Long QT syndrome
Long QT syndrome (LQTS) is a heart rhythm disorder that could cause rapid irregular heartbeats. These heartbeats can cause the patient to faint suddenly. Certain people suffering from the condition experience seizures. In certain instances, LQTS can cause sudden death.
Certain people have an inherited mutation that can cause Long QT Syndrome (congenital Long QT Syndrome). Long QT syndrome could result from certain drugs minerals, imbalances in mineral levels, or medical illnesses (acquired Long QT Syndrome).
Long QT syndrome can be treated. It is possible to limit or take certain medicines to reduce the risk of heartbeat events. Sometimes the treatment of long QT syndrome requires surgical intervention or the use of implantable devices♥.
Symptoms
Shedding light on dangerous faints
A lot of people with long QT syndrome do not show any symptoms or signs. You may be aware of the condition due to:
- The results are from electrocardiograms (ECG) taken in connection with an unrelated cause
- An ancestral history is associated with QT syndrome
- Genetic test results
The most frequent manifestation of the long QT syndrome.
Fainting (syncope) is when the heart beats in an irregular manner. It is possible to faint when stressed, angry, or scared or when you exercise. Things that frighten you like an alarm clock, could cause you to fall asleep. A fainting or shaky feeling due to prolonged QT syndrome could be experienced with no warning. Some individuals may have an early warning sign that is the feeling of lightheadedness, heart palpitations blurred vision or weakness.
Seizures can also occur in those who suffer from LQTS.
In general, the heart will return back to a normal beat. If this doesn’t happen itself or if an external defibrillator doesn’t work at the time needed to bring your heart’s beat in a normal way, then sudden death could take place.
Many people suffering from indications of symptoms of QT syndrome experience their first episode before the age of 40. However congenital long QT syndrome symptoms and symptoms may be seen in newborns in the first weeks or months following birth, or even in early childhood or later. A few people suffering from congenital QT syndrome don’t show any symptoms or signs.
Signs and symptoms of QT syndrome can manifest in sleep.
When is the best time to seek medical help?
Contact your physician if you suddenly experience a fainting sensation during exercise in the midst of emotional turmoil or following the use of any new medication. If you are a family member in the first degree (parent or sibling) who suffers from prolonged QT syndrome, it’s vital to inform your doctor. Long QT syndrome is a common occurrence in families.
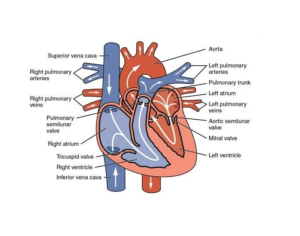
Long QT syndrome is a heart rhythm disorder triggered by heart-related issues with the electrical recharge system. The heart’s structure is normal.
The heart normally sends blood to the body with each heartbeat. The chambers in the heart expand and relax to circulate blood. It is controlled through the cardiac electrical circuit. The electrical signals (impulses) flow between the upper and bottom of your heart to cause it to beat and contract. Following each heartbeat, the heart system recharges itself to prepare for the next heartbeat.
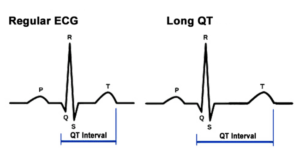
In the case of long QT syndrome, your heart’s electrical system is taking longer than usual to recharge between heart beats. This is the delay that is visible in the electrocardiogram (ECG) is known as an extended QT interval.
Long QT syndrome is usually divided into two types, based on the reason.
- If you’re born with this condition, it’s known as congenital Long QT syndrome. Certain types that are a result of QT syndrome are caused by genetic mutations that are transmitted via the families (inherited).
- If an unrelated medical issue or medication causes it, it’s known as an acquired Long QT Syndrome. This kind of long QT syndrome can be reversed once the root cause has been discovered.
The causes of congenital long QT syndrome
Over 17 genes are associated with the long QT syndrome as of now Researchers have discovered hundreds of mutations in these genes.
Doctors have identified two types of congenital long QT syndrome.
- Romano Ward syndrome (autosomal dominant variant). This more frequent form is found in those who only inherit a single mutation in the gene in one of their parents.
- Jervell as well as Lange-Nielsen Syndrome (autosomal recessive variant). This rare type usually manifests later and can be more serious. In this form, children are born with defective genes that are passed down from their parents. Children have been given the long QT syndrome as well as deafness.
What causes acquired QT syndrome
More than 100 drugs some of which are commonly used may prolong the QT interval in healthy individuals and lead to the development of long QT syndrome.
The medications that may cause long QT syndrome in the acquired form can cause it. These include:
- Certain commonly used antibiotics, like erythromycin (Eryc, Erythrocin, other) azithromycin (Zithromax, Zmax), and others.
- Certain antifungal medications that are administered by mouth can be used in treating yeast infections
- Diuretics that can cause an unbalanced electrolyte (low potassium levels, commonly)
- Heart rhythm medications (especially anti-arrhythmic medicines that increase your QT time)
- Certain antidepressants and antipsychotic drugs
- A few anti-nausea medicines
If your problem is due to medication, it can be referred to as drug-induced long QT syndrome. Be sure to inform your doctor of any medication you are taking and even those you purchase without a prescription.
Other causes of the acquired QT syndrome can be attributed to:
- Low potassium levels (hypokalemia)
- Low calcium levels (hypocalcemia)
- Low magnesium levels (hypomagnesemia)
- COVID-19 infection
Risk factors
Certain factors can increase the risk of developing acquired or congenital long QT syndrome, or its manifestations:
- A previous history of cardiac arrest
- Being a first-degree relative (parent sibling) with the long QT syndrome
- Utilizing medicines that have been proven to prolong QT intervals
- Being a woman and taking heart medication
- Excessive vomiting or diarrhea
- Disorders of eating, like anorexia, can result in electrolyte imbalances
Sexual relations don’t seem to carry a high risk for people suffering from the syndrome of long QT. Pregnancy and birth aren’t associated with a risk increase of developing symptoms in women who have been diagnosed with the syndrome. If you do have the disorder and are pregnant the doctor will be sure to closely monitor you both during and after the pregnancy.
Complications
The right medical treatment and lifestyle modifications can reduce the risk of complications due to long QT syndrome.
Complications of the long QT syndrome can include:
- Torsades de Pointes (‘twisting between the points’). This is a serious form of arrhythmias of the ventricular type. The heart’s lower chambers (ventricles) beat quickly and in a chaotic manner, creating waves in an ECG monitor that look twisted. The heart pumps less blood. The absence of blood supply to the brain can cause your body to collapse suddenly and, in many cases, without warning. If the episode continues for an extended period, the episode of fainting could lead to an entire body seizure. If the risky rhythm is not corrected a life-threatening arrhythmia known as ventricular fibrillation can occur. Other arrhythmias have also been reported.
- Ventricular fibrillation. This condition causes the ventricles to beat at such a rate that the heart quivers and ceases pumping blood. Unless your heart is stimulated back to a normal rhythm using a defibrillator ventricular fibrillation could cause brain injury and death in a flash.
- The sudden death. It’s now known that long QT syndrome may cause sudden death among young people who appear otherwise healthy.
- Unexplained seizures, drownings, faintings or other accidents. Long QT syndrome may be responsible for a number of unsolved deaths of children and young adults.
Prevention
Congenital Long QT syndrome is caused by a genetic mutation. There is no cure. But, with the right care, it is possible to reduce heartbeats that are dangerous and could cause prolonged QT syndrome-related problems.
It is possible to avoid health issues that can cause some forms of long QT syndrome acquired by having regular health checks and regular communication with your physician. It is particularly important to stay clear of medications that could alter your heart rate and lead to a prolongation of that QT-QT interval.
Diagnosis
To identify the long QT syndrome, your physician will conduct a physical examination and will ask questions regarding the symptoms of your child or you and the family and medical history. Your doctor will utilize a stethoscope for listening to your heart.
Electrocardiograms are the most frequently used test to determine the presence of long QT syndrome.
Electrocardiogram (ECG or EKG)
An electrocardiogram is a fast and painless test that captures the electrical signals inside your heart. You could be suffering from an ECG when you are at rest, or at rest or while exercising on a treadmill, while at rest or on a stationary bicycle. If you are unable to safely exercise or rest, you might be offered an epinephrine-based medication (Adrenalin) which stimulates your heart’s activity in a manner like an exercise.
During an ECG the sticky patch (electrodes) can be placed over your chest to capture the electrical signals generated by your heart that trigger your heartbeat. The signals are displayed in waves on a printer or monitor for a computer.
An ECG It is possible to determine if you’re experiencing a prolonged QT. The test categorizes your heart’s electrical signals as five waves with the letters P Q, Q, and S. You can also tell if you are experiencing a prolonged QT interval. The waves that are labelled Q-T indicate the electrical activity that occurs in the lower chambers of your heart (ventricles).
The time between the start of the Q wave to the conclusion of the T-wave is called the QT interval. It takes time for the heart’s muscles to relax and fill with blood prior to beating again.
What’s normal for you is contingent on your age of you, gender, and heart rate. Your doctor will look into this information. If the interval is longer than usual to happen this is known as an extended QT interval.
Remote ECG monitoring
If your lengthy QT symptoms are prone to appear or go away, it might not be able to be spotted during the course of a typical ECG recording. In this instance, your doctor might recommend either continuous or remote ECG monitoring. There are many different kinds of monitoring.
- Holter monitor. A Holter monitor is a tiny, wearable device that captures an ongoing ECG generally for between 24 and 48 hours.
- Event monitor. This portable device is like a Holter monitor, however, it only records at specific dates for a short period at one time. It is possible to wear it for longer than the Holter monitor, but typically for 30 days. It is typically a matter of pressing the button whenever you experience symptoms. Certain devices automatically record the moment an abnormal rhythm is observed.
Genetic testing
A genetic test to determine the cause of long QT syndrome is available and is recommended by numerous physicians to establish the presence of the condition. Contact your insurance company to determine if the test is covered.
It is important to know that tests for genetic causes of long QT syndrome aren’t able to detect all cases of inherited lengthy QT syndrome. It is recommended that families talk to a genetic counsellor prior to and after the test.
If you’ve been able to confirm a DNA test to detect the long QT syndrome, your physician might recommend that any of the other members of your family also test to find out if they have this gene.
Treatment
The treatment for the long QT syndrome includes lifestyle changes as well as medications. It could also involve surgical procedures or other treatments.
The purpose of treatment is to stop irregular heartbeats and sudden deaths. The doctor will go over with you the best treatment options based on the symptoms you are experiencing and the type of QT syndrome. Your doctor may suggest treatments even though you don’t notice any signs or symptoms.
If you are suffering from drug-induced QT syndrome Stopping the medication that causes the symptoms could be the only thing needed to manage the problem. Your physician will be able to tell you how to do this.
In other instances of acquired long QT disorder, treatment of the cause is required. Treatment is different but can include magnesium and other fluids prescribed by IV to balance electrolytes.
Medications
Medicines won’t fix long QT syndrome, However, they can safeguard against potentially life-threatening changes in the heart rhythm.
Treatment options for the long QT syndrome can include:
- Beta blockers. These heart drugs are the most common treatment option for patients suffering from Long QT Syndrome. They reduce heart rate and make lengthy QT incidents less common. Beta-blockers are prescribed in treating QT conditions comprise the nadolol (Corgard) as well as propranolol (Inderal LA, InnoPran XL).
- Mexiletine. Taking this heart rhythm drug in conjunction with a beta-blocker may reduce the QT interval and lower your chance of fainting, seizures, and sudden demise.
Always take the medication prescribed by your physician as directed.
Other procedures or surgeries
Based on your specific symptoms, your physician may look into other QT syndrome treatments that may be appropriate for you, such as:
- left cardiac sympathetic denervation (LCSD) procedure. In this procedure surgeons cut off certain nerves that lie on to the spine’s left inside your chest. These nerves form part of the sympathetic nervous system of your body that helps regulate your heart rate. It is usually reserved for those with a prolonged QT or persistent heart rhythm issues with a high risk of developing symptoms and who are unable to use or tolerate beta blockers. It isn’t a cure for long QT syndrome however it can help lower the risk of sudden death.
- Implantable cardioverter-defibrillator (ICD). An ICS is Implanted under the chest’s skin and constantly detects the heartbeat. It could stop a life-threatening arrhythmia. When it detects an irregular heart rhythm when it detects an irregular heartbeat, it releases electrical shocks that reset the heart to normal. Many people with long QT syndrome don’t require an ICD. However, it can be carried out in athletes in order to allow them to athletes to return to competitive sports. The choice to implant an ICD in particular, in children, should be considered with care. Implanting an ICD is a significant procedure that can cause unintentional shocks or other issues.
Lifestyle and home solutions for home and lifestyle
Alongside recommending medication or surgical procedures, your physician may suggest changes in your lifestyle to decrease your risk of suffering a prolonged QT syndrome-related fainting spell, or sudden heart attack.
- Find out what sports you can play safely. It may be feasible to be fully engaged in sport, including competition, after studying the risks and benefits with your physician. It is generally accepted that those with long QT syndrome shouldn’t swim by themselves. It is likely that recreational activities will be fine if you have a companion in the event of an episode of fainting.
- Conduct a sound test. Turn down the volume on doorbells, as well as others (such as phones) which could wake you, particularly during sleeping.
- Keep your emotions in check. Being very excited or in awe of someone else’s reaction could trigger changes in heart rate in people suffering from long QT syndrome.
- Be sure to check your medications. Avoid drugs that may cause prolonged QT intervals. If you’re not certain, ask your physician. It’s recommended to inform your doctor about every medication and supplement you use, even the ones you purchase without a prescription.
- Check-ups are scheduled regularly. During your appointment make sure to inform your doctor of the modifications in the symptoms you experience or your condition. Your doctor might modify treatments or offer other therapies for you.
Helping to cope and providing support
Being concerned about potentially dangerous heart rhythms that are associated with the long QT syndrome can create stress for both you and your family members. Do your best to aid your loved ones to know how they can support you and help your needs in case of emergency.
- Let other people know. Make family, teachers, friends, and your neighbors, as well as any other person who has frequent contact with you, aware of your heart condition as well as the symptoms. You should wear a health alert ID to inform others about your heart condition.
- Prepare for emergencies. Family members may be interested in learning about cardiopulmonary resuscitation to be able to offer immediate resuscitation in the event that you require it. In certain circumstances, it is appropriate to own or be able to quickly access an automated external defibrillator.
- Find support or counsel. Some people find it beneficial by joining a group in which they can discuss their experiences and emotions with others and their families who are aware of the disorder. Families who have genetically inherited long QT syndrome may consider it beneficial to speak with an expert in genetics.

Wow, fantastic weblog structure! How lengthy have you been blogging for?
you made blogging glance easy. The full look of your site
is magnificent, as neatly as the content! You can see similar here sklep online
Hey there! Do you know if they make any plugins to assist with
SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing
very good gains. If you know of any please share.
Kudos! You can read similar blog here: Najlepszy sklep
It’s very interesting! If you need help, look here: ARA Agency
Good day! Do you know if they make any plugins to assist with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Appreciate it! You can read similar
text here: Sklep internetowy
Good day! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get my blog to rank for some targeted keywords
but I’m not seeing very good gains. If you know of any please
share. Thanks! You can read similar text here: Dobry sklep
Hi there! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to
get my blog to rank for some targeted keywords but I’m not
seeing very good gains. If you know of any please share.
Cheers! I saw similar art here: Scrapebox List
Howdy! Do you know if they make any plugins to
assist with Search Engine Optimization? I’m trying to get my website to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Cheers! I saw
similar art here: Auto Approve List
Hi! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get
my website to rank for some targeted keywords but I’m
not seeing very good gains. If you know of any please share.
Thanks! You can read similar article here: Auto Approve List
Wow, marvelous blog format! How long have you ever been blogging for?
you made running a blog look easy. The whole glance of your site is
magnificent, let alone the content material!
You can see similar here dobry sklep
Your blog is a wealth of information. I always learn something new from your posts. This one was particularly enlightening. Great job!blogpulse
You consistently produce high-quality content that is both informative and enjoyable to read. This post was no exception. Keep it up!pulsepeak
There couple of fascinating points at some point in this posting but I don’t determine if them all center to heart. There may be some validity but I’ll take hold opinion until I investigate it further. Excellent write-up , thanks and that we want much more! Added to FeedBurner also
Many thanks for this particular info I has been checking all Yahoo to come across it!
I just added this weblog to my google reader, great stuff. Cannot get enough!
There are some fascinating closing dates on this article however I don know if I see all of them heart to heart. There’s some validity however I will take maintain opinion till I look into it further. Good article , thanks and we would like more! Added to FeedBurner as properly
Oh my goodness! an incredible article dude. Thank you Nevertheless I’m experiencing subject with ur rss . Don know why Unable to subscribe to it. Is there anyone getting an identical rss downside? Anybody who knows kindly respond. Thnkx
Wow! This can be one particular of the most helpful blogs We’ve ever arrive across on this subject. Actually Excellent. I’m also a specialist in this topic therefore I can understand your effort.
Amazing the following manual is incredible it really helped me and also my children, many thanks!
I was suggested this web site via my cousin. I’m not certain whether this submit is written through him as no one else realize such targeted about my problem. You are incredible! Thank you!
It looks like there exists a trouble with your internet site utilising Opera web browser.
This is actually a good affecting approach to this specific point. Thanks, I’m really happy you shared your thoughts in addition to techniques and I find that i am in agreement. I certainly appreciate your very clear writing additionally , the effort you’ve spent with this posting. A great many thanks for that great work also very good luck with your internet site, I’m awaiting new subjects within the future.
It is in reality a great and useful piece of information. I am happy that you just shared this useful information with us. Please keep us up to date like this. Thanks for sharing.
of course we need to know our family history so that we can share it to our kids“
Some truly howling work on behalf of the owner of this website , dead great subject matter.
I couldn’t resist writing comments. “All successful people men and women are big dreamers. They imagine what their future could be, ideal in every respect, and then they work every day toward their distant vision, that goal or purpose.” by Brian Tracy..
Only a few blogger would discuss this topic the way you do.~::`:
The when I just read a weblog, I am hoping who’s doesnt disappoint me up to brussels. I am talking about, I know it was my substitute for read, but I just thought youd have some thing interesting to express. All I hear is really a handful of whining about something that you could fix when you werent too busy searching for attention.
Thanks for the sensible critique. Me & my neighbor were just preparing to do a little research about this. We got a grab a book from our area library but I think I learned more from this post. I’m very glad to see such fantastic information being shared freely out there.
Hey this can be a great looking site, is wordpress? Forgive me for the dumb question – but if so, what theme is? Thanks!
Utterly written articles , Really enjoyed looking at .
“Quality is everything, so we need to ensure that there are values on what we are sharing to keep our subscribers interested. ” CHECK THIS
I was really lucky to find this internet site on bing, just what I was searching for : D likewise saved to favorites .
A formidable share, I just given this onto a colleague who was doing a bit of analysis on this. And he the truth is bought me breakfast because I discovered it for him.. smile. So let me reword that: Thnx for the treat! But yeah Thnkx for spending the time to debate this, I feel strongly about it and love reading more on this topic. If doable, as you turn into expertise, would you thoughts updating your weblog with more details? It’s extremely helpful for me. Massive thumb up for this weblog submit!
Spot on with this write-up, I must say i believe this excellent website needs much more consideration. I’ll probably be once again to learn a great deal more, many thanks that information.
Hey! I know this is kinda off topic however , I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog post or vice-versa? My blog covers a lot of the same topics as yours and I believe we could greatly benefit from each other. If you are interested feel free to send me an e-mail. I look forward to hearing from you! Superb blog by the way!
wide-web website together with your website will undoubtedly be one in every of my fresh favorite types. I’m keen on this amazing website given and has now
I loved as much as you’ll receive carried out right here. The sketch is attractive, your authored subject matter stylish. nonetheless, you command get bought an impatience over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly a lot often inside case you shield this increase.
fapturbo review Hello! I just want to make a large thumbs up for the fantastic info you’ve here on this post. I’ll be returning to your site to get more detailed soon.
Hi there! I know this is kind of off topic but I was wondering if you knew where I could locate a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having trouble finding one? Thanks a lot!
There are extremely a great deal of details that way to think about. That is a fantastic denote talk about. I provide thoughts above as general inspiration but clearly there are actually questions such as the one you talk about in which the most essential thing will be in honest very good faith. I don?t determine if best practices have emerged about items like that, but I am sure that your chosen job is clearly known as a fair game. Both youngsters feel the impact of merely a moment’s pleasure, for the remainder of their lives.
I have a question that is kind of related. What is the easiest way to get high volume keywords? Best!
I’d have to talk with you here. Which isn’t something I usually do! I spend time reading a post which will get people to believe. Also, many thanks for allowing me to comment!
As I web site possessor I believe the content material here is rattling magnificent , appreciate it for your hard work. You should keep it up forever! Good Luck.
investing is tricky, sometimes you win and sometimes you loss. Risk takers win of course”
we have collectibles at home that we display in our living room. they are quite nice,
Good day! This post could not be written any better! Reading this post reminds me of my good old room mate! He always kept chatting about this. I will forward this page to him. Fairly certain he will have a good read. Thank you for sharing!
I think so. I think your article will give those people a good reminding. And they will express thanks to you later
Oh my goodness! an excellent post dude. Many thanks However We are experiencing problem with ur rss . Don’t know why Not able to sign up to it. Could there be anybody getting identical rss dilemma? Anyone who knows kindly respond. Thnkx
I have been exploring for a little for any high quality articles or blog posts on this kind of area . Exploring in Yahoo I at last stumbled upon this web site. Reading this info So i’m happy to convey that I have an incredibly good uncanny feeling I discovered exactly what I needed. I most certainly will make certain to do not forget this site and give it a glance on a constant basis.
There are a handful of intriguing points with time here but I do not know if I see these people center to heart. There is certainly some validity but I’ll take hold opinion until I take a look at it further. Good post , thanks and we want a lot more! Added to FeedBurner also
I like what you guys are creating here. Such smart work and writing! Carry on with the superb works guys. I have incorporated your site into my blogroll and my website about HCG. I think it will improve the value of my websiteand the traffic too.
The following the five information you should do remember so you can manage to produce your particular successful world-wide-web. survey reviews
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get several e-mails with the same comment. Is there any way you can remove me from that service? Cheers!
Hey! Do you know if they make any plugins to assist with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Kudos! I saw similar blog here: Choose escape room
I feel that is among the so much important info for me. And i’m satisfied studying your article. However wanna commentary on some normal things, The site taste is ideal, the articles is actually nice . Good task, cheers.
very good put up, i definitely love this web site, keep on it
We are a group of volunteers and starting a new scheme in our community. Your website provided us with valuable info to work on. You’ve done a formidable job and our whole community will be thankful to you.
You have noted very interesting details ! ps nice site.
whoah this weblog is excellent i love reading your articles. Stay up the good paintings! You already know, lots of persons are looking round for this info, you can aid them greatly.
Individuals are often shedding desire or even squandering the occasion by means of getting a best condo they will have because they lack knowledge or ideas on where to locate these types of qualities immediately.
LCD TVs can really save you from high electricity bills and office space*
Can I just say what a relief to find someone who really is aware of what theyre speaking about on the internet. You undoubtedly know methods to carry a problem to gentle and make it important. Extra people must learn this and understand this aspect of the story. I cant imagine youre not more widespread because you positively have the gift.
Yo!. Certainly liked reading your post. It was very informative and helpful. I hope you do not mind me blogging concerning this post on my personal blog. Will definitely link back to you. Nice site theme! Salamat.
I’d should talk to you here. Which is not some thing I do! I quite like reading a post which will make people believe. Also, many thanks permitting me to comment!
I just have my browsers (Firefox and Opera) start from where they left off, ie with all the tabs as I left them.
Cheap Handbags Wholesale You should think about doing growing this web site to a major authority in this particular market. You clearly contain a grasp handle in the topics so many people are looking for on this website anyways therefore you could indisputably even create a dollar or two off of some advertising. I’d explore following recent topics and raising how many write ups putting up and i guarantee you???d begin seeing some awesome web traffic in the near future. Simply a thought, all the best in whatever you do!
There is perceptibly a lot to identify about this. I believe you made various good points in features also.
You’re the best, wonderful blog… really enjoy it and put into my social bookmarks. Keep up the good work
Attention ! I just found an error in your article! Check if your theme is set right!
The next occasion I just read a blog, Hopefully which it doesnt disappoint me about this one. I mean, Yes, it was my option to read, but I just thought youd have something intriguing to say. All I hear is a lot of whining about something you could fix in the event you werent too busy in search of attention.
When I originally commented I clicked the -Notify me when new comments are added- checkbox and now each time a comment is added I receive four emails with the same comment. Can there be however you possibly can get rid of me from that service? Thanks!
we cant think courtney cox as well as donald arquette are getting a divorce! they were with each other with regard to Eleven years!
I was very pleased to discover this page. I wanted to thank you for ones time for this fantastic read!! I definitely enjoyed every part of it and I have you book marked to check out new information on your web site.
Glad to be one of many visitants on this awing web site : D.
Nice post , this is my first time i read this blog and i found it very interesting , nice job .
There is noticeably big money to comprehend this. I assume you have made particular nice points in features also.
I’d should consult you here. Which is not some thing I usually do! I spend time reading an article that should get people to feel. Also, thanks for allowing me to comment!
forty people that work with all the services Oasis provides, and he is a very busy man, he
light and make it fundamental. More many people really need to read this and have an understanding of this side of the story. I cant believe youre not more
The next time I read a weblog, I really hope who’s doesnt disappoint me approximately this one. I mean, I know it was my choice to read, but When i thought youd have something intriguing to convey. All I hear is really a few whining about something that you could fix if you werent too busy searching for attention.
Incredible this kind of guideline is incredible it truly helped me and also my family, cheers!
You lost me, friend. What i’m saying is, I imagine I am what youre saying. I am aware what you’re saying, however, you just appear to have forgotten that might be another folks inside the world who view this issue for which it truly is and may even perhaps not go along with you. You may well be turning away many people that may have been lovers of your website.
I found your article very thought provoking. The way it was written made me look at things from a different angle and think about what I originaly thought, why not visit us .I will definately be back again.
You’ll notice several contrasting points from New york Weight reduction eating plan and every one one may be useful. The first point will probably be authentic relinquishing on this excessive. lose weight
I like what you guys are up also. Such smart work and reporting! Keep up the superb works guys I’ve incorporated you guys to my blogroll. I think it will improve the value of my website .
This web-site is actually a walk-through rather than the data you wanted with this and didn’t know who need to. Glimpse here, and you’ll definitely discover it.
I am curious to find out what blog platform you happen to be working with? I’m experiencing some minor security problems with my latest blog and I would like to find something more secure. Do you have any recommendations?
Great story it is definitely. My girlfriend has been awaiting for this information.
Optimal humanity messages, because toasts. are hands down sent out certain times in the evening reception and therefore are supposed to end entertaining, amusing furthermore useful what’s more. best man speaches
Hi, have you ever pondered to write regarding Nintendo Dsi handheld?
Not sure about this text. It seems to be all right, but something is missing
That put up appears to be get numerous website visitors. Will you support it? That it offers a sweet specific forget on the subject of problems. Man enduring one thing accurate and / or maybe a lot of to deliver facts about is essential task.
there are many bargain priced home-for-sale in our city, i was considering buying one.
This site is usually a walk-through you discover the details you wished with this and didn’t know who must. Glimpse here, and you’ll absolutely discover it.
Many thanks taking a few minutes to discuss this unique, I find myself passionately with this and also adoration looking over on that problem. Just in case likely, since complete specialist knowledge, on earth would you feelings modernizing your main internet page along with other facts? This is very helpful for me.
Nice post. I discover something very complicated on different blogs everyday. It will always be stimulating to study content from other writers and rehearse something there. I’d want to apply certain using the content on my small weblog regardless of whether you don’t mind. Natually I’ll supply you with a link for your internet weblog. Appreciate your sharing.
You should be a part of a contest for just one of the best blogs on the net. I’ll recommend this website!
Fabulous piece of writing! Genuinely savored often the examining. I hope to study significantly more away from you. In my opinion you may have amazing information and even imaginative and prescient vision. I’m greatly fascinated this particular answers.
Hi, do you have a facebook fan page for your blog?.~”-~
Great post, you have pointed out some great points, I besides believe this is a very wonderful website.
you have a very excellent weblog here! if you’d like to earn some invite posts in my small blog?
Nice post. I learn something tougher on different blogs everyday. Most commonly it is stimulating to learn to read content using their company writers and exercise a specific thing there. I’d would rather use some with all the content on my own blog regardless of whether you don’t mind. Natually I’ll provide a link in your web weblog. Thank you for sharing.
in China, they do not respect intellectual property at all. too many software and movie pirates out there`
Everything is very open with a clear clarification of the challenges. It was definitely informative. Your site is very useful. Many thanks for sharing!
With the amount of money being spent on addiction you would think there would be a cure. Just the time lost at work should be sufficient enough to get this thing fixed. drugs addictions
i love funny stuffs, but i specially like funny movies and funny videos on the internet..
It was virtually any exhilaration discovering your website yesterday. I came here today searching new things. I was definitely not frustrated. Your ideas following fresh techniques with this thing happen to be useful additionally a good outstanding help individually. All of us value you leaving out time for you to create these products and also for uncovering your ideas.
I merely picked up your blog post a couple weeks ago i have actually been perusing this tool always. An individual has a lot of helpful tips at this point we absolutely love your lifestyle of a internet sites actually. Stick to the nice perform!
As far as me being a member here, I wasn’t aware that I was a member for any days, actually. When the article was published I received a username and password, so that I could participate in Comments, That would explain me stumbuling upon this post. But we’re certainly all members in the world of ideas.
Your blog never ceases to amaze me, it is very well written and organized.~*:`-
Can I say thats a relief to discover a person that actually knows what theyre discussing on the web. You definitely have learned to bring a problem to light and earn it important. More and more people need to look at this and appreciate this side of the story. I cant believe youre less common as you definitely contain the gift.
Enjoyed looking at this, very good stuff, thanks .
One thing I’d really like to comment on is that fat reduction plan fast is possible by the correct diet and exercise. Your size not merely affects appearance, but also the overall quality of life. Self-esteem, depressive disorder, health risks, along with physical capabilities are affected in excess weight. It is possible to do everything right and at the same time having a gain. If this happens, a condition may be the reason. While a lot food but not enough workout are usually accountable, common health concerns and traditionally used prescriptions may greatly increase size. Kudos for your post in this article.
The greatest tribute to Roy’s skill and a sign of his attention to the human side of things is that he gets her to the wedding, after a few car explosions and chases and dozens of dead bodies.
Dead pent subject material , Really enjoyed examining .
Some genuinely terrific work on behalf of the owner of this site, absolutely great written content .
A few things i have constantly told people is that when searching for a good on-line electronics retail outlet, there are a few variables that you have to remember to consider. First and foremost, you need to make sure to choose a reputable as well as reliable retail store that has got great opinions and scores from other shoppers and business world professionals. This will make sure that you are getting along with a well-known store that can offer good assistance and assistance to their patrons. Thank you for sharing your notions on this weblog.
hi. I observe that you’re most likely interested in generating quality backlinks and stuff. I’m promoting scrapebox auto approve link lists. Do you want to trade ?
To say that I like Tom Cruise personally would be a lie, but dammit, he makes entertaining films.
i like wireless internet because you can surf anywhere and you can avoid those ethernet cables,
wireless routers are very necessary nowadays because we do not want so many wires running around the home*
Thank you for the sensible critique. Me & my friend were just preparing to do a little research about this. We got a book from our area library but I think I learned better from this post. I am very glad to see such wonderful info being shared freely out there…
When I originally commented I clicked the -Notify me when new surveys are added- checkbox and from now on whenever a comment is added I purchase four emails sticking with the same comment. Perhaps there is by any means you may get rid of me from that service? Thanks!
When I originally commented I clicked the -Notify me when new surveys are added- checkbox and from now on every time a comment is added I am four emails using the same comment. Is there however it is possible to eliminate me from that service? Thanks!
I had been honored to receive a call from my friend as soon as he found out the important tips shared on your own site. Studying your blog publication is a real excellent experience. Thanks again for taking into account readers at all like me, and I want for you the best of success as being a professional topic.
Some truly wonderful work on behalf of the owner of this web site , perfectly great content .
I needed to say thanks a lot just as before wrist watches dazzling web-site you can have written reading this. It will be jam-packed with smart ideas if you’re contemplating the following make any difference, mainly this type of really quite article. You’re in fact every single one fully fantastic a great bonus accommodating coming from all blog writers for a few incontrovertible fact result your blog site comments is a fantastic pleasure when camping. Also good job on a substantial current! Serta and have hype in your inspirations in doing what came across get in most calendar months. Our new home listing should be a extended distance particularly long together with thoughts rrs going to be offer ideal purposes.
I truly appreciate this post. I have been looking all over for this! Thank goodness I found it on Bing. You have made my day! Thx again
Even though We came up through this web site, My partner and i remarked that not merely can be my own computer not necessarily demonstrating the particular Feed correct though the one inch the kitchen at home is just too… Oh as well as webe gas grills master
Free games… […]Do you mind if I quote a few of your articles as long as I provide credit and sources back to your website? My blog is in the exact same area of interest as yours and my visitors would truly benefit from a lot of the information you present here. …
I really like your writing style, excellent information, appreciate it for putting up : D.
You are so awesome! I do not think I’ve truly read through a single thing like that before. So nice to discover somebody with unique thoughts on this topic. Really.. many thanks for starting this up. This website is one thing that’s needed on the web, someone with a little originality.
This blog was… how do I say it? Relevant!! Finally I have found something that helped me. Many thanks!
Right here is the right site for anyone who hopes to understand this topic. You know so much its almost tough to argue with you (not that I personally will need to…HaHa). You certainly put a brand new spin on a subject that’s been discussed for ages. Wonderful stuff, just great.
Hello, I do think your blog might be having internet browser compatibility problems. Whenever I take a look at your website in Safari, it looks fine but when opening in Internet Explorer, it’s got some overlapping issues. I merely wanted to give you a quick heads up! Other than that, wonderful site!
Good day! Do you know if they make any plugins to help with Search
Engine Optimization? I’m trying to get my blog to rank for some
targeted keywords but I’m not seeing very good success.
If you know of any please share. Cheers! I saw similar text here
An interesting discussion is value comment. I believe that it’s best to write extra on this subject, it may not be a taboo topic but usually individuals are not sufficient to speak on such topics. To the next. Cheers
The Zune concentrates on being a Portable Media Player. Not a web browser. Not a game machine. Maybe in the future it’ll do even better in those areas, but for now it’s a fantastic way to organize and listen to your music and videos, and is without peer in that regard. The iPod’s strengths are its web browsing and apps. If those sound more compelling, perhaps it is your best choice.
I really like your writing style, wonderful information, thankyou for posting : D.
Folks have no idea that this exists. I know this must be here but I eventually got lucky and the search phrases worked. You’ve contributed to my exploration in your posting.
Great info. Lucky me I found your website by accident (stumbleupon). I have book-marked it for later!
I think one of your advertisings caused my browser to resize, you might want to put that on your blacklist.
‘Thank you for this blog. That’s all I can say. You most definitely have made this blog into something that’s eye opening and important. You clearly know so much about the subject, youve covered so many bases. Great stuff from this part of the internet. Again, thank you for this blog.”
When I originally commented I clicked the -Notify me when new surveys are added- checkbox and after this every time a comment is added I recieve four emails using the same comment. Could there be in whatever way you may eliminate me from that service? Thanks!
I simply wanted to appreciate you again. I’m not certain the things that I might have sorted out without these tips revealed by you relating to such subject. It absolutely was a distressing situation in my circumstances, however , coming across the well-written tactic you handled that took me to leap for fulfillment. Now i’m thankful for your information as well as trust you recognize what a great job you are undertaking instructing the mediocre ones via your websites. More than likely you haven’t encountered any of us.
Oh my goodness! Incredible article dude! Thank you so much, However I am experiencing difficulties with your RSS. I don’t know the reason why I cannot join it. Is there anybody else getting similar RSS issues? Anybody who knows the answer will you kindly respond? Thanx!!
There is noticeably a lot of money to know about this. I suppose you made particular nice points in functions also.
Hi there, just became aware of your blog through Google, and found that it’s truly informative. I’ll be grateful if you continue this in future. Lots of people will benefit from your writing. Cheers!
howdy, I’ve been havin a tough time attempting to rank well for the words “victorias secret coupon codes”… Pls approve my comment!!
That is certainly when I commenced contemplating learn how to do anything at once. I commenced rearranging facts on my blog in order to provide my loyal guests the capability to comment and obtain do-follow backlinks and virtually remove all of the automated comment posting as soon as and for all.
I see your site on google. I searching something about research statistic and I find it in your site. Thank a lot.
Having read this I thought it was really enlightening. I appreciate you spending some time and energy to put this information together. I once again find myself spending a significant amount of time both reading and leaving comments. But so what, it was still worthwhile!
I never let this go…….But i can’t find the words to tell you|Angiie_Rockss|
finance is really critical when it comes to the future of businesses and trade. i also took finance during my college days”
“Cold Case” is definitely one of the best detective tv shows that you can watch on TV. the story is great“
Oh my goodness! an excellent article dude. Thank you Nonetheless We’re experiencing problem with ur rss . Do not know why Not able to register for it. Could there be everyone getting identical rss problem? Anybody who knows kindly respond. Thnkx
Associations are typically powerful. Custom made is in fact extraordinarily vital, in addition to alter arrives rarely along with slowly. There’s pretty smaller division linked with job in to distinct responsibilities. As an alternative, every particular person is in fact very likely to execute a terrific number of duties, whilst duties differs somewhere between your genders.
Incredible! This blog looks exactly like my old one! It’s on a totally different subject but it has pretty much the same layout and design. Excellent choice of colors!
Nice post. I find out some thing very complicated on diverse blogs everyday. Most commonly it is stimulating to see content from other writers and employ a little something at their store. I’d choose to use some while using the content in my small blog no matter whether you don’t mind. Natually I’ll supply you with a link on your web blog. Many thanks for sharing.
I was on Google looking for bulk shirts activewear forum, when I found a link to this blog, glad I stopped by!!! Thanks!!!!
Greetings, Can I grab that photo and implement that on my blog?
I like the helpful info you provide in your articles. I’ll bookmark your weblog and check again here regularly. I’m quite sure I will learn plenty of new stuff right here! Good luck for the next!
there are many hobbies out there but there is no other hobby like fishing, fishing is every enjoyable.
I wanted to thank you for this great read!! I definitely enjoying every little bit of it I have you bookmarked to check out new stuff you post…
I enjoyed reading your pleasant website. I see you offer priceless info. stumbled into this website by chance but I’m sure glad I clicked on that link. You definitely answered all the questions I’ve been dying to answer for some time now. Will definitely come back for more of this.
A fascinating discussion is definitely worth comment. I do believe that you ought to write more about this issue, it may not be a taboo subject but generally folks don’t talk about such topics. To the next! Cheers!
Can I merely say such a relief to find a person that actually knows what theyre speaking about over the internet. You definitely have learned to bring a challenge to light to make it essential. Lots more people need to check out this and appreciate this side on the story. I cant believe youre not more popular because you definitely have the gift.
I always visit new blog everyday and i found your blog.*~~;~
Bardzo pouczający blog na temat SEO! Dzięki za podzielenie się nim.
This design is steller! You obviously know how to keep a reader amused. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Excellent job. I really loved what you had to say, and more than that, how you presented it. Too cool!
Ten blog to cenne źródło informacji dla każdego, kto myśli o SEO.
Dzięki za szczegółowy przewodnik po tym, czego można oczekiwać podczas wdrażania SEO.
Great article. I will be experiencing a few of these issues as well..
Dziękuję za podkreślenie znaczenia profesjonalnego podejścia do SEO.
Bardzo pouczający blog na temat SEO! Dzięki za podzielenie się nim.
Ten blog bardzo mi pomógł w zrozumieniu potrzeby SEO.
Ten blog dostarczył mi dużo jasności na temat SEO. Dzięki!
Doceniam nacisk na bezpieczeństwo i profesjonalizm w SEO.
Dzięki za krok po kroku wyjaśnienie procesu SEO.
Świetne wskazówki dotyczące znalezienia wiarygodnych usług SEO. Dzięki!
Ten blog to cenne źródło informacji dla każdego, kto myśli o SEO.
Dzięki za szczegółowy przegląd procedur SEO.
Dzięki za świetne porady na temat SEO. Bezpieczeństwo jest kluczowe!
Doceniam skupienie się na ochronie zdrowia i bezpieczeństwa podczas SEO.
Bardzo pouczające. Na pewno będę monitorować SEO mojej strony.
SEO wydaje się trudne, ale Twój blog sprawia, że staje się bardziej zrozumiałe. Dzięki!
Cieszę się, że natrafiłem na ten blog przed rozpoczęciem jakichkolwiek działań SEO.
Great paintings! That is the type of info that are meant to be shared around the web. Shame on Google for no longer positioning this submit higher! Come on over and seek advice from my site . Thanks =)
Can I take part of your post to my blog
I simply could not go away your website prior to suggesting that I really loved the standard information an individual provide for your visitors? Is going to be again ceaselessly to investigate cross-check new posts
I’ve recently been wondering about the very same point myself recently. Happy to see someone on the same wavelength! Nice article.
I like this website because so much utile stuff on here : D.
I like what you guys are up also. Such clever work and reporting! Carry on the excellent works guys I have incorporated you guys to my blogroll. I think it will improve the value of my website rentacar kosovo
As far as me being a member here, I wasn’t aware that I was a member for any days, actually. When the article was published I received a notification, so that I could participate in the discussion of the post, That would explain me stumbuling upon this post. But we’re certainly all members in the world of ideas.
My friend sent me here and I thought I’d say hi, great blog.
You made some decent points there. I looked over the internet for the issue and found most people will go in addition to with your website.
There is noticeably a bundle to comprehend this. I assume you’ve made specific nice points in functions also.
Magnificent beat ! I would like to apprentice while you amend your site, how can i subscribe for a blog site? The account aided me a applicable deal. I had been a little bit acquainted of this your broadcast provided bright clear concept.
Labor party talking heads are on claiming the meeja is agin’ them.
you can always say that Dan Aykroyd is a very talented actor and a nice comedian.,
This design is wicked! You definitely know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Excellent job. I really loved what you had to say, and more than that, how you presented it. Too cool!
You should take part in a contest for one of the best blogs on the web. I will recommend this site!
I your writing style really enjoying this site.
A well written post, I just given this onto a colleague who was doing slightly analysis on that. And he indeed purchased me breakfast because I discovered it for him .. thus let me reword that: Thankx for the treat! however yeah Thnx for spending the time to talk concerning this, I feel strongly concerning it and revel in reading a lot of on this topic. If potential, as you become expertise, would you mind updating your blog with a lot of info? it’s very useful on behalf of me. two thumb up for this blog!
Hi there, I just stumbled your blog and wanted to say that I’ve truly enjoyed browsing your blog posts. After all I’ll be subscribing to your feed and I hope you write again very soon!
dj equipments that are built by Sennheiser are the best in my opinion, we always use them when we have a gig.,
You’re the best, I was doing a google search and your site came up for bank owned homes in Winter Springs, FL but anyway, I have had a pleasant time reading it, keep it up!
Thank you for sharing with us, I think this website truly stands out : D.
You should join in a contest first of the greatest blogs on the web. I will recommend this web site!
Hey – nice blog, just wanting around some blogs, seems a reasonably nice platform You Are using. I’m presently using Drupal for a couple of of my sites but looking to change one in every of them over to a platform very a lot the identical to yours as a trial run. Anything specifically you’d recommend about it?
Spot lets start work on this write-up, I actually believe this site needs much more consideration. I’ll apt to be once again to read a lot more, many thanks that info.
I’m not positive the place you are getting your information, but great topic. I needs to spend a while finding out much more or understanding more. Thank you for excellent information I was looking for this information for my mission.
This will be the proper blog if you hopes to discover this topic. You already know a lot its practically difficult to argue on hand (not that I actually would want…HaHa). You certainly put a whole new spin over a topic thats been written about for a long time. Wonderful stuff, just wonderful!
Hiya, I’m really glad I’ve found this information. Nowadays bloggers publish only about gossips and net and this is actually frustrating. A good web site with interesting content, that’s what I need. Thanks for keeping this web-site, I will be visiting it. Do you do newsletters? Can’t find it.
I have been exploring for a little bit for any high quality articles or weblog posts in this kind of area . Exploring in Yahoo I finally stumbled upon this web site. Studying this information So i am glad to express that I’ve a very good uncanny feeling I discovered exactly what I needed. I most certainly will make certain to do not fail to remember this web site and provides it a glance regularly.
The thing i like about your blog is that you always post direct to the point info.~’”**
construction jobs are on the rise again these days because the recession is almost over**
for kitchen knife, i would always use ceramic kitchen knifes because they are sharper and tougher than steel knifes.,
I love reading your blog because it has very interesting topics.:.:~’
As I web site possessor I believe the content material here is rattling magnificent , appreciate it for your hard work. You should keep it up forever! Good Luck.
Excellent blog here! Also your web site loads up fast! What host are you using? Can I get your affiliate link to your host? I wish my web site loaded up as fast as yours lol
Okay, Let’s Say I’m An Eighteen Old Country Boy Living On A Farm Looking For A Great Way To Make Money Online?: An
I’ve been with the entire content of this weblog that’s extremely educational and educated stuff”
I conceive you have mentioned some very interesting points , appreciate it for the post.
I know this really is genuinely dull and you’re missing to another comment, but I merely desired to toss a large thank you — a person resolved the main things individually!
Really great info. I’m very happy to read this article. Thanks for sharing us nice articles.
I’m sure there is a downside to your web blog making use of Safari internet browser.
Howdy! I just wish to give an enormous thumbs up for the great information you have got right here on this post. I can be coming again to your weblog for extra soon.
I have been reading out many of your articles and i must say pretty good stuff. I will surely bookmark your site
I like the efforts you have put in this, thanks for all the great blog posts.
An intriguing discussion might be priced at comment. I do believe you should write much more about this topic, it will not be considered a taboo subject but usually people are there are not enough to talk on such topics. To the next. Cheers
I am not able to view this particular internet site properly on opera I really feel there is certainly an issue
hi, I’m having bad luck attempting to rank high for the words “victorias secret coupon codes”… Please approve my comment!!
Perfect work you have done, this web site is really cool with good information.
Thank you for taking the time to discuss the idea, I find myself intently with it and additionally real love looking at more about this kind of theme. In the event capability, mainly because you arrive at mastery, on earth do you insights upgrading your primary webpage utilizing indepth important info? This is useful for all of us.
It’s perfect time to make some plans for the future and it is time to be happy. I’ve read this post and if I could I wish to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I want to read more things about it!
I feel very lucky to have encountered your web page and look forward to tons of more brilliant times reading here. Thank you again for all the details.
Thank you, I have recently been searching for info approximately this topic for ages and yours is the greatest I’ve came upon till now. But, what concerning the bottom line? Are you certain concerning the supply?
This internet site is often a walk-through its the details you wanted in regards to this and didn’t know who to ask. Glimpse here, and you’ll undoubtedly discover it.
I think you have remarked some very interesting details , appreciate it for the post.
the TV Stands that i bought online is made of lighweight aluminum, i like aluminum because it can be anodized**
Fantastic guide! Chatting about how treasured the entire digesting. I hope to learn from way more away from you. I know you’ve awesome look and additionally view. I happen to be very much contented using data.
I really like your blog.. very nice colors & theme. Did you make this website yourself or did you hire someone to do it for you? Plz reply as I’m looking to design my own blog and would like to find out where u got this from. cheers
Being grateful for for your post. I know that throughout today’s complicated world, folks have many beliefs and this has made it to be very difficult for learners much like me. However, you have made it very easy for me to fully grasp and I now have in mind the correct thing. Your continued reputation as one of the top experts on this topic may be increased through words with appreciation from visitors like me. Thanks, again.
when i was a kid, i love to receive an assortment of birthday presents like teddy bears and mechanical toys,
It¡¦s really a cool and useful piece of information. I¡¦m satisfied that you shared this useful information with us. Please keep us up to date like this. Thank you for sharing. Pristina Travel
에볼루션 파싱알
Pretty nice post, thanks for the awesome article. I’m having troubles subscribing to your blogs feed. Thought I’d let you know
This is a good tip especially to those fresh to the blogosphere. Simple but very precise info… Appreciate your sharing this one. A must read post!
After I originally commented I appear to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I receive 4 emails with the exact same comment. Perhaps there is a way you can remove me from that service? Thanks a lot.
This website was… how do I say it? Relevant!! Finally I have found something that helped me. Kudos!
Good information. Lucky me I ran across your website by accident (stumbleupon). I have bookmarked it for later.
Hello! I could have sworn I’ve been to this web site before but after looking at a few of the posts I realized it’s new to me. Regardless, I’m definitely delighted I stumbled upon it and I’ll be bookmarking it and checking back regularly.
This is a great tip especially to those new to the blogosphere. Simple but very precise information… Thanks for sharing this one. A must read post!
Your style is really unique in comparison to other folks I have read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I’ll just bookmark this blog.
I resonate deeply with your conclusions.대출 이자 계산기
Your approach is refreshing.대학생 대출
This is exactly the kind of discussion we need.프라그마틱 무료게임
Greetings! Very helpful advice within this post! It is the little changes that make the greatest changes. Many thanks for sharing!
I really like looking through a post that will make men and women think. Also, thanks for permitting me to comment.
I love reading through an article that can make men and women think. Also, thanks for allowing for me to comment.
Wonderful article! We are linking to this great post on our website. Keep up the great writing.
Howdy! I simply would like to offer you a big thumbs up for the excellent information you have got right here on this post. I am coming back to your blog for more soon.
I am always thought about this, appreciate it for putting up.
Way cool! Some very valid points! I appreciate you penning this post plus the rest of the website is extremely good.
hi there, your website is discount. Me thank you for do the job
You created some decent points there. I looked online for your issue and located most people go along with together with your web site.
Yikes this definitely takes me back, i’ve been wondering about this subject for a while.
Saved as a favorite, I love your blog.
Some genuinely interesting info , well written and broadly speaking user pleasant.
Couldn´t be written any kind of far better. Reading this post reminds me of my old room mate! He always kept talking about this. I can forward that article to him. Extremely sure he definitely will possess a excellent read. Thanks for sharing!
The facts on your blog site is seriously informative and good, it served me to clear up my problem and responses are also handy. Men you can go by means of this blog site and it helps you a ton.
Exceptional content! I absolutely demonstrated a going through. I’m hoping to learn to read added away from you. There’s no doubt you’ll have beneficial awareness not to mention dream. My group is seriously pleased just for this important info.
Very good info. Lucky me I recently found your site by chance (stumbleupon). I’ve book marked it for later.
I am usually to blogging and i actually appreciate your site content. This great article has truly peaks my interest. I will bookmark your internet site and keep checking for first time details.
Spot on with this write-up, I really believe that this site needs much more attention. I’ll probably be returning to read more, thanks for the advice.
An impressive share! I have just forwarded this onto a co-worker who has been doing a little research on this. And he in fact ordered me lunch because I discovered it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanx for spending some time to talk about this issue here on your internet site.
Pretty! This has been an extremely wonderful article. Thanks for providing this info.
When I originally left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I recieve 4 emails with the exact same comment. Is there a means you can remove me from that service? Many thanks.
I’m very pleased to uncover this web site. I want to to thank you for your time just for this wonderful read!! I definitely savored every bit of it and i also have you bookmarked to see new information on your web site.
Greetings! Very helpful advice within this article! It is the little changes that produce the greatest changes. Thanks for sharing!
I wanted to thank you for this good read!! I definitely loved every bit of it. I have you bookmarked to check out new things you post…
After I initially left a comment I seem to have clicked on the -Notify me when new comments are added- checkbox and now whenever a comment is added I get 4 emails with the same comment. Perhaps there is a means you are able to remove me from that service? Thanks a lot.
https://artdaily.com/news/171650/Mp3Juice-Review–The-Pros-and-Cons-You-Need-to-Know
Hi, I do believe this is a great site. I stumbledupon it 😉 I will revisit yet again since I bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to help other people.
Your style is very unique in comparison to other people I have read stuff from. Thanks for posting when you’ve got the opportunity, Guess I will just bookmark this site.
Good day! I could have sworn I’ve been to your blog before but after browsing through a few of the articles I realized it’s new to me. Anyhow, I’m certainly happy I stumbled upon it and I’ll be bookmarking it and checking back frequently!
It’s hard to come by educated people for this topic, but you seem like you know what you’re talking about! Thanks
I was excited to discover this page. I need to to thank you for ones time just for this fantastic read!! I definitely savored every little bit of it and I have you saved as a favorite to see new stuff on your web site.
You made some really good points there. I checked on the web to find out more about the issue and found most people will go along with your views on this web site.
Hello there! This article couldn’t be written much better! Reading through this post reminds me of my previous roommate! He constantly kept talking about this. I most certainly will forward this article to him. Pretty sure he’s going to have a good read. Thank you for sharing!
Good post. I learn something totally new and challenging on sites I stumbleupon every day. It will always be helpful to read articles from other writers and practice a little something from other sites.
There’s certainly a lot to learn about this issue. I like all the points you’ve made.
You have made some decent points there. I checked on the internet to find out more about the issue and found most people will go along with your views on this website.
That is a really good tip particularly to those new to the blogosphere. Simple but very precise information… Many thanks for sharing this one. A must read post!
I blog often and I genuinely thank you for your content. Your article has really peaked my interest. I am going to bookmark your site and keep checking for new details about once per week. I opted in for your RSS feed as well.
You have made some decent points there. I checked on the net to learn more about the issue and found most people will go along with your views on this site.
Everything is very open with a clear explanation of the issues. It was truly informative. Your website is very helpful. Thanks for sharing.
It’s hard to find educated people on this topic, however, you sound like you know what you’re talking about! Thanks
This blog was… how do I say it? Relevant!! Finally I have found something that helped me. Cheers!
The next time I read a blog, Hopefully it does not disappoint me just as much as this one. I mean, Yes, it was my choice to read, however I actually believed you’d have something helpful to talk about. All I hear is a bunch of complaining about something you can fix if you were not too busy seeking attention.
Right here is the perfect webpage for everyone who wishes to find out about this topic. You realize so much its almost hard to argue with you (not that I really will need to…HaHa). You definitely put a new spin on a subject that’s been written about for ages. Great stuff, just excellent.
Very nice blog post. I absolutely appreciate this website. Stick with it!
I could not refrain from commenting. Exceptionally well written.
Good post! We will be linking to this great article on our site. Keep up the great writing.
You are so interesting! I do not suppose I’ve read through anything like this before. So nice to discover somebody with genuine thoughts on this issue. Seriously.. thanks for starting this up. This web site is one thing that is required on the internet, someone with some originality.
There is certainly a lot to know about this topic. I love all the points you made.
Very good info. Lucky me I recently found your website by accident (stumbleupon). I’ve saved as a favorite for later.
Hi, I do think this is a great blog. I stumbledupon it 😉 I am going to revisit yet again since I saved as a favorite it. Money and freedom is the best way to change, may you be rich and continue to help other people.
I like it whenever people get together and share views. Great blog, keep it up!
Way cool! Some very valid points! I appreciate you writing this post plus the rest of the site is extremely good.
This is such an important topic—thanks for covering it.백링크 프로그램
The next time I read a blog, Hopefully it does not fail me as much as this one. I mean, I know it was my choice to read through, nonetheless I actually believed you would have something helpful to talk about. All I hear is a bunch of moaning about something that you could possibly fix if you weren’t too busy looking for attention.
bookmarked!!, I like your blog.
Your writing style is so engaging and clear.백링크 사이트
You’re so interesting! I don’t think I’ve truly read through anything like this before. So great to discover another person with a few original thoughts on this subject. Seriously.. thanks for starting this up. This website is something that is required on the web, someone with a little originality.
Can I just say what a comfort to uncover somebody who truly knows what they are discussing on the web. You definitely realize how to bring a problem to light and make it important. More and more people must check this out and understand this side of your story. I can’t believe you are not more popular given that you most certainly have the gift.
This is the right web site for anybody who hopes to find out about this topic. You realize a whole lot its almost hard to argue with you (not that I really will need to…HaHa). You certainly put a fresh spin on a subject that’s been discussed for ages. Excellent stuff, just great.
Hi, I do believe this is an excellent site. I stumbledupon it 😉 I’m going to revisit yet again since I bookmarked it. Money and freedom is the best way to change, may you be rich and continue to guide others.
This is a very good tip particularly to those fresh to the blogosphere. Simple but very accurate information… Many thanks for sharing this one. A must read post!
You made some decent points there. I checked on the internet for more information about the issue and found most people will go along with your views on this site.
The very next time I read a blog, Hopefully it won’t disappoint me just as much as this one. I mean, Yes, it was my choice to read, but I really thought you would probably have something interesting to say. All I hear is a bunch of moaning about something you could possibly fix if you were not too busy searching for attention.
I’m amazed, I have to admit. Seldom do I come across a blog that’s both educative and amusing, and without a doubt, you’ve hit the nail on the head. The issue is something which not enough people are speaking intelligently about. Now i’m very happy that I stumbled across this in my search for something relating to this.
bookmarked!!, I love your site.
I was able to find good advice from your content.
I blog quite often and I seriously thank you for your content. This great article has really peaked my interest. I’m going to take a note of your site and keep checking for new details about once a week. I opted in for your Feed as well.
Good post. I will be facing many of these issues as well..
It’s hard to find educated people for this subject, however, you sound like you know what you’re talking about! Thanks
I like it when people come together and share ideas. Great blog, stick with it!
An intriguing discussion is definitely worth comment. I do believe that you need to write more on this topic, it may not be a taboo matter but usually people don’t speak about these subjects. To the next! All the best!
I love it whenever people get together and share views. Great blog, keep it up!
It’s nearly impossible to find well-informed people for this topic, however, you seem like you know what you’re talking about! Thanks
Next time I read a blog, Hopefully it won’t disappoint me just as much as this particular one. After all, I know it was my choice to read through, nonetheless I truly believed you’d have something interesting to talk about. All I hear is a bunch of moaning about something that you can fix if you were not too busy searching for attention.
An interesting discussion is worth comment. I think that you ought to publish more on this subject matter, it may not be a taboo subject but generally people don’t discuss such issues. To the next! Many thanks.
After checking out a number of the blog articles on your blog, I really appreciate your way of writing a blog. I added it to my bookmark site list and will be checking back soon. Please check out my website as well and tell me what you think.
Your style is very unique in comparison to other people I’ve read stuff from. I appreciate you for posting when you have the opportunity, Guess I will just book mark this blog.
After exploring a few of the blog articles on your site, I truly appreciate your technique of writing a blog. I saved as a favorite it to my bookmark webpage list and will be checking back in the near future. Please check out my web site too and let me know how you feel.
That is a great tip especially to those fresh to the blogosphere. Brief but very precise information… Appreciate your sharing this one. A must read post!
I’m impressed, I must say. Rarely do I come across a blog that’s both educative and entertaining, and without a doubt, you have hit the nail on the head. The issue is something too few folks are speaking intelligently about. Now i’m very happy that I came across this during my hunt for something concerning this.
I really love your site.. Pleasant colors & theme. Did you develop this site yourself? Please reply back as I’m wanting to create my very own website and would love to know where you got this from or exactly what the theme is called. Thank you!
Greetings! Very useful advice in this particular article! It’s the little changes which will make the most important changes. Many thanks for sharing!
Saved as a favorite, I really like your site.
Can I simply say what a comfort to find somebody that actually knows what they’re discussing on the net. You actually know how to bring an issue to light and make it important. A lot more people need to check this out and understand this side of the story. It’s surprising you aren’t more popular given that you surely possess the gift.
Nice post. I learn something new and challenging on sites I stumbleupon every day. It’s always interesting to read through content from other authors and practice a little something from other websites.