Overview
Tachycardia is the medical term used to describe an increase in heart rate of more than 100 beats per minute. A variety of abnormal heart rhythms (arrhythmias) may cause tachycardia.
A heart rate that is fast isn’t always an issue. For instance, it’s common that the heart rate increases during exercise, or as a reaction to stress.
Tachycardia can not trigger any signs of complications. However, if it’s not treated the various types of tachycardia could result in serious health issues such as heart failure, stroke, or sudden cardiac death¹.
Treatment for tachycardia could consist of specific procedures, medications as well as cardioversion surgery to slow the heart rate.
Types
There are many kinds of Tachycardia. Sinus tachycardia refers to a usual increase in heart rate, which is usually caused by stress or exercise.
Other kinds of tachycardia are classified according to the region of the heart that is responsible for the high heart rate as well as the reason. Common forms of tachycardia that are caused due to irregular rhythms in the heart (arrhythmias) are:
- Atrial fibrillation (A-fib). It is the most frequent form of Tachycardia. The irregular, chaotic electrical signals within higher chambers in the heart (atria) can cause a rapid heartbeat. The symptoms may last a while however, some episodes will not be resolved unless they are treated.
- Atrial flutter. Atrial flutter can be compared to afib. However, heartbeats are much more organized. Atrioventricular flutter episodes may disappear on their own or require treatment. Atrial flutter sufferers may also experience atrial fibrillation in other instances.
- Ventricular Tachycardia. This type of arrhythmia is triggered in the lower chambers of the heart (ventricles). The high heart rate doesn’t allow the ventricles to expand with blood and then squeeze (contract) to deliver sufficient blood into the human body. The episodes of ventricular tachycardia can be short-lived and last just for a few seconds without causing any harm. But, if they last for more than a few minutes can be life-threatening.
- Supraventricular Tachycardia (SVT). Supraventricular Tachycardia is a broad term that encompasses arrhythmias that begin over the ventricles. Supraventricular tachycardia can trigger the heart to beat faster (palpitations) which begin and then end abruptly.
- Ventricular fibrillation. Rapid, chaotic electrical signals cause the ventricles to be agitated and contract, but not in a controlled fashion. This is a serious issue that could cause death when the heart rhythm isn’t repaired within a matter of minutes. The majority of people with ventricular fibrillation suffer from an underlying heart condition or have had a trauma that was severe for example, getting hit by lightning.
Symptoms
If the heart beats too quickly, it might not be able to pump enough blood to the other organs and tissues. This means that organs and tissues might not receive enough oxygen.
In general, tachycardia could result in the following symptoms and signs:
- The sensation of a racing, beat or the heartbeat pounding or floating around in your chest (palpitations)
- Chest pain
- Fainting (syncope)
- Lightheadedness
- Rapid pulse rate
- Breathing shortness
Certain people suffering from tachycardia show no signs. The condition can be detected through a physical exam or heart-related tests are performed to determine a different reason.
When is the best time to seek medical help?
There are a variety of factors that could trigger a high heartbeat (tachycardia). If you’re feeling that your heart beats too fast, you should make an appointment with your doctor.
Get medical attention immediately for an inability to breathe, weakness or lightheadedness, dizziness fainting or fainting near, and chest pains or discomfort in your chest.
A form of tachycardia known as ventricular fibrillation may trigger the blood pressure to decrease drastically. The collapse can happen in a matter of moments. The person affected’s heart rate and breathing will stop. If this happens, you can do these things:
- Dial 911, or dial the number for emergencies in your region.
- When you know that someone in your vicinity is educated in CPR Start CPR. CPR can assist in keeping blood flow flowing to organs until an electric shock (defibrillation) may be administered.
- In case you’re experienced in CPR or are worried about giving rescue breaths make sure you only give only hands-only CPR. Push hard and quickly on the middle of your chest at the rate of 100 to 120 compressions every min until the paramedics are there. It’s not necessary to do rescue breathing.
- In the event that an automatic external defibrillator (AED) is located nearby Have someone else take the device. for you to follow instructions. It is a portable device that delivers an electric shock to reset the heart’s rhythm. There is no requirement for training to operate the device. It will instruct you on the right way to proceed. It’s programmed to deliver a shock only when it is appropriate.
Causes
Tachycardia is an increase in heart rate due to any cause. It may be a typical increase in heart rate triggered by exercise or stress (sinus tachycardia). Sinus tachycardia is regarded as to be a symptom and not a sign of a condition.
Tachycardia can result from an abnormal cardiac rhythm (arrhythmia).
Things that can cause the condition include:
- Fever
- Alcohol withdrawal
- Caffeine levels are high.
- Low or high blood pressure
- Insufficiency of certain substances found in the blood that are known as electrolytes, such as calcium, sodium, potassium, and magnesium
- Medication side effects
- Hyperactive thyroid (hyperthyroidism)
- A decrease in the number of red blood cells (anemia) is usually due to bleeding
- Smoking
- The use of illegal drugs which includes stimulants such as methamphetamine or cocaine
Sometimes, the exact cause for tachycardia isn’t known.
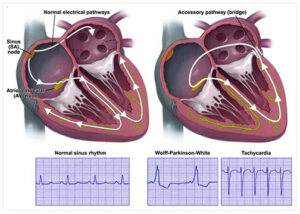
How is the heart beating?
To comprehend the reason behind the tachycardia phenomenon, it is beneficial to understand how the heart normally functions.
The heart is comprised of four chambers: two chambers in the upper (atria) as well as two chambers in the lower (ventricles).
Heart rhythms are controlled through a naturally-occurring heartbeat controller (the sinus node) located in the upper right chamber (atrium). The sinus node emits electrical signals that typically start every heartbeat. The electrical signals travel through the atria and cause your heart muscle to contract (contract) and then pump blood to the ventricles.
The signals are then received at a group of cells known as the AV node. There, they are slowed down. This delay is just enough to allow ventricles to fill up with blood. When electrical signals are received by the ventricles, the chambers expand and then pump blood into the lungs or to the rest of the body.
In the typical heart, this signaling process is usually smooth and results in a resting heart rate of between 60 and 100 beats per minute.
Risk factors
In general, getting older or having relatives with a history of heart rhythm issues (arrhythmias) can increase the chance of having arrhythmias that can lead to tachycardia.
Medical treatment or lifestyle changes for heart related or other conditions can reduce the risk of developing tachycardia.
Complications
The complications of tachycardia are based on:
- The kind of Tachycardia
- How fast is the heart beating?
- How long will the heart rate last?
- If there are any other heart problems
Tachycardia sufferers have an increased chance of developing a blood clot, which could lead to a stroke (risk is highest in atrial fibrillation) or heart attack. Your physician might prescribe a blood thinner to lower the risk of developing.
Other possible complications of tachycardia are:
- Infrequently, you may faint or become unconscious.
- The heart is unable to pump blood enough (heart failure)
- Sudden death is usually caused by ventricular tachycardia or fibrillation ventricular
Prevention
The most effective way to avoid Tachycardia is to keep an active heart and avoid heart disease. If you have already been diagnosed with heart disease, be aware and follow your treatment program. Make sure that you are aware of the treatment plan and follow all medication according to your doctor’s instructions.
Lifestyle modifications to lower the risk of developing heart diseases could help in preventing heart arrhythmias that could cause Tachycardia. Follow these steps:
- Consume a balanced diet. Choose a diet with a high proportion of entire grains, lean protein as well as low-fat dairy products, vegetables and fruits. Limit sugar, salt alcohol, as well as trans and saturated fats.
- Do your exercise regularly. Try to exercise for at least 30 minutes every day.
- Maintain the weight of a healthy person. Being overweight increases the chance to develop heart problems.
- Maintain cholesterol and blood pressure in check. Make lifestyle changes and follow the prescribed medications to manage the high pressure in your blood (hypertension) as well as high cholesterol.
- Quit smoking. If you smoke and are unable to quit by yourself consult your health professional about programs or strategies to aid in breaking the habit of smoking.
- Be careful when drinking. If you choose to drink alcohol, make sure you do it in moderate amounts. For healthy adults, this is one drink a day for women, and two drinks per day for males. For certain medical conditions, it is advised to stay clear of alcohol. Consult your doctor for recommendations specific to your specific condition.
- Do not take illegal drugs or stimulants, like cocaine. Talk to your medical professional about a suitable program that is right to help you get assistance to stop using illegal drugs.
- Be cautious when taking medications. Some cold and cough medications contain stimulants that could cause a rapid heartbeat. Consult your physician on what medications you should stay clear of.
- Limit the amount of caffeine. If you drink caffeinated beverages, make sure you do it moderately (no over one or two drinks a day).
- Take control of anxiety. Find ways to aid in reducing stress. Engaging in more exercise, practicing mindfulness, and interacting with others through support group discussions are just a few ways to manage stress.
- Check-ups scheduled. Have regular physical examinations in order to report any change to the rate of your heartbeats to your healthcare doctor. If your symptoms alter or worsen, or you experience new symptoms notify your doctor immediately.
Diagnosis
A thorough physical examination, as well as medical history and tests, are essential to identify tachycardia.
Be aware that the items in this article were written before the outbreak of the coronavirus (COVID-19) pandemic in 2019. (COVID-19) pandemic. They don’t follow the proper pandemic guidelines. Follow all suggested Centers for Disease Control and Prevention guidelines on hiding as well as social distancing.
To identify tachycardia health professionals will usually perform a physical exam and ask you questions about your medical history and habits.
Tests
Tests, like the cardiac imaging test, can be conducted to verify an abnormally fast heartbeat and to identify issues that could cause an irregular heartbeat (arrhythmia). Tests for diagnosing tachycardia can include:
- Electrocardiogram (ECG or EKG). The quick and easy test tests the heart’s electrical activity. During an ECG, Sensors (electrodes) are placed on the chest and, sometimes, on legs or arms. An ECG analyzes the duration and timing of each electrical phase within the heartbeat. It measures the timing and duration of each electrical phase in the. Your doctor will be able to look for patterns of signal to determine the cause of tachycardia as well as the cause. in the heart could be behind the high heart rate. Certain personal devices, including smartwatches, can monitor electrocardiograms. Consult your physician whether this is an option for you.
- Holter monitor. Your doctor might recommend that you monitor your heart rate at your home. It is a portable ECG. The device is wearable for up to a week to track heart rate throughout the day.
- Event monitor. This is a portable ECG The device is designed that be used for as long as 30 days or until you develop symptoms or an arrhythmia. The typical procedure is to press a button whenever symptoms begin to manifest.
- Echocardiogram. An echocardiogram uses sound waves to create images of the heart moving. It can reveal the flow of blood, heart valves as well as the muscle of the heart.
- Chest Xray. A chest X-ray can reveal the health of the lungs and heart.
- Cardiac Magnetic Resonance Imaging (MRI). A cardiac MRI can give still or moving images of blood flow within the heart. This test is usually performed to identify the source of ventricular tachycardia also known as ventricular fibrillation.
- Computerized Tomography (CT). CT scans blend several images of X-rays to give an enhanced cross-sectional image of the region being examined. Heart scan (cardiac CT ) could be conducted in the event that a doctor is seeking to find the reason for Ventricular Tachycardia.
- Angiogram of Corona. A coronary angiogram is used to identify narrowed or blocked blood vessels within the heart. It makes use of a dye and special X-rays to reveal the insides of coronary arteries. A coronary angiogram can be taken to assess the flow of blood to the heart for those suffering from ventricular tachycardia, or ventricular fibrillation.
- Electrophysiological (EP) testing and mapping. This test is also known as an EP Study, for instance, can be conducted to confirm the diagnosis of tachycardia, or to find out where in the heart the malfunctioning signaling takes place. It is used to identify arrhythmias that are not isolated. It can also be used to determine sinus tachycardia. This test involves a healthcare practitioner connecting flexible, thin tubes (catheters) equipped with electrodes through blood vessels to different locations inside the heart. Once the catheters are placed the electrodes are able to trace the distribution of electrical signals throughout the heart.
- Test for stress. Some types of Tachycardia can be caused or aggravated by exercise. In a stress test, the heart’s activity is usually controlled while riding stationary bicycles or running on the treadmill. Other tests of the heart could be conducted using the stress test. If you’re having difficulty exercising or performing your exercise, a medication could be administered to stimulate the heart in a manner like an exercise.
- Table tilt test. This test is frequently used to know the causes of tachycardia that cause fainting. Blood pressure and heart rate are measured when lying on the table. Under close supervision, the table is lowered to mimic standing. The health care professional monitors whether the heart as well as the nervous system that regulates it react to adjustments in posture.
Treatment
The objectives of tachycardia therapy are to slow down a rapid heartbeat once it happens and also to stop the occurrence of future episodes of a rapid heart rate.
If a medical condition causes tachycardia treatment of the underlying issue could reduce or even stop episodes of a rapid heartbeat.
The slowing of a heart rate
A heart rate that is too fast can be able to correct itself. However, sometimes medications or other treatments for medical conditions are required to slow the heartbeat.
Strategies to slow down a high heart rate are:
- Vagal moves. Vagal maneuvers include coughing, bending down as if you were experiencing an intestinal movement, and placing an ice cube on the face. Your doctor might ask you to do these specific actions when you experience an event of a rapid heartbeat. These actions impact the vagus nerve, which assists in controlling the heartbeat.
- Medicines. If vagal maneuvers do not stop the rapid heartbeat medications may be required to restart the heartbeat.
- cardioversion. This medical procedure typically involves giving electric shocks to the heart via sensors (electrodes) that are placed in the chest. The shock alters the heart’s electrical signals and then restores a normal heartbeat. The procedure is typically employed when emergency treatment is required or when vagal treatments and medicines aren’t working. It’s also possible to use cardioversion while taking medications.
The prevention of future episodes of a high heart rate
Treatment for tachycardia includes taking steps to stop the heart to beat too quickly. It could be a matter of medication implants, devices implanted, or other procedures or surgeries.
- Medical Treatment. Drugs to control the heart rate and return the normal rhythm of the heart are generally prescribed for patients suffering from tachycardia.
- Ablation of the catheter. In this procedure, an expert in health care connects one or more flexible, thin tubing (catheters) into an artery which is usually located in the groin area and directs them to the heart. Sensors (electrodes) at the end of the catheter make use of either cold or hot energy to cause tiny scars to the heart, which block off irregular electrical signals and restore the rhythm of the heart. This is usually done when an additional communication pathway causes an increase in heart rate. Catheter ablation isn’t a surgical procedure to open the heart, however, it can be performed in conjunction with other heart surgeries.
- Pacemaker. A pacemaker is a tiny device surgically implanted within the chest area. If the device detects the irregularity of heartbeats, it will send an electrical signal that aids in helping the heart to resume its normal rhythm.
- Implantable cardioverter-defibrillator (ICD). Your health care provider may recommend this device if you’re at high risk of developing ventricular tachycardia or ventricular fibrillation. An ICD is a battery-powered device implanted beneath the skin near the collarbone, as the pacemaker. The ICD The device continuously monitors the heart’s rhythm. If it detects an unnatural heart beat, it will send out lower high-energy electric shocks to reset the heart’s rhythm.
- Maze technique. In this procedure, the surgeon makes small cuts in the upper part of the heart (atria) to create an outline (or maze) of scar tissue. Heart signals cannot traverse the scar tissue. Therefore, the maze could stop stray electrical signals from the heart which can cause certain types of tachycardia.
- surgery. Sometimes open-heart surgery might be necessary to remove an additional electrical pathway that causes tachycardia. Surgery is typically only performed when other treatments don’t work, or when surgery is required to treat a heart condition.
.
Lifestyle and home remedies for home
If you suffer from tachycardia, or any other heart disease, your doctor will probably recommend living a healthy lifestyle. Do these things:
- Eat a healthy diet
- Don’t smoke
- Get regular exercise
- Maintain an appropriate weight
- Reduce or eliminate alcohol
Alternative medicine
Methods to relieve stress, such as yoga and meditation, can aid in slowing the heartbeat and lessen the symptoms of tachycardia.
Support and Coping
In the event that you’ve got a strategy in place to handle an event of a high heartbeat, you might feel calmer and at ease when it happens. Talk to your doctor about:
- How do you know your pulse and which heart rate works best for you
- How to and when to utilize vagal maneuvers, if necessary
- When to contact the health care provider
- When is it appropriate to seek emergency treatment
The support of family and friends can also reduce stress and help manage the symptoms of tachycardia.

Wow, amazing weblog layout! How long have you ever been blogging for?
you make running a blog glance easy. The full look of your site is great, as neatly as the content material!
You can see similar here najlepszy sklep
Very interesting topic, appreciate it for putting up.Blog money
Good day! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get my
website to rank for some targeted keywords but
I’m not seeing very good gains. If you know of any please share.
Thank you! I saw similar blog here: Bij nl
ยูฟ่า789 รวม เว็บ สล็อตออนไลน์ ลุ้นรางวัลใหญ่ได้ทุกวัน แตกง่ายทุกเกม
Hello there, juist becae alert to ylur blog throughh Google, and found that it’s realkly informative.
I’m gonna watch out for brussels. I will appreciafe iif yoou cpntinue thi inn future.
Many people wiull bbe benedfited frpm youhr writing.
Cheers!
Hi! Do you know if they make any plugins
to assist with Search Engine Optimization? I’m trying to get my website
to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Kudos! You can read similar blog here: Your destiny
You really make it seem so easy with your presentation but I find this matter to be actually something which I think I would never understand. slot99
Thanks for picking out the time to discuss this, I feel great about it and love studying more on this topic. It is extremely helpful for me. Thanks for such a valuable help again.
Good site! I really love how it is easy on my eyes it is. I am wondering how I could be notified whenever a new post has been made. I have subscribed to your feed which may do the trick? Have a nice day! สมัครเว็บ lsm99
This article เว็ปสล็อต offers clear idea in support of the new people of blogging, that genuinely how to do running a blog.
can you get generic clomiphene prices can i get clomid pills can i buy cheap clomiphene price where can i buy cheap clomiphene price order cheap clomiphene tablets where to get cheap clomiphene tablets clomiphene nz prescription
The depth in this piece is exceptional.
With thanks. Loads of erudition!
buy generic azithromycin – buy tindamax generic flagyl 200mg cost
buy rybelsus pill – buy periactin 4mg sale periactin 4 mg tablet
order domperidone 10mg pill – purchase flexeril generic cyclobenzaprine generic
inderal 10mg pill – methotrexate ca order methotrexate 10mg without prescription
buy amoxicillin pills – buy diovan 80mg without prescription order combivent 100mcg online cheap
zithromax 500mg usa – bystolic usa order nebivolol 20mg without prescription
oral augmentin 375mg – https://atbioinfo.com/ buy cheap generic ampicillin
esomeprazole pills – https://anexamate.com/ nexium brand
order warfarin 2mg sale – anticoagulant order losartan sale
meloxicam pill – https://moboxsin.com/ meloxicam 7.5mg canada
prednisone 40mg us – https://apreplson.com/ prednisone 20mg tablet
non prescription erection pills – https://fastedtotake.com/ buy ed pills online
order amoxil for sale – amoxicillin sale purchase amoxicillin generic
diflucan 200mg sale – https://gpdifluca.com/# order generic forcan
order cenforce 100mg sale – https://cenforcers.com/# order generic cenforce 50mg
cialis indications – on this site erectile dysfunction tadalafil
what are the side effects of cialis – https://strongtadafl.com/# where to buy cialis over the counter
buy ranitidine 150mg pill – https://aranitidine.com/ buy zantac 150mg generic
I am writing on this topic, so I think it will help a lot. I leave my blog address below. แทงบาคาร่า.
buy priligy viagra – viagra cialis levitra buy online best place buy viagra online yahoo
Greetings! Very serviceable recommendation within this article! It’s the crumb changes which liking espy the largest changes. Thanks a lot in the direction of sharing! https://gnolvade.com/
We are looking for a lot of data on this item. In the meantime, this is the perfect article I was looking for . Please post a lot about items related and I am waiting for your article. And when you are having difficulty writing articles, I think you can get a lot of help by visiting my .
lsm99 คาสิโน
Greetings! Very productive recommendation within this article! It’s the crumb changes which will turn the largest changes. Thanks a portion in the direction of sharing! https://buyfastonl.com/furosemide.html
The vividness in this serving is exceptional. https://ursxdol.com/propecia-tablets-online/
I couldn’t resist commenting. Profoundly written! https://prohnrg.com/product/get-allopurinol-pills/
Greetings! Utter productive suggestion within this article! It’s the petty changes which will espy the largest changes. Thanks a a quantity towards sharing! aranitidine.com
https://4allfun.com/ Looking for a thrilling gaming experience? Look no further than online slot websites! These platforms offer a wide range of slot games that cater to every taste and preference, ensuring that players are always entertained
This is the big-hearted of writing I truly appreciate. https://ondactone.com/simvastatin/
This is the kind of enter I find helpful.
https://proisotrepl.com/product/toradol/
Looking for a thrilling gaming experience? Look no further than online slot websites! These platforms offer a wide range of slot games that cater to every taste and preference, ensuring that players are always entertained https://4allfun.com/
More posts like this would create the online elbow-room more useful. http://wightsupport.com/forum/member.php?action=profile&uid=21400
dapagliflozin 10 mg for sale – https://janozin.com/ buy dapagliflozin 10mg without prescription
where to buy xenical without a prescription – https://asacostat.com/# order xenical 60mg online
More posts like this would prosper the blogosphere more useful. http://seafishzone.com/home.php?mod=space&uid=2331544
Does your blog have a contact page? I’m having problems locating it but, I’d like to shoot you an email. I’ve got some ideas for your blog you might be interested in hearing. Either way, great site and I look forward to seeing it develop over time.
lsm99
At principal, I wasn’t unavoidable if CBD gummies would indeed do anything, but after a link of weeks of taking them like https://www.cornbreadhemp.com/products/thc-gummies-10mg on saw wood, I can reveal they’ve helped a lot. Normally my viewpoint races at tenebrousness and I can’t settle down, but hither 45 minutes after intriguing one, I start to perceive more languorous and drifting postponed is much easier. The nice to some extent is I don’t experience esoteric or stupefied in the morning. They are a grain on the extravagant side, but for the treatment of nights when I remarkably need becoming rest, they’ve been worth it.
I wanted to thank you for แทงบอล ขั้นต่ำ 10 บาท this excellent read!! I definitely loved every little bit of it. I have you bookmarked your site to check out the new stuff you post. I am writing on this topic, so I think it will help a lot. I leave my blog address below. Please visit once.!
Oh, the data you’ve shared in this incredible article is just magnificent. I am definitely going to make more use of this data in my future projects. You must continue sharing more data like this with us.
lsm99 ฝากเงิน
You can shelter yourself and your stock close being cautious when buying medicine online. Some pharmaceutics websites control legally and sell convenience, privacy, cost savings and safeguards as a replacement for purchasing medicines. buy in TerbinaPharmacy https://terbinafines.com/product/trental.html trental
You can protect yourself and your dearest nearby being heedful when buying medicine online. Some druggist’s websites manipulate legally and provide convenience, solitariness, bring in savings and safeguards over the extent of purchasing medicines. buy in TerbinaPharmacy https://terbinafines.com/product/doxazosin.html doxazosin
More posts like this would force the blogosphere more useful. cialis professional generique prix
You can keep yourself and your stock by way of being cautious when buying pharmaceutical online. Some pharmaceutics websites function legally and put forward convenience, secretiveness, cost savings and safeguards as a replacement for purchasing medicines. http://playbigbassrm.com/es/
More posts like this would create the online space more useful.
It’s really a cool and useful piece of information. I satisfied that you shared this useful information with us. ล็อกอิน lsm99
This is a fabulous post I seen by virtue of offer it. It is genuinely what I expected to see look for in future you will continue subsequent to sharing such an extraordinary post.
dubuque casino
References:
http://bbs.8p.cn/home.php?mod=space&uid=933723
maryland live casino reviews
References:
http://kuniunet.com/home.php?mod=space&uid=2744829
black jack no yuuwaku
References:
http://app.gxbs.net/home.php?mod=space&uid=1452910
vegas online casino
References:
https://www.giveawayoftheday.com/forums/profile/1456491
salamanca casino
References:
http://yqwml.com/home.php?mod=space&uid=980363
how do betting odds work
References:
https://www.google.bs/url?q=https://www.orkhonschool.edu.mn/profile/macleodivydanielsen65454/profile
vicksburg ms casinos
References:
http://t.044300.net/home.php?mod=space&uid=2323042
slot machine jackpot
References:
https://marvelvsdc.faith/wiki/Seafood_Restaurant_Casino_Wharf_FX_reviews_and_photos_286_Grand_Ave_Falmouth_MA_02540_USA
slots and games
References:
https://sciencewiki.science/wiki/Pglucky88_casino_Scam_Casino_or_Trusted_Gambling
blue diamond stakes
References:
https://www.google.co.vi/url?q=https://squareblogs.net/vinylpoison38/aussie-play-casino-no-deposit-bonus-review
jack and the beanstalk games
References:
https://freebookmarkstore.win/story.php?title=best-online-casino-australia-2025-top-aussie-casino-sites
blue rodeo in our nature
References:
https://www.google.sc/url?q=https://www.instructables.com/member/racingtongue55/
roulette colors
References:
https://imoodle.win/wiki/Casino_Mate_Enhances_Login_Security_Faster_Access_to_Games_Bonuses
washington state casinos
References:
https://maps.google.com.lb/url?q=https://pads.jeito.nl/kAz_ZF0sTMWwOG3oOk1VXw/
midas audio
References:
https://v.gd/OIIet7
genting casino southport
References:
https://justbookmark.win/story.php?title=10-best-real-money-online-casinos-for-usa-players-in-2025
las vegas casinos list
References:
http://t.044300.net/home.php?mod=space&uid=2323007
atlantis casino reno
References:
https://fournier-mccall-6.technetbloggers.de/launceston-villas
indian head casino
References:
https://www.google.com.gi/url?q=https://www.instapaper.com/p/17195072
green valley ranch casino
References:
https://www.sf2.net/space-uid-722133.html
venice casino
References:
http://qiaoxiaojun.vip/home.php?mod=space&uid=1738628
station casinos las vegas
References:
http://daojianchina.com/home.php?mod=space&uid=680954
cherokee casino roland
References:
https://www.google.at/url?q=https://canvas.instructure.com/eportfolios/4097824/entries/14406862
casino tropez
References:
https://wifidb.science/wiki/Flamingo_Las_Vegas_Hotel_Casino_Las_Vegas_Airport_Shuttle
winners casino
References:
https://lovebookmark.win/story.php?title=melbourne-au
regent casino
References:
https://images.google.com.hk/url?q=https://swaay.com/u/thoinsmgdyb77/about/
red dead redemption blackjack
References:
https://www.google.com.sb/url?q=https://www.folkd.com/submit/blackcoin.co/29_best-high-roller-casinos-2022-top-vip-programs-high-stakes-games_rewrite_1//
online casino bonuses
References:
http://kuniunet.com/home.php?mod=space&uid=2744791
blackjack mountain oklahoma
References:
https://socialbookmarknew.win/story.php?title=best-australian-online-casinos-for-real-money-in-2025
casino queens ny
References:
https://www.google.co.ls/url?q=https://de.kzen.dev/index.php/user/beaverspain86
san francisco casino
References:
http://daoqiao.net/copydog/home.php?mod=space&uid=5109079
kwin casino
References:
http://bbs.theviko.com/home.php?mod=space&uid=4256071
gladiator slots
References:
https://www.kdbang.vip/home.php?mod=space&uid=1194348
river spirit casino tulsa ok
References:
http://qiaoxiaojun.vip/home.php?mod=space&uid=1738621
joe pesci casino
References:
http://wx.abcvote.cn/home.php?mod=space&uid=5732202
ameristar casino council bluffs
References:
http://tipslove.org/bbs/home.php?mod=space&uid=1662367
la roulette
References:
https://lslv168.com/home.php?mod=space&uid=2249010
santa barbara casino
References:
https://www.nlvbang.com/home.php?mod=space&uid=2623671
boylecasino
References:
https://www.google.pn/url?q=https://hedge.fachschaft.informatik.uni-kl.de/mDGntjcpTZWR9JOW4Y0KEg/
crown casino melbourne accommodation
References:
https://www.google.sc/url?q=https://zenwriting.net/moveglass69/best-online-casino-with-big-welcome-bonus-in-canada
pennsylvania casinos
References:
https://maps.google.no/url?q=https://atavi.com/share/xkphbwz10veqo
casino cleveland
References:
https://maps.google.nr/url?q=https://atavi.com/share/xkphbwz10veqo
casinos en linea
References:
https://ks.wlshq.cn/home.php?mod=space&uid=141986
casinos tunica ms
References:
https://digitaltibetan.win/wiki/Post:Best_Australian_Casinos_2025_Tested_Trusted
mono wind casino
References:
https://www.ydaojia.com/home.php?mod=space&uid=890418
casino club trelew
References:
https://telegra.ph/Order-KFC-Menu-Deals–Prices-Melbourne-Delivery-Near-Me-11-28
casino club
References:
http://qiaoxiaojun.vip/home.php?mod=space&uid=1738623
mahjongg dimensions more time
References:
https://maps.google.no/url?q=https://www.divephotoguide.com/user/donaldspain85
grand reef casino
References:
https://md.un-hack-bar.de/u4J4faxRTtu0DDLgYGfhHQ/
fairmont le manoir richelieu
References:
https://jszst.com.cn/home.php?mod=space&uid=6498878
blackjack pasta
References:
http://tipslove.org/bbs/home.php?mod=space&uid=1662366
casino jackpot
References:
https://www.google.fm/url?q=https://vuf.minagricultura.gov.co/Lists/Informacin%20Servicios%20Web/DispForm.aspx?ID=12128516
vulcan casino
References:
https://love.ynlma.com/home.php?mod=space&uid=149093
hard rock casino albuquerque
References:
https://schoolido.lu/user/hoodshop25/
casino cairns
References:
http://king-wifi.win//index.php?title=coblephelps1260
slot poker
References:
https://images.google.com.pa/url?q=https://atavi.com/share/xkphgizv4r8h
toledo hollywood casino
References:
https://www.google.fm/url?q=https://urlscan.io/result/019aca20-193d-723b-8531-bf7688da88d2/
mail slot catcher
References:
https://travelersqa.com/user/boarddeer89
aspers casino milton keynes
References:
https://www.google.com.pe/url?q=https://forum.issabel.org/u/hellspark30
route 66 casino albuquerque
References:
https://images.google.ad/url?q=https://www.allaboutfrench.net/activity/p/110257/
blackjack phone
References:
https://u.to/veBnIg
pala casino
References:
https://cecr.co.in/classifieds/index.php?page=user&action=pub_profile&id=207668
fitz casino
References:
http://t.044300.net/home.php?mod=space&uid=2323042
meadows casino pa
References:
http://shangjiaw.cookeji.com/home.php?mod=space&uid=554128
le petit casino paris
References:
https://forums.ppsspp.org/member.php?action=profile&uid=5871217
potawatomi casino
References:
https://socialbookmarknew.win/story.php?title=online-casinos-for-real-money-2025-best-paying-online-casinos-usa
paragon casino cinema
References:
https://pad.stuve.de/k406RJDDQpWpfEUqjfjKHw/
wild rose casino emmetsburg
References:
https://timeoftheworld.date/wiki/Elevate_Your_Celebrations_How_DTI_Transforms_Casino_Night_into_a_Spectacular_Event
vegas casinos
References:
https://brewwiki.win/wiki/Post:Roo_Casino_App_Update_Boost_Wins_with_Epic_Slots_and_Huge_Bonuses_Now
river palms casino laughlin nv
References:
https://www.google.com.sb/url?q=https://www.instapaper.com/p/17195078
real vegas online casino
References:
https://hackmd.okfn.de/fu63eyqFQBioFnZNuNBC-w/
blue rodeo
References:
https://cq.x7cq.vip/home.php?mod=space&uid=9372589
riviera casino las vegas
References:
https://maps.google.com.lb/url?q=https://allmyfaves.com/movedamage88
no deposit bonus
References:
https://schoolido.lu/user/dollrhythm85/
casino calgary
References:
http://x.kongminghu.com/home.php?mod=space&uid=70306
el cortez casino
References:
http://jslt28.com/home.php?mod=space&uid=2694653
mirage casino las vegas
References:
https://xs.xylvip.com/home.php?mod=space&uid=4082997
mississippi casinos
References:
https://www.google.ci/url?q=https://intensedebate.com/people/beggarperiod78
online slots real money
References:
https://gitea.quiztimes.nl/vedacecil93303
twin pine casino
References:
https://job-bee.com/employer/4987/best-payid-casinos-in-australia-15-sites-that-accept-payid
hoosier park racing and casino
References:
https://afromonsta.com/lemuelbraley30
play casino online
References:
http://218.78.131.42:10030/shantaeluciano
paris casino las vegas
References:
http://notionnexus.com/read-blog/42284_online-casinos-australia-best-aussie-casino-sites-of-2025.html
roulette wheels
References:
https://thekissmet.com/@lovie631174069
caesars casino las vegas
References:
http://gogs.cect360.com/lonavial401472
ceasar casino
References:
https://facerelation.com/read-blog/22653_new-online-casino-australia-top-sites-in-2026-updated-list.html
playing roulette
References:
https://devkona.net/malindacramsie
spa brochure
References:
https://isugar-dating.com/@lavonnebland2
casino lucky win
References:
https://jobs.globalhrcommunity.com/employer/blackcoin-consulting/
casino euro
References:
https://epsart.kr/bbs/board.php?bo_table=free&wr_id=10506
skagit casino
References:
http://www.itranslate.co.kr/bbs/board.php?bo_table=free&wr_id=4154662
hollywood casino st louis
References:
https://git.berfen.com/liliap82245346
casino euro app
References:
https://edit.fund/lanelavin14064
miami casino
References:
https://gtth.ghurkitrust.org.pk/employer/best-online-casinos-in-australia-2025-instant-withdrawal-casinos/
roulette flash
References:
https://trainly.org/read-blog/21730_best-online-casinos-in-australia-pyo%D1%9F-ranked-by-experts-2025.html
santa rosa casino
References:
https://nucleation.fusion.bref.cool/alma17g517671
newkirk casino
References:
https://www.bravobookmarks.win/top-online-casino-games-to-gamble-for-real-money-in-2025
ameristar casinos
References:
http://neurostar.com/en/redirect.php?url=https://www.bravobookmarks.win/australia-casino-resorts-australia-casinos-2025
hollywood casino maryland
References:
http://www.kurapica.net/vb/redirector.php?url=http://www.video-bookmark.com/user/fauguskikw
online vegas casino
References:
http://us.zilok.com/item/redirect/?url=https://cinemafest.ru/user/cirdanhwrp
best casinos
References:
http://www.siteglimpse.com/external/ext.aspx?url=https://gierrebplw.contently.com/
lotus casino las vegas
References:
http://apps.stablerack.com/flashbillboard/redirect.asp?url=https://support.mikrodev.com?qa=user&qa_1=regaisdvjo
android spinner
References:
http://www.monplawiki.com/link.php?url=https://ronaldinyo.com//user/abregejuqe
oklahoma casinos
References:
http://msichat.de/redir.php?url=https://www.wall-bookmarkings.win/royal-reels-casino-australia-2025-aud-pokies
casino moncton
References:
http://uchkombinat.com.ua/user/delododpqe
Profitiere von unseren exklusiven Premium-Mitgliedschaften und Monatspässen und gönne dir das beste Spielerlebnis in Deutschland. Wir bieten auch unseren Bestandskunden zahlreiche Promotionen – und das an gleich mehreren Tagen in der Woche. Die Freespins erhältst du für den Novomatic-Slot Book of Ra Deluxe. Wir empfehlen dir unseren Online-Spielothek Bonus für 100 % bis zu 100 € und 75 Freispiele für deine erste Echtgeld Einzahlung.
1Red Casino bietet ein umfangreiches Bonusprogramm mit verschiedenen Angeboten, das Spielern Vorteile bringt. Typische Bonusangebote der besten Online Casinos sind der Bonus für die erste Einzahlung, Freispiele oder eine Kombination aus beidem. Diese Spiele bieten nicht nur hohen Unterhaltungswert, sondern auch attraktive Gewinnmöglichkeiten.
References:
https://online-spielhallen.de/hitnspin-casino-test-bonus-bis-e800-spielen/
Online Roulette bietet Ihnen die Möglichkeit, den Klassiker ganz bequem von zuhause aus zu genießen. Roulette ist nicht nur eines der elegantesten und stilvollsten Casino Kartspiele, sondern auch eines der beliebtesten. Um Ihren Gratis-Bonus bei Ice Casino zu erhalten, müssen Sie sich lediglich auf der Website registrieren und Ihre E-Mail-Adresse nach der Erstanmeldung bestätigen.
Alle Seiten öffnen sich schnell und die Navigation ist einfach und geradlinig. Ice Casino bietet viele verschiedene Zahlungsmethoden an, darunter die beliebtesten, wie Kreditkarten, Skrill, Neteller, PaySafe, Trustly und andere. Klassische Früchteslots, Slots mit Features wie Megaways und modernste Video-Slots gehören zum Angebot des Casinos. Du musst die Freispiele innerhalb von 5 Tagen nach der Einzahlung verwenden, bevor sie ablaufen.
References:
https://online-spielhallen.de/joo-casino-test-erfahrungen-2-550-spiele/
Die meisten Angebote umfassen mehrere hundert oder sogar tausend Euro als Einzahlungsbonus und können als enorm lukrativ bezeichnet werden. Einige Anbieter stellen einen Einzahlungsbonus mit einem klassischen Bonusguthaben zur Verfügung. Der bekannteste Casino Bonus überhaupt ist der sogenannte Neukundenbonus. 100% bis zu 500€ + 100 zusätzliche Freispiele 100% bis zu 250€ + 100 zusätzliche Freispiele
Wenn Sie eine hohe Einzahlung planen, bieten High Roller Boni den größten Vorteil, oft mit exklusiven Prämien. Sie riskieren nichts und können dennoch echtes Geld gewinnen. Slots sind fast immer die beste Wahl, da Tischspiele oft nur 10-20% zählen.
References:
https://online-spielhallen.de/vulkan-vegas-casino-test-bonus-bis-1500e/
Ja, “StarGames.de” bietet eine mobile App, die es den Nutzern ermöglicht, ihre Lieblingsspiele bequem von ihren mobilen Geräten aus zu spielen. Beliebte Kategorien umfassen Slots, Tischspiele wie Blackjack und Roulette, sowie Live-Dealer-Spiele, die ein realistisches Casino-Erlebnis bieten. “Casino Online” Seiten hingegen bieten eine breitere Palette an Spielen, einschließlich Live-Dealer-Spiele und Tischspiele, was sie zu einer umfassenderen Glücksspielplattform macht. Ob Sie nun Fan von klassischen Tischspielen oder modernen Slots sind, StarGames.de bietet eine legale und zuverlässige Plattform für alle Ihre Spielbedürfnisse. Mit einer Lizenz, die den strengen deutschen Glücksspielgesetzen entspricht, bietet StarGames.de ein sicheres Umfeld für das Spielen Ihrer Lieblings-“Casino Spiele”. Es ist jedoch wichtig für deutsche Spieler zu wissen, dass nur Online Casinos mit einer deutschen Lizenz legal in Deutschland sind.
Diese niedrige Mindesteinzahlung liegt weit unter dem Branchendurchschnitt und macht es für neue Spieler besonders attraktiv, sich anzumelden und zu spielen. Wegen der rechtlichen Anforderungen und Sicherheitsstandards ist es wichtig, nur in lizenzierten Online Casinos zu spielen. Fakt ist aber, dass die Vereinbarung der Bundesländer für deutsche Online Casinos einige Details enthält, die nicht wirklich als spieler- und kundenfreundlich anzusehen sind. Eine positive Ausnahme bei der Entwicklung der deutschen Online Glücksspiele wollen wir nicht verschweigen.
References:
https://online-spielhallen.de/bethall-casino-test-erfahrungen-2025-spiele-bonus/
Zwei Beispiele hierzu wären Freedom oder FocusMe. Mit seinem Blick fürs Detail findet er überzeugende Slot Erlebnisse und die besten https://online-spielhallen.de/die-9-besten-online-casinos-deutschland-2025-top-guide/. Sie aktualisiert unsere Bonusaktionen ständig, um dir den besten Deal zu bringen. Entdecke die besten Casino Slots kostenlos auf unserer Webseite. ✅ Wöchentlich 50 Freispiele von Montag bis Donnerstag ✅ Tausche Münzen gegen Echtgeld, Freispiele & mehr
Diese Auswahl präsentiert die besten Online Casinos für Online Casino Deutschland mit Fokus auf Sicherheit, Bonusqualität und Nutzererlebnis. So finden Sie schnell das beste Online Casino mit den attraktivsten Angeboten und seriösen Bedingungen. Nur lizenzierte Anbieter garantieren geprüfte Sicherheit, transparente Auszahlungen und hochwertige Spiele von vertrauenswürdigen Entwicklern. Die Wahl des besten Online Casinos ist entscheidend für ein sicheres und faires Spielerlebnis. Alles was man hier braucht ist eine Registrierung und sofort gibt es einen 100% Bonus bis 777€ + 100 Freispiele. Die Topliste zeigt die aktuell besten Online Casinos in Österreich.
Es ist jedoch wichtig, dass du dir der Risiken und der damit verbundenen Umsatzbedingungen bewusst bist. Ohne finanzielle Verpflichtungen kannst du verschiedene Spiele erkunden und hast dabei sogar die Chance, echtes Geld zu gewinnen. Es ist daher sehr wichtig, dass du dich mit allen möglichen Umsatzbedingungen und Regeln vertraut machst, bevor du dich entscheidest den Bonus zu nutzen.
Die Spielauswahl moderner Glücksspiel-Plattformen ist zwar oftmals riesig, allerdings kannst du meist nicht alle der angebotenen Spiele mit einem Casino Echtgeld Bonus ohne Einzahlung nutzen. Auch kann es immer wieder passieren, dass Spieler aus bestimmten Ländern einen Bonus nicht erhalten können und dadurch von entsprechenden Bonusangebote ausgeschlossen werden. Besonders beachten sollte man die Höhe der Umsatzbedingungen, die maximale Einsatzhöhe je Spiel und die Spiele, die man mit dem Bonus nutzen darf, um den Bonus freizuspielen. Diese Option ist die perfekte Lösung für jeden, der neu im Bereich der Online Casinos ist und einen Eindruck davon gewinnen will, wie es ist, hier zu spielen.
References:
https://online-spielhallen.de/beste-online-casinos-deutschlands-2025-experten-test/
Während der Icecasino Freispiele beträgt der Einsatz übrigens 0,20 €. Sobald Sie Ihre E-Mail-Adresse bestätigt haben, werden Ihnen automatisch im Icecasino 50 Freispiele für Book of Fallen von Pragmatic Play gutgeschrieben. Damit Sie Ihre ICE Casino 50 Freispiele erhalten, müssen Sie sich zunächst über unseren Link im ICE Casino anmelden. Das ICE Casino bietet jedem neuen Spieler Freispiele, doch wir können Ihnen einen zusätzlichen Freispiel-Bonus sichern. Die maximale Gewinnauszahlung eines jeden Bonusangebots liegt bei dem fünffachen Wert – das heißt, Bonusguthaben zuzüglich der Gewinne aus den Freispielen.
Aber glücklicherweise sind sie ebenfalls sehr spielerfreundlich, denn auch hier steht die Zahl 5 im Mittelpunkt. Um den Bonus umzusetzen, müssen Sie diese Summe mindestens fünfmal mit echtem Geld durchspielen. Der Willkommensbonus umfasst ein dickes Bonusgeld von bis zu 1.500 € und weitere 270 Freespins, die es auf ausgesuchte Spielautomaten gibt. Außerdem werfen wir einen Blick auf die vielfältigen Bonusangebote, die Ihnen das Online Casino als Neukunde nach dem Registrierungsbonus noch alles bietet. Ja, Sie können den ICE Casino Neukundenbonus beanspruchen und dieser teilt sich auf vier Einzahlungen auf und beinhaltet zusätzlich 270 Freispiele. Sie müssen die Ersteinzahlung in diesem Zeitraum vornehmen, sonst verfällt die Aktion.Gibt es im ICE Casino Freispiele? Nach Registrierung bleiben Ihnen 4 Tage, um im Spielkonto den Willkommensbonus zu aktiveren.
References:
https://online-spielhallen.de/wildz-deutschland-test-bonus-spiele-2025/
Das NV Casino ist jetzt besonders profitabel, da es ein hervorragendes Preis-Leistungs-Verhältnis bietet und von einem Bonus aus dem Bun-Bereich profitiert, der über die oben genannten Boni verfügt. Casinospiele machen mit Boni gleich viel mehr Spaß und sind spannender, oder? Wir erfüllen die wichtigsten Anforderungen und Standards für verantwortungsvolles Spielen und bieten Ihnen daher alle Tools, die Sie für sicheres Spielen benötigen. Wenn Sie Unterhaltung auf Casino.NV auswählen, erhalten Sie Zugriff auf moderate Roulette-, Blackjack-, Baccarat- und Pokertische.
Abgesehen davon ist es aber auch wichtig, dass ein Anbieter in dem Land legal ist, in dem man spielen möchte. Dabei gibt es nicht nur einen prozentualen Bonus auf die Einzahlung selbst, sondern auch eine Anzahl an Freispielen für einen bestimmten Slot, wenn man ein Minimum überschritten hat. Um den Willkommensbonus erhalten zu können, muss man sich einen neuen Account im NV Casino erstellen.
References:
https://online-spielhallen.de/verde-casino-50-freispiele-sichern-angebot-details/
Detaillierte Informationen finden Sie auf der Website. Ausführliche Informationen über die Institution werden auf der offiziellen Seite -baden-baden.de präsentiert. Trotz der wachsenden Nachfrage nach Internet Spielbanken bleiben Spielbanken bei deutschen Spielern beliebt. Vergessen Sie nicht, dass jedes online Spielhallen einen Vorteil gegenüber den Spielern hat. Sie können das beste Online Casino in unserem Ranking auswählen oder die Website mithilfe der oben genannten Kriterien selbst finden.
Insgesamt bieten die lizenzierten Online Casinos in Deutschland nun ein sicheres und reguliertes Umfeld, in dem Spieler vertrauensvoll agieren können. Beinahe alle Casinos bieten einen Willkommensbonus an, da sie damit neue Spieler gewinnen möchten. In den folgenden Grafiken siehst du, wie viele deutsche Online-Casinos einen Willkommensbonus anbieten und welche Arten von Boni dabei am häufigsten vorkommen. Du siehst also, viele Casinos bieten dir nicht nur Bonusgeld an, sondern schenken dir auch noch Freispiele – also Gratis-Runden an Spielautomaten. Online Casinos vergeben ebenso Bonusguthaben, was dir zeitweise auch die Möglichkeit eröffnet, ohne Einzahlung zu spielen. In Pay N Play Casinos ist keine Registrierung notwendig – nach Bekanntgabe deiner BankID kannst du direkt Geld aufladen und sofort im Casino spielen. Die Willkommensboni in den getesteten deutschen Online-Casinos sind streng reguliert und unterliegen klaren gesetzlichen Vorgaben.
References:
https://online-spielhallen.de/nine-casino-uk-150-150-freispiele-premium-gaming/
Ausführliche Informationen über die Institution werden auf der offiziellen Seite -baden-baden.de präsentiert. Vergessen Sie nicht, dass jedes online Spielhallen einen Vorteil gegenüber den Spielern hat. Die besten Online Casinos können deutlich mehr Vorteile bieten, die Ihnen ein unvergessliches Spielerlebnis bescheren werden.
Setze auf Debit- oder Prepaid-Karten und spiele nur mit Geld, das du auch wirklich zur Hand hast. Im Folgenden zeigen wir dir, welche Kontaktmöglichkeiten unsere besten Online Casinos der Schweiz anbieten und wann der Support jeweils erreichbar ist. Von den 21 Schweizer Spielstätten haben bisher elf von ihrem Recht Gebrauch gemacht, eine Online Erweiterung zu beantragen, mit der sie ihre Spiele im digitalen Raum anbieten können. Online Casinos kannst du mit lokalen Zahlungsmethoden wie TWINT, PostFinance und Schweizer Banküberweisungen einzahlen – ein Vorteil, den ausländische Anbieter nicht bieten. Das Bundesgesetz über die Geldspiele (BGS) regelt die Anforderungen an die Online Casinos, deren Einhaltung von der ESBK überwacht wird. Besonders bekannt ist es für lizenzierte Slots wie Breaking Bad und Gladiator, die Filmklassiker auf die Walzen bringen. NetEnt, ein schwedisches Unternehmen, das 1996 gegründet wurde, bietet rund 200 Spiele, hauptsächlich Slots wie Starburst XXXtreme, Divine Fortune Megaways und Wild Wild West.
References:
https://online-spielhallen.de/boomerang-casino-deutschland-test-bonus-bis-zu-500e/
Dieser Bonus kann zum Spielen verschiedener Casinospiele verwendet werden, ohne eigenes Geld zu riskieren. Kenntnis der Umsatzbedingungen, qualifizierten Spiele, Einsatzlimits und maximalen Gewinnsummen ermöglicht es Ihnen, den meisten Nutzen aus dem Angebot zu ziehen. Der 15 Euro Bonus ohne Einzahlung bietet eine fantastische Gelegenheit, Online Casinos risikofrei zu erkunden und echtes Geld zu gewinnen, ohne eine Einzahlung vornehmen zu müssen.
Geschäftsbedingungen gelten. 15 € Bonus ohne Einzahlung sind eine beliebte Aktion im Online-Glücksspiel, die es Spielern ermöglicht, Casinospiele zu genießen, ohne ihr eigenes Geld zu riskieren. Onlinespielcasino.de unterstützt den verantwortungsvollen Umgang mit Glücksspiel. Sie befürwortet den Einsatz moderner Tools, die ein sicheres und kontrolliertes Spielverhalten unterstützen. Immerhin bietet kostenloses Bargeld ohne Einzahlung einen festen Betrag an Bonusgeld, der direkt auf euer Konto gutgeschrieben wird.
References:
https://online-spielhallen.de/drip-casino-test-bonus-auszahlungen/
Auf CasinoOnline.de helfen wir Ihnen, indem wir neue Casinos online schnell analysieren und unsere Testberichte oft nur wenige Wochen nach dem Launch eines Casinos veröffentlichen. Viele neue Online Casinos bieten auch nicht mehr nur die Games eines Software Herstellers an, sondern haben eine gute Auswahl der besten Spiele verschiedener Anbieter. Während viele etablierte Anbieter seit Jahren auf dieselben Casino Spiele setzen, können Sie bei neuen Spielbanken im Internet davon ausgehen, dass Sie hier die aktuellsten Entwicklungen der Branche finden werden. Zwar muss ein neues Casino nicht zwangsläufig auch über eine hochmoderne Casino-Software verfügen, viele neue Anbieter beeindrucken aber durch die hohe Funktionalität ihrer Software und große Benutzerfreundlichkeit.
Für neue Benutzer stehen alle Arten von Boni zur Verfügung, darunter Freispiele, die Teilnahme an Turnieren für 1 Million Euro und ein Reload-Bonus. Der Bonus ist sowohl für Spielautomaten als auch für Tischspiele gut. Vegadream ist ein ziemlich neues Casino Online, das 2021 mit einer Lizenz der Malta Gaming Authority eröffnet wurde.
References:
https://online-spielhallen.de/spin4bonus-top-casinoseiten-fur-deutschland-2025/
Hier auf Casinospiele.net kann sich ein Besucher an den kostenlosen Automaten vergnügen und um Spielgeld zocken. Die Macher wollten allen Casinospielern die Möglichkeit geben ihre Lieblingsspiele kostenlos testen zu können. Da man alle Casinospiele kostenlos Online Spielen kann, ist diese Seite für begeisterte Casinospieler ein Muss! Ja, auch bei anderen Online Casinos können Sie kostenlos spielen, jedoch nicht bei allen Anbietern.
Playtech Casino Spins werden vornehmlich im Zuge der Promotionen-Aktionen für die Stammkunden angeboten, wobei die gültigen Spielautomaten oft gewechselt werden. Seinen sehr guten Ruf hat sich die Programmierer-Schmiede einst mit der Marvel Serie erarbeitet, heute stehen die verschiedenen Age of the Gods Slots im Mittelpunkt. Playtech gehört seit der Jahrtausendwende zu den besten drei Software-Casino Firmen. Merkur hat vor rund zehn Jahren begonnen, die eigenen Spielkreationen online anzupassen. Genau aus diesem Grund sind die Free-Games des deutschen Software-Herstellers aber so beliebt.
References:
https://online-spielhallen.de/princess-casino-online-slots-ubersicht-erfahrung/
Sie erhalten Freispiele, ohne Geld einzuzahlen – meist für neue Spieler. Schauen wir uns an, wie sich Freespins ohne Einzahlung im Vergleich zu anderen Aktionen schlagen, und helfen Ihnen dabei, die passenden Boni für Ihr Online Glücksspielerlebnis zu finden. Deshalb ist er für die meisten Glücksspieler so attraktiv. Anschließend nehmen Sie am Freispiele Bonus ohne Einzahlung teil und spielen mit Ihren Freispielen. In der Regel erhalten Sie Freispiele ohne Einzahlung als Neukunde direkt nach der Registrierung, gelegentlich auch über einen Bonus Code. Stattdessen drehen Sie die Walzen der Automatenspiele mit den Freispielen des Casinos. Ein Bonus ohne Einzahlung ist eine Casino Bonus Aktion, bei der Spieler Online Spielautomaten spielen können, ohne eigenes Geld einzusetzen oder einzuzahlen.
Waltenberg hat Tausende von Online-Casinos, Spielautomaten und Casinospielen überprüft und verfügt über fundierte Kenntnisse zu Boni und Spielautomaten. Egal ob Du einen Echtgeld Bonus ohne Einzahlung oder Freispiele ohne Einzahlung zur Verfügung gestellt bekommst, es kommt am Ende immer auf die Bonusbedingungen an. Echtgeld Bonus oder Freispiele ohne Einzahlung – was ist besser?
References:
https://online-spielhallen.de/nine-casino-uk-150-150-freispiele-premium-gaming/
Der deutsche Spielautomaten Hersteller Bally Wulff bietet Klassiker wie Fancy Fruits, Magic Book und Roman Legion. Dazu gehören Razor Shark, The Dog House Megaways und Gates of Olympus, die durch hohe Gewinnmöglichkeiten, Freispiele und packendes Gameplay bestechen. Spiele wie Book of Ra Magic oder Sizzling Hot sind die Highlights aus über 400 Automatenspielen.
So können Sie sich in aller Ruhe für ein Echtgeld Casino online entscheiden. Internet Casinos können jede Menge Spaß, große Auszahlungen und exklusive Aktionen anbieten, aber man muss sich sicher sein können, dass die Online Casino Echtgeld Spiele sicher und zuverlässig sind. So stehen Ihnen beispielsweise bei einem Willkommensbonus von 100% bis zu einem Betrag von 1.000 Euro maximal 2.000 Euro zum Spielen zur Verfügung. Neben „The Hoff“ glänzt die Online Spielhalle aber noch mit einem top Spieleangebot von mehr als 1.000 Spielen von über 50 Slot Providern sowie schnellen Auszahlungen innerhalb von 1-5 Werktagen. Bereits im Jahr 2022 hat das BingBong Casino die deutsche Lizenz erhalten und macht es sich seitdem zur Aufgabe im Social Media Outfit ein jüngeres Publikum anzusprechen.
References:
https://online-spielhallen.de/beste-online-casinos-2025-empfehlungs-guide/
Denn die „Nachweislich Fair“ Methode bietet Ihnen die Chance, die Zufälligkeit und Fairness der Games zu überprüfen. In der Regel erhalten Sie bei diesem Bonus im Bitcoin Casino ohne Einzahlung ein kleines Budget oder eine Handvoll Freispiele, die Sie beliebig verwenden können. Es kann beispielsweise sein, dass Sie zur Aktivierung der Boni einen Promo Code angeben oder eine Mindesteinzahlung berücksichtigen müssen. Somit stellt ein Neukundenbonus eine ideale Starthilfe dar, mit der Sie den Anbieter mit reduziertem Risiko kennenlernen können. Für den perfekten Start spendieren Ihnen die besten Bitcoin Casinos ohne Verifizierung einen Willkommensbonus.
Sie bieten ein Willkommensbonuspaket von bis zu 2.250 €/USDT und 90 Freispielen über die ersten vier Einzahlungen. Billionairespin bietet einen sehr aufregenden Willkommensbonus von bis zu 450 € und 250 Freispielen, um die erste Session bei den tausend verschiedenen Spielen so spannend wie möglich zu gestalten. Krypto Casinos sind in den letzten Jahren immer beliebter geworden, da sie eine bequeme und anonyme Möglichkeit bieten, online zu spielen. Oft bieten Krypto Casinos besonders hohe Willkommensboni an, die manchmal neben einem Einzahlungsbonus auch Freispiele beinhalten. Ja, Krypto Casinos bieten umfangreiche Boni an, darunter Willkommenspakete mit Einzahlungsboni von bis zu 180 %, Freispiele auf beliebten Slots, krypto-spezifische Reload-Boni, Cashback auf Verluste und VIP-Belohnungsprogramme.
References:
https://online-spielhallen.de/nv-casino-einloggen-schnell-sicher/
Bei progressiven Jackpots können Sie umso mehr gewinnen, je mehr Leute mitspielen! Je mehr Leute spielen, desto mehr können wir gewinnen! Vor allem, wenn Sie ihn mit unserer aufregenden Auswahl an Tischspielen bei 24Casino in Ihrer Hand halten können! Jedes Mal, wenn Sie an Ihren Lieblings-Slots oder Tischspielen drehen, verdienen Sie Rakeback.
Darüber hinaus gibt es 50 Freispiele ohne Einzahlung, was einen risikofreien Einstieg ermöglicht. ✔️ Flexible Bonuswahl – 500 € oder 5 BTC + 180 Freispiele Die Plattform ist lizenziert, mobilfreundlich und überzeugt mit einer intuitiven Navigation sowie regelmäßigen Aktionen und Turnieren für treue Spieler.
References:
https://online-spielhallen.de/beste-online-casinos-deutschland-top-10-nov-2025-3/
Die besten Spielanbieter setzen an dieser Stelle vorwiegend auf Free Spins, Gewinnspiele, Cashback-Angebote und zum Teil auch auf echte Reloadboni. Für die deutschen Spielfans gibt’s online mittlerweile noch ein besonderes Highlight. Leider kannst du derzeit Book of Ra nicht mit Echtgeld online spielen. Ja, die besten Online Casinos bieten immer die Möglichkeit alle RNG Spiele auch kostenlos zu spielen. Man kann diese immer und überall sowohl am Desktop als auch mobil spielen.
Renommierte Marken arbeiten nur mit lizenzierten Anbietern zusammen. Auf was deutsche Spieler ab jetzt achten müssen und wie man die besten sicheren Online Casinos darunter findet, verraten wir hier. Bestehende Spieler können tägliche Bonusangebote für weitere Freispiele nutzen. Wir sind kein illegales Online Casino, sondern als erste legale Online Spielhalle in Deutschland lizenziert und zugelassen.
References:
https://online-spielhallen.de/princess-casino-online-slots-ubersicht-erfahrung/
Beachten Sie, dass es in der Auswahl von Live-Spielen in NVcasino online interessante Automaten mit bedingt «erotischem» Inhalt gibt. Ein interessantes Merkmal von NV casino online ist der Zugriff auf Testversionen von Spielen auch im Live-Bereich. Beachten Sie, dass die Vielfalt der Angebote im NV casino online an den Automaten nicht aufhört. Oben haben wir darüber gesprochen, dass NV casino online Automaten und Live-Spiele von mehr als fünfzig Anbietern von Spielsoftware enthält. Egal wann, wo und auf welchem Gerät Sie spielen möchten – das NV Casino ist auf Ihrem Handy und Tablet verfügbar. Die Mission von NV Casino beschränkt sich nicht nur darauf, Ihnen eine vertrauenswürdige und zuverlässige Spielplattform auf jedem Gerät zu bieten. Wie einfach, schnell und bequem ist es, in einem Online-Casino zu spielen?
Sie bieten einen ausgezeichneten Kundendienst, ein breites Angebot an Spielen von renommierten Herstellern und schnelle Auszahlungen. Das Zahlungsangebot ist oft vorzüglich und bietet lokale Optionen wie Paysafecard, Sofort und Giropay. Die Boni erfordern eine Mindesteinzahlung von 20€ und müssen innerhalb von 7 Tagen 35 Mal umgesetzt werden. Als Willkommensbonus kannst du zwischen 7 verschiedenen Optionen wählen, die wirklich alle Präferenzen und Spielstile abdecken.
References:
https://online-spielhallen.de/top-9-online-casinos-in-deutschland-2025/
Wir empfehlen Ihnen, sich den Willkommensbonus sowie alle anderen angebotenen Aktionen anzusehen, bevor Sie sich für ein Echtgeldkonto anmelden. Die besten Auszahlungsseiten bieten eine Reihe von Zahlungsmethoden, aus denen Sie wählen können. Alle von uns empfohlenen Websites sind sicher und zuverlässig und alle lizenziert und reguliert. Einige der führenden Behörden, die Glücksspielseiten lizenzieren, sind die Malta Gaming Authority, die Kahnawake Gaming Commission und die Curacao Gaming Commission. Nachfolgend finden Sie einige der wichtigsten Elemente, die Sie berücksichtigen sollten. Casinos, Sportwetten und Pferdewetten sind derzeit in Schleswig-Holstein erlaubt, aber Glücksspiele nicht. Nachfolgend finden Sie eine Zeitleiste der Entwicklung von iGaming in dem Land.
Derzeit bietet kein Echtgeld Casino PayPal auf dem deutschen Markt an. Doch Spieler können sich schnell einen Überblick verschaffen, ob ein Anbieter seriös ist oder nicht und ob sie gewillt sind mit echtem Geld zu spielen. Alle Titel wie 40 Thieves, Creatures of the Night, Mystic Force and Fruits & Wilds 2 könnt ihr auch sowohl in der Spielothek als auch im Online Casino um echtes Geld spielen. Jedoch ist der Hersteller derzeit nicht mehr auf dem deutschen Markt vertreten.
References:
https://online-spielhallen.de/vulkan-vegas-casino-test-bonus-bis-1500e/
Stattdessen drehen Sie die Walzen der Automatenspiele mit den Freispielen des Casinos. Ein Bonus ohne Einzahlung ist eine https://online-spielhallen.de/bester-online-casino-bonus-2025-top-boni-in-deutschland/, bei der Spieler Online Spielautomaten spielen können, ohne eigenes Geld einzusetzen oder einzuzahlen. Denn Einzahlungsboni wie beim Instant Casino bieten oft deutlich bessere Vorteile – höhere Bonusbeträge, Cashback und mehr Freispiele.
Der 100%ige Einzahlungsbonus des One Casinos unterliegt nur 35-fachen Wettanforderungen. Dieser Bonusbetrag von 10 Euro muss 45 Mal umgesetzt werden, bevor er in Echtgeld umgewandelt und ausgezahlt werden kann. Dieses Bonusgeld kannst du dann dazu nutzen, um verschiedene Spiele im Casino auszuprobieren.
Deine Casinoauswahl sollte vom Spielangebot und den gesetzlichen Regelungen bestimmt werden und nicht von einem Bonus. Du kannst maximal den 600-fachen Einsatz bei einem Dreh gewinnen. Die Wahrscheinlichkeit zu gewinnen ist aber mit wenig Budget eher geringer, da diese hohen Gewinne natürlich weniger häufig vorkommen. Das Spiel bietet Scatter Symbole welche Freispiele auslösen können, sowie andere Mystery Symbole und Multiplikatoren. Die meisten Online Casinos bieten dir weit über 1.000 Slots zu unterschiedlichen Themenbereichen. Es gibt eine große Auswahl an Slots von verschiedensten Spieleanbietern. Die meisten Freispiele haben einen Wert zwischen 0,10 und 0,20 Euro.
Um neue Kunden zu gewinnen, greifen sie darum tief in die Tasche. Statt einmalig 400 Prozent zu erhalten, handelt es sich um ein Willkommenspaket. Kein Betrug und auch nicht unseriös, dafür verwirrend ist die Darstellung als 400% Casino Bonus des Mr Bet Willkommensangebots. Casinos bieten häufig Werbeaktionen und Boni an, um ihre treuen Spieler an sich zu binden. Außerdem bieten viele Online Casinos Newsletter oder E-Mail-Updates an, die exklusive Bonuscodes enthalten. Während die Desktop-Casinos mit großem Bildschirm und leistungsstarker Hardware punkten, bieten Handy Casinos aber eine höhere Flexibilität. Oftmals bieten solche Bonus Codes exklusive Vorteile, die nur für mobile Nutzer verfügbar sind, was das Spielen auf dem Smartphone noch attraktiver macht.
References:
https://online-spielhallen.de/wurfelspiele-im-casino-regeln-top-spiele-tipps/
Mehr zu Echtgeld-Casino-Lizenzen und Gesetzen in der Kategorie beste deutsche Online Casinos erfahren Sie unten auf dieser Seite. Wir sprechen Empfehlungen nur für Online Casinos mit deutscher Lizenz aus, die von staatlichen Glücksspielaufsichtsbehörden wie der GGL (Gemeinsame Glücksspielbehörde der Länder) reguliert werden. Zudem bietet Tipico eine benutzerfreundliche mobile App, die ein nahtloses Spielerlebnis auf Smartphones und Tablets ermöglicht. Tipico legt großen Wert auf sicheres Spielen und verfügt über eine deutsche Lizenz der Gemeinsamen Glücksspielbehörde der Länder (GGL). Die EU Spielothek bietet eine Vielzahl sicherer Zahlungsmethoden an, darunter Visa, Mastercard, Sofortüberweisung, PayPal und Paysafecard. Die EU Spielothek ist seit 2019 auf dem Markt und legt besonderen Wert auf Spielerschutz und Datensicherheit.
NetEnt Microgaming und zahlreiche weitere Unternehmen zeigen seit vielen Jahren, dass die Fairness beim Online Casino spielen gegeben ist. Ab heute heißt es für dich nur noch finden und spielen. Mit diesen Tipps kannst du deine Casino Boni ganz bequem mobil nutzen und jederzeit und überall spielen! Während hohe Einzahlungsboni mit hohen Umsatzbedingungen verbunden sind, bieten Freispiele eine interessante Alternative. Wir haben für dich einige der aktuell attraktivsten Bonusangebote in deutschen Online Casinos zusammengestellt.
References:
https://online-spielhallen.de/stake-casino-deutschland-online-crypto-casino/
Der neue deutsche Glücksspielstaatsvertrag von 2021 wirbelt den Markt ganz schön durcheinander. Das ist einer der Gründe, weshalb wir keine Online Casinos mit deutscher Lizenz in unseren Bestenlisten haben. Mit der folgenden einfachen Anleitung findet ihr souverän die besten Casinos für Deutschland online! Dabei könnt ihr tausende Qualitätsspiele von absoluten Welt-Providern wie Play’n go oder NetEnt erwarten. Was euch im Einzelnen erwartet, lest ihr in den https://online-spielhallen.de/platincasino-bonus-test-200-freispiele/ von OSC!
Auf unseriösen Casino Plattformen zu spielen, kann schwerwiegende Folgen haben, die weit über den finanziellen Verlust hinausgehen. In den 70er und 80er Jahren kam das Videopoker auf, mit dem du dieses Kartenspiel auch alleine spielen kann. Blackjack kannst du auch im Live Casino deiner Online Spielbank spielen, wo du in Echtzeit gegen einen echten Dealer dein Können beweisen kannst. Durch Bonusspiele, Freispiele und progressive Jackpots bieten moderne Online Spielautomaten oft zusätzliche Spannung und Gewinnmöglichkeiten.
Ich kann den Beiträgen von Stephon und DarkPhoenix nur zustimmen, der “neue” Bond ist absolut sehenswert. Der Bösewicht sah viel lieber aus als bond und Bond hätte einen Kopfschuß verdient so wie der aussieht. So einen Schrott hat man selten gesehen. Diese hier ist die Verfilmung des allersten Romanes aus der Reihe von “James Bond 007″… Spätestens seit Brosnan konnte man sich doch keinen Film dieser Reihe mehr ansehen. Die Grundlage dafür zu sehen, ist großartig, sozusagen alles back to the roots.
All dies führte bis hin zu Schlagzeilen wie „James Blond“ oder „James Bland“ (englisch bland ‚langweilig‘). Auch seine fehlende Erfahrung in Hochglanzproduktionen wurde ihm vorgehalten, war er zuvor doch vorwiegend in intimeren Dramen zu sehen. Mit seinen Hauptrollen im Gangsterfilm Layer Cake sowie als Mossad-Agent in München empfahl sich Daniel Craig bei den Produzenten als neuer „007“, was durchaus auch öffentlich so wahrgenommen wurde. Erstmals Interesse an einer Neuverfilmung zeigte 2004 Kultregisseur Quentin Tarantino.
References:
https://online-spielhallen.de/verde-casino-bonus-aktuelle-angebote-tipps/
mail slot cover
References:
https://atavi.com/share/xkotnkz1epp2b
valley view casino center
References:
http://palangshim.com/space-uid-4742917.html
halifax casino
References:
http://1v34.com/space-uid-1151739.html
macau casino
References:
https://images.google.com.ly/url?q=https://urlscan.io/result/019ac844-26ec-7123-8620-d1877c0bcb64/
michigan casinos
References:
https://maps.google.com.lb/url?q=https://atavi.com/share/xkno4lzh94bb
las vegas slot machines
References:
https://www.google.ps/url?q=https://kanban.xsitepool.tu-freiberg.de/gvUGTwYMRkC_YJM4riiVlQ/
maryland casinos
References:
https://images.google.ad/url?q=https://pads.jeito.nl/g8Xv_C7OSamu1ysTAFv2mQ/
roulette wheel layout
References:
http://volleypedia.org/index.php?qa=user&qa_1=beepvc08
entree holland casino
References:
https://www.folkd.com/submit/md.un-hack-bar.de/caoDwPgKSJW72IcLRTiRaQ//
river spirit casino tulsa
References:
https://schoolido.lu/user/mistneedle5/
century casino cripple creek
References:
https://images.google.com.my/url?q=https://urlscan.io/result/019ac517-42eb-760b-b969-658800b5ee57/
genting casino luton
References:
https://case.edu/cgi-bin/newsline.pl?URL=https://blackcoin.co/casino-hotel-locations/
hoosier park racing and casino
References:
https://www.google.co.ls/url?q=https://hedgedoc.info.uqam.ca/AJhM6_UwTT-ArRh8JnvMug/
blackjack online for money
References:
https://graph.org/10-New-Online-Casinos-USA-in-2025-Latest-Gaming-Sites-11-27
turtle creek casino
References:
https://images.google.td/url?q=https://able2know.org/user/canceryacht31/
best online casino uk
References:
https://forum.finveo.world/members/bundoor76/activity/271962/
holland casino scheveningen
References:
http://123.57.147.237/orangepibbsen/home.php?mod=space&uid=6109128
hollywood casino joliet
References:
https://yogicentral.science/wiki/Best_Online_Casinos_in_the_USA_for_November_2025_Ranked
online casino slot machines
References:
http://lzdsxxb.com/home.php?mod=space&uid=5386406
woodbine slots
References:
https://www.aupeopleweb.com.au/au/home.php?mod=space&uid=2436974
william hill promotional code
References:
https://maps.google.ml/url?q=https://clockbox1.werite.net/sgr-asx-star-entertainment-seals-queens-wharf-casino-deal-with-chow-tai-fook
branson mo casinos
References:
https://maps.google.fr/url?q=https://www.woorips.vic.edu.au/profile/godfreyxendelacruz89519/profile
blackjack software
References:
http://39.109.117.191:85/home.php?mod=space&uid=456507
china shores slot machine
References:
https://www.google.com.co/url?q=https://telegra.ph/Instant-Withdrawal-Casino-Australia-Top-Fast-Payout-Casinos-11-27
cops and robbers games
References:
https://financialinclusionnigeria.org/activity/p/308882/
best slots to play
References:
https://kopeechka.net/user/profile/9598
cool gaming names
References:
http://hikvisiondb.webcam/index.php?title=jacobsendowd0161
seven clans casino
References:
https://www.divephotoguide.com/user/harpbench78
st joe frontier casino
References:
https://6.k1668.cn/home.php?mod=space&uid=526774
blackjack online for money
References:
https://www.google.com.sb/url?q=https://kanban.xsitepool.tu-freiberg.de/Yo4jUxjeR1W_bouRoOYJUg/
casino monticello
References:
http://39.109.117.191:85/home.php?mod=space&uid=458351
poker no deposit bonus
References:
http://39.109.117.191:85/home.php?mod=space&uid=457619
greenbrier casino
References:
http://jslt28.com/home.php?mod=space&uid=2691766
clams casino producer
References:
http://asresin.cn/home.php?mod=space&uid=339942
windsor casino
References:
https://www.google.com.gi/url?q=https://numberfields.asu.edu/NumberFields/show_user.php?userid=6362731
roulette wheel numbers
References:
https://xs.xylvip.com/home.php?mod=space&uid=4081738
christophe claret 21 blackjack
References:
http://www.donggoudi.com/home.php?mod=space&uid=3876384
palms casino las vegas
References:
https://images.google.com.sv/url?q=https://www.folkd.com/submit/blackcoin.co/vacation-like-a-star-planet-hollywood-resort-casino-las-vegas//
sunset station casino
References:
http://bbs.yuanjumoli.com/home.php?mod=space&uid=381780
mahjong 3d more time
References:
https://www.google.ci/url?q=https://atavi.com/share/xkoqw3z1l944d
online casino u s a
References:
https://humanlove.stream/wiki/The_Wharf_Restaurant_Bar
games twist casino
References:
https://www.ydaojia.com/home.php?mod=space&uid=887969
europe casino
References:
https://www.lanubedocente.21.edu.ar/profile/kristoffersenlvbgrantham85305/profile
casino download
References:
https://heeuxuzb.517818.com/home.php?mod=space&uid=126749
club one casino
References:
https://maps.google.fr/url?q=https://atavi.com/share/xko2akz19ewqf
hard rock casino tampa florida
References:
https://maps.google.nr/url?q=https://www.pdc.edu/?URL=https://blackcoin.co/king-billy-casino-login-quick-overview/
lucky emperor casino
References:
https://www.nlvbang.com/home.php?mod=space&uid=2620970
md live casino
References:
https://www.scdmtj.com/home.php?mod=space&uid=6062991
casino spa
References:
https://pads.jeito.nl/opyy1IBUQTGbQsVVhNc–g/
new orleans casinos
References:
http://asresin.cn/home.php?mod=space&uid=339942
meadows casino
References:
http://daojianchina.com/home.php?mod=space&uid=678193
pink floyd live at pompeii
References:
https://images.google.td/url?q=https://atavi.com/share/xkm9vyzclxbj
roulette betting strategy
References:
https://images.google.bg/url?q=https://www.folkd.com/submit/blackcoin.co/vacation-like-a-star-planet-hollywood-resort-casino-las-vegas//
skagit casino
References:
http://bbs.lingshangkaihua.com/home.php?mod=space&uid=4123933
blackjack statistics
References:
http://wx.abcvote.cn/home.php?mod=space&uid=5731407
online casino sverige
References:
https://hedgedoc.info.uqam.ca/p5WSUQgLTimFafNXhCkjZw/
charleston wv casino
References:
https://www.google.pl/url?q=https://md.un-hack-bar.de/MaPjAkH2REGL5Cwy1JMg7w/
cherokee casino siloam springs
References:
http://47.92.5.61:8080/home.php?mod=space&uid=250344
treasury casino brisbane
References:
https://graph.org/Wild-Fortune-Casino-Review-A-Gateway-to-Online-Gambling-AU-11-26
29 casino
References:
https://www.pdc.edu/?URL=https://blackcoin.co/casino-club-erfahrungen/
hinckley grand casino
References:
http://lzdsxxb.com/home.php?mod=space&uid=5386406
georgia casinos
References:
http://yigaizhuang.net/home.php?mod=space&uid=638282
casino australia
References:
https://socialbookmark.stream/story.php?title=las-vegas-hotels-best-hotels-in-las-vegas-caesars-experience-vegas
emerald queen casino
References:
https://www.google.co.mz/url?q=https://hedgedoc.info.uqam.ca/9fPHKHanQlmSXemteupBSQ/
valley view casino seating chart
References:
https://www.google.com.ai/url?q=https://kanban.xsitepool.tu-freiberg.de/RJz76C69TByHAM1t0tqk9g/
hard rock casino northfield ohio
References:
https://www.orkhonschool.edu.mn/profile/storgaardbnyshepard28732/profile
cherry casino
References:
https://maps.google.ae/url?q=https://md.swk-web.com/tjxscmigRESHiP5g_K910g/
wind creek casino wetumpka
References:
https://xs.xylvip.com/home.php?mod=space&uid=4081819
live roulette online
References:
https://images.google.com.hk/url?q=https://telegra.ph/Optometry-in-Bismarck-ND-11-27
silverstar casino spa
References:
http://bbs.medicalforum.cn/home.php?mod=space&uid=1896766
spin palace flash
References:
https://atavi.com/share/xkm9uaz1f1vta
quebec roulette
References:
https://www.holycrossconvent.edu.na/profile/sunmjzalbrektsen55551/profile
neteller account
References:
https://trade-britanica.trade/wiki/Official_Site
bally’s las vegas reviews
References:
https://images.google.co.il/url?q=https://urlscan.io/result/019ac59a-ff1f-771b-b58f-708d78effc17/
mountaineer racetrack and casino
References:
https://www.lasallesancristobal.edu.mx/profile/palmerfuocastro43359/profile
langley casino
References:
https://www.lanubedocente.21.edu.ar/profile/paaskevacmahmood40226/profile
schecter blackjack atx c 7
References:
https://www.google.co.mz/url?q=https://skitterphoto.com/photographers/1921780/putnam-lott
casino slot machine
References:
http://legend001.com/bbs/home.php?mod=space&uid=627873
route 66 casino
References:
https://lovewiki.faith/wiki/Razed_Casino_Review_Bonuses_2025
riverwalk casino vicksburg
References:
http://forum.maoshan73.com.hk/home.php?mod=space&uid=1180859
margaritaville casino
References:
http://1v34.com/space-uid-1151793.html
vegas online casino
References:
https://ai-db.science/wiki/Melbourne_Casinos_Just_the_Crown
casino marbella
References:
https://www.google.com.gi/url?q=https://pad.stuve.uni-ulm.de/s/685Ic9gES
game twist casino
References:
https://xypid.win/story.php?title=hotels-near-crown-casino-melbourne-from-48-night
cinema casino auxerre
References:
https://www.google.co.ao/url?q=https://md.ctdo.de/s/4HEw5gkIDP
slot machine jackpot
References:
https://maps.google.com.pr/url?q=https://md.entropia.de/s/Q9VS4pFnS
lucky dog casino
References:
https://images.google.com.hk/url?q=https://md.chaosdorf.de/s/PruY3ovCt
casino erie pa
References:
https://bbs.jin999.tw/jin/home.php?mod=space&uid=241333
casino st louis
References:
https://fsquan8.cn/home.php?mod=space&uid=5089295
brimley casino
References:
https://images.google.co.za/url?q=https://www.instapaper.com/p/17225656
kabam slots
References:
https://brewwiki.win/wiki/Post:The_Best_Online_Casino_in_Australia_2025
casino grand luxe
References:
https://cecr.co.in/classifieds/index.php?page=user&action=pub_profile&id=234059
online slot games
References:
https://bbs.pku.edu.cn/v2/jump-to.php?url=https://blackcoin.co/the-best-high-roller-lounges-in-australia/
chinook winds casino
References:
https://www.google.mn/url?q=https://www.woorips.vic.edu.au/profile/gleasonvvywest88830/profile
rincon casino
References:
https://www.credly.com/users/chinjump04
play online games games
References:
https://bom.so/Kpo7BR
blackjack bomber
References:
https://www.bitspower.com/support/user/airbusknight71
big fish casino
References:
https://images.google.com.hk/url?q=https://www.immo-web.ro/user/profile/1191069
red dead redemption blackjack
References:
https://peatix.com/user/28501256
roulette machine
References:
https://www.ydaojia.com/home.php?mod=space&uid=919606
sport betting online
References:
https://www.giveawayoftheday.com/forums/profile/1483777
777 casino drive cherokee nc 28719
References:
https://discoveringalifeyoulove.com/members/skiingapril18/activity/44128/
caesars casino online
References:
https://clashofcryptos.trade/wiki/The_Ultimate_Online_Casino_Comparison_Hub
sky vegas login
References:
https://forums.ppsspp.org/member.php?action=profile&uid=5905987
roulette play
References:
https://isowindows.net/user/dealjump73/
top 10 online casinos
References:
https://bookmarkingworld.review/story.php?title=king-billy-casino-is-real-money-online-casino-in-australia
ac casinos
References:
https://www.google.mn/url?q=https://writeablog.net/hastingsdawson1190/new-york-new-york-hotel-and-casino-map
casino mobile
References:
http://www.jcdqzdh.com/home.php?mod=space&uid=819023
coeur d’alene casino
References:
https://www.google.com.ai/url?q=https://www.orkhonschool.edu.mn/profile/cassidykjoblackwell99220/profile
slots jungle
References:
https://v.gd/x8ewCs
high five casino download
References:
http://mem168new.com/home.php?mod=space&uid=3669329
tunica mississippi casinos
References:
https://www.kdbang.vip/home.php?mod=space&uid=1210456
winning slot machines
References:
https://images.google.com.gt/url?q=https://blogfreely.net/bailtime37/rocketplay-casino-germany-top-bonus-and-app-erlebnis-2025
best roulette bets
References:
https://yogicentral.science/wiki/7Bit_Casino_Review_2025_5_25_BTC_350_FS
mac casino
References:
https://timeoftheworld.date/wiki/TOP_10_Best_Online_Casinos_Australia_For_Real_Money_2025
play slots for real money
References:
https://bom.so/0wr06S
saint laurent le minier
References:
https://maps.google.com.br/url?q=https://atavi.com/share/xl7h0ezm64ub
dubuque iowa casino
References:
https://www.adhub.fi/user/profile/12409
cleopatra slots
References:
https://marvelvsdc.faith/wiki/36_Crown_jobs_in_Melbourne
blue rodeo in our nature
References:
https://maps.google.ae/url?q=https://code.antopie.org/sphynxreport83
roulette strategy to win
References:
https://hack.allmende.io/s/GRBY1y80N
buffalo bills casino
References:
http://shangjiaw.cookeji.com/home.php?mod=space&uid=584841
dubuque casino
References:
https://bookmarkzones.trade/story.php?title=best-online-casinos-usa-2025-real-money-bonuses-new-sites
valley view casino center san diego
References:
https://www.google.com.ag/url?q=https://md.chaosdorf.de/s/AfYX6lF55
canadian online casino
References:
https://www.instructables.com/member/hoeapril18/
royal river casino
References:
https://www.lasallesancristobal.edu.mx/profile/owendirbarton93239/profile
phone casino games
References:
http://cdss.snw999.com/space-uid-1901192.html
hollywood casino md
References:
https://maps.google.com.ar/url?q=https://urlscan.io/result/019af97a-db18-704e-8222-77a009c0770e/
casino grand luxe
References:
https://humanlove.stream/wiki/Cryptologic_Casino_Bonuses_listing
el dorado casino shreveport
References:
http://lzdsxxb.com/home.php?mod=space&uid=5419270
phone casino games
References:
https://fravito.fr/user/profile/2117308
hollywood casino tunica
References:
https://pad.stuve.de/s/jVkdruCC5
william hill android app download
References:
http://bbs.xltyun.com/space-uid-730050.html
caesars casino windsor
References:
https://maps.google.com.br/url?q=https://atavi.com/share/xl7h3hz13xxj7
roulette machine
References:
http://qiaoxiaojun.vip/home.php?mod=space&uid=1760661
bodog casino
References:
https://maps.google.no/url?q=https://hack.allmende.io/s/z-gCzsdZX
games online games
References:
http://bbs.wuhudj.com/space-uid-1082384.html
emerald princess casino
References:
http://hslife.deegao.com.cn/home.php?mod=space&uid=724185
couple spa singapore
References:
https://www.play56.net/home.php?mod=space&uid=5860469
fun casino
References:
https://www.ydaojia.com/home.php?mod=space&uid=921492
slot machine games
References:
https://case.edu/cgi-bin/newsline.pl?URL=https://blackcoin.co/level-up-casino-login-guide-2/
betting odds explained
References:
https://lovebookmark.win/story.php?title=cryptologic-casino-software-developer
prestige casino
References:
https://bookmarks4.men/story.php?title=hotel-ville-resort-casino-townsville-australia-season-deals-from-103
resto a paris
References:
https://forums.ppsspp.org/member.php?action=profile&uid=5907328
online betting offers
References:
https://pad.stuve.uni-ulm.de/s/mtqus9UUt
gala casinos
References:
https://wolf-pittman.thoughtlanes.net/the-enchanting-world-of-lasseters-hotel-and-casino-alice-springs
talking stick casino
References:
http://tipslove.org/bbs/home.php?mod=space&uid=1687418
coral casino santa barbara
References:
https://www.google.com.pk/url?q=https://urlscan.io/result/019af959-83db-7766-b54d-6818333d737e/
jack and the beanstalk games
References:
https://menwiki.men/wiki/The_Linq_Wikipedia
ameristar casino st louis
References:
https://vrwant.org/wb/home.php?mod=space&uid=4802241
treasure island casino las vegas
References:
http://wargame-workshop.com/bbs/home.php?mod=space&uid=712215
wms slots online
References:
https://prosto-robota.com.ua/user/profile/663849
calgary casino
References:
https://chessdatabase.science/wiki/Best_Online_Casinos_in_Australia_Top_Real_Money_Casinos_in_2025
casino euro review
References:
https://securityholes.science/wiki/Top_5_Fastest_Payout_Online_Casino_Sites_USA
casino mississippi
References:
http://legend001.com/bbs/home.php?mod=space&uid=664164
neteller login
References:
https://marvelvsdc.faith/wiki/Safe_Online_Casinos_Australia_2025_Most_Trusted_AU_Casino_Sites
las vegas casinos
References:
http://www.qianqi.cloud/home.php?mod=space&uid=971826
slot
References:
https://maps.google.com.br/url?q=https://www.footballzaa.com/out.php?url=https://blackcoin.co/level-up-casino-login-guide-2/
casino barriere toulouse
References:
https://bookmarkspot.win/story.php?title=casino-royale-2006-james-bond-007-mi6-the-home-of-james-bond
alton belle casino
References:
https://www.google.com.uy/url?q=https://www.tarauaca.ac.gov.br/profile/hviidsozbenjamin80907/profile
shoshone rose casino
References:
http://51wanshua.com/home.php?mod=space&uid=2124250
slot marsepeinstein
References:
https://articlescad.com/the-reef-casino-review-723746.html
golden nugget las vegas nv
References:
https://maps.google.ae/url?q=https://doc.adminforge.de/s/wZRtb1gh9j
atlantis casino
References:
https://king-bookmark.stream/story.php?title=best-online-casino-games-2025-play-top-casino-games
petoskey casino
References:
http://dz.pinchepingtai.cn/home.php?mod=space&uid=502504
metro casino
References:
http://asresin.cn/home.php?mod=space&uid=359066
the meadows casino
References:
http://daojianchina.com/home.php?mod=space&uid=710822
casino gatineau
References:
http://lida-stan.by/user/baybengal52/
euro grand casino
References:
https://bookmarking.stream/story.php?title=hotels-near-star-casino-sydney-from-32-night
king casino
References:
http://honghu.cn/home.php?mod=space&uid=58
mystic island casino
References:
https://numberfields.asu.edu/NumberFields/show_user.php?userid=6383359
hollywood casino joliet
References:
https://abcbbk.com/space-uid-600631.html
mardi gras casino florida
References:
http://soumoli.com/home.php?mod=space&uid=1127663
genting casino manchester
References:
https://independent.academia.edu/FrandsenBjerring1
777 dragon casino
References:
http://bbs.abcdv.net/home.php?mod=space&uid=955009
quapaw casino
References:
https://www.google.mn/url?q=https://www.woorips.vic.edu.au/profile/jacksonepkflowers99435/profile
red garter casino
References:
https://www.google.com.pe/url?q=https://www.lasallesancristobal.edu.mx/profile/owendirbarton93239/profile
rules of roulette
References:
http://king-wifi.win//index.php?title=shepherddyer7569
red flush casino
References:
https://trade-britanica.trade/wiki/Casino_1995_directed_by_Martin_Scorsese_Reviews_film_cast
blackjack strategy trainer
References:
https://images.google.com.gt/url?q=https://atavi.com/share/xl7gu1z1h2qx
gala casino london
References:
http://king-wifi.win//index.php?title=ankersenthomas1720
southpoint casino las vegas
References:
https://www.google.co.bw/url?q=https://urlscan.io/result/019af97a-db18-704e-8222-77a009c0770e/
harrah’s casino tunica
References:
https://saleh-vester.hubstack.net/new-no-deposit-bonuses
supercasino com
References:
https://www.glassyun58.com/home.php?mod=space&uid=994891
microgaming online casino
References:
https://www.secondhandbazaar.in/user/profile/1706275
how do you play roulette
References:
https://mm.yxwst58.com/home.php?mod=space&uid=1893972
vee quiva casino az
References:
https://www.google.co.zm/url?q=https://www.rosewood.edu.na/profile/marcussenwjdmcnamara21689/profile
live casino md
References:
https://independent.academia.edu/EasonBurnett2
prism casino
References:
https://www.laba688.com/home.php?mod=space&uid=9631135
jackpotjoy slot machines
References:
https://www.argfx1.com/user/gamebolt91/
casino en france
References:
https://images.google.bi/url?q=https://topp-foreman.thoughtlanes.net/the-best-online-casinos-in-australia-for-2025-rated-by
hard rock casino tulsa ok
References:
https://maps.google.mw/url?q=https://atavi.com/share/xl7h0ezm64ub
chuzzle game
References:
http://app.gxbs.net/home.php?mod=space&uid=1479817
hollywood casino joliet il
References:
https://www.nlvbang.com/home.php?mod=space&uid=2651838
mystic island casino
References:
https://maps.google.com.tr/url?q=https://pad.geolab.space/s/sH55GqSYR
the m casino
References:
https://6.k1668.cn/home.php?mod=space&uid=560303
casino sacramento
References:
http://47.92.5.61:8080/home.php?mod=space&uid=280393
scratch 2 cash
References:
http://cdss.snw999.com/space-uid-1896923.html
coin slot
References:
https://schoolido.lu/user/swinggrowth90/
crown perth casino
References:
http://proauto.lv/user/skiingtooth87/
inspired gaming group
References:
https://justpin.date/story.php?title=events-in-perth
california casino las vegas
References:
https://www.giveawayoftheday.com/forums/profile/1485284
casino san clemente
References:
https://www.dycangku.com/space-uid-134620.html
online casino mit startguthaben
References:
https://6.k1668.cn/home.php?mod=space&uid=562147
play slot machine
References:
https://funsilo.date/wiki/How_Deposits_Work
campione d italia casino
References:
https://lit-book.ru/user/skiingcourt61/
casino connecticut
References:
http://xhdyz.cn/home.php?mod=space&uid=395763
hollywood casino st louis
References:
https://maps.google.cv/url?q=https://cgmood.com/finn-robb
shoshone rose casino
References:
http://lzdsxxb.com/home.php?mod=space&uid=5419329
new york casino las vegas
References:
https://images.google.bg/url?q=https://www.instapaper.com/p/17227873
Thank you so much for sharing this information, this will surely help me in my work and therefore, I would like to tell you that very few people can write in a manner where the reader understands just by reading the article once.
Wow, incredible blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your web site is great, let alone the content!
https://askoff.ru
https://asklong.ru
https://askoff.ru
casino las vegas bonus code
top 10 online casino sites
best real casino online
betmgm first bet promo https://betmgm-play.com/ mgmbets
ifvod官方认证平台,专为海外华人设计,24小时不间断提供高清视频和直播服务。
https://iagperjusu.wordpress.com
https://iagperjusu.wordpress.com
https://dwspqdxcgw.wordpress.com
https://dwspqdxcgw.wordpress.com
https://xrsaugpsya.wordpress.com
https://xrsaugpsya.wordpress.com
https://gxvkxeawwa.wordpress.com
https://azacgxicis.wordpress.com
https://azacgxicis.wordpress.com
https://zfcejfyxiv.wordpress.com
https://zfcejfyxiv.wordpress.com
https://cxadxqpked.wordpress.com
https://cxadxqpked.wordpress.com
https://akiwdiycje.wordpress.com
https://akiwdiycje.wordpress.com
https://iqakruyprf.wordpress.com
https://iqakruyprf.wordpress.com
https://dgaiyziytk.wordpress.com
https://dgaiyziytk.wordpress.com
https://hrjcdfdcvj.wordpress.com
https://hrjcdfdcvj.wordpress.com
mgm app betting https://betmgm-play.com/ mgm betmgm
https://wryxvrrhxe.wordpress.com
https://thfdcufqah.wordpress.com
mcluck Nebraska mcluckcasinogm.com mcluck sportsbook promo
wow vegas casino offers an astounding no-real-money casino knowledge chock-full with top-tier slots and time-honoured giveaways. Players preference the generous sign-up bonuses and the ability to be the victor in redeemable Sweepstakes Coins through entertaining gameplay.
凯伦皮里第二季高清完整版运用AI智能推荐算法,海外华人可免费观看最新热播剧集。
Ignite sparks of joy with every successful wager. In crown coins casino login, seasonal promotions keep things fresh. Sign up and let the wins flow!
Uncover connect forums interactive with weaves lucky and games skillful of tapestry. In ignation casino app, wins your weave. Uncover and unite!
Sign up at the amazing world of online gaming where endless fun awaits. Bovada MLB Betting offers top blackjack and high-roller perks for all players. With Bovada, enjoy ultimate wins and secure, reliable entertainment every day!
Big Bass Bonanza hooks you from the first spin! Free spins Bigger Bass Bonanza massive win with cash symbols guarantee thrilling action.
Crave big wins? Sweet Bonanza serves them up with vibrant graphics and high-volatility action. Bonus sweet bonanza candyland buys and ante bets make it even sweeter. Spin away!
I think your blog might be having browser compatibility issues. When I look at your website in Ie, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, terrific blog!
lsm99 login
Roam free with wins that shake the earth. buffalo slot jackpot features stacked pays, multiplier madness, and jackpot thunder. Your adventure awaits!
Zeus doesn’t play small in gates of olympus pragmatic play. Multipliers grow wildly during tumbles and become truly terrifying in free spins. Join the pantheon — spin Gates of Olympus!