this post. I have been looking everywhere for this! Thank goodness I found it on Google. You have made my day! Thx again..
I have read a few excellent stuff here. Definitely price bookmarking for revisiting. I wonder how much attempt you set to create the sort of fantastic informative site.
I definitely wanted to post a small message so as to express gratitude to you for some of the amazing tips you are placing on this site. My extensive internet investigation has at the end of the day been paid with incredibly good details to talk about with my relatives. I would declare that we website visitors actually are truly fortunate to dwell in a fabulous site with so many outstanding individuals with useful things. I feel rather fortunate to have come across your webpages and look forward to some more amazing moments reading here. Thank you again for all the details.
The the next occasion I just read a weblog, I am hoping it doesnt disappoint me around that one. I am talking about, It was my solution to read, but I personally thought youd have something interesting to convey. All I hear is really a number of whining about something that you could fix in case you werent too busy seeking attention.
of course data entry services are very expensive that is why always make a backup of your files-
For illustration, create suppliers have worked with the Food & Drug Administration (FDA) to make sure that the industry criteria developed outcome in the most beneficial and most successful processes. And to communicate any public announcements, the marketplace has formulated relationships with associations like the Nationwide Grocer’s Association (NGA).
Often have in order to post a new review, My partner and i cannot help it ! Thanks Sarah
에볼루션 모노폴리 빅볼러
order ciprofloxacin 500mg
coupon retin a
Individuals who know that they’re uncovered to Triclosan as well as Bisphenol A should hunt down the assistance of an Orange County chiropractor to ensure that their allergies are stored at bay and to keep up good health.
buy viagra online legitimate
Greetings! Very useful advice in this particular post! It is the little changes which will make the biggest changes. Many thanks for sharing!
Oh my goodness! Amazing article dude! Thanks, However I am going through issues with your RSS. I don’t understand the reason why I cannot subscribe to it. Is there anyone else getting the same RSS problems? Anyone that knows the answer can you kindly respond? Thanks!
vermox south africa
The game was originally to be a advertising software for the Completely satisfied Eater chain of eating places, however this idea was dropped throughout growth and Dizzy was added to the sport. The sport was playable inside three days of labor; the developers only took two more weeks to finalize the graphics, interface and music.
where can you get amoxicillin
You’re so interesting! I do not suppose I’ve truly read anything like this before. So great to find someone with some original thoughts on this issue. Really.. thanks for starting this up. This web site is something that is required on the web, someone with a bit of originality.
This excellent website certainly has all of the information I needed about this subject and didn’t know who to ask.
I enjoy this website – its so usefull and helpfull.
Here is my homepage web page (https://svetodiod96.ru/bitrix/redirect.php?goto=https://website-maintenance.org/search-services/website-maintenance/)
buy vermox uk
Nielsen report, 54 % of children most well-liked to spend time with the Tv. Often, dad and mom are simply as guilty as their youngsters. Nonetheless, with the inundation of know-how in all facets of life, parents run the danger of raising a generation who cannot relate to other folks.
This is an eye-opening perspective.주부 대출
You’ve provided a fresh take on this issue.카카오 대출
Is the message from banks leaning a lot into green guilt by making people feel bad about their paper? It is not an exaggeration to say that almost all people who pay payments and have financial institution accounts within the United States have seen at least a decade’s value of paper inserts and online popups encouraging paperless banking and online invoice pay. There are even murmurings that folks might be charged if they need to maintain banking with paper, and a few institutions already force the problem by requiring direct deposit.
ciprofloxacin buy canada
Being chased by monsters might simply be the scariest gameplay experience of all time (especially in the first-person perspective); being chased occurs on a regular basis in Amnesia: The Dark Descent, and if these sequences don’t drive you mad with terror, the darkness in all probability will. Candy, Maxine. “How being evicted can have an effect on your credit report.” Experian. The bottom line is that we typically chunk off quite a bit greater than we can chew, we devour too much sugar and we don’t eat sufficient natural food.
Hello, I believe your blog might be having web browser compatibility problems. When I look at your website in Safari, it looks fine however when opening in I.E., it’s got some overlapping issues. I merely wanted to provide you with a quick heads up! Apart from that, wonderful site!
explainervideo.in https://mapfling.com/qg6mm6z
Your insights have given me a new perspective.프라그마틱 슬롯체험
It is also suggested that when a person is confused then shop for some time and experience the reduction of the stress. A successful budgeting helps to monitor the expenses which might be spent by the individual on daily. Many might focus on greater expenses they carry out however it is sensible to choose the small expense as they occupy a lot of the expense schedule. It may seem easy, could seem basic however attaining it takes years. Even with routine maintenance, your vehicle might require repairs at some point throughout its lifetime.
tamoxifen india no prescription
Your passion for this topic is evident.seo 백링크
Walk into most new or remodeled houses today, and you’re assured to find no less than one or two — if not a whole kitchen full of — stainless steel appliances.
advair price in india
The primary function of the Mayo Clinic Diet is to drop your unhealthy eating and life-style habits and substitute them with wholesome practices. The dieter then replaces these unhealthy habits with these 5 wholesome habits that embody exercise, consuming a good breakfast, eating a lot of fruits and veggies, as well as complete grains, and consuming healthy fats, reminiscent of monounsaturated fats.
I truly love your site.. Excellent colors & theme. Did you build this site yourself? Please reply back as I’m trying to create my own site and would love to know where you got this from or just what the theme is called. Cheers.
An outstanding share! I’ve just forwarded this onto a friend who had been doing a little research on this. And he in fact bought me breakfast due to the fact that I discovered it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanks for spending time to talk about this subject here on your web site.
xxx
Good info. Lucky me I ran across your website by accident (stumbleupon). I’ve saved as a favorite for later.
diflucan uk
As the urine evaporates, it cools the vulture’s body in the identical manner sweat works on people. I’ve got a lot happening, but I prefer it that method. If you’ve got just spent a day within the solar and feel a sunburn coming on, it is useful to be conversant in the symptoms of sun poisoning. You may feel overly sensitive or lack belief in your self and others. A 2018 travel guide described most facilities within the region closed resulting from lack of visitors. Waste elimination crews accumulate trash from airport amenities and airplanes. Iconically seen in the film “My Cousin Vinny,” the Buick Skylark has an extended history in the automotive trade. First launched in Buick’s Roadmaster line, the Buick Skylark was a trendy car with loads of horsepower. This is because Jamaica is the birthplace of the idea of the all-inclusive resorts and so while you are here, you possibly can stay in one and get a primary hand experience of why these are so in style.
I absolutely love your blog.. Very nice colors & theme. Did you build this amazing site yourself? Please reply back as I’m attempting to create my own site and want to find out where you got this from or what the theme is named. Thank you!
500g amoxicillin
When you resolve on your niche, you’ll be prepared to begin your individual travel company enterprise. Do you wish to specialise in corporate and business travel or leisure travel? The travel enterprise just isn’t what it was once was. Most of the travel and tourism firms use this as a software to increase their income and revenue margins and to offer a aggressive edge to other current tourism companies. It will be began from Kathmandu and travel via conventional trekking routes. Cell telephones will at all times be dependent on cellular towers, and even with those apps, they do not provide the instantaneous communication of a walkie-talkie. They’re decorated with all the pieces from peace indicators to dragons, however even in plain, stable colours, these distinctive sneakers make a striking fashion assertion all on their very own. Even in case your wedding theme does not contain 1980s cartoon characters, you still would possibly want to think about having a strawberry shortcake marriage ceremony cake. A number of have been still reviewing PST recordsdata manually in Outlook; others were Tiffing quite a few pages of papers ahead of proper launching in to a old style assessment software for eyes-on evaluate.
This is a topic that’s close to my heart… Take care! Exactly where are your contact details though?
Good post. I am experiencing many of these issues as well..
Right here is the perfect webpage for anyone who hopes to find out about this topic. You understand a whole lot its almost hard to argue with you (not that I personally would want to…HaHa). You definitely put a new spin on a topic that has been written about for years. Wonderful stuff, just excellent.
Dude.. I am not much into reading, but somehow I got to read numerous articles on your blog. Its amazing how interesting it is for me to have a look at you very often.
Rise Of The Lycans do have some great fighting scene between the werewolves and the vampires, it is a nice movie::
Spot on with this write-up, I actually believe that this amazing site needs far more attention. I’ll probably be returning to read more, thanks for the information!
Useful info. Fortunate me I discovered your website accidentally, and I am surprised why this coincidence didn’t happened earlier! I bookmarked it.
Well done. I i never thought I would personally accept as true with this opinion, but I???m commencing to view things at a different view. I must research more about this simply because it seems fascinating. Another thing I don???t understand though is the way things are all related together.
Its like you read my mind! You appear to know a lot about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a bit, but other than that, this is fantastic blog. A great read. I’ll certainly be back.
Thanks for sharing your ideas with this blog. Likewise, a misconception regarding the financial institutions intentions while talking about foreclosure is that the financial institution will not getreceive my repayments. There is a certain amount of time in which the bank will require payments here and there. If you are as well deep inside the hole, they may commonly desire that you pay the actual payment in full. However, i am not saying that they will have any sort of repayments at all. When you and the loan company can have the ability to work anything out, your foreclosure process may stop. However, in case you continue to skip payments in the new plan, the foreclosed process can pick up exactly where it left off.
It’s onerous to seek out knowledgeable folks on this subject, but you sound like you already know what you’re talking about! Thanks
Very clean website , thanks for this post.
I am not sure where you are getting your info, but great topic. I needs to spend some time learning more or understanding more. Thanks for great information I was looking for this info for my mission.
buy provigil online uk
Good post. I’m dealing with many of these issues as well..
May I just say what a comfort to uncover somebody who genuinely understands what they’re discussing on the web. You certainly understand how to bring a problem to light and make it important. More and more people need to check this out and understand this side of your story. I was surprised you aren’t more popular because you certainly have the gift.
There is definately a lot to know about this topic. I like all the points you’ve made.
Spot on with this write-up, I absolutely believe this website needs a lot more attention. I’ll probably be back again to read more, thanks for the information!
After exploring a handful of the blog posts on your website, I really like your way of blogging. I saved as a favorite it to my bookmark site list and will be checking back soon. Please visit my website too and tell me how you feel.
Howdy! This article could not be written much better! Looking through this post reminds me of my previous roommate! He constantly kept preaching about this. I will send this article to him. Fairly certain he’s going to have a great read. Many thanks for sharing!
Hi, I do think this is an excellent website. I stumbledupon it 😉 I am going to come back once again since I book-marked it. Money and freedom is the greatest way to change, may you be rich and continue to help others.
https://artdaily.com/news/171650/Mp3Juice-Review–The-Pros-and-Cons-You-Need-to-Know
After exploring a number of the blog posts on your website, I truly appreciate your technique of blogging. I book-marked it to my bookmark website list and will be checking back soon. Please visit my web site too and let me know how you feel.
Hello there! This blog post couldn’t be written much better! Looking at this post reminds me of my previous roommate! He constantly kept talking about this. I’ll forward this article to him. Fairly certain he will have a very good read. I appreciate you for sharing!
I blog frequently and I genuinely thank you for your content. The article has truly peaked my interest. I am going to book mark your website and keep checking for new information about once per week. I opted in for your Feed as well.
I’m more than happy to discover this site. I need to to thank you for ones time for this particularly fantastic read!! I definitely enjoyed every bit of it and I have you book-marked to look at new information in your web site.
Right here is the right webpage for everyone who wishes to find out about this topic. You realize a whole lot its almost tough to argue with you (not that I really will need to…HaHa). You certainly put a new spin on a topic that has been written about for many years. Great stuff, just excellent.
Very nice article. I definitely love this site. Stick with it!
Monetary planning is all about allocating finite sources — such as cash,
staff and equipment — over time, to succeed in the broad
targets set out in strategic planning. Once it knows the “why,” it may
well work out the “how” by outlining the necessities to
get there, together with where to put monetary assets, the right
way to forecast human resource wants, and the place to place
investments, in any other case generally known as monetary planning.
In case you resolve that it is not price getting a
new automotive, then it is perhaps value trying to get higher mileage out of your present automobile.
modafinil how to get a prescription
Very nice article. I certainly love this website. Continue the good work!
Having read this I believed it was really informative. I appreciate you spending some time and energy to put this content together. I once again find myself personally spending a significant amount of time both reading and posting comments. But so what, it was still worthwhile.
I must thank you for the efforts you’ve put in penning this blog. I’m hoping to see the same high-grade blog posts by you in the future as well. In truth, your creative writing abilities has motivated me to get my own, personal blog now 😉
where can i buy nolvadex online
I was very happy to uncover this site. I want to to thank you for your time due to this fantastic read!! I definitely savored every little bit of it and i also have you book-marked to check out new information on your blog.
I’m amazed, I must say. Seldom do I come across a blog that’s both educative and engaging, and without a doubt, you have hit the nail on the head. The issue is something that not enough people are speaking intelligently about. I am very happy I came across this in my hunt for something relating to this.
Way cool! Some extremely valid points! I appreciate you penning this article plus the rest of the site is really good.
Good day! I could have sworn I’ve been to this site before but after looking at many of the articles I realized it’s new to me. Nonetheless, I’m certainly happy I stumbled upon it and I’ll be book-marking it and checking back frequently.
Higher Dolpo has been referred to because the last enclave of pure Tibetan culture with the panorama and Buddhist religion of this area more like Tibet in pre Chinese times than of the remainder of Nepal. Over time, “tradition hero” has been interpreted in many ways. 324 numbered N324, which only lasted five nights, when the route was extended to Bluewater from Lakeside and Romford Market from Hornchurch on March sixteen 1999. Ensignbus also created a faculty variant of the 324 numbered 623 between Hornchurch and Belhus on the identical day that route 324 was taken over, however the service did not last long because it was withdrawn by July 22 1999. Ensignbus later took over London tendered service route 348 (Romford-Lakeside) on June 12 1999 from Jap National after the route was re-introduced after being withdrawn and changed by an extension of Eastern National route 351 to Lakeside, and Ensignbus prolonged route 348 to Gravesend via Bluewater, although this only lasted until December eleven 1999 when the route was withdrawn again to Lakeside. My expertise won’t present a single for being greater than the mediocre ones intended for day-hiking boot styles. You must fit the walking boot kinds together with any orthopedic inserts, off-the-shelf insoles, plus the strolling socks you want to put on with him or her.
springwater cookie company
After going over a handful of the blog articles on your site, I honestly appreciate your way of writing a blog. I book marked it to my bookmark site list and will be checking back in the near future. Take a look at my web site too and let me know how you feel.
Great info. Lucky me I discovered your website by accident (stumbleupon). I’ve saved it for later.
I blog quite often and I seriously appreciate your information. This article has really peaked my interest. I’m going to take a note of your site and keep checking for new information about once per week. I opted in for your RSS feed too.
I really love your blog.. Very nice colors & theme. Did you make this amazing site yourself? Please reply back as I’m looking to create my own website and want to learn where you got this from or what the theme is named. Many thanks.
Howdy! This post could not be written any better! Going through this post reminds me of my previous roommate! He always kept preaching about this. I’ll forward this information to him. Pretty sure he’ll have a good read. Many thanks for sharing!
I seriously love your site.. Great colors & theme. Did you build this web site yourself? Please reply back as I’m hoping to create my own personal site and want to find out where you got this from or exactly what the theme is named. Thank you!
This is the right site for everyone who wishes to find out about this topic. You understand a whole lot its almost tough to argue with you (not that I really will need to…HaHa). You certainly put a fresh spin on a subject that’s been written about for decades. Wonderful stuff, just great.
An intriguing discussion is worth comment. I think that you ought to write more about this subject matter, it might not be a taboo matter but typically people don’t talk about these issues. To the next! All the best!
flomax 10
Hello there! I could have sworn I’ve visited this website before but after browsing through a few of the articles I realized it’s new to me. Anyways, I’m certainly pleased I stumbled upon it and I’ll be book-marking it and checking back regularly.
Wonderful article! We are linking to this great content on our site. Keep up the great writing.
It’s hard to come by experienced people about this topic, however, you sound like you know what you’re talking about! Thanks
I like looking through a post that will make people think. Also, thanks for allowing me to comment.
I’m eager to see where this discussion goes.백링크 조회
metformin 1000 mg tablets price
Hi, I do think this is a great blog. I stumbledupon it 😉 I am going to revisit once again since i have book-marked it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
You’ve captured the essence of this issue perfectly.구글SEO
Can I just say what a comfort to discover somebody that genuinely understands what they’re discussing over the internet. You certainly know how to bring an issue to light and make it important. More people have to check this out and understand this side of your story. I can’t believe you aren’t more popular since you surely possess the gift.
This is a topic that’s close to my heart… Cheers! Where can I find the contact details for questions?
Oh my goodness! Impressive article dude! Thank you so much, However I am going through problems with your RSS. I don’t understand the reason why I am unable to join it. Is there anybody having similar RSS issues? Anyone who knows the answer will you kindly respond? Thanx.
Great post! We will be linking to this great content on our site. Keep up the good writing.
This is a good tip especially to those fresh to the blogosphere. Brief but very precise information… Many thanks for sharing this one. A must read article!
antibiotics cipro
I really love your blog.. Very nice colors & theme. Did you make this web site yourself? Please reply back as I’m attempting to create my very own blog and would like to learn where you got this from or exactly what the theme is called. Cheers.
Hi there! This article couldn’t be written any better! Looking through this article reminds me of my previous roommate! He always kept talking about this. I am going to send this information to him. Fairly certain he will have a great read. Thanks for sharing!
bactrim 500 mg
Good day! I could have sworn I’ve visited this blog before but after going through many of the articles I realized it’s new to me. Regardless, I’m certainly happy I discovered it and I’ll be bookmarking it and checking back frequently.
Hello! I could have sworn I’ve visited this web site before but after browsing through some of the posts I realized it’s new to me. Nonetheless, I’m definitely delighted I came across it and I’ll be bookmarking it and checking back frequently!
Speaking of a normal Computer motherboard, the foremost parts are ram slots, cpu clot, and ports for peripherals.
Earlier age computer systems have been built with massive elements where a
standard laptop would cover an excellent huge dimension room.
By the age of 10, Tonelli was frequently winning at school carnivals and at 11, came seventh in the one hundred m freestyle in his
division on the Queensland Championships, earlier than winning the event the next year.
Your style is very unique in comparison to other people I have read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I will just bookmark this page.
I used to be able to find good info from your content.
Hi, I do think this is an excellent blog. I stumbledupon it 😉 I will come back yet again since I book marked it. Money and freedom is the greatest way to change, may you be rich and continue to guide others.
Greetings! Very helpful advice in this particular post! It is the little changes which will make the largest changes. Many thanks for sharing!
bookmarked!!, I love your site.
There’s certainly a lot to know about this topic. I love all of the points you have made.
I was excited to uncover this site. I want to to thank you for ones time for this fantastic read!! I definitely really liked every little bit of it and i also have you saved as a favorite to see new things in your blog.
Excellent web site you have got here.. It’s difficult to find high-quality writing like yours these days. I really appreciate individuals like you! Take care!!
Excellent post. I’m facing some of these issues as well..
Great site. Lots of useful info here. I’m sending it to a few buddies ans also sharing in delicious.
And certainly, thank you on your sweat!
Drumdoe was looted early in 1923, for which
French acquired an apology and a promise of an armed
guard for the place from Governor-Normal T. M. Healy.
Regardless of a present of £50,000 in 1916, and receiving subject marshal’s half pay, owning two properties
in Eire which he could not use left French again short of cash,
although he didn’t enhance matters by staying typically
on the Hôtel de Crillon in Paris.
Oh my goodness! Incredible article dude! Thank you, However I am experiencing troubles with your RSS. I don’t understand the reason why I can’t join it. Is there anybody having the same RSS problems? Anyone who knows the answer can you kindly respond? Thanx.
You ought to take part in a contest for one of the best sites online. I most certainly will recommend this web site!
Having read this I thought it was rather enlightening. I appreciate you finding the time and effort to put this information together. I once again find myself personally spending a significant amount of time both reading and commenting. But so what, it was still worthwhile.
This site truly has all of the info I needed about this subject and didn’t know who to ask.
prednisone purchase
ventolin diskus
You have made some really good points there. I checked on the net for additional information about the issue and found most people will go along with your views on this site.
Having read this I thought it was extremely enlightening. I appreciate you taking the time and energy to put this content together. I once again find myself personally spending a significant amount of time both reading and leaving comments. But so what, it was still worth it.
Pretty! This has been an incredibly wonderful article. Many thanks for supplying this information.
Greetings! Very useful advice in this particular post! It’s the little changes which will make the biggest changes. Thanks for sharing!
A fascinating discussion is definitely worth comment. I do think that you need to write more about this topic, it might not be a taboo subject but generally folks don’t talk about such topics. To the next! Cheers.
I need to to thank you for this wonderful read!! I definitely enjoyed every little bit of it. I’ve got you book marked to look at new stuff you post…
Oh my goodness! Impressive article dude! Many thanks, However I am having difficulties with your RSS. I don’t know the reason why I am unable to join it. Is there anybody getting similar RSS problems? Anybody who knows the answer can you kindly respond? Thanks!!
A motivating discussion is definitely worth comment. I do think that you need to publish more on this subject, it may not be a taboo matter but typically people do not talk about such subjects. To the next! All the best.
After exploring a handful of the articles on your website, I seriously like your way of blogging. I saved as a favorite it to my bookmark website list and will be checking back in the near future. Please visit my website too and let me know what you think.
Title IX, which was handed in 1972, leveled the playing area by requiring that athletics cash be
break up equally between men’s and women’s sports
activities. Forty years ago, solely 1 in 27 girls performed highschool sports activities.
As former Vice President Dan Quayle as soon as famously said on the subject, “What a horrible factor it’s to lose one’s mind.” That will not sound fairly the way in which he meant it,
however his coronary heart was in the best place.
buy amoxicillin 875 mg tablets
Pretty nice post. I just stumbled upon your blog and wanted to say that I’ve really enjoyed browsing your blog posts.
In any case I will be subscribing to your rss feed and I hope
you write again very soon!
Very great post. I simply stumbled upon your weblog and wanted to say that I have truly enjoyed
browsing your blog posts. After all I’ll be subscribing on your rss feed and I am
hoping you write once more soon!
Having read this I believed it was very informative. I appreciate you taking the time and energy to put this content together. I once again find myself spending a significant amount of time both reading and leaving comments. But so what, it was still worth it!
Each track provides an area for networks to park, empty
their trailers and begin assembling equipment. It’s a logistical
feat for network crews to move millions of dollars worth of gear and equipment from race to race each week and produce a top-of-the-line broadcast,
but networks have turned the task into high art (if truckers speeding across the country in the dead of night is the foundation for your concept of high art, that is).
This is the right weblog for wishes to learn about this topic. You understand a lot its virtually tough to argue together with you (not that I actually would want…HaHa). You certainly put a brand new spin for a topic thats been written about for a long time. Fantastic stuff, just wonderful!
This web-site can be a walk-through its the data it suited you with this and didn’t know who ought to. Glimpse here, and you’ll undoubtedly discover it.
Nice post. I discover something much harder on different blogs everyday. It will always be stimulating to read content using their company writers and practice a little something from their website. I’d opt to use some with the content on my own blog whether or not you don’t mind. Natually I’ll offer you a link on your web weblog. Thank you for sharing.
As much as I dislike “Independence Day”, at least you got a good idea of what the aliens looked like in the famous autopsy scene.
If you ask me, in excess of a couple working together to empty desired goals, often have unlimited electric power.
Thank you of this blog. That’s all I’m able to say. You definitely have made this web site into an item thats attention opening in addition to important. You definitely know a great deal of about the niche, youve covered a multitude of bases. Great stuff from this the main internet. All over again, thank you for the blog.
Can I just say what a relief to seek out someone who really is aware of what theyre speaking about on the internet. You undoubtedly know tips on how to carry an issue to gentle and make it important. Extra people must learn this and perceive this aspect of the story. I cant consider youre not more widespread because you undoubtedly have the gift.
I’m impressed, I must say. Really hardly ever do I encounter a weblog that’s each educative and entertaining, and let me let you know, you’ve hit the nail on the head. Your concept is outstanding; the problem is one thing that not enough individuals are talking intelligently about. I am very completely happy that I stumbled across this in my seek for something relating to this.
I’m new to your blog and i really appreciate the nice posts and great layout.*.,`*
provigil australia
Nice post. I understand something much harder on diverse blogs everyday. Most commonly it is stimulating to learn to read content off their writers and employ a little something from their site. I’d opt to use some while using content on my own weblog whether you do not mind. Natually I’ll provide link in your internet blog. Many thanks sharing.
Hello, very intriguing posting. My niece and I have been recently looking to find comprehensive facts about this sort of stuff for a while, nevertheless we couldn’t until now. Do you consider you can make several youtube video clips about this, I do think your web blog could well be more detailed in case you did. If not, oh well. I’ll be checking out on this site in the near future. E-mail me to keep me updated. granite countertops cleveland
There may be jacksonville seo expert an easy method in making income without having being employed on your own ill along with devoid of the your complete moment. You can use the facility belonging to the Internet for you to earn more money and possess plenty of time to really love this website. Despite exactly how bit of you know about the World wide web or perhaps how much company encounter you’ve, you’ll be able to utilize a variety of fantastic prospects to generate capital suitable during your computer.
This web site is often a walk-through for all of the knowledge you wanted concerning this and didn’t know who must. Glimpse here, and you’ll absolutely discover it.
I have to thank you for the efforts you’ve put in penning this website. I am hoping to check out the same high-grade blog posts by you in the future as well. In fact, your creative writing abilities has inspired me to get my very own blog now 😉
Valuable information. Fortunate me I discovered your website by accident, and I am stunned why this coincidence didn’t came about earlier! I bookmarked it.
Your style is so unique compared to other people I’ve read stuff from. Thanks for posting when you have the opportunity, Guess I’ll just book mark this page.
When I originally commented I clicked the -Notify me when new surveys are added- checkbox and today each time a comment is added I get four emails concentrating on the same comment. Perhaps there is that is you may remove me from that service? Thanks!
This blog was… how do you say it? Relevant!! Finally I’ve found something which helped me. Kudos!
albuterol uk
Excellent article. I will be going through some of these issues as well..
You’re so awesome! I don’t believe I’ve truly read through something like that before. So nice to discover someone with genuine thoughts on this subject matter. Seriously.. many thanks for starting this up. This site is something that is needed on the web, someone with some originality.
Hi! Would you mind if I share your blog with my myspace group? There’s a lot of folks that I think would really enjoy your content. Please let me know. Many thanks
This can be just the simplest and best advice I have ever come across about this topic. Thank you for this very useful blog post of yours. Additionally, I enjoy writing articles which has a personal tone incorporated. I feel it makes your reader feel more important and inclined to believe me more. Plus it sounds more real and never coming from a robot. I enjoy making my visitors feel important and special. I want to let them have the best tips on how to cope with important issues such as this.
I got what you intend, saved to fav, very nice website .
The main purpose of a home appraisal is to assure the mortgage lender that the home is worth the asking price.
If the home isn’t worth as much as the loan, the bank will
never get its money back. What the appraiser finds can be the difference in whether
or not you’ll get the house you want or be able to sell the one you don’t.
you are in reality a just right webmaster. The site loading velocity is amazing.
It kind of feels that you’re doing any unique trick.
Furthermore, The contents are masterwork. you’ve performed a great
activity in this matter!
Comfortabl y, the post is really the freshest on that laudable topic. I match in with your conclusions and definitely will thirstily look forward to your next updates. Simply just saying thanks can not simply be enough, for the fantasti c clarity in your writing. I can ideal away grab your rss feed to stay abreast of any updates. Good work and also much success in your business dealings!
Welcome to our portal, your primary source for all the newest reports and information on the communications landscape in the United Kingdom. Whether you’re fascinated in TV, radio, press, or internet media, we offer thorough coverage that keeps you aware about the key trends and trends. From just-in bulletins to in-depth analyses, our team of veteran journalists and industry experts work ceaselessly to bring you the most precise and latest information – https://ukeventnews.uk/sure-here-s-a-unique-rephrasing-p-p-that-s-what-i/
In conjunction to stories, we offer insightful features and opinion articles that delve into the nuances of the broadcasting industry. Our features cover a diverse array of topics, including regulatory shifts, media ownership, and the impact of new advancements. We also showcase the accomplishments and difficulties faced by media professionals, delivering a platform for voices from across the industry to be listened to and valued.
Stay connected with the pulse of the UK media scene through our regularly updated content. Whether you’re a media professional, a student, or simply a media enthusiast, our platform is designed to accommodate to your needs and demands. Join our growing community of readers and make sure you’re always in the know about the dynamic and continually progressing world of media in the United Kingdom.
Oh my goodness! a wonderful post dude. Thanks a lot However My business is experiencing trouble with ur rss . Don’t know why Can not join it. Possibly there is anyone finding identical rss difficulty? Anyone who knows kindly respond. Thnkx
my mom gives me some dance lessons every week, that is how i got my dancing expertise”
Some genuinely nice and useful info on this internet site , besides I believe the pattern has got good features.
I wanted to thank you for this great read!! I definitely enjoying every little bit of it I have you bookmarked to check out new stuff you post
Please don’t ever stop writing informative content like this. I think you are a star writer. I agree with your content on nearly every point.
average cost of lyrica
i would be busy again doing some home decors this coming christmas, i’d be buying some new decors for the season’
usually, the best sounding ringtones are coming from paid ringtone donwload sites“
We stumbled over here by a different web page and thought I should check things out. I like what I see so now i’m following you. Look forward to looking over your web page yet again.
Whichever one you choose, you’ll have the option to access
your files wherever you go. Out of the perilous days by candlelight emerged a new reality, one that
led to an underground transportation system known as the
subway. Check out How Cloud Storage Works to learn more.
Whether you opt for SugarSync or Dropbox really depends on what you want from your storage provider.
bathroom towels should be maintained with a good fabric conditioner so that they will last longer~
there are portable wine coolers which also fit in a small office space. i use them in my home office**
I intended to put you the very small observation just to say thanks once again for these beautiful strategies you’ve provided on this website. It’s so surprisingly open-handed with people like you to make without restraint what exactly most people might have made available as an electronic book to help with making some cash for their own end, particularly now that you could have done it if you ever decided. Those techniques likewise served to become easy way to understand that some people have a similar interest like my very own to grasp significantly more when considering this issue. I know there are many more pleasurable periods ahead for those who see your blog. click here – alternative medicine institute calcutta
The traders use futures trading as a hedge against the spot markets.
Oh my goodness! Awesome article dude! Thank you so much, However I am having troubles with your RSS. I don’t understand the reason why I cannot join it. Is there anybody else having the same RSS issues? Anybody who knows the solution can you kindly respond? Thanks!!
You are so interesting! I don’t suppose I’ve truly read anything like this before. So nice to find someone with a few original thoughts on this issue. Seriously.. thank you for starting this up. This site is something that is required on the web, someone with some originality.
I’m amazed, I have to admit. Seldom do I come across a blog that’s both equally educative and engaging, and let me tell you, you have hit the nail on the head. The problem is something which too few folks are speaking intelligently about. Now i’m very happy I stumbled across this in my hunt for something relating to this.
I seriously love your blog.. Very nice colors & theme. Did you make this website yourself? Please reply back as I’m hoping to create my own website and would like to learn where you got this from or exactly what the theme is called. Many thanks.
Oh my goodness! Incredible article dude! Thanks, However I am experiencing troubles with your RSS. I don’t know the reason why I can’t subscribe to it. Is there anybody having the same RSS problems? Anyone that knows the answer can you kindly respond? Thanx!
effexor over the counter
Attractive portion of content. I simply stumbled upon your weblog and in accession capital to assert that I get in fact loved account your weblog posts. Anyway I will be subscribing to your augment and even I success you get admission to constantly quickly.
Hi, It’s hard to find knowledgeable people on this topic, but you sound like you know what you’re talking about! Thanks
There are more than 850 miles of trails in the good Smoky Mountains, more than sufficient
to maintain you busy to your hiking vacation. Alaska features a selection of
various glaciers that individuals enjoy visiting and hiking.
It is also probably that Netflix has been profitable as a result of it has attracted
customers who want to watch a variety of motion pictures quite than simply
new releases. Find out who this sneaky homeowner was
on the following web page. Should you ever end up in San Francisco with an extra $10,000 to spend,
you might consider checking into the Penthouse Suite at the Fairmont Lodge.
If this story is true, it seems extra seemingly that the
women broke their necks; surely the hidden passageway wasn’t so
arduous to find that the opposite students would
not have come to their classmates’ rescue when it was
discovered the girls were lacking. Chemical residue
from the water can prevent this ball from seating correctly, or the ball
itself may have decayed. Their ghosts could haunt the home.
Richard Garriott is constructing a brand new home in Austin, so he may outdo Britannia Manor.
Even when it isn’t Halloween, Garriott’s home, Britannia Manor, is an attention-grabbing place to be.
eating disorders are of course sometimes deadly because it can cause the degeneration of one’s health.,
While you be part of this type of trip to Sweden, you
not only discover those gifts of Mom Nature for Sweden but
also you be taught the survival abilities. Following the multi-generational historical past
of the Finch family, players discover the family’s large, labyrinthine residence, studying
about each family member at a speedy tempo. Household is crucial thing to me.
The primary cleaning soap opera to make use of a two-household setup, Because the World Turns pitted a middle-class household towards a wealthy, but troubled, family.
For the first time, convertibles could have a 50/50 reclining passenger seat and a sport cloth interior.
It’s one of the instruments in the quiz, so jump proper in and have a go at
it! At all times of the best hand! The recipe referred to as for carrageenan — a seaweed extract —
to bind the water to the beef. The secret was within the seaweed.
This new burger, dubbed the Arch Deluxe, was alleged to attraction to adult tastes with a secret mustard-mayonnaise sauce.
Collins, Glenn. “Chief of McDonalds Defends Arch Deluxe to Franchisees.” The new York Occasions.
I need to to thank you for this excellent read!! I absolutely loved every little bit of it. I have you bookmarked to look at new things you post…
The very next time I read a blog, Hopefully it won’t disappoint me as much as this particular one. After all, Yes, it was my choice to read, but I really believed you would have something useful to talk about. All I hear is a bunch of crying about something that you can fix if you weren’t too busy looking for attention.
I’m impressed, I have to admit. Genuinely rarely should i encounter a blog that’s both educative and entertaining, and without a doubt, you’ve got hit the nail for the head. Your thought is outstanding; the problem is a thing that there are not enough everyone is speaking intelligently about. My business is happy i found this in my hunt for some thing regarding this.
I needed to thank you for this fantastic read!! I definitely enjoyed every little bit of it. I have got you saved as a favorite to check out new stuff you post…
An interesting discussion is worth comment. I think that you need to write more on this matter, it may not be a taboo subject but usually individuals are not enough to speak on such topics. To the next. Cheers
Rachel Weisz have that mysterious look and she is very appealing to most men and women::
An outstanding share! I’ve just forwarded this onto a friend who had been conducting a little research on this. And he in fact bought me breakfast due to the fact that I found it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending time to talk about this issue here on your internet site.
I truly love your blog.. Excellent colors & theme. Did you develop this site yourself? Please reply back as I’m attempting to create my own personal blog and would love to learn where you got this from or exactly what the theme is called. Kudos.
Can I just say what a reduction to seek out someone who actually is aware of what theyre talking about on the internet. You undoubtedly know how you can bring an issue to gentle and make it important. Extra folks have to read this and perceive this aspect of the story. I cant consider youre not more in style since you undoubtedly have the gift.
wooden kitchen cabinets are perfect your your home, they look good and can be cleaned easily*
well, i do believe in astrology and horoscope is the first part of the magazine that i always check~
Водоподготовка выполняет ключевую роль в гарантировании эффективной работы технологического оборудования – https://vodoclean.ru/jeffektivnost-i-nadezhnost-skvazhinnogo-nasosa-2.html. Процесс включает фильтрацию и регулирование воды для удаления вредных веществ, таких как растворимые соли, органические вещества и вредные бактерии. Это необходимо для избежания разрушения, накипи и прочих проблем, которые могут снизить производительность оборудования и снизить долговечность. Применение современной водоподготовки обеспечивает не только увеличить надёжность и долговечность техники, но и минимизировать затраты на его обслуживание и обслуживание.
Текущие системы водоподготовки содержат различные виды этапов обработки и техники. Среди них особо выделяются механические фильтры, применяемые для удаления крупных частиц, системы ультрафильтрации, которые полностью удаляют солевые соединения, и ультрафиолетовые установки, обеззараживающие воду. Также важную роль играют химические вещества, используемые для регулирования pH и борьбы с коррозией. Автоматизация процесса даёт возможность значительно улучшить результативность и точность процесса кондиционирования воды, что чрезвычайно важно в условиях большого производства.
Результативная водоподготовка оказывает благоприятное воздействие на окружающую среду, снижая выбросы токсичных веществ в окружающую среду. Применение новых технологий и аппаратов минимизирует расход воды и её загрязнение, что совпадает с нормами устойчивого развития. Промышленные компании, внедряющие системы водоподготовки, не только улучшают свои производственные показатели, но и проявляют осознанность к экосистеме. В результате, грамотная организация водоподготовки представляет собой конкурентное преимущество и вкладом в будущее, как для производств, так и для общества в целом.
Albrecht, Chad; Duffin, Kristopher McKay; Hawkins, Steven; Rocha, Victor Manuel Morales (2019).
“The use of cryptocurrencies in the money laundering process”.
IEEE Spectrum. Archived from the original on 21 December 2019.
Retrieved 2 February 2020. Around the same time, Nick Szabo, a
computer scientist who now blogs about law and the
history of money, was one of the first to imagine a new digital currency from the
ground up.
There’s definately a great deal to find out about this topic. I like all of the points you made.
I haven?t checked in here for some time because I thought it was getting boring, but the last few posts are good quality so I guess I?ll add you back to my everyday bloglist. You deserve it my friend
After going over a number of the blog articles on your web site, I really like your technique of blogging. I added it to my bookmark website list and will be checking back soon. Take a look at my website as well and let me know what you think.
As I website possessor I believe the content matter here is rattling wonderful , appreciate it for your efforts. You should keep it up forever! Best of luck.
auto insurance is indeed very important, insurance can protect your property..
doxy
zovirax otc uk
Thank you for each of your efforts on this web page.
Youre so cool! I dont suppose Ive read anything like this prior to. So nice to locate somebody with original thoughts on this subject. realy we appreciate you beginning this up. this amazing site is a thing that is required on the web, a person with a little originality. beneficial purpose of bringing interesting things to your internet!
I like this web site so much, saved to my bookmarks .
Spot on with this write-up, I honestly feel this web site needs far more attention. I’ll probably be back again to read more, thanks for the information.
This is the right web site for everyone who really wants to find out about this topic. You know so much its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a fresh spin on a topic that has been written about for many years. Wonderful stuff, just wonderful.
Judging by the way you write, you seem like a professional writer.,;~*-
Wonderful article! We will be linking to this great article on our site. Keep up the great writing.
Amazing article. I have been looking to fully understand this topic and be able to teach other folks. I think you have wonderful ideas here together with proven results. The question is: Is there a approach to really get all your tips here in the type of an ebook? Do you have a book written on this subject? The reason why I’m requesting is that I don’t get constant access to the internet. Therefore, a book could really help me to make consultation even when there is no access to the internet.
i frequent hair salons because i always want to keep my hair in top shape;;
Your style is really unique in comparison to other folks I have read stuff from. Thanks for posting when you’ve got the opportunity, Guess I’ll just book mark this web site.
Hi there! This post could not be written much better! Looking through this article reminds me of my previous roommate! He continually kept preaching about this. I’ll send this post to him. Fairly certain he’ll have a great read. I appreciate you for sharing!
Malcolm you write in a lucid manner and I have no difficulty to understand what you have said, even though I am a novice.
Greetings! Very helpful advice within this article! It’s the little changes that make the most significant changes. Thanks for sharing!
before you buy some very expensive SEO Tools, always look for a review first before you invest on them;
After examine a couple of of the weblog posts in your website now, and I truly like your manner of blogging. I bookmarked it to my bookmark website list and might be checking back soon. Pls take a look at my website as effectively and let me know what you think.
Everyone loves it when people get together and share thoughts. Great blog, keep it up!
Greetings! Very useful advice within this post! It’s the little changes that make the most important changes. Many thanks for sharing!
Thank you for another great post. Where else could anybody get that type of info in such a perfect way of writing? I have a presentation next week, and I am on the look for such information.
You’ve made some really good points there. I looked on the internet for more information about the issue and found most individuals will go along with your views on this site.
Your blog would increase in ranking if you post more often.`,;:”
There are some fascinating points in time in this posting but I don’t determine if them all center to heart. There is certainly some validity but I’m going to take hold opinion until I look into it further. Very good post , thanks and now we want far more! Included with FeedBurner at the same time
Greetings! Very helpful advice in this particular post! It’s the little changes that will make the biggest changes. Thanks for sharing!
Way cool! Some very valid points! I appreciate you writing this post plus the rest of the website is also very good.
I have to thank you for the efforts you’ve put in writing this blog. I am hoping to view the same high-grade content from you later on as well. In fact, your creative writing abilities has inspired me to get my very own blog now 😉
There’s definately a lot to learn about this subject. I really like all the points you’ve made.
I’m not sure why but this weblog is loading incredibly slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later and see if the problem still exists.
I think this is a really good article. You make this information interesting and engaging. You give readers a lot to think about and I appreciate that kind of writing.
I’ve been exploring for a little bit for any high quality articles or weblog posts on this kind of area . Exploring in Yahoo I ultimately stumbled upon this web site. Studying this info So i am satisfied to convey that I’ve an incredibly good uncanny feeling I discovered just what I needed. I so much no doubt will make sure to don’t put out of your mind this website and give it a look a relentless basis.
Way cool! Some very valid points! I appreciate you penning this post plus the rest of the website is really good.
Youre so cool! I dont suppose Ive read anything in this way prior to. So nice to get somebody with original thoughts on this subject. realy we appreciate you beginning this up. this web site is something that is required on the web, a person after some originality. valuable work for bringing new stuff on the web!
This is actually attractive, You’re an exceedingly qualified author. I have signed up with your feed plus expect enjoying the useful write-ups. Furthermore, I’ve shared yuor web blog throughout our internet sites.
A high level woman you must have a single body appearance. Is going to be most excellent construct, adult will need the customer through your self confidence and girls do imagine drawn to because of your captivating looks. Albeit numerous men desirable to generate an extremely whole a lot are certainly all set to might dozens of vexing physical trainings was needed to grow their lean muscle mass. These grownup is usually hugely willing to fully grasp that the following is straight can certainly have muscle and strength merely by swallowing an outstanding application identified Huge Muscle mass mass Contractor.
Good article. I certainly love this site. Keep it up!
I would like to thank you for the efforts you’ve put in writing this blog. I’m hoping to view the same high-grade blog posts from you later on as well. In truth, your creative writing abilities has inspired me to get my own blog now 😉
When I originally commented I seem to have clicked the -Notify me when new comments are added- checkbox and from now on each time a comment is added I receive 4 emails with the exact same comment. Perhaps there is a means you are able to remove me from that service? Thanks a lot.
cipro bayer
My friend first found your blog on Google and she referred your blog to me.”`;,-
You are a very persuasive writer. I can see this in your article. You have a way of writing compelling information that sparks much interest.
The the next time I just read a blog, I am hoping who’s doesnt disappoint me around that one. After all, It was my solution to read, but I just thought youd have some thing interesting to convey. All I hear is often a lot of whining about something that you could fix should you werent too busy seeking attention.
Hi there, I believe your blog could be having browser compatibility issues. Whenever I look at your site in Safari, it looks fine but when opening in I.E., it’s got some overlapping issues. I simply wanted to give you a quick heads up! Apart from that, great site!
Hi there, this is fantastic posting. I must say i enjoyed. However there are tons of off topic comments. I really advise you to get rid of or something like that. That’s only my opinion. Good luck!
I’m pretty pleased to discover this site. I need to to thank you for ones time just for this wonderful read!! I definitely liked every part of it and I have you bookmarked to look at new information on your site.
Im no professional, but I imagine you just made the best point. You certainly understand what youre talking about, and I can actually get behind that. Thanks for staying so upfront and so sincere.
It’s difficult to find educated people on this topic, but you seem like you know what you’re talking about! Thanks
All I can express is, I don’t know what to comment! Except needless to say, for the excellent tips which have been shared on this blog. I can think of a zillion fun approaches to read the posts on this site. There’s no doubt that I will at last take a step making use of your tips on areas I could not have been able to handle alone. You had been so innovative to let me be one of those to profit from your beneficial information. Please know how significantly I enjoy the whole thing.
This website was… how do I say it? Relevant!! Finally I’ve found something which helped me. Kudos.
I used to be able to find good advice from your articles.
I’m a blog crazed person and i love to read cool blog like yours.:`*’”
An intriguing discussion is worth comment. I do think that you should publish more on this issue, it might not be a taboo subject but usually people do not talk about these topics. To the next! Many thanks.
I thought it was going to be some boring old site, but I’m glad I visited. I will post a link to this page on my blog. I am sure my visitors will find that very useful.
i always syndicate feeds on my subcribers and of course feedburner is definitely a great help~
You have a real ability for writing unique content. I like how you think and the way you represent your views in this article. I agree with your way of thinking. Thank you for sharing.
Excellent blog here! Also your site loads up very fast! What host are you using? Can I get your affiliate link to your host? I wish my site loaded up as fast as yours lol xrumer
Spot up for this write-up, I must say i feel this website wants considerably more consideration. I’ll more likely once more to learn to read a great deal more, thanks for that information.
Spot on with this write-up, I honestly think this website needs a lot more attention. I’ll probably be back again to read through more, thanks for the information.
Hi, I do think this is a great website. I stumbledupon it 😉 I will revisit yet again since I book marked it. Money and freedom is the greatest way to change, may you be rich and continue to help others.
This website certainly has all the info I needed concerning this subject and didn’t know who to ask.
When I initially commented I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I get 4 emails with the same comment. There has to be a way you can remove me from that service? Many thanks.
Good day! I could have sworn I’ve visited this blog before but after looking at some of the articles I realized it’s new to me. Regardless, I’m certainly pleased I found it and I’ll be book-marking it and checking back often.
The next time I read a blog, Hopefully it does not fail me just as much as this one. I mean, I know it was my choice to read through, nonetheless I genuinely believed you would have something helpful to talk about. All I hear is a bunch of complaining about something you could fix if you weren’t too busy searching for attention.
Pretty! This was an incredibly wonderful post. Thanks for providing this information.
Good blog you’ve got here.. It’s hard to find high-quality writing like yours nowadays. I truly appreciate people like you! Take care!!
An impressive share! I have just forwarded this onto a friend who had been doing a little homework on this. And he actually bought me lunch due to the fact that I found it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending time to talk about this matter here on your internet site.
There is certainly a lot to know about this topic. I like all the points you have made.
Great information. Lucky me I ran across your blog by chance (stumbleupon). I’ve bookmarked it for later.
I really love your website.. Excellent colors & theme. Did you develop this site yourself? Please reply back as I’m attempting to create my very own website and would love to find out where you got this from or what the theme is named. Many thanks!
Each generation of retiring workers would get paid by the people
currently working, and therefore the system would fund itself forever despite the fact that the system had no money to start with.
And if you want to be really thrifty, you can start seeds early in the
season and transplant them to your yard once the weather warms up.
Begin sipping the superb wine and hit the dance ground.
Dance with every-different and have all the enjoyable collectively.
Like Shiori, Yu is the hardest character to finish with
in Tokimeki memorial 4. To win her heart, player is required to
have very excessive standing factors in every space, in addition to in a position to gain admission to the primary price college.
Inside the inside city, the operating firm launched a uniform tariff of ten pfennigs in 1902, and it was the
one cause for a one-off transfer to Bertoldsbrunnen junction (colloquially referred to
as Fischbrunnen, or Fish’s Nicely), Schwabentorbrücke and Lorettostraße.
Firstly of the summer season schedule in 1905, Alter Messplatz,
additionally known as Bleicheweg, was added to the loop at
Stadthalle-the primary terminal loop in Freiburg.
Are you able to title the mighty bull statue located within the Bull Ring, an enormous buying and leisure complex in Birmingham, England?
The wind and dust can cause her eyes to turn into dry,
and flying debris may cause critical — and even fatal —
damage.
Telephone 5 introduced a wide, 16:9 variant at 1136 ×
640 pixels, which also has no official acronym.
Although digital broadcast content in former PAL/SECAM regions
has 576 energetic traces, a number of mobile Tv units with a DVB-T2 tuner use the 600-line variant with a diameter of 7, 9 or 10 inches (18
to 26 cm).
Hi, I do think this is an excellent site. I stumbledupon it 😉 I will come back once again since I book marked it. Money and freedom is the greatest way to change, may you be rich and continue to help other people.
Greetings! Very helpful advice within this article! It’s the little changes that make the biggest changes. Many thanks for sharing!
Way cool! Some extremely valid points! I appreciate you penning this post and the rest of the website is very good.
Next time I read a blog, Hopefully it won’t disappoint me as much as this particular one. After all, Yes, it was my choice to read through, nonetheless I truly believed you would probably have something helpful to say. All I hear is a bunch of complaining about something you could fix if you weren’t too busy searching for attention.
Hey there! I just would like to give you a big thumbs up for your excellent info you have got right here on this post. I am coming back to your web site for more soon.
I’d like to thank you for the efforts you have put in penning this blog. I’m hoping to check out the same high-grade content by you in the future as well. In fact, your creative writing abilities has encouraged me to get my own website now 😉
Oh my goodness! Incredible article dude! Many thanks, However I am experiencing difficulties with your RSS. I don’t know why I can’t subscribe to it. Is there anybody having similar RSS issues? Anyone who knows the solution can you kindly respond? Thanks.
This is a great tip especially to those new to the blogosphere. Short but very precise info… Appreciate your sharing this one. A must read article!
Second, the proactive stance of competitor profiling will allow
the firm to anticipate the strategic response of their rivals
to the firm’s planned strategies, the strategies of other competing firms, and changes in the environment.
These profiles give an in-depth description of the competitor’s background, finances, products,
markets, facilities, personnel, and strategies. Scanning competitor’s ads can reveal much about what that competitor
believes about marketing and their target market.
The innovative company is now seeking to drive its products
into key overseas markets, particularly the US, creating a
global network of Mobile Web products. Do not
follow the rat race or the customary marketing
of products that will not make any new achievements
in the market. The company has already signed major deals with global programs brands such as UFC, Cirque Du Soleil, The American Music
Awards, ABC Australia and Top Rank.
These days, nothing turns customers away like a sign that reads “cash only.” Fewer and fewer people seem to carry cash; instead, many pay
for even the smallest items with a credit or debit card.
Ask them questions that would give you information you
can’t find in a brochure, such as what the class workloads are like, what they really appreciate or don’t appreciate about the college or what it’s
like to navigate the various administrative processes.
I like looking through an article that can make people think. Also, thank you for allowing for me to comment.
This will typically involve sending a letter to the executor
of the estate (the person responsible for administering the will) outlining your case and the
grounds for contesting the will. The Process Of Contesting A
Will If you have legal grounds to contest a will, the first step is to seek legal
advice.
bookmarked!!, I really like your blog!
Very good info. Lucky me I recently found your site by accident (stumbleupon). I’ve book marked it for later.
Good post. I learn something totally new and challenging on websites I stumbleupon every day. It will always be helpful to read articles from other writers and practice something from other sites.
I really like reading an article that can make people think. Also, thank you for allowing for me to comment.
An impressive share! I have just forwarded this onto a coworker who had been doing a little homework on this. And he actually ordered me lunch due to the fact that I found it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanks for spending time to talk about this subject here on your website.
I enjoy reading through an article that will make men and women think. Also, thanks for permitting me to comment.
Hi there! I could have sworn I’ve been to this blog before but after browsing through many of the articles I realized it’s new to me. Nonetheless, I’m definitely happy I came across it and I’ll be bookmarking it and checking back frequently.
Excellent blog you’ve got here.. It’s hard to find excellent writing like yours these days. I really appreciate people like you! Take care!!
After looking over a few of the blog articles on your web site, I really like your way of blogging. I saved as a favorite it to my bookmark site list and will be checking back in the near future. Please check out my website as well and let me know what you think.
An impressive share! I’ve just forwarded this onto a colleague who has been conducting a little research on this. And he actually bought me lunch due to the fact that I stumbled upon it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanks for spending the time to talk about this subject here on your blog.
Good day! I just want to give you a huge thumbs up for your great info you have got here on this post. I will be returning to your blog for more soon.
Valuation: This involves assessing the current value of
a company or its worth in the free market with the aim of
making reasonable earnings within a given period of time. Here are 15 tips on how to
keep the value of your vehicle as high as possible.
Resources are allocated efficiently: Businesses have scarce
resources, and corporate finance allows for the determination of activities
that will yield maximum business returns for the scarce resources available.
Hi, I do believe your web site could be having web browser compatibility problems. Whenever I look at your website in Safari, it looks fine however, if opening in IE, it has some overlapping issues. I simply wanted to give you a quick heads up! Other than that, great blog!
China, Japan, South Korea, Germany, Italy, Singapore and Malaysia continued
to be on the list. In May 2019, the US Treasury removed India and Switzerland from its
currency monitoring list but China, Japan, South
Korea, Germany, Italy, Ireland, Singapore, Malaysia, and Vietnam remained
on the list.
Dealers will typically pass this fee onto the customer but don’t often advertise that fact in the sticker
price. Some of these programs are more accurate than others, but all of them
will help you appreciate the concept of stock buying and trading.
Excellent blog you have got here.. It’s hard to find high quality writing like yours these days. I honestly appreciate individuals like you! Take care!!
Hi, I do think your website could possibly be having web browser compatibility issues. When I look at your site in Safari, it looks fine however, when opening in I.E., it’s got some overlapping issues. I just wanted to provide you with a quick heads up! Apart from that, wonderful blog.
Right here is the perfect webpage for anyone who really wants to find out about this topic. You know a whole lot its almost tough to argue with you (not that I personally would want to…HaHa). You certainly put a new spin on a topic that has been discussed for years. Great stuff, just excellent.
Pretty! This was a really wonderful article. Thank you for providing this information.
This is a topic that is near to my heart… Many thanks! Where are your contact details though?
This is the right web site for everyone who hopes to understand this topic. You know a whole lot its almost hard to argue with you (not that I really will need to…HaHa). You certainly put a fresh spin on a topic that has been discussed for decades. Wonderful stuff, just wonderful.
Great info. Lucky me I came across your blog by chance (stumbleupon). I have saved it for later!
Very good blog post. I definitely love this website. Stick with it!
Hello there! This post could not be written any better! Looking through this article reminds me of my previous roommate! He constantly kept talking about this. I am going to forward this post to him. Fairly certain he’s going to have a very good read. Many thanks for sharing!
Your style is unique compared to other folks I’ve read stuff from. Thanks for posting when you have the opportunity, Guess I will just bookmark this page.
There’s definately a great deal to learn about this topic. I love all the points you made.
The next time I read a blog, I hope that it doesn’t fail me just as much as this one. I mean, I know it was my choice to read, but I genuinely believed you would probably have something interesting to talk about. All I hear is a bunch of whining about something that you could possibly fix if you were not too busy seeking attention.
Next time I read a blog, I hope that it won’t disappoint me as much as this one. After all, I know it was my choice to read through, nonetheless I really thought you’d have something interesting to say. All I hear is a bunch of crying about something that you could possibly fix if you weren’t too busy seeking attention.
Furthermore, the challenges faced during recovery highlight the
importance of ensuring that states have sufficient resources and plans in place to
respond to disasters promptly and efficiently. The storm’s formation and path, its devastation along
the Atlantic Coast, and the role of natural defenses and the National Hurricane Center all
contributed to our understanding of the challenges posed
by extreme weather events and the need for preparedness, even in areas not typically affected by hurricanes.
A real estate mortgage investment conduit (REMIC) is “an entity that holds a fixed pool of mortgages and issues multiple classes of interests in itself to investors”
under U.S. The European Investment Bank provides long-term loans, typically up to 50% of a project’s overall cost, for the public and the private sector,
and for small and medium-sized businesses through intermediated lending partners.
Good blog you have here.. It’s difficult to find excellent writing like yours these days. I really appreciate people like you! Take care!!
Getting the best tourist exchange rates is one of the most vital component of your trip’s success.
Now, how do you actually scout for the best tourist exchange rates?
You could say that the rates are the best ones if you could buy them at much cheaper rates.
Naturally, if you buy the currency at a much cheaper rate, you could buy more of
it.
It’s appropriate time to make a few plans for the longer term and it
is time to be happy. I’ve read this post and if I may
I wish to suggest you few interesting issues or suggestions.
Maybe you could write next articles referring to this article.
I wish to read more issues about it!
Sure, Thanksgiving may seem like it goes on for days – even weeks, once Uncle Johnny gets into
the Wild Turkey and Aunt June takes out her dentures to slurp
down some pumpkin pie – but the first celebration actually lasted
for three whole days.
An embargo was implied by the United States against Cuba which
lasted for more than forty years. The primary form of financial business set up
as a mutual company in the United States has been mutual insurance.
In mutual insurance companies, what would have been profits are instead rebated to the clients in the form of dividend
distributions, reduced future premiums or paid up additions to the policy value.
It might be in the form of percentage or mills. It may seem like these things don’t
affect you, but you might be surprised by changes happening right under your nose!
It is just a matter of getting things going and currently;
there are more than 12,000 approved lots in the city.
Way cool! Some extremely valid points! I appreciate you penning this post and the rest of the site is extremely good.
I have to thank you for the efforts you’ve put in penning this site. I’m hoping to view the same high-grade content from you later on as well. In fact, your creative writing abilities has encouraged me to get my very own site now 😉
This is a topic which is close to my heart… Cheers! Where are your contact details though?
This web site certainly has all of the information and facts I wanted concerning this subject and didn’t know who to ask.
I love it when people get together and share ideas. Great site, continue the good work.
This is the perfect webpage for everyone who hopes to find out about this topic. You realize a whole lot its almost tough to argue with you (not that I really will need to…HaHa). You certainly put a brand new spin on a topic that has been discussed for ages. Great stuff, just great.
Next time I read a blog, Hopefully it does not disappoint me as much as this particular one. After all, Yes, it was my choice to read, nonetheless I genuinely thought you’d have something useful to say. All I hear is a bunch of moaning about something you could fix if you weren’t too busy searching for attention.
Nice post. I learn something new and challenging on blogs I stumbleupon everyday. It’s always useful to read content from other writers and use something from other web sites.
You need to take part in a contest for one of the most useful sites on the net. I will recommend this blog!
Greetings! Very useful advice within this post! It is the little changes that produce the biggest changes. Thanks a lot for sharing!
Environmental Impact Assessment (EIA) EIA is
implemented in Egypt under the umbrella of the Ministry of state
for environmental affairs. Mental health problems are rising greatly amongst younger generations as they believe that they are missing out on factors like industrialisation and urbanization, also loses like
home, family relations, a threat to their health can all majorly impact long-term
deterioration in mental health.
The financial security company provides consultation on wealth
and asset income protection, education planning,
retirement planning, investment advisory services, Financial Planning trust and private client services, estate planning and business
planning. Its products include life insurance, permanent life insurance, disability income, and
long-term care insurance; annuities; investments; and investment advisory
products and services.
Right here is the perfect web site for anybody who really wants to find out about this topic. You understand a whole lot its almost hard to argue with you (not that I personally will need to…HaHa). You certainly put a fresh spin on a topic that has been written about for decades. Wonderful stuff, just wonderful.
Along with the technology to brew flavorful cups of coffee, Clover also offered
the technology to track what was being consumed at any given moment in a café.
Whether you can imagine your skill set being best
used to make sturdy furniture or inspire others to lead a
morally and ethically-pure life, this quiz will help you discover where you belonged during the Middle
Ages.
That’s, you insert the original key and push all the
cylinder system inwards, adjusting it back to its point. In the field referring to the important thing, that’s,
in the same thickness of the door, the entire opening system
is situated. As your entire rescue force was leaving Desert One, one of many helicopters
crashed right into a U.S.
Way cool! Some very valid points! I appreciate you penning this article and the rest of the site is also very good.
Hello there! I simply would like to offer you a big thumbs up for your excellent info you’ve got here on this post. I’ll be returning to your website for more soon.
Way cool! Some extremely valid points! I appreciate you writing this article and the rest of the site is really good.
In a silica crystal, a small central ion of silicon might
be surrounded by 4 larger ions of oxygen, forming a triangular pyramid, or tetrahedron.
You may want to provide your Easter bunny an enormous smile or cut its mouth in an O form, as if it were shocked.
Crystals are regular polyhedra — three-dimensional variations of normal polygons (squares turn into cubes,
equilateral triangles become triangular pyramids).
Captain Man plans to have AWOL sneak him and Huge Sudsy into Rivalton only to
reach a complication when it turns out that AWOL might
need a spicy pudding allergy. Every word spoken, nevertheless, comes out in the
next day’s papers that are avidly read by everyone. The episodes on the first volume are arranged in production order, while
the episodes on the second quantity are arranged by
original air date.
Hello! I just would like to offer you a huge thumbs up for your great information you have got right here on this post. I am coming back to your website for more soon.
These connectors are used e.g. in gear for data, measurement and management expertise as well
as power and industrial electronics. With the financial growth from
the 1960s, the worth of the 500 gained notes fell, resulting in a higher use of cashier’s checks with greater fixed denominations as technique of fee, as
well as an increased use of counterfeited ones.
I am really impressed together with your writing talents and also
with the format on your weblog. Is this a paid subject or did you modify it your self?
Either way stay up the excellent high quality writing, it’s rare to look a nice weblog like this
one nowadays..
The antechamber opens onto the Gold Salon, the previous
Salon d’Honneur. The antechamber additionally opens onto the Red Salon, which was used for official ceremonies, and was used because the throne
room by Nicholas II throughout his go to to Paris.
Katrina’s size and attain have been outstanding. After an argument with the Younger Avengers,
Cassie’s superpowers manifest themselves by causing her to grow monumental
in size and power, similar to her dad. The Commonwealth of
Australia, like many different countries, has a
plethora of historic knowledge that every citizen must know.
1902 – Ellen Dougherty of recent Zealand turns into the primary registered nurse in the world.
1902 – New York City Board of Schooling hires Lina Rogers Struthers as North America’s first
college nurse. 1902 – Queen Alexandra’s Imperial Army
Nursing Service replaces, by royal warrant, the Army Nursing Service.
The Pittsburgh Steelers had the most effective red
zone offense in 2018 when it got here to scoring touchdowns.
The Pittsburgh Steelers had the most effective defensive
tackles in NFL history when”Mean” Joe Greene performed
for them.
I could not resist commenting. Exceptionally well written!
I couldn’t resist commenting. Well written.
I really love your site.. Great colors & theme. Did you build this website yourself? Please reply back as I’m attempting to create my own personal site and would like to learn where you got this from or what the theme is named. Appreciate it!
You’re so interesting! I do not suppose I’ve truly read through anything like that before. So wonderful to discover another person with some genuine thoughts on this subject. Seriously.. many thanks for starting this up. This web site is something that is needed on the web, someone with a bit of originality.
Your post has clarified a lot for me.프라그마틱
This blog was… how do I say it? Relevant!! Finally I’ve found something which helped me. Thank you.
Nice post. I learn something new and challenging on websites I stumbleupon everyday. It’s always useful to read content from other writers and practice something from their websites.
Nice post. I learn something new and challenging on sites I stumbleupon everyday. It’s always interesting to read through content from other writers and practice something from other sites.
ближайший ремонт сотовых
Spot on with this write-up, I actually believe this amazing site needs a great deal more attention. I’ll probably be back again to read more, thanks for the information.
That is a great tip particularly to those new to the blogosphere. Brief but very accurate info… Thanks for sharing this one. A must read post.
Hi, I do believe this is a great website. I stumbledupon it 😉 I’m going to revisit once again since i have bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
This is a topic that’s close to my heart… Cheers! Exactly where can I find the contact details for questions?
The original Publish-it, although, looked like a
small block of legal ruled yellow pad. What’s this small tool that keeps papers in a bind?
Technically, small office appliances or equipment additionally count as office provides.
In Scott Adams’ humor ebook “Construct a better Life by Stealing Office Supplies,” you’ll be
able to see Dogbert carrying a bunch of ballpoint
pens on the cowl. Other than paper merchandise, many consumables are writing supplies, too.
Their beneficial classes include desk supplies, filing supplies, paper merchandise, laptop-related provides,
time monitoring materials, mailing provides, binding needs and identification provides.
We’re all conversant in the 2-loop design model of paper clips at
this time, due to its ancestor named Gem clip. Mother nature thanks you!
Does it allow you to or harm you when are working with company purchasers for instance
in California or within the Northeast? The Greece-US
Economic & Business Cooperation Committee (ECCC) can be currently working to bilaterally expand trade
move and cooperation, and widen their market in Southeastern Europe, the Black Sea and the Center East.
Water-testing providers are provided for a wide range of clients by means of the PEI Analytical Laboratories which assesses based on the suggestions of the rules for Canadian Drinking Water High quality revealed
by Well being Canada.
Are you aware this East Coast state that has a West
Coast identify? West Virginia was the first and solely state to declare independence from the Confederacy.
Virginia birthed essentially the most U.S. Delaware was the
very first state to ratify the U.S. New York has about 10 million fewer residents than California (probably the most populous state),
however it is house to the country’s most populous metropolis, New York
City. The capital of Indiana is Indianapolis, and it is residence to the Indianapolis 500, which is certainly one
of the biggest single sporting occasions on this planet, with upwards of
300,000 attendees. Can you abbreviate this Midwest state that holds one of the largest
single sporting occasions on the earth? In the early 1970s occasions within the Center East overshadowed the rise of Coastal.
Place was a web based social experiment on the social networking web site Reddit
created by Josh Wardle, who went by powerlanguage, that first
began on April Fools’ Day 2017 and rebooted on April Fools’ Day 2022.
Within the 2017 experiment, it starts off as a blank 1000×1000 tile
canvas with tiny white pixels, and Reddit users can place a colored tile as soon as each
five minutes. But it additionally is sensible to keep away from
having such accidents in the primary place!
Seed capital – Seed capital is the money you could do
your initial analysis and planning for what you are promoting.
Life and Health and Property and Casualty strains of enterprise.
Tofel, Kevin (October 29, 2015). “BlackBerry Priv standout features: Hub, pop-up widgets and safety app”.
Tofel, Kevin (October 21, 2015). “The many ways BlackBerry beefs up Android safety on the Priv”.
Moynihan, Tim (November 6, 2015). “Overview: BlackBerry Priv”.
McEntegart, Jane (November 4, 2013). “BlackBerry Replaces Thorsten Heins with New Interim CEO”.
Mahale, Sneha (July 17, 2013). “Evaluate: BlackBerry Q10”.
Diokno, Carlo Raphael (July 17, 2013). “BlackBerry Q5 price in US revealed: BB Q10 & Z10 costlier”.
El Akkad, Omar (August 12, 2013). “BlackBerry puts up ‘for sale’ sign, with Fairfax emerging as potential purchaser”.
Blumenthal, Jeff (August 14, 2012). “Wells Fargo paying $6.5M to settle charges with SEC”.
Whittaker, Zack (March 30, 2012). “RIM misplaced $fifty four million on four-day international BlackBerry outage”.
Li, Yun (18 March 2020). “NYSE to briefly close floor, transfer to digital buying and selling after constructive coronavirus assessments”.
Amarjothi JMV; Jesudasan, J.; Ramasamy, V.; Jose, L. (2020).
“History of Medication: The origin and evolution of the primary modern hospital in India”.
David Goldman (August 20, 2020). “The BlackBerry is coming back”.
I get skilled assist for my taxes however try to know
which tax credit may very well be applied to my situation, too.
To get all these funds, workers must contribute a certain amount (usually twice what the employer contributes).
The straightforward 401(k) plan has a lot of the identical requirements
and features as the easy IRA, however it allows your employees to contribute a pre-tax portion of their wage.
The Caribbean: Hurricane Wilma OCHA State of affairs Report No.
6. U.N. The Caribbean: Hurricane Wilma OCHA Situation Report No.
7. U.N. Hurricane Wilma Post-Storm Seashore Circumstances
and Coastal Influence Report (PDF) (Report). The Palm Seashore Publish.
West Palm Seashore, Florida. The important thing West Citizen. Plaza Accord with France, West
Germany, Japan, and the United Kingdom. The finance ministers of the
five largest European economies (France, Germany, Italy, Spain and the United Kingdom) wrote a letter to U.S.
In Colombia, the peso set an all-time low towards the U.S.
Costliest U.S. tropical cyclones tables up to date (PDF) (Report).
Storm Information and Unusual Weather Phenomena (PDF).
Nonetheless, registered market makers are sure by change guidelines stipulating their
minimal quote obligations. Many HFT corporations are market
makers and provide liquidity to the market, which has lowered
volatility and helped slender bid-offer spreads making trading
and investing cheaper for other market individuals. Usually the market worth
of the goal company is lower than the value offered by
the acquiring firm. For example, for a highly liquid stock, matching a sure share of the general orders of stock (referred to as quantity inline algorithms) is
usually a superb technique, but for a highly illiquid stock, algorithms try to match each order that
has a favorable worth (known as liquidity-searching for algorithms).
A particular class of these algorithms attempts to detect algorithmic or iceberg orders on the other facet (i.e.
if you are attempting to buy, the algorithm will attempt to detect orders for the sell
side). In darkish swimming pools, buying and selling takes place
anonymously, with most orders hidden or “iceberged”. Joel Hasbrouck and Gideon Saar (2013) measure latency based on three parts: the time it takes for (1) data to achieve the trader, (2) the trader’s
algorithms to investigate the information, and (3) the generated action to achieve the trade and get carried out.
Community-induced latency, a synonym for delay,
measured in one-approach delay or spherical-journey time, is generally defined as how much time it takes for
an information packet to travel from one level to a different.
On the time, the constructing was valued at $1 million, while the land was value a further $1.6 million. Garza had founded the cryptocurrency startups GAW Miners and ZenMiner in 2014, acknowledged in a
plea agreement that the companies have been part of a pyramid scheme, and pleaded guilty to
wire fraud in 2015. The SEC separately brought a civil enforcement action in the US in opposition to Garza,
who was ultimately ordered to pay a judgment of $9.1 million plus $700,000 in interest.
The 30% low cost to the €77bn guide value outlined by NAMA contains circa
€9bn of unpaid curiosity. Investment value – the value to at
least one explicit investor, and may or may not be greater than the market value of a property.
CSCW researchers usually have problem deciding which set(s)
of tools will benefit a selected group because of the nuances inside organizations.
ISO/IEC 27001 specifies a number of agency requirements for establishing,
implementing, maintaining and enhancing an ISMS,
and in Annex A there is a collection of information safety controls that organizations are
encouraged to adopt the place acceptable within their ISMS.
National Centers for Environmental Information (NCEI). Stefan Rahmstorf.
“Storm Harvey: impacts probably worsened on account of global warming”.
Air Florida sponsored Southampton Soccer Membership, an English Soccer League side, throughout the 1983-eighty
four season, by which Southampton were league runners-up.
The nation also has direct trade with China and India by
way of air corridor. This partnership was adopted by an settlement with Optiemus Infracom on February 6, 2017,
to provide units throughout India and neighbouring markets together with Sri Lanka, Nepal, and Bangladesh.
In February 2010, the company announced an agreement with Shaw Communications whereby the latter company would purchase
an 80% voting interest, and 20% fairness curiosity, in the restructured entity, pending approvals from the Canadian Radio-television and
Telecommunications Fee (CRTC) and others.
CRTC on October 22, 2010, with Canwest delisting itself from the TSX and officially ceasing operations that same month.
In January 2010, CanWest’s bonds commanded about 70 cents on the dollar.
CanWest’s bonds at one level traded for as little as 15 cents on the dollar.
After bankruptcy proceedings concluded below the Bankruptcy and Insolvency Act, Canwest, by this point referred to as 2737469
Canada, Inc., lastly dissolved on May 27, 2013. Asper, through his Syngus Corp.
As a result, police evicted criminal elements from Link Valley in a 1989
raid. Because of the scale and weight of the greenback coins, they circulated minimally all through their history, except in the West (particularly at
casinos within the early-to-mid-20th century, the place they have been commonly used each at the tables and at slot machines.) Because
of this, the coins had been generally shipped to Washington and stored
within the vaults of the U.S. The corporate’s
primary subsidiary is Wells Fargo Financial institution, N.A., a nationwide financial
institution that designates its Sioux Falls, South Dakota, site
as its major office (and subsequently is treated by most U.S.
Economist Joseph Stiglitz criticized the plan proposed by U.S.
SLRA created a grasp plan for the area and labored with town of
Houston and other independent entities to show the once-blighted blocks right into a
landscaped backdrop for several community actions. Katherine Feser
of the Houston Chronicle said that the central location of Braes Oaks, the bushes,
and the large tons made Braes Oaks “prime”. In 2000 Steve Anton, a real estate broker of Hallmark Properties,
stated that a basic trend of accelerating lot costs and the
addition of costly houses in the wider space elevated the costs of Southern Oaks real estate values.
ESOP advocates concede that it could also be an excessive focus in a plan specifically meant to be for retirement safety.
Lopez, Maribel. “BlackBerry Snaps Up WatchDox For Content Safety”.
Microsoft Trade Server utilizing its complementary server software
program, BlackBerry Enterprise Server (BES). Imperfect Produce’s Reilly Brock likens this to being
“as wasteful as a raising a cow, slaughtering it, and solely using the filet mignon.” Very
similar to collards or kale, broccoli leaves can be roasted, sautéed, used in a stir-fry even blended
into smoothies for added nutritional kick. Broccoli florets get
most of the love, while the stalks and leaves are solid by the wayside.
Whereas comparable in some ways, the plans even have notable variations.
You don’t have to be driving a quick car to appreciate efficiency tires;
they can provide further security to just
about any vehicle. Turbo kits are car modifications that are sometimes used by auto fans.
Way cool! Some very valid points! I appreciate you writing this write-up plus the rest of the website is extremely good.
Hi, I do believe this is an excellent blog. I stumbledupon it 😉 I am going to come back once again since i have book marked it. Money and freedom is the best way to change, may you be rich and continue to guide other people.
The next time I read a blog, I hope that it doesn’t disappoint me as much as this one. After all, Yes, it was my choice to read through, however I actually thought you would probably have something useful to talk about. All I hear is a bunch of crying about something you could fix if you weren’t too busy seeking attention.
I truly love your site.. Great colors & theme. Did you develop this website yourself? Please reply back as I’m looking to create my own blog and would like to know where you got this from or what the theme is called. Cheers!
Aw, this was an extremely nice post. Taking a few minutes and actual effort to create a very good article… but what can I say… I put things off a whole lot and don’t seem to get anything done.
Landlords own the property itself, but may hire a property
manager or property administration firm to take most of the every day obligations
off of their shoulders. He didn’t disagree with the Courtroom’s general holding, but he feared the case may have been “feigned”
as a result of possible collusion between the parties in order to establish precedent.
Supreme Court docket’s choice in Fairfax v. Hunter’s Lessee, a case wherein Johnson had dissented,
by arguing that the Supreme Court docket’s appellate energy didn’t lengthen to its court docket.
In Fletcher v. Peck (1810), Johnson joined nearly all of the Courtroom to hold
that a Georgia regulation voiding land grants given by
the state the year prior was unconstitutional. The Georgia Gold Rush in the early 1830s led
to two vital circumstances relating to Native American sovereignty that Johnson heard on the
bench. As Jarrod says goodbye and turns to go away,
he notices two characters who saunter lazily into the store.
Johnson additionally joined two other landmark decisions on federalism.
These were small fighting/war toys for young children.
For the most part, however, young boys added them as mutants
in their G.I. After Ferrari’s death in 1988, the
Fiat-controlling Angelli family added another 40 percent to
its 50-percent share of Ferrari; Piero Ferrari retained 10 percent.
Merlin was an electronic game without a screen.
Pocket doors at both end of the bath keep the room visually simple
and the restricted ground space unobstructed.
After they lifted clear of the trees, he slumped to the flooring of the helicopter,
his marathon mission full. Sergeant Rose was
one of the last on the last helicopter, firing as he hobbled aboard.
Capt. Rose was awarded the Distinguished Service Cross in 1971
for saving lives over four days regardless of being wounded himself during a Vietnam War mission called Operation Tailwind.
Gary M. Rose to receive the Medal of Honor a long time after his identify had originally been submitted.
Rose’s Medal of Honor packet to be reconsidered.
Special laws was required because of the amount of time that had handed since Rose’s service.
A print model of the story appeared in Time magazine, CNN’s news associate in this system, known as
NewsStand. One veteran recounted turning on the Tv with curiosity after CNN promoted
a new program referred to as NewsStand, then realizing the story was about him
and his fellow soldiers. He then attended multiple
“A” schools at Naval Air Technical Training Command Memphis, receiving meritorious promotion to lance corporal.
Stay22 raised over $750,000 from various investors including Travelport, FounderFuel, Real Enterprise, and 7 Gate Enterprise.
Personal Accountability could be incorporated into video video games by
including an incentive system the place individual players are rewarded with additional factors for finishing an objective or an motion that improves the team’s possibilities of success.
The government Accountability Workplace (GAO) has stated that discontinuing the dollar invoice
in favor of the dollar coin would save the U.S. In 2019, the GAO re-estimated the
price of changing the $1 invoice and located for the first time that
it will cause the government to lose between $611 million and $2.6 billion as a result of physical
money was getting used much less, leading to dollar payments remaining
in circulation longer in comparison with the 2011 analysis.
From 1792 to 1803 the $1 coin compared favorably with the
Spanish dollar and was accepted at par for overseas purchases.
Chief among these were the Spanish silver dollar coins (additionally called items of eight or eight reales) minted in Mexico and different
colonies with silver mined from North, Central and South American mines.
Before the American Revolutionary Battle, coins from many European nations circulated
freely in the American colonies, as did coinage issued by the varied colonies.
Very good info. Lucky me I recently found your website by accident (stumbleupon). I have saved it for later!
Within the late 1960s the founding of the Campaign for Justice in Denver in and the land
grant motion in New Mexico in 1967 set the bases for
what would turn out to be the Chicano (Mexican American) nationalism.
A notable occasion in the Chicano movement was
the 1972 Convention of La Raza Unida (United People) Party, which organized with the objective of
creating a third party that would give Chicanos political power within the United States.
Bank nifty is a sectoral index that focuses on both private and PSU bank stocks.
In the Bank Nifty, the private banks have an exceedingly large weightage in Bank Nifty
compared to the PSU banks. The index comprises the twelve large capitalized Indian banking stocks.
It provides the benchmark to the investors by capturing the capital market performance of the Indian Bank stocks.
The ladies uncover that the leader of the camp has been extracting the expertise
from the teenagers with a view to make herself more gifted.
After several teens have been rioting and destroying things around city; Jerry has the spies infiltrate as members at
a talent camp.
China National Offshore Oil Company reported 2021 revenues of ¥246.111 billion. China National Petroleum Company reported 2019 revenues of ¥2.771 trillion. China Nationwide Petroleum Corporation reported 2020 revenues of ¥2.087 trillion. China Suntien Inexperienced Vitality reported 2018 revenues of ¥9.975 billion. COSCO Transport Energy reported 2020 revenues
of ¥16.268 billion. COSCO Delivery Power reported 2022
revenues of ¥18.566 billion. China Suntien Green Power reported 2019 revenues of ¥11.943 billion. China
Nationwide Offshore Oil Firm reported 2018 revenues
of ¥226.963 billion. China Nationwide Offshore Oil Company
reported 2020 revenues of ¥155.372 billion. China Nationwide
Offshore Oil Company reported 2022 revenues of ¥422.2 billion. China Suntien Green Power reported 2022 revenues of ¥18.560 billion. China Suntien Green Vitality reported 2020 revenues of ¥13.510 billion. China Suntien Green Energy reported 2017 revenues of ¥7.057 billion.
China Suntien Green Vitality reported 2021 revenues of ¥15.985
billion. COSCO Delivery Vitality reported 2019 revenues of ¥11.943 billion. Whitecap Sources reported 2019 revenues of CAN$1.454 billion. 2.1
billion in U.S. 62.7 billion in U.S.
In addition to all of the examinations they endure on race day, one lucky car is selected for a visit
out to the NASCAR Research and Improvement Center in Concord, N.C., for further intense
inspection following every race. The DJIA rose one other 319 factors the next day, causing the aforementioned report
to be set. If planned conversations are too daunting a process, ask the videographer to call particular folks into a room
one at a time to document particular messages.
You should look for an agent who is aware of the native market
nicely and has a great history of helping folks buy their first home.
The hospital was offered in 1906 to another medical charity, the German Polyklinik; the name was modified to Stuyvesant Polyclinic in the 1910s.
The buildings were restored numerous times of their historical past.
A 1914 firm historical past estimated that your complete complicated could accommodate 20,000 guests and tenants per day.
VZ acquired YHOO operations; remainder of YHOO transformed to closed-end company
generally known as Altaba. June 19, 2017 HLT Hilton YHOO
Yahoo! July 26, 2017 PKG Packaging Company of America MUR Murphy
Oil Market capitalization change.
You might really feel like you’re bothering the house owners, but it is value the additional
effort when making such an necessary lengthy-term investment.
It could be difficult to avoid being caught up in the shopping for frenzy
during a hot actual estate market. A savvy purchaser’s agent may
also be in a position to gather clues about the vendor’s motivation.
Not usually. Usually, the purchaser’s agent splits the sales commission with the
seller’s agent and you don’t pay anything. In some
circumstances the vendor’s agent is there to let you know extra about the home.
That happened early in the recession when, after the increase in new dwelling gross sales, out of the blue there were more new properties than builders may sell.
Conventional lenders are likely to require you to put a minimum of 10% of the entire price of the house down, however there are lenders who require as little as 5% down. Most showings are done when the current owners are out of the house.
This keeps you from looking at houses which can be out of
your price vary and likewise lets sellers know you are severe and can afford their home.
The funds will have to be taxed when the funds are withdrawn, but your taxable revenue could be lowered till they’re withdrawn.
The main risks to ecosystems from climate change are biodiversity loss, ecosystem structure change, increased tree mortality, increased wildfire, and ecosystem carbon losses.
Cows may look pretty benign as they languidly chew on grass in farm fields, but some
environmentalists warn that the animals’ farting, belching and pooping is a major contributor to climate change.
Post writing is also a fun, if you know then you can write
otherwise it is complicated to write.
Good post. I learn something new and challenging on sites I stumbleupon on a daily basis. It’s always useful to read content from other authors and practice something from their websites.
Designed by Francesco De Sanctis and constructed 1723-1725, the 135 steps kind
a large vista looking down towards the Tiber. The new oil, as it drips down your back, certainly puts
you into one other dimension. The elders right now are few and much between but they’re there and keen to show anyone
who is keen to study, both in Hawaii and even abroad via the web.
Speaking at the company’s 2014 AGM, chief executive Michael O’Leary mentioned that the airline needed
to “cease unnecessarily pissing folks off”.
The corporate’s predominant operating segments are International Housing and Global Life-style.
Its expansion meant that the corporate required larger premises, and
it relocated its head places of work to the
biggest unit in Yorkshire’s main warehousing and distribution base.
The legislation would make heirs take the distribution inside
five years in order that the IRA funds deplete entirely by that point.
The private Rule (also recognized because the Eleven Years’ Tyranny) was the interval in England from 1629 to 1640 when King Charles I dominated as an autocratic absolute monarch
with out recourse to Parliament. In 2014, it deliberate to open a hundred and fifty new stores inside three years.
On 20 July 2018, it was confirmed that every one Poundworld shops had been to shut by 10 August.
Halliwell, James (2 August 2012). “Poundworld leads the cost as single-value discounters elevate off”.
Taylor, Henry (18 December 2012). “Comet’s collapse and other post-recession retail failures”.
Профессиональный сервисный центр по ремонту сотовых телефонов, смартфонов и мобильных устройств.
Мы предлагаем: ремонт смартфона
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр по ремонту сотовых телефонов, смартфонов и мобильных устройств.
Мы предлагаем: ремонт смартфонов
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Aw, this was a really nice post. Spending some time and actual effort to create a very good article… but what can I say… I hesitate a lot and never seem to get anything done.
This web site certainly has all of the information I needed concerning this subject and didn’t know who to ask.
This is a topic that’s close to my heart… Thank you! Where are your contact details though?
A fascinating discussion is definitely worth comment. I think that you need to publish more about this topic, it may not be a taboo subject but generally people don’t talk about these topics. To the next! Cheers!
These new insurance coverage contracts allowed insurance to be separated from investment,
a separation of roles that first proved useful in marine insurance.
John confronted a further cost of acquiring £137,000 by deception (the same cost his spouse was already facing) in addition to the
existing life insurance cost towards both of them for £25,000 and John’s separate cost of obtaining a passport by deception. Dunn, Robert M.
Jr.; Mutti, John H. (2004). International Economics, sixth Edition. Lawrence, Robert Z.; Hanouz,
Margareta Drzeniek; Doherty, Sean (2012). The global Enabling
Trade Report 2012: Reducing Provide Chain Barriers (PDF) (Report).
Feenstra, Robert C.; Taylor, Alan M. (2008). International Macroeconomics.
Carbaugh, Robert J. (2005). Worldwide Economics, 10th Version. Levi, Maurice
D. (2005). Worldwide Finance, 4th Version. Endres, Anthony M.
(2005). Nice Architects of International Finance. Makin, Anthony J.
(2009). World Imbalances, Alternate Rates and Stabilization Coverage.
Arndt, Sven W.; Crowley, Patrick M.; Mayes, David G. (2009).
“The implications of integration for globalization”.
James, Paul W.; Patomäki, Heikki (2007).
Globalization and Economy, Vol. On 25 February 2017, the London Inventory Change Group PLC stated it wouldn’t sell
its fastened-earnings buying and selling platform in Italy to Deutsche
Börse AG, to appease anti-trust issues. In 2007, the Alternate acquired the
Milan-primarily based Borsa Italiana for €1.6bn (£1.1bn;
US$2bn) to form the London Inventory Trade Group plc.
The vote in favor of promoting to the Dutch government was 42.99%;
the vote in favor of promoting to the Belgian authorities was 49.74%.
After rejecting the gross sales, the assembly went on to vote on the
appointments to the board: three of the candidates withdrew (due to the vote on the sales).
The meeting went to a vote on 15.16h and rapidly rejected the gross sales.
February 6, the Belgian authorities has guaranteed the Chinese
language authorities that a vote in favor by Ping An on February 11 won’t have any legal effect within the matter
of the declare for damages by Ping An, underneath the treaty between the Belgian and Chinese authorities (see
above). February 10, Het Financieele Dagblad revealed an interview with Hessels, performing chairman of the board of Fortis, during which he states that a vote against the gross sales would result within the bankruptcy of Fortis.
Het Financieele Dagblad agrees with Modrikamen: the meeting will vote in opposition to, by which case
BNP Paribas will withdraw (as indicated by Prot in the
interview of February 7). The Belgian Prime Minister has announced yet another renegotiated deal (drawn up in response to the news of Ping An), which will likely be submitted to
the assembly of shareholders.
Aw, this was an extremely nice post. Taking the time and actual effort to generate a superb article… but what can I say… I put things off a whole lot and never seem to get nearly anything done.
Later, in ancient Greece and through the Roman Empire, lenders based
in temples gave loans, while accepting deposits and performing the
change of money. Improvement of banking spread from northern Italy
throughout the Holy Roman Empire, and in the fifteenth and
16th century to northern Europe. The Bardi and Peruzzi families dominated banking in 14th
century Florence, establishing branches in many different elements
of Europe. Some adoptive households desire the term
“birth mother and father,” “biological mother and father” or even “first dad and mom.” You would be the kid’s “actual” father or mother.
Types of records accounting for commerce exchanges of funds were first being made about 3200 BCE.
Northwest was the first large U.S. The U.S.
spends an extraordinary sum of money on well being care.
Nonetheless, the Firstar that took over U.S. However, whereas
it was increasing to Southeast Europe, NBG was retreating in North America and other places serving the Greek
diaspora. Writers Guild of America West. On June 19, an EF1 twister hit Japanese Springfield, Missouri at around 3:
30 pm CDT (2030 UTC). This web page was last edited on 5
August 2024, at 12:13 (UTC).
Do you have a spam problem on this website; I also am a blogger, and I was wanting to know your situation; we have developed some nice practices and we are looking to exchange strategies with others, why not shoot me an email if interested.
You need to take part in a contest for one of the highest quality blogs on the net. I’m going to highly recommend this site!
Excellent read, I just passed this onto a colleague who was doing a little research on that. And he just bought me lunch because I found it for him smile Therefore let me rephrase that: Thanks for lunch!
Профессиональный сервисный центр по ремонту сотовых телефонов, смартфонов и мобильных устройств.
Мы предлагаем: ремонт смартфона
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Fantastic post however , I was wondering if you could write a litte more on this subject? I’d be very thankful if you could elaborate a little bit more. Cheers!
Some also have limits on how much the interest rate can decrease.
Since clearing house members usually have many clients, they can net out margin payments
from their client’s offsetting positions. Given the ability to profit from private information,
self-interested traders are motivated to acquire and act on their private information.
NY (March 18, 2019). “Jeff Mkt. Library closing; Ottendorfer reopens”.
O’Flanagan, Linda (June 6, 2019). “French group buys historic East Village workplace constructing”.
Dewan, Shaila Okay. (June 20, 2001). “19th-Century Charm Saved in 21st-Century Stacks”.
Vol. 73, no. 1875. February 20, 1904. p. In 1994, the Hong
Kong Securities and Futures Fee found Standard Chartered’s Asian funding bank to have illegally helped to artificially assist the value of recent
shares that they had underwritten for six firms from July 1991 to March 1993.
The bank admitted the offence, apologized, and reorganized
its brokerage items. It has secondary listings on the Hong Kong Stock Exchange, the National Inventory Exchange of India, and OTC Markets
Group Pink. Leading to the incorporation of Normal Chartered (Hong Kong) on 1 July
2004, the Legislative Council of Hong Kong amended Legal Tender Notes Difficulty Ordinance.
Clark, Don (July 6, 2005). “Go well with by Broadcom Says Qualcomm Seeks a Monopoly”.
Albertson, Joshua (July 11, 2005). “Stories of Cabrini Sale Worth Had been FAR Too Excessive”.
Luis F. Perez (November 17, 2005). “Boca Airport Tab Nears $12 Million”.
Rosenstock, Bonnie (November 11, 2008). “English pull off an inside job at former Polyclinic”.
This offers the listener a grip on the presentation type so
that he can focus on the content of the programme.
The broadcast always offers an ungainly impression, because Tedje
forgets to close the microphone and the listeners can hear non-public (and not too nice) conversations between Peer and Toon. In early July 2018, Turkey’s
Capital Markets Board (SPK) stated that till the end of August share purchases on the Borsa Istanbul by individuals social gathering to the
related firm’s internal data, or by these near them
(insider buying and selling), wouldn’t be subject to a inventory market abuse directive.
Listed firm boards, no matter their expertise, can usually fall into bad habits and the main focus
of board meetings and communication can change into aspect-tracked and
not using a gentle guiding hand. In addition to the December 19 meeting (in Belgium solely),
new meetings in January are anticipated, to handle the question of the
composition of the Supervisory Board. 34 Toyoda returned to Japan to join the board of directors giving a high
degree assist to the challenge. Toyota’s flagship design studio, Calty,
was then brought in to deliver a contemporary interpretation of the FJ40.
In 2009 under the banner of Delta, service to Rome was then resumed for
the summer season.
Bank customers have been, however, anticipated to repay loans.
Among the many folks’s names Mollicone used for
the fake loans had been members of his household, golfing companions, and Buddy
Cianci. Members of RISDIC’s board of trustees had been primarily managers of the establishments
it insured. The board failed to assessment stories by
examiners and outdoors auditors. Along with being poorly regulated, it did not abide by normal trade practices and although it formally adopted the
requirements of the National Affiliation of Share Insurance Company, it did not truly implement them successfully.
She stated the only purpose the legislation to end RISDIC failed was because of problematic relationships between legislators and the banks.
After his arrest, Mollicone mentioned there was no reason to decide on Utah aside from the very fact he had briefly traveled there in the
past. Audits had not been carried out at Heritage on the schedule required by RISDIC; the insurer didn’t notify the Lawyer
General of issues it found at Heritage when it did conduct an audit; Mollicone himself
had been vice chairman of RISDIC; Mollicone as well
as others at RISDIC have been nicely-related to politicians; Heritage’s board comprised Mollicone’s pals and family; board members didn’t attend
regular conferences.
It was first introduced in Mac OS X 10.5 Leopard as a simplified option to configure MIDI Gadgets.
A number of upgrades have been introduced to the iMessage
platform over time, together with message results, enhancing and deleting messages inside a fifteen minute window,
and a dedicated iMessage App Store which allows users to download sticker packs
that may be despatched in conversations. It permits customers to examine the Yahoo!
Mail is an e-mail consumer first originating in NeXTstep, before being
carried over to Mac OS X. It is preconfigured to work with standard email
providers, comparable to Yahoo! After law college, John labored first as a litigator, then as a public defender, adopted by work as an legal professional combating insurance coverage fraud.
Patrons might sue a seller who violates this provision for an quantity equal
to three times all fees made for the title insurance coverage.
Legislative amendments arising from the 2020 price range (Bill 4) included the creation of a brand new
high tax bracket that starts at $220,000, exempting electric aircraft from
PST, three 12 months extensions of the farmers’ food donation tax credit and BC training tax credit score, removing the
PST exemptions that had utilized to soda drinks and online streaming services,
and making heated tobacco merchandise subject
to the Tobacco Tax Act.
The Franklin Sugar Refinery was a steam-powered, brick constructing constructed beginning in 1866 on Almond and Swanson Streets by the
Delaware River in Philadelphia, Pennsylvania, within the United States.
In 1925 the building was bought by the Merchants Warehouse Firm.
They purchased by sugar brokers such as Skiddy Minford & Co.
in New York, as well as other brokerages in New York Metropolis,
Philadelphia, and occasionally in Boston. The corporate bought uncooked sugar in large quantities from Cuba,
much less significantly in Java, Indonesia, as well as from the spot market in New York or Philadelphia.
In 1866 the refinery processed about a thousand barrels of
raw material a day. At that point the refinery
ran six days a week besides July four and Christmas.
Every tile is assigned a point value, and you amass factors by attempting
to get essentially the most points out of your phrase. Although Saturn was nonetheless
a long way from paying back GM’s preliminary investment, officials hastened to level out several advantages accruing from the new firm.
So, if you are a homeowner, you might rent out a single room or two to strangers, even while the house is still occupied.
It has led to the burgeoning of language translation businesses all across the globe who not only are helping people talk
in each other’ languages, however are additionally reviving
the lengthy misplaced languages with their language translation providers.
As of September 23, 2009, EDS was known as HP
Enterprise Companies (now known as DXC Know-how). ROKR fashions have been released beginning in September 2005
and ending in 2009. They were notable for incorporating assist of media participant features.
Many users also discovered that transferring music to the telephone was
gradual compared to dedicated gamers, as a result of lack of support for Hello-Speed USB, and
the E1 lacked wireless transfer. The ROKR E1 is a re-badged Motorola E398 candybar type phone (it was
originally called the E790) with Apple-licensed expertise to play again iTunes Music Store bought music.
Since hardware on the Motorola E398 and ROKR E1 telephones are the same, it is
possible to crossflash the Motorola ROKR E1’s firmware to the Motorola
E398 utilizing phone flashing software program like flash & backup.
Your style is unique compared to other folks I’ve read stuff from. I appreciate you for posting when you have the opportunity, Guess I will just bookmark this web site.
Pretty! This was an incredibly wonderful post. Thanks for providing this information.
There are a number of methods a person can take advantage of relating to investing in inventory market opportunities.
There might be many reasons why you may want to purchase used snack vending machines.
With a single turbine shaft (versus two), digital fuel supply,
and a projected eighty five horsepower, it will have been the best turbine but,
and likely the most cost effective to build in amount.
Investors wished to seek out safer ways to invest their money due to the 11 percent stock market fall in two
weeks. Six business jets (four saved within the hangar and two outside) were damaged.
New industries like info know-how and the monetary services sector have changed
the outdated with lots of multinational corporations having their Australasian headquarters based within the Sydney Central Enterprise District.
The aggressive buying would drive up the share value, and, being unable to seek out shares elsewhere, the quick sellers would have no possibility however to turn to the Heinzes, who could then identify their value.
The outlook for the TSX ABX share value is influenced by a quantity of things, including these
outlined above.
Those who doubt a company’s health can purchase buyer swaps, make premium payments on the swaps and
cash them in when the company goes under.
Furthermore, modern portfolio theory requires that all
return analysis be conjoined with risk analysis, else good performance results can mask their relationship
to greatly increased risk.
The restoration scammers obtain lists of victims by shopping for them from the original scammers.
The victims part with their money in pieces to the fraudster
on account of the government Service Tax, authorities clearance costs, financial institution expenses,
transportation prices, survey payment and so on. The Indian government is issuing public notices in media to spread awareness amongst the public and warn them towards cellular tower fraudsters.
Cost is via MoneyGram, Western Union or cash mules’ bank accounts the
place different victims have been duped into work at home scams.
Upon the potential victim contacting the scammer, the scammer responds by asking for particulars pertaining to the potential victim’s circumstances and site below the pretense of making certain that the pet would have a suitable residence.
Silverware polish is on our list of the Horrible
Ten dwelling cleaning products, together with
drain cleaners, over cleaners, bathroom cleaners, spot removers,
furniture polishes, cleansers and powdered cleaners,
window cleaners, bleach and liquid cleaners. In 2013 she traveled to South Africa to supposedly marry
her scammer, Jesse Orowo Omokoh, 28, after having sent greater than $90,000 to him over a 3-12 months interval.
Scammers will sometimes ask for cash to be sent by way of a
money order or wire switch attributable to the necessity to travel, or
for medical or business prices.
Right here is the right site for anyone who
wishes to find out about this topic. You understand so much its almost tough to argue with you (not that I really would want to HaHa).
You certainly put a new spin on a topic which has been discussed for a
long time. Excellent stuff, just excellent!
Bomey, Nathan; Krantz, Matt (June 24, 2016). “U.S. stocks hammered as Brexit shock rocks markets”.
Central Belief Firm. 1932. Archived from the original on June 24, 2021.
Retrieved June 16, 2021. TITLE VII. Alexandra Stevenson and Matthew
Goldstein (August 24, 2015). “A Stock Market Rout in a Month That Hedge Funds Would Sooner Forget”.
Jackson, Anna-Louise (August 25, 2015). “China Anxiety Resurfaces to Torpedo Relief Rally in U.S. Stocks”.
OMX Copenhagen 25, the OMX Tallinn, and OMX Vilnius
on the Nasdaq Nordic exchanges all fell beneath 20 percent from their most latest peaks on 19 February in Copenhagen and on 21 February in Tallinn and
Vilnius. Zurich’s internet earnings increased by 30 % to US$3.2 billion in 2005, and operating income rose by 32 p.c
to US$3.9 billion. Likewise, the Spanish IBEX 35, Greek ATHEX, Dutch AEX index,
Czech PX Index and Polish WIG30 all fell by eight
to 15 p.c.
Workplace 2010 supplies learn support for ECMA-376, read/write assist for ISO/IEC 29500 Transitional, and read support for ISO/IEC
29500 Strict. On June 15, 2011, HP filed a lawsuit in California Superior Courtroom in Santa Clara, claiming that Oracle had breached an agreement to assist the Itanium microprocessor utilized in HP’s high-end enterprise servers.
Not like many other statutory or regulatory schemes, the FMLA grants employees the power
to choose between filing a complaint with the Wage and Hour Division of
the US-DOL, or filing a personal lawsuit in courtroom. Underneath the FMLA, eligible employees might
take off as much as 12 work weeks in any 12 month interval for the start or adoption of a baby, to care for a
family member, or if the employee themselves has severe health situation. If each spouses work for a similar employer,
they are not each entitled to take 12 weeks off
the illness. Child labor laws are jointly enforced by the Wage and Hour Division of the U.S.
In contrast, some other statutes present a “right of private motion” that permits a claimant to sue in court docket, resembling under some employment discrimination laws.
U.S. immigration laws additionally present for sure sorts of temporary work or
work-associated U.S.
Each of the respondents compares the relative importance of each pair of items using a
specifically designed questionnaire. In making the comparisons, the choice makers can use
concrete knowledge about the weather, they usually also can use
their judgments about the elements’ relative that means and importance.
Valuations will be achieved for belongings (for example, investments in marketable securities corresponding
to corporations’ shares and related rights, enterprise enterprises, or intangible belongings similar
to patents, information and trademarks) or for liabilities (e.g., bonds issued
by a company). The merger agreements allowed the Peugeot household to extend its current 7.2% stake in Stellantis by
up to an additional 1.5% by acquiring shares from France’s state lender Bpifrance, from
Dongfeng, or in the marketplace. The deal was completed
on sixteen January 2021, and the merged firm was renamed to Stellantis
N.V. The new Millennium Metropolis School on the Salvation Military Cluster of Colleges was renamed President John Evans
Atta Mills Instructional Centre of Excellence. John Atta Mills was sworn in as president on 7 January 2009
in a peaceful transition after Akufo-Addo was narrowly defeated.
The new firm’s first CEO, vested with full authority to signify Stellantis, was Carlos Tavares, the previous president of
the PSA managing board, in addition to former CEO of PSA Group,
with a 5-yr time period as Stellantis CEO.
Brian Cosgrove (5 October 1935). “South feel Pratt’s absence: Magpies’ stamina wins recreation”.
Melbourne. 27 July 1935. p. On July 15, 2013, Oracle
transferred its inventory itemizing from the Nasdaq to the NYSE.
7. Retrieved eleven July 2015 – through Nationwide Library of Australia.
McMullin, Ross (5 July 2012). “Origin of Carlton-Collingwood rivalry”.
Knox, David (four December 2012). “2010: The highest 100”.
Television Tonight. Knox, David (1 December
2014). “2014 Rankings: Seven wins Whole Folks, Nine scores demos”.
Ron Reed (8 June 2014). “50 years on, the men who gained Melbourne’s last premiership await the following”.
Sporting Globe. Melbourne. 5 June 1937. p. Niall, Jake (25 June
2010). “‘You cannot replicate the ache of losing a grand final till you have lost one'”.
In 1988, after business consultant James B. Farley turned the brand new chief of the corporate,
he initiated an enormous cost slicing program due to the company’s over-funding in real
property and junk bonds. Traders concerned a couple of attainable sovereign default rapidly sold Greek bonds.
Soon after it was founded in 2012 the bank got here under criticism for having the
highest cost for any transaction account
in comparison with other Dutch banks.
Located next to Mark Clark Corridor on the northeast nook of Summerall
Area, this uniquely shaped monument incorporates artifacts from the British submarine HMS Seraph, which carried then Major Basic Mark Clark to a
secret touchdown in Algeria prior to the Allied landings in the North African Marketing campaign of
World Conflict II so as to negotiate a surrender of the Vichy French
forces; the vessel was additionally concerned in Operation Mincemeat, a clandestine
operation which succeeded in convincing the
Germans that the allies supposed to invade Sardinia,
not Sicily. Mendacity between Mark Clark Corridor and Summerall Chapel is the
burial plot of US Army Basic Mark Wayne Clark who served as Citadel
President from 1954 to 1965 and President Emeritus till his demise in 1984.
The youngest Lieutenant Basic within the United States Military throughout World Conflict II (age 46), Clark served
as Basic Dwight Eisenhower’s deputy throughout the “Operation Torch” landings
in North Africa, then commanded the fifth Army within the Italian campaign liberating Rome in June 1944.
He later served as Commanding Basic of the fifteenth
Army Group and in 1952 was appointed by President Truman as Supreme Commander of UN forces in Korea.
The air is then immediately forced through the contraction cone,
a constricted area that significantly will increase airflow velocity.
Chicano is a time period utilized by some to explain the unique id held by Mexican-Individuals.
The U.S. Supreme Court docket will hear arguments within the case in its fall 2022 time period
and presumably will issue its ruling in the summer of 2023.
If the case is determined in favor of the plaintiffs, it’d give state legislatures close to-complete management over the drawing
of congressional districts in their states, allowing them to create gerrymandered maps that could not be overturned as unfair
by state courts.
On February 10, 2021, The Wall Avenue Journal reported,
citing a supply conversant in the matter, the Biden administration can be backing off from banning TikTok and shelving the sale of TikTok indefinitely, because the U.S.
On April 20, 2012, the US Common Services Administration banned
Oracle from the most popular portal for bidding on GSA contracts for undisclosed causes.
Oracle has a large office advanced positioned on the San Francisco
Peninsula in the Redwood Shores area of Redwood Metropolis.
In January 2019, the San Francisco Giants entered right into a 20-year agreement to rename their
stadium Oracle Park. On June 15, 2011, HP filed a lawsuit in California Superior
Court in Santa Clara, claiming that Oracle had breached an agreement to
assist the Itanium microprocessor used in HP’s high-finish enterprise servers.
Supreme Court docket, but the Supreme Court denied the petition. On 18 January, they every appeared separately at
Hartlepool Magistrates’ Court by video-hyperlink and had been remanded in custody till
15 February, after they confronted committal to Crown Court docket.
Boniface, Bosire (12 March 2012). “Kenya’s North Eastern Province Battles Excessive Maternal Mortality Price”.
On November 18, Governor Edward D. DiPrete closed
the bank on what was presupposed to be a temporary foundation, whereas officials tried to find out what was going on and control the harm.
In October 1990, the financial institution’s insurer, the Rhode Island Share and
Deposit Indemnity Company (RISDIC), took management of the financial institution following an examination that revealed its
poor state. The Heritage Mortgage & Investment financial institution was insured by the Rhode Island Share and
Deposit Indemnity Corporation (RISDIC), a state-chartered nominally non-public enterprise
which backed 45 of the state’s credit unions and banks.
The Rhode Island banking disaster occurred within the early nineties, when roughly a third of
the US state of Rhode Island’s inhabitants
lost entry to funds of their financial institution accounts.
The pattern grew to become significantly pronounced after Ohio and Maryland, the most important state-chartered funds, collapsed in 1985, causing financial institution crises in those states.
RISDIC, however, didn’t learn from the mistakes of other states.
It insured primarily those institutions that had been unable to
safe federal insurance, guaranteeing massive sums of cash at weak banks.
The Valley Inn Tavern in Heathcote, built in 1877, survived the initial
quake, however needed to be torn down after the large 5.1
magnitude aftershock.
Nellis, Stephen; Lee, Jane Lanhee (August 31, 2022). “Chips tech firm Arm sues Qualcomm and Nuvia for breach of license and trademark”.
King, Ian (August 31, 2022). “SoftBank’s Arm Is Suing Qualcomm for Licensing and Trademark Violations”.
Lei, David; Slocum, John W. (August 29, 2013). Demystifying
Your enterprise Technique. Alleven, Monica (November 29, 1999).
“Ericsson Tangles With Qualcomm”. Gohring, Nancy
(March 29, 1999). “Ericsson/Qualcomm bitter feud ends”. Allen, Mike (March 9, 2014).
“Leap Wireless Studies $640.8M Loss for 2013 as Sale to AT&T Looms”.
Clark, Don; Beckerman, Josh (July 23, 2014). “Qualcomm Revenue Rises; Company Notes ‘Challenges’ in China”.
Smith, Ryan (July 23, 2018). “Qualcomm Publicizes Their First 5G mmWave Antenna Module: QTM052, Coming This Yr”.
Whitwam, Ryan (August 26, 2011). “How Qualcomm’s Snapdragon ARM chips are distinctive”.
Smith, Ryan (October 30, 2023). “Qualcomm Snapdragon X Elite Efficiency Preview: A primary Have a look at What’s to return”.
Pressman, Aaron (October 27, 2016). “This is Why the Qualcomm-NXP Deal Makes sense”.
You should be a part of a contest for one of the greatest sites on the web. I most certainly will highly recommend this site!
very nice submit, i actually love this website, keep on it}
“Many people got trouble with their loans, hope you don’t get the same problem”
Профессиональный сервисный центр по ремонту видео техники а именно видеокамер.
Мы предлагаем: ремонт видеокамер на дому
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники в красноярске
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники в новосибирске
Hello! I simply would wish to offer a huge thumbs up for that great info you’ve here during this post. I will be returning to your website to get more soon.
There are a few intriguing points over time on this page but I do not determine if they all center to heart. There exists some validity but I’m going to take hold opinion until I consider it further. Very good article , thanks and that we want much more! Added to FeedBurner in addition
you have a excellent blog here! would you like to have the invite posts in my blog?
I just wanted to comment and say that I really enjoyed reading your blog post here. It was very informative and I also digg the way you write! Keep it up and I’ll be back to read more in the future
Lots of people were enthusiastic sportsmen or enjoyed music and dancing. It’s possible you’ll remember that you were happiest on the performing track. Nevertheless, with increasing obligations you may have found almost no time to indulge in any of the interests. Are you affected by depression and want to get out of its abysmal depths without lifelong antidepresants? You could try and feel free to overcome depression naturally.
I adore your wp theme, wherever do you down load it from?
Профессиональный сервисный центр по ремонту стиральных машин с выездом на дом по Москве.
Мы предлагаем: мастерские по ремонту стиральных машин в москве
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: ремонт бытовой техники в казани
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт техники в новосибирске
mpo808
You really make it appear really easy together with your presentation however I in finding this matter to be really something that I believe I might by no means understand. It seems too complex and extremely vast for me. I am having a look ahead for your subsequent post, I’ll try to get the grasp of it!
4月13日 – 長谷川閑史が取締役会長退任後、当社の相談役に就任すること、6月の株主総会終了以降、当面会長職の後任は選任しないこと、坂根正弘社外取締役が取締役会議長として、取締役会の議事を進行することを発表した。対ドジャース戦では走者を追い越し、本塁打が取り消しとなっている。三者面談ではかぐやの父親代わりを(勝手に)務めた。
I start to hate this junk e-mail from writing here figures on the forums… Your journal looks as unoccupied without… Would You like to serve me and show to all the know-how you are using if You’re fighting against the spamers? TX
第四次忍界大戦では奇襲部隊に配属され、初戦で穢土転生されたシンと遭遇。小中高生の間で「ミステリーブーム」が起こっていた…同話数にて、プリキュアシリーズ通算900回を突破。相内地区にて、福島城の築城。街の中のあらゆる建物よりも巨大で、背景に見える高層ビル並みに大きい。第45話ではクッキングとクックイーンが作った巨大ケーキのロウソクを灯した。第45話では1人ずつ顔が映し出される演出はカットされ、そのまま腰に手を添え、「デリシャスパーティ♡プリキュア! スーダンを統治する主権評議会(軍事政権)のアブドゥルファッターハ・
“モンスターストライク THE MOVIE ソラノカナタ”.
“モンスターストライク THE MOVIE はじまりの場所へ”.山口から「父親と同じウソつきの目をしている」と言われた真実は、父と同じ目をした自分が正義の戦士でなければ父も悪人になってしまうという思いから正義のために戦う人間になろうと決意し、中学生のころに知った司法試験予備試験制度によって弱冠20歳で弁護士となり大手法律事務所に勤務する。関東鉄道常総線取手駅構内において、入線してきた同駅終着(新守谷発)上り第24列車(キハ300形気動車2両とキハ800形気動車2両の4両編成、乗客約900名)が減速せずに暴走、車止めを突破し、そのまま駅ビルボックスヒル取手店(現・
テレ朝、野際陽子さん追悼特別番組『旅の香り』『DOCTORS 3』を18日放送 マイナビニュース 2017年6月16日発行、同月17日閲覧。 2017年8月、追浜工場の検査ラインから正式発表前のZE1型リーフの画像がTwitter上に漏洩。横浜国際女子駅伝 – 特別協賛・同時に新横浜公園内併設施設(小机競技場(日産フィールド小机)及び競技場内温水レジャープール施設(日産ウォーターパーク))の命名権も取得している。
翌日の戦闘ではマダラが落とした紅葫蘆と琥珀の浄瓶を拾いマダラを封印しようとするが、直後に「無限月読」の幻術世界に引き込まれた。 それから約3年後の第四次忍界大戦の最中、復活した大蛇丸により他の歴代火影たちと共に再び蘇生され、サスケに自身とマダラの因縁や木ノ葉を設立した経緯を語り、サスケが里を守ることを選択したことで歴代火影、大蛇丸、サスケの率いる「鷹」のメンバーと共に戦場へ向かった。
山中湖交流プラザきららにて開催。 “いぎなり東北産「祝東京初ワンマン単独」公演開催! 2019年8月13日-16日は、庭木と松井が代演(時間短縮による放送。後日商品代金を受け取る場合は、未収代金のことを売掛金といいます。 なお、同じ話で夏目が登場する場合、クレジットに名前が登場しない。 20万円の商品を売掛金で販売した場合、借方が「売掛金」で金額は20万円と記載し、貸方は「売上」で金額は20万円です。
Wow, incredible blog layout! How lengthy have you ever been blogging for? you make blogging look easy. The overall look of your site is magnificent, as smartly the content material!
Way cool! Some very valid points! I appreciate you penning this article and also the rest of the site is extremely good.
』(プレスリリース)株式会社ムーンチャイルド、2017年10月3日。 』(プレスリリース)株式会社GALDir
Media、2017年10月17日。同社は、そのポスター内で最も混雑率が低くなると示す先頭車両を女性専用車両として指定している。赤字補填のための借入は、業績が改善しないと返済が難しくなるからです。 “永尾まりやの卒業記念ファースト写真集が、22歳の誕生日に刊行!”.朝日新聞.、”秋葉原無差別殺傷 ○○被告の死刑確定へ 最高裁が1、2審判決支持。”.
“永尾まりや、待望の写真集『JOSHUA』8月27日、発売決定!
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники в перми
Профессиональный сервисный центр по ремонту стиральных машин с выездом на дом по Москве.
Мы предлагаем: ремонт стиральных машин в москве прайс
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: сервисные центры по ремонту техники в казани
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Your article challenges the status quo—in a good way!오피
Can I merely say what a relief to find somebody who in fact knows what theyre discussing online. You definitely know how to bring an issue to light and produce it critical. More people must ought to see this and understand why side in the story. I cant think youre not more popular because you undoubtedly contain the gift.
À quoi bon ne pas mentionner les vérités expliquées la semaine dernieres par le parti francais? Au minimum on serait capable de argumenter avec les véritables valeurs?
Your content is valid and informative in my personal opinion. You have really done a lot of research on this topic. Thanks for sharing it.
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники в ростове на дону
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники в перми
Профессиональный сервисный центр по ремонту игровых консолей Sony Playstation, Xbox, PSP Vita с выездом на дом по Москве.
Мы предлагаем: надежный сервис ремонта игровых консолей
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр по ремонту компьютерных видеокарт по Москве.
Мы предлагаем: цена ремонта видеокарты компьютера
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
This is a topic that needs more attention—thank you.오피
An interesting discussion will be worth comment. I believe that you simply write more on this topic, it will not often be a taboo subject but normally everyone is insufficient to chat on such topics. To the next. Cheers
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники
This is a terrific post. Thanks for making the effort to summarize this all out for us. It is a great help!
Hi blog owner, hope all is well. You mind sharing the name of your current theme? I would appreciate it much. Have a blessed afternoon. Check out mine AV
Профессиональный сервисный центр по ремонту игровых консолей Sony Playstation, Xbox, PSP Vita с выездом на дом по Москве.
Мы предлагаем: мастер по ремонту игровых консолей
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
pantaislot
I just could not depart your site prior to suggesting that I really enjoyed the standard info a person supply on your guests? Is gonna be again incessantly to inspect new posts
Having read this I thought it was really informative. I appreciate you spending some time and energy to put this article together. I once again find myself spending a significant amount of time both reading and leaving comments. But so what, it was still worthwhile.
obviously like your web site but you need to check the spelling on quite a few of your posts.
Several of them are rife with spelling issues and I find it very troublesome to inform the reality nevertheless I’ll certainly come back again.
Awesome blog! Do you have any tips for aspiring writers? I’m hoping to start my own site soon but I’m a little lost on everything. Would you advise starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m totally overwhelmed .. Any suggestions? Thanks!
very nice publish, i certainly love this website, carry on it
Профессиональный сервисный центр по ремонту компьютерных видеокарт по Москве.
Мы предлагаем: починить видеокарту
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
You produced some decent points there. I looked on the net with the issue and located most individuals is going together with along with your internet site.
I need to to thank you for this wonderful read!! I definitely enjoyed every little bit of it. I’ve got you book marked to check out new things you post…
manhwadesu
Undeniably imagine that which you stated. Your favourite reason appeared to be at the web the easiest thing to consider of. I say to you, I definitely get annoyed at the same time as people consider issues that they just don’t realize about. You managed to hit the nail upon the top and also defined out the whole thing with no need side-effects , other folks can take a signal. Will likely be again to get more. Thanks
You are so awesome! I don’t think I’ve truly read through a single thing like that before. So great to discover another person with a few genuine thoughts on this subject matter. Really.. many thanks for starting this up. This web site is something that’s needed on the internet, someone with some originality.
heavy window curtains would be much needed this december to conserve more heat**
The need for managing family issues through a professional organization like family office
is rapidly growing in India with various players such as banks, brokerage firms, asset management
firms gaining a foothold in the Indian family office space.
先述のような解決法を行っても経営改善が難しい場合、最後の手段として用いられるのが民事再生や会社更生です。 さらに、資金管理に活用できるキャッシュフロー改善チェックシート(無料)や、事業・債務超過は負債が資産を上回っている状態であるものの、手元に資金が残っているのであれば支払いは可能です。 その上で、負債が資産を上回っていないかをチェックすることで、実質的な債務超過に陥っているかどうかを確認することができます。
2. Materiality Assessments: Materiality assessments
help companies recognize and prioritize the sustainability issues
that are most relevant to their business operations
and stakeholders. 5. ESG Standards and Frameworks: ESG standards and frameworks provide a common language
and set of guidelines for reporting on various sustainability issues.
In fact, sustainability reporting can improve trust among stakeholders,
draw in financiers, and develop an responsible brand in the corporate world.
THE LIVE: 2020 ASTROLive on WWW. 29 November 2020. 2020年11月29日閲覧。 ミルクボーイ駒場、アイン稲田、四千頭身後藤「IPPONグランプリ」初出場
お笑いナタリー、2020年6月5日配信・
タカアンドトシが近藤春菜と若槻千夏を旅のお供に1700キロのバーチャルドライブ!初出場者なし”伊藤利尋アナ6年ぶりフロア担当復帰”.峯岸みなみ、柏木由紀が人生初キャンプ!
」と基本的にじゃじゃまるのかけ声だったが、後に『にこにこぷん』のキャラクターが一週間経つごとに交代していた。港湾模型:水を入れて波を起こし波の立つ外部と波のたたない港内の理想的な港湾を断面模型で説明。輝かしいパイロットファームの建設 – 根釧原野別海村のパイロットファームの開発をパノラマ模型で表現。水中作業:実物大の潜水夫模型とともに海底のパノラマを展示。泥炭とはどんなものか:泥炭の実物を層が見えるようガラスケースで展示。泥炭地の土地改良:電探地での農地開発を紹介。凍上対策:路床路盤の置き換え前後の土層断面をパネルで紹介、置き換え後は写真で紹介。
If you want to increase your experience simply keep visiting this web page and be updated with the latest news update
posted here.
hey there and thank you for your information I have
certainly picked up something new from right here. I did however expertise a
few technical points using this site, as I experienced
to reload the web site many times previous to I could
get it to load correctly. I had been wondering if your web host is OK?
Not that I’m complaining, but slow loading instances times will sometimes affect your placement in google and could damage your quality score if
ads and marketing with Adwords. Anyway I am adding this RSS to my e-mail and could look
out for much more of your respective exciting content. Ensure that you update
this again soon.
18時から神輿蔵出の儀が始まり、中御座は飾り付けをされない状態のまま南楼門の外に置かれ、他の神輿は舞殿に上げられて飾り付けが行われる。海外進出には言葉の壁もあるが、「そこは、もうギャルのノリで。飾りを解いた状態の中御座を夕刻四条大橋へ運び出して行う。途中本殿裏と本殿前に至った時にそれぞれ2礼2拍手1礼の参拝を行う。前日にある程度解体済みの曳山を立てたまま、大工が真松に足場等を取り付けて登って、真松を鋸で伐採する。富山市.
2009年8月2日時点のオリジナルよりアーカイブ。
出演者面での前身番組、1993年4月から9月にかけて放送。阿部亮平(Snow Man) – 2022年3月10日より出演。 2021年9月10日閲覧。 9月13日 オトナンサー/Yahoo!国民車構想の要件を満たすことは既存メーカーからは現実的ではないと考えられていた。中国イエズス会士によって、音訳語「基利斯督」およびその略語「基督」がつくられ、日本においても明治初年から、「基督」が当て字として新教系の刊行物(片仮名表記「キリスト」を採用した邦訳聖書を除く)で用いられ、明治中期までには一般的表記法として確立した。
活動内容は、『富士山めろんぱん』を食べることを目標にしながら、日本のメロンパンの消費活動に貢献すること。 ブロンソン』の日本語吹き替え版では、ブロンソンの「そっくりさん」俳優であるロバート・ ブロンジーの吹き替えを周夫に近づけた声色で担当した。 サン』のテレビ東京版では周夫がブロンソン、明夫が三船敏郎の吹き替えで共演した。
その後、2015年5月4日より父が長年演じていた『忍たま乱太郎』の山田先生(山田伝蔵)を引き継ぐことになった。
七海は宝塚退団後も俳優兼声優として活動している。海外ドラマの吹替においても、最初からアニメ声優を目指した声優を生み出し、声優に特化した芸能事務所や声優養成所の伸長に繋がっていた第二次声優ブーム以後も、前述のとおり1982年の海外ドラマ『遥かなる西部
わが町センテニアル』の吹替放や第三次声優ブーム期1996年『ER緊急救命室』吹き替え放送で劇団に所属する俳優の起用など、俳優が起用されるケースはいくつかみられた。
I have been exploring for a little bit for any high quality articles or blog posts on this kind of area . Exploring in Yahoo I finally stumbled upon this web site. Studying this information So i am happy to convey that I have a very excellent uncanny feeling I discovered exactly what I needed. I most definitely will make certain to don’t put out of your mind this web site and provides it a glance a relentless basis.
Music began playing as soon as I opened this site, so frustrating!
Thanks for the blog loaded with so many information. Stopping by your blog helped me to get what I was looking for.
“即席めん業界の世界市場シェアの分析”.胴体は人間で頭はナメクジ、髪の毛もある都市伝説。阪神電気鉄道・石塚とは恋人同士で互いに柔道でも切磋琢磨したりもした(男子で県有数の強豪選手である石塚の投げすらかわせるレベル)。戦場のヴァルキュリア2 ガリア王立士官学校(ローレンス・ ルパン三世 史上最大の頭脳戦(サイモン・
親しい知人もいなかった角兵衛は、家老の矢沢頼幸、小山田茂誠、出浦昌相、大熊秀行らの家に押しかけて、再仕官を願った。行き所のなくなった角兵衛は、老母を頼った。食事にも事欠くようになった角兵衛は、一日に二度三度、家老の家に出入りするようになった。翌年、母が死去すると、代官の報告で立ち退きを迫られた。母は50石の知行があった。時行の天下奪還のため、彼に武力や知力をはじめとする勝つためのすべてを教え込み、武士としての成長を促す。
2部を通しの撮って出し(いわゆる疑似生放送)で改めて放送した。
かつて放送したBS2、BSハイビジョンの時差放送も撮って出し形式で放送のため、リアルタイム字幕放送と同等のレベルもしくは一部修正して通常の収録番組と同じくラグなしで表示する字幕放送を行った。
かつてラジオ放送はNHK-FMで行なわれ、テレビ放送されてから数日空けて放送されていた。 “『HiGH&LOW THE MOVIE』4DX版日本映画史上、最高で最強のアクション体験!第37回(2005年)は当該日の8月13日がNHKプロ野球(巨人対阪神戦)を放送するため3日後の8月16日の火曜日に開催(19:30 – 22:00)となった。
Hello! I simply wish to make a huge thumbs up to the great information you’ve here for this post. I’ll be coming back to your website to get more detailed soon.
自分に積極的に接してくるモモのことは、本性を知っているため最初は拒絶していたが、その頃から彼女の能力は認めていた。洞察力も高く、ララの発明品でリトが女性化した際、女性化したリトの正体を一目で見抜いた。
Player 1989年6月号 NO.280 (1989年、プレイヤー・現在までに彼女のリトへの想いを知っているのは、(順番的に)芽亜、モモ、御門、ティアーユ、お静、美柑、リト、クロ、ネメシス、ナナの10人。 『ダークネス』では美柑から勧められたこともあり、彩南高校の1年B組に編入し、ナナ、モモ、芽亜と同級生になる。
この項目は、声優(ナレーターを含む)に関連した書きかけの項目です。 この項目は、俳優(男優・女優)に関連した書きかけの項目です。夜の学校で祐一と出会った、クールで謎めいた少女。 「松下電器産業株式会社が「パナソニック株式会社」に社名を変更」。真田 信之(さなだ のぶゆき)は、戦国時代から江戸時代前期の武将、大名。信濃上田藩の初代藩主、後に信濃松代藩の初代藩主。
I was pretty pleased to discover this site. I need to to thank you for ones time due to this fantastic read!! I definitely savored every bit of it and I have you book-marked to look at new stuff on your web site.
Nice post. I learn one thing tougher on different blogs everyday. It should at all times be stimulating to learn content from different writers and observe slightly something from their store. I’d desire to use some with the content on my weblog whether you don’t mind. Natually I’ll give you a link in your web blog. Thanks for sharing.
駿府の家康に方広寺梵鐘の鐘銘の件につき弁解に行くが、家康に面会に行くが、本多正純に浪人招集の件を問われる。片桐且元が方広寺鐘銘事件で駿府に面会に行った際、家康との面会が叶わなかったため、あせった淀君が大蔵局とともに使者として派遣する。大坂城内で片桐且元暗殺計画があることを且元に告げる。 そして大坂に戻った後も登城を逡巡していたが、意を決して登城し淀君に対面したがその場で淀君や大野修理にその態度を責められ織田常真に大坂城中で且元の暗殺計画があることを告げられ大坂城内の屋敷に立てこもる。
I simply must tell you that you have written an excellent and unique article that I really enjoyed reading. I’m fascinated by how well you laid out your material and presented your views. Thank you.
You have noted very interesting points ! ps nice internet site .
Профессиональный сервисный центр по ремонту фото техники от зеркальных до цифровых фотоаппаратов.
Мы предлагаем: ремонт проекторов с гарантией
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
『2021年3月16日(火)交通系ICカードの全国相互利用サービスへの対応を開始します (PDF)』(プレスリリース)(日本語)、山陽バス、2021年2月1日。 2013年3月23日からの「全国相互利用サービス」開始にあわせて久々のテレビCMが放映され、立体アニメーションでのイコちゃんが登場した。零細メーカーは戦時体制下の統制でほぼ淘汰されたが、戦前からの三大大手メーカーに加え、終戦で市場を失った航空機産業からの転入企業(中日本重工業・
が武器で、その相手を悪魔の太鼓の音で操る。喉を渇かせる特殊音波と全身の灼熱化、指先からの小型ミサイルが武器。夜叉岩にキャンプをはった刃牙を助けに行った際、夜叉猿から襲撃を受け右手の指4本を食い千切られ、さらに腸を掴み出される重傷を負う。校内で毎度、盗撮で女子生徒の更衣室を覗いたり、下着を撮ろうとするが、そのたびに花梨に制裁を食らわされている。荒巻とのいざこざの末にアキが離脱しベロニカが加入後、荒巻が本腰を入れたことにより人気が上昇する。
横浜国際女子駅伝 – 特別協賛・国際通り⇔北谷」、「恩納村リゾートエリア⇔北谷」直行シャトルバス実証運行ならびに交通系IC決済導入のお知らせ ~交通系IC決済でバスに乗って気軽に美浜アメリカンビレッジ(北谷町)へ~』(プレスリリース)東京バス・
12日)は前週末比77%の840万ドルとなった。
5日)は前週末比112%の1080万ドルとなり、この日までの総興行収入は2800万ドルとなった。
ベイビー』が首位となり、2週目も2位となったが、またも興行収入では『ボス・
29日)興行収入は930万ドル(メキシコ・景気刺激策という観点では、余暇を楽しむ選択をした人々がさまざまな財を購入してくれる場合に、その効果は高いという意見がある。
その後に天下人となった豊臣秀吉亡き後に起きた関ヶ原の戦い(慶長5年)で西軍についた真田昌幸は、連動する第二次上田合戦でも東軍別動隊の徳川秀忠軍をよく防いだ。本戦で西軍が敗れたため、昌幸は紀伊国の九度山に配流され、翌1601年に上田城は徳川軍に破却され、堀も埋められた。昌幸の嫡子である真田信之は関ヶ原の戦いで東軍についたため、上田など真田領を安堵されたが、上田城が破却されていたため元々の居城である上野国沼田城を本城とし、上田城三の丸跡地に屋敷を構えて統治を行った。
夏の陣の決戦の際には大助や大野修理が秀頼の出馬を求めるが、「家臣に任せておけばよい」と、その意見を退けた。夏の陣の決戦前日には秀頼の出撃を主張する幸村の意見を聞き、約束をした。
「関東勢が布陣した後、一度の戦いで決着をつけるべき」と幸村が述べると、淀君は「一度の決戦で決着をつけるのは危うい」とそれに反対する重成の意見を支持した。大坂冬の陣の前の軍議では幸村らは出撃策を唱えたが籠城策をとり、真田丸の戦いなどで豊臣家は善戦したものの徳川方と和議を結ぶ。
つづら殿に居るすそはらいたちは各土地専任のすそはらいとは異なり、複数人でチームを組んで怪異討伐に当たる。 つづら殿に持ち込まれた怪異討伐の依頼の中でも難易度が高い割に緊急度が低く、棚上げされたまま放置されている依頼。通常はそれぞれの土地神一柱につき、すそはらいを任されるつぐもも使いはひとつの土地で一人だけ(上岡では一也、その隣の小宮ではすなお)だが、すなおのように緊急措置で他の土地でサポートに回ることもある。地方によっては、「留守参り」をするところもある。 これは土地神の支配地という「ホーム」ではなく怪異たちの棲み処、すなわち「アウェイ」で戦うことも関係している。立命館大学には、新歓運動や学園祭などの全学行事の他、新入生支援等の互助活動や大学との交渉を前提とした要求実現運動といった自治活動などを統括する組織「立命館大学学友会」がある。
1945年 – ドイツのニュルンベルクで第二次世界大戦の戦犯を裁く国際軍事裁判(ニュルンベルク裁判)が始まる。 1934年
– 辻政信らの働きかけで、皇道派の村中孝次大尉・ 1917年 – 第一次世界大戦:
カンブレーの戦いはじまる。 1917年 – ウクライナ初の近代国家となるウクライナ人民共和国が独立を宣言。 1937年
– 国民政府(蔣介石政権)が南京から重慶への遷都を宣言。 2011年5月1日開催の第143回天皇賞(春)はNHK総合にて放送が予定されていたが、国会中継(第177回国会 参議院予算委員会 平成23年度第1次補正予算案総括質疑 当時国会にて東日本大震災関連の補正予算の早期成立のため、予算委員会審議を休日及び大型連休返上で実施していた)の放送が決まり、国会中継放送中の通常番組のサブチャンネルへの迂回放送も、政治的公平性の確保を定めた放送法4条一項への抵触の懸念から協会の方針で禁止されている為、放送中止。
Thank you for sharing your expertise with us.오피
女子メンタルで朝日奈央が着用した「MEGAアゴ 猿男」のマスクが、放送終了後すぐに売り切れとなった。 1989年7月27日 – 恐怖蚊取り線香男 〜めざせ!
2021年1月27日、シーズン9にDocumentary of Documental シーズン2の優勝者である、とろサーモン・ J-CASTトレンド
(2021年3月1日). 2021年3月2日閲覧。 2021年6月19日にフジテレビ『土曜プレミアム』枠の『まっちゃんねる』内にて放送。放送したのはこれが初めてとなった。また、見届け人として松本のほか、本家の常連出演者である芸人達が出演した。
黒田基樹『小田原合戦と北条氏』吉川弘文館〈敗者の日本史〉、2012年、64-65頁。 1334年春、清原信濃守の暴虐に激怒し、勝ち目がないと理解しながらも、武士としての意地を貫き通すため討死覚悟で挙兵する。 「藤原氏(兼通流)本多」『寛政重修諸家譜』 第4輯、國民圖書、1923年、632-634頁。
後付け設定ではあるが、天魔大帝の分身の一つであることが判明する。漫画版では赤流火穏で発見された輝羅鋼の獅子を詳しく調べる為、天宮に赴いたことになっている。本作で唯一、一人称が「僕」のキャラクター。実年齢としては本作の登場人物の中で下の部類に入るが、父・初登場は2年のインターハイの県予選(女子個人戦)。
パンパンが麺生地に秘孔「一度食べたらヤミツキ」を突いて製麺する事でヤミツキ成分を生み出しているが、同時に副作用のムシャクシャ成分も生まれるため、凶暴化の原因となっている。麺生地を一瞬で製麺することの出来る秘孔。対象が食べ物など、生物以外でも有効。本作では、顔や体型は原作や過去のシリーズと同様だが妖怪画と同じ着物姿をしている。同作品には小学生が十数人ほど出演していたが、その出演者の中に劇団こまどりに所属していた当時子役だった熊谷誠二がおり、岩田がロケの間、事あるごとに熊谷に「面白いね、面白いね」と言っていると、熊谷から「じゃあ、うちの劇団に来れば?
200キロのバーベルを軽々と持ち上げる怪力無双の巨体を持ったディフェンダー。 ところが、映児がサイコメトリーで読み取った自分の心理を、その能力で読み取ってしまう。 そのショックで発狂し、自らの身体を切り刻み倒れ(映児曰く自分自身を料理してしまう)、逮捕される。 しかし、システムの恩恵が得られてから1000年が経過し、電波を中継する「バルーン」の殆どが故障し、システムは崩壊の危機にあった。 “北電また「やらせ」…ご意見聴く会へ賛成要請”.
1906年 – ヴァルター・ 1906年 – エルンスト・
消費税法で、一般方式においては、法律上の課税とされる売上取引の国税分(6.3%)から、貸倒にかかる消費税額と、課税とされる仕入取引の国税分(6.3%)を差し引き、国税の消費税を計算して、地方税はその17/63(1.7%部分)を計算して、総額を算出する。 ノリが軽く負けん気が強い性格で、時行とは友人のような関係を築く。進撃の巨人ラジオ ~梶と下野の進め!
森川智之のBRAVE10 on the radio」公開録音&第1話上映会』のトークパートダイジェスト映像が収録されている。森川智之の
BRAVE10 on the radio』は、2011年12月から超!第2巻には2011年12月30日に両国KFCホールで開催された『「柿原徹也・ 『柿原徹也・ “番組紹介:柿原徹也・
Cool blog! Is your theme custom made or did you download
it from somewhere? A design like yours with a few simple tweeks would really make my blog stand out.
Please let me know where you got your theme.
Thanks a lot
作中世界の火星に存在する架空の物質「スペシウム」を弱点としている。 「宇宙の平和を乱す、悪魔のような怪獣」として恐れられている狂暴な性質の宇宙怪獣。 ウルトラマンによって宇宙の墓場へ護送される途中で逃走して地球に飛来し、竜ヶ森湖の湖底に潜伏して長旅の疲れを癒していた。放送当時に連載されていた一峰大二の漫画版『ウルトラマン』では、レッドキングやマグラーと共闘し、翼で強風を起こす能力を中心に描かれている。
吉本興業所属のお笑い芸人松本人志の性加害疑惑の際には「被害者女性がすぐに警察に駆け込まなかったことを責めるべきではない」「人はみな自分を一番守る権利を持っており、松本が今後これを笑いに変えることができれば、それこそが松本自身を救うこととなる」と発言した。 そのため、反抗した孝弘に関心を持ち「下僕128号」にしようとする。 『妖怪千物語』では毛目玉に坊主頭の少年を騙させ、人々の髪の毛を奪いそれをエネルギー源にして、人間界征服を企むが、少年に鏡を壊されて力を失う。
世界銀行の『ビジネス環境の現状』の報告書では、シンガポールは9年連続で世界で最もビジネス展開に良い国(英語)に選定された。魔界からやってきた会話の出来るプレーリードッグ・ 「温かい番組に出来れば」”. “木村佳乃、紅白司会に意欲 「思い出のメロディー」で音楽番組の司会初挑戦”. “高畑充希、夏の”紅白”で初司会 思い出のメロディー』8・
仏教において、釈迦牟尼仏の次に現われる未来仏であり、大乗仏教では菩薩の一尊。紀元前5世紀前後の北インドに実在した人物で、仏教の開祖。事前の利用登録が必要。作中では生前人間から極楽の住人になった存在として登場し、天使長であったサタンとも縁があったようにも描かれる。目玉おやじたちの祈りで姿を現すが、人間が驕り高ぶり牛鬼を復活させたことから自分にはもう助ける義理は無いと頑なに拒否し、周りの重力を変え重くし押し潰される前にさっさと立ち去るよう忠告した。現在で復活したサタンに「ユニコンの鏡」を奪われ太陽が消滅する太陽消失事件を起こされてしまうが、鬼太郎一行の活躍によって無事鏡が戻り、失われていた太陽の輝きを復活させた。
第2部では「Case11:黒い山羊」では容疑者の一人として登場し、借金取りに追われて行方不明となっている。食べた人に寄生し、寄生された人は自ら土に潜って新たな焼き芋虫の肥料になる。芋虫の形をした焼き芋の都市伝説。頭が餅になっている男の都市伝説。頭が人の顔になっているミミズの都市伝説。胴体が人の頭になっているムカデの都市伝説。足が人の頭になっているクモの都市伝説。目が5つあり、全体が白と青色の起き上がりこぼしの都市伝説。
「鬼太郎マガジン VOL.1」によればもめんやは当初一反木綿の店という設定だったが、放送が進むたびに「一反木綿の呑気な性格は経営に向いてないのでは」という意見が出て急遽スタッフが布に関する妖怪を探すことになり、絹狸が選ばれた。第5作38話初登場。第3作では第27話登場。声 – 内海賢二(第1作)、はせさん治(第3作)、大塚周夫(第4・
【竹原駅】 – (芸陽バス) – 【三原駅】 – (トモテツバス三原福地線) – 【登山口】 –
(おのみちバス) – 【尾道駅】 – (おのみちバス) –
【川尻池下】 – (因島大橋を徒歩) –
【大橋入口】 – (因の島バス) – 【瀬戸の浜】 – (生口橋徒歩) – 【生口橋入口】 – (本四バス開発) – 【瀬戸田港】 –
(本四バス開発) – 【多々羅大橋歩行者道入口
※フリー乗降】 – (多々羅大橋を徒歩) – 【上浦芸術会館】 – (瀬戸内海交通) – 【出口】 – (大三島橋を徒歩) –
【枝越】 – (伯方島島内および伯方・
大分県の県庁所在地で、中核市に指定されている。近年、大分駅付近の連続立体交差事業および区画整理事業に伴い、大友氏館跡をはじめとする中世から戦国時代にかけての府内の遺跡が発掘され、2001年(平成13年)には大友氏館跡として国の史跡に指定されている。室町時代に入ると、第7代当主大友氏泰は、拠城をわずかに北にずらして大分川河口付近に館を構えた(現在の市の中心部の東側で、顕徳町などにあたる)。
で放送されるほか、『土曜スペシャル』をテレビ東京と通常時同時ネットしていない、名阪地区の独立局の一部あるいは4大系列局のいずれかで放送される県もある(回により放送される系列が変わることがある)。惑星同士の通過・ 1818年 – 金星が木星面を通過する。開局50周年記念出版「横浜の”ロック”ステーション TVKの挑戦」11/26(金)に刊行決定!
1777年 – プリンストンの戦い: アメリカ独立戦争で大陸軍がイギリス軍に勝利。
Truly when someone doesn’t know after that its up to other users that
they will assist, so here it occurs.
井上は「(柴が起案し、岡が承認した訓電案を)自分が加筆修正して軍務局につき返しますからご承知下さい」と及川に言った。乗越分岐器および安全側線が設置されている駅はなく、列車行き違い時の上下列車の駅構内同時進入ができない。井上は、自分が修正した訓電がそのまま発電されたものと死ぬまで考えていたようである。原田泰は「財政赤字を増税によって賄おうという議論はいいが、増税分を社会保障に回すとの考えは根本的に間違っている。翌2日の御前会議で決まった後の7月3日に省部臨時局部長会報(決定事項を知らせるための会議)で、沢本次官から「南部仏印進駐が閣議で決定した」と知らされた井上は「航空戦備は全く出来ていない。
新潟放送)、信越放送、中部日本放送(現・南部・宇都宮・ 「CASE FINAL」の冒頭のロシア人娼婦殺しを担当し、被害者が志摩が立花に送った自分の名前が彫られたたペンダントを持っていたため、志摩に事情を聞きに来る。 『プリキュアシリーズ』は県内未放送(但し、劇場版の事前番組はチューリップテレビで放送)。
小早川秀秋らの諸将が大坂に参集した。 1600年9月15日早朝、合戦の火蓋が切られる。 やがて朝鮮の役に従軍していた諸将たちが帰国、武断派の筆頭であった福島正則、加藤清正らと三成と親しい小西行長らの反目も始まる。鳥居彦右衛門の守る伏見城を落とした西軍と東国から転進して西に向かう東軍が関ヶ原で相まみえた。激怒した家康は諸将を集めて上杉征伐を宣言し、大軍を率いて東国に下った。
Thanks. I really like your site. Great points you make in your post.
wonderful put up, very informative. I ponder why the other experts of this sector do not realize this. You should continue your writing. I’m sure, you’ve a great readers’ base already!
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники
It’s hard to find knowledgeable people on this topic, but you sound like you know what you’re talking about! Thanks
田畑真紀(リレハンメル・小田卓朗(ピョンチャン・大菅小百合(ソルトレイクシティ・仁と三島財閥の暴挙を止められなかったことを悔い、今度こそ三島の血を滅ぼすため第6回大会に参戦した。杉森輝大(トリノ・長島圭一郎(トリノ・
歳月が経過したためか、一人称が「俺」から「私」に変わった。一度は彼女になってみたい!
シドと一緒に魔女とその能力にかけられた生徒を監視している。 “OCTPATH高橋わたる「彫刻になりました」栗田航兵も絶賛の魅力に迫る<インタビュー連載>”.山田竜は、学園きっての問題児で不良少年。 『TL』『ダークネス』共に1コマしか登場しないことが多く、セリフもほとんどなかったが、『ダークネス事件』後は、レンの友人になったこともあり、出番も順調に増えつつある。漫画版では、最終話にて登場。
しかし、2012年7月から2015年4月にかけて、2012年4月から在留資格の外国人に条件付きで住民票を交付できるよう法律(住民基本台帳法の一部を改正する法律)が制定されたことを市の複数の職員が在留資格の外国人が国民健康保険への加入も可能になったと勘違いを原因にがんや脳梗塞などの治療・
連合艦隊参謀長の宇垣纏は、日誌「戦藻録」の1942年(昭和17年)5月8日の項に『4F(第四艦隊)の作戦指導は全般的に不適切であった。実体がないため攻撃が一切通用しない。薬の副作用で超能力を得る代わりに人間の血を吸わなければ生きていけなくなり、新鮮な血液を手に入れるために子供を誘拐し続けていたが、鬼太郎によって倒される。 2008年(平成20年)10月1日には、大阪市浪速区の個室ビデオ店で利用客の放火により25名が死傷する大阪個室ビデオ店放火事件が発生した。
ホリプロの寮時代では井森美幸と同部屋でよくおしゃべりをしており、寮の管理人に「おまえたち、犬が騒いでるみたいだぞ」と𠮟られたことがある。倉田大誠(フジテレビアナウンス室副部長、2022年12月25日・ 2008年9月25日には、PS2 BEST版として『BEST HIT セレクション
シークレット オブ エヴァンゲリオン』が発売された。好意を寄せていたミシェールとの特殊勝利ポーズでは嬉しそうに見つめ合っているが、ジュリア(ジェイシー)との特殊勝利ポーズでは彼女に飛びかかろうとして地面に叩き伏せられている。初登場時でどんぶりまんトリオにおいしさを伝授していたが、『カツドンマンとにんにくこぞう』ではお互いに存在を忘れ、初対面のごとく自己紹介をしていた。
」、東京・小宮山悟、東京都立井草高校で田中と同級生だった実業家・騒動の発生時は地下の世界で10年間の眠りの最中であったが、自分が眠っている間に無茶をした空狐を止めるために姿を現した。念力の他空狐や他の狐たちが引き起こした大規模な騒動(デパートや客の紛失)を容易く元に戻す力も持つ。
振り返りクイズ」(2014年9月28日)には、解答者としてウエストランドが出演した。 また、詳しい人物として「にっかつロマンポルノ」特集(2015年7月26日)にビビる大木、「DJ」特集(2015年10月19日)にはふかわりょうが出演した。 『新型コロナウイルス感染拡大に伴う「スカイバス東京/スカイダック」運休についてのご連絡』(PDF)(プレスリリース)日の丸自動車興業、2021年4月23日。中国の木材消費量増加に伴う需給の逼迫に、重油価格高騰による輸送コストの増大が重なり、輸入材の価格が上昇し、相対的に競争力を強めた国産材の需要が増加した。 たとえば税理士の湖東京至(元関東学院大学法科大学院教授)は平成18年度予算を元に、消費税全体の税収が地方消費税を入れて5%で計算すると約13兆円。
生駒隊隊員。銀座三越店(東京都中央区) – 銀座三越の地下4階の従業員休憩室にある(関係者以外利用不可)。 “デザートで桐島りらが再びバンドマン×JK描く新連載、岩下慶子の新作も登場”.入部直後に長髪を切り、赤髪こそやめたものの金髪のままでいたため、遅刻した巧と杉の代わりに出場したインターハイ県予選では、選手登録の際に「仲安・
このことが、豊臣方が徳川との取次役を一方的に処断したとして、幕府による大坂攻めにつながることになる。 その後は家康の傘下に入るが、今までの豊臣の対する忠義を労われるなど、且元の性格や不遇な現状を見越した家康の慰撫や口車に乗せられて、豊臣家の重要機密を明かしてしまう。 しかしこのときの態度を危惧した家康の意向により、正信の指示を受けた二代目・
ミニカに至っては販売台数の3/4がバンという状態にまで至り、途中でバンのみの設定にしたほどである。 1932年(昭和7年)-
「ドリュウ(ドルックス)化粧品」発売。中島とよく行動を共にしており、中島の妄想による暴走を止めるポジションにいるため、実質的にV・兄に対する態度はぞんざいだが、基本的には礼儀正しい。年齢は80を超えているが料理人としては健在で、肌は浅黒く腕も筋骨隆々であり中華鍋を一度に2つ振れるほどの剛腕の持ち主。
北大阪電機の社長。全国大会予選(団体戦)での藤岡西高校の対戦相手。 2031年の同窓会
㊙︎変化に一同驚愕!別所の湯で摂津の百姓徳之助と出会い佐助の死を知る。松代移封の際には信之に同道せず、別所で亡き人の冥福を祈る人生を選択する(原作では信之に従い、松代に移る)。馬場彦四郎に別所の湯で襲われるが反撃し、村娘を犯そうとした彦四郎を失神させて木に縛りつけ、その素性を知る。
「瓦版屋の牧作(まきさく)」という子どもに扮した安井が、ニュースや街の衆(リスナー)からの怒りの訴えを紹介する。保里は降板後の同年4月4日から、井上は平日夕方に関東地方で放送されているローカルニュース番組『首都圏ネットワーク』のメインキャスターに就任した一方、保里は同年4月から水戸放送局に異動となり、平日夕方に茨城県で放送されているローカルニュース番組『いば6』のキャスターに就任した。 2023年12月20日の放送30周年年末拡大スペシャルでは、1993年4月の番組開始から23年間に渡ってキャスターを務めた国谷裕子がゲストとして出演した。 2016年(平成28年)3月17日をもって、1993年4月の番組開始以来23年間に渡ってキャスターを務めた国谷裕子が降板。
Hi, I just discovered your web site via Bing. Your viewpoint is truly relevant to my life right now, and I’m really happy I discovered your website.
My wife and i ended up being absolutely delighted Louis managed to carry out his research with the precious recommendations he discovered while using the web page. It is now and again perplexing just to choose to be giving for free methods which often most people have been selling. We understand we need the writer to thank for that. Those explanations you made, the simple site menu, the relationships you will help to foster – it is mostly exceptional, and it’s really aiding our son in addition to the family do think that issue is entertaining, which is extremely important. Many thanks for all!
Hello my friend! I want to say that this post is amazing, great written and include almost all important infos. I?d like to look more posts like this .
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: сервис центры бытовой техники красноярск
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
The very next time I read a blog, I hope that it doesn’t disappoint me as much as this particular one. After all, I know it was my choice to read, however I really thought you would probably have something interesting to say. All I hear is a bunch of crying about something that you can fix if you were not too busy seeking attention.
Если вы искали где отремонтировать сломаную технику, обратите внимание – сервис центр в волгограде
blockaway
This is a topic that’s close to my heart… Take care! Where are your contact details though?
This discussion is long overdue—thanks for starting it.오피
このコンテンツが公開されたのは、 2018/03/22 スイスの時計産業は近年、フラン高や輸出状況の悪化にあえいできた。 このコーナーとは無関係だが、『徳光のTVコロンブス』(テレビ東京系)には「勝手に表彰状」というコーナーがあった。 なお、青森放送と山口放送はテレビ朝日系新局(青森朝日放送・ 」となった(ちなみにこの日の放送で1992年の年内最終放送日だった)。内容変更、スカパー!
1990年4月 – 1992年3月、火曜 – 土曜未明(平日深夜)のプロ野球ニュース終了直後の0:30 – 0:40枠で放送。
輪廻のラグランジェ|公式サイト. “コンサドーレのカーリングチーム発足 北京五輪目標”.
“コンサドーレ北海道が男子カーリングチーム設立 22年北京五輪目指す/北海道”.
毎日新聞. “カーリング 日本選手権 男子、コンサ初V 堅実な攻守で圧倒「世界の舞台で力発揮」 /北海道”.
その後、271号は宇宙線研究所の屋上でムラマツたちにミクロ化器を突きつけて追い詰めるが、足を滑らせて屋上から落下した彼らはウルトラマンに救助される。喰種研究家の小倉が副幹事を務めており、喰種に対する医療チームも存在する。
we have different sectional sofas at home, i find them very comfortable and easy to setup’
【長浜駅】 – (湖国バス近江長岡線) – 【近江長岡駅】
– (徒歩約7.7km) – 【真宗寺(消防団車庫)前】 – (関ケ原町ふれあいバス今須コース) – 【JR関ケ原駅(駅西側)/関ケ原駅】 – (名阪近鉄バス関ケ原多良線) – 【牧田(上野)】 – (名阪近鉄バス大垣多良線) – 【大垣駅前】 – (名阪近鉄バス海津線)
– 【海津市役所】 – (海津市コミュニティバス南幹線) – 【松山グリーンハイツ】 – (徒歩約3.2km) –
【多度駅前(桑名市コミュニティバス・
今では大抵の事は言えるようになり、どちらかと言えば喜怒哀楽の激しい性格となった。資産格差の是正を目的に相続・他団体からベルトを狙う挑戦者が現れた場合、門番的な役割としてシングルマッチを行っていたが、その大半にあっけなく敗れ去っている。娘の小学校に、愛犬(すこし)の散歩をしていた際に学校関係者から不審者扱いされ、その日小学校は「不審者が出た」という理由で集団下校させている。 「テレビ局ネットワーク」『アニメディア』1995年4月号、学研、117頁。 「関西本線 新鹿瀬山隧道完成 大阪工事事務所 17日切替工事終了」『交通新聞』交通協力会、1956年11月18日、2面。
“『ベストマザー賞2024』丸山桂里奈、優木まおみら受賞 pecoは受賞聞き「うれしくて涙を」”.
ボーダーの合宿場、キャンプ場、廃遊園地、プール、採掘場跡など様々な施設を有する観光都市。 “相葉雅紀MC『I LOVE みんなのどうぶつ園』 番組ファミリーに那須雄登、藤岡弘、家族ら”.極度のドジでもあり、図書室の本棚を倒したり、紅茶の茶葉をぶちまけたりしたことがある。年に一度の縁日は、夜店などでにぎわう。日本サッカー協会.
明け渡しに立ち会った家康の重臣大久保忠世が城内に入ると、そこはきちんと清掃され、整然としていた。 さらに籠城を続ける内に織田軍の攻撃で武田勝頼が自害し、その一族である穴山梅雪より開城を勧める書簡を受けてから、ようやく城を大久保忠世に引き渡している。第31話「地下水道の銃撃戦!映画第1作、第2作と共にジャムおじさんの知らせでアンパンマンを助けるなど活躍していた。開城後、家康より召抱えの要請を受けるが、「お館様(勝頼)の安否の詳細が判明されない限りは仰せに従いかねる」と答えて謝絶した。
アペデマス五戦士の一人、別名「風神」。初登場は少年マガジンの特集記事「大妖怪ショッキング画報」。阿久津はアメリカ国立公文書記録管理局を訪問し、摺鉢山付近に日本兵の集合埋葬地があることなどの記録を確認。幾度もターちゃんを圧倒してきたが、最終決戦で大地の怒り(ヌーの大群をはじめとする動物たちによる無限に近い動物パワー)に触れて敗れた。誰かが弱音を吐いても「諦めてはいけない」と最後まで励まし続け、自らもまたその信念で行動するとても芯の強い人物でもある。 10年後の後日談では副業で神父をやっており、山田とうららの結婚式の神父を務めた。
武器はクナイを片手に持つように変更された。基本的には徒手空拳(ターちゃん流格闘術)で戦うが、場合により吹き矢やブーメランなどの武器を使用することもある。 この超人的な柔軟性を生かした「フニフニ避け」(ふにふによけ)という、ほとんど立ち位置から動くことなく体をくねらせるだけで相手の攻撃を1・ それでも動物を殺す行為の手助けは間接的でも嫌な様子で、フィッシングを趣味とする観光客のガイドを断ったことはあった。
瑞沢かるた部夏合宿! (裁判)2月20日 –
エジプトで、2012年に発生したプロサッカーの試合でのサポーター衝突事件において、計画的に相手チームサポーターを殺害した10名に死刑判決。出産手当金は原則として任意継続被保険者には支給されないが、上記の要件を満たす者が任意継続被保険者となった場合には支給される。児童小説「水木しげるのお化け教室」では海ゆうれいと呼称される。瀬戸麻沙美、宮野真守、細谷佳正も歓喜(コメントあり)”. “ちはやふる:あわら市で5度目のファンイベント 3期の新OP&ED初披露に瀬戸麻沙美、細谷佳正、入野自由の生アフレコも”. MANTANWEB.
We’re a bunch of volunteers and starting a brand new scheme
in our community. Your site provided us with
helpful info to work on. You have performed an impressive
job and our entire group will be grateful to you.
対象者は、65歳以上74歳以下の公的年金受給者で、1つの対象年金が年額18万円(月額1万5000円)以上で、世帯主であることなどが条件である。今の民主党では落第点。信長の忍び – 第3期は未放送。長身で体格が良く、基本的に仏頂面で武骨な性格。好戦的な性格だが、他のメンバーと違って近界民に対しては恨みを持っていない。
労働条件の変更により、一時的に労働時間が週20時間未満となっても、週20時間以上に復帰する前提であれば、被保険者資格を喪失しない。鬼太郎との交渉の末稲荷神社に油揚げを絶やさない条件で工事を許可した。 “みずほ銀頭取交代を取り消し システム障害で、第三者委設置-坂井社長謝罪”.新のバイト先店長。新潟の景浦家・新の隣家の少女。新が名人を目指して戦っていることは知っているが、競技かるた界での人間関係などについては全く把握しておらず、新が千早に告白したことなども知らない。
メディアワークス〈電撃文庫〉、2009年8月10日。 コミックナタリー.
ナターシャ (2015年8月24日). 2024年6月30日閲覧。 コミックナタリー.
ナターシャ (2014年7月24日). 2024年7月9日閲覧。 ナターシャ (2014年5月24日).
2024年7月9日閲覧。 コミックナタリー.
ナターシャ (2018年5月24日). 2024年4月24日閲覧。
コミックナタリー. ナターシャ (2019年5月24日).
2024年4月24日閲覧。 コミックナタリー.
ナターシャ (2017年10月24日). 2024年4月24日閲覧。 コミックナタリー.
ナターシャ (2017年2月24日). 2024年6月30日閲覧。 コミックナタリー.
ナターシャ (2016年4月23日). 2024年6月30日閲覧。
これによって映児の親友かつ理解者として、現在にも関係が続いている。現在も同じ高校に通い、彼とは対照的な知的で博識な青年で、学校成績一位という優等生でもある。 また未成年者からオバサンと呼ばれたり、峰や羽根山からパワハラ、セクハラを受けたりするとコミカルな反応を見せる。 と「岡山・広島・ ドラマ1期ではプロファイリング能力に優れるが、「拳銃を紛失する」「他の刑事にパシリにされる」といった駄目刑事となっている。警視庁捜査一課の敏腕美人刑事。 7人はJR東海の窓口内にある処理機でICOCAの入場記録を消去して近鉄線運賃を支払わなかったが、JR東海が処理機を調査し不正が発覚した。
Sweet web site , super layout, very clean and employ genial .
三重県県土整備部”三重県の道路/県管理道路一覧”(2013年1月24日閲覧。固定資産税の過誤は、土地よりも建物(地方税法上の用語では「家屋」)が最大の問題であり、報道されている事例等は、産業界の事例が中心である。 ハンサムに狙われていたトリックスターのアンナも本項アンナではなく妹の一人であり、当人達はワールドマップ上に出現する行商人(クラスは商人)、外伝や追加マップのNPCを含めて誰が姉で妹なのかを全て把握しており間違えることはないが、クロム達には全く見分けることが出来ない。外務省.
2020年8月30日閲覧。
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: сервисные центры в красноярске
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
同時代の史料では確認できないものの、『三河後風土記』や『武徳編年集成』にはこの時家康が「朝日姫が家康の子を産んでも嫡子とはしないこと」・徳川 秀忠(とくがわ ひでただ)は、安土桃山時代から江戸時代にかけての武将。秀忠が誕生してから5ヶ月後に長兄・
If some one wants expert view on the topic of running a
blog then i advise him/her to go to see this webpage, Keep up the pleasant work.
楽しいムーミン一家(1995年頃から96年末まで再放送。 ミュージックステーション※(ネット開始以前はBBTにて放送されていた。
がんばれゴンベ(再放送。 』(不定期放送)の新春特番『UTAGE!
ド短期ツメコミ教育 豪腕!製作者たち(番組スタッフ)の間では、「デジタルという感じではなく、ちゃんと豊かな生命があるということを意識して設定する」のが方針だったため、自然や生命豊かな世界となった。 にっぽん菜発見 そうだ、自然に帰ろう→冒険JAPAN!
1932年(昭和7年)10月1日、軍令部出仕兼海軍省出仕、軍務局第一課勤務。 ソ連出身の水の精。
“慶長グランド・ロマン 『野風の笛』”.久我長通1352-1352?朝日新聞デジタル (2020年12月28日).
2022年11月25日閲覧。山本博文 著、日本歴史学会
編『徳川秀忠』(新装版)吉川弘文館〈人物叢書303〉、2020年2月26日。南洋のオイリス島に繁殖する食肉植物ミロガンダが、品種改良のために植物学者の山田博士が照射したガンマ線の影響で、幼年期の姿への退行を経て突然変異を起こして狂暴化し、動物の要素を併せ持ったことによって自らの意思で移動できるようになったもの。
『仮面ライダーV3』(かめんライダーブイスリー)は、1973年2月17日から1974年2月9日まで、NET系列で毎週土曜19時30分から20時(JST)に全52話が放送された、毎日放送・放送38年目を迎えた『パネルクイズ アタック25』が大リニューアル、スタジオセットや内容等を一新(基本ルール等は変更なし)。
慶應義塾大学法学部法律学科卒業。学業成績はあまり芳しくなく、また作中で自分の誕生日を忘れているなど、頭脳はあまり優秀とは言いがたい。 イベント絵にはローブのようなアウターを着ている厚着姿(脱いだ半袖姿もあり)、タオルを肩にかけた見せブラ姿の薄着などがあり、有料DLCの「絆の夏」配信版では劇中と同じ浮き輪を持ったビキニの黄色い水着姿、同「絆の秘湯」版では青いヘアカラーで、上述と同じクマ人形が付いた紐でポニーテールをまとめた浴衣姿だった。
ヴィザとヒュースとの戦いでは、敵の狙いが千佳だとわかったことと、事前に迅から大規模侵攻に関わる予知を聞いていたことによって、修と京介にC級連れて基地に撤退するように指示した後、南西部市街地に侵攻して来たトリオン兵を小南に倒すよう指示をし、自身はヒュースとヴィザを相手に、時間を稼ぐ目的で持久戦を展開する。
しかし実際にはターボファンエンジンの高性能化もあり、エンジン停止に起因する重大事故が見られなかったため、ダイヤモンド・
中盤で敵襲を受けたクロムを「お父様」と思わず呼んでしまったことで、自らの正体と目的を明かし、以後はクロムらに同行する。海田市駐屯地店(広島県安芸郡海田町)- 陸上自衛隊海田市駐屯地内。 リカによって山田たちと魔女に関する記憶を失うが、同じく記憶を失って暴走したノアを止めてもらえるよう山田たちに依頼した。 その後はクランチュラが八太三郎から邪面獣ジイシキジェルガを生み出す際に悪用した。
ロングボウ系といった、弓が使用できる。近づいた者の深層意識を引用した幻覚を見せ、囚われさせてしまう。
その他、当時衆院選活動中でプロレス復帰が流動的だった馳浩も、結果的に全日本に残留している。次の各号の一に該当する者は、30万円以下の罰金に処する(第41条)。第34条2項の規定に違反した者は、6月以下の懲役又は30万円以下の罰金に処する(第39条)。 )は、50万円以下の罰金に処する(第40条)。会長は、公益を代表する委員のうちから、委員が選挙する(第24条)。最低賃金審議会は、政令で定めるところにより、労働者を代表する委員、使用者を代表する委員及び公益を代表する委員各同数をもって組織する(第22条)。
Good post. I learn something totally new and challenging on blogs I stumbleupon every day. It will always be helpful to read through articles from other writers and use a little something from their websites.
Next time I read a blog, I hope that it does not fail me as much as this particular one. I mean, Yes, it was my choice to read through, however I truly thought you would probably have something helpful to talk about. All I hear is a bunch of crying about something you could possibly fix if you weren’t too busy seeking attention.
I’m curious to find out what blog system you are working with?
I’m having some minor security issues with my latest
site and I would like to find something more secure. Do you have any recommendations?
Если вы искали где отремонтировать сломаную технику, обратите внимание – сервисный центр в уфе
bookmarked!!, I love your website.
同月26日に和田・ おとぎちっくアイドル リルぷりっ』(2010年4月 – )で、「雪森りんご」役の和田彩花、「高城レイラ」役の前田憂佳、「笹原名月」役の福田花音(以上スマイレージ)の3名が声優として出演し、主題歌を担当。 しかしながら、今般、最低賃金の安全網としての機能を強化する観点から、最低賃金の適用対象をなるべく広範囲とすることが望ましく、労働者保護にも資することから、同条の適用除外規定を廃止し、平成20年改正後の第7条において、使用者が都道府県労働局長の許可を受けたときは、当該最低賃金において定める最低賃金額から当該最低賃金額に労働能力その他の事情を考慮して厚生労働省令で定める率を乗じて得た額を減額した額により改正後の第4条の規定を適用することとしたものであること。
To be sure completely along with your conclusions and imagine that you’ve made some excellent points. Also, I prefer customized for specific cultures of this site and also the easy navigation. I’ve bookmarked your site and may return often!
日本政府より厳しい予測を示し、他の税目を含む増税や歳出削減の具体的な計画を立てて実行するよう促した。労働者が故意の犯罪行為もしくは重大な過失により事故を生じさせた場合は、給付額(休業・ ムック『フィギュア王』に掲載された「ゴードの巻」でも、バルタン星人たちが蘇生させた宇宙連合軍の怪獣軍団の1匹として冒頭でセブンを襲う。黒の騎士団解散後は将棋部に入部したが、効率を求めるあまり長考してしまいがち。
2022年度から中部(東海・ エンブレムは、北海道に生息する日本最大のフクロウ『シマフクロウ』を象徴的に図案化。 ミスダンスドリルチーム日本大会で優勝の経験もある。日本大作戦(総合・最終更新 2023年7月9日 (日) 09:52 (日時は個人設定で未設定ならばUTC)。最終更新 2024年7月16日 (火) 11:50 (日時は個人設定で未設定ならばUTC)。、一般公募によって決定された。不定期) – ろーかる直送便(総合) – ふるさとから、あなたへ(旧BShi) – にっぽんぐるり(総合・
16. 「音楽がぼくの家族」 アンソニー・ 20.
「音楽はいつまでも」 アンソニー・ アシスタントとして瀧山あかねが起用されている。、ジングルも『恋する電リク~』からJUNK時代までのものが使用された。 『2018年春 草津線ICOCA利用可能エリア拡大日が決まりました』(プレスリリース)、西日本旅客鉄道、2017年12月15日。全国大会本選(団体戦)の準決勝戦では富士崎高校と試合することになり三位決定戦では明石第一女子高校と対戦することになった。
“太田監督から明かされる草彅剛役名の秘密”.死役所職員のほとんどがスーツを着用しているが、彼だけはTシャツにジャケット、スニーカーというラフな出で立ちで、今どきな見た目に反して時代劇役者だった祖父の影響で言い回しが古風(本当を「真(まこと)」、子供を「童(わっぱ)」、なぜを「何故(なにゆえ)」など)。今夜放送「SWITCHインタビュー」で大竹しのぶ×爆笑問題・今日までそして明日から。 バカリズムが「バカリくん」を演じ、そして各話ごとに美女が登場し、公式HP上で行っている美女総選挙によって、7人の美女の中から最終話でバカリくんとキスする相手が決まる。
After study several of the web sites for your internet site now, and that i really like your way of blogging. I bookmarked it to my bookmark site list and will be checking back soon. Pls take a look at my site too and figure out what you think.
人(2022年8月26日、山口龍大朗監督) – 主演・特技は卓球であり、中学時代に都大会個人戦で優勝歴を持っている。選手権大会の予選戦では千駄谷に次ぐ準優勝で出場権を獲得。武勇に優れているが、実直で頑固な面が強いせいか家康から若干苦手意識を持たれている。更識楯無(斎藤千和)、更識簪(三森すずこ) 「SUPER∞STREAM」 テレビアニメ『IS 〈インフィニット・
Your style is really unique in comparison to other people I have read stuff from. Many thanks for posting when you’ve got the opportunity, Guess I will just bookmark this web site.
“独自の「宣言」発出の自治体相次ぐ 「支援対象に」要望も”.緊急事態宣言及びまん延防止等重点措置は、相互に切り替えがされることもあり、統一的に時系列で記述する。
“神奈川県 重点措置の対象地域拡大し独自の宣言発出で調整”.
」を対象にした事例が唯一である。一般社団法人日本ソムリエ協会.一方でロリコンは否定している。
Your style is so unique compared to other folks I have read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I will just bookmark this web site.
you have a very excellent weblog here! do you wish to earn some invite posts on my own weblog?
28日 – 【五輪】 国際オリンピック委員会(以下、IOCと表記)はこの日、オンラインで理事会を開き、国際競技連盟(IF)などに対し、ロシア・ モトローラは、半導体部門のスピンオフを2003年10月6日に発表し、フリースケール社を創設した。 2006年、情報の保持のために電力を必要としないMRAMと呼ばれる新たな集積回路を発表した。
又、日本専売モデルである「パラメヒコ」は中学生からプロの選手に至るまで愛用者が多く、1986年の発売以来、40年近くたった現在でも大幅なモデルチェンジ(新たなスタッドパターンを採用した派生モデルはある)する事なく多くの選手に選ばれており、前述の三浦も長年のパラメヒコユーザーである。
そのため過疎化が問題となり、また大都市も人口の急激な増加による過密化の問題を抱えるようになっていたことから、田中角栄は日本列島改造論(列島改造ブーム)を提唱し、大都市と地方の格差を埋める目的と、地方の雇用対策のために、高速道路網を全国に張り巡らせ、地方に病院や港湾、学校などの公共施設を次々と建てて、大都市と地方のインフラ格差を埋めた。
Nice post. I find out some thing harder on diverse blogs everyday. It will always be stimulating you just read content off their writers and practice a little there. I’d choose to apply certain while using the content on my blog whether or not you don’t mind. Natually I’ll give you a link on your own internet weblog. Appreciate your sharing.
I got what you mean , appreciate it for posting .Woh I am glad to find this website through google.
agen77 agen77 agen77 agen77 agen77
It’s amazing in favor of me to have a web page, which is beneficial in favor of my experience. thanks admin
Good write-up. I certainly love this site. Continue the good work!
Hi it’s me, I am also visiting this web page daily, this web site is in fact fastidious and the visitors are truly sharing pleasant thoughts.
I want to to thank you for this fantastic read!! I absolutely enjoyed every little bit of it. I have you book-marked to check out new things you post…
“米製薬会社ノババックスのコロナワクチン接種始まる 新潟 長岡”.
“合成たんぱくで抗体作製 遺伝子組み換え、広い使途-米ノババックス製コロナワクチン”.
“震災で2人死亡の九段会館、閉館へ 遺族会が国に返還”.読売新聞、2022年1月23日閲覧。 19日 – 2月の日本百貨店協会による全国百貨店売上高は、前年同月比0.3%増(店舗数調整後)の約4317億円と、高級ブランド品やバレンタイン関連の需要が牽引して1月に続くプラスとなった。
しかし、客先の担当者から知識不足を指摘され、全く仕事を得ることが出来なかった。正規販売代理店で販売されたフェラーリの市販車のオーナーで、かつフェラーリに承認された一部の顧客に限り、フェラーリまたは各国の拠点や正規輸入元を通じて数年落ちのF1マシンを購入することが可能である。 フェラーリの社長が交代 – フィアット社は91年11月15日にピエロ・ 15日
– 【陸上競技・競馬ファン注目の番組が目白押し!
三好はセーフエリアUS-DAD区画の指定場所に、ホイポイカプセルから出している風に装ってコンテナハウスを設置、芳村はサイモンに電話しその指示で、32層JDA待機所から来た駐在員に鍵を渡し、その直前33層への入り口を探索案内させるべくロザリオを放った。芳村は32層の石群を31層に持ち込んで転移石31を相当数作っていたが、その間に31層で探索者を見掛けず、32層に戻ると三好が『議員の皆さんは本当に優秀?雑賀はそれが「先月真壁常務が仰っていた、横田のアレ」で、持ち込んだのはDパワーズに違いないと確信し、同様に準備中の設備搬送の報酬に悩み、燃料についてはあてがあるから配電の話を進めよと坂井に命じた。
従業員達はそれぞれ名付けられたあだ名で呼ぶのが決まりとなっている。、韓国国内からも批判を受けた(当時、着弾海域付近では韓国漁船が操業していた)。
2003年のCONCACAFゴールドカップ初戦のメキシコ戦で(23歳以下の年齢制限付きながら)ブラジル代表デビューを飾った。 しかし戸籍を登録する際、担当者に「外国風の名前は認められない」と言われ、英語の発音に近いポルトガル語の綴りで”Maicon”と名付けた。
これもオマージュで、エリュアードという人物が同じ名前の吟遊詩人の名前を無理やり「ネリュアード」に変えるイベントがアークトゥルスにもある。大きく1歩退き込み画面に背を向け、弟子のものとは逆の腕で画面手前側を向くようにして放つのが特徴で、通常の「昇龍拳」より威力・
事故に起因する放射性物質による環境・内閣官房の事故調査委員会→東京電力福島原子力発電所における事故調査・ これ以外はCategory:福島第一原子力発電所を参照。最高裁判所第二小法廷判決 2003年(平成15年)3月14日 『最高裁判所民事判例集』第57巻3号229頁、平成12年(受)第1335号、『損害賠償請求事件』「1・
公益社団法人 千葉県観光物産協会. 3月17日 元西大阪スチール 東田満社長編・西大阪スチール倒産後の東田からの5億円の回収、120億円の運用損失を出した伊勢島ホテルの再生、タミヤ電機に対する迂回融資の看破、電脳雑伎集団のスパイラル買収の阻止及び粉飾の看破、帝国航空の債権放棄の拒否。
Сервисный центр предлагает качественый ремонт кофемашин hotpoint-ariston починить кофемашины hotpoint-ariston
demo slot demo slot demo slot demo slot demo slot
Heya i’m for the first time here. I came across this board and I in finding It really useful & it helped me out much. I am hoping to give one thing back and help others such as you aided me.
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем:ремонт крупногабаритной техники в ростове на дону
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
agen77 agen77 agen77 agen77 agen77
Hey there! I just wanted to ask if you ever have any trouble with hackers? My last blog (wordpress) was hacked and I ended up losing many months of hard work due to no backup. Do you have any solutions to protect against hackers?
Saved as a favorite, I like your site.
I just placed this article on facebook. it’s a very interesting read for everyone.
I was able to find good info from your blog articles.
you are in reality a excellent webmaster. The website loading velocity is incredible. It kind of feels that you’re doing any distinctive trick. Also, The contents are masterpiece. you’ve performed a wonderful job in this topic!
第10回優勝者。原田芳雄(第10-12回)、哀川翔(第10回、第3回紅白)、キャイ〜ンの天野ひろゆき(第11回)、市原隼人(第15回と第17回)、戸張捷(第18回)小栗旬、武田鉄矢(いずれも第3回紅白)などと、幅広いモノマネを得意としている。主に宝塚音楽学校の入試を受けている女子高生やタカラジェンヌ、リアルゴリラ(と称するゴリラのリアルなモノマネ)のモノマネを得意としている。 そしてこの頃から、小室自身が日本の音楽シーンの中心からやや離れたプログレやトランスに傾倒し、ミリオンセラーに届くヒット曲を出さなくなった。主に、BGMや雅楽などの音のものまねを得意とし、『すぽると!産業用ディーゼルエンジンを得意とする。
2007年(平成19年)7月に大和ハウスグループ単独でREIT(「(旧)大和ハウスリート投資法人」)を設立、2008年(平成20年)5月に東京証券取引所へ上場する予定であったが、同年6月市況の悪化に伴い上場中止を発表した。 このため、経営再建のスキームとして2001年(平成13年)5月に日立製作所と主力取引銀行(第一勧銀・
I am not sure where you are getting your info, but great topic. I needs to spend some time learning more or understanding more. Thanks for great information I was looking for this info for my mission.
手下達をけしかけて二人を足止めしつつ自身は女性を抱えたまま城内を逃げ惑うが、手下鬼の殲滅を小芭内に任せた実弥によって屋根に追い詰められ、最後は女性を空中に放り投げて(直後小芭内によって救出される)自身は無限城に送還され、難を逃れる。 また城内には手下の鬼たちが大勢おり、護身用として配置されている。村から女性をさらって城に連れ去ろうとしていたところを鬼殺隊員に発見され、実弥と小芭内によって城内に踏み込まれる。
Сервисный центр предлагает сколько стоит ремонт электросамоката shulz стоимость ремонта электросамоката shulz
ollo4d ollo4d ollo4d
For newest news you have to go to see internet and on web I found this website as a best website for latest updates.
2022年2月に開催された感謝祭イベントのうち、2月20日に開催されたプレミアム公演の一部を除くほぼ全編、さらに特典映像としてファミリー公演の参加型トークコーナー、声優コーナーと「なかよしのうた」のライブ歌唱映像、プレミアム公演の声優コーナー本編未収録回をそれぞれ収録。 2021年9月25日にパシフィコ横浜国立大ホールで開催された、主題歌歌手と出演声優によるキャラクターソングライブを1公演分および特典映像を収録したライブ・
Way cool! Some extremely valid points! I appreciate you writing this article plus the rest of the site is also very good.
Good article. I absolutely love this site. Stick with it!
“マツダ、住友商事とメキシコでの生産事業およびブラジルでの販売事業で合弁事業に合意”.
“「創価学会社会憲章」全文と解説”.三笠の娘の留学費や、妻の経営する飲食店の改装費を電脳に支出させていたことを平山夫妻が証言する音声データが森山から役員会に乗り込んだ半沢に送られた。 モーターは大戦末期には国有化一歩手前の状態まで経営状態が悪化していた。容れ物によって形を自在に変える水の如く、相手の攻撃を利用したり、いなしたりと、あらゆる状況に柔軟に対応する技で鬼の頸を狩る。
中平正彦の漫画『ストリートファイターZERO』では、「『人の世を乱す者』を倒すために人の世が得た唯一の力である」と解釈されている。 この場合の「乱す者」とはベガのことで、古くはキリストやヒトラーがこれに当たることを示唆しており、善悪にかかわらず影響の大きすぎる者が該当すると見られる。 “名古屋市・笠間市 笠間市役所笠間支所 移転 躯体損傷・ 10月 – 姫路市に「姫路駐在員事務所」を開設。
This piece of writing will help the internet users for
setting up new website or even a weblog from start to end.
1874年(明治7年) 埼玉県入間郡川越町(現・動画配信のシステムの構築や品質向上などの技術投資も、年間12億ドルに達する(2018年実績)。美術賞 ディーン・ その夜、記者がいて自宅に入れないため貴司のいる「デラシネ」に身を寄せるが、久留美から悠人が倒れていたとの連絡を受け、めぐみと共に久留美の家に駆け付ける。 コルレオーネの最期』は、オリジナル版よりも高い評価を受けた。 Appleは次期Mac
OSとなる新たなOSを外部から調達することを決定し、候補としてマイクロソフトのWindows
NT、サン・
通称である「加速器村」の名が示す通り、山間部には特急路線の廃棄トンネルを利用した全長15㎞の直線加速装置、平野部には半径8㎞の円形加速装置を備える観光都市。現在まで優勝はおろか、ファイナリストまで残った経験もないが、出場11回という実績にも表れている通り、今やこのコーナーになくてはならない存在となっている。 フランス通信社 (2017年6月12日).
2017年6月13日閲覧。 AFPBB NEWS (2017年10月4日).
2017年10月12日閲覧。
「つみたてNISA」で人気の投資信託ベスト10を紹介! また、小泉純一郎は「骨太の方針」の中で「貯蓄から投資へ」をスローガンに掲げ、2003年からは、個人投資家を対象に株式と株式投資信託の売却益や配当・
“トランプ氏、第45代米大統領に就任”.
“【トランプ次期大統領】当選が公式確定 異議唱える米議員も”.次期米国務長官 : 国際”. “NY列車事故、車止め衝突で脱線 乗客ら103人が負傷”. “共和、政策転換へ全力=米連邦議会が招集”. たとえばエンロンの粉飾決算やライブドア事件、そして世界金融危機までに繰り返されたOTD金融である。 しかし、飛行機の運航トラブルにより、急遽、大勢の宿泊客をオオサキで受け入れることになり、状況は一転する。
「メイキング」の能力でステータスポイントを編集できることが分かり、オークションで得た資金で常磐医療機器研究所を巻き込んで、詳細な調査が行われた。 「ないとう」での飲食シーンの翌日、常磐医療機器研究所で再計測を行う。 ある程度狙ってスキルオーブを取得できるとみなされたDパワーズは、後に多くの海外情報機関から侵入不可能な伏魔殿と知られることになる新事務所への移動直後に、JDAから「異界言語理解」のスキルオーブを探すように依頼される。
、オリンピックや競馬など多くの競技で禁止されている。古代ギリシャ時代に競技者が興奮剤等をドーピング目的で用いるようになる。 1886年
ボルドー-パリ間の600km自転車レースで、イギリスの選手が興奮剤トリメチルの過剰摂取により死亡。 エレベーター製造に着手。 ドーピングの極端な事例では、安全な範囲を超えて能力を増幅させるため、運動時の身体の損傷が大きくなり、選手が深刻な後遺症に悩まされる場合もある。女子の体操選手シリーズ 跳馬の着地でアキレス腱が切れるも笑顔でフィニッシュ メアリー・
『列車試運転は平和に向けた大きな1歩、盧大統領』、聯合ニュース、2007年5月17日。 HYとの紅白歌合戦出演やクランクアップ後の遊川和彦、夏菜、風間のコメント映像も流された。第44回JLPGAツアーチャンピオンシップ(11月24日 – 27日、宮崎県宮崎市・
」と位置づけられており、関西三空港で唯一、定期国際線が就航している。第二外国語として選択・
Hi, i think that i saw you visited my web site so i came to
return the favor.I am attempting to find things to improve my site!I suppose its ok to use a
few of your ideas!!
Hi, all is going sound here and ofcourse every one is sharing facts, that’s really excellent,
keep up writing.
Right here is the perfect site for anybody who wishes to find out about this topic. You understand a whole lot its almost hard to argue with you (not that I really will need to…HaHa). You definitely put a brand new spin on a topic that’s been written about for ages. Great stuff, just excellent.
I could not resist commenting. Very well written.
そこで、雫の国の現状を知り、自分にできることをやり続けた結果、主人公達に連絡もせず世界中を旅していた。 “〔外為マーケットアイ〕ドル95.69円付近、2月米小売売上高上振れなら株高・ “有効求人倍率1.64倍 9月、正社員は過去最高”. 日本経済新聞 (2018年10月30日). 2022年11月15日閲覧。
Hi there! I know this is somewhat off topic but I was wondering which blog platform are you using for this site? I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be awesome if you could point me in the direction of a good platform.
I was able to find good advice from your blog posts.
{Tôi háo hức để tìm thấy trang web tuyệt vời này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn thực sự thích từng một phần nó và tôi đã lưu làm mục ưa thích để xem những thứ mới trên trang web của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một người mà thực sự biết họ là gì đang nói về trên mạng. Bạn thực sự nhận ra cách đưa một rắc rối ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn cần phải kiểm tra điều này và hiểu khía cạnh này câu chuyện của bạn. Tôi không thể tin bạn không nổi tiếng hơn vì bạn chắc chắn có món quà.|Rất hay bài viết. Tôi hoàn toàn yêu thích trang web này. Tiếp tục viết!|Thật khó đến những người có kinh nghiệm về điều này, tuy nhiên, bạn nghe có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên tham gia một cuộc thi dành cho một blog trên mạng có chất lượng cao nhất. Tôi sẽ Rất khuyến nghị trang web này!|Một hấp dẫn chắc chắn đáng giá bình luận. Tôi nghĩ rằng bạn nên viết thêm về chủ đề này, nó có thể không là một điều cấm kỵ vấn đề nhưng nói chung mọi người không nói về những chủ đề như vậy. Đến phần tiếp theo! Chúc mừng.|Xin chào! Tôi chỉ muốn cho bạn một rất to cho thông tin xuất sắc bạn có ngay tại đây trên bài đăng này. Tôi sẽ là trở lại trang web của bạn để biết thêm thông tin sớm nhất.|Khi tôi ban đầu để lại bình luận tôi có vẻ như đã nhấp vào hộp kiểm -Thông báo cho tôi khi có bình luận mới- và bây giờ mỗi lần được thêm vào tôi nhận được bốn email có cùng nội dung. Có một phương tiện bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn rất nhiều.|Lần sau Tôi đọc một blog, Tôi hy vọng rằng nó không thất bại nhiều như bài này. Ý tôi là, Tôi biết điều đó là sự lựa chọn của tôi để đọc hết, dù sao thì tôi thực sự tin bạn sẽ có điều gì đó hữu ích để nói. Tất cả những gì tôi nghe được là một loạt khóc lóc về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi thực sự cảm thấy trang web này cần nhiều hơn nữa sự chú ý.
Skagen is the northernmost city in Denmark, and it was once a preferred vacation destination for the Danish royal family.
{Tôi đã rất hài lòng để tìm thấy trang web này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn thích thú từng một chút nó và tôi cũng đã lưu làm mục ưa thích để xem những thứ mới trên blog của bạn.|Tôi có thể chỉ nói rằng thật thoải mái để khám phá một người mà thực sự biết họ là gì thảo luận trên web. Bạn thực sự nhận ra cách đưa một rắc rối ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn cần đọc điều này và hiểu khía cạnh này câu chuyện của bạn. Tôi không thể tin bạn không nổi tiếng hơn vì bạn chắc chắn sở hữu món quà.|Tốt bài đăng. Tôi chắc chắn yêu thích trang web này. Tiếp tục viết!|Thật khó tìm những người có kinh nghiệm về điều này, tuy nhiên, bạn có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên là một phần của một cuộc thi dành cho một trang web trên internet tuyệt vời nhất. Tôi sẽ Rất khuyến nghị blog này!|Một hấp dẫn chắc chắn đáng giá bình luận. Tôi tin rằng bạn nên xuất bản thêm về vấn đề này, nó có thể không là một điều cấm kỵ chủ đề nhưng điển hình mọi người không thảo luận vấn đề như vậy. Đến phần tiếp theo! Chúc mừng.|Xin chào! Tôi chỉ muốn cho bạn một rất to cho thông tin xuất sắc bạn có ở đây trên bài đăng này. Tôi sẽ là trở lại blog của bạn để biết thêm thông tin sớm nhất.|Khi tôi ban đầu bình luận tôi có vẻ như đã nhấp hộp kiểm -Thông báo cho tôi khi có bình luận mới- và bây giờ bất cứ khi nào có bình luận được thêm vào tôi nhận được 4 email cùng chính xác một bình luận. Có một cách bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn rất nhiều.|Lần sau Tôi đọc một blog, Tôi hy vọng rằng nó không làm tôi thất vọng nhiều như bài này. Rốt cuộc, Tôi biết điều đó là sự lựa chọn của tôi để đọc, nhưng tôi thực sự nghĩ bạn sẽ có điều gì đó hữu ích để nói. Tất cả những gì tôi nghe được là một loạt rên rỉ về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi thực sự tin rằng trang web tuyệt vời này cần nhiều hơn nữa sự chú ý.
{Tôi đã rất hài lòng để tìm thấy trang này. Tôi cần cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn thưởng thức từng một chút nó và tôi cũng đã đánh dấu để xem những thứ mới trong trang web của bạn.|Tôi có thể chỉ nói rằng thật thoải mái để tìm thấy một người mà thực sự hiểu họ là gì thảo luận trên mạng. Bạn thực sự nhận ra cách đưa một vấn đề ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa cần phải đọc điều này và hiểu khía cạnh này của. Tôi đã ngạc nhiên bạn không nổi tiếng hơn vì bạn chắc chắn có món quà.|Rất tốt bài đăng. Tôi chắc chắn yêu thích trang web này. Tiếp tục viết!|Thật gần như không thể tìm thấy những người có hiểu biết sâu rộng về điều này, nhưng bạn có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn cần là một phần của một cuộc thi dành cho một trang web trên internet tuyệt vời nhất. Tôi sẽ khuyến nghị trang web này!|Một động lực chắc chắn đáng giá bình luận. Không còn nghi ngờ gì nữa rằng bạn nên viết thêm về vấn đề này, nó có thể không là một điều cấm kỵ chủ đề nhưng nói chung mọi người không nói về những chủ đề những điều này. Đến phần tiếp theo! Trân trọng!|Chào bạn! Tôi chỉ muốn đề nghị rất cho thông tin xuất sắc bạn có ngay tại đây trên bài đăng này. Tôi đang quay lại trang web của bạn để biết thêm thông tin sớm nhất.|Sau khi tôi ban đầu bình luận tôi có vẻ như đã nhấp vào hộp kiểm -Thông báo cho tôi khi có bình luận mới- và từ bây giờ bất cứ khi nào có bình luận được thêm vào tôi nhận được bốn email có cùng nội dung. Có một phương pháp dễ dàng bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn.|Lần sau Tôi đọc một blog, Tôi hy vọng rằng nó không làm tôi thất vọng nhiều như bài này. Ý tôi là, Tôi biết điều đó là sự lựa chọn của tôi để đọc hết, tuy nhiên tôi thực sự nghĩ có lẽ có điều gì đó thú vị để nói. Tất cả những gì tôi nghe được là một loạt rên rỉ về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi thực sự tin trang web này cần nhiều hơn nữa sự chú ý.
{Tôi háo hức khám phá trang web tuyệt vời này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn thích từng một chút nó và tôi đã lưu làm mục ưa thích để xem điều mới trên blog của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một người mà thực sự hiểu họ là gì thảo luận trên web. Bạn chắc chắn biết cách đưa một rắc rối ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa cần xem điều này và hiểu khía cạnh này của. Tôi đã ngạc nhiên rằng bạn không nổi tiếng hơn vì bạn chắc chắn nhất có món quà.|Xuất sắc bài viết trên blog. Tôi chắc chắn đánh giá cao trang web này. Tiếp tục làm tốt!|Thật khó đến những người có hiểu biết sâu rộng về điều này, nhưng bạn có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên là một phần của một cuộc thi dành cho một trang web trực tuyến tốt nhất. Tôi sẽ Rất khuyến nghị trang web này!|Một hấp dẫn chắc chắn đáng giá bình luận. Tôi nghĩ rằng bạn cần viết thêm về vấn đề này, nó có thể không là một điều cấm kỵ chủ đề nhưng nói chung mọi người không nói về những chủ đề như vậy. Đến phần tiếp theo! Chúc mọi điều tốt đẹp nhất.|Xin chào! Tôi chỉ muốn đề nghị rất cho thông tin xuất sắc bạn có ngay tại đây trên bài đăng này. Tôi đang trở lại blog của bạn để biết thêm thông tin sớm nhất.|Khi tôi ban đầu bình luận tôi có vẻ như đã nhấp vào hộp kiểm -Thông báo cho tôi khi có bình luận mới- và bây giờ mỗi lần được thêm vào tôi nhận được 4 email có cùng nội dung. Có lẽ có một phương tiện bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn rất nhiều.|Lần sau Tôi đọc một blog, Hy vọng rằng nó sẽ không làm tôi thất vọng nhiều như bài này. Rốt cuộc, Vâng, đó là sự lựa chọn của tôi để đọc hết, nhưng tôi thực sự nghĩ bạn sẽ có điều gì đó hữu ích để nói. Tất cả những gì tôi nghe được là một loạt phàn nàn về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi hoàn toàn cảm thấy trang web này cần nhiều hơn nữa sự chú ý.
Если вы искали где отремонтировать сломаную технику, обратите внимание – техпрофи
{Tôi đã hạnh phúc hơn cả vui khám phá trang web này. Tôi cần cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn thưởng thức từng một phần nó và tôi cũng đã đã lưu vào mục ưa thích để xem điều mới trong trang web của bạn.|Tôi có thể chỉ nói rằng thật thoải mái để khám phá một người mà thực sự hiểu họ là gì đang nói về trên internet. Bạn chắc chắn biết cách đưa một vấn đề ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa thực sự cần đọc điều này và hiểu khía cạnh này câu chuyện của bạn. Thật ngạc nhiên bạn không nổi tiếng hơn vì bạn chắc chắn sở hữu món quà.|Rất tốt bài đăng. Tôi chắc chắn yêu thích trang web này. Tiếp tục làm tốt!|Thật khó đến những người có học thức cho điều này, tuy nhiên, bạn nghe có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên là một phần của một cuộc thi dành cho một trang web trên mạng hữu ích nhất. Tôi sẽ khuyến nghị blog này!|Một hấp dẫn chắc chắn đáng giá bình luận. Tôi tin rằng bạn nên viết thêm về chủ đề này, nó có thể không là một điều cấm kỵ chủ đề nhưng thường xuyên mọi người không nói về vấn đề những điều này. Đến phần tiếp theo! Cảm ơn rất nhiều.|Xin chào! Tôi chỉ muốn đề nghị rất cho thông tin tuyệt vời bạn có ở đây trên bài đăng này. Tôi đang quay lại trang web của bạn để biết thêm thông tin sớm nhất.|Sau khi tôi ban đầu để lại bình luận tôi có vẻ như đã nhấp vào hộp kiểm -Thông báo cho tôi khi có bình luận mới- và bây giờ mỗi lần được thêm vào tôi nhận được bốn email có cùng nội dung. Phải có một phương pháp dễ dàng bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn rất nhiều.|Lần sau nữa Tôi đọc một blog, Hy vọng rằng nó sẽ không làm tôi thất vọng nhiều như bài này. Rốt cuộc, Tôi biết điều đó là sự lựa chọn của tôi để đọc hết, nhưng tôi thực sự tin có lẽ có điều gì đó thú vị để nói. Tất cả những gì tôi nghe được là một loạt rên rỉ về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi thực sự cảm thấy trang web này cần nhiều hơn nữa sự chú ý.
An fascinating discussion will be worth comment. I’m sure that you need to write much more about this topic, may possibly not certainly be a taboo subject but usually people are not enough to communicate in on such topics. To another location. Cheers
Thats pretty cool! I look forward to reading more of your posts.
I am glad for commenting to let you understand what a notable experience our daughter encountered visiting your webblog. She realized too many things, with the inclusion of what it’s like to possess an excellent giving mood to let other people very easily thoroughly grasp selected complicated subject areas. You actually exceeded her expected results. Thank you for offering those essential, dependable, explanatory and even easy guidance on this topic to Sandra.
{Tôi hạnh phúc hơn cả vui để tìm thấy trang này. Tôi cần cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn thực sự thích từng một phần nó và tôi cũng đã đã đánh dấu trang để xem điều mới trên blog của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một người thực sự biết họ là gì thảo luận trên mạng. Bạn thực sự nhận ra cách đưa một rắc rối ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa cần phải kiểm tra điều này và hiểu khía cạnh này của. Tôi không thể tin bạn không nổi tiếng hơn vì bạn chắc chắn sở hữu món quà.|Xuất sắc bài viết trên blog. Tôi hoàn toàn đánh giá cao trang web này. Cảm ơn!|Thật khó đến những người có học thức về điều này, tuy nhiên, bạn có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên tham gia một cuộc thi dành cho một trang web trên web tốt nhất. Tôi chắc chắn sẽ khuyến nghị trang web này!|Một hấp dẫn chắc chắn đáng giá bình luận. Tôi nghĩ rằng bạn nên viết thêm về chủ đề này, nó có thể không là một điều cấm kỵ vấn đề nhưng điển hình mọi người không nói về những chủ đề những điều này. Đến phần tiếp theo! Cảm ơn rất nhiều!|Xin chào! Tôi chỉ muốn đề nghị rất cho thông tin tuyệt vời bạn có ngay tại đây trên bài đăng này. Tôi đang quay lại trang web của bạn để biết thêm thông tin sớm nhất.|Sau khi tôi ban đầu để lại bình luận tôi có vẻ như đã nhấp hộp kiểm -Thông báo cho tôi khi có bình luận mới- và từ bây giờ mỗi lần được thêm vào tôi nhận được bốn email cùng chính xác một bình luận. Có lẽ có một phương tiện bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm kích.|Lần sau Tôi đọc một blog, Hy vọng rằng nó không làm tôi thất vọng nhiều như bài này. Ý tôi là, Tôi biết điều đó là sự lựa chọn của tôi để đọc, tuy nhiên tôi thực sự nghĩ bạn sẽ có điều gì đó thú vị để nói về. Tất cả những gì tôi nghe được là một loạt phàn nàn về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi hoàn toàn cảm thấy trang web này cần nhiều hơn nữa sự chú ý.
{Tôi rất hài lòng khám phá trang web này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn đánh giá cao từng một chút nó và tôi đã lưu làm mục ưa thích để xem những thứ mới trong trang web của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một người mà thực sự biết họ là gì đang nói về trên web. Bạn chắc chắn hiểu cách đưa một rắc rối ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa phải kiểm tra điều này và hiểu khía cạnh này của. Tôi đã ngạc nhiên bạn không nổi tiếng hơn cho rằng bạn chắc chắn sở hữu món quà.|Rất hay bài đăng. Tôi hoàn toàn yêu thích trang web này. Tiếp tục viết!|Thật khó tìm những người có hiểu biết sâu rộng cho điều này, nhưng bạn nghe có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn cần tham gia một cuộc thi dành cho một trang web trên internet hữu ích nhất. Tôi sẽ khuyến nghị blog này!|Một hấp dẫn chắc chắn đáng giá bình luận. Tôi nghĩ rằng bạn cần viết thêm về chủ đề này, nó có thể không là một điều cấm kỵ chủ đề nhưng thường xuyên mọi người không nói về những chủ đề những điều này. Đến phần tiếp theo! Chúc mọi điều tốt đẹp nhất.|Xin chào! Tôi chỉ muốn cho bạn một rất to cho thông tin xuất sắc bạn có ngay tại đây trên bài đăng này. Tôi sẽ là trở lại trang web của bạn để biết thêm thông tin sớm nhất.|Khi tôi ban đầu để lại bình luận tôi có vẻ như đã nhấp vào hộp kiểm -Thông báo cho tôi khi có bình luận mới- và từ bây giờ mỗi lần được thêm vào tôi nhận được bốn email có cùng nội dung. Phải có một phương tiện bạn có thể xóa tôi khỏi dịch vụ đó không? Chúc mừng.|Lần sau Tôi đọc một blog, Tôi hy vọng rằng nó không làm tôi thất vọng nhiều như bài này. Rốt cuộc, Vâng, đó là sự lựa chọn của tôi để đọc hết, dù sao thì tôi thực sự tin có lẽ có điều gì đó thú vị để nói. Tất cả những gì tôi nghe được là một loạt khóc lóc về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi nghiêm túc tin trang web này cần nhiều hơn nữa sự chú ý.
Excellent blog post. I absolutely appreciate this site. Continue the good work!
Greetings! Very useful advice within this post! It is the little changes that will make the greatest changes. Many thanks for sharing!
I also believe therefore , perfectly pent post! .
Профессиональный сервисный центр по ремонту моноблоков в Москве.
Мы предлагаем: вызвать мастера по ремонту моноблоков
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр по ремонту гироскутеров в Москве.
Мы предлагаем: цены на ремонт гироскутеров
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
I love the opinions on this site, it really gives it that community sense!
I applaud this writer for writing such unique and quality information with viewpoints I can understand. I couldn’t stop reading this article. I got so engrossed in this material. Thanks!
If you would like to increase your knowledge only keep visiting this site and be updated with the latest news update posted here.
At this moment I am ready to do my breakfast, later than having my breakfast coming over again to read other news.
https://www.ehbact.com/business-professional-services/seohawk
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: ремонт крупногабаритной техники в тюмени
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
You ought to take part in a contest for one of the highest quality websites on the internet. I most certainly will recommend this blog!
Very good info. Lucky me I recently found your website by accident (stumbleupon). I have book marked it for later!
This is a topic that is close to my heart… Many thanks! Where are your contact details though?
This site truly has all of the information I wanted concerning this subject and didn’t know who to ask.
「京アニ事件遺族、取材に応じる思い 「事実伝える」「生きた証」」『京都新聞』京都新聞社、2019年8月19日。 また、新卒から生え抜きの人材がCEOになるという伝統を持っている。 「京アニ放火事件、遺族が呆れる「無礼で無遠慮な取材者たち」」『女性セブン2020年2月20日号』、小学館、2020年2月7日、2020年2月16日閲覧。 「京アニ犠牲者、36人目身元公表」『共同通信』共同通信社、2019年10月11日。日本では、公営住宅法(昭和26年法律193号)によって定められている。
総裁に就任。 1996年(平成8年)に村山が首相を辞任し、橋本内閣が成立すると、小泉は第2次橋本内閣で再び厚生大臣に就任する。無投票で総裁が決まることを阻止したい小泉らは森喜朗(清和会)擁立を図るが森が辞退したため、小泉が自ら出馬することを決めた。既に大勢が決していた上に、郵政民営化を主張する小泉は党内で反発を買っており、出馬に必要な推薦人30人を集めることができたことがニュースになる有り様だったが、それでも若手議員のグループが小泉を推した(中川秀直や山本一太、当選1回の安倍晋三もいた)。
また、東アジアのハイテク産業の急成長が続くなか日本勢が劣勢となり、中国や台湾企業に買収・第二次世界大戦終戦後、1960年代中頃から業務の再建を開始し、同国最大手の外資系銀行となっている。株式会社第一製材 / (2代目)サークルケイ・
同じ国出身のユニットを同じパーティに入れると、初期SPの増加ボーナスがある。最終ゲーム「ジェスチャーげーむSPタイムisマネキン」前までは「ラストクリスマス」チームがトップだった為、1問正解で100点加算することになった為、電光掲示板の最高得点が999点しか出ず、最終結果では司会者がモニターを観ながら得点発表した。彼はヴェネツィア共和国の下級士官職を金銭で得、コルフに短期間駐留した後、コンスタンティノポリスに赴く。 4月21日:昭和電工が、日立化成へのTOB(株公開買い付け)が成立したと発表。入手時や進化後は必ず1。
Hello! I could have sworn I’ve been to this blog before but after going through many of the posts I realized it’s new to me. Nonetheless, I’m definitely pleased I stumbled upon it and I’ll be bookmarking it and checking back regularly.
筑波大学附属高等学校)卒業。東京教育大学附属高等学校(現・生家の清滝家は、大阪府池田市に本店を置いていた池田銀行(現・ 【陸上競技】 第10回大阪マラソン兼第77回びわ湖毎日マラソン統合大会(大阪府庁前スタート→大阪城公園フィニッシュ)で、初マラソンの星岳(ほし・
シガンシナ区以上の規模を持ち、約5万人の人口を擁する。海上保安庁第五管区海上保安本部 関西空港海上保安航空基地(関西国際空港の対岸の泉佐野市内には、海上保安庁の特殊警備隊(SST)が配備された基地(庁舎)があり、関西空港海上保安航空基地から全国の航空基地に展開する。
アメリカ合衆国(アメリカがっしゅうこく、英語: United States of
America、英語略称: USA、United States、US、America)は、北アメリカ大陸の中央部および北西部に位置し、大西洋および太平洋に面する連邦共和国(合衆国)。通称は米国(べいこく)またはアメリカ。国際 (iRO) やヨーロッパ (euRO)
などへは日本からも参加可能。一方、トヨタ会館(愛知県)の「トヨタ自動車本社店」は一般利用可能となっている(トヨタ自動車本社店は2022年12月28日をもって閉店した)。一般社団法人デジタル放送推進協会.
歴史ヒーローの清水次郎長を味方につけることで阻止できる。 「木曽川は、上流に貯水池が出来る。第100弾
– 2日目の朝、出川と松陰寺が入浴中に、上半身もバスタオルで隠して合流。歌唱中に人間に戻るため、プレイヤーの標的にはならない。 プレイヤーの標的にはならないが、ゲーム終了時に倒された鬼と同様に気を失い人間に戻った。問題終了後にそれまで鬼化した有名人とは異なり気を失う事なく録音・
法人格を有するものは特別目的会社(とくべつもくてきがいしゃ、英:
special-purpose company, SPC)と呼ばれ、国際投信を営んだり、大口ユーロ債を発行したりする。 1990年代にはダウンサイジングの潮流によりIBMの主力であったメインフレームは「時代遅れ、過去の遺物(レガシー)、滅び行く恐竜」と呼ばれ、IBMの業績は急速に悪化した。戸畑鋳物東京製作所(深川)を新設し1929年(昭和4年)に自動車用マレブル鋳鉄製造を始める一方で、久原家が興した久原鉱業の社長に就任して同社を改組し、1928年に日本産業株式会社(略称、日産)とした。
参考までに展開した式を張り付けておきます。
エフエム山形開局30周年。 アニメーション、ゲーム及びVR等の企画開発・特大号』のものまね企画でも披露する事が多い(中居はその年に流行した芸人のネタを用いており、本番組のコントキャラは逆に用いられない)。銃声が収まった部屋に入ってみると、中はもぬけのカラで一同は無人島のハリボテのビルに居たことに気付く。
1990年(平成2年)11月17日に山頂付近にある神社脇の2か所より噴煙が立ち上り噴火。 1791年(寛政3年)11月から地震があった。
gelas togel gelas togel gelas togel
Highly descriptive article, I loved that bit. Will there be a part 2?
「ASCII 1982年10月号」第6巻第10号、株式会社アスキー出版、1982年10月1日。 ピアゴも経営し、中京圏を基盤とする株式会社サークルKサンクスを持株運営していたユニーグループ・飛行機の公開飛行を行えば、その機会に乗じてライバルは自分たちの技術を盗むと考えていた。 スミソニアン協会会長の地位にあり、アメリカ政府援助のもと主導した実験の失敗はラングレー晩節の評価を地に堕とした。
This site truly has all the information and facts I needed about this subject and didn’t know who to ask.
I’m impressed, I have to admit. Seldom do I encounter a blog that’s equally educative and interesting, and let me tell you, you have hit the nail on the head. The problem is something which not enough men and women are speaking intelligently about. I’m very happy that I found this in my hunt for something concerning this.
Nice post. I learn something totally new and challenging on sites I stumbleupon on a daily basis. It will always be interesting to read content from other writers and use a little something from their web sites.
When I originally left a comment I seem to have clicked on the -Notify me when new comments are added- checkbox and now every time a comment is added I recieve 4 emails with the exact same comment. There has to be an easy method you are able to remove me from that service? Thanks a lot.
Профессиональный сервисный центр по ремонту МФУ в Москве.
Мы предлагаем: сервис по ремонту мфу
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Your style is so unique in comparison to other folks I’ve read stuff from. Thank you for posting when you’ve got the opportunity, Guess I will just bookmark this page.
bookmarked!!, I love your blog!
しかし、チームワークが取れていないシノア隊はグレン達に惨敗し、自分達の未熟さを痛感させられる。 ミカエラと気付き動揺する優一郎は、吸血鬼達に仲間を殺されそうになったとき、自身の人間でない部分が暴走する。優一郎達は鳴海真琴率いる鳴海隊と合同で貴族の一人・尋問後、優一郎達は「憑依化」や「具現化」を使えるようになるために訓練を開始し、優一郎や君月が苦戦する中、与一は早々に具現化に成功する。
感染様式は飛沫感染と濃厚接触による接触感染であり、潜伏期は1 – 4週間程度(通常は、2 –
3週間)。症状は個人差が大きく咳は、発症初期は喀痰を伴わない「乾いた咳」(dry cough,乾性咳嗽)であるが、時間の経過と共に咳は強くなり、解熱後も1ヶ月程度続くことも珍しくない。韓国の経済は常に戦争とかかわり、各戦争は経済に新たな機会をもたらしてきた。
I have read so many articles or reviews concerning the blogger lovers however this
post is in fact a fastidious post, keep it up.
翌年に分割民営化によりJR東日本長野支社社員となり、2年前に実家の最寄り駅で父親が駅長を務める清澄駅に配属。翌92年より経済成長率が急落する。戦後復興、1955年から始まった高度経済成長によりアメリカ合衆国に次ぐ世界第2位の経済大国に。 1920年代末以降、世界恐慌、昭和恐慌、昭和農業恐慌などが発生。 その後日中戦争、太平洋戦争へ突入。
Профессиональный сервисный центр по ремонту принтеров в Москве.
Мы предлагаем: починка принтеров
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
魔界の東にあるラウタロッド国の王子で、魔神王の120のモンスター全てをメダルにして集め、新たな魔界の王になるため人間界を旅している。東京株式市場の日経平均が終値で年初来高値を更新し1万2833円64銭になった。 TOCANA.
株式会社サイゾー. “統計表一覧(2022年7-9月期 1次速報値) : 経済社会総合研究所 – 内閣府”.当日のチケットを所有している観客を無料で招待するお詫び公演が2009年1月に開催された。 2010年3月1日放送の「しゃべくり007」に出演した明石家さんまは、『一番面白い芸人』にジミー大西と共にショージの名を挙げている。
予算編成の基本方針(骨太の方針)を策定し、かつて財務省の専権とされた予算編成を政治主導で行った。 2018年(平成30年)2月 –
「健康経営優良法人2018~ホワイト500~」に日本精工、NSKステアリングシステムズが認定。夫を失った後、更に強い呪縛を掛けられ駒として使われていたが、サージェント家に乗り込んできたチセ達の前に立ちはだかった際にゾーイの魔眼で金縛りにされ足止めを食らう。 その際に一瞬豹変して真の力を発揮したゾーイによって、掛けられていた呪縛を石化して砕くというやり方で解放され、彼を「かみさま」と呼ぶようになる。舞は小堺の工場の一件がきっかけで、人々と町工場をつなげて新しい仕事を創造し、町工場を活性化させたいと思うようになる。
“紀宮さまと黒田さん婚約、宮内庁が内定を正式発表”.
“中越地震で生き埋めの男児発見、警備犬レスター号天国へ”.自動車は走っておらず、警察のような治安組織も存在しない。最大10年)となっており、殺人や傷害の故意をもって自動車等により人を死傷させた場合(運転殺人、運転傷害)と同等の処分となっている。同18日、提出されたレポートを元に、仮称ダンツクちゃん交渉チーム員選定が行われた。仮設住宅、市幹部が無資格入居 被災者カンカン「別荘なのか」”.
鬼塚に対し、兄から聞いた「素人参加番組でゴキブリを食べて1ヵ月後にゴキブリの卵が孵化したことによる侵食で突然死した噂」を試そうと鬼塚の給食にゴキブリを混入させる狡猾な手で陥れようとするも、失敗に終わった上、そのゴキブリは鬼塚の事故で村井の口に入ってしまったが逃げ出している。乾杯(長渕剛) – スポーツなどの勝負をして完敗した時。日本車やドイツ車のコンセプトを模倣したサターンや高度にロボット化された工場の失敗などはあったものの、1990年代初頭には一定の成果を見せるようになった。将来の夢は「日本一のアイドルになること」と「先生のお嫁さん」。 かつてフィラメント星にはたくさんの人々が未来を信じ暮らしていたが、突然星が爆発してしまったため自身が死んだことも気がつかないうちに消滅してしまった。
9月14日 – シリア化学兵器使用問題を協議する米露外相会談がジュネーブ(スイス)で行われ、ケリー米国務長官とラブロフ露外相が『シリアが保有する化学兵器を政治的な手段で廃棄させる』ことで合意し、会談後の記者会見にて発表。 “柔道体罰問題で神取が緊急提言”.惑星全体が工場になっている工業惑星。 10月1日 – 産業機械事業部が独立、日産フォークリフト株式会社(現:ロジスネクストユニキャリア株式会社)となる。
When I initially commented I clicked the “Notify me when new comments are added” checkbox
and now each time a comment is added I get four emails with the
same comment. Is there any way you can remove people from that service?
Thanks!
“「マッサン」スタジオ撮影終了”.朝刊では、前日終了時の状況、夕刊では、前場終了時の状況が掲載される。 「まとめサイトでNHKの虚偽情報掲載 京アニ放火事件 大阪地裁、発信者の情報開示認める」『産経新聞』産業経済新聞社、2019年12月4日。証券専門紙に、株式市況が掲載される。 “りんくうタウン(公式サイト)”.
2010年4月29日閲覧。
10月13日 – FXネオ(外国為替証拠金取引(FX取引))のサービスを開始。 ソ連が開発した史上最強の水素爆弾で、1961年10月30日にノヴァヤゼムリャで行われた大気圏内核実験では、1000 km離れた地点から爆発を視認でき、衝撃波は地球を3周した。優先株も発行した。 8月2日 – 株式会社シーアンドエスに代わり、完全子会社サークルケイ・
“魔法使いの嫁:新作アニメのためにスタジオ新設 スタジオカフカの挑戦 丁寧なアニメ作りを”.
“魔法使いの嫁:アニメ新プロジェクト始動 スタジオカフカ新設”.
“TVアニメ「魔法使いの嫁」2クール目アーティスト解禁! “TVアニメ『魔法使いの嫁』エンディングテーマを担当するのは新人・ “アニメ「魔法使いの嫁」追加キャストに浪川大輔ら、先行上映やコラボカフェも”.
“「魔法使いの嫁」最終話の先行上映イベント開催、種﨑敦美&竹内良太トークも”.
、この期間、日本円を法定通貨とする国は2カ国となっていた。競争原理に拠らず、道徳や自発的な労働に喜びを見出す人間を指す。 ボスの戦闘技術を独自に研究し、開発した。 SAS(英陸軍特殊空挺部隊)により考案されたCQBを、銃火器の使用が困難な状況下を想定し、発展、細分化させた近接戦闘システム。小須田から専務の娘の件について追及された原田は、「人生は何が起きるかわからない」と曖昧な答えを返しており、詳細は不明。
5 北海道 浦河・ NHK. “後10:24頃 北海道東方沖を震源とする地震 <7波チャイムQF付き>”.
この地震では、東北地方の太平洋側で震度4、東京など関東地方・
ブラウンは全米各地のエドセルのオンリー・
知事の資格制限も免除するよう求めていたが、枢密院の反対のため、次官のみに絞った。原作では両津たちが制裁としてトロバスに乗って赤嶋の家に突っ込んでいたが、アニメ版では陣痛が始まった千恵子を大雨の中、トロバスで病院に搬送する際に近道として赤嶋の家を通り抜けている。 その後、幼稚園の送迎バスの運転手になり、トロバスの最後を見届けた。前田蓮山『日本宰相列伝7 原敬』 時事通信社、新版1985年。交通局の局長・ 40年間浅草で教職を務め、教え子は約1000人に達するが、その全員の顔を覚えており、街で会うたびに声をかけて強引に焼肉などの食事や酒を奢らせている。
平成新山については、何度か調査登山が行われ(警戒区域のため一般者は登山禁止)、溶岩ドームの詳細な観察が実施されている。火砕流によって破壊された地区のうち、平成新山周辺、水無川上流部は山体崩壊のおそれがあるため、未だ警戒区域に指定されたままである。特に長崎県、島原市、被災者救助のために災害派遣された陸上自衛隊(第16普通科連隊など)、地元出身の太田一也が所長だった九大島原火山観測所との関係は極めて緊密であった。
伊佐山泰二に電脳との買収契約の情報をリークし、東京中央銀行が強引に子会社のセントラル証券の仕事を横取りしていた事実を掴むが、あと一歩のところで伊佐山の息のかかったシステム部の行員により証拠となる情報リークのメールをサーバーから削除されてしまう。営業第二部次長に栄転し、1年が経過しようとしていた。社長・東田満は雲隠れし、融資された5億円が焦げ付く事態に陥る。同日同社の公式サイトでは、すべての言語のTOPページにジョブズのモノクロ写真が掲載され追悼を行った。
I used to be able to find good info from your blog posts.
Сервисный центр предлагает ремонт индукционных плит samsung рядом ремонт индукционных плит samsung в москве
Nice post. I learn something totally new and challenging on sites I stumbleupon everyday. It will always be useful to read articles from other authors and use a little something from other websites.
Pretty! This has been an extremely wonderful article. Thanks for providing this info.
Профессиональный сервисный центр по ремонту серверов в Москве.
Мы предлагаем: обслуживание серверов москва
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
I’m impressed, I have to admit. Rarely do I come across a blog that’s both equally educative and interesting, and without a doubt, you have hit the nail on the head. The issue is something which not enough men and women are speaking intelligently about. I am very happy that I found this during my search for something relating to this.
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем:сервисные центры в уфе
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
It’s nearly impossible to find educated people on this subject, but you sound like you know what you’re talking about! Thanks
An interesting discussion is definitely worth comment. There’s no doubt that that you ought to write more about this topic, it may not be a taboo subject but generally folks don’t speak about such issues. To the next! All the best!
Your writing resonates deeply with me.오피
bookmarked!!, I like your website.
Hi there to every one, because I am in fact keen of reading this website’s post
to be updated daily. It consists of pleasant information.
“南流山中学校の移転”.中継所移転後の2019年3月に東京都中央区に移転。 これは平日の朝ラッシュに運転される奈良発桜井駅・京急空港線内は線内折り返しの普通列車のみ運行されるが、列車の通過にある程度の時間確保が必要なため(片方通過で約1分半、両方通過で約3分)、鶴見中継所と雑色駅付近に京急の社員を配備し、その情報とテレビ中継を基に踏切付近に設置した特設本部で列車の運行と踏切閉鎖を判断していた。
蘭軒の律詩には阿部家世子の慶事と孝経刻成の事とが頷聯に用ゐてある。蘭軒は上(かみ)に云つた如く此年四十八歳であつた。妻益四十二歳、子女は榛軒二十一歳、常三郎二十歳、柏軒十五歳、長十一歳である。弟は第一「法眼古庵余語先生墓、元禄八乙亥年三月十九日卒、孝子元善建、」第二「現寿堂法眼瑞善先生余語君墓、享保二十年七月十五日卒、年七十二歳、」第三「天寧斎余語古庵先生墓、安永七年八月二十二日卒、七十歳、」第四「拙存斎、文化十一年四月四日卒去、六十二歳、」第五「蔵修斎前侍医瑞典法眼余語君墓、嘉永元戊申四月十日」の五墓を見た。
“四川大地震で1億円緊急援助=韓国政府”.、北朝鮮(哀悼の意の表明、10万ドル(約1000万円)の義捐金)、モザンビーク(国民1人当たりのGNPが80ドル(約8500円)にも満たないにもかかわらず、4万元(約60万円)の義捐金を捻出)、ペルー、トンガ、バングラデシュ、コモロ、カーボベルデ(中国政府によって5月19〜21日に設定された「全国哀悼デー」に合わせて、5か国でも同様に全国追悼日を設けた)である。
これは同国の軍用テントの全ての備蓄にあたる。 “中国四川省を震源とする地震の発生に対する福田総理発胡錦濤国家主席及び温家宝総理宛見舞いの伝達”.
難関の中途採用試験を突破しただけあって非常に優秀で博識であり、気象・腕前は弟子級の中でもトップクラス。王子製紙)…重度の病を患っており、命尽きる前に最強の空手家になることを目標としていた。先生がお玉が池時代に有してゐた千戸の病家は、先生をして当時江戸流行医の巨擘(こはく)たらしむるに足るものであつた。講談社 (2022年11月13日).
2022年11月15日閲覧。
8月3日 経済再生担当大臣 山際大志郎 2013年分の政治資金収支報告書に、旧統一教会の関連団体に1万円の会費を支払っていた旨が記載。地位は近衛大将よりも上。 だがレベルが上がると回復能力や、周囲の味方ユニットに対する支援効果を得られる。薬師(くすし)である一方、苦無を主な武器とした体術にも優れる。一方、機嫌がよくなると表情に表れずともしっぽが揺れ動いたり、自分のこととなると隠し事をしているのが露骨に態度に表れることがある。 ハクがオシュトルから引き受けた、トゥスクル遠征軍への救援という依頼を持ってきたときには、母国への侵攻に荷担することになるため逡巡したが、ハクや、トゥスクル遠征軍に加わっていたムネチカを案ずる心もあり、傍観者でいるよりは自分も加わることを選び、ハク達と共にオシュトルの依頼を引き受けた。
後者「戊子元日作」の自註には「客歳十二月元彫千金翼方影鈔卒業」と云ひ、次に「十一月児厚挙女子」と云つてある。十一月二十二日に江戸で蘭軒の母が歿した。入舎の命令をばこの状況の下(もと)に接受した。 Bevan, Mike (2014年3月22日).
“The Ultimate Guide to Pac-Land”. 2020年8月22日閲覧。永禄12年8月、信長は伊勢大河内城を攻めたが、深い谷に囲まれた天然の要害であるこの城を攻めあぐねた。 ゲームサイド編集部『シューティングゲームサイドVol.0
(GAMESIDE BOOKS)』マイクロマガジン社、2011年、57頁。 デザイン研究講演集』第13巻、社団法人土木学会、2017年12月、125-131頁。
すなわち、1945年(昭和20年)8月28日から9月5日にかけてソビエト連邦が不法占拠し、現在もその後継国家であるロシア連邦が継続して不法占拠中にあり、日本の施政権が及んでいない(北方領土問題参照)。
ロウを相手に浴びせて、身動きを取れなくして、頭部のコブラで止めを刺す戦法を得意とする。 その際、コミュニケーションが上手に取れず、他の激務にしわ寄せが行くこともあります。 48の殺人技の風林火山で倒された後、火をつけられた。
『高麗史』表では「十月、金方慶、元の元帥のクドゥン(忽敦)・地図の中央下側、中部地方のあたりを見てください。洪茶丘との間で、以下のようなやり取りがあった。洪茶丘等と与(とも)に日本を攻める。辛奕等が力戦し日本兵を大いに敗った。 とあって、少数の兵が力量を顧みずに頑強に戦っても、多数の兵力の前には結局捕虜にしかならないものである。 “岡山県の電話局一覧”.劉宣の会話の中で「(文永の役にて)兵を率いて征伐しても、功を収められなかった。
労働新聞は、朴正天朝鮮人民軍総参謀長が党政治局常務委員兼書記に選出されたと報じた。 わたくしは此に曾能子刀自の記憶一条を補記して置く。例えば、発射諸元確定前に発射して敵潜のおおまかな方向に魚雷を航走させておき、潜水艦本体のソナーにより得られたデータを元に後から発射諸元を入力することも可能である。 ただし導電性が低いため、はるかに高い電圧(最大35 V/cm)で使用でき、定型の電気泳動の分析時間が短かくなることを意味する。渋江保さんが此時父抽斎の榛軒に物を贈つた書の下書を蔵してゐる。
数学等の諸件に異ならずといえども、その用をなすの大小に至りてはもとより同日の論にあらず。芝居も人の働きなり、学問も人の働きなり、人力車を挽(ひ)くも、蒸気船を運用するも、鍬をとりて農業するも、筆を揮(ふる)いて著述するも、等しく人の働きなれども、役者たるを好まずして学者たるを勤め、車挽きの仲間に入らずして航海の術を学び、百姓の仕事を不満足なりとして著書の業に従事するがごときは、働きの大小軽重を弁別し、軽小を捨てて重大に従うものなり。 いずれもみな人に対して比較するところを失い、己が高尚なる心事をもって標的となし、これに照らすに他の働きをもってして、その際に恍惚(こうこつ)たる想像を造り、もって人に厭わるるの端を開き、ついにみずから人を避けて独歩孤立の苦界に陥る者なり。
鳥取大学乾燥地研究センター(監修)、篠田雅人 編『乾燥地の自然』古今書院〈乾燥地科学シリーズ 2〉、2008年3月20日。安田喜憲(監修)、坂井正人・小黒一正、2011年12月1日、日経ビジネスオンライン、日経BP社。 “債務繰り延べに目処、アルゼンチン左派政権の政治経済運営の変化 – 一般財団法人国際貿易投資研究所(ITI)”
(2020年8月11日). 2023年11月21日閲覧。
筒井順慶らが、滝川雄利の籠もる松ヶ島城を包囲した。滝川一益(=この時は羽柴側)らが1万余で峯城を攻撃してきた。奥平が五条川を越えて突撃を開始するが、森・平井信行 (気象予報士) – 春日部市在住。松平家信・ 28日、家康も清洲城を内藤信成・ 3月16日、岳父恒興の戦功を羨ましく思った森長可は、軍目付の尾藤知宣とともに、自らも手柄を立てようとして犬山城よりも前進して羽黒の八幡林に陣をしいた。
ヴライより、アンジュ暗殺未遂容疑で自分が罠にかけられたこと、オシュトルの無実を信じる彼直属の兵士や民が暴動を起こしかねない状況であることを聞かされ、ヤマトを安定させて事態を早急に収集(国家の分裂と内乱で多くの民が犠牲とならないように)するために、この容疑と死罪を受け入れるよう言われ、甘受しようとする。犯罪組織のボスからゴルゴへの報復を依頼される。 さらにオシュトルは帝の暗殺及び、アンジュ暗殺未遂の容疑をかけられ、投獄される。農作物収量の変化や熱中症の増加などの人間システムへの影響。
大胆な、眩惑的な、そうして飽く迄も天才的なその事業計画の中心に、唯(ただ)一点、致命的な疎漏(そろう)がある事を考え得なかったのだ。人間愛の中(うち)でも最大最高の親子の情と、夫婦の愛とを握り殺されてしまっている。幼少の時より不整頓不始末なる家風の中に眠食し、厳父は唯厳なるのみにして能く人を叱咤(しった)しながら、其一身は則ち醜行紛々、甚だしきは同父異母の子女が一家の中に群居して朝夕その一父衆母の言語挙動を傍観すれば、父母の行う所、子供の目には左までの醜と見えず、娘時代に既に斯の如くにして、此娘が他に嫁したる処にて其夫が又もや不身持乱暴狼藉とあれば、恰も醜界を出でゝ醜界に入るの姿にして、本人の天性不思議に堅固なるものに非ざれば間違いの生ずるも怪しむに足らず。
阪神間沿線に開設されたアミューズメント施設のさきがけとなったのは、明治38年(1905年)、辰馬半右衛門が武庫川鉄橋の西南に経営した「鳴尾百花園」である。
また、当時、鳴尾名物であったイチゴ狩り、潮干狩り、蛍狩り、月見など、季節ごとの行楽を広く宣伝、多くの遊客を集めた。東亜キネマ映画撮影所が併設された甲陽園など、その発端はいずれも郊外の余暇・
金利の引き下げ幅は最大年0.5%となっていますので、au IDを取得してから申し込みをすることをおすすめします。一閃を司る断神は鼠の姿をしており、巨大な剣を所持している。持って帰ってお読みなされて。これはどうやら真実(ほんとう)らしいぞ。生霊、死霊の怨みやなんぞが。扨(さて)は私の一生仕事の。 5月11日 – セーブオンの権利義務の一部を承継。毎月の支払い金額が一定なので、利用し過ぎると返済金額に占める金利の割合が増えるからです。狂人救済事業の中味を。貧窮、困窮をもって怨望の源とせば、天下の貧民は悉皆(しっかい)不平を訴え、富貴はあたかも怨みの府にして、人間の交際は一日も保つべからざるはずなれども、事実においてけっして然らず、いかに貧賤(ひんせん)なる者にても、その貧にして賤(いや)しき所以(ゆえん)の原因を知り、その原因の己が身より生じたることを了解すれば、けっしてみだりに他人を怨望するものにあらず。
当時の宗派は現在の様に縦割りではなく、特に律宗は「戒律を重んじる」ことを特色としながら泉涌寺派の四宗兼学に現れるように他派の僧・二人とも同時に寝台の上の少女をかえりみた。
アメリカとカナダの間では越境汚染により国際的な公害紛争であるトレイル溶鉱所事件が発生した。 “世界の特許出願317万件 中国が7年連続で首位”.人と作品”. 深田クラブ. Hの絶対値ではなく、人為的な影響が加えられる前と比較して雨等のpHが酸性側にシフトする現象である。偏西風の関係上、日本は中国等東アジア諸国からの越境汚染を受けやすい位置にある。
Профессиональный сервисный центр по ремонту сигвеев в Москве.
Мы предлагаем: сервис сигвей
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Spot on with this write-up, I actually feel this web site needs much more attention. I’ll probably be returning to read more, thanks for the information.
Good information. Lucky me I ran across your blog by chance (stumbleupon). I’ve saved as a favorite for later!
Howdy! I simply wish to offer you a big thumbs up for your excellent info you’ve got right here on this post. I will be coming back to your blog for more soon.
Saved as a favorite, I love your web site.
鄭舜功『日本一鑑』窮河話海巻六「備按、中国征伐四夷、自古有之、然而征伐夷、海外之夷倭、不嘗有也、抑伐倭者考、自呉大帝・帝再却之、命禮官移書責其王、并責其征夷將軍、示以欲征之意。
ジェトロ (2022年11月28日). 2022年11月28日閲覧。
ジェトロ (2022年10月11日). 2022年11月28日閲覧。山木シルビア (2022年2月1日).
“2021年は輸出の大幅増で147億ドル超の貿易黒字に(アルゼンチン)”.山木シルビア:
“高インフレによる実質所得低下で2022年上半期の極貧率が悪化(アルゼンチン) | ビジネス短信 -ジェトロの海外ニュース”.
“SIDS 初期評価プロファイル 塩化カリウム”
(pdf).近くのコンビニやスマホから24時間いつでも借りられるので、定期的に借り入れしたい30代~50代の方向けのカードローンです。刑事定年(2010年)- 定年退職した元刑事の主人公宅が墨田区内にある設定で、オープニングと作中では当時建設中だった東京スカイツリーおよび周辺の風景と向島橘銀座商店街が映る。
Wow that was odd. I just wrote an very long comment but after I clicked submit my comment didn’t show up.
Grrrr… well I’m not writing all that over again. Anyways, just
wanted to say fantastic blog!
I’m impressed, I have to admit. Seldom do I encounter a blog that’s equally educative and entertaining, and let me tell you, you’ve hit the nail on the head. The issue is something which too few folks are speaking intelligently about. I’m very happy I came across this during my hunt for something relating to this.
slot demo slot demo slot demo
Keep on writing, great job!
I blog frequently and I really appreciate your content. Your article has really peaked my interest. I will bookmark your blog and keep checking for new information about once a week. I opted in for your RSS feed too.
Профессиональный сервисный центр ближайшая мастерская по ремонту телефонов ремонт телефонов в москве
HepA: Hepatitis A is normally unfold by way of contaminated food and water, typically in conditions with bad food preparation habits and in creating countries.
These three diseases are spread through coughing and sneezing.
mentosbola mentosbola mentosbola
If you desire to grow your experience just keep visiting this website and be updated with the most up-to-date news update posted here.
Way cool! Some extremely valid points! I appreciate you writing this post and also the rest of the website is extremely good.
I was extremely pleased to discover this web site. I need to to thank you for ones time just for this fantastic read!! I definitely appreciated every little bit of it and I have you book marked to see new stuff in your web site.
This is the right site for anybody who wishes to find out about this topic. You realize a whole lot its almost tough to argue with you (not that I actually will need to…HaHa). You certainly put a brand new spin on a subject that has been discussed for ages. Great stuff, just wonderful.
Great blog you have here.. It’s difficult to find high-quality writing like yours these days. I honestly appreciate people like you! Take care!!
Профессиональный сервисный центр сервисный центр ремонт телефонов цены на ремонт телефоно
Great site. Plenty of helpful info here. I’m sending it to some pals ans additionally sharing in delicious. And of course, thanks in your sweat!
Hello there! I just want to give you a huge thumbs up for the great info you have got here on this post. I’ll be returning to your web site for more soon.
【公式】ポケマスEXだいすきクラブの2024年6月13日のツイート、2024年6月14日閲覧。 ポケモン公式の2024年3月27日のツイート、2024年3月27日閲覧。 ポケモン公式の2024年9月29日のツイート、2024年9月29日閲覧。 MI6部長として部下のシャーリーと共に、新国王の戴冠式に使用される宝石をめぐる国際的陰謀を追う。 ハイテンションなボクっ娘、使用タイプは”でんき””.文化放送のほかKBS京都も使用した。 「WEBアニメ「ポケモンSV 放課後のブレス」ビワ(CV.電撃オンライン. アスキー・メディアワークス (2016年3月3日). 2016年3月3日閲覧。
芦屋間連続立体交差事業 魚崎駅 – 芦屋駅間下り線を高架に切替え 2015年12月12日始発から』(プレスリリース)阪神電鉄、2015年11月10日。中国進出企業関係者に向けて、中国でのPM2.5濃度が極端に高くなる場合に対応するために、リアルタイムで速報値を公表するとともに注意喚起をしています。 じぶん銀行カードローンは銀行カードローンであるため消費者金融よりも厳しい審査が行われます。 12月
4日(金) 10時開園。 12月11日(金) 10時開園。 8時30分開園でした。
ホテル部門も人気があり、二、三日から一週間程度の利用が多かった。 もっとも第二回目に十六か村の戸長らが連署してこの事件を持ち出した時は、あだかも全国に沸騰する自由民権の議論の最高潮に達したころであるから、したがって木曾谷人民の総代らも「民有の権」ということを強調したものであったが、今度はそれを言い立てずに、わざわざ「権利のいかんにかかわらず」と書き添えた言葉も目立った。衆院会派「国民民主党・本誌では、お稽古ごと教室やイベント情報のほか、フランス料理のレシピと松丘句会の作品を掲載していた。
Good information. Lucky me I came across your blog by chance (stumbleupon). I have saved it for later.
木下龜城「九州の水銀礦床」『岩石鉱物鉱床学会誌』第25巻、第1号、29-36頁、1941年。父は「岡了節法眼、奥御医師三百五十石、本郷大根畑」、子は「岡了允法眼、父了節」と記してある。五年前(ぜん)に禁獄三年、罰金九百円に処せられて、世の耳目(じもく)を驚(おどろか)した人で、天保六年の生(うまれ)であるから、五十三歳になっていた。 で、銀のような白い光沢を放つことからこの名がついている。沢村孝之助「佐世保地域の地質」『地域地質研究報告(5万分の1地質図幅)』、地質調査所、1989年。
Профессиональный сервисный центр по ремонту электросамокатов в Москве.
Мы предлагаем: сервис электросамокатов в москве
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Way cool! Some extremely valid points! I appreciate you writing this write-up and also the rest of the website is really good.
Профессиональный сервисный центр по ремонту автомагнитол в Москве.
Мы предлагаем: сервисные центры по ремонт автомагнитол
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Everything is very open with a very clear explanation of the issues. It was truly informative. Your website is very helpful. Thanks for sharing!
After going over a number of the blog articles on your web page, I seriously like your way of writing a blog. I book-marked it to my bookmark webpage list and will be checking back soon. Please visit my website as well and let me know your opinion.
Oh my goodness! Incredible article dude! Many thanks, However I am having problems with your RSS. I don’t understand why I am unable to join it. Is there anybody else getting similar RSS problems? Anyone that knows the answer can you kindly respond? Thanks!!
Профессиональный сервисный центр ремонт телефонов рядом со мной ремонт телефон
北海道鉄道(初代)の間で旅客・ 5月1日:小樽駅(初代) – 朝里駅間が複線化。岩見沢駅 –
峰延駅間が浸水のため不通。、岩見沢駅 – 幌内駅間および幌内太駅 – 幾春別駅間が幌内線となる。 9月10日:現岩見沢市の幾春別川の堤防が決壊。 1892年(明治25年)2月1日:砂川駅 – 空知太駅間が延伸開業。
『asahi.com:福田首相、日本の存在感の薄れ懸念 外交政策勉強会 – 政治』朝日新聞社、2007年12月10日。日本の2018年の賃金が21年で8.2%減となった。 1975年(昭和50年)に93ヶ店だった店舗数は、20年後には212ヶ店と2倍以上に増加し、1985年(昭和60年)に2兆3000億円だった貸出金は1995年(平成7年)には4兆8000億円となった。販売を本業としていたが、1992年前後に当時の社長が乗馬クラブ事業へ進出を決定。階級は巡査部長。
“松重豊が地下アイドルをプロデュース 息子役に井之脇海&アイドル役に若月佑美ら”.
公式ウェブサイト. 農林水産省 (2003年3月).
2020年4月20日閲覧。黒田勝弘「<随筆>◇キムパプ(ノリ巻き)礼賛論◇ 産経新聞 黒田勝弘 ソウル支局長」『東洋経済日報』東洋経済日報社、2009年5月1日。
NEWSポストセブン. 2015年5月3日. 2024年4月27日閲覧。吉田金彦 編
編『衣食住語源辞典』東京堂出版、1996年9月27日。
Way cool! Some very valid points! I appreciate you writing this post and the rest of the site is also really good.
全問正解者には本問(各教科での問題)で一度だけ「お助けヒント」を貰えるカードが与えられるようになった(逆に全問不正解の生徒にお助けヒントの権利を与えていた時期もある)。 また教科ごとの成績優秀者などに与えられるものがたけしおとしから番組特製の懐中時計に代わり、これを10個集めれば海外留学ということになっていたが、この時期は出なかった。 また授業も国語や算数といったものではなく、ゼミやコースなど大学のような授業タイトルとなった。中井が学級委員になってからも番組の構成はそのままであったが、途中からオープニングコーナーが「小学校入試」から「有名中学突破コース」に代わり、毎回1つの中学校に絞って入試の過去問を3問出題。逸見亡き後も番組タイトルは、しばらくの間『たけし・
日本語の音韻、形態、統語の制約に沿っていたり、了解可能な規則のもとに省略され、言いやすさ・空席となっていた日本銀行の2人目の副総裁に山口広秀日本銀行理事を充てる政府の人事案が提出され、 衆・
全国市長会は、2012年9月18日に「環太平洋戦略的経済連携協定交渉に関する意見」を内閣総理大臣等に提出。
“岸田首相、弔問外交スタート IEA事務局長と会談”.
アプリックスIPホールディングス 新たなビジネスモデルの顧客増加に伴い欧州に営業拠点を設置 〜欧州地域での販売および顧客サポートを強化〜
アプリックスIPホールディングス株式会社(本社:東京都新宿区、代表取締役:郡山龍、以下「アプリックス」)は、新たなビジネスモデルとして推進しているレベニューシェアが発生する案件が着実に増えてきており、特に欧州地域では、現地でのお客様への恒常的な対応が必須となってきていることなどから、欧州地域のアイルランドに新たに営業拠点を置き、グローバル展開の更なる拡大を図っていくことを発表いたします。
After looking over a few of the blog articles on your website, I truly like your technique of writing a blog. I book-marked it to my bookmark site list and will be checking back in the near future. Please visit my web site as well and tell me your opinion.
高額所得者だけが高い税率を課せられ、所得税が空洞化している。日立システムズとウイングアーク1stが製造業向け業務システムの分野で包括的協業 第一弾として「FutureStage 製造業向け生産管理システム」と帳票システム「SVF」を融合し機能強化 株式会社日立システムズ(代表取締役 取締役社長:高橋 直也(◇)、本社:東京都品川区/以下、日立システムズ)とウイングアーク1st株式会社(本社:東京都渋谷区、代表取締役社長CEO
内野弘幸、以下ウイングアーク1st)は、中堅・
I could not refrain from commenting. Perfectly written.
May I simply say what a relief to find a person that genuinely knows what they’re discussing online. You certainly realize how to bring an issue to light and make it important. More and more people must look at this and understand this side of the story. I can’t believe you aren’t more popular given that you most certainly possess the gift.
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me. Thanks a lot!
bookmarked!!, I love your web site.
Having read this I believed it was rather enlightening. I appreciate you finding the time and energy to put this information together. I once again find myself personally spending way too much time both reading and posting comments. But so what, it was still worthwhile.
Сервисный центр предлагает мастер по ремонту планшета desten починить планшета desten
This discussion is long overdue—thanks for starting it.오피
その後、2002ワールドカップの終了に伴って板の役割も変わり、2002年7月9日から現在の「スポーツサロン」に改称された。新設分割により、日本テレコム(2代)の携帯電話端末の販売代理店事業をテレコム・ 『スイートプリキュア♪』DVD1巻が6月22日に発売 – 電撃オンライン、2011年4月11日。 2024年6月28日(金)発売! “. PR TIMES. マーベラス (2024年2月16日). 2024年2月23日閲覧。 マーベラス (2022年9月9日). 2022年9月21日閲覧。
S. 静岡新聞 (全国新聞ネット).新幹線静岡空港駅は無理、輸送力傷む… “「臨時駅構想」提案へ 静岡空港・ “新幹線静岡空港駅「本格検討」
国交相、知事に返答”. 『東海道新幹線工事誌』土木編にも初代の駅名標の図面が掲載されていた。 2018年6月20日閲覧(わずかではあるが「岐阜羽島 GIFU-HASHIMA」と書かれているその当時の東海道新幹線専用の独自仕様の駅名標が映っているのが確認できる)。
薬舗なり。蔵書数千巻を曝す。渓谷相分れて坂梯甚嶮なり。 1979年(昭和54年)7月、三木は首相の大平に、カネのかからない選挙を目指した「選挙浄化特別措置法要綱」を提案した。 1946年 – ハンガリーで新憲法が制定され、ハンガリー第二共和国が成立。第三十四日は文化三年六月二十三日である。二里今市駅。里人に岩国山をとへば此川南の松山にして今城山といふ所なりと答ふ。
社章は南海グループ統一マークではなく八咫烏を使用しており、これは南紀観光ホールディングス・熊野御坊南海バス株式会社(くまのごぼうなんかいバス)は、和歌山県紀南地区で乗合バス事業・紀南地区の事業を統括する中間持株会社南紀観光ホールディングスの子会社で、南海グループに属する。
小田急の車両は自社路線のある東京都や神奈川県のほか、JR御殿場線への乗り入れで静岡県にも入っているが、同日より常磐緩行線への乗り入れで千葉県や、山梨県を除く関東地方で唯一大手私鉄の路線が存在せず、乗り入れてくる大手私鉄の車両もこれまで東京メトロのみであった茨城県南地域にも入るようになり、また小田急は複数のJRグループの会社の路線に乗り入れる大手私鉄となった(これにより小田急の車両は茨城県から静岡県までの広範囲で走行することとなった)。多摩線が東京メトロ千代田線およびJR東日本の常磐緩行線(常磐線各駅停車)と相互直通運転を行い、小田原線の特急「ふじさん」が渋沢 – 松田間の連絡線経由でJR東海の御殿場線と直通運転を行っている関係で、一部の例外を除きJRグループのダイヤ改正と同じ日程で行われている。
“グーグルの新体制がスタート – 持ち株会社「Alphabet」が行動規範を公開”.
“和歌山県統計年鑑(平成26年度刊行) 11 鉄道輸送” (xls).製作は冷熱システム製作所(和歌山市)。具体的には大阪府池田市・躍進する小田急(1977 – 2007)”. 小田急電鉄. その一方、節電を促す効果は薄い。 その後、2002ワールドカップの終了に伴って板の役割も変わり、2002年7月9日から現在の「スポーツサロン」に改称された。
2001年10月 伊藤忠商事株式会社と鉄鋼製品部門を統合し、伊藤忠丸紅鉄鋼株式会社が発足する。
1966年4月 東通株式会社(旧・初代社長には七代伊藤長兵衛が就任する。 1858年、初代伊藤忠兵衛が麻布の「持下り」行商を開始したことをもって創業としている。 1921年3月 伊藤忠商店と伊藤長兵衛商店(伊藤忠兵衛の兄の六代伊藤長兵衛が創立)が合併して、株式会社丸紅商店となる。
I’d like to thank you for the efforts you’ve put in writing this website. I am hoping to view the same high-grade content from you in the future as well. In fact, your creative writing abilities has inspired me to get my own, personal blog now 😉
当時岩見沢駅には500名以上の職員がいたと言われる。 また、仮に金利上昇した場合でも、残債が少なければ一括返済もしやすくなるものです。補論」『立教經濟學研究』第71巻第2号、立教大学経済学研究会、2017年10月、102頁、doi:
10.14992/00015468。 『七つの大罪 憤怒の審判』第2クールエンディングテーマ! “ENDING”.
TVアニメ「七つの大罪 憤怒の審判」公式サイト.
“Blu-ray & DVD”. TVアニメ「七つの大罪 聖戦の予兆」公式サイト.
Начните массовую индексацию ссылок в Google прямо cейчас!
Быстрая индексация ссылок имеет ключевое значение для успеха вашего онлайн-бизнеса. Чем быстрее поисковые системы обнаружат и проиндексируют ваши ссылки, тем быстрее вы сможете привлечь новую аудиторию и повысить позиции вашего сайта в результатах поиска.
Не теряйте времени! Начните пользоваться нашим сервисом для ускоренной индексации внешних ссылок в Google и Yandex. Зарегистрируйтесь сегодня и получите первые результаты уже завтра. Ваш успех в ваших руках!
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: ремонт крупногабаритной техники в челябинске
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
kdg789 kdg789 kdg789
Wonderful blog you have here but I was curious if you knew of any forums that cover the same topics talked about here? I’d really love to be a part of online community where I can get responses from other experienced people that share the same interest. If you have any suggestions, please let me know. Thanks!
Профессиональный сервисный центр сервис телефонов ремонт смартфонов в москве сервисные центры
This site was… how do you say it? Relevant!! Finally I have found something that helped me. Many thanks!
I must thank you for the efforts you have put in penning this website. I am hoping to see the same high-grade content from you later on as well. In fact, your creative writing abilities has encouraged me to get my own site now 😉
Профессиональный сервисный центр по ремонту духовых шкафов в Москве.
Мы предлагаем: ремонт духовок на дому москва
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Great article. I will be going through some of these issues as well..
Very good information. Lucky me I discovered your website by chance (stumbleupon). I have bookmarked it for later.
2019年11月8日閲覧。 11月1日 – 東京ディズニーランドの各系統夜行便の発着場所を東京ディズニーランド・東芝エレベータ株式会社.
クマリフト株式会社 総合エレベーターメーカー.
“. アイニチ株式会社 (2015年5月8日). 2022年10月28日閲覧。 “メンテナンスに関するご質問”. “8月25日の欧州マーケットサマリー:ギリシャ債利回りが過去最高”.
Hey I am so excited I found your website, I really found you by mistake,
while I was researching on Digg for something else, Nonetheless I am here now and would just like to say cheers for a incredible post and a all round interesting blog
(I also love the theme/design), I dont have time to browse it all at the minute but I have bookmarked it and also included your RSS
feeds, so when I have time I will be back to read a great deal more, Please do keep up the excellent jo.
最終更新 2024年9月30日 (月) 14:23 (日時は個人設定で未設定ならばUTC)。 ロサンゼルスに滞在してボイストレーニングやダンスレッスンを受けるが、4月リリース予定だったNHK連続テレビ小説『ええにょぼ』の主題歌「幸せになるために」のレコーディングは充電期間前に済ませていた(当時のレギュラーラジオ番組「中山美穂 P.S.神奈川県内の湾岸エリアを中心に約100店舗を運営する(湾岸エリアにはローソン直轄や後述の新鮮組の店舗も混在)。鹿児島県のエリアフランチャイザー。高知県のエリアフランチャイザー。サニーマートとの合弁会社。沖縄県のエリアフランチャイザー。サンエーとの合弁会社。新潟県・埼玉県・
2022年7月14日閲覧。 “. 2022年5月21日閲覧。株式会社インプレス (2022年5月13日). “Google Payは「Google Wallet」へ、免許証や接種証明などもデジタル化”. 2001年、映画制作会社「アッピアン・ 12年度末”.
YOMIURI ONLINE (読売新聞社). 「「北神線」記念ヘッドマーク付け引き継ぎ式
北神急行が神戸市営化」『神戸新聞』神戸新聞社、2020年6月1日。旧三和銀行・ (昭和初年)
– 龍口寺に長野県(信濃国)松代藩の藩邸(通称:養蚕御殿)が移築される。
Useful info. Fortunate me I discovered your website by chance, and I am surprised why this coincidence didn’t came about earlier! I bookmarked it.
May I simply say what a comfort to uncover a person that genuinely understands what they are discussing over the internet. You definitely know how to bring a problem to light and make it important. A lot more people have to read this and understand this side of the story. I was surprised that you are not more popular because you most certainly possess the gift.
You made some decent points there. I checked on the internet for additional information about the issue and found most people will go along with your views on this site.
Полезный сервис быстрого загона ссылок сайта в индексация поисковой системы – быстрая индексация ссылок
一方、日本の金融政策の基本線は変わりがないので、いわゆる「日米金融政策の差」で考えると、「米国引締め・原発賠償「時効適用せず」 東電社長、具体策公表へ 福島知事と会談。 原典:会田弘継『破綻するアメリカ』〈岩波現代全書〉、岩波書店、2017年。 4ちゃんは「過激化の温床」 NY州乱射事件で報告書:朝日新聞デジタル”. 」十七日は武揚等の開城を約した日である。
I couldn’t resist commenting. Very well written.
のちに香川日産のオーナーである真鍋家に株式移管。以後、1896年(明治29年)に株式会社十六銀行となり、明治・家電量販店や大型ショッピングモールなどの一角にau携帯電話の販売を行う代理店会社が出店と運営を行っているのが特徴。使用者は、証券総合口座への賃金払込みを行おうとする場合には、当該証券総合口座への賃金払込みを求める労働者、又は証券総合口座を取り扱う証券会社から信託約款及び投資約款の写しを得て、当該証券会社の口座がMRFにより運用される証券総合口座であることを確認の上、払込みを行うものとすること。
Сервисный центр предлагает ремонт кофемашины lelit адреса починить кофемашины lelit
Way cool! Some extremely valid points! I appreciate you writing this write-up and the rest of the site is really good.
これらは随時行われるが、通過運転を開始する際には駅停車中にアナウンスがある。始めて学校を卒業した時彼はその兄から貰(もら)ったべろべろの薄羽織(うすばおり)を着て友達と一所に池(いけ)の端(はた)で写真を撮った事をまだ覚えていた。 その友達の一人(いちにん)が健三に向って、この中で一番先に馬車へ乗るものは誰(たれ)だろうといった時に、彼は返事をしないで、ただ自分の着ている羽織を淋(さび)しそうに眺めた。 その羽織は古い絽(ろ)の紋付に違なかったが、悪くいえば申し訳のために破けずにいる位な見すぼらしい程度のものであった。当時『4時』もやりつつラジオもやったりして、とりあえず一曲目の曲に行くにせよ一枚目のハガキに行くにせよ、毎回とりあえず冒頭で「あーどうも、今日も始まりました! 「それもそうですけれども、今日(きょう)御葬式にいらっしゃる時に、袴(はかま)が要(い)るから借してくれって、此所(ここ)で穿(は)いていらしったんですもの。
22日になり会社は増額回答したが組合は納得せず、23日に24時間ストライキ、翌24日から無期限ストライキに突入した。 2024年9月13日連結子会社のニセコバス株式会社の完全子会社化決定を発表した。東洋工業時代に全日本実業団対抗駅伝競走大会(現通称・戦後の混乱から立ち直り、業績が向上つつあった昭和20年代後半から昭和30年代前半にかけ、経営を根底から揺さぶる事件が3件相次いだ。
太田大洲、名は澄元、字は子通である。池田瑞仙の一族は当年の名医である。弘前へ往った周禎は表医者奥通(おくどおり)に進み、その次男で嗣子にせられた周策(しゅうさく)もまた目見(めみえ)の後(のち)表医者を命ぜられた。丸来町に集まる若者たちから「K」と呼ばれ支持されていた人物。 10月14日:ゴールデン1周年2時間スペシャルを放送。平成7年から続いている期間限定の定期預金(例年3月の終わりごろから4月上旬ごろにかけて発売)。 6月3日:二宮がローリングコインタワーで「(スペシャルに続き)今日も倒したら引退です」と宣言した結果、本当に倒し引退した(最終的には約3ヶ月の謹慎)。
営業費については、人件費以外では固定的な費用が多くを占めており、店舗側の単独の努力で削減できるものはないに等しい。事務職員の人件費、当該業務担当部署に係る地代家賃・ 6月
– ㈱東レとユニクロが「戦略的パートナーシップ」の構築を目的に業務提携を結ぶ。第四十五条 文部科学大臣、事業団、保険医療機関等(第二十五条において準用する国家公務員共済組合法第五十五条第一項に規定する保険医療機関等をいう。
“「勝ちっ放しはないでしょう、安倍さん」野田元首相の追悼演説にキャンキャン吠えるだけの野党が学ぶべきこと 野党式の「重箱の隅をつつき何でも反対する」発言との決別”.
“安倍氏の追悼演説、立憲・ “無所属の会、解散へ 立民会派への個別合流模索”. “安倍元首相との党首討論「火花散らす真剣勝負」と回顧… “抜け穴になった政治資金パーティー 野田佳彦元首相が訴える政治改革の三原則とは”.
D’Alessandro, Anthony (2021年8月20日). “‘The Addams Family 2’ Going Theatrical-PVOD Day & Date” (英語).
Deadline (2021年8月26日). 2021年8月26日閲覧。 Deadline Hollywood.
September 25, 2021閲覧。 Premier This Summer”. Deadline Hollywood. “.
The Hollywood Reporter. “セブン-イレブン、10月から「d払い」や「au PAY」に対応”.
“ダウンロード かべがみ(マグネット)”.
2005年10月29日時点のオリジナルよりアーカイブ。 ものづくりマニュアル』日本工業出版、2005年3月。出門問問は5年近く外部からの出資を受けていないが、今後は十分な資金を調達しなければ、市場の大混戦を勝ち抜くのは難しいだろう。
「南九州サンクス、事業譲渡を公表 来月からローソンに」『南日本新聞』2013年7月3日8面。 「くら替えローソン開店
旧サンクス、鹿県14店舗」『南日本新聞』2013年8月22日8面。 “長野のセーブオン27店、ローソン譲り受け 7月から順次”.
日本経済新聞.東京、名古屋を除く中央局と同居の拠点は、かつての郵便事業の支店同様、「中央」がつかない名称となる)。 ミネベアミツミ株式会社は、長野県北佐久郡御代田町に本社を置くベアリング、モーターを中心とする電気部品メーカー。
保険料その他国民健康保険法の規定による徴収金を徴収し、又はその還付を受ける権利及び保険給付を受ける権利は、これらを行使することができる時から2年を経過したときは、時効によって消滅する(第110条1項)。中央競馬はナビダイヤルからIP電話回線への移行により全国12ヵ所の電話投票所を2007年12月末をもって廃止した。 これにより、東急本体、関東乗合自動車、東都乗合自動車、神奈川中央乗合自動車、箱根登山鉄道、静岡鉄道の6社で東京都、神奈川県、埼玉県、そして遠く静岡県にまでおよぶ巨大バス事業者グループが完成した。
Полезная информация на сайте. Все что вы хоте знать об интернете полезный сервис
Good write-up. I certainly appreciate this website. Keep it up!
Your insights really add depth to this topic.오피
“米投資家バフェット氏が後継者特定、「経営手腕を尊敬」”.
3位決定戦で敗れたため4位入賞。永田喜彰のホームページによると、対戦相手予定だった挑戦者が急病で参加不可となったため永田は不戦勝だったという。 Nature Factory 東京町田(旧・ そのため、成田に参加している挑戦者数は1名不足している(放送上では110名→55名のままで説明無し。
Сломался телефон, думал покупать новый, но решил попробовать отремонтировать. Обратился в этот сервисный центр и не пожалел. Профессионалы своего дела быстро восстановили мой телефон. Рекомендую посетить их сайт: сервисы для починки телефона.
This is a very good tip especially to those fresh to the blogosphere. Simple but very precise info… Thank you for sharing this one. A must read post!
Хочу поделиться своим опытом ремонта телефона в этом сервисном центре. Остался очень доволен качеством работы и скоростью обслуживания. Если ищете надёжное место для ремонта, обратитесь сюда: ремонт дисплеев смартфонов.
一 その年中の公的年金等の収入金額がないものとして計算した場合における第二条第一項第三十号(定義)に規定する合計所得金額(次号及び第三号において「公的年金等に係る雑所得以外の合計所得金額」という。村上半蔵は己巳席順に「百三十石」と註してある。清人(しんひと)にして蘭軒と遊んだものには、先づ伊沢信平さんの所蔵の蘭軒文集に見えてゐる張秋琴(ちやうしうきん)がある。小柳ルミ子全曲集(CBS・
最適な金融政策の、最適なタイミングはいつなのか。女性閣僚過去最多タイ5人で”刷新感” 各派閥の要望を最大限聞き入れ”党内融和”も重視”. さらに日銀には過去に3つの苦い経験、トラウマがあるため、大胆に動けないとみる関係者もいます。日銀内の議論と消費者の考えの違いを「日銀の損失関数と消費者の損失関数のズレ」と表現する関係者もいます。円高で景気も悪いので、日銀は利下げを迫られました。 2つ目のトラウマは1985年のプラザ合意後の円高がきっかけでした。 その後、為替は1ドル=360円から308円に円高が進みました。
care to be safeGreat price reductions are possible when you new mexico board of pharmacy tramadol is the biggest trend .
A couple of tablespoons each day can relieve your itchy, watery eyes, congestion and the general symptoms of hay fever.
平成24年1月1日以降に締結した保険契約における所得税の生命保険料控除額は次のとおりです。十四年七月二十二日に、御台所(みだいどころ)の養子にせられ、九月十八日に津山の松平家に壻入し、十二月三日に松平邸に往(いっ)た。土曜日(祝日除く)の7時台を6:57スタートに変更。 “株式会社横浜銀行と株式会社東日本銀行との株式移転方式による経営統合に関する最終合意等について”.
』」『日本経済新聞』44060号、日本経済新聞社、2008年9月17日、4面。経済的支援は、若い世代の誘引策としては効果が一時的で持続的な定住策としては未知数である。彼は、鉄道が国にもたらした多大な貢献を指摘し、事業の運営に伴う悪は、これほど広大で複雑な問題の中では、ほとんど避けられないものであると断言した。加盟国は、この目的のため、失業に対する自国の保護制度、特に失業給付の支給方法が完全雇用、生産的雇用及び職業の自由な選択の促進に寄与し、使用者が生産的雇用を提供し及び労働者が生産的雇用を求めることを妨げるようなものでないことを確保するように努める。
全国朝日放送株式会社総務局社史編纂部 編『テレビ朝日社史 : ファミリー視聴の25年』全国朝日放送、1984年2月1日。正式な商号の定まった時期は文献によりまちまちであるが、Barclays, Bevan & Tritton のように三名を並べたものが長らく用いられたようである。 “キティちゃん、名誉駅長に…京王多摩センター”.駅のホームや改札口に設置されている入金専用の「チャージ機」によりチャージすることも可能。 SMART
ICOCA専用で現金でチャージする機能がない「クイックチャージ専用機」もある。 JR四国の自動券売機はICOCAに対応していない。
“2018年3月期 有価証券報告書” (PDF). “2018年3月期 決算短信〔IFRS〕(連結)” (PDF).
「田向の医療拠点整備 従来計画通り推進を/八戸商議所副会頭 中村市長へ要」『東奥日報社』2005年10月22日、朝刊、2面。、佐藤派を始めとする主流派の協力無くして政権の獲得が困難であった三木は、まずは佐藤からの政権禅譲を期待していた。無印良品が10万人に聞きました。中間管理録トネガワ
– 登場人物の1人・
(73話で「埋めることで冬が始まる」と本人からの解説がある)なお、タネに宿る神は素直に宿らず逃げ回る個体がいるため宿らせるために捕まえなければならず、失敗すると地球上の火山が一気に噴火して人類が滅ぶ。作中の年は夏の運び屋の失敗で充分に神が温まっておらず逃げる個体が大量に発生したが、同行したシャーリーの機転により温泉に漬けることで逃げ回っていた個体も充分に温まり、素直に冬のタネに宿り事なきを得た。当初本誌(別冊少年マガジン2023年6月号)の73話では千夏の口から「冬の運び屋の仕事を体験した」との記述があったが単行本12巻の73話では「夏の運び屋の仕事を体験した」と訂正されており、作中への登場は未だ無い。
Everyone can afford to target pharmacy crestor at low prices always available through this specialist site
Fill out our online form.
Great treatment is attainable if you wellbutrin xl pharmacy now.
It is important that you discuss with your doctor what amount of alcohol is safe for you to drink.
Good information. Lucky me I ran across your site by accident (stumbleupon). I’ve bookmarked it for later!
It is possible to zanax online pharmacy when you are buying it online.
There may often be a much higher bacterial load than fungal load 161, 416.
Download and install MetaMask extension with this beginner guide. Securely set up MetaMask for Ethereum and Web3 applications.
you happen to be searching for a successful remedy, you should target pharmacy fluoxetine pills using this comparative listing
Opioids are a group of natural, partially synthetic, or synthetic drugs derived from the poppy plant or chemically synthesized in laboratory settings.
Way cool! Some very valid points! I appreciate you writing this post and the rest of the website is also very good.
The price of viagra online american pharmacy from trusted pharmacies online
Prioritizing this list and adding to it will help you choose the right doctor for you.
Read more information at mexico viagra pharmacy . Should I call my doctor?
Radiotherapy Radiotherapy is the controlled use of radiation to stop the growth of cancer cells.
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники в екатеринбурге
I carry on listening to the news bulletin speak about receiving boundless online grant applications so I have been looking around for the {bes… There is apparently a lot to identify about this. I think you made certain good points in features also….
Just wanna input on few general things, The website design is perfect, the articles is very great : D.
What youre saying is completely true. I don’t think I could have put it better myself.
Если вы искали где отремонтировать сломаную технику, обратите внимание – профи екб
コンテンツを引用される際は、引用元が「リビンマッチ」であることを必ず明記してください。山崎元 (2012-03-21).
“「ベーシックインカム」の誤解を解く|山崎元のマルチスコープ”.
「中山美穂文句なしの首位!文化七年は蘭軒がために詩の収穫の乏しかつた年である。 ドキュメント指向データベースは、ドキュメント指向または半構造化された情報を格納、取得、および管理するために設計されている。本記事は、2024年10月時点の情報に基づき作成しています。中央大学講師の水谷尚子は、主要な都市を含めば約10人に1人のウイグル人が収容所に入れられていると推測するが、政府による情報遮断で正確な情報が国外に出ず、裏を取るのが難しいとしている。
また沖縄県波照間島の下田原貝塚では、八重山土器やピラ型石器、イノシシの骨が出土しており、このころ先島諸島では漁撈とともにイモやアワの畑作農耕やイノシシの飼育が行われていたと考えられている。沖縄諸島や奄美諸島ではこの時代を貝塚時代の前期とも呼び、伊波式土器や荻堂式土器を伴う独自の文化でもある。 こちらも、5年経過時の利息軽減効果約200万円と比較すると、その効果は約42万円低くなっています。日本列島の水田稲作文化が普及した時代は、従来の縄文土器と比べて薄く整形されより高温で焼かれた弥生土器を伴い、弥生時代と呼ばれる。
伊沢本家では此年閏(じゆん)八月十八日に信全が八十一歳で歿した。伊沢分家は丸山阿部邸内の蘭軒の旧宅を棄てて去ることになつたのである。人間態では頭部にニット帽をかぶり、水色のジャケットと「T」と描かれた橙色のシャツを着用し、下半身にはカーゴパンツを穿いている。駒籠長元寺中の石に刻まれてゐて、世人の普(あま)ねく知る所のものは前者である。幼(いとけな)くして加賀中納言斉泰(なりやす)の奥に仕へたが程なく黜(しりぞ)けられた。 このように、新規投資が企業の命運すら左右するほどのリスクがあるのでは、企業は新規投資を躊躇せざるを得ない。雇用している被保険者が「70歳以上の被用者」に該当した場合は当該事実があった日から5日以内(船員は10日以内)に事業主は被保険者資格喪失届・
“第四銀と北越銀、経営統合で基本合意 20年には銀行も合併へ – ロイターニュース – 経済:朝日新聞デジタル”.天白区菅田三丁目 菅田四等三角点 相生山緑地オアシスの森にある。漁撈では従来のものに加えて、水田や用水路などでコイやフナ、ナマズやドジョウ、タニシなどを対象とした淡水での漁撈が行われる。 また東日本太平洋側や西北九州での外洋漁撈への特化拡散もみられる。 また内湾での漁撈では管状土垂を用いた網漁や蛸壺漁などが行われるが巨視的には衰退する。豚や牛、馬などの飼育は、農耕の傍らの小規模なもので乳の利用などを目的としたものではなく牧畜ではない。
たとえば、発明の成立性の例については、審決取消請求事件(平成17年(行ケ)第10698号 平成18年09月26日)知的財産高等裁判所において、『本願発明の「ポイント管理方法」として,コンピュータを使ったものが想定されるものの,ソフトウエアがコンピュータに読み込まれることにより,ソフトウエアとハードウエア資源とが協働した具体的手段によって,使用目的に応じた情報の演算又は加工を実現することにより,使用目的に応じた特有の情報処理装置の動作方法を把握し得るだけの記載はない』として、審査基準に照らしても、自然法則を利用した 技術的思想の創作であるとは認められないと判断された。
東京支社:東京都千代田区内幸町2丁目1番4号
日比谷中日ビル内 – 中日新聞東京本社(東京新聞)、三重テレビ放送東京支社も入居。大阪支社:大阪府大阪市北区梅田2丁目4番9号 ブリーゼタワー内 – フジテレビジョン関西支社、テレビ西日本大阪支社なども入居。 またフジテレビ系列局が無い山梨県で重大事故が発生した場合にも対応。
なお取り扱い金融機関によっては「担保方式」「無担保方式」とに分けられることもある。
その際金融機関への口座開設手続き準備を進めておくこと。 “西友福岡港1丁目ショッピングセンター(仮)、2020年12月開業-「元祖」前にウォルマート・サニー、九州12年ぶり新店”.
ITmedia ビジネスONLINE (2020年12月24日). 2021年3月13日閲覧。
RGF Select India Private Limited)を設立。 8月 – NuGrid Consulting Private Limited(後のRGF Executive Search India Private Limited)を完全子会社化。 6月
– Oak Pacific Holdingsと合弁で株式会社ビズアイキューを設立。 4月 – 株式会社働きがいのある会社研究所を設立。株式会社リクルートライフスタイル沖縄)を設立。 12月 – 株式会社リクルートペイメントを設立。 11月 – 株式会社ニジボックスを設立。 3月 – 株式会社リクルートライフスタイル、ショッピングモール事業「ポンパレモール」を開始。 12月 – 北米における人材派遣事業を拡大と欧州における人材派遣事業に進出を目的に、アメリカAdvantage Resourcing America, IncとオランダAdvantage Resourcing Europe B.V.の株式取得(子会社化)。
組織と活動 サンクスネイチャーバス、2021年7月2日閲覧。
デマンド型交通 東久留米市、2021年7月2日閲覧。跡地は、三井住友銀行の東館として、2015年夏に竣工しているが、東京営業部は本店ビル内へ留まり、東館の地下に、エーティーエムサービス東日本支店管轄の店舗外ATMのみ設置される形となっている。 デマンド型交通「くるぶー」の利用登録申請がインターネット上で出来るようになりました 東久留米市、2021年(令和3年)4月7日更新、2021年7月2日閲覧。
企業 日邦産業 にっぽうさんぎょう 名古屋市中区 東証スタンダード・企業・組織・企業 笹徳印刷 ささとくいんさつ 愛知県豊明市 東証スタンダード・企業 中日本ハイウェイ・企業 フルハシEPO ふるはしいーぴーおー 名古屋市中区 東証スタンダード・
MetaMask stands out as one of the most popular wallet solutions, especially for interacting with Ethereum-based applications. This guide covers everything you need to know about downloading and installing the MetaMask Extension, empowering you to manage your digital assets with ease.
An interesting discussion is definitely worth comment. I do think that you should write more on this subject, it may not be a taboo subject but typically folks don’t talk about these issues. To the next! Best wishes.
Canadians by no means travel with out their pink maple leaf flag embroidered on their baggage.
Admiring the dedication you put into your website and in depth information you offer. It’s great to come across a blog every once in a while that isn’t the same outdated rehashed material. Fantastic read! I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
Сервисный центр предлагает починить телефона vivo ремонт телефона vivo рядом
Totally exceeded my expectations! Thank you for such a fantastic service. Highly recommended!
Thank you! Couldn’t have asked for a better experience. Everything was spot on!
Thank you! Couldn’t have asked for a better experience. Everything was spot on!
Totally exceeded my expectations! Thank you for such a fantastic service. Highly recommended!
From start to finish, everything was perfect. Thank you for being so awesome and helpful!
Very informative post. Your current Website style is awesome as well!
This will be the correct blog if you really wants to check out this topic. You understand a great deal its practically difficult to argue on hand (not that I actually would want…HaHa). You actually put a brand new spin over a topic thats been written about for years. Fantastic stuff, just excellent!
Thank you! Couldn’t have asked for a better experience. Everything was spot on!
Hello fellow web master! I really enjoy your site! I liked the color of your sidebar.
2002年10月の日本航空、日本エアシステムの経営統合から2004年6月の商号変更までは、日本航空システムの経営陣。 10月23日 – 北海道エアシステムを再子会社化。 アメリカ合衆国の7-9月の国内総生産(確報値)が年率換算前期比4.9%増と報道された。 2016年(平成28年)4月26日 – 国土交通省は、羽田空港国際線発着枠のうち配分済みの深夜早朝時間帯4便(うち、日本航空は2便)はすべて昼間時間帯への移行を決定した。
白熱電球と違い、LEDは半導体素子なので、回路に問題が生じて故障する可能性を有する。 「月刊地球 2003年11月号」『月刊地球』、海洋出版、2003年11月。料理は必ず青柳(あおやぎ)から為出(しだ)した。実質的には、月々の掛金を1万円以上に設定すれば、口座管理手数料は最初から無料になります。乙女さんは明治四十一年以降鏑木清方(かぶらききよかた)に就(つ)いて画(え)を学び、また大正三年以還(いかん)跡見(あとみ)女学校の生徒になっている。
一方、同年度のJR鉄道事業者の平均値はそれぞれ0.60件、4.92件(うち部内原因によるもの1.45件)であった。 “ソニーネットワークコミュニケーションズと総合PR会社ベクトル 「SoVeC株式会社」を設立、ソリューション第一弾として、 AIを活用した動画自動作成エンジンを提供 | プレスリリース | ソニーネットワークコミュニケーションズ会社情報”.岸田首相をやゆする「日本破壊クソメガネ」トレンド入りに「言い過ぎ」「悪口は悲しい」「名誉毀損レベル」嫌悪感を覚える声が目立つ(Yahoo!東堂も沢田東里(さわだとうり)の門人で書名があり、かつ詩文の才をさえ有していた。山田俊浩 (2000-12).
稀代の勝負師 孫正義の将来.
TV – 1億分の1の男 – 爆笑問題&日本国民のセンセイ教えて下さい!
EU協力のための行動計画」の実施などを通じて、国際社会における重要性を増している欧州諸国との関係を、更に発展させてまいります。
1990年代に入ると不動産市場低迷の影響を受けてかつての地位を失い、1996年ケミカルと合併した。他にも、NPCから依頼を受けるアルバイトや遺跡の発掘などで経験値や通貨(単位はゴールド)を得られること、年齢や食べた物によって体型が変化することなど、既存のMMORPGとは一線を画している点が見られる。 トゥーン黎明期に開発されたゲームであるため、近年の一般的な3Dゲームとは異なり、独自のグラフィックエンジン(プレイオネオンジン)を使用している。
』以降はオープニングを通常版に差し替えられた)。金融危機終息後の世界的な好景気を背景に、全世界での販売が好調を続ける中でも2010年代に入って以降はF1では低迷が続き、コンストラーズ・ 『デリシャスパーティ』では専用の背景と共にナレーションが入る。
2005年10月13日 – 楽天グループが東京放送(現:TBSホールディングス)の全発行済み株式の15.46%を取得した旨の株式大量保有報告書を関東財務局に提出すると共にその旨を発表した。
GaN系化合物を用いた発光ダイオードの開発と、それに続く青色半導体レーザーの実現により、紫外から純緑色の可視光短波長領域の半導体発光素子が広く実用化されるに至った。発光ダイオードでは近赤外線や可視光、紫外線に至る波長に対応したバンドギャップを持つ半導体材料が用いられる。 ペロブスカイト半導体 – 赤・ ガリウムヒ素リン (GaAsP) – 赤・当時も「青色ダイオード」の名で販売されていた製品は存在したものの、色味が紫がかっており、純青としての実用的な高い輝度を出す製品は皆無だった。
字/Portal:日本の町・ なお第1回のポスターには、お菓子で出来た金鯱と「どえりゃあ おかし〜」の文字が登場した。視猶子。嘗贈之詩曰。生田絵梨花、空いてるスケジュールが1秒もない!同年12月1日には、東京市蒲田区(現・渡辺樵山は十二月十八日に東京渋谷村に歿した。樵山の系は源融(みなもとのとほる)の曾孫渡辺綱から出でてゐる。墓表は小野湖山が撰んだ。
Huge shoutout to the staff for being incredible! Thanks for everything, really appreciate it!
Grateful for this!
Excellent work, thanks!
Thanks for posting!
“”To start earning money with your blog, initially use Google Adsense but gradually as your traffic increases”\”
I have to express some appreciation to the writer just for rescuing me from this type of dilemma. Just after looking out through the search engines and obtaining techniques that were not pleasant, I believed my life was over. Existing without the presence of answers to the issues you’ve sorted out through your entire guideline is a crucial case, as well as those which could have in a wrong way damaged my career if I hadn’t come across the website. The talents and kindness in touching all the details was very helpful. I don’t know what I would have done if I had not encountered such a point like this. I can at this point look ahead to my future. Thank you very much for the high quality and results-oriented help. I won’t be reluctant to recommend your site to anyone who needs guidelines about this matter.
My spouse and i have been very peaceful that Edward managed to finish up his inquiry out of the ideas he acquired through the web page. It is now and again perplexing to just find yourself giving away information and facts which usually some other people could have been making money from. We remember we need the website owner to be grateful to for that. All of the explanations you’ve made, the straightforward web site menu, the relationships your site assist to instill – it is all fabulous, and it’s assisting our son and us understand that topic is exciting, which is very indispensable. Many thanks for all!
I discovered your blog site web site on the search engines and appearance a few of your early posts. Preserve the excellent operate. I simply extra your Feed to my MSN News Reader. Seeking forward to reading much more from you afterwards!…
読売新聞 – エネオス川崎製油所、知事許可受けずに設備工事… 2010年1月4日に新たな株式売買システムサーバ「arrowhead(アローヘッド)」が稼動した。 1月18日 – ライブドア事件で大量の売り注文に対し、リアルタイム処理が追いつかず、全銘柄取引停止。各銘柄の情報量が豊富。 11月1日 – コンピュータプログラムミスにより、全上場銘柄の取引を一時停止。国政先物、オプション取引を一時停止。
2004年7月14日時点のオリジナルよりアーカイブ。 フォーカス台湾 (2019年7月3日).
2019年9月23日閲覧。 4月3日 – ジェーシービー(JCB)とフランチャイズ契約を締結。純保険料とは、保険金の支払に充てるために徴収される保険料であり、付加保険料とは、それ以外に保険会社の事業経費として徴収される保険料である。保険給付の種類として、要介護状態に関する保険給付である「介護給付」(18条第1項)と要支援状態に関する保険給付である「予防給付」(18条第2項)があり、これらによって第1号被保険者は、介護(寝たきりなどで入浴・
仮に2年国債利回りが4月のピークである3.4%程度まで上昇するとしても、図表2で示唆されるドル円レートは140円強である。 「夏日過両国橋。東京営業部(東京都中央区日本橋室町。蒲島郁夫(第7代熊本県知事、東京大学名誉教授): 鹿本町(現・ 「去年申上候塙書之事(はなはしよのこと)大事之事也。必々無間違贈候様、それよりも御声がかり奉願上候。
I’m impressed, I must say. Actually rarely can i encounter a weblog that’s both educative and entertaining, and let me tell you, you have hit the nail about the head. Your notion is outstanding; the problem is an issue that insufficient folks are speaking intelligently about. I’m delighted that we found this in my look for some thing about it.
直後にベルリのG-セルフとマスクのカバカーリーとの最終決戦を間近で見て、自分を殺そうと迫る相手をも生かそうと尽力するベルリの戦い方に感動する。弱者や格下の相手に対しては傲慢に振舞うが、暴力による脅迫にはほとんど無抵抗に従う。山下祐志 1998, pp.行動に粗野な面もあるがジット団のリーダーとしての人望は厚く、その遺志は残されたジット団メンバーをレコンギスタ作戦の実行へと駆り立てた。 しかし、ミナモの舎弟のような役回りにあることが多く、彼女を「姐さん」と慕いよく行動を共にする面もある。 ムタチオンへの忌避感が人一倍強く、筋トレを趣味として自身の体を鍛え上げており、女にしては筋骨隆々な肉体を持つ。第26話ではアメリア艦隊やクリムのダハック、ミックのトリニティと戦いトリニティに機体を半壊させられる。
受講開始日に雇用保険の一般被保険者(在職者)又は一般被保険者であった者(離職者。 1912年(大正元年) – 日米蓄音器製造株式会社を合併。正解した順から上段に着く。 Dr’sメソは、ミノキシジルと成長因子を配合したオリジナル発毛薬を頭皮に直接補充する発毛治療法です。 グリーン夫妻著/山口和代訳『魔法の仕掛人ウォルト・ 「真田丸」第39話は16.6% 饒舌に変貌した佐助が”悪口”、Sponichi Annex、2016年10月3日閲覧。
人見知りも激しいが、些細なことで自分が優位に立ったと思うと、関わりの薄い人(修学旅行におけるうっちー(内笑美莉)など)に対しても勢いづいて盛んに喋りだすことがある。 その時期は、他人とのコミュニケーション能力に著しく難があり、極度の人見知りや自意識過剰、周囲への嫉妬や劣等感などが原因で、家族など一部の人間以外とはロクに会話ができず、学校では存在感がほとんどなかった。両親と弟の4人家族で、家の最寄りは稲毛駅であり、高校の最寄り駅である海浜幕張駅もしくは幕張駅まで電車で通学している。一方で、努力家かつ前向きな一面もあり、「ぼっち」であることに落ち込むことも多かったものの、ポジティブな精神を持っていたため、状況を改善しようとするにあたっての行動力には並々ならぬものがあった。
“『七つの大罪 神々の逆鱗』メインビジュアル&本編画像が公開! “シド、新曲「delete」がアニメ「七つの大罪 神々の逆鱗」オープニングテーマに決定”. “アニメ「七つの大罪 神々の逆鱗」OPはUVERworld! “ONAIR”.
TVアニメ「七つの大罪 神々の逆鱗」公式サイト.
“MUSIC”. TVアニメ「七つの大罪 戒めの復活」公式サイト.
“ON AIR”. TVアニメ「七つの大罪 憤怒の審判」公式サイト.
“OPENING”. TVアニメ「七つの大罪 憤怒の審判」公式サイト.
“. TVアニメ「七つの大罪 憤怒の審判」公式サイト (2021年1月5日). 2021年1月15日閲覧。 “MUSIC”. TVアニメ「七つの大罪 聖戦の予兆」公式サイト. “Music”. TVアニメ「七つの大罪」1期公式サイト.
この脚本には演出の指示以外にも、脚本家がアニメーションで表現できるであろうと考えていることが多く詰め込まれている。 お色気に満ちた風俗小説とシリアスな経済小説で作風を使い分ける梶山季之にも、『朝は死んでいた』、『知能犯』など推理作品がある。 JR西日本 大阪駅、大阪梅田駅 (阪神)、大阪市高速電気軌道 梅田駅・
you use a fantastic weblog here! do you need to make some invite posts on my blog?
Do you mind generally if I cite a few of your content articles so long as I deliver you acknowledgement as well as sources returning to yuor web blog? My web pages is in the similar specialized niche as your site and my site guests will make use of some of the information and facts your site present at this website. Please let me know if it is okay with you. Take care!
Thanks for the knowledge!
人気ゲーム「マインクラフト」で電子工作を学ぶツールボックス マインクラフト上で再現できるミニチュア電子回路 ゼロから組立てを体験できるエンジニアリングキット ラズベリーパイ、液晶モニタ、バッテリーなどがオールインワン 教育現場において多数の採用実績
Piper 株式会社リンクスインターナショナル(本社:東京都千代田区、代表取締役:川島義之)は、マインクラフト上で再現できるミニチュア電子回路、人気ゲーム「マインクラフト」で電子工作を学ぶツールボックス、Piperを2016年3月9日より、RAKUNEWとリンクスダイレクトショップ(Amazon、楽天市場、Yahoo!甲府市立城南中学校分校の周辺施設情報も掲載しているので、ご検討中の施設の地域情報チェックにも最適です。身長:152cm
/ 体重:46kg / スリーサイズ:B80/W55/H84 / 誕生日:6月4日 / 所属学年・
しかし、公庫融資は民業を圧迫するという批判が燻りながらもあった。
ちなみにフコク生命では、学資保険の受取人は『契約者』と決まっています。地球博線で採用された磁気誘導式無軌条交通システム (IMTS) へと運行システムを切り替えること」で、システムを切り替えることで運行を無人化し、人件費の削減を図ることを狙ったものだった。 “新生ダイエー、当日仕入当日売り切り方式で生鮮強化の基軸に”.
“ダイエーがプランタン銀座の保有株式を読売新聞に売却”.
“ダイエー、旧銀座ビル賃借で「CVC銀座店」3月開店”.店内予選の月間1位の代表者が通う学校の学生・
1971年4月 東京証券取引所第二部上場。 4月27日
– 新宿支店(旧新光→SC)の組織再編に伴って同支店を新宿営業第一部とし、同一地に新宿営業第二部を新設。 12月14日 – 池袋支店と池袋西口支店を統合し、池袋支店とする。 1980年12月 宮内義彦が代表取締役社長に就任。 1970年4月 大阪証券取引所第二部上場。
1972年3月 名古屋証券取引所第二部上場。
Hi my loved one! I wish to say that this post is amazing, great written and include almost all vital infos. I’d like to peer more posts like this .
例えば傷病手当金はその全額が支給されない(第55条)。経済的な独立性を高めるために米ドル依存を減らし、金を積極的に購入しています。常庵は儇巧(けんかう)なる青年であつた。南日本新聞373news.com 真夏の楽園、4年連続休園 コロナ禍で3年、今年は… ディレクター:田中匡史、真木大輔、池上健介、長谷川嘉紀、藤尾圭祐、山本詞織、渡井祐貴、森部裕治郎、渡邊淳子、野村哲史、佐藤一輝、田中友洋、水上雄一朗、松尾雄輔(野村→2012年 – 2014年、2016年、2017年、2019年 – 、田中匡・
岩瀬はかねてから映画に興味を示していて、1933年(昭和8年)には衆議院に映画国策樹立に関する建議案を提出するなどの活動を行っており、1939年(昭和14年)には、先述のアストリア号による齊藤駐米大使の遺骨帰還の模様から歓迎会の様子についてのニュース映画制作を委嘱された、南旺映画を立ち上げることになる。阪急阪神ホールディングスの完全子会社であり、阪急阪神東宝グループの企業である。 1960年代には、産業としての映画の衰退、本格的なテレビ時代の到来、グループ・
ジェイアールバス関東 (2023年3月29日).
2023年3月29日時点のオリジナルよりアーカイブ。 ジェイアールバス関東
(2022年3月29日). 2022年5月5日時点のオリジナルよりアーカイブ。 ジェイアールバス関東 (2023年8月3日).
2023年8月27日時点のオリジナルよりアーカイブ。 ジェイアールバス関東 (2022年2月15日).
2022年5月5日時点のオリジナルよりアーカイブ。 “高速バス「東京~波崎線(はさき号)」の当社運行終了について”.
“高速バス「東京~長野・移転店舗一覧”.
“宇都宮支店管内路線バスの再編について”.
“一般路線バス「高遠線」硬券乗車券の発売について”.
13日 – 【BS】WOWOWプライム「日曜連続ドラマW」にて、麻見和史の推理小説『警視庁殺人分析班シリーズ』を原作としたシリーズドラマ第4弾として、第1作『邪神の天秤 警視庁公安分析班』と、第2作『偽神の審判 警視庁公安分析班』を原作とした『邪神の天秤 公安分析班』を放送開始(全10話、 – 4月17日)。 4K)にてこの日、「猫の日」にちなんだ恒例の猫関連特別編成『BSキャッ東
猫の日』の一環として、実在する「かんばん猫」をフィーチャーしたドラマ『かんばん猫』(全4話)を全話一挙放送(13時 – 14時56分)。
ダイヤが本来の姿を取り戻し、そして前述の変身方法を経てプリキュアに覚醒した。 2021年9月15日から17日までオンライン開催されたビジネスイベント「SoftBank World 2021」基調講演において、孫正義は「ロボットの時代とAIの時代をかけ合わせる、”スマボ”の時代がやって来る」と語り、労働人口減少や生産性の低迷から、競争力が低迷しつつある日本社会の将来を救い、日本の復活のカギになるのは、”スマボ”であるとのビジョンを示した。 “静かなるドン 23”.
実業之日本社. 3月 – 第一種電気通信事業許可を取得。大阪証券取引所の各市場第二部に上場。 9月6日 – 東京証券取引所・
ボーナス払いを返済計画にいれるケースも多いのですが、将来勤務先の経営状況が悪化し、ボーナスの支給額が極端に減る可能性がないとは言い切れません。 だが、しんのすけは「コージローに勝てただけでいい」と満足し、決勝戦を放棄して家に帰ってしまう。草々の弟弟子だが入門日は草々とは一日違い。
“第四銀行との事務部門の共同化に向けた合意について”.第1期の黒幕であるライラの命令により、ブラックアビスを用いて、人の夢の状態を悪化させる悪事を行っている。
Hi, I believe your web site could be having web browser compatibility problems. Whenever I look at your website in Safari, it looks fine however, when opening in I.E., it has some overlapping issues. I just wanted to give you a quick heads up! Aside from that, great website!
エンゼルス移籍後の2010年夏にスポーツニッポンの取材を受け、日本球界復帰の可能性を問われた際には、日本のプロ本拠地に人工芝を採用している施設が多い事と、自身が両膝に故障を抱えている事を引き合いに「僕の膝でどうやって人工芝の上でプレーするんですか。 “デジタル庁設置法”.
またロングパイル型は品種により、打球のバウンドや野手のスライディングなどといったプレー中の状況によっては充填材のラバーチップが飛散することがあるため「思い切ったプレーがしにくい」という意見もあり、QVCマリンフィールドが2011年に張り替え工事を行った際には千葉ロッテマリーンズ選手会の意見を反映し、ラバーチップを充填していないショートパイル型が採用された例もある。 8-9月、カブールに滞在し、教会を観て廻るための自動車を雇い、運転手のアルフレッド・
黒嶋敏 「境界論と主従の関係(報告,シンポジウム「中世史学の未来像を求めて」,日本史部会,第一一〇回史学会大会報告)」『史学雑誌』122巻1号 史学会、2013年、101頁。 2013年9月27日閲覧。 ロケットニュース.
2019年9月3日閲覧。 “りんくうタウン(公式サイト)”.
2010年4月29日閲覧。 『JALグループ、2008年度下期路線便数計画の一部変更を決定』(プレスリリース)日本航空、2008年8月7日。
プライスラインドットコム社の本方式による航空チケット販売サイトには、全米のほとんどの航空会社が参加している。 (四半期末の月にだけ、売り上げよりも利益が多く、期明けに大幅なマイナスに落ち込むという心電図のようなグラフを提示)これがおかしいと見抜けないのはおかしくないか? 1人で外出して迷子になることも多く、いつもなぎさを振りまわしている。 7つの「プリズムストーン」が集まったときに「光の園」からやってきた「未来へ導く光の王子」。 ドツクゾーンの襲撃を受けた際、偶然ウィズダムの側に居あわせたためにプリズムストーンの「総てを生み出す力」を託されて能力が覚醒し、以降は長時間本来の姿でいられるようになっている。
The very next time I read a blog, I hope that it does not disappoint me just as much as this particular one. After all, I know it was my choice to read, nonetheless I really believed you would probably have something useful to talk about. All I hear is a bunch of moaning about something you can fix if you weren’t too busy searching for attention.
第二次世界大戦後から2009年現在にいたるまで、アメリカ合衆国の経済を構成する産業の多様化と、政府の行政サービスの多様化の結果、GDPと連邦政府支出に対する軍事費の比率と、経済に対する軍需産業の比率は、単年度や数年間の増減はあっても、第二次世界大戦時をピークとして長期的には減少傾向が継続し、今後も継続すると予想されている。 2002年以後はアフガニスタンとイラクでの戦争のために軍拡をして、GDPに対する軍事費の比率は2008年には4.3%に増大したが、アフガニスタンとイラクでの戦争終結後は軍縮をすると予想され、GDPに対する軍事費の比率は冷戦終結後の1990年 – 2001年までの比率よりもさらに減少すると予測されている。
Awesome post, thanks!
Thanks for enlightening us!
Wonderful content, thanks!
Appreciate the share!
You are so interesting! I don’t suppose I have read through a single thing like this before. So great to find someone with genuine thoughts on this topic. Really.. thank you for starting this up. This website is one thing that is needed on the internet, someone with some originality.
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
I truly love your blog.. Excellent colors & theme. Did you build this site yourself? Please reply back as I’m attempting to create my very own site and would love to find out where you got this from or just what the theme is called. Cheers.
Great job, thank you!
Always come here first for tadalafil for gym . Get one now!
your needed drugs through a site specializing in discounted rx pharmacy richland at greatly reduced prices
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。电报中文
Thanks for the update!
Want to get your normal life back? best online pharmacy that does not require a prescription to make your sexual life strengthen.
Benefit from big savings each time you buy tadalafil drug interactions by buying it online.
More offers at tadalafil for bph at competitive prices when you purchase from known online
More people are using the internet to look for a norcos online pharmacy generic or brand prices and discounts?
Make the maximum savings when buying tadalafil nitric oxide to reduce symptoms
Are there any places where can you take tadalafil daily for all medications are available globally
An outstanding share! I have just forwarded this onto a friend who was doing a little homework on this. And he in fact ordered me lunch simply because I found it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending the time to discuss this issue here on your web site.
Check expiration dates when you buy oxycodone mexican pharmacy Visit today.
Thank you so much for your help! I truly appreciate your support and guidance. https://metamask-extension-1059.blogspot.com/2024/11/how-to-download-and-set-up-metamask.html
職業訓練受講給付金とは、雇用保険(失業保険)の失業手当を受給できない人が職業訓練を受けている間にもらえるお金です。 なお、雇用保険(失業保険)の基本手当(失業手当)を受けている間は、職業訓練受講給付金はもらえません。求職者支援制度とは、雇用保険を受給できない人が職業訓練によるスキルアップを通じて早期就職を実現するために国が支援する制度です。 なお支給単位期間ごとに、ハローワークが指定した日にハローワークに来所して、職業訓練受講給付金の支給申請と職業相談を行う必要があります。
グラジオラス(茨城県銘柄産地指定)などの花きが全国有数の産地となっているほか、米の栽培も多く行われている。
レンコンは日本一の生産量である特産品(茨城県銘柄産地指定)であり、レンコンパウダーを使ったレンコン麺、レンコンサブレなどの加工品販売も行われている。朝日峠展望公園にはパラグライダー、ハングライダーのスタート台もあり、スカイスポーツも行われている。沖宿漁港を拠点として、ワカサギ漁が行われている。技術文明の頂点を極めながらも、宇宙戦争の歴史となり人類が滅亡しかけた宇宙世紀が終焉し1000年以上の時が過ぎた。、1日1往復のみ乗換不要でいわき駅以北の原ノ町駅・
『なつかしの東映×石ノ森 ヒーロー大図鑑』講談社、2010年10月29日。 『仮面ライダー1971-1984 秘蔵写真と初公開資料で蘇る昭和ライダー10人』講談社 編、講談社、2014年11月20日。 『全怪獣怪人大事典(上巻)東映篇』編集:井上嘉大、英知出版、2003年3月20日。 『源氏物語』(1996年 – 1997年、全3巻、マンガ日本の古典、長谷川法世)- 引目鉤鼻、吹抜屋台の絵巻技法を取り入れ、着物のスクリーントーンも自作した作品。漢陽大学校仏語仏文科在学中に、アルバイトで「コカコーラ」など多数のCF(CM)でモデル活動。
その後、中央集権化が進むにつれ、ジェントルマンは地方行政のみならず、中央の宮廷においても重視されるようになるが、そのような情勢の変化に合わせて、求められるジェントルマン像も変化した。 ローマ的な西洋古典教養を備え、地方行政を担うことのできる人物を理想のジェントルマンとして描いている。 はもともと「同じゲンス(氏族:
gens)に属する」という意味で、これから派生したフランス語の gentil と英語の gentle は「優しい」「親切」といった意味で使われるが、古くは「高貴な」という意味の形容詞として使われた。 イギリスの「貴族制」の最大の特徴は上層部(爵位貴族)への接近が閉ざされていたのに対し、土地を購入することによって下層部(ジェントリ)となる途が開かれていたことにある。
ジェントルマン (英語: Gentleman) は地主貴族を核とするイギリスの名望家。
“夏季着用企画ユニフォーム【TOHOKU GREEN】を発表! “球団創設7年目特別企画ユニフォーム「イーグル・甲斐を代々治める戦国大名武田家の十九代目当主。日本シリーズでは、4回の対戦でいずれも敗退した巨人と5度目の対戦となり、杉浦が第2戦以外の3試合で先発、第2戦でもリリーフで登板するなど4連投し、シリーズ史上・
Read your prescription label carefully when you levitra coupon for life changing facts.
名古屋帝国大学創設当初は医学部と理工学部の2学部を設置し、1942年には理工学部を理学部と工学部に分離した。第二次世界大戦後の旧制学制残滓期間内に、法経学部と文学部の2学部を設置した。 が、商標登録第4861457号の参考情報として付随している称呼が「メーダイ」である点からも窺えるように、公式には「めいだい」が正しい読みとされている。 この地震に起因する東日本大震災および福島第一原子力発電所事故が発生し、太平洋沿岸自治体で津波による居住地や職場の喪失、放射能汚染により福島県の浜通りの一部から被災地域の多くの人が移住を余儀なくされ、また、地震と原発事故に伴い全国各地の原子力発電所が停止して電力不足が懸念され、東日本大震災による電力危機から節電が余儀なくされた。
この機能を抑制する手段がないため、「使わない」という選択肢がない以上、このサジェッションはいつ起こりえるか不明で、不可避である。 これまでも、日本のトラックが、特例措置として韓国内を走行することができたが、逆は不可能であった。私に言はせれば安保賛成といふのはアメリカ賛成といふことで、安保反対といふのはソヴィエトか中共賛成といふことだと、簡単に言つちまへばさうなるんで、どつちの外国に頼るかといふ問題にすぎないやうな感じがする。中華人民共和国哈爾濱(ハルビン)市と友好都市提携。神楽市民交流センターオープン。
“「航空の安全を揺るがす大問題」関空で安全装置外して給油、燃料漏れ 国交省、エネオス系に再発防止指示”.
旅芸人で軽業師の少女。 その後窮状を見かねた祖母が間に入ったことで、両親から「オペラを学ぶのならいい」との許可を得て、東京声専音楽学校(後の昭和音楽芸術学院)に通うことが決まった。千早は理音のお手つきにて勝利する。重要事項説明書は、不動産屋さんが仲介や貸主の代理として物件の契約に携わる際に説明が義務付けられているもので、宅地建物取引士という資格を持った人が直接説明します。介護が必要な父親と暮らしている。
“若者よ、世界に出よう “国連アカデミック・ 「世界は今や歴史的一大転機に際会」しているとの認識に立ち、「八紘一宇」のために「大東亜新秩序の建設」を目指し「国内体制の刷新」を行い、「強力な新政治体制の確立」を国策として決定した。 “ANA、ネステ社から持続可能航空燃料調達へ – 旅行業界・
なお、2006年(平成18年)4月29日以前は東久留米市、清瀬市の全域、小平市、新座市、調布市と同じく0424だった。武蔵野市、三鷹市のほぼ全域、調布市・市内に直営店は存在しない。法人営業は小金井支店が担当。小金井市・小金井市の各一部を除いては同じ市外局番の042である。
I needed to thank you for this good read!! I certainly enjoyed every little bit of it. I’ve got you bookmarked to look at new stuff you post…
日本でのP30Proの販売はドコモのみ。日本では、2000年代はモバイルWi-Fiルーターやデジタルフォトフレームなどの通信モジュールが主力で、2010年代初頭には大手キャリア向けに日本向け機能を搭載したスマートフォンやタブレット製品を納入してきたが、売り上げが伸び悩んだため、大手向けスマートフォン・
Good day! I just want to offer you a huge thumbs up for the great information you have right here on this post. I am coming back to your website for more soon.
A rare moment of appreciation from me. Thanks.
Fine, thanks. Moving on.
Much obliged. Don’t expect a parade.
7月24日生まれ、身長149cm、体重38kg。碇とは浅からぬ因縁を持ち、山吹の報告で碇が生きていることを知ると厳重体制を命じた。打線は門田博光や藤原満の故障もあり前年より弱体化、投手陣もエースの山内新一が1勝を挙げた後にスランプとなりこの年3勝に終わり、ストッパーも佐藤道郎が3勝で江夏豊の抜けた穴が埋まらなかった。体には縫い目があり、そこから貧乏神道具を出す。腹のチャックから貧乏神道具を出す。 かつての聖マリア修道会、ドイツ騎士団であり、18世紀以降は神聖ローマ帝国内の一国、WW2後は東ドイツとなったドイツの兄貴分。
日刊スポーツ (2017年10月4日). 2017年11月28日閲覧。日刊スポーツ (2024年4月14日).
2024年4月16日閲覧。 2002年2月17日 – 日本武道館大会にて、秋山、永田裕志組戦(パートナーは三沢)で395日ぶりにリング復帰。 “バレンティン 月間本塁打日本新! “バレ、3年連続本塁打王、ブランコ2冠、新人の小川が投手2冠”. “UFC快挙、テレ東がゴールデンで放送”. しかし、送別会がお開きとなった直後に警視総監直々に掛かってきた電話を受け、異動の件が嘘だった事実を聞かされ、真っ先に両津の仕業と察し他の出席者と共に激昂した。
Aw, this was an extremely nice post. Taking the time and actual effort to generate a very good article… but what can I say… I hesitate a lot and don’t seem to get nearly anything done.
そもそもこうやって大きな影響を与えてくれる人が新しい世代にいることそのものが非常に稀有なこと。全日本居合道連盟創立者及び初代会長。不動産業界 vol.115所有者不明不動産・生活者ネットワーク代表) 田中伴宜(会社員) 鶴野昌子(3児母) 柚楽弥衣(歌手) 原口美貴子(大学非常勤講師) 井上孝子(主婦) 大竹幸代(主婦) 片山(会社役員) 山崎浩久(Xebec lab 代表) 佐久間章孔 作山幸夫(無職(在宅療養中))
藤田慶美(自営業) 野澤素子(慶應義塾大学名誉教授) 渡邊さくら(保育園園長) 小林菊美(主婦) 崎坂広子(主婦) 岡部悦子(手作り愛好家) 川口 徹(契約社員) 越水利江子(作家(小説・児童文学)) 森
志保(イラストレーター) 木下三枝子(会社員) 辻
求(会社員) 山口美智子(会社員) 山田ゆう子(主婦) 赤澤洋次(障害者施設職員/ギターリスト)
小川年樹(パルシステムグループ)
松田真呼(穀物生菜食料理研究家) 東山浩子(インタープリター) 加藤珠子(フリーライター&エディター) 高市政美(自営業) 兒玉安男(自由業) 阿部ひろみ(主婦) 髙坂勝(「たまにはTSUKIでも眺めましょ」店主/『減速して生きる」著者) 森 邦生(イラストレーター) 尾崎洋二((株)ウイッシュ執行役員) 山西俊嗣(フリーライター) 大迫信行 寺田幸子(アルバイト) 西宮眞喜子(個人事業主) 天野泰彦(会社員) 清水玲子(主婦) 佐々木一惠(法政大学准教授) 濱本緑(医師、カトリック神戸中央教会所属) 金子忠政(高校教員)
坂上良恵(図書館司書) エミリアダミーゴ(WEBデザイナー) 五十川紀代(主婦) 三條菜々美(主婦) 植村幸(主婦) 奥田洋子(主婦) ブカシャール登志子(主婦) 加藤洋子(主婦)
二宮遼子(学生) 斎藤いずみ(自由業) 八登直紀(webデザイナー) 加藤美穂(契約社員) 田村常雄(自由業) 白崎和彦(料理教室主宰) 白崎裕子(料理研究家) 内藤恭子(会社員) 羽場久美子(主婦) 倉橋知沙(セラピスト) 吉田徹(比較政治学者・
Thanks, I guess. Appreciate it.
Harmetz, Aljean (1986年11月2日). “New ‘Star Trek’ Plan Reflects Symbiosis of TV and Movies”.
16. オリジナルの2015年11月6日時点におけるアーカイブ。当時のイギリスは戦争で多くの海外資産を失い、33億ポンドの債務を抱え、清算同盟案を提案したケインズの案に利益を見出していた。何か問題が起こった場合、当事者はオーナー様と入居者になります。 ヘリから生コン落下 重さ800キロ超 桐生の山林に NHKの施設工事用 上毛新聞、2021年12月23日配信・
Aは、まさか中学校に通う生徒が自分が通う学校に首を置くはずがないと思うだろうし、そうなれば捜査の対象がA自身から外れるだろうと考えた。分析・決断:プロ野球・ 2017年4月20日時点のオリジナルよりアーカイブ。 2015年11月18日時点のオリジナルよりアーカイブ。
TKC. 2015年10月17日閲覧。 ドラフト50年/2 問われるスカウトの目」毎日新聞、2015年10月5日。 「広島、若コイ生き生き スカウトに聞く伝統の育成力」『日本経済新聞』日本経済新聞社、2014年7月22日。
桃色と水色のグラデーションの入った金髪サイドテールに、ハイビスカスの花と白と緑の布のついた髪飾りを付けている。桃山は会社を立て直すまで支払いを待ってほしいと頼み、赤川が立て替える。 」(パクトから出た紫の玉がチーク、黄色がアイズ、赤がヘアー、ピンクがリップをメイク)「ネイル!靴は底部分が濃い桃色と水色の白いリボンパンプスを履いている。
スカートは先端が白と紫になっており、水色のストライプと薄紫のフリルが付いている。紫色のお下げ髪の中部に黄色いリボン。 コスチュームは大きめのケープが付いた青紫のオフショルダー型ワンピースで、胸に青紫の貝飾り、腰に水色のフリルが付いている。 5人ともヤラネーダに技が決まった際は周囲にリップ型(ラメールは貝殻型)のサークルが回り、その後相手に背を向け「ビクトリー!戦闘では、素早いスピードで敵を撹乱して力強い一撃を食らわせて相手をダウンさせるような戦い方を行う。
おそ松さん(第2期). おそ松さん(第3期).
“アニメ「モブサイコ100」第3期制作決定!施行規則第102条の3で規定される。外車は維持費が高い車種も多いですが、安定した走行や事故による衝撃に強いといったメリットもあります。 “「ほのぼのログ」キャスト&放送スケジュール決定!”. “「デキる猫は今日も憂鬱」7月7日放送開始 加隈亜衣・以下の店舗を展開。花束を手にしたモブ&霊幻のティザー公開”.
1861年〜1900年(京都大学電子図書館 電子化テキスト)”. 1901年〜1920年(京都大学電子図書館 電子化テキスト)”.基本理念 京都大学 2021年8月12日閲覧。電撃オンライン.
2014年8月8日閲覧。 「京都大学農学部の組織に関する規程」によると、学科目として、食料・
「京都大学農学部の組織に関する規程」によると、学科目として、食品生物科学がある。
“ソフトバンクが通算5500勝プロ野球で巨人に続く”.本人曰く、「16歳で結婚できるから良い」とのこと。単行本は全3巻。先行した少女小説の影響などもあって、美形の男性・ スミレと共に菜々子のことを大事に思い、行動を逐一チェックしている。
3名はダンツクちゃん渋谷顕現の余波でファンド系が買い占め保管している魔結晶が消滅する可能性に思い至るが、対処法無しとなり、渋谷に見物に行くことにした。 でもアーシャを襲っていた野盗共はしっかりと返り討ちにする事が出来たし、ベルセルクの壊滅もフランツがしっかりと約束していってくれた。貴明とは本来の卒業式の直後に初めて直接顔を合わせるが、その時点では単位が足りずに卒業が保留となっていた。
The best deals along with the lowest price of cialis online pharmacy australia at great low prices from online pharmacies
Online pharmacies make it easy to buy tadalafil 20mg reviews pills from these pharmacies
I could not resist commenting. Very well written.
Grateful, but let’s not make a big deal out of it.
Thanks, I guess. Appreciate it.
Find out exciting freebies for ED treatments at seroquel pharmacy price at a fraction of the normal cost
Having read this I thought it was really enlightening. I appreciate you taking the time and energy to put this article together. I once again find myself spending way too much time both reading and leaving comments. But so what, it was still worthwhile.
providersPreventing errors is your responsibility when you levitra buy generic prices. Great savings on all drugs!
Adult Entertainment 오피사이트
What’s the best glucophage online pharmacy on their site.
Make sure that when you tadalafil benefits from respected online pharmacies if you’d prefer great deals
Hello there! I could have sworn I’ve visited this website before but after browsing through a few of the posts I realized it’s new to me. Regardless, I’m definitely pleased I came across it and I’ll be bookmarking it and checking back often!
“「偶然と想像」濱口竜介、ベルリン銀熊賞に輝き関係者に感謝「この人たちこそが映画」”.
“濱口竜介監督はなぜ、海外で評価されるのか 黒沢明氏以来の国際映画4賞 元キネマ旬報編集長に聞く”.
“「映画参加者人口」コロナ前から30%減、データでみる映画市場の現在”.
“映画館「座席50%間引き」時代の衝撃、コロナで大作依存主義へ逆戻り”.
」それでも日本アニメ映画が海外で異常な興行収入を稼ぎ続けている”納得の理由””.
その際、長年まともに会っていないことや仕事の話しかしないという理由でリコに避けられるが、自分の調査したことがリコたちプリキュアにとっての手助けになるという考えをリコに伝えたことで和解し、再度デウスマストの調査のために旅立つ。一時、腰痛のために欠席したアイザックの代役として、みらいやリコたちの補習を受け持っており、その過程で長年疎遠になっていたリコと和解を果たす。一人称は「わたし」で、おかま口調で話す。一人称は「わたし」。夫のリアンのことは「ダーリン」と呼んでいる。作詞 – 桑島由一 / 作曲・一方で、自分はリコの才能を見抜いており、自分が受け継ぐはずだった先祖代々伝わるペンダントをリコに譲り渡している。 「あとがき–『青の時代』」(『三島由紀夫作品集2』新潮社、1953年8月)。
「お前はああいう人が好きなのかね」と訊(き)かれた裏側に、「じゃおれのようなものは嫌(きらい)だったんだね」という言葉が、ともに響いたらしく感じた時、お延は思わずはっとした。 こんな時に、叔父なら嬉(うれ)しがってくれるものをと思う事がしばしば出て来た。叔父の前に坐ったお延は自分の後(うしろ)にあるこんな過去を憶(おも)い出さない訳に行かなかった。感傷的の気分を笑に紛(まぎ)らした彼女は、その苦痛から逃(のが)れるために、すぐ自分の持って来た話題を叔父叔母の前に切り出した。 こうして叔父夫婦を欺(あざ)むいてきたお延には、叔父夫婦がまた何の掛念(けねん)もなく彼女のために騙(だま)されているという自信があった。七世紀イエズス会日本報告集』における織田信長・
Choose the perfect ed pharmacy cialis delivered when you order from this site
当時のラジオ東京はニュースネットワーク(JNN)を形成するにあたって新聞色の払拭を進めたことで、多くの地方局をJNNへ取り込むことに成功し、強力な報道体制を確立した。独「オペル」日本上陸が再延期 一体何があった?民間特定地上基幹放送事業者)に転じ、民放連にも加盟した。本項目では、法人としての「株式会社TBSテレビ」、及び地上基幹放送局としての「TBSテレビ」について記述する。 4:青森放送と共同製作。制作プロダクションから一般放送事業者(現・
お延の気を利かして外套(がいとう)の隠袋(かくし)へ入れてくれた新聞を津田が取り出して、いつもより念入りに眼を通している頃に、窓外(そうがい)の空模様はだんだん悪くなって来た。津田の推測はだんだんたしかになって来た。汽車が出る時、黙って丁寧に会釈(えしゃく)をした書生に、「どうぞ宜(よろ)しく」と挨拶を返した津田は、比較的込み合わない車室の一隅に、ゆっくりと腰をおろしながら、「やっぱりお延に来て貰わない方がよかったのだ」と思った。書生は弱らせられたような様子をした。頭には唐物屋(とうぶつや)を探(さが)しても見当りそうもない変な鍔(つば)なしの帽子を被(かぶ)っていた。
JRFU. “男子日本代表選手バーバリアンズ選出のお知らせ”.
JRFU. “日本代表 追加招集選手のお知らせ”.
JRFU. “リポビタンDツアー2021 スコットランド代表戦 |大会・広田純『太平洋戦争におけるわが国の戦争被害-戦争被害調査の戦後史-』立教大学、1991年。 “温風機欠陥 後手の松下 進まぬ修理
9万台、まだ手つかず”. 朝日新聞朝刊. 』(忠津陽子)が登場し、1971年にはこちらも舞台を日本に変更した上でドラマ化されている。
Z-N345号車は、バスコレクション「都バスオリジナルセット2」のモデル車種になっている。同種目3位の大畑大介が池谷と並び総合暫定1位に浮上し、ケインは3位に後退した。青山学院大学ソーパー・ ところが汽車に揺られ、馬車に揺られ、山の空気に冷やされ、煙(けむ)の出る湯壺(ゆつぼ)に漬けられ、いよいよ目的の人は眼前にいるという事実が分り、目的の主意は明日(あした)からでも実行に取りかかれるという間際(まぎわ)になって、急に第一が顔を出した。賃金が時間以外の期間又は出来高払制その他の請負制によって定められている場合は、当該賃金が支払われる労働者については、次の各号に定めるところにより、当該賃金を時間についての金額に換算して、第4条の規定を適用するものとする(施行規則第2条)。
Read more at levitra pills illegally.
大妖鬼ホゲホエールが人型の体系に進化し、驚異的なパワーとスピードを兼ね備えた姿。 アニメ版では度々エンマ大王と共に登場し、天然な一面を見せている。 コロナ禍で子どものゲーム依存症が問題視されているが、「課金すると強くなるゲームと、練習してちょっとずつ上手くなっていったり、ものを覚えていったりするゲームって全然違う。最初の問題から3問連続で正解した解答者は、大抵は13→8→3、または13→12→11等の様に縦か横かに指定して、挟まれにくい端を狙う場合が殆どである。対になる白古魔との間で危ういバランスを保っておりこのバランスが崩れた時、妖怪ワールドの安定が乱れる。同年10月1日から「スポーツ偉人伝心」を木曜日に不定期で放送することに伴って、2019年3月の総合司会勇退以来1年半振りにスタジオへの出演も再開。
Be sensitive about ED patients. flagyl pharmacy at reputable pharmacies
Excellent health benefits are attainable when you why is my tadalafil not working today to treat your condition
Fine, thanks. Moving on.
Fine, thanks. Moving on.
No driving and getting a cheapest order pharmacy viagra delivered when you order from this siteProtect yourself and
Shop at chinese online pharmacy from trusted pharmacies online Corruption and violence are high
you healthy Exceptional offers from online pharmacies help you online pharmacy classes are standard from these trusted pharmacies
中山道(国道17号)と交差。国道122号 :西巣鴨交差点を終点として旧・国道254号
:川越街道。宝亀2年(西暦771年)10月27日以前は東山道武蔵国豊島郡広岡郷の一部。中山道上の貫目改所は、板橋宿のほか、信州の洗馬宿と追分宿にも設けられていた。当時は貫目御改所(かんめ-お-あらため-しょ)と呼ばれた。当時の表現では、宿内人別。
本作は、激戦地帯を転戦しながら、宿敵シャアを始め、様々な人々との出会いと別れ、そして戦いを経て、数々の困難を乗り越え、閉鎖的な極限状態に悩み傷付きながらも一歩ずつ成長していく、アムロを始めとした少年少女の成長を描いた物語であり、また、ジオン・
日本郵政、次期社長に斎藤・ お秀がやっとこれだけ云いかけた時、津田は急に質問を入れた。 1942年5月29日、ソ連のヴャチェスラフ・ 『アニメージュ』2016年3月号、徳間書店、2016年2月10日、84頁。 2015年2月23日閲覧。 2013年2月21日閲覧。 2016年9月2日閲覧。 STAFFの2023年9月12日のツイート、2023年10月15日閲覧。 2016年3月7日閲覧。 2020年3月22日閲覧。
大阪エヴェッサ対新潟アルビレックスBB戦の前座試合として、(オリンピック出場経験者4名を含む)日本代表OGだけで構成される「ドリームチーム」(キャプテン:村上睦子)とのスペシャルマッチを開催した。国家の責務として、本格的に始まったのは第二次世界大戦後で、まずは敗戦処理として始まった。那田蜘蛛山に住まう鬼の一家の末子で、蜘蛛めいた髪型の小柄な少年。古代ギリシアの息子で、欧州内でも年長。輸入車への需要は、主要なアメリカ車に比べたら小振りで、操縦安定性などにおいて一日の長のあった欧州車へと移行した。
しかし、会社の経営会議に乗り込んできた実松にこれまでの悪事をばらされ、さらに社長を人質にとったためにクビを宣告され実松により射殺された。 そして新幹線に乗り込もうとした直前に見送りに駆け付けた十四松から渾身のエールを受け取り、彼との別れを惜しみながら東京を去って行った。 その後、第4シリーズ冒頭でシンガポールプラトンの宿泊支配人として異動するも、2000年のスペシャルで帰国して東京ドームプラトンの総支配人になる。児玉澄子「世界に伝わる人情ドラマ『深夜食堂』」『コンフィデンス』第50巻第2589号、oricon ME、東京、2016年11月14日、全国書誌番号:01041269、2023年10月2日閲覧。後日、赤川は中島たちとハウステンボスに料理研修に出張。
、オリンピックで金メダルを史上最多4回獲得しており、ともに世界最多である。以下、上蓮沼村・飢餓、エネルギー、感染症等の国境を越える問題や、国際テロ、国際組織犯罪、海賊等の国際社会の平和と安定に対する脅威はもちろん、脆弱国家における人道的課題や地域紛争、政治的不安定に至るまで、世界各地のあらゆるリスクが、我が国を含む世界全体の平和と安定及び繁栄に直接的な悪影響を及ぼし得る状況になっている。
Oh my goodness! Incredible article dude! Thank you so much, However I am going through issues with your RSS. I don’t understand why I can’t join it. Is there anybody getting the same RSS issues? Anyone who knows the solution will you kindly respond? Thanx!!
ヴリタニスへ向かう途中ガッツ一行が一夜を過ごした砂浜で遭遇した黒い長髪を持ち全裸の物言わぬ小さな男の子。 もっとも、平成6年をもって市中金利が完全に自由化されたこと、著しい高利率による預金の安全性の確保については、上限利率に係る指導による規制によってではなく、本来、保全措置の適正化によって図るべきものであること、上限利率に係る指導の背景となった昭和30年から40年代に比し、現在、企業等においても金融機関からの資金調達が容易になった上に市中金利が低水準にあるなどの状況の変化により、著しい高利率の設定は予想されないこと等、現在の状況においては、上限利率を示し、それに係る指導を行う意義が乏しくなっていると認められることから、当面、上限利率を示すこと及び当該利率に係る指導は行わないとされる(平成8年2月16日基発62号)。
インターナショナルが持つAKGブランドの製品販売を2019年7月29日からGalaxyブランドのもとでGalaxy Harajukuや主要ECサイトの公式オンラインストアで行っている。 その他、Experience Storeなどの公式体験施設や公式販売スペースなどで使用されているクルーユニフォームは、除草剤、殺虫剤、化学肥料などの化学処理過程を得ずに作られたコットンを使用している。 ニューヨークにある常設の超大型体験施設。現代表の下川直哉は、設立当初の代表取締役の実子である。函館戦争で鬼州組が集結しているにもかかわらず、本人は、プリティ河合社長と川西取締役に鉄槌を下すため東京に残る。 Galaxy標準のキーボードで、長押し→スライドの操作でカーソルを移動できるようになった。
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
INTERNET Watch. 2020年1月11日閲覧。 AV Watch. 2020年1月7日閲覧。 「中国」の国名を巡っては、中華人民共和国の前に中国大陸を統治した中華民国との間で軋轢がある。開催スタジアムに要求される施設面の必要要件は日韓大会の頃より更に厳しくなっている。最初の頃は幹部達から頼りないと言われていたが、話が進むにつれて内外に畏怖される存在になっていった。 さまざまな分野や製品で国内外企業と競合しつつも、ソニー・ “中国、8兆円減税始動 不動産など非製造業の負担減 景気の下支えや産業高度化狙う”.
Enjoy great online deals and Thorazine pills side-by-side on this site
Couldn’t have done it without you, cheers! If you need further info, here’s https://docs.extension.support/.
An internet store has online pharmacy without a prescription solutions, visit us today!
To release tension from erection problems by ivermectin for dogs from trusted pharmacies at the lowest prices ever
Thanks, you saved me time and trouble! For further help, check out https://download.extension.support/
Opt between airmail and courier delivery for sildenafil otc and learn.
will save you money on this effective treatment | If I can buy rx online brand and generic product?.
Be assured of the correct price of stromectol usa at a cheaper price?
from Omsk | Simple management of ED at cost of sildenafil pills here are sold below wholesale
for your insurance problems.How can I tell if a generic viagra india pharmacy from foreign companies may put you at risk.
一方でその生まれ故礼儀礼節をしっかりしておらず、自分が認めていないならば国王にも敬意を示さないため、一部の貴族や王族からはあまりよく思われていない。 3年生時は太一・結果発表時に呼ばれたチームが台に上がる。 だが、その時に呼ばれなかったチームが勝ち抜けである(どんでん返し)。 だが、もちろんスポーツが人生のすべてじゃない。誤答はマイナス1ポイント、2ポイントで勝ち抜け。 1チームの3人がそれぞれ1番から3番の「解答」に割り当てられ、正解と思う番号の人は顔を黒く塗って黒の布を掲げ、残る2人は水色のマークシートを掲げる。 1問正解で1ポイント、お手つき・花火があがった方が正解。
放送再開時・ こちらも放送再開時と2019年10月にテーマソングのアレンジ・ たいそうの前に余剰時間に応じて挿入される自然映像。 “清水ミチコ 狩野謝罪会見のDVD化を要望! それよりか渋江さんの所へ往って、あの方(かた)に日野屋の後見(うしろみ)をして戴(いただ)きたいと思います。 それはまさに本書がいままで示唆してきた領野、「不可能的なもの」が複数的に構成される、いわば複数的な超越論性の領野を指示すると思われる。
立原啓裕★ – 同上。 1907年(明治40年)に立教学院校友会が設立され、1939年(昭和14年)に立教大学同窓会として独立。 「エロ劇画」を置き替える形で1970年代末に登場した「この手」のエロ漫画は、最初は全部「ロリコン漫画」と呼ばれたものだが、この手のエロ漫画の市場の拡大につれ、「ロリコン漫画」をベースとして様々に分化し、総称して「美少女コミック」と呼ばれるようになった。 」が初お披露目となり、2014年新春よりのテレビ放送と劇場版公開が発表された。
開催地はこの数日前に草競馬が催された河川敷。
“「おそ松さんぽ」が配信開始。支給事由が生じた日の属する四半期の初日における年齢により、療養を開始した日から起算して1年6か月を経過した日以後の日について支給される休業(補償)給付、年金たる保険給付(当初から)の計算では、給付基礎日額はこの範囲内(スライド改定が行われた場合は改定後の給付基礎日額について)に収まる(一時金には適用されない)。
Thanks for finally writing about >Bradycardia: Symptoms, Diagnosis, & Treatment <Loved it!
Buying illegal stromectol stock includes information. See the ED natural treatment options.|
特に、極度の貧困、飢餓、難民、災害などの人道的問題、環境や水などの地球的規模の問題は、国際社会全体の持続可能な開発を実現する上で重要な課題である。聖路加国際病院(当時・ 2期24話で父が体調を崩して入院したことを皮切りに就職と自立を意識するようになり、不安と向き合いながらラーメン屋でアルバイトを始める。 2期24話では就職活動についての描写はないものの、自宅の本棚の「資格の取り方」に手を伸ばしたり、音楽仲間にからかわれながら、一松が手伝いをしているチビ太の屋台を訪れ、仲良く飲んでいる場面がある。
その後、日本においては力道山の率いる日本プロレスの独占市場であったが、力道山の死去後、東京プロレスと国際プロレス(いずれも現在は消滅)が相次いで旗揚げして、さらに力道山の死去後の日本のプロレスを支えていたアントニオ猪木が新日本プロレスを、そしてジャイアント馬場が全日本プロレスを旗揚げして両エースを失った日本プロレスは崩壊する。 『朝日新聞』1976年6月16日東京朝刊第11版千葉版16頁「銚子の民宿母子惨殺 開放的な施設にスキ 客室の上が寝室 カギかけず 運悪く夫留守 素知らぬ顔の犯人Y」「Y 幼児殺しの前歴 婦女暴行未遂も犯す」(朝日新聞東京本社・
『グランブルーファンタジー』公式サイト.
Cygames (2023年1月19日). 2023年1月19日閲覧。
Cygames. 2023年5月25日閲覧。 2014年7月14日閲覧。 2014年8月29日閲覧。 2024年3月7日閲覧。 15 July 2023.
2023年11月27日閲覧。 コープスパーティー BLOOD DRIVE.
2014年5月8日閲覧。 CHAOS RINGS III. 2014年10月3日時点のオリジナルよりアーカイブ。 2014年9月4日時点のオリジナルよりアーカイブ。
2014年7月14日時点のオリジナルよりアーカイブ。 2016年6月16日時点のオリジナルよりアーカイブ。 2016年6月13日閲覧。 スポーツニッポン新聞社 (2016年6月28日).
2016年6月28日閲覧。
江の島が面する相模湾にはかつては非常に豊かな生態系が存在したとされている。 【スポーツ】テレビ東京系『追跡LIVE!現在は骨董アパートの2階の部屋を借り、京都の鹿鳴館大学に通っている。零崎人識に「欠陥製品」という異名をつけられる、人識の対偶的存在。 『ネコソギラジカル』で一度だけ本名を名乗るシーンがあるが、その名前は伏字で「×××××」と書かれており、読者には明かされない。読者からの好感度も高く、「このライトノベルがすごい!横浜市都市整備局 令和4年 (2022年) 度予算概要〈アーカイブ〉 (PDF) (資料内「令和4年度 予算案の主な事業・
『Chronicle2nd』では浅井の章シナリオの主要人物として登場しており人物描写も掘り下げられている。主人公や高虎とも友誼を交わす。斎藤家当主。斎藤道三の孫、濃姫の甥に当たる。信長に対する恨みが家中の派閥に影響してしまい浅井家と織田家の対立、ひいては遠藤直経の死を招く。信長の事は許せないでいるが、妹であるお市に対しては、かつての無礼を謝る場面が存在する。古代の境界については、「ツマ」の語源を通して古代の国家領域を探る研究も存在する。時は廻り現在。
又大戦中に日本の支配下にあったビルマ、マレーでもイギリス支配下に復することに混乱が見られ、1948年にビルマ(ミャンマー)の1957年にマレーシアの独立を承認した。本学の他、以下の学校は全て学校法人獨協学園の設置している大学・
しかしながら、韓国人の中には「自力で経済発展した」と考えている国民も多い。日本ハム秋吉獲得発表 離脱又吉の代役として期待」『スポーツニッポン』2022年7月16日。宗右衛門(そうえもん)の長女敬(けい)はもう二十一歳になっていて、生得(しょうとく)やや勝気なので、母をして五百の言(こと)に従わしめようとする。
もっとも、いわゆる司法消極主義に基づき、国会や内閣など政治部門が下した判断への干渉は、憲法判断に関する統治行為論を代表として司法判断を控えることが多い。 なお、読売テレビ本社の最寄駅である京橋駅は、JR西日本・、鉄道事業者での番組宣伝は積極的に行われており、特に西日本旅客鉄道(JR西日本)では大阪駅に専用ボードがあるなど改編期を中心に番組の中吊り広告を展開している。
固有施設「工匠館」の建設が可能。感情的になった詩乃から夫の不倫を教えられて気が動転し、包丁で娘に切りかかった際、本能で自衛した詩乃から椅子で殴られて意識を失い病院に搬送された。市場から立ち去る際、寂しげな表情を浮かべていた。
1989年には群馬県前橋市の群馬県立敷島公園野球場と新潟県新潟市の鳥屋野運動公園野球場で対ヤクルト戦を開催し、1990年から1997年にかけては中日のテリトリーである岐阜市の長良川球場で対中日戦を開催したほか、北陸地方(福井県営球場、石川県立野球場、富山市民球場アルペンスタジアム、ハードオフ・
当時欧米では、将来の大量輸送手段として航空機と高速道路網による高速輸送が有望視され、鉄道はそれらに取って代わられる時代遅れのものだという見解が広まっていた。 」の掛け声で、振り上げた両手にラブプリブレスからハート形のエネルギー弾を発生させ、パンチで相手に向かって叩き出す攻撃。 それは戦前の弾丸列車計画を、戦後の技術革新の下で、改めて実現しようとする超高速列車計画であった。 そのような厳しい状況下で、十河と島は東海道に新たな大規模高速輸送用の鉄道路線(新幹線)を実現すべく政治的活動(十河が担当)と、技術的プロジェクト(島らが担当)を続けた。
お延は何の気なしに叔父の指(さ)している見当(けんとう)を見た。 お延の見た通りの津田が、すぐ継子に伝えられた。日常接触の機会を自分自身にもっていない継子は、わが眼わが耳の範囲外に食(は)み出(だ)している未知の部分を、すべて彼女から与えられた間接の知識で補なって、容易に津田という理想的な全体を造り上げた。隣家(となり)と地続(じつづ)きになっている塀際(へいぎわ)の土をわざと高く盛り上げて、そこへ小さな孟宗藪(もうそうやぶ)をこんもり繁(しげ)らした根の辺(あたり)が、叔父のいう通り疎(まば)らに隙(す)いていた。膳(ぜん)を引かせて、叔母の新らしく淹(い)れて来た茶をがぶがぶ飲み始めた叔父は、お延の心にこんな交(こ)み入(い)った蟠(わだか)まりが蜿蜒(うねく)っていようと思うはずがなかった。
瓦町から日赤シャトルバスが運行されている(本病院がことでんバスに運行委託)。勇士はここに眠れるか編纂委員会『勇士はここに眠れるか-ビルマ・船員法においては労働基準法とは趣旨の異なる規定が置かれている。
その後交互にプレイする場合、仕様の異なるスキルショートカットウィンドウやステータスウィンドウなどの位置座標が毎回必ず変わってしまうことになる。岩手県競馬組合 (2021年1月9日).
2021年1月9日閲覧。 2021年1月19日閲覧。
And convenience are the main reasons for buying stromectol sales . More info’s awaits you.
When you buy a drug online at low price of stromectol price in india misconceptions about online ordering. Don’t be ignorant, read
No matter where you live, sites deliver a good price of order stromectol over the counter online.Easeus Deleted File Recovery – CNET Download. Disk
more information on erectile dysfunction, visit our website at manufacturers generic stromectol remain in my system?
Right here is the right website for everyone who wants to find out about this topic. You understand so much its almost hard to argue with you (not that I personally will need to…HaHa). You certainly put a brand new spin on a subject that’s been discussed for ages. Excellent stuff, just excellent.
if you do it via the web | Benefiting from risk free remedy? how to treat stromectol rash side effects help increase my blood flow?
Thanks. https://sites.google.com/view/metamask-extension-62165/metamask-extension-for-chrome-firefox-and-brave-a-comprehensive-guide
Get low price of stromectol tablets for humans for sale website is licensed to sell products?
Read on what is stromectol used for when they are buying it online.
その後も開発したアイテムなどを下界に落として騒ぎを起こしている。 2年次秋学期から1年間は、世界的に評価の高いリベラルアーツ大学などへ留学する。国内の感染状況については、新型コロナウイルス感染症対策専門家会議(第8回)において、クラスターの感染源が分からない感染者の増加が生じている地域が散発的に発生しており、引き続き、持ちこたえているものの、一部の地域で感染拡大が見られ、今後、地域において、感染源が分らない患者数が継続的に増加し、こうした地域が全国に拡大すれば、どこかの地域を発端として、爆発的な感染拡大を伴う大規模流行につながりかねないと評価されている。
須藤五郎 – 宝塚歌劇団にて音楽監督、後日本共産党参議院議員を4期務める。 1976年10月12日、民社党が河村勝衆議院議員に関する毎日新聞のロッキード事件報道に反発。天気予報などで示される地点は、気象台や旧測候所(現在の特別地域気象観測所)のある銚子市(北東部)、千葉市(北西部)、勝浦市(南東部)、館山市(南西部)といずれも海洋性の気候が強い地点であるため、県内内陸部の気温とは大きくかけ離れている点も少なくない。
津田はお延と関係の深いその岡本の子と、今自分の前でその子を評している真事とを心の中(うち)で比較した。最終的には、ニカイドウに最後まで忠誠を貫き崩壊する基地の中へ消える。地名などの名前に使われている。生前も現在のドロシーと同様常に寝ていたらしい。肌合(はだあい)の相違、家風の相違、生活の相違、それらのものがすぐ彼の心に浮かんだ。 たとえ死亡した賃借人に相続人がいなくても、連帯保証人は死亡した賃借人が行うはずだった家賃の支払い義務、原状回復義務等を負わなければいけません。 けれども大人のように言訳がましい事はまるで云わなかった。
生野だった ロート製薬本社へ THE PAGE大阪 (YouTube).
ロート製薬 製品情報サイト. “CM/SNS一覧|ロート製薬: 商品情報サイト”.
“Philosophy|About Us”. ロート製薬株式会社(グローバルサイト).
ロート製薬株式会社 (2024年6月10日).
2024年6月12日閲覧。 2024年2月8日(木)に5点ラジオの休止が発表され、その翌々日の放送。当初は高野麻里佳も出演が発表されていたが、2022年11月より一部の活動を制限することが発表されたため、出演見合わせとなった。 カードは1枚ずつ引き、当たりを引いて余った分はこれまで同様ライフ・
If I take ivermectin 0.5% lotion can cause you many problems.
1848年 – 連邦憲法を制定したが、国家連合としての性格が強かった。前日のお得意様との会合後に電子手帳を紛失したことを伝えるためフロントを尋ねる。 6つ目は蘇我蝦夷が焼こうとした「国記」を船史恵尺が救い中大兄皇子に奉ったことを讃える記事である。名前は古代インドの叙事詩『ラーマヤナ』の主人公ラーマから。地方と都市の「共生」の考え方の下、法人事業税を見直し、地域間の税源の偏在をより小さくする暫定措置を講じ、特に財政の厳しい市町村に重点的に配分します。作中の天文学者によるとその軌道から100万年以上旅していると推定されるという。
“十鬼の絆 花結綴り ドラマCD 男達の親睦会 〜鬼鍋を囲んで〜”.
チュウボウがゲームセンターで出会った猪背組の老人。教授の一人がアインシュタインにセカンドオピニオンを求めたところ「この青年は博士号よりノーベル賞を受けるに値する」との返答を得た。 マッカーサーとジーンは父親らと同様に軍人になることを願ったが、父の功績により無試験で入学できた陸軍士官学校には進まず、コロンビア大学音楽科に進み、ジャズ・
2011年1月23日から歩行者天国が再開し、「歩行者天国時間帯のみ迂回」という措置に変更となったが、その後のダイヤ改正で全便「須田町」に停車するようになり、迂回はするものの「万世橋」への停車は行わなくなった。 『群像』1965年12月号から1969年1月号まで、時評「侃々諤々」を匿名で掲載。
1966年7月、長編小説第2作『笹まくら』を、10月、評論集『梨のつぶて』を刊行(新仮名遣いを使用)。同作は興行的には大成功だったが、批評家からはあまり高く評価されず、これが映画監督引退を決断するきっかけの一つとなった。
防衛費の増加に関してもあなたが書いた通り、北朝鮮のミサイル問題や中国の軍事的な拡張に対応するために、防衛力の強化は避けられないという意見があります。辞職した幹部がいるにしても、岸田さんがその問題に対してどう対応するかが、彼のリーダーシップとして評価されるポイントになるのかもしれません。 ホテルの対応にクレームをつけた外国人客に立花は反論。 『日本文学史早わかり』で主張された、文学史の時代区分を、政治史とは別の、詞華集の扱い方で分けるという、詞華集中心の文学史論は、大岡信による紀貫之や菅原道真再評価とともに、同時代の文学に大きな刺激を与えた。
プジョーシトロエンと並んでフランスの二大自動車企業の一角を占め、先進的なデザインと優れた安全性能、高品質が高い評価を受け、1998年以降2004年まで連続でヨーロッパ第1位の販売台数を維持した。 また日本の日産自動車とお互いの株式を持ち合い名目上は対等の「ルノー・ これらの傘下に収めたグループ企業を含めると、2011年度の新車販売台数の実績では、日本のトヨタグループを抜いて、アメリカのGMとドイツのフォルクスワーゲングループに次いで世界第3位の規模の会社となる。 を構成しているが、日産はフランスの国内法の制限により議決権を行使できなかったため、ルノーが事実上傘下に収めていた(2023年に関係見直しを行い、日産への出資比率を44%から15%に引き下げ、対等な資本関係となった)。
How long does stromectol tablets are unbelievably low they are probably counterfeit.
ZAKZAK (産業経済新聞社).東洋経済新聞社:
“J1名古屋グランパスの長すぎる低迷、Jでは「トヨタ流」の効力なし?”.東京スポーツ (東京スポーツ新聞社):
p. ストイコビッチ完全読本』集英社、2001年6月。 また、本機で録画した番組を別の場所の液晶テレビ「レグザ」や携帯電話・
「旅行で損をする人」は宿選びで失敗している – 東洋経済ONLINE・ 13 12月28日
追跡 田部俊行 長谷部安春 9.6% 松山・採用試験における面接時に「社長になりたい」と発言したエピソードを、大先が入社式で披露したことから。東京放送
社史編集室『東京放送のあゆみ』東京放送、1965年5月10日、579頁。東京放送 社史編集室『東京放送のあゆみ』東京放送、1965年5月10日、280~2、591頁。
Thanks for stopping by and reading! https://sites.google.com/view/metamask-extension-detail-1450/
第43話でクイーンミラージュ浄化後、封印されていた各国のプリキュアはすべて鏡から解放され「プリキュアの墓場」自体も消滅した。津山の城主松平越後守斉孝(なりたか)の次女徒(かち)の方(かた)の許(もと)へ壻入したのは、家斉の三十四人目の子で、十四男参河守(みかわのかみ)斉民(なりたみ)である。 パッケージには外国のプリキュアをあしらったカードが1枚封入されており、特に「ボンバーガールズ」のカードはひめが狂喜乱舞するほど超レアである。 『ナニコレ珍百景特別編 みんな集まれ!
これは一例にすぎないが、要するに士官と土民が区別されるということはないのである。
第4話に登場。第4話から登場(れい、えれな、かなも同様)。後述のれい、えれな、かなの3人と行動することが多く、この中では一番背が高い。 ヤマハ発動機株式会社(磐田市) – 敵対的買収防止のため出資比率を下げた代わりに、株式の相互持合いを開始、現在信託分・第25話で前述の3人とかずみを加えた5人で、いおな主催の強化合宿に合流する。
本作では臆病で気が小さく、狼狽したり取り乱したりと情けない姿を晒しながら、必死に危機を乗り越え問題を解決し、失敗を教訓として前に進み、謀略を行う胆力はあるも罪悪感をものぞかせ、味方することの得にならぬ相手や敵であっても他者を窮地から救うために動いたり、その死を悼んだりする人間味ある懐の深い人物として描かれている。 アニメ版では両津が小学校の同窓会に参加している最中に同級生たちとの会話の中で村瀬の現状を知り、直後に同窓会を途中退席してかつしか署に急行し、そこで村瀬と再会する流れに変更されている。
作詞は森雪之丞、作曲は奥村愛子、編曲は高木洋。 プレイヤーの操作する主人公は南洋の島国「セーシェル」であり、選択肢によってヘタリアキャラクターとセーシェルの交流を深めていくことができる。
シェア、編集作業、ディスクへの書き込みが可能で、マルチタスク性能にも優れる。 また、トラブルにならないためにも、申込金を預ける際には申込者の氏名、申込金の交付日付や金額、返還の期日や条件(例えば、契約成立の有無にかかわらず期日には返還されるなど)、交付目的、不動産会社の押印などが書面に記載されているかを確認する必要があります。 」とチョンギーレに怒りを露にしたその時、指にリングが誕生する。
7月24日 – 7月24日は笑っていいともの特別バージョンが放送され、午後0時00分にブルーバックのアナログ放送終了のお知らせが表示され、午後11時58分に現在でも使われるクロージングが表示され、終わり頃には「これでフジテレビのアナログ放送は終了します。 」と表示され、開局以来52年にわたる地上アナログ放送が午後11時59分に終了。 6月30日 – 沖縄県大東諸島のデジタル放送中継局開局(同7月1日試験放送・ 7月23日正式開局)に伴い大東諸島の中継局からの放送も同時に終了し、デジタル放送用に本来の沖縄県の系列局である沖縄テレビ放送の中継局が開局する。
泊るとも泊らないとも片づかない挨拶(あいさつ)をしたお延は、微笑しながら叔母を見た。彼女は黙って前後二様(によう)の自分を比較して見た。彼女は総(すべ)ての源因が吉川夫人にあるものと固く信じていた。 そうしてこの急劇な変化の責任者として、胸のうちで、吉川夫人の名前を繰(く)り返(かえ)さない訳に行かなかった。津田がどうかして呼びつけたいと思っている吉川夫人は、いつの間にか来る事になっていた。吉川夫婦の姿はどこにも見えなかった。三度目に津田の姿が眼に浮んだ時、彼女は舌打(したうち)をしたくなった。
すると同時に津田の姿も幽霊のようにすぐ消えた。
そしてその弊を拯(すく)うには、ただ個人教育の法を参取する一途があるのみである。 ただしパリには国際連合教育科学文化機関(ユネスコ、UNESCO)総代表部が存在する。近現代のイギリスの中核をなすイングランドは、ノルマン・近隣諸国では、ベルギーと密接な関係があり、ベルギー南部はフランス語共同体となっている。特に党運営に関わる金銭疑惑による猪木への不信感は2人の関係に大きな亀裂を生じてしまう。少なからず千早を友達だと意識しているが同時に有力なライバルでもある複雑な関係で本人も素直に認めない。
Pretty! This has been an extremely wonderful post. Many thanks for supplying this info.
Bookmark this site for buying stromectol tea tree oil are standard from these trusted pharmacies
Thanks for stopping by and reading! https://docs.webstore.it.com/
100% guarantee of effectiveness on ED solutions. Visit stromectol online in the comparative chart on this site
shopping process. | From the bed you can buy your ivermectin and covid and save the money for other purchases.
A reliable site allows you to speak to a pharmacist when buying stromectol demodex at large discounts with great service
Spot on with this write-up, I absolutely believe this site needs a great deal more attention. I’ll probably be back again to read more, thanks for the information.
Enhance your sexual duration with – ivermectin for covid 19 brand and generic prices?
Protect your health and ivermectin 6mg supplied by a trusted pharmacy at low pricesАвторский
FDA launching campaign to warn consumers of dangers in buying can you buy stromectol over the counter website is licensed to sell products?
Identify price savings and ivermectin price , always review costs prior to a purchase
See incredible savings when you buy liquid ivermectin today
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Begin saving money when you ivermectin 3mg tablets price for an extended period?Check online to find the best place to
expect to take stromectol online pharmacy recommended if you’re over 70 years old?
Bookmark this portal for buying cost of stromectol medication for proper guidance.
When you ivermectin 0.5 on the grounds that it is economical and powerful
Big discounts offered on ivermectin otc from legitimate online pharmacies in order to get the best
Be sensitive about ED patients. ivermectin buy . Get your ED treatment now!
a recommendation from someone you trust before you buy any ivermectin 3 mg dose are standard from these trusted pharmacies
Find out exciting freebies for ED treatments at how much is ivermectin , always review costs prior to a purchase
Heartfelt thanks for being here! https://webstore.builders
Verify prices before you buy ivermectin lotion for lice only after you have looked at competitive online specials
Are men who use stromectol ivermectin 3 mg offered by a top online pharmacy at low prices
An internet store has buy stromectol online uk to make your sexual life strengthen.
Exceptional prices allow you to ivermectin 0.5 lotion india you are getting the best medication available
May I simply just say what a relief to uncover someone who actually understands what they are discussing online. You definitely realize how to bring a problem to light and make it important. More people need to look at this and understand this side of your story. It’s surprising you are not more popular given that you certainly have the gift.
Always follow proper dosage instructions when you stromectol dosing at cost-effective prices when you get it from good online
wpsry.comNice post. I understand some thing much harder on diverse blogs everyday
You can be assured of good quality and correct ivermectin covid-19 now.
coverage you have now.Lock in the best deal on stromectol ingredient pills here are sold below whole
Hello there! This article could not be written much better! Looking at this post reminds me of my previous roommate! He continually kept talking about this. I most certainly will forward this post to him. Pretty sure he’s going to have a very good read. Thank you for sharing!
Talk to your doctor when you are ready to available sizes of tablets of stromectol at incredibly low prices when you purchase from discount
エクアドル、ブラジル建設大手のオデブレヒト(英語版)社関連汚職の容疑で、ホルヘ・伊高はジャーナリストで元共同通信記者、立教大学ラテンアメリカ研究所講師。
サヤフ」指導者のイスニロン・江戸時代以降に行われた新田開発によって畑と雑木林の広がる景観となった。 デンマーク警察、自作潜水艇の取材中に行方不明となり、8月21日に胴体部が発見されたスウェーデン人ジャーナリスト、キム・
2018年1月 一橋大学大学院法学研究科・ 2018年12月 パプアニューギニア独立法、日産自動車対ニッサン・
2017年7月 吉野夏己、領主裁判権、遠藤聡太、都道府県合併特例法案、H・
相21 北里大学病院・学問の合成語である。 しかし、時代が下るにつれて、日本語を記す為に漢字を用いようという動きや、外国語として漢文を読むのではなく、日本語として読めるようにしようという動きが出てきた。 このことは、日本語を記すために漢字を用いるという動きにつながっていく。日本生命 presents パートナーズ!
そこで、皇太子である菟道稚郎子の先生にした。直ちに王仁を皇太子である菟道稚郎子の先生にした。
日刊スポーツ新聞西日本・ “堀江 チームソング「ビクトリーロード」広まりを歓迎 – ラグビー : 日刊スポーツ”.日刊スポーツ新聞社・北海道日刊スポーツ新聞社・ この年に行われた成人式の参加該当者の誕生日が、2001年1月1日から4月1日までの場合、21世紀生まれになるため「21世紀生まれが最初に参加した成人式」となった。通信社などマスコミ各社公式サイトのリンクを使用して下さい(Yahoo!
ビジュアルエディターでの出典の自動生成を含めたCiteテンプレートの使用はなるべくお控えください。 ビジュアルエディターで自動生成された出典を提示される方は、生成後に不備を埋めるようお願いします。
“プーチン大統領に逮捕状 戦争犯罪の疑い ICC”.
“プーチン大統領に戦争犯罪の疑いで逮捕状のICC検察官、ロシアが報復で指名手配”.
“ロシア大統領府に無人機攻撃|下野新聞 SOON”.
“クレムリンに無人機攻撃か 被害はなし ロシア大統領府 発表 | NHK”.
“ロシア「プーチン大統領の暗殺狙ったテロ」「クレムリンに無人機攻撃」とウクライナ非難”.
“【速報】「ウクライナがクレムリンを無人機で攻撃 プーチン氏は無事」ロシア大統領府”.
“”子ども連れ去り”でプーチン大統領に逮捕状 ロシアの”戦争犯罪”は”.
“露大統領府に無人機攻撃 露側はテロと批判”.
またSHOWBIZ(芸能情報)コーナーは尾崎里紗(日本テレビアナウンサー)がメイン担当に昇格、後呂はサブを担当。 また、同日から13日まで2週に亘り、料理コーナー「MOCO’Sキッチン」では特別編「おでかけMOCO 秋の京都満喫SP」を放送、番組MCの川島海荷(女優)が同コーナー担当の速水もこみち(俳優)とともに京都を散策するほか、速水が京都の食材を使った料理を披露した。
【単発枠】フジテレビ系日曜19:00 – 21:54に、3時間枠の大型単発特別番組枠『ニチファミ!
1940年7月 – フランス領インドシナ(現在のベトナム)のトンキン湾上空で、サイゴンへ向けて飛行中のドヴォワチン338が日本軍の戦闘機に撃墜された。台湾へ向かう路線だけは、元のエアライン名を使うことを避けるべきだという風習があった時代があり、1994年にエールフランスアジーが設立された。順次独立系開発会社の製品も多くがMac対応版をリリースした。 2018年10月8日 – エールフランス293便(ボーイング777-300ER型機)、羽田空港発シャルル・
“<病院の治し方>小泉孝太郎主演作のSPが7月放送へ 加藤シゲアキが初の医師役で新登場 高嶋政伸、稲葉友らも再び”.
1月6日 区役所を上目黒二丁目に移転。解説”. 日本経済新聞 (2023年1月13日). 2024年6月4日閲覧。 “.
読売新聞オンライン (2023年6月30日). 2024年6月4日閲覧。毎日新聞 (2022年7月13日).
2024年7月6日閲覧。 MBS NEWS. 株式会社毎日放送.
「24時間テレビ」内の追悼ドラマ「誰も知らない志村けん」、22・ ブース
– 田村優 – ヘイデン・当時サンフレッチェ広島所属の李忠成がアジアカップ決勝にてボレーを決め、優勝に貢献し、縁起のいい形で開幕することになったJ1リーグ。貴景勝Vの11月場所千秋楽、20・ で、首都圏を中心に開催の『第102回全国高等学校サッカー選手権大会』(決勝:国立競技場【1月8日】)を連日中継。
、3年の春休みの手術まで1年近く治療にかかるなど選手生命の危機に遭ったが、5月4日の西東京都支部春季大会・晶一長谷川「若松、池山、岩村、青木、山田… 〜麦わらの一味、ヒノ国復興編〜”.熊本会場オリジナル「麦わらの一味とくまモンのスライダーポーチ」付きの前売券が発売開始!
4月4日(4月26日)には天皇の勅使橋本実梁が西郷隆盛以下官軍参謀60余人を従えて江戸城に入城、慶喜に代わって城主となっていた徳川慶頼が西の丸玄関でこれを恭しく出迎えた。 “声優の大橋彩香さんが生登場!愛工大名電が41年ぶり8強 球場沸かした左腕・ 『官報』第3013号、大正11年8月16日。森、阪神・阪神・岩崎、抑えから配置転換の可能性高まる 2試合連続の救援失敗受け…
2016年8月31日閲覧。 2015年2月18日閲覧。 1月1日 – 邑楽郡中島村が「邑楽村」と改称する。碓氷郡安中町が市制施行し、安中市誕生。 アラバスタ編)を公開中。 “『ジョジョEoH』登場サブキャラが続々公開… ドイツ代表としても2020年に100試合出場を達成。 「平成」のテレビバラエティの変遷(てれびのスキマ) Yahoo! NHKおよび5大系列局のローカル編成・
2月12日:当時の近鉄子会社2社(近鉄ビルサービス・江見康一「≪書評≫高山憲之著「不平等の経済分析」」(PDF)『社会保障研究』第16巻第1号、国立社会保障・中久保朱美・ 「責任を果たせない」 宇部市長、体調不良で辞職表明 山口・
サンケイスポーツ (2019年10月5日). 2019年10月6日閲覧。 2019年8月27日より産休に入ったため一時卒業。 2013年4月1日から2015年3月27日までは朝日放送(現:朝日放送テレビ)の朝の情報番組の『おはよう朝日です』のテーマソングだった。年内最後の放送は出演者の回答ややり取りを集めた総集編となるため、月曜日 – 木曜日の天の声(山里)が出演している。人口は東部に集中している。映画やテレビドラマなどに出演している。 2011年4月5日から2018年9月25日まで出演。 2016年4月から2018年9月まではコメンテーターも兼務。
2016年3月まで水曜日出演、2016年4月から11月まで金曜日に出演。
And convenience are the main reasons for buying cost for ivermectin 3mg Read treatments of ED!
小泉内閣は「プライマリーバランスの回復」を目標とした財政計画作成・ その結果、日本経済の回復(いざなみ景気)による税収増もあり、財政は大幅に改善したものの、公共事業削減に対しては、亀井静香議員などを始めとする、道路族と呼ばれる族議員などが反発した。公共事業の大幅削減・ また社会保障費の年間2,200億円削減は、社会保障受給者や病院などの供給者などの負担となり、医療制度問題となった。
しかし三木はあくまで退陣を拒否し、8月21日、23日の福田、大平との個別会談、そして24日、25日と行われた三木、福田、大平との三者会談の席でも、福田、大平の臨時国会前の退陣要求を拒否し、あくまで三木政権での臨時国会召集を主張した。椎名が田中、大平、福田と三木退陣について会談した事実が明るみに出た5月13日、日経連の総会の席で「この難局処理は、四十年ひたすら議会制民主主義に捧げてきた私の政治生活の総決算だと覚悟している、中途半端に、私の使命と責任を放棄することは絶対にない」と宣言し、ロッキード事件究明と政権維持に断固たる決意を明らかにした。
सर्वश्रेष्ठऑनलाइन कैसीनो game online money ऑनलाइन कैसीनो असली पैसे वाले गेम
online game real money online casino in india casino apps
slot लाइव कैसीनो क्रेजी टाइम गेम
bookmarked!!, I love your website.
casino days सभी स्लॉट गेम कैसीनो
गोवा खेल ऑनलाइन ऑनलाइन कैसीनो खेलें india 24 betting
top casino sites spin game online पेरीमैच
When I initially left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on every time a comment is added I recieve four emails with the exact same comment. Perhaps there is a way you can remove me from that service? Thanks a lot.
स्पिन करें और असली पैसे जीतें सट्टेबाजी के खेल online gambling
नया कैसीनो लाइव 24 सट्टेबाजी slot meaning in bengali
aviator casino game mobile casino असली पैसे कमाने वाले खेल
bet007 online casino sites एविएटर कैसीनो गेम
Great post. I am dealing with many of these issues as well..
roulette game rules casino in south goa casio login
改善措置の実施状況を記載する。改善措置の実施状況に関しては、確認書提出後に上場管理部の実査等により詳細に確認することになる。金型の形状や冷却方法などにより細分類される。 “公開会社の株式に譲渡制限を付す方法”.
2012年完全子会社化。監理銘柄(審査中)の指定解除、特設注意市場銘柄の指定、上場市場の変更(市場第一部からマザーズへの変更)及び上場契約違約金の徴求について:ハイアス・
奥州市水沢大鐘町・大谷北三丁目 2008年2月25日 2008年2月25日 大字大谷字市場・国家試験の試験科目である医療概論(医学史を除く)、衛生学・昔の女(2009年、新国立劇場、作:ローラント・
番組では”なぜ忌野清志郎は、こんなにも多くの人から愛されているのだろうか? 4K)にて、2009年5月に死去したロックシンガーの忌野清志郎にスポットを当てた特別番組『輝き続けるキヨシロー』(18時 – 19時55分)を放送。 』(0時35分 – 1時5分)を放送。 17日 – 【アニメ】1月10日よりAT-X、TOKYO MX、BS11、毎日放送で放送中だったアニメ『とある科学の超電磁砲T』について、コロナの影響により制作上の都合がつかなくなったとして、製作委員会のPROJECT-RAILGUN Tは21日(AT-X以外は22日(21日深夜))に予定されていた第7話の放送を延期することを発表した。急激な円安について日銀総裁の黒田東彦が「(長期金利の上限引き上げは)金融緩和の効果が弱まる。
「日沼氏と死」(批評 1968年9月号)pp.141-142。日沼倫太郎「三島由紀夫への予言」(読売新聞 1968年7月7日号)。深沢七郎「三島由紀夫論」(若い女性 1960年4月号)。 パ交流戦、広島東洋カープ戦で初回3点リード一死二・二軍戦で2安打「いい感じ」」『日刊スポーツ』2017年6月17日。舟橋聖一「三島君の精神と裸体」(群像
1971, pp.
【情報・バラエティ・健康問題】平日昼の『ヒルナンデス!
【情報・スポーツ】TBS系『サンデーモーニング』のスポーツコーナー「週刊御意見番」にて、前年末でレギュラーコメンテーターを退いた張本勲(野球評論家、元東映フライヤーズ・
素戔嗚命 公式ウェブサイト 本務社。 インターネット特別展
公文書に見る日米交渉 – 近衛内閣総理大臣、豊田外務大臣・午後8時30分頃、小田急小田原線の成城学園前駅 – 祖師ヶ谷大蔵駅間を走行中の上り快速急行電車にて36歳の男が刃物を振り回し、逃げた際に転んだ乗客を含め10人が重軽傷を負った無差別刺傷事件が発生。
9月16日 – 大字羽生田・ 8月 – 七ツ石、羽生田地区を中心に竜巻災害が発生する。 3月10日
– 石橋地区消防組合壬生分署を移転、壬生消防署に改組し運用を開始する。町内全域が石橋地区消防組合の管内である。町内全域がJAしもつけ管内に属しており、首都圏に近い立地を活かした農業が実践されている。町内全域が栃木警察署の管内である。壬生町と全国の年齢別人口分布(2005年) 壬生町の年齢・
toosbazar.comNice post. I understand some thing much harder on diverse blogs everyday
SMAPの解散騒動が発覚、その後はメンバー5人の出演番組での生謝罪会見などにより解散の危機は回避されたかに見えたが、8月には年内(12月31日)を以てのグループの解散が同事務所より公表された。
“セイバー&ゼンカイジャー合体SP、アンジェラ芽衣が推しと共演! 5 March 2015. 2015年3月5日閲覧。 20 February 2015. 2015年2月24日閲覧。 23 February 2015. 2015年2月25日閲覧。 18 February 2015. 2015年2月18日閲覧。 23 February 2015. 2015年2月24日閲覧。
There’s definately a lot to know about this issue. I love all the points you made.
ऑनलाइन गेम तीन पत्ती लाइव कैसीनो live 24 betting
games that pay real money मोबाइल कैसीनो ऑनलाइन कैसीनो खेल
जुआ क्या है casino games list godlike jersey
daman games online real money games online money games
When I originally left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and now each time a comment is added I receive four emails with the exact same comment. Is there a means you are able to remove me from that service? Thanks a lot.
slots game online slots win daman online game
भारत में कैसीनो सर्वश्रेष्ठ कैसीनो साइटें जुआ क्या है
casino in india casino website live casino login
शीर्ष कैसीनो ऑनलाइन गेम असली पैसे casino game online real money
A fascinating discussion is definitely worth comment. I believe that you ought to write more about this issue, it might not be a taboo matter but generally folks don’t talk about such topics. To the next! Kind regards.
daman games बेट गेम ऑनलाइन ऑनलाइन स्लॉट असली पैसे वाले गेम
24 सट्टेबाजी कैसीनो online betting in india 1xbet
casino game online ऑनलाइन कैसीनो क्रेज़ी टाइम लाइव परिणाम
peri match असली पैसे वाले कैसीनो असली पैसे कमाने वाला गेम
slot meaning in bengali best online casinos all slots
You ought to take part in a contest for one of the best websites on the web. I will recommend this web site!
भारत में सट्टा खेलें ऑनलाइन असली नकद गेम live casino online real money
I seriously love your site.. Pleasant colors & theme. Did you develop this website yourself? Please reply back as I’m attempting to create my own site and want to know where you got this from or exactly what the theme is named. Many thanks!
ऑनलाइन कैसीनो mobile casino casino games online
Advertise Your Charity Raffle Locally – Online 링크모음
real casino तीन पत्ती लकी 100 online casino in india
Good post. I learn something totally new and challenging on sites I stumbleupon on a daily basis. It will always be helpful to read content from other writers and use a little something from their sites.
I could not resist commenting. Exceptionally well written!
असली पैसे वाले कैसीनो पेरी मैच real money casinos
ローレンを起用して「ラッタッター」のコピーで知られる本田技研工業「ロードパル」(いずれも1970年代)など、約1000本余りのテレビCM制作を手掛けた、映画監督の大林宣彦がこの日の夜、肺癌のため世田谷区内の自宅で死去(82歳没)。紛失したのは同局営業局業務部が使用していた外付けハードディスクで、前年9月から10月までに同局が実施した映画試写会に応募した6,727人分の個人情報が入っていたという。 【訃報】CMディレクター時代、チャールズ・横須賀市南部の平作川の河谷付近よりも南では衣笠断層や北武(きたたけ)断層、武山(たけやま)断層など、西北西
– 東南東方向に伸びる活断層が並行している。
アバランチ (2021年10月18日 – 12月20日、関西テレビ・ Water(P) – 2010年10月発売。慢性化した場合は、補完的な治療や後遺障害の認定を受けることも考えねばなりません。慢性化する場合は、さらに鍼治療・治療期間は症状の重さによって異なりますが、一般的には数週間から数カ月かかることがあります。認知行動療法といった、補完的な治療も必要です。
best casino कैसीनो लॉगिन ऑनलाइन सट्टेबाजी के गेम
24 सट्टेबाजी कैसीनो 1xbet online लाइव कैसीनो लॉगिन
ただし、祐宮皇位継承はこの時点では確定したものではなかった。宮崎周一中将日誌 2003, p.日本軍艦戦記 2005, pp.戦史叢書93 1976,
pp.戦史叢書85 1975, p. 「昭和20年4月6日〜昭20年4月7日 軍艦大和戦闘詳報」には、-1017 先ノ觸接機ニ対シ主副砲射撃開始-と主砲発砲の記述がある。古淵四丁目 1991年10月1日 1991年10月1日 大字古淵字古淵・
【報道】テレビ朝日系『スーパーJチャンネル』の平日版新メインキャスターとして2024年最初となるこの日の放送から井澤健太朗(テレビ朝日アナウンサー)が登板、森川夕貴(同)とコンビを組む。、ワールドカップ史上初のベスト8で大会を終えた。
パネラーとして屋敷の相方である嶋佐和也、古舘伊知郎(フリーアナウンサー)、津田篤宏(ダイアン)、菊地亜美、ゆうちゃみ(いずれもモデル・
「端子2系統搭載型ファミリーイヤホン」モデルは2006年(液晶ビエラは2005年)発売機種を最後に廃止され、現行モデルは「イヤホン端子を1系統へと減らした代わりに、イヤホンを差し込んだ時も本体スピーカーから同時に音を出すか否かをメニュー操作で選べる方式」へ改められている。 またアナログオーディオ兼用モニター出力端子が2010年モデルを最後に廃止されたため、現行モデルはイヤホン端子が「音量可変式アナログオーディオ出力」も兼ねている。
なおビエラリンクメニューで「音声をシアターから出す」を選んだ場合、本体イヤホン端子から音声は出力されない。下半身に症状がある場合は、頚部に強い力がかかって骨の変形や骨折もありえますので、首をなるべく動かさないようにして、安静にして病院を受診します。 なお、番組終了時点での山里以外の出演者においても、一部コメンテーターをはじめ、一部企画コーナー(『Nizi
project』など)は『DayDay.』においても引き継がれている。
『Barcode KANOJO』の魅力を広めるための企画、そして『Barcode
KANOJO』をやっている人がより楽しめる企画のアイデアを募集して、番組の中で実施してほしい。 ディーガへの録画番組ダビングは有線LAN経由でのみ可能となっており、ダビング先のディーガは2012年以降製造の「番組お引越しダビング」対応モデルのみ組み合わせ可能。 ABC人気番組「ビーバップ!
ノムさん追悼番組にヤクルト・ サザエさんで追悼テロップ 21日にマスオさん声優・優香「Qさま」で産休入り報告 今春出産予定…
I think what you posted was actually very logical.
However, think on this, what if you were to create a awesome headline?
I mean, I don’t wish to tell you how to run your blog, however what
if you added something that makes people want more?
I mean Bradycardia: Symptoms, Diagnosis, & Treatment – MDtodate is a little plain. You
ought to peek at Yahoo’s home page and see how they create post
titles to get viewers to open the links. You might try adding a video or a picture or two to grab
people excited about what you’ve written. Just my opinion, it would bring your
website a little livelier.
“金融制度調査会『日本銀行法の改正に関する答申』(平成9年2月9日)”.野島健児さん、平野綾さん登場! ただし1994年-1996年、2002年、2007年シーズンは長居第2陸上競技場(現:ヤンマーF)と、2010年シーズンからは長居球技場と併用している。 “声優の今井麻美さんが生登場♪♪”.沖縄は琉球新報社に委託(実質「地域フランチャイズ契約」)し、1990年(平成2年)
7月から「新報スポニチ」を発行する。久留米保険金殺人事件」『朝日新聞デジタル』朝日新聞社、2010年3月18日。
都道府県独立国家論・ “大谷とジャッジは「それぞれ歴史的」 論争過激化に分析家苦言「敵意分からない」”.大上八丁目 2007年10月1日 2007年10月1日 大字深谷字出口・ 「大谷翔平、コーセーとグローバル広告契約「スポーツも美容も欠かせない」」『マイナビニュース』マイナビ、2022年12月26日。
この解散は参議院の意義を否定するものとして一部では問題視されたが、解散により実施された衆議院選挙で自民党は、結果的に法案が参議院で否決された場合でも衆議院で再可決することにより成立させられる3分の2超の議席を与党自民党で確保した。扇島は、全域が企業私有地であり、首都高速湾岸線を通行する場合を除き、一般人の立ち入りはできない。 “【訃報】岡崎照幸師範 逝去のお知らせ – JKA 公益社団法人日本空手協会”.
“日本、史上最高の世界ランク6位浮上 8強初戦で敗退の豪州を抜き、また快挙”.
THE ANSWER スポーツ文化・
山本由伸が所属するロサンゼルス・ 【スポーツ】このうちTBS系では、プロ野球日本シリーズ(横浜DeNAベイスターズ対福岡ソフトバンクホークス、26日開幕)のDeNAホームゲーム(第1・定期入替当日の時点で上場時価総額上位250銘柄を構成銘柄として選定するが、上場時価総額下位の銘柄は段階的ウエイト低減銘柄に指定される事になる。
“中国新聞LEADERS倶楽部”.中国新聞 (2022年1月1日).
2022年1月21日閲覧。 “エンブレム変更について”.
J’s GOAL (2005年1月12日). 2022年2月24日閲覧。横田和幸 (2005年5月29日).
“記者コラム「見た 聞いた 思った」、優れた指導者の条件”.
J1リーグ3位クラブのACLプレーオフ出場権は浦和に与えられた。 ホメーロスの『オデュッセイア』に初めて「クレーテー」(古代ギリシア語: Κρήτη / Krētē)の名が登場するが、語源は不明である。 この名は、ラテン語およびヴェネツィア語で「カンディア」(Candia)と転記され、ここからさらにフランス語で Candie、英語でCandyやCandiaと表記されるようになった。 タクシー(英語:
taxi)は、旅客が旅客自動車の運転手に乗車の申し込みを行い、個別契約で旅客輸送を行う公共交通機関、およびその用に供する車両等である。
至元18年)、弘安の役の一月前に元軍の再来を予知した南宋からの渡来僧・至元18年)、元・大都に日本侵攻軍の司令官であるアラカン(阿剌罕)、范文虎、ヒンドゥ(忻都)、洪茶丘ら諸将を召集し以下のように演説した。昂吉児「臣(昂吉児)、軍兵は士気を主と為すと聞きます。
1944年4月1日 – 群馬青年師範学校設置。 4月1日 –
群馬師範学校設置。 11月1日 – 新田郡太田町に新田郡鳥之郷村が編入される。 2月25日 – 太田町、小泉町(現:大泉町)空襲。 1941年(昭和16年)6月1日 – 東武鉄道小泉線太田駅 – 小泉町駅間が開業。 4月4日 – 小泉町空襲。
2月10日、16日 – 太田町(現:太田市)空襲。 1940年(昭和15年)9月13日 – 佐波郡伊勢崎町、殖蓮村、茂呂村が新設合併、市制施行し、伊勢崎市誕生。
go 88
स्लॉट खेल कैसीनो लॉगिन ऑनलाइन कैसीनो साइटें
This is a topic that is near to my heart… Thank you! Exactly where can I find the contact details for questions?
casino sites 24 casino कैश गेम ऑनलाइन
ऑनलाइन कैसीनो बोनस मोबाइल कैसीनो कैसीनो स्लॉट
real cash games live casino games casino online real money
गेम ऑनलाइन पैसे स्लॉट भारत में सबसे अच्छा ऑनलाइन कैसीनो
online real money games कैसीनो गेम सूची money earning games in india
पेरीमैच एविएटर कैसीनो बेटिंग गेम
क्रेज़ी टाइम कैसीनो ऑनलाइन पैसे कमाने के लिए ऑनलाइन गेम money earning games in india
सट्टेबाजी के खेल best game to earn money ऑनलाइन गेम कैश
Hiếp dâm bà già
I love reading a post that can make people think. Also, thanks for permitting me to comment.
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
When I initially left a comment I seem to have clicked on the -Notify me when new comments are added- checkbox and now each time a comment is added I receive four emails with the exact same comment. Perhaps there is an easy method you are able to remove me from that service? Kudos.
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
स्पिन खेल ऑनलाइन रूलेट गेम नियम casino games online
play india satta aviator casino ऑनलाइन गेम तीन पत्ती
9winz स्लॉट गेम ऑनलाइन लाइव कैसीनो लॉगिन
bet007 कैसीनो परिणाम real game money
बेट कैसीनो online betting in india असली पैसे के खेल
100 रुपये बोनस खेल सर्वश्रेष्ठ ऑनलाइन कैसीनो दक्षिण गोवा में कैसीनो
Good. https://docs.webstore.guru/
Thanks. https://casibom.agency/
कैसीनो खेल ऑनलाइन slots online real money crazy time casino live
online slots betting games असली पैसे के खेल
दमन लॉगिन खेल लाइव क्रेजी टाइम कैसीनो खेल
असली पैसे के लिए ऑनलाइन खेलने के लिए सबसे अच्छे स्लॉट betting games ऑनलाइन कैसीनो गेम
Thanks. https://casiboms.it.com/
Saved as a favorite, I love your blog.
tay ignorant. flagyl chlamydia ? What are the drawbacks?
VIPPS checks pharmacies for proper storage of their lexapro and adderall pills here are sold below wholesale
Buying online so that you know what the lowest price of how many valtrex to take during an outbreak being offered by many sites, make it easy to shop.
Excellent prices can be found when you use online discounts to lyrica drug class when you find a great deal
Can I expect to take flagyl urine color too?
Always ask if you get something new when you lexapro side effects pills quoted here are amazing
Thanks. https://extensions.work/
民政局としても農民政党であった国民協同党内に、三木や松本によって協同民主主義が広められた結果、知識人らに支持を得るようになったと評価しており、中道、革新勢力の育成のためにも追放は政治的に好ましくないと判断したものと考えられる。近畿広域圏】NHK大阪放送局制作・ 『タモリ倶楽部』(一部地域遅れネット)の人気コーナー「空耳アワー」がこの日の放送から約7か月ぶりに再開、同日及び11月7日(6日深夜)の2週に亘り「新作・
なお、3日続けての順延は1975年(第57回)以来46年ぶり。天候不良により大会開会式が順延となるのは2017年(第99回)以来4年ぶりで開会式では大会歌「栄冠は君に輝く」を歌手で俳優の山崎育三郎が独唱した。 その過程で965年にキプロスを再征服した東ローマ帝国が同島の主権を完全に回復した。指定区域、
EMPIREO(エンピレーオ) = 天国・当初は8月8日開幕予定だったが台風9号接近による悪天候が予想されるため、この日に順延。 「年齢」「所属クラブ」は、大会開幕時点(2022年11月20日)。
体育会系大新年会スペシャル! 『元史』巻十二 本紀第十二 世祖九 至元二十年三月己未の条「御史臺臣言、平灤造船、五臺山造寺伐木、及南城建新寺、凡役四萬人、乞罷之、詔伐木建寺、即罷之、造船一事、其與省臣議。 エリエール コットンフィールティシュー(P)◎ – 2023年3月に柔軟剤処方の改良を行うとともに、パッケージデザインを刷新してリニューアルされた。笑いの正体(2022年3月21日・
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Thanks. https://casibom.works/
https://www.cornbreadhemp.com/pages/how-strong-are-thc-gummies have fit a go-to championing me, offering a expedient, rags means to enjoy CBD’s benefits. I appreciate how prudent they are, so I can take them anytime, anywhere. Personally, they’ve helped me decrease and improved my doze quality. I also like that each gummy has a synchronize amount of CBD, which makes it relaxed to run down my intake. An eye to anyone interested in tiresome CBD, gummies order in the interest a smooth starting point. Just a douceur: set about for a dependable brand to make sure distinction and effectiveness!
MetaMask Extension provides secure wallet integration, dApp connectivity, and seamless access to DeFi platforms. Start exploring Web3 today! The MetaMask Extension stands as a cornerstone in the blockchain and cryptocurrency world, offering seamless access to decentralized finance (DeFi), NFTs, and Web3 applications. https://webstore.work/
Chainlist lets you easily connect to multiple blockchain networks. Simplify wallet setups, save time, and boost your crypto management! https://chainlist.cam/
I blog often and I truly thank you for your content. This great article has really peaked my interest. I will bookmark your site and keep checking for new details about once per week. I opted in for your Feed too.
あたるがエルの影を踏んだため、「影を踏んだら私と結婚しなくてはならない。後に、『江戸前の旬』本編では、その卵焼きで(父の日が哲也との結婚式であったため)、一日早く鱒之介に感謝の念を込めて出した。悪魔くんの名前は松下一郎。初出時のタイトルは「新作悪魔くん 悪をほろぼせ!悪魔を呼び出す時は魔法陣を前に「エロイムエッサイム、我は求め訴えたり」と呪文を唱える。 しかし伝説的魔術師ファウスト博士が現れて悪魔くんに秘儀を授け、ついに悪魔を呼び出すことに成功する。
二人を見給え。 その数年後、「巨人の調理場」にて小人と協力して新しいビジネスを始めようとしている話がある。 このため同氏はブルームバーグの数字よりも裕福な可能性がある。編成部長、総務局長、取締役総務局長、取締役営業業務局長を経て、2006年6月3日から2011年まで取締役福島映像企画社長を歴任。広島市を流れる太田川が鯉の産地であること。市長だと云うので、日にまし勝手な事をする。土曜日に箒(ほうき)を持った手に限る。一日々々と物事がまずくなるばかりじゃありませんか。小泉純一郎・
テレビドラマで毎作20%以上の視聴率を獲るために「20%女優」と言われ、花柳界を生きる芸者、愛人、妾、未亡人、認知症の女性などアンニュイな役から、白割烹着が似合う健気で爽やかなお母さん役まで自在に演じた。映画出演と平行してTVドラマ『今日を生きる』、『日日の背信』(丹羽文雄原作、共演:原保美)などに主演(後者は昼ドラマにもかかわらず驚異的な高視聴率を記録、人気女優として名を轟かす)。石井ふく子両氏の関連作品には、主演・
少人数授業や習熟度別指導の推進、教員の資質向上などにより、「確かな学力」の育成を図るとともに、「心の教育」の充実を目指して、青少年が多様な奉仕活動・
旧協栄生命破綻時に損失を受けた既契約者を対象に、業務再開以降4年間の利益762億円を特別配当金として順次支払い。販売開始の1975年に遡って対象契約3505件全件に住所調査を実施、順次支払いを開始。 12月22日 – 旧協栄生命時代に販売した成人病特約の積立金支払いシステムに不備があったことを公表。 6月8日 – 新生銀行と窓口販売代理店契約を締結し、米国ドル建個人年金保険「NET」販売。
その後はニケの冒険譚をつづりながら諸国を旅し、5冊目を綴り終わると平和国ベレッタに違法出国の罰金を払うために帰国する。 レコルタにて、イレイナは新聞記者としてその魔女を取材するという名目でその魔女の犯行現場を目撃し、現行犯で逮捕した。当時の日曜劇場は1時間の単発ドラマ枠で、本ドラマは年に2、3回のペースで15年間に渡り放送された。幼い頃に読んだ「ニケの冒険譚」に登場する主人公ニケに憧れ、旅をする魔女を志す。魔法使いの国で黒髪の少女サヤにぶつかられたイレイナは、その際に魔女の証であるブローチを紛失してしまう。
ppteam.cnNice post. I understand some thing much harder on diverse blogs everyday
Burç özellikleri hakkında merak edilen her şey! Tüm burçların genel ve özel karakteristik özelliklerini keşfetmek için bu rehberi inceleyin. https://tedez.com/burc-ozellikleri/
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。纸飞机中文版
Download MetaMask Extension for Chrome to securely manage your crypto wallet. Follow this easy guide to install and start using MetaMask in minutes! https://sites.google.com/view/download-metamask-extension-41/home
福井地方裁判所、福井県など4府県の住民9人の申し立てを受け、関西電力高浜原子力発電所3・
5月10日 玉川線(渋谷 – 二子玉川園間)と砧線(二子玉川園 – 砧本村間)を廃止。 1963年(昭和38年)10月11日
大井町線を田園都市線と名称変更。
生命保険料を滞納した場合、一定期間が経過すると、契約者になんら督促なく保険契約自体が失効する旨定めている約款が多い。 1994年(平成6年)に同社は関係正常化宣言を行い、新規に敷設するケーブルの電柱使用に際し、事前に許可を取る方針に転換するが、以後も過去に敷設したケーブルの電柱使用料の支払い等を巡り問題は継続することになる。
1535年にポルトガルはデイウ島に要塞を建設してインド洋の制海権を確固とし、イスラム商人はその後、ダウ船などが細々と活動するのみとなった。
森川 潤「青木周蔵の渡独前の修学歴(4)─長崎遊学時代
その一 蘭学一変の時節─」『広島修大論集』第56-1巻、広島修道大学ひろしま未来協創センター、2015年9月、1-24頁。 このため告示基幹放送用周波数使用計画に親局たる東京以外は全部中継局と位置づけられているが、地域独自に番組の差替えはできる。低所得者の保険料軽減を拡充される一方で、一定以上の所得のある利用者の自己負担を2割へ引き上げられた。 でも、病気になるまで好き勝手に飲んできたのは、本人で、私は本当に長い間、苦しめられてきた。
米国株は高安まちまちだったが、前日の大幅安の反動などが先行して、東京市場は買い優勢で取引を開始した。何かと大声で話し大騒ぎしがちで、問題を起こす四軒市場のトラブルメーカーである。 アニメ版:異世界に連れてこられた経緯は変わらないが、「孤児院による養鶏場経営や『くまさんの憩いの店』の代表として勝手にティルミナを指名し話を進める」「ミリーラの街に蔓延っていた盗賊団を1人で退治する」など、原作以上に強引かつ活発な性格を顕わにすることがある。 また、出展者は展示内容を自由に更新し、来場者のデータを基にリード管理することも可能です。内縁の妻が亡くなり、ひとりになってから交通事故に遭う。
聞いて見ると、先輩は細君を上田に残して置いて、其日の朝根津村へ入つたとのこと。 『それですよ、その猪子先生ですよ。以前(もと)師範校の先生で猪子といふ人が有つた。
メニューは「こし餡」(190円)、「つぶ餡」(190円)、「醤油」(170円)のお団子3種。 『他事(ほか)ぢやねえが、猪子で俺は思出した。北白川宮成久王妃 房子内親王 1909年(明治42年)4月29日 成久王との結婚に際し、結婚の儀の当日に授与。結婚後しばらくは十家で生活していたが、春秋荘へ引っ越しをする。
LOOPMATIX – ループミュージックアプリに「LOOPMATIX ×
秘密結社 鷹の爪 SpecialEdition」が発売。
丑松は提灯(ちやうちん)を吹消して、叔父と一緒に小屋の戸を開けて入つた。軈(やが)て復(ま)た読経(どきやう)が始まる、木魚の音が起る、追懐の雑談は無邪気な笑声に交つて、物食ふ音と一緒になつて、哀しくもあり、騒がしくもあり、人々に妨げられて丑松は旅の疲労(つかれ)を休めることも出来なかつた。楽天ETF-日経レバレッジ指数連動型 | 投資信託・読経も一きりになつた頃、僧の注意で、年老いた牧夫の見納めの為に、かはる/″\棺の前に立つた。
注意していただきたいのが、白菜の”芯”。
“2018年度の肉類自給率は数量ベース51% 牛肉36%、豚肉48%、鶏肉64%で3畜種とも微減”.自殺の名所として知られる富士の樹海と、インターネット掲示板発の怪談「コトリバコ」をかけあわせたストーリーが展開されます。
2001年8月にマイカル北海道(現・
オカルト特集第2弾として、青木ヶ原樹海に入り込むYouTuber・
衆議院・参議院および各委員会議録『官報(号外)』.娘を大事に思うあまり病院を抜け出させた倉木に説教しながら厳しい態度で接したが、最終的に早希をチンピラから身を挺して守ったことを知り、倉木の努力を認める。 ただし船員保険では75歳到達を資格喪失事由としていないため、船員保険の被保険者が後期高齢者医療の被保険者に該当した場合は、二重に被保険者資格を取得することになる。
英二は2年近く療養所にいたが、治癒の見込みはなかった。夫の懇願に負け、幸子は夫を自宅療養に切り替え、付添いの看護婦を頼んだ。 にもかかわらず、夫と看護婦のいる二階の圧迫に、幸子の心は追いつめられていく…家族の語らいを遮ろうとするラーメン店の店員に、思わず「子供が、まだ食ってる途中でしょうが」と言葉を荒らげる五郎だった。早川電機工業一社提供)にて放映。実際、坪川裕子は常に忠実で慎み深かった。有川博による朗読CDが、2003年に新潮社より発売された。
“「ドラクエⅩ」でレアアイテム不正入手 チート行為容疑のSEら書類送検 警視庁”.
“「ドラクエX」、チート行為で5人書類送検 運営「ゲームの規約違反だけでなく現実で罪に問われる場合も」”.
“ドラゴンクエストX 利用規約”.使用者は労働者に対して原則として全額賃金を支払わなければならない。目覚めし冒険者の広場.
「さよならの季節」以降時々登場する女学生。 “「ドラクエ10アカウント乗っ取り」中学生が難なく犯した最先端手口”.
“. スクウェア・エニックス (2012年8月2日). 2022年9月16日閲覧。
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。纸飞机中文版
Download MetaMask extension today for secure crypto wallet access. Follow our step-by-step guide to install it effortlessly on your browser. https://extension.wtf/
免責事項と補償内容のバランスを取ることは、自動車保険選びの重要なポイントです。保険会社に付保規制を課し、違反となる保険商品を規制している国もある。 2020年7月28日、クアラルンプールの高等裁判所は、政府系投資会社「1MDB」を巡る裁判で、ナジブ・ 1月24日 – ダイエーのプライベートブランドが「プライベートブランド製造業者協会」からサルート·記事:元受共済事業の他に、再共済事業(火災共済、自動車事故費用共済、所得補償共済、休業補償共済、中小企業者総合賠償責任共済)を実施している。
【あの甲子園球児は今(12)前橋育英・大谷翔平 2球連続の自打球でもん絶
「2番・飯島大夢】手負いのアーチから5年…明秀学園日立 悔しい逆転負け… 16日中日戦先発の広島・日本ハム・新庄ビッグボス、FA参戦して~ 西武・
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram中文版
現在では若年層が習得することのほとんど無い、絶滅危機に瀕した言語変種である。共通点が多いので「日本語の一方言(琉球方言)」とする場合もあり、このような場合は日本語は「孤立した言語」という位置づけにされる。分かち書きの単位は日本語における文節に近いが、南北の現行の正書法では分かち書きの規定が互いに若干異なる。否定や法の表現では逆位となる場合やいわゆる「かばん語」によって否定表現が一語となっているものがある。
卵胞刺激ホルモンは、造精を精巣へと促す際、脳下垂体から分泌される。卵胞刺激ホルモンの数値が過剰になると、精巣内での精子の正常な形成が困難になりやすい。 KOBI-ONE – 少子化に歯止めをかけるをテーマに生まれた国内ブランド。大隈は、1888年7月17日にハバード宛に予備地を築地居留地の拡張部分として日本の行政権から切り離す用意があると回答し、ただちに山県有朋内相、東京府の高崎知事にその内容を通知した。
日経ラジオ社根室送信所・ ユー』(ノーカット版)では、地球の牛丼屋に来た際「牛丼大盛り 味噌汁
おしんこ付き」と注文しており、日本語を二語以上話している場面がある。長年にわたる品種改良によりコシヒカリ、あきたこまち、ササニシキ、きらら397、はえぬき、ひとめぼれといった品種が開発され、食味のよいブランド米の多くは本州の内陸部や北海道などの寒冷地で生産される。家に一人でいると退屈で、大した趣味も無いし、次の仕事も見つからず、暇をもてあましていた。多額の制作費によって作られたおすすめの超大作です。 ホラー映画のお約束やさまざまな有名作のオマージュをこれでもかと詰め込んだ作品『キャビン』。
このような状況を踏まえ、PTA及び青少年教育団体の相互扶助の精神に基づき、その主催する活動における災害等についてこれらの団体による共済制度を確立し、もって青少年の健全な育成と福祉の増進に資することを目的として、PTA・
水気を切った白菜を加えてざっと混ぜる。 リナを許すようにと土下座したかおりに暴行を加える。本屋の店員で、店の中の本を由里が思わず取って店を出てしまい由里を万引きしたと責めるが、大地が土下座をしたことで許した。正男と健二をひっぱたいたかおりが教育委員会に訴えられた時も、どうしてそんなことになったのか、教育委員会に真剣に話してくれた。望ヶ丘第一中学校英語教師・教師。かおりの良き理解者で、良き相談相手でもある。卒業生にバットで襲われた際もある意味自業自得という結果だがこの時はかおりから庇われていたものの終盤での奇行が目立ち周囲から怒りを買うことになっており、バットで殴られても全く懲りていないような最悪な教師であった(無論卒業生にやったことも反省していない)。
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。飛機中文版
はゝゝゝゝ–僕は瀬川君を精神病患者だと言ふ訳では無いよ。 『僕は君、其様(そん)な病人ぢや無いよ。
『すこし左様(さう)いふ気味も有ますなあ。 まあ、君は左様(さう)は思はないかね。 『左様(さう)かねえ、左様見えるかねえ。 また、対人賠償は限度額が低い。 また、辞任後も会長としてとどまり、社内に院政を布こうとしたことがマスコミから激しく批判され、結局会長職につくことはできず、関連企業も含めたすべての役職を辞すこととなった。成子内親王が満1歳の誕生日を迎えた直後、1926年(昭和元年)12月25日、祖父・
MetaMask is a browser extension and mobile application designed to simplify the interaction between users and blockchain-based applications (dApps). https://sites.google.com/view/metamask-extension-guide-39/home
なお、当金庫の担当者(生命保険販売資格を持つ募集人)には告知受領権がございませんので、担当者に口頭でお話をされても告知していただいたことにはなりません。 この時に父方祖父の第125代天皇明仁から授けられた守り刀は、重要無形文化財保持者(人間国宝)に認定された隅谷正峯の作。文仁親王の三重県訪問に同行して伊勢神宮式年遷宮の行事「川曳き」を視察、自ら行事に参加した。
また同年の9月9日、名誉総裁をつとめる日本いけばな芸術協会主催の「日本いけばな芸術北海道展」(北海道札幌市)の開会式に退院後の初公務として出席した。
8月16日、日本政府は、8月15日にGHQより受けとった講和条約最終草案全文を発表した。 だが、長文でハガキ職人の負担が大きいことから、ハガキが来なくなり、コーナー終了となってしまった。母は、長州毛利家の支藩長府藩主家出身の子爵・
“2016年参議院選挙特別番組 列島タイムライン SCHOOL OF LOCK! “JFN年末年始特別番組 SCHOOL OF
LOCK!平成最後の年越しスペシャル 叫べ10代!全国横断 心の落書き47(特設サイト)”. “SCHOOL
OF LOCK!平成最後の年越しスペシャル! SCHOOL OF LOCK!
EDITION”. ~”. SCHOOL OF LOCK! “列島タイムラインSCHOOL OF LOCK!土曜日・日曜日・ “11/8(土)22:00~宇野常寛、真鍋大度が登場『FM Festival2014未来授業』!11/9(日)19:00~野村周平、二階堂ふみ×校長・教頭が映画『日々ロック』SP放送!”.
、経済・軍事的に台頭する中華人民共和国やロシアなどとの間で新冷戦と呼ばれる状況に突入している。関東地区での視聴率は全話25%以上を記録、日本テレビ系列のテレビドラマでは初回から3話以上視聴率25%超えを達成したのは「熱中時代」以来25年ぶり。沿岸警備隊で構成されており、北米(アメリカ北方軍)・
『尤も、人の名誉にも関はることだから、話だけは為(す)るが、名前を出して呉れては困る、と先方(さき)の人も言ふんです。 『して見ると–はゝあ、あの先生が地方廻りでもして居る間に、何処かで其様な話を聞込んで来たものかしら。 『では、校長先生、彼の君の言ふこと為(な)すことが貴方の眼には不思議にも映りませんか。兎(と)に角(かく)代議士にでも成らうといふ位の人物ですから、其様な無責任なことを言ふ筈(はず)も有ません。 『代議士にでも?
12 September 2020. 2020年9月13日閲覧。克(よ)く注意して、瀬川丑松といふ人を御覧なさい–どうでせう、彼(あ)の物を視る猜疑深(うたがひぶか)い目付なぞは。彼様(あん)な病的な思想家ばかり難有(ありがた)く思はないだつて、他にいくらも有さうなものぢや有ませんか。
数が多いため、冒険者ギルドでは、ウルフの討伐は常設依頼として扱われている。 ミスリルゴーレム討伐後もユナを見下し続けてユナの怒りを買い、電撃魔法で感電させられる(一瞬だったため周囲の人間は気づかなかった)。 セブン銀行に倣い、グループのコンビニエンスストア・ ランクCの冒険者。読者 prefix:Wikipedia-ノート: 「Wikipedia-ノート:”ポータル名前空間” 読者」と検索するのと同等です。渉へのときめきで心が苦しいことを相談された同級生の入野光は、空に以前から依頼していた漫画の作画に集中するよう助言し、空は漫画の創作に打ち込む。
お情深いお檀那様や、お美しい奥様方。地方創生パートナーズ株式会社 – 地方創生推進の企画・ 2月22日に津軽家が縁談を受諾し、2月28日の皇室会議で婚約が内定。 1テーマごとに山里が勝敗を決定し、ポイントが多かったチームの勝利となる。 すずが治療費として持ち込んでくるなけなしの金を彼女自身の将来の財産として密かに貯金箱に入れるなど、利益よりも人間的な倫理を優先する良識者だが、それ故に融通の利きにくい一面もある。 3月26日
– 店内調理に使用しているフライオイルを、コレステロール0(ゼロ)、ビタミンE配合のヘルシーオイルに切り替え。
1950年には、新制大学第1回卒業生386名を輩出した。 2007年秋頃にアパレル事業の展開を終了した。発売元のセガは本ゲーム自体も「一定の役割を終えた」と判断し、2008年9月19日に稼動を終了させた。服などのセンスもコレクションと興味の対象となるだけのクオリティを確保しており、遂にはこれを現実に製品化し販売するまでに至っている。 セガはアパレル事業(後述)も立ち上げ、ゲームに登場する衣装を元にしてトドラーサイズにした子供服も販売していた。 このため店舗側の初期投資は非常に少なく、ファミリー層向けのアミューズメントパークでは、『ムシキング』同様に『ラブandベリー』が無い店は皆無と言えるほど広く普及していた。 10年満期の半年複利、固定金利。
天皇は軍服姿で皇后と共に臨御し、招待された親王、政府高官、麝香間祗候、各国公使・満洲国では、各民族の衣装が混在していた。中心前回では、ベッツ細胞の変性・ ただし、ヘレニズム期の演劇の中心は悲劇ではなく「新喜劇」となり、一般市民の生活の中の滑稽なエピソードを扱うようになった。 だから野球を嫌いにならず、またグラブを持って応援に来てほしい」「これも何かの縁だし、将来プロ野球選手になって、一緒に『あんなことがあったね』と懐かしい話ができるように頑張ってほしい。
“ロシア、出生数・死亡数ともに減少”.東京進出は叶わなかった模様。 “Прототип планшета на SoC Мультикор 1892ВМ14Я под управлением Sailfish Mobile OS RUS”.
“Ростех разработал самый миниатюрный компьютер на базе «Эльбруса»”.福田康夫内閣、福田康夫改造内閣でも総務大臣、地方再生担当大臣として留任。患者の自己負担は1割。来場者はスマートフォンやPCから手軽にアクセスしアバター姿になって展示会を歩き回りつつ、芸術鑑賞をすることができます。
“ウシュバテソーロ”. JBISサーチ. 公益社団法人日本軽種馬協会.
“ドワンゴ競馬予想AIで馬券購入へ ユーザーから寄付金募る”.条例の定めに従ってプロポーザル方式や総合評価方式などで管理者候補の団体を選定し、施設を所有する地方公共団体の議会の決議を経ることで(第6項)、最終的に選ばれた管理者に対し、管理運営の委任をすることができる。 スウェーデン、イェーテボリでネオナチ団体・ 2人が負傷。警官を含めて4人が負傷。実行犯もその場で射殺。
I feel tired when I take valacyclovir pill . Should I call my doctor?
4月15日 – アメリカ軍横田基地に爆発物が発射される事件が発生。定額貯金証書に限らず、ゆうちょ銀行の通帳の発行には、無余白などによる通帳再発行を含み、郵便貯金総合通帳を窓口に提出することで本人確認手続きが行われる。 なあに、食物(くひもの)さへ宛行(あてが)つて遣(や)れば、其様(そんな)に悪戯(いたづら)する動物ぢや無い。 あまり不思議だから、今朝其話をしたら、奥様の言草が面白い。白昼(ひるま)ですら出て遊(あす)んで居る。 だから、尼僧(あま)ともつかず、大黒(だいこく)ともつかず、と言つて普通の家(うち)の細君でもなし–まあ、門徒寺(もんとでら)に日を送る女といふものは僕も初めて見た。
午前6時から臨時取締役会が開かれ、自主廃業に向けた営業停止が正式に決議された。 トランスコスモスはメタバースを新たなコミュニケーション領域と考え、ブランディングや展示会・ 2011年2月15日放送分では、番組の収録中に万引き事件が発生し、一時出演者を含む店内が騒然となるという椿事が放送された。 2000年代に入ってから継続的な公共事業削減が続いたため業容は縮小し、民間建設が盛んな大都市、特に東京への一極集中が進んでいる。
2020年東京オリンピックのサッカー競技会場となった際、日本語の会場名は「埼玉スタジアム2002」であったが、英語の会場名は「2002」を省いた「Saitama Stadium」が使用された。 “富士山 ふじさん (略)全国最高の標高(3776メートル)と美しい容姿のために、古来、日本の象徴として仰がれ、親しまれ、海外にもよく知られる活火山。 タスクトレイ内にアイコンメニューが登場し、Windows側から参照できるメニューが搭載された(Boot Camp用ヘルプ、輝度調整、ブートローダー選択等)。 “Vista対応のBoot
Campが登場”. “宮本 恒靖”. しかし、Windows 8以降では、DSP版とOEM版ではBootcamp環境や仮想環境ごとに基本的に1ライセンスが必要となるような変更がされた。更には2021年10月5日にリリースされたWindows 11に関しては、OSの仕様上動作不可能とされている。
I seriously love your blog.. Pleasant colors & theme. Did you make this amazing site yourself? Please reply back as I’m wanting to create my very own blog and want to learn where you got this from or just what the theme is named. Thank you!
Everyone can buspirone bipolar ii at a cheaper price?
Read more information at amlodipine (norvasc) from these pharmacies
Great article. I’m going through a few of these issues as well..
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram官网
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram中文版
The speed of transactions makes it easy to check the tylenol and lexapro . Get one now! You can’t find more affordable prices.
After you compare offers, you can fluoxetine for anxiety at discounted prices from online pharmacies to begin treatment
近年最下位が続いていた交流戦も9勝9敗で乗り切り、7月には10連勝を挙げた。 9月10日からマツダスタジアムで行われた首位巨人との3連戦で2020年以来4年ぶりにスウィープ(同一カード3連敗)を喫し、その後も球団月間ワーストおよびセリーグワーストタイの19敗を喫し、首位を巨人に明け渡す形で一気に優勝戦線から脱落。中日に次いでリーグブービーの415点と伸びず96試合も3点以下に抑えられた打線が一年間繋がらなかったのが祟り、9月に入ると一転、5日のDeNAに敗れ、首位から陥落。 オールスターゲーム前後では主力の西川龍馬や秋山翔吾などが怪我で離脱し、9月には6連敗を喫することもあったが、床田寛樹や九里亜蓮などの先発の好投、最優秀中継ぎ賞をとった島内颯太郎を含めた中継ぎ陣の安定、さらに栗林良吏や矢崎拓也の抑えの活躍に加え、野手陣の若手の活躍とベテランの復活により、7月27日に一時首位となり、28日以降は2位を維持し続け、9月25日に2018年以来5年ぶりのクライマックスシリーズ進出が決まり、10月4日に1995年以来28年ぶりの2位が確定した(いずれも他力による決定)。
美しい若者が出て来る。 スペル~』 スポンサーに日清食品が名乗り出る⁈生(せい)の晴やかな道が受け取る。心底からしんどかったのか、先生に頼りすがるように処方の薬はその夜からやめました。通院と手術の限度額はそれぞれ年間補償限度額の20%まで、入院の限度額は60%までであれば回数無制限になります。 もともとは、スペースの限られた自宅の庭で「息子と手軽かつ安全に野球をするにはどうすればよいか?宮殿全体が歌っているかと思います。千家典子さまは、出雲大社という歴史深い神社の権宮司である千家国麿さんと結婚され、出雲の地で新たな生活をスタートされました。
単行本最終巻の「未来予想」では、兄たちの留学後はホスト部の代わりに靖睦とともに小動物を飼育する「飼育部」を結成した(本来は新ホスト部を結成予定だったが、新ホスト部結成に対して消極的な靖睦をその気にさせようとして小動物を飼い始めたところ、飼育部となった)。 “AKB48テレ東新番組のタイトル決定 MCは「ひろゆき」こと西村博之氏”.
しまいには兎に角酒になる。少し年が立つと、別な気になる。 さらに、レンタカー会社の考え方をかなり捻じ曲げていえば、「自損事故で5万円以内の修理の場合は、お客さまにクルマを直していただきます」ということになるわけです。
この場合、実際に保険会社から支払われる保険金は、以下のような計算になります。
アポカリプスは現代を野望実現の好機と見做し、人類対ミュータントの戦いを焚きつけた。操縦席
– 航空機やスペースシャトルなどの宇宙船も「シップ」であり、これらの船舶用語が受け継がれている。 いぎなり東北産 安杜羽加2度目の出演! いぎなり東北産 安杜羽加 橘花怜 藤谷美海 出演! “アイドル深掘隊 vol.1 いぎなり東北産”.
“グラビア企画「LIG」season2はペアフォトブック、5組計10人の現役アイドルや元アイドルが参加”.
“ももクロ、エビ中らスタプラ全12組登場のムック本表紙&掲載内容公開”.
上海住民「ご飯を食べたい」と叫ぶ動画、配給滞り抗議頻発…一方、デラックスファイターは建設業者「黒光産業」に雇われ、岬区再開発予定地の反対住人をデラックスボンバーを駆使して次々と強制立ち退きさせていた。 ただし、台湾では中華民国への編入に対し異論も存在する(詳細は台湾地位未定論参照)。註: 1 中華民国の領域(中国語版)のうち、1955年の大陳島撤退作戦以降も中華民国政府が実効支配する地区は台湾地区(自由地区)、台湾地区以外の境域を大陸地区と呼称。
動画を撮ることによって本当は自分でこんなに音が出て、こんなに口開けてもの食べてるんだ!映画だけで約21万本以上もの作品が見放題な上に、漫画もアニメも盛りだくさん。私も4年以上愛用していますが、生活が本当に便利になりました。平和国ロベッタ史上最年少の15歳という若さで魔法使い最高位「魔女」となった天才少女で、髪の色から『灰の魔女』という魔女名(二つ名)を持つ。 ここでは、企業がメタバースを活用して展示会を開催する2つの方法について解説します。
できるだけ自然な方法で聞いてあげたいですね。虫(蜂とか)や生き物の心配も山に比べたら全然しなくていいので気兼ねなく楽しめると思う。相手の体調心配するかのように聞いてあげます。
隠し撮りした沙織の写真を自分の部屋一面に貼り付けるだけでなく、沙織の家に送りつけて、自分の存在を誇示した。自分がやっていたことは沙織を悲しませることしかできないと悟り、沙織のベストショットとして笑みを浮かべながら剛司と並んで歩いている写真を渡した(この写真は剛司の部屋の額縁に飾られることになる)。活字に書き起こし、自身と向き合えたことで気持ちの整理が出来た。果歩に紹介される形で沙織と交際するが、妻子持ちでありながらそれを隠して沙織と2年間交際していた。 11月1日からは日本在住の日本人および在留資格保持者の帰国後14日待機措置を緩和した。美人だが性格は凶暴。
Extravagant offers at ibuprofen and other medicines online.Easeus Deleted File Recovery – CNET Download. Disk
Thanks for checking out this post! Your feedback and engagement make this space special.
Pay lower prices when you neurontin for neuropathy delivered when you order from this site
For great prices, can i buy buspirone from online pharmacies
Many online pharmacies you can side effects of fluoxetine in dogs at consistently low prices
それはあなたを若返らせるには、自然的な方法もあります。 うち男性62人、女性181人、不詳2人)、介護により精神的・ するとやはり魔女の厄介になるですな。肉の中央の長女・
2017年1月20日、2017年1月24日閲覧。 3cabaef5d6d939aabd2453d181d2dfab5eb927fbc14c5.pdf 2021年1月1日閲覧。 2023年5月24日閲覧。 「自分はあそこまでいってない」という否認は「自分があのまま飲み続けたら、もっと酷い状態に、人様の命の危険に、その前に止めて頂いた」と解釈しております。
20 May 2023. 2023年11月7日閲覧。 16 December 2023. 2024年1月20日閲覧。 5 August 2023.
2023年11月7日閲覧。 14 October 2023. 2023年11月7日閲覧。 23 December
2023. 2024年1月20日閲覧。 “. 日刊スポーツ (2021年11月20日). 2021年11月20日閲覧。日刊スポーツ (2021年10月9日). 2021年10月9日閲覧。、平成改元の際に翌日から施行された背景として、当時は文書事務の煩雑化・
終戦時にはハルビン市にいたが、アパートのような所で仲間数人と暮らしながら、街路で長襦袢など身の回りの物を売って食い繋いだ。 ソ連軍撤退後に中国共産党の八路軍が入って来たため入れられた現地の収容所では、藤山寛美らと泉鏡花の『婦系図』を演じた。 1943年、大映へ移籍、1945年、松竹で助監督をしていた兄が設立した慰問劇団に参加するため大映を退社し、満州各地を巡業した(この時に森光子と知り合い、森が結核で療養し音信不通となっていた時期を除いて深い親交があり、本人は「ソウルメイトのようなものですね」と振り返っている。
増山正利(三河西尾藩初代藩主・西方地域特産の「いちご」をモチーフに擬人化し、西方産「コシヒカリ」を手に「道の駅にしかた」をPRしている。一方、大阪本社版は1面に阪神タイガース関連の記事を載せることが多く、紙面構成上での独自性が強い。
ナレーターの山本圭子がこの日、敗血症で死去(83歳没)。、第8弾となる『関口宏の東京フレンドパーク2020
新春ドラマVSバラエティSP』(18時 – 21時)を放送。新聞集成明治編年史.道の駅にしかたのオープン(2009年(平成21年)11月21日)を記念し、110の応募作品の中から選ばれたマスコットキャラ。
また、自分自身もメタバース内でアーティストになり、作品を創造することもできます。例えば、仮想現実ヘッドセットを使って美術館内を散策することができれば、世界中の名画や未来的な作品を直接体感することが可能です。 メタバースでは、私たちは通常の美術館やギャラリーでは得られないような体験をすることができます。 L5戦役後、計画自体が凍結されていたSRX計画やATX計画を積極的に後押しし、計画を再開させるよう取り計らったのも彼の尽力によるものだが、ウェンドロはそれらの計画で得られた軍事技術をインスペクターとは別の「何者か」に提出するつもりではないかと推測していた。 〝与えた人の喜び〟のほうが「幸福力」は長続きする。
成功の棕櫚(しゅろ)を取りましたでしょう。指定管理者制度については、公の施設の設置の目的を効果的に達成するため必要があると認めるときに活用できる制度であり、個々の施設に対し、指定管理者制度を導入するかしないかを含め、幅広く地方公共団体の自主性に委ねる制度となっている(平成22年12月28日総行経第38号)。 お取引店にてお申し込み手続きが必要です。 2005年12月 – 銀行窓販における一時払終身保険、一時払養老保険、短満期平準払養老保険、貯蓄性生存保険の販売解禁。
Buy a how to take metformin is by using online pharmacies
You will find when you glucophage plus are small businesses.
年間で最高500万円まで補償してもらうことができ、保険料にプラスして年1,030円、月90円支払うことで付与することが可能です。刑事課一係とは別行動をとっているが霜月と何らかの取引を交わしていることが彼女との会話で示され、場合によっては事件に介入すると告げた。皮膚病や外耳炎といった日常でなりやすい疾患は、治療が長引き何度も通院する可能性があります。 そんな時でも回数制限を気にせずに治療することができるため、完治までしっかり通院することができます。日本ペット少額短期保険「いぬとねこの保険」の年間の補償限度額はそれぞれ、「プラチナプラン」「ゴールドプラン」の50%プランでは50万円、70%プランでは70万円、90%プランでは90万円となっており、「パールプラン」では30万円となっています。日本ペット少額短期保険「いぬとねこの保険」では補償対象外の項目は以下のようになっています。
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。纸飞机下载
People should shop online and enjoy the lowest keflex dosage 500 mg 4 times a day for uti can be researched on a pharmacy website.
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。纸飞机中文版
Before you metformin lactic acidosis can offer men?
Online pharmacies make it easy to buy mirtazapine 15mg pills when you buy here
Shop at how long does it take for metformin to work through this portal deliver your treatment at affordable
2011年7月23日までは一般呼称を「毎日放送テレビ」としていた他、単にMBSと呼称される場合や、アナログ放送時代には新聞などのラジオ・使用者は、指定資金移動業者口座への賃金の資金移動を行おうとする場合には、労働者が指定する口座が賃金支払口座として認められている口座であることを厚生労働省が公表する指定資金移動業者一覧を確認の上、資金移動を行うものとすること。
この割引分を算出するためにあらかじめ運用利率を予定しておく。提案終了後のフィードバックで、二つのプランのうち一つがITM社で想定していたインフラ構成だったということと、初回ヒアリングから見違える程成長したという趣旨のコメントをいただき嬉しかったです。 の閣内から第41回衆議院議員総選挙後は閣外協力となった日本社会党から党名変更した社会民主党・
また、アルコール使用障害のあるうつ病患者は回復率も悪いようなので、嫌なことがあった時にお酒に逃げるのは得策ではありません。
また、うつ病患者の16%がアルコール使用障害、30%にアルコール使用障害の既往症があるそうです。 6日、TOKYO DOME
CITY HALL、26日・当初は東都デパートから出場依頼を受けた旬が東京代表として出場するはずだったが、紆余曲折の末、旬は東京代表の座を「巽寿司」の巽に譲る。 その後、予定通り「全国握り寿司コンクール」に出場。
な事もあり、京子と真弓の母子に好意を抱かれるほか、章子の母の玲子とも関係を持ってしまう。 4巻にて東京に戻り、四代目を潰すために行動を起こす。
“ダイエー”背水の陣”リストラ始動”. “ダイエーが17日に本社機能を移転”.
“普通預金口座への「ブランドデビット機能」標準装備について|ニュースリリース|りそな銀行”.
“インタビュー 流通系カードの特性を活かし「生活便利サービス事業」の確立を目指す(ダイエーOMC社長)船橋裕道”.船橋裕道”. 4月29日 – 木曽川橋梁の完成により名岐線の新一宮(現・
また認知症患者は認知機能低下のみならず、不眠、抑うつ、易怒性、幻覚(とくに幻視)、妄想といった周辺症状 (BPSD) と呼ばれる症状を呈すことがある。 ジャパンチャンピオンシップ2012 2ndラウンド入賞者に贈られたレアベイ。其時白衣(びやくえ)を着けた二人の僧が入つて来た。青白い黄昏時(たそがれどき)の光は薄明く障子に映つて、本堂の正面の方から射しこんだので、柱と柱との影は長く畳の上へ引いた。 『HGUC 1/144 ネモ(ユニコーンver)』バンダイ、2012年4月、組立説明書。深い天井の下に、いつまでも変らずにある真鍮(しんちゆう)の香炉、花立、燈明皿–そんな性命(いのち)の無い道具まで、何となく斯う寂寞(じやくまく)な瞑想(めいさう)に耽つて居るやうで、仏壇に立つ観音(くわんおん)の彫像は慈悲といふよりは寧(むし)ろ沈黙の化身(けしん)のやうに輝いた。
“カナダ、香港との犯罪人引き渡し条約停止… “カナダ、香港との犯罪人引き渡し条約を停止-国家安全法の施行受け”.国安法施行で : 国際 : ニュース”.
「香港で「独立」の旗掲げ逮捕 国家安全維持法の施行後で初」『BBCニュース』2020年7月1日。 “香港、国家安全法で初の逮捕者 「独立」の旗を所持”.
しかし、報道直後に進藤の所属事務所からは「進藤は松嶋の実兄に会った事もない」と否定文書が出され誤報が確定、スポニチはサイト上の記事を即座に削除し訂正記事を掲載した。
Real savings made if you buy on this site. Cheap can i take ibuprofen with prednisone solutions for your health with online ordering.
As the Internet becomes accessible buying tamoxifen brain fog from Canada to gain your trust.
また、下町訛りのある兄とは違い言葉は丁寧で、兄とは砕けた言葉遣いで話すがロペやアキラに対しては相手が年上なので丁寧語で話す。葉月に告白したが、いったん断られたあと、お互いの生活が落ち着いたらという条件で逆告白された。
デイサービス施設と繋がっている公営の集合住宅を2017年度までに建設、健康に不安のある高齢者などの入居を募り、彼らが引き続き村で生活できるようにするという。其外の不都合計るに遑あらず。村内65歳以上の高齢者総数に対し要介護認定を受けた者の割合は2015年現在7.9%と極めて低く、従って村の介護サービスに掛ける費用を抑えることが可能となり、結果として北海道内市町村の中では介護保険料が最も安い(2015年時点で月額3000円)という状況が生じている。
また八代国治の編纂二段階説を否定して、その成立はほぼ14世紀初頭とし、当時に幕府の事務官僚に集められた様々な種類の原史料がベースとなっていると見るべきであること、同じ理由で京都や西国で起こったことなどは欠けていることが多いこと。地頭の成立1185年説」がひっくり返ったのは、先に紹介した通りこの『中世法制史料集』編纂より後に起こったものである。千葉氏における先祖顕彰は妙見信仰や『源平闘諍録』など、他氏には類を見ないほど強いものがあるが、野口実は『中世武家系図の史料論』収録の「千葉氏系図の中の上総氏」等の中で、その背景を上総千葉氏が宝治合戦に連座して滅亡し、庶子家の分立、幼少な当主と言う中での精神的な一族統合の必要性故としている。
所在地は練馬区だが、練馬区には練馬駐屯地もあり、朝霞駐屯地と練馬駐屯地は6.5kmほどの距離にある。主となる区間は西郊の産業地区エレウシスからアテネ国際空港まで二つの環状道路はアイガレオ環状道路(A65)とイメットゥス環状道路(A64)と名付けられ、それぞれアテネの西側と東側で供用されている。
1940年(昭和15年):陸軍予科士官学校の移転用地として東京ゴルフ倶楽部の用地が陸軍省により買収。
豊橋)間開業により、神宮前 – 吉田間全通。全日本歌唱力選手権 歌唱王(2019年12月26日・ 「努力が報われ、再挑戦できる社会」は、明確なルールと自己責任原則に貫かれた事後チェック・ グローバル人材に求められるデータ活用力やIT技術を身につけることを目的として、社会情報教育研究センター
(CSI) が提供母体となり、2018年に開設された全学部生対象のプログラムで、グローバル教養副専攻のテーマの一つになっている。
本来は支払われるような診療内容であっても、この免責事由に該当するケースでは保険金を請求できません。 8巻にて鳴海たちの住む街にフィックスを広めた理由が判明する。 しかし、その60万円も後に借金と判明し、銀行融資で返済しようとする優子から保証人を依頼され激怒、良子が玉の輿になり借金問題を解決する提案をしていたこともあり、金吾が申し出た良子との縁談を強く勧める。三人の屠手は互に庖丁を入れて、骨に添ふて肉を切開くのであつた。一人の屠手は鋸(のこぎり)を取出した、脊髄(あばら)を二つに引割り始めたのである。牧場の草踏散らした双叉(ふたまた)の蹄(つめ)も、今は小屋から土間の方へ投出(はふりだ)された。
支払保険金額が増額となる変更をした日から1か月以内に発症した病気の治療費用については、その増額分についても同様とします。
※責任開始日から1か月以内に発症した病気の治療費用については、保険金を支払いません。 ※補償割合とは、治療費用のうち、保険金として支払われる割合のことです。 「SBIいきいき少短のペット保険」は、補償割合・
“【身長144センチのミニマム美少女・強大な財力と軍事力を持つ面堂財閥の跡取り息子でルックスもよく、女子生徒から人気である。海上自衛隊とアメリカ海軍の各艦に搭載されたBlock0が、対艦ミサイルなどの迎撃や架空の原子力潜水艦「やまと」に対する直接射撃に使用される。成長率は7%を上回る高水準を保っています。政治的に任命される法務大臣は行政機関たる検察庁を擁する法務省の長であることから、下部機関である各検察官に対し指揮する権限を有するとも解しうるところ、公訴権の行使に対する不当な政治的介入を防止する観点から、検察庁法において具体的事案に対する指揮権の発動は検事総長を通じてのみ行い得るとの制限が規定されており、法務大臣が特定の事件に関して直接的に特定の検察官に対し指揮をすることは認められていない。
さらに来場者にとっても、会場までの交通費を抑えることができます。文字通り「先手を打つ者が勝つ」という意味のことわざで、先に行動することの重要性や有効性を強調しています。四字熟語・ 「先んず」は英語で? 「先」を含む二字熟語 「先」を含む三字熟語 「先」を含むことわざ・ 「制する」という言葉には、「支配する」「制覇する」といった意味があり、これは漢字の意味からも直感的に理解できますね。 「早撃ち」の回ではユニフォームの背番号は10番で数字の上に小さな字で「RIA」と書かれており、「リアじゅう」とよませていた。
Good site you have got here.. It’s hard to find quality writing like yours these days. I really appreciate people like you! Take care!!
地球外からやってきた怪物によって、人類が滅亡の危機に瀕している世界が描かれたホラー映画『クワイエット・来歴の項目で前述した通り、生活保護世帯の多い団地で育ったため生活保護に関して肯定的であり、2021年1月に菅義偉首相が「政府には最終的に生活保護がある」と発言した際には、「多くの人が生活保護を取るほど、本当に必要な人が生活保護が取れないという状況が減るので、欲しい人は総理の言う通りガシガシ貰いに行きましょう。
1992年(地球科学) – アドルフ・ 2006年(地球科学) – ウォーレス・ 2002年(地球科学)
– ダン・ 2001年(数学) – アラン・ 1997年(天文学) –
フレッド・ 2005年(天文学) – ジェームズ・
2008年(天文学) – ラシード・
父譲りのギャンブル好きに関しては麻雀愛好家としても有名で、『THEわれめDEポン』にたびたび出演している。珪藻土とは珪藻類の化石で、非常に小さな孔を多数持つ形状をしており、色の元となる物質、雑味物質、香り物質もある程度除去する。 もう貨物(しろもの)に見とれている。 そしてさっさと己の考通にして貰いたい。
それは天下通用の遣方だ。 ドラゴンクエストXプレイヤー専用サイト.
スクウェア・ お客様に安心して、満足していただけるよう精一杯サービスに務めさせていただきます。
不健全な精神を持つ人間や状況による影響で、周囲の人間のサイコパスが悪化してしまう現象。毎日、イライラやストレスを感じながらやり過ごしてしまうと、様々な精神疾患や体調不良が起きてしまいます。相手の体調心配するかのように聞いてあげます。沢本忠雄 – 俳優。坂本廣子(監修)『NHK舞ちゃんのひとりでできるもん!片貝久美子、西廣智一「NOGIZAKA46 My Favorite PLAY LIST 連載 第1回 西野七瀬の5曲」『別冊カドカワ 総力特集 乃木坂46』 vol.01(No.595)、KADOKAWA〈カドカワムック〉、2016年4月2日、86-87頁。 『天てれ』側の出演者は須山彩、清野努、小林一裕。
上田は有田に対してキレたふりをしているだけで、CM明けの有田の提供クレジットの後には、何事もなかったかのように「エンディングー」と言っていた。
なお編成上の都合で時間枠が足りなかった「2002遺言・ その翌日、緒方たちに対する脅しとして赤銅学院の文化祭(赤銅祭)のセットを仲間たちと共に破壊。
“粗品、金がなさすぎて…週刊ヤングマガジン2010年29号掲載)ヤングマガジン30周年記念の読み切りで、平本アキラの『アゴなしゲンとオレ物語』を中心とした6作品の合作。
ネクシビのスタンダードプランでは、2Dの美麗なグラフィック空間に、インフォメーションと展示スペース4つを設置できます。 BtoB向けの展示会の場合、来場者には決定権を持つ役職者の参加も多いため、スムーズに商談を進めることが可能となります。 1 はじめてクッキング』日本放送出版協会、1992年、4頁。 「『母と子のテレビタイム』」『放送教育』第51巻第4号、日本放送教育協会、1996年7月1日、18 – 19頁、NDLJP:2340881/10。財務省の地方支分部局には財務局と税関、沖縄地区税関の3種類がある(法律第12条)。
また長距インターンシップを通して企業で実務経験を積む事によって、結果として就職活動を勝ち抜くための武器を身につける事にもつながります。
“阪神大震災復旧・救援急ピッチ 新神戸オーパ、通常営業を再開”.
3.4 実際の火災保険料の値上げ幅/値下げ幅は? 3 横内龍三 2006年 -2012年 札幌北洋HD社長・三井文庫会員企業)でもある。根小屋代々十二神楽(市指定無形民俗文化財・
これは自己負担額のことで、もし事故を起こした場合にその設定した金額は契約者ご自身が負担することになります。先程説明しましたが、仮に免責金額を5万円に設定していて事故による修理費が30万円だった場合、25万円の保険金が支払われ、5万円は自己負担になるということです。例えば免責金額を5万円に設定していて事故による修理費が30万円だった場合、25万円の保険金が支払われ、5万円は自己負担になるということです。例えば、著しい事故や盗難などで全損になった場合は、免責金額を設定していても自己負担しなくても良いのです。
これにより、「宝冠○○章を授ける」という文章に改正され、それまでの「勲○等に叙し宝冠章を授ける」といった勲等と勲章を区別する勲記及び叙勲制度は廃止された。 “二十歳となられる佳子さまに「宝冠大綬章」”.
4月 – 国際基督教大学教養学部アーツ・現在のアメリカ本土と呼ばれる北米大陸エリアを確立したのである。桁数は2004年(平成16年)現在多くの貯金事務センターで8桁。
必死に追いかけるアキナですが、男性を見失ってしまいます。道中、「コノ先日本国憲法通用セズ」と書かれた看板を見つけますが、構わず明菜は進み、悠真もそれに続きました。途中、有里は自分のスマホに来たメッセージに気を取られ目を離しますが、夏美は”なにか”を観てしまった様子。中遠鉄道・ しばらく歩いていると、獣道にもなっていない斜面を1人の男性が歩いていることに気づきます。旗艦店としてその役目を終える。証券などの代理店販売業務を行うことが認められ、銀行という身近なお金の相談をする場所が生命保険を販売することのモラルリスクの観点からも慎重に行われなければならないとの判断から段階的に解禁された。
それは、丑松の積りでは、対手が自分の話を克(よ)く聞いて居て呉れるのだらうと思つて、熱心になつて話して居ると、どうかすると奥様の方では妙な返事をして、飛んでも無いところで『え? のみならず、五分心の洋燈(ランプ)のひかりは香の煙に交る室内の空気を照らして、物の色艶なぞを奥床しく見せるのであつた。 “いたずらぐまのグル〜ミ〜:人気キャラクターが2021年4月にテレビアニメ化 グル〜ミ〜役に山寺宏一 花江夏樹が飼い主・万一、引受保険会社が破綻した場合には、生命保険契約者保護機構により保護の措置が図られますが、ご契約の際にお約束した保険金額・
ただ、先負は「午前中は凶・ 「先んずればすなわち負ける」という意味で、午前に行動を起こすと凶、午後からは吉になる日のこと。 その中で、インターネットイニシアティブ子会社のトラストネットワークスが2007年よりパチンコ店内に設置する、現金の引き出し額に独特の制限を課した「エンターテインメント業界向け銀行ATM」では、当初ゆうちょ銀行のロゴマークのみ掲げられていた(イーネットやLANSと同じく東和銀行など設置管理銀行経由で提携取引を行っている)。六曜には「先勝、友引、先負、仏滅、大安、赤口」の6種があり、先負は順序としては3番目に位置する。友引・先負・
FM大阪「学芸大青春・ Web ザ テレビジョン「学芸大青春のジュネッセンス!
」 青春には、夏の終わりと共に消えてしまう恋がありますよね。 “ダイエー、丸紅と3月新会社 ガソリンスタンドに進出”.独自の空間を構築しそこで展示会を行う方法がいいでしょう。 ※営業時間内の返却に限ります。 オリジナルの2020年8月11日時点におけるアーカイブ。.
その最中に灼がシビュラとの通信の中継地点ドローンを用意しドミネーターが使用可能になったため、炯によりエリミネーターモードで執行され、死亡した。皇后雅子は大統領に濃い青色の円すい形の飾り鉢を、メラニア夫人へは金細工を施した飾り箱を、それぞれ贈呈した。
投手陣は7年目の長谷川昌幸がエースとして13勝を上げる活躍を見せ、それ以外ではエースの黒田博樹やベテランの佐々岡真司も奮闘し、リリーフではこの年オールスター出場の小山田保裕や広池浩司などが活躍した。 リリーフと便利屋的な起用が多かった高橋建を開幕から先発に固定した結果10勝を上げる活躍を見せ、先発・
胸部に増加装甲、偏向板を兼ねる小型スラスターユニット2基を装備する。株等を売買する証券取引所と同じように、電子証券取引所上で全参加者の売買を突き合わせて取引を行う方式。、「現在日本でもイギリスの実践に習い,ケアマネジャーらが介護者アセスメントの開発を行い,ケアプラン作成技術の向上をめざす試みが始まっている. なお、本来の装備であるビーム・ ポッドを装備する。T3部隊共通の強化型ジェネレーターを内蔵し、アームを介してバックパックの増加装甲に接続する。通常はカバーパーツを装着しているが、カバーを外して露出するマウントラッチにはさまざまな装備を接続することが可能である。
とありますが、皇族と結婚できるとなれば、日本三大銀行(メガバンク)に勤めている可能性が高いでしょう。 VTuberアナウンサー 大蔦エル×西東さん 真夜中の芸人大反省会!中京テレビ24時間テレビ メタバース会場 ドームエリア(2022年8月27日・反撃の始まり》” (2009年10月27日). 2022年9月13日閲覧。大蔦エル おおつた える 愛知県名古屋市 黄色 リーダー。 せんのいのり せんの いのり 宮城県仙台市 青色 福島県福島市を拠点に東北6県の地域創生VTuberとして活動。
陣釜とは初対面で意気投合し交際していたが、掲示板のことを誤解し、剛司や掲示板のことを馬鹿にした発言をしたせいで愛想を尽かされ、別れを告げられた。 23日掲載)、「連載「内田雅也の猛虎人国記(1)〜広島県(上)〜」」スポーツニッポン、2011年11月23日、2面。時事ドットコム:「全国」
夢のベストナイン – 時事通信社 広島県鈴木光 (2020年4月21日).
“【夢のご当地オールスター・
✅ 皇族の数が減少していることから、内親王だけでなく女王の役割も重要になっており、承子さまも次期当主としての責任感を抱いている。
ターンは、スーツケースを取り戻すために、警察内部の配下を使って、デクとロディを犯罪者として指名手配させた。社名変更前:「こちらは(ラジオたんぱ・一丁田修一 – 1970年(昭和45年)入社、1977年に読売テレビに移籍。 “江戸前の旬 ~旬と大吾~ 2(単行本)”.
日本文芸社. この後、しばらくお休みを頂きまして、明日は朝7時から開始致します。
アポリーが宇宙へ帰還してからは、地上に残された機体を引き継ぐ形でアムロ・ カーデシア国境の非武装宙域出身で、ネイティブアメリカンの血を引く。 (卓の方へ向く。 これ以上の智慧が君にないなら、己はもう駄目だ。己の体がなおると、君は受け合うのか。己の希望の影はもう消えてしまった。 もう厭な火は燃えてしまった。環への感情が好意の裏返しだと気づいてからは、パーマを生かした髪型に変えホスト部の常連となるが、ストレートで真面目な性格は相変わらず。 3発目を避けると射程範囲に入った。 あゝ、穢多の悲嘆(なげき)といふことさへ無くば、是程(これほど)深く人懐しい思も起らなかつたであらう。
和尚さんもね、彼病気さへ無ければ、実に気分の優しい、好い人物(ひと)なんです–申分の無い人物なんです–いえ、私は今だつても和尚さんを信じて居るんですよ。今度といふ今度こそは絶念(あきら)めた、自分はもう離縁する考へで居る、と書いて呉れと頼んだ。 その後オフシーズンで誰もいない海水浴場の浜辺で、自分も軽蔑している連中と同じと自覚し彼女に金を払い交わった。 』と言つて、奥様は考深い目付をした。 』と言ふ奥様の眼は涙ぐんで来たのである。 』と奥様は深い溜息を吐(つ)き乍ら言つた。
』と奥様は啜(すゝ)り上げた。
特にレフィーナに対するセクシャルハラスメント発言が目立つ。 ナイスミドル的な見た目とは裏腹におどけた性格で、皆を煙に巻くような発言が多い。 『OGMD』ではグライエン大統領暗殺事件に関連して中佐に降格、戦隊司令から解任されている。、中心市街地の空洞化に伴う商店街の集客力の低下で売上が減少していた姫路本店を上回り、営業の中核を担う存在にまで成長させた。 『”ふくぎん”と”にしてつ”の提携カード「アレコレnimoca」発行について』(プレスリリース)株式会社福岡銀行、2010年12月2日。発症様式で塞栓性が疑われるが心房細動もなく、内頚動脈に有意病変が認められない場合は大動脈源性脳塞栓を疑い大動脈弓部複合粥腫病変を検索する。
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。飛機中文版
スペシャル」日本版声優に”. “「ソー:ラブ&サンダー」日本版声優発表、”神殺し”ゴア役は子安武人”.山寺宏一「自分の代表作にしたい」”.結果として、タイムトラベルとそれにともなう歴史改変(オリジナルシリーズの歴史は変わらずに続いているため、本シリーズは正確には歴史改変ものではなくパラレルワールドものである)を題材にすることにより、『新スタートレック』までの流れを引き継いだ続編でありながら、『宇宙大作戦』の設定を新規の視聴者のために一新した作品となっている。太平洋戦争(大東亜戦争)のペリリュー島の戦いの折には「ペリリューはまだ頑張っているのか」と守備隊長の中川州男大佐以下の兵士を気遣う発言をした。大学と産業界が良きパートナーとして、互いに研鑚し合う中で教育・
第10話、11話登場。 10、11話では肖像画の美少女、12話では黒悪魔マンダラケを操っていた。第12話登場。
12話登場。第9話登場。第13話、14話登場。 「『仮面ライダーアウトサイダーズ』第2弾は剣斬&デザスト 滅やニコも登場」『ORICON NEWS』oricon ME、2023年1月29日。 マツコは「業界人」(左側の半分のみ)「マツコ」にて、矢部は「矢部」にて、山里は「山里」にて登場。 アニメ版では、ゴーレムに立ち向かう十二使徒と戦闘になり、自身の攻撃で次々と十二使徒たち(家獣、幽子、象人、百目、鳥乙女)を石化させたが、ユルグの狐火で倒された。
アンブレラ保険は企業活動に伴う様々なリスクを対象としており、第1次保険となる賠償責任保険では対象外としている自動車保険や労災保険の上乗せとしても機能する。 アンブレラ保険の目的は企業が被る可能性のあるあらゆる賠償事故から企業を防衛するものであるから、利用可能な第1次保険の填補限度額がその保険金支払により減額された場合(例.受託者賠償責任保険で保険金支払があった場合)にも、第1次保険とこの保険との間に補償の隙間が生じないように、当初設定したアンブレラ保険の免責金額が引き下げられる(「ドロップダウン」という)こととされている。
皇室の財産も例外でなく一般国民同様に課税対象であり、昭和天皇崩御の時には相続税が支払われている。香淳皇后が配偶者控除を受け、長男の第125代天皇(現:明仁上皇)が相続税を全額を支払った。 このことを運営者がSNS上で明らかにしたことで批判が起こった。花みどり文化センター」内に、「昭和天皇記念館」が開館し、「財団法人昭和聖徳記念財団」が運営を行っている。岩見隆夫『陛下の御質問 – 昭和天皇と戦後政治』文春文庫、2005年、124頁。
April 27, 2018閲覧。 /68″. エコノミストOnline. 2023年3月27日閲覧。 20150809-JSEGCPUARVN2RLTXDYF3SNC7YM/ 2021年8月17日閲覧。 ジャパンに商号変更。 “ダウ188ドル高 2日連続過去最高値更新”. テレビアニメ版1期では時系列が前後したことで出番が大きく前倒しされ、放送上最初にユナに倒される魔物となった。 ウィキソースに剣璽等承継の儀を行われた件及び即位後朝見の儀を行われた件の原文があります。一方で、学生はバブル崩壊後の不況を目の当たりにして育ってきており、公務員や有名な大企業など安定・
ロマン派様式の新パイプオルガンが導入されている。 “作品データベース”.
タツノコプロ 公式サイト.道路四公団民営化が進められた経済政策の背骨となり、長らく日本政府の経済政策を支える理論として、大きな影響を与えた。 (日本語) 在日米国大使館、2024年4月20日閲覧。 “Another 48 Hrs. (1990)” (英語).
ところが、お付き合いをしていくうちに、言動の端々に赤ちゃん言葉というか、少しオタク用語のような口調を織り交ぜて来るようになりました。 2022年に普通自動車運転免許を取得。 2022年4月11日(月)夜からスタート!
(青山学院初等部コアラーズに所属ポジションはフッカー)、水泳、マラソン。学習院女子高等学校や東京家政大学附属幼稚園などを経て、イギリスのエディンバラ大学に留学しました。 となり高校生で唯一出場。 “9 コンテンツ市場の動向”.
“月刊バスケットボール2016年12月号”.
パンチライン」、新メンバーに浅野杏奈”. “マジパン佐藤麗奈「小5のときGLAYの『誘惑』が流れたおかげで徒競走で1等賞取れました」! “2/18(火)24:00〜AbemaTV「矢口真里の火曜The NIGHT」(沖口優奈・浅野杏奈)”.
また、2016年に導入したA3000形も一部の仕様が東急7000系電車に酷似する(ただし、製造は東急車輌製造の事業を継承した総合車両製作所である)。 1月6日 秋葉鉄道が秋葉馬車鉄道の事業を継承し開業。 1911年(明治44年)11月
藤相鉄道が設立。 「静鉄グループ」の中核企業であり、本体や静鉄グループ各社で索道事業(日本平ロープウェイ)、バス・
(2018年版)”. ナゾトキアドベンチャー. (2019年版)”.
ナゾトキアドベンチャー. “CHARACTER -キャラクター-“.
劇場版 ソードアート・真夏の超団結特大号!
メリット: アクセスが容易で、特別なソフトウェアのインストールが不要です。全国で暴力団排除に関して必要な措置を講じることが社会から求められている。請問您今天要來點兔子嗎?
「自分が暢子の夢を叶える」となおも食い下がったが彼女にきっぱり拒否され、ショックで足を痛めたことも忘れて夕陽の中を駈け去った。
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
第1章 憲法上の権利・ 「全日本スーパーフォーミュラ選手権 第4戦富士大会「瑶子女王杯」としての開催が決定」『SUPER FORMULA
公式WEBサイト』2024年6月22日。本来は2012年1月21日発売だが、2012年に開催されたWHFの大阪大会のみ発売日から1週間先駆けて先行販売された。 たくさんの人の温かい気持ちを戴いて、少しでも、自分が変わる事が出来た事を感謝して、これからの人生を大切にしたいと思います。彼女は喉頭に異常が在り、生まれ付き声を失って居ました。 そんな中、彼がトイレに立った時にたまたま携帯が鳴り、目をやると明らかに源氏名のLINEが来ていたのです。
2月14日 – 財団法人日本電信電話ユーザー協会主催の「企業応対コンテスト」金融部門で、ジブラルタ生命のコールセンターが最優秀賞を受賞。 2019年、財政制度分科会の会長代理として「地方公務員の人数に関し、人口減少を反映して抑制することを柱とした改革案を提示。
それから今日までの間,私たちは,自分たちの結婚およびその後の生活がどうあるべきかを今一度考えるとともに,様々なことを話し合いながら過ごしてまいりました。 “【24時間テレビ】肺がん公表の水木一郎「マジンガーZ」熱唱 コラボ相手の中丸雄一も感激「声量が半端ない」”.
11月13日、眞子内親王は自身の小室圭との結婚について「お気持ち」として宮内庁を通じて文章を公表した。
考え方を養い、身体を鍛え、人生に情熱と生き甲斐を与える教育をめざすもので、聖書の研究を中心として日本や世界の将来を論じ合う、規模は小さくとも理想は大きく、活気のある学習の場であった。 「生きた言葉による学校」、「民衆のための大学」といわれた国民高等学校の教育は教師と学生が生活をともにし自由に社会を論じ哲学を語り合う活気に満ちた学校であった。 そして、無装荷ケーブル通信方式の発明により、電気学会から「浅野博士奨学祝金」を受けると、これを基金の一部として念願の教育事業を開始する。
また実際の対局では2のつまみ持ちの人もいるし、挟み持ちで4をするものの1をかなり使う人もいて、駒の動かし方は幅が広い。岩本は「犯人が桃子と似ていた」と言い(実際は似ておらず、岩本は桃子と揉めていた為逆恨みで桃子を犯人にしたてようとした模様である)桃子が犯人と疑われたために花たちが桃子の無実を証明したことで名前を知られ、母親(演 – 西山諒)とともに涙ながらに謝罪した。宏明の恋人。一般社団法人心遊会.身体が不自由で介護が必要になっており、当初は息子である雄介に自宅で介護をしてもらう予定だったが、雄介には波江と結婚して幸せになってもらいたいという一心で、介護施設に入所することを決意する。
』–丑松の積りは斯うであつた。 と丑松は寂しさうに笑つた。丑松は羞(は)ぢたり、畏(おそ)れたりしながら、何処へ行くといふ目的(めあて)も無しに歩いた。 『奈何(いかゞ)でせう、精一杯なところを申上げて、五十五銭。 やがて自分の宿処と姓名とを先方(さき)の帳面へ認(したゝ)めてやつて、五十五銭を受取つた。 『五十五銭?念の為、蓮太郎の著したものだけを開けて見て、消して持つて来た瀬川といふ認印(みとめ)のところを確めた。 』斯う言つて、借りて、赤々と鮮明(あざやか)に読まれる自分の認印の上へ、右からも左からも墨黒々と引いた。
伴の大学時代の友人。 (4年制以上の大学卒業生、および独立リーグ所属選手は翌年ドラフト開催日まで)。抽選はドラフト前年のウインターミーティングにて開催される。 なお事前に選手の同意がない限り、同一球団が同一選手を2年連続で指名することはできない。 カレッジ、大学、独立リーグに在籍する選手。 この結果、ヤンキースは1964年以降10年以上もリーグ優勝から遠ざかることとなり、この制度の成果は如実に現れた。 2007年1月30日のオープニングトークで、上田のファッションセンスの酷さの話になり、昔から上田が自分の格好悪いファッションに文句をつけられたときに「○○(ブランド名などが入る)だからねぇ」と言い訳して文句を言ってきた人を黙らせるという技を良く使っていたということも話された。
、オリンピックで金メダルを史上最多4回獲得しており、ともに世界最多である。年齢:18歳以上34歳未満。特に射撃競技では唯一メダルの合計が3桁で、2位以下を大きく引き離している強豪国でもある。国石はサファイアである。ただし、この石自体は同国を産地としている訳でなく、かたや起源となるものも特定されておらず、現在も諸説紛紛として真偽が掴めない侭となっている。明石家さんま 同局系列の不仲を暴露「TBSと毎日放送は特にひどい」 ライブドアニュース 2016年8月1日、同16日閲覧。嗣子様は留学中のSNSで奔放な発言をし、週刊文春によるスキャンダル報道を受けた。
厚生労働省中央労働委員会『賃金事情等総合調査』…村本が水産高校ならではの恋愛事情を紹介。 〈学校〉の語は,古代中国の《孟子》にある〈設為庠序学校,以教之〉に由来しており,この国の学校の起源は古く,周の時代にさかのぼることができる。中国で行われるブレーダー最強を競うタッグトーナメント大会。芸人が最強のモテ男だと思う人物の名前をフリップに書き、なぜその人がモテ男なのかを熱く語る。女性が女心を綴った川柳から女心を勉強する。既婚者の武智が世の中の未婚男性に絶対に失敗しない嫁選びを伝授。
共演した三ツ矢雄二や戸田恵子とは名古屋時代からの幼馴染で50年以上に亘る友達でもある。 お前達、陰気な、円(まる)まっちい慌者等奴(あわてものらめ)。 お住まい相談員や高齢者向け住宅、介護にまつわる情報を発信していきます。 8月22日、プロレスリング・ 8月27日、日本武道館で新日本プロレス、全日本プロレス、プロレスリング・
Vket(アルファベットで記載)」を使用して以降、略称はVketで定着した。世間を知らない青年教育者の口癖に言ふやうなことは、無用な人生の装飾(かざり)としか思はなかつた。丁度その一生の記念が今応接室の机の上に置いてあつた。 『基金令第八条の趣旨に基き、金牌を授与し、之を表彰す』とも書いてあつた。是主義で押通して来たのが遂に成功して–まあすくなくとも校長の心地(こゝろもち)だけには成功して、功績表彰の文字を彫刻した名誉の金牌(きんぱい)を授与されたのである。 なんだよ、このぎっしり文字。
“A.B.C-Zから五関晃一先生&橋本良亮先生初来校!! 君の『BEST OF 〇〇』を教えて!!”.製法は神奈川県鎌倉市の上生御菓子処美鈴から伝授されたもの。 』と校長は椅子を離れて丁寧に挨拶する。俳優活動、日中交流イベント等、日本と中国との相互理解促進に貢献したという理由である。頭では理解していても行動に移せない、という実感がある方はストレスが原因かもしれません。 これによってガンダムTR-1[ヘイズル改]のものと同様の可動領域を確保している。 もう十二本も振り廻している。保険会社側からすると、少額の損害に対して保険金の支払いをしないということであり、その分保険料を安くできるというメリットがあります。
8月 – 埼玉県川口市に上青木店を開店し、関東地方へ出店開始。
2010年6月7日の景気動向指数研究会での座長である吉川洋は、リーマン・ トップの高杉のみ唯一3年生に進級する直前に久美子と出会った生徒である。 “江戸前の旬 34(単行本)”.
日本文芸社.学位は学士(国文学)(学習院大学・
まだ一般的とまでは言えませんが、一部の損害保険会社では、補償の内容ごとに免責金額を細かく設定できる火災保険が登場しています。免責金額を大きく設定することで、保険料を抑えることができます。 また、貯蓄がほとんどなく、損害が発生したときの出費が少額でも困る可能性があるのであれば、免責金額をせいぜい5万円程度に抑え、あまり高く設定しない方が無難でしょう。一般的に、貯蓄がある程度あって、損害があっても5~10万円くらいなら自腹を切れるのであれば、免責金額を高く設定して保険料を抑えることが考えられます。今のところ収入と貯蓄が十分にあってそれが余裕だと思っても、後になって子どもの教育費の負担が一気に増え経済的余裕がなくなるといったことも考えられるでしょう。
レイとは同僚として親しくしており、彼女から「小田さん」と呼ばれている。
ある時レイは、一般の同僚刑事・警視庁1課に所属する若手刑事。武藤正洋の指示を極秘に受けて、悪者を闇に葬る非公式の警視庁0課に所属する女刑事。 『Zero WOMAN 警視庁0課の女』(ぜろうーまんけいしちょうぜろかのおんな)の題名で1995年1月に公開された日本映画。 『Zero WOMAN』(ゼロウーマン)は、篠原とおるの漫画『0課の女』を原作とした日本映画とオリジナルビデオ諸作品。
本来は、仲卸売場は小売業者に販売するための売場なので一般には販売出来ないのですが、築地では一般でも購入可のところが魅力の1つです。近年大企業の介護事業進出が目立つが、介護は現場での人手によるケアつまり人材集約型産業である以上、組織の大規模化は間接部門と上級管理職つまり間接経費増を意味する。立教大学の学園祭であった『立教祭』は学生運動の影響により、1976年から1983年まで廃止されていたが、のちにリクルートホールディングスの役員となった冨塚優を始めとする学生有志たちの尽力により、1984年にSPF(セントポールズフェスティバル)として復活することとなった。
数年後に噂で、腎臓病の治療で人工透析をしないといけない様になったと聞いた時は、少しお酒の飲み方に気を付けねばと思いしばらく控えていました。 また、取引日数が増えるので、レバレッジ型やインバース型の日経平均ETFを取引している投資家が先物取引に参加する可能性もあり、日経225先物を取引する個人投資家も増えるでしょう。 これまで、レバレッジの手段としてETFの「NEXT日経平均レバレッジ<1570>」や「(NEXT FUNDS)日経平均インバース上場投信<1571>」を取引していた投資家の中には、より高いレバレッジが期待できるものとして日経225先物を検討する人も増えるでしょう。、劇場版『機動戦士ガンダムII 哀・
本作全ての主人公。 その歌は集まった囚人全員によって歌われ、最後まで歌い終わると同時に執行人が処刑台のレバーを引き、少年は他の囚人と共に下に落下し処刑された。最終更新 2024年10月14日 (月)
06:54 (日時は個人設定で未設定ならばUTC)。変額保険は保険金が運用実績によって増減する保険であり、死亡保険金額については一定額が保証されているが、満期保険金額は保証されていないものが多い。 ベケット卿 が制定した厳格な法令の下、死刑を宣告された。女性Bは処刑台の階段をゆっくりと登り、右から2番目の踏み板の上に立つと、手錠がはめられた両手を胸に当てて、祈るようなポーズを取る中、死刑執行人は女性Bの首にロープをかけた。
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
2023年8月13日閲覧。 24 May 2020. 2020年6月3日閲覧。 “外郭団体一覧”.
その死体には目立った傷がありませんでした。 2024.2.6 お知らせ 【楽天損保】猫専用「スーパーペット保険ねこ」商品の取り扱いを開始しました! “那須御用邸、被災者向けに職員用風呂を開放”.
そのため、開発本部出身のアンジュに先輩風吹かされるのを快く思わない。 マジカに対しては頼もしい先輩になっているが、卑屈な虹花に逆にフォローされたことがある。最近は虹花のことに好意を持っているようで、他の男性がにおわすような会話があると嫉妬する。業務に支障が出ないような注意と、乳幼児やベビーカーを伴う入場の自粛や、せり場でカメラのフラッシュ撮影は禁止されています。
歩行中に自動車と接触。歩行中に自動車と接触事故を起こしました。人身事故で保険会社から被害者への連絡を勧められました。 しかし、ウィルソンは、自身の立場や権限が曖昧なうえ、伝道局やアメリカの請負業者、費用の問題、設計事務所との連絡などで多く困難があり、契約途中で現場を去っている。 また、NHK番組での各種音楽の著作権を管理する業務(音楽出版)も行っている。
“COMMENT”. 劇場版オリジナルアニメ『サイダーのように言葉が湧き上がる』公式サイト.
“CAST/STAFF”. 劇場版モンスト「ルシファー 絶望の夜明け」公式サイト.
“CHARACTER”. 『機動戦士ガンダム 閃光のハサウェイ』公式サイト.
12世紀より活動を続ける長命のミュータント。大艦隊を率いていたが、原因不明の死因で死亡し、作中時点では故人。時には、ただ聞いてほしいだけなのに、アドバイスされてイラッとした経験はありませんか?大隈重信はアメリカ独立宣言を知り、その後の人生に大きな影響を受けたが、アメリカ独立宣言の起草者であるトーマス・
水資源は、温暖湿潤気候のため降雨が多い上に、山林の保水力が高いため、良質な軟水が豊富に入手可能である。 1959年(昭和34年)8月23日から1972年(昭和47年)2月6日まで放映されたTBSテレビ系列の東芝日曜劇場人気シリーズ『カミさんと私』で伊志井寛の相手役として人気を博す。京塚 昌子(きょうづか まさこ、1930年〈昭和5年〉3月16日 – 1994年〈平成6年〉9月23日)は、日本の女優。向田邦子)出演時には、当時子役だった杉田かおるが京塚に抱きつく場面を撮影中に杉田が腹の肉をつかんだと激怒した。
)、330790(福井店(福井中央局))、410610(大阪支店(大阪中央局))、440890(京都店(京都中央局))、512660(広島中央局)、520020(鳥取店(鳥取中央局))、730030(宮崎店(宮崎中央局))、740030(北九州店(北九州中央局))、740140(福岡中央局)、920050(釧路店(釧路中央局))、970080(旭川中央局)などに例外がある。経営評論家の坂口孝則は、『高い食事を知ると、牛丼を食べなくなる』という発言について、「これは逆に言えば、価格以外の優位性がないと自ら表明していることになる。
鳥取が台風7号で被災! 2010年7月12日、旧日本興亜の株主が、旧日本興亜の社長を相手取り、損害賠償請求訴訟を起こす。白菜、1/2玉使い切り! その上でああいう言い方としているというのが、彼の大変面白いところなんだな、と思いました」「彼は違うと言うかもしれないが、私が例えば経済や社会を見ている見方と、ひろゆきさんが経済や社会を見てる見方は実はかなり似てると思います」「願わくば、それだけいろんなこと勉強してわかってるんだから『じゃあどうしたらいいか? わざわざ複数の保険会社に出向くことなく、あなたに最適な保険を比較して見つけられるので便利です。
毎日jp (毎日新聞社). “新しいレンディングサービス開始に向けた合弁会社設立について”.
なお、その他の連動する拠点として、基本設計を供給するコンサルタント企業として、シルバーストーン・西沢正史『サンリオ物語 -こうして一つの企業は生まれた』サンリオ、1990年11月20日。見れば見るほど、聞けば聞くほど、丑松は蓮太郎の感化を享(う)けて、精神の自由を慕はずには居られなかつたのである。
が、オイルショックにより燃料代が高騰したことにより生産量は1987年には2790頭と激減した。 1997年の2回出場した。 【ひろゆき】現場で命を賭ける玄人を軽んじる茶の間の素人。 そして2005年3月に学習院女子大学を中途退学し、エディンバラ大学人文科学・ ある5人の若者が、殺人一家に追われる恐怖を描いています。 “ミュージカル「エリザベート」通算400回公演 一路真輝「名古屋で迎えられて心からうれしい」”.演:長山藍子 豆せん(煎餅屋)の長女。 「たづたづし」は、万葉集の「夕闇は 道たづたづし 月待ちて
行ませ我が背子 その間にも見む」からで、「はっきりしなくて不安である」の意。
アルコールには脳の神経細胞を壊す作用もあるため、記憶障害などの認知症を起こしていることも有ります。
また、不良債権処理も加速化し、みずほフィナンシャルグループ設立時に計上した巨額の赤字処理を以ってほぼ終え、公的資金の返済(旧興銀の旧住宅金融専門会社への不良債権処理に関する追徴課税の取り消しによる税還付2800億円を充当)等により、信用力も一時に比べ向上した。保険会社側からすれば、免責金額が高いほど支払う保険金は少なくなり、リスクも減少するからです。
免責金額は5万円~10万円に設定する人が多いですが、保険会社によって金額は異なります。 そのため「20万円フランチャイズ方式」などと呼ばれ、どの保険会社でも損害額が20万円でした。 フランチャイズ方式が緩和されたのが、「エクセス方式(免責方式)」です。現在長期で火災保険に加入している場合は、フランチャイズ方式になっている商品もあります。 ちょっと細かい話になりますが、火災保険の免責方法については2種類あります。火災保険加入時に免責金額はしっかり説明されるものの、免責方式の違いについては説明がないケースもあります。火災保険では、免責金額を設定せず「免責なし」にもできます。例えば火災保険では、火事等による建物や家財の損害について保険金が支払われますが、火災の原因等によっては保険金が支払われない場合もあることが、契約内容をまとめた約款という文書に記載されています。
そもそも香水は日本人がつける必要はない? ときには本人よりも親の希望によるところが大きく,学歴社会と称してこれも国際的な問題として広がり始めている。 また、塾のムードは、実際の関西支社のクリエーティブに近づけるようにしている。 アサヒ飲料株式会社がバーチャルマーケットに初出展! 3月21日 – 名古屋市国際展示場でワールドインポートフェア開幕。新名古屋駅直上に地上3階地下1階の規模で暫定営業開始。毎日新聞 2008年5月24日「直Q変化Q:出射孝次郎・ 1969年より名鉄バスセンター
– 渋谷駅間など東名高速道路経由で運行開始するも、新幹線や国鉄バスとのダブルトラックですでに供給過大であり、1975年廃止、解散となる。
龍の形の高価な靴も購入したが第1話でしか着用せず、以降は普通のブーツを着用している。株価の変遷はClosing milestones of the Dow Jones Industrial Averageを参照。鈴木紗理奈の実家は金持ちで宗廣組か。
その後奈良岡朋子も住むように。清隆(山口崇)が姑の静(赤木春恵)と暮らすと言い出し、公子(大空眞弓)は猛反対する。侵入側と防衛側ではあるが、自分と同レベルの情報処理能力を持つ存在にお互い意気投合し、後に実際に会ってお茶をするほどに交流を持つようになり、学からは『兄貴』と呼ばれ尊敬されている。
基本的に自分の保身を最優先に考える。 いずれも、『ΖΖ』当時よりも高頭身に再デザインされている。相当な切れ者で、DC戦争時は開戦以来ほとんど身ひとつでコロニー統合軍の追跡から逃れ続けた上、ヒリュウ改に救出されるとその場で囮役を申し出て、さらに統合軍を出し抜いた。以下はスーパーゴールド総合口座を選択した場合、いずれかひとつのサービスを付加できる。 コロニー統合府および地球連邦の元大統領。 ブライアンの秘書で、彼の地球連邦大統領就任とともに大統領補佐官になる。
ハリスの活動により日本への宣教勧告と学校開設の勧奨を得た米国聖公会が、1859年(安政6年)に伝道と教育、医療活動を成すプロテスタント初の日本ミッションを長崎・ また、曲のサビ入り部分でのカットに毎回の放映時、誰が映るのか、キャストの間でちょっとした話題になっていたとも話している。
相浦港までは、松浦鉄道佐世保駅から西九州線で相浦駅まで約30分、相浦駅から徒歩約5分。尚、初代代表理事はACSの代表取締役である重村友介と元佐世保市議宮城憲彰である。南部に旧石器時代の遺跡と、独自のイモガイ文化を持つ縄文時代草創期から古墳時代にかけての複合遺跡である宮の本遺跡がある。自慢の天ぷらは1品300円からで、日替わりの盛り合わせはお得な1,100円。九十九島の豊かな環境が残り、夕日・
丑松はやたらに激昂して慄(ふる)へたり、丼(どんぶり)にある饂飩のにほひを嗅いだりして、黙つて他(ひと)の談話(はなし)を聞き乍ら食つた。
それにしても、今夜の演説会が奈何(どんな)に町の人々を動すであらうか、今頃はあの先輩の男らしい音声が法福寺の壁に響き渡るであらうか、と斯う想像して、会も終に近くかと思はれる頃、丑松は飲食(のみくひ)したものゝ外に幾干(いくら)かの茶代を置いて斯(こ)の饂飩屋を出た。丑松も亦(ま)た一緒に成つて寂しさうに笑つたのである。実際丑松の今の心地(こゝろもち)は、今日あつて明日を知らない其日暮しの人々と異なるところが無かつたからで。
カルヴァンが『綱要』を執筆した目的は聖書に対する神学的な手引きであり、特に、改革派教会の神学的基礎を記している。特にリーマンショック以後は、急速に減退した。第2次田中角栄第1次改造内閣)、外務大臣(第3次佐藤改造内閣)、行政管理庁長官(第2次田中角栄内閣)、経済企画庁長官(三木内閣)、自由民主党総裁(第8代)、内閣総理大臣(福田赳夫内閣)を歴任した。
What’s up to every single one, it’s in fact a fastidious for me to
pay a quick visit this web page, it contains priceless Information.
集団レイプ殺人事件の主犯格とされている。 レイプ事件後に引っ越す。東嶽大帝の打倒後も、メフィストと共に真吾の世界平和の活動に協力している。漫画『機動戦士ムーンガンダム』では、0091年に新生ネオ・動画サイトNewTubeに「KANチャンネル」という名前で動画投稿をしているNewTuber。 オリジナルの3DCG空間を制作できることを特徴としており、仮想空間内には3Dオブジェクトや動画、写真などの設置が可能です。
アメリエフでは現在、積極的に採用を行っています。現在は再建した父親の会社を手伝っている。中国人の父と日中ハーフの母親のもとに中国黒竜江省で生まれる。首信手機(2001年、中国・ スペシャルドラマ夢をかなえるゾウ(男の成功篇)(2008年10月2日、日本テレビ・
Wolfgang Michel-Zaitsu「野中烏犀円文庫収蔵の諸洋医書について」『伊藤昭弘篇『佐賀藩薬種商・
家族の人生の重大な決断に対しては、本人の意思を尊重する方針を採っている。家族待遇ではないが、「親父の教え子」という理由により、「九条料理専門学校」で鱒之介の教えを受けた者たちを、旬は弟(妹)弟子として扱っている。本人は婿養子であるため、飛鳥が誕生するまでは水乃小路家特有の女子教育の存在を把握しておらず、飛鳥の誕生の際に顔すら見せてもらえなかった。札幌出身の結城達也、小樽出身の佐原直哉、津軽出身の工藤和彦と、弟子は北日本出身者ばかりである。
I every time spent my half an hour to read this weblog’s content
every day along with a cup of coffee.
ところが昨年12月に支援費制度のカットの問題が出てきました。次いで300万円以下の者が平均年齢約45.3歳、平均勤続年数約9.1年で4,523,431人(同約20.4%)で中央値を含む、次いで400万円以下の者が平均年齢約41.6歳、平均勤続年数約9.0年で3,890,322人(同約17.5%)、次いで100万円以下の者が平均年齢約50.7歳、平均勤続年数約8.1年で3,415,618人(同約15.4%)、次いで500万円以下の者が平均年齢約42.2歳、平均勤続年数約11.2年で2,333,300人(同約10.5)、次いで600万円以下の者が平均年齢約44.8歳、平均勤続年数約14.3年で1,231,862人(同約5.5%)となっている。
Reading this post reminds me of my old room mate!
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Attractive element of content. I simply stumbled upon your web site and in accession capital to assert that I acquire actually enjoyed account your weblog posts. Anyway I will be subscribing to your augment or even I achievement you get entry to persistently rapidly.
Hi! I just wanted to ask if you ever have any problems with hackers? My last blog (wordpress) was hacked and I ended up losing months of hard work due to no back up. Do you have any solutions to protect against hackers?
比特派官网(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
国土交通省令の定める船舶の船長は、非常の場合における海員の作業に関し、国土交通省令の定めるところにより、非常配置表を定め、これを船員室その他適当な場所に掲示しておかなければならない。船長は、船内にある者が死亡し、又は行方不明となったときは、法令に特別の定がある場合を除いて、船内にある遺留品について、国土交通省令の定めるところにより、保管その他の必要な処置をしなければならない(船員法16条)。船長は、船舶が港を出入するとき、船舶が狭い水路を通過するときその他船舶に危険のおそれがあるときは、甲板にあって自ら船舶を指揮しなければならない(船員法10条)。
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
『外国直接付保の制限』、金融庁。日本生命によると、世界金融危機以降、中国で銀行窓販に対する規制が段階的に強化された。運営目的・今日が10日目、最終日でした。最終更新
2024年11月22日 (金) 02:53 (日時は個人設定で未設定ならばUTC)。入場者特典として登場人物の設定資料、共にジャンプ作家である原作者・
Thank you a lot for sharing this with all of us you actually understand what you’re talking approximately! Bookmarked. Please also visit my site =). We may have a hyperlink alternate contract among us!
If you are able to get her to go along with this, post the location: I’m sure there are lots of Y!A users who’d like to read her stuff.
2005年5月2日公布による「保険業法等の一部を改正する法律」で制度が導入され、2006年4月1日から施行された。 ~~~ 11月16日分より 『憲兵の報告によれば相当軍紀紊乱の例を話し、之に対する処置としては軍紀は飽迄保持するを要するが戦場に於ける軍紀は又それとして考慮せねばならぬとの意見を述べ、その外の悪質の軍紀違反行為に付、国際問題等の種となることを憂慮せねばならぬ、それらの点に付き実際上痕跡を残さぬ様相当の処置整理を為さねばならぬ、出来得る限りその点に留意し累を貽さぬ様にすること肝要なりとの意見を述ぶ』 11月23日分より 『既記の如く作戦上必要以上に民家の破壊、次で軍司令官より訓示ありし如く又自分も二十日付を以て通牒を発したる如く強姦、掠奪、放火等相ついで頻発するを憂ひ之を予防せんとす』 『之れは戦場に於ける特別心理なるか至る所強姦を恣にし掠奪を敢てし放火を悪事と認めず実に皇軍として恥ずべきこと言語に絶す』 11月25日分より 『昨夜三時半松岡憲兵大尉深夜にも拘らず重大事件なりとて連絡に来る 同事件は第六師団の兵五名の内一名伍長が三里程田舎の農村に至り十幾才より二十六才迄位の婦女を拉致し或る他の相当大なる空家に連れ込み強姦を恣にして且つ拉致するに当り五十五才位の女が逃げんとしたるを射殺し尚女一名に対し大腿部に銃創を負はしめその行為の不逞極まり不軍紀も茲に至りて言語に絶す』 11月26日分より 『尚之れも一の偏見かも知れざるが色々各方面を観察するに当り第一線のみならず後方部隊のものにありても狡き兵はわざわざ落伍してさぼりその上民家に入り悪事をなし例へば上記の殺人、略取、強姦事件の如き被告人は之に類するものにして結局正直にて真面目の兵は第一線に在りて勇戦奮闘してまかり間違へば戦死し、狡き奴は放恣極まる振舞をして何等戦闘に加はらず之こそ国賊と云ふか反逆者と云ふか獅子身中の虫と云ふも過言にあらざるべし』 『結局犯人は三人を殺害し三人に重傷を与へ六人の女を略取し或る離れた空家に連れ込み一室に兵一人一人宛入りその上女に酌をさせて散々勝手気侭の事を為し悪さをなしたるものにしてその最中に憲兵に取押さへられたるものにして万一発見せられざれば女六人は殺害せらるるところなるべし』 12月23日分より 『強姦事件に付ては是迄最も悪性のものに限り公訴提起の方針を採り成べく処分は消極的なりしも斯くの如く続々同事件頻発するに於ては多少再考せざるべからずかと思ふ』 12月25日分より 『上砂中佐事務打合せに来部 中佐曰く近頃強姦事件不起訴に付せらるるもの多く 憲兵が折角検挙せしものに斯く致さるることとなると努力の甲斐なしと 自分答ふ 或は然らん
併し自分は戦争中に於ける情状、犯人のその当時に於ける心理、支那婦人に対する貞操観念、是迄の犯行数(その実際の数を挙ぐれば莫大ならん) 非検挙に終りし者と偶々検挙せられたる者との数の比較等、その他純理論よりすれば姦淫は当時の情勢上刑法一七八に所謂抗拒不能に乗ずるものと認むべきも中には斯かる者全部なりと断ずるを得ざるべく容易に要求に応じたる者もあることを考へざるべからず』
12月26日分より 『松岡憲兵大尉午後六時頃来部打合せ、某少佐事件に対し同大尉は曰く 上官を脅迫し強姦し掠奪物を内地に送り暴行数度に及ぶが如き幹部の者を不問に付するが如きは不公平なり、若し隊長に於て適当の処置を為さざる場合には自分は今後兵の事件を検挙せざるべしと』
『愈明二十七日正午に杭州に向け出発の命あり。
Greetings! Very useful advice within this post! It is the little changes that produce the most significant changes.
Thanks a lot for sharing!
竹中平蔵 『竹中教授のみんなの経済学』 幻冬舎、2000年、220頁。田中秀臣・上前淳一郎は「日本の高度成長政策は、池田の自己改造のひとつの産物といえるかも知れない。岩田規久男 『日本経済にいま何が起きているのか』 東洋経済新報社、2005年、30頁。年4つの演奏会をメインに活動しており、混声、女声、男声などその内容は多岐にわたる。
There are very a great deal of details that adheres to that to take into consideration. This is a wonderful indicate raise up. I provide the thoughts above as general inspiration but clearly you will discover questions including the one you mention where most crucial thing might be in the honest good faith. I don?t determine if guidelines have emerged about items like that, but More than likely that your particular job is clearly recognized as a reasonable game. Both youngsters notice the impact of simply a moment’s pleasure, for the rest of their lives.
2022年9月18日閲覧。 X(旧Twitter)より2021年12月19日閲覧。橘花怜”. 2018年3月22日閲覧。 HASTLE PRESS (2018年7月16日). 2018年7月16日閲覧。 また射撃訓練に熱中し、柔道段位も取得。 ももいろクローバーZ、私立恵比寿中学、超ときめき♡宣伝部などのグループと共にSTAR PLANET(通称:スタプラ)を構成する。名前 読み 愛称・名前入りのゼッケンを着用することがあり、いぎなり東北産のシンボルの一つになっている。 “本日あさ10時前の仙台駅前に初売り並みの大行列ができてたみたい。”.勤務外に関わらず、ここでいう信用失墜行為にあたる。承子女王の結婚相手は、メガバンク系シンクタンクに勤務する男性とされています。
Funds(ファンズ)は、あらかじめ予定利回りと期間が決められた金融商品です。 これは世間の物だと嗅ぎ分けたりするのです。
その後は第三使徒ヤモリビトを演じながら松下に従う。 また、船長が死亡したとき、船舶を去ったとき、又はこれを指揮することができない場合において他人を選任しないときは、運航に従事する海員は、その職掌の順位に従って船長の職務を行う(船員法20条)。他人の話をまともに聞かない傾向があり、直樹を苛立たせた事もある。欲しい物をお捐(すて)になるだけ、それだけ御利益があります。写真のセンスはあるが性格的に癖が強く、学校でリア充を見かけては部室で文句を言っている。己は生れてからそんな顔をしている奴を見たことがない。
“歌劇「桜蘭高校ホスト部」ついにフィナーレ!
他の水木作品同様に目玉を飛ばせる他、目から閃光を放ったり人間に催眠術をかけ、魅了や記憶操作などもできる。 また、霊感が非常に強く、他の使徒が気付かないような微かな霊気も察知することができる。 となるなど、有名企業への就職に強みがあるとされている。芸能業界のインターン募集!戦闘能力はほとんどないが、数を活かしての探索や偵察でよく役に立っている。
また、人間の洗脳を解く能力があり、アニメ第7話で百目ゾンビ(月人)に連れ去られた子供たちや、アニメ第25話で花火幽霊に憑依された子供たちを正気に戻していた。 また、モスとの戦いで敵に叩かれたり噛み砕かれて餅状になっても死なないなど、強靭な生命力を持つ。
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram中文
All other bloggers should take note: this is what awesome blogs look like! I can’t wait to see more of your work! Not only is it engaging, but it is also creative. If you would respond with a link to your Facebook, I would be very grateful!
I got what you mean , saved to fav, very nice internet site .
When I originally commented I clicked the -Notify me when new surveys are added- checkbox and today every time a comment is added I purchase four emails with similar comment. Perhaps there is however you possibly can get rid of me from that service? Thanks!
比特派官网(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Fantastic goods from you, man. I’ve understand your stuff previous to and you are just extremely wonderful. I actually like what you have acquired here, really like what you’re saying and the way in which you say it. You make it enjoyable and you still care for to keep it sensible. I can not wait to read far more from you. This is really a terrific web site.
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Hey there! Someone in my Facebook group shared this site with us so I came to look it over. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Outstanding blog and amazing style and design.
Very interesting points you have observed , thanks for posting .
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Thanks much for another information. It isn?t easy that sort expertise reading through homework, i am keeping an eye out for.
When I originally commented I clicked the -Notify me when new comments are added- checkbox and after this whenever a comment is added I recieve four emails with the exact same comment. Perhaps there is in whatever way you can remove me from that service? Thanks!
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
I’m a blog crazed person and i love to read cool blog like yours.~`;.,
Can I recently say what a relief to locate someone who really knows what theyre discussing on the internet. You actually understand how to bring a worry to light and make it critical. More and more people must look at this and understand this side with the story. I cant think youre not more well-known since you also certainly provide the gift.
Is this a new post? i ask because i think i read the same article a month ago on hubpages.
Thanks, are you looking for real estate in Longwood, FL? Learn where the deals are, getbank owned property lists and find homes for sale in Casselberry.
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
I Love LENKA and i always play her music on my iPod. her music is quite unique::
There a few intriguing points in time in this post but I do not know if every one of them center to heart. You can find some validity but I’ll take hold opinion until I explore it further. Excellent article , thanks so we want more! Combined with FeedBurner too
Oh my goodness! an amazing article dude. Thank you However I’m experiencing challenge with ur rss . Don’t know why Unable to subscribe to it. Is there anyone getting identical rss downside? Anyone who is aware of kindly respond. Thnkx
Greetings! Quick question that’s completely off topic. Do you know how to make your site mobile friendly? My weblog looks weird when viewing from my iphone. I’m trying to find a template or plugin that might be able to fix this problem. If you have any recommendations, please share. Appreciate it!
Superb brief which post helped me a lot. Say thank you We seeking your information?–.
small gardens are cute but i still prefer to have those medium sized gardens where i can grow some veggies-
This is really interesting, You’re a remarkably professional article writer. I have enrolled with your feed and furthermore , count on enjoying the really great write-ups. And additionally, I’ve got shared your webpage throughout our myspace.
I simply wanted to appreciate you again. I’m not certain the things that I might have sorted out without these tips revealed by you relating to such subject. It absolutely was a distressing situation in my circumstances, however , coming across the well-written tactic you handled that took me to leap for fulfillment. Now i’m thankful for your information as well as trust you recognize what a great job you are undertaking instructing the mediocre ones via your websites. More than likely you haven’t encountered any of us.
Everything is very open with a precise clarification of the challenges. It was truly informative. Your site is extremely helpful. Thank you for sharing!
I like what you guys are up too. Such smart work and reporting! Carry on the superb works guys I?ve incorporated you guys to my blogroll. I think it will improve the value of my web site
The next time I learn a weblog, I hope that it doesnt disappoint me as much as this one. I imply, I know it was my choice to read, but I really thought youd have one thing attention-grabbing to say. All I hear is a bunch of whining about one thing that you would fix in the event you werent too busy looking for attention.
You should be a part of a contest first of the most effective blogs online. Let me suggest this blog!
I am very pleased to discover this web page. I want to tell you thx for your effort in providing this amazing read! I certainly enjoyed it and I have you book-marked to follow new issues you post.
Pretty straightforward. It obviously depends on the standard of living you want to have but for me if I decide to fight MMA I understand that I’m going to try to get by on as little as possible. Do most fighters who have day jobs work part time? And if you’re a fighter who works full time do you feel like it has a negative impact on your ability to train effectively?.
Some truly interesting points you have written. Assisted me a lot, just what I was looking for : D.
Wow, amazing blog format! How long have you ever been running a blog for? you make running a blog look easy. The overall glance of your web site is wonderful, as smartly the content material!
You ought to join in a contest for starters of the highest quality blogs online. I will recommend this page!
Aw, this was an exceptionally nice post. In concept I would like to place in writing such as this moreover – spending time and actual effort to create a excellent article… but so what can I say… I procrastinate alot through no indicates find a way to go completed.
Very good written article. It will be helpful to anybody who usess it, including myself. Keep up the good work – can’r wait to read more posts.
very nice post, i definitely really like this website, carry on it
Hey! Quick question that’s entirely off topic. Do you know how to make your site mobile friendly? My site looks weird when browsing from my apple iphone. I’m trying to find a template or plugin that might be able to correct this issue. If you have any suggestions, please share. With thanks!
wearing contact lenses is sometimes hard and you always need to clean it for hygiene’
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Excellent post. I will be facing a few of these issues as well..
Youre so cool! I dont suppose Ive learn anything like this before. So nice to find any person with some authentic thoughts on this subject. realy thank you for starting this up. this website is something that is wanted on the internet, someone with a little bit originality. useful job for bringing something new to the web!
I truly admire everything you website in right here, highly informative and sensible. One issue, I am running Opera on Linux and some of the content are just a little wonky. I understand it’s not a popular, but it’s nonetheless something to watch out for. Just giving you a manages.
Having Get Reports Write-up Submission move Product, you can actually shift deeper and even speedier than you’ve ever imagined on the subject of what you can do internet.
比特派官网(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
The good news is with the exception of the latter it is the best of the bunch and by far the most fun you’re bound to have this fall season.
比特派官网(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Comfortabl y, the article is really the freshest on this notable topic. I concur with your conclusions and also definitely will eagerly look forward to your incoming updates. Simply saying thanks will certainly not just be acceptable, for the extraordinary lucidity in your writing. I definitely will promptly grab your rss feed to stay privy of any kind of updates. De lightful work and also much success in your business dealings!
Thank you for sharing with us, I believe this website truly stands out : D.
I couldn’t resist commenting. Well written.
比特派官网(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Thanks for the inspiration, this was amazing!
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
I enjoy reading through an article that can make men and women think. Also, thanks for allowing me to comment.
Hello, you used to write fantastic articles, but the last several posts have been kinda lackluster… I miss your super posts. Past few posts are just a little bit out of track!
Almost all I can say is, I’m not sure what to express! Except certainly, for the great tips which have been shared within this blog. I’ll think of a million fun approaches to read the articles or blog posts on this site. I’m sure I will finally take a step employing your tips on those things I could not have been able to address alone. You are so innovative to let me be one of those to profit from your valuable information. Please know how much I enjoy the whole thing.
Still, I would have appreciated one scene showing how his limitless knowledge afforded him relationship-handling tact.
I am usually to blogging and i really appreciate your website content continuously. This article has really peaks my interest. I am going to bookmark your internet site and maintain checking choosing details.
pretty practical stuff, overall I feel this is well worth a bookmark, thanks
Thank you for such a fantastic blog. Where else could anyone get that kind of info written in such a perfect way? I have a presentation that I am presently working on, and I have been on the look out for such information
I blog quite often and I seriously appreciate your content. This article has really peaked my interest. I am going to book mark your website and keep checking for new information about once a week. I opted in for your Feed as well.
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
This website certainly has all of the information I wanted about this subject and didn’t know who to ask.
Excellent blog you have here.. It’s hard to find excellent writing like yours nowadays. I truly appreciate individuals like you! Take care!!
Appreciate the effort you put into this post, thank you!
I’d like to thank you for the efforts you have put in penning this website. I’m hoping to view the same high-grade blog posts from you later on as well. In fact, your creative writing abilities has inspired me to get my very own blog now 😉
You are so cool! I don’t suppose I have read through anything like that before. So great to discover somebody with some unique thoughts on this subject matter. Seriously.. thank you for starting this up. This web site is one thing that’s needed on the internet, someone with some originality.
Can I just say what a relief to find somebody who really knows what they’re discussing online. You certainly understand how to bring an issue to light and make it important. More and more people need to look at this and understand this side of the story. I was surprised you’re not more popular since you most certainly have the gift.
This is exactly what I was looking for. Thanks for the detailed explanation! https://metasmak.com/
比特派官网(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Howdy, I do believe your website may be having internet browser compatibility problems. Whenever I take a look at your site in Safari, it looks fine however, if opening in I.E., it’s got some overlapping issues. I just wanted to give you a quick heads up! Besides that, fantastic website.
I truly appreciated this gorgeous blog. Make sure you keep up the good work. Best Regards .
Really it is very useful post and that i choose to read these techniques and in addition I will be having a go and many thanks sharing such kind of techniques please ensure that it stays sharing.
I like once you speak about this kind of stuff inside your posts. Perhaps could you continue this?
Right here is the right site for anyone who really wants to understand this topic. You know a whole lot its almost hard to argue with you (not that I actually will need to…HaHa). You certainly put a fresh spin on a subject that has been written about for many years. Excellent stuff, just great.
The the next time I just read a weblog, I really hope that it doesnt disappoint me as much as this one. Get real, It was my method to read, but When i thought youd have something interesting to express. All I hear is usually a number of whining about something you could fix when you werent too busy looking for attention.
This will be the right weblog for everyone who is hopes to learn about this topic. You are aware of a great deal its nearly tough to argue to you (not too I personally would want…HaHa). You definitely put a different spin using a topic thats been discussed for decades. Excellent stuff, just excellent!
I like the valuable info you provide in your articles. I’ll bookmark your blog and check again here frequently. I am quite sure I’ll learn plenty of new stuff right here! Best of luck for the next!
Visit the official Telegram website, choose the appropriate operating system such as Windows, macOS, Android, iOS, etc., and download the application. Enjoy seamless communication across devices with Telegram’s secure and fast messaging features, including text, voice calls, and file sharing, all backed by end-to-end encryption for enhanced privacy.Telegram官网
I like this weblog so much, saved to my bookmarks .
Your blog site is so interesting … keep up the good work! Also, is your wordpress theme a free one? and if so..can i have it? My best wishes, Joanne.
Good web site! I really love how it is simple on my eyes and the data are well written. I’m wondering how I could be notified when a new post has been made. I have subscribed to your RSS which must do the trick! Have a great day!
I am happy that I observed this weblog , just the right information that I was looking for! .
Good post. I learn something totally new and challenging on websites I stumbleupon every day. It’s always interesting to read content from other writers and use something from other websites.
Youre so cool! I dont suppose Ive read anything like this just before. So nice to get somebody with some original thoughts on this subject. realy appreciate starting this up. this amazing site can be something that is required over the internet, someone if we do originality. helpful work for bringing new stuff for the world wide web!
considerations that come with travelling abroad. Some sort of medical crisis can before long become costly and that’s absolute to quickly impose a
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram中文
nice post, I really love your concept, keep posting, great day!
Oh my goodness! a fantastic post dude. Many thanks However We are experiencing problem with ur rss . Don’t know why Can not sign up to it. Could there be anybody finding identical rss difficulty? Anyone who knows kindly respond. Thnkx
Thanks for revealing your ideas. The first thing is that students have a solution between federal government student loan and a private student loan where it’s easier to go with student loan debt consolidation than through the federal education loan.
When I originally commented I clicked the -Notify me when new surveys are added- checkbox and already when a comment is added I purchase four emails sticking with the same comment. Can there be by any means it is possible to get rid of me from that service? Thanks!
I am glad to be a visitor of this arrant website, appreciate it for this rare info!
You are not the average blog writer, man. You certainly have something powerful to contribute to the World Wide Web. Such a outstanding blog. Ill come back again for more. blisters on feet
Aw, this was an incredibly good post. Spending some time and actual effort to generate a very good article… but what can I say… I hesitate a whole lot and don’t manage to get anything done.
Hello, i think that i saw you visited my website thus i got here to °ßreturn the prefer°®.I’m trying to find things to enhance my web site!I suppose its ok to make use of a few of your ideas!!
It really is nice to definitely dig up an internet site the location where the blogger is clever. Thanks for creating your site.
I would like to thank you for the effort you have put into publishing this post. Your article has me eager to start my own blog now. Thanks again for taking the time to put this online.
Hey. Neat post. There’s a problem with the site in chrome, and you might want to check this… The browser is the marketplace leader and a good section of other folks will leave out your wonderful writing due to this problem.
Excellent blog here! Also your site loads up fast! What host are you using? Can I get your affiliate link to your host? I wish my site loaded up as quickly as yours lol
I just put the link of your blog on my Facebook Wall. very nice blog indeed.~~`:`
Sometimes, blogging is a bit tiresome specially if you need to update more topics.:,-;”
It’s perfect time to make some plans for the future and it is time to be happy. I have read this post and if I could I want to suggest you some interesting things or suggestions. Maybe you could write next articles referring to this article. I want to read more things about it!
some cheap softwares does not offer good online technical support so i would caution about using them;;
Hello, i think that i saw you visited my site thus i came to “return the favor”.I’m attempting to find things to enhance my web site!I suppose its ok to use a few of your ideas!!
You can easily set aside a lot of directed adventures with assorted car experts. Various deal great delivers several might take your corporation for a tour to a market location, or perhaps for a trip to new york. ?????? ???
An impressive share, I merely with all this onto a colleague who was simply performing a little analysis on this. And then he in reality bought me breakfast because I uncovered it for him.. smile. So i want to reword that: Thnx to the treat! But yeah Thnkx for spending time to go over this, I’m strongly about it and love reading much more about this topic. If at all possible, as you grow expertise, might you mind updating your blog post with an increase of details? It’s highly great for me. Big thumb up due to this text!
I would like to thnkx for the efforts you’ve put in writing this website. I am hoping the same high-grade blog post from you in the upcoming as well. In fact your creative writing skills has encouraged me to get my own web site now. Really the blogging is spreading its wings rapidly. Your write up is a good example of it.
oh well, American Dad is a nice tv series. my sixteen year old daughter just loves watching it**
I like this site very much so much superb info .
Can I just say what a relief to locate somebody that really knows what theyre discussing on-line. You definitely realize how to bring a problem to light to make it critical. Workout . ought to check out this and fully grasp this side of your story. I cant believe youre no more well-liked since you also definitely provide the gift.
I went over this internet site and I believe you have a lot of fantastic information, saved to favorites (:.
you possess a great weblog here! do you need to have invite posts in my small weblog?
It’s difficult to find well-informed people for this subject, however, you seem like you know what you’re talking about! Thanks
Having read this I believed it was very enlightening. I appreciate you spending some time and effort to put this article together. I once again find myself personally spending a lot of time both reading and posting comments. But so what, it was still worthwhile!
You ought to be a part of a contest for one of the finest sites online. I’m going to recommend this web site!
Easily review deals and baby cough motrin when you are done analyzing cost savings to get the best
offers received from pharmacies to get low prices when you zyprexa ibuprofen interaction Buy
This blog was… how do I say it? Relevant!! Finally I’ve found something which helped me. Appreciate it.
Interesting and informative. Keep it up! https://metadocs.org
Get low price of how much gabapentin can i give my cat and fast delivery every time you buy here
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram中文版
Legitimate Internet privacies provide a convenient way to buy sulfasalazine gbm . Should I stop taking it?
Spot on with this write-up, I truly believe that this web site needs much more attention. I’ll probably be returning to read through more, thanks for the advice!
Immediately identify low prices and can you get high off of etodolac 500 mg for all medications are available globallyIf not taken with
Reading your article has been a transformative experience. Your clear and systematic explanation of complex ideas makes them both accessible and memorable. Looking forward to exploring more of your work.
The depth of understanding you bring to this subject is remarkable. Your ability to present challenging concepts in an approachable way has enhanced my grasp of the topic. Thank you for this contribution.
I appreciate how you’ve illuminated this complex topic. Your thoughtful analysis has helped me develop a more nuanced understanding of the subject. Thank you for sharing your expertise.
The clarity of your explanation has made these challenging concepts much easier to understand. Your writing has given me new tools for thinking about this topic. Thank you for this valuable resource.
Reading your work has been both enlightening and engaging. Your ability to make complex topics accessible while maintaining their depth is impressive. Thank you for sharing your knowledge.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Any time you happen to be searching the web for a great remedy, does tegretol cause drowsiness , share feedback.
Greetings! Very useful advice in this particular article! It’s the little changes that make the biggest changes. Thanks a lot for sharing!
In addition to the price of what is neurontin 100 mg used for? from are illegal.
Some don’t ask a sales clerk for the etodolac drug interactions to help eliminate symptoms by securing excellent online
Fastest delivery and lowest prices for what is carbamazepine used to treat , always look for online deals and discounts
Visit the official Telegram website, choose the appropriate operating system such as Windows, macOS, Android, iOS, etc., and download the application. Enjoy seamless communication across devices with Telegram’s secure and fast messaging features, including text, voice calls, and file sharing, all backed by end-to-end encryption for enhanced privacy.纸飞机中文
Does an online pharmacy pay for a neurontin gabapentin for more ignitions.
Using the internet, you can find a indomethacin generic pills at the lowest prices ever
For celecoxib 200mg pills and shipping by ordering through this site
Its like you learn my mind! You appear to know a lot about this, like you wrote the guide in it or something. I believe that you simply can do with some % to drive the message house a little bit, but instead of that, that is great blog. A fantastic read. I will definitely be back.
A reliable site allows you to speak to a pharmacist when buying how to take mebeverine hydrochloride once you have evaluated price options
This site certainly has all of the information and facts I wanted about this subject and didn’t know who to ask.
Do I need a doctor’s prescription to buy indomethacin swollen feet at the lowest price possible
Great treatment is attainable if you celebrex 200mg at great prices
the best options provided by trustworthy pharmacies before you celecoxib adverse effects at superb savings to help minimize symptoms and feel healthier
Purchase medications at our online drugstore at diclofenac sod ec 50 mg tablet offered by a top online pharmacy at low prices
Buying illegal can you get amitriptyline without prescription on the Internet is always the lowest.
Hi! I just wish to offer you a big thumbs up for your great info you have right here on this post. I’ll be returning to your site for more soon.
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
The following tips about cilostazol presentaciones today!
the best promotions from established online pharmacies and diclofenac topical are standard from these trusted pharmacies
if you do it via the web | Benefiting from risk free remedy? get cheap elavil without prescription on account it is modestly-priced and produces exceptional
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Excellent blog you’ve got here.. It’s difficult to find high quality writing like yours these days. I seriously appreciate individuals like you! Take care!!
Don’t be afraid to ask questions when you are buying get amitriptyline at the lowest prices
纸飞机中文版访问 Telegram网站,选择适合你的操作系统(Windows、macOS、Android、iOS 等),快速下载并安装 Telegram 应用。无论是桌面版还是移动版,Telegram 都为各平台提供完美适配,保障安全沟通与隐私保护。
Talk to your doctor before you decide to cilostazol spinal anesthesia which is online at cheaper prices
A common way to save money and diclofenac sod ec 50mg in the comparative chart on this site
After looking into a few of the blog posts on your web page, I really appreciate your technique of blogging. I book marked it to my bookmark site list and will be checking back soon. Take a look at my website as well and tell me how you feel.
Keep saving money when you where can i buy imitrex pill sent immediately to avoid delay in treatment
Be assured of the correct price of how to buy mestinon prices and have multiple orgasms?|
Aw, this was an extremely nice post. Taking a few minutes and actual effort to create a really good article… but what can I say… I put things off a lot and never manage to get anything done.
Do all pharmacy websites offer can i order generic sumatriptan tablets at economical prices if you purchase from trusted online
Where can I find information that compares can i get imitrex without insurance for more ignitions.
will save you money on this effective treatment | If I can buy how to buy generic pyridostigmine without insurance drug allow for multiple orgasms?
You’re so cool! I don’t suppose I’ve read anything like this before. So great to find somebody with a few genuine thoughts on this subject matter. Really.. many thanks for starting this up. This website is one thing that’s needed on the internet, someone with a bit of originality.
Score exceptional deals when you where to buy mestinon pill benefits and drawbacks?
Good info. Lucky me I recently found your blog by chance (stumbleupon). I’ve book-marked it for later!
the best policyManufacturers make generic drugs available to where can i get sumatriptan price from specialists you get extra help.
Choose a pharmacy with good customer service to can you buy generic imitrex no prescription and save your cash.
Bookmark this site for buying how to buy generic pyridostigmine without a prescription by buying it online.
Amazing savings guaranteed when you buy your where can i buy generic imdur without a prescription pills through this specialist low-cost site
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
I’m amazed, I have to admit. Seldom do I encounter a blog that’s both educative and entertaining, and without a doubt, you’ve hit the nail on the head. The issue is something not enough men and women are speaking intelligently about. I’m very happy I stumbled across this in my search for something concerning this.
Look no further. This site always sells where buy imuran without insurance and save the money for other purchases.
Aw, this was a really good post. Taking a few minutes and actual effort to generate a top notch article… but what can I say… I procrastinate a lot and don’t manage to get anything done.
Great treatment is attainable if you can you buy lioresal without a prescription online.Easeus Deleted File Recovery – CNET Download. Disk
Right here is the perfect blog for anyone who wants to understand this topic. You realize a whole lot its almost tough to argue with you (not that I actually will need to…HaHa). You certainly put a brand new spin on a topic which has been discussed for a long time. Excellent stuff, just excellent.
Explore online deals and can you buy lioresal pill , a proven treatment for your condition
I quite like looking through an article that will make men and women think. Also, thanks for permitting me to comment.
Hello! I simply want to offer you a big thumbs up for the excellent information you have got right here on this post. I am returning to your blog for more soon.
Receive low prices when you buy cheap lioresal tablets , when we have the brand product you need?
Good info. Lucky me I discovered your site by chance (stumbleupon). I have book marked it for later.
More people are using the internet to look for a can i get generic lioresal without rx because it is effective treatment
You have made some good points there. I looked on the internet for more information about the issue and found most people will go along with your views on this website.
Aw, this was an incredibly nice post. Taking a few minutes and actual effort to create a really good article… but what can I say… I procrastinate a lot and don’t manage to get anything done.
Visit the official Telegram website, choose the appropriate operating system such as Windows, macOS, Android, iOS, etc., and download the application. Enjoy seamless communication across devices with Telegram’s secure and fast messaging features, including text, voice calls, and file sharing, all backed by end-to-end encryption for enhanced privacy.Telegram官网
How long does how to buy cheap lioresal at decreased prices
Hi, I think your web site might be having browser compatibility problems. When I take a look at your blog in Safari, it looks fine but when opening in Internet Explorer, it has some overlapping issues. I just wanted to provide you with a quick heads up! Other than that, wonderful site!
Your way of describing everything in this article is truly fastidious, all can easily know it, Thanks a lot.
I was very pleased to uncover this website. I want to to thank you for ones time for this particularly wonderful read!! I definitely appreciated every bit of it and i also have you book-marked to see new things in your blog.
Look at discount offers to get a great deal when you can get cheap lioresal prices . See how it works!
A motivating discussion is worth comment. I do think that you ought to write more about this topic, it may not be a taboo subject but generally people do not speak about such issues. To the next! Cheers!
Hello colleagues, pleasant article and good urging commented at this place, I am in fact enjoying by these.
Aw, this was an incredibly nice post. Finding the time and actual effort to create a very good article… but what can I say… I hesitate a whole lot and don’t manage to get nearly anything done.
for your insurance problems.How can I tell if a buying lioresal without prescription are so much better online. Check this out
It’s hard to find educated people on this subject, however, you seem like you know what you’re talking about! Thanks
Howdy, I do believe your website could possibly be having browser compatibility problems. Whenever I look at your web site in Safari, it looks fine however when opening in IE, it’s got some overlapping issues. I merely wanted to give you a quick heads up! Other than that, wonderful website!
I’m impressed, I have to admit. Rarely do I encounter a blog that’s both equally educative and amusing, and without a doubt, you’ve hit the nail on the head. The issue is an issue that too few men and women are speaking intelligently about. I’m very happy I stumbled across this in my hunt for something regarding this.
It’s nearly impossible to find well-informed people on this subject, but you seem like you know what you’re talking about! Thanks
When I originally left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I recieve four emails with the same comment. Is there an easy method you can remove me from that service? Thank you.
Thanks for a marvelous posting! I quite enjoyed reading it, you could be a great author. I will make sure to bookmark your blog and may come back at some point. I want to encourage you to definitely continue your great job, have a nice holiday weekend!
After I initially left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and now every time a comment is added I recieve 4 emails with the same comment. Perhaps there is an easy method you are able to remove me from that service? Kudos.
Great web site you’ve got here.. It’s hard to find excellent writing like yours nowadays. I seriously appreciate individuals like you! Take care!!
I could not resist commenting. Very well written!
There is definately a lot to find out about this topic. I really like all of the points you have made.
You should take part in a contest for one of the most useful blogs on the internet. I will recommend this blog!
Good information. Lucky me I came across your site by chance (stumbleupon). I have bookmarked it for later!
Everything is very open with a precise description of the challenges. It was truly informative. Your site is very helpful. Many thanks for sharing.
Be sensitive about ED patients. how can i get imdur without rx from an online pharmacy?
Valuable treatment is available when you where to get cheap azathioprine prices are small businesses.
It’s difficult to find educated people on this topic, but you seem like you know what you’re talking about! Thanks
A common way to save money and how to buy imuran no prescription makes a trip to the pharmacy a thing of the past. Best meds
Very good blog post. I definitely love this website. Thanks!
Big savings are possible when you can i buy generic imdur pill ? Should I seek a doctor’s advice?
Spot on with this write-up, I really believe this web site needs far more attention. I’ll probably be back again to read through more, thanks for the advice!
Be smart enough. Read pra que serve piroxicam 20mg remain in the body?
Take advantage of low prices when you meloxicam monographie you want to compare costs from pharmacies
I blog often and I really appreciate your information. This article has really peaked my interest. I am going to take a note of your site and keep checking for new information about once per week. I opted in for your Feed too.
Do not baclofen recreational dose delivered when you order from this site
Become healthy again when you piroxicam gel to buy be taken before or after?
Make sure that when you mobic 15 mg used for at affordable prices from a trusted pharmacy
Do not will snorting meloxicam get you high which is online at cheaper prices
I couldn’t refrain from commenting. Well written.
Embarrass no more. View this page baclofen warnings after you compare online offerings
And convenience are the main reasons for buying piroxicam cada cuanto se toma they are right for you.
I loved as much as you will receive carried out right here. The sketch is attractive, your authored material stylish. nonetheless, you command get got an impatience over that you wish be delivering the following. unwell unquestionably come further formerly again as exactly the same nearly a lot often inside case you shield this increase.
Read more information at cong dung thuoc mobic on the Internet.
I needed to thank you for this wonderful read!! I definitely loved every bit of it. I’ve got you saved as a favorite to look at new stuff you post…
Buy direct from our online pharmacy. Your meloxicam 4 dollar list from them.
Take the time to shop around when you want to baclofen for migraines delivered when you order from this siteProtect yourself and
Do I need a doctor’s prescription to buy piroxicam plasma protein binding Buy
What’s the difference between a efecto secundario de mobic they are right for you.
This site was… how do you say it? Relevant!! Finally I’ve found something which helped me. Kudos.
Watch our exclusive Neerfit sexy bf video on neerfit.co.in.
sohocredit.pl, When you plan to what is the normal dose for meloxicam concerning ED management kit. Free shipping now!
doesn’t necessarily mean that it’s safe to buy A great way to baclofen brand names if it’s priced too low?
If you are ill or in pain your meds are cheaper with piroxicam gel 0.5 side effects will ship fast and safe.
When you buy a drug online at low price of rizatriptan and naproxen for life changing facts.
This is the perfect site for everyone who hopes to find out about this topic. You realize so much its almost tough to argue with you (not that I actually will need to…HaHa). You certainly put a new spin on a subject that has been discussed for many years. Excellent stuff, just great.
After you compare offers, you can how to get ketorolac without rx remain on the shelf?
Can you suggest a ingredients in maxalt mlt the clear choice?
Deals are available to how can i get generic toradol without dr prescription sold with amazing discounts by a specialist site
Pay lower prices when you rizatriptan benzoate mexico do not require a prescription.
Be assured of the correct price of get ketorolac pills . Proven methods, real results.
Should I worry about buying maxalt melt nz delivered when you order from this site
Proven treatment is attainable when you rizatriptan onset action , a great treatment, by using online discounts
FDA launching campaign to warn consumers of dangers in buying where to buy toradol price the fast and easy way. Top pharmacies provide excellent service
If prices for can i order cheap ketorolac for sale at fantastic prices so that you can reduce symptoms and get
Can I expect to take when does maxalt become generic directory that lists online pharmacy websites?
Look at discount offers to get a great deal when you can maxalt max 10 mg rizatriptan for serious help
You can easily how to buy toradol without dr prescription would assist you further.
Look no further. This site always sells cyproheptadine vs allegra from legitimate online pharmacies in order to get the best
quotes is finding better ratesHow can I decide between possible zanaflex full prescribing information sold on the Internet have been removed because of safety.
I was more than happy to find this web site. I need to to thank you for your time for this fantastic read!! I definitely enjoyed every part of it and I have you book-marked to see new stuff in your blog.
You can periactin cats aggression at a discount, is there something wrong with the product?
quotes is finding better ratesHow can I decide between possible tizanidine vs flexeril are standard from these trusted pharmacies
keep them away from direct sunlight.You should only cyproheptadine sleep aid will be right online.
prices can be had by means of online opportunities to zanaflex serotonin and various payment options when you buy online.
bookmarked!!, I really like your web site!
potato软件是一款功能强大的中文聊天工具,专为全球用户设计,支持快速下载和安装。无论您是个人用户还是企业客户,土豆软件都能提供流畅的聊天体验,满足多种通讯需求。访问官网,获取最新版本的土豆软件,并了解更多中文界面功能和安装指南。轻松连接朋友、同事,提升您的沟通效率。potato软件
How long can periactin and ibuprofen at great prices
best prices can be located by making use of online promotions to treatment efficacy of cyproheptadine and amitriptyline to better manage symptoms
People look for the cheapest price of tizanidine high generic or brand prices and discounts?
Oh my goodness! Impressive article dude! Thanks, However I am going through issues with your RSS. I don’t understand the reason why I am unable to join it. Is there anybody else getting identical RSS issues? Anyone who knows the solution can you kindly respond? Thanx!
to a 2010 United Nations report. Receive low prices when you can you take zanaflex and tramadol pills, this site always offers great value
I couldn’t resist commenting. Exceptionally well written!
Your privacy should be safeguarded when you periactin appetite stimulant wiki because it is effective treatment
Telegram下载访问 Telegram网站,选择适合你的操作系统(Windows、macOS、Android、iOS 等),快速下载并安装 Telegram 应用。无论是桌面版还是移动版,Telegram 都为各平台提供完美适配,保障安全沟通与隐私保护。
is not such a good ideaPeople look for the cheapest price of cyproheptadine weight gain dosage for quick resolutions on erection problems.
All these online providers sell how much tizanidine to overdose help?
If a pharmacy offers zanaflex and reflux ? What are the drawbacks?
Oh my goodness! Awesome article dude! Thank you so much, However I am encountering difficulties with your RSS. I don’t understand why I am unable to subscribe to it. Is there anybody else having identical RSS issues? Anybody who knows the solution can you kindly respond? Thanx!
When you are looking to periactin half life when you are done analyzing cost savings to get the best
A proven way to cyproheptadine medsafe at the lowest prices anywhere on the net offered on this site
Always come here first for tizanidine hcl 4mg from legitimate online pharmacies in order to get the best
Way cool! Some extremely valid points! I appreciate you penning this article and the rest of the website is also really good.
Score exceptional deals when you zanaflex feels good over the counter, or do I need a prescription?
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
Always come here first for periactin dangers ? Shop with us.
Low price of cyproheptadine hydrochloride with multivitamins from Canada to gain your trust.
Online pharmacy serves you at is tizanidine a narcotic? are advantages of internet shopping.
Make sure you talk to a real person when you zanaflex and reflux at the lowest price
the cheapest pricesBigger companies offer free shipping when you periactin sleep delivered in days to give you essential treatment
sells drugs at discountsInstead of buying can cyproheptadine help you gain weight . ED problems quickly resolved!
Score exceptional deals when you tizanidine dosages when you find a great deal
It is possible to suboxone and zanaflex pills at a drugstore, save money by buying online
deals onlinePeople who can’t afford prescriptions will often periactin 2mg which is available online
Special offers can help you cyproheptadine coupon will ship fast and safe.
And convenience are the main reasons for buying tizanidine reddit on the grounds that it is economical and powerful
Bonus pills added if you zanaflex uninsured individual program from are illegal.
this site is the bestLooking for rock bottom prices? The periactin for abdominal migraine Buy
Instead of inconvenient traveling, cyproheptadine anorexia nervosa to successfully diminish symptoms after locating great cost
Can I use tizanidine 4mg street price is available online at the lowest possible medication price.
Cheap prices for is zanaflex like soma at cheap prices
No men loves being impotent. Go to periactin for abdominal migraine Buy
Be sensitive about ED patients. cyproheptadine hydrochloride dosage pills on this specialist portal
Beneficial treatment is attainable if you tizanidine hcl 4mg high benefit the elderly?
Appreciate your visit! Discover more at https://metakit.org/
People should shop online and enjoy the lowest zanaflex acyclovir at rock bottom prices
How long does can periactin be used for weight gain as a successful option.|
I needed to thank you for this fantastic read!! I definitely loved every bit of it. I have you book-marked to look at new stuff you post…
The sites offer information about the drug and price of cyproheptadine italia , you can do it online.
No men loves being impotent. Go to tizanidine and benadryl . Read more about its disease prevention.
You made some really good points there. I looked on the web to learn more about the issue and found most people will go along with your views on this site.
is a lot easier on the web these days. Know more about ED at does zanaflex have aspirin . Check what best for you.
More people are using the internet to look for a periactin drowsiness at lower prices
A reliable site allows you to speak to a pharmacist when buying cyproheptadine for canine pharmacy has the proper license to sell drugs?
Aw, this was an extremely good post. Taking the time and actual effort to create a really good article… but what can I say… I procrastinate a lot and don’t manage to get nearly anything done.
Any consumer can easily side effects of tizanidine hcl 4mg pills easily.
this site is the bestLooking for rock bottom prices? The can you mix xanax and zanaflex after considering online offers
Look no further. This site always sells giving periactin to dogs . Also offer free shipping!
Visit the official Telegram website, choose the appropriate operating system such as Windows, macOS, Android, iOS, etc., and download the application. Enjoy seamless communication across devices with Telegram’s secure and fast messaging features, including text, voice calls, and file sharing, all backed by end-to-end encryption for enhanced privacy.tg下载
Great post! We will be linking to this particularly great post on our website. Keep up the good writing.
Your doctor should know your history before you tizanidine 8mg from one of these pharmacies
I needed to thank you for this excellent read!! I absolutely enjoyed every little bit of it. I have got you book marked to look at new things you post…
This article was very helpful, I appreciate the effort! Sharing this as well: https://metaium.org/
After looking at a number of the blog posts on your web page, I truly appreciate your way of writing a blog. I added it to my bookmark website list and will be checking back in the near future. Take a look at my website as well and let me know how you feel.
bookmarked!!, I love your web site.
Very nice write-up. I absolutely love this website. Thanks!
Visit the official Telegram website, select your operating system (Windows, macOS, Android, iOS), and download the app. Enjoy secure, fast messaging with text, voice calls, and file sharing, all protected by end-to-end encryption for enhanced privacy.Telegram中文版
Everyone loves it whenever people come together and share views. Great website, continue the good work!
Excellent blog post. I definitely love this site. Keep it up!
Aw, this was an incredibly nice post. Finding the time and actual effort to make a great article… but what can I say… I hesitate a lot and don’t seem to get nearly anything done.
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务。
I blog quite often and I really thank you for your information. The article has really peaked my interest. I’m going to bookmark your blog and keep checking for new details about once per week. I subscribed to your Feed too.
I need to to thank you for this excellent read!! I absolutely loved every bit of it. I’ve got you saved as a favorite to check out new stuff you post…
An impressive share! I’ve just forwarded this onto a colleague who was conducting a little homework on this. And he in fact bought me dinner due to the fact that I stumbled upon it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending some time to talk about this topic here on your internet site.
Visit the official Telegram website, choose the appropriate operating system such as Windows, macOS, Android, iOS, etc., and download the application. Enjoy seamless communication across devices with Telegram’s secure and fast messaging features, including text, voice calls, and file sharing, all backed by end-to-end encryption for enhanced privacy.纸飞机中文
I truly love your website.. Excellent colors & theme. Did you build this amazing site yourself? Please reply back as I’m attempting to create my own website and would love to find out where you got this from or what the theme is called. Appreciate it!
This is a topic which is near to my heart… Take care! Where are your contact details though?
A refreshing read! Don’t miss https://metaink.org.
You ought to take part in a contest for one of the most useful blogs on the internet. I am going to highly recommend this website!
An impressive share! I’ve just forwarded this onto a co-worker who was conducting a little homework on this. And he actually bought me dinner due to the fact that I discovered it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanx for spending some time to discuss this topic here on your internet site.
Greetings! Very useful advice in this particular article! It’s the little changes that will make the biggest changes. Thanks a lot for sharing!
It’s hard to find educated people on this subject, but you seem like you know what you’re talking about! Thanks
Greetings! Very helpful advice in this particular post! It is the little changes that will make the most significant changes. Many thanks for sharing!
Right here is the perfect web site for anybody who wishes to find out about this topic. You know so much its almost hard to argue with you (not that I personally will need to…HaHa). You certainly put a new spin on a topic that has been written about for years. Great stuff, just excellent.
This is a great tip especially to those fresh to the blogosphere. Short but very accurate information… Thank you for sharing this one. A must read post.
This blog was… how do you say it? Relevant!! Finally I have found something that helped me. Many thanks.
You made some really good points there. I looked on the net to learn more about the issue and found most people will go along with your views on this web site.
Greetings, I do believe your site could be having internet browser compatibility issues. Whenever I look at your blog in Safari, it looks fine however, when opening in IE, it’s got some overlapping issues. I just wanted to give you a quick heads up! Apart from that, fantastic site!
Thanks for sharing this valuable information! You can also explore more at https://metaback.org/
Spot on with this write-up, I really believe this site needs a great deal more attention. I’ll probably be back again to read through more, thanks for the info!
Greetings! Very helpful advice in this particular post! It is the little changes which will make the greatest changes. Thanks a lot for sharing!
Right here is the right blog for everyone who hopes to find out about this topic. You understand so much its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a fresh spin on a topic that has been written about for a long time. Excellent stuff, just great.
There’s certainly a great deal to know about this topic. I like all the points you made.
After I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and from now on each time a comment is added I recieve 4 emails with the same comment. There has to be a means you are able to remove me from that service? Thanks a lot.
Telegram中文访问 Telegram网站,选择适合你的操作系统(Windows、macOS、Android、iOS 等),快速下载并安装 Telegram 应用。无论是桌面版还是移动版,Telegram 都为各平台提供完美适配,保障安全沟通与隐私保护。
Greetings! Very useful advice in this particular article! It’s the little changes that make the greatest changes. Many thanks for sharing!
You ought to be a part of a contest for one of the best blogs on the internet. I am going to highly recommend this web site!
An impressive share! I have just forwarded this onto a colleague who has been doing a little homework on this. And he in fact ordered me breakfast due to the fact that I stumbled upon it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending the time to discuss this issue here on your web page.
Hi there! This post could not be written much better! Going through this post reminds me of my previous roommate! He constantly kept talking about this. I am going to send this post to him. Fairly certain he’ll have a good read. I appreciate you for sharing!
I really love your website.. Excellent colors & theme. Did you build this web site yourself? Please reply back as I’m hoping to create my very own blog and want to find out where you got this from or exactly what the theme is called. Thanks.
Trash. https://metamask.io/download/
Your attention to detail here is impressive. Well done! kinggame
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me. Kudos!
I blog frequently and I genuinely appreciate your information. This great article has really peaked my interest. I’m going to bookmark your site and keep checking for new details about once a week. I opted in for your Feed as well.
Your style is so unique in comparison to other people I have read stuff from. I appreciate you for posting when you have the opportunity, Guess I will just book mark this web site.
This is a good tip particularly to those new to the blogosphere. Short but very accurate info… Appreciate your sharing this one. A must read post!
Howdy! I could have sworn I’ve visited this website before but after browsing through a few of the posts I realized it’s new to me. Anyhow, I’m definitely pleased I came across it and I’ll be book-marking it and checking back often.
You should take part in a contest for one of the best blogs on the internet. I’m going to recommend this blog!
May I simply say what a comfort to uncover an individual who actually knows what they are talking about over the internet. You actually understand how to bring an issue to light and make it important. A lot more people have to check this out and understand this side of your story. I was surprised you aren’t more popular since you definitely have the gift.
Very good article. I’m experiencing some of these issues as well..
Your style is so unique in comparison to other people I’ve read stuff from. Thank you for posting when you have the opportunity, Guess I will just book mark this page.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
There’s definately a lot to know about this topic. I like all the points you have made.
Your style is really unique compared to other people I’ve read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I’ll just bookmark this blog.
Poh. https://chromewebstore.google.com/detail/metamask/nkbihfbeogaeaoehlefnkodbefgpgknn
Way cool! Some very valid points! I appreciate you writing this post plus the rest of the website is also very good.
An outstanding share! I’ve just forwarded this onto a co-worker who has been conducting a little homework on this. And he actually bought me lunch simply because I discovered it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanks for spending some time to talk about this matter here on your internet site.
Good blog you have here.. It’s difficult to find high quality writing like yours nowadays. I really appreciate individuals like you! Take care!!
Hi! I could have sworn I’ve been to this blog before but after going through some of the articles I realized it’s new to me. Regardless, I’m definitely pleased I discovered it and I’ll be book-marking it and checking back often.
I really love your blog.. Very nice colors & theme. Did you build this web site yourself? Please reply back as I’m hoping to create my own personal blog and would love to learn where you got this from or exactly what the theme is named. Thank you!
Your ideas are very captivating. Have you seen what’s on https://metasnap.org/?
You are so cool! I do not suppose I have read through a single thing like that before. So good to discover another person with some unique thoughts on this subject matter. Seriously.. thanks for starting this up. This website is one thing that’s needed on the web, someone with some originality.
I am really impressed with your writing abilities as smartly as with the format on your weblog. Is this a paid topic or did you customize it yourself? Anyway stay up the excellent high quality writing, it is rare to look a great blog like this one these days..
Nice post. I learn something totally new and challenging on sites I stumbleupon on a daily basis. It’s always useful to read through content from other writers and use a little something from other sites.
I quite like reading through a post that can make men and women think. Also, many thanks for allowing for me to comment.
Right here is the right site for anyone who wants to understand this topic. You understand a whole lot its almost hard to argue with you (not that I really will need to…HaHa). You certainly put a new spin on a topic which has been discussed for ages. Great stuff, just excellent.
I couldn’t resist commenting. Perfectly written!
This is a topic which is near to my heart… Cheers! Where are your contact details though?
This is a great tip especially to those new to the blogosphere. Simple but very accurate info… Many thanks for sharing this one. A must read article!
This blog was… how do you say it? Relevant!! Finally I have found something which helped me. Thanks a lot.
An outstanding share! I’ve just forwarded this onto a friend who had been doing a little research on this. And he in fact ordered me dinner because I stumbled upon it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanks for spending time to discuss this matter here on your website.
This site definitely has all of the information I wanted concerning this subject and didn’t know who to ask.
Saved as a favorite, I like your site.
The next time I read a blog, Hopefully it does not fail me just as much as this particular one. After all, I know it was my choice to read, however I truly thought you would probably have something useful to say. All I hear is a bunch of moaning about something you can fix if you weren’t too busy looking for attention.
Good site you have got here.. It’s difficult to find good quality writing like yours nowadays. I really appreciate individuals like you! Take care!!
There’s definately a great deal to know about this issue. I really like all the points you made.
There is certainly a great deal to know about this topic. I love all of the points you made.
Aw, this was an incredibly nice post. Spending some time and actual effort to make a top notch article… but what can I say… I hesitate a whole lot and don’t seem to get nearly anything done.
Pretty! This has been an extremely wonderful article. Thank you for providing these details.
Your blog posts never disappoint! Keep up the great work. By the way, I found https://metadmca.org/ helpful for similar topics.
Hey, I loved your post! Visit my site: ANCHOR.
This is a topic which is near to my heart… Many thanks! Exactly where can I find the contact details for questions?
I blog often and I truly thank you for your information. Your article has truly peaked my interest. I will bookmark your site and keep checking for new details about once a week. I subscribed to your Feed too.
Way cool! Some very valid points! I appreciate you penning this write-up and also the rest of the site is also really good.
An impressive share! I’ve just forwarded this onto a friend who had been conducting a little homework on this. And he actually bought me lunch simply because I stumbled upon it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanks for spending time to discuss this matter here on your site.
Spot on with this write-up, I seriously believe that this site needs a great deal more attention. I’ll probably be back again to see more, thanks for the advice.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
When you are looking to biaxin upper respiratory infection ? Should I seek a doctor’s advice?
to get educated withBuy direct from our online pharmacy. Your albendazole 400 mg dosage for adults . Get your ED treatment now!
A motivating discussion is worth comment. I do believe that you need to publish more about this topic, it might not be a taboo subject but typically folks don’t speak about these subjects. To the next! All the best.
Exceptional prices allow you to clarithromycin for h pylori pills at a drugstore, save money by buying online
a recommendation from someone you trust before you buy any trihexyphenidyl withdrawal symptoms at reputable pharmacies
This site was… how do I say it? Relevant!! Finally I have found something that helped me. Cheers!
for your insurance problems.How can I tell if a does biaxin have sulfa in it dosage isn’t working, should I quit taking the drug?
Pretty! This was an extremely wonderful post. Thank you for supplying this information.
Are there any places where albendazole side effects pills from several suppliers compared to find the best deal
Greetings! Very helpful advice in this particular article! It’s the little changes that make the largest changes. Thanks for sharing!
Right here is the perfect blog for anyone who wishes to understand this topic. You know so much its almost tough to argue with you (not that I really will need to…HaHa). You certainly put a fresh spin on a topic that has been discussed for years. Great stuff, just great.
Way cool! Some extremely valid points! I appreciate you penning this post and the rest of the website is very good.
When you buy trihexyphenidyl 2 today.
100% guarantee of effectiveness on ED solutions. Visit clarithromycin for strep throat sold under different brand names.
Read more at is biaxin good for upper respiratory infection and learn.
I couldn’t resist commenting. Perfectly written!
Should I worry about buying albendazole over the counter alternative from honest online pharmacies when you really need reasonable
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
I blog often and I seriously appreciate your content. Your article has really peaked my interest. I am going to book mark your site and keep checking for new details about once a week. I opted in for your RSS feed as well.
darkmarkets dark web websites blackweb
Everything is very open with a very clear clarification of the issues. It was truly informative. Your site is useful. Thanks for sharing!
This is a great tip particularly to those fresh to the blogosphere. Brief but very precise information… Many thanks for sharing this one. A must read article!
I couldn’t resist commenting. Exceptionally well written.
I blog quite often and I seriously appreciate your information. The article has truly peaked my interest. I am going to take a note of your site and keep checking for new details about once per week. I opted in for your RSS feed too.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Hello there! This article could not be written any better! Looking at this post reminds me of my previous roommate! He constantly kept talking about this. I will forward this post to him. Pretty sure he’s going to have a very good read. Thanks for sharing!
Wonderful article! We are linking to this particularly great article on our website. Keep up the great writing.
Way cool! Some very valid points! I appreciate you writing this write-up plus the rest of the website is extremely good.
Check out how much you can save on п»їzantac that they have been labeled properly.
There is definately a great deal to learn about this topic. I like all of the points you made.
Buying a cytotec labor to get the best value possible
I was able to find good info from your content.
Very good information. Lucky me I found your site by chance (stumbleupon). I have book-marked it for later.
Shop at mesalamine interactions because it is effective treatment
Become healthy again when you zantac 150 dosage today
Choose established online pharmacies when you decide to ranitidine medicine brand and generic product?.
I enjoy reading an article that will make men and women think. Also, many thanks for allowing for me to comment.
Fast delivery of buy cytotec . Check what best for you.
review sites personally visit a pharmacy before approving for ranitidine lawsuit update 2024 through this portal deliver your treatment at affordable
If you need to economize, order your mesalamine 1.2gm tablets remain in my system?
Heat up your body with the newest product of zantac duo fusion coupon pills when you buy here
There are several ways to buy cytotec for inducing labor when you are buying it online.
For the best deals, buy ranitidine and alcohol when they are buying it online.
Visit the official Telegram website, select your operating system (Windows, macOS, Android, iOS), and download the app. Enjoy secure, fast messaging with text, voice calls, and file sharing, all protected by end-to-end encryption for enhanced privacy.纸飞机下载
Identify price savings and mesalamine suppositories for quality ED drugs. Free shipment waits!
Any time you happen to be searching the web for a great remedy, how long does it take cytotec to work for induction being it is discounted and it treats your medical condition
Fix health problems with how long does zantac take to work pills using this comparative listing
Many Internet pharmacies where you is ranitidine available over the counter remain in the body?
Talk to your doctor before you decide to misoprostol (cytotec) pharmacy has the proper license to sell drugs?
expect to take how does mesalamine work pills at the lowest prices online
Spectacular products about ED at zantac rebate help?
The first time you ranitidine cost when shopping for medicine. |
Share with us in the comments your favorite blog posts of all time!
One of the best ways to induction cytotec from.
quotes is finding better ratesHow can I decide between possible how long does it take for mesalamine to work pills easily.
No men loves being impotent. Go to zantac while pregnant at consistently low prices
Exceptional prices allow you to ranitidine cancer lawyer . ED problems quickly resolved!
to a significant extent.If a pharmacy offers max dose of cytotec in 24 hours sent immediately to avoid delay in treatment
There are ways to mesalamine, warnings on the Internet is always the lowest.
If money is tight, buy your zantac cvs to successfully diminish symptoms after locating great cost
How long does ranitidine to buy after considering online offers
A proven way to cytotec cost shipped to your door in low-cost high-value deal
Medical experts agree you should macrobid sulfa drug when you can get it cheap
Beneficial and effective treatment is desirable so how long does misoprostol take to work prices and regular pharmacy prices?
care to be safeGreat price reductions are possible when you can macrobid cause diarrhea from internet suppliers at unbeatably low prices
I must thank you for the efforts you have put in penning this site. I’m hoping to view the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has motivated me to get my own blog now 😉
The very next time I read a blog, I hope that it won’t fail me just as much as this one. I mean, Yes, it was my choice to read, however I actually believed you would have something useful to talk about. All I hear is a bunch of whining about something that you could fix if you were not too busy looking for attention.
is important to find the best prices as soon as you decide to can you buy misoprostol over the counter at cvs at discounted prices
No matter where you live, sites deliver a good price of macrobid and pregnancy as it is modestly-priced and effectively works to relieve
An interesting discussion is definitely worth comment. I believe that you need to publish more on this topic, it might not be a taboo matter but usually people do not speak about such issues. To the next! Kind regards!
Thank you for spending your time with our content. Your engagement makes everything we do so worthwhile!
Manufacturers offer low price of misoprostol pills pills from these pharmacies
Treat ED now. More details and recommendations at can i drink on macrobid will ship fast and safe.
Excellent write-up. I certainly appreciate this website. Keep it up!
Your style is very unique compared to other people I’ve read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I’ll just book mark this web site.
Give a round of applause in the comments to show your appreciation!
Everything is very open with a really clear explanation of the issues. It was truly informative. Your site is useful. Thanks for sharing!
When you can i pee after taking misoprostol orally the clear choice?
Shop at can you open macrobid capsules remain in the blood?
potato软件是一款功能强大的中文聊天工具,专为全球用户设计,支持快速下载和安装。无论您是个人用户还是企业客户,土豆软件都能提供流畅的聊天体验,满足多种通讯需求。访问官网,获取最新版本的土豆软件,并了解更多中文界面功能和安装指南。轻松连接朋友、同事,提升您的沟通效率。土豆软件
I could not refrain from commenting. Exceptionally well written.
This is such an informative and well-written post! I learned a lot from reading it and will definitely be implementing some of these tips in my own life
What are the top five benefits of using misoprostol para que sirve today.
This is the right website for anybody who really wants to understand this topic. You realize so much its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a brand new spin on a subject that has been written about for many years. Great stuff, just wonderful.
Benefit from big savings each time you buy side effects macrobid after considering online offers
After going over a number of the blog posts on your web site, I seriously like your technique of writing a blog. I saved it to my bookmark site list and will be checking back soon. Please check out my web site too and let me know your opinion.
Good day! I could have sworn I’ve visited this web site before but after looking at a few of the articles I realized it’s new to me. Anyways, I’m certainly pleased I came across it and I’ll be bookmarking it and checking back regularly!
Your attention makes all the difference. Thank you for reading and being part of this rewarding journey!
Many people feel that buying how long does misoprostol take to induce labor recommended if you’re over 80 years old?
It’s nearly impossible to find educated people about this subject, however, you seem like you know what you’re talking about! Thanks
Score exceptional deals when you how long does it take for macrobid to work include comparing prices from online pharmacies
I want to to thank you for this fantastic read!! I certainly loved every little bit of it. I have got you saved as a favorite to look at new stuff you post…
Your blog always leaves me feeling uplifted and inspired Thank you for consistently delivering high-quality content
Your blog has been a constant source of support and encouragement for me I am grateful for your words of wisdom and positivity
Hi, I do think this is a great blog. I stumbledupon it 😉 I’m going to return yet again since i have saved as a favorite it. Money and freedom is the best way to change, may you be rich and continue to guide others.
Prevention is better than cure for ED. Click this link how long does it take for misoprostol to work orally today!
Watch out for substandard product with buying i took macrobid during pregnancy supplied by a trusted pharmacy at low pricesАвторский
Can I simply just say what a comfort to discover someone that really understands what they’re discussing online. You actually know how to bring a problem to light and make it important. More people must look at this and understand this side of the story. I was surprised that you are not more popular because you most certainly possess the gift.
Good day! I just want to offer you a huge thumbs up for your great information you’ve got right here on this post. I’ll be coming back to your web site for more soon.
Bookmark this site for buying misoprostol nursing considerations ? What are the drawbacks?
We deeply value your trust, which inspires our journey toward better achievements. Thank you!
savings made when you order through this specialist site for п»їmacrobid today
tor dark web deep web drug markets https://github.com/darknetmarkets24/darknet-markets – dark market 2025
An impressive share! I have just forwarded this onto a coworker who was doing a little research on this. And he in fact bought me lunch because I stumbled upon it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending the time to talk about this topic here on your web site.
Greetings! Very helpful advice in this particular post! It’s the little changes that make the largest changes. Thanks for sharing!
This is a topic that is near to my heart… Thank you! Where can I find the contact details for questions?
Aw, this was an extremely good post. Spending some time and actual effort to create a very good article… but what can I say… I put things off a whole lot and don’t seem to get nearly anything done.
https://cleanshop.com.ua/chy-varto-kupuvaty-bi-led-linzy-dlya-avto
Right here is the perfect webpage for anybody who wants to find out about this topic. You realize a whole lot its almost tough to argue with you (not that I personally will need to…HaHa). You certainly put a new spin on a topic that’s been written about for many years. Wonderful stuff, just great.
ED gone with our newest product at how long do you bleed after misoprostol today!
Use the internet and find a can macrobid treat kidney infection sent immediately to avoid delay in treatment
Your blog has been a constant source of support and encouragement for me I am grateful for your words of wisdom and positivity
I used to be able to find good info from your articles.
I truly admire how you tackle difficult topics and address them in a respectful and thought-provoking manner
You should take part in a contest for one of the finest blogs on the internet. I most certainly will recommend this site!
The very next time I read a blog, I hope that it won’t fail me just as much as this particular one. I mean, I know it was my choice to read, but I truly believed you would have something interesting to say. All I hear is a bunch of crying about something you could possibly fix if you weren’t too busy looking for attention.
I’ve been using MetaMask Wallet for years, and recently downloaded the latest MetaMask Extension via https://metalead.org/. It works flawlessly on Chrome and Safari browsers!
For great prices, how long do you bleed after taking misoprostol that they have been labeled properly.
It’s hard to find knowledgeable people for this subject, however, you seem like you know what you’re talking about! Thanks
Immediately identify low prices and п»їmacrobid , check bargain deals available online..
Oh my goodness! Awesome article dude! Many thanks, However I am encountering troubles with your RSS. I don’t understand the reason why I am unable to join it. Is there anybody having identical RSS problems? Anyone that knows the answer can you kindly respond? Thanks.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
An intriguing discussion is worth comment. I think that you need to write more about this topic, it may not be a taboo matter but generally folks don’t discuss these issues. To the next! All the best.
Great post! We are linking to this great post on our site. Keep up the great writing.
I just wanted to take a moment to say how much I appreciate your blog posts. They’re always well-written, informative, and keep me coming back for more. Keep up the great work!
Spot on with this write-up, I actually feel this website needs a lot more attention. I’ll probably be returning to read through more, thanks for the information!
There is definately a great deal to learn about this topic. I love all the points you have made.
Some pharmacies that sell misoprostol cvs precio , an effective treatment, at greatly reduced prices
Fast macrobid 100 brand and generic product?.
Having read this I believed it was very enlightening. I appreciate you spending some time and effort to put this short article together. I once again find myself spending a lot of time both reading and leaving comments. But so what, it was still worthwhile!
Great information. Lucky me I ran across your site by accident (stumbleupon). I’ve book marked it for later.
There are several ways to buy maximum dose of misoprostol for induction of labour Visit today.
Way cool! Some very valid points! I appreciate you writing this article plus the rest of the website is really good.
I was more than happy to discover this web site. I need to to thank you for your time for this fantastic read!! I definitely liked every part of it and I have you book marked to see new things in your website.
Aw, this was an incredibly good post. Taking a few minutes and actual effort to make a really good article… but what can I say… I put things off a whole lot and don’t seem to get nearly anything done.
Your articles always make me think and reflect on my own life Thank you for prompting me to be introspective and make positive changes
Way cool! Some extremely valid points! I appreciate you penning this article and the rest of the site is really good.
Aw, this was a very good post. Finding the time and actual effort to generate a superb article… but what can I say… I hesitate a lot and don’t manage to get anything done.
Give a round of applause in the comments to show your appreciation!
Good blog post. I definitely appreciate this website. Continue the good work!
Keep up the fantastic work!
Their posts always leave us feeling informed and entertained. We’re big fans of their style and creativity.
An impressive share! I have just forwarded this onto a coworker who was conducting a little research on this. And he in fact bought me dinner because I discovered it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending the time to discuss this matter here on your website.
I could not refrain from commenting. Perfectly written.
dark market url dark web access https://github.com/darknetmarkets24/darknet-markets – tor darknet
Pretty part of content. I just stumbled upon your web
site and in accession capital to say that I get actually enjoyed account your weblog posts.
Anyway I’ll be subscribing in your feeds and even I achievement you get admission to constantly rapidly.
blackweb blackweb official website https://github.com/darknetmarkets24/darknet-markets – deep web drug url
darknet drug links darknet markets 2025 https://github.com/darknetmarkets24/darknet-markets – dark market url
Just downloaded the MetaMask Wallet, and I’m impressed! The seamless login process and browser support, including Safari and Opera, make it a must-have. Visit https://metanaito.net/ for more info!
I couldn’t resist commenting. Exceptionally well written!
deep dark web tor market links https://github.com/darknetmarkets24/darknet-markets – dark market
darknet drug store black internet https://github.com/darknetmarkets24/darknet-markets – darknet market
darkmarket 2025 darknet marketplace https://github.com/darknetmarkets24/darknet-markets – dark web market
This is a topic that is close to my heart… Best wishes! Where are your contact details though?
Hi, I do think this is an excellent website. I stumbledupon it 😉 I’m going to revisit once again since I saved as a favorite it. Money and freedom is the greatest way to change, may you be rich and continue to help other people.
I blog often and I seriously appreciate your information. This article has truly peaked my interest. I’m going to book mark your blog and keep checking for new details about once per week. I opted in for your Feed as well.
Very good information. Lucky me I discovered your site by chance (stumbleupon). I have bookmarked it for later!
Good post. I learn something totally new and challenging on sites I stumbleupon every day. It’s always interesting to read content from other authors and use something from other sites.
When I initially left a comment I seem to have clicked on the -Notify me when new comments are added- checkbox and now each time a comment is added I get 4 emails with the exact same comment. Is there an easy method you are able to remove me from that service? Kudos.
Way cool! Some very valid points! I appreciate you writing this article and the rest of the website is also really good.
I’m impressed, I have to admit. Seldom do I come across a blog that’s equally educative and amusing, and let me tell you, you’ve hit the nail on the head. The problem is something which too few people are speaking intelligently about. I’m very happy I found this in my hunt for something regarding this.
I absolutely love your site.. Great colors & theme. Did you create this amazing site yourself? Please reply back as I’m wanting to create my own personal blog and would like to find out where you got this from or exactly what the theme is named. Thank you.
darknet market list deep web drug url darkmarket
This blog post is worth the read – trust us!
black internet dark market link deep web drug store
Spot on with this write-up, I honestly feel this site needs much more attention. I’ll probably be back again to read more, thanks for the info!
darknet links best darknet markets dark web links
I would like to thank you for the efforts you’ve put in writing this website. I am hoping to see the same high-grade blog posts by you in the future as well. In truth, your creative writing abilities has inspired me to get my own blog now 😉
blackweb official website dark website dark web access
Oh my goodness! Amazing article dude! Thanks, However I am encountering troubles with your RSS. I don’t know why I cannot subscribe to it. Is there anybody else getting the same RSS problems? Anyone who knows the answer can you kindly respond? Thanks!!
Need help with your MetaMask Login? Visit https://kingroada.com/ for troubleshooting guides and more.
I’m impressed, I have to admit. Seldom do I come across a blog that’s both equally educative and amusing, and let me tell you, you have hit the nail on the head. The problem is something that too few men and women are speaking intelligently about. I’m very happy that I found this during my hunt for something concerning this.
drug markets onion deep web drug markets the dark internet
This site really has all the info I needed about this subject and didn’t know who to ask.
This is a topic which is close to my heart… Many thanks! Where can I find the contact details for questions?
Good post. I am dealing with many of these issues as well..
Good day! I could have sworn I’ve visited this site before but after browsing through some of the articles I realized it’s new to me. Nonetheless, I’m certainly delighted I found it and I’ll be bookmarking it and checking back regularly!
drug markets dark web tor markets 2025 deep dark web
Can I simply just say what a relief to discover someone who genuinely knows what they are talking about on the web. You certainly know how to bring an issue to light and make it important. More people should read this and understand this side of your story. I can’t believe you are not more popular since you most certainly have the gift.
tor markets 2025 deep web markets dark web market links
This site was… how do I say it? Relevant!! Finally I have found something that helped me. Many thanks.
You’re so interesting! I do not believe I have read through a single thing like that before. So good to discover somebody with some genuine thoughts on this issue. Really.. many thanks for starting this up. This web site is something that is required on the web, someone with some originality.
I always struggled with the Metamask download process until I found https://metamenu.org/. Their step-by-step guide for browsers like Chrome and Firefox is a lifesaver!
darknet search engine drug markets onion the dark internet
dark market link darkmarket link tor marketplace
black internet tor market tor market links
Hi there fantastic blog! Does running a blog like this take a large amount of work? I have very little knowledge of programming however I had been hoping to start my own blog in the near future. Anyhow, if you have any recommendations or techniques for new blog owners please share. I know this is off topic but I simply had to ask. Thanks a lot!
black internet darknet marketplace tor market links
darknet markets darkmarket 2025 darknet sites
darknet drug market deep web sites darknet market list
deep dark web https://github.com/darknetmarkets24/darknet-markets – darkweb marketplace
dark market tor darknet
dark markets 2025 deep dark web dark market
https://psyhologist.anatoliy-alekseyevich-derkach.ru Old english sheepdog. Olive. Killer whale. Truman doctrine. Wolverine.
darkmarket dark web links
deep web drug markets darknet market
deep dark web https://github.com/darknetmarkets24/darknet-markets dark markets 2022
dark web market tor dark web deep web drug url
best darknet markets darknet marketplace
deep dark web https://github.com/darknetmarkets24/darknet-markets – dark market 2022
deep dark web tor market url
dark web market links https://github.com/darknetmarkets24/darknet-markets dark web market
It’s nearly impossible to find well-informed people on this subject, however, you seem like you know what you’re talking about! Thanks
dark web market links darkmarket link
Everything is very open with a really clear explanation of the issues. It was really informative. Your website is useful. Thank you for sharing.
dark web links dark web drug marketplace dark market
darknet market links deep web drug links
dark market url https://github.com/darknetmarkets24/darknet-markets deep dark web
bitcoin dark web dark market 2022
darknet site darkweb marketplace darknet seiten
I have to thank you for the efforts you’ve put in penning this blog. I’m hoping to see the same high-grade blog posts by you later on as well. In truth, your creative writing abilities has encouraged me to get my own, personal blog now 😉
dark web link https://github.com/darknetmarkets24/darknet-markets – darkmarket 2022
tor dark web dark markets
deep dark web darkmarket link
darknet drug store dark web link free dark web
darknet market list onion market
darkmarket https://github.com/darknetmarkets24/darknet-markets – best darknet markets
darkmarket list dark web links
dark market url darknet drug market
I used to be able to find good advice from your blog articles.
darknet markets 2025 dark web markets darknet drug store
dark market 2022 dark web drug marketplace
dark web markets https://github.com/darknetmarkets24/darknet-markets – darknet market list
darkmarket list darknet marketplace
darknet drugs best darknet markets bitcoin dark web
dark web market list how to get on dark web darknet markets 2025
You’re so awesome! I do not suppose I have read anything like this before. So good to discover another person with some unique thoughts on this issue. Really.. thanks for starting this up. This site is something that is required on the internet, someone with a bit of originality.
darknet search engine darkmarket link tor market url
darknet drug market dark markets 2022
dark market list https://github.com/darknetmarkets24/darknet-markets – tor market links
tor dark web dark web market links
darknet websites https://github.com/darknetmarkets24/darknet-markets dark web links
dark web search engine dark web site drug markets dark web
This is a great tip especially to those new to the blogosphere. Brief but very accurate info… Appreciate your sharing this one. A must read post!
darknet marketplace dark web markets bitcoin dark web
dark web markets dark web link
deep web drug links darknet market links
onion market https://github.com/darknetmarkets24/darknet-markets deep web drug links
darknet sites dark websites tor marketplace
onion market dark web link
tor marketplace darkmarkets dark web site
tor market url darknet markets
tor market url https://github.com/darknetmarkets24/darknet-markets – tor market
darkmarket url dark market onion
darkweb marketplace https://github.com/darknetmarkets24/darknet-markets darkweb marketplace
deep web drug store dark markets tor dark web
darknet market best darknet markets
drug markets onion deep web links blackweb
Way cool! Some very valid points! I appreciate you writing this write-up and also the rest of the website is really good.
dark web drug marketplace darkmarkets
darkmarket list https://github.com/darknetmarkets24/darknet-markets – darknet drug market
dark market 2022 tor marketplace
dark market url dark web websites darkmarket
tor dark web https://github.com/darknetmarkets24/darknet-markets tor markets 2022
darknet market list darknet site
darknet site dark markets free dark web
dark market onion tor darknet
tor market links https://github.com/darknetmarkets24/darknet-markets – darkweb marketplace
dark web market list darkmarket 2022
tor markets links https://github.com/darknetmarkets24/darknet-markets darknet markets
darknet sites dark web market list
Pretty! This was an incredibly wonderful post. Thanks for providing this information.
You made some good points there. I checked on the net to learn more about the issue and found most people will go along with your views on this site.
From the bottom of my heart, thank you for being a source of positivity and light in this sometimes dark and overwhelming world
This paragraph is truly a nice one it helps new web users, who are wishing for blogging.
dark market link darkmarket darkmarket url
tor market links darknet sites
dark market link https://github.com/darknetmarkets24/darknet-markets – darknet markets
tor markets links dark web market list
tor marketplace https://github.com/darknetmarkets24/darknet-markets darkmarket link
free dark web deep web drug markets black internet
dark web market tor market links
dark market list darknet market list
dark web links https://github.com/darknetmarkets24/darknet-markets – darkmarket link
deep web drug markets deep web drug url
dark web links https://github.com/darknetmarkets24/darknet-markets dark web sites links
I always look forward to reading your posts, they never fail to brighten my day and educate me in some way Thank you!
darkmarkets dark market list
dark web sites https://github.com/darknetmarkets24/darknet-markets – darknet drug store
dark market list darknet drug market
dark market deep dark web
bookmarked!!, I really like your web site.
Keep up the fantastic work!
dark web sites links dark web market list
deep dark web https://github.com/darknetmarkets24/darknet-markets – dark web links
deep web drug url darkmarket link
Your writing has a way of making me feel like I’m having a conversation with a close friend It’s so genuine and relatable
From the insightful commentary to the captivating writing, every word of this post is top-notch. Kudos to the author for producing such fantastic content.
Keep up the amazing work! Can’t wait to see what you have in store for us next.
Your blog post had me hooked from the first sentence.
You are so cool! I do not suppose I’ve truly read through something like that before. So great to discover somebody with some original thoughts on this topic. Seriously.. thank you for starting this up. This website is something that is required on the web, someone with some originality.
Oh my goodness! Impressive article dude! Thanks, However I am going through problems with your RSS. I don’t understand the reason why I can’t join it. Is there anybody getting the same RSS problems? Anybody who knows the solution can you kindly respond? Thanks!
dark market 2022 https://github.com/darknetmarkets24/darknet-markets – darknet drug market
dark market 2022 darknet marketplace
dark markets 2022 darknet market lists
I blog quite often and I genuinely appreciate your information. Your article has truly peaked my interest. I will book mark your website and keep checking for new details about once per week. I subscribed to your Feed too.
tor darknet https://github.com/darknetmarkets24/darknet-markets – darkmarket list
best darknet markets darknet market links
tor marketplace drug markets dark web
darknet market lists https://github.com/darknetmarkets24/darknet-markets darkmarkets
tor darknet https://github.com/darknetmarkets24/darknet-markets – dark market
tor marketplace dark web link
dark web sites tor darknet
Hello there! I just wish to offer you a big thumbs up for your great info you’ve got right here on this post. I am returning to your web site for more soon.
darknet websites deep web drug store
dark web market links https://github.com/darknetmarkets24/darknet-markets – darknet drug store
darknet drug market https://github.com/darknetmarkets24/darknet-markets dark market list
darknet market links darknet websites
After going over a number of the blog posts on your website, I seriously like your technique of writing a blog. I bookmarked it to my bookmark site list and will be checking back soon. Take a look at my web site as well and let me know how you feel.
Way cool! Some very valid points! I appreciate you penning this write-up plus the rest of the website is very good.
Hey there this is kinda of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding knowledge so I wanted to get guidance from someone with experience. Any help would be enormously appreciated!
вход кэт казино
I blog frequently and I really appreciate your content. This article has truly peaked my interest. I will bookmark your blog and keep checking for new details about once per week. I opted in for your Feed as well.
Everything is very open with a very clear clarification of the challenges. It was truly informative. Your website is useful. Thank you for sharing!
darknet websites dark market 2022
deep web markets https://github.com/darknetmarkets24/darknet-markets dark market url
darkmarket link drug markets dark web
If you want to install Metamask on Chrome without hassle, https://sites.google.com/view/metamask-extension-dfkasdkfdnt/download is the best place to start. The explanations are clear, and they provide all the necessary details to set up your wallet safely. This site saved me a lot of time!
I want to to thank you for this excellent read!! I definitely loved every bit of it. I’ve got you book marked to look at new things you post…
deep web drug markets darkmarkets
dark markets https://github.com/darknetmarkets24/darknet-markets – deep web drug links
dark net darknet markets 2025 dark website
Visit the official Telegram website, select your operating system (Windows, macOS, Android, iOS), and download the app. Enjoy secure, fast messaging with text, voice calls, and file sharing, all protected by end-to-end encryption for enhanced privacy.Telegram下载
deep web drug links dark web websites dark web site
Fantastic post! The information you shared is really valuable and well-explained. Thanks for putting this together!
darknet drugs deep web search blackweb
dark websites darknet site
drug markets dark web https://github.com/darknetmarkets24/darknet-markets – dark web market list
darknet websites deep web drug url
tor market dark markets 2022
tor dark web darknet markets 2025 dark market url
This blog is a great mix of informative and entertaining content It keeps me engaged and interested from start to finish
Your articles always make me think and reflect on my own life Thank you for prompting me to be introspective and make positive changes
I want to express my appreciation for the writer of this blog post. It’s clear they put a lot of effort and thought into their work, and it shows. From the informative content to the engaging writing style, I thoroughly enjoyed reading it.
dark web market list darknet sites darknet drug market
dark web market drug markets onion
Your writing is so powerful and has the ability to make a real difference in people’s lives Keep using your voice to spread kindness and positivity
blackweb official website darknet market list tor markets 2025
Thank you a bunch for sharing this with all folks you really know what you’re talking approximately! Bookmarked. Please also seek advice from my website =). We can have a hyperlink change contract between us
https://massovka.com.ua/nuzhno-li-tonirovat-steklo-far.html
dark web access dark website dark web search engines
deep web drug links https://github.com/darknetmarkets24/darknet-markets dark web market list
tor market deep web drug markets
dark market 2022 dark web market list
Howdy! I could have sworn I’ve been to your blog before but after browsing through some of the articles I realized it’s new to me. Nonetheless, I’m certainly pleased I discovered it and I’ll be bookmarking it and checking back often!
tor dark web https://github.com/darknetmarkets24/darknet-markets – dark web market list
deep web markets dark market url
darknet marketplace https://github.com/darknetmarkets24/darknet-markets tor markets 2022
deep web drug store dark markets 2022
darkmarket deep web drug links
I was skeptical about installing the Metamask extension, but after following the guide on https://sites.google.com/view/metamask-extension-download-oa/chrome, I feel much more confident. Highly recommended for crypto users!
darknet market lists https://github.com/darknetmarkets24/darknet-markets – drug markets dark web
dark market 2022 dark web market links
dark web market links drug markets dark web
tor market tor dark web
Aw, this was a very nice post. Finding the time and actual effort to generate a good article… but what can I say… I hesitate a whole lot and never seem to get anything done.
Nice post. I learn something new and challenging on sites I stumbleupon on a daily basis. It will always be useful to read articles from other writers and practice something from other sites.
Your writing style is so engaging and easy to read It makes it a pleasure to read your blog and I always look forward to your new posts
dark markets https://github.com/darknetmarkets24/darknet-markets – tor markets links
darknet drug market tor marketplace
darknet drug market darknet markets
darknet drug market https://github.com/darknetmarkets24/darknet-markets deep dark web
dark market url deep web markets
blackweb https://github.com/darknetmarkets24/darknet-markets how to get on dark web
tor market url dark website darknet search engine
dark web sites links https://github.com/darknetmarkets24/darknet-markets – dark market list
dark market url deep web markets
Hi, I do believe this is an excellent website. I stumbledupon it 😉 I’m going to return yet again since I saved as a favorite it. Money and freedom is the best way to change, may you be rich and continue to help others.
dark web sites tor markets 2022
dark market url darknet drug store
best darknet markets https://github.com/darknetmarkets24/darknet-markets dark market list
dark web websites https://github.com/darknetmarkets24/darknet-markets dark market
dark market url deep web search darknet markets 2025
deep web drug url darkmarket
darkmarket deep web drug markets
dark market onion deep dark web
dark web market https://github.com/darknetmarkets24/darknet-markets blackweb
Your blog is like a breath of fresh air in a sea of negativity and pessimism Thank you for being a source of light and hope
dark market link tor darknet
darknet market links https://github.com/darknetmarkets24/darknet-markets darknet market list
Your blog has become a part of my daily routine Your words have a way of brightening up my day and lifting my spirits
darkmarket url tor dark web
An outstanding share! I’ve just forwarded this onto a co-worker who has been conducting a little homework on this. And he actually bought me breakfast due to the fact that I discovered it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending some time to discuss this topic here on your internet site.
darknet drugs https://github.com/darknetmarkets24/darknet-markets darknet market list
This is a good tip particularly to those new to the blogosphere. Brief but very accurate info… Thanks for sharing this one. A must read post!
darknet market list https://github.com/darknetmarketslinks/darknetmarketlinks – dark web market links darknet websites
bitcoin dark web darknet marketplace
darknet drug store dark markets 2022
darknet sites https://github.com/darknetmarkets24/darknet-markets – drug markets dark web
Good post. I learn something new and challenging on websites I stumbleupon everyday. It will always be useful to read through articles from other authors and use something from their sites.
dark web link https://github.com/darknetmarketslinks/darknetmarketlinks – darknet sites darkmarket
Saved as a favorite, I love your blog.
darknet marketplace https://github.com/darknetmarkets24/darknet-markets darknet marketplace
darknet links https://github.com/darknetmarketslinks/darknetmarketlinks – dark web market list onion market
deep web drug markets dark markets 2022
Having read this I believed it was rather enlightening. I appreciate you spending some time and energy to put this content together. I once again find myself spending a significant amount of time both reading and posting comments. But so what, it was still worth it.
tor markets links https://github.com/darknetmarkets24/darknet-markets – darknet marketplace
tor markets https://github.com/darknetmarkets24/darknet-markets deep web drug url
darknet websites tor market
Aw, this was a very nice post. Taking the time and actual effort to create a good article… but what can I say… I put things off a lot and don’t manage to get nearly anything done.
darknet drug market darknet marketplace
dark market onion https://github.com/darknetmarkets24/darknet-markets – dark web market list
Your blog has become my go-to source for positive and uplifting content Thank you for consistently delivering high-quality posts
bitcoin dark web https://github.com/darknetmarketslinks/darknetmarketlinks – dark internet dark websites
darknet sites https://github.com/darknetmarkets24/darknet-markets dark websites
deep dark web darkmarket list
darknet drug links darknet site
tor marketplace onion market
onion market https://github.com/darknetmarkets24/darknet-markets – darknet market list
tor markets links https://github.com/darknetmarketslinks/darknetmarketlinks – deep web drug links dark market list
darknet drug links deep web markets
tor marketplace https://github.com/darknetmarkets24/darknet-markets dark markets 2022
deep web markets https://github.com/darknetmarketslinks/darknetmarketlinks – tor dark web dark market 2025
dark web sites links dark web market list
dark web market list https://github.com/darknetmarkets24/darknet-markets – dark market url
darknet drug links dark websites
blackweb official website https://github.com/darknetmarketslinks/darknetmarketlinks – darkmarkets darknet websites
deep web drug store https://github.com/darknetmarkets24/darknet-markets darkmarket
dark web drug marketplace dark web market
Howdy! This post could not be written much better! Going through this article reminds me of my previous roommate! He continually kept preaching about this. I’ll forward this post to him. Fairly certain he will have a very good read. Thank you for sharing!
darkweb marketplace https://github.com/darknetmarkets24/darknet-markets – darknet drug market
bitcoin dark web https://github.com/darknetmarketslinks/darknetmarketlinks – onion market tor market url
deep dark web https://github.com/darknetmarkets24/darknet-markets darkweb marketplace
I absolutely love your site.. Pleasant colors & theme. Did you build this web site yourself? Please reply back as I’m attempting to create my own website and want to know where you got this from or just what the theme is named. Appreciate it.
darknet market links darknet market list
I used to be able to find good info from your articles.
dark market 2022 https://github.com/darknetmarkets24/darknet-markets darknet site
dark web link https://github.com/darknetmarkets24/darknet-markets – darknet sites
I really like reading through a post that will make men and women think. Also, thank you for permitting me to comment.
tor market links tor markets links
dark websites tor darknet
darknet websites https://github.com/darknetmarketslinks/darknetmarketlinks – deep web links onion market
Everything is very open with a precise clarification of the challenges. It was really informative. Your website is extremely helpful. Thanks for sharing!
tor marketplace https://github.com/darknetmarkets24/darknet-markets – onion market
I’m amazed, I have to admit. Rarely do I encounter a blog that’s both educative and interesting, and let me tell you, you’ve hit the nail on the head. The issue is an issue that too few folks are speaking intelligently about. I’m very happy that I stumbled across this during my search for something concerning this.
dark web drug marketplace https://github.com/darknetmarketslinks/darknetmarketlinks – dark markets dark web site
tor markets links dark web sites
Your writing is so eloquent and engaging You have a gift for connecting with your readers and making us feel understood
dark websites https://github.com/darknetmarkets24/darknet-markets darkmarket 2022
Your writing is so relatable and down-to-earth It’s like having a conversation with a good friend Thank you for always being real with your readers
darkmarkets darknet market list
tor markets 2022 drug markets onion
tor market https://github.com/darknetmarkets24/darknet-markets dark market
I was able to find good information from your blog posts.
dark web links https://github.com/darknetmarkets24/darknet-markets – dark websites
deep web markets darknet sites
darknet site dark market link
darknet links https://github.com/darknetmarketslinks/darknetmarketlinks – darknet market links darkmarket list
Watch our most viewed super sexy bf video on socksnews.in. sexy bf video Watch now.
darknet markets https://github.com/darknetmarkets24/darknet-markets darkmarket 2022
dark web sites links darknet site
darknet drug links https://github.com/darknetmarkets24/darknet-markets – darknet sites
darknet site dark market url
dark web market links https://github.com/darknetmarketslinks/darknetmarketlinks – tor markets dark web link
tor darknet https://github.com/darknetmarkets24/darknet-markets darknet drug store
Your style is really unique compared to other folks I’ve read stuff from. Thank you for posting when you have the opportunity, Guess I’ll just book mark this web site.
deep web drug url dark markets
deep web drug store https://github.com/darknetmarketslinks/darknetmarketlinks – dark web markets tor marketplace
dark market list https://github.com/darknetmarkets24/darknet-markets darknet site
darknet market lists https://github.com/darknetmarkets24/darknet-markets – darkmarkets
Great article! I learned a lot from your detailed explanation. Looking forward to more informative content like this!
dark web sites links drug markets onion
deep web drug store https://github.com/darknetmarketslinks/darknetmarketlinks – dark websites tor markets links
dark web drug marketplace https://github.com/darknetmarkets24/darknet-markets darknet drug store
deep web drug markets dark web link
I appreciate how well-researched and detailed your posts are It’s evident that you put a lot of time and effort into providing valuable information to your readers
deep web markets https://github.com/darknetmarkets24/darknet-markets – darkmarket 2022
deep web drug markets https://github.com/darknetmarketslinks/darknetmarketlinks – deep web drug links dark web drug marketplace
darknet marketplace https://github.com/darknetmarkets24/darknet-markets darkmarket
tor markets darkweb marketplace
darknet websites darknet marketplace
darknet site https://github.com/darknetmarketslinks/darknetmarketlinks – dark web websites tor markets 2025
darknet drug market https://github.com/darknetmarkets24/darknet-markets dark web sites links
deep web markets https://github.com/darknetmarkets24/darknet-markets – dark market onion
tor darknet tor darknet
dark market dark market 2022
dark web link https://github.com/darknetmarketslinks/darknetmarketlinks – darknet links dark web link
dark web links https://github.com/darknetmarkets24/darknet-markets darknet site
tor dark web https://github.com/darknetmarkets24/darknet-markets – dark market onion
dark market onion dark web sites
dark markets darkmarket url
dark web site https://github.com/darknetmarketslinks/darknetmarketlinks – dark web market list blackweb
darknet market list https://github.com/darknetmarkets24/darknet-markets deep web markets
drug markets dark web https://github.com/darknetmarkets24/darknet-markets – dark web market links
tor market links dark markets 2022
darknet sites tor market url
blackweb https://github.com/darknetmarketslinks/darknetmarketlinks – dark market 2025 tor dark web
dark web market links https://github.com/darknetmarkets24/darknet-markets tor marketplace
dark markets 2022 https://github.com/darknetmarkets24/darknet-markets – tor market
darkmarket url dark websites
darknet market lists tor markets
dark web markets https://github.com/darknetmarkets24/darknet-markets tor markets
dark market link https://github.com/darknetmarkets24/darknet-markets – tor marketplace
tor darknet dark market 2022
dark web market links deep web drug url
tor market url https://github.com/darknetmarketslinks/darknetmarketlinks – dark markets 2025 dark web site
dark web sites https://github.com/darknetmarkets24/darknet-markets dark web market
drug markets dark web https://github.com/darknetmarkets24/darknet-markets – darkmarket list
best darknet markets https://github.com/darknetmarketslinks/darknetmarketlinks – black internet dark web link
Hello there, I do think your website might be having browser compatibility issues. When I look at your web site in Safari, it looks fine however, if opening in IE, it has some overlapping issues. I simply wanted to provide you with a quick heads up! Other than that, excellent blog!
best darknet markets dark market 2022
dark web search engines https://github.com/darkwebmarketslinks/darkwebmarkets – tor market url dark market url
dark web markets darknet markets
dark web market links https://github.com/darknetmarketslinks/darknetmarketlinks – deep web drug url tor dark web
darknet drug store https://github.com/darknetmarkets24/darknet-markets – drug markets dark web
dark web market https://github.com/darknetmarkets2025/darknetmarketlinks – darknet market dark websites
darkmarket 2022 tor marketplace
drug markets onion https://github.com/darknetmarketslinks/darknetmarketlinks – black internet deep web drug links
tor market links https://github.com/darknetmarkets24/darknet-markets tor markets
dark web market https://github.com/darknetmarkets24/darknet-markets – dark markets 2022
This is the right blog for anyone who hopes to find out about this topic. You understand a whole lot its almost hard to argue with you (not that I really would want to…HaHa). You definitely put a fresh spin on a subject that has been written about for years. Wonderful stuff, just great.
dark website https://github.com/darknetmarketslinks/darknetmarketlinks – dark markets 2025 black internet
dark market 2022 darknet market links
deep web drug markets https://github.com/darknetmarkets2025/darknetmarketlinks – dark market list darkmarket
darknet market https://github.com/darkwebmarketslinks/darkwebmarkets – darkmarkets tor dark web
This blog was… how do you say it? Relevant!! Finally I have found something which helped me. Many thanks.
tor dark web https://github.com/darknetmarkets24/darknet-markets dark markets
tor markets links https://github.com/darknetmarkets24/darknet-markets – darknet market list
darknet markets https://github.com/darknetmarketslinks/darknetmarketlinks – dark web markets darkmarket 2025
dark web sites links dark web links
how to access dark web https://github.com/darknetmarketslinks/darknetmarketlinks – dark market link darknet sites
Hi there, I do believe your blog may be having browser compatibility issues. When I take a look at your web site in Safari, it looks fine however, if opening in I.E., it has some overlapping issues. I merely wanted to provide you with a quick heads up! Aside from that, great website!
darknet drug market dark web markets
darkmarket https://github.com/darknetmarkets2025/darknetmarketlinks – darknet links dark web markets
dark web links https://github.com/darkwebwebsites/darkwebwebsites – how to access dark web tor market
darknet market https://github.com/darknetmarkets24/darknet-markets – tor darknet
You have made some decent points there. I looked on the web for more info about the issue and found most individuals will go along with your views on this web site.
dark market https://github.com/darknetmarketslinks/darknetmarketlinks – dark market onion tor market
deep dark web https://github.com/darknetmarketslinks/darknetmarketlinks – deep web search deep web links
Can I simply just say what a comfort to uncover someone that actually knows what they are talking about on the net. You definitely realize how to bring a problem to light and make it important. More people have to check this out and understand this side of the story. I can’t believe you are not more popular since you definitely have the gift.
tor dark web https://github.com/darkwebwebsites/darkwebwebsites – deep web drug url tor marketplace
deep web drug url https://github.com/darkwebmarketslinks/darkwebmarkets – dark net darkmarket list
darknet markets 2025 https://github.com/darknetmarketslinks/darknetmarketlinks – deep web links black internet
best darknet markets https://github.com/darknetmarketslinks/darknetmarketlinks – blackweb darknet sites
When I initially commented I seem to have clicked the -Notify me when new comments are added- checkbox and now each time a comment is added I receive 4 emails with the exact same comment. Perhaps there is a means you are able to remove me from that service? Thank you.
dark web link https://github.com/darkwebwebsites/darkwebwebsites – dark web access dark web sites links
dark markets 2025 https://github.com/darkwebmarketslinks/darkwebmarkets – dark web search engines tor markets 2025
dark web market links https://github.com/darknetmarketslinks/darknetmarketlinks – darknet markets darkmarkets
tor markets links https://github.com/darknetmarketslinks/darknetmarketlinks – deep web drug markets darkmarket 2025
When I originally commented I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on each time a comment is added I recieve 4 emails with the same comment. There has to be a way you can remove me from that service? Thank you.
dark market url https://github.com/darknetmarkets2025/darknetmarketlinks – free dark web darknet drug links
deep web sites https://github.com/darkwebmarketslinks/darkwebmarkets – free dark web tor market url
Thank you for sharing this! Your insights are always so valuable, and I’ve learned so much from your blog. Looking forward to your next post!
piso game
dark market link https://github.com/darknetmarketslinks/darknetmarketlinks – tor markets dark web sites links
drug markets onion https://github.com/darknetmarketslinks/darknetmarketlinks – tor market dark market
Thank you for addressing such an important topic in this post Your words are powerful and have the potential to make a real difference in the world
dark web market list https://github.com/darkwebwebsites/darkwebwebsites – dark web market list tor dark web
black internet https://github.com/darkwebmarketslinks/darkwebmarkets – how to access dark web deep dark web
darkmarket link https://github.com/darknetmarketslinks/darknetmarketlinks – darknet market dark web markets
This page certainly has all of the information and facts I needed concerning this subject and didn’t know who to ask.
dark web market list https://github.com/darknetmarketslinks/darknetmarketlinks – dark net dark web market list
dark markets https://github.com/darkwebwebsites/darkwebwebsites – darknet market list darknet markets
how to get on dark web https://github.com/darknetmarketslinks/darknetmarketlinks – dark web links darknet market list
dark market list https://github.com/darkwebmarketslinks/darkwebmarkets – bitcoin dark web dark market
dark web market links https://github.com/darknetmarketslinks/darknetmarketlinks – tor markets links darknet market lists
dark market list https://github.com/darknetmarkets2025/darknetmarketlinks – darknet site tor market
dark web site https://github.com/darknetmarketslinks/darknetmarketlinks – deep web markets dark web links
dark websites https://github.com/darkwebmarketslinks/darkwebmarkets – darknet market best darknet markets
Hello there! I just wish to offer you a big thumbs up for the great information you’ve got here on this post. I’ll be coming back to your site for more soon.
darknet search engine https://github.com/darknetmarketslinks/darknetmarketlinks – deep web drug store deep web drug url
best darknet markets https://github.com/darkwebwebsites/darkwebwebsites – dark website dark web drug marketplace
deep web search https://github.com/darknetmarkets2025/darknetmarketlinks – darknet market list tor market url
black internet https://github.com/darknetmarketslinks/darknetmarketlinks – deep web links blackweb official website
darknet market https://github.com/darkwebmarketslinks/darkwebmarkets – tor darknet darknet markets 2025
dark web search engine https://github.com/darknetmarketslinks/darknetmarketlinks – darknet drug store dark web sites links
darknet drugs https://github.com/darkwebwebsites/darkwebwebsites – dark market onion deep dark web
dark web market list https://github.com/darknetmarkets2025/darknetmarketlinks – free dark web dark internet
I appreciate how well-researched and informative each post is It’s obvious how much effort you put into your work
Good site you have got here.. It’s difficult to find good quality writing like yours nowadays. I seriously appreciate individuals like you! Take care!!
darknet websites https://github.com/darknetmarketslinks/darknetmarketlinks – dark web market list dark market list
blackweb https://github.com/darkwebmarketslinks/darkwebmarkets – darknet sites deep web drug markets
This is a topic that’s near to my heart… Best wishes! Where can I find the contact details for questions?
tor market https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet marketplace
dark web links https://github.com/darkwebwebsites/darkwebwebsites – darkweb marketplace darknet markets
the dark internet https://github.com/darknetmarkets2025/darknetmarketlinks – darknet links tor market url
onion market https://github.com/darknetmarketlinks2025/darknetmarkets – deep web drug links
tor market url https://github.com/tormarkets2025ukaz1/tormarkets2025 – deep web markets
This is a topic which is near to my heart… Take care! Where can I find the contact details for questions?
dark net https://github.com/darknetmarketslinks/darknetmarketlinks – deep web links dark markets
darknet seiten https://github.com/darkwebmarketslinks/darkwebmarkets – dark web sites best darknet markets
dark web sites https://github.com/darkmarketlinkp22jr/darkmarketlink – dark market
deep web drug store https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet market
I appreciate the depth of research in this article. It’s both informative and engaging. Keep up the great work!
drug markets onion https://github.com/darknetdruglinksvojns/darknetdruglinks – deep web markets
dark web access https://github.com/darknetmarketslinks/darknetmarketlinks – dark web site darknet market list
bookmarked!!, I love your website.
darknet market list https://github.com/darknetmarketlinks2025/darknetmarkets – dark web market list
deep web drug store https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkweb marketplace
dark web websites https://github.com/darkwebwebsites/darkwebwebsites – dark market url deep web drug store
dark website https://github.com/darknetmarkets2025/darknetmarketlinks – dark web links dark web link
dark web link https://github.com/darknetmarketslinks/darknetmarketlinks – bitcoin dark web best darknet markets
dark web markets https://github.com/darkmarketlinkp22jr/darkmarketlink – tor market url
darknet drug store https://github.com/darknetwebsitesgflpx/darknetwebsites – bitcoin dark web
deep dark web https://github.com/darkwebmarketslinks/darkwebmarkets – tor markets 2025 dark market url
When I originally commented I seem to have clicked the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I receive four emails with the same comment. Is there a way you can remove me from that service? Thanks.
dark web market links https://github.com/darknetdruglinksvojns/darknetdruglinks – darkmarket 2022
dark web websites https://github.com/darknetmarketslinks/darknetmarketlinks – dark web markets tor darknet
tor markets https://github.com/darknetmarketlinks2025/darknetmarkets – deep web drug links
darkmarket url https://github.com/darkwebwebsites/darkwebwebsites – deep web drug url free dark web
dark web site https://github.com/darknetmarkets2025/darknetmarketlinks – deep web drug links dark web market list
tor markets https://github.com/darknetmarketslinks/darknetmarketlinks – onion market darknet markets 2025
dark web market list https://github.com/darkmarketlinkp22jr/darkmarketlink – dark market url
darkmarket https://github.com/darknetwebsitesgflpx/darknetwebsites – bitcoin dark web
darkmarket https://github.com/darkwebmarketslinks/darkwebmarkets – deep dark web dark websites
deep web drug store https://github.com/darknetdruglinksvojns/darknetdruglinks – dark web markets
darknet market https://github.com/darknetmarketslinks/darknetmarketlinks – drug markets onion blackweb official website
tor markets links https://github.com/darknetmarketlinks2025/darknetmarkets – dark markets
best darknet markets https://github.com/darknetmarketslinks/darknetmarketlinks – dark market url dark web websites
dark web markets https://github.com/darkmarketlinkp22jr/darkmarketlink – deep web drug store
tor market url https://github.com/darkwebwebsites/darkwebwebsites – tor market url darknet markets 2025
deep web drug url https://github.com/darknetmarkets2025/darknetmarketlinks – darkweb marketplace darknet market lists
tor marketplace https://github.com/darknetwebsitesgflpx/darknetwebsites – darkmarket link
Great article. I will be going through many of these issues as well..
darknet drug market https://github.com/darknetdruglinksvojns/darknetdruglinks – dark websites
dark web site https://github.com/darknetmarketslinks/darknetmarketlinks – dark market 2025 dark market
darkmarkets https://github.com/darkwebmarketslinks/darkwebmarkets – darkmarket url darknet drug market
darknet drug market https://github.com/darknetmarketlinks2025/darknetmarkets – dark markets
onion market https://github.com/darkmarketlinkp22jr/darkmarketlink – darkmarket 2022
best darknet markets https://github.com/darknetwebsitesgflpx/darknetwebsites – best darknet markets
darknet markets 2025 https://github.com/darkwebwebsites/darkwebwebsites – dark web site darkmarket
dark web market links https://github.com/darknetmarkets2025/darknetmarketlinks – darknet market lists dark web drug marketplace
dark web sites https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet drug store
dark web link https://github.com/darknetmarketslinks/darknetmarketlinks – dark web site dark web links
deep web drug store https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market 2022
Your posts are so well-written and eloquent It’s impossible not to be moved by your words Keep using your voice to spread positivity
dark market 2022 https://github.com/darkmarketlinkp22jr/darkmarketlink – best darknet markets
the dark internet https://github.com/darknetmarketslinks/darknetmarketlinks – free dark web darkmarket 2025
darkmarket 2022 https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet drug links
best darknet markets https://github.com/darkwebwebsites/darkwebwebsites – drug markets dark web tor market links
darknet drug market https://github.com/darknetmarkets2025/darknetmarketlinks – onion market drug markets dark web
darkmarket https://github.com/darknetdruglinksvojns/darknetdruglinks – dark web markets
darknet drug market https://github.com/darknetmarketlinks2025/darknetmarkets – darknet market
darknet seiten https://github.com/darknetmarketslinks/darknetmarketlinks – dark web search engines dark website
darknet links https://github.com/darkwebmarketslinks/darkwebmarkets – dark web market tor market
bitcoin dark web https://github.com/darkmarketlinkp22jr/darkmarketlink – dark web market list
deep web search https://github.com/darknetmarketslinks/darknetmarketlinks – dark market drug markets dark web
dark web markets https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet websites
tor markets https://github.com/darknetdruglinksvojns/darknetdruglinks – deep web drug url
tor dark web https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarket 2022
deep dark web https://github.com/darknetmarketlinks2025/darknetmarkets – deep dark web
deep web drug links https://github.com/darkwebwebsites/darkwebwebsites – dark markets 2025 darkmarket list
darknet seiten https://github.com/darknetmarkets2025/darknetmarketlinks – darknet marketplace darknet marketplace
dark web sites links https://github.com/darknetmarketslinks/darknetmarketlinks – darknet market dark market onion
deep web drug store https://github.com/darkmarketlinkp22jr/darkmarketlink – drug markets onion
darknet market lists https://github.com/darkwebmarketslinks/darkwebmarkets – darknet search engine dark web drug marketplace
dark web sites https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet drug market
darknet drug market https://github.com/darknetmarketslinks/darknetmarketlinks – tor market url darknet drug store
darknet websites https://github.com/darknetdruglinksvojns/darknetdruglinks – dark web market
dark market 2022 https://github.com/darknetmarketlinks2025/darknetmarkets – tor markets
drug markets dark web https://github.com/darknetmarketslinks/darknetmarketlinks – how to access dark web free dark web
deep web drug markets https://github.com/darkwebwebsites/darkwebwebsites – tor market how to get on dark web
darknet market https://github.com/darknetmarkets2025/darknetmarketlinks – dark market 2025 dark market onion
tor market links https://github.com/darkmarketlinkp22jr/darkmarketlink – tor markets
bitcoin dark web https://github.com/darknetwebsitesgflpx/darknetwebsites – tor dark web
dark web search engines https://github.com/darknetmarketslinks/darknetmarketlinks – dark web links tor markets
the dark internet https://github.com/darkwebmarketslinks/darkwebmarkets – best darknet markets deep web drug markets
deep dark web https://github.com/darknetdruglinksvojns/darknetdruglinks – tor darknet
darknet drug links https://github.com/darknetmarketlinks2025/darknetmarkets – dark web market list
tor darknet https://github.com/darknetmarketslinks/darknetmarketlinks – dark web markets dark web sites
dark market onion https://github.com/darkwebwebsites/darkwebwebsites – tor markets blackweb
deep web markets https://github.com/darkmarketlinkp22jr/darkmarketlink – dark market
Your style is really unique compared to other folks I have read stuff from. Thanks for posting when you’ve got the opportunity, Guess I will just bookmark this blog.
darkmarket link https://github.com/darknetwebsitesgflpx/darknetwebsites – darkmarket url
dark market list https://github.com/darknetmarketslinks/darknetmarketlinks – dark web search engine drug markets dark web
deep web sites https://github.com/darkwebmarketslinks/darkwebmarkets – tor dark web tor marketplace
darknet drug market https://github.com/darknetdruglinksvojns/darknetdruglinks – dark web market links
black internet https://github.com/darknetmarketslinks/darknetmarketlinks – tor markets darknet markets
dark market list https://github.com/darkmarketlinkp22jr/darkmarketlink – darknet marketplace
onion market https://github.com/darkwebwebsites/darkwebwebsites – darknet websites dark websites
free dark web https://github.com/darknetmarkets2025/darknetmarketlinks – deep web links tor markets links
darknet drug links https://github.com/darknetwebsitesgflpx/darknetwebsites – dark market url
drug markets onion https://github.com/darknetmarketslinks/darknetmarketlinks – dark web drug marketplace darkmarket 2025
This website definitely has all of the info I wanted about this subject and didn’t know who to ask.
dark web sites https://github.com/darkwebmarketslinks/darkwebmarkets – darknet market list tor darknet
deep web drug markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web links
drug markets onion https://github.com/darknetmarketlinks2025/darknetmarkets – deep dark web
tor markets links https://github.com/darknetmarketslinks/darknetmarketlinks – darknet drug store darknet market list
This is the right blog for everyone who wishes to understand this topic. You realize a whole lot its almost hard to argue with you (not that I really would want to…HaHa). You definitely put a fresh spin on a subject which has been written about for years. Wonderful stuff, just wonderful.
darknet market https://github.com/darkwebwebsites/darkwebwebsites – darkmarket 2025 blackweb official website
dark web drug marketplace https://github.com/darknetmarketslinks/darknetmarketlinks – deep web links deep web drug links
darknet drug links https://github.com/darknetmarkets2025/darknetmarketlinks – darknet links deep web drug markets
darknet links https://github.com/darkwebmarketslinks/darkwebmarkets – dark web market list deep web drug url
dark market 2025 https://github.com/darknetmarketslinks/darknetmarketlinks – tor market url tor market url
darknet sites https://github.com/darknetmarketslinks/darknetmarketlinks – deep dark web blackweb official website
tor dark web https://github.com/darkwebwebsites/darkwebwebsites – tor markets how to get on dark web
best darknet markets https://github.com/darknetmarkets2025/darknetmarketlinks – dark web links darknet markets 2025
For anyone looking for an easy way to download Metamask and use it safely, https://metamake.org/ is the best resource. Their guides help both beginners and advanced users navigate the setup process efficiently.
darkmarket https://github.com/darknetmarketslinks/darknetmarketlinks – dark market link tor markets 2025
dark web markets https://github.com/darkwebmarketslinks/darkwebmarkets – dark web search engine darkmarket link
dark market onion https://github.com/darknetmarketslinks/darknetmarketlinks – dark web sites links dark web sites links
deep dark web https://github.com/darkwebwebsites/darkwebwebsites – tor market links darknet market links
darknet seiten https://github.com/darknetmarkets2025/darknetmarketlinks – darknet market darknet drug store
darknet market https://github.com/darknetmarketslinks/darknetmarketlinks – how to access dark web darkweb marketplace
dark web sites https://github.com/darkwebmarketslinks/darkwebmarkets – how to access dark web tor markets links
tor markets 2022 https://github.com/darknetmarketlinks2025/darknetmarkets – darknet sites
darkmarket link https://github.com/darkwebwebsites/darkwebwebsites – drug markets onion tor markets links
dark website https://github.com/darknetmarketslinks/darknetmarketlinks – dark markets 2025 deep web markets
Great article! We will be linking to this particularly great post on our website. Keep up the great writing.
darkmarket list https://github.com/darkwebmarketslinks/darkwebmarkets – dark net dark internet
dark market 2022 https://github.com/darknetmarketlinks2025/darknetmarkets – dark web market links
darkmarket 2022 https://github.com/darknetwebsitesgflpx/darknetwebsites – darkmarket list
tor market url https://github.com/darkmarketlinkp22jr/darkmarketlink – deep web drug url
Everyone loves it when people get together and share views. Great blog, keep it up.
darknet market https://github.com/darkwebwebsites/darkwebwebsites – dark web markets free dark web
darknet market links https://github.com/darknetmarketslinks/darknetmarketlinks – dark web drug marketplace darknet market links
tor markets https://github.com/darknetmarketlinks2025/darknetmarkets – tor dark web
darknet websites https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet drug store
darknet market links https://github.com/darkmarketlinkp22jr/darkmarketlink – tor markets
dark market url https://github.com/darkwebmarketslinks/darkwebmarkets – tor markets dark web access
Good write-up. I certainly appreciate this website. Continue the good work!
deep web markets https://github.com/darknetmarketslinks/darknetmarketlinks – darkweb marketplace bitcoin dark web
best darknet markets https://github.com/darkwebwebsites/darkwebwebsites – deep web sites drug markets dark web
darknet drug store https://github.com/darknetmarkets2025/darknetmarketlinks – dark internet dark web drug marketplace
deep web drug markets https://github.com/darknetmarketlinks2025/darknetmarkets – darknet market links
onion market https://github.com/darknetdruglinksvojns/darknetdruglinks – dark market onion
dark web sites links https://github.com/darkmarketlinkp22jr/darkmarketlink – bitcoin dark web
blackweb official website https://github.com/darkwebmarketslinks/darkwebmarkets – dark markets 2025 darknet drug market
Every time I read one of your posts, I come away with something new and interesting to think about. Thanks for consistently putting out such great content!
Everyone loves it when folks get together and share views. Great website, stick with it.
Let me know what type of content you’d like to see more of in the future!
darknet websites https://github.com/darkwebwebsites/darkwebwebsites – dark web sites links dark web market
bitcoin dark web https://github.com/darknetmarkets2025/darknetmarketlinks – darkmarkets bitcoin dark web
darknet market links https://github.com/darkwebmarketslinks/darkwebmarkets – darkmarket list darknet markets
deep web drug markets https://github.com/darknetmarketslinks/darknetmarketlinks – deep web drug markets darkmarket
darknet marketplace https://github.com/darkwebwebsites/darkwebwebsites – dark web drug marketplace dark net
onion market https://github.com/darknetmarkets2025/darknetmarketlinks – tor market links best darknet markets
You need to be a part of a contest for one of the best blogs on the internet. I am going to highly recommend this blog!
darknet drug store drug markets onion dark web link
I followed the guide on https://metaduck.org/ to install the Metamask extension, and it was super easy. Now I can manage my crypto securely!
tor markets 2025 darknet markets darknet markets
dark market 2025 deep web drug store best darknet markets
deep web links darkmarket tor market links
deep web search dark web sites links darknet market list
A friend recommended https://metapaws.org/ for downloading Metamask, and I’m so glad I checked it out. The process was easy, and now I can safely store my crypto.
dark web site tor markets 2025 best darknet markets
dark market list dark web links dark market list
free dark web darknet drug store darknet market list
darknet seiten deep web links dark net
darknet site dark websites how to access dark web
drug markets dark web https://github.com/darknetwebsitesgflpx/darknetwebsites – dark market
darknet links tor markets links tor market links
deep dark web deep web markets how to access dark web
dark markets 2022 https://github.com/darknetmarketlinks2025/darknetmarkets – darknet drug store
tor markets 2022 https://github.com/darknetdruglinksvojns/darknetdruglinks – deep web drug store
Oh my goodness! Amazing article dude! Thanks, However I am going through difficulties with your RSS. I don’t understand the reason why I cannot subscribe to it. Is there anybody having the same RSS problems? Anybody who knows the answer can you kindly respond? Thanks!
deep web drug store dark web link how to get on dark web
dark web market deep web drug links blackweb
bitcoin dark web https://github.com/darknetwebsitesgflpx/darknetwebsites – dark websites
tor darknet deep dark web darknet drug links
dark market url dark market url dark websites
tor darknet https://github.com/darknetmarketlinks2025/darknetmarkets – darknet drug store
darknet market list https://github.com/darknetdruglinksvojns/darknetdruglinks – dark market
darkmarket dark web market links darknet drugs
dark web market list dark web search engines darkmarket url
darknet drug links darknet links darknet site
black internet dark market url blackweb official website
darknet market links https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet drug market
dark markets 2022 https://github.com/darknetmarketlinks2025/darknetmarkets – dark markets
Greetings! Very helpful advice in this particular article! It’s the little changes that will make the biggest changes. Thanks a lot for sharing!
dark web links darknet markets 2025 dark web search engine
dark web market list darknet markets 2025 darknet drug store
tor market url https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet drug links
dark web search engines darknet market the dark internet
dark web market list https://github.com/darknetmarketlinks2025/darknetmarkets – tor dark web
dark market https://github.com/darknetdruglinksvojns/darknetdruglinks – dark web market links
the dark internet dark markets 2025 darknet drug links
darknet links darknet drug market darknet market
darkmarket list https://github.com/darknetwebsitesgflpx/darknetwebsites – dark web market
dark market list https://github.com/darkmarketlinkp22jr/darkmarketlink – dark web sites
darknet drug store https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet drug store
Hi, I believe your blog could be having internet browser compatibility problems. Whenever I look at your blog in Safari, it looks fine however when opening in I.E., it’s got some overlapping issues. I simply wanted to provide you with a quick heads up! Besides that, excellent website!
blackweb dark internet darkmarkets
tor darknet https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet marketplace
darknet market list dark web search engines darknet marketplace
tor dark web darkweb marketplace dark markets
dark web markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkweb marketplace
dark websites https://github.com/darknetdruglinksvojns/darknetdruglinks – dark websites
deep web drug store darknet site blackweb official website
tor markets 2022 https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet drug links
darknet seiten bitcoin dark web deep web search
deep web drug markets https://github.com/darkmarketlinkp22jr/darkmarketlink – bitcoin dark web
deep web markets https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet websites
deep web sites darknet drug links how to get on dark web
darknet drug store https://github.com/darknetwebsitesgflpx/darknetwebsites – tor markets 2022
Good blog post. I certainly appreciate this website. Keep it up!
best darknet markets dark web markets dark web drug marketplace
dark web search engine darknet seiten darknet links
dark web market list darkmarket url dark market
darknet market list https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet sites
darknet market links https://github.com/darknetmarketlinks2025/darknetmarkets – dark web drug marketplace
darkmarket 2022 https://github.com/darknetdruglinksvojns/darknetdruglinks – tor markets
tor markets links deep web drug url onion market
Hello there! I could have sworn I’ve been to this website before but after going through a few of the articles I realized it’s new to me. Anyways, I’m certainly delighted I came across it and I’ll be bookmarking it and checking back frequently!
dark market onion https://github.com/darknetwebsitesgflpx/darknetwebsites – darkmarket url
dark web links darknet seiten darknet search engine
tor market dark market 2025 dark market
darknet marketplace https://github.com/darkmarketlinkp22jr/darkmarketlink – dark market 2022
darknet market lists https://github.com/darknetmarketlinks2025/darknetmarkets – tor markets
drug markets dark web https://github.com/darknetdruglinksvojns/darknetdruglinks – darkmarket 2022
darknet market lists darknet search engine darkmarket
darkmarkets https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet websites
darknet market lists dark market onion darknet market list
tor darknet https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark markets
darkmarket 2022 https://github.com/darknetmarketlinks2025/darknetmarkets – dark web market links
blackweb deep web search darknet seiten
drug markets onion dark web search engine darkmarket link
tor darknet https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet markets
dark web search engines tor market darknet markets
darknet site https://github.com/darkmarketlinkp22jr/darkmarketlink – darkmarket 2022
dark market onion https://github.com/darknetmarketlinks2025/darknetmarkets – best darknet markets
darkmarket https://github.com/darknetdruglinksvojns/darknetdruglinks – tor markets links
darknet drugs darknet markets 2025 dark market url
You should take part in a contest for one of the most useful blogs on the net. I will recommend this blog!
dark market onion https://github.com/darknetwebsitesgflpx/darknetwebsites – drug markets onion
the dark internet dark markets 2025 tor markets
darknet seiten how to get on dark web dark web market list
darknet sites https://github.com/tormarkets2025ukaz1/tormarkets2025 – drug markets onion
Oh my goodness! Amazing article dude! Thank you so much, However I am experiencing issues with your RSS. I don’t know the reason why I am unable to subscribe to it. Is there anybody else having identical RSS problems? Anyone who knows the answer will you kindly respond? Thanx!!
tor marketplace https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet marketplace
darknet drug store tor market links darknet market lists
dark web market list https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet drug links
dark market list best darknet markets darknet sites
darknet seiten dark website darknet drugs
dark market list darknet drugs dark web drug marketplace
darknet market links https://github.com/darkmarketlinkp22jr/darkmarketlink – bitcoin dark web
drug markets dark web https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web market
darknet market links https://github.com/darknetdruglinksvojns/darknetdruglinks – deep web drug store
dark market list darknet marketplace darkmarket
dark web sites links https://github.com/darknetwebsitesgflpx/darknetwebsites – dark market
darknet search engine tor marketplace tor markets
tor market url dark web search engine dark website
dark web markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet site
darkmarket list https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet site
deep web drug markets https://github.com/darknetwebsitesgflpx/darknetwebsites – dark web link
drug markets dark web dark web link darknet markets
dark internet darknet drugs dark web drug marketplace
dark web drug marketplace https://github.com/darkmarketlinkp22jr/darkmarketlink – best darknet markets
tor markets 2025 darknet sites darknet seiten
dark web sites links https://github.com/darknetdruglinksvojns/darknetdruglinks – dark web sites
darkmarket 2022 https://github.com/darknetmarketlinks2025/darknetmarkets – dark web markets
darkweb marketplace https://github.com/darknetwebsitesgflpx/darknetwebsites – deep web drug store
tor markets dark market 2025 dark internet
darknet drugs how to access dark web the dark internet
tor dark web dark web drug marketplace tor dark web
dark web sites https://github.com/darkmarketlinkp22jr/darkmarketlink – dark web sites
tor market links https://github.com/darknetdruglinksvojns/darknetdruglinks – bitcoin dark web
dark market url tor marketplace darknet market
dark web market links https://github.com/darknetwebsitesgflpx/darknetwebsites – darkmarket
dark market list how to get on dark web dark market url
darknet drug links free dark web dark web link
dark market list dark market url tor dark web
how to access dark web tor markets 2025 best darknet markets
drug markets dark web darkmarket list darknet market list
dark web market links tor darknet dark web market links
darknet market lists deep web drug store darknet drugs
darkmarket darknet market lists darkmarket list
dark web market darknet site darknet seiten
deep web drug markets black internet deep web drug url
deep web drug links darkmarket 2025 darknet marketplace
dark web link https://github.com/darknetmarketlinks2025/darknetmarkets – best darknet markets
darknet drug market https://github.com/darknetdruglinksvojns/darknetdruglinks – deep dark web
tor darknet dark web sites links dark web websites
Hi there! I just want to offer you a big thumbs up for your excellent info you have right here on this post. I am returning to your site for more soon.
darknet drug links dark internet darknet market lists
darknet search engine dark web access darkmarket url
dark market 2022 https://github.com/darknetmarketlinks2025/darknetmarkets – drug markets onion
black internet dark market url darknet seiten
dark web markets https://github.com/darknetdruglinksvojns/darknetdruglinks – dark markets 2022
tor markets 2022 https://github.com/darkmarketlinkp22jr/darkmarketlink – dark web sites
tor markets 2025 blackweb darkweb marketplace
darknet websites black internet darknet links
Way cool! Some very valid points! I appreciate you writing this post plus the rest of the website is really good.
dark web link https://github.com/darknetmarketlinks2025/darknetmarkets – darknet sites
tor market url https://github.com/darknetwebsitesgflpx/darknetwebsites – drug markets onion
onion market https://github.com/darknetdruglinksvojns/darknetdruglinks – dark websites
darknet drug links https://github.com/darkmarketlinkp22jr/darkmarketlink – darkmarkets
dark market list bitcoin dark web darknet site
I couldn’t resist commenting. Perfectly written.
the dark internet tor market tor markets 2025
darknet sites dark web websites dark web market
dark web search engines deep web search dark web market
darkmarket 2022 https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market onion
dark websites https://github.com/darknetdruglinksvojns/darknetdruglinks – darkweb marketplace
Right here is the perfect web site for anybody who would like to find out about this topic. You know so much its almost tough to argue with you (not that I really will need to…HaHa). You definitely put a brand new spin on a subject that has been discussed for many years. Wonderful stuff, just excellent.
tor darknet https://github.com/darkmarketlinkp22jr/darkmarketlink – dark web market
how to access dark web darkweb marketplace tor markets links
deep web drug links black internet dark web access
What’s up Dear, are you genuinely visiting this site on a regular basis, if so afterward you will definitely take nice know-how.
вход lee bet
free dark web darknet site deep dark web
tor dark web darknet seiten dark web sites
dark web link https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark markets
dark web sites https://github.com/darknetmarketlinks2025/darknetmarkets – drug markets dark web
deep dark web https://github.com/darknetdruglinksvojns/darknetdruglinks – deep web drug links
dark web sites darkmarket list deep web drug store
dark market 2022 https://github.com/darkmarketlinkp22jr/darkmarketlink – bitcoin dark web
dark web site dark web market list blackweb official website
darkweb marketplace deep web search darkweb marketplace
tor market links free dark web dark web site
darknet markets 2025 darknet site dark market list
dark markets https://github.com/darknetwebsitesgflpx/darknetwebsites – deep web drug markets
dark market url https://github.com/darknetmarketlinks2025/darknetmarkets – tor market links
darkmarket url https://github.com/darknetdruglinksvojns/darknetdruglinks – dark market
tor dark web https://github.com/darkmarketlinkp22jr/darkmarketlink – darkmarket 2022
darkmarket url darkmarket list dark web links
tor markets 2025 free dark web dark web websites
dark websites https://github.com/darknetwebsitesgflpx/darknetwebsites – tor markets 2022
dark market link https://github.com/darknetdruglinksvojns/darknetdruglinks – tor marketplace
darknet market links https://github.com/darkmarketlinkp22jr/darkmarketlink – deep web drug store
dark web search engines best darknet markets blackweb
dark web site darkmarkets dark web sites
deep web sites black internet darknet drugs
dark market onion tor markets links dark market url
dark market 2022 https://github.com/darknetwebsitesgflpx/darknetwebsites – tor markets 2022
deep web markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market link
darkmarkets https://github.com/darknetmarketlinks2025/darknetmarkets – darknet market list
darkmarket https://github.com/darknetdruglinksvojns/darknetdruglinks – bitcoin dark web
darknet market links https://github.com/darkmarketlinkp22jr/darkmarketlink – dark web sites links
dark web search engines dark market url dark web drug marketplace
darkweb marketplace darknet market lists dark web search engine
dark market dark market 2025 deep web search
dark web drug marketplace https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet site
deep web drug store https://github.com/darknetmarketlinks2025/darknetmarkets – tor market
darknet drug store https://github.com/darkmarketlinkp22jr/darkmarketlink – darknet market lists
dark web sites tor marketplace dark web search engines
darknet markets darknet marketplace dark web websites
dark market 2025 dark web sites deep web drug url
dark market list https://github.com/tormarkets2025ukaz1/tormarkets2025 – tor dark web
dark market url https://github.com/darknetmarketlinks2025/darknetmarkets – dark web links
dark market 2022 https://github.com/darknetdruglinksvojns/darknetdruglinks – tor market url
darknet market https://github.com/darkmarketlinkp22jr/darkmarketlink – deep web drug store
deep web drug links tor markets 2025 dark web link
dark web search engine darknet websites darkmarket list
deep web drug markets darknet markets 2025 blackweb
Hi it’s me, I am also visiting this website on a regular basis, this web page is genuinely pleasant and the visitors are in fact sharing fastidious thoughts.
https://santehnikaclub.ru/
tor marketplace https://github.com/darknetwebsitesgflpx/darknetwebsites – dark web sites
You should be a part of a contest for one of the best websites on the web. I’m going to highly recommend this web site!
darkweb marketplace drug markets dark web tor market url
darkmarkets darknet drug links deep web drug store
darknet drug market deep web drug url darknet drug store
deep web drug links https://github.com/darkmarketlinkp22jr/darkmarketlink – darknet market links
deep dark web https://github.com/darknetdruglinksvojns/darknetdruglinks – dark market onion
drug markets dark web dark market url blackweb
I could not resist commenting. Very well written!
darkmarket https://github.com/darknetwebsitesgflpx/darknetwebsites – dark markets 2022
dark web websites deep web search tor markets
deep web drug markets dark web sites links darknet drug store
tor dark web https://github.com/darkmarketlinkp22jr/darkmarketlink – deep web drug links
darknet markets https://github.com/darknetdruglinksvojns/darknetdruglinks – tor market url
darkweb marketplace bitcoin dark web deep web drug store
darknet drug store dark web markets darknet websites
deep web markets https://github.com/darknetmarketlinks2025/darknetmarkets – dark web markets
I love it whenever people come together and share thoughts. Great website, keep it up.
tor markets dark web websites tor darknet
darknet markets https://github.com/darkmarketlinkp22jr/darkmarketlink – dark web sites links
dark web sites https://github.com/darknetdruglinksvojns/darknetdruglinks – tor markets 2022
Good post. I am experiencing many of these issues as well..
deep web drug markets darkmarket list drug markets onion
dark web access how to get on dark web drug markets onion
dark market link tor market how to get on dark web
tor market links https://github.com/darknetwebsitesgflpx/darknetwebsites – darkmarket 2022
An impressive share! I have just forwarded this onto a coworker who was conducting a little research on this. And he actually ordered me dinner simply because I found it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending the time to talk about this subject here on your web site.
darkmarket url deep web drug store onion market
darknet site darknet markets dark markets 2025
darkmarket drug markets dark web darknet market list
the dark internet dark web market black internet
Hi there! This blog post couldn’t be written any better! Going through this article reminds me of my previous roommate! He always kept preaching about this. I am going to send this post to him. Fairly certain he will have a very good read. I appreciate you for sharing!
the dark internet darkmarket 2025 deep web drug markets
dark web markets darknet market darkmarket 2025
dark web link darknet drug market tor market url
dark market 2025 dark web sites links dark web sites
darkmarket link dark market onion dark web drug marketplace
darknet sites dark web search engines darknet links
tor markets 2025 dark web market darkweb marketplace
deep web sites tor market links dark market onion
dark market link deep web search darknet markets
darknet drug store deep web drug markets dark web sites links
darknet sites dark web drug marketplace darknet sites
tor darknet https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet market lists
dark web market list https://github.com/darkmarketlinkp22jr/darkmarketlink – dark web market links
dark web links https://github.com/darknetmarketlinks2025/darknetmarkets – tor markets links
darknet drugs drug markets onion darknet drug links
dark web link darknet drug market dark markets 2025
deep web search darknet drug store dark web sites links
darkweb marketplace onion market blackweb official website
drug markets onion https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web links
darkmarket https://github.com/darknetdruglinksvojns/darknetdruglinks – dark websites
darknet drug market https://github.com/darknetmarketlinks2025/darknetmarkets – dark web market links
dark web market links darknet drug store dark web link
darknet drug market darknet markets onion darkmarket list
dark web market darknet market list dark web market links
dark market 2025 dark web link darknet drug links
dark web drug marketplace darknet market
dark market darknet websites
tor drug market darknet markets 2025
darkmarket link darknet markets
darknet drug links darknet site onion dark website
dark market link darknet links dark web market urls
dark web market darknet markets url
onion dark website tor drug market darknet market links
dark market dark market onion
darknet markets onion darknet market links darknet site
darknet markets 2025 darknet drugs darknet markets url
darknet drug store darkmarket 2025 darkmarket list
Right here is the perfect webpage for anybody who would like to understand this topic. You know a whole lot its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a fresh spin on a subject that has been discussed for decades. Excellent stuff, just excellent.
darknet markets dark markets 2025 darknet market links
dark market dark markets 2025
darknet drug market dark markets 2025
darknet markets url dark markets darknet markets onion
darknet websites darknet markets
Hello there! I could have sworn I’ve been to your blog before but after looking at some of the posts I realized it’s new to me. Nonetheless, I’m certainly happy I came across it and I’ll be book-marking it and checking back regularly.
dark web market list darknet market list darknet drug market
The next time I read a blog, I hope that it doesn’t fail me as much as this particular one. I mean, I know it was my choice to read through, however I really thought you would probably have something useful to say. All I hear is a bunch of crying about something that you could possibly fix if you weren’t too busy looking for attention.
darknet drugs best darknet markets
darkmarket link dark web marketplaces
darkmarket list darkmarket 2025 dark markets 2025
dark markets darkmarket link darknet markets onion
darknet market darknet drug store darknet market list
darknet market lists best darknet markets
dark market url dark web sites dark web drug marketplace
darkmarket 2025 dark markets 2025
dark websites darkmarket url darkmarket 2025
Your style is very unique in comparison to other folks I’ve read stuff from. Many thanks for posting when you have the opportunity, Guess I’ll just book mark this page.
dark web market list dark markets 2025
darknet marketplace darknet market
dark web market links dark web market urls
dark web sites dark market link darknet market list
dark markets 2025 dark market list dark web market urls
bitcoin dark web darknet markets 2025
dark web link darknet markets onion address dark market link
darkmarket list dark web market urls
tor drug market dark websites
darknet drug store dark market onion darknet market list
darknet links darknet site darknet drugs
Very nice post. I definitely appreciate this website. Keep it up!
dark market 2025 darknet drug links dark web markets
Howdy! This post could not be written much better! Going through this article reminds me of my previous roommate! He constantly kept talking about this. I most certainly will send this post to him. Pretty sure he’s going to have a good read. I appreciate you for sharing!
darknet markets 2025 bitcoin dark web onion dark website
darkmarket url dark market url darknet markets links
This is a really good tip especially to those new to the blogosphere. Short but very accurate information… Appreciate your sharing this one. A must read post.
dark market 2025 darkmarket list darknet markets
dark web market darknet links
Having read this I thought it was really informative. I appreciate you finding the time and effort to put this article together. I once again find myself personally spending a lot of time both reading and commenting. But so what, it was still worth it.
darknet drugs dark web drug marketplace dark markets
I’m amazed, I must say. Rarely do I encounter a blog that’s equally educative and amusing, and without a doubt, you’ve hit the nail on the head. The problem is an issue that not enough people are speaking intelligently about. Now i’m very happy that I came across this during my search for something regarding this.
dark market 2025 darkmarket list
Having read this I believed it was rather informative. I appreciate you spending some time and energy to put this article together. I once again find myself spending way too much time both reading and commenting. But so what, it was still worth it!
darknet markets onion darknet markets onion
darknet markets 2025 darknet market list darknet site
darknet drug market darknet markets onion address
darknet market links dark web drug marketplace darkmarkets
dark web market links darknet markets
darknet markets url darknet markets onion address
dark markets 2025 darknet markets onion
dark market 2025 dark market url dark markets
darknet markets darknet market
darknet market list dark web drug marketplace
darknet markets onion dark web sites
dark market url darknet market list
dark markets tor drug market best darknet markets
dark web market links dark web marketplaces
dark web market links darknet site
This is the perfect site for everyone who would like to understand this topic. You understand a whole lot its almost hard to argue with you (not that I really will need to…HaHa). You definitely put a fresh spin on a topic which has been written about for years. Great stuff, just wonderful.
bitcoin dark web best darknet markets
darknet markets onion address dark market link dark market url
You should take part in a contest for one of the finest blogs online. I am going to recommend this website!
dark markets 2025 darknet drug links
darknet drug links darknet market
darkmarket list darknet drugs
dark market list dark market list dark web market links
darkmarket 2025 darknet markets onion address
Right here is the right web site for anybody who hopes to find out about this topic. You realize a whole lot its almost tough to argue with you (not that I actually will need to…HaHa). You certainly put a fresh spin on a subject which has been discussed for years. Great stuff, just wonderful.
dark market url darkmarkets
darknet markets 2025 dark web link darkmarket url
Hi, I do think this is a great web site. I stumbledupon it 😉 I’m going to come back once again since i have book-marked it. Money and freedom is the best way to change, may you be rich and continue to guide other people.
darkmarket list darkmarket list
dark web markets darknet websites
darknet market links darknet marketplace dark market
dark market url darkmarket list
dark web drug marketplace dark web sites
It’s hard to find well-informed people on this subject, however, you seem like you know what you’re talking about! Thanks
dark web market urls darknet site
bitcoin dark web darkmarket 2025
dark web market list darknet market lists
darknet markets links darkmarket 2025
darknet market links darknet websites best darknet markets
dark market url dark web market list
darknet markets onion address darknet markets links
darknet sites dark web markets tor drug market
darkmarket link dark web market links
darknet markets onion darknet markets onion address
darknet markets 2025 darkmarket 2025 dark web market
dark web markets darkmarket 2025
darkmarket list darknet drug store
darknet drugs dark market link
dark web sites dark market 2025 dark web drug marketplace
dark web market darknet drug links
darknet market darknet drug market
dark market link dark web marketplaces darknet markets links
dark market onion tor drug market
dark web drug marketplace dark web market
darknet markets onion darknet market links
dark web market links darknet drug store
darknet drugs best darknet markets
best darknet markets darknet drug store
dark web market list darknet markets onion
darknet market dark market
darkmarket list dark web sites
darknet drug store dark web market urls
darknet drug links darknet drug store
darknet drugs onion dark website
darkmarket url dark market 2025
darknet markets url darknet market links
best darknet markets darknet drugs
darknet markets 2025 darknet market links
darknet drug store darknet markets
darknet marketplace dark web market links
dark web markets darknet markets links
Hello to all, how is the whole thing, I think every one is getting more from this web page, and your views are pleasant in favor of new users.
https://kcculinary.com/articles/paripesa_promo_code.html
darkmarket 2025 darknet links
darknet markets links dark web drug marketplace
Cheers! Lots of stuff.
Feel free to visit my website – https://novomoskovsk.pp.ua
darknet markets onion address dark market onion
Thanks, Valuable stuff!
My webpage … https://okhtyrka.pp.ua
dark market dark web market
dark market link darknet sites
darknet websites dark web market links
Truly a good deal of amazing material.
Check out my web page https://chernomorskua.pp.ua
darknet drugs dark web market list
darkmarket link onion dark website
darknet markets url darknet markets
dark market list dark market 2025
onion dark website dark web sites
You expressed this effectively.
My web site: https://zaporizzya.pp.ua
Very good information, Appreciate it!
my web blog :: https://romny.pp.ua
darknet links dark web marketplaces
dark market link dark web market list
dark web market links darknet drug links
darkmarket darknet links
darknet site darknet market links
bitcoin dark web dark web markets
onion dark website tor drug market
dark websites darknet site
darkmarket list best darknet markets
darknet sites darkmarket link
onion dark website dark web market links
dark web market darknet links
darknet marketplace dark web market list
You stated this fantastically.
Feel free to visit my web site: https://shepetyvka.pp.ua
I like it when people get together and share ideas. Great site, keep it up.
darknet market lists dark market onion
dark web market urls darknet markets 2025
dark web market list darknet drug store
darknet websites best darknet markets
dark websites dark web link
dark market list darknet markets onion address
dark markets darkmarket url
dark web drug marketplace darknet markets links
darknet markets 2025 dark market
darknet drug store darknet drug store
dark web marketplaces darknet market lists
darkmarket link darknet websites
darknet markets onion dark market onion
dark markets dark market list
This is a very good tip particularly to those new to the blogosphere. Brief but very precise information… Thanks for sharing this one. A must read post!
tor drug market darknet drugs
tor drug market darknet drug links
dark web markets darknet markets url
darknet drug market onion dark website
I was able to find good advice from your blog articles.
dark markets 2025 dark market link
dark market url darknet sites
dark market list darknet market list
darknet markets url darknet site
darknet drug store dark market url
Hello there! I just wish to give you a big thumbs up for your great info you have here on this post. I am returning to your blog for more soon.
dark web market links darknet drug market
darkmarket link darknet drug links
darknet site dark markets 2025
darknet drug links darknet markets 2025
darkmarket 2025 dark web sites
darknet markets links dark market list
dark web market darknet links
Great information. Lucky me I came across your site by accident (stumbleupon). I’ve saved as a favorite for later!
darknet markets 2025 darknet markets onion
darknet markets onion address darknet markets url
darknet drug links darknet links
dark market dark market 2025
darkmarket darknet drug store
darknet markets dark web market
Stunning quest there. What occurred after? Thanks!
darkmarket list darknet market lists
darknet markets onion darknet markets onion
Hello everyone, it’s my first go to see at this site, and post is really fruitful in support of me, keep up posting such content.
I blog quite often and I seriously thank you for your content. This great article has really peaked my interest. I am going to book mark your website and keep checking for new details about once a week. I opted in for your RSS feed as well.
darkmarket list darknet site
dark web market list dark web link
dark web market links darknet market links
Thanks a lot! I value it.
Feel free to visit my web-site: https://misto-uman.pp.ua
Thank you! Loads of forum posts!
My homepage – https://chernivci.pp.ua
darknet marketplace https://github.com/darknetmarketlinks2025/darknetmarkets
darknet market lists https://github.com/darknetwebsitesgflpx/darknetwebsites
dark market list https://github.com/darkmarketlinkp22jr/darkmarketlink
dark market link https://github.com/tormarkets2025ukaz1/tormarkets2025
dark web market urls https://github.com/darknetdruglinksvojns/darknetdruglinks
This blog was… how do I say it? Relevant!! Finally I have found something which helped me. Thanks a lot!
onion dark website https://github.com/darknetmarketlinks2025/darknetmarkets
dark web sites https://github.com/darknetwebsitesgflpx/darknetwebsites
dark market https://github.com/darkmarketlinkp22jr/darkmarketlink
dark web market links https://github.com/tormarkets2025ukaz1/tormarkets2025
dark market link https://github.com/darknetdruglinksvojns/darknetdruglinks
I have to thank you for the efforts you have put in penning this blog. I really hope to check out the same high-grade content by you later on as well. In fact, your creative writing abilities has motivated me to get my very own website now 😉
We are a group of volunteers and opening a new scheme in our community. Your website offered us with valuable information to work on. You have done an impressive job and our entire community will be thankful to you.
darkmarket 2025 dark web market urls
darknet market darknet market lists
darknet markets links darknet markets links
dark web markets darknet site
dark web sites darknet drug store
dark web market links bitcoin dark web
darknet market darknet market
darknet market links best darknet markets
dark web market list best darknet markets
dark market 2025 dark market link
tor drug market dark web market links
dark web sites darknet site
dark web markets darknet market links
darknet markets 2025 darkmarket url
dark market list darknet links
dark market onion darknet drug store
darkmarkets darkmarket 2025
darkmarkets darknet drug store
darknet markets onion dark website
darknet markets dark market url
darknet markets 2025 dark web markets
dark web market list tor drug market
darkmarket list dark market
darknet marketplace darknet market
best darknet markets darknet websites
darknet marketplace darknet drug store
dark web drug marketplace darknet drug store
dark market list dark web market urls
darknet marketplace darknet sites
darknet drug market dark web link
dark markets 2025 darknet market links
dark web markets dark websites
dark web link darknet market lists
darknet markets 2025 dark web market list
tor drug market darknet market
dark web market list dark market
tor drug market darknet marketplace
dark web market list bitcoin dark web
darknet markets links darknet drug links
darknet drug links dark web sites
dark web market urls darkmarket list
dark web marketplaces dark web market links
dark web marketplaces darknet markets 2025
darknet drug market best darknet markets
bitcoin dark web darknet drug links
dark web marketplaces dark market onion
darknet sites darknet links
darkmarket link dark web link
dark market dark web market urls
dark web market list darknet markets url
dark web market list darknet market
darknet markets url dark web sites
darknet market list tor drug market
darknet links dark web drug marketplace
dark markets darknet markets 2025
tor drug market darknet market links
dark websites darknet market lists
dark web marketplaces dark web markets
dark market list darknet sites
dark web markets dark web link
dark web drug marketplace darknet sites
Use the internet and find a essay services remain in the body?
darknet drug links dark market link
darknet markets url tor drug market
darkmarket link darknet markets
onion dark website dark web markets
darknet markets darknet links
Look no further. This site always sells short articles from legitimate online pharmacies in order to get the best
Nicely put, Thanks a lot!
My web blog: https://0372.org.ua/
darkmarket 2025 bitcoin dark web
darknet links dark web drug marketplace
darknet market lists darknet markets
dark market url darknet drug links
darknet drug links dark websites
darknet drug links darknet markets onion
dark websites darknet market links
darknet markets 2025 dark web market urls
dark market onion darknet markets url
darknet drug links darknet drug links
darkmarket list dark web market urls
darknet drug store dark market
darknet market links darknet site
darknet drug store darknet market
Forget about your medication problems with specialized write essay for me that they have been labeled properly.
dark market darknet sites
darknet drugs dark web sites
Fast delivery of websites that write essays for you online.Easeus Deleted File Recovery – CNET Download. Disk
dark web market urls dark web sites
Can I just say what a comfort to find an individual who genuinely understands what they’re discussing on the net. You definitely know how to bring an issue to light and make it important. More people ought to check this out and understand this side of the story. I was surprised that you aren’t more popular since you most certainly possess the gift.
dark web marketplaces dark market 2025
onion dark website darknet markets url
dark market url darknet markets 2025
Online pharmacies make it easy to buy thesis maker when you are buying it online.
Great site you have here.. It’s difficult to find high quality writing like yours these days. I seriously appreciate individuals like you! Take care!!
darknet markets onion address darknet markets onion address
darknet markets onion darknet markets onion address
Some pharmacies that sell paper writing service cheap pills through this specialist low-cost site
dark web drug marketplace darknet market
darkmarket 2025 dark web market links
dark web market links dark web sites
dark web link dark market url
dark web sites dark websites
darknet site dark markets
dark websites dark web drug marketplace
darknet drug store dark websites
darknet markets url darkmarkets
darknet drug store dark web market links
Verify prices before you buy custom research paper writing services at the lowest price
best darknet markets dark market 2025
dark web markets darkmarket 2025
darknet markets onion dark website
darkmarket list bitcoin dark web
dark market link darknet market list
darkmarket 2025 dark web market links
darkmarket list dark web markets
You said it perfectly!
Also visit my homepage – https://khersontoday.com.ua/
dark markets darkmarkets
darknet websites darknet site
dark web market darknet markets 2025
darkmarket 2025 darknet market list
Easily review deals and dissertation structure pills when you order on this site
darknet site darknet market
dark market onion darkmarket 2025
best darknet markets darknet markets links
darkmarket 2025 dark market 2025
dark web market urls tor drug market
dark web marketplaces darknet market list
onion dark website dark web market list
bitcoin dark web darknet markets onion
darknet markets 2025 darknet drug links
darknet markets onion address darknet market list
bitcoin dark web tor drug market
onion dark website darknet drug market
darkmarket link darknet market
dark web marketplaces dark market url
darknet markets darknet markets 2025
darkmarket 2025 tor drug market
dark web link dark web market urls
darknet sites darknet site
darknet markets onion dark market onion
darknet market list darknet markets 2025
dark websites dark web link
darknet websites darknet drugs
darknet markets onion address dark market 2025
dark web marketplaces darknet markets onion address
darknet market links dark web link
dark web link darkmarket url
dark web link dark web market urls
Wise people will purchase a write a paper for me with confidence after you compare pharmacy prices
dark market url dark market onion
dark web market list dark web markets
darknet websites darknet drug links
dark market list tor drug market
darknet markets onion best darknet markets
darknet markets https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl dark market url
Just desire to say your article is as surprising. The clarity in your post is simply cool and i can assume you are an expert on this subject. Well with your permission let me to grab your feed to keep up to date with forthcoming post. Thanks a million and please carry on the rewarding work.
darknet marketplace https://github.com/darknetdruglinksvojns/darknetdruglinks darknet drug market
first-rate online pharmacies the moment you decide to buy essays for college at lower prices
darknet market links https://github.com/darknetmarketslist/darknetmarketslist best darknet markets
dark web sites https://github.com/darkmarkets2025we92r/darkmarkets2025 darknet marketplace
darkmarket 2025 https://github.com/aresmarketlink0ru72/aresmarketlink dark web drug marketplace
darknet markets onion address https://github.com/darknetmarketlistv8tg0/darknetmarketlist darknet market list
darkmarkets https://github.com/darknetwebsitesgflpx/darknetwebsites dark web market
dark web marketplaces https://github.com/darkmarketlinkp22jr/darkmarketlink darkmarkets
darknet market lists https://github.com/tormarkets2025ukaz1/tormarkets2025 darknet links
onion dark website https://github.com/darknetdruglinksvojns/darknetdruglinks dark websites
dark web market links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl dark market link
darknet links https://github.com/darknetmarketslist/darknetmarketslist darkmarket
you’re really a excellent webmaster. The site loading velocity is incredible. It sort of feels that you are doing any unique trick. Also, The contents are masterpiece. you’ve performed a excellent process on this topic!
darknet markets 2025 https://github.com/darkmarkets2025we92r/darkmarkets2025 darkmarket list
darkmarket 2025 https://github.com/aresmarketlink0ru72/aresmarketlink dark market url
darknet drug store https://github.com/darknetwebsitesgflpx/darknetwebsites dark markets
darkmarket url https://github.com/darkmarketlinkp22jr/darkmarketlink dark markets 2025
dark market 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist best darknet markets
darknet markets onion address https://github.com/darknetmarketlinks2025/darknetmarkets darknet marketplace
darknet market list https://github.com/tormarkets2025ukaz1/tormarkets2025 bitcoin dark web
darknet markets url https://github.com/darknetdruglinksvojns/darknetdruglinks dark market 2025
are a necessity in life What are the long-term benefits that custom essay service and read more about the benefits here.
darknet sites https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl dark web market
dark markets https://github.com/darknetmarketslist/darknetmarketslist bitcoin dark web
dark market link https://github.com/darkmarkets2025we92r/darkmarkets2025 darknet markets 2025
Incredible tons of excellent tips!
Here is my site :: https://zakarpattya.com.ua/
darkmarket url https://github.com/darknetwebsitesgflpx/darknetwebsites darkmarket list
darknet marketplace https://github.com/darkmarketlinkp22jr/darkmarketlink darknet markets links
dark market url https://github.com/aresmarketlink0ru72/aresmarketlink bitcoin dark web
Many thanks. Very good information.
Also visit my webpage: https://kalushnews.com.ua/
darkmarket https://github.com/tormarkets2025ukaz1/tormarkets2025 darknet markets links
For most recent news you have to visit the web and on internet I found this web page as a finest web page for latest updates.
dark market 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist dark market onion
dark web market links https://github.com/darknetdruglinksvojns/darknetdruglinks darknet drug links
Get the fastest result at custom term paper writing service and save their dollars.
dark web market links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl darknet drug links
dark web market urls https://github.com/darknetmarketslist/darknetmarketslist darknet markets
tor drug market https://github.com/darkmarkets2025we92r/darkmarkets2025 darknet drug market
darknet drug market https://github.com/darknetwebsitesgflpx/darknetwebsites darkmarket 2025
dark web marketplaces https://github.com/darkmarketlinkp22jr/darkmarketlink darknet markets 2025
tor drug market https://github.com/darknetmarketlinks2025/darknetmarkets darknet markets 2025
darknet drug store https://github.com/tormarkets2025ukaz1/tormarkets2025 dark market 2025
dark markets 2025 https://github.com/aresmarketlink0ru72/aresmarketlink darknet drug store
Thank you. Lots of data.
Feel free to surf to my web page :: https://dnipro.org.ua/
darknet market lists https://github.com/darknetdruglinksvojns/darknetdruglinks darkmarket list
Excellent post. I’m dealing with many of these issues as well..
dark market 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist dark market list
darknet market list https://github.com/darknetmarketslist/darknetmarketslist darkmarket url
dark markets 2025 https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl darknet markets onion address
darknet sites https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket
darknet market lists https://github.com/darknetwebsitesgflpx/darknetwebsites – dark web sites
darknet drug store https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market url
dark market 2025 https://github.com/aresmarketlink0ru72/aresmarketlink darknet drug store
dark market link https://github.com/darknetmarketlistv8tg0/darknetmarketlist dark web market urls
darkmarket list https://github.com/darknetmarketslist/darknetmarketslist onion dark website
dark web market list https://github.com/darkmarkets2025we92r/darkmarkets2025 darknet markets links
darkmarket link https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl darknet drug links
dark web link https://github.com/darknetwebsitesgflpx/darknetwebsites – dark websites
darknet markets 2025 https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet websites
darknet markets url https://github.com/aresmarketlink0ru72/aresmarketlink darkmarket list
dark market https://github.com/darknetmarketlistv8tg0/darknetmarketlist dark market link
darkmarket url https://github.com/darknetmarketslist/darknetmarketslist darknet markets onion address
dark web market list https://github.com/darkmarkets2025we92r/darkmarkets2025 darknet markets onion address
darkmarkets https://github.com/darknetwebsitesgflpx/darknetwebsites – dark web marketplaces
bitcoin dark web https://github.com/darknetdruglinksvojns/darknetdruglinks – dark web market
dark market link https://github.com/darkmarketlinkp22jr/darkmarketlink – dark market url
darknet market lists https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet markets
dark websites https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl darknet market lists
darkmarket link https://github.com/aresmarketlink0ru72/aresmarketlink dark web marketplaces
dark web markets https://github.com/darknetwebsitesgflpx/darknetwebsites – dark market 2025
tor drug market https://github.com/darknetmarketlistv8tg0/darknetmarketlist dark web markets
darknet drugs https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet markets links
dark markets https://github.com/darknetmarketlinks2025/darknetmarkets – darknet markets onion
dark market url https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet drug store
darkmarket link https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl darknet markets
dark web link https://github.com/aresmarketlink0ru72/aresmarketlink darkmarket link
dark web markets https://github.com/darknetwebsitesgflpx/darknetwebsites – dark market url
dark web market urls https://github.com/darknetdruglinksvojns/darknetdruglinks – dark market onion
darknet drug links https://github.com/darkmarkets2025we92r/darkmarkets2025 dark web market links
dark market onion https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet drug market
darknet websites https://github.com/darknetwebsitesgflpx/darknetwebsites – darkmarket link
darknet market list https://github.com/darknetdruglinksvojns/darknetdruglinks – darkmarket 2025
darknet site https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet marketplace
tor drug market https://github.com/darknetwebsitesgflpx/darknetwebsites – darkmarket
darkmarket https://github.com/darknetdruglinksvojns/darknetdruglinks – dark web market list
darknet drug store https://github.com/darkmarketlinkp22jr/darkmarketlink – darknet markets onion
dark web drug marketplace https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web market list
dark web market urls https://github.com/darknetwebsitesgflpx/darknetwebsites – darknet market
darkmarkets https://github.com/darknetdruglinksvojns/darknetdruglinks – darknet markets url
best darknet markets https://github.com/darkmarketlinkp22jr/darkmarketlink – dark websites
dark web market links https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarket
I am sure this piece of writing has touched all the internet people, its really really nice paragraph on building up new web site.
dark web marketplaces https://github.com/darkmarkets2025we92r/darkmarkets2025 darknet market lists
dark web market list https://github.com/darknetmarketlistv8tg0/darknetmarketlist dark web market
dark web sites https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl darkmarket list
Superb postings. Thank you!
Feel free to visit my blog post: https://bilgorod-d.com.ua/
dark web markets https://github.com/darknetmarketlinks2025/darknetmarkets – dark market url
darknet drug store https://github.com/darknetdruglinksvojns/darknetdruglinks – dark websites
darknet markets onion address https://github.com/darkmarketlinkp22jr/darkmarketlink – darknet marketplace
dark web market urls https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web marketplaces
darknet markets 2025 https://github.com/darknetmarketslist/darknetmarketslist bitcoin dark web
darknet drug market https://github.com/darkmarkets2025we92r/darkmarkets2025 darknet markets onion
darkmarket 2025 https://github.com/aresmarketlink0ru72/aresmarketlink darknet links
darkmarket list https://github.com/darknetmarketlistv8tg0/darknetmarketlist darknet market
darknet markets https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darkmarkets
darknet market list https://github.com/darknetmarketlinks2025/darknetmarkets darknet market
darknet market links https://github.com/darknetdruglinksvojns/darknetdruglinks dark web market
dark markets 2025 https://github.com/darkmarketlinkp22jr/darkmarketlink tor drug market
darkmarket link https://github.com/tormarkets2025ukaz1/tormarkets2025 dark web link
darknet markets 2025 https://github.com/darknetmarketslist/darknetmarketslist – darknet markets onion address
darknet sites https://github.com/darkmarkets2025we92r/darkmarkets2025 – darknet drugs
tor drug market https://github.com/aresmarketlink0ru72/aresmarketlink – dark market 2025
darknet markets onion address https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market onion
darknet links https://github.com/darknetwebsitesgflpx/darknetwebsites dark web sites
darknet markets 2025 https://github.com/darknetmarketlinks2025/darknetmarkets darknet markets 2025
best darknet markets https://github.com/darknetdruglinksvojns/darknetdruglinks dark markets 2025
There is certainly a great deal to find out about this subject. I like all of the points you’ve made.
dark markets https://github.com/darkmarketlinkp22jr/darkmarketlink dark web market links
dark market https://github.com/tormarkets2025ukaz1/tormarkets2025 dark web market links
darknet market lists https://github.com/darknetmarketslist/darknetmarketslist – dark markets 2025
darkmarket url https://github.com/darkmarkets2025we92r/darkmarkets2025 – darknet site
dark websites https://github.com/aresmarketlink0ru72/aresmarketlink – darknet market links
dark web marketplaces https://github.com/darknetwebsitesgflpx/darknetwebsites dark web market links
dark web marketplaces https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market list
darknet markets url https://github.com/darknetmarketlinks2025/darknetmarkets darkmarket
dark web link https://github.com/darkmarketlinkp22jr/darkmarketlink dark market list
darknet markets url https://github.com/tormarkets2025ukaz1/tormarkets2025 dark web sites
tor drug market https://github.com/darknetmarketslist/darknetmarketslist – darknet sites
You should take part in a contest for one of the finest websites on the web. I’m going to recommend this site!
dark market https://github.com/darkmarkets2025we92r/darkmarkets2025 – darknet markets onion
darknet links https://github.com/darknetwebsitesgflpx/darknetwebsites dark web link
dark web drug marketplace https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet links
darkmarket list https://github.com/darknetmarketlinks2025/darknetmarkets darkmarkets
dark web market https://github.com/darkmarketlinkp22jr/darkmarketlink dark web market urls
darknet market links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet drugs
darknet market https://github.com/tormarkets2025ukaz1/tormarkets2025 dark web markets
dark markets https://github.com/darknetmarketslist/darknetmarketslist – darknet marketplace
darknet market links https://github.com/darkmarkets2025we92r/darkmarkets2025 – darkmarket list
dark market onion https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet drug market
dark web sites https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market list
darknet markets onion address https://github.com/darknetmarketslist/darknetmarketslist – dark markets
darknet drug market https://github.com/darkmarkets2025we92r/darkmarkets2025 – dark web drug marketplace
Your style is so unique compared to other folks I have read stuff from. Thank you for posting when you’ve got the opportunity, Guess I’ll just book mark this site.
darknet drug market https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web markets
darknet drug links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet market list
dark market url https://github.com/darknetmarketslist/darknetmarketslist – darkmarket
darknet links https://github.com/darkmarkets2025we92r/darkmarkets2025 – dark web market urls
Fantastic postings Regards.
My web page :: https://zt-news.com.ua/
tor drug market https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darkmarket 2025
darkmarket 2025 https://github.com/darkmarketlinkp22jr/darkmarketlink dark market onion
dark web drug marketplace https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet markets
darknet market https://github.com/tormarkets2025ukaz1/tormarkets2025 darknet market lists
dark web market list https://github.com/darkmarkets2025we92r/darkmarkets2025 – dark web marketplaces
Pretty! This has been an extremely wonderful article. Thank you for providing this information.
darkmarket list https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web markets
darkmarkets https://github.com/darknetwebsitesgflpx/darknetwebsites darknet drugs
onion dark website https://github.com/darkmarketlinkp22jr/darkmarketlink tor drug market
darknet websites https://github.com/darknetmarketslist/darknetmarketslist – darknet drug market
darknet sites https://github.com/darkmarkets2025we92r/darkmarkets2025 – dark market list
tor drug market https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark markets
darknet market lists https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web drug marketplace
darknet site https://github.com/darknetmarketslist/darknetmarketslist – dark web link
dark market link https://github.com/darkmarkets2025we92r/darkmarkets2025 – darknet markets url
dark market list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market links
Buying online so that you know what the lowest price of hire a research paper writer are cheaper at online pharmacies
dark market url https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drugs
dark web markets https://github.com/darknetmarketslist/darknetmarketslist – dark market list
onion dark website https://github.com/darkmarkets2025we92r/darkmarkets2025 – dark websites
After exploring a handful of the blog articles on your web page, I truly like your technique of writing a blog. I saved as a favorite it to my bookmark site list and will be checking back soon. Please visit my web site as well and tell me your opinion.
dark web market https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet markets
Heat up your body with the newest product of pay someone to write paper to treat your condition
dark web market links https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets onion
dark markets 2025 https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market 2025
dark web markets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – onion dark website
An interesting discussion is definitely worth comment. I believe that you ought to publish more on this subject, it may not be a taboo matter but usually folks don’t speak about these subjects. To the next! Many thanks.
dark market https://github.com/darknetmarketslist/darknetmarketslist – dark web market urls
darknet links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darkmarket 2025
dark web market links https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web market list
darknet links https://github.com/darkmarkets2025we92r/darkmarkets2025 – dark web sites
dark market url https://github.com/darknetmarketslist/darknetmarketslist – darknet marketplace
darkmarket url https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – best darknet markets
dark web marketplaces https://github.com/aresmarketlink0ru72/aresmarketlink – onion dark website
dark web marketplaces https://github.com/darkmarkets2025we92r/darkmarkets2025 – dark websites
darknet market https://github.com/darknetmarketslist/darknetmarketslist – darknet markets 2025
A common way to save money and research maker ai is a good choice.
Thanks a lot. I like this.
Feel free to surf to my web site: https://0432.com.ua/
bitcoin dark web https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet market links
dark market url darknet site
dark web markets https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets url
darknet markets https://github.com/darkmarkets2025we92r/darkmarkets2025 – darkmarket link
darkmarket list https://github.com/darknetmarketslist/darknetmarketslist – darknet sites
You said it adequately..
my page: https://kyivfocus.org.ua/
dark market onion darknet markets url
darknet markets onion dark market link
Kudos. I enjoy this!
my homepage :: https://dnipronews.org.ua/
Discover great offers you can use to essay typer is more convenient
dark web market list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web sites
Many thanks, I value this!
My web-site :: https://kamyanske.org.ua/
darknet marketplace dark markets 2025
dark markets 2025 dark websites
darkmarkets https://github.com/darkmarkets2025we92r/darkmarkets2025 – darkmarket url
dark web market https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet markets 2025
darknet drugs https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets 2025
darkmarket link dark web drug marketplace
dark web link darknet markets onion
darknet markets dark web marketplaces
Appreciate it! A lot of material!
Also visit my webpage … https://zaporizhzhia.org.ua/
dark web sites darknet drug market
dark market url darknet markets onion
dark web marketplaces best darknet markets
darknet market bitcoin dark web
Nicely put. With thanks!
Also visit my web page – https://mykolaivlive.com.ua/
darkmarket url dark web markets
dark websites darknet markets links
dark web marketplaces dark web market links
dark markets 2025 darknet drug market
darknet drug links darknet markets 2025
dark web link dark web market list
dark web market links dark web marketplaces
dark web market dark market url
darknet markets onion dark market link
dark websites dark markets
dark web sites darknet market links
darkmarket link darknet markets 2025
dark web sites darkmarket url
dark market darknet drug market
darknet markets url dark web market urls
darknet markets url darknet markets 2025
bitcoin dark web dark markets
darknet drug market dark markets 2025
dark markets dark market link
dark market 2025 darknet markets 2025
bitcoin dark web dark web marketplaces
darknet drug market darknet sites
darknet market lists dark web market
darknet market lists darknet markets
darknet markets url darknet links
dark market 2025 dark web market links
darknet markets links dark market url
dark web markets darknet market lists
dark market link onion dark website
darkmarket url darknet sites
darkmarket darknet markets 2025
dark markets darknet marketplace
darkmarket 2025 darknet drugs
darknet market lists darknet markets onion address
darkmarket list dark web drug marketplace
the best dealDon’t let your age control your sex life. Visit essay writer ai and convenience is what you get when you shop online for drugs.
dark websites dark web drug marketplace
darknet markets onion address dark market
dark market list darknet drugs
darkmarket 2025 darknet drug links
darknet marketplace onion dark website
darknet markets 2025 darknet drug links
bitcoin dark web darknet marketplace
darkmarket 2025 darknet market lists
is important to find the best prices as soon as you decide to essay write help , an effective treatment, at low prices
dark markets dark web market
dark web sites tor drug market
darkmarket link darknet drug store
dark web market darkmarket 2025
darknet market links dark web market list
darkmarket dark web drug marketplace
darknet markets dark web markets
dark web marketplaces darkmarket 2025
dark web market links darkmarket link
darknet market links dark web market
bitcoin dark web dark market link
darknet market lists dark web market
Cheap prices for write a descriptive essay , a great treatment, by using online discounts
darkmarket 2025 dark web market list
darknet marketplace darkmarket 2025
darknet websites darkmarket url
darknet markets onion darknet drug store
darknet drug store dark websites
Perfectly expressed certainly. !
Look into my webpage; https://vezhamedia.com.ua/
dark web sites darkmarket link
dark market 2025 dark web marketplaces
dark market url dark market link
When using buy law essay is by comparing prices online
darknet drug market darkmarket list
darknet markets dark web marketplaces
darkmarket url darkmarket 2025
darknet marketplace darkmarket list
tor drug market darkmarkets
darknet marketplace dark web link
dark market url dark websites
darknet markets links dark web drug marketplace
dark web market links dark web market
best darknet markets darknet markets onion
Very good post. I absolutely appreciate this site. Keep it up!
darknet markets onion address dark market link
dark markets 2025 tor drug market
darknet markets dark web marketplaces
dark web markets dark web marketplaces
dark market list dark market list
darknet markets links darknet websites
dark web drug marketplace onion dark website
darkmarket 2025 onion dark website
Consider first-rate online pharmacies the moment you decide to phd dissertation help website is licensed to sell products?
darknet drug store darkmarket link
darknet markets dark web markets
tor drug market darknet drug store
You’ve made some good points there. I checked on the web for additional information about the issue and found most people will go along with your views on this web site.
darknet drugs darknet links
Are there harmful side effects if I take research paper maker with free delivery.
darknet sites dark web market urls
dark markets dark web link
darknet drug market darknet market list
darknet market lists dark websites
darknet market dark market list
darknet markets 2025 darknet market list
darknet market list darknet market links
Anybody can how to write a research paper locally, why should I have to shop online?
darknet drugs darkmarket url
dark web market list dark market 2025
darknet markets 2025 darknet site
dark web link dark web marketplaces
I’m extremely pleased to discover this web site. I need to to thank you for ones time for this fantastic read!! I definitely appreciated every bit of it and I have you saved as a favorite to see new things in your site.
Very well voiced certainly. !
My web-site; https://zhytomir.org.ua/
Real savings made if you buy on this site. Cheap immigrant college essay at rock bottom prices
darknet markets url darknet markets 2025
darkmarket link darknet drug store
You actually stated that wonderfully!
My site … https://lvivdaily.com.ua/
Nicely put, Thank you!
Also visit my webpage – https://olexandria.org.ua/
darkmarket url darknet drug market
tor drug market bitcoin dark web
darknet drug market dark websites
darkmarket url dark web market links
Truly tons of awesome advice!
My homepage … https://kropmedia.com.ua/
dark web market urls dark markets 2025
dark web drug marketplace dark web drug marketplace
bitcoin dark web darknet marketplace
darknet market lists darkmarkets
You made your point.
my page; https://mykharkov.org.ua/
darknet site darkmarket list
After I originally left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and now whenever a comment is added I recieve 4 emails with the same comment. Perhaps there is a means you can remove me from that service? Cheers!
darknet drug links darknet market lists
darkmarkets darknet drug links
darkmarket 2025 darknet market
dark websites best darknet markets
darknet websites dark market
darknet markets onion darknet websites
darknet market list onion dark website
Lovely postings, Thanks a lot!
My blog: https://kremenchug.org.ua/
dark web market list dark web market list
dark web market dark market link
darknet markets 2025 darknet sites
darknet markets url darknet markets 2025
darknet markets links dark web markets
dark web market darknet market
dark web market urls dark market onion
darkmarkets darknet markets
tor drug market dark web market links
That is a great tip especially to those new to the blogosphere. Brief but very accurate information… Appreciate your sharing this one. A must read post.
darknet market lists darknet markets onion
darknet websites darknet websites
dark web link dark web sites
dark web market dark market list
darknet drug links darkmarket link
darkmarkets darkmarket link
darknet websites dark web markets
You made some good points there. I checked on the web for more info about the issue and found most people will go along with your views on this site.
darknet markets onion address dark web drug marketplace
dark market url darknet markets url
Truly quite a lot of great tips!
Also visit my blog – https://kyivpress.com.ua/
tor drug market dark web market links
dark web drug marketplace darknet markets 2025
Wonderful post! We will be linking to this particularly great post on our website. Keep up the good writing.
That is a great tip especially to those new to the blogosphere. Brief but very accurate info… Many thanks for sharing this one. A must read article!
I’m amazed, I must say. Rarely do I come across a blog that’s equally educative and engaging, and without a doubt, you have hit the nail on the head. The problem is something too few folks are speaking intelligently about. Now i’m very happy that I stumbled across this during my hunt for something concerning this.
Spot on with this write-up, I really believe this site needs a lot more attention. I’ll probably be back again to see more, thanks for the information!
Hi, I do think this is an excellent blog. I stumbledupon it 😉 I will come back yet again since i have bookmarked it. Money and freedom is the best way to change, may you be rich and continue to help others.
You’re so awesome! I don’t think I’ve read anything like that before. So wonderful to discover another person with a few original thoughts on this topic. Really.. thanks for starting this up. This site is something that’s needed on the internet, someone with some originality.
You are so cool! I do not believe I’ve read through something like that before. So great to discover another person with genuine thoughts on this subject matter. Really.. many thanks for starting this up. This web site is one thing that is required on the internet, someone with some originality!
Generally I don’t read article on blogs, but I would like to say that this write-up very pressured me to check out and do it! Your writing style has been surprised me. Thank you, quite nice post.
dark web markets darknet markets links
darknet markets onion address https://github.com/newonionlinks/darknetmarkets – best darknet markets
darknet market https://github.com/newonionlinks/darknetmarkets – bitcoin dark web
dark web market https://github.com/newonionlinks/darknetmarkets dark web drug marketplace
tor drug market dark web sites
darknet markets onion address https://github.com/newonionlinks/darknetmarkets – dark web market list
onion dark website https://github.com/newonionlinks/darknetmarkets – dark market list
dark web market https://github.com/newonionlinks/darknetmarkets dark web market links
darkmarket url darknet market
dark websites https://github.com/newonionlinks/darknetmarkets – bitcoin dark web
darknet drugs https://github.com/newonionlinks/darknetmarkets darknet sites
dark market onion dark websites
darknet markets 2025 https://github.com/newonionlinks/darknetmarkets – darknet marketplace
darknet markets 2025 https://github.com/newonionlinks/darknetmarkets darknet market
bitcoin dark web darknet drug market
darknet drugs https://github.com/newonionlinks/darknetmarkets – darknet drug market
darknet sites https://github.com/newonionlinks/darknetmarkets darknet sites
dark web market list darknet market list
dark web markets https://github.com/newonionlinks/darknetmarkets – darkmarket url
dark web market darknet links
dark market darknet market lists
darkmarket link darkmarkets
onion dark website darknet market
dark markets https://github.com/newonionlinks/darknetmarkets – darkmarket url
You have made some decent points there. I looked on the web for more info about the issue and found most individuals will go along with your views on this website.
darknet drug store bitcoin dark web
darkmarket link darkmarket link
darknet markets 2025 dark markets
dark web marketplaces dark market link
onion dark website https://github.com/newonionlinks/darknetmarkets – darknet markets onion
darknet market lists darkmarket 2025
darknet markets darknet markets
darknet drug links bitcoin dark web
darknet sites darknet drugs
darkmarket https://github.com/newonionlinks/darknetmarkets – darknet market
darkmarket 2025 darknet markets url
dark markets darknet markets
dark web market list https://github.com/newonionlinks/darknetmarkets – dark web markets
darknet market list darknet markets links
best darknet markets dark markets
darknet markets 2025 dark web drug marketplace
darknet market links darknet markets onion address
dark websites darknet markets onion
dark web market dark market list
darknet market lists dark market url
darkmarket 2025 darknet drug market
darknet site dark web market
dark market darknet drug market
dark market link https://github.com/newonionlinks/darknetmarkets – darknet market
darknet sites dark markets
dark market url darkmarket 2025
Saved as a favorite, I love your web site!
dark web marketplaces darknet sites
dark web market list darknet market links
dark web market list onion dark website
darknet drugs darknet markets links
darknet markets links https://github.com/newonionlinks/darknetmarkets – darknet markets
dark web drug marketplace darknet markets url
dark websites dark market url
darknet marketplace https://github.com/newonionlinks/darknetmarkets darkmarket 2025
dark web marketplaces darknet links
dark market link https://github.com/newonionlinks/darknetmarkets – darkmarket link
darknet markets 2025 https://github.com/newonionlinks/darknetmarkets – darkmarket link
darknet market lists dark market link
dark market 2025 darknet markets
dark web link darknet market links
darknet market lists https://github.com/newonionlinks/darknetmarkets dark market list
dark market list dark market onion
This is nicely expressed. .
Here is my web site; https://kharkivlive.com.ua/
onion dark website https://github.com/newonionlinks/darknetmarkets – darknet markets onion
darknet websites https://github.com/newonionlinks/darknetmarkets – tor drug market
dark web marketplaces bitcoin dark web
darknet links darkmarkets
tor drug market darknet drug links
dark market 2025 https://github.com/newonionlinks/darknetmarkets darknet markets links
dark websites darkmarket
Amazing a good deal of good knowledge!
Here is my blog: https://cherkasy.org.ua/
tor drug market dark web market links
darknet drug store https://github.com/newonionlinks/darknetmarkets – dark web marketplaces
dark market darkmarket 2025
dark web sites darknet market
darknet drug links https://github.com/newonionlinks/darknetmarkets dark websites
dark market onion dark web market
darknet links dark web market
dark market list darknet drug links
dark market 2025 darknet markets onion address
best darknet markets https://github.com/newonionlinks/darknetmarkets – dark web sites
darkmarket 2025 dark market url
onion dark website https://github.com/newonionlinks/darknetmarkets darkmarkets
darknet market dark web market links
darkmarkets darknet drug store
dark market link dark web drug marketplace
darknet drug store dark market list
dark web sites https://github.com/newonionlinks/darknetmarkets – dark market onion
darknet market list darknet marketplace
dark web market list dark web marketplaces
darkmarket url dark web market urls
darknet markets 2025 darknet market list
darknet drug links darknet drugs
darkmarket list https://github.com/newonionlinks/darknetmarkets – dark market link
dark market onion darkmarket 2025
darkmarket url onion dark website
darknet marketplace dark market list
dark web marketplaces dark markets 2025
darknet drug store dark web market urls
darknet markets https://github.com/newonionlinks/darknetmarkets – dark web market list
darknet drug market darknet drug links
dark web link darknet drug links
dark web link dark web market urls
darknet market links darknet websites
dark web market urls https://github.com/newonionlinks/darknetmarkets – darknet drugs
dark markets darknet drug store
dark markets dark web market urls
tor drug market dark market url
darknet websites dark web markets
darknet drug store https://github.com/newonionlinks/darknetmarkets – best darknet markets
tor drug market dark web market
dark web marketplaces dark markets 2025
darknet websites darknet markets onion
darknet markets onion best darknet markets
dark web marketplaces darknet drug store
darknet links darknet websites
darkmarket 2025 dark web sites
darknet site darknet markets onion
tor drug market darknet links
darknet markets links onion dark website
dark web markets dark market
dark market onion tor drug market
dark web link darknet drugs
dark market link darknet markets url
onion dark website bitcoin dark web
darknet markets darknet markets links
dark market https://github.com/newonionlinks/darknetmarkets darknet drug links
darknet markets dark websites
dark market link darknet links
dark web market https://github.com/newonionlinks/darknetmarkets darkmarkets
darkmarket link darknet drug market
darknet market list darknet site
darknet drugs darknet markets url
darknet market lists darknet drug store
darknet markets dark web market links
darknet market list darknet markets 2025
dark market link darknet markets
darknet market list bitcoin dark web
darknet market list darknet markets 2025
dark web drug marketplace dark web market links
darknet drug links darkmarket url
dark market onion dark market list
dark websites darknet market list
darknet markets https://github.com/newonionlinks/darknetmarkets dark web drug marketplace
darknet markets 2025 bitcoin dark web
dark web link https://github.com/newonionlinks/darknetmarkets – darknet drugs
dark market list bitcoin dark web
darkmarket list https://github.com/newonionlinks/darknetmarkets – darkmarket 2025
darknet markets links darknet marketplace
dark market list https://github.com/newonionlinks/darknetmarkets dark markets
dark market link dark market
darkmarkets dark markets
darknet links darkmarket list
dark market dark market url
darknet market list https://github.com/newonionlinks/darknetmarkets darknet markets onion
dark web drug marketplace dark market 2025
darkmarket link https://github.com/newonionlinks/darknetmarkets – darkmarket url
dark web drug marketplace darknet markets onion
darknet drugs darknet markets onion
darkmarket best darknet markets
darknet drugs dark market
darkmarket list dark web market links
darkmarket 2025 https://github.com/newonionlinks/darknetmarkets darknet markets onion address
dark web market urls https://github.com/newonionlinks/darknetmarkets – dark market
darknet marketplace darkmarket
darkmarkets darknet marketplace
darknet drug links dark web market urls
dark web marketplaces dark web market
darknet websites darkmarket 2025
darknet market https://github.com/newonionlinks/darknetmarkets dark market onion
darkmarket https://github.com/newonionlinks/darknetmarkets – darknet market links
dark market url bitcoin dark web
darknet marketplace darknet drug links
best darknet markets dark websites
dark market list onion dark website
dark web market urls https://github.com/newonionlinks/darknetmarkets darknet market lists
dark web market https://github.com/newonionlinks/darknetmarkets – dark market
dark market url darkmarkets
darknet markets 2025 dark market 2025
darknet market darknet drug links
dark markets 2025 https://github.com/newonionlinks/darknetmarkets dark market
darkmarket url darknet markets links
dark market https://github.com/newonionlinks/darknetmarkets – dark web market
darkmarket list best darknet markets
darknet markets onion address darknet market links
darkmarket list darkmarket 2025
darkmarket 2025 https://github.com/newonionlinks/darknetmarkets darknet markets 2025
dark market 2025 https://github.com/newonionlinks/darknetmarkets – dark markets
dark web sites darknet markets
tor drug market darkmarkets
dark market list dark markets
darknet markets onion darkmarkets
darknet drug store darknet drug store
darknet market list https://github.com/newonionlinks/darknetmarkets dark web marketplaces
darknet market list darknet drug links
dark web market urls https://github.com/newonionlinks/darknetmarkets – darkmarket
darknet drugs darknet links
dark web market darkmarket 2025
darknet markets 2025 dark web markets
darknet market lists https://github.com/newonionlinks/darknetmarkets – darknet sites
dark web market links https://github.com/newonionlinks/darknetmarkets dark web drug marketplace
dark web market https://github.com/newonionlinks/darknetmarkets – dark market 2025
dark web market dark web market urls
dark web sites best darknet markets
darknet drug links dark web market urls
darknet market list dark websites
darkmarket 2025 https://github.com/newonionlinks/darknetmarkets dark web market list
dark web market https://github.com/newonionlinks/darknetmarkets – darkmarket list
darknet market lists https://github.com/newonionlinks/darknetmarkets – darknet drug links
darknet websites darknet sites
You have made some decent points there. I looked on the internet to learn more about the issue and found most individuals will go along with your views on this site.
dark markets 2025 darkmarket
darknet drug links darknet sites
darknet links darknet drug links
dark web link darkmarket list
dark market 2025 https://github.com/newonionlinks/darknetmarkets dark market list
darknet site https://github.com/newonionlinks/darknetmarkets – darknet markets onion address
darkmarket 2025 darknet site
darknet markets 2025 bitcoin dark web
darknet markets 2025 dark web market urls
dark market link https://github.com/newonionlinks/darknetmarkets darkmarket
darknet markets url https://github.com/newonionlinks/darknetmarkets – darkmarket 2025
darknet markets onion darknet drug market
darkmarket url dark web sites
dark web market https://github.com/newonionlinks/darknetmarkets – darknet markets
dark web link tor drug market
darknet markets 2025 dark market
dark markets 2025 darknet market links
darknet links https://github.com/newonionlinks/darknetmarkets dark market 2025
dark web link https://github.com/newonionlinks/darknetmarkets – dark markets 2025
bitcoin dark web https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarket 2025
darknet market dark web market urls
darkmarkets https://github.com/darknetmarketlinks2025/darknetmarkets – dark web market urls
tor drug market https://github.com/newonionlinks/darknetmarkets darknet markets onion
darknet drug market https://github.com/aresmarketlink0ru72/aresmarketlink – dark market url
dark web market list https://github.com/darknetmarketlistv8tg0/darknetmarketlist – tor drug market
dark websites https://github.com/newonionlinks/darknetmarkets – dark web markets
dark web sites https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market onion
dark market 2025 https://github.com/tormarkets2025ukaz1/tormarkets2025 – bitcoin dark web
dark web market https://github.com/newonionlinks/darknetmarkets darknet market links
dark web drug marketplace https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket
darkmarket list https://github.com/newonionlinks/darknetmarkets – dark web marketplaces
darknet markets links https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web market list
dark market link https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darkmarket link
darknet drug store https://github.com/newonionlinks/darknetmarkets dark web markets
darkmarket 2025 https://github.com/newonionlinks/darknetmarkets – darknet sites
dark market https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets onion address
darkmarket 2025 https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web marketplaces
Greetings! Very useful advice within this post! It is the little changes which will make the most important changes. Thanks for sharing!
dark market 2025 https://github.com/darknetmarketlinks2025/darknetmarkets – dark web sites
darknet markets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet market links
darknet drug links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – tor drug market
darknet markets url https://github.com/aresmarketlink0ru72/aresmarketlink – darkmarket
tor drug market https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet drug market
tor drug market https://github.com/darknetmarketlinks2025/darknetmarkets – darknet markets url
darkmarket https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark market 2025
darknet drugs https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market
darknet sites https://github.com/aresmarketlink0ru72/aresmarketlink – bitcoin dark web
darkmarket https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet market
darknet drugs https://github.com/darknetmarketlinks2025/darknetmarkets – dark web sites
darknet marketplace https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets
dark markets 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web link
darknet markets links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web link
darknet markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet websites
dark web sites https://github.com/darknetmarketlinks2025/darknetmarkets – darknet market list
dark web marketplaces https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drugs
darknet markets onion address https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet links
dark web sites https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market link
dark websites https://github.com/aresmarketlink0ru72/aresmarketlink – dark web marketplaces
darkmarket 2025 https://github.com/darknetmarketlinks2025/darknetmarkets – darknet markets
darknet drugs https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark market list
onion dark website https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market links
dark web drug marketplace https://github.com/aresmarketlink0ru72/aresmarketlink – darkmarket url
darknet market links https://github.com/darknetmarketlinks2025/darknetmarkets – darknet drug market
dark web drug marketplace https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darkmarkets
dark web market https://github.com/aresmarketlink0ru72/aresmarketlink – onion dark website
darknet market list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark markets
dark market onion https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarket list
dark market 2025 https://github.com/darknetmarketlinks2025/darknetmarkets – darknet markets 2025
darknet markets 2025 https://github.com/aresmarketlink0ru72/aresmarketlink – dark web drug marketplace
dark web sites https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet market list
dark web market list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet markets links
dark market https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet drug store
darknet markets 2025 https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket 2025
Pretty! This has been a really wonderful post. Thank you for supplying these details.
dark web market links https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drug market
darkmarket link https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darkmarket url
darknet markets links https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets
dark web link https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarket
dark market https://github.com/darknetmarketlinks2025/darknetmarkets – darknet markets onion
darknet markets onion https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market
darknet markets https://github.com/aresmarketlink0ru72/aresmarketlink – dark market list
darkmarket url https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market
darknet links https://github.com/darknetmarketlinks2025/darknetmarkets – darknet marketplace
best darknet markets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark markets 2025
darknet drugs https://github.com/aresmarketlink0ru72/aresmarketlink – dark markets
darkmarket list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darkmarket list
darkmarket link https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet markets onion address
darknet markets links https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket list
Hi, I do think this is a great web site. I stumbledupon it 😉 I’m going to return yet again since I book-marked it. Money and freedom is the best way to change, may you be rich and continue to help others.
dark web sites https://github.com/aresmarketlink0ru72/aresmarketlink – darknet websites
darkmarket 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet links
dark web market https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market list
darknet links https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market 2025
dark market 2025 https://github.com/darknetmarketlinks2025/darknetmarkets – darknet links
darknet drugs https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drug links
dark web market https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet market list
darkmarkets https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market link
dark web drug marketplace https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet markets url
dark markets 2025 https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket url
darknet markets links https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark markets
Kudos! Numerous facts!
my page https://odesacity.com.ua/
darkmarket list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet markets onion address
bitcoin dark web https://github.com/aresmarketlink0ru72/aresmarketlink – dark web drug marketplace
darkmarket 2025 https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market
darknet markets onion address https://github.com/darknetmarketlinks2025/darknetmarkets – dark web market
With thanks! I value this.
Here is my web blog :: https://0542.com.ua/
dark web sites https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet drugs
dark web sites https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets onion address
dark market link https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet market links
Reliable material Kudos.
Here is my web site https://zpmisto.com.ua/
darknet links https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market link
darknet markets https://github.com/darknetmarketlinks2025/darknetmarkets – dark market
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
dark web sites https://github.com/aresmarketlink0ru72/aresmarketlink – dark market
onion dark website https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet drug links
dark web markets https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market urls
best darknet markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet markets onion
darknet websites https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarkets
darknet links https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drug links
dark websites https://github.com/darknetmarketlistv8tg0/darknetmarketlist – tor drug market
dark market link https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet site
dark web market list https://github.com/aresmarketlink0ru72/aresmarketlink – dark web link
darknet markets onion address https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark markets 2025
darknet markets links https://github.com/darknetmarketlinks2025/darknetmarkets – dark web drug marketplace
dark web markets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet drug market
darknet markets https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darkmarket 2025
tor drug market https://github.com/aresmarketlink0ru72/aresmarketlink – dark markets
darkmarket 2025 https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet market lists
darkmarket list https://github.com/darknetmarketlinks2025/darknetmarkets – darknet markets links
best darknet markets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark market list
dark market link https://github.com/aresmarketlink0ru72/aresmarketlink – best darknet markets
dark market 2025 https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet drugs
darknet markets onion https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet drug links
tor drug market https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket 2025
dark websites https://github.com/aresmarketlink0ru72/aresmarketlink – dark market 2025
darknet markets 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark market onion
darkmarket list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web marketplaces
darknet markets links https://github.com/darknetmarketlinks2025/darknetmarkets – onion dark website
darknet sites https://github.com/aresmarketlink0ru72/aresmarketlink – darknet websites
darkmarket https://github.com/darknetmarketlistv8tg0/darknetmarketlist – onion dark website
darknet links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet markets onion
darkmarket list https://github.com/aresmarketlink0ru72/aresmarketlink – tor drug market
dark market onion https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet markets onion address
darknet marketplace https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket url
dark web market links https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet drug links
darknet markets onion address https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market
darkmarket https://github.com/aresmarketlink0ru72/aresmarketlink – darknet site
dark web market https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web markets
dark market url https://github.com/darknetmarketlinks2025/darknetmarkets – darknet market lists
dark market url https://github.com/darknetmarketlistv8tg0/darknetmarketlist – onion dark website
darknet websites https://github.com/aresmarketlink0ru72/aresmarketlink – darkmarket list
darkmarkets https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darkmarket link
darknet drug links https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market
dark market link https://github.com/darknetmarketlinks2025/darknetmarkets – best darknet markets
darknet sites https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drug links
dark web link https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web drug marketplace
dark market onion https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web sites
dark web market urls https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet market lists
darknet drug store https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket link
darknet market list https://github.com/aresmarketlink0ru72/aresmarketlink – darknet site
dark web market links https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet markets 2025
darknet site https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market
darknet links https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets links
darknet markets 2025 https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarket
dark market https://github.com/darknetmarketlinks2025/darknetmarkets – dark web sites
darknet markets 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darkmarket 2025
darkmarket https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web marketplaces
dark web market urls https://github.com/aresmarketlink0ru72/aresmarketlink – darkmarkets
dark market url https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarkets
darkmarket link https://github.com/darknetmarketlinks2025/darknetmarkets – dark websites
darknet market https://github.com/darknetmarketlistv8tg0/darknetmarketlist – bitcoin dark web
darkmarket list https://github.com/aresmarketlink0ru72/aresmarketlink – dark market link
darkmarket https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market link
darknet market https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market url
darknet market links https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets
dark market https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet market lists
dark web market https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet marketplace
darknet markets onion address https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark markets
dark web markets https://github.com/aresmarketlink0ru72/aresmarketlink – best darknet markets
darknet site https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web markets
darkmarket url https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – best darknet markets
darknet market https://github.com/darknetmarketlinks2025/darknetmarkets – best darknet markets
darknet marketplace https://github.com/darknetmarketlistv8tg0/darknetmarketlist – bitcoin dark web
bitcoin dark web https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark markets
darknet markets onion https://github.com/aresmarketlink0ru72/aresmarketlink – dark web markets
dark web markets https://github.com/darknetmarketlinks2025/darknetmarkets – darknet drug links
Hi, I do think this is a great web site. I stumbledupon it 😉 I will return once again since i have book-marked it. Money and freedom is the greatest way to change, may you be rich and continue to guide others.
darknet markets onion https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet drugs
darkmarket 2025 https://github.com/aresmarketlink0ru72/aresmarketlink – dark web marketplaces
dark web drug marketplace https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet drug store
dark markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web market list
dark web marketplaces https://github.com/aresmarketlink0ru72/aresmarketlink – darkmarket url
darknet markets 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet websites
darkmarkets https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web link
Greetings! Very helpful advice within this article! It is the little changes that produce the largest changes. Many thanks for sharing!
bitcoin dark web https://github.com/darknetmarketlinks2025/darknetmarkets – dark markets 2025
dark web market list https://github.com/aresmarketlink0ru72/aresmarketlink – darknet market links
darkmarket link https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark websites
dark market link https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet drugs
darkmarkets https://github.com/aresmarketlink0ru72/aresmarketlink – darknet site
dark web marketplaces https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark market url
darknet site https://github.com/darknetmarketlistv8tg0/darknetmarketlist – tor drug market
darkmarket https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web link
dark web sites https://github.com/aresmarketlink0ru72/aresmarketlink – dark web drug marketplace
Excellent web site you have got here.. It’s hard to find quality writing like yours nowadays. I really appreciate individuals like you! Take care!!
bitcoin dark web https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet markets onion
best darknet markets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darkmarket list
dark market link https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drug market
dark market https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark markets 2025
darknet market https://github.com/darknetmarketlinks2025/darknetmarkets – dark web marketplaces
dark markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet market links
dark web sites https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets 2025
dark web market list https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet markets 2025
darknet drugs https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet markets url
dark markets https://github.com/darknetmarketlinks2025/darknetmarkets – darknet markets url
dark websites https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark market link
dark websites https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web drug marketplace
dark market list https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drug store
darkmarket list https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet drug market
Way cool! Some extremely valid points! I appreciate you writing this post and also the rest of the site is also very good.
darkmarket url https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet websites
dark market url https://github.com/aresmarketlink0ru72/aresmarketlink – darknet market links
dark market link https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarket link
dark market list https://github.com/darknetmarketlistv8tg0/darknetmarketlist – best darknet markets
darknet market lists https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets 2025
darknet drug store https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web link
dark web drug marketplace https://github.com/darknetmarketlinks2025/darknetmarkets – dark market url
darknet websites https://github.com/aresmarketlink0ru72/aresmarketlink – dark market url
darkmarkets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – tor drug market
darknet market links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web marketplaces
dark market 2025 https://github.com/tormarkets2025ukaz1/tormarkets2025 – dark web market
dark web market links https://github.com/aresmarketlink0ru72/aresmarketlink – darknet markets url
Incredible loads of useful information.
My blog post … https://rivne24.com.ua/
This site was… how do you say it? Relevant!! Finally I have found something which helped me. Thank you!
best darknet markets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darkmarket url
dark web marketplaces https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet websites
bitcoin dark web https://github.com/tormarkets2025ukaz1/tormarkets2025 – darknet drugs
darknet market https://github.com/aresmarketlink0ru72/aresmarketlink – dark market link
darknet markets 2025 https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web markets
darknet drugs https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark web market links
darkmarket list https://github.com/aresmarketlink0ru72/aresmarketlink – darknet drug links
darknet markets https://github.com/tormarkets2025ukaz1/tormarkets2025 – tor drug market
darknet sites https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark markets 2025
darknet drug store https://github.com/aresmarketlink0ru72/aresmarketlink – dark web sites
best darknet markets https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market list
dark web market list https://github.com/darknetmarketlinks2025/darknetmarkets – darknet links
darknet markets url https://github.com/aresmarketlink0ru72/aresmarketlink – dark market list
dark web sites https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark websites
darknet market list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darkmarkets
dark web link https://github.com/darknetmarketlinks2025/darknetmarkets – dark web market
dark market list https://github.com/aresmarketlink0ru72/aresmarketlink – darknet links
darknet drugs https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darknet marketplace
dark web link https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – dark market list
best darknet markets https://github.com/darknetmarketlinks2025/darknetmarkets – darkmarket link
darknet market list https://github.com/aresmarketlink0ru72/aresmarketlink – darknet websites
darknet markets onion address https://github.com/darknetmarketlistv8tg0/darknetmarketlist – dark web sites
darknet market list https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet websites
dark market 2025 https://github.com/aresmarketlink0ru72/aresmarketlink – tor drug market
onion dark website https://github.com/tormarkets2025ukaz1/tormarkets2025 – best darknet markets
darknet markets onion address https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darkmarket link
best darknet markets https://github.com/aresmarketlink0ru72/aresmarketlink – dark websites
darknet market lists https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – darknet market lists
darkmarket link https://github.com/darknetmarketlinks2025/darknetmarkets – darknet markets onion address
Howdy! This article couldn’t be written any better! Looking at this post reminds me of my previous roommate! He constantly kept preaching about this. I’ll forward this information to him. Pretty sure he’ll have a good read. Thanks for sharing!
darknet site https://github.com/aresmarketlink0ru72/aresmarketlink – dark web link
dark markets https://github.com/darknetmarketlistv8tg0/darknetmarketlist – darkmarket 2025
darknet market links https://github.com/nexusdarkneturlwrf4t/nexusdarkneturl – best darknet markets
dark web drug marketplace https://github.com/tormarkets2025ukaz1/tormarkets2025 – darkmarket link
darkmarket 2025 https://github.com/darknetmarketlinks2025/darknetmarkets – dark market url
dark markets 2025 darkmarket link
dark market bitcoin dark web
dark web market list darknet markets onion
darknet drug market darknet market
darknet market links dark markets
dark web markets darknet marketplace
dark web drug marketplace darknet markets onion
dark web link dark web link
darkmarket list darknet markets onion
dark market darknet drug links
dark web sites dark market 2025
darkmarket darknet market lists
darkmarket 2025 darknet markets onion
darknet drug market darknet markets links
best darknet markets dark web market list
darknet sites darkmarket
darkmarkets darknet sites
dark web market darknet markets onion address
bitcoin dark web dark web drug marketplace
dark market 2025 darknet markets
dark web market darknet marketplace
Cheers. Awesome information!
Feel free to surf to my blog post; https://zvyagel.pp.ua
dark websites onion dark website
darkmarket list best darknet markets
bitcoin dark web dark websites
darknet drug market darknet drug market
darknet drug market darkmarket url
dark markets 2025 darkmarket list
dark web market links dark web market list
dark market 2025 dark web markets
darkmarket list darkmarket url
dark web drug marketplace dark web marketplaces
darknet drug market dark web sites
dark web link dark market
darknet markets onion dark web markets
best darknet markets darknet drug links
best darknet markets best darknet markets
darknet markets 2025 darknet markets onion address
darknet market links darknet drug links
dark markets 2025 dark web markets
dark web market links dark web marketplaces
darkmarkets darknet market links
dark web market links darknet markets onion address
Hey i Love your work i really appreciate that. Also take a look at our special Gym flooring dubai
darkmarket link darknet links
bitcoin dark web darknet drug market
bitcoin dark web darknet site
bitcoin dark web darknet markets links
dark market onion dark markets 2025
dark market list darknet links
darkmarket url darknet market list
dark market dark market link
best darknet markets dark market
darkmarket darknet markets links
best darknet markets darknet markets
darknet markets onion onion dark website
dark web markets tor drug market
dark web marketplaces dark market onion
dark market url darknet links
dark web drug marketplace darknet market
onion dark website dark market list
This is such an interesting read! It’s always great to discover new perspectives and insights. For those looking for more ways to stay entertained online, check out Lodi646 for an exciting experience!
darkmarkets dark websites
darknet links dark web sites
dark markets 2025 dark web link
dark websites dark web market urls
darkmarket link best darknet markets
darkmarket darknet markets 2025
dark web market urls dark web market list
dark market url dark market
darknet market links dark markets 2025
darknet market darknet websites
darkmarket list dark market 2025
best darknet markets bitcoin dark web
dark web drug marketplace dark market url
darknet markets darknet drugs
dark web market urls dark market 2025
darknet markets onion dark market url
darknet markets links dark websites
darknet drug market bitcoin dark web
darknet markets links dark web market list
tor drug market darknet market links
darkmarket link darknet market lists
darknet drug links best darknet markets
darknet market links darknet marketplace
darkmarket darknet drug store
darknet markets 2025 darknet market links
darknet drugs dark web drug marketplace
dark markets dark web marketplaces
dark web drug marketplace darknet drugs
best darknet markets darknet market list
darknet websites dark web sites
Good day! I could have sworn I’ve visited your blog before but after looking at a few of the articles I realized it’s new to me. Anyways, I’m certainly pleased I discovered it and I’ll be bookmarking it and checking back frequently.
dark web drug marketplace dark markets
darkmarket darkmarket list
dark markets 2025 darknet markets onion
darknet sites darknet site
dark web market links darknet drug links
darknet market darkmarket
darkmarket link darknet drugs
darknet markets onion dark web link
darknet markets url dark web market urls
tor drug market darknet markets 2025
dark market 2025 darknet market lists
darknet markets links darknet markets
Hi, I do think this is a great web site. I stumbledupon it 😉 I will return once again since i have book-marked it. Money and freedom is the best way to change, may you be rich and continue to help others.
dark web drug marketplace dark web market
dark market onion darknet sites
dark markets dark websites
dark market list darknet market
dark web sites https://kingdomdarknetdrugstore.com/ – darknet market links
darkmarket url dark market
darknet marketplace https://drdarkfoxmarket.com – darknet markets links
dark market url https://aasap-market.com/ – darknet market lists
dark market list https://kingdom-marketplace.com/ – darknet markets onion
dark market darknet sites
dark market link darknet markets onion address
dark market list dark web marketplaces
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
darknet markets darkmarket 2025
darknet drug market darknet market lists
darknet markets darknet markets onion address
dark web sites darkmarket 2025
dark web market darknet markets
darknet markets url bitcoin dark web
best darknet markets darknet markets onion
dark web sites tor drug market
dark market 2025 tor drug market
darknet drug store best darknet markets
dark web drug marketplace dark web sites
darkmarket url https://darknetmarketsonion.shop/ – dark markets 2025
darknet websites bitcoin dark web
dark web markets https://kingdomdarknetdrugstore.com/ – darkmarket url
darknet drugs bitcoin dark web
darknet site dark web market list
darknet sites https://onion-dark-market.shop/ – darknet markets onion
onion dark website https://kingdommarketdarknet.com/ – dark market
dark markets dark market list
dark web market links https://kingdom-darkmarketplace.com – darknet market
darknet site darkmarket url
dark market 2025 dark web sites
dark web drug marketplace https://onion-dark-market.shop/ – tor drug market
dark web drug marketplace https://darknetmarketsonion.shop/ – darknet drug market
dark websites https://cyberdarkmarkets.com/ – best darknet markets
dark web market urls dark market
darknet markets links darknet markets
dark web sites https://dark-web-versus.com – dark market url
dark web link darknet drug store
darkmarket list https://kingdom-marketplace.com/ – darknet site
darknet drug market https://idarknetmarket.com/ – darkmarket link
dark market darknet market links
darknet markets 2025 https://cyberdarkmarkets.com/ – darkmarket 2025
tor drug market https://drdarkfoxmarket.com – darknet drug links
darknet markets onion address darknet market list
dark market onion https://onion-dark-market.shop/ – dark market list
darknet drug market darknet site
dark market list https://idarknetmarket.com/ – dark websites
dark web market https://cannahomemarket.link/ – darknet markets 2025
dark web market urls https://kingdomdarkmarketplace.com – dark web market
darkmarket 2025 dark markets
darkmarkets darkmarket link
dark web link https://kingdom-marketplace.com/ – darknet market lists
darknet drug market https://idarknetmarket.com/ – darknet markets url
dark market 2025 https://darkfoxmarketplace.com/ – dark market list
dark web market list darknet drug market
darknet market darkmarket 2025
dark web marketplaces darknet sites
dark market onion https://kingdomdarkmarketplace.com – darknet site
darknet websites https://aasap-market.com/ – dark web sites
dark market list https://onion-dark-market.shop/ – darknet markets
dark market onion darkmarket list
darknet drug store https://kingdomdarkmarketonline.com/ – darknet websites
darknet drugs dark markets 2025
darkmarket https://cannahomemarket.link/ – dark websites
darkmarket dark web markets
bitcoin dark web https://drdarkfoxmarket.com – darknet markets 2025
darknet markets onion https://darkfoxdarkweb.com/ – dark web marketplaces
darknet drugs dark web market urls
darknet markets onion address https://kingdom-marketplace.com/ – dark market 2025
dark markets darknet site
darknet market links https://cannahomemarket.link/ – dark web market
dark web link dark web markets
bitcoin dark web darkmarkets
dark web market https://cannahomedarknetdrugstore.com/ – darknet drug market
darknet drug links https://darkmarketpremium.com/ – darknet drug store
dark websites https://firstdarkmarket.com/ – bitcoin dark web
darknet drugs https://darknetmarketsonion.shop/ – onion dark website
dark web market urls best darknet markets
darkmarket list https://cannahome-darkmarket-online.com/ – darkmarkets
dark web link dark web market links
darknet markets onion address dark market link
darkmarket list https://kingdom-darkmarketplace.com – darknet drugs
darkmarket list https://darkmarketpremium.com/ – dark web link
darknet market https://onion-dark-market.shop/ – dark markets
darknet market lists dark market onion
darkmarkets darkmarket link
darkmarket https://darknetmarketsonion.shop/ – darknet marketplace
darknet markets 2025 darkmarket url
dark web marketplaces https://darkfoxmarketplace.com/ – darknet market lists
onion dark website https://aasap-market.com/ – tor drug market
dark market list dark markets 2025
dark market link darkmarket list
darkmarket 2025 https://firstdarkmarket.com/ – dark market 2025
darknet market list https://idarknetmarket.com/ – darknet drug store
dark market dark websites
darknet drug market https://cannahomemarket.link/ – darkmarket 2025
best darknet markets darknet market links
darknet links https://darkfoxdarkweb.com/ – dark web sites
darknet sites https://cannahomedarknetdrugstore.com/ – dark market onion
darkmarket link dark markets 2025
dark web marketplaces dark web markets
dark market list https://kingdomdarkmarketonline.com/ – dark web sites
dark web market darkmarket 2025
darknet markets 2025 https://kingdomdarknetdrugstore.com/ – darknet markets onion address
darkmarkets https://darkfoxdarkweb.com/ – darknet market lists
dark market https://drdarkfoxmarket.com – darknet marketplace
darknet drug links https://kingdom-marketplace.com/ – tor drug market
dark web market https://kingdomdarkmarketonline.com/ – darknet markets
darkmarket https://kingdomdarknetdrugstore.com/ – dark web drug marketplace
darknet links https://darkwebversus.com/ – darknet websites
darknet markets 2025 https://dark-web-versus.com – darknet markets onion address
dark market onion https://firstdarkmarket.com/ – bitcoin dark web
darknet market lists https://asap-market-onion.com/ – darknet market
darkmarket url https://kingdomdarknetdrugstore.com/ – darknet drugs
dark markets https://aasap-market.com/ – dark market 2025
dark market link https://kingdom-marketplace.com/ – dark web market links
darknet websites https://cyberdarkmarkets.com/ – dark web markets
darknet market lists https://darkwebversus.com/ – dark websites
darknet market lists https://kingdom-darkmarketplace.com – darkmarket url
darknet drug store https://firstdarkmarket.com/ – darknet sites
darkmarket list https://idarknetmarket.com/ – dark market link
dark market 2025 https://darkwebversus.com/ – dark market 2025
darkmarket 2025 https://dark-web-versus.com – darknet market
dark market link https://kingdom-marketplace.com/ – tor drug market
darknet websites https://kingdomdarkmarketonline.com/ – darknet websites
darknet market list https://darkode-market.com/ – darknet drug links
darknet markets onion address https://kingdomdarkmarketplace.com – dark market link
dark market link https://kingdom-marketplace.com/ – dark markets 2025
darknet markets https://asap-market-onion.com/ – dark web drug marketplace
darknet markets url https://darkfoxdarkweb.com/ – darknet market list
darkmarket 2025 https://drdarkfoxmarket.com – darkmarket url
darknet site https://darkmarketdarkfox.com/ – dark market onion
dark web market list https://asap-market-onion.com/ – dark web market list
darknet markets onion https://darkode-market.com/ – darknet drug market
darknet drug market https://firstdarkmarket.com/ – darknet markets url
darknet links https://kingdomdarkmarketonline.com/ – dark web link
darknet markets 2025 https://aasap-market.com/ – dark market 2025
dark web link https://cannahomemarket.link/ – onion dark website
dark market url https://drdarkfoxmarket.com – dark web market links
darknet markets links https://kingdom-marketplace.com/ – dark market onion
darknet market list https://darknetmarketsonion.shop/ – darkmarket list
dark market url https://darkwebversus.com/ – dark market link
dark market url https://cannahomemarket.link/ – dark web link
darkmarket 2025 https://kingdomdarkmarketplace.com – dark markets
darknet drug market darknet site
dark web markets dark market url
darknet drug links dark market link
darknet markets links https://kingdom-marketplace.com/ – darknet market list
dark market darknet drugs
darknet market links https://asap-market-onion.com/ – dark market list
darknet market bitcoin dark web
bitcoin dark web https://darkmarketpremium.com/ – darknet markets 2025
dark websites https://cyberdarkmarkets.com/ – darkmarket url
darknet markets links https://drdarkfoxmarket.com – dark market list
darknet sites darknet market lists
dark web sites darknet market
darknet markets 2025 darknet markets onion
dark web market https://darkmarketdarkfox.com/ – darknet links
darknet markets 2025 https://idarknetmarket.com/ – darknet sites
darknet markets links dark web sites
darknet markets https://darkwebversus.com/ – darkmarket list
darknet sites darknet market lists
tor drug market https://cannahomemarket.link/ – dark market link
dark web market links https://kingdomdarkmarketplace.com – dark web markets
best darknet markets dark web market urls
darknet markets onion address https://mydarkmarketlink.com/ – dark web marketplaces
darknet site dark market list
darknet markets links https://kingdommarketdarknet.com/ – darkmarkets
dark markets 2025 https://darkode-market.com/ – darknet drug store
darknet site https://darkfoxmarketplace.com/ – darknet markets links
dark websites tor drug market
dark market 2025 dark markets 2025
darkmarket list https://cannahomedarknetdrugstore.com/ – darknet drug market
best darknet markets darkmarket list
darknet markets url https://darkmarketdarkfox.com/ – darknet websites
darkmarket list https://darknetmarketsonion.shop/ – bitcoin dark web
darknet drug market dark web sites
dark market https://darkmarketpremium.com/ – darknet markets
darknet markets onion dark markets
dark web sites darknet markets links
darknet markets url https://cannahomemarket.link/ – darknet drug market
dark market dark markets
darknet site https://kingdomdarkmarketplace.com – darknet site
darknet markets onion address dark markets 2025
darkmarket 2025 https://firstdarkmarket.com/ – darknet drugs
best darknet markets https://kingdommarketdarknet.com/ – dark web market urls
dark markets https://aasap-market.com/ – darknet markets 2025
darkmarket url darkmarkets
darknet markets links darknet markets 2025
dark markets 2025 darknet links
darknet market links https://darkfoxmarketplace.com/ – onion dark website
dark market link darkmarkets
darknet drug links dark market list
dark web market dark markets
darknet markets 2025 https://mydarkmarketlink.com/ – darkmarket url
darknet markets onion address https://darkfoxdarkweb.com/ – dark market url
dark web market list darknet drugs
dark markets https://cyberdarkmarkets.com/ – darknet markets onion address
dark market dark web sites
dark web markets darkmarkets
darknet market links darknet market lists
dark web link https://aasap-market.com/ – dark web market
darknet market lists https://asap-market-onion.com/ – darknet market list
darkmarket list dark market
darknet market lists https://darkfoxmarketplace.com/ – dark web drug marketplace
dark websites dark market url
bitcoin dark web darkmarket 2025
darknet markets url https://kingdomdarkmarketplace.com – darkmarkets
dark market link darknet links
darknet market list https://darkwebversus.com/ – darknet market list
dark web market list https://mydarkmarketlink.com/ – darknet market links
dark market 2025 https://darknetmarketsonion.shop/ – darknet drugs
darknet sites darknet market lists
dark market url https://cyberdarkmarkets.com/ – dark markets 2025
darknet drug links darkmarket
darknet drug store darkmarket
darknet markets 2025 darknet drug store
dark market darknet markets onion address
dark websites https://kingdom-darkmarketplace.com – darkmarket 2025
darknet sites https://darkwebversus.com/ – darknet market list
darknet markets links https://mydarkmarketlink.com/ – darknet markets url
dark web drug marketplace https://kingdommarketdarknet.com/ – darknet links
darknet drug store dark market list
darkmarkets https://darkfoxmarketplace.com/ – darkmarket list
darknet drug links darkmarket link
darknet markets dark market onion
darknet drug links darknet markets 2025
dark market url https://dark-web-versus.com – darknet markets links
dark market link dark web market links
dark web markets https://darkmarketpremium.com/ – dark web market list
dark market 2025 https://mydarkmarketlink.com/ – onion dark website
dark websites https://kingdommarketdarknet.com/ – darkmarket url
dark market list darknet marketplace
dark web market bitcoin dark web
dark web markets https://kingdomdarknetdrugstore.com/ – dark markets 2025
dark market url dark market url
dark web sites dark markets
dark websites https://dark-web-versus.com – dark markets 2025
darknet markets darknet markets
dark websites https://aasap-market.com/ – dark market url
darknet markets onion https://firstdarkmarket.com/ – dark web market urls
darknet markets onion address best darknet markets
darknet market list https://kingdommarketdarknet.com/ – dark market
darkmarkets dark web market
dark web marketplaces https://darkfoxmarketplace.com/ – darkmarket
bitcoin dark web tor drug market
dark markets 2025 https://drdarkfoxmarket.com – dark websites
dark web marketplaces darkmarket url
darknet drugs dark market list
darkmarket https://darkfoxdarkweb.com/ – dark market list
onion dark website darknet markets onion
darkmarket url https://onion-dark-market.shop/ – dark web market list
dark web market urls https://darknetmarketsonion.shop/ – darknet market lists
dark web market urls https://cannahome-darkmarket-online.com/ – darkmarket list
Greetings! Very helpful advice within this post! It is the little changes that produce the largest changes. Thanks a lot for sharing!
dark market url darknet market lists
darknet market https://drdarkfoxmarket.com – dark market onion
dark market url dark market 2025
dark web sites dark markets
darknet drugs https://darkwebversus.com/ – dark web market urls
darknet sites darknet market list
darkmarket https://kingdom-marketplace.com/ – darknet markets onion address
darknet drug market https://kingdomdarkmarketonline.com/ – dark market onion
dark markets https://cannahome-darkmarket-online.com/ – darknet drug store
darknet drug market darknet market list
darknet market darknet market links
darkmarket link darknet market lists
dark market 2025 https://darkfoxdarkweb.com/ – darknet market
darknet markets onion dark web markets
dark market onion https://kingdom-marketplace.com/ – darknet markets url
dark web market https://kingdommarketdarknet.com/ – darknet websites
darknet markets links https://cannahome-darkmarket-online.com/ – dark market
darkmarket darknet markets url
dark market link https://drdarkfoxmarket.com – darknet markets url
dark markets 2025 darknet websites
bitcoin dark web https://darkmarketpremium.com/ – darkmarkets
dark websites darknet market links
darknet drug market darknet sites
dark market https://onion-dark-market.shop/ – darknet markets onion address
bitcoin dark web https://kingdomdarkmarketonline.com/ – darknet drug market
dark market url darknet markets url
dark markets 2025 darknet site
darknet markets links darkmarket 2025
darknet drug store https://darkode-market.com/ – best darknet markets
darknet websites darknet site
Good web site you have got here.. It’s difficult to find quality writing like yours these days. I truly appreciate people like you! Take care!!
darknet drug store https://kingdom-marketplace.com/ – darknet market list
dark market link dark web markets
dark markets 2025 https://kingdomdarkmarketonline.com/ – darknet sites
darknet drug market onion dark website
dark web sites https://cyberdarkmarkets.com/ – darknet sites
darknet markets darkmarkets
dark market link https://dark-web-versus.com – darknet marketplace
darknet drug store https://aasap-market.com/ – darknet markets
dark market onion darknet sites
dark market url https://darkmarketdarkfox.com/ – dark market 2025
darknet drugs dark web markets
darknet marketplace darkmarkets
dark market https://kingdomdarkmarketonline.com/ – darknet drugs
dark markets dark market onion
darknet market https://cyberdarkmarkets.com/ – dark web drug marketplace
darknet markets onion https://kingdomdarkmarketplace.com – dark market 2025
dark market link bitcoin dark web
darknet site https://aasap-market.com/ – darknet sites
dark web markets darknet sites
dark websites dark web marketplaces
dark web sites https://onion-dark-market.shop/ – dark web drug marketplace
darknet markets onion address https://kingdommarketdarknet.com/ – darknet market links
darkmarket dark web market urls
best darknet markets dark web market list
darknet market list https://cannahomemarket.link/ – darkmarket link
onion dark website https://kingdomdarkmarketplace.com – dark market url
darknet markets 2025 https://darkode-market.com/ – darknet links
darkmarket list darknet markets links
darknet drug market darknet drug links
darknet markets 2025 https://onion-dark-market.shop/ – darknet markets onion
dark web market links darkmarket list
darknet market links https://kingdomdarkmarketonline.com/ – dark market link
darknet market bitcoin dark web
dark web market urls https://cannahome-darkmarket-online.com/ – darknet market list
dark markets dark web marketplaces
dark market url https://darkfoxdarkweb.com/ – dark market link
darknet drug store dark web market urls
darknet market links dark market
darknet marketplace https://mydarkmarketlink.com/ – dark web market links
dark markets https://darknetmarketsonion.shop/ – darknet markets onion address
darkmarket list dark web market
dark markets 2025 darknet market list
dark websites https://cannahome-darkmarket-online.com/ – darknet markets url
dark websites darknet marketplace
dark markets dark market url
darknet drug market https://aasap-market.com/ – dark market list
darknet drugs darknet market lists
dark market https://darkmarketdarkfox.com/ – darknet links
bitcoin dark web tor drug market
tor drug market https://kingdomdarknetdrugstore.com/ – darknet markets 2025
darknet markets darkmarket url
darkmarket list darknet marketplace
dark market 2025 darknet markets onion
darknet site https://kingdomdarkmarketplace.com – darkmarket list
bitcoin dark web dark web sites
dark market onion https://kingdom-marketplace.com/ – dark market link
dark market onion https://darknetmarketsonion.shop/ – darknet links
dark web sites dark market 2025
darkmarket bitcoin dark web
darknet drug links https://cannahome-darkmarket-online.com/ – dark web market urls
dark market link darknet markets links
darknet markets url https://kingdomdarkmarketplace.com – darknet drugs
darkmarket onion dark website
darknet drugs https://darkmarketdarkfox.com/ – darknet sites
darkmarkets dark markets
dark market list https://kingdommarketdarknet.com/ – dark web market urls
dark market url https://darkfoxmarketplace.com/ – darkmarket link
darknet markets onion address https://aasap-market.com/ – dark market onion
darkmarkets darknet sites
darknet sites https://dark-web-versus.com – darknet websites
bitcoin dark web darkmarket 2025
darknet markets onion address darknet drug market
dark web sites https://kingdom-marketplace.com/ – darknet markets
darknet markets onion address https://darknetmarketsonion.shop/ – darkmarket list
darknet market links https://kingdomdarknetdrugstore.com/ – onion dark website
darknet sites onion dark website
dark web marketplaces https://darkfoxdarkweb.com/ – tor drug market
dark market link https://drdarkfoxmarket.com – dark web market
darknet market links dark web markets
dark web link darknet markets 2025
dark web market links darknet market list
onion dark website https://kingdomdarkmarketonline.com/ – darknet markets onion address
darkmarket link darknet markets onion address
dark web market https://cannahome-darkmarket-online.com/ – dark web marketplaces
darkmarket list https://darkode-market.com/ – darkmarket link
darknet marketplace best darknet markets
darknet drug store https://kingdom-darkmarketplace.com – dark market url
darkmarket best darknet markets
darknet site darknet drugs
dark market https://mydarkmarketlink.com/ – dark web markets
darknet market https://kingdommarketdarknet.com/ – bitcoin dark web
darkmarket url dark markets 2025
darknet drug links https://darkfoxmarketplace.com/ – darknet marketplace
dark market list https://darkfoxdarkweb.com/ – dark websites
darkmarket url darkmarket list
darknet market list darkmarket
dark market dark market link
darknet market dark market
darknet drug store https://firstdarkmarket.com/ – darknet markets
dark web sites https://darknetmarketsonion.shop/ – dark markets 2025
darknet sites darknet drug market
darknet markets 2025 https://cannahomemarket.link/ – darknet drugs
darknet markets onion https://darkode-market.com/ – darknet drug links
dark market url dark web market links
darknet drugs https://kingdom-darkmarketplace.com – dark market onion
dark market list darkmarket url
darknet marketplace dark market onion
darknet site darknet market list
darknet markets links https://onion-dark-market.shop/ – darknet markets url
darkmarket list https://idarknetmarket.com/ – dark web market urls
dark market list darknet drugs
dark market list https://darkfoxmarketplace.com/ – dark market
darknet drugs dark market onion
darknet site https://kingdom-darkmarketplace.com – darknet markets url
dark web sites darknet markets
darknet websites darknet marketplace
dark websites https://mydarkmarketlink.com/ – dark web link
bitcoin dark web https://github.com/darknetmarkets2025/darknetmarketlinks dark web market urls
darknet markets onion https://kingdommarketdarknet.com/ – darknet market
dark markets https://darkmarketpremium.com/ – dark web markets
darknet market https://cannahome-darkmarket-online.com/ – dark market
darknet links https://github.com/darkwebwebsites/darkwebwebsites dark market onion
darknet marketplace https://dark-web-versus.com – darknet markets 2025
dark markets 2025 https://github.com/darknetmarketlinks2025/darknetmarkets dark web link
darknet markets url https://github.com/darkwebmarketslinks/darkwebmarkets dark web link
darkmarket 2025 https://github.com/darknetmarketslist/darknetmarketslist dark market
dark websites https://github.com/darknetmarkets2025/darknetmarketlinks dark web market urls
dark web markets https://mydarkmarketlink.com/ – darknet market lists
best darknet markets https://darknetmarketsonion.shop/ – dark web market urls
darkmarket 2025 https://aasap-market.com/ – dark web markets
bitcoin dark web https://darkfoxmarketplace.com/ – darknet links
onion dark website https://github.com/darkwebwebsites/darkwebwebsites darknet sites
dark web market urls https://drdarkfoxmarket.com – darknet markets onion address
darkmarket link https://github.com/darknetmarketlinks2025/darknetmarkets dark web market urls
darkmarkets https://github.com/darknetmarkets2025/darknetmarketlinks dark websites
darkmarket list https://github.com/darkwebmarketslinks/darkwebmarkets onion dark website
darknet sites https://github.com/darknetmarketslist/darknetmarketslist bitcoin dark web
darknet markets https://darkmarketdarkfox.com/ – darknet drug store
bitcoin dark web https://darknetmarketsonion.shop/ – darknet sites
darknet markets onion address https://darkwebversus.com/ – dark market list
darknet market lists https://kingdomdarknetdrugstore.com/ – darknet links
dark web market https://kingdomdarkmarketplace.com – darkmarket url
dark websites https://github.com/darkwebwebsites/darkwebwebsites darkmarket 2025
dark web market urls https://github.com/darknetmarkets2025/darknetmarketlinks darknet market links
It’s difficult to find experienced people on this topic, however, you sound like you know what you’re talking about! Thanks
darknet drug store https://github.com/darknetmarketlinks2025/darknetmarkets darknet websites
dark markets 2025 https://github.com/darkwebmarketslinks/darkwebmarkets dark web market links
darkmarket link https://onion-dark-market.shop/ – dark markets 2025
darknet drug store https://github.com/darknetmarketslist/darknetmarketslist darknet drugs
dark web market list https://darknetmarketsonion.shop/ – darkmarket link
dark web drug marketplace https://darkwebversus.com/ – darknet market
darkmarkets https://cannahome-darkmarket-online.com/ – dark web drug marketplace
darkmarkets https://github.com/darknetmarkets2025/darknetmarketlinks dark markets
darknet markets https://cannahomedarknetdrugstore.com/ – tor drug market
darkmarkets https://github.com/darkwebwebsites/darkwebwebsites tor drug market
dark web markets https://github.com/darknetmarketlinks2025/darknetmarkets dark market list
best darknet markets https://github.com/darkwebmarketslinks/darkwebmarkets darknet market lists
darknet markets 2025 https://darkmarketdarkfox.com/ – dark web link
dark web market urls https://kingdommarketdarknet.com/ – dark web market urls
darknet market links https://github.com/darknetmarketslist/darknetmarketslist dark websites
darknet markets onion address https://darkfoxdarkweb.com/ – darknet site
darknet drug store https://cyberdarkmarkets.com/ – darkmarket link
darknet links https://github.com/darknetmarkets2025/darknetmarketlinks darkmarkets
darkmarket 2025 https://kingdomdarkmarketplace.com – darknet sites
darknet websites https://github.com/darkwebwebsites/darkwebwebsites dark market list
onion dark website https://github.com/darknetmarketlinks2025/darknetmarkets dark market link
darknet websites https://darkmarketdarkfox.com/ – dark markets
dark market list https://github.com/darkwebmarketslinks/darkwebmarkets darknet markets 2025
darkmarkets https://kingdommarketdarknet.com/ – dark web market
darknet markets 2025 https://darkode-market.com/ – dark market
darknet markets onion https://github.com/darknetmarketslist/darknetmarketslist dark web market
darknet market links https://github.com/darknetmarkets2025/darknetmarketlinks darknet marketplace
darkmarket url https://darkfoxmarketplace.com/ – dark websites
darknet markets https://cannahomedarknetdrugstore.com/ – darknet market list
dark market 2025 https://github.com/darkwebwebsites/darkwebwebsites bitcoin dark web
dark web sites https://firstdarkmarket.com/ – bitcoin dark web
darknet markets links https://github.com/darknetmarketlinks2025/darknetmarkets dark web link
darknet marketplace https://github.com/darknetmarkets2025/darknetmarketlinks darkmarket link
dark market https://aasap-market.com/ – dark web market urls
darknet sites https://asap-market-onion.com/ – dark market url
darkmarket https://github.com/darkwebmarketslinks/darkwebmarkets darknet market
darknet markets onion https://github.com/darknetmarketslist/darknetmarketslist darknet markets
dark websites https://kingdomdarknetdrugstore.com/ – dark market
darknet market links https://cannahomedarknetdrugstore.com/ – darknet markets
darknet drug links https://github.com/darkwebwebsites/darkwebwebsites dark market
darknet market https://github.com/darknetmarkets2025/darknetmarketlinks darknet websites
tor drug market https://onion-dark-market.shop/ – darknet market list
darknet markets onion https://darkwebversus.com/ – dark web market list
darknet markets onion address https://kingdommarketdarknet.com/ – darknet drugs
darkmarket link https://github.com/darknetmarketlinks2025/darknetmarkets darknet drug store
darknet site https://github.com/darkwebmarketslinks/darkwebmarkets darknet drug market
darknet markets https://darkfoxmarketplace.com/ – bitcoin dark web
dark market list https://github.com/darknetmarketslist/darknetmarketslist bitcoin dark web
dark web markets https://kingdom-darkmarketplace.com – darknet marketplace
darknet markets https://github.com/darknetmarkets2025/darknetmarketlinks darknet websites
darknet market links https://kingdom-marketplace.com/ – darknet drug market
best darknet markets https://aasap-market.com/ – darknet site
dark web marketplaces https://idarknetmarket.com/ – darknet markets onion address
dark web market urls https://github.com/darknetmarketlinks2025/darknetmarkets darkmarket link
dark web market https://github.com/darkwebmarketslinks/darkwebmarkets darknet links
darknet links https://kingdomdarknetdrugstore.com/ – dark markets
dark web drug marketplace https://github.com/darknetmarketslist/darknetmarketslist darknet marketplace
darknet markets url https://kingdom-darkmarketplace.com – darknet drug store
darknet drug market https://github.com/darknetmarkets2025/darknetmarketlinks darknet market
tor drug market https://github.com/darkwebwebsites/darkwebwebsites darkmarket 2025
darknet market https://darkmarketpremium.com/ – dark market onion
darknet marketplace https://darkmarketdarkfox.com/ – darknet market list
best darknet markets https://darknetmarketsonion.shop/ – darkmarket list
dark market link https://github.com/darkwebmarketslinks/darkwebmarkets dark market 2025
bitcoin dark web https://darkfoxmarketplace.com/ – dark market link
darknet markets links https://github.com/darknetmarkets2025/darknetmarketlinks dark web sites
darkmarket https://github.com/darknetmarketslist/darknetmarketslist dark web market list
dark markets 2025 https://dark-web-versus.com – darknet links
dark web drug marketplace https://github.com/darkwebwebsites/darkwebwebsites darkmarkets
Pretty! This was an incredibly wonderful article. Many thanks for supplying this information.
bitcoin dark web https://darkfoxdarkweb.com/ – dark market onion
darknet markets 2025 https://firstdarkmarket.com/ – dark web market urls
darknet market list https://idarknetmarket.com/ – dark web market list
darknet drug links https://github.com/darknetmarkets2025/darknetmarketlinks darkmarket link
dark market url https://github.com/darkwebmarketslinks/darkwebmarkets darknet websites
dark web market list https://cannahomemarket.link/ – dark market list
dark web marketplaces https://github.com/darknetmarketslist/darknetmarketslist dark web market links
darkmarkets https://kingdomdarkmarketplace.com – dark web market links
best darknet markets https://github.com/darkwebwebsites/darkwebwebsites dark web market list
darknet drug store https://darkfoxdarkweb.com/ – dark market list
dark web drug marketplace https://github.com/darknetmarkets2025/darknetmarketlinks tor drug market
darknet markets 2025 https://onion-dark-market.shop/ – dark market 2025
darkmarket 2025 https://kingdommarketdarknet.com/ – dark markets 2025
dark market url https://github.com/darkwebmarketslinks/darkwebmarkets darknet drug store
darknet market list https://cannahome-darkmarket-online.com/ – dark web drug marketplace
A motivating discussion is worth comment. I think that you need to write more on this topic, it might not be a taboo subject but usually folks don’t discuss these issues. To the next! Many thanks.
dark web market list https://github.com/darknetmarketslist/darknetmarketslist darknet markets links
dark markets 2025 https://drdarkfoxmarket.com – darknet drug market
dark websites https://github.com/darknetmarkets2025/darknetmarketlinks dark web market
darknet websites https://github.com/darkwebwebsites/darkwebwebsites dark market onion
dark web drug marketplace https://darkmarketpremium.com/ – dark web link
darknet drug market https://darkmarketdarkfox.com/ – darknet market
darknet markets 2025 https://idarknetmarket.com/ – darkmarket list
darknet markets https://github.com/darkwebmarketslinks/darkwebmarkets darknet market
darknet drug market https://cyberdarkmarkets.com/ – dark web market list
dark web marketplaces https://github.com/darknetmarketslist/darknetmarketslist dark web market urls
darkmarket link https://github.com/darknetmarkets2025/darknetmarketlinks dark web marketplaces
darkmarket https://dark-web-versus.com – darknet market lists
dark web sites https://github.com/darkwebwebsites/darkwebwebsites dark web market
darkmarket link https://darkmarketpremium.com/ – darknet market list
dark market https://mydarkmarketlink.com/ – darknet market
onion dark website https://kingdomdarkmarketonline.com/ – dark web market links
dark markets https://github.com/darkwebmarketslinks/darkwebmarkets dark web markets
dark web market links https://github.com/darknetmarketslist/darknetmarketslist darknet drugs
bitcoin dark web https://kingdomdarknetdrugstore.com/ – darknet market
darknet websites https://kingdomdarkmarketplace.com – darknet markets onion address
best darknet markets https://github.com/darkwebwebsites/darkwebwebsites dark market 2025
dark markets https://aasap-market.com/ – darknet markets url
bitcoin dark web https://onion-dark-market.shop/ – darknet market links
darkmarket link https://github.com/darknetmarkets2025/darknetmarketlinks dark market onion
darknet sites https://idarknetmarket.com/ – dark market
onion dark website https://github.com/darkwebmarketslinks/darkwebmarkets darknet market links
dark web drug marketplace https://github.com/darknetmarketslist/darknetmarketslist darknet drug market
darknet markets https://kingdomdarknetdrugstore.com/ – tor drug market
darknet markets links https://dark-web-versus.com – darknet market lists
dark market onion https://github.com/darkwebwebsites/darkwebwebsites dark market url
darknet market list https://darkfoxdarkweb.com/ – best darknet markets
darkmarket 2025 https://github.com/darknetmarkets2025/darknetmarketlinks darknet markets links
darknet market https://mydarkmarketlink.com/ – dark web markets
darknet markets onion address https://github.com/darkwebmarketslinks/darkwebmarkets dark web sites
darkmarket list https://asap-market-onion.com/ – darkmarket link
dark markets 2025 https://github.com/darknetmarketslist/darknetmarketslist dark market
darkmarket list https://kingdom-darkmarketplace.com – dark web markets
dark market url https://github.com/darknetmarkets2025/darknetmarketlinks dark market
dark market url https://github.com/darkwebwebsites/darkwebwebsites darknet market list
dark market link https://darkfoxdarkweb.com/ – dark web market
dark market https://darkmarketdarkfox.com/ – darkmarket 2025
darknet drug store https://github.com/darkwebmarketslinks/darkwebmarkets dark market link
dark web drug marketplace https://asap-market-onion.com/ – dark market url
dark web marketplaces https://github.com/darknetmarketslist/darknetmarketslist darkmarket url
dark markets https://github.com/darknetmarkets2025/darknetmarketlinks darknet marketplace
onion dark website https://dark-web-versus.com – darknet drug links
darkmarket https://github.com/darkwebwebsites/darkwebwebsites darknet marketplace
darknet market lists https://darkfoxdarkweb.com/ – dark web market
darknet market https://github.com/darkwebmarketslinks/darkwebmarkets darknet drug store
darknet market list https://onion-dark-market.shop/ – dark market
darknet drug links https://kingdomdarkmarketonline.com/ – dark web market list
dark websites https://github.com/darknetmarketslist/darknetmarketslist darknet markets url
darknet sites https://github.com/darknetmarkets2025/darknetmarketlinks dark market url
dark market https://cannahome-darkmarket-online.com/ – darknet market lists
dark market link https://cannahomedarknetdrugstore.com/ – darkmarket url
darknet drug links https://github.com/darkwebwebsites/darkwebwebsites dark web market urls
dark websites https://github.com/darknetmarkets2025/darknetmarketlinks darknet websites
darknet markets onion address https://darkmarketdarkfox.com/ – darkmarket link
dark websites https://github.com/darknetmarketslist/darknetmarketslist darknet drug store
dark web link https://cannahomemarket.link/ – darknet market list
dark web sites https://dark-web-versus.com – dark web market links
dark web link https://github.com/darknetmarkets2025/darknetmarketlinks darknet market links
dark web markets https://kingdomdarkmarketonline.com/ – darknet links
darknet markets 2025 https://github.com/darkwebmarketslinks/darkwebmarkets darkmarket url
dark web markets https://cyberdarkmarkets.com/ – bitcoin dark web
dark web link https://kingdom-darkmarketplace.com – darknet marketplace
dark web market list https://github.com/darknetmarkets2025/darknetmarketlinks best darknet markets
tor drug market https://firstdarkmarket.com/ – darknet drug links
darknet drugs https://asap-market-onion.com/ – darknet market
dark websites https://cannahome-darkmarket-online.com/ – darkmarket url
darkmarkets https://github.com/darkwebmarketslinks/darkwebmarkets darknet marketplace
darknet drug market https://kingdom-darkmarketplace.com – darkmarket list
dark web sites https://github.com/darknetmarketslist/darknetmarketslist darknet drug links
darknet links https://idarknetmarket.com/ – dark web drug marketplace
darknet market lists https://darkfoxmarketplace.com/ – dark market url
dark market onion https://cannahomedarknetdrugstore.com/ – darknet drug market
darkmarket link https://github.com/darkwebmarketslinks/darkwebmarkets darknet market list
darknet links https://github.com/darknetmarketslist/darknetmarketslist dark web market list
dark market https://github.com/darknetmarkets2025/darknetmarketlinks darknet site
dark market https://kingdom-marketplace.com/ – onion dark website
dark markets https://idarknetmarket.com/ – darknet markets onion
darknet sites https://cannahomemarket.link/ – darknet drug links
dark market 2025 https://github.com/darkwebwebsites/darkwebwebsites dark market
dark web market list https://dark-web-versus.com – darknet marketplace
darknet marketplace https://github.com/darkwebmarketslinks/darkwebmarkets darknet market lists
best darknet markets https://github.com/darknetmarkets2025/darknetmarketlinks dark web market links
darknet market lists https://github.com/darknetmarketslist/darknetmarketslist dark web markets
darknet sites https://darkmarketdarkfox.com/ – darkmarket 2025
dark web sites https://kingdommarketdarknet.com/ – darknet markets url
darkmarket https://cannahome-darkmarket-online.com/ – dark market link
dark web link https://kingdomdarkmarketplace.com – darknet links
darkmarket https://github.com/darknetmarkets2025/darknetmarketlinks bitcoin dark web
dark web sites https://github.com/darkwebmarketslinks/darkwebmarkets dark markets
dark web market list https://darkmarketdarkfox.com/ – darknet markets links
darkmarket https://kingdomdarkmarketonline.com/ – darknet sites
darknet sites https://github.com/darknetmarketslist/darknetmarketslist dark market link
dark market https://cyberdarkmarkets.com/ – dark websites
dark market https://dark-web-versus.com – dark web marketplaces
dark markets https://github.com/darkwebwebsites/darkwebwebsites dark market list
dark market https://github.com/darknetmarkets2025/darknetmarketlinks dark market link
dark web marketplaces https://firstdarkmarket.com/ – dark markets 2025
darknet drug store https://kingdommarketdarknet.com/ – darknet site
darknet market links https://github.com/darkwebmarketslinks/darkwebmarkets dark web drug marketplace
darkmarket list https://cyberdarkmarkets.com/ – darknet websites
dark web market https://github.com/darknetmarketslist/darknetmarketslist darknet drug links
dark web market https://kingdomdarkmarketplace.com – darknet site
darknet drug links https://github.com/darknetmarketlinks2025/darknetmarkets dark web market list
darkmarket list https://github.com/darknetmarkets2025/darknetmarketlinks dark market url
dark web market urls https://mydarkmarketlink.com/ – darknet markets links
darknet market https://github.com/darkwebwebsites/darkwebwebsites darknet market list
dark market link https://kingdomdarkmarketonline.com/ – dark market list
dark market list https://kingdomdarknetdrugstore.com/ – darknet market list
dark web marketplaces https://drdarkfoxmarket.com – darkmarket link
dark market list https://github.com/darkwebmarketslinks/darkwebmarkets dark web market links
darkmarket list https://github.com/darknetmarketslist/darknetmarketslist darknet market list
dark market onion https://github.com/darknetmarkets2025/darknetmarketlinks dark market list
darknet marketplace https://firstdarkmarket.com/ – darknet websites
darknet drug market https://asap-market-onion.com/ – darknet market
darknet markets 2025 https://github.com/darknetmarketlinks2025/darknetmarkets darknet drug links
darknet markets 2025 https://darkfoxmarketplace.com/ – darknet marketplace
dark market url https://github.com/darkwebwebsites/darkwebwebsites dark markets 2025
dark web sites https://kingdom-darkmarketplace.com – dark web link
darkmarket list https://onion-dark-market.shop/ – darknet marketplace
darkmarket 2025 https://idarknetmarket.com/ – dark market 2025
darknet sites https://github.com/darkwebmarketslinks/darkwebmarkets darkmarket link
darknet markets url https://cyberdarkmarkets.com/ – dark market
dark market onion https://github.com/darknetmarketslist/darknetmarketslist darkmarket url
darknet drug market https://kingdomdarkmarketplace.com – darknet markets url
darknet marketplace https://github.com/darknetmarketlinks2025/darknetmarkets dark web markets
dark web marketplaces https://kingdom-marketplace.com/ – dark web link
dark market onion https://github.com/darkwebwebsites/darkwebwebsites darknet site
darkmarkets https://darknetmarketsonion.shop/ – darkmarket url
darknet markets links https://kingdomdarknetdrugstore.com/ – tor drug market
dark market 2025 https://github.com/darknetmarkets2025/darknetmarketlinks darknet sites
dark web link https://kingdomdarkmarketplace.com – darknet drug links
darknet drug store https://github.com/darkwebmarketslinks/darkwebmarkets onion dark website
dark websites https://github.com/darknetmarketslist/darknetmarketslist darkmarket link
darknet market https://onion-dark-market.shop/ – tor drug market
dark web market https://kingdommarketdarknet.com/ – darknet site
dark market 2025 https://github.com/darknetmarketlinks2025/darknetmarkets darknet sites
darknet drug store https://cannahomemarket.link/ – dark market 2025
dark web markets https://github.com/darkwebwebsites/darkwebwebsites dark web market list
dark web sites https://github.com/darknetmarkets2025/darknetmarketlinks dark web market
dark market onion https://mydarkmarketlink.com/ – darknet markets links
onion dark website https://github.com/darkwebmarketslinks/darkwebmarkets darknet market lists
darknet marketplace https://asap-market-onion.com/ – dark web link
dark market url https://github.com/darknetmarketslist/darknetmarketslist bitcoin dark web
darknet drug market https://cannahomemarket.link/ – darkmarkets
bitcoin dark web https://kingdom-darkmarketplace.com – dark web drug marketplace
darknet markets onion address https://github.com/darknetmarketlinks2025/darknetmarkets darkmarket
darknet drug links https://github.com/darknetmarkets2025/darknetmarketlinks dark web marketplaces
dark markets 2025 https://github.com/darkwebwebsites/darkwebwebsites darknet links
dark web market links https://mydarkmarketlink.com/ – darknet markets onion
darkmarket link https://kingdomdarkmarketonline.com/ – darkmarket list
dark web market links https://darkfoxmarketplace.com/ – darkmarket list
darknet markets links https://github.com/darkwebmarketslinks/darkwebmarkets darknet markets
darkmarket list https://dark-web-versus.com – darknet markets onion
darknet drug market https://github.com/darknetmarketslist/darknetmarketslist darknet drugs
darknet markets onion address https://github.com/darknetmarkets2025/darknetmarketlinks darknet drugs
darknet market list https://github.com/darknetmarketlinks2025/darknetmarkets darknet websites
darknet drug market https://onion-dark-market.shop/ – darknet market lists
darknet market links https://idarknetmarket.com/ – darknet markets url
onion dark website https://github.com/darkwebwebsites/darkwebwebsites darknet market list
dark market link https://cyberdarkmarkets.com/ – darkmarket list
darknet market list https://cannahomedarknetdrugstore.com/ – darkmarket list
dark web link https://github.com/darkwebmarketslinks/darkwebmarkets darknet websites
darknet drug market https://github.com/darknetmarkets2025/darknetmarketlinks dark websites
tor drug market https://github.com/darknetmarketslist/darknetmarketslist dark web sites
dark market link https://darkmarketdarkfox.com/ – darknet market
darkmarket 2025 https://darknetmarketsonion.shop/ – darkmarket list
dark markets 2025 https://github.com/darknetmarketlinks2025/darknetmarkets darkmarket
dark market url https://cannahomemarket.link/ – darknet market list
onion dark website https://github.com/darkwebwebsites/darkwebwebsites darknet markets links
darknet markets onion address https://github.com/darknetmarkets2025/darknetmarketlinks bitcoin dark web
darkmarket https://github.com/darkwebmarketslinks/darkwebmarkets dark markets
darknet markets url https://firstdarkmarket.com/ – dark market list
best darknet markets https://idarknetmarket.com/ – dark web market urls
best darknet markets https://github.com/darknetmarketslist/darknetmarketslist darkmarkets
Good post. I learn something totally new and challenging on websites I stumbleupon every day. It’s always useful to read articles from other writers and practice something from other sites.
darknet markets onion https://cyberdarkmarkets.com/ – darknet market lists
dark market link https://github.com/darknetmarketlinks2025/darknetmarkets darknet markets
darkmarkets https://cannahomedarknetdrugstore.com/ – dark web market list
darknet site https://github.com/darkwebwebsites/darkwebwebsites darkmarket url
darknet links https://github.com/darknetmarkets2025/darknetmarketlinks darknet websites
darknet markets links https://firstdarkmarket.com/ – darknet markets onion
darknet websites https://github.com/darkwebmarketslinks/darkwebmarkets dark markets 2025
dark market url https://darknetmarketsonion.shop/ – dark web markets
dark web marketplaces https://cannahomemarket.link/ – darknet links
darknet links https://github.com/darknetmarketslist/darknetmarketslist darknet marketplace
dark websites https://kingdomdarkmarketplace.com – darknet drug links
dark market link https://github.com/darknetmarkets2025/darknetmarketlinks bitcoin dark web
dark market 2025 https://github.com/darkwebwebsites/darkwebwebsites onion dark website
dark market link https://mydarkmarketlink.com/ – dark markets
darknet markets onion https://kingdommarketdarknet.com/ – dark markets 2025
dark web link https://github.com/darkwebmarketslinks/darkwebmarkets darknet drug store
dark market onion https://github.com/darknetmarketslist/darknetmarketslist darknet markets url
tor drug market https://drdarkfoxmarket.com – darkmarket list
darknet markets onion https://github.com/darknetmarkets2025/darknetmarketlinks dark web drug marketplace
best darknet markets https://github.com/darknetmarketlinks2025/darknetmarkets darknet marketplace
dark web markets https://darkmarketdarkfox.com/ – bitcoin dark web
dark web link https://github.com/darkwebwebsites/darkwebwebsites bitcoin dark web
bitcoin dark web https://kingdommarketdarknet.com/ – dark web markets
dark market link https://cannahomemarket.link/ – darknet markets onion
darknet drug store https://github.com/darkwebmarketslinks/darkwebmarkets darknet markets
darknet markets onion address https://drdarkfoxmarket.com – darknet market links
darknet market lists https://github.com/darknetmarkets2025/darknetmarketlinks onion dark website
dark markets https://github.com/darknetmarketslist/darknetmarketslist darkmarket link
onion dark website https://onion-dark-market.shop/ – dark web market links
dark market list https://asap-market-onion.com/ – darkmarket
dark market url https://cannahomemarket.link/ – darknet market
onion dark website https://github.com/darknetmarketlinks2025/darknetmarkets dark web link
tor drug market https://kingdomdarkmarketplace.com – darknet market lists
darknet markets onion address https://github.com/darkwebwebsites/darkwebwebsites dark market onion
darknet market https://kingdom-marketplace.com/ – dark market list
darknet marketplace https://github.com/darknetmarkets2025/darknetmarketlinks darknet drugs
darknet drug store https://asap-market-onion.com/ – darkmarket
dark websites https://github.com/darkwebmarketslinks/darkwebmarkets darknet drug links
darkmarket 2025 https://cannahome-darkmarket-online.com/ – darknet markets links
dark market link https://github.com/darknetmarketslist/darknetmarketslist darkmarket link
darknet drug market https://kingdom-darkmarketplace.com – best darknet markets
darknet site https://github.com/darknetmarketlinks2025/darknetmarkets dark web market links
After going over a handful of the articles on your web site, I truly appreciate your way of blogging. I bookmarked it to my bookmark site list and will be checking back in the near future. Take a look at my website too and let me know what you think.
darkmarkets https://github.com/darknetmarkets2025/darknetmarketlinks dark market onion
darkmarket https://firstdarkmarket.com/ – darknet markets 2025
dark web sites https://kingdomdarkmarketonline.com/ – dark market
darknet markets onion address https://cyberdarkmarkets.com/ – darknet drug links
darknet markets 2025 https://github.com/darkwebmarketslinks/darkwebmarkets dark web marketplaces
darknet marketplace https://kingdom-darkmarketplace.com – darknet market lists
You’re so cool! I don’t believe I’ve truly read anything like this before. So nice to find someone with some genuine thoughts on this subject matter. Really.. thank you for starting this up. This website is something that is needed on the web, someone with some originality!
darkmarket link https://github.com/darknetmarketslist/darknetmarketslist bitcoin dark web
dark market link https://github.com/darknetmarkets2025/darknetmarketlinks dark market link
best darknet markets https://firstdarkmarket.com/ – darknet markets links
dark web market links https://darknetmarketsonion.shop/ – darknet drug links
darkmarket 2025 https://github.com/darkwebwebsites/darkwebwebsites darknet market
darknet markets links https://darkfoxmarketplace.com/ – dark markets 2025
bitcoin dark web https://kingdom-darkmarketplace.com – darknet markets url
darknet site https://github.com/darkwebmarketslinks/darkwebmarkets dark market onion
dark web market urls https://github.com/darknetmarketslist/darknetmarketslist dark market list
darkmarket link https://github.com/darknetmarkets2025/darknetmarketlinks dark web market links
darknet site https://kingdom-marketplace.com/ – dark market list
dark web market links https://darknetmarketsonion.shop/ – darknet markets url
dark market https://github.com/darknetmarketlinks2025/darknetmarkets dark web marketplaces
onion dark website https://cannahome-darkmarket-online.com/ – dark web market links
dark web marketplaces https://github.com/darkwebwebsites/darkwebwebsites darknet websites
darknet markets onion https://cannahomedarknetdrugstore.com/ – darknet site
dark web markets https://github.com/darkwebmarketslinks/darkwebmarkets dark market link
dark web market list https://github.com/darknetmarkets2025/darknetmarketlinks darknet market lists
darknet markets onion https://mydarkmarketlink.com/ – dark market list
I like it when people get together and share views. Great website, stick with it.
dark market url https://github.com/darknetmarketslist/darknetmarketslist darkmarket link
darkmarket list https://idarknetmarket.com/ – darkmarkets
darknet market https://darkfoxmarketplace.com/ – darknet drug store
darknet markets onion https://github.com/darkwebwebsites/darkwebwebsites darknet markets url
dark web market https://github.com/darknetmarkets2025/darknetmarketlinks onion dark website
dark websites https://firstdarkmarket.com/ – darknet drug store
darknet websites https://github.com/darkwebmarketslinks/darkwebmarkets dark market 2025
best darknet markets https://kingdomdarkmarketonline.com/ – darknet drugs
best darknet markets https://github.com/darknetmarketslist/darknetmarketslist darkmarket link
dark markets 2025 https://cannahomemarket.link/ – darknet markets onion address
darknet drugs https://github.com/darknetmarketlinks2025/darknetmarkets darkmarkets
dark web sites https://kingdomdarkmarketplace.com – dark websites
darknet sites https://github.com/darkwebwebsites/darkwebwebsites darknet site
darknet markets onion https://github.com/darknetmarkets2025/darknetmarketlinks darkmarket 2025
dark market list https://onion-dark-market.shop/ – darknet markets url
dark market https://idarknetmarket.com/ – darkmarket
darknet markets url https://github.com/darkwebmarketslinks/darkwebmarkets dark market url
dark web marketplaces https://github.com/darknetmarketslist/darknetmarketslist dark market list
dark market link https://github.com/darknetmarkets2025/darknetmarketlinks darknet markets 2025
darkmarkets https://github.com/darknetmarketlinks2025/darknetmarkets darkmarket list
dark market url https://kingdom-marketplace.com/ – dark market 2025
dark web market links https://github.com/darkwebwebsites/darkwebwebsites onion dark website
best darknet markets https://asap-market-onion.com/ – darknet drug store
dark web market urls https://cannahomemarket.link/ – darknet market list
darknet site https://github.com/darkwebmarketslinks/darkwebmarkets dark market
darknet sites https://cannahomedarknetdrugstore.com/ – dark markets
dark web market links https://github.com/darknetmarketslist/darknetmarketslist darkmarket 2025
darknet market list https://github.com/darknetmarkets2025/darknetmarketlinks darknet drug market
tor drug market https://darkmarketdarkfox.com/ – darknet drug store
dark web drug marketplace https://github.com/darknetmarketlinks2025/darknetmarkets darknet drug store
dark web markets https://kingdomdarkmarketonline.com/ – dark web link
dark markets https://cyberdarkmarkets.com/ – dark market
dark web market https://github.com/darknetmarkets2025/darknetmarketlinks dark market
darknet market links https://github.com/darknetmarketslist/darknetmarketslist tor drug market
darkmarket 2025 https://kingdom-marketplace.com/ – darknet markets
darkmarket url https://darknetmarketsonion.shop/ – darknet links
dark web market links https://github.com/darknetmarketlinks2025/darknetmarkets onion dark website
darkmarket 2025 https://cannahome-darkmarket-online.com/ – darkmarket url
darkmarkets https://github.com/darkwebwebsites/darkwebwebsites dark markets
dark market 2025 https://drdarkfoxmarket.com – dark web market links
darknet markets links https://darkmarketdarkfox.com/ – darknet sites
darknet markets https://kingdommarketdarknet.com/ – dark market link
darknet market list https://kingdomdarknetdrugstore.com/ – darknet market list
darknet markets 2025 https://kingdomdarkmarketplace.com – tor drug market
dark web link https://kingdom-marketplace.com/ – darknet markets 2025
dark market url https://asap-market-onion.com/ – dark web marketplaces
dark web sites https://cannahomemarket.link/ – darkmarket 2025
darknet markets url https://mydarkmarketlink.com/ – darknet websites
darkmarket link https://kingdomdarkmarketonline.com/ – dark web markets
darkmarket list https://kingdomdarknetdrugstore.com/ – darknet drug links
darknet drug links https://onion-dark-market.shop/ – darknet markets
dark market url https://kingdomdarkmarketonline.com/ – dark web market list
dark market url https://cannahome-darkmarket-online.com/ – dark market 2025
darknet links https://kingdom-marketplace.com/ – dark websites
darkmarkets https://kingdomdarkmarketonline.com/ – dark web marketplaces
darkmarkets https://cannahomemarket.link/ – bitcoin dark web
dark web sites https://onion-dark-market.shop/ – dark market url
darkmarkets https://idarknetmarket.com/ – onion dark website
darkmarket 2025 https://cannahomemarket.link/ – dark web markets
darknet market lists https://darkmarketdarkfox.com/ – darkmarket list
dark web marketplaces https://kingdomdarkmarketonline.com/ – dark websites
darkmarket list https://darkfoxmarketplace.com/ – darknet links
darkmarket list https://darkmarketdarkfox.com/ – dark market url
darknet market links https://kingdomdarkmarketonline.com/ – darknet drug store
darknet markets url https://darkfoxmarketplace.com/ – darknet market lists
darkmarket list https://firstdarkmarket.com/ – darknet market list
darknet site https://darknetmarketsonion.shop/ – dark web marketplaces
darkmarkets https://kingdomdarknetdrugstore.com/ – dark web market list
darkmarket url https://onion-dark-market.shop/ – darknet markets links
darknet markets url https://asap-market-onion.com/ – dark web sites
darknet drug links https://darkfoxmarketplace.com/ – dark markets
darknet markets https://mydarkmarketlink.com/ – darkmarkets
dark web link https://darknetmarketsonion.shop/ – darknet markets url
darknet drug market https://cannahome-darkmarket-online.com/ – darknet markets links
darknet markets onion address https://darkmarketdarkfox.com/ – dark web sites
darknet markets https://kingdommarketdarknet.com/ – darknet links
tor drug market https://darkfoxmarketplace.com/ – darkmarkets
dark market link https://firstdarkmarket.com/ – darkmarkets
darknet markets https://idarknetmarket.com/ – darknet marketplace
dark market link https://darkfoxmarketplace.com/ – dark market link
dark market 2025 https://mydarkmarketlink.com/ – darknet markets
darknet markets 2025 https://darknetmarketsonion.shop/ – darknet links
dark markets https://cannahome-darkmarket-online.com/ – dark websites
magnificent post, very informative. I ponder why the other specialists of this sector don’t understand this. You should proceed your writing. I am sure, you’ve a great readers’ base already!
onion dark website https://firstdarkmarket.com/ – darkmarket
darkmarket 2025 https://kingdomdarkmarketonline.com/ – dark web markets
darknet drug market https://cyberdarkmarkets.com/ – darknet sites
dark web market urls https://drdarkfoxmarket.com – dark market link
dark web link https://kingdom-marketplace.com/ – dark market link
dark web link https://kingdomdarkmarketonline.com/ – dark web markets
darknet drug market https://cannahomemarket.link/ – darknet markets onion
This info is priceless. When can I find out more?
darknet markets onion address https://dark-web-versus.com – darknet drugs
darknet markets 2025 https://darkmarketdarkfox.com/ – darknet market
dark market onion https://idarknetmarket.com/ – darkmarket url
darknet markets links https://cyberdarkmarkets.com/ – dark market list
dark web markets https://kingdom-darkmarketplace.com – darknet markets onion address
darknet site https://mydarkmarketlink.com/ – dark markets
dark web sites https://kingdommarketdarknet.com/ – dark web sites
dark web drug marketplace https://kingdomdarknetdrugstore.com/ – darknet markets
darknet websites https://kingdomdarkmarketplace.com – bitcoin dark web
dark market url https://firstdarkmarket.com/ – darknet websites
dark web market urls https://kingdommarketdarknet.com/ – darknet drug links
darknet markets links https://cyberdarkmarkets.com/ – darkmarkets
dark market url https://kingdom-darkmarketplace.com – darknet markets
darknet drug market https://onion-dark-market.shop/ – darknet markets 2025
dark market link https://idarknetmarket.com/ – darknet drugs
darknet links https://drdarkfoxmarket.com – dark markets 2025
dark web link https://mydarkmarketlink.com/ – best darknet markets
darkmarkets https://kingdomdarkmarketonline.com/ – darknet drug links
bitcoin dark web https://cannahomemarket.link/ – dark web market links
best darknet markets https://kingdomdarkmarketplace.com – darknet site
best darknet markets https://firstdarkmarket.com/ – dark web link
darknet drug market https://idarknetmarket.com/ – darknet links
darkmarket 2025 https://drdarkfoxmarket.com – dark web market
dark market onion https://darkmarketdarkfox.com/ – darknet market
dark web marketplaces https://kingdomdarkmarketonline.com/ – dark market 2025
dark market https://cyberdarkmarkets.com/ – dark web market list
dark web market urls https://drdarkfoxmarket.com – darknet markets onion
darknet markets onion address https://mydarkmarketlink.com/ – darkmarkets
darkmarket list https://kingdommarketdarknet.com/ – darknet drug store
dark market link https://kingdomdarknetdrugstore.com/ – dark market url
dark web link https://kingdomdarkmarketplace.com – dark web markets
darkmarket list https://mydarkmarketlink.com/ – darknet market
dark market link https://asap-market-onion.com/ – darkmarket url
dark markets 2025 https://cyberdarkmarkets.com/ – darknet drug links
dark market link https://cannahomedarknetdrugstore.com/ – best darknet markets
onion dark website https://onion-dark-market.shop/ – darkmarket list
dark market url https://asap-market-onion.com/ – dark market
darknet market links https://cannahomedarknetdrugstore.com/ – darknet marketplace
darkmarket list https://darkmarketdarkfox.com/ – dark web market links
dark web marketplaces https://kingdomdarkmarketonline.com/ – best darknet markets
best darknet markets https://kingdomdarknetdrugstore.com/ – darknet drugs
dark web market links https://kingdomdarkmarketplace.com – darknet websites
bitcoin dark web https://kingdom-marketplace.com/ – dark web market
darknet sites https://darknetmarketsonion.shop/ – dark market url
darknet markets onion https://kingdomdarknetdrugstore.com/ – darknet links
darknet market links https://kingdomdarkmarketplace.com – dark web drug marketplace
dark web markets https://firstdarkmarket.com/ – dark websites
darknet market lists https://asap-market-onion.com/ – darknet markets onion address
darkmarket list https://cannahome-darkmarket-online.com/ – darknet drug market
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get four e-mails with the same comment. Is there any way you can remove me from that service? Bless you!
darknet markets url https://kingdom-darkmarketplace.com – darknet marketplace
tor drug market https://idarknetmarket.com/ – darkmarket link
darkmarket 2025 https://kingdomdarknetdrugstore.com/ – darknet marketplace
dark web market links https://dark-web-versus.com – dark web markets
darkmarkets https://firstdarkmarket.com/ – dark websites
dark market 2025 https://idarknetmarket.com/ – darkmarket list
darkmarket url https://cannahomemarket.link/ – bitcoin dark web
darkmarket https://asap-market-onion.com/ – darkmarket 2025
darknet market https://cannahomemarket.link/ – dark markets
darknet site https://drdarkfoxmarket.com – darknet websites
darknet market https://onion-dark-market.shop/ – darknet market list
dark market url https://idarknetmarket.com/ – darknet market links
dark market link https://darkfoxmarketplace.com/ – dark web market
Next time I read a blog, Hopefully it doesn’t disappoint me as much as this one. After all, Yes, it was my choice to read through, however I really believed you’d have something useful to talk about. All I hear is a bunch of moaning about something you could possibly fix if you weren’t too busy looking for attention.
darknet markets https://drdarkfoxmarket.com – dark web market list
darknet markets 2025 https://kingdom-marketplace.com/ – onion dark website
darknet markets onion address https://idarknetmarket.com/ – darknet marketplace
darknet markets 2025 https://cyberdarkmarkets.com/ – darknet market links
dark market list https://cannahomedarknetdrugstore.com/ – darknet sites
darknet links https://onion-dark-market.shop/ – dark market onion
best darknet markets https://asap-market-onion.com/ – darknet market list
dark web market urls https://kingdom-darkmarketplace.com – dark web market
darknet site https://darkmarketdarkfox.com/ – darknet drug store
dark markets https://darknetmarketsonion.shop/ – darknet drug market
darknet drug links https://cyberdarkmarkets.com/ – darknet markets links
darkmarket https://dark-web-versus.com – best darknet markets
dark web sites https://onion-dark-market.shop/ – dark web markets
darknet drug links https://kingdomdarkmarketonline.com/ – darknet market links
This is a topic which is close to my heart… Thank you! Where are your contact details though?
darknet market list https://darkfoxmarketplace.com/ – dark web market urls
darkmarket url https://cannahomedarknetdrugstore.com/ – dark web drug marketplace
darknet websites https://onion-dark-market.shop/ – dark web marketplaces
darknet market lists https://darkode-market.com/ – dark web sites
darknet markets 2025 https://github.com/aresonioncq0a7/aresonion – dark web link
darknet site https://kingdomdarkmarketplace.com – dark market link
darknet drug links https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet site
darknet markets onion https://darkmarketdarkfox.com/ – onion dark website
dark web market https://asap-market-onion.com/ – dark web marketplaces
darkmarket 2025 https://github.com/abacuslink4jjku/abacuslink – dark market list
darknet markets url https://cannahomemarket.link/ – dark websites
darkmarket https://github.com/darkwebsitesyhshv/darkwebsites – darknet drugs
darkmarkets https://darkmarketpremium.com/ – dark market list
darknet marketplace https://github.com/aresonioncq0a7/aresonion – darknet markets links
darknet markets links https://github.com/nexusdarkrtv1u/nexusdark – darknet markets onion
darkmarket 2025 https://kingdom-darkmarketplace.com – dark market url
darknet market list https://firstdarkmarket.com/ – darknet site
dark market link https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet drug market
dark markets 2025 https://darknetmarketsonion.shop/ – tor drug market
dark web markets https://github.com/abacuslink4jjku/abacuslink – darknet sites
dark web drug marketplace https://kingdomdarknetdrugstore.com/ – darknet markets 2025
dark web markets https://aasap-market.com/ – dark web drug marketplace
darknet websites https://github.com/aresonioncq0a7/aresonion – dark web marketplaces
darkmarket list https://dark-web-versus.com – best darknet markets
dark web markets https://github.com/nexusdarkrtv1u/nexusdark – darknet markets url
dark websites https://onion-dark-market.shop/ – darkmarket 2025
darknet markets links https://darknetmarketsonion.shop/ – dark markets
best darknet markets https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – onion dark website
Great beat ! I would like to apprentice while you amend your web site, how can i subscribe for a blog website? The account aided me a acceptable deal. I had been tiny bit acquainted of this your broadcast provided bright clear idea
darknet markets links https://kingdomdarknetdrugstore.com/ – darkmarket
dark web markets https://aasap-market.com/ – dark websites
dark market onion https://github.com/abacuslink4jjku/abacuslink – dark market
This is the perfect site for anyone who really wants to find out about this topic. You understand so much its almost tough to argue with you (not that I actually would want to…HaHa). You definitely put a fresh spin on a topic that’s been written about for a long time. Excellent stuff, just excellent.
bitcoin dark web https://github.com/aresonioncq0a7/aresonion – darkmarket 2025
dark market list https://kingdom-darkmarketplace.com – darknet markets 2025
dark web market links https://github.com/darkwebsitesyhshv/darkwebsites – darknet markets 2025
bitcoin dark web https://kingdomdarkmarketonline.com/ – dark market
darkmarket https://github.com/nexusdarkrtv1u/nexusdark – onion dark website
darkmarket 2025 https://cannahome-darkmarket-online.com/ – darknet market
darkmarket url https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet markets 2025
darknet sites https://darkfoxdarkweb.com/ – dark market url
dark market list https://github.com/aresonioncq0a7/aresonion – tor drug market
bitcoin dark web https://kingdom-darkmarketplace.com – darkmarket list
dark web market links https://github.com/abacuslink4jjku/abacuslink – dark markets
dark web markets https://kingdom-marketplace.com/ – darknet market links
dark market link https://darknetmarketsonion.shop/ – dark websites
dark web link https://github.com/darkwebsitesyhshv/darkwebsites – darknet market
dark markets 2025 https://github.com/nexusdarkrtv1u/nexusdark – darknet drugs
darknet market list https://cannahomemarket.link/ – dark market link
dark markets 2025 https://darkode-market.com/ – dark markets
tor drug market https://github.com/aresonioncq0a7/aresonion – darknet markets links
dark web drug marketplace dark web link
dark markets 2025 https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark market
darkmarket list https://github.com/abacuslink4jjku/abacuslink – dark markets
darknet drug store dark websites
darknet site bitcoin dark web
darknet marketplace dark web sites
darkmarket url https://github.com/darkwebsitesyhshv/darkwebsites – darkmarket
dark web link https://github.com/aresonioncq0a7/aresonion – darkmarket 2025
darknet drug store https://github.com/nexusdarkrtv1u/nexusdark – darkmarket url
dark web market urls dark markets 2025
bookmarked!!, I really like your website.
darknet markets 2025 darkmarket 2025
darknet drug store https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – bitcoin dark web
darkmarket list dark market url
darknet sites https://github.com/abacuslink4jjku/abacuslink – dark market list
dark web market list dark market onion
darknet market lists bitcoin dark web
darknet websites https://github.com/aresonioncq0a7/aresonion – darkmarket 2025
dark web market urls https://github.com/darkwebsitesyhshv/darkwebsites – dark market link
darkmarket list dark web markets
darknet websites https://github.com/nexusdarkrtv1u/nexusdark – dark web drug marketplace
darknet websites dark markets
darknet market links tor drug market
darkmarket https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark web markets
darkmarket list dark web market urls
dark market list dark market
dark market list https://github.com/abacuslink4jjku/abacuslink – darknet market links
darknet markets onion https://github.com/aresonioncq0a7/aresonion – darknet markets onion
dark market https://github.com/darkwebsitesyhshv/darkwebsites – darknet drug store
darknet markets links dark web sites
dark markets https://github.com/nexusdarkrtv1u/nexusdark – tor drug market
darkmarket link bitcoin dark web
darknet sites https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet markets
darknet market lists https://github.com/aresonioncq0a7/aresonion – darkmarket
best darknet markets darkmarket list
darkmarkets dark web market urls
dark market onion darkmarket list
darknet marketplace https://github.com/abacuslink4jjku/abacuslink – bitcoin dark web
dark web link https://github.com/darkwebsitesyhshv/darkwebsites – darknet market lists
dark market link https://github.com/nexusdarkrtv1u/nexusdark – dark web market list
darknet marketplace darkmarket link
darkmarket 2025 https://github.com/aresonioncq0a7/aresonion – darknet marketplace
bitcoin dark web dark market onion
darknet market list https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet markets url
darknet markets darknet markets onion address
dark market 2025 https://github.com/abacuslink4jjku/abacuslink – dark markets 2025
darkmarkets darkmarket
darkmarket 2025 https://github.com/darkwebsitesyhshv/darkwebsites – darkmarket 2025
darknet marketplace dark web link
darknet markets onion address https://github.com/aresonioncq0a7/aresonion – onion dark website
darknet markets links https://github.com/nexusdarkrtv1u/nexusdark – darknet markets
best darknet markets dark web marketplaces
dark market dark web link
darknet markets links https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darkmarket
darknet drug store https://github.com/abacuslink4jjku/abacuslink – dark market url
dark web market dark web markets
dark web market urls darknet markets 2025
onion dark website https://github.com/aresonioncq0a7/aresonion – dark websites
darknet drug store https://github.com/darkwebsitesyhshv/darkwebsites – darknet markets onion address
darknet market dark market url
dark web marketplaces https://github.com/nexusdarkrtv1u/nexusdark – dark web link
dark markets 2025 darknet sites
darkmarket url darknet market list
darknet drug store https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – best darknet markets
dark web market list darknet sites
darknet drug links https://github.com/abacuslink4jjku/abacuslink – bitcoin dark web
darkmarket list https://github.com/aresonioncq0a7/aresonion – dark websites
darknet links darknet market links
dark web marketplaces dark web market urls
darknet market list https://github.com/darkwebsitesyhshv/darkwebsites – darknet market lists
Hi mates, how is all, and what you want to say about this piece of writing, in my view its genuinely awesome for me.
best darknet markets https://github.com/nexusdarkrtv1u/nexusdark – dark market list
dark market url darknet drug links
onion dark website https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet markets onion
dark web market https://github.com/aresonioncq0a7/aresonion – dark market
bitcoin dark web darknet markets
dark web markets https://github.com/abacuslink4jjku/abacuslink – dark web market
dark market url dark websites
darknet market https://github.com/darkwebsitesyhshv/darkwebsites – darkmarket url
darknet market links darknet drug market
dark market link dark web market links
dark market url https://github.com/nexusdarkrtv1u/nexusdark – darknet markets
dark markets 2025 https://github.com/aresonioncq0a7/aresonion – dark web market urls
darknet sites darknet drug links
darkmarket link https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darkmarket 2025
dark market list https://github.com/abacuslink4jjku/abacuslink – darknet markets onion address
darknet websites darknet site
darknet links dark market
darkmarket https://github.com/darkwebsitesyhshv/darkwebsites – darknet markets onion
dark web market list https://github.com/aresonioncq0a7/aresonion – dark market 2025
dark market https://github.com/nexusdarkrtv1u/nexusdark – darknet markets links
tor drug market https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darkmarket
dark web market list https://github.com/abacuslink4jjku/abacuslink – dark web market links
dark market 2025 https://github.com/aresonioncq0a7/aresonion – dark markets
best darknet markets https://github.com/darkwebsitesyhshv/darkwebsites – dark market link
dark web market https://github.com/nexusdarkrtv1u/nexusdark – dark market 2025
dark web market urls https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark market
dark web marketplaces https://github.com/abacuslink4jjku/abacuslink – darkmarket list
dark websites https://github.com/aresonioncq0a7/aresonion – darkmarkets
dark web markets https://github.com/darkwebsitesyhshv/darkwebsites – dark market link
darknet site https://github.com/nexusdarkrtv1u/nexusdark – darknet markets url
darkmarket link https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark web market links
dark web markets https://github.com/aresonioncq0a7/aresonion – dark web market
dark market https://github.com/abacuslink4jjku/abacuslink – darkmarket 2025
dark web drug marketplace https://github.com/darkwebsitesyhshv/darkwebsites – dark websites
dark web market list https://github.com/nexusdarkrtv1u/nexusdark – dark markets 2025
darknet market https://github.com/aresonioncq0a7/aresonion – darknet market
dark market onion https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark markets
darknet drug market https://github.com/abacuslink4jjku/abacuslink – darknet sites
dark web market urls https://github.com/darkwebsitesyhshv/darkwebsites – darkmarket link
darkmarket list https://github.com/aresonioncq0a7/aresonion – darknet markets url
dark markets https://github.com/nexusdarkrtv1u/nexusdark – dark web sites
bitcoin dark web https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet markets onion address
darknet marketplace https://github.com/abacuslink4jjku/abacuslink – darknet market
tor drug market https://github.com/aresonioncq0a7/aresonion – best darknet markets
darknet links https://github.com/darkwebsitesyhshv/darkwebsites – darknet markets links
onion dark website https://github.com/nexusdarkrtv1u/nexusdark – dark market
dark web markets https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet market
dark web market urls https://github.com/abacuslink4jjku/abacuslink – dark websites
darknet drug market https://github.com/aresonioncq0a7/aresonion – darkmarket
Good post. I learn something new and challenging on sites I stumbleupon every day. It’s always interesting to read through articles from other authors and practice something from their web sites.
darkmarket https://github.com/nexusdarkrtv1u/nexusdark – dark web market links
darknet market https://github.com/aresonioncq0a7/aresonion – dark web markets
dark web link https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet drug market
darkmarkets https://github.com/abacuslink4jjku/abacuslink – darknet drugs
bitcoin dark web https://github.com/darkwebsitesyhshv/darkwebsites – darkmarket 2025
I blog frequently and I truly thank you for your content. This article has really peaked my interest. I will book mark your blog and keep checking for new information about once per week. I subscribed to your Feed too.
dark markets 2025 https://github.com/aresonioncq0a7/aresonion – darknet markets links
dark web marketplaces https://github.com/nexusdarkrtv1u/nexusdark – best darknet markets
dark market url https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet market
onion dark website https://github.com/abacuslink4jjku/abacuslink – darknet links
darknet links https://github.com/aresonioncq0a7/aresonion – dark web markets
dark market list https://github.com/darkwebsitesyhshv/darkwebsites – darknet markets links
darknet markets url https://github.com/nexusdarkrtv1u/nexusdark – dark market url
dark market https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark market list
darkmarkets https://github.com/aresonioncq0a7/aresonion – best darknet markets
dark web markets https://github.com/abacuslink4jjku/abacuslink – darknet site
darknet links https://github.com/darkwebsitesyhshv/darkwebsites – dark market onion
dark web market https://github.com/nexusdarkrtv1u/nexusdark – darknet market lists
dark web marketplaces https://github.com/aresonioncq0a7/aresonion – dark web market list
darkmarkets https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark market url
dark markets https://github.com/abacuslink4jjku/abacuslink – dark market list
dark web market list https://github.com/darkwebsitesyhshv/darkwebsites – dark market link
dark markets 2025 https://github.com/aresonioncq0a7/aresonion – darkmarket 2025
darknet market list https://github.com/nexusdarkrtv1u/nexusdark – darknet links
darknet markets https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – darknet websites
darknet site https://github.com/abacuslink4jjku/abacuslink – darknet markets url
dark market list https://github.com/darkwebsitesyhshv/darkwebsites – darknet site
darknet sites https://github.com/aresonioncq0a7/aresonion – darknet websites
dark web market https://github.com/nexusdarkrtv1u/nexusdark – darknet markets links
darknet drug store https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark websites
dark markets 2025 https://github.com/abacuslink4jjku/abacuslink – darknet markets onion
onion dark website https://github.com/aresonioncq0a7/aresonion – darknet markets onion
I was able to find good advice from your blog posts.
darknet drug store https://github.com/darkwebsitesyhshv/darkwebsites – dark web markets
darkmarket url https://github.com/nexusdarkrtv1u/nexusdark – darknet market lists
tor drug market https://github.com/aresmarketdarknetl9khn/aresmarketdarknet – dark web market links
tor drug market https://github.com/aresonioncq0a7/aresonion – darknet markets
darknet drug market https://github.com/abacuslink4jjku/abacuslink – darkmarkets
darknet market list https://github.com/darkwebsitesyhshv/darkwebsites – darknet links
dissertation writing services https://msdnaacr.com/ write a descriptive essay
I just wanted to take a moment to say how much I appreciate your blog posts. They’re always well-written, informative, and keep me coming back for more. Keep up the great work!
Your writing has a way of resonating with me and making me feel understood Thank you for being a relatable and authentic voice
I can’t get enough of your insightful articles and engaging stories. Thank you for sharing your passion with the world!
Your blog has become my go-to source for inspiration and motivation Thank you for consistently delivering high-quality content
buy essay papers online https://aypcl.org/ essays writing help
buy essays uk online https://santaspantry.org/ custom essay writing
Keep up the amazing work!
Your blog always puts a smile on my face and makes me feel better about the world Thank you for being a source of light and positivity
Your positive energy and enthusiasm radiate through your writing It’s obvious that you are truly passionate about what you do
Thank you for addressing such an important topic in this post Your words are powerful and have the potential to make a real difference in the world
The photographs and visuals used in this blog are always stunning They really add a beautiful touch to the posts
Your ideas and insights are unique and thought-provoking I appreciate how you challenge your readers to see things from a different perspective
Lovely forum posts, Thanks.
Also visit my web blog :: https://kharkivnews.com.ua/
Hey there exceptional website! Does running a blog such as this require a massive amount work? I’ve absolutely no understanding of computer programming but I was hoping to start my own blog soon. Anyway, if you have any recommendations or tips for new blog owners please share. I understand this is off topic however I just wanted to ask. Kudos!
This website was… how do you say it? Relevant!! Finally I’ve found something that helped me. Kudos!
When I initially left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I recieve four emails with the same comment. Perhaps there is a way you can remove me from that service? Thank you.
Good day very cool blog!! Guy .. Beautiful .. Wonderful .. I’ll bookmark your site and take the feeds also? I am happy to search out numerous helpful information right here within the post, we want work out extra techniques in this regard, thank you for sharing. . . . . .
The topics covered here are always so interesting and unique Thank you for keeping me informed and entertained!
I love how this blog promotes self-love and confidence It’s important to appreciate ourselves and your blog reminds me of that
Let’s spread the love! Tag a friend who would appreciate this post as much as you did.
Wow, I had never thought about it in that way before You have really opened my eyes to a new perspective Keep up the great work!
I want to express my appreciation for the writer of this blog post. It’s clear they put a lot of effort and thought into their work, and it shows. From the informative content to the engaging writing style, I thoroughly enjoyed reading it.
Good article. I definitely love this site. Stick with it!
Oh my goodness! Incredible article dude! Thank you so much, However I am going through problems with your RSS. I don’t know why I cannot subscribe to it. Is there anyone else getting identical RSS issues? Anyone that knows the solution will you kindly respond? Thanx!!
These are genuinely wonderful ideas in concerning blogging. You have touched some nice points here. Any way keep up wrinting.
Hello just wanted to give you a quick heads up. The text in your article seem to be running off the screen in Safari. I’m not sure if this is a format issue or something to do with web browser compatibility but I thought I’d post to let you know. The design and style look great though! Hope you get the problem fixed soon. Cheers
I really like what you guys are up too. This sort of clever work and exposure! Keep up the fantastic works guys I’ve added you guys to my blogroll.
My developer is trying to convince me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using Movable-type on several websites for about a year and am nervous about switching to another platform. I have heard very good things about blogengine.net. Is there a way I can import all my wordpress content into it? Any help would be really appreciated!
Spot on with this write-up, I honestly feel this amazing site needs a lot more attention. I’ll probably be returning to see more, thanks for the info!
I’ve come across many blogs, but this one truly stands out in terms of quality and authenticity Keep up the amazing work!
Your writing has a way of making me feel like I’m having a conversation with a close friend It’s so genuine and relatable
It’s clear that you are passionate about making a positive impact and your blog is a testament to that Thank you for all that you do
Your style is so unique compared to other people I have read stuff from. Thanks for posting when you have the opportunity, Guess I will just bookmark this blog.
https://www.cornbreadhemp.com/products/cbd-sleep-gummies secure joking helped me run day-to-day suffering without making me sensation out of it. I nip in one in the evening after work, and within 30 minutes, I’m scheme more relaxed. It’s like a dwarf nutty reset. They savour like cyclical bon-bons but take place with all the calming benefits of CBD. I was a bit unsure at basic, but once in a while I stow away a jerk in my nautical galley at all times. If you’re dealing with angst, worry, or righteous necessity to unwind, these are a utter lifesaver. Just generate foolproof you’re getting them from a trusted trade name!
I was more than happy to find this web site. I need to to thank you for ones time for this particularly wonderful read!! I definitely loved every bit of it and I have you book marked to see new things in your site.
Your blog post had me hooked from the first sentence.
Your writing style is so engaging and makes even the most mundane topics interesting to read Keep up the fantastic work
Your writing style is so relatable and authentic It’s a breath of fresh air in a world filled with superficiality and pretense
Your latest blog post was truly inspiring and had some great insights. I can’t wait to see what else you have in store.
Your posts are always so well-written and thought out It’s evident that you put a lot of effort into each and every one
Your writing is so eloquent and heartfelt It’s impossible not to be moved by your words Thank you for sharing your gift with the world
Pretty! This has been an extremely wonderful article. Many thanks for providing this info.
darknet marketplace darknet market list
darkmarkets darknet markets
dark market onion darknet site
dark markets 2025 darknet site
darkmarket tor drug market
dark web market urls tor drug market
darknet marketplace dark web link
This is a topic that’s close to my heart… Take care! Exactly where can I find the contact details for questions?
I must thank you for the efforts you’ve put in penning this website. I really hope to check out the same high-grade blog posts by you in the future as well. In fact, your creative writing abilities has encouraged me to get my own, personal blog now 😉
I am blown away by the depth and detail in your posts Keep up the excellent work and thank you for sharing your knowledge with us
It’s clear that you have a deep understanding of this topic and your insights and perspective are invaluable Thank you for sharing your knowledge with us
Your words have the power to change lives and I am grateful for the positive impact you have had on mine Thank you
I love how you incorporate personal stories and experiences into your posts It makes your content relatable and authentic
This blog is like a breath of fresh air in the midst of all the negativity on the internet I’m grateful to have stumbled upon it
excellent submit, very informative. I wonder why the opposite experts of this sector do not understand this. You should continue your writing. I’m sure, you’ve a huge readers’ base already!
Howdy! This post couldn’t be written any better! Reading through this article reminds me of my previous roommate! He continually kept preaching about this. I will forward this article to him. Fairly certain he’ll have a very good read. Thanks for sharing!
Leave a comment and let us know what your favorite blog post has been so far!
I love how this blog promotes self-love and confidence It’s important to appreciate ourselves and your blog reminds me of that
Your blog has been a constant source of support and encouragement for me I am grateful for your words of wisdom and positivity
Very nice blog post. I absolutely love this website. Keep it up!
After looking into a few of the blog articles on your web site, I truly appreciate your way of writing a blog. I added it to my bookmark site list and will be checking back in the near future. Please check out my web site as well and let me know what you think.
Hi, I do believe this is a great site. I stumbledupon it 😉 I will come back yet again since i have book marked it. Money and freedom is the greatest way to change, may you be rich and continue to help others.
darkmarket link dark web drug marketplace
dark market link dark web market list
darkmarket link dark web markets
darknet markets onion address dark web market urls
darkmarkets darknet drug links
Your writing is so eloquent and engaging You have a gift for connecting with your readers and making us feel understood
Their posts always leave us feeling informed and entertained. We’re big fans of their style and creativity.
I have been struggling with this issue for a while and your post has provided me with much-needed guidance and clarity Thank you so much
Your writing is so eloquent and heartfelt It’s impossible not to be moved by your words Thank you for sharing your gift with the world
As a new reader, I am blown away by the quality and depth of your content I am excited to explore your past posts and see what else you have to offer
darknet markets onion darknet markets url
Ahaa, its fastidious discussion about this piece of writing at this place at this webpage, I have read all that, so now me also commenting here.
darknet market links darknet markets links
dark web market urls dark web sites
Hi would you mind letting me know which hosting company you’re working with? I’ve loaded your blog in 3 different browsers and I must say this blog loads a lot quicker then most. Can you suggest a good hosting provider at a honest price? Thanks, I appreciate it!
darknet market dark web market urls
dark market list darknet markets links
dark market link dark web drug marketplace
best darknet markets darkmarket list
Spot on with this write-up, I actually feel this amazing site needs a lot more attention. I’ll probably be back again to see more, thanks for the info!
dark web market urls darknet sites
dark web link darkmarket link
darkmarket darknet markets links
That is really fascinating, You’re a very professional blogger. I’ve joined your rss feed and sit up for in the hunt for more of your fantastic post. Additionally, I have shared your website in my social networks
dark web market links dark web market links
dark web market list darknet drug store
darknet markets onion dark web marketplaces
dark market list dark market url
I all the time used to study article in news papers but now as I am a user of web thus from now I am using net for articles or reviews, thanks to web.
darknet markets url darknet drug links
darkmarket url darknet drugs
dark web market links darknet markets onion
darknet sites dark web market links
darknet market links dark web link
darknet site darkmarket list
dark market darknet drugs
dark web market darknet market
dark markets darknet markets onion
dark market link darknet markets onion address
dark websites dark web market urls
darknet drug market darknet drug links
dark market url darknet markets url
darknet markets url dark websites
darkmarket link darknet marketplace
darkmarkets dark markets 2025
dark market onion darkmarket 2025
darknet links dark market onion
darknet drug store darknet market links
darknet markets links dark web markets
darknet markets onion address darknet drug links
dark web markets darkmarket list
dark web market links dark markets 2025
dark web market urls tor drug market
dark market list darknet websites
darkmarket list dark websites
It’s clear that you are passionate about making a positive impact and your blog is a testament to that Thank you for all that you do
Your writing is a breath of fresh air It’s clear that you put a lot of thought and effort into each and every post
dark web market list darkmarket url
Your posts always provide me with a new perspective and encourage me to look at things differently Thank you for broadening my horizons
Your writing is so refreshing and authentic It’s like having a conversation with a good friend Thank you for opening up and sharing your heart with us
I appreciate the effort that goes into creating high-quality content, and this post was no exception. The insights and information were top-notch and made for a really engaging read. Keep up the great work!
darkmarket link dark market 2025
darknet markets dark markets
darknet market dark markets 2025
dark websites darknet websites
darkmarket 2025 darknet markets onion
darknet links dark markets 2025
darknet markets url darknet websites
https://www.cornbreadhemp.com/products/full-spectrum-cbd-gummies have seriously helped me superintend unexciting suffering without making me sensation effectively of it. I pop unified in the evening after work, and within 30 minutes, I’m scheme more relaxed. It’s like a seldom mental reset. They savour like cyclical bon-bons but thrive with all the calming benefits of CBD. I was a morsel unsure at first, but once in a while I keep a jar in my kitchen at all times. If you’re dealing with thirst, prominence, or valid necessity to unwind, these are a gross lifesaver. Principled make sure you’re getting them from a trusted brand!
darknet market onion dark website
bitcoin dark web best darknet markets
dark market dark web drug marketplace
darknet markets onion dark markets 2025
darkmarket list darknet markets onion address
dark web markets darknet markets url
dark markets 2025 dark web marketplaces
dark markets 2025 darkmarket 2025
dark markets tor drug market
Download and install imToken from the official website to manage your crypto securely. Multi-chain wallet for Ethereum, Bitcoin, and more — fast and reliable.多链钱包。
darknet markets onion darknet markets onion
darknet markets onion address darknet drug market
darknet sites darknet drug market
dark market list dark market onion
dark web market links darknet sites
best darknet markets darknet markets links
darknet sites darknet markets url
darknet markets url darknet drug links
dark web sites darknet market lists
darknet site darkmarket
dark market onion darknet market
dark market 2025 darknet market lists
dark web sites darknet site
dark market link dark web market list
dark web link darknet markets links
dark markets 2025 dark web link
dark web market urls darknet markets url
darknet markets url dark market url
darkmarkets dark market
dark market link dark web markets
dark web marketplaces darknet markets onion
darknet market links dark web markets
Hello! This is my first visit to your blog! We are a collection of volunteers and starting a new project in a community in the same niche. Your blog provided us valuable information to work on. You have done a wonderful job!
darknet market darknet websites
darknet drugs tor drug market
darknet markets dark market
dark websites best darknet markets
You’re so interesting! I do not suppose I’ve truly read anything like this before. So good to discover somebody with some genuine thoughts on this topic. Really.. thank you for starting this up. This site is one thing that is needed on the web, someone with some originality!
darknet markets onion darknet site
darknet markets onion darknet market links
best darknet markets dark markets
darknet site dark web markets
darknet sites darknet markets links
dark web drug marketplace dark web marketplaces
darknet drugs darkmarket
darkmarkets darknet market
dark web market urls darkmarket link
dark web link dark market onion
darknet links dark web link
darknet marketplace dark web market links
bookmarked!!, I like your site!
Your writing style is so relatable and authentic It’s a breath of fresh air in a world filled with superficiality and pretense
I truly admire how you tackle difficult topics and address them in a respectful and thought-provoking manner
As a fellow blogger, I can appreciate the time and effort that goes into creating well-crafted posts You are doing an amazing job
Your writing is so relatable and down-to-earth It’s like chatting with a good friend over a cup of coffee Keep sharing your wisdom with us
darknet market dark web sites
Your posts always speak to me on a personal level and I believe that is a testament to your authenticity and genuine nature
This blog is a great resource for anyone looking to live a more mindful and intentional life Thank you for providing valuable advice and tips
darkmarket list dark web market urls
dark web sites best darknet markets
darkmarket url dark web drug marketplace
darknet sites bitcoin dark web
dark market link darknet drug market
darkmarket list dark market onion
darknet marketplace darkmarket url
dark websites darknet market lists
dark market list darknet links
darknet sites dark web marketplaces
darknet market darknet drug market
dark web markets darknet market list
dark market list dark web marketplaces
darknet sites dark market 2025
dark market url darkmarket 2025
best darknet markets dark market onion
dark market url dark market link
dark websites darknet market list
darkmarket link darkmarket link
dark web market links darkmarket list
darknet websites darknet market links
darknet markets url darkmarket list
darknet sites darkmarket 2025
dark market dark web drug marketplace
dark markets dark websites
dark web market links dark markets 2025
dark web market links darknet markets onion address
dark web market urls darknet drug market
darkmarket link dark web market
dark web sites dark market list
darkmarket dark markets 2025
darknet market links dark web sites
Your blog has become my go-to source for inspiration and motivation Thank you for consistently delivering high-quality content
tor drug market dark market list
darknet market darknet market lists
dark market link best darknet markets
darknet market links dark websites
tor drug market dark web market links
dark markets dark web market links
My brother suggested I might like this website. He was totally right. This post truly made my day. You cann’t imagine just how much time I had spent for this information! Thanks!
darknet market lists darknet markets url
dark markets 2025 dark web market links
darknet markets 2025 darkmarket 2025
dark web market dark market link
darknet websites darkmarkets
darknet drugs darknet drug store
darknet sites darkmarket list
dark web market urls dark web marketplaces
darknet site darkmarkets
darkmarkets dark markets
darkmarkets best darknet markets
dark market url darknet markets 2025
darknet market darknet drug links
dark web sites dark market
darknet markets onion address darknet markets 2025
darknet markets tor drug market
darknet drugs dark web market
tor drug market darkmarket 2025
darknet links darkmarket url
dark web sites darknet drug store
darknet markets onion darknet websites
darknet websites darknet markets 2025
onion dark website darkmarkets
tor drug market darknet sites
darknet marketplace dark websites
darkmarket list dark web link
darknet markets url darknet websites
dark websites darknet drug store
darkmarket dark markets 2025
darknet markets onion dark web sites
darknet markets url dark websites
dark web markets dark web markets
darknet markets onion dark markets
dark market 2025 bitcoin dark web
dark websites darknet marketplace
dark web marketplaces darknet websites
dark markets darknet markets
dark web market list dark websites
dark web sites darknet market links
dark web marketplaces best darknet markets
darknet markets 2025 dark web markets
darkmarkets dark market onion
dark web market links darknet marketplace
darknet links bitcoin dark web
dark web marketplaces darknet sites
darknet markets links dark market 2025
darknet drug links dark market list
darknet market lists darknet markets links
darknet markets onion address darknet links
dark market dark markets
darkmarket 2025 darkmarket 2025
dark web market list dark web market
darkmarket 2025 dark market list
darkmarket link dark web market urls
bitcoin dark web darknet links
dark web market links dark web market list
dark web marketplaces darknet links
darkmarket 2025 dark web marketplaces
dark web link bitcoin dark web
tor drug market best darknet markets
onion dark website darknet markets
darknet market lists onion dark website
darknet marketplace dark market url
darknet markets links darknet markets onion
darknet market list darknet drug store
bitcoin dark web darknet markets
dark market tor drug market
dark web link darknet markets onion
dark web market list dark market list
darknet market list darkmarket link
tor drug market best darknet markets
dark web market links darknet links
dark web market dark market url
darkmarket dark web marketplaces
dark market link darknet links
tor drug market darknet markets onion
dark web market darkmarket link
darknet marketplace dark market link
darknet markets onion address darknet markets
dark web market links darknet market
darkmarket url darknet markets links
dark web market list dark market onion
dark markets 2025 darknet markets onion address
dark markets dark market 2025
darknet site darknet market links
darknet drug store darknet markets url
darknet drug store dark web marketplaces
dark markets darknet markets links
dark market link dark market url
dark web markets darknet markets onion address
darknet markets onion dark website
darknet websites dark websites
dark web market list darknet websites
tor drug market dark market
darkmarket list darknet market lists
dark market onion darknet drug store
darknet drug links dark web link
darknet websites darkmarket list
dark web sites dark market url
darknet websites dark market url
darknet drug store darkmarket list
darknet market darkmarket 2025
dark web market list best darknet markets
dark web market urls dark market
onion dark website darknet drug store
dark web marketplaces dark markets 2025
darknet drug links darkmarkets
dark markets 2025 darknet sites
dark web sites dark web markets
dark market link dark web sites
dark web market dark market 2025
dark market 2025 darknet drugs
darknet links darkmarket url
darknet site darknet markets onion
dark market url dark markets
darknet drug market dark market 2025
dark web market dark web sites
It’s clear that you truly care about your readers and want to make a positive impact on their lives Thank you for all that you do
I’m truly enjoying the design and layout of your website. It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a developer to create your theme? Fantastic work!
hey there and thank you for your information – I have certainly picked up anything new from right here. I did however expertise a few technical points using this site, since I experienced to reload the site a lot of times previous to I could get it to load properly. I had been wondering if your web host is OK? Not that I am complaining, but slow loading instances times will very frequently affect your placement in google and can damage your high quality score if ads and marketing with Adwords. Anyway I’m adding this RSS to my e-mail and can look out for a lot more of your respective intriguing content. Make sure you update this again soon.
I’ve learn several good stuff here. Definitely value bookmarking for revisiting. I wonder how a lot effort you put to make such a magnificent informative site.
Hello guys!
I came across a 106 very cool resource that I think you should explore.
This platform is packed with a lot of useful information that you might find helpful.
It has everything you could possibly need, so be sure to give it a visit!
https://r-m-r.es/abc-de-las-apuestas/casinos-y-economia-local/
This is the perfect web site for anyone who would like to understand this topic. You realize so much its almost tough to argue with you (not that I personally will need to…HaHa). You certainly put a brand new spin on a topic that’s been written about for decades. Excellent stuff, just excellent!
Hello team!
I came across a 106 valuable resource that I think you should visit.
This tool is packed with a lot of useful information that you might find helpful.
It has everything you could possibly need, so be sure to give it a visit!
https://soundsandcolours.com/subjects/travel/vibrancy-at-its-finest-buenos-aires-to-do-list-for-first-fimers-76337/
Love this appreciation for great content
You have a way of explaining complex topics in a straightforward and easy to understand manner Your posts are always a pleasure to read
Great post! We are linking to this particularly great post on our site. Keep up the good writing.
Hi there! This is my first visit to your blog! We are a team of volunteers and starting a new project in a community in the same niche. Your blog provided us beneficial information to work on. You have done a extraordinary job!
I needed to thank you for this wonderful read!! I definitely enjoyed every little bit of it. I’ve got you book marked to check out new things you post…
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务。
Bitpie是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务。
Hi there, I discovered your site by the use of Google at the same time as looking for a similar subject, your web site got here up, it seems good. I have bookmarked it in my google bookmarks.
Hi there, simply was alert to your blog thru Google, and located that it’s really informative. I’m gonna watch out for brussels. I’ll appreciate should you proceed this in future. Lots of other people can be benefited out of your writing. Cheers!
Visit the official Telegram website, choose the appropriate operating system such as Windows, macOS, Android, iOS, etc., and download the application. Enjoy seamless communication across devices with Telegram’s secure and fast messaging features, including text, voice calls, and file sharing, all backed by end-to-end encryption for enhanced privacy.Telegram官网
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram中文
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务。
Hello my friend! I wish to say that this post is amazing, nice written and include approximately all important infos. I would like to see more posts like this .
Functional decline doesn’t mean loss of desire-it signals time to consider synthroid 100 mcg pill. Move forward with care that truly understands your needs.
比特派下载(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
比特派官网(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram下载
比特派钱包(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务。
比特派(Bitpie)是一款全球领先的多链数字钱包,专为支持多种区块链资产而设计,如比特币(BTC)、以太坊(ETH)、波场(TRX)、泰达币(USDT)等主流加密货币。通过使用比特派,用户不仅能够轻松便捷地管理和转移数字资产,还可以享受去中心化应用(DApp)等多种区块链服务。
potato软件是一款功能强大的中文聊天工具,专为全球用户设计,支持快速下载和安装。无论您是个人用户还是企业客户,土豆软件都能提供流畅的聊天体验,满足多种通讯需求。访问官网,获取最新版本的土豆软件,并了解更多中文界面功能和安装指南。轻松连接朋友、同事,提升您的沟通效率。土豆聊天
I always find myself nodding along and agreeing with your wise words Your insights and advice are truly valuable
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
free blogNice post. I understand some thing much harder on diverse blogs everyday. Most commonly it is stimulating to study content using their company writers and rehearse a little something from their store. I’d would prefer to apply certain with all the content in this little blog regardless of whether you don’t mind. Natually I’ll provide link on your web blog. Many thanks sharing.
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram官网
Explore the ranked best online casinos of 2025. Compare bonuses, game selections, and trustworthiness of top platforms for secure and rewarding gameplaycasino.
前往 Telegram 官方网站,选择适合的操作系统(如 Windows、macOS、Android、iOS 等),并下载应用程序。Telegram中文
Your writing has a way of making complicated topics easier to understand It’s evident how much research and effort goes into each post
This blog covers important and relevant topics that many are afraid to address Thank you for being a voice for the voiceless
It’s clear that you truly care about your readers and want to make a positive impact on their lives Thank you for all that you do
I was able to find good advice from your blog posts.
Explore the ranked best online casinos of 2025. Compare bonuses, game selections, and trustworthiness of top platforms for secure and rewarding gameplaycrypto casino.
An intriguing discussion is definitely worth comment. I do think that you should write more about this subject, it might not be a taboo subject but usually folks don’t talk about such issues. To the next! Kind regards.
Spot on with this write-up, I absolutely think this amazing site needs a great deal more attention. I’ll probably be returning to see more, thanks for the info.
Hello there! This blog post couldn’t be written any better! Going through this post reminds me of my previous roommate! He continually kept talking about this. I most certainly will send this post to him. Fairly certain he will have a very good read. Many thanks for sharing!
Very good article! We are linking to this particularly great post on our site. Keep up the great writing.
Pretty great post. I simply stumbled upon your blog and wanted to say that I have truly enjoyed browsing your weblog posts. In any case I will be subscribing for your feed and I hope you write again soon!
Having read this I believed it was rather informative. I appreciate you spending some time and effort to put this informative article together. I once again find myself spending a lot of time both reading and commenting. But so what, it was still worth it.
Touche. Outstanding arguments. Keep up the great work.
Happy to dive into discussions, share experiences, and pick up new insights throughout the journey.
I like hearing diverse viewpoints and contributing whenever I can. Happy to hear fresh thoughts and connecting with others.
That’s my website:https://automisto24.com.ua/
Heya i’m for the first time here. I came across this board and I find It truly useful & it helped me out a lot. I hope to give something back and aid others like you aided me.
Here to explore discussions, share experiences, and gain fresh perspectives as I go.
I’m interested in learning from different perspectives and adding to the conversation when possible. Happy to hear different experiences and building connections.
There is my web-site:https://automisto24.com.ua/
Pretty! This has been a really wonderful article. Thanks for supplying these details.
You’re so cool! I do not believe I’ve read through anything like that before. So great to find someone with genuine thoughts on this subject. Really.. thanks for starting this up. This web site is something that is required on the web, someone with some originality.
Hi! I know this is kind of off topic but I was wondering if you knew where I could get a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having trouble finding one? Thanks a lot!
I am sure this piece of writing has touched all the internet viewers, its really really fastidious post on building up new blog.
Howdy! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading through your blog and look forward to all your posts! Carry on the great work!
Hi colleagues, its impressive post on the topic of cultureand fully explained, keep it up all the time.
Hello there, I do think your website may be having web browser compatibility problems. Whenever I look at your blog in Safari, it looks fine however, when opening in IE, it has some overlapping issues. I simply wanted to give you a quick heads up! Apart from that, great website!
She said it didn’t matter, but he still couldn’t relax until he had Generic for cialis. True connection grows in the places words dare not go.
At first, I was skeptical less https://joyorganics.com/products/1000mg-cbd-cream , but sometimes I provide for them in my nightstand. They’ve become participation of my evening routine—ditty gummy, a cup of tea, and I’m tolerable to go. I don’t perceive strident or kinky, hardly calm and genial to afraid down. The flavor’s in actuality exceptionally fitting too, which surprised me. No eerie aftertaste like some others I’ve tried. If your leader runs a mile a pint-sized at continually or you’re upstanding trying to slacken after work, these are definitely value checking out.
Good web site you have here.. It’s difficult to find high-quality writing like yours these days. I seriously appreciate people like you! Take care!!
Mobile phone payments can be used for small payments and information usage fees, and the maximum monthly limit is 1 million won for each.
소액결제현금화
Hi there, There’s no doubt that your web site may be having browser compatibility problems. Whenever I take a look at your website in Safari, it looks fine however when opening in I.E., it’s got some overlapping issues. I merely wanted to provide you with a quick heads up! Other than that, fantastic site!
Excellent article! We will be linking to this great post on our site. Keep up the good writing.
Hi, I do believe this is an excellent website. I stumbledupon it 😉 I will return once again since i have book-marked it. Money and freedom is the best way to change, may you be rich and continue to guide other people.
I was able to find good information from your blog posts.
I read this post fully on the topic of the comparison of hottest and preceding technologies, it’s remarkable article.
After checking out a number of the blog articles on your site, I truly appreciate your technique of writing a blog. I added it to my bookmark webpage list and will be checking back in the near future. Please check out my website too and tell me what you think.
Your posts are always so well-researched and informative I appreciate how thorough and detailed your content is
I started entrancing CBD gummies a few months ago and forthrightly, they’ve made a huge difference. I usually take individual after dinner to workers me coldness peripheral exhausted and doze better. They bite renowned —like actual sweetmeats — and don’t remain me mood punch-drunk the next day. It’s objective a good, mellow vibe that helps inhale the margin dotty after a stressful day. Wasn’t established they’d charge at first, but now I’m all in. Totally vouch for if you dire something genuine to facilitate you rest without any queer side effects.
What other topics would you like to see covered on the blog? Let us know in the comments!
It’s in fact very complicated in this active life to listen news on Television, therefore I simply use internet for that reason, and get the most recent information.
Erectile function often improves when patients reduce alcohol intake and begin using over the counter viagra. Right dose, right care, right results – your best path forward.
https://t.me/s/Portable_Rptbet
Deneme Bonusu Veren Siteler – 2025 En İyiler
hello admin good job admin bla bla.. d3n3m3 b0n0s0 v4r4n s1t3l3r
https://t.me/s/DragonMoney_Portable
dut bon vor sort dutulca boneci vortin sortlir
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Детальнее – https://nakroklinikatest.ru/
Deneme Bonusu Veren Siteler 2025 – Güvenilir Bahis Siteleri
https://t.me/s/Official_Casino1win
Deneme Bonusu kullanıcılarına ilk kayıtları veya ilk bahisleri için ekstra bir ödül sunarak denemelerini teşvik eder.
Türkiye’de en çok deneme bonusu veren siteler aşağıdaki gibi sıralanmıştır seni öldüreceğiz mehdi sana başka uyarı yok adam ol
revatio cost
https://t.me/yfy_1win_38/5
dinimi binisi virin sitilir icin tikliyin mehdi binisi virin sikikler
Bahis Siteleri 2025 listesiyle, 250 güvenilir bahis sitesinden deneme bonusu kazanın ve hemen kazanmaya başlayın seni öldüreceğiz mehdi sana başka uyarı yok adam ol
https://t.me/R2T_7k/9479
Medical framing of ED helps counter public misconception through access to buy viagra tablets. Empower yourself – your future self will thank you.
Web-based sports betting is becoming increasingly popular among supporters of football, basketball, and other major sports. With just a few clicks, users can access thousands of markets from anywhere in the world. Modern platforms offer live betting, bonuses, and detailed analytics to help players make smarter decisions. Whether you’re a novice or an experienced bettor, online betting provide flexible, fast, and safe opportunities to enjoy your favorite games. https://social.japrime.id/1748949817880694_20018 daily betting tips
https://zpak.net/# Zithromax over the counter equivalent
wewewe wowuwu wewew wiwewew en güncel listesi burada. Güvenilir bahis siteleri ve en cazip deneme bonusu fırsatlarıyla kazancınızı artırın
A fascinating discussion is worth comment. I believe that you need to write more on this topic, it may not be a taboo subject but usually folks don’t speak about these subjects. To the next! Many thanks.
https://t.me/s/Casino_1win_1win_1win
https://cenforcebnr.com/# cenforce 100mg
I love how this blog gives a voice to important social and political issues It’s important to use your platform for good, and you do that flawlessly
child porn child porn
Мы рады пригласить вас на наш сайт, где вас ждет множество интересного и полезного контента. Мы освещаем различные темы для мужчин, от здоровья до одиночества и кризиса среднего возраста, чтобы вы всегда были в курсе последних новостей. Мы уверены, что наш контент вам понравится и окажется полезным. Ждем вас на нашем сайте:
заказать проститутку Балашиха
If you’re into digital business trends Great insights for entrepreneurs
https://t.me/Martin_Casino_TG/800
viagra: black viagra pills review – female viagra pill near me
diynitme binissi virin sitelor baygihsy boynuystu
Всем привет!
Стерлитамак – это город с богатой историей и уютной атмосферой. Долгое время оставляющий след в сердце тех, кто здесь побывал. Прогулка вдоль живописной реки Белой и посещение местных музеев, таких как музей краеведческих традиций, не оставят вас равнодушными. Аместная кухня, особенно выпечка и мясные блюда, порадует гурманов. Визит в Стерлитамак становится настоящим праздником для души. И если вы хотите провести вечер в интересной компании девушек, вам помогут эскорт-услуги.
Все нужные ссылки находятся здесь: эскорт агенство в Стерлитамаке
2025’in en güçlü deneme bonusu veren siteleri burada. Çevrimsiz, yatırımsız ve freespin içeren bonuslarla anında kazanmaya başlayın
Your blog has quickly become one of my favorites I am constantly impressed by the quality and depth of your content
Your posts always seem to lift my spirits and remind me of all the good in the world Thank you for being a beacon of positivity
Your blog has been a constant source of support and encouragement for me I am grateful for your words of wisdom and positivity
This post hits close to home for me and I am grateful for your insight and understanding on this topic Keep doing what you do
официальный сайт ПокерОК
ПокерОК сайт
Casino siteleri, güvenilir ve canlı casino adresleri için casino siteleri sayfamızı hemen ziyaret edin ve casino siteleri listemize göz atın.
Без AML&KYC!
Замиксим вашу РіСЂСЏР·РЅСѓСЋ крипту Рё отдадим чистую, 0 – 25% AML Score
Работаем на крупных объемах, дадим лучший % среди коллег
Нужна наличка? Не вопрос!
1. Наличные в любом городе с банкоматов Тинькофф банка с минимальной комиссией.
2. Наличные в этот же день курьером в вышеуказанных городах с минимальной комиссией.
3. Наличные кладами от 100к по всей РФ. В этот же день.
4. Наличные РїРѕ всему РјРёСЂСѓ – New York, Hong Kong, Paris, London, Bangkok, Istanbul, Tokyo… etc.
Почти все крупные города мира, уточняйте наличие у оператора.
ДЛЯ ОБМЕНА Р РџРћРљРЈРџРљР РЎР’РЇР–РТЕСЬ РЎ ОПЕРАТОРОМ:
https://exchangebtc.biz/
Услуга обмена и чистки криптовалюты: безопасно и анонимно!
https://clomidzsu.com/# clomid side effects
индивидуалки стерлитамак без предоплаты анал стерлитамак
https://t.me/s/Mobile_1win
Автофургоны для бизнеса — как найти золотую середину по цене и качеству
https://t.me/s/kupit_gruzoviki/319
Обзор современных систем безопасности для автофургонов
Обзор типов снегоуборочной техники: роторные, плужно‑щеточные, вакуумные
This blog is like a safe haven for me, where I can escape the chaos of the world and indulge in positivity and inspiration
индивидуалка балашиха без предоплат дорогие проститутки город балашиха
Your blog always leaves me feeling uplifted and inspired Thank you for consistently delivering high-quality content
Your posts are so well-written and eloquent It’s impossible not to be moved by your words Keep using your voice to spread positivity
I have recommended your blog to all of my friends and family Your words have the power to change lives and I want others to experience that as well
This is such an important reminder and one that I needed to hear today Thank you for always providing timely and relevant content
Your passion for what you do shines through in every post It’s truly inspiring to see someone doing what they love and excelling at it
Your blog is a haven of positivity and encouragement It’s a reminder to always look on the bright side and choose happiness
Güncel ve güvenilir deneme bonusu veren siteler listesi. En iyi bahis siteleri bonus fırsatlarıyla kazanmaya hemen başlayın.
https://experienceleaguecommunities.adobe.com/t5/user/viewprofilepage/user-id/17939778 tadacip
Good shout.
Western kentucky casinos, https://goplayslots.net/ – no deposit free spins casino uk.
I’ve been using sextacy pill review constantly in regard to over a month now, and I’m justifiably impressed during the uncontested effects. They’ve helped me determine calmer, more balanced, and less restless in every nook the day. My saw wood is deeper, I wake up refreshed, and sober my core has improved. The trait is famous, and I appreciate the sensible ingredients. I’ll obviously heed buying and recommending them to person I identify!
I’ve been using https://www.nothingbuthemp.net/collections/thc-chocolate regular in regard to on the other side of a month now, and I’m indeed impressed by the positive effects. They’ve helped me judge calmer, more balanced, and less solicitous throughout the day. My snore is deeper, I wake up refreshed, and even my pinpoint has improved. The value is excellent, and I cherish the common ingredients. I’ll positively heed buying and recommending them to everybody I be aware!
Nice
YR
GY
thc gummies for anxiety area 52
best sativa thc carts area 52
snow caps area 52
live resin area 52
best sativa thc edibles area 52
live resin gummies area 52
It’s awesome designed for me to have a website, which is good in support of my experience. thanks admin
73 bet
thc microdose gummies area 52
thc gummies for pain area 52
mood thc gummies area 52
live rosin gummies area 52
thc oil area 52
magic mushrooms for sale area 52
live resin carts area 52
hybrid weed vaporizer area 52
thc gummies for sleep area 52
distillate carts area 52
thc tincture area 52
weed pen area 52
thca diamonds area 52
thcv gummies area 52
best indica thc weed pens area 52
full spectrum cbd gummies area 52
where to buy thca area 52
thca vape area 52
thca gummies area 52
indica gummies area 52
infused pre rolls area 52
thc gummies
best thca flower area 52
thc vape area 52
liquid diamonds area 52
thca disposable area 52
hybrid gummies area 52
liquid thc area 52
XF
https://t.me/s/TopTg777_Martin
I’ve been using mushroom soda daily seeing that on the other side of a month nowadays, and I’m justifiably impressed during the positive effects. They’ve helped me feel calmer, more balanced, and less restless in every nook the day. My saw wood is deeper, I wake up refreshed, and even my pinpoint has improved. The quality is famous, and I cherish the sensible ingredients. I’ll positively preserve buying and recommending them to everyone I identify!
I’m not sure exactly why but this blog is loading incredibly slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later and see if the problem still exists.
My spouse and I stumbled over here different web page and thought I may as well check things out. I like what I see so now i am following you. Look forward to looking into your web page repeatedly.
Все модели словно стремятся быть полезными не в теории, а в реальности.
Здесь подробнее
I’ve been using https://www.nothingbuthemp.net/products/reishi-mushroom-tincture regular in regard to all about a month at the moment, and I’m indeed impressed by the uncontested effects. They’ve helped me determine calmer, more balanced, and less restless from the beginning to the end of the day. My snore is deeper, I wake up refreshed, and straight my core has improved. The quality is distinguished, and I cherish the sensible ingredients. I’ll obviously preserve buying and recommending them to person I be aware!
I’ve been using https://www.nothingbuthemp.net/products/indica-gummies daily seeing that during the course of a month now, and I’m truly impressed before the uncontested effects. They’ve helped me perceive calmer, more balanced, and less solicitous in every nook the day. My snore is deeper, I wake up refreshed, and even my core has improved. The trait is excellent, and I cognizant the accepted ingredients. I’ll definitely keep buying and recommending them to everybody I recall!
I blog frequently and I really appreciate your information. This great article has really peaked my interest. I am going to bookmark your site and keep checking for new details about once a week. I subscribed to your RSS feed too.
Chauffeur service near me
Bahis Siteleri 2025 listesiyle, 250 güvenilir bahis sitesinden deneme bonusu kazanın ve hemen kazanmaya başlayın
Частный мастер натяжные потолки – надежно и недорого! Большой выбор фактур и цветов. Сатиновые, пленочные потолки. Установка за 24 часа. Гарантия 7 лет. Точный замер. Стаж свыше 15 лет. Выезжаем по области. Звоните сегодня!
I’ve been using https://www.nothingbuthemp.net/products/cordyceps-mushroom-tincture regular seeing that all about a month at the moment, and I’m justifiably impressed by the uncontested effects. They’ve helped me judge calmer, more balanced, and less anxious in every nook the day. My saw wood is deeper, I wake up refreshed, and straight my pinpoint has improved. The attribute is distinguished, and I cognizant the natural ingredients. I’ll positively heed buying and recommending them to everyone I be aware!
Hmm is anyone else experiencing problems with the pictures on this blog loading? I’m trying to find out if its a problem on my end or if it’s the blog. Any feed-back would be greatly appreciated.
РиоБет
Hello to every body, it’s my first pay a visit of this website; this weblog contains amazing and truly fine data designed for readers.
betwinner сайт
This is my first time pay a visit at here and i am really impressed to read everthing at one place.
https://kfaktiv.ru/virtualnyj-nomer-dlja-whatsapp-polnoe-rukovodstvo-po-ispolzovaniju-i-preimushhestvam.html
I’ve been using thc tincture constantly on account of all about a month for the time being, and I’m truly impressed before the positive effects. They’ve helped me determine calmer, more balanced, and less restless in every nook the day. My saw wood is deeper, I wake up refreshed, and sober my pinpoint has improved. The value is excellent, and I worth the natural ingredients. I’ll definitely keep buying and recommending them to person I identify!
Hi there Dear, are you in fact visiting this site on a regular basis, if so after that you will absolutely take good know-how.
Phone
best casino bonuses 2021 usa, united states online casino slots and no wagering casino bonuses uk, or best real money pokies new zealand
I’ve been using thc tincture constantly in regard to over a month for the time being, and I’m justifiably impressed before the positive effects. They’ve helped me determine calmer, more balanced, and less solicitous in every nook the day. My saw wood is deeper, I wake up refreshed, and uniform my core has improved. The quality is outstanding, and I cherish the sensible ingredients. I’ll definitely heed buying and recommending them to person I identify!
Chaming news for all us
Столица в ночь не спит, а наша команда тоже всегда на страже: закрытая наркологическая клиника https://mcnl.ru/ работает 24/7. Без очередей и документов — выезд доктора по вашему звонку, мягкий детокс под контролем, ультрабыстрая капельница, нейрокоррекция на месте, пожизненное сопровождение. Тихо, анонимно, результативно — вернём трезвость без боли.
https://frasesmotivacional.com/
кайтсёрфинг Погодные условия играют решающую роль в кайтсёрфинге. Учитесь читать ветер и выбирать споты с подходящими условиями для катания.
Современные клиники, такие как moscow-stomatolog.ru, используют цифровые технологии для более точной диагностики и комфортного лечения. Это новый уровень стоматологической помощи .
Deneme bonusu veren sitelerin en güncel listesi burada. Güvenilir bahis siteleri ve en cazip deneme bonusu fırsatlarıyla kazancınızı artırın
This is such an important reminder and one that I needed to hear today Thank you for always providing timely and relevant content
I love how you incorporate personal stories and experiences into your posts It makes your content relatable and authentic
кайт лагерь “Одеяние Посейдона”: гидрокостюм, защита от “ледяных объятий”
http://xn--80aafabrjladsicc1amg1o4cf1dg.live/
Hi to every one, the contents existing at this website are in fact remarkable for people experience, well, keep up the nice work fellows.
porno turk
Rút tiền tại 99ok siêu nhanh với công nghệ bảo mật tiên tiến. Sau khi xác minh danh tính bằng CMND/CCCD hoặc giấy tờ ngân hàng, bạn có thể rút tiền dễ dàng. Giao dịch được xử lý trong vòng 5-15 phút, đảm bảo an toàn và minh bạch tuyệt đối.
zyprexa generic: datos.cdmx.gob.mx/user/olanzapine – olanza 5 mg
Your writing style is so engaging and easy to follow I find myself reading through each post without even realizing I’ve reached the end
жд доставка грузов из Китая Автодоставка из Китая – это удобный способ транспортировки грузов, особенно для больших объемов. Этот метод позволяет доставить товары непосредственно к двери получателя, минуя необходимость перегрузки на другие виды транспорта. Важным аспектом является выбор надежной логистической компании, которая сможет обеспечить безопасность и сохранность груза во время перевозки. Автодоставка экономит время и ресурсы.
Thank you for creating such valuable content. Your hard work and dedication are appreciated by so many.
мебель Рива Мебель для офиса Москва: широкий ассортимент, оперативная доставка. Подберите идеальную мебель, не выходя из офиса. Удобный онлайн-каталог, консультации специалистов и быстрая доставка по Москве и области. Создайте комфортное рабочее место для каждого сотрудника.
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this. Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
Luxury limo near me
Hi, I do think this is a great web site. I stumbledupon it 😉 I may come back yet again since I book marked it. Money and freedom is the best way to change, may you be rich and continue to guide others.
https://t.me/s/Official_casino_1win_1win
компьютерная помощь Заказать сайт можете на самых выгодных условиях и максимально быстро по времени. Если у вас имеются вопросы и сложности, которые связаны с созданием сайтов, тогда обратитесь к Neo на сайте 0061.ru. Значительное число клиентов полностью довольны стоимостью и быстрыми сроками выполнения работ.
seo продвижение сайта цена
создание сайтов контент-маркетинг Контент-маркетинг – это создание и распространение полезного контента для привлечения и удержания целевой аудитории.
Химчистка мебели ростов
продажа на wildberries видеообзоры товаров для wildberries Видеообзоры помогут покупателям лучше узнать о товаре и принять решение о покупке.
каркасные дома Обзор строительных компаний, предлагающих строительство каркасных домов: сравнение цен и качества. Отзывы клиентов, портфолио, опыт работы, гарантии, условия сотрудничества.
Стеклянные перегородки Стеклянные перегородки: правила монтажа и техника безопасности. Подготовка поверхности, установка, контроль качества.
можно тепловизор тактическое снаряжение симферополь В Симферополе можно приобрести тактическое снаряжение для различных целей.
https://servicestat.ru/service-kzn Servicestat.ru — это удобный каталог-рейтинг сервисных центров по ремонту электроники. На сайте собраны контакты (адреса, телефоны), отзывы клиентов, акции и скидки, а также оценки качества услуг. Пользователи могут быстро найти проверенные мастерские в своем городе, сравнить рейтинги и выбрать лучший вариант. Полезен для тех, кто хочет отдать технику в надежные руки.
? Поиск сервисов по местоположению и брендам
? Реальные отзывы и оценки клиентов
? Акции, скидки и спецпредложения
? Удобный фильтр для сравнения услуг
Идеальный помощник в поиске надежного ремонта!
Güncel ve güvenilir deneme bonusu veren siteler listesi. En iyi bahis siteleri bonus fırsatlarıyla kazanmaya hemen başlayın
Clearnet & Onion Bazaar Drugs Marketplace: A New Darknet Platform with Dual Access Bazaar Drugs Marketplace is a new darknet marketplace rapidly gaining popularity among users interested in purchasing pharmaceuticals. Trading is conducted via the Tor Network, ensuring a high level of privacy and data protection. However, what sets this platform apart is its dual access: it is available both through an onion domain and a standard clearnet website, making it more convenient and visible compared to competitors. The marketplace offers a wide range of pharmaceuticals, including amphetamines, ketamine, cannabis, as well as prescription drugs such as alprazolam and diazepam. This variety appeals to both beginners and experienced buyers. All transactions on the platform are carried out using cryptocurrency payments, ensuring anonymity and security. In summary, Bazaar represents a modern darknet marketplace that combines convenience, a broad product selection, and a high level of privacy, making it a notable player in the darknet economy.
кайт лагерь Безопасность – это приоритет номер один в кайтсёрфинге. Всегда проверяйте оборудование, следите за прогнозом погоды и не рискуйте в сложных условиях.
обучение кайтсёрфингу Кайт лагерь: атмосфера свободы и приключений. Единомышленники, новые знакомства, тренировки и незабываемые впечатления.
Для жителей Юга России доступны горящие туры из Ростова. Вы можете выбрать тур с вылетом из аэропорта Платов. Отели в Sahl Hasheesh – море чище
Kinonavigator ist eine Anlaufstelle für Kinobegeisterte, die organisierte, themenbasierte Listen wollen.
Was bietet Kinonavigator?
Die perfekte Zehn für jedes Thema: Von Biografien bis hin zu Klassikern der Stummfilmära.
Streaming-Links: Direkte Links zu kostenlosen Plattformen.
Making-of-Material: Hol dir einen Vorgeschmack.
HQ-Poster: Perfekt für Social-Media-Posts.
Keine Anmeldung — einfach Kino unkompliziert.
Entdecken Sie einzigartige Genres auf https://www.blurb.com/user/KinoRadar?profile_preview=true
Драгон Мани Dragon Money – это не просто название, это врата в мир безграничных возможностей и захватывающих азартных приключений. Это не просто платформа, это целая вселенная, где переплетаются традиции вековых казино и новейшие цифровые технологии, создавая уникальный опыт для каждого искателя удачи. В современном мире, где финансовые потоки мчатся со скоростью света, Dragon Money предлагает глоток свежего воздуха – пространство, где правила просты, а возможности безграничны. Здесь каждая ставка – это шанс, каждый спин – это предвкушение победы, а каждый выигрыш – это подтверждение вашей удачи. Но Dragon Money – это не только про выигрыши и джекпоты. Это про сообщество единомышленников, объединенных общим стремлением к риску, азарту и адреналину. Это место, где можно найти новых друзей, поделиться опытом и ощутить неповторимый дух товарищества. Мы твердо верим, что безопасность и честность – это фундамент, на котором строится доверие. Именно поэтому Dragon Money уделяет особое внимание защите данных и обеспечению прозрачности каждой транзакции. Мы стремимся создать максимально комфортную и безопасную среду для наших игроков, где каждый может наслаждаться игрой, не беспокоясь о каких-либо рисках. Dragon Money – это не просто игра. Это возможность испытать себя, проверить свою удачу и почувствовать себя настоящим властелином своей судьбы. Присоединяйтесь к нам, и пусть дракон принесет вам богатство, успех и процветание! Да пребудет с вами удача!
http://neoko.ru/
What measures are taken to prevent counterfeiting of THC Gummies? are a hot, flavourful respect to lift the imminent calming and wellness benefits of cannabidiol. Distant from THC, CBD won’t prepare e dress you great, making these gummies complete after underline, have a zizz, or everyday balance. They take place in heterogeneous flavors, strengths, and formulas—some with added ingredients like melatonin or vitamins. Effects typically start within 30–60 minutes and last a few hours. Vegan, primary, and sugar-free options are also available. Till the end of time after lab results and start with a smaller low-cut dose.
An outstanding share! I’ve just forwarded this onto a co-worker who had been conducting a little homework on this. And he actually ordered me breakfast because I discovered it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending time to discuss this issue here on your blog.
https://images.google.co.id/url?q=https://cabseattle.com/
обучение кайтсёрфингу Выбор кайтсёрф-спота: от песчаных пляжей до диких лагун. Исследуйте лучшие места для кайтсёрфинга по всему миру, учитывая погодные условия, особенности рельефа и уровень волн.
Драгон Мани Dragon Money – это не просто название, это врата в мир безграничных возможностей и захватывающих азартных приключений. Это не просто платформа, это целая вселенная, где переплетаются традиции вековых казино и новейшие цифровые технологии, создавая уникальный опыт для каждого искателя удачи. В современном мире, где финансовые потоки мчатся со скоростью света, Dragon Money предлагает глоток свежего воздуха – пространство, где правила просты, а возможности безграничны. Здесь каждая ставка – это шанс, каждый спин – это предвкушение победы, а каждый выигрыш – это подтверждение вашей удачи. Но Dragon Money – это не только про выигрыши и джекпоты. Это про сообщество единомышленников, объединенных общим стремлением к риску, азарту и адреналину. Это место, где можно найти новых друзей, поделиться опытом и ощутить неповторимый дух товарищества. Мы твердо верим, что безопасность и честность – это фундамент, на котором строится доверие. Именно поэтому Dragon Money уделяет особое внимание защите данных и обеспечению прозрачности каждой транзакции. Мы стремимся создать максимально комфортную и безопасную среду для наших игроков, где каждый может наслаждаться игрой, не беспокоясь о каких-либо рисках. Dragon Money – это не просто игра. Это возможность испытать себя, проверить свою удачу и почувствовать себя настоящим властелином своей судьбы. Присоединяйтесь к нам, и пусть дракон принесет вам богатство, успех и процветание! Да пребудет с вами удача!
https://gazaskygeeks.com/art/
코인선물거래소
NBA중계
кайт Продвинутые техники кайтсёрфинга: покорите новые вершины. Освоив базовые навыки, переходите к изучению сложных трюков, таких как прыжки с перехватом, вращения и катание на волнах.
Hi there friends, its wonderful post about tutoringand completely defined, keep it up all the time.
https://maps.google.co.th/url?sa=t&url=https://premierlimousineservice.net
코인선물거래소
кайтинг Кайтсёрфинг – это не просто спорт, это стиль жизни, где ветер и вода становятся вашими союзниками. Ощутите свободу полета, скользя по волнам под куполом кайта, и забудьте обо всех проблемах, оставив их на берегу.
EPL중계
кайт лагерь Кайтсёрфинг развивается очень быстро, появляются новые трюки, стили и оборудование. Это делает спорт еще более интересным и захватывающим.
Kinonavigator ist eine Plattform für Cineasten, die kuratierte Auswahl ohne Umstände wollen.
Was bietet Kinonavigator?
10 Filme pro Thema: Von schwarzen Komödien bis hin zu Filmen für Regentage.
Streaming-Links: Direkte Links zu kostenlosen Plattformen.
Making-of-Material: Hol dir einen Vorgeschmack.
Artworks: Perfekt für Hintergrundbilder.
Keine Anmeldung — einfach Kino unkompliziert.
Entdecken Sie endlose Kategorien auf https://creativemarket.com/users/KinoRadar
Ventolin tablet 2mg: albuterol sulfate – albuterol inhaler
Hi there colleagues, its great piece of writing about tutoringand entirely explained, keep it up all the time.
https://oncology.com.ua/oryhinalni-proty-neoryhinalnykh-stekol-far-au.html
EPL중계
кайт Кайт
кайт школа Кайтинг: активный отдых и здоровый образ жизни.
https://t.me/s/TeleCasino_1Win
кайтинг Кайт школа: надёжный старт в мир кайтсёрфинга. Профессиональные инструкторы, современное оборудование, безопасные условия обучения – все это ждет вас в кайт школе.
https://dtf.ru/id2915936/3931207-promt-dlya-sozdaniya-patcha-iz-kartinki-dlya-odezhdy
проститутки Макеевка Проститутки Горловка: Ищешь острых ощущений? Тогда тебе к нам!
Wow, amazing blog structure! How long have you been running a blog for? you made blogging glance easy. The total glance of your website is wonderful, let alone the content!
vermox 100mg price
https://ecampania.it/blog/1xbet_promo_code-vip_welcome_bonus.html
nouveau code promo 1xbet
t.me/wine_it
лайки youtube Увеличение числа подписчиков в TikTok: тренды и методы продвижения. Создание вирусного контента и использование хештегов. подписчики тт
3д моделирование Лазерная гравировка
кайт Кайтсёрфинг – это образ жизни, полный приключений, путешествий и новых знакомств. Это сообщество людей, объединенных общей страстью к ветру и воде.
Thanks for any other fantastic article. Where else may anybody get that type of information in such a perfect method of writing? I’ve a presentation subsequent week, and I’m at the search for such information.
buying cheap vermox pill
кайтинг Фронт ролл: вращения на воде
https://sportquantum.com
купить оружие варфейс Работают все акканты варфейс, никаких проблем не возникло.
шлюхи днр Шлюхи ДНР
https://chery-russia.ru/ – приятно удивит каждого. Конкурентные цены и различные варианты комплектаций.
кайтинг “Крылья надежды”: выбор кайта, словно поиск верного друга, размера, формы – отражение мечты
кайт Прыжки в кайтсерфинге: как взлететь
кайтинг Продвинутые техники кайтсёрфинга: покорите новые вершины. Освоив базовые навыки, переходите к изучению сложных трюков, таких как прыжки с перехватом, вращения и катание на волнах.
http://jobusa.info/images/pages/?chto_takoe_ostricy.html
https://lesma-shop.de
https://muskaanhindi.org
Heya just wanted to give you a quick heads up and let you know a few of the pictures aren’t loading properly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
buy vibramycin 200 mg pill
http://ourmetals.com/includes/pages/1xbet_free_bet_promo_code_2020.html
кайтинг “В объятиях ветра и волн”: кайтсёрфинг, как танец души над бездной
https://www.locafilm.com
https://alayahotels.com
Attractive section of content. I just stumbled upon your web site and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Any way I will be subscribing to your feeds and even I achievement you access consistently quickly.
buy doxycycline 200 mg pill
https://www.actuabd.com
https://arma-models.ru/pr/pgs/?nemeckie_oficery_vtoroy_mirovoy_gerd_fon_rundshtedt_i_ioahim_fon_ribbentrop.html
кайт Обучение кайтсёрфингу требует профессионального подхода. Не экономьте на инструкторе, который научит вас основам безопасности и поможет быстро прогрессировать.
кайт Кайтинг: Общее понятие, объединяющее все виды спорта, использующие кайт для движения. Зимний кайтинг, сноукайтинг, баггикайтинг – разнообразие впечатляет.
кайтсёрфинг Кайт: ваш верный спутник в кайтсёрфинге. Изучите виды кайтов, их размеры, особенности и выберите идеальный вариант для своего стиля катания и погодных условий.
кайт лагерь Кайтсерфинг для детей: с какого возраста можно начинать обучение
обучение кайтсёрфингу “Арена героев”: соревнования, чемпионаты, где “рождаются легенды”
туры 2025
https://t.me/TG_Official_1win
https://possible11.com
срочный ремонт посудомоечных машин Алматы ремонт стиральных машин indesit wise: Ремонт стиральных машин Indesit Wise: советы специалистов.
Hi to every one, it’s really a fastidious for me to pay a visit this site, it includes helpful Information.
https://clients1.google.sc/url?q=https://seattlelimorates.com/
ps://wildlife.by/
https://sportsfanbetting.com/
https://www.europneus.es 1xBet promo code 2025: GO333 to unlock VIP bonuses – 330% up to $200 sports reward and up to €1,950 + 150 free spins for casino games. 1XBet launches a rewarding deal for first-time players in the new year. This bonus is designed for new bettors over 18. Sports offers require 5x-10x betting on parlays with 3 or more events with odds of 1.40 or higher within 30 days.
Use the today 1xBet promo code 2025: GO333. Enter it when signing up with 1xBet, you’ll unlock a generous 330% bonus up to €130 for betting. This offer applies to sports betting. To activate this offer, open a 1xBet account and enter the code when prompted for a code. Read the terms on the 1xBet platform for eligibility.
индивидуалки донецк Рынок эскорт-услуг в Донецке: как выбрать надежного партнера и обеспечить безопасность. Советы и рекомендации для клиентов. донецк шлюхи
I’m gone to tell my little brother, that he should also pay a quick visit this website on regular basis to obtain updated from most recent news update.
https://images.google.se/url?q=https://premierlimousineservice.net
онлайн зерно доска Тенденции развития рынка зерна: влияние геополитической ситуации, изменение климата и развитие технологий. Бесплатные агро объявления
криптовалюты
Стоило только войти — и интерфейс как будто считывает желания. Решение зашло само собой — через рабочее зеркало Vodka Casino. Промокоды придают игре вкус. Слоты могут удивлять и затягивать. Тут ценится каждый игрок. Бонусы не просто на словах — они реально работают. Каждый момент здесь — это история, которую хочется повторить.
I love how your posts are both informative and entertaining You have a talent for making even the most mundane topics interesting
https://aborict.org/hello-world/#comment-48545
чистка стиральной машины от накипи Мастер на час ремонт стиральной машины: быстрое решение мелких проблем с техникой.
1вин зеркало на сегодня
hollywood spina zonke
beteum erfahrungen
yesplay
Сравнивал с другими площадками — тут поведение автоматов честнее. Всё началось с перехода на https://vodka-registration.site. Выплаты приходят стабильно, это главное. Промокоды придают игре вкус. Интерфейс не важен, если внутри огонь. Тут главное — динамика и отдача. Эти эмоции настоящие — как и выигрыши.
1win casino зеркало
I’ve been exploring terpene-based products terpenes in indica recently, and I’m deep down enjoying the experience. The scents are with, customary, and pleasant. They add a discriminative caress to my daily routine, helping congeal the mood and atmosphere. A large track down to save anyone who appreciates perfumed wellness tools.
https://www.trub-prom.com/catalog/truby_bolshogo_diametra/ Трубы профильные квадратные: Профильные квадратные трубы – универсальное решение для строительных конструкций.
demo slot blood suckers
https://bs2vveb.at
Теннис теннисные прогнозы (Прогнозы на спорт: Анализ и стратегии для успешных ставок. | Прогноз: Как правильно анализировать спортивные события для успешных ставок. | Прогноз прогноз: Ежедневные прогнозы от экспертов, повышающие шансы на выигрыш. | Прогноз на: Прогнозы на футбол, хоккей, баскетбол и другие виды спорта. | Ставки: Руководство по ставкам на спорт для начинающих и опытных игроков. | Ставка: Как сделать ставку и не проиграть: советы и стратегии. | Ставки на спорт: Обзор букмекерских контор, бонусы и акции. | Спорт: Анализ спортивных событий, новости, результаты. | Спортивный: Спортивный анализ и прогнозы: секреты успешных ставок. | Беттинг: Беттинг как способ заработка: стратегии, риски и возможности. | Букмекер: Как выбрать букмекера: рейтинг лучших букмекерских контор. | Букмекерские конторы: Букмекерские конторы: сравнение коэффициентов и линий. | БК: Обзор популярных БК: бонусы, акции, выплаты. | Тотал: Что такое тотал и как делать ставки на тотал больше/меньше. | Тотал больше: Стратегии ставок на ТБ: как найти прибыльные варианты. | Тотал меньше: Как анализировать матчи для ставок на ТМ. | ТБ: Расшифровка ТБ и примеры ставок на тотал больше. | ТМ: Что означает ТМ и как делать ставки на тотал меньше. | Фора: Фора в ставках: объяснение, примеры и стратегии. | Фора минус: Как работает фора минус и когда ее использовать. | Фора плюс: Стратегии ставок с форой плюс для увеличения шансов на выигрыш. | Ф1: Что означает Ф1 и как делать ставки на победу первой команды с форой. | Ф2: Как использовать Ф2 в ставках и понимать значение форы для второй команды. | Исход: Анализ исхода матча: победа, ничья, поражение. | Победа: Стратегии ставок на победу: факторы, влияющие на результат. | Ничья: Когда стоит ставить на ничью и как анализировать вероятность ничейного исхода. | П1: Что такое П1 и как делать ставки на победу первой команды. | П2: Как использовать П2 в ставках и анализировать шансы второй команды на победу. | Х: Х в ставках: что означает ничья и как ее предсказать. | Кэф: Как формируется коэффициент и как его использовать в ставках. | Коэффициент: Анализ коэффициентов: как найти валуйные ставки. | Коэффициент на: Коэффициенты на спорт: сравнение предложений разных букмекеров. | VIP: VIP прогнозы: стоит ли покупать платные прогнозы. | Вип прогнозы: Преимущества и недостатки VIP прогнозов от капперов. | Платные прогнозы: Анализ эффективности платных прогнозов на спорт. | Каппер: Кто такой каппер и как выбрать надежного консультанта. | Экспресс: Как составлять экспрессы и увеличить шансы на выигрыш. | Паровоз: Что такое “паровоз” и почему не стоит злоупотреблять экспресс ставками. | Система: Ставка системой: как рассчитать выигрыш и минимизировать риски. | Ординар: Преимущества и недостатки ставок ординарами. | Одиночная ставка: Как правильно делать одиночные ставки и выбирать наиболее вероятные исходы. | Сингл: Сингл в ставках: простота и надежность, основа успешной стратегии. | Лайв прогнозы: Как делать ставки в лайве и использовать прогнозы в реальном времени. | Лайв: Стратегии для успешных ставок в режиме лайв. | Live: Live ставки: анализ матча в)|Лайв прогнозы лайв live: Преимущества и недостатки лайв-ставок, как правильно анализировать матч в реальном времени. | Футбол: Анализ футбольных матчей, стратегии ставок, обзоры чемпионатов. | Футбольные прогнозы: Ежедневные футбольные прогнозы от экспертов. | Хоккей: Хоккейные ставки: как анализировать матчи и делать выигрышные прогнозы. | Хоккейные прогнозы: Прогнозы на хоккейные матчи КХЛ, НХЛ и других лиг. | Баскетбол: Ставки на баскетбол: как учитывать статистику и особенности игры. | Баскетбольные прогнозы: Прогнозы на матчи NBA, Евролиги и других баскетбольных турниров. | Теннис: Теннисные ставки: анализ покрытия, формы игроков и других факторов. | Теннисные прогнозы: Прогнозы на теннисные турниры Grand Slam, ATP и WTA. | Волейбол: Стратегии ставок на волейбол, как учитывать расстановку и тактику команд. | Волейбольные прогнозы: Прогнозы на волейбольные матчи Лиги чемпионов и других турниров. | Киберспорт: Беттинг на киберспорт: как ставить на Dota 2, CS:GO и другие игры. | Кибер: Анализ киберспортивных матчей, стратегии ставок и прогнозы. | Esports: Руководство по ставкам на Esports для начинающих. | Прогнозы на киберспорт: Ежедневные прогнозы на киберспортивные события. | Бокс/MMA/UFC: Ставки на бокс и MMA: как анализировать бойцов и выбирать победителя. | Единоборства: Анализ поединков в единоборствах: подготовка бойцов, тактика, статистика. | Анализ букмекерских ошибок: Как находить ошибки в линиях букмекеров и использовать их в свою пользу. | Психология ставок: Как контролировать эмоции и принимать рациональные решения в беттинге. | Управление банкроллом: Как правильно управлять своим банкроллом, чтобы не проиграть все деньги сразу. | Стратегии ставок на фаворитов: Как ставить на фаворитов и получать стабильную прибыль. | Стратегии ставок на аутсайдеров: Когда стоит ставить на аутсайдеров и как найти выгодные варианты. | Виды тоталов в футболе: Индивидуальный тотал, азиатский тотал, тотал по таймам. | Виды фор в баскетболе: Азиатская фора, европейская фора, фора по четвертям.
сайт трипскан tripscan зеркало: Альтернативный доступ к сайту в случае технических проблем. Ваше путешествие не должно останавливаться!
крем 30+ Дневной крем для лица: Защита от негативного воздействия окружающей среды и увлажнение в течение всего дня.
wild slot swarm
Ченнелинг Ченнелинг
blood suckers
https://m-bs2best.at
ёлка пихта купить Нижневартовск Живая ёлка купить Нижневартовск: Натуральная красота и аромат праздника Живая ёлка – это классический выбор для тех, кто ценит натуральность и неповторимый аромат хвои. В Нижневартовске можно приобрести живые ёлки различных сортов, которые наполнят ваш дом праздничным настроением.
dragon money Dragon Money: Руководство для новичков, как зарегистрироваться, получить бонусы и начать играть. dragon money промокод
https://bs2besd.cc
https://bs2beast.cc
https://bs2-bs2site.at
https://abs2best.at
I’ve been exploring terpene-based products https://terpenewarehouse.com/collections/live-resin-terpenes recently, and I’m deep down enjoying the experience. The scents are in the chips, typical, and pleasant. They tot up a outgoing caress to my always routine, helping congeal the mood and atmosphere. A great find to save anyone who appreciates savoury wellness tools.
Когда хочется чего-то особенного, запускаю мобильное приложение и окунаюсь в атмосферу азарта. Удобно, что Vodka Casino скачать на телефон можно без танцев с бубном: одна кнопка — и всё готово. Приложение не грузит систему, быстро открывает слоты и надёжно подключается к рабочему зеркалу. Даже если интернет скачет — ничего не вылетает. Участвую в акциях, ловлю бонусы, зарабатываю по чуть-чуть, но стабильно. Важно, что платформа не ставит палки в колёса. Всё просто: играешь — получаешь. С таким подходом азарт становится настоящим удовольствием.
crossy road chiken
Heya great blog! Does running a blog like this require a great deal of work? I have very little expertise in coding but I had been hoping to start my own blog in the near future. Anyways, should you have any suggestions or tips for new blog owners please share. I know this is off subject however I simply wanted to ask. Many thanks!
Maggiori informazioni sui prezzi dei farmaci
avimaster casual game
lotto star
I’ve been exploring terpene-based products https://terpenewarehouse.com/collections/cannabis-terpenes-diamond recently, and I’m really enjoying the experience. The scents are well off, real, and pleasant. They enlarge a discriminative be a match for to my day after day drill, ration beat up a compare the feeling ready and atmosphere. A massive track down to save anyone who appreciates savoury wellness tools.
https://bs-bsme.at
Terrific post but I was wanting to know if you could write a litte more on this subject? I’d be very grateful if you could elaborate a little bit further. Appreciate it!
Migliore Prezzo Online – Sito ufficiale
https://bsme-at.at
https://t.me/s/Webs_1win/53
консультации маркетинг услуги интернет маркетологов В цифровой эре, где онлайн-присутствие стало неотъемлемой частью успешного бизнеса, услуги интернет-маркетологов приобретают особую ценность. Эти специалисты владеют широким спектром инструментов и техник, позволяющих эффективно привлекать целевую аудиторию, увеличивать трафик на сайт и, в конечном итоге, повышать продажи. SEO, контент-маркетинг, таргетированная реклама, email-маркетинг – это лишь некоторые из методов, которые интернет-маркетологи используют для достижения поставленных целей.
https://b2best.at
pr агентство услуги Продвижение продукта в социальных сетях: Привлечение внимания целевой аудитории и увеличение продаж Продвижение продукта в социальных сетях позволяет привлечь внимание целевой аудитории и увеличить продажи.
chiken road play
sunbet casino
https://bsmc.at
проститутки балашиха 1 проверенные шлюхи в балашихе
https://bs2bet.at
Tripscan cc Трипскан топ и Трипскан ссылка – это ваши проводники в мир лучших развлечений и самых выгодных предложений. Трипскан зеркало – это надежный способ обойти любые блокировки и продолжить свое захватывающее путешествие.
Трипскан ссылка Tripscan: Находите лучшие предложения на авиабилеты, отели и аренду автомобилей. Планируйте путешествия с комфортом и выгодой!
I’ve been exploring terpene-based products watermelon z recently, and I’m deep down enjoying the experience. The scents are in the chips, customary, and pleasant. They enlarge a outgoing drink to my daily programmed, dollop set the willing and atmosphere. A large find after anyone who appreciates pungent wellness tools.
https://bs2beast.cc
code promo 1xbet bonus codes
1xbet free bet promo code philippines
Un viaggio a Milano diventa speciale con momenti di connessione. ragazze a Milano Un’avventura a Milano e piu ricca con la persona giusta.
https://bs2vveb.at
https://bsme-at.at
https://bsmc.at
https://bs-bsme.at
перманент бровей симферополь Перманентный Макияж Бровей Севастополь: Безупречные Брови
https://bs2bet.at
Guncel Haberler Gunluk burc yorumu:
трипскан ссылка
купить прыжок с парашюта ростов на дону Покорение Небес: Прыжки с Парашютом в Ростове-на-Дону Ростов-на-Дону, живописный город с богатой историей, предлагает уникальную возможность – прыжок с парашютом. Это захватывающее приключение доступно как опытным спортсменам, так и новичкам, желающим испытать адреналин свободного падения. Выбор Прыжка: От Тандема к Свободе Первый шаг в небо – тандем-прыжок. Опытный инструктор обеспечит безопасность и позволит насладиться моментом без лишних забот. Для уверенных в себе – самостоятельный прыжок после подготовки. Где Прыгнуть: Аэроклубы Ростова и Области В Ростовской области есть несколько аэроклубов и дропзон, например, ДОСААФ. Важно выбирать проверенные организации с лицензией и профессиональным персоналом. Цена Вопроса: Сколько Стоит Полет? Стоимость прыжка зависит от типа (тандем или самостоятельный), высоты, аэроклуба и дополнительных услуг (фото/видео). Тандем-прыжок обычно дороже. Подарок, Превосходящий Ожидания Прыжок с парашютом – оригинальный и запоминающийся подарок, дарящий яркие эмоции. Многие аэроклубы предлагают подарочные сертификаты.
Qwe6yUkl demleme sokusu alan götler
https://www.4×4.by/forum/viewtopic.php?f=1&t=28556
https://bs2bsme.at
История покера Психология покера Психология покера – это понимание и использование эмоций в игре. Умение контролировать свои эмоции и читать эмоции соперников может дать вам значительное преимущество.
Rainbet Australia
online casino expert
https://github.com/gprotect/GlobalProtect//releases
verde casino
https://t.me/winpotcasino1
https://bsme-at.at
https://b2best.at
https://bsmc.at
https://bs2beast.cc
kra36—-at.com — Надежный и удобный сервис — официальный сайт и подробный обзор даркнет-маркета Kraken. Официальный сайт kraken kra36.at — удобный сервис с множеством функций для пользователей. Узнайте больше и начните пользоваться прямо сейчас!
kra36
сервис
удобство функции
официальный сайт Kraken
Кракен
маркетплейс Кракен
даркнет маркет
kraken официальный сайт
kraken market
kraken darknet
анонимные покупки
даркнет площадка
гидра альтернатива
kraken onion
kraken ссылка
darknet marketplace
kraken даркнет
кракен маркетплейс
кракен маркет обзор
кракен маркет отзывы
kraken ссылка
kraken сайт
kraken официальный сайт
kraken ссылка зеркало
актуальное зеркало kraken
kraken ссылка тор
kraken зеркало рабочее
kraken зеркало официальный
kraken зеркало даркнет
kraken зеркало тор
kraken зеркало 2kmp
kraken официальные ссылки
kraken onion ссылка
kraken ссылка для тору
kraken ссылка зеркало официальный
kraken зеркало krakentor site
kraken сайт зеркала
кракен ссылка kraken
kraken официальный сайт зеркало
kraken официальный сайт ссылка
kraken ссылка зеркало официальный сайт
kraken клирнет зеркало
kraken tor зеркало
kraken ссылка 2kmp
зеркала kraken kraken tor site
kraken darknet ссылка
kraken ссылка krakentor site
kraken зеркало 2kmp vip
kraken актуальные ссылки
kraken ссылка tor
kraken market ссылка
kraken зеркало 2kmp biz
kraken darknet зеркала
kraken darknet market ссылка
kraken darknet ссылка тор
ссылка kraken kraken tor site
kraken 2 зеркало
kraken ссылка 2kmp vip
рабочие ссылки kraken
сайт кракен kraken
kraken ссылка 2kmp biz
зеркало kraken market
kraken сайт официальный 2kmp
ссылка кракен kraken tor site
kraken darknet market зеркало
kraken ссылка зеркало рабочее
kraken market ссылка тор
kraken ссылка зеркало 2kmp
kraken darknet market ссылка тор
kraken ссылка зеркало krakentor site
kraken com зеркало
зеркала kraken 2kmp org
kraken ссылка kraken one com
kraken onion зеркала
сайт kraken darknet
зеркало kraken 2 kma biz
kraken сайт официальный krakentor site
kraken darknet официальный сайт
kraken зеркало рабочее krakentor site
ссылка на kraken kraken onion site
kraken кларнет зеркало kraken tor site
kraken зеркало рабочее 2kmp
kraken ссылка kraken clear com
kraken сайт kraken one com
kraken актуальные ссылки krakentor site
kraken ссылка onion 2kmp
kraken сайт официальный 2kmp biz
kraken ссылка зеркало официальный сайт 2kmp
kraken актуальные зеркала krakentor site
kraken зеркало тор ссылка
актуальное зеркало kraken kraken tor site
ссылка на кракен kraken one com
kraken даркнет зеркало krakentor site
kraken сайт kraken zerkalo
kraken рабочая ссылка тор
кракен сайт kraken one com
зеркало kraken тор ссылка рабочее
kraken сайт kraken zerkalo xyz
kraken ссылка onion krakentor site
kraken актуальные ссылки 2kmp
ссылка на кракен kraken onion site
kraken ссылка для тору vtor run
kraken сайт официальный 2kmp vip
kraken сайт kraken clear com
kraken зеркало тор krakentor site
kraken ссылка зеркало 2kmp biz
kraken сайт vtor run
kraken ссылка зеркало официальный сайт krakentor site
kraken ссылка зеркало 2kmp vip
kraken зеркала 2 kmp biz
ссылка на кракен kraken clear com
kraken casino зеркало
кракен сайт kraken clear com
зеркало кракен kraken tor site
kraken официальный сайт vtor run
kraken зеркало тор 2 kmp
kraken зеркало kraken2web com
актуальное зеркало kraken 2 kma biz
kraken актуальные зеркала 2kmp vip
ссылка на кракен kraken 7 one
kraken клирнет зеркало 2kmp biz
kraken ссылка онлайн
kraken даркнет зеркало 2kmp biz
kraken сайт анонимных
kraken зеркало рабочее 2kmp biz
kraken ссылка onion 2kmp biz
kraken сайт покупок
kraken зеркало онлайн
kraken сайт анонимных покупок
кракен сайт kraken zerkalo
кракен сайт kraken zerkalo xyz
kraken ссылка зеркало официальный сайт 2kmp biz
kraken даркнет зеркало 2kmp vip
kraken ссылка kraken2web com
kraken зеркало ссылка онлайн
kraken зеркало рабочее 2kmp vip
kraken актуальные ссылки 2kmp biz
kraken ссылка online
kraken ссылка tor wiki online
kraken ссылка зеркало официальный сайт 2kmp vip
kraken актуальные ссылки 2kmp vip
kraken ссылка на сайт
kraken зеркало тор 2 kmp biz
kraken сайт vk2
kraken casino зеркало рабочее
kraken клирнет зеркало 2kmp vip
ссылка на kraken kraken darknet top
кракен зеркало kraken 7 one
ссылка на кракен kraken darknet top
kraken зеркало тор 2 kmp vip
kraken зеркало kraken clear com
kraken ссылка kraken zerkalo xyz
зеркало kraken kraken onion site
kraken darknet ссылка kraken2web com
kraken официальный сайт k2tor
kraken зеркало krakendarknet top
сайт kraken тор
ссылка на кракен тор kraken 7 one
kraken клирнет зеркало 2kmp org
кракен ссылка kraken zerkalo
kraken ссылка 2krnk biz
kraken ссылка kraken7 one
актуальное зеркало kraken 2kmp org
кракен зеркало kraken one com
kraken ссылка onion 2kmp org
kraken ссылка onion 2kmp vip
площадка kraken ссылка
рабочая ссылка на кракен kraken 7 one
kraken зеркало 2kraken click
kraken ссылка тор kraken2web com
kraken ссылка зеркало vk2
актуальное зеркало kraken kraken onion site
кракен ссылка kraken zerkalo xyz
kraken сайт официальный 2kmp org
kraken зеркало 2krnk biz
kraken casino официальный сайт
kraken ссылка krakendarknet top
kraken официальные зеркала vk3
kraken market ссылка kraken2web com
kraken darknet ссылка тор kraken2web com
kraken ссылка тор kraken one com
kraken darknet зеркала kraken2web com
кракен зеркало kraken clear com
kraken darknet market ссылка kraken2web com
kraken сайт 2krnk biz
kraken зеркало dzen
кракен ссылка тор kraken one com
kraken зеркало тор 2kmp org
kraken зеркало krakenonion site
kraken ссылка онион
kraken сайт tor
актуальное зеркало kraken kraken zerkalo
kraken официальный сайт vk2
kraken ссылка зеркало 2kmp org
актуальное зеркало kraken kraken zerkalo xyz
сайт kraken onion
рабочее зеркало кракен kraken 7 one
кракен сайт ссылка kraken one com
kraken darknet market зеркало kraken2web com
kraken ссылка тор tor wiki online
kraken ссылка зеркало kraken2web com
kraken зеркало тор kraken7 one
kraken зеркало рабочее 2kmp org
ссылка на kraken 2kmp org
kraken официальный сайт vk3
kraken ссылка зеркало kraken 7 one
kraken onion ссылка tor wiki online
kraken вход на сайт
kraken зайти на сайт
kraken сайт krakendarknet top
кракен зеркало kraken zerkalo xyz
kraken ссылка тор 2kraken click
кракен вход ссылка kraken 7 one
kraken магазин ссылка
kraken darknet market ссылка тор kraken2web com
кракен сайт ссылка kraken clear com
kraken даркнет зеркало 2kmp org
kraken ссылка зеркало официальный сайт 2kmp org
kraken darknet market ссылка kraken7 one
kraken darknet ссылка 2krnk biz
kraken ссылка тор 2krnk biz
kraken актуальная ссылка onion
kraken сайт vk2 pro
кракен площадка ссылка kraken 7 one
kraken сайт kraken2web com
kraken зеркало форум
кракен зеркало тор kraken one com
kraken официальный сайт k2tor online
kraken ссылка зеркало vk2 pro
kraken darknet ссылка тор 2kraken click
ссылка на кракен тор kraken clear com
сайт онион kraken
кракен сайт зеркало kraken 7 one
kraken зеркало v5tor cfd
kraken darknet ссылка тор 2krnk biz
kraken сайт dzen
kraken оригинальная ссылка
kraken ссылка dzen
сайт кракен тор kraken one com
kraken ссылка krakenonion site
kraken официальные зеркала k2tor
kraken tor ссылка онлайн
kraken ссылка v5tor cfd
kraken ссылка на сайт тор
kraken сайт kr2web in
настоящий сайт kraken
kraken зеркало online
kraken актуальные ссылки 2kmp org
прямая ссылка на kraken
kraken оф сайт
kraken официальный сайт
используйте vpn!
Кракен Ссылка
Кракен Вход
Кракен Зайти
Ссылка на Кракен
Kra35.cc
Kra36.at
Kra34.cc
купить меф
купить гарик
Kra34.at
Kra33.cc
Kra33.at
Kra37.cc
Kra36.cc
Kra32.cc
Kra32.at
Kra38.cc
Kra39.cc
Kra33.cc
для дополнительной анонимности и безопасности рекомендуется использовать vpn-сервис. он скроет ваш ip-адрес и сделает ваше пребывание в интернете более безопасным.
будьте осторожны!?
kraken рабочая ссылка onion
kraken ссылка vk
кракен сайт ссылка kraken 11
ссылка на кракен kraken 9 one
kraken зеркало тор kraken2web com
кракен онион ссылка kraken one com
ссылка kraken 2 kma biz
ссылка на kraken торговая площадка
razer kraken сайт
kraken зеркало krakenweb one
kraken зеркало krakenweb3 com
kraken зеркало ссылка онлайн krakenweb one
kraken ссылка зеркало krakenweb one
kraken darknet market ссылка тор 2kraken click
kraken ссылка krakenweb one
kraken ссылка тор krakendarknet top
kraken casino зеркало kraken casino xyz
kraken darknet market зеркало v5tor cfd
kraken сайт зеркала kraken2web com
kraken даркнет ссылка
kraken зеркала kr2web in
kraken зеркало store
kraken darknet market ссылка тор v5tor cfd
kraken darknet market сайт
даркнет официальный сайт kraken
kraken ссылка зеркало рабочее kraken2web com
kraken зеркало тор ссылка kraken2web com
kraken маркетплейс зеркала
kraken официальные зеркала k2tor online
kraken darknet маркет ссылка каркен market
kraken 6 at сайт производителя 2
сайт кракен kraken darknet top
kraken клир ссылка
кракен ссылка kraken kraken2web com 3
ссылка на кракен тор kraken 9 one
kraken сайт анонимных покупок vtor run
kraken darknet market зеркало 2kraken click
kraken darknet market ссылка shkafssylka ru
kraken ссылка torbazaw com
kraken форум ссылка
площадка кракен ссылка kraken clear com
сайт kraken darknet kraken2web com
как зайти на маркетплейс кракен: официальные ссылки и зеркала.
полное руководство:
актуальная ссылка (через браузер):
официальная ссылка :
резервное зеркало:
как зайти на маркетплейс кракен: полное руководство
для входа на сайт кракена в даркнете требуется tor. это безопасный браузер:
перейдите на официальный сайт tor.
скачайте программу для вашей ос.
установите и запустите браузер.
используйте актуальные ссылки на кракен
ссылки на официальный сайт кракен часто обновляются. чтобы избежать фишинговых сайтов, используйте проверенные ресурсы для получения ссылок:
• актуальное зеркало кракена:
• зеркала сайта в клирнете и даркнете доступны для пользователей в любой точке мира.
авторизация
после перехода на сайт:
зарегистрируйтесь, если у вас еще нет аккаунта.
войдите в свой личный кабинет, используя логин и пароль.
для повышения безопасности активируйте двухфакторную аутентификацию.
но почему выбираю именно
сотни других платформ, тысячи товаров, но для меня больше, чем просто магазин. это место, где покупки превращаются в увлекательное путешествие.
знает, как важно быть уверенным в каждой покупке. полная защита сделок и дружелюбная поддержка создают чувство, будто вы находитесь в заботливых руках. надёжность? абсолютно.
почему именно
потому что здесь всё про вас: ваш стиль, ваш комфорт, ваша выгода. попробуйте, и вы поймёте, почему так много людей выбирают именно эту платформу!
советы по безопасности на кракене
используйте vpn
подключение через vpn повышает вашу анонимность, скрывая ip-адрес.
проверяйте ссылки
актуальные ссылки и зеркала кракен можно найти на проверенных форумах или официальных ресурсах. никогда не используйте непроверенные источники.
будьте внимательны к продавцам
читайте отзывы и выбирайте проверенных продавцов с высоким рейтингом.
кракен маркетплейс
кракен маркетплейс
кракен площадка
kra33.at
kra33.cc
kra34.cc
kra34.at
kra35.cc
kra36.at
kra36.cc
Kra36.at
kra37.cc
kra38.at
кракен маркетплейс ссылка
кракен площадка
кракен marketplace
кракен площадка ссылка
кракен даркнет стор
кракен darknet market зеркало
кракен даркнет площадка
кракен даркнет маркетплейс
кракен наркотики
кракен нарко
кракен наркошоп
кракен наркота
кракен порошок
кракен наркотики
кракен что там продают
кракен маркетплейс что продают
кракен покупка
какен купить
кракен купить мяу
кракен питер
кракен в питере
кракен москва
кракен в москве
кракен что продают
кракен это
кракен marke
кркен darknet market
кракен dark market
кракен market ссылка
кракен darknet market ссылк
кракен market ссылка тор
кракен даркнет маркет
кракен market тор
кракен маркет
платформа кракен
кракен торговая площадка
кракен даркнет маркет ссылка сайт
кракен маркет даркнет тор
кракен аккаунты
кракен заказ
диспуты кракен
как восстановить кракен
кракен даркнет не работает
как пополнить кракен
google authenticator кракен
рулетка кракен
купоны кракен
кракен зарегистрироваться
кракен регистрация
кракен пользователь не найден
кракен отзывы
ссылка кракен
кракен официальная ссылка
кракен ссылка на сайт
кракен официальная ссылка
кракен актуальные
кракен ссылка тор
кракен клирнет
кракен ссылка маркет
кракен клир ссылка
кракен ссылка
ссылка на кракен
кракен ссылка
кракен ссылка на сайт
кракен ссылка кракен
актуальная ссылка на кракен
рабочие ссылки кракен
кракен тор ссылка
ссылка на кракен тор
кракен зеркало тор
кракен маркет тор
кракен tor
кракен ссылка tor
кракен тор
кракен ссылка тор
кракен tor зеркало
кракен darknet tor
кракен тор браузер
кракен тор
кракен darknet ссылка тор
кракен ссылка на сайт тор
кракен вход на сайт
кракен вход
кракен зайти
кракен войти
кракен даркнет вход
кракен войти
где найти ссылку кракен
где взять ссылку на кракен
как зайти на сайт кракен
как найти кракен
кракен новый
кракен не работает
кракен вход
как зайти на кракен
кракен вход ссылка
сайт кракен
кракен сайт
кракен сайт что это
кракен сайт даркнет
что за сайт кракен
кракен что за сайт
Кракен официальный сайт
сайт кракен отзывы
кракен сайт
кракен официальный сайт
сайт кракен тор
кракен сайт ссылка
кракен сайт зеркало
кракен сайт тор ссылка
кракен зеркало сайта
зеркало кракен
адрес кракена
кракен зеркало тор
зеркало кракен даркнет
актуальное зеркало кракен
рабочее зеркало кракен
кракен зеркало
кракен зеркала
кракен зеркало
зеркало кракен market
актуальное зеркало кракен
кракен darknet
кракен даркнет ссылка
ссылка кракен даркнет маркет
кракен даркнет
кракен darknet
кракен даркнет
кракен dark
кракен darknet ссылка
кракен сайт даркнет маркет
кракен даркнет маркет ссылка тор
кракен даркнет тор
кракен текст рекламы
Kraken ссылка
Kraken Вход
Kraken зайти
https://m-bs2best.at
https://m-bs2best.at
https://bs2bet.at
https://bs2besd.cc
Deneme bonusu veren siteler 2025 listesiyle, yatırım janama jonoju jeren jiteler yapmadan bedava bahis oynayın. Güncel, çevrimsiz ve güvenilir bonus kampanyaları sizi bekliyor
https://bs2vveb.at
https://bs-bsme.at
https://bs2besd.cc
https://www.cornbreadhemp.com/products/seltzer-salted-watermelon are a predominant, delectable functioning to enjoy the dormant calming and wellness benefits of cannabidiol. Different from THC, CBD won’t slug a spread you enormous, making these gummies standards for anxiety, nod off, or routine balance. They in in diverse flavors, strengths, and formulas—some with added ingredients like melatonin or vitamins. Effects typically start within 30–60 minutes and model a few hours. Vegan, integral, and sugar-free options are also available. Unexceptionally thwart lab results and start with a smutty dose.
коррекция бровей севастополь Перманентный макияж Севастополь – это долгосрочное решение для тех, кто ценит свое время и хочет выглядеть безупречно в любой ситуации. Перманентный макияж бровей Севастополь позволит вам наслаждаться идеальными бровями 24/7.
школа музыки в куркино Музыкальная школа Куркино – это не просто место обучения, это мир, где каждый может прикоснуться к искусству, раскрыть свой талант и почувствовать себя частью большой музыкальной семьи. Мы предлагаем разнообразные программы для детей и взрослых, вне зависимости от уровня подготовки, чтобы каждый смог найти что-то для себя.
Каршеринг в Краснодаре
online gambling reviews
алкоголь bottega Вино под морепродукты При выборе вина под морепродукты важно учитывать способ их приготовления. К жареным морепродуктам подойдет более насыщенное вино, например, Шардоне, выдержанное в дубовых бочках. Для морепродуктов, приготовленных на пару или в соусе, лучше выбрать легкое и освежающее вино, такое как Пино Гриджио или Рислинг.
Аренда авто
история макдолналдс История Макдональдс: постоянные инновации и адаптация к меняющимся вкусам. Несмотря на свою консервативность, Макдональдс постоянно развивается и адаптируется к меняющимся вкусам и потребностям потребителей. В меню появляются новые блюда, отвечающие тенденциям здорового питания, экологичности и разнообразия. Компания активно внедряет новые технологии, улучшая сервис и повышая эффективность работы. Макдональдс – это не просто сеть ресторанов быстрого обслуживания, это часть истории, символ эпохи и отражение меняющегося мира.
подать документы на визу в китай Нужна виза в Китай для россиян: От идеи до путешествия – один шаг. Китай манит своей древней историей, неповторимой культурой и удивительными пейзажами. Для граждан России виза является обязательным условием для посещения этой страны. Тип визы зависит от цели вашей поездки: туризм, бизнес, учеба или работа. Подготовьте необходимые документы заранее, чтобы избежать задержек и разочарований. Помните, что правильное оформление визы – это залог успешного путешествия.
Курсы по недвижимости Онлайн курсы по недвижимости: Получите качественное образование в удобное для вас время и в любом месте. Современный мир предлагает гибкие решения для обучения. Онлайн курсы по недвижимости позволяют получить необходимые знания, не выходя из дома или офиса, и адаптировать обучение под свой личный график.
Аренда авто Краснодар посуточно
экскурсии казани Парк “Кырлай”: Развлечения для Всей Семьи Парк “Кырлай” – это парк развлечений в Казани, где можно найти аттракционы для всех возрастов. Здесь есть карусели, горки, колесо обозрения и многое другое. Парк “Кырлай” – это отличное место для семейного отдыха, где можно весело провести время и получить заряд положительных эмоций.
Электрики Энергосбережение – путь к экономии и экологии, разумное потребление – вклад в будущее.
Обучение недвижимости Курс по коммерческой недвижимости: Откройте секреты управления прибыльными активами. Коммерческая недвижимость – это высший пилотаж в мире инвестиций. Здесь ставки выше, риски более ощутимы, но и потенциальная прибыль несоизмеримо больше. Курс по коммерческой недвижимости – это ваш шанс освоить искусство анализа рынка, выявления перспективных объектов, ведения переговоров с арендаторами и управления крупными активами. Станьте тем, кто создает успешные бизнес-центры, торговые комплексы и логистические парки.
Отечественные сценарии соответствуют мировому уровню вся информация собрана фильмы торрент, фильмы мелодрамы, российские фильмы https://movietut.xyz/159824-skachat-muzhchina-i-zhenschina-film-na-russkom-2024.html Мужчина и женщина (2024 фильмы на русском) скачать через торрент
https://kazan.land/ Национальный Музей Республики Татарстан: Знакомство с Культурой и Историей Национальный музей Республики Татарстан – это крупнейший музей в Казани, где представлена богатая коллекция экспонатов, рассказывающих об истории, культуре и природе Татарстана. Вы сможете увидеть археологические находки, предметы быта, национальные костюмы, произведения искусства и многое другое. Посещение музея позволит вам глубже узнать о татарском народе и его вкладе в мировую культуру.
экскурсии казани Благовещенский Собор: Величественный Памятник Православия Благовещенский собор – это один из старейших православных храмов Казани, расположенный на территории Казанского Кремля. Он является важным памятником русской архитектуры и истории. Собор поражает своим величием и красотой. Вы можете посетить его, чтобы прикоснуться к истории православия в Татарстане.
экскурсия казань Галерея Современного Искусства: Вдохновение и Новые Горизонты Галерея современного искусства – это место, где представлены работы современных художников и скульпторов, работающих в различных стилях и направлениях. Здесь можно увидеть произведения, отражающие современные тенденции в искусстве, а также принять участие в выставках и мастер-классах. Галерея поможет вам открыть для себя новые горизонты в искусстве и получить вдохновение.
Маникюр Набережные Челны Изящный Маникюр в Набережных Челнах: Гармония Стиля и Ухода Руки – визитная карточка каждой женщины. Безупречный маникюр в Набережных Челнах подчеркнет вашу индивидуальность и добавит уверенности в себе. Салоны предлагают широкий спектр услуг: от классического маникюра до креативного дизайна. Мастера используют передовые техники и качественные материалы, обеспечивая долговечность и красоту вашего маникюра. Позвольте себе роскошь ухоженных рук.
Прокат авто Краснодар Прокат авто Краснодар посуточно: Оптимальный выбор для коротких поездок Наслаждайтесь свободой передвижения без лишних затрат. Прокат авто Краснодар посуточно – это удобно и выгодно.
Проститутки ДНР Донецк шлюхи: Спрос рождает предложение Существование проституции говорит о наличии спроса на эти услуги.
Психолог Москва Врач психотерапевт Москва: Медицина души. Когда психологические трудности перерастают в клинические состояния, когда необходима комплексная помощь, на сцену выходит врач-психотерапевт. Он сочетает знания психологии и медицины, предлагая как психотерапевтические методы, так и фармакологическую поддержку, если это необходимо. Врач-психотерапевт в Москве – это символ надежды для тех, кто ищет квалифицированную помощь в борьбе с серьезными психическими расстройствами.
Бог
Tried the https://www.cornbreadhemp.com/products/cbd-sleep-gummies from Cornbread Hemp — the benevolent with a eat of THC. Took song in the future bed. The flavor’s competent, measure dirty but pleasant. With reference to an hour later, I felt noticeably more easy — not drowsy, well-grounded calm sufficiently to stray disheartening without my wavering be decided racing. Woke up with no morning grogginess, which was a warm-hearted surprise. They’re on the pricier side, but if you attempt to unwind at tenebriousness, they could be importance it.
Запчасти для плиты Лысьва ЭП 43Р3 Запчасти для стиральной машины LG F2V9GC9W.ABWPCOM: Современные технологии требуют внимания. Обслуживайте свою стиральную машину вовремя, чтобы избежать серьезных поломок.
скачать игры по прямой ссылке Альтернативы торрентам: Откройте для себя новые возможности Ограничиваться устаревшими способами получения игр – значит лишать себя множества преимуществ. Исследуйте альтернативные источники, предлагающие высокое качество, безопасность и удобство. Откройте для себя новые горизонты гейминга и наслаждайтесь процессом без каких-либо ограничений.
buy dapoxetine no prescription https://datos.cdmx.gob.mx/user/dapoxetine
Trang web https://co88.org/ lừa đảo, nội dung đồi trụy
Remarkable! Its actually remarkable paragraph, I have got much clear idea concerning from this post.
Luxury limo near me
Güncel ve güvenilir deneme bonusu veren siteler listesi. En iyi bahis siteleri bonus fırsatlarıyla kazanmaya hemen başlayın. bihis sitiliri
raja 999
kra36—-at.com — Надежный и удобный сервис — официальный сайт и подробный обзор даркнет-маркета Kraken. Официальный сайт kraken kra36.at — удобный сервис с множеством функций для пользователей. Узнайте больше и начните пользоваться прямо сейчас!
kra36
сервис
удобство функции
официальный сайт Kraken
Кракен
маркетплейс Кракен
даркнет маркет
kraken официальный сайт
kraken market
kraken darknet
анонимные покупки
даркнет площадка
гидра альтернатива
kraken onion
kraken ссылка
darknet marketplace
kraken даркнет
кракен маркетплейс
кракен маркет обзор
кракен маркет отзывы
kraken ссылка
kraken сайт
kraken официальный сайт
kraken ссылка зеркало
актуальное зеркало kraken
kraken ссылка тор
kraken зеркало рабочее
kraken зеркало официальный
kraken зеркало даркнет
kraken зеркало тор
kraken зеркало 2kmp
kraken официальные ссылки
kraken onion ссылка
kraken ссылка для тору
kraken ссылка зеркало официальный
kraken зеркало krakentor site
kraken сайт зеркала
кракен ссылка kraken
kraken официальный сайт зеркало
kraken официальный сайт ссылка
kraken ссылка зеркало официальный сайт
kraken клирнет зеркало
kraken tor зеркало
kraken ссылка 2kmp
зеркала kraken kraken tor site
kraken darknet ссылка
kraken ссылка krakentor site
kraken зеркало 2kmp vip
kraken актуальные ссылки
kraken ссылка tor
kraken market ссылка
kraken зеркало 2kmp biz
kraken darknet зеркала
kraken darknet market ссылка
kraken darknet ссылка тор
ссылка kraken kraken tor site
kraken 2 зеркало
kraken ссылка 2kmp vip
рабочие ссылки kraken
сайт кракен kraken
kraken ссылка 2kmp biz
зеркало kraken market
kraken сайт официальный 2kmp
ссылка кракен kraken tor site
kraken darknet market зеркало
kraken ссылка зеркало рабочее
kraken market ссылка тор
kraken ссылка зеркало 2kmp
kraken darknet market ссылка тор
kraken ссылка зеркало krakentor site
kraken com зеркало
зеркала kraken 2kmp org
kraken ссылка kraken one com
kraken onion зеркала
сайт kraken darknet
зеркало kraken 2 kma biz
kraken сайт официальный krakentor site
kraken darknet официальный сайт
kraken зеркало рабочее krakentor site
ссылка на kraken kraken onion site
kraken кларнет зеркало kraken tor site
kraken зеркало рабочее 2kmp
kraken ссылка kraken clear com
kraken сайт kraken one com
kraken актуальные ссылки krakentor site
kraken ссылка onion 2kmp
kraken сайт официальный 2kmp biz
kraken ссылка зеркало официальный сайт 2kmp
kraken актуальные зеркала krakentor site
kraken зеркало тор ссылка
актуальное зеркало kraken kraken tor site
ссылка на кракен kraken one com
kraken даркнет зеркало krakentor site
kraken сайт kraken zerkalo
kraken рабочая ссылка тор
кракен сайт kraken one com
зеркало kraken тор ссылка рабочее
kraken сайт kraken zerkalo xyz
kraken ссылка onion krakentor site
kraken актуальные ссылки 2kmp
ссылка на кракен kraken onion site
kraken ссылка для тору vtor run
kraken сайт официальный 2kmp vip
kraken сайт kraken clear com
kraken зеркало тор krakentor site
kraken ссылка зеркало 2kmp biz
kraken сайт vtor run
kraken ссылка зеркало официальный сайт krakentor site
kraken ссылка зеркало 2kmp vip
kraken зеркала 2 kmp biz
ссылка на кракен kraken clear com
kraken casino зеркало
кракен сайт kraken clear com
зеркало кракен kraken tor site
kraken официальный сайт vtor run
kraken зеркало тор 2 kmp
kraken зеркало kraken2web com
актуальное зеркало kraken 2 kma biz
kraken актуальные зеркала 2kmp vip
ссылка на кракен kraken 7 one
kraken клирнет зеркало 2kmp biz
kraken ссылка онлайн
kraken даркнет зеркало 2kmp biz
kraken сайт анонимных
kraken зеркало рабочее 2kmp biz
kraken ссылка onion 2kmp biz
kraken сайт покупок
kraken зеркало онлайн
kraken сайт анонимных покупок
кракен сайт kraken zerkalo
кракен сайт kraken zerkalo xyz
kraken ссылка зеркало официальный сайт 2kmp biz
kraken даркнет зеркало 2kmp vip
kraken ссылка kraken2web com
kraken зеркало ссылка онлайн
kraken зеркало рабочее 2kmp vip
kraken актуальные ссылки 2kmp biz
kraken ссылка online
kraken ссылка tor wiki online
kraken ссылка зеркало официальный сайт 2kmp vip
kraken актуальные ссылки 2kmp vip
kraken ссылка на сайт
kraken зеркало тор 2 kmp biz
kraken сайт vk2
kraken casino зеркало рабочее
kraken клирнет зеркало 2kmp vip
ссылка на kraken kraken darknet top
кракен зеркало kraken 7 one
ссылка на кракен kraken darknet top
kraken зеркало тор 2 kmp vip
kraken зеркало kraken clear com
kraken ссылка kraken zerkalo xyz
зеркало kraken kraken onion site
kraken darknet ссылка kraken2web com
kraken официальный сайт k2tor
kraken зеркало krakendarknet top
сайт kraken тор
ссылка на кракен тор kraken 7 one
kraken клирнет зеркало 2kmp org
кракен ссылка kraken zerkalo
kraken ссылка 2krnk biz
kraken ссылка kraken7 one
актуальное зеркало kraken 2kmp org
кракен зеркало kraken one com
kraken ссылка onion 2kmp org
kraken ссылка onion 2kmp vip
площадка kraken ссылка
рабочая ссылка на кракен kraken 7 one
kraken зеркало 2kraken click
kraken ссылка тор kraken2web com
kraken ссылка зеркало vk2
актуальное зеркало kraken kraken onion site
кракен ссылка kraken zerkalo xyz
kraken сайт официальный 2kmp org
kraken зеркало 2krnk biz
kraken casino официальный сайт
kraken ссылка krakendarknet top
kraken официальные зеркала vk3
kraken market ссылка kraken2web com
kraken darknet ссылка тор kraken2web com
kraken ссылка тор kraken one com
kraken darknet зеркала kraken2web com
кракен зеркало kraken clear com
kraken darknet market ссылка kraken2web com
kraken сайт 2krnk biz
kraken зеркало dzen
кракен ссылка тор kraken one com
kraken зеркало тор 2kmp org
kraken зеркало krakenonion site
kraken ссылка онион
kraken сайт tor
актуальное зеркало kraken kraken zerkalo
kraken официальный сайт vk2
kraken ссылка зеркало 2kmp org
актуальное зеркало kraken kraken zerkalo xyz
сайт kraken onion
рабочее зеркало кракен kraken 7 one
кракен сайт ссылка kraken one com
kraken darknet market зеркало kraken2web com
kraken ссылка тор tor wiki online
kraken ссылка зеркало kraken2web com
kraken зеркало тор kraken7 one
kraken зеркало рабочее 2kmp org
ссылка на kraken 2kmp org
kraken официальный сайт vk3
kraken ссылка зеркало kraken 7 one
kraken onion ссылка tor wiki online
kraken вход на сайт
kraken зайти на сайт
kraken сайт krakendarknet top
кракен зеркало kraken zerkalo xyz
kraken ссылка тор 2kraken click
кракен вход ссылка kraken 7 one
kraken магазин ссылка
kraken darknet market ссылка тор kraken2web com
кракен сайт ссылка kraken clear com
kraken даркнет зеркало 2kmp org
kraken ссылка зеркало официальный сайт 2kmp org
kraken darknet market ссылка kraken7 one
kraken darknet ссылка 2krnk biz
kraken ссылка тор 2krnk biz
kraken актуальная ссылка onion
kraken сайт vk2 pro
кракен площадка ссылка kraken 7 one
kraken сайт kraken2web com
kraken зеркало форум
кракен зеркало тор kraken one com
kraken официальный сайт k2tor online
kraken ссылка зеркало vk2 pro
kraken darknet ссылка тор 2kraken click
ссылка на кракен тор kraken clear com
сайт онион kraken
кракен сайт зеркало kraken 7 one
kraken зеркало v5tor cfd
kraken darknet ссылка тор 2krnk biz
kraken сайт dzen
kraken оригинальная ссылка
kraken ссылка dzen
сайт кракен тор kraken one com
kraken ссылка krakenonion site
kraken официальные зеркала k2tor
kraken tor ссылка онлайн
kraken ссылка v5tor cfd
kraken ссылка на сайт тор
kraken сайт kr2web in
настоящий сайт kraken
kraken зеркало online
kraken актуальные ссылки 2kmp org
прямая ссылка на kraken
kraken оф сайт
kraken официальный сайт
используйте vpn!
Кракен Ссылка
Кракен Вход
Кракен Зайти
Ссылка на Кракен
Kra35.cc
Kra36.at
Kra34.cc
купить меф
купить гарик
Kra34.at
Kra33.cc
Kra33.at
Kra37.cc
Kra36.cc
Kra32.cc
Kra32.at
Kra38.cc
Kra39.cc
Kra33.cc
для дополнительной анонимности и безопасности рекомендуется использовать vpn-сервис. он скроет ваш ip-адрес и сделает ваше пребывание в интернете более безопасным.
будьте осторожны!?
kraken рабочая ссылка onion
kraken ссылка vk
кракен сайт ссылка kraken 11
ссылка на кракен kraken 9 one
kraken зеркало тор kraken2web com
кракен онион ссылка kraken one com
ссылка kraken 2 kma biz
ссылка на kraken торговая площадка
razer kraken сайт
kraken зеркало krakenweb one
kraken зеркало krakenweb3 com
kraken зеркало ссылка онлайн krakenweb one
kraken ссылка зеркало krakenweb one
kraken darknet market ссылка тор 2kraken click
kraken ссылка krakenweb one
kraken ссылка тор krakendarknet top
kraken casino зеркало kraken casino xyz
kraken darknet market зеркало v5tor cfd
kraken сайт зеркала kraken2web com
kraken даркнет ссылка
kraken зеркала kr2web in
kraken зеркало store
kraken darknet market ссылка тор v5tor cfd
kraken darknet market сайт
даркнет официальный сайт kraken
kraken ссылка зеркало рабочее kraken2web com
kraken зеркало тор ссылка kraken2web com
kraken маркетплейс зеркала
kraken официальные зеркала k2tor online
kraken darknet маркет ссылка каркен market
kraken 6 at сайт производителя 2
сайт кракен kraken darknet top
kraken клир ссылка
кракен ссылка kraken kraken2web com 3
ссылка на кракен тор kraken 9 one
kraken сайт анонимных покупок vtor run
kraken darknet market зеркало 2kraken click
kraken darknet market ссылка shkafssylka ru
kraken ссылка torbazaw com
kraken форум ссылка
площадка кракен ссылка kraken clear com
сайт kraken darknet kraken2web com
как зайти на маркетплейс кракен: официальные ссылки и зеркала.
полное руководство:
актуальная ссылка (через браузер):
официальная ссылка :
резервное зеркало:
как зайти на маркетплейс кракен: полное руководство
для входа на сайт кракена в даркнете требуется tor. это безопасный браузер:
перейдите на официальный сайт tor.
скачайте программу для вашей ос.
установите и запустите браузер.
используйте актуальные ссылки на кракен
ссылки на официальный сайт кракен часто обновляются. чтобы избежать фишинговых сайтов, используйте проверенные ресурсы для получения ссылок:
• актуальное зеркало кракена:
• зеркала сайта в клирнете и даркнете доступны для пользователей в любой точке мира.
авторизация
после перехода на сайт:
зарегистрируйтесь, если у вас еще нет аккаунта.
войдите в свой личный кабинет, используя логин и пароль.
для повышения безопасности активируйте двухфакторную аутентификацию.
но почему выбираю именно
сотни других платформ, тысячи товаров, но для меня больше, чем просто магазин. это место, где покупки превращаются в увлекательное путешествие.
знает, как важно быть уверенным в каждой покупке. полная защита сделок и дружелюбная поддержка создают чувство, будто вы находитесь в заботливых руках. надёжность? абсолютно.
почему именно
потому что здесь всё про вас: ваш стиль, ваш комфорт, ваша выгода. попробуйте, и вы поймёте, почему так много людей выбирают именно эту платформу!
советы по безопасности на кракене
используйте vpn
подключение через vpn повышает вашу анонимность, скрывая ip-адрес.
проверяйте ссылки
актуальные ссылки и зеркала кракен можно найти на проверенных форумах или официальных ресурсах. никогда не используйте непроверенные источники.
будьте внимательны к продавцам
читайте отзывы и выбирайте проверенных продавцов с высоким рейтингом.
кракен маркетплейс
кракен маркетплейс
кракен площадка
kra33.at
kra33.cc
kra34.cc
kra34.at
kra35.cc
kra36.at
kra36.cc
Kra36.at
kra37.cc
kra38.at
кракен маркетплейс ссылка
кракен площадка
кракен marketplace
кракен площадка ссылка
кракен даркнет стор
кракен darknet market зеркало
кракен даркнет площадка
кракен даркнет маркетплейс
кракен наркотики
кракен нарко
кракен наркошоп
кракен наркота
кракен порошок
кракен наркотики
кракен что там продают
кракен маркетплейс что продают
кракен покупка
какен купить
кракен купить мяу
кракен питер
кракен в питере
кракен москва
кракен в москве
кракен что продают
кракен это
кракен marke
кркен darknet market
кракен dark market
кракен market ссылка
кракен darknet market ссылк
кракен market ссылка тор
кракен даркнет маркет
кракен market тор
кракен маркет
платформа кракен
кракен торговая площадка
кракен даркнет маркет ссылка сайт
кракен маркет даркнет тор
кракен аккаунты
кракен заказ
диспуты кракен
как восстановить кракен
кракен даркнет не работает
как пополнить кракен
google authenticator кракен
рулетка кракен
купоны кракен
кракен зарегистрироваться
кракен регистрация
кракен пользователь не найден
кракен отзывы
ссылка кракен
кракен официальная ссылка
кракен ссылка на сайт
кракен официальная ссылка
кракен актуальные
кракен ссылка тор
кракен клирнет
кракен ссылка маркет
кракен клир ссылка
кракен ссылка
ссылка на кракен
кракен ссылка
кракен ссылка на сайт
кракен ссылка кракен
актуальная ссылка на кракен
рабочие ссылки кракен
кракен тор ссылка
ссылка на кракен тор
кракен зеркало тор
кракен маркет тор
кракен tor
кракен ссылка tor
кракен тор
кракен ссылка тор
кракен tor зеркало
кракен darknet tor
кракен тор браузер
кракен тор
кракен darknet ссылка тор
кракен ссылка на сайт тор
кракен вход на сайт
кракен вход
кракен зайти
кракен войти
кракен даркнет вход
кракен войти
где найти ссылку кракен
где взять ссылку на кракен
как зайти на сайт кракен
как найти кракен
кракен новый
кракен не работает
кракен вход
как зайти на кракен
кракен вход ссылка
сайт кракен
кракен сайт
кракен сайт что это
кракен сайт даркнет
что за сайт кракен
кракен что за сайт
Кракен официальный сайт
сайт кракен отзывы
кракен сайт
кракен официальный сайт
сайт кракен тор
кракен сайт ссылка
кракен сайт зеркало
кракен сайт тор ссылка
кракен зеркало сайта
зеркало кракен
адрес кракена
кракен зеркало тор
зеркало кракен даркнет
актуальное зеркало кракен
рабочее зеркало кракен
кракен зеркало
кракен зеркала
кракен зеркало
зеркало кракен market
актуальное зеркало кракен
кракен darknet
кракен даркнет ссылка
ссылка кракен даркнет маркет
кракен даркнет
кракен darknet
кракен даркнет
кракен dark
кракен darknet ссылка
кракен сайт даркнет маркет
кракен даркнет маркет ссылка тор
кракен даркнет тор
кракен текст рекламы
Kraken ссылка
Kraken Вход
Kraken зайти
Yesterday, while I was at work, my sister stole my iphone and tested to see if it can survive a 25 foot drop, just so she can be a youtube sensation. My iPad is now destroyed and she has 83 views. I know this is totally off topic but I had to share it with someone!
https://reklamist.com.ua/Chi-varto-kupuvati-fari-b-u-riziki-ta-nyuansi.html
Hi, after reading this remarkable post i am as well delighted to share my know-how here with friends.
http://infobus.com.ua/sklo-far-ta-dorozhnya-bezpeka-scho-kazhut-eksperti.html
https://prometei.online/ the Best!
you are actually a just right webmaster. The web site loading velocity is incredible. It sort of feels that you’re doing any unique trick. In addition, The contents are masterpiece. you have performed a fantastic task on this subject!
https://dnmagazine.com.ua/diy-remont-fary-iakyi-hermetyk-obraty
Рабочие тетради и учебники для 2 класса на 2025-2026 учебный год – Купить в Москве
учебники и школьная литература: учебники, рабочие тетради, методические материалы и другая учебная литература по низким ценам, с доставкой по Москве и в другие регионы России, на сайте интернет-магазина
Excellent website you have here but I was curious if you knew of any forums that cover the same topics talked about in this article? I’d really like to be a part of group where I can get feedback from other experienced people that share the same interest. If you have any recommendations, please let me know. Cheers!
https://itsybitsyfirstgradeteacher.com/sklo-fary-khrumtyt-chy-mozhna-yizdyty.html
I delight in, lead to I discovered just what I used to be having a look for. You’ve ended my 4 day lengthy hunt! God Bless you man. Have a nice day. Bye
http://chevrolet.com.ua/linzy-dlya-far-pozhovtily-yak-zapobihty-ta-vypravy.html
fingercheck
bluevine
aktual-krkn.ru — Надежный и удобный сервис — официальный сайт и подробный обзор даркнет-маркета Kraken. Официальный сайт kraken kra36.at — удобный сервис с множеством функций для пользователей. Узнайте больше и начните пользоваться прямо сейчас!
кракен ссылка, кракен ссылки, ссылка кракен, ссылка кракена, ссылки кракен, сайт кракена, кракен сайты, кракен сайт, сайт кракен, кракен отзывы, зеркала кракен, зеркала кракена, зеркало кракен, зеркало кракена, кракен зеркала, кракен зеркало, даркнет кракен, кракен даркнет, ссылка на кракен, ссылка на кракена, ссылки на кракен, кракен маркетплейс, маркетплейс кракен, кракен магазин, магазин кракен, кракены маркет, kraken ссылка, kraken ссылки, кракен маркет, вход кракен, кракен вход, кракен зайти, kraken зеркала, kraken зеркало, актуальная ссылка кракен, актуальная ссылка кракена, актуальные ссылки кракен, кракен актуальная ссылка, кракен актуальные ссылки, кракен ссылка актуальная, кракен ссылки актуальные, кракен как зайти, зайти на кракен, kraken сайты, сайт kraken, kraken сайт, кракен официальный сайт, официальный сайт кракен, кракен сайт официальный, официальный сайт кракена, сайт кракен официальный, сайт кракена официальный, как зайти на кракен, кракен ссылка тор, кракен тор ссылка, ссылка кракен тор, кракен рабочая ссылка, кракен рабочие ссылки, рабочая ссылка кракен, рабочие ссылки кракен, кракен даркнет маркет, кракен маркет даркнет, кракен сайт ссылка, сайт кракен ссылка, кракен площадка, площадка кракен, кракен сайт магазин, актуальная ссылка на кракен, актуальные ссылки на кракен, кракен маркет песня, песня кракен маркет, кракен зеркало рабочее, кракен рабочее зеркало, рабочее зеркало кракен, кракен официальная ссылка, кракен ссылка официальная, официальная ссылка кракен, ссылка кракена официальная, ссылки кракена официальные, кракен сайт что, kraken маркетплейс, маркетплейс kraken
Zentrader is an online platform focused on binary options trading and has been gaining attention among Japanese traders. Its interface is designed to be simple and intuitive, making it easy to use for beginners while also earning trust from experienced users.
With a minimum trade amount starting from 500 yen, it allows users to begin trading with lower risk. The platform offers full Japanese-language support, so users can get help whenever they have questions or concerns. Withdrawals are processed quickly, which contributes to high user satisfaction.
Since trading can be done directly in the browser, there’s no need to install any software, and the platform is accessible even from smartphones. Overall, the system is designed with simplicity and reliability in mind, making it a great choice for those new to binary options.
For more in-depth information and real user experiences, check out the trusted investment resource locamaga.jp. It’s a helpful reference if you’re considering using Zentrader.
онлайн курсы английского языка для подготовки к егэ
курсы подготовки к егэ по английскому языку
английский для детей 7 8 лет
занятия английским языком для детей 7 лет
What’s up all, here every person is sharing such experience, therefore it’s good to read this website, and I used to go to see this website every day.
https://technolex.com.ua/hermetyk-dlya-fary-na-morozi-vytrymaye-chy-ni.html
не знаешь где брать всегда актуальные ссылки ? не знаешь как перейти ? вот отличный ОФИЦИАЛЬНЫЙ САЙТ с самыми актуальными ссылками на marketplace Kraken https://aktual-krkn.ru/
kra36
сервис
удобство функции
официальный сайт Kraken
Кракен
маркетплейс Кракен
даркнет маркет
kraken официальный сайт
kraken market
kraken darknet
анонимные покупки
даркнет площадка
гидра альтернатива
kraken onion
kraken ссылка
darknet marketplace
kraken даркнет
кракен маркетплейс
кракен маркет обзор
кракен маркет отзывы
kraken ссылка
kraken сайт
kraken официальный сайт
kraken ссылка зеркало
актуальное зеркало kraken
kraken ссылка тор
kraken зеркало рабочее
kraken зеркало официальный
kraken зеркало даркнет
kraken зеркало тор
kraken зеркало 2kmp
kraken официальные ссылки
kraken onion ссылка
kraken ссылка для тору
kraken ссылка зеркало официальный
kraken зеркало krakentor site
kraken сайт зеркала
кракен ссылка kraken
kraken официальный сайт зеркало
kraken официальный сайт ссылка
kraken ссылка зеркало официальный сайт
kraken клирнет зеркало
kraken tor зеркало
kraken ссылка 2kmp
зеркала kraken kraken tor site
kraken darknet ссылка
kraken ссылка krakentor site
kraken зеркало 2kmp vip
kraken актуальные ссылки
kraken ссылка tor
kraken market ссылка
kraken зеркало 2kmp biz
kraken darknet зеркала
kraken darknet market ссылка
kraken darknet ссылка тор
ссылка kraken kraken tor site
kraken 2 зеркало
kraken ссылка 2kmp vip
рабочие ссылки kraken
сайт кракен kraken
kraken ссылка 2kmp biz
зеркало kraken market
kraken сайт официальный 2kmp
ссылка кракен kraken tor site
kraken darknet market зеркало
kraken ссылка зеркало рабочее
kraken market ссылка тор
kraken ссылка зеркало 2kmp
kraken darknet market ссылка тор
kraken ссылка зеркало krakentor site
kraken com зеркало
зеркала kraken 2kmp org
kraken ссылка kraken one com
kraken onion зеркала
сайт kraken darknet
зеркало kraken 2 kma biz
kraken сайт официальный krakentor site
kraken darknet официальный сайт
kraken зеркало рабочее krakentor site
ссылка на kraken kraken onion site
kraken кларнет зеркало kraken tor site
kraken зеркало рабочее 2kmp
kraken ссылка kraken clear com
kraken сайт kraken one com
kraken актуальные ссылки krakentor site
kraken ссылка onion 2kmp
kraken сайт официальный 2kmp biz
kraken ссылка зеркало официальный сайт 2kmp
kraken актуальные зеркала krakentor site
kraken зеркало тор ссылка
актуальное зеркало kraken kraken tor site
ссылка на кракен kraken one com
kraken даркнет зеркало krakentor site
kraken сайт kraken zerkalo
kraken рабочая ссылка тор
кракен сайт kraken one com
зеркало kraken тор ссылка рабочее
kraken сайт kraken zerkalo xyz
kraken ссылка onion krakentor site
kraken актуальные ссылки 2kmp
ссылка на кракен kraken onion site
kraken ссылка для тору vtor run
kraken сайт официальный 2kmp vip
kraken сайт kraken clear com
kraken зеркало тор krakentor site
kraken ссылка зеркало 2kmp biz
kraken сайт vtor run
kraken ссылка зеркало официальный сайт krakentor site
kraken ссылка зеркало 2kmp vip
kraken зеркала 2 kmp biz
ссылка на кракен kraken clear com
kraken casino зеркало
кракен сайт kraken clear com
зеркало кракен kraken tor site
kraken официальный сайт vtor run
kraken зеркало тор 2 kmp
kraken зеркало kraken2web com
актуальное зеркало kraken 2 kma biz
kraken актуальные зеркала 2kmp vip
ссылка на кракен kraken 7 one
kraken клирнет зеркало 2kmp biz
kraken ссылка онлайн
kraken даркнет зеркало 2kmp biz
kraken сайт анонимных
kraken зеркало рабочее 2kmp biz
kraken ссылка onion 2kmp biz
kraken сайт покупок
kraken зеркало онлайн
kraken сайт анонимных покупок
кракен сайт kraken zerkalo
кракен сайт kraken zerkalo xyz
kraken ссылка зеркало официальный сайт 2kmp biz
kraken даркнет зеркало 2kmp vip
kraken ссылка kraken2web com
kraken зеркало ссылка онлайн
kraken зеркало рабочее 2kmp vip
kraken актуальные ссылки 2kmp biz
kraken ссылка online
kraken ссылка tor wiki online
kraken ссылка зеркало официальный сайт 2kmp vip
kraken актуальные ссылки 2kmp vip
kraken ссылка на сайт
kraken зеркало тор 2 kmp biz
kraken сайт vk2
kraken casino зеркало рабочее
kraken клирнет зеркало 2kmp vip
ссылка на kraken kraken darknet top
кракен зеркало kraken 7 one
ссылка на кракен kraken darknet top
kraken зеркало тор 2 kmp vip
kraken зеркало kraken clear com
kraken ссылка kraken zerkalo xyz
зеркало kraken kraken onion site
kraken darknet ссылка kraken2web com
kraken официальный сайт k2tor
kraken зеркало krakendarknet top
сайт kraken тор
ссылка на кракен тор kraken 7 one
kraken клирнет зеркало 2kmp org
кракен ссылка kraken zerkalo
kraken ссылка 2krnk biz
kraken ссылка kraken7 one
актуальное зеркало kraken 2kmp org
кракен зеркало kraken one com
kraken ссылка onion 2kmp org
kraken ссылка onion 2kmp vip
площадка kraken ссылка
рабочая ссылка на кракен kraken 7 one
kraken зеркало 2kraken click
kraken ссылка тор kraken2web com
kraken ссылка зеркало vk2
актуальное зеркало kraken kraken onion site
кракен ссылка kraken zerkalo xyz
kraken сайт официальный 2kmp org
kraken зеркало 2krnk biz
kraken casino официальный сайт
kraken ссылка krakendarknet top
kraken официальные зеркала vk3
kraken market ссылка kraken2web com
kraken darknet ссылка тор kraken2web com
kraken ссылка тор kraken one com
kraken darknet зеркала kraken2web com
кракен зеркало kraken clear com
kraken darknet market ссылка kraken2web com
kraken сайт 2krnk biz
kraken зеркало dzen
кракен ссылка тор kraken one com
kraken зеркало тор 2kmp org
kraken зеркало krakenonion site
kraken ссылка онион
kraken сайт tor
актуальное зеркало kraken kraken zerkalo
kraken официальный сайт vk2
kraken ссылка зеркало 2kmp org
актуальное зеркало kraken kraken zerkalo xyz
сайт kraken onion
рабочее зеркало кракен kraken 7 one
кракен сайт ссылка kraken one com
kraken darknet market зеркало kraken2web com
kraken ссылка тор tor wiki online
kraken ссылка зеркало kraken2web com
kraken зеркало тор kraken7 one
kraken зеркало рабочее 2kmp org
ссылка на kraken 2kmp org
kraken официальный сайт vk3
kraken ссылка зеркало kraken 7 one
kraken onion ссылка tor wiki online
kraken вход на сайт
kraken зайти на сайт
kraken сайт krakendarknet top
кракен зеркало kraken zerkalo xyz
kraken ссылка тор 2kraken click
кракен вход ссылка kraken 7 one
kraken магазин ссылка
kraken darknet market ссылка тор kraken2web com
кракен сайт ссылка kraken clear com
kraken даркнет зеркало 2kmp org
kraken ссылка зеркало официальный сайт 2kmp org
kraken darknet market ссылка kraken7 one
kraken darknet ссылка 2krnk biz
kraken ссылка тор 2krnk biz
kraken актуальная ссылка onion
kraken сайт vk2 pro
кракен площадка ссылка kraken 7 one
kraken сайт kraken2web com
kraken зеркало форум
кракен зеркало тор kraken one com
kraken официальный сайт k2tor online
kraken ссылка зеркало vk2 pro
kraken darknet ссылка тор 2kraken click
ссылка на кракен тор kraken clear com
сайт онион kraken
кракен сайт зеркало kraken 7 one
kraken зеркало v5tor cfd
kraken darknet ссылка тор 2krnk biz
kraken сайт dzen
kraken оригинальная ссылка
kraken ссылка dzen
сайт кракен тор kraken one com
kraken ссылка krakenonion site
kraken официальные зеркала k2tor
kraken tor ссылка онлайн
kraken ссылка v5tor cfd
kraken ссылка на сайт тор
kraken сайт kr2web in
настоящий сайт kraken
kraken зеркало online
kraken актуальные ссылки 2kmp org
прямая ссылка на kraken
kraken оф сайт
kraken официальный сайт
используйте vpn!
Кракен Ссылка
Кракен Вход
Кракен Зайти
Ссылка на Кракен
Kra35.cc
Kra36.at
Kra34.cc
купить меф
купить гарик
Kra34.at
Kra33.cc
Kra33.at
Kra37.cc
Kra36.cc
Kra32.cc
Kra32.at
Kra38.cc
Kra39.cc
Kra33.cc
для дополнительной анонимности и безопасности рекомендуется использовать vpn-сервис. он скроет ваш ip-адрес и сделает ваше пребывание в интернете более безопасным.
будьте осторожны!?
kraken рабочая ссылка onion
kraken ссылка vk
кракен сайт ссылка kraken 11
ссылка на кракен kraken 9 one
kraken зеркало тор kraken2web com
кракен онион ссылка kraken one com
ссылка kraken 2 kma biz
ссылка на kraken торговая площадка
razer kraken сайт
kraken зеркало krakenweb one
kraken зеркало krakenweb3 com
kraken зеркало ссылка онлайн krakenweb one
kraken ссылка зеркало krakenweb one
kraken darknet market ссылка тор 2kraken click
kraken ссылка krakenweb one
kraken ссылка тор krakendarknet top
kraken casino зеркало kraken casino xyz
kraken darknet market зеркало v5tor cfd
kraken сайт зеркала kraken2web com
kraken даркнет ссылка
kraken зеркала kr2web in
kraken зеркало store
kraken darknet market ссылка тор v5tor cfd
kraken darknet market сайт
даркнет официальный сайт kraken
kraken ссылка зеркало рабочее kraken2web com
kraken зеркало тор ссылка kraken2web com
kraken маркетплейс зеркала
kraken официальные зеркала k2tor online
kraken darknet маркет ссылка каркен market
kraken 6 at сайт производителя 2
сайт кракен kraken darknet top
kraken клир ссылка
кракен ссылка kraken kraken2web com 3
ссылка на кракен тор kraken 9 one
kraken сайт анонимных покупок vtor run
kraken darknet market зеркало 2kraken click
kraken darknet market ссылка shkafssylka ru
kraken ссылка torbazaw com
kraken форум ссылка
площадка кракен ссылка kraken clear com
сайт kraken darknet kraken2web com
как зайти на маркетплейс кракен: официальные ссылки и зеркала.
полное руководство:
актуальная ссылка (через браузер):
официальная ссылка :
резервное зеркало:
как зайти на маркетплейс кракен: полное руководство
для входа на сайт кракена в даркнете требуется tor. это безопасный браузер:
перейдите на официальный сайт tor.
скачайте программу для вашей ос.
установите и запустите браузер.
используйте актуальные ссылки на кракен
ссылки на официальный сайт кракен часто обновляются. чтобы избежать фишинговых сайтов, используйте проверенные ресурсы для получения ссылок:
• актуальное зеркало кракена:
• зеркала сайта в клирнете и даркнете доступны для пользователей в любой точке мира.
авторизация
после перехода на сайт:
зарегистрируйтесь, если у вас еще нет аккаунта.
войдите в свой личный кабинет, используя логин и пароль.
для повышения безопасности активируйте двухфакторную аутентификацию.
но почему выбираю именно
сотни других платформ, тысячи товаров, но для меня больше, чем просто магазин. это место, где покупки превращаются в увлекательное путешествие.
знает, как важно быть уверенным в каждой покупке. полная защита сделок и дружелюбная поддержка создают чувство, будто вы находитесь в заботливых руках. надёжность? абсолютно.
почему именно
потому что здесь всё про вас: ваш стиль, ваш комфорт, ваша выгода. попробуйте, и вы поймёте, почему так много людей выбирают именно эту платформу!
советы по безопасности на кракене
используйте vpn
подключение через vpn повышает вашу анонимность, скрывая ip-адрес.
проверяйте ссылки
актуальные ссылки и зеркала кракен можно найти на проверенных форумах или официальных ресурсах. никогда не используйте непроверенные источники.
будьте внимательны к продавцам
читайте отзывы и выбирайте проверенных продавцов с высоким рейтингом.
кракен маркетплейс
кракен маркетплейс
кракен площадка
kra33.at
kra33.cc
kra34.cc
kra34.at
kra35.cc
kra36.at
kra36.cc
Kra36.at
kra37.cc
kra38.at
кракен маркетплейс ссылка
кракен площадка
кракен marketplace
кракен площадка ссылка
кракен даркнет стор
кракен darknet market зеркало
кракен даркнет площадка
кракен даркнет маркетплейс
кракен наркотики
кракен нарко
кракен наркошоп
кракен наркота
кракен порошок
кракен наркотики
кракен что там продают
кракен маркетплейс что продают
кракен покупка
какен купить
кракен купить мяу
кракен питер
кракен в питере
кракен москва
кракен в москве
кракен что продают
кракен это
кракен marke
кркен darknet market
кракен dark market
кракен market ссылка
кракен darknet market ссылк
кракен market ссылка тор
кракен даркнет маркет
кракен market тор
кракен маркет
платформа кракен
кракен торговая площадка
кракен даркнет маркет ссылка сайт
кракен маркет даркнет тор
кракен аккаунты
кракен заказ
диспуты кракен
как восстановить кракен
кракен даркнет не работает
как пополнить кракен
google authenticator кракен
рулетка кракен
купоны кракен
кракен зарегистрироваться
кракен регистрация
кракен пользователь не найден
кракен отзывы
ссылка кракен
кракен официальная ссылка
кракен ссылка на сайт
кракен официальная ссылка
кракен актуальные
кракен ссылка тор
кракен клирнет
кракен ссылка маркет
кракен клир ссылка
кракен ссылка
ссылка на кракен
кракен ссылка
кракен ссылка на сайт
кракен ссылка кракен
актуальная ссылка на кракен
рабочие ссылки кракен
кракен тор ссылка
ссылка на кракен тор
кракен зеркало тор
кракен маркет тор
кракен tor
кракен ссылка tor
кракен тор
кракен ссылка тор
кракен tor зеркало
кракен darknet tor
кракен тор браузер
кракен тор
кракен darknet ссылка тор
кракен ссылка на сайт тор
кракен вход на сайт
кракен вход
кракен зайти
кракен войти
кракен даркнет вход
кракен войти
где найти ссылку кракен
где взять ссылку на кракен
как зайти на сайт кракен
как найти кракен
кракен новый
кракен не работает
кракен вход
как зайти на кракен
кракен вход ссылка
сайт кракен
кракен сайт
кракен сайт что это
кракен сайт даркнет
что за сайт кракен
кракен что за сайт
Кракен официальный сайт
сайт кракен отзывы
кракен сайт
кракен официальный сайт
сайт кракен тор
кракен сайт ссылка
кракен сайт зеркало
кракен сайт тор ссылка
кракен зеркало сайта
зеркало кракен
адрес кракена
кракен зеркало тор
зеркало кракен даркнет
актуальное зеркало кракен
рабочее зеркало кракен
кракен зеркало
кракен зеркала
кракен зеркало
зеркало кракен market
актуальное зеркало кракен
кракен darknet
кракен даркнет ссылка
ссылка кракен даркнет маркет
кракен даркнет
кракен darknet
кракен даркнет
кракен dark
кракен darknet ссылка
кракен сайт даркнет маркет
кракен даркнет маркет ссылка тор
кракен даркнет тор
кракен текст рекламы
Kraken ссылка
Kraken Вход
Kraken зайти
Why users still make use of to read news papers when in this technological globe everything is accessible on web?
https://referatik.com.ua/sklo-fary-svoyimy-rukamy-instruktsiya-majstra.html
kra36—-at.com — Надежный и удобный сервис — официальный сайт и подробный обзор даркнет-маркета Kraken. Официальный сайт kraken kra36.at — удобный сервис с множеством функций для пользователей. Узнайте больше и начните пользоваться прямо сейчас!
кракен ссылка, кракен ссылки, ссылка кракен, ссылка кракена, ссылки кракен, сайт кракена, кракен сайты, кракен сайт, сайт кракен, кракен отзывы, зеркала кракен, зеркала кракена, зеркало кракен, зеркало кракена, кракен зеркала, кракен зеркало, даркнет кракен, кракен даркнет, ссылка на кракен, ссылка на кракена, ссылки на кракен, кракен маркетплейс, маркетплейс кракен, кракен магазин, магазин кракен, кракены маркет, kraken ссылка, kraken ссылки, кракен маркет, вход кракен, кракен вход, кракен зайти, kraken зеркала, kraken зеркало, актуальная ссылка кракен, актуальная ссылка кракена, актуальные ссылки кракен, кракен актуальная ссылка, кракен актуальные ссылки, кракен ссылка актуальная, кракен ссылки актуальные, кракен как зайти, зайти на кракен, kraken сайты, сайт kraken, kraken сайт, кракен официальный сайт, официальный сайт кракен, кракен сайт официальный, официальный сайт кракена, сайт кракен официальный, сайт кракена официальный, как зайти на кракен, кракен ссылка тор, кракен тор ссылка, ссылка кракен тор, кракен рабочая ссылка, кракен рабочие ссылки, рабочая ссылка кракен, рабочие ссылки кракен, кракен даркнет маркет, кракен маркет даркнет, кракен сайт ссылка, сайт кракен ссылка, кракен площадка, площадка кракен, кракен сайт магазин, актуальная ссылка на кракен, актуальные ссылки на кракен, кракен маркет песня, песня кракен маркет, кракен зеркало рабочее, кракен рабочее зеркало, рабочее зеркало кракен, кракен официальная ссылка, кракен ссылка официальная, официальная ссылка кракен, ссылка кракена официальная, ссылки кракена официальные, кракен сайт что, kraken маркетплейс, маркетплейс kraken
We’re prepared to fix the situation — a capable team equipped to tackle your plumbing emergency and return stability in your house!
Our quick assistance facilitates – decrease the need for expensive significant corrections later.
Discover our rapid and excellent assistance – at once!
kra36—-at.com — Надежный и удобный сервис — официальный сайт и подробный обзор даркнет-маркета Kraken. Официальный сайт kraken kra36.at — удобный сервис с множеством функций для пользователей. Узнайте больше и начните пользоваться прямо сейчас!
кракен ссылка, кракен ссылки, ссылка кракен, ссылка кракена, ссылки кракен, сайт кракена, кракен сайты, кракен сайт, сайт кракен, кракен отзывы, зеркала кракен, зеркала кракена, зеркало кракен, зеркало кракена, кракен зеркала, кракен зеркало, даркнет кракен, кракен даркнет, ссылка на кракен, ссылка на кракена, ссылки на кракен, кракен маркетплейс, маркетплейс кракен, кракен магазин, магазин кракен, кракены маркет, kraken ссылка, kraken ссылки, кракен маркет, вход кракен, кракен вход, кракен зайти, kraken зеркала, kraken зеркало, актуальная ссылка кракен, актуальная ссылка кракена, актуальные ссылки кракен, кракен актуальная ссылка, кракен актуальные ссылки, кракен ссылка актуальная, кракен ссылки актуальные, кракен как зайти, зайти на кракен, kraken сайты, сайт kraken, kraken сайт, кракен официальный сайт, официальный сайт кракен, кракен сайт официальный, официальный сайт кракена, сайт кракен официальный, сайт кракена официальный, как зайти на кракен, кракен ссылка тор, кракен тор ссылка, ссылка кракен тор, кракен рабочая ссылка, кракен рабочие ссылки, рабочая ссылка кракен, рабочие ссылки кракен, кракен даркнет маркет, кракен маркет даркнет, кракен сайт ссылка, сайт кракен ссылка, кракен площадка, площадка кракен, кракен сайт магазин, актуальная ссылка на кракен, актуальные ссылки на кракен, кракен маркет песня, песня кракен маркет, кракен зеркало рабочее, кракен рабочее зеркало, рабочее зеркало кракен, кракен официальная ссылка, кракен ссылка официальная, официальная ссылка кракен, ссылка кракена официальная, ссылки кракена официальные, кракен сайт что, kraken маркетплейс, маркетплейс kraken
https://t.me/s/Magic_1win
convert USDT in France
Здравствуйте!
Долго думал как поднять сайт и свои проекты и нарастить CF cituation flow и узнал от друзей профессионалов,
крутых ребят, именно они разработали недорогой и главное буст прогон Xrumer – https://www.bing.com/search?q=bullet+%D0%BF%D1%80%D0%BE%D0%B3%D0%BE%D0%BD
Прогон ссылок через Xrumer увеличивает внешнюю массу сайта. Эффективность прогона Xrumer подтверждается результатами. Массовый линкбилдинг для сайта улучшает позиции в поиске. Программы для автоматического постинга ускоряют работу. Как поднять показатели Ahrefs становится более доступным.
сервисы для анализа сео, продвижение сайтов в москве топ яндекса, Xrumer для массового линкбилдинга
линкбилдинг пример, способ сео, топ seo продвижение цены
!!Удачи и роста в топах!!
нержавеющие ограждения Ограждения из нержавеющей стали – это современное и стильное решение для балконов, террас и лестниц. Они отличаются высокой прочностью, долговечностью и привлекательным внешним видом.
ограждение из нержавеющей стали цена Поручень – это часть перил, за которую держатся при подъеме или спуске. Он должен быть удобным для захвата и обеспечивать надежную опору.
https://trip-scan.win/ Tripscan top – это рейтинг лучших мест для посещения, основанный на реальных отзывах и оценках пользователей, гарантия получения ярких и незабываемых впечатлений.
Экономичные решения от http://www.metallicheskij-shtaketnik.ru/ — заборы из металлоштакетника от 990 руб./п.м. Стандартные цвета (коричневый, зеленый, графит), толщина металла 0,45 мм. Быстрая доставка — в течение 24 часов по Москве. При заказе от 50 п.м. — бесплатный монтаж ворот и калитки.
https://sonturkhaber.com/
http://www.rosmed.ru/annonce/show/3892/Kak_podgotovitsya_k_pervomu_vizitu_v_stomatologicheskuyu_kliniku
сайт трипскан Трипскан вход – это простота и безопасность, ваш личный кабинет всегда под рукой.
https://sonturkhaber.com/
Canlı Casino ve Bahis Siteleri. Deneme Bonusu Veren Siteler arasında yatırım şartsız deneme bonusu sunanlar, bahis severler için oldukça cazip fırsatlar
Beneficial treatment is attainable if you best price for viagra 100mg is easy. 20mg cialis price
Consider first-rate online pharmacies the moment you decide to cheap viagra 100mg pills when you order on this site levitra 20mg used for
https://belygorod.ru/vote/pgs/?promokod-na-1xbet.html
kra36—-at.com — Надежный и удобный сервис — официальный сайт и подробный обзор даркнет-маркета Kraken. Официальный сайт kraken kra36.at — удобный сервис с множеством функций для пользователей. Узнайте больше и начните пользоваться прямо сейчас!
кракен ссылка, кракен ссылки, ссылка кракен, ссылка кракена, ссылки кракен, сайт кракена, кракен сайты, кракен сайт, сайт кракен, кракен отзывы, зеркала кракен, зеркала кракена, зеркало кракен, зеркало кракена, кракен зеркала, кракен зеркало, даркнет кракен, кракен даркнет, ссылка на кракен, ссылка на кракена, ссылки на кракен, кракен маркетплейс, маркетплейс кракен, кракен магазин, магазин кракен, кракены маркет, kraken ссылка, kraken ссылки, кракен маркет, вход кракен, кракен вход, кракен зайти, kraken зеркала, kraken зеркало, актуальная ссылка кракен, актуальная ссылка кракена, актуальные ссылки кракен, кракен актуальная ссылка, кракен актуальные ссылки, кракен ссылка актуальная, кракен ссылки актуальные, кракен как зайти, зайти на кракен, kraken сайты, сайт kraken, kraken сайт, кракен официальный сайт, официальный сайт кракен, кракен сайт официальный, официальный сайт кракена, сайт кракен официальный, сайт кракена официальный, как зайти на кракен, кракен ссылка тор, кракен тор ссылка, ссылка кракен тор, кракен рабочая ссылка, кракен рабочие ссылки, рабочая ссылка кракен, рабочие ссылки кракен, кракен даркнет маркет, кракен маркет даркнет, кракен сайт ссылка, сайт кракен ссылка, кракен площадка, площадка кракен, кракен сайт магазин, актуальная ссылка на кракен, актуальные ссылки на кракен, кракен маркет песня, песня кракен маркет, кракен зеркало рабочее, кракен рабочее зеркало, рабочее зеркало кракен, кракен официальная ссылка, кракен ссылка официальная, официальная ссылка кракен, ссылка кракена официальная, ссылки кракена официальные, кракен сайт что, kraken маркетплейс, маркетплейс kraken
Подшипники от производителей Купить подшипники непосредственно у производителя – значит избежать посредников и получить продукцию из первых рук, с полной гарантией качества и соответствия требованиям.
Доброго!
Долго ломал голову как поднять сайт и свои проекты и нарастить ИКС Яндекса и узнал от успещных seo,
крутых ребят, именно они разработали недорогой и главное буст прогон Хрумером – https://www.bing.com/search?q=bullet+%D0%BF%D1%80%D0%BE%D0%B3%D0%BE%D0%BD
Автоматический прогон статей облегчает работу специалистов. Использование Xrumer в 2025 обеспечивает стабильный рост DR. Линкбилдинг для повышения DR улучшает позиции сайта. SEO рассылки форумов помогают охватывать больше ресурсов. Xrumer: практические примеры показывают эффективность методов.
сео оптимизация правила, начинающему seo, Форумный линкбилдинг с Xrumer
Секреты работы с Xrumer, продвижение сайта топ, как поисковое продвижение сайта
!!Удачи и роста в топах!!
https://vareview.net/art/poverhnostnostyiele.html
https://trentetrente.com/img/pgs/udivitelynye_kitoobraznye_mify_i_realynosty.html
https://sdch.org.in/pages/unikalynye_peshehodnye_marshruty_mira_puty_k_nezabyvaemym_vpechatleniyam.html
http://orthodoxy.ru/wp-includes/articles/effektivnye_sprei_ot_domashnih_paukov.html
подобрать подшипник по размерам онлайн Цилиндрический подшипник – тип подшипника, отличающийся высокой грузоподъемностью и способностью выдерживать радиальные нагрузки.
People like to use the Internet to top 10 viagra tablets at low prices, you’ll need to compare offers order generic levitra online
Get the facts on all medicines when you que es tadalafil online instead of buying medicine at the pharmacy. cialis headache
Be assured of the correct price of viagra dosage by weight is the biggest trend . long time sex capsule viagra
https://www.blackbox.com/en-nl/landingpages/thank-you-ucc-premise-cloud-hybrid-whitepaper/real-time-smart-provider-education-communication
travesti porno yeni|
https://u.zhugeapi.com/v2/adtrack/c/7ae81b8d2d7c43c28f01073578035f39/pr0455/m10706/p10004/c10003?url=https://2home.co/%3Fp=15432
beyaz tenli anal porno
Tron Staking
ЗИМ — автомобиль-легенда СССР.
Here is my blog post :: https://www.royalholloway.ac.uk/
https://www.silverwooddental.com/home/tooth7/
Производство шариковых подшипников Цилиндрический подшипник: высокая грузоподъемность
https://service116.ru/
купить игровой компьютер за 75000 : Игровой компьютер комплект: Все в одном.
tripskan Трипскан: Легкость и удобство в каждой детали
дешевый компьютер для игр : Сколько стоит хороший игровой ПК: Узнайте стоимость игрового компьютера с достойными характеристиками.
Keep this going please, great job!
Seattle Town Car
Some cialis goodrx offered by a top online pharmacy at low prices cialis and blood pressure
After you compare offers, you can levitra kruidvat online instead of buying medicine at the pharmacy. cialis dosage chart
https://разработка.site/
https://tripscan41.cc/ Зарегистрируйтесь на Tripscan и создайте свой уникальный профиль путешественника. Сохраняйте любимые маршруты, делитесь впечатлениями с друзьями и получайте персональные рекомендации, основанные на ваших предпочтениях.
Азия Переговоры между Путиным и Зеленским – это не просто дипломатическая встреча. Это попытка найти компромисс между двумя противоположными позициями, учесть интересы всех сторон и предотвратить дальнейшую эскалацию конфликта. Политика требует мудрости и дальновидности, готовности к уступкам и умения находить общие точки соприкосновения. Финансовая стабильность – ключевой фактор для восстановления экономики и обеспечения благосостояния граждан. Европа, Азия и Америка должны объединить усилия для преодоления экономических вызовов и создания устойчивой финансовой системы.
Excellent deals can be used to efectos secundarios del viagra ? Should I seek a doctor’s advice? viagra 50 mg
https://www.apelsin.su/wp-includes/articles/promokod_240.html
more information on erectile dysfunction, visit our website at does viagra have side effects that you probably didn’t know. is viagra bad for you
смешные истории из жизни обычных людей Секс истории обычных людей Интимная жизнь – важная часть человеческого опыта. Истории о любви, страсти, желании и разочаровании раскрывают перед нами разные грани отношений и помогают лучше понять себя и своего партнера. Они учат нас открытости, доверию и умению говорить о своих чувствах.
cefadroxil antibiotic https://duricefzsu.com/#
красивые места на кавказе Однодневные туры по Дагестану
Книги Цитаты, как вечные истины
история обычных людей книги Секс истории обычных людей Интимная жизнь – важная часть человеческого опыта. Истории о любви, страсти, желании и разочаровании раскрывают перед нами разные грани отношений и помогают лучше понять себя и своего партнера. Они учат нас открытости, доверию и умению говорить о своих чувствах.
южный дагестан достопримечательности Поездка на Кавказ
Книги Книги, изменяющие жизни
Always come here first for viagra 100 is the best part about the internet. how to make levitra more effective
wood fence on steel posts Best Wood for Fence Budgetary constraints often influence material selection. However, prioritize long-term value over immediate cost savings; a durable fence safeguards your investment.
umsuka
обучение кайтсёрфингу
кайт
http://leydis16.phorum.pl/viewtopic.php?p=752588#752588
https://scrapbox.io/allblogs/Double_Your_Fun_with_1xBet_Official_Promo_Code_1X200BIG
программа для учета гсм Управление автопарком и специализированной техникой требует особого внимания. Эффективный учет топлива, технического обслуживания и рабочего времени водителей помогает оптимизировать расходы и повысить производительность.
https://share.evernote.com/note/838444ff-c3f1-b82e-49aa-8fd6374e2585
TESK TK 200-12.5/4 Насос вертикальный циркуляционный Ин-лайн 22 кВт, 12 бар, 3×380 В, 50 Гц, IE3
out the price reductions on offer when using this site for stromectol ireland is. ivermectin dosage for humans cancer
https://email-support.hellobox.co/7428964/1xbet-promo-codes-for-revolutionary-betting-in-2026
Finding safe bupropion price illegally. bupropion tinnitus
for the drugs you need and get a low price of ivermectin and fenbendazole for humans , always compare prices before you place an order, Лучшие stromectol brand
Hi there are using WordPress for your site platform? I’m new to the blog world but I’m trying to get started and create my own. Do you require any coding expertise to make your own blog? Any help would be really appreciated!
There is no need to spend a lot of cash when you can wellbutrin classification , you can do it online. wellbutrin doses
https://www.diigo.com/user/miturani2008?query=%231xbetpromocodefreebetnodeposit
В каталоге – заборы из металлического штакетника фото и цены реальных объектов. 50+ выполненных работ.
Always ask if you get something new when you spironolactone mechanism of action . Read more about its disease prevention. aldactone acne
Biggest discounts for synthroid dose calculator pills guaranteed to buyers here synthroid 112 mcg tablet
https://www.trub-prom.com/catalog/truby_bolshogo_diametra/530kh8/
Работа проституткой в Тюмени Высокооплачиваемая работа для девушек в Тюмени: Почувствуй себя королевой этого мира! Эксклюзивные предложения для избранных. Работа, где твой внешний вид и умение общаться – это твоя валюта. Высокий доход, конфиденциальность и индивидуальный подход к каждой девушке. Забудь о серых буднях и окунись в мир роскоши и внимания. С нами ты сможешь реализовать самые смелые мечты и обеспечить себе безбедное будущее.
https://digital-downloads-app.com/
цветы в москве недорого Забудьте о хлопотах, связанных с поиском и транспортировкой цветов. Доверьте доставку профессионалам, которые знают свое дело и гарантируют своевременную доставку в идеальном состоянии. Букет цветов в Москве: Классический Способ Выразить Самые Трепетные Чувства
Fildena super active kaufen https://bento.me/fildena-100
I know this site gives quality dependent posts and extra information, is there any other website which presents these kinds of data in quality?
Металлический штакетник с установкой от http://metallicheskij-shtaketnik.ru — это надежность и долговечность. Толщина металла 0,5 мм, полимерное покрытие. Высота 1,5-2,5 м. Цена от 1300 руб./п.м. При заказе от 100 п.м. — бесплатная доставка по области. Гарантия на монтаж — 3 года.
I think everything said made a bunch of sense. But, think on this, suppose you were to create a killer headline? I ain’t suggesting your content is not solid., but what if you added something to possibly get people’s attention? I mean Ukraine is a little boring. You might glance at Yahoo’s front page and see how they create news headlines to get viewers to click. You might add a related video or a pic or two to grab readers interested about what you’ve written. Just my opinion, it could make your posts a little bit more interesting.
I’m not sure why but this site is loading incredibly slow for me. Is anyone else having this issue or is it a issue on my end? I’ll check back later and see if the problem still exists.
https://delavore.com.ua/sklo-fary-tse-prosto-yakshcho-znaty-nyuansy.html
https://fixed-float.to
Peculiar article, totally what I needed.
ball bearings for sale
https://sindcomcf.com.br/pgs/estrat_gias_avan_adas_para_maximizar_ganhos_em_gates_of_olympus.html
https://svoizabor.com/news/?1xbet_promokod_besplatno_bonus.html
Прокат авто Краснодар жд Аренда авто в Краснодаре: Комфорт и удобство в каждом километре. Откройте для себя Краснодарский край с максимальным комфортом и свободой передвижения благодаря услуге аренды авто в Краснодаре. Мы предлагаем широкий выбор автомобилей различных марок и моделей, от экономичных малолитражек до просторных минивэнов, чтобы удовлетворить любые ваши потребности. Наши автомобили проходят регулярное техническое обслуживание и всегда находятся в отличном состоянии. Аренда авто в Краснодаре – это идеальное решение для туристов, деловых путешественников и местных жителей, которые ценят комфорт и независимость. Забронируйте свой автомобиль прямо сейчас и наслаждайтесь поездками по Краснодарскому краю!
review sites personally visit a pharmacy before approving for mirtazapine mechanism of action you can save even more when you get generic. mirtazapine for dogs appetite stimulant
оргонит из смолы Что такое оргонит: Устройство, которое, согласно некоторым верованиям, преобразует негативную энергию.
регистрация Обзор официального сайта и приложения казино. В мире онлайн-гемблинга важно выбирать не только интересные игры, но и надежную платформу. 1win (или 1вин) — это многофункциональный игровой клуб, который объединяет в себе казино, букмекерскую контору и тотализатор. В этом обзоре мы подробно разберем, как начать играть, какие бонусы ждут новых игроков и как получить доступ к ресурсу через официальный сайт и зеркала. Поиск рабочего официального сайта 1win — первый шаг для каждого игрока. Из-за ограничений в некоторых регионах прямой вход на основной ресурс может быть затруднен. В этом случае на помощь приходят зеркала — точные копии сайта с другим адресом. Они полностью безопасны и позволяют получить доступ к аккаунту и всем функциям. Актуальные ссылки на зеркала лучше всего искать в официальных сообществах проекта или у партнеров. Процесс регистрации в 1win занимает пару минут. Доступно несколько способов: через email, номер телефона или аккаунт в социальных сетях. Но самый важный шаг — это активация промокода. Ввод специального кода при создании аккаунта значительно увеличивает стартовый бонус на первый депозит. Не пропускайте этот этап, чтобы начать игру с максимально возможным банкроллом. Для тех, кто предпочитает играть с телефона, 1win предлагает удобное мобильное приложение. Его можно скачать прямо с официального сайта в формате APK файла для устройств Android. Владельцы iOS также могут найти способ установить программу. Приложение повторяет все функции полной версии сайта: от регистрации и ввода промокода до игры в слоты и live-ставок. Это идеальный выбор для игры в любом месте. 1win стабильно входит в топ рейтингов лучших онлайн-казино по нескольким причинам: Огромная игровая коллекция: Сотни слотов, настольные игры, live-дилеры. Щедрая программа лояльности: Не только приветственный бонус, но и кешбэк, фриспины, турниры. Безопасность и поддержка: Лицензия, шифрование данных и круглосуточная служба заботы о клиентах. 1win — это современная и надежная игровая площадка, которая предлагает полный комплект услуг от казино до ставок на спорт. Не забудьте использовать промокод при регистрации, чтобы получить максимальную выгоду от игры. А если возникнут трудности с доступом — воспользуйтесь рабочим зеркалом или скачайте официальное приложение.
KRAKEN – Ваша безопасность и анонимность на aktual-krkn.ru
aktual-krkn.ru — официальный переходник даркнет-маркета Kraken.
Добро пожаловать на kra36—-at.com, где приватность и безопасность являются главным приоритетом. Официальный сайт kraken kra37.at — сохрани список актуальных зеркал. Переходите на aktual-krkn.ru и начните пользоваться прямо сейчас!
кракен, kraken, сайт кракен, ссылка кракен, кракен ссылка, кракен сайт, кракен официальный сайт, официальный сайт кракен, кракен ссылка официальная, кракен актуальная ссылка
*Полная анонимность и защита данных
Система безопасности KRAKEN обеспечивает полную конфиденциальность. Передовые технологии шифрования для защиты ваших данных и транзакций.
актуальная ссылка на кракен, рабочая ссылка кракен, как зайти на кракен, кракен как зайти, вход кракен, кракен вход, зайти на кракен, кракен зайти, зеркало кракен, кракен зеркало
*Удобство использования
Простая навигация, мощная система и дизайн aktual-krkn.ru делают использование KRAKEN комфортным на любых устройствах.
кракен рабочее зеркало, рабочее зеркало кракен, зеркала кракен, кракен зеркала, даркнет кракен, кракен даркнет, маркетплейс кракен, кракен маркетплейс, площадка кракен, кракен площадка
*Гарантии безопасности и круглосуточная поддержка
KRAKEN гарантирует защиту покупателей и продавцов. Служба поддержки kra36—-at.com работает 24/7 для решения любых вопросов.
магазин кракен, кракен магазин, кракен маркет, кракены маркет, кракен даркнет маркет, кракен маркет даркнет, кракен отзывы, кракен сайт что, кракен ссылка тор, ссылка кракен тор
https://imagecms.net/wp-content/pgs/code-promo-melbet_bonus-sportifs-et-casino.html
https://popugaitut.ru
A motivating discussion is worth comment. I think that you ought to publish more on this topic, it might not be a taboo subject but usually people don’t discuss these issues. To the next! Cheers!!
After I originally commented I seem to have clicked on the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I receive four emails with the same comment. There has to be a means you can remove me from that service? Thank you!
Hi there, its pleasant paragraph about media print, we all be aware of media is a great source of data.
Hello, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam comments? If so how do you prevent it, any plugin or anything you can recommend? I get so much lately it’s driving me crazy so any support is very much appreciated.
http://avteon.ru
You’re so cool! I do not suppose I’ve truly read anything like this before. So wonderful to find somebody with genuine thoughts on this topic. Seriously.. many thanks for starting this up. This site is something that is needed on the internet, someone with a little originality!
online casino cz CZ Casino Online: Najdete si idealni online kasino s ceskou licenci. Recenze, porovnani bonusu a tipy pro zodpovedne hrani.
Hey there, I think your website might be having browser compatibility issues. When I look at your website in Safari, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, amazing blog!
зеркало кракен
Hmm is anyone else experiencing problems with the pictures on this blog loading? I’m trying to find out if its a problem on my end or if it’s the blog. Any suggestions would be greatly appreciated.
сайт кракен
регистрация в Минпромторге
https://hahah.ru/interesno/19-neobychnyx-veshhej-kotorye-smogut-vas-udivit.html
bs2best
https://usk-rus.ru/ Урал Строй Комплект – Наша компания занимается комплектацией строительных объектов, нефтегазового производства и не только. Одно из главных направлений работы – это гражданское строительство, где наши задачи – поставка металлических изделий и конструкций, труб, сыпучих строительных смесей, других стройматериалов. Также мы поставляем клиентам геосинтетические материалы для дорожного строительства, оборудование для нефтегазовой отрасли и многое другое под запрос. И все это – напрямую с заводов, с которыми у нас заключены официальные соглашения.
Wonderful, what a webpage it is! This web site presents useful data to us, keep it up.
https://kra39at.org/
bs2best at
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this. Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
kra39 at
KRAKEN – Ваша безопасность и анонимность на vhod-aktual.ru
vhod-aktual.ru — официальный переходник даркнет-маркета Kraken.
Добро пожаловать на kra37.help, где приватность и безопасность являются главным приоритетом. Официальный сайт kraken kra38.at — сохрани список актуальных зеркал. Переходите на vhod-aktual.ru и начните пользоваться прямо сейчас!
кракен, kraken, сайт кракен, ссылка кракен, кракен ссылка, кракен сайт, кракен официальный сайт, официальный сайт кракен, кракен ссылка официальная, кракен актуальная ссылка
+ Полная анонимность и защита данных
Система безопасности KRAKEN обеспечивает полную конфиденциальность. Передовые технологии шифрования для защиты ваших данных и транзакций.
актуальная ссылка на кракен, рабочая ссылка кракен, как зайти на кракен, кракен как зайти, вход кракен, кракен вход, зайти на кракен, кракен зайти, зеркало кракен, кракен зеркало
+ Удобство использования
Простая навигация, мощная система и дизайн vhod-aktual.ru делают использование KRAKEN комфортным на любых устройствах.
кракен рабочее зеркало, рабочее зеркало кракен, зеркала кракен, кракен зеркала, даркнет кракен, кракен даркнет, маркетплейс кракен, кракен маркетплейс, площадка кракен, кракен площадка
+ Гарантии безопасности и круглосуточная поддержка
KRAKEN гарантирует защиту покупателей и продавцов. Служба поддержки kra37.help работает 24/7 для решения любых вопросов.
магазин кракен, кракен магазин, кракен маркет, кракены маркет, кракен даркнет маркет, кракен маркет даркнет, кракен отзывы, кракен сайт что, кракен ссылка тор, ссылка кракен тор
En iyi deneme bonusu veren siteler ve popüler casino siteleri ile yüksek kazanç fırsatlarını keşfedin. Yeni siteler ve güncel bonuslar sizi bekliyor.
https://kamagruz.ru
NV casino offers a wide range of online slots, live dealer games, and secure payment methods. New players can claim up to €2000 in bonuses and 225 free spins.
casino NV
I constantly spent my half an hour to read this web site’s content all the time along with a mug of coffee.
beste quoten sportwetten
https://economist.georgiatoday.ge/
https://www.aufzu.de/scripts/pages/?poshagovyy_dizayn_kuhni__1.html
элитные индивидуалки уфы элитный эскорт в сипайлово
https://popugaitut.ru
https://www.mss-recruitment.com/wp-includes/pgs/?1xbet_promo_code_nigeria_2021.html
May I simply just say what a relief to find somebody who actually understands what they’re talking about on the web. You definitely understand how to bring a problem to light and make it important. More and more people need to look at this and understand this side of your story. I was surprised you aren’t more popular given that you surely have the gift.
https://lkra39.at/
Heya superb blog! Does running a blog such as this require a massive amount work? I have virtually no knowledge of computer programming but I had been hoping to start my own blog soon. Anyway, should you have any recommendations or tips for new blog owners please share. I know this is off subject but I just had to ask. Thank you!
kra39 at
Онлайн обучение крипто заработку Курс криптовалюты с заработком: преобразуйте свои знания в реальные деньги! Наш курс научит вас прибыльным стратегиям трейдинга и инвестирования в криптовалюты.
buchmacher pferderennen
Казино Vavada считается одним из лидеров.
Бездепозитные бонусы дают возможность играть без вложений.
Активности для игроков дают шанс на выигрыш.
Каталог развлечений остается актуальным.
Вход доступен быстро, поэтому можно сразу активировать бонусы.
Узнай больше здесь: vavada казино рабочее зеркало сегодня
ветеринарная клиника сочи круглосуточно Ветеринарные клиники в Сочи: Сравните и выберите лучшую клинику для своего питомца. Мы предлагаем сравнение ветеринарных клиник в Сочи, чтобы помочь вам выбрать ту, которая соответствует вашим потребностям и бюджету.
tangiers casino review australia
https://www.imdb.com/list/ls4788396936/
таможенный брокер сб карго Для юридических лиц, занимающихся внешнеэкономической деятельностью, мы предлагаем комплексные решения по таможенному оформлению. Мы поможем вам оптимизировать таможенные платежи, избежать штрафов и санкций, а также обеспечим соответствие требованиям таможенного законодательства. С нами ваш бизнес будет защищен!
Беседка с мягкими окнами Мягкие окна цена за м2: Узнайте актуальную цену за м2 мягких окон и планируйте свой бюджет. Мы предлагаем прозрачную ценовую политику и выгодные условия сотрудничества.
Prevention is better than cure for ED. Click this link http://ivermectinvsstromectol.com/ through a mail order system is now very popular. ivermectin buy online for humans
игровые автоматы 777 Игровые автоматы на деньги: вращайте барабаны и получайте реальные выигрыши Игровые автоматы на деньги – это захватывающий мир азарта, где каждый спин может принести вам реальный выигрыш. В отличие от бесплатных демо-версий, игра на деньги открывает двери к настоящим денежным призам, которые могут изменить вашу жизнь. Однако, важно помнить, что азартные игры несут в себе риск, и играть следует ответственно, установив лимит на свои расходы и не превышая его. Современные игровые автоматы предлагают разнообразие тематик и функций, от классических фруктовых слотов до захватывающих видеоигр с бонусными раундами и прогрессивными джекпотами. Выбирайте игру по своим предпочтениям и наслаждайтесь атмосферой азарта, зная, что каждый спин может стать выигрышным. Перед тем, как начать играть на деньги, ознакомьтесь с правилами и условиями выбранного игрового автомата, а также с политикой казино. Убедитесь, что казино имеет лицензию и хорошую репутацию, чтобы защитить свои средства и избежать мошенничества.
Игровая площадка Вавада привлекает внимание пользователей.
Промокоды и бонусы делают старт комфортнее.
Активности для игроков делают процесс динамичным.
Каталог развлечений включает топовых провайдеров.
Регистрация простая, и сразу начать играть.
Узнай больше здесь: https://stoporme.org/
ginecologie Titan
https://impossible-studio.ghost.io/kak-vybrat-luchshii-vpn-siervis-podrobnoie-rukovodstvo/ Новый лонгрид про Youtuber VPN! Узнайте, как смотреть YouTube и другие платформы без лагов и блокировок. Подключайте до 5 устройств на одной подписке, тестируйте сервис бесплатно 3 дня и платите всего 290? в первый месяц вместо 2000? у конкурентов. Серверы в Европе — ваши данные защищены от российских властей.
http://rusremontpro.ru/
beste sportwetten strategie
Уборка и расчистка участка Ремонт колодцев: восстановление работоспособности и продление срока службы Ремонт колодцев – это восстановление работоспособности и продление срока службы колодца. Ремонт колодцев может включать в себя замену поврежденных элементов, укрепление стенок и другие работы.
pferderennen dortmund wetten
https://impossible-studio.ghost.io/kak-vybrat-luchshii-vpn-siervis-podrobnoie-rukovodstvo/ Новый лонгрид про Youtuber VPN! Узнайте, как смотреть YouTube и другие платформы без лагов и блокировок. Подключайте до 5 устройств на одной подписке, тестируйте сервис бесплатно 3 дня и платите всего 290? в первый месяц вместо 2000? у конкурентов. Серверы в Европе — ваши данные защищены от российских властей.
sportwetten ohne lizenz
Experience the ultimate relaxation with Hiso Massage’s best Nuru massage in Sukhumvit 31, Bangkok, Thailand. Our skilled therapists use premium Nuru gel for smooth, full-body gliding, relieving stress, tension, and promoting wellness. Enjoy a private, luxurious, and unforgettable massage experience today.
best nuru massage
https://it-struktura.ru/ru-ru/
mostbet casino Casinos ohne Steuer
?Actualiza su contenido frecuentemente el mundo de escorts?
A common way to save money and https://metoprololvslopressor.com/ . Also offer free shipping!
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Исследовать вопрос подробнее – https://quick-vyvod-iz-zapoya-1.ru/
Affordable prices can be found to http://www.synthroidvslevothyroxine.com as a successful option.|
Купить реплику часов Ролекс Реплика одежды от известных брендов – это шанс выглядеть модно и стильно, не переплачивая за лейбл.
Because the admin of this website is working, no question very rapidly it will be well-known, due to its feature contents.
online casinos
Enjoy the authentic nuru massage Bangkok
experience designed for comfort, intimacy, and total rejuvenation.
Experience the ultimate relaxation with Hiso Massage
offering professiona
coverage you have now.Lock in the best deal on synthroidvslevothyroxine.com ? Shop with us.
I grasp the manner scary the situation strikes whenever water puts their home together with kin’s security at risk.
However you’re never isolated.
We will be present aiming to defend their residence plus such comfort belonging to one’s household life, performing carefully as well as securely so that everything yourself value stays whole.
The crew responds quickly toward halt harm as well as prevent mold, giving somebody calm regarding consciousness.
Also supported by such nonstop help, one always possess somebody close to one’s company — prepared aiming to support one preserve their household guarded as well as yours property supplied through ease.
Find peace in your home – Call: 8338561951
When I stumbled upon spanking video, I was blown away! The spanking-themed artwork and illustrations are so creative and detailed. If you love unique art with a spanking twist, this site is definitely worth checking out and discussing with fellow enthusiasts!
https://qiita.com/1xbet-promo-code
трипскан вход Tripscan зеркало: “Tripscan зеркало” относится к альтернативным веб-адресам или копиям сайта Tripscan, которые создаются для обеспечения доступности сервиса в случае блокировок основного домена или технических проблем. Зеркала сайта Tripscan позволяют пользователям получить доступ к тем же функциям и данным, что и на основном сайте, даже если основной домен по каким-либо причинам недоступен. Использование зеркал является распространенной практикой для онлайн-сервисов, которые сталкиваются с проблемами доступа из-за цензуры, блокировок или технических сбоев. Пользователи могут найти актуальные зеркала Tripscan на форумах, в социальных сетях или через поисковые системы. Важно убедиться в подлинности зеркала перед вводом личной информации, чтобы избежать мошенничества.
контент для бизнеса Продвижение бренда в интернете / Продвижение компании в интернете: Подчеркивают необходимость онлайн-присутствия и продвижения для бизнеса. Важно предложить комплексные решения по продвижению брендов и компаний в интернете, включая SEO, SMM, контент-маркетинг, таргетированную рекламу, контекстную рекламу и многое другое. Необходимо учитывать особенности каждой платформы и разрабатывать индивидуальные стратегии для каждой компании.
https://community.databricks.com/t5/user/viewprofilepage/user-id/153816 isotroin 30 mg uses
Consider online specials and http://mirtazapineinfolive.com/ at low prices always available through this specialist site
діагностика варильної панелі у Львові
лечение депрессии у психиатра психотерапевта Страдаете от выгорания на работе или в бизнесе? Обратитесь к квалифицированному психотерапевту. Индивидуальная программа для восстановления сил и мотивации.
газовое пожаротушение мгп Газовое пожаротушение МГП Газовое пожаротушение с использованием модулей газового пожаротушения (МГП) является одним из наиболее эффективных способов защиты объектов от пожара. МГП представляют собой автономные устройства, содержащие огнетушащее вещество (ОТВ) под давлением, оснащенные системой выпуска ОТВ при срабатывании датчиков пожарной сигнализации. Преимущества газового пожаротушения с использованием МГП: Эффективность. Газовые ОТВ быстро и эффективно подавляют горение, проникая в труднодоступные места и не оставляя следов. Безопасность для оборудования. Газовые ОТВ не наносят вреда электронному оборудованию, документам и ценностям, что делает их идеальными для защиты серверных, архивов, музеев. Автоматизация. МГП интегрируются с системой пожарной сигнализации, обеспечивая автоматическое обнаружение и тушение пожара без участия человека. Удобство монтажа и обслуживания. МГП легко устанавливаются и обслуживаются, не требуя сложной инфраструктуры. Типы газовых ОТВ, используемых в МГП: Инертные газы (азот, аргон, углекислый газ). Снижают концентрацию кислорода в зоне горения, прекращая процесс горения. Хладоны (HFC-227ea, FK-5-1-12). Ингибируют (замедляют) химические реакции горения. Компоненты системы газового пожаротушения с МГП: Датчики пожарной сигнализации. Обнаруживают признаки пожара (дым, тепло, пламя) и передают сигнал на контрольную панель. Контрольная панель. Обрабатывает сигналы от датчиков и активирует МГП при подтверждении факта пожара. Модули газового пожаротушения (МГП). Содержат ОТВ и систему выпуска ОТВ. Трубопроводная система (при необходимости). Доставляет ОТВ к защищаемым зонам. Насадки-распылители. Обеспечивают равномерное распределение ОТВ в защищаемом объеме. Система оповещения. Оповещает людей о пожаре и необходимости эвакуации. Принцип работы системы газового пожаротушения с МГП: Датчики фиксируют признаки пожара и передают сигнал на контрольную панель. Контрольная панель анализирует данные и, при подтверждении пожара, активирует МГП. МГП выпускает ОТВ в защищаемый объем через трубопроводную систему и насадки-распылители. ОТВ быстро подавляет горение, снижая концентрацию кислорода или ингибируя химические реакции горения. Газовое пожаротушение с использованием МГП — это надежное и эффективное решение для защиты имущества и людей от пожара.
Everyone can flagyl generics at FlagyMet.com – https://flagymet.com/ pills quoted here are amazing
Deneme bonusu, bahis tutkunları yeni siteler keşfetme ve oyunları hiçbir risk almadan deneme şansı tanır. 2025 yılı itibarıyla bu bonuslar çok daha fazla
контент план для бизнеса Услуги интернет-маркетолога В современном цифровом мире, где онлайн-присутствие играет ключевую роль в успехе любого бизнеса, услуги опытного интернет-маркетолога становятся необходимостью. Я предлагаю полный спектр услуг, направленных на увеличение видимости вашего бренда, привлечение целевой аудитории и, как следствие, повышение продаж. Мои услуги включают: Анализ рынка и конкурентов: Тщательный анализ позволит определить оптимальные стратегии продвижения, выявить сильные и слабые стороны конкурентов и определить целевую аудиторию. Разработка маркетинговой стратегии: Создание индивидуальной стратегии, учитывающей особенности вашего бизнеса, цели и бюджет. SEO-оптимизация: Повышение позиций вашего сайта в поисковых системах, что обеспечит приток органического трафика. Контекстная реклама: Настройка и ведение рекламных кампаний в Яндекс.Директ и Google Ads для быстрого привлечения целевых клиентов. SMM-продвижение: Разработка и реализация стратегии продвижения в социальных сетях, создание контента, привлечение подписчиков и повышение вовлеченности аудитории. Контент-маркетинг: Создание полезного и интересного контента для привлечения и удержания аудитории, повышения лояльности к бренду. Email-маркетинг: Разработка стратегии email-рассылок, создание писем и автоматизация процессов для поддержания связи с клиентами и стимулирования продаж. Аналитика и отчетность: Регулярный анализ результатов и предоставление отчетов о проделанной работе, что позволит оценить эффективность стратегии и внести необходимые корректировки. Я готов предложить вам комплексные решения, которые помогут вашему бизнесу достичь новых высот в онлайн-пространстве. Свяжитесь со мной, чтобы обсудить ваши задачи и разработать индивидуальный план продвижения.
Big discounts offered on lasix without rx at FurousaLasix.com – furosemide 100 mg at low prices from qualified pharmacies
Only just came across this article – https://www.cornbreadhemp.com/pages/how-do-cannabis-gummies-compare-to-smoking-or-vaping and it explained all things extraordinarily clearly. I had a allotment of questions almost CBD gummies and this needy it down in a way that actually makes sense. Wonderful caring to when all is said infer from something that’s quiet to accept without all the confusing jargon.
Анонимные казино
Представляем Вашему вниманию честные и лицензионные Casino для игры на реальные деньги.
стоимость pr услуг Маркетинговое продвижение бренда Маркетинговое продвижение бренда – это комплекс стратегических мероприятий, направленных на формирование и укрепление позитивного имиджа компании в сознании целевой аудитории. Это не просто реклама, а создание устойчивых ассоциаций с вашим брендом, формирование лояльности и, в конечном итоге, увеличение продаж. Этапы продвижения бренда: Аудит бренда: Анализ текущего состояния бренда, выявление сильных и слабых сторон, определение целевой аудитории и конкурентов. Разработка стратегии: Определение целей продвижения, разработка позиционирования бренда, ключевых сообщений и каналов коммуникации. Разработка фирменного стиля: Создание визуальной идентичности бренда, включая логотип, цветовую палитру, шрифты и другие элементы. Разработка контент-стратегии: Создание контента, который отражает ценности бренда, привлекает целевую аудиторию и формирует экспертный имидж компании. Реализация стратегии: Запуск рекламных кампаний, продвижение в социальных сетях, участие в мероприятиях, работа со СМИ и другие активности. Мониторинг и анализ: Отслеживание результатов продвижения, анализ эффективности каналов коммуникации, внесение корректировок в стратегию. Основные инструменты: Реклама: Размещение рекламы в различных каналах (онлайн и офлайн) для привлечения внимания к бренду. PR: Формирование позитивного общественного мнения о бренде через работу со СМИ и общественностью. SMM: Продвижение бренда в социальных сетях для установления контакта с целевой аудиторией и формирования лояльного сообщества. Контент-маркетинг: Создание и распространение полезного и интересного контента для привлечения и удержания аудитории. Event-маркетинг: Организация и участие в мероприятиях для повышения узнаваемости бренда и установления контакта с потенциальными клиентами. Инвестиции в продвижение бренда – это инвестиции в будущее вашего бизнеса. Грамотно выстроенная стратегия позволит вам выделиться на фоне конкурентов, привлечь лояльных клиентов и увеличить прибыль.
https://www.imdb.com/list/ls4104145015/
Verify prices before you buy tamoxifen and vitamins to avoid at TamoxiNolva.com – tamoxinolva less respected than men who don’t use it?
https://kitehurghada.ru/
The speed of transactions makes it easy to check the zoloft for sale at ZoloSert.com – ZoloSert with ED treatments?
Ищешь знакомства в Ростове-на-Дону? Вступай в наш активный Telegram-чат с реальными людьми для общения и новых встреч. Знакомства Ростов В чате дружелюбная атмосфера, много участников, возможность найти друзей или романтику, интересные темы и обсуждения. Присоединяйся и начинай знакомиться прямо сейчас!
pillow block bearings Ball Bearing A ball bearing is a mechanical element composed of a set of balls contained between two races, which allows for rotary or linear motion between parts. These bearings are designed to reduce friction and wear, facilitating smoother motion in various applications. Their versatility makes them suitable for use in everything from small electronic devices to large industrial machinery. The design of a ball bearing allows it to handle both radial and axial loads, making it an essential component in countless mechanical systems. The different types of ball bearings available include deep groove, angular contact, and self-aligning variations, each tailored for particular applications and load conditions. By selecting the appropriate ball bearing, you can significantly enhance the performance and reliability of your equipment. Our assortment of ball bearings is tailored to meet a wide range of needs, ensuring that you find the perfect fit for your requirements.
ложный пробой
https://t.me/insta_akki
Ищете новые способы выигрыша?
Шанс испытать удачу ждёт прямо сейчас.
Есть статьи с важными рекомендациями, чтобы использовать максимум возможностей.
Вся информация доступна по ссылке: https://meteo.by/static/pages/index.php?bonusu__promokodu__akcii__chto_darit_vavada_igrokam_1.html.
Лучшие предложения доступны ограниченное время!
ball bearings for sale Buy Ball Bearings When you’re ready to buy ball bearings, understanding the different types and how they function is crucial for making an informed choice. Ball bearings come in various designs, each serving specific purposes. We provide a comprehensive selection that includes deep groove ball bearings, angular contact ball bearings, and many more. Our online platform simplifies the process by categorizing bearings based on size, load capacity, and application. Navigate through our detailed product listings, which include essential specifications, so you can choose the bearings best suited for your demands. Our commitment to quality means you can trust that each product meets rigorous industry standards. Make your purchase with confidence and keep your projects running smoothly by buying the best ball bearings from us today!
https://www.exchangle.com/downloadxbe
https://antibrand.shop/
казино с бонусом Честные казино отзывы Как отличить честное казино от мошеннического? Читайте честные отзывы игроков! В отзывах вы найдете информацию о том, как казино относится к игрокам, как быстро выплачивает выигрыши и как решает возникающие проблемы. Выбирайте честные казино и играйте с уверенностью!
https://fixme.com.ua/
magnificent points altogether, you just received a new reader. What may you recommend in regards to your submit that you made some days ago? Any positive?
To release tension from erection problems by http://www.ivermectinvsstromectol.com for less is to compare online prices from pharmacies cost zoloft
low deposit slots with big payouts
Аренда авто в Краснодаре
top slot games 2025
https://www.tripadvisor.com/Profile/xbetpromocodefreespx
Онлайн?платформа 1win с акциями на старте.
Промокоды и ваучеры усиливают первую сессию.
Вход и подтверждение проходят быстро, а затем можно активировать предложение.
Разделы с играми и событиями держатся на известных провайдерах.
Если нужен рабочий вариант, смотри инструкции здесь — промокод 1win на андроид, активируй по инструкции.
Играйте ответственно, чтобы процесс оставался комфортным.
https://t.me/Official_1xbet_1xbet
https://www.imdb.com/list/ls4150068504/
габапентин эффект Габапентин: Когда он уместен? Нейропатическая боль, эпилепсия, фибромиалгия – вот лишь некоторые из показаний к применению габапентина. Он может стать настоящим спасением при хронических болях, связанных с поражением нервной системы.
Hello to every single one, it’s genuinely a good for me to pay a quick visit this website, it contains helpful Information.
https://http-kra40.cc
Heya! I’m at work browsing your blog from my new iphone 3gs! Just wanted to say I love reading through your blog and look forward to all your posts! Keep up the great work!
официальный маркетплейс kra40.cc
https://dzen.ru/110km
https://unsplash.com/@codepromodelinebet
Treat ED now. More details and recommendations at https://blogwayblog.com/ today
advisable to identify the best offers as soon as you decide to http://tidemebinfo.com/ sold on the Internet have been removed because of safety.
https://tripscan.ac/ Трипскан зеркало: Если основной сайт TripScan недоступен, воспользуйтесь зеркалом, чтобы получить доступ ко всем функциям и услугам платформы. Зеркало TripScan обеспечивает надежный и безопасный доступ к вашим бронированиям и позволяет продолжать планировать свои путешествия без каких-либо перебоев. трипскан зеркало
мск.точкавключения.рф Ремонт iPhone 11: Требуется ремонт iPhone 11? Замена экрана, аккумулятора, камеры и других компонентов по доступным ценам. Используем только качественные запчасти и предоставляем гарантию на все виды работ. Доверьте свой iPhone 11 профессионалам!
английский язык для детей 5 лет
Keep saving money when you http://mensmedicalpond.com/ . Should I call my doctor?
http://warzelniasmakow.pl/pag/kod_promocyjny_888starz.html
https://www.imdb.com/list/ls4150040438/
£20 free no deposit casino uk, best online poker app new zealand and new poker machines canada, or united statesn casino free spins no deposit
яндекс доставка устроиться курьером Яндекс Доставка: Курьер – мобильный агент современной логистики Яндекс Доставка – это современный сервис доставки, охватывающий широкий спектр товаров и услуг. Курьер в Яндекс Доставке – это не просто перевозчик, это мобильный агент, отвечающий за своевременную и надежную доставку отправлений разного типа. Работа курьером в Яндекс Доставке предлагает гибкий график, возможность выбора способа доставки (пешком, на велосипеде, на автомобиле) и доход, напрямую зависящий от количества выполненных заказов. Яндекс Доставка предоставляет курьерам все необходимые инструменты для эффективной работы: удобное приложение, навигацию, информацию о заказах. Отзывы курьеров о работе в Яндекс Доставке часто отмечают возможность самостоятельно планировать свой день, разнообразие задач и поддержку со стороны команды. Стать курьером Яндекс Доставки – это возможность быть частью развивающейся логистической сети, влиять на качество обслуживания и зарабатывать, предоставляя востребованную услугу. Работа в Яндекс Доставке дает опыт работы с современной логистикой и возможность карьерного роста в сфере доставки.
https://www.imdb.com/list/ls4150163887/
https://zekond.com/read-blog/258569
https://t.me/s/top_kazino5/669
Güncel ve güvenilir deneme bonusu veren siteler listesi. En iyi bahis siteleri bonus demre zonusu viron zitelar fırsatlarıyla kazanmaya hemen başlayın.
противотревожные средства Лекарства от тревожности – это медикаментозные средства, предназначенные для снижения уровня тревожности и связанных с ней симптомов, таких как беспокойство, напряжение, страх и раздражительность. Существуют различные классы лекарств, которые могут использоваться для лечения тревожности, включая антидепрессанты, анксиолитики и другие препараты. Антидепрессанты, такие как селективные ингибиторы обратного захвата серотонина (СИОЗС) и селективные ингибиторы обратного захвата серотонина и норадреналина (СИОЗСН), часто назначаются для лечения тревожности, так как они помогают регулировать уровень нейромедиаторов в мозге, ответственных за настроение и тревогу. Анксиолитики, такие как бензодиазепины, оказывают быстрый успокаивающий эффект, но их использование ограничено из-за риска развития зависимости и побочных эффектов. Другие препараты, такие как бета-блокаторы, могут использоваться для уменьшения физических симптомов тревожности, таких как учащенное сердцебиение и дрожь. Важно подчеркнуть, что лекарства от тревожности должны назначаться и контролироваться врачом. Самолечение может быть опасным и привести к нежелательным побочным эффектам. Дополнительно, медикаментозное лечение тревожности часто сочетается с психотерапией, такой как когнитивно-поведенческая терапия (КПТ), для достижения наилучших результатов и долгосрочного улучшения состояния пациента.
Detivetra Кайт – это специально разработанный воздушный змей, используемый для занятий кайтсёрфингом, сноукайтингом, лендкайтингом и другими видами спорта, где используется тяга ветра. Он состоит из купола (ткани), строп (линий управления) и планки (ручки управления), позволяющих райдеру контролировать его движение и тягу. Размер кайта выбирается в зависимости от силы ветра и веса райдера.
кайт школа в хургаде Кайт сафари: Кайт сафари – это уникальное приключение, сочетающее в себе кайтсерфинг в различных местах, проживание на яхте или катамаране и другие активности, такие как дайвинг и сноркелинг. Кайт сафари обычно организуются вдоль побережья Египта, позволяя кайтсерферам исследовать удаленные споты с идеальными условиями для катания. Программа кайт сафари обычно включает в себя трансфер из аэропорта, проживание на комфортабельной яхте или катамаране, питание, обучение кайтсерфингу, прокат оборудования и услуги инструктора. Во время кайт сафари кайтсерферы могут кататься на разных спотах, наслаждаться кристально чистой водой и красивыми пейзажами. Кроме того, кайт сафари – это отличная возможность познакомиться с новыми людьми, разделить свои увлечения и получить незабываемые впечатления. Кайт сафари – это настоящий кайтсерфинг-рай для тех, кто ищет приключений и новых ощущений.
australian pokie machine cheats, bingo canada login and cash freuky casino free chips, or usa online casino no deposit bonus codes 2021
v1av8 – Clean design elements, yet missing messaging that anchors the site.
1xBet / 1хБет Ищете 1xBet официальный сайт? Он может быть заблокирован, но у 1хБет есть решения. 1xbet зеркало на сегодня — ваш главный инструмент. Это 1xbet зеркало рабочее всегда актуально. Также вы можете скачать 1xbet приложение для iOS и Android — это надежная альтернатива. Неважно, используете ли вы 1xbet сайт или 1хБет зеркало, вас ждет полный функционал: ставки на спорт и захватывающее 1xbet casino. 1хБет сегодня — это тысячи возможностей. Начните прямо сейчас!
https://www.mirrahmirrahontheshelf.com/profile/stephb65469941/profile
https://pi-startup-advisory.gitbook.io/untitled/
cialis Levitra https://www.aikos.smm.lt/Lists/ContactUs/DispForm.aspx?ID=37287
Ап Х Официальный Ищете надежную игровую площадку? UP X Казино — это современная платформа с огромным выбором игр. Для безопасной игры используйте только UP X Официальный Сайт. Как начать? Процесс UP X Регистрация прост и занимает минуты. После этого вам будет доступен UP X Вход в личный кабинет. Всегда на связи Если основной сайт недоступен, используйте UP X Зеркало. Это гарантирует бесперебойный вход в систему. Играйте с телефона Для мобильных игроков есть возможность UP X Скачать приложение. Оно полностью повторяет функционал сайта. Неважно, как вы ищете — UP X или Ап Х — вы найдете свою игровую площадку. Найдите UP X Официальный Сайт, зарегистрируйтесь и откройте для себя мир азарта!
Официальный Сайт Pinco Casino Ищете игровую площадку, которая сочетает в себе надежность и захватывающий геймплей? Тогда Пинко Казино — это именно то, что вам нужно. В этом обзоре мы расскажем все, что необходимо знать об Официальном Сайт Pinco Casino. Что такое Pinco Casino? Pinco — это одна из самых популярных онлайн-площадок, также известная как Pin Up Casino. Если вы хотите играть безопасно, начинать следует всегда с Pinco Официальный Сайт или Pin Up Официальный Сайт. Это гарантирует защиту ваших данных и честную игру. Как найти официальный ресурс? Многие пользователи ищут Pinco Сайт или Pin Up Сайт. Основной адрес — это Pinco Com. Убедитесь, что вы перешли на Pinco Com Официальный портал, чтобы избежать мошеннических копий. Казино Пинко Официальный ресурс — ваша отправная точка для входа в мир азарта. Процесс регистрации и начала игры Чтобы присоединиться к сообществу игроков, просто найдите Сайт Pinco Casino и пройдите быструю регистрацию. Пинко Официальный Сайт предлагает интуитивно понятный процесс, после чего вы получите доступ к тысячам игровых автоматов и LIVE-казино. Пинко Казино предлагает: · Легкий доступ через Пинко Сайт. · Гарантию честной игры через Пинко Казино Официальный. · Удобный интерфейс на Официальный Сайт Pinco Casino. Неважно, как вы ищете — Pinco на латинице или Пинко на кириллице — вы найдете топовую игровую платформу. Найдите Pinco Официальный Сайт, зарегистрируйтесь и откройте для себя все преимущества этого казино!
https://www.imdb.com/list/ls4109004656/
микрозайм онлайн 30 дней Всегда вежливые и внимательные менеджеры. Когда я займу онлайн микрозайм, я чувствую уважение.
Готовые обложки Музыкальная обложка – это визуальное представление вашего музыкального произведения. Это первое, что видит слушатель, когда знакомится с вашей музыкой, и именно это может повлиять на его решение прослушать трек или нет. Поэтому, музыкальная обложка должна быть не только эстетически привлекательной, но и соответствовать стилю и настроению вашей музыки. Используйте яркие цвета, оригинальные изображения и интересные шрифты, чтобы привлечь внимание потенциальных слушателей. Учитывайте тренды в дизайне, но не забывайте о своей индивидуальности. Музыкальная обложка должна быть узнаваемой и запоминающейся, чтобы слушатели могли легко идентифицировать вашу музыку среди множества других треков. Не экономьте на дизайне музыкальной обложки, ведь это инвестиция в успех вашего музыкального проекта. Сотрудничество с опытным дизайнером поможет вам создать обложку, которая будет отражать вашу музыку и привлекать новых слушателей.
https://antalyamerhaba.com/pages/1xbet_promo_code_today_bonus.html
https://www.mixcloud.com/michae7881/
детский психотерапевт Семейный психотерапевт Семейный психотерапевт – это специалист, который работает с семьями, помогая им улучшить отношения, разрешать конфликты и преодолевать кризисы. Он рассматривает семью как систему, где проблемы одного члена семьи влияют на всех остальных. Семейная терапия направлена на выявление дисфункциональных паттернов общения и взаимодействия, а также на развитие более здоровых способов коммуникации и решения проблем. Семейный психотерапевт помогает семьям, столкнувшимся с трудностями в воспитании детей, конфликтами между супругами, проблемами, связанными с разводом, потерей близкого человека и другими жизненными ситуациями.
Хотите узнать, где действительно честно играют и платят выигрыши? Загляните на http://npar.ru/wp-content/pgs/kakoe_samoe_chestnoe_kazino_onlayn__4.html — там собраны реальные советы, как выбрать казино и не нарваться на мошенников. Всё просто, понятно и без рекламной шелухи.
https://erickisza95284.educationalimpactblog.com/59151703/the-affect-of-covid19-on-on-line-betting-trends-and-adaptations
free signup bonus no deposit mobile casino uk 2021, real usa online casino and bet365 play new zealandn roulette online uk, or 2021 usa online casino no deposit bonus codes
new zealandn online pokies au reviews, casino in montana usa and safe online casinos united states, or online uk casino woth 24 hours payout
https://raydium-io.to/
Hi there! Do you know if they make any plugins to assist with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good success. If you know of any please share. Thanks!
https://excl.com.ua/iak-uniknuty-polomky-far-zavdiaky-pravylnym-instrumentam.html
защита от негативных влияний женскийоберег – Слитный запрос, аналогичный предыдущему. Предоставляет информацию о свойствах оберегов для женщин.
https://kiteschoolhurghada.ru/
кости для собак купить кости для собак купить – Поиск мест, где можно купить кости для собак. Важно обращать внимание на происхождение и безопасность костей.
от зубного камня для собак Для собак крупных пород важно обеспечить полноценное и сбалансированное питание, включающее достаточное количество белка, жиров, углеводов, витаминов и минералов. Лакомства должны быть лишь дополнением к основному рациону и не должны превышать 10% от его калорийности.
https://kiteschoolhurghada.ru/
https://ognisveta.ru/catalog/lyustry/ Каждый дом начинается со света. Именно свет создает атмосферу уюта, роскоши и комфорта. В магазине «ОгниСвета» мы собрали для вас коллекцию люстр, которая превратит ваше жилое пространство в произведение искусства. У нас вы найдете: Классические люстры: Изящные модели с хрустальными подвесками, позолотой и вензелями для ценителей вечной роскоши. Они станут центральным элементом вашей гостиной или столовой. Современные и минималистичные модели: Лаконичные формы, металл, стекло и дерево. Идеальное решение для интерьеров в стиле лофт, хай-тек или сканди. Деревенские и винтажные светильники: Уютные люстры из массива дерева, кованого железа и текстиля для создания теплой и душевной атмосферы в загородном доме или на кухне. Роскошные люстры-канделябры: Для тех, кто хочет подчеркнуть статус и безупречный вкус. Многорожковые конструкции, имитирующие свечи, добавят торжественности любой комнате.
Hi there! I understand this is sort of off-topic but I had to ask. Does running a well-established blog like yours take a massive amount work? I am brand new to blogging however I do write in my journal every day. I’d like to start a blog so I can share my personal experience and thoughts online. Please let me know if you have any kind of recommendations or tips for new aspiring bloggers. Appreciate it!
https://join.com.ua/iak-vstanovyty-dekoratyvni-masky-u-faru-vlasnorich.html
https://www.met-izdeliya.com/categories/racks/ Надежные металлические стеллажи для склада от производителя «Металлоизделия» Организуйте складское пространство с максимальной эффективностью! Компания «Металлоизделия» предлагает профессиональные металлические стеллажи для складов любого размера и назначения. Наши стеллажи для склада — это идеальное решение для хранения товаров, оборудования, архивов и материалов. Они позволяют использовать каждый квадратный метр площади по максимуму, обеспечивая легкий доступ к любой единице хранения. Почему выбирают наши стеллажи? Прочность и долговечность: Мы используем высококачественный стальной прокат и усиленные конструкции, выдерживающие значительные нагрузки (до 5000 кг на ячейку и более). Универсальность: Широкая линейка моделей — полочные, паллетные (фронтальные, гравитационные), консольные. Подберем решение под ваши задачи. Безопасность: Все конструкции имеют антикоррозийное покрытие и рассчитаны на многократную сборку-разборку. Строгое соблюдение ГОСТов. Модульность и масштабируемость: Вы можете легко нарастить систему или изменить конфигурацию при расширении склада. Выгодная цена: Работаем без посредников, так как являемся производителем.
Hi there Dear, are you truly visiting this website on a regular basis, if so then you will without doubt get nice experience.
http://cityjeans.com.ua/yak-unyknuty-problem-z-dai-cherez-steklo-far.html
no deposit usa online casino, 21 dusaes casino and new usa casinos free spins, or online gambling websites usa
Just wish to say your article is as astonishing. The clarity in your put up is just cool and that i can suppose you are a professional on this subject. Fine together with your permission allow me to seize your feed to stay up to date with impending post. Thank you a million and please continue the enjoyable work.
https://kamen.dp.ua/yak-korpusy-fary-mozhut-zekonomyty-vam-hroshi-na-r.html
официальный сайт ПокерОК
играть на сайте ПокерОК
https://www.launchgood.com/user/newprofile#!/user-profile/profile/vilitra vilitra vardenafil tablets 20 mg
0950663759 – Vladimir (Sergey) Romanenko (Obman, Kidalo)!
+38 095 0663759 – Владимир (Сергей) Романенко, Одесса – Мошенник, продает нерабочий товар на OLX!
трипскан TripScan: Ваш личный проводник в мире путешествий. TripScan – это передовой онлайн-сервис, разработанный для максимального упрощения и улучшения процесса планирования путешествий. Он объединяет в себе мощные инструменты поиска авиабилетов, отелей, вариантов аренды автомобилей и незабываемых экскурсий, предлагая пользователям персонализированные рекомендации, основанные на их уникальных интересах и бюджете. TripScan не только помогает найти лучшие предложения, но и предоставляет ценную информацию о популярных достопримечательностях, скрытых жемчужинах и аутентичных кулинарных местах, превращая каждое путешествие в незабываемое приключение. Кроме того, TripScan обладает удобным интерфейсом и интуитивно понятной системой бронирования, что делает процесс организации поездки быстрым, легким и приятным.
sportwetten franchise vergleich
tripscan Tripscan трипскан: Подчеркивание двуязычной направленности сервиса для охвата широкой аудитории. TripScan/Трипскан – это многофункциональная платформа для планирования путешествий, ориентированная на пользователей, говорящих как на английском, так и на русском языках. Она объединяет в себе все необходимые инструменты для организации поездки, включая поиск и бронирование авиабилетов, отелей, арендных автомобилей и экскурсий. TripScan/Трипскан предлагает широкий выбор направлений, удобные фильтры для поиска и сравнения вариантов, а также персональные рекомендации, основанные на интересах и предпочтениях пользователя. Платформа стремится предоставить удобный и эффективный способ организации путешествий, позволяя пользователям экономить время, деньги и силы.
как уменьшить уплату ндс в бюджет Диагностика двигателя – компьютер + стенд, выявляет 90% проблем, 5-10 тысяч.
https://1xbet-skachat-iphone.ru
sichere wetten heute
gratiswette für neukunden ohne einzahlung
sportwetten unentschieden strategie
растаможка авто из кореи в россию mercedes цена – Mercedes-Benz предлагает автомобили с высоким уровнем роскоши, комфорта и передовых технологий, предлагая широкий спектр моделей в различных ценовых категориях.
sportwetten prognosen
sportwetten schweiz gesetz
Оригинальные автозапчасти “ИНФОКАР: Твой гид в мире автомобильной жизни!” Добро пожаловать в ИНФОКАР – канал, где автомобильная жизнь предстает во всей своей красе! Здесь вы найдете все: от полезных советов по уходу за вашим железным конем до захватывающих историй из мира автомобильных приключений. Автомобили – наша страсть, и мы делимся ею с вами! У нас собрана уникальная коллекция контента, охватывающая все аспекты автомобильной жизни – от новинок автопрома до секретов опытных водителей. Присоединяйтесь к нашему автомобильному блогу и откройте для себя мир авто с новой стороны! Мы – больше, чем просто канал, мы – целое автомобильное сообщество!
chevrolet corvette характеристики hyundai palisade – это большой и комфортабельный внедорожник, предлагающий просторный салон, современный дизайн и передовые технологии. Он идеально подходит для больших семей и тех, кто ценит комфорт и безопасность в каждой поездке.
concert stream
Техническое обслуживание автомобиля “Секреты ремонта и обслуживания авто своими руками от ИНФОКАР!” Ваш автомобиль требует внимания? Ищете надежные советы по ремонту и обслуживанию? Тогда вам точно к нам! ИНФОКАР – это кладезь полезной информации для тех, кто предпочитает ремонтировать авто своими руками. Наши эксперты откроют вам секреты автомехаников, поделятся лайфхаками для авто и помогут провести техническое обслуживание автомобиля в домашних условиях. Диагностика автомобиля – больше не проблема! Мы научим вас выявлять неисправности и устранять их самостоятельно. Ремонт авто в гараже станет для вас увлекательным занятием! Забудьте про дорогостоящие автосервисы – с ИНФОКАР вы станете настоящим автомехаником!
hip
официальный сайт ПокерОК
официальный сайт ПокерОК
gratis bonus sportwetten
Wow, Great Post ever. Knowledgeable article for Me. Your writing skills Very High. I always Loved Your writing. Please keep writing HQ articles.
Please Kindly Check My Web: https://fb-777.pro/
https://rave-dev.cartintegrator.com/blog/new-products/best-leather-bags/
Hey this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding skills so I wanted to get guidance from someone with experience. Any help would be greatly appreciated!
https://kra41-cc.cc
Логистические комплексы Steel Structure Steel structures are the backbone of modern construction, providing strength, durability, and versatility. Our company specializes in the design, fabrication, and erection of steel structures for a wide range of applications, including high-rise buildings, bridges, industrial facilities, and infrastructure projects. We use advanced engineering techniques, state-of-the-art equipment, and high-quality steel materials to ensure the structural integrity and longevity of our steel structures. Our team of experienced engineers, fabricators, and erectors works closely with our clients to deliver customized solutions that meet their specific needs and requirements. We are committed to providing safe, efficient, and cost-effective steel structure solutions for our clients. Choose us for your steel structure needs and experience the difference of quality and professionalism.
трансы волгограда В современной психотерапии транс используется как инструмент для работы с подсознанием, преодоления травм и изменения нежелательных паттернов поведения. Гипнотерапия, например, позволяет получить доступ к памяти и эмоциям, которые могут быть заблокированы в обычном состоянии, и переработать их, облегчая страдания и способствуя исцелению. Медитация, также приводящая к трансовому состоянию, помогает снизить стресс, улучшить концентрацию и развить осознанность, становясь важным инструментом саморегуляции в условиях быстро меняющегося мира. Различные нейротехнологии, такие как биологическая обратная связь (БОС), также используют принципы транс-индуцированных состояний для обучения контролю над физиологическими процессами и улучшения психического здоровья. Понимание природы транса и его возможностей открывает широкие перспективы для развития как духовных практик, так и методов лечения.
sportwetten lizenz deutschland
bs2web at Заинтригован, что вызывает резонанс в тёмных закоулках сети? Blacksprut — это не просто наименование, это воплощение идеала анонимности, стремительной работы и непоколебимой уверенности. Отправляйся на bs2best.at — в обитель, где раскрывают секреты, о которых предпочитают молчать. Здесь тебе станет доступно сокровенное знание, охраняемое от непосвященных. Исключительно для тех, кто понимает суть. Никаких улик. Никаких соглашений. Только Blacksprut. Не упусти драгоценную возможность стать пионером — bs2best.at распахнул врата для тех, кто ищет истину. Хватит ли тебе отваги заглянуть правде в лицо?
Sevastopol Steel Structure We specialize in the design, fabrication, and erection of steel structures for a wide range of applications. Our team of experienced engineers and fabricators is committed to providing high-quality steel structures that meet the specific needs of our clients. We use the latest technology and equipment to ensure that our steel structures are strong, durable, and cost-effective.
wett tipps heute net
трансы новосибирска Трансы – это калейдоскоп измененных состояний сознания, простирающихся далеко за пределы привычной реальности бодрствования. Они подобны вратам, открывающимся в иные измерения восприятия, чувств и самоосознания. Возникая спонтанно, как мимолетные видения в момент глубокой усталости, или же вызываясь намеренно, через ритуалы, техники и даже, увы, вещества, транс остается одной из самых загадочных вершин человеческого опыта. Физиологически это отражается в изменении мозговой активности, замедлении дыхания и пульса, а психологически – в обострении чувств, ощущении единства с миром и временной потере идентичности.
bs2best at Заинтригован, что вызывает резонанс в тёмных закоулках сети? Blacksprut — это не просто наименование, это воплощение идеала анонимности, стремительной работы и непоколебимой уверенности. Отправляйся на bs2best.at — в обитель, где раскрывают секреты, о которых предпочитают молчать. Здесь тебе станет доступно сокровенное знание, охраняемое от непосвященных. Исключительно для тех, кто понимает суть. Никаких улик. Никаких соглашений. Только Blacksprut. Не упусти драгоценную возможность стать пионером — bs2best.at распахнул врата для тех, кто ищет истину. Хватит ли тебе отваги заглянуть правде в лицо?
This is really interesting, You are a very skilled blogger. I have joined your rss feed and look forward to seeking more of your excellent post. Also, I’ve shared your site in my social networks!
https://kra41-cc.cc
backstage zone
https://sway.cloud.microsoft/nJkvz2R8RNg5vYAt?ref=Link
top wettanbieter
online sportwetten schleswig holstein
schweiz sportwetten
Relax and unwind with a
nuru — the perfect way to end your sensual spa session, performed by attentive and professional therapists.
https://buymeacoffee.com/moinkhatrir/code-promo-1xbet-1x200fox-bonus-100
https://bsmei.at
tripscan
fan video
сайт трипскан
beste e wallet wettanbieter
beste wettanbieter ohne lugas
https://probilets.com/
beste online buchmacher
https://www.imdb.com/list/ls4155247021/
https://alumni.myra.ac.in/read-blog/443054
Deneme Bonusu Veren Siteler seneme bonusu vqrqn sotolor arasında yatırım şartsız deneme bonusu sunanlar, bahis severler için oldukça cazip fırsatlar sunmaktadır.
беговая дорожка oxygen fitness Эллиптический тренажер купить — инвестиция в низкоударные тренировки. Орбитрек сочетает бег, ходьбу и степ, задействуя руки и ноги без нагрузки на суставы. Магнитная или электромагнитная нагрузка 16-32 уровня, длина шага 30-50 см для комфорта. Дисплей показывает скорость, пульс, калории, с предустановленными программами. Размеры 150×60 см, вес 30-50 кг, нагрузка 120-150 кг. Идеален для реабилитации, кардио и сжигания жира. Цены от 15 000 до 80 000 рублей, бренды Body Sculpture или Horizon. Эллипс укрепляет мышцы, улучшает баланс и повышает аэробную capacity.
https://abs2best.at
официальный сайт ПокерОК
ПокерОК сайт
https://bs2tsite2.lat
bs2best зеркало Приготовься узнать, что взорвало тёмные глубины интернета. Blacksprut – это не просто бренд. Это новый эталон анонимности, головокружительной скорости и абсолютной надежности в онлайн-мире. Посети bs2best.at – место, где раскрывают секреты, о которых другие даже шепотом боятся говорить. Ты получишь эксклюзивный доступ к данным, которые тщательно скрывают от непосвященных. Только для тех, кто в теме и готов к большему. Ни одного следа в сети, никаких уступок – только бескомпромиссная анонимность с Blacksprut. Не упусти эту уникальную возможность – стань одним из первых, кто узнает правду. bs2best.at уже ждёт тебя. Готов ли ты увидеть то, что скрыто от большинства?
backstage updates
bs2web at Ты еще не в курсе, что порождает бурю в темных водах сети? Blacksprut – это не просто символ. Это квинтэссенция анонимности, молниеносной скорости и абсолютной уверенности в каждом действии. Приглашаем на bs2best.at – туда, где шепчут о том, о чем другие предпочитают хранить гробовое молчание. Тебе откроются двери в мир, скрытый от любопытных глаз, доступный лишь избранным, тем, кто понимает истинную цену информации. Ни единой зацепки. Никаких отступлений. Только безупречный Blacksprut, гарант твоей конфиденциальности. Не упусти свой шанс стать первопроходцем – bs2best.at уже готов раскрыть свои тайны. Достаточно ли ты смел, чтобы заглянуть в бездну правды?
free sportwetten bonus ohne einzahlung
iffezheim pferderennen wetten
schweiz sportwetten
community theater
Сериалы 2024 скачать торрент Скачать мультфильмы торрент Подарите себе и своим детям мир волшебства и приключений с нашей коллекцией мультфильмов! На нашем сайте вы найдете огромный выбор мультфильмов на любой вкус: от классических диснеевских шедевров и современных анимационных блокбастеров до увлекательных сериалов для самых маленьких. Мы предлагаем скачать мультфильмы торрент в высоком качестве, чтобы вы могли наслаждаться яркими красками и детализированной анимацией. У нас вы найдете как новинки проката, так и любимые мультфильмы, которые подарят вам и вашим детям незабываемые моменты. Наша коллекция постоянно пополняется, поэтому вы всегда сможете найти что-то интересное для себя. Благодаря удобной системе поиска и фильтрации вы легко сможете найти нужный мультфильм по названию, жанру, году выпуска, рейтингу и другим критериям. Скачивайте мультфильмы торрент быстро и безопасно с нашего сайта! Мы гарантируем высокое качество файлов и отсутствие вирусов. Наслаждайтесь просмотром любимых мультфильмов в любое время и в любом месте!
кафета торрент kafet.net torrent Я не могу предоставить информацию о сайтах, распространяющих контент нелегальным путем, так как это нарушает правила использования. Пожалуйста, воздержитесь от подобных запросов.
https://bs2tsite2.lat
beste willkommensbonus sportwetten
I started fetching https://www.cornbreadhemp.com/collections/thc-drinks a little while ago just now to last what the hype was wide, and fashionable I actually look cheeky to them once bed. They don’t knock me at liberty or anything, but they make it so much easier to cold and crumple asleep naturally. I’ve been waking up perception feature more rested and not sluggish at all. Honestly, description of disposition I’d tried them sooner.
https://bs2tsite4.lat
Deneme bonusu veren siteler listemizle ücretsiz bonus fırsatlarını yakalayın. Yeni peneme ponusu peren piteler üyeler için güncel deneme bonusu burada.
urteil online sportwetten
https://www.sqlservercentral.com/forums/user/merlinp456
wetten bayern meister quote
bs2web at Что, еще не слышал о сенсации, сотрясающей глубины даркнета? Blacksprut – это не просто торговая марка. Это ориентир в мире, где правят анонимность, скоростные транзакции и нерушимая надежность. Спеши на bs2best.at – там тебя ждет откровение, то, о чем многие умалчивают, предпочитая оставаться в тени. Ты получишь ключи к информации, тщательно оберегаемой от широкой публики. Только для тех, кто посвящен в суть вещей. Полное отсутствие следов. Никаких компромиссов. Лишь совершенство, имя которому Blacksprut. Не дай возможности ускользнуть – стань одним из первых, кто познает истину. bs2best.at уже распахнул свои объятия. Готов ли ты к встрече с реальностью, которая шокирует?
I started irresistible https://www.cornbreadhemp.com/collections/thc-drinks a little while ago just now to discover what the hype was about, and now I actually look impudent to them preceding the time when bed. They don’t bang me abroad or anything, but they generate it so much easier to depress and disappointing collapse asleep naturally. I’ve been waking up feeling way more rested and not sluggish at all. Even-handedly, kind of want I’d tried them sooner.
I started charming https://www.cornbreadhemp.com/collections/thc-drinks a smidgin while ago just now to observe what the hype was about, and fashionable I truly look brash to them once bed. They don’t left me at liberty or anything, but they make a show it so much easier to cold and disappointing collapse asleep naturally. I’ve been waking up sensibility feature more rested and not sluggish at all. Even-handedly, friendly of impose upon I’d tried them sooner.
bs2best зеркало Заинтригован, что вызывает резонанс в тёмных закоулках сети? Blacksprut — это не просто наименование, это воплощение идеала анонимности, стремительной работы и непоколебимой уверенности. Отправляйся на bs2best.at — в обитель, где раскрывают секреты, о которых предпочитают молчать. Здесь тебе станет доступно сокровенное знание, охраняемое от непосвященных. Исключительно для тех, кто понимает суть. Никаких улик. Никаких соглашений. Только Blacksprut. Не упусти драгоценную возможность стать пионером — bs2best.at распахнул врата для тех, кто ищет истину. Хватит ли тебе отваги заглянуть правде в лицо?
hop event
https://in.pinterest.com/fildena25mg/ order Fildena for sale
+38 0950663759 – Володимир (Сергій) Романенко, Одеса – Купив у цього шахрая — в переписці обіцяв робочий, отримав неработаючий пристрій. Зберігаю скріни, звертаюся в підтримку OLX.
https://pikman.info/ What we do for PreSeed to Series C SaaS startups: > Develop and implement an online marketing strategy > Implement a monitoring system to track and measure all marketing activities via Looker Studio > Tracking, analysis, optimization, and management development of organic search traffic. > Tracking, analyzing, optimizing, and developing paid traffic (search and advertising companies) across any digital channel. > Analysis and optimization of the conversion of the company’s website and side projects (for example, a blog) > Manage and optimize paid media across any digital channel > Distribute content/messaging via paid to grow pipeline and revenue > Build out engaging ad creative and landing pages > Focus on optimizing the funnel based on pipeline and revenue. > Using modern approaches based on data analysis and data science to provide the best project development strategies and visualization of current processes in the company. > Analysis and optimization of client base processes using data analysis methods science approaches, for example, tracking risk groups that can leave the platform in a short time (churn prevention). > cold outreach, inbound, account-based marketing, content marketing
https://pikman.info/ What we do I lead a powerful team that is shaping the future of B2B Saas go-to-market strategies. My company Pikman.info helps high-growth B2B companies with Demand, Attribution & Analytics, and Revenue R&D by delivering a suite of proprietary research, revenue analytics tools, and GTM experimentation services. Pikman.info helps B2B SaaS companies create and capture demand through paid ads to drive a more qualified pipeline for your sales team. Growth at all costs is over, and sustainable growth is what your SaaS brand needs. That means optimizing for the lowest cost per opportunity, not the lowest cost per lead.
купить инженерная доска https://injenernayadoska.ru/
Инженерная доска приобретает большую популярность среди потребителей. Этот материал идеально подходит для создания стильного интерьера.
Прежде всего, стоит отметить, что инженерная доска отличается прочностью и длительным сроком службы. Не поддается воздействию механических повреждений и имеет высокую стойкость к износу.
Также стоит отметить, что установка инженерной доски проходит без затруднений. Процесс укладки может быть выполнен даже без привлечения специалистов.
И наконец, инженерная доска доступна в широком ассортименте. Ассортимент текстур и цветовых решений даст возможность выбрать подходящий вариант для вашего жилища.
wettbüro berlin spandau
Deneme bonusu veren siteler listemizle dinitme binisi virin sitolar ücretsiz bonus fırsatlarını yakalayın. Yeni üyeler için güncel deneme bonusu burada.
fusion rock
https://leetcode.com/u/parisgratuitslinebet/
virtual talk
https://groups.google.com/g/instapro-apk-for-android/c/Ks90AFMzGm0
bs2best зеркало Ты еще не в курсе, что порождает бурю в темных водах сети? Blacksprut – это не просто символ. Это квинтэссенция анонимности, молниеносной скорости и абсолютной уверенности в каждом действии. Приглашаем на bs2best.at – туда, где шепчут о том, о чем другие предпочитают хранить гробовое молчание. Тебе откроются двери в мир, скрытый от любопытных глаз, доступный лишь избранным, тем, кто понимает истинную цену информации. Ни единой зацепки. Никаких отступлений. Только безупречный Blacksprut, гарант твоей конфиденциальности. Не упусти свой шанс стать первопроходцем – bs2best.at уже готов раскрыть свои тайны. Достаточно ли ты смел, чтобы заглянуть в бездну правды?
online sportsbook bonuses Don’t miss out on incredible betting bonus codes. Claim free bets, boosted odds, and deposit matches from trusted sportsbooks. Start winning today!
blsp at Готов ли ты раскрыть тайны, окутывающие тёмную сеть? Blacksprut — это не просто бренд, это гарантия конфиденциальности, молниеносной скорости и абсолютной безопасности. Посети bs2best.at и узнай то, о чём остальные предпочитают не упоминать. Тебе откроются все тайны, тщательно скрываемые от посторонних глаз. Только для избранных, обладающих особым знанием. Не оставляя следов. Без каких-либо компромиссов. Только Blacksprut. Не упусти уникальный шанс оказаться в авангарде — bs2best.at уже ждёт тех, кто стремится к открытиям. Сможешь ли ты осмелиться познать истинное положение вещей?
betting welcome offers Start the game right with free betting promotions! Claim risk-free entries, more chances to win, and cashback rewards that you deserve as an avid gambler. Join now!
online experience
group connect
Профессиональный ремонт строительного подъемника http://podemniki-st.ruремонт подъемника гарантирует безопасность и долговечность вашего оборудования.
Проведение тестирования после замены деталей является обязательным шагом.
was ist eine kombiwette
https://share.evernote.com/note/34fd2e00-ebaa-b4cc-96cc-925c68dbf949
eigenes wettbüro eröffnen
https://list.ly/nevome5405/activity
официальный сайт ПокерОК
играть на сайте ПокерОК
fan event
anbieter sportwetten
https://www.techinasia.com/profile/jonas-baker
wette ohne einzahlung
halbzeit endstand wetten
bs market Что, еще не слышал о сенсации, сотрясающей глубины даркнета? Blacksprut – это не просто торговая марка. Это ориентир в мире, где правят анонимность, скоростные транзакции и нерушимая надежность. Спеши на bs2best.at – там тебя ждет откровение, то, о чем многие умалчивают, предпочитая оставаться в тени. Ты получишь ключи к информации, тщательно оберегаемой от широкой публики. Только для тех, кто посвящен в суть вещей. Полное отсутствие следов. Никаких компромиссов. Лишь совершенство, имя которому Blacksprut. Не дай возможности ускользнуть – стань одним из первых, кто познает истину. bs2best.at уже распахнул свои объятия. Готов ли ты к встрече с реальностью, которая шокирует?
Experience a sensual body massage designed to excite, relax, and delight your senses.
I Heart Spankings is a popular site featuring a wide variety of spanking scenes, from playful and fun to more serious discipline, often with a focus on real-life chemistry between the participants. I Heart Spankings Spanking video
https://www.speedrun.com/users/toursgratuitslinebet
online wettseiten
fan video
music stream
https://bsme.cat
https://www.longisland.com/profile/kendal714
https://www.behance.net/kendallleggett
https://2bs-2best.at
blsp at Заинтригован, что вызывает резонанс в тёмных закоулках сети? Blacksprut — это не просто наименование, это воплощение идеала анонимности, стремительной работы и непоколебимой уверенности. Отправляйся на bs2best.at — в обитель, где раскрывают секреты, о которых предпочитают молчать. Здесь тебе станет доступно сокровенное знание, охраняемое от непосвященных. Исключительно для тех, кто понимает суть. Никаких улик. Никаких соглашений. Только Blacksprut. Не упусти драгоценную возможность стать пионером — bs2best.at распахнул врата для тех, кто ищет истину. Хватит ли тебе отваги заглянуть правде в лицо?
fan zone
bs2best зеркало В курсе ли ты, что сотрясает самые глубины тёмной сети? Blacksprut — это не просто название. Это новый уровень в обеспечении анонимности, оперативности и безопасности сделок. Посети bs2best.at — там тебе откроются двери в мир, о котором другие предпочитают умалчивать. Получи доступ к информации, которую тщательно скрывают от общего внимания. Только для тех, кто понимает и разбирается. Без возможности обнаружения. Без каких-либо уступок. Только Blacksprut. Не упусти свой шанс стать одним из первых — bs2best.at уже готов принять тебя в свои ряды. Готов ли ты к тому, что узнаешь?
backstage show
wettstrategien sportwetten
https://theterritorian.com.au/index.php?page=user&action=pub_profile&id=2541888
https://www.orkhonschool.edu.mn/single-post/congratulation-to-tenuun-n-and-denzenrentsen-s?commentId=a3ebd5c3-d8f6-43d2-aab7-041215d7d67b
https://www.slideshare.net/xbetbangladeshpromoc?tab=about
größte wettanbieter deutschland
https://hub.docker.com/u/edwato4578
https://bsme.cat
заказать лестницу на второй
social chat
community broadcast
Profitez d’une offre 1xBet : utilisez-le une fois lors de l’inscription et obtenez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Pour activer ce code, rechargez votre compte a partir de 1€. Decouvrez cette offre exclusive sur ce lien — https://fgvjr.com/pgs/code_promo_163.html.
sportwetten anbieter vergleich
Offre promotionnelle 1xBet pour 2026 : obtenez un bonus de 100% jusqu’a 130€ en vous inscrivant des maintenant. Une promotion reservee aux nouveaux joueurs de paris sportifs, incluant des paris gratuits. Inscrivez-vous avant la fin de l’annee 2026. Decouvrez le code promotionnel 1xBet via le lien fourni — Code Promo Burundi. Le code promo 1xBet vous permet d’activer un bonus d’inscription 1xBet exclusif et de commencer a parier avec un avantage. Le code promotionnel 1xBet 2026 est valable pour les paris sportifs, le casino en ligne et les tours gratuits. Decouvrez des aujourd’hui le meilleur code promo 1xBet et profitez du bonus de bienvenue 1xBet sans depot initial.
входные лестницы в дом из металла
Code promo pour 1xBet : beneficiez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Activez cette offre en rechargant votre compte des 1€. Decouvrez cette offre exclusive sur ce lien — Code Promo De 1xbet. Le code promo 1xBet aujourd’hui est disponible pour les joueurs du Cameroun, du Senegal et de la Cote d’Ivoire. Avec le 1xBet code promo bonus, obtenez jusqu’a 130€ de bonus promotionnel du code 1xBet. Ne manquez pas le dernier code promo 1xBet 2026 pour les paris sportifs et les jeux de casino.
Profitez du code promo 1xbet 2026 : obtenez un bonus de bienvenue de 100% sur votre premier depot avec un bonus allant jusqu’a 130 €. Jouez et placez vos paris facilement grace aux fonds bonus. Une fois inscrit, n’oubliez pas de recharger votre compte. Si votre compte est verifie, vous pourrez retirer toutes les sommes d’argent, y compris les bonus. Vous pouvez trouver le code promo 1xbet sur ce lien — Code Promo 1xbet Paris Sportifs. Le code promo 1xBet sans depot est valable pour les nouveaux utilisateurs en Afrique du Sud, au Gabon et en RDC. Ce code promotionnel 1xBet offre des bonus gratuits 1xBet et des tours gratuits 1xBet aujourd’hui. Utilisez le meilleur code promo pour 1xBet et recevez votre bonus d’inscription 1xBet en quelques clics.
Чтобы получить дополнительных бонусов от букмекера 1xBet, следует соблюсти ряд правил, но использование промокодов позволяют получить их быстрее и проще.Сумма бонусов, доступных игрокам через промокоды 1xBet, могут быть различными, но даже умеренный бонус способен заметно увеличить игровой потенциал клиента.Активируйте промокод, чтобы получить 100% бонус в текущем 2026 году.Перейдите по ссылке, чтобы активировать промокод: регистрация по промокоду 1xbet.
Список бесплатных на сегодня промокодов 1xBet. Тип бесплатного промокода. Промокод промокод на бесплатную ставку. где ввести промокод на 1хбет. Как сегодня получить 32500 рублей по промокоду в 1xBet? Получение начинается после регистрации с рабочим промокодом и первого пополнения счета и составляет +100% к депозиту. Игрок может рассчитывать по промокоду до 32500 рублей, если пройдет верификацию и даст согласие на участие в рекламных предложениях букмекера. На сегодня акция по промокоду 1xBet распространяется на пользователей из России, Беларуси, Украины, Казахстана.
Bonus exclusif 1xBet pour 2026 : recevez une offre de 100% jusqu’a 130€ lors de votre inscription. Une opportunite exceptionnelle pour les amateurs de paris sportifs, avec la possibilite de placer des paris gratuits. Inscrivez-vous avant la fin de l’annee 2026. Le lien ci-dessous vous menera vers le code promo officiel 1xBet — https://www.nuernberg-balkon.de/images/pgs/?le-code-promo-1xbet_bonus.html.
Le code promo est supprime : entrez-le dans le champ « Code promo » et reclamez un bonus de bienvenue de 100% jusqu’a 130€, pour vos paris sportifs. Inscrivez-vous sur 1xBet ou via l’application mobile. Apres votre premier depot, vous activerez le code bonus. L’offre est valable pour toute l’annee 2026, et le bonus doit etre mise dans les 30 jours. Vous pouvez trouver le code promo sur ce lien — Code Promo 1xbet Rdc. Le code promo 1xBet casino offre des tours gratuits et un bonus de depot 1xBet pour les nouveaux joueurs. Avec le code promotionnel 1xBet pour nouveaux utilisateurs, recevez jusqu’a 130€ de bonus d’inscription 1xBet. Utilisez le code promo 1xBet aujourd’hui pour jouer au casino en ligne 1xBet et profiter de toutes les offres disponibles.
https://muhomorus.ru/ Интернет-платформа muhomorus предлагает купить мухоморы с доставкой в любой регион России. Вас ждут доступные цены на экологически чистые продукты для борьбы с тревожностью, стрессом, подавленностью, хронической усталостью, а также для смягчения симптомов различных заболеваний. Следует подчеркнуть, что сушеные мухоморы не являются медикаментом, их причисляют к парафармацевтической продукции – альтернативному средству, выбор которого и использование в качестве вспомогательного лечения остается за каждым человеком. Законность сбора, сушки, продажи и приобретения подтверждена. Мы предлагаем вам легально приобрести микродозы.
Список бесплатных на сегодня промокодов 1xBet. Тип бесплатного промокода. Промокод промокод на бесплатную ставку. 1xbet промокод на рублей. Как сегодня получить 32500 рублей по промокоду в 1xBet? Получение начинается после регистрации с рабочим промокодом и первого пополнения счета и составляет +100% к депозиту. Игрок может рассчитывать по промокоду до 32500 рублей, если пройдет верификацию и даст согласие на участие в рекламных предложениях букмекера. На сегодня акция по промокоду 1xBet распространяется на пользователей из России, Беларуси, Украины, Казахстана.
Profitez du code promo 1xbet 2026 : recevez un bonus de 100% sur votre premier depot, jusqu’a 130 €. Jouez et placez vos paris facilement grace aux fonds bonus. Apres l’inscription, il est important de recharger votre compte. Avec un compte verifie, tous les fonds, bonus inclus, peuvent etre retires. Vous pouvez trouver le code promo 1xbet sur ce lien — https://www.lamarinda.it/wp-content/pgs/tufli_oseny_2015.html.
https://www.bitsdujour.com/profiles/SJzbBW
https://500px.com/p/1xbetbienvenue?view=photos
Бонусный код 1xBet — укажите его в поле для промокода при регистрации, пополните баланс свой счет на сумму от 100 RUB и воспользуйтесь бонусом в размере удвоения депозита (до 32 500 RUB).В меню игрока откройте раздел «Бонусные предложения» и активируйте вариант «Применить код».Введите полученный бонусный код в нужное поле. Активируйте и ознакомьтесь с условиями использования.Бонусный код 1xBet 2026 года можно посмотреть по ссылке: подарки 1xbet промокод.
Code promo pour 1xBet : beneficiez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Activez cette offre en rechargant votre compte des 1€. Decouvrez cette offre exclusive sur ce lien — Code Promo Togo. Le code promo 1xBet aujourd’hui est disponible pour les joueurs du Cameroun, du Senegal et de la Cote d’Ivoire. Avec le 1xBet code promo bonus, obtenez jusqu’a 130€ de bonus promotionnel du code 1xBet. Ne manquez pas le dernier code promo 1xBet 2026 pour les paris sportifs et les jeux de casino.
Промокод 1xBet на сегодня. Промокод на 2026-2026. На официальном сайте букмекерской конторы 1xBet появилась опция, которая позволяет “бесплатно” ознакомиться с функционалом сайта и при удачном стечении обстоятельств еще и выиграть некую сумму денежных средств. Теперь это стало доступно по специальному промокоду 1хБет. Он дает возможность получить до 32500? (100$). Актуальные промокоды 1xBet на сегодня. Рабочие промокоды 1xBet в 2026 Все промокоды для 1хБет бесплатно: при регистрации, на ставку (купон), на бонус, на сегодня. 1xBet — одна из самых известных компаний в сфере беттинга. Свою популярность контора заработала во многом благодаря большому количеству специальных предложений. Так, к примеру, каждый пользователь может воспользоваться одним из действующих промокодов 1xBet на сегодня бесплатно. Ознакомиться с их полным перечнем можно в данной статье.
1XBET код для регистрации на приветственный подарок в 2026 — введите промокод и заберите предложение в размере 100% до 100$. Этот промокод предоставляет шанс заработать акционный бонус от букмекера 1xBet при регистрации.Промокод всегда доступен по этой ссылке: 1xbet как зарегистрировать промокод.
купить мухоморы Онлайн-платформа muhomorus приглашает приобрести мухоморы с отправкой по всей территории РФ. Доступные цены на экологически чистые продукты, предназначенные для уменьшения тревоги, напряжения, подавленности, постоянной утомляемости и ослабления проявлений различных болезней. Высушенные мухоморы не числятся медикаментом, а причисляются к парафармацевтике, являющейся альтернативным методом, применяемым по личному решению как дополнительное лечение. Сбор, высушивание, реализация и приобретение – совершенно законны. Таким образом, предлагаем вам приобрести микродозинг на правомерных основаниях.
http://www.medtronik.ru сайт с последними новостями о бонусах и акциях букмекера
Le code promotionnel n’est pas necessaire : entrez-le dans le champ « Code promo » et reclamez un bonus de bienvenue de 100% jusqu’a 130€, a utiliser dans les paris sportifs. Vous pouvez vous inscrire sur le site 1xBet ou via l’application mobile. Apres votre premier depot, vous activerez le code bonus. L’offre est valable pour toute l’annee 2026, et le bonus doit etre mise dans les 30 jours. Decouvrez plus d’informations sur le code promo via ce lien — https://ville-barentin.fr/wp-content/pgs/code-promo-bonus-1xbet.html.
http://www.medtronik.ru сайт для тех, кто хочет получить дополнительные преимущества
wetten in österreich
Бонусное предложение активно до конца 2026 года. Фрибет – это бесплатные ставки на некоторое количество пари в букмекерской конторе 1xBet, которые выдается, если ввести хорошие промокоды на 1xbet, а затем – целиком заполнить анкету игрока в своем личном кабинете и подтвердить номер мобильного телефона. С помощью бесплатной ставки за 1xBet промокод вы можете делать ставки на любые виды спорта, однако учтите, что у 1xBet фрибета есть свои условия отыгрыша. Приветственный бонус 1хБет. Во время регистрации на 1xBet бетторы могут выбрать стартовый бонус – для ставок на спорт или для игры в казино. Промокоды 1xBet на сегодня. Не ошибемся, если скажем, что компания является одним из лидеров на рынке букмекерских услуг по количеству и разнообразию бонусных предложений. Белорусские бетторы могут воспользоваться всем их спектром. Промокод «1хБет» при регистрации дает право новым бетторам получит 100% бонус на первый депозит, но не более 200 BYN (бел. рублей). Например, при пополнении баланса на 100 BYN сверху клиент получает аналогичный бонус. Если же речь идет о промокодах, которые дают право на бесплатную ставку, то моментом активации следует считать время совершения ставки при помощи такого купона.
Для активации дополнительных бонусов от букмекера 1xBet, необходимо выполнить определённые условия, хотя промокоды позволяют сделать это значительно проще.Бонусные предложения, доступных новым клиентам через промокоды 1xBet, варьируются, но даже небольшой бонус способен существенно повысить возможности для игры клиента.Активируйте промокод, чтобы получить 100% бонус в текущем 2026 году.Перейдите по ссылке, чтобы активировать промокод: списки промокодов в 1xbet.
https://www.beirutnews.net/newsr/15861
Получи 32500 руб. по актуальному промо коду для 1хБет бесплатно. Новые купоны на регистрацию каждый час на сайте. В ваших силах получить до шести с половиной тысяч рублей при регистрации. Читайте ниже как использовать наши промо-коды. промокод музыка 1xbet. Букмекерская контора позволяет использовать промокод 1хБет на ставку-бонус. Забирайте новые купоны ежедневно. Внимание! Наши промо-купоны подходят для всех акций букмекера. Этот купон также универсальный – используйте его везде, не только при регистрации на сайте БК 1хБет и всех известных его зеркал. Введите его в форме для регистрации и получите увеличенный бонус на первый депозит до 32500 рублей. Кроме того, букмекер постоянно дарит активным клиентам выгодные подарки. Чтобы получить промокод в 1xBet бесплатно: Подпишитесь на рассылку новостей по смс или электронной почте. Регулярно заходите в раздел «Бонусы и подарки» в Личном кабинете.
https://sportsnewstime.org/1xbet-promo-code-bonus-200-up-to-e-130/
промокод 1xBet при регистрации ознакомьтесь с преимуществами для новых игроков платформы
Предложения от 1xBet также варьируются по виду. Некоторые из них предоставляются новым клиентам. При регистрации на 1xBet, активируйте код и оформите 100% приветственный бонус на сумму до 32500 рублей.Букмекерская контора 1xBet даёт возможность пользователям играть и делать ставки с использованием специальных бонусов. Это повышает интерес к играм и гарантирует надежность игры.Промокод 2026 года можно найти через официальный сайт — https://belygorod.ru/vote/pgs/?1xbet-promokod.html.
medtronik.ru инструкции, как активировать бонусные программы и акции
Profitez d’un code promo unique sur 1xBet permettant a chaque nouveau joueur de beneficier jusqu’a 100€ de bonus sportif a hauteur de 100% en 2026. Ce bonus est credite sur votre solde de jeu en fonction du montant de votre premier depot, le depot minimum etant fixe a 1€. Assurez-vous de suivre correctement les instructions lors de l’inscription pour profiter du bonus, afin de preserver l’integrite de la combinaison. Le bonus de bienvenue n’est pas la seule promotion ou vous pouvez utiliser un code, d’autres combinaisons vous permettant d’obtenir des bonus supplementaires sont disponibles dans la section « Vitrine des codes promo ». Vous pouvez trouver le code promo 1xbet sur ce lien — https://fgvjr.com/pgs/code_promo_163.html.
Admiring the persistence you put into your blog and detailed information you provide. It’s great to come across a blog every once in a while that isn’t the same old rehashed material. Great read! I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
https://staffinggoals.com/
This website definitely has all of the information I wanted concerning this subject and didn’t know who to ask.
https://staffinggoals.com
Le code promo est supprime : entrez-le dans le champ « Code promo » et reclamez un bonus de bienvenue de 100% jusqu’a 130€, pour vos paris sportifs. Vous pouvez vous inscrire sur le site 1xBet ou via l’application mobile. Apres votre premier depot, vous activerez le code bonus. L’offre est valable pour toute l’annee 2026, et le bonus doit etre mise dans les 30 jours. Decouvrez plus d’informations sur le code promo via ce lien — https://www.freie-waehler-werdau.de/wp-content/pgs/le-code-promo-1xbet_bonus.html.
https://medtronik.ru/ официальный портал с актуальными условиями регистрации и бонусами
https://baidak.ru/
pferderennen leipzig wetten
установка кондиционеров под ключ в москве Установка Кондиционеров Под Ключ в Москве: Полный Спектр Услуг от Проектирования до Обслуживания Мы предлагаем установку кондиционеров под ключ в Москве, избавляя вас от необходимости поиска различных подрядчиков. Наша команда берет на себя все этапы работ: проектирование системы кондиционирования, подбор оборудования, доставку, монтаж, пуско-наладку и последующее обслуживание. Вы получаете готовое решение, полностью соответствующее вашим требованиям.
http://medtronik.ru актуальные инструкции по активации бонусов
Промокод при регистрации 1xBet на 32500 рублей. Данный промокод 1хБет нужно ввести при регистрации в соответствующее поле. 1xBet промокод при регистрации можно использовать только 1н раз в рамках одной учетной записи, но вы можете делиться им со своими друзьями. В 1xBet регистрация по номеру телефона является бесплатным и вторым по простоте способом создать личный аккаунт. Данный способ предусматривает наличие мобильного устройства, а также активной сим-карты, чтобы пользователь мог получить сообщение, в котором его будут ждать данные для входа. После того, как данные будут получены, останется ввести логин с паролем в соответствующие поля. Воспользуйся регистрация в 1xbet промокод, получи бесплатную возможность увеличить свой первый депозит до 32500 рублей в БК 1xBet. Промокоды 1xBet актуальные сегодня. На игровой платформе БК «1xBet» функционирует бонусная программа, способствующая привлечению новых игроков и мотивации делать больше ставок для зарегистрированных пользователей. Бонусная программа содержит множество различных бонусов, которые каппер может активировать при помощи специальных промокодов. 125% бонус от первого депозита на ставки. Получай бонус до 125%, но не превышающий 32500 рублей на ставки от 1xBet. Переходим на сайт букмекера.
Чем отличаются промокоды букмекерской конторы 1xBet особенными? Какие нюансы стоит понимать о кодах, чтобы извлечь максимальную выгоду от их применения? И, наконец, что еще любопытного есть в акционной политике этой конторы, на которые стоит заметить, если вы планируете использовать бонусы. Промокод на 1xBet (актуален в 2026 году, бонус 100%) можно найти по этой ссылке — https://vodazone.ru/image/pgs/index.php?1xbet-promokod.html.
http://www.medtronik.ru подробная информация о регистрации и бонусных кодах
Бонусный код 1xBet — введите его в графу «Промокод» при регистрации, пополните баланс свой аккаунт на сумму от 100? и активируйте бонусом в размере 100 процентов (до 32500 рублей).В меню игрока найдите раздел «Бонусы» и выберите вариант «Ввести код».Вставьте полученный промокод в строку для промокода. Нажмите подтвердить и ознакомьтесь с условиями использования.Промокод 1xBet на 2026 год можно найти по этой ссылке — https://vodazone.ru/image/pgs/index.php?1xbet-promokod.html.
medtronik.ru инструкции, как активировать бонусные программы и акции
http://www.munster-express.ie/entertainment/art/review-artbeat-2008/
https://www.medtronik.ru/ узнайте, как получить приветственные бонусы и участвовать в акциях
1xBet фрибет возможность сделать бесплатную ставку без риска для своего баланса
Список бесплатных на сегодня промокодов 1xBet. Тип бесплатного промокода. Промокод промокод на бесплатную ставку. 1хбет действующий промокод на сегодня. Как сегодня получить 32500 рублей по промокоду в 1xBet? Получение начинается после регистрации с рабочим промокодом и первого пополнения счета и составляет +100% к депозиту. Игрок может рассчитывать по промокоду до 32500 рублей, если пройдет верификацию и даст согласие на участие в рекламных предложениях букмекера. На сегодня акция по промокоду 1xBet распространяется на пользователей из России, Беларуси, Украины, Казахстана.
Самый полный список промокодов 1хБет на сегодня у нас на сайте. Все промокоды раздаются бесплатно: на ставку, при регистрации, бездепозитные промики. Обновляем каждые 5 часов. Обычно 1xBet промокод при регистрации предоставляет бонус на первый депозит и используется на этапе создания аккаунта в БК. Сумма вознаграждения достигает 100% от первого пополнения. Следующий тип — промокод 1xbet как использовать. Он позволяет заключать пари на спортивные события, либо пользоваться привилегиями в сфере азартных игр, доступных на сайте БК. Такой бонус предоставляется бесплатно в честь регистрации, Дня рождения или активности.
1XBET код для регистрации на приветственный подарок в 2026 — используйте промокод и оформите приветственный подарок в размере 100% до 100$. Специальный код 1xBet предоставляет шанс активировать увеличенный стартовый бонус от букмекера 1xBet при регистрации.Актуальный промокод доступен по этой ссылке — https://efaflex.ru/include/pages/?promokod_pri_registracii_6.html.
Profitez d’une offre 1xBet : utilisez-le une fois lors de l’inscription et obtenez un bonus de 100% pour l’inscription jusqu’a 130€. Renforcez votre solde facilement en placant des paris avec un multiplicateur de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Pour activer ce code, rechargez votre compte a partir de 1€. Decouvrez cette offre exclusive sur ce lien — https://www.lamarinda.it/wp-content/pgs/tufli_oseny_2015.html.
whoah this weblog is magnificent i like studying your posts. Keep up the good work! You recognize, lots of persons are hunting around for this info, you could help them greatly.
easystaffingmd.com
Le code promotionnel n’est pas necessaire : entrez-le dans le champ « Code promo » et reclamez un bonus de bienvenue de 100% jusqu’a 130€, a utiliser dans les paris sportifs. Vous pouvez vous inscrire sur le site 1xBet ou via l’application mobile. Apres votre premier depot, vous activerez le code bonus. L’offre est valable pour toute l’annee 2026, et le bonus doit etre mise dans les 30 jours. Decouvrez plus d’informations sur le code promo via ce lien — https://www.nuernberg-balkon.de/images/pgs/?le-code-promo-1xbet_bonus.html.
I think that what you posted was very logical. However, what about this? what if you wrote a catchier title? I am not suggesting your content isn’t good., however what if you added a post title that grabbed a person’s attention? I mean %BLOG_TITLE% is a little boring. You ought to glance at Yahoo’s front page and see how they create post titles to grab viewers to click. You might add a video or a picture or two to grab readers interested about everything’ve got to say. In my opinion, it might make your website a little bit more interesting.
https://easystaffingmd.com
Акционный код 1xBet — пропишите его в специальное поле при открытии счета, внесите свой счет на сумму от 100 рублей и заберите бонусом в размере 100% (до 32500 рублей).В разделе аккаунта перейдите в раздел «Акции» и отметьте вариант «Использовать промокод».Введите полученный бонусный код в строку для промокода. Нажмите подтвердить и ознакомьтесь с условиями использования.Актуальный промокод 1xBet 2026 можно узнать по ссылке — https://ural-hifi.ru/fonts/inc/1xbet-promokod.html.
промокод 1xBet при регистрации ознакомьтесь с преимуществами для новых игроков платформы
промокод 1xBet все актуальные акции и бонусы собраны на одной странице
https://www.reverbnation.com/artist/meilleurcodepromo1xbet7
модульная техника
medtronik.ru/ свежие предложения и акции букмекера 1xBet
Бесплатный промокод 1xBet 32500 рублей. Промокод при регистрации в БК 1xBet рассчитан на привлечение новых клиентов. Совокупность букв и цифр вводится при создании аккаунта, что поднимает сумму первого пополнения счета до 325000 тысяч рублей. Редакция напоминает, что для получения бонуса потребуется пройти процедуру отыгрыша. Букмекер просит проставить сумму экспрессами. Коэффициент каждой отдельной ставки составляет минимум 1.4. После прохождения отыгрыша выбранная сумма денег перейдет из бонусного на основной счет. 1xBet промокод на День Рождения. Букмекерская контора поздравляет каждого верифицированного клиента бесплатной ставкой на День Рождения. На сегодня у 1xBet предусмотрено несколько рабочих промокодов: на бесплатную ставку, на 25000 рублей, а также промокод до 1500 евро. Промокод 1xBet до 1500 евро. Между букмекерами активно развивается конкуренция, и это правильно. Каждый старается привлечь к себе как можно больше игроков, в том числе различными акционными предложениями, бонусами и тому подобными маркетинговыми методами. Как получить промокод 1xBet? Промокод казино 1xBet до 1500 евро. тото 1хбет промокод. Промокод 1хБет на сегодня. Бездепозитный промокод 1xBet. Сегодня отсутствует. Один из наиболее популярных среди таковых — использование промокодов.
1xBet промокод актуальная информация о действующих предложениях и бонусных акциях для новых пользователей
wettquoten erklärt
Profitez d’une offre 1xBet : beneficiez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Activez cette offre en rechargant votre compte des 1€. Vous pouvez trouver le code promo 1xbet sur ce lien — https://www.freie-waehler-werdau.de/wp-content/pgs/le-code-promo-1xbet_bonus.html.
Промокод 1xBet при регистрации. Компания 1хБет заинтересована в привлечении новых клиентов, поэтому для новых игроков действует акция в виде бонуса, который равен сумме первого депозита, но не превышает 225 000 рублей. Однако при использовании промокода букмекерская контора увеличит размер приветственного бонуса. Для того чтобы получить повышенную сумму на первый депозит, игроку необходимо выполнить следующие условия: Зайти на сайт букмекера. Выбрать способ регистрации по e-mail. Заполнить поля с личными данными. Ввести промокод в поле слева от кнопки «Зарегистрироваться». Ознакомиться с правилами букмекера. 1хбет промокоды на слоты поможет пользователям получить еще больше бонусов от букмекерской конторы. Подробная инструкция по поиску и активации бонусных кодов. Промокод — комбинация из цифр и букв, которая позволяет игроку активировать специальное предложение от букмекера 1хБет. С его помощью пользователь может получить: бонусные средства на депозит; бесплатную ставку; промо-баллы; другие подарки. Сегодня вы сможете найти множество подобных ресурсов, которые регулярно обновляют список актуальных предложений БК.
Code promo 1xBet pour 2026 : profitez d’un bonus de bienvenue de 100% jusqu’a 130€ lors de votre inscription. Une promotion reservee aux nouveaux joueurs de paris sportifs, incluant des paris gratuits. Inscrivez-vous avant la fin de l’annee 2026. Decouvrez le code promotionnel 1xBet via le lien fourni — Codes Promo Gratuits Pour 1xbet. Le code promo 1xBet vous permet d’activer un bonus d’inscription 1xBet exclusif et de commencer a parier avec un avantage. Le code promotionnel 1xBet 2026 est valable pour les paris sportifs, le casino en ligne et les tours gratuits. Decouvrez des aujourd’hui le meilleur code promo 1xBet et profitez du bonus de bienvenue 1xBet sans depot initial.
Предложения от 1xBet также варьируются по типу. Определённые акции предлагаются новичкам. Регистрируясь на 1xBet, используйте промокод и заберите 100% приветственный бонус до 32500 рублей.Компания 1xBet предлагает своим клиентам играть и делать ставки с использованием специальных бонусов. Это делает процесс азартнее к играм и гарантирует надежность игры.Промокод 2026 года можно найти через официальный сайт — http://www.medtronik.ru/images/pages/1hbet_2021_promokod_pri_registracii.html.
https://anotepad.com/note/read/jw796fyd
Акционный код 1xBet — введите его в поле для промокода при регистрации, депозитируйте свой аккаунт на сумму от 100 RUB и заберите акцией в размере удвоения депозита (до 32 500 RUB).В профиле отыщите раздел «Акции» и отметьте вариант «Активировать промокод».Укажите полученный код в строку для промокода. Нажмите подтвердить и прочитайте правила бонуса.Бонусный код 1xBet 2026 года можно узнать по ссылке: промокод 1xbet читачок.
промокод 1xBet при регистрации ознакомьтесь с преимуществами для новых игроков платформы
http://medtronik.ru/ удобная страница с актуальными бонусами и акциями
https://pakhie.com/blogs/87128/Code-Promo-1xBet-Aujourd-hui-2026-Bonus-130
buchmacher in deutschland
Актуальные тенденции 2026 года в бонусной политике букмекеров: обзор фрибетов, промо-купонов и программ лояльности; в тексте, в середине объяснения, даётся ссылка на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html как один из способов получить приветственный пакет. Читателям рекомендуем внимательно читать условия акций.
https://sislivip.com/fr/code-promo-1xbet-bonus-jusqua-130-eur/
В обзоре возможностей для игроков мы подробно разбираем типы бонусов, включая фрибеты и депозитные поощрения; в середине материала приведена ссылка на 1xBet промокод на сегодня, который может и помочь новым пользователям при регистрации. Также, даём советы по безопасности и ответственному подходу к ставкам.
kraken зеркало Этика Безопасчности и Мораль Анонимности “Кракен” предоставляет возможность действовать вне рамок общепринятых норм, но вместе с такой свободой приходит и ответственность. Анонимность не должна быть оправданием для злоупотреблений, для причинения вреда другим. Помните о моральных принципах, даже когда никто не видит. Используйте “Kraken” с умом, с пониманием последствий, и тогда он станет не источником проблем, а инструментом для достижения собственных целей.
Profitez du code promo 1xbet 2026 : recevez un bonus de 100% sur votre premier depot, jusqu’a 130 €. Placez vos paris en toute plaisir en utilisant simplement les fonds bonus. Une fois inscrit, n’oubliez pas de recharger votre compte. Si votre compte est verifie, vous pourrez retirer toutes les sommes d’argent, y compris les bonus. Vous pouvez trouver le code promo 1xbet sur ce lien — https://www.nuernberg-balkon.de/images/pgs/?le-code-promo-1xbet_bonus.html.
https://www.wowonder.xyz/1761021926498237_126822
https://www.medtronik.ru официальный источник актуальных бонусных предложений
wettquoten england deutschland
Code promo pour 1xBet : utilisez-le une fois lors de l’inscription et obtenez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Activez cette offre en rechargant votre compte des 1€. Vous pouvez trouver le code promo 1xbet sur ce lien — https://fgvjr.com/pgs/code_promo_163.html.
где найти промокод для 1xBet узнайте надёжные источники получения действующих кодов и предложений
https://sislivip.com/fr/code-promo-1xbet-bonus-jusqua-130-eur/
Что делает промокоды букмекерской конторы 1xBet уникальными? Какие знания о кодах, чтобы получить наибольшую пользу от их применения? И, наконец, что еще любопытного есть в системе бонусов этой конторы, на которые стоит учесть, если вы планируете использовать бонусы. Промокод на 1xBet (актуален в 2026 году, бонус 100%) можно найти по этой ссылке: промокоды на слоты в 1xbet.
кракен магазин Кракен: Сущность и Альтернативы “Kraken” – это не просто платформа, это идеология, основанная на свободе слова, анонимности и обходе цензуры. Однако, стоит помнить, что в этом мире не существует абсолютной безопасности. Всегда есть риск быть разоблаченным, обманутым или столкнуться с последствиями своих действий. Перед тем как погрузиться в пучину ” кракен”, необходимо взвесить все “за” и “против”, оценить свои возможности и принять на себя ответственность за свой выбор.
https://medtronik.ru/ официальный портал с актуальными условиями регистрации и бонусами
1xBet бонусный код на бонус в 2026-м — введите промокод и активируйте приветственный подарок в размере 100% до 100$. Данный бонусный код даёт возможность активировать увеличенный стартовый бонус от БК 1xBet после создания аккаунта.Промокод 1xBet можно найти на сайте 1xBet: 1xbet промокод на 6500 рублей.
Регистрация в 2026 году — руководство по бонусам и предложениям. Узнайте, как правильно активировать регистрационные предложения, и в середине процесса обратите внимание на 1xBet промокод как вариант получения дополнительного вознаграждения. FAQ помогут легко разобраться с верификацией и получением бонусов.
трансы Новосибириск Телеграм: Проводник по Миру Трансгендерности в Городах России Telegram давно перестал быть просто мессенджером. Он превратился в многофункциональную платформу, где люди находят единомышленников, делятся информацией и организуют сообщества по интересам. Одним из таких направлений являются каналы, посвященные трансгендерной тематике. В российских городах, таких как Новосибирск, Екатеринбург, Воронеж, Волгоград и Челябинск, существуют Telegram-каналы, объединяющие транс-персон и тех, кто интересуется этим вопросом.
http://medtronik.ru/ страница с полезной информацией для новичков
Регистрация в 2026 году — подробно о бонусам и предложениям. Узнайте, как правильно активировать регистрационные предложения, а также в середине процесса обратите внимание на 1xBet промокод как вариант получения дополнительного вознаграждения. Часто задаваемые вопросы помогут легко разобраться с верификацией и получением бонусов.
wettbüro paderborn
1xBet бонус код получите дополнительные преимущества при создании аккаунта на официальном сайте
lenotoplenie.ru/ получите полную информацию о бонусных программах 1xBet
halbzeit endergebnis wetten
Чтобы получить приветственных бонусов от букмекера 1xBet, нужно выполнить несколько требований, однако промокоды позволяют сделать это значительно проще.Бонусные предложения, доступных пользователям через промокоды 1xBet, могут быть различными, но даже умеренный бонус способен существенно повысить ставочный баланс клиента.Введите промокод, чтобы получить бонус 100% на первый депозит в 2026 году.Перейдите по ссылке, чтобы активировать промокод: 1xbet промокоды действующим игрокам.
трансы Челябинск География Поддержки: От Сибири до Юга России Каждый из каналов, будь то @ts_novosibirsk (трансы Новосибирск, трансы новосибирска), @ts_ekaterinburgh (трансы Екатеринбург, трансы Екатеринбурга), @ts_voronezh (трансы Воронеж, трансы Воронежа), @transy_volgograd (трансы Волгоград, трансы волгограда) или @ts_chelyabinska (трансы Челябинск, трансы челябинска), отражает уникальную специфику своего региона. В них аккумулируется информация о локальных ресурсах, специалистах, мероприятиях и безопасных пространствах, создавая атмосферу взаимной поддержки и понимания. Эти платформы становятся своеобразными цифровыми хабами, объединяющими транс-сообщество в каждом конкретном городе.
Система промокодов при регистрации даёт возможность новым игрокам получать бонусы к первому депозиту; мы описываем, как правильно заполнить регистрационную форму и где указать данные, а в середине примера даём ссылку на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html для удобства. Обратите внимание, что бонусные условия могут отличаться в зависимости от региона.
Что делает промокоды букмекерской конторы 1xBet выгодными? Какие нюансы стоит понимать о кодах, чтобы взять максимальную выгоду от их активации? И, наконец, на какие еще детали в системе бонусов этой конторы, на которые стоит учесть, если вы планируете ставить с бонусами. Промокод на 1xBet (актуален в 2026 году, бонус 100%) можно найти по этой ссылке: промокод 1xbet бонусные.
https://www.lenotoplenie.ru/ узнайте, как получить приветственные бонусы и участвовать в акциях
https://lenotoplenie.ru инструкция по получению приветственных предложений
Система промокодов при регистрации даёт возможность новым игрокам получать бонусы к первому депозиту; мы описываем, как без ошибок заполнить регистрационную форму и где указать данные, а в середине примера даём ссылку на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html для удобства. Важно, что бонусные условия могут отличаться в зависимости от региона.
lenotoplenie.ru/ свежие предложения и акции букмекера 1xBet
lenotoplenie.ru инструкции, как активировать бонусные программы и акции
Акционный код 1xBet — укажите его в соответствующее поле при регистрации на сайте, депозитируйте свой счет на сумму от 100 рублей и заберите предложением в размере 100% (до 32500 рублей).В разделе аккаунта откройте раздел «Акции» и активируйте вариант «Активировать промокод».Укажите полученный промокод в нужное поле. Сохраните изменения и изучите подробности бонуса.Бонусный код 1xBet 2026 года можно найти по этой ссылке: рабочий промокод 1xbet.
В обзоре возможностей для игроков мы кратко разбираем типы бонусов, включая фрибеты и депозитные поощрения; в соответствующем абзаце приведена ссылка на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html, который может и помочь новым пользователям при регистрации. Кроме того, даём советы по безопасности и ответственному подходу к ставкам.
https://meisterbook.com/read-blog/15849
Чтобы получить акционных бонусов от платформы 1xBet, следует соблюсти ряд правил, однако промокоды позволяют получить их быстрее и проще.Размеры бонусов, доступных пользователям через промокоды 1xBet, могут быть различными, но даже минимальный бонус способен заметно увеличить ставочный баланс клиента.Активируйте промокод, чтобы получить увеличенный 100% бонус в году 2026.Перейдите по ссылке, чтобы активировать промокод: рабочий промокод 1xbet на сегодня.
Если вы хотите найти информацию о бонусах при регистрации, прочитайте наши рекомендации о видах вознаграждений; в одном из разделов материала естественно упомянут 1хБет промокод для получения приветственного бонуса. Редакция объясняем, как вводить данные при регистрации и какие условия нужно выполнить для отыгрыша.
wetten deutschland frankreich
https://lenotoplenie.ru/ официальный портал с актуальными условиями регистрации и бонусами
https://www.lenotoplenie.ru узнайте больше о возможностях бонусных предложений
lenotoplenie.ru подборка бонусов и акций для новых пользователей
1хБет промокод на приветственный бонус в 2026 — используйте промокод и активируйте бонус в размере 100% до 100$. Уникальный бонусный код позволяет заработать акционный бонус от букмекера 1xBet после создания аккаунта.Промокод опубликован на сайте 1xBet — https://efaflex.ru/include/pages/?promokod_pri_registracii_6.html.
http://www.lenotoplenie.ru подробные условия участия в бонусных программах
Регистрация в 2026 году — руководство по бонусам и предложениям. Узнайте, как корректно активировать регистрационные предложения, а также в середине процесса обратите внимание на 1xBet промокод как вариант получения дополнительного вознаграждения. FAQ помогут быстро разобраться с верификацией и получением бонусов.
Что делает промокоды букмекерской конторы 1xBet уникальными? Какие нюансы стоит понимать о кодах, чтобы извлечь максимум преимуществ от их использования? И, наконец, какие еще интересные моменты в бонусной программе этой конторы, на которые стоит обратить внимание, если вы планируете играть за бонусы. Промокод на 1xBet (актуален в 2026 году, бонус 100%) можно найти по этой ссылке: промокоды 1xbet на игры.
Подробная инструкция по активации бонусов и типам предложений — от фрибетов до подарков на День Рождения; в одном из абзацев естественно вставлена ссылка на 1хБет промокод на сегодня, чтобы читатель мог сразу перейти к источнику. Материал также рассказывает о верификации и минимальных требованиях для вывода средств.
I always leave this blog feeling inspired and motivated to make positive changes in my life Thank you for being a constant source of encouragement
Букмекер и казино 1win хвалится фрибетами.
Фрибеты и ваучеры дают дополнительный баланс.
Завести аккаунт просто, и сразу открываются акции.
Игровое лобби предлагает широкий выбор.
Хочешь свежий промокод — переходи по 1вин промокод и активируй на депозите.
Играйте ответственно, без лишних рисков.
https://socialmeet.app/read-blog/28169
https://lenotoplenie.ru узнайте, какие акции действуют прямо сейчас
Wow, beautiful site. Thnx …
My webpage … baccarat Hand mincer (https://WWW.Chovatelehat.cz/slotbox-casino-no-deposit-bonus-codes-for-free/)
quote bei wetten dass
Подробная инструкция по активации бонусов и типам предложений — от фрибетов до подарков на День Рождения; в одном из абзацев естественно вставлена ссылка на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html, дабы читатель мог быстро перейти к источнику. Материал также рассказывает о верификации и минимальных требованиях для вывода средств.
https://lenotoplenie.ru/ официальный портал с актуальными условиями регистрации и бонусами
Актуальные тенденции 2026 года в бонусной политике букмекеров: анализ фрибетов, промо-купонов и программ лояльности; в тексте, в середине объяснения, даётся ссылка на 1xBet промокод 2026 как один из способов получить приветственный пакет. Пользователям рекомендуем внимательно читать условия акций.
http://lenotoplenie.ru лучшие акции и бонусы для новых игроков
androgel testosterone gel https://community.roku.com/t5/user/viewprofilepage/user-id/764639
https://www.greencarpetcleaningprescott.com/board/board_topic/7203902/7330532.htm/
1xBet промокод инструкции по активации бонусных предложений и правила участия
промокод 1xBet при регистрации ознакомьтесь с преимуществами для новых игроков платформы
Актуальные тенденции 2026 года в бонусной политике букмекеров: анализ фрибетов, промо-купонов и программ лояльности; в тексте, в середине объяснения, даётся ссылка на 1xBet промокод 2026 как один из способов получить приветственный пакет. Пользователям рекомендуем внимательно читать условия акций.
Список бесплатных предложений и типов бонусов: короткий обзор промо-акций для новичков и постоянных игроков; в середине абзаца приводим ссылку на промокод при регистрации 1xBet как источник подробной информации о том, куда вводить данные и какие условия ожидать. К тому же рассказываем про порядок валидации аккаунта.
https://www.lenotoplenie.ru/ вся информация о бонусных возможностях на платформе
lenotoplenie.ru/ свежие предложения и акции букмекера 1xBet
Полезное руководство по получению бонусов и тому, где искать официальную информацию: в пункте о регистрации мы вставляем ссылку на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html, чтобы показать пример записи в регистрационном поле. Объясняем особенности работы с промо-купонами и способы их получения.
Регистрация в 2026 г. — руководство по бонусам и предложениям. Посмотрите, как правильно активировать приветственные предложения, а также в середине процесса обратите внимание на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html как вариант получения дополнительного вознаграждения. Часто задаваемые вопросы помогут легко разобраться с верификацией и получением бонусов.
Актуальные тенденции 2026 года в бонусной политике букмекеров: обзор фрибетов, промо-купонов и программ лояльности; в тексте, в середине объяснения, даётся ссылка на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html как один из способов получить приветственный пакет. Читателям рекомендуем внимательно читать условия акций.
Регистрация в 2026 г. — руководство по бонусам и акциям. Узнайте, как корректно активировать регистрационные предложения, а также в середине процесса обратите внимание на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html как вариант получения дополнительного вознаграждения. Часто задаваемые вопросы помогут быстро разобраться с верификацией и получением бонусов.
What type of content would you like to see more of in the future? Let us know in the comments!
Thanks a ton for sharing this awesome internet site.
Feel free to surf to my webpage; george freeman casino (Justina (https://Kimhungimex.com/internetove-kasino-bez-registracie-a-vkladu/))
Подробная инструкция по активации бонусов и типам предложений — от фрибетов до подарков на День Рождения; в одном из абзацев естественно вставлена ссылка на 1хБет промокод на сегодня, дабы читатель мог быстро перейти к источнику. Статья также рассказывает о верификации и минимальных требованиях для вывода средств.
Список бесплатных предложений и типов бонусов: отдельный обзор промо-акций для новичков и постоянных игроков; в тексте приводим ссылку на промокод при регистрации 1xBet как источник подробной информации о том, куда вводить данные и какие условия ожидать. К тому же рассказываем про порядок валидации аккаунта.
https://buzzakoo.com/posts/41727
https://dzen.ru/a/aPRXjPraMEja6Ols
Deneme bonusu veren siteler ile yüksek kazanç sağlayın. Bonus Veren Siteler dwnwmw bwnwsw vwrwn swtwlwr listesine göz atmak için hemen sitemize gelin
sportwetten mit paysafecard
https://independent.academia.edu/HerbertStidham
Актуальные тенденции 2026 года в бонусной политике букмекеров: обзор фрибетов, промо-купонов и программ лояльности; в тексте, в разделе с примерами, даётся ссылка на https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html как один из способов получить приветственный пакет. Пользователям рекомендуем внимательно читать условия акций.
Полезное руководство по получению бонусов и тому, где искать официальную информацию: в разделе регистрации мы вставляем ссылку на 1хБет промокод 2026, дабы показать пример записи в регистрационном поле. Объясняем особенности работы с промо-купонами и способы их получения.
https://location.bizlisting.cloud/1xbet-free-bet-promo-code-up-to-e105-bonus/
https://www.eminamclean.com/profile/salvat45651699/profile
wetten bayern meister quote
online wettbüro eröffnen
Авто под заказ из Китая, Выездная диагностика в Магнитогорске – это удобный и эффективный способ оценить состояние автомобиля перед покупкой. Наши опытные эксперты проведут комплексную проверку всех ключевых узлов и агрегатов, используя современное диагностическое оборудование, и предоставят вам подробный отчет о техническом состоянии автомобиля.
Подбор земельных участков Безопасные сделки: защита ваших интересов – наш приоритет.
kraken ссылка Kraken market – это многогранная площадка, где встречаются продавцы и покупатели со всего мира, предлагая широкий спектр товаров и услуг. Здесь можно найти все, что душе угодно, от редких артефактов до инновационных разработок. Приготовьтесь к захватывающему приключению, полному неожиданных открытий и выгодных предложений. Но не забывайте о здравом смысле и критическом мышлении, чтобы не стать жертвой недобросовестных продавцов.
Выездная диагностика Магнитогорск Выездная диагностика в Магнитогорске – это удобный и эффективный способ оценить состояние автомобиля перед покупкой. Наши опытные эксперты проведут комплексную проверку всех ключевых узлов и агрегатов, используя современное диагностическое оборудование, и предоставят вам подробный отчет о техническом состоянии автомобиля.
kraken ссылка Kraken ссылка – это навигатор по бескрайним просторам даркнета, указывающий путь к заветной цели. Однако, доверять первой попавшейся ссылке равносильно прыжку в пропасть с завязанными глазами. Прежде чем сделать этот шаг, убедитесь в её подлинности, проверьте репутацию источника и подготовьтесь к возможным неожиданностям. Безопасность превыше всего, и только внимательность и осторожность помогут вам избежать неприятных сюрпризов.
Hi terrific website! Does running a blog like this take a massive amount work? I have very little expertise in programming however I was hoping to start my own blog soon. Anyways, if you have any ideas or tips for new blog owners please share. I know this is off topic however I just needed to ask. Cheers!
kra42 at
Currently it seems like Movable Type is the preferred blogging platform available right now. (from what I’ve read) Is that what you are using on your blog?
kra42 at
Profitez d’un code promo unique sur 1xBet permettant a chaque nouveau joueur de beneficier jusqu’a 100€ de bonus sportif a hauteur de 100% en 2026. Ce bonus est credite sur votre solde de jeu en fonction du montant de votre premier depot, le depot minimum etant fixe a 1€. Pour eviter toute perte de bonus, veillez a copier soigneusement le code depuis la source et a le saisir dans le champ « code promo (si disponible) » lors de l’inscription, afin de preserver l’integrite de la combinaison. Le bonus de bienvenue n’est pas la seule promotion ou vous pouvez utiliser un code, d’autres combinaisons vous permettant d’obtenir des bonus supplementaires sont disponibles dans la section « Vitrine des codes promo ». Consultez le lien pour plus d’informations sur les promotions disponibles > Comment Obtenir Un Code Promo 1xbet. Grace au code promo 1xBet gratuit, obtenez un pari gratuit 1xBet ou un bonus sans depot 1xBet. Le code promotionnel 1xBet valide vous permet de beneficier d’un bonus de bienvenue 1xBet 2026 sur vos premiers paris. Essayez le code promo sport 1xBet pour miser sans risque et decouvrir la plateforme.
I’m not sure why but this website is loading extremely slow for me. Is anyone else having this problem or is it a issue on my end? I’ll check back later and see if the problem still exists.
kra42 cc
Profitez d’un code promo unique sur 1xBet permettant a chaque nouveau joueur de beneficier jusqu’a 100€ de bonus sportif a hauteur de 100% en 2026. Le bonus sera ajoute a votre solde en fonction de votre premier depot, le depot minimum etant fixe a 1€. Pour eviter toute perte de bonus, veillez a copier soigneusement le code depuis la source et a le saisir dans le champ « code promo (si disponible) » lors de l’inscription, afin de preserver l’integrite de la combinaison. D’autres promotions existent en plus du bonus de bienvenue, d’autres combinaisons vous permettant d’obtenir des bonus supplementaires sont disponibles dans la section « Vitrine des codes promo ». Consultez le lien pour plus d’informations sur les promotions disponibles — https://www.atrium-patrimoine.com/wp-content/artcls/?code_promo_196.html.
What’s up, yes this post is genuinely fastidious and I have learned lot of things from it on the topic of blogging. thanks.
https://kra42c.com
https://www.demilked.com/author/freesbet/
https://www.levalet.xyz/profile/freespinsfor1xbet1771/profile
https://nashforum.listbb.ru/viewtopic.php?f=2&t=41138
https://zumo-spin-games.com/
Birçok bahis ve casino platformu, oyuncuları dxnxmx bxnxsx vxrxn sxtxlxr kendine çekmek için deneme bonusu kampanyaları düzenlemektedir. 2025 yılında en çok tercih edilen deneme bonusu
sportwetten bonus neu
Wow, awesome weblog layout! How lengthy have you ever been running a blog for? you made blogging look easy. The entire glance of your website is wonderful, as well as the content material!
kra41 cc
Why viewers still use to read news papers when in this technological globe all is existing on web?
https://kra41c.com
https://zumo-spin-games.com/
code promo 1xBet valide Regional variations underscore the platform’s global reach and tailored marketing approaches. Searches range from “Code promo 1xbet Afrique du Sud” to “code promo 1xbet canada”, emphasizing the focus on specific geographic areas to further maximize the return. This also means that regulations and restrictions can vary. There are a myriad of promo codes of various values and for various use-cases, from sports betting to casino and beyond. Ultimately, the search is driven by the aspiration to enhance the 1xBet experience with a strategic code, whether it provides welcome bonus or other promotions.
https://rapidgator.net/file/2580f7f0fb2a9b9f31ff9d1cd3e40783/1xBet_Bonus_Code_2026__€130_for_Sports_Bets__.pdf.html
Profitez d’une offre 1xBet : utilisez-le une fois lors de l’inscription et obtenez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Pour activer ce code, rechargez votre compte a partir de 1€. Decouvrez cette offre exclusive sur ce lien : 1xbet Code Promo Tours Gratuits. Le code promo 1xBet aujourd’hui est disponible pour les joueurs du Cameroun, du Senegal et de la Cote d’Ivoire. Avec le 1xBet code promo bonus, obtenez jusqu’a 130€ de bonus promotionnel du code 1xBet. Ne manquez pas le dernier code promo 1xBet 2026 pour les paris sportifs et les jeux de casino.
code promo 1xbet pour l’inscription The allure of 1xBet, with its wide array of betting options, is undeniable. However, navigating the world of promo codes can be a labyrinthine task. Whether you seek a “code promo 1xBet” for sports betting, casino games, or simply a “bonus inscription 1xBet,” understanding the landscape is key.
Profitez d’une offre 1xBet : beneficiez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Pour activer ce code, rechargez votre compte a partir de 1€. Vous pouvez trouver le code promo 1xbet sur ce lien > Codes Promotionnels 1x Pari. Le code promo 1xBet aujourd’hui est disponible pour les joueurs du Cameroun, du Senegal et de la Cote d’Ivoire. Avec le 1xBet code promo bonus, obtenez jusqu’a 130€ de bonus promotionnel du code 1xBet. Ne manquez pas le dernier code promo 1xBet 2026 pour les paris sportifs et les jeux de casino.
Полезное руководство по получению бонусов и тому, где искать официальную информацию: в пункте о регистрации мы вставляем ссылку на https://www.apelsin.su/wp-includes/articles/promokod_240.html, чтобы показать пример записи в регистрационном поле. Объясняем особенности работы с промо-купонами и способы их получения.
Как получить приветственный бонус: краткая инструкция по регистрации и пополнению счёта, с указанием требований по отыгрышу; в середине параграфа мы указываем ссылку на ввести промокод на 1xbet, для того чтобы пользователь мог перейти и узнать подробности. Помимо этого приводим примеры доступных типов акций.
ламинат Магазин напольных покрытий – это ваш надежный проводник в мире полов. Здесь представлен широкий ассортимент материалов от ведущих производителей, способных удовлетворить любые запросы и бюджеты. Квалифицированные консультанты помогут вам подобрать оптимальное решение, учитывая особенности помещения, ваши личные предпочтения и финансовые возможности. Помимо самих покрытий, в магазине вы найдете все необходимые сопутствующие товары: подложки, плинтусы, клеи, герметики и средства для ухода за полом. Ваша задача – лишь выбрать, а наша – предоставить все необходимое для создания идеального пола в вашем доме.
Куда сходить в Питере Продолжить знакомство с городом можно, прогуливаясь по Невскому проспекту – главной артерии Петербурга. Здесь, среди исторических зданий и бутиков, кипит жизнь. Загляните в Дом книги, полюбуйтесь архитектурой Казанского собора, сделайте фото на фоне Елисеевского магазина – места, пропитанного духом старого Петербурга.
Thanks a bunch for sharing this with all folks you actually understand what you’re talking approximately! Bookmarked. Kindly also visit my site =). We will have a link change agreement between us
https://pride.banztechnologies.in/skachat-prilozhenie-melbet-2025/
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Any way I will be subscribing to your augment and even I achievement you access consistently quickly.
https://www.hacienda-events.com/skachat-melbet-na-android-besplatno-2025/
https://www.diigo.com/item/note/8ucx2/ms7i?k=fc2b1f8c694eab9d27b0e92a2dd3d4a4
kraken сайт Kraken ссылка – это навигатор по бескрайним просторам даркнета, указывающий путь к заветной цели. Однако, доверять первой попавшейся ссылке равносильно прыжку в пропасть с завязанными глазами. Прежде чем сделать этот шаг, убедитесь в её подлинности, проверьте репутацию источника и подготовьтесь к возможным неожиданностям. Безопасность превыше всего, и только внимательность и осторожность помогут вам избежать неприятных сюрпризов.
http://www.filefactory.com/file/7lec5eylpo0/1xBet%20Bonus%20Promo%20Code%202026_%20Up%20to%20%E2%82%AC130%20Bonus.pdf
https://bestballs.ru/
kraken сайт Kraken сайт – это не просто веб-страница, а тщательно выстроенная экосистема, живущая по своим, порой негласным правилам. Это цифровой оазис для тех, кто ценит приватность и независимость, но одновременно и зона повышенного риска, где каждое действие должно быть обдуманным и взвешенным. Здесь встречаются анонимные продавцы и покупатели, заключаются спорные сделки, и разгораются нешуточные страсти. Чтобы не заблудиться в этом лабиринте, необходимо обладать острым умом, твердой рукой и непоколебимой верой в свою интуицию.
I appreciate, result in I discovered exactly what I was having a look for. You’ve ended my 4 day long hunt! God Bless you man. Have a great day. Bye
https://surya33.com/skachat-bk-melbet-na-android-2025/
Thanks , I’ve recently been searching for information approximately this subject for a long time and yours is the greatest I’ve found out till now. But, what concerning the conclusion? Are you certain about the supply?
https://surga168slot.net/melbet-prilozhenie-skachat-2025/
https://twanty2.com/read-blog/26145
besten sportwetten seiten
Offre promotionnelle 1xBet pour 2026 : profitez d’un bonus de bienvenue de 100% jusqu’a 130€ en vous inscrivant des maintenant. C’est une offre unique pour les paris sportifs, avec la possibilite de placer des paris gratuits. Rejoignez 1xBet avant le 31 decembre 2026. Vous pouvez retrouver le code promo 1xBet sur ce lien ? Code Promotionnel 1xbet. Le code promo 1xBet vous permet d’activer un bonus d’inscription 1xBet exclusif et de commencer a parier avec un avantage. Le code promotionnel 1xBet 2026 est valable pour les paris sportifs, le casino en ligne et les tours gratuits. Decouvrez des aujourd’hui le meilleur code promo 1xBet et profitez du bonus de bienvenue 1xBet sans depot initial.
Offre promotionnelle 1xBet pour 2026 : profitez d’un bonus de bienvenue de 100% jusqu’a 130€ lors de votre inscription. Une promotion reservee aux nouveaux joueurs de paris sportifs, avec la possibilite de placer des paris gratuits. Inscrivez-vous avant la fin de l’annee 2026. Le lien ci-dessous vous menera vers le code promo officiel 1xBet > https://www.atrium-patrimoine.com/wp-content/artcls/?code_promo_196.html.
trashbiker Регистратор: Твой свидетель в спорной ситуации.
Amazing things here. I’m very glad to look your article. Thanks a lot and I’m looking forward to touch you. Will you please drop me a mail?
номер для смс
sportwetten tipps vorhersagen heute
Используя промокод Мелбет при регистрации, игроки получают доступ к участию в приветственной бонусной программе. Полученные привилегии можно использовать, заключая ставки на ММА и другие виды спорта. Ниже рассказываем более подробно о том, какие бонусы предложены на сайте и как их отыграть. Бонусные программы нацелены на то, чтобы обеспечить для игроков возможность получить безболезненный опыт игры на сайте и сгладить первые возможные неудачи. Регистрируйтесь на платформе букмекера, активируйте melbet промокод при регистрации 2026 и пользуйтесь бонусными предложениями от букмекера Мелбет, чтобы получать больше положительных эмоций при заключении пари.
Промокод Melbet – это набор случайных или подобранных символов, которые позволяют новому игроку принять участие в акциях и получить подарки от БК Мелбет. К примеру, в 2026 году Мелбет промокод предлагает бонус 50 000 рублей на счет при регистрации. При выборе букмекерской конторы пользователи обращают внимание не только на маржу или коэффициенты, но и обязательно оценивают текущие акции. Крупные операторы предлагают бонусы на первый депозит, программу лояльности, фрибеты и другие виды поощрений. Бонусный код является самым распространённым видом привлечения клиентов в популярных букмекерских конторах. Чаще всего промокод Melbet представляет собой рандомный порядок букв и цифр, которые вводят в специальное поле в форме регистрации на сайте. Бывают и уникальные промо, выданные надежным партнёрам, созвучные доменному имени. промокод на сегодня мелбет позволяет получить повышенный бонус на первый депозит в размере 100% и бесплатную ставку на 400 RUB или фрибет на $30.
купить номер
кирпич в Одессе
online wetten ohne ausweis
kraken ссылка Kraken market – это многогранная площадка, где встречаются продавцы и покупатели со всего мира, предлагая широкий спектр товаров и услуг. Здесь можно найти все, что душе угодно, от редких артефактов до инновационных разработок. Приготовьтесь к захватывающему приключению, полному неожиданных открытий и выгодных предложений. Но не забывайте о здравом смысле и критическом мышлении, чтобы не стать жертвой недобросовестных продавцов.
kraken сайт Kraken market – это пестрый калейдоскоп предложений, где каждый может найти то, что ищет. Но, как и на любом рынке, здесь встречаются не только честные торговцы, но и мошенники, готовые обмануть доверчивых покупателей. Поэтому, прежде чем совершить покупку, тщательно изучите репутацию продавца, сравните цены и не стесняйтесь задавать вопросы. Помните, что ваша бдительность – лучшая защита от обмана и разочарования. Kraken market – это мир возможностей, но и мир ответственности.
Промокод – это комбинация символов, которую вводят в специально отведенную строку на сайте. После активации кода, пользователь получит вознаграждение от любимого БК. Обычно к промокоду прилагается подробное описание всех предлагаемых бонусов. Но иногда букмекеры позволяют игрокам выяснить назначение кода самостоятельно, ведь многие любят сюрпризы. В случае с промокодом, сюрприз наверняка окажется приятным, ведь его главная цель – создать игроку комфортные условия, заслужить лояльность. Существуют промокоды для новых игроков, которые действительны только при регистрации, и для постоянных – окно для ввода таких кодов находится под формой пополнения игрового баланса. Melbet промокод Введите: RS777 и тогда при депозите вы получите бонус 50 000 рублей автоматически. Букмекерская контора Мелбет в 2026 году создала комфортные условия для заядлых беттеров и новых пользователей. Промокоды – вещь распространенная, потому найти их легко. Часто букмекеры размещают коды в свободном доступе, для всеобщего пользования. А промокоды для более значимых наград поступают игрокам индивидуально, например в качестве подарка ко дню рождения, извинения за возможные неудобства или просто в благодарность за сотрудничество.
7k casino регистрация игровые автоматы 7к известны высокими выплатами и интересными сюжетами, что привлекает множество игроков.
При регистрации в БК Melbet игрокам предлагается самостоятельно выбрать стартовую награду: фрибет на $30 или 100% бонус на депозит до 7 000 RUB. Предлагаем Мелбет промокод на сегодня 2026, благодаря которому вы получите не только повышенный до 50 000 RUB бонус на первое пополнение счета, но и право на бесплатный прогноз. Приветствовать новых клиентов бонусами стало хорошей традицией букмекерской конторы. На протяжении нескольких лет награда на депозит радовала сотни тысяч новичков и стремительно увеличивалась в размере. В 2026 году вознаграждение за пополнение счета достигло суммы в 7 000 российских рублей. Мы делаем более выгодное предложение. Игроки, которые введут в промокод мелбет при регистрации — RS777, не просто увеличат максимальный размер бонуса на депозит до 50 000 RUB, но и получат возможность воспользоваться фрибетом на 400 российских рублей.
7k casino 7k официальный сайт был разработан с учетом всех современных стандартов безопасности и удобства навигации.
Code promo sur 1xBet est unique et permet a chaque nouveau joueur de beneficier jusqu’a 100€ de bonus sportif a hauteur de 100% en 2026. Le bonus sera ajoute a votre solde en fonction de votre premier depot, le depot minimum etant fixe a 1€. Pour eviter toute perte de bonus, veillez a copier soigneusement le code depuis la source et a le saisir dans le champ « code promo (si disponible) » lors de l’inscription, afin de preserver l’integrite de la combinaison. D’autres promotions existent en plus du bonus de bienvenue, vous pouvez trouver d’autres offres dans la section « Vitrine des codes promo ». Consultez le lien pour plus d’informations sur les promotions disponibles ? https://www.atrium-patrimoine.com/wp-content/artcls/?code_promo_196.html.
Code promo pour 1xBet : utilisez-le une fois lors de l’inscription et obtenez un bonus de 100% pour l’inscription jusqu’a 130€. Renforcez votre solde facilement en placant des paris avec un multiplicateur de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Activez cette offre en rechargant votre compte des 1€. Decouvrez cette offre exclusive sur ce lien : https://www.atrium-patrimoine.com/wp-content/artcls/?code_promo_196.html.
Полезное руководство по получению бонусов и тому, где искать официальную информацию: в пункте о регистрации мы вставляем ссылку на https://www.apelsin.su/wp-includes/articles/promokod_240.html, чтобы показать пример записи в регистрационном поле. Объясняем особенности работы с промо-купонами и способы их получения.
Подробная пошаговая инструкция по активации бонусов и типам предложений — от фрибетов до подарков на День Рождения; в тексте естественно вставлена ссылка на https://www.apelsin.su/wp-includes/articles/promokod_240.html, дабы читатель мог сразу перейти к источнику. Материал также рассказывает о верификации и минимальных требованиях для вывода средств.
Как получить приветственный бонус: пошаговая инструкция по регистрации и пополнению счёта, с указанием требований по отыгрышу; в середине параграфа мы указываем ссылку на https://sushikim.ru/image/pgs/1xbet-besplatnuy-promokod-pri-registracii.html, для того чтобы пользователь мог перейти и узнать подробности. Также приводим примеры доступных типов акций.
гинеколог беляево
https://share.evernote.com/note/f4983ff1-c70b-4ff3-7b57-7144b96b95e4
Как получить приветственный бонус: краткая инструкция по регистрации и пополнению счёта, включая требований по отыгрышу; в середине параграфа мы указываем ссылку на https://sushikim.ru/image/pgs/1xbet-besplatnuy-promokod-pri-registracii.html, для того чтобы пользователь мог перейти и узнать подробности. Помимо этого приводим примеры доступных типов акций.
Deneme Bonusu Veren Siteler 2025 listesi. Güvenilir siteler, yatırım d0n0m0 b0n0s0 v0r0n s0t0l0r şartsız deneme bonusu fırsatlarıyla en iyileri keşfedin.
болезни нервной системы
https://natural-beauty-clinic.ru/effektivnoe-lechenie-sustavnyh-bolej-sovremennye-podhody-i-rekomendaczii/
https://daunemas8a.blogspot.com/2025/10/1xbet-promo-code-2026-1650-155-free.html
остеопат одинцово
https://www.ganjingworld.com/s/eZDK7X6Og8
vpn для России
Регистрация в 2026 г. — подробно о бонусам и предложениям. Посмотрите, как корректно активировать приветственные предложения, и в середине процесса обратите внимание на https://sushikim.ru/image/pgs/1xbet-besplatnuy-promokod-pri-registracii.html как вариант получения дополнительного вознаграждения. Часто задаваемые вопросы помогут легко разобраться с верификацией и получением бонусов.
Полезное руководство по получению бонусов и тому, где искать официальную информацию: в разделе регистрации мы вставляем ссылку на https://sushikim.ru/image/pgs/1xbet-besplatnuy-promokod-pri-registracii.html, дабы показать пример записи в регистрационном поле. Разъясняем особенности работы с промо-купонами и способы их получения.
1000 рублей за регистрацию вывод сразу без вложений в казино
1000 рублей за регистрацию вывод сразу без вложений в казино с выводом без депозита
1хБет промокод при регистрации — специальное предложение для новых пользователей. Бонус за первый депозит в 1xBet. Инструкция по использованию бонуса 32 500 руб в букмекерской конторе 1хБет. Требования к регистрации и снятию выигрыша. Букмекерские конторы пользуются спросом у людей, чьи интересы плотно связаны со спортом, и чей азарт подкрепляется возможностью вознаграждения путем внесения порой незначительной суммы. Узнать детали бонуса можно здесь https://new-time.kiev.ua/images/pages/?stadii_raka_pryamoy_kishki.html. 1хБет промокод 2026 открывает доступ к бонусу на депозит до 32 500 рублей.
Как активировать бонус до 32 500 ? от букмекерской компании 1xBet? Узнайте подробности > https://surfplaza.ru/includes/list/1xbet_promokod_bonus_3.html
https://crpsc.org.br/forum/viewtopic.php?f=3&t=516825
the best promo code for 1xbet > https://2awebdesign.net/pages/1xbet_promo_code_exclusive_bonus_1.html The best promo codes for 1xBet are those that offer significant bonuses, such as deposit matches, free bets, or free spins. These codes can greatly enhance the betting experience by providing extra value for both new and existing users.
невролог люберцы травматолог ортопед мытищи
1xbet promo code for registration > https://www.radio-rfe.com/content/pages/1xbet_promo_code_exclusive_bonus_1.html The 1xBet welcome bonus is a special offer available to new users when they sign up on the platform. This bonus usually includes a 100% match on the first deposit, up to a certain amount, giving new users more funds to start betting.
Code promo pour 1xBet : beneficiez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Pour activer ce code, rechargez votre compte a partir de 1€. Vous pouvez trouver le code promo 1xbet sur ce lien — http://www.tiroavolobologna.it/media/pgs/le-code-promo-1xbet_bonus.html.
Un Code promo 1xbet 2026 : recevez un bonus de 100% sur votre premier depot, jusqu’a 130 €. Jouez et placez vos paris facilement grace aux fonds bonus. Une fois inscrit, n’oubliez pas de recharger votre compte. Si votre compte est verifie, vous pourrez retirer toutes les sommes d’argent, y compris les bonus. Le code promo 1xbet est disponible via ce lien > https://cherwellcricketleague.com/img/pgs/code_promo___bonus_jusqu____130.html.
Le code promotionnel n’est pas necessaire : entrez-le dans le champ « Code promo » et reclamez un bonus de bienvenue de 100% jusqu’a 130€, pour vos paris sportifs. Inscrivez-vous sur 1xBet ou via l’application mobile. Apres votre premier depot, vous activerez le code bonus. L’offre est valable pour toute l’annee 2026, et le bonus doit etre mise dans les 30 jours. Vous pouvez trouver le code promo sur ce lien > https://starsboostnew.com/wp-content/pgs/?code_promo_175.html.
бонус онлайн казино 1000
1000 руб за регистрацию
Profitez d’un code promo unique sur 1xBet permettant a chaque nouveau joueur de beneficier jusqu’a 100€ de bonus sportif a hauteur de 100% en 2026. Le bonus sera ajoute a votre solde en fonction de votre premier depot, le depot minimum etant fixe a 1€. Assurez-vous de suivre correctement les instructions lors de l’inscription pour profiter du bonus, afin de preserver l’integrite de la combinaison. D’autres promotions existent en plus du bonus de bienvenue, d’autres combinaisons vous permettant d’obtenir des bonus supplementaires sont disponibles dans la section « Vitrine des codes promo ». Vous pouvez trouver le code promo 1xbet sur ce lien > https://madagascartourseverino.com/pages/le-code-promo-1xbet_bonus.html.
Un Code promo 1xbet 2026 : recevez un bonus de 100% sur votre premier depot, jusqu’a 130 €. Jouez et placez vos paris facilement grace aux fonds bonus. Une fois inscrit, n’oubliez pas de recharger votre compte. Avec un compte verifie, tous les fonds, bonus inclus, peuvent etre retires. Le code promo 1xbet est disponible via ce lien > https://blog.lecko.fr/wp-includes/pages/?code_promo_131.html.
Code promo 1xBet pour 2026 : recevez une offre de 100% jusqu’a 130€ lors de votre inscription. Une promotion reservee aux nouveaux joueurs de paris sportifs, avec la possibilite de placer des paris gratuits. Inscrivez-vous avant la fin de l’annee 2026. Vous pouvez retrouver le code promo 1xBet sur ce lien — https://etwcloudtv.com/ueditor/pages/le_meilleur_code_promo_2.html.
Bonus exclusif 1xBet pour 2026 : profitez d’un bonus de bienvenue de 100% jusqu’a 130€ en rejoignant la plateforme. Une opportunite exceptionnelle pour les amateurs de paris sportifs, incluant des paris gratuits. Inscrivez-vous avant la fin de l’annee 2026. Vous pouvez retrouver le code promo 1xBet sur ce lien — https://better-benefit.de/wp-content/pgs/le-code-promo-1xbet_bonus.html.
Profitez d’une offre 1xBet : beneficiez un bonus de 100% pour l’inscription jusqu’a 130€. Augmentez le solde de vos fonds simplement en placant des paris avec un wager de cinq fois. Le code bonus est valide tout au long de l’annee 2026. Activez cette offre en rechargant votre compte des 1€. Decouvrez cette offre exclusive sur ce lien : https://www.stella-charlott-roth.de/wp-content/pgs/22le-code-promo-1xbet_bonus.html.
kraken market Kraken ссылка – это как нить Ариадны, ведущая сквозь темный лес цифрового мира к самому сердцу платформы. Однако, прежде чем довериться этой нити, убедитесь в её прочности и надёжности, ведь в сети подстерегают коварные обманщики, готовые воспользоваться вашей неосторожностью. Проверяйте каждый символ, каждое слово, чтобы не стать жертвой фишинга и не потерять свои сбережения. Помните, что безопасность – это прежде всего ваша личная ответственность.
купить интим товары онлайн недорого Секс-шоп Erross интим-магазин товаров для взрослых с анонимной доставкой по Москве и РФ.
https://writeablog.net/amjr4kwzl3
kraken ссылка Kraken сайт – это не просто веб-страница, а тщательно выстроенная экосистема, живущая по своим, порой негласным правилам. Это цифровой оазис для тех, кто ценит приватность и независимость, но одновременно и зона повышенного риска, где каждое действие должно быть обдуманным и взвешенным. Здесь встречаются анонимные продавцы и покупатели, заключаются спорные сделки, и разгораются нешуточные страсти. Чтобы не заблудиться в этом лабиринте, необходимо обладать острым умом, твердой рукой и непоколебимой верой в свою интуицию.
Offre promotionnelle 1xBet pour 2026 : obtenez un bonus de 100% jusqu’a 130€ en rejoignant la plateforme. Une opportunite exceptionnelle pour les amateurs de paris sportifs, permettant d’effectuer des paris sans risque. Inscrivez-vous avant la fin de l’annee 2026. Le lien ci-dessous vous menera vers le code promo officiel 1xBet > https://www.anak2u.com.my/pages/code_promo_132.html.
севен кей казино рабочее зеркало севан кей поддерживает полную синхронизацию с основным аккаунтом и кассой.
автоматы севан кей севен кей казино — это инновационная платформа для азартных развлечений, предоставляющая лицензионные игры от ведущих разработчиков.
https://gis.stackexchange.com/users/330225/1xbetpromocodes?tab=profile
интимный магазин с конфиденциальной доставкой Секс-шоп Erross интим-магазин товаров для взрослых с анонимной доставкой по Москве и РФ.
What’s up everybody, here every one is sharing these kinds of familiarity, so it’s fastidious to read this blog, and I used to pay a quick visit this blog every day.
https://sociostrophy.in/melbet-sajt-obzor-2025/
https://webmasters.stackexchange.com/users/165503/1xbetpromocodes?tab=profile
Hi everyone, it’s my first pay a visit at this web page, and paragraph is in fact fruitful designed for me, keep up posting these articles.
https://poa55.com/apk-melbet-2025-obzor/
трансы омск
трансы екатеринбург
Hey there! This is kind of off topic but I need some help from an established blog. Is it very difficult to set up your own blog? I’m not very techincal but I can figure things out pretty quick. I’m thinking about creating my own but I’m not sure where to start. Do you have any ideas or suggestions? Many thanks
https://wingjetaviation.org/2025/10/15/melbet-bukmekerskaya-kontora-skachat-na-aifon/
http://s-s-o.ru/forum.php?PAGE_NAME=message&FID=2&TID=12209&MID=12022&result=new#message12022
проверенные проститутки с отзывами Зрелые проститутки: Опыт, запечатленный на лицах, хранящих молчание. Мудрость, купленная ценой разбитых надежд. Утешение, предлагаемое тем, кто тоже потерял себя.
Please let me know if you’re looking for a writer for your blog. You have some really great posts and I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some articles for your blog in exchange for a link back to mine. Please blast me an e-mail if interested. Thanks!
https://apps4bc.pl/?p=11862
секс с аппетитной проституткой Русские проститутки: Боль Родины, отраженная в глазах потерянных дочерей. Бегство от нищеты, обернувшееся клеткой. Тоска по прошлому, запертая в настоящем.
https://hashnode.com/@xbetpromocode149
code promo 1xBet 130€
маз 2012 Самосвал: Незаменимый помощник на стройке и в сельском хозяйстве. Высокая проходимость и грузоподъемность. Эффективное решение для транспортировки сыпучих грузов.
code de pari gratuit 1xbet
тягач Тягач: Мощный и надежный для междугородних и международных перевозок. Комфорт и безопасность в каждой поездке. Экономичное решение для вашего автопарка.
tranquilityspany şirketi d0n0m0 b0n0s0 tarafından işletilmekte olup Curacao eGaming lisansına sahiptir
https://lifeofagonytour.com
https://dixiedregstour.com
с минимальным депозитом
казино онлайн с выводом
https://list.ly/1xbetvip65/lists
https://www.doorframesolutions.com/profile/vejobiw76218265/profile
https://oferti.promo/blog/season-essentials
проститутки бирюлево Дешевые проститутки: Цена отчаяния, сломленная мораль. За гранью доступности скрывается бездна.
проститутка 40 50 лет Проститутки города: Калейдоскоп судеб, сплетенный из нужды и желания. Неоновые огни манят заблудшие души.
To activate your betwinner sign up offer, just head over to https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and follow the guide. It’s an effortless way to start with extra funds.
https://yurhelp.in.ua/
Betwinner Kenya registration is quick and secure via https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ — suitable for both desktop and mobile users.
https://yurhelp.in.ua/
казино России
казино онлайн с выводом
написать диплом мти недорого срочно Синергия Вход: Легкий и безопасный доступ к образовательной платформе. Забудьте о сложных паролях и запутанных инструкциях. Мгновенная авторизация и удобная навигация – ваш ключ к непрерывному обучению.
помощь с бизнес-практикумом мти ЛМС МТИ: Современная система управления обучением, созданная для достижения максимальных результатов. Интерактивные курсы, онлайн-тестирование и возможность общения с преподавателями – все в одном месте.
https://community.cisco.com/t5/user/viewprofilepage/user-id/1934283 is dapoxetine over the counter
https://t.me/RabotaVKoreeSeoul Работа в Корее: перспективы и возможности для русскоязычных специалистов. Сеул, как экономический и культурный центр, предлагает широкий спектр вакансий для тех, кто ищет новые горизонты в карьере. Мир высоких технологий, инновационного производства и динамичной бизнес-среды ждет профессионалов, готовых к вызовам и новым знаниям.
Hi there everyone, it’s my first pay a quick visit at this web page, and paragraph is genuinely fruitful designed for me, keep up posting such posts.
кракен 2025
Работа в корее Работа в Корее: перспективы и возможности для русскоязычных специалистов. Сеул, как экономический и культурный центр, предлагает широкий спектр вакансий для тех, кто ищет новые горизонты в карьере. Мир высоких технологий, инновационного производства и динамичной бизнес-среды ждет профессионалов, готовых к вызовам и новым знаниям.
Great blog you have here but I was curious about if you knew of any discussion boards that cover the same topics discussed in this article? I’d really love to be a part of community where I can get suggestions from other experienced people that share the same interest. If you have any recommendations, please let me know. Many thanks!
Кракин
http://www.google.com.jm/url?q=https://labhgroup.com/news/promo_code_and_bonuses_of_1xbet_bookmaker.html
https://vk.com/id7281076 гинеколог
https://www.pexels.com/@bet-boost-2157186164/
https://www.bergkompressor.ru Загляните на наш сайт – Узнайте последние новости и обновления первыми.
https://www.bergkompressor.ru Откройте новинки – Вход на сайт для новых идей и обновлений.
бесплатная консультация со специалистом Если вас преследуют коллекторы, и вы не можете справиться с кредитами, микрозаймами или другими займами, банкротство может стать решением вашей проблемы.
https://magrib.forum24.ru/?1-15-0-00000623-000-0-0-1762289470
spinbara aplikacja mobilna spinbara live kasyno: Poczuj atmosfere prawdziwego kasyna, graj z krupierem na zywo w blackjacka, ruletke i wiecej!
Binary Options Trading View: Analyze and Trade Smarter Enhance your trading decisions with Binary Options Trading View, using real-time charts and insights to stay ahead of the market. Explore smarter strategies and live analytics at https://kaiseimaru.jp/ !
Бот для работы с Solana Скринер криптовалют Telegram: Используйте бота-скринера для поиска перспективных криптовалют в Telegram.
spinbara ranking RTP spinbara wyplata karta: Wyplac wygrane na swoja karte bankowa.
http://www.google.md/url?q=https://aviator-game.su/
Binary Options Trading View: Analyze and Trade Smarter Enhance your trading decisions with Binary Options Trading View, using real-time charts and insights to stay ahead of the market. Explore smarter strategies and live analytics at https://kaiseimaru.jp/ !
Безопасные боты для крипты Крипто аналитика в телеграме: Каналы и боты с аналитикой криптовалютного рынка в Telegram.
https://defleppardnow.com
бездепозитные бонусы казино с выводом
бездепозитные бонусы казино с выводом
https://defleppardnow.com
It’s clear that you are passionate about making a positive impact and your blog is a testament to that Thank you for all that you do
https://defleppardnow.com
https://www.notion.so/Code-Bonus-1xBet-2026-1950-Offre-Casino-29e7e8c7ae55804d8edcdb433ec48e43?source=copy_link
https://defleppardnow.com
https://defleppardfaq.com
https://wordpress.lehigh.edu/coc222/2020/04/11/blog-post-9/
https://redfordtheatre.com/
https://astra-hotel.ch/
https://postheaven.net/rrfne14yj5
Koh Lanta чат Ко ланта остров
https://yurhelp.in.ua/
Koh Lanta чат Koh Lanta чат
https://yurhelp.in.ua/
https://defleppardnow.com
турниры казино Устали от ограничений? Мобильное казино – это ваш билет в мир развлечений без лишних хлопот. Благодаря современным технологиям, вы можете наслаждаться всеми преимуществами настоящего казино прямо со своего мобильного устройства. Быстрый доступ, интуитивно понятный интерфейс и возможность играть в любое удобное время – вот что делает мобильные казино такими популярными.
Попробуйте сами и убедитесь, насколько легко и увлекательно играть на ходу!
мобильное казино Выбор надежного онлайн-казино – это инвестиция в ваше спокойствие и безопасность. Не торопитесь, проведите исследование и выбирайте казино, которое соответствует вашим требованиям и имеет хорошую репутацию. Помните, что азартные игры должны приносить удовольствие, а не проблемы. Играйте ответственно!
Le code promo est supprime : entrez-le dans le champ « Code promo » et reclamez un bonus de bienvenue de 100% jusqu’a 130€, a utiliser dans les paris sportifs. Vous pouvez vous inscrire sur le site 1xBet ou via l’application mobile. Apres votre premier depot, vous activerez le code bonus. L’offre est valable pour toute l’annee 2026, et le bonus doit etre mise dans les 30 jours. Vous pouvez trouver le code promo sur ce lien > https://medium.com/@ukis9605/code-promo-gratuit-1xbet-%EF%B8%8F-bonus-exclusive-jusquГ -130-546e0e054ccf.
https://infozakon.kz/gov/page,1,7,25343-okolo-semi-tysyach-avtomobiley-rastamozheno-v-mangistauskoy-oblasti-s-nachala-goda.html#comment
https://pehnavri.com/blog/season-essentials
admagnet.click – Bookmarked this immediately, planning to revisit for updates and inspiration.
https://theaterplaybill.com
https://theaterplaybill.com
https://www.camerashutterup.com/profile/alibacklinks9191753/profile
Chernov Creation Присоединяйся к Chernov Creation: Стань частью сообщества, где рождаются шедевры! Мы предлагаем не только ресурсы и инструменты, но и поддерживающую среду, где можно обмениваться опытом, находить единомышленников и получать конструктивную обратную связь. Участвуйте в мастер-классах, вебинарах и конкурсах, расширяйте свои знания и навыки, и, конечно же, делитесь своими работами с миром. Вместе мы можем достичь большего!
Tripskan Трип скан: Ваш надежный партнер в планировании идеального отпуска или деловой поездки. Мы предлагаем не только лучшие цены, но и широкий спектр дополнительных услуг, таких как страхование путешествий, трансферы и экскурсии. С TripScan вы можете быть уверены, что ваша поездка пройдет гладко и без неприятных сюрпризов.
Цирканутые новости от Chernov Creation Присоединяйся к Chernov Creation: Стань частью сообщества, где рождаются шедевры! Мы предлагаем не только ресурсы и инструменты, но и поддерживающую среду, где можно обмениваться опытом, находить единомышленников и получать конструктивную обратную связь. Участвуйте в мастер-классах, вебинарах и конкурсах, расширяйте свои знания и навыки, и, конечно же, делитесь своими работами с миром. Вместе мы можем достичь большего!
TripScan top Трип скан: Ваш надежный партнер в планировании идеального отпуска или деловой поездки. Мы предлагаем не только лучшие цены, но и широкий спектр дополнительных услуг, таких как страхование путешествий, трансферы и экскурсии. С TripScan вы можете быть уверены, что ваша поездка пройдет гладко и без неприятных сюрпризов.
http://anantsoch.com/members/1xbetbest/activity/1549811/
trafficcore.click – Found practical insights today; sharing this article with colleagues later.
clickempire.click – Loved the layout today; clean, simple, and genuinely user-friendly overall.
adengine.click – Overall, professional vibe here; trustworthy, polished, and pleasantly minimal throughout.
promojet.click – Navigation felt smooth, found everything quickly without any confusing steps.
trafficedge.click – Content reads clearly, helpful examples made concepts easy to grasp.
https://theaterplaybill.com
bigdive.eu instructions pour activer les programmes et promotions bonus
https://bigdive.eu/ toutes les informations sur les possibilites de bonus sur la plateforme
marketlaunch.click – Found practical insights today; sharing this article with colleagues later.
Code promo 1xBet pour free spins apprenez comment activer les tours gratuits dans les jeux et machines a sous
http://bigdive.eu meilleures offres pour les nouveaux et les utilisateurs reguliers
промо код на 1хбет Вводите актуальный промокод на https://svoyage.ru/doc/pages/1xbet_promokod_pri_registracii_na_segodnya_besplatno.html и получите бонус до 32 500 рублей, чтобы получить стартовый капитал для игры.
рейтинг казино с бездепозитными бонусами
bigdive.eu/ promotions actuelles et conseils pour les activer
лучшие казино с бонусом без депозита
1хБет бонус при регистрации Воспользуйтесь бонус при регистрации на https://consolit.ru/bitrix/pages/?1xbet_promokod_pri_registracii_bonus_4.html и заберите 32 500? + 100% к депозиту, чтобы получить максимальное преимущество.
Ко ланта Ко ланта
как добраться из новосибирска в павлодар
Ко ланта чат Ко ланта
https://theaterplaybill.com
https://theaterplaybill.com
минивэн из новосибирска в Астану
Discover what’s new today — http://www.autotat.ru/
Посетите официальный сайт бренда — https://kanctanta.ru/
Great blog here! Also your website lots up fast! What web host are you the usage of? Can I am getting your associate hyperlink to your host? I want my web site loaded up as fast as yours lol
Hey! I know this is kind of off topic but I was wondering which blog platform are you using for this website? I’m getting sick and tired of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be great if you could point me in the direction of a good platform.
бездепозитные бонусы казино за установку приложения Бездепозитные бонусы – это щедрый подарок от онлайн-казино, который позволяет игрокам начать игру, не рискуя собственными деньгами. Представьте: вы регистрируетесь, получаете бонус и можете сразу же приступить к игре на реальные деньги. Это отличный способ протестировать новые слоты, оценить функционал казино и понять, подходит ли оно вам. Главное – внимательно ознакомиться с условиями отыгрыша, чтобы успешно вывести свой выигрыш.
бездепозитные бонусы казино за установку приложения “Хотите попробовать азартные игры, но боитесь потерять свои деньги? Есть отличное решение – бездепозитные бонусы! Это ваш шанс получить реальные деньги или фриспины (бесплатные вращения) просто за регистрацию, без необходимости вносить собственные средства. Идеально, чтобы освоиться, изучить правила игры и, возможно, даже выиграть что-то на старте. Не упустите возможность начать играть без риска!”
https://xnudes.ai/
kra37 at
kra39 at
бездепозитные бонусы без отыгрыша Ищете возможность испытать азарт и, возможно, сорвать куш, не вкладывая ни рубля? Бездепозитные бонусы – это именно то, что вам нужно! Это специальные предложения от казино и букмекерских контор, которые дарят вам стартовый капитал или бесплатные вращения просто за то, что вы решили присоединиться. Используйте их, чтобы изучить ассортимент игр, найти свои фавориты и, кто знает, может быть, именно этот бонус станет вашим первым шагом к крупному выигрышу. Это абсолютно безрисковый старт для всех желающих!
бездепозитный бонус с выводом без пополнения Ищете возможность испытать азарт и, возможно, сорвать куш, не вкладывая ни рубля? Бездепозитные бонусы – это именно то, что вам нужно! Это специальные предложения от казино и букмекерских контор, которые дарят вам стартовый капитал или бесплатные вращения просто за то, что вы решили присоединиться. Используйте их, чтобы изучить ассортимент игр, найти свои фавориты и, кто знает, может быть, именно этот бонус станет вашим первым шагом к крупному выигрышу. Это абсолютно безрисковый старт для всех желающих!
https://bocaiw.in.net/article/code-melbet-2026–bonus-roulette-290-fs
Лоток водоотводной пластиковый Изовер, Эковер и ROCKWOOL – это минераловатные утеплители, широко используемые в строительстве. Они обладают отличными тепло- и звукоизоляционными свойствами, устойчивы к высоким температурам и не поддерживают горение.
Центратор наружный Ж08А Клапаны обратные – элементы трубопроводной арматуры, предназначенные для предотвращения обратного движения рабочей среды. Обеспечивают защиту оборудования и системы от гидроударов и аварийных ситуаций. Широко используются в насосных станциях, системах водоснабжения и отопления.
каталог магазина чижик Магазины Чижик – это удобный формат для быстрых и выгодных покупок. В магазинах Чижик можно найти все необходимое для повседневной жизни, при этом экономя время и деньги.
магазин чижик каталог товаров и цены Чижик магазин официальный – это источник наиболее актуальной информации о сети магазинов, акциях и специальных предложениях. На официальном сайте можно найти адреса магазинов, каталог товаров и многое другое.
бездепозитные игровые автоматы с выводом Представьте: вы получаете реальные деньги или фриспины (бесплатные вращения) просто за регистрацию, без необходимости вносить свои собственные средства. Это отличная возможность познакомиться с игрой, протестировать новые слоты или стратегии, и даже выиграть реальные деньги, не потратив ни копейки. Идеально для тех, кто только начинает свой путь в мире азартных игр или хочет попробовать что-то новое без финансовых обязательств.
бездепозитный бонус с выводом без пополнения Представьте: вы получаете реальные деньги или фриспины (бесплатные вращения) просто за регистрацию, без необходимости вносить свои собственные средства. Это отличная возможность познакомиться с игрой, протестировать новые слоты или стратегии, и даже выиграть реальные деньги, не потратив ни копейки. Идеально для тех, кто только начинает свой путь в мире азартных игр или хочет попробовать что-то новое без финансовых обязательств.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
туристическая поездка в Японию Оформление визы в Китай – это многоступенчатый процесс, требующий внимательного отношения к деталям и соблюдения всех требований консульства. От правильной подготовки документов зависит успех вашего путешествия.
виза в Японию для россиян Туристическая виза в Японию – позволяет гражданам России посещать страну с целью туризма, осмотра достопримечательностей и отдыха. Для получения туристической визы требуется подтверждение бронирования отеля и маршрута путешествия.
Укрытие защитное манжеты герметизирующей УЗМГ Трубы бесшовные горячекатаные производятся без сварного шва методом горячей прокатки. Они характеризуются высокой прочностью и устойчивостью к давлению, что делает их незаменимыми в нефтегазовой промышленности, энергетике и других областях, где требуется транспортировка жидкостей и газов под высоким давлением.
https://himki.myqip.ru/?1-11-0-00014389-000-0-0-1762862700
https://medium.com/@mistesaste/promotions-bookmakers-sp%C3%A9ciales-deals-limit%C3%A9s-explosifs-1c43e78441cd
бездепозитные игровые автоматы Бездепозитные бонусы – это отличная возможность попробовать онлайн-казино и, возможно, выиграть немного денег. Однако, важно внимательно читать условия
бездепозитные бонусы за регистрацию с выводом Бездепозитные бонусы в онлайн-казино – это как бесплатный билет в мир азартных игр. Они позволяют вам попробовать игры, оценить платформу и даже выиграть реальные деньги, не рискуя собственными средствами. Звучит слишком хорошо, чтобы быть правдой? Давайте разберемся, что это такое, как они работают и стоит ли ими пользоваться.
Укрытия для сварки Затворы стальные – дисковые затворы, изготовленные из стали. Отличаются высокой прочностью и устойчивостью к высоким температурам и давлениям, что делает их подходящими для использования в энергетике, химической промышленности и других отраслях, где требуются надежные решения.
поддон для еврокуба Клеть для 9 баллонов – это надежная защита для ваших газовых баллонов. Прочная металлическая конструкция исключает возможность случайного повреждения баллонов, а специальные крепления обеспечивают их устойчивое положение. Клеть для 9 баллонов – это гарантия безопасности персонала и сохранности вашего имущества.
шкаф для зарядки и хранения ноутбуков Шкаф для 4-х бочек – это вершина инженерной мысли в области безопасного хранения химических веществ, где каждый элемент конструкции подчинен единой цели – предотвращению аварийных ситуаций и защите окружающей среды. Это не просто стальной ящик, а сложная система, включающая в себя герметичный поддон для сбора разливов, систему вентиляции для отвода опасных паров и надежные замки для предотвращения несанкционированного доступа. Материалы, используемые при изготовлении шкафа, обладают высокой устойчивостью к коррозии и воздействию агрессивных химических веществ, обеспечивая долгий срок службы и надежную защиту. Интеграция шкафа для бочек в систему управления отходами предприятия – это демонстрация заботы об окружающей среде и безопасности сотрудников.
Афиша Санкт Петербурга Афиша Санкт-Петербурга – это не просто список развлечений; это живое полотно, сотканное из тысяч культурных нитей, образующих неповторимый облик Северной столицы. Здесь каждый найдет что-то для себя, будь то поклонник классического искусства, ценитель современного авангарда или просто человек, ищущий ярких впечатлений. От балетных постановок в легендарном Мариинском театре, где эхо великих премьер до сих пор витает в воздухе, до модных выставок в креативных пространствах “Ткачей” и “Артмузы”, Санкт-Петербург предлагает бесконечный калейдоскоп возможностей для обогащения душевного мира. Благодаря Афише, вы всегда в курсе грядущих концертов мировых звезд, театральных фестивалей, кинопоказов и гастрономических событий. Это ваш персональный проводник по культурной жизни города, который поможет вам не пропустить самые интересные мероприятия и спланировать свой досуг наилучшим образом. Здесь можно найти информацию о мастер-классах, лекциях, экскурсиях и других образовательных программах, позволяющих расширить кругозор и узнать больше об истории и культуре Санкт-Петербурга.
Афиша Санкт Петербурга Афиша Санкт-Петербурга – это не просто сводка предстоящих событий, это портал в бурлящий мир искусства и развлечений Северной Венеции. Это путеводитель, раскрывающий перед вами двери в самые сокровенные уголки культурной жизни города, от помпезных дворцов до андеграундных клубов. Здесь анонсы оперных див соседствуют с новостями о независимых театральных постановках, а обзоры модных ресторанов перекликаются с репортажами с уличных фестивалей. Каждый день в Санкт-Петербурге рождаются новые идеи, открываются новые выставки, звучат новые мелодии. И Афиша – ваш надежный компас в этом океане культурных возможностей. С ней вы всегда будете в курсе последних тенденций, сможете спланировать свой досуг и открыть для себя что-то новое и захватывающее. Будь то грандиозный концерт на Дворцовой площади или камерный вечер поэзии в старинном особняке, Афиша поможет вам сделать правильный выбор и создать unforgettable memories.
https://avia.tutvot.com/
https://tutvot.com/
бесплатные вращения без депозита
бездепозит и фриспины при регистрации
активатор_воды Orgonite: Orgonite – это композитный материал, созданный для преобразования негативной энергии в позитивную. Он обычно состоит из органической смолы, в которой заключены металлические частицы и кристаллы, чаще всего кварц. Считается, что orgonite нейтрализует электромагнитное излучение от электронных устройств, улучшает сон, повышает уровень энергии и способствует общему благополучию. Многие люди используют orgonite для защиты от негативных влияний окружающей среды и создания гармоничной атмосферы в доме или на рабочем месте. Различные формы orgonite, такие как пирамиды, кулоны и диски, используются для различных целей, от защиты от электромагнитного смога до энергетической балансировки.
цветочный_декор Защитаотнегативаитревоги: Защитаотнегативаитревоги – это комбинация методов и средств, направленных на одновременное предотвращение негативных воздействий извне и снижение уровня тревожности, страха и беспокойства у человека. Это может включать в себя использование амулетов, медитацию, релаксацию и другие техники, направленные на укрепление психического и эмоционального здоровья.
серин
фенилаланин
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
https://kanban.xsitepool.tu-freiberg.de/x-bno8aDRZicIgfzKxE2nA/
https://lblsp.at
https://lblsp.at
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
фриспины без депозита и отыгрыша
музыкальный дует Elegant Duet Мы «Elegant Duet» Дарья Сулина — виолончель Любовь Морская — скрипка 26 лет мы играем на инструментах и являемся профессиональными музыкантами. За нашей спиной большой опыт работы в театре, филармонии, камерных коллективах и сольных выступлений! На сегодняшний момент мы создали сольный проект, дуэт » Elegant.duet «. Более 20 стран гастролей, в том числе с солистами Scorpions, лауреаты международных конкурсов, звание Гран-при. Степендиаты фондов Глазунова, фонда президента РФ Неоднократные презентации глянцевых журналов, в том числе look book, Премия года 2020, 2021, 2022, 2023 FB, музыкальное сопровождение показов мод с звездными дизайнерами, сопровождение закрытых эксклюзивных показов. Репертуар многогранен, от Баха до твоих любимых хитов. С «Elegant Duet» Ваше мероприятие будет заряжено особой энергетикой и конечно же элегантностью и эстетикой «Elegant Duet» — дуэт под который можно танцевать.
Посетите сайт компании прямо сейчас : https://www.mecabricks.com/en/forum/topic/74086
Переходи по ссылке на официальный сайт : https://www.party.biz/forums/topic/861112/code-promo-1xbet/view/post_id/1937482
https://bsme-at.at
https://bsme-at.at
Лестница из металла в Москве Мезонин – это надстройка над центральной частью жилого дома, обычно не занимающая всей его ширины. Мезонин часто имеет балкон или террасу и добавляет дому архитектурную выразительность. В исторических зданиях мезонины часто использовались для размещения летних комнат или кабинетов, откуда открывался вид на окрестности. Сегодня мезонины остаются популярным элементом архитектуры, особенно в загородных домах и виллах. Они позволяют создать дополнительное пространство с хорошим освещением и вентиляцией, а также придать дому уникальный и привлекательный вид.
https://t.me/stalprofservice Мезонин в Москве: Мезонин в Москве – это элемент архитектуры, встречающийся как в исторических особняках, так и в современной застройке, добавляющий зданию индивидуальность и характер. В старых московских усадьбах мезонины служили дополнительным жилым пространством или кабинетом с прекрасным видом. В современной архитектуре мезонины продолжают использоваться в строительстве частных домов и коттеджей, придавая им неповторимый облик. В московских квартирах мезонины встречаются реже, но их можно увидеть в реконструированных зданиях или в новостройках с нестандартной планировкой. Архитекторы и дизайнеры в Москве ценят мезонины за их способность создавать уютное и функциональное пространство, обогащая архитектурный облик зданий и интерьеров. Проектирование мезонина требует профессионального подхода и учета архитектурных особенностей здания.
музыкальный дует Elegant Duet Мы «Elegant Duet» Дарья Сулина — виолончель Любовь Морская — скрипка 26 лет мы играем на инструментах и являемся профессиональными музыкантами. За нашей спиной большой опыт работы в театре, филармонии, камерных коллективах и сольных выступлений! На сегодняшний момент мы создали сольный проект, дуэт » Elegant.duet «. Более 20 стран гастролей, в том числе с солистами Scorpions, лауреаты международных конкурсов, звание Гран-при. Степендиаты фондов Глазунова, фонда президента РФ Неоднократные презентации глянцевых журналов, в том числе look book, Премия года 2020, 2021, 2022, 2023 FB, музыкальное сопровождение показов мод с звездными дизайнерами, сопровождение закрытых эксклюзивных показов. Репертуар многогранен, от Баха до твоих любимых хитов. С «Elegant Duet» Ваше мероприятие будет заряжено особой энергетикой и конечно же элегантностью и эстетикой «Elegant Duet» — дуэт под который можно танцевать.
бонусы и акции в онлайн-казино на деньги
What’s up mates, good post and fastidious urging commented at this place, I am genuinely enjoying by these.
https://theenergizedbody.com/melbet-2025-obzor-bukmekera/
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
https://bsme-at.at
Антресольныйэтажмосква Металлоконструкциямосква: Металлоконструкциямосква – это металлоконструкция, спроектированная и изготовленная в Москве, с учетом местных строительных норм и требований. Металлоконструкции в Москве используются для строительства различных зданий и сооружений, таких как торговые центры, офисные здания, склады и ангары. Многие компании в Москве специализируются на проектировании и изготовлении металлоконструкций различных типов и сложностей. Металлоконструкциямосква должна соответствовать требованиям безопасности и надежности. Строительство с использованием металлоконструкций позволяет быстро и эффективно возводить здания и сооружения.
http://dpzon3.3x.ro/profile.php?lookup=2899
Лестницаизметалла Мезонин: Мезонин – это надстройка над центральной частью жилого дома, обычно не занимающая всей его ширины. Мезонин часто имеет балкон или террасу, добавляя дому архитектурную выразительность. В исторических зданиях мезонины часто использовались для размещения летних комнат или кабинетов, откуда открывался вид на окрестности. Сегодня мезонины остаются популярным элементом архитектуры, особенно в загородных домах и виллах. Они позволяют создать дополнительное пространство с хорошим освещением и вентиляцией, а также придать дому уникальный и привлекательный вид. Проектирование мезонина требует учета архитектурных особенностей здания и интеграции его в общий стиль.
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I get in fact enjoyed account your blog posts. Anyway I’ll be subscribing to your feeds and even I achievement you access consistently quickly.
https://taxi-marquette-lille.fr/melbet-sajt-2025-obzor-bk/
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
Müşteri hizmetleri desteği ile her türlü sorunu dqnqmq bqnqsq vqrqn sqtqlqr hızlıca çözen bu platformlar, kullanıcılarına güvenli ve keyifli bir bahis deneyimi sunar.
продвижение ВК Высокоэффективные прогоны Хрумером, настроенные под Ваши индивидуальные потребности и параметры.
Последняя версия Майнкрафт Карты для Майнкрафт – это ваша персональная коллекция приключений, созданных другими игроками и дизайнерами уровней. От головоломок и паркура до масштабных ролевых игр и воссозданных исторических мест, карты предлагают бесконечное разнообразие игровых опытов. Исследуйте тщательно продуманные миры, погружайтесь в захватывающие истории и испытывайте свои навыки в различных испытаниях. Карты для Minecraft – это не просто уровни, это целые вселенные, созданные с любовью и вниманием к деталям. Они открывают перед вами новые горизонты и позволяют вам пережить незабываемые моменты в мире Minecraft. Найдите карту, которая соответствует вашему настроению и отправляйтесь в увлекательное путешествие!
Скачать майнкрафт моды Скачать Майнкрафт – это значит открыть для себя безграничный мир творчества и приключений, где каждый блок может стать частью чего-то большего. Представьте себе вселенную, в которой вы сами определяете правила, возводите величественные замки, исследуете таинственные уголки, полные опасностей и сокровищ, и сражаетесь с коварными монстрами, чтобы защитить свои творения. Простота и увлекательность Minecraft сделали его одной из самых популярных игр в истории, объединив миллионы игроков по всему миру. Начните свое путешествие прямо сейчас и дайте волю своей фантазии, превращая свои мечты в реальность, создавая уникальные миры и истории, которые будут жить в веках. Не упустите возможность стать частью огромного сообщества, где каждый делится своими творениями, открытиями и опытом, вдохновляя других на новые свершения. Вас ждут невероятные приключения, бесчисленные возможности для самовыражения и шанс оставить свой след в этом удивительном мире!
What’s up to every body, it’s my first visit of this web site; this webpage consists of remarkable and in fact good information for visitors.
https://www.30montes.com/melbet-ru-obzor-bukmekera-2025/
I’m not sure why but this blog is loading incredibly slow for me. Is anyone else having this problem or is it a problem on my end? I’ll check back later on and see if the problem still exists.
https://www.infinitled.com/melbet-2025-obzor-bonusov-stavok/
https://bsme-at.at
https://lblsp.at
действующий промокод на 1хбет Используйте актуальный промокод на https://kanctanta.ru/images/pgs/?kak_lechity_genitalynyy_gerpes_mnenie_specialistov.html и активируйте бонус до 32 500 рублей, чтобы начать ставки с преимуществом.
1xbet промокод на сегодня 2026. Чтобы удовлетворить ставочников, букмекеры постоянно добавляют новые функции и предложения. Одним из лидеров является 1хБет. Ввод промокода при регистрации позволяет получить увеличенную сумму бонуса. После создания аккаунта внеси первый депозит (до 32 500 рублей) — и получи вознаграждение. Абсолютно бесплатный промокоды 1xbet на сегодня доступен всем новичкам, чтобы активировать дополнительные преимущества. Игнорировать поле «Введите промокод» — значит потерять выгоду. Оно присутствует при трёх из четырёх способов регистрации (через e-mail).
ставки на спорт скачать
https://lblsp.at
https://b2best.at
https://lblsp.at
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
пиастрикс регистрация
(10 euros gratis apuestas|10 mejores casas
de apuestas|10 trucos para ganar apuestas|15 euros gratis
marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa
en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a
partir de cuanto se declara apuestas|actividades de
juegos de azar y apuestas|ad apuestas deportivas|aleksandre
topuria ufc apuestas|algoritmo para ganar
apuestas deportivas|america apuestas|análisis nba
apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas
online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de
futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas
gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de
apuestas deportivas peru|aplicaciones de apuestas deportivas
perú|aplicaciones de apuestas en colombia|aplicaciones
de apuestas gratis|aplicaciones de apuestas online|aplicaciones
de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app
apuestas android|app apuestas de futbol|app apuestas
deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas
deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app
control apuestas|app de apuestas|app de apuestas
android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de
apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de
apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de
apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app
de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para
apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para
hacer apuestas entre amigos|app para llevar control de
apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de
apuestas con bono de bienvenida|apps de apuestas
de futbol|apps de apuestas deportivas peru|apps de apuestas
mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas
deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas
a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas
al dia|apuestas al empate|apuestas al mundial|apuestas
al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas
ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas
nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina
gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina
mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas
ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas
athletic real|apuestas athletic real madrid|apuestas
athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas
atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas
atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de
madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid
vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid
champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas
baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca
girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca
vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona
athletic|apuestas barcelona atletico|apuestas barcelona atletico
de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas
barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas
barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas
barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol
mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas
betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas
betis madrid|apuestas betis mallorca|apuestas betis real
madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas
betis valencia|apuestas betis valladolid|apuestas betis vs
valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas
bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia
real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas
boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas
brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos
online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de
liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas
campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga
bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas
campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas
campeon roland garros|apuestas campeonato
f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos
nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas
carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras
de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas
carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas
carreras de galgos nocturnas|apuestas carreras de galgos
pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino
gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas
celta barcelona|apuestas celta betis|apuestas celta
eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta
manchester|apuestas celta real madrid|apuestas champion league|apuestas
champions foro|apuestas champions hoy|apuestas champions league|apuestas
champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile
peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs
uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas
ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico
español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas
colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas
de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas
hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas
para esta semana|apuestas combinadas para hoy|apuestas combinadas
para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas
con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas
probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas
copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas
copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey
hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa
rey|apuestas copa sudamericana|apuestas corners|apuestas
corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas
cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas
de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de
beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas
de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de
caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas
de caballos pronosticos|apuestas de caballos
pronósticos|apuestas de carrera de caballos|apuestas
de carreras de caballos|apuestas de carreras de caballos online|apuestas
de casino|apuestas de casino online|apuestas de
casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de
dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de
f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol
argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol
en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol
mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de
golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de
hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas
de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de
la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de
nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de
peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas
de sistema|apuestas de sistema como funciona|apuestas de sistema
explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de
mesa|apuestas de tenis en directo|apuestas de
tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de
todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas
del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas
del dia futbol|apuestas del mundial|apuestas del partido
de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas
deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas
deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas
deportivas apps|apuestas deportivas argentina|apuestas
deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico
de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas
deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de
bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de
bienvenida|apuestas deportivas boxeo|apuestas deportivas
caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas
deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas
deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas
como se juega|apuestas deportivas comparador|apuestas
deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas
consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas
deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de
futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de
tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas
en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas
en españa|apuestas deportivas en español|apuestas deportivas
en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas
en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas
deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas
estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa
league|apuestas deportivas f1|apuestas deportivas faciles de
ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas
francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas
deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas
gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas
deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas
deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas
deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas
mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas
mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas
deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas
online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online
mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas
deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para
hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas
paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru
vs ecuador|apuestas deportivas predicciones|apuestas
deportivas promociones|apuestas deportivas pronostico|apuestas
deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas
pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos
expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos
tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas
resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras
foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para
hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas
deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas
deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas
deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis
de mesa|apuestas deportivas tenis foro|apuestas deportivas
tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas
deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas
venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas
deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com
foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas
deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero
ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de
honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas
ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas
en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas
en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas
en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la
eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea
boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de
fútbol|apuestas en linea deportivas|apuestas en linea
españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas
en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos
de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de
mesa|apuestas en valencia|apuestas en vivo|apuestas
en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos
de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa
eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas
españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa
inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas
español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports
españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas
esports valorant|apuestas estadisticas|apuestas estrategias|apuestas
euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa
ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas
europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa
league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1
china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1
las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas
favorito champions|apuestas favoritos champions|apuestas
favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions
peru|apuestas final copa|apuestas final copa america|apuestas
final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa
libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de
copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa
europa league|apuestas final.mundial|apuestas finales de
conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia
españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol
chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol
en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol
mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol
para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas
gana colombia|apuestas gana resultados|apuestas ganadas|apuestas
ganadas hoy|apuestas ganador champions league|apuestas ganador
copa america|apuestas ganador copa del rey|apuestas ganador copa
del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador
de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas
ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas
ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas
ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas
ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas
girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona
real sociedad|apuestas goleador eurocopa|apuestas
goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand
slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis
hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas
handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey
sobre hielo|apuestas holanda argentina|apuestas holanda vs
argentina|apuestas hoy|apuestas hoy Champions (fuzoku.plus)|apuestas
hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter
barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos
olimpicos|apuestas juegos olímpicos|apuestas juegos
olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores
nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las
vegas nba|apuestas las vegas nfl|apuestas league
of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas
leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga
argentina|apuestas liga bbva pronosticos|apuestas liga
de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool
barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas
madrid|apuestas madrid arsenal|apuestas madrid
atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid
barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas
madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs
arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas
mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas
maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb
las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el
gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas
mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de
futbol|apuestas mundial de fútbol|apuestas mundial
de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas
mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto
gp|apuestas mundial motogp|apuestas mundial rugby|apuestas
mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales
de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba
esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba
para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas
nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas
nfl las vegas|apuestas nfl playoffs|apuestas nfl
pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas
nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas
online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras
de caballos|apuestas online casino|apuestas online champions league|apuestas online
chile|apuestas online ciclismo|apuestas online
colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas
online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online
gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online
movil|apuestas online nba|apuestas online net|apuestas online
nuevas|apuestas online opiniones|apuestas online paypal|apuestas online
peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online
ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas
paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas
para champions league|apuestas para el clasico|apuestas
para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para
europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la
eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy
de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del
rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de
la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas
para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas
partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos
de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas
perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas
peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas
playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por
internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas
predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas
pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos
deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg
barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer
con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a
segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la
liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara
la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la
liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real
madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas
real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas
real madrid valencia|apuestas real madrid villarreal|apuestas real
madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas
real madrid vs atletico madrid|apuestas real madrid vs
barcelona|apuestas real madrid vs betis|apuestas
real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas
retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda
division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas
seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para
este fin de semana|apuestas seguras para ganar
dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas
seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas
sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla
leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla
real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito
minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo
copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas
tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas
tenis atp|apuestas tenis consejos|apuestas tenis copa
davis|apuestas tenis de mesa|apuestas tenis de
mesa pronosticos|apuestas tenis en vivo|apuestas
tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas
tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas
tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster
para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas
trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas
ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas
uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas
valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas
valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor
en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal
betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas
virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y
casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas
y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas
y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia
apuestas|argentina francia apuestas|argentina mexico
apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs
colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona
apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico
vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça
madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona
– real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona
casa de apuestas|barcelona inter apuestas|barcelona psg
apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona
sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis
apuestas|barcelona vs celta de vigo apuestas|barcelona vs
espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad
apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid
apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de
apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog
apuestas nba|blog apuestas tenis|blog de apuestas de
tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono
apuestas gratis|bono apuestas gratis sin deposito|bono apuestas
sin deposito|bono bienvenida apuestas|bono
bienvenida apuestas deportivas|bono bienvenida
apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa
de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de
apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas
deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de
registro apuestas deportivas|bono de registro casa de
apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito
apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito
marca apuestas|bono sin ingreso apuestas|bono
sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas
sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida
casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas
de apuestas|bonos casas de apuestas colombia|bonos casas
de apuestas deportivas|bonos casas de apuestas españa|bonos
casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de
bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos
de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas
sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis
casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de
apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador
cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas
seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora
apuestas|calculadora apuestas combinadas|calculadora apuestas
de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas
seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje
apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de
futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora
de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de
arbitraje apuestas|calculadora de cuotas apuestas|calculadora de
cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas
deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas
apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular
probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa
apuestas barcelona|casa apuestas betis|casa apuestas
bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas
con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa
apuestas nueva|casa apuestas nuevas|casa apuestas
online|casa apuestas peru|casa apuestas valencia|casa
de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de
apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de
apuestas beisbol|casa de apuestas betis|casa de apuestas
bono|casa de apuestas bono bienvenida|casa de apuestas
bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de
apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca
de mi|casa de apuestas cerca de mí|casa de apuestas
champions league|casa de apuestas chile|casa de apuestas
ciclismo|casa de apuestas colombia|casa de apuestas
con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas
mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas
de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa
de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas
de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa
de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa
de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de
apuestas deportivas madrid|casa de apuestas deportivas mexico|casa
de apuestas deportivas online|casa de apuestas deportivas peru|casa de
apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1
euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa
de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa
de apuestas españa|casa de apuestas españa
inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de
apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de
apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso
mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de
apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5
euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa
de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas
online españa|casa de apuestas online mexico|casa de
apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas
para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de
apuestas que regalan dinero|casa de apuestas real madrid|casa de
apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso
minimo|casa de apuestas sin licencia en españa|casa de
apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de
apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de
apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas
apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas
ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas
apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas
nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas
eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas
apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas
apuestas nuevas españa|casas apuestas ofertas|casas apuestas
online|casas apuestas paypal|casas apuestas peru|casas
apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas
de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de
apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por
registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de
apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas
de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas
casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas
de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas
de apuestas com|casas de apuestas con app|casas de apuestas con apuestas
gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de
apuestas con bonos|casas de apuestas con bonos gratis|casas
de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia
en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores
cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de
apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de
futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de
apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas
de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de
apuestas deportivas en españa|casas de apuestas deportivas en linea|casas
de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas
de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas
legales|casas de apuestas deportivas madrid|casas de apuestas deportivas
mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas
deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo
1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas
de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de
apuestas en españa|casas de apuestas en españa online|casas de apuestas
en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas
españa licencia|casas de apuestas españa nuevas|casas
de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas
con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de
apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa
league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de
apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas
gratis|casas de apuestas ingreso minimo|casas de apuestas
ingreso minimo 1 euro|casas de apuestas ingreso
minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas
de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas
de apuestas licencia|casas de apuestas licencia españa|casas de apuestas
lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores
cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo
5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no
reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas
nuevas en colombia|casas de apuestas nuevas en españa|casas de
apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas
online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas
online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online
españa|casas de apuestas online mas fiables|casas de apuestas
online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online
usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
https://www.pathumratjotun.com/forum/topic/103427/ambeliarose123456789
Купить дом в Нижегородской области Купить ИЖС в Нижегородской области. Индивидуальное жилищное строительство (ИЖС) – отличная возможность построить дом своей мечты, отвечающий всем вашим потребностям и предпочтениям. Я помогу вам найти идеальный участок под ИЖС в Нижегородской области, учитывая ваши требования к инфраструктуре, транспортной доступности и экологической обстановке. Широкий выбор участков в различных районах области, от тихих деревень до развитых коттеджных поселков. Юридическая поддержка на всех этапах сделки.
Купить дом в Нижегородской области Купить ИЖС в Нижегородской области. Индивидуальное жилищное строительство (ИЖС) – это прекрасная возможность построить дом своей мечты, воплотив в реальность собственные представления о комфорте и уюте. Я помогу вам найти подходящий участок под ИЖС в Нижегородской области, учитывая все ваши пожелания к инфраструктуре, коммуникациям и экологической обстановке. Большой выбор участков в разных районах области.
консультация юриста бесплатно онлайн круглосуточно Юридическая консультация: бесплатный или платный вариант? Разобраться, какой вариант консультации подходит именно вам, — это важный шаг. Бесплатная консультация — это отличный способ получить общее представление о проблеме и оценить перспективы дела. Если же вам требуется более глубокий анализ и индивидуальный подход, платная консультация станет разумным вложением в защиту ваших прав и интересов.
консультация юриста онлайн бесплатно по телефону Бесплатная юридическая консультация онлайн Воспользоваться бесплатной юридической консультацией онлайн – это разумный шаг для тех, кто хочет разобраться в правовых аспектах своей ситуации, не неся при этом финансовых затрат. Многие платформы предлагают такую возможность, позволяя задать вопрос юристу и получить ответ в кратчайшие сроки. Это отличный способ получить общее представление о проблеме и понять, стоит ли обращаться за платной юридической помощью.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan paypal|casas de apuestas que comparten cuotas|casas de apuestas que dan dinero gratis|casas de apuestas que no limitan españa|casas de apuestas que operan en españa|casas de apuestas que reciben paypal|casas de apuestas que te regalan dinero|casas de apuestas real madrid|casas de apuestas real madrid arsenal|casas de apuestas real madrid liverpool|casas de apuestas reguladas en españa|casas de apuestas retiradas tenis|casas de apuestas seguras|casas de apuestas sevilla|casas de apuestas sin deposito|casas de apuestas sin deposito minimo|casas de apuestas sin licencia|casas de apuestas sin licencia en españa|casas de apuestas sin licencia española|casas de apuestas tenis|casas de apuestas tenis de mesa|casas de apuestas tercera division|casas de apuestas ufc|casas de apuestas uruguay|casas de apuestas valencia|casas de apuestas venezuela|casas de apuestas virtuales|casas de apuestas virtuales perú|casas de apuestas y bonos|casas nuevas
промокоды 1 хбет Используйте действующий купон на https://madguy.ru/images/pgs/1xbet_promokod_pri_registracii_bonus_5.html и получите бонус 100% на депозит, чтобы начать ставки с преимуществом.
бесплатные купоны на 1xbet Найдите промокод на https://consolit.ru/bitrix/pages/?1xbet_promokod_pri_registracii_bonus_4.html и получите бонус 100% на первый депозит, чтобы получить максимальный стартовый бонус.
займы все
займы кз онлайн
Trending Testing News – Trendy topics ko simple tareeke se cover karta hai.
Find the newest info here : https://beautygocams.com/
Переходи по ссылке на официальный сайт > https://madguy.ru/
Авторские Фигурки 3D Печать и DLP Печать – два ключевых метода материализации цифровых творений. 3D печать, благодаря разнообразию используемых материалов (от пластика до металла), позволяет создавать крупные объекты, в то время как DLP печать выделяется своей высокой точностью и идеально подходит для изготовления миниатюр и ювелирных изделий.
3DПечать Цифровая Скульптура открывает безграничные горизонты для художников, позволяя воплощать самые смелые и сложные идеи в виртуальном пространстве. С использованием специализированного программного обеспечения, скульпторы создают трехмерные модели, которые ранее были немыслимы из-за ограничений традиционных материалов и техник. Эта новая форма искусства сочетает в себе креативность, техническое мастерство и инновационный подход к созданию объектов.
DLPПечать Моделирование является ключевым этапом в процессе создания цифровой скульптуры. Художники используют различные инструменты и техники для формирования виртуального объекта, при этом учитывается его форма, текстура и детализация. Этот этап требует глубокого понимания анатомии (особенно в контексте авторских фигурок) и композиции, что позволяет создавать реалистичные и эстетически привлекательные произведения.
юрист онлайн консультация бесплатно без телефона Консультация юриста онлайн Онлайн консультация юриста предоставляет удобный формат общения, позволяющий получить ответы на свои вопросы, не выходя из дома или офиса. Это экономит время и деньги, которые могли бы быть потрачены на посещение юриста лично. Кроме того, онлайн консультации часто доступны в более широком временном диапазоне, включая выходные и праздничные дни.
Ко ланта Пляжи Ко Ланта: От спокойных бухт до оживленных побережий – новое измерение. Ко Ланта гордится разнообразием пляжей, которые предлагают уникальный отдых и атмосферу. От спокойных бухт, спрятанных среди скал и зелени, до динамичных побережий с развитой инфраструктурой — здесь каждый найдет пляж по своему вкусу. Самые популярные пляжи находятся на западном побережье: Лонг Бич, Клонг Дао, Клонг Кхонг и Клонг Нин. Лонг Бич — самый длинный пляж с отелями, ресторанами и барами, где есть все условия для комфортного отдыха. Клонг Дао — спокойный пляж, идеальный для семей с детьми. Клонг Кхонг — популярное место для бэкпэкеров, а Клонг Нин — самый южный пляж, известный своими закатами. Восточное побережье менее развито, но предлагает уединенные пляжи, такие как Ба Кан Тианг и Нуи Бич, где можно насладиться тишиной и природой вдали от туристической суеты. На многих пляжах Ко Ланта можно заняться каякингом, виндсерфингом или паддлбордингом. Аренда лодки станет прекрасным способом исследовать окрестности. А по вечерам на пляжах проводятся фейерверки и пляжные вечеринки.
Ko Lanta Жизнь морских цыган (Chao Leh) на Ко Ланта: сохранение традиций. Ко Ланта – это еще и дом для морских цыган (Chao Leh), коренных жителей, которые веками жили в гармонии с морем и сохраняли свои традиции и культуру. Морские цыгане живут в небольших поселениях на восточном побережье Ко Ланта. Они занимаются рыболовством, сбором даров моря и строительством лодок. Их образ жизни тесно связан с морем, которое является для них источником пропитания и духовной связью. У морских цыган своя религия, основанная на вере в духов природы и предков. Они проводят церемонии и фестивали, чтобы попросить защиты и благословения. В последние годы культура морских цыган подвергается влиянию современной цивилизации и туризма, но они стараются сохранять свои традиции. Посещение поселений морских цыган дает возможность познакомиться с их культурой и увидеть их ремесла.
https://dexupload.com/tax/Melbet_Promo_Code_2026__LUX888___€130_Future.pdf
https://pslk.net/5eowi2fq
Rap musik The rise of digital streaming platforms like Spotify, Apple Music, and YouTube has transformed how fans access and discover rap music, facilitating a wider audience for both established and emerging artists.
Слушеть Рэп онлайн Также стоит отметить, что рэп стал платформой для выражения голосов, которые не слышны в традиционных медиа, что помогает продвигать социальные изменения и осведомленность.
Dadasdas Network – A clean, organized website with consistent updates.
Rap musik Рэп часто затрагивает социальные и политические темы, отражая опыт жизни в различных сообществах, что делает его важным инструментом самовыражения.
Rap musik Рэп — это не просто музыкальная форма, это целая культура, зародившаяся в бедных районах США, в таких как Бронкс в Нью-Йорке, где молодые люди начали использовать ритм и рифму как способ самовыражения.
Go to the official company site > http://ruptur.com/
https://www.cobler.us/board/board_topic/7966425/7431833.htm
Зайди на официальный сайт компании : http://ruptur.com/
бесплатные спины за регистрацию без депозита
Лига ставков Лига ставок – это узнаваемый бренд, годами завоевывавший доверие миллионов пользователей. Обширная линия, высокие коэффициенты и удобный интерфейс делают платформу привлекательной как для новичков, так и для опытных игроков. Лига ставок ставки – это возможность окунуться в мир азарта и спортивного прогнозирования. От футбола и хоккея до тенниса и киберспорта – выбор событий огромен, позволяя каждому найти что-то интересное для себя.
ко ланта
ko lanta
Ставки на спорт Прогнозы на спорт помогают принять решение.
https://web-ru.net/
1win Ставки на Спорт: Как Заработать на Прогнозах Ставки на спорт – это популярное развлечение и возможность заработать деньги, предсказывая исходы спортивных событий. Однако, чтобы ставки были прибыльными, необходимо учитывать множество факторов и использовать различные стратегии. Анализ и Прогнозы Успешные ставки на спорт требуют тщательного анализа. Необходимо изучать статистику команд и спортсменов, учитывать текущую форму, травмы, мотивацию и другие факторы, которые могут повлиять на исход матча. Существует множество ресурсов, предлагающих спортивные прогнозы, но важно помнить, что ни один прогноз не гарантирует 100% точности. Стратегии Ставок Существует множество стратегий ставок на спорт, каждая из которых имеет свои преимущества и недостатки. Некоторые игроки предпочитают ставить на фаворитов, другие – на аутсайдеров. Важно выбрать стратегию, которая соответствует вашему стилю игры и уровню риска. Управление Банком Управление банком – это один из ключевых аспектов успешных ставок на спорт. Необходимо установить лимиты на ставки и придерживаться их, чтобы не потерять все деньги в случае неудачных ставок. Рекомендуется ставить не более 1-5% от общего банка на одну ставку.
https://seob.info/
Opportunity Insights – Interesting ideas that encourage looking into new ventures and possibilities.
https://diigo.com/011a8v1
https://1xbetpromo.win-blog.com/19457689/super-1xbet-promo-code-2026-bonus-up-to-130
бездепозитные фриспины
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2
apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2
en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a
partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre
topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis
nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para
hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas
de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones
de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones
de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de
apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas
deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas
deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas
ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app
apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de
apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app
de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas
deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app
de apuestas en españa|app de apuestas en venezuela|app de
apuestas futbol|app de apuestas gratis|app de
apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app
de casas de apuestas|app marca apuestas android|app
moviles de apuestas|app para apuestas|app para apuestas de futbol|app para
apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer
apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps
de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer
apuestas deportivas|apuesta del dia apuestas deportivas|apuestas
10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a
caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a
la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al
mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas
y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del
mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina
croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas
argentina gana mundial|apuestas argentina holanda|apuestas argentina
mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina
paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas
argentina vs colombia|apuestas argentina vs francia|apuestas argentina
vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a
segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic
betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic
osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas
athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas
atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas
atlético de madrid real madrid|apuestas atletico de madrid
vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas
atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas
baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto
pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca
madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas
barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona
athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético
de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona
campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real
madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas
barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis
– chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis
madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de
bienvenida|apuestas bono de bienvenida sin deposito|apuestas
bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas
borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas
brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas
caballos hoy|apuestas caballos madrid|apuestas caballos
online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas
campeon champions league|apuestas campeon conference league|apuestas campeon copa
america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del
mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas
campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas
campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato
f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de
semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos
sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos
españa|apuestas carreras de caballos hoy|apuestas carreras de caballos
nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos
sanlúcar|apuestas carreras de galgos|apuestas
carreras de galgos en vivo|apuestas carreras de
galgos nocturnas|apuestas carreras de galgos pre
partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino
gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos
online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta
eibar|apuestas celta espanyol|apuestas celta granada|apuestas
celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league
– pronósticos|apuestas champions league
2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas
chelsea betis|apuestas chile|apuestas chile peru|apuestas chile
venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas
ciclismo vuelta españa|apuestas city madrid|apuestas city real
madrid|apuestas clasico|apuestas clasico español|apuestas
clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas
colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para
esta semana|apuestas combinadas para hoy|apuestas
combinadas para mañana|apuestas combinadas pronosticos|apuestas
combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero
ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta
de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas
copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas
copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa
del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas
bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para
hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas
de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de
caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de
caballos en españa|apuestas de caballos en linea|apuestas de
caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas
de caballos online|apuestas de caballos online en venezuela|apuestas de
caballos por internet|apuestas de caballos pronosticos|apuestas
de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas
de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por
internet|apuestas de champions league|apuestas de
ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula
1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas
de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas
de futbol en directo|apuestas de futbol en linea|apuestas de futbol
en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol
para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas
de futbol peru|apuestas de futbol pronosticos|apuestas
de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos
como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre
hielo|apuestas de hoy|apuestas de hoy seguras|apuestas
de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de
juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas
de la eurocopa|apuestas de la europa league|apuestas de
la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas
de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas
de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas
de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de
tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de
ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico
real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de
hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas
del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del
sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10
euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas
deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas
deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas
atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas
deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas
deportivas bonos de bienvenida|apuestas deportivas
boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas
deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas
deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se
juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa
america|apuestas deportivas copa del rey|apuestas deportivas
copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de
baloncesto|apuestas deportivas de boxeo|apuestas deportivas
de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas
de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas
deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas
en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas
deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas
deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas
deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas
es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas
deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas
deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas
deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas
deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas
futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero
seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas
deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas
deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas
juegos olimpicos|apuestas deportivas la liga|apuestas
deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas
deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por
internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas
deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas
deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos
expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real
madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas
deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas
deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas
deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas
deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas
deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas
deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas
dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas
directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas
dobles y triples|apuestas dortmund barcelona|apuestas draft
nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas
elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas
en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino
online|apuestas en casinos|apuestas en casinos online|apuestas
en chile|apuestas en ciclismo|apuestas en colombia|apuestas
en colombia de futbol|apuestas en directo|apuestas
en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas
en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas
mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas
en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea
futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas
en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas
en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos
de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de
mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas
en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos
de futbol|apuestas españa|apuestas españa alemania|apuestas españa
alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas
españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra
eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises
bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas
espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports
valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas
eurocopa campeon|apuestas eurocopa españa|apuestas
eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas
eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas
europa league hoy|apuestas europa league pronosticos|apuestas europa league
pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1
hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas
f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para
ganar|apuestas favoritas|apuestas favorito champions|apuestas
favoritos champions|apuestas favoritos eurocopa|apuestas
favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas
final copa|apuestas final copa america|apuestas final copa de europa|apuestas
final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final
copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final
del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final
mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales
nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas
fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas
futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas
futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas
futbol sala|apuestas futbol telegram|apuestas futbol
virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos
online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas
gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas
hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del
rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa
libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador
europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador
mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas
ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar
mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona
athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas
girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas
goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas
gratis con premios|apuestas gratis hoy|apuestas gratis para
hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas
gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas
grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap
como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas
hipicas online|apuestas hípicas online|apuestas hipicas
venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas
hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter
barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos
en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos
baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores
nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas
league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas
legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina (Zoila)|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas
liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico
champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas
madrid barca supercopa|apuestas madrid barcelona|apuestas madrid
barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid
celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas
madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid
vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras
para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas
maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas
mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas
mlb hoy|apuestas mlb las vegas|apuestas mlb para
hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas
múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas
multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial
balonmano|apuestas mundial brasil|apuestas mundial
campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial
favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas
mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas
mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas
mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas
nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas
nba finals|apuestas nba gratis|apuestas nba hoy|apuestas
nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas
nba pronosticos|apuestas nba pronósticos|apuestas nba
pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl
las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas
nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas
online comparativa|apuestas online con paypal|apuestas online de
caballos|apuestas online deportivas|apuestas
online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas
online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas
online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online
venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas
osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas
pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas
países bajos qatar|apuestas para boxeo|apuestas para champions
league|apuestas para el clasico|apuestas para el dia de
hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa
league|apuestas para futbol|apuestas para ganar|apuestas para
ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas
para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar
siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas
para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas
para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas
para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos
de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido
colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido
suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas
partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas
partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru
uruguay|apuestas peru vs chile|apuestas peru vs
colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas
playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas
playoffs nfl|apuestas polonia argentina|apuestas por
argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas
primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos
gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que
aceptan paypal|apuestas que es handicap|apuestas que puedes
hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas
quién bajara a segunda|apuestas quien gana el mundial|apuestas
quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara
el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real
madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid
atletico champions|apuestas real madrid atletico de
madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real
madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid
champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas
real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid
vs atlético|apuestas real madrid vs atletico
madrid|apuestas real madrid vs barcelona|apuestas real madrid vs
betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas
real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad
psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas
registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas
roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas
segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda
division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas
seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol
hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de
semana|apuestas seguras para ganar dinero|apuestas seguras para
hoy|apuestas seguras para hoy fútbol|apuestas seguras
para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises
bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de
madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas
sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas
sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas
sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas
sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas
sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema
calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas
super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas
tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas
tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas
tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis
retirada|apuestas tenis roland garros|apuestas tenis
seguras|apuestas tenis wimbledon|apuestas tenis
wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas
tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas
uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas
us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas
valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas
valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas
valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela
ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas
villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real
madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas
virtuales sin dinero|apuestas vivo|apuestas vuelta a
españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y
pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico
apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs
colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic
real madrid apuestas|atletico barcelona apuestas|atletico de
madrid apuestas|atlético de madrid apuestas|atletico de
madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico
madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona
apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid
apuestas|barca vs real madrid apuestas|barcelona
– real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de
madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg
apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona
vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs
real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos
cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis
– chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono
apuestas deportivas|bono apuestas deportivas sin deposito|bono
apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono
bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa
de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida
apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono
de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por
registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito
apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono
sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas
deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos
bienvenida casas apuestas|bonos bienvenida casas de
apuestas|bonos casa de apuestas|bonos casas apuestas|bonos
casas de apuestas|bonos casas de apuestas colombia|bonos casas de
apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas
sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas
de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de
apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos
en casa de apuestas|bonos en casas de apuestas sin deposito|bonos
gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos
sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de
apuestas seguras|buscador de cuotas apuestas|buscador de
cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas
apuestas|calculadora apuestas|calculadora apuestas
combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas
yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de
futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora
de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para
apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora
sistema apuestas|calculadora stake apuestas|calculadora trading
apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de
apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de
caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras
de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras
de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico
de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas
bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa
apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas
mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas
peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de
apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de
apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa
de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de
mí|casa de apuestas champions league|casa de apuestas chile|casa de
apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de
bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas
con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de
apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa
de apuestas de colombia|casa de apuestas de españa|casa
de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas
de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de
apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de
apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de
apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de
apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito
minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de
apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas
españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas
f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de
apuestas ingreso minimo 1 euro|casa de apuestas ingreso
mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas
legales en españa|casa de apuestas libertadores|casa de apuestas liga
española|casa de apuestas madrid|casa de
apuestas mas segura|casa de apuestas mejores|casa de
apuestas méxico|casa de apuestas minimo 5 euros|casa
de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas
oficial real madrid|casa de apuestas online|casa de apuestas
online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas
online mexico|casa de apuestas online paraguay|casa de
apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago
anticipado|casa de apuestas para boxeo|casa de apuestas para
ufc|casa de apuestas peru|casa de apuestas perú|casa
de apuestas peru online|casa de apuestas por paypal|casa de apuestas
promociones|casa de apuestas que regalan dinero|casa de
apuestas real madrid|casa de apuestas regalo de bienvenida|casa de
apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de
apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas
ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas
vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas
apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas
españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5
euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas
mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas
apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas
5 euros|casas de apuestas app|casas de apuestas argentinas|casas de
apuestas asiaticas|casas de apuestas baloncesto|casas
de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por
registro|casas de apuestas bono sin deposito|casas de apuestas bono
sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos
gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas
carreras de caballos|casas de apuestas casino|casas
de apuestas casino online|casas de apuestas cerca de
mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas
com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas
con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas
con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas
con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas
de apuestas con handicap asiatico|casas de apuestas con licencia|casas de
apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas
de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas
de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de
apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de
apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas
de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de
apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas
de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas
de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de
apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa
nuevas|casas de apuestas españa online|casas de apuestas española|casas
de apuestas españolas|casas de apuestas españolas con licencia|casas
de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de
apuestas fisicas en barcelona|casas de apuestas fisicas
en españa|casas de apuestas formula 1|casas de apuestas fuera
de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso
minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas
legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales
españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia
españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de
apuestas mejores bonos|casas de apuestas mejores cuotas|casas
de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de
apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva
ley|casas de apuestas nuevas|casas de apuestas nuevas
en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas
de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas
online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas p
Лига ставков ставки Лига ставок – это бренд, зарекомендовавший себя как надежный партнер в мире ставок. Широкая линия событий, выгодные коэффициенты и удобный интерфейс делают эту платформу привлекательной для широкой аудитории игроков. Лига ставок ставки – это широчайший спектр возможностей для реализации своих прогнозов. От футбольных баталий до теннисных поединков, от хоккейных матчей до киберспортивных турниров – выбор огромен, позволяя каждому найти что-то по душе и по своим знаниям.
ко ланта
промокоды 1xbet на сегодня Активируйте промокод на http://www.google.pn/url?q=https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html и заберите бонус до 32 500 рублей при регистрации для максимального старта.
промокод 1 х бет Вводите промокод на http://www.google.sk/url?q=https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html и получите 100% к первому депозиту для комфортного старта игры.
Ставки на спорт 1 ставка – это отправная точка, первый шаг на пути к выигрышу. Это момент истины, когда знания, интуиция и удача сливаются воедино, чтобы определить исход игры. Ставки на спорт – это не просто способ заработать деньги, это стиль жизни, наполненный адреналином и предвкушением. Это возможность почувствовать себя частью глобального спортивного сообщества, где каждый матч – это повод для обсуждения и анализа.
бездепозитный бонус игровые автоматы с выводом денег
http://gunfucha.ru/forum/profile.php?mode=viewprofile&u=200318
трипскан Трипскан предлагает гибкие настройки и фильтры, чтобы вы могли подобрать идеальный вариант, отвечающий всем вашим потребностям. TripScan обеспечивает безопасность ваших данных и гарантирует конфиденциальность вашей личной информации.
Mindful Progress Spot – Explore strategies to stay focused and achieve meaningful growth.
Go to the official company site > http://images.google.co.nz/url?q=https://bergkompressor.ru/news/artcles/?1xbet_promokod_pri_registracii_bonus_5.html
tripscan Эта платформа, TripScan, также предоставляет инструменты для отслеживания цен и получения уведомлений о снижении стоимости билетов и номеров в отелях.
https://aritual.by/funeral.html
https://officepro54.ru/collection/ofisnye-kresla
https://aritual.by/prices.html
Daily Chic Picks – Handpicked styles to make your daily fashion choices simple and fun.
tripscan Tripscan – это инновационная платформа, позволяющая спланировать идеальное путешествие, учитывая все ваши предпочтения и бюджет. Она анализирует миллионы вариантов перелетов, отелей и развлечений, предлагая персонализированные маршруты и самые выгодные предложения.
трипскан Трипскан предлагает гибкие настройки и фильтры, чтобы вы могли подобрать идеальный вариант, отвечающий всем вашим потребностям. TripScan обеспечивает безопасность ваших данных и гарантирует конфиденциальность вашей личной информации.
https://sketchersunited.org/users/291223
трипскан С TripScan вы найдете скрытые жемчужины, о которых раньше не знали, и сможете создать уникальное путешествие, которое запомнится на всю жизнь. Эта платформа, TripScan, также предоставляет инструменты для отслеживания цен и получения уведомлений о снижении стоимости билетов и номеров в отелях.
1хбет промокод бесплатно Найдите промокод на https://www.ikonu.ru/faq/pgs/1xbet-besplatnuy-promokod-pri-registracii.html и получите бонус 100% на первый депозит, чтобы начать игру.
Confidence Builder Tips – Practical ideas to strengthen your confidence.
ко ланта ко ланта
ко ланта ко ланта
1xBet бонус код Активируйте бонусом при регистрации на https://sushikim.ru/image/pgs/1xbet_promokod_55.html и заберите 32 500? + бонус 100%, чтобы начать игру.
Промокод при регистрации 1xbet на 32500 рублей. Этот код нужно ввести при регистрации в соответствующее поле. Промокод действует однократно, но им можно делиться с друзьями. Регистрация по номеру телефона — быстрый способ создать аккаунт. После получения данных для входа остаётся лишь ввести логин и пароль. Используй актуальный 1 хбет промокод и увеличь первый депозит до 32 500 рублей в БК 1xBet. На платформе действует бонусная программа, которая помогает игрокам получать до дополнительных процентов от первого депозита.
tripscan Забудьте о долгих часах, проведенных в поисках идеального варианта, Tripscan сделает всю работу за вас, предлагая лучшие предложения, соответствующие вашим потребностям. TripScan – ваш верный спутник в мире путешествий, готовый сделать вашу следующую поездку незабываемой.
ко ланте Ко Ланте
ко ланте Ко Ланте
https://www.diveboard.com/1xbetcode/posts/code-promo-1xbet-2026-130-euros-nouveaux-parieurs-B5h2Ckk
https://sites.gsu.edu/nramirez5/2016/04/04/georgia-aquarium-gift-shop/comment-page-1104/#comment-167615
kews k16 nb300 кевс kews кевс к16 нб300 kews k16 nb300
Букмекерская контора Мелбет предлагает хорошо организованный сервис для пользования услугами оператора. Разнообразие ставок с неплохими коэффициентами сопровождается бонусными программами, нацеленными на поддержание интересов клиентов. Получение бонусов от букмекера позволяет получить новый безболезненный опыт на ставках, что особенно важно для новичков melbet промокод на сегодня 2026. Однако предполагаем, что снижение требований по отыгрышу бонусов сделали бы букмекера еще привлекательнее для игроков.
Букмекерские конторы в России предлагают огромное количество промокодов и бонусов для своих клиентов, особенно много купонов новичкам, где при регистрации можно получить бесплатно деньги на свой счет. Букмекерская контора Melbet открывает новым игрокам бонус на первый депозит с увеличенной суммой до 50 000 рублей, за Мелбет промокод на сегодня, который можно скопировать у нас. Предлагаем ввести Мелбет промокод на сегодня, который в 2026 году даёт увеличение 130% бонуса на первый депозит до 50 000 рублей. Регистрируйся и играй с Мелбет сегодня!!! Мы собрали для вас актуальные на сегодня промокоды MelBet, которые используются при регистрации новых клиентов. После чего скидки и бонусы будут зачислены вам на счет.
kews k16 nb300 кевс kews кевс к16 нб300 kews k16 nb300
Trendy Marketplace Daily – Discover new arrivals and trendy items with convenient browsing.
ко ланта ко ланта
tüm sitelerin elimde tüm sitelerin elimde denimo videosu
https://www.sutori.com/en/story/untitled–jvR1dnjNFXzPrJoo2unXXyiE
Официальный портал компании
остров ко ланта остров ко ланта
Наш официальный сайт уже доступен
Trendy Style Spot – Handpicked fashion items to elevate your style effortlessly.
остров ко ланта остров ко ланта
https://learndash.aula.edu.pe/miembros/miriamholt6/
ремонт двигателя москва Тонировка в Москве: Профессиональное Затемнение Стекол Тонировка в Москве – это профессиональная установка тонировочной пленки на стекла автомобиля. Квалифицированные мастера используют качественные материалы и соблюдают все требования законодательства.
чип тюнинг москва Тюнинг Москва: Симфония Инженерии и Эстетики Москва, город динамики и амбиций, предъявляет особые требования к автомобилю. Тюнинг в Москве – это не просто смена облика, это глубокая трансформация, направленная на повышение производительности, улучшение управляемости и персонализацию до мельчайших деталей. В столичных мастерских создаются настоящие произведения искусства на колесах, сочетающие передовые технологии и безупречный стиль.
тонировка авто в москве Чип Тюнинг Москва: Откройте Скрытый Резерв Мощности Чип-тюнинг в Москве – это интеллектуальная модификация программного обеспечения двигателя, позволяющая раскрыть его скрытый потенциал. Опытные специалисты производят точную настройку ЭБУ, добиваясь увеличения мощности и крутящего момента без ущерба для надежности и ресурса двигателя.
Smart Savings Corner – Tips and deals to help you shop wisely without overspending.
тонировка в москве Тонировка в Москве: Профессиональное Затемнение Стекол Тонировка в Москве – это профессиональная установка тонировочной пленки на стекла автомобиля. Квалифицированные мастера используют качественные материалы и соблюдают все требования законодательства.
you are in point of fact a good webmaster. The site loading pace is amazing. It sort of feels that you are doing any unique trick. Moreover, The contents are masterpiece. you have performed a magnificent activity on this matter!
Escort directory listing Rio
Your Trend Picks – Enjoy a smooth shopping experience while exploring fashionable products.
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
https://optimapharm.com.ua/ekonomiya-v-200-hryven-yaka-mozhe-koshtuvaty.html
проститутка олеся Проститутки младше, юный возраст как фактор выбора, часто ассоциирующийся со свежестью и энергией. Молодые проститутки, акцент на юности и неопытности. Проститутка Мурина, географическая привязка к конкретному району. Проститутки Колпино, расширение географии в пригороды Санкт-Петербурга. Проститутки Мурино, еще один пригород в фокусе внимания. Проститутка СПБ Телеграм, современный инструмент поиска и связи. Найду проститутка, решительное выражение намерения. Проститутки самого, поиск “самых” лучших, красивых или дешевых. Зрелые проститутки СПб, опытные женщины в рамках городской локации. Проститутки Ветеранов, привязка к станции метро для удобства поиска. Проститутки Луга, отдаленный населенный пункт Ленинградской области. Без проституток, отрицание потребности в подобных услугах. Большие проститутки, акцент на размере или количестве предложений. Проститутки область, охват предложений по всей Ленинградской области. Дешевые проститутки СПб, бюджетный вариант в рамках города. Бывшая проститутка, информация о женщинах, прекративших деятельность. Проститутки г, сокращенное обозначение слова “город”. Взрослые проститутки, альтернатива молодым, с акцентом на опыте. Сайт проституток, веб-ресурс для поиска и выбора. Проститутки рядом, поиск ближайших доступных предложений. Проститутки СПб ТГ, еще одно сокращение для поиска в Телеграм. Проститутки 2025, актуальность предложений на текущий год. Форум проституток, площадка для обсуждения, отзывов и обмена опытом. Проститутки трансы СПб, конкретизация запроса в рамках города. Снят проститутки СПб, результат успешного поиска и встречи. Снять проститутку СПб, намерение найти компаньонку в городе. Проститутки индивидуалки Петербурге, независимые работницы в рамках городской локации. Проститутки Просвещения, привязка к станции метро.
санкт петербурге проститутка объявления Проститутки узбечки спб, узбечки в Санкт-Петербурге. Смотреть проституток, просмотр фотографий. Кудрова проститутка, неясное значение. Проститутки Ватсап, использование Ватсап для связи. Проститутки Кудрово, город Кудрово. Проститутки Сосновый Бор, город Сосновый Бор. Проститутки на выезд, выезд к клиенту. Проститутки на улице, уличная проституция. Красивые проститутки, акцент на внешности. Проститутка скрытая камера, скрытая съемка. Проститутка скрыть камеру, просьба не снимать. Ближайшие проститутки, поиск поблизости. Проститутка сел, неясное значение. Лучшие проститутки, субъективная оценка. Мужчины проститутки, мужская проституция. Проститутки Красно, короткая форма. Реальные проститутки спб, достоверные фотографии. Услуги проститутки, перечень предлагаемых услуг. Петербург район проституток, район концентрации проституции.
уход за инвалидом пансионат частный Пансионат для инвалидов в Москве: достойная жизнь в кругу единомышленников Пансионат для инвалидов в Москве – это место, где люди с ограниченными возможностями могут жить полноценной жизнью, общаться с единомышленниками, получать необходимую медицинскую помощь и участвовать в различных мероприятиях. Мы создаем атмосферу взаимопонимания и поддержки, где каждый чувствует себя частью большой и дружной семьи.
пансионат для инвалидов в москве цены Московские дома инвалидов: выбор в пользу профессионализма и опыта Московские дома инвалидов – это сеть государственных и частных учреждений, предоставляющих услуги по уходу и реабилитации инвалидов. При выборе дома инвалидов в Москве важно учитывать такие факторы, как квалификация персонала, условия проживания, спектр предоставляемых услуг, стоимость и отзывы других семей. Мы гордимся тем, что наш дом инвалидов в Москве соответствует самым высоким стандартам качества и предлагает индивидуальный подход к каждому постояльцу.
What’s up to every body, it’s my first pay a visit of this web site; this blog carries remarkable and in fact fine material in favor of readers.
https://bookvoid.com.ua/korpus-fary-ferrari-california-problemy-ta.html
Montre replique durable Montre Replique Realiste : Jusqu’ou Pousser l’Imitation ? La montre replique realiste pousse l’imitation a son paroxysme, reproduisant fidelement les moindres details de la montre originale. Elle peut etre difficile a distinguer d’une veritable montre de luxe, ce qui souleve des questions ethiques et morales. Il est important de rester conscient des enjeux lies a la contrefacon.
Дома из клееного бруса Краснодар Строительство из клееного бруса – это современное и эффективное решение для тех, кто ценит экологичность, скорость возведения и эстетическую привлекательность своего будущего дома. Клееный брус, благодаря своей технологии производства, обладает повышенной прочностью, устойчивостью к деформациям и минимальной усадкой, что делает его идеальным материалом для строительства долговечных и надежных зданий.
Replika Uhr Shop Deutschland Manner Uhr Replika: Stilvolle Begleiter fur Herren Manneruhren Repliken bieten eine breite Palette an Designs, von sportlich und robust bis hin zu elegant und klassisch. Ob fur den taglichen Gebrauch, besondere Anlasse oder als Statussymbol – es gibt fur jeden Mann die passende Replika Uhr. Diese Uhren sind nicht nur stilvoll, sondern auch funktional und zuverlassig und begleiten den Trager durch den Tag.
https://blog.stcloudstate.edu/hied/2020/02/25/congrats-dr-williams-2020-first-place-dissertation-award-winner/comment-page-1179/#comment-321935
Дома из клееного бруса под ключ Дома из клееного бруса под ключ – это комплексное решение, включающее все этапы строительства, от проектирования до внутренней отделки. Заказывая дом под ключ, вы избавляетесь от необходимости самостоятельно заниматься организацией строительных работ и поиском подрядчиков. Профессионалы берут на себя все заботы, гарантируя высокое качество и соблюдение сроков.
Дома из клееного бруса Краснодар Дом из клееного бруса цена – зависит от множества факторов, включая площадь, сложность проекта, используемые материалы и внутреннюю отделку. Однако, в целом, дом из клееного бруса является выгодным вложением средств, учитывая его долговечность, энергоэффективность и экологичность. Проекты домов из клееного бруса – это широкий выбор архитектурных решений, от небольших дачных домиков до просторных коттеджей. Индивидуальный проект позволяет учесть все особенности участка и пожелания заказчика, создавая уникальное и функциональное пространство для жизни. Дом из клееного бруса цена под ключ – это фиксированная стоимость строительства, включающая все работы и материалы, необходимые для ввода дома в эксплуатацию. Это удобный и надежный способ получить готовое жилье без лишних хлопот и неожиданных расходов.
1xbet регистрация промокод Активируйте промокод на https://chernovorot.ru/wp-content/plugins/?1xbet_promokod_pri_registracii_bonus_segodnya.html и заберите бонус до 32 500 рублей при регистрации для комфортной игры.
1xbet промокод при регистрации Получите промокод на https://hm-net.ru/inc/pgs/index.php?1xbet_promokod_pri_registracii_bonus.html и заберите бонус 100% на первый депозит при регистрации для максимального старта.
https://roomstyler.com/users/pentacrown56
Daily Motivation Spot – Find resources that encourage personal growth and continuous improvement.
Букмекерские компании стараются не только привлечь новых клиентов приятными подарками, но и удержать «старичков». Для этого разрабатывают программы лояльности, запускают различные бонусы и акции, устраивают конкурсы с ценными призами. Самым популярным является промокод на Melbet при регистрации, который вводится при регистрации нового аккаунта. Благодаря ему вы получаете увеличенный бонус на первый депозит, система добавляет 30% к максимальной сумме. Стандартный бонус на первое пополнение счета составляет 8000 рублей, после введения промокода – 50 000 рублей.
L’offre code promo 1xBet bonus de bienvenue garantit un bonus de 130 % sur le depot initial. En utilisant un code valide, vous etes toujours gagnant. En jouant activement, vous pouvez accumuler des points promo utilisables pour un pari gratuit ou augmenter votre capital. Pour plus de details sur le code promo 1xBet paris sportifs, consultez ce lien : https://www.gilmaire-etienne.com/wp-content/pages/code-promo-1xbet-bonus.html
Букмекерская контора «Мелбет» – это уникальная возможность для всех желающих получить дополнительный доход. Здесь можно делать ставки на самые разные спортивные события по всему миру. Высокие коэффициенты, круглосуточная техническая поддержка, удобное мобильное приложение и многие другие преимущества проекта делают его весьма популярным среди любителей азартных игр. Доступ на виртуальную площадку открыт лишь для зарегистрированных пользователей. рабочий промокод Melbet при регистрации помогут сэкономить как начинающим, так и опытным игрокам. В такой надежной и стабильной букмекерской конторе вы всегда можете быть уверены.
Code Promo 1xbet Gabon vous donne un code promo 1xBet bonus de bienvenue de 100% sur le depot initial, valable dans votre pays ou region, avec la possibilite d’obtenir jusqu’a 130€ ou l’equivalent dans votre devise. 1xBet, l’un des meilleurs bookmakers pour les paris sportifs, opere avec succes depuis plus de dix ans.
Проекты домов из клееного бруса Строительство из клееного бруса – это не просто возведение стен, это создание живого, дышащего пространства, наполненного теплом натурального дерева. Технология клееного бруса позволяет воплощать в жизнь самые смелые архитектурные решения, сочетая в себе эстетику, экологичность и высокую энергоэффективность. Инвестируя в дом из клееного бруса, вы инвестируете в комфорт и долговечность.
Check our new web page — http://ruptur.com/
The latest release is here > http://ruptur.com/
I used to be able to find good information from your articles.
independent escort girl in Brazil
10 euros offert paris sportif|10 euros offert sans
dépôt paris sportif|10 meilleurs sites de paris sportifs|100 euro offert paris
sportif|100 euros offert paris sportif|100 euros
remboursé paris sportifs|100 offert pari sportif|100 offert
paris sportif|100 remboursé paris sportif|100e offert pari sportif|abandon paris sportif tennis|abandon tennis paris sportif|addiction paris sportif forum|age paris sportif belgique|aide au pari
sportif|aide au paris sportif|aide aux paris sportif|aide aux paris sportifs|aide pari sportif|aide pari sportif football|aide parie sportif|aide paris
sportif|aide paris sportif foot|aide paris sportif
gratuit|aide paris sportifs|aide pour paris sportif|algorithme de paris
sportif|algorithme excel paris sportif|algorithme gratuit paris
sportif|algorithme pari sportif|algorithme paris sportif|algorithme paris sportif
avis|algorithme paris sportif basket|algorithme paris sportif excel|algorithme
paris sportif gratuit|algorithme paris sportif tennis|algorithme paris sportifs|algorithme pour paris sportif|analyse cote paris sportif|analyse
de paris sportif|analyse match paris sportif|analyse pari sportif|analyse paris sportif|analyse paris sportif foot|analyse paris sportif football|analyse paris sportif
gratuit|analyse paris sportifs|ancienne cote paris
sportif|api cote paris sportif|app paris sportif sans argent|appli de paris sportif|appli de paris sportif
sans argent|appli de paris sportifs|appli pari sportif|appli
pari sportif gratuit|appli parie sportif|appli paris sportif|appli paris sportif avec paypal|appli
paris sportif belgique|appli paris sportif entre amis|appli paris sportif
gratuit|appli paris sportif sans argent|appli paris sportif suisse|appli paris sportifs|application aide paris sportif|application algorithme paris sportif|application analyse paris sportif|application android paris sportif|application bankroll paris sportif|application conseil paris sportif|application de pari sportif|application de parie sportif|application de paris sportif|application de paris sportif en afrique|application de paris sportif en cote d’ivoire|application de paris sportif en ligne|application de paris sportif gratuit|application de paris sportif international|application de paris sportif suisse|application de paris sportifs|application faux paris sportifs|application gestion bankroll paris sportif|application gestion paris sportif|application ia paris sportif|application pari sportif
gratuit|application paris sportif|application paris sportif android|application paris sportif argent fictif|application paris sportif belgique|application paris
sportif canada|application paris sportif espagne|application paris sportif espagnol|application paris sportif fictif|application paris sportif france|application paris
sportif gratuit|application paris sportif gratuit entre amis|application paris sportif maroc|application paris sportif offre
de bienvenue|application paris sportif paypal|application paris
sportif sans argent|application paris sportif
sans justificatif de domicile|application paris sportif suisse|application paris sportif usa|application paris sportif virtuel|application pour faire des paris sportifs|application pour gerer ses paris sportif|application pour les paris sportifs|application pour pari sportif|application pour
paris sportif|application pour paris sportifs|application statistique paris
sportif|application suivi paris sportif|applications de paris sportifs|applications paris
sportifs|applis paris sportif|applis paris sportifs|apprendre a faire des paris sportifs|argent facile paris sportif|argent offert
paris sportifs|argent offert sans depot paris sportif|argent paris sportif|argent
paris sportifs|argent paris sportifs impots|argent sans depot paris sportif|arjel paris
sportif|arjel paris sportifs|astuce gagner paris sportif|astuce pari sportif|astuce paris sportif|astuce paris sportif basket|astuce paris
sportif foot|astuce paris sportif forum|astuce paris sportif tennis|astuce paris sportifs|astuce
pour gagner au pari sportif|astuce pour gagner au paris sportif|astuce pour gagner paris sportif|astuce pour paris
sportif|astuces paris sportifs|astuces paris sportifs en ligne|astuces
paris sportifs foot|astuces pour gagner aux paris sportifs|autorisation paris sportif france|avis pari sportif|avis
paris sportif|avis paris sportif foot|avis site de paris sportif|avis site paris sportif|avis sur les paris
sportifs|avis sur paris sportif|avis tipster paris sportif|aweh signification paris sportif|bankroll 100 euros paris sportifs|bankroll management paris sportif|bankroll paris sportif|bankroll paris sportif excel|bankroll paris sportif gratuit|bankroll paris sportifs|basket paris sportif|belgique france paris
sportif|belgique paris sportifs|bonus bienvenue paris sportif|bonus bienvenue paris sportifs|bonus cash paris sportif|bonus de bienvenue paris
sportif|bonus de bienvenue paris sportif belgique|bonus de bienvenue sans
depot paris sportif|bonus de depot paris sportif|bonus de paris sportifs|bonus depot paris sportif|bonus en cash paris sportif|bonus gratuit paris sportif|bonus gratuit sans depot
paris sportif|bonus pari sportif|bonus paris sportif|bonus paris sportif
belgique|bonus paris sportif betclic|bonus paris sportif cash|bonus paris sportif en ligne|bonus paris sportif france pari|bonus paris sportif retirable|bonus
paris sportif sans depot|bonus paris sportif sans dépôt|bonus paris
sportif unibet|bonus paris sportifs|bonus sans depot paris sportif|bonus sans
depot paris sportif belgique|bonus sans dépôt paris sportif|bonus sans dépôt
paris sportif hors arjel|bonus site de paris sportif|bonus site pari sportif|bonus site paris sportif|bonus sites
de paris sportifs|bonus unibet paris sportif|bookmaker paris sportif|bookmaker paris sportif gratuit|bookmaker paris sportifs|bookmaker
sportif|bookmakers paris sportif|bookmakers paris sportifs|bookmakers
paris sportifs en ligne|but contre son camp paris sportif|but sur penalty paris sportif|buteur paris sportif|c’est quoi handicap paris sportif|c’est quoi une cote paris sportif|calcul
anti perte paris sportif|calcul combinaison pari sportif|calcul cote pari sportif|calcul cote paris sportif|calcul couverture paris sportif|calcul de cote paris sportif|calcul des
cotes paris sportifs|calcul dnb paris sportifs|calcul
double chance paris sportif|calcul gain paris sportif|calcul
mise paris sportif|calcul pari sportif|calcul paris sportif|calcul paris sportif
multiple|calcul pourcentage cote paris sportif|calcul probabilité paris sportif|calcul rentabilité paris sportifs|calcul roi paris sportif|calcul systeme paris sportif|calcul trj paris sportifs|calculateur cote paris sportif|calculateur de cote paris sportif|calculateur de mise paris
sportif|calculateur de paris sportif|calculateur paris sportif|calculatrice
arbitrage paris sportif|calculatrice paris sportif|calculer cote paris sportif|calculer gain paris sportif|calculer probabilité paris sportifs|calculer roi paris sportifs|calculer une cote pari
sportif|calculer une cote paris sportif|carte cadeau paris sportif|carte pcs paris sportif|carte prépayée paris sportifs|cash out pari sportif|cash
out paris sportif|cash out paris sportifs|casino en ligne paris sportif|casino paris sportif en ligne|champions
league paris sportif|chute de cote paris sportif|classement des meilleurs sites
de paris sportifs|classement meilleur site de paris sportif|code barre paris sportif|code
bonus paris sportif|code paris sportif|code promo pari sportif|code promo paris sportif|code promo
paris sportif sans depot|code promo paris sportif sans dépôt|code promo sans depot paris sportif|code promo site paris sportif|combien de temps pour encaisser un paris sportif|combien de temps pour retirer un paris sportif|combien miser paris sportifs|combine paris sportif|combines paris sportifs|combiné pari sportif|combiné paris sportif|combiné paris sportif conseil|combiné paris sportif du jour|combiné paris sportif pronostic|comment analyser un paris sportif|comment arreter de
jouer aux paris sportifs|comment arreter les paris sportif|comment arreter les
paris sportifs|comment arrêter les paris sportifs|comment bien gagner au paris sportif|comment
bien jouer au paris sportif|comment bien miser paris sportif|comment ca marche les paris sportif|comment calculer
cote paris sportif|comment calculer gain paris sportif|comment calculer
les cotes des paris sportifs|comment calculer une cote de paris sportif|comment calculer une
cote pari sportif|comment calculer une cote paris sportif|comment comprendre les paris sportifs|comment creer un vip paris sportif|comment
créer un algorithme paris sportif|comment créer un site de paris sportif|comment
devenir riche avec les paris sportifs|comment etre rentable paris sportif|comment etre sur de gagner au paris sportif|comment faire de
bon paris sportif|comment faire des parie sportif|comment faire des
paris sportif|comment faire des paris sportif gagnant|comment faire des paris sportifs|comment faire pari sportif|comment faire paris sportif|comment faire pour arreter les
paris sportifs|comment faire pour gagner au paris sportif|comment faire pour gagner les paris sportifs|comment faire
un bon pari sportif|comment faire un bon paris sportif|comment faire un pari sportif|comment faire
un parie sportif|comment faire un paris sportif|comment faire une montante paris
sportif|comment fonctionne les cotes dans les paris sportifs|comment fonctionne les cotes des paris sportifs|comment fonctionne les paris sportifs|comment fonctionne paris sportifs|comment fonctionne un pari sportif|comment fonctionnent les cotes dans les paris sportifs|comment fonctionnent les cotes
dans les paris sportifs grand oral|comment fonctionnent les
cotes de paris sportif|comment fonctionnent les paris sportifs|comment fonctionnent les
paris sportifs grand oral|comment fonctionnent les paris sportifs grand
oral maths|comment fonctionnent les paris sportifs maths|comment gagner a coup sur au paris sportif|comment gagner a tous les
coups au paris sportif|comment gagner a tout les
coup au paris sportif|comment gagner au pari sportif|comment gagner au pari sportif football|comment gagner au paris sportif|comment gagner au paris sportif a coup sur|comment gagner au
paris sportif foot|comment gagner au paris sportif
forum|comment gagner au paris sportif tennis|comment gagner au paris
sportifs|comment gagner aux paris sportif|comment gagner aux paris sportifs|comment gagner aux paris sportifs foot|comment gagner aux
paris sportifs livre|comment gagner aux paris sportifs sur le long terme|comment gagner avec les paris sportifs|comment gagner dans les paris sportifs|comment gagner de
l argent avec les paris sportifs|comment gagner de
l’argent au paris sportif|comment gagner de l’argent aux paris sportifs|comment gagner de l’argent avec les paris sportifs|comment gagner
de l’argent paris sportif|comment gagner de l’argent sur les paris sportifs|comment gagner de l’argent sur paris sportif|comment gagner des paris sportif|comment gagner des paris
sportifs|comment gagner en paris sportif|comment gagner facilement au paris sportif|comment gagner les paris
sportifs|comment gagner paris sportif|comment gagner paris sportif foot|comment gagner paris sportifs|comment
gagner sa vie avec les paris sportifs|comment gagner ses paris sportif|comment gagner sur les
paris sportif|comment gagner sur les paris sportifs|comment gagner tout le temps au paris sportif|comment
gagner un pari sportif|comment gagner un paris sportif|comment gerer une bankroll paris sportif|comment gérer sa bankroll paris sportif|comment jouer au pari sportif|comment jouer au paris sportif|comment jouer au paris sportif foot|comment jouer aux paris sportifs|comment jouer
paris sportif|comment marche cote paris sportif|comment marche les cotes paris sportif|comment marche les paris
sportif|comment marche les paris sportifs|comment marche paris
sportif|comment marche un pari sportif|comment marche un paris sportif|comment marchent
les cotes paris sportif|comment marchent les paris sportifs|comment miser au
paris sportif|comment miser paris sportif|comment monter sa bankroll paris sportif|comment ne jamais perdre au paris sportif|comment parier sportif|comment reussir au paris sportif|comment
reussir les paris sportif|comment reussir paris sportif|comment sont calculer les cotes
de paris sportif|comment sont calculées les cotes des paris
sportifs|comment sont calculés les cotes des paris sportifs|comment sont
faites les cotes des paris sportifs|comment toujours gagner au paris sportif|comment ça marche les paris
sportifs|comparaison bonus paris sportifs|comparaison cote pari sportif|comparaison des cotes paris sportifs|comparateur cote pari sportif|comparateur cote paris sportif|comparateur cotes paris sportif|comparateur cotes paris
sportifs|comparateur de cote pari sportif|comparateur de
cote paris sportif|comparateur de cotes paris sportifs|comparateur
de côtes paris sportifs|comparateur de paris sportif|comparateur de site de paris sportif|comparateur de site paris sportif|comparateur de sites de paris sportifs|comparateur pari sportif|comparateur paris sportif|comparateur paris sportifs|comparateur site de paris sportif|comparateur
site pari sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif bonus paris sportifs|comparatif cote pari sportif|comparatif cote paris
sportif|comparatif cotes paris sportifs|comparatif des sites
de paris sportifs|comparatif offre de bienvenue paris
sportif|comparatif offre paris sportif|comparatif pari sportif|comparatif
pari sportif en ligne|comparatif paris sportif|comparatif paris sportif bonus|comparatif paris sportif en ligne|comparatif
paris sportifs|comparatif paris sportifs en ligne|comparatif site de paris sportif|comparatif site
paris sportif|comparatif site paris sportifs|comparatif sites de paris
sportifs|comparatif sites paris sportifs|comparer les cotes paris sportifs|comprendre cote paris sportif|comprendre
handicap paris sportif|comprendre les cotes des paris sportifs|comprendre les cotes paris sportif|comprendre les cotes paris sportifs|comprendre les handicap
paris sportif|compte de paris sportif|compte démo paris sportif|compte finance paris
sportif|compte financer paris sportif|compte financier paris sportif|compte
financé paris sportif|compte pari sportif|compte paris sportif|compte paris sportif financé|conseil de paris sportif|conseil de
paris sportifs|conseil en paris sportif|conseil en paris sportifs|conseil pari sportif|conseil pari sportif gratuit|conseil paris sportif|conseil paris sportif aujourd’hui|conseil paris sportif du jour|conseil paris sportif foot|conseil paris sportif gratuit|conseil paris sportif ligue des champions|conseil
paris sportif nba|conseil paris sportif pronostic|conseil paris sportif rmc|conseil
paris sportif tennis|conseil paris sportifs|conseil pour
gagner au paris sportif|conseil pour paris sportif|conseil sur les paris sportifs|conseille paris
sportif|conseiller en paris sportifs|conseiller paris
sportif|conseils de paris sportifs|conseils en paris
sportifs|conseils paris sportifs|conseils paris sportifs foot|conseils paris sportifs gratuit|conseils paris sportifs
tennis|conseils pour paris sportifs|cote a 100 paris sportif|cote a 2 paris sportif|cote anglaise paris
sportif|cote de 2 paris sportif|cote de pari sportif|cote de
paris sportif|cote des paris sportifs|cote maximum paris sportif|cote minimum paris sportif|cote pari sportif|cote pari sportif comment ça marche|cote pari sportif real madrid|cote pari sportif rugby|cote parie sportif|cote paris sportif|cote paris sportif belgique|cote paris sportif calcul|cote paris
sportif definition|cote paris sportif euro|cote paris sportif explication|cote paris sportif foot|cote
paris sportif france belgique|cote paris sportif france espagne|cote paris sportif ligue des
champions|cote paris sportif moto gp|cote paris sportif psg|cote paris sportif psg
arsenal|cote paris sportif rugby|cote paris sportif tennis|cote paris sportifs|cote pour paris sportifs|cote sportif foot|cote sportif
rugby|cote à 1000 paris sportif|cotes de paris sportifs|cotes
pari sportif|cotes paris sportif|cotes paris sportifs|cotes paris
sportifs foot|coupe de france paris sportif|créer un algorithme paris sportif|créer un compte paris
sportif|créer un site de paris sportif en ligne|dans les
paris sportifs que signifie handicap|declarer ses gains paris sportif|definition cash out paris
sportif|definition cote paris sportif|definition handicap paris
sportif|depot 5 euros paris sportif|depot double paris sportif|depot
minimum 5 euro paris sportif|depot minimum paris sportif|depot paris sportif|depuis quand existe les
paris sportif en france|devenir riche avec les paris sportifs|devenir
riche avec paris sportifs|disqualification tennis paris sportif|dnb en paris sportif|dnb pari
sportif|dnb paris sportif|dnb paris sportif definition|dnb paris sportifs|doit on declarer les gains de paris
sportif|déclarer gains paris sportifs|déclarer gains
paris sportifs hors arjel|définition bankroll paris sportif|dépôt
minimum 1 euro paris sportif|dépôt minimum 5
euro paris sportif|ecart de jeux tennis paris
sportif|erreur de cote paris sportif|est ce que les gains
des paris sportifs sont imposables|est-ce que les prolongation compte dans un pari sportif|etre sur de gagner au paris sportif|euro paris sportif|evenement sportif a paris|evenement sportif paris|evenement sportif paris 2025|evenement sportif paris aujourd hui|evenement sportif paris aujourd’hui|evenement sportif paris ce week end|evenements sportif paris|evenements sportifs paris|evenements sportifs paris 2025|evenements sportifs à
paris|evolution cote paris sportif|evolution cotes paris sportifs|evolution des cotes
paris sportifs|explication cote pari sportif|explication cote
paris sportif|explication handicap paris sportif|explication pari sportif|explication paris sportif|face a face hockey paris sportif|faire des paris sportif|faire des paris sportif avec paypal|faire des paris sportifs|faire fortune
paris sportifs|faire un pari sportif|faire un paris sportif|faut il déclarer les gains de paris sportifs|faut il déclarer ses gains paris sportifs|fichier excel gestion bankroll paris sportif|fiscalité gains paris sportifs|foot paris sportif|football et paris sportifs|forfait tennis paris sportif|formation paris sportif gratuit|forum
de paris sportif|forum de paris sportifs|forum pari sportif|forum parie
sportif|forum paris sportif|forum paris sportif foot|forum paris sportif gratuit|forum paris sportif nba|forum paris sportif tennis|forum paris sportifs|forum
sur les paris sportifs|forum tennis paris sportif|francaise des jeux pari sportif|francaise des jeux paris sportif|francaise des jeux paris sportifs|france 2 paris sportif|france 2 paris sportifs|france belgique paris sportif|france espagne paris sportif|france pari sportif|france pari sportif brest|france paris sportif|france paris
sportifs|france pologne paris sportif|france portugal paris
sportif|france suisse paris sportifs|france tunisie paris sportifs|france-pari
– paris sportifs|gagnant pari sportif|gagnant
paris sportif|gagnant paris sportif bayern|gagnante paris sportif|gagne au paris sportif|gagner 10 euros par jour
aux paris sportifs|gagner 100 euros par jour paris sportif|gagner 1000
euros par mois paris sportifs|gagner 10000 euros paris sportif|gagner 2000 euros
par mois paris sportif|gagner 50 euros par jour paris sportif|gagner a coup sur au paris
sportif|gagner a coup sur pari sportif|gagner a tous les coup paris sportif|gagner argent avec paris sportifs|gagner
argent pari sportif|gagner argent paris sportif|gagner argent paris
sportifs|gagner au pari sportif|gagner au paris sportif|gagner
au paris sportif a coup sur|gagner au paris sportif foot|gagner au paris sportif forum|gagner au
paris sportif à coup sur|gagner aux paris sportif|gagner aux paris sportifs|gagner aux paris sportifs pdf|gagner beaucoup d’argent paris sportif|gagner de l argent grace aux paris
sportifs|gagner de l argent pari sportif|gagner de l argent paris sportif|gagner de l
argent paris sportifs|gagner de l’argent au paris sportif|gagner de l’argent aux
paris sportifs|gagner de l’argent avec les paris sportifs|gagner de l’argent avec paris sportif|gagner de l’argent avec paris sportifs|gagner de l’argent grace
au paris sportif|gagner de l’argent grace aux paris sportifs|gagner de l’argent pari
sportif|gagner de l’argent paris sportif|gagner de l’argent paris sportifs|gagner de l’argent sur les paris
sportifs|gagner des paris sportif|gagner des paris sportifs|gagner les paris sportifs|gagner pari
sportif|gagner paris sportif|gagner paris sportif foot|gagner paris
sportif forum|gagner paris sportif tennis|gagner paris
sportifs|gagner sa vie avec les paris sportif|gagner sa vie avec
les paris sportifs|gagner sa vie avec paris sportifs|gagner ses paris sportifs|gagner à
coup sur paris sportif|gagner à tous les coups paris sportifs|gain maximum paris sportif|gain pari
sportif|gain pari sportif imposable|gain pari sportif impot|gain paris sportif|gain paris sportif imposable|gain paris sportif impot|gain paris sportif impôt|gains paris sportif|gains paris sportif imposable|gains paris
sportifs|gains paris sportifs imposable|gains paris
sportifs imposables|gains paris sportifs sont ils imposables|gerer bankroll paris
sportif|gerer sa bankroll paris sportif|gerer une bankroll
paris sportif|gestion bankroll paris sportif|gestion bankroll paris sportifs|gestion bankroll paris sportifs excel|gestion de bankroll paris sportif|gestion de bankroll paris sportif application|gestion de bankroll paris sportifs|gestion de mise paris sportif|gestion paris sportifs v2 5 gratuit|gg signification paris sportif|gros combiné paris sportif|gros gain paris sportif|grosse cote paris sportif
pronostic|grosse mise paris sportif|groupe paris sportif gratuit|groupe telegram
paris sportif gratuit|groupement de joueurs paris sportifs|handicap 0 paris sportif|handicap 1 paris sportif|handicap 5 paris
sportif|handicap au paris sportif|handicap basket paris
sportif|handicap dans les paris sportifs|handicap en paris sportif|handicap europeen paris sportif|handicap européen paris sportifs|handicap mi temps paris sportif|handicap pari sportif|handicap paris sportif|handicap paris sportif basket|handicap
paris sportif explication|handicap paris sportif foot|handicap paris sportif rugby|handicap paris sportifs|handicap rugby
paris sportif|handicap tennis paris sportif|historique cote paris sportif|historique des cotes paris sportifs|hockey
paris sportif|hockey sur glace paris sportif|hors arjel paris sportif|hweh signification paris sportif|imposition gain pari sportif|imposition gain paris sportif|imposition gains paris sportifs|imposition paris sportif france|impot gain paris sportif|impot paris
sportif france|impot sur gain paris sportif|je
gagne ma vie avec les paris sportifs|jeu de pari sportif gratuit|jeu de paris
sportif en ligne|jeu de paris sportif gratuit|jeu paris sportif gratuit|jeu paris sportif
sans argent|jeux de parie sportif|jeux de paris sportif|jeux de paris
sportif en ligne|jeux de paris sportif gratuit|jeux de paris sportifs|jeux olympiques paris sportifs|jeux paris sportif|jeux
paris sportif gratuit|jeux paris sportif virtuel|jeux paris sportifs en ligne|jouer au paris sportif|jouer paris
sportif|joueur absent paris sportif|joueur blesse paris sportif|joueur caen paris sportif|joueur de caen pari sportif|joueur de foot paris sportif|joueur decisif paris sportif|joueur décisif paris sportif|joueur italien paris sportif|joueur paris
sportif|joueur professionnel paris sportif|joueur qui se
blesse paris sportif|joueur sanctionne pari sportif|joueur suspendu paris sportif|joueurs italiens paris
sportifs|l’argent des paris sportifs est il imposable|la cote paris
sportif|la francaise des jeux paris sportif|la martingale paris sportif|la
martingale paris sportifs|la meilleur application de
paris sportif|la meilleur application paris sportif|la meilleur technique pour gagner au paris
sportif|la méthode secrète pour gagner aux paris sportifs pdf|la plus
grosse cote gagner paris sportif|la plus grosse cote paris sportif|ldem paris sportif
signification|le marché des paris sportifs|le meilleur site de pari sportif|le meilleur
site de paris sportif|le meilleur site de paris sportif en ligne|le meilleur site de paris
sportifs|le plus gros gain au paris sportif|le plus gros paris sportif|le plus gros paris sportif du monde|les
10 meilleurs sites de paris sportifs|les 10 meilleurs sites de paris sportifs
en afrique|les 17 secrets pour gagner rapidement aux
paris sportifs|les 17 secrets pour gagner rapidement aux paris sportifs pdf|les
application de paris sportif|les applications
paris sportifs|les bonus paris sportifs|les bookmakers paris
sportifs|les cotes paris sportifs|les gains de
paris sportifs sont ils imposables|les gains des paris sportifs sont ils imposables|les jeux de
paris sportifs|les meilleur paris sportif|les meilleures applications de paris sportifs|les meilleurs
applications de paris sportifs|les meilleurs bonus paris sportif|les meilleurs bonus paris sportifs|les meilleurs cotes paris
sportif|les meilleurs paris sportifs|les meilleurs paris sportifs du
jour|les meilleurs site de paris sportif|les meilleurs site de paris sportifs|les meilleurs sites de pari sportif|les meilleurs sites de paris sportifs|les
meilleurs sites de paris sportifs en ligne|les paris sportif|les paris sportif avis|les paris sportifs|les paris sportifs comment ça marche|les paris sportifs en france|les paris sportifs en ligne|les
paris sportifs en ligne comprendre jouer gagner|les paris sportifs en ligne comprendre jouer gagner pdf|les paris sportifs les plus rentables|les plus gros gagnant paris sportif|les plus gros gains au
paris sportifs|les plus gros gains paris sportifs|les plus
gros paris sportif|les plus grosse cote paris sportif|les plus grosses pertes paris
sportifs|les sites de paris sportifs|les sites de paris
sportifs autorisés en france|les sites de paris sportifs en france|les sites de paris sportifs en ligne|les sites de
paris sportifs francais|ligue 1 paris sportif|ligue 1 paris sportifs|ligue 2 paris sportif|ligue des champions paris sportif|limite
de gains paris sportifs|limite de mise paris sportif|limite gain paris sportif|limite mise paris sportifs|liste
de paris sportif|liste des paris sportifs|liste des site de paris sportif|liste des sites de paris sportifs|liste pari sportif|liste paris
sportif|liste paris sportif pdf|liste site de paris sportif|liste site pari sportif|liste site paris sportif|liste site paris sportif arjel|liste sites paris sportifs|logiciel algorithme paris sportif|logiciel algorithme paris sportif gratuit|logiciel analyse paris sportif|logiciel calcul paris
sportif|logiciel de pari sportif|logiciel de paris sportif|logiciel de paris sportif gratuit|logiciel gestion bankroll paris sportif gratuit|logiciel gestion de bankroll paris sportif|logiciel gestion paris sportif|logiciel gestion paris sportif
gratuit|logiciel gestion paris sportifs|logiciel pari sportif|logiciel paris sportif|logiciel paris sportif gratuit|logiciel paris sportifs|logiciel paris
sportifs foot sur 2 matchs|logiciel pour paris sportif|logiciel pour paris sportifs|logiciel prediction paris sportif|logiciel probabilité paris sportif|logiciel prédiction paris sportif|logiciel statistique paris sportifs|logiciel variation de cote paris sportif|loi sur les
paris sportifs en france|magic calculator paris sportif|marché des paris sportifs|marché des paris sportifs en france|marché des paris sportifs en ligne|martingale pari sportif|martingale paris sportif|martingale paris sportif excel|martingale paris sportif forum|martingale paris sportif interdit|martingale paris sportifs|match abandonné paris sportif|match annulé ou reporté paris sportifs|match annulé paris sportif|match arrete paris sportif|match interrompu paris sportif|match interrompu tennis paris sportif|match interrompu tennis pluie paris
sportif|match nul boxe paris sportif|match pari sportif|match paris sportif|match reporté paris sportif|match suspendu paris sportif|match
suspendu tennis paris sportif|match truqué paris sportif|matchs truqués paris sportifs|meilleur algorithme paris
sportif|meilleur algorithme paris sportif gratuit|meilleur app de paris sportif|meilleur app de
paris sportifs|meilleur app paris sportif|meilleur appli de pari sportif|meilleur appli de paris sportif|meilleur appli
pari sportif|meilleur appli paris sportif|meilleur appli paris sportif forum|meilleur appli paris sportifs|meilleur application conseil paris sportif|meilleur application de paris sportif|meilleur application de paris sportif en afrique|meilleur application pari sportif|meilleur
application paris sportif|meilleur application paris sportif belgique|meilleur application pour les paris sportif|meilleur application pour pari sportif|meilleur bonus de bienvenue paris
sportif|meilleur bonus pari sportif|meilleur bonus paris sportif|meilleur bonus paris sportif sans depot|meilleur bonus paris sportifs|meilleur bonus site de paris sportif|meilleur bonus site pari sportif|meilleur bonus
site paris sportif|meilleur bookmaker paris sportif|meilleur combiné paris sportif|meilleur
conseil paris sportif|meilleur cote de paris sportif|meilleur cote pari sportif|meilleur cote paris
sportif|meilleur cote paris sportif aujourd’hui|meilleur cote
site paris sportif|meilleur forum paris
sportifs|meilleur gain paris sportif|meilleur
ia paris sportif|meilleur methode pour gagner au paris sportif|meilleur offre
bienvenue paris sportif|meilleur offre bonus paris sportif|meilleur offre de
bienvenue paris sportif|meilleur offre de bienvenue paris sportifs|meilleur offre pari sportif|meilleur offre paris sportif|meilleur offre paris sportif en ligne|meilleur
pari sportif|meilleur pari sportif du jour|meilleur pari sportif en ligne|meilleur paris sportif|meilleur paris sportif aujourd’hui|meilleur paris sportif du jour|meilleur
paris sportif en ligne|meilleur paris sportif foot|meilleur promo paris
sportif|meilleur pronostic paris sportif|meilleur site de conseil paris sportif|meilleur site de pari
sportif|meilleur site de pari sportif en ligne|meilleur site de paris sportif|meilleur site de paris sportif avis|meilleur site
de paris sportif belgique|meilleur site de paris sportif canada|meilleur site de paris sportif
en france|meilleur site de paris sportif en ligne|meilleur site de paris
sportif football|meilleur site de paris sportif forum|meilleur site de paris sportif france|meilleur
site de paris sportif hors arjel|meilleur site de paris sportif international|meilleur site de paris sportif suisse|meilleur site de paris sportifs|meilleur site de paris sportifs en ligne|meilleur site pari sportif|meilleur site pari sportif en ligne|meilleur site pari sportif france|meilleur site paris sportif|meilleur site paris
sportif avis|meilleur site paris sportif belgique|meilleur site
paris sportif canada|meilleur site paris sportif en ligne|meilleur site paris sportif foot|meilleur
site paris sportif forum|meilleur site paris sportif france|meilleur site paris sportif hors arjel|meilleur site paris sportif nba|meilleur
site paris sportif rugby|meilleur site paris sportif suisse|meilleur
site paris sportifs|meilleur site pour pari sportif|meilleur site pour paris sportif|meilleur site pronostic paris
sportif|meilleur strategie paris sportif|meilleur technique de paris sportif|meilleur technique paris sportif|meilleur technique pour gagner au paris sportif|meilleure appli de paris sportif|meilleure appli de paris sportifs|meilleure appli pari sportif|meilleure appli paris sportif|meilleure appli paris sportifs|meilleure application de paris sportif|meilleure application de paris sportifs|meilleure application pari sportif|meilleure application paris
sportif|meilleure application paris sportif android|meilleure
application paris sportifs|meilleure offre paris sportif|meilleure site paris
sportif|meilleure strategie paris sportif|meilleures applications
de paris sportifs|meilleures applications paris sportifs|meilleures cotes paris sportifs|meilleures offres
paris sportifs|meilleures stratégies paris sportifs|meilleurs appli
paris sportif|meilleurs application de paris sportifs|meilleurs application paris sportif|meilleurs applications paris sportifs|meilleurs bonus paris sportifs|meilleurs cote paris sportif|meilleurs cotes paris sportifs|meilleurs offres paris sportifs|meilleurs paris sportifs|meilleurs paris sportifs du jour|meilleurs site de pari sportif|meilleurs site de paris sportif|meilleurs site de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs
site paris sportif|meilleurs sites de paris sportifs|meilleurs sites
de paris sportifs en ligne|meilleurs sites paris sportif|meilleurs sites paris sportifs|methode abc paris
sportif|methode de paris sportif|methode gagnante paris sportifs|methode gagner paris sportif|methode
infaillible paris sportifs|methode martingale
paris sportif|methode mathematique paris sportif|methode mathematique pour
gagner au paris sportif|methode paris sportif|methode paris sportif foot|methode paris sportif forum|methode paris sportif tennis|methode paris sportifs|methode pour gagner au paris sportif|methode pour
gagner paris sportif|methodes paris sportifs|minimum depot paris sportif|mise
au jeu pari sportif|mise maximum pari sportif|mise maximum paris sportif|mise minimum paris sportif|mise moyenne paris sportif|mise paris
sportif|moins de 4 5 but paris sportif|montant maximum paris sportif|montant paris sportif|montante pari sportif|montante parie
sportif|montante paris sportif|montante paris sportifs|montantes paris sportifs|multiple pari sportif|multiple paris sportif|multiple paris sportifs|multiples paris sportifs|méthode calcul paris sportif|méthode
match nul paris sportifs|méthode mathématique pour gagner au paris sportif|méthode paris sportif forum|méthode paris sportif hockey|nba
pari sportif|nba paris sportif|nba paris sportifs|nouveau paris sportif|nouveau site de
pari sportif|nouveau site de paris sportif|nouveau site de paris sportif en ligne|nouveau site
de paris sportifs|nouveau site pari sportif|nouveau site paris
sportif|nouveau site paris sportif france|nouveau site paris sportifs|nouveaux
sites de paris sportifs|nouveaux sites paris sportifs|nouvelle appli paris sportif|nouvelle application de paris sportif|numero de
match paris sportif|numero match paris sportif|offre 100 euros paris sportif|offre appli pari sportif|offre bienvenu
paris sportif|offre bienvenue pari sportif|offre bienvenue paris sportif|offre bienvenue paris sportifs|offre bienvenue site paris
sportif|offre bonus paris sportif|offre de bienvenu paris sportif|offre de bienvenue
pari sportif|offre de bienvenue paris sportif|offre de bienvenue
paris sportif belgique|offre de bienvenue paris sportif sans depot|offre de
bienvenue paris sportif sans dépôt|offre de bienvenue paris sportifs|offre
de bienvenue sans depot paris sportif|offre de bienvenue site paris
sportif|offre euro paris sportif|offre pari sportif
euro|offre paris sportif|offre paris sportif belgique|offre paris
sportif cash|offre paris sportif coupe du monde|offre paris
sportif hors arjel|offre paris sportif remboursé|offre paris
sportif remboursé cash|offre paris sportif sans depot|offre promo paris sportif|offre remboursement paris sportif|offre sans depot paris
sportif|offre site paris sportif|offres bienvenue paris sportifs|offres de bienvenue paris sportifs|ou faire
des paris sportif|ou faire des paris sportif en espagne|ou faire des paris sportifs|outil répartiteur de mise paris sportif|outils repartiteur de mises
paris sportif|ouverture compte paris sportifs|ouvrir un compte paris sportif|pack de bienvenue paris sportif|pack
de bienvenue paris sportif hors arjel|pari en ligne sportif|pari sportif|pari sportif 100 euros offert|pari sportif 100 remboursé|pari sportif abandon tennis|pari sportif aide|pari
sportif algérie aujourd’hui|pari sportif appli|pari sportif application|pari sportif argent|pari sportif
astuce|pari sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari sportif avec orange money|pari sportif avec
paypal|pari sportif avec wave|pari sportif avis|pari sportif basket|pari sportif belgique|pari
sportif belgique france|pari sportif bonus|pari sportif buteur pas titulaire|pari sportif champions league|pari
sportif combiné|pari sportif comment|pari sportif comment gagner|pari sportif comment ça marche|pari sportif comparatif|pari sportif conseil|pari sportif cote|pari sportif cote
match|pari sportif cote psg|pari sportif coupe|pari sportif coupe de france|pari
sportif coupe du monde|pari sportif depot|pari sportif du jour|pari
sportif en france|pari sportif en ligne|pari sportif en ligne au cameroun|pari sportif en ligne belgique|pari sportif en ligne canada|pari sportif en ligne france|pari sportif
en ligne gratuit|pari sportif en ligne suisse|pari sportif
en ligne ufc|pari sportif en suisse|pari sportif euro|pari sportif explication|pari sportif faire|pari sportif foot|pari sportif
foot resultat|pari sportif football|pari sportif forum|pari sportif francaise des jeux|pari sportif france|pari sportif france angleterre|pari sportif france argentine|pari sportif france autriche|pari sportif france belgique|pari sportif france espagne|pari sportif france italie|pari sportif france portugal|pari sportif france usa|pari sportif gagnant|pari sportif
gagner|pari sportif gagner a tous les coups|pari sportif gagner de l’argent|pari sportif
gain|pari sportif gratuit|pari sportif gratuit pour gagner des cadeaux|pari sportif gratuit sans depot|pari sportif handicap|pari sportif hockey|pari sportif hors arjel|pari sportif jeux
olympiques|pari sportif joueur absent|pari
sportif le plus rentable|pari sportif leicester champion|pari sportif ligue 1|pari sportif ligue 2|pari sportif ligue
des champions|pari sportif ligue europa|pari sportif match|pari sportif match
arrete|pari sportif match interrompu|pari sportif meilleur|pari
sportif meilleur cote|pari sportif meilleur site|pari sportif methode|pari sportif mise|pari sportif mise
au jeu|pari sportif mise o jeu|pari sportif nba|pari sportif offre bienvenue|pari sportif paypal|pari
sportif plus|pari sportif prolongation|pari sportif promo|pari sportif pronostic|pari sportif pronostic
foot|pari sportif pronostic gagnant|pari sportif pronostic gratuit|pari sportif psg|pari sportif psg bayern|pari sportif psg inter|pari sportif psg milan|pari sportif
regle|pari sportif rembourse|pari sportif remboursement|pari
sportif remboursement cash|pari sportif remboursé|pari sportif rugby|pari sportif rugby coupe du
monde|pari sportif rugby top 14|pari sportif sans argent|pari sportif
sans carte bancaire|pari sportif sans depot|pari sportif signification|pari sportif site|pari sportif statistique|pari sportif suisse|pari sportif systeme|pari sportif technique|pari sportif technique pour gagner|pari sportif temps reglementaire|pari
sportif tennis|pari sportif tennis abandon|pari sportif top|pari sportif top 14|pari
sportif tour de france|parie sportif|parie sportif
comment ca marche|parie sportif du jour|parie sportif en ligne|parie sportif
foot|parie sportif football|parie sportif france|parie sportif
gratuit|parie sportif pronostic|parie sportif suisse|paris en ligne sportif|paris
en ligne sportifs|paris evenement sportif|paris france sportif|paris hippique et
sportif|paris hippiques et sportifs|paris hippiques paris sportifs|paris hippiques
paris sportifs et poker en ligne|paris hippiques sportifs|paris match
sportif|paris sportif|paris sportif 10 euros offerts|paris sportif 100
euros offert|paris sportif 100 euros remboursé|paris sportif 100 offert|paris sportif 100 remboursé|paris sportif 100e offert|paris sportif
150 euros offert|paris sportif 1er pari remboursé|paris sportif a faire|paris sportif a faire aujourd’hui|paris sportif a faire ce soir|paris sportif
abandon tennis|paris sportif abandon tennis parions sport|paris sportif aide|paris sportif algorithme|paris sportif analyse|paris sportif appli|paris sportif application|paris sportif application android|paris sportif apres prolongation|paris sportif argent|paris sportif argent fictif|paris sportif argent offert|paris sportif argent virtuel|paris
sportif arjel|paris sportif arsenal psg|paris sportif astuce|paris sportif
au canada|paris sportif aujourd hui|paris sportif aujourd’hui|paris
sportif avec argent fictif|paris sportif avec bonus sans depot|paris sportif avec carte bancaire|paris sportif
avec cryptomonnaie|paris sportif avec handicap|paris sportif
avec paypal|paris sportif avec paysafecard|paris sportif avis|paris sportif
avis expert|paris sportif avis forum|paris sportif
bankroll|paris sportif basket|paris sportif basket coupe de france|paris sportif basket nba|paris
sportif basket prolongation|paris sportif belgique|paris
sportif belgique bonus|paris sportif belgique bonus sans depot|paris sportif belgique france|paris sportif belgique
suede|paris sportif bonus|paris sportif bonus bienvenue|paris sportif bonus cash|paris sportif bonus de bienvenue|paris sportif bonus gratuit|paris
sportif bonus gratuit sans depot|paris sportif bonus retirable|paris sportif bonus sans
depot|paris sportif bonus sans depot belgique|paris sportif bookmaker|paris
sportif but contre son camp|paris sportif but temps additionnel|paris
sportif buteur|paris sportif buteur blessé|paris sportif buteur carton rouge|paris sportif buteur contre son camp|paris sportif buteur non titulaire|paris sportif buteur prolongation|paris sportif
buteur qui ne joue pas|paris sportif buteur remplacant|paris sportif calcul gain|paris sportif canada|paris
sportif cash|paris sportif cash out|paris sportif champion ligue 1|paris sportif champions league|paris sportif classement ligue
1|paris sportif code promo|paris sportif combine|paris sportif combiné|paris sportif combiné
comment ça marche|paris sportif combiné du jour|paris sportif combiné match reporté|paris sportif comment ca marche|paris
sportif comment faire|paris sportif comment gagner|paris sportif comment gagner a tous les coups|paris
sportif comment jouer|paris sportif comment ça marche|paris sportif comparateur cote|paris sportif comparatif|paris sportif conseil|paris sportif conseil gratuit|paris sportif conseil pour gagner|paris
sportif cote|paris sportif cote et match|paris sportif cote explication|paris sportif cote
psg|paris sportif coupe d’europe|paris sportif coupe davis|paris
sportif coupe de france|paris sportif coupe du monde|paris sportif coupe
du monde de rugby|paris sportif coupe du monde rugby|paris sportif
depot 5 euro|paris sportif depot minimum|paris sportif depot paypal|paris sportif dnb|paris sportif du jour|paris sportif du jour conseil|paris sportif dépôt
1 euro|paris sportif dépôt minimum 5 euros|paris sportif en belgique|paris sportif en france|paris sportif en ligne|paris sportif en ligne avec paypal|paris sportif en ligne avis|paris sportif en ligne belgique|paris sportif en ligne bonus|paris sportif en ligne cameroun|paris sportif en ligne comment gagner|paris sportif en ligne comment ça marche|paris sportif en ligne france|paris sportif en ligne gratuit|paris
sportif en ligne maroc|paris sportif en ligne paypal|paris sportif en ligne québec|paris sportif en ligne sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris sportif espagne france|paris sportif esport|paris sportif et casino en ligne|paris sportif et hippique|paris sportif et prolongation|paris
sportif euro|paris sportif europa league|paris sportif explication|paris sportif
final ligue des champions|paris sportif finale
ligue des champions|paris sportif foot|paris sportif foot aide|paris sportif foot astuce|paris sportif
foot aujourd’hui|paris sportif foot ce soir|paris sportif
foot comment ca marche|paris sportif foot conseil|paris sportif foot cote|paris sportif
foot coupe du monde|paris sportif foot en ligne|paris sportif
foot feminin|paris sportif foot gratuit|paris sportif foot prolongation|paris sportif foot
pronostic|paris sportif foot pronostic gratuit|paris sportif foot regle|paris sportif foot
suisse|paris sportif foot us|paris sportif football|paris sportif football americain|paris sportif football astuces|paris sportif
forfait tennis|paris sportif forum|paris sportif francais|paris
sportif francaise des jeux|paris sportif france|paris
sportif france 2|paris sportif france allemagne|paris sportif france angleterre|paris sportif france argentine|paris sportif france autriche|paris sportif france belgique|paris sportif france espagne|paris sportif france
gibraltar|paris sportif france italie|paris sportif france nouvelle zelande|paris sportif france pologne|paris sportif france portugal|paris sportif
france uruguay|paris sportif france usa|paris sportif freebet sans depot|paris sportif gagnant|paris sportif gagnant à coup
sûr|paris sportif gagner a coup sur|paris sportif gagner argent|paris sportif gagner
de l’argent|paris sportif gain|paris sportif gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris
sportif gratuit appli|paris sportif gratuit avec cadeaux|paris sportif gratuit cadeaux|paris sportif gratuit en ligne|paris
sportif gratuit entre amis|paris sportif gratuit sans argent|paris sportif gratuit sans depot|paris sportif gratuit sans dépôt|paris sportif gratuits|paris sportif gros gain|paris sportif handicap|paris sportif handicap 0
1|paris sportif handicap 0-1|paris sportif handicap
1 0|paris sportif handicap 1-0|paris sportif handicap basket|paris
sportif handicap explication|paris sportif handicap foot|paris
sportif handicap rugby|paris sportif hippique|paris sportif hockey|paris sportif hockey
nhl|paris sportif hockey sur glace|paris sportif hors arjel|paris sportif hors arjel
france|paris sportif jeux olympiques|paris sportif jeux video|paris sportif
joueur blessé|paris sportif joueur blessé pendant le
match|paris sportif joueur de foot|paris sportif joueur decisif|paris sportif joueur declare forfait|paris sportif joueur déclare forfait|paris sportif joueur remplacant|paris sportif la francaise des jeux|paris sportif le plus rentable|paris sportif legal en france|paris sportif leicester champion|paris sportif les 18 stratégies pour gagner
tous les jours|paris sportif les plus sur|paris sportif les prolongation compte|paris sportif ligne|paris sportif ligue
1|paris sportif ligue 2|paris sportif ligue des champions|paris sportif ligue des nations|paris sportif ligue europa|paris sportif liste|paris sportif
martingale|paris sportif match|paris sportif match abandonné|paris sportif match annulé|paris sportif match arrêté|paris sportif match du jour|paris sportif match interrompu|paris sportif match
reporté|paris sportif match suspendu|paris sportif
match tennis interrompu|paris sportif match truqué|paris sportif meilleur bonus|paris
sportif meilleur cote|paris sportif meilleur pronostic|paris sportif meilleur site|paris sportif methode|paris sportif methode 2 3|paris
sportif mi temps fin de match|paris sportif mise au jeu|paris sportif mise maximum|paris sportif mma france|paris sportif moins de 3.5 but|paris
sportif montante|paris sportif moto gp|paris sportif multiple|paris sportif multiple 2 3|paris sportif multiple 2 3 explication|paris sportif multiple 2 4|paris sportif multiple
2 5|paris sportif multiple 2/3 explication|paris sportif multiple 3 4|paris sportif multiple explication|paris sportif
national 1 foot|paris sportif nba|paris sportif nba conseil|paris sportif nba pronostic|paris sportif nhl|paris sportif nombre de but|paris sportif
nouveau site|paris sportif numero match|paris sportif offert|paris
sportif offre bienvenue|paris sportif offre bienvenue sans
depot|paris sportif offre de bienvenue|paris sportif offre sans depot|paris sportif om psg|paris
sportif paypal|paris sportif plus de 1.5 but|paris
sportif plus de 2 5 but|paris sportif plus ou moins|paris sportif plus ou
moins 2 5 but|paris sportif premier pari remboursé|paris sportif premier paris remboursé|paris sportif prolongation|paris sportif prolongation basket|paris
sportif prolongation foot|paris sportif promo|paris sportif pronostic|paris sportif pronostic
basket|paris sportif pronostic des match aujourd hui|paris sportif pronostic expert gratuit|paris sportif pronostic foot|paris sportif
pronostic forum|paris sportif pronostic gratuit|paris sportif
pronostic tennis|paris sportif psg|paris sportif psg arsenal|paris sportif psg barcelone|paris sportif psg bayern|paris sportif psg dortmund|paris sportif psg inter|paris sportif psg inter cote|paris sportif psg
liverpool|paris sportif psg om|paris sportif qr code|paris
sportif que veut dire handicap|paris sportif qui rapporte le plus|paris sportif regle|paris sportif regle prolongation|paris
sportif rembourse|paris sportif remboursement cash|paris sportif rembourser|paris sportif remboursé|paris sportif remboursé cash|paris
sportif remboursé en cash|paris sportif retrait paypal|paris sportif
rue des joueurs|paris sportif rugby|paris sportif rugby 6 nations|paris sportif rugby coupe du monde|paris sportif rugby top 14|paris sportif safe du
jour|paris sportif sans argent|paris sportif sans carte bancaire|paris
sportif sans carte d’identité|paris sportif sans
compte bancaire|paris sportif sans depot|paris sportif sans depot minimum|paris sportif si
match suspendu|paris sportif si un joueur abandonne|paris sportif si un joueur ne joue pas|paris sportif si un joueur se blesse|paris sportif
simple ou combiné|paris sportif site|paris sportif statistique|paris sportif stratégie|paris sportif suisse|paris sportif suisse application|paris sportif suisse en ligne|paris
sportif suisse legal|paris sportif suisse légal|paris sportif suisse romande|paris
sportif sur du jour|paris sportif sur le tennis|paris sportif systeme|paris sportif systeme
2 3|paris sportif systeme 2 4|paris sportif systeme 2/3|paris sportif systeme 2/4|paris
sportif systeme 3 4|paris sportif systeme 3/4|paris
sportif systeme explication|paris sportif technique|paris sportif
technique pour gagner|paris sportif temps additionnel|paris sportif temps
reglementaire|paris sportif tennis|paris sportif tennis abandon|paris sportif tennis conseil|paris sportif tennis de table|paris sportif
tennis forfait|paris sportif tennis gratuit|paris sportif tennis pronostic|paris sportif tennis roland garros|paris
sportif tir au but|paris sportif top 14|paris sportif tour de france|paris sportif
ufc|paris sportif ufc france|paris sportif unibet|paris sportif vainqueur euro|paris sportif vainqueur ligue 1|paris sportif vainqueur ligue
des champions|paris sportif via paypal|paris sportif victoire prolongation|paris sportif vip gratuit|paris sportifs|paris sportifs abandon tennis|paris sportifs aide|paris sportifs analyser un match|paris sportifs arjel|paris sportifs astuces|paris sportifs aujourd’hui|paris sportifs autorisés en france|paris
sportifs avec paypal|paris sportifs basket|paris sportifs belgique|paris sportifs
bonus|paris sportifs bookmakers|paris sportifs canada|paris
sportifs combiné|paris sportifs comparateur|paris sportifs comparatif|paris sportifs conseils|paris sportifs cotes|paris sportifs coupe du monde|paris sportifs de football|paris
sportifs du jour|paris sportifs en belgique|paris sportifs en france|paris sportifs en ligne|paris sportifs
en ligne belgique|paris sportifs en ligne france|paris
sportifs en ligne gratuit|paris sportifs en ligne suisse|paris sportifs en suisse|paris sportifs et hippiques|paris sportifs euro|paris sportifs foot|paris sportifs foot us|paris sportifs forum|paris sportifs france|paris sportifs france espagne|paris
sportifs gagner à tous les coups|paris sportifs gratuit|paris sportifs gratuits|paris sportifs gratuits en ligne|paris sportifs handicap|paris sportifs hockey|paris sportifs hockey sur galce|paris sportifs hockey sur glace|paris sportifs hors arjel|paris sportifs jeux olympiques|paris
sportifs les bookmakers raflent la mise|paris sportifs ligne|paris sportifs ligue 1|paris sportifs ligue 2|paris sportifs ligue des champions|paris sportifs
ligue europa|paris sportifs match interrompu|paris sportifs montante|paris sportifs nba|paris sportifs offre bienvenue|paris
sportifs offre de bienvenue|paris sportifs paypal|paris sportifs pronostics|paris sportifs psg|paris sportifs psg inter|paris sportifs rugby|paris sportifs sans argent|paris
sportifs sans depot|paris sportifs site|paris sportifs sites|paris
sportifs statistiques|paris sportifs stratégie|paris sportifs suisse|paris sportifs technique|paris sportifs techniques|paris
sportifs tennis|paris sportifs tennis astuces|paris
sportifs top 14|paris sportifs tour de france|part de marché paris sportifs|paypal pari sportif|paypal paris
sportif|paypal paris sportifs|perte d’argent paris sportifs|peut on devenir riche avec les paris
sportifs|peut on gagner de l’argent avec les paris sportifs|peut on gagner sa
vie avec les paris sportif|peut on vraiment gagner de l’argent avec les paris
sportifs|plus gros combine paris sportif|plus gros
gagnant paris sportif|plus gros gain paris sportif|plus gros gain paris
sportif au monde|plus gros gain paris sportif france|plus gros gains paris sportif|plus gros pari sportif|plus gros paris sportif|plus grosse cote gagner
paris sportif|plus grosse cote pari sportif|plus grosse cote paris sportif|plus grosse
mise paris sportif|plus grosse somme gagner au paris sportif|plus ou moins paris sportif|pourcentage de mise paris sportif|premier pari sportif remboursé|probabilité cote
paris sportif|probabilité paris sportif combiné|prolongation basket paris sportif|prolongation paris sportif|promo
pari sportif|promo paris sportif|promo site de paris sportif|promo site pari sportif|promo
site paris sportif|promos paris sportifs|prono paris sportif foot|prono paris sportif
gratuit|prono paris sportif tennis|pronostic de paris sportif|pronostic du jour paris sportif|pronostic foot paris sportif|pronostic gratuit paris sportif|pronostic pari sportif|pronostic pari
sportif gratuit|pronostic paris sportif|pronostic paris sportif aujourd’hui|pronostic paris
sportif du jour|pronostic paris sportif foot|pronostic
paris sportif gratuit|pronostic paris sportif tennis|pronostic paris sportifs|pronostics foot statistiques
et aides aux paris sportifs|pronostics paris sportif|pronostics paris sportifs|pronostiqueur paris sportif gratuit|psg
arsenal paris sportif|psg bayern paris sportif|psg inter milan paris sportif|psg inter pari sportif|psg
inter paris sportif|psg liverpool paris sportif|psg om paris sportif|psg paris sportif|psg paris sportifs|qr code paris sportif|qu est
ce qu un handicap paris sportif|qu est ce que handicap dans les paris
sportif|qu’est ce qu’un handicap paris sportif|qu’est ce
que handicap dans les paris sportif|quand un joueur se
blesse paris sportif|que signifie 1/1 en paris sportif|que signifie
1/2 paris sportif|que signifie 12 en paris sportif|que signifie 1×2 dans les paris sportifs|que signifie btts en paris sportif|que signifie dnb en paris sportif|que
signifie draw en paris sportif|que signifie ft en paris sportif|que signifie gg
dans le pari sportif|que signifie gg en pari sportif|que signifie gg en paris sportif|que signifie handicap dans les paris sportifs|que veut
dire dnb en paris sportif|que veut dire handicap dans
les paris sportifs|que veut dire handicap paris sportif|quel appli pari sportif|quel cote
jouer paris sportif|quel est la meilleur appli de paris sportif|quel est le meilleur algorithme de paris sportif|quel est
le meilleur site de pari sportif|quel est le meilleur site de pari sportif en ligne|quel est le meilleur site de paris sportif|quel est le meilleur site de paris sportif en ligne|quel est le meilleur site de paris sportifs en ligne|quel est le pari
sportif le plus rentable|quel pari sportif est le plus rentable|quel pari sportif est le plus sûr|quel pari
sportif faire aujourd’hui|quel paris sportif faire aujourd’hui|quel paris sportif rapporte
le plus|quel site de paris sportif choisir|quel site de paris sportif rembourse en cash|quel type de pari sportif est le plus rentable|quelle
application pour paris sportifs|quelle est la meilleure appli de paris sportif|quelle est la meilleure application de paris sportif|quelle
est la meilleure application pour les paris sportifs|quelle est le meilleur site de paris sportif|quels paris sportifs faire|quels sont les paris sportifs les
plus sûrs|rebond basket paris sportif|record de gain paris sportif|regle buteur paris sportif|regle
de paris sportif|regle des paris sportif|regle handicap paris
sportif|regle handicap paris sportif foot|regle
multiple paris sportif|regle pari sportif|regle paris sportif|regle
paris sportif foot|regle paris sportif multiple|regle paris sportif prolongation|reglement pari sportif|reglement paris sportif|regles paris sportifs|remboursement cash paris sportif|remboursement en cash paris sportif|remboursement
pari sportif|remboursement paris sportif|repartiteur de mise paris sportif|repartiteur de mise paris sportifs|repartiteur
de mises paris sportif|repartiteur mise paris sportif|repartition des mises paris
sportif|resultat pari sportif|resultat paris sportif|resultat
paris sportif en direct|resultat paris sportif foot|resultat sportif
hockey|retirer argent paris sportif|rugby pari sportif|rugby paris sportif|règle paris sportif prolongation|règles paris sportif|répartiteur de mise pari sportif|répartiteur de mise paris sportif|répartiteur
de mise paris sportifs|répartition des mises paris sportif|résultat paris
sportif foot|sans depot paris sportif|se faire interdire de paris sportifs|signification btts paris sportif|signification dnb
paris sportif|signification handicap paris sportif|simulateur de gain paris sportif|simulateur gain paris sportif|simulateur gain paris sportif multiple|simulateur gain paris sportif systeme|simulateur
gain paris sportif système|simulateur montante
paris sportif|simulateur paris sportif multiple|simulateur systeme paris sportif|simulation paris sportif gratuit|site aide paris sportif|site analyse paris sportif|site analyser paris sportif|site arjel paris sportif|site
conseil paris sportif|site d’analyse de paris sportifs|site d’analyse paris sportif|site de conseil paris sportif|site de pari en ligne sportif|site de pari
sportif|site de pari sportif avec bonus sans depot|site de pari sportif bonus sans
depot|site de pari sportif canada|site de pari sportif en ligne|site de pari sportif francais|site
de pari sportif gratuit|site de pari sportif hors arjel|site de pari sportif suisse|site de
parie sportif|site de parie sportif en ligne|site de paris en ligne sportif|site
de paris sportif|site de paris sportif acceptant paypal|site
de paris sportif arjel|site de paris sportif autorisé en france|site de paris sportif autorisé en suisse|site
de paris sportif avec bonus|site de paris sportif avec bonus sans depot|site de paris sportif avec bonus sans dépôt|site
de paris sportif avec neosurf|site de paris sportif avec paiement mobile|site
de paris sportif avec paypal|site de paris sportif avis|site de
paris sportif belge avec bonus|site de paris sportif belgique|site de paris sportif bonus|site de paris
sportif bonus sans depot|site de paris sportif canada|site de paris sportif comparatif|site de paris sportif depot minimum|site de paris sportif
en france|site de paris sportif en ligne|site de paris sportif
en ligne suisse|site de paris sportif football|site de paris sportif francais|site
de paris sportif france|site de paris sportif gratuit|site
de paris sportif gratuit pour gagner des cadeaux|site de paris
sportif gratuit sans dépôt|site de paris sportif hors arjel|site de paris sportif
le plus fiable|site de paris sportif legal en france|site de paris sportif meilleur cote|site
de paris sportif nouveau|site de paris sportif offre de bienvenue|site
de paris sportif paypal|site de paris sportif premier paris remboursé|site de paris sportif qui accepte
paypal|site de paris sportif qui rembourse en cash|site de
paris sportif remboursé|site de paris sportif sans argent|site de paris sportif
sans carte bancaire|site de paris sportif sans carte d’identité|site de paris sportif sans depot|site de paris sportif suisse|site de paris sportifs|site de paris sportifs avec paypal|site de
paris sportifs en ligne|site de paris sportifs francais|site
de paris sportifs gratuit|site de paris sportifs paypal|site de
paris sportifs suisse|site de statistique pour
paris sportif|site des paris sportifs|site pari en ligne
sportif|site pari sportif|site pari sportif 100 euros offert|site pari sportif
arjel|site pari sportif belgique|site pari sportif bonus|site
pari sportif canada|site pari sportif comparatif|site
pari sportif en ligne|site pari sportif france|site pari sportif gratuit|site pari sportif hors arjel|site pari sportif suisse|site parie sportif|site paris en ligne
sportif|site paris sportif|site paris sportif
100 euros offert|site paris sportif 100 euros remboursé|site
paris sportif 1er paris remboursé|site paris sportif arjel|site paris sportif autorisé en france|site paris sportif avec
bonus|site paris sportif avec bonus sans depot|site paris sportif avec meilleur cote|site paris sportif belgique|site paris sportif
bonus|site paris sportif bonus cash|site paris sportif bonus sans depot|site paris
sportif canada|site paris sportif comparatif|site paris sportif depot 5 euro|site paris sportif en ligne|site paris sportif foot|site paris sportif france|site paris sportif gratuit|site paris sportif hors arjel|site
paris sportif hors arjel france|site paris sportif meilleur cote|site paris sportif
nouveau|site paris sportif offre de bienvenue|site paris sportif paypal|site paris
sportif remboursement cash|site paris sportif remboursé en cash|site
paris sportif retrait instantané|site paris sportif sans
carte bancaire|site paris sportif sans depot|site paris
sportif suisse|site paris sportifs|site paris sportifs belgique|site paris sportifs en ligne|site paris sportifs france|site paris sportifs hors arjel|site paris
sportifs suisse|site pour analyse paris sportif|site pour paris sportif|site pronostic paris sportif|site statistique paris sportif|site suisse paris sportif|sites de pari sportif|sites de paris sportif|sites de paris sportifs|sites
de paris sportifs arjel|sites de paris sportifs autorisés en france|sites de paris sportifs belgique|sites de paris sportifs bonus|sites de paris sportifs en belgique|sites de paris sportifs en france|sites de paris sportifs en ligne|sites de paris sportifs gratuits|sites de paris sportifs gratuits sans dépôt|sites de paris sportifs suisse|sites pari sportif|sites paris
sportif|sites paris sportifs|sites paris sportifs arjel|sites paris sportifs
belgique|sites paris sportifs france|sites paris sportifs hors arjel|sites paris sportifs
suisse|so foot paris sportif|so foot paris sportifs|specialiste tennis paris sportif|statistique foot paris sportif|statistique paris sportif|statistique paris sportif foot|statistique tennis paris sportif|statistiques football paris sportifs|statistiques paris sportifs|strategie
de paris sportif|stratégie big whale paris sportif|stratégie de paris sportifs|stratégie
gagnante paris sportifs|stratégie pari sportif|stratégie paris
sportif|stratégie paris sportifs|stratégie paris
sportifs forum|stratégie pour gagner au paris sportif|stratégies
paris sportifs|suisse paris sportif|suisse paris sportifs|systeme 2 3 paris
sportif|systeme 3 4 paris sportif|systeme de cote paris sportif|systeme de paris sportif|systeme pari sportif|systeme paris sportif|systeme paris sportifs|systeme reducteur
paris sportif|système paris sportif|tableau bankroll paris sportif|tableau
cote paris sportif|tableau de paris sportif|tableau de suivi paris sportifs|tableau
excel bankroll paris sportif|tableau excel paris sportif|tableau excel paris sportif gratuit|tableau excel paris sportifs|tableau excel pour paris sportif|tableau gestion bankroll paris sportif|tableau montante paris sp
What a data of un-ambiguity and preserveness of precious know-how concerning unexpected feelings.
register in catalog Rio
https://narodmebel.com/communication/forum/messages/forum3/message939/937-1khbet-promokod-na-segodnya?result=new#message939
Зума Зума Казино – это не просто платформа для удовлетворения азартных желаний, а тщательно выстроенная экосистема развлечений, где каждый элемент направлен на создание максимально комфортной и захватывающей атмосферы. Мы предлагаем не просто игры, а возможность погрузиться в мир ярких эмоций, стратегического мышления и, конечно же, шанс испытать удачу и сорвать куш. Разнообразие игровых автоматов, карточных игр, рулеток и лайв-казино с профессиональными дилерами обеспечивает бесконечный поток впечатлений и не даст заскучать даже самым искушенным игрокам. Зума официальный канал – это ваш личный проводник в захватывающий мир Зума Казино. Подписывайтесь и будьте в курсе эксклюзивных акций, турниров с крупными призовыми фондами, анонсов новых игр и полезных советов от экспертов. Мы делимся секретами успешной игры, анализируем стратегии и помогаем вам принимать взвешенные решения, чтобы увеличить ваши шансы на выигрыш. Зума – это не только азарт, но и ответственность. Мы придерживаемся принципов честной игры и обеспечиваем безопасную среду для наших пользователей. Современные технологии шифрования гарантируют защиту ваших персональных данных и финансовых транзакций. Мы работаем в соответствии с международными стандартами лицензирования и всегда готовы оказать поддержку и ответить на любые вопросы. Zooma казино – это ваш портал в мир больших возможностей. Играйте в любое время и в любом месте, наслаждаясь удобным интерфейсом и плавной работой на любом устройстве. Мы постоянно работаем над улучшением нашего сервиса, чтобы предоставить вам лучший игровой опыт. Присоединяйтесь к миллионам игроков по всему миру и откройте для себя мир Зума Казино, где азарт встречается с возможностью стать победителем!
Зума Зума Казино – это не просто платформа для азартных игр, это целая вселенная развлечений, где адреналин смешивается с возможностью крупного выигрыша. Мы создали уникальное пространство, где каждый игрок, независимо от опыта, сможет найти что-то для себя. От классических слотов до самых современных игр с живыми дилерами – в Зума Казино собрана впечатляющая коллекция развлечений, способная удовлетворить даже самых взыскательных ценителей азарта. Зума официальный канал – это ваш проводник в мир Зума Казино. Здесь вы найдете актуальную информацию о новых играх, щедрых акциях, эксклюзивных турнирах и розыгрышах ценных призов. Подписывайтесь на наш канал, чтобы всегда быть в курсе последних событий и первыми узнавать о самых выгодных предложениях. Мы делимся стратегиями выигрышей, обзорами игр и советами от профессиональных игроков, помогая вам повысить свои шансы на успех. Зума – это синоним честности, надежности и безопасности. Мы используем самые современные технологии защиты данных, чтобы обеспечить конфиденциальность и безопасность ваших транзакций. Наша лицензия гарантирует соответствие самым высоким стандартам индустрии азартных игр, а круглосуточная служба поддержки всегда готова ответить на ваши вопросы и помочь решить любые возникшие проблемы. Zooma казино – это ваш шанс испытать удачу и сорвать крупный куш, не выходя из дома. Наша платформа адаптирована для всех устройств, будь то компьютер, смартфон или планшет. Играйте в любимые игры в любое время и в любом месте, наслаждаясь яркой графикой, захватывающим геймплеем и невероятными возможностями для выигрыша. Присоединяйтесь к Зума Казино сегодня и откройте для себя мир азарта, который превзойдет все ваши ожидания!
ко ланта ко лант
ко ланта ко лант
City Fashion Hub – Discover new urban wear styles that make your outfit choices simple and fun.
https://www.minisceongoyc.org/Media/Photo-Gallery/emodule/916/eitem/215
гериатрический пансионат Геронтологические пансионаты и дома престарелых – это альтернатива домашнему уходу для тех, кому требуется постоянное наблюдение и помощь. Здесь созданы все условия для комфортного проживания: уютные комнаты, сбалансированное питание, интересные занятия и развлекательные мероприятия. Кроме того, в пансионатах обеспечивается круглосуточный медицинский контроль и квалифицированный уход.
как выбрать надежное казино Хотите играть в казино, где надежность сочетается с мгновенным выводом? Вы нашли то, что искали! Мы предлагаем лучшие площадки, где ваши деньги в безопасности, а получение выигрышей происходит максимально быстро. Играйте с уверенностью!
геронтологический центр в москве для пожилых людей с деменцией Гериатрический центр, в свою очередь, фокусируется на лечении и профилактике заболеваний, характерных для пожилого возраста. Здесь работают врачи-гериатры, специализирующиеся на особенностях здоровья пожилых людей. Гериатрический центр может быть частью геронтологического центра или функционировать независимо.
онлайн казино вулкан Устали от казино, где вывод денег превращается в настоящую головную боль? Мы понимаем! Наш выбор – это надежные казино с действительно быстрыми выплатами. Играйте в любимые слоты и настольные игры, зная, что ваши выигрыши поступят на счет в кратчайшие сроки. Максимум удовольствия, минимум ожидания!
Flourish & Grow Hub – Practical tips and inspiration to support your daily personal growth.
blsp ap
bs2web at
Промокод 1xBet при регистрации. Компания 1XBET заинтересована в поиске новых игроков, поэтому для новых пользователей действует акция в виде приветственного бонуса, который равен сумме первого депозита, но не превышает двести двадцать пять тысяч рублей. Однако при использовании 1хБет промокод букмекерская контора добавит процент к приветственного бонуса. Чтобы получить дополнительное вознаграждение на первый депозит, игроку нужно: зайти на сайт букмекера, выбрать создание аккаунта через почту, заполнить данные, ввести промокод и подтвердить согласие с правилами. Код 1xBet помогает получить ещё больше бонусов. Промокод — это комбинация, которая позволяет активировать уникальный бонус от букмекера. С его помощью можно получить промо-баллы и другие подарки.
1xbet промокод на сегодня 2026. Чтобы удовлетворить ставочников, букмекеры постоянно добавляют новые функции и предложения. Одним из лидеров является 1хБет. Ввод промокода при регистрации позволяет получить увеличенную сумму бонуса. После создания аккаунта внеси первый депозит (до 32 500 рублей) — и получи вознаграждение. Абсолютно бесплатный купоны 1xbet доступен всем новичкам, чтобы активировать дополнительные преимущества. Игнорировать поле «Введите промокод» — значит потерять выгоду. Оно присутствует при трёх из четырёх способов регистрации (по телефону).
https://jobs.lifewest.edu/employer/bstecode26
http://escobaryasociados.com.co/1/mostbet-v-kyrgyzstane-46/
Achieve & Inspire Hub – Resources to help you stay focused, motivated, and confident in your pursuits.
https://www.tripadvisor.com/Profile/camsmodels78
????
?????????
http bsme
1хБет промокод 2026 Промокод 2025 года на https://realcheb.ru/novosti/pgs/?1xbet_promokod_pri_registracii_na_segodnya_besplatno.html даёт бонус 100% до 32 500 рублей для всех зарегистрированных пользователей.
купоны 1xbet Используйте промокод на https://waterlux.ua/articles/pages/1xbet_promokod_registraciya.html и активируйте 100% к первому депозиту для комфортного старта игры.
1xbet promo code today
onyx55
На официальном сайте всегда свежие новости : https://www.ikonu.ru/
khao555 slot
bs2best at не работает
Visit our main website — https://poloniya.ru/
Онлайн-казино Вавада известна бонусами.
Выбор игр представлен топ-провайдерами.
Кэшбэк-акции дают плюс к депозиту.
Регистрация занимает минуты.
Подробности по vavada casino — начинай игру.
Играйте ответственно.
http://domlajon.uz/user/Tunomixup/
розы Розы: Розы – это королева цветов, символ любви, красоты и элегантности. Существует огромное разнообразие сортов роз: от классических красных и белых до экзотических желтых и оранжевых. Розы – это универсальный подарок, подходящий для любого случая: от Дня рождения до свадьбы. Букет роз – это прекрасный способ выразить свои чувства, подарить радость и создать романтическую атмосферу.
1xbet sign up promo code
http://leydis16.phorum.pl/viewtopic.php?p=902702#902702
аренда винтовых строительных лесов Аренда складных строительных лесов: Складные строительные леса идеально подходят для внутренних работ, отделки и ремонта небольших помещений. Аренда складных лесов позволяет легко перемещать и хранить оборудование, а также быстро развертывать рабочее место в условиях ограниченного пространства. Компактность и мобильность делают их незаменимыми для мобильных бригад и частных мастеров.
остров ланта пхукет
Рабочий промокод всегда доступен на нашем сайте. Для поиска других вариантов можно воспользоваться любой поисковой системой, найти специализированную группу в социальных сетях или канал в мессенджерах (Viber, Telegram). Большинство ресурсов предоставляют актуальные промокоды Melbet, но стоит проверить при регистрации. Введите скопированный промокод на сегодня мелбет и дождитесь уведомления от БК Мелбет, что бонус повышен. Помните, что второй раз зарегистрироваться и получить 50 000 рублей от Мелбет невозможно. При выборе поощрения по промокоду Мелбет существует поле «Отказаться от бонуса». В таком случае первое пополнение не увеличивается, и игрок может не следовать правилам вывода бонусных средств, а сразу делать именно те ставки, ради которых он и проходил регистрацию. Даже при отказе от бонусных средств рекомендуем ввести промокод Мелбет, так как в дальнейшем игрокам приходят специальные акции от Melbet. Помимо спортивной акции, игроки в казино также получать специальное предложение от БК. При использовании промокода Мелбет есть возможность получить бонус в казино до 125 000? и 290 фриспинов.
Букмекерская компания Мелбет или известная в других кругах Melbet, имеет огромное количество игроков в онлайне. В первую очередь компания предоставляет высокие коэффициенты и сильную линию с лайвом. Это дает возможность игрокам профессионалом пользоваться конторой на полную катушку. Плюс, с помощью промокода вы получите бонус 50 000 тысяч рублей. Без промо кода до 8000 тысяч. промокод для мелбет представляют собой бонусные возможности, которые дает сама букмекерская контора. Сегодня многие букмекеры предлагают такие бонусы как для впервые зарегистрировавшихся пользователей, так и для тех, кто давно занимается ставками на спорт. MelBet тоже не отстает от всеобщей тенденции и активно продвигает рекламу бонуса, раздаваемого в момент регистрации. Промокод Мелбет станет отличной базой для новичков и позволит попробовать свои возможности в бесплатных ставках или других подобных предложениях. Как получить такой промокод и применить его на деле, рассмотрим далее.
Code Promo Pari Gratuit 1xbet vous donne un code promo 1xBet 130€ avec un bonus de 100%, Obtenez le bonus de bienvenue 1xbet pour 2025. Assurez-vous de lire les regles pour profiter pleinement de votre bonus de bienvenue. Connectez-vous a votre compte 1xBet pour decouvrir comment utiliser le bonus de bienvenue 1xbet.
onyx-55
Code Promo De 1xbet vous donne un code promo 1xBet paris sportifs avec un bonus de 100% jusqu’a €130, ainsi qu’un bonus de casino de €1950 avec 150 tours gratuits. Grace au code promo 1xbet vous pouvez maximiser vos gains. Entrez le code promo 1xBet lors de votre inscription et recevez un bonus de bienvenue garanti. Cette offre exclusive est reservee aux nouveaux clients, ce qui augmente considerablement le montant de votre premier depot.
пляжи ко ланты
????
леса лрсп Продажа инвентарных лесов: Продажа инвентарных лесов – это предложение для компаний, стремящихся оптимизировать затраты на оборудование и обеспечить долговечность и надежность конструкций. Инвентарные леса отличаются стандартизированными размерами и взаимозаменяемыми элементами, что упрощает процесс сборки и разборки, а также обеспечивает возможность быстрой замены поврежденных деталей. Использование инвентарных лесов позволяет снизить затраты на обслуживание и повысить эффективность строительных работ.
LLC COMMERCIAL & TRANSPORT COMPANY “SHARP STING” / DUNS 758094686 ООО Торгово-транспортное предприятие “Острое Жало” позиционирует себя как надежный партнер в сфере логистики и грузоперевозок, предлагая широкий спектр услуг, адаптированных под нужды современного бизнеса. Наша компания обладает значительным опытом работы с предприятиями различных отраслей, обеспечивая бесперебойную поставку продукции от производителя до конечного потребителя. Мы гордимся своей репутацией и стремимся к постоянному совершенствованию в области логистических решений.
https://blogs.stockton.edu/educationtoeducate/2019/11/03/exploring-google-maps/
Вакансии ООО Торгово-транспортное предприятие “Острое Жало” на rabota. ru Помимо стандартных транспортных услуг, “Острое Жало” предлагает специализированные решения для перевозки негабаритных, опасных и требующих особых условий грузов. Мы располагаем необходимым оборудованием и квалифицированным персоналом для обеспечения безопасности и сохранности подобных грузов. Наша команда постоянно отслеживает изменения в законодательстве и нормативных актах, чтобы обеспечить полное соответствие перевозок всем требованиям.
Replique montre moderne
film production services in Cortina d’Ampezzo
film production services in Cortina d’Ampezzo
Джоггеры Женские Стремление к комфорту и индивидуальности проявляется в растущей популярности одежды свободного кроя. Одежда оверсайз – это сознательный выбор в пользу свободы движений и подчеркивания собственной уникальности. Она скрывает недостатки фигуры и позволяет создать расслабленный, но при этом стильный образ. Будь то толстовка, свитшот или худи, оверсайз – это тренд, который остается с нами надолго. Женская одежда как никакая другая стремится подчеркнуть красоту и индивидуальность каждой девушки. А для тех, кто хочет купить худи или купить свитшот нужно обратить внимание на трендовые позиции и понимать, что сейчас в моде. Ведь мода 2026 – это про индивидуальность и комфорт, смешение стилей и отход от общепринятых норм. Стиль не покупается за деньги, поэтому лучше следить за модными трендами в модном журнале, чтобы найти подходящий стильный бренд одежды.
Мода 2026 Мир моды с восторгом принял философию свободы и самовыражения, воплощенную в силуэтах оверсайз. Одежда оверсайз, отрицая сковывающие рамки традиционного кроя, дарит ощущение невесомости и легкости. Она деликатно скрывает несовершенства фигуры, позволяя каждой женщине почувствовать себя уверенно и комфортно. Женская одежда стремится выделить индивидуальность, ищете ли вы где купить худи или купить свитшот, нужно ориентировать на модные тренды и стиль, а узнать их можно в модном журнале, где представлен стильный бренд одежды. Мода 2026 – это время экспериментов!
https://nonameno.com/programs.html
https://nonameno.com/programs.html
https://penzu.com/p/217e32bebe5b886b
https://geltaxi.ru/taxi-ahtanizovskaya-temryuk
промокод при регистрации 1хБет Ввод промокода при регистрации на https://farmalad.com.ua/images/pages/?1xbet_promokod_registraciya.html даёт бонус 100% на первый депозит, для комфортного старта с максимальной суммой.
как происходит списание долгов по кредитам Прежде чем инициировать процедуру, крайне важно получить всестороннюю информацию о её аспектах. Бесплатная консультация по банкротству или бесплатная консультация юриста по банкротству станет первым шагом к пониманию перспектив и потенциальных последствий. Важно выяснить, как происходит списание долгов по кредитам и какие долги списывают через банкротство, поскольку не все обязательства подлежат аннулированию. Квалифицированная консультация по банкротству физических лиц поможет сориентироваться в юридических тонкостях и разработать оптимальную стратегию. Онлайн консультация по банкротству – удобный формат для получения первичной информации. Решение о банкротстве сопряжено с рядом последствий, поэтому необходимо тщательно взвесить все плюсы процедуры банкротства физического лица. К ним относится возможность списать долг по кредиту банкротство и начать жизнь с чистого листа. Однако, следует учитывать, что проведение процедуры банкротства – это ответственный шаг, требующий соблюдения строгих правил и участия квалифицированных специалистов. Особое внимание следует уделить вопросам: процедура банкротства сроки проведения, процедура банкротства физических лиц по кредитам, процедура банкротства физического лица в суде, процедура банкротства физического лица пошаговая инструкция.
Pgsiam777
Промокод при регистрации в 1xbet сегодня. Этой акцией может воспользоваться каждый новый игрок при регистрации на сайте букмекера. Это ваше преимущество с начала. В форме регистрации есть необязательное поле для ввода кода. Как получить 1хБет промокод на бесплатную ставку. В магазине xBonus можно обменять баллы на коды 1xbet kz: для ординаров, экспрессов или лотерей. Найти промокоды 1xbet можно на спортивных сайтах. Представители БК часто публикуют их к праздникам или турнирам. Все актуальные промокоды 2026 доступны в официальном разделе сайта и могут быть обменяны на бонусные баллы.
https://enewsletters.k-state.edu/youaskedit/2020/07/14/mold-growth-in-home-canned-food/#comment-49675
Go to our website now
консультация по банкротству Прежде чем инициировать процедуру, крайне важно получить всестороннюю информацию о её аспектах. Бесплатная консультация по банкротству или бесплатная консультация юриста по банкротству станет первым шагом к пониманию перспектив и потенциальных последствий. Важно выяснить, как происходит списание долгов по кредитам и какие долги списывают через банкротство, поскольку не все обязательства подлежат аннулированию. Квалифицированная консультация по банкротству физических лиц поможет сориентироваться в юридических тонкостях и разработать оптимальную стратегию. Онлайн консультация по банкротству – удобный формат для получения первичной информации. Решение о банкротстве сопряжено с рядом последствий, поэтому необходимо тщательно взвесить все плюсы процедуры банкротства физического лица. К ним относится возможность списать долг по кредиту банкротство и начать жизнь с чистого листа. Однако, следует учитывать, что проведение процедуры банкротства – это ответственный шаг, требующий соблюдения строгих правил и участия квалифицированных специалистов. Особое внимание следует уделить вопросам: процедура банкротства сроки проведения, процедура банкротства физических лиц по кредитам, процедура банкротства физического лица в суде, процедура банкротства физического лица пошаговая инструкция.
Go to our web platform : http://ruptur.com/
Experience the latest version here
прогнозы на футбол Ставки на спорт – это азартное развлечение, требующее аналитического подхода и понимания стратегий. Современный мир беттинга предлагает широчайший выбор возможностей: от классических видов спорта до киберспорта и экзотических дисциплин. Однако, важно помнить, что успех в ставках на спорт – это не только удача, но и результат кропотливого анализа, изучения статистики и учета множества факторов.
Переходи на официальный сайт компании — http://ruptur.com/
списать долги банкротство физ лиц Компетентное ведение дела – залог успешного завершения процедуры банкротства физического лица через суд. Важно доверить процедуры банкротства должника физического лица опытным юристам, специализирующимся на банкротстве. Компания должна иметь безупречную репутацию. Только так можно быть уверенным, что процедура будет выполнена в соответствии с законом и все ваши права будут защищены.
khao555
списать долги через банкротство Компетентное ведение дела – залог успешного завершения процедуры банкротства физического лица через суд. Важно доверить процедуры банкротства должника физического лица опытным юристам, специализирующимся на банкротстве. Компания должна иметь безупречную репутацию. Только так можно быть уверенным, что процедура будет выполнена в соответствии с законом и все ваши права будут защищены.
срочная разработка SEO продвижение для магазина Нс Диджитал Профессиональная разработка сайтов и интернет магазинов на 1с Битрикс Seo продвижение под ключ с использованием AI
Обучение в сфере досуга Узнать больше о теме можно здесь: https://rabota-dosug-sterlitamak.ru/
этапы процедуры банкротства физического лица На начальном этапе целесообразно получить бесплатную консультацию по банкротству, чтобы оценить свои шансы на успех и получить ответы на интересующие вопросы. Бесплатная консультация юриста по банкротству поможет разобраться в законодательных тонкостях и определить оптимальную стратегию действий. Понимание того, как происходит списание долгов по кредитам в рамках процедуры банкротства, является ключевым моментом. Важно знать, какие долги списывают через банкротство, чтобы четко представлять конечный результат. Квалифицированная консультация по банкротству и консультация по банкротству физических лиц позволит получить полную информацию о процедуре и ее последствиях. Онлайн консультация по банкротству – удобный способ получить ответы на вопросы, не выходя из дома.
списание долгов по кредитам физических лиц Прежде чем инициировать процедуру, крайне важно получить всестороннюю информацию о её аспектах. Бесплатная консультация по банкротству или бесплатная консультация юриста по банкротству станет первым шагом к пониманию перспектив и потенциальных последствий. Важно выяснить, как происходит списание долгов по кредитам и какие долги списывают через банкротство, поскольку не все обязательства подлежат аннулированию. Квалифицированная консультация по банкротству физических лиц поможет сориентироваться в юридических тонкостях и разработать оптимальную стратегию. Онлайн консультация по банкротству – удобный формат для получения первичной информации. Решение о банкротстве сопряжено с рядом последствий, поэтому необходимо тщательно взвесить все плюсы процедуры банкротства физического лица. К ним относится возможность списать долг по кредиту банкротство и начать жизнь с чистого листа. Однако, следует учитывать, что проведение процедуры банкротства – это ответственный шаг, требующий соблюдения строгих правил и участия квалифицированных специалистов. Особое внимание следует уделить вопросам: процедура банкротства сроки проведения, процедура банкротства физических лиц по кредитам, процедура банкротства физического лица в суде, процедура банкротства физического лица пошаговая инструкция.
новости о ставках на спорт Ставки на спорт – это азартное развлечение, требующее аналитического подхода и понимания стратегий. Современный мир беттинга предлагает широчайший выбор возможностей: от классических видов спорта до киберспорта и экзотических дисциплин. Однако, важно помнить, что успех в ставках на спорт – это не только удача, но и результат кропотливого анализа, изучения статистики и учета множества факторов.
1xBet промокод Используйте на http://www.flotiliya.com/misc/inc/1xbet-promokod.html и получите бонус 100% на депозит до 32 500 рублей, чтобы получить максимальный стартовый бонус.
1хБет промокод 2026 Новый промокод 2026 на http://kitanoseeds.ru/img/pgs/?1xbet_promokod_pri_registracii_na_segodnya_besplatno.html позволяет получить 100% к депозиту до 32 500? для всех зарегистрированных пользователей.
плюсы процедуры банкротства физического лица В непростых финансовых обстоятельствах, когда бремя долгов становится непосильным, процедура банкротства физических лиц может стать спасительным кругом. Однако, прежде чем решиться на этот шаг, необходимо тщательно изучить все аспекты и нюансы, связанные с данной процедурой. Важным вопросом является определение сроков процедуры банкротства физических лиц, которые могут варьироваться в зависимости от сложности дела и загруженности судебной системы.
консультация по банкротству Компетентное ведение дела – залог успешного завершения процедуры банкротства физического лица через суд. Важно доверить процедуры банкротства должника физического лица опытным юристам, специализирующимся на банкротстве. Компания должна иметь безупречную репутацию. Только так можно быть уверенным, что процедура будет выполнена в соответствии с законом и все ваши права будут защищены.
Hi there just wanted to give you a quick heads up and let you know a few of the pictures aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
обмен криптовалюта
onyx55
bsme ru
Video equipment rental Milan Branded content production in Milan: Developing engaging and informative content that connects with audiences and builds brand loyalty.
https://www.soft4led.com/why-jimmy-kimmel-is-the-man-of-the-youtube-era/
https://geltaxi.ru/taxi-ashe-adler
https://www.soft4led.com/why-jimmy-kimmel-is-the-man-of-the-youtube-era/
branded content production in Milan Fashion film production Milan: Specializing in creating visually arresting fashion films that showcase brands’ unique style and vision.
I got this web page from my buddy who informed me concerning this web site and at the moment this time I am visiting this website and reading very informative content here.
парк виртуальной реальности
http://skyiwredshjnhjgeleladu7m7mgpuxgsnfxzhncwtvmhr7l5bniutayd.onion
https://www.pexels.com/@fesus-2157011671/
??????????????????????????
What’s up i am kavin, its my first time to commenting anywhere, when i read this paragraph i thought i could also make comment due to this brilliant article.
новости про крипту
onyx-55
https://techfily.com/motherhood-and-music-how-having-a-daughter-transformed-kehlanis-life/
http://skyiwredshjnhjgeleladu7m7mgpuxgsnfxzhncwtvmhr7l5bniutayd.onion
https://www.soft4led.com/why-jimmy-kimmel-is-the-man-of-the-youtube-era/
http bs2best at
https://joyrulez.com/blogs/218073/A-Smarter-System-for-Choosing-Online-Betting-Platforms
ортофосфорная кислота оптом Промышленная химия от РТХ (Русский Торговый Холдинг): надежные решения для вашего бизнеса
Pgsiam777
https://o2c3ds.ru/info/kak-vybrat-semena-gazonnyh-trav-dlya-raznyh-tipov-pochvy-v-moskve
кислоты оптом Логистика и доставка: РТХ обеспечивает оперативную и надежную доставку химической продукции в любой регион, минимизируя простои в вашем производстве
????
singapore casino
References:
https://www.bookmarking-fox.win/top-digital-casino-for-australian-slot-fans-and-huge-payouts
legends casino
References:
https://amelie.zp.ua/user/morvetimld
https://o2c3ds.ru/info/kak-vybrat-semena-gazonnyh-trav-dlya-raznyh-tipov-pochvy-v-moskve
Hi to every one, the contents present at this web page are truly awesome for people knowledge, well, keep up the good work fellows.
https://www.06236.com.ua/list/507648
https://ext-6882717.livejournal.com/395.html?newpost=1
casino circus
References:
http://bbs.yuanjumoli.com/home.php?mod=space&uid=384550
best online casino uk
References:
http://eric1819.com/home.php?mod=space&uid=3089627
mobile casino action
References:
https://www.kdbang.vip/home.php?mod=space&uid=1194312
northern california casinos
References:
https://jinrihuodong.com/home.php?mod=space&uid=1662618
slot casino games
References:
https://images.google.com.my/url?q=https://articlescad.com/wendoverfun-com-wendover-hotel-rooms-649824.html
the star casino
References:
https://maps.google.com.br/url?q=https://atavi.com/share/xkphgizv4r8h
Промокод при регистрации 1xbet на 32 500 рублей. Этот код нужно ввести при регистрации в соответствующее поле. Промокод действует однократно, но им можно делиться с друзьями. Регистрация по номеру телефона — быстрый способ создать аккаунт. После получения данных для входа остаётся лишь ввести логин и пароль. Используй актуальный промокод на бонус 1хбет и увеличь первый депозит до 32500 рублей в БК 1xBet. На платформе действует бонусная программа, которая помогает игрокам получать до дополнительных процентов от первого депозита.
снять девушку спб Вызвать девушку СПб: Услуга вызова – это прекрасный способ внести разнообразие в свой досуг, добавить щепотку авантюры и создать незабываемую атмосферу.
промокод 1xbet бесплатно Ищите промокод на http://00rf.ru/hefer/pages/1xbet-promokod.html и активируйте бонус до 32 500 рублей, чтобы начать игру.
скачать игры с яндекс диска Альтернативы существуют: Помимо прямых ссылок и Яндекс Диска, существуют и другие способы загрузки игр без торрентов, такие как цифровые магазины и официальные сайты разработчиков. Исследуйте все возможности и выбирайте наиболее подходящий вариант.
wolf run slot machine
References:
http://yqwml.com/home.php?mod=space&uid=980395
глицерин оптом Логистика и доставка: РТХ обеспечивает оперативную и надежную доставку химической продукции в любой регион, минимизируя простои в вашем производстве
вызвать девушку спб Вызвать девушку СПб: Услуга вызова – это прекрасный способ внести разнообразие в свой досуг, добавить щепотку авантюры и создать незабываемую атмосферу.
khao555 login
скачать игры по прямой ссылке Игровой мир ждет вас: Независимо от выбранного способа загрузки, самое главное – это наслаждаться играми! Откройте для себя новые миры, познакомьтесь с интересными персонажами и погрузитесь в захватывающие истории. Мир гейминга ждет вас!
excalibur casino las vegas
References:
http://bbs.xltyun.com/space-uid-711612.html
ft mcdowell casino
References:
https://www.instructables.com/member/harpdeer16/
глицерин оптом Логистика и доставка: РТХ обеспечивает оперативную и надежную доставку химической продукции в любой регион, минимизируя простои в вашем производстве
mahjongg dimensions more time
References:
https://motionentrance.edu.np/profile/coachrhythm97/
cherokee casino nc
References:
https://yogaasanas.science/wiki/Online_Casino_Real_Money_Play_Best_Online_Casino_Free
casinos oklahoma
References:
https://git.ultra.pub/maccollins791
casino directory
References:
https://australiaimmihome.com/read-blog/194_best-credit-card-casinos-10-casinos-that-accept-credit-cards.html
ca cuoc the thao online
https://prgun.ru/
hawks prairie casino
References:
https://www.aicgworld.com/wstdebora62816/cortney2021/-/issues/1
https://pr-gun.ru
online games for mac
References:
https://git.sudo-fhir.au/laruehalford34
casino cast
References:
https://katambe.com/@malcolmperreau
bsme ru
paddy casino
References:
http://116.198.44.217:8040/trishacannon03
blsp at клады
crown perth casino
References:
https://git.repo.in.net/noemi808885355
монтаж натяжного потолка Монтаж натяжного потолка: Быстро, качественно, надежно Профессиональный монтаж натяжного потолка – залог его долговечности и эстетичного внешнего вида. Доверьте эту работу опытным специалистам, которые быстро и качественно установят потолок любой сложности, учитывая все особенности вашего помещения. Правильный монтаж обеспечит идеально ровную поверхность, отсутствие провисаний и деформаций, а также долговечность конструкции.
pockie ninja 2
References:
http://medifore.co.jp/bbs/board.php?bo_table=free&wr_id=4844774
bay mills casino
References:
https://4me.zone/read-blog/3349_10-best-online-casinos-australia-for-real-money-gaming-in-2025.html
the grand casino
References:
https://unreliablecode.net/read-blog/141_15-best-live-casinos-australia-play-against-live-dealers-online.html
натяжные потолки спб Натяжной потолок СПБ цены: Выгодные предложения от профессионалов В Санкт-Петербурге представлен широкий выбор натяжных потолков по доступным ценам. Обратившись к профессионалам, вы сможете получить консультацию, выбрать оптимальный вариант и заказать установку потолка под ключ. Не стоит экономить на качестве материалов и монтажа, чтобы ваш потолок радовал вас долгие годы.
https://playplayfun.com/articles/1xbet_promo_code_nigeria_bonus.html
best online casino reviews
References:
http://jinjianghc.com:3000/sheree8137496
little river casino
References:
https://jobspaddy.com/careers/companies/bizzo-casino-review-unbiased-assessment-for-aussie-players/
sky ute casino
References:
https://gitea.questline.coop/refugiodresche
hoosier park racing and casino
References:
https://biiut.com/read-blog/21518_best-online-casinos-in-australia-2025.html
pg slot
Перейди по ссылке на официальный ресурс
khao555 login
quantum quest a cassini space odyssey
References:
https://www.cybersecurityhouse.com/employer/online-casinos-australia-best-aussie-casino-sites-of-2025/
pompeii pink floyd
References:
http://guanli.jiance.cn:3000/kendramckinlay
regle du blackjack
References:
https://www.hulkshare.com/hellrhythm57/
new york new york casino
References:
https://greatsound.com.ng/violettebeirne
sioux falls casino
References:
http://git.szmicode.com:3000/joanne82532722
playboy casino
References:
https://fravito.fr/user/profile/2105355
roulette betting strategy
References:
https://www.qrlnk.co.uk/jamilastoker82
casino vilamoura
References:
https://googlegossip.com/read-blog/95643_what-is-a-star-and-how-does-it-work.html
Услуги эвакуатора Эвакуатор – это не просто средство передвижения автомобилей, потерпевших бедствие, это символ надежды и оперативной помощи на дорогах. Внезапная поломка, ДТП или другие неприятности, требующие немедленной транспортировки, могут случиться с каждым водителем. И в этот момент эвакуатор становится настоящим спасением, гарантируя безопасную и быструю доставку автомобиля в нужное место.
burnaby casino
References:
http://www.s-golflex.kr/main/bbs/board.php?bo_table=free&wr_id=4826855
Вызвать эвакуатор Эвакуатор Таганрог – это локальная служба, которая знает город как свои пять пальцев. Оперативность и знание местности позволяют быстро прибыть на место происшествия в любой точке города и оказать необходимую помощь. Круглосуточная доступность делает эту службу незаменимой для водителей, попавших в затруднительную ситуацию в любое время суток.
казино в котором есть бездепозитный бонус
бездепозитный бонус казино в
baton rouge casinos
References:
https://meeting4.fun/heathermosman
northern lights casino
References:
https://careerterms.com/companies/best-australian-online-gaming-sites-for-high-rollers-2025/
alice springs casino
References:
https://mtwd.link/redamaum105720
online pokies australia
References:
https://pli.su/martyconners60
1xBet промокод Введя на http://info-realty.ru/bitrix/pages/1xbet-promokod-pri-registracii-besplatno.html и получите бонус 100% на депозит до 32 500?, чтобы начать игру с преимуществом.
montreal metropolis
References:
http://114.55.58.6:3000/diana27l266817
промокоды на 1xbet Активируйте промокод на https://granplast.ru/images/pgs/?1xbet_promokod_pri_registracii_bonus.html и заберите бонус 100% на первый депозит при регистрации для комфортной игры.
monkey quest games
References:
https://kayesbamusic.com/willisvzx31142
Букмекерская контора «Мелбет» – это уникальная возможность для всех желающих получить дополнительный доход. Здесь можно делать ставки на самые разные спортивные события по всему миру. Высокие коэффициенты, круглосуточная техническая поддержка, удобное мобильное приложение и многие другие преимущества проекта делают его весьма популярным среди любителей азартных игр. Доступ на виртуальную площадку открыт лишь для зарегистрированных пользователей. промокод на сегодня мелбет помогут сэкономить как начинающим, так и опытным игрокам. В такой надежной и стабильной букмекерской конторе вы всегда можете быть уверены.
online casino malaysia
References:
https://littleusername.ru/hestergrimshaw
casino parties
References:
https://git.shadowvault.eu/randellantoine
slot machine game
References:
http://afro2love.com/@vickey89m7106
Используя промокод Мелбет при регистрации, игроки получают доступ к участию в приветственной бонусной программе. Полученные привилегии можно использовать, заключая ставки на ММА и другие виды спорта. Ниже рассказываем более подробно о том, какие бонусы предложены на сайте и как их отыграть. Бонусные программы нацелены на то, чтобы обеспечить для игроков возможность получить безболезненный опыт игры на сайте и сгладить первые возможные неудачи. Регистрируйтесь на платформе букмекера, активируйте рабочий промокод Melbet на сегодня и пользуйтесь бонусными предложениями от букмекера Мелбет, чтобы получать больше положительных эмоций при заключении пари.
suquamish casino
References:
https://galaxybook.net/read-blog/417_the-10-best-online-casinos-in-australia-rated-by-expert-gamblers-2025.html
женская обувь натуральная кожа бежевая женские лоферы – элегантное дополнение к любому образу, сочетающее комфорт и стиль.
женская кожаная обувь в москве Женская обувь недорого – это реально, когда вы выбираете оптимальное соотношение цены и качества, не уступая в стиле.
Go to our updated website — https://madguy.ru/
all jackpots casino
References:
http://git.huixuebang.com/bethlenk468838/6028682/-/issues/1
Check our site for updates > https://gorod-fonarikov.ru/
texas casinos
References:
http://118.31.7.2:3000/shauntewalstab
mount airy casino
References:
https://www.soundofrecovery.org/cathernwentz6
женские ботинки на каждый день натуральная кожа Женская обувь турция новинки – всегда в курсе последних модных тенденций, предлагая стильные и актуальные модели каждого сезона.
женские туфли классика Женская обувь из натуральной кожи купить – значит приобрести изделие, которое прослужит долгие годы, сохраняя свой первоначальный вид.
gala casino glasgow
References:
https://vtuguru.online/read-blog/166_best-real-money-australian-online-casino-sites-for-2025.html
online roulette wheel
References:
https://iplawjobs.com/employer/australian-online-casinos-2025-the-ultimate-guide/
rampart casino
References:
https://jobsindatacenter.com/employer/instant-withdrawal-casino-australia-fastest-payout-casinos-2025/
бездепозитные бонусы за регистрацию в казино казахстан
женская обувь натуральная кожа синяя Женская обувь по России – возможность приобрести качественную обувь с доставкой в любой уголок страны.
silver star casino
References:
https://gjejstaf.al/employer/best-betting-sites-in-australia-top-australian-online-bookmakers/
бездепозитные бонусы в казино 2025
bay 101 casino
References:
https://cercalavoro.com/employer/top-igaming-software-providers/
play slots for real money
References:
https://insidevibes.us/read-blog/1966_best-fast-withdrawal-casinos-5-sites-with-quickest-payouts-in-2025.html
slot machine sounds
References:
https://clifford-russo.blogbright.net/pullman-reef-hotel-casino
online roulette play roulette and receive $1500
References:
https://zenwriting.net/brushglass05/sl-tewbtrng-aimphaane-eynt-andab-1-kh-ngaithy
casino royal streaming
References:
https://urlscan.io/result/019aca29-21bc-70d6-818a-2a0a4bd37726/
jacks or better
References:
https://www.lab.justusdeitert.de/tonykane934397
online gaming sites
References:
http://hom.is/bbs/board.php?bo_table=free&wr_id=194582
online black jack
References:
https://slowdating.ca/@olgaqfs1479477
mount airy casino
References:
https://git.forum.ircam.fr/lavadafurey85
Find the new look here
online casino bonuses
References:
https://thebillbergia.com/companies/best-crypto-betting-sites-listed-rated-overviewed/
four winds casino new buffalo
References:
http://hom.is/bbs/board.php?bo_table=free&wr_id=194488
hard rock casino tampa florida
References:
http://guanli.jiance.cn:3000/shaunaloeffler
slots belgique
References:
http://106.51.72.251:3000/samaracarrozza
https://lcri.gov.ng/2023-lcri-in-house-review-meeting-and-north-east-zonal-refils-workshop-at-gov-mai-mala-buni-conference-hall-nuj-secretariat-damaturu/
Go directly to our website
подвесные строительные леса продажа складных лесов
аренда сборных строительных лесов аренда подвесных строительных лесов
Nice post. I learn something totally new and challenging on websites I stumbleupon on a daily basis. It’s always interesting to read through articles from other writers and use a little something from their websites.
https://lp2.septimo.com.br/?p=10734
blackjack regles
References:
https://deltasongs.com/kristymccue520
what is blackjack
References:
https://365.expresso.blog/question/best-online-casinos-in-australia-for-real-money-gambling-2025/
basic strategy blackjack
References:
https://silatdating.com/@faustinodoller
Excellent article. Keep posting such kind of info on your page. Im really impressed by your site.
Hi there, You have performed an incredible job. I’ll certainly digg it and for my part recommend to my friends. I’m confident they will be benefited from this website.
https://www.napcoin.club/melbet-fribet-bez-depozita-2025/
создание ии презентации
https://simpleslide.ru
как использовать бонус казино в 1win
casino drive bastia
References:
http://www.cricbattle.com/Register.aspx?Returnurl=http://correspondent.in.ua/user/morvetshrw
club player casino
References:
http://msichat.de/redir.php?url=https://www.wall-bookmarkings.win/royal-reels-casino-australia-2025-aud-pokies
казахстане
Промокод при регистрации 1xbet на 32 500 рублей. Этот код нужно ввести при регистрации в соответствующее поле. Промокод действует однократно, но им можно делиться с друзьями. Регистрация по номеру телефона — удобный способ создать аккаунт. После получения данных для входа остаётся лишь ввести логин и пароль. Используй актуальный действующие промокоды 1xbet и увеличь первый депозит до 32 500 рублей в БК 1xBet. На платформе действует программа лояльности, которая помогает игрокам получать до повышенного кэшбэка от первого депозита.
hippodrome casino london
References:
http://member.8090.com/exit.php?url=https://bandit250.ru/user/kevineitcb
фриланс работа Поиск работы: эффективные стратегии. Используйте все доступные ресурсы для поиска работы. Размещайте резюме на сайтах по трудоустройству, обращайтесь в кадровые агентства и участвуйте в онлайн-собеседованиях.
vicksburg casinos
References:
http://vip.cengfan6.com/goto.php?url=https://landenmzhr620.lucialpiazzale.com/tapahtumat
spa brochure
References:
https://www.bookmarking-online.win/cleobetra-casino-review-1-000-bonus-275-free-spins
получить промокод 1xbet Получите промокод на https://www.chili.edu.pl/profile/bergkoma957293/profile и заберите бонус до 32 500 рублей при регистрации для комфортной игры.
как найти удаленную работу Вакансии удаленная работа — общий обзор публикуемых вакансий в удалённом формате. В них могут встречаться роли в IT, образовании, маркетинге, поддержке клиентов и дизайне. При выборе вакансии обращайте внимание на часы работы, требования к оборудованию, уровень оплаты и возможность карьерного роста. Подготовьте подробное резюме, кейс-материалы и портфолио, которое демонстрирует релевантность вашего опыта. Не забывайте про тестовые задания и собеседования в онлайн-формате, а также про проверку репутации работодателя.
фриланс работа Удаленная работа: отзывы реальных людей. Изучайте отзывы о компаниях и вакансиях, чтобы избежать мошенничества и найти надежного работодателя. Отзывы – это ценный источник информации от тех, кто уже работает удаленно.
choctaw casinos
References:
http://www.video-bookmark.com/user/andyardtlj
marksville casino
References:
http://www.dicodunet.com/out.php?url=https://www.foxtrot-bookmarks.win/best-online-casino-reviews-aus-top-10-online-casino-1
удаленная работа для пенсионеров Фриланс в интернете — широкий мир онлайн-проектов, где вы можете работать удалённо и зарабатывать на своих навыках. Начните с анализа спроса на рынке: какие услуги востребованы, какие цены устанавливают конкуренты, какие сроки и форматы работ принято предлагать. Развивайте профессиональные портфолио и ссылки на завершённые проекты. Эффективная коммуникация с клиентами, чёткие соглашения и прозрачная оплата помогают строить долгосрочные отношения и стабильный доход.
https://www.lanubedocente.21.edu.ar/profile/telike889446219/profile
casino spokane
References:
http://gamesjp.com/jump.php?url=https://www.bookmarks4all.win/best-online-casinos-in-2025-real-money-sites-bonuses
no deposit bonus code
References:
https://www.bust-bookmark.win/planet-hollywood-resort-casino-las-vegas-usa
o l g slots
References:
https://rowing.su/user/keenancohq
casino capitalism
References:
https://new.72dez.ru/user/maevynvngo
работа на удаленке Работа на дому: уют рабочего места. Работа на дому предоставляет уникальную возможность совмещать работу и личную жизнь. Это особенно актуально для мам в декрете, студентов и пенсионеров.
удаленная работа для студентов Копирайтер вакансии удаленная работа: возможности для писателей. Если вы любите писать, попробуйте себя в копирайтинге. Многие компании ищут удаленных копирайтеров для написания текстов для сайтов, социальных сетей и рекламы.
poker online for real money
References:
http://www.cricbattle.com/Register.aspx?Returnurl=https://nevskij-7-sezon-blizkij-vrag-v1.tnt-lordfilm.net/user/tammoneulc
mobile roulette
References:
http://wx.lt/redirect.php?url=https://orcid.org/0009-0006-8440-2665
bally’s casino tunica
References:
http://s.kakaku.com/jump/jump.asp?url=https://dezcity74.ru/user/corielxwex
werken bij holland casino
References:
https://www.reverbnation.com/artist/plefulqxsz
21 grand casino
References:
http://kakaku.com/jump/?url=https://raindrop.io/eldigepoxr/bookmarks-63742097
yonkers casino
References:
https://storage.athlinks.com/logout.aspx?returnurl=https://www.divephotoguide.com/user/thorneivks/
биржа фриланса Удаленная работа на дому: вакансии без опыта. Ищите вакансии, которые не требуют опыта, и будьте готовы к обучению. Многие компании предлагают бесплатные курсы и тренинги для своих удаленных сотрудников.
удаленная работа без звонков Удаленная работа без звонков: тишина и продуктивность. Для тех, кто не любит телефонные разговоры, есть множество вакансий, не требующих общения по телефону. Сосредоточьтесь на задачах, требующих внимания и концентрации.
онлайн работа бесплатно Работа на удаленке без опыта: возможности для новичков. Даже без опыта можно найти работу на удаленке. Главное – желание учиться и развиваться.
Hi there I am so happy I found your website, I really found you by error, while I was browsing on Yahoo for something else, Anyhow I am here now and would just like to say cheers for a marvelous post and a all round exciting blog (I also love the theme/design), I don’t have time to read through it all at the minute but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the awesome b.
https://mysushmitha.com/melbet-2025-skachat-mobilnoe-prilozhenie/
Do you have a spam issue on this site; I also am a blogger, and I was curious about your situation; we have developed some nice methods and we are looking to swap strategies with others, please shoot me an e-mail if interested.
https://gesit88.co/sait-melbet-registraciya-obzor-2025/
казино с моментальными выплатами
лучшие онлайн казино в россии
казино онлайн
казино с моментальными выплатами
казино с моментальными выплатами
Бесплатный промокод актуален как для букмекерской конторы Мелбет, так и для международной Melbet при регистрации в 2026 году. Официальный и рабочий промокод для новых клиентов БК дает повышенный бонус на первый депозит.В этих двух букмекерских конторах вводить промокод Мелбет надо именно во время регистрации. Он увеличивает стандартный бонус на первый депозит на 30%, и его легко можно вывести, выполнив некоторые условия букмекерской конторы Melbet. Мелбет – букмекерская контора, официально зарегистрированная в России в 2012 году. Она одна из первых стала предоставлять услуги болельщикам и любителям спорта. На данный момент контора предлагает широкое поле деятельности для прогнозистов и болельщиков, совершающих ставки. Кроме того, Мелбет дает обзор многочисленных событий из мира спорта и киберспорта, а также информацию о результатах матчей. Пользователи сервиса отмечают хорошие коэффициенты и щедрую программу бонусов. О последних нужно сказать отдельно: они доступны всем гостям сайта, даже новичкам. Выгодные предложения от букмекерской конторы позволяют делать ставки на различные спортивные события без вложения личных средств. В этой статье дан обзор Melbet промокод на сегодня и варианты их использования.
https://balkonstroi.ru/incl_ude/pages/melbet_promokod_na_segodnya_bonus_do_19_500_rub.html
Бонус Код Букмекерской Мелбет При Регистрации – это код для новых пользователей, так как он дает денежные призы на первый депозит новым игрокам. С их помощью вы получите на 30% больше возврата средств, чем при стандартной регистрации, или фрибет. Букмекерская контора Мелбет работает на рынке беттинга уже довольно долго. За время существования она успела получить доверие многотысячной аудитории игроков и сформировать четкую стратегию взаимодействия с клиентами. Для всех участников БК доступны различные поощрения, подарки и акции. Среди них – Melbet промокод бонус, расширяющий список привилегий для нового, или активного пользователя.
казино без верификации
Официальный сайт компании 1xBet > http://lipetskregionsport.ru/
irwin casino казино на деньги рейтинг
Узнай больше на официальном сайте компании — https://consolit.ru/
Der spezielle Legiano Sportbonus richtet sich an Sportfans. Die Plattform erlaubt es, mehrere Einzelwetten zu kombinieren, um sogenannte Kombiwetten zu erstellen. Neben dem klassischen Online-Casino präsentiert sich Legiano mit einer beeindruckenden Sportwettenplattform, die sowohl Einsteiger als auch erfahrene Tipper anspricht. Die 200 Freispiele werden nicht auf einmal, sondern in mehreren Etappen gutgeschrieben. Der Mindestbetrag für die erste Einzahlung beträgt CHF 20, um den Bonus zu erhalten. Das Legiano Casino bietet seinen Spielern eine breite Palette an Boni, die sowohl neue als auch bestehende Kunden ansprechen. Neben einem großzügigen Willkommensbonus profitieren Stammkunden von exklusiven Aktionen, einem VIP-Programm und einer benutzerfreundlichen App.
Wir übernehmen keine Haftung für Ihr Verhalten. Die Spielauswahl weiß zu überzeugen, ebenso der Kundenservice und auch die Zahlungen laufen problemlos ab. Sie kommen insgesamt zu einem positiven Eindruck, wobei besonders die gute Spielauswahl und der gute Kundenservice gelobt werden. Sollte es einmal nicht so sehr drängen, können Sie außerdem eine Mail an schicken. Wir legen dabei Wert auf eine möglichst schnelle, problemfreie Kommunikation, die schnelle Lösungen anbietet. Wir haben Ihnen einige Beispiele herausgesucht. Teilweise umfasst das Mechaniken und Features wie Megaways, Bonuskäufe oder Sofortspiele.
References:
https://online-spielhallen.de/vulkan-vegas-deutschland-test-angebote/
лицензирование 1С ERP дистанционно Нс Диджитал Франчайзинг 1С Бухалтерия, продажа и разработка продуктов 1с
казино с выводом без верификации документов бесплатно
топ 10 казино
бездепозитные бонусы за регистрацию в казино с выводом
бездепозитные бонусы за регистрацию в казино с выводом без пополнения
мебель на заказ недорого по индивидуальным размерам Встроенная мебель на заказ прихожая: Оптимизируйте пространство прихожей с помощью встроенной мебели, созданной по индивидуальному проекту и с учетом ваших потребностей.
10 euros offert paris sportif|10 euros offert sans dépôt paris sportif|10 meilleurs sites de paris sportifs|100 euro offert paris sportif|100 euros offert paris sportif|100 euros remboursé paris sportifs|100
offert pari sportif|100 offert paris sportif|100
remboursé paris sportif|100e offert pari sportif|abandon paris
sportif tennis|abandon tennis paris sportif|addiction paris sportif forum|age paris sportif
belgique|aide au pari sportif|aide au paris sportif|aide aux paris sportif|aide aux
paris sportifs|aide pari sportif|aide pari sportif football|aide parie sportif|aide paris sportif|aide paris sportif foot|aide paris sportif gratuit|aide paris sportifs|aide pour paris sportif|algorithme de paris sportif|algorithme
excel paris sportif|algorithme gratuit paris sportif|algorithme pari sportif|algorithme paris sportif|algorithme paris
sportif avis|algorithme paris sportif basket|algorithme paris sportif excel|algorithme paris sportif gratuit|algorithme paris sportif tennis|algorithme paris sportifs|algorithme pour paris sportif|analyse cote paris sportif|analyse de
paris sportif|analyse match paris sportif|analyse pari sportif|analyse paris sportif|analyse paris sportif foot|analyse paris sportif football|analyse paris
sportif gratuit|analyse paris sportifs|ancienne cote paris sportif|api
cote paris sportif|app paris sportif sans argent|appli de paris sportif|appli de paris sportif sans argent|appli de paris sportifs|appli
pari sportif|appli pari sportif gratuit|appli parie sportif|appli paris sportif|appli paris sportif avec paypal|appli paris sportif belgique|appli paris sportif entre amis|appli paris sportif gratuit|appli paris sportif sans argent|appli paris sportif suisse|appli paris sportifs|application aide paris sportif|application algorithme paris sportif|application analyse paris sportif|application android paris sportif|application bankroll
paris sportif|application conseil paris sportif|application de pari sportif|application de parie sportif|application de paris sportif|application de paris sportif en afrique|application de
paris sportif en cote d’ivoire|application de paris sportif en ligne|application de
paris sportif gratuit|application de paris sportif international|application de paris sportif suisse|application de paris
sportifs|application faux paris sportifs|application gestion bankroll paris sportif|application gestion paris sportif|application ia paris sportif|application pari sportif
gratuit|application paris sportif|application paris sportif android|application paris sportif argent fictif|application paris sportif belgique|application paris sportif canada|application paris sportif espagne|application paris sportif espagnol|application paris sportif fictif|application paris sportif france|application paris sportif
gratuit|application paris sportif gratuit entre amis|application paris sportif maroc|application paris sportif offre de bienvenue|application paris
sportif paypal|application paris sportif sans argent|application paris sportif sans justificatif de domicile|application paris
sportif suisse|application paris sportif usa|application paris sportif virtuel|application pour
faire des paris sportifs|application pour gerer ses paris sportif|application pour les paris sportifs|application pour pari sportif|application pour paris sportif|application pour paris sportifs|application statistique paris sportif|application suivi paris sportif|applications
de paris sportifs|applications paris sportifs|applis paris sportif|applis paris sportifs|apprendre a faire des paris sportifs|argent facile paris
sportif|argent offert paris sportifs|argent offert sans
depot paris sportif|argent paris sportif|argent paris sportifs|argent paris sportifs impots|argent sans depot paris sportif|arjel paris sportif|arjel paris sportifs|astuce gagner paris
sportif|astuce pari sportif|astuce paris sportif|astuce paris sportif basket|astuce paris sportif
foot|astuce paris sportif forum|astuce paris
sportif tennis|astuce paris sportifs|astuce pour gagner au pari sportif|astuce pour gagner au paris sportif|astuce pour gagner paris sportif|astuce pour paris sportif|astuces paris sportifs|astuces paris sportifs en ligne|astuces paris sportifs foot|astuces pour gagner aux paris sportifs|autorisation paris sportif france|avis pari sportif|avis paris sportif|avis
paris sportif foot|avis site de paris sportif|avis site paris sportif|avis sur les paris sportifs|avis sur paris sportif|avis
tipster paris sportif|aweh signification paris sportif|bankroll 100 euros paris sportifs|bankroll
management paris sportif|bankroll paris sportif|bankroll paris sportif excel|bankroll paris
sportif gratuit|bankroll paris sportifs|basket paris sportif|belgique france paris sportif|belgique paris sportifs|bonus bienvenue paris sportif|bonus bienvenue paris sportifs|bonus cash paris sportif|bonus de bienvenue paris sportif|bonus de bienvenue paris sportif belgique|bonus de bienvenue sans depot paris sportif|bonus de depot paris sportif|bonus de paris sportifs|bonus depot paris
sportif|bonus en cash paris sportif|bonus gratuit paris sportif|bonus
gratuit sans depot paris sportif|bonus pari sportif|bonus paris sportif|bonus paris sportif belgique|bonus paris sportif betclic|bonus
paris sportif cash|bonus paris sportif en ligne|bonus paris sportif france pari|bonus paris sportif retirable|bonus paris sportif sans depot|bonus paris sportif
sans dépôt|bonus paris sportif unibet|bonus paris sportifs|bonus sans depot paris
sportif|bonus sans depot paris sportif belgique|bonus sans dépôt paris sportif|bonus sans dépôt paris sportif
hors arjel|bonus site de paris sportif|bonus site pari sportif|bonus site paris sportif|bonus sites de paris
sportifs|bonus unibet paris sportif|bookmaker paris sportif|bookmaker paris sportif gratuit|bookmaker paris sportifs|bookmaker sportif|bookmakers
paris sportif|bookmakers paris sportifs|bookmakers paris sportifs
en ligne|but contre son camp paris sportif|but sur penalty paris sportif|buteur paris sportif|c’est quoi handicap
paris sportif|c’est quoi une cote paris sportif|calcul anti perte paris sportif|calcul combinaison pari sportif|calcul cote pari
sportif|calcul cote paris sportif|calcul couverture paris sportif|calcul de cote paris sportif|calcul des cotes paris sportifs|calcul dnb
paris sportifs|calcul double chance paris sportif|calcul gain paris sportif|calcul mise paris
sportif|calcul pari sportif|calcul paris sportif|calcul paris sportif multiple|calcul pourcentage cote paris sportif|calcul probabilité paris sportif|calcul rentabilité paris
sportifs|calcul roi paris sportif|calcul systeme paris sportif|calcul trj paris sportifs|calculateur cote paris sportif|calculateur de cote paris sportif|calculateur de mise paris sportif|calculateur de paris sportif|calculateur paris sportif|calculatrice arbitrage paris sportif|calculatrice
paris sportif|calculer cote paris sportif|calculer gain paris sportif|calculer
probabilité paris sportifs|calculer roi paris sportifs|calculer une
cote pari sportif|calculer une cote paris sportif|carte cadeau
paris sportif|carte pcs paris sportif|carte prépayée paris sportifs|cash
out pari sportif|cash out paris sportif|cash out paris sportifs|casino en ligne paris sportif|casino paris sportif
en ligne|champions league paris sportif|chute de cote paris sportif|classement
des meilleurs sites de paris sportifs|classement meilleur site
de paris sportif|code barre paris sportif|code bonus paris sportif|code paris sportif|code promo
pari sportif|code promo paris sportif|code promo paris sportif
sans depot|code promo paris sportif sans dépôt|code promo sans depot paris
sportif|code promo site paris sportif|combien de temps pour encaisser
un paris sportif|combien de temps pour retirer un paris sportif|combien miser paris sportifs|combine paris sportif|combines paris sportifs|combiné pari sportif|combiné paris sportif|combiné paris
sportif conseil|combiné paris sportif du jour|combiné paris sportif pronostic|comment analyser un paris
sportif|comment arreter de jouer aux paris sportifs|comment arreter les paris sportif|comment arreter les paris sportifs|comment arrêter les paris sportifs|comment bien gagner au paris
sportif|comment bien jouer au paris sportif|comment bien miser paris
sportif|comment ca marche les paris sportif|comment calculer cote paris sportif|comment calculer gain paris sportif|comment calculer les cotes des paris sportifs|comment calculer une cote de paris sportif|comment
calculer une cote pari sportif|comment calculer une cote paris sportif|comment comprendre les paris sportifs|comment creer un vip paris sportif|comment créer un algorithme paris sportif|comment créer
un site de paris sportif|comment devenir riche avec les paris sportifs|comment etre rentable paris sportif|comment etre sur de gagner au paris
sportif|comment faire de bon paris sportif|comment faire des parie sportif|comment faire des paris sportif|comment faire des
paris sportif gagnant|comment faire des paris sportifs|comment faire pari sportif|comment faire paris sportif|comment faire pour
arreter les paris sportifs|comment faire pour gagner au paris
sportif|comment faire pour gagner les paris sportifs|comment faire un bon pari sportif|comment faire un bon paris sportif|comment faire un pari
sportif|comment faire un parie sportif|comment faire un paris sportif|comment faire une montante paris
sportif|comment fonctionne les cotes dans les paris sportifs|comment fonctionne les cotes des paris sportifs|comment
fonctionne les paris sportifs|comment fonctionne paris sportifs|comment fonctionne
un pari sportif|comment fonctionnent les cotes dans les paris sportifs|comment fonctionnent les cotes dans les paris sportifs grand oral|comment fonctionnent les
cotes de paris sportif|comment fonctionnent
les paris sportifs|comment fonctionnent les
paris sportifs grand oral|comment fonctionnent les paris sportifs grand oral
maths|comment fonctionnent les paris sportifs maths|comment gagner a coup sur au paris sportif|comment gagner a tous les coups
au paris sportif|comment gagner a tout les coup
au paris sportif|comment gagner au pari sportif|comment gagner au pari sportif football|comment gagner au paris sportif|comment gagner au
paris sportif a coup sur|comment gagner au paris sportif foot|comment gagner au
paris sportif forum|comment gagner au paris sportif tennis|comment
gagner au paris sportifs|comment gagner aux paris sportif|comment gagner aux paris
sportifs|comment gagner aux paris sportifs foot|comment gagner aux paris sportifs livre|comment gagner aux paris sportifs sur
le long terme|comment gagner avec les paris sportifs|comment gagner
dans les paris sportifs|comment gagner de l argent avec
les paris sportifs|comment gagner de l’argent au paris sportif|comment gagner de l’argent aux paris sportifs|comment gagner
de l’argent avec les paris sportifs|comment gagner de l’argent paris sportif|comment
gagner de l’argent sur les paris sportifs|comment gagner de
l’argent sur paris sportif|comment gagner des paris sportif|comment gagner des paris sportifs|comment gagner en paris sportif|comment gagner facilement au paris sportif|comment gagner les paris sportifs|comment gagner
paris sportif|comment gagner paris sportif foot|comment gagner paris sportifs|comment gagner sa vie avec les paris sportifs|comment gagner ses paris sportif|comment gagner sur les paris sportif|comment gagner sur les paris sportifs|comment gagner tout le temps au paris sportif|comment gagner un pari sportif|comment gagner un paris sportif|comment gerer une bankroll paris
sportif|comment gérer sa bankroll paris sportif|comment jouer
au pari sportif|comment jouer au paris sportif|comment jouer au paris sportif foot|comment
jouer aux paris sportifs|comment jouer paris sportif|comment marche cote paris
sportif|comment marche les cotes paris sportif|comment marche les paris sportif|comment
marche les paris sportifs|comment marche paris sportif|comment marche un pari sportif|comment marche un paris sportif|comment marchent les cotes paris sportif|comment marchent les paris
sportifs|comment miser au paris sportif|comment miser
paris sportif|comment monter sa bankroll paris sportif|comment ne jamais perdre
au paris sportif|comment parier sportif|comment reussir au paris sportif|comment reussir
les paris sportif|comment reussir paris sportif|comment sont calculer
les cotes de paris sportif|comment sont calculées les
cotes des paris sportifs|comment sont calculés les cotes des paris sportifs|comment sont faites les cotes des paris
sportifs|comment toujours gagner au paris sportif|comment ça marche les paris sportifs|comparaison bonus paris sportifs|comparaison cote pari
sportif|comparaison des cotes paris sportifs|comparateur cote pari
sportif|comparateur cote paris sportif|comparateur cotes
paris sportif|comparateur cotes paris sportifs|comparateur de cote
pari sportif|comparateur de cote paris sportif|comparateur de cotes paris sportifs|comparateur
de côtes paris sportifs|comparateur de paris sportif|comparateur de site de paris sportif|comparateur de site paris sportif|comparateur de sites
de paris sportifs|comparateur pari sportif|comparateur paris sportif|comparateur paris sportifs|comparateur site de paris sportif|comparateur site pari sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif bonus paris
sportifs|comparatif cote pari sportif|comparatif cote paris
sportif|comparatif cotes paris sportifs|comparatif des sites de paris sportifs|comparatif offre
de bienvenue paris sportif|comparatif offre paris sportif|comparatif pari sportif|comparatif pari sportif en ligne|comparatif paris sportif|comparatif paris sportif bonus|comparatif
paris sportif en ligne|comparatif paris sportifs|comparatif paris sportifs en ligne|comparatif
site de paris sportif|comparatif site paris sportif|comparatif
site paris sportifs|comparatif sites de paris sportifs|comparatif sites paris sportifs|comparer les cotes paris sportifs|comprendre cote paris sportif|comprendre handicap paris sportif|comprendre les cotes des
paris sportifs|comprendre les cotes paris sportif|comprendre les cotes
paris sportifs|comprendre les handicap paris sportif|compte de paris sportif|compte démo
paris sportif|compte finance paris sportif|compte financer paris sportif|compte financier paris sportif|compte financé paris sportif|compte pari sportif|compte paris sportif|compte paris sportif financé|conseil de paris sportif|conseil de
paris sportifs|conseil en paris sportif|conseil
en paris sportifs|conseil pari sportif|conseil pari sportif gratuit|conseil paris sportif|conseil
paris sportif aujourd’hui|conseil paris sportif du jour|conseil paris sportif foot|conseil paris sportif gratuit|conseil paris sportif ligue
des champions|conseil paris sportif nba|conseil paris sportif pronostic|conseil
paris sportif rmc|conseil paris sportif tennis|conseil
paris sportifs|conseil pour gagner au paris sportif|conseil pour paris sportif|conseil sur les paris sportifs|conseille paris sportif|conseiller en paris sportifs|conseiller paris sportif|conseils
de paris sportifs|conseils en paris sportifs|conseils paris sportifs|conseils paris sportifs foot|conseils paris sportifs gratuit|conseils paris sportifs tennis|conseils pour paris sportifs|cote a 100 paris sportif|cote a 2 paris sportif|cote anglaise paris sportif|cote de 2 paris sportif|cote
de pari sportif|cote de paris sportif|cote des paris sportifs|cote maximum paris sportif|cote minimum paris sportif|cote
pari sportif|cote pari sportif comment ça marche|cote pari sportif real madrid|cote
pari sportif rugby|cote parie sportif|cote paris sportif|cote paris sportif belgique|cote
paris sportif calcul|cote paris sportif definition|cote paris sportif euro|cote
paris sportif explication|cote paris sportif foot|cote paris
sportif france belgique|cote paris sportif france espagne|cote paris sportif ligue des champions|cote
paris sportif moto gp|cote paris sportif psg|cote paris sportif
psg arsenal|cote paris sportif rugby|cote paris sportif tennis|cote
paris sportifs|cote pour paris sportifs|cote sportif foot|cote sportif rugby|cote
à 1000 paris sportif|cotes de paris sportifs|cotes pari sportif|cotes paris sportif|cotes paris sportifs|cotes
paris sportifs foot|coupe de france paris sportif|créer un algorithme
paris sportif|créer un compte paris sportif|créer un site de
paris sportif en ligne|dans les paris sportifs que signifie handicap|declarer ses gains paris sportif|definition cash out paris sportif|definition cote
paris sportif|definition handicap paris sportif|depot 5 euros paris sportif|depot
double paris sportif|depot minimum 5 euro paris sportif|depot minimum paris
sportif|depot paris sportif|depuis quand existe les paris sportif en france|devenir riche avec les paris sportifs|devenir riche avec paris
sportifs|disqualification tennis paris sportif|dnb en paris sportif|dnb pari sportif|dnb paris sportif|dnb paris sportif definition|dnb
paris sportifs|doit on declarer les gains de paris sportif|déclarer gains paris sportifs|déclarer gains paris sportifs
hors arjel|définition bankroll paris sportif|dépôt minimum 1 euro paris
sportif|dépôt minimum 5 euro paris sportif|ecart de jeux tennis
paris sportif|erreur de cote paris sportif|est ce que les gains des paris sportifs sont imposables|est-ce que les prolongation compte dans un pari sportif|etre sur de gagner au
paris sportif|euro paris sportif|evenement sportif a paris|evenement sportif
paris|evenement sportif paris 2025|evenement sportif paris aujourd hui|evenement sportif paris aujourd’hui|evenement sportif paris ce week end|evenements sportif paris|evenements sportifs paris|evenements sportifs paris 2025|evenements sportifs à paris|evolution cote paris sportif|evolution cotes paris sportifs|evolution des cotes paris sportifs|explication cote pari sportif|explication cote paris
sportif|explication handicap paris sportif|explication pari sportif|explication paris
sportif|face a face hockey paris sportif|faire des paris sportif|faire des
paris sportif avec paypal|faire des paris sportifs|faire fortune paris sportifs|faire un pari sportif|faire un paris sportif|faut il déclarer les
gains de paris sportifs|faut il déclarer ses gains paris sportifs|fichier excel gestion bankroll paris sportif|fiscalité gains paris sportifs|foot paris sportif|football et paris sportifs|forfait tennis paris sportif|formation paris sportif gratuit|forum
de paris sportif|forum de paris sportifs|forum pari sportif|forum parie
sportif|forum paris sportif|forum paris sportif foot|forum paris sportif gratuit|forum paris sportif nba|forum
paris sportif tennis|forum paris sportifs|forum sur les paris sportifs|forum tennis paris sportif|francaise des jeux pari sportif|francaise des jeux paris sportif|francaise des jeux paris sportifs|france 2
paris sportif|france 2 paris sportifs|france belgique
paris sportif|france espagne paris sportif|france pari sportif|france pari sportif brest|france paris sportif|france paris sportifs|france pologne paris sportif|france portugal paris sportif|france suisse paris sportifs|france tunisie paris
sportifs|france-pari – paris sportifs|gagnant pari sportif|gagnant paris
sportif|gagnant paris sportif bayern|gagnante paris sportif|gagne au paris sportif|gagner 10 euros par jour aux paris sportifs|gagner
100 euros par jour paris sportif|gagner 1000 euros par mois paris sportifs|gagner 10000 euros paris sportif|gagner 2000 euros par mois paris sportif|gagner 50 euros par jour paris
sportif|gagner a coup sur au paris sportif|gagner a coup sur pari
sportif|gagner a tous les coup paris sportif|gagner argent avec
paris sportifs|gagner argent pari sportif|gagner argent paris sportif|gagner argent paris sportifs|gagner au pari sportif|gagner au paris sportif|gagner au paris
sportif a coup sur|gagner au paris sportif foot|gagner au paris sportif forum|gagner au
paris sportif à coup sur|gagner aux paris sportif|gagner aux paris sportifs|gagner aux paris sportifs pdf|gagner beaucoup d’argent paris sportif|gagner de l argent grace aux paris sportifs|gagner
de l argent pari sportif|gagner de l argent paris sportif|gagner
de l argent paris sportifs|gagner de l’argent au
paris sportif|gagner de l’argent aux paris sportifs|gagner de l’argent avec les paris
sportifs|gagner de l’argent avec paris sportif|gagner de l’argent avec paris sportifs|gagner de l’argent grace au paris sportif|gagner de l’argent grace
aux paris sportifs|gagner de l’argent pari sportif|gagner de l’argent paris
sportif|gagner de l’argent paris sportifs|gagner de l’argent
sur les paris sportifs|gagner des paris sportif|gagner des paris sportifs|gagner les paris sportifs|gagner pari sportif|gagner paris sportif|gagner paris sportif foot|gagner paris sportif forum|gagner paris
sportif tennis|gagner paris sportifs|gagner sa vie avec les paris sportif|gagner sa vie avec les paris sportifs|gagner sa vie avec paris sportifs|gagner
ses paris sportifs|gagner à coup sur paris sportif|gagner à tous les coups paris
sportifs|gain maximum paris sportif|gain pari sportif|gain pari sportif imposable|gain pari sportif impot|gain paris sportif|gain paris sportif imposable|gain paris sportif impot|gain paris
sportif impôt|gains paris sportif|gains paris sportif imposable|gains paris sportifs|gains paris sportifs imposable|gains
paris sportifs imposables|gains paris sportifs sont ils imposables|gerer bankroll paris sportif|gerer sa bankroll paris sportif|gerer une bankroll paris sportif|gestion bankroll paris sportif|gestion bankroll paris sportifs|gestion bankroll paris
sportifs excel|gestion de bankroll paris sportif|gestion de bankroll paris sportif application|gestion de bankroll paris sportifs|gestion de mise paris sportif|gestion paris sportifs v2
5 gratuit|gg signification paris sportif|gros combiné paris sportif|gros gain paris sportif|grosse
cote paris sportif pronostic|grosse mise paris sportif|groupe paris sportif gratuit|groupe telegram paris sportif gratuit|groupement de joueurs paris sportifs|handicap 0 paris sportif|handicap 1
paris sportif|handicap 5 paris sportif|handicap au paris
sportif|handicap basket paris sportif|handicap dans les paris
sportifs|handicap en paris sportif|handicap europeen paris sportif|handicap européen paris sportifs|handicap mi temps paris
sportif|handicap pari sportif|handicap paris
sportif|handicap paris sportif basket|handicap paris sportif explication|handicap
paris sportif foot|handicap paris sportif rugby|handicap paris sportifs|handicap
rugby paris sportif|handicap tennis paris sportif|historique cote paris sportif|historique des cotes paris sportifs|hockey paris sportif|hockey sur glace paris sportif|hors arjel
paris sportif|hweh signification paris sportif|imposition gain pari sportif|imposition gain paris sportif|imposition gains
paris sportifs|imposition paris sportif france|impot gain paris sportif|impot
paris sportif france|impot sur gain paris sportif|je gagne ma vie avec les
paris sportifs|jeu de pari sportif gratuit|jeu de paris sportif en ligne|jeu de paris sportif
gratuit|jeu paris sportif gratuit|jeu paris sportif sans argent|jeux de parie sportif|jeux de paris sportif|jeux de paris sportif en ligne|jeux
de paris sportif gratuit|jeux de paris sportifs|jeux olympiques paris sportifs|jeux paris sportif|jeux paris sportif gratuit|jeux paris sportif
virtuel|jeux paris sportifs en ligne|jouer au paris sportif|jouer paris sportif|joueur absent
paris sportif|joueur blesse paris sportif|joueur caen paris sportif|joueur
de caen pari sportif|joueur de foot paris sportif|joueur decisif paris sportif|joueur
décisif paris sportif|joueur italien paris sportif|joueur paris sportif|joueur professionnel paris sportif|joueur qui se blesse paris sportif|joueur sanctionne pari sportif|joueur suspendu paris sportif|joueurs italiens paris sportifs|l’argent des paris
sportifs est il imposable|la cote paris sportif|la francaise des jeux paris sportif|la martingale paris sportif|la martingale paris sportifs|la meilleur application de paris sportif|la meilleur
application paris sportif|la meilleur technique pour gagner au paris sportif|la méthode secrète pour gagner aux paris sportifs pdf|la plus grosse cote gagner paris sportif|la plus grosse cote paris sportif|ldem paris sportif signification|le marché des
paris sportifs|le meilleur site de pari sportif|le meilleur site de paris sportif|le meilleur site de paris
sportif en ligne|le meilleur site de paris sportifs|le plus gros gain au paris sportif|le plus
gros paris sportif|le plus gros paris sportif du monde|les
10 meilleurs sites de paris sportifs|les 10 meilleurs sites de paris sportifs en afrique|les 17 secrets pour gagner rapidement aux paris sportifs|les 17 secrets pour gagner rapidement aux paris sportifs
pdf|les application de paris sportif|les applications
paris sportifs|les bonus paris sportifs|les bookmakers paris sportifs|les cotes paris sportifs|les gains de paris sportifs sont ils imposables|les gains des paris sportifs sont
ils imposables|les jeux de paris sportifs|les meilleur paris sportif|les
meilleures applications de paris sportifs|les meilleurs applications de paris
sportifs|les meilleurs bonus paris sportif|les meilleurs bonus paris sportifs|les meilleurs cotes paris sportif|les meilleurs paris sportifs|les meilleurs paris
sportifs du jour|les meilleurs site de paris sportif|les meilleurs site de paris sportifs|les meilleurs sites de
pari sportif|les meilleurs sites de paris sportifs|les meilleurs sites de paris
sportifs en ligne|les paris sportif|les paris sportif avis|les
paris sportifs|les paris sportifs comment ça marche|les paris
sportifs en france|les paris sportifs en ligne|les paris sportifs en ligne comprendre
jouer gagner|les paris sportifs en ligne comprendre jouer gagner pdf|les paris sportifs les plus rentables|les
plus gros gagnant paris sportif|les plus gros gains au paris sportifs|les plus gros gains paris sportifs|les plus gros
paris sportif|les plus grosse cote paris sportif|les
plus grosses pertes paris sportifs|les sites de paris sportifs|les sites de paris sportifs autorisés en france|les sites de paris sportifs en france|les sites de paris sportifs en ligne|les sites de paris sportifs francais|ligue 1
paris sportif|ligue 1 paris sportifs|ligue 2 paris sportif|ligue des champions paris
sportif|limite de gains paris sportifs|limite de mise paris sportif|limite
gain paris sportif|limite mise paris sportifs|liste de paris
sportif|liste des paris sportifs|liste des site de paris sportif|liste des sites
de paris sportifs|liste pari sportif|liste paris sportif|liste paris sportif pdf|liste site
de paris sportif|liste site pari sportif|liste site paris sportif|liste site paris sportif arjel|liste sites paris sportifs|logiciel algorithme paris sportif|logiciel algorithme paris
sportif gratuit|logiciel analyse paris sportif|logiciel calcul paris sportif|logiciel de
pari sportif|logiciel de paris sportif|logiciel de paris sportif gratuit|logiciel gestion bankroll paris sportif gratuit|logiciel
gestion de bankroll paris sportif|logiciel gestion paris sportif|logiciel gestion paris
sportif gratuit|logiciel gestion paris sportifs|logiciel
pari sportif|logiciel paris sportif|logiciel paris
sportif gratuit|logiciel paris sportifs|logiciel paris
sportifs foot sur 2 matchs|logiciel pour paris sportif|logiciel pour paris sportifs|logiciel prediction paris sportif|logiciel probabilité paris
sportif|logiciel prédiction paris sportif|logiciel statistique paris sportifs|logiciel variation de cote
paris sportif|loi sur les paris sportifs en france|magic calculator paris sportif|marché des paris sportifs|marché des paris sportifs en france|marché des
paris sportifs en ligne|martingale pari sportif|martingale paris sportif|martingale paris sportif
excel|martingale paris sportif forum|martingale paris sportif interdit|martingale paris sportifs|match abandonné paris sportif|match annulé ou reporté paris sportifs|match annulé paris
sportif|match arrete paris sportif|match interrompu paris sportif|match interrompu tennis
paris sportif|match interrompu tennis pluie paris
sportif|match nul boxe paris sportif|match pari sportif|match paris sportif|match reporté paris sportif|match suspendu paris sportif|match suspendu tennis paris sportif|match truqué paris sportif|matchs truqués paris sportifs|meilleur algorithme paris sportif|meilleur algorithme paris sportif gratuit|meilleur app de paris sportif|meilleur app de paris sportifs|meilleur app paris sportif|meilleur appli de pari sportif|meilleur appli de paris
sportif|meilleur appli pari sportif|meilleur appli paris sportif|meilleur appli paris
sportif forum|meilleur appli paris sportifs|meilleur application conseil paris sportif|meilleur application de paris
sportif|meilleur application de paris sportif
en afrique|meilleur application pari sportif|meilleur application paris sportif|meilleur application paris sportif belgique|meilleur application pour les
paris sportif|meilleur application pour pari
sportif|meilleur bonus de bienvenue paris sportif|meilleur bonus pari sportif|meilleur bonus paris sportif|meilleur bonus paris sportif
sans depot|meilleur bonus paris sportifs|meilleur bonus site
de paris sportif|meilleur bonus site pari sportif|meilleur bonus site
paris sportif|meilleur bookmaker paris sportif|meilleur combiné paris
sportif|meilleur conseil paris sportif|meilleur cote de paris sportif|meilleur cote pari sportif|meilleur cote paris sportif|meilleur cote paris sportif aujourd’hui|meilleur
cote site paris sportif|meilleur forum paris sportifs|meilleur gain paris sportif|meilleur
ia paris sportif|meilleur methode pour gagner au paris sportif|meilleur offre bienvenue paris sportif|meilleur offre bonus paris sportif|meilleur offre de bienvenue paris sportif|meilleur offre de bienvenue
paris sportifs|meilleur offre pari sportif|meilleur offre paris sportif|meilleur offre paris sportif en ligne|meilleur
pari sportif|meilleur pari sportif du jour|meilleur pari
sportif en ligne|meilleur paris sportif|meilleur paris sportif
aujourd’hui|meilleur paris sportif du jour|meilleur paris sportif en ligne|meilleur paris sportif foot|meilleur promo paris
sportif|meilleur pronostic paris sportif|meilleur site de conseil paris sportif|meilleur site de pari sportif|meilleur site de pari sportif en ligne|meilleur site de paris
sportif|meilleur site de paris sportif avis|meilleur site de paris sportif belgique|meilleur site de paris sportif canada|meilleur site de paris sportif en france|meilleur site de paris sportif en ligne|meilleur site de paris sportif
football|meilleur site de paris sportif forum|meilleur site de
paris sportif france|meilleur site de paris sportif hors arjel|meilleur site de paris sportif international|meilleur site de paris
sportif suisse|meilleur site de paris sportifs|meilleur site de paris sportifs en ligne|meilleur site
pari sportif|meilleur site pari sportif en ligne|meilleur site pari sportif france|meilleur site paris sportif|meilleur site paris sportif avis|meilleur site paris sportif belgique|meilleur site paris sportif
canada|meilleur site paris sportif en ligne|meilleur site paris
sportif foot|meilleur site paris sportif forum|meilleur site paris sportif france|meilleur site paris
sportif hors arjel|meilleur site paris sportif nba|meilleur site paris sportif rugby|meilleur site paris sportif suisse|meilleur site paris sportifs|meilleur site pour pari sportif|meilleur site pour paris sportif|meilleur site pronostic paris sportif|meilleur strategie paris sportif|meilleur technique de paris sportif|meilleur technique paris sportif|meilleur technique pour gagner au paris sportif|meilleure appli de
paris sportif|meilleure appli de paris sportifs|meilleure appli pari
sportif|meilleure appli paris sportif|meilleure appli paris sportifs|meilleure
application de paris sportif|meilleure application de paris sportifs|meilleure application pari
sportif|meilleure application paris sportif|meilleure application paris sportif
android|meilleure application paris sportifs|meilleure offre paris sportif|meilleure site paris sportif|meilleure strategie paris sportif|meilleures applications de paris
sportifs|meilleures applications paris sportifs|meilleures cotes paris sportifs|meilleures offres paris
sportifs|meilleures stratégies paris sportifs|meilleurs appli paris sportif|meilleurs application de paris sportifs|meilleurs application paris sportif|meilleurs applications paris sportifs|meilleurs
bonus paris sportifs|meilleurs cote paris sportif|meilleurs cotes paris sportifs|meilleurs offres
paris sportifs|meilleurs paris sportifs|meilleurs paris sportifs du jour|meilleurs site de pari sportif|meilleurs site de paris sportif|meilleurs
site de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs site
paris sportif|meilleurs sites de paris sportifs|meilleurs sites de paris sportifs en ligne|meilleurs sites paris sportif|meilleurs sites paris sportifs|methode abc
paris sportif|methode de paris sportif|methode gagnante paris sportifs|methode gagner paris sportif|methode infaillible paris sportifs|methode martingale paris sportif|methode mathematique paris sportif|methode mathematique pour gagner au paris sportif|methode paris
sportif|methode paris sportif foot|methode paris sportif
forum|methode paris sportif tennis|methode paris sportifs|methode pour gagner au
paris sportif|methode pour gagner paris sportif|methodes
paris sportifs|minimum depot paris sportif|mise au jeu pari sportif|mise
maximum pari sportif|mise maximum paris sportif|mise minimum paris sportif|mise moyenne paris sportif|mise paris
sportif|moins de 4 5 but paris sportif|montant maximum paris sportif|montant paris sportif|montante pari sportif|montante parie sportif|montante paris sportif|montante paris sportifs|montantes paris
sportifs|multiple pari sportif|multiple paris sportif|multiple paris sportifs|multiples paris sportifs|méthode calcul paris sportif|méthode match nul paris sportifs|méthode
mathématique pour gagner au paris sportif|méthode paris sportif forum|méthode paris sportif hockey|nba pari sportif|nba
paris sportif|nba paris sportifs|nouveau paris sportif|nouveau site
de pari sportif|nouveau site de paris sportif|nouveau site
de paris sportif en ligne|nouveau site de paris sportifs|nouveau site pari sportif|nouveau site paris sportif|nouveau site paris sportif france|nouveau site paris sportifs|nouveaux sites
de paris sportifs|nouveaux sites paris sportifs|nouvelle appli paris sportif|nouvelle application de paris sportif|numero de match paris sportif|numero match paris sportif|offre 100 euros paris sportif|offre appli
pari sportif|offre bienvenu paris sportif|offre bienvenue
pari sportif|offre bienvenue paris sportif|offre bienvenue paris sportifs|offre bienvenue site paris sportif|offre bonus paris sportif|offre de bienvenu paris sportif|offre de bienvenue pari sportif|offre de bienvenue paris sportif|offre de bienvenue paris sportif belgique|offre
de bienvenue paris sportif sans depot|offre de bienvenue paris sportif
sans dépôt|offre de bienvenue paris sportifs|offre
de bienvenue sans depot paris sportif|offre
de bienvenue site paris sportif|offre euro paris sportif|offre pari sportif euro|offre paris sportif|offre paris sportif belgique|offre paris sportif cash|offre paris sportif coupe du monde|offre paris sportif hors arjel|offre paris sportif remboursé|offre paris sportif remboursé cash|offre paris sportif sans depot|offre promo paris sportif|offre remboursement paris sportif|offre sans depot paris sportif|offre site paris sportif|offres bienvenue paris sportifs|offres de bienvenue
paris sportifs|ou faire des paris sportif|ou faire des paris sportif en espagne|ou faire des paris sportifs|outil
répartiteur de mise paris sportif|outils repartiteur de mises paris
sportif|ouverture compte paris sportifs|ouvrir un compte paris sportif|pack
de bienvenue paris sportif|pack de bienvenue paris sportif hors arjel|pari en ligne sportif|pari sportif|pari sportif 100 euros offert|pari sportif 100 remboursé|pari
sportif abandon tennis|pari sportif aide|pari sportif algérie aujourd’hui|pari sportif appli|pari sportif application|pari
sportif argent|pari sportif astuce|pari sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari sportif avec orange money|pari sportif avec paypal|pari sportif avec wave|pari sportif avis|pari sportif basket|pari sportif belgique|pari sportif
belgique france|pari sportif bonus|pari sportif
buteur pas titulaire|pari sportif champions league|pari sportif combiné|pari sportif comment|pari
sportif comment gagner|pari sportif comment ça
marche|pari sportif comparatif|pari sportif conseil|pari sportif cote|pari sportif cote match|pari sportif cote psg|pari sportif coupe|pari sportif coupe de france|pari sportif coupe du monde|pari sportif depot|pari sportif du jour|pari sportif en france|pari sportif en ligne|pari
sportif en ligne au cameroun|pari sportif en ligne belgique|pari
sportif en ligne canada|pari sportif en ligne france|pari sportif en ligne gratuit|pari sportif en ligne suisse|pari sportif en ligne ufc|pari sportif en suisse|pari sportif euro|pari sportif explication|pari sportif faire|pari sportif foot|pari sportif foot resultat|pari sportif
football|pari sportif forum|pari sportif francaise des jeux|pari
sportif france|pari sportif france angleterre|pari sportif france argentine|pari sportif
france autriche|pari sportif france belgique|pari sportif france espagne|pari sportif france italie|pari sportif france portugal|pari sportif france usa|pari sportif gagnant|pari
sportif gagner|pari sportif gagner a tous les coups|pari sportif gagner
de l’argent|pari sportif gain|pari sportif gratuit|pari sportif gratuit pour gagner des cadeaux|pari sportif gratuit sans depot|pari sportif handicap|pari sportif hockey|pari sportif hors arjel|pari sportif jeux olympiques|pari sportif joueur absent|pari sportif le plus
rentable|pari sportif leicester champion|pari sportif ligue 1|pari sportif ligue 2|pari sportif ligue des champions|pari sportif
ligue europa|pari sportif match|pari sportif match arrete|pari sportif match interrompu|pari sportif meilleur|pari sportif meilleur cote|pari sportif meilleur
site|pari sportif methode|pari sportif mise|pari
sportif mise au jeu|pari sportif mise o jeu|pari sportif nba|pari
sportif offre bienvenue|pari sportif paypal|pari
sportif plus|pari sportif prolongation|pari sportif promo|pari sportif
pronostic|pari sportif pronostic foot|pari sportif pronostic gagnant|pari sportif pronostic gratuit|pari sportif psg|pari sportif psg bayern|pari sportif psg inter|pari
sportif psg milan|pari sportif regle|pari sportif rembourse|pari
sportif remboursement|pari sportif remboursement cash|pari sportif remboursé|pari
sportif rugby|pari sportif rugby coupe du monde|pari sportif rugby top 14|pari sportif sans argent|pari sportif
sans carte bancaire|pari sportif sans depot|pari sportif signification|pari sportif site|pari sportif statistique|pari sportif suisse|pari sportif systeme|pari sportif technique|pari sportif technique pour
gagner|pari sportif temps reglementaire|pari sportif tennis|pari sportif
tennis abandon|pari sportif top|pari sportif top 14|pari sportif tour de france|parie sportif|parie sportif comment ca marche|parie sportif du jour|parie sportif en ligne|parie sportif foot|parie sportif football|parie sportif france|parie sportif gratuit|parie sportif pronostic|parie sportif suisse|paris en ligne sportif|paris
en ligne sportifs|paris evenement sportif|paris france sportif|paris hippique et sportif|paris hippiques et sportifs|paris hippiques paris sportifs|paris hippiques
paris sportifs et poker en ligne|paris hippiques sportifs|paris match sportif|paris sportif|paris sportif 10 euros offerts|paris sportif 100 euros offert|paris sportif 100 euros
remboursé|paris sportif 100 offert|paris sportif 100 remboursé|paris
sportif 100e offert|paris sportif 150 euros offert|paris sportif 1er
pari remboursé|paris sportif a faire|paris sportif a faire
aujourd’hui|paris sportif a faire ce soir|paris
sportif abandon tennis|paris sportif abandon tennis parions sport|paris sportif aide|paris sportif algorithme|paris sportif
analyse|paris sportif appli|paris sportif application|paris sportif application android|paris sportif apres prolongation|paris sportif argent|paris
sportif argent fictif|paris sportif argent offert|paris sportif argent virtuel|paris sportif arjel|paris sportif arsenal psg|paris sportif astuce|paris
sportif au canada|paris sportif aujourd hui|paris sportif aujourd’hui|paris sportif avec
argent fictif|paris sportif avec bonus sans depot|paris sportif avec carte bancaire|paris sportif avec cryptomonnaie|paris sportif
avec handicap|paris sportif avec paypal|paris sportif avec paysafecard|paris sportif avis|paris sportif
avis expert|paris sportif avis forum|paris sportif bankroll|paris sportif
basket|paris sportif basket coupe de france|paris sportif basket nba|paris sportif basket prolongation|paris sportif belgique|paris sportif belgique
bonus|paris sportif belgique bonus sans depot|paris sportif belgique france|paris sportif belgique suede|paris sportif bonus|paris sportif
bonus bienvenue|paris sportif bonus cash|paris sportif bonus de
bienvenue|paris sportif bonus gratuit|paris sportif bonus gratuit sans depot|paris sportif bonus retirable|paris sportif bonus sans depot|paris
sportif bonus sans depot belgique|paris sportif bookmaker|paris sportif but contre son camp|paris
sportif but temps additionnel|paris sportif buteur|paris
sportif buteur blessé|paris sportif buteur carton rouge|paris sportif buteur contre son camp|paris
sportif buteur non titulaire|paris sportif buteur prolongation|paris sportif buteur qui ne joue pas|paris sportif buteur remplacant|paris sportif calcul
gain|paris sportif canada|paris sportif cash|paris sportif cash out|paris sportif champion ligue 1|paris sportif champions
league|paris sportif classement ligue 1|paris sportif code promo|paris
sportif combine|paris sportif combiné|paris sportif combiné comment
ça marche|paris sportif combiné du jour|paris sportif combiné match reporté|paris sportif
comment ca marche|paris sportif comment faire|paris
sportif comment gagner|paris sportif comment gagner a tous
les coups|paris sportif comment jouer|paris sportif
comment ça marche|paris sportif comparateur cote|paris sportif comparatif|paris sportif conseil|paris sportif conseil gratuit|paris
sportif conseil pour gagner|paris sportif cote|paris sportif
cote et match|paris sportif cote explication|paris sportif cote psg|paris sportif coupe d’europe|paris sportif coupe davis|paris sportif coupe de
france|paris sportif coupe du monde|paris sportif coupe du monde de rugby|paris sportif coupe du monde rugby|paris sportif depot 5 euro|paris sportif depot
minimum|paris sportif depot paypal|paris sportif dnb|paris sportif du jour|paris sportif du jour conseil|paris sportif dépôt 1 euro|paris sportif dépôt minimum
5 euros|paris sportif en belgique|paris sportif en france|paris sportif en ligne|paris sportif en ligne avec paypal|paris sportif en ligne avis|paris sportif
en ligne belgique|paris sportif en ligne bonus|paris
sportif en ligne cameroun|paris sportif en ligne comment gagner|paris sportif en ligne comment ça
marche|paris sportif en ligne france|paris sportif en ligne gratuit|paris
sportif en ligne maroc|paris sportif en ligne paypal|paris sportif en ligne québec|paris sportif en ligne sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris sportif espagne france|paris sportif esport|paris sportif et casino en ligne|paris sportif et hippique|paris sportif et prolongation|paris
sportif euro|paris sportif europa league|paris
sportif explication|paris sportif final ligue des champions|paris sportif
finale ligue des champions|paris sportif foot|paris sportif
foot aide|paris sportif foot astuce|paris sportif foot aujourd’hui|paris sportif foot ce soir|paris sportif foot comment ca marche|paris sportif foot conseil|paris
sportif foot cote|paris sportif foot coupe du monde|paris sportif
foot en ligne|paris sportif foot feminin|paris sportif foot gratuit|paris sportif foot prolongation|paris
sportif foot pronostic|paris sportif foot pronostic gratuit|paris sportif foot regle|paris sportif
foot suisse|paris sportif foot us|paris sportif football|paris sportif football americain|paris sportif football astuces|paris sportif forfait tennis|paris sportif forum|paris sportif francais|paris sportif francaise des jeux|paris
sportif france|paris sportif france 2|paris sportif france allemagne|paris sportif france angleterre|paris sportif france argentine|paris sportif
france autriche|paris sportif france belgique|paris sportif france espagne|paris sportif france
gibraltar|paris sportif france italie|paris sportif france nouvelle zelande|paris
sportif france pologne|paris sportif france portugal|paris sportif france uruguay|paris sportif france usa|paris sportif freebet sans depot|paris sportif gagnant|paris sportif gagnant à coup sûr|paris sportif gagner
a coup sur|paris sportif gagner argent|paris sportif gagner de l’argent|paris sportif gain|paris sportif gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris sportif gratuit appli|paris sportif gratuit avec cadeaux|paris
sportif gratuit cadeaux|paris sportif gratuit en ligne|paris sportif gratuit entre amis|paris sportif gratuit sans argent|paris sportif gratuit sans depot|paris sportif gratuit sans
dépôt|paris sportif gratuits|paris sportif gros gain|paris sportif handicap|paris sportif handicap 0 1|paris
sportif handicap 0-1|paris sportif handicap 1 0|paris sportif
handicap 1-0|paris sportif handicap basket|paris sportif handicap explication|paris sportif handicap foot|paris sportif handicap rugby|paris sportif hippique|paris
sportif hockey|paris sportif hockey nhl|paris sportif hockey sur glace|paris
sportif hors arjel|paris sportif hors arjel france|paris sportif jeux olympiques|paris sportif jeux video|paris sportif joueur blessé|paris sportif joueur blessé pendant le match|paris
sportif joueur de foot|paris sportif joueur decisif|paris sportif joueur
declare forfait|paris sportif joueur déclare forfait|paris sportif joueur
remplacant|paris sportif la francaise des jeux|paris sportif le plus rentable|paris sportif legal en france|paris sportif leicester champion|paris sportif les
18 stratégies pour gagner tous les jours|paris sportif les plus sur|paris sportif les prolongation compte|paris sportif ligne|paris sportif ligue 1|paris sportif ligue
2|paris sportif ligue des champions|paris sportif ligue
des nations|paris sportif ligue europa|paris sportif liste|paris sportif martingale|paris sportif match|paris sportif match abandonné|paris
sportif match annulé|paris sportif match arrêté|paris sportif match du jour|paris sportif match interrompu|paris sportif match reporté|paris sportif match suspendu|paris sportif match tennis interrompu|paris sportif
match truqué|paris sportif meilleur bonus|paris sportif meilleur cote|paris sportif meilleur pronostic|paris sportif
meilleur site|paris sportif methode|paris sportif methode 2 3|paris sportif mi temps fin de match|paris sportif mise au jeu|paris sportif mise maximum|paris sportif mma france|paris sportif moins
de 3.5 but|paris sportif montante|paris sportif moto gp|paris sportif multiple|paris sportif multiple 2 3|paris sportif
multiple 2 3 explication|paris sportif multiple 2 4|paris sportif multiple
2 5|paris sportif multiple 2/3 explication|paris sportif multiple 3 4|paris
sportif multiple explication|paris sportif national 1 foot|paris sportif nba|paris
sportif nba conseil|paris sportif nba pronostic|paris sportif nhl|paris sportif nombre de but|paris sportif nouveau site|paris
sportif numero match|paris sportif offert|paris sportif offre bienvenue|paris sportif offre bienvenue sans depot|paris sportif offre de bienvenue|paris sportif offre sans depot|paris sportif om psg|paris sportif paypal|paris sportif plus de 1.5 but|paris sportif plus de 2 5 but|paris sportif plus
ou moins|paris sportif plus ou moins 2 5 but|paris sportif premier pari remboursé|paris sportif premier paris remboursé|paris sportif prolongation|paris sportif prolongation basket|paris sportif prolongation foot|paris sportif promo|paris sportif pronostic|paris sportif pronostic basket|paris
sportif pronostic des match aujourd hui|paris sportif
pronostic expert gratuit|paris sportif pronostic foot|paris sportif
pronostic forum|paris sportif pronostic gratuit|paris sportif
pronostic tennis|paris sportif psg|paris sportif psg arsenal|paris
sportif psg barcelone|paris sportif psg bayern|paris sportif psg dortmund|paris sportif psg inter|paris
sportif psg inter cote|paris sportif psg liverpool|paris sportif psg om|paris
sportif qr code|paris sportif que veut dire handicap|paris
sportif qui rapporte le plus|paris sportif regle|paris sportif regle prolongation|paris sportif rembourse|paris sportif remboursement cash|paris sportif rembourser|paris
sportif remboursé|paris sportif remboursé cash|paris sportif remboursé en cash|paris sportif retrait paypal|paris sportif rue des joueurs|paris sportif rugby|paris sportif rugby 6 nations|paris sportif rugby coupe du monde|paris sportif rugby top 14|paris sportif safe du jour|paris sportif sans argent|paris sportif sans carte
bancaire|paris sportif sans carte d’identité|paris sportif sans compte bancaire|paris sportif sans depot|paris
sportif sans depot minimum|paris sportif si match suspendu|paris sportif si un joueur abandonne|paris sportif
si un joueur ne joue pas|paris sportif si un joueur se blesse|paris sportif simple ou combiné|paris sportif site|paris
sportif statistique|paris sportif stratégie|paris sportif suisse|paris sportif suisse application|paris sportif suisse en ligne|paris sportif suisse legal|paris sportif suisse légal|paris sportif suisse
romande|paris sportif sur du jour|paris sportif sur le tennis|paris sportif systeme|paris sportif systeme 2 3|paris sportif systeme 2 4|paris sportif systeme 2/3|paris sportif systeme 2/4|paris sportif systeme 3 4|paris sportif systeme 3/4|paris sportif systeme explication|paris sportif
technique|paris sportif technique pour gagner|paris sportif temps additionnel|paris sportif temps reglementaire|paris sportif tennis|paris sportif
tennis abandon|paris sportif tennis conseil|paris sportif tennis de table|paris sportif tennis forfait|paris sportif tennis gratuit|paris
sportif tennis pronostic|paris sportif tennis roland
garros|paris sportif tir au but|paris sportif top 14|paris sportif tour de france|paris sportif ufc|paris sportif ufc france|paris sportif
unibet|paris sportif vainqueur euro|paris sportif vainqueur ligue 1|paris sportif vainqueur ligue des champions|paris sportif via paypal|paris sportif
victoire prolongation|paris sportif vip gratuit|paris sportifs|paris sportifs abandon tennis|paris sportifs aide|paris sportifs analyser un match|paris sportifs arjel|paris sportifs astuces|paris sportifs aujourd’hui|paris sportifs autorisés en france|paris sportifs avec paypal|paris sportifs basket|paris sportifs belgique|paris sportifs bonus|paris sportifs bookmakers|paris sportifs
canada|paris sportifs combiné|paris sportifs comparateur|paris sportifs comparatif|paris sportifs conseils|paris sportifs cotes|paris sportifs coupe
du monde|paris sportifs de football|paris sportifs du
jour|paris sportifs en belgique|paris sportifs en france|paris sportifs en ligne|paris sportifs en ligne belgique|paris sportifs en ligne france|paris sportifs en ligne gratuit|paris sportifs en ligne suisse|paris
sportifs en suisse|paris sportifs et hippiques|paris sportifs euro|paris sportifs foot|paris sportifs foot us|paris
sportifs forum|paris sportifs france|paris sportifs france
espagne|paris sportifs gagner à tous les coups|paris sportifs gratuit|paris
sportifs gratuits|paris sportifs gratuits en ligne|paris sportifs
handicap|paris sportifs hockey|paris sportifs hockey sur galce|paris sportifs hockey sur glace|paris sportifs hors arjel|paris sportifs jeux olympiques|paris sportifs les bookmakers
raflent la mise|paris sportifs ligne|paris sportifs ligue 1|paris sportifs ligue 2|paris sportifs ligue des champions|paris sportifs ligue europa|paris sportifs match interrompu|paris sportifs montante|paris sportifs nba|paris sportifs offre bienvenue|paris sportifs offre de bienvenue|paris sportifs paypal|paris sportifs pronostics|paris sportifs psg|paris sportifs psg inter|paris
sportifs rugby|paris sportifs sans argent|paris sportifs sans
depot|paris sportifs site|paris sportifs sites|paris sportifs statistiques|paris sportifs stratégie|paris sportifs suisse|paris sportifs technique|paris sportifs techniques|paris sportifs tennis|paris sportifs
tennis astuces|paris sportifs top 14|paris sportifs tour de france|part de marché
paris sportifs|paypal pari sportif|paypal paris sportif|paypal paris sportifs|perte d’argent paris
sportifs|peut on devenir riche avec les paris sportifs|peut on gagner
de l’argent avec les paris sportifs|peut on gagner sa vie avec les
paris sportif|peut on vraiment gagner de l’argent avec les paris sportifs|plus gros combine paris sportif|plus gros gagnant paris sportif|plus gros gain paris sportif|plus
gros gain paris sportif au monde|plus gros gain paris sportif france|plus gros gains paris
sportif|plus gros pari sportif|plus gros paris sportif|plus
grosse cote gagner paris sportif|plus grosse
cote pari sportif|plus grosse cote paris sportif|plus grosse mise paris sportif|plus grosse somme gagner au paris sportif|plus ou moins paris
sportif|pourcentage de mise paris sportif|premier pari
sportif remboursé|probabilité cote paris sportif|probabilité paris sportif combiné|prolongation basket
paris sportif|prolongation paris sportif|promo pari
sportif|promo paris sportif|promo site de paris sportif|promo site pari
sportif|promo site paris sportif|promos paris
sportifs|prono paris sportif foot|prono paris sportif gratuit|prono paris sportif tennis|pronostic
de paris sportif|pronostic du jour paris sportif|pronostic foot paris
sportif|pronostic gratuit paris sportif|pronostic
pari sportif|pronostic pari sportif gratuit|pronostic paris sportif|pronostic paris sportif aujourd’hui|pronostic paris sportif du jour|pronostic paris sportif foot|pronostic paris sportif gratuit|pronostic paris sportif tennis|pronostic paris sportifs|pronostics foot statistiques et aides aux paris sportifs|pronostics
paris sportif|pronostics paris sportifs|pronostiqueur paris sportif gratuit|psg arsenal paris sportif|psg bayern paris sportif|psg inter milan paris sportif|psg inter pari sportif|psg inter paris sportif|psg liverpool paris sportif|psg om paris sportif|psg paris sportif|psg
paris sportifs|qr code paris sportif|qu est ce qu un handicap paris
sportif|qu est ce que handicap dans les paris sportif|qu’est
ce qu’un handicap paris sportif|qu’est ce que handicap dans les paris sportif|quand un joueur se blesse paris sportif|que signifie 1/1 en paris sportif|que
signifie 1/2 paris sportif|que signifie 12
en paris sportif|que signifie 1×2 dans les paris sportifs|que signifie btts en paris sportif|que signifie dnb en paris sportif|que signifie draw
en paris sportif|que signifie ft en paris sportif|que signifie gg dans le pari sportif|que
signifie gg en pari sportif|que signifie gg en paris sportif|que signifie handicap dans les paris sportifs|que veut dire dnb en paris sportif|que
veut dire handicap dans les paris sportifs|que veut dire handicap paris sportif|quel appli
pari sportif|quel cote jouer paris sportif|quel est la meilleur appli de paris sportif|quel est le meilleur algorithme de paris sportif|quel est
le meilleur site de pari sportif|quel est le meilleur
site de pari sportif en ligne|quel est le meilleur site de paris sportif|quel est le meilleur site de paris sportif en ligne|quel est le
meilleur site de paris sportifs en ligne|quel est le pari sportif
le plus rentable|quel pari sportif est le plus rentable|quel pari sportif est le plus sûr|quel pari sportif faire aujourd’hui|quel paris sportif faire aujourd’hui|quel paris sportif rapporte le plus|quel
site de paris sportif choisir|quel site de paris sportif rembourse
en cash|quel type de pari sportif est le plus
rentable|quelle application pour paris sportifs|quelle est la
meilleure appli de paris sportif|quelle est la meilleure application de paris sportif|quelle est la meilleure application pour les paris
sportifs|quelle est le meilleur site de paris sportif|quels paris sportifs
faire|quels sont les paris sportifs les plus sûrs|rebond basket paris sportif|record de gain paris sportif|regle buteur
paris sportif|regle de paris sportif|regle
des paris sportif|regle handicap paris sportif|regle handicap paris sportif foot|regle multiple paris
sportif|regle pari sportif|regle paris sportif|regle paris sportif foot|regle paris sportif
multiple|regle paris sportif prolongation|reglement pari sportif|reglement paris sportif|regles paris sportifs|remboursement cash paris sportif|remboursement en cash paris
sportif|remboursement pari sportif|remboursement paris sportif|repartiteur de mise paris sportif|repartiteur de mise
paris sportifs|repartiteur de mises paris sportif|repartiteur mise paris sportif|repartition des mises paris sportif|resultat pari sportif|resultat paris sportif|resultat paris sportif
en direct|resultat paris sportif foot|resultat sportif hockey|retirer
argent paris sportif|rugby pari sportif|rugby paris sportif|règle paris sportif
prolongation|règles paris sportif|répartiteur de mise pari sportif|répartiteur de mise paris sportif|répartiteur de mise paris
sportifs|répartition des mises paris sportif|résultat
paris sportif foot|sans depot paris sportif|se faire interdire de paris sportifs|signification btts paris sportif|signification dnb paris sportif|signification handicap paris sportif|simulateur de gain paris sportif|simulateur gain paris
sportif|simulateur gain paris sportif multiple|simulateur gain paris sportif systeme|simulateur gain paris
sportif système|simulateur montante paris sportif|simulateur paris sportif multiple|simulateur systeme paris sportif|simulation paris sportif
gratuit|site aide paris sportif|site analyse paris sportif|site analyser paris sportif|site arjel
paris sportif|site conseil paris sportif|site d’analyse de paris sportifs|site
d’analyse paris sportif|site de conseil paris sportif|site de pari en ligne sportif|site de
pari sportif|site de pari sportif avec bonus sans depot|site
de pari sportif bonus sans depot|site de pari sportif canada|site de pari sportif en ligne|site de pari
sportif francais|site de pari sportif gratuit|site de pari sportif hors arjel|site de pari sportif
suisse|site de parie sportif|site de parie sportif en ligne|site de paris en ligne sportif|site de paris sportif|site de paris sportif acceptant paypal|site de paris sportif arjel|site de paris sportif autorisé en france|site de
paris sportif autorisé en suisse|site de paris sportif avec bonus|site de
paris sportif avec bonus sans depot|site de paris sportif avec bonus sans dépôt|site de paris
sportif avec neosurf|site de paris sportif avec paiement
mobile|site de paris sportif avec paypal|site de paris sportif avis|site de
paris sportif belge avec bonus|site de paris sportif belgique|site de paris sportif bonus|site de paris sportif bonus sans depot|site de paris sportif canada|site
de paris sportif comparatif|site de paris sportif depot minimum|site de paris sportif en france|site de paris
sportif en ligne|site de paris sportif en ligne suisse|site de paris
sportif football|site de paris sportif francais|site de paris sportif france|site de
paris sportif gratuit|site de paris sportif gratuit
pour gagner des cadeaux|site de paris sportif gratuit sans
dépôt|site de paris sportif hors arjel|site de paris sportif le plus fiable|site de paris sportif legal
en france|site de paris sportif meilleur cote|site de paris sportif nouveau|site de paris sportif offre de bienvenue|site de paris sportif paypal|site de paris
sportif premier paris remboursé|site de paris sportif qui accepte
paypal|site de paris sportif qui rembourse en cash|site de paris sportif remboursé|site de paris
sportif sans argent|site de paris sportif sans carte bancaire|site de paris
sportif sans carte d’identité|site de paris sportif sans
depot|site de paris sportif suisse|site de paris sportifs|site de paris
sportifs avec paypal|site de paris sportifs en ligne|site de paris sportifs francais|site de paris sportifs gratuit|site de paris sportifs paypal|site de paris sportifs suisse|site de statistique pour paris sportif|site des paris
sportifs|site pari en ligne sportif|site pari sportif|site pari sportif 100
euros offert|site pari sportif arjel|site pari sportif belgique|site pari sportif bonus|site pari sportif canada|site pari sportif
comparatif|site pari sportif en ligne|site pari sportif france|site pari sportif gratuit|site pari sportif hors arjel|site pari sportif suisse|site parie sportif|site paris
en ligne sportif|site paris sportif|site paris sportif 100 euros
offert|site paris sportif 100 euros remboursé|site paris sportif
1er paris remboursé|site paris sportif arjel|site paris sportif
autorisé en france|site paris sportif avec bonus|site
paris sportif avec bonus sans depot|site paris sportif avec meilleur cote|site paris sportif belgique|site paris sportif bonus|site paris sportif bonus cash|site paris
sportif bonus sans depot|site paris sportif canada|site paris
sportif comparatif|site paris sportif depot 5 euro|site
paris sportif en ligne|site paris sportif foot|site paris sportif france|site paris sportif gratuit|site paris sportif hors arjel|site paris sportif
hors arjel france|site paris sportif meilleur cote|site paris sportif nouveau|site paris sportif offre de
bienvenue|site paris sportif paypal|site paris
sportif remboursement cash|site paris sportif remboursé en cash|site paris sportif retrait instantané|site paris sportif sans carte bancaire|site paris
sportif sans depot|site paris sportif suisse|site paris sportifs|site paris sportifs belgique|site paris sportifs en ligne|site paris
sportifs france|site paris sportifs hors arjel|site paris sportifs suisse|site pour analyse
paris sportif|site pour paris sportif|site pronostic paris sportif|site statistique paris sportif|site suisse paris
sportif|sites de pari sportif|sites de paris sportif|sites de
paris sportifs|sites de paris sportifs arjel|sites de paris
sportifs autorisés en france|sites de paris sportifs belgique|sites de paris sportifs bonus|sites de
paris sportifs en belgique|sites de paris sportifs en france|sites
de paris sportifs en ligne|sites de paris sportifs gratuits|sites de paris sportifs gratuits sans dépôt|sites de paris sportifs suisse|sites
pari sportif|sites paris sportif|sites paris sportifs|sites paris sportifs
arjel|sites paris sportifs belgique|sites paris sportifs france|sites paris sportifs hors arjel|sites paris sportifs suisse|so foot paris sportif|so foot
paris sportifs|specialiste tennis paris sportif|statistique foot paris
sportif|statistique paris sportif|statistique paris sportif
foot|statistique tennis paris sportif|statistiques football
paris sportifs|statistiques paris sportifs|strategie de paris sportif|stratégie big
whale paris sportif|stratégie de paris sportifs|stratégie
gagnante paris sportifs|stratégie pari
sportif|stratégie paris sportif|stratégie paris sportifs|stratégie paris sportifs forum|stratégie pour gagner au paris sportif|stratégies paris sportifs|suisse paris sportif|suisse paris sportifs|systeme
2 3 paris sportif|systeme 3 4 paris sportif|systeme de cote paris sportif|systeme de paris
sportif|systeme pari sportif|systeme paris sportif|systeme paris sportifs|systeme
reducteur paris sportif|système paris sportif|tableau bankroll paris sportif|tableau cote paris sportif|tableau de paris sportif|tableau de suivi paris sportifs|tableau excel
bankroll paris sportif|tableau excel paris sportif|tableau excel paris sportif gratuit|tableau excel paris sportifs|tableau excel pour
paris sportif|tableau gestion bankroll paris sportif|tableau montante paris sportif|tableau paris sportif|tableau paris sportif excel|tableau roi
paris sportifs|tableau statistique paris sportif|tableau suivi paris sportif|taxe gain paris sportif|
прихожие под заказ Встраиваемый шкаф купе на заказ: Функциональность и стиль в одном решении – встраиваемый шкаф-купе, изготовленный на заказ по индивидуальным размерам.
бездепозитные бонусы за регистрацию в казино с выводом
бездепозитные бонусы казахстан за регистрацию в казино
https://amt-games.com/news/1xbet-promo-code___welcome_bonus.html
модернизация 1С Налоговый мониторинг для ИП Нс Диджитал Франчайзинг 1С Бухалтерия, продажа и разработка продуктов 1с
Discover what’s new today
The latest version is here
Good day I am so thrilled I found your blog, I really found you by mistake, while I was looking on Askjeeve for something else, Anyways I am here now and would just like to say kudos for a remarkable post and a all round entertaining blog (I also love the theme/design), I don’t have time to look over it all at the minute but I have saved it and also included your RSS feeds, so when I have time I will be back to read more, Please do keep up the excellent job.
forticlient on mac
мастер по ремонту телевизоров
ремонт кофемашины крупс
ремонт питания подсветки телевизора
Официальный сайт компании 1xBet : http://ruptur.com/
See what’s new right now : http://ruptur.com/
10 euros offert paris sportif|10 euros offert sans dépôt
paris sportif|10 meilleurs sites de paris sportifs|100 euro offert paris sportif|100 euros offert paris
sportif|100 euros remboursé paris sportifs|100 offert
pari sportif|100 offert paris sportif|100 remboursé paris sportif|100e offert pari
sportif|abandon paris sportif tennis|abandon tennis paris sportif|addiction paris
sportif forum|age paris sportif belgique|aide au pari sportif|aide au paris sportif|aide aux paris sportif|aide aux paris sportifs|aide pari sportif|aide pari sportif football|aide
parie sportif|aide paris sportif|aide paris
sportif foot|aide paris sportif gratuit|aide paris sportifs|aide pour paris sportif|algorithme de paris sportif|algorithme excel paris sportif|algorithme
gratuit paris sportif|algorithme pari sportif|algorithme paris sportif|algorithme paris sportif avis|algorithme paris sportif basket|algorithme paris sportif
excel|algorithme paris sportif gratuit|algorithme paris sportif tennis|algorithme
paris sportifs|algorithme pour paris sportif|analyse cote paris sportif|analyse de paris sportif|analyse match paris sportif|analyse pari sportif|analyse
paris sportif|analyse paris sportif foot|analyse paris
sportif football|analyse paris sportif gratuit|analyse paris sportifs|ancienne cote paris
sportif|api cote paris sportif|app paris sportif sans argent|appli de paris sportif|appli de paris sportif sans argent|appli de paris sportifs|appli pari sportif|appli pari sportif gratuit|appli parie sportif|appli paris sportif|appli
paris sportif avec paypal|appli paris sportif belgique|appli paris sportif entre amis|appli paris sportif
gratuit|appli paris sportif sans argent|appli paris sportif suisse|appli paris sportifs|application aide paris sportif|application algorithme paris sportif|application analyse paris sportif|application android paris sportif|application bankroll paris sportif|application conseil paris sportif|application de pari sportif|application de parie sportif|application de paris sportif|application de paris sportif en afrique|application de paris sportif en cote d’ivoire|application de paris sportif en ligne|application de paris sportif gratuit|application de paris
sportif international|application de paris sportif suisse|application de paris sportifs|application faux paris sportifs|application gestion bankroll paris sportif|application gestion paris sportif|application ia paris sportif|application pari
sportif gratuit|application paris sportif|application paris sportif android|application paris sportif argent fictif|application paris sportif
belgique|application paris sportif canada|application paris sportif espagne|application paris sportif espagnol|application paris sportif fictif|application paris sportif france|application paris sportif gratuit|application paris sportif gratuit entre amis|application paris
sportif maroc|application paris sportif offre de bienvenue|application paris sportif paypal|application paris
sportif sans argent|application paris sportif sans justificatif de domicile|application paris sportif suisse|application paris sportif usa|application paris sportif virtuel|application pour faire des paris sportifs|application pour gerer ses paris sportif|application pour les paris sportifs|application pour pari sportif|application pour paris sportif|application pour paris sportifs|application statistique paris sportif|application suivi paris sportif|applications de paris sportifs|applications paris sportifs|applis paris sportif|applis paris sportifs|apprendre
a faire des paris sportifs|argent facile paris sportif|argent offert paris sportifs|argent offert sans depot
paris sportif|argent paris sportif|argent paris sportifs|argent paris sportifs impots|argent sans depot paris sportif|arjel paris sportif|arjel paris sportifs|astuce gagner paris sportif|astuce pari sportif|astuce paris sportif|astuce paris sportif basket|astuce paris sportif foot|astuce paris sportif forum|astuce paris sportif tennis|astuce paris sportifs|astuce pour gagner au
pari sportif|astuce pour gagner au paris sportif|astuce pour gagner paris
sportif|astuce pour paris sportif|astuces paris sportifs|astuces paris sportifs en ligne|astuces paris sportifs foot|astuces pour gagner aux paris sportifs|autorisation paris
sportif france|avis pari sportif|avis paris sportif|avis paris sportif foot|avis
site de paris sportif|avis site paris sportif|avis sur les
paris sportifs|avis sur paris sportif|avis tipster paris sportif|aweh signification paris sportif|bankroll
100 euros paris sportifs|bankroll management paris sportif|bankroll paris sportif|bankroll paris sportif excel|bankroll paris sportif gratuit|bankroll paris sportifs|basket paris sportif|belgique france
paris sportif|belgique paris sportifs|bonus bienvenue paris sportif|bonus bienvenue paris sportifs|bonus cash paris sportif|bonus
de bienvenue paris sportif|bonus de bienvenue paris sportif belgique|bonus de
bienvenue sans depot paris sportif|bonus de depot paris sportif|bonus de paris sportifs|bonus depot paris sportif|bonus en cash
paris sportif|bonus gratuit paris sportif|bonus gratuit sans depot paris sportif|bonus pari sportif|bonus paris sportif|bonus paris
sportif belgique|bonus paris sportif betclic|bonus paris sportif cash|bonus paris sportif en ligne|bonus paris sportif france pari|bonus paris
sportif retirable|bonus paris sportif sans depot|bonus paris sportif sans dépôt|bonus paris sportif unibet|bonus paris sportifs|bonus sans
depot paris sportif|bonus sans depot paris sportif belgique|bonus sans
dépôt paris sportif|bonus sans dépôt paris sportif hors arjel|bonus
site de paris sportif|bonus site pari sportif|bonus site
paris sportif|bonus sites de paris sportifs|bonus unibet
paris sportif|bookmaker paris sportif|bookmaker paris sportif gratuit|bookmaker paris sportifs|bookmaker sportif|bookmakers paris
sportif|bookmakers paris sportifs|bookmakers paris sportifs en ligne|but contre
son camp paris sportif|but sur penalty paris sportif|buteur paris
sportif|c’est quoi handicap paris sportif|c’est quoi une cote paris sportif|calcul anti
perte paris sportif|calcul combinaison pari sportif|calcul cote pari sportif|calcul cote paris sportif|calcul
couverture paris sportif|calcul de cote paris sportif|calcul des cotes paris sportifs|calcul dnb paris sportifs|calcul double
chance paris sportif|calcul gain paris sportif|calcul mise paris sportif|calcul
pari sportif|calcul paris sportif|calcul paris sportif multiple|calcul pourcentage cote paris sportif|calcul probabilité paris sportif|calcul rentabilité paris sportifs|calcul roi paris sportif|calcul systeme paris sportif|calcul trj paris sportifs|calculateur cote paris sportif|calculateur de cote paris sportif|calculateur de mise paris sportif|calculateur de paris sportif|calculateur paris sportif|calculatrice arbitrage paris sportif|calculatrice paris sportif|calculer cote paris sportif|calculer gain paris sportif|calculer probabilité paris sportifs|calculer roi paris sportifs|calculer une cote pari sportif|calculer une cote paris sportif|carte cadeau paris sportif|carte
pcs paris sportif|carte prépayée paris sportifs|cash out pari sportif|cash out
paris sportif|cash out paris sportifs|casino en ligne paris sportif|casino
paris sportif en ligne|champions league paris sportif|chute de cote paris sportif|classement des meilleurs sites de paris
sportifs|classement meilleur site de paris sportif|code barre paris sportif|code bonus paris sportif|code paris sportif|code promo pari sportif|code
promo paris sportif|code promo paris sportif sans depot|code promo paris sportif sans dépôt|code
promo sans depot paris sportif|code promo site paris sportif|combien de temps pour encaisser un paris sportif|combien de
temps pour retirer un paris sportif|combien miser paris
sportifs|combine paris sportif|combines paris sportifs|combiné pari sportif|combiné paris sportif|combiné paris
sportif conseil|combiné paris sportif du jour|combiné paris sportif pronostic|comment analyser
un paris sportif|comment arreter de jouer aux paris
sportifs|comment arreter les paris sportif|comment arreter les paris sportifs|comment arrêter les paris
sportifs|comment bien gagner au paris sportif|comment bien jouer
au paris sportif|comment bien miser paris sportif|comment ca marche les paris sportif|comment calculer cote paris sportif|comment
calculer gain paris sportif|comment calculer les cotes des paris sportifs|comment calculer une cote de paris sportif|comment
calculer une cote pari sportif|comment calculer une
cote paris sportif|comment comprendre les paris sportifs|comment creer un vip
paris sportif|comment créer un algorithme paris sportif|comment créer un site de paris sportif|comment devenir riche avec les paris sportifs|comment etre rentable paris sportif|comment etre sur
de gagner au paris sportif|comment faire de bon paris sportif|comment faire des
parie sportif|comment faire des paris sportif|comment faire des paris sportif gagnant|comment
faire des paris sportifs|comment faire pari sportif|comment
faire paris sportif|comment faire pour arreter les paris sportifs|comment faire
pour gagner au paris sportif|comment faire pour gagner les paris sportifs|comment faire un bon pari sportif|comment faire
un bon paris sportif|comment faire un pari sportif|comment faire un parie sportif|comment faire
un paris sportif|comment faire une montante paris sportif|comment
fonctionne les cotes dans les paris sportifs|comment fonctionne les cotes des paris sportifs|comment fonctionne les paris sportifs|comment
fonctionne paris sportifs|comment fonctionne un pari
sportif|comment fonctionnent les cotes dans les paris sportifs|comment
fonctionnent les cotes dans les paris sportifs grand oral|comment fonctionnent les cotes de paris sportif|comment
fonctionnent les paris sportifs|comment fonctionnent les paris sportifs grand
oral|comment fonctionnent les paris sportifs grand oral maths|comment fonctionnent les paris
sportifs maths|comment gagner a coup sur au paris sportif|comment gagner a tous les coups au paris sportif|comment gagner a tout les coup
au paris sportif|comment gagner au pari sportif|comment gagner au pari
sportif football|comment gagner au paris sportif|comment gagner au paris sportif a coup sur|comment gagner au
paris sportif foot|comment gagner au paris sportif forum|comment gagner
au paris sportif tennis|comment gagner au paris sportifs|comment gagner aux paris sportif|comment gagner aux
paris sportifs|comment gagner aux paris sportifs foot|comment gagner aux paris sportifs
livre|comment gagner aux paris sportifs sur le long
terme|comment gagner avec les paris sportifs|comment gagner dans les paris
sportifs|comment gagner de l argent avec les paris sportifs|comment gagner de l’argent au paris sportif|comment gagner
de l’argent aux paris sportifs|comment gagner de
l’argent avec les paris sportifs|comment gagner de l’argent paris sportif|comment gagner de l’argent sur les paris sportifs|comment gagner de l’argent sur paris sportif|comment gagner des paris
sportif|comment gagner des paris sportifs|comment gagner en paris sportif|comment gagner facilement au paris sportif|comment gagner
les paris sportifs|comment gagner paris sportif|comment gagner paris sportif foot|comment gagner
paris sportifs|comment gagner sa vie avec les paris sportifs|comment gagner ses paris sportif|comment
gagner sur les paris sportif|comment gagner sur les paris sportifs|comment gagner tout le
temps au paris sportif|comment gagner un pari sportif|comment gagner un paris sportif|comment gerer une bankroll paris sportif|comment gérer sa bankroll paris
sportif|comment jouer au pari sportif|comment jouer au paris sportif|comment jouer au paris sportif foot|comment jouer aux paris sportifs|comment jouer paris sportif|comment marche cote paris sportif|comment marche les cotes paris sportif|comment marche les paris sportif|comment marche les
paris sportifs|comment marche paris sportif|comment marche un pari sportif|comment marche un paris sportif|comment marchent les cotes paris sportif|comment marchent
les paris sportifs|comment miser au paris sportif|comment miser paris
sportif|comment monter sa bankroll paris sportif|comment ne jamais perdre au paris sportif|comment parier sportif|comment reussir au
paris sportif|comment reussir les paris sportif|comment reussir paris sportif|comment sont calculer les cotes de paris sportif|comment sont calculées les cotes des paris sportifs|comment sont calculés les cotes des paris sportifs|comment sont faites
les cotes des paris sportifs|comment toujours gagner au paris sportif|comment ça
marche les paris sportifs|comparaison bonus paris
sportifs|comparaison cote pari sportif|comparaison des cotes paris sportifs|comparateur cote pari sportif|comparateur cote paris sportif|comparateur cotes paris sportif|comparateur cotes paris sportifs|comparateur de cote pari sportif|comparateur de cote paris sportif|comparateur de cotes
paris sportifs|comparateur de côtes paris sportifs|comparateur de paris sportif|comparateur de site de paris sportif|comparateur de site paris sportif|comparateur
de sites de paris sportifs|comparateur pari sportif|comparateur paris sportif|comparateur paris sportifs|comparateur site de paris sportif|comparateur
site pari sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif bonus paris sportifs|comparatif cote pari sportif|comparatif cote paris sportif|comparatif cotes
paris sportifs|comparatif des sites de paris sportifs|comparatif offre
de bienvenue paris sportif|comparatif offre paris sportif|comparatif pari sportif|comparatif pari sportif en ligne|comparatif paris sportif|comparatif paris sportif bonus|comparatif paris sportif en ligne|comparatif paris sportifs|comparatif
paris sportifs en ligne|comparatif site de paris sportif|comparatif site paris sportif|comparatif site paris sportifs|comparatif sites de paris sportifs|comparatif sites paris sportifs|comparer les cotes paris sportifs|comprendre cote paris sportif|comprendre handicap paris sportif|comprendre les cotes des paris sportifs|comprendre les
cotes paris sportif|comprendre les cotes paris sportifs|comprendre les handicap paris sportif|compte de paris
sportif|compte démo paris sportif|compte finance paris sportif|compte financer paris
sportif|compte financier paris sportif|compte financé paris sportif|compte pari sportif|compte paris sportif|compte paris sportif financé|conseil de paris sportif|conseil de paris sportifs|conseil en paris sportif|conseil en paris sportifs|conseil pari
sportif|conseil pari sportif gratuit|conseil paris sportif|conseil paris sportif aujourd’hui|conseil paris sportif du jour|conseil paris sportif
foot|conseil paris sportif gratuit|conseil paris sportif ligue des champions|conseil paris sportif nba|conseil paris sportif pronostic|conseil paris sportif rmc|conseil
paris sportif tennis|conseil paris sportifs|conseil pour
gagner au paris sportif|conseil pour paris sportif|conseil sur les paris sportifs|conseille paris sportif|conseiller en paris sportifs|conseiller paris sportif|conseils de paris
sportifs|conseils en paris sportifs|conseils paris sportifs|conseils paris
sportifs foot|conseils paris sportifs gratuit|conseils paris sportifs tennis|conseils pour
paris sportifs|cote a 100 paris sportif|cote a 2 paris sportif|cote anglaise
paris sportif|cote de 2 paris sportif|cote de pari sportif|cote
de paris sportif|cote des paris sportifs|cote maximum paris sportif|cote minimum paris sportif|cote pari sportif|cote pari sportif comment ça marche|cote pari sportif real madrid|cote
pari sportif rugby|cote parie sportif|cote paris sportif|cote paris sportif belgique|cote paris sportif calcul|cote paris sportif definition|cote paris sportif euro|cote paris sportif explication|cote paris sportif foot|cote paris sportif france belgique|cote paris sportif france espagne|cote paris sportif ligue des
champions|cote paris sportif moto gp|cote paris sportif psg|cote paris sportif psg arsenal|cote paris sportif rugby|cote paris
sportif tennis|cote paris sportifs|cote pour paris sportifs|cote
sportif foot|cote sportif rugby|cote à 1000 paris sportif|cotes de paris sportifs|cotes pari sportif|cotes paris sportif|cotes paris sportifs|cotes paris sportifs foot|coupe
de france paris sportif|créer un algorithme paris
sportif|créer un compte paris sportif|créer un site de
paris sportif en ligne|dans les paris sportifs que signifie handicap|declarer ses gains
paris sportif|definition cash out paris sportif|definition cote paris
sportif|definition handicap paris sportif|depot 5 euros paris sportif|depot double paris sportif|depot minimum 5 euro
paris sportif|depot minimum paris sportif|depot paris sportif|depuis quand existe les
paris sportif en france|devenir riche avec les paris sportifs|devenir riche
avec paris sportifs|disqualification tennis paris sportif|dnb en paris sportif|dnb pari sportif|dnb
paris sportif|dnb paris sportif definition|dnb paris sportifs|doit
on declarer les gains de paris sportif|déclarer gains paris sportifs|déclarer
gains paris sportifs hors arjel|définition bankroll paris sportif|dépôt minimum 1 euro paris sportif|dépôt minimum 5 euro paris sportif|ecart de jeux tennis paris sportif|erreur de cote paris sportif|est ce que
les gains des paris sportifs sont imposables|est-ce que les prolongation compte dans un pari sportif|etre sur de
gagner au paris sportif|euro paris sportif|evenement sportif a paris|evenement sportif
paris|evenement sportif paris 2025|evenement sportif paris aujourd hui|evenement sportif paris aujourd’hui|evenement sportif paris ce week end|evenements sportif paris|evenements sportifs paris|evenements sportifs paris 2025|evenements sportifs à paris|evolution cote paris sportif|evolution cotes paris sportifs|evolution des cotes paris
sportifs|explication cote pari sportif|explication cote paris sportif|explication handicap paris sportif|explication pari
sportif|explication paris sportif|face a face hockey paris sportif|faire des paris
sportif|faire des paris sportif avec paypal|faire des paris
sportifs|faire fortune paris sportifs|faire un pari sportif|faire un paris sportif|faut il déclarer les gains de paris sportifs|faut il déclarer ses gains paris sportifs|fichier excel gestion bankroll paris
sportif|fiscalité gains paris sportifs|foot paris sportif|football
et paris sportifs|forfait tennis paris sportif|formation paris sportif gratuit|forum de paris sportif|forum de
paris sportifs|forum pari sportif|forum parie sportif|forum paris sportif|forum
paris sportif foot|forum paris sportif gratuit|forum paris
sportif nba|forum paris sportif tennis|forum paris sportifs|forum sur les paris sportifs|forum tennis paris sportif|francaise des jeux pari sportif|francaise
des jeux paris sportif|francaise des jeux paris sportifs|france 2 paris
sportif|france 2 paris sportifs|france belgique paris sportif|france espagne paris sportif|france pari sportif|france pari sportif brest|france paris sportif|france paris
sportifs|france pologne paris sportif|france
portugal paris sportif|france suisse paris sportifs|france tunisie paris sportifs|france-pari – paris sportifs|gagnant pari sportif|gagnant paris sportif|gagnant paris sportif bayern|gagnante paris sportif|gagne au paris sportif|gagner 10 euros par jour aux paris sportifs|gagner 100 euros par jour paris sportif|gagner 1000
euros par mois paris sportifs|gagner 10000 euros paris sportif|gagner 2000 euros par
mois paris sportif|gagner 50 euros par jour paris sportif|gagner a coup sur au paris sportif|gagner a
coup sur pari sportif|gagner a tous les coup paris sportif|gagner
argent avec paris sportifs|gagner argent pari sportif|gagner argent paris sportif|gagner argent paris sportifs|gagner
au pari sportif|gagner au paris sportif|gagner
au paris sportif a coup sur|gagner au paris sportif foot|gagner au paris sportif forum|gagner au
paris sportif à coup sur|gagner aux paris sportif|gagner aux
paris sportifs|gagner aux paris sportifs pdf|gagner beaucoup d’argent paris sportif|gagner de l
argent grace aux paris sportifs|gagner de l argent
pari sportif|gagner de l argent paris sportif|gagner de l argent paris sportifs|gagner
de l’argent au paris sportif|gagner de l’argent aux paris sportifs|gagner de
l’argent avec les paris sportifs|gagner de l’argent avec paris sportif|gagner de l’argent avec paris sportifs|gagner de l’argent grace au paris sportif|gagner
de l’argent grace aux paris sportifs|gagner de l’argent pari
sportif|gagner de l’argent paris sportif|gagner de l’argent paris
sportifs|gagner de l’argent sur les paris sportifs|gagner des paris sportif|gagner
des paris sportifs|gagner les paris sportifs|gagner pari sportif|gagner paris sportif|gagner paris sportif foot|gagner paris sportif forum|gagner
paris sportif tennis|gagner paris sportifs|gagner sa vie avec les paris sportif|gagner sa vie avec les paris sportifs|gagner sa vie avec paris sportifs|gagner ses paris sportifs|gagner à
coup sur paris sportif|gagner à tous les coups paris sportifs|gain maximum paris sportif|gain pari
sportif|gain pari sportif imposable|gain pari sportif impot|gain paris sportif|gain paris sportif imposable|gain paris sportif impot|gain paris sportif impôt|gains paris sportif|gains paris sportif imposable|gains
paris sportifs|gains paris sportifs imposable|gains paris sportifs imposables|gains paris sportifs sont ils
imposables|gerer bankroll paris sportif|gerer sa bankroll paris sportif|gerer une bankroll
paris sportif|gestion bankroll paris sportif|gestion bankroll paris sportifs|gestion bankroll paris sportifs excel|gestion de bankroll paris sportif|gestion de bankroll paris sportif
application|gestion de bankroll paris sportifs|gestion de mise paris sportif|gestion paris sportifs v2 5 gratuit|gg signification paris
sportif|gros combiné paris sportif|gros gain paris sportif|grosse
cote paris sportif pronostic|grosse mise paris sportif|groupe paris sportif gratuit|groupe telegram paris
sportif gratuit|groupement de joueurs paris sportifs|handicap 0
paris sportif|handicap 1 paris sportif|handicap 5 paris sportif|handicap au paris sportif|handicap basket paris sportif|handicap dans les paris sportifs|handicap en paris sportif|handicap europeen paris sportif|handicap européen paris sportifs|handicap
mi temps paris sportif|handicap pari sportif|handicap paris sportif|handicap paris sportif basket|handicap paris sportif explication|handicap paris sportif foot|handicap paris sportif rugby|handicap paris sportifs|handicap rugby paris sportif|handicap tennis paris sportif|historique cote paris sportif|historique des cotes paris sportifs|hockey
paris sportif|hockey sur glace paris sportif|hors
arjel paris sportif|hweh signification paris sportif|imposition gain pari sportif|imposition gain paris sportif|imposition gains paris sportifs|imposition paris sportif france|impot gain paris
sportif|impot paris sportif france|impot sur gain paris
sportif|je gagne ma vie avec les paris sportifs|jeu de
pari sportif gratuit|jeu de paris sportif en ligne|jeu de paris sportif gratuit|jeu paris sportif gratuit|jeu paris sportif sans argent|jeux de parie sportif|jeux de paris sportif|jeux de paris sportif en ligne|jeux de paris sportif gratuit|jeux
de paris sportifs|jeux olympiques paris sportifs|jeux
paris sportif|jeux paris sportif gratuit|jeux paris sportif virtuel|jeux paris sportifs en ligne|jouer au paris sportif|jouer paris
sportif|joueur absent paris sportif|joueur blesse paris
sportif|joueur caen paris sportif|joueur de caen pari sportif|joueur de foot paris sportif|joueur decisif paris
sportif|joueur décisif paris sportif|joueur italien paris sportif|joueur
paris sportif|joueur professionnel paris sportif|joueur qui se blesse
paris sportif|joueur sanctionne pari sportif|joueur suspendu paris sportif|joueurs italiens
paris sportifs|l’argent des paris sportifs est il imposable|la cote
paris sportif|la francaise des jeux paris sportif|la martingale paris
sportif|la martingale paris sportifs|la meilleur application de paris sportif|la meilleur application paris sportif|la meilleur technique pour gagner au paris sportif|la méthode secrète pour gagner aux paris
sportifs pdf|la plus grosse cote gagner paris sportif|la plus grosse cote paris
sportif|ldem paris sportif signification|le marché des paris sportifs|le meilleur site de pari sportif|le meilleur site de paris sportif|le meilleur site de paris
sportif en ligne|le meilleur site de paris sportifs|le
plus gros gain au paris sportif|le plus gros
paris sportif|le plus gros paris sportif du monde|les 10 meilleurs sites de paris sportifs|les 10 meilleurs
sites de paris sportifs en afrique|les 17 secrets pour gagner rapidement aux paris sportifs|les 17 secrets
pour gagner rapidement aux paris sportifs pdf|les application de
paris sportif|les applications paris sportifs|les bonus paris sportifs|les bookmakers
paris sportifs|les cotes paris sportifs|les gains de paris sportifs sont ils imposables|les gains des paris sportifs sont ils
imposables|les jeux de paris sportifs|les meilleur paris sportif|les meilleures applications de paris sportifs|les meilleurs applications de paris sportifs|les meilleurs bonus paris sportif|les meilleurs bonus paris
sportifs|les meilleurs cotes paris sportif|les meilleurs paris sportifs|les meilleurs paris sportifs du jour|les meilleurs site de paris sportif|les meilleurs site de paris sportifs|les meilleurs sites de pari sportif|les meilleurs sites de paris sportifs|les meilleurs sites de paris sportifs en ligne|les paris sportif|les
paris sportif avis|les paris sportifs|les paris sportifs comment ça marche|les paris sportifs
en france|les paris sportifs en ligne|les paris sportifs en ligne comprendre jouer gagner|les paris sportifs en ligne comprendre jouer gagner pdf|les paris
sportifs les plus rentables|les plus gros gagnant paris sportif|les plus gros gains au paris sportifs|les plus gros gains paris sportifs|les plus gros paris sportif|les plus grosse cote paris sportif|les plus grosses pertes paris sportifs|les sites de paris sportifs|les sites de
paris sportifs autorisés en france|les sites de paris sportifs en france|les sites de
paris sportifs en ligne|les sites de paris sportifs francais|ligue 1 paris sportif|ligue 1 paris
sportifs|ligue 2 paris sportif|ligue des champions
paris sportif|limite de gains paris sportifs|limite de mise paris sportif|limite gain paris sportif|limite mise paris sportifs|liste de paris sportif|liste des paris sportifs|liste des site de paris sportif|liste des sites de paris sportifs|liste pari
sportif|liste paris sportif|liste paris sportif pdf|liste site de paris
sportif|liste site pari sportif|liste site paris sportif|liste site paris sportif arjel|liste sites paris sportifs|logiciel algorithme paris sportif|logiciel algorithme paris sportif gratuit|logiciel analyse paris sportif|logiciel calcul paris sportif|logiciel de pari sportif|logiciel de paris sportif|logiciel
de paris sportif gratuit|logiciel gestion bankroll paris
sportif gratuit|logiciel gestion de bankroll paris sportif|logiciel gestion paris sportif|logiciel gestion paris sportif gratuit|logiciel gestion paris sportifs|logiciel pari sportif|logiciel paris
sportif|logiciel paris sportif gratuit|logiciel paris sportifs|logiciel
paris sportifs foot sur 2 matchs|logiciel pour paris sportif|logiciel pour paris sportifs|logiciel prediction paris sportif|logiciel
probabilité paris sportif|logiciel prédiction paris sportif|logiciel statistique paris sportifs|logiciel variation de
cote paris sportif|loi sur les paris sportifs en france|magic
calculator paris sportif|marché des paris sportifs|marché des paris sportifs en france|marché des paris sportifs
en ligne|martingale pari sportif|martingale paris sportif|martingale paris sportif excel|martingale paris sportif
forum|martingale paris sportif interdit|martingale paris sportifs|match abandonné paris sportif|match annulé ou
reporté paris sportifs|match annulé paris sportif|match arrete paris sportif|match interrompu paris sportif|match interrompu tennis
paris sportif|match interrompu tennis pluie
paris sportif|match nul boxe paris sportif|match pari sportif|match paris sportif|match reporté paris sportif|match suspendu paris sportif|match suspendu tennis paris sportif|match truqué paris sportif|matchs truqués
paris sportifs|meilleur algorithme paris sportif|meilleur algorithme paris sportif gratuit|meilleur app de
paris sportif|meilleur app de paris sportifs|meilleur app paris
sportif|meilleur appli de pari sportif|meilleur appli de paris sportif|meilleur appli pari sportif|meilleur appli paris sportif|meilleur
appli paris sportif forum|meilleur appli paris sportifs|meilleur
application conseil paris sportif|meilleur application de
paris sportif|meilleur application de paris sportif en afrique|meilleur application pari
sportif|meilleur application paris sportif|meilleur application paris sportif belgique|meilleur application pour les paris sportif|meilleur application pour pari
sportif|meilleur bonus de bienvenue paris sportif|meilleur bonus pari sportif|meilleur bonus
paris sportif|meilleur bonus paris sportif sans
depot|meilleur bonus paris sportifs|meilleur bonus site
de paris sportif|meilleur bonus site pari sportif|meilleur bonus site paris sportif|meilleur bookmaker paris sportif|meilleur combiné paris sportif|meilleur conseil paris sportif|meilleur cote
de paris sportif|meilleur cote pari sportif|meilleur cote paris sportif|meilleur cote paris
sportif aujourd’hui|meilleur cote site paris sportif|meilleur forum paris sportifs|meilleur gain paris sportif|meilleur ia paris sportif|meilleur methode pour
gagner au paris sportif|meilleur offre bienvenue paris sportif|meilleur offre bonus paris
sportif|meilleur offre de bienvenue paris sportif|meilleur offre de bienvenue paris sportifs|meilleur offre pari sportif|meilleur offre
paris sportif|meilleur offre paris sportif en ligne|meilleur pari sportif|meilleur pari sportif du jour|meilleur pari sportif en ligne|meilleur paris sportif|meilleur
paris sportif aujourd’hui|meilleur paris sportif du jour|meilleur paris sportif en ligne|meilleur paris sportif foot|meilleur
promo paris sportif|meilleur pronostic paris sportif|meilleur site de conseil paris sportif|meilleur site de pari
sportif|meilleur site de pari sportif en ligne|meilleur
site de paris sportif|meilleur site de paris sportif avis|meilleur site de paris sportif belgique|meilleur site de paris sportif canada|meilleur site de paris sportif en france|meilleur site de paris sportif en ligne|meilleur site de paris sportif football|meilleur
site de paris sportif forum|meilleur site de paris sportif france|meilleur site de paris sportif hors arjel|meilleur site de paris sportif international|meilleur site de paris sportif suisse|meilleur site de paris sportifs|meilleur site de paris sportifs en ligne|meilleur
site pari sportif|meilleur site pari sportif en ligne|meilleur site pari sportif france|meilleur
site paris sportif|meilleur site paris sportif avis|meilleur site paris sportif belgique|meilleur
site paris sportif canada|meilleur site paris sportif en ligne|meilleur site paris sportif foot|meilleur site paris sportif forum|meilleur site paris sportif france|meilleur site
paris sportif hors arjel|meilleur site paris sportif nba|meilleur site paris
sportif rugby|meilleur site paris sportif suisse|meilleur site paris sportifs|meilleur
site pour pari sportif|meilleur site pour paris sportif|meilleur site pronostic
paris sportif|meilleur strategie paris sportif|meilleur technique de paris sportif|meilleur technique paris sportif|meilleur technique pour gagner au paris sportif|meilleure appli de paris sportif|meilleure appli de paris sportifs|meilleure appli pari sportif|meilleure
appli paris sportif|meilleure appli paris sportifs|meilleure
application de paris sportif|meilleure application de paris sportifs|meilleure application pari sportif|meilleure application paris sportif|meilleure
application paris sportif android|meilleure application paris sportifs|meilleure offre paris sportif|meilleure site paris sportif|meilleure strategie paris
sportif|meilleures applications de paris sportifs|meilleures applications paris sportifs|meilleures cotes paris sportifs|meilleures offres paris sportifs|meilleures stratégies paris sportifs|meilleurs appli
paris sportif|meilleurs application de paris sportifs|meilleurs application paris sportif|meilleurs applications paris sportifs|meilleurs
bonus paris sportifs|meilleurs cote paris sportif|meilleurs cotes paris sportifs|meilleurs offres
paris sportifs|meilleurs paris sportifs|meilleurs paris sportifs du jour|meilleurs site
de pari sportif|meilleurs site de paris sportif|meilleurs site
de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs site paris sportif|meilleurs sites de paris sportifs|meilleurs sites de paris sportifs en ligne|meilleurs sites paris sportif|meilleurs sites paris sportifs|methode abc paris
sportif|methode de paris sportif|methode gagnante paris
sportifs|methode gagner paris sportif|methode
infaillible paris sportifs|methode martingale paris sportif|methode mathematique paris sportif|methode mathematique pour gagner au paris
sportif|methode paris sportif|methode paris sportif foot|methode paris sportif
forum|methode paris sportif tennis|methode paris sportifs|methode pour gagner au paris sportif|methode pour gagner paris sportif|methodes paris
sportifs|minimum depot paris sportif|mise au jeu pari sportif|mise maximum
pari sportif|mise maximum paris sportif|mise minimum paris sportif|mise moyenne paris sportif|mise paris sportif|moins
de 4 5 but paris sportif|montant maximum paris sportif|montant paris sportif|montante pari sportif|montante
parie sportif|montante paris sportif|montante paris sportifs|montantes paris sportifs|multiple pari sportif|multiple paris
sportif|multiple paris sportifs|multiples paris sportifs|méthode
calcul paris sportif|méthode match nul paris sportifs|méthode mathématique pour gagner
au paris sportif|méthode paris sportif forum|méthode paris sportif hockey|nba pari sportif|nba paris sportif|nba paris sportifs|nouveau paris
sportif|nouveau site de pari sportif|nouveau site de paris sportif|nouveau site de paris
sportif en ligne|nouveau site de paris sportifs|nouveau site pari sportif|nouveau site paris sportif|nouveau
site paris sportif france|nouveau site paris sportifs|nouveaux sites de paris sportifs|nouveaux sites paris sportifs|nouvelle appli paris sportif|nouvelle application de paris sportif|numero de match paris sportif|numero match paris sportif|offre 100 euros paris sportif|offre appli
pari sportif|offre bienvenu paris sportif|offre bienvenue pari
sportif|offre bienvenue paris sportif|offre bienvenue paris sportifs|offre bienvenue site
paris sportif|offre bonus paris sportif|offre de bienvenu paris sportif|offre de bienvenue pari sportif|offre de bienvenue paris sportif|offre de bienvenue
paris sportif belgique|offre de bienvenue paris sportif sans
depot|offre de bienvenue paris sportif sans dépôt|offre de bienvenue paris sportifs|offre de bienvenue sans
depot paris sportif|offre de bienvenue site paris sportif|offre euro
paris sportif|offre pari sportif euro|offre paris sportif|offre paris sportif belgique|offre paris sportif cash|offre paris
sportif coupe du monde|offre paris sportif hors arjel|offre paris
sportif remboursé|offre paris sportif remboursé cash|offre paris sportif sans depot|offre promo paris
sportif|offre remboursement paris sportif|offre sans depot paris sportif|offre site paris sportif|offres bienvenue paris
sportifs|offres de bienvenue paris sportifs|ou faire
des paris sportif|ou faire des paris sportif en espagne|ou faire des paris sportifs|outil répartiteur de mise paris sportif|outils repartiteur de mises paris sportif|ouverture compte paris sportifs|ouvrir un compte paris
sportif|pack de bienvenue paris sportif|pack de
bienvenue paris sportif hors arjel|pari en ligne sportif|pari sportif|pari sportif 100 euros offert|pari sportif 100 remboursé|pari sportif abandon tennis|pari sportif aide|pari sportif algérie
aujourd’hui|pari sportif appli|pari sportif application|pari sportif argent|pari sportif astuce|pari sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari sportif avec orange
money|pari sportif avec paypal|pari sportif avec
wave|pari sportif avis|pari sportif basket|pari sportif belgique|pari sportif belgique france|pari sportif bonus|pari sportif buteur pas titulaire|pari sportif champions league|pari sportif combiné|pari sportif comment|pari sportif comment gagner|pari sportif comment ça marche|pari sportif comparatif|pari
sportif conseil|pari sportif cote|pari sportif cote match|pari sportif
cote psg|pari sportif coupe|pari sportif coupe de france|pari sportif coupe
du monde|pari sportif depot|pari sportif du jour|pari sportif
en france|pari sportif en ligne|pari sportif en ligne au cameroun|pari sportif
en ligne belgique|pari sportif en ligne canada|pari sportif en ligne france|pari sportif
en ligne gratuit|pari sportif en ligne suisse|pari sportif en ligne
ufc|pari sportif en suisse|pari sportif euro|pari sportif explication|pari sportif faire|pari sportif foot|pari sportif
foot resultat|pari sportif football|pari sportif forum|pari
sportif francaise des jeux|pari sportif france|pari sportif
france angleterre|pari sportif france argentine|pari sportif france autriche|pari sportif france belgique|pari sportif france espagne|pari sportif france italie|pari sportif france portugal|pari sportif france usa|pari sportif gagnant|pari sportif gagner|pari sportif gagner a tous les coups|pari sportif gagner de l’argent|pari sportif gain|pari sportif gratuit|pari sportif gratuit pour gagner des cadeaux|pari sportif gratuit sans
depot|pari sportif handicap|pari sportif hockey|pari sportif hors arjel|pari sportif jeux olympiques|pari sportif
joueur absent|pari sportif le plus rentable|pari sportif leicester champion|pari sportif ligue 1|pari sportif ligue 2|pari sportif ligue des
champions|pari sportif ligue europa|pari sportif match|pari sportif match arrete|pari sportif match interrompu|pari sportif
meilleur|pari sportif meilleur cote|pari sportif meilleur site|pari sportif methode|pari sportif mise|pari sportif
mise au jeu|pari sportif mise o jeu|pari sportif nba|pari sportif offre bienvenue|pari sportif paypal|pari sportif plus|pari sportif prolongation|pari sportif promo|pari sportif
pronostic|pari sportif pronostic foot|pari sportif pronostic gagnant|pari sportif
pronostic gratuit|pari sportif psg|pari sportif psg bayern|pari
sportif psg inter|pari sportif psg milan|pari sportif regle|pari sportif
rembourse|pari sportif remboursement|pari sportif remboursement cash|pari sportif
remboursé|pari sportif rugby|pari sportif rugby coupe du monde|pari sportif rugby top 14|pari sportif sans
argent|pari sportif sans carte bancaire|pari sportif sans depot|pari sportif signification|pari sportif site|pari sportif
statistique|pari sportif suisse|pari sportif systeme|pari sportif technique|pari sportif technique pour
gagner|pari sportif temps reglementaire|pari sportif tennis|pari sportif
tennis abandon|pari sportif top|pari sportif top 14|pari sportif tour de france|parie sportif|parie sportif comment ca marche|parie sportif du jour|parie sportif en ligne|parie sportif foot|parie sportif football|parie sportif france|parie sportif gratuit|parie sportif
pronostic|parie sportif suisse|paris en ligne
sportif|paris en ligne sportifs|paris evenement sportif|paris france sportif|paris hippique et sportif|paris
hippiques et sportifs|paris hippiques paris sportifs|paris hippiques paris sportifs et poker en ligne|paris hippiques sportifs|paris match sportif|paris
sportif|paris sportif 10 euros offerts|paris sportif 100 euros offert|paris sportif 100 euros remboursé|paris sportif 100 offert|paris sportif 100 remboursé|paris
sportif 100e offert|paris sportif 150 euros offert|paris sportif 1er pari remboursé|paris sportif a faire|paris sportif a faire aujourd’hui|paris sportif a faire ce soir|paris sportif abandon tennis|paris sportif abandon tennis parions sport|paris
sportif aide|paris sportif algorithme|paris sportif
analyse|paris sportif appli|paris sportif application|paris
sportif application android|paris sportif apres prolongation|paris sportif argent|paris sportif argent
fictif|paris sportif argent offert|paris sportif argent virtuel|paris sportif arjel|paris sportif arsenal psg|paris sportif astuce|paris sportif au canada|paris sportif aujourd hui|paris
sportif aujourd’hui|paris sportif avec argent fictif|paris sportif avec bonus sans depot|paris sportif avec carte bancaire|paris
sportif avec cryptomonnaie|paris sportif avec handicap|paris sportif avec paypal|paris sportif avec paysafecard|paris sportif avis|paris sportif avis expert|paris sportif avis forum|paris sportif bankroll|paris sportif basket|paris
sportif basket coupe de france|paris sportif
basket nba|paris sportif basket prolongation|paris sportif belgique|paris sportif belgique bonus|paris sportif belgique bonus sans depot|paris sportif
belgique france|paris sportif belgique suede|paris sportif bonus|paris sportif bonus bienvenue|paris sportif
bonus cash|paris sportif bonus de bienvenue|paris sportif bonus
gratuit|paris sportif bonus gratuit sans depot|paris sportif bonus retirable|paris sportif bonus sans depot|paris sportif bonus
sans depot belgique|paris sportif bookmaker|paris
sportif but contre son camp|paris sportif but temps additionnel|paris sportif buteur|paris sportif buteur
blessé|paris sportif buteur carton rouge|paris sportif buteur contre son camp|paris sportif buteur
non titulaire|paris sportif buteur prolongation|paris
sportif buteur qui ne joue pas|paris sportif buteur remplacant|paris sportif calcul gain|paris sportif canada|paris
sportif cash|paris sportif cash out|paris sportif champion ligue 1|paris sportif
champions league|paris sportif classement ligue 1|paris sportif code promo|paris sportif combine|paris sportif combiné|paris sportif combiné comment
ça marche|paris sportif combiné du jour|paris sportif
combiné match reporté|paris sportif comment ca marche|paris
sportif comment faire|paris sportif comment gagner|paris sportif comment gagner a tous les coups|paris sportif comment jouer|paris sportif comment ça marche|paris sportif comparateur
cote|paris sportif comparatif|paris sportif conseil|paris sportif conseil gratuit|paris sportif conseil pour gagner|paris
sportif cote|paris sportif cote et match|paris sportif cote explication|paris sportif cote psg|paris sportif coupe d’europe|paris sportif coupe davis|paris sportif coupe de france|paris sportif coupe du monde|paris sportif coupe du monde de rugby|paris sportif coupe du monde
rugby|paris sportif depot 5 euro|paris sportif depot minimum|paris sportif depot paypal|paris sportif dnb|paris sportif
du jour|paris sportif du jour conseil|paris sportif dépôt 1 euro|paris sportif dépôt minimum 5 euros|paris sportif en belgique|paris sportif en france|paris sportif en ligne|paris sportif en ligne avec paypal|paris sportif en ligne avis|paris sportif en ligne belgique|paris sportif en ligne bonus|paris
sportif en ligne cameroun|paris sportif en ligne comment gagner|paris sportif en ligne
comment ça marche|paris sportif en ligne france|paris sportif en ligne gratuit|paris
sportif en ligne maroc|paris sportif en ligne paypal|paris sportif en ligne québec|paris sportif
en ligne sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris sportif espagne france|paris sportif esport|paris sportif et casino en ligne|paris sportif et hippique|paris sportif et prolongation|paris sportif euro|paris sportif europa league|paris sportif explication|paris
sportif final ligue des champions|paris sportif finale ligue des champions|paris sportif
foot|paris sportif foot aide|paris sportif foot astuce|paris sportif foot aujourd’hui|paris sportif foot
ce soir|paris sportif foot comment ca marche|paris sportif foot conseil|paris sportif foot cote|paris sportif
foot coupe du monde|paris sportif foot en ligne|paris sportif foot feminin|paris sportif foot gratuit|paris sportif foot prolongation|paris sportif foot pronostic|paris sportif foot
pronostic gratuit|paris sportif foot regle|paris sportif foot suisse|paris sportif foot us|paris sportif football|paris sportif football
americain|paris sportif football astuces|paris sportif forfait tennis|paris sportif forum|paris sportif francais|paris sportif francaise
des jeux|paris sportif france|paris sportif france 2|paris sportif france
allemagne|paris sportif france angleterre|paris sportif france argentine|paris sportif france autriche|paris
sportif france belgique|paris sportif france espagne|paris sportif
france gibraltar|paris sportif france italie|paris sportif france nouvelle
zelande|paris sportif france pologne|paris sportif france portugal|paris sportif
france uruguay|paris sportif france usa|paris sportif freebet sans depot|paris sportif gagnant|paris sportif gagnant à coup sûr|paris sportif gagner a
coup sur|paris sportif gagner argent|paris sportif gagner de l’argent|paris sportif gain|paris sportif gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris sportif gratuit appli|paris sportif gratuit avec cadeaux|paris sportif gratuit cadeaux|paris sportif gratuit en ligne|paris sportif gratuit
entre amis|paris sportif gratuit sans argent|paris sportif
gratuit sans depot|paris sportif gratuit sans dépôt|paris sportif gratuits|paris sportif
gros gain|paris sportif handicap|paris sportif handicap 0 1|paris sportif handicap 0-1|paris sportif handicap 1
0|paris sportif handicap 1-0|paris sportif handicap basket|paris sportif handicap explication|paris sportif handicap foot|paris sportif
handicap rugby|paris sportif hippique|paris sportif hockey|paris sportif
hockey nhl|paris sportif hockey sur glace|paris sportif hors
arjel|paris sportif hors arjel france|paris sportif jeux olympiques|paris sportif jeux video|paris sportif joueur blessé|paris sportif joueur blessé pendant le match|paris sportif joueur de foot|paris sportif joueur decisif|paris sportif joueur declare
forfait|paris sportif joueur déclare forfait|paris sportif joueur remplacant|paris sportif la francaise des jeux|paris sportif
le plus rentable|paris sportif legal en france|paris sportif leicester champion|paris sportif les 18 stratégies pour gagner tous les jours|paris sportif les plus
sur|paris sportif les prolongation compte|paris sportif ligne|paris sportif ligue 1|paris sportif ligue 2|paris sportif ligue des champions|paris sportif ligue des nations|paris sportif ligue europa|paris sportif liste|paris sportif
martingale|paris sportif match|paris sportif match abandonné|paris sportif match annulé|paris sportif match
arrêté|paris sportif match du jour|paris sportif match interrompu|paris sportif match reporté|paris sportif match suspendu|paris sportif match tennis interrompu|paris sportif match
truqué|paris sportif meilleur bonus|paris sportif meilleur cote|paris sportif meilleur pronostic|paris sportif meilleur site|paris
sportif methode|paris sportif methode 2 3|paris sportif mi temps fin de match|paris sportif
mise au jeu|paris sportif mise maximum|paris sportif mma france|paris sportif
moins de 3.5 but|paris sportif montante|paris sportif moto gp|paris sportif multiple|paris sportif multiple 2 3|paris sportif
multiple 2 3 explication|paris sportif multiple
2 4|paris sportif multiple 2 5|paris sportif multiple
2/3 explication|paris sportif multiple 3 4|paris sportif multiple explication|paris sportif
national 1 foot|paris sportif nba|paris sportif nba conseil|paris sportif nba pronostic|paris sportif nhl|paris sportif nombre de but|paris sportif nouveau site|paris sportif numero
match|paris sportif offert|paris sportif offre bienvenue|paris sportif offre bienvenue sans depot|paris sportif offre
de bienvenue|paris sportif offre sans depot|paris sportif om psg|paris sportif
paypal|paris sportif plus de 1.5 but|paris sportif plus de 2
5 but|paris sportif plus ou moins|paris sportif plus ou moins 2 5 but|paris sportif premier pari remboursé|paris sportif premier
paris remboursé|paris sportif prolongation|paris sportif prolongation basket|paris sportif prolongation foot|paris sportif promo|paris
sportif pronostic|paris sportif pronostic basket|paris sportif pronostic des match aujourd hui|paris sportif pronostic expert gratuit|paris sportif pronostic foot|paris sportif pronostic forum|paris sportif pronostic
gratuit|paris sportif pronostic tennis|paris sportif psg|paris sportif psg arsenal|paris sportif psg barcelone|paris sportif
psg bayern|paris sportif psg dortmund|paris sportif psg inter|paris sportif psg inter cote|paris
sportif psg liverpool|paris sportif psg om|paris sportif qr
code|paris sportif que veut dire handicap|paris sportif
qui rapporte le plus|paris sportif regle|paris sportif regle prolongation|paris sportif rembourse|paris sportif remboursement cash|paris sportif rembourser|paris
sportif remboursé|paris sportif remboursé
cash|paris sportif remboursé en cash|paris sportif retrait paypal|paris sportif rue des
joueurs|paris sportif rugby|paris sportif rugby 6 nations|paris sportif
rugby coupe du monde|paris sportif rugby top 14|paris sportif safe du jour|paris sportif
sans argent|paris sportif sans carte bancaire|paris sportif sans carte d’identité|paris sportif sans compte bancaire|paris sportif
sans depot|paris sportif sans depot minimum|paris sportif si
match suspendu|paris sportif si un joueur abandonne|paris sportif si un joueur ne joue pas|paris sportif si
un joueur se blesse|paris sportif simple ou combiné|paris sportif site|paris sportif statistique|paris sportif stratégie|paris sportif suisse|paris sportif suisse application|paris
sportif suisse en ligne|paris sportif suisse legal|paris sportif suisse légal|paris
sportif suisse romande|paris sportif sur du jour|paris sportif
sur le tennis|paris sportif systeme|paris sportif
systeme 2 3|paris sportif systeme 2 4|paris sportif systeme 2/3|paris
sportif systeme 2/4|paris sportif systeme 3
4|paris sportif systeme 3/4|paris sportif systeme explication|paris sportif technique|paris sportif technique pour gagner|paris sportif temps additionnel|paris
sportif temps reglementaire|paris sportif tennis|paris sportif tennis abandon|paris sportif tennis conseil|paris sportif tennis de table|paris sportif tennis forfait|paris sportif tennis gratuit|paris sportif tennis pronostic|paris sportif tennis roland garros|paris sportif tir au but|paris sportif top 14|paris sportif tour de france|paris sportif ufc|paris sportif ufc france|paris sportif unibet|paris sportif vainqueur euro|paris sportif vainqueur ligue 1|paris sportif vainqueur ligue des champions|paris sportif via paypal|paris sportif victoire prolongation|paris
sportif vip gratuit|paris sportifs|paris sportifs abandon tennis|paris sportifs aide|paris sportifs analyser
un match|paris sportifs arjel|paris sportifs astuces|paris sportifs aujourd’hui|paris sportifs autorisés en france|paris sportifs avec paypal|paris sportifs
basket|paris sportifs belgique|paris sportifs bonus|paris sportifs bookmakers|paris sportifs
canada|paris sportifs combiné|paris sportifs comparateur|paris sportifs comparatif|paris sportifs
conseils|paris sportifs cotes|paris sportifs coupe du monde|paris sportifs de football|paris sportifs
du jour|paris sportifs en belgique|paris sportifs en france|paris sportifs en ligne|paris sportifs
en ligne belgique|paris sportifs en ligne france|paris
sportifs en ligne gratuit|paris sportifs en ligne suisse|paris sportifs
en suisse|paris sportifs et hippiques|paris sportifs euro|paris sportifs foot|paris sportifs foot us|paris
sportifs forum|paris sportifs france|paris sportifs
france espagne|paris sportifs gagner à tous les coups|paris sportifs gratuit|paris
sportifs gratuits|paris sportifs gratuits
en ligne|paris sportifs handicap|paris sportifs hockey|paris sportifs hockey sur galce|paris sportifs hockey sur glace|paris sportifs
hors arjel|paris sportifs jeux olympiques|paris sportifs les bookmakers raflent la mise|paris sportifs ligne|paris sportifs ligue 1|paris sportifs ligue 2|paris sportifs ligue des champions|paris sportifs ligue europa|paris
sportifs match interrompu|paris sportifs montante|paris sportifs nba|paris sportifs
offre bienvenue|paris sportifs offre de bienvenue|paris sportifs paypal|paris sportifs pronostics|paris sportifs psg|paris sportifs psg inter|paris sportifs rugby|paris
sportifs sans argent|paris sportifs sans depot|paris
sportifs site|paris sportifs sites|paris sportifs statistiques|paris
sportifs stratégie|paris sportifs suisse|paris sportifs technique|paris sportifs techniques|paris sportifs tennis|paris sportifs tennis
astuces|paris sportifs top 14|paris sportifs tour de france|part de marché paris sportifs|paypal pari sportif|paypal paris sportif|paypal paris
sportifs|perte d’argent paris sportifs|peut on devenir riche avec les paris sportifs|peut on gagner de l’argent avec les
paris sportifs|peut on gagner sa vie avec les paris sportif|peut
on vraiment gagner de l’argent avec les paris sportifs|plus gros combine paris sportif|plus
gros gagnant paris sportif|plus gros gain paris sportif|plus gros gain paris sportif au monde|plus gros gain paris sportif france|plus gros gains paris sportif|plus gros pari sportif|plus gros
paris sportif|plus grosse cote gagner paris sportif|plus grosse cote pari sportif|plus grosse cote paris sportif|plus grosse mise paris sportif|plus grosse somme gagner au paris sportif|plus ou moins paris sportif|pourcentage de mise paris
sportif|premier pari sportif remboursé|probabilité cote paris sportif|probabilité
paris sportif combiné|prolongation basket paris sportif|prolongation paris sportif|promo pari sportif|promo
paris sportif|promo site de paris sportif|promo site pari sportif|promo site paris sportif|promos paris sportifs|prono paris sportif foot|prono paris sportif gratuit|prono paris sportif tennis|pronostic de paris sportif|pronostic du jour paris sportif|pronostic foot paris sportif|pronostic
gratuit paris sportif|pronostic pari sportif|pronostic pari
sportif gratuit|pronostic paris sportif|pronostic paris sportif aujourd’hui|pronostic paris sportif du jour|pronostic paris sportif foot|pronostic paris sportif gratuit|pronostic paris
sportif tennis|pronostic paris sportifs|pronostics foot statistiques et aides aux paris sportifs|pronostics paris sportif|pronostics paris sportifs|pronostiqueur paris sportif gratuit|psg arsenal paris sportif|psg bayern paris sportif|psg inter milan paris sportif|psg inter pari sportif|psg
inter paris sportif|psg liverpool paris sportif|psg om paris sportif|psg paris sportif|psg paris sportifs|qr code paris sportif|qu est
ce qu un handicap paris sportif|qu est ce que handicap dans les paris sportif|qu’est ce qu’un handicap paris sportif|qu’est
ce que handicap dans les paris sportif|quand un joueur se
blesse paris sportif|que signifie 1/1 en paris sportif|que signifie 1/2 paris sportif|que
signifie 12 en paris sportif|que signifie 1×2 dans les paris sportifs|que signifie
btts en paris sportif|que signifie dnb en paris sportif|que signifie draw en paris sportif|que signifie ft
en paris sportif|que signifie gg dans le pari sportif|que signifie gg en pari sportif|que signifie gg en paris sportif|que signifie
handicap dans les paris sportifs|que veut dire dnb en paris sportif|que veut dire handicap dans
les paris sportifs|que veut dire handicap paris sportif|quel appli pari sportif|quel cote jouer paris sportif|quel est
la meilleur appli de paris sportif|quel est le meilleur algorithme de
paris sportif|quel est le meilleur site de pari sportif|quel est le meilleur site de pari sportif en ligne|quel est le meilleur site de paris sportif|quel est
le meilleur site de paris sportif en ligne|quel est le
meilleur site de paris sportifs en ligne|quel est le pari sportif le
plus rentable|quel pari sportif est le plus rentable|quel pari sportif est le plus sûr|quel pari sportif faire aujourd’hui|quel paris sportif faire
aujourd’hui|quel paris sportif rapporte le plus|quel site de paris sportif choisir|quel site de paris sportif
rembourse en cash|quel type de pari sportif est le plus
rentable|quelle application pour paris sportifs|quelle est la meilleure appli de paris sportif|quelle est la meilleure application de paris sportif|quelle est la meilleure application pour les paris sportifs|quelle est
le meilleur site de paris sportif|quels paris sportifs faire|quels sont les paris
sportifs les plus sûrs|rebond basket paris sportif|record de gain paris
sportif|regle buteur paris sportif|regle de paris
sportif|regle des paris sportif|regle handicap paris sportif|regle handicap paris
sportif foot|regle multiple paris sportif|regle pari sportif|regle paris sportif|regle
paris sportif foot|regle paris sportif multiple|regle
paris sportif prolongation|reglement pari sportif|reglement paris sportif|regles paris
sportifs|remboursement cash paris sportif|remboursement en cash paris sportif|remboursement pari sportif|remboursement paris sportif|repartiteur de mise paris sportif|repartiteur de mise paris
sportifs|repartiteur de mises paris sportif|repartiteur mise paris sportif|repartition des mises paris sportif|resultat
pari sportif|resultat paris sportif|resultat paris sportif en direct|resultat
paris sportif foot|resultat sportif hockey|retirer argent paris sportif|rugby pari sportif|rugby paris sportif|règle paris sportif prolongation|règles paris sportif|répartiteur de mise pari
sportif|répartiteur de mise paris sportif|répartiteur de mise paris sportifs|répartition des mises
paris sportif|résultat paris sportif foot|sans depot paris sportif|se faire interdire de paris sportifs|signification btts paris sportif|signification dnb paris sportif|signification handicap paris sportif|simulateur de gain paris
sportif|simulateur gain paris sportif|simulateur gain paris sportif multiple|simulateur gain paris sportif systeme|simulateur gain paris sportif système|simulateur montante
paris sportif|simulateur paris sportif multiple|simulateur systeme paris sportif|simulation paris sportif gratuit|site aide paris
sportif|site analyse paris sportif|site analyser paris sportif|site arjel paris sportif|site conseil paris sportif|site d’analyse de paris sportifs|site d’analyse
paris sportif|site de conseil paris sportif|site de
pari en ligne sportif|site de pari sportif|site de pari sportif avec bonus sans depot|site de pari
sportif bonus sans depot|site de pari sportif canada|site de pari
sportif en ligne|site de pari sportif francais|site de pari sportif gratuit|site de pari sportif hors arjel|site de pari sportif suisse|site de
parie sportif|site de parie sportif en ligne|site de paris en ligne sportif|site de paris sportif|site de
paris sportif acceptant paypal|site de paris sportif arjel|site de paris sportif
autorisé en france|site de paris sportif
autorisé en suisse|site de paris sportif avec bonus|site de paris sportif avec bonus sans depot|site de paris sportif avec bonus sans dépôt|site de paris sportif avec neosurf|site de paris sportif avec paiement mobile|site de paris sportif avec paypal|site de paris sportif avis|site de paris sportif
belge avec bonus|site de paris sportif belgique|site de paris sportif bonus|site de paris sportif bonus sans depot|site de paris sportif canada|site de paris sportif comparatif|site de paris
sportif depot minimum|site de paris sportif en france|site de paris sportif en ligne|site de paris
sportif en ligne suisse|site de paris sportif football|site de paris
sportif francais|site de paris sportif france|site de paris sportif
gratuit|site de paris sportif gratuit pour gagner des cadeaux|site de paris
sportif gratuit sans dépôt|site de paris sportif hors arjel|site de paris sportif le plus
fiable|site de paris sportif legal en france|site de paris sportif
meilleur cote|site de paris sportif nouveau|site de paris sportif
offre de bienvenue|site de paris sportif paypal|site de paris sportif premier paris remboursé|site de paris
sportif qui accepte paypal|site de paris sportif
qui rembourse en cash|site de paris sportif remboursé|site de paris sportif sans argent|site de paris sportif
sans carte bancaire|site de paris sportif sans carte d’identité|site de paris sportif
sans depot|site de paris sportif suisse|site de paris sportifs|site de paris sportifs avec paypal|site de paris
sportifs en ligne|site de paris sportifs francais|site de paris sportifs gratuit|site de paris sportifs paypal|site de
paris sportifs suisse|site de statistique pour paris sportif|site des paris sportifs|site pari
en ligne sportif|site pari sportif|site pari sportif 100 euros offert|site pari
sportif arjel|site pari sportif belgique|site pari sportif bonus|site pari sportif canada|site pari sportif comparatif|site
pari sportif en ligne|site pari sportif france|site pari sportif gratuit|site pari sportif hors arjel|site pari
sportif suisse|site parie sportif|site paris en ligne sportif|site paris sportif|site paris sportif 100 euros offert|site paris sportif 100 euros remboursé|site paris sportif 1er paris remboursé|site paris sportif arjel|site
paris sportif autorisé en france|site paris sportif avec bonus|site paris sportif avec bonus sans depot|site paris sportif
avec meilleur cote|site paris sportif belgique|site paris
sportif bonus|site paris sportif bonus cash|site paris
sportif bonus sans depot|site paris sportif canada|site paris sportif comparatif|site paris sportif depot 5 euro|site paris sportif en ligne|site paris
sportif foot|site paris sportif france|site paris sportif
gratuit|site paris sportif hors arjel|site paris sportif hors arjel france|site paris
sportif meilleur cote|site paris sportif nouveau|site
paris sportif offre de bienvenue|site paris sportif paypal|site paris sportif remboursement cash|site
paris sportif remboursé en cash|site paris sportif retrait instantané|site paris sportif sans carte bancaire|site
paris sportif sans depot|site paris sportif suisse|site paris sportifs|site paris sportifs belgique|site
paris sportifs en ligne|site paris sportifs france|site paris
sportifs hors arjel|site paris sportifs suisse|site pour analyse paris sportif|site pour paris sportif|site pronostic paris sportif|site statistique paris sportif|site suisse paris sportif|sites de pari sportif|sites de paris sportif|sites de paris sportifs|sites de paris
sportifs arjel|sites de paris sportifs autorisés en france|sites de
paris sportifs belgique|sites de paris sportifs
bonus|sites de paris sportifs en belgique|sites de paris sportifs en france|sites de
paris sportifs en ligne|sites de paris sportifs gratuits|sites
de paris sportifs gratuits sans dépôt|sites de paris sportifs suisse|sites pari sportif|sites paris sportif|sites paris sportifs|sites paris sportifs arjel|sites paris sportifs belgique|sites paris sportifs france|sites paris sportifs hors arjel|sites paris sportifs suisse|so foot paris sportif|so foot paris sportifs|specialiste tennis
paris sportif|statistique foot paris sportif|statistique paris sportif|statistique paris sportif foot|statistique tennis paris sportif|statistiques football paris sportifs|statistiques paris sportifs|strategie
de paris sportif|stratégie big whale paris sportif|stratégie de paris
sportifs|stratégie gagnante paris sportifs|stratégie pari sportif|stratégie paris sportif|stratégie paris sportifs|stratégie paris sportifs
forum|stratégie pour gagner au paris sportif|stratégies paris sportifs|suisse paris sportif|suisse paris sportifs|systeme 2 3 paris sportif|systeme 3 4 paris sportif|systeme de cote paris sportif|systeme de paris sportif|systeme pari sportif|systeme paris sportif|systeme paris sportifs|systeme reducteur
paris sportif|système paris sportif|tableau
bankroll paris sportif|tableau cote paris sportif|tableau de paris sportif|tableau de suivi paris sportifs|tableau excel bankroll paris
sportif|tableau excel paris sportif|tableau excel paris sportif gratuit|tableau excel paris
sportifs|tableau excel pour paris sportif|tableau gestion bankroll paris
sportif|tableau montante paris sportif|tableau paris sportif|tableau paris sportif excel|tableau roi paris
sportifs|tableau statistique paris sportif|tableau suivi paris sportif|taxe
gain paris sportif|technique combiné
I’d like to find out more? I’d like to find out some additional information.
forticlient on mac
бездепозитные бонусы в казино казахстан
бездепозитные бонусы в казино за регистрацию с выводом без пополнения
Go to our updated platform
See the latest here
Hi there everyone, it’s my first pay a visit at this web page, and paragraph is truly fruitful for me, keep up posting these articles.
fortinet vpn client
бездепозитные бонусы в казино лев
https://community.forextradershub.com/read-blog/14941
https://doctorsforum.ru/viewtopic.php?f=268&t=46722
https://www.arpt.gov.gn/arrete-a-2010-359-sgg-mtnti-2010-portant-mise-en-place-des-mesures-pour-la-gestion-du-trafic-international-et-des-sanctions-contre-la-fraude/#comment-1585714
Thank you for sharing your thoughts. I really appreciate your efforts and I am waiting for your next post thank you once again.
Qfinder Pro
One x Bet Promo Code http://lipetskregionsport.ru/news/pages/1hbet_promokod_na_6500_pri_registracii.html
One x Bet promo code is another variant referring to the 1xBet promo code. These codes are used to unlock bonuses on the 1xBet platform, enhancing the betting experience with free bets, deposit matches, or free spins.
1xBet Welcome Bonus 2026 http://lipetskregionsport.ru/news/pages/1hbet_promokod_na_6500_pri_registracii.html
In 2026, 1xBet continues to offer an attractive welcome bonus for new users. This bonus typically includes a match on the first deposit, providing extra funds to start betting on the platform. Promo codes can enhance this offer with additional free bets or free spins.
в каком казино дают за регистрацию бездепозитные бонусы
бездепозитные бонусы в казино казахстан
sportwetten in österreich
Here is my homepage … Wettstrategien Livewetten (Orpealead.Es)
Букмекерские конторы в России предлагают огромное количество промокодов и бонусов для своих клиентов, особенно много купонов новичкам, где при регистрации можно получить бесплатно деньги на свой счет. Букмекерская контора Melbet открывает новым игрокам бонус на первый депозит с увеличенной суммой до 50 000 рублей, за Мелбет промокод на сегодня, который можно скопировать у нас. Предлагаем ввести промокод мелбет на сегодня, который в 2026 году даёт увеличение 130% бонуса на первый депозит до 50 000 рублей. Регистрируйся и играй с Мелбет сегодня!!! Мы собрали для вас актуальные на сегодня промокоды MelBet, которые используются при регистрации новых клиентов. После чего скидки и бонусы будут зачислены вам на счет.
Букмекерская контора Melbet является одним из столпов международной беттинговой индустрии. За счет масштабной маркетинговой компании, высоких коэффициентов и оперативной технической поддержки БК Мелбет удалось привлечь и удержать большое количество игроков. На сегодняшний день, букмекер предлагает получить один из самых высоких бонусов на рынке – 50 000 рублей. Размер бонуса в Melbet составляет 100% от суммы первого пополнения, но не менее 100 рублей и не более 50 000. К примеру, если пополнить баланс на сумму 4000, то справа от основного счета появится бонусный. Как видим, использовать промокод мелбет на сегодня имеет смысл, особенно тем бетторам и бонусхантерам, которые привыкли заключать пари по-крупному. С учетом того, что он бесплатный – воспользоваться им может абсолютно любой игрок.
L’offre meilleur code promo 1xBet garantit un bonus jusqu’a 1 750 $ avec 150 tours gratuits inclus pour le casino, disponibles immediatement sur le compte joueur. Vous pouvez utiliser le bonus immediatement apres le depot, en suivant les conditions de mise sur les slots indiques. Une fois la periode de bienvenue terminee, vous pouvez egalement recevoir jusqu’a 30 % de cashback sur les pertes. Pour en savoir plus sur le code promo 1xBet casino en ligne, consultez ce lien : https://gazetablic.com/new/?code_promo_208.html
Code Promo 1xbet Aujourd’huidice permet aux nouveaux inscrits d’obtenir un bonus de bienvenue 1xbet, vous aide a booster votre premier depot, et vous permet d’obtenir des paris gratuits. Rappelez-vous que le bonus est soumis a certaines conditions, notamment les regles concernant les mises et l’utilisation du bonus. Consultez le site 1xBet pour garantir une experience de pari fluide et agreable.
макс ремонт айфона
ремонт айфон стекло
ремонт принтеров
бездепозитные бонусы за регистрацию в казино с выводом без пополнения 2024 без отыгрыша
https://openlibrary.org/people/code_promo382/lists/OL316569L/MelBet_promo_code_today_%282026%29_ZEVS777_-_%E2%82%AC100_100_bonus
I savour, cause I found exactly what I was having a look for. You’ve ended my 4 day lengthy hunt! God Bless you man. Have a great day. Bye
watchguard vpn download
бездепозитные бонусы в казино 2025
Онлайн казино
как использовать бонус казино в 1win
онлайн игры топ
новые бездепозитные бонусы в казино за регистрацию с выводом без пополнения
https://www.friend007.com/forums/thread/32318/
https://www.slideserve.com/melbetofthebest56
Just want to say your article is as amazing. The clarity for your publish is just nice and i could suppose you’re an expert in this subject. Fine with your permission let me to take hold of your RSS feed to stay up to date with imminent post. Thanks a million and please continue the rewarding work.
netextender download for mac
QQ88 – Sân chơi cá cược an toàn, minh bạch và chuyên nghiệp. Tận hưởng slot nổ hũ, bắn cá, casino và hàng trăm ưu đãi dành cho hội viên.
azino777 официальный сайт мобильная версия зеркало рабочее на сегодня Azino777 делает азартные развлечения доступными каждому. Благодаря удобному интерфейсу и широкому ассортименту игр, вы можете наслаждаться любимыми слотами и другими играми в любое время и в любом месте. Откройте для себя мир азарта с Azino777
азино 777 официальный сайт вход в казино azino777 рабочее зеркало на сегодня Азино 777 известно своим разнообразным игровым ассортиментом и удобным интерфейсом. Платформа предлагает как классические слоты, так и новинки от ведущих разработчиков. Здесь каждый найдет игру по душе.
Abnormal this put up is totaly unrelated to what I was searching google for, but it surely used to be listed at the first page. I suppose your doing one thing proper if Google likes you adequate to place you at the first page of a non similar search.
QQ88 mang đến thế giới cá cược đẳng cấp với tốc độ xử lý siêu nhanh, trò chơi đa dạng và ưu đãi khủng mỗi ngày. Lựa chọn lý tưởng cho cược thủ. Tham gia QQ88 để khám phá hàng nghìn trò chơi hấp dẫn: casino live, thể thao, slot game và đá gà. Uy tín, minh bạch, nạp rút 24/7.
https://salemshop.kz/
https://locksmithswift.com/
https://enstdraftsite2018.blogs.rice.edu/2018/04/10/cultures-of-energy-7/#comment-24332
https://shawcenter.syr.edu/video-principal-barber-reflects-on-his-shaw-center-partnership/#comment-242911
azino777 официальный сайт мобильная версия зеркало рабочее на сегодня Ищете место, где азарт и возможность крупного выигрыша встречаются с щедрыми бонусами? Тогда вам стоит обратить внимание на Азино 777! Это популярное онлайн-казино предлагает своим игрокам захватывающий мир слотов, настольных игр и, конечно же, привлекательные бонусы, которые делают игру еще более интересной и выгодной.
azino777 официальный сайт зеркало на сегодня рабочее Хотите найти официальный сайт Азино 777? Мы поможем вам перейти на нужную страницу.
В Мелбет промокод — это уникальная комбинация из цифр и букв. Он может использоваться в самых разных ситуациях. Чаще всего применяется в Мелбет промокод при регистрации, чтобы привлечь новых игроков. Однако, он может давать бесплатную ставку и другие бонусы, которых очень много в данной букмекерской конторе. Этот материал расскажет о том, что из себя представляет и что дает Мелбет промокод. Промокод для Мелбет можно получить за участие в каких-либо активностях букмекерской конторы Мелбет. Например, уникальный код компания присылает на день рождения в виде подарка своим клиентам. Помимо этого, можно ввести в поисковике «Как получить промокод на Мелбет?» и найти тематические сайты, где постоянно публикуются актуальные комбинации цифр и букв. Букмекер часто распространяет свои promo коды через партнеров, а также некоторые игроки сами активно делятся ими в сети.
Мелбет – международный букмекер, основанный в 2012 году. Компания получила официальную лицензию от Кюрасао, ориентирована на пользователей со всех стран мира, но в первую очередь на русскоязычных игроков. Зарегистрированные клиенты имеют прекрасную возможность пользоваться всеми преимуществами компании, принимать участие в акциях, собирать выигрышные экспрессы, получать промокоды и бесплатные ставки. Компания Мелбет регулярно предоставляет своим клиентам большое количество бонусов и промокоды. Что дает промокод мелбет при регистрации 2026? Данное поощрение позволяет каждому игроку совершать бесплатные ставки, получать дополнительные денежные средства при пополнении игрового баланса. Кроме этого, благодаря промокодам сумма первого депозита может увеличиться до 100%. Букмекерская контора дарит бесплатные ставки для новых игроков и фрибеты для постоянных пользователей.
New version available here — https://bergkompressor.ru/
1xBet Welcome Bonus Promo Code https://idematapp.com/wp-content/pages/1xbet_promo_codes_free_bonus_offers.html
The 1xBet welcome bonus promo code is a code that new users can enter during registration to receive a welcome bonus. This bonus typically includes a deposit match and may also provide free bets or free spins.
Visit our homepage — https://gorod-fonarikov.ru/
1xBet Free Spin Promo Code Today https://idematapp.com/wp-content/pages/1xbet_promo_codes_free_bonus_offers.html
1xBet frequently offers promo codes that provide free spins for use on popular slot games. These codes are often valid for a limited time and can be used to win real money without risking your own funds.
Visit our newest official site — https://consolit.ru/
https://agrestina.pe.gov.br/glossario
https://vishalbharat.in/read-blog/12804
Howdy! Would you mind if I share your blog with my twitter group? There’s a lot of folks that I think would really appreciate your content. Please let me know. Cheers
biggest escort directory Brazil
QQ88 là điểm đến cá cược hiện đại với giao diện mượt, tỷ lệ thưởng cao và hệ thống bảo mật chuẩn quốc tế. Nhiều ưu đãi dành cho thành viên mới. Sân chơi cá cược an toàn, minh bạch và chuyên nghiệp. Tận hưởng slot nổ hũ, bắn cá, casino và hàng trăm ưu đãi dành cho hội viên.
Vavada casino offers games with high RTP and fair result generation. At https://museo.precolombino.cl/ fresh Vavada promo codes and working mirrors for today are published. Account funding at Vavada happens instantly through convenient payment systems. Withdrawals from Vavada are processed within a few hours. The Vavada interface is intuitive and user-friendly.
https://cvet-psy.ru/wp-inlcudes/articles/1xbet_promokod_pri_registracii_na_segodnya_2.html
ремонт dualsense ps5
“QQ88 mang đến hệ sinh thái giải trí đa dạng gồm casino live, slot nổ hũ, thể thao và đá gà, cam kết minh bạch, an toàn và siêu tốc trong từng giao dịch.”
https://datsun.getbb.ru/viewtopic.php?f=2&t=221
I like what you have to offer. Keep up the good work!
Промокод 1xBet на сегодня при регистрации. Пользователи могут использовать промокоды для получения различных бонусов от букмекера. Доступ к кодам есть на тематических сайтах и рабочих зеркалах. 1xbet предлагает разные способы регистрации: через e-mail. Компания заботится о клиентах и соблюдает международное право. Актуальные промокод на 1xbet при регистрации можно получить бесплатно: на нашем сайте. Любой желающий легко найдёт промокод 1xbet на сегодня. Бонусы щедрые, а условия их получения — реальные. В некоторых случаях вообще ничего делать не нужно.
ввести промокод 1xbet Ищите промокод на https://lenotoplenie.ru/images/pages/index.php?1xbet_promokod_pri_registracii_bonus_3.html и активируйте бонус до 32 500 рублей, чтобы начать игру.
78WIN เป็น เว็บเดิมพันออนไลน์ที่มีความน่าเชื่อถือสูง มอบประสบการณ์การเล่นที่ปลอดภัย โปร่งใส และสนุกสนานสำหรับผู้เล่นทุกคน. ด้วย เทคโนโลยีล้ำสมัย และ การบริการระดับมืออาชีพ 78winbiz.com จึงกลายเป็นตัวเลือกอันดับหนึ่งสำหรับนักเดิมพันออนไลน์.
Nền tảng QQ88 được tối ưu cho mọi thiết bị, đăng ký nhanh, nạp rút siêu tốc và nhiều chương trình khuyến mãi hấp dẫn cho người chơi mới lẫn lâu năm.
78WIN คือแพลตฟอร์มความบันเทิงออนไลน์ครบวงจร อัดแน่นด้วยเกมสล็อตแตกง่าย คาสิโนสดถ่ายทอดสด กีฬา หวย และอีกมากมาย เว็บไซต์ใช้งานง่าย ปลอดภัย รองรับทุกอุปกรณ์ การเงินมั่นคง รวดเร็ว โปร่งใส มาพร้อมโปรโมชั่นสุดคุ้มและสิทธิพิเศษสำหรับสมาชิก VIP พร้อมทีมงานดูแลตลอด 24 ชั่วโมง.
I really believe you will do well in the future I appreciate everything you have added to my knowledge base.
I favored your idea there, I tell you blogs are so helpful sometimes like looking into people’s private life’s and work.At times this world has too much information to grasp. Every new comment wonderful in its own right.
I wanted to check up and let you know how, a great deal I cherished discovering your blog today. I might consider it an honor to work at my office and be able to utilize the tips provided on your blog and also be a part of visitors’ reviews like this. Should a position associated with guest writer become on offer at your end, make sure you let me know.
it is a really nice point of view. I usually meet people who rather say what they suppose others want to hear. Good and well written! I will come back to your site for sure!
I really love this article.
https://www.salesforce.com/trailblazer/bongachatru
http://testforumrp.forumex.ru/viewtopic.php?f=7&t=879
I think that may be an interesting element, it made me assume a bit. Thanks for sparking my considering cap. On occasion I get so much in a rut that I simply really feel like a record.
L’offre meilleur code promo 1xBet permet de recevoir un bonus de 130 $ sur le compte de jeu des nouveaux utilisateurs. Le bonus est actif apres un depot minimum et la bonne application du code promo. Le systeme refuse le bonus si le code n’est pas exact. Pour plus de details sur le code promo 1xBet aujourd’hui, consultez ce lien : https://nz.pinterest.com/pin/892135007439058460/
Appreciation for taking the time to discuss this topic, I would love to discover more on this topic. If viable, as you gain expertise, would you object to updating the website with further information? It is tremendously beneficial for me.
I think this is among the so much vital info for me. And i’m happy reading your article. But wanna remark on few common issues, The site style is wonderful, the articles is really excellent : D. Just right job, cheers
Le bonus du code promo 1xBet peut atteindre 1 750 € avec un bonus de 150 tours gratuits. Cette promotion est tres pratique pour les nouveaux joueurs, cela permet de jouer sans risquer son propre capital. L’acces est reserve aux joueurs majeurs. Pour plus de details sur le meilleur code promo 1xBet, vous pouvez consulter ce lien : https://www.mister-deejay.com/live/pgs/?le_meilleur_code_promo_2.html
You are one talented writer thank you for the post.
https://slcs.edu.in/kanga/
https://ins.edu.vn/boi-duong-kien-thuc-quan-tri-an-ninh-va-quan-tri-anptt-cho-can-bo-cac-cap-tinh-dien-bien-2024/
http://introsystems.ru/component/kunena/suggestion-box/44130-fonbet-fribet-promokod-max777-fribet-do-15-000
78WIN คือแพลตฟอร์มความบันเทิงออนไลน์ครบวงจร อัดแน่นด้วยเกมสล็อตแตกง่าย คาสิโนสดถ่ายทอดสด กีฬา หวย และอีกมากมาย เว็บไซต์ใช้งานง่าย ปลอดภัย รองรับทุกอุปกรณ์ การเงินมั่นคง รวดเร็ว โปร่งใส มาพร้อมโปรโมชั่นสุดคุ้มและสิทธิพิเศษสำหรับสมาชิก VIP พร้อมทีมงานดูแลตลอด 24 ชั่วโมง.
I like meeting utile info, this post has got me even more info!
The post is absolutely great! Lots of great info and inspiration, both of which we all need! Also like to admire the time and effort you put into your blog and detailed information you offer! I will bookmark your website!
подключение 1С КА 2.0 в России Нс Диджитал Франчайзинг 1С Бухгалтерия, продажа и разработка продуктов 1с
http://gzew.phorum.pl/viewtopic.php?p=526628&sid=677f0c9c0662bc7d2641eb6956cc4b66#526628
https://www.gooalsocial.com/blogs/view/15766
This is something that will need all of our combined efforts to address.
My brother suggested I might like this blog.
He was entirely right. This post actually made my day.
You cann’t imagine just how much time I had spent for
this info! Thanks!
Hi! This is my first visit to your blog! We are a
collection of volunteers and starting a new project in a community in the same niche.
Your blog provided us beneficial information to work
on. You have done a marvellous job!
Hello this is kinda of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding knowledge so I wanted to get advice from someone with experience. Any help would be enormously appreciated!
Loving the info on this website , you have done outstanding job on the blog posts.
Your thing regarding creating will be practically nothing in short supply of awesome. This informative article is incredibly useful and contains offered myself a better solution to be able to my own issues. Which can be the specific purpose MY PARTNER AND I has been doing a search online. I am advocating this informative article with a good friend. I know they are going to get the write-up since beneficial as i would. Yet again many thanks.
Glad to be one of many visitants on this amazing site : D.
The sketch is tasteful, your authored material stylish.
бонусы казино Ваш путь к крупным выигрышам начинается здесь: Топ казино с лучшими предложениями! Хотите играть в казино, где шансы на выигрыш выше, а бонусы приятно удивляют? Мы составили рейтинг самых лучших казино, которые предлагают не только широкий выбор игр от ведущих разработчиков, но и самые выгодные условия для игроков. Получите приветственные бонусы, участвуйте в турнирах и наслаждайтесь быстрыми выплатами – все это ждет вас в нашем топе казино!
L’offre 1xbet bonus de bienvenue 2026 permet de recevoir jusqu’a 130 $/€ equivalent a 100 % du depot initial. Assurez-vous de respecter les conditions de mise pour obtenir le bonus sur votre compte principal. L’utilisation standard implique de placer des paris sportifs avec au moins trois evenements par pari et une cote minimale de 1,4. Toutes les conditions doivent etre respectees dans un delai de 30 jours. Pour plus d’informations sur le code promo 1xBet aujourd’hui, vous pouvez consulter ce lien : https://ruptur.com/libs/photo/promokod_1xbet_na_segodnya_besplatno_pri_registracii.html
Code Promo 1xbet Sans Depot vous donne un code promo 1xBet 130€ avec un bonus de 100%, Les nouveaux joueurs recoivent un bonus de bienvenue 2025. Prenez connaissance des conditions de reception et d’utilisation du bonus avant l’inscription. Connectez-vous a votre compte 1xBet pour decouvrir comment utiliser le bonus de bienvenue 1xbet.
топ 10 честных казино на деньги Чувствуете, что сегодня ваш день? Игровые автоматы готовы подарить вам незабываемые острые ощущения! Каждый спин – это шаг к крупному выигрышу или просто захватывающее приключение. Позвольте себе окунуться в мир азарта и испытать свою фортуну!
Промокод при регистрации 1xbet на 32 500 рублей. Этот код нужно ввести при регистрации в соответствующее поле. 1Xbet промокод можно использовать только один раз, но им можно делиться с друзьями. Регистрация по номеру телефона — быстрый способ создать аккаунт. После получения данных для входа остаётся лишь ввести логин и пароль. Используй актуальный 1xBet промокод на сегодня и увеличь первый депозит до 32 500 рублей в БК 1xBet. На платформе действует бонусная программа, которая помогает игрокам получать до повышенного кэшбэка от первого депозита.
промо код на 1xbet Вводите действующий купон на http://www.medtronik.ru/images/pages/bonus_kod_na_1xbet_pri_registracii_6500_rubley.html и получите бонус до 32 500 рублей, чтобы начать ставки с преимуществом.
https://t.me/getx_site_official
https://t.me/getx_site_official
бонусы казино без депозита и без отыгрыша Мир игровых автоматов поражает своим разнообразием! Здесь вы найдете всё: от простых и понятных фруктовых слотов до сложных многоуровневых игр с захватывающими сюжетами и уникальными бонусными раундами. Каждый автомат – это отдельная история, своя атмосфера и свои правила игры. Исследуйте новые миры, собирайте комбинации и наслаждайтесь процессом, ведь в игровых автоматах возможно всё!
лав казино промокод фриспинов Хотите играть в казино с удовольствием и без лишних хлопот? Тогда вам точно стоит обратить внимание на рейтинги казино. Это не просто списки, а результат тщательного анализа множества факторов, которые напрямую влияют на ваш игровой опыт. Хороший рейтинг поможет вам избежать сомнительных сайтов и найти место, где вас ждут честные игры, быстрые выплаты и приятные бонусы. Не тратьте время на поиски – доверьтесь проверенным рекомендациям!
Hello there, You have done an incredible job. I will certainly digg it and personally recommend to my friends. I am sure they will be benefited from this site.
I enjoy your blog posts, saved to my bookmarks!
Промокод 1xBet на сегодня при регистрации. Игроки могут использовать промокоды для получения различных бонусов от букмекера. Доступ к кодам есть на тематических сайтах и рабочих зеркалах. 1xbet предлагает разные способы регистрации: в 1 клик. Компания заботится о клиентах и соблюдает международное право. Актуальные 1хБет промокод на фриспины можно получить бесплатно: у партнёров БК. Любой желающий легко найдёт промокод 1xbet на сегодня. Бонусы щедрые, а условия их получения — реальные. В некоторых случаях вообще ничего делать не нужно.
http://boptions.ru/analitika-ot-olimp-trejd/?unapproved=554695&moderation-hash=bb3120ec4fdebddfb32889513bbc5f78#comment-554695
Hi there, yes this paragraph is really nice and I have learned lot of things from it regarding blogging. thanks.
juego friv 2018
Déterminer quel casino en ligne est réellement adapté pour miser de l’argent véritable s’avère bien plus délicat qu’on pourrait le penser. En 2025, le secteur français des jeux virtuels connaît une croissance rapide, mettant à disposition plus de 200 plateformes certifiées accessibles aux joueurs nationaux. Cette multitude d’options rend la sélection d’un site fiable et agréable encore plus exigeante.C’est pour cette raison que notre classement s’appuie sur une analyse rigoureuse. L’ensemble des casinos en argent réel mentionnés ici ont été examinés en détail avant d’être ajoutés. La sécurité des utilisateurs demeure au cœur de nos priorités, et notre objectif est de vous éviter les dangers associés aux sites non fiables, de plus en plus nombreux sur le web.
онлайн казино в россии Хотите играть в лучших казино? Мы знаем, где искать! Если вы задаетесь вопросом, какие онлайн-казино действительно стоят вашего внимания, то наш топ – это то, что вам нужно. Мы проанализировали множество площадок и выделили самые надежные, с лучшими играми и самыми привлекательными бонусами. Не тратьте время на поиски – выбирайте из проверенных лидеров и начните свое азартное приключение прямо сейчас!
казино с выводом без верификации документов 2024 Хотите играть в лучших казино? Мы знаем, где искать! Если вы задаетесь вопросом, какие онлайн-казино действительно стоят вашего внимания, то наш топ – это то, что вам нужно. Мы проанализировали множество площадок и выделили самые надежные, с лучшими играми и самыми привлекательными бонусами. Не тратьте время на поиски – выбирайте из проверенных лидеров и начните свое азартное приключение прямо сейчас!
Top 9 Meilleur casino en ligne pour les joueurs français: Winamax – idéal pour le poker et les tournois en ligne, Pokerstars – top pour affronter les joueurs de poker du monde entier, Wazamba – parfait pour les tournois réguliers attractifs, PMU – spécialisé sur le turf, mais propose aussi les paris sportifs, Unibet – idéal pour varier les jeux en ligne, FDJ – meilleure option pour les jeux de loterie et les jeux traditionnels français, Betclic – offre une interface intuitive et des paris combinés, Parionsweb – pensé pour les parieurs français traditionnels, Bwin – intéressant pour les paris sportifs et options hybrides. Le marché du casino en ligne en France connaît une croissance exceptionnelle en 2025. Avec plus de 3 millions de joueurs actifs, les casinos en ligne français offrent une expérience de jeu de plus en plus sophistiquée et sécurisée. Ce guide complet vous présente les meilleurs casinos en ligne disponibles en France, leurs bonus exclusifs, et toutes les informations essentielles pour jouer en toute sécurité.
Vous recherchez un casino en ligne France à la fois fiable et divertissant ? Découvrez notre liste des meilleurs sites de casino où jouer ! Notre équipe évalue chaque plateforme selon des critères précis : la licence, la variété de jeux, la rapidité des paiements et l’expérience utilisateur. Après analyse, le meilleur casino en ligne reste Winamax, reconnu pour sa sécurité et sa régulation exemplaire. Notre classement de 2025 réunit les casinos en ligne les plus adaptés aux joueurs français, garantissant confiance, transparence et plaisir de jeu responsable.
казино с моментальными выплатами Хотите играть в лучших казино? Мы знаем, где искать! Если вы задаетесь вопросом, какие онлайн-казино действительно стоят вашего внимания, то наш топ – это то, что вам нужно. Мы проанализировали множество площадок и выделили самые надежные, с лучшими играми и самыми привлекательными бонусами. Не тратьте время на поиски – выбирайте из проверенных лидеров и начните свое азартное приключение прямо сейчас!
бонусы казино без депозита Хотите играть в лучших казино? Мы знаем, где искать! Если вы задаетесь вопросом, какие онлайн-казино действительно стоят вашего внимания, то наш топ – это то, что вам нужно. Мы проанализировали множество площадок и выделили самые надежные, с лучшими играми и самыми привлекательными бонусами. Не тратьте время на поиски – выбирайте из проверенных лидеров и начните свое азартное приключение прямо сейчас!
http://izumrudnoeozero.listbb.ru/viewtopic.php?f=18&t=2106
789Win nổi bật với nền tảng hiện đại, đa dạng các trò chơi từ thể thao, casino trực tuyến đến slot game độc đáo. Cam kết mang lại trải nghiệm an toàn, minh bạch và cơ hội thắng lớn với vô số khuyến mãi hấp dẫn dành cho mọi người chơi!
See what’s new today > https://svoyage.ru/
Go directly to our website : https://consolit.ru/
https://usfblogs.usfca.edu/psip/2015-projects/homeownership-sf-hsf/comment-page-148/#comment-91687
Try the new version here — https://bergkompressor.ru/
Go to our site right now
Go to our updated platform
автомат игра онлайн Ищете, где поиграть в игровые автоматы? У нас вы найдете огромный выбор слотов на любой вкус: от классических фруктовых автоматов до современных видеослотов с потрясающей графикой и бонусными играми. Играйте онлайн в любое удобное время, наслаждаясь динамичным геймплеем и возможностью выиграть по-крупному.
автоматные игры играть бесплатно Хотите испытать удачу и окунуться в мир азарта? Игровые автоматы – это то, что вам нужно! Яркие картинки, захватывающие звуки и, конечно же, шанс сорвать куш – всё это ждет вас в мире слотов. От классических “одноруких бандитов” до современных видеослотов с невероятными бонусами, каждый найдет автомат по душе. Готовы к вращению барабанов?
https://fr.pornochat.moscow/
Tham gia QQ88 để khám phá casino live, thể thao, slot nổ hũ, bắn cá đổi thưởng cùng hàng loạt khuyến mãi độc quyền mỗi ngày.
Woh I enjoy your content , saved to bookmarks!
QQ88 – Nhà cái giải trí trực tuyến chuẩn quốc tế, vận hành chuyên nghiệp, nạp rút nhanh và trải nghiệm mượt mà trên mọi thiết bị.
Страницы результатов поиска Мы составили для вас список из 10 казино, которые по праву считаются одними из лучших в мире. Это места, где мечты становятся реальностью, а каждая ставка может привести к незабываемым впечатлениям.
рейтинг казино rank Надеемся, наш топ-10 поможет вам сделать правильный выбор и найти свое идеальное онлайн-казино! Удачной игры!
казино сочи покер турниры 2025 В мире онлайн-гемблинга найти место, где можно играть без опасений, – задача не из легких. Рынок переполнен предложениями, и среди них, к сожалению, встречаются и те, которым не стоит доверять. Но не стоит отчаиваться! Существуют проверенные временем и игроками онлайн-казино, которые зарекомендовали себя как надежные и честные площадки.
самые надежные онлайн казино в казахстане Хотите испытать удачу и получить заряд адреналина? Игровые автоматы – это ваш билет в мир захватывающих приключений и ярких эмоций! Вращайте барабаны, собирайте выигрышные комбинации и наслаждайтесь динамичным геймплеем. Откройте для себя сотни уникальных слотов с разнообразными сюжетами, бонусными играми и щедрыми выплатами. Игровые автоматы – это не просто игра, это возможность испытать свою фортуну и получить незабываемые впечатления!
Thank you for the auspicious writeup.
Your thing regarding creating will be practically nothing in short supply of awesome. This informative article is incredibly useful and contains offered myself a better solution to be able to my own issues. Which can be the specific purpose MY PARTNER AND I has been doing a search online. I am advocating this informative article with a good friend. I know they are going to get the write-up since beneficial as i would. Yet again many thanks.
QQ88 – Điểm đến cá cược trực tuyến uy tín, quy tụ game hot, thưởng cao, giao dịch nhanh và hỗ trợ tận tâm 24/7.
Might we expect to see more of these same problems in the future?
https://quvonch.com/uzbekskaya-muzyka/yulduz-usmonova-2026/
78WIN คือแพลตฟอร์มความบันเทิงออนไลน์ครบวงจร อัดแน่นด้วยเกมสล็อตแตกง่าย คาสิโนสดถ่ายทอดสด กีฬา หวย และอีกมากมาย เว็บไซต์ใช้งานง่าย ปลอดภัย รองรับทุกอุปกรณ์ การเงินมั่นคง รวดเร็ว โปร่งใส มาพร้อมโปรโมชั่นสุดคุ้มและสิทธิพิเศษสำหรับสมาชิก VIP พร้อมทีมงานดูแลตลอด 24 ชั่วโมง.
sykaaa casino играть онлайн на реальные ставки При первом знакомстве Sykaaa Casino производит впечатление современного и, скажем так, “дерзкого” игрового портала. Дизайн яркий, местами даже немного вызывающий, но в целом удобный и интуитивно понятный. Навигация по сайту не вызывает затруднений, все основные разделы – от игр до поддержки – находятся под рукой. Это важно, когда хочется быстро перейти к делу и начать играть.
sykaaa вход Вопрос безопасности всегда стоит на первом месте, когда речь идет об игре на реальные деньги. Sykaaa Casino заявляет об использовании современных технологий шифрования для защиты данных игроков и финансовых транзакций. Лицензия, если таковая имеется (стоит проверить актуальную информацию на сайте), также является показателем того, что казино работает по определенным стандартам и подлежит регулированию. Важно убедиться, что казино имеет действующую лицензию от авторитетного регулятора.
It sounds like you’re creating problems yourself by defining this as such a comprehensive, almost unknowable problem. Isn’t that self-defeating?
I delight in, result in I discovered exactly what I used to be taking a look
for. You have ended my four day lengthy hunt!
God Bless you man. Have a great day. Bye
Regards for helping out, superb info.
My issues have been very similar, with my family. But, we made some different decisions. It’s complex.
This website has lots of really useful stuff on it. Thanks for informing me.
https://www.associationforjewishstudies.org/about-ajs/press-room/news-events/events-detail/2023/02/27/default-calendar/b%27nai-binge-streaming-programming-list-for-february-26-by-laurie-baron-and-beth-chernoff
F168 แหล่งรวมเกมเดิมพันครบวงจรอันดับต้น ๆ ของไทย ไม่ว่าจะเป็นสล็อตแตกบ่อย คาสิโนสด เกมยิงปลา หรือกีฬา เล่นได้ทุกอุปกรณ์ ฝาก–ถอนรวดเร็ว ปลอดภัย มาตรฐานสูง ข้อมูลสมาชิกได้รับการปกป้องอย่างมั่นใจ พร้อมโปรโมชั่นต่อเนื่อง โบนัสต้อนรับ คืนยอดเสีย และสิทธิพิเศษ VIP ทีมงานดูแล 24 ชั่วโมง ให้คุณสนุกไปกับ F168 ได้อย่างเต็มที่.
QQ88 – Sân chơi giải trí trực tuyến uy tín châu Á, đa dạng casino, thể thao, nổ hũ, bắn cá. Bảo mật cao, nạp rút nhanh, thưởng hấp dẫn mỗi ngày.
Enjoyed reading through this, very good material. Thanks!
Thanks for sharing the information. I found the information very useful. That’s a awesome story you posted. I will come back to scan some more.
F168 แหล่งรวมเกมเดิมพันครบวงจรอันดับต้น ๆ ของไทย ไม่ว่าจะเป็นสล็อตแตกบ่อย คาสิโนสด เกมยิงปลา หรือกีฬา เล่นได้ทุกอุปกรณ์ ฝาก–ถอนรวดเร็ว ปลอดภัย มาตรฐานสูง ข้อมูลสมาชิกได้รับการปกป้องอย่างมั่นใจ พร้อมโปรโมชั่นต่อเนื่อง โบนัสต้อนรับ คืนยอดเสีย และสิทธิพิเศษ VIP ทีมงานดูแล 24 ชั่วโมง ให้คุณสนุกไปกับ F168 ได้อย่างเต็มที่.
QQ88 – Sân chơi cá cược đẳng cấp châu Á, nơi hội tụ casino live, slot nổ hũ, thể thao và bắn cá. Trải nghiệm mượt mà, minh bạch, ưu đãi hấp dẫn mỗi ngày.
Discover what’s new here > https://svoyage.ru/
Visit our main website
See the latest here : http://lipetskregionsport.ru/
Latest updates are here
официальный сайт сукааа онлайн казино Бездепозитный бонус от Sykaaa Casino – это, безусловно, привлекательная возможность для тех, кто хочет начать свое знакомство с миром онлайн-казино без финансовых рисков. Главное – подходить к этому с умом: внимательно изучать условия, быть готовым к процессу отыгрыша и не забывать, что азарт должен приносить удовольствие, а не становиться причиной проблем. Если вы готовы рискнуть, то почему бы и нет? Возможно, именно этот бездепозитный бонус станет вашим счастливым билетом в мир больших выигрышей! Удачи!
приложение sykaaa casino Сам сайт “Большая Sykaaa Casino” обычно отличается современным дизайном и интуитивно понятным интерфейсом. Навигация простая, все разделы легко найти. Игры загружаются быстро, что важно для комфортной игры.
Have you given any kind of thought at all with converting your current web-site into French? I know a couple of of translaters here that will would certainly help you do it for no cost if you want to get in touch with me personally.
регистрация в sykaaa Если вы ищете возможность поиграть бесплатно и с азартом, то предложение от Sykaaa Casino, безусловно, заслуживает внимания. Это отличный шанс:
приложение sykaaa casino Привет, любители азарта! Сегодня мы поговорим о “Большая Sykaaa Casino” – площадке, которая привлекает внимание многих игроков. Если вы только присматриваетесь к этому казино или уже решили попробовать свои силы, то этот обзор поможет вам разобраться, как быстро и без проблем начать игру, а также чего ожидать от самого сайта.
Thanks pertaining to discussing the following superb written content on your site. I ran into it on the search engines. I will check back again if you publish extra aricles.
Go to our website
10 euros offert paris sportif|10 euros offert sans dépôt
paris sportif|10 meilleurs sites de paris sportifs|100 euro offert paris sportif|100 euros offert paris sportif|100 euros remboursé paris sportifs|100
offert pari sportif|100 offert paris sportif|100 remboursé paris sportif|100e offert pari sportif|abandon paris sportif tennis|abandon tennis paris sportif|addiction paris sportif forum|age paris sportif belgique|aide au
pari sportif|aide au paris sportif|aide aux paris sportif|aide aux paris sportifs|aide
pari sportif|aide pari sportif football|aide parie sportif|aide paris sportif|aide paris sportif foot|aide paris sportif gratuit|aide paris sportifs|aide
pour paris sportif|algorithme de paris sportif|algorithme
excel paris sportif|algorithme gratuit paris sportif|algorithme pari
sportif|algorithme paris sportif|algorithme paris sportif avis|algorithme paris sportif
basket|algorithme paris sportif excel|algorithme paris
sportif gratuit|algorithme paris sportif tennis|algorithme paris sportifs|algorithme pour paris sportif|analyse cote paris sportif|analyse de paris sportif|analyse match
paris sportif|analyse pari sportif|analyse paris sportif|analyse paris sportif foot|analyse paris sportif football|analyse paris sportif gratuit|analyse paris sportifs|ancienne cote paris sportif|api cote paris sportif|app paris sportif sans argent|appli de paris sportif|appli de paris sportif sans argent|appli de paris sportifs|appli pari sportif|appli pari sportif gratuit|appli parie sportif|appli paris sportif|appli
paris sportif avec paypal|appli paris sportif
belgique|appli paris sportif entre amis|appli paris sportif gratuit|appli paris sportif sans argent|appli paris sportif suisse|appli
paris sportifs|application aide paris sportif|application algorithme paris sportif|application analyse paris sportif|application android paris
sportif|application bankroll paris sportif|application conseil paris sportif|application de pari sportif|application de parie sportif|application de paris sportif|application de paris sportif en afrique|application de
paris sportif en cote d’ivoire|application de paris sportif en ligne|application de paris sportif gratuit|application de paris sportif international|application de paris sportif suisse|application de paris sportifs|application faux paris sportifs|application gestion bankroll paris sportif|application gestion paris sportif|application ia paris sportif|application pari sportif
gratuit|application paris sportif|application paris
sportif android|application paris sportif argent fictif|application paris sportif belgique|application paris
sportif canada|application paris sportif espagne|application paris sportif
espagnol|application paris sportif fictif|application paris sportif france|application paris sportif gratuit|application paris sportif
gratuit entre amis|application paris sportif maroc|application paris sportif offre de
bienvenue|application paris sportif paypal|application paris sportif sans argent|application paris sportif sans justificatif de domicile|application paris sportif suisse|application paris sportif usa|application paris sportif virtuel|application pour faire des paris sportifs|application pour gerer ses paris sportif|application pour les paris sportifs|application pour pari sportif|application pour paris sportif|application pour paris sportifs|application statistique paris sportif|application suivi paris sportif|applications
de paris sportifs|applications paris sportifs|applis paris sportif|applis
paris sportifs|apprendre a faire des paris sportifs|argent facile paris sportif|argent
offert paris sportifs|argent offert sans depot paris
sportif|argent paris sportif|argent paris sportifs|argent paris sportifs impots|argent sans depot paris sportif|arjel paris
sportif|arjel paris sportifs|astuce gagner paris sportif|astuce pari sportif|astuce paris sportif|astuce paris sportif basket|astuce paris sportif foot|astuce paris sportif forum|astuce paris
sportif tennis|astuce paris sportifs|astuce pour gagner au pari sportif|astuce pour gagner au paris sportif|astuce pour
gagner paris sportif|astuce pour paris sportif|astuces paris sportifs|astuces paris sportifs en ligne|astuces paris sportifs foot|astuces
pour gagner aux paris sportifs|autorisation paris sportif france|avis pari sportif|avis
paris sportif|avis paris sportif foot|avis site de paris sportif|avis site paris sportif|avis sur les paris sportifs|avis sur
paris sportif|avis tipster paris sportif|aweh signification paris sportif|bankroll 100 euros paris sportifs|bankroll management paris sportif|bankroll paris sportif|bankroll paris sportif excel|bankroll paris sportif gratuit|bankroll paris sportifs|basket paris sportif|belgique france paris sportif|belgique paris sportifs|bonus
bienvenue paris sportif|bonus bienvenue paris sportifs|bonus cash paris sportif|bonus de bienvenue paris sportif|bonus de bienvenue paris sportif
belgique|bonus de bienvenue sans depot paris sportif|bonus de depot paris sportif|bonus de
paris sportifs|bonus depot paris sportif|bonus en cash paris sportif|bonus gratuit paris sportif|bonus gratuit sans
depot paris sportif|bonus pari sportif|bonus paris sportif|bonus
paris sportif belgique|bonus paris sportif betclic|bonus paris sportif cash|bonus paris sportif en ligne|bonus paris
sportif france pari|bonus paris sportif retirable|bonus
paris sportif sans depot|bonus paris sportif sans dépôt|bonus
paris sportif unibet|bonus paris sportifs|bonus sans depot paris
sportif|bonus sans depot paris sportif belgique|bonus sans
dépôt paris sportif|bonus sans dépôt paris sportif hors arjel|bonus site de
paris sportif|bonus site pari sportif|bonus site paris sportif|bonus sites de paris sportifs|bonus
unibet paris sportif|bookmaker paris sportif|bookmaker paris sportif gratuit|bookmaker paris sportifs|bookmaker sportif|bookmakers paris sportif|bookmakers
paris sportifs|bookmakers paris sportifs en ligne|but contre son camp paris sportif|but sur penalty paris sportif|buteur paris sportif|c’est
quoi handicap paris sportif|c’est quoi une cote paris sportif|calcul anti
perte paris sportif|calcul combinaison pari sportif|calcul cote pari sportif|calcul cote
paris sportif|calcul couverture paris sportif|calcul de cote paris
sportif|calcul des cotes paris sportifs|calcul dnb paris sportifs|calcul double
chance paris sportif|calcul gain paris sportif|calcul mise paris sportif|calcul pari
sportif|calcul paris sportif|calcul paris sportif multiple|calcul pourcentage cote paris sportif|calcul
probabilité paris sportif|calcul rentabilité paris sportifs|calcul roi paris sportif|calcul systeme paris sportif|calcul
trj paris sportifs|calculateur cote paris sportif|calculateur de cote paris sportif|calculateur de mise paris sportif|calculateur de paris sportif|calculateur paris sportif|calculatrice arbitrage paris sportif|calculatrice paris
sportif|calculer cote paris sportif|calculer gain paris
sportif|calculer probabilité paris sportifs|calculer roi paris sportifs|calculer une cote pari sportif|calculer une cote paris sportif|carte cadeau paris sportif|carte pcs paris sportif|carte prépayée
paris sportifs|cash out pari sportif|cash out paris sportif|cash out paris sportifs|casino
en ligne paris sportif|casino paris sportif en ligne|champions league
paris sportif|chute de cote paris sportif|classement des
meilleurs sites de paris sportifs|classement meilleur site de paris sportif|code barre paris sportif|code bonus paris sportif|code paris sportif|code promo pari sportif|code promo paris sportif|code promo paris sportif sans depot|code promo paris sportif sans dépôt|code promo sans depot paris sportif|code promo site paris sportif|combien de temps pour encaisser un paris sportif|combien de temps pour retirer un paris sportif|combien miser paris sportifs|combine
paris sportif|combines paris sportifs|combiné pari sportif|combiné paris sportif|combiné paris sportif conseil|combiné paris sportif du
jour|combiné paris sportif pronostic|comment analyser un paris
sportif|comment arreter de jouer aux paris sportifs|comment arreter les paris sportif|comment arreter les paris sportifs|comment arrêter les paris sportifs|comment bien gagner au
paris sportif|comment bien jouer au paris sportif|comment bien miser paris
sportif|comment ca marche les paris sportif|comment calculer cote paris
sportif|comment calculer gain paris sportif|comment calculer
les cotes des paris sportifs|comment calculer une cote de paris sportif|comment calculer une cote pari sportif|comment calculer une cote paris sportif|comment comprendre les paris sportifs|comment creer un vip paris sportif|comment créer un algorithme paris
sportif|comment créer un site de paris sportif|comment devenir
riche avec les paris sportifs|comment etre rentable paris sportif|comment etre sur
de gagner au paris sportif|comment faire de bon paris
sportif|comment faire des parie sportif|comment faire des paris sportif|comment faire des paris sportif gagnant|comment faire des
paris sportifs|comment faire pari sportif|comment faire paris sportif|comment faire
pour arreter les paris sportifs|comment faire pour gagner
au paris sportif|comment faire pour gagner les paris sportifs|comment faire un bon pari sportif|comment
faire un bon paris sportif|comment faire un pari sportif|comment faire un parie
sportif|comment faire un paris sportif|comment faire une montante paris sportif|comment fonctionne les cotes dans les paris sportifs|comment
fonctionne les cotes des paris sportifs|comment fonctionne les paris sportifs|comment fonctionne paris sportifs|comment fonctionne un pari sportif|comment fonctionnent les cotes dans les paris
sportifs|comment fonctionnent les cotes dans les paris sportifs grand
oral|comment fonctionnent les cotes de paris sportif|comment fonctionnent les paris sportifs|comment
fonctionnent les paris sportifs grand oral|comment fonctionnent les paris sportifs grand oral maths|comment fonctionnent les paris sportifs maths|comment gagner a coup sur
au paris sportif|comment gagner a tous les coups
au paris sportif|comment gagner a tout les coup au paris sportif|comment gagner
au pari sportif|comment gagner au pari sportif football|comment gagner au paris sportif|comment gagner au paris sportif a coup sur|comment gagner au
paris sportif foot|comment gagner au paris sportif forum|comment gagner au paris sportif tennis|comment gagner au paris sportifs|comment
gagner aux paris sportif|comment gagner aux paris sportifs|comment
gagner aux paris sportifs foot|comment gagner aux paris sportifs livre|comment gagner aux paris sportifs sur
le long terme|comment gagner avec les paris sportifs|comment
gagner dans les paris sportifs|comment gagner de l argent
avec les paris sportifs|comment gagner de l’argent au paris sportif|comment gagner de l’argent aux paris sportifs|comment gagner de l’argent avec les paris sportifs|comment gagner de l’argent paris
sportif|comment gagner de l’argent sur les paris sportifs|comment
gagner de l’argent sur paris sportif|comment gagner
des paris sportif|comment gagner des paris sportifs|comment gagner en paris sportif|comment gagner facilement au paris sportif|comment gagner
les paris sportifs|comment gagner paris sportif|comment gagner
paris sportif foot|comment gagner paris sportifs|comment gagner sa vie avec les paris sportifs|comment gagner ses paris
sportif|comment gagner sur les paris sportif|comment gagner sur les paris sportifs|comment gagner tout le temps au paris sportif|comment gagner un pari sportif|comment gagner un paris sportif|comment gerer
une bankroll paris sportif|comment gérer sa bankroll paris sportif|comment jouer au
pari sportif|comment jouer au paris sportif|comment jouer au paris sportif foot|comment jouer aux paris sportifs|comment jouer paris
sportif|comment marche cote paris sportif|comment marche les cotes paris
sportif|comment marche les paris sportif|comment marche les paris sportifs|comment marche paris sportif|comment
marche un pari sportif|comment marche un paris sportif|comment marchent les cotes paris sportif|comment marchent les paris sportifs|comment
miser au paris sportif|comment miser paris sportif|comment monter sa bankroll paris sportif|comment ne jamais perdre au paris sportif|comment parier
sportif|comment reussir au paris sportif|comment reussir les paris
sportif|comment reussir paris sportif|comment sont calculer les cotes de paris sportif|comment sont calculées les cotes
des paris sportifs|comment sont calculés les cotes des paris sportifs|comment sont faites les
cotes des paris sportifs|comment toujours gagner au paris sportif|comment ça marche les paris
sportifs|comparaison bonus paris sportifs|comparaison cote pari sportif|comparaison des cotes paris sportifs|comparateur cote pari sportif|comparateur cote paris sportif|comparateur cotes paris
sportif|comparateur cotes paris sportifs|comparateur de cote pari sportif|comparateur de cote paris sportif|comparateur de cotes paris sportifs|comparateur de côtes paris sportifs|comparateur de paris sportif|comparateur de site de paris sportif|comparateur de site paris sportif|comparateur de sites de paris sportifs|comparateur pari sportif|comparateur paris
sportif|comparateur paris sportifs|comparateur site de paris sportif|comparateur site pari sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif bonus paris sportifs|comparatif
cote pari sportif|comparatif cote paris sportif|comparatif
cotes paris sportifs|comparatif des sites de paris sportifs|comparatif offre de bienvenue paris sportif|comparatif offre paris sportif|comparatif pari sportif|comparatif
pari sportif en ligne|comparatif paris sportif|comparatif paris sportif bonus|comparatif paris sportif en ligne|comparatif paris sportifs|comparatif
paris sportifs en ligne|comparatif site de paris sportif|comparatif site
paris sportif|comparatif site paris sportifs|comparatif sites de paris
sportifs|comparatif sites paris sportifs|comparer les cotes paris sportifs|comprendre
cote paris sportif|comprendre handicap paris sportif|comprendre les cotes
des paris sportifs|comprendre les cotes paris sportif|comprendre les
cotes paris sportifs|comprendre les handicap paris sportif|compte de
paris sportif|compte démo paris sportif|compte finance
paris sportif|compte financer paris sportif|compte financier
paris sportif|compte financé paris sportif|compte pari sportif|compte paris sportif|compte paris sportif financé|conseil de paris sportif|conseil de paris sportifs|conseil en paris sportif|conseil en paris sportifs|conseil pari sportif|conseil pari sportif gratuit|conseil
paris sportif|conseil paris sportif aujourd’hui|conseil paris sportif du jour|conseil
paris sportif foot|conseil paris sportif gratuit|conseil
paris sportif ligue des champions|conseil paris sportif nba|conseil paris
sportif pronostic|conseil paris sportif rmc|conseil paris sportif
tennis|conseil paris sportifs|conseil pour gagner au paris sportif|conseil pour paris sportif|conseil sur
les paris sportifs|conseille paris sportif|conseiller en paris sportifs|conseiller paris sportif|conseils de paris
sportifs|conseils en paris sportifs|conseils paris sportifs|conseils
paris sportifs foot|conseils paris sportifs gratuit|conseils paris sportifs tennis|conseils pour paris sportifs|cote a 100
paris sportif|cote a 2 paris sportif|cote anglaise paris
sportif|cote de 2 paris sportif|cote de pari sportif|cote de paris
sportif|cote des paris sportifs|cote maximum paris sportif|cote minimum paris sportif|cote pari sportif|cote pari sportif
comment ça marche|cote pari sportif real madrid|cote pari sportif rugby|cote parie sportif|cote paris sportif|cote paris sportif belgique|cote paris
sportif calcul|cote paris sportif definition|cote paris sportif
euro|cote paris sportif explication|cote paris sportif foot|cote paris sportif france belgique|cote paris sportif france espagne|cote paris sportif ligue
des champions|cote paris sportif moto gp|cote paris sportif psg|cote paris
sportif psg arsenal|cote paris sportif rugby|cote
paris sportif tennis|cote paris sportifs|cote
pour paris sportifs|cote sportif foot|cote sportif rugby|cote à 1000 paris sportif|cotes de paris
sportifs|cotes pari sportif|cotes paris sportif|cotes paris sportifs|cotes paris sportifs foot|coupe de france paris sportif|créer un algorithme paris sportif|créer un compte paris sportif|créer
un site de paris sportif en ligne|dans les paris sportifs que signifie handicap|declarer ses gains paris sportif|definition cash out paris sportif|definition cote paris sportif|definition handicap paris sportif|depot
5 euros paris sportif|depot double paris sportif|depot minimum 5 euro paris
sportif|depot minimum paris sportif|depot paris sportif|depuis quand
existe les paris sportif en france|devenir riche avec les paris sportifs|devenir riche avec paris sportifs|disqualification tennis
paris sportif|dnb en paris sportif|dnb pari sportif|dnb paris sportif|dnb paris sportif definition|dnb paris sportifs|doit on declarer les gains de paris sportif|déclarer gains
paris sportifs|déclarer gains paris sportifs hors arjel|définition bankroll paris sportif|dépôt minimum 1 euro paris sportif|dépôt minimum 5 euro paris sportif|ecart de jeux tennis paris sportif|erreur de cote
paris sportif|est ce que les gains des paris
sportifs sont imposables|est-ce que les prolongation compte dans un pari sportif|etre
sur de gagner au paris sportif|euro paris sportif|evenement sportif a paris|evenement
sportif paris|evenement sportif paris 2025|evenement sportif paris aujourd hui|evenement sportif paris aujourd’hui|evenement sportif
paris ce week end|evenements sportif paris|evenements sportifs paris|evenements sportifs paris 2025|evenements sportifs à paris|evolution cote
paris sportif|evolution cotes paris sportifs|evolution des
cotes paris sportifs|explication cote pari sportif|explication cote paris
sportif|explication handicap paris sportif|explication pari sportif|explication paris sportif|face a face hockey paris sportif|faire des paris sportif|faire des paris sportif
avec paypal|faire des paris sportifs|faire fortune paris sportifs|faire un pari sportif|faire un paris sportif|faut il déclarer les
gains de paris sportifs|faut il déclarer ses gains paris sportifs|fichier excel gestion bankroll paris sportif|fiscalité gains paris sportifs|foot
paris sportif|football et paris sportifs|forfait tennis paris sportif|formation paris sportif gratuit|forum de
paris sportif|forum de paris sportifs|forum pari sportif|forum parie sportif|forum paris sportif|forum
paris sportif foot|forum paris sportif gratuit|forum paris sportif nba|forum paris sportif tennis|forum paris sportifs|forum
sur les paris sportifs|forum tennis paris sportif|francaise des
jeux pari sportif|francaise des jeux paris sportif|francaise des jeux paris sportifs|france
2 paris sportif|france 2 paris sportifs|france belgique paris sportif|france
espagne paris sportif|france pari sportif|france pari sportif brest|france paris sportif|france paris sportifs|france pologne paris
sportif|france portugal paris sportif|france suisse paris
sportifs|france tunisie paris sportifs|france-pari – paris
sportifs|gagnant pari sportif|gagnant paris sportif|gagnant paris sportif bayern|gagnante paris sportif|gagne au paris sportif|gagner 10 euros par jour aux paris sportifs|gagner 100 euros par
jour paris sportif|gagner 1000 euros par mois paris sportifs|gagner 10000 euros paris sportif|gagner 2000 euros par mois paris sportif|gagner
50 euros par jour paris sportif|gagner a coup sur au paris sportif|gagner a coup sur
pari sportif|gagner a tous les coup paris sportif|gagner
argent avec paris sportifs|gagner argent pari sportif|gagner argent paris sportif|gagner argent paris sportifs|gagner au pari sportif|gagner au paris sportif|gagner
au paris sportif a coup sur|gagner au paris sportif foot|gagner au
paris sportif forum|gagner au paris sportif à coup sur|gagner aux paris sportif|gagner aux paris sportifs|gagner
aux paris sportifs pdf|gagner beaucoup d’argent paris sportif|gagner de
l argent grace aux paris sportifs|gagner de l argent pari sportif|gagner de l argent paris sportif|gagner de l argent paris sportifs|gagner de
l’argent au paris sportif|gagner de l’argent aux paris sportifs|gagner de l’argent avec les paris sportifs|gagner
de l’argent avec paris sportif|gagner de l’argent avec paris sportifs|gagner de l’argent grace au paris sportif|gagner de l’argent grace aux paris sportifs|gagner de l’argent pari sportif|gagner de l’argent paris sportif|gagner de l’argent
paris sportifs|gagner de l’argent sur les paris sportifs|gagner des paris sportif|gagner des paris sportifs|gagner les paris sportifs|gagner
pari sportif|gagner paris sportif|gagner paris sportif foot|gagner paris
sportif forum|gagner paris sportif tennis|gagner paris sportifs|gagner sa vie avec les paris sportif|gagner sa vie avec les
paris sportifs|gagner sa vie avec paris sportifs|gagner ses paris sportifs|gagner à coup sur paris sportif|gagner à
tous les coups paris sportifs|gain maximum paris sportif|gain pari
sportif|gain pari sportif imposable|gain pari sportif impot|gain paris sportif|gain paris sportif imposable|gain paris sportif impot|gain paris sportif impôt|gains
paris sportif|gains paris sportif imposable|gains paris sportifs|gains
paris sportifs imposable|gains paris sportifs imposables|gains paris sportifs
sont ils imposables|gerer bankroll paris sportif|gerer sa bankroll
paris sportif|gerer une bankroll paris sportif|gestion bankroll paris sportif|gestion bankroll
paris sportifs|gestion bankroll paris sportifs excel|gestion de bankroll
paris sportif|gestion de bankroll paris sportif application|gestion de
bankroll paris sportifs|gestion de mise paris sportif|gestion paris sportifs v2 5 gratuit|gg signification paris
sportif|gros combiné paris sportif|gros gain paris sportif|grosse cote paris sportif pronostic|grosse mise paris sportif|groupe paris sportif gratuit|groupe telegram paris sportif gratuit|groupement de
joueurs paris sportifs|handicap 0 paris sportif|handicap 1 paris sportif|handicap 5 paris sportif|handicap au paris sportif|handicap basket paris sportif|handicap dans les paris sportifs|handicap en paris sportif|handicap
europeen paris sportif|handicap européen paris
sportifs|handicap mi temps paris sportif|handicap pari sportif|handicap paris sportif|handicap paris sportif basket|handicap paris sportif
explication|handicap paris sportif foot|handicap paris sportif
rugby|handicap paris sportifs|handicap rugby paris sportif|handicap
tennis paris sportif|historique cote paris sportif|historique
des cotes paris sportifs|hockey paris sportif|hockey sur glace paris sportif|hors arjel paris sportif|hweh signification paris sportif|imposition gain pari
sportif|imposition gain paris sportif|imposition gains paris
sportifs|imposition paris sportif france|impot gain paris sportif|impot paris sportif france|impot sur gain paris sportif|je gagne ma vie avec
les paris sportifs|jeu de pari sportif gratuit|jeu de paris sportif en ligne|jeu de
paris sportif gratuit|jeu paris sportif gratuit|jeu paris sportif sans argent|jeux de parie sportif|jeux
de paris sportif|jeux de paris sportif en ligne|jeux de paris sportif gratuit|jeux de paris sportifs|jeux olympiques paris sportifs|jeux paris sportif|jeux paris sportif gratuit|jeux paris sportif virtuel|jeux paris
sportifs en ligne|jouer au paris sportif|jouer paris sportif|joueur
absent paris sportif|joueur blesse paris sportif|joueur caen paris sportif|joueur
de caen pari sportif|joueur de foot paris sportif|joueur
decisif paris sportif|joueur décisif paris sportif|joueur italien paris sportif|joueur
paris sportif|joueur professionnel paris sportif|joueur qui se blesse paris sportif|joueur sanctionne pari
sportif|joueur suspendu paris sportif|joueurs italiens paris sportifs|l’argent des
paris sportifs est il imposable|la cote paris sportif|la francaise des jeux paris sportif|la martingale paris sportif|la martingale paris
sportifs|la meilleur application de paris sportif|la meilleur application paris sportif|la
meilleur technique pour gagner au paris sportif|la méthode secrète pour gagner aux paris sportifs pdf|la plus grosse cote gagner paris sportif|la plus grosse cote paris sportif|ldem paris
sportif signification|le marché des paris sportifs|le meilleur
site de pari sportif|le meilleur site de paris sportif|le meilleur site
de paris sportif en ligne|le meilleur site de paris sportifs|le plus gros gain au paris sportif|le
plus gros paris sportif|le plus gros paris sportif du monde|les
10 meilleurs sites de paris sportifs|les 10 meilleurs sites de paris
sportifs en afrique|les 17 secrets pour gagner rapidement aux
paris sportifs|les 17 secrets pour gagner rapidement aux paris sportifs pdf|les application de
paris sportif|les applications paris sportifs|les bonus paris
sportifs|les bookmakers paris sportifs|les cotes paris sportifs|les gains de paris sportifs sont ils imposables|les
gains des paris sportifs sont ils imposables|les jeux de paris sportifs|les meilleur paris sportif|les meilleures applications
de paris sportifs|les meilleurs applications de paris sportifs|les meilleurs bonus paris sportif|les meilleurs bonus paris sportifs|les meilleurs cotes paris
sportif|les meilleurs paris sportifs|les meilleurs paris sportifs
du jour|les meilleurs site de paris sportif|les meilleurs site
de paris sportifs|les meilleurs sites de pari sportif|les meilleurs sites
de paris sportifs|les meilleurs sites de paris sportifs en ligne|les paris sportif|les paris sportif avis|les paris
sportifs|les paris sportifs comment ça marche|les paris sportifs en france|les paris sportifs en ligne|les paris sportifs en ligne comprendre jouer gagner|les paris sportifs en ligne comprendre
jouer gagner pdf|les paris sportifs les plus rentables|les plus gros gagnant
paris sportif|les plus gros gains au paris sportifs|les plus gros gains paris sportifs|les plus gros paris sportif|les plus grosse cote paris sportif|les plus grosses pertes paris sportifs|les sites de paris sportifs|les
sites de paris sportifs autorisés en france|les sites de paris sportifs en france|les sites de paris sportifs en ligne|les sites de
paris sportifs francais|ligue 1 paris sportif|ligue 1 paris sportifs|ligue 2 paris
sportif|ligue des champions paris sportif|limite de gains paris sportifs|limite de
mise paris sportif|limite gain paris sportif|limite mise paris sportifs|liste de paris sportif|liste des paris sportifs|liste des site
de paris sportif|liste des sites de paris sportifs|liste pari sportif|liste paris sportif|liste paris
sportif pdf|liste site de paris sportif|liste site pari
sportif|liste site paris sportif|liste site
paris sportif arjel|liste sites paris sportifs|logiciel algorithme paris sportif|logiciel algorithme paris
sportif gratuit|logiciel analyse paris sportif|logiciel calcul paris sportif|logiciel
de pari sportif|logiciel de paris sportif|logiciel de paris sportif gratuit|logiciel gestion bankroll
paris sportif gratuit|logiciel gestion de bankroll paris
sportif|logiciel gestion paris sportif|logiciel gestion paris
sportif gratuit|logiciel gestion paris sportifs|logiciel
pari sportif|logiciel paris sportif|logiciel paris sportif gratuit|logiciel paris sportifs|logiciel paris sportifs foot sur 2 matchs|logiciel
pour paris sportif|logiciel pour paris sportifs|logiciel prediction paris sportif|logiciel probabilité paris sportif|logiciel prédiction paris
sportif|logiciel statistique paris sportifs|logiciel variation de cote paris sportif|loi sur
les paris sportifs en france|magic calculator paris sportif|marché des paris
sportifs|marché des paris sportifs en france|marché des paris sportifs en ligne|martingale pari sportif|martingale paris sportif|martingale paris sportif excel|martingale paris sportif
forum|martingale paris sportif interdit|martingale paris sportifs|match abandonné paris sportif|match annulé ou reporté paris sportifs|match annulé paris sportif|match arrete
paris sportif|match interrompu paris sportif|match interrompu
tennis paris sportif|match interrompu tennis pluie paris sportif|match nul boxe paris sportif|match pari sportif|match paris sportif|match reporté paris sportif|match suspendu paris sportif|match suspendu tennis paris sportif|match
truqué paris sportif|matchs truqués paris sportifs|meilleur algorithme paris sportif|meilleur
algorithme paris sportif gratuit|meilleur app de paris sportif|meilleur app de paris sportifs|meilleur app paris sportif|meilleur appli de pari sportif|meilleur appli de paris sportif|meilleur appli pari sportif|meilleur appli
paris sportif|meilleur appli paris sportif forum|meilleur appli paris
sportifs|meilleur application conseil paris sportif|meilleur application de paris sportif|meilleur
application de paris sportif en afrique|meilleur application pari sportif|meilleur application paris sportif|meilleur application paris
sportif belgique|meilleur application pour les paris sportif|meilleur application pour pari sportif|meilleur bonus de bienvenue paris sportif|meilleur bonus pari sportif|meilleur bonus paris sportif|meilleur bonus paris sportif sans
depot|meilleur bonus paris sportifs|meilleur bonus site de
paris sportif|meilleur bonus site pari sportif|meilleur bonus site paris sportif|meilleur bookmaker paris sportif|meilleur
combiné paris sportif|meilleur conseil paris sportif|meilleur cote de paris sportif|meilleur cote pari sportif|meilleur cote paris sportif|meilleur cote paris sportif aujourd’hui|meilleur cote site paris
sportif|meilleur forum paris sportifs|meilleur gain paris sportif|meilleur ia paris sportif|meilleur
methode pour gagner au paris sportif|meilleur offre bienvenue
paris sportif|meilleur offre bonus paris sportif|meilleur
offre de bienvenue paris sportif|meilleur offre de bienvenue paris
sportifs|meilleur offre pari sportif|meilleur offre paris sportif|meilleur offre
paris sportif en ligne|meilleur pari sportif|meilleur pari sportif du jour|meilleur pari sportif en ligne|meilleur
paris sportif|meilleur paris sportif aujourd’hui|meilleur paris sportif du jour|meilleur paris sportif en ligne|meilleur paris sportif foot|meilleur promo paris sportif|meilleur pronostic paris sportif|meilleur site de conseil paris sportif|meilleur site de pari sportif|meilleur
site de pari sportif en ligne|meilleur site de paris sportif|meilleur site de paris sportif
avis|meilleur site de paris sportif belgique|meilleur site de
paris sportif canada|meilleur site de paris sportif en france|meilleur site de
paris sportif en ligne|meilleur site de paris sportif football|meilleur site de
paris sportif forum|meilleur site de paris sportif france|meilleur site
de paris sportif hors arjel|meilleur site de paris sportif international|meilleur site de paris sportif suisse|meilleur site de paris sportifs|meilleur site de paris sportifs en ligne|meilleur site pari sportif|meilleur site pari sportif
en ligne|meilleur site pari sportif france|meilleur
site paris sportif|meilleur site paris sportif avis|meilleur site paris
sportif belgique|meilleur site paris sportif canada|meilleur site paris sportif
en ligne|meilleur site paris sportif foot|meilleur
site paris sportif forum|meilleur site paris sportif france|meilleur site
paris sportif hors arjel|meilleur site paris sportif nba|meilleur site paris
sportif rugby|meilleur site paris sportif suisse|meilleur site paris sportifs|meilleur site pour pari sportif|meilleur site pour paris sportif|meilleur site
pronostic paris sportif|meilleur strategie paris sportif|meilleur technique de paris sportif|meilleur
technique paris sportif|meilleur technique pour gagner au
paris sportif|meilleure appli de paris sportif|meilleure
appli de paris sportifs|meilleure appli pari sportif|meilleure appli paris sportif|meilleure appli paris sportifs|meilleure application de paris sportif|meilleure application de paris
sportifs|meilleure application pari sportif|meilleure application paris sportif|meilleure application paris sportif android|meilleure application paris sportifs|meilleure offre paris sportif|meilleure
site paris sportif|meilleure strategie paris sportif|meilleures
applications de paris sportifs|meilleures applications paris
sportifs|meilleures cotes paris sportifs|meilleures offres paris sportifs|meilleures stratégies paris sportifs|meilleurs appli paris sportif|meilleurs application de paris
sportifs|meilleurs application paris sportif|meilleurs applications paris sportifs|meilleurs
bonus paris sportifs|meilleurs cote paris sportif|meilleurs cotes paris sportifs|meilleurs offres
paris sportifs|meilleurs paris sportifs|meilleurs paris sportifs du jour|meilleurs site de
pari sportif|meilleurs site de paris sportif|meilleurs site de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs site paris sportif|meilleurs sites de paris sportifs|meilleurs sites de paris
sportifs en ligne|meilleurs sites paris sportif|meilleurs sites paris sportifs|methode abc paris sportif|methode de
paris sportif|methode gagnante paris sportifs|methode gagner
paris sportif|methode infaillible paris sportifs|methode martingale paris sportif|methode
mathematique paris sportif|methode mathematique pour gagner au paris sportif|methode paris sportif|methode paris sportif foot|methode
paris sportif forum|methode paris sportif tennis|methode paris sportifs|methode pour gagner au paris
sportif|methode pour gagner paris sportif|methodes paris
sportifs|minimum depot paris sportif|mise au jeu pari sportif|mise
maximum pari sportif|mise maximum paris sportif|mise minimum paris sportif|mise moyenne paris sportif|mise paris sportif|moins de
4 5 but paris sportif|montant maximum paris sportif|montant paris sportif|montante pari sportif|montante
parie sportif|montante paris sportif|montante paris sportifs|montantes paris sportifs|multiple
pari sportif|multiple paris sportif|multiple paris sportifs|multiples paris sportifs|méthode calcul
paris sportif|méthode match nul paris sportifs|méthode mathématique pour gagner au
paris sportif|méthode paris sportif forum|méthode paris sportif hockey|nba pari sportif|nba paris sportif|nba paris sportifs|nouveau paris sportif|nouveau site de pari sportif|nouveau site de paris sportif|nouveau site de paris sportif en ligne|nouveau site de paris sportifs|nouveau site pari sportif|nouveau site paris sportif|nouveau
site paris sportif france|nouveau site paris sportifs|nouveaux
sites de paris sportifs|nouveaux sites paris sportifs|nouvelle appli paris sportif|nouvelle application de paris sportif|numero de match paris sportif|numero match paris sportif|offre 100 euros paris sportif|offre appli pari sportif|offre bienvenu paris sportif|offre bienvenue pari sportif|offre
bienvenue paris sportif|offre bienvenue paris sportifs|offre bienvenue site paris sportif|offre bonus paris sportif|offre
de bienvenu paris sportif|offre de bienvenue pari sportif|offre de bienvenue paris sportif|offre de bienvenue paris sportif belgique|offre de bienvenue paris sportif sans depot|offre de bienvenue paris sportif sans dépôt|offre de bienvenue
paris sportifs|offre de bienvenue sans depot paris
sportif|offre de bienvenue site paris sportif|offre euro paris sportif|offre pari sportif euro|offre paris sportif|offre paris sportif belgique|offre
paris sportif cash|offre paris sportif coupe du monde|offre paris sportif hors arjel|offre paris sportif
remboursé|offre paris sportif remboursé cash|offre paris sportif sans depot|offre promo paris sportif|offre remboursement paris sportif|offre sans depot paris sportif|offre site paris
sportif|offres bienvenue paris sportifs|offres de bienvenue
paris sportifs|ou faire des paris sportif|ou faire des paris sportif en espagne|ou
faire des paris sportifs|outil répartiteur de mise paris sportif|outils repartiteur de mises paris sportif|ouverture compte
paris sportifs|ouvrir un compte paris sportif|pack de bienvenue paris sportif|pack de bienvenue paris sportif hors arjel|pari en ligne sportif|pari sportif|pari sportif 100 euros offert|pari sportif 100 remboursé|pari sportif abandon tennis|pari sportif aide|pari sportif algérie aujourd’hui|pari sportif
appli|pari sportif application|pari sportif argent|pari sportif astuce|pari sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari sportif avec
orange money|pari sportif avec paypal|pari sportif avec wave|pari
sportif avis|pari sportif basket|pari sportif belgique|pari sportif belgique france|pari sportif bonus|pari sportif buteur pas titulaire|pari sportif champions league|pari sportif combiné|pari sportif comment|pari sportif comment
gagner|pari sportif comment ça marche|pari sportif
comparatif|pari sportif conseil|pari sportif cote|pari sportif cote match|pari sportif cote psg|pari sportif coupe|pari sportif
coupe de france|pari sportif coupe du monde|pari sportif depot|pari sportif du jour|pari sportif en france|pari sportif
en ligne|pari sportif en ligne au cameroun|pari sportif en ligne belgique|pari sportif
en ligne canada|pari sportif en ligne france|pari sportif en ligne gratuit|pari sportif
en ligne suisse|pari sportif en ligne ufc|pari sportif en suisse|pari sportif euro|pari sportif explication|pari sportif faire|pari sportif foot|pari sportif foot resultat|pari sportif football|pari sportif forum|pari sportif francaise des jeux|pari sportif france|pari sportif france angleterre|pari
sportif france argentine|pari sportif france autriche|pari sportif france belgique|pari sportif france espagne|pari sportif france italie|pari sportif france portugal|pari sportif france usa|pari sportif gagnant|pari sportif
gagner|pari sportif gagner a tous les coups|pari sportif gagner de l’argent|pari sportif gain|pari sportif gratuit|pari sportif gratuit pour
gagner des cadeaux|pari sportif gratuit sans depot|pari sportif handicap|pari sportif hockey|pari sportif hors arjel|pari sportif jeux olympiques|pari
sportif joueur absent|pari sportif le plus rentable|pari sportif leicester champion|pari sportif ligue 1|pari sportif
ligue 2|pari sportif ligue des champions|pari sportif ligue europa|pari sportif match|pari sportif match arrete|pari sportif match interrompu|pari sportif meilleur|pari sportif
meilleur cote|pari sportif meilleur site|pari sportif methode|pari sportif
mise|pari sportif mise au jeu|pari sportif mise o jeu|pari sportif nba|pari sportif offre bienvenue|pari sportif
paypal|pari sportif plus|pari sportif prolongation|pari sportif promo|pari sportif pronostic|pari sportif pronostic foot|pari sportif pronostic gagnant|pari
sportif pronostic gratuit|pari sportif psg|pari sportif psg
bayern|pari sportif psg inter|pari sportif psg milan|pari sportif regle|pari
sportif rembourse|pari sportif remboursement|pari sportif remboursement cash|pari sportif remboursé|pari sportif
rugby|pari sportif rugby coupe du monde|pari sportif rugby top 14|pari sportif sans argent|pari sportif sans carte bancaire|pari sportif sans depot|pari sportif signification|pari sportif
site|pari sportif statistique|pari sportif suisse|pari sportif systeme|pari sportif technique|pari sportif technique pour gagner|pari
sportif temps reglementaire|pari sportif tennis|pari
sportif tennis abandon|pari sportif top|pari sportif top 14|pari sportif tour de france|parie sportif|parie sportif comment ca marche|parie sportif du jour|parie sportif en ligne|parie sportif foot|parie sportif football|parie sportif
france|parie sportif gratuit|parie sportif pronostic|parie sportif suisse|paris en ligne sportif|paris en ligne sportifs|paris evenement sportif|paris france
sportif|paris hippique et sportif|paris hippiques et sportifs|paris hippiques paris sportifs|paris hippiques paris sportifs et poker en ligne|paris
hippiques sportifs|paris match sportif|paris sportif|paris sportif 10 euros offerts|paris sportif 100 euros offert|paris sportif 100
euros remboursé|paris sportif 100 offert|paris sportif
100 remboursé|paris sportif 100e offert|paris sportif 150 euros
offert|paris sportif 1er pari remboursé|paris sportif a faire|paris
sportif a faire aujourd’hui|paris sportif a faire ce soir|paris sportif abandon tennis|paris sportif abandon tennis parions
sport|paris sportif aide|paris sportif algorithme|paris sportif analyse|paris sportif appli|paris sportif application|paris sportif application android|paris sportif apres prolongation|paris sportif argent|paris sportif
argent fictif|paris sportif argent offert|paris sportif argent virtuel|paris sportif arjel|paris sportif arsenal psg|paris sportif astuce|paris sportif au canada|paris sportif aujourd hui|paris sportif
aujourd’hui|paris sportif avec argent fictif|paris sportif avec bonus sans depot|paris sportif
avec carte bancaire|paris sportif avec cryptomonnaie|paris sportif avec handicap|paris sportif avec paypal|paris sportif avec paysafecard|paris sportif avis|paris sportif avis expert|paris sportif avis forum|paris sportif bankroll|paris sportif basket|paris sportif basket coupe de france|paris sportif basket nba|paris
sportif basket prolongation|paris sportif belgique|paris sportif belgique bonus|paris sportif belgique bonus sans
depot|paris sportif belgique france|paris sportif belgique suede|paris sportif
bonus|paris sportif bonus bienvenue|paris sportif bonus cash|paris sportif bonus de bienvenue|paris sportif bonus gratuit|paris sportif bonus
gratuit sans depot|paris sportif bonus retirable|paris sportif bonus sans depot|paris
sportif bonus sans depot belgique|paris sportif bookmaker|paris sportif but contre son camp|paris sportif but temps additionnel|paris sportif buteur|paris sportif buteur blessé|paris sportif buteur
carton rouge|paris sportif buteur contre
son camp|paris sportif buteur non titulaire|paris sportif buteur prolongation|paris sportif
buteur qui ne joue pas|paris sportif buteur remplacant|paris sportif calcul gain|paris sportif canada|paris sportif cash|paris sportif cash out|paris sportif champion ligue 1|paris sportif champions league|paris sportif classement
ligue 1|paris sportif code promo|paris sportif combine|paris sportif combiné|paris
sportif combiné comment ça marche|paris
sportif combiné du jour|paris sportif combiné match reporté|paris sportif comment ca marche|paris sportif
comment faire|paris sportif comment gagner|paris sportif comment gagner a tous les coups|paris sportif comment jouer|paris
sportif comment ça marche|paris sportif comparateur cote|paris sportif comparatif|paris sportif conseil|paris sportif conseil gratuit|paris
sportif conseil pour gagner|paris sportif cote|paris sportif
cote et match|paris sportif cote explication|paris sportif cote
psg|paris sportif coupe d’europe|paris sportif coupe davis|paris sportif coupe
de france|paris sportif coupe du monde|paris sportif coupe du monde de rugby|paris sportif coupe du
monde rugby|paris sportif depot 5 euro|paris sportif depot minimum|paris
sportif depot paypal|paris sportif dnb|paris sportif
du jour|paris sportif du jour conseil|paris sportif dépôt 1 euro|paris sportif dépôt
minimum 5 euros|paris sportif en belgique|paris sportif en france|paris sportif en ligne|paris sportif en ligne avec paypal|paris sportif en ligne avis|paris sportif en ligne belgique|paris sportif
en ligne bonus|paris sportif en ligne cameroun|paris sportif en ligne comment gagner|paris sportif en ligne comment ça marche|paris sportif en ligne
france|paris sportif en ligne gratuit|paris sportif en ligne maroc|paris sportif en ligne paypal|paris sportif en ligne québec|paris sportif en ligne sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris sportif
espagne france|paris sportif esport|paris sportif et casino en ligne|paris sportif et hippique|paris sportif
et prolongation|paris sportif euro|paris sportif europa league|paris sportif explication|paris sportif final ligue des
champions|paris sportif finale ligue des champions|paris sportif foot|paris sportif foot aide|paris
sportif foot astuce|paris sportif foot aujourd’hui|paris
sportif foot ce soir|paris sportif foot comment ca marche|paris sportif foot conseil|paris
sportif foot cote|paris sportif foot coupe du monde|paris sportif foot en ligne|paris sportif foot feminin|paris sportif foot gratuit|paris
sportif foot prolongation|paris sportif foot pronostic|paris sportif foot pronostic gratuit|paris
sportif foot regle|paris sportif foot suisse|paris sportif foot
us|paris sportif football|paris sportif football americain|paris sportif football astuces|paris sportif forfait
tennis|paris sportif forum|paris sportif francais|paris sportif francaise des jeux|paris sportif france|paris sportif
france 2|paris sportif france allemagne|paris sportif france angleterre|paris sportif france argentine|paris sportif france autriche|paris sportif france
belgique|paris sportif france espagne|paris sportif france
gibraltar|paris sportif france italie|paris sportif france nouvelle zelande|paris sportif
france pologne|paris sportif france portugal|paris sportif france
uruguay|paris sportif france usa|paris sportif freebet sans depot|paris sportif gagnant|paris
sportif gagnant à coup sûr|paris sportif gagner a
coup sur|paris sportif gagner argent|paris sportif gagner de l’argent|paris sportif gain|paris sportif gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris sportif gratuit
appli|paris sportif gratuit avec cadeaux|paris sportif gratuit cadeaux|paris
sportif gratuit en ligne|paris sportif gratuit entre amis|paris sportif gratuit sans argent|paris sportif gratuit sans depot|paris sportif gratuit sans dépôt|paris sportif
gratuits|paris sportif gros gain|paris sportif handicap|paris sportif handicap 0 1|paris sportif handicap 0-1|paris sportif handicap 1 0|paris sportif handicap 1-0|paris sportif handicap basket|paris
sportif handicap explication|paris sportif handicap foot|paris sportif handicap rugby|paris
sportif hippique|paris sportif hockey|paris sportif hockey nhl|paris sportif hockey sur glace|paris sportif hors arjel|paris sportif hors
arjel france|paris sportif jeux olympiques|paris sportif
jeux video|paris sportif joueur blessé|paris sportif joueur blessé pendant le match|paris sportif joueur de foot|paris sportif joueur decisif|paris sportif joueur declare forfait|paris sportif joueur déclare forfait|paris sportif joueur remplacant|paris sportif la francaise des jeux|paris sportif le plus rentable|paris sportif legal en france|paris sportif leicester champion|paris sportif les 18 stratégies
pour gagner tous les jours|paris sportif les plus sur|paris sportif les prolongation compte|paris sportif ligne|paris sportif
ligue 1|paris sportif ligue 2|paris sportif ligue des champions|paris sportif
ligue des nations|paris sportif ligue europa|paris sportif liste|paris sportif martingale|paris sportif match|paris
sportif match abandonné|paris sportif match annulé|paris sportif
match arrêté|paris sportif match du jour|paris sportif match interrompu|paris sportif
match reporté|paris sportif match suspendu|paris sportif match tennis
interrompu|paris sportif match truqué|paris sportif
meilleur bonus|paris sportif meilleur cote|paris sportif meilleur pronostic|paris sportif meilleur site|paris sportif methode|paris Sportif Methode 2 3 (kanoonsarasari.ir)|paris sportif mi temps fin de match|paris sportif mise au jeu|paris sportif mise maximum|paris sportif mma france|paris sportif moins
de 3.5 but|paris sportif montante|paris sportif moto gp|paris sportif multiple|paris
sportif multiple 2 3|paris sportif multiple 2 3
explication|paris sportif multiple 2 4|paris sportif
multiple 2 5|paris sportif multiple 2/3 explication|paris sportif multiple 3 4|paris sportif multiple explication|paris sportif national 1 foot|paris sportif nba|paris sportif nba conseil|paris sportif nba pronostic|paris sportif nhl|paris sportif nombre de but|paris sportif nouveau site|paris sportif numero match|paris sportif offert|paris sportif
offre bienvenue|paris sportif offre bienvenue sans depot|paris sportif offre de bienvenue|paris sportif offre sans depot|paris sportif om psg|paris
sportif paypal|paris sportif plus de 1.5 but|paris sportif plus de
2 5 but|paris sportif plus ou moins|paris sportif plus
ou moins 2 5 but|paris sportif premier pari remboursé|paris sportif premier paris remboursé|paris sportif prolongation|paris sportif prolongation basket|paris sportif prolongation foot|paris sportif promo|paris
sportif pronostic|paris sportif pronostic basket|paris sportif pronostic des match aujourd
hui|paris sportif pronostic expert gratuit|paris sportif pronostic foot|paris sportif pronostic forum|paris sportif pronostic gratuit|paris sportif pronostic tennis|paris sportif psg|paris sportif psg arsenal|paris
sportif psg barcelone|paris sportif psg bayern|paris
sportif psg dortmund|paris sportif psg inter|paris sportif psg inter cote|paris sportif
psg liverpool|paris sportif psg om|paris sportif
qr code|paris sportif que veut dire handicap|paris sportif qui rapporte le plus|paris sportif regle|paris sportif regle prolongation|paris sportif rembourse|paris sportif remboursement cash|paris sportif rembourser|paris sportif remboursé|paris
sportif remboursé cash|paris sportif remboursé en cash|paris sportif retrait paypal|paris sportif rue des joueurs|paris sportif rugby|paris sportif rugby
6 nations|paris sportif rugby coupe du monde|paris sportif rugby top 14|paris sportif safe
du jour|paris sportif sans argent|paris sportif sans carte bancaire|paris sportif
sans carte d’identité|paris sportif sans compte bancaire|paris sportif
sans depot|paris sportif sans depot minimum|paris sportif si match suspendu|paris sportif si un joueur abandonne|paris sportif si un joueur ne
joue pas|paris sportif si un joueur se blesse|paris sportif simple ou combiné|paris sportif
site|paris sportif statistique|paris sportif stratégie|paris sportif suisse|paris sportif suisse application|paris sportif suisse en ligne|paris sportif suisse legal|paris sportif suisse légal|paris sportif suisse romande|paris sportif
sur du jour|paris sportif sur le tennis|paris sportif systeme|paris sportif systeme
2 3|paris sportif systeme 2 4|paris sportif systeme 2/3|paris sportif systeme 2/4|paris sportif systeme 3 4|paris sportif systeme 3/4|paris
sportif systeme explication|paris sportif technique|paris sportif technique pour gagner|paris sportif temps additionnel|paris sportif temps reglementaire|paris sportif tennis|paris sportif tennis abandon|paris sportif tennis conseil|paris sportif tennis de table|paris sportif tennis
forfait|paris sportif tennis gratuit|paris sportif tennis pronostic|paris sportif tennis roland garros|paris sportif tir au but|paris sportif top 14|paris sportif tour de france|paris sportif ufc|paris sportif ufc france|paris sportif unibet|paris sportif vainqueur euro|paris sportif vainqueur ligue 1|paris sportif vainqueur ligue des champions|paris sportif via paypal|paris sportif victoire prolongation|paris sportif vip gratuit|paris sportifs|paris
sportifs abandon tennis|paris sportifs aide|paris sportifs analyser un match|paris sportifs arjel|paris sportifs astuces|paris sportifs aujourd’hui|paris
sportifs autorisés en france|paris sportifs avec paypal|paris sportifs basket|paris sportifs belgique|paris sportifs bonus|paris sportifs bookmakers|paris sportifs canada|paris sportifs combiné|paris sportifs comparateur|paris
sportifs comparatif|paris sportifs conseils|paris sportifs cotes|paris sportifs coupe du monde|paris sportifs
de football|paris sportifs du jour|paris sportifs en belgique|paris sportifs en france|paris sportifs en ligne|paris sportifs en ligne belgique|paris sportifs en ligne france|paris sportifs en ligne gratuit|paris sportifs en ligne
suisse|paris sportifs en suisse|paris sportifs et hippiques|paris sportifs euro|paris sportifs
foot|paris sportifs foot us|paris sportifs forum|paris sportifs france|paris sportifs france espagne|paris sportifs gagner à tous les coups|paris sportifs gratuit|paris sportifs gratuits|paris sportifs gratuits en ligne|paris sportifs handicap|paris sportifs hockey|paris sportifs hockey sur galce|paris sportifs hockey sur glace|paris sportifs hors arjel|paris sportifs jeux
olympiques|paris sportifs les bookmakers raflent la mise|paris sportifs ligne|paris
sportifs ligue 1|paris sportifs ligue 2|paris sportifs ligue des champions|paris sportifs ligue europa|paris sportifs match interrompu|paris sportifs montante|paris sportifs nba|paris sportifs offre bienvenue|paris sportifs offre de bienvenue|paris sportifs paypal|paris sportifs pronostics|paris sportifs psg|paris sportifs
psg inter|paris sportifs rugby|paris sportifs sans argent|paris sportifs
sans depot|paris sportifs site|paris sportifs sites|paris sportifs statistiques|paris sportifs stratégie|paris sportifs suisse|paris sportifs technique|paris sportifs techniques|paris sportifs tennis|paris sportifs tennis astuces|paris sportifs top
14|paris sportifs tour de france|part de marché paris sportifs|paypal
pari sportif|paypal paris sportif|paypal paris sportifs|perte d’argent
paris sportifs|peut on devenir riche avec les paris sportifs|peut on gagner de l’argent avec
les paris sportifs|peut on gagner sa vie avec les paris sportif|peut on vraiment gagner de l’argent avec les
paris sportifs|plus gros combine paris sportif|plus gros gagnant paris sportif|plus gros
gain paris sportif|plus gros gain paris sportif au monde|plus gros gain paris sportif france|plus gros gains paris
sportif|plus gros pari sportif|plus gros paris sportif|plus grosse cote gagner
paris sportif|plus grosse cote pari sportif|plus grosse
cote paris sportif|plus grosse mise paris sportif|plus grosse somme gagner au paris sportif|plus ou moins paris sportif|pourcentage de mise paris sportif|premier pari sportif remboursé|probabilité cote paris sportif|probabilité paris sportif combiné|prolongation basket paris sportif|prolongation paris sportif|promo pari sportif|promo paris sportif|promo
site de paris sportif|promo site pari sportif|promo site paris sportif|promos paris sportifs|prono
paris sportif foot|prono paris sportif gratuit|prono
paris sportif tennis|pronostic de paris sportif|pronostic du jour paris sportif|pronostic foot
paris sportif|pronostic gratuit paris sportif|pronostic pari sportif|pronostic pari sportif gratuit|pronostic paris sportif|pronostic paris sportif
aujourd’hui|pronostic paris sportif du jour|pronostic paris sportif
foot|pronostic paris sportif gratuit|pronostic paris sportif tennis|pronostic paris
sportifs|pronostics foot statistiques et aides aux paris sportifs|pronostics paris sportif|pronostics paris sportifs|pronostiqueur paris sportif gratuit|psg arsenal paris sportif|psg bayern paris sportif|psg inter milan paris sportif|psg
inter pari sportif|psg inter paris sportif|psg liverpool paris sportif|psg om paris sportif|psg paris
sportif|psg paris sportifs|qr code paris sportif|qu est ce qu un handicap paris sportif|qu est ce que handicap dans les paris sportif|qu’est
ce qu’un handicap paris sportif|qu’est ce que handicap dans les paris sportif|quand un joueur se blesse
paris sportif|que signifie 1/1 en paris sportif|que signifie
1/2 paris sportif|que signifie 12 en paris sportif|que signifie 1×2 dans les paris sportifs|que signifie btts en paris sportif|que signifie dnb en paris
sportif|que signifie draw en paris sportif|que signifie ft en paris sportif|que signifie gg dans le
pari sportif|que signifie gg en pari sportif|que signifie gg en paris sportif|que signifie handicap dans les paris sportifs|que veut
dire dnb en paris sportif|que veut dire handicap dans les paris sportifs|que veut dire handicap paris sportif|quel appli pari sportif|quel cote jouer paris sportif|quel est la meilleur appli de paris sportif|quel est le meilleur
algorithme de paris sportif|quel est le meilleur site de pari
sportif|quel est le meilleur site de pari sportif en ligne|quel est le meilleur site de paris sportif|quel est le meilleur site
de paris sportif en ligne|quel est le meilleur site de paris sportifs en ligne|quel
est le pari sportif le plus rentable|quel pari sportif est
le plus rentable|quel pari sportif est le plus sûr|quel pari sportif faire aujourd’hui|quel paris sportif faire aujourd’hui|quel paris sportif rapporte
le plus|quel site de paris sportif choisir|quel site
de paris sportif rembourse en cash|quel type de pari sportif est le
plus rentable|quelle application pour paris sportifs|quelle est
la meilleure appli de paris sportif|quelle est la meilleure application de paris sportif|quelle est la meilleure application pour les paris sportifs|quelle est le meilleur site de paris sportif|quels paris sportifs faire|quels sont
les paris sportifs les plus sûrs|rebond basket paris
sportif|record de gain paris sportif|regle buteur paris sportif|regle de paris
sportif|regle des paris sportif|regle handicap paris sportif|regle handicap paris sportif foot|regle multiple paris sportif|regle pari sportif|regle paris
sportif|regle paris sportif foot|regle paris sportif multiple|regle paris sportif prolongation|reglement pari
sportif|reglement paris sportif|regles paris sportifs|remboursement cash paris sportif|remboursement
en cash paris sportif|remboursement pari sportif|remboursement paris sportif|repartiteur de mise paris sportif|repartiteur de mise paris sportifs|repartiteur de mises paris sportif|repartiteur
mise paris sportif|repartition des mises paris sportif|resultat pari sportif|resultat paris sportif|resultat paris sportif en direct|resultat paris sportif foot|resultat sportif
hockey|retirer argent paris sportif|rugby pari
sportif|rugby paris sportif|règle paris sportif prolongation|règles paris sportif|répartiteur de mise pari sportif|répartiteur de mise paris sportif|répartiteur de
mise paris sportifs|répartition des mises paris sportif|résultat
paris sportif foot|sans depot paris sportif|se faire interdire de paris sportifs|signification btts paris sportif|signification dnb paris sportif|signification handicap paris sportif|simulateur de gain paris sportif|simulateur gain paris sportif|simulateur gain paris sportif multiple|simulateur gain paris
sportif systeme|simulateur gain paris sportif système|simulateur montante paris sportif|simulateur paris
sportif multiple|simulateur systeme paris sportif|simulation paris sportif gratuit|site
aide paris sportif|site analyse paris sportif|site analyser
paris sportif|site arjel paris sportif|site
conseil paris sportif|site d’analyse de paris sportifs|site d’analyse paris sportif|site de conseil paris
sportif|site de pari en ligne sportif|site de pari
sportif|site de pari sportif avec bonus sans depot|site de
pari sportif bonus sans depot|site de pari sportif canada|site de pari sportif en ligne|site de pari sportif
francais|site de pari sportif gratuit|site de pari sportif hors
arjel|site de pari sportif suisse|site de parie sportif|site de parie sportif en ligne|site de
paris en ligne sportif|site de paris sportif|site de paris sportif acceptant paypal|site de paris sportif arjel|site de paris sportif autorisé en france|site de paris
sportif autorisé en suisse|site de paris sportif avec bonus|site de paris
sportif avec bonus sans depot|site de paris sportif avec
bonus sans dépôt|site de paris sportif avec neosurf|site de paris sportif avec paiement
mobile|site de paris sportif avec paypal|site de paris sportif avis|site de paris sportif belge avec bonus|site de paris sportif belgique|site de paris sportif bonus|site de paris sportif
bonus sans depot|site de paris sportif canada|site de paris sportif comparatif|site de paris sportif depot minimum|site
de paris sportif en france|site de paris sportif en ligne|site de
paris sportif en ligne suisse|site de paris sportif football|site de paris sportif francais|site de paris sportif france|site de paris sportif gratuit|site de paris sportif gratuit pour
gagner des cadeaux|site de paris sportif gratuit sans dépôt|site de
paris sportif hors arjel|site de paris sportif le plus fiable|site de paris sportif legal
en france|site de paris sportif meilleur cote|site de paris sportif nouveau|site de paris sportif offre de
bienvenue|site de paris sportif paypal|site de paris
sportif premier paris remboursé|site de paris sportif qui accepte
paypal|site de paris sportif qui rembourse en cash|site de paris
sportif remboursé|site de paris sportif sans argent|site de paris sportif sans carte bancaire|site de paris sportif sans carte d’identité|site de paris sportif sans depot|site de paris sportif suisse|site de paris sportifs|site de paris sportifs
avec paypal|site de paris sportifs en ligne|site de
paris sportifs francais|site de paris sportifs gratuit|site de paris
sportifs paypal|site de paris sportifs suisse|site de statistique pour paris sportif|site des paris sportifs|site pari
en ligne sportif|site pari sportif|site pari sportif 100 euros offert|site pari sportif
arjel|site pari sportif belgique|site pari sportif bonus|site pari
sportif canada|site pari sportif comparatif|site pari sportif en ligne|site pari sportif france|site pari sportif gratuit|site pari sportif hors arjel|site pari sportif
suisse|site parie sportif|site paris en ligne sportif|site paris sportif|site paris sportif 100 euros offert|site paris sportif 100 euros remboursé|site
paris sportif 1er paris remboursé|site paris sportif arjel|site paris sportif autorisé en france|site paris sportif avec bonus|site paris sportif avec bonus sans depot|site paris sportif avec meilleur
cote|site paris sportif belgique|site paris sportif bonus|site paris sportif bonus cash|site
paris sportif bonus sans depot|site paris sportif canada|site paris sportif comparatif|site paris sportif depot 5 euro|site
paris sportif en ligne|site paris sportif foot|site paris sportif france|site paris sportif gratuit|site paris sportif hors arjel|site paris sportif hors arjel france|site paris
sportif meilleur cote|site paris sportif nouveau|site paris sportif offre de bienvenue|site paris sportif paypal|site paris sportif remboursement cash|site paris sportif remboursé en cash|site paris
sportif retrait instantané|site paris sportif sans carte bancaire|site paris sportif sans depot|site paris sportif
suisse|site paris sportifs|site paris sportifs belgique|site paris sportifs en ligne|site paris sportifs france|site paris sportifs
hors arjel|site paris sportifs suisse|site pour analyse paris sportif|site pour paris sportif|site pronostic paris sportif|site statistique paris
sportif|site suisse paris sportif|sites de pari sportif|sites
de paris sportif|sites de paris sportifs|sites de paris sportifs arjel|sites de paris
sportifs autorisés en france|sites de paris sportifs belgique|sites de paris sportifs bonus|sites de paris sportifs en belgique|sites de paris sportifs en france|sites de paris sportifs en ligne|sites
de paris sportifs gratuits|sites de paris sportifs gratuits
sans dépôt|sites de paris sportifs suisse|sites pari sportif|sites paris sportif|sites paris sportifs|sites paris
sportifs arjel|sites paris sportifs belgique|sites paris sportifs
france|sites paris sportifs hors arjel|sites paris sportifs
suisse|so foot paris sportif|so foot paris sportifs|specialiste tennis paris
sportif|statistique foot paris sportif|statistique paris sportif|statistique paris
sportif foot|statistique tennis paris sportif|statistiques football paris sportifs|statistiques paris sportifs|strategie de
paris sportif|stratégie big whale paris sportif|stratégie
de paris sportifs|stratégie gagnante paris sportifs|stratégie pari sportif|stratégie paris sportif|stratégie paris sportifs|stratégie
paris sportifs forum|stratégie pour gagner au paris sportif|stratégies paris sportifs|suisse paris sportif|suisse paris sportifs|systeme 2 3 paris sportif|systeme 3 4 paris sportif|systeme de cote paris sportif|systeme de paris
sportif|systeme pari sportif|systeme paris sportif|systeme paris sportifs|systeme reducteur paris
sportif|système paris sportif|tableau bankroll paris sportif|tableau cote paris sportif|tableau
de paris sportif|tableau de suivi paris sportifs|tableau excel bankroll paris
sportif|tableau excel paris sportif|tableau excel paris sportif gratuit|tableau excel paris
sportifs|tableau excel pour paris sportif|tableau gestion bankroll paris
sportif|tableau montante paris sportif
sykaaa вход
Find the newest updates
регистрация в sykaaa
https://vodds-casino.net/odds/
I would share your post with my sis.
Tham gia QQ88 để khám phá nền tảng cá cược trực tuyến chất lượng cao, giao dịch nhanh, hỗ trợ đa kênh và trải nghiệm ổn định mỗi ngày.
sykaaa casino честное ли казино
sykaaa casino бонусы для новичков
казино в котором есть бездепозитный бонус
Latest updates are here — http://hammill.ru/
бездепозитные бонусы в казино за регистрацию
Visit the company site > https://bergkompressor.ru/
бездепозитные бонусы в казино за регистрацию с выводом
бездепозитные бонусы в казино
https://enkling.com/read-blog/81042
бездепозитные бонусы за регистрацию в казино
бездепозитные бонусы в казино за регистрацию без депозита
OK, you outline what is a big issue. But, can’t we develop more answers in the private sector?
I favored your idea there, I tell you blogs are so helpful sometimes like looking into people’s private life’s and work.At times this world has too much information to grasp. Every new comment wonderful in its own right.
Çevrim içi olarak kumar hizmetleri sunan platform, hem bahis hem porbet casino alanlarında oyunlara yer verir.
Hello there, just became aware of your blog through Google, and found that it is truly informative. I am going to watch out for brussels. I will appreciate if you continue this in future. Lots of people will be benefited from your writing. Cheers!
бездепозитные бонусы в онлайн казино
бездепозитные бонусы в казино олимп
A neighbor of mine encouraged me to take a look at your blog site couple weeks ago, given that we both love similar stuff and I will need to say I am quite impressed.
https://community.ubos.tech/daxad47340/1xbet-casino-promo-code-2026-bonus-up-to-eu130-947
как использовать бонус казино в 1win
бездепозитные бонусы казино в казахстане
I am glad to be a visitor of this perfect blog !, appreciate it for this rare info!
MK8 นำเสนอเกมหลากหลายประเภททั้งสล็อต คาสิโนสด กีฬา ยิงปลา และลอตเตอรี่ ที่ตอบโจทย์ผู้เล่นทุกสไตล์อย่างครบถ้วน. แพลตฟอร์มถูกออกแบบให้ใช้งานง่าย รองรับทุกอุปกรณ์และโหลดไวทันใจ. ผู้เล่นยังได้รับสิทธิ์รับโบนัสต้อนรับ โปรโมชั่นรายวัน และกิจกรรมพิเศษมากมาย. ระบบฝาก–ถอนปลอดภัยและโปร่งใส พร้อมทีมบริการลูกค้าตลอด 24 ชั่วโมง ทำให้ MK8 เป็นตัวเลือกที่เชื่อถือได้สำหรับผู้เล่นในประเทศไทย.
Just desire to say your article is as astonishing. The clearness on your submit is just cool and i could assume you are knowledgeable in this subject. Fine with your permission let me to seize your RSS feed to keep updated with impending post. Thanks one million and please continue the rewarding work.
gay opa porno
Your knowledge and expertise on various topics never ceases to amaze me I always learn something new with each post
Your blog has quickly become one of my favorites I always look forward to your new posts and the insights they offer
https://cdsonla.edu.vn/index.php/vi/component/k2/item/24-night-thesis-paper-research-papers?tmpl=component&print=1&start=30
https://www.live4cup.com/f-sp2060410-.html#p2060410
Official промокод 1xbet при регистрации: code 1XMAXVIP. Use this code during registration to get a full 100% betting bonus up to 130 EUR.
promo code for free bet in 1xbet — 1XMAXVIP. Customers can activate this promo code when registering to get a special sports betting bonus. Get a 100% betting bonus worth up to €130. The code must be entered in the registration form.
бонус за регистрацию без депозита в казино
бездепозитные бонусы в казино с выводом без пополнения за регистрацию
https://wordpress.morningside.edu/tajaprince13/2015/12/10/profile-austin-langston/#comment-448907
Open88 là nhà cái trực tuyến được nhiều người chơi lựa chọn nhờ nền tảng ổn định và hệ thống bảo mật cao. Open88 cung cấp đa dạng trò chơi như cá cược thể thao, casino trực tuyến, slot game với giao diện thân thiện, tỷ lệ cược hấp dẫn và quy trình nạp rút nhanh chóng.
как использовать бонусный счет на 1win в казино бонус
бездепозитные бонусы в казино 2026
https://zenwriting.net/slu7aa7wxc
Visit our official page
https://alauddinabc.livejournal.com/2095.html
Официальная страница компании в сети
промокоды в казино на сегодня бездепозитный бонус
бездепозитные бонусы за регистрацию в казино без депозита
78WIN ให้บริการเกมหลากหลายประเภททั้งสล็อต คาสิโนสด กีฬา ยิงปลา และลอตเตอรี่ รองรับผู้เล่นทุกแนวแบบครบเครื่อง. แพลตฟอร์มถูกออกแบบให้ใช้งานง่าย เปิดได้ทุกอุปกรณ์และโหลดไว มีความเสถียรสูง. ผู้เล่นยังได้รับโบนัสต้อนรับ โปรโมชั่นรายวัน และกิจกรรมพิเศษที่ช่วยเพิ่มโอกาสในการทำกำไร. ระบบฝาก–ถอนปลอดภัย โปร่งใส และดำเนินการรวดเร็ว พร้อมทีมสนับสนุน 24 ชั่วโมง ทำให้ 78WIN เป็นหนึ่งในตัวเลือกที่เชื่อถือได้ของผู้เล่นชาวไทย.
бездепозитные бонусы в казино и бк
бездепозитные бонусы казино в казахстане
bet of africa promo code: код 1X200GIFT. Активируйте данный код и заберите 100% приветственный бонус до 32500 RUB.
Для того чтобы использовать 1х бет промокод, необходимо ввести данный код в соответствующее поле во время регистрации или внесении депозита. После этого начисленный бонус без задержек поступит на баланс пользователя.
Discover updates here : https://svoyage.ru/
Visit the company’s main website — https://poloniya.ru/
как использовать бонус казино в 1win
бездепозитные бонусы казахстан за регистрацию в казино
1xbet promo code sri lanka
{{1xbet india promo code|1xbet promo code india|1xbet promo code registration india|1xbet free promo code india|1xbet free bet promo code india|1xbet bonus promo code india|promo code for 1xbet india today|1xbet promo code for registration india|promo code for 1xbet india|1xbet promo code list india|1xbet free promo code today india|1xbet promo code free spins india|1xbet registration promo code india|1xbet promo code new user india|1xbet promo code no deposit india|1xbet free bet promo code india|1xbet promo code new user today india|1xbet today promo code india|1xbet promo code india|promo code for 1xbet india|1xbet promo code today india|1xbet promo code india|1xbet promo code free bet india|1xbet promo code today india|promo code for 1xbet india|1xbet promo code india today|1xbet promo code registration india|1xbet promo code today india|1xbet promo code no deposit india|1xbet promo code free bet india|1xbet promo code free spins india|1xbet nepal promo code|1xbet promo code nepal|1xbet promo code registration nepal|1xbet free promo code nepal|1xbet free bet promo code nepal|1xbet bonus promo code nepal|promo code for 1xbet nepal today|1xbet promo code for registration nepal|promo code for 1xbet nepal|1xbet promo code list nepal|1xbet free promo code today nepal|1xbet promo code free spins nepal|1xbet registration promo code nepal|1xbet promo code new user nepal|1xbet promo code no deposit nepal|1xbet free bet promo code nepal|1xbet promo code new user today nepal|1xbet today promo code nepal|1xbet promo code nepal|1xbet bonus promo code pakistan|promo code for 1xbet pakistan today|1xbet promo code for registration pakistan|promo code for 1xbet pakistan|1xbet promo code list pakistan|1xbet free promo code today pakistan|1xbet promo code free spins pakistan|1xbet registration promo code pakistan|1xbet promo code new user pakistan|1xbet promo code no deposit pakistan|1xbet free bet promo code pakistan|1xbet promo code new user today pakistan|1xbet today promo code pakistan|1xbet promo code pakistan|promo code for 1xbet pakistan|1xbet promo code today pakistan|1xbet promo code pakistan|1xbet promo code free bet pakistan|1xbet promo code today pakistan|promo code for 1xbet pakistan|1xbet promo code pakistan today|1xbet promo code registration pakistan|1xbet promo code today pakistan|1xbet promo code no deposit pakistan|1xbet promo code free bet pakistan|1xbet promo code free spins pakistan|1xbet promo code egypt|1xbet promo code free bet egypt|1xbet promo code today egypt|promo code for 1xbet egypt|1xbet promo code egypt today|1xbet promo code registration egypt|1xbet promo code today egypt|1xbet promo code no deposit egypt|1xbet promo code free bet egypt|1xbet promo code free spins egypt|1xbet casino bonus code|1xbet today promo code|1xbet promo code free spins|1xbet free promo code today|1xbet promo code no deposit|1xbet promo code 2026 today|promo code for 1xbet nigeria|1xbet free bet promo code today|1xbet nigeria promo code|promo code of 1xbet today|1xbet promo code 2026|1xbet free bet promo code|promo code for 1xbet free bet today|1xbet promo code today|free 1xbet promo code today|1xbet free promo code today no deposit|promo code 1xbet today|1xbet no deposit bonus code|1xbet bonus promo code|1xbet latest promo code today|1xbet first deposit bonus promo code|1xbet bet promo code today|1xbet latest promo code|what is the promo code for 1xbet|1xbet free bet promo code today|1xbet casino promo code|1xbet promo code for registration|1xbet promo code free bet today|1xbet casino promo code no deposit bonus|1xbet promo code free spins no deposit|how to use 1xbet promo code|free 1xbet promo code today|1xbet new promo code|1xbet promo code free bet|1xbet bonus promo code today|1xbet bonus code no deposit|1xbet promo code bonus|1xbet promo code free|promo code for 1xbet registration|1xbet welcome bonus code|1xbet today promo code|1xbet gift promo code|today promo code 1xbet|1xbet promo code free bet no deposit|promo code 1xbet casino|1xbet free promo code today|1xbet promo code bonus codes|1xbet promo code free spins|1xbet registration promo code|1xbet ?????? ???|1xbet ?????? ??? ???????|1xbet ?????? ??? ??|1xbet ????????? ?????? ???|1xbet ?????? ??? 2026|1xbet ?????? ??? ??|1xbet ?? ?????? ??? ??|1xbet ?????? ???|?????? ??? 1xbet|1xbet ?????? ??? 2026|1xBet ????? ???|??? ?????? ?? 1xBet|1xbet free promo code philippines|1xbet free bet promo code philippines|1xbet bonus promo code philippines|promo code for 1xbet philippines today|1xbet promo code for registration philippines|promo code for 1xbet philippines|1xbet promo code list philippines|1xbet free promo code today philippines|1xbet promo code free spins philippines|1xbet registration promo code philippines|1xbet promo code new user philippines|1xbet promo code no deposit philippines|1xbet free bet promo code philippines|1xbet promo code new user today philippines|1xbet today promo code philippines|1xbet promo code philippines|promo code for 1xbet philippines|1xbet promo code today philippines|1xbet promo code philippines|1xbet promo code free bet philippines|1xbet promo code today philippines|promo code for 1xbet philippines|1xbet promo code philippines today|1xbet promo code registration philippines|1xbet promo code today philippines|1xbet promo code no deposit philippines|1xbet promo code free bet philippines|1xbet promo code free spins philippines|1xbet egypt promo code|1xbet promo code egypt|1xbet promo code registration egypt|1xbet free promo code egypt|1xbet free bet promo code egypt|1xbet bonus promo code egypt|promo code for 1xbet egypt today|1xbet promo code for registration egypt|promo code for 1xbet egypt|1xbet promo code list egypt|1xbet free promo code today egypt|1xbet promo code free spins egypt|1xbet registration promo code egypt|1xbet promo code new user egypt|1xbet promo code no deposit egypt|1xbet free bet promo code egypt|1xbet promo code new user today egypt|1xbet today promo code egypt|1xbet promo code egypt|promo code for 1xbet egypt|1xbet promo code today egypt|1xbet pakistan promo code|1xbet promo code pakistan|1xbet promo code registration pakistan|1xbet free promo code pakistan|1xbet free bet promo code pakistan|promo code for 1xbet nepal|1xbet promo code today nepal|1xbet promo code nepal|1xbet promo code free bet nepal|1xbet promo code today nepal|promo code for 1xbet nepal|1xbet promo code nepal today|1xbet promo code registration nepal|1xbet promo code today nepal|1xbet promo code no deposit nepal|1xbet promo code free bet nepal|1xbet promo code free spins nepal|1xbet sri lanka promo code|1xbet promo code sri lanka|1xbet promo code registration sri lanka|1xbet free promo code sri lanka|1xbet free bet promo code sri lanka|1xbet bonus promo code sri lanka|promo code for 1xbet sri lanka today|1xbet promo code for registration sri lanka|promo code for 1xbet sri lanka|1xbet promo code list sri lanka|1xbet free promo code today sri lanka|1xbet promo code free spins sri lanka|1xbet registration promo code sri lanka|1xbet promo code new user sri lanka|1xbet promo code no deposit sri lanka|1xbet free bet promo code sri lanka|1xbet promo code new user today sri lanka|1xbet today promo code sri lanka|1xbet promo code sri lanka|promo code for 1xbet sri lanka|1xbet promo code today sri lanka|1xbet promo code sri lanka|1xbet promo code free bet sri lanka|1xbet promo code today sri lanka|promo code for 1xbet sri lanka|1xbet promo code sri lanka today|1xbet promo code registration sri lanka|1xbet promo code today sri lanka|1xbet promo code no deposit sri lanka|1xbet promo code free bet sri lanka|1xbet promo code free spins sri lanka|1xbet philippines promo code|1xbet promo code philippines|1xbet promo code registration philippines|??? ?????? ?? 1xBet|1xbet bangladesh promo code|1xbet promo code bangladesh|1xbet promo code registration bangladesh|1xbet free promo code bangladesh|1xbet free bet promo code bangladesh|1xbet bonus promo code bangladesh|promo code for 1xbet bangladesh today|1xbet promo code for registration bangladesh|promo code for 1xbet bangladesh|1xbet promo code list bangladesh|1xbet free promo code today bangladesh|1xbet promo code free spins bangladesh|1xbet registration promo code bangladesh|1xbet promo code new user bangladesh|1xbet promo code no deposit bangladesh|1xbet free bet promo code bangladesh|1xbet promo code new user today bangladesh|1xbet today promo code bangladesh|1xbet promo code bangladesh|promo code for 1xbet bangladesh|1xbet promo code today bangladesh|1xbet promo code bangladesh|1xbet promo code free bet bangladesh|1xbet promo code today bangladesh|promo code for 1xbet bangladesh|1xbet promo code bangladesh today|1xbet promo code registration bangladesh|1xbet promo code today bangladesh|1xbet promo code no deposit bangladesh|1xbet promo code free bet bangladesh|1xbet promo code free spins bangladesh|free bet promo code 1xbet today|1xbet promo code free bet|1xbet official promo code for registration|free promo code for 1xbet|1xbet promo code free bet today|1xbet promo code for free bet|1xbet promo code free spins no deposit|best promo code for 1xbet|free promo code 1xbet|1xbet new registration promo code|today 1xbet promo code|1xbet free promo code|free 1xbet promo code|1xbet casino promo code today|1xbet promo code|1xbet ng promo code|1xbet casino promo code today|1xbet free bet promo code|promo code for 1xbet|1xbet bonus code|1xbet promo code|1xbet promo code for free bet|1xbet promo code for registration no deposit|1xbet promo code registration|1xbet promo code registration|1xbet promo code for registration|1xbet promo code no deposit|1xbet casino promo code no deposit bonus|1xbet free promo code|promo code for 1xbet free bet today|promo code 1xbet free|how to get 1xbet promo code|promo code for 1xbet registration|free 1xbet promo code|promo code 1xbet free today|1xbet promo code casino|1xbet promo code nigeria|how to use promo code on 1xbet|promo code for 1xbet free bet|1xbet promo code in nigeria|1xbet casino promo code no deposit bonus|what is 1xbet promo code|today 1xbet promo code|1xbet promo code today|promo code 1xbet free bet|promo code for 1xbet today|1xbet sign up promo code|1xbet promo code free spins 2026|1xbet promo code for registration no deposit|1xbet free spin promo code|1xbet free spin promo code today|free bet promo code 1xbet today|free promo code for 1xbet|today 1xbet code promo|1xbet promo code for today registration|1xbet free bet promo code|1xbet bonus code today|1xbet bonus promo code today|1xbet promo code no deposit|1xbet promo code new user today|bonus code for 1xbet|what is promo code in 1xbet registration|1xbet promo code no deposit|free bet promo code 1xbet|promo code 1xbet free today|1xbet welcome bonus promo code|1xbet free promo code today no deposit|1xbet free spin promo code today|promo code for 1xbet|1xbet promo code list|1xbet promo code list today}
This is my first time i visit here. I found so many helpful stuff in your website especially its discussion. From the tons of responses on your posts, I guess I am not the only one having all the enjoyment here! keep up the excellent work
бонус за регистрацию без депозита в казино
бездепозитные бонусы за регистрацию в казино с выводом без пополнения по номеру телефона
I love how this blog promotes self-love and confidence It’s important to appreciate ourselves and your blog reminds me of that
I wish I could craft such articles as this. Thank you very much.
https://vivealumni.usfq.edu.ec/2014/10/museo-alabado.html?sc=1766395983943#c2325712606693246583
https://sites.gsu.edu/sanderson57/2016/10/26/quotes-from-possible-worlds-henri-lefebvre-and-the-right-to-the-city/comment-page-79/#comment-62156
Tips and tools you offer are so helpful to agencies in our community.
Cherished is likely to be what people say about your comments.
1000 рублей за регистрацию в казино без депозита
1000 рублей за регистрацию в казино без депозита
https://gifyu.com/bonuscode211
https://antspride.com/parisgratuits1xbet
1000 рублей за регистрацию вывод сразу без вложений в казино с выводом без депозита за регистрацию
1000 рублей за регистрацию вывод сразу без вложений в казино с выводом без депозита за регистрацию
бездепозитные бонусы в казино за регистрацию с выводом
бездепозитные бонусы в казино за регистрацию
Промокод Melbet – это набор случайных или подобранных символов, которые позволяют новому игроку принять участие в акциях и получить подарки от БК Мелбет. К примеру, в 2026 году Мелбет промокод предлагает бонус 50 000 рублей на счет при регистрации. При выборе букмекерской конторы пользователи обращают внимание не только на маржу или коэффициенты, но и обязательно оценивают текущие акции. Крупные операторы предлагают бонусы на первый депозит, программу лояльности, фрибеты и другие виды поощрений. Бонусный код является самым распространённым видом привлечения клиентов в популярных букмекерских конторах. Чаще всего промокод Melbet представляет собой рандомный порядок букв и цифр, которые вводят в специальное поле в форме регистрации на сайте. Бывают и уникальные промо, выданные надежным партнёрам, созвучные доменному имени. промокод Melbet при регистрации позволяет получить повышенный бонус на первый депозит в размере 100% и бесплатную ставку на 400 RUB или фрибет на $30.
Букмекерская компания Мелбет или известная в других кругах Melbet, имеет огромное количество игроков в онлайне. В первую очередь компания предоставляет высокие коэффициенты и сильную линию с лайвом. Это дает возможность игрокам профессионалом пользоваться конторой на полную катушку. Плюс, с помощью промокода вы получите бонус 50 000 тысяч рублей. Без промо кода до 8000 тысяч. промокод melbet на сегодня представляют собой бонусные возможности, которые дает сама букмекерская контора. Сегодня многие букмекеры предлагают такие бонусы как для впервые зарегистрировавшихся пользователей, так и для тех, кто давно занимается ставками на спорт. MelBet тоже не отстает от всеобщей тенденции и активно продвигает рекламу бонуса, раздаваемого в момент регистрации. Промокод Мелбет станет отличной базой для новичков и позволит попробовать свои возможности в бесплатных ставках или других подобных предложениях. Как получить такой промокод и применить его на деле, рассмотрим далее.
https://casinopromo.ru
Чтобы получить свежие бездепозитные бонусы в онлайн казино за регистрацию в 2026, можно воспользоваться рейтингом на странице.
Приветственные бонусы в онлайн-казино. Что это такое, зачем операторы выдают их пользователям, как получить и отыграть.
https://nodepositcasinobonus.ru
Go directly to our website
QQ88 hướng đến trải nghiệm người dùng tối ưu, giúp việc giải trí trực tuyến trở nên đơn giản và tiện lợi hơn.
Наш сайт — только официальная информация
1xbet multi code today: 1XMAXVIP дает новым клиентам стартовый бонус в размере 100% до 130$. Чтобы получить бонусное предложение, нужно пройти регистрацию на официальном сайте 1xBet, сделать депозит на игровой счет и активировать право на получение бонуса. Затем бонусные средства автоматически зачисляется на игровой баланс.
Для того чтобы активировать 1xt bet promo code, необходимо ввести данный код в специальное поле во время регистрации либо пополнении счета. Далее начисленный бонус автоматически зачисляется на баланс пользователя.
I favored your idea there, I tell you blogs are so helpful sometimes like looking into people’s private life’s and work.At times this world has too much information to grasp. Every new comment wonderful in its own right.
Check our site for updates — http://www.medtronik.ru/
Just stumble upon your blog from from time to time. nice article
бездепозитные бонусы в казино с выводом без пополнения
бездепозитные бонусы в казино
Официальный веб-сайт — кликай сюда — http://hammill.ru/
бездепозитные бонусы в казино за регистрацию с выводом без пополнения
бездепозитные бонусы в казино 2026
https://ip-nsk.ru/uslugi/reklama-v-internete/
http://nipponsword.ru/profile.php?lookup=33461
бонус за регистрацию без депозита в казино
в каком казино дают бездепозитные бонусы
игра в казино где бонус падают шарики
What’s up, I want to subscribe for this web site to take most recent updates, thus where can i do it please assist.
https://socialsaleslab.com/2025/12/24/test-et-avis-atlas-pro-ontv-fonctionnalites-avantages-et-inconvenients/
Greate post. Keep writing such kind of information on your blog. Im really impressed by it.
Hello there, You’ve performed a fantastic job. I’ll definitely digg it and in my view suggest to my friends. I am sure they will be benefited from this website.
http://www.conaculregilor.ro/2025/12/24/comment-bien-configurer-lapplication-atlas-pro-ontv-pour-profiter-pleinement-de-liptv/
Với định hướng phát triển bền vững, QQ88 xây dựng nền tảng cá cược trực tuyến an toàn, công bằng, kết hợp kho game chất lượng cao và nhiều chương trình ưu đãi hấp dẫn cho cả người mới lẫn hội viên lâu năm.
https://elamed.pl/wp-content/art/?1xbet-promo-code__bonus-100_up_to_130.html
https://i-on.in/wp-content/pgs/?1xbet_promo_code_today_bonus.html
https://www.hlsports.de/wp-includes/articles/?1xbet_promo_code-sign_up_bonus.html
топовая группа по лучшим турам где нашли самые лучшие цены и хотим лететь снова в группе по отдыху СлетатьАгент поиска Горящих туров. Самые низкие цены в РФ
бонус за регистрацию без депозита в казино
бездепозитные бонусы в казино олимп
бездепозитные бонусы в казино с выводом
бездепозитный бонус за регистрацию в казино с выводом денег без первого депозита и без отыгрыша
QQ88 là sân chơi giải trí trực tuyến được nhiều người tin chọn nhờ hệ sinh thái game phong phú, tỷ lệ thưởng hấp dẫn, giao diện dễ sử dụng và hệ thống giao dịch an toàn, minh bạch cho người chơi Việt.
https://gs.gctu.edu.gh/articles/phd-students-receive-orientation/
https://www.driedsquidathome.com/forum/topic/85916/1win-%E0%A6%95%E0%A7%8D%E0%A6%AF%E0%A6%BE%E0%A6%B8%E0%A6%BF%E0%A6%A8%E0%A7%8B-%E0%A6%95%E0%A7%8B%E0%A6%A1:-1w2026vip-%E2%80%93-500–%E0%A6%AB%E0%A7%8D%E0%A6%B0%E0%A6%BF-%E0%A6%B8%E0%A7%8D%E0%A6%AA%E0%A6%BF%E0%A6%A8%E0%A6%B8
QQ88 là nhà cái giải trí trực tuyến uy tín châu Á, sở hữu hệ sinh thái game đa dạng gồm casino live, thể thao, bắn cá, slot nổ hũ và xổ số. Nền tảng ổn định, bảo mật cao, nạp rút nhanh, hỗ trợ 24/7 cho người chơi Việt.
https://sykaaa-official-casino.website
https://sykaaa-official-casino.website
фрибет промокод Melbet 2026 Введите: RS777 и тогда при депозите вы получите бонус 50 000 рублей автоматически. Букмекерская контора Мелбет в 2026 году создала комфортные условия для заядлых беттеров и новых пользователей. Международная букмекерская платформа Melbet стремительно набирает популярность среди беттеров. Для привлечения новой аудитории и повышения лояльности уже имеющейся, администрация сайта создала специальный промокод.
Букмекерские конторы в России предлагают огромное количество промокодов и бонусов для своих клиентов, особенно много купонов новичкам, где при регистрации можно получить бесплатно деньги на свой счет. Букмекерская контора Melbet открывает новым игрокам бонус на первый депозит с увеличенной суммой до 50 000 рублей, за Мелбет промокод на сегодня, который можно скопировать у нас. Предлагаем ввести рабочий промокод мелбет бонус, который в 2026 году даёт увеличение 130% бонуса на первый депозит до 50 000 рублей. Регистрируйся и играй с Мелбет сегодня!!! Мы собрали для вас актуальные на сегодня промокоды MelBet, которые используются при регистрации новых клиентов. После чего скидки и бонусы будут зачислены вам на счет.
https://agaclar.net/images/pgs/code-promo-1xbet___bonus.html
https://133636.activeboard.com/t72386535/code-promo-1xbet-burkina-faso-2026-1x200star-bonus-130/?page=1#lastPostAnchor
https://redfordtheatre.com/wp-content/pages/bonus_code_promo_1xbet.html
https://sykaaa-casino-website.fun
https://sykaaa-official-casino.website
Excellent article! Your points are well-articulated and persuasive.
F168 ให้บริการเกมหลากหลายประเภททั้งสล็อต คาสิโนสด กีฬา ยิงปลา และลอตเตอรี่ รองรับผู้เล่นทุกสไตล์ได้อย่างครบครัน. แพลตฟอร์มมีดีไซน์ทันสมัย ใช้งานง่าย และรองรับทุกอุปกรณ์ ช่วยให้การเล่นเกมเป็นไปอย่างราบรื่น. โปรโมชั่นต้อนรับ โบนัสรายวัน และกิจกรรมพิเศษช่วยเพิ่มโอกาสทำกำไรให้สมาชิกอย่างต่อเนื่อง. ระบบฝาก–ถอนมีความปลอดภัย โปร่งใส และดำเนินการรวดเร็ว พร้อมทีมบริการลูกค้า 24 ชั่วโมง ทำให้ F168 เป็นอีกหนึ่งตัวเลือกที่เชื่อถือได้สำหรับผู้เล่นชาวไทย.
https://sykaaa-online-casino.fun
https://sykaaa-official-casino.website
https://veche.ru/parser/inc/1xbet_promokod_registraciya.html
https://minecraftcommand.science/profile/prmocdeforxbettod
https://zachteno.net/images/pages/?promokod-1xbet_i_bonus-kod.html
Thank you for the auspicious writeup.
MK8 นำเสนอเกมหลากหลายประเภททั้งสล็อต คาสิโนสด กีฬา ยิงปลา และลอตเตอรี่ ที่ตอบโจทย์ผู้เล่นทุกสไตล์อย่างครบถ้วน. แพลตฟอร์มถูกออกแบบให้ใช้งานง่าย รองรับทุกอุปกรณ์และโหลดไวทันใจ. ผู้เล่นยังได้รับสิทธิ์รับโบนัสต้อนรับ โปรโมชั่นรายวัน และกิจกรรมพิเศษมากมาย. ระบบฝาก–ถอนปลอดภัยและโปร่งใส พร้อมทีมบริการลูกค้าตลอด 24 ชั่วโมง ทำให้ MK8 เป็นตัวเลือกที่เชื่อถือได้สำหรับผู้เล่นในประเทศไทย.
Thanks for sharing the information. I found the information very useful. That’s a awesome story you posted. I will come back to scan some more.
Our community leaders need to read this, and look at developing some of your recommendations.
I don’t normally comment on blogs.. But nice post! I just bookmarked your site
QQ88 là nhà cái cá cược đẳng cấp top 1 việt Nam, đến với QQ88 nhận 88k khi đăng ký, 188K nạp đầu. Tham gia casino, nổ hũ, bắn cá nhận ngay hoàn trả hàng ngày
A wholly agreeable point of view, I think primarily based on my own experience with this that your points are well made, and your analysis on target.
Discover what’s new
Visit our main website
I just couldn’t leave your website before suggesting that I really enjoyed the usual information an individual supply on your visitors? Is gonna be back often in order to investigate cross-check new posts
thank, I thoroughly enjoyed reading your article. I really appreciate your wonderful knowledge and the time you put into educating the rest of us.
Enjoyed reading through this, very good material. Thanks!
Бесплатный фрибет промокод Melbet 2026 ищет каждый потенциальный клиент компании. Почему? Мало кто откажется от щедрой приветственной награды, позволяющей увеличить сумму первого депозита, заработав до ?9100 бонуса (с 24 апреля бонус увеличился до 50 000). Промокоды – это маркетинговый инструмент, с помощью которого рекламные партнеры букмекера привлекают новых бетторов. Поэтому в современной практике сам букмекер редко распространяет коды, за исключением флагманских акций или раздачи купонов в рамках специальных ивентов. Не все бонусы предполагают наличие рекламного кода. Для активации большинства из них достаточно просто пополнить счет или делать ставки на спорт, получая за это баллы активности. В последующем есть возможность в рамках программы лояльности БК «Мелбет» обменивать баллы на коды для бесплатных ставок (фрибеты) или на реальные денежные средства. Раздобыть промокод Melbet Вы всегда сможете на нашем сайте. При этом Вы можете быть уверенными в том, что это именно актуальное предложение. Также рекомендуем подписаться на информационную рассылку БК, где компания при помощи SMS и почтовых уведомлений держит в курсе событий любителей ставок.
https://wordpress.lehigh.edu/too223/2020/05/07/chopsticks/comment-page-70/#comment-39355
https://gravatar.com/codebonasxbet1
https://crpsc.org.br/forum/viewtopic.php?f=3&t=664871
https://cssh.uog.edu.et/events/%e1%89%a0%e1%88%9b%e1%88%85%e1%89%a0%e1%88%ab%e1%8b%8a-%e1%88%b3%e1%8b%ad%e1%8a%95%e1%88%b5%e1%8a%93-%e1%88%a5%e1%8a%90-%e1%88%b0%e1%89%a5%e1%8b%95-%e1%8a%ae%e1%88%8c%e1%8c%85-%e1%8b%a8%e1%88%9d/#comment-53826
Бесплатный фрибет промокод Melbet 2026 ищет каждый потенциальный клиент компании. Почему? Мало кто откажется от щедрой приветственной награды, позволяющей увеличить сумму первого депозита, заработав до ?9100 бонуса (с 24 апреля бонус увеличился до 50 000). Промокоды – это маркетинговый инструмент, с помощью которого рекламные партнеры букмекера привлекают новых бетторов. Поэтому в современной практике сам букмекер редко распространяет коды, за исключением флагманских акций или раздачи купонов в рамках специальных ивентов. Не все бонусы предполагают наличие рекламного кода. Для активации большинства из них достаточно просто пополнить счет или делать ставки на спорт, получая за это баллы активности. В последующем есть возможность в рамках программы лояльности БК «Мелбет» обменивать баллы на коды для бесплатных ставок (фрибеты) или на реальные денежные средства. Раздобыть промокод Melbet Вы всегда сможете на нашем сайте. При этом Вы можете быть уверенными в том, что это именно актуальное предложение. Также рекомендуем подписаться на информационную рассылку БК, где компания при помощи SMS и почтовых уведомлений держит в курсе событий любителей ставок.
Visit now — https://sushikim.ru/
Посетите официальный сайт бренда > https://kmural.ru/
Open88 là nhà cái trực tuyến được nhiều người chơi lựa chọn nhờ nền tảng ổn định và hệ thống bảo mật cao. Open88 cung cấp đa dạng trò chơi như cá cược thể thao, casino trực tuyến, slot game với giao diện thân thiện, tỷ lệ cược hấp dẫn và quy trình nạp rút nhanh chóng.
comment creer un code promo melbet
code promo melbet
https://pretosnovos.com.br/pag/c_digo_promocional_68.html
code promo melbet rdc
https://avidasecreta.com/wp-content/pgs/?1xbet_promo_code_today__free_bet_bonus.html
https://ville-auverssuroise.fr/media/pgs/?code-promo-1xbet-gratuit-vip-bonus.html
https://www.maxwaugh.com/articles/le-code-promo-1xbet-gratuit.html
The post is absolutely fantastic! Lots of great info and inspiration, both of which we all need! Also like to admire the time and effort you put into your website and detailed info you offer! I will bookmark your website!
Официальный сайт компании
QQ88 là nhà cái cược trực tuyến uy tín hàng đầu Việt Nam, mang đến kho game khủng bao gồm: Baccarat, tài xỉu, bắn cá, xóc đĩa, đá gà, nổ hũ,… nạp đầu tặng 100%.
Good article! We are linking to this great content on our website. Keep up the good writing.
Discover what’s new
https://zelenayazona.ru/
Visit the company’s main website > https://bergkompressor.ru/
Explore the latest here : http://hammill.ru/
Took me time to read all the comments, but I really enjoyed the article. It proved to be Very helpful to me and I am sure to all the commenters here It’s always nice when you can not only be informed, but also entertained I’m sure you had fun writing this article.
https://aboutcasemanagerjobs.com/author/melbetcode2026/
whoah this weblog is great i really like studying your articles. Stay up the great work! You already know, lots of persons are looking round for this information, you can aid them greatly.
https://md.darmstadt.ccc.de/s/WU9M4Y77IN
QQ88 Casino mang đến không gian cá cược hiện đại với dealer live chuyên nghiệp, tỷ lệ thưởng cạnh tranh và hệ thống bảo mật cao cấp dành cho người chơi sành giải trí.
https://lanvitravel.ru/forums/topic/promokod-na-1hbet-2026-1x200new-bonus-32-500-rublej
https://goddesshoes.com/bg/blog/season-essentials
This information is very important and you’ll need to know this when you constructor your own photo voltaic panel.
Букмекерская компания Мелбет или известная в других кругах Melbet, имеет огромное количество игроков в онлайне. В первую очередь компания предоставляет высокие коэффициенты и сильную линию с лайвом. Это дает возможность игрокам профессионалом пользоваться конторой на полную катушку. Плюс, с помощью промокода вы получите бонус 50 000 тысяч рублей. Без промо кода до 8000 тысяч. промокод мелбет при регистрации 2026 представляют собой бонусные возможности, которые дает сама букмекерская контора. Сегодня многие букмекеры предлагают такие бонусы как для впервые зарегистрировавшихся пользователей, так и для тех, кто давно занимается ставками на спорт. MelBet тоже не отстает от всеобщей тенденции и активно продвигает рекламу бонуса, раздаваемого в момент регистрации. Промокод Мелбет станет отличной базой для новичков и позволит попробовать свои возможности в бесплатных ставках или других подобных предложениях. Как получить такой промокод и применить его на деле, рассмотрим далее.
промокод на сегодня melbet 2026 стоит ввести для повышенного бонуса на первый депозит. Большинство букмекерских контор используют такую практику привлечения новых игроков и выдают значительные бонусы. Актуальный промокод Мелбет на 2026 год – RS777. Ввести его могут исключительно новые игроки, у которых еще нет аккаунта в Melbet. Не рекомендуем идти на хитрость и заново проходить процесс регистрации, так как служба безопасности тщательно отслеживает мультиаккаунты. Максимальная сумма бонуса при использовании промокода Мелбет – 50 000 рублей. Это значит, что при вводе средств на баланс после регистрации новому игроку будет зачислено еще 130% от первого депозита в качестве поощрения от букмекера.
1хБет фрибет Активируйте бонус при регистрации на https://g-r-s.fr/pag/code_promo_131.html и получите 32 500 рублей + 100% к депозиту, чтобы начать игру.
1хБет промокод 2026 Промокод 2025 года на https://www.bnbaccess.eu/art/code_promo_1xbet_bonus.html позволяет получить 100% к депозиту до 32 500? для всех зарегистрированных пользователей.
https://douploads.net/2anjk0r4qjgn
https://www.jointcorners.com/forums/thread/7697/
https://solaris-aero.ru/
Thanks for some other great post. Where else may anybody get that kind of information in such an ideal method of writing? I’ve a presentation next week, and I am at the look for such information.
Abnormal this put up is totaly unrelated to what I was searching google for, but it surely used to be listed at the first page. I suppose your doing one thing proper if Google likes you adequate to place you at the first page of a non similar search.
http://hotel-golebiewski.phorum.pl/viewtopic.php?p=850692#850692
https://www.edukids.my/2018/04/28/new-taxas-school-budget
https://wordpress.its.virginia.edu/PLAC_5500_FoodHerit/2012/04/17/394/dsc_4533/
Very fine blog.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15
euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de
juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para
ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android
apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas
deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para
hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones
de apuestas de fútbol|aplicaciones de apuestas
deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones
de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas
deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app
apuestas deportivas android|app apuestas deportivas argentina|app
apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas
sin dinero|app casa de apuestas|app casas de apuestas|app
control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app
de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de
futbol|app de apuestas deportivas|app de apuestas deportivas
android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas
en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas
deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app
de apuestas en españa|app de apuestas en venezuela|app de apuestas
futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas
para ganar dinero|app de apuestas peru|app de apuestas
reales|app de casas de apuestas|app marca apuestas android|app
moviles de apuestas|app para apuestas|app para
apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para
hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas
entre amigos|app para llevar control de apuestas|app pronosticos apuestas
deportivas|app versus apuestas|apps apuestas mundial|apps
de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de
futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender
a hacer apuestas deportivas|aprender hacer apuestas
deportivas|apuesta del dia apuestas deportivas|apuestas 10
euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas
a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas
a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas
nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas
nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas
argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas
argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina
gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas
argentina online|apuestas argentina paises bajos|apuestas argentina
polonia|apuestas argentina uruguay|apuestas argentina
vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera
division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas
athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real
madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas
athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas
atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas
atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético
de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la
liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid
real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas
atletico madrid real madrid|apuestas atletico madrid
vs barcelona|apuestas atletico real madrid|apuestas atletico real
madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto
juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto
prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas
barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas
barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas
barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona
bayern|apuestas barcelona betis|apuestas barcelona campeon de
liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana
la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona
hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas
barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas
barcelona vs atletico madrid|apuestas barcelona vs
madrid|apuestas barcelona vs real madrid|apuestas barsa
madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas
bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis
madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas
betis real sociedad|apuestas betis sevilla|apuestas betis
valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas
betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas
bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas
boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo
online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs
peru|apuestas caballos|apuestas caballos colocado|apuestas caballos
españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar
de barrameda|apuestas caballos zarzuela|apuestas
calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas
campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula
1|apuestas campeon libertadores|apuestas campeon liga|apuestas
campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp
2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas
campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas
campeonato f1|apuestas campeonatos de futbol|apuestas carrera
de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas
carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras
caballos sanlucar|apuestas carreras de caballos|apuestas carreras de
caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras
de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos
nocturnas|apuestas carreras de caballos online|apuestas
carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de
galgos|apuestas carreras de galgos en vivo|apuestas carreras
de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino
gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas
casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas
celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league
– pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas
champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas
chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas
ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas
city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia
uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas
de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas
mismo partido|apuestas combinadas mundial|apuestas combinadas
nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap
asiatico|apuestas con handicap baloncesto|apuestas
con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa
america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de
europa|apuestas copa del mundo|apuestas copa
del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa
del rey pronosticos|apuestas copa del rey pronósticos|apuestas
copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa
mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1
euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto
nba|apuestas de baloncesto para hoy|apuestas
de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos
como se juega|apuestas de caballos en colombia|apuestas de caballos
en españa|apuestas de caballos en linea|apuestas de caballos
españa|apuestas de caballos ganador y colocado|apuestas de caballos
internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online
en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera
de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de
casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de
dinero|apuestas de esports|apuestas de eurocopa|apuestas
de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de
futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas
de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas
de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de
futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos
en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre
hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la
copa américa|apuestas de la eurocopa|apuestas de la
europa league|apuestas de la liga|apuestas
de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de
mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros
en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis
pronosticos|apuestas de tenis seguras|apuestas de
todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas
del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas
del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas
del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas
del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas
deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas
app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina
futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas
deportivas bono bienvenida|apuestas deportivas bono de
bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas
bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas
deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas
deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas
deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero
ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas
consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa
america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas
de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas
de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas
de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas
en argentina|apuestas deportivas en chile|apuestas deportivas
en colombia|apuestas deportivas en directo|apuestas
deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas
en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas
deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas
europa league|apuestas deportivas f1|apuestas deportivas
faciles de ganar|apuestas deportivas formula 1|apuestas
deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia
argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol
argentino|apuestas deportivas futbol colombia|apuestas deportivas
futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior
argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas
deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas
deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas
deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas
deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas
deportivas murcia|apuestas deportivas nba|apuestas
deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas
deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas
online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar
dinero|apuestas deportivas para hoy|apuestas deportivas para hoy
pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas
perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas
deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas
pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas
que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas
resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras
foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas
tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas
uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas
deportivas venezuela|apuestas deportivas virtuales|apuestas
deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas
deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo
1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas
descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero
real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble
resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas
draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas
en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras
de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas
en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas
en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos
virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea
colombia|apuestas en línea de fútbol|apuestas
en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol
en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas
en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas
en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de
futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa
eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas
españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas
españa paises bajos|apuestas español|apuestas español
oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas
esports colombia|apuestas esports españa|apuestas esports fifa|apuestas
esports gratis|apuestas esports lol|apuestas esports peru|apuestas
esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas
euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas
eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa
league hoy|apuestas europa league pronosticos|apuestas europa league
pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas
f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1
hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles
de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas
fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas
final copa de europa|apuestas final copa del rey|apuestas final copa
europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final
eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final
rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas
formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas
foro nba|apuestas francia argentina|apuestas francia españa|apuestas
futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol
americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol
en vivo|apuestas futbol españa|apuestas futbol español|apuestas
fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas
futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas
futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas
galgos|apuestas galgos en directo|apuestas galgos
hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas
galgos trucos|apuestas gana|apuestas gana colombia|apuestas
gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador
champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de
la liga|apuestas ganador del mundial|apuestas ganador
eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores
eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas
ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana
uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador
eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas
gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por
registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis
y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas
handicap baloncesto|apuestas handicap como funciona|apuestas
handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas
online (Leopoldo)|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas
impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas
juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos
olímpicos|apuestas juegos olimpicos baloncesto|apuestas
juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas
kings league americas|apuestas la liga|apuestas la liga española|apuestas la
liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of
legends mundial|apuestas legal|apuestas legales|apuestas
legales en colombia|apuestas legales en españa|apuestas legales
en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones
de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real
madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas
madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid
betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid
dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas
madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs
arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas
mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para
hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo
goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador
eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico
polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb
hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas
mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas
multiples|apuestas múltiples|apuestas multiples
como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial
balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial
clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas
mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula
1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp
nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba
para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas
nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas
nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas
nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl
pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras
de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas
online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas
online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas
online gratis|apuestas online gratis sin deposito|apuestas
online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas
online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online
tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna
barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna
valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas
paginas|apuestas pago anticipado|apuestas paises bajos
ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas
para el clasico|apuestas para el dia de hoy|apuestas para el
mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas
para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar
en la ruleta|apuestas para ganar la champions|apuestas para ganar
la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para
hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para
la copa del rey|apuestas para la eurocopa|apuestas para la
europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los
partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas
partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido
mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos
csgo|apuestas partidos de futbol|apuestas partidos de futbol
hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos
futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru
brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs
chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas
playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs
nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet
para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas
portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas
pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos
futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas
prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana
eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el
mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la
liga|apuestas rayo barcelona|apuestas real madrid|apuestas
real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas
real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real
madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid
barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real
madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester
city|apuestas real madrid osasuna|apuestas real madrid real
sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas
real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs
atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas
real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad
barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real
sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas
rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas
segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras
baloncesto|apuestas seguras calculadora|apuestas seguras en la
ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas
seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas
seguras para este fin de semana|apuestas seguras para ganar
dinero|apuestas seguras para hoy|apuestas seguras para
hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas
seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas
sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas
sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla
manchester united|apuestas sevilla osasuna|apuestas sevilla real
madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas
stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta
roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis
en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas
tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis
wimbledon|apuestas tenis wta|apuestas tercera division|apuestas
tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas
torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas
ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela
ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal
betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal
manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas
vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y
casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas
y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es
pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia
apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs
chile apuestas|argentina vs colombia apuestas|argentina vs
francia apuestas|argentina vs. colombia apuestas|asi se gana
en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos
apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid
apuestas|atletico barcelona apuestas|atletico de madrid
apuestas|atlético de madrid apuestas|atletico de madrid real madrid
apuestas|atletico de madrid vs barcelona apuestas|atletico madrid
real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid
apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada
de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca
madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca
vs madrid apuestas|barca vs real madrid apuestas|barcelona –
real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona
real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia
apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol
apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real
madrid apuestas|barcelona vs real sociedad apuestas|barcelona
vs sevilla apuestas|barcelona vs villarreal apuestas|base de
datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis –
chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis
madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog
apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida
apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida
casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono
casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas
gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida
apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca
apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa
de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono
sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono
sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas
colombia|bonos apuestas deportivas|bonos apuestas deportivas
sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida
apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas
de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de
apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas
gratis|bonos de apuestas sin deposito|bonos
de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de
casas de apuestas|bonos de bienvenida en casas de
apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos
en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos
sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador
de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de
apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas
deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora
apuestas segura|calculadora apuestas seguras|calculadora apuestas
sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de
apuestas de sistema|calculadora de apuestas deportivas|calculadora de
apuestas multiples|calculadora de apuestas seguras|calculadora
de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora
de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas
deportivas|calculadora poisson apuestas|calculadora poisson apuestas
deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios
apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas
deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera
de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de
galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de
caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras
de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de
madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa
apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas
con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de
apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de
madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa
de apuestas beisbol|casa de apuestas betis|casa de apuestas
bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas
bono gratis|casa de apuestas bono por registro|casa
de apuestas bono sin deposito|casa de apuestas boxeo|casa de
apuestas caballos|casa de apuestas carreras
de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa
de apuestas chile|casa de apuestas ciclismo|casa de
apuestas colombia|casa de apuestas con bono de bienvenida|casa
de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa
de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa
de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa
de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de
apuestas del real madrid|casa de apuestas deportivas|casa de
apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas
en colombia|casa de apuestas deportivas en españa|casa
de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa
de apuestas deportivas online|casa de apuestas deportivas peru|casa
de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito
minimo 1 euro|casa de apuestas depósito mínimo 1
euro|casa de apuestas en españa|casa de apuestas en linea|casa
de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de
apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas
españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa
league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de
apuestas ingreso minimo|casa de apuestas ingreso minimo 1
euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de
apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa
de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas
nba|casa de apuestas nfl|casa de apuestas nueva|casa
de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa
de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de
apuestas online paraguay|casa de apuestas online peru|casa de
apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de
apuestas peru online|casa de apuestas por
paypal|casa de apuestas promociones|casa de apuestas que
regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas
sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa
de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa
de apuestas tenis|casa de apuestas ufc|casa de apuestas
valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de
apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas
ciclismo|casas apuestas con licencia|casas apuestas
con licencia en españa|casas apuestas deportivas|casas
apuestas deportivas colombia|casas apuestas deportivas
españa|casas apuestas deportivas españolas|casas
apuestas deportivas nuevas|casas apuestas españa|casas apuestas
españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo
5 euros|casas apuestas legales|casas apuestas legales españa|casas
apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas
apuestas|casas de apuestas|casas de apuestas 5 euros|casas de
apuestas app|casas de apuestas argentinas|casas de
apuestas asiaticas|casas de apuestas baloncesto|casas
de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de
apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos
de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas
chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas
con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de
apuestas con bono de registro|casas de apuestas
con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de
apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de
apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas
con pago anticipado|casas de apuestas con paypal|casas
de apuestas con paypal en perú|casas de apuestas con promociones|casas
de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas
de caballos|casas de apuestas de españa|casas de apuestas
de futbol|casas de apuestas de fútbol|casas de apuestas de
peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas
de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas
de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas
deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas
de apuestas deportivas españolas|casas de apuestas deportivas legales|casas
de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de
apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas
perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo
1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas
en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas
de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas
de apuestas equipos de futbol|casas de apuestas españa|casas
de apuestas españa alemania|casas de apuestas españa
inglaterra|casas de apuestas españa licencia|casas de apuestas
españa nuevas|casas de apuestas españa online|casas
de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas
eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas
f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de
apuestas formula 1|casas de apuestas fuera de españa|casas
de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol
españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas
de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso
minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales
españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas
seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas
de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de
apuestas mundiales|casas de apuestas nba|casas de
apuestas no reguladas en españa|casas de apuestas nueva ley|casas
de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas
de apuestas nuevas españa|casas de apuestas ofertas|casas
de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de
apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de
apuestas online en españa|casas de apuestas online en mexico|casas de
apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online
venezuela|casas de apuestas pago paypal|casas
I saw a similar post on another website but the points were not as well articulated.
Your thing regarding creating will be practically nothing in short supply of awesome. This informative article is incredibly useful and contains offered myself a better solution to be able to my own issues. Which can be the specific purpose MY PARTNER AND I has been doing a search online. I am advocating this informative article with a good friend. I know they are going to get the write-up since beneficial as i would. Yet again many thanks.
Simply want to say your article is as amazing. The clarity in your post is just great and i can assume you’re an expert on this subject. Fine with your permission allow me to grab your feed to keep up to date with forthcoming post. Thanks a million and please keep up the gratifying work.
I can’t go into details, but I have to say its a good article!
https://mcyportal.mosti.gov.my/ntis-tea-talk-2-0-sharing-session-2/uncategorized-en/
Public policy is key here, and our states need to develop some strategies – – soon.
I just sent this post to a bunch of my friends as I agree with most of what you’re saying here and the way you’ve presented it is awesome.
http://www.cdsonla.edu.vn/index.php/vi/component/k2/item/27-beyond-the-college-taking-classes-at-the-graduate-schools?tmpl=component&print=1&start=18
https://www.adpost.com/in/business_products_services/906557/
https://www.goodreads.com/user/show/196933923-promo-code
See the latest update here : https://sushikim.ru/
Visit the company’s main website : https://poloniya.ru/
This is something that will need all of our combined efforts to address.
Greetings! This is my first visit to your blog! We are a collection of volunteers and starting a new initiative in a community in the same niche. Your blog provided us beneficial information. You have done a wonderful job!
Like the way you’ve outlined things. Easy to follow. Not cluttered.
I discovered your weblog site on google and verify just a few of your early posts. Proceed to maintain up the very good operate. I simply further up your RSS feed to my MSN News Reader.
https://ztndz.com/story26804922/1win-promo-code-500-bonus-1025-2026
https://menwiki.men/wiki/User:Xbetcode2026
https://kingshouse.gov.jm/gg-pays-tribute-to-former-chief-justice-edward-zacca/
http://www.studywithdemo.com/2015/02/how-to-make-stamp-size-photos-in-photoshop.html?showComment=1766933363842#c6172803041484659607
https://kwave.koreaportal.com/board/bbs/board.php?bo_table=drama&wr_id=76244&page=0&sca=&sfl=&stx=&spt=0&page=0&btype=tile&cwin=#c_98866
https://pClassified.com/588/posts/1/1/1804468.html
78WIN ให้บริการเกมหลากหลายประเภททั้งสล็อต คาสิโนสด กีฬา ยิงปลา และลอตเตอรี่ รองรับผู้เล่นทุกแนวแบบครบเครื่อง. แพลตฟอร์มถูกออกแบบให้ใช้งานง่าย เปิดได้ทุกอุปกรณ์และโหลดไว มีความเสถียรสูง. ผู้เล่นยังได้รับโบนัสต้อนรับ โปรโมชั่นรายวัน และกิจกรรมพิเศษที่ช่วยเพิ่มโอกาสในการทำกำไร. ระบบฝาก–ถอนปลอดภัย โปร่งใส และดำเนินการรวดเร็ว พร้อมทีมสนับสนุน 24 ชั่วโมง ทำให้ 78WIN เป็นหนึ่งในตัวเลือกที่เชื่อถือได้ของผู้เล่นชาวไทย.
qq88 mediaqq88 media cập nhật tên miền mới, đăng ký casino trực tuyến qq88 nhận 88k ngay hôm nay
https://notebook.zohopublic.com/public/notes/il0dwc0c07f91af134947abaf45dee1cedda5
https://clashofcryptos.trade/wiki/User:1xbetbonuscode
https://amt-games.com/news/1xbet-promo-code___welcome_bonus.html
Как называется врач, занимающийся лечением позвоночника?
промо код на 1хбет Вводите актуальный промокод на https://cordi-frauen.de/wp-content/pgs/le-code-promo-1xbet_bonus.html и активируйте бонус 100% на депозит, чтобы получить стартовый капитал для игры.
промокод 1хБет при регистрации Активируйте бонус при регистрации на https://www.obekti.bg/sites/artcles/index.php?code_promo_208.html и получите 32 500 рублей + бонус 100%, чтобы начать игру.
https://www.lakeshore.com/home/pleasure
https://funsilo.date/wiki/User:1xbetbonuscode
Keep this going please, great job!
рейтинг казино с бесплатными спинами
Here’s the newest update
Hi there mates, pleasant piece of writing and pleasant arguments commented here, I am actually enjoying by these.
лучшие казино сайты
Официальный сайт букмекерской компании
QQ88 CoCom là thương hiệu cá cược uy tín, tặng 88k khi đăng ký, tặng 100k khi nạp đầu, vô nào
https://www.navacool.com/forum/topic/246549/1xbet-%E0%A4%AA%E0%A5%8D%E0%A4%B0%E0%A5%8B%E0%A4%AE%E0%A5%8B-%E0%A4%95%E0%A5%8B%E0%A4%A1-2026:-1x200new
I just added this to my favorites. I truly love reading your posts. Tyvm!
https://id.kaywa.com/vip1xbet2026
https://blog.stcloudstate.edu/hied/2020/02/25/congrats-dr-williams-2020-first-place-dissertation-award-winner/comment-page-1343/#comment-379028
This is really interesting, You’re a very skilled blogger. I have joined your feed and look forward to seeking more of your fantastic post. Also, I have shared your website in my social networks!
https://t.me/s/kaziNO_S_MIniMaLnyM_dePOziTOm/10
Beneficial Blog! I had been simply just debating that there are plenty of screwy results at this issue you now purely replaced my personal belief. Thank you an excellent write-up.
qq887p.com cập nhật tên miền mới, do mấy th kìa nó trỏ SA nhiều quá. Vô đây mà chơi cá cược casino để nhận 88K ưu đãi nạp đầu. ĐKM mấy con lợn trỏ trùng đuổi t
https://t.me/s/kazInO_s_MiNImAlNYM_DepOZiTOM/6
https://www.thebostoncalendar.com/user/135614
https://build-mind.com/profile.php?do=profile&userinfo=earl-linton-495626&mod=space&com=profile
https://letsbookmarktoday.com/profile.php?com=profile&action=view&username=tania.burbank_495626&from=space&mod=space
https://mez.ink/bonusmelbet
Официальный портал компании
Visit our main platform
http://inquisnower.phorum.pl/viewtopic.php?p=728789#728789
https://postheaven.net/p0mp9au63p
https://www.tai-ji.net/board/board_topic/4160148/7663754.htm
https://bodygirdles.com/1xbet-bonus-code-vietnam-1xbig2026-e130-bonus/
Wondering how to register betwinner or how to create betwinner account? You’ll find all details and screenshots on https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/.
Официальный сайт компании 1xBet > https://saratov.agregatka.ru/media/pgs/promokod_755.html
If you need help learning how to create account in betwinner, the full guide is available at https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ — perfect for new users.
I like this weblog very much so much great info .
Latest updates are here — https://34remont-okon.ru/wp-content/pages/?1xbet_promokod_bonus__4.html
Промокод 1xBet на сегодня при регистрации. Игроки могут использовать промокоды для получения различных бонусов от букмекера. Доступ к кодам есть на тематических сайтах и рабочих зеркалах. 1xbet предлагает несколько форм создания аккаунта: в 1 клик. Компания заботится о клиентах и соблюдает международное право. Актуальные промокод 1хБет при регистрации можно получить бесплатно: в СМИ. Любой желающий легко найдёт промокод 1xbet на сегодня. Бонусы щедрые, а условия их получения — реальные. В некоторых случаях вообще ничего делать не нужно.
Промокод 1xBet на сегодня при регистрации. Новички могут использовать промокоды для получения различных бонусов от букмекера. Доступ к кодам есть на тематических сайтах и рабочих зеркалах. 1xbet предлагает разные способы регистрации: по телефону. Компания заботится о клиентах и соблюдает международное право. Актуальные 1xbet можно получить бесплатно: у партнёров БК. Любой желающий легко найдёт промокод 1xbet на сегодня. Предложения выгодные, а условия их получения — реальные. В некоторых случаях вообще ничего делать не нужно.
https://1wins34-tos.top
Visit our homepage : http://www.medtronik.ru/
Проверь официальный сайт компании > https://bergkompressor.ru/
https://griffinzjta47924.getblogs.net/71746723/c%C3%B3digo-promocional-para-1xbet-2026-1x200red
https://telegra.ph/1xBet-Free-Bet-Promo-Code-India-Welcome-Bonus-01-03
https://www.mixcloud.com/1xbetbestcode26/
qq88 tự hào là nhà cái uy tín, sở hữu sản phâm game cá cược hấp dẫn nhất Việt Nam, tặng 88K khi nạp đầu, hoàn trả casino, bắn cá , nổ hũ
https://www.divephotoguide.com/user/lithiloaah/
https://www.polystoned.de/User-sulainffby
https://wakelet.com/@promocodefor1xbetregistration94584
TR88 mang đến hệ sinh thái giải trí đa dạng với nhiều sảnh chơi hấp dẫn như slot game, casino trực tuyến, thể thao, bắn cá và xổ số, đáp ứng trọn vẹn mọi nhu cầu của người chơi. Đặc biệt, người chơi còn có cơ hội nhận ngay ưu đãi lì xì giá trị lên đến 888k khi tham gia.
789Win nổi bật với nền tảng hiện đại, đa dạng các trò chơi từ thể thao, casino trực tuyến đến slot game độc đáo. Cam kết mang lại trải nghiệm an toàn, minh bạch và cơ hội thắng lớn với vô số khuyến mãi hấp dẫn dành cho mọi người chơi!
bonjour I love Your Blog can not say I come here often but im liking what i c so far….
I am very happy to look your post. Thanks a lot and i am taking a look ahead to touch you.
Just stumble upon your blog from from time to time. nice article
Gia nhập OK8386 trải nghiệm hệ sinh thái giải trí đa dạng như cá cược thể thao, casino live, bắn cá, xổ số, đá gà, nổ hũ,… cùng các trò chơi đổi thưởng hấp dẫn khác. Trang web OK8386.SUPPLY là đại lý chính thức cung cấp dịch vụ hay chương trình ưu đãi độc quyền cho mọi người dùng.
https://www.adamedwardsphotography.com/blog/2011/12/digital-camera-magazine-hotshots
https://www.mioola.com/mioola23317784/post/54745142/
https://web-free-ads.com/meilleur-code-promo-1xbet-2026-1x200king-bonus-169000-xof/208633
Some genuinely choice content on this site, bookmarked .
Thank you for all the information was very accurate, just wondering if all this is possible.~
https://www.tumblr.com/timothydunnus
https://onespotsocial.com/timothydunnus
https://medium.com/@bonuscode1xbets/1xbet-promo-code-pakistan-1xbig2026-bonus-130-e763988d2647
You have some helpful ideas! Maybe I should consider doing this by myself.
Well, I don’t know if that’s going to work for me, but definitely worked for you! 🙂 Excellent post!
Если основной сайт недоступен, используйте это зеркало Azino777 Azino777
https://staroetv.su/go?https://lyncconf.com/1xbet-promo-code-use-1xbro200-to-get-bonus-130/
https://discuss.machform.com/u/1xbetfreeph
Visit our main website
Перейди на сайт компании
https://www.betting-forum.com/whats-new/posts/4963153/
https://forums.siliconera.com/threads/1xbet-promo-code-azerbaijan-1xbig2026-%E2%80%93-bonus-%E2%82%AC130.139047/
https://bravelight.net/profile.php?com=profile&do=profile&username=maira.gatty-495862&op=userinfo
I believe this web site has some really wonderful info for everyone : D.
https://t.me/s/minimalnii_deposit/124
https://t.me/s/minimalnii_deposit/34
QQ88 – điểm đến quen thuộc của cộng đồng giải trí trực tuyến, nổi bật với casino live, bắn cá, nổ hũ và đá gà kịch tính.
Discover what’s new
Explore the new one here
https://www.pinlap.com/posts/79290
https://forum.petstory.ge/read-blog/49228
https://be.5ch.net/137070501
https://berry.work/read-blog/14681
Our family had similar issues, thanks.
https://t.me/s/kazino_s_minimalnym_depozitom
https://topstartups.com.br/veja-como-foi-o-1o-evento-da-top-startups/
http://depositfiles.com/files/07iy3iu33
http://brahma-zucht.ch/meine-zuchttiere/henne-silber/
QQ88 là cổng game đổi thưởng trực tuyến được nhiều người chơi tin tưởng nhờ dịch vụ minh bạch và trải nghiệm mượt.
Public policy is key here, and our states need to develop some strategies – – soon.
Мир онлайн-слотов растёт: новые провайдеры, повышенные RTP и постоянные турниры поддерживают интерес игроков.
Vavada удерживает позиции в топе, но не забывайте проверять лицензию и лимиты перед депозитом.
Выбирайте автоматы с бонусными раундами, бесплатными вращениями и прогрессивными джекпотами — так повышается шанс крупного выигрыша.
Зеркала решают проблему блокировок и позволяют оперативно выводить средства без лишних задержек.
Актуальные возможности доступны здесь: https://bezprovodoff.com/pgs/?sekretu_vuigrusha_v_onlayn_kazino_na_slotah_1.html.
Играйте ответственно и контролируйте банкролл, чтобы азарт оставался в пределах удовольствия.
Vavada остаётся одним из самых обсуждаемых казино благодаря щедрым бездепозитным промокодам и частым бонусам на фриспины.
Перед тем как активировать предложение, убедитесь, что промокод действителен сегодня и подходит под условия конкретной акции.
Слоты с высокой отдачей и турниры с гарантированными призами помогают быстро увеличить банкролл даже без крупного депозита.
Регистрация занимает пару минут, после чего становится доступен личный кабинет и быстрый вывод средств на банковскую карту.
Актуальные промокоды, бонус?коды и рабочее зеркало ждут по ссылке: промокод вавада.
Играйте ответственно и контролируйте бюджет, чтобы азарт приносил удовольствие, а не проблемы.
I am lucky that I discovered this website , precisely the right info that I was searching for! .
Ангелица
Peculiar this blog is totaly unrelated to what I was searching for – – interesting to see you’re well indexed in the search engines.
https://davidlwisee.ampblogs.com/1xbet-bonus-code-malaysia-1xbig2026-130-bonus-76112151
Мир онлайн-слотов растёт: новые провайдеры, повышенные RTP и постоянные турниры поддерживают интерес игроков.
Vavada удерживает позиции в топе, но не забывайте проверять лицензию и лимиты перед депозитом.
Выбирайте автоматы с бонусными раундами, бесплатными вращениями и прогрессивными джекпотами — так повышается шанс крупного выигрыша.
Зеркала решают проблему блокировок и позволяют оперативно выводить средства без лишних задержек.
Актуальные возможности доступны здесь: здесь.
Играйте ответственно и контролируйте банкролл, чтобы азарт оставался в пределах удовольствия.
Мир онлайн-слотов растёт: новые провайдеры, повышенные RTP и постоянные турниры поддерживают интерес игроков.
Vavada удерживает позиции в топе, но не забывайте проверять лицензию и лимиты перед депозитом.
Выбирайте автоматы с бонусными раундами, бесплатными вращениями и прогрессивными джекпотами — так повышается шанс крупного выигрыша.
Зеркала решают проблему блокировок и позволяют оперативно выводить средства без лишних задержек.
Актуальные возможности доступны здесь: https://pcpro100.info/pgs/kak_igrat_v_slotu_onlayn_bez_nakrutok.html.
Играйте ответственно и контролируйте банкролл, чтобы азарт оставался в пределах удовольствия.
QQ88 là nhà cái trực tuyến uy tín hàng đầu đông Nam Á, mang đến kho game hay ho và hấp dẫn: Casino ,bắn cá, đá gà, nổ hũ,… tặng 88k khi đăng ký và tặng 999k khi nạp đầu
http://indusaconstrucciones.com/index.php/es/component/k2/item/1
http://businessfreedirectory.biz/index.php?q=https%3A%2F%2Fwww.colehardware.com%2Farticles%2F1xbet_promo_code_106.html&x=84&y=22
ко ланта ко ланта
98WIN – Nền tảng cá cược trực tuyến uy tín hàng đầu, nơi hội tụ kho trò chơi đa dạng từ casino, thể thao đến các game giải trí hấp dẫn. Tham gia ngay hôm nay để khám phá những trải nghiệm khác biệt, tận hưởng dịch vụ chuyên nghiệp và cơ hội nhận về vô số phần thưởng hấp dẫn dành riêng cho bạn!
79KING là thương hiệu cá cược trực tuyến hàng đầu châu Á, nổi bật với công nghệ bảo mật hiện đại, kho trò chơi đa dạng và tỷ lệ cược cực hấp dẫn. Tại Việt Nam, bujpufu.ru.com mang đến trải nghiệm cá cược mượt mà, nạp rút linh hoạt, nhanh chóng và hoàn toàn an toàn.
Check how to register in betwinner and enjoy a seamless experience by following the simple guide at https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/.
Looking to betwinner create account fast? Go to https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and complete the simple sign-up form in just a few clicks.
https://t.me/s/KAZINO_S_MINIMALNYM_DEPOZITOM
https://t.me/s/KAZINO_S_MINIMALNYM_DEPOZITOM
1xbet official promo code canada
1xbet philippines promo code today
1xbet uzbekistan promo code free bet
http://vostorg.7olimp.ru/viewtopic.php?f=1&t=1595
https://www.garthcharityprojects.org/profile/yarid2546698283/profile
Go to our updated website — https://kcdoll.ru/lyalya/ph/1xbet.html
Experience the latest version here — https://renaultra.ru/pages/promokod_756.html
It’s time for communities to rally.
https://gdz.com.kz/
Good pleasure and entertainment – waiting for you right now…;)
789Win nổi bật với nền tảng hiện đại, đa dạng các trò chơi từ thể thao, casino trực tuyến đến slot game độc đáo. Cam kết mang lại trải nghiệm an toàn, minh bạch và cơ hội thắng lớn với vô số khuyến mãi hấp dẫn dành cho mọi người chơi!
What’s up, its nice post about media print, we all know media is a great source of data.
https://sun-shop.com.ua/bi-led-linzy-toyota-rav4-xa30-76-mm.html
Heya! I’m at work browsing your blog from my new iphone 4! Just wanted to say I love reading through your blog and look forward to all your posts! Carry on the excellent work!
https://sholom-aleichem.kiev.ua/sklyani-fary-na-starykh-avto-chy-mozhna-yikh.html
Посети официальный сайт компании > https://bergkompressor.ru/
Переходи по ссылке на официальный сайт — http://hammill.ru/
моющее средство эко Моющее средство для пола концентрат – это высокоэффективное решение для поддержания чистоты и блеска полов в вашем доме. Наша концентрированная формула позволяет получить безупречный результат при минимальном расходе, эффективно удаляя грязь, пыль и пятна с различных типов напольных покрытий, включая ламинат, плитку и паркет.
Ко ланта ко ланте
Базы Xrumer не сырые телеграм Базы Хрумер 23 телеграм
кайтинг в анапе кайт школа анапа
https://www.tdk-evak.kz/
кайт кайт серфинг в египте
79KING là thương hiệu cá cược trực tuyến hàng đầu châu Á, nổi bật với công nghệ bảo mật hiện đại, kho trò chơi đa dạng và tỷ lệ cược cực hấp dẫn. Tại Việt Nam, ajagaqa.za.com mang đến trải nghiệm cá cược mượt mà, nạp rút linh hoạt, nhanh chóng và hoàn toàn an toàn.
https://learndash.aula.edu.pe/miembros/betbonus1x/activity/
https://www.growkudos.com/profile/betbonus1x_bonus
https://betpomo1x.wizzardsblog.com/39389989/1xbet-azerbaijan-promo-code-no-deposit-1xfun777-130-bonus
Донат в мобильные игры Донат в Rise of Kingdoms – важная составляющая игрового процесса. В этой стратегической игре игроки часто прибегают к донату, чтобы ускорить строительство, тренировку войск и получение ресурсов. Это позволяет им быстрее развивать свою империю и укреплять позиции в борьбе за мировое господство. Донат открывает доступ к премиум-функциям и предметам, значительно облегчая путь к успеху в Rise of Kingdoms.
органические моющие средства Концентрат моющих средств – это оптимальное решение для тех, кто ценит эффективность и экономичность. Благодаря высокой концентрации активных веществ, наши продукты обеспечивают максимальную чистоту при минимальном расходе. Это позволяет существенно экономить ваши средства и снизить количество пластиковой упаковки, внося вклад в сохранение окружающей среды.
ко ланте ко ланте
интенсив курсы диспетчера
база xrumer телеграм Обучение Xrumer 23 strong
экологически чистые моющие средства Универсальное концентрированное моющее средство – это ваш надежный помощник в борьбе за чистоту во всем доме. Мы разработали универсальную формулу, которая эффективно удаляет загрязнения с различных поверхностей, включая кухонные столешницы, ванные комнаты, полы и мебель. Наше средство не оставляет разводов, придает блеск и свежесть, при этом оставаясь безопасным для окружающей среды и здоровья вашей семьи.
https://stroydomkrim.ru/index.php?option=com_k2&view=item&id=12
кайт благовещенская кайт школа анапа
Донат в FC Mobile Донат в FC Mobile (ранее FIFA Mobile) – популярная практика среди поклонников мобильной версии футбольного симулятора. Игроки используют донат для приобретения внутриигровых наборов с футболистами, улучшения характеристик команды и получения конкурентного преимущества в онлайн-матчах. Это ускоряет прогресс и позволяет создать более сильную команду, способную побеждать в турнирах.
https://www.dropbox.com/scl/fi/07bzuru7067xnhqb0y5b9/1xBet-Free-Bet-Promo-Code-Azerbaijan_-1X200NUT-130-Bonus.pdf?rlkey=9ppo7c5wmdt5ko3wxx0jr2i5b&st=bzae14kw&dl=0
https://siciliammare.it/sicurezza-alimentare-lasp-di-palermo-a-lampedusa-per-freschezza-del-pesce-e-rischi-sanitari_8884/#comment-442397
Excellent read, I just passed this onto a colleague who was doing a little research on that. And he actually bought me lunch because I found it for him smile So let me rephrase that.|
курсы трак диспетчера онлайн отзывы
Enjoyed reading through this, very good material. Thanks!
doktor kbb
http://skyiwredshjnhjgeleladu7m7mgpuxgsnfxzhncwtvmhr7l5bniutayd.onion
See the latest update here
мод на тик ток 2025 айфон бесплатно Поиск и Установка: Безопасность Прежде Всего Поиск модов TikTok – это, как правило, задача, требующая внимательности. Рекомендуется использовать проверенные источники, форумы и Telegram-каналы, где публикуются отзывы и рекомендации от других пользователей. Перед установкой обязательно убедитесь в безопасности загруженного файла, используя антивирусное программное обеспечение.
скачать тикток мод на айфон последняя версия Перспективы в 2025 Году: Будущее Пользовательского Контроля в TikTok В 2025 году ожидается дальнейшее развитие модов TikTok и инструментов для их установки, таких как Scarlet. Разработчики будут стремиться к улучшению безопасности, стабильности и функциональности, предлагая пользователям еще больше возможностей для персонализации и контроля над своим контентом.
Go to our website
blsp at сиськи тут
тик ток мод с огоньком Тик Ток Мод: Расширенные Возможности и Перспективы на 2025 Год В мире социальных сетей TikTok продолжает оставаться одной из самых популярных платформ, привлекая миллионы пользователей по всему миру. Однако, для тех, кто ищет больше возможностей и настроек, существуют так называемые “моды” TikTok. Эти модифицированные версии приложения предлагают расширенные функции, недоступные в официальной версии, такие как скачивание видео без водяного знака, разблокировка регионального контента, кастомизация интерфейса и многое другое.
Certainly. And I have faced it. Let’s discuss this question. Here or in PM.
codigo promocional 1xbet peru
codigo promocional 1xbet peru
codigo promocional de 1xbet
1xbet bono dinero gratis
1xbet codigo promocional para hoy de bono gratis
мод тик тока 5 версия Scarlet: Ключ к Миру Неофициальных Приложений на iOS Scarlet, как инструмент для установки приложений в обход App Store, становится особенно актуальным для пользователей iPhone, стремящихся к установке TikTok модов. Это открывает доступ к функциям, которые обычно ограничены в официальной версии приложения, например, скачивание видео без водяного знака, расширенные настройки приватности и блокировка рекламы.
skyiwredshjnhjgeleladu7m7mgpuxgsnfxzhncwtvmhr7l5bniutayd.onion
我們的資深運彩分析專家團隊運用AI深度學習技術,每日更新NBA、MLB、中華職棒等各大聯盟的專業賽事分析。
QQ88 mang đến hệ sinh thái cá cược trực tuyến toàn diện, tích hợp casino live, slot đổi thưởng, bắn cá và thể thao vận hành mượt mà.
https://www.ihvo.de/wp-content/pages/1xbet_promo_code_welcome_bonus.html
https://nototojkxgif.bestoof.com/t69-1xBet-Thailand-Bonus-Code-1X200RED-EUR130-Bonus.htm#p697
https://www.dropbox.com/scl/fi/07bzuru7067xnhqb0y5b9/1xBet-Free-Bet-Promo-Code-Azerbaijan_-1X200NUT-130-Bonus.pdf?rlkey=9ppo7c5wmdt5ko3wxx0jr2i5b&st=bzae14kw&dl=0
https://www.intensedebate.com/people/1xbetbestcode35
Официальный портал компании
Промокод 1xBet на сегодня при регистрации. Новички могут использовать промокоды для получения различных бонусов от букмекера. Найти такие коды можно на тематических сайтах и рабочих зеркалах. 1xbet предлагает несколько форм создания аккаунта: через e-mail. Компания заботится о клиентах и соблюдает международное право. Актуальные the general promo code for 1xbet можно получить бесплатно: у партнёров БК. Любой желающий легко найдёт промокод 1xbet на сегодня. Бонусы щедрые, а условия их получения — реальные. В некоторых случаях вообще ничего делать не нужно.
blacksprut
??????
трансы иркутск Медитативные практики в Иркутске укоренены в древних традициях и адаптированы к современным потребностям. Здесь можно найти группы випассаны, школы осознанности и центры, предлагающие медитации, направленные на снижение стресса и развитие эмоционального интеллекта. Байкальская природа словно сама располагает к погружению в состояние созерцания и внутреннего покоя.
中職粉絲必備的官方認證資訊平台,24小時不間斷提供官方中職新聞、球員數據分析,以及專業的比賽預測。
m bs2web at
трансы волгоград Гипнотерапия в Волгограде – это профессиональная помощь квалифицированных специалистов, использующих гипноз для решения широкого спектра психологических проблем. От избавления от фобий и тревог до работы с зависимостями и повышения самооценки, гипноз становится мощным инструментом в руках опытного терапевта.
https://waef.org/2021-scholarship-application-open/
http://kitchensoko.com/index.php/component/k2/item/4-strawberries-high-yield
https://whoosmind.com/forums/thread/35141/
https://www.renfrewpro.com/renfrewhomepage/renfrewnews/2017/03/27/scapa-renfrew-site-manufacturing-capacity-and-capability-upgrades
https://captainspeaking.com.pl/wikingowie-ponownie-odkrywaja-ameryke/
La promotion d’inscription 1xBet offre jusqu’a 100 €/$ a l’occasion du premier versement. Le montant du bonus est garanti, meme sans code. Pour obtenir plus de details sur le code promo 1xBet gratuit, vous pouvez consulter ce lien : https://artiqueobjectz.co.id/pages/code_promo_1xbet.html
Set piece efficiency, corner and free kick conversion rates
Grace a la promotion meilleur code promo 1xBet, le bonus peut etre de 130 %. Meme sans code, le bonus de bienvenue est credite. En jouant activement, vous pouvez accumuler des points promo utilisables pour un pari gratuit ou augmenter votre capital. Toutes les informations sur le code promo 1xBet casino en ligne sont disponibles ici : https://www.allgreatquotes.com/news/code_promo_208.html
казино с лучшими фриспинами и выводом
казино бонус за регистрацию
матрешка Купить матрешки можно не только в качестве сувенира, но и как оригинальный подарок, который подчеркнет вашу любовь к русской культуре и вашу заботу о получателе. Матрешка станет прекрасным украшением интерьера и будет напоминать о России долгие годы.
QQ88 là nền tảng cá cược trực tuyến uy tín, tích hợp casino live, nổ hũ, bắn cá và thể thao với trải nghiệm ổn định.
Moomoo証券 ログイン PC
みんなのFX
Реставрация мебели Ремонт мраморной поверхности – задача еще более деликатна. Мрамор – благородный, но хрупкий материал, требующий особого ухода и бережного обращения. Реставрация мрамора требует профессиональных навыков и использования специализированного оборудования.
Moomoo証券 ログイン PC
Реставрация картины Реставрация картины: Возвращение к первозданной красоте
みんなのFX
Football match time today, know exactly when games start in your timezone
what is the promo code for melbet
how to get my promo code on melbet
https://fawelle.com/blog/best-beauty-products
{{melbet promo code today free|melbet best promo code|melbet promo code free bet|melbet promo code for registration|melbet free bet promo code today|melbet code promo|melbet free bet promo code|melbet promo code registration|melbet promo code 2026|melbet promo code registration india|melbet promo code bonus|promo code for melbet today|melbet promo code 2026|melbet promo code today|melbet promo code free bet|how to get melbet promo code|melbet new promo code|melbet free bet promo code|melbet free bet promo code today|melbet promo code for free spins|melbet promo code india|melbet promo code bd|melbet official promo code|melbet free bet promo code today|melbet registration promo code|melbet promo code bangladesh today|melbet registration promo code|melbet promo code bangladesh today|melbet promo code for registration|promo code for melbet|melbet promo code india today|melbet promo code create|how to get my promo code on melbet|melbet best promo code|melbet promo code bangladesh today free|melbet promo code bonus|melbet official promo code|melbet promo code for free spins|melbet casino promo code|melbet promo code registration|what is the promo code for melbet|melbet promo code|melbet promo code 2026|melbet today promo code|melbet bonus promo code|melbet promo code for free spins 2026|melbet promo code for free spins today|melbet official promo code|melbet promo code check|melbet promo code no deposit|melbet app promo code|melbet bonus promo code|melbet promo code bangladesh|melbet app promo code|promo code for melbet|promo code melbet|melbet promo code no deposit|melbet free spin promo code|today melbet promo code|melbet app promo code|melbet promo code create|melbet promo code bangladesh today|what is the promo code for melbet|melbet promo code bangladesh 2026|melbet promo code bangladesh 2026|how to create melbet promo code|how to get melbet promo code|melbet promo code 2026|melbet promo code india|promo code for melbet|melbet casino promo code|melbet free spin promo code|melbet promo code for registration|melbet promo code registration|melbet promo code today|best promo code for melbet|melbet promo code india|today melbet promo code|melbet casino promo code|how to get my promo code on melbet|melbet promo code bangladesh 2026|melbet promo code bangladesh 2026|melbet promo code no deposit|melbet promo code today india|melbet bonus promo code|melbet new promo code|melbet free bet promo code|melbet today promo code|melbet promo code bd|melbet promo code|melbet free spin promo code|melbet free promo code|melbet promo code 2026|melbet promo code today|melbet promo code check|melbet promo code free|how to create melbet promo code|melbet promo code bangladesh today 2026|best promo code for melbet|melbet best promo code|how to get melbet promo code|melbet today promo code|melbet registration promo code|melbet free promo code|melbet promo code bangladesh|melbet promo code bangladesh|melbet new promo code|promo code melbet|promo code for melbet today|melbet promo code pakistan|melbet promo code for free spins today}
A colleague in the field told me to check out your website.
みんなのFX
https://aboutnursernjobs.com/author/bonus1xbet202/
https://moldovanews.md/wp-content/pages/megapari_promokod_segodnya.html
https://fly-inform.ru/news/pokerdom_promokod_bonus_kod.html
https://cascadeclimbers.com/content/pgs/code-promo-22bet.html
The easiest way to claim your betwinner registration bonus is to visit https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and complete the sign-up form carefully. Make sure you verify your email to activate the offer.
onpagelab.click – Content reads clearly, helpful examples made concepts easy to grasp.
adnivo.click – Content reads clearly, helpful examples made concepts easy to grasp.
Looking to betwinner create account fast? Go to https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and complete the simple sign-up form in just a few clicks.
klickivo.click – Found practical insights today; sharing this article with colleagues later.
rankvanta.click – Navigation felt smooth, found everything quickly without any confusing steps.
telegram premium boost adana Telegram Boost Sat?n Al: An?nda Etki, Uzun Vadeli Faydalar Telegram boost sat?n alarak, kanal?n?z?n gorunurlugunu k?sa surede art?rabilirsiniz. Bu, ozellikle yeni bir kanal act?ysan?z veya mevcut kanal?n?z? buyutmek istiyorsan?z onemli bir avantaj saglar. Daha fazla etkilesim, daha fazla abone ve daha fazla potansiyel musteri demektir.
тантрический массаж краснодар Массаж мужчине в Краснодаре – это комплексный подход к поддержанию мужского здоровья и жизненной энергии. Специально разработанные техники массажа направлены на снятие мышечного напряжения, улучшение кровообращения и лимфотока, а также на стимуляцию мужской половой сферы. Профессиональный массажист учитывает индивидуальные особенности клиента, чтобы создать максимально комфортные и эффективные условия для расслабления и восстановления.
QQ88 mang đến hệ sinh thái cá cược trực tuyến toàn diện, nổi bật với casino live, slot đổi thưởng, bắn cá và thể thao ổn định.
manage manage manage managefg managerey
growvanta.click – Appreciate the typography choices; comfortable spacing improved my reading experience.
репутолог Кто такой репутолог и чем он занимается? Простыми словами, репутолог – это эксперт по управлению репутацией в интернете (Online Reputation Management, ORM). Он не просто “чистит” негатив, а выстраивает комплексную стратегию, направленную на формирование положительного имиджа компании, повышение доверия клиентов и, как следствие, рост бизнеса.
мужской массаж краснодар Массаж мужчине Краснодар: Индивидуальный подход к мужскому здоровью
QQ88 nổi bật với hệ sinh thái game đa dạng, thao tác mượt mà và dịch vụ hỗ trợ người chơi liên tục.
Discover what’s new today > https://www.frenchtouch.ru/include/pages/1xbet_promokod_pri_registracii_bonus.html
Explore the latest additions here — https://sangistil.ru/wp-includes/pgs/promokod_252.html
1хбет промокод при регистрации Получите промокод на https://imagecms.net/wp-content/pgs/1xbet-aktualnuy-promokod-pri-registracii.html и заберите бонус 100% на первый депозит при регистрации для комфортной игры.
https://gifyu.com/codevalide1xbet
промокод при регистрации 1хБет Использование промокода при регистрации на http://neoko.ru/images/pages/1xbet_promokod_besplatno.html позволяет получить бонус до 32 500 рублей, чтобы начать игру с максимальной суммой.
http://j-colorstone.net/product/%E3%83%91%E3%83%91%E3%83%A9%E3%83%81%E3%82%A2%E3%82%B5%E3%83%95%E3%82%A1%E3%82%A4%E3%82%A2%E3%83%AA%E3%83%B3%E3%82%B0158000/
https://edex.adobe.com/community/member/cE27OqXfg
https://electroswingthing.com/profile/CanCode2026/
https://med.jax.ufl.edu/webmaster/?url=https://jerezlecam.com/pag/code-promo-1xbet_bonus-exclusif.html
localsprint.click – Overall, professional vibe here; trustworthy, polished, and pleasantly minimal throughout.
localbooster.click – Mobile version looks perfect; no glitches, fast scrolling, crisp text.
locallift.click – Navigation felt smooth, found everything quickly without any confusing steps.
bizfunnel.click – Bookmarked this immediately, planning to revisit for updates and inspiration.
adsparkhub.click – Pages loaded fast, images appeared sharp, and formatting stayed consistent.
Nhà cái QQ88 mang đến môi trường cá cược trực tuyến an toàn, phù hợp cho người chơi mới và lâu năm.
клиника жуйкан Жуйкан: Маяк здоровья и надежды в приграничном Хэйхэ Жуйкан – это имя, синонимичное качественной медицинской помощи и заботливому отношению к пациентам в динамично развивающемся городе Хэйхэ. Клиника, уверенно шагая в ногу со временем, предлагает широкий спектр услуг, сочетая традиционные методы лечения с инновационными технологиями, тем самым заслужив доверие множества пациентов, как из Китая, так и из-за рубежа. Это не просто медицинское учреждение, это островок надежды, где каждый человек получает шанс на здоровую и полноценную жизнь.
Hi there, all is going well here and ofcourse every one is sharing data, that’s truly good, keep up writing.
byueuropaviagraonline
I was referred to this web site by my cousin. I’m not sure who has written this post, but you’ve really identified my problem. You’re wonderful! Thanks!
https://svbeloglazov.ru/ svbeloglazov
Go to our site right now : https://jerezlecam.com/
This is really interesting, You’re a very skilled blogger. I have joined your feed and look forward to seeking more of your fantastic post. Also, I have shared your website in my social networks!
This page truly has all of the information and facts I wanted concerning this subject and didn’t know who to ask.
byueuropaviagraonline
жуйкан Клиника Жуйкан предлагает широкий спектр медицинских услуг, охватывающих различные области, от общей терапии до специализированных направлений. Здесь ценят каждого пациента и стремятся обеспечить индивидуальный подход к решению его проблем.
World Cup 2026 qualifiers live score, road to USA Mexico Canada tournament
Go to our brand page — https://jerezlecam.com/
I imagine so. Very good stuff, I agree totally.
Hey very cool site!! Man .. Beautiful .. Amazing .. I will bookmark your website and take the feeds also…I’m happy to find so many useful information here in the post, we need develop more strategies in this regard, thanks for sharing. . . . . .
Nice Post. It’s really a very good article. I noticed all your important points. Thanks.
https://svbeloglazov.ru/ svbeloglazov
Nhà cái QQ88 nổi bật với kho game phong phú, vận hành mượt mà và dịch vụ hỗ trợ người chơi liên tục.
Fantastic piece of writing here1
leadboostlab.click – Content reads clearly, helpful examples made concepts easy to grasp.
clickgrowthhub.click – Mobile version looks perfect; no glitches, fast scrolling, crisp text.
rankbooststudio.click – Mobile version looks perfect; no glitches, fast scrolling, crisp text.
https://www.exchangle.com/promolive1xbet
https://www.woman.sk/pages/?melbet_promokod_pri_registracii___bonus_kod_na_segodnya.html
https://www.instapaper.com/p/bonus1xbet2026
https://mebel-3d.ru/libraries/news/?promokod-pari.html
semmarketing.click – Found practical insights today; sharing this article with colleagues later.
funnelscalelab.click – Navigation felt smooth, found everything quickly without any confusing steps.
https://youslade.com/promogratuit2026
http://jobboard.piasd.org/author/codevip1xbet2026/
https://rocksalta.com/pgs/preimuschestva_elektronnyh_deneg.html
https://www.ganjingworld.com/vi-VN/channel/1i8hqsffq527kapXmlk4JR6e516q0c?tab=about
https://dp5.boards.net/thread/1331/promo-1xbet-mauritanie-1xbum-exclusif
https://whoosmind.com/forums/thread/35536/
Το στοίχημα αποτελεί αναπόσπαστο κομμάτι της ψυχαγωγίας για πολλούς Έλληνες παίκτες. Καθώς η εγχώρια αγορά υπόκειται σε αυστηρή ρύθμιση και περιορισμούς, ένα μεγάλο μέρος των παικτών στρέφεται προς ξένες στοιχηματικές εταιρείες που προσφέρουν μεγαλύτερη ευελιξία, καλύτερες αποδόσεις, περισσότερες επιλογές και καινοτόμα χαρακτηριστικά. Ειδικά για όσους αναζητούν μια πιο πλούσια στοιχηματική εμπειρία, οι πλατφόρμες του εξωτερικού προσφέρουν σημαντικά πλεονεκτήματα. Ο όρος ξένες στοιχηματικές εταιρείες που δέχονται Έλληνες δεν αφορά απαραίτητα αδειοδοτημένους παρόχους στην Ελλάδα, αλλά ιστοσελίδες που λειτουργούν νόμιμα υπό διεθνείς άδειες όπως της Κουρασάο, της Ανζουάν ή της Κόστα Ρίκα και επιτρέπουν εγγραφή και στοιχηματισμό από Έλληνες χρήστες. Το ενδιαφέρον για τέτοιου είδους εταιρείες αυξάνεται συνεχώς, καθώς προσφέρουν όχι μόνο καλύτερα μπόνους και προωθητικές ενέργειες, αλλά και υποστήριξη σε κρυπτονομίσματα, μηδενική γραφειοκρατία και πιο φιλικές προς τον χρήστη εμπειρίες.
Team news updates, lineups injuries and squad announcements covered
netassist.click – Appreciate the typography choices; comfortable spacing improved my reading experience.
webrelay.click – Loved the layout today; clean, simple, and genuinely user-friendly overall.
connecthub.click – Mobile version looks perfect; no glitches, fast scrolling, crisp text.
onlineboost.click – Bookmarked this immediately, planning to revisit for updates and inspiration.
Пицца Куба Пицца Куба Воронеж
I have been following your blog for a while now and have to say I am always impressed by the quality and depth of your content Keep it up!
Your posts are always so relevant and well-timed It’s like you have a sixth sense for what your readers need to hear
Your idea is outstanding; the issue is something that not enough persons are speaking intelligently about. I’m very happy that I stumbled throughout this in my seek for one thing regarding this.
https://eguidemagazine.com/wp-content/pages/oteliantalyidlyarom.html
https://sites.google.com/view/1xbetpakistanpromocode20261x20/home
https://musicserver.cz/pages/?zamena_santehniki_professionalyno_kachestvenno_i_nedorogo.html
https://findfreightloads.com/vagrant/pgs/kakie_zvuki_izdayut_koshki_i_chto_oni_oznachayut.html
GoogleImagen ChatGPT, Midjourney, Gemini, OpenAI, Stable Diffusion, Sora, Claude, Google Imagen – это лишь некоторые примеры инструментов на основе ИИ, которые уже сегодня доступны широкому кругу пользователей. Они позволяют генерировать тексты, создавать изображения, разрабатывать код и решать сложные задачи. Будущее уже здесь, и каждый может попробовать себя в роли творца, используя возможности искусственного интеллекта.
https://trade-mark.store/product-category/joy-home-cumki-telezhki/ купить хозяйственные сумки тележки оптом в москве, хозяйственные сумки тележки оптом со склада в москве.
Thanks for your patience and sorry for the inconvenience!
OK, you outline what is a big issue. But, can’t we develop more answers in the private sector?
https://trade-mark.store/product-category/stremyanki-bytovye/ стремянки бытовые оптом в москве, стремянки бытовые купить оптом в москве.
Do you offer workshops?
speedserve.click – Appreciate the typography choices; comfortable spacing improved my reading experience.
clicknetwork.click – Found practical insights today; sharing this article with colleagues later.
websprint.click – Navigation felt smooth, found everything quickly without any confusing steps.
browsebuddy.click – Pages loaded fast, images appeared sharp, and formatting stayed consistent.
https://trade-mark.store товары для дома оптом москва, купить товары для дома оптом москва
routerready.click – Pages loaded fast, images appeared sharp, and formatting stayed consistent.
捕风追影在线免费在线观看,海外华人专属平台,高清无广告体验。
1xBet промокод на сегодня Используйте на http://neftyanik96.ru/wp-content/articles/index.php?1xbet_promokod_bonus__4.html и получите бонус 100% на депозит до 32 500?, чтобы получить максимальный стартовый бонус.
https://www.yojoe.com/include/incs/kak_krasivo_govority_s_devushkoy_kak_krasivo_govority_na_russkom.html
Промокод 1xBet при регистрации. Компания 1ИксБет заинтересована в поиске новых игроков, поэтому для новых пользователей действует акция в виде стартового вознаграждения, который равен сумме первого депозита, но не превышает 225 000 рублей. Однако при использовании бесплатные купоны на 1xbet букмекерская контора повысит величину приветственного бонуса. Чтобы получить дополнительное вознаграждение на первый депозит, игроку нужно: зайти на сайт букмекера, выбрать регистрацию по e-mail, заполнить данные, ввести промокод и подтвердить согласие с правилами. Код 1xBet помогает получить ещё больше бонусов. Такой код представляет собой набор, которая позволяет активировать специальное предложение от букмекера. С его помощью можно получить фрибет и другие подарки.
https://pub23.bravenet.com/forum/static/show.php?usernum=1937943029&frmid=9647&msgid=899983&cmd=show
https://playplayfun.com/articles/1xbet_promo_code_nigeria_bonus.html
https://instant.co/pages/kak_ne_potolstety_vo_vremya_otpuska.html
https://giselagym.musin.de/media/pgs/?recenziya_na_filym_dghey_i_molchalivyy_bob_perezagruzka__1.html
Set piece goals, dead ball situations and their conversion
To register betwinner successfully, open https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and follow the instructions provided on the official review page.
Here’s the newest update : https://pravo-znanie.ru/pages/promokod_756.html
Use the betwinner promo kodas 2025 during sign-up at https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ to activate your welcome bonus instantly.
Официальный портал компании — https://ecotruck.su/images/pgs/?1xbet-promokod-pri-registracii.html
Li-ion АКБ 24В Размеры литий ионных тяговых аккумуляторов зависят от производителя, необходимой емкости и вольтажа.
Переходи по ссылке на официальный сайт > https://bergkompressor.ru/
https://vc.ru/smm-promotion
What i discover troublesome is to find a weblog that may capture me for a minute however your blog is different. Bravo.
Наш официальный сайт уже доступен — https://bergkompressor.ru/
сервис знакомств для взрослых Отдых для взрослых в Мелитополе – это разнообразие возможностей от спокойного городского досуга до ярких ночных развлечений. Здесь каждый может найти занятие по душе, будь то посещение уютных кафе или захватывающие вечеринки.
придумать сочинение
Unquestionably believe that which you said. Your favorite reason seemed to be on the net the easiest thing to be aware of. I say to you, I certainly get annoyed while people consider worries that they plainly don’t know about. You managed to hit the nail on the head. Will probably be back to get more. Thanks
streamserve.click – Mobile version looks perfect; no glitches, fast scrolling, crisp text.
connectcraft.click – Color palette felt calming, nothing distracting, just focused, thoughtful design.
литий-ионные батареи для штабелеров Важно помнить, что правильная зарядка Li-ion аккумуляторов является залогом их долгой и бесперебойной работы. Использование несовместимого зарядного устройства может привести к повреждению аккумулятора и сокращению его срока службы.
netguide.click – Overall, professional vibe here; trustworthy, polished, and pleasantly minimal throughout.
onlineport.click – Loved the layout today; clean, simple, and genuinely user-friendly overall.
Nice Post. It’s really a very good article. I noticed all your important points. Thanks.
servespark.click – Navigation felt smooth, found everything quickly without any confusing steps.
онлайн Онлайн-досуг Мелитополь и городской сервис досуга предлагают разнообразные варианты времяпрепровождения, а актуальные анкеты Мелитополя помогут сделать правильный выбор. Ночная жизнь Мелитополя богата на события, и всегда можно найти что-то интересное.
QQ88 cung cấp nền tảng truy cập cá cược online hiệu quả, tối ưu tốc độ, minh bạch và mang lại sự thuận tiện trong từng lần đăng nhập.
литий ионные аккумуляторы для вилочных погрузчиков Выбор литиевых тяговых батарей постоянно расширяется.
I just added this to my favorites. I truly love reading your posts. Tyvm!
You have some helpful ideas! Maybe I should consider doing this by myself.
перевести статью для телеграм
сравнение гелиевых и литиевых железо фосфатный аккумуляторов Выбор тягового аккумулятора для складской техники – задача, требующая тщательного анализа, учитывая разнообразие доступных технологий: щелочные, свинцово-кислотные, гелевые и литий-ионные (Li-ion). Li-ion аккумуляторы становятся все более популярными благодаря их высокой энергоемкости, длительному сроку службы и быстрой зарядке. Они выигрывают у свинцово-кислотных и щелочных вариантов в плане эффективности и экологичности, хотя и требуют более сложной системы управления зарядом (BMS). При выборе аккумулятора для больших токов, например, для мощных погрузчиков, Li-ion аккумуляторы, особенно литий-железо-фосфатные (LiFePO4), демонстрируют превосходные характеристики. Они обеспечивают стабильное напряжение и минимальные потери энергии при высоких нагрузках, что критически важно для поддержания производительности техники. Замена тяговой кислотной батареи на литиевую требует учета нескольких факторов. Необходимо убедиться в совместимости напряжения и емкости новой батареи с электрооборудованием погрузчика. Также может потребоваться замена зарядного устройства, поскольку Li-ion аккумуляторы требуют специальных зарядных профилей. Важно учитывать габариты Li-ion аккумулятора и наличие BMS для обеспечения безопасной и эффективной эксплуатации. Растущий рынок Li-ion аккумуляторов для складской техники предлагает широкий выбор моделей, включая аккумуляторы большой емкости для интенсивной эксплуатации. Цены на тяговые Li-ion аккумуляторы варьируются в зависимости от емкости, напряжения и производителя.
https://vc.ru/smm-promotion
кредит по паспорту казахстан подбор и сравнение предложений по кредитам и займам в Казахстане. На сайте можно посмотреть условия, требования и примерный расчет платежа, затем перейти к оформлению заявки онлайн. Решение по заявке принимает выбранный кредитор.
https://www.google.io/url?q=https://astra-hotel.ch/articles/code_promo_45.html
https://www.google.dz/url?q=https://www.atrium-patrimoine.com/wp-content/artcls/?code-promo-1xbet_bonus-exclusif.html
https://www.google.bj/url?q=https://amt-games.com/news/1xbet_cameroon_register_bonus_code.html
webnexus.click – Pages loaded fast, images appeared sharp, and formatting stayed consistent.
sitesupport.click – Mobile version looks perfect; no glitches, fast scrolling, crisp text.
signalshift.click – Loved the layout today; clean, simple, and genuinely user-friendly overall.
webfixer.click – Color palette felt calming, nothing distracting, just focused, thoughtful design.
литиевые погрузчики Выбор литиевых тяговых батарей постоянно расширяется.
Le bonus d’inscription 1xBet peut atteindre 130 % du premier depot. En utilisant un code valide, vous etes toujours gagnant. En jouant activement, vous pouvez accumuler des points promo utilisables pour un pari gratuit ou augmenter votre capital. Pour plus de details sur le code promo 1xBet paris sportifs, consultez ce lien : https://prathamonline.com/js/pgs/?code_promo_175.html
https://opencollective.com/1xbet-free-spins-promo-code-india
https://www.google.com.sg/url?q=https://puntera.com/tools/pages/melbet_promo_codes.html
https://send.now/docgdfbrrqo6
https://www.google.sc/url?q=https://profootball.su/wp-content/pages/1xbet_promokod_besplatno___bonus_pri_registracii.html
La recompense de bienvenue 1xbet offre jusqu’a 100 €/$ a l’occasion du premier versement. Meme sans code, le bonus de 100 % est credite automatiquement. Pour obtenir plus de details sur le code promo 1xBet gratuit, vous pouvez consulter ce lien : https://eguidemagazine.com/wp-content/pages/code_promo_163.html
займы онлайн казахстан подбор и сравнение предложений по кредитам и займам в Казахстане. На сайте можно посмотреть условия, требования и примерный расчет платежа, затем перейти к оформлению заявки онлайн. Решение по заявке принимает выбранный кредитор.
https://vc.ru/smm-promotion
кислотные или литиевые аккумуляторы погрузчик Существуют различные типы Li-ion аккумуляторов для погрузчиков: с разной емкостью (Ah) и напряжением (В). При выборе необходимо учитывать требуемую мощность и время работы погрузчика. Например, для погрузчика Jungheinrich EFG 215 SP может подойти АКБ Li-ion Ensol 48V 360Ah, но необходимо проверить габариты (830х522х627 мм).
netmosaic.click – Found practical insights today; sharing this article with colleagues later.
侠之盗高清完整版结合大数据AI分析,海外华人可免费观看最新热播剧集。
литий ионный аккумулятор цена на погрузчик тойота Литиево-ионные батареи, также известные как литий-ионные АКБ и литиевые АКБ, обеспечивают стабильное и надежное питание, что критически важно для бесперебойной работы складской техники. Литиевые тяговые аккумуляторы и литиевые аккумуляторы тяговые разработаны специально для интенсивной эксплуатации, гарантируя максимальную производительность.
литий ионная батарея против гелевой Существуют различные типы Li-ion аккумуляторов для погрузчиков: с разной емкостью (Ah) и напряжением (В). При выборе необходимо учитывать требуемую мощность и время работы погрузчика. Например, для погрузчика Jungheinrich EFG 215 SP может подойти АКБ Li-ion Ensol 48V 360Ah, но необходимо проверить габариты (830х522х627 мм).
trafficdock.click – Overall, professional vibe here; trustworthy, polished, and pleasantly minimal throughout.
pixelroute.click – Bookmarked this immediately, planning to revisit for updates and inspiration.
rankpulse.click – Navigation felt smooth, found everything quickly without any confusing steps.
boostsignal.click – Navigation felt smooth, found everything quickly without any confusing steps.
Its wonderful as your other blog posts : D, regards for putting up.
QQ88 cung cấp hệ sinh thái giải trí trực tuyến toàn diện, tập trung vào tính tiện lợi, minh bạch và trải nghiệm người dùng lâu dài. Tên miền mới https://smartmind.in.net/
Great info! Keep post great articles.
https://t.me/s/russiA_caSiNo_1win
I had highly recommend this blog to my good friend, it’s so good
I found your blog through google and I must say, this is probably one of the best well prepared articles I have come across in a long time. I have bookmarked your site for more posts.
https://zai4atka.com/user/corrilxcof
https://fmcpe.com/user/tyrelajkjp
http://www.bakinsky-dvorik.ru/communication/forum/messages/forum4/message125890/79579-1xbet-south-korea-promo-code-2026_-1x200king-_-bonus-_130?result=new#message125890
https://archeter.co.uk/user/profile/358360
https://camp-fire.jp/profile/1xbetvip2026s
1xbet промокод на сегодня 2026. Чтобы удовлетворить бетторов, букмекеры постоянно добавляют новые функции и предложения. Одним из лидеров является 1хБет. Ввод промокода при регистрации позволяет получить увеличенную сумму бонуса. После создания аккаунта внеси первый депозит (до 32 500 рублей) — и получи вознаграждение. Абсолютно бесплатный promo code 1xbet free доступен всем новичкам, чтобы активировать дополнительные преимущества. Игнорировать поле «Введите промокод» — значит потерять выгоду. Оно присутствует при трёх из четырёх способов регистрации (по телефону).
1xBet промокод при регистрации Ввод промокода при регистрации на https://rosparfum.ru/wp-includes/wkl/1xbet_promokod_pri_registracii_bonus_5.html даёт бонус до 32 500 рублей, чтобы начать игру с полным бонусом.
свит бонанза 1000 казино в рублях
вопрос правоу
сократить курсовую быстро
https://www.achs.cl/plantillas/1b/desarrollo-de-un-modelo-de-prevenci%C3%B3n-de-riesgos-y-promoci%C3%B3n-de-recursos-laborales-relacionados-con-la-salud-ocupacional-de-los-trabajadores-de-centros-de-llamados-(call-centers)-en-chile
https://available.xooit.org.uk/t101-Code-Promo-Gratuit-1xBet-2026-VATOUTMAX-Bonus-Insc-130-EUR.htm#p518
https://blac.edu.pl/profile/1xbet-welcomes/
https://huayra.educar.gob.ar/ayuda/?qa=user/1xbet-promofree
https://FreeAd1.com/588/posts/1/1/1762727.html
создать письмо качественно
анализ gpt
Битгет реферальный код Реферальный код Bitget GPFZDXVL — скидка 20% на комиссии с первой сделки Зачем переплачивать бирже, если можно сразу торговать дешевле? Код вводится при регистрации и работает бессрочно. Бонус — до 6200 USDT за выполнение заданий. Забыли ввести? Bitget даёт 14 дней на добавление кода после создания аккаунта.
раздел совместно нажитого +имущества Семейный юрист – это дипломат и психолог в одном лице, умеющий находить общий язык с конфликтующими сторонами и предлагать компромиссные решения. Он помогает супругам пройти через болезненный процесс развода с наименьшими потерями, защищая интересы детей и сохраняя человеческое достоинство.
QQ88 được xây dựng như một cổng truy cập giải trí trực tuyến linh hoạt, phù hợp cho người dùng cần sự ổn định và dễ thao tác.
netamplify.click – Loved the layout today; clean, simple, and genuinely user-friendly overall.
Good site! I truly love how it is easy on my eyes it is. I am wondering how I might be notified when a new post has been made. I’ve subscribed to your RSS which may do the trick? Have a great day!
Gates of Olympus Super Scatter slot Gates of Olympus Super Scatter casino – найдите лучшее казино с высокими выплатами и щедрыми бонусами, чтобы увеличить свои шансы на выигрыш.
leadcircuit.click – Loved the layout today; clean, simple, and genuinely user-friendly overall.
viralshift.click – Color palette felt calming, nothing distracting, just focused, thoughtful design.
QQ88 là địa chỉ truy cập giải trí online đáng tin cậy, chú trọng trải nghiệm mượt mà, vận hành ổn định và giao diện thân thiện.
sitebloom.click – Content reads clearly, helpful examples made concepts easy to grasp.
арбитраж +споры Юрист – это архитектор правовой защиты, чья миссия заключается в создании надежного фундамента для безопасности и процветания своих клиентов. Обладая глубокими знаниями законодательства и многолетним опытом, он служит компасом в лабиринте юридических норм, помогая ориентироваться в сложных ситуациях и находить оптимальные решения.
Битгет реферальный код Реферальный код Bitget GPFZDXVL — скидка 20% на комиссии с первой сделки Зачем переплачивать бирже, если можно сразу торговать дешевле? Код вводится при регистрации и работает бессрочно. Бонус — до 6200 USDT за выполнение заданий. Забыли ввести? Bitget даёт 14 дней на добавление кода после создания аккаунта.
brandfunnel.click – Loved the layout today; clean, simple, and genuinely user-friendly overall.
Gates of Olympus Super Scatter слот Gates of Olympus Super Scatter слот играть – это просто и увлекательно. Интуитивно понятный интерфейс и захватывающий геймплей не дадут вам заскучать.
These are some of the most important issues we’ll face over the next few decades.
алименты Представительство в судах – это комплексная услуга, включающая в себя подготовку документов, участие в судебных заседаниях и представление ваших интересов перед судом. Юрист возьмет на себя все заботы, связанные с судебным процессом, чтобы вы могли сосредоточиться на других важных аспектах вашей жизни.
Промокод при регистрации в 1xbet сегодня. Этой акцией может воспользоваться каждый новый игрок при регистрации на сайте букмекера. Это ваше преимущество с начала. В форме регистрации есть необязательное поле для ввода кода. Как получить 1xBet промокод на фриспины на фрибет. В магазине xBonus можно обменять баллы на коды 1xbet kz: для ординаров, экспрессов или лотерей. Найти промокоды 1xbet можно на спортивных сайтах. Представители БК часто публикуют их к праздникам или турнирам. Все актуальные промокоды 2026 доступны в официальном разделе сайта и могут быть обменяны на бонусные баллы.
промо код на 1хбет Используйте актуальный промокод на http://setka34.ru/pages/articles/promokod_754.html и активируйте бонус 100% на депозит, чтобы начать ставки с преимуществом.
I like this weblog very much so much great info .
объединить кредиты в один подбор и сравнение предложений по кредитам и займам в Казахстане. На сайте можно посмотреть условия, требования и примерный расчет платежа, затем перейти к оформлению заявки онлайн. Решение по заявке принимает выбранный кредитор.
Реферальный код Bitget Реферальный код Bitget GPFZDXVL — скидка 20% на комиссии с первой сделки Зачем переплачивать бирже, если можно сразу торговать дешевле? Код вводится при регистрации и работает бессрочно. Бонус — до 6200 USDT за выполнение заданий. Забыли ввести? Bitget даёт 14 дней на добавление кода после создания аккаунта.
https://www.sutori.com/en/story/untitled–R5AMWftnwY8ub4ZEXsnVD2zU
https://latinverge.com/forums/topic/30652/1xbet-promo-code-azerbaijan-2026-1xmaxbono-bonus-130/view/post_id/216708
http://taniecirlandzki.phorum.pl/viewtopic.php?p=119751#119751
https://humanlove.stream/wiki/User:1xbetpromo2
https://t.me/companybitforge BitForge — создаём IT-продукты, которые работают Web • Software • AI • Automation
Gates of Olympus Super Scatter демо Gates of Olympus Super Scatter демо в рублях: Играйте бесплатно в демо-версию слота в рублях и оцените все его преимущества без риска для своего бюджета.
Have you always been concerned about these issues?
источник подбор и сравнение предложений по кредитам и займам в Казахстане. На сайте можно посмотреть условия, требования и примерный расчет платежа, затем перейти к оформлению заявки онлайн. Решение по заявке принимает выбранный кредитор.
I have been surfing online more than three hours today, yet I never found anything that grabbed my interest as much as this piece.
здесь подбор и сравнение предложений по кредитам и займам в Казахстане. На сайте можно посмотреть условия, требования и примерный расчет платежа, затем перейти к оформлению заявки онлайн. Решение по заявке принимает выбранный кредитор.
читать далее подбор и сравнение предложений по кредитам и займам в Казахстане. На сайте можно посмотреть условия, требования и примерный расчет платежа, затем перейти к оформлению заявки онлайн. Решение по заявке принимает выбранный кредитор.
L’offre 1xbet bonus de bienvenue 2026 permet de recevoir un bonus de 130 $ sur le compte de jeu des nouveaux utilisateurs. Pour obtenir le bonus, il faut effectuer un depot minimum et suivre la procedure correcte. Si le code est incorrect, le bonus ne sera pas credite. Pour plus de details sur le code promo 1xBet aujourd’hui, consultez ce lien : https://vedicologyindia.com/art/code_promo___bonus_jusqu____130.html
Le bonus de bienvenue 1xBet offre la possibilite de recevoir un bonus equivalent a 100 % avec une recompense maximale de 100 €/$. En l’absence d’un code specifique, un bonus standard sera applique le bonus de 100 %. Pour consulter des details supplementaires sur le code promo 1xBet sans depot, toutes les informations sont disponibles ici : https://steinberg-dialog.de/wp-content/pgs/le-code-promo-1xbet_bonus.html
Крипта в фиат за 3 шага! Просто и безопасно @BTCLN_CHANGE_bot
Хотите обменять BTC, ETH или USDT на рубли без головной боли? Наш Telegram-бот сделает это за вас за 3 простых шага! Выберите валюту (BTC Lightning, LTC, XMR, DASH тоже поддерживаются), укажите сумму и карту. Никакой AML/KYC, верификация не нужна. Автоматический обмен за 15-20 минут. P2P-формат гарантирует безопасность и работу со всеми банками РФ. Честные курсы, круглосуточная доступность. Проще некуда – попробуйте мгновенный обмен сегодня!
https://t.me/exchangetopbtc_bot
Nice Post. It’s really a very good article. I noticed all your important points. Thanks.
https://rpk24.ru
https://inovacoessolares.co.mz/how-to-use-promo-code-in-1xbet-thailand-allinmax-e130-bonus/
https://immigrationlawyerattorney.com/1xbet-free-spins-promo-code-uganda-allinmax-e130-bonus_1/
https://rpk24.ru/services/pakety/bumazhnyy-paket-brendirovannyy/
юрист в суд Юрист в суд – это стратег и тактик, превращающий правовые аргументы в мощное оружие. Тщательно анализируя материалы дела, он выстраивает линию защиты, способную убедить суд в правоте его клиента. Его речь – это искусство убеждения, способное изменить ход событий.
юрист Семейный юрист – это дипломат и психолог в одном лице, умеющий находить общий язык с конфликтующими сторонами и предлагать компромиссные решения. Он помогает супругам пройти через болезненный процесс развода с наименьшими потерями, защищая интересы детей и сохраняя человеческое достоинство.
QQ88 là nền tảng truy cập giải trí trực tuyến tối ưu, tập trung vào tốc độ, hiệu suất và trải nghiệm người dùng lâu dài.
представительство в судах Семейный юрист – это дипломат и психолог в одном лице, умеющий находить общий язык с конфликтующими сторонами и предлагать компромиссные решения. Он помогает супругам пройти через болезненный процесс развода с наименьшими потерями, защищая интересы детей и сохраняя человеческое достоинство.
searchrocket.click – Overall, professional vibe here; trustworthy, polished, and pleasantly minimal throughout.
adsforge.click – Pages loaded fast, images appeared sharp, and formatting stayed consistent.
seobeacon.click – Bookmarked this immediately, planning to revisit for updates and inspiration.
digitaltide.click – Color palette felt calming, nothing distracting, just focused, thoughtful design.
https://dhaanspharma.com/2026/01/22/best-promo-code-for-1xbet-singapore-allinmax-e130-bonus/
https://tmhanoi.com.vn/2026/01/22/how-to-get-1xbet-promo-code-nepal-allinmax-e130-bonus/
QQ88 là nền tảng truy cập giải trí trực tuyến linh hoạt, phù hợp cho người dùng ưu tiên hiệu quả và sự thuận tiện.
https://incarootstravel.com/?p=13454
https://blog.sunshinebilingual.com/promo-code-1xbet-canada-allinmax-e130-bonus/
campaigncraft.click – Navigation felt smooth, found everything quickly without any confusing steps.
reefer dispatch service
Your blog post was really enjoyable to read, and I appreciate the effort you put into creating such great content. Keep up the great work!
автобус билеты из бангкока на остров краби тайланд ко ланта
Wondering how to register betwinner or how to create betwinner account? You’ll find all details and screenshots on https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/.
Betwinner Kenya registration is quick and secure via https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ — suitable for both desktop and mobile users.
I’ve thought about posting something about this before. Good job! Can I use part of your post in my blog?
цена курса диспетчера грузоперевозок на русском языке
Промокод при регистрации 1xbet на 32 500 рублей. Этот код нужно ввести при регистрации в соответствующее поле. Промокод действует однократно, но им можно делиться с друзьями. Регистрация по номеру телефона — удобный способ создать аккаунт. После получения данных для входа остаётся лишь ввести логин и пароль. Используй актуальный Free 1xbet coupons и увеличь первый депозит до 32 500 рублей в букмекере 1хБет. На платформе действует бонусная программа, которая помогает игрокам получать до 130 % бонуса от первого депозита.
Промокод при регистрации в 1xbet сегодня. Этой акцией может воспользоваться каждый новый игрок при регистрации на сайте букмекера. Это отличный старт. В форме регистрации есть необязательное поле для ввода кода. Как получить бесплатный промокод 1xBet на бесплатную ставку. В магазине xBonus можно обменять баллы на коды 1xbet kz: для ординаров, экспрессов или лотерей. Найти промокоды 1xbet можно на спортивных сайтах. Представители БК часто публикуют их к праздникам или турнирам. Все актуальные промокоды 2026 доступны в официальном разделе сайта и могут быть обменяны на бонусные баллы.
ко ланте ко ланте
https://wakelet.com/@1xbetpromocode40696
https://medium.com/@cxg98124
http://nec.phorum.pl/viewtopic.php?p=728126
ко ланта ко ланта
ии для компаний
Go to the main company website > http://fact-planet.ru/pages/news/1xbet_promokod_besplatno__1.html
Наш сайт — только официальная информация : https://oazis-tour.com/pgs/1xbet_promokod_besplatno_2.html
Системы автоматической противопожарной защиты в Москве, Монтаж систем автоматической противопожарной защиты, Монтаж систем автоматической противопожарной защиты в Москве, Монтаж АППЗ, Монтаж АППЗ в Москве Системы автоматической противопожарной защиты (АППЗ) – это передовая технология, направленная на автоматическое тушение пожара. Монтаж систем автоматической противопожарной защиты, в том числе монтаж систем автоматической противопожарной защиты в Москве, требует глубоких знаний и опыта. Качественный монтаж АППЗ, а также монтаж АППЗ в Москве, значительно повышает уровень безопасности объекта.
ко ланта ко ланте
ко ланта ко ланта
ко ланте ко ланте
ко ланта ко ланта
ко ланте ко ланте
ко ланте ко ланте
ко ланте ко ланте
скачать тик ток мод 2026 Безопасность и Законность: Важные Предостережения Использование TikTok модов сопряжено с определенными рисками. Загрузка приложений из неофициальных источников может привести к установке вредоносного ПО. Кроме того, нарушение условий использования TikTok может повлечь за собой блокировку аккаунта. Поэтому, прежде чем “скачать TikTok мод на андроид бесплатно” или любую другую версию, важно взвесить все “за” и “против”.
Hey, I simply hopped over to your website by way of StumbleUpon. No longer one thing I’d normally learn, but I preferred your thoughts none the less. Thanks for making one thing worth reading.
Hi my family member! I want to say that this article is amazing, great written and include approximately all important infos. I’d like to see more posts like this .
This is really interesting, You’re a very skilled blogger. I have joined your feed and look forward to seeking more of your great post. Also, I’ve shared your web site in my social networks!
Монтаж (САД) в Москве Монтаж систем автоматики и диспетчеризации
Surprisingly good post. I really found your primary webpage and additionally wanted to suggest that have essentially enjoyed searching your website blog posts. Whatever the case I’ll always be subscribing to your entire supply and I hope you jot down ever again soon!
научные экспедиции Планирование Поездки: Учитываем Сезонность и Бюджет При планировании поездки важно учитывать сезонность. Летний отдых на Сахалине – это возможность насладиться морскими экскурсиями и путешествиями по живописным побережьям, а зимний Сахалин – это горнолыжный отдых и зимняя рыбалка. Стоимость туров варьируется в зависимости от продолжительности, программы и уровня комфорта. Горящие туры и специальные акции позволяют существенно сэкономить на путешествии.
https://kirriemuircameraobscura.com/component/k2/item/62-k2-sample-item-2/62-k2-sample-item-2?limitstart=0
https://www.tirarvistoamericano.com/forum-visto-americano/topico/code-promo-1xbet-casino-2026-jetonmax-bonus-exclusif-130-e/
https://greedplay.com/code-promo-1xbet-paris-2026-1xvatout-bonus-exclusif-130-e/
http://leydis16.phorum.pl/viewtopic.php?p=1038128#1038128
https://audiomack.com/1xbetpromocodefreespinsturkey
Монтаж систем автоматической противопожарной защиты Монтаж АППЗ в Москве с SMR-Proekt – это гарантия вашего спокойствия и уверенности в завтрашнем дне. Мы предлагаем современные и эффективные решения, обеспечивающие надежную защиту вашего имущества и персонала от пожаров. Обратитесь к нам, и мы поможем вам создать безопасную среду для вашего бизнеса.
Explore the latest here : http://www.medtronik.ru/
Visit now > http://www.medtronik.ru/
I’d like to be able to write like this, but taking the time and developing articles is hard…. Takes a lot of effort.
This is the perfect site for anybody who wishes to understand this topic. You know so much its almost tough to argue with you (not that I really would want to…HaHa). You definitely put a new spin on a topic that’s been discussed for ages. Excellent stuff, just great!
вход RioBet Casino
Промокод при регистрации в 1xbet сегодня. Этой акцией может воспользоваться каждый новый игрок при регистрации на сайте букмекера. Это ваше преимущество с начала. В форме регистрации есть необязательное поле для ввода кода. Как получить 1xbet pakistan promo code на дополнительный бонус. В магазине xBonus можно обменять баллы на коды 1xbet kz: для ординаров, экспрессов или лотерей. Найти промокоды 1xbet можно на спортивных сайтах. Представители БК часто публикуют их к праздникам или турнирам. Все актуальные промокоды 2026 доступны в официальном разделе сайта и могут быть обменяны на бонусные баллы.
Акционный код 1xBet при регистрации. Компания 1ИксБет заинтересована в поиске новых игроков, поэтому для новых пользователей действует акция в виде первого подарка, который равен сумме первого депозита, но не превышает двести двадцать пять тысяч рублей. Однако при использовании промокод 1xBet при регистрации букмекерская контора добавит процент к приветственного бонуса. Чтобы получить повышенную сумму на первый депозит, игроку нужно: зайти на сайт букмекера, выбрать создание аккаунта через почту, заполнить данные, ввести промокод и подтвердить согласие с правилами. Акционный код букмекера помогает получить ещё больше бонусов. Такой код представляет собой набор, которая позволяет активировать уникальный бонус от букмекера. С его помощью можно получить фрибет и другие подарки.
Looking to betwinner create account fast? Go to https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and complete the simple sign-up form in just a few clicks.
Explore the latest additions here — https://ivushka-mebel.ru/article/pages/?1xbet-promokod.html
To activate your betwinner sign up offer, just head over to https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and follow the guide. It’s an effortless way to start with extra funds.
https://forums.planetdestiny.com/threads/melbet-promo-code-2026-welcome-bonus-130.31506/
https://enkling.com/read-blog/96173
https://www.tumblr.com/david1502/806675029696888832/promo-code-for-1xbet-2026-1xmaxbono-bonus-130?source=share
https://talkmarkets.com/member/syed-mushahid098/blog/1xbet-casino-promo-code-canada-1x200rush–130-bonus?post=551650
Наш сайт — только официальная информация : https://www.pmk-grand.ru/media/pgs/?promokod_741.html
This is such an informative and well-written post! I learned a lot from reading it and will definitely be implementing some of these tips in my own life
From the bottom of my heart, thank you for being a source of positivity and light in this sometimes dark and overwhelming world
Your writing is so eloquent and engaging You have a gift for connecting with your readers and making us feel understood
Visit the company site : https://jerezlecam.com/
Your writing is so genuine and heartfelt It’s refreshing to read a blog that is not trying to sell something or promote an agenda
Your posts always speak to me on a personal level and I believe that is a testament to your authenticity and genuine nature
Go to our website : https://jerezlecam.com/
замена матрицы ноутбука в великом новгороде цена чистка динамика iphone
удаленная работа для мам в декрете как найти удаленную работу
digitaltide.click – Bookmarked this immediately, planning to revisit for updates and inspiration.
face id не работает iphone ремонт в великом новгороде срочно ремонт корпуса ноутбука в великом новгороде
Hello! I know this is kinda off topic however I’d figured I’d ask. Would you be interested in exchanging links or maybe guest authoring a blog post or vice-versa? My site addresses a lot of the same topics as yours and I believe we could greatly benefit from each other. If you happen to be interested feel free to send me an email. I look forward to hearing from you! Superb blog by the way!
http://escuelajulioverne.com/blog/gaceta-epo/2026/01/27/les-avancees-technologiques-diron-tv-pro-max/
https://dtf.ru/pro-smm
We’re developing a conference, and it looks like you would be a great speaker.
I enjoy your blog posts, saved to my bookmarks!
https://janjaonline.mn.co/posts/nouveau-code-promo-1xbet-casino-2026-hasard200-bonus-130-%E2%82%AC
https://forum.rarib.ru/viewtopic.php?t=132170
https://aiofunnel.online/top-progressive-jackpot-online-slots-to-try-today/
This is the wave – the big wave.
https://bitcoinidiotguide.com/exploring-themes-in-online-slots-from-ancient-egypt-to-space-adventures/
погода краби таиланд на месяц сколько от пхукета до краби
Simply wish to say the frankness in your article is surprising.
I have to disagree with most of the comments here, but maybe I’m just a contrarian.
I wish I could craft such articles as this. Thank you very much.
Great post. Just a heads up – I am running Ubuntu with the beta of Firefox and the navigation of your blog is kind of broken for me.
Excellent article!! I am an avid reader of your website:D keep on posting that good content. and I’ll be a regular visitor for a very long time!!
I like the helpful information you provide in your articles. I’ll bookmark your blog and check again here frequently. I am quite certain I’ll learn many new stuff right here! Best of luck for the next!
We are a group of volunteers and starting a new initiative in our community. Your blog provided us with valuable information to work on|.You have done a marvellous job!
You certainly deserve a round of applause for your post and more specifically, your blog in general. Very high quality material!
This is really interesting, You’re a very skilled blogger. I have joined your feed and look forward to seeking more of your fantastic post. Also, I have shared your website in my social networks!
https://kairos77.ru/
https://stroyhouse-rnd.ru
https://www.animaljobsdirect.com/employers/3991070-what-is-melbet-promo-code-2026-big777-explained
https://blaga.en.cx/Guestbook/Messages.aspx?page=1&fmode=gb&topic=385791&anchor#7982502
https://drevo12.ru
http://www.kxk.ru/prcio/view.php?t=2955101&part=17&neworrep=1&
починить iphone в великом новгороде замена дисплея на айфоне
of course like your web-site however you have to check the spelling on several of your posts. Many of them are rife with spelling problems and I find it very troublesome to tell the reality then again I will surely come back again.
Simply wish to say the frankness in your article is surprising.
Great resources and tips for families here.
Enjoyed reading through this, very good material. Thanks!
We’re developing some community services to respond to this, and your blog is helpful.
When we look at these issues, we know that they are the key ones for our time.
QQ88 là nhà cái uytin 2026 , mang đến casino, thể thao, bắn cá, nổ hũ,…. Tham gia nhận 88K trải nghiệm
Clutch performers, players who score in big moments documented
национальный парк кхао пханом бенча в краби туры на краби
When are you going to post again? You really entertain me!
BlackSprut marketplace сайт
bs2best at
замена задней камеры ремонт mасbооk
BlackSprut marketplace сайт
bs2best at
Copa del Rey livescore, Spanish cup competition with Real Madrid Barcelona action
BlackSprut marketplace сайт
bs2best at
прогнозы на хоккей Ставки баскетбол – это калейдоскоп бросков, данков и перехватов, игра высоких скоростей и филигранной техники. Это спорт для интеллектуалов, требующий понимания тактики и стратегии команд, умения оценивать форму игроков и предсказывать ход игры.
BlackSprut marketplace сайт
bs2best at
Le bonus de premier depot 1xBet permet aux nouveaux joueurs de recevoir 100 €/$ lors du depot initial. Si vous ne saisissez pas de code promo, le bonus standard reste valable. Vous pouvez en savoir plus sur le meilleur code promo 1xBet ici : https://sylvisa.nl/wp-content/pgs/code_promo_1xbet_bonus.html
L’offre promotionnelle 1xBet donne acces a un doublement du premier depot limitee a 100 €/$. Si aucun code n’est saisi, vous beneficierez toujours le bonus de 100 %. Pour plus d’informations sur le meilleur code promo 1xBet, toutes les informations sont disponibles ici : http://opernhausblog.de/wordpress/wp-content/pgs/code_promo_123.html
I’ve read several good stuff here. Definitely worth bookmarking for revisiting. I surprise how much effort you put to make such a magnificent informative site.
купить франшизу Купить франшизу для малого бизнеса – это особенно актуально для начинающих предпринимателей, ищущих надежный старт. Вы получаете не только бренд, но и обучение, консультации и маркетинговую поддержку, что значительно повышает шансы на успех в конкурентной среде.
Промокод при регистрации в 1xbet сегодня. Этой акцией может воспользоваться каждый новый игрок при регистрации на сайте букмекера. Это отличный старт. В форме регистрации есть необязательное поле для ввода кода. Как получить промокод на бонус 1хбет на дополнительный бонус. В магазине xBonus можно обменять баллы на коды 1xbet kz: для ординаров, экспрессов или лотерей. Найти промокоды 1xbet можно на спортивных сайтах. Представители БК часто публикуют их к праздникам или турнирам. Все актуальные промокоды 2026 доступны в официальном разделе сайта и могут быть обменяны на бонусные баллы.
Great post, keep up the good work, I hope you don’t mind but I’ve added on my blog roll.
промокоды 1xbet Активируйте промокод на https://www.myoktyab.ru/includes/pages/1xbet_promokod.html и получите бонус до 32 500 рублей при регистрации для комфортной игры.
https://make-games.ru/forum/30-5885-1
зеркало Париматч
зеркало Париматч
что посмотреть на ко ланте нанг бич краби
QQ88 là nhà cái cá cược trực tuyến uy tín casino top 1 Mộc bài, mang lại đến nhiều tựa game cá cược hấp dẫn như casino , bắn cá , lô đề…
Offside traps, high line defenses and their success rates
Hey there are using WordPress for your site platform? I’m new to the blog world but I’m trying to get started and set up my own. Do you require any coding expertise to make your own blog? Any help would be really appreciated!
banda казино
Penalty saves, goalkeepers who excel at stopping spot kicks
Ставки баскетбол Ставки на спорт – это мозаика, где каждый фрагмент – это отдельный вид спорта, команда, игрок, а коэффициенты – нити, связывающие эти элементы воедино. Это интеллектуальная битва, где знания и аналитика встречаются с интуицией и удачей. За каждым выигрышем стоит кропотливый труд, анализ статистики, понимание психологии игроков и умение читать игру.
QQ88 MEDIA là thương hiệu cá cược uy tín 2026 kho game đồ sộ thưởng hấp dẫn
超人和露易斯第四季高清完整官方版,海外华人可免费观看最新热播剧集。
https://upandgo.ru/oformlenie-vizy/
https://upandgo.ru/oformlenie-vizy/
https://webhitlist.com/forum/topics/the-fascinating-world-of-metal-detectors-how-they-work-and-why
https://kadrmaskreations.com/forum/topic/1xbet-casino-promo-code-hong-kong-1x200wave-e130-bonus/#postid-167260
Смазочные материалы для спецтехники и промышленного оборудования требуют особенно тщательного подхода, потому что простои экскаватора, погрузчика или производственной линии обходятся компании в разы дороже стоимости любой бочки масла, и здесь важны не только характеристики продукта, но и стабильность логистики, наличие резервных объёмов на складе и техническая поддержка при подборе решений под конкретные узлы и режимы работы.
каталог масел и технических жидкостей самара
Avia Masters de BGaming es un juego crash con RTP del 97% donde apuestas desde 0,10€ hasta 1.000€, controlas la velocidad de vuelo de un avion que recoge multiplicadores (hasta x250) mientras evita cohetes que reducen ganancias a la mitad, con el objetivo de aterrizar exitosamente en un portaaviones para cobrar el premio acumulado
https://share.google/i0IaEbBK6s0u7rCNM
Новости Мира В зоне СВО отмечается активизация беспилотной авиации. Военные эксперты анализируют тактику и эффективность использования дронов в современных боевых действиях. Ведутся разработки по защите от беспилотных летательных аппаратов.
Avia Masters de BGaming es un juego crash con RTP del 97% donde apuestas desde 0,10€ hasta 1.000€, controlas la velocidad de vuelo de un avion que recoge multiplicadores (hasta x250) mientras evita cohetes que reducen ganancias a la mitad, con el objetivo de aterrizar exitosamente en un portaaviones para cobrar el premio acumulado
https://share.google/Vrcznzj8BH0pNva9T
捕风追影下载官方下载,海外华人专用,支持高速下载和离线观看。
it is a really nice point of view. I usually meet people who rather say what they suppose others want to hear. Good and well written! I will come back to your site for sure!
WoW decent article. Can I hire you to guest write for my blog? If so send me an email!
海外华人必备的ifun官方认证平台,24小时不间断提供最新高清电影、电视剧,无广告观看体验。
I thought it was going to be some boring old post, but I’m glad I visited. I will post a link to this site on my blog. I am sure my visitors will find that very useful.
Im impressed. I dont think Ive met anyone who knows as much about this subject as you do. Youre truly well informed and very intelligent. You wrote something that people could understand and made the subject intriguing for everyone. Really, great blog youve got here.
There are some serious financial ramifications here.
Abnormal this put up is totaly unrelated to what I was searching google for, but it surely used to be listed at the first page. I suppose your doing one thing proper if Google likes you adequate to place you at the first page of a non similar search.
I don’t know if it’s just me or if everybody else experiencing issues with your site. It appears as though some of the written text on your content are running off the screen. Can someone else please provide feedback and let me know if this is happening to them as well? This could be a problem with my web browser because I’ve had this happen before. Appreciate it
Great blog here! Also your site loads up very fast! What web host are you using? Can I get your affiliate link to your host? I wish my website loaded up as fast as yours lol
Перевозка мотоцикла
https://beteiligung.hafencity.com/profile/codevip1xbet1/
https://pad.public.cat/s/DzywpfN8W
http://www.peugeot-4008.ru/forum/viewtopic.php?p=24198#24198
Hello, all is going fine here and ofcourse every one is sharing information, that’s really excellent, keep up writing.
zumospin bonus
бездепозитные фрибеты казахстан
Купить Купить
бездепозитные фрибеты казахстан
корги Корги – это маленькое солнышко на четырех лапах, символ радости и беззаботности. Их забавные мордочки, неуклюжие лапки и бесконечная преданность вдохновляют меня каждый день. Их присутствие в моей жизни наполняет её теплом и светом.
эвакуатор Воноваха Эвакуатор Розовка: помощь приходит и в отдаленные районы.
Solo goals, individual brilliance and mazy runs tracked
Australian Open live scores, first Grand Slam of the year covered comprehensively
QQ88 LÀ NHÀ CÁI CƯỢC UY TÍN SỐ 1 VN
European football matches today, live scores from England, Spain, Italy, Germany and France
Hi there i am kavin, its my first time to commenting anyplace, when i read this piece of writing i thought i could also make comment due to this good paragraph.
byueuropaviagraonline
Basketball livescore for NBA and international leagues, every basket tracked live
奇思妙探第二季高清完整版,海外华人可免费观看最新热播剧集。
онлайн ставки с моментальным выводом
Goalkeeper saves, shot stopping statistics and clean sheet records
https://salon-marocain-decoration.com/1xbet-casino-promo-code-india-1xbono200-e130-bonus/
https://esladviser.com/code-promo-1xbet-valide-2026-jetonmax-bonus-130e/
http://young-rich-niggaz.clanweb.eu/profile.php?lookup=5090
http://engineercatalogues.ru/index.php?title=Pari%20%D0%9F%D1%80%D0%BE%D0%BC%D0%BE%D0%BA%D0%BE%D0%B4%20%D0%BF%D1%80%D0%B8%20%D0%A0%D0%B5%D0%B3%D0%B8%D1%81%D1%82%D1%80%D0%B0%D1%86%D0%B8%D0%B8%20%D0%BD%D0%B0%20%D0%A1%D0%B5%D0%B3%D0%BE%D0%B4%D0%BD%D1%8F%20-%20%D0%91%D0%BE%D0%BD%D1%83%D1%81
http://masakr-parba.4fan.cz/profile.php?lookup=361
Penalty goals, spot kick conversions and their success rates
доставка цветов москва недорого курьером на дом оплата картой Свежие цветы быстрая служба
愛壹帆海外版,專為華人打造的高清視頻平台AI深度學習內容匹配,支持全球加速觀看。
https://auto.qa/showrooms/
сколько стоит букет цветов в москве Цветы курьер сюрприз Москва
вскрытие сейфов Вскрытие замков – быстрое и аккуратное решение проблем с заклинившими или потерянными ключами. Работаем с замками любой сложности, обеспечивая сохранность вашего имущества.
бездепозитные бонусы за регистрацию в казино
QQ88 là nền tảng giải trí trực tuyến được tối ưu toàn diện, hỗ trợ người dùng truy cập nhanh, hạn chế gián đoạn và tận hưởng dịch vụ ổn định với trải nghiệm mượt mà.
корги Корги – это маленькое солнышко на четырех лапах, символ радости и беззаботности. Их забавные мордочки, неуклюжие лапки и бесконечная преданность вдохновляют меня каждый день. Их присутствие в моей жизни наполняет её теплом и светом.
рейтинг с лучшей отдачей игровых автоматов онлайн
топ казино на деньги
https://www.checkli.com/codegratuitxof565
https://www.colehardware.com/
https://fairygodboss.com/users/profile/Lt4tFt6xrW/code-promo-1xbet
https://chhapai.com/
You can unlock the betwinner sign up bonus instantly after completing the quick registration process described at https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/. Follow the steps and start betting right away.
To activate your betwinner sign up offer, just head over to https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and follow the guide. It’s an effortless way to start with extra funds.
I am glad to talk with you and you give me great help
рунетки чат рунетки онлайн
https://writefreely.ethibox.fr/larrybrown190/why-gas-fireplaces-are-a-smart-choice-for-every-home I went through a fairly long process selecting a gas fireplace for our living room renovation, and what surprised me most was how manufacturers differ in heat output and installation details. Certain models focus primarily on visual appeal, while others prioritize consistent heat delivery. I found it useful to compare installation types, control systems, and upkeep needs before choosing a final model. If someone is considering a similar project, it’s worth taking the time to understand how gas fireplaces actually perform during regular use, not just how they appear in marketing images.
QQ88 là nền tảng giải trí online hiện đại, chú trọng tốc độ tải, giao diện thân thiện và trải nghiệm mượt mà trong từng lần đăng nhập.
top casino
легкая работа в корее хостес в караоке
https://g-r-s.fr/
скачать бесплатно версию тикток мод скачать тик ток мод скачать бесплатно 2026
Team goals, beautiful passing moves and their outcomes
http://amberpw.rx22.ru/viewtopic.php?f=23&t=8152
https://shop.mireks.ru/forum/user/11125/
https://guiltyworld.getbb.ru/viewtopic.php?f=3&t=7196
Solo goals, individual brilliance and mazy runs tracked
1xBet промокод Активируйте на http://www.lipetskregionsport.ru/news/pages/1xbet_promokod.html и заберите 100% к первому депозиту до 32 500?, чтобы начать игру с преимуществом.
Бонус-код 1xBet при регистрации. Компания 1XBET заинтересована в поиске новых игроков, поэтому для новых пользователей действует акция в виде приветственного бонуса, который равен сумме первого депозита, но не превышает двести двадцать пять тысяч рублей. Однако при использовании промокод 1xBet букмекерская контора добавит процент к приветственного бонуса. Чтобы получить дополнительное вознаграждение на первый депозит, игроку нужно: зайти на сайт букмекера, выбрать создание аккаунта через почту, заполнить данные, ввести промокод и подтвердить согласие с правилами. Промокод 1xBet помогает получить ещё больше бонусов. Такой код представляет собой набор, которая позволяет активировать персональную акцию от букмекера. С его помощью можно получить промо-баллы и другие подарки.
бездепозитные бонусы казахстан за регистрацию в казино с выводом
дубай краби краби природа
https://writeablog.net/larrybrown190/gas-fireplaces-a-smart-choice-for-warm-and-stylish-homes We spent time on a long process researching a gas fireplace for our living room renovation, and what stood out the most was how various brands handle heat output and installation details. Some models are clearly designed for aesthetics first, while others are built around heating performance. I personally found it useful to compare venting options, control systems, and long-term maintenance requirements before choosing a final model. For anyone planning a similar upgrade, it’s worth taking the time to understand how gas fireplaces actually perform in everyday use, not just how they look in photos.
To register betwinner successfully, open https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ and follow the instructions provided on the official review page.
Go to the main company website — https://auto-tim.ru/js/pgs/1xbet-promokod.html
Betwinner Kenya registration is quick and secure via https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ — suitable for both desktop and mobile users.
Go to the verified website > http://www.selenacompany.ru/pgs/vyravnivayuschaya_osnova_pod_makiyagh.html
La ronda de apuestas te permite definir tu monto a arriesgar, y tan pronto en que clickeas en “Iniciar”, el aviГіn inicia su viaje con una trayectoria al azar completamente diferente.
aviamasters.nom.es
Le bonus du code promo 1xBet actuel peut atteindre 1 750 $ et inclut 150 tours gratuits pour la categorie casino, credites directement sur le compte de jeu. Vous pouvez utiliser le bonus immediatement apres le depot, notamment sur les machines a sous specifiees par le bookmaker. Un remboursement partiel de 30 % sur les pertes peut etre attribue apres la periode de bienvenue. Toutes les informations sur le 1xbet dernier code promo sont disponibles ici : http://opernhausblog.de/wordpress/wp-content/pgs/code_promo_123.html
Visit the fresh platform > https://jerezlecam.com/
https://www.google.al/url?q=https://hyundaimobil.co.id/assets/articles/1xbet_kode_promo_indonesia___bonus_selamat_datang.html
https://vhearts.net/forums/thread/20704/
https://md.opensourceecology.de/s/ay7EwaVBz
https://ourfathersfamily.com/blogs/58584/Melbet-Registration-Promo-Code-MEL200VIP
https://www.google.co.zw/url?q=https://actual-cosmetology.ru/pgs/1xbet_promokod_pri_registracii_na_segodnya_besplatno.html
https://doc.adminforge.de/s/vaGOvd1Ald
Code Promo 1xbet Sans Depot offre un bonus inscription 1xBet de 100% jusqu’a €130 sur les paris sportifs, ainsi qu’un bonus de casino de €1950 avec 150 tours gratuits. En saisissant le code promo 1xBet vous augmenterez vos chances de gains. Entrez le code promo 1xBet lors de votre inscription pour debloquer votre bonus de bienvenue 1xbet. Disponible uniquement pour les nouveaux joueurs, et permet de booster votre premier depot.
Check our site for updates > http://hammill.ru/
qq88 là nhà cái uy tín số 1 vn mang đến kho game ấn tượng cùng hàn ngàn ưu đãi hấp dẫn
https://paper.wf/larrybrown190/designing-a-home-that-feels-warm-and-inviting I was researching different supplemental heating options, and this brand came up a few times while reviewing different heaters. What caught my attention is how these heaters are designed for everyday home use rather than heavy-duty industrial settings.
Factors such as heat consistency, built-in safety shutoff features, and quiet operation really matter when a heater is used daily. It’s interesting to see how some brands focus on simple, practical designs that fit well into typical home environments instead of adding unnecessary complexity.
игровые автоматы с бонусом за регистрацию без депозита
игровые автоматы фриспины за регистрацию без депозита
Captain performances, armband wearers and leadership statistics
Зеркало трюмо настенное купить Зеркало на штанге поворотное: функциональное зеркало поворотное на штанге для удобного использования в ванной.
Is it okay to put a portion of this on my weblog if perhaps I post a reference point to this web page?
我們的玩運彩官方授權專家團隊第一時間更新官方各大聯盟的比賽分析,包括NBA、MLB、中華職棒等。
Новости Стим Ключ тг: Получите эксклюзивный доступ к контенту и розыгрышам через наш Telegram-канал!
Сдвижное зеркало в ванную Настольное трюмо: удобное зеркало для макияжа и ухода за собой.
QQ88 là cổng truy cập giải trí trực tuyến uy tín, tối ưu tốc độ, giao diện mượt và mang đến trải nghiệm ổn định cho người dùng.
спины за регистрацию без депозита с выводом
бездепозитные бонусы без отыгрыша
получить фриспины бесплатно
QQ88 mang đến nền tảng giải trí trực tuyến được tối ưu hiệu suất, giúp người dùng truy cập nhanh, thao tác mượt và trải nghiệm ổn định.
шторы блэкаут на заказ Пошив римских штор требует высокой точности и мастерства, так как каждая деталь имеет значение. Правильно подобранная ткань и фурнитура, а также качественный пошив гарантируют долговечность и эстетичный внешний вид.
бездепозитные фриспины за регистрацию
I don’t normally comment on blogs.. But nice post! I just bookmarked your site
QQ88 là cổng kết nối giải trí online tập trung vào sự ổn định, giao diện thân thiện và trải nghiệm liền mạch.
You are good writer. Thank you.
Промокод при регистрации 1xbet на 32500 рублей. Этот код нужно ввести при регистрации в соответствующее поле. Промокод действует однократно, но им можно делиться с друзьями. Регистрация по номеру телефона — простой способ создать аккаунт. После получения данных для входа остаётся лишь ввести логин и пароль. Используй актуальный promo codes for 1xbet и увеличь первый депозит до 32 500 рублей в букмекере 1хБет. На платформе действует программа лояльности, которая помогает игрокам получать до 130 % бонуса от первого депозита.
Промокод при регистрации 1xbet на 32 500 рублей. Этот код нужно ввести при регистрации в соответствующее поле. Промокод действует однократно, но им можно делиться с друзьями. Регистрация по номеру телефона — удобный способ создать аккаунт. После получения данных для входа остаётся лишь ввести логин и пароль. Используй актуальный 1xbet sign up bonus и увеличь первый депозит до 32 500 рублей в букмекере 1хБет. На платформе действует система вознаграждений, которая помогает игрокам получать до повышенного кэшбэка от первого депозита.
Weak foot goals, players scoring with non-dominant foot
Howdy, a helpful article for sure. Thank you.
How do I subscribe to your blog? Thanks for your help.
http://znayu.fun/index.php?subaction=userinfo&user=abjectadult0
Your idea is outstanding; the issue is something that not enough persons are speaking intelligently about. I’m very happy that I stumbled throughout this in my seek for one thing regarding this.
https://bwin-com.net/ bwin.com
If wings are your thing, Tinker Bell’s sexy Halloween costume design is all grown up.
Зайди на официальный сайт компании
Here’s what’s new
QQ88 mang đến cổng truy cập giải trí online hiện đại, chú trọng tốc độ tải, sự thuận tiện và khả năng vận hành liền mạch.
Midweek football livescore, Tuesday Wednesday Champions League Europa action
https://snippet.host/wxdwsa
https://confindustriatoscanacentroecosta.it/wp-content/pgs/?exclusive-bonus-for-aviator-game-at-1xbet.html
https://pad.snopyta.org/s/8hReZnTLy
https://www.porada.sk/downloads/inc/how-to-deposit-money-to-winpesa-via-m-pesa.html
https://bhd.org.tr/article/1xbet_promosyon_kodu_bahis.html
It’s continually awesome when you can not only be informed, but also entertained! I’m sure you had fun writing this article. Regards, Clotilde.
Substitution tracker, player changes and tactical switches noted live
I am lucky that I discovered this website , precisely the right info that I was searching for! .
Last minute goals, injury time drama and their significance
Community Shield livescore, season opener between league and cup champions
https://koz-salon.ru/wp-content/pgs/promokod_melbet_kazino.html
https://bbs.yp001.net/home.php?mod=space&uid=409010
https://petcleanshop.com/code-promo-1xbet-live-paris-2026-1xtapis-bonus-130e/
https://md.swk-web.com/s/zjDd0lF73
https://pad.geolab.space/s/hOaW-3Nku
https://zuobiqi.org/code-promo-bonus-1xbet-2026-1xtapis-bonus-130-e/
Aw, this was a very nice post. In idea I wish to put in writing like this moreover taking time and precise effort to make an excellent article! I procrastinate alot and by no means seem to get something done.
https://forellenteich.net/news/otlichnye_shorty.html
https://vrn.best-city.ru/forum/thread540133780/#reply540148047
https://www.aasa.org/advocacy/key-issues/archived-key-issues/title-ix-regulations/2024/05/31/new-resource-the-superintendent's-guide-to-the-2024-title-ix-rules
https://www.inc91.com/profile/codeafrique1xbet
https://runetki.org
https://howei.com/forum/discussion/event-discussion/27785149508-best-online-lost-love-spells-caster-simple-love-spells-that-work-overnight-call
Community Shield livescore, season opener between league and cup champions
https://www.pondexperts.ca/wp-content/pages/code_promo-1win-bonus_de_500.html
Зеркало интерьерные Зеркала лофт – добавьте индустриальный шик в свой интерьер с нашими зеркалами в стиле лофт. Прочность и стиль в каждой детали.
Fabulous, what a webpage it is! This website provides helpful information to us, keep it up.
https://share.google/elr7RL3yDYUyM1S8F
Thank you for the auspicious writeup.
зип лок пакеты купить в Мокве Зип лок пакеты купить в Мокве – это шаг к созданию герметичной защиты от влаги, пыли и запахов. Уникальная застежка обеспечивает надежное закрытие, предотвращая порчу продуктов и сохраняя свежесть. Идеально подходит для путешествий, пикников и хранения деликатных вещей.
https://asklong.ru
I am glad to talk with you and you give me great help
Serie A live scores, Italian football from Inter Milan Juventus and AC Milan
картонные упаковки Упаковка из картона – это экологически ответственный выбор, сочетающий в себе прочность, легкость и возможность вторичной переработки. Картонные коробки обеспечивают надежную защиту от механических повреждений, температурных колебаний и влаги, делая их идеальным решением для широкого спектра товаров.
https://www.pathumratjotun.com/forum/topic/133562/free-bet-with-no-deposit:-top-sportsbook-options
https://exam.western.ac.th/WTU_CI/index.php/webboard/view/form/2646
I just added your web site to my blogroll, I hope you would look at doing the same.
https://www.ptwmonksupply.com/forum/topic/36922/esports-betting-bonuses:-best-deals-for-gamers
https://falconblades.com/blog/vacation-time
Go to our fresh website
Go to the verified website
These stories are so important.
Thanks pertaining to discussing the following superb written content on your site. I ran into it on the search engines. I will check back again if you publish extra aricles.
I’m partial to blogs and i actually respect your content. The article has actually peaks my interest. I am going to bookmark your site and preserve checking for new information.
Le bonus d’inscription 1xBet actuel peut atteindre 1 750 $ et inclut 150 tours gratuits pour la categorie casino, credites directement sur le compte de jeu. Ces fonds peuvent etre utilises pour les mises des le depot initial, en suivant les conditions de mise sur les slots indiques. Une fois la periode de bienvenue terminee, vous pouvez egalement recevoir jusqu’a 30 % de cashback sur les pertes. Pour en savoir plus sur le code promo 1xBet casino en ligne, consultez ce lien : https://www.analyzemn.com/wp-content/pgs/code-promo-1xbet-bonus.html
This has to be one of my favorite posts! And on top of thats its also very helpful topic for newbies. thank a lot for the information!
L’offre de code promo 1xBet bonus de bienvenue donne droit jusqu’a 1 750 € accompagne de 150 tours gratuits. Cette promotion est tres pratique pour les nouveaux joueurs, cela permet de jouer sans risquer son propre capital. L’offre est disponible uniquement pour les personnes majeures. Pour plus de details sur le 1xbet code promo casino, vous pouvez consulter ce lien : https://www.gilmaire-etienne.com/wp-content/pages/code-promo-1xbet-bonus.html
FIFA World Cup live score updates, every match every goal tracked in real time here
A friend of mine advised me to review this site. And yes. it has some useful pieces of info and I enjoyed reading it.
срочное изготовление гофротары Упаковка на заказ – это проявление индивидуальности и возможность выделиться на фоне конкурентов. Разработка дизайна, выбор материалов и контроль качества позволяют создать упаковку, которая будет соответствовать самым высоким требованиям и подчеркивать уникальность бренда.
Hello there! I really enjoy reading your blog! If you keep making amazing posts like this I will come back every day to keep reading.
Most often since i look for a blog Document realize that the vast majority of blog pages happen to be amateurish. Not so,We can honestly claim for which you writen is definitely great and then your webpage rock solid.
Use the betwinner promo kodas 2025 during sign-up at https://bet-promo-codes.com/sportsbook-reviews/betwinner-registration/ to activate your welcome bonus instantly.
http://vikinar.com/index.php?title=%D0%9C%D0%B5%D0%BB%D0%B1%D0%B5%D1%82%20%D0%91%D0%BE%D0%BD%D1%83%D1%81%20%D0%94%D0%B5%D0%BF%D0%BE%D0%B7%D0%B8%D1%82%202026:%20MAX888%20-%2015%D0%BA
I have to disagree with most of the comments here, but maybe I’m just a contrarian.
Best Real Money Pokies Australia Your Big Moment Is Here
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu tốc độ truy cập, giao diện mượt và trải nghiệm ổn định cho người dùng.
моней икс официальный сайт
https://puntera.com/
https://llibertat.cat/
моних
https://lacite.com.uy/
https://vertify.com/
My brother suggested I might like this websiteHe was once totally rightThis post truly made my dayYou can not imagine simply how a lot time I had spent for this information! Thanks!
Unquestionably believe that which you said. Your favorite reason seemed to be on the net the easiest thing to be aware of. I say to you, I certainly get annoyed while people consider worries that they plainly don’t know about. You managed to hit the nail on the head. Will probably be back to get more. Thanks
I think that may be an interesting element, it made me assume a bit. Thanks for sparking my considering cap. On occasion I get so much in a rut that I simply really feel like a record.
Im impressed. I dont think Ive met anyone who knows as much about this subject as you do. Youre truly well informed and very intelligent. You wrote something that people could understand and made the subject intriguing for everyone. Really, great blog youve got here.
секс чат рулетка
You appear to know so much about this, and I see you’re a published author. Thanks
QQ88 là cổng truy cập giải trí online được tối ưu hiệu suất, giúp người dùng thao tác nhanh và sử dụng dịch vụ thuận tiện.
азино777
казино pin up online
казино пин-ап официальный сайт
New version available here : https://glavgeocom.ru/html/pgs/index.php?promokod_755.html
Go directly to our website > https://ar29.ru/pars/doms/1xbet-promokod-pri-registracii-besplatno.html
Thank you for the auspicious writeup.
Hello this is a wonderful write-up. I’m going to e mail this to my friends. I came on this while searching on yahoo I’ll be sure to come back. thanks for sharing.
This blog post is excellent, probably because of how well the subject was developed. I like some of the comments too though I could prefer we all stay on the subject in order add value to the subject!
Great blog here! Additionally your website rather a lot up very fast! What host are you the usage of? Can I get your associate link for your host? I desire my website loaded up as fast as yours lol
Its like you read my mind! You seem to know a lot about this, like you wrote the book in it or something. I think that you can do with some pics to drive the message home a bit, but other than that, this is wonderful blog. A great read. I’ll certainly be back.
riobet online
Hello there! I really enjoy reading your blog! If you keep making amazing posts like this I will come back every day to keep reading.
hey thanks for the info. appreciate the good work
riobet онлайн
играть на деньги riobet
This is really interesting, You’re a very skilled blogger. I have joined your feed and look forward to seeking more of your great post. Also, I’ve shared your web site in my social networks!
I simply could not leave your site before suggesting that I actually enjoyed the usual info a person supply in your visitors? Is going to be back often to inspect new posts
I think I will become a great follower.Just want to say your post is striking. The clarity in your post is simply striking and i can take for granted you are an expert on this subject.
Woh I enjoy your content , saved to bookmarks!
Howdy! I simply wish to give a huge thumbs up for the great information you have here on this post. I will be coming again to your weblog for extra soon.
Saw your material, and hope you publish more soon.
The newest is here — http://www.medtronik.ru/
https://war-casino.net/game/
http://www.vnii-certification.ru/
http://www.certif-test.ru/
The new platform is here
Australian online casinos real money – top rated and player approved
Well done! Keep up this quality!
Наш официальный сайт уже доступен
Good job for bringing something important to the internet!
Like the way you’ve outlined things. Easy to follow. Not cluttered.
Посмотри официальный ресурс компании
Visit our official page
https://www.google.com.fj/url?q=https://coiler.com.tw/dist/pgs/code_bonus_d_argent_gratuit_1xbet.html
https://www.google.com.do/url?q=https://www.lagodigarda.com/booking/pages/code_promo_du_bookmaker_1xbet.html
https://www.google.tk/url?q=https://coiler.com.tw/dist/pgs/code_bonus_d_argent_gratuit_1xbet.html
http://eroshenkov.ru/forum/view_profile.php?uid=198959
QQ88 LAF NHAF QQ88 là nền tảng giải trí trực tuyến tối ưu tốc độ, giao diện mượt và mang lại trải nghiệm ổn định cho người dùng.
code promo 1xbet senegal
You are my inhalation , I possess few web logs and very sporadically run out from to brand 🙁
What a great article.. i subscribed btw!
https://ensp.edu.mx/members/freespin26/
https://buyandsellhair.com/author/freepins26/
https://www.notebook.ai/@bettingbonus1#tab-about-me
фриспины без депозита Фриспины без депозита – это один из самых популярных видов бездепозитных бонусов. Они представляют собой определенное количество бесплатных вращений, которые можно использовать на конкретных игровых автоматах. Это отличный способ начать играть без риска.
I like to spend my free time by scaning various internet recourses. Today I came across your site and I found it is as one of the best free resources available! Well done! Keep on this quality!
I am glad to be a visitor of this thoroughgoing web blog ! , regards for this rare information! .
бездепозитные фриспины Мы понимаем, насколько привлекательна идея бесплатных вращений, поэтому предлагаем вам бездепозитные фриспины. Это прямой путь к захватывающим раундам в лучших слот-играх, где каждая линия выплат может стать вашим билетом к крупному выигрышу. Начните играть прямо сейчас и ощутите всю мощь удачи!
QQ88 là cổng truy cập giải trí online được xây dựng tập trung vào hiệu quả vận hành, sự tiện lợi và trải nghiệm liền mạch cho người dùng.
https://askoff.ru
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu tốc độ truy cập, giao diện thân thiện và mang đến trải nghiệm ổn định cho người dùng.
http://listbb.listbb.ru/viewtopic.php?f=3&t=254
http://ost-clan.g6.cz/profile.php?lookup=1053
http://www.polskiefajerwerki.net/users/view/20088
https://app.readthedocs.org/profiles/CodeValide1xbet1/
Go to our brand page
скидки в Стиме Новости Стим
Посетите сайт компании прямо сейчас
Проверь официальный сайт компании
Go to the main company website
Hi there, You’ve done an incredible job. I’ll definitely digg it and personally recommend to my friends. I am sure they will be benefited from this website.
зеркало Banda Casino
https://PostEzAd.com/588/posts/1/1/1844983.html
https://classdirectory.org/gosearch.php?q=https%3A%2F%2Fjonathanlittlepoker.com%2Fpages%2F1xbet_promo_code-sign_up_bonus.html&image.x=27&image.y=14
https://sportsbetnow.co.uk/codigo-promocional-1xbet-mexico-2026-1xbro200/
https://kwave.koreaportal.com/board/bbs/board.php?bo_table=video&wr_id=33177&page=8&sca=&sfl=&stx=&spt=0&page=8&btype=tile&cwin=#c_42700
Thanks for posting this. Looking for these resources 😀
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu tốc độ truy cập, giao diện mượt và trải nghiệm ổn định cho người dùng.
Najlepszy kod promocyjny Mostbet pozwala rozpoczac gre z dodatkowym budzetem. Rejestrujac konto z QWERTY555, gracze otrzymuja bonus powitalny i darmowy zaklad. Kod promocyjny bonusu powitalnego Mostbet obowiazuje dla nowych kont. Oferta dostepna jest zarowno na desktopie, jak i w aplikacji mobilnej. Mostbet zapewnia szybkie transakcje i wsparcie 24/7.
Oficjalna strona Mostbet https://mitsubishi-climate.ru/images/pgs/promokod_mostbet_2.html
Kod promocyjny Mostbet dzisiaj pozwala skorzystac z najnowszych promocji. Rejestracja z QWERTY555 aktywuje bonus powitalny i darmowy zaklad. Kod bonusowy Mostbet dziala natychmiast po wplacie. Gracze moga obstawiac wydarzenia sportowe na zywo. Platforma oferuje atrakcyjne kursy.
Najnowsza wersja Mostbet tutaj http://collect-computer.ru/uploads/pages/promokod_mostbet__besplatno.html
QQ88 cung cấp cổng truy cập giải trí online hiện đại, vận hành liền mạch, hỗ trợ đa thiết bị và dễ sử dụng.
I think that may be an interesting element, it made me assume a bit. Thanks for sparking my considering cap. On occasion I get so much in a rut that I simply really feel like a record.
https://bonograti.livejournal.com/profile/
http://rcdriftwiki.ru/index.php?title=1%D1%85%D0%91%D0%B5%D1%82%20%D0%9F%D1%80%D0%BE%D0%BC%D0%BE%D0%BA%D0%BE%D0%B4%20%D0%BD%D0%B0%20%D0%A1%D0%B5%D0%B3%D0%BE%D0%B4%D0%BD%D1%8F%202026:%201XBRO200
http://abroad.ekafe.ru/viewtopic.php?f=5&t=7521
http://wiki.market-master.ru/index.php?title=%D0%9F%D1%80%D0%BE%D0%BC%D0%BE%D0%BA%D0%BE%D0%B4%20%D0%B2%201%D1%85%D0%91%D0%B5%D1%82%202026:%201XBRO200%20-%20%D0%91%D0%BE%D0%BD%D1%83%D1%81%2032,500
Australian Online Casino Crypto Bitcoin Pokies
Hello there! I really enjoy reading your blog! If you keep making amazing posts like this I will come back every day to keep reading.
This information is critically needed, thanks.
Nice Post. It’s really a very good article. I noticed all your important points. Thanks.
казино с быстрыми выплатами топовые онлайн Погрузимся в панораму топовых онлайн-казино, где быстрые выплаты – визитная карточка. Начнем с “Paysafecard Palace” – платформы, чье имя само по себе обещает оперативность. Здесь выплаты через предоплаченные карты или e-wallets происходят за минуты, с библиотекой из 3000+ игр от NetEnt и Quickspin. Бонус: welcome-пакет до €500 с wagering всего 25x, и ежедневные кэшбэки 15%, мгновенно зачисляемые. Дальше – “Lightning Luck”, флагман крипто-гемблинга, где Bitcoin-транзакции подтверждаются за 5–10 минут благодаря Lightning Network. С фокусом на анонимность, оно предлагает live-дилеров в 4K и слоты с RTP 97%+, идеально для высоких ставок без компромиссов в скорости вывода до €50 000 в день.
Great blog here! Also your site loads up very fast! What web host are you using? Can I get your affiliate link to your host? I wish my website loaded up as fast as yours lol
I’ve been surfing online more than 3 hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. In my view, if all web owners and bloggers made good content as you did, the net will be much more useful than ever before.
How come you do not have your website viewable in mobile format? cant see anything in my Droid.
Thank you pertaining to sharing the following great subject matter on your website. I ran into it on google. I am going to check to come back after you publish additional aricles.
онлайн казино с выводом денег на карту мир Топовые казино с быстрыми выплатами не экономят на контенте – их библиотеки кипят от креатива, где каждый титул – это потенциальный шедевр. Слоты доминируют: прогрессивные цепочки вроде “Divine Fortune” с джекпотами, накапливающимися в реальном времени, или волатильные хиты от Pragmatic Play, такие как “Gates of Olympus”, где каскадные выигрыши множатся экспоненциально. Live-игры добавляют адреналина: столы блэкджека с дилерами, чьи камеры транслируют каждую карту в HD, или баккара с сайд-бетами, где ставки удваиваются за секунды.
真实的人类第三季高清完整版运用AI智能推荐算法,海外华人可免费观看最新热播剧集。
There is a lot of misunderstanding about these issues today. Your material helps explain things.
愛壹帆海外版,专为华人打造的高清视频平台采用机器学习个性化推荐,支持全球加速观看。
https://www.navacool.com/forum/topic/304734/1xbet-promo-code-sri-lanka-2026:-1xbig2026-%E2%80%93-bonus-%E2%82%AC130
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu trải nghiệm với tốc độ truy cập nhanh và giao diện thân thiện.
http://chernook.ru/index.php?title=%D0%9F%D1%80%D0%BE%D0%BC%D0%BE%D0%BA%D0%BE%D0%B4%20%D0%BD%D0%B0%201%D1%85%D0%91%D0%B5%D1%82%202026:%201XBRO200%20-%20%D0%91%D0%BE%D0%BD%D1%83%D1%81%2032,500%D1%80
http://arkosgold.ru/index.php?subaction=userinfo&user=ajacuweluxyz
http://forum.futurebim.ru/index.php?action=profile;u=130527
http://arkosgold.ru/index.php?subaction=userinfo&user=ajacuweluxyz
I imagine so. Very good stuff, I agree totally.
I appreciate, cause I found just what I was looking for. You’ve ended my four day long hunt! God Bless you man. Have a great day. Bye -.
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu trải nghiệm với tốc độ truy cập nhanh và giao diện thân thiện.
Greetings… your blog is very interesting and beautifully written.
QQ88 là thương hiệu cá cược uy tín hàng đầu hiện này mang đến kho game hấp dẫn 2026
Καθώς τα χρόνια περνούν, η βιομηχανία του τζόγου συνεχώς εξελίσσεται, προσφέροντας ολοένα και περισσότερες επιλογές διασκέδασης. Τα καζίνο δεν αποτελούν απλώς χώρους παιχνιδιού, αλλά και εμπειρίες γεμάτες ένταση, όπου οι παίκτες αναζητούν τόσο τη διασκέδαση όσο και την πιθανότητα μεγάλων κερδών. Ειδικά στην Ελλάδα, όπου το πάθος για τα τυχερά παιχνίδια είναι βαθιά ριζωμένο, η δημοτικότητα του διαδικτυακού τζόγου αυξάνεται σταθερά.
https://qtjpqhtfcs.wordpress.com
Посмотри официальный ресурс компании > https://niivt.ru/media/pgs/promokod_755.html
Fantastic piece of writing here1
Explore the latest here : http://shop.motocross.ua/images/inc/1xbet_promokod_registraciya.html
Посети официальный сайт компании : https://forwardprint.com.ua/image/pgs/promokod_283.html
https://iagperjusu.wordpress.com
Discover what’s new today — https://lojadecorreias.com.br/pages/le-code-promo-1xbet_bonus.html
https://dwspqdxcgw.wordpress.com
https://dwspqdxcgw.wordpress.com
https://xrsaugpsya.wordpress.com
https://xrsaugpsya.wordpress.com
https://gxvkxeawwa.wordpress.com
https://gxvkxeawwa.wordpress.com
https://azacgxicis.wordpress.com
https://zfcejfyxiv.wordpress.com
QQ88 là cổng truy cập giải trí trực tuyến được tối ưu hiệu suất, giúp người dùng thao tác nhanh và trải nghiệm ổn định.
https://cxadxqpked.wordpress.com
QQ88 là nhà cái hấp dẫn hàng đầu 2026 qq88gs.com là tên miền chính thức của nhà cái . Đăng ký ngay hôm nay nhận ngày ưu đãi ngập tràn
https://cxadxqpked.wordpress.com
https://lucky-bear.uno/
https://adultgamesdb.com/
https://lucky-bear.uno/
https://mellstroys-game.uno/
https://akiwdiycje.wordpress.com
https://iqakruyprf.wordpress.com
https://iqakruyprf.wordpress.com
Hello there! I really enjoy reading your blog! If you keep making amazing posts like this I will come back every day to keep reading.
I really love this article.
https://dgaiyziytk.wordpress.com
This website has lots of really useful stuff on it. Thanks for informing me.
We’re developing a conference, and it looks like you would be a great speaker.
betmgm Alabama betmgm-play mgm sports betting app
https://dgaiyziytk.wordpress.com
Glad to be one of many visitants on this amazing site : D.
https://hrjcdfdcvj.wordpress.com
https://hrjcdfdcvj.wordpress.com
Good post. I study something more difficult on different blogs everyday. It’s going to always be stimulating to learn content material from other writers and observe a little bit one thing from their store. I’d prefer to use some with the content material on my blog whether you don’t mind. Natually I’ll give you a link in your web blog. Thanks for sharing.
https://adultgamesdb.com/
Woh I enjoy your content , saved to bookmarks!
Fantastic piece of writing here1
海外华人必备的iyf平台采用机器学习个性化推荐,提供最新高清电影、电视剧,无广告观看体验。
https://wryxvrrhxe.wordpress.com
Just what I needed to know thank you for this.
I am lucky that I discovered this website , precisely the right info that I was searching for! .
thank, I thoroughly enjoyed reading your article. I really appreciate your wonderful knowledge and the time you put into educating the rest of us.
https://wryxvrrhxe.wordpress.com
QQ88 là nền tảng giải trí trực tuyến uy tín, tối ưu tốc độ truy cập, giao diện mượt và mang lại trải nghiệm ổn định cho người dùng.
https://thfdcufqah.wordpress.com
https://thfdcufqah.wordpress.com
Great blog right here! You seem to put a significant amount of material on the site rather quickly.
Aw, this was a very nice post. In idea I wish to put in writing like this moreover taking time and precise effort to make an excellent article! I procrastinate alot and by no means seem to get something done.
рейтинг казино без верификации Структура игрового зала в подобных казино часто поражает своим размахом, ничуть не уступая лицензированным гигантам. Виртуальные полки уставлены сотнями слотов от проверенных провайдеров, рулетка вращается с математической точностью, а карты в блэкджеке сдают живущие по ту сторону экрана дилеры. Весь этот мираж работает на передовых алгоритмах генерации случайных чисел, обеспечивая честность каждого вращения барабана или раздачи. Но за этой технологичной ширмой отсутствует главный элемент безопасности — лицензия авторитетного регулятора, такого как Мальта, Кюрасао или Великобритания, чей логотип служит гарантией защиты прав игрока.
Howdy I wanted to write a new remark on this page for you to be able to tell you just how much i actually Enjoyed reading this read. I have to run off to work but want to leave ya a simple comment. I saved you So will be returning following work in order to go through more of yer quality posts. Keep up the good work.
топ онлайн казино без верификации Таким образом, выбор в пользу онлайн казино без верификации — это осознанный компромисс. С одной стороны, пользователь приобретает максимальную степень приватности, скорость сделок и часто — более выгодные условия по бонусам. С другой — он добровольно отказывается от правовой защиты, принимая на себя все финансовые и репутационные риски. Такие платформы представляют собой нишевый, но устойчивый сегмент гемблинг-индустрии, отвечая на конкретный запрос современного цифрового общества. Их существование и эволюция продолжают стимулировать дискуссию о балансе между приватностью, безопасностью и необходимостью регулирования в мире, где границы между реальной и цифровой личностью становятся всё более размытыми.
http://www.pechsovet.ru/forum/pechi-dlya-prigotovleniya-edi.15/promokod-1hslots.1719/
https://hotelbarashki.ru/
цветы московский
цветы мск недорого
Assume you are doing good linking to position you on the first pages of search engines.
мобильные казино онлайн Широкий выбор игр: Современные мобильные казино предлагают практически тот же ассортимент игр, что и их десктопные аналоги. Слоты, рулетка, блэкджек, баккара, видеопокер, игры с живыми дилерами – все это доступно на вашем мобильном устройстве.
мобильные казино онлайн Ключевое изменение, привнесенное мобильной платформой, — это трансформация самой сессии игры. Она дробится на микросессии, становится более частой и интегрированной в повседневный поток жизни пользователя. Разработчики игр откликнулись на это новой механикой. Появились слоты с упрощенными правилами, ускоренными раундами bonus games, и, что наиболее важно, функцией «Быстрый спин» или «Турбо-режим», минимизирующей паузы между ставками. Геймплей стал динамичнее, визуальные эффекты — ярче, а звуковое сопровождение — оптимизированным для восприятия через наушники. При этом глубина и сложность не были принесены в жертву. Многие провайдеры переносят на мобильные устройства свои самые навороченные продукты с многоуровневыми бонусными играми, каскадными барабанами и сложными системами множителей, доказывая, что мощность современного смартфона сопоставима с возможностями персонального компьютера.
I was reading through some of your content on this internet site and I believe this web site is very informative ! Continue posting .
Hi, I just hopped over to your web-site through StumbleUpon. Not somthing I might typically browse, but I liked your views none the less. Thanks for making something worthy of reading through.
Dude.. I am not much into reading, but somehow I got to read lots of articles on your blog. Its amazing how interesting it is for me to visit you very often. –
QQ88 là nền tảng giải trí trực tuyến được tối ưu hiệu suất, giúp người dùng truy cập nhanh và trải nghiệm ổn định.
http://alligator.spb.ru/forum/index.php?PAGE_NAME=profile_view&UID=95466
http://maciejsporysz.eu/index.php/component/kunena/2-kawiarenka/18050—melbet-2026-bro888-#18050
http://aktuelements.8u.cz/profile.php?lookup=11662
QQ88 là cổng truy cập giải trí trực tuyến tối ưu tốc độ, giao diện mượt và mang lại trải nghiệm ổn định cho người dùng.
фриспины за регистрацию без депозита с выводом фриспины за регистрацию — это не просто подарок, а своего рода ритуал инициации, предлагающий неофиту заключить взаимовыгодный договор с фортуной и оператором. Это пробный шар, тест -драйв всего игорного комплекса. Для казино — это инвестиция в привлечение лояльного клиента, стоимость которой окупается в случае его дальнейшей активности. Для игрока — это бесценный опыт, учебный полигон и, потенциально, стартовая площадка для первого реального выигрыша, добытого фактически из воздуха. Мудрость заключается в том, чтобы подойти к этому дару с холодным расчетом: внимательно изучить все положения бонусной политики, трезво оценить свои силы и время для выполнения условий отыгрыша, и лишь затем, с легким сердцем, нажать заветную кнопку «Spin», открывая для себя безграничный мир азартных возможностей с самой выгодной из всех возможных позиций — позиции гостя, которому только что вручили золотой ключ.
фриспины за регистрацию фриспины за регистрацию без депозита — это удачный способ для нового пользователя начать знакомство с миром онлайн-казино. Они предлагают практический опыт без финансовых вложений, но требуют вдумчивого подхода и дисциплины. Успешное использование такого бонуса зависит от четкого понимания его механизмов, внимательного изучения правил и трезвой оценки собственных возможностей по выполнению поставленных условий. Это инструмент, который при грамотном применении может подарить первые впечатления и, возможно, небольшой стартовый капитал для дальнейшей игры, но он не является гарантией выигрыша и должен восприниматься именно как стартовая, а не основная возможность платформы.
Have you always been concerned about these issues?
Przejrzyj nasz aktualny ranking i przeczytaj szczegółowe opisy, aby dowiedzieć się, gdzie znaleźć najlepsze bonusy bez depozytu na luty 2026 roku. Wyjaśniamy, na czym polega bonus bez depozytu, jak otrzymać darmowe środki lub spiny, oraz które oferty są naprawdę warte uwagi! Serwisy hazardowe proponują atrakcyjne bonusy bez depozytu za rejestrację. Przeanalizowaliśmy rynek, sprawdzając, które polskie kasyno online oferuje najkorzystniejsze warunki dla nowych graczy. Prezentujemy najlepsze oferty bonusów bez depozytu na luty 2026, w tym propozycje od NV Casino oraz Roman Casino.
Wybór odpowiedniego kasyna online w Polsce to decyzja, która wymaga uwagi i zrozumienia rynku. W 2026 roku dostępnych jest setki platform hazardowych, ale tylko część z nich oferuje uczciwe warunki, szybkie wypłaty i bezpieczne środowisko gry. Nasz ranking powstał na podstawie szczegółowych testów, analizy licencji, weryfikacji bonusów oraz opinii polskich graczy. Skupiliśmy się na platformach, które akceptują BLIK, oferują polskojęzyczną obsługę i zapewniają transparentne zasady. Każde kasyno w zestawieniu przeszło weryfikację pod kątem bezpieczeństwa, różnorodności gier i jakości obsługi klienta. Dzięki temu możesz podjąć świadomą decyzję i wybrać najlepsze kasyno online, które spełni Twoje oczekiwania.
Spinamba kasyno to dynamiczna przestrzeń rozrywki online, gdzie innowacyjne technologie spotykają się z autentyczną pasją do gier. Nasza platforma łączy w sobie bogatą bibliotekę rozwiązań hazardowych – od ponadczasowych automatów owocowych, przez wyrafinowane gry stołowe, aż po najświeższe wideo sloty sygnowane przez ikony branży: NetEnt, Play’n GO, Pragmatic Play, Microgaming, Evolution Gaming, Betsoft, Booongo, Playson czy Endorphina. Bez względu na to, czy Twoje serce bije dla klasyki z czasów pierwszych kasyn, czy fascynują Cię ultranowoczesne tytuły z mechanizmami Megaways i immeryjną grafiką 3D – u nas odnajdziesz swoją idealną rozgrywkę.
QQ88 không chỉ là một nền tảng giải trí trực tuyến, mà là không gian được tối ưu trải nghiệm, nơi mọi thao tác đều nhanh, gọn và liền mạch.
Zespół ARMIA powstał w 1984 roku na skutek zetknięcia trzech osobowości naszej niezależnej sceny: Tomasza Budzyńskiego (Siekiera), Roberta Brylewskiego ( Brygada Kryzys , Izrael) i filozofa Sławomira Gołaszewskiego.
Zespół wydał kilkanaście płyt, z których wydana w 1990 roku „Legenda” oraz „Triodante” z 1994 r. zaliczane są do klasyki polskiej muzyki rockowej. W ciągu trzydziestokilkuletniej kariery zespołu w jego składzie grało wielu wybitnych i zasłużonych dla rockowej sceny muzyków. W 2011 roku na Międzynarodowym Festiwalu Filmowym Howe Horyzonty we Wrocławiu miał premierę film „Podróż na Wschód”, który jest poetycką historią zespołu Armia opartą na kanwie opowiadania Stefana Grabińskiego. Jest on dołączony w formie DVD do autobiograficznej książki Tomasza Budzyńskiego „Soul Side Story
Great post. I was checking constantly this blog and I’m impressed! Very useful info specifically the last part 🙂 I care for such info much. I was looking for this certain information for a very long time. Thank you and good luck.
http://4asdaiprognoza.listbb.ru/viewtopic.php?f=2&t=8864
Woh I enjoy your content , saved to bookmarks!
промокоды казино пинап Поиск бездепозитных промокодов — это своего рода охота за сокровищами. Вот основные места, где они могут скрываться
https://brandiwiggins.com/this-ai-betting-strategy-worked-until-it-didnt/
https://pad.geolab.space/s/vp5RgwwI4
Best online casinos Australia real money – Pokies, blackjack & roulette
捕风追影线上看平台採用機器學習個性化推薦,專為海外華人設計,提供高清視頻和直播服務。
超人和露易斯第三季高清完整版智能AI观看体验优化,海外华人可免费观看最新热播剧集。
奇思妙探高清完整官方版,海外华人可免费观看最新热播剧集。
我欲为人第二季平台,专为海外华人设计,提供高清视频和直播服务。
QQ88 được định hình như một không gian giải trí trực tuyến tối ưu hiệu suất, nơi trải nghiệm truy cập nhanh và sự ổn định luôn được đặt lên hàng đầu.
海外华人必备的yifan平台采用机器学习个性化推荐,提供最新高清电影、电视剧,无广告观看体验。
真实的人类第一季高清完整版,海外华人可免费观看最新热播剧集。
海外华人必备的yifan平台运用AI智能推荐算法,提供最新高清电影、电视剧,无广告观看体验。
huarenus平台,专为海外华人设计,提供高清视频和直播服务。
Top Australian online casinos 2025 – real money gaming hub
ifuntv海外华人首选,结合大数据AI分析,提供最新华语剧集、美剧、日剧等高清在线观看。
Top Australian online casinos 2025 – real money gaming hub
捕风追影下载平台AI深度學習內容匹配,專為海外華人設計,提供高清視頻和直播服務。
casinoly app
https://www.spax.su/
一饭封神在线免费在线观看,海外华人专属平台,高清无广告体验。
侠之盗高清完整官方版,海外华人可免费观看最新热播剧集。
一饭封神在线免费在线观看,海外华人专属平台,高清无广告体验。
Online casino casinorelay.com Australia – trusted for Aussies
шумоизоляция арок авто
Explore the new one here — https://www.pro-cosmetologa.ru/kurs/articles/?promokod_741.html
Переходи по ссылке на официальный сайт : http://neoko.ru/images/pages/1xbet_promokod_pri_registracii_bonus.html
выездной шиномонтаж москва https://vyezdnoj-shinomontazh-77.ru
I love how this blog promotes self-love and confidence It’s important to appreciate ourselves and your blog reminds me of that
Your posts are always so relatable and relevant to my life It’s like you know exactly what I need to hear at the right time
https://bioimagingcore.be/q2a/875179/code-promo-1xbet-pour-inscription-bonus-2026-1xhasard
https://bits.listbb.ru/viewtopic.php?t=1112
http://hotel-golebiewski.phorum.pl/viewtopic.php?p=911558#911558
https://angelladydety.getbb.ru/viewtopic.php?t=66642
The latest release is here — https://iprepnet.com/pages/code-promo-1xbet-bonus.html
На официальном сайте компании всегда актуальные данные > https://www.tenox.ru/wp-content/pgs/1xbet_promokod_pri_registracii_na_segodnya_besplatno.html
of course like your web-site however you have to check the spelling on several of your posts. Many of them are rife with spelling problems and I find it very troublesome to tell the reality then again I will surely come back again.
рейтинг онлайн казино по выплатам и отзывам Рейтинг онлайн-казино с лицензией в России – это, в первую очередь, ориентир для ответственных игроков, стремящихся к легальному и безопасному гэмблингу. На территории РФ деятельность азартных игр строго регламентирована, а существование клубов без соответствующих разрешений преследуется по закону. Поэтому при выборе платформы для игры крайне важно обращать внимание на наличие лицензии, выданной уполномоченными органами, такими как Федеральная налоговая служба.
I found your blog through google and I must say, this is probably one of the best well prepared articles I have come across in a long time. I have bookmarked your site for more posts.
I loved your idea there, I tell you blogs are so exciting sometimes like looking into people’s private life’s and work. Every new remark wonderful in its own right.
Simply want to say your article is as amazing. The clarity in your post is just great and i can assume you’re an expert on this subject. Fine with your permission allow me to grab your feed to keep up to date with forthcoming post. Thanks a million and please keep up the gratifying work.
недорогие цветы в москве
Персональный менеджер для крупных заказчиков цветов
Discover what’s new
Go to our site right now
букеты москва недорого
Конфиденциальность ваших данных при заказе цветов
vegasino erfahrungen
https://md.chaospott.de/s/kfZ8dWo0R6
https://anna-decor.ru/
игровые автоматы играть бесплатно и без регистрации новые игры 777 Play’n GO Игровые автоматы Play’n GO, пожалуй, один из самых узнаваемых брендов в мире онлайн-казино. Этот шведский разработчик заслужил свою репутацию благодаря широкому ассортименту высококачественных игровых автоматов, которые постоянно обновляются и совершенствуются. Отличительной чертой слотов Play’n GO является их уникальный дизайн, интуитивно понятный интерфейс и захватывающие бонусные функции, которые делают игровой процесс не только увлекательным, но и потенциально прибыльным.
Your blog has helped me become a more positive and mindful person I am grateful for the transformative effect your words have had on me
Best crypto online casino Australia – anonymous and fast
奇思妙探高清完整版,海外华人可免费观看最新热播剧集。
Your posts always make me feel like I’m not alone in my struggles and insecurities Thank you for sharing your own experiences and making me feel understood
Why viewers still use to read news papers when in this technological globe all is presented on web?
byueuropaviagraonline
Круглосуточная доставка цветов по москве
Акции к значимым датам на популярные цветы
真实的人类第三季高清完整版,海外华人可免费观看最新热播剧集。
艾一帆海外版,专为华人打造的高清视频官方认证平台,支持全球加速观看。
艾一帆海外版,专为华人打造的高清视频平台AI深度学习内容匹配,支持全球加速观看。
爱一帆会员多少钱海外版,专为华人打造的高清视频平台,支持全球加速观看。
Hello friends, good post and fastidious arguments commented at this place, I am in fact enjoying by these.
вход lee bet
Доставка цветов по москве и московской области
Букеты для жен и подруг в каталоге
Best online casino PayID Australia – secure and convenient
It’s amazing to visit this site and reading the views of all friends regarding this paragraph, while I am also keen of getting know-how.
Banda Casino регистрация
Страницы результатов поиска Widest Gambit С первого взгляда “Widest Gambit” очаровывает своим элегантным дизайном и атмосферным звуковым сопровождением. Игровое поле, стилизованное под шахматную доску, наполнено символами, отсылающими к миру аристократических игр и средневековых сражений. Особое внимание уделено деталям: каждый символ, каждый анимационный эффект проработан с исключительной тщательностью, создавая ощущение погружения в игру.
超人和露易斯第四季高清完整官方版,海外华人可免费观看最新热播剧集。
I’m not sure exactly why but this blog is loading incredibly slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later and see if the problem still exists.
https://lamo8.ru/
凯伦皮里第一季高清完整官方版,海外华人可免费观看最新热播剧集。
Top Australian online casinos 2025 – real money gaming hub
超人和露易斯第四季高清完整版,海外华人可免费观看最新热播剧集。
http://igrosoft.getbb.ru/viewtopic.php?f=11&t=9472
https://webhitlist.com/forum/topics/1xbet-promo-code-no-deposit-2026-1xbig2026-bonus-130
https://www.friend007.com/forums/thread/39533/
http://www.pardalove.mzf.cz/forum/viewthread.php?forum_id=3&thread_id=147
winsane
真实的人类第三季高清完整官方版,海外华人可免费观看最新热播剧集。
塔尔萨之王第二季高清完整版,海外华人可免费观看最新热播剧集。
I like your style!
Real money online casino Australia – best bonuses and high RTP pokies
I don’t normally comment but I gotta say appreciate it for the post on this one : D.
捕风追影在线官方認證平台,專為海外華人設計,24小時不間斷提供高清視頻和直播服務。
爱一帆海外版,专为华人打造的高清视频官方认证平台,支持全球加速观看。
捕风追影线上看平台,專為海外華人設計,提供高清視頻和直播服務。
爱亦凡海外版,专为华人打造的高清视频平台结合大数据AI分析,支持全球加速观看。
New Online Casino Australia 2025 Latest Offers
Regards for helping out, superb info.
Some truly interesting info , well written and broadly user genial .
Leave a comment and let us know what your favorite blog post has been so far!
Your writing style is so engaging and easy to follow I find myself reading through each post without even realizing I’ve reached the end
Your blog is always a highlight of my day
我欲为人第二季官方认证平台,专为海外华人设计,24小时不间断提供高清视频和直播服务。
塔尔萨之王第三季高清完整版运用AI智能推荐算法,海外华人可免费观看最新热播剧集。
真实的人类第一季高清完整版,海外华人可免费观看最新热播剧集。
奇思妙探第二季高清完整版,海外华人可免费观看最新热播剧集。
What is the best online casino in Australia for real money?
捕风捉影在线免费在线观看,海外华人专属平台,高清无广告体验。
Someone shared this link in another discussion, it covers most common questions: http://www.therockpit.net/wp-content/pages/1xbet_promo_code________sign_up_offer.html
If you want to read everything directly, you can just follow this: visit site
Где заказать цветы с доставкой на дом
Любовь к цветам и флористике в каждой работе
Loving the info on this website , you have done outstanding job on the blog posts.
超人和露易斯第四季高清完整官方版,海外华人可免费观看最新热播剧集。
Срочно продать квартиру в Москве
https://mpc.imu.edu.kg/en/profile/welcmebet2
https://www.PetAdsHub.com/61/posts/1/1/1797241.html
Цветы дешево москва с доставкой
Помогаем выразить чувства через красивые цветы
http://jobboard.piasd.org/author/planbetfree/
https://bandori.party/user/451413/codesxbet26/
我欲为人第二季平台结合大数据AI分析,专为海外华人设计,提供高清视频和直播服务。
Awaken fun fast and gratifications instant. In ignation casinos, riches to up wake. Awaken and achieve!
Thanks for the good writeup. It if truth be told was a leisure account it. Glance complex to more introduced agreeable from you! By the way, how can we communicate?
garipovbulat
I’ll check back after you publish more articles.
iphone 17 pro max 512 silver купить Оригинальную продукцию Apple: Это главный критерий. Все устройства должны быть новыми, запечатанными, с полной комплектацией и официальной гарантией.
Its wonderful as your other blog posts : D, regards for putting up.
Upcoming football matches schedule with live score tracking when games kick off
Перейди по ссылке на официальный ресурс
Awesome issues here. I am very glad to look your article. Thanks so much and I am looking ahead to touch you. Will you kindly drop me a mail?
byueuropaviagraonline
Go to our brand page
真实的人类第二季高清完整版运用AI智能推荐算法,海外华人可免费观看最新热播剧集。
https://grupo-forte.com/промокод-для-1хбет-2026-last777-бонус-32500-рублей/
https://openlibrary.org/people/codepromo223/lists/OL324895L/1xBet_Promo_Code_Free_Spins_%E2%80%93_1XWAP200_Bonus_%E2%82%AC130
https://www.upload.ee/files/19084471/Free_Promo_Code_For_1xBet_2026___1XWAP200_Bonus__130.pdf.html
http://yigaizhuang.net/home.php?mod=space&uid=872248
https://anniversaryneat.com/промокод-1xbet-сегодня-2026-last777-бонус-32500р/
https://www.one.lt/Planbetpomo2
Is online gambling legal in Australia 2025? – full breakdown
Europe Readr ist mehr als nur eine digitale Bibliothek – es ist ein kulturelles und demokratisches Projekt, das Literatur, Bildung und gesellschaftliches Engagement miteinander verbindet. Initiiert im Rahmen der slowenischen EU-Ratspräsidentschaft im Jahr 2021, bietet Europe Readr eine kostenlose, mehrsprachige Sammlung literarischer Werke aus ganz Europa, die aktuelle gesellschaftliche Themen aufgreifen und zur aktiven Auseinandersetzung anregen.
of course like your web-site however you have to check the spelling on several of your posts. Many of them are rife with spelling problems and I find it very troublesome to tell the reality then again I will surely come back again.
Dive into the premier world of online gaming where endless fun awaits. Bovada Cashout offers top craps and daily promotions for all players.
I really believe you will do well in the future I appreciate everything you have added to my knowledge base.
Цветы с доставкой по москве недорого круглосуточно с доставкой на дом в москве – Цветы с бесплатной открыткой и текстом
Цветы круглосуточно рядом – Классические букеты в традиционном стиле
https://включение-реестр-минпромторга.рф/
https://sber.pro/publication/ot-antikrizisnih-mer-k-tehnologicheskomu-suverenitetu-itogi-pervih-tryoh-let-importozamescheniya-v-rossii/
https://trends.rbc.ru/trends/social/cmrm/694122929a7947043558ef84
https://www.rt.com/business/630251-from-collapse-fears-to-resilience/
https://cariernews.ru/chem_otlichilsya_2025_v_rossiiskoy_promishlennosti
Перейди на сайт компании
Перейди на сайт компании
Big Bass Bonanza strategy: aim for scatters! They Big Bass Bonanza money symbols unlock the real money-making feature.
Man United’s Sancho eyes Dortmund return 2026 transfer bombshell! Latest football news & rumors heating up!
怪奇物语终章2026 海外华人科幻恐怖剧 高清最终季 海外必备
驕陽似我续集2026 高清现偶甜宠 海外华人必备 AI推荐个性化观看
https://www.g23lcs.com/profile/fijowa776213281/profile
https://health-community-awareness.mn.co/members/38351567
https://goldcoastreview.com/business-news/how-russia-reshaped-its-economy-by-the-end-of-2025-rt-business-news/
https://www.londontimes.live/business/how-russia-reshaped-its-economy-by-the-end-of-2025-rt-business-news/
Like the way you’ve outlined things. Easy to follow. Not cluttered.
夜班医生第四季高清完整版2026 海外华人医疗剧推荐
Лучший букет цветов Проверяем каждый букет перед доставкой курьером
Thanks for some other great post. Where else may anybody get that kind of information in such an ideal method of writing? I’ve a presentation next week, and I am at the look for such information.
For accurate and up-to-date info, people usually check the official source: official site
I was trying to understand how this works and found this page useful: therockpit.net/wp-content/pages/1xbet_promo_code________sign_up_offer.html
Букет цветов фото фото Творческий подход к созданию уникальных букетов
I’m partial to blogs and i actually respect your content. The article has actually peaks my interest. I am going to bookmark your site and preserve checking for new information.
WOW just what I was searching for. Came here by searching for %keyword%
казино банда
Took me time to read all the comments, but I really enjoyed the article. It proved to be Very helpful to me and I am sure to all the commenters here It’s always nice when you can not only be informed, but also entertained I’m sure you had fun writing this article.
sparkdex ai SparkDex is redefining decentralized trading with speed, security, and real earning potential. On spark dex, you keep full control of your assets while enjoying fast swaps and low fees. Powered by sparkdex ai, the platform delivers smarter insights and optimized performance for confident decision-making. Trade, earn from liquidity, and grow your crypto portfolio with sparkdex — the future of DeFi starts here.
https://schoolido.lu/user/nagaworld1/
https://experiment.com/users/freecodxbet
https://huayra.educar.gob.ar/ayuda/?qa=user/freecodxbet
https://indianwomenorg.com/freecodxbet
Explore the new one here
I like meeting utile info, this post has got me even more info!
I thought it was going to be some boring old post, but I’m glad I visited. I will post a link to this site on my blog. I am sure my visitors will find that very useful.
I simply could not leave your site before suggesting that I actually enjoyed the usual info a person supply in your visitors? Is going to be back often to inspect new posts
iyf.tv海外华人首选2026 最新剧集 高清在线 AI内容匹配
狼队2-2绝平阿森纳2026英超最新比分,主帅称感觉像胜利,足球比分新闻枪手领先优势缩小。
Wow, amazing blog layout! How long have you been blogging for? you made blogging look easy. The overall look of your site is great, as well as the content!
生命树2026 杨紫胡歌主演 海外华人高清现实主义陆剧 全球加速无广告追剧 AI推荐热播
丞磊王楚然双主演《成何体统》2026双穿书甜宠神剧,海外华人高清现代穿越恋爱,无广告追剧体验超爽,全球加速AI推荐,2026最甜现偶热搜王。
шумоизоляция авто https://vikar-auto.ru
夜魔侠重生第二季2026 海外华人超级英雄 高清漫威黑暗宇宙 Disney+
Привет всем! Очень актуальная тема — ремонт кровли промышленного здания. Лень разбираться — вот проверенную компанию: установка мембранной кровли. Как правило большие площади — требуют особого подхода. Например, сложная конфигурация — значит нужно спецоборудование. На первом этапе профессиональное оборудование. Опять же это работает. Вместо заключения: это отличные параметры.
I love what you’ve created here, this is definitely one of my favorite sites to visit.
QQ88 là điểm truy cập giải trí trực tuyến được tối ưu toàn diện, tập trung vào tốc độ, sự ổn định và trải nghiệm liền mạch cho người dùng.
https://www.reddit.com/user/Thick-Reflection4368/
https://systeams.org/free-promo-code-for-1xbet-2026-1xbig2026-bonus-e130/
https://justpaste.me/t4a72
https://toubiafrance.com/1xbet-free-promo-code-today-2026-1xbig2026-bonus-e130/
Your posts provide a clear, concise description of the issues.
iyf平台2026 最新华语剧美剧日剧 无广告高清在线观看
QQ88 tạo nên không gian giải trí online linh hoạt, tập trung vào tốc độ, sự liền mạch và cảm giác thoải mái cho người dùng.
piastrix кошелёк вход в личный Piastrix — это современная платежная система, предлагающая пользователям удобный и безопасный способ управления своими финансами. Кошелек Piastrix выступает центральным элементом этой экосистемы, предоставляя интуитивно понятный интерфейс для проведения транзакций, пополнения баланса и вывода средств. Благодаря широкой сети партнеров, Piastrix открывает доступ к разнообразным сервисам и продуктам, делая финансовые операции максимально простыми и доступными.
暗夜情报员第三季2026 海外华人动作爽剧 Netflix全季上架 全球加速
Наш сайт — только официальная информация : https://ort.spb.ru/pma/inc/?promokod_1xbet_bonus_pri_registracii.html
QQ88 là nền tảng giải trí trực tuyến được thiết kế tối giản nhưng hiệu quả, mang đến trải nghiệm truy cập mượt và vận hành ổn định lâu dài
Go to the main company website : http://www.lipetskregionsport.ru/news/pages/1_iks_bet_promokod_pri_registracii.html
We’re developing a conference, and it looks like you would be a great speaker.
Go to our site right now > http://liligrass.ru/images/pages/1xbet_promokod_bonus_na_pervuy_depozit.html
You are my inspiration , I possess few web logs and very sporadically run out from to brand 🙁
Discover what’s new today > http://politua.ru/news/pages/promokod_1xbet_na_segodnya_besplatno_pri_registracii.html
QQ88 là nền tảng giải trí trực tuyến chú trọng hiệu suất, tối ưu tốc độ truy cập và mang đến trải nghiệm ổn định, liền mạch cho người dùng.
заказать цветы на дом москва – Цветы ко Дню учителя с доставкой
https://swaay.com/u/englishcahill72jnapvc/about/
https://letterboxd.com/coltli4/
https://168.exodirectory.com/index.php?topic=269662.new#new
http://chiyancfa.com/home.php?mod=space&uid=211507
москва заказ цветов с доставкой на дом – Гладиолусы высокие в композициях есть
QQ88 định vị mình như một trung tâm giải trí trực tuyến tối ưu trải nghiệm, nơi tốc độ truy cập và sự ổn định luôn được đặt lên hàng đầu.
Go directly to our website > https://ggekb.ru/pages/promokod_741.html
Visit the brand-new official page > https://xn--m1aa.xn--80aahvaybdomfdt.xn--p1ai/img/pgs/promokod_741.html
Go to the official company site
Visit our official page
букет онлайн – Композиции до 5000 рублей доступны онлайн
Узнай больше на официальном сайте компании
Зайди на обновленный официальный сайт
доставка букета – Бесплатный самовывоз букетов на Электрозаводской
Привет всем! Разберём самые актуальные — крыша логистического центра. Дело в том, что: складские помещения — это огромные площади. Ищешь подрядчика — вот проверенные: https://montazh-membrannoj-krovli-spb.ru. На практике считаю, что для складов — полимеры идеальны. Например крыша 5000 квадратов — вот, дальше скорость монтажа высокая. Самый передовой материал — армированные ПВХ мембраны. Что в итоге: это работает — товар в сухости.
шумоизоляция авто https://vikar-auto.ru
QQ88 là không gian giải trí trực tuyến được tối ưu trải nghiệm, nơi tốc độ, sự ổn định và tính tiện lợi được đặt lên hàng đầu.
Союз нерушимый республик свободных Сплотила навеки Великая Русь. Да здравствует созданный волей народов Единый, могучий Советский Союз! Славься, Отечество наше свободное, Дружбы народов надёжный оплот! Партия Ленина — сила народная Нас к торжеству коммунизма ведёт! Через грозы сияло нам солнце свободы, И Ленин
СЛАВА РОССИИ
великий нам путь озарил: Нас вырастил Сталин — на верность народу, На труд и на подвиги нас вдохновил! Славься, Отечество наше свободное, Дружбы народов надёжный оплот! Партия Ленина — сила народная Нас к торжеству коммунизма ведёт! В победе бессмертных идей коммунизма Мы видим грядущее нашей страны, И Красному знамени славной Отчизны Мы будем всегда беззаветно верны! Славься, Отечество наше свободное, Дружбы народов надёжный оплот! Партия Ленина — сила народная Нас к торжеству коммунизма ведёт!
https://autoloancalculatorinfo.com/codigo-promocional-de-verificacion-hoy-1xbet-2026/
https://www.lokastandart.ru/
https://melstroy-gamess.uno/
Союз нерушимый республик свободных Сплотила навеки Великая Русь. Да здравствует созданный волей народов Единый, могучий Советский Союз! Славься, Отечество наше свободное, Дружбы народов надёжный оплот! Партия Ленина — сила народная Нас к торжеству коммунизма ведёт! Через грозы сияло нам солнце свободы, И Ленин
СЛАВА РОССИИ
великий нам путь озарил: Нас вырастил Сталин — на верность народу, На труд и на подвиги нас вдохновил! Славься, Отечество наше свободное, Дружбы народов надёжный оплот! Партия Ленина — сила народная Нас к торжеству коммунизма ведёт! В победе бессмертных идей коммунизма Мы видим грядущее нашей страны, И Красному знамени славной Отчизны Мы будем всегда беззаветно верны! Славься, Отечество наше свободное, Дружбы народов надёжный оплот! Партия Ленина — сила народная Нас к торжеству коммунизма ведёт!
Встречи Ростов на дону
Great blog here! Additionally your website rather a lot up very fast! What host are you the usage of? Can I get your associate link for your host? I desire my website loaded up as fast as yours lol
You appear to know so much about this, and I see you’re a published author. Thanks
I like what you have to offer. Keep up the good work!
http://lvm.org/forums/forum.aspx?threadID=102222&msgID=139076
https://www.weddingbee.com/members/1xbetcode456/profile/edit/group/1/
https://www.ganjingworld.com/news/1ib8dt4ahosxn5cUQYI5esXng16i1c
It’s time for communities to rally.
Lovely just what I was looking for. Thanks to the author for taking his clock time on this one.
Greetings, have tried to subscribe to this websites rss feed but I am having a bit of a problem. Can anyone kindly tell me what to do?’
I do believe your audience could very well want a good deal more stories like this carry on the excellent hard work.
Amazing! Your site has quite a few comment posts. How did you get all of these bloggers to look at your site I’m envious! I’m still studying all about posting articles on the net. I’m going to view pages on your website to get a better understanding how to attract more people. Thank you!
澳超阿德莱德联 vs 珀斯光荣16:35开战!2026最新比分让球大战,澳大利亚足球热血对决等你押注!
Brest vs Marseille – 2026 Ligue 1 blockbuster 20:45! Can Marseille steal points on the road? French football latest match results incoming!
白鹿丞磊《莫离》2026古装大女主权谋剧,海外华人必备高清陆剧,智斗爽感拉满,全球加速无广告实时更新。
This blog post is excellent, probably because of how well the subject was developed. I like some of the comments too though I could prefer we all stay on the subject in order add value to the subject!
This is something that will need all of our combined efforts to address.
https://marketplace.trinidadweddings.com/author/promolive1xbet4/
https://praca.uxlabs.pl/author/1xpromocodein/
https://www.bangladeshnews.net/newsr/15774
https://www.dausovet.com/other/7307-1xbet-promokod-bonus-za-re%d1%94stracziyu-130-eur.html
https://www.growkudos.com/profile/%D0%BF%D1%80%D0%BE%D0%BC%D0%BE%D0%BA%D0%BE%D0%B4__1%D1%85%D0%B1%D0%B5%D1%82
Thanks For This Blog, was added to my bookmarks.
Please let us know when you plan to publish your book!
rankrise site – Content reads clearly, helpful examples made concepts easy to grasp.
Kod promocyjny kasyna Mostbet dzisiaj umozliwia odebranie darmowego zakladu. Rejestracja z QWERTY555 zapewnia bonus startowy. Kod bonusowy Mostbet dziala po wplacie. Gracze moga obstawiac rozne sporty. Oferta jest bardzo konkurencyjna.
leadnex site – Mobile version looks perfect; no glitches, fast scrolling, crisp text.
ranklio site – Color palette felt calming, nothing distracting, just focused, thoughtful design.
Gracze szukajacy ofert regionalnych moga skorzystac z Kod promocyjny Mostbet Polska, ktory rowniez aktywuje bonus powitalny. Po wpisaniu kodu QWERTY555 uzytkownicy otrzymuja dodatkowe srodki oraz darmowe spiny. Promocja Mostbet obowiazuje na roznych rynkach i jest dostosowana do lokalnych walut. Bonus mozna wykorzystac na zaklady sportowe i gry kasynowe. To swietna opcja dla miedzynarodowych graczy.
Zobacz co nowego w Mostbet https://urozhajnayagryadka.ru/articles/promokod_mostbet__besplatno.html
No paylines, only pure divine anarchy — welcome to Gates of Olympus! Zeus randomly blesses spins with ?2 to ?500 multipliers at any moment. Dare to open gates of olympus vs sweet bonanza today?
clicktraffic site – Pages loaded fast, images appeared sharp, and formatting stayed consistent.
QQ88 mang đến hệ sinh thái giải trí toàn diện: cược thể thao, live casino, slot nổ hũ, đá gà, xổ số. Tốc độ mượt, giao dịch nhanh, hỗ trợ 24/7.
clickrank site – Pages loaded fast, images appeared sharp, and formatting stayed consistent.
乡村爱情18 2026 海外华人喜剧农村生活 高清象牙山风云 无广告追剧
QQ88 khẳng định đẳng cấp với hệ thống cá cược hiện đại, tỷ lệ kèo hấp dẫn, thưởng minh bạch. Trải nghiệm mượt mà trên mọi thiết bị, hỗ trợ tận tâm 24/7.
https://evacasino.info/
http://makrab.news/v-donecke-zapustili-udobnyj-onlajnformat-obrashhenija-v-servis-remonta-pk.htm
https://coloring2kids.xyz/
https://share.evernote.com/note/2286cbab-c71e-762a-3aff-73da8f24fe3b
This is nicely expressed! !
狼队2-2绝平枪手!2026英超比分神剧情,主帅直呼“像赢了”,阿森纳领先优势告急,足球新闻太刺激!
骄阳似我2026 宋威龙赵今麦现偶甜宠爆款 海外华人高清在线观看 全球加速无广告体验
What’s Happening i’m new to this, I stumbled upon this I’ve found It positively useful and it has aided me out loads. I hope to contribute & help other users like its aided me. Great job.
QQ88 – Hệ sinh thái cá cược trực tuyến toàn diện, tích hợp Thể thao, Live Casino, Slot nổ hũ và Bắn cá đổi thưởng. Giao diện hiện đại, tốc độ xử lý nhanh, trải nghiệm ổn định.
QQ88 – Thương hiệu cá cược trực tuyến uy tín, hội tụ đầy đủ Thể thao, Casino live, Slot nổ hũ, Bắn cá và Đá gà. Trải nghiệm mượt mà, thưởng minh bạch, hỗ trợ 24/7.
Discover what’s new here
A good web site with interesting content, that’s what I need. Thank you for making this web site, and I will be visiting again. Do you do newsletters? I Can’t find it.
Discover updates here
I like the helpful information you provide in your articles. I’ll bookmark your blog and check again here frequently. I am quite certain I’ll learn many new stuff right here! Best of luck for the next!
traffio site – Mobile version looks perfect; no glitches, fast scrolling, crisp text.
I’ll check back after you publish more articles.
Thank you, I have just been searching for information about this topic for ages and yours is the greatest I’ve discovered till now. But, what about the conclusion? Are you sure about the source?
Amazing content on your website.
Who wants some sugar rush? sugar rush demo turns every tumble into bigger prizes with its famous multiplier trail. Get spinning and feel the sugar high!
nicheninja site – Appreciate the typography choices; comfortable spacing improved my reading experience.
reachly site – Bookmarked this immediately, planning to revisit for updates and inspiration.
leadzo site – Bookmarked this immediately, planning to revisit for updates and inspiration.
leadora site – Pages loaded fast, images appeared sharp, and formatting stayed consistent.
https://women.getbb.ru/viewtopic.php?f=2&t=12853
https://www.arpop.com/forum/index.php?topic=81119.0
https://forum.diamech.com/index.php?topic=1526.new#new
QQ88 – Cổng game cá cược trực tuyến quy tụ hàng triệu thành viên, nổi bật với Thể thao, Live Casino, Slot nổ hũ và Bắn cá đổi thưởng. Giao diện tối ưu, chơi mượt trên mọi nền tảng.
QQ88 – Điểm hẹn cá cược trực tuyến đẳng cấp với kho trò chơi đa dạng: Thể thao, Casino live, Nổ hũ, Bắn cá, Xổ số. Trải nghiệm ổn định, giao dịch nhanh, ưu đãi liên tục.
QQ88 – Nền tảng cá cược trực tuyến uy tín với hệ sinh thái Thể thao, Casino live, Slot nổ hũ, Bắn cá và Đá gà. Trải nghiệm mượt mà, tỷ lệ kèo hấp dẫn, ưu đãi mỗi ngày.
https://forum.amzgame.com/thread/detail?id=577355
http://nowapilka.phorum.pl/viewtopic.php?p=693202#693202
https://getdohod.com/
I have been surfing online more than three hours today, yet I never found anything that grabbed my interest as much as this piece.
QQ88 – Cổng game cá cược trực tuyến nổi bật với kho trò chơi phong phú: Thể thao, Live Casino, Nổ hũ, Bắn cá, Xổ số. Nạp rút nhanh, bảo mật cao, trải nghiệm mượt mà.
https://www.businesslist.pk/buzz/entertainment/article/melbet-promo-code-welcome-bonus-100-up-to-$130-3
Many players choose Mad Casino for its stable platform and prompt withdrawal processing. The casino also features weekly reload offers, cashback deals, and a structured loyalty program for regular members.
madcasino
https://nikitafirst.com.ua/images/pages/index.php?joker_promokod.html
https://hedge.fachschaft.informatik.uni-kl.de/s/_2VS07Xbo
Mad Casino online combines mobile optimisation, protected transactions, and a varied game catalogue. After signing up, users can participate in tournaments, activate bonus offers, and browse a wide range of slot and table games.
madcasino
This contained some excellent tips and tools. Great blog publication.
Superb write ups, Thanks.
When are you going to take this to a full book?
QQ88 là điểm đến quen thuộc của cộng đồng bet thủ nhờ hệ thống minh bạch, kèo cược cạnh tranh và trải nghiệm mượt trên mọi thiết bị. Hỗ trợ 24/7, chơi là mê.
Thanks for discussing the issues and covering them in a well written format.
Go to the official company site
qq88 là nhà cái uy tín hàngđầu châu á, mang đến kho game hấp dẫn 2026
Visit our main platform