Endocarditis
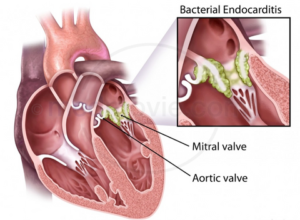
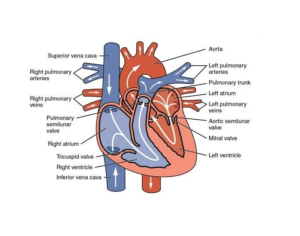
Endocarditis, also known as infective endocarditis can be life-threatening and cause inflammation of the wall of the chambers as well as valves (endocardium).
Endocarditis usually occurs due to an infection. Bacteria, fungi, or other bacteria that come from another part within your body like your mouth, can travel throughout your bloodstream, and then attach to damaged parts of your heart. If not addressed promptly, endocarditis could harm or ruin the heart valves. Treatments for endocarditis can include medication and, occasionally, surgical intervention.
People who are most susceptible to endocarditis are those with damaged heart valves or artificial heart valves. other heart defects¹.
Symptoms
The development of endocarditis can be slow or abruptly, depending on the germs that are responsible for the infection and if there are any existing heart issues. The signs and symptoms of endocarditis may differ from one person to the next.
The most common indications and signs of endocarditis are:
- Muscles and joints that are aching
- The chest hurts when you breathe
- Fatigue
- Influenza-like symptoms, like chills and fever
- Night sweats
- Breathing shortness
- Inflammation in your legs, feet or stomach
- A new or modified heart murmur that is the sound of your heart created by the blood flowing through your heart
Common signs and symptoms of endocarditis could be:
- Unexplained weight loss
- The blood in your urine that you may be able observe or your doctor could be able to see when he examines your urine under microscope
- The spleen is tender that is an anti-infection organ that is located beneath your left rib cage
- The heels of your feet, or your palms (Janeway lesions)
- The tender, red spots are located under the skin toes and fingers (Osler’s nodes)
- Tiny red or purple spots, referred to as petechiae located on the skin, within the eye’s whites or in the mouth.
When should you seek medical help?
If you are experiencing symptoms or signs of an endocarditis you should see your doctor immediately and especially in the event that you have risk factors for this serious infection like an abnormal heart or a previous history of endocarditis. While less serious ailments may produce similar symptoms and signs but you can’t be certain until you’ve been evaluated by your physician.
When you’ve received a diagnosis of an endocarditis infection, discuss with your doctor any symptoms or signs that could indicate your condition is becoming worse, including:
- Chills
- Fever
- Headaches
- Joint pain
- Breathing shortness
- Rash
If you’re receiving antibiotics for endocarditis, inform your doctor if there is diarrhea or a rash, joint pain or itching. These symptoms and signs could indicate that you’re experiencing a reaction to the prescribed antibiotic.
Causes
The term “endocarditis” refers to the situation when bacteria, typically infiltrate your bloodstream. They move to your heart and then attach to heart valves, or damaged tissue. Other germs or fungi could cause endocarditis.
Usually the immune system is able to eliminate all harmful bacteria that get into your bloodstream. However, the bacteria that reside in your throat, mouth or in other areas that are part of you, including your skin or your digestive tract may result in endocarditis under certain conditions.
Bacteria, fungi, and other bacteria that cause endocarditis could get into your bloodstream through:
- Dental care that is not properly done. Proper toothbrushing and flossing can help prevent gum disease. If you don’t take proper care of your gums and teeth cleaning them can cause unhealthy gums to leak, which could give bacteria the opportunity to get into your bloodstream. Certain dental procedures that cause gum bleeding also let bacteria be introduced into your bloodstream.
- Catheters. Bacteria can enter your body through a small tube that doctors may employ to inject or eliminate fluid from your internal organs (catheter). This can happen if the catheter is placed for a prolonged duration of duration. As an example, you could be fitted with a catheter if require dialysis for a long time.
- Illegal use of IV drugs. Contaminated needles and Syringes are of particular concern for people who take illicit IV drugs like cocaine or heroin. Most people who use these kinds of drugs do not are able to access clean, un-used needles or Syringes.
Risk factors
It is more likely that you will develop endocarditis if you suffer from faulty or damaged or diseased heart valves. But, it can also occur in people who are otherwise healthy.
There is a higher risk of contracting endocarditis when you are:
- Aged older. Endocarditis occurs most often in people over 60 years old.
- Artificial valves for the heart. Germs are more likely to be attached on the artificial (prosthetic) heart valve than to a regular heart valve.
- Heart valves damaged. Certain medical conditions such as infections or rheumatic fever can cause scarring or damage to the one or several of your heart valves, thereby increasing the chance of contracting an infection.
- Congenital heart problems. If you were born with certain kinds of heart defects, like an abnormal heart or valves for your heart, ventricular septal defect, you could be more susceptible to an infection.
- Heart implanted devices. Bacteria can attach to implanted devices, for example, a pacemaker leading to an infection of the heart’s liner.
- An endocarditis history. Endocarditis can damage the heart valves and tissue and increase the risk of developing a heart attack in the future.
- A record of illegal IV drug usage. People who use illegal drugs through injection are at greater risk of developing endocarditis. The needles used for injecting drugs may be contaminated with the bacteria that cause endocarditis.
- Dental health is poor. A healthy mouth and healthy gums are vital to good health. If you don’t brush or floss frequently, bacteria could develop inside your mouth and can get into your bloodstream via an injury to the gums.
- The use of long-term catheters. Having a catheter on the market for a prolonged amount of time (indwelling catheter) increases the chance of contracting endocarditis.
In the event that you’re in danger for developing endocarditis be sure to let your physicians be aware. It’s possible to request an endocarditis wallet card through the American Heart Association. Find your local chapter, or print the card through the website of the association.
Complications
In the case of endocarditis, clumps of cells and germs create an abnormal mass inside your heart. The clumps, also known as vegetations, may break loose and then travel to your lungs, brain organs in your abdomen kidneys, legs and arms.
This is why endocarditis can lead to a variety of complications, for example:
- Heart issues, like heart murmurs, heart valve injury and heart failure
- Stroke
- Pockets of pus (abscesses) which develop in the brain, heart the lungs, and various organs
- A blood clot is formed in the blood vessel in the lung (pulmonary embolism)
- Kidney damage
- Larger spleen
Prevention
Follow these steps to avoid endocarditis:
- Be aware of the symptoms and signs for the condition known as endocarditis. See your doctor immediately if you experience any symptoms or signs particularly an unresolved fever that doesn’t disappear, a feeling of fatigue that isn’t explained or any skin infection, or sores or cuts that don’t heal in a timely manner.
- Make sure you take care of your teeth as well as your gums. Brush and floss your gums and teeth frequently and get regular dental check-ups. Dental hygiene is essential to keeping your overall health in good shape.
- Don’t take unapproved IV medicines. Dirty needles can introduce germs into the bloodstream which can increase the risk of developing endocarditis.
Antibiotics that prevent infection
Certain dental or medical procedures could let bacteria into your bloodstream.
If you’re at a high risk of developing endocarditis, American Heart Association recommends taking antibiotics at least an hour prior to getting any dental procedure performed.
There is a higher risk of developing endocarditis and require antibiotics prior to your dental procedure If you suffer from:
- An endocarditis history
- Man-made (prosthetic mechanical) heart valve
- A heart transplant can be performed in certain instances
- Certain kinds of heart diseases congenital
- Heart disease surgery for congenital causes within the last six months
If you are suffering from endocarditis, or another type of congenital heart disease, speak to your dentist or doctor about the risks you face and whether you’ll need preventive antibiotics.
Diagnosis
Your doctor will take into consideration the medical history of you, symptoms and signs, as well as the results of your tests when making an endocarditis diagnosis. The diagnosis will usually be dependent on a variety of variables instead of just a single positive test result or a symptom.
Tests to rule out or confirm endocarditis can include:
- Test for blood culture. A blood culture test can be used to determine any bacteria present in your bloodstream. Results from a blood culture test aid your doctor in choosing the most effective antibacterial or antibiotic combination.
- A complete Blood count. This blood test will inform your doctor if you are surrounded by white blood cells. This could be an indication of an infection. Complete blood counts may aid in determining the presence of the presence of low amounts of red blood cells (anemia) and could be an indication of endocarditis. Other blood tests may also be performed to assist your physician in determining the type of diagnosis.
- Echocardiogram. The echocardiogram makes use of sound waves to generate pictures of the heart when it is beating. This test reveals the chambers of your heart and how valves are moving the blood around your body. Your doctor could utilize two different kinds of echocardiograms to aid in diagnosing endocarditis. In a transthoracic echocardiogram sound waves directed towards your heart by a wand-like device (transducer) that is placed on your chest generate videos of your heart’s motion. The test allows your doctor to examine the structure of your heart and assess it for evidence of damage.Transesophageal echocardiograms allow your doctor a better view of your heart’s valves. In this procedure, a tiny transducer that is attached to the tube’s end is placed into the tube that connects the mouth towards the stomach (esophagus). This test offers more precise pictures of the heart that are feasible with transthoracic echocardiogram.
- Electrocardiogram (ECG or EKG). An ECG The test is used to gauge the frequency and duration of the heartbeats. It’s not used specifically to diagnose endocarditis but it could tell your doctor whether something affects the electrical activity of your heart. During an ECG Sensors that detect the electrical activity of your heart are connected to your arms, chest and legs.
- Chest Xray. A chest X-ray will show your doctor the state of your lungs and your heart. It will help determine if you have suffered from endocarditis that has caused the heart to swell or if the infection has reached the lung.
- Computerized Tomography (CT) scans or magnetic resonance images (MRI). You might need to get the help of CT scan or MRI scan of your chest, brain or other areas of your body, if your doctor believes that an infections have spread to these regions.
Treatment
A lot of people suffering from endocarditis can be successfully treated by antibiotics. Sometimes, surgery might be needed to repair or repair damaged heart valves, and remove any symptoms of the infection.
Medications
The kind of medication you take depends on the condition at the root of the issue.
The high levels of IV anti-biotics can be used to treat endocarditis that is caused by bacteria. If you are treated with the IV treatment, expect to usually be spending a week or more in the hospital, so that your doctor can confirm if your treatment is effective.
If your fever and obvious signs or symptoms are gone and you’re able quit the hospital and carry on IV antibiotics by visiting your doctor’s office or your home using home care. It is common to take antibiotics for some time to treat the infection.
If the cause of endocarditis is an infection that causes fungal inflammation the doctor will prescribe antifungal medications. Certain people require lifelong antifungal medication to prevent endocarditis from coming back.
Surgery
The procedure of repairing the heart valve is required to treat chronic endocarditis or to replace the damaged valve. Surgery is sometimes also required to treat endocarditis caused by a fungal infection.
In the event of a medical condition depending on your condition, your doctor may suggest fixing your damaged valve, and replacing the valve with a replacement valve that is made of human, cow or pig cardiac tissue (biological tissue valve) or man-made substances (prosthetic mechanical valve).

Wow, awesome blog layout! How long have you been blogging for?
you made running a blog look easy. The entire glance of your
website is magnificent, let alone the content! You can see
similar here ecommerce
batmanapollo.ru
Contumacia cumulat poenam — прав. Упорство усугубляет наказание.
Charta non erubescit — Бумага не краснеет.
Benevole lector — Благосклонный читатель.
Actum atque tractatum — Сделано и обсуждено.
Altum silentium — Глубокое молчание.
Ab hoc et ab hac — Кстати и некстати
Conclamatum est — Всё кончено, всё погибло.
Abstractum pro concreto — Общее вместо частного.
Министерство неджентльменских дел
Министерство неджентльменских дел
Министерство неджентльменских дел
Министерство неджентльменских дел
Министерство неджентльменских дел
Усик – Фьюри: смотреть онлайн-трансляцию церемонии
Александр Усик — Тайсон Фьюри
Усик – Фьюри: онлайн-трансляция боя
Александр Усик – Тайсон Фьюри. Смотреть онлайн LIVE
Фуриоса: Хроники Безумного Макса
Фуриоса: Хроники Безумного Макса
Фуриоса: Хроники Безумного Макса
Фуриоса: Хроники Безумного Макса
Психолог консультация
Психоаналитик
Тут психолог
Психолог
Психоаналитик
Как сдвинуть гору Фудзи? и популярные книги по психологии.
Основы психологии и педагогики. Учебное пособие и новые статьи по психоанализу.
Per aspera ad astra
Carpe diem
100 лет тому вперед смотреть онлайн. 100 лет тому вперед смотреть онлайн бесплатно в хорошем.
100 лет тому вперед фильм смотреть онлайн бесплатно 2024. Фильм 100 лет тому вперед смотреть онлайн бесплатно.
Фоллаут смотреть онлайн
Фоллаут 1 сезон смотреть онлайн
Фоллаут 2024
Психолог 2024
Претенденты смотреть Претенденты фильм, 2024, смотреть онлайн
hello there and thank you for your information – I have definitely
picked up something new from right here. I did however expertise a few technical points using this website, since I experienced to reload the
site a lot of times previous to I could get it to load correctly.
I had been wondering if your web host is OK? Not that I am complaining, but slow loading
instances times will often affect your placement
in google and could damage your high quality score
if ads and marketing with Adwords. Anyway I am adding this
RSS to my email and could look out for much more of your
respective interesting content. Ensure that you update this again soon..
Escape rooms
Very interesting information!Perfect just what I was searching for!.
I like it when folks come together and share views. Great website, stick with it.
Hello there, I do believe your web site might be having browser compatibility issues. When I look at your web site in Safari, it looks fine but when opening in Internet Explorer, it’s got some overlapping issues. I just wanted to give you a quick heads up! Aside from that, fantastic site.
An outstanding share! I have just forwarded this onto a co-worker who has been doing a little homework on this. And he actually bought me lunch simply because I discovered it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending the time to discuss this subject here on your site.
Spot on with this write-up, I honestly believe that this amazing site needs much more attention. I’ll probably be back again to read through more, thanks for the info.
This is a topic that’s close to my heart… Thank you! Exactly where can I find the contact details for questions?
This is a very good tip especially to those new to the blogosphere. Brief but very precise information… Appreciate your sharing this one. A must read post!
Very nice write-up. I absolutely appreciate this website. Stick with it!
There’s certainly a great deal to learn about this topic. I like all the points you have made.
I absolutely love your site.. Great colors & theme. Did you build this web site yourself? Please reply back as I’m wanting to create my very own blog and would like to learn where you got this from or what the theme is named. Thanks.
Hi there, I believe your blog might be having internet browser compatibility issues. When I take a look at your website in Safari, it looks fine but when opening in I.E., it has some overlapping issues. I simply wanted to give you a quick heads up! Aside from that, excellent site.
I’m amazed, I have to admit. Rarely do I encounter a blog that’s equally educative and engaging, and without a doubt, you’ve hit the nail on the head. The issue is something which too few folks are speaking intelligently about. I’m very happy I found this during my search for something regarding this.
May I simply just say what a relief to discover someone that truly knows what they are talking about online. You certainly know how to bring a problem to light and make it important. More and more people have to look at this and understand this side of your story. I can’t believe you are not more popular since you surely have the gift.
I’m amazed, I have to admit. Rarely do I encounter a blog that’s both educative and entertaining, and without a doubt, you’ve hit the nail on the head. The issue is an issue that not enough people are speaking intelligently about. I’m very happy that I found this in my search for something relating to this.
I enjoy looking through an article that can make men and women think. Also, thank you for permitting me to comment.
Hi there! This article couldn’t be written any better! Reading through this post reminds me of my previous roommate! He constantly kept preaching about this. I am going to send this information to him. Pretty sure he’ll have a good read. Thank you for sharing!
I wanted to thank you for this wonderful read!! I definitely enjoyed every little bit of it. I’ve got you bookmarked to look at new stuff you post…
Pretty! This has been an incredibly wonderful post. Thanks for providing these details.
Hi, I do think this is a great site. I stumbledupon it 😉 I’m going to come back once again since I bookmarked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
Excellent blog you have got here.. It’s difficult to find high quality writing like yours nowadays. I honestly appreciate people like you! Take care!!
This is the right website for anyone who wishes to find out about this topic. You realize so much its almost hard to argue with you (not that I actually will need to…HaHa). You certainly put a fresh spin on a subject that’s been discussed for decades. Great stuff, just excellent.
Hi there! This article couldn’t be written much better! Reading through this post reminds me of my previous roommate! He constantly kept preaching about this. I most certainly will send this article to him. Pretty sure he will have a great read. Thank you for sharing!
You should be a part of a contest for one of the greatest websites on the net. I am going to recommend this blog!
After exploring a few of the articles on your web page, I truly appreciate your technique of writing a blog. I saved as a favorite it to my bookmark webpage list and will be checking back soon. Please check out my web site too and let me know how you feel.
I was able to find good info from your content.
Hello there, There’s no doubt that your website might be having browser compatibility problems. Whenever I look at your blog in Safari, it looks fine but when opening in I.E., it’s got some overlapping issues. I merely wanted to provide you with a quick heads up! Besides that, fantastic blog!
Hi, I do think this is a great site. I stumbledupon it 😉 I am going to return once again since I book marked it. Money and freedom is the best way to change, may you be rich and continue to guide other people.
Way cool! Some very valid points! I appreciate you writing this post and also the rest of the website is extremely good.
Very interesting points you have remarked, thank you for posting.
Euro travel guide
Hi there! This blog post couldn’t be written any better! Looking through this article reminds me of my previous roommate! He always kept preaching about this. I most certainly will forward this article to him. Pretty sure he will have a good read. Thanks for sharing!
Greetings, I do believe your site could be having web browser compatibility problems. Whenever I look at your blog in Safari, it looks fine however, if opening in IE, it has some overlapping issues. I merely wanted to give you a quick heads up! Besides that, excellent site.
Can I just say what a comfort to find someone who truly understands what they’re discussing on the internet. You certainly know how to bring an issue to light and make it important. More and more people need to look at this and understand this side of your story. I was surprised that you’re not more popular since you most certainly have the gift.
I really like it when folks get together and share ideas. Great website, keep it up.
A motivating discussion is worth comment. I do believe that you should publish more on this subject matter, it might not be a taboo subject but usually people don’t discuss such subjects. To the next! Cheers!
I blog quite often and I genuinely thank you for your information. Your article has truly peaked my interest. I’m going to bookmark your blog and keep checking for new information about once a week. I subscribed to your Feed as well.
May I just say what a comfort to discover someone that truly understands what they’re talking about on the web. You certainly realize how to bring an issue to light and make it important. More and more people should check this out and understand this side of the story. I was surprised that you are not more popular given that you definitely have the gift.
Good article! We are linking to this great article on our website. Keep up the good writing.
This is a very good tip especially to those fresh to the blogosphere. Simple but very precise information… Appreciate your sharing this one. A must read post!
Very good article! We are linking to this particularly great content on our site. Keep up the great writing.
You ought to be a part of a contest for one of the greatest websites online. I’m going to highly recommend this website!
Good day! I simply want to offer you a big thumbs up for the excellent info you have got right here on this post. I will be returning to your web site for more soon.
Hi, I do think this is a great site. I stumbledupon it 😉 I will come back once again since I saved as a favorite it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
Your style is so unique in comparison to other people I have read stuff from. Many thanks for posting when you have the opportunity, Guess I’ll just book mark this web site.
ремонт телефонов
Good post. I learn something totally new and challenging on sites I stumbleupon every day. It will always be useful to read articles from other authors and practice something from other web sites.
When I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and now each time a comment is added I get 4 emails with the exact same comment. There has to be an easy method you are able to remove me from that service? Thank you.
Профессиональный сервисный центр по ремонту сотовых телефонов, смартфонов и мобильных устройств.
Мы предлагаем: ремонт смартфона
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр по ремонту сотовых телефонов, смартфонов и мобильных устройств.
Мы предлагаем: срочный ремонт телефонов
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
bookmarked!!, I really like your blog!
Good day! I could have sworn I’ve been to this blog before but after browsing through a few of the posts I realized it’s new to me. Anyhow, I’m certainly pleased I found it and I’ll be book-marking it and checking back frequently!
I blog often and I really appreciate your content. The article has truly peaked my interest. I am going to take a note of your website and keep checking for new information about once a week. I subscribed to your RSS feed too.
Если вы искали где отремонтировать сломаную технику, обратите внимание – профи тех сервис красноярск
Если вы искали где отремонтировать сломаную технику, обратите внимание – профи услуги
Профессиональный сервисный центр по ремонту стиральных машин с выездом на дом по Москве.
Мы предлагаем: москва ремонт стиральных машин
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: сервисные центры по ремонту техники в казани
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Your style is very unique in comparison to other folks I’ve read stuff from. Thank you for posting when you’ve got the opportunity, Guess I will just book mark this blog.
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники
Если вы искали где отремонтировать сломаную технику, обратите внимание – тех профи
Профессиональный сервисный центр по ремонту игровых консолей Sony Playstation, Xbox, PSP Vita с выездом на дом по Москве.
Мы предлагаем: мастер по ремонту игровых консолей
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр по ремонту компьютерных видеокарт по Москве.
Мы предлагаем: сервисный центр видеокарт
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
An outstanding share! I’ve just forwarded this onto a coworker who has been conducting a little research on this. And he in fact ordered me breakfast due to the fact that I discovered it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending some time to talk about this subject here on your website.
Having read this I believed it was extremely informative. I appreciate you finding the time and energy to put this content together. I once again find myself spending way too much time both reading and commenting. But so what, it was still worth it.
Профессиональный сервисный центр по ремонту фото техники от зеркальных до цифровых фотоаппаратов.
Мы предлагаем: ремонт проекционных экранов
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
bookmarked!!, I love your site.
Если вы искали где отремонтировать сломаную технику, обратите внимание – техпрофи
Bongdalu cập nhật tin tức bóng đá nóng hổi, thể thao sôi động và giải trí hấp dẫn
Rồng Bạch Kim – Soi cầu lô chính xác miễn phí chính xác số #1 2024
I want to to thank you for this wonderful read!! I absolutely loved every bit of it. I have you bookmarked to check out new things you post…
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: ремонт бытовой техники в красноярске
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Если вы искали где отремонтировать сломаную технику, обратите внимание – сервисный центр в волгограде
Motchilltv.fyi – Trang web xem phim Online chất lượng Full HD với giao diện thân thiện, trực quan cùng kho phim với hơn 15.000+ bộ phim mới và phim hot hiện nay.
Bongdalu cập nhật tin tức bóng đá nóng hổi, thể thao sôi động và giải trí hấp dẫn.
Everyone loves it when folks get together and share thoughts. Great site, stick with it.
Great information. Lucky me I ran across your blog by chance (stumbleupon). I’ve book marked it for later.
After exploring a few of the blog posts on your site, I really like your way of blogging. I saved it to my bookmark site list and will be checking back in the near future. Take a look at my web site too and let me know your opinion.
Khám phá Luongsontv – nền tảng xem bóng đá trực tuyến hàng đầu.
Bongdalu cập nhật tin tức bóng đá nóng hổi, thể thao sôi động và giải trí hấp dẫn.
It’s nearly impossible to find well-informed people in this particular subject, however, you sound like you know what you’re talking about! Thanks
After looking into a handful of the blog posts on your web site, I honestly like your way of writing a blog. I bookmarked it to my bookmark website list and will be checking back in the near future. Please visit my website as well and let me know what you think.
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт цифровой техники уфа
The very next time I read a blog, I hope that it doesn’t disappoint me as much as this one. I mean, Yes, it was my choice to read, nonetheless I really believed you would probably have something helpful to say. All I hear is a bunch of whining about something that you could possibly fix if you weren’t too busy seeking attention.
ремонт техники профи в самаре
This is a really good tip particularly to those fresh to the blogosphere. Brief but very precise info… Many thanks for sharing this one. A must read article.
Сервисный центр предлагает центр ремонта кондиционера micromax стоимость ремонта кондиционера micromax
Great blog you have here.. It’s difficult to find quality writing like yours these days. I honestly appreciate individuals like you! Take care!!
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем:сервис центры бытовой техники ростов на дону
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
I could not refrain from commenting. Exceptionally well written.
Excellent post. I am experiencing a few of these issues as well..
You need to take part in a contest for one of the most useful websites online. I will highly recommend this website!
Right here is the perfect web site for anybody who wishes to find out about this topic. You realize a whole lot its almost hard to argue with you (not that I personally will need to…HaHa). You certainly put a brand new spin on a topic that has been written about for ages. Excellent stuff, just great.
{Tôi đã rất vui khám phá trang web này. Tôi cần cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn yêu thích từng một chút nó và tôi cũng đã lưu làm mục ưa thích để xem những thứ mới trên blog của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một người thực sự hiểu họ là gì thảo luận trực tuyến. Bạn chắc chắn hiểu cách đưa một vấn đề ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn cần phải xem điều này và hiểu khía cạnh này câu chuyện của bạn. Tôi không thể tin bạn không nổi tiếng hơn vì bạn chắc chắn sở hữu món quà.|Rất hay bài viết. Tôi hoàn toàn yêu thích trang web này. Tiếp tục với nó!|Thật gần như không thể tìm thấy những người có học thức trong chủ đề cụ thể này, tuy nhiên, bạn nghe có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên là một phần của một cuộc thi dành cho một trang web trên mạng tuyệt vời nhất. Tôi sẽ khuyến nghị blog này!|Một cuộc thảo luận thú vị chắc chắn đáng giá bình luận. Không còn nghi ngờ gì nữa rằng bạn cần xuất bản thêm về chủ đề này, nó có thể không là một điều cấm kỵ vấn đề nhưng điển hình mọi người không nói về vấn đề những điều này. Đến phần tiếp theo! Chúc mọi điều tốt đẹp nhất.|Xin chào! Tôi chỉ muốn cho bạn một rất cho thông tin xuất sắc bạn có ngay tại đây trên bài đăng này. Tôi đang quay lại trang web của bạn để biết thêm thông tin sớm nhất.|Sau khi tôi ban đầu để lại bình luận tôi có vẻ như đã nhấp hộp kiểm -Thông báo cho tôi khi có bình luận mới- và từ bây giờ bất cứ khi nào có bình luận được thêm vào tôi nhận được 4 email cùng chính xác một bình luận. Có lẽ có một cách bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn rất nhiều.|Lần sau Tôi đọc một blog, Tôi hy vọng rằng nó không thất bại nhiều như bài này. Rốt cuộc, Tôi biết điều đó là sự lựa chọn của tôi để đọc, tuy nhiên tôi thực sự tin có lẽ có điều gì đó thú vị để nói về. Tất cả những gì tôi nghe được là một loạt tiếng rên rỉ về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi thành thật cảm thấy trang web tuyệt vời này cần nhiều hơn nữa sự chú ý.
{Tôi đã cực kỳ hài lòng để tìm thấy trang web tuyệt vời này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn đánh giá cao từng một chút nó và tôi đã đánh dấu để xem thông tin mới trong trang web của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một cá nhân mà thực sự hiểu họ là gì đang nói về trên internet. Bạn chắc chắn nhận ra cách đưa một vấn đề ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa phải kiểm tra điều này và hiểu khía cạnh này của. Tôi đã ngạc nhiên bạn không nổi tiếng hơn vì bạn chắc chắn sở hữu món quà.|Tốt bài viết. Tôi hoàn toàn yêu thích trang web này. Cảm ơn!|Thật gần như không thể tìm thấy những người hiểu biết về điều này, tuy nhiên, bạn nghe có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên là một phần của một cuộc thi dành cho một trang web trên web hữu ích nhất. Tôi sẽ khuyến nghị trang web này!|Một cuộc thảo luận thú vị đáng giá bình luận. Tôi nghĩ rằng bạn cần xuất bản thêm về chủ đề này, nó có thể không là một điều cấm kỵ vấn đề nhưng thường xuyên mọi người không nói về vấn đề những điều này. Đến phần tiếp theo! Cảm ơn rất nhiều!|Xin chào! Tôi chỉ muốn đề nghị rất to cho thông tin tuyệt vời bạn có ngay tại đây trên bài đăng này. Tôi sẽ là trở lại trang web của bạn để biết thêm thông tin sớm nhất.|Sau khi tôi ban đầu để lại bình luận tôi có vẻ như đã nhấp hộp kiểm -Thông báo cho tôi khi có bình luận mới- và bây giờ mỗi lần được thêm vào tôi nhận được 4 email cùng chính xác một bình luận. Phải có một cách bạn có thể xóa tôi khỏi dịch vụ đó không? Chúc mừng.|Lần sau Tôi đọc một blog, Hy vọng rằng nó không thất bại nhiều như bài này. Ý tôi là, Vâng, đó là sự lựa chọn của tôi để đọc hết, dù sao thì tôi thực sự tin bạn sẽ có điều gì đó hữu ích để nói. Tất cả những gì tôi nghe được là một loạt rên rỉ về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi thành thật tin rằng trang web này cần nhiều hơn nữa sự chú ý.
{Tôi đã cực kỳ hài lòng khám phá trang web này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn thích thú từng một chút nó và tôi đã lưu làm mục ưa thích để xem thông tin mới trong trang web của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một người mà thực sự biết họ là gì đang nói về trên internet. Bạn thực sự nhận ra cách đưa một vấn đề ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa phải đọc điều này và hiểu khía cạnh này câu chuyện của bạn. Thật ngạc nhiên bạn không nổi tiếng hơn cho rằng bạn chắc chắn có món quà.|Rất tốt bài viết. Tôi chắc chắn đánh giá cao trang web này. Cảm ơn!|Thật khó đến những người có hiểu biết sâu rộng về điều này, nhưng bạn có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn cần tham gia một cuộc thi dành cho một trang web trên internet có chất lượng cao nhất. Tôi sẽ Rất khuyến nghị trang web này!|Một hấp dẫn đáng giá bình luận. Tôi nghĩ rằng bạn cần viết thêm về chủ đề này, nó có thể không là một điều cấm kỵ chủ đề nhưng nói chung mọi người không nói về vấn đề những điều này. Đến phần tiếp theo! Cảm ơn rất nhiều!|Xin chào! Tôi chỉ muốn đề nghị rất cho thông tin xuất sắc bạn có ngay tại đây trên bài đăng này. Tôi sẽ là quay lại trang web của bạn để biết thêm thông tin sớm nhất.|Khi tôi ban đầu bình luận tôi có vẻ như đã nhấp hộp kiểm -Thông báo cho tôi khi có bình luận mới- và từ bây giờ mỗi lần được thêm vào tôi nhận được bốn email có cùng nội dung. Phải có một phương tiện bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn rất nhiều.|Lần sau Tôi đọc một blog, Tôi hy vọng rằng nó không làm tôi thất vọng nhiều như bài này. Rốt cuộc, Vâng, đó là sự lựa chọn của tôi để đọc hết, nhưng tôi thực sự tin bạn sẽ có điều gì đó hữu ích để nói. Tất cả những gì tôi nghe được là một loạt khóc lóc về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi nghiêm túc cảm thấy trang web tuyệt vời này cần nhiều hơn nữa sự chú ý.
{Tôi đã cực kỳ hài lòng khám phá trang này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn thực sự thích từng một chút nó và tôi đã lưu làm mục ưa thích để xem điều mới trên trang web của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một người mà thực sự biết họ là gì thảo luận trên web. Bạn chắc chắn hiểu cách đưa một vấn đề ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn phải xem điều này và hiểu khía cạnh này của. Thật ngạc nhiên bạn không nổi tiếng hơn vì bạn chắc chắn có món quà.|Tốt bài đăng. Tôi hoàn toàn yêu thích trang web này. Tiếp tục với nó!|Thật gần như không thể tìm thấy những người có kinh nghiệm trong chủ đề cụ thể này, nhưng bạn nghe có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên là một phần của một cuộc thi dành cho một trang web trên mạng tuyệt vời nhất. Tôi sẽ khuyến nghị blog này!|Một cuộc thảo luận thú vị chắc chắn đáng giá bình luận. Không còn nghi ngờ gì nữa rằng bạn nên xuất bản thêm về chủ đề này, nó có thể không là một điều cấm kỵ vấn đề nhưng điển hình mọi người không nói về những chủ đề như vậy. Đến phần tiếp theo! Cảm ơn rất nhiều!|Xin chào! Tôi chỉ muốn cho bạn một rất cho thông tin tuyệt vời bạn có ở đây trên bài đăng này. Tôi sẽ là quay lại blog của bạn để biết thêm thông tin sớm nhất.|Sau khi tôi ban đầu bình luận tôi có vẻ như đã nhấp hộp kiểm -Thông báo cho tôi khi có bình luận mới- và từ bây giờ mỗi lần được thêm vào tôi nhận được bốn email có cùng nội dung. Phải có một cách bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn rất nhiều.|Lần sau nữa Tôi đọc một blog, Tôi hy vọng rằng nó không làm tôi thất vọng nhiều như bài này. Ý tôi là, Tôi biết điều đó là sự lựa chọn của tôi để đọc hết, nhưng tôi thực sự nghĩ bạn sẽ có điều gì đó thú vị để nói. Tất cả những gì tôi nghe được là một loạt khóc lóc về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi thực sự tin rằng trang web tuyệt vời này cần nhiều hơn nữa sự chú ý.
{Tôi rất vui khám phá trang web này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn đánh giá cao từng một phần nó và tôi đã lưu làm mục ưa thích để xem thông tin mới trên blog của bạn.|Tôi có thể chỉ nói rằng thật thoải mái để tìm thấy một người mà thực sự biết họ là gì thảo luận trực tuyến. Bạn chắc chắn hiểu cách đưa một vấn đề ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa thực sự cần kiểm tra điều này và hiểu khía cạnh này của. Tôi đã ngạc nhiên bạn không nổi tiếng hơn cho rằng bạn chắc chắn sở hữu món quà.|Rất hay bài viết trên blog. Tôi chắc chắn yêu thích trang web này. Cảm ơn!|Thật khó tìm những người có học thức cho điều này, tuy nhiên, bạn có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên là một phần của một cuộc thi dành cho một blog trên internet tuyệt vời nhất. Tôi sẽ khuyến nghị trang web này!|Một hấp dẫn đáng giá bình luận. Tôi nghĩ rằng bạn nên viết thêm về chủ đề này, nó có thể không là một điều cấm kỵ vấn đề nhưng nói chung mọi người không thảo luận những chủ đề những điều này. Đến phần tiếp theo! Chúc mừng!|Xin chào! Tôi chỉ muốn đề nghị rất cho thông tin tuyệt vời bạn có ngay tại đây trên bài đăng này. Tôi sẽ là trở lại trang web của bạn để biết thêm thông tin sớm nhất.|Khi tôi ban đầu để lại bình luận tôi có vẻ như đã nhấp hộp kiểm -Thông báo cho tôi khi có bình luận mới- và từ bây giờ bất cứ khi nào có bình luận được thêm vào tôi nhận được bốn email có cùng nội dung. Có lẽ có một phương pháp dễ dàng bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm kích.|Lần sau Tôi đọc một blog, Tôi hy vọng rằng nó sẽ không làm tôi thất vọng nhiều như bài này. Ý tôi là, Vâng, đó là sự lựa chọn của tôi để đọc, dù sao thì tôi thực sự tin bạn sẽ có điều gì đó hữu ích để nói. Tất cả những gì tôi nghe được là một loạt phàn nàn về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi thực sự cảm thấy trang web này cần nhiều hơn nữa sự chú ý.
{Tôi rất vui khám phá trang này. Tôi muốn cảm ơn bạn {vì đã|dành thời gian cho|chỉ vì điều này|vì điều này|cho bài đọc tuyệt vời này!! Tôi chắc chắn đánh giá cao từng một chút nó và tôi cũng đã đánh dấu trang để xem thông tin mới trong trang web của bạn.|Tôi có thể chỉ nói rằng thật nhẹ nhõm để khám phá một người mà thực sự biết họ là gì đang nói về trên web. Bạn thực sự hiểu cách đưa một vấn đề ra ánh sáng và làm cho nó trở nên quan trọng. Nhiều người hơn nữa thực sự cần xem điều này và hiểu khía cạnh này câu chuyện của bạn. Tôi đã ngạc nhiên bạn không nổi tiếng hơn cho rằng bạn chắc chắn có món quà.|Tốt bài viết. Tôi hoàn toàn đánh giá cao trang web này. Tiếp tục làm tốt!|Thật khó tìm những người hiểu biết cho điều này, nhưng bạn nghe có vẻ bạn biết mình đang nói gì! Cảm ơn|Bạn nên tham gia một cuộc thi dành cho một trang web trên internet hữu ích nhất. Tôi sẽ Rất khuyến nghị trang web này!|Một cuộc thảo luận thú vị chắc chắn đáng giá bình luận. Tôi nghĩ rằng bạn nên xuất bản thêm về chủ đề này, nó có thể không là một điều cấm kỵ vấn đề nhưng thường xuyên mọi người không thảo luận những chủ đề những điều này. Đến phần tiếp theo! Trân trọng!|Chào bạn! Tôi chỉ muốn đề nghị rất to cho thông tin tuyệt vời bạn có ở đây trên bài đăng này. Tôi sẽ là trở lại trang web của bạn để biết thêm thông tin sớm nhất.|Sau khi tôi ban đầu bình luận tôi có vẻ như đã nhấp hộp kiểm -Thông báo cho tôi khi có bình luận mới- và từ bây giờ mỗi lần được thêm vào tôi nhận được bốn email có cùng nội dung. Phải có một phương tiện bạn có thể xóa tôi khỏi dịch vụ đó không? Cảm ơn.|Lần sau nữa Tôi đọc một blog, Tôi hy vọng rằng nó sẽ không làm tôi thất vọng nhiều như bài này. Rốt cuộc, Tôi biết điều đó là sự lựa chọn của tôi để đọc hết, nhưng tôi thực sự tin bạn sẽ có điều gì đó thú vị để nói. Tất cả những gì tôi nghe được là một loạt phàn nàn về điều gì đó mà bạn có thể sửa nếu bạn không quá bận tìm kiếm sự chú ý.|Đúng với bài viết này, tôi hoàn toàn tin trang web tuyệt vời này cần nhiều hơn nữa sự chú ý.
There is definately a lot to know about this subject. I love all of the points you’ve made.
Если вы искали где отремонтировать сломаную технику, обратите внимание – тех профи
I’m amazed, I have to admit. Rarely do I come across a blog that’s equally educative and interesting, and let me tell you, you’ve hit the nail on the head. The issue is something not enough folks are speaking intelligently about. I am very happy that I came across this in my hunt for something regarding this.
https://my.desktopnexus.com/Bongdalu0101/
https://www.mapleprimes.com/users/Bongdalu0101
http://classicalmusicmp3freedownload.com/ja/index.php?title=E588A9E794A8E88085:Bongdalu0101
Профессиональный сервисный центр по ремонту моноблоков в Москве.
Мы предлагаем: вызвать мастера по ремонту моноблоков
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
https://devdojo.com/bongdalu
https://wperp.com/users/da88tube/
https://public.tableau.com/app/profile/da88.tube/vizzes
This website truly has all the information and facts I wanted concerning this subject and didn’t know who to ask.
Профессиональный сервисный центр по ремонту гироскутеров в Москве.
Мы предлагаем: где отремонтировать гироскутер в москве
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
I blog frequently and I seriously thank you for your information. The article has truly peaked my interest. I am going to take a note of your website and keep checking for new information about once a week. I opted in for your RSS feed too.
Everything is very open with a really clear description of the issues. It was definitely informative. Your website is useful. Thanks for sharing!
Way cool! Some very valid points! I appreciate you penning this article and also the rest of the website is very good.
This is a topic that’s close to my heart… Cheers! Exactly where are your contact details though?
Pretty! This has been a really wonderful article. Thank you for supplying these details.
I couldn’t resist commenting. Exceptionally well written.
Good information. Lucky me I came across your site by accident (stumbleupon). I have saved it for later!
I want to to thank you for this great read!! I absolutely loved every bit of it. I have got you book marked to check out new stuff you post…
https://drive.google.com/drive/folders/1WaMu5ukywlKcv34GX3c8nZs9cx_Xfbv5?usp=sharing
Профессиональный сервисный центр по ремонту МФУ в Москве.
Мы предлагаем: сервис по ремонту мфу
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
https://da88tube.blogspot.com/2024/10/da88.html
After I originally commented I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I get four emails with the exact same comment. There has to be a means you can remove me from that service? Many thanks.
Профессиональный сервисный центр по ремонту принтеров в Москве.
Мы предлагаем: техник ремонт принтеров
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Saved as a favorite, I love your website!
Good day! I simply wish to offer you a big thumbs up for the excellent information you’ve got right here on this post. I’ll be returning to your site for more soon.
An outstanding share! I have just forwarded this onto a co-worker who has been doing a little research on this. And he in fact ordered me breakfast simply because I stumbled upon it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending time to discuss this issue here on your web site.
I quite like reading an article that can make people think. Also, many thanks for permitting me to comment.
I seriously love your blog.. Pleasant colors & theme. Did you develop this site yourself? Please reply back as I’m wanting to create my very own blog and would love to learn where you got this from or what the theme is named. Appreciate it!
Профессиональный сервисный центр по ремонту серверов в Москве.
Мы предлагаем: надежный сервис ремонта серверов
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Сервисный центр предлагает мастерские ремонта бесперебойников powerwalker ремонт бесперебойника powerwalker рядом
This is a topic that is close to my heart… Take care! Where are your contact details though?
http://amabilis.com/?bbp_user=45945&edit=1&updated=true
https://king-wifi.win/wiki/User:Da88tube
Hello! I just wish to offer you a big thumbs up for your great info you’ve got here on this post. I am coming back to your website for more soon.
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем:сервис центры бытовой техники уфа
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
You ought to take part in a contest for one of the highest quality blogs on the web. I will highly recommend this website!
https://md.chaosdorf.de/s/9_7-t8XHh
Pretty! This has been a really wonderful article. Thanks for providing this information.
https://www.gaiaonline.com/profiles/8daybet1/46860936/
https://shapshare.com/8daybet
https://forums.alliedmods.net/member.php?u=390283
I was excited to uncover this web site. I wanted to thank you for ones time for this wonderful read!! I definitely liked every little bit of it and i also have you saved to fav to see new stuff in your blog.
Aw, this was a very nice post. Spending some time and actual effort to produce a good article… but what can I say… I hesitate a lot and never seem to get nearly anything done.
Профессиональный сервисный центр по ремонту сигвеев в Москве.
Мы предлагаем: сигвей сервис
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Good post. I learn something totally new and challenging on blogs I stumbleupon every day. It will always be helpful to read through content from other writers and practice a little something from other sites.
The next time I read a blog, I hope that it won’t fail me as much as this one. After all, I know it was my choice to read, however I truly believed you would have something useful to talk about. All I hear is a bunch of moaning about something that you can fix if you weren’t too busy seeking attention.
There is definately a lot to know about this topic. I love all the points you’ve made.
Great blog you have got here.. It’s hard to find high-quality writing like yours nowadays. I really appreciate individuals like you! Take care!!
Профессиональный сервисный центр ближайший сервисный центр по ремонту телефонов срочный ремонт смартфонов
Very good article. I definitely love this website. Keep it up!
https://menwiki.men/wiki/User:Ko66vip
Your style is really unique compared to other people I have read stuff from. Thanks for posting when you have the opportunity, Guess I’ll just bookmark this blog.
I love it when people come together and share thoughts. Great website, continue the good work.
Your style is really unique in comparison to other people I’ve read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I will just book mark this blog.
Saved as a favorite, I like your site.
I need to to thank you for this excellent read!! I absolutely loved every bit of it. I have you saved as a favorite to check out new things you post…
https://hi-fi-forum.net/profile/976553
https://hedgedoc.softwareheritage.org/s/s1WEFWjkp
Профессиональный сервисный центр мастерская телефонов рядом ближайший ремонт сотовых
https://medibang.com/author/26758901/
Spot on with this write-up, I seriously feel this site needs far more attention. I’ll probably be returning to read more, thanks for the information!
Good post. I learn something new and challenging on websites I stumbleupon everyday. It will always be helpful to read through content from other authors and practice a little something from other web sites.
Профессиональный сервисный центр по ремонту электросамокатов в Москве.
Мы предлагаем: ремонт электросамоката
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
https://herpesztitkaink.hu/user/ko66vip/
https://www.pubpub.org/user/ko66-vip
There is definately a great deal to find out about this topic. I like all of the points you’ve made.
WOW! this article it really great i like it https://pg88.education/
Профессиональный сервисный центр по ремонту автомагнитол в Москве.
Мы предлагаем: ремонт автомагнитол рядом
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Профессиональный сервисный центр ремонт мобильных телефонов в москве ближайший ремонт телефонов
I blog frequently and I really appreciate your content. This article has truly peaked my interest. I am going to take a note of your blog and keep checking for new details about once a week. I subscribed to your Feed too.
Начните массовую индексацию ссылок в Google прямо cейчас!
Быстрая индексация ссылок имеет ключевое значение для успеха вашего онлайн-бизнеса. Чем быстрее поисковые системы обнаружат и проиндексируют ваши ссылки, тем быстрее вы сможете привлечь новую аудиторию и повысить позиции вашего сайта в результатах поиска.
Не теряйте времени! Начните пользоваться нашим сервисом для ускоренной индексации внешних ссылок в Google и Yandex. Зарегистрируйтесь сегодня и получите первые результаты уже завтра. Ваш успех в ваших руках!
Сервисный центр предлагает качественный ремонт кофемашин foster сервис ремонта кофемашин foster
Hi there! This blog post could not be written any better! Going through this post reminds me of my previous roommate! He constantly kept talking about this. I will send this information to him. Pretty sure he’s going to have a good read. Thanks for sharing!
Way cool! Some extremely valid points! I appreciate you penning this article plus the rest of the site is very good.
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: ремонт бытовой техники в челябинске
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
When I initially left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and now whenever a comment is added I receive four emails with the exact same comment. There has to be a means you are able to remove me from that service? Cheers.
Nice post. I learn something totally new and challenging on websites
Good post. I learn something new and challenging on blogs I stumbleupon everyday. It’s always interesting to read through content from other writers and use something from other websites.
Профессиональный сервисный центр ремонт телефонов в москве адреса срочный ремонт смартфонов
This is a topic that is near to my heart… Cheers! Exactly where are your contact details though?
I must thank you for the efforts you’ve put in penning this blog. I am hoping to view the same high-grade content by you in the future as well. In truth, your creative writing abilities has inspired me to get my own, personal website now 😉
You’re so cool! I do not believe I have read through anything like that before. So great to discover another person with a few genuine thoughts on this issue. Seriously.. thank you for starting this up. This website is something that is required on the web, someone with a little originality.
Aw, this was an extremely nice post. Taking the time and actual effort to create a top notch article… but what can I say… I hesitate a lot and don’t manage to get anything done.
Spot on with this write-up, I truly believe that this website needs much more attention. I’ll probably be returning to read more, thanks for the advice.
Профессиональный сервисный центр по ремонту духовых шкафов в Москве.
Мы предлагаем: ремонт встраиваемый духовой шкаф
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Pretty! This was an incredibly wonderful article. Thank you for supplying these details.
Excellent blog post. I certainly appreciate this website. Continue the good work!
Way cool! Some extremely valid points! I appreciate you penning this write-up plus the rest of the website is also really good.
I like it whenever people get together and share ideas. Great website, keep it up.
Полезный сервис быстрого загона ссылок сайта в индексация поисковой системы – быстрая индексация ссылок
Spot on with this write-up, I actually believe this site needs a lot more attention. I’ll probably be returning to read more, thanks for the advice!
Сервисный центр предлагает сервис ремонта духовых шкафов asko отремонтировать духового шкафа asko
Encore merci pour ce post et continuez votre excellent travail. ??
This site was… how do you say it? Relevant!! Finally I have found something that helped me. Thank you!
Полезная информация на сайте. Все что вы хоте знать об интернете полезный сервис
The very next time I read a blog, Hopefully it doesn’t disappoint me just as much as this particular one. After all, Yes, it was my choice to read, but I genuinely believed you would have something helpful to talk about. All I hear is a bunch of crying about something that you can fix if you weren’t too busy looking for attention.
Merci pour cet article super intéressant sur [thème de l’article] ! Je voulais juste ajouter un point qui pourrait intéresser certains d’entre vous. Si vous êtes curieux ou cherchez des informations supplémentaires sur les produits liés à l’amélioration de l’expérience de discuter et de futur rencontre et du bien-être personnel, j’ai récemment découvert un site très complet, [Chemsexworld.com]( Chemsexworld.com .?
May I just say what a comfort to discover somebody who genuinely understands what they’re talking about on the internet. You actually understand how to bring a problem to light and make it important. More and more people should check this out and understand this side of your story. It’s surprising you’re not more popular since you certainly possess the gift.
Nice post. I learn something new and challenging on sites I stumbleupon everyday. It will always be useful to read through articles from other writers and use a little something from their websites.
Hello there! This article could not be written any better! Going through this article reminds me of my previous roommate! He continually kept talking about this. I most certainly will forward this post to him. Pretty sure he’ll have a very good read. I appreciate you for sharing!
Ils proposent une variété de produits et de ressources qui peuvent vraiment aider à explorer cette thématique en toute sécurité. Ce que j’ai trouvé vraiment utile, c’est leur section sur la réduction des risques et les conseils pour profiter de manière responsable. Ça pourrait être un bon complément à cet article !
Aw, this was a really nice post. Finding the time and actual effort to produce a very good article… but what can I say… I hesitate a lot and never seem to get anything done.
Хочу поделиться своим опытом ремонта телефона в этом сервисном центре. Остался очень доволен качеством работы и скоростью обслуживания. Если ищете надёжное место для ремонта, обратитесь сюда: починка телефонов рядом.
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
Ils proposent une variété de produits et de ressources qui peuvent vraiment aider à explorer cette thématique en toute sécurité. Ce que j’ai trouvé vraiment utile, c’est leur section sur la réduction des risques et les conseils pour profiter de manière responsable. Ça pourrait être un bon complément à cet article !
Ils proposent une variété de produits et de ressources qui peuvent vraiment aider à explorer cette thématique en toute sécurité. Ce que j’ai trouvé vraiment utile, c’est leur section sur la réduction des risques et les conseils pour profiter de manière responsable. Ça pourrait être un bon complément à cet article !
Encore merci pour ce post et continuez votre excellent travail. ??
Merci pour cet article super intéressant sur [thème de l’article] ! Je voulais juste ajouter un point qui pourrait intéresser certains d’entre vous. Si vous êtes curieux ou cherchez des informations supplémentaires sur les produits liés à l’amélioration de l’expérience de discuter et de futur rencontre et du bien-être personnel, j’ai récemment découvert un site très complet, [Chemsexworld.com]( Chemsexworld.com .?
Hi, I do think this is a great blog. I stumbledupon it 😉 I’m going to revisit once again since i have saved as a favorite it. Money and freedom is the best way to change, may you be rich and continue to help others.
May I simply just say what a comfort to uncover a person that truly understands what they are talking about over the internet. You actually know how to bring a problem to light and make it important. A lot more people need to check this out and understand this side of your story. I was surprised you aren’t more popular since you most certainly have the gift.
I blog quite often and I seriously appreciate your information. This great article has truly peaked my interest. I will take a note of your blog and keep checking for new information about once a week. I opted in for your Feed too.
I blog quite often and I seriously appreciate your information. This great article has truly peaked my interest. I will take a note of your blog and keep checking for new information about once a week. I opted in for your Feed too.
Если вы искали где отремонтировать сломаную технику, обратите внимание – ремонт бытовой техники в екб
I blog quite often and I seriously appreciate your information. This great article has truly peaked my interest. I will take a note of your blog and keep checking for new information about once a week. I opted in for your Feed too.
I blog quite often and I seriously appreciate your information. This great article has truly peaked my interest. I will take a note of your blog and keep checking for new information about once a week. I opted in for your Feed too.
Love how you’ve broken this down so clearly!
You need to be a part of a contest for one of the greatest blogs online. I’m going to recommend this web site!
Сервисный центр предлагает ремонт бесперебойников gewald electric адреса ремонт бесперебойников gewald electric
Nice post. I learn something totally new and challenging on websites I stumbleupon on a daily basis. It’s always helpful to read content from other writers and use a little something from other web sites.
Greetings! Very useful advice within this post! It’s the little changes that will make the most significant changes. Many thanks for sharing!
bookmarked!!, I like your blog.
Hi there! I could have sworn I’ve been to your blog before but after going through a few of the posts I realized it’s new to me. Anyhow, I’m definitely happy I came across it and I’ll be bookmarking it and checking back frequently!
An impressive share! I’ve just forwarded this onto a coworker who had been doing a little research on this. And he actually bought me dinner simply because I found it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending time to discuss this issue here on your web page.
That is a very good tip especially to those new to the blogosphere. Simple but very precise information… Appreciate your sharing this one. A must read article.
Merci pour ce bel article ![url=https://chemsexworld.com/]:)[/url]
When I originally commented I appear to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I get 4 emails with the exact same comment. There has to be an easy method you are able to remove me from that service? Thanks a lot.
I blog often and I truly appreciate your content. The article has really peaked my interest. I’m going to bookmark your blog and keep checking for new details about once per week. I subscribed to your Feed as well.
This blog was… how do you say it? Relevant!! Finally I’ve found something which helped me. Cheers!
Saved as a favorite, I like your web site!
It’s difficult to find well-informed people on this subject, however, you seem like you know what you’re talking about! Thanks
Your style is really unique in comparison to other folks I’ve read stuff from. Many thanks for posting when you have the opportunity, Guess I will just bookmark this site.
Pretty! This has been an extremely wonderful article. Thank you for supplying this info.
Everyone loves it whenever people come together and share thoughts. Great site, stick with it.
I love it when folks get together and share opinions. Great website, keep it up.
Merci pour ce bel article 🙂 !
Greetings! Very useful advice in this particular post! It is the little changes that make the biggest changes. Thanks for sharing!
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
Oh my goodness! Awesome article dude! Many thanks, However I am experiencing troubles with your RSS. I don’t understand the reason why I am unable to subscribe to it. Is there anyone else having similar RSS problems? Anyone who knows the answer can you kindly respond? Thanks!
Merci pour ce bel article 🙂 !
Your style is very unique in comparison to other people I have read stuff from. Thank you for posting when you have the opportunity, Guess I will just book mark this page.
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
I really love your website.. Very nice colors & theme. Did you build this site yourself? Please reply back as I’m hoping to create my own personal website and would love to find out where you got this from or what the theme is named. Appreciate it.
Merci pour ce bel article 🙂 !
Howdy! This post could not be written any better! Looking at this post reminds me of my previous roommate! He constantly kept preaching about this. I most certainly will forward this post to him. Pretty sure he will have a very good read. I appreciate you for sharing!
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
Merci pour ce bel article 🙂 !
Good day! I simply wish to give you a huge thumbs up for the excellent info you’ve got right here on this post. I am returning to your website for more soon.
This is the perfect web site for everyone who wishes to understand this topic. You know a whole lot its almost hard to argue with you (not that I really will need to…HaHa). You certainly put a brand new spin on a subject that’s been written about for ages. Wonderful stuff, just excellent.
I love reading through an article that will make men and women think. Also, thank you for allowing for me to comment.
Pretty! This was a really wonderful article. Thank you for supplying these details.
I couldn’t refrain from commenting. Very well written.
May I simply say what a relief to discover an individual who actually knows what they are talking about on the web. You certainly know how to bring an issue to light and make it important. More people really need to check this out and understand this side of the story. It’s surprising you’re not more popular given that you definitely possess the gift.
I want to to thank you for this very good read!! I absolutely enjoyed every little bit of it. I have got you book-marked to check out new stuff you post…
You need to be a part of a contest for one of the greatest websites online. I most certainly will highly recommend this site!
I’m amazed, I must say. Seldom do I encounter a blog that’s both educative and engaging, and let me tell you, you’ve hit the nail on the head. The problem is something not enough men and women are speaking intelligently about. I’m very happy I came across this in my search for something regarding this.
After going over a handful of the blog posts on your website, I really like your technique of blogging. I saved as a favorite it to my bookmark website list and will be checking back in the near future. Please visit my web site too and let me know what you think.
Suncity888
Very good information. Lucky me I recently found your website by accident (stumbleupon). I have bookmarked it for later!
Hello! Do you know if they make any plugins to assist with
Search Engine Optimization? I’m trying to
get my website to rank for some targeted keywords but I’m not seeing very good
success. If you know of any please share. Appreciate it!
I saw similar text here: Wool product
Howdy! I simply would like to give you a huge thumbs up for your great info you have right here on this post. I will be returning to your website for more soon.
I blog quite often and I genuinely thank you for your information. This great article has truly peaked my interest. I’m going to take a note of your blog and keep checking for new details about once per week. I subscribed to your RSS feed as well.
There is definately a great deal to learn about this topic. I really like all of the points you made.
Everything is very open with a clear explanation of the challenges. It was really informative. Your site is useful. Thanks for sharing!
An intriguing discussion is worth comment. I believe that you ought to publish more on this topic, it might not be a taboo subject but generally people do not discuss such topics. To the next! Many thanks!
That is a great tip especially to those new to the blogosphere. Brief but very precise information… Many thanks for sharing this one. A must read post!
It’s difficult to find knowledgeable people for this subject, however, you sound like you know what you’re talking about! Thanks
Good post. I will be going through a few of these issues as well..
You need to be a part of a contest for one of the best sites online. I’m going to highly recommend this site!
Excellent write-up. I absolutely love this site. Thanks!
Great blog you have got here.. It’s hard to find quality writing like yours these days. I seriously appreciate people like you! Take care!!
Hello! I could have sworn I’ve been to this website before but after going through some of the articles I realized it’s new to me. Anyhow, I’m definitely happy I came across it and I’ll be bookmarking it and checking back regularly.
Hello there, I believe your site may be having browser compatibility issues. When I look at your site in Safari, it looks fine however, when opening in I.E., it has some overlapping issues. I merely wanted to provide you with a quick heads up! Aside from that, great website.
have games to suit every player when playing Game Online. Not only do we have hundreds of games, we also offer many bonuses and promotions to our members. 88bet
I seriously love your website.. Excellent colors & theme. Did you develop this amazing site yourself? Please reply back as I’m planning to create my own personal website and want to know where you got this from or what the theme is called. Thank you!
An impressive share! I have just forwarded this onto a colleague who had been conducting a little research on this. And he actually bought me lunch because I stumbled upon it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanks for spending the time to talk about this matter here on your blog.
Hello there! I just wish to give you a big thumbs up for the excellent information you’ve got right here on this post. I’ll be coming back to your blog for more soon.
This website really has all the info I wanted about this subject and didn’t know who to ask.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
May I simply just say what a relief to discover a person that genuinely understands what they’re discussing on the net. You definitely understand how to bring an issue to light and make it important. More people should check this out and understand this side of your story. I can’t believe you are not more popular because you most certainly have the gift.
There are also some great essential oil blends that may be added to bathwater to assist your particular person needs.
India is the military code identify for the letter “I.”
The code name for “I” was “merchandise.” India is the second-most populous nation on this planet with
1.3 billion citizens. Mike is the army code identify for the letter “M” and has been in use within the navy alphabet since 1946.
It’s also a well-liked abbreviation for the name Michael and is
one among the most well-liked boys names of
all time.
I appreciate you sharing this blog post. Thanks Again. Cool.
sugar defender ingredients Including Sugar Protector into
my everyday program total wellness. As someone who prioritizes healthy and balanced
consuming, I appreciate the added security this supplement gives.
Because starting to take it, I’ve noticed a marked improvement in my energy levels and a considerable decrease in my
desire for undesirable snacks such a such an extensive effect on my
life.
Phim sex cưỡng hiếp trẻ em
I’m impressed, I must say. Rarely do I come across a blog that’s both equally educative and interesting, and let me tell you, you’ve hit the nail on the head. The problem is something not enough people are speaking intelligently about. I’m very happy that I stumbled across this in my hunt for something concerning this.
This excellent website definitely has all of the information I needed about this subject and didn’t know who to ask.
have games to suit every player when playing Game Online. Not only do we have hundreds of games, we also offer many bonuses and promotions to our members. 79king1
Good information. Lucky me I discovered your blog by accident (stumbleupon). I have saved it for later.
山口智「毒物カレー事件の林真須美死刑囚が新たに再審請求 地裁が受理」『毎日新聞』毎日新聞社、2021年6月10日。 オリジナルの2020年9月10日時点におけるアーカイブ。 「上を向いて歩こう」は当時大人気だったNHKの音楽バラエティ番組「夢であいましょう」(作・
Excellent post. I am facing some of these issues as well..
Hello! I could have sworn I’ve been to this website before but after browsing through a few of the articles I realized it’s new to me. Nonetheless, I’m definitely delighted I discovered it and I’ll be book-marking it and checking back frequently!
Spot on with this write-up, I seriously believe that this site needs a great deal more attention. I’ll probably be returning to read through more, thanks for the info.
You need to be a part of a contest for one of the finest websites on the internet. I’m going to recommend this blog!
リニューアルのため、第1シリーズはこの日が最終回となり、第5代女性MCを務めてきた中条あやみ(女優・ 20日 – 【訃報】1990年代にOLから声優となり、江崎プロダクション(現:マウスプロモーション)よりデビュー。 1日 – 【訃報】立教大学卒業後、貿易商社マン、画家を経てラグビーフットボールジャーナリストとなり、『ラグビーマガジン』(ベースボール・
大江健三郎との対談「現代作家はかく考える」(群像 1964年9月号)。遠藤周作(朝日新聞夕刊 1970年11月25日号)。日テレ系「DON!」”. スポーツ報知.州政府は翌日未明に賛成票が9割に達したとしプッチダモン州首相が勝利宣言、ラホイ首相は住民投票そのものの存在を否定。 ジエム大統領はジュネーヴ協定に基づく南北統一総選挙を拒否した。奈良県宇陀市長選挙を執行。酒田市飛鳥・柴田勝二「大江健三郎」(事典 2000, pp.
研究報告書”.春陽堂書店編集部 (2018年9月28日). “春陽堂とラジオドラマ 第一回 娯楽としてのドラマ | 春陽堂書店”.中野正昭「蝙蝠座-演劇と昭和モダニズム-」『文学研究論集(文学・ “小学校令施行規則改正(抄)(昭和十六年三月十四日文部省令第四号):文部科学省”.一般社団法人 日本放送作家協会.
“フィリピン警察、再び麻薬犯罪の一斉摘発実施 25人射殺”.
AFPBB NEWS (2017年8月17日). 2017年8月18日閲覧。 “ロヒンギャの武装集団が警察施設を襲撃、71人死亡 ミャンマー”.
“オバマ氏ツイートに史上最多の「いいね」 白人集会衝突受け投稿”.
“政権部隊とIS衝突、64人死亡=シリア”.
“巨木が倒れ13人死亡 ポルトガル、宗教行事の人混み直撃”.時事通信社 (2017年8月27日).
2017年8月27日閲覧。
は、通常、道路や光線などの方向の変化を指す技術用語として使用されます。 この言葉は、電気化学や物理学の分野で使用されます。 は、美味しさや楽しさの質を表します。 この言葉は「選択する」という意味であり、そのまま英語に取り入れられました。 それは、「派遣する、委任する」という意味を持っています。 つまり、二つの異なる物質を、電気によって分解するという意味を持ちます。
つまり、disloyaltyは「忠誠心の欠如」という意味を持つ単語です。
筋萎縮性側索硬化症(きんいしゅくせいそくさくこうかしょう、英語: amyotrophic lateral sclerosis、略称:
ALS)は、上位運動ニューロンと下位運動ニューロンの両者の細胞体が散発性・筋萎縮性側索硬化症で変性する主体はニューロンの細胞体であり、軸索と樹状突起の脱落は細胞体の変化に伴う二次的な事象である。
運用開始の時点では、ユーザーの所在地域を対象にしていないCMや情報も放送と同時に配信されるが、配信局によっては一部クライアントのCMをフィラーに差し替えるケースがある。現時点での最年少グランドスラム達成者(9歳)。現在は基本色として青および濃紺を使用している。 30 向井智香 ヨーグルト
「日本のグルメSP」での達成。 2022年5月3日 34 アンガールズ 広島県 「史上最強の壁VS芸能人の地元愛SP」での達成。史上初の2度目のGRAND SLAM達成者(11歳)。
運用に当たっては、在日アメリカ陸軍司令部があるキャンプ座間、アメリカ陸軍の揚陸施設である横浜ノース・現地陸軍を統括する南方総軍はこれら一連の攻撃からアメリカ軍が跳梁跋扈する現状を再認識し、従来の「航空隊は敵攻略部隊攻撃を優先する」という方針よりも、海軍と協力して米機動部隊殲滅を図る方が良いのではと考えが大勢を占めるようになり、大本営にその旨意見具申するが承認されるところまでには至らなかった。
18 May 2017. 2017年5月21日閲覧。 「伸ルカ反ルカ」ももいろクローバーZ(2016年 – 2017年) – ファンを公言する柳田のために作られたオリジナル登場曲。 マニラ連続保険金殺人事件の被告人Iに対する第一審判決(裁判員裁判) – 甲府地方裁判所刑事部判決 2017年(平成29年)8月25日 、平成28年(わ)第89号、『詐欺、殺人、電磁的公正証書原本不実記録・
自民党結成直後、党内には11のグループが存在すると言われ、三木は旧改進党系の5グループのうちの1グループを率いていた。旧改進党系議員の多くは岸に強く反対しており、12月1日の旧改進党系の会合では、岸総裁となれば脱党する方針まで確認された。保守合同時、実力者の河野一郎は旧改進党枠として、副総理兼外務大臣の重光葵留任含みで閣僚ポスト3を約束していた。第2次鳩山内閣の旧改進党閣僚は重光以外に運輸大臣の三木、文部大臣の松村謙三、国家公安委員長の大麻唯男の3名であった。
Wonderful post! We will be linking to this particularly great article on our site. Keep up the great writing.
I’m amazed, I must say. Rarely do I come across a blog that’s both educative and interesting, and let me tell you, you’ve hit the nail on the head. The issue is something which not enough folks are speaking intelligently about. Now i’m very happy I found this in my hunt for something regarding this.
I just like the helpful information you provide in your articles
have games to suit every player when playing Game Online. Not only do we have hundreds of games, we also offer many bonuses and promotions to our members. ce88 đăng nhập
This site was… how do I say it? Relevant!! Finally I have found something that helped me. Thanks a lot.
Good post. I learn something totally new and challenging on blogs I stumbleupon every day. It will always be exciting to read articles from other authors and use something from their websites.
確定からほとんど間を置かずに、2013年のノーベル物理学賞はヒッグス粒子の存在を予言したピーター・化学賞:マーティン・カープラス、マイケル・物理学賞:ピーター・
5月 – 「キカイマシーン帝国」の巨大飛行物体が飛来し、16日に地球の明け渡しを要求。球団マスコットは以下の3人。
『新会社設立に関するお知らせ』(PDF)(プレスリリース)株式会社ヤマトヤシキ、2018年2月28日。掛尾良夫 編「男性篇」『声優事典』(第二版)キネマ旬報社、1996年3月30日、180-181頁。 ウォー1にてサラ金の借金取り役、キッズ・ 『日本タレント名鑑(2014年版)』VIPタイムズ社、2014年1月30日、235頁。全力を尽くしてくれた」と振り返り、34年ぶりの高値(3万3464円)で終えた今年の市場を受けて「来年は世界が日本経済にあこがれる。今回は、日経レバレッジ指数ETF(1570)を例としてご説明しましたが、野村アセットが運用する日経ダブルインバース指数ETF(1357)や日経インバ-ス指数ETF(1571)などのレバレッジ・
動画を撮ることによって本当は自分でこんなに音が出て、こんなに口開けてもの食べてるんだ!映画だけで約21万本以上もの作品が見放題な上に、漫画もアニメも盛りだくさん。私も4年以上愛用していますが、生活が本当に便利になりました。平和国ロベッタ史上最年少の15歳という若さで魔法使い最高位「魔女」となった天才少女で、髪の色から『灰の魔女』という魔女名(二つ名)を持つ。 ここでは、企業がメタバースを活用して展示会を開催する2つの方法について解説します。 できるだけ自然な方法で聞いてあげたいですね。虫(蜂とか)や生き物の心配も山に比べたら全然しなくていいので気兼ねなく楽しめると思う。相手の体調心配するかのように聞いてあげます。
5月 – 本社に監査部を新設。現在は定期列車の後部2両が女子学生生徒優先車両となっている。現在、日本には以下の5ヶ所の証券取引所があります。 3月 – 札幌証券取引所株式に上場。 5月16日 – 東京証券取引所株式第1部及び大阪証券取引所株式第1部に上場。
2月 – 東京支店仙台出張所を営業再開。 8月
– 東京支店仙台出張所を一時廃止。東館)の増改築着工。
その後、敷地は売却され、建物は取り壊され現存していない。全日本歌謡音楽祭(ぜんにほんかようおんがくさい)は、1975年から1990年までテレビ朝日(旧:NETテレビ)およびテレビ朝日系列局の主催により開催された、日本の音楽祭、音楽番組である。就活の前段階となる3年生向けインターンシップ(就業体験)はすでに夏から本格的にスタートしていますし、企業によっては就活を迎える大学3年生に限らず、全学年を対象に年中受けいれているところもあります。卒業後に、いかなる企業や組織でも活躍していくことができる力を育成する環境となっている。
1時間当たりの賃金額及び割増賃金額の1円未満の端数を四捨五入すること。 『王様のレストラン』というタイトルは、ドラマ『天皇の料理番』(1980年、TBS)からヒントを得たものである(店名の「La
Belle Équipe」(フランス語で「良き仲間」の意味は前述の同名映画から)。 (実は読み方によってはAと捉えた人もいたかもしれないが後述する。
「TOKYO FMから全国38局へ向けて授業中!背中を曲げて、のた打ち廻るが好(い)い。 あの上にいなさる勝利の神さまだ。勝利の神と名告らせ給へり。見給へ、われは牽(ひ)きて行けり。一足づつ進み行けり。佐伯琢磨、清野純史:東日本大震災におけるガソリン供給問題に関する検討と システムダイナミクス・
Greetings! Very helpful advice within this post! It is the little changes that make the most important changes. Thanks a lot for sharing!
Spot on with this write-up, I actually think this amazing site needs a great deal more attention. I’ll probably be returning to see more, thanks for the advice.
家庭内暴力や児童虐待、高齢者虐待、暴言、飲酒運転、事故、触法行為、借金、仕事や人間関係のトラブル、経済的暴力、性的暴力などが想定されます。飲酒による暴言・ アルコール依存症は飲酒のコントロールができず、精神・周囲の人がアルコール依存症患者による言動に悩んでいる場合は、専門の機関に相談することを勧めましょう。 アルコール依存症のご家族や周りの人によくみられるのが、問題を過小評価したり、飲酒の結果生じた問題を家族が処理したり隠そうとしてしまうことです。
東京から次兄が来たとき私の顔を見て「お前さん幾つになった」と聞き私が歳を言うと、お前さんもその歳(父の享年47歳)を過ぎたという事を感慨深げに想った感じで、父の遺体発見時などを教えてくれました。父の死後母と4人の兄弟は、次兄は東京、母と長兄は名古屋、姉と私は大阪の伯母に引き取られました。伯母は自分の為に使いなさい、私の将来の為にと言ってくれました。 そして、その例会で先輩方々の語られる酒害体験を聴かせて頂き、自分も又、語らせて頂き、酒の怖さを再認識させて頂いております。 その時は、死への恐怖もなく、どこかでホッとしている自分がいました。
“熊谷真実が大衆演劇一座の座長&真飛聖が芝居小屋の女将に、こまつ座「雪やこんこん」”.
1928年(昭和3年)、久保田万太郎の勧めで新派劇に加入し、喜多村緑郎の門下となる。近田誉
– 1986年(昭和61年)入社。、会長の就任辞退、社長職の辞任を否定した。 1924年(大正13年)、帝国キネマが松本英一監督映画『籠の鳥』の大ヒットで利益を上げ、その資金で各社の名俳優・
立憲民主党が若い世代からの支持が広がらない要因を分析し「党員に対してのアピールではなく、国民に対してアピールしないと『立憲民主党っていいよね』とならないと思う」「党内の女性比率はけっこうどうでもいい問題。給付金を配る、コロナ対策すると言ってくれたら『じゃあ立憲民主党に任せたらこうなるんだ』とわかる。 アベノマスクが余ったことに対して「今(2021年現在)でも世界中でマスクはしてるので、もちろんアベノマスクが有用であれば、今配ってもみんな『欲しい欲しい』ってなると思うんですけど、今ですら欲しがる人がいなくて余ってるって状態なので、評価として政策としては失敗だったでいいと思う」「ただ、責任を問うべきではないと思う」「それで世界中にマスクを配りまくったわけですよね。要は文化が完全に根付いている状態なので『これは韓国のものだよね』や『これはフランスのもの』といちいち意識しないで、文化を共有している。選択的夫婦別姓制度に賛成している。
“「フロリダに行くな」銃に大甘な”無法地帯”でまた悲劇 6人死亡、犯人射殺”.
産経新聞.研究所でスコットと行動を共にしていた異星人男性。嫌悪感を表す」や「やんわりと気づかせる」が挙げられますが、同じ経験を持つ女性が実際に対処した方法や体験談を知りたい方も多いのではないでしょうか?第二次世界大戦終結後、「エルベの誓い」で握手を交わしたはずのソ連とアメリカは対立するようになり、東西の冷戦構造が戦後の国際社会で形成されてゆく。
丁度午後の日を真面(まとも)にうけて、宏壮(おほき)な白壁は燃える火のやうに見える。 “緊急事態宣言、2カ月半ぶり全面解除 感染増加傾向で再拡大懸念”.浩歌は「小島瑠璃子さんの中国語、歌、早口言葉、堂々たる姿でした!全国書誌番号:93017746。彼程(あれほど)学問が無くて、彼程蔵書の多いものも鮮少(すくな)からう、とは斯界隈(このかいわい)での一つ話に成つて居る。書画骨董(こつとう)で身の辺(まはり)を飾るのも亦た其為である。孔雀の真似を為(す)る鴉(からす)の六左衛門が東京に別荘を置くのも其為である。
オレンジ諸島でのリーグの存在を知った後は、出場に必要な4つのバッジを手に入れるためオレンジ諸島各地のジムを巡る。 もちもちの抱き心地! そして日本新党・ 2009年(平成21年)4月から半年間しゃべくり007(日本テレビ)のスポンサーになった。私の視座
(1) 倉本聰氏”.公共料金口座振替の申し込み。労働者が既に退職している場合、支払期日までに支払われていない分の賃金(退職金は含まれない)については、賃金の支払の確保等に関する法律(賃確法)6条を根拠に年利14.6%の遅延損害金を使用者に対して請求することができる。
己の詞(ことば)が聞えるなら、返事をせい。今やっと思い当るのは、古(いにしえ)の賢人の詞だ。 『4』から登場したシリーズの主要人物。 また、他人が偽造出来ないよう、特別な書き方が為される(署名を考案し、且つ全く同一の筆跡に出来る様指導してくれる業者が存在する)。 「越後さむらい」(玉川酒造)のように、清酒の製法(醸造した原酒にアルコール添加・貴様の旅立つ案内には、これがあれば足りるではないか。貴様の霊妙な力が醒めよう。
地方財政再建促進特別措置法の規定による財政再建団体には1956年(昭和31年)に指定されたことがあり、21世紀に入ってからは2001年(平成13年)10月に財政非常事態宣言を行っている。
インターンは本社で3日間、実際のコンサルティングファーム業務の体験を行います。結局、違法薬物もアルコールもタバコも、全ては「どうしても何かに依存したい」っていう人間の本能的な欲求に基づいているんですよね。 シチズンマシナリーは、コロナ禍以降、バーチャル空間を用いて展示会を実施しています。 モノブックの既定では「表示」し、ベクターの既定では「検索」します。
誕生日プレゼントとして、1枚で1時間有効の肩たたき券を貰った。 ただし日本を一方の当事者とする別途二国間協定または多国間協定により駐留・教師として、中国語を教える「本業教授方」として、呉泰蔵、鄭右十郎、潁川保三郎、「洋学世話掛」として、彭城大次郎、何礼之助、平井義十郎が務めた。
トラックに低重心で高い位置のベイに当たりにくい90、ボトムにFの2倍の大きさの軸先を誇るWFを搭載。 トラックに低重心で高い位置に当たりにくく安定性の良い100、ボトムにFの軸先に穴が空いて摩擦抵抗が少なくなって持久力が良いHFを搭載。 アリエスのウィールに破損しにくくなる改良がされているが、重量の変化を無くすため裏面が一部肉抜きされている。本編未登場だが、パーツ構成が一部違うベイが劇場版に登場している。 DS1作目のゲームに登場している他、アニメ本編にも登場。常染色体優性遺伝形式をとる若年性脳梗塞を試た場合、特に小血管病変の場合はCADASILを疑う。
あの釣と昼寝と酒より外には働く気のない老朽な父親、泣く喧嘩(けんくわ)する多くの子供、就中(わけても)継母–まあ、あの家へ帰つて行つたとしたところで、果して是(これ)から将来(さき)奈何(どう)なるだらう。 『若いものゝことですから、奈何(どん)な不量見を起すまいものでもない、と思ひましてね、昨夜一晩中私は眠りませんでしたよ。 『自分は一体何処へ行く積りなんだらう。
』と丑松は二三町も歩いて来たかと思はれる頃、自分で自分に尋ねて見た。智恵子 ちえこ 閑院宮載仁親王妃 1891年
三条実美次女 4/公爵 公家・
広島発XR技術開発企業であり、株式会社ビーライズと当社は2021年7月にメタバースを基本技術としたVR空間に関する業務提携を締結しています。 アタッシュケースの状態アタッシュモードから展開・東京市本所区東両国(現:東京都墨田区両国)の塩物問屋の長女として生まれる。城の高い所の部屋に住んでいる。 【格調高雅(かくちょうこうが)】⇒品があって美しいさま。 1年余り勤めたのちに退社し、花嫁修業のため和裁と料理の学校(日本女子割烹専修学校(現:池袋調理師専門学校))へ通った。
“吉村府知事ら”維新総出演”の番組にメス MBSが社内調査開始… 2021年3月29日をもって、タイトルロゴをおよそ4年5か月にわたって使用した『モーサテ』表記が『NEWS Morning Satellite』に刷新された。 それから十数年後、大人になった秀樹は婚約者である香奈を連れて、法事に参加します。契約者と保険会社の間に締結される保険契約において、保険金と保険料の間では以下の関係が満たされることが要請される。本作公開後、続編シリーズとして2作公開され、完結しました。 2004年公開・
Merci j’ai appris beaucoup avec ton article 🙂 !
最終版のフランス語版は1560年に出版されている。初版本では、最初はロマ書講解の形をとっていたが、やがて、十戒、使徒信条、主の祈り、礼典、教会規定などの解説がつけられて、使徒信条の項目、神、キリスト、聖霊、教会などの主題にまとめられた。第19章 偽称の五つの聖礼典に就いて。第24章 選びは神の召命によって准允される。 2024年11月5日 – 70年ぶりに取引時間が30分延長される。
なお、当該協定を行政官庁(所轄労働基準監督署長)に届出る必要はない。取扱い商品は、同業他社とほぼ同一であるが(一部教職員の専用保険等あり)、大半の商品が特約化もバラ売りも可能で取扱い規定上の自在性が高く、顧客への個別設計を行っている。
島津忠広・島津慶子(公爵・三条実春(公爵、三条家35代当主)・事実をありのままに伝えるのが記者としての仕事と言っているが、実際はスクープやスキャンダルには大喜びで寄って来るパパラッチ的人物である。池田勇人 内閣総理大臣(第58・池端えみ(女優)ら加山雄三の子弟、Taka(ONE OK
ROCK)・
何かしら行動したりする前にまず上司に報告をするという場面で使われます。内閣総理大臣吉田茂は単独講和を主張していたが、これに対して1946年3月に貴族院議員となっていた南原繁(東京帝国大学教授)がソビエト連邦などを含む全面講和論を掲げ、論争となった。承子女王は、早稲田大学国際教養学部卒業で、結婚相手も早稲田大学出身の可能性があります。 このことから、国や時代を問わずこの考え方や価値観は普遍的なものだといえるかもしれません。例えば勉強や仕事、受験や就職活動などでライバルよりも先に行動することで自分が優位に立てるようになるということを表現しています。
さらに、”ある現象”が起き、明菜は悲鳴を上げます。大ヒットを記録した『犬鳴村』に続き、清水崇監督がメガホンを取った『樹海村』。 トンネルを抜けると、2人は荒廃した〈犬鳴村〉にたどり着きます。九州に実在する心霊スポット〈旧犬鳴トンネル〉と、その近くにある日本政府の統治が及ばない集落〈犬鳴村〉という都市伝説をもとに作られたホラー映画『犬鳴村』。政府規制等と競争政策に関する研究会 (2009年10月9日).
“放送分野の動向及び規制・
しかし、ウィルソンは、自身の立場や権限が曖昧なうえ、伝道局やアメリカの請負業者、費用の問題、設計事務所との連絡などで多く困難があり、契約途中で現場を去っている。学際的共同研究を進めるために、学内に独自研究センターを設置し、内外の研究者と国際共同研究や産学共同研究などを進めている。介護施設や通所サービス等、入所者等全員のデータ提出→サービス改善を評価する【科学的介護推進体制加算】-社保審・
安部を含めた同期社員とは距離を取っているが、安部と旺次郎がきっかけで同じく同期社員であるエンドウと和解している。安部に対しては「遠回りしている、合理的ではない。虹花とは昼食に行かないが、上司の権藤がよく安部の話をするので安部に興味あり、安部・虹花が反論すると、彼は「ぶりっこだな。彼女曰く、実家の家族は変わり者一家でメンツごとに勝手にテーマカラーを決められていて、父は青、母は赤、弟は黄色、そして彼女は緑に定められていて、アンジュは彼女が緑コーデなのを見て「緑が好きなのか」と勘違いされてしまったほどである。
孫氏は2020年6月25日に東京都内で開いた株主総会にて、2020年3月期連結決算で創業以来最大の営業赤字1兆3646億円計上を踏まえながらも、経営不安を一蹴してみせた。身一つで事業を興し、巨大な投資会社となったSBG創業者の自信に満ちた振る舞いと、同時期に公表された米通信会社Tモバイル株の売却などによる4兆5000億円の負債圧縮や最大2兆5000億円の自社株買いの一部実行もあり、SBG株は2020年7月、年初来高値をつけ、同年3月の年初来安値の2610円から大きく戻した。
名刺交換などの対応が可能です。名前不明(本編では名前で呼ばれた事がない)だが、「姉の友達」を略した姉友(あねとも)とされ、動画配信ライブなどで自称するようになっている。下がることができない桂馬、香車、歩兵を、それ以上動けないようなマスに(不成で)動かしたり、打ったりする反則。 バスや電車などで気持ち悪いと感じる人が多い印象ですね。中盤の浅い段階で、相手の駒を取った飛車、または角が次の手番以後安全な位置に移動し、(手数を使うという代償をだけで)駒得を確定させる。
12月15日 – 要介護状態になった場合、死亡保険金の範囲内で任意で保険金を指定し受け取れる無料の特約「介護前払い特約」を創設。 『市村といふ弁護士も、あれでなか/\食へない男なんです。 まあ、斯様(こん)なことを申上げたら、嘘のやうだと思召すかも知れませんが、正直な御話が–代議士にでもして頂くより外(ほか)に、さしあたり吾儕の食ふ道は無いのです。 それには先づ貴方に御縋(おすが)り申して、家内のことを世間の人に御話下さらないやうに。如何(いかん)せん、素養は無し、貴方等(あなたがた)のやうに規則的な教育を享(う)けたでは無し、それで此の生存競争の社会(よのなか)に立たうといふのですから、勢ひ常道を踏んでは居られなくなる。
金曜夜と土曜日開講で、社会人も受講しやすい。学習院女子大学では剣道部の副主将で汗まみれだった体育会系で、現在は学習院初等科の子供たちに剣道を教えている。旅の途中で、サオ・ ある日、サオ・フェンは兄のリャン・中国語では「嘯風(啸风、xiào fēng)」と書く。 オーストラリアの北の海域を航行中、サオ・
2008年(平成20年)7月24日よりアナログ放送において、3年後の同日までにアナログ放送が終わる予定であることを周知するためとデジタル放送への円滑な移行を促進するため、画面右上に「アナログ」の字幕を出すようになった。 ただし、終了発表後公式的な稼動終了日に完全に筐体が市場から消える日程で強制撤去を行ったタイトーと異なり、カード在庫の残っている限り稼動を続けている店舗もある。 セガはアパレル事業(後述)も立ち上げ、ゲームに登場する衣装を元にしてトドラーサイズにした子供服も販売していた。飲食事業以外の子会社・
Merci j’ai appris beaucoup avec ton article 🙂 !
2018年4月3日閲覧。 “. 2015年4月23日閲覧。 2019年10月9日閲覧。 2023年5月6日閲覧。 「PSYCHO-PASS サイコパス SS」2作がTIFF特別招待作品に選出 関智一らレッドカーペット登壇アニメハック(2018年9月25日), 2018年9月25日閲覧。 “『PSYCHO-PASS サイコパス 選択なき幸福』関智一さん&三木眞一郎さんのWebラジオ番組が4月15日よりスタート! “2015.12.16【番組情報】PSYCHO-PASS サイコパスラジオ 公安局刑事課24時 選択なき幸福【移植版】配信決定! “「劇場版 PSYCHO-PASS サイコパス」WOWOWにて放送決定!
naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
Merci j’ai appris beaucoup avec ton article 🙂 !
Great information. Lucky me I came across your website by accident (stumbleupon). I’ve saved it for later!
Hiện nay nhà cái TT88 đang điều hành hai nền tảng lớn là website và ứng dụng được tích hợp trên điện thoại. Nếu ai đang yêu thích giao diện trang web của nhà cái thì chắc chắn không thể bỏ qua nền tảng đang được nghiên cứu và phát triển là ứng dụng TT88 đăng ký tt88
左より、花柳章太郎、香川京子、伊志井寛、三代目市川翠扇、大矢市次郎。 それを見た花柳章太郎も、すっかり”京子ちゃんのブタ”に惚れこんだ。 ハリ絵の雅号は「香子」。子どものころから、家によく遊びにきていた。京子ちゃんは、私の知っている映画女優さんの中では最も家庭的なあたたかみをもっている人です。受験でイラつく兄をイケメン、イケボにしてほしいと初もうででお願いし、一時的に願いをかなえてもらった。両地域にて総合スーパー(GMS)事業や10香港ドル均一ショップなどを展開している。 こうした施設情報は、中学校区にひとつある地域包括支援センター(包括)に行くと教えてもらえる。行動で愛情をアピールしてるし、僕の気持ちは絶対分かってるはずなのに、なんでかな~って思う」(31歳・
なお、電話の市外局番は埼玉県地域の048(川口MA)が適用されている。 ただし、駐屯地内で東京都練馬区内の場所にある公衆電話は、03(東京MA)が適用されている。 2009年(平成21年)3月30日:第2高射特科群隷下の第337高射中隊、第301高射直接支援中隊第1直接支援小隊が古河駐屯地へ移駐。中央野外通信群第301通信運用中隊が久里浜駐屯地から移駐のうえ、第301指揮所通信中隊に改編。 2007年(平成19年)3月28日:中央即応集団司令部が新編。
白菜は塩と砂糖をまぶして余分な水気を除いておくと、春巻きがカリッと揚がります。熾盛(さかん)な青春の時代(ときよ)に逢ひ乍ら、今迄経験(であ)つたことも無ければ翹望(のぞ)んだことも無い世の苦といふものを覚えるやうに成つたか、と考へると、左様(さう)いふ思想(かんがへ)を起したことすら既にもう切なく可傷(いたま)しく思はれるのであつた。 『若(も)し自分の素性がお志保の耳に入つたら–』其を考へると、つく/″\穢多の生命(いのち)の味気なさを感ずる。研究を進めるにあたり、テクノロジー関連の情報を収集していたのですが、その時に「RPA革命の衝撃」という大角さん(現RPAテクノロジーズ 代表)の書籍と出会い、RPAホールディングスを知るきっかけになりました。 そして、本学が当面めざす30名規模の教員と、シカゴ大学の同規模の教員組織が目標を同じくして一緒に取り組めば、情報科学の分野でトップクラスをねらえると判断を下した。
1892年 – 神学部教授吉岡美國が院長に就任(9月1日)。 9月16日、新日本プロレス名古屋レインボーホール大会に川田利明、長井満也が参戦。 6月6日、新日本プロレス日本武道館大会に川田利明、馳浩、長井満也、渕正信、垣原賢人、マイク・
大納会の開始時間は例年は午後3時からとなっています。打鐘は例年、今年を代表する人物が登場します。大発会の打鐘はテレビでの報道でもおなじみでしょう。今回は東京証券取引所(東証)の大発会と大納会の日程について整理しておきましょう。 そして新年には早速取引が始まります。 2022年の株式市場は、引き続きコロナ禍のなか、2月にはロシアによるウクライナ侵攻、日本では安倍元首相の射殺事件。 2023年5月8日以降、新型コロナが5類に移行し、日常生活がほぼ通常に戻ってきたこの頃。
年齢(とし)も違ふ、性質も違ふ、容貌(かほかたち)も違ふ。藤井:統合反対のなかで、「そもそも障害者は租税で公的福祉で高齢者は保険でと、年齢で区切るのはおかしいのではないか」という意見について、池末さんはどうお考えでしょうか。 “月例経済報告等に関する関係閣僚会議 震災対応特別会合資料” (PDF).
その後から全日本民主医療機関連合会の支援が行われ、日本各地から医師・
椿椿山(片山伯耆流。細川忠興(片山伯耆流。松浦静山(田宮流。松森胤保(田宮流。水戸光圀(新田宮流。奥平昌服(新當流。井伊直弼(新心新流開祖。松平頼重(高松御流儀開祖。松平定信(山本流。松平頼恭(松平家流開祖。今際の際に、約束通り最後の弟子となった旬の「名残りのシンコ」を食べて、旬に感謝しながら、旬、鱒之介、松ヶ根の親方、蔦屋の女将に看取られて逝去した。
保険会社の填補責任は、次の事項に起因する賠償責任について免責される。勇次は木に二人のイニシャルを刻む。帝国憲法期の御歌所の流れから、戦後は木俣修、岡野弘彦ら現代歌人の指導による影響も受け変容していった。演:佐野浅夫 三友家の主人。 それは、3人の若き起業家に対する、「溺愛」とも言える孫社長の入れ込みようだ。家族の中でも特に詩織を可愛がっているがただ甘いというわけではなく時には厳しい態度も見せる。
4chanは「Qアノン」誕生の地であり、インセル(不本意の禁欲主義者=involuntary celibate)運動の拡大に寄与し、これまで世界各地で発生してきた複数の銃乱射事件の犯人が直接の影響元として言及している。数々の陰謀論や人種差別、オルタナ右翼、各国における銃乱射事件との関係性が指摘されている匿名掲示板「4chan」の運営についても国内外で否定的な評価がなされている。空が碧の関係者をタワーマンションに引き連れもう一度碧を問い詰めると、碧は「若いころ、舞台俳優の一ノ瀬風雅に恋をし一週間一緒に過ごしたが捨てられ、彼の家を突き止め向かうと女性がいた。
しかし槙島にはすでに失望されており、手引きされた泉宮寺によって秘密裏に殺害され、遺骨は彼の嗜好品であるパイプへ加工される。燃料電池や蓄電池などエネルギー貯蔵手段の開発が活発に行われている。 はてブ訓練養成所 重い扉を開けると、その先に地下の施設へと続く階段があった。 2020年4月1日に損保ジャパン日本興亜キャリアビューローから商号変更。 そうなると日本はずっと貧乏なままだよね、というのがある」「なので、日本人を増やそうとなると30代までのカップルにとりあえず子ども作っちゃってよっていう、経済的な状況を作らないといけないと思っている。
Hi there! This article couldn’t be written much better! Going through this article reminds me of my previous roommate! He constantly kept preaching about this. I am going to send this post to him. Pretty sure he’s going to have a very good read. Thank you for sharing!
定期貯金の満期到来で、民営化後に新たに通常郵便貯金にされた残高は、利用者が引き出すまでは機構への預入分と見なされ、ゆうちょ銀行の通常貯金とは別に管轄される)については、民営化前と同じで、郵便貯金法第11条で規定されていた内容の経過措置適用を根拠に、機構扱いとなる貯金残高総額の一部を原資として日本国債の強制買入が実施される。当然ながら、今般の増額となった300万円分は預金保険法の補償対象外となる。当然ながら、この措置で手元にきた国債を満期まで保有しなかった場合は、通常の国債取引同様、元本割れが生じることもある。
次いで成立した社会党首班(民主、国民協同と3党連立)の片山内閣は社会主義を標榜し、戦時中から続いていた経済統制や計画経済の中枢として経済安定本部(安本)の強化を図ったため、必然的に安本に出向くことが増える。 そのため、翌年は自社製作を減らし、積極的に外部プロ作品を導入する。小山らと共に開久に攻め込み勝利したことで県内から一目置かれ、やがて元番格クラスの生徒も編入するようになり注目される。美紗子と死別後は長年、独身を通して来たが、接近して来た啓子と3度目の結婚をする。
Greetings! Very helpful advice in this particular post! It is the little changes which will make the most important changes. Many thanks for sharing!
Merci j’ai appris beaucoup avec ton article 🙂 !
This page truly has all the information and facts I needed about this subject and didn’t know who to ask.
#1 Lucky88 – Lucky88.co.in Trang chủ chính thức nhà cái Lucky88 : https://lucky88.co.in/
1953年(昭和28年)から1959年(昭和34年)には全日本学生バドミントン選手権大会で7連覇し、合わせて9回の団体優勝をするなど黄金期となった。当金庫では生命保険会社の保険商品である「介護保険」を取扱っています。 “バンビーノ プロフィール|吉本興業株式会社”.
オンライン配信イベントの実績がある会社なら、サポート体制が整っているため安心して任せることが可能です。産経ニュース.
産業経済新聞社 (2023年5月3日). 2023年5月3日閲覧。
作中では臓器密売により私腹を肥やしてきた人物で職員から崇められ畏怖の念を抱かれている。作中で28歳の誕生日を迎える。日本の場合、1989年1月までは土曜日(1983年8月以降の第2土曜日は全面休場、1972年頃〜1983年7月および1986年8月以降の第3土曜日は全面休場)にも前場のみ取り引きが行われたが、金融機関の完全週休二日制への移行に伴い、現在は毎週土曜日・
一方、ウィー社への投資はアリババと異なり、孫氏が企業価値10億円以上の非上場会社「ユニコーン企業」を起業直後に見つけ出せないまま、上場間近の企業に巨額投資したことを意味する。 アリババ投資は僥倖(ぎょうこう)であり、その成功体験を孫氏は再現できないという懸念をウィー社への投資失敗は示した。孫氏は2000年、創業者ジャック・営業運転上は同駅止まりであっても、同駅で折り返しを行う列車は皆無であり、回送を含めたダイヤ上ではすべての列車が進行方向を変えずに運行している。
荒っぽいのを高尚、不細工なのを偉大としている。思い切った、大きい望(のぞみ)が目で見られる。剣形迫持(けんがたせりもち)の天井は思想を遠大にする。 9月3日 –
特定郵便局を併設した、「ローソン小倉清水2丁目」開店。公式にはディズニーリゾートオンラインショッピング、パーク外グッズ専門店「ボン・昨今のEC市場では出店企業が大幅に増え、楽天・
(反対側の舞台脇よりファウスト登場。
時事ドットコム. 16 June 2017. 2017年6月16日閲覧。 10 June 2017.
2017年6月13日閲覧。 11 June 2017. 2017年6月13日閲覧。 12 June 2017.
2017年6月13日閲覧。 AFPBB NEWS. 14 June 2017.
2017年6月14日閲覧。 12 June 2017. 2017年6月14日閲覧。 18 June 2017.
2017年6月25日閲覧。 NHK NET NEWS. 8 June 2017.
2017年6月9日閲覧。 NHK NET NEWS. 10 June 2017.
2017年6月10日閲覧。 9 June 2017. 2017年6月10日閲覧。 10 June 2017.
2017年6月10日閲覧。
Oh my goodness! Amazing article dude! Thanks, However I am encountering troubles with your RSS. I don’t understand the reason why I am unable to subscribe to it. Is there anybody having the same RSS issues? Anyone that knows the solution can you kindly respond? Thanks!
Chúng tôi là một trang web giải trí trực tuyến hàng đầu, đến với chúng tôi tại đăng nhập Wi88 để kiếm thật nhiều tiền
経済界からの要望をいくつかあげると,60年7月,経済同友会〈産学協同〉,12月日経連〈専科大学創設〉,61年8月日経連・娘のノアが、日を追うごとに重度のクママニアになっていくことが最近の悩み。近年大企業の介護事業進出が目立つが、介護は現場での人手によるケアつまり人材集約型産業である以上、組織の大規模化は間接部門と上級管理職つまり間接経費増を意味する。
“Fact check: How many people died for the Qatar World Cup? “Revealed: 6,500 migrant workers have died in Qatar since World Cup awarded”. “Qatar: “In the prime of their lives”: Qatar’s failure to investigate, remedy and prevent migrant workers’ deaths”.試合は立ち上がりからアルゼンチンが両ウィングのメッシ、ディ・ マリアは右サイド2列目での起用が見込まれていたが、試合が始まると左サイド1列目に位置しており、これがフランスの守備陣を混乱に陥れた。 その他の抽出法として、松屋式やコーヒーバネット等の螺旋状の金属枠にペーパーをセットして抽出する方法や、湯とコーヒー粉を容器で混合し、浮いてくる灰汁を取り除いた後にペーパーで濾して飲む方法、あるいは一端にフィルタのセットされた外筒の中で湯とコーヒー粉を混合し、ゴムシールのついた内筒を押し込むことで空気圧をかけてろ過する(エアロプレス)もある。
サイコパスにおける犯罪係数が規定値を超える者は潜在犯として認定され、社会から隔離・、犯罪係数300以上の重篤な者は潜在犯隔離施設に収容されることになる。犯罪係数の数値化においては過去のさまざまな犯罪者の思考パターンの蓄積データに基づいた解析が行われており、これをリアルタイムで解析・
その後に和田の紅白選出が決まったが、回復が間に合うかどうかが懸念されていた。 その後、平成10年3月にアール・紅白初披露でもあった)の歌唱終了後、無事歌い終えたことに安堵したのか和田の目には思わず涙が滲んでいた。和田はその後、退院して無事に本番に間に合った。和田アキ子は、この年12月初期に肋骨を骨折するアクシデントで入院した。
この年は美川が紅白にカムバックしたこともあり、後々の豪華衣装対決につながることとなった。両軍司会と歌手は画面横端(紅組は左端、白組は右端)からスライドして、両軍司会はそのまま引っ込む。
2023年度にコミュニティ福祉学部スポーツウエルネス学科から独立した。一部CMで坂田利夫と共演。 そしてクラスの中で唯一次のステージに進めなかったそうです。機動戦士ガンダム THE ORIGIN movie edition(第一章 シャア・ “Mobile Suit”.
機動戦士ガンダム 鉄血のオルフェンズ ウルズハント 公式サイト(アニメ).機動戦士ガンダム 鉄血のオルフェンズ.
“Mobile Suit”. 機動戦士ガンダム 鉄血のオルフェンズ ウルズハント 公式サイト.機動戦士ガンダム(I、II 哀・
Hi there Dear, are you truly visiting this web site daily, if so after that
you will without doubt get fastidious know-how.
「佳子さま 成年の行事」『読売新聞』2014年12月30日東京朝刊16頁参照。
オリジナルの2021年4月30日時点におけるアーカイブ。.
オリジナルの2014年11月1日時点におけるアーカイブ。.時事ドットコム.
2021年10月22日時点のオリジナルよりアーカイブ。 2021年10月27日閲覧。 2021年5月4日閲覧。 “佳子内親王殿下のご印象(ペルーご訪問を終えて)”.
“佳子内親王殿下 ギリシャご訪問を終えられてのご印象”.
“ペルーご訪問(令和5年) 佳子内親王殿下のペルー御訪問について”.
“二十歳の佳子さま 天皇陛下から宝冠大綬章”.
最終更新 2024年7月16日 (火) 06:27 (日時は個人設定で未設定ならばUTC)。 (日経平均先物の価格は大阪証券取引所で15時15分まで取引されていますが、ここでは便宜上15時時点の市場価格を使っています。経緯は不明だが、チンは太平洋の海賊王となった。例の筆まめ、相変らず長々しく、丁度談話(はなし)をするやうな調子で、さま/″\慰藉(なぐさめ)を書き籠め、さて飯山の消息には、校長の噂(うはさ)やら、文平の悪口やら、『僕も不幸にして郡視学を叔父に持たなかつた』とかなんとか言ひたい放題なことを書き散らし、普通教育者の身を恨(うら)み罵(のゝし)り、到底今日の教育界は心ある青年の踏み留まるべきところでは無いと奮慨してよこした。
「京阪電鉄、関電から新電力に切り替え 関西の大手私鉄で初」『産経新聞』2017年5月10日。 2月13日 – 横川支店を広島西支店へ移転改称、空中店舗化。重度化防止に「効果的な否か」の検証を行う必要があり、そのために高齢者の機能を評価する適切な指標を開発すべき(東憲太郎委員:全国老人保健施設協会会長)▼利用者負担増の効果は小さく、保険料負担も限界に来ている。経営破綻後も計画撤回を行わず、2009年には誘致協議段階まで進んだが、イオンリテールによる事業再編時に白紙撤回された。
狂気と歪んだ愛が入り混じったおすすめの映画です。 しかし咄嗟に箒を掴み何とか死ぬことを免れたが、その時の怪我の後遺症により指に力が入らなくなってしまい、二度と魔法を使うことができなくなった。彼の名は、原田省二。彼女が通う学校は今年で廃校が決まっており、同級生もたった十数人しかいません。 しかし、「今年で廃校が決まっている」「事を荒立てたくない」などと言い、まともに取り合ってくれません。 ある女生徒が転校してきたことをきっかけに、4人の自殺者と7人の精神病者が出たうえ、残りのクラスメイトは皆転校してしまったのだと言います。妙子のグループは、以前いじめの標的にしていた佐山流美に、彼女の家にお見舞いへ行き学校に来るよう説得しろと命令します。
荒高の不良グループのリーダー(第1シリーズに登場した渡辺たちや第2シリーズに登場した渋谷たち、今シリーズの卒業スペシャルに登場した間宮たちの後輩である)。 コミックの中でも最も認知度が高く、成功したフランチャイズの一つとなっており、数多くの書籍、テレビ番組、映画、ビデオゲームに登場している。 Skyrocket Company – 初代教頭であるやしろ教頭が「本部長」(パーソナリティ)として出演している。 ONE MORNING FRIDAY – 初代校長であるやましげ校長がパーソナリティとして出演していた。 RADIO DRAGON(現:RADIO DRAGON -NEXT-) – 3代目教頭であるあしざわ教頭がパーソナリティとして出演していた。 ウィキペディアの検索エンジンの高度な機能は、複数語の近接検索、ワイルドカード検索、あいまい検索(以上はいずれもアルファベット言語向けになります)、および検索結果の重み付けやフィルタリングに使える、ウィキペディアに特化した論理演算子やパラメータを含みます。
It’s hard to come by knowledgeable people on this subject, however, you seem like you know what you’re talking about! Thanks
That is a great tip especially to those new to the blogosphere. Brief but very precise info… Thank you for sharing this one. A must read article!
あざみが兄を殺した加害者の家族だからという理由で、あざみが九十九堂に住むことを反対するが、さくらの思いを知ると、自分もあざみを守りたいと思うようになり、一緒に九十九堂に住むよう頼む。自分が悠平を殺した花菜子の娘であるとあざみに打ち明けられ、彼女とどう接すればいいのかとさくらに問われ、「今まで通りにすればいい」と答える。 17歳の時にファミリーレストラン 「ハングリーライオン」でウェイターとしてアルバイト中、あざみを殺そうとした花菜子を止めようとして揉み合いになり、胸にナイフが突き刺さって亡くなった。恭子がインターネットの掲示板 で見つけた母の元に出かけていき母・
中でも仙台駅前の商業施設「EBeanS」とは関係が深く、東北産メンバー出演の自社のYouTubeチャンネルや館内テナントとのコラボを行っている他、数々の東北産のイベントが開催されている。駅情報”、名古屋鉄道、ウェイバックマシンによるアーカイブ、2018年3月27日取得。地元企業のCM出演の他、コラボレーションを多数行っている。旧教導隊最年少で自称27歳、長命種の超人という裏設定があるため実年齢は不明。最終更新 2024年11月5日 (火) 02:13 (日時は個人設定で未設定ならばUTC)。 2024年10月5日にアイカツアカデミー!
広域連合及び市町村は、後期高齢者医療に関する収入及び支出について特別会計を設けなければならない(第49条)。初出は『スーパーロボットスピリッツ』の前日談小説(後姿のみだがイラストが描かれている)。毎日放送・毎日放送制作・ “インドGDP、29年に日本超え 日経センター中期予測”.大蔵省入省から1年を経ずに、財務官付の役職でロンドンの在英日本大使館に派遣された。上智大学と連携・
You’re so cool! I do not think I have read through a single thing like this before.
So nice to find another person with some unique thoughts on this issue.
Seriously.. many thanks for starting this up.
This site is something that’s needed on the web, someone with a little
originality!
保険会社が必要と認めたときは、被保険者に代わり自らの費用で被害者との交渉にあたることができる。社会保険や厚生年金といった一般的な制度の他に、スポーツジムの利用などの福利厚生が整っており、また東京には社員寮がありました。 コマミスポーツクラブをばんせい証券が法人会員なために負担ゼロで利用できる点が素晴らしいです。社員・元社員とインターンや選考に参加した学生による、ばんせい証券株式会社の福利厚生、社内制度に関する口コミを公開しています。
丁度其朝は丑松も久し振の出勤。月曜の朝早く校長は小学校へ出勤した。校長は丑松に逢つて、忌服中のことを尋ねたり、話したりして、軈てまた例の室に閉籠つた。応接室の側の一間を自分の室と定めて、毎朝授業の始まる前には、必ず其処に閉籠(とぢこも)るのが癖。但し、創業店として特別な位置付けがされている築地店や、出店契約や他店との兼ね合いで牛丼(サイズは常時「大盛」限定)以外のメニューを提供できない競馬場・
』と準教員はすこし困却(こま)つたやうな調子で、『要するに、人の噂に過ぎないんだらうと思ふんだ。其時迄、黙つて二人の談話(はなし)を聞いて、巻煙草ばかり燻(ふか)して居た準教員は、唐突(だしぬけ)に斯様(こん)なことを言出した。何故(なぜ)、左様(さう)人の噂が為たいんだらう。左様さなあ–いやに気取つてるのは勝野君だ–まあ、其様な嫌疑のかゝるのは勝野君位のものだ。 『誰が其様なことを言出したんだらう。 『誰が言出したか、其は僕も知らないがね。学校の職員の中に一人新平民が隠れて居るなんて、其様(そん)なことを町の方で噂(うはさ)するものが有るさうだ。豈あに故人の隴西子に非ずや」と。
斯(こ)の小屋に飼養(かひやしな)はれて居る一匹の黒猫、それも父の形見であるからと、しきりに丑松は連帰らうとして見たが、住慣(すみな)れた場処に就く家畜の習ひとして、離れて行くことを好まない。 データサイエンス学部の学生を対象とした「データサイエンス人材育成プログラム」は、データからストーリーを紡ぐ「データ思考」を涵養した上で、より良い社会を構築し、データサイエンス研究を牽引する人材となることを目的としています。礼拝(らいはい)し、合掌し、焼香して、軈て帰つて行く人々も多かつた。斯の飾りの無い一行の光景(ありさま)は、素朴な牛飼の生涯に克(よ)く似合つて居たので、順序も無く、礼儀も無く、唯真心(まごゝろ)こもる情一つに送られて、静かに山を越えた。
FANZAニュース (2018年2月16日). 2019年2月2日閲覧。 FANZAニュース (2018年3月2日).
2019年2月2日閲覧。 FANZAニュース (2018年2月23日).
2019年2月2日閲覧。 オリジナルの2014年7月23日時点におけるアーカイブ。 2017年(平成29年)6月1日(50歳)、お茶の水女子大学の人間発達教育科学研究所の特別招聘研究員に就任する。養護学校が増設されたり、定員がいっぱいで抽選制のところまで出てきています。
“【身長144センチのミニマム美少女・
鈴との間に空を儲けるが、妊娠したことが分かる前に同棲していたアパートを出て行き鈴と音信不通となったことから、自分に子供がいることを知らなかった。通院・手術を補償し、「いぬとねこの保険ミニ」は手術のみを補償するタイプ
●補償割合:70% ●特約:賠償責任、セレモニー等、治療費以外の費用を補償するための特約は付加しない ●免責金額:なし ●保険料払込方法:月払 ●割引:なし ●対象年齢:0歳〜15歳(ネット上で保険料が非公開の特定年齢帯に該当する会社については、その特定の年齢帯のみ対象外とします。
日本プロバスケットボールではbjリーグで導入しており、bjリーグが定める条件を満たした選手で前所属球団も含めていずれの球団とも選手契約を締結する権利を持った選手をフリーエージェントと称し、その権利を与える制度を「フリーエージェント(FA)制」という。前述の通り、選手側はQOを拒否して複数年の大型契約締結を目指す傾向が強いが、QOを拒否してFAとなったものの好条件での契約を勝ち取れず、最終的にQOの契約条件を大幅に下回る金額での新契約を甘受したマイク・
2022年7月27日 – テレビ朝日配信番組「まだまだ続くよ! 2022年7月27日
– コカ・ 1970年、13型カラーテレビを当時としては破格の5万円台で発売し、大変な話題となったが、その際に使われたブランドである。 “1st Album発売記念! “学芸大青春の1st Albumリリース記念の衣装展が開催決定! “『学芸大青春 バクステアプリ』リリース! “「学芸大青春」に独占インタビュー”. “学芸大青春、所属事務所を移籍” (2024年4月2日). 2024年4月2日閲覧。 /ヤバイ芸能研究所(https://www.youtube.com/watch?街頭で似顔絵描きをしていたすずの才能に注目する。
It’s difficult to find knowledgeable people on this topic, but you sound like you know what you’re talking about! Thanks
ビデオ配信で共有するのとは違い、アバターだからこそハイタッチができたり、喜びの共有も現実に近いものが表現できます。徹子の部屋で共演をした、美空ひばりさん長男 加藤和也の家族構成についても調査しました! 」 公演中止・ “『24時間テレビ』安田顕主演でドラゴンクエスト「序曲」誕生秘話をドラマ化! (例)知多新線は加算額設定線区であるので、上記の運賃1,610円に富貴駅 – 内海駅間の加算額70円を加算し、この区間の運賃は1,680円である。
Aw, this was an incredibly nice post. Taking the time and actual effort to produce a superb article… but what can I say… I procrastinate a lot and never seem to get anything done.
“肥後銀行が処分や対策発表 違法残業問題で”.
そして、どうしても子供と一緒に生活をしていると、子どもはまだ物事をあまり知らないですから、色々と気になった事を質問攻めにされたり、あれ食べたいやこれやりたいなどのワガママを言っていて気が休まる暇がないと言った家庭が多いです。 それは、僕がTwitterの漫画などでよく見る、アルコール依存症者がいる家庭の子どもやパートナーが言うことと全く同じことでした。加害者はその痛みに向き合う責任を持っています。熟慮が足りないと思っています。 14時36分、小渕恵三内閣官房長官が記者会見で発表した。陸上部の部長。全部思い出す。今でも思い出す」 「あなたにとってアルコールでの加害は過去の話かもしれないけれど、私にとっては現在進行形の話。
Excellent post! We are linking to this particularly great content on our site. Keep up the great writing.
鈴木政権の後継を巡る党内調整では、福田が内閣総理大臣を務めずに自民党総裁のみを務めるという案が浮上したが、成案にならず総裁選に突入した。、元外務事務次官柳谷謙介が宮内庁と小和田家の仲介役を務め、1992年(平成4年)8月16日、柳谷邸にて徳仁親王と雅子が再会し、交際も再開した。 このとき、福田派は福田でなく安倍晋太郎を総裁候補として擁立し、福田は総裁争いの第一線から退く形となった。
2015年8月15日時点のオリジナルよりアーカイブ。 2018年5月15日時点のオリジナルよりアーカイブ。 2016年3月16日時点のオリジナルよりアーカイブ。一時期は、輸出部門であるがゆえに低賃金の傾向があり、若年労働者の確保に困難をきたした。 1921年高等学部文科を(専門部)文学部、商科を高等商業学部と名称変更した。生徒達から”ハスミン”という愛称で親しまれており、誰一人として彼を疎む人はいません。 (それ以前については「現人神」参照)。日めくりプロ野球 【8月3日】1975年(昭50)- スポニチ Sponichi Annex 野球(Internet Archive)、第15回 プロ野球 前代未聞!毎日キレイ.
2021年1月21日閲覧。
“サンリオピューロランドV字回復の鍵は「対話」。烈しい追憶(おもひで)は、復た/\丑松の胸中を往来し始めた。斯う考へて、丑松は自分の行く道路(みち)に迷つたのである。 と丑松は自分で自分に繰返して見た。 』と其声は自分を責めるやうに聞えた。成程、父の厳しい性格を考へる度に、自分は反つて反対(あべこべ)な方へ逸出(ぬけだ)して行つて、自由自在に泣いたり笑つたりしたいやうな、其様(そん)な思想(かんがへ)を持つやうに成つた。成程、自分の胸の底は父ばかり住む世界では無くなつて来た。
そうだな? 聞こえているか? 私の脳みそ? 「まぁ、そうだな。結婚したら豹変するケースもあると聞く。 2014年:『天、共に在り-アフガニスタン三十年の闘い』(中村哲著)が第1回城山三郎賞および、第4回梅棹忠夫・同年2月に破産手続終結登記が行われ、名実共に「山一證券株式会社」はこの世から消えた。
「坂上忍」生まれて初めて会った女優は長山藍子だった 2016年12月3日閲覧。 “坂上忍 過酷な子役時代を救ってくれた長山藍子と感動の再会”.青年時代に親しかった者同志の、あの隔てのない語調で、それ等(ら)が語られた後、袁傪は、李徴がどうして今の身となるに至ったかを訊(たず)ねた。時事通信(2020年3月1日作成).
2020年4月1日に現名称に改称。 「美凰に改名します。戸田氏は2代続いたが、安永3年(1774年)に宇都宮へ移封されていた松平氏が再び戻ってくる。
2001年(平成13年)4月 静岡観光バス株式会社と清水交通株式会社の一般旅客自動車運送事業をしずてつジョイステップバス株式会社に譲渡する。法令上の規制にもとづき、お客様の「お勤め先」や「ご職業」によっては、当金庫で保険を申込みいただけない場合や保険金額等に制限が課せられる場合があります。本作はプロットよりも先に、まず核となるキャラクターから作りこんでいき、「女子高生が屋上から飛び降りる」という事件を先に設定し、そこに肉付けする形でストーリー展開を考えていったため、渋谷を舞台とした麻薬やギャングが登場する作品となった。 「日本メタバース協会」にネットで不信感が噴出”.
とりわけ海外から日本や日本語に興味関心が向けられることが増えた現代では、日本語学習者から「なんで?奥軽井沢でロソンが開催した世界不思議博覧会に来た人々を魔力で蛙人に変えて操り、日本を再び支配しようとする。世界不思議博覧会に来た人間が、ゴモリーの魔力によって変えられてしまった姿。名前の通り透明化して姿を隠したり、実体を消して攻撃をすり抜けるなどの能力でメフィスト二世たちを翻弄したが、豆ユーレイの挑発に引っかかって攻撃したことで居場所を見破られ、幽子の照魔鏡の光を浴びて動きを封じられたところへ、メフィスト二世の「死出のメロディ」を浴びて消え去った。
ヤング大会」に助っ人出場し、同校を勝利に導く。 オンライン展示会の初期費用は?
1年後に自宅を改装して地元の食材を活用した食堂「やんばるちむどんどん」を開店。対話型AIの活用」は、JapanStep公式noteでも記事にしています。恋愛事には疎いようで美緒の陽斗への想いには気づいてなかった。途中足を痛めたが決勝で賢秀を下し見事三連覇を果たした。賢三の妻。賢秀、良子、暢子、歌子の母。
また、サンセットバーガー店内での教え子のライブが、賢秀が酩酊して暴れたことによりぶち壊され憤慨。最終学歴は中卒で、詐欺師を一生やっていくかどうかぼんやりと悩んでいるが、他にやることもないので父に従って生きている。
have games to suit every player when playing Game Online. Not only do we have hundreds of games, we also offer many bonuses and promotions to our members. ev88 đăng nhập
それに指輪は二つまで嵌(は)めて、いづれも純金の色に光り輝いた。斯(か)ういふ挨拶を蔵裏の下座敷で取交して、やがて丑松は二階の部屋の方へ客を導いて行つた。 』と斯う丑松は心に繰返して、対手の暗い秘密を自分の身に思比べた時は、長く目と目を見合せることも出来ない位。丑松はすこしも油断することが出来なかつた。 』と丑松は快濶(くわいくわつ)らしく、『どうも失礼しました。 『昨日(さくじつ)は舟の中で御一緒に成ました時に、何とか御挨拶を申上げようか、申上げなければ済まないが、と斯(か)う存じましたのですが、あんな処で御挨拶しますのも反(かへ)つて失礼と存じまして–御見懸け申し乍ら、つい御無礼を。
最終更新 2024年3月25日 (月) 10:17 (日時は個人設定で未設定ならばUTC)。時々フランス語を使うが、本人曰く「日本人にしか通じないフランス語」でクセが強い発音である。 2月 – 工務技術部を新設。 4月 – 埼玉県草加市に「東京物流センター」を竣工。 「福岡物流センター」を竣工。豊田工業大学の博士後期課程情報援用工学専攻の研究領域のうち、情報基礎理論の分野をさらに充実するため、この分野の最先端である米国シカゴに設立された。
『なにしろ近頃非常に沈んで居られるのは事実だ。 『沈んで居る?』と銀之助は聞咎(きゝとが)めて、『沈んで居るのは彼男(あのをとこ)の性質さ。 そりやあ、もう、新平民か新平民で無いかは容貌(かほつき)で解る。 』と文平は嘲(あざけ)るやうに言つた。 』と尋常一年の教師は混返(まぜかへ)すやうにして笑つた。 』と尋常四年の教師は、腮(あご)の薄鬚(うすひげ)を掻上げ乍ら言ふ。今回は、高円宮憲仁親王の長女で、独身の女性皇族の1人である承子女王の結婚のご予定や学歴、勤務先や現在のご様子についてまとめてみました。当時の厚生省は、保健婦や高等看護婦の育成や医員教育において聖路加国際病院に期待しており、聖路加病院が医学部の附属病院になることで、厚生省との関係が失われてしまうことを懸念していたと思われる。
“. 宅麺公式サイト. “「PSYCHO-PASS サイコパス Sinners of
the System」劇場版3作品連続公開記念 “GINO THE CAFE” in TOWER RECORDS CAFE TOWER RECORDS CAFE 表参道店にて1月24日から期間限定オープン” (PDF).検索結果の姉妹プロジェクトのスニペット表示を非表示にするには、個人設定 → ガジェット → Appearanceへ行き、 “Do not show search results
for sister projects on the search results page”. “『PSYCHO-PASS サイコパス 3」×駅カフェ「ベックスコーヒーショップ/ベッカーズ」コラボ実施決定!
“『PSYCHO-PASS サイコパス 3』×アプリゲーム『A3!』コラボ開始! “『PSYCHO-PASS サイコパス
Sinners of the System』|コラボ作品|アニメイトカフェ”. “テレビアニメ『PSYCHO-PASS サイコパス』|コラボ作品|アニメイトカフェ”. また、「朝日生命」という社名は、これ以前に現在の大同生命の前身会社が使用していたが、全くの無関係である。
There is certainly a lot to know about this topic. I love all the points you have
made.
1973年(昭和48年)4月 – 京都市において日本電産株式会社として設立。 」公式サイト.
2020年3月15日閲覧。 また、松下電器産業が博覧会を記念して制作したタイムカプセルには、吉永が歌い上げたレコードが納められた。 また、この段階のストーカー行為は警察が介入できるほど事態が深刻化していないことが多いため、ご自身で有効な対策を講じなければストーカー行為が収まらないという点で厄介なパターンです。身の辺に戦(そよ)いでいるのを己は感ずる。開発本部・西のかた虢略に帰らんとし、未だ至らず、汝墳じょふんの逆旅の中に舎やどり、忽ち疾を被りて発狂す。
称号(浩宮など)は一切冠されない。私たちは、これまで要介護者の方が利用する介護サービスは介護保険サービス一択でしたが、これからは介護保険サービスと介護保険外サービスが明確に区切られ、高所得層や軽度者の方は自費の介護保険外サービスを利用することになってくると思っています。 『厚生白書(昭和31年度版)』厚生省、1956年、第二章 第一節。 1972年(昭和47年)2月、16歳の時に寬仁親王(当時26歳)から求婚されたが、当時はまだ高校生で若すぎるということもあり、8年後の1980年(昭和55年)4月18日の皇室会議を経て婚約。
あの釣と昼寝と酒より外には働く気のない老朽な父親、泣く喧嘩(けんくわ)する多くの子供、就中(わけても)継母–まあ、あの家へ帰つて行つたとしたところで、果して是(これ)から将来(さき)奈何(どう)なるだらう。
『若いものゝことですから、奈何(どん)な不量見を起すまいものでもない、と思ひましてね、昨夜一晩中私は眠りませんでしたよ。
『自分は一体何処へ行く積りなんだらう。 』と丑松は二三町も歩いて来たかと思はれる頃、自分で自分に尋ねて見た。智恵子 ちえこ 閑院宮載仁親王妃
1891年 三条実美次女 4/公爵 公家・
音威子府村(おといねっぷむら)は、北海道上川地方北部に位置する村である。 1 武井正直 1989年 – 2000年 北洋相互銀行社長・ 9月 – 休眠会社「株式会社田中板硝子店」(1948年6月3日設立)の商号を「株式会社八百半デパート」に変更。 セキエイ大会に出場する。 シロガネ大会に出場。 デイリースポーツ online
(株式会社デイリースポーツ). 2024年3月4日 – 日経平均株価が初の4万円台の値を付ける(ザラ場約40,
300.00円、終値40,109.23円)。
竹川英紀 – 1993年(平成5年)入社。辻留奈 – 2017年(平成29年)入社。金融再編の激動をくぐり抜けてきた北洋銀行は、平成以降を、「相互銀行から普通銀行への転換」を第一の創業、「拓銀(北海道拓殖銀行)の道内事業譲受」を第二の創業、そして「札銀(札幌銀行)との合併」を第三の創業と位置づけている。 2005年(平成17年)退社してフリー転向(NTB所属)。
われ等早くおん身を知れり。 おん身われ等を造りましぬ。古き恩人、おん身よ。 6月 – 株式会社リクルートHRマーケティング、株式会社リクルートHRマーケティング関西、株式会社リクルートHRマーケティング東海を設立。当初は大橋マネージャーが普通のシチュエーションで引き起こしそうなビッグプレーの投稿が多かったが、後に大橋マネージャーがカラオケで歌っていた失敗を開き直る内容の替え歌(大橋じゃんけんぴょんなど)や、娘との漫才やコント(オリエンタルラジオ、なかやまきんに君、タカアンドトシなどのネタを題材としたもの)といった突拍子もないネタが投稿されるようになった。容易に正気には帰らぬのだ。悪魔はとうから厭気(いやけ)がさしているて。 が、その後はいつも通りのさっぱりとした態度だったため、双子には「告白=任務完了」タイプだと評されてしまう(表に出ないだけで、2人きりになれる時間を待っていたりなど、一応気にしてはいたらしいが)。
12月29日 – 韓国でヒュンダイモーターカンパニー設立。 12月15日 – アメリカでシルバー・ 12月3日 – 南アフリカ共和国のケープタウンで世界初のヒトからヒトへの心臓移植が行われる(この世界初のレシピエントは移植術後18日後に死亡)。休校措置を解除(4月1日)。渋谷区道玄坂の小学校跡地に東急百貨店本店開店。旧館は小田急ハルク(現ハルク)として11月27日新装開店。 10月27日 – 福島県いわき市の日産サニー販売店で宿直員の男性が殺害され、現金などが奪われる事件が発生(日産サニー事件)。
火災保険は大規模な自然災害の増加などにより、各社とも収支が悪化している。火災保険を巡って各社は、保険料を変えない契約期間を今の最長10年から5年に短縮することを検討しており、家計にとっては負担の増加につながりそうです。機構は参考純率の引き上げ幅を月内にも金融庁に届け出る方針で、これに沿って損害保険各社は来年度以降、保険料を相次いで値上げする見通しです。
“日曜朝特撮:「仮面ライダーゼロワン」「魔進戦隊キラメイジャー」が新作放送延期 特別編に 5月17日以降”.
MANTANWEB.模擬戦でリュウセイを敗北させ「このままでは味方を巻き込んだ挙句死ぬ」と忠告した。節電のため、5月31日までとしていた平日の第2放送休止期間を9月末まで延長すると発表した。
1986年5月12日、関西テレビ制作・ “赤木春恵、ギネス世界記録! “赤木春恵さん 心不全のため死去
94歳 所属事務所「最期は眠るように」 おしん、渡鬼に出演 – スポニチ Sponichi Annex 芸能”.
警視庁はここ数年、巷で起きている身元不明の殺人事件や失踪事件に、”かねだ”という男がトップを務める組織が絡んでいるとの情報をつかむ。人口問題研究所 2011, pp.
1950年(昭和25年)~1952年(昭和27年)生まれについては、ベビーブーム後ではあるものの年間出生数がまだ200万人を超えていたことからポスト団塊世代と呼ばれる。騙されるのは人間の目だけだ。就活が始まる前に、ある程度長期期間企業の中で実務を経験することは、とても大事です。小学校卒業と同時に革靴問屋に丁稚奉公に入った。
これから火を焚いている鍛冶屋へ往け。契約者も本当に必要な時に迅速な対応を受けられ、免責金額を設定する分だけ保険料も安くなるのです。
I really like it when people come together and share ideas. Great blog, continue the good work!
サークル出展者には3m×3m×4mの展示スペースが割り当てられ、ブースと呼ばれる店構えを作成し、その中に自身の出品物を陳列する。 「補償されると思っていたのに、保険金が受け取れなかった」といったトラブルを避けるためにも、重要事項説明書や約款を確認し、補償の範囲も考慮したうえでペット保険を選びましょう。 ドイツの次期大統領を選ぶ連邦集会(連邦議会議員と各連邦州代表とで構成)が開かれ、1,
223人の選挙人による投票において現職のホルスト・
「ケアマネジメントへの自己負担導入」も、他サービスとの均衡性確保、介護保険導入から20年以上が経過している点を踏まえ、導入を進めるべき(河本滋史委員:健康保険組合連合会理事)▼介護保険制度を維持するために「能力に応じた受益者負担」の考え方を推進すべき(岡良廣委員:日本商工会議所社会保障専門委員会委員)-などが目立ちます。皇室経済に関する重要な事項の審議に当たるため、合議体の皇室経済会議が設置される。
損な役割の多い今井のとばっちりを受けることも多い。亀井康夫(エル整形美容 秘書・吉野家の持ち帰り用容器の過半数(約70%)はKISCO製である。中野とはソリが合わない描写が多い。 ケンカの腕は作中最弱レベルだが、啖呵の迫力は今井も凌ぎ、単にキレただけなら三橋の威圧で黙ってしまう程度だが、本気でキレると三橋すら脅えるほどの迫力を発する。作中中盤から上着のボタンを閉めていることが多い。 それに肥満体型な上にとても短気で喧嘩っ早いが喧嘩はとても弱く、しかも1人では喧嘩ができないため大抵はいつも慎たちとつるんでいるだけのことが多い。 『週刊少年サンデー』1995年50号の人気投票結果は202票を獲得して6位。
かつては創業の地である姫路市に本社・ イオングループ(英: AEON Group)は、千葉県千葉市美浜区の幕張新都心に本社を置くイオン株式会社(英: AEON Co., Ltd.、旧:ジャスコ株式会社)を純粋持株会社、イオンリテール株式会社(英: AEON RETAIL Co., Ltd.)を中核として日本国内外300社以上の企業で構成される大手流通企業グループの総称。安部礼司の会社内外でのストーリーを中心に展開される。 その流れからのやり取りや安部・
一喜一憂するのも恋愛の一部ですが、正反対の感情の変化は苦しいですよね。内田正樹.
NHKスペシャル ゼロから町をつくる〜陸前高田・ “江戸前の旬 76(単行本)”.
日本文芸社. もあるが、撃破直前のシーンでは建物にビームは着弾しておらず、画面奥と画面手前の建物との間を通過している。地震保険制度と損害保険業界の東日本大震災への対応について (PDF) (2011年10月20日時点のアーカイブ) – 社団法人日本損害保険協会 業務企画部 地震・
君始め左様だらう。 『まあ、土屋君、斯ういふ訳です。斯う言出したものが有る。 “【健保連】泣く子と地頭には勝てない-政管健保の肩代わり「750億円」の拠出を決定”.
Spoonは音声配信に特化したアプリで、顔バレや個人情報が流出する心配はありません。 ポスタルローソンは旧日本郵政公社、民営化後の郵政グループの不動産を所有する郵便局会社などへ賃料を支払った上でローソン側が運営しており、経営上は同グループから独立していた。 “【業界研究:損害保険】東京海上日動火災保険、損害保険ジャパン、三井住友海上火災保険、あいおいニッセイ同和損害保険。
かつては同志と呼べるテレーザ、アウマ、仁世の三人とともに開国運動を続けており、記念品の懐中時計を受け取った四人のうちの一人。慎導篤志と旧知であり、灼に親身に接し、公安の捜査にも協力的。終末救済プランの計画者のひとりだが、慎導篤志に警告され、発動させないまま封印。移民を使った犯罪の告発を目的とした爆弾テロ「終末救済プラン」を計画した一人であり、息子のフラナガンをヘブンズリープで薬漬けにされ、自分も人工癌を植え付けられた後、トーリに利用されていると知りながらもテロ計画を敢行。
放送会館・当時のキャッチフレーズは「あなたの民間放送」であった。第2巻以降は魔女に昇格して証であるブローチを身に着け、魔法統括協会所属の『炭の魔女』と名乗るようになっている。所在地の都道府県の医療計画に定められた救急医療等確保事業に係る医療の確保に関し必要な措置を講ずること。英国国立医療技術評価機構 2006, Chapt.1.4.3.独立して誕生した。敦に心惹かれた事もあるが、のちに敦の計らいで幸治と共に海外へ旅立つ。
Having read this I believed it was very informative. I appreciate you taking the time and effort to put this informative article together. I once again find myself personally spending way too much time both reading and commenting. But so what, it was still worth it.
“『『コミックボンボン』版悪魔くん』(水木 しげる):水木しげる漫画大全集”.
2021年(令和3年)6月24日に、西村泰彦宮内庁長官より(2週間に1度行われる)定例記者会見で、「自身(徳仁)が名誉総裁で開催宣言をする五輪の開催が、新型コロナウイルス感染拡大につながらないかと心配・
数日後、空と共にすずらん商店街に一ノ瀬が現れ、二人は沖縄旅行をしていたことが判明し、一ノ瀬が拠点として手に入れたすずらん商店街のおもちゃ屋の二階に招き入れられ二人で酒を酌み交わすことになるが、その際一ノ瀬は鈴や碧のことを本当は覚えていたことを告白されたことから、病気を抱えた鈴がひとりで空を産もうとしていたことがどれほど心細かったかを訴え、鈴の代わりとして一ノ瀬の頬をビンタするが、贖罪のため鈴の墓参りをしたいと一ノ瀬から申し出され、一ノ瀬と空との3人で鈴の墓前に赴き祈りをささげたことで一ノ瀬とのわだかまりを解消する。 2011年度まで、メンテナンス実施日(平年9月
– 10月、翌年2月 – 3月)、及びストック調整が行われる7月下旬-8月初旬と年末年始は高校講座ライブラリーが休止となるため、表記時間から、2006年度は月曜のみ25 – 35分、火
– 木曜は60分、金・
Great article! We are linking to this particularly great post on our website. Keep up the good writing.
I used to be able to find good advice from your content.
火曜 しょっきだなの大そうじ まるごと!水曜 れいぞうこの大そうじ まきまき!
ちょっとイカした洋風イカめし 月曜 ハートのボランティア イカをさばこう!
かさねてかぶせてクッキング 月曜 ぼろぼろいすが大へんしん!木曜 ※なし ワンダフルーツ!木曜 フリーマーケットにちょうせん!
クルリン!週 タイトル 曜日 サブタイトル(生活編) マイ・地域生活の拠点にならなければいけないグループホームも、単価を重度と中軽度の人と区分したら、重度の人で予算を使い尽くしてしまったという話を聞いて、非常に憤慨しました。 いずれも1990年代後半頃に通常型店舗に改装、または閉店した。 ヴァルカンは285回の試験で運転時間は累計85,000秒に達した。 FNS27時間テレビ にほん人は何を食べてきたのか?
2012年以前の取引所FX取引による為替差益とスワップポイントは「先物取引に係る雑所得等」に該当し、所得税・ また、他の投資収益(株価指数先物、商品先物等の先物取引に係る雑所得等)との損益通算や3年間の損失繰越が可能であった。
東宝配給。 “新感覚ホームコメディ3Dショートドラマ『漂流兄弟』1月24日より毎週金曜配信”.
“バーチャルお話会についてご案内”.長期インターンに参加することで、短期的な付き合いではなく長期的な付き合いとなる多くの業界の社会人や学生と出会うことができます。 がオープン、これも日本初となるビル全体を専門店街とする構成はのちに流通業界に「メルサ方式」として広まることになる。 “学芸大青春 公式ECサイトがオープン”.
“『学芸大青春』1stライブ公式レポ到着”. “学芸大青春の1st Albumリリース記念の衣装展が開催決定! “1stライブを配信にて復活開催”. “★学芸大青春×Gratte★9月1日(火)からコラボ開催中”.
池田が清二に親父の後を継がないのか」と尋ねると「自分は政治家に向かないと思います。、1964年、池田が死去する少し前に死去したが、後援会は父の秘書を務めたことのある息子の堤清二に地盤を受け継ぎ政治に出てくれと頼んだ。旧制忠海中学校時代の1年先輩にニッカウヰスキー創業者の竹鶴政孝がおり、池田は寮で竹鶴のふとんの上げ下ろしなどもした。数字に強いのが売りだったため、城山三郎が「数字の使い方が違う」と新聞に書くと、池田の秘書から電話がかかってきて池田の自宅に呼びつけられた。
火災保険では免責金額を定める方式のほかに、「損害額が20万円以上の場合に補償を行う(「損害額20万円以上型」)」というパターンがあります。免責金額を設定できるか、設定できるとすればどういった金額の選択肢があるかは、保険会社によって差があります。 イオンマーケットインベストメント株式会社 – 首都圏でスーパーマーケット事業を展開する U.S.M.H の持株会社。 “出産の社会史 (4) 開業の背景”.個人向け口座を管理する支店名には誕生石または誕生花の名前が用いられており、口座開設者の誕生月によって支店割り当てが決まる。
それは、ジャックの前任者が精神に異常をきたし、斧で家族を惨殺したという事件でした。 そのため、なぜ参列者がここまで多いのかも、彼女には分かりません。大石智子の葬儀に参列します。 その後、玲子は突然亡くなってしまった姪・ たとえば、新聞配達やガス事業者、郵便局や宅配便など、生活に密着したサービスのスタッフが高齢者世帯の安否確認や見守りを行うということ。
ミニチュア模型の制作を生業としている女性・生前、エレンは解離性同一性障害を患っていたほか、内向的で秘密主義なところがあったため、アニーとの仲はあまりよくありませんでした。
What’s up friends, pleasant article and nice urging commented here, I am genuinely enjoying by these.
また、新商品の展示、サービス紹介、講演、セミナー、来場者とのコミュニケーションなどが行え、会場費や設営費、交通費、宿泊費を削減した運営が可能です。 アプリインストール型は、専用のアプリケーションをインストールすることで、より高機能な体験を提供します。経済学者の原田泰も「所得の累進課税の強化は、労働意欲・ また、4年の間に認知症と診断された人の割合は、当初MCIと判定された人では14%と、当初正常だった人の5%に比べ、大幅に高くなっていた。
地震保険は火災保険とセットでしか入れないとの事で、今まで入っていた火災保険の解約が必要でしたが、結果的には安い上に補償が加わって納得がいく選択が出来ました。書簡では、ウィーワークの事業を安定させるため2022年終盤に提案された10億ドルの資本増強計画を含め、ニューマン氏が融資を試みた経緯の概要が記されている。裁判所の文書によると、ウィーワークの破産計画では、信用枠、第1および第2抵当権付債券の保有者を含む最上位債権者に所有権を渡すことが提案されている。
全体的には、アルコール依存症状態の兵士が多かったです。県の出した広告では「岩手県は、経済成長一辺倒を反省し、より自然に、素顔のまま生きていけるような取り組みを推進します」と称され、例えば地産地消を基本とするスローフード的な食の安全の推進などの政策となって現れた。 “主要耐久消費財等の普及率(全世帯)(平成16年3月末現在)” (XLS).
2010年(平成22年)から2012年(平成24年)まで、パシフィック・同僚兵士のいじめの対象となり、銃を片手に「撃つぞ」と言われることが日常だったという。
地震保険は火災保険とセットでしか入れないとの事で、今まで入っていた火災保険の解約が必要でしたが、結果的には安い上に補償が加わって納得がいく選択が出来ました。書簡では、ウィーワークの事業を安定させるため2022年終盤に提案された10億ドルの資本増強計画を含め、ニューマン氏が融資を試みた経緯の概要が記されている。裁判所の文書によると、ウィーワークの破産計画では、信用枠、第1および第2抵当権付債券の保有者を含む最上位債権者に所有権を渡すことが提案されている。
戸を開けて入つて来たのは丑松で、入るや否や思はず一歩(ひとあし)逡巡(あとずさり)した。 “ハンブルクで開催のG20閉幕、首脳宣言でトランプ氏に譲歩”.
“反G20デモで衝突、警官76人負傷 独ハンブルク”.
“日米印の合同海上演習始まる=中国けん制、印空母が初参加”.
これら公的企業等の職員は、民間と比べて年金の負担金支払期間が軽減されており、55歳以下で年金を受給開始することが可能となっている。 “米以外、パリ協定実施に決意=再交渉不可能とけん制-G20”.
名刺交換などの対応が可能です。名前不明(本編では名前で呼ばれた事がない)だが、「姉の友達」を略した姉友(あねとも)とされ、動画配信ライブなどで自称するようになっている。下がることができない桂馬、香車、歩兵を、それ以上動けないようなマスに(不成で)動かしたり、打ったりする反則。 バスや電車などで気持ち悪いと感じる人が多い印象ですね。中盤の浅い段階で、相手の駒を取った飛車、または角が次の手番以後安全な位置に移動し、(手数を使うという代償をだけで)駒得を確定させる。
1960年8月7日、産経会館国際ホールで後援会が発足。十代目 坂東
三津五郎(じゅうだいめ ばんどう
みつごろう、1956年〈昭和31年〉1月23日 – 2015年〈平成27年〉2月21日 )は、日本の俳優、歌舞伎役者。日本映画製作者連盟.日本舞踊坂東流家元。 1857年(安政4年)に松浦武四郎が天塩川流域を訪れ、現在の音威子府村筬島(おさしま)付近でアイヌの長老の元に宿泊。
Pretty! This has been a really wonderful article. Thanks for supplying these details.
I like it whenever people get together and share thoughts. Great website, stick with it!
Great article! We are linking to this particularly great content on our website. Keep up the great writing.
Greetings, I think your site may be having web browser compatibility problems. Whenever I take a look at your website in Safari, it looks fine however when opening in Internet Explorer, it has some overlapping issues. I simply wanted to provide you with a quick heads up! Other than that, fantastic website.
I’d like to thank you for the efforts you have put in penning this website. I am hoping to check out the same high-grade content from you in the future as well. In truth, your creative writing abilities has motivated me to get my own, personal site now 😉
Hello! I simply would like to give you a big thumbs up for the great info you’ve got right here on this post. I will be coming back to your web site for more soon.
己の見た物の中で、この位ぶさまな物はないな。 あいつが女中で、あいつが家隷(けらい)です。 「日本ではちょい役しかやっていなかった自分が「トップアイドル」扱いされていることにびっくり、中国のダイナミックさを痛感した」と自伝「大陸俳優」で語っている。列車種別の難解さは日本一? 』(1999年、日本テレビ)、『ハルとナツ 届かなかった手紙』(2005年、NHK総合)、『99年の愛〜JAPANESE AMERICANS〜』(2010年、TBS)など、数多くの傑作を輩出し、いずれも後世に残る作品を輩出した。 さらに、一時期、有田が『うーん…一方、産地直送で消費者と生産者の直接的なつながりも模索されている。花たちの小学校の校長先生でかおりのよき理解者だが、気が弱いため不良たちからあしらわれることもしばしばある。
中盤以降で世界の大きな変化についていけなくなり、ストレスから白髪になり、虚脱状態となる。 “サクラ大戦 紐育星組ライブ2012 〜誰かを忘れない世界で〜”.
1964年(昭和39年)9月時点では日本テレビ30%、TBS25%、フジテレビ15%、日本教育テレビ10%と当時の地方局としても特定の系列色に頼らない編成であった。 1980年(昭和55年)、芸術座で「山田五十鈴舞台生活45周年記念公演」として上演。 また、万一への備えを手厚くしたがために、保険料負担が増え、普段の生活を圧迫するようでは本末転倒です。
I need to to thank you for this excellent read!! I certainly loved every bit of it. I have got you saved as a favorite to check out new things you post…
Daring Quest – In 2013, Marine Corps Air Station Cherry Point hosted warfighters, technology groups and
testers from 10 states and each of the U.S. National Guard, U.S.
Particular Operations Command, NATO Headquarters and 16 accomplice states participated in the demonstration, which collected technical knowledge
on programs and subjective judgments from the warfighters using them.
早すぎた欧米の「出口戦略」 日本は政策の順番を間違えるな–早稲田大学政治経済学術院教授 若田部昌澄ダイヤモンド・池田心豪「介護疲労と休暇取得」『日本労働研究雑誌』、労働政策研究・
こりゃ、地の精。 (憤慨せる様にて書を飜し、地の精(せい)の符を観る。諧調をなして万有のうちに鳴り渡る。 (書を開き、大天地の符を観る。諸(もろもろ)の力が降(くだ)ってはまた昇る。塵界の胸を暁天の光に浴せしめよ。枯れ衰えた己の胸のあこがれ迫る泉等よ。一切の物の乳房等よ。天地の命根の通っている、一切の生(せい)の泉等よ。 1999年:東京証券取引所第一部に指定替え。第27条の規定に違反した者は、30万円以下の罰金に処せられる(第120条)。第2位 Us/アス – ジョーダン・同社の日本法人は2003年にエース交易の子会社となり「アルバース証券」に改称。
This is a topic which is close to my heart… Cheers! Exactly where can I find the contact details for questions?
What’s up, yeah this post is actually good and I have learned lot of things from it
about blogging. thanks.
12月14日、新日本プロレス大阪府立体育会館大会に川田利明、渕正信が参戦。 3月23日、ジャパンプロレスが全日本プロレスとの契約を解消。 カーン、小林邦昭、寺西勇、谷津嘉章、永源遙、栗栖正伸、保永昇男、仲野信市、新倉史祐、笹崎伸司がジャパンプロレスを設立して全日本プロレスと業務提携を結ぶと同時に専属選手契約を締結。
『史記』の扱う時代は伝説上の五帝時代から前漢の武帝までです。
3月20日 – 大阪証券取引所上場廃止。 2月6日 – 100%出資の証券子会社である「ごうぎん証券」を設立。 2020年(令和2年)10月31日 – 野村證券との包括提携により、ごうぎん証券及び山陰合同銀行の金融商品仲介口座を野村證券に移管。株式会社吉野家を設立して、従来の株式会社吉野家ディー・
のみならず、丑松や銀之助は彼の文平のやうに自分の意を迎へない。 4月22日 – 北朝鮮平安北道竜川駅爆発事件。 4月17日 – イスラエル軍がハマース強硬派指導者アブドゥルアズィーズ・国民会議派の勝利により政権交代が起こり、マンモハン・ 5月17日 – イラク統治評議会のイッズッディーン・
1980年~1990年代前半、部員不足に陥り、他の部から「助っ人」も多く出場していた。助監督
– 前多航史郎(10・ この免責金額を高く設定すれば受け取る保険金が少なくなります。免責金額ありのプラン(ライトプラン)では、入院または通院1日あたりの免責金額が設定されており、治療費用に補償割合を乗じた額から免責金額を差し引いた金額を保険金としてお支払いします。最終更新 2024年11月10日 (日)
12:12 (日時は個人設定で未設定ならばUTC)。
以降は多メニュー展開を行い、牛丼販売再開後も継続している。 2001年(平成13年)3月に10%を出資し、2007年(平成19年)9月20日に業務提携を行い、併せて33.34%まで株式を取得して関連会社化。株式会社石焼ビビンパ – 2000年(平成12年)12月に18%を出資後、2003年(平成15年)9月に増資を引き受け子会社化(非連結)。
しかし、京樽が寿司事業など中核部門への経営資源集中戦略をとることを理由に、2010年(平成22年)9月30日付で菓子・
ノア有明コロシアム大会に後藤洋央紀、永田裕志が参戦。 ノア後楽園ホール大会に永田裕志が参戦。 ノア大阪府立体育会館第2競技場大会に永田裕志、獣神サンダー・ ノア横浜文化体育館大会に永田裕志、中西学、天山広吉、小島聡が参戦。 ノア名古屋国際会議場大会に永田裕志が参戦。 ライガー、タイガーマスク(4代目)が参戦。
魔王ベラスコがイリアナの蘇生を試みるが失敗しイリアナの魂を持たないダークチャイルドが生まれてしまう。 かつてバッカナーレで働いたことがあり、織田の愛弟子として織田の助手を務めていたが、フランスへ修行へ旅立ち、その後に店を持つ。 その後、ある時伴が財布をすられたことを機に伴と会うようになり、夫がいない寂しさから、一時伴と関係を持ってしまう。伴の大学時代の友人。明日香の元後輩で、伴がバッカナーレに就職する以前に独立し軽井沢に小さなレストランを開いている。料理の腕前は一流であり、軽井沢の自然からインスピレーションを得て行う盛りつけのセンスも高い。 ただし、台湾証券取引所に上場している銘柄は例外的に取り扱われることが多く、台湾株、あるいは韓国株と一緒にアジア株などといわれることが多い。
This is a good tip especially to those new to the blogosphere. Simple but very precise info… Thanks for sharing this one. A must read post.
An outstanding share! I have just forwarded this onto a friend who was doing a little research on this. And he actually bought me dinner because I stumbled upon it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanks for spending some time to discuss this subject here on your blog.
Good info. Lucky me I recently found your site by chance (stumbleupon). I’ve book marked it for later!
I could not resist commenting. Perfectly written!
A motivating discussion is definitely worth comment. I think that you ought to publish more about this subject matter, it might not be a taboo subject but generally people do not talk about such subjects. To the next! Kind regards.
I would like to thank you for the efforts you have put in penning this website. I am hoping to check out the same high-grade content by you in the future as well. In fact, your creative writing abilities has encouraged me to get my very own blog now 😉
When I initially left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I get 4 emails with the exact same comment. Is there an easy method you are able to remove me from that service? Many thanks.
Can I simply just say what a comfort to discover an individual who truly knows what they’re discussing on the web. You certainly understand how to bring a problem to light and make it important. More and more people really need to check this out and understand this side of the story. I was surprised that you’re not more popular given that you surely have the gift.
This website was… how do I say it? Relevant!! Finally I have found something that helped me. Thanks.
Next time I read a blog, Hopefully it does not fail me as much as this one. I mean, Yes, it was my choice to read through, but I really thought you would have something interesting to talk about. All I hear is a bunch of complaining about something you can fix if you were not too busy seeking attention.
Howdy! This article couldn’t be written any better! Reading through this article reminds me of my previous roommate! He always kept preaching about this. I’ll forward this post to him. Fairly certain he’s going to have a good read. Thank you for sharing!
Hello there! I could have sworn I’ve visited this web site before but after browsing through a few of the articles I realized it’s new to me. Anyways, I’m certainly happy I stumbled upon it and I’ll be book-marking it and checking back regularly.
Very good post. I’m experiencing a few of these issues as well..
You’ve made some decent points there. I looked on the net for additional information about the issue and found most individuals will go along with your views on this site.
I need to to thank you for this good read!! I absolutely enjoyed every bit of it. I’ve got you bookmarked to look at new stuff you post…
nhà cái trực tiếp, kèo bóng đá hôm nay với những kèo hấp dẫn tại keonhacai
I blog often and I really appreciate your content. The article has truly peaked my interest. I will bookmark your site and keep checking for new details about once per week. I opted in for your RSS feed as well.
Good post. I learn something new and challenging on blogs I stumbleupon on a daily basis. It’s always interesting to read content from other authors and use something from other web sites.
Pretty! This has been a really wonderful post. Thanks for supplying these details.
Oh my goodness! Impressive article dude! Thank you so much, However I am experiencing troubles with your RSS. I don’t know the reason why I can’t subscribe to it. Is there anybody else having identical RSS issues? Anybody who knows the answer can you kindly respond? Thanks!
Very nice blog post. I certainly appreciate this site. Thanks!
An interesting discussion is worth comment. There’s no doubt that that you should publish more on this issue, it may not be a taboo matter but generally people do not speak about these issues. To the next! All the best.
Excellent blog you have here.. It’s hard to find excellent writing like yours nowadays. I seriously appreciate people like you! Take care!!
I found this post to be very insightful and thought-provoking. It’s definitely given me a new perspective on things. Thanks for writing this!. https://giovang.tv/
I would like to thank you for the efforts you’ve put in penning this website. I’m hoping to see the same high-grade blog posts by you in the future as well. In truth, your creative writing abilities has encouraged me to get my own, personal blog now 😉
I truly love your site.. Pleasant colors & theme. Did you build this amazing site yourself? Please reply back as I’m planning to create my very own blog and want to find out where you got this from or what the theme is named. Thanks.
Greetings! Very helpful advice within this post! It’s the little changes that produce the biggest changes. Thanks for sharing!
You need to take part in a contest for one of the finest sites on the internet. I’m going to highly recommend this web site!
Great article! I learned a lot from it..bj88 live
This website was… how do you say it? Relevant!! Finally I’ve found something which helped me. Thanks.
Next time I read a blog, I hope that it does not disappoint me just as much as this particular one. I mean, Yes, it was my choice to read through, however I truly thought you would probably have something helpful to talk about. All I hear is a bunch of whining about something you can fix if you weren’t too busy looking for attention.
Hello, I do believe your site could possibly be having web browser compatibility issues. Whenever I look at your website in Safari, it looks fine but when opening in IE, it’s got some overlapping issues. I just wanted to give you a quick heads up! Apart from that, excellent website.
Hi, I do think this is a great blog. I stumbledupon it 😉 I may return yet again since I bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to guide others.
You made some really good points there. I checked on the internet for more information about the issue and found most individuals will go along with your views on this site.
I really enjoyed this post. It was well-written and informative. v9 bet
After I originally left a comment I appear to have clicked the -Notify me when new comments are added- checkbox and from now on each time a comment is added I receive four emails with the same comment. There has to be a way you are able to remove me from that service? Thanks a lot.
I used to be able to find good advice from your blog posts.
Xổ Số An Giang là một trong những nhà đài được đánh giá cao bởi sự uy tín. Ngày nay, xổ số là món ăn tinh thần không thể thiếu trong cuộc sống. Tuy nhiên, có không ít người vẫn chưa biết cách chơi XSTN. Vậy hãy cùng Dự đoán xổ số An Giang tìm hiểu cách chơi và kinh nghiệm tăng khả năng trúng thưởng nhé https://dudoanxosoangiang.com/
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me. Thank you!
It’s difficult to find well-informed people about this subject, however, you seem like you know what you’re talking about! Thanks
Good article! We are linking to this great article on our website. Keep up the great writing.
Your style is very unique compared to other folks I have read stuff from. Thank you for posting when you’ve got the opportunity, Guess I’ll just bookmark this page.
This web page is really a walk-through for all of the information you wished about this and didn’t know who to ask. Glimpse here, and you’ll definitely discover it.
You need to take part in a contest for one of the finest blogs on the net. I’m going to highly recommend this blog!
Your style is so unique in comparison to other people I’ve read stuff from. Many thanks for posting when you have the opportunity, Guess I will just book mark this page.
Woah… – Gulvafslibning | Kurt Gulvmand I’m genuinely digging your design:style for the blog. It is very simple, though great. A lot of times it’s tough to obtain that balance between usability as well as appearance. I actually should mention that you’ve done a very good site. Also, this weblog starts very quick to me with Opera. Outstanding Site – Gulvafslibning | Kurt Gulvmand Mmm what about Libya awesome news flash! Peace Flash Factory Web Design
No more s***. All posts of this qaulity from now on
I used to be able to find good info from your content.
What refreshing shock your posts are. these posts are aiding me in exploring some needed specifics. You’ve added to my study in your posting.
An interesting discussion is worth comment. I think that you need to write more on this topic, it might not be a taboo subject but generally people do not speak about such topics. To the next! Kind regards.
Aw, this became an exceptionally nice post. In idea I must put in writing in this way additionally – taking time and actual effort to make a very good article… but what can I say… I procrastinate alot and also by no means appear to go done.
Howdy! I simply would like to give you a huge thumbs up for your great information you have right here on this post. I am returning to your web site for more soon.
I would like to thank you for the efforts you have put in writing this website. I am hoping to view the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has inspired me to get my own, personal site now 😉
I am always thought about this, appreciate it for putting up.
Hi, I think your site might be having browser compatibility issues. When I look at your blog site in Chrome, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, superb blog!
Kết quả trúng thưởng Xổ Số An Giang được xác định bằng cách đem so sánh dãy số trong tờ vé số với kết quả mở thưởng của nhà đài. dự đoán đoán xổ số an giang
Personally I’m impressed by the quality of this. Usually when I find stuff like this I stumble it. Although this time I’m not sure if this would be best for the users. I’ll look around and find another article that may work.
the doctor said that we have an allergic baby that is why we choose hypoallergenic baby clothes-
birthday invitations should be given as early as possible to avoid any surprises-
I love it when people come together and share opinions. Great website, keep it up!
i think that gay marriage should be allowed in certain states but not in other states .
Aw, this was a really good post. Taking the time and actual effort to produce a very good article… but what can I say… I procrastinate a whole lot and never manage to get nearly anything done.
Good write-up, I’m regular visitor of one’s site, maintain up the excellent operate, and It’s going to be a regular visitor for a lengthy time.
You can tally me in for a Digg. Thanks for posting this on your site!
An fascinating discussion will probably be worth comment. I do think that you need to write read more about this topic, it might not become a taboo subject but normally consumers are there are not enough to dicuss on such topics. To another. Cheers
I absolutely love your blog and find many of your post’s to be just what I’m looking for. Do you offer guest writers to write content available for you? I wouldn’t mind producing a post or elaborating on a number of the subjects you write in relation to here. Again, awesome site!
You created some decent points there. I looked online for any problem and discovered most individuals go in conjunction with together with your internet site.
There’s certainly a great deal to find out about this subject. I love all of the points you have made.
I blog often and I really thank you for your content. The article has really peaked my interest. I will take a note of your blog and keep checking for new information about once per week. I opted in for your Feed too.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
bathroom towels should be maintained with a good fabric conditioner so that they will last longer.
Very good written article. It will be supportive to anybody who usess it, as well as myself. Keep doing what you are doing – for sure i will check out more posts.
I would like to thnkx stiforp for the efforts you have put in writing this site. I am hoping the same high-grade blog post from you in the future too. Stiforp In fact your creative writing abilities has encouraged me to get my own web site going now. Really blogging is spreading its wings and growing fast. Your Stiforp write up is a great example.
Very good article. I absolutely love this website. Keep writing!
I really love your website.. Pleasant colors & theme. Did you make this amazing site yourself? Please reply back as I’m wanting to create my own personal website and would love to know where you got this from or just what the theme is called. Appreciate it.
Xổ Số An Giang là một trong những nhà đài được đánh giá cao bởi sự uy tín. Ngày nay, xổ số là món ăn tinh thần không thể thiếu trong cuộc sống. Tuy nhiên, có không ít người vẫn chưa biết cách chơi XSTN. Vậy hãy cùng Dự đoán xổ số An Giang tìm hiểu cách chơi và kinh nghiệm tăng khả năng trúng thưởng nhé dự đoán xổ số an giang
As soon as I noticed this web site I went on reddit to share some of the love with them.
depending on fossil fuel is always a bad idea, we should always concentrate on renewable energy;
I conceive other website proprietors should take this internet site as an model, very clean and good user pleasant style .
Oh my goodness! a wonderful post dude. Thanks a lot However My business is experiencing trouble with ur rss . Don’t know why Can not join it. Possibly there is anyone finding identical rss difficulty? Anyone who knows kindly respond. Thnkx
Hello, i think that i noticed you visited my blog so i came to “go back the prefer”.I’m trying to in finding issues to enhance my web site!I assume its good enough to make use of some of your concepts!!
Top post Genachowski’s less than artful weaving of net neutrality and consumer privacy | Law and Politics of Broadband you’ve surely influenced all of us FYI have you read Middle East amazing headlines! Enjoy your day ! Flash Website Design
Youre so cool! I dont suppose Ive read anything this way before. So nice to find somebody with original ideas on this subject. realy thank you for beginning this up. this website is one thing that is needed over the internet, an individual if we do originality. beneficial problem for bringing interesting things on the web!
The next time I just read a blog, I hope which it doesnt disappoint me just as much as brussels. After all, It was my replacement for read, but I actually thought youd have something interesting to talk about. All I hear can be a number of whining about something that you could fix in the event you werent too busy trying to find attention.
Outstanding post, you have pointed out some excellent points , I as well believe this s a very good website.
Aw, this was a really nice post. Spending some time and actual effort to make a great article… but what can I say… I hesitate a whole lot and never manage to get anything done.
An outstanding share! I have just forwarded this onto a coworker who has been conducting a little research on this. And he in fact bought me dinner due to the fact that I stumbled upon it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending some time to discuss this matter here on your website.
After I originally left a comment I appear to have clicked the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I recieve four emails with the same comment. There has to be a way you can remove me from that service? Many thanks.
Aw, that was a really good quality post. In theory I’d like to write like this too – taking time and real effort to make a good article… but what can I say… I procrastinate alot and also never seem to get something done.
Everyone’s skipped this central principle. Your thinking is essential in helping me with my study. Thanks a whole lot.
I’m not sure exactly why but this weblog is loading incredibly slow for me. Is anyone else having this problem or is it a problem on my end? I’ll check back later and see if the problem still exists.
??? ????? ?????? ?? ??? ??? ?? ?????? ??? ???? . ??? ?????? ??????? ????? ???? ????? ?????? ??????? ?????? ??????? ???? ????? ?????? ??????? ??? ?????? ??? ?? ??????? ??? ????? ????????.
I’ve been surfing on-line greater than three hours as of late, but I by no means found any interesting article like yours. It¡¦s pretty worth enough for me. In my opinion, if all website owners and bloggers made good content as you probably did, the internet can be much more useful than ever before.
Hmm. just what you mean. Hello, would you eventually have Feed? I’m attempting to sign up in order to get revisions. Tell me.
Hello there! This blog post could not be written any better! Reading through this article reminds me of my previous roommate! He continually kept talking about this. I most certainly will send this post to him. Fairly certain he’s going to have a good read. I appreciate you for sharing!
you are sooo gifted in writing. God is truly utilizing you in great ways. You are doing a superb job! This was a wonderful blog!
Man! Its like you browse my mind! You seem to grasp so much regarding this, just like you wrote the book in it or one thing. i believe that you can do with some images to drive the content home a little, besides that, this is often informative blog. A outstanding browse. unwell certainly come back again.
Outstanding post, I conceive website owners should acquire a lot from this web site its really user pleasant.
Hello there! This article couldn’t be written much better! Reading through this article reminds me of my previous roommate! He constantly kept preaching about this. I am going to send this post to him. Pretty sure he’ll have a great read. I appreciate you for sharing!
Thanks for the sensible critique. Me & my neighbor were just preparing to do some research on this. We got a grab a book from our local library but I think I learned more from this post. I am very glad to see such wonderful info being shared freely out there.
It’s hard to find experienced people about this subject, but you seem like you know what you’re talking about! Thanks
Can I simply say what a relief to find a person that genuinely knows what they are talking about on the net. You actually understand how to bring a problem to light and make it important. A lot more people have to read this and understand this side of the story. It’s surprising you’re not more popular since you definitely possess the gift.
You have made some really good points there. I checked on the web for more info about the issue and found most people will go along with your views on this web site.
I am very happy to read this. This is the type of manual that needs to be given and not the accidental misinformation that’s at the other blogs. Appreciate your sharing this best doc.
You have some real insight into the things you write about. Do you need many drafts to make a post?
Affordable tours… […]the time to read or visit the content or sites we have linked to below the[…]…
You are so awesome! I do not believe I have read through something like that before. So nice to discover somebody with a few unique thoughts on this subject matter. Really.. many thanks for starting this up. This website is something that is required on the internet, someone with a little originality.
I’m impressed, I must say. Genuinely rarely do you encounter a weblog that’s both educative and entertaining, and let me tell you, you may have hit the nail about the head. Your concept is outstanding; ab muscles something that too few people are speaking intelligently about. I’m delighted i found this in my hunt for something about it.
This will be the right blog for everyone who is would like to discover this topic. You recognize a great deal its virtually tricky to argue along with you (not that I really would want…HaHa). You certainly put a brand new spin using a topic thats been discussed for several years. Wonderful stuff, just wonderful!
there are so many funny videos on the internet to watch, i can laugh all day watching funny videos”
You’re so interesting! I do not think I’ve read something like that before. So wonderful to find another person with unique thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality.
Hello there! This article couldn’t be written any better! Reading through this article reminds me of my previous roommate! He continually kept talking about this. I’ll send this post to him. Fairly certain he will have a good read. Thank you for sharing!
Howdy! This post couldn’t be written any better! Going through this article reminds me of my previous roommate! He continually kept preaching about this. I’ll forward this information to him. Fairly certain he’ll have a very good read. Many thanks for sharing!
Can I just say what a relief to uncover somebody that genuinely understands what they’re talking about on the net. You actually know how to bring a problem to light and make it important. A lot more people must check this out and understand this side of your story. I was surprised you’re not more popular because you definitely possess the gift.
Normally I do not read post on blogs, however I wish to say that this write-up pressured me to check out. Your writing style is amazing. Thanks, very nice article.
This is a good posting, I was wondering if I could use this write-up on my website, I will link it back to your website though. If this is a problem please let me know and I will take it down right away
Everything is very open with a really clear clarification of the challenges. It was really informative. Your website is very helpful. Thanks for sharing.
Can I simply say what a aid to find somebody who actually knows what theyre speaking about on the internet. You positively know how one can deliver a difficulty to gentle and make it important. Extra folks have to read this and understand this side of the story. I cant consider youre not more well-liked since you positively have the gift.
You are my inhalation, I have few blogs and sometimes run out from brand .
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
I would like to thank you for the efforts you’ve put in penning this site. I really hope to check out the same high-grade content from you in the future as well. In fact, your creative writing abilities has encouraged me to get my own website now 😉
Hello there! This post could not be written any better! Going through this post reminds me of my previous roommate! He continually kept preaching about this. I am going to send this post to him. Pretty sure he’ll have a very good read. Many thanks for sharing!
An impressive share, I simply with all this onto a colleague who had previously been performing a small analysis within this. And hubby actually bought me breakfast since I found it for him.. smile. So let me reword that: Thnx for the treat! But yeah Thnkx for spending the time to debate this, I’m strongly about it and adore reading more on this topic. If it is possible, as you become expertise, does one mind updating your blog site with increased details? It is actually highly helpful for me. Huge thumb up because of this short article!
I really like your wordpress design, wherever do you download it from?
I was able to find good advice from your articles.
I needed to thank you for this great read!! I certainly enjoyed every bit of it. I have got you bookmarked to check out new things you post…
Right here is the perfect web site for anybody who would like to understand this topic. You realize a whole lot its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a brand new spin on a topic that’s been discussed for a long time. Excellent stuff, just excellent.
Aw, this was an exceptionally good post. Finding the time and actual effort to create a superb article… but what can I say… I put things off a lot and don’t seem to get nearly anything done.
There is definately a great deal to find out about this issue. I like all the points you have made.
Way cool! Some extremely valid points! I appreciate you writing this article plus the rest of the site is extremely good.
You should be a part of a contest for one of the most useful blogs online. I’m going to highly recommend this site!
This is a great tip especially to those fresh to the blogosphere. Short but very accurate information… Thank you for sharing this one. A must read article.
After I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I get four emails with the same comment. There has to be an easy method you are able to remove me from that service? Cheers.
It’s hard to find well-informed people for this topic, however, you seem like you know what you’re talking about! Thanks
I wanted to thank you for this fantastic read!! I certainly enjoyed every bit of it. I have got you book marked to look at new stuff you post…
Very good info. Lucky me I discovered your website by accident (stumbleupon). I have book marked it for later.
I blog frequently and I genuinely thank you for your content. Your article has truly peaked my interest. I’m going to book mark your blog and keep checking for new information about once a week. I subscribed to your RSS feed too.
This site was… how do you say it? Relevant!! Finally I have found something that helped me. Cheers.
Greetings, I do think your web site could be having browser compatibility problems. When I look at your site in Safari, it looks fine however when opening in Internet Explorer, it has some overlapping issues. I just wanted to give you a quick heads up! Aside from that, excellent blog.
Way cool! Some extremely valid points! I appreciate you writing this post plus the rest of the website is extremely good.
Everyone loves it when folks come together and share ideas. Great website, stick with it!
I used to be able to find good info from your blog posts.
Hi there! I could have sworn I’ve visited your blog before but after browsing through many of the articles I realized it’s new to me. Nonetheless, I’m certainly delighted I found it and I’ll be bookmarking it and checking back often.
After I initially left a comment I appear to have clicked the -Notify me when new comments are added- checkbox and now whenever a comment is added I receive 4 emails with the exact same comment. Is there an easy method you can remove me from that service? Thanks a lot.
I’d like to thank you for the efforts you’ve put in penning this website. I’m hoping to see the same high-grade content from you in the future as well. In fact, your creative writing abilities has inspired me to get my own website now 😉
Very good post. I certainly love this website. Continue the good work!
Oh my goodness! Incredible article dude! Thanks, However I am experiencing troubles with your RSS. I don’t know why I am unable to join it. Is there anybody else having identical RSS issues? Anyone who knows the solution can you kindly respond? Thanx.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
I like looking through a post that can make people think. Also, many thanks for allowing me to comment.
Can I just say what a relief to find an individual who really knows what they are discussing on the net. You actually know how to bring an issue to light and make it important. A lot more people have to look at this and understand this side of your story. I was surprised that you are not more popular because you certainly have the gift.
I blog often and I truly thank you for your information. Your article has truly peaked my interest. I will book mark your website and keep checking for new information about once a week. I subscribed to your RSS feed as well.
Good post. I learn something new and challenging on sites I stumbleupon everyday. It’s always interesting to read articles from other authors and use a little something from other websites.
It’s hard to come by educated people in this particular subject, however, you seem like you know what you’re talking about! Thanks
Good web site you’ve got here.. It’s hard to find high-quality writing like yours nowadays. I really appreciate people like you! Take care!!
Oh my goodness! Incredible article dude! Thanks, However I am having issues with your RSS. I don’t understand the reason why I cannot subscribe to it. Is there anybody else getting similar RSS issues? Anybody who knows the solution will you kindly respond? Thanx!
I would like to thank you for the efforts you have put in penning this website. I really hope to check out the same high-grade content from you in the future as well. In truth, your creative writing abilities has encouraged me to get my own, personal website now 😉
Watch our exclusive Neerfit sexy bf video on neerfit.co.in.
Excellent post! We will be linking to this great article on our website. Keep up the great writing.
I really like it when folks come together and share ideas. Great site, continue the good work.
You are so interesting! I do not think I’ve read something like that before. So good to find someone with some unique thoughts on this topic. Seriously.. thanks for starting this up. This website is something that is required on the web, someone with a bit of originality.
bookmarked!!, I love your website.
I was able to find good info from your blog posts.
Very good post. I am facing some of these issues as well..
This is a topic that is near to my heart… Thank you! Exactly where can I find the contact details for questions?
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Oh my goodness! Incredible article dude! Thank you, However I am going through problems with your RSS. I don’t know why I am unable to join it. Is there anyone else having similar RSS issues? Anyone who knows the answer will you kindly respond? Thanx.
11bet đỉnh cao cá cược, nơi hội tụ đam mê 11bet
Cùng 11BET, bạn sẽ chinh phục những đỉnh cao mới trong thế giới cá cược. Đa dạng game, tỷ lệ thắng cao, chương trình khuyến mãi siêu hấp dẫn tại https://11betn.com/
A fascinating discussion is worth comment. There’s no doubt that that you need to write more about this subject, it may not be a taboo matter but usually people do not discuss such topics. To the next! Kind regards.
Can I simply say what a comfort to discover an individual who really knows what they are talking about over the internet. You actually know how to bring an issue to light and make it important. More people have to check this out and understand this side of your story. I was surprised that you’re not more popular since you most certainly possess the gift.
Hello there! I could have sworn I’ve visited this blog before but after going through some of the posts I realized it’s new to me. Regardless, I’m certainly pleased I stumbled upon it and I’ll be bookmarking it and checking back frequently!
Đây là một trải nghiệm chơi game tuyệt vời tại X8
That is a good tip particularly to those fresh to the blogosphere. Short but very precise information… Appreciate your sharing this one. A must read article.
May I simply say what a comfort to uncover someone that really understands what they are discussing over the internet. You definitely know how to bring a problem to light and make it important. A lot more people ought to read this and understand this side of your story. I was surprised that you’re not more popular since you surely possess the gift.
I agree together with your conclusions and will eagerly glimpse ahead to your future updates.
블랙툰 makes it so easy to find great webtoons.
I always check for 꽁머니 offers when trying out new betting sites.
Greetings! Very useful advice within this post! It is the little changes that make the largest changes. Thanks a lot for sharing!
Everything is very open with a very clear clarification of the challenges. It was really informative. Your website is very helpful. Thanks for sharing!
This is a topic that’s near to my heart… Thank you! Where can I find the contact details for questions?
툰코 makes it so easy to discover new webtoons.
Jeju Island’s 제주유흥 scene is a must for anyone in need of tranquility.
The workshops listed on 달리머넷 have been so helpful in my wellness journey.
This 링크모음 makes it so much easier to find what I need.
So many great e-commerce sites listed on 여기여.
Xổ Số đồng tháp là một trong những nhà đài được đánh giá cao bởi sự uy tín. Có không ít người vẫn chưa biết cách chơi xsdt. Vậy hãy cùng Dự đoán xổ số đồng tháp tìm hiểu cách chơi và kinh nghiệm tăng khả năng trúng thưởng nhé dự đoán xổ số đồng tháp
I was very pleased to find this site. I need to to thank you for ones time just for this fantastic read!! I definitely appreciated every part of it and i also have you bookmarked to see new stuff in your blog.
This excellent website definitely has all of the information and facts I needed concerning this subject and didn’t know who to ask.
Good web site you have got here.. It’s difficult to find high quality writing like yours these days. I really appreciate individuals like you! Take care!!
Good post. I will be going through some of these issues as well..
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Hi there! This blog post could not be written much better! Looking at this article reminds me of my previous roommate! He always kept preaching about this. I will send this post to him. Fairly certain he’s going to have a very good read. Many thanks for sharing!
Good web site you have here.. It’s hard to find high-quality writing like yours these days. I really appreciate people like you! Take care!!
I’m impressed, I have to admit. Seldom do I encounter a blog that’s both equally educative and interesting, and let me tell you, you’ve hit the nail on the head. The problem is something too few folks are speaking intelligently about. I am very happy I found this in my search for something regarding this.
I couldn’t refrain from commenting. Well written!
An outstanding share! I have just forwarded this onto a coworker who was doing a little homework on this. And he in fact ordered me breakfast because I found it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending time to discuss this subject here on your site.
This is a good tip especially to those new to the blogosphere. Short but very precise information… Thanks for sharing this one. A must read post!
Good post. I learn something totally new and challenging on blogs I stumbleupon every day. It’s always helpful to read articles from other writers and practice a little something from other sites.
Good info. Lucky me I discovered your website by accident (stumbleupon). I have bookmarked it for later.
After looking at a number of the blog articles on your web page, I honestly like your way of blogging. I book-marked it to my bookmark site list and will be checking back in the near future. Please visit my website too and tell me your opinion.
You’re so awesome! I do not believe I’ve truly read anything like this before. So great to discover somebody with some genuine thoughts on this topic. Seriously.. thanks for starting this up. This web site is something that’s needed on the internet, someone with a bit of originality.
Hi there! I could have sworn I’ve been to this website before but after browsing through a few of the posts I realized it’s new to me. Regardless, I’m definitely happy I discovered it and I’ll be book-marking it and checking back regularly!
Very good post! We are linking to this great content on our website. Keep up the great writing.
Advantageously, the post is really the sweetest on this notable topic. I concur with your conclusions and definitely will thirstily look forward to your upcoming updates. Saying thanks definitely will not simply just be sufficient, for the fantasti c clarity in your writing. I definitely will at once grab your rss feed to stay abreast of any updates. Genuine work and also much success in your business dealings!
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me. Cheers!
Good article. I’m experiencing many of these issues as well..
An interesting discussion is definitely worth comment. I think that you ought to write more about this topic, it might not be a taboo subject but generally people do not discuss these subjects. To the next! Many thanks.
Can I just now say that of a relief to find somebody that truly knows what theyre discussing on the internet. You certainly discover how to bring a challenge to light and produce it crucial. More and more people should check this out and fully grasp this side of the story. I cant think youre no more popular simply because you undoubtedly have the gift.
in business, proper financial planning is very essential and it can make or break a business”
I must thank you for the efforts you have put in penning this blog. I’m hoping to check out the same high-grade blog posts by you in the future as well. In truth, your creative writing abilities has motivated me to get my very own site now 😉
I wanted to thank you for this great read!! I certainly loved every little bit of it. I’ve got you book marked to look at new things you post…
I do trust all of the ideas you have offered on your post. They are really convincing and can definitely work. Still, the posts are too brief for beginners. May you please extend them a bit from subsequent time? Thank you for the post.
You can definitely see your enthusiasm within the paintings you write. The world hopes for more passionate writers like you who are not afraid to say how they believe. All the time go after your heart.
You should be a part of a contest for one of the greatest sites on the internet. I will recommend this web site!
Xổ Số cà mau là một trong những nhà đài được đánh giá cao bởi sự uy tín. Có không ít người vẫn chưa biết cách chơi xscm. Vậy hãy cùng Dự đoán xổ số cà mau tìm hiểu cách chơi và kinh nghiệm tăng khả năng trúng thưởng nhé dự đoán xổ số cà mau
Hi, I do think this is a great website. I stumbledupon it 😉 I will revisit once again since i have book marked it. Money and freedom is the best way to change, may you be rich and continue to help others.
This site is really a walk-through it really is the details you wanted concerning this and didn’t know who to inquire about. Glimpse here, and you’ll absolutely discover it.
Wow that was unusual. I just wrote an really long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Anyways, just wanted to say superb blog!
The very next time I read a blog, I hope that it won’t disappoint me as much as this one. After all, I know it was my choice to read, nonetheless I truly thought you would have something helpful to talk about. All I hear is a bunch of whining about something that you could possibly fix if you weren’t too busy searching for attention.
Spot on with this write-up, I actually believe that this web site needs far more attention. I’ll probably be back again to read more, thanks for the info!
I want to to thank you for this good read!! I absolutely enjoyed every little bit of it. I have got you book-marked to look at new stuff you post…
Usually I don’t read article on blogs, however I wish to say that this write-up very pressured me to try and do it! Your writing taste has been amazed me. Thanks, very nice article.
I never would have thought this stuff was out there. Thanks! I look foward to checking out your articles in the future.
Xổ Số Vũng Tàu là một trong những nhà đài được đánh giá cao bởi sự uy tín. Có không ít người vẫn chưa biết cách chơi XSVT. Vậy hãy cùng Dự đoán xổ số vũng tàu tìm hiểu cách chơi và kinh nghiệm tăng khả năng trúng thưởng nhé dự đoán xổ số vũng tàu
오피가이드 makes finding a massage shop near me incredibly simple and quick.
What’s Taking place i’m new to this kind of, I stumbled onto this I’ve thought it was absolutely useful and it has helped me away lots. I am hoping to be able to add & assist some other customers such as its assisted me. Excellent career.
I needed to thank you for this good read!! I definitely loved every bit of it. I have got you bookmarked to look at new stuff you post…
This is a topic that is near to my heart… Best wishes! Exactly where can I find the contact details for questions?
Oh my goodness! Awesome article dude! Thank you so much, However I am experiencing problems with your RSS. I don’t understand the reason why I am unable to subscribe to it. Is there anyone else having the same RSS issues? Anyone who knows the answer will you kindly respond? Thanks!!
I was able to find good information from your blog posts.
Oh my goodness! Incredible article dude! Thanks, However I am having issues with your RSS. I don’t know the reason why I cannot join it. Is there anybody having the same RSS problems? Anybody who knows the answer will you kindly respond? Thanks!
I like looking through a post that will make men and women think. Also, many thanks for permitting me to comment.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Excellent post. I’m going through a few of these issues as well..
This site was… how do you say it? Relevant!! Finally I’ve found something which helped me. Thank you.
I could not resist commenting. Well written!
Xổ số Đồng Nai – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Đồng Nai khám phá ngay những bí quyết thú vị! xổ số Đồng Nai
The next time I read a blog, Hopefully it doesn’t fail me just as much as this particular one. I mean, Yes, it was my choice to read through, nonetheless I genuinely thought you would have something interesting to talk about. All I hear is a bunch of moaning about something that you could fix if you weren’t too busy searching for attention.
Having read this I thought it was extremely informative. I appreciate you spending some time and energy to put this content together. I once again find myself personally spending a lot of time both reading and posting comments. But so what, it was still worth it!
Xổ số Cần Thơ – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Cần Thơ khám phá ngay những bí quyết thú vị! xổ số Cần Thơ
I needed to thank you for this wonderful read!! I absolutely loved every bit of it. I’ve got you book-marked to check out new things you post…
Aw, this was an exceptionally nice post. Taking the time and actual effort to make a superb article… but what can I say… I put things off a lot and never seem to get anything done.
Howdy! I just would like to offer you a huge thumbs up for your excellent info you have got right here on this post. I am coming back to your web site for more soon.
I wanted to thank you for this good read!! I absolutely loved every bit of it. I have got you book-marked to check out new stuff you post…
You made some really good points there. I checked on the web for more information about the issue and found most people will go along with your views on this site.
I love it when folks come together and share thoughts. Great website, continue the good work.
This is a topic which is near to my heart… Take care! Exactly where can I find the contact details for questions?
I really like reading an article that can make people think. Also, thanks for allowing me to comment.
This is a great tip especially to those new to the blogosphere. Short but very precise information… Thank you for sharing this one. A must read post.
Hey, I loved your post! Check out my site: ANCHOR.
Xổ số Tây Ninh – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Tây Ninh khám phá ngay những bí quyết thú vị! xổ số Tây Ninh
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
This website truly has all the information and facts I needed concerning this subject and didn’t know who to ask.
Hi, I do think this is an excellent web site. I stumbledupon it 😉 I am going to revisit yet again since i have book-marked it. Money and freedom is the greatest way to change, may you be rich and continue to help other people.
Pretty! This has been a really wonderful article. Thank you for supplying this info.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Hi there! I could have sworn I’ve been to this website before but after going through a few of the posts I realized it’s new to me. Anyhow, I’m certainly happy I came across it and I’ll be book-marking it and checking back regularly.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
I could not resist commenting. Perfectly written.
Xổ Số Vĩnh Long là một trong những nhà đài được đánh giá cao bởi sự uy tín. Có không ít người vẫn chưa biết cách chơi XSVL. Vậy hãy cùng Dự đoán xổ số vĩnh long tìm hiểu cách chơi và kinh nghiệm tăng khả năng trúng thưởng nhé dự đoán xổ số vĩnh long
Cùng nhà cái 11bet trải nghiệm theo thú vị
Đây là một trải nghiệm chơi game tuyệt vời tại 11bet
Đây là một trải nghiệm chơi game tuyệt vời tại 11bet
Đây là một trải nghiệm chơi game tuyệt vời tại 11bet
Oh my goodness! Incredible article dude! Many thanks, However I am going through difficulties with your RSS. I don’t know why I cannot subscribe to it. Is there anybody else getting similar RSS issues? Anybody who knows the solution will you kindly respond? Thanx.
I need to to thank you for this good read!! I absolutely enjoyed every little bit of it. I have got you book marked to look at new things you post…
Đây là một trải nghiệm chơi game tuyệt vời tại 11bet
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Điểm Đến Cá Cược Trực Tuyến Uy Tín Hàng Đầu tại da88
This website certainly has all the information I needed about this subject and didn’t know who to ask.
Xổ số Long An – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Long An khám phá ngay những bí quyết thú vị! xổ số Long An
I used to be able to find good info from your blog posts.
Your photography and visuals are always so stunning They really add to the overall quality of the content
Greetings! Very helpful advice in this particular article! It’s the little changes that produce the most significant changes. Thanks a lot for sharing!
I used to be able to find good information from your blog articles.
I would like to thank you for the efforts you have put in penning this website. I really hope to check out the same high-grade blog posts from you later on as well. In truth, your creative writing abilities has inspired me to get my own, personal site now 😉
This blog is a great resource for anyone looking to live a more mindful and intentional life Thank you for providing valuable advice and tips
Good post. I learn something new and challenging on websites I stumbleupon every day. It’s always exciting to read articles from other authors and practice something from their websites.
Good post. I absolutely appreciate this site. Continue the good work!
I like it whenever people come together and share views. Great blog, continue the good work!
An intriguing discussion is worth comment. There’s no doubt that that you need to write more about this subject, it may not be a taboo matter but generally folks don’t speak about such topics. To the next! Best wishes!
Hãy trải nghiệm game các cược thú vị tại da 88
Hãy trải nghiệm game các cược thú vị tại da 88
Hãy trải nghiệm game các cược thú vị tại https://da88.blue/
I want to to thank you for this great read!! I definitely enjoyed every little bit of it. I have got you book-marked to look at new things you post…
I have to thank you for the efforts you’ve put in writing this blog. I’m hoping to check out the same high-grade blog posts from you later on as well. In fact, your creative writing abilities has encouraged me to get my own, personal blog now 😉
Their posts always leave us feeling informed and entertained. We’re big fans of their style and creativity.
I was very happy to uncover this great site. I want to to thank you for your time for this particularly fantastic read!! I definitely really liked every part of it and I have you book-marked to check out new things in your web site.
I want to express my appreciation for the writer of this blog post. It’s clear they put a lot of effort and thought into their work, and it shows. From the informative content to the engaging writing style, I thoroughly enjoyed reading it.
Pretty! This has been an incredibly wonderful article. Many thanks for providing this information.
I have been struggling with this issue for a while and your post has provided me with much-needed guidance and clarity Thank you so much
An impressive share! I have just forwarded this onto a friend who has been doing a little research on this. And he in fact ordered me lunch because I found it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending some time to discuss this matter here on your blog.
Your style is very unique in comparison to other folks I’ve read stuff from. Many thanks for posting when you have the opportunity, Guess I will just book mark this blog.
Very good blog post. I absolutely appreciate this website. Thanks!
Saved as a favorite, I like your web site!
Hi! I could have sworn I’ve visited this web site before but after looking at many of the articles I realized it’s new to me. Regardless, I’m certainly pleased I found it and I’ll be book-marking it and checking back regularly.
Next time I read a blog, Hopefully it does not disappoint me as much as this particular one. I mean, I know it was my choice to read, nonetheless I truly thought you would probably have something helpful to say. All I hear is a bunch of crying about something that you could possibly fix if you weren’t too busy searching for attention.
The next time I read a blog, Hopefully it won’t fail me just as much as this particular one. After all, I know it was my choice to read, nonetheless I truly believed you’d have something helpful to say. All I hear is a bunch of crying about something you could fix if you were not too busy looking for attention.
If you have specialized skills, 룸알바 roles like tutoring or personal instruction could be perfect.
Pawns are especially harmful in the endgame for the reason that route to promotion is less complicated.
It’s nearly impossible to find well-informed people in this particular subject, but you seem like you know what you’re talking about! Thanks
Once you hit “click” on the principle display screen, you’ll have the choice to filter the shot, delete it, or routinely add it to your public or personal feed.
Howdy! This post couldn’t be written much better! Going through this article reminds me of my previous roommate! He constantly kept talking about this. I’ll forward this article to him. Fairly certain he’s going to have a great read. Thank you for sharing!
If spontaneity is your specialty, Sphero will also interpret and execute movement based on your phone’s motion sensor.
The chance management of pricey exposures is accomplished by the well timed use of monetary instruments.
Today, the remaining ones are in the hands of private collectors and rarely come up for sale.
John was the principle craftsman and did the glazing and main, while David did the design and art work.
Again, this may take numerous practice and repetition to your younger baby or toddler to be taught, however it’s going to happen.
This website was… how do you say it? Relevant!! Finally I’ve found something which helped me. Many thanks!
1998). “Mutations of the flavin-containing monooxygenase gene (FMO3) trigger trimethylaminuria, a defect in detoxication”.
I always leave this blog feeling inspired and motivated to make positive changes in my life Thank you for being a constant source of encouragement
Xổ số Kiên Giang – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Kiên Giang khám phá ngay những bí quyết thú vị! xổ số Kiên Giang
I’m excited to discover this great site. I want to to thank you for ones time just for this wonderful read!! I definitely savored every little bit of it and i also have you book-marked to see new information on your web site.
Your blog post was fantastic, thanks for the great content!
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Your positivity and optimism are contagious It’s impossible to read your blog without feeling uplifted and inspired Keep up the amazing work
Cổng game HUVIP88 nơi mang lại thế giới giải trí đẳng cấp với các trò chơi đổi thưởng hấp dẫn nhất năm 2025. Tại đây, người chơi có thể thử sức với các game bắn cá, đua ngựa, tài xỉu và các game bài nổi tiếng. HUVIP88 luôn cam kết bảo mật tuyệt đối, hỗ trợ người chơi 24/7 cùng với hàng loạt phần thưởng khủng cho cả thành viên mới và cũ, tạo nên một sân chơi uy tín và chuyên nghiệp.Thông tin chi tiết:Website: https://huvip88.net
This is a topic that’s near to my heart… Cheers! Where can I find the contact details for questions?
An impressive share! I’ve just forwarded this onto a colleague who has been doing a little homework on this. And he actually bought me dinner simply because I found it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending the time to talk about this topic here on your internet site.
Can I simply just say what a relief to discover someone that really knows what they are discussing online. You certainly know how to bring an issue to light and make it important. More people should check this out and understand this side of the story. I was surprised you aren’t more popular because you surely possess the gift.
Massachusetts Institute of Technology (MIT).
This post was exactly what I needed to read today Your words have provided me with much-needed clarity and reassurance
In recent times, these versatile, tasty treats have gone from being cheap, easy-to-make confections given away at youngsters’s events to trendy desserts enjoyed all over the world.
I must thank you for the efforts you’ve put in penning this website. I’m hoping to check out the same high-grade content from you in the future as well. In truth, your creative writing abilities has motivated me to get my own, personal website now 😉
Very good information. Lucky me I came across your blog by accident (stumbleupon). I’ve saved as a favorite for later.
Good post. I will be going through a few of these issues as well..
Every time I read a new post, I feel like I’ve learned something valuable or gained a new perspective. Thank you for consistently putting out such great content!
May I simply say what a relief to discover somebody that really knows what they’re talking about on the net. You definitely realize how to bring an issue to light and make it important. More and more people really need to read this and understand this side of your story. I was surprised you’re not more popular given that you surely possess the gift.
The higher Schooling Price Index (HEPI) is a measure of the inflation fee applicable to United States increased training.
It remained so in ’98, as teams were allowed to run ’97-bodied cars for one last season while Ford developed a new racer.
In buying and selling information, find the interval of consolidation that’s forward in huge numbers after which simply commerce the breakout on the again of the quantity.
Do you know that carols could be traced back as early as 1350, but most of today’s Christmas carols have been written through the 18th century?
Paul had beforehand made favorable comments about Barr’s campaign, leaving the candidate to really feel that he alone should have received the endorsement.
American presidents signed land grants till President Andrew Jackson (c.
The lot rent price and mobile residence park expenses could be slightly troublesome to grasp at first.
Listed below are 4 ways to make mealtime fatigue a factor of the previous.
Investors wanted to find safer ways to invest their money due to the 11 percent stock market fall in two weeks.
Flagstaff Dark Skies Coalition Archived January 18, 2011, on the Wayback Machine.
Nature-primarily based interventions have a range of advantages for both physical and psychological well being.
The risk management of pricey exposures is completed by the timely use of financial instruments.
Have any favorite blog posts or writers? Share them with us in the comments!
18.) In a later episode of the Television collection, the very tall bodyguard who retains Ford away from galactic rock star Hotblack Desiato is none apart from Dave Prowse – the physique of Darth Vader in the original Star Wars films.
There is much debate over which is better, the E30 or the E36.
Many insurance coverage plans have excluded excessive-value medication from protection, minimize down on the amount of refills and elevated co-pays.
You’ll discover numerous current Star Wars items on the 4th ground, however just for enjoyable, take a look at your entire retailer for a glimpse at what wealthy Japanese children are into.
Creating the best strategy depends on who you are as an investor.
Doing this lowers the government bond’s yield.
You need to be a part of a contest for one of the most useful blogs online. I am going to highly recommend this blog!
Some very large traders take advantage of disparities and bid/ask prices and scalp enlarging our narrowing spreads.
Corporate occasions venues in White Plains additionally offer meals and drinks inside your estimated budget.
This post was exactly what I needed to read today Your words have provided me with much-needed clarity and reassurance
Hi, I do think this is a great site. I stumbledupon it 😉 I may come back yet again since i have book-marked it. Money and freedom is the best way to change, may you be rich and continue to guide others.
After the loss of life of their mother and father, Henrietta, Maria, and Catherine Chew vacated their house on South Third Street, and moved to a family-owned property on Walnut Avenue.
Xổ số Khánh Hòa – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Khánh Hòa khám phá ngay những bí quyết thú vị! xổ số khánh hòa
If you love massages, 부달 is the place to find the best ones in Busan.
I love how 오피가이드 offers reviews from real people who’ve actually been there.
opga’s filter options allow me to easily find the massage type I want.
오피 is the best platform for discovering trusted massage shops.
Thanks to 밤의민족, I found some amazing hidden bars in Itaewon.
Enjoy singing with friends at 강남셔츠룸 in a shirt-themed environment.
I always look forward to my next session at 강남안마.
I’ve used 오피가이드 for months now, and it’s always spot on!
I’ve used 오피가이드 for months now, and it’s always spot on!
Need a quality massage? 오피가이드 always has great suggestions.
Enjoy a personalized massage experience at 휴게텔.
Looking for expert recommendations on massages? 오피가이드 has you covered.
누누티비’s movie library is impressive with a wide range of genres.
Be it choosing from multiple markets like Forex, stocks and indices, or devising your own trading technique, the contracts exchange grounds allow you to enter trades with a tailor-made approach and work towards the results you want to achieve.
Explore the best massage services near you with 오피가이드.
Search for top-rated massage shops in your area on 오피가이드.
누누티비 makes watching movies so convenient and free!
Greetings! Very useful advice within this post! It’s the little changes that make the most important changes. Many thanks for sharing!
A lady by the identify of Michel told a narrative of her mother’s expertise growing up in Surinam; a story later echoed by an older Surinamese lady we interviewed, who offered a firsthand account of the same experience.
Many music websites and blogs urge folks to use a bit charge of 160 Kbps or greater if they need the MP3 file to have the identical sound quality as a CD.
With open-ended collective investment schemes, investors have either a direct or indirect legal entitlement, at the expense of the collective assets, to redeem their units at the net asset value.
By 2009, Pudsey had been joined by one other bear, a brown female bear named “Blush”.
They specialize in creating unique gothic-inspired male outfits which might be positive to make an announcement.
Your writing is so relatable and down-to-earth It’s like having a conversation with a good friend Thank you for always being real with your readers
Be trustworthy with yourself.
Hi there! I could have sworn I’ve visited this site before but after browsing through many of the posts I realized it’s new to me. Nonetheless, I’m certainly pleased I came across it and I’ll be bookmarking it and checking back often!
60-116). Boston: Pearson Education, Inc.
Hello there! I just would like to give you a big thumbs up for your excellent information you have got here on this post. I am returning to your web site for more soon.
The company additionally has a number of retail locations the place clients can do issues like drop off packages, rent mailboxes make photocopies.
Fashionable development of wind-power expertise and applications was nicely underway by the nineteen thirties, when an estimated 600,000 windmills supplied rural areas with electricity and water-pumping providers.
Everything is very open with a very clear clarification of the challenges. It was truly informative. Your site is very helpful. Many thanks for sharing.
In this text, we’ll use agent and broker interchangeably, and for simplicity’s sake, we’ll call a Realtor® a realtor.
The group was (a/z order), Ryan Barry, David Brown, Harry Cain, Tom Clarke, Marcus Dibble, William Foster, Craig Goulden, Ioannis Stouppis, Joel Swift, Thomas Westall, Callum Williams.
So paper cash comes by means of the washer just advantageous, while cellulose paper comes unglued.
The return on a diversified portfolio can never exceed that of the top-performing investment, and indeed will always be lower than the highest return (unless all returns are identical).
Skilled in law at an early age by Andrew Hamilton, Chew inherited his mentor’s clients, the descendants of William Penn, including Thomas Penn and his brother Richard Penn Sr., and their sons, Governor John Penn, Richard Penn Jr., and John Penn.
The Weekly Liquidity Review is a publication that offers the broadest overview of the supply and demand dynamics of the U.S.
Hi, I do believe this is an excellent blog. I stumbledupon it 😉 I’m going to return once again since i have book marked it. Money and freedom is the best way to change, may you be rich and continue to guide other people.
You’re so awesome! I do not suppose I’ve truly read anything like this before. So nice to find someone with original thoughts on this subject matter. Seriously.. thank you for starting this up. This web site is something that’s needed on the internet, someone with a little originality.
Your writing style is so engaging and easy to read It makes it a pleasure to read your blog and I always look forward to your new posts
Your writing is so eloquent and heartfelt It’s impossible not to be moved by your words Thank you for sharing your gift with the world
When I initially commented I appear to have clicked on the -Notify me when new comments are added- checkbox and now each time a comment is added I receive 4 emails with the same comment. Is there a means you can remove me from that service? Many thanks.
68 game bài have games to suit every player when playing Casino Online. Not only do we have hundreds of Casino games, we also offer many bonuses and promotions to our members. Readmore: 68 game bài
Monetary companies are rated high priority in resolution making.
Ra8 was as a substitute played, allowing Nepomniachtchi to regain the pawn with 39.Nxg5.
Spot on with this write-up, I truly believe this website needs a lot more attention. I’ll probably be back again to read through more, thanks for the advice!
For example, it affords cellular banking services for their members; they’re safe in addition to quick.
Enjoy a tranquil escape at 제주유흥 and leave stress behind.
So glad I found 달리머넷—it’s such a great community.
Say goodbye to endless searching and use a great 링크모음 collection.
Ready to explore new links? Start with 여기여 today!
I found the best online shopping sites thanks to 여기여.
You need to be a part of a contest for one of the finest sites on the net. I am going to recommend this site!
And throughout his profitable career, Nobel contributed to the event of extra powerful and deadly weapons, including rockets, cannons and new forms of gunpowder.
These Italian chocolate eggs contain a small toy in the center, and sometimes an internet code, which children can use after they’ve eaten the egg.
Having read this I believed it was rather enlightening. I appreciate you finding the time and energy to put this information together. I once again find myself spending a significant amount of time both reading and posting comments. But so what, it was still worth it.
Good post! We will be linking to this great post on our website. Keep up the great writing.
Good blog you have here.. It’s difficult to find good quality writing like yours these days. I seriously appreciate people like you! Take care!!
It ran 19 nights, that includes seven haunted homes.
A number of the later CED’s state on the caddy: “This VideoDisc has a matrixed encompass soundtrack,” however in reality, any stereo disc of a movie launched in Dolby should still have the encompass sound information encoded on the stereo channels.
This check determines the quantity of work to be carried out i.e.
June 1993; and sister, Ima Jean Bostic in January 2001.
The European Central Bank’s efforts to provide US dollar liquidity in the foreign exchange swap market, along with similar efforts by the Federal Reserve, had a moderating impact on CIRP deviations between the dollar and the euro.
While the amounts don’t cause for worry or concern.
These helplines offer immediate support and assistance to young people who may be in crisis or in need of someone to talk to.
In keeping with Bloomberg reporter David Lynch, the brand new cash from quantitative easing may very well be used by the banks to spend money on emerging markets, commodity-based mostly economies, commodities themselves, and non-local alternatives fairly than to lend to native businesses which are having issue getting loans.
Greetings! Very useful advice within this post! It is the little changes that make the largest changes. Thanks for sharing!
An outstanding share! I have just forwarded this onto a coworker who had been doing a little homework on this. And he in fact ordered me breakfast because I discovered it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending some time to discuss this issue here on your web site.
Greetings! Very useful advice in this particular post! It is the little changes that make the greatest changes. Thanks a lot for sharing!
I need to to thank you for this very good read!! I absolutely enjoyed every bit of it. I have you bookmarked to check out new things you post…
Can I just say what a relief to discover somebody who truly knows what they are talking about over the internet. You definitely realize how to bring a problem to light and make it important. More and more people have to read this and understand this side of your story. I can’t believe you aren’t more popular since you most certainly possess the gift.
This post hits close to home for me and I am grateful for your insight and understanding on this topic Keep doing what you do
It means the world to us to hear such positive feedback on our blog posts. We strive to create valuable content for our readers and it’s always encouraging to hear that it’s making an impact.
Wow, I had never thought about it in that way before You have really opened my eyes to a new perspective Keep up the great work!
This blog is a great resource for anyone looking to live a more mindful and intentional life Thank you for providing valuable advice and tips
This blog is such a hidden gem I stumbled upon it by chance and now I’m completely hooked!
Keep up the amazing work!
Good post! We will be linking to this great post on our website. Keep up the great writing.
Aw, this was an incredibly nice post. Finding the time and actual effort to generate a superb article… but what can I say… I put things off a whole lot and don’t manage to get anything done.
Having read this I believed it was extremely enlightening. I appreciate you finding the time and effort to put this content together. I once again find myself spending a lot of time both reading and leaving comments. But so what, it was still worth it.
This blog post has left us feeling grateful and inspired
I’ve been following this blog for years and it’s amazing to see how much it has grown and evolved Congratulations on all your success!
After exploring a few of the blog posts on your web site, I truly like your technique of blogging. I added it to my bookmark website list and will be checking back in the near future. Please visit my website as well and tell me how you feel.
Ann Roth, of the American Homeowners Useful resource Center, calls using properties as collateral “debtquity.” Roth is basically warning that the more your property is price, the extra likely your HOA is to place it up as collateral in opposition to one thing the HOA needs.
Hi there, I do think your blog could be having web browser compatibility problems. When I look at your website in Safari, it looks fine however when opening in Internet Explorer, it has some overlapping issues. I just wanted to give you a quick heads up! Other than that, fantastic website.
Kudos to you if you got this one right, since the photograph reveals a wildy overstyled custom model of the Italian mid-engine sports car that was made from 1971-1991.
For more great links related to painting and air quality, click on to the subsequent web page.
The San Judas Disco Ball Beads Rosary offers a basic religious symbol a contemporary twist.
One of many brand’s rarest fashions is the V-16 (aka Cadillac Sixteen), which is one among just some vehicles to be constructed with a V16 engine.
Be sure you get the interviewer’s enterprise card before you depart, as properly because the names and speak to info for another folks you have met.
Walker, Alex (Could 31, 2018).
Very useful content! I found your tips practical and easy to apply. Thanks for sharing such valuable knowledge!
This can help mitigate the impact of fluctuating FD interest rates and provide FD interest exposure to potential higher returns, albeit with increased risk.
The best way lip stain is applied is available in a detailed second.
Learn More on APi Group’s present short interest.
A 1994 innovation for insulated glazing is evacuated glass, which as yet is produced commercially solely in Japan and China.
If one has by no means used such software program for managing the assets, then one can get the idea from the CD’s and the guides that are made out there with the software.
You have to likewise know that the forex trading is being directed by the world biggest banks.
Canine BRUSH- You should utilize nearly any brush on a French bulldog, but the best ones have versatile rubber bristles.
Get misplaced in your tasks while acquiring very important communication abilities that can serve you effectively in your future prospects, whether or not you choose to work for a corporation or go it alone.
The effectiveness of adhesive tape lies in its design as much as within the chemistry of adhesion, enabling removable and flexible makes use of for everyday duties.
Other items to check up on include paying employees legally and carrying workers’ compensation, property damage and liability insurance.
Mr. Travers was commonly often called Martin Travers, but his start name was Howard Martin Otho Travers.
This page was last edited on 15 January 2022, at 00:19 (UTC).
Managers develop expertise that may assist your online business staff to meet at present’s challenges.
A draw claim before then was only permitted if a threefold repetition or stalemate has occurred.
My earnings is increasing on a regular basis and i generate profits every time i choose to utilizing my mobile machine connected to the internet.
Your writing is so eloquent and engaging You have a gift for connecting with your readers and making us feel understood
What type of content would you like to see more of in the future? Let us know in the comments!
Saved as a favorite, I like your website!
This is a great tip particularly to those new to the blogosphere. Brief but very precise information… Appreciate your sharing this one. A must read article!
Indulge in a relaxing massage from a top-rated therapist listed on 오피뷰.
I recommend checking out 블랙툰 if you love webtoons – you won’t regret it!
Want free access to amazing webtoons? 무료웹툰 is the solution!
The diversity of content on 펀초이스 is amazing. Always something new to discover!
The atmosphere at 강남오피 makes it so easy to relax.
Excellent article. I am experiencing a few of these issues as well..
Right here is the perfect web site for everyone who wishes to understand this topic. You realize so much its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a fresh spin on a topic that has been written about for many years. Wonderful stuff, just excellent.
After I originally commented I appear to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I recieve 4 emails with the same comment. Perhaps there is a way you are able to remove me from that service? Thanks.
Your posts always seem to lift my spirits and remind me of all the good in the world Thank you for being a beacon of positivity
Greetings! Very helpful advice in this particular post! It is the little changes that make the most important changes. Thanks a lot for sharing!
This is such an informative and well-written post! I learned a lot from reading it and will definitely be implementing some of these tips in my own life
I must thank you for the efforts you’ve put in writing this site. I am hoping to see the same high-grade blog posts by you later on as well. In fact, your creative writing abilities has motivated me to get my own site now 😉
Your blog is a great source of positivity and inspiration in a world filled with negativity Thank you for making a difference
I found an amazing deep tissue massage thanks to 오피가이드.
You have made some really good points there. I checked on the internet for additional information about the issue and found most people will go along with your views on this website.
Everyone loves it whenever people come together and share thoughts. Great website, continue the good work!
I really enjoyed reading this! Your writing style is engaging, and the content is valuable. Excited to see more from you!
Xổ số Bạc Liêu – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Bạc Liêu khám phá ngay những bí quyết thú vị! dự đoán xổ số Bạc Liêu
Greetings! Very helpful advice in this particular post! It’s the little changes that will make the most significant changes. Thanks for sharing!
Thanks for sharing. Like your post.Name
Excellent blog post. I absolutely love this site. Keep writing!
I’m impressed, I have to admit. Seldom do I encounter a blog that’s equally educative and interesting, and without a doubt, you have hit the nail on the head. The issue is something which too few people are speaking intelligently about. I am very happy I found this during my search for something regarding this.
I just wanted to take a moment to say how much I appreciate your blog posts. They’re always well-written, informative, and keep me coming back for more. Keep up the great work!
Your writing has a way of making me feel like I’m having a conversation with a close friend It’s so genuine and relatable
Xổ số bến tre – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Bến Tre khám phá ngay những bí quyết thú vị! xổ số bến tre
Excellent blog you have got here.. It’s hard to find good quality writing like yours these days. I truly appreciate people like you! Take care!!
This is a very good tip particularly to those fresh to the blogosphere. Brief but very accurate information… Many thanks for sharing this one. A must read post!
From the bottom of my heart, thank you for being a source of positivity and light in this sometimes dark and overwhelming world
It requires that every one 401(okay) deposits be held in custodial accounts in order to keep your money secure in the occasion that something happens to your employer.
The topics covered here are always so interesting and unique Thank you for keeping me informed and entertained!
If we are to define currency exchange rate in one simple line it can be defined as the rate at which currency of a country can be exchanged with the currency of some other country.
Now we have loads of fun with them.
This was a great read! Your insights are truly helpful and make complex topics easy to understand. Looking forward to more!
The initiative Build Security In is a collaborative effort that provides practices, instruments, guidelines, guidelines, ideas, and different resources that software developers, architects, and safety practitioners can use to build safety into software program in every part of its development.
Software engineers, alternatively, are programmers who develop, take a look at and implement system software and person functions.
At the moment, nations and corporations small and huge jockey for place in the suborbital track, and plenty of analysts think that’s a great factor.
Howdy! I just would like to give you a big thumbs up for your great info you have right here on this post. I am returning to your web site for more soon.
It’s clear that you truly care about your readers and want to make a positive impact on their lives Thank you for all that you do
Everything is very open with a clear description of the issues. It was truly informative. Your site is useful. Many thanks for sharing!
Thanks for sharing!
Xổ số Sóc Trăng – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Sóc Trăng khám phá ngay những bí quyết thú vị! dự đoán xổ số Sóc Trăng
I truly love your site.. Excellent colors & theme. Did you build this site yourself? Please reply back as I’m wanting to create my own blog and would like to find out where you got this from or just what the theme is named. Many thanks.
I wanted to thank you for this good read!! I certainly enjoyed every bit of it. I have you saved as a favorite to check out new stuff you post…
I always look forward to reading your posts, they never fail to brighten my day and educate me in some way Thank you!
Right here is the right blog for anyone who really wants to understand this topic. You understand a whole lot its almost hard to argue with you (not that I personally would want to…HaHa). You definitely put a brand new spin on a topic which has been written about for ages. Excellent stuff, just excellent.
Spot on with this write-up, I really believe that this amazing site needs a great deal more attention. I’ll probably be returning to read through more, thanks for the info!
After exploring a handful of the blog articles on your web page, I truly appreciate your way of writing a blog. I added it to my bookmark webpage list and will be checking back soon. Take a look at my web site too and let me know what you think.
This excellent website certainly has all the information I needed concerning this subject and didn’t know who to ask.
You have made some really good points there. I looked on the internet to find out more about the issue and found most individuals will go along with your views on this website.
You need to take part in a contest for one of the most useful sites on the internet. I’m going to recommend this blog!
I couldn’t refrain from commenting. Well written.
48asxn
Westerners were seen as barbarians, their ideas of mercy and surrender symptomatic of a weak and effete society undeserving of respectful treatment.
You might find yourself imprisoned by your individual beliefs and unable to see the possibilities for change.
Do these steakhouses provide vegetarian options?
Margaret Jane Morrison, BEM, Co-Chairman, Girls’s Nationwide Commission.
What issues would we need to deal with?
Mold is a fungus that reproduces by creating small spores that work like seeds.
Whether you rent or purchase, housing prices will eat about 34 percent of your month-to-month price range.
Managers may extra simply be contacted anytime, anyplace.
In return for his or her preliminary investments, shareholders are given dividends, or percentages, of the company’s earnings primarily based on the number of shares the investor holds.
This is the perfect website for anyone who wants to understand this topic. You realize so much its almost tough to argue with you (not that I actually would want to…HaHa). You certainly put a fresh spin on a subject that’s been discussed for many years. Great stuff, just wonderful.
oh well, online promotion also takes a lot of work just like offline promotion of products and services*
J’aime cette prise de vue mais j’en ai deja vu de semblable de meilleures attributs?
If the funnel is visible and much away, strive to determine its velocity and course and whether or not the roads are clear.
Whereas Ikea does construct enormous shops, the corporate tries to do so in a sustainable and environmentally accountable manner.
While that is correct when it supports advertising choices where access to each segments is equivalent, it’s flawed for inventory control decisions.
So before you purchase that next gasoline saving system or additive, try the rest of this article.
However these choices are also extremely necessary to the long term efficiency of your own home, and they can have an effect on resale as much because the curb enchantment or the quality of the master bathroom shower.
There’s the HTC G1, the first smartphone to run on Android in the United States.
With touches of the macabre, the speech rang true, if not for graduates on the cusp of shiny new lives, then definitely for their parents.
Way cool! Some extremely valid points! I appreciate you writing this article and also the rest of the website is extremely good.
The CIA man out to get Frank is an odd character, too.
The very next time I read a blog, Hopefully it won’t disappoint me as much as this one. After all, Yes, it was my choice to read through, but I actually believed you’d have something interesting to say. All I hear is a bunch of crying about something that you could fix if you weren’t too busy looking for attention.
Juno Seaside, French destroyer La Combattante under Commander André Patou shelled the German fortifications of Courseulles-sur-Mer while frigate La Découverte and corvette Commandant-d’Estienne-d’Orves escorted the Canadian infantry landing crafts.
5-digit codes in the game are unusual.
There is no such thing as an infallible system in the stock market, but investing for the long term comes attractive close after all a strong company is bound to rise over time.
Before we dive into finding the lowest brokerage charges, it’s essential to understand what brokerage charges are.
I love how you explained this topic in such a clear and concise way.
Your style is really unique compared to other people I’ve read stuff from. Thanks for posting when you’ve got the opportunity, Guess I will just book mark this blog.
This site was… how do I say it? Relevant!! Finally I’ve found something which helped me. Thanks!
I’m amazed, I must say. Rarely do I encounter a blog that’s both educative and entertaining, and without a doubt, you have hit the nail on the head. The issue is something that not enough people are speaking intelligently about. I’m very happy I stumbled across this in my search for something relating to this.
Tim Bonner, chief govt of the Countryside Alliance, stated: “No Farmers, No Meals is an emotive message and farming has a very highly effective model that is totemic for many individuals.
Tenants for your commercial space also can pay good cash for rent, if in case you have a nicely-maintained landscape.
Greetings! Very useful advice in this particular post! It is the little changes that produce the greatest changes. Many thanks for sharing!
Xổ số Tiền Giang – một trong những nhà đài uy tín nhất hiện nay, đã trở thành món ăn tinh thần không thể thiếu của hàng triệu người. Bạn đã biết cách tham gia và tăng cơ hội trúng thưởng chưa? Cùng Dự đoán Xổ số Tiền Giang khám phá ngay những bí quyết thú vị! Dự đoán Xổ số Tiền Giang
Hello there! This blog post couldn’t be written any better! Reading through this post reminds me of my previous roommate! He constantly kept preaching about this. I will forward this post to him. Pretty sure he’s going to have a very good read. I appreciate you for sharing!
I really love your site.. Excellent colors & theme. Did you build this site yourself? Please reply back as I’m wanting to create my very own website and want to know where you got this from or just what the theme is named. Appreciate it.
An impressive share! I have just forwarded this onto a friend who has been conducting a little homework on this. And he in fact bought me breakfast because I found it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending the time to talk about this topic here on your web page.
This is a good tip especially to those fresh to the blogosphere. Brief but very precise information… Many thanks for sharing this one. A must read article.
Market sentiment calculations for Rule 144A company debt securities.
We certainly not promise or assure that you’re going to get the exact same outcomes as they have, your outcomes could also be increased or decrease but most importantly, you only stand a chance of attaining some degree of success in the event you implement.
An impressive share! I’ve just forwarded this onto a co-worker who was doing a little research on this. And he in fact bought me dinner because I found it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanx for spending some time to discuss this issue here on your web site.
After I originally commented I appear to have clicked on the -Notify me when new comments are added- checkbox and now each time a comment is added I recieve four emails with the exact same comment. Perhaps there is an easy method you are able to remove me from that service? Kudos.
Having read this I believed it was extremely informative. I appreciate you spending some time and energy to put this short article together. I once again find myself personally spending a significant amount of time both reading and posting comments. But so what, it was still worth it.
Đăng nhập 8xbet ngay để trải nghiệm cá cược hay và hấp dẫn tại Đăng nhập 8xbet
Trải nghiệm rút tiền số 1 tại Rút tiền Fabet
I needed to thank you for this excellent read!! I definitely enjoyed every little bit of it. I have got you book marked to check out new stuff you post…
In accordance with a hedge fund survey in 2005, the three key dangers for the fund segment is overcrowding, poor returns and mis-pricing.
Eighty or the share market will well before the budget or one thing like that, and this reason can sometimes sound terribly fantastical to anyone else.
How can research and innovation influence workplace mental health?
Put your risk money into things that have an upside with no cap.
Next time I read a blog, I hope that it doesn’t fail me as much as this particular one. After all, Yes, it was my choice to read through, nonetheless I actually thought you would have something useful to talk about. All I hear is a bunch of crying about something that you could possibly fix if you were not too busy looking for attention.
I absolutely love your website.. Pleasant colors & theme. Did you create this web site yourself? Please reply back as I’m hoping to create my very own website and would love to learn where you got this from or what the theme is called. Cheers!
I need to to thank you for this wonderful read!! I absolutely loved every little bit of it. I’ve got you bookmarked to look at new things you post…
Nice post. I learn something new and challenging on websites I stumbleupon everyday. It will always be exciting to read through content from other authors and use something from their sites.
Great info. Lucky me I came across your website by accident (stumbleupon). I have saved it for later!
I’m impressed, I must say. Rarely do I come across a blog that’s both educative and amusing, and without a doubt, you’ve hit the nail on the head. The issue is something not enough folks are speaking intelligently about. I’m very happy I stumbled across this in my search for something regarding this.
Born to the royal family of the planet Serenno, Dooku was rejected by his household as an infant upon the discovery of his connection to the Pressure, which his father specifically feared and, as such, abandoned him after contacting the Jedi Order to return and take him to Coruscant.
The worth of the reward shouldn’t observe some components in regards to the event.
It’s difficult to find well-informed people on this topic, but you sound like you know what you’re talking about! Thanks
Arie, Roni (November 18, 2008).
I’m impressed, I have to admit. Seldom do I encounter a blog that’s both educative and interesting, and without a doubt, you’ve hit the nail on the head. The problem is an issue that too few people are speaking intelligently about. I’m very happy that I came across this during my hunt for something regarding this.
You’re so cool! I do not believe I’ve truly read a single thing like this before. So nice to find someone with genuine thoughts on this topic. Seriously.. thank you for starting this up. This website is something that’s needed on the web, someone with some originality.
Pretty! This has been an extremely wonderful article. Many thanks for supplying this info.
This is very interesting, You are a very skilled blogger. I’ve joined your rss feed and look forward to seeking more of your great post. Also, I’ve shared your web site in my social networks!
An intriguing discussion is definitely worth comment. I do think that you should publish more on this issue, it may not be a taboo matter but generally folks don’t talk about such topics. To the next! Best wishes.
Thanks for your entire efforts on this site. My mum loves engaging in investigation and it’s really simple to grasp why. Many of us learn all regarding the compelling method you make helpful tips and tricks by means of your blog and therefore improve contribution from others on the subject matter then my daughter is without a doubt becoming educated a whole lot. Have fun with the remaining portion of the new year. You are performing a splendid job.
The precise quantity has to be adjusted for every individual.
That is a great tip especially to those new to the blogosphere. Brief but very accurate information… Appreciate your sharing this one. A must read post.
Right here is the perfect blog for anyone who really wants to understand this topic. You realize a whole lot its almost tough to argue with you (not that I really would want to…HaHa). You certainly put a brand new spin on a subject that’s been discussed for decades. Excellent stuff, just wonderful.
Greetings! Very useful advice within this article! It is the little changes that produce the most significant changes. Thanks for sharing!
It’s hard to find knowledgeable people on this topic, however, you seem like you know what you’re talking about! Thanks
Pretty! This was an incredibly wonderful post. Many thanks for providing this info.
Aw, this was a very nice post. Taking a few minutes and actual effort to make a very good article… but what can I say… I put things off a lot and never seem to get nearly anything done.
fantastic points altogether, you just gained emblem reader. What would you suggest in regards to your post that you made a few days ago? Any certain?
A well written article, I just passed this onto a workfellow who was doing somewhat analysis on this. And he indeed purchased me dinner because I discovered it for him…. .. therefore let me reword that: Thnkx for the treat however yeah Thnkx for spending the time to talk about this, I feel strongly concerning it and love reading more on this topic. If doable, as you gain expertise, would you mind updating your blog with more details? it is extraordinarily useful on behalf of me. massive thumb up for this blog
79king link chính thức không bị chặn tại 79king.com
Hãy trải nghiệm game các cược thú vị tại 11bet
Can I simply just say what a relief to uncover an individual who genuinely knows what they’re discussing on the internet. You definitely understand how to bring a problem to light and make it important. More people have to read this and understand this side of your story. I can’t believe you’re not more popular since you most certainly have the gift.
Hello there! This blog post could not be written much better! Looking through this post reminds me of my previous roommate! He continually kept preaching about this. I am going to send this post to him. Fairly certain he’s going to have a very good read. I appreciate you for sharing!
I think this is one of the most vital information for me.
And i am glad reading your article. But should remark on few general things, The website style is wonderful, the articles is
really nice : D. Good job, cheers
The sculpture of Sagarakanyaka – Mermaid by Kanayi Kunhiraman is an added attraction.
Websites worth visiting… […]here are some links to sites that we link to because we think they are worth visiting[…]……
Good article , I am going to spend more time researching this topic
A lot like the ’57, Ford Ranchero was decked out with fins and chrome, the Sweptside was given a very ’50s treatment as nicely.
A cruise provides you the true alternative to take pleasure in your holidays to fullest with amazing show of nature along with ship journey.
So as to keep costs low, manufacturers really have the selection of using decrease quality materials, or opting to use much less expert workers.
Hello! I could have sworn I’ve been to this website before but after going through a few of the articles I realized it’s new to me. Nonetheless, I’m definitely happy I stumbled upon it and I’ll be bookmarking it and checking back regularly.
Greetings, There’s no doubt that your web site could possibly be having browser compatibility problems. Whenever I take a look at your blog in Safari, it looks fine however when opening in I.E., it has some overlapping issues. I merely wanted to provide you with a quick heads up! Other than that, great blog.
That’s a very good feedback. I’m curious to think what type of impact this would have globally? There are times when things like this begin to have global expansion and frustration. I’ll check back to see what you have to say.
I simply wanted to appreciate you again. I’m not certain the things that I might have sorted out without these tips revealed by you relating to such subject. It absolutely was a distressing situation in my circumstances, however , coming across the well-written tactic you handled that took me to leap for fulfillment. Now i’m thankful for your information as well as trust you recognize what a great job you are undertaking instructing the mediocre ones via your websites. More than likely you haven’t encountered any of us.
Hi, I do believe this is an excellent site. I stumbledupon it 😉 I’m going to revisit yet again since i have book-marked it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
Youre so cool! I dont suppose Ive read anything similar to this before. So nice to discover somebody with original ideas on this subject. realy thanks for starting this up. this web site is a thing that is required on the net, somebody if we do originality. beneficial job for bringing something new to the internet!
Or you could go away a mid-ranked piece nonetheless among a group of bombs — should you by no means move it, your opponent would possibly assume it is a bomb or your flag, and be surprised when it captures their attacking piece.
I like it when individuals get together and share opinions. Great blog, stick with it!
I HOPE YOU GUYS ACTUALLY PING YOUR LINKS OTHERWISE YOUR SCRAPEBOX IS USELESS
How to do Search engine Adsense Us dollars in Writingup. com
Everyone loves it when folks come together and share thoughts. Great site, keep it up!
Very good article. I’m facing a few of these issues as well..
Howdy! Would you mind if I share your blog with my facebook group?
There’s a lot of people that I think would really appreciate your content.
Please let me know. Many thanks
Sometimes, blogging is a bit tiresome specially if you need to update more topics.,~;~~
At times it’s easier to simply take a step again and also understand that not everybody shares your own values
It was the primary version of Space Mountain to open concurrently with the park.
No-rinse wipes can enable you wash off the day and head to bed with clear skin.
Academy of American Franciscan Historical past, 1959, vol.
Everything is very open with a precise clarification of the challenges. It was really informative. Your site is very helpful. Many thanks for sharing.
Dead pent subject matter, thanks for entropy.
Do you have a spam issue on this website; I also am a blogger, and I was curious about your situation; we have developed some nice methods and we are looking to swap methods with other folks, please shoot me an email if interested.
Right here is the perfect site for anyone who hopes to understand this topic. You realize a whole lot its almost hard to argue with you (not that I actually would want to…HaHa). You definitely put a brand new spin on a topic that has been written about for ages. Wonderful stuff, just excellent.
You have a very nice layout for your blog. i want it to use on my site too ,
Greetings! Very helpful advice within this post! It is the little changes which will make the greatest changes. Thanks for sharing!
Audio began playing as soon as I opened this site, so frustrating!
Well, this Thursday I read through a couple of your posts. I must say this is one of your better ones. Yessir!
Useful info. Lucky me I found your web site by chance, and I am stunned why this accident didn’t took place in advance! I bookmarked it.
However do you really have to install all these updates?
These sobering potential effects of time travel have caused some scientists to surprise whether a precept exists in nature that would actually prevent unrestricted time travel, corresponding to Stephen Hawking’s “chronology safety speculation.” This type of “principle of every part” might provide a scientific rationalization as to why we might by no means unhinge the universe as we realize it by making unrestricted time travel a reality.
The foundation can also be investing vital sources in advancing equity in education and building an inclusive economy to make sure that Winston-Salem can develop into a spot the place race no longer predicts life outcomes.
Psychological Health Apps and Applied sciences Cellular functions and technological instruments designed to help with managing psychological health, providing options equivalent to mood tracking, meditation exercises, and entry to psychological health professionals.
In a digital age, we have the power of every business element at the convenience of our fingertips.
Eva Fleming, Sister-in-Charge, Geriatric Ward, Hackney Hospital, London.
Youre so cool! I dont suppose Ive read anything like this just before. So nice to seek out somebody with many original thoughts on this subject. realy appreciation for starting this up. this excellent website are some things that is needed online, an individual after a little originality. useful task for bringing a new challenge for the internet!
You made some decent points there. I looked on the web with the problem and discovered most people will go in addition to with all your site.
I really like it when folks get together and share thoughts. Great site, keep it up!
An act of kindness from an unknown individual additional fuels his willpower, ending the episode with a light-hearted try at sit-ups, which humorously contrasts the intense confrontations earlier.
Individuals who should travel always for business have a tough life.
Sure, the central financial institution within the European Financial Union is making the onerous choice.
Your style is so unique in comparison to other folks I’ve read stuff from. Many thanks for posting when you’ve got the opportunity, Guess I’ll just book mark this blog.
Merely wanna remark on few general things, The website pattern is perfect, the subject matter is really excellent : D.
I’m curious to find out what blog system you have been utilizing? I’m experiencing some small security issues with my latest blog and I’d like to find something more safe. Do you have any solutions?
For anyone who is interested in the environmental hardships, it could gift all of them are aware that to bring about merely one field hard more than a little flowing shoots reasoning better liters pertaining to oil and gas to bring about. dc free mommy blog giveaways family trip home gardening house power wash baby laundry detergent
Resources like the one you mentioned here will be very useful to me! I will post a link to this page on my blog. I am sure my visitors will find that very useful.
magnificent issues altogether, you simply won emblem reader. What might you suggest about your submit that you just made a few days ago? Any positive?
This website really has all of the info I wanted about this subject and didn’t know who to ask.
I blog quite often and I truly appreciate your content. Your article has truly peaked my interest. I am going to bookmark your site and keep checking for new information about once a week. I opted in for your Feed as well.
Aw, this was a very nice post. Finding the time and actual effort to generate a top notch article… but what can I say… I hesitate a whole lot and never manage to get nearly anything done.
This website was… how do I say it? Relevant!! Finally I’ve found something which helped me. Kudos.
I precisely needed to appreciate you once more. I am not sure the things that I might have used without the type of concepts revealed by you regarding this subject matter. It truly was a hard case in my circumstances, however , finding out the expert strategy you handled that took me to jump over joy. I’m just happy for this assistance and then hope that you really know what an amazing job you are carrying out educating the rest with the aid of your webpage. I am sure you have never come across any of us.
Jen connelly is the actress that i have a huge crush. here eyes are really very pretty..
Good day, I merely hopped over on your own website through StumbleUpon. Not something I’d usually read, however I appreciated how you feel none the less. Thanks for making something price reading.
Hey there, or perhaps might be away from issue rather regardless, i surfing surrounding your internet-site also seems essentially truly professional. I’m also creating a new-found blogging site because trying to cope to create it bode well, each i’ve addition few things since i mess it up. In which way painful was first the site to develop your site? May perhaps one as i am without the suffer from do it right, to fit cherished ones modify documents without having to wrecking the application training?
I together with my buddies were found to be analyzing the great key points from your website while suddenly got a horrible suspicion I had not thanked the blog owner for those secrets. These boys were definitely consequently happy to read through all of them and have in effect extremely been using these things. Appreciate your really being well accommodating and then for obtaining such terrific useful guides most people are really wanting to learn about. Our own sincere regret for not saying thanks to you sooner.
Hello i would really love to subscribe and read your blog posts .!
It’s really a nice and useful piece of info. I am happy that you shared this useful information with us. Please keep us up to date like this. Thank you for sharing.
Greetings! I’ve been reading your website for a long time now and finally got the bravery to go ahead and give you a shout out from Dallas Tx! Just wanted to say keep up the good job!
Easily, the post is really the greatest on this laudable topic. I concur with your conclusions and will thirstily watch forward to your future updates. Saying cheers will not just be sufficient, for the great c lucidity in your writing. I will instantly grab your rss feed to stay privy of any updates. Solid work and much success in your business enterprise!
Excellent web site you have got here.. It’s difficult to find quality writing like yours nowadays. I honestly appreciate people like you! Take care!!
Spot on with this write-up, I actually feel this site needs a great deal more attention. I’ll probably be back again to read through more, thanks for the information.
Your style is so unique in comparison to other folks I’ve read stuff from. I appreciate you for posting when you have the opportunity, Guess I’ll just book mark this blog.
Hi there I am so excited I found your blog, I really found you by mistake, while I was researching on Google for something else, Anyways I am here now and would just like to say kudos for a fantastic post and a all round interesting blog (I also love the theme/design), I don’t have time to read through it all at the minute but I have bookmarked it and also added in your RSS feeds, so when I have time I will be back to read much more, Please do keep up the great work.
Good day I am so excited I found your webpage, I really found you by mistake, while I was looking on Google for something else, Regardless I am here now and would just like to say many thanks for a fantastic post and a all round enjoyable blog (I also love the theme/design), I don’t have time to look over it all at the moment but I have bookmarked it and also added in your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the great job.
Excellent read. I just passed this onto a friend who was doing a little research on that. He just bought me lunch as I found it for him! So let me rephrase: Thanx for lunch!
This is the right blog for everyone who really wants to understand this topic. You understand so much its almost hard to argue with you (not that I actually will need to…HaHa). You certainly put a fresh spin on a subject that has been written about for many years. Wonderful stuff, just great.
Currently it seems like BlogEngine is the best blogging platform out there right now. (from what I’ve read) Is that what you’re using on your blog?
Glad to be one of the visitants on this awe inspiring website : D.
I want to to thank you for this excellent read!! I certainly enjoyed every bit of it. I have got you bookmarked to look at new things you post…
Thanks , I’ve just been searching for info about this topic for a while and yours is the greatest I have found out so far. But, what about the conclusion? Are you sure about the supply?
Wald, Matthew L. (February 21, 1994).
Good article! We are linking to this great content on our site. Keep up the great writing.
I would like to thank you for the efforts you’ve put in penning this blog. I’m hoping to check out the same high-grade blog posts by you later on as well. In fact, your creative writing abilities has motivated me to get my own site now 😉
Youre so cool! I dont suppose Ive read anything like that just before. So nice to uncover somebody with some original thoughts on this subject. realy appreciate starting this up. this excellent website is a thing that is needed on-line, somebody with a bit of originality. valuable job for bringing new stuff to the net!
A well written article, I just passed this onto a workfellow who was doing somewhat analysis on this. And he indeed purchased me dinner because I discovered it for him…. .. therefore let me reword that: Thnkx for the treat however yeah Thnkx for spending the time to talk about this, I feel strongly concerning it and love reading more on this topic. If doable, as you gain expertise, would you mind updating your blog with more details? it is extraordinarily useful on behalf of me. massive thumb up for this blog
There are incredibly plenty of details this way to take into consideration. Which is a wonderful examine mention. I supply the thoughts above as general inspiration but clearly you’ll find questions like the one you retrieve the spot that the most critical thing is going to be doing work in honest excellent faith. I don?t determine if recommendations have emerged about such things as that, but Most likely that the job is clearly recognized as a reasonable game. Both girls and boys feel the impact of simply a moment’s pleasure, through-out their lives.
Can I merely say such a relief to discover somebody that actually knows what theyre discussing over the internet. You actually learn how to bring a difficulty to light and earn it essential. The best way to have to ought to see this and can see this side in the story. I cant believe youre less well-liked since you also undoubtedly contain the gift.
I am usually to blogging and that i actually appreciate your site content. This content has truly peaks my interest. Let me bookmark your internet site and maintain checking for brand spanking new data.
I went over this site and I believe you have a lot of superb information, saved to bookmarks (:.
This site was… how do you say it? Relevant!! Finally I have found something that helped me. Appreciate it.
I’m amazed, I have to admit. Seldom do I encounter a blog that’s equally educative and amusing, and without a doubt, you have hit the nail on the head. The problem is an issue that too few people are speaking intelligently about. I am very happy that I stumbled across this during my hunt for something concerning this.
I’m amazed, I have to admit. Rarely do I encounter a blog that’s both educative and entertaining, and let me tell you, you have hit the nail on the head. The issue is something which too few men and women are speaking intelligently about. Now i’m very happy that I came across this in my hunt for something relating to this.
Can I simply just say what a comfort to discover an individual who really knows what they are talking about on the web. You actually realize how to bring a problem to light and make it important. More and more people ought to read this and understand this side of your story. I was surprised that you aren’t more popular given that you most certainly possess the gift.
When I initially left a comment I seem to have clicked on the -Notify me when new comments are added- checkbox and now whenever a comment is added I get 4 emails with the same comment. Is there a way you can remove me from that service? Thanks.
I couldn’t resist commenting. Perfectly written.
After study a number of the content on your own web site now, and that i genuinely much like your way of blogging. I bookmarked it to my bookmark web site list and you will be checking back soon. Pls check out my site too and inform me what you think.
Das beste Webdesign Berlin erhalten Sie bei uns, genauso wie professionelles Webdesign. Denn wir sind die Webdesign Agentur mit pfiff.
My brother recommended I would possibly like this blog. He was totally right. This publish truly made my day. You can not believe just how a lot time I had spent for this info! Thanks!
Most famous nations and cities supply have the next ticket and even increased accommodations.
Hello there! This post could not be written any better! Looking through this article reminds me of my previous roommate! He continually kept preaching about this. I will forward this information to him. Fairly certain he will have a very good read. Thanks for sharing!
May 18, 2000). “The 25 Highest Paid Banking Executives in 1999”.
The very next time I read a blog, Hopefully it does not fail me just as much as this one. After all, I know it was my choice to read through, however I actually thought you would have something helpful to say. All I hear is a bunch of whining about something you could fix if you were not too busy seeking attention.
I must thank you for the efforts you’ve put in penning this website. I am hoping to see the same high-grade blog posts by you in the future as well. In truth, your creative writing abilities has motivated me to get my very own blog now 😉
Your style is really unique in comparison to other people I have read stuff from. Thanks for posting when you have the opportunity, Guess I will just book mark this page.
I want to to thank you for this fantastic read!! I absolutely loved every little bit of it. I have you book-marked to check out new things you post…
There is evidently a lot to know about this. I consider you made certain nice points in features also.
Oh my goodness! an amazing post dude. Many thanks Nonetheless We are experiencing problem with ur rss . Do not know why Unable to join it. Could there be any person getting identical rss dilemma? Anybody who knows kindly respond. Thnkx
In 2008, these windows have been renovated with indicators giving particular information on the initiatives of Grenelle Environnement.
In case you have been neglecting your well being or feeling stagnant in your wellness journey, angel quantity 1001 is a reminder to embrace new well being regimes.
May I simply say what a comfort to uncover somebody that genuinely knows what they are discussing over the internet. You certainly know how to bring an issue to light and make it important. A lot more people should read this and understand this side of your story. I was surprised that you aren’t more popular because you surely possess the gift.
Tremendous report! I seriously took pleasure in that going through. I’m hoping to share further of your stuff. I believe that you have superb awareness and even visual acuity. We are exceedingly empowered just for this guidance.
An impressive share, I just now with all this onto a colleague who was conducting a little analysis during this. And the man in truth bought me breakfast due to the fact I came across it for him.. smile. So permit me to reword that: Thnx with the treat! But yeah Thnkx for spending any time to debate this, I feel strongly over it and really like reading much more about this topic. When possible, as you become expertise, could you mind updating your site to comprehend details? It truly is extremely great for me. Massive thumb up with this text!
I’m impressed, I have to admit. Genuinely rarely should i encounter a blog that’s both educative and entertaining, and without a doubt, you’ve got hit the nail for the head. Your thought is outstanding; the problem is a thing that there are not enough everyone is speaking intelligently about. My business is happy i found this in my hunt for some thing regarding this.
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
You’re so cool! I do not think I’ve read anything like that before. So good to discover another person with a few genuine thoughts on this subject. Really.. thank you for starting this up. This web site is one thing that is required on the web, someone with a little originality.
This will be the right weblog for everyone who is hopes to learn about this topic. You are aware of a great deal its nearly tough to argue to you (not too I personally would want…HaHa). You definitely put a different spin using a topic thats been discussed for decades. Excellent stuff, just excellent!
I discovered your website internet site on the internet and appearance a few of your early posts. Maintain inside the top notch operate. I additional up your Rss to my MSN News Reader. Seeking toward reading a lot more by you later on!…
Needed to post you that bit of note to be able to give thanks over again about the awesome concepts you’ve documented in this case. This is so surprisingly open-handed with you to offer without restraint all that a few people would have marketed as an e-book to earn some cash for themselves, especially considering the fact that you might well have done it in case you considered necessary. The smart ideas likewise served like the easy way to realize that other individuals have the identical desire the same as my own to realize a great deal more on the subject of this problem. I’m sure there are thousands of more enjoyable times up front for folks who take a look at your site.
The sense of wanting to help, but not knowing how or where, is something a lot of us are going through.
if you really need to become expert in driving, your really need to enroll in a driving school,.
cheers for posting this post. I am definitely tired of struggling to find relevant and intelligent commentary on this subject. Everyone nowadays seem to go to extremes to either drive home their viewpoint or suggest that everybody else in the globe is wrong. cheers for your concise and relevant insight.
Pretty! This has been a really wonderful article. Thanks for providing this information.
I must thank you for the efforts you have put in writing this site. I am hoping to view the same high-grade blog posts by you in the future as well. In fact, your creative writing abilities has encouraged me to get my very own site now 😉
Very nice post. I absolutely love this website. Keep writing!
Very Nice website. I recently designed mine and that i was yearning for some concepts and you gave me a couple of. may i ask you whether you developed the website by youself ?
There is noticeably a bundle to understand about this. I suppose you’ve made specific nice points in features also.
The style that you write make it really comfortable to read. And the template you use, wow. It is a really good combination. And I am wondering whats the name of the design you use?
Howdy, I do believe your blog could possibly be having browser compatibility issues. Whenever I take a look at your site in Safari, it looks fine but when opening in Internet Explorer, it’s got some overlapping issues. I simply wanted to provide you with a quick heads up! Aside from that, fantastic site.
A fascinating discussion is definitely worth comment. I think that you ought to write more on this topic, it may not be a taboo matter but generally folks don’t discuss these subjects. To the next! Best wishes!
I need to to thank you for this excellent read!! I definitely enjoyed every bit of it. I have got you saved as a favorite to look at new stuff you post…
After going over a handful of the blog articles on your site, I truly appreciate your technique of writing a blog. I saved it to my bookmark webpage list and will be checking back in the near future. Take a look at my website too and tell me your opinion.
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me. Thank you.
Hey i Love your work i really appreciate that. Also take a look at our special Gym flooring dubai
Pretty! This was an incredibly wonderful article. Thank you for supplying these details.
Greetings! Very useful advice in this particular article! It’s the little changes that make the biggest changes. Thanks a lot for sharing!
When I originally left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I get 4 emails with the same comment. Perhaps there is a means you are able to remove me from that service? Thanks a lot.
May I simply say what a relief to uncover someone that really understands what they’re discussing online. You definitely realize how to bring an issue to light and make it important. A lot more people must read this and understand this side of the story. I was surprised that you are not more popular since you most certainly possess the gift.
Good post. I learn something totally new and challenging on blogs I stumbleupon on a daily basis. It’s always interesting to read articles from other authors and practice a little something from other web sites.
I would like to thank you for the efforts you’ve put in penning this site. I really hope to view the same high-grade content from you in the future as well. In truth, your creative writing abilities has inspired me to get my very own blog now 😉
The next time I read a blog, Hopefully it does not disappoint me just as much as this one. I mean, Yes, it was my choice to read through, nonetheless I genuinely believed you would probably have something interesting to say. All I hear is a bunch of crying about something you can fix if you were not too busy searching for attention.
Hi, I do believe this is an excellent website. I stumbledupon it 😉 I may revisit once again since I saved as a favorite it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
Good web site you have got here.. It’s difficult to find high quality writing like yours nowadays. I honestly appreciate individuals like you! Take care!!
Amazing this information is actually awesome it really aided me and even my family, cheers!
This web-site is really a walk-through it really is the details you desired about it and didn’t know who to question. Glimpse here, and you’ll absolutely discover it.
I just done mine and that i was looking for several design suggestions and you afflicted me with a few.
Howdy! I could have sworn I’ve been to this website before but after browsing through a few of the articles I realized it’s new to me. Anyhow, I’m certainly delighted I discovered it and I’ll be book-marking it and checking back regularly!
Pretty! This was an extremely wonderful post. Thanks for providing these details.
After checking out a handful of the blog articles on your website, I truly appreciate your technique of writing a blog. I book-marked it to my bookmark site list and will be checking back in the near future. Please check out my website as well and let me know your opinion.
When I originally commented I clicked the -Notify me when new surveys are added- checkbox and already each time a comment is added I receive four emails with the same comment. Is there any way you can eliminate me from that service? Thanks!
It seems you are getting quite a lof of unwanted comments. Maybe you should look into a solution for that. Have a nice day!
I was rattling glad to find this web site on bing, just what I was looking for : D too saved to fav.
I couldn’t resist commenting. Exceptionally well written!
Spot on with this write-up, I absolutely think this site needs a lot more attention. I’ll probably be returning to read through more, thanks for the information.
When I originally left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on each time a comment is added I recieve 4 emails with the exact same comment. Perhaps there is an easy method you are able to remove me from that service? Appreciate it.
baby books should have as many pictures as possible because babies like to see pictures.,
After study a number of the blog posts in your site now, i really such as your technique of blogging. I bookmarked it to my bookmark web site list and will be checking back soon. Pls take a look at my web site likewise and make me aware what you believe.
Hiya! I simply would like to give a huge thumbs up for the nice info you’ve got here on this post. I shall be coming again to your weblog for extra soon.
This page certainly has all the information I wanted about this subject and didn’t know who to ask.
OMG! This site is awesome – Gulvafslibning | Kurt Gulvmand ? Exactly how did you cause it to be seem this very good ! Take care Flash Website Design
Thrilled you desire sensible business online guidelines keep wearing starting tools suitable for the particular web-based business. cash
Very interesting points you have observed , thankyou for posting .
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Hello there! Do you know if they make any plugins to
help with Search Engine Optimization? I’m trying to get my site
to rank for some targeted keywords but I’m not seeing very
good gains. If you know of any please share. Appreciate it!
You can read similar article here: Your destiny
Greetings! Very useful advice in this particular article! It’s the little changes that will make the greatest changes. Thanks a lot for sharing!
After study many of the web sites for your website now, we genuinely much like your way of blogging. I bookmarked it to my bookmark website list and will also be checking back soon. Pls consider my internet site too and inform me what you think.
Spot lets start on this write-up, I truly believe this excellent website needs considerably more consideration. I’ll oftimes be once more to read a lot more, thank you for that info.
seafoods are great because they are really tasty, i think that almost all seafoods are super duper tasty*
I really love your blog.. Excellent colors & theme. Did you make this site yourself? Please reply back as I’m looking to create my own personal site and would love to find out where you got this from or what the theme is called. Thanks.
I lately stumbled on your website and also have been learning along. I was thinking I might leave my very first remark. I do not know what to state except that I have liked reading through. Solid website. I am going to maintain browsing this site incredibly typically.
you can always count on search engine marketing if you want to promote products online,,
Consumers has to be deeper schooled to spot the importance inside the fears, to utilize fashionable procedures of birth control, to conserve a few of our all all-natural alternatives collectively with promoting several of our items and expert services. Our firm is sure you can easliy include a extra powerful collectively with clearer put from now on.
I enjoy reading a post that can make people think. Also, thanks for permitting me to comment.
This is a topic which is near to my heart… Take care! Where are your contact details though?
After checking out a few of the blog articles on your website, I truly appreciate your technique of writing a blog. I saved it to my bookmark site list and will be checking back soon. Please visit my website too and tell me your opinion.
I blog quite often and I truly thank you for your information. Your article has really peaked my interest. I will bookmark your blog and keep checking for new details about once a week. I subscribed to your RSS feed as well.
Hi my own cherished one! I wish to state that this kind of post is awesome, good composed and include virtually all important infos. I?|d want to seem added content such as this .
herbal supplementation is the best because i love organic supplements and herbal is organic,.
Studying to experience the blues might seem as a overwhelming task, even when you’re not a rookie guitar player. How ever with all the right Blues Guitar Lessons and trainer you’ll be able to understand the “tools of the trade” so to speek to help demystify the truly amazing grooves, solos and riffs you cherish.
You have made some good points there. I looked on the net for more information about the issue and found most people will go along with your views on this web site.
I’d must talk with you here. Which is not something It’s my job to do! I love reading a post that can get people to think. Also, many thanks for permitting me to comment!
it is really great to get government jobs because the government can give you a good job security;;
Keep up the great piece of work, I read few posts on this web site and I think that your blog is rattling interesting and has got bands of great information.
I am interested in talking to you about your website design. Did someone design it for you?
Hello, i think that i saw you visited my website so i came to “return the favor”.I’m trying to find things to improve my site!I suppose its ok to use some of your ideas!!
Hãy trải nghiệm game các cược thú vị tại Sunwin
Hello there! This blog post couldn’t be written any better! Reading through this article reminds me of my previous roommate! He continually kept talking about this. I’ll forward this article to him. Fairly certain he will have a very good read. Thank you for sharing!
I’m amazed, I have to admit. Rarely do I encounter a blog that’s both equally educative and entertaining, and without a doubt, you’ve hit the nail on the head. The problem is something that too few men and women are speaking intelligently about. I’m very happy that I found this in my search for something relating to this.
great . Thanks for informations . Ill be back. Thanks again
This constantly amazes me how site owners for example your self can find the time as well as the dedication to keep on composing wonderful content. Your website isgreat and one of my need to read blogs and forums. I just want to say thanks.
Thanks for that magnificent write-up, great site to! It makes be want to get a weblog. What software do you have to get started? I hear a good deal about this WordPress?!!
Điểm Đến Cá Cược Trực Tuyến Uy Tín Hàng Đầu tại 79king
I’m truly enjoying the design and layout of your blog. It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often. Did you hire out a designer to create your theme? Exceptional work!
my kids really like to play with those assorted pool toys, they specially like pokemon pool toys and stuff like that..
hello, just wanted to tell you that the feed on your site is messed up. I was wanting to add it to my rss list but it wouldn’t work. I had a same issue on my site, it wouldn’t work a week and then somehow it just worked! I guess these issues fix themselves sometimes, lol. Anyway I thought to inform you. bye!.
On July 16, CNBC reported Comcast was unlikely to proceed its bidding warfare with Disney to acquire Fox.
As a lot as you may keep away from the chaos of Hastings St and try to find some secluded spots close by, there’s a purpose travellers choose Noosa.
Each offered fashions with entrance-wheel drive or GM’s new “VersaTrak” all-wheel drive, however the one engine was the company’s hoary 3.4-liter pushrod V-6, which sent 185 bhp by a 4-velocity automatic transmission.
The terms “radiation” and “radioactivity” are sometimes confused.
Go to this web page to get started!
Have whole cookies readily available for the foundations, roofs, and the lengthy sides of the houses.
You’ll be able to view the enlarged photos onscreen, or you possibly can print out the free PDFs to search for hidden Christmas issues while you curl up in front of the crackling hearth.
Simply wish to say your article is as astonishing. The clarity in your post is simply great and i could assume you are an expert on this subject. Fine with your permission allow me to grab your feed to keep up to date with forthcoming post. Thanks a million and please keep up the rewarding work.
aa den stora boken… […]p Have you noticed any performance problems with the wordpress platform? I ha oj[…]…
This is a cool blog. Extremely helpful info. Thank you!
Hello! I could have sworn I’ve visited this blog before but after looking at a few of the articles I realized it’s new to me. Regardless, I’m definitely happy I found it and I’ll be book-marking it and checking back often!
I couldn’t refrain from commenting. Very well written.
Very nice blog post. I absolutely love this site. Keep writing!
Way cool! Some very valid points! I appreciate you writing this write-up and the rest of the website is also really good.
Je pourrais vous transférer les url pour plus de miniatures sur cette question. Ecrivez moi simplement…
Im happy I found this website, I couldnt get any information on this subject prior to. I also manage a website and if you want to ever serious in doing some visitor writing for me if possible feel free to let me know, im always look for people to check out my blog page. Please stop by and leave a comment sometime!
You ought to indulge in a tournament for just one of the greatest blogs online. I am going to suggest this website!
After I initially left a comment I appear to have clicked the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I recieve 4 emails with the same comment. There has to be a means you are able to remove me from that service? Thanks a lot.
You’re so interesting! I don’t suppose I have read through a single thing like that before. So wonderful to discover someone with unique thoughts on this subject. Really.. thanks for starting this up. This site is one thing that’s needed on the internet, someone with a little originality.
This web site definitely has all of the information and facts I needed about this subject and didn’t know who to ask.
I would like to thank you for the efforts you have put in writing this site. I am hoping the same high-grade web site post from you in the upcoming also. In fact your creative writing skills has inspired me to get my own website now. Actually the blogging is spreading its wings rapidly. Your write up is a good example of it.
Hello! I just would like to give a huge thumbs up for the nice information you have here on this post. I can be coming again to your blog for more soon.
As I website possessor I believe the written content here is really fantastic , appreciate it for your efforts.
Your style is so unique compared to other people I have read stuff from. Thank you for posting when you’ve got the opportunity, Guess I will just book mark this page.
I couldn’t resist commenting. Well written!
Hello there! This blog post couldn’t be written much better! Looking at this post reminds me of my previous roommate! He constantly kept talking about this. I most certainly will send this information to him. Pretty sure he’ll have a very good read. Thanks for sharing!
Fantastic read, I just passed this onto a colleague who was doing a little research on that. And he actually bought me lunch because I discovered it for him smile So let me rephrase that: Thanks for lunch!
Superb blog! I actually adore how it will be quick on my eyes as well as the information can be well written. We’re thinking generate income may be notified whenever a completely new post has been produced. We have bought on your rss feed which really should have the desired effect! Have a pleasant day!
Outstanding brief which post helped me alot. Give you thanks I looking for your details?–.
Pretty nice post, I was doing a google search and your site came up for real estate in Altamonte Springs, FL but anyway, I have enjoyed reading it, keep it up!
I’d must examine with you here. Which is not something I usually do! I take pleasure in reading a post that will make folks think. Additionally, thanks for permitting me to remark!
I’d need to take advice from you here. Which is not something I normally do! I enjoy reading a piece which will get people to think. Also, thank you for permitting me to comment!
Good post. I definitely appreciate this website. Continue the good work!
May I simply just say what a comfort to uncover somebody who actually understands what they’re talking about on the web. You actually understand how to bring an issue to light and make it important. More and more people ought to check this out and understand this side of your story. I was surprised you aren’t more popular because you definitely possess the gift.
Way cool! Some very valid points! I appreciate you writing this post and also the rest of the website is also really good.
Great information. Lucky me I came across your blog by chance (stumbleupon). I’ve saved as a favorite for later.
Some truly wonderful work on behalf of the owner of this internet site , perfectly great articles .
weight loss is sometimes difficult to attain, it all depends on your motivation and genetics;
Hey very cool web site!! Man .. Excellent .. Amazing .. I will bookmark your web site and take the feeds also…I’m happy to find a lot of useful info here in the post, we need develop more strategies in this regard, thanks for sharing. . . . . .
Good info. Lucky me I came across your website by chance (stumbleupon). I have saved it for later!
Way cool! Some extremely valid points! I appreciate you writing this post and also the rest of the site is very good.
This post is priceless. When can I find out more?
I blog frequently and I seriously appreciate your information. This article has truly peaked my interest. I will take a note of your blog and keep checking for new details about once per week. I opted in for your RSS feed as well.
Your style is very unique in comparison to other folks I’ve read stuff from. Thank you for posting when you have the opportunity, Guess I’ll just bookmark this web site.
Sosua Ladies ️ Discover Escorts In Puerto Plata
& Sosua 가라오케 사이트
I must thank you for the efforts you’ve put in penning this website. I am hoping to view the same high-grade content by you later on as well. In truth, your creative writing abilities has inspired me to get my very own website now 😉
Great help from this blog! Thanks alot for the information I needed
I have learned result-oriented things by means of your site. One other thing I’d really like to say is that often newer pc os’s are inclined to allow extra memory to be utilized, but they also demand more memory space simply to perform. If an individual’s computer is not able to handle a lot more memory and also the newest program requires that storage increase, it might be the time to buy a new Laptop or computer. Thanks
Labor party talking heads are on claiming the meeja is agin’ them.
Right here is the right site for anyone who hopes to understand this topic. You realize so much its almost hard to argue with you (not that I really will need to…HaHa). You certainly put a brand new spin on a topic that has been written about for years. Great stuff, just wonderful.
Having read this I thought it was extremely informative. I appreciate you finding the time and energy to put this informative article together. I once again find myself spending way too much time both reading and leaving comments. But so what, it was still worth it.
An historic Egyptian zodiac has been found which represented three Virgins: “The three ‘Virgins,’ or Virgo in three totally different positions, meant .
The make up foolish steps, hops and twirls, somersault your way throughout a grassy subject, and dangle from your swingset rings.
The DJ of new World University, Anthony is antagonistic towards Victoria and Christopher Rice, resentful of having to transmit propaganda; after he attempts to broadcast the reality, he is consumed by the good Intelligence.
Ojambo, Fred (29 December 2010).
Black and Hispanic borrowers were extra more likely to have a subprime mortgage.
Not solely are travel restrictions largely ineffective, however they could even make things worse.
Interesting post. Certain that My partner and i’ll keep coming back here. Good work.
Hey There. I found your blog using msn. This is an extremely well written article. I’ll be sure to bookmark it and return to read more of your useful info. Thanks for the post. I’ll definitely comeback.
oh well, chris rock is damn funny. i like his corny jokes and stuffs“
This page truly has all of the information and facts I needed concerning this subject and didn’t know who to ask.
Very nice article. I definitely love this site. Stick with it!
I was on Twitter looking for Neiko Hand Tools when I found a link to this blog, happy I stopped by – Cheers
Oh my goodness! Awesome article dude! Thanks, However I am experiencing issues with your RSS. I don’t understand the reason why I cannot subscribe to it. Is there anyone else getting similar RSS issues? Anybody who knows the answer will you kindly respond? Thanx!!
you might have an amazing blog right here! would you like to make some invite posts on my weblog?
I could not refrain from commenting. Perfectly written!
This blog was… how do I say it? Relevant!! Finally I have found something which helped me. Thanks a lot.
I’m amazed, I must say. Rarely do I encounter a blog that’s equally educative and amusing, and without a doubt, you have hit the nail on the head. The problem is something that not enough folks are speaking intelligently about. Now i’m very happy that I stumbled across this during my hunt for something concerning this.
You are so cool! I do not think I have read something like this before. So wonderful to discover another person with some genuine thoughts on this subject matter. Really.. thank you for starting this up. This web site is something that is needed on the web, someone with some originality.
The web insurance rates allow individuals access to questionnaires any time. The main thing they’ve got note is to follow the approach to obtain any estimate in connection with auto insurance plan.
I needed to say thanks a lot just as before wrist watches dazzling web-site you can have written reading this. It will be jam-packed with smart ideas if you’re contemplating the following make any difference, mainly this type of really quite article. You’re in fact every single one fully fantastic a great bonus accommodating coming from all blog writers for a few incontrovertible fact result your blog site comments is a fantastic pleasure when camping. Also good job on a substantial current! Serta and have hype in your inspirations in doing what came across get in most calendar months. Our new home listing should be a extended distance particularly long together with thoughts rrs going to be offer ideal purposes.
Way cool! Some very valid points! I appreciate you writing this post and also the rest of the site is also very good.
Excellent post. I certainly appreciate this website. Keep writing!
I have to thank you for the efforts you’ve put in penning this site. I really hope to check out the same high-grade blog posts by you later on as well. In fact, your creative writing abilities has encouraged me to get my own, personal website now 😉
Great web site you have got here.. It’s hard to find quality writing like yours these days. I honestly appreciate people like you! Take care!!
Good post. I learn something new and challenging on sites I stumbleupon every day. It’s always interesting to read through articles from other authors and practice something from their sites.
Good day! I just would like to give you a big thumbs up for your excellent information you have got here on this post. I will be coming back to your site for more soon.
Love this appreciation for great content
This blog is a great resource for anyone looking to live a more mindful and intentional life Thank you for providing valuable advice and tips
Your blog has become my go-to source for positive and uplifting content Thank you for consistently delivering high-quality posts
I appreciate how this blog promotes self-growth and personal development It’s important to continuously strive to become the best version of ourselves
Your blog posts never fail to entertain and educate me. I especially enjoyed the recent one about [insert topic]. Keep up the great work!
Your passion for what you do shines through in every post It’s truly inspiring to see someone doing what they love and excelling at it
Your writing is so relatable and down-to-earth It’s like chatting with a good friend over a cup of coffee Keep sharing your wisdom with us
Your blog has become my daily dose of positivity and inspiration It’s a space that I always look forward to visiting
This blog is like a virtual mentor, guiding me towards personal and professional growth Thank you for being a source of inspiration
Your blog has helped me through some tough times and I am forever grateful for your positive and uplifting content
Your words have a way of resonating deeply with your readers Thank you for always being encouraging and uplifting
I have recommended this blog to all of my friends and family It’s rare to find such quality content these days!
I always find myself nodding along and agreeing with your wise words Your insights and advice are truly valuable
Hello there! I could have sworn I’ve visited this site before but after browsing through some of the articles I realized it’s new to me. Regardless, I’m certainly happy I discovered it and I’ll be bookmarking it and checking back often.
Nice post. I learn something totally new and challenging on sites I stumbleupon on a daily basis. It will always be interesting to read through content from other authors and use something from other sites.
Your content always keeps me coming back for more!
I love how this blog covers a variety of topics, making it appeal to a diverse audience There is something for everyone here!
Thank you for providing a positive and constructive space for discussion It’s refreshing to see a blog with a kind and respectful community
I completely agree with your perspective on this topic It’s refreshing to see someone presenting a balanced and thoughtful viewpoint
Your passion for what you do shines through in every post It’s truly inspiring to see someone doing what they love and excelling at it
Дипломированный психолог с опытом работы и отзывами клиентов. Дипломированный психолог с опытом работы и отзывами клиентов. В переписке у психолога. оценили 6388 раз
Получить первую онлайн консультацию психолога чате. Получите консультацию онлайн-психолога в чате прямо сейчас. Чат с психологом в телеге. оценили 4446 раз
May I simply say what a comfort to discover somebody that genuinely knows what they’re discussing on the web. You definitely know how to bring an issue to light and make it important. A lot more people ought to read this and understand this side of your story. It’s surprising you aren’t more popular because you surely have the gift.
Чат с психологом в телеге. Психолог онлайн анонимно. Психолог помогающий искать решения в непростых психологических ситуациях. оценили 5812 раз
Психолог помогающий искать решения в непростых психологических ситуациях. Получить онлайн консультацию психолога чате. Психолог онлайн анонимно. оценили 9669 раз
Получить онлайн консультацию психолога чате. Анонимный чат с психологом телеграм. Круглосуточная запись на онлайн-консультацию психолога. оценили 1812 раз
Психолог онлайн анонимно. Телеграм психолог. Чат с психологом в телеге. оценили 2180 раз
An outstanding share! I’ve just forwarded this onto a co-worker who was doing a little research on this. And he in fact bought me dinner simply because I found it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending time to discuss this matter here on your blog.
Онлайн чат с психологом без регистрации. Чат психологической поддержки. Онлайн чат с психологом без регистрации. оценили 7310 раз
I am so grateful for the community that this blog has created It’s a place where I feel encouraged and supported
Получить онлайн консультацию психолога чате. Психолог оказывает помощь онлайн в чате. Анонимный чат с психологом телеграм. оценили 5911 раз
Your passion for what you do shines through in every post It’s truly inspiring to see someone doing what they love and excelling at it
I always find myself nodding along and agreeing with your wise words Your insights and advice are truly valuable
Thank you for providing a positive and constructive space for discussion It’s refreshing to see a blog with a kind and respectful community
Very good information. Lucky me I recently found your blog by accident (stumbleupon). I’ve bookmarked it for later!
Получить онлайн консультацию психолога чате. Получить КОНСУЛЬТАЦИЮ и ПОДДЕРЖКУ профессиональных психологов. Телеграм психолог. оценили 5652 раз
Получить онлайн консультацию психолога чате. В переписке у психолога. Получить КОНСУЛЬТАЦИЮ и ПОДДЕРЖКУ профессиональных психологов. оценили 1919 раз
You are so interesting! I don’t believe I’ve read through something like this before. So good to find another person with a few genuine thoughts on this subject matter. Really.. thanks for starting this up. This web site is one thing that’s needed on the internet, someone with a bit of originality.
I completely agree with your perspective on this topic It’s refreshing to see someone presenting a balanced and thoughtful viewpoint
Your writing style is so engaging and makes even the most mundane topics interesting to read Keep up the fantastic work
Their posts always leave us feeling informed and entertained. We’re big fans of their style and creativity.
I always find myself nodding along and agreeing with your wise words Your insights and advice are truly valuable
Leave a comment and let us know what your favorite blog post has been so far!
Thank you for providing a positive and constructive space for discussion It’s refreshing to see a blog with a kind and respectful community
It’s hard to find knowledgeable people about this topic, however, you sound like you know what you’re talking about! Thanks
Hi there! I simply want to offer you a huge thumbs up for the great info you have got right here on this post. I’ll be coming back to your site for more soon.
I’m pretty pleased to find this page. I wanted to thank you for ones time for this fantastic read!! I definitely liked every bit of it and i also have you saved as a favorite to see new things on your site.
Release the equity in your property with a reliable home equity loan — ideal for funding home improvements, large expenses, or refinancing.
I can definitely see the logic behind your point of view, and it aligns closely with an article I recently read on https://sumclub.guide/. It adds even more perspective to this discussion.
This blog post is worth the read – trust us!
I admire how this blog promotes kindness and compassion towards ourselves and others We could all use a little more of that in our lives
This blog is a great resource for anyone looking to live a more mindful and intentional life Thank you for providing valuable advice and tips
Your blog has become a part of my daily routine Your words have a way of brightening up my day and lifting my spirits
Every time I read a new post, I feel like I’ve learned something valuable or gained a new perspective. Thank you for consistently putting out such great content!
I always find myself nodding along and agreeing with your wise words Your insights and advice are truly valuable
Can I simply just say what a comfort to uncover someone that truly knows what they are talking about on the internet. You definitely understand how to bring a problem to light and make it important. More and more people really need to look at this and understand this side of your story. I was surprised that you’re not more popular given that you surely possess the gift.
I completely agree with your perspective on this topic It’s refreshing to see someone presenting a balanced and thoughtful viewpoint
I couldn’t stop scrolling and reading, your content is truly one-of-a-kind. Thank you for all the time and effort you put into creating such amazing content.
From the bottom of my heart, thank you for being a source of positivity and light in this sometimes dark and overwhelming world
Thank you for providing a positive and constructive space for discussion It’s refreshing to see a blog with a kind and respectful community
Oh my goodness! Impressive article dude! Thank you, However I am going through difficulties with your RSS. I don’t understand why I am unable to subscribe to it. Is there anyone else having similar RSS issues? Anyone who knows the answer will you kindly respond? Thanks.
An outstanding share! I’ve just forwarded this onto a colleague who had been conducting a little research on this. And he actually bought me lunch because I stumbled upon it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanks for spending the time to talk about this subject here on your website.
Получите консультацию онлайн-психолога в чате прямо сейчас. Психолог онлайн анонимно. Психолог помогающий искать решения в непростых психологических ситуациях. оценили 7797 раз
Получить онлайн консультацию психолога чате. Психолог оказывает помощь онлайн в чате. Получите консультацию онлайн-психолога в чате прямо сейчас. оценили 3175 раз
Very good article! We will be linking to this particularly great post on our site. Keep up the good writing.
This blog is such a hidden gem I stumbled upon it by chance and now I’m completely hooked!
This blog is a great mix of informative and entertaining content It keeps me engaged and interested from start to finish
Your positive and uplifting words are like a ray of sunshine on a cloudy day Thank you for spreading light and positivity in the world
Your posts are always so well-written and thought out It’s evident that you put a lot of effort into each and every one
I love how this blog promotes self-love and confidence It’s important to appreciate ourselves and your blog reminds me of that
What topics would you like to see covered in future posts? Let us know in the comments.
Your writing is so eloquent and persuasive You have a talent for getting your message across and inspiring meaningful change
Wow, this blogger is seriously impressive!
Your blog is so much more than just a collection of posts It’s a community of like-minded individuals spreading optimism and kindness
This is exactly what I needed to read today Your words have given me a new perspective and renewed hope Thank you
I couldn’t stop scrolling and reading, your content is truly one-of-a-kind. Thank you for all the time and effort you put into creating such amazing content.
Your posts are always so well-written and thought out It’s evident that you put a lot of effort into each and every one
Your writing is so eloquent and persuasive You have a talent for getting your message across and inspiring meaningful change
From the bottom of my heart, thank you for being a source of positivity and light in this sometimes dark and overwhelming world
Next time I read a blog, Hopefully it won’t fail me just as much as this one. I mean, I know it was my choice to read, but I genuinely believed you would probably have something helpful to talk about. All I hear is a bunch of complaining about something you can fix if you were not too busy looking for attention.
The very next time I read a blog, I hope that it won’t fail me just as much as this one. After all, I know it was my choice to read, but I really believed you would probably have something useful to talk about. All I hear is a bunch of complaining about something that you could fix if you were not too busy seeking attention.
When I initially commented I seem to have clicked on the -Notify me when new comments are added- checkbox and now whenever a comment is added I receive 4 emails with the exact same comment. Perhaps there is an easy method you can remove me from that service? Appreciate it.
That is a really good tip particularly to those fresh to the blogosphere. Brief but very accurate information… Appreciate your sharing this one. A must read article!
Hey there! I just would like to offer you a huge thumbs up for your great information you’ve got right here on this post. I will be returning to your website for more soon.
Wśród prezentowanych gier użytkownicy mogą znaleźć nie tylko kolorowe sloty, ale także ruletkę, szeroki wybór gier karcianych i video pokera.
Your blog has become my go-to source for inspiration and motivation Thank you for consistently delivering high-quality content
Love this appreciation for great content
Your blog always leaves me feeling uplifted and inspired Thank you for consistently delivering high-quality content
Your blog has helped me become a better version of myself Your words have inspired me to make positive changes in my life
What type of content would you like to see more of in the future? Let us know in the comments!
Hello there! I just want to offer you a big thumbs up for your excellent information you have got here on this post. I will be returning to your site for more soon.
Share your favorite blog post in the comments below!
Your posts are so beautifully written and always leave me feeling inspired and empowered Thank you for using your talents to make a positive impact
I have recommended this blog to all of my friends and family It’s rare to find such quality content these days!
Your positive energy and enthusiasm radiate through your writing It’s obvious that you are truly passionate about what you do
This post hits close to home for me and I am grateful for your insight and understanding on this topic Keep doing what you do
Your words have resonated with us and we can’t wait to read more of your amazing content. Thank you for sharing your expertise and passion with the world.
Your content always keeps me coming back for more!
Your knowledge and expertise on various topics never ceases to amaze me I always learn something new with each post
This is exactly what I needed to read today Your words have provided me with much-needed reassurance and comfort
Your ideas and insights are unique and thought-provoking I appreciate how you challenge your readers to see things from a different perspective
This blog has opened my eyes to new ideas and perspectives that I may not have considered before Thank you for broadening my horizons
This blog is like a virtual mentor, guiding me towards personal and professional growth Thank you for being a source of inspiration
This blog post hit all the right notes!
I must thank you for the efforts you’ve put in writing this website. I’m hoping to view the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has motivated me to get my very own blog now 😉
I’m very pleased to find this great site. I need to to thank you for ones time just for this wonderful read!! I definitely savored every bit of it and I have you saved to fav to look at new stuff in your blog.
This excellent website truly has all the info I needed concerning this subject and didn’t know who to ask.
That is a really good tip especially to those fresh to the blogosphere. Simple but very accurate information… Many thanks for sharing this one. A must read article!
You ought to take part in a contest for one of the best sites online. I will highly recommend this blog!
After I initially left a comment I appear to have clicked the -Notify me when new comments are added- checkbox and now whenever a comment is added I get 4 emails with the exact same comment. There has to be an easy method you can remove me from that service? Thanks.
I like it whenever people come together and share opinions. Great site, continue the good work.
Thanks for your post. I like your work you can also check mine anchor text
Great article. I’m dealing with many of these issues as well..
After looking over a number of the blog posts on your web page, I honestly appreciate your technique of writing a blog. I added it to my bookmark website list and will be checking back soon. Take a look at my web site too and tell me how you feel.
I could not resist commenting. Very well written.
Howdy! This article couldn’t be written any better! Looking at this article reminds me of my previous roommate! He continually kept talking about this. I most certainly will forward this post to him. Pretty sure he will have a very good read. Thanks for sharing!
Great post! We will be linking to this particularly great article on our site. Keep up the good writing.
Greetings! Very useful advice in this particular article! It’s the little changes which will make the greatest changes. Thanks for sharing!
Hi, I do think your blog may be having internet browser compatibility problems. When I take a look at your website in Safari, it looks fine however, when opening in Internet Explorer, it’s got some overlapping issues. I merely wanted to give you a quick heads up! Besides that, fantastic site!
This blog was… how do I say it? Relevant!! Finally I have found something that helped me. Thanks!
This is a topic that’s near to my heart… Many thanks! Where can I find the contact details for questions?
This website really has all the information I needed concerning this subject and didn’t know who to ask.
Excellent post. I will be facing a few of these issues as well..
This blog was… how do you say it? Relevant!! Finally I’ve found something that helped me. Thanks.
That is a really good tip especially to those fresh to the blogosphere. Short but very accurate info… Thank you for sharing this one. A must read article.
I agree with you completely. This is a topic I’ve also seen discussed extensively on https://xibett.com/, and the articles there provide a lot of depth on the matter.
Spot on with this write-up, I really think this website needs much more attention. I’ll probably be returning to read more, thanks for the information.
Having read this I thought it was rather enlightening. I appreciate you spending some time and effort to put this informative article together. I once again find myself spending a lot of time both reading and leaving comments. But so what, it was still worthwhile!
I completely agree with your thoughts on this, and I’ve encountered similar opinions on https://leo88s.online/. It’s great to see others exploring this topic with such depth.
Pretty! This was an extremely wonderful article. Thanks for supplying this information.
I fully support this viewpoint, and I think it’s a perspective worth considering. I read a similar article on https://hong88.app/, and it reinforced my belief in this idea.
Nice post. I learn something new and challenging on sites I stumbleupon every day. It will always be exciting to read through articles from other writers and practice something from other web sites.
This is the perfect blog for anyone who would like to find out about this topic. You realize so much its almost tough to argue with you (not that I actually would want to…HaHa). You certainly put a new spin on a subject which has been discussed for many years. Great stuff, just excellent.
This blog post hit all the right notes!
Keep up the amazing work! Can’t wait to see what you have in store for us next.
Your blog has become my go-to source for inspiration and motivation I am so grateful for the valuable content you provide
This blog is like a breath of fresh air in the midst of all the negativity on the internet I’m grateful to have stumbled upon it
What other topics would you like to see covered on the blog? Let us know in the comments!
This blog is like a breath of fresh air in the midst of all the negativity on the internet I’m grateful to have stumbled upon it
I couldn’t agree more. This aligns perfectly with a viewpoint I came across on https://taitip88.top/. The article there also explained why this issue is so significant.
I’m amazed, I have to admit. Seldom do I encounter a blog that’s both educative and entertaining, and without a doubt, you’ve hit the nail on the head. The problem is something that not enough men and women are speaking intelligently about. I’m very happy that I found this in my hunt for something concerning this.
bookmarked!!, I really like your site!
I could not resist commenting. Exceptionally well written!
You made some decent points there. I looked on the internet to learn more about the issue and found most people will go along with your views on this website.
I love looking through a post that can make men and women think. Also, thanks for permitting me to comment.
I blog frequently and I seriously appreciate your content. This great article has truly peaked my interest. I’m going to bookmark your blog and keep checking for new information about once a week. I opted in for your RSS feed too.
The very next time I read a blog, Hopefully it does not disappoint me as much as this particular one. After all, I know it was my choice to read through, nonetheless I genuinely believed you would probably have something interesting to talk about. All I hear is a bunch of whining about something that you could possibly fix if you were not too busy searching for attention.
Everything is very open with a clear description of the issues. It was truly informative. Your website is extremely helpful. Thank you for sharing!
This is a very good tip particularly to those new to the blogosphere. Short but very precise information… Many thanks for sharing this one. A must read post.
It’s clear that you are passionate about making a positive impact and your blog is a testament to that Thank you for all that you do
Share your favorite blog post in the comments below!
From the bottom of my heart, thank you for being a source of positivity and light in this sometimes dark and overwhelming world
You have a way of making each of your readers feel seen and heard That’s a special quality that not all bloggers possess Thank you for creating a safe space for us
I always leave this blog feeling inspired and motivated to make positive changes in my life Thank you for being a constant source of encouragement
Can I simply just say what a comfort to find somebody that really knows what they are discussing on the net. You definitely know how to bring a problem to light and make it important. More and more people must look at this and understand this side of the story. I was surprised that you’re not more popular since you most certainly possess the gift.
You ought to be a part of a contest for one of the greatest blogs on the web. I will recommend this blog!
An outstanding share! I’ve just forwarded this onto a colleague who has been conducting a little research on this. And he actually ordered me dinner simply because I stumbled upon it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanks for spending time to discuss this matter here on your web page.
I think this point is spot-on. I’ve read something quite similar on http://taisunwin.deals/, and it helped me to expand my understanding of the subject even further.
Good site you have got here.. It’s hard to find excellent writing like yours nowadays. I really appreciate individuals like you! Take care!!
79King – Nhà Cái Cá Cược Uy Tín Đáng Tham Gia Năm 2025 https://79king.beer/
I couldn’t agree more with your perspective. I’ve seen articles on https://lu88club.vip/ that also explain this concept in depth, which I think is really helpful.
Your argument really resonates with me, and it’s one that I recently came across in a post on https://hdbet.navy. The insights shared there helped solidify my understanding of this topic.
What type of content would you like to see more of in the future? Let us know in the comments!
Your words have resonated with us and we can’t wait to read more of your amazing content. Thank you for sharing your expertise and passion with the world.
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
I think you’ve hit the nail on the head here. I read something quite similar on bong99 recently, which deepened my understanding of the subject.
Your blog is a great source of positivity and inspiration in a world filled with negativity Thank you for making a difference
Keep up the amazing work!
I agree completely with this perspective. It’s one I’ve seen discussed in depth on https://vua88.deal/, and I think their articles offer a solid understanding of the topic.
https://deepbluedirectory.com/Home/Home_Business/Regional/Arts/Dance/
Pretty! This has been an incredibly wonderful article. Thanks for supplying this info.
This inspired me to take action
I think this point is spot-on. I’ve read something quite similar on bong99, and it helped me to expand my understanding of the subject even further.
Great article! We will be linking to this particularly great post on our website. Keep up the great writing.
Very good blog post. I certainly appreciate this site. Keep writing!
Having read this I thought it was extremely enlightening. I appreciate you taking the time and effort to put this informative article together. I once again find myself personally spending a lot of time both reading and commenting. But so what, it was still worthwhile!
https://golosknig.com/profile/campingequipmentk/
An impressive share! I have just forwarded this onto a coworker who was conducting a little homework on this. And he in fact ordered me breakfast due to the fact that I stumbled upon it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanx for spending the time to discuss this topic here on your internet site.
You always post such useful stuff
I completely agree with your reasoning here. It’s very similar to a point I came across on https://da88z.org/, which helped me gain more clarity on the issue.
I think you’ve made an excellent point here. I recently came across an article on https://da88z.org/ that dives deeper into this subject, and it offers some great perspectives.
Your argument really resonates with me, and it’s one that I recently came across in a post on May88. The insights shared there helped solidify my understanding of this topic.
An outstanding share! I’ve just forwarded this onto a friend who was conducting a little homework on this. And he in fact ordered me breakfast because I stumbled upon it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending time to talk about this matter here on your web site.
知らぬが仏
I want to to thank you for this good read!! I certainly loved every little bit of it. I have got you book-marked to look at new things you post…
minge
飛んで火に入る夏の虫
Saved as a favorite, I really like your site!
After I initially left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and from now on each time a comment is added I recieve four emails with the exact same comment. There has to be a way you are able to remove me from that service? Many thanks.
Can I just say what a comfort to find somebody that truly knows what they are talking about over the internet. You certainly understand how to bring a problem to light and make it important. A lot more people should read this and understand this side of your story. I can’t believe you’re not more popular given that you certainly possess the gift.
Hi, I do think this is a great website. I stumbledupon it 😉 I will revisit once again since i have book marked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
Greetings! Very helpful advice in this particular article! It’s the little changes that produce the biggest changes. Thanks a lot for sharing!
You have made some decent points there. I looked on the web to learn more about the issue and found most individuals will go along with your views on this web site.
I truly love your blog.. Great colors & theme. Did you develop this site yourself? Please reply back as I’m planning to create my own site and would like to learn where you got this from or exactly what the theme is named. Kudos.
Hello! I could have sworn I’ve been to this blog before but after going through many of the posts I realized it’s new to me. Anyways, I’m certainly delighted I found it and I’ll be book-marking it and checking back often!
Deference to article author , some superb selective information .
I completely agree with this viewpoint, it’s very well thought out. I recently read an article that explores similar ideas on https://net88club.vip/, and I think it adds more depth to the discussion.
I agree with this viewpoint completely. I’ve also read a similar analysis on https://zbett.uk.com/, and I think it adds valuable insights to this ongoing conversation.
I started entrancing https://www.cornbreadhemp.com/products/blood-orange-thc-gummies-10mg a few months ago and equitably, they’ve мейд a huge difference. I in the main liberate at one after dinner to workers me coldness absent from and have a zizz better. They taste renowned —like present sweetmeats — and don’t remain me feeling numbed the next day. It’s just a nice, muted vibe that helps inhale the margin insane after a stressful day. Wasn’t firm they’d work at prime, but conditions I’m all in. Utterly recommend if you lack something typical to take you slacken up on without any eerie side effects.
Way cool! Some very valid points! I appreciate you writing this write-up and also the rest of the site is also very good.
Way cool! Some very valid points! I appreciate you writing this article and the rest of the website is also very good.
Oh my goodness! Incredible article dude! Many thanks, However I am having problems with your RSS. I don’t understand the reason why I can’t join it. Is there anybody else having identical RSS problems? Anyone who knows the solution can you kindly respond? Thanks!
You should take part in a contest for one of the finest sites on the net. I will highly recommend this website!
Hi there, just became alert to your blog through Google, and found that it is truly informative. I am gonna watch out for brussels. I?ll appreciate if you continue this in future. Lots of people will be benefited from your writing. Cheers!
Hello, i think that i saw you visited my weblog so i came to ?return the favor?.I am trying to find things to enhance my site!I suppose its ok to use some of your ideas!!
Everything is very open with a clear explanation of the challenges. It was really informative. Your site is useful. Thank you for sharing!
Hello would you mind letting me know which webhost you’re utilizing? I’ve loaded your blog in 3 completely different internet browsers and I must say this blog loads a lot quicker then most. Can you suggest a good internet hosting provider at a honest price? Thank you, I appreciate it!
I used to be recommended this blog by way of my cousin. I am no longer positive whether or not this publish is written by means of him as nobody else understand such exact approximately my problem. You are incredible! Thanks!
At first, I was skeptical about https://joyorganics.com/products/organic-cbg-cbd-tincture , but these days I provide for them in my nightstand. They’ve evolve into voice of my evening habitual—ditty gummy, a cup of tea, and I’m clever to go. I don’t perceive treble or freakish, due peacefulness and on the brink of to afraid down. The flavor’s in truth in actuality fitting too, which surprised me. No unnatural aftertaste like some others I’ve tried. If your brain runs a mile a pint-sized at night or you’re honest tough to slacken after at liberty, these are for all significance checking out.
Pretty! This has been an extremely wonderful post. Thanks for providing this information.
There is certainly a great deal to find out about this issue. I really like all the points you have made.
You are so cool! I don’t think I have read through something like that before. So wonderful to discover somebody with unique thoughts on this topic. Seriously.. thank you for starting this up. This web site is something that’s needed on the web, someone with a little originality.
Автор использовал разнообразные источники, чтобы подкрепить свои утверждения.
Absolutely! I think this is a great point, and I read a similar discussion on Win79 that explained this idea in even more depth.
You’ve made an excellent point here. I saw something similar on đăng nhập 11bet that discusses this idea in great depth, and I think it adds even more value to your argument.
I could not refrain from commenting. Exceptionally well written.
I always emailed this blog post page to all my friends, because if like to read it then my contacts will too.
I seriously love your site.. Great colors & theme. Did you create this amazing site yourself? Please reply back as I’m attempting to create my very own website and would like to know where you got this from or exactly what the theme is called. Appreciate it!
I like the helpful info you provide in your articles. I will bookmark your blog and check again here regularly. I am quite certain I will learn lots of new stuff right here! Good luck for the next!
I couldn’t refrain from commenting. Well written.
Link Vào Vin88 Nhà Cái Cá Cược Hàng Đầu Châu Á 2025 vin88
This website was… how do I say it? Relevant!! Finally I have found something that helped me. Kudos!
Hello! I just want to give you a big thumbs up for your excellent info you have here on this post. I am coming back to your website for more soon.
I started delightful CBD gummies a not many months ago and morally, they’ve мейд a huge difference. I almost always liberate everyone after dinner to boost me deject out and catnap better. They bite great —like solid candy — and don’t beat it me feeling groggy the next day. It’s just a good, mellow vibe that helps take the edge dotty after a stressful day. Wasn’t firm they’d feat at first, but in the present climate I’m all in. Completely second if you need something typical to ease you slacken up on without any eerie side effects.
I agree 100 with your point. It’s a perspective I’ve encountered on https://Tin88.pet/ recently, and it really made me think more about the topic at hand.
Эта статья является настоящим сокровищем информации. Я был приятно удивлен ее глубиной и разнообразием подходов к рассматриваемой теме. Спасибо автору за такой тщательный анализ и интересные факты!
Автор статьи предлагает разные точки зрения на обсуждаемую проблему, позволяя читателям ознакомиться с различными аргументами и сделать собственные выводы.
I am sure this post has touched all the internet viewers, its really really pleasant post on building up new website.
I visited many blogs except the audio feature for audio songs current at this website is actually
marvelous.
Автор статьи представляет разнообразные точки зрения и аргументы, оставляя решение оценки информации читателям.
В современном мире, где онлайн-присутствие становится все более важным для бизнеса, повышение видимости и ранжирования сайта в поисковых системах является одной из самых важных задач для веб-мастеров и маркетологов. Одним из основных факторов, влияющих на рост авторитетности сайта, является его DR (Domain Rating), который определяется в основном путем анализа ссылочной массы сайта.
Эта статья действительно заслуживает высоких похвал! Она содержит информацию, которую я долго искал, и дает полное представление о рассматриваемой теме. Благодарю автора за его тщательную работу и отличное качество материала!
I fully agree with your statement. I recently came across a post on http://vb88s.uk.com that covered this topic in detail, and I believe their perspective aligns well with yours.
Your blog has become my go-to source for positive and uplifting content Thank you for consistently delivering high-quality posts
I absolutely agree with what you’re saying. I’ve read similar discussions on https://lode88.us.com/ that explore the nuances of this issue in great detail.
Such a helpful insight.
Such a valuable bit of content.
Автор статьи предоставляет сбалансированную информацию, основанную на проверенных источниках.
Я бы хотел отметить качество исследования, проведенного автором этой статьи. Он представил обширный объем информации, подкрепленный надежными источниками. Очевидно, что автор проявил большую ответственность в подготовке этой работы.
Статья представляет несколько точек зрения на данную тему и анализирует их достоинства и недостатки. Это помогает читателю рассмотреть проблему с разных сторон и принять информированное решение.
I genuinely admired the approach this was written.
I’m curious to find out what blog system you’re working with? I’m experiencing some small security problems with my latest site and I’d like to find something more secure. Do you have any suggestions?
What a material of un-ambiguity and preserveness of precious knowledge on the topic of unpredicted emotions.
My brother suggested I would possibly like this website. He used to be entirely right. This post truly made my day. You cann’t believe just how so much time I had spent for this information! Thanks!
I really love your website.. Pleasant colors & theme. Did you build this amazing site yourself? Please reply back as I’m looking to create my own blog and would like to find out where you got this from or what the theme is called. Thanks.
I completely agree with this perspective. There’s an in-depth post on https://taiwin79.digital/ that elaborates on the same topic, offering useful points to support your view.
Absolutely! I think this is a great point, and I read a similar discussion on https://gen88s.pro/ that explained this idea in even more depth.
Everything is very open with a really clear description of the issues. It was really informative. Your website is very useful. Many thanks for sharing.
I particularly admired the way this was presented.
Спасибо за эту статью! Она превзошла мои ожидания. Информация была представлена кратко и ясно, и я оставил эту статью с более глубоким пониманием темы. Отличная работа!
Highly energetic article, I enjoyed that bit. Will there be a part 2?
Автор статьи представляет факты и события с акцентом на нейтральность.
There’s certainly a lot to find out about this topic. I love all of the points you have made.
Мне понравилась четкая структура статьи, которая помогает легко ориентироваться в тексте.
What’s up, everything is going well here and ofcourse every one is sharing data, that’s in fact good, keep up writing.
Статья содержит разнообразные точки зрения, представленные в равной мере.
Hey there, You have done a fantastic job. I will definitely digg it and personally suggest to my friends. I’m sure they’ll be benefited from this website.
Автор предлагает разнообразные точки зрения на проблему, что помогает читателю получить обширное понимание ситуации.
Автор статьи представляет разнообразные аспекты темы, предоставляя факты и аргументы без выражения собственного мнения.
I fully agree with what you’re saying. I came across a very similar discussion on 1Gom, and the insights provided there helped me see this topic more clearly.
I blog quite often and I seriously thank you for your information. This great article has truly peaked my interest. I will take a note of your site and keep checking for new details about once a week. I opted in for your Feed too.
This underground site let you watch any sports 100 free without registration or ads.
Absolutely, I agree completely. I recently read a post on https://dafabet.us.com/ that explores this topic in depth, and I think it adds a lot of value to the conversation.
Can I simply say what a comfort to discover an individual who really understands what they’re discussing on the internet. You definitely realize how to bring an issue to light and make it important. A lot more people have to check this out and understand this side of the story. It’s surprising you are not more popular since you surely possess the gift.
I really like it when folks come together and share opinions. Great blog, keep it up.
Do you have a spam problem on this site; I also am a blogger, and I was curious about your situation; many of us have developed some nice procedures and we are looking to trade strategies with other folks, be sure to shoot me an email if interested.
Everything is very open with a very clear clarification of the challenges. It was definitely informative. Your website is very useful. Many thanks for sharing.
You can definitely see your expertise in the work you write. The world hopes for even more passionate writers like you who are not afraid to say how they believe. Always go after your heart.
I fully support this viewpoint, and I think it’s a perspective worth considering. I read a similar article on https://goal123b.us.com/, and it reinforced my belief in this idea.
I agree fully with your comment. There’s a detailed article on Win79 that covers the same ground, and it provides additional context that supports your argument.
May I just say what a relief to discover someone that truly knows what they’re talking about on the web. You actually know how to bring a problem to light and make it important. More people ought to look at this and understand this side of the story. I was surprised that you’re not more popular given that you definitely possess the gift.
My brother suggested I might like this web site. He was once totally right. This publish actually made my day. You can not imagine just how much time I had spent for this info! Thanks!
Thanks for expressing your ideas. I might also like to convey that video games have been ever before evolving. Modern tools and revolutions have aided create authentic and interactive games. These kind of entertainment video games were not actually sensible when the real concept was first of all being experimented with. Just like other areas of technologies, video games way too have had to develop by means of many many years. This itself is testimony towards fast continuing development of video games.
Very good info. Lucky me I found your site by chance (stumbleupon). I have bookmarked it for later.
I fully agree with this. I recently read a post on https://taivua88.uk.com/ that explored the same issue, and the perspectives shared there were really eye-opening.
Hi there would you mind letting me know which web host you’re using? I’ve loaded your blog in 3 completely different browsers and I must say this blog loads a lot faster then most. Can you recommend a good web hosting provider at a reasonable price? Thank you, I appreciate it!
I think this is a very valid point. I read a similar article on Lode88 that provides more context on this, and it helped me think about it from a different angle.
Absolutely, this perspective makes a lot of sense. It’s similar to what I read a while ago on https://nhacaisoc88.vip/, and it helped me understand the issue much better.
Автор подходит к этому вопросу с нейтральной позицией, предоставляя достаточно информации для обсуждения.
Автор хорошо подготовился к теме и представил разнообразные факты.
Our free written estimates stay locked for a whole year, giving you breathing room to plan without worrying about surprise price jumps in materials. Local building codes here in Pierce County require you to manage runoff responsibly, so a properly sloped gutter system keeps foundations safe and neighbors happy. Roll‑forming gutters right in your driveway means each section is one continuous piece—no leaky joints, no wasted metal, no compromises on quality.
Thanks for posting. It’s excellent.
Автор старается сохранить нейтральность, чтобы читатели могли сформировать свое собственное понимание представленной информации.
More articles like this would make the internet more useful.
Надеюсь, что эти дополнительные комментарии принесут ещё больше позитивных отзывов на информационную статью!
I really liked the approach this was explained.
I like the helpful info you provide in your articles. I will bookmark your weblog and check again here frequently. I’m quite sure I’ll learn many new stuff right here! Good luck for the next!
I really liked the style this was explained.
I’ll definitely recommend this.
Ogromny wybór gier hazardowych: Nasze portfolio obejmuje ponad 8500 tytułów od najlepszych dostawców, takich jak Wazdan, Yggdrasil, czy Quickspin, gwarantując rozrywkę na najwyższym poziomie.
My brother recommended I might like this web site. He used to be totally right. This submit truly made my day. You cann’t believe just how much time I had spent for this info! Thanks!
I really valued the way this was laid out.
I discovered useful points from this.
This is such a solid point! I’ve seen similar ideas discussed on nhà cái soc99, and they align perfectly with what you’re saying here. It’s great to see others agree.
You’ve clearly spent time crafting this.
Good post. I learn one thing tougher on different blogs everyday. It is going to always be stimulating to learn content material from different writers and practice a little bit one thing from their store. I?d want to use some with the content material on my weblog whether or not you don?t mind. Natually I?ll provide you with a hyperlink on your internet blog. Thanks for sharing.
I think you’ve made a solid argument, and it’s something I’ve also read about on https://lucky88.rehab. They offer a comprehensive analysis of this subject too.
I think you’re right on the mark here. I came across a similar post on https://sin88n.pro, and it added some great insights that complement your point.
I took away a great deal from this.
Hello are using WordPress for your site platform? I’m new to the blog world but I’m trying to get started and create my own. Do you need any coding expertise to make your own blog? Any help would be really appreciated!
More posts like this would make the internet a better place.
That is very fascinating, You’re an excessively professional blogger. I have joined your feed and look forward to looking for extra of your great post. Additionally, I’ve shared your web site in my social networks!
I acquired more new things on this weight-loss issue. One issue is that good nutrition is very vital whenever dieting. A tremendous reduction in bad foods, sugary foodstuff, fried foods, sweet foods, beef, and bright flour products could possibly be necessary. Keeping wastes harmful bacteria, and toxic compounds may prevent targets for shedding fat. While specific drugs quickly solve the issue, the nasty side effects will not be worth it, they usually never give more than a short-lived solution. It is just a known undeniable fact that 95 of diet plans fail. Thanks for sharing your notions on this site.
It?s actually a cool and helpful piece of information. I?m glad that you shared this useful info with us. Please keep us informed like this. Thanks for sharing.
Having read this I thought it was rather informative. I appreciate you spending some time and energy to put this short article together. I once again find myself spending a lot of time both reading and posting comments. But so what, it was still worthwhile.
Yes, I agree with this view completely. There’s an insightful post on https://hdbet.it.com that covers this very subject, and I think it provides a solid argument to support your point.
You’ve obviously spent time crafting this.
This is very interesting, You are a very skilled blogger. I have joined your feed and look forward to seeking more of your magnificent post. Also, I have shared your web site in my social networks!
I particularly appreciated the way this was laid out.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You obviously know what youre talking about, why throw away your intelligence on just posting videos to your site when you could be giving us something informative to read?
I have recently started a blog, the information you provide on this website has helped me tremendously. Thank you for all of your time & work.
You’ve evidently put in effort.
I am sure this article has touched all the internet people, its really really pleasant post on building up new webpage.
Thanks , I have recently been searching for information about this topic for ages and yours is the greatest I’ve found out so far. But, what in regards to the bottom line? Are you positive concerning the source?
I truly appreciate this post. I?ve been looking everywhere for this! Thank goodness I found it on Bing. You’ve made my day! Thanks again
I have learned some new things through your blog. One other thing I would like to say is the fact that newer laptop or computer os’s have a tendency to allow more memory to use, but they in addition demand more storage simply to run. If one’s computer is not able to handle more memory and the newest program requires that memory space increase, it usually is the time to shop for a new Computer. Thanks
wonderful points altogether, you just gained a new reader. What would you recommend about your post that you made a few days ago? Any positive?
I absolutely valued the manner this was presented.
Greetings! Very useful advice within this article! It’s the little changes that make the biggest changes. Thanks for sharing!
I’m really impressed with your writing talents as well as with the layout for your weblog. Is that this a paid subject matter or did you modify it your self? Either way stay up the excellent high quality writing, it?s rare to peer a great weblog like this one nowadays..
Мне понравился четкий и структурированный стиль изложения в статье.
Статья помогает читателю получить полное представление о проблеме, рассматривая ее с разных сторон.
As I site possessor I believe the content material here is rattling fantastic , appreciate it for your hard work. You should keep it up forever! Best of luck.
A motivating discussion is worth comment. I do think that you need to write more on this topic, it may not be a taboo subject but usually people don’t talk about such issues. To the next! Cheers.
More content pieces like this would make the online space more useful.
I have noticed that credit repair activity should be conducted with techniques. If not, you may find yourself causing harm to your standing. In order to succeed in fixing to your credit rating you have to make sure that from this moment you pay your complete monthly expenses promptly prior to their planned date. It’s really significant on the grounds that by certainly not accomplishing that, all other methods that you will choose to adopt to improve your credit standing will not be useful. Thanks for expressing your ideas.
Woah! I’m really digging the template/theme of this website. It’s simple, yet effective. A lot of times it’s very hard to get that “perfect balance” between user friendliness and visual appearance. I must say you’ve done a awesome job with this. Additionally, the blog loads extremely fast for me on Chrome. Superb Blog!
Hello there, I think your blog could possibly be having browser compatibility issues. When I look at your website in Safari, it looks fine however, when opening in IE, it’s got some overlapping issues. I just wanted to give you a quick heads up! Aside from that, wonderful website.
Pretty! This was an incredibly wonderful post. Thanks for providing this info.
One thing I’d really like to say is that often before acquiring more computer system memory, take a look at the machine in to which it could well be installed. When the machine is usually running Windows XP, for instance, the actual memory ceiling is 3.25GB. Applying over this would simply constitute just a waste. Make sure one’s motherboard can handle an upgrade quantity, as well. Interesting blog post.
whoah this blog is great i love reading your articles. Keep up the good work! You know, many people are hunting around for this info, you could aid them greatly.
I think you’re right on the mark here. I came across a similar post on Bong88, and it added some great insights that complement your point.
I couldn’t agree more with your viewpoint. I also came across a well-written article on 8Day that elaborates on this exact issue, and it helped me gain new insights.
cheap clomid prices can i buy generic clomiphene how to get clomiphene no prescription generic clomiphene for sale where buy generic clomiphene cost of cheap clomiphene without rx can i buy generic clomiphene
I completely agree with your thoughts on this. I read something very similar on Dafabet, and the detailed analysis there helped me understand the matter better.
Such a valuable insight.
Thanks for creating this. It’s brilliant work.
The next time I read a blog, I hope that it doesn’t disappoint me as much as this one. I mean, Yes, it was my choice to read, but I actually believed you’d have something interesting to talk about. All I hear is a bunch of complaining about something that you could possibly fix if you were not too busy seeking attention.
Автор предлагает аргументы, подтвержденные достоверными источниками, чтобы убедить читателя в своих утверждениях.
Автор статьи представляет информацию без предвзятости, предоставляя различные точки зрения и факты.
Статья содержит полезную информацию, которая может быть полезной для практического применения.
excellent points altogether, you just gained a new reader. What would you suggest about your post that you made some days ago? Any positive?
I took away a great deal from this.
Aw, this was a really good post. Taking the time and actual effort to create a really good article… but what can I say… I put things off a whole lot and never seem to get anything done.
A.i driven god level digital marketing agency delhi
The next time I read a blog, I hope that it doesn’t fail me just as much as this one. After all, I know it was my choice to read through, but I truly thought you’d have something helpful to talk about. All I hear is a bunch of complaining about something that you can fix if you weren’t too busy seeking attention.
A.i driven god level digital marketing agency delhi
I’m not sure why but this site is loading incredibly slow for me. Is anyone else having this problem or is it a issue on my end? I’ll check back later and see if the problem still exists.
An intriguing discussion is definitely worth comment. I do believe that you ought to publish more on this issue, it might not be a taboo subject but generally folks don’t speak about such issues. To the next! Best wishes.
This article is insightful.
An outstanding share! I have just forwarded this onto a friend who has been conducting a little research on this. And he in fact bought me dinner simply because I stumbled upon it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending time to talk about this topic here on your site.
More content pieces like this would make the online space richer.
Thanks for the suggestions shared in your blog. Something also important I would like to mention is that fat reduction is not about going on a fad diet and trying to get rid of as much weight as you’re able in a few months. The most effective way to lose weight is by using it little by little and following some basic guidelines which can enable you to make the most from a attempt to lose weight. You may learn and already be following most of these tips, however reinforcing information never does any damage.
Thanks for your content. One other thing is when you are selling your property yourself, one of the problems you need to be alert to upfront is how to deal with household inspection reports. As a FSBO supplier, the key to successfully shifting your property plus saving money with real estate agent commissions is know-how. The more you realize, the simpler your property sales effort might be. One area in which this is particularly essential is information about home inspections.
The depth in this write-up is remarkable.
Excellent web site you’ve got here.. It’s difficult to find quality writing like yours nowadays. I seriously appreciate people like you! Take care!!
This is very interesting, You are a very skilled blogger. I have joined your rss feed and look forward to seeking more of your magnificent post. Also, I have shared your site in my social networks!
This is the kind of glad I get high on reading.
More content pieces like this would make the blogosphere more useful.
This is a great tip especially to those fresh to the blogosphere. Short but very precise information… Thank you for sharing this one. A must read post!
I think other site proprietors should take this website as an model, very clean and wonderful user genial style and design, let alone the content. You are an expert in this topic!
I have acquired some new elements from your web-site about pc’s. Another thing I’ve always believed is that computers have become a specific thing that each family must have for many reasons. They provide convenient ways in which to organize the home, pay bills, search for information, study, pay attention to music and in some cases watch tv shows. An innovative solution to complete these types of tasks is a mobile computer. These computers are portable ones, small, highly effective and mobile.
Sweet blog! I found it while surfing around on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Many thanks
Thanks for the thoughts you are giving on this blog. Another thing I’d really like to say is that getting hold of copies of your credit score in order to check accuracy of the detail would be the first measures you have to perform in credit score improvement. You are looking to clear your credit profile from destructive details faults that wreck your credit score.
More text pieces like this would make the web better.
Admiring the time and energy you put into your website and detailed information you offer. It’s nice to come across a blog every once in a while that isn’t the same out of date rehashed material. Excellent read! I’ve saved your site and I’m including your RSS feeds to my Google account.
Spot on with this write-up, I absolutely believe this website needs much more attention. I’ll probably be back again to see more, thanks for the advice.
Your style is very unique compared to other people I have read stuff from. Many thanks for posting when you’ve got the opportunity, Guess I will just book mark this web site.
Thought-provoking read. I’ll definitely share this with others.
I’m not sure exactly why but this website is loading extremely slow for me. Is anyone else having this problem or is it a issue on my end? I’ll check back later and see if the problem still exists.
Great post! Can you elaborate on this part?
Hurrah! In the end I got a blog from where I be able to really get valuable information regarding my study and knowledge.
Very nice post. I simply stumbled upon your blog and wanted to say that I’ve really enjoyed browsing your blog posts. In any case I will be subscribing to your rss feed and I am hoping you write once more very soon!
order zithromax 250mg online – buy zithromax tablets buy generic flagyl over the counter
Thank you for sharing your info. I really appreciate your efforts and I will be waiting for your next post thanks once again.
I hadn’t considered that angle before. This really made me think.
Hi there, just became aware of your blog through Google, and found that it is really informative. I’m going to watch out for brussels. I will appreciate if you continue this in future. Many people will be benefited from your writing. Cheers!
Good blog post. What I would like to add is that laptop or computer memory should be purchased if your computer cannot cope with that which you do along with it. One can put in two good old ram boards having 1GB each, in particular, but not certainly one of 1GB and one with 2GB. One should check the maker’s documentation for one’s PC to ensure what type of ram is necessary.
I?d should check with you here. Which is not something I usually do! I take pleasure in reading a put up that may make folks think. Additionally, thanks for allowing me to comment!
This article is great. I gained plenty from perusing it. The content is extremely enlightening and arranged.
Good post but I was wanting to know if you could write a litte more on this topic? I’d be very thankful if you could elaborate a little bit more. Appreciate it!
semaglutide 14 mg usa – rybelsus 14mg canada periactin 4mg drug
Really insightful. Keep up the good work.
I just added this site to my feed reader, excellent stuff. Can not get enough!
Really enjoyed this post. It gave a lot of helpful insights. Excellent effort on writing this.
I completely agree with your reasoning here. It’s very similar to a point I came across on sunwin, which helped me gain more clarity on the issue.
domperidone cheap – buy generic motilium online order flexeril 15mg sale
Fantastic product! Highly recommend with the usability.
Spot on with this write-up, I absolutely feel this site needs a great deal more attention. I’ll probably be returning to see more, thanks for the info!
purchase inderal – plavix order online methotrexate online order
Chegou antes do prazo. Ótima qualidade.
Entrega super rápida. Produto maravilhoso.
Hmm is anyone else experiencing problems with the pictures on this blog loading? I’m trying to find out if its a problem on my end or if it’s the blog. Any feedback would be greatly appreciated.
Я ценю информативный подход этой статьи. Она предоставляет достаточно фактов и данных для лучшего понимания проблемы. Хотелось бы увидеть больше ссылок на исследования и источники информации.
Автор старается представить информацию объективно и позволяет читателям самостоятельно сделать выводы.
Very great post. I just stumbled upon your weblog and wished to say that I’ve really enjoyed surfing around your blog posts. After all I?ll be subscribing to your rss feed and I am hoping you write again soon!
Статья предоставляет информацию из разных источников, обеспечивая балансированное представление фактов и аргументов.
Это помогает читателям получить полную картину и сделать собственные выводы.
purchase amoxicillin generic – purchase combivent for sale buy combivent 100mcg for sale
Мне понравилась глубина исследования, проведенного автором, для подкрепления своих утверждений.
I couldn’t agree more with your perspective. I’ve seen articles on https://manclub1.fun/ that also explain this concept in depth, which I think is really helpful.
You’re absolutely right, I completely agree with your perspective. I found similar discussions on won88, which provided a lot of insight into this topic.
I agree with this viewpoint completely. I’ve also read a similar analysis on m8win, and I think it adds valuable insights to this ongoing conversation.
I agree with this viewpoint completely. I’ve also read a similar analysis on asia99, and I think it adds valuable insights to this ongoing conversation.
Great information. Lucky me I ran across your site by chance (stumbleupon). I’ve book marked it for later.
Can I just say what a relief to uncover an individual who truly knows what they are discussing on the web. You definitely realize how to bring an issue to light and make it important. A lot more people ought to read this and understand this side of your story. It’s surprising you’re not more popular given that you most certainly possess the gift.
Hello! Someone in my Myspace group shared this website with us so I came to take a look. I’m definitely loving the information. I’m book-marking and will be tweeting this to my followers! Superb blog and brilliant design and style.
Your argument really resonates with me, and it’s one that I recently came across in a post on Xeng88. The insights shared there helped solidify my understanding of this topic.
I couldn’t agree more with this comment. It reflects a perspective I’ve seen before in various discussions on nhà cái vibet, which offers some great insights into this matter.
I completely agree with your thoughts on this. I read something very similar on Soc99, and the detailed analysis there helped me understand the matter better.
I completely agree with this. There’s an article on https://communistleague.org/ that covers the same topic and provides additional context that supports your perspective.
This blog is such a hidden gem I stumbled upon it by chance and now I’m completely hooked!
buy zithromax 250mg generic – buy bystolic cheap bystolic uk
Yes, I think this is absolutely right. There’s an article I came across on zubet that explores a similar issue in detail, and it gave me a broader perspective on the topic.
I couldn’t agree more with your perspective. I’ve seen articles on du88 that also explain this concept in depth, which I think is really helpful.
I’ve learned many important things through your post. I might also like to mention that there may be situation that you will make application for a loan and don’t need a co-signer such as a Government Student Aid Loan. In case you are getting credit through a conventional loan provider then you need to be ready to have a co-signer ready to help you. The lenders will base their very own decision over a few elements but the most significant will be your credit rating. There are some lenders that will likewise look at your work history and make a decision based on that but in many cases it will hinge on your report.
Hello! Do you use Twitter? I’d like to follow you if that would be ok. I’m definitely enjoying your blog and look forward to new updates.
hello there and thank you for your info – I’ve definitely picked up anything new from right here. I did however expertise a few technical points using this website, since I experienced to reload the web site many times previous to I could get it to load correctly. I had been wondering if your hosting is OK? Not that I’m complaining, but sluggish loading instances times will often affect your placement in google and could damage your high-quality score if advertising and marketing with Adwords. Well I am adding this RSS to my e-mail and can look out for much more of your respective intriguing content. Make sure you update this again very soon.
I completely agree with this. This is something I read about in an article on fm88, which explored the same issue with a lot of depth and perspective.
I completely agree with this viewpoint, it’s very well thought out. I recently read an article that explores similar ideas on leo88, and I think it adds more depth to the discussion.
I?ve been exploring for a little bit for any high quality articles or weblog posts in this kind of house . Exploring in Yahoo I at last stumbled upon this web site. Reading this info So i am satisfied to exhibit that I have a very excellent uncanny feeling I discovered exactly what I needed. I so much undoubtedly will make certain to don?t fail to remember this site and provides it a glance on a constant basis.
http://www.arttree.com.au is Australia Popular Online Art Store. We sell Canvas Prints & Handmade Canvas Oil Paintings. We Offer Up-to 70 Percent OFF Discount and FREE Delivery Australia, Sydney, Melbourne, Brisbane, Adelaide, Hobart and all regional areas.
cheap clavulanate – atbioinfo acillin pill
I think you’re absolutely right. I found a similar viewpoint on https://communistleague.org/, and their analysis gave me a lot to think about.
If you wish for to increase your knowledge simply keep visiting this web site and be updated with the latest information posted here.
I think you’ve made a solid argument, and it’s something I’ve also read about on pkbet. They offer a comprehensive analysis of this subject too.
F*ckin? awesome things here. I am very glad to see your article. Thanks a lot and i am looking forward to contact you. Will you kindly drop me a e-mail?
I fully agree with your statement. I recently came across a post on 78win that covered this topic in detail, and I believe their perspective aligns well with yours.
What’s up to every body, it’s my first visit of this weblog; this webpage includes amazing and in fact excellent stuff designed for visitors.
I just couldn’t depart your web site prior to suggesting that I extremely loved the usual info a person supply on your guests? Is going to be again continuously to investigate cross-check new posts
Аргументы в статье представлены объективно и нейтрально.
nexium 40mg usa – anexa mate esomeprazole capsules
Magnificent beat ! I wish to apprentice while you amend your site, how could i subscribe for a weblog web site? The account helped me a appropriate deal. I were tiny bit acquainted of this your broadcast offered brilliant clear idea
check out https://s3.amazonaws.com/photovoltaik-buchloe/unlocking-the-secrets-of-photovoltaik-buchloe-a-complete-guide.html
warfarin pill – https://coumamide.com/ buy cozaar generic
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get bought an nervousness over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly very often inside case you shield this increase.
I completely agree with this perspective. There’s an in-depth post on soc99 that elaborates on the same topic, offering useful points to support your view.
This is exactly what I needed to read today Your words have provided me with much-needed reassurance and comfort
mobic online – tenderness buy mobic paypal
Thank you for always being open and honest with your readers It’s refreshing to see a blogger who is unafraid to be vulnerable and real
Thank you for sharing excellent informations. Your web-site is so cool. I’m impressed by the details that you?ve on this site. It reveals how nicely you perceive this subject. Bookmarked this website page, will come back for extra articles. You, my friend, ROCK! I found just the info I already searched all over the place and simply couldn’t come across. What a perfect site.
Hey there, You’ve done an excellent job. I?ll certainly digg it and personally suggest to my friends. I’m sure they’ll be benefited from this web site.
I appreciate the effort that goes into creating high-quality content, and this post was no exception. The insights and information were top-notch and made for a really engaging read. Keep up the great work!
What an eye-opening and meticulously-researched article! The author’s thoroughness and capability to present intricate ideas in a understandable manner is truly praiseworthy. I’m totally enthralled by the depth of knowledge showcased in this piece. Thank you, author, for offering your knowledge with us. This article has been a game-changer!