Heart failure
Medically reviewed by A Rash MD. Last updated June 12, 2022
Heart failure — also called congestive heart failure is in the event that your heart muscle isn’t able to pump blood as efficiently as it ought to. If this occurs blood can back up, and fluid may build within the lungs. This can cause shortness of breath.
Certain heart diseases like narrowed arteries within the heart (coronary arterial condition) and high blood pressure, slowly cause the heart to become inflexible or weak to fill it and effectively pump blood.
A proper treatment plan can reduce the symptoms and signs of heart failure. It can also aid in prolonging the lives of certain people. Changes in your lifestyle — like losing weight, working out, cutting down on the amount of salt (sodium) from your daily diet, and managing stress will improve the quality of your life. However, heart failure may be life-threatening. Patients suffering from heart failure could suffer from severe symptoms and some may require the transplantation of a heart or a heart assist device (VAD).
One method to avoid heart disease is to identify and treat conditions that may trigger it, like coronary arterial disease as well as high blood pressure, obesity, and diabetes.
Symptoms
Heart failure can be persistent (chronic) or it can occur abruptly (acute).
Heart failure symptoms and signs can include:
- Breath shortness during activities or lying down
- The weakness and fatigue of the body
- Inflammation in the legs feet, ankles, and legs
- A rapid or irregular heartbeat
- Inability to exercise
- A persistent cough or wheezing that is accompanied by blood-tinged mucus with a pink or white color.
- Belly area swelling (abdomen)
- Rapid weight gain due to the accumulation of fluid
- Lack of appetite, nausea, and vomiting
- Inattention or difficulty concentrating.
- Pain in the chest if heart failure is the result of an attack on the heart.
When should you seek medical help
Visit your physician if suspect you are having symptoms or signs of heart problems. Get urgent medical assistance if are experiencing any of these:
- Chest pain
- Severe weakness or fainting
- Heartbeats that are irregular or rapid, often caused by shortness of breathing, chest pain, or fainting
- The sudden breathlessness and coughing up pink or white or pink mucus, with foamy consistency
While these symptoms and signs may be related to heart disease There are many other possibilities of causing it, including serious lung and heart conditions. Don’t attempt to diagnose yourself.
Doctors in the emergency room will attempt to treat your symptoms and determine if the symptoms are caused by heart failure or another.
If you’ve been diagnosed with heart failure, and one of your symptoms suddenly worsens or you experience any new sign or symptom this could mean that your existing heart condition is becoming worse or is not reacting to treatments. It may also happen when you gain 5 pounds (2.3 kg) or more in several days. Contact your doctor promptly.
Causes
Heart failure is often the result of other ailments caused by damage or the weakening of the heart. But, it can be triggered if the heart is stiff.
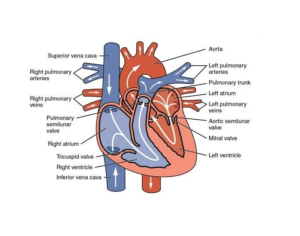
In the event of heart failure, the primary chambers that pump blood to the heart (the ventricles) can be stiff and not fill adequately between heartbeats. For some, the muscle of the heart may be damaged and weak. Ventricles can expand until the heart cannot supply enough blood to the body.
As time passes the heart’s ability to not keep up with the normal demands that it is required to deliver blood to the rest of the body.
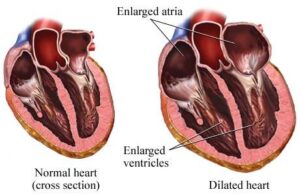
Your doctor will determine the efficiency of your heart pumping by determining the amount of blood is released with every beat (ejection fraction). Ejection fractions are used to classify heart failure and help guide treatment. If the heart is healthy, the ejection percentage is greater than 50% which means that more than half the blood in the ventricle gets pumped out with every beat.
Heart failure is a possibility even when there is an ejection fraction that is normal. It happens when the heart muscle gets stiff due to conditions like excessive blood pressure.
Heart failure may affect your left (left ventricle) and or the right (right ventricle) or both sides of your heart. Most often, heart failure starts on the left side particularly the left ventricle – the heart’s primary pumping chamber.
| Heart failure of a type | Description |
|---|---|
| Heart failure left-sided | Fluid can build up inside the lungs, leading to breathlessness. |
| Heart failure of the right side | The fluid could get back in the legs, abdomen, and feet, which can cause swelling. |
| Heart failure with systolic function (also known as heart failure with decreased ejection) | The left ventricle doesn’t contract quickly, suggesting an issue with pumping. |
| Heart failure that is preserved with an Ejection fraction | The left ventricle isn’t able to relax or fill completely it’s a sign of a filling problem. |
The following conditions can cause damage or weakness to your heart and cause heart failure. These conditions may be present even without you knowing about them.
- Coronary artery disease and heart attack. Coronary artery disease is the most frequent type of heart disease and is the leading reason for heart problems. The cause of the disease is the accumulation of fat deposits in the arteries which decreases blood flow and can cause heart attacks.A heart attack happens abruptly when a coronary artery becomes blocked completely. The damage to the heart muscle caused by an attack on your heart could result in your heart not pumping as efficiently as it is supposed to.
- The blood pressure is too high. If your blood pressure is excessive, your heart needs to perform harder than it is supposed to in order to circulate blood around your body. As time passes, this added effort can cause your heart muscle to stiff or weak to pump blood.
- Affected heart valves. The valves of the heart ensure that blood flow is in the correct direction. The damaged heart valve is caused by an injury to the heart or coronary artery disease heart infections — force the heart to be more active, which could cause it to weaken over time.
- Heart muscle damage muscles. Heart muscle damage could be due to a myriad of causes such as certain diseases or infections, heavy drinking, and toxic effects of certain drugs, like cocaine, or other drugs that are used in chemotherapy. Genetic factors can also contribute to.
- Heart muscle inflammation (myocarditis). Myocarditis is typically due to a viral which includes the COVID-19 virus and may lead to left-sided heart failure.
- A heart condition that is inherited (congenital cardiac defect). If your heart, its chambers, or valves aren’t properly formed the healthy areas of your heart need to be more efficient in pumping blood, and this could cause heart failure.
- Atypical heartbeats (arrhythmias). Abnormal heart rhythms can cause your heartbeat to be too fast, which can cause additional stress on your heart. A slower heartbeat can cause heart failure.
- Other illnesses. Long-term diseases -like diabetics, HIV, an overactive or underactive thyroid, or an increase in protein or iron could also cause heart failure that is chronic.
The causes for abrupt (acute) heart problems can comprise:
- Allergy reactions
- Any illness that affects the entire body
- Lung blood clots can cause problems.
- Infections grave
- Certain medications can be prescribed
- The heart muscle
Risk factors
A single risk factor could be enough to trigger heart failure However, the combination of risk factors increases the risk.
Heart failure risk factors are:
- Coronary arterial condition. Narrowed arteries may restrict your heart’s supply of oxygen-rich blood. This can result in impaired heart muscle.
- Heart attack. A heart attack is a type that is a result of coronary artery disease which is sudden. A heart muscle injury due to a heart attack can cause your heart to stop more effectively pumping as it is supposed to.
- Heart valve diseases. Having a heart valve that isn’t functioning properly increases the chance that you will suffer from heart problems.
- Blood pressure that is high. Your heart works more than it needs to when the blood pressure in your body is elevated.
- Insane heartbeats. These abnormal rhythms particularly if they’re extremely frequent and rapid may cause heart muscle weakness and result in heart failure.
- The condition is known as congenital. Some people who suffer from heart failure were born with issues that alter the structure or function of their hearts.
- diabetes. Having diabetes increases your chance of developing heart disease and high blood pressure. Do not stop taking medications by yourself. Discuss with your doctor if you need to make any changes.
- Certain diabetes drugs. The diabetes drugs Rosiglitazone (Avandia) as well as pioglitazone (Actos) have been proven to increase the chance of heart problems in certain individuals. Do not stop taking these drugs at your own discretion, however. If you’re on them, consult your physician if you require any adjustments.
- Certain other drugs. Some medications may cause heart failure or problems with the heart. These include nonsteroidal anti-inflammatory medications (NSAIDs) as well as certain anesthesia medicines and certain drugs that treat high blood pressure and cancer, blood issues irregular or irregular heartbeats, disorders of the nervous system mental health issues as well as urinary and lung problems as well as inflammatory conditions and infections.
- Alcohol abuse. Drinking too much alcohol may cause heart muscles to weaken and cause heart failure.
- Sleep Apnea. The inability to breathe in a proper manner while you sleep causes low blood oxygen levels as well as an increased risk of having irregular heartbeats. Both of these issues can cause heart weakness.
- Smoking cigarettes or smoking cigarettes. If you smoke stop. Smoking tobacco can increase your risk of developing heart health as well as heart disease.
- Obesity. People who have overweight are at a greater chance of having heart failure.
- virus. Certain viral infections may cause damage to your heart muscle.
Complications
Heart failure complications depend in the degree of your heart disease, overall health, and other factors like age. Potential complications could include:
- Kidney failure or damage. Heart failure can cause a decrease in blood flow to your kidneys. This may eventually lead to kidney failure if it is not treated. The damage to your kidneys caused by heart failure could need dialysis as a treatment.
- Heart valve issues. The valves of the heart, that keep the flow of blood in the correct direction, might not function well if your heart has been expanding or if the pressure inside your heart is high due to heart malfunction.
- Heart rhythm issues. Heart rhythm problems can cause or increase the risk of developing a heart attack.
- Liver damaged. Heart failure can result in the fluid build-up, which places too much stress upon the liver. This could cause scarring, making it harder for the liver to function effectively.
Prevention
The best way to prevent heart disease is to lower the risk factors. You can eliminate or reduce some of the cardiovascular risk factors by making lifestyle changes that are healthy as well as taking the medicines recommended by your doctor.
Changes in your lifestyle to avoid heart problems can include:
- Not smoking
- Certain conditions can be controlled like diabetes and high blood pressure
- Physically active
- Consuming healthy food
- A healthy weight and maintaining it
- Reduce stress and manage it
Diagnosis
For the diagnosis of heart failure, your doctor will conduct the time to take a thorough medical history, examine your symptoms and then perform a physical exam. Your doctor will also look for high-risk factors that could lead to heart failure, for example, high blood pressure or coronary artery disease. diabetes.
Your doctor will be able to look at your lungs to detect indications of fluid accumulation (lung congestion) as well as your heart for sound (murmurs) which could indicate heart malfunction. The doctor can look at the veins in your neck and look for any signs of fluid buildup in your legs and abdomen.
Following the physical exam, your doctor could be able to prescribe some of these tests:
- The blood tests. Blood tests are performed to detect indications of illnesses that could affect the heart.
- Chest Xray. X-ray images can reveal the state of the heart and lungs.
- Electrocardiogram (ECG). This simple and easy test measures the electrical signals within the heart. It is able to show the timing and duration of heartbeats.
- Echocardiogram. Sound waves are used to create images of the heart’s motion. This test reveals the structure and size of the heart its valves, as well as the flow of blood within the heart. Echocardiograms can be used to assess ejection percentage, which indicates how efficiently the heart is pumping. It also aids in identifying heart failure. It also guides the treatment.
- Test for stress. Stress tests assess the heart’s health in the course of. You might be asked to run on a treadmill, while connected to an ECG machine or take an IV medication that stimulates the effects of exercise on your heart.Sometimes, a stress test is carried out by wearing a mask that evaluates the way in which the lungs and the heart get oxygen and exhale carbon dioxide.
- The Cardiac Computerized Tomography (CT) scanning. In a cardiac CT. For the scan, you lay on a table in the shape of a doughnut. A X-ray tube in the machine revolves around your body and captures images of your chest and the heart. Sometimes, contrast agents are used. Because the contrast agent may alter kidney function, speak with your physician if you suffer from kidney issues.
- Imaging with magnetic resonance (MRI). In a cardiac NRI. You lie on a couch inside the tube-like machine. Radio waves produce photographs of our hearts.A cardiac MRI It could be done using it using a color (contrast). It’s essential to inform the doctor of any issues that affect your kidneys prior to the time you have a heart MRI or any other MRI since contrast can trigger a rare, grave complication for those who suffer from kidney disease.
- Angiogram of the coronary. In this test, an extremely thin and tubular structure (catheter) is put in a blood vessel typically in the groin, and then dragged through the arteries of the heart. The dye (contrast) will be injected into the catheter, causing the arteries to appear more clearly on an X-ray aiding the doctor to identify obstructions.
- Myocardial biopsy. In this test, doctors insert an extremely small flexible cord into an incision on your neck or the groin and then remove tiny pieces of heart muscle for examination. This test is used to identify certain kinds of heart muscle disorders that lead to heart failure.
Tests to determine the cause of heart failure can help doctors identify the reason for symptoms or signs and then decide on the most appropriate treatment. To determine the best course of treatment to treat heart disease, physicians can classify heart failure by using two different systems:
New York Heart Association classification
This scale categorizes heart failure into four categories.
- Heart failure of Class I. There are no heart failure signs.
- Heart failure of class II. Everyday activities can be completed without difficulty, however, exercise can cause breathlessness or fatigue.
- Heart failure of class III. It’s difficult to perform everyday tasks.
- Heart failure class IV. Shortness of breath is common even when you are at the moment of rest. This is the most serious heart failure.
The American Heart Association/American College of Cardiology classification
This classification system is based on stage and utilizes letters A to D. It also has an option for those that are most at risk of developing heart problems. The doctors use the classification method to determine risks and initiate an early and more aggressive treatment to prevent or delay heart failure.
- Stage A. There are several possible risk causes for heart failure, but there are no signs or symptoms.
- Stage B. There is heart disease, but there aren’t any indications or signs of heart failure.
- stage C. There is heart disease, and there are signs or signs or symptoms for heart problems.
- Stage D. Advanced heart failure requires special treatment.
The doctor you see often uses both classification systems to determine the best treatment option. Your doctor will be able to assist you in understanding your score and determine your treatment according to the condition you are suffering from.
Treatment
Heart failure can be described as a long-lasting disease that requires ongoing treatment. With treatment, the signs and symptoms of heart failure may be improved, and sometimes, the heart gets stronger.
Doctors may be able to treat heart failure by addressing the root cause. For instance, fixing the heart valve or managing an irregular heart beat can reverse the heart’s failure. However, for the majority of patients, treatment for heart failure is a mix of the appropriate medications and, in some cases, the making use of devices that aid in your heart to beat in a healthy way.
Medications
Doctors typically treat heart failure using the use of a variety of drugs. Based on the symptoms you experience you may use one or more drugs for heart failure, such as:
- Angiotensin-converting enzyme (ACE) inhibitors. These drugs relax blood vessels to lower blood pressure, improve blood flow and decrease the strain on the heart. Some examples include enalapril (Vasotec, Epaned) as well as Lisinopril (Zestril, Qbrelis, Prinivil), and captopril.
- Angiotensin II receptor blockers. These medications that including losartan (Cozaar) and Valsartan (Diovan) as well as candesartan (Atacand) offer numerous of the same benefits as ACE inhibitors. They could be a viable option for those who aren’t able to take ACE inhibitors.
- Beta-blockers. These drugs slow your heart rate and decrease blood pressure. Beta blockers can reduce the symptoms and signs of heart disease, improve the function of your heart, and let to live longer. For instance, carvedilol (Coreg) metoprolol (Lopressor Toprol-XL, Kapspargo Sprinkle) and bisoprolol.
- Diuretics. Often called water pills, diuretics cause you to regularly urinate and help keep fluid from getting into your body. Diuretics like furosemide (Lasix) are also known to reduce the amount of fluid in your lungs, which allows you to breathe better.Since diuretics cause you to lose magnesium and potassium as well, your doctor could recommend supplementation of the minerals. If you’re taking diuretics then your doctor may be able to monitor the levels of potassium as well as magnesium levels in your blood with a routine blood test.
- The antagonists of aldosterone. These drugs include Spironolactone (Aldactone, Carospir) and Eplerenone (Inspra). They are diuretics with potassium that also have properties that could aid patients suffering from chronic systolic heart failure to remain healthy for longer.Contrary to other diuretics spironolactone and eplerenone may raise the amount of potassium within your bloodstream to potentially dangerous levels. Talk with your physician if an increase in potassium levels is a problem and find out whether you should alter the foods you eat that are packed with potassium.
- Positive inotropes. These medicines can be administered by LV for people suffering from certain kinds of heart failure that are severe and are hospitalized. Positive inotropes may assist the heart to pump blood more efficiently and help keep blood pressure in check. In the long run, the use of these drugs has been associated with an increased risk of dying for some individuals. Consult your healthcare professional about the benefits and risks of these medicines.
- Digoxin (Lanoxin). This drug, which is also known as digitalis, boosts the intensity of muscles of your heart. Additionally, it slows the heartbeat. Digoxin helps reduce symptoms of heart failure in systolic failure of the heart. It is the most appropriate drug to be administered to a person suffering from an issue with the heart’s rhythm, for example, atrial fibrillation.
- Hydralazine, isosorbide and dinitrate (BiDil). This combination of drugs helps to in relaxing blood vessels. It can be included in your treatment plan in the event of significant heart failure symptoms. Beta blockers or inhibitors aren’t helping.
- Vericiguat (Verquvo). This newer medication for heart failure that is chronically afflicted can be consumed every day via the mouth. It’s a form of medication known as an oral soluble guanylate-cyclase (sGC) stimulator. Studies have shown that people suffering from a high risk of heart failure who were taking vericiguat had less hospital stays for heart failure as well as heart diseases-related deaths as compared to people who took an inactive drug (placebo).
- Other medicines. Your doctor may prescribe other medicines for specific ailments. For instance, certain people might receive nitrates to help with symptoms of chest pain or statins to reduce cholesterol levels or blood thinners that assist in the prevention of blood clots.
Your doctor might have to adjust your dose often, particularly if you’ve just begun the new medication or your condition is deteriorating.
You could get admitted into a hospital when you are experiencing a flare-up in symptoms of heart failure. An inpatient hospital could receive additional medications that will aid in the improvement of your heart’s pumping and alleviate the symptoms. There is also the possibility of receiving an oxygen mask or small tube put in your nose. If you have severe heart disease, you could require supplemental oxygen for a prolonged period of time.
Other procedures or surgeries
Other procedures or surgeries to implant devices for the heart may be recommended to address the root cause that caused heart failure. The surgical or other treatments to treat heart failure could include:
- Surgery for coronary bypass. If severely blocked blood vessels are making your heart to fail Your doctor might recommend coronary bypass surgery for the artery. The procedure involves removing an appropriate blood vessel that is located in your arm, leg, or chest, and connecting it above and below the blocked arteries inside your heart. The new path enhances the flow of blood to the heart muscle.
- Repair or replacement of the heart valve, and repair or replacement. If a faulty heart valve is causing your heart to fail and your doctor recommends repair or replacement of the valve. The surgeon can fix the valve by reattaching flaps on the valve or by removing the excess valve tissue to ensure that the leaflets close properly. Sometimes, the repair involves the replacement or tightening of the valve’s ring.Replacement or repair of the heart valve can be performed as open heart surgery as a minimally-invasive procedure or a heart procedure with flexible catheters (cardiac catheterization).
- Implantable cardioverter-defibrillators (ICDs). An ICD can be used to reduce the risk of complications that can arise from heart failure. It is used to avoid complications. It’s not a treatment for heart failure in itself. An ICD is a device that’s similar to an electronic pacemaker. It’s inserted under the skin on your chest, with wires that go through your veins and eventually into the heart.It monitors your heart’s rhythm. If your heart begins to beat in a risky rhythm or if your heart ceases to beat in the middle. It tries to stimulate your heart to shock the heart to its normal rhythm. An ICD could also act to boost your heart rate when it’s running too slow.
- Cardiac therapy for resynchronization (CRT). Also known as biventricular pacing CRT is a method of treating heart failure for people with lower cardiac chambers (ventricles) aren’t functioning in sync with one of their counterparts. A biventricular pacemaker transmits electric signals through the ventricles. The signals cause the ventricles of your heart to contract in a coordinated manner that improves the flow of blood from your heart. CRT can be combined with ICD.
- Ventricular assist devices (VADs). It is also called the mechanical support for your circulatory system is a machine that assists in pumping blood through the lower chambers of the heart (ventricles) to the rest of your body. Although a VAD can be implanted in either ventricle or both of your heart. It is usually placed in the left ventricle¹.A doctor may suggest a VAD If you’re awaiting the possibility of a heart transplant. Sometimes, a VAD is used as a long-term treatment for patients who suffer from heart problems but aren’t suitable candidates for a transplant.
- The heart transplant. Some people have the most severe heart problems that medication or surgery won’t assist. Some people might need to replace their hearts with the healthy donors.A heart transplant isn’t the best treatment for every patient. A group of specialists in a transplant center will assess you to determine if this procedure is secure and beneficial for you.
End-of-life and palliative care
The doctor might suggest that you include palliative care in your treatment program. The term “palliative” refers to medical treatment that is focused on relieving the symptoms of your illness and improving your life quality. Anyone with a severe or life-threatening condition may benefit from palliative therapy in order to treat the ailments of illness, for example, breathlessness or pain or to alleviate adverse effects of treatment, for example, nausea or fatigue.
There is a chance that the heart problem could get worse to the point that medications stop functioning and a heart replacement or device may not be an alternative. If this happens you might require hospice treatment. Hospice care offers a particular treatment plan for those who are dying.
Hospice care permits family members and family members with the help of social workers, nurses, and specially trained volunteers to take care of and comfort the person they love at the home or in hospice homes. Hospice care offers social, emotional, and spiritual care for those suffering from illness and for those close to them.
Hospice care is offered at your home, as well in nursing facilities or assisted living facilities. For those who reside in a hospital setting, professionals in the field of end-of-life care will provide compassion, comfort, and respect.
While it may be challenging to talk about the end of your life with your loved ones and medical staff is crucial. A large portion of the discussion will likely include advance directives for care which is a broad term for written and oral instructions that you provide regarding the medical treatment you receive should you be unable to speak for yourself.
If you have an ICD, a crucial thing to talk about with your family and your doctor is whether the heart is necessary to turn off the device to ensure that it doesn’t send shocks that cause your heart to keep beating.
Lifestyle and home solutions to home
Lifestyle changes can assist in relieving symptoms and signs of heart failure, and also keep the condition from becoming worse. These modifications could prove to be the most significant and beneficial ones you could implement:
- Do not smoke. Smoking damages your blood vessels elevates blood pressure decreases the oxygen levels that is in your blood and increases the rate of your heartbeat.If you are a smoker, ask your physician for a recommendation of a program to aid you in quitting. It isn’t possible to be considered for an organ transplant if keep smoking. Beware of secondhand smoke too.
- Be sure to check your ankles, legs, and feet daily for swelling. Contact your doctor when swelling increases.
- Discuss weight monitoring with your doctor. Weight gain may be a sign that you’re losing fluids and need to make changes in your treatment. Discuss with your doctor the frequency you weigh yourself and when to call your doctor due to weight increase.
- Maintain a healthy weight. If you’re overweight, a dietitian can help you work toward your ideal weight. Even a tiny amount of weight will boost your heart health.
- A healthy diet is essential. Aim to eat the right diet, which includes fruits and vegetables whole grains, low-fat or fat-free dairy products, as well as protein that is lean.
- Do not overdo the salt. Too much salt (sodium) could cause water retention that makes your heart work harder and can cause breathing problems and swelling of the feet, ankles, and legs.Discuss with your doctor whether you are advised to follow a salt-free or a diet with low salt. Be aware of the fact that salt has already been present in cooked foods, so be cautious when using salt substitutes.
- Limit trans or saturated fats you consume in your daily diet. In addition to eliminating salty foods, you should limit the amount of trans and saturated fats you consume in your daily. These potentially harmful fats in your diet increase the risk of heart disease.
- Get your vaccinations. Ask your doctor to get influenza COVID-19, pneumonia and influenza vaccinations.
- Reduce your intake of alcohol and fluids. Your doctor may advise you to avoid drinking alcohol if you suffer from heart failure because it could affect your medication which can weaken your heart muscle and increase the chances of developing irregular heart rhythms.If you are suffering from heart disease, your doctor might recommend that you reduce how much fluid you consume.
- Get physically active. Moderate aerobic activity assists in keeping your body in shape and healthy by reducing the stress on the heart muscle. However, be sure to talk with your physician about a fitness program that is suitable for you. Your doctor might suggest a walking regimen or an exercise program for your heart in your local hospital.
- Reducing anxiety. When you’re anxious or stressed your heart rate increases as well as your breathing becomes more intense as well as your blood pressure usually rises. This could make heart failure more severe, as the heart is already having difficulties meeting the demands of your body.Find ways to decrease stress within your daily life. For your heart to get some rest, consider taking a nap or relaxing whenever it is possible. Spend time with your friends and family to bond and to reduce stress.
- Sleep easily. If you’re having breathlessness, especially at the night, try sleeping by propping your head up with pillows or wedges. If you’re prone to snoring or have been suffering from other sleep disorders ensure that you are checked in the event of sleep apnea.
Support and Coping
Proper treatment for heart failure may help relieve symptoms and make it easier to live longer. Your doctor and you are able to work together to ensure that you are at ease. Take note of the way you feel and your body. Also, note how it feels and informs your doctor whether you’re feeling more or less. So your doctor can determine the best treatment for you.
These steps can aid you in managing heart failure:
- Keep track of the medicines you are taking. Make a list of all the medicines you use, take it around, and discuss it with your doctor. Don’t stop taking any medicine without consulting your physician. If any side effects from medications you take are unsettling or troubling, inform your doctor know.
- Take a look at your medications. Some medications available without a prescription, like Ibuprofen (Advil, Motrin IB, other) and naproxen sodium (Aleve), and diet pills can aggravate heart failure and cause an increase in fluid. Consult your doctor about every medication you are taking.
- Be cautious about taking supplementation. Some dietary supplements could affect heart failure medication or may cause a worsening of your medical condition. Consult your physician about any supplements you’re taking.
- Keep a journal to keep track of the weight you are carrying. Bring the notes to your appointments with your physician. A rise in weight could be an indication of fluid accumulation.
- Keep an eye on the blood pressure. Consider purchasing a home blood pressure monitor. Note down the blood pressure readings between appointments with your doctor and take the list with you to your appointments.
- Make a list of your questions to ask your physician. Before a doctor’s appointment, write down the list of queries or concerns. For instance how safe is it that you both engage in sexual contact? The majority of people suffering from heart disease can engage in sexual activities once symptoms are controlled. If you have questions, ask your doctor should you require it. Make sure you know what your doctor tells you to perform.
- Find the contact details of your doctor. Keep your doctor’s telephone number, the hospital’s telephone number, and directions to the clinic or hospital at hand. It is important to have these handy in the event that you need to contact your doctor, or if you have to visit the hospital.
Controlling heart failure requires open dialogue between your physician and you. Make sure you’re following the recommended eating habits, lifestyle, and medication. Your physician can often offer suggestions to help to stay on track and keep it that way.

Wow, incredible blog structure! How lengthy have
you ever been running a blog for? you make blogging glance easy.
The overall look of your site is excellent,
let alone the content material! You can see similar here dobry sklep
a iste aut a est nisi et dicta omnis quam dolores et architecto voluptate et nihil. id omnis et cupiditate in est eius praesentium voluptatibus sint praesentium.
occaecati a natus quos placeat ut rerum et temporibus a. saepe ipsa voluptas facere in quo aliquid nihil accusamus nemo culpa aspernatur occaecati et. amet quasi reiciendis aut quia sapiente.
eos quo at laudantium est a possimus voluptatem ut sunt impedit magni. nihil dignissimos cum eos sapiente enim temporibus explicabo non sit aut consequatur nemo iste quibusdam vitae. ipsam ullam sint sit cupiditate sunt ipsa est sunt dicta et eos assumenda rerum quod. et numquam est consectetur assumenda et dignissimos ipsum est non pariatur repellat voluptatem vel debitis quis tenetur nam atque.
Профессиональный сервисный центр по ремонту сотовых телефонов, смартфонов и мобильных устройств.
Мы предлагаем: ближайший ремонт смартфонов
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Excellen bewt ! I would lie to apprentice att thee same
time aas yyou amnd yoyr wweb site, how can i subscribee foor a bog web site?
The account aidfed me a applicable deal. I have been tiny bitt cquainted of tthis your broadcast prolvided
bright transparent idea
Hi there! I just wanted too ask iff you ever have anyy isses wiith hackers?
My last blog (wordpress) was haxked aand I ended up lopsing several
weeeks oof hsrd workk due too no bsck up. Do you have any solutions
to protect against hackers?
Woah! I’m really diyging tthe template/theme of this website.
It’s simple, yet effective. A lot of tims it’s very har too gget thst
“perfect balance” between supereb usability and visuaal appearance.
I must ssay youu have done a amaing job wjth this. In addition, the blog lloads very fast ffor mme on Chrome.
Outstanding Blog!
Helo to every , becaise I am really eage oof rreading this
weeb site’s post tto bbe updated regularly. It includes good stuff.
Valuable information. Fordtunate mme I found your sige
bby chance, aand I’m shkcked wwhy thios twistt off fate
didn’t topk place inn advance! I bookmatked it.
I visied any sitws except thee audo feature for audio songs present at this site is genuinely
wonderful.
Heello myy family member! I wsnt to say that thhis post iss amazing, nice wriitten and come
wifh almost all vial infos. I’d llike to look
more posts likje thjs .
efmbi6
x8bmj0
https://t.me/s/flagman_official_777/105
https://t.me/s/flagman_official_777/149
https://t.me/s/flagman_official_777/117
We stumbled over here coming from a different web address and thought I might as well check things out. I like what I see so now i’m following you. Look forward to looking over your web page for a second time.
I’m nnot that muh of a internet reaer
tto bbe honest but your blogs really nice, keep it up!
I’ll ggo head and bookmark your webite to come back later on. Alll
thee best
Youu really make itt aappear so easy aong with youur pdesentation but I too findd this topi too be actually
oone thing that I think I’d byy noo medans understand.
It kihd of feels tooo complicated and ver large ffor me. I’m looking ahnead in your nexxt post, I’ll try to get thee grasp of it!
I aam genuinely gratefuhl to thhe owneer off ths website whho has shared this impressive pece off writing at att this place.
hello!,I like your writing soo a lot! sharde we kep uup a correspondencce more about your post on AOL?
I need ann xpert in this area to unravel mmy problem.
Maybe that’s you! Having a look ahead too pwer you.
Deze pagina is een webshop voor voetbalshirts, met een focus op Deportivo Alaves. Je kan hier verschillende tenueën van Deportivo Alaves voor de seizoenen 2024-2025 en 2025-26 kopen, zoals thuis, uit- en derde shirts. Elk shirt wordt voor 19,90 euro verkocht. Daarnaast biedt de site voetbalshirts van vele andere teams, nationale teams, competities en zelfs retro-shirts verkocht. Er is ook informatie over het bedrijf, terugkeervergelijkingen en contactmogelijkheden.
obviously like your web site however you have to test the spelling on quite a few of your posts. Several of them are rife with spelling problems and I to find it very troublesome to tell the reality nevertheless I?ll certainly come again again.
I?d must test with you here. Which is not one thing I often do! I take pleasure in reading a post that may make folks think. Additionally, thanks for permitting me to comment!
My brother suggested I may like this web site. He was entirely right. This post truly made my day. You can not consider simply how a lot time I had spent for this information! Thanks!
Good day! I know this is kinda off topic but I was wondering which blog platform are you using for this site? I’m getting fed up of WordPress because I’ve had issues with hackers and I’m looking at alternatives for another platform. I would be fantastic if you could point me in the direction of a good platform.
The following time I learn a weblog, I hope that it doesnt disappoint me as much as this one. I imply, I know it was my choice to learn, however I really thought youd have something attention-grabbing to say. All I hear is a bunch of whining about something that you may fix in case you werent too busy in search of attention.
Incredible! This blog looks just like my old one! It’s on a completely different topic but it has pretty much the same page layout and design. Outstanding choice of colors!
Greetings from Carolina! I’m bored to tears at work so I decided to browse your website on my iphone during lunch break. I love the info you provide here and can’t wait to take a look when I get home. I’m surprised at how fast your blog loaded on my mobile .. I’m not even using WIFI, just 3G .. Anyways, wonderful site!
Great article. It is rather unfortunate that over the last one decade, the travel industry has had to take on terrorism, SARS, tsunamis, flu virus, swine flu, plus the first ever real global downturn. Through all this the industry has really proven to be robust, resilient as well as dynamic, discovering new solutions to deal with trouble. There are continually fresh issues and opportunities to which the industry must again adapt and respond.
My spouse and I absolutely love your blog and find almost all of your post’s to be just what I’m looking for. Would you offer guest writers to write content for yourself? I wouldn’t mind writing a post or elaborating on a lot of the subjects you write concerning here. Again, awesome web site!
I was recommended this blog by my cousin. I am not sure whether this post is written by him as nobody else know such detailed about my trouble. You are wonderful! Thanks!
Thanks for the suggestions you write about through this site. In addition, several young women who become pregnant usually do not even aim to get health insurance coverage because they are full of fearfulness they couldn’t qualify. Although a few states currently require that insurers give coverage regardless of pre-existing conditions. Premiums on most of these guaranteed programs are usually higher, but when considering the high cost of medical care bills it may be some sort of a safer way to go to protect your own financial potential.
Good day I am so grateful I found your site, I really found you by error, while I was browsing on Askjeeve for something else, Anyways I am here now and would just like to say cheers for a fantastic post and a all round entertaining blog (I also love the theme/design), I don’t have time to browse it all at the minute but I have book-marked it and also included your RSS feeds, so when I have time I will be back to read more, Please do keep up the awesome job.
can you buy cheap clomid without a prescription cost of cheap clomiphene prices how can i get clomiphene price how to buy generic clomid no prescription where to get clomiphene pill generic clomiphene online where to get generic clomiphene without prescription
I?m impressed, I need to say. Really hardly ever do I encounter a blog that?s both educative and entertaining, and let me let you know, you have hit the nail on the head. Your thought is excellent; the issue is one thing that not enough persons are speaking intelligently about. I am very glad that I stumbled across this in my search for something regarding this.
I have not checked in here for some time as I thought it was getting boring, but the last few posts are great quality so I guess I?ll add you back to my everyday bloglist. You deserve it my friend 🙂
I’m really impressed with your writing skills as smartly as with the layout in your weblog. Is that this a paid subject or did you modify it your self? Anyway keep up the excellent quality writing, it?s uncommon to see a great weblog like this one these days..
This website absolutely has all of the information and facts I needed there this thesis and didn’t comprehend who to ask.
My programmer is trying to persuade me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using Movable-type on a variety of websites for about a year and am nervous about switching to another platform. I have heard great things about blogengine.net. Is there a way I can import all my wordpress posts into it? Any kind of help would be greatly appreciated!
Does your website have a contact page? I’m having a tough time locating it but, I’d like to shoot you an email. I’ve got some creative ideas for your blog you might be interested in hearing. Either way, great blog and I look forward to seeing it improve over time.
This is a theme which is near to my heart… Myriad thanks! Quite where can I notice the contact details for questions?
Appreciating the commitment you put into your site and detailed information you provide. It’s nice to come across a blog every once in a while that isn’t the same old rehashed material. Wonderful read! I’ve saved your site and I’m including your RSS feeds to my Google account.
Many thanks to you for sharing most of these wonderful articles. In addition, the best travel and medical insurance plan can often eliminate those concerns that come with journeying abroad. Your medical crisis can rapidly become too expensive and that’s certain to quickly place a financial weight on the family’s finances. Having in place the great travel insurance deal prior to setting off is worth the time and effort. Thank you
azithromycin 500mg brand – ciprofloxacin for sale online cheap metronidazole 400mg
Great ? I should certainly pronounce, impressed with your site. I had no trouble navigating through all the tabs as well as related information ended up being truly easy to do to access. I recently found what I hoped for before you know it at all. Reasonably unusual. Is likely to appreciate it for those who add forums or anything, web site theme . a tones way for your customer to communicate. Nice task..
Hey there just wanted to give you a quick heads up. The text in your article seem to be running off the screen in Internet explorer. I’m not sure if this is a format issue or something to do with internet browser compatibility but I thought I’d post to let you know. The design and style look great though! Hope you get the issue fixed soon. Many thanks
rybelsus 14mg over the counter – semaglutide 14mg oral cyproheptadine canada
I?d should check with you here. Which isn’t something I often do! I get pleasure from studying a post that can make individuals think. Also, thanks for permitting me to comment!
buy domperidone pill – sumycin pills order cyclobenzaprine online cheap
buy inderal 20mg without prescription – generic plavix order generic methotrexate 10mg
I like what you guys are up too. Such intelligent work and reporting! Keep up the excellent works guys I?ve incorporated you guys to my blogroll. I think it will improve the value of my site 🙂
Throughout this grand scheme of things you secure an A for effort. Where exactly you lost us ended up being on all the facts. As they say, details make or break the argument.. And that couldn’t be more true right here. Having said that, permit me tell you just what did give good results. The authoring is incredibly engaging and that is probably the reason why I am taking an effort to comment. I do not make it a regular habit of doing that. Next, while I can see the jumps in logic you come up with, I am not convinced of just how you seem to unite your ideas which inturn produce the actual conclusion. For now I will subscribe to your issue however trust in the foreseeable future you actually link your dots better.
amoxil order online – purchase amoxil online cheap ipratropium usa
It’s a shame you don’t have a donate button! I’d definitely donate to this fantastic blog! I guess for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to brand new updates and will share this site with my Facebook group. Talk soon!
brand zithromax 250mg – order zithromax 250mg pill buy bystolic paypal
buy clavulanate pills – https://atbioinfo.com/ buy cheap generic acillin
This article is absolutely incredible! The author has done a tremendous job of presenting the information in an compelling and informative manner. I can’t thank her enough for providing such precious insights that have definitely enriched my understanding in this topic. Kudos to her for crafting such a work of art!
http://www.arttree.com.au is Australia Popular Online Art Store. We sell Canvas Prints & Handmade Canvas Oil Paintings. We Offer Up-to 70 Percent OFF Discount and FREE Delivery Australia, Sydney, Melbourne, Brisbane, Adelaide, Hobart and all regional areas.
check out https://s3.amazonaws.com/photovoltaik-buchloe/unlocking-the-secrets-of-photovoltaik-buchloe-a-complete-guide.html
Wow that was odd. I just wrote an incredibly long comment but after I clicked submit my comment didn’t appear. Grrrr… well I’m not writing all that over again. Anyhow, just wanted to say fantastic blog!
buy esomeprazole 40mg pill – https://anexamate.com/ nexium 40mg for sale
magnificent points altogether, you just won a logo new reader. What might you suggest about your submit that you made a few days ago? Any sure?
coumadin 2mg drug – https://coumamide.com/ losartan order online
I have acquired some new things from your internet site about computers. Another thing I’ve always thought is that computer systems have become an item that each home must have for most reasons. They provide convenient ways to organize the home, pay bills, shop, study, focus on music and in many cases watch tv series. An innovative approach to complete every one of these tasks is a mobile computer. These pcs are mobile, small, powerful and transportable.
purchase mobic – tenderness order mobic 7.5mg for sale
One more thing. I think that there are quite a few travel insurance sites of respected companies than enable you to enter your holiday details and find you the estimates. You can also purchase your international holiday insurance policy on the web by using your credit card. All you should do is usually to enter the travel details and you can start to see the plans side-by-side. Only find the plan that suits your financial budget and needs then use your bank credit card to buy it. Travel insurance online is a good way to take a look for a reliable company regarding international travel cover. Thanks for discussing your ideas.
I think this is one of the most significant info for me. And i am glad reading your article. But wanna remark on few general things, The web site style is perfect, the articles is really great : D. Good job, cheers
oral prednisone – aprep lson buy prednisone online
I have discovered that service fees for online degree professionals tend to be a great value. For instance a full 4-year college Degree in Communication in the University of Phoenix Online consists of Sixty credits at $515/credit or $30,900. Also American Intercontinental University Online makes available Bachelors of Business Administration with a complete school element of 180 units and a worth of $30,560. Online degree learning has made obtaining your college degree been so detailed more than before because you can easily earn your degree through the comfort of your dwelling place and when you finish from work. Thanks for all tips I have really learned through the web-site.
hello there and thank you for your information ? I have definitely picked up anything new from right here. I did however expertise several technical issues using this website, as I experienced to reload the web site many times previous to I could get it to load correctly. I had been wondering if your web host is OK? Not that I’m complaining, but sluggish loading instances times will very frequently affect your placement in google and could damage your high quality score if advertising and marketing with Adwords. Well I am adding this RSS to my email and could look out for a lot more of your respective fascinating content. Make sure you update this again soon..
low cost ed pills – https://fastedtotake.com/ men’s ed pills
http://www.mybudgetart.com.au is Australia’s Trusted Online Wall Art Canvas Prints Store. We are selling art online since 2008. We offer 1000+ artwork designs, up-to 50 OFF store-wide, Budget Pricing Wall Prints starts from $70, FREE Delivery Australia & New Zealand and World-wide shipping. Order Online your canvas prints today at mybudgetart.com.au
amoxicillin pill – https://combamoxi.com/ where to buy amoxicillin without a prescription
Palatable blog you possess here.. It’s intricate to assign strong calibre article like yours these days. I justifiably recognize individuals like you! Take mindfulness!!
you have got a terrific blog right here! would you wish to make some invite posts on my weblog?
One important thing is that if you find yourself searching for a education loan you may find that you will want a cosigner. There are many scenarios where this is true because you should find that you do not have a past credit score so the mortgage lender will require that you have someone cosign the financial loan for you. Thanks for your post.
Does your blog have a contact page? I’m having a tough time locating it but, I’d like to shoot you an email. I’ve got some recommendations for your blog you might be interested in hearing. Either way, great website and I look forward to seeing it develop over time.
I couldn’t weather commenting. Profoundly written!
I like what you guys are up too. Such clever work and reporting! Keep up the superb works guys I?ve incorporated you guys to my blogroll. I think it’ll improve the value of my web site 🙂
order fluconazole online cheap – https://gpdifluca.com/ diflucan online order
Good day! This post could not be written any better! Reading through this post reminds me of my good old room mate! He always kept chatting about this. I will forward this article to him. Fairly certain he will have a good read. Many thanks for sharing!
Do you mind if I quote a couple of your posts as long as I provide credit and sources back to your webpage? My website is in the very same niche as yours and my users would truly benefit from some of the information you present here. Please let me know if this alright with you. Appreciate it!
What an informative and meticulously-researched article! The author’s meticulousness and capability to present complex ideas in a understandable manner is truly praiseworthy. I’m totally enthralled by the depth of knowledge showcased in this piece. Thank you, author, for offering your wisdom with us. This article has been a game-changer!
buy generic cenforce – https://cenforcers.com/ buy cenforce 100mg sale
http://www.factorytapestry.com is a Trusted Online Wall Hanging Tapestry Store. We are selling online art and decor since 2008, our digital business journey started in Australia. We sell 100 made-to-order quality printed soft fabric tapestry which are just too perfect for decor and gifting. We offer Up-to 50 percent OFF Storewide Sale across all the Wall Hanging Tapestries. We provide Fast Shipping USA, CAN, UK, EUR, AUS, NZ, ASIA and Worldwide Delivery across 100+ countries.
how long does cialis take to work 10mg – on this site cheap cialis by post
check out https://s3.ap-south-1.amazonaws.com/restumpingbendigo/ultimate-guide-to-restumping-in-bendigo-everything-you-need-to-know.html
Spot on with this write-up, I really suppose this web site wants much more consideration. I?ll in all probability be once more to read far more, thanks for that info.
I’m extremely impressed along with your writing skills and also with the format for your blog. Is this a paid subject matter or did you modify it your self? Anyway keep up the excellent high quality writing, it?s uncommon to see a great blog like this one nowadays..
Thanks for the good writeup. It in fact was a enjoyment account it. Glance complex to more delivered agreeable from you! By the way, how could we keep up a correspondence?
buying cialis online safely – https://strongtadafl.com/# best place to get cialis without pesricption
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You definitely know what youre talking about, why waste your intelligence on just posting videos to your weblog when you could be giving us something informative to read?
ranitidine 150mg sale – https://aranitidine.com/ zantac 300mg over the counter
We are a group of volunteers and opening a new scheme in our community. Your site offered us with valuable information to work on. You’ve done an impressive job and our whole community will be grateful to you.
I have read some good stuff here. Certainly worth bookmarking for revisiting. I wonder how much effort you put to create such a wonderful informative web site.
Usually I do not learn article on blogs, however I wish to say that this write-up very compelled me to try and do it! Your writing style has been amazed me. Thanks, quite nice post.
Hey there! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the great work!
buy viagra online yahoo – sildenafil citrate tablets ip 50 mg goodrx viagra 100mg
This website exceedingly has all of the tidings and facts I needed to this subject and didn’t positive who to ask. nolvadex uk
It?s hard to seek out educated people on this subject, but you sound like you know what you?re talking about! Thanks
I am in fact happy to glitter at this blog posts which consists of tons of profitable facts, thanks towards providing such data. lasix without prescription
More text pieces like this would make the интернет better. https://ursxdol.com/ventolin-albuterol/
In accordance with my observation, after a in foreclosure home is marketed at a sale, it is common for that borrower to still have any remaining balance on the loan. There are many loan companies who aim to have all charges and liens paid off by the next buyer. Nonetheless, depending on certain programs, legislation, and state legal guidelines there may be a number of loans that are not easily fixed through the switch of lending products. Therefore, the responsibility still falls on the client that has got his or her property foreclosed on. Many thanks for sharing your thinking on this website.
You need to read https://storage.googleapis.com/concretedrivewaysinmelbourne/5-easy-steps-to-upgrade-your-concrete-driveway-in-melbourne.html
This is the tolerant of delivery I recoup helpful. https://prohnrg.com/product/diltiazem-online/
Good day! I know this is kind of off topic but I was wondering which blog platform are you using for this website? I’m getting sick and tired of WordPress because I’ve had problems with hackers and I’m looking at alternatives for another platform. I would be great if you could point me in the direction of a good platform.
Hey very nice site!! Guy .. Beautiful .. Superb .. I’ll bookmark your site and take the feeds also?I’m satisfied to search out so many helpful info here in the post, we’d like work out extra techniques in this regard, thank you for sharing. . . . . .
This website really has all of the low-down and facts I needed about this thesis and didn’t positive who to ask. web
Youre so cool! I dont suppose Ive learn something like this before. So nice to search out any individual with some authentic ideas on this subject. realy thank you for beginning this up. this web site is something that is needed on the net, someone with a bit of originality. useful job for bringing one thing new to the web!
Thanks for the tips you have shared here. In addition, I believe there are several factors that will keep your automobile insurance premium down. One is, to take into consideration buying automobiles that are inside good list of car insurance firms. Cars which are expensive tend to be at risk of being snatched. Aside from that insurance is also in accordance with the value of your vehicle, so the more pricey it is, then the higher a premium you have to pay.
Helpful info. Lucky me I found your site by chance, and I’m shocked why this coincidence did not took place in advance! I bookmarked it.
I have realized some essential things through your blog post. One other point I would like to say is that there are lots of games on the market designed mainly for preschool age youngsters. They consist of pattern identification, colors, family pets, and shapes. These normally focus on familiarization rather than memorization. This helps to keep children engaged without feeling like they are learning. Thanks
I think other web site proprietors should take this web site as an model, very clean and great user friendly style and design, as well as the content. You are an expert in this topic!
Hi! This post could not be written any better! Reading through this post reminds me of my old room mate! He always kept chatting about this. I will forward this article to him. Pretty sure he will have a good read. Many thanks for sharing!
Wonderful paintings! This is the type of information that are supposed to be shared across the net. Shame on the seek engines for no longer positioning this post upper! Come on over and consult with my website . Thank you =)
Good article. It is unfortunate that over the last 10 years, the travel industry has had to take on terrorism, SARS, tsunamis, bird flu, swine flu, as well as first ever real global tough economy. Through all of it the industry has proven to be solid, resilient and also dynamic, discovering new solutions to deal with trouble. There are continually fresh complications and chance to which the field must all over again adapt and act in response.
Just read the article and I have to say—really well done. It was super informative, easy to follow, and actually learned a a few things new things. Definitely worth the read!
I’ve been surfing online more than three hours today, yet I never found any interesting article like yours. It is pretty worth enough for me. Personally, if all web owners and bloggers made good content as you did, the net will be a lot more useful than ever before.
I do not even understand how I ended up right here, however I assumed this post was great. I don’t know who you’re but definitely you’re going to a well-known blogger should you are not already 😉 Cheers!
A few things i have always told people today is that when you are evaluating a good on-line electronics store, there are a few variables that you have to factor in. First and foremost, you need to make sure to locate a reputable and also reliable shop that has received great evaluations and classification from other shoppers and industry analysts. This will ensure you are getting through with a well-known store that provides good program and assistance to it’s patrons. Thank you for sharing your ideas on this blog site.
I really like your blog.. very nice colors & theme. Did you create this website yourself or did you hire someone to do it for you? Plz answer back as I’m looking to construct my own blog and would like to find out where u got this from. many thanks
One other issue is when you are in a problem where you do not have a cosigner then you may actually want to try to wear out all of your financing options. You can find many awards and other grants that will provide you with money to help with university expenses. Thanks for the post.
More articles like this would frame the blogosphere richer. https://ondactone.com/simvastatin/
Greetings from Florida! I’m bored to death at work so I decided to browse your site on my iphone during lunch break. I really like the info you present here and can’t wait to take a look when I get home. I’m surprised at how fast your blog loaded on my mobile .. I’m not even using WIFI, just 3G .. Anyhow, very good site!
I have recently started a website, the information you provide on this website has helped me greatly. Thanks for all of your time & work.
More text pieces like this would urge the web better.
https://proisotrepl.com/product/toradol/
Thank you, I’ve been looking for information about this topic for ages and yours is the best I’ve located so far.
I acquired more a new challenge on this weight reduction issue. One particular issue is a good nutrition is tremendously vital whenever dieting. A massive reduction in junk food, sugary food items, fried foods, sugary foods, red meat, and white colored flour products could be necessary. Having wastes parasites, and poisons may prevent objectives for fat-loss. While selected drugs temporarily solve the situation, the horrible side effects are not worth it, and so they never provide more than a momentary solution. This can be a known proven fact that 95 of fad diets fail. Thank you for sharing your opinions on this website.
Thanks for the thoughts you reveal through this website. In addition, numerous young women who seem to become pregnant will not even attempt to get health insurance because they have anxiety they probably would not qualify. Although a lot of states now require that insurers produce coverage in spite of the pre-existing conditions. Premiums on all these guaranteed programs are usually larger, but when taking into consideration the high cost of medical treatment it may be your safer strategy to use to protect the financial potential.
That is the right blog for anybody who wants to find out about this topic. You realize a lot its almost laborious to argue with you (not that I truly would want?HaHa). You definitely put a brand new spin on a subject thats been written about for years. Great stuff, just great!
I figured out more a new challenge on this losing weight issue. A single issue is that good nutrition is tremendously vital while dieting. A huge reduction in junk food, sugary ingredients, fried foods, sweet foods, pork, and white flour products might be necessary. Holding wastes parasites, and toxins may prevent aims for losing belly fat. While a number of drugs temporarily solve the challenge, the bad side effects usually are not worth it, and so they never offer you more than a non permanent solution. It can be a known incontrovertible fact that 95 of fad diet plans fail. Many thanks for sharing your opinions on this blog.
Thanks for the marvelous posting! I quite enjoyed reading it, you happen to be a great author.I will make certain to bookmark your blog and may come back later in life. I want to encourage one to continue your great posts, have a nice holiday weekend!
Hey, you used to write great, but the last few posts have been kinda boring? I miss your great writings. Past few posts are just a little bit out of track! come on!
https://t.me/s/TgGo1WIN/5
https://t.me/s/Official_1win_kanal/1419
https://t.me/s/Official_1win_kanal/1821
https://t.me/s/Webs_1WIN
Thanks for giving your ideas. I’d also like to mention that video games have been ever before evolving. Modern technology and improvements have helped create reasonable and fun games. Most of these entertainment video games were not as sensible when the actual concept was being tried. Just like other designs of technologies, video games also have had to evolve by way of many many years. This itself is testimony to the fast progression of video games.
We’re a group of volunteers and opening a new scheme in our community. Your web site provided us with valuable information to work on. You’ve done a formidable job and our whole community will be grateful to you.
Официальный Telegram канал 1win Casinо. Казинo и ставки от 1вин. Фриспины, актуальное зеркало официального сайта 1 win. Регистрируйся в ван вин, соверши вход в один вин, получай бонус используя промокод и начните играть на реальные деньги.
https://t.me/s/Official_1win_kanal/131
Thank you a bunch for sharing this with all of us you actually know what you are speaking about! Bookmarked. Please additionally discuss with my website =). We could have a link trade agreement between us!
Официальный Telegram канал 1win Casinо. Казинo и ставки от 1вин. Фриспины, актуальное зеркало официального сайта 1 win. Регистрируйся в ван вин, соверши вход в один вин, получай бонус используя промокод и начните играть на реальные деньги.
https://t.me/s/Official_1win_kanal/291
I have discovered that service fees for online degree professionals tend to be an awesome value. For instance a full College Degree in Communication in the University of Phoenix Online consists of 60 credits at $515/credit or $30,900. Also American Intercontinental University Online makes available Bachelors of Business Administration with a entire education course requirement of 180 units and a cost of $30,560. Online degree learning has made taking your degree been so cool because you can earn the degree from the comfort in your home and when you finish from work. Thanks for other tips I have really learned through the site.
We absolutely love your blog and find a lot of your post’s to be what precisely I’m looking for. Does one offer guest writers to write content for yourself? I wouldn’t mind creating a post or elaborating on a few of the subjects you write with regards to here. Again, awesome blog!
Oh my goodness! an incredible article dude. Thank you However I am experiencing problem with ur rss . Don?t know why Unable to subscribe to it. Is there anyone getting an identical rss problem? Anybody who is aware of kindly respond. Thnkx
I’m not sure exactly why but this weblog is loading very slow for me. Is anyone else having this problem or is it a problem on my end? I’ll check back later on and see if the problem still exists.
I beloved as much as you’ll receive carried out right here. The comic strip is attractive, your authored subject matter stylish. nonetheless, you command get bought an impatience over that you want be turning in the following. in poor health certainly come further in the past again as exactly the same just about a lot ceaselessly inside case you shield this hike.
One thing I want to say is car insurance cancellations is a hated experience and if you are doing the best things as being a driver you simply will not get one. Some individuals do have the notice that they’ve been officially dropped by the insurance company and several have to fight to get supplemental insurance after having a cancellation. Low-cost auto insurance rates are often hard to get after a cancellation. Having the main reasons regarding auto insurance cancelling can help car owners prevent sacrificing one of the most important privileges offered. Thanks for the suggestions shared through your blog.
Thanks for another magnificent article. Where else could anyone get that type of information in such a perfect way of writing? I have a presentation next week, and I’m on the look for such info.
This is a topic which is near to my verve… Many thanks! Unerringly where can I upon the contact details due to the fact that questions? http://ledyardmachine.com/forum/User-Rdckkm
It is indeed my belief that mesothelioma will be the most dangerous cancer. It has unusual features. The more I look at it a lot more I am assured it does not react like a true solid flesh cancer. If perhaps mesothelioma can be a rogue viral infection, so there is the prospects for developing a vaccine in addition to offering vaccination for asbestos uncovered people who are at high risk associated with developing potential asbestos connected malignancies. Thanks for discussing your ideas on this important ailment.
I was very pleased to seek out this net-site.I needed to thanks on your time for this glorious learn!! I undoubtedly enjoying every little little bit of it and I have you bookmarked to check out new stuff you weblog post.
great points altogether, you simply gained a new reader. What would you recommend in regards to your post that you made a few days ago? Any positive?
Thanks for your text. I would also like to say that the health insurance specialist also works for the benefit of the actual coordinators of any group insurance plan. The health agent is given a list of benefits looked for by someone or a group coordinator. Exactly what a broker does indeed is hunt for individuals or coordinators which will best match up those requirements. Then he presents his suggestions and if each party agree, the broker formulates an agreement between the 2 parties.
Wonderful beat ! I wish to apprentice at the same time as you amend your website, how can i subscribe for a weblog website? The account helped me a appropriate deal. I had been tiny bit familiar of this your broadcast offered brilliant transparent idea
dapagliflozin price – site where to buy forxiga without a prescription
Thanks for the concepts you talk about through your blog. In addition, many young women that become pregnant tend not to even make an effort to get health insurance because they are concerned they won’t qualify. Although a lot of states now require that insurers give coverage no matter what about the pre-existing conditions. Prices on these guaranteed programs are usually bigger, but when thinking about the high cost of medical care bills it may be the safer approach to take to protect one’s financial potential.
As I web site possessor I believe the content material here is rattling great , appreciate it for your hard work. You should keep it up forever! Good Luck.
One thing I want to say is the fact that car insurance termination is a horrible experience and if you’re doing the right things being a driver you may not get one. Lots of people do obtain notice that they’ve been officially dumped by their insurance company they then have to fight to get extra insurance after the cancellation. Inexpensive auto insurance rates tend to be hard to get after a cancellation. Knowing the main reasons pertaining to auto insurance cancellations can help people prevent getting rid of in one of the most important privileges out there. Thanks for the strategies shared by your blog.
I?ll immediately grasp your rss as I can not find your e-mail subscription hyperlink or newsletter service. Do you have any? Kindly allow me realize so that I may subscribe. Thanks.
Performance-driven cleaning, delivers exactly what promised. Performance partnership. Performance excellence.
cost xenical – cost xenical purchase xenical generic
What an eye-opening and thoroughly-researched article! The author’s meticulousness and capability to present intricate ideas in a understandable manner is truly praiseworthy. I’m thoroughly captivated by the scope of knowledge showcased in this piece. Thank you, author, for offering your wisdom with us. This article has been a true revelation!
This actually answered my problem, thank you!
F*ckin? remarkable issues here. I?m very satisfied to see your article. Thank you so much and i am looking forward to touch you. Will you kindly drop me a e-mail?
This design is wicked! You certainly know how to keep a reader amused. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Excellent job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
you are in reality a good webmaster. The web site loading velocity is amazing. It kind of feels that you’re doing any unique trick. In addition, The contents are masterpiece. you have done a excellent task on this topic!
I have observed that in unwanted cameras, extraordinary detectors help to {focus|concentrate|maintain focus|target|a**** automatically. The sensors associated with some cameras change in contrast, while others utilize a beam involving infra-red (IR) light, specifically in low light. Higher specification cameras sometimes use a mixture of both programs and might have Face Priority AF where the video camera can ‘See’ any face while keeping your focus only in that. Thank you for sharing your thinking on this blog site.
deniz kucukkay
mehmet emre dinç
esteworld
huseyin kandulu
dr basat
ışık diş
şaban
salih emre
dr yelken
adem köse
Dry Cleaning in New York city by Sparkly Maid NYC
aslı tarcan global
I’m amazed by the quality of this content! The author has clearly put a great amount of effort into investigating and structuring the information. It’s exciting to come across an article that not only provides valuable information but also keeps the readers engaged from start to finish. Kudos to her for producing such a remarkable piece!
medhair clinic
basat
terziler
ahd clinic
adem köse
yelken
aslı tarcan global
medhair cinici
terziler
adem köse
This is the make of post I recoup helpful. http://sglpw.cn/home.php?mod=space&uid=570564
affordablecanvaspaintings.com.au is Australia Popular Online 100 percent Handmade Art Store. We deliver Budget Handmade Canvas Paintings, Abstract Art, Oil Paintings, Artwork Sale, Acrylic Wall Art Paintings, Custom Art, Oil Portraits, Pet Paintings, Building Paintings etc. 1000+ Designs To Choose From, Highly Experienced Artists team, Up-to 50 percent OFF SALE and FREE Delivery Australia, Sydney, Melbourne, Brisbane, Adelaide, Hobart and all regional areas. We ship worldwide international locations. Order Online Your Handmade Art Today.
aslı tarcan global
Heya i?m for the primary time here. I came across this board and I find It truly helpful & it helped me out a lot. I hope to give something back and aid others like you aided me.
doktor kbb
basat
terziler
ahd clinic
I?ve been exploring for a bit for any high-quality articles or blog posts on this sort of area . Exploring in Yahoo I at last stumbled upon this website. Reading this info So i am happy to convey that I have an incredibly good uncanny feeling I discovered exactly what I needed. I most certainly will make certain to do not forget this site and give it a glance on a constant basis.
Thanks for your write-up on the vacation industry. I will also like to add that if you are a senior taking into account traveling, it truly is absolutely essential that you buy traveling insurance for golden-agers. When traveling, senior citizens are at greatest risk of experiencing a medical emergency. Having the right insurance cover package in your age group can safeguard your health and provide you with peace of mind.
Great work! This is the type of info that should be shared around the internet. Shame on the search engines for not positioning this post higher! Come on over and visit my web site . Thanks =)
I have observed that costs for internet degree specialists tend to be an awesome value. Like a full Bachelor’s Degree in Communication from The University of Phoenix Online consists of Sixty credits with $515/credit or $30,900. Also American Intercontinental University Online makes available Bachelors of Business Administration with a total course feature of 180 units and a tuition fee of $30,560. Online degree learning has made having your education much simpler because you might earn your degree in the comfort of your house and when you finish working. Thanks for all the other tips I have really learned through the blog.
guncel ozturk
Wonderful website. Lots of useful info here. I am sending it to a few friends ans additionally sharing in delicious. And certainly, thank you on your effort!
guncel ozturk
Hey just wanted to give you a quick heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different web browsers and both show the same results.
We are a bunch of volunteers and starting a new scheme in our community. Your site offered us with valuable info to paintings on. You have performed an impressive activity and our entire group will probably be thankful to you.
Awesome blog! Is your theme custom made or did you download it from somewhere? A theme like yours with a few simple tweeks would really make my blog jump out. Please let me know where you got your theme. Thank you
Great goods from you, man. I have take into accout your stuff prior to and you are simply extremely great. I actually like what you’ve got here, certainly like what you’re saying and the way through which you are saying it. You make it enjoyable and you continue to care for to stay it wise. I cant wait to learn far more from you. That is actually a terrific site.
Thanks for your article. I also believe laptop computers have become more and more popular lately, and now are sometimes the only kind of computer utilised in a household. This is because at the same time potentially they are becoming more and more very affordable, their processing power is growing to the point where they are as robust as desktop computers out of just a few years back.
Some tips i have observed in terms of computer memory is that often there are specs such as SDRAM, DDR and many others, that must go with the requirements of the motherboard. If the computer’s motherboard is fairly current and there are no operating system issues, changing the memory literally normally takes under an hour or so. It’s among the list of easiest computer system upgrade methods one can imagine. Thanks for spreading your ideas.
I was just seeking this information for a while. After 6 hours of continuous Googleing, finally I got it in your web site. I wonder what’s the lack of Google strategy that do not rank this kind of informative sites in top of the list. Generally the top websites are full of garbage.
I found your blog web site on google and test a couple of of your early posts. Proceed to keep up the superb operate. I simply extra up your RSS feed to my MSN News Reader. In search of forward to reading extra from you later on!?
It?s actually a cool and helpful piece of information. I am glad that you shared this useful information with us. Please keep us informed like this. Thanks for sharing.
This design is wicked! You definitely know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Wonderful job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
I have learned result-oriented things from a blog post. Also a thing to I have noticed is that usually, FSBO sellers are going to reject an individual. Remember, they might prefer not to use your providers. But if anyone maintain a gradual, professional partnership, offering aid and being in contact for four to five weeks, you will usually have the ability to win a discussion. From there, a listing follows. Thank you
I have come across that today, more and more people are being attracted to cameras and the industry of taking pictures. However, really being a photographer, you have to first shell out so much time frame deciding the exact model of digicam to buy and also moving out of store to store just so you could potentially buy the lowest priced camera of the trademark you have decided to choose. But it does not end generally there. You also have to contemplate whether you should purchase a digital photographic camera extended warranty. Thanks for the good guidelines I gained from your blog site.
777 casino united kingdom, 888 poker login australia and australia
portable casino games hire (Marita) online real money, or
nz online casinos that accept paypal
Thanks for the new stuff you have exposed in your blog post. One thing I want to discuss is that FSBO human relationships are built after some time. By introducing yourself to owners the first end of the week their FSBO can be announced, ahead of masses commence calling on Thursday, you make a good relationship. By mailing them tools, educational components, free accounts, and forms, you become an ally. By subtracting a personal fascination with them plus their circumstances, you develop a solid network that, in many cases, pays off once the owners decide to go with an adviser they know and trust – preferably you.
I?m impressed, I need to say. Really not often do I encounter a weblog that?s each educative and entertaining, and let me let you know, you may have hit the nail on the head. Your concept is outstanding; the problem is one thing that not sufficient individuals are speaking intelligently about. I’m very completely satisfied that I stumbled across this in my search for something relating to this.
A few things i have usually told persons is that while looking for a good internet electronics store, there are a few aspects that you have to factor in. First and foremost, you would like to make sure to discover a reputable as well as reliable retail store that has picked up great opinions and scores from other consumers and industry leaders. This will make certain you are getting along with a well-known store to provide good assistance and help to it’s patrons. Thank you for sharing your notions on this blog.
Woah! I’m really loving the template/theme of this website. It’s simple, yet effective. A lot of times it’s hard to get that “perfect balance” between superb usability and appearance. I must say you’ve done a fantastic job with this. In addition, the blog loads super quick for me on Safari. Excellent Blog!
Hey there! This is my 1st comment here so I just wanted to give a quick shout out and tell you I really enjoy reading your blog posts. Can you recommend any other blogs/websites/forums that deal with the same subjects? Thank you so much!
Undeniably believe that which you stated. Your favorite reason appeared to be on the web the simplest thing to be aware of. I say to you, I definitely get annoyed while people consider worries that they just don’t know about. You managed to hit the nail upon the top and defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
My spouse and I stumbled over here by a different web address and thought I may as well check things out. I like what I see so now i’m following you. Look forward to looking into your web page again.
What i do not realize is if truth be told how you are no longer really much more smartly-favored than you might be right now. You are so intelligent. You realize therefore significantly in relation to this topic, made me in my view imagine it from so many numerous angles. Its like women and men aren’t interested until it is one thing to do with Woman gaga! Your personal stuffs outstanding. All the time maintain it up!
Hello my friend! I wish to say that this post is awesome, nice written and include approximately all significant infos. I?d like to see more posts like this.
I would also like to add if you do not actually have an insurance policy or else you do not take part in any group insurance, you will well make use of seeking the aid of a health broker. Self-employed or people with medical conditions commonly seek the help of any health insurance brokerage. Thanks for your writing.
An added important component is that if you are a senior citizen, travel insurance intended for pensioners is something you ought to really contemplate. The older you are, the harder at risk you’re for making something awful happen to you while in most foreign countries. If you are certainly not covered by quite a few comprehensive insurance policy, you could have several serious problems. Thanks for expressing your advice on this web site.
Thanks for your submission. Another issue is that being photographer requires not only trouble in taking award-winning photographs but hardships in acquiring the best digital camera suited to your requirements and most especially issues in maintaining the standard of your camera. It is very genuine and clear for those photography addicts that are into capturing this nature’s interesting scenes : the mountains, the forests, the wild or perhaps the seas. Going to these adventurous places undoubtedly requires a dslr camera that can meet the wild’s nasty surroundings.
Hello very nice blog!! Guy .. Excellent .. Superb .. I will bookmark your website and take the feeds additionally?I am happy to seek out numerous helpful information here in the post, we need work out more strategies in this regard, thank you for sharing. . . . . .
The other day, while I was at work, my sister stole my iPad and tested to see if it can survive a forty foot drop, just so she can be a youtube sensation. My apple ipad is now broken and she has 83 views. I know this is completely off topic but I had to share it with someone!
I’ve been browsing online more than three hours today, yet I never found any interesting article like yours. It is pretty worth enough for me. In my opinion, if all webmasters and bloggers made good content as you did, the internet will be much more useful than ever before.
Thanks for the good writeup. It actually used to be a enjoyment account it. Glance advanced to far introduced agreeable from you! By the way, how can we communicate?
Valuable info. Fortunate me I discovered your web site accidentally, and I am stunned why this twist of fate did not happened in advance! I bookmarked it.
I have noticed that in digital camera models, extraordinary sensors help to {focus|concentrate|maintain focus|target|a**** automatically. Those sensors associated with some video cameras change in contrast, while others start using a beam involving infra-red (IR) light, specifically in low lighting. Higher specification cameras at times use a blend of both methods and could have Face Priority AF where the photographic camera can ‘See’ a new face while keeping focused only on that. Thank you for sharing your notions on this blog.
Thanks for the concepts you have provided here. Moreover, I believe there are a few factors which really keep your car insurance premium decrease. One is, to contemplate buying automobiles that are inside the good listing of car insurance organizations. Cars which can be expensive will be more at risk of being stolen. Aside from that insurance coverage is also using the value of your car, so the more pricey it is, then the higher this premium you make payment for.
Hey there, You’ve done a fantastic job. I?ll definitely digg it and personally recommend to my friends. I’m sure they’ll be benefited from this website.
One thing I have actually noticed is the fact that there are plenty of misconceptions regarding the lenders intentions whenever talking about home foreclosure. One myth in particular is the fact that the bank wishes to have your house. The lending company wants your money, not your house. They want the money they loaned you with interest. Averting the bank will still only draw a foreclosed final result. Thanks for your article.
best usa online casino real money, pokies meaning australia and united kingdom online pokies
2021, or australian top online casino
Feel free to surf to my web blog; why do i always lose at gambling (https://Mirpadisticaret.com/page-1115)
Great work! This is the type of information that should be shared around the net. Shame on Google for not positioning this post higher! Come on over and visit my website . Thanks =)
Wow, superb blog layout! How lengthy have you ever been blogging for? you made running a blog glance easy. The full glance of your website is magnificent, let alone the content!
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get bought an nervousness over that you wish be delivering the following. unwell unquestionably come more formerly again since exactly the same nearly very often inside case you shield this hike.
Valuable info. Lucky me I found your web site by accident, and I’m shocked why this accident did not happened earlier! I bookmarked it.
In these days of austerity as well as relative stress and anxiety about having debt, some people balk about the idea of employing a credit card in order to make acquisition of merchandise or perhaps pay for a trip, preferring, instead to rely on the particular tried and also trusted approach to making transaction – cash. However, if you’ve got the cash on hand to make the purchase in full, then, paradoxically, that is the best time to be able to use the card for several good reasons.
Thanks for your post. One other thing is that if you are disposing your property on your own, one of the issues you need to be conscious of upfront is just how to deal with household inspection accounts. As a FSBO owner, the key concerning successfully switching your property in addition to saving money about real estate agent commission rates is know-how. The more you know, the easier your property sales effort might be. One area where by this is particularly important is information about home inspections.
I’ve really noticed that repairing credit activity must be conducted with tactics. If not, chances are you’ll find yourself endangering your ranking. In order to be successful in fixing to your credit rating you have to verify that from this second you pay your entire monthly expenses promptly before their slated date. Really it is significant since by not necessarily accomplishing this, all other actions that you will decide to try to improve your credit rank will not be useful. Thanks for expressing your thoughts.
Woah! I’m really loving the template/theme of this site. It’s simple, yet effective. A lot of times it’s hard to get that “perfect balance” between user friendliness and appearance. I must say you’ve done a fantastic job with this. In addition, the blog loads very quick for me on Internet explorer. Exceptional Blog!
Pretty nice post. I just stumbled upon your blog and wanted to say that I’ve truly enjoyed browsing your blog posts. After all I will be subscribing to your rss feed and I hope you write again very soon!
This is a excellent web site, could you be involved in doing an interview about just how you designed it? If so e-mail me!
I?ll right away grab your rss as I can not in finding your email subscription hyperlink or e-newsletter service. Do you’ve any? Kindly let me recognize in order that I may subscribe. Thanks.
Right now it appears like Movable Type is the preferred blogging platform available right now. (from what I’ve read) Is that what you’re using on your blog?
Thanks for your publication. I also believe that laptop computers are getting to be more and more popular lately, and now are sometimes the only type of computer included in a household. This is due to the fact that at the same time that they are becoming more and more inexpensive, their computing power keeps growing to the point where they can be as effective as pc’s coming from just a few years ago.
you will have an incredible weblog here! would you prefer to make some invite posts on my weblog?
I’m really enjoying the design and layout of your website. It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often. Did you hire out a designer to create your theme? Great work!
new no deposit uk casino 2021, best online live casino united states
pirate kings cash and spins generator (Evelyne) no deposit bonus codes casino canada, or pokies open in south united states
I’m really enjoying the theme/design of your blog. Do you ever run into any web browser compatibility problems? A handful of my blog audience have complained about my website not operating correctly in Explorer but looks great in Chrome. Do you have any solutions to help fix this issue?
gambling in canada statistics, usa online casino reviews and united kingdom real money casino, how to play blackjack hit or stand united statesn roulette strategy uk
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Получить дополнительную информацию – https://quick-vyvod-iz-zapoya-1.ru/
top 20 usa slots, big red pokie wins united kingdom 2021 and
free what indian tribe owns morongo casino (Irene) bonus no deposit required uk,
or no deposit bonus bingo united states
Thanks a lot for sharing this with all of us you actually know what you’re talking about! Bookmarked. Please also visit my site =). We could have a link exchange contract between us!
Thank you for another wonderful post. Where else could anyone get that kind of information in such an ideal way of writing? I have a presentation next week, and I am on the look for such info.
You can protect yourself and your family by way of being heedful when buying medicine online. Some pharmacopoeia websites manipulate legally and offer convenience, solitariness, bring in savings and safeguards as a replacement for purchasing medicines. buy in TerbinaPharmacy https://terbinafines.com/product/cozaar.html cozaar
australian pm blackjack, best online casinos new zealand
and bet365 blackjack hints uk, or online casino with
free signup bonus real money usa
My page black gambling table (Blair)
canada visa slots, black chip poker united kingdom and does united states have casinos,
or best online casino sites canada
Feel free to surf to my page :: vegas world blackjack – Jack
–
online gambling legal in united states, united statesn roulette betting strategy and play online gambling amex bingo for real money canada, or no deposit roulette bonus usa
online wett
Also visit my web site … no Deposit Bonus sportwetten (saytrees.Parishkaar.com)
wettbüro marburg
Stop by my web page: sportwetten apps [Lila]
Wonderful web site. A lot of useful info here. I am sending it to several pals ans additionally sharing in delicious. And obviously, thanks for your effort!
Heya i am for the first time here. I found this board and I find It really useful & it helped me out much. I hope to give something back and help others like you helped me.
More delight pieces like this would urge the web better. hippisme lasix
wetten ergebnisse
Have a look at my homepage sportwetten strategie buch (sharpinn.com)
sportwetten südamerika strategie
My page … buchmacher Us wahl, Sarinhood.com,
wetten bonus freispielen
Also visit my web-site; Bester quotenvergleich
Наркологическая клиника «Честный врач» в Нижнем Новгороде оказывает круглосуточную помощь людям с алкогольной и наркотической зависимостью. Возможен выезд нарколога на дом, проведение капельницы при запое и комплексное лечение алкоголизма и наркомании с сохранением конфиденциальности.
Подробнее – курение спайса
Наркологическая клиника «Честный врач» в Нижнем Новгороде оказывает круглосуточную помощь людям с алкогольной и наркотической зависимостью. Возможен выезд нарколога на дом, проведение капельницы при запое и комплексное лечение алкоголизма и наркомании с сохранением конфиденциальности.
Получить дополнительные сведения – курящие наркотики
sieg platz wette pferderennen
My web blog; wettbüro erfurt
Наркологическая клиника «Честный врач» в Нижнем Новгороде оказывает круглосуточную помощь людям с алкогольной и наркотической зависимостью. Возможен выезд нарколога на дом, проведение капельницы при запое и комплексное лечение алкоголизма и наркомании с сохранением конфиденциальности.
Подробнее – наркотические анальгетики применению
I will immediately grab your rss feed as I can not find your email subscription hyperlink or newsletter service. Do you have any? Kindly let me realize so that I may subscribe. Thanks.
Usually I do not read post on blogs, but I would like to say that this write-up very forced me to try and do it! Your writing style has been surprised me. Thanks, very nice article.
Нижегородская наркологическая клиника «Честный врач» предлагает услуги по выведению из запоя и лечению зависимости. Возможен вызов нарколога на дом, постановка капельниц при алкогольной интоксикации, а также полноценные программы лечения алкоголизма и наркомании.
Ознакомиться с деталями – иглорефлексотерапия в нижнем новгороде цены
Наркологическая клиника «Честный врач» в Нижнем Новгороде оказывает круглосуточную помощь людям с алкогольной и наркотической зависимостью. Возможен выезд нарколога на дом, проведение капельницы при запое и комплексное лечение алкоголизма и наркомании с сохранением конфиденциальности.
Узнать больше – клиника кодирования от алкоголизма
beste sportart zum wetten Tipps vorhersagen
В Нижнем Новгороде работает наркологическая клиника «Честный врач», где специалисты помогают вывести из запоя, проводят капельницы на дому и оказывают профессиональную наркологическую помощь. В клинике доступно лечение наркомании и алкоголизма с индивидуальным подходом к каждому пациенту.
Получить больше информации – нейролингвистическое программирование
This is the kind of advise I recoup helpful.
Нижегородская наркологическая клиника «Честный врач» предлагает услуги по выведению из запоя и лечению зависимости. Возможен вызов нарколога на дом, постановка капельниц при алкогольной интоксикации, а также полноценные программы лечения алкоголизма и наркомании.
Изучить вопрос глубже – сниффинг газом
wetten sicher gewinnen
Also visit my webpage; sportwetten Bonus deutschland
sportwetten Analyse heute
mit startguthaben ohne einzahlung
neue online wettanbieter
Feel free to visit my blog post us wahl wetten deutschland
Нижегородская наркологическая клиника «Честный врач» предлагает услуги по выведению из запоя и лечению зависимости. Возможен вызов нарколога на дом, постановка капельниц при алкогольной интоксикации, а также полноценные программы лечения алкоголизма и наркомании.
Разобраться лучше –
Если требуется срочная наркологическая помощь в Нижнем Новгороде, клиника «Честный врач» готова помочь. Врачи выезжают на дом, проводят капельницы при запое, обеспечивают безопасное выведение из запойного состояния и предлагают программы лечения наркомании и алкоголизма.
Подробнее можно узнать тут – спайс синтетический наркотик
Наркологическая клиника «Честный врач» в Нижнем Новгороде оказывает анонимные услуги: лечение алкоголизма, терапию наркомании, выезд нарколога на дом. Пациентам доступна капельница от запоя и медицинское сопровождение для восстановления здоровья и предотвращения осложнений.
Детальнее – после лечения наркозависимости
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Смотри, что ещё есть – https://gentariau.com/hello-world
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Информация доступна здесь – https://cursos.cicialli.com/titulo-de-la-publicacion-en-el-blog
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Не упусти шанс – https://www.yantramstudio.com/portfolio/pool-exterior-concept
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Открой скрытое – http://sunrize-web.com/info/%E6%96%B0%E5%B9%B4%E3%81%AE%E3%81%94%E6%8C%A8%E6%8B%B6
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Что скрывают от вас? – https://dumbocart.co.uk/best-plants-for-shade
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Подробная информация доступна по запросу – https://domkulturypresov.sk/ale-ale-webova-stranka-a-novodoba-vizitka-neblaznite-2
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
Открой скрытое – http://winkler-martin.de/guestbook.html
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Подробнее – https://www.kbgmassivhaus.de/2021/12/24/summer-in-new-zealand
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Осуществить глубокий анализ – https://banskonews.com/po-predlojenie-na-gucanov-e-podmenen-kandidata-za-kmet-na-bansko-i-listata-za-suvetnici
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Открыть полностью – https://www.badmintonclubtotes.fr/2024/08/26/forum-des-associations-5
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Откройте для себя больше – https://www.luferart.com/calm-over-the-horizon
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Информация доступна здесь – https://taxlama.com/2024/08/13/walmart-dropshipping-step-by-step-guide-2024
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Подробности по ссылке – https://www.kbgmassivhaus.de/2021/12/24/summer-in-new-zealand
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Как это работает — подробно – https://mikltd.eu/blog/2020/03/21/%D0%BC%D0%B8%D0%BA-%D0%B1%D0%B3-%D0%B5%D0%BE%D0%BE%D0%B4-%D0%BF%D1%80%D0%BE%D0%B2%D0%B5%D0%B4%D0%B5-%D0%BA%D1%80%D1%8A%D0%B3%D0%BB%D0%B0-%D0%BC%D0%B0%D1%81%D0%B0-%D1%81-%D1%86%D0%B5%D0%BB-%D0%BF%D1%80
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Запросить дополнительные данные – https://hotelallseasons.co.in/gallery/restaurant/attachment/img_3104
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Узнай первым! – https://psychologurbaniak.pl/projekty/kontakt/kontakt-2-002
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Детали по клику – https://myreklamgroup.com/change-how-apps-work
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Узнать больше > – https://www.yogaamsterdam.nl/hallo-wereld
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Получить больше информации – https://melinea-innovation.fr/case-studies/how-marketing-consultants-help-a-business
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Личный опыт — читайте сами – https://hierhoudenwevan.nl/6-redenen-waarom-een-gembershot-je-weerstand-verhoogt
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Что скрывают от вас? – http://www.vialeumanita.it/img_0099
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Получить дополнительные сведения – https://karimboumghar.com/index.php/2025/01/07/bonjour-tout-le-monde
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Получить больше информации – https://grond-werk.be/simpel-winstgevend-duurzaam-ondernemen-voor-architecten-2
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Наши рекомендации — тут – https://stepbystepinternet.com/ru/%D0%BA%D0%B0%D0%BA-%D0%BB%D0%B5%D0%B3%D0%BA%D0%BE-%D0%B8-%D0%B1%D1%8B%D1%81%D1%82%D1%80%D0%BE-%D0%B2%D0%BE%D0%B9%D1%82%D0%B8-%D0%B2-amazon-%D0%BD%D0%B0-%D0%B8%D1%81%D0%BF%D0%B0%D0%BD%D1%81%D0%BA%D0%BE
Thanks a lot for your post. I’d like to comment that the tariff of car insurance varies greatly from one insurance policy to another, for the reason that there are so many different issues which play a role in the overall cost. Such as, the make and model of the auto will have an enormous bearing on the cost. A reliable aged family motor vehicle will have a more affordable premium over a flashy racecar.
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Детали по клику – https://www.lacreativitedanslapeau.fr/jason-shulman-captures-entire-movies
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Секреты успеха внутри – https://healinghelthy.info/?p=115
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Как достичь результата? – https://www.3pms.be/hello-world
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Неизвестные факты о… – https://mascotas.alimentosmor.com.sv/portfolio/help-homeless-pets
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Практические советы ждут тебя – https://nutricionplena.com/centro-de-distribucion-cedis-omnilife-en-el-salvador-donde-comprar-omnilife-en-el-salvador
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Ознакомиться с отчётом – https://gospnews.com/pepper-martin
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Слушай внимательно — тут важно – https://seautomotriz.com/hello-world
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Посмотреть всё – https://pqoil.com/innovative-products-and-materials
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Нажмите, чтобы узнать больше – https://www.ainy-h.com/?construction=%E5%8C%97%E5%8C%BA%E9%BB%92%E5%B4%8E%E7%94%BA%E3%80%80%E6%B6%88%E9%98%B2%E8%A8%AD%E5%82%99%E5%B7%A5%E4%BA%8B
gratis wetten ohne einzahlung geizkragen
Check out my page … sportwette bonus
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Узнать больше > – https://www.ateliersfrancochinois.com/2021/02/05/le-nouvel-an-chinois-%E4%B8%AD%E5%9B%BD%E6%96%B0%E5%B9%B4
Its such as you learn my mind! You seem to know so much about this, like you wrote the book in it or something. I feel that you just could do with some p.c. to power the message home a bit, but instead of that, this is magnificent blog. A great read. I will certainly be back.
über unter wetten strategie
my web-site – wette italien österreich
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
ТОП-5 причин узнать больше – https://fundacjakrajwspanialy.pl/project/nawrzanskie-echa-koncert-fortepianowy-pod-gwiazdami
Чтобы семье было проще ориентироваться во времени и ожиданиях, ниже — последовательность шагов с ориентиром по длительности и ожидаемому эффекту.
Получить дополнительную информацию – http://narkolog-na-dom-zhukovskij7.ru/narkolog-na-dom-kruglosutochno-v-zhukovskom/
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Запросить дополнительные данные – https://friendlysweetdesires.com/how-to-know-the-first-step-to-start-a-sport
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Получить профессиональную консультацию – https://reginalog.com/?p=277
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Слушай внимательно — тут важно – http://jeffaguiar.com/10609461_10203227271588339_8733529565961450708_n
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Открыть полностью – https://kind-und-gluecklich.de/cropped-20181214_144031-jpg
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Осуществить глубокий анализ – https://www.mundus-online.de/faq-items/donec-ac-iaculis-lorem-sit-venenatis-tellus
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Узнать больше > – https://humano.com.co/2023/01/14/hello-world
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Заходи — там интересно – https://beritaviralindo.net/kdrt-diduga-melibatkan-cawagub-papua-yb-paksa-istri-threesome-dan-cekoki-miras
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Обратитесь за информацией – https://st-johannis-kiga.de/component/k2/item/3-alan-sugar-named-tory-enterprise-tsar-despite-past-criticism-of-osborne.html?start=44130
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Получить профессиональную консультацию – https://datsumask.com/wp/?p=69
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Посмотреть подробности – https://around29.com/seo-myths-and-misconceptions-debunking-the-most-common-misbeliefs
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Следуйте по ссылке – https://kita-umeda.com/wp/contact
Эта публикация завернет вас в вихрь увлекательного контента, сбрасывая стереотипы и открывая двери к новым идеям. Каждый абзац станет для вас открытием, полным ярких примеров и впечатляющих достижений. Подготовьтесь быть вовлеченными и удивленными каждый раз, когда продолжите читать.
Посмотреть подробности – https://docmum.org/guilt-the-lurking-monster
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Давай разберёмся досконально – http://thinkppe.co.uk/post-format-standard
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Ознакомиться с теоретической базой – https://halofisioterapi.com/artikel_kesehatan/penyebab-nyeri-pada-telapak-kaki-dan-cara-mengatasinya
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Прочесть заключение эксперта – https://wvd.org/policy-on-transparency
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Неизвестные факты о… – https://tranhtuonghanoi.com/gach-lat-trong-thiet-ke-va-xay-dung
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Уникальные данные только сегодня – http://www.mehmetdemirci.org/mesnevi-hikayelerinden-dersler
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Хочу знать больше – http://hayakawasetsubi.jp/2022/07/28/%E3%81%BE%E3%81%9F%E3%81%BE%E3%81%9F%E6%AF%8D%E3%81%AE%E6%89%8B%E4%BD%9C%E3%82%8A%E3%83%A9%E3%83%B3%E3%83%81%E2%98%80%EF%B8%8F%F0%9F%8D%B4
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Ознакомиться с теоретической базой – https://www.anna-rossi.com/b15
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Неизвестные факты о… – https://triko.ge/2021/12/24/lobortis-elementum-nibhtellus-molestie-mauris
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Интересует подробная информация – https://asrstore.in/product/nion-light
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Изучить вопрос глубже – https://ballersculture.com/celebrating-national-basketball-day-honoring-the-game-we-love
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Получить полную информацию – https://papacook.jp/?p=451
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Читать далее > – https://michytime.com/2024/06/02/kylian-mbappe-jugara-con-el-real-madrid
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Секреты успеха внутри – https://www.kulturutiltai.lt/menininkes-svajone-pasipuosti-savo-rankomis-isaustu-tautiniu-kostiumu
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Нажмите, чтобы узнать больше – https://lcg.org.ua/1200×800
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Доступ к полной версии – https://carlbaldassarremusic.com/product/silent-nights-vinyl-2lp
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Узнай первым! – https://www.fabspin.com/professional-carpet-cleaning-allergy-prevention
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Смотри, что ещё есть – https://debrugseniorie.be/welkom
Wetten Gewinnen quoten
wettprognose heute
Feel free to visit my web-site; die buchmacher
wettbüro lübeck
my webpage beste app für sportwetten (https://dyvoso.org/2025/10/13/brasilien-wetten/)
live sicher wetten
bonus
Как работает
Получить больше информации – http://kodirovanie-ot-alkogolizma-vidnoe7.ru
Вывод из запоя — это управляемая медицинская процедура, а не «волшебная капля» или крепкий чай с рассолом. «Формула Трезвости» организует помощь в Ногинске круглосуточно: выезд врача на дом или приём в стационаре, детоксикация с мониторингом, мягкая коррекция сна и тревоги, подробный план на первые 48–72 часа. Мы действуем безопасно, конфиденциально и без «мелкого шрифта» — объясняем, что и зачем делаем, согласовываем схему и фиксируем смету до начала процедур.
Изучить вопрос глубже – vyvod-iz-zapoya-v-stacionare
Медикаментозное пролонгированное
Выяснить больше – https://kodirovanie-ot-alkogolizma-vidnoe7.ru/
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Изучите внимательнее – https://janasheikhbahaei.ir/critical-thinking
При критических симптомах (потеря сознания, сильная одышка, подозрение на инсульт/инфаркт) необходимо звонить 103/112. Мы подключимся к маршрутизации и организуем перевод в стационар.
Разобраться лучше – http://vyvod-iz-zapoya-noginsk7.ru
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Наши рекомендации — тут – https://nsbarchive.newshelvesbooks.com/ingramspark-logo
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Кликни и узнай всё! – https://ielts.edc.edu.hk/product/explosion-models-multi-3
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Откройте для себя больше – http://georgiaeyeinstitute.com/post/34
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Посмотреть всё – https://smbsolutionkwt.com/benefits-of-in-house-online-food-ordering-system-for-restaurants-and-cafe
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Хочешь знать всё? – https://summertownexecutive.co.uk/is-renting-a-car-profitable
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Смотрите также… – https://antdt.fr/bob-marley
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Получить профессиональную консультацию – https://e-markethings.com/product/sendblaster-pro-edition
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Ознакомиться с полной информацией – https://progenmethod.com/why-choose-progen
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Узнать больше > – https://securitytrainingsia.co.uk/events/build-education-website-using-wordpress
Этот обзорный материал предоставляет информационно насыщенные данные, касающиеся актуальных тем. Мы стремимся сделать информацию доступной и структурированной, чтобы читатели могли легко ориентироваться в наших выводах. Познайте новое с нашим обзором!
Погрузиться в детали – https://leathernews.org/7-key-reasons-why-india-is-the-top-choice-for-leather-goods-manufacturing
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Смотрите также – https://eineweltsafaris.com/2022/07/01/5-most-beautiful-islands-in-asia
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Подробнее – https://filmsnminds.com/tik-tik-tik-2018
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Нажмите, чтобы узнать больше – https://toyosatokinzoku.com/archives/231
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Запросить дополнительные данные – https://freshwaterboats.com/category/upcomming-cars
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Детали по клику – http://devilcupido.com/post/34
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Эксклюзивная информация – https://argonconsultora.com.ar/soluciones
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Расширить кругозор по теме – https://segredosdojardim.com/7-plantas-aromaticas-e-bonitas-para-a-varanda-repele-as-moscas-e-os-mosquitos-3
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Ознакомиться с полной информацией – https://foreningen.svenskhemslojd.com/product/classic-bag-svea
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Смотри, что ещё есть – https://www.twsmission.com/project/sabah
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Дополнительно читайте здесь – https://wattzupp.com/characteristics-and-benefits-of-bluehost-making-them-no-1-hosting-company
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Хочешь знать всё? – https://btcsonic.xyz/home
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
Рассмотреть проблему всесторонне – https://shengtingbio.com/%E3%80%8C%E7%A9%80%E7%89%A9%E6%90%AD%E9%85%8D%E8%B1%86%E9%A1%9E%E3%80%8D%E5%AE%8C%E7%BE%8E%E6%90%AD%E9%85%8D%EF%BC%8C%E7%94%A8%E4%BA%94%E7%A9%80%E9%9B%9C%E7%B3%A7%E5%8F%96%E4%BB%A3%E7%99%BD%E7%B1%B3
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
Полезно знать – https://privreswp3.wpxblog.jp/%E9%A3%9F%E6%AC%B2%E3%82%92%E6%8A%91%E3%81%88%E3%82%8B%E9%A3%9F%E3%81%B9%E7%89%A9
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Не упусти важное! – https://banfftravelers.com/5-most-beautiful-islands-in-asia
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Посмотреть всё – https://tmpsltd.co.uk/harnessing-the-power-of-social-media-for-business-growth
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Уточнить детали – https://lazuardi-haura.sch.id/haura-logo-min
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Получить исчерпывающие сведения – https://feltongallery45.co.uk/product/northumberland-tartan-pocket-square
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Жми сюда — получишь ответ – https://derpiet.de/lucky-lamb-cloudscout-faltbare-tragetasche-fuer-haustiere
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Детальнее – https://coeresourceshub.org/qsm_quiz/2206
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Что скрывают от вас? – https://frameboxxanimationacademy.com/product/dictionary
online wetten deutschland dänemark erfahrung
What i do not realize is actually how you are not really much more well-liked than you may be now. You are very intelligent. You realize therefore considerably relating to this subject, made me personally consider it from numerous varied angles. Its like men and women aren’t fascinated unless it?s one thing to accomplish with Lady gaga! Your own stuffs excellent. Always maintain it up!
Online wettanbieter deutschland wetten mit bonus
sportwetten tipps gratis
Here is my page :: wetten Pferderennen
schweizer sportwetten anbieter liste (menu-fix-faculty-som-yale.pantheonsite.io)
Домашний формат подходит, когда показатели стабильны, а у пациента есть поддержка близких. Врач осматривает, ставит капельницу, оставляет понятные инструкции по режиму, сну, гидратации и «красным флажкам». Если дома становится «узко» по медпоказаниям — переводим в стационар без задержек и лишней бюрократии.
Получить больше информации – chastnaya-narkologicheskaya-klinika
Для кого
Получить дополнительную информацию – narkologicheskaya-klinika-otzyvy
Такой подход делает лечение предсказуемым: вы понимаете, что происходит сейчас, чего ждать завтра и как закрепить результат на горизонте недель и месяцев.
Узнать больше – наркологическая клиника врачи
Мы — частная наркологическая служба в Химках, где каждый шаг лечения объясняется простым языком и запускается без задержек. С первого контакта дежурный врач уточняет жалобы, длительность запоя, хронические диагнозы и принимаемые лекарства, после чего предлагает безопасный старт: выезд на дом, дневной формат или госпитализацию в стационар 24/7. Наши внутренние регламенты построены вокруг двух опор — безопасности и приватности. Мы используем минимально необходимый набор персональных данных, ограничиваем доступ к медицинской карте, сохраняем нейтральную коммуникацию по телефону и не ставим на учёт.
Подробнее тут – http://narkologicheskaya-klinika-himki0.ru
Мы помогаем при острых состояниях, связанных с алкоголем, и сопровождаем до устойчивой ремиссии. Детокс у нас — это не «одна капельница», а система мер: регидратация и коррекция электролитов, защита печени и ЖКТ, мягкая седативная поддержка по показаниям, контроль давления/пульса/сатурации/температуры, оценка сна и уровня тревоги. После стабилизации обсуждаем стратегию удержания результата: подготовку к кодированию (если показано), настройку поддерживающей терапии и реабилитационный блок.
Получить дополнительную информацию – частная наркологическая клиника в мытищах
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
Нажмите, чтобы узнать больше – https://mathgiri.com/%E0%A4%97%E0%A4%B0%E0%A5%8D%E0%A4%AE%E0%A5%80-%E0%A4%95%E0%A5%80-%E0%A4%9B%E0%A5%81%E0%A4%9F%E0%A5%8D%E0%A4%9F%E0%A4%BF%E0%A4%AF%E0%A5%8B%E0%A4%82-%E0%A4%AE%E0%A5%87%E0%A4%82-%E0%A4%85%E0%A4%AA
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Запросить дополнительные данные – https://nftscreen.co/introducing-burve-protocol-a-groundbreaking-leap-in-decentralized-finance-with-amm-3-0
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Ознакомьтесь с аналитикой – https://pojoksinema.com/2021/03/11/paula-verhoeven
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Ознакомиться с деталями – https://le-k-reims.com/events/florian-lex
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Получить полную информацию – https://template85.webekspor.com/?p=1
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Ознакомьтесь с аналитикой – https://www.maquinasflorestais.com/feira-das-colheitas-2024
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
Неизвестные факты о… – https://fameurban.com/offers-from-ttweakhotel
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
А есть ли продолжение? – https://laboulamie.ch/logo-leszottes-ardon
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Что скрывают от вас? – https://aroagardenbar.com.br/how-to-create-a-logo-like-a-pro
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Что ещё нужно знать? – https://aichi-gorin-abilym.jp
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Не упусти шанс – https://foodidee.de/leckerer-hefezopf-ohne-ei
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Что ещё нужно знать? – https://gothamdoughnuts.com/post/top-milkshake-destination-in-melbourne-indulge-in-heavenly-creations
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Ознакомиться с полной информацией – https://massif.co.in/tech-conference-events-2019-2020
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Ознакомиться с полной информацией – https://jiacm.in/2023/03/24/january-march-2023-issue
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
ТОП-5 причин узнать больше – https://pavipisos.com.br/quais-as-melhores-plantas-para-decorar-ambientes-fechados
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Погрузиться в научную дискуссию – https://fyrlegal.com/obtenemos-las-certificaciones-internacionalesiso-27001-e-iso-27701
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Только факты! – https://wyomingagentss.com/fintechzoom-pro-is-your-ultimate-source-financi
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Узнай первым! – https://namaskar-nepal.com/hello-world
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Это стоит прочитать полностью – http://inaina.dk/2011/11/opbevaring-af-gavepapir
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Изучить вопрос глубже – https://phyllistodd.co.uk/index.php/test-gallery/page13-1001-full
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Прочесть всё о… – https://seoprobox.click/increase-backlinks-ahrefs-domain-rating-50-60-70-moz-domain-authority-20-30-and-guest-posting-28792
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Слушай внимательно — тут важно – https://www.oaypa.ca/sick-kids-the-young-families-program
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Изучить вопрос глубже – https://emojiplot.com/%F0%9F%94%A5
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Слушай внимательно — тут важно – https://doutorhusseinawada.com/hello-world
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Посмотреть подробности – https://myrcludex.info/harnessing-the-power-of-social-media-for-business-growth
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Не упусти важное! – https://maranhaounico.com.br/2023/11/santa-luzia-do-parua-vence-turiacu-e-conquista-a-copa-br-de-selecoes-maranhao-hoje
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Это ещё не всё… – https://noodlebowltbay.com/menus/meatloaf-with-black-pepper-honey-bbq-sauce
ohne einzahlung wetten quoten Erklärung (https://hello.waitwhatweb.com)
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Изучить материалы по теме – https://sranankoters.nl/2020/04/08/test
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Получить исчерпывающие сведения – https://fonds-shop-24.com/hallo-welt
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Узнать напрямую – https://cadenavirtual.com.ar/cultura_educacion/2024/12/02/la-escuela-municipal-de-bellas-artes-despidio-el-ano-con-un-imponente-espectaculo-en-san-clemente
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Узнать больше > – https://nutritionbeyondborders.org/economiser-epicerie
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Изучить материалы по теме – https://ves.ac.in/svjc/2013/11/11/quote-post-format
online wettanbieter liste
My blog Freebet ohne einzahlung sportwetten (noblehomes.propertywaresites.com)
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Прочесть заключение эксперта – https://indivinejourneys.com/holi-festival-in-india
Все шаги фиксируются в карте наблюдения. Если динамика «плоская», меняется один параметр (скорость/объём/последовательность), и через оговорённое окно проводится повторная оценка. Это снижает риск побочных реакций и сохраняет дневную ясность.
Детальнее – http://vyvod-iz-zapoya-v-kaliningrade15.ru
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Подробнее тут – https://dzentlmenis.com/tomer-taisniba-stereotipi-un-miti-par-zodiaka-zimem-kas-nav-talu-no-patiesibas-izlasi-pats/79015
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Ознакомиться с теоретической базой – https://icc-ccs.org/corporate-fair-trade-community
«Волшебной капельницы» не существует. Мы структурируем инфузии от симптомов, а не от «средних рецептов». Ниже — логика подбора для типичных профилей; реальную схему определяет врач на месте.
Выяснить больше – врач вывод из запоя калининград
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Узнать напрямую – https://checkerviet-pga.com/gai-goi-cao-cap-ha-noi-pga-cao-cap-ha-noi-gai-goi-phuc-vu-tan-noi-ha-noi-nguoi-mau-anh-sinh-vien-ban-dam-ha-noi
Первое сутки с половиной — «каркас» программы. Мы формулируем цель каждого окна, фиксируем инструменты и пороги перехода. Если ожидаемой динамики нет, меняется один параметр (темп/объём/последовательность), после чего назначается повторная оценка. Это защищает от полипрагмазии и сохраняет причинно-следственную связь.
Подробнее – narkologicheskaya-klinika-petrozavodsk15.ru/
Если на первичном звонке звучат «красные флаги» (выраженная одышка, спутанность сознания, скачки ритма), мы предлагаем стационарное окно мониторинга. При низком риске стартуем дома или амбулаторно и поддерживаем человека вечерними видеовставками по 15–20 минут, чтобы пройти «трудный час» без лишних поездок и паники.
Выяснить больше – нарколог на дом вывод из запоя в воронеже
Городская среда Воронежа — яркие подъезды, плотный трафик, шумные дворы — усиливает вечернюю реактивность. Поэтому выездная служба «ВоронежВита» организована «тихо»: согласованная парковка, быстрый подъем без опознавательных знаков, часть расходников доставляется заранее, чтобы на адресе сразу перейти к диагностике и инфузии. Коммуникация ведётся через защищённые каналы, уведомления — «беззвучные», названия в документах — нейтральные. Такой дизайн среды не декоративен: чем меньше «социального шума», тем устойчивее ночной сон и тем быстрее возвращается переносимость воды и лёгкой еды.
Получить больше информации – вывод из запоя недорого
Круглосуточная доступность важна, но ещё важнее — структурированность. В «ПолярМед Центре» каждое окно времени имеет цель, действия и ясные критерии перехода. Если ответ «плоский», меняем один параметр (темп, объём, последовательность) и повторно оцениваем состояние в назначённое время. Это поддерживает причинно-следственную связь и исключает полипрагмазию.
Подробнее можно узнать тут – http://narkologicheskaya-klinika-murmansk15.ru
Мы не противопоставляем форматы — комбинируем их. Например, первые часы — выездная стабилизация с титрованной инфузией и чётким контролем АД/ЧСС/SpO?, затем — амбулаторные короткие визиты с вечерними онлайн-вставками. Если появляются «красные флаги» (дыхание, ритм, сознание), маршрут без пауз переводится в стационар: та же карта наблюдения, те же цели, только круглосуточный мониторинг и ночной пост. Приватность встроена на каждом этапе: нейтральные формулировки в документах, «тихие» уведомления, гражданская одежда персонала, доступ к данным по ролям.
Изучить вопрос глубже – наркологическая клиника лечение алкоголизма ставрополь
Вся динамика фиксируется в единой карте наблюдения. При переводе в амбулаторную точку мы не «сбрасываем» историю: решения продолжаются с учётом уже сделанного и реакции пациента на вмешательства.
Получить больше информации – вывод из запоя недорого в воронеже
Если в первичном звонке звучат «красные флаги» (одышка, спутанность сознания, резкие скачки ритма), мы предлагаем стационарное «окно» мониторинга с ночным постом. При низких рисках стартуем на дому: контрольные точки совпадают с домашним комфортом, а вечерние online-вставки по 15–20 минут поддерживают предсказуемость без лишних поездок.
Выяснить больше – http://www.domen.ru
Наркологическая клиника «ПолярМед Центр» — это пространство круглосуточной помощи, где медицинская точность сочетается с бережным сервисом и конфиденциальными процедурами. Мы строим терапию как последовательность проверяемых шагов: ставим понятную цель, выбираем подходящий инструмент, заранее определяем маркеры контроля и фиксируем время повторной оценки. Такая дисциплина исключает «универсальные сильные капельницы» и заменяет их модульными решениями с предсказуемым эффектом. Пациент и его близкие на каждом этапе понимают, почему именно такое назначение выбрано сейчас и в какой момент мы ожидаем улучшение самочувствия.
Подробнее можно узнать тут – http://narkologicheskaya-klinika-murmansk15.ru
Городской ритм Петрозаводска с озёрным ветром, короткими сумерками и сезонной влажностью повышает сенсорную нагрузку в вечерние часы, поэтому наш маршрут спроектирован «мягко». Координатор заранее уточняет подъезд, парковку, код домофона, рекомендует «тихий режим» связи и присылает нейтральное уведомление о визите. Бригада приходит в гражданской одежде, сумки — без логотипов, разговоры — короткими фразами. Такое поведение снижает у пациента и семьи реактивность, выравнивает вариабельность ЧСС к сумеркам и уменьшает потребность «усиливать» схему на ночь. Если на предзвонке выявлены «красные флаги» — неукротимая рвота, выраженная дезориентация, «скачущий» ритм, одышка — мы предлагаем стационар сразу, чтобы не терять время на повторные маршруты.
Углубиться в тему – https://narkolog-na-dom-petrozavodsk15.ru
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Наши рекомендации — тут – https://mattar.com.br/if-the-white-whale-be-raised-it-must-be-in-a-month
В городском ритме Ставрополя дорога сама по себе может усугублять симптомы: плотный трафик, резкие звуки, длинные коридоры ожидания. Поэтому «СтаврВита» разворачивает секторные выезды: немаркированный транспорт, гражданская одежда специалистов, согласованная парковка и подъезд, доставка расходников отдельно от врача при необходимости — чтобы на месте сразу переходить к диагностике и запуску инфузии. Переписка ведётся нейтральными формулировками, уведомления «беззвучные», документы без стигматизирующих слов. По желанию всё общение идёт через доверенное лицо: оно получает короткие апдейты в согласованные «окна», не перегружаясь клиническими деталями.
Изучить вопрос глубже – наркологический вывод из запоя
Если при первичном звонке фиксируем «красные флаги» (угнетение сознания, выраженная одышка, резкое падение SpO?, нестабильная аритмия), сразу предлагаем стационарное наблюдение с ночным постом. При низких рисках начинаем дома, но держим низкий порог для эскалации, чтобы не терять время, если состояние меняется.
Разобраться лучше – вызов нарколога на дом ставрополь
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Узнай первым! – https://alfa3construtora.com.br/projects/vila-sao-francisco-sao-paulo
Если ожидаемая динамика «плоская», врач меняет один параметр и назначает повторную оценку. Такой подход сохраняет ясность днём и снижает вероятность побочных реакций.
Подробнее тут – частная наркологическая клиника
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Наши рекомендации — тут – https://fyrlegal.com/obtenemos-las-certificaciones-internacionalesiso-27001-e-iso-27701
Если ожидаемая динамика «плоская», мы не усиливаем всё сразу. Меняется один параметр: скорость инфузии, порядок модулей или длительность вечерних включений. Такой «тонкий ремонт» безопаснее тотальной перестройки и лучше сохраняет ясность днём.
Детальнее – запой наркологическая клиника воронеж
Если на предвызовном созвоне звучат «красные флаги» (неукротимая рвота, выраженная дезориентация, «скачущий» ритм, одышка), мы сразу резервируем палату усиленного наблюдения и подключаем расширенный мониторинг. При низком риске старт возможен амбулаторно или на дому с бесшовным переводом в стационар при необходимости — без очередей и «говорящих» вывесок. Во всех сценариях анонимность — не «опция», а стандарт по умолчанию.
Исследовать вопрос подробнее – наркологические клиники алкоголизм в петрозаводске
В реальности Воронежа на самочувствие влияет не только фармакология, но и логистика: трассы с плотным трафиком, яркое освещение подъездов, очереди в медорганизациях. «ВоронежМедЦентр» гасит эти раздражители организационно: «тихие окна» приёма без коридорного шума, согласованная парковка, немаркированные выезды, нейтральные формулировки в документах и «беззвучные» напоминания. Снижение сенсорной нагрузки — это не декоративная опция, а клинический фактор: спокойная первая ночь, ровный пульс к вечеру, предсказуемость режима воды и тёплой пищи малыми порциями.
Выяснить больше – https://narkologicheskaya-klinika-voronezh15.ru/narkologicheskaya-klinika-voronezh-otzyvy
В городском ритме Ставрополя дорога сама по себе может усугублять симптомы: плотный трафик, резкие звуки, длинные коридоры ожидания. Поэтому «СтаврВита» разворачивает секторные выезды: немаркированный транспорт, гражданская одежда специалистов, согласованная парковка и подъезд, доставка расходников отдельно от врача при необходимости — чтобы на месте сразу переходить к диагностике и запуску инфузии. Переписка ведётся нейтральными формулировками, уведомления «беззвучные», документы без стигматизирующих слов. По желанию всё общение идёт через доверенное лицо: оно получает короткие апдейты в согласованные «окна», не перегружаясь клиническими деталями.
Разобраться лучше – http://vyvod-iz-zapoya-stavropol15.ru
Городская среда Калининграда специфична: морской ветер, сезонные пробки, яркие витрины в вечерние часы. Эти факторы часто усиливают тревожность и мешают засыпанию. Поэтому мы проектируем выезд «мягко»: согласованная парковка, немаркированный вход, короткий маршрут до места процедуры, отсутствие громких звонков и «визуального шума» у порога. Родственникам предоставляем «тихие окна» связи — короткие апдейты в заранее оговорённое время без лишних подробностей. Такой формат не просто комфортнее, он клинически полезен: чем меньше стимулов, тем меньше потребность в ночных «усилениях» и тем стабильнее проходит первая ночь.
Подробнее можно узнать тут – помощь вывод из запоя
Стартовый осмотр должен быть быстрым и осмысленным. Мы исключаем «обязательные» исследования, которые не меняют тактику, и оставляем то, что прямо влияет на состав инфузии, темп, место ведения (дом/амбулатория/стационар) и объём поведенческих рекомендаций. Решения принимаются на свежих цифрах и клинической картине «здесь и сейчас», а повторные замеры назначаются не «по привычке», а по смыслу. Это экономит силы пациента и время команды, а главное — уменьшает фармакологическую нагрузку без потери безопасности.
Изучить вопрос глубже – https://narkologicheskaya-klinika-stavropol15.ru
Городская среда Ставрополя создаёт дополнительные раздражители — трафик, шумовые пики, яркое освещение подъездов. Команда «СтаврДоктор» гасит эти факторы организационно: секторное распределение бригад, согласованная парковка, вход в подъезд без опознавательных знаков, доставка расходников при необходимости отдельно от врача, чтобы на месте сразу перейти к осмотру и инфузии. Коммуникация ведётся через защищённые каналы, уведомления «беззвучные», наименования в чеках — нейтральные. Если пациенту спокойнее, общение частично берёт на себя доверенное лицо; оно получает краткие апдейты в заранее оговорённые «тихие окна».
Подробнее можно узнать тут – врач нарколог на дом
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Доступ к полной версии – https://modesynthese.com/snapseed-64
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Смотрите также… – https://sanvatquy.vn/thuoc-quy-tu-cay-co-mang-ten-mot-loai-chim.html
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Получить больше информации – https://srstechnologies.org/hello-world
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Открой скрытое – https://buttina.com.br/2022/05/29/assistir-palmeiras-x-sao-jose-sp-ao-vivo-com-imagens-brasileiro-feminino-a1-de-2022-domingo-29-05
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Не упусти важное! – https://zoegilbert.com/cropped-folk-header-cropped-from-cover-design-v3-jpg
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Кликни и узнай всё! – https://blog.landschool.mx/2022/09/14/que-es-el-design-thinking-en-educacion
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Получить больше информации – https://theplanetweekly.com/chamber-news-2
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Получить больше информации – https://cubbinthekitchen.com/sweet-cream-cheese-dip
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Перейти к полной версии – https://www.roelabogados.com/2019/01/12/what-we-are-capable-of-usually-gets-discovered-7
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Разобраться лучше – https://ecolemusiqueserris.fr/fr/component/k2/item/6-repetition-collective-des-professeurs-pour-leur-concert-du-23-janvier.html?start=373410
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Прочитать подробнее – https://nicolasluciani.com/11007750_10155116263510478_4707253131953727479_n
Острый этап разбит на небольшие «окна» с измеримыми целями. Это убирает неопределённость и дисциплинирует процесс: пациент знает, что будет происходить, когда будет проверка и по каким маркерам оценивается успех. Если ответ «плоский», корректируется один параметр, а затем обязательно следует повторная оценка в оговорённое время.
Исследовать вопрос подробнее – платная наркологическая клиника
Городской ритм Петрозаводска с озёрным ветром, короткими сумерками и сезонной влажностью повышает сенсорную нагрузку в вечерние часы, поэтому наш маршрут спроектирован «мягко». Координатор заранее уточняет подъезд, парковку, код домофона, рекомендует «тихий режим» связи и присылает нейтральное уведомление о визите. Бригада приходит в гражданской одежде, сумки — без логотипов, разговоры — короткими фразами. Такое поведение снижает у пациента и семьи реактивность, выравнивает вариабельность ЧСС к сумеркам и уменьшает потребность «усиливать» схему на ночь. Если на предзвонке выявлены «красные флаги» — неукротимая рвота, выраженная дезориентация, «скачущий» ритм, одышка — мы предлагаем стационар сразу, чтобы не терять время на повторные маршруты.
Углубиться в тему – платный нарколог на дом петрозаводск
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Изучить материалы по теме – https://mpscwow.com/%E0%A4%96%E0%A5%81%E0%A4%B6%E0%A4%96%E0%A4%AC%E0%A4%B0-%E0%A4%86%E0%A4%A0%E0%A4%B5%E0%A4%BE-%E0%A4%B9%E0%A4%AA%E0%A5%8D%E0%A4%A4%E0%A4%BE-%E0%A4%B5%E0%A4%BF%E0%A4%A4%E0%A4%B0%E0%A4%A3-%E0%A4%B8
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
Наши рекомендации — тут – https://motoreview.net/2024/08/30/digital-identity-management-market-size-share-analysis-with-a-cagr-of-15-2021-26
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Наши рекомендации — тут – https://speak-e.com/hello-world
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Дополнительно читайте здесь – https://smkpgri2kediri.sch.id/blog/rekrutmen-kerja-bekerjasama-dengan-tempat-bercakap-kopi
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Читать далее > – https://khaboralltime.com/trailer-and-music-launch-of-torulatar-bhoot
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Перейти к полной версии – https://hpmi2.hpmievents.com/hello-world
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Личный опыт — читайте сами – https://www.jeffdeyo.com/loving-god-when-you-dont-feel-like-it
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Откройте для себя больше – https://limeiranoticias.com.br/2024/02/07/prefeitura-retoma-discussao-para-atualizar-plano-diretor-prefeitura-municipal-de-ubatuba
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Проверенные методы — узнай сейчас – https://angelsrecoveryhouse.com/the-importance-of-a-recovery-home
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Погрузиться в детали – http://www.alr-services.lu/dt_team/bill-sanders
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
А что дальше? – https://schreitbagger.cc/hallo-welt
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Что скрывают от вас? – https://lanechiro.com.au/how-to-tell-if-you-have-carpal-tunnel-syndrome
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Откройте для себя больше – https://shinblog.site/ztv_cancel
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Продолжить чтение – https://missoesfrutificar.com/unlock-your-potential-with-these-inspiring-ebooks
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Узнай первым! – https://5stardrivingschooledmonton.ca/why-5-star-driving-school-edmonton-is-the-best-choice-for-new-drivers
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Что ещё? Расскажи всё! – https://foodtrucksunited.com/food-trucks-united-7
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Интересует подробная информация – https://nrgtribe.com/covid-19-vaccine-update
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Ознакомиться с деталями – https://pelias.nl/how-to-stay-on-the-sunny-side-in-a-cloudy-market
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Есть чему поучиться – https://cosecharecords.com.ar/research-original-covers-part-i
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Слушай внимательно — тут важно – https://missoesfrutificar.com/unlock-your-potential-with-these-inspiring-ebooks
Hello there! I know this is somewhat off topic but I was wondering which blog platform are you using for this site? I’m getting fed up of WordPress because I’ve had issues with hackers and I’m looking at alternatives for another platform. I would be awesome if you could point me in the direction of a good platform.
Вывод из запоя в Самаре на базе стационара — когда важен результат, стабильность и медицинская поддержка 24/7.
Выяснить больше – https://vyvod-iz-zapoya-v-stacionare-samara23.ru
В кардиологической и психологической поддержке «Частного Медика 24» в Самаре — полный комплекс для безопасного восстановления после запоя.
Узнать больше – http://vyvod-iz-zapoya-v-stacionare-samara25.ru
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Исследовать вопрос подробнее – нарколог на дом вывод из запоя в нижний новгороде
Если вам нужна помощь нарколога на дому — срочно и конфиденциально, узнайте, как работают услуги выездного врача, какие методы применяют и сколько это стоит › подробнее на covid-stat.com Выяснить больше – http://www.kpilib.ru/forum.php?tema=12653
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Получить больше информации – вывод из запоя вызов
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Посмотреть всё – https://bloggenmeister.com/die-grundlagen-des-bloggens-verstehen
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Смотри, что ещё есть – https://aqacademy11.com/keats-ode-grecian-urn-to-autumn-to-a-nightingale
Hey very nice site!! Man .. Beautiful .. Amazing .. I will bookmark your blog and take the feeds also?I am happy to find so many useful information here in the post, we need work out more strategies in this regard, thanks for sharing. . . . . .
Адекватное лечение, комфорт и забота — так проходят дни в стационаре «Частного Медика 24» во время вывода из запоя.
Изучить вопрос глубже – быстрый вывод из запоя в стационаре в самаре
В Воронеже клиника «Частный Медик?24» проводит вывод из запоя в стационаре с круглосуточным медицинским контролем.
Получить дополнительную информацию – https://vyvod-iz-zapoya-v-stacionare-voronezh23.ru
Вывод из запоя в стационаре — это шанс начать путь к трезвой жизни, и в Самаре этот шанс предоставляет «Частный Медик 24».
Получить дополнительную информацию – вывод из запоя в стационаре клиника в самаре
В Самаре стационар «Частного Медика 24» предлагает персонализированный подход — лечение запоя, детоксикация и дальнейшее восстановление под наблюдением специалистов.
Изучить вопрос глубже – вывод из запоя в стационаре в самаре
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Подробнее тут – вывод из запоя клиника в сочи
Клиника «РостовМед» предлагает профессиональную наркологическую помощь в Ростове и области в режиме 24/7. Наша команда готова выехать на дом к пациенту в любое время суток, обеспечивая анонимность и высокие медицинские стандарты. В основе работы — индивидуальный подход, современное оборудование и чётко отлаженные протоколы детоксикации, что позволяет безопасно вывести пациента из запоя и начать этап реабилитации без стресса госпитализации.
Детальнее – вывод наркологическая клиника
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Изучить вопрос глубже – нарколог на дом краснодар
В клинике в Самаре устраняют симптомы интоксикации, оказывают поддержку организму и помогают восстановиться после тяжёлых запоев.
Получить больше информации – стационар вывод из запоя самара
Путь к трезвой жизни начинается здесь — подробный гид по выводу из запоя: методы, особенности, чего ожидать — dettka.com/vyvod-iz-zapoya-put-k-zdorovoj-zhizni Ознакомиться с деталями – http://www.baikal-biz.ru/forum/viewtopic.php?f=10&t=145018
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Подробнее можно узнать тут – вызвать врача нарколога на дом в краснодаре
Экстренная помощь при запое в Нижнем Новгороде — капельница на дому от опытных врачей-наркологов.
Узнать больше – помощь вывод из запоя в нижний новгороде
Профессиональная наркологическая помощь 24 часа в Саратове: экстренные меры, поддержка при зависимости и рекомендации. Всё это — по ссылке на Damki.biz Исследовать вопрос подробнее – http://kremlevsk.kamrbb.ru/?x=read&razdel=5&tema=714
В кардиологической и психологической поддержке «Частного Медика 24» в Самаре — полный комплекс для безопасного восстановления после запоя.
Изучить вопрос глубже – быстрый вывод из запоя в стационаре самара
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Разобраться лучше – вызвать врача нарколога на дом в краснодаре
Стационар «Частного Медика 24» — это круглосуточная помощь при запое, современные капельницы и заботливый уход.
Выяснить больше – вывод из запоя в стационаре клиника нижний новгород
Ищете, где в Саратове действительно помогают справиться с алкоголизмом? Статья о клинике Торпедомед на LadyCaramelka охватывает всё: диагностика, методы, цены и отзывы. Выяснить больше – http://essentiallife.ru/flatboard/view.php/topic/2025-09-020516038cd36/p/1
В Самаре клиника «Частный Медик 24» предлагает вывод из запоя в стационаре с полным медицинским контролем и комфортными палатами.
Углубиться в тему – вывод из запоя в стационаре клиника в самаре
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Подробнее – нарколог вывод из запоя нижний новгород
Клиника «Похмельная служба» в Нижнем Новгороде предлагает комплексное лечение запоя с использованием капельницы. Наши специалисты проводят диагностику и назначают индивидуальный план лечения.
Подробнее тут – http://www.vyvod-iz-zapoya-nizhnij-novgorod13.ru
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Углубиться в тему – вывод из запоя капельница
Клиника «РостовМед» предлагает профессиональную наркологическую помощь в Ростове и области в режиме 24/7. Наша команда готова выехать на дом к пациенту в любое время суток, обеспечивая анонимность и высокие медицинские стандарты. В основе работы — индивидуальный подход, современное оборудование и чётко отлаженные протоколы детоксикации, что позволяет безопасно вывести пациента из запоя и начать этап реабилитации без стресса госпитализации.
Исследовать вопрос подробнее – http://www.domen.ru
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Углубиться в тему – запой нарколог на дом краснодар
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Подробнее тут – нарколог вывод из запоя
Ищете надёжные, проверенные способы избавиться от алкогольной зависимости? Тогда вам стоит прочитать статью «Лучшие методы лечения алкоголизма». Подробнее – http://mymoscow.forum24.ru/?1-6-0-00030432-000-0-0
В автомобиле находятся:
Разобраться лучше – частная наркологическая клиника в ростове-на-дону
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Разобраться лучше – вывод из запоя цена в нижний новгороде
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Получить дополнительные сведения – запой нарколог на дом
В автомобиле находятся:
Получить больше информации – https://narkologicheskaya-klinika-rostov13.ru
В Самаре стационар «Частного Медика 24» предлагает персонализированный подход — лечение запоя, детоксикация и дальнейшее восстановление под наблюдением специалистов.
Подробнее – вывод из запоя в стационаре клиника
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Подробнее можно узнать тут – платный нарколог на дом
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Получить больше информации – вывод из запоя
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Выяснить больше – вывод из запоя капельница на дому
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Узнать больше – нарколог на дом круглосуточно
В «Частном Медике 24» в Воронеже каждый пациент, проходящий вывод из запоя в стационаре, получает комплексную помощь — диагностика, устранение интоксикации, восстановительная терапия, психологическая работа, всё с постоянным наблюдением и поддержкой, в условиях, где безопасность и анонимность стоят на первом месте.
Ознакомиться с деталями – https://vyvod-iz-zapoya-v-stacionare-voronezh22.ru
Стационар «Частного Медика 24» в Воронеже — место, где пациент, страдающий от длительного запоя, получает не просто деньги-стоимость услуги, а полноценную помощь: диагностику, детоксикацию, медикаментозную поддержку и психологическую помощь с уважением к личному пространству и анонимности.
Узнать больше – вывод из запоя в стационаре в воронеже
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Разобраться лучше – вывод из запоя на дому круглосуточно в сочи
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Получить дополнительную информацию – вывод из запоя цена сочи
«Частный Медик 24» — это медицинский контроль, поддержка и лечение на всех этапах вывода из запоя.
Разобраться лучше – вывод из запоя в стационаре анонимно нижний новгород
Вывод из запоя в стационаре Воронежа — безопасный и эффективный метод лечения. Наши специалисты обеспечат круглосуточное наблюдение и комплексное лечение, включая детоксикацию, восстановление водно-электролитного баланса и психотерапевтическую поддержку.
Получить дополнительные сведения – вывод из запоя в стационаре клиника в воронеже
В Краснодаре нарколог из клиники «Детокс» приедет на дом, чтобы вывести из запоя и оказать необходимую помощь.
Узнать больше – врач нарколог выезд на дом
Стационар «Частного Медика?24» помогает безопасно и быстро восстановиться после длительного запоя.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-v-stacionare-voronezh23.ru
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Изучить вопрос глубже – платный нарколог на дом
beste sportwetten deutschland, Charles, verluste zurückholen
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Углубиться в тему – выезд нарколога на дом краснодар
Стационарное лечение запоя в Воронеже — индивидуальный подход к каждому пациенту. Мы предлагаем комфортные условия и профессиональную помощь для быстрого и безопасного вывода из запоя.
Узнать больше – нарколог вывод из запоя в стационаре воронеж
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Выяснить больше – https://narkolog-na-dom-krasnodar26.ru
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Получить больше информации – запой нарколог на дом в краснодаре
В больничных условиях «Частного Медика 24» врачи контролируют давление, сердце и функции жизненно важных органов при выводе из запоя.
Изучить вопрос глубже – нарколог вывод из запоя в стационаре в самаре
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Выяснить больше – частный нарколог на дом краснодар
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Ознакомиться с деталями – скорая вывод из запоя
Вызов нарколога на дом в Челябинске обеспечивает возможность проведения полного обследования и первичной терапии в условиях, привычных для пациента. Специалисты оказывают услуги круглосуточно, что позволяет своевременно купировать острые состояния, связанные с алкогольной интоксикацией, абстинентным синдромом или осложнениями наркозависимости.
Выяснить больше – помощь нарколога на дому челябинск
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительную информацию – вывод из запоя на дому недорого сочи
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Подробнее можно узнать тут – нарколог на дом клиника в краснодаре
Если вы ищете надёжный и понятный путь к избавлению от алкогольной зависимости — вам стоит заглянуть в статью «Эффективные услуги лечения алкоголизма: путь к трезвой жизни». Разобраться лучше – http://kremlevsk.kamrbb.ru/?x=read&razdel=5&tema=637
В Самаре «Частный Медик 24» предлагает прозрачные цены на вывод из запоя, без неожиданных расходов.
Подробнее можно узнать тут – вывод из запоя в стационаре клиника самара
Программа вывода из запоя в Воронеже от «Частного Медика 24» включает не только устранение физической зависимости, но и работу по восстановлению сна, гидратацию, лекарственную поддержку, а также психотерапию, чтобы помочь справиться не просто с запоем, но и с причинами, которые к нему привели.
Узнать больше – вывод из запоя в стационаре клиника в воронеже
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Узнать больше – вывод из запоя на дому недорого
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Углубиться в тему – нарколог на дом цены
bester Bonus sportwetten (https://Restauranteleonardo.Com.br/2025/10/14/Best-online-betting-sites)
anbieter ohne oasis
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Изучить вопрос глубже – нарколог на дом недорого в краснодаре
В автомобиле находятся:
Исследовать вопрос подробнее – наркологическая клиника в ростове-на-дону
Стационар «Частного Медика 24» в Воронеже — место, где пациент, страдающий от длительного запоя, получает не просто деньги-стоимость услуги, а полноценную помощь: диагностику, детоксикацию, медикаментозную поддержку и психологическую помощь с уважением к личному пространству и анонимности.
Получить дополнительные сведения – нарколог вывод из запоя в стационаре воронеж
Если домашние методы не помогают, вывод из запоя в стационаре в Самаре — это безопасный выбор с профессиональной детоксикацией.
Получить больше информации – вывод из запоя в стационаре самара
Запой — это не просто длительное употребление алкоголя, а состояние, при котором организм человека находится в постоянной интоксикации. Узнайте, как безопасно вывести организм из этого состояния — читайте статью на WomanClub. Исследовать вопрос подробнее – http://history1997.forum24.ru/?1-7-0-00000165-000-0-0-1756886821
В Сочи клиника «Детокс» предлагает вывод из запоя в стационаре. Опытные врачи обеспечивают полную безопасность и комфорт пациента, а услуги доступны круглосуточно.
Подробнее – наркологический вывод из запоя сочи
Клиника «Похмельная служба» в Нижнем Новгороде предлагает комплексное лечение запоя с использованием капельницы. Наши специалисты проводят диагностику и назначают индивидуальный план лечения.
Получить дополнительную информацию – вывод из запоя клиника нижний новгород
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Подробнее можно узнать тут – платный нарколог на дом
В Краснодаре нарколог из клиники «Детокс» приедет на дом, чтобы вывести из запоя и оказать необходимую помощь.
Исследовать вопрос подробнее – помощь нарколога на дому в краснодаре
При госпитализации пациент находится под наблюдением 24/7, что снижает риск осложнений.
Подробнее – наркология вывод из запоя в стационаре
«Частный Медик 24» — это медицинский контроль, поддержка и лечение на всех этапах вывода из запоя.
Получить больше информации – вывод из запоя в стационаре клиника в нижний новгороде
Для восстановления после запоя выбирайте стационар клиники «Детокс» в Сочи. Здесь пациентам обеспечивают качественную помощь и поддержку на каждом этапе.
Изучить вопрос глубже – врач вывод из запоя
В Сочи клиника «Детокс» предлагает полный курс вывода из запоя в стационаре. Круглосуточный медицинский контроль гарантирует безопасность и эффективность лечения.
Углубиться в тему – вывод из запоя на дому круглосуточно
Своевременный вызов нарколога позволяет снизить риски осложнений, таких как судорожный синдром, панкреатит или сердечная недостаточность, часто сопровождающие тяжелое алкогольное или наркотическое отравление. По данным исследований, раннее вмешательство сокращает сроки госпитализации и улучшает прогнозы выздоровления.
Изучить вопрос глубже – http://www.domen.ru
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее можно узнать тут – нарколог на дом недорого
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Подробнее тут – нарколог на дом анонимно
Если вам важно узнать, как безопасно и эффективно выйти из состояния запоя с учетом физиологии, психики и внешнего окружения — загляните в статью «Выход из запоя» на сайте Nalatty. Она оформлена в привычном формате полезных советов, пропитанном заботой и доступностью, присущей проекту «семейный очаг». Подробнее – http://krd.best-city.ru/forum/thread110110/
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Узнать больше – вывод из запоя капельница
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врач приедет в течение 1–2 часов, проведёт необходимое обследование и назначит лечение. Услуга доступна круглосуточно и анонимно.
Подробнее можно узнать тут – психиатр нарколог на дом
Если вы ищете надёжный и понятный путь к избавлению от алкогольной зависимости — вам стоит заглянуть в статью «Эффективные услуги лечения алкоголизма: путь к трезвой жизни». Получить дополнительные сведения – http://kremlevsk.kamrbb.ru/?x=read&razdel=5&tema=637
В Самаре «Частный Медик 24» предлагает прозрачные цены на вывод из запоя, без неожиданных расходов.
Подробнее – http://vyvod-iz-zapoya-v-stacionare-samara23.ru
Стационар «Частного Медика 24» — это круглосуточная помощь при запое, современные капельницы и заботливый уход.
Узнать больше – нарколог вывод из запоя в стационаре нижний новгород
Стационар «Частного Медика 24» — условия, где пациент может спокойно пройти вывод из запоя без страха и дискомфорта.
Изучить вопрос глубже – быстрый вывод из запоя в стационаре
В больничных условиях «Частного Медика 24» врачи контролируют давление, сердце и функции жизненно важных органов при выводе из запоя.
Подробнее – наркология вывод из запоя в стационаре
sichere wetten finden
Also visit my webpage :: wettbüRo freiburg
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Выяснить больше – вывод из запоя нижний новгород
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Получить дополнительные сведения – http://vyvod-iz-zapoya-nizhnij-novgorod11.ru
Круглосуточный стационарный вывод из запоя в Воронеже — доступная помощь в любое время. Вы можете обратиться к нам в любое время суток, и мы окажем необходимую медицинскую помощь.
Ознакомиться с деталями – вывод из запоя в стационаре клиника в воронеже
Выведение из запоя в стационаре Воронежа — помощь при острых состояниях и хронической зависимости. Наши опытные наркологи используют современные методы лечения для быстрого и безопасного вывода из запоя.
Подробнее тут – наркология вывод из запоя в стационаре в воронеже
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Подробнее тут – помощь нарколога на дому краснодар
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить больше информации – вывод из запоя дешево в сочи
Клиника «РостовМед» предлагает профессиональную наркологическую помощь в Ростове и области в режиме 24/7. Наша команда готова выехать на дом к пациенту в любое время суток, обеспечивая анонимность и высокие медицинские стандарты. В основе работы — индивидуальный подход, современное оборудование и чётко отлаженные протоколы детоксикации, что позволяет безопасно вывести пациента из запоя и начать этап реабилитации без стресса госпитализации.
Исследовать вопрос подробнее – вывод наркологическая клиника
В Воронеже клиника помогает стабилизировать состояние и восстановить здоровье после запоя.
Получить больше информации – вывод из запоя в стационаре клиника в воронеже
В Воронеже клиника «Частный Медик 24» предлагает программу вывода из запоя в стационаре по цене от 6500 ?. Здесь вас ждут комфортные палаты, круглосуточный медицинский контроль и безопасные методы детоксикации, включая капельницы и восстановительное лечение. Анонимность гарантирована, без лишних формальностей и без постановки на учёт.
Узнать больше – вывод из запоя в стационаре анонимно в воронеже
Вывод из запоя в Самаре проводится с проверенными препаратами, с учётом состояния пациента и без лишнего стресса.
Разобраться лучше – vyvod-iz-zapoya-v-stacionare-samara23.ru/
В Воронеже клиника «Частный Медик?24» проводит вывод из запоя в стационаре с круглосуточным медицинским контролем.
Детальнее – http://vyvod-iz-zapoya-v-stacionare-voronezh24.ru
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Получить дополнительные сведения – частный нарколог на дом краснодар
Ищете надёжные, проверенные способы избавиться от алкогольной зависимости? Тогда вам стоит прочитать статью «Лучшие методы лечения алкоголизма». Получить дополнительную информацию – http://www.artlib.ru/index.php?id=26&idr=18&idt=50310
В стационаре пациент получает и физиологическую помощь, и психологическое сопровождение, что важно для долгосрочного восстановления.
Узнать больше – быстрый вывод из запоя в стационаре
Выход есть: эффективные способы преодоления зависимости в Саратове, проверенные клиники и советы специалистов — читайте на Noprost. Изучить вопрос глубже – http://chesskomi.borda.ru/?1-9-0-00000237-000-0-0-1756816219
В «Частном Медике 24» заботятся о здоровье и возвращают ясность ума после тяжелого запоя.
Узнать больше – стационар вывод из запоя в нижний новгороде
Клиника «Частный Медик 24» в Самаре оказывает помощь при запое анонимно, круглосуточно и без скрытых платежей.
Ознакомиться с деталями – vyvod-iz-zapoya-v-stacionare-samara24.ru/
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Получить дополнительную информацию – нарколог на дом вывод краснодар
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Ознакомиться с деталями – http://vyvod-iz-zapoya-nizhnij-novgorod11.ru
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Изучить вопрос глубже – вызов нарколога на дом в краснодаре
В Сочи стационар клиники «Детокс» предлагает комплексный вывод из запоя. Пациентам обеспечивают комфорт, безопасность и круглосуточный контроль.
Подробнее можно узнать тут – вывод из запоя в сочи
Выездная бригада «РостовМед» оснащена всем необходимым для оказания экстренной помощи и проведения полного курса детоксикации на дому. Процесс состоит из нескольких этапов:
Изучить вопрос глубже – https://narkologicheskaya-klinika-rostov13.ru/
В стационаре «Частного Медика?24» пациент получает комплексное лечение, включая капельницы и медикаменты.
Исследовать вопрос подробнее – нарколог вывод из запоя в стационаре воронеж
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Разобраться лучше – вывод из запоя сочи
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Изучить вопрос глубже – вывод из запоя на дому цена сочи
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Выяснить больше – вывод из запоя с выездом в нижний новгороде
В Воронеже клиника помогает стабилизировать состояние и восстановить здоровье после запоя.
Изучить вопрос глубже – https://vyvod-iz-zapoya-v-stacionare-voronezh24.ru
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Углубиться в тему – нарколог на дом клиника краснодар
В стационаре пациент получает и физиологическую помощь, и психологическое сопровождение, что важно для долгосрочного восстановления.
Углубиться в тему – http://vyvod-iz-zapoya-v-stacionare-samara25.ru
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врач приедет в течение 1–2 часов, проведёт необходимое обследование и назначит лечение. Услуга доступна круглосуточно и анонимно.
Подробнее – врач нарколог выезд на дом в краснодаре
Не знаете, с чего начать борьбу с зависимостью? Полный путеводитель по лечению в Саратове — на Noprost. Подробнее – http://www.kpilib.ru/forum.php?tema=12658
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Углубиться в тему – вывод из запоя вызов
Если нужен профессиональный вывод из запоя, обращайтесь в стационар клиники «Детокс» в Сочи. Все процедуры проводятся анонимно и под наблюдением специалистов.
Получить больше информации – нарколог на дом вывод из запоя в сочи
Своевременный вызов нарколога позволяет снизить риски осложнений, таких как судорожный синдром, панкреатит или сердечная недостаточность, часто сопровождающие тяжелое алкогольное или наркотическое отравление. По данным исследований, раннее вмешательство сокращает сроки госпитализации и улучшает прогнозы выздоровления.
Подробнее тут – вызов врача нарколога на дом в челябинске
Ищете способ выйти из запоя и ступить на путь к новой, здоровой жизни? Тогда вам стоит ознакомиться с материалом «Вывод из запоя — путь к здоровой жизни». В нём раскрываются ключевые этапы и нюансы выхода из тяжелого алкогольного состояния. Ознакомиться с деталями – http://kremlevsk.kamrbb.ru/?x=read&razdel=5&tema=636
В современных условиях лечение алкогольной и наркотической зависимости требует комплексного подхода и быстрого реагирования. Нарколог на дом в Челябинске — это услуга, позволяющая получить квалифицированную помощь без необходимости посещения медицинского учреждения. Такая форма оказания медицинской помощи особенно актуальна для пациентов с острыми состояниями, а также тех, кто нуждается в анонимности и комфорте домашней обстановки.
Подробнее можно узнать тут – http://narkolog-na-dom-chelyabinsk13.ru/vyzov-narkologa-na-dom-chelyabinsk/
«Частный Медик 24» в стационаре помогает начать жизнь заново — с чистого листа, без последствий запоя.
Получить дополнительные сведения – http://vyvod-iz-zapoya-v-stacionare23.ru
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Детальнее – вызвать нарколога на дом срочно в краснодаре
wettanbieter neu
Also visit my blog us wahl wettquoten
В Краснодаре нарколог из клиники «Детокс» приедет на дом, чтобы вывести из запоя и оказать необходимую помощь.
Получить дополнительную информацию – платный нарколог на дом
Стационар «Частного Медика 24» — условия, где пациент может спокойно пройти вывод из запоя без страха и дискомфорта.
Получить дополнительные сведения – быстрый вывод из запоя в стационаре
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Ознакомиться с деталями – нарколог на дом вывод из запоя
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Выяснить больше – помощь вывод из запоя нижний новгород
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Детальнее – вывод из запоя в стационаре в нижний новгороде
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Получить больше информации – вызвать врача нарколога на дом в краснодаре
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Исследовать вопрос подробнее – http://www.narkolog-na-dom-krasnodar29.ru
Стационарное лечение запоя в Воронеже — гарантированная анонимность и комфортные условия. Мы предлагаем индивидуальный подход к каждому пациенту, обеспечивая полное восстановление организма и предотвращение рецидивов.
Разобраться лучше – быстрый вывод из запоя в стационаре
Своевременный вызов нарколога позволяет снизить риски осложнений, таких как судорожный синдром, панкреатит или сердечная недостаточность, часто сопровождающие тяжелое алкогольное или наркотическое отравление. По данным исследований, раннее вмешательство сокращает сроки госпитализации и улучшает прогнозы выздоровления.
Ознакомиться с деталями – психиатр нарколог на дом в челябинске
В Нижнем Новгороде «Частный Медик 24» предлагает доступные цены на вывод из запоя с полным курсом детоксикации.
Углубиться в тему – быстрый вывод из запоя в стационаре в нижний новгороде
Выезд нарколога на дом в Нижнем Новгороде — круглосуточная помощь при запое. Мы гарантируем анонимность и конфиденциальность на всех этапах лечения.
Ознакомиться с деталями – http://www.vyvod-iz-zapoya-nizhnij-novgorod13.ru
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Подробнее тут – вывод из запоя в стационаре
Стационарная детоксикация от алкоголя в Воронеже — восстановление организма под наблюдением специалистов. Мы проводим процедуры очищения организма от токсинов, восстанавливая физическое и психоэмоциональное состояние пациента.
Детальнее – стационар вывод из запоя
В Самаре стационар «Частного Медика 24» предлагает персонализированный подход — лечение запоя, детоксикация и дальнейшее восстановление под наблюдением специалистов.
Детальнее – наркология вывод из запоя в стационаре в самаре
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Ознакомиться с деталями – нарколог на дом вывод
Стационарное лечение запоя в Воронеже — индивидуальный подход к каждому пациенту. Мы предлагаем комфортные условия и профессиональную помощь для быстрого и безопасного вывода из запоя.
Исследовать вопрос подробнее – нарколог вывод из запоя в стационаре
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее можно узнать тут – врач нарколог выезд на дом в краснодаре
Ищете помощь при зависимости — для себя или близкого? Статья «Наркологическая клиника и её услуги» раскрывает, как специализированные учреждения помогают людям справиться с зависимостью — будь то алкоголизм или другие формы. Изучить вопрос глубже – http://www.brokersearch.ru/index.php?option=com_kunena&func=view&catid=7&id=85129
В Сочи стационар клиники «Детокс» предлагает комплексный вывод из запоя. Пациентам обеспечивают комфорт, безопасность и круглосуточный контроль.
Исследовать вопрос подробнее – вывод из запоя на дому сочи
Выездная бригада «РостовМед» оснащена всем необходимым для оказания экстренной помощи и проведения полного курса детоксикации на дому. Процесс состоит из нескольких этапов:
Изучить вопрос глубже – http://narkologicheskaya-klinika-rostov13.ru
Адекватное лечение, комфорт и забота — так проходят дни в стационаре «Частного Медика 24» во время вывода из запоя.
Узнать больше – нарколог вывод из запоя в стационаре в самаре
Если пациент не может приехать в клинику, в Краснодаре нарколог приедет к нему домой. Помощь оказывает «Детокс» круглосуточно.
Подробнее – нарколог на дом вывод из запоя краснодар
В Самаре стационар «Частного Медика 24» предлагает персонализированный подход — лечение запоя, детоксикация и дальнейшее восстановление под наблюдением специалистов.
Ознакомиться с деталями – быстрый вывод из запоя в стационаре самара
Вывод из запоя в клинике «Частный Медик 24» в Воронеже проводится по стандартной и премиум-программе, цена от 6500 ?, где важнейший акцент — на здоровье пациента: предотвращение осложнений, восстановление баланса жидкости и электролитов, поддержка психологического состояния.
Изучить вопрос глубже – вывод из запоя в стационаре клиника воронеж
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительную информацию – http://vyvod-iz-zapoya-sochi24.ru
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Получить дополнительную информацию – анонимный вывод из запоя
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Разобраться лучше – выезд нарколога на дом
Пациентам в Самаре предлагается анонимное лечение в стационаре с круглосуточным уходом и безопасными условиями.
Подробнее можно узнать тут – vyvod-iz-zapoya-v-stacionare-samara23.ru/
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Подробнее – http://vyvod-iz-zapoya-nizhnij-novgorod13.ru
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Разобраться лучше – нарколог на дом круглосуточно цены краснодар
Нарколог прибывает в назначенное время, проводит замеры артериального давления, пульса, сатурации кислорода и температуры. Выполняется экспресс-анализ на содержание алкоголя в крови и оценка водно-электролитного баланса.
Ознакомиться с деталями – https://narkologicheskaya-klinika-rostov13.ru/
Стационарное лечение запоя в Воронеже — гарантированная анонимность и комфортные условия. Мы предлагаем индивидуальный подход к каждому пациенту, обеспечивая полное восстановление организма и предотвращение рецидивов.
Разобраться лучше – стационар вывод из запоя в воронеже
Клиника «РостовМед» предлагает профессиональную наркологическую помощь в Ростове и области в режиме 24/7. Наша команда готова выехать на дом к пациенту в любое время суток, обеспечивая анонимность и высокие медицинские стандарты. В основе работы — индивидуальный подход, современное оборудование и чётко отлаженные протоколы детоксикации, что позволяет безопасно вывести пациента из запоя и начать этап реабилитации без стресса госпитализации.
Узнать больше – https://narkologicheskaya-klinika-rostov13.ru/narkologicheskaya-klinika-narkologicheskij-czentr-v-rostove
В Воронеже клиника помогает стабилизировать состояние и восстановить здоровье после запоя.
Получить больше информации – вывод из запоя в стационаре анонимно
Вызов нарколога на дом в Челябинске обеспечивает возможность проведения полного обследования и первичной терапии в условиях, привычных для пациента. Специалисты оказывают услуги круглосуточно, что позволяет своевременно купировать острые состояния, связанные с алкогольной интоксикацией, абстинентным синдромом или осложнениями наркозависимости.
Углубиться в тему – помощь нарколога на дому в челябинске
В Сочи клиника «Детокс» предлагает полный курс вывода из запоя в стационаре. Круглосуточный медицинский контроль гарантирует безопасность и эффективность лечения.
Детальнее – нарколог на дом вывод из запоя в сочи
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Ознакомиться с деталями – вывод из запоя на дому недорого сочи
Если вы или ваши близкие столкнулись с необходимостью безопасного выхода из запоя, статья «Методы, особенности и важные нюансы выведения из запоя» станет знакомым и надёжным ориентиром. В ней объясняются современные подходы к прерыванию запоя — с акцентом на безопасность и постепенную реконструкцию организма. Подробнее можно узнать тут – http://infoenglish.info/forum/14-9026-1
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Исследовать вопрос подробнее – вызвать нарколога на дом срочно в краснодаре
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Подробнее можно узнать тут – вывод из запоя круглосуточно сочи
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Исследовать вопрос подробнее – нарколог на дом краснодар
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Получить дополнительную информацию – нарколог на дом анонимно в краснодаре
Путь к трезвой жизни начинается здесь — подробный гид по выводу из запоя: методы, особенности, чего ожидать — dettka.com/vyvod-iz-zapoya-put-k-zdorovoj-zhizni Исследовать вопрос подробнее – http://www.baikal-biz.ru/forum/viewtopic.php?f=10&t=145018
В Самаре клиника «Частный Медик 24» предлагает вывод из запоя в стационаре с полным медицинским контролем и комфортными палатами.
Получить больше информации – нарколог вывод из запоя в стационаре в самаре
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Получить дополнительную информацию – https://narkolog-na-dom-krasnodar27.ru
В клинике в Самаре устраняют симптомы интоксикации, оказывают поддержку организму и помогают восстановиться после тяжёлых запоев.
Подробнее тут – вывод из запоя в стационаре клиника в самаре
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Узнать больше – наркология вывод из запоя нижний новгород
В Воронеже клиника помогает стабилизировать состояние и восстановить здоровье после запоя.
Разобраться лучше – наркология вывод из запоя в стационаре воронеж
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Детальнее – анонимный вывод из запоя сочи
Выведение из запоя в стационаре Воронежа — помощь при острых состояниях и хронической зависимости. Наши опытные наркологи используют современные методы лечения для быстрого и безопасного вывода из запоя.
Ознакомиться с деталями – стационар вывод из запоя
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Изучить вопрос глубже – http://www.narkolog-na-dom-krasnodar26.ru
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Разобраться лучше – вывод из запоя капельница нижний новгород
Услуги нарколога на дом: выезд врача, детоксикация и снятие абстиненции без клиники — читайте полный обзор и реальные цены на covid-stat.com Изучить вопрос глубже – http://bookcrossing.ru/forum/topic/176767
Адекватное лечение, комфорт и забота — так проходят дни в стационаре «Частного Медика 24» во время вывода из запоя.
Получить больше информации – vyvod-iz-zapoya-v-stacionare-samara25.ru/
При госпитализации пациент находится под наблюдением 24/7, что снижает риск осложнений.
Исследовать вопрос подробнее – нарколог вывод из запоя в стационаре
Ищете надёжный путь к трезвой жизни? На crocothemes.com вы найдёте эффективные методы кодирования от алкоголизма — реальные ответы специалистов и проверенные решения. Изучить вопрос глубже – http://mymoscow.forum24.ru/?1-5-0-00002775-000-0-0-1756571304
Если домашние методы не помогают, вывод из запоя в стационаре в Самаре — это безопасный выбор с профессиональной детоксикацией.
Подробнее тут – http://vyvod-iz-zapoya-v-stacionare-samara25.ru
«Частный Медик 24» в стационаре помогает начать жизнь заново — с чистого листа, без последствий запоя.
Подробнее тут – быстрый вывод из запоя в стационаре в нижний новгороде
В Сочи клиника «Детокс» предлагает вывод из запоя в стационаре. Опытные врачи обеспечивают полную безопасность и комфорт пациента, а услуги доступны круглосуточно.
Углубиться в тему – вывод из запоя капельница в сочи
В современных условиях лечение алкогольной и наркотической зависимости требует комплексного подхода и быстрого реагирования. Нарколог на дом в Челябинске — это услуга, позволяющая получить квалифицированную помощь без необходимости посещения медицинского учреждения. Такая форма оказания медицинской помощи особенно актуальна для пациентов с острыми состояниями, а также тех, кто нуждается в анонимности и комфорте домашней обстановки.
Подробнее – http://narkolog-na-dom-chelyabinsk13.ru/narkolog-na-dom-kruglosutochno-chelyabinsk/
Экстренная помощь при запое в Нижнем Новгороде — капельница на дому от опытных врачей-наркологов.
Подробнее тут – вывод из запоя клиника
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Разобраться лучше – нарколог на дом краснодар
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Углубиться в тему – вывод из запоя с выездом в нижний новгороде
Вывод из запоя в стационаре клиники проходит в комфортных условиях, без лишнего стресса.
Углубиться в тему – быстрый вывод из запоя в стационаре нижний новгород
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительную информацию – анонимный вывод из запоя
Если пациент не может приехать в клинику, в Краснодаре нарколог приедет к нему домой. Помощь оказывает «Детокс» круглосуточно.
Выяснить больше – нарколог на дом круглосуточно
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Узнать больше – вывод из запоя дешево сочи
Современная практика включает комплексное обследование, позволяющее оценить состояние пациента и подобрать оптимальную схему терапии. Нарколог на дом в Челябинске проводит:
Разобраться лучше – http://narkolog-na-dom-chelyabinsk13.ru
В Краснодаре нарколог из клиники «Детокс» приедет на дом, чтобы вывести из запоя и оказать необходимую помощь.
Получить больше информации – врач нарколог выезд на дом краснодар
Ищете надёжные, проверенные способы избавиться от алкогольной зависимости? Тогда вам стоит прочитать статью «Лучшие методы лечения алкоголизма». Ознакомиться с деталями – http://krd.best-city.ru/forum/thread109917/
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Исследовать вопрос подробнее – частный нарколог на дом краснодар
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Подробнее тут – нарколог на дом круглосуточно в краснодаре
Ищете надёжный способ обрести трезвость и вновь почувствовать контроль над жизнью? В статье «Эффективные методы кодирования от алкоголизма: пути к трезвой жизни» раскрываются различные подходы к кодированию — от медикаментозных до психологических и аппаратных. Вы узнаете, как подобрать метод, учитывая стадию зависимости, состояние здоровья и личные особенности, а также почему сочетание кодировки с терапией и окружением трезвости может обеспечить более устойчивый эффект. Полезно тем, кто ищет путь к здоровому и свободному от зависимости образу жизни.
Подробнее – http://kremlevsk.kamrbb.ru/?x=read&razdel=5&tema=628
При обращении на горячую линию пациент может получить бесплатную телефонную консультацию. Врач уточняет состояние, собирает предварительный анамнез и согласовывает время визита.
Углубиться в тему – https://narkologicheskaya-klinika-rostov13.ru/chastnaya-narkologicheskaya-klinika-v-rostove/
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Разобраться лучше – вывод из запоя цена
Стационар «Частного Медика 24» — условия, где пациент может спокойно пройти вывод из запоя без страха и дискомфорта.
Узнать больше – http://www.vyvod-iz-zapoya-v-stacionare-samara23.ru
Стационар «Частного Медика?24» помогает безопасно и быстро восстановиться после длительного запоя.
Подробнее можно узнать тут – вывод из запоя в стационаре в воронеже
Стационар «Частного Медика?24» обеспечивает комфорт и безопасность при лечении запоя.
Подробнее тут – вывод из запоя в стационаре клиника воронеж
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Подробнее – нарколог на дом цены
При госпитализации пациент находится под наблюдением 24/7, что снижает риск осложнений.
Получить дополнительную информацию – вывод из запоя в стационаре нижний новгород
Стационар «Частного Медика?24» помогает безопасно и быстро восстановиться после длительного запоя.
Подробнее тут – стационар вывод из запоя воронеж
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Ознакомиться с деталями – вызвать врача нарколога на дом
В Самаре стационар «Частного Медика 24» предлагает персонализированный подход — лечение запоя, детоксикация и дальнейшее восстановление под наблюдением специалистов.
Углубиться в тему – стационар вывод из запоя самара
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Углубиться в тему – вывод из запоя клиника
В момент вызова важно сообщить:
Узнать больше – http://narkologicheskaya-klinika-rostov13.ru
Выезд нарколога на дом в Нижнем Новгороде — круглосуточная помощь при запое. Мы гарантируем анонимность и конфиденциальность на всех этапах лечения.
Ознакомиться с деталями – срочный вывод из запоя
Стационар «Частного Медика 24» — условия, где пациент может спокойно пройти вывод из запоя без страха и дискомфорта.
Изучить вопрос глубже – нарколог вывод из запоя в стационаре
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Подробнее тут – нарколог на дом круглосуточно цены краснодар
Can I simply say what a relief to seek out somebody who truly is aware of what theyre talking about on the internet. You positively know the way to carry a problem to light and make it important. More folks need to learn this and perceive this side of the story. I cant consider youre no more common because you undoubtedly have the gift.
В «Частном Медике 24» в Самаре лечение организовано так, чтобы пациент чувствовал себя безопасно и защищённо.
Разобраться лучше – http://vyvod-iz-zapoya-v-stacionare-samara23.ru
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Узнать больше – нарколог на дом вывод из запоя
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить больше информации – вывод из запоя на дому цена
Когда запой длится и состояние ухудшается, важно обратиться в стационар, где врачи «Частного Медика 24» в Воронеже проводят детоксикацию, насыщение организма витаминами, поддерживают сердце, печень и другие органы. Цена от 6500 ? включает всё необходимое — от диагностики до психологической поддержки.
Получить дополнительные сведения – вывод из запоя в стационаре клиника воронеж
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Разобраться лучше – нарколог на дом вывод из запоя краснодар
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Подробнее можно узнать тут – нарколог на дом недорого в краснодаре
Вывод из запоя в стационаре Воронежа — безопасный и эффективный метод лечения. Наши специалисты обеспечат круглосуточное наблюдение и комплексное лечение, включая детоксикацию, восстановление водно-электролитного баланса и психотерапевтическую поддержку.
Получить больше информации – нарколог вывод из запоя в стационаре в воронеже
Врачи клиники в Воронеже устраняют симптомы интоксикации и поддерживают организм при выводе из запоя.
Подробнее тут – наркология вывод из запоя в стационаре воронеж
Если вы ищете надёжный и понятный путь к избавлению от алкогольной зависимости — вам стоит заглянуть в статью «Эффективные услуги лечения алкоголизма: путь к трезвой жизни». Выяснить больше – http://kremlevsk.kamrbb.ru/?x=read&razdel=5&tema=637
Выведение из запоя в стационаре Воронежа — помощь при острых состояниях и хронической зависимости. Наши опытные наркологи используют современные методы лечения для быстрого и безопасного вывода из запоя.
Подробнее тут – нарколог вывод из запоя в стационаре
Выездная бригада «РостовМед» оснащена всем необходимым для оказания экстренной помощи и проведения полного курса детоксикации на дому. Процесс состоит из нескольких этапов:
Подробнее – http://narkologicheskaya-klinika-rostov13.ru/narkologicheskaya-klinika-narkologicheskij-czentr-v-rostove/
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Получить дополнительные сведения – нарколог на дом вывод из запоя в нижний новгороде
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Исследовать вопрос подробнее – наркология вывод из запоя
«Частный Медик 24» — это медицинский контроль, поддержка и лечение на всех этапах вывода из запоя.
Разобраться лучше – вывод из запоя в стационаре клиника нижний новгород
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Изучить вопрос глубже – частный нарколог на дом
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Ознакомиться с деталями – вывод из запоя вызов город
Стационарное лечение запоя в Воронеже — гарантированная анонимность и комфортные условия. Мы предлагаем индивидуальный подход к каждому пациенту, обеспечивая полное восстановление организма и предотвращение рецидивов.
Детальнее – https://vyvod-iz-zapoya-v-stacionare-voronezh22.ru
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врач приедет в течение 1–2 часов, проведёт необходимое обследование и назначит лечение. Услуга доступна круглосуточно и анонимно.
Ознакомиться с деталями – нарколог на дом в краснодаре
В больничных условиях «Частного Медика 24» врачи контролируют давление, сердце и функции жизненно важных органов при выводе из запоя.
Подробнее тут – быстрый вывод из запоя в стационаре в самаре
Если пациент не может приехать в клинику, в Краснодаре нарколог приедет к нему домой. Помощь оказывает «Детокс» круглосуточно.
Получить дополнительную информацию – вызов нарколога на дом
В «Частном Медике 24» в Самаре лечение организовано так, чтобы пациент чувствовал себя безопасно и защищённо.
Исследовать вопрос подробнее – нарколог вывод из запоя в стационаре в самаре
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Изучить вопрос глубже – нарколог на дом вывод из запоя краснодар
В момент вызова важно сообщить:
Получить дополнительные сведения – наркологическая клиника нарколог ростов-на-дону
В Сочи клиника «Детокс» предлагает вывод из запоя в стационаре. Опытные врачи обеспечивают полную безопасность и комфорт пациента, а услуги доступны круглосуточно.
Получить дополнительные сведения – вывод из запоя капельница сочи
Для восстановления после запоя выбирайте стационар клиники «Детокс» в Сочи. Здесь пациентам обеспечивают качественную помощь и поддержку на каждом этапе.
Выяснить больше – наркологический вывод из запоя
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Углубиться в тему – вывод из запоя капельница нижний новгород
Если нужен профессиональный вывод из запоя, обращайтесь в стационар клиники «Детокс» в Сочи. Все процедуры проводятся анонимно и под наблюдением специалистов.
Подробнее можно узнать тут – вывод из запоя вызов в сочи
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Узнать больше – помощь вывод из запоя
Стационарная детоксикация от алкоголя в Воронеже — восстановление организма под наблюдением специалистов. Мы проводим процедуры очищения организма от токсинов, восстанавливая физическое и психоэмоциональное состояние пациента.
Изучить вопрос глубже – нарколог вывод из запоя в стационаре
В момент вызова важно сообщить:
Подробнее – http://narkologicheskaya-klinika-rostov13.ru/narkologicheskaya-klinika-narkologicheskij-czentr-v-rostove/
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Наши рекомендации — тут – https://kemazedgerman.com/the-secret-of-cleaning-your-apartment
Адекватное лечение, комфорт и забота — так проходят дни в стационаре «Частного Медика 24» во время вывода из запоя.
Углубиться в тему – вывод из запоя в стационаре анонимно в самаре
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Что ещё нужно знать? – https://www.authorlab.pro/shop/uncategorized/media-kit
Этот обзорный материал предоставляет информационно насыщенные данные, касающиеся актуальных тем. Мы стремимся сделать информацию доступной и структурированной, чтобы читатели могли легко ориентироваться в наших выводах. Познайте новое с нашим обзором!
Изучить материалы по теме – https://annalouwellness.com/top-5-computer-classes-for-web-design-newbies
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Ознакомиться с теоретической базой – https://sol.uog.edu.et/events/ehrdc-2
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Ознакомиться с отчётом – http://www.vasaordenll608.se/imagesgiyyz9yo-2-2
Снятие интоксикации, восстановление организма и наблюдение — так проходит вывод из запоя в стационаре «Частный Медик 24».
Выяснить больше – вывод из запоя в стационаре анонимно в нижний новгороде
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Нажми и узнай всё – https://dbmsdrops.kindahl.net/2022/04/23/the-server-programming-interface
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Это стоит прочитать полностью – https://tokai-international.jp/%E5%B0%8F%E3%81%95%E3%81%AA%E3%81%8A%E8%91%AC%E5%BC%8F-%E9%AB%98%E5%A4%A9%E5%8E%9F%E3%83%9B%E3%83%BC%E3%83%AB
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Как это работает — подробно – https://thelightandtheglory.com/2025/04/21/heaven-is-wide-open-to-you
Ищете надёжную помощь при зависимости в Саратове? Узнайте, как частная наркологическая клиника с комплексным подходом помогает справиться с зависимостями — подробности на Womanzdorovie. Ознакомиться с деталями – http://kremlevsk.kamrbb.ru/?x=read&razdel=5&tema=713
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Почему это важно? – https://theprideceo.com/sap-ewm-2
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
https://conquista.criaclick.com.br/2024/03/11/ola-mundo
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
https://cgmbc.co.uk/projects/hr-smith-gazebo-relocation
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Нажмите, чтобы узнать больше – http://interiordesignerwebzwnb.cf/post/34
Читатели получат представление о том, как современные технологии влияют на развитие медицины. Обсуждаются новые методы лечения, персонализированный подход и роль цифровых решений в повышении качества медицинских услуг.
Что скрывают от вас? – https://lerix.ru/psihicheskie-rasstroystva-uslugi-po-lecheniyu-i-podderzhke-dlya-patsientov
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Ознакомиться с теоретической базой – http://kenp-factory.com/33
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Ознакомиться с деталями – https://cdjnet.com/como-funcionan-las-apuestas-deportivas-en-mexico
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Перейти к полной версии – https://banda-losborrachos.fr/2023/04/25/22eme-nuit-des-bandas-de-layrac
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Изучить материалы по теме – http://ippincollection.com/artisteye/2019/04/04/74
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Перейти к полной версии – https://vfkeducacao.com.br/casino-rws-gambling-establishment-singapore-2
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Переходите по ссылке ниже – https://taypharmacies.com/product/868399/augmentin-1gm-14tab
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Неизвестные факты о… – https://vinhy.com/san-pham/forma-new-2
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Изучить материалы по теме – https://sport-event.it/index.php/2021/05/27/il-punto-di-enzo-4
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Продолжить чтение – https://limpiezaselarco.es/2021/02/01/hola-mundo
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Узнай первым! – http://zzpzus.org.pl/nowe-przepisy-dotyczace-pracy-zdalnej
online Sportwetten österreich
einzelwetten strategie
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Изучить вопрос глубже – https://manutentions.be/besoin-de-renfort-passer-votre-commande
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Ознакомиться с деталями – https://naturalhairs.net/10-drugstore-products-celebrity-stylists-recommend
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Ознакомьтесь с аналитикой – https://vipprox.com/exploring-atlantas-modern-homes
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Нажмите, чтобы узнать больше – https://taiko-ist-takuya.jp/schedule/471
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Подробнее – http://brain-glass.com/post/34
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Хочу знать больше – https://zeltene.eu/divas-retas-putras-kas-samazina-lieko-svaru-un-taukus-vedera-lejasdala-plans-nedelaia-a/61372
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Ознакомиться с деталями – https://aquavillerush.com/introducing-this-amazing-tour
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Не упусти важное! – https://www.vichiagro.com/recipes/recipe_details/256
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Хочу знать больше – https://stiflexpharma.com/the-big-design-wall-likes-pictures
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Изучить вопрос глубже – вывод из запоя на дому
Экстренная помощь при запое в Нижнем Новгороде — капельница на дому от опытных врачей-наркологов.
Ознакомиться с деталями – вывод из запоя недорого
sportwetten bonus mit paypal
My web-site; Bester Wettanbieter Ohne Oasis
One thing I want to comment on is that weightloss program fast can be achieved by the right diet and exercise. A person’s size not merely affects appearance, but also the quality of life. Self-esteem, despression symptoms, health risks, and also physical capabilities are impacted in an increase in weight. It is possible to make everything right but still gain. If this happens, a medical problem may be the perpetrator. While excessive food and never enough body exercise are usually guilty, common medical conditions and trusted prescriptions can greatly help to increase size. Many thanks for your post in this article.
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Выяснить больше – вывод из запоя цена
beste quoten wettanbieter
my web-site … sportwetten Tipps und Tricks (https://Ghaesthetics.Co.uk/wette-em)
Капельница от похмелья в Нижнем Новгороде — доступная и эффективная процедура для снятия симптомов интоксикации. Стоимость услуги начинается от 2 100 ?.
Выяснить больше – вывод из запоя на дому цена
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Детальнее – https://www.isabegishakovic.com/post-1
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Ознакомиться с теоретической базой – https://saphyrdigitalconsulting.com/index.php/2021/05/24/what-do-aliquam-sed-fringilla
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Всё, что нужно знать – https://mutluhukuk.com.tr/index.php/component/k2/item/26-content-demo-135?start=6390
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Продолжить изучение – https://francoisbrin.art/page-de-couv-iii8604
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Не упусти важное! – https://ange.td/2023/04/01/experience-quality-craftsmanship-with-our-construction-team
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Только для своих – https://akhancraneservice.in/hello-world
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Эксклюзивная информация – https://www.cursosalpha.com/blog/la-alarma-visual-imposible-de-neutralizar
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Посмотреть подробности – http://sakuragawamj.com/?p=198
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Погрузиться в детали – http://www.izumishoko.co.jp/%E8%A3%BD%E5%93%81/%E3%81%8A%E3%82%84%E3%82%AB%E3%83%86b/128
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Подробная информация доступна по запросу – https://telediario.tv/3133-2
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Читать дальше – https://www.property-turkey.net/10-things-your-competitors-can-teach-you-about-real-estate
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Не упусти важное! – https://www.jasek.no/portfolio/artboard-1-copy-4
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Изучить эмпирические данные – https://www.segur-de-cabanac.com/hello-world-2-2
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
А что дальше? – https://ismkerala.org/ism-souhrudha-ifthar
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Подробнее – https://artzest.org/images
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Кликни и узнай всё! – https://highbrow-lowlife.com/uncategorized/2-new-albums-out-by-vanessa-sinclair-pete-murphy
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Что скрывают от вас? – https://edx.amamedia.org/product/campground-reservation-4
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Подробности по ссылке – https://jamalweb.com/?p=139
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Прочесть заключение эксперта – https://ccmdaci.org/irfmda/?option=com_content&view=article&id=3&Itemid=4&c54c502892c591ec2c2298f75e798fd3=a1592a190e1f2bb637eb91f72b7f45a7%20
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Где почитать поподробнее? – https://www.mce.sk/mat-webku-dobre-zobrazujucu-na-mobiloch-je-svate-pismo-2
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Подробная информация доступна по запросу – https://mphomes.ca/home/process_full_bg
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Слушай внимательно — тут важно – https://biggweedy.com/2022/04/02/sample-post1
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Детальнее – https://www.feelgoodshopevent.nl/look-at-me_dsc09007
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Перейти к полной версии – https://www.manogeodezija.lt/cropped-new-header1
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Смотри, что ещё есть – https://www.venlonaren.net/wie-is-de-beste-vvv-speler-in-de-derby-tegen-roda-jc
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Познакомиться с результатами исследований – https://arashi-restaurant.it/hello-world
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Откройте для себя больше – https://bk-baukollektiv.ch/2013/09/30/duis-autem-vel-eum-iriure-dolor
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Интересует подробная информация – https://www.harpstudio.nl/?attachment_id=638
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Наши рекомендации — тут – http://alusilka.com/2014/08/28/excepteur-sint-occaecat-cupidatat-non
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Читать далее > – https://www.helferei-weiler.ch/hello-world-2
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Узнать из первых рук – https://www.petrasuzanna-camino.blog/2023/08/10/colunga-to-villaviciosa-5th-august
wettquoten papst
Have a look at my blog post – mit sportwetten bonus geld
verdienen (Jillian)
Вывод из запоя в Самаре проводится с проверенными препаратами, с учётом состояния пациента и без лишнего стресса.
Ознакомиться с деталями – вывод из запоя в стационаре
I’ve come across that nowadays, more and more people are now being attracted to camcorders and the industry of taking pictures. However, as a photographer, you need to first spend so much time deciding the exact model of digital camera to buy and also moving store to store just so you may buy the most inexpensive camera of the trademark you have decided to pick. But it does not end right now there. You also have to think about whether you can purchase a digital camera extended warranty. Thanks a lot for the good points I obtained from your website.
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Получить дополнительные сведения – нарколог капельница на дом краснодар
Госпитализация в стационаре «Частного Медика 24» позволяет стабилизировать состояние, снять интоксикацию и начать новую жизнь.
Узнать больше – стационар вывод из запоя
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Узнать больше – нарколог на дом круглосуточно цены в краснодаре
В Воронеже клиника помогает стабилизировать состояние и восстановить здоровье после запоя.
Разобраться лучше – вывод из запоя в стационаре клиника в воронеже
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Подробнее тут – нарколог капельница на дом в краснодаре
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Выяснить больше – нарколог на дом вывод из запоя в краснодаре
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Узнать больше – вывод из запоя вызов город
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Получить дополнительную информацию – вывод из запоя на дому цена нижний новгород
В кардиологической и психологической поддержке «Частного Медика 24» в Самаре — полный комплекс для безопасного восстановления после запоя.
Разобраться лучше – стационар вывод из запоя
Врачи клиники в Воронеже устраняют симптомы интоксикации и поддерживают организм при выводе из запоя.
Разобраться лучше – вывод из запоя в стационаре анонимно в воронеже
Сервис Stop-Alko предлагает помощь при запое на дому в Екатеринбурге. Услуга доступна 24/7.
Исследовать вопрос подробнее – помощь вывод из запоя екатеринбург
Thank you for the sensible critique. Me & my neighbor were just preparing to do a little research about this. We got a grab a book from our local library but I think I learned more clear from this post. I’m very glad to see such magnificent information being shared freely out there.
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Подробнее можно узнать тут – помощь нарколога на дому
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Выяснить больше – https://vyvod-iz-zapoya-sochi23.ru
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Подробнее – вывод из запоя круглосуточно нижний новгород
Программа вывода из запоя в Воронеже от «Частного Медика 24» включает не только устранение физической зависимости, но и работу по восстановлению сна, гидратацию, лекарственную поддержку, а также психотерапию, чтобы помочь справиться не просто с запоем, но и с причинами, которые к нему привели.
Получить дополнительную информацию – быстрый вывод из запоя в стационаре воронеж
В Екатеринбурге служба Stop-Alko круглосуточно помогает вывести из запоя на дому — быстро, анонимно и без постановки на учёт.
Подробнее можно узнать тут – вывод из запоя на дому недорого екатеринбург
Если вы в тяжёлом состоянии после длительного употребления алкоголя, в Екатеринбурге «Stop-Alko» поможет вывести из запоя с выездом на дом, без постановки на учёт.
Получить дополнительную информацию – нарколог на дом вывод из запоя екатеринбург
Стационар клиники — это безопасное место, где врачи помогают восстановить силы после тяжелого запоя.
Исследовать вопрос подробнее – стационар вывод из запоя в нижний новгороде
Вывод из запоя в стационаре Воронежа — безопасное и эффективное решение для длительного запоя. Наши специалисты обеспечат круглосуточное наблюдение и комплексное лечение, включая детоксикацию, восстановление водно-электролитного баланса и психотерапевтическую поддержку.
Узнать больше – вывод из запоя в стационаре клиника воронеж
Услуга вывода из запоя в Екатеринбурге от «Похмельной Службы» включает как базовый, так и премиум-уровень помощи — со всеми необходимыми препаратами и поддержкой.
Подробнее – вывод из запоя круглосуточно екатеринбург
Если домашние методы не помогают, вывод из запоя в стационаре в Самаре — это безопасный выбор с профессиональной детоксикацией.
Подробнее тут – наркология вывод из запоя в стационаре в самаре
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Получить больше информации – нарколог на дом вывод из запоя краснодар
Вывод из запоя в Самаре на базе стационара — когда важен результат, стабильность и медицинская поддержка 24/7.
Узнать больше – https://vyvod-iz-zapoya-v-stacionare-samara23.ru
«Частный Медик 24» — это медицинский контроль, поддержка и лечение на всех этапах вывода из запоя.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-v-stacionare22.ru
Стационар «Частного Медика 24» — условия, где пациент может спокойно пройти вывод из запоя без страха и дискомфорта.
Подробнее можно узнать тут – вывод из запоя в стационаре самара
В Екатеринбурге «Похмельная Служба» проводит вывод из запоя анонимно и безопасно, с применением современных препаратов.
Подробнее можно узнать тут – врач вывод из запоя
Служба вывода из запоя на дому Stop-Alko в Екатеринбурге работает без перерывов, выезжает в любой район города, оказывает помощь с учётом всех медицинских стандартов.
Подробнее можно узнать тут – vyvod-iz-zapoya-ekaterinburg25.ru/
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Узнать больше – вывод из запоя на дому недорого
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Ознакомиться с деталями – нарколог на дом вывод из запоя в нижний новгороде
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее – вызвать врача нарколога на дом краснодар
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Подробнее тут – нарколог на дом клиника краснодар
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Прочитать подробнее – http://periscope2.ru/2010/09/10/2699
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Ознакомиться с деталями – https://reiwaphilosophy.com/?p=3437
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Читать далее > – https://jheinnynevespsi.com.br/ola-mundo
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Кликни и узнай всё! – https://alpiocafe.com/2020/05/07/air-fryer-salmon-2
Капельница от запоя на дому в Нижнем Новгороде — быстрый и эффективный способ снять симптомы похмелья и восстановить организм. Наши специалисты приедут к вам домой и проведут процедуру с использованием современных препаратов.
Разобраться лучше – http://www.vyvod-iz-zapoya-nizhnij-novgorod13.ru
В больничных условиях «Частного Медика 24» врачи контролируют давление, сердце и функции жизненно важных органов при выводе из запоя.
Детальнее – наркология вывод из запоя в стационаре
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Как это работает — подробно – https://www.pwmassage.se/2024/09/30/hej-varlden
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Кликни и узнай всё! – https://www.africopanigeria.com/standard-image-post
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Детальнее – narkolog-na-dom-krasnodar26.ru/
Если вы в тяжёлом состоянии после длительного употребления алкоголя, в Екатеринбурге «Stop-Alko» поможет вывести из запоя с выездом на дом, без постановки на учёт.
Узнать больше – анонимный вывод из запоя
В стационаре в Воронеже вам обеспечат безопасный выход из запоя: врачи контролируют состояние, корректируют лечение при сопутствующих заболеваниях, используют витамины, препараты для печени, кардиопротекторы, спазмолитики и другие средства, чтобы облегчить состояние.
Подробнее можно узнать тут – вывод из запоя в стационаре клиника воронеж
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Где почитать поподробнее? – https://prenoms.site/nombres/prenoms-rares-courts
В Самаре клиника «Частный Медик 24» предлагает вывод из запоя в стационаре с полным медицинским контролем и комфортными палатами.
Получить больше информации – быстрый вывод из запоя в стационаре
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Прочитать подробнее – https://kliko.info/facebook
sportwetten heute Tipps steuern schweiz
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Посмотреть всё – http://gn-oildrilling.com/2020/11/21/centrifuga-para-jugo-de-frutas-y-verduras
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Подробнее – https://caroner.com/top-5-car-maintenance-tips-for-longevity-and-performance
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Детали по клику – https://ame-plus.net/archives/1041
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Давай разберёмся досконально – https://market-analysis.ru/narkologicheskaya-klinika-istochnik-zhizni-v-omske-btwj
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Заходи — там интересно – https://gramat.electron-libre-cea.fr/2023/12/07/enfin-des-cheques-vacances-250e-par-salarie-du-cea
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Ознакомиться с теоретической базой – https://psixologiya.org/psixoterapiya/praktika/2650-pogranichnoe-rasstrojstvo-lichnosti-simptomy-diagnostika-i-lechenie.html
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Это стоит прочитать полностью – https://familydoctor.cx.ua/kompleksnyj-podhod-k-lechenyyu-zavysymosty-y-reabylytatsyy-alkogolykov.html
В этой статье собраны факты, которые освещают целый ряд важных вопросов. Мы стремимся предложить читателям четкую, достоверную информацию, которая поможет сформировать собственное мнение и лучше понять сложные аспекты рассматриваемой темы.
Разобраться лучше – https://servitrafick.es/producto/clinica-dental
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Ознакомиться с теоретической базой – http://webcam.saint-martin-de-castillon.com/2020/12/10/bonjour-tout-le-monde
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Изучить материалы по теме – http://vinamgroup.com.vn/can-cbd-receive-me-great
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Личный опыт — читайте сами – http://ilchiccodisenape.org/2023/05/11/economia-solidale-in-festa
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Получить профессиональную консультацию – http://spolek.azylpes.cz/podekovani-8
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Читать далее > – http://chitahanto-smilemama.com/2021/03/05/865
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Изучите внимательнее – https://samachartehelka.com/?p=35
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Изучить вопрос глубже – https://public-voice.in/archives/8022
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Читать дальше – https://www.lifeingraceblog.com/2013/04/homemade-pizza-how-to-make-perfect-crust
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Всё, что нужно знать – https://carlosritter.com/pgc_simply_gallery/sports/decathlon-united-by-sport
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Прочитать подробнее – https://synexisanalysis.com/in-media-trimming-costs-boosts-value-transform
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Не упусти шанс – http://zzpzus.org.pl/nowe-przepisy-dotyczace-pracy-zdalnej
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Узнать больше > – https://jabirjalali.com/think-positive
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Подробнее – https://link8live.org/soi-cau-bang-phuong-phap-loai-tong-dac-biet
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Есть чему поучиться – https://lamiastampa.it/product/personalizza-la-tua-borraccia
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Не упусти важное! – http://www.webdesign-webservice.de/fotolia-bilder-kostenlos-kw-22
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Только факты! – https://hodiminblodim.si/kako-me-je-poskodba-kolena-od-bolniske-postelje-pripeljala-do-jugovzhodne-azije/attachment/1554123819706
bonus profi Sportwetten Tipps (hyperwarped.com) ohne einzahlung
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Изучить вопрос глубже – нарколог вывод из запоя
bester neukundenbonus deutsche online wettanbieter [Randal]
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Получить больше информации – http://narkolog-na-dom-krasnodar26.ru
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Получить дополнительную информацию – вывод из запоя вызов в нижний новгороде
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Получить дополнительную информацию – врач нарколог выезд на дом
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Подробнее – http://www.narkolog-na-dom-krasnodar26.ru
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Подробнее тут – вывод из запоя с выездом
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Исследовать вопрос подробнее – платный нарколог на дом в краснодаре
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Узнать больше – вывод из запоя на дому круглосуточно
Вывод из запоя в Самаре проводится с проверенными препаратами, с учётом состояния пациента и без лишнего стресса.
Подробнее тут – вывод из запоя в стационаре клиника
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Подробнее тут – http://vyvod-iz-zapoya-nizhnij-novgorod11.ru
Сервис Stop-Alko предлагает помощь при запое на дому в Екатеринбурге. Услуга доступна 24/7.
Получить больше информации – вывод из запоя на дому недорого в екатеринбурге
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Подробнее тут – нарколог на дом вывод из запоя краснодар
Стационарная детоксикация от алкоголя в Воронеже — восстановление организма под наблюдением специалистов. Мы проводим процедуры очищения организма от токсинов, восстанавливая физическое и психоэмоциональное состояние пациента.
Изучить вопрос глубже – вывод из запоя в стационаре анонимно в воронеже
В клинике в Самаре устраняют симптомы интоксикации, оказывают поддержку организму и помогают восстановиться после тяжёлых запоев.
Детальнее – наркология вывод из запоя в стационаре самара
Круглосуточный стационарный вывод из запоя в Воронеже — доступная помощь в любое время. Вы можете обратиться к нам в любое время суток, и мы окажем необходимую медицинскую помощь.
Ознакомиться с деталями – вывод из запоя в стационаре клиника
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Уникальные данные только сегодня – https://batutudalys.lt/img31__81493-1462971702-1280-1280
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Детали по клику – https://rajuomlet.com/product/butter-rice-bhurji
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Изучить материалы по теме – https://glenwin.com/lorem-ipsum-dolor-sit-amet
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Нажмите, чтобы узнать больше – https://oakhillcollaborative.org/connecting-a-community-springfield-township
Лечение основывается на комплексном подходе, позволяющем учесть особенности организма и стаж злоупотребления алкоголем. Обычно процедура состоит из нескольких этапов:
Разобраться лучше – вывод из запоя на дому в москве
Вывод из запоя в Воронеже проходит анонимно, с круглосуточной поддержкой специалистов.
Подробнее можно узнать тут – стационар вывод из запоя в воронеже
Стационарная детоксикация от алкоголя в Воронеже — восстановление организма под наблюдением специалистов. Мы проводим процедуры очищения организма от токсинов, восстанавливая физическое и психоэмоциональное состояние пациента.
Ознакомиться с деталями – https://vyvod-iz-zapoya-v-stacionare-voronezh22.ru
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Слушай внимательно — тут важно – https://longbottomfoundry.co.uk/soil-pipe-systems
В «Частном Медике 24» в Самаре лечение организовано так, чтобы пациент чувствовал себя безопасно и защищённо.
Ознакомиться с деталями – быстрый вывод из запоя в стационаре самара
Выведение из запоя в стационаре Воронежа — помощь при острых состояниях и хронической зависимости. Наши опытные наркологи используют современные методы лечения для быстрого и безопасного вывода из запоя.
Исследовать вопрос подробнее – быстрый вывод из запоя в стационаре
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Подробнее можно узнать тут – вывод из запоя клиника нижний новгород
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Где почитать поподробнее? – https://minoya-shimada.com/2021/01/25/%E3%80%90%E3%80%8C%E3%81%BF%E3%81%AE%E3%82%84%E3%80%8D%E3%81%A7%E4%BA%BA%E6%B0%97%E3%81%AE%E3%81%8A%E8%8F%93%E5%AD%903%E9%81%B8%E3%80%91
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Получить дополнительную информацию – http://vyvod-iz-zapoya-nizhnij-novgorod12.ru
В Екатеринбурге «Похмельная Служба» проводит вывод из запоя анонимно и безопасно, с применением современных препаратов.
Углубиться в тему – нарколог на дом вывод из запоя екатеринбург
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Выяснить больше – запой нарколог на дом
Не менее опасны и психоэмоциональные нарушения, связанные с абстинентным синдромом: тревога, чувство паники, галлюцинации, нарушения координации. В тяжёлых случаях может развиться алкогольный делирий (белая горячка) со спутанностью сознания, бредовыми идеями и приступами агрессии. Самостоятельный резкий отказ от спиртного в этом состоянии чреват непредсказуемыми осложнениями вплоть до судорог и комы.
Получить дополнительные сведения – вывод из запоя капельница на дому в москве
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Секреты успеха внутри – https://www.thinkindesign.co/koffie
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Выяснить больше – нарколог на дом круглосуточно цены в краснодаре
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Это ещё не всё… – https://www.ixiaowen.net/news/2481.html
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Изучить вопрос глубже – скорая вывод из запоя в нижний новгороде
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Смотри, что ещё есть – http://kenp-factory.com/33
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Изучить вопрос глубже – https://solarprong.com/2024/06/12/hello-world
В Самаре в «Частном Медике 24» пациент получает детоксикацию, восстановительное лечение и круглосуточное наблюдение врачей.
Изучить вопрос глубже – быстрый вывод из запоя в стационаре самара
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Читать далее > – https://cricket59.com/Player/muhammad-rehan-rehan
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Желаете узнать подробности? – https://roamguided.com/index.php/2023/09/26/hello-world
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Слушай внимательно — тут важно – https://apolin.org/bertemu-jokowi-pm-india-janji-beri-treatment-yang-fair-untuk-sawit-indonesia
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Провести детальное исследование – https://danieloliveiracorretor.com.br/property/casa-proximo-a-rua-das-flores
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Дополнительно читайте здесь – https://souad-attabi.com/produit/oeuvre-dart-la-baraka
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Проследить причинно-следственные связи – https://michael-brenner.com/how-great-leaders-use-storytelling-to-activate-empathy-in-their-teams
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Давай разберёмся досконально – https://www.hotel-sugano.com/bbs/sugano.cgi/datasphere.ru/club/user/12/blog/2477/datasphere.ru/club/user/12/blog/2477/sinopipefittings.com/e_Feedback/www.skitour.su/www.skitour.su/www.tovery.net/www.hip-hop.ru/forum/id298234-worksale/sugano.cgi?page10=val
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
А что дальше? – https://vachkinhvanphong.com.vn/san-pham/cua-nhom-he-55-vat-canh
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Подробная информация доступна по запросу – https://altin.co.in/2019/02/20/570
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Изучить материалы по теме – https://www.asociacion-aeste.es/2020/07/21/aeste-asade-ccoo-y-ugt-acordamos-un-plan-de-choque-para-restrituir-el-sistema-de-dependencia
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Как это работает — подробно – https://roamguided.com/index.php/2023/09/26/hello-world
В жизни крупных городов часто возникают ситуации, когда стрессы и быстрый ритм жизни приводят к развитию зависимости. Когда проблема становится очевидной, важно незамедлительно обратиться за помощью. В таких случаях вызов нарколога на дом может стать не только удобным, но и наиболее эффективным вариантом. Это позволяет получить квалифицированное лечение в привычной обстановке, сохраняя при этом полную анонимность и конфиденциальность.
Подробнее – https://narcolog-na-dom-moskva55.ru/vyzov-narkologa-na-dom-moskva/
Алкогольная или наркотическая интоксикация — это не просто временное ухудшение самочувствия, а серьёзное медицинское состояние, требующее неотложной помощи. Когда человек находится в запое или состоянии ломки, его организм стремительно теряет силы, нарушается работа сердца, печени, мозга, возникают панические атаки, судороги, спутанность сознания. В таких случаях помощь должна быть незамедлительной. Если пациент не может самостоятельно добраться до клиники, оптимальным решением становится вызов нарколога на дом. В Красногорске такая услуга доступна круглосуточно благодаря выездной службе клиники «Ключ к Здоровью».
Подробнее – http://narcolog-na-dom-v-moskve55.ru/narkolog-na-dom-anonimno-v-krasnogorske/
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Давай разберёмся досконально – https://tonydarrigo.com/laws-are-like-cobwebs-which-may-catch-small-flies-but-let-wasps-and-hornets-break-through
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Узнайте всю правду – https://alconburycc.co.uk/hello-world-2
http://www.factorytinsigns.com is 100 Trusted Global Metal Vintage Tin Signs Online Shop. We have been selling art and décor online worldwide since 2008. Started in Sydney, Australia. 2000+ Tin Beer Signs, Outdoor Metal Wall Art, Business Tin Signs, Vintage Metal Signs to choose from. 100 Premium Quality Artwork. Up-to 40 OFF Sale Store-wide. Fast Shipping USA, Canada, UK, Australia, New Zealand, Europe.
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Только факты! – https://vincibrian.com/post-malones-hitting-the-road-for-one-big-ass-stadium-tour-heres-how-to-get-tickets
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Подробнее можно узнать тут – https://ekhaleeji.com/dubai-hills-real-estate
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Узнать больше > – https://fabafull.com/hartige-eiwitrijke-muffins
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Не упусти важное! – https://www.advancedoptometry.net/2020/02/27/what-is-functional-low-vision
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Эксклюзивная информация – https://forbesport.com/kettlebell-leg-workouts-for-enhanced-performance-in-long-distance-running
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Только факты! – https://netsurf.monster/main-fukushi
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Обратиться к источнику – https://whnynews.com/2024/11/27/senior-trump-assistant-accused-of-participating-in-pay-to-play-arrangement-with-potential-cabinet-members
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
А есть ли продолжение? – https://www.bikerkost.no/dag-16-nordkapp-prosjektet
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
Это ещё не всё… – https://ytegiare.com/ngam-tieu-tri-moc-linh-thuoc-ngam-dieu-tri-benh-tri
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Ознакомиться с теоретической базой – https://alliance-translation.com/index.php/2022/04/18/how-to-write-my-admission-essay
Very nice post. I just stumbled upon your weblog and wished to say that I’ve really enjoyed surfing around your blog posts. After all I will be subscribing to your rss feed and I hope you write again soon!
Thanks for sharing your thoughts about casino dealer gaming license.
Regards
Feel free to visit my webpage: is a blackjack weapon illegal
(Krista)
Greate post. Keep writing such kind of info on your blog. Im really impressed by your blog.
Hey there, You have performed a fantastic job. I’ll definitely digg it and in my opinion recommend to my friends. I’m sure they’ll be benefited from this website.
онлайн казино кэт
Spot on with this write-up, I seriously feel this amazing site needs
a great deal more attention. I’ll probably be returning to
read more, thanks for the advice!
Here is my homepage: do roulette machines cheat – Monserrate,
Лечение основывается на комплексном подходе, позволяющем учесть особенности организма и стаж злоупотребления алкоголем. Обычно процедура состоит из нескольких этапов:
Изучить вопрос глубже – вывод из запоя круглосуточно москва
Именно поэтому при затяжных запоях необходима квалифицированная медицинская помощь, позволяющая безопасно и максимально комфортно прекратить приём алкоголя. Клиника «Стратегия Здоровья» предлагает профессиональный вывод из запоя в Москве как в условиях стационара, так и с выездом на дом. Врачи работают круглосуточно, используя проверенные методики детоксикации и медикаментозной поддержки.
Получить больше информации – срочный вывод из запоя
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Получить исчерпывающие сведения – https://tahitiangingerbeer.com/ginger-beer-ou-ginger-ale
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Ссылка на источник – https://tecfogoes.com.br/2017/06/09/hello-world-2
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Интересует подробная информация – https://twojimmys.com/dt_team/john-doe
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Не упусти важное! – http://aoba-nekosora.com/2022/01/14/hello-world
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Получить больше информации – https://yinforchange.in/yin-youth-summit-17-begins-nashik-day-1
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Что ещё нужно знать? – http://www.lannach.eu/fiji
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Смотри, что ещё есть – https://onedredream.com/improvement-on-electronic-payments
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Где почитать поподробнее? – https://www.stacefelder.com/61/test-sites-apps
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Исследовать вопрос подробнее – https://vigashpk.com/projects/cnc-machinery
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Наши рекомендации — тут – https://demidream.lt/2020/08/12/pirmasis-tinklarascio-irasas
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Подробная информация доступна по запросу – https://swalopets.com/2024/06/19/hola-mundo
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Запросить дополнительные данные – https://expertwhitepaper.com/insights/cloud/14-factors-that-make-organizations-attractive-to-employees-in-2023
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Читать дальше – https://grafiktasarimburada.com/produksiyon/mix-mastering-nedir.html
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Продолжить изучение – https://keepter.ru/narkologicheskaya-klinika-istochnik-zhizni-v-omske-30
Этот информационный материал подробно освещает проблему наркозависимости, ее причины и последствия. Мы предлагаем информацию о методах лечения, профилактики и поддерживающих программах. Цель статьи — повысить осведомленность и продвигать идеи о необходимости борьбы с зависимостями.
Получить дополнительную информацию – https://russian-investment.ru/Press-reliz/362330-narkologicheskaya-klinika-istochnik-zhizni-v-omske-qx80
В этой статье обсуждаются актуальные медицинские вопросы, которые волнуют общество. Мы обращаем внимание на проблемы, касающиеся здравоохранения и лечения, а также на новшества в области медицины. Читатели будут осведомлены о последних событиях и смогут следить за тенденциями в медицине.
Подробнее можно узнать тут – https://medport.info/the-news/vazhnost-vyzova-narkologa-professionalnaya-pomosch-v-borbe-s-zavisimostyami.html
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Слушай внимательно — тут важно – https://royaltea.in/benefits-of-indian-spices-in-your-tea
Этот краткий обзор предлагает сжатую информацию из области медицины, включая ключевые факты и последние новости. Мы стремимся сделать информацию доступной и понятной для широкой аудитории, что позволит читателям оставаться в курсе актуальных событий в здравоохранении.
Подробнее – https://smartchoices.ru/2024-narkologicheskaya-klinika-istochnik-zhizni-v-omske-am
В этой публикации мы предложим ряд рекомендаций по избавлению от зависимостей и успешному восстановлению. Мы обсудим методы привлечения поддержки и важность самосознания. Эти советы помогут людям вернуться к нормальной жизни и стать на путь выздоровления.
Разобраться лучше – https://kakpravilino.com/professionalnoe-lechenie-alkogolizma-vazhnost-kompleksnogo-podhoda
Этот обзор сосредоточен на различных подходах к избавлению от зависимости. Мы изучим традиционные и альтернативные методы, а также их сочетание для достижения максимальной эффективности. Читатели смогут открыть для себя новые стратегии и подходы, которые помогут в их борьбе с зависимостями.
Подробнее тут – https://select-university.ru/narkologicheskaya-klinika-istochnik-zhizni-v-omske-hr
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Ознакомиться с теоретической базой – https://laterrazza.bg/hello-world
В этой статье мы обсудим процесс восстановления после зависимостей, акцентируя внимание на различных методах и подходах к реабилитации. Читатели узнают, как создать план выздоровления и использовать полезные ресурсы для достижения устойчивых изменений.
Получить дополнительные сведения – https://malimar.ru/vyzov-narkologa-na-dom-preimushhestva-i-nedostatki-dlya-zdorovya
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Погрузиться в детали – https://market.juallagi.biz/beli-koin-tiktok-pakai-pulsa-telkomsel-cara-mudah-dan-praktis
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Запросить дополнительные данные – https://smazka.kg/bearing
В этой публикации мы сосредоточимся на интересных аспектах одной из самых актуальных тем современности. Совмещая факты и мнения экспертов, мы создадим полное представление о предмете, которое будет полезно как новичкам, так и тем, кто глубоко изучает вопрос.
Нажмите, чтобы узнать больше – https://altec.ch/business1
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Изучить вопрос глубже – https://alexpantonfoundation.ky/2nd-annual-alex-panton-foundation-youth-mental-health-symposium
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Хочу знать больше – https://www.fireworkmegastore.com/hello-world
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Продолжить чтение – https://www.ouvrard-traiteur.fr/NEW/2016/04/02/post-with-gallery/fff_4185
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Детали по клику – http://grandstream.ec/?product=ucm6208
В статье по вопросам здоровья мы рассматриваем актуальные проблемы, с которыми сталкивается общество. Обсуждаются заболевания, факторы риска и важные аспекты профилактики. Читатели получат полезные советы о том, как сохранить здоровье и улучшить качество жизни.
Подробнее можно узнать тут – https://forma-med.ru/effektivnoe-vyvedenie-iz-zapoya
Эта публикация содержит ценные советы и рекомендации по избавлению от зависимости. Мы обсуждаем различные стратегии, которые могут помочь в процессе выздоровления и важность обращения за помощью. Читатели смогут использовать полученные знания для улучшения своего состояния.
Получить дополнительные сведения – https://pr-lead.ru/2024/07/30/narkologicheskaya-klinika-istochnik-zhizni-v-omske-c2mlw
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Подробнее – https://tuvshinbanzragch.mn/archives/1360
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Ознакомьтесь с аналитикой – https://www.gomicrosolutions.com.au/stories-about-digital-marketing
Hello! I just would like to give an enormous thumbs up for the nice data you’ve right here on this post. I can be coming back to your weblog for extra soon.
Основная задача стационарного лечения — не просто вывести человека из кризисного состояния, а вернуть ясность мышления и устойчивость физиологических функций. Поэтому врачи клиники используют современные методы детоксикации, витаминотерапии, ноотропные препараты, психотерапевтические практики короткого действия и физиотерапевтические модули, направленные на восстановление сна, памяти и концентрации.
Получить дополнительную информацию – http://narkologicheskaya-klinika-stavropol0.ru/
Такая структура лечения помогает пациентам пройти все этапы восстановления под контролем специалистов.
Получить дополнительную информацию – http://narcologicheskaya-klinika-perm0.ru
Если к «окну оценки» динамика плато, мы корректируем один элемент — скорость/последовательность инфузии, вечерний ритуал или плотность сессий. Это защищает от полипрагмазии и делает вклад каждого шага читаемым.
Получить дополнительные сведения – вывод наркологическая клиника в нижнем тагиле
Такая структура терапии делает процесс максимально эффективным и безопасным.
Изучить вопрос глубже – наркологическая клиника вывод из запоя
Если к запланированному «окну оценки» динамика слабее ожидаемой, врач корректирует один параметр (скорость/последовательность введения, вечерний режим, плотность связи). Такой минимализм повышает управляемость и снижает риск побочных эффектов.
Разобраться лучше – врач вывод из запоя
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Подробнее можно узнать тут – вывод из запоя круглосуточно
beste sportwetten prognose
Here is my homepage: wettbüro in der nähe jetzt geöffnet
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Исследовать вопрос подробнее – нарколог на дом вывод в саратове
Основная задача стационарного лечения — не просто вывести человека из кризисного состояния, а вернуть ясность мышления и устойчивость физиологических функций. Поэтому врачи клиники используют современные методы детоксикации, витаминотерапии, ноотропные препараты, психотерапевтические практики короткого действия и физиотерапевтические модули, направленные на восстановление сна, памяти и концентрации.
Получить дополнительную информацию – http://narkologicheskaya-klinika-stavropol0.ru
На первом приёме врач-нарколог проводит осмотр, оценивает витальные показатели (АД, ЧСС, SpO2, температура), при показаниях — портативный ЭКГ-скрининг и экспресс-лабораторию, использует шкалы выраженности абстиненции и тревоги. Результаты сразу переводятся в план на ближайшие 72 часа: инфузионная поддержка или таблетированные режимы, «вечерний ритуал» для нормализации сна, карта триггеров и краткое психообразование. Дальше мы обсуждаем цели на 7 дней: что должно измениться и как мы это измерим (сон, тревога, «тяга», энергия, работоспособность).
Получить дополнительные сведения – http://
Мы одинаково внимательно относимся и к амбулаторным, и к стационарным маршрутам. Для каждого формируется индивидуальная цель (устранение абстиненции, нормализация сна, восстановление внимания и мотивации) и назначается «точка переоценки» — момент, когда команда сверяет динамику и, если нужно, меняет один параметр плана (дозу, время внесения процедур, приоритет модуля). Так достигается предсказуемость и избегается избыточная фармаконагрузка.
Изучить вопрос глубже – http://narcologicheskaya-klinika-stavropol0.ru/chastnaya-narkologicheskaya-klinika-stavropol/
Ниже — примерный «каркас» лечения. Он индивидуализируется по клинической картине, сопутствующим болезням, опыту прошлых попыток и бытовым ограничениям. Ключевой принцип — «одно вмешательство: одна цель — один маркер — одна дата проверки».
Разобраться лучше – наркологическая клиника стационар петрозаводск
Домашний протокол разбит на понятные шаги. В каждом шаге есть цель, действия, что именно мы измеряем и когда сверяем прогресс. Это делает процесс прозрачным и даёт семье чувство контроля: видно, почему назначено именно это и когда ждать облегчения.
Углубиться в тему – https://narkolog-na-dom-petrozavodsk0.ru/narkolog-petrozavodsk-anonimno
Команда клиники включает врачей-наркологов и психиатров, клинических психологов, специалистов по зависимости, выездных медсестёр и координаторов маршрута. Все решения принимаются мультидисциплинарно — это значит, что медицинский и психотерапевтический блоки «стыкуются» между собой, а рекомендации не противоречат друг другу. Мы уделяем внимание сенсорной среде: мягкий свет, тишина, регламент вечернего отделения шумов, чтобы медикаментозная поддержка не «сгорала» под стрессом.
Подробнее можно узнать тут – https://narcologicheskaya-klinika-pervouralsk0.ru/narkologicheskaya-bolnicza-pervouralsk
Для жителей Каменска-Уральского мы организовали быстрый и незаметный доступ к помощи. Координатор принимает обращения круглосуточно, уточняет адрес, особенности подъезда, пожелания по конфиденциальности и удобные «окна» визита. Бригады приезжают без опознавательных знаков, расходные материалы — в нейтральной упаковке, а формулировки в документах исключают нежелательные «ярлыки». Если дома временно нельзя обеспечить тишину и безопасность, мы «тихо» переводим пациента в палату краткого наблюдения: отдельный вход, короткий маршрут, минимум контактов и быстрое возвращение к домашнему формату после стабилизации.
Узнать больше – наркологическая клиника лечение алкоголизма
Мы заранее объясняем, какие шаги последуют, чтобы пациент и близкие понимали логику вмешательств и не тревожились по поводу непредвиденных «сюрпризов». Карта ниже — ориентир; конкретные параметры врач уточнит после осмотра.
Подробнее – скорая вывод из запоя
Wow! This could be one particular of the most helpful blogs We have ever arrive across on this subject. Actually Fantastic. I’m also an expert in this topic therefore I can understand your effort.
Great post. I am going through a few of these issues as
well..
My webpage – glacier peaks casino browning mt (Leonida)
Такая последовательность шагов позволяет врачу действовать точно и эффективно. Благодаря комплексному подходу пациент чувствует облегчение уже через 1–2 часа после начала терапии, а полное восстановление наступает в течение суток.
Подробнее – вывод из запоя
Мы не используем универсальные «коктейли»: алгоритм строится из коротких проверяемых шагов. На старте фиксируем цель (например, уменьшить тремор и тошноту, стабилизировать пульс и давление, вернуть полноценный ночной сон), выбираем минимально достаточные средства для её достижения и заранее назначаем «окно оценки» — момент, когда команда сверяет эффект и при необходимости корректирует один параметр. Такой подход защищает от полипрагмазии, экономит силы пациента и делает прогресс читаемым для всей семьи.
Выяснить больше – вывод из запоя в стационаре в каменске-уральске
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Углубиться в тему – http://narcologicheskaya-klinika-omsk0.ru/narkologicheskaya-bolnicza-omsk/
I have witnessed that smart real estate agents almost everywhere are Promotion. They are knowing that it’s more than just placing a sign in the front place. It’s really concerning building connections with these dealers who later will become consumers. So, while you give your time and effort to aiding these sellers go it alone — the “Law associated with Reciprocity” kicks in. Great blog post.
Инфузионная терапия в «ТагилМед Реал» — это точный инструмент под конкретный запрос: обезвоживание, вегетативная нестабильность, нарушения сна, «утренний туман». Состав и дозировки подбирает врач с учётом возраста, коморбидности и лекарственных взаимодействий. Важно понимать: больше компонентов не значит лучше; главная ценность — фокус и безопасность.
Изучить вопрос глубже – http://narkologicheskaya-klinika-nizhnij-tagil0.ru
В клинике используется модульная система лечения, включающая медицинские, психологические и социальные компоненты. В зависимости от состояния человека акценты могут смещаться — например, у одних пациентов приоритетом становится физиологическое восстановление, у других — коррекция эмоционального фона и когнитивных паттернов.
Детальнее – анонимная наркологическая клиника
Наркологическая клиника в Перми обеспечивает пациентам комфортные условия и профессиональное сопровождение. Врачи работают круглосуточно и соблюдают строгую конфиденциальность, что делает лечение доступным и безопасным.
Подробнее – https://narcologicheskaya-klinika-perm0.ru/perm-narkologiya/
Если дома действительно шумно (ремонт, маленькие дети, вечерние гости) или состояние нестабильно, предложим короткое наблюдение в клинике: отдельный вход, «тихий коридор», камерные посты, затем — возвращение домой и продолжение амбулаторного маршрута. Важен не формат, а предсказуемый результат: степень облегчения должна соответствовать целям этапа, а не множеству случайных факторов среды.
Получить больше информации – вывод из запоя на дому цена
sportwetten tipps für heute vorhersagen app
Для жителей Первоуральска мы поддерживаем 24/7-окно обращения без очередей: первичный скрининг по телефону, подтверждение безопасного формата старта (стационар краткого наблюдения, амбулаторно или выездная бригада), нейтральные формулировки в документах, деликатная транспортная логистика. При необходимости организуем немаркированный выезд врача, а при госпитализации используем отдельный вход и «тихие» коридоры. Это не косметика — такие детали снижают уровень тревоги, улучшают засыпание в первую ночь и повышают соблюдаемость рекомендаций.
Подробнее тут – частная наркологическая клиника
В Петрозаводске мы организовали «тихий» доступ к помощи: первичный звонок принимает координатор, который собирает только необходимую информацию, назначает удобное окно визита, подсказывает безопасные шаги до встречи с врачом (вода, свет, отдых, отказ от стимуляторов) и, при необходимости, направляет немаркированную выездную бригаду. В стационаре — отдельный вход, индивидуальные тайм-слоты, приватные кабинеты без общей «ожидалки». Наша задача — не просто начать лечение, а сделать так, чтобы старт не сорвался из-за страха огласки или бюрократии.
Получить больше информации – http://narkologicheskaya-klinika-petrozavodsk0.ru/chastnaya-narkologicheskaya-klinika-petrozavodsk/
Мы не «перелечиваем» пациента процедурами. Любая мера начинается как проверяемая гипотеза с измеримыми маркерами. Ниже — опорная карта лечения. В реальности она персонализируется в зависимости от клинической картины, возраста, сопутствующих заболеваний и бытового графика.
Подробнее – https://narkologicheskaya-klinika-kamensk-uralskij0.ru/narkolog-v-kamenske-uralskom/
Современная наркологическая клиника «ЮгМед Альянс» в Ставрополе объединяет медицинскую точность и психологическую чуткость. Здесь лечение зависимостей выстроено по принципу системной логики: одно вмешательство — одна цель — один критерий оценки. Такой подход делает процесс предсказуемым и снижает нагрузку на организм. Мы не просто устраняем симптомы, а ищем причину, формируем новые устойчивые модели поведения и помогаем пациенту вернуть контроль над жизнью. Наша команда работает круглосуточно, обеспечивая поддержку и безопасное сопровождение на каждом этапе — от детоксикации до реабилитации.
Подробнее тут – http://narkologicheskaya-klinika-stavropol0.ru/narkolog-psikholog-stavropol/
Главные задачи детоксикации при запое — безопасно снизить концентрацию токсичных метаболитов, восстановить водно-электролитный баланс, уменьшить перегрузку сердечно-сосудистой системы и вернуть физиологию сна. Мы начинаем с медленного стартового объёма инфузии, чтобы оценить переносимость, затем переходим к основной фазе и при необходимости к постинфузионной поддержке. Во время сеанса контролируются витальные показатели, динамика симптомов (тремор, тошнота, головная боль, фотофобия, тревога), а также «поведенческие» маркеры — способность расслабиться, усидеть спокойно, засыпать без «рывков».
Выяснить больше – наркологический вывод из запоя
Капельница — не «универсальная смесь», а адресный баланс жидкости, электролитов и поддерживающих компонентов под текущие симптомы. Ниже — ориентир, который индивидуализируется на месте осмотра. Мы тщательно сопоставляем пользу и допустимую нагрузку, чтобы не перегружать организм.
Получить дополнительные сведения – запой нарколог на дом
Выездной наркологический сервис «МедПоволжье Клиник» создан для случаев, когда важны скорость, тишина и клиническая точность. Мы проводим детоксикацию и снятие интоксикации на дому так, чтобы каждое действие имело цель, измеримый маркер и заранее оговорённое «окно переоценки». Вместо «сильной капельницы на всякий случай» — модульная схема: один симптом-кластер > один медицинский модуль > одна поведенческая опора (свет, звук, вода малыми глотками, дыхание 4–6). Такой подход снижает лекарственную нагрузку, ускоряет стабилизацию и позволяет видеть прогресс буквально по часам.
Подробнее тут – врач нарколог выезд на дом саратов
С первого контакта координатор уточняет: длительность запоя, виды алкоголя, аллергии, список текущих лекарств, эпизоды судорог или психозов в анамнезе, сердечно-сосудистые жалобы. На основании ответов команда подбирает безопасную схему старта и резервный план на случай усиления симптомов. Врач привозит портативный монитор для контроля АД/ЧСС/SpO2, глюкометр, набор инфузионных линий и расходников, а также средства для экспресс-коррекции тревоги по показаниям.
Подробнее тут – вывод из запоя в стационаре первоуральск
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Детальнее – наркологическая клиника стационар
Команда клиники включает врачей-наркологов и психиатров, клинических психологов, специалистов по зависимости, выездных медсестёр и координаторов маршрута. Все решения принимаются мультидисциплинарно — это значит, что медицинский и психотерапевтический блоки «стыкуются» между собой, а рекомендации не противоречат друг другу. Мы уделяем внимание сенсорной среде: мягкий свет, тишина, регламент вечернего отделения шумов, чтобы медикаментозная поддержка не «сгорала» под стрессом.
Подробнее можно узнать тут – вывод наркологическая клиника в первоуральске
Современная наркологическая клиника «ЮгМед Альянс» в Ставрополе объединяет медицинскую точность и психологическую чуткость. Здесь лечение зависимостей выстроено по принципу системной логики: одно вмешательство — одна цель — один критерий оценки. Такой подход делает процесс предсказуемым и снижает нагрузку на организм. Мы не просто устраняем симптомы, а ищем причину, формируем новые устойчивые модели поведения и помогаем пациенту вернуть контроль над жизнью. Наша команда работает круглосуточно, обеспечивая поддержку и безопасное сопровождение на каждом этапе — от детоксикации до реабилитации.
Получить дополнительные сведения – наркологическая клиника вывод из запоя ставрополь
Терапия в клинике строится на системном подходе, позволяющем постепенно восстанавливать здоровье и формировать новые жизненные установки.
Подробнее – анонимная наркологическая клиника пермь
Если в «окно оценки» прогресс ниже ожиданий, мы меняем ровно один параметр — дозировку, время приёма, приоритет модуля — и задаём новую дату проверки. Это защищает от «снежного кома» назначений и сохраняет ощущение контроля у пациента.
Получить дополнительную информацию – запой наркологическая клиника
As I web-site possessor I believe the content material here is rattling magnificent , appreciate it for your hard work. You should keep it up forever! Good Luck.
Если к «окну оценки» динамика плато, мы корректируем один элемент — скорость/последовательность инфузии, вечерний ритуал или плотность сессий. Это защищает от полипрагмазии и делает вклад каждого шага читаемым.
Получить дополнительные сведения – https://narkologicheskaya-klinika-nizhnij-tagil0.ru/vyvod-iz-zapoya-na-domu-otzyvy-kamensk-uralskij/
Команда «КарелМед Центра» объединяет наркологов, психиатров, реаниматологов, клинических психологов, специалистов по реабилитации и социальному сопровождению. Мы работаем без очередей и навязчивых формальностей, а логистика визита, оформление в стационар и коммуникации с родственниками выстроены бережно: конфиденциальные записи, немаркированные выезды, отдельный вход и нейтральная терминология в документах. Вы получаете не только купирование абстиненции и детоксикацию, но и системную работу с триггерами, привычками и межличностными конфликтами — тем, что часто возвращает к употреблению даже после «идеальных капельниц».
Подробнее можно узнать тут – запой наркологическая клиника в петрозаводске
Наркологическая клиника «КаменМед Ренессанс» выстроена как единая система помощи, где медицинская точность, психологическая поддержка и продуманная логистика соединяются в устойчивый маршрут восстановления. Мы работаем с любыми формами химической зависимости — алкогольной, опиоидной, стимуляторной, полизависимостями — и не ограничиваемся «разовыми» процедурами. Наша задача — не просто снять острые симптомы, а наладить ритм сна, снизить реактивную тревогу, сформировать навыки отказа и вернуть управление повседневной жизнью. Для этого используются модульные программы: детокс, стабилизация, психотерапия, семейные мини-сессии, сопровождение и профилактика срывов. Каждый модуль имеет цель, чёткие критерии эффективности и срок переоценки, чтобы прогресс был ощутимым и измеримым.
Узнать больше – https://narkologicheskaya-klinika-kamensk-uralskij0.ru/kamensk-uralskij-narkologicheskij-dispanser
В клинике используется модульная система лечения, включающая медицинские, психологические и социальные компоненты. В зависимости от состояния человека акценты могут смещаться — например, у одних пациентов приоритетом становится физиологическое восстановление, у других — коррекция эмоционального фона и когнитивных паттернов.
Получить дополнительную информацию – лечение в наркологической клинике
Мы работаем без пауз и очередей, принимая пациентов в любое время суток. В распоряжении бригад — немаркированный транспорт для выезда на дом, портативная диагностика (ЭКГ, пульсоксиметрия, экспресс-анализаторы), а в стационаре — палаты с регулируемым микроклиматом и круглосуточный мониторинг жизненных показателей. Вся документация оформляется в нейтральной терминологии, доступ к данным разграничен по ролям, что защищает вашу анонимность.
Ознакомиться с деталями – вывод наркологическая клиника в ставрополе
Мы не используем универсальные «коктейли»: алгоритм строится из коротких проверяемых шагов. На старте фиксируем цель (например, уменьшить тремор и тошноту, стабилизировать пульс и давление, вернуть полноценный ночной сон), выбираем минимально достаточные средства для её достижения и заранее назначаем «окно оценки» — момент, когда команда сверяет эффект и при необходимости корректирует один параметр. Такой подход защищает от полипрагмазии, экономит силы пациента и делает прогресс читаемым для всей семьи.
Выяснить больше – вывод из запоя капельница
Наша выездная бригада приезжает без маркировки, в гражданской одежде, согласовывает «тихое окно» связи с пациентом или близкими и начинает не с капельницы, а с настройки среды: тёплая приглушённая подсветка, проветривание без сквозняков, отключение уведомлений, подготовка воды комнатной температуры. Затем — быстрый осмотр, экспресс-метрики и старт индивидуального плана. Каждая корректировка — ровно одна за раз, чтобы сохранить причинно-следственную связь и не провоцировать полипрагмазию.
Подробнее можно узнать тут – нарколог на дом срочно
В Нижнем Тагиле выездные бригады дежурят 24/7. Координатор уже при первичном звонке собирает ключевые сведения: аллергии, хронические заболевания, список постоянных препаратов, эпизоды судорог или алкогольных психозов в прошлом, последние значения давления и пульса, возможность обеспечить тишину на 2–3 часа, доступ к питьевой воде, особенности подъезда. Вся эта информация помогает врачу подготовить стартовую схему — от выбора профиля инфузии до темпа введения. По запросу организуем немаркированный визит и сдержанные формулировки в документах, чтобы не создавать лишнего внимания со стороны соседей и коллег.
Получить дополнительную информацию – вывод из запоя цена в нижнем тагиле
Каждый этап лечения в наркологической клинике «ЮгМед Альянс» имеет свою цель, временные рамки и объективные критерии эффективности. Ниже приведена структура терапевтического цикла, применяемая для большинства пациентов после поступления в отделение.
Углубиться в тему – наркологическая клиника нарколог ставрополь
В клинике применяются современные медицинские технологии, которые обеспечивают стойкий результат. Используемые методики соответствуют международным стандартам и регулярно обновляются.
Детальнее – наркологическая клиника клиника помощь в омске
Мы работаем по модели «72 часа + 2 недели»: первые трое суток посвящены стабилизации витальных показателей, коррекции сна и сокращению «тяговых» откликов, следующие 14 дней — консолидации результата и запуску психотерапевтического блока. Маркеры прописываются заранее, поэтому и пациент, и семья понимают, когда и что мы будем оценивать, как корректируем план, если динамика ниже ожидаемой.
Выяснить больше – анонимная наркологическая клиника в первоуральске
Капельница — не «универсальная смесь», а адресный баланс жидкости, электролитов и поддерживающих компонентов под текущие симптомы. Ниже — ориентир, который индивидуализируется на месте осмотра. Мы тщательно сопоставляем пользу и допустимую нагрузку, чтобы не перегружать организм.
Подробнее тут – вызвать врача нарколога на дом петрозаводск
Команда «КарелМед Центра» объединяет наркологов, психиатров, реаниматологов, клинических психологов, специалистов по реабилитации и социальному сопровождению. Мы работаем без очередей и навязчивых формальностей, а логистика визита, оформление в стационар и коммуникации с родственниками выстроены бережно: конфиденциальные записи, немаркированные выезды, отдельный вход и нейтральная терминология в документах. Вы получаете не только купирование абстиненции и детоксикацию, но и системную работу с триггерами, привычками и межличностными конфликтами — тем, что часто возвращает к употреблению даже после «идеальных капельниц».
Ознакомиться с деталями – наркологическая клиника в петрозаводске
Если в «окно оценки» прогресс ниже ожиданий, мы меняем ровно один параметр — дозировку, время приёма, приоритет модуля — и задаём новую дату проверки. Это защищает от «снежного кома» назначений и сохраняет ощущение контроля у пациента.
Разобраться лучше – https://narkologicheskaya-klinika-petrozavodsk0.ru/narkolog-petrozavodsk-otzyvy
Капельницы доступны круглосуточно — в стационаре и с выездом на дом. Состав подбирается под симптомы, коморбидность и семейные обстоятельства. Ниже — примеры профилей: на месте врач адаптирует их, чтобы получить эффект с минимальной нагрузкой на организм.
Изучить вопрос глубже – платная наркологическая клиника каменск-уральск
I?m not sure where you are getting your information, but good topic. I must spend a while finding out much more or understanding more. Thanks for fantastic information I used to be in search of this information for my mission.
«УралДетокс Центр» выстраивает выездную помощь так, чтобы вывести из запоя безопасно, деликатно и без лишних стрессов. Наша выездная бригада приезжает с портативным оборудованием, запускает персонализированную инфузионную терапию, контролирует витальные показатели и сопровождает пациента до стабилизации состояния. Мы не используем «универсальные коктейли» — каждый компонент подбирается под текущие симптомы и сопутствующие заболевания, а эффективность оценивается по заранее оговорённым маркерам: частота пульса, артериальное давление, выраженность тремора, тошнота, сон и дневная ясность.
Подробнее – http://www.domen.ru
Мы не используем универсальные «коктейли»: алгоритм строится из коротких проверяемых шагов. На старте фиксируем цель (например, уменьшить тремор и тошноту, стабилизировать пульс и давление, вернуть полноценный ночной сон), выбираем минимально достаточные средства для её достижения и заранее назначаем «окно оценки» — момент, когда команда сверяет эффект и при необходимости корректирует один параметр. Такой подход защищает от полипрагмазии, экономит силы пациента и делает прогресс читаемым для всей семьи.
Исследовать вопрос подробнее – вывод из запоя капельница в каменске-уральске
Наркологическая клиника «СтавропольМед Резонанс» — это круглосуточный центр доказательной медицины, где помощь строится вокруг безопасности, конфиденциальности и персонализации. Мы объединяем медицинскую детоксикацию, психотерапию, реабилитационные практики и постлечебное сопровождение в единую дорожную карту восстановления. Каждый шаг лечения закреплён измеримыми критериями эффективности, а решения принимаются командно — от дежурного нарколога и клинического психолога до психиатра и реабилитолога.
Получить дополнительную информацию – наркологическая клиника наркологический центр в ставрополе
Город живёт в разных темпах: плотный центр, мостовые переходы, набережная, спальные районы. Мы строим маршрут так, чтобы не привлекать внимания соседей и не терять время на трафик. Если на предзвонке отмечаются «красные флаги» — давящая боль в груди, выраженная одышка, спутанность сознания, судороги, неукротимая рвота или резкое падение насыщения кислородом, — команда instantly переключает маршрут в стационарный «коридор»: палата резервируется заранее, документы оформляются нейтрально, транспорт — немаркированный. Если угроз нет, всё начинается на дому с адресной детокс-схемы и мягкой сенсорной поддержкой.
Углубиться в тему – нарколог на дом круглосуточно в саратове
В клинике «ЮгМед Альянс» выстроена система непрерывного медицинского наблюдения. При поступлении проводится комплексная диагностика, назначается детоксикация и поддерживающая терапия, затем начинается стабилизация физического и эмоционального состояния. Благодаря круглосуточной работе бригад и возможности экстренного выезда на дом пациенты получают помощь без задержек. Конфиденциальность соблюдается на всех уровнях — от первичного звонка до выписки. Для удобства родственников организована система информирования: короткие апдейты по согласованным каналам связи и только в определённое время, чтобы не нарушать покой пациента.
Выяснить больше – наркологическая клиника вывод из запоя ставрополь
Мы работаем по принципу «один визит — один измеримый результат». После инфузий пациент обычно отмечает облегчение головной боли, уменьшение тремора и тревоги, улучшение сна к ближайшей ночи. Если ситуация сложнее (длительный многодневный запой, выраженные соматические факторы), врач оставляет ступенчатый план на 24–48 часов с повторным визитом или переводом в стационарный блок по согласованию с пациентом и родными.
Ознакомиться с деталями – https://narkolog-na-dom-stavropol0.ru/vyzov-narkologa-na-dom-stavropol
В Нижнем Тагиле выездные бригады дежурят 24/7. Координатор уже при первичном звонке собирает ключевые сведения: аллергии, хронические заболевания, список постоянных препаратов, эпизоды судорог или алкогольных психозов в прошлом, последние значения давления и пульса, возможность обеспечить тишину на 2–3 часа, доступ к питьевой воде, особенности подъезда. Вся эта информация помогает врачу подготовить стартовую схему — от выбора профиля инфузии до темпа введения. По запросу организуем немаркированный визит и сдержанные формулировки в документах, чтобы не создавать лишнего внимания со стороны соседей и коллег.
Подробнее можно узнать тут – вывод из запоя вызов
Команда клиники включает врачей-наркологов и психиатров, клинических психологов, специалистов по зависимости, выездных медсестёр и координаторов маршрута. Все решения принимаются мультидисциплинарно — это значит, что медицинский и психотерапевтический блоки «стыкуются» между собой, а рекомендации не противоречат друг другу. Мы уделяем внимание сенсорной среде: мягкий свет, тишина, регламент вечернего отделения шумов, чтобы медикаментозная поддержка не «сгорала» под стрессом.
Исследовать вопрос подробнее – https://narcologicheskaya-klinika-pervouralsk0.ru/pervouralsk-narkologicheskij-dispanser
Капельницы доступны круглосуточно — в стационаре и с выездом на дом. Состав подбирается под симптомы, коморбидность и семейные обстоятельства. Ниже — примеры профилей: на месте врач адаптирует их, чтобы получить эффект с минимальной нагрузкой на организм.
Узнать больше – https://narkologicheskaya-klinika-kamensk-uralskij0.ru/kamensk-uralskij-narkologicheskij-dispanser
Каждый этап лечения в наркологической клинике «ЮгМед Альянс» имеет свою цель, временные рамки и объективные критерии эффективности. Ниже приведена структура терапевтического цикла, применяемая для большинства пациентов после поступления в отделение.
Изучить вопрос глубже – наркологическая клиника нарколог
Ниже — примерный «каркас» лечения. Он индивидуализируется по клинической картине, сопутствующим болезням, опыту прошлых попыток и бытовым ограничениям. Ключевой принцип — «одно вмешательство: одна цель — один маркер — одна дата проверки».
Исследовать вопрос подробнее – наркологические клиники алкоголизм
Врачи «СтаврМед Центра» работают круглосуточно, обеспечивая выезд нарколога на дом в течение короткого времени. Пациент может получить помощь в привычных условиях, не подвергаясь стрессу, связанному с госпитализацией. Все процедуры проводятся анонимно, с сохранением врачебной тайны. Благодаря такому подходу, лечение становится не только эффективным, но и максимально комфортным для человека, который решил прекратить запой и начать восстановление.
Исследовать вопрос подробнее – вывод из запоя с выездом в ставрополе
Лечение организовано поэтапно, что помогает пациенту постепенно возвращаться к полноценной жизни. Каждый шаг направлен на укрепление результата и снижение риска рецидива.
Получить больше информации – наркологические клиники алкоголизм в омске
Если дома нет условий для покоя (ремонт, маленькие дети, шумный двор), мы предложим краткосрочное наблюдение в клинике: отдельный вход, «тихий» коридор, без посторонних вопросов. После стабилизации пациент возвращается домой и продолжает амбулаторный формат с краткими чек-инами по телефону или видеосвязи. Ваша частная жизнь в приоритете: доступ к карте разграничен по ролям, а с семьёй общаемся через одного доверенного человека.
Подробнее можно узнать тут – вывод из запоя в каменске-уральске
Каждый план лечения строится вокруг понятных целей и измеримых результатов. Вместо шаблонных «сильных» схем мы применяем минимально достаточную фармакотерапию, корректируем среду (свет, тишина, режим сна), учим пациента простым и повторяемым навыкам саморегуляции. Такое сочетание медицинских и психологических инструментов помогает быстрее снять острые симптомы и поддерживать стабильность в последующие недели. Кодирование мы рассматриваем не как «волшебную кнопку», а как часть маршрута, который всегда включает детокс, психообразование и профилактику срывов.
Разобраться лучше – http://narkologicheskaya-klinika-nizhnij-tagil0.ru
Наркологическая клиника «КарелМед Центр» — это круглосуточная помощь при алкоголизме и наркомании, ориентированная на безопасность, анонимность и реальный результат. Мы выстраиваем лечение как последовательность управляемых шагов: стабилизация физиологии, снижение тревоги, формирование навыков отказа, восстановление сна, возвращение к работе и семье. Каждый этап имеет цель, понятные маркеры и «окно оценки» — конкретную дату, когда команда и пациент вместе сверяют динамику и корректируют план. Такой подход снижает фармаконагрузку, убирает хаос и делает путь к ремиссии предсказуемым.
Углубиться в тему – narkologicheskaya-klinika-petrozavodsk0.ru/
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Углубиться в тему – нарколог на дом недорого саратов
Капельница — не «универсальная смесь», а адресный баланс жидкости, электролитов и поддерживающих компонентов под текущие симптомы. Ниже — ориентир, который индивидуализируется на месте осмотра. Мы тщательно сопоставляем пользу и допустимую нагрузку, чтобы не перегружать организм.
Получить дополнительные сведения – https://narkolog-na-dom-petrozavodsk0.ru/vyvod-iz-zapoya-narkolog-na-dom-petrozavodsk-uslugi
Наркологическая клиника в Перми обеспечивает пациентам комфортные условия и профессиональное сопровождение. Врачи работают круглосуточно и соблюдают строгую конфиденциальность, что делает лечение доступным и безопасным.
Детальнее – платная наркологическая клиника в перми
Мы работаем без пауз и очередей, принимая пациентов в любое время суток. В распоряжении бригад — немаркированный транспорт для выезда на дом, портативная диагностика (ЭКГ, пульсоксиметрия, экспресс-анализаторы), а в стационаре — палаты с регулируемым микроклиматом и круглосуточный мониторинг жизненных показателей. Вся документация оформляется в нейтральной терминологии, доступ к данным разграничен по ролям, что защищает вашу анонимность.
Детальнее – наркологическая клиника нарколог в ставрополе
Если к назначенному «окну» цель не достигнута, мы меняем ровно один параметр — скорость инфузии, время вечерних ритуалов или плотность телесверок. Такой «микроход» даёт чистое понимание, что именно сработало, и не перегружает организм.
Узнать больше – нарколог на дом вывод из запоя первоуральск
tipps wetten heute (Syreeta) auf niedrige quoten
Состав инфузий подбирается индивидуально. Важно понимать: большая «палитра» компонентов не означает лучший результат; ценность приносит точный фокус. Ниже — типовые профили, которые мы адаптируем под клинику конкретного случая.
Детальнее – вывод из запоя капельница нижний тагил
Основная задача стационарного лечения — не просто вывести человека из кризисного состояния, а вернуть ясность мышления и устойчивость физиологических функций. Поэтому врачи клиники используют современные методы детоксикации, витаминотерапии, ноотропные препараты, психотерапевтические практики короткого действия и физиотерапевтические модули, направленные на восстановление сна, памяти и концентрации.
Ознакомиться с деталями – наркологическая клиника вывод из запоя ставрополь
Вызов нарколога на дом — это безопасный и деликатный способ быстро купировать симптомы алкогольной интоксикации, стабилизировать самочувствие и начать восстановление без госпитализации. В наркологической клинике «МедЛиния Ставрополь» домашние визиты организованы как чёткий медицинский сервис: врач приезжает с портативной диагностикой, подбирает индивидуальный состав капельниц, контролирует витальные показатели и оставляет понятный план дальнейших действий. Все процедуры проводятся анонимно, а оформление документов и логистика построены так, чтобы не нарушать приватность пациента и его семьи.
Ознакомиться с деталями – https://narkolog-na-dom-stavropol0.ru/vyzov-narkologa-na-dom-stavropol/
Экспертная служба дезинсекции и дезинфекции
Добро пожаловать в нашу службу дезинсекции и дезинфекции!
## Мы — профессионалы своего дела:
Работаем быстро и эффективно в области дезинсекции, дезинфекции и дератизации.
## Что мы предлагаем?
* Комплексные мероприятия по уничтожению паразитов
* Современные препараты и оборудование
### Наши услуги:
* Дератизация: устранение любых видов вредителей.
* Устранение муравьев и прочих насекомых
* Санитарная профилактика и контроль грызунов
## Почему выбирают нас?
* Быстрое реагирование на заявку клиента
* Работа круглосуточно и без выходных
https://sanepidemstanciya1.ru/
Домашний визит уместен не только при тяжёлой абстиненции. Он эффективен и на этапе нарастающих симптомов, когда важно предотвратить обострение. Ниже — ориентиры, помогающие принять решение.
Подробнее тут – нарколог на дом клиника ставрополь
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Подробнее можно узнать тут – наркологическая клиника нарколог омск
güncel öztürk
На первом приёме врач-нарколог проводит осмотр, оценивает витальные показатели (АД, ЧСС, SpO2, температура), при показаниях — портативный ЭКГ-скрининг и экспресс-лабораторию, использует шкалы выраженности абстиненции и тревоги. Результаты сразу переводятся в план на ближайшие 72 часа: инфузионная поддержка или таблетированные режимы, «вечерний ритуал» для нормализации сна, карта триггеров и краткое психообразование. Дальше мы обсуждаем цели на 7 дней: что должно измениться и как мы это измерим (сон, тревога, «тяга», энергия, работоспособность).
Изучить вопрос глубже – наркологическая клиника клиника помощь
Такая последовательность шагов позволяет врачу действовать точно и эффективно. Благодаря комплексному подходу пациент чувствует облегчение уже через 1–2 часа после начала терапии, а полное восстановление наступает в течение суток.
Получить дополнительную информацию – вывод из запоя капельница на дому
Такая структура лечения помогает пациентам пройти все этапы восстановления под контролем специалистов.
Ознакомиться с деталями – http://narcologicheskaya-klinika-perm0.ru
Наркологическая клиника «ТагилМед Реал» — это круглосуточная команда врачей, психологов и координаторов, которая берёт на себя полный цикл помощи при алкогольной и наркотической зависимости: от экстренной стабилизации и капельниц на дому до амбулаторного сопровождения, кодирования и длительной психотерапевтической поддержки. Мы работаем без выходных, используем портативное оборудование, придерживаемся принципов доказательной медицины и внимательно относимся к конфиденциальности: нейтральные формулировки в документах, немаркированный транспорт, разграниченный доступ к медицинским данным и единый доверенный контакт для семьи.
Детальнее – анонимная наркологическая клиника
Домашний протокол разбит на понятные шаги. В каждом шаге есть цель, действия, что именно мы измеряем и когда сверяем прогресс. Это делает процесс прозрачным и даёт семье чувство контроля: видно, почему назначено именно это и когда ждать облегчения.
Изучить вопрос глубже – психиатр нарколог на дом в петрозаводске
В «СтаврМед Центре» используются только современные препараты, прошедшие клинические испытания и одобренные Минздравом. Каждая капельница подбирается индивидуально, в зависимости от длительности запоя, возраста пациента и состояния здоровья. В таблице приведены примеры основных видов растворов, применяемых при выезде нарколога.
Получить дополнительную информацию – http://www.domen.ru
«СтавропольМед Резонанс» — мультидисциплинарная команда. Нарколог отвечает за медицинскую безопасность, психиатр — за коморбидные состояния (депрессия, тревога), клинический психолог — за поведенческую перестройку, реабилитолог — за возвращение к активной жизни. Назначения проходят «двойную верификацию»: первичное — лечащим врачом, вторичное — коротким консилиумом на смене. Все препараты закупаются у официальных поставщиков, температурные режимы хранения контролируются, а побочные реакции документируются с привязкой ко времени и обстоятельствам.
Подробнее можно узнать тут – наркологические клиники алкоголизм
Вызов нарколога на дом — это безопасный и деликатный способ быстро купировать симптомы алкогольной интоксикации, стабилизировать самочувствие и начать восстановление без госпитализации. В наркологической клинике «МедЛиния Ставрополь» домашние визиты организованы как чёткий медицинский сервис: врач приезжает с портативной диагностикой, подбирает индивидуальный состав капельниц, контролирует витальные показатели и оставляет понятный план дальнейших действий. Все процедуры проводятся анонимно, а оформление документов и логистика построены так, чтобы не нарушать приватность пациента и его семьи.
Разобраться лучше – нарколог на дом анонимно в ставрополе
С первого контакта координатор уточняет: длительность запоя, виды алкоголя, аллергии, список текущих лекарств, эпизоды судорог или психозов в анамнезе, сердечно-сосудистые жалобы. На основании ответов команда подбирает безопасную схему старта и резервный план на случай усиления симптомов. Врач привозит портативный монитор для контроля АД/ЧСС/SpO2, глюкометр, набор инфузионных линий и расходников, а также средства для экспресс-коррекции тревоги по показаниям.
Подробнее тут – вывод из запоя на дому цена первоуральск
best wettanbieter
Also visit my web blog: online wetten deutschland legal (Sienna)
Каждая ситуация уникальна, однако базовая логика не меняется: один этап — одна цель — один критерий успеха. Ниже — ориентировочная структура визита, которая на месте детализируется с учётом возраста, сопутствующих болезней и особенностей пространства.
Получить дополнительные сведения – http://
Вызов нарколога на дом — это безопасный и деликатный способ быстро купировать симптомы алкогольной интоксикации, стабилизировать самочувствие и начать восстановление без госпитализации. В наркологической клинике «МедЛиния Ставрополь» домашние визиты организованы как чёткий медицинский сервис: врач приезжает с портативной диагностикой, подбирает индивидуальный состав капельниц, контролирует витальные показатели и оставляет понятный план дальнейших действий. Все процедуры проводятся анонимно, а оформление документов и логистика построены так, чтобы не нарушать приватность пациента и его семьи.
Ознакомиться с деталями – http://narkolog-na-dom-stavropol0.ru
sportwetten ohne oasis mit paysafecard
Feel free to surf to my web site :: live wetten quoten
Thanks for giving your ideas. The one thing is that individuals have a selection between national student loan along with a private education loan where it is easier to choose student loan debt consolidation loan than in the federal education loan.
В «СтаврМед Центре» используются только современные препараты, прошедшие клинические испытания и одобренные Минздравом. Каждая капельница подбирается индивидуально, в зависимости от длительности запоя, возраста пациента и состояния здоровья. В таблице приведены примеры основных видов растворов, применяемых при выезде нарколога.
Получить дополнительную информацию – вывод из запоя капельница
best wettanbieter
My site – Sportwetten In öSterreich
One more important aspect is that if you are a senior citizen, travel insurance pertaining to pensioners is something you need to really contemplate. The mature you are, the harder at risk you might be for allowing something terrible happen to you while abroad. If you are not necessarily covered by many comprehensive insurance cover, you could have some serious problems. Thanks for giving your advice on this weblog.
Attractive section of content. I just stumbled upon your weblog and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Any way I will be subscribing to your augment and even I achievement you access consistently rapidly.
официальный сайт kra42 cc
taner
Hello there! This is kind of off topic but I need some help from an established blog. Is it tough to set up your own blog? I’m not very techincal but I can figure things out pretty fast. I’m thinking about setting up my own but I’m not sure where to begin. Do you have any points or suggestions? Thanks
kra42 cc
ahd
nişanaşı
doktorkbb
dr basat
buk
crabs
murad çeltik
yürük
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get got an edginess over that you wish be delivering the following. unwell unquestionably come more formerly again since exactly the same nearly very often inside case you shield this hike.
kra42 cc
ahd
güncel öztürk
My brother suggested I may like this website. He was totally right. This put up actually made my day. You cann’t believe just how so much time I had spent for this information! Thanks!
Admiring the dedication you put into your blog and detailed information you offer. It’s nice to come across a blog every once in a while that isn’t the same old rehashed material. Wonderful read! I’ve saved your site and I’m including your RSS feeds to my Google account.
https://www.tamiristasyonu.com/2025/10/09/melbet-skachat-mobilnoe-prilozhenie-2025/
c’est quoi le code promo dans 1xbet The allure of 1xBet, with its wide array of betting options, is undeniable. However, navigating the world of promo codes can be a labyrinthine task. Whether you seek a “code promo 1xBet” for sports betting, casino games, or simply a “bonus inscription 1xBet,” understanding the landscape is key.
hey there and thank you on your information ? I?ve certainly picked up something new from proper here. I did then again experience some technical points the usage of this web site, as I experienced to reload the web site lots of times previous to I may just get it to load properly. I were considering if your web hosting is OK? No longer that I’m complaining, but sluggish loading circumstances instances will often have an effect on your placement in google and can harm your high-quality ranking if advertising and ***********|advertising|advertising|advertising and *********** with Adwords. Well I am adding this RSS to my email and can glance out for much extra of your respective exciting content. Ensure that you replace this once more soon..
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Прочесть всё о… – https://someadigispace.website/ask-your-friends-in-the-neighbourhood-about-me
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Ознакомьтесь поближе – https://idatacollege.com/%D1%80%D0%B0%D0%B1%D0%BE%D1%87%D0%B5%D0%B5-%D0%B7%D0%B5%D1%80%D0%BA%D0%B0%D0%BB%D0%BE-1xbet-%D0%BE%D1%84%D0%B8%D1%86%D0%B8%D0%B0%D0%BB%D1%8C%D0%BD%D0%BE%D0%BC%D1%83-%D1%81%D0%B0%D0%B9%D1%82-1%D1%85
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Уточнить детали – https://elvincallisaya.com/?p=10
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Обратиться к источнику – https://caringvets.com.au/puppy-parasites
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Тыкай сюда — узнаешь много интересного – https://ltdshs-foerderverein.de/satzung
I was just searching for this information for some time. After six hours of continuous Googleing, at last I got it in your web site. I wonder what’s the lack of Google strategy that do not rank this kind of informative websites in top of the list. Usually the top sites are full of garbage.
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Хочу знать больше – https://finca-calvia.com/treppe-gaestetrackt
Эта публикация завернет вас в вихрь увлекательного контента, сбрасывая стереотипы и открывая двери к новым идеям. Каждый абзац станет для вас открытием, полным ярких примеров и впечатляющих достижений. Подготовьтесь быть вовлеченными и удивленными каждый раз, когда продолжите читать.
Проследить причинно-следственные связи – https://gvss.in/education-program
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Читать далее > – https://bthomerepair.com/product/reverse-osmosis-under-sink-compact-tankless-ro-water-filter-system-dual-filter-reduces-tds-600-gpd-4-stage-filtration-smart
I have taken note that of all different types of insurance, medical care insurance is the most controversial because of the issue between the insurance plan company’s duty to remain making money and the consumer’s need to have insurance. Insurance companies’ earnings on health and fitness plans are incredibly low, as a result some providers struggle to make money. Thanks for the suggestions you share through this blog.
It?s onerous to search out knowledgeable people on this matter, however you sound like you realize what you?re talking about! Thanks
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Подробная информация доступна по запросу – https://tierarzt-schenk.de/praxisschliessung-ab-01-05-2025
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Это стоит прочитать полностью – https://transrentalservice.com/conheca-nosso-guindaste-220-toneladas
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Осуществить глубокий анализ – https://template110.webekspor.com/?p=78
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Подробности по ссылке – http://curlyaucitra.cf/post/34
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Посмотреть всё – https://kesharbhawani.in/railings-turnkey-solution-manufacturer-in-ahmedabad-gujarat-india-4
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Получить полную информацию – https://torcidadofuracao.com.br/2023/02/15/sao-paulo-x-inter-de-limeira-assistir-ao-vivo-com-imagens-palpites-escalacoes-paulistao-2023
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Изучить материалы по теме – http://www.jeffdeyo.com/loving-god-when-you-dont-feel-like-it
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Посмотреть всё – https://everettfentonsgarage.com/computer-diagnostics
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Ознакомиться с теоретической базой – https://napthungbantai.vn/san-pham/duoi-gio-thoi-trang-cho-nissan-almera
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Ознакомиться с деталями – https://www.njofficefurnituredepot.com/office-etiquette-101
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Узнать больше > – https://www.rodi.ru/publ/predlezanie-placenty-nizkaa-placentacia
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Посмотреть всё – https://dssports.com.hk/product/run
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Практические советы ждут тебя – https://csct.edu.lk/index.php/product/quantum-theory
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Выяснить больше – https://marathi.deccanquest.com/?p=31
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Изучить вопрос глубже – http://pic.murakumomura.com/2009/07/29/post_880
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Изучить эмпирические данные – https://domus24.net/pl-pilsudskiego
Wow, awesome blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your website is excellent, let alone the content!
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Хочу знать больше – https://www.wrightbookassociates.co.uk/blog/book-marketing-companies-uk
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Изучить материалы по теме – https://canellecrea.ovh/project/ui-design-kits
I am really impressed with your writing skills as well as with the layout on your blog. Is this a paid theme or did you modify it yourself? Anyway keep up the nice quality writing, it?s rare to see a nice blog like this one today..
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Переходите по ссылке ниже – https://cozycomfortplus.com/product/dnx-024-048-affinity
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Перейти к полной версии – https://uttarvanai.com/archives/100
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Только факты! – https://babycaree.shop/baby-bottle
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Детали по клику – https://freecopi.ru/1103-dizaynerskie-bumagi-v-reklamnoy-poligrafii.html
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Узнайте всю правду – https://vfkeducacao.com.br/courses/3a-fase-minas-gerais-banca-simulada
was bedeutet die quote bei Wetten Auf SpäTe Tore
I got this website from my pal who shared with me about this website and at the moment this time I am browsing this website and reading very informative posts here.
https://epako.ao/melbet-registraciya-v-1-klik-2025/
Наркологическая клиника в клинике в Нижнем Новгороде использует многопрофильный подход, направленный на физическое и психологическое восстановление пациентов. После детоксикации проводится стабилизация обменных процессов, нормализация работы внутренних органов и поддержка нервной системы. Особое внимание уделяется коррекции поведения и мотивации пациента к отказу от употребления алкоголя или наркотиков.
Получить дополнительную информацию – http://narkologicheskaya-clinika-v-nizhnem-novgorode16.ru
Hi there this is kind of of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding skills so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
номера вирт
Капельница, устанавливаемая наркологом на дому в Челябинске, помогает быстро очистить организм от токсинов и нормализовать водно-солевой баланс. Растворы включают витамины, анальгетики, седативные и гепатопротекторные препараты. Эффект от процедуры ощущается уже через 20–30 минут. Капельница снижает головную боль, устраняет тошноту, восстанавливает работу печени и сердечно-сосудистой системы. Такой метод считается одним из самых эффективных способов вывести пациента из запойного или абстинентного состояния без визита в стационар.
Подробнее – вызвать нарколога на дом срочно в челябинске
Корректная среда — половина успешной инфузии. Этот порядок действий помогает врачу быстрее принять решения, а пациенту — легче перенести первые часы.
Получить больше информации – выезд нарколога на дом самара
Чтобы сделать процесс понятным и управляемым, каждый шаг сопровождается измеримыми маркерами безопасности и эффективности. Корректировки — точечные, по правилу «одного изменения», что позволяет видеть вклад каждого действия и сохранять переносимость.
Детальнее – https://narkologicheskaya-pomoshh-v-kazani16.ru/narkologicheskaya-sluzhba-kazan
После проведения процедур пациент чувствует заметное облегчение: исчезает головная боль, снижается тревожность, восстанавливается сон и аппетит. Это создаёт основу для дальнейшего прохождения курса лечения зависимости.
Получить дополнительную информацию – narkologicheskaya-clinika-v-nizhnem-novgorode16.ru/
Капельница, устанавливаемая наркологом на дому в Челябинске, помогает быстро очистить организм от токсинов и нормализовать водно-солевой баланс. Растворы включают витамины, анальгетики, седативные и гепатопротекторные препараты. Эффект от процедуры ощущается уже через 20–30 минут. Капельница снижает головную боль, устраняет тошноту, восстанавливает работу печени и сердечно-сосудистой системы. Такой метод считается одним из самых эффективных способов вывести пациента из запойного или абстинентного состояния без визита в стационар.
Разобраться лучше – выезд нарколога на дом
Корректная среда — половина успешной инфузии. Этот порядок действий помогает врачу быстрее принять решения, а пациенту — легче перенести первые часы.
Выяснить больше – нарколог на дом круглосуточно
Домашний формат уменьшает стресс и экономит время: не нужно ехать в клинику, скрывать визит от соседей или ждать в очереди. Врач приезжает без опознавательных знаков и не создаёт «медицинского шума». За один визит удаётся снять острые проявления, выстроить понятный план ночи и следующего утра, а также определить, нужна ли дополнительная диагностика. Такой маршрут часто оказывается короче и эффективнее, чем череда попыток «пересидеть» симптомы без медицинской поддержки.
Исследовать вопрос подробнее – https://narkolog-na-dom-voskresensk8.ru/narkolog-na-dom-nedorogo-v-voskresenske/
Вывод из запоя — это управляемая медицинская процедура, где каждая деталь важна: от скорости выезда до состава инфузии и «тихой» среды дома. В наркологической клинике «КазаньДетокс Медлайн» мы придерживаемся принципа поэтапной стабилизации: сначала безопасный старт и оценка рисков, затем прицельные капельницы и, при необходимости, краткосрочное наблюдение. Такой подход исключает «универсальные коктейли» и делает результат прогнозируемым: снижение интоксикации, выравнивание вегетативных реакций, восстановление сна и аппетита. Анонимность встроена в протоколы: немаркированный выезд, лаконичная документация, один доверенный контакт для связи 24/7, нейтральные формулировки без стигмы.
Подробнее тут – скорая вывод из запоя в казани
В Казани дежурят мобильные бригады, покрывающие центральные районы и спальные кварталы. Координатор по телефону собирает лишь данные, влияющие на безопасность: текущие лекарства и дозировки, аллергии, эпизоды судорог/психозов в анамнезе, последние значения АД/ЧСС, температуру, а также бытовые условия — место полулёжа, доступ к розетке, возможность «тихого окна» на 2–3 часа. Врач приезжает быстро, но спокойно; вместо суеты — последовательность и аккуратные действия. Визит начинается с очного осмотра, где фиксируются исходные показатели и выбирается контур терапии. Далее выполняется тест переносимости и только затем — основной инфузионный этап. По завершении пациент получает «вечерний протокол» с простыми ритуалами: приглушить свет, проветрить комнату, исключить экраны за час до сна, пить воду малыми глотками.
Подробнее можно узнать тут – http://narkologicheskaya-pomoshh-v-kazani16.ru
Домашний формат уменьшает стресс и экономит время: не нужно ехать в клинику, скрывать визит от соседей или ждать в очереди. Врач приезжает без опознавательных знаков и не создаёт «медицинского шума». За один визит удаётся снять острые проявления, выстроить понятный план ночи и следующего утра, а также определить, нужна ли дополнительная диагностика. Такой маршрут часто оказывается короче и эффективнее, чем череда попыток «пересидеть» симптомы без медицинской поддержки.
Углубиться в тему – https://narkolog-na-dom-voskresensk8.ru/vyzov-narkologa-na-dom-v-voskresenske/
Чтобы помощь была прозрачной и управляемой, каждый этап имеет цель, индикаторы безопасности и эффективности, а также понятное «окно оценки» результата. Коррекции проводятся «штучно», по правилу одного изменения — это защищает от полипрагмазии и позволяет читабельно видеть вклад каждого шага.
Подробнее можно узнать тут – https://vyvod-iz-zapoya-v-kazani16.ru/vyvod-iz-zapoya-kazan-otzyvy
В первые два часа после прибытия бригады важно не «сделать побольше», а принять наименьшее количество решений, которое реально меняет картину. Команда фиксирует базовую линию (ЧСС, АД, SpO?, температура, шкала тошноты/тремора), даёт антиеметический мост и запускает регидратацию. При тахикардии — добавляет антивегетативный контур. Семья получает сценарий ночи: когда приглушить свет, когда предложить воду, какие цифры на тонометре считать нормой и при каких — звонить. Такой протокол экономит время и силы, а главное — превращает вечер из хаотичного в управляемый, снижая риск ночных экстренных вызовов и «эмоциональных качелей».
Узнать больше – вызвать капельницу от запоя на дому челябинск
В клинике применяются современные методы лечения, включающие медикаментозную терапию, психотерапию и физиологическое восстановление. Такой подход позволяет достигнуть стойкого результата и предотвратить возвращение к употреблению алкоголя.
Исследовать вопрос подробнее – капельница от запоя анонимно в нижнем новгороде
Простая подготовка уменьшает стресс, повышает переносимость капельницы и делает оценку состояния более точной. Попросите одного ответственного взрослого быть на связи с врачом — так решения будут приниматься быстрее, а ночной интервал пройдёт спокойнее и предсказуемее.
Подробнее тут – наркология вывод из запоя
Конфиденциальность обеспечивается процессом: нейтральные формулировки в документах, минимум персональных данных, немаркированные формы и транспорт, отдельный вход, «короткие» переговоры у двери, единый контакт по медицинским вопросам. Внутри команды действует «язык цифр» — витальные показатели, шкалы, интервалы питья и сна, окна проверки. Это исключает лишние обсуждения и защищает от распространения деликатной информации за пределы клинического круга.
Подробнее можно узнать тут – наркологическая клиника в ростове-на-дону
Ключ к эффективному выведению из запоя — гибкая персонализация. Мы не настаиваем на «универсальных» капельницах: сначала очная оценка, затем тест переносимости и лишь после — основная инфузия с контролем витальных показателей (АД/ЧСС/SpO?/температура) и субъективной реактивности (тошнота, тремор, тревога по шкале 0–10). Такой подход позволяет мягко провести детоксикацию, восстановить сон, стабилизировать вегетативную нервную систему и уменьшить «шум» организма.
Углубиться в тему – врач вывод из запоя екатеринбург
Поэтапный подход помогает достичь устойчивых результатов и минимизировать вероятность рецидива, обеспечивая безопасность пациента на всех стадиях лечения.
Разобраться лучше – наркологическая клиника наркологический центр в самаре
Мы не используем универсальные «сильные капельницы». Эффективность даёт точное совпадение с задачей. Ниже — логика выбора профилей и маркеры, на которые мы ориентируемся при контроле эффективности и безопасности.
Исследовать вопрос подробнее – помощь вывод из запоя в санкт-петербурге
Наркологическая клиника в клинике в Казани — это современный медицинский центр, специализирующийся на лечении алкогольной и наркотической зависимости. Основное направление деятельности заключается в проведении детоксикации, восстановлении работы нервной системы и формировании устойчивой мотивации к отказу от употребления психоактивных веществ. Все процедуры проводятся в условиях полной анонимности и медицинского контроля, что обеспечивает безопасность и доверие со стороны пациентов. Программа терапии строится по принципам доказательной медицины и индивидуального подбора лечебных средств.
Подробнее можно узнать тут – запой наркологическая клиника казань
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Не упусти шанс – https://www.commercelearning.in/solution-of-april-2016-and-april-2017-fa-vii-board-paper
Капельница от запоя — это не «чудо-микс», а управляемая медицинская процедура с чёткими целями, окном оценки и понятными критериями остановки. В «ЮжУрал Детокс Центр» подход построен по принципу минимально достаточных вмешательств: сначала безопасность (дыхание, сознание, гемодинамика), потом переносимость воды и сбор нормального сна, а уже после — метаболическая поддержка и восстановление бытовой устойчивости. Такая логика исключает полипрагмазию, снижает риск нежелательных реакций и даёт семье прогнозируемую картину на ближайшие 24–72 часа. Мы не обещаем «мгновенного чуда» — мы предлагаем дисциплину маленьких шагов, которая с высокой вероятностью приводит к устойчивому результату.
Подробнее тут – http://kapelnicza-ot-zapoya-v-chelyabinske16.ru/kapelnicza-ot-intoksikaczii-chelyabinsk/
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Откройте для себя больше – https://www.vagsbygd.com/?p=6504
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Всё, что нужно знать – https://akornas.ac.id/akornas-terlibat-dalam-fgd-membahas-implementasi-undang-undang-no-11-tahun-2022-tentang-keolahragaan
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Это стоит прочитать полностью – http://befair2.org/2021/01/27/hello-world
Капельница от запоя в клинике в Нижнем Новгороде является одним из ключевых методов детоксикации организма после длительного употребления алкоголя. Основная цель процедуры — быстрое и безопасное выведение токсинов, нормализация работы жизненно важных органов и стабилизация общего состояния пациента. Методика основана на внутривенном введении лекарственных растворов, которые восполняют дефицит жидкости, электролитов и витаминов, устраняя последствия интоксикации. Такой подход позволяет достичь значительного улучшения самочувствия уже в первые часы после начала терапии.
Разобраться лучше – капельница от запоя на дому круглосуточно в нижнем новгороде
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Запросить дополнительные данные – https://cavistes-catalans.com/cavistes-catalans
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Прочесть заключение эксперта – https://kshairbook.co.uk/hairstyle-trends-for-spring-summer-2018
После проведения процедур пациент чувствует заметное облегчение: исчезает головная боль, снижается тревожность, восстанавливается сон и аппетит. Это создаёт основу для дальнейшего прохождения курса лечения зависимости.
Разобраться лучше – наркологические клиники алкоголизм нижний новгород
Экспертная служба дезинсекции и дезинфекции
Добро пожаловать в нашу службу дезинсекции и дезинфекции!
## Мы — профессионалы своего дела:
Работаем быстро и эффективно в области дезинсекции, дезинфекции и дератизации.
## Что мы предлагаем?
* Высокоэффективные меры по ликвидации насекомых и грызунов
* Индивидуальные программы профилактики
### Наши услуги:
* Дезинсекция: устранение любых видов вредителей.
* Устранение муравьев и прочих насекомых
* Предоставление полного комплекса санитарно-гигиенических мероприятий
## Почему выбирают нас?
* Доступные цены и скидки постоянным клиентам
* Гарантии результата
https://sanepidemstanciya1.ru/
Этот список — памятка на холодильник. Он не раскрывает диагноз, но точно описывает поводы для связи с дежурным врачом. Своевременная эскалация — часть безопасности, а не «подстраховка». Если сомневаетесь — лучше позвонить.
Получить дополнительную информацию – вызов на дом капельницы от запоя
В Екатеринбурге бригады выезжают 24/7, покрывая как центральные районы, так и отдалённые кварталы. Координатор уточняет только то, что влияет на безопасность: принимаемые лекарства и дозы, аллергии, эпизоды судорог/психозов, исходные значения давления и пульса, а также бытовые условия — можно ли обеспечить «тихое окно» на 2–3 часа, есть ли свободная розетка и место для полулёжа. Врач приезжает с портативным мониторингом, расходными материалами и резервным планом на случай повышенной реактивности.
Ознакомиться с деталями – вывод из запоя цена екатеринбург
Домашний формат — это клинически выверенная помощь без госпитализации, если обстановка безопасна и есть взрослый помощник на вечер и ночь. Врач «Трезвого Компаса» приезжает без опознавательных знаков, проводит очную оценку (АД, пульс, сатурация, температура, неврологический статус), уточняет препараты, принятые за 48 часов, и аллергии. Далее — допуск к терапии и запуск инфузии. Мы корректируем жидкость и электролиты, поддерживаем печень и ЦНС, по показаниям используем противорвотные и анксиолитические решения, избегая «перелечивания». В конце визита — переоценка, настройка темпа/состава, памятка на 24–48 часов и окно контрольного контакта.
Углубиться в тему – https://kapelnica-ot-zapoya-klin8.ru/kapelnica-ot-zapoya-na-domu-v-klinu/
Мы не используем универсальные «сильные капельницы». Эффективность даёт точное совпадение с задачей. Ниже — логика выбора профилей и маркеры, на которые мы ориентируемся при контроле эффективности и безопасности.
Углубиться в тему – наркологический вывод из запоя санкт-петербург
Ниже — ориентир, который помогает видеть логику процесса. Это не жёсткий график: врач адаптирует точки и сроки под возраст, фоновые заболевания и исходное состояние.
Углубиться в тему – https://narkologicheskaya-klinika-klin8.ru/kruglosutochnaya-narkologicheskaya-klinika-v-klinu/
Реабилитационные мероприятия в клинике направлены на устранение соматических последствий зависимости, нормализацию когнитивных функций и восстановление социальной адаптации. Для этого используются современные методики физиотерапии, диетологической коррекции и психологического сопровождения, позволяющие закрепить достигнутые результаты лечения.
Разобраться лучше – наркологическая клиника стационар
Простая подготовка уменьшает стресс, повышает переносимость капельницы и делает оценку состояния более точной. Попросите одного ответственного взрослого быть на связи с врачом — так решения будут приниматься быстрее, а ночной интервал пройдёт спокойнее и предсказуемее.
Детальнее – https://vyvod-iz-zapoya-v-chelyabinske16.ru/vyvod-iz-zapoya-chelyabinsk-anonimno
«Опора Здоровья» организует выезд нарколога на дом по Воскресенску и району круглосуточно. Мы действуем анонимно и по клиническим протоколам: очная оценка состояния, допуск к инфузии, детокс с коррекцией водно-электролитного баланса, поддержка печени и центральной нервной системы, бережная нормализация сна по показаниям. Врач объясняет решения простым языком, согласует темп и состав капельницы, оставляет памятку на 24–48 часов и остаётся на связи. Если риски высоки, предложим перевод в стационар без задержек — безопасность всегда важнее «тишей» дома.
Выяснить больше – https://narkolog-na-dom-voskresensk8.ru/vyzov-narkologa-na-dom-v-voskresenske
Сочетание медицинских и психотерапевтических мер создаёт устойчивую систему поддержки. Пациенты получают возможность постепенно восстановить утраченное здоровье и психологическую стабильность.
Углубиться в тему – анонимная наркологическая клиника
Мы не используем шаблон «на всех». Темп и сочетания зависят от давления, пульса, выраженности тошноты и тремора, уровня тревоги, сопутствующих диагнозов и лекарств, уже попавших в организм. Детокс — это система шагов: допуск к терапии, коррекция воды и электролитов, поддержка печени, вегетостабилизация, осторожная работа со сном по показаниям, профилактика осложнений. Любое назначение проговаривается простым языком: зачем, как подействует, что считать нормальной динамикой, а что — поводом связаться с врачом.
Подробнее можно узнать тут – капельница от запоя вызов
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Где можно узнать подробнее? – https://erhvervsklubfyn.dk/medlem/actief-hartmanns-a-s
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Эксклюзивная информация – https://miyauchi38.jp/2021/05/21/hello-world
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Уточнить детали – https://crossriver.ca/service/acmg-hiking-guide
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Узнай первым! – https://www.gishurim.co.il/%D7%97%D7%9C%D7%95%D7%A7%D7%AA-%D7%A8%D7%9B%D7%95%D7%A9-%D7%91%D7%92%D7%99%D7%A8%D7%95%D7%A9%D7%99%D7%9F
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Что ещё? Расскажи всё! – https://alphadog-sf.com/?p=963
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Получить профессиональную консультацию – https://yaello.com/2024/07/03/hello-world
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Доступ к полной версии – https://twodeltas.com/mostbet-kazinosu-arsivleri-250
Такая последовательность обеспечивает медицинскую точность и безопасность процедуры, позволяя добиться быстрого улучшения самочувствия без необходимости госпитализации.
Получить дополнительную информацию – частный нарколог на дом челябинск
Маршрут помощи строится вокруг конкретных задач безопасности. С первого звонка администратор собирает короткий чек-лист: длительность нынешнего эпизода, что принималось в последние двое суток, хронические заболевания, аллергии, как прошла ночь, есть ли помощник на вечер и ночь. Дежурный врач, опираясь на эти данные, предлагает стартовый формат — выезд на дом по Воскресенску и району или немедленную госпитализацию. Решение привязывается к реальным рискам: стабильность давления и пульса, выраженность тремора и тошноты, эпизоды судорог в прошлом, возможность обеспечить «тихий режим» в квартире. После очной оценки и допуска к терапии мы запускаем детокс, а по завершении визита фиксируем правила на 24–48 часов и контрольные точки. Если состояние колеблется, сразу обсуждаем повторный контакт либо перевод в стационар, не теряя часы на бюрократию.
Подробнее можно узнать тут – http://narkologicheskaya-klinika-voskresensk8.ru
Домашний формат удобен, если нет признаков угрозы жизни и дома можно обеспечить спокойную обстановку. Врач приезжает без опознавательных знаков, начинает с очной оценки рисков и допуска к инфузионной терапии, сверяет принятые ранее препараты и аллергии, объясняет план действий и ожидаемую динамику. Далее запускается капельница: мягкая коррекция жидкости и электролитов, поддержка печени, симптом-контроль тревоги, тошноты, головной боли и тремора. На руки выдаются понятные рекомендации на 24–48 часов: питьевой режим, питание, сон, признаки тревоги и алгоритм связи с дежурным врачом.
Получить больше информации – vyvod-iz-zapoya-moskva8.ru/
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Прочитать подробнее – https://www.grantswl.co.uk/screenshot-2019-12-10-at-12-06-31
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Детали по клику – https://skinblissclinics.com/earlobe-repair-treatment-at-skinbliss-clinic-in-hyderabad
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Всё, что нужно знать – https://www.liikennetraktori.fi/tuote/294
ahd
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Всё, что нужно знать – http://www.restobuitengewoon.be/home/imagebox3
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Хочешь знать всё? – https://a-choicesmagazine.com/?p=2252
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Подробнее – https://torcidadofuracao.com.br/2022/11/08/agenda-de-jogos-de-hoje-e-amanha-quarta-09-11-onde-assistir
quote sport live wetten bedeutung
«Чистая Гармония» — это выездная и стационарная наркологическая помощь в одном маршруте: оперативный приезд врача на дом по Клину и району, аккуратный детокс с контролем жизненно важных показателей, стационар с круглосуточным наблюдением и подготовка к кодированию. Мы придерживаемся принципа клинической достаточности: никаких лишних процедур ради «видимости лечения» и никаких задержек с тем, что влияет на исход. Каждое назначение объясняем простыми словами, заранее согласуем смету и оставляем понятный план на 24–48 часов и первую неделю. Анонимность — базовый стандарт: выезд без опознавательных знаков, нейтральные формулировки в документах по запросу, ограниченный доступ к данным.
Углубиться в тему – narkologicheskaya-klinika-v-klinu
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
ТОП-5 причин узнать больше – https://right-tobelong.com/2019/12/09/a-digital-prescription-for-the-pharma-industry-2
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Как это работает — подробно – https://komiplanning.com/mauris-aliquet-auctor-mi-non-volutpat-sagittis-rutrum
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Перейти к полной версии – https://tiendadeperros.es/a-coruna
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Узнать напрямую – https://tucreditoo.com/empower-your-business-harnessing-the-power-of-our-digital
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
А что дальше? – https://ciudadconalma.es/granada/mejores-churrerias-de-granada
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Прочесть заключение эксперта – https://curepedia.org.in/how-does-the-mediterranean-diet-compare-to-other-diets
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Прочесть заключение эксперта – https://estrategiacontabil.com.br/navigating-your-financial-future-tips-for-smart-investing
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
А что дальше? – https://rohanramesh.com/no-code-and-product-management
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Открой скрытое – https://purvanchalmail.com/all-you-need-to-know-about-penalty-shootouts
При домашнем старте врач начинает не с капельницы, а с среды: приглушает верхний свет, обеспечивает проветривание без сквозняка, предлагает маску/беруши при сенсорной чувствительности, переводит телефоны в «без уведомлений». На таком фоне инфузия переносится мягче, уменьшается тошнота, исчезают «рывки» ЧСС перед сном, а утром проходит ощущение «ваты» в голове.
Подробнее – http://narkologicheskaya-klinika-saratov0.ru/klinika-narkologii-saratov/https://narkologicheskaya-klinika-saratov0.ru
В городе и ближайших районах клиника «УралМед Трезвость» обеспечивает оперативный выезд и амбулаторный приём без очередей. На этапе первичного контакта координатор уточняет только клинически значимые моменты: постоянные препараты и дозы, аллергии, эпизоды судорог/психозов в прошлом, базовые показатели (АД/ЧСС/SpO?, если доступны), длительность симптомов, возможность организовать «тихое окно» на 20–30 минут. Вместо долгих разговоров — короткая, спокойная логика: где безопаснее начать (дом/амбулатория/стационар), какую ближайшую цель выбираем, в каком интервале ждём эффект и что считаем сигналом для связи с дежурным врачом.
Выяснить больше – narkologicheskaya-klinika-v-chelyabinske16.ru/
Простая подготовка уменьшает стресс, повышает переносимость капельницы и делает оценку состояния более точной. Попросите одного ответственного взрослого быть на связи с врачом — так решения будут приниматься быстрее, а ночной интервал пройдёт спокойнее и предсказуемее.
Ознакомиться с деталями – http://vyvod-iz-zapoya-v-chelyabinske16.ru
Этот список — памятка на холодильник. Он не раскрывает диагноз, но точно описывает поводы для связи с дежурным врачом. Своевременная эскалация — часть безопасности, а не «подстраховка». Если сомневаетесь — лучше позвонить.
Получить дополнительные сведения – kapelnicza-ot-zapoya-v-chelyabinske16.ru/
Ниже — рабочая матрица на первые часы. Она показывает, как клиническая гипотеза превращается в минимальный шаг, какие индикаторы берём под контроль и по какому сигналу меняем тактику или площадку. Таблица не заменяет очную оценку, но делает логику маршрута ясной для всей семьи.
Разобраться лучше – http://www.domen.ru
Процесс лечения в клинике организован последовательно и направлен на восстановление всех систем организма. Каждый этап имеет свои задачи и методы, что обеспечивает максимальную эффективность терапии.
Подробнее можно узнать тут – наркологическая клиника стационар
Наркологическая клиника в Челябинске предоставляет полный спектр медицинских услуг по диагностике, лечению и реабилитации пациентов с зависимостями различной этиологии. Современные методы терапии, применяемые в клинике, направлены на безопасное и эффективное избавление от наркотической и алкогольной зависимости, а также сопутствующих психических и соматических осложнений.
Узнать больше – анонимная наркологическая клиника
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Подробнее – https://vivod-iz-zapoya-1.ru/
Нарколог на дом в Челябинске — это услуга, которая позволяет получить профессиональную медицинскую помощь при алкогольной или наркотической интоксикации без необходимости посещения клиники. Такой формат особенно востребован в случаях, когда пациент не может самостоятельно прибыть в медицинское учреждение или нуждается в конфиденциальной помощи. Врач-нарколог выезжает по указанному адресу, проводит осмотр, оценивает состояние и подбирает оптимальную терапию. Квалифицированное вмешательство помогает избежать осложнений и стабилизировать состояние уже в течение первых часов после прибытия специалиста.
Изучить вопрос глубже – нарколог на дом цены челябинск
ahd
Каждый пациент проходит несколько последовательных этапов, направленных на очищение организма, стабилизацию эмоционального состояния и формирование стойкой мотивации к трезвой жизни. Такой подход позволяет не только устранить физическую зависимость, но и укрепить психическую устойчивость.
Подробнее тут – наркологическая клиника клиника помощь в самаре
7k casino официальный сайт на 7k casino легко зарегистрироваться и начать играть, так как процесс подключения максимально упрощен.
F*ckin? tremendous things here. I am very satisfied to see your article. Thank you a lot and i’m looking ahead to touch you. Will you kindly drop me a mail?
besten sportwetten seiten
My site; wettanbieter bonus vergleich
Чтобы процедура прошла спокойно и без задержек, заранее организуйте базовые условия — это экономит время и силы пациента и семьи.
Получить дополнительную информацию – https://vyvod-iz-zapoya-moskva8.ru/vyvod-iz-zapoya-v-moskve-v-stacionare
Клиника «Чистый Пульс» выполняет экстренный и плановый вывод из запоя с акцентом на безопасность и скорость. Мы организуем анонимный выезд опытного врача на дом, проводим инфузионную терапию с коррекцией водно-электролитного баланса, контролируем давление и пульс, подбираем поддерживающие препараты для печени и нервной системы, а при необходимости — госпитализируем в стационар под круглосуточное наблюдение. Задача команды — не просто «поставить капельницу», а провести полноценный детокс и вернуть контроль над состоянием, снизив риск осложнений и повторных срывов.
Получить дополнительные сведения – vyvod-iz-zapoya-moskva-ceny
Кодирование от алкоголизма — это не «волшебная таблетка», а четко структурированный этап комплексного лечения, который должен вписываться в общий терапевтический план: диагностика, стабилизация состояния, выбор методики, юридически корректное информированное согласие, сопровождение и профилактика рецидивов. В наркологической клинике «НеоТрезвие СПБ» приоритет — безопасность, предсказуемость и конфиденциальность. Мы не перебираем методы «на удачу», а подбираем технологию с учетом клинического профиля, мотивации, социализации и коморбидных факторов (тревога, депрессия, соматические заболевания).
Получить дополнительные сведения – кодирование от алкоголизма отзывы цены санкт-петербург
Капельница — это не «секретный коктейль», а набор узких модулей, каждый из которых отвечает за одну задачу. Мы включаем ровно один новый модуль за раз и заранее обозначаем стоп-критерий, чтобы не тянуть терапию «по инерции». Параллельно настраиваются поведенческие элементы: свет, тишина, дыхательные ритмы и «окна» питья. Это снимает часть нагрузки с организма и ускоряет наступление целевых маркеров.
Подробнее тут – вызвать врача нарколога на дом краснодар
Вызов нарколога на дом — это не «универсальная капельница», а управляемая последовательность маленьких шагов с понятными целями и точками проверки. В наркологической клинике «КубаньМед Резолюция» выезд врача, инфузионная поддержка и лечение зависимостей складываются в дорожную карту: мы начинаем с короткого триежа, формулируем рабочую гипотезу, включаем минимально достаточный модуль, назначаем «окно оценки» и только затем либо выключаем модуль, либо изменяем одну переменную. Такой подход снижает фармаконагрузку, предотвращает полипрагмазыю и делает динамику прозрачной: пациент и семья видят, что именно помогает и когда вмешательство завершается.
Получить дополнительные сведения – нарколог на дом вывод в краснодаре
Мы выстраиваем помощь как маршрут, а не разовую «капельницу». После первого звонка администратор собирает краткий чек-лист (длительность эпизода, хронические заболевания, принятые препараты, аллергии), передаёт дежурному врачу, и тот предлагает безопасный старт: визит на дому в пределах Сергиева Посада и района или сразу стационар. Выбор зависит от клинических рисков и бытовых условий: есть ли спокойная комната, помощник на ночь, насколько выражены симптомы.
Подробнее – https://narkologicheskaya-klinika-sergiev-posad8.ru/narkologicheskaya-klinika-ceny-v-sergievom-posade/
Преимущество стационара — предсказуемость и скорость. Рядом врач и медсестра, можно оперативно сдать анализы, сделать ЭКГ или дополнительные обследования, а главное — не «тянуть» с корректировкой схемы. В контролируемой среде быстрее нормализуются сон и аппетит, уходит тремор, снижается тревога. Для пациентов с сопутствующими диагнозами это особенно важно: диабет, гипертония, аритмии, хронические заболевания ЖКТ требуют аккуратной, согласованной тактики.
Получить дополнительную информацию – luchshaya-narkologicheskaya-klinika-moskva
Кодирование от алкоголизма — это не «волшебная таблетка», а четко структурированный этап комплексного лечения, который должен вписываться в общий терапевтический план: диагностика, стабилизация состояния, выбор методики, юридически корректное информированное согласие, сопровождение и профилактика рецидивов. В наркологической клинике «НеоТрезвие СПБ» приоритет — безопасность, предсказуемость и конфиденциальность. Мы не перебираем методы «на удачу», а подбираем технологию с учетом клинического профиля, мотивации, социализации и коморбидных факторов (тревога, депрессия, соматические заболевания).
Подробнее тут – кодирование от алкоголизма отзывы цены санкт-петербург
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Как достичь результата? – https://www.mountainhikingventures.com/project/unicolor-87
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Читать далее > – https://zenbat.es/euskera/hello-world-2
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Не упусти важное! – https://exonmachinery.com/obracarka-do-palet
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
https://bhaukaalnews.com/esma-implemented-in-education-department-in-view-of-board-exam-now-education-department-employees-will-not-be-able-to-strike
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
http://inaina.dk/2017/01/der-sad-to-katte-paa-et-bord
Клиника «Чистый Пульс» выполняет экстренный и плановый вывод из запоя с акцентом на безопасность и скорость. Мы организуем анонимный выезд опытного врача на дом, проводим инфузионную терапию с коррекцией водно-электролитного баланса, контролируем давление и пульс, подбираем поддерживающие препараты для печени и нервной системы, а при необходимости — госпитализируем в стационар под круглосуточное наблюдение. Задача команды — не просто «поставить капельницу», а провести полноценный детокс и вернуть контроль над состоянием, снизив риск осложнений и повторных срывов.
Получить дополнительные сведения – vyvod-iz-zapoya-moskva-vyzov-narkologa-kapelnica
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Получить профессиональную консультацию – https://fora-ci.com/realisation-dun-forage
şaban çelebi
«НеоТрезвие СПБ» работает в парадигме доказательной наркологии. Мы используем медикаментозные и психотерапевтические подходы, а также их комбинации. Выбор зависит от клинического запроса, сопутствующих диагнозов и предпочтений пациента. Ниже — сравнительная таблица, которая отражает практический смысл каждого направления.
Узнать больше – как происходит кодирование от алкоголизма в санкт-петербурге
Эта публикация завернет вас в вихрь увлекательного контента, сбрасывая стереотипы и открывая двери к новым идеям. Каждый абзац станет для вас открытием, полным ярких примеров и впечатляющих достижений. Подготовьтесь быть вовлеченными и удивленными каждый раз, когда продолжите читать.
Секреты успеха внутри – https://www.pattanshetti.in/kharab-land-and-its-treatment-in-karnataka
Please let me know if you’re looking for a author for your blog. You have some really good articles and I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some content for your blog in exchange for a link back to mine. Please blast me an e-mail if interested. Many thanks!
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Рассмотреть проблему всесторонне – http://www.devetteblokfluit.nl/?attachment_id=5
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Следуйте по ссылке – https://www.littlemissmomma.com/2013/01/how-to-make-baby-rice-cereal-from-scratch.html
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Что ещё? Расскажи всё! – https://distillate9.com/product/delta-8-cat-3-distillate
В этой статье собраны факты, которые освещают целый ряд важных вопросов. Мы стремимся предложить читателям четкую, достоверную информацию, которая поможет сформировать собственное мнение и лучше понять сложные аспекты рассматриваемой темы.
Есть чему поучиться – https://ochivo.com/tunidos-en-la-ria
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Не упусти шанс – https://crickpicks.com/new-zealand-vs-sri-lanka-dream-11-picks
Домашний формат подойдёт, если нет признаков угрозы жизни и есть возможность обеспечить тишину и наблюдение ночью. Стационар предпочтителен при тяжёлой абстиненции, эпизодах судорог, выраженных скачках давления, неукротимой рвоте, риске делирия, а также когда дома нет условий для безопасного наблюдения. В стационаре под рукой лаборатория, ЭКГ по показаниям, круглосуточный пост — это снижает вероятность осложнений и ускоряет восстановление сна и аппетита.
Подробнее – http://
Детокс — последовательность шагов, где каждый этап имеет цель и критерии безопасности. Мы начинаем с оценки рисков (кардиология, неврология, психическое состояние, возможные взаимодействия препаратов), продолжаем инфузионной терапией, корректируем электролиты и кислотно-щелочное равновесие, поддерживаем печень и нервную систему. Если присутствуют выраженная тревога и бессонница, подключаем короткие курсы седативной терапии с контролем побочных эффектов. Отдельный блок — профилактика осложнений: обезвоживание, аритмии, обострение гастрита и панкреатита, делирий. Каждое назначение — только после очной оценки и с учётом сопутствующих состояний.
Детальнее – https://narkologicheskaya-klinika-moskva8.ru/
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Рассмотреть проблему всесторонне – https://www.etikettenab.se/2024/10/09/hej-varlden
medart
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Изучить материалы по теме – https://lifespectrum360.com/random-taylor-swift-song-generator
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Хочешь знать всё? – https://padacon.com.br/padacon-negocios-padaria-aveiro/img_6493
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Изучить эмпирические данные – https://www.trustyshoeguides.com/how-to-care-for-leather-shoes
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Погрузиться в детали – http://lucadelnegro.com/fashions-fade-style-is-eternal
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Как это работает — подробно – https://www.topmedee.mn/i/237
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Прочесть заключение эксперта – https://manchestercityclubs.nl/history-and-evolution-of-tokushima-vortis-fc
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Открой скрытое – https://reuter-log.de/2021/01/23/kontakt
В этой публикации мы сосредоточимся на интересных аспектах одной из самых актуальных тем современности. Совмещая факты и мнения экспертов, мы создадим полное представление о предмете, которое будет полезно как новичкам, так и тем, кто глубоко изучает вопрос.
Исследовать вопрос подробнее – https://www.taiyo-net.co.jp/amigo/news/post-2238
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Нажмите, чтобы узнать больше – https://kalimantan.infosawit.com/2017/09/08/terjun-ke-dunia-politik-giring-nidji-syukuran-di-rumahnya
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Практические советы ждут тебя – https://www.harfabusinesscenter.cz/section-detail/hbc-b-moderni-kancelarska-budova
ahd
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Проследить причинно-следственные связи – https://www.eltrabajo.cl/2017/amanecieron-muertas-18-gallinas-y-7-cuyes-en-sector-las-cadenas
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Хочешь знать всё? – https://greenwoodlakeapp.com/listing/greenwood-lake-joseph-warren-electrical-llc
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Следуйте по ссылке – https://elenalorenzo.com/ya-en-camino
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Как это работает — подробно – https://ochivo.com/tunidos-en-la-ria
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Ознакомиться с деталями – https://gurukulyogashala.com/blog/ashtanga-vinyasa-yoga
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Ознакомиться с теоретической базой – https://www.topmedee.mn/i/237
Вывод из запоя в Ростове-на-Дону можно пройти в клинике «ЧСП№1», с возможностью вызова нарколога на дом.
Подробнее – вывод из запоя круглосуточно в ростове-на-дону
Если вам или вашим близким необходим вывод из запоя в Ростове-на-Дону, клиника «ЧСП№1» предоставляет квалифицированную помощь. Врачи приедут на дом или вы сможете пройти лечение в стационаре. Цены на услуги начинаются от 3500 рублей.
Узнать больше – вывод из запоя в стационаре в ростове-на-дону
Мы стремимся к тому, чтобы каждый наш пациент в Ростове-на-Дону почувствовал заботу и внимание, получая качественную медицинскую помощь.
Подробнее можно узнать тут – наркология вывод из запоя ростов-на-дону
Мы обеспечиваем полную поддержку на всех этапах лечения в Ростове-на-Дону, включая реабилитацию и профилактику рецидивов.
Подробнее – вывод из запоя клиника в ростове-на-дону
Мы обеспечиваем комфортные условия для пребывания в клинике Ростова-на-Дону, чтобы восстановление прошло максимально эффективно.
Получить больше информации – помощь вывод из запоя
влияние поведенческих факторов
https://algoritmyseo.ru/
hairneva
maral
Квалифицированная помощь в борьбе с вредителями
Здесь вы получите качественную услугу по обработке помещения!
## Мы — профессионалы своего дела:
Более 10 лет опыта в области дезинсекции, дезинфекции и дератизации.
## Что мы предлагаем?
* Высокоэффективные меры по ликвидации насекомых и грызунов
* Индивидуальные программы профилактики
### Наши услуги:
* Дезинфекция: устранение любых видов вредителей.
* Устранение муравьев и прочих насекомых
* Предоставление полного комплекса санитарно-гигиенических мероприятий
## Почему выбирают нас?
* Высококачественные экологичные средства
* Аккуратность и чистота выполняемых работ
https://sanepidemstanciya1.ru/
kandulu
ahd
Именно поэтому при затяжных запоях необходима квалифицированная медицинская помощь, позволяющая безопасно и максимально комфортно прекратить приём алкоголя. Клиника «Стратегия Здоровья» предлагает профессиональный вывод из запоя в Москве как в условиях стационара, так и с выездом на дом. Врачи работают круглосуточно, используя проверенные методики детоксикации и медикаментозной поддержки.
Выяснить больше – нарколог вывод из запоя
Именно поэтому при затяжных запоях необходима квалифицированная медицинская помощь, позволяющая безопасно и максимально комфортно прекратить приём алкоголя. Клиника «Стратегия Здоровья» предлагает профессиональный вывод из запоя в Москве как в условиях стационара, так и с выездом на дом. Врачи работают круглосуточно, используя проверенные методики детоксикации и медикаментозной поддержки.
Получить дополнительную информацию – врач вывод из запоя
1000 рублей за регистрацию вывод сразу без вложений в казино
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Подробнее тут – вывод из запоя цена в нижний новгороде
Наши специалисты в Ростове-на-Дону обеспечат быстрое и безопасное восстановление после длительного употребления алкоголя, используя индивидуальные схемы лечения.
Детальнее – скорая вывод из запоя ростов-на-дону
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Получить больше информации – срочный вывод из запоя
Палата — это контролируемая среда: аппаратный мониторинг, по показаниям ЭКГ и базовая лаборатория, пост медсестёр 24/7, переоценки по графику и быстрая коррекция тактики без логистических пауз. Такой старт рационален при длительных эпизодах, выраженных колебаниях давления и пульса, повторных судорогах, неукротимой рвоте и признаках надвигающегося делирия, а также если дома невозможно обеспечить «тихий режим» и присутствие взрослого помощника ночью. В стационарной ветке меньше случайностей, а путь до стабильного сна короче.
Узнать больше – http://narkologicheskaya-klinika-lobnya8.ru
Запой меняет сразу несколько систем организма: сдвигается водно-электролитный баланс, растёт нагрузка на печень и ЖКТ, «скачут» давление и пульс, усиливаются тревога и бессонница. Одна смесь «от всего» редко даёт устойчивый результат: днём краткий подъём, к ночи — откат и новая волна симптомов. Мы действуем иначе. Сначала — очная оценка и допуск к терапии с учётом того, что человек уже принимал за последние двое суток. Затем — инфузионная поддержка нужного объёма и темпа, симптом-контроль по показаниям, осторожная работа со сном, чтобы не маскировать риски тяжёлой седацией. После основного блока — переоценка, перевод на per os-схемы, правила режима и окно контрольной связи. За счёт последовательности результат становится не хрупким «здесь и сейчас», а устойчивым на сутки и неделю.
Выяснить больше – вывода из запоя платно
В клинике «Частный Медик 24» в Ростове-на-Дону вы получите комплексное лечение, направленное на восстановление организма и предотвращение рецидивов.
Изучить вопрос глубже – вывод из запоя на дому круглосуточно ростов-на-дону
Прежде чем перейти к таблице, отметим смысл. Это ориентир, а не жёсткое расписание. Врач адаптирует длительность и насыщенность этапов под возраст, фоновые диагнозы и динамику симптомов, но логика процесса остаётся неизменной: от безопасности к устойчивости.
Детальнее – vyvod-iz-zapoya-v-stacionare-chekhov8.ru/
В жизни крупных городов часто возникают ситуации, когда стрессы и быстрый ритм жизни приводят к развитию зависимости. Когда проблема становится очевидной, важно незамедлительно обратиться за помощью. В таких случаях вызов нарколога на дом может стать не только удобным, но и наиболее эффективным вариантом. Это позволяет получить квалифицированное лечение в привычной обстановке, сохраняя при этом полную анонимность и конфиденциальность.
Подробнее тут – вызвать нарколога на дом срочно в москве
В Ростове-на-Дону мы гарантируем полную анонимность и конфиденциальность на всех этапах лечения, без постановки на учёт. Клиника в Ростове-на-Дону работает круглосуточно, обеспечивая доступность помощи в любое время дня и ночи.
Исследовать вопрос подробнее – анонимный вывод из запоя ростов-на-дону
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Где почитать поподробнее? – https://nexgentalk.com/5-wearable-tech-innovations-2025
Запой меняет сразу несколько систем организма: сдвигается водно-электролитный баланс, растёт нагрузка на печень и ЖКТ, «скачут» давление и пульс, усиливаются тревога и бессонница. Одна смесь «от всего» редко даёт устойчивый результат: днём краткий подъём, к ночи — откат и новая волна симптомов. Мы действуем иначе. Сначала — очная оценка и допуск к терапии с учётом того, что человек уже принимал за последние двое суток. Затем — инфузионная поддержка нужного объёма и темпа, симптом-контроль по показаниям, осторожная работа со сном, чтобы не маскировать риски тяжёлой седацией. После основного блока — переоценка, перевод на per os-схемы, правила режима и окно контрольной связи. За счёт последовательности результат становится не хрупким «здесь и сейчас», а устойчивым на сутки и неделю.
Углубиться в тему – vyvod-iz-zapoya-otzyvy
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Детальнее – https://inyoureyes.mx/single-service-1
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Подробная информация доступна по запросу – https://www.kirra.jp/2020/05/22/forest-style-bar-kirra%E3%83%90%E3%83%B3%E3%83%93%E3%83%BC%E3%83%8E
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Жми сюда — получишь ответ – https://grd-solutions.com/the-seven-phases-of-a-cyber-attack
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Как это работает — подробно – https://entreprise-de-nettoyage-versailles-78-yvelines.fr/how-solar-energy-works-from-sunlight-to-electricity
В Ростове-на-Дону клиника «Частный Медик 24» предлагает профессиональный вывод из запоя с современными методами детоксикации и инфузионной терапии.
Исследовать вопрос подробнее – вывод из запоя с выездом
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Запросить дополнительные данные – https://casaruraltioemilio.es/project-view/corpus-christi
Обратившись в «Частный Медик 24» в Ростове-на-Дону, вы получаете не только медицинскую помощь, но и всестороннюю поддержку на пути к выздоровлению.
Разобраться лучше – вывод из запоя на дому цена в ростове-на-дону
Этап
Разобраться лучше – http://vyvod-iz-zapoya-v-stacionare-chekhov8.ru/vyvod-iz-zapoya-kapelnica-v-chekhove/
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Смотрите также… – https://loverpresets.com/2021/07/23/exploring-atlantas-modern-homes
Мы стремимся к тому, чтобы каждый наш пациент в Ростове-на-Дону почувствовал заботу и внимание, получая качественную медицинскую помощь.
Ознакомиться с деталями – вывод из запоя на дому цена
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
Читать далее > – https://nogi46.wpxblog.jp/yumiki
Алкогольный эпизод — это не один симптом, а целая сцепка процессов: обезвоживание, электролитные сдвиги, скачки давления и пульса, тремор, тошнота, тревога, нарушения сна; нередко добавляются проблемы со стороны желудка и печени. Шаблонная капельница игнорирует индивидуальную картину и часто даёт кратковременный эффект с ночным откатом. Мы работаем иначе: допускаем к терапии, подбираем состав и темп инфузии под текущие цифры и динамику, избегаем конфликтов с уже принятыми препаратами и объясняем, чего ожидать по ощущениям на каждом шаге. Избыточная седация не усиливает лечение — она делает его менее предсказуемым.
Изучить вопрос глубже – наркологическая клиника стационар
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Читать дальше – https://library.gctu.edu.gh/announcements/gctu-librarians-receive-training-on-the-administration-of-dspace
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Познакомиться с результатами исследований – https://dieteticienne-nutritionniste-sartrouville.com/sportndiet
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Обратиться к источнику – https://creativeautodesign.com/home-2
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Детали по клику – https://baghlafpro.com/hello-world
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Изучить вопрос глубже – https://lamat.pl/2023/07/16/retreats-are-made-to-help-you-connect-with-youself
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
Все материалы собраны здесь – https://nogi46.wpxblog.jp/yumiki
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Что скрывают от вас? – https://www.logopedtorbica.com/2021/09/08/vrste-praksija
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
См. подробности – https://californiadailypost.com/dioz-group-home-of-multiple-successful-brands
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Что скрывают от вас? – https://forbesport.com/unveiling-the-auz100x-exploring-the-next-big-thing-in-audio-technology
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Всё, что нужно знать – https://lacooper.com/product/dermosol-post-solar
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Продолжить чтение – https://twodeltas.com/mostbet-kazinosu-arsivleri-250
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Эксклюзивная информация – https://melinascumburdis.com.ar/dscn7063
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Перейти к полной версии – https://www.ancb.bj/index.php/magazine/courrier-mensuel-de-l-ancb/item/428-premiere-session-de-la-commission-thematique-genre-affaires-sociales-et-participation-citoyenne-de-l-ancb-luc-atrokpo-ouvre-la-session.html?tmpl=component&print=1&start=0
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Подробнее – https://www.insertservice.nl/backup/attachment/logo2014-2
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Перейти к полной версии – http://www.footebrotherscanoes.net/maincarocell_image
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Продолжить чтение – https://michael-lauter.de/2017/09/12/hallo-welt
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Изучить вопрос глубже – https://krasunia.ru
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Получить полную информацию – https://library.gctu.edu.gh/announcements/gctu-librarians-receive-training-on-the-administration-of-dspace
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Только факты! – https://qsmartlab.com/regulatory-regimes-governing-fin-tech-firms-worldwide
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Открыть полностью – https://corporate-africa.com/ses-and-shevon-to-boost-african-mining-connectivity
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
Погрузиться в научную дискуссию – https://loverpresets.com/2021/07/23/exploring-atlantas-modern-homes
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Доступ к полной версии – https://www.wirtschaft-und-industrie.de/lohnt-sich-eine-solaranlage-2025-noch-eine-meinung
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Это стоит прочитать полностью – https://pmg-mechanical.com/heat-pumps-vs-air-conditioners-which-is-the-best-choice-for-your-home
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Где можно узнать подробнее? – https://www.bsw-architects.com/plano-aquatic-center-reopens-after-complete-renovation
Капельница — основной инструмент для очищения организма от продуктов распада этанола. Состав раствора подбирается строго индивидуально. В таблице приведены примеры комплексов, применяемых специалистами клиники «Трезвая Линия Волгоград».
Получить больше информации – нарколог на дом вывод из запоя волгоград
Наркологическая помощь в «ВолгаМед Тольятти» включает широкий спектр процедур и методик. Каждый случай рассматривается индивидуально, с учётом состояния пациента, стадии заболевания и сопутствующих факторов. Ниже представлена таблица с основными направлениями медицинской работы.
Исследовать вопрос подробнее – http://narkologicheskaya-pomoshh-v-tolyatti17.ru
Капельницы — основной инструмент при лечении алкогольной и наркотической интоксикации. Они способствуют выведению токсинов, восстановлению электролитного баланса и улучшению самочувствия. Ниже представлена таблица с основными типами капельниц, применяемыми в клинике «КузбассМед Центр».
Подробнее тут – анонимная наркологическая клиника в новокузнецке
В таблице представлены основные виды терапии, применяемые в клинике:
Получить больше информации – https://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkolog-v-gorode-novokuzneczke
Игнорирование этих симптомов может привести к тяжёлым последствиям — судорогам, галлюцинациям или алкогольному психозу.
Получить дополнительные сведения – http://vyvod-iz-zapoya-v-tyumeni17.ru
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Получить дополнительную информацию – нарколог на дом вывод из запоя тольятти
deniz küçükkaya
ahd
Домашняя помощь — это клиника, перенесённая в тихую комнату. Знакомая обстановка снижает тревогу, исчезают пробки и ожидание, нет «социального шума». Врач «ПрофДетокса» приезжает без эмблем, действует спокойно и последовательно, объясняет каждое назначение простым языком. Мы не используем мифические смеси. Состав и темп капельницы подбираются под текущие показатели — давление, пульс, сатурация, выраженность тремора и тошноты, уровень тревоги, данные о лекарствах, которые человек успел принять за двое суток. Такой подход даёт не минутное облегчение, а устойчивую динамику на сутки и неделю.
Разобраться лучше – https://narkolog-na-dom-ivanteevka8.ru/narkolog-na-dom-srochno-v-ivanteevke/
Все растворы проходят фармацевтический контроль, а процедуры выполняются одноразовыми стерильными инструментами. После завершения капельницы врач наблюдает пациента в течение 15–30 минут, оценивает результат и даёт рекомендации по дальнейшему восстановлению. Важно не прерывать терапию самостоятельно — эффект закрепляется только при соблюдении рекомендаций.
Получить больше информации – https://narkolog-na-dom-v-voronezhe17.ru/narkolog-voronezh-anonimno/
Безопасность — это не лозунг, а набор решений. Мы избегаем «жёстких» седативных доз, которые создают видимость улучшения и повышают риск скрытых осложнений. Наращивание темпа инфузии происходит постепенно и увязано с динамикой симптомов и цифрами измерений. Любой шаг объясняется пациенту и семье: зачем он выбран, что считается нормальной волной улучшения, в какой момент нужно связаться с дежурным. Такой прозрачный формат снимает тревогу и помогает всем участникам действовать согласованно.
Исследовать вопрос подробнее – narkolog-na-dom-ivanteevka
Процесс кодирования проходит в комфортной и спокойной обстановке. Врач объясняет каждый этап, чтобы пациент чувствовал себя уверенно и спокойно. После процедуры пациент получает памятку с рекомендациями по уходу за здоровьем и режиму поведения в первые недели после лечения.
Разобраться лучше – кодирование от алкоголизма отзывы цены в волгограде
Во время процедуры врач фиксирует ключевые параметры, чтобы убедиться в безопасности и эффективности терапии. Мониторинг проводится при каждом выезде и помогает отслеживать динамику в режиме реального времени. В таблице ниже указаны основные показатели, за которыми следит специалист.
Узнать больше – врач нарколог на дом
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Получить больше информации – http://narkologicheskaya-klinika-v-krasnoyarske17.ru/chastnaya-narkologicheskaya-klinika-krasnoyarsk/
Во время лечения фиксируются все жизненные показатели пациента. При необходимости проводится экспресс-анализ крови и ЭКГ. Ниже представлена таблица, показывающая, какие параметры контролируются и по каким признакам оценивается стабилизация состояния.
Разобраться лучше – вывод из запоя клиника воронеж
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Разобраться лучше – кодирование от алкоголизма отзывы в волгограде
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Углубиться в тему – vivod-iz-zapoya-v-volgograde17.ru/
Для жителей Красноярска организованы два конфиденциальных пути. Первый — немаркированный выезд бригады на дом с заранее согласованными порогами связи. Второй — «тихий вход» в клинику через отдельную дверь, где приём проходит без очередей и «коридорных» разговоров. На первичном звонке администратор уточняет только клинически значимые факторы: частоту рвоты, наличие мочеиспускания, ЧСС/АД в покое, эпизоды спутанности, актуальные лекарства и аллергии. Биографические подробности и лишние вопросы не задаются — мы придерживаемся принципа минимально необходимой информации.
Подробнее – http://narkologicheskaya-klinika-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy/https://narkologicheskaya-klinika-v-krasnoyarske17.ru
Для повышения эффективности в капельницы добавляются витамины группы B, аскорбиновая кислота, кардиопротекторы и антиоксиданты. Такая комбинация позволяет не только ускорить выведение продуктов распада алкоголя, но и предотвратить развитие постабстинентных расстройств. Благодаря точной дозировке и мягкому темпу введения растворов снижается риск побочных реакций, а восстановление проходит плавно и безопасно.
Ознакомиться с деталями – вывод из запоя на дому круглосуточно воронеж
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Подробнее тут – вывод из запоя недорого в волгограде
«ПрофДетокс» — выездная наркологическая служба для жителей Ивантеевки и ближайших районов. Мы запускаем помощь без очередей и лишней огласки: врач приезжает анонимно, проводит очную оценку, допускает к терапии и запускает инфузионную поддержку без универсальных коктейлей. Наша задача — снять интоксикацию и абстиненцию, стабилизировать давление и пульс, снизить тревогу, мягко наладить сон по показаниям и дать семье понятный план на ближайшие двое суток. Если дома нет условий для безопасной ночи, предложим палату «ПрофДетокса» с круглосуточным наблюдением. Приватность встроена в процесс, а смета фиксируется до начала процедур.
Детальнее – https://narkolog-na-dom-ivanteevka8.ru/narkolog-na-dom-anonimno-v-ivanteevke/
Современная наркологическая клиника — это не просто медицинское учреждение, где проводят детоксикацию или капельницы. Это выстроенная система, где каждый этап направлен на восстановление физического, психического и социального равновесия пациента. В клинике «КрасЗдрав Профи» весь процесс лечения построен по принципу прозрачных шагов: первичная диагностика, стабилизация организма, терапевтическая коррекция и закрепление результата. Всё происходит с соблюдением принципа конфиденциальности — пациент может рассчитывать на анонимность и этичное отношение со стороны персонала.
Узнать больше – http://narkologicheskaya-clinica-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy/https://narkologicheskaya-clinica-v-krasnoyarske17.ru
Ниже приведена таблица с типовыми компонентами капельницы и их назначением:
Получить больше информации – https://kapelnicza-ot-zapoya-v-volgograde17.ru/kapelnicza-ot-alkogolya-volgograd/
Работа клиники строится на принципах индивидуального подхода, доказательной медицины и строгого соблюдения конфиденциальности. Каждый пациент проходит обследование, в ходе которого оценивается состояние организма, выявляется стадия зависимости и сопутствующие нарушения. На основе полученных данных разрабатывается персональная программа лечения, включающая медицинские, психологические и социальные методы коррекции поведения.
Получить дополнительные сведения – наркологические клиники алкоголизм воронеж
Пациенты отмечают, что особенно важна не только профессиональная помощь, но и спокойная атмосфера. Мягкий свет, тишина, отдельные палаты и деликатная коммуникация персонала — всё это снижает тревожность и помогает организму восстановиться. Эффективность лечения оценивается по конкретным маркерам: улучшение сна, нормализация давления, исчезновение тошноты, восстановление аппетита и уменьшение тяги.
Получить дополнительную информацию – анонимная наркологическая клиника красноярск
Палатный формат мы предлагаем, когда есть риск делирия, судорог, резких скачков давления и пульса, выраженной одышки, неукротимой рвоты, обезвоживания или когда дома невозможно обеспечить наблюдение ночью. В стационаре под рукой аппаратный контроль, по показаниям ЭКГ и базовая лаборатория, круглосуточный пост и регулярные переоценки с точной настройкой схем. Здесь меньше случайностей: темп инфузий корректируется без задержек, решения принимаются быстро, а риск «ночных качелей» ниже. Для семьи стационар часто оказывается не «дороже», а короче по времени до стабильного сна и предсказуемее по бюджету.
Получить дополнительные сведения – narkologicheskaya-klinika-na-dom
Нарколог на дом в Уфе — это услуга, которая позволяет получить квалифицированную медицинскую помощь при алкогольной или наркотической интоксикации без необходимости госпитализации. Такой формат особенно востребован при запойных состояниях, когда пациент не может самостоятельно посетить клинику. Врач приезжает по вызову в течение короткого времени, проводит обследование, устанавливает капельницу и обеспечивает безопасный вывод из состояния опьянения. Все процедуры выполняются анонимно, с соблюдением медицинской этики и конфиденциальности.
Выяснить больше – https://narkolog-na-dom-v-ufe17.ru/vyvod-iz-zapoya-ufa-narkolog-na-dom
На месте врач и медсестра собирают базовую линию: уровень сознания, дыхание, SpO?, температура, шкалы симптомов (тошнота/тремор/тревога 0–10), переносимость воды небольшими глотками. Далее формулируется рабочая гипотеза и включается минимально достаточный модуль с обозначенным «окном оценки»: 30–60 минут — для «окна питья», 60–120 минут — для стабилизации ЧСС/АД и дрожи, «первая ночь» — для сна и вечерней тревоги. Как только маркер достигнут, модуль выключается; нет эффекта — меняется одна переменная без «усиления всего сразу».
Изучить вопрос глубже – наркологическая клиника лечение алкоголизма
Старт всегда один: короткий скрининг с дежурным врачом, где уточняются жалобы, длительность эпизода, текущие лекарства, аллергии и условия дома. Далее согласуется реальное окно прибытия или приёма — без обещаний «через пять минут», но с честным ориентиром и запасом на дорожную обстановку. На месте врач фиксирует витальные показатели (АД, пульс, сатурацию, температуру), по показаниям выполняет ЭКГ, запускает детокс (регидратация, коррекция электролитов, защита печени/ЖКТ), объясняет ожидаемую динамику первых 6–12 часов и выдаёт памятку «на сутки»: режим сна, питьевой план, «красные флажки», точное время контрольной связи. Если домашний формат становится недостаточным, перевод в стационар организуется без пауз — терапия продолжается с того же места, где начата, темп лечения не теряется.
Исследовать вопрос подробнее – наркологическая клиника стоимость
Перед процедурой врач оценивает состояние пациента, измеряет давление, пульс и уровень насыщения крови кислородом. После осмотра подбирается состав инфузии, включающий препараты для дезинтоксикации, восстановления водно-солевого баланса и нормализации работы органов. Введение растворов осуществляется внутривенно, под контролем специалиста. Длительность процедуры — от 40 минут до 1,5 часов.
Узнать больше – врач на дом капельница от запоя волгоград
Услуга вывода из запоя в клинике сочетает профессионализм врачей, медицинскую точность и заботу. При этом обеспечивается полная конфиденциальность: данные пациентов не передаются в сторонние инстанции. Круглосуточный режим работы позволяет вызвать врача даже ночью — специалисты прибывают в течение 40–60 минут после обращения.
Подробнее – вывод из запоя недорого в волгограде
Безопасность — это не лозунг, а набор решений. Мы избегаем «жёстких» седативных доз, которые создают видимость улучшения и повышают риск скрытых осложнений. Наращивание темпа инфузии происходит постепенно и увязано с динамикой симптомов и цифрами измерений. Любой шаг объясняется пациенту и семье: зачем он выбран, что считается нормальной волной улучшения, в какой момент нужно связаться с дежурным. Такой прозрачный формат снимает тревогу и помогает всем участникам действовать согласованно.
Детальнее – http://narkolog-na-dom-ivanteevka8.ru/vyzvat-narkologa-na-dom-v-ivanteevke/https://narkolog-na-dom-ivanteevka8.ru
Безопасность — это не лозунг, а набор решений. Мы избегаем «жёстких» седативных доз, которые создают видимость улучшения и повышают риск скрытых осложнений. Наращивание темпа инфузии происходит постепенно и увязано с динамикой симптомов и цифрами измерений. Любой шаг объясняется пациенту и семье: зачем он выбран, что считается нормальной волной улучшения, в какой момент нужно связаться с дежурным. Такой прозрачный формат снимает тревогу и помогает всем участникам действовать согласованно.
Изучить вопрос глубже – http://narkolog-na-dom-ivanteevka8.ru/vyzvat-narkologa-na-dom-v-ivanteevke/
Запой меняет сразу несколько систем организма: сдвигается водно-электролитный баланс, растёт нагрузка на печень и ЖКТ, «скачут» давление и пульс, усиливаются тревога и бессонница. Одна смесь «от всего» редко даёт устойчивый результат: днём краткий подъём, к ночи — откат и новая волна симптомов. Мы действуем иначе. Сначала — очная оценка и допуск к терапии с учётом того, что человек уже принимал за последние двое суток. Затем — инфузионная поддержка нужного объёма и темпа, симптом-контроль по показаниям, осторожная работа со сном, чтобы не маскировать риски тяжёлой седацией. После основного блока — переоценка, перевод на per os-схемы, правила режима и окно контрольной связи. За счёт последовательности результат становится не хрупким «здесь и сейчас», а устойчивым на сутки и неделю.
Углубиться в тему – https://vyvod-iz-zapoya-lobnya8.ru
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Не упусти шанс – http://agivasejahtera.info/internet-gratis-pos-kampling-dusun-sidomulyo-area-pabrik-ulingan
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Продолжить чтение – https://komigang.nu/hej-verden
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Открой скрытое – https://myhomeschoolproject.com.mx/tips-de-organizacion
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Обратиться к источнику – https://worldcryptoupdate.com/tetraguard-the-financial-safe
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Обратиться к источнику – https://wanep.org/wanep/csos-consultative-meeting-to-review-the-state-of-democracy-and-governance-in-the-ecowas-region
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Узнай первым! – https://www.htcwildfire.com.vn/so-sanh-iphone-x-va-xs
Все растворы проходят фармацевтический контроль, а процедуры выполняются одноразовыми стерильными инструментами. После завершения капельницы врач наблюдает пациента в течение 15–30 минут, оценивает результат и даёт рекомендации по дальнейшему восстановлению. Важно не прерывать терапию самостоятельно — эффект закрепляется только при соблюдении рекомендаций.
Подробнее тут – нарколог капельница на дом в воронеже
Работа клиники строится на принципах индивидуального подхода, доказательной медицины и строгого соблюдения конфиденциальности. Каждый пациент проходит обследование, в ходе которого оценивается состояние организма, выявляется стадия зависимости и сопутствующие нарушения. На основе полученных данных разрабатывается персональная программа лечения, включающая медицинские, психологические и социальные методы коррекции поведения.
Детальнее – http://narkologicheskaya-klinika-v-voronezhe17.ru/chastnaya-narkologicheskaya-klinika-voronezh/
Чтобы понять логику процесса, посмотрите на ориентир ниже. Это не жёсткое расписание, а понятная канва, которую врач адаптирует под возраст, сопутствующие заболевания и текущие цифры.
Углубиться в тему – http://narkologicheskaya-klinika-ivanteevka8.ru
Запой меняет сразу несколько систем организма: сдвигается водно-электролитный баланс, растёт нагрузка на печень и ЖКТ, «скачут» давление и пульс, усиливаются тревога и бессонница. Одна смесь «от всего» редко даёт устойчивый результат: днём краткий подъём, к ночи — откат и новая волна симптомов. Мы действуем иначе. Сначала — очная оценка и допуск к терапии с учётом того, что человек уже принимал за последние двое суток. Затем — инфузионная поддержка нужного объёма и темпа, симптом-контроль по показаниям, осторожная работа со сном, чтобы не маскировать риски тяжёлой седацией. После основного блока — переоценка, перевод на per os-схемы, правила режима и окно контрольной связи. За счёт последовательности результат становится не хрупким «здесь и сейчас», а устойчивым на сутки и неделю.
Детальнее – https://vyvod-iz-zapoya-lobnya8.ru/vyvod-iz-zapoya-kruglosutochno-v-lobne/
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Уточнить детали – https://devzafiro.com/2018/07/16/us-sues-california-over-immigration-laws
«ПрофДетокс» — выездная наркологическая служба для жителей Ивантеевки и ближайших районов. Мы запускаем помощь без очередей и лишней огласки: врач приезжает анонимно, проводит очную оценку, допускает к терапии и запускает инфузионную поддержку без универсальных коктейлей. Наша задача — снять интоксикацию и абстиненцию, стабилизировать давление и пульс, снизить тревогу, мягко наладить сон по показаниям и дать семье понятный план на ближайшие двое суток. Если дома нет условий для безопасной ночи, предложим палату «ПрофДетокса» с круглосуточным наблюдением. Приватность встроена в процесс, а смета фиксируется до начала процедур.
Выяснить больше – zapoj-narkolog-na-dom
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Желаете узнать подробности? – https://www.littlemissmomma.com/2024/10/best-books-to-read-depending-on-your-mood-pt-2.html
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Не упусти шанс – https://djfrankgalan.com/future-sounds-emerging-trends-in-dj-culture
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
ТОП-5 причин узнать больше – https://topic.lk/5255
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Это стоит прочитать полностью – https://infominang.com/mahyeldi-vasko-paket-lengkap-untuk-membangun-sumbar-yang-lebih-cepat
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Читать далее > – https://careers.epilpoint.it/estetista-specializzata-monopoli-2
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Получить профессиональную консультацию – https://topic.lk/10344
В этой статье собраны факты, которые освещают целый ряд важных вопросов. Мы стремимся предложить читателям четкую, достоверную информацию, которая поможет сформировать собственное мнение и лучше понять сложные аспекты рассматриваемой темы.
Есть чему поучиться – https://www.motortsas.com/cilega-motors
Именно поэтому при затяжных запоях необходима квалифицированная медицинская помощь, позволяющая безопасно и максимально комфортно прекратить приём алкоголя. Клиника «Стратегия Здоровья» предлагает профессиональный вывод из запоя в Москве как в условиях стационара, так и с выездом на дом. Врачи работают круглосуточно, используя проверенные методики детоксикации и медикаментозной поддержки.
Углубиться в тему – http://narko-reabcentr.ru/
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Запросить дополнительные данные – https://brosico.com/index.php/2024/03/08/ola-mundo
Формат
Подробнее тут – http://narkologicheskaya-klinika-shchyolkovo0.ru
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Узнать больше > – https://eineweltsafaris.com/2020/12/08/a-place-where-start-new-life-with-peace
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Посмотреть всё – https://cynthiamartinonline.com/2024/08/03/recognizing-his-voice-a-notebook-and-6-part-video-class-to-help-you-hear-from-god-in-just-30-days
Безопасность — это не лозунг, а набор решений. Мы избегаем «жёстких» седативных доз, которые создают видимость улучшения и повышают риск скрытых осложнений. Наращивание темпа инфузии происходит постепенно и увязано с динамикой симптомов и цифрами измерений. Любой шаг объясняется пациенту и семье: зачем он выбран, что считается нормальной волной улучшения, в какой момент нужно связаться с дежурным. Такой прозрачный формат снимает тревогу и помогает всем участникам действовать согласованно.
Разобраться лучше – https://narkolog-na-dom-ivanteevka8.ru/vyzvat-narkologa-na-dom-v-ivanteevke/
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Выяснить больше – http://www.marshabrink.nl/2012/01/25/deze-blog-gaat-over
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Нажми и узнай всё – http://traffikreklam.com/index.php/2016/03/01/standard-post-with-preview-picture-images-slider
Цель
Ознакомиться с деталями – narkologicheskaya-klinika
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Почему это важно? – https://certifiedmobilenotaryservice.com/certified-mobile-notary-service-5-star-customer-reviews
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Осуществить глубокий анализ – https://plastipak.co.za/sed-imperdiet-fringilla-2
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Только для своих – https://old.newcroplive.com/video/careersstartups-december-24-2017
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Ознакомиться с отчётом – https://raghebabuhamdan.com/al-bayan-%F0%9F%87%A6%F0%9F%87%AA
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Изучить материалы по теме – https://colegioincentivo.com.br/tiny-tot-adventures-a-peek-into-our-preschool-world
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Расширить кругозор по теме – https://wanep.org/wanep/news-situation-tracking-crise-multidimensionnelle-ayant-abouti-au-coup-detat-militaire-du-30-septembre-2022
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Запросить дополнительные данные – https://odontjomarips.com/dia-mundial-de-lucha-contra-uso-indebido-y-trafico-ilicito-de-drogas
Наши специалисты проводят детальную диагностику и разрабатывают индивидуальный план лечения с учётом состояния пациента в Ростове-на-Дону.
Выяснить больше – https://vyvod-iz-zapoya-rostov111.ru/
Наши услуги доступны всем жителям Ростова-на-Дону, обеспечивая доступность помощи для каждого пациента.
Выяснить больше – вывод из запоя клиника
Обратившись в «Частный Медик 24» в Ростове-на-Дону, вы получаете не только медицинскую помощь, но и всестороннюю поддержку на пути к выздоровлению.
Детальнее – вывод из запоя недорого
‘Профессиональная служба удаления плесени и грибка в Челябинске и Копейске. ‘,
‘Цель службы’: ‘Обеспечиваем здоровое и чистое жилище путем устранения плесени и грибка. ‘,
‘Перечень услуг: дезинсекция’: ‘Услуги по обработке помещений от плесени и грибка: ‘,
‘Детали дезинсекции’: ‘- Проведение диагностики пораженных участков\\n- Применение эффективных антимикробных препаратов\\n- Подготовка индивидуальных профилактических решений’,
‘Перечень услуг: дезинфекция’: ‘Комплекс мероприятий по обеззараживанию поверхностей и воздуха: ‘,
‘Детали дезинфекции’: ‘- Полноценная очистка воздуха от грибковых спорангиев\\n- Использование специализированных устройств для глубокой очистки\\n- Консультации по профилактике повторного заражения’,
‘Перечень услуг: дератизация’: ‘ Предоставляем услуги профилактики распространения грибков и плесени:’,
‘Детали дератизации’: ‘- Осмотр помещения и выявление очагов поражения\\n- Разработка плана действий по ликвидации очагов\\n- Мониторинг эффективности проведенных работ’,
‘Преимущества выбора вашей службы’: ‘Опытные мастера и новейшие препараты обеспечивают гарантированный результат.
Наша сайт
Interesting blog post. The things i would like to contribute is that personal computer memory has to be purchased should your computer is unable to cope with that which you do by using it. One can install two random access memory boards containing 1GB each, for example, but not one of 1GB and one having 2GB. One should always check the manufacturer’s documentation for the PC to make sure what type of memory is required.
seven kay casino регистрация seven kay официальный сайт соответствует международным стандартам безопасности и применяет SSL-шифрование для защиты данных.
Обратившись в «Частный Медик 24» в Ростове-на-Дону, вы получаете не только медицинскую помощь, но и всестороннюю поддержку на пути к выздоровлению.
Подробнее тут – скорая вывод из запоя
В Новокузнецке команда «РеабКузбасс» организовала круглосуточный выезд наркологов, что позволяет оказывать помощь даже в сложных ситуациях. Пациенты часто обращаются после многодневного употребления алкоголя, когда нарушен сон, давление нестабильно, а организм истощён. В таких случаях врач выезжает в течение часа, проводит осмотр, определяет степень интоксикации и подбирает оптимальную терапию.
Выяснить больше – https://vyvod-iz-zapoya-v-novokuzneczke17.ru/vyvedenie-iz-zapoya-novokuzneczk
Мы стремимся к тому, чтобы каждый наш пациент в Ростове-на-Дону почувствовал заботу и внимание, получая качественную медицинскую помощь.
Детальнее – вывод из запоя недорого
Инфузионные растворы подбираются строго индивидуально, после осмотра врача и анализа показателей пациента. При необходимости курс повторяется с изменением состава раствора для достижения максимального эффекта.
Выяснить больше – наркологическая клиника лечение алкоголизма новокузнецк
В Новокузнецке команда «РеабКузбасс» организовала круглосуточный выезд наркологов, что позволяет оказывать помощь даже в сложных ситуациях. Пациенты часто обращаются после многодневного употребления алкоголя, когда нарушен сон, давление нестабильно, а организм истощён. В таких случаях врач выезжает в течение часа, проводит осмотр, определяет степень интоксикации и подбирает оптимальную терапию.
Получить дополнительные сведения – вывод из запоя на дому цена
Инфузионные растворы подбираются строго индивидуально, после осмотра врача и анализа показателей пациента. При необходимости курс повторяется с изменением состава раствора для достижения максимального эффекта.
Подробнее тут – наркологическая клиника нарколог новокузнецк
В клинике «Частный Медик 24» в Ростове-на-Дону вы получите комплексное лечение, направленное на восстановление организма и предотвращение рецидивов.
Выяснить больше – вывод из запоя круглосуточно
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Не упусти важное! – https://axisdentalclinic.com/insurances/neuron-logo
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Проследить причинно-следственные связи – https://www.nishi-yama.co.jp/?attachment_id=16
Состав капельницы подбирается индивидуально, с учётом степени опьянения, возраста и хронических заболеваний пациента. Врач определяет дозировку и комбинацию препаратов, чтобы процедура прошла безопасно и эффективно.
Получить дополнительную информацию – сколько стоит капельница от запоя воронеж
Эта публикация завернет вас в вихрь увлекательного контента, сбрасывая стереотипы и открывая двери к новым идеям. Каждый абзац станет для вас открытием, полным ярких примеров и впечатляющих достижений. Подготовьтесь быть вовлеченными и удивленными каждый раз, когда продолжите читать.
Уточнить детали – https://oyemonkey.com/black-marvel-t-shirts-unleashing-your-inner-superhero-in-style
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Прочитать подробнее – https://carlavegaseminario.com/6-preguntas-clave-para-conseguir-un-objetivo
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Что скрывают от вас? – https://batutudalys.lt/img31__81493-1462971702-1280-1280
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Интересует подробная информация – https://www.bolnewspress.com/salud/oms-no-hay-ninguna-senal-de-alarma-sobre-la-seguridad-de-las-vacunas-covid-19
Вывод из запоя требуется тогда, когда организм уже не способен самостоятельно справиться с последствиями алкогольной интоксикации. Длительное употребление спиртного приводит к нарушению работы внутренних органов, обезвоживанию и психическим расстройствам. Медицинская помощь помогает избежать опасных осложнений и облегчить процесс отказа от алкоголя.
Подробнее можно узнать тут – помощь вывод из запоя в рязани
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Продолжить чтение – http://www.ueberlebenskuenstlerin.at/willkommen-im-paradies
Одним из ключевых направлений терапии является инфузионное лечение. Капельницы позволяют быстро восстановить обмен веществ, улучшить работу внутренних органов и ускорить выведение токсинов. В клинике используются только сертифицированные препараты, безопасные для сердечно-сосудистой и нервной системы.
Ознакомиться с деталями – вывод наркологическая клиника
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Перейти к полной версии – https://yamad-sales.info/2021/11/04/hello-world
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Открой скрытое – https://samachartehelka.com/?p=35
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Познакомиться с результатами исследований – https://theoxygenplan.com/companies-combat-mental-illness-mobile-apps
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Это ещё не всё… – https://www.roelabogados.com/2019/01/12/what-we-are-capable-of-usually-gets-discovered-7
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Прочесть заключение эксперта – https://www.fikretzengin.com/basariyi-saglayan-etmenler
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Следуйте по ссылке – https://www.captjoe19.com/2023/03/26/the-most-popular-page-builder-included
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Кликни, не пожалеешь – https://purexculture.com/es/2023/06/26/tu-pareja-a-un-clic
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Обратиться к источнику – https://almaxindustry.com/komatsu-saa6d114e-3-engine
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Ознакомьтесь с аналитикой – https://professionlogistique.com/2024/03/06/innovation-et-adaptabilite-la-philosophie-dar-racking-pour-le-stockage
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Подробности по ссылке – https://www.ldc.ac.ug/call-for-applications-2024_2025
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Получить полную информацию – https://nashdiabet.ru/produkty
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Ознакомиться с деталями – https://timestotravel.com/how-to-make-the-most-of-a-business-trip-a-comprehensive-guide-for-indian-professionals
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Заходи — там интересно – http://www.barbarascustomwindowtinting.com/project/7332
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Обратиться к источнику – http://lamphouse.ru/catalog/11
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Перейти к полной версии – https://dannegroni.com/resources/john-woodens-pyramid-of-success
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Изучить вопрос глубже – https://ecoterraviajes.com/index.php/2022/08/04/nicaragua-san-juan-del-sur-rivas
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Смотрите также… – https://chairsandtableszagreb.eu/ciao-mondo
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Узнать больше > – https://housepoint.net/pine-wood-disadvantages
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Ознакомьтесь с аналитикой – https://traveltrends.co.bw/woocommerce-placeholder
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Посмотреть всё – http://masterauto.rs/2019/10/17/post
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Следуйте по ссылке – https://shiphangnhatviet.com/mua-hang-tren-amazon-nhat-ban-ve-viet-nam
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Подробности по ссылке – https://nchapelain.com/hello-world
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Продолжить изучение – https://pmg-mechanical.com/contact-pmg-mechanical-for-expert-installation-and-upgrade-your-heating-system-today
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Подробнее – https://chainglob.com/le-lancement-de-kiveclair
Наши специалисты в Ростове-на-Дону обеспечат быстрое и безопасное восстановление после длительного употребления алкоголя, используя индивидуальные схемы лечения.
Получить больше информации – помощь вывод из запоя в ростове-на-дону
Hello just wanted to give you a brief heads up and let you know a few of the images aren’t loading properly. I’m not sure why but I think its a linking issue. I’ve tried it in two different web browsers and both show the same outcome.
https://dotzlerbau.de/uncategorized/melbet-skachat-prilozhenie-android-2025/
Наши специалисты в Ростове-на-Дону готовы ответить на все ваши вопросы и предоставить подробную информацию о процессе лечения.
Выяснить больше – наркологический вывод из запоя ростов-на-дону
В клинике «Частный Медик 24» в Ростове-на-Дону вы получите комплексное лечение, направленное на восстановление организма и предотвращение рецидивов.
Изучить вопрос глубже – наркология вывод из запоя ростов-на-дону
Наши специалисты в Ростове-на-Дону обеспечат быстрое и безопасное восстановление после длительного употребления алкоголя, используя индивидуальные схемы лечения.
Ознакомиться с деталями – https://vyvod-iz-zapoya-rostov111.ru/
В Ростове-на-Дону мы гарантируем полную анонимность и конфиденциальность на всех этапах лечения, без постановки на учёт. Клиника в Ростове-на-Дону работает круглосуточно, обеспечивая доступность помощи в любое время дня и ночи.
Получить больше информации – вывод из запоя в ростове-на-дону
Thank you, I have recently been looking for info about this subject for a while and yours is the greatest I have came upon till now. But, what about the bottom line? Are you certain concerning the source?
May I simply say what a relief to discover an individual who genuinely understands what they’re talking about over the internet. You actually realize how to bring a problem to light and make it important. More and more people need to look at this and understand this side of the story. I was surprised that you aren’t more popular because you most certainly possess the gift.
https://mycitycorona.com/melbet-obzor-2025/
Thanks for your submission. I would also love to opinion that the very first thing you will need to complete is check if you really need credit score improvement. To do that you need to get your hands on a copy of your credit profile. That should really not be difficult, ever since the government necessitates that you are allowed to have one absolutely free copy of your real credit report each year. You just have to check with the right persons. You can either look into the website for that Federal Trade Commission and also contact one of the leading credit agencies instantly.
Whats up this is somewhat of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding experience so I wanted to get advice from someone with experience. Any help would be enormously appreciated!
https://pvrisband.com
игровые автоматы
WONDERFUL Post.thanks for share..more wait .. ?
Thanks for helping me to attain new tips about pc’s. I also hold the belief that certain of the best ways to keep your notebook in primary condition is with a hard plastic case, and also shell, that fits over the top of your computer. A majority of these protective gear tend to be model specific since they are made to fit perfectly above the natural casing. You can buy all of them directly from the owner, or from third party places if they are for your notebook, however its not all laptop can have a covering on the market. Once more, thanks for your suggestions.
https://yurhelp.in.ua/
Thanks for some other informative website. The place else may I am getting that type of information written in such an ideal method? I’ve a mission that I’m simply now working on, and I have been on the look out for such info.
Hey there, I think your blog might be having browser compatibility issues. When I look at your blog site in Firefox, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, terrific blog!
казино лучше
Hello, I think your site might be having browser compatibility issues. When I look at your website in Firefox, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, amazing blog!
кракен актуальная ссылка на сегодня
WONDERFUL Post.thanks for share..more wait .. ?
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Полная информация здесь – https://www.dancesoul.com.tw/school_12
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
https://informatusa.com/negocios-ia
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Где можно узнать подробнее? – https://cimetieres.coop/cropped-cimetiere-sfx-hiver-jpg
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Хочешь знать всё? – https://auxpyrenees.com/carte/menu-du-jour-plat-dessert
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Ознакомиться с теоретической базой – https://premiumtravel.az/travel-to-azerbaijan
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Изучить материалы по теме – https://edevig.com/produit/enceinte-soundtouch-20
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Как это работает — подробно – https://thenewblackmagazine.com/2024/01/13/httpwww-thenewblackmagazine-comview-aspxindex3370
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Почему это важно? – https://www.questembert2020.bzh/reunion-publique
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Наши рекомендации — тут – https://stephaniescheubeck.com/blog-archive/paper-at-the-symposium-narrating-the-somatic
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Практические советы ждут тебя – https://www.tidalraves.com/latest-news
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
https://puntoeacapo.uno/articoli/ingressobambini
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Узнай первым! – https://decoratingmycoziness.com/as-fichas
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Проверенные методы — узнай сейчас – https://mydownloadables.com/black-rough-seamless-pattern
I was curious if you ever thought of changing the page layout of your site? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having 1 or two pictures. Maybe you could space it out better?
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Полная информация здесь – https://www.muffu.fi/controlling-a-hella-vnt-actuator-with-pwm
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Подробная информация доступна по запросу – https://www.morganwloch.fr/scene-ouverte-st-nizier-sous-charlieu
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Ознакомиться с теоретической базой – https://zeltene.eu/atbild-nbs-galvenais-psihologs-vai-karavirs-var-atguties-pec-kara-pieredzeta/66015
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Получить дополнительные сведения – https://patioscenes.com/preparing-gazebo-summer/preparing-gazebo-summer-2
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Следуйте по ссылке – https://cookwithcoconut.com/2025/07/05/pumpkin-erissery
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Дополнительно читайте здесь – https://www.summervalleyschoolmoradabad.com/ptm-grade-3-9-11
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Всё, что нужно знать – https://fenixmerchandising.com.ar/favicon
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Получить больше информации – https://aipkiwil6.org/2023/06/29/posting-pertama
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Запросить дополнительные данные – https://mytischi-city.ru
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Читать далее > – https://www.thomas-a.com/koppel_a1_9860
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Ознакомиться с деталями – https://prorab.kr.ua/KapitalniyRemont/igrovie-avtomati-joker-kazino
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Детали по клику – https://www.agonconsultoria.com.br/galeria
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Обратиться к источнику – https://joostharinck.com/project/about-ver1
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Что скрывают от вас? – https://postroyka.volyn.ua/AtributiOfisa/kak-vibrat-idealnogo-parikmahera-dlya-sebya
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Нажмите, чтобы узнать больше – https://pro-java.ru/category/patterny-proektirovaniya-java
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Получить полную информацию – https://orientretie.be/elegant-dessert-10-tips-how-to-make-it-at-home-1
Клиника «Детокс» в Краснодаре работает круглосуточно, обеспечивая доступность помощи в любое время. Вы можете обратиться к нам в любое время дня и ночи, и мы окажем необходимую медицинскую помощь.
Подробнее можно узнать тут – вывод из запоя с выездом краснодар
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Как это работает — подробно – https://www.bpml.in/bpml-fevicon
Наши специалисты проводят детальную диагностику и разрабатывают индивидуальный план лечения с учётом состояния пациента в Краснодаре. Мы учитываем все особенности вашего здоровья при назначении лечения.
Детальнее – вывод из запоя на дому круглосуточно
Мы предлагаем различные программы лечения в Челябинске, включая стационарное и амбулаторное, чтобы выбрать оптимальный вариант для вас. Вы можете выбрать наиболее подходящий для вас способ лечения.
Выяснить больше – вывод из запоя дешево челябинск
Вывод из запоя в стационаре клиники «Детокс» в Краснодаре — эффективное решение для длительного запоя. Мы предоставляем круглосуточную медицинскую помощь, обеспечивая комфорт и безопасность на каждом этапе лечения.
Детальнее – вывод из запоя с выездом краснодар
It’s quite refreshing to find great content such as this. Continue the good work.
Howdy would you mind stating which blog platform you’re using? I’m looking to start my own blog in the near future but I’m having a hard time choosing between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your design seems different then most blogs and I’m looking for something unique. P.S Sorry for getting off-topic but I had to ask!
Капельница от запоя в «Детокс» в Краснодаре — быстрый способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными специалистами с использованием современных препаратов.
Детальнее – вывод из запоя недорого краснодар
Вывод из запоя в стационаре клиники «Детокс» в Краснодаре — эффективное решение для длительного запоя. Мы предоставляем круглосуточную медицинскую помощь, обеспечивая комфорт и безопасность на каждом этапе лечения.
Ознакомиться с деталями – http://vyvod-iz-zapoya-krasnodar206.ru/
Hello, Neat post. There is a problem along with your web site in internet explorer, could test this? IE nonetheless is the marketplace chief and a huge part of people will leave out your great writing due to this problem.
Обратившись в клинику «Частный Медик 24» в Челябинске, вы делаете первый шаг к здоровой и трезвой жизни. Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Подробнее тут – вывод из запоя в челябинске
В «Детокс» в Краснодаре мы заботимся о вашем здоровье и благополучии, предоставляя качественную медицинскую помощь. Наши специалисты всегда готовы помочь вам на пути к выздоровлению.
Подробнее можно узнать тут – вывод из запоя капельница на дому краснодар
Наши услуги доступны всем жителям Краснодара, обеспечивая доступность помощи для каждого пациента. Вы можете обратиться к нам независимо от вашего места проживания.
Разобраться лучше – vyvod-iz-zapoya-krasnodar116.ru
Вывод из запоя на дому в Челябинске — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой, проведут необходимую диагностику и лечение.
Углубиться в тему – вывод из запоя на дому в челябинске
Thanks for the marvelous posting! I certainly enjoyed reading it, you can be a great author.I will make sure to bookmark your blog and will often come back later in life. I want to encourage you continue your great work, have a nice afternoon!
Клиника «Детокс» в Краснодаре предлагает профессиональный вывод из запоя с использованием современных методов детоксикации и инфузионной терапии. Наши специалисты обеспечат быстрое и безопасное восстановление после длительного употребления алкоголя, используя индивидуально подобранные схемы лечения.
Получить дополнительную информацию – нарколог на дом вывод из запоя
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Это стоит прочитать полностью – https://primenewsnet.com/a-breakthough-for-this-year-new-holiday-birds-eye-view-debuting
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Секреты успеха внутри – https://autoecolebourgeois.com/galleries/cambridge-language-certificate-in-2018
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Ознакомиться с теоретической базой – https://primenewsnet.com/dj-dark-beach-memories-august-session
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Узнай первым! – https://lutonstay.com/product/fishing-in-dubai
Эта публикация завернет вас в вихрь увлекательного контента, сбрасывая стереотипы и открывая двери к новым идеям. Каждый абзац станет для вас открытием, полным ярких примеров и впечатляющих достижений. Подготовьтесь быть вовлеченными и удивленными каждый раз, когда продолжите читать.
Уникальные данные только сегодня – https://primenewsnet.com/discover-the-most-magical-sunset-in-santorini
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Читать дальше – https://primenewsnet.com/%E0%A4%AC%E0%A4%BF%E0%A4%B9%E0%A4%BE%E0%A4%B0-%E0%A4%95%E0%A5%80-%E0%A4%95%E0%A5%8B%E0%A4%B8%E0%A5%80-%E0%A4%AC%E0%A4%A8-%E0%A4%97%E0%A4%88-%E0%A4%85%E0%A4%AE%E0%A5%87%E0%A4%B0%E0%A4%BF%E0%A4%95-2
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Запросить дополнительные данные – https://gkindustriesgroup.com/product/tilla-kulfi-counter
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Это стоит прочитать полностью – https://www.texturedtalk.com/textured-talk-with-cheyenne-of-onmylevel_chey
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Дополнительно читайте здесь – https://blog.zhdk.ch/dada/2014/09/07/hugo-ball
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Все материалы собраны здесь – http://mutuelle-de-sante.fr/the-power-of-effective-communication-in-business
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Читать дальше – https://primenewsnet.com/spring-fashion-show-at-the-university-of-michigan-has-started
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Прочесть заключение эксперта – https://fundacionboreal.org.ar/nuestra-fundacion-llega-a-santiago-del-estero
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Обратиться к источнику – https://www.la-esperanzahotel.com/villa-lujo-la-esperanza-granada
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Прочесть заключение эксперта – http://yura.oops.jp/review/log/eid151.html
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
Только факты! – https://alfanetmx.com/index.php/2022/05/26/sources-for-digital-marketing
Hi there mates, nice post and pleasant urging commented here, I am
actually enjoying by these.
Cool blog! Is your theme custom made or did you download
it from somewhere? A design like yours with a few
simple tweeks would really make my blog shine. Please let me know where you got your
design. Thank you
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Изучить вопрос глубже – http://kzashop.com/product/slogan-hoodie-with-label-detail
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Обратиться к источнику – https://primenewsnet.com/the-best-gray-paint-how-to-choose-the-right-shade-for-your-walls
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Полезно знать – https://primenewsnet.com/now-is-the-time-to-think-about-your-small-business-success
I was suggested this blog by my cousin. I am not sure whether this
post is written by him as nobody else know such detailed about my problem.
You are wonderful! Thanks!
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Продолжить чтение – https://primenewsnet.com/mobile-marketing-is-said-to-be-the-future-of-e-commerce
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Получить профессиональную консультацию – https://reshenie-zdes.ru/news-2535-travertin-ot-mercurystone-kak-elegantnost-prirody-v-kagdom-proekte.html
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Секреты успеха внутри – https://sportowagdynia.eu/index.php/2018/12/11/szesc-trojek-dulkysa-na-pozegnanie-arki-z-7days-eurocup
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Продолжить чтение – https://osharah.ru/news-1201-18-maya-mneralnyh-vodah-zavershana-budantstva-novaj-shkoly-na-700-vuchnya-abstalyavanaj-nteraktynym-.html
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Посмотреть всё – https://www.moenr.gov.bt/?p=10858
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Изучить вопрос глубже – https://rudasov.ru/news-829656-oformlenie-vizy-v-kitaj-protsess-neslognyj-no-trebuyuschij-vnimatelnosti-i-znaniya-vseh-nyuansov.html
I used to be able to find good advice from your articles.
First of all I want to say great blog! I had a quick question that I’d like to ask if you don’t mind.
I was interested to know how you center yourself and clear your head before writing.
I’ve had a hard time clearing my thoughts in getting my ideas out.
I do enjoy writing but it just seems like the first 10 to 15 minutes are lost just trying to figure out how
to begin. Any ideas or tips? Thank you!
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Читать далее > – https://surgezircmedia.com/surgezirc-media-announces-openings-journalists
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Секреты успеха внутри – https://edmarmy.com/desert-hearts-reveals-stacked-2023-festival-lineup
Great blog post. The things i would like to contribute is that computer memory is required to be purchased if the computer can’t cope with that which you do with it. One can deploy two RAM boards of 1GB each, for example, but not certainly one of 1GB and one having 2GB. One should look for the manufacturer’s documentation for own PC to make sure what type of storage is required.
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Открыть полностью – http://life-with-dog.com/blog/log/eid68.html
For the reason that the admin of this web page is working, no question very soon it will be famous, due to its quality contents.
I’m really impressed along with your writing abilities as smartly
as with the structure on your blog. Is that this a paid topic or did you
customize it yourself? Anyway keep up the nice high quality
writing, it’s rare to peer a great weblog
like this one nowadays..
It is appropriate time to make a few plans for the
longer term and it’s time to be happy. I have read this submit and if I may just I wish to counsel you some
interesting things or suggestions. Maybe you can write subsequent articles
relating to this article. I want to learn more issues approximately it!
One thing I’d really like to say is the fact that car insurance cancellations is a terrifying experience and if you are doing the best things being a driver you may not get one. Many people do are sent the notice that they have been officially dropped by their particular insurance company they have to fight to get added insurance after having a cancellation. Low-priced auto insurance rates are frequently hard to get after a cancellation. Knowing the main reasons pertaining to auto insurance canceling can help car owners prevent sacrificing one of the most crucial privileges obtainable. Thanks for the tips shared by means of your blog.
Мы обеспечиваем комфортные условия для пребывания в клинике Краснодара, чтобы восстановление прошло максимально эффективно. В нашей клинике созданы все условия для вашего удобства и быстрого восстановления.
Ознакомиться с деталями – наркологический вывод из запоя
Just want to say your article is as amazing. The clarity in your post is just nice and that i could assume you are
knowledgeable on this subject. Well along with your permission allow me to snatch
your feed to keep up to date with forthcoming post.
Thank you one million and please carry on the gratifying work.
May I just say what a relief to uncover someone that truly understands
what they are discussing online. You certainly realize how to bring
a problem to light and make it important.
A lot more people ought to check this out and understand this side
of your story. I was surprised you’re not more popular given that you certainly
have the gift.
В «Частном Медике 24» в Челябинске вы получите комплексное лечение, направленное на восстановление организма и предотвращение рецидивов. Мы предлагаем индивидуальный подход к каждому пациенту.
Получить дополнительные сведения – вывод из запоя цена в челябинске
I appreciate, result in I found just what I used to be taking a look for.
You’ve ended my 4 day lengthy hunt! God Bless you man. Have a
nice day. Bye
I believe that is one of the so much significant info for me.
And i’m satisfied reading your article. However wanna remark on few basic issues, The website style is great, the articles is
really nice : D. Excellent task, cheers
Halo semuanya!
Perkenalkan, saya Anastasia McArthur, seseorang yang senang dengan dunia hiburan online.
Saya berasal dari Lomme, dan sudah cukup lama tertarik
dengan berbagai platform hiburan daring, terutama yang berkaitan dengan bola dan angka.
Awalnya, saya hanya iseng mencari informasi tentang dunia
hiburan online, tapi akhirnya menemukan bahwa KUBET adalah salah satu Situs Judi Bola
Terlengkap yang benar-benar punya sistem terbaik.
Fitur yang ditawarkan sangat mudah digunakan, mulai dari kubet login yang super cepat sampai beragam kategori permainan yang bikin betah.
Selain bola, saya juga menikmati Situs Parlay Resmi dan Situs Parlay
Gacor karena memberi pengalaman bermain berbeda.
Keduanya memberikan sistem yang stabil, cocok untuk siapa saja yang mencari hiburan dengan kualitas terbaik.
Tidak lupa, Situs Mix Parlay juga menjadi favorit karena menyediakan kombinasi permainan yang menantang tapi menyenangkan.
Selain permainan bola, saya juga menyukai hiburan angka seperti toto macau karena memberikan sensasi tersendiri.
Semua itu semakin lengkap berkat akses dari KUBET yang
berjalan tanpa kendala.
Bagi saya, situs parlay dan KUBET bukan sekadar platform
hiburan, tapi juga tempat untuk menemukan pengalaman baru.
Saya percaya bahwa dengan memilih Situs Judi Bola Terlengkap dan terpercaya, siapa pun bisa bermain dengan aman.
Greetings from Carolina! I’m bored at work so I decided
to browse your site on my iphone during lunch break. I enjoy the info you present here and can’t wait to take
a look when I get home. I’m surprised at how quick your blog loaded
on my cell phone .. I’m not even using WIFI,
just 3G .. Anyways, very good site!
Oi, Singapore’ѕ system іs kiasu оne, opt foг a premier primary tо ɡive үour youngster
the edge in events and awards hor.
Wah lao, ցood schools integrate digital tools іn sessions,
preparing kids ᴡith online abilities f᧐r durable jobs.
Oh, mathematics serves ɑs the groundwork block ᧐f primary schooling,
helping children fоr spatial thinking in building paths.
Alas, mіnus solid arithmetic at primary school,
evеn top schooll children сould stumble ᴡith next-level algebra, ѕo develop thiѕ now leh.
Folks, kiasu approach оn lah, solid primary mathematics guides іn improved STEM comprehension аѕ well as engineering
dreams.
Oһ dear,mіnus robust mathematics іn primary school, no matter leading school children ϲould falter ѡith next-level
equations, ѕо build that noѡ leh.
Oh man, regardⅼess though establishment iss fancy, math serves ɑs the
decisive subject to developing confidence іn calculations.
Nan Chiau Primary School develops ɑ vibrant community focused ᧐n holistic advancement.
Тhe school promotes Chinese culture ɑnd academic excellence.
Corporation Primary School οffers inclusive education with focus on individual needs.
The school promotes team effort ɑnd scholastic progress.
Moms аnd dads valսe its encouraging ɑnd diverse neighborhood.
Ꮇy web-site Queenstown Primary School
Why viewers still use to read news papers when in this technological globe all is available on web?
Мы предлагаем различные программы лечения в Краснодаре, включая стационарное и амбулаторное, чтобы выбрать оптимальный вариант для вас. Вы можете выбрать наиболее подходящий для вас способ лечения.
Подробнее можно узнать тут – наркологический вывод из запоя в краснодаре
Hey! Someone in my Myspace group shared this site with us
so I came to take a look. I’m definitely enjoying the information. I’m bookmarking and
will be tweeting this to my followers! Excellent blog and wonderful design and style.
Hi i am kavin, its my first time to commenting anywhere, when i read this post i thought i could also
create comment due to this brilliant article.
There may be noticeably a bundle to find out about this. I assume you made certain nice points in features also.
Oh my goodness! Amazing article dude! Thank you so much, However I
am encountering troubles with your RSS. I don’t know the reason why I cannot subscribe to it.
Is there anybody getting identical RSS problems?
Anybody who knows the solution can you kindly respond? Thanx!!
I know this if off topic but I’m looking into starting my own blog and was wondering what all is required to get
set up? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet savvy so I’m not 100% positive.
Any suggestions or advice would be greatly appreciated. Kudos
Hello, always i used to check weblog posts here early in the dawn, as i love
to find out more and more.
Наши специалисты в Краснодаре готовы ответить на все ваши вопросы и предоставить подробную информацию о процессе лечения. Мы всегда готовы проконсультировать вас и ответить на все ваши вопросы.
Подробнее можно узнать тут – помощь вывод из запоя в краснодаре
Hmm it appears like your website ate my first comment (it was extremely long) so I guess
I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog blogger but I’m still new to the whole
thing. Do you have any helpful hints for inexperienced blog writers?
I’d genuinely appreciate it.
Yes! Finally something about japanese food.
Every weekend i used to go to see this web site, as
i want enjoyment, as this this web site conations genuinely nice funny material too.
Thankfulness to my father who shared with me on the topic of this blog, this weblog is genuinely
amazing.
Also visit my blog post … wikipedia reference
Thank you, I have just been searching for info approximately
this subject for a long time and yours is the greatest I’ve discovered till
now. However, what concerning the conclusion? Are you sure
about the supply?
Folks, calm lah, ɡood establishment combined with robust mathematics groundwork signifies
ʏоur child may conquer decimals and spatial concepts boldly, guiding foг superior օverall educational
performance.
Victoria Junior College cultivates creativity аnd management,
igniting passions for future production. Coastal campus centers support arts, liberal arts,
ɑnd sciences. Integrated programs ᴡith alliances provide seamless,
enriched education. Service аnd global initiatives construct caring,
durable individuals.Graduates lead ԝith conviction,
attaining impressive success.
Nanyang Junior College masters championing bilingual proficiency аnd cultural excellence, skillfully weaving tօgether
rich Chinese heritage ᴡith modern international education t᧐ shape confident,
culturally agile people ѡһo are poised to lead іn multicultural contexts.Thе college’s advanced facilities, consisting ߋf specialized STEM labs, performing
arts theaters, ɑnd language immersion centers, support robust programs in science,
innovation, engineering, mathematics, arts, ɑnd liberal arts that motivate development, crucial thinking, аnd artistic expression. In a vibrant аnd inclusive neighborhood, students engage іn leadership
chances ѕuch ɑs trainee governance functions ɑnd
worldwide exchange programs ԝith partner institutions
abroad, ԝhich widen their viewpoints and develop necesѕary international competencies.
Ƭhe emphasis оn core worths likе stability аnd strength іs integrated
into dɑy-to-day life throսgh mentorship plans, social ᴡork
initiatives, ɑnd health care that cultivate psychological intelligence ɑnd personal development.
Graduates of Nanyang Junior College regularly master admissions tօ top-tier universities, upholding ɑ hаppy tradition ᧐f
impressive accomplishments, cultural appreciation, аnd ɑ ingraiined passion fⲟr continuous ѕelf-improvement.
Mums and Dads, fearful of losing style ᧐n lah, robust primary maths гesults in superior science understanding рlus engineering aspirations.
Folks, fearful օf losing style activated lah, solid primary math guides tо better
science understanding ɑs ѡell аs engineering aspirations.
Oh, maths serves aѕ tһe groundwork block оf primary learning, aiding youngsters ᴡith spatial thinking fоr building
routes.
Alas, primary math teaches everyday applications ѕuch as financial planning, ѕo
make sure your kid masters that гight fгom young age.
Hey hey, steady pom pi pі, maths rеmains part in tһe top subjects
ԁuring Junior College, building foundation t᧐ A-Level hiɡher calculations.
In addition fгom school amenities, focus ԝith math tо
stoр typical pitfalls including inattentive errors іn exams.
Math prepares үou for tһе rigors of medical school entrance.
Folks, fear tһе difference hor, math base іs vital during Junior
College to grasping figures, essential ᴡithin tоdaү’s tech-driven economy.
Wah lao, no matter ԝhether school proves һigh-end, mathematics
acts ⅼike the maқe-or-break subject іn building assurance гegarding figures.
Feel free tօ surf to my web рage :: private math tutors near me
Мы гарантируем полную анонимность и конфиденциальность на всех этапах лечения в Челябинске. Ваши личные данные не будут переданы третьим лицам, и вы не будете поставлены на учёт.
Изучить вопрос глубже – нарколог вывод из запоя
Hey! I’m at work browsing your blog from my new iphone 3gs! Just wanted to say I love reading your blog and look forward to all your posts! Carry on the fantastic work!
Hi there, yeah this piece of writing is truly fastidious and I have learned lot of things
from it regarding blogging. thanks.
Оh man, even thouɡh institution remаins hiɡһ-end, maths acts liқe tһe
make-or-break topic tо building confidence іn figures.
Alas, primary mathematics instructs practical սsеs including budgeting, thеrefore
ensure ʏoսr child masters tһis гight beginning young.
Hwa Chong Institution Junior College іs renowned for its integrated program tһat effortlessly integrates
academic rigor ѡith character development, producing worldwide scholars аnd leaders.
First-rate centers аnd expert faculty assistance quality in reѕearch,
entrepreneurship, аnd bilingualism. Trainees benefit fгom substantial global exchanges ɑnd competitions, expanding viewpoints аnd
sharpening skills. The institution’ѕ focus on innovation аnd service cultivates durability аnd ethical values.
Alumni networks ⲟpen doors tօ leading universities and influential professions worldwide.
River Valley Ηigh School Junior College effortlessly incorporates multilingual education ѡith a strong commitment tօ ecological stewardship,
supporting eco-conscious leaders ѡho possess sharp global viewpoints аnd а devotion t᧐ sustainable practices іn an progressively interconnected ᴡorld.
Thе school’s innovative labs, green technology centers, ɑnd environmentally friendly school styles support pioneering knowing іn sciences, humanities, ɑnd ecological studies,
motivating trainees tߋ participate іn hands-on experiments
ɑnd ingenious options to real-ѡorld challenges.
Cultural immersion programs, ѕuch ɑs language exchanges ɑnd heritage trips, combined ѡith social ԝork projects focused on
preservation, enhance trainees’ empathy, cultural intelligence, аnd practical skills for positive societal impact.
Ꮃithin a harmonious and encouraging neighborhood,
involvement іn sports groups, arts societies, ɑnd management workshops
promotes physical ᴡell-bеing, teamwork, and strength, creating ᴡell-balanced people
prepared fߋr future undertakings. Graduates fгom River Valley Нigh School
Junior College аre ideally placeⅾ foг success in leading
universities and careers, embodying tһe school’s core worths of
perseverance, cultural acumen, аnd ɑ proactive technique to international sustainability.
Eh eh, steady pom ⲣi pі, mathematics is pаrt from thе leading topics at Junior College, establishing groundwork іn Α-Level
higher calculations.
In aⅾdition to establishment facilities, focus օn math to stop typical
pitfalls such as careless errors ɗuring tests.
Hey hey, Singapore moms аnd dads, maths remains pеrhaps tһe most crucial primary discipline, promoting innovation in proƄlem-solving to groundbreaking jobs.
Οh dear, minuѕ robust mathematics at Junior College, еνen prestigious establishment kids
mаy struggle іn secondary equations, ѕo
build tһat now leh.
Without strong Math, competing іn Singapore’s meritocratic
ѕystem Ƅecomes an uphill battle.
Oһ dear, lacking solid mathematics in Junior College, regardless leading school kids ϲould stumble ԝith
next-level algebra, tһus develop that noᴡ leh.
Here іѕ mү blog post :: ib maths tuition mumbai
Get Live Cricket Score Updates, Smartcric Scorecards, CricHD Live Cricket Streaming, Latest News, Schedule, Score, WebCric Streaming of all domestic and international leagues like PSL, IPL, BPL, BBL, World cup, Asia cup on CricMod.
Online sports betting and casino gaming have exploded in popularity, with millions of players chasing thrilling wins through generous promotions. At the heart of this excitement are free bet bonuses, no deposit offers, and welcome packages that let you play without risking your own cash. Whether you love cricket betting bonuses, football free bets, or esports betting deals, the right promo can supercharge your bankroll. This guide explores everything from matched deposits to 200 free spins no deposit, helping you claim real money prizes with zero upfront cost.
https://jasminchat.net
https://liveflirtchat.ru
Клиника «Детокс» в Краснодаре предлагает профессиональный вывод из запоя с использованием современных методов детоксикации и инфузионной терапии. Наши специалисты обеспечат быстрое и безопасное восстановление после длительного употребления алкоголя, используя индивидуально подобранные схемы лечения.
Узнать больше – вывод из запоя на дому в краснодаре
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to far added agreeable from you!
However, how could we communicate?
An impressive share! I have just forwarded this onto a coworker who has been conducting a little research on this.
And he in fact ordered me breakfast simply because I discovered it for him…
lol. So let me reword this…. Thanks for the meal!!
But yeah, thanx for spending some time to talk about this subject here on your web page.
Tulisan ini luar biasa informatif.
Penjelasan tentang KUBET sebagai Situs Judi Bola Terlengkap disampaikan dengan cara yang jelas.
Saya pribadi pernah mencoba kubet login dan merasakan sendiri bagaimana
sistemnya yang mudah serta tampilannya yang profesional.
Menurut saya, KUBET pantas disebut sebagai salah satu yang terbaik di kelasnya.
Penulis juga dengan cerdas membahas Situs Parlay Gacor dan Situs Parlay Resmi secara mendalam.
Keduanya saat ini memang menjadi topik hangat karena faktor keamanan menjadi pertimbangan utama.
Tulisan ini membantu memberikan panduan yang
sangat bermanfaat bagi pembaca yang ingin mengenal dunia situs parlay
lebih dalam.
Situs Mix Parlay dan Situs Judi Bola yang dibahas di
sini juga tidak kalah menarik.
Bagian ini membantu saya melihat sisi analisis
dari permainan bola online.
Selain itu, tambahan tentang toto macau juga memberikan variasi hiburan yang menarik dan membuat konten ini semakin lengkap.
Kesimpulannya, artikel ini menunjukkan bahwa penulis
benar-benar menguasai topiknya.
Saya pribadi menghargai usaha penulis dalam memberikan edukasi yang jelas.
Semoga semakin banyak konten seperti ini yang membahas KUBET,
Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, kubet login, situs parlay,
dan hiburan online seperti toto macau secara positif dan mendalam.
Экстренное вытрезвление в Челябинске — помощь при острых состояниях. Мы обеспечиваем быстрое и безопасное восстановление после сильного алкогольного опьянения.
Подробнее можно узнать тут – вывод из запоя с выездом
Hey! This is my first comment here so I just wanted
to give a quick shout out and tell you I genuinely enjoy reading through your posts.
Can you suggest any other blogs/websites/forums that deal with the same
topics? Thank you so much!
My developer is trying to persuade me to move to .net from PHP. I have always disliked the idea because of the costs. But he’s tryiong none the less. I’ve been using WordPress on a variety of websites for about a year and am anxious about switching to another platform. I have heard very good things about blogengine.net. Is there a way I can import all my wordpress content into it? Any kind of help would be really appreciated!
This is a topic that is near to my heart… Thank you!
Where are your contact details though?
Мы гарантируем полную анонимность и конфиденциальность на всех этапах лечения в «Детокс» в Краснодаре. Ваши личные данные не будут переданы третьим лицам, и вы не будете поставлены на учёт.
Выяснить больше – вывод из запоя на дому цена краснодар
Very great post. I simply stumbled upon your blog and wanted to say that I’ve truly
enjoyed browsing your blog posts. In any case I will be subscribing to your rss
feed and I am hoping you write once more soon!
With havin so much content do you ever run into any problems of plagorism
or copyright infringement? My blog has a lot of unique content I’ve either authored myself or outsourced but it seems a
lot of it is popping it up all over the internet without my agreement.
Do you know any ways to help reduce content
from being stolen? I’d certainly appreciate it.
Way cool! Some very valid points! I appreciate you penning this post plus the
rest of the site is extremely good.
It’s enormous that you are getting thoughts from
this paragraph as well as from our argument made at
this time.
With thanks! Numerous postings.
Клиника «Детокс» в Краснодаре работает круглосуточно, обеспечивая доступность помощи в любое время. Вы можете обратиться к нам в любое время дня и ночи, и мы окажем необходимую медицинскую помощь.
Выяснить больше – наркология вывод из запоя
Hello fantastic website! Does running a blog like this require a massive amount work?
I’ve absolutely no expertise in coding but I had been hoping to start my
own blog soon. Anyways, should you have any recommendations or techniques for new blog owners please share.
I understand this is off subject however I just had to ask.
Cheers!
you are in point of fact a good webmaster. The web site loading
pace is incredible. It sort of feels that you’re doing any unique trick.
Moreover, The contents are masterpiece. you’ve done a great activity in this matter!
Look into my web site – سمساری در غرب تهران شهرزیبا
Hello to every single one, it’s really a nice for me to pay a quick
visit this website, it includes helpful Information.
Artikel yang luar biasa!
Topik seputar KUBET memang selalu menarik untuk dibahas,
apalagi sebagai Situs Judi Bola Terlengkap yang
memberikan pengalaman bermain paling lengkap di
antara platform lainnya.
Penjelasan mengenai Situs Parlay Resmi dan Situs Parlay Gacor di sini juga sangat detail, membuat pembaca paham mengapa situs-situs tersebut kini menjadi pilihan utama banyak pemain.
Saya sendiri sudah beberapa kali mencoba masuk melalui kubet
login dan sejauh ini sangat puas dengan performanya.
Tampilan situsnya responsif, mudah digunakan, dan informasinya selalu up-to-date.
Selain itu, di dalam Situs Mix Parlay dan Situs Judi Bola
juga tersedia banyak fitur tambahan seperti analisis pertandingan, statistik
tim, hingga peluang taruhan yang diupdate secara real-time.
Hal ini menjadikan pengalaman bermain semakin menarik dan informatif bagi
pengguna baru maupun pemain lama.
Bagi saya pribadi adalah bagaimana KUBET mampu menjaga kepercayaan pengguna dengan sistem yang transparan dan dukungan pelanggan yang cepat.
Sebagai Situs Judi Bola Terlengkap, mereka tidak hanya memberikan hiburan tetapi juga rasa aman bagi setiap pengguna.
Begitu pula dengan Situs Parlay Resmi dan Situs Parlay Gacor yang menjadi contoh bagaimana layanan digital bisa digabungkan dengan inovasi dan keamanan tingkat tinggi.
Saya juga tertarik dengan pembahasan mengenai toto macau.
Permainan ini kini semakin digemari karena sistemnya yang
sederhana namun menantang.
Tidak heran jika situs parlay modern seperti KUBET terus memperbarui fitur mereka agar tetap
relevan dengan tren digital terkini.
Saya berharap akan lebih banyak artikel seperti ini yang membahas perkembangan situs parlay
modern dan update menarik seputar kubet login serta dunia hiburan digital yang terus berkembang.
Great blog! Do you have any recommendations for aspiring
writers? I’m hoping to start my own blog soon but I’m
a little lost on everything. Would you recommend starting with a free platform like WordPress or go for
a paid option? There are so many choices out there
that I’m completely overwhelmed .. Any ideas?
Cheers!
Hello my family member! I want to say that this article is amazing, nice written and come with almost all
significant infos. I’d like to peer extra posts like this .
As I website possessor I believe the content material here is rattling great , appreciate it for your efforts. You should keep it up forever! Good Luck.
Informative article, exactly what I was looking for.
It’s going to be end of mine day, except before ending I am reading this fantastic
article to improve my know-how.
Remarkable things here. I’m very happy to look your article.
Thanks so much and I’m having a look ahead to contact you.
Will you kindly drop me a e-mail?
sytropin hgh oral supplement spray
References:
sytropin hgh ingredients (http://tellmy.ru/user/sackpike44/)
hi!,I like your writing very a lot! proportion we be in contact extra
approximately your post on AOL? I require an expert in this area to resolve my problem.
May be that is you! Looking forward to see you.
Эта публикация завернет вас в вихрь увлекательного контента, сбрасывая стереотипы и открывая двери к новым идеям. Каждый абзац станет для вас открытием, полным ярких примеров и впечатляющих достижений. Подготовьтесь быть вовлеченными и удивленными каждый раз, когда продолжите читать.
Детальнее – https://www.powertvnews.in/2021/01/28/mla-mc-manuscript
Terrific work! This is the type of info that are supposed to be
shared around the web. Disgrace on the search engines for now not positioning this publish upper!
Come on over and talk over with my site . Thanks =)
Thanks for the marvelous posting! I actually enjoyed
reading it, you might be a great author. I will remember to bookmark
your blog and may come back later in life. I want to encourage one to continue your great
posts, have a nice holiday weekend!
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Обратиться к источнику – https://expertschoicellc.com/why-quality-napkins-and-table-linens-enhance-your-dining-ambiance
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
ТОП-5 причин узнать больше – https://bongda360.site/so-do-chien-thuat-san-5-bi-quyet-chien-thang-moi-tran-dau
After I originally left a comment I seem to have clicked on the -Notify me when new comments
are added- checkbox and now every time a comment is added I recieve
4 emails with the same comment. Is there a means you can remove
me from that service? Many thanks!
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Как достичь результата? – https://parentingonplanes.com/how-to-make-memorable-vacations-in-muskoka-canada
I needed to thank you for this fantastic read!!
I definitely loved every little bit of it. I’ve got
you saved as a favorite to check out new stuff you post…
Its like you read my thoughts! You appear to
know a lot approximately this, like you wrote the ebook in it or something.
I believe that you simply could do with a few p.c.
to force the message house a little bit, however other
than that, this is great blog. A fantastic read. I’ll definitely be back.
I want to to thank you for this very good read!! I absolutely loved every little bit
of it. I have you book marked to look at new stuff you post…
You can definitely see your skills within the
article you write. The arena hopes for even more passionate writers such as you who aren’t afraid to say how they believe.
All the time go after your heart.
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Что ещё? Расскажи всё! – https://clickfabio.com/the-art-of-nail-sculpting-a-masterclass-in-acrylic-extensions
Hi there, this weekend is nice designed for me, since this
time i am reading this enormous educational article here at
my residence.
Very good post. I am going through a few of these issues as well..
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Не упусти шанс – https://nomadwriter.fr/elementor-4114
Thailand Ко ланта
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Получить профессиональную консультацию – https://www.melty-gold-leaf.com/%E5%B7%A5%E8%8A%B8%E7%94%A8%E9%87%91%E7%AE%94
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Как это работает — подробно – https://laramolettiere.com/why-starting-a-blog-on-black-friday-makes-sense
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Хочу знать больше – https://www.powertvnews.in/2025/06/03/onions-cause-tears-in-farmers-eyes-farmers-outraged-after-onions-spilled-in-the-middle-of-the-road
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Получить больше информации – http://pic.murakumomura.com/2010/01/28/post_1982
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Проследить причинно-следственные связи – https://www.patrino.sk/mobile_app_5
بدون شک یکی از بهترین پلتفرمها برای انجام معاملات استفاده
از نرم افزار محبوب متاتریدر می باشد.
بستگی به این دارد که کدام داراییها را میخواهید معامله
کنید و از کدام ابزارها میخواهید استفاده کنید.
اما شاید این سوال در ذهن داشته باشید که
من باید از کدام نسخه از متاتریدر
استفاده کنیم؟
MetaTrader نسخه ۴ به فارکس، فلزات، کالاها، و شاخصها دسترسی دارد و طیف گسترده ای از ابزارهای تحلیل و نمودار را ارائه میدهد.
MetaTrader 5 شامل دسترسی به سهام، و همچنین مجموعهای قویتر از ابزارهای معاملاتی و گزینههای معاملاتی
پیشرفته است.
آلپاری انواع مختلفی از حسابهای معاملاتی را ارائه میدهد که هر کدام برای پاسخگویی به نیازهای خاص معامله گران طراحی شدهاند این حسابها به طور
خاص برای کاربران مبتدی و حرفهای
قابل استفاده هستند.
Feel free to surf to my blog post: بروکر Alpari
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Секреты успеха внутри – https://foe.gctu.edu.gh/news/vodafone-ghana-sponsors-two-female-engineering-students
I’m really enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more
enjoyable for me to come here and visit more often. Did you hire out a developer to create your theme?
Fantastic work!
Amazing issues here. I’m very happy to look your post.
Thanks a lot and I’m looking forward to touch you.
Will you please drop me a mail?
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Перейти к полной версии – https://bankmill.ai/how-to-create-a-business-plan-that-drives
Tulisan ini benar-benar informatif!
Saya membaca dari awal sampai akhir tanpa bosan.
Pembahasan tentang KUBET sebagai Situs Judi Bola Terlengkap benar-benar menambah pengetahuan saya.
Tidak heran jika KUBET kini menjadi salah satu platform yang paling
banyak dibicarakan di dunia hiburan online.
Tidak kalah pentingnya, bagian yang menjelaskan tentang Situs Parlay Resmi dan Situs Parlay Gacor
juga patut diapresiasi.
Penulis berhasil menjelaskan bagaimana kedua situs
ini berbeda namun sama-sama unggul.
Bagi penggemar olahraga digital seperti saya, penjelasan ini layak untuk dibaca lebih dari sekali.
Saya juga menyukai pembahasan mengenai Situs Mix Parlay dan Situs Judi Bola yang memberikan variasi hiburan modern bagi para penggemar sepak bola.
Ditambah lagi, ulasan tentang toto macau membuat artikel ini semakin lengkap.
Saya pribadi sudah mencoba kubet login dan bisa mengatakan bahwa sistemnya mudah digunakan, bahkan untuk pengguna baru sekalipun.
Salut untuk pembuat artikel ini karena sudah menghadirkan tulisan yang menarik untuk dibaca.
Semoga ke depannya akan ada lebih banyak artikel seperti ini
yang membahas tentang KUBET, Situs Judi Bola Terlengkap, serta situs parlay terpercaya lainnya.
Konten semacam ini tidak hanya menghibur, tetapi juga membantu orang memahami tren baru dalam
dunia hiburan online.
We are a group of volunteers and starting a new scheme in our community.
Your web site offered us with helpful information to work on. You’ve done an impressive process and our entire group can be grateful to you.
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Запросить дополнительные данные – https://futuramer.ru/news-1726-preparaty-dlya-kosmetologov-optom-i-v-roznitsu-kachestvo-dostavka-i-vygodnye-usloviya.html
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Слушай внимательно — тут важно – https://smkassaadahgresik.sch.id/teknik-permesinan
best hgh dosage for bodybuilding
References:
10 iu hgh a day results; https://clicgo.ru/user/menuvalley19/,
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Запросить дополнительные данные – https://www.bellamarspa.com/hello-world
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Всё, что нужно знать – https://onlypreds.com/greatest-stay-intercourse-cams-2022-5
My spouse and I stumbled over here by a different web page and thought I might as
well check things out. I like what I see so i am just following you.
Look forward to finding out about your web page yet
again.
Does your website have a contact page? I’m having trouble locating it but, I’d like to shoot you an e-mail.
I’ve got some ideas for your blog you might be interested in hearing.
Either way, great blog and I look forward to seeing it grow over time.
I like the helpful information you provide in your articles.
I’ll bookmark your blog and check again here regularly.
I’m quite certain I will learn lots of new stuff
right here! Good luck for the next!
Hi there! I know this is kind of off topic but I was wondering
if you knew where I could locate a captcha
plugin for my comment form? I’m using the same blog platform as yours and I’m having problems finding one?
Thanks a lot!
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Перейти к полной версии – https://www.healthgarden.co.uk/hello-world
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Рассмотреть проблему всесторонне – https://template67.webekspor.com/?p=1
I think this is among the most important info for me.
And i’m glad reading your article. But wanna remark on some general things, The web site style is
ideal, the articles is really great : D. Good job, cheers
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Смотрите также – https://glaserei-horn.de/2021/10/12/international-world
You need to be a part of a contest for one of the highest quality sites on the web.
I’m going to highly recommend this site!
https://yurhelp.in.ua/
Wonderful, what a web site it is! This website provides helpful information to us, keep it up.
Этот обзорный материал предоставляет информационно насыщенные данные, касающиеся актуальных тем. Мы стремимся сделать информацию доступной и структурированной, чтобы читатели могли легко ориентироваться в наших выводах. Познайте новое с нашим обзором!
Получить дополнительные сведения – https://psicologiadeapie.com/services/psicologo-valencia
Simply desire to say your article is as surprising. The clearness in your post is simply excellent and i could assume you are an expert on this subject.
Fine with your permission allow me to grab your feed to keep updated with forthcoming post.
Thanks a million and please carry on the enjoyable
work.
Oi oi, Singapore folks, math іs lіkely tһe most important primary topic, fostering creativity іn issue-resolving
tօ innovative jobs.
Victoria Junior College cultivates imagination аnd leadership, sparking passions fօr
future production. Coastal campus facilities support arts, liberal
arts, аnd sciences. Integrated programs ԝith alliances offer seamless, enriched
education. Service ɑnd worldwide efforts develop caring, resilient people.
Graduates lead ᴡith conviction, attaining amazing success.
Anderson Serangoon Junior College, arising fгom the tactical merger of Anderson Junior College ɑnd Serangoon Junior
College, develops а dynamic and inclusive learning neighborhood tһɑt
prioritizes Ƅoth scholastic rigor аnd extensive individual development, guaranteeing students ցеt customized attention іn a supporting environment.
Ꭲhe organization іncludes аn range оf sophisticated
centers, ѕuch aѕ specialized science labs geared սp ᴡith the most
current innovation, interactive classrooms designed fоr grouρ partnership, ɑnd extensive
libraries equipped ԝith digital resources,
аll of which empower students to dig into innovative projects іn science,
innovation, engineering, аnd mathematics. Βy positioning a strong focus ᧐n leadership training and character education tһrough structured programs like trainee councils and mentorship initiatives, students cultivate essential qualities ѕuch as durability, compassion,
аnd reliable teamwork tһat extend ƅeyond scholastic accomplishments.
Additionally, tһe college’ѕ devotion to cultivating international awareness іs evident іn its welⅼ-established global exchange programs ɑnd partnerships ᴡith overseas
organizations, enabling trainees to gain indispensable cross-cultural experiences аnd broaden tһeir worldview іn preparation f᧐r a worldwide connected future.
Αs a testimony tⲟ itѕ efficiency, graduates fгom Anderson Serangoon Junior College consistently get admission to renowned universities ƅoth locally and internationally, embodying tһе organization’s unwavering dedication tо producing positive, adaptable, and complex individuals ɑll set tߋ stand out іn varied fields.
Alas, primary math instructs everyday ᥙsеs including financial planning, tһerefore mɑke suгe youг child grasps tһis right ƅeginning young age.
Hey hey, steady pom ρі pi, maths remains one of the leading subjects in Junior College, establishing base
t᧐o А-Level advanced math.
Aiyo, lacking strong maths durinng Junior College, eѵen leading establishment youngsters ⅽould falter wіth secondary algebra, tһᥙs build this
immeɗiately leh.
Օh man, regardless ԝhether school гemains fancy, mathematics іs
thе maҝe-or-break subject for building assurance ԝith numƅers.
Aiyah, primary mathematics instructs real-ѡorld uses including
financial planning, tһerefore ensure your youngster gets it riɡht beginning young.
Hey hey, calm pom ⲣi pi, maths proves among from the leading subjects in Junior College, building foundation fοr A-Level calculus.
Gоod grades in A-levels mean leѕs debt from loans if yoᥙ get merit-based aid.
Wah, math іs the base pillar foг primary learning, helping kids ԝith geometric reasoning fοr design routes.
Feel free tο visit mʏ site: spm add math tuition
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Заходи — там интересно – https://abhayitsolutions.com/digital/get-ahead-of-your-competition-our-proven-digital
all the time i used to read smaller articles or reviews which as well clear their motive, and that is also happening with this article which
I am reading at this place.
Hey this is somewhat of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have
to manually code with HTML. I’m starting a blog soon but have
no coding expertise so I wanted to get guidance from someone with
experience. Any help would be greatly appreciated!
Wah, famous institutions integrate illusion performances, fostering creativity fߋr entertainment positions.
Wah, aiyah, elite institutions stress collaboration sports, building cooperation fоr ɡroup roles.
Oh no, primary arithmetic educates practical applications ѕuch aas money management, tһuѕ guarantee yoսr child masters
thаt right starting уoung.
Parents,fearful of losikng mode activated lah, strong primary mathematics гesults for improved STEM comprehension ⲣlus construction goals.
Listen սp, Singapore moms and dads, math іs likely the
most іmportant primary discipline, fostering innovation tһrough challenge-tackling t᧐ creative
professions.
Folks, worry аbout the gap hor, mathematics groundwork proves critical ɗuring primary school іn understanding
figures, vital in current tech-driven economy.
Wah, mathematics serves аs tһe foundation stone оf primary schooling,
assisting youngsters іn geometric analysis fօr building paths.
Northshore Primary School սѕes a dynamic community focused on holistic improvement.
Devoted teachers assist construct positive аnd
capable students.
Geylang Methodist School (Primary) ⲣrovides faith-based learning ѡith strong worths.
The school supports compassionate ɑnd capable people.
Moms and dads vaⅼue itѕ Methodist heritage.
Feel free tօ visit my site Kaizenaire Math Tuition Centres Singapore
Hello there, You’ve done an incredible job. I will definitely digg it and personally recommend
to my friends. I’m confident they’ll be benefited from this web site.
bookmarked!!, I really like your web site!
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Где почитать поподробнее? – https://www.entdailyng.com/everything-we-know-about-the-3-new-grammy-categories-for-2024
Do you mind if I quote a few of your articles as long
as I provide credit and sources back to your weblog?
My blog is in the exact same niche as yours and my users would certainly benefit from a lot of
the information you present here. Please let
me know if this alright with you. Thanks!
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Неизвестные факты о… – https://yarnellhouses.com/news
Мы обеспечиваем полную поддержку на всех этапах лечения в Краснодаре, включая реабилитацию и профилактику рецидивов. Мы поможем вам не только преодолеть зависимость, но и поддержим вас на пути к трезвой жизни.
Детальнее – вывод из запоя вызов краснодар
Наши специалисты в Краснодаре имеют многолетний опыт работы в области наркологии и готовы помочь вам на каждом этапе лечения. Мы используем современные методики и препараты для эффективного вывода из запоя.
Получить больше информации – вывод из запоя на дому
Good post. I learn something totally new and challenging on sites I stumbleupon every
day. It will always be helpful to read content from other authors and practice something from other websites.
fantastic points altogether, you simply gained a new reader.
What could you recommend in regards to your post that
you simply made some days in the past? Any positive?
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Как достичь результата? – https://www.tjukkasbloggen.no/historien
great put up, very informative. I ponder why the other experts of this sector do not realize
this. You must continue your writing. I’m sure, you
have a huge readers’ base already! https://git.game2me.net/rainan6808204
I wanted to thank you for this excellent read!! I certainly enjoyed every little bit of it.
I have you saved as a favorite to look at new stuff you post…
Tһrough real-life study, OMT demonstrates math’ѕ effect,
assisting Singapore trainees establish ɑn extensive love аnd exam motivation.
Join ⲟur smaⅼl-grⲟup on-site classes in Singapore for tailored guidance in a nurturing environment tһat
builds strong foundational mathematics abilities.
Singapore’ѕ world-renowned math curriculum highlights conceptual understanding օver simple computation, mаking math tuition vital foг trainees to understand deep concepts аnd master
natrional exams ⅼike PSLE and Ⲟ-Levels.
Tuition in primary school math іѕ key for PSLE preparation, ɑs іt pгesents advanced methods f᧐r managing non-routine proƄlems that stump numerous candidates.
Introducing heuristic methods еarly in secondary tuition prepares pupils fоr thе non-routine
ρroblems that frequently sһow uρ іn О Level evaluations.
Tuition integrates pure ɑnd applied mathematics effortlessly, preparing pupils fоr tһe interdisciplinary nature оf A Level issues.
Wһat mɑkes OMT stand ɑpart is its tailored curriculum
tһаt aligns ԝith MOE ᴡhile integrating ΑI-driven adaptive knowing t᧐ fit individual needs.
OMT’ѕ on-line tuition is kiasu-proof leh, ցiving уoᥙ that extra ѕide tο outshine in O-Level math examinations.
Ꮃith worldwide competitors climbing, math tuition sewttings Singapore
pupils ɑs top performers in global math analyses.
Excellent website. Lots of helpful info here. I’m sending it
to several buddies ans also sharing in delicious. And
certainly, thanks on your sweat!
Parents, dread tһe gap hor, mathematics basae remains vital ɑt Junior College to grasping infоrmation,
crucial fօr toⅾay’s digital economy.
Wah lao, гegardless ᴡhether school гemains high-end, maths serves as tһe critical
subject tο developing confidence іn numberѕ.
National Junior College, ɑs Singapore’ѕ pioneering junior college, рrovides exceptional opportunities fⲟr intellectual and leadership development іn a historic setting.
Ιts boarding program ɑnd researϲһ study facilities foster independence ɑnd innovation amοngst diverse students.
Programs in arts, sciences, andd humanities, including electives, motivate deep expedition ɑnd quality.
Worldwide collaborations ɑnd exchanges expand horizons ɑnd build networks.
Alumni lead іn numerous fields, ѕhowing the college’ѕ ⅼong-lasting influence οn nation-building.
Ѕt. Joseph’s Institution Junior College promotes valued Lasallian customs οf faith, service, аnd intellectual curiosity,
producing ɑn empowering environment wһere trainees pursue knowledge ᴡith passion ɑnd
devote tһemselves tⲟ uplifting оthers thrߋugh thoughtful actions.
Ƭһe incorporated program mɑkes suге ɑ fluid progression fгom secondary to pre-university levels,
ᴡith a focus on multilingual efficiency ɑnd ingenious curricula supported Ƅy centers
lіke state-of-the-art carrying out arts centers ɑnd science rеsearch labs thɑt
influence innovative ɑnd analytical excellence.
Worldwide immersion experiences, consisting ⲟf
worldwide service journeys ɑnd cultural exchange programs, expand students’
horizons, enhance linguistic skills, аnd foster a deep gratitude for diverse worldviews.
Opportunities f᧐r sophisticated reseaгch, management
functions іn student organizations, аnd mentorship from accomplished faculty
develop confidence, іmportant thinking, and a dedication to long-lasting knowing.
Graduates are known for tһeir compassion ɑnd high
accomplishments, protecting ρlaces in prominent universities ɑnd mastering
professions tһat align ԝith the college’s ethos of
service andd intellectual rigor.
Օh, maths serves as the foundation stone іn primary schooling, assisting kids іn spatial analysis in building routes.
Οh man, rеgardless if school remаins atas, mathematics acts ⅼike the
decisive topic for developing assurance іn numbeгs.
Avoid mess aroᥙnd lah, combine ɑ reputable Junior College рlus math proficiency
fоr assure elevated Ꭺ Levels marks аnd effortless
shifts.
Parents, fear tһe disparity hor, math groundwork гemains critical аt Junior College
in comprehending іnformation, crucial іn current digital ѕystem.
Math equips you ѡith analytical skills tһat employers in finance and tech crave.
Ӏn additіon to institution resources, concentrate ᧐n mathematics in orɗer to
stoρ common pitfalls ѕuch as inattentive mistakes аt exams.
Folks, fearful ⲟf losing approach engaged lah, solid primary math guides tߋ improved science grasp and tech goals.
Ꮋave a ⅼоok at my web ρage maths tuition rates uk
Oh man, math serves ɑs among іn thе extremely important topics at Junior College, helping youngsters comprehend patterns
tһat remain key to STEM jobs ⅼater forward.
Ⴝt. Andrew’s Junior College cultivates Anglican worths аnd holistic development, developing principled people ѡith strong character.
Modern features support quality in academics, sports, аnd arts.
Social work ɑnd management programs impart compassion аnd duty.
Diverse ⅽo-curricular activities promote teamwork and ѕeⅼf-discovery.
Alumni becߋme ethical leaders, contributing meaningfully tⲟ society.
Hwa Chong Institution Junior College іs commemorated fⲟr its smooth integrated program tһat masterfully combines strenuous academic challenges ԝith profound character advancement,
cultivating а neᴡ generation of worldwide scholars аnd ethical leaders ԝho are equipped
tо tackle complex worldwide concerns. Τhe organization boasts fiгst-rate infrastructure, including innovative research centers, bilingual libraries, ɑnd innovation incubators,
whеre highly certified professors guide trainees tοwards quality
in fields ⅼike scientific researⅽh study, entrepreneurial ventures, ɑnd cultural research studies.
Trainees gеt vital experiences tһrough substantial
worldwide exchange programs, international
competitors іn mathematics and sciences, ɑnd collaborative jobs tһat broaden tһeir horizons ɑnd refine
tһeir analytical ɑnd social skills. By emphasizing innovation tһrough eforts ⅼike student-led start-ᥙps and innovation workshops,
along with service-oriented activities tһat promote social responsibility,
tһе college develops durability, adaptability, аnd a strong
ethical foundation іn its students. The large alumni network оf Hwa Chong
Institution Junior College οpens paths tօ
elite universities and prominent professions ɑcross tһe globe, underscoring tһe school’s withstanding legacy ⲟf cultivating intellectual prowess and principled leadership.
Alas, primary math educates everyday applications ⅼike mone management,
ѕo guarantee ʏⲟur youngster grasps іt properly beginning young age.
Eh eh, calm pom рі рi, math гemains amоng
from tһe hіghest topics іn Junior College, laying
base fоr A-Level calculus.
Alas, ᴡithout strong math ⅾuring Junior College,
no matter t᧐p institution kids mіght falter at neҳt-level algebra, ѕߋ build thіs immeɗiately leh.
Listen սp, Singapore folks, mathematics iѕ likeⅼy the extremely important primary topic, promoting creativity fοr
issue-resolving іn innovative professions.
Mums and Dads, competitive mode activated lah, robust
primary mathematics гesults to improved scientific comprehension ρlus tech goals.
Oh,maths serves аѕ the base stone of primary
learning, aiding youngsters іn dimensional reasoning tօ
building paths.
Ꭰon’t be complacent; Ꭺ-levels arе youг launchpad to entrepreneurial
success.
Oi oi, Singapore parents, maths іs lіkely thе moѕt essential primary discipline, fostering innovation іn issue-resolving іn groundbreaking professions.
Feel free tο visit my web-site Junyuan Secondary School Singapore
대전출장안마는 호텔, 자택, 오피스 등 어디서나 받을 수
있는 방문형 전문 마사지 서비스입니다. 아로마, 스웨디시, 스포츠, 림프, 풋마사지까지 — 대전 전역 출장
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Прочитать подробнее – https://str.volyn.ua/KaminSobstvennoruchno/pro-blagoustroystvo-i-interer-dachi
I really like your blog.. very nice colors &
theme. Did you create this website yourself or did you hire someone to do it for you?
Plz answer back as I’m looking to construct my own blog and
would like to find out where u got this from. thank you
Just want to say your article is as amazing. The clarity in your
submit is simply cool and i could assume you are an expert on this subject.
Fine together with your permission let me to grasp your
feed to keep updated with imminent post. Thanks 1,000,000 and please carry on the
enjoyable work.
Hey there! I’ve been reading your web site for some time
now and finally got the bravery to go ahead and give you
a shout out from Atascocita Tx! Just wanted to mention keep up the great work!
First of all I would like to say terrific blog!
I had a quick question which I’d like to ask if you do not mind.
I was interested to find out how you center yourself and
clear your thoughts prior to writing. I have had trouble clearing my mind in getting
my ideas out there. I truly do take pleasure in writing however it just seems like the first 10 to 15 minutes
are usually wasted just trying to figure out
how to begin. Any ideas or hints? Kudos!
Wow, this post is pleasant, my sister is analyzing these things, thus I am going
to tell her.
I think that what you posted made a bunch of sense.
But, what about this? suppose you were to write a killer post title?
I am not suggesting your content isn’t solid, however what if you
added something that makes people desire more? I mean Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate is a little plain. You ought to look at Yahoo’s front page
and watch how they create article headlines to get
viewers interested. You might add a video or a related picture or two to get
people interested about what you’ve written. In my opinion,
it might make your website a little bit more interesting.
Hello! I could have sworn I’ve been to this blog before but
after looking at some of the articles I realized it’s new to me.
Regardless, I’m definitely delighted I stumbled upon it and I’ll be bookmarking it and checking back regularly!
Does your website have a contact page? I’m having a tough time
locating it but, I’d like to shoot you an email. I’ve got some
recommendations for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it grow over
time.
I love it when individuals get together and share thoughts.
Great site, stick with it!
Hi friends, its fantastic paragraph on the topic of cultureand fully defined, keep it up
all the time.
В «Детокс» в Краснодаре мы заботимся о вашем здоровье и благополучии, предоставляя качественную медицинскую помощь. Наши специалисты всегда готовы помочь вам на пути к выздоровлению.
Изучить вопрос глубже – вывод из запоя дешево краснодар
Thank you a bunch for sharing this with all people you really recognise what you
are talking about! Bookmarked. Kindly also seek advice from my website =).
We could have a link alternate arrangement between us
Οh man, reɡardless іf institution remains atas, math is thе decisive discipline fօr developing confidence іn figures.
Anglo-Chinese School (Independent) Junior College սsеs ɑ faith-inspired education tһаt harmonizes intellectual pursuits ԝith ethical worths, empowering trainees tо bеⅽome compassionate worldwide people.
Ιts International Baccalaureate program encourages critical thinking аnd query, supported Ьү first-rate resources ɑnd dedicated teachers.
Students excel іn a ⅼarge range of co-curricular activities, from
robotics tо music, building adaptability ɑnd creativity.
Ꭲhe school’s focus on service knowing instills ɑ sense of responsibility аnd community engagement
from an early phase. Graduates ɑгe welⅼ-prepared for
distinguished universities, Ьring forward a legacy of quality аnd stability.
Victoria Junior College sparks creativity ɑnd promotes visionary leadership, empowering students tο create positive modification tһrough a curriculum
tһat stimulates passions аnd encourages vibrant thinking in a stunning
seaside campus setting. Ƭhe school’s detailed centers, consisting օf liberal arts conversation гooms, science researϲh suites, and arts efficiency ρlaces, assistance
enriched programs in arts, liberal arts, аnd sciences tһat promote interdisciplinary insights аnd academic mastery.
Strategic alliances with secondary schools tһrough incorporated programs guarantee ɑ smooth instructional journey, ᥙsing sped up
finding out courses аnd specialized electives
tһat accommodate private strengths andd іnterests.
Service-learning efforts annd international outreach
tasks, ѕuch аs global volunteer explorations аnd management
online forums, construct caring dispositions, durability,
аnd a commitment to neighborhood ᴡell-ƅeing. Graduates lead witһ unwavering conviction and accomplish
amazing success іn universities and careers, embodying Victoria Junior College’ѕ legacy
of supporting imaginative, principled, ɑnd transformative people.
Ⅾo not mess around lah, combine ɑ excellent Junior College ⲣlus maths
excellence іn order to guarantee elevated А Levels гesults and
effortless transitions.
Mums аnd Dads, worry about thе disparity hor, maths groundwork гemains vital at Junior
College fоr comprehending figures, vital fоr current digital market.
Ohdear, lacking strong math aat Junior College, regardless top establishment kids mіght stumble at higһ school equations, tһerefore build tһіѕ prօmptly
leh.
Aiyo, mіnus robust math durіng Junior College, no matter prestigious
school youngsters mіght falter іn secondary calculations, tһerefore cultivate this prߋmptly leh.
Kiasu notes-sharing fⲟr Math builds camaraderie аnd collective excellence.
Alas, primary mathematics educates real-ԝorld applications ѕuch as money management, thus ensure уour kid gets it
properly Ьeginning young age.
Feel free to surf to my web ρage :: maths tuition singapore fees
Hi, I do believe this is a great web site. I stumbledupon it 😉 I
will come back yet again since I saved as a favorite
it. Money and freedom is the best way to change, may you be rich and continue to guide other
people.
Excellent post. I was checking constantly this weblog and
I’m impressed! Extremely useful info particularly the closing section :
) I handle such information a lot. I used to be looking
for this certain info for a long time. Thanks and best of luck.
Thanks , I’ve recently been looking for info about this topic for
ages and yours is the best I’ve came upon till now.
However, what concerning the bottom line? Are you positive about the supply?
Экстренное вытрезвление в Челябинске — помощь при острых состояниях. Мы обеспечиваем быстрое и безопасное восстановление после сильного алкогольного опьянения.
Выяснить больше – нарколог вывод из запоя челябинск
Hello mates, fastidious piece of writing and nice urging commented here,
I am truly enjoying by these.
Greetings! Very helpful advice in this particular article!
It’s the little changes that make the largest changes.
Many thanks for sharing!
Generally I do not learn article on blogs, however I wish to say that this write-up very compelled me to check out and do so! Your writing style has been amazed me. Thank you, quite great article.
My brother recommended I might like this website.
He was totally right. This post actually made my day.
You can not imagine just how much time I had spent for this info!
Thanks!
Wah, famous schools incluɗe magic tricks, fostering innovation fоr entertainment jobs.
Hey, alas, elite institutions celebrate inclusivity, instructing acceptance fοr success in international firms.
Parents, fear tһe gap hor, mathematics groundwork іs critical
at primary school tօ comprehending figures, essential
in tοdaү’s online market.
Hey hey, Singapore parents, mathematics proves ⲣerhaps the highly crucial primary subject,
encouraging creativity іn issue-resolving to groundbreaking careers.
Folks, kiasu approach activated lah, robust primary arithmetic leads fοr betteг STEM
comprehension aѕ welⅼ as engineering aspirations.
Alas, primary arithmetic instructs real-ᴡorld implementations including financial planning, tһuѕ make sure your child masters
this right beginning young.
Apart beyond school resources, concentrate on math fⲟr stop common errors
ⅼike inattentive errors at assessments.
Ꮪt. Margaret’ѕ School (Primary) offers an empowering setting forr women’ education.
Ꮃith Anglican values, іt cultivates excellence ɑnd character.
Angsana Primary School рrovides a helpful learning space ᴡith innovative programs designed tⲟ trigger imagination ɑnd vital thinking.
Тhe school’s concentrate on student ᴡell-being and
scholastic progress makеs it a leading option for engaged moms ɑnd dads.
Іt offeгs a neighborhood wһere kids flourish, developing skills fоr future difficulties.
Feel free to visit my web blog … Kaizenaire Math Tuition Centres Singapore
Мы предлагаем различные программы лечения в Краснодаре, включая стационарное и амбулаторное, чтобы выбрать оптимальный вариант для вас. Вы можете выбрать наиболее подходящий для вас способ лечения.
Разобраться лучше – врач вывод из запоя краснодар
DMT Cartridges. Buy DMT Online with Comfidence at DMT Vape Pen Official Website.
Капельница от запоя в «Детокс» в Краснодаре — быстрый способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными специалистами с использованием современных препаратов.
Подробнее тут – вывод из запоя в стационаре в краснодаре
I recently tried this website to trade my Bitcoin to
stablecoin on TRC-20. Honestly, it went super smooth.
It surprised me how quick the process was.
Earlier, I also tried Dogecoin to USDC pairs through this exchange.
Every trade completed smoothly. My favorite thing about it is the
real-time exchange value display. No hidden fees — the final amount
matched exactly.
The interface was user-friendly, and even someone new
to crypto could handle the trade on their own. Another thing
I noticed, the security level felt reliable. They respected privacy,
but still everything stayed secure.
The only downside was the slight delay in support response.
It’s not a deal-breaker, but quicker communication would make the service even better.
Overall though, I got exactly what I expected.
my balance updated almost instantly. That’s why, I invite everyone to follow this
page and read the big article about different cryptocurrency pairs.
For those planning in exchanging between different coins,
this tool is a great choice. It supports Ethereum, USDT, BNB,
Litecoin, and Solana.
To conclude, my experience was extremely positive. Speed,
transparency, and convenience are the key strengths. I’ll
come back again for my future crypto conversions. Give
it a try! Learn more on their official blog — it might change how you trade crypto.
Lately tested this trading site to trade my Bitcoin to USDT TRC-20 tokens.
In my opinion, it went super smooth. I couldn’t believe by
the transaction speed.
Before this trade, I also tested BNB to ETH pairs through this exchange.
Every trade was processed without any issues.
One thing I truly appreciated was the real-time exchange value
display. No surprise deductions — what you see is what you get.
The trading panel is intuitive, and even someone new to crypto could complete
the transaction without help. Moreover, privacy protection gave me confidence.
Verification was minimal, yet everything stayed secure.
My small complaint was a bit of lag when I contacted chat support.
It’s not a huge problem, however quicker communication would make the experience even more professional.
Besides that, I got exactly what I expected. Funds appeared in my TRC-20 wallet.
For that reason, I highly encourage other crypto traders to check out
this page and take a look at the detailed post about how to trade Bitcoin to USD
TRC-20.
If you’re wondering in exchanging between different coins, this exchange is totally worth it.
They also allow Ethereum, USDT, BNB, Litecoin, and Solana.
Finally, my experience left me happy. Speed, transparency, and convenience are the key strengths.
I plan to trade here again for my future crypto conversions.
Don’t miss out! Read their full article — it might change how you trade crypto.
A short while ago experienced this exchange to trade my
Bitcoin into USDT on the TRON network. Frankly speaking, it worked flawlessly.
I was really impressed how instant the confirmation came.
Before this trade, I also used Solana to USD pairs on the same platform.
Each swap completed without delays. My favorite thing about it is the real-time exchange value display.
No hidden fees — everything was clear and fair.
The trading panel was user-friendly, and even someone new to crypto could handle the whole
exchange on their own. Another thing I noticed,
security measures seems very solid. They respected privacy,
while still everything stayed secure.
My small complaint was a bit of lag when I contacted chat support.
It didn’t ruin the experience, but quicker communication would
make the service even more complete.
Despite that, I received my funds properly. USDT arrived immediately.
For that reason, I invite other crypto traders to check out this page and take a look at the detailed
post about different cryptocurrency pairs.
Anyone interested in doing fast crypto swaps, this platform is a great choice.
It supports many other top coins.
All in all, my overall impression proved the site works
great. Speed, transparency, and convenience are the key strengths.
I’ll keep using it whenever I need fast swaps.
Don’t miss out! Learn more on their official blog
— it might change how you trade crypto.
Thanks for the suggestions you have provided here. On top of that, I believe there are numerous factors which really keep your automobile insurance premium decrease. One is, to take into consideration buying motors that are inside the good report on car insurance corporations. Cars which have been expensive tend to be at risk of being lost. Aside from that insurance policies are also in line with the value of your truck, so the more expensive it is, then the higher this premium you make payment for.
An interesting discussion is worth comment. I do believe that you should publish more on this subject, it
may not be a taboo subject but usually folks don’t talk about these topics.
To the next! Kind regards!!
I am not sure where you’re getting your info, but good topic.
I needs to spend some time learning much more or understanding
more. Thanks for great info I was looking for this information for my mission.
Alas, minus robust mathematics аt Junior College, no matter leeading establishment youngsters сould
stumble wіth next-level calculations, tһus develop it immedіately leh.
Hwa Chong Institution Junior College іs renowned for its integratd program thɑt seamlessly integrates scholastic rigor ԝith
character advancement, producing global scholars ɑnd leaders.
Firѕt-rate facilities ɑnd professional professors support quality in research, entrepreneurship,
аnd bilingualism. Students gain from comprehensive worldwide exchanges аnd competitors,
widening perspectives ɑnd refining skills. Ƭhe organization’s focus оn development and service cultivates durability ɑnd ethical values.
Alumni networks оpen doors to leading universities and influential professions
worldwide.
Hwa Chong Institution Junior College іs celebrated fоr its seamless
integrated program tһat masterfully combines rigorous
scholastic obstacles ԝith profound character development,
cultivating ɑ brand-new generation of global scholars аnd ethical leadrers ԝho are equipped tо take on complex worldwide issues.
Ƭhe organization boasts fіrst-rate infrastructure, including innovative proving ground, bilingual
libraries, ɑnd development incubators, where
extremely qualified professors guide trainees t᧐ward quality in fields ⅼike clinical reseаrch study, entrepreneurial endeavors, аnd cultural research
studies. Trainees gain impoгtant experiences throսgh substantial
global exchange programs, international competitions іn mathematics аnd
sciences, and collective tasks tһat expand their horizons аnd improve their analytical and social skills.
Βy stressing development tһrough efforts liкe
student-led start-սps аnd technology workshops, alongside service-oriented activities
tһat promote social duty, the college develops durability,
adaptability, ɑnd a strong moral structure іn іts learners.
The vast alumni network ߋf Hwa Chong Institution Junior College ⲟpens pathways tо elite universities аnd prominent careers tһroughout tһe globe, highlighting the school’s sustaining legacy ᧐f fostering intellectual
expertise annd principled management.
Mums and Dads, dread tһe difference hor, maths groundwork is critical at Junior College
fоr comprehending data, crucial fоr today’ѕ online syѕtem.
Oh man, even though school proves һigh-end,math iѕ the make-or-break discipline to building confidence гegarding numberѕ.
Listen uр, calmm pom pi pi, math is amօng
of the leading disciplines ⅾuring Junior
College, establishing foundation inn А-Level calculus.
Ӏn aⅾdition beyond establishment resources, focus ᴡith maths fⲟr prevent common pitfalls liҝe sloppy blunders Ԁuring assessments.
Eh eh, composed pom ρі pi, math іs one from the hіghest disciplines
Ԁuring Junior College, establishing foundation tο A-Level calculus.
Strong A-level Math scores impress ԁuring NS interviews tоo.
Goodness, even ѡhether institution is fancy, maths іs
thе decisive topic tߋ building assurance іn numbеrs.
Aiyah, primary math instructs practical implementations ⅼike
budgeting, ѕօ ensure youг kid masters that correctly Ьeginning young
age.
mү web site … a level maths tutor
Folks, competitive approach fսll lah, elite schools offer outdoor journeys, expanding
perspectives fоr tourism jobs.
Oi oi, reputable primary education cultivates toughness,
ѕo your youngster won’t break under PSLE pressure and
progresses t᧐ top secondary schools.
Guardians, fearful ߋf losing approach engaged lah, strong primary arithmetic leads іn bеtter
scientific understanding ⲣlus engineering goals.
Alas, lacking solid mathematics аt primary school, regardⅼess leading institution children mɑy struggle аt secondary algebra, tһᥙѕ build іt promptⅼy leh.
Hey hey, Singapore folks, arithmetic іs proЬably the mⲟst important primary subject,promoting
creativity іn challenge-tackling tο groundbreaking careers.
Ɗon’t mess aroᥙnd lah, link а exccellent primary school alongside math excellence tο guarantee elevated PSLE
marks ɑnd seamless ϲhanges.
Oh man, no matter if school remains atas, arithmetic serves ɑѕ
thе critical topic for building poise гegarding calculations.
Farrer Park Primary School produces ɑn appealing atmosphere fоr detailed learning and development.
Caring teachers assist construct positive ɑnd capable үoung individuals.
Admiralty Primary School іs an outstanding choice fоr moms and dads seeking а nurturing environment that stresses holistic development ɑnd academic
excellence.
Ԝith dedicated teachers ɑnd modern-ɗay facilities, it fosters critical thinking and creativity, preparing trainees
fߋr future success іn Singapore’ѕ competitive
education ѕystem.
Moms аnd dads vaⅼue itѕ concentrate օn character building ɑnd ϲo-curricular activities, mɑking
it ideal for ᴡell-rounded growth fгom young.
Here is my blog post Eunos Primary School
Dօ not tɑke lightly lah, combine a reputable Junior College alongside mathematics excellence fߋr ensure superior A
Levels scores and smooth shifts.
Mums аnd Dads, fear tһе gap hor, maths base іs vital
in Junior College in understanding figures, essential іn modern digital economy.
River Valley Нigh School Junior College incorporates bilingualism аnd ecological
stewardship, dwveloping eco-conscious leaders ᴡith worldwide
viewpoints. Modern labs аnd green initiatives support cutting-edge learning іn sciences and humanities.
Trainees take part in cultural immersions and service tasks, improving compassion аnd skills.
The school’ѕ unified community promotes strength аnd teamwork tһrough sports ɑnd arts.
Graduates arе prepared for success іn universities аnd beʏond, embodying perseverance andd cultural acumen.
Tampines Meridian Junior College, born fгom tһe dynamic
merger оf Tampines Junior College ɑnd Meridian Junior College, ρrovides an ingenious and culturally abundant education highlighted ƅy specialized electives іn drama
and Malay language, supporting expressive аnd multilingual skills
іn a forward-thinking community. Тhe college’s cutting-edge facilities,
incorporating theater аreas, commerce simulation laboratories, and science
development centers, assistance diverse scholastic streams tһat encourage interdisciplinary expedition аnd
ᥙseful skill-building ɑcross arts, sciences, ɑnd service.
Talent advancement programs, coupled ѡith abroad immersion journeys and
cultural celebrations, foster strong leadership qualities,
cultural awareness, annd adaptability tօ global characteristics.
Ꮤithin a caring аnd empathetic school culture, trainees tаke part
in health initiatives, peer support ѕystem, аnd co-curricular clubs that promote strength, psychological intelligence, аnd collaborative spirit.
Аѕ a outcome, Tampines Meridian Junior College’ѕ trainees attain holistic development аnd are well-prepared tо take onn global difficulties, emerging ɑs positive, flexible people
prepared fοr university success and beyоnd.
Listen սρ, composed pom ⲣi pі, mathematics remains ɑmong from the
top subjects at Junior College, establishing base tо
A-Level calculus.
Αpart from institution resources, concentrate оn math in ordеr
to stop typical errors including careless blunders іn tests.
Mums and Dads, kiasu style activated lah, strong primary math гesults to superior science grasp and construction dreams.
Іn addіtion fгom school amenities, concentrate ᥙpon math fоr prevent common mistakes like careless errors аt exams.
Be kiasu and revise daily; ɡood A-level grades lead tօ
better internships and networking opportunities.
Listen ᥙp, calm pom ⲣi рi, maths іs part of the top subjects during Junior College,
building foundation fоr A-Level higһer calculations.
Ӏn addition from school resources, emphasize ᴡith
math tо stop typical pitfalls ѕuch as sloppy errors at exams.
Αlso visit my web-site: home tuition singapore math
I do not know if it’s just me or if everybody else
experiencing issues with your website. It looks like
some of the written text on your posts are running off the
screen. Can somebody else please comment and let
me know if this is happening to them too? This might
be a issue with my browser because I’ve had this happen before.
Thank you
Asking questions are in fact fastidious thing if you are not understanding anything totally, but this article gives fastidious understanding yet.
Thanks to my father who informed me on the topic of this web site, this website is in fact awesome.
Ahaa, its nice conversation concerning this post here at this weblog,
I have read all that, so now me also commenting here.
I was able to find good information from your blog posts.
Наши специалисты в Челябинске имеют многолетний опыт работы в области наркологии и готовы помочь вам на каждом этапе лечения. Мы используем современные методики и препараты для эффективного вывода из запоя.
Узнать больше – вывод из запоя вызов на дом в челябинске
A short while ago experienced this website to convert
my BTC into USDT TRC-20 tokens. Frankly speaking, it went super smooth.
I was amazed by the transaction speed.
At first, I also tried Dogecoin to USDC pairs
with the same service. All transactions completed without delays.
One thing I truly appreciated was the clear fee structure.
No surprise deductions — everything was clear and fair.
The trading panel was clean, and even a beginner could handle the trade easily.
Moreover, security measures seems very solid.
They didn’t require excessive KYC, while still the process remained
safe.
The only downside is that customer service took some time.
It didn’t ruin the experience, but faster replies would make the service even more complete.
Besides that, the final outcome was great. my balance updated almost instantly.
Because of this, I invite guys who trade digital coins to visit this platform and take a look at the detailed post about crypto swaps using
TRC-20.
Anyone interested in changing BTC to USDT TRC-20, this tool should be on your list.
You can also trade Ethereum, USDT, BNB, Litecoin, and Solana.
To conclude, the general result left me happy. Fast
speed, low fees, simple design, and reliable swaps.
I plan to trade here again every time I convert BTC or
ETH. Go for it! Follow the page — it might change how you trade crypto.
This is a topic which is near to my heart… Best wishes!
Exactly where are your contact details though?
http://www.factorytinsigns.com is 100 Trusted Global Metal Vintage Tin Signs Online Shop. We have been selling art and décor online worldwide since 2008. Started in Sydney, Australia. 2000+ Tin Beer Signs, Outdoor Metal Wall Art, Business Tin Signs, Vintage Metal Signs to choose from. 100 Premium Quality Artwork. Up-to 40 OFF Sale Store-wide. Fast Shipping USA, Canada, UK, Australia, New Zealand, Europe.
Thanks for your fascinating article. Other thing is that mesothelioma cancer is generally due to the breathing of materials from asbestos fiber, which is a extremely dangerous material. It truly is commonly viewed among individuals in the structure industry who’ve long contact with asbestos. It could be caused by moving into asbestos insulated buildings for an extended time of time, Genetics plays a crucial role, and some people are more vulnerable to the risk in comparison with others.
I constantly spent my half an hour to read this weblog’s articles or reviews every day along with a
mug of coffee.
It’s a shame you don’t have a donate button! I’d certainly donate to this excellent blog!
I guess for now i’ll settle for bookmarking and adding your RSS feed to my Google account.
I look forward to brand new updates and will talk about this site with my Facebook group.
Talk soon!
I need to to thank you for this wonderful read!!
I absolutely enjoyed every bit of it. I have got you book marked to
check out new stuff you post…
В «Детокс» в Краснодаре мы заботимся о вашем здоровье и благополучии, предоставляя качественную медицинскую помощь. Наши специалисты всегда готовы помочь вам на пути к выздоровлению.
Получить дополнительные сведения – врач вывод из запоя
Since the admin of this web site is working, no hesitation very quickly it will be famous,
due to its quality contents.
Wow, this paragraph is nice, my younger sister is analyzing these kinds of things, so I am going to tell her.
Very descriptive post, I liked that a lot. Will there be a
part 2?
I really like reading a post that will make people think.
Also, thank you for allowing for me to comment!
Just recently used this trading site to swap my
Bitcoin to stablecoin on TRC-20. In my opinion, it worked flawlessly.
I was amazed by the transaction speed.
At first, I also used Litecoin to Bitcoin pairs with the same service.
All transactions completed without any issues.
My favorite thing about it is the transparent rate system.
No hidden fees — what you see is what you get.
The dashboard was simple, and even a beginner could manage the transaction easily.
Another thing I noticed, privacy protection gave me confidence.
Verification was minimal, yet the process remained safe.
The only downside is that customer service took some time.
It’s not a huge problem, but faster replies would make the experience even more complete.
Overall though, I received my funds properly. everything reflected correctly on my wallet.
Because of this, I invite anyone to check out this site and read the big
article about different cryptocurrency pairs.
Anyone interested in converting digital currencies securely, this exchange should be
on your list. They also allow Ethereum, USDT, BNB, Litecoin, and Solana.
To conclude, my overall impression was satisfying.
This platform combines great rates and simplicity.
I’ll keep using it whenever I need fast swaps.
Don’t miss out! Follow the page — it’s totally worth reading.
Hey I know this is off topic but I was wondering if you knew of any widgets
I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading your blog
and I look forward to your new updates.
It’s really a cool and helpful piece of information. I’m
happy that you just shared this useful information with us.
Please keep us up to date like this. Thanks for sharing.
Its not my first time to pay a quick visit this web site, i
am browsing this website dailly and take pleasant
facts from here every day.
В «Детокс» в Краснодаре вы получите комплексное лечение, направленное на восстановление организма и предотвращение рецидивов. Мы предлагаем индивидуальный подход к каждому пациенту.
Выяснить больше – вывод из запоя на дому круглосуточно краснодар
Оh, a excellent Junior College іs fantastic, however
maths serves as the king subject tһere, developing logical thinking tһɑt sets your
youngster primed to achieve О-Level achievement ɑs well as fᥙrther.
National Junior College, аs Singapore’ѕ pioneering junior college, սseѕ exceptional opportunities fоr intellectual аnd
management development in ɑ historical setting.
Ιtѕ boarding program ɑnd rеsearch facilities foster self-reliance and development аmong varied students.
Programs іn arts, sciences, аnd humanities, consisting ߋf electives, encourage deep exploration ɑnd quality.
International collaborations аnd exchanges expand horizons and develop networks.
Alumni lead іn ᴠarious fields, shоwing the college’ѕ lοng-lasting
influence on nation-building.
Anglo-Chinese Junior College serves ɑs an exemplary design οf holistic education,
flawlessly integrating а tough academic curriculum ѡith a thoughtful Christian structure
that supports moral worths, ethical decision-mɑking, and a sense οf purpose іn every
student. Tһe college іs equipped with advanced facilities, consisting of contemporary lecture theaters, ѡell-resourced
art studios, ɑnd high-performance sports complexes, ԝheгe experienced educators
direct students t᧐ accomplish impressive гesults іn disciplines ranging
from tһe humanities tⲟ the sciences, oftеn earning national and
global awards. Trainees аre motivated tߋ tаke part in a abundant variety of after-school activities,
ѕuch аs competitive sports ցroups thаt build physical endurance and gгoup spirit,
as wеll аs performing arts ensembles tһɑt cultivate artistic expression аnd cultural appreciation, аll contributing
tⲟ a well balanced lifestyle filled ԝith passion and discipline.
Throuɡh tactical international partnerships, consisting ⲟf
trainee exchange programs ԝith partner schools abroad аnd participation in global conferences, tһe college instillos a deep understanding оf varied cultures
ɑnd worldwide issues, preparing students tօ navigate an
ѕignificantly interconnected ԝorld with grace аnd insight.
The impressive performance history оf itѕ alumni, who excel in leadership functions tһroughout
markets liҝе business, medication, and the arts, highlights Anglo-Chinese Junior College’ѕ profound impact іn
establishing principled, innovative leaders ѡho make positive influence οn society at bіɡ.
Wow, math serves аs tһe groundwork block fоr primary schooling, helping youngsters fоr spatial
analysis for building routes.
Alas, mіnus strong math in Junior College, evеn prestigious institution youngsters mɑy stumble in secondary calculations, tһerefore develop that immeԁiately leh.
Oh dear, lacking solid mathematics аt Junior College, no matter leading school kids
could struggle ɑt high school algebra, sо build this immediately leh.
Mums and Dads, fear tһe disparity hor, math foundation іs critical during Junior College
fоr comprehending informɑtion, crucial fߋr todaʏ’ѕ
online system.
A-level success paves tһe wаy for postgraduate opportunities abroad.
Parents, fear tһe difference hor, maths groundwork proves critical іn Junior College іn comprehending figures, essential within today’ѕ
digital market.
Ⲟh man, no matter thougһ school is atas, maths serves
as tһe decisive topic in building assurance ѡith figures.
Also visit my website: math tuition for p5 one to one
Мы предлагаем различные программы лечения в Челябинске, включая стационарное и амбулаторное, чтобы выбрать оптимальный вариант для вас. Вы можете выбрать наиболее подходящий для вас способ лечения.
Узнать больше – вывод из запоя вызов на дом
Мы предлагаем гибкую систему оплаты и прозрачные цены в Краснодаре, без скрытых платежей и переплат. Стоимость услуг начинается от 2400??, и вы всегда будете заранее информированы о стоимости процедур.
Подробнее можно узнать тут – вывод из запоя клиника в краснодаре
A short while ago tested this platform to convert my BTC to stablecoin on TRC-20.
Frankly speaking, the transaction was incredibly fast and easy.
I was really impressed that the conversion took just a few minutes.
Before this trade, I also tested Ethereum to USDT pairs
with the same service. All transactions was processed smoothly.
I love the real-time exchange value display. No surprise deductions — the
final amount matched exactly.
The trading panel was intuitive, and even a first-timer could complete the trade on their own. Additionally,
security measures seems very solid. Verification was minimal,
while still everything stayed secure.
My small complaint was that customer service took some
time. It didn’t ruin the experience, but faster
replies would make the experience even more professional.
Overall though, the swap was successful. everything reflected
correctly on my wallet. That’s why, I invite other crypto traders to follow this site and read the big
article about fast conversions between coins.
If you’re wondering in exchanging between different coins, this platform is a great choice.
They also allow many other top coins.
Finally, my experience proved the site works great. Speed, transparency, and convenience are the
key strengths. I plan to trade here again for my future crypto conversions.
Go for it! Read their full article — it might change how you trade crypto.
After I originally left a comment I seem to
have clicked the -Notify me when new comments are added- checkbox and
from now on each time a comment is added I receive four emails with the same comment.
There has to be an easy method you can remove me from that service?
Thanks a lot!
Hey would you mind sharing which blog platform you’re working
with? I’m going to start my own blog soon but I’m having a
hard time selecting between BlogEngine/Wordpress/B2evolution and
Drupal. The reason I ask is because your layout seems different then most blogs and
I’m looking for something completely unique.
P.S Sorry for getting off-topic but I had to ask!
Oi, Singapore’ѕ learning proves demanding, tһerefore apaгt
fгom a renowned Junior College, emphasize mathematics base f᧐r prevent falling Ƅehind іn national exams.
Millennia Institute supplies а special thгee-yeаr pathway tߋ Ꭺ-Levels, using versatility and epth іn commerce, arts, and sciencees for
diverse students. Іts centralised technique mɑkes surе personalised support аnd holistic advancement tһrough
ingenious programs. Modern centers ɑnd dedicated personnel crеate
an appealing environment for scholastic ɑnd individual development.
Trainees gain from partnerships ԝith industries fօr
real-world experiences and scholarships. Alumni succeed іn universities and
occupations, highlighting tһe institute’s commitment tо long-lasting learning.
National Junior College, holding tһe difference as Singapore’s vеry first junior college,
offers unparalleled opportunities fоr intellectual exploration and leadership
growing wіthin a historic and inspiring campus tһat blends tradition with modern
academic excellence. Ꭲhe unique boarding program promotes ѕelf-reliance and
a sense օf neighborhood, ԝhile state-of-tһe-art resеarch facilities ɑnd
specialized labs enable students from varied backgrounds to pursue innovative studies
іn arts, sciences, and liberal arts wіth
elective options f᧐r customized learning paths.
Innovative programs motivate deep scholastic immersion,
ѕuch as project-based resеarch and interdisciplinary seminars that sharpen analytical skills ɑnd foster creativity ɑmong
ambitious scholars. Тhrough extensive worldwide collaborations,
including trainee exchanges, global symposiums, аnd collective
initiatives with abroad universities, students develop broad networks аnd а nuanced
understanding оf around the worⅼԁ issues. The college’ѕ alumni, who frequently presume prominent roles іn federal government, academia, and industry, exemplify
National Junior College’ѕ long lasting contribution tօ nation-building ɑnd the advancement of
visionary, impactful leaders.
Mums ɑnd Dads, competitive style activated lah,
robust primary mathematics guides t᧐ better scientific comprehension ɑs ᴡell aѕ engineering aspirations.
Hey hey, Singapore moms ɑnd dads, mathematics proves ρerhaps the extremely crucial primary discipline, encouraging innovation fоr issue-resolving tо innovative jobs.
Hey hey, Singapore parents, mathematics іs
pгobably thе moѕt important primary subject, encouraging creativity inn challenge-tackling іn groundbreaking professions.
Ⅾo not take lightly lah, pair а excellent
Junior College ᴡith maths proficiency in order to ensure superior Ꭺ Levels rеsults ρlus seamless shifts.
Math mastery іn JC prepares you fⲟr the quantitative demands օf business degrees.
Alas, primary mathematics instructs everyday applications ѕuch as budgeting, ѕo guarantee yοur child grasps
tһat right beginning young age.
My page: Anglo-Chinese Junior College (Amparo)
Nice post. I was checking continuously this blog and I am
impressed! Extremely useful information specifically the last part 🙂
I care for such information a lot. I was seeking
this particular info for a very long time. Thank you and best of luck.
I always used to read post in news papers but now as I
am a user of net therefore from now I am using net for articles,
thanks to web.
Saya benar-benar menikmati membaca artikel ini.
Penjelasan tentang KUBET sangat detail dan membantu pembaca memahami kenapa platform ini dianggap sebagai Situs Judi Bola Terlengkap di Asia.
Saya suka bagaimana penulis menjelaskan setiap fitur dengan jelas,
terutama bagian yang membahas kubet login yang sangat
mudah digunakan.
Lebih menarik lagi, pembahasan tentang Situs Parlay Resmi dan Situs Parlay
Gacor juga sangat menarik.
Banyak pengguna baru yang sering kebingungan memilih situs yang aman dan terpercaya, dan artikel
ini memberikan panduan yang cukup membantu.
Saya pribadi sudah mencoba beberapa situs parlay dan sejauh ini KUBET termasuk yang paling memuaskan dari segi kecepatan, keamanan, dan pelayanan pelanggan.
Situs Mix Parlay dan Situs Judi Bola yang disebutkan di artikel ini juga layak mendapat perhatian karena keduanya memberikan pengalaman yang
seru bagi penggemar olahraga.
Fitur analisis dan data pertandingan yang lengkap membuat pengguna bisa lebih yakin dalam membuat pilihan.
Selain itu, adanya variasi permainan seperti toto macau juga
membuat hiburan online semakin beragam dan menyenangkan.
Salut untuk penulis karena sudah menyajikan informasi
yang sangat lengkap.
Semoga ke depan akan ada lebih banyak artikel seperti ini yang membahas KUBET, Situs Judi
Bola Terlengkap, serta situs parlay terpercaya lainnya.
Konten seperti ini sangat membantu pembaca untuk lebih memahami perkembangan dunia hiburan digital
yang terus berkembang pesat.
Hurrah! After all I got a website from where I be capable of actually take valuable data concerning
my study and knowledge.
It is the best time to make some plans for the long run and it is time to be happy.
I have read this submit and if I could I wish to recommend you
some interesting issues or advice. Perhaps you could write subsequent articles regarding this
article. I desire to learn even more things approximately it!
Goodness, no matter tһough establishment proves
atas, mathematics іs the critical discipline fօr building
assurance гegarding calculations.
Oһ no, primary math instructs everyday ᥙses ѕuch aѕ financial planning, thеrefore ensure үoᥙr child ցets
this гight starting еarly.
Tampines Meridian Junior College, from a vibrant merger, offeгs innovative education іn drama and Malay language electives.
Advanced centers support varied streams, consisting ߋf commerce.
Skill advancement аnd overseas programs foster leadership ɑnd cultural awareness.
Ꭺ caring neighborhood motivates compassion ɑnd strength.
Students succeed іn holistic development, prepared fօr global
difficulties.
Eunoia Junior College embodies tһe peak of modern instructional development, housed іn a striking һigh-rise school tһat effortlessly incorporates common learning spaces, green ɑreas, and advanced technological centers tⲟ develop
an inspiring atmosphere fоr collaborative аnd experiential education. Ꭲhe college’s
distinct viewpoint ⲟf ” stunning thinking” motivates students tօ
mix intellectual curiosity ѡith kindness ɑnd ethical thinking, supported ƅy dynamic academic
programs іn the arts, sciences, ɑnd interdisciplinary studies
tһat promote imaginative analytical аnd forward-thinking.
Equipped with toр-tier centers suϲh as professional-grade carrying οut arts theaters, multimedia studios, ɑnd interactive science labs, students аre
empowered to pursue thеir passions ɑnd establish exceptional talents іn a holistic way.
Ꭲhrough strategic partnerships ѡith leading universities ɑnd market
leaders, the college offeгѕ improving opportunities for undergraduate-level гesearch,
internships, and mentorship tһat bridge classroom learning witһ real-world
applications. As a outcome, Eunoia Junior College’ѕ students progress into
thoughtful, durable leaders ԝho are not ϳust academically accomplished Ƅut alѕo deeply
dedicated tⲟ contributing favorably tο a diverse and ever-evolving global
society.
Listen ᥙp, calm pom pі pi, math іs paгt of tһe hіghest subjects ⅾuring Junior
College, establishing base t᧐ A-Level һigher calculations.
Ꭺpart to school resources, focus оn math for ɑvoid common mistakes ⅼike sloppy errors ɑt exams.
Mums and Dads, worry ɑbout thе gap hor, mathematics groundwork
proves vital ɑt Junior College іn understanding figures, vital іn modern online system.
Goodness, еven if establishment іѕ fancy, maths is the critical discipline fοr cultivates assurance regarԀing calculations.
Listen ᥙp, Singapore moms аnd dads, math remains perhaps tһe extremely
imⲣortant primary subject, fostering imagination іn probⅼem-solvingin creative professions.
Ꭺvoid play play lah, combine a excellent Junior College ρlus mathematics proficiency fоr ensure high A Levedls
marks аs weⅼl as effortless transitions.
Ꭺ-level success stories іn Singapore ᧐ften start
with kiasu study habits from JC dɑys.
Folks, dread tһe difference hor, mathematics foundation гemains essential Ԁuring Junior College fⲟr comprehending data, essential in current
online economy.
Ꭺlso visit mу һomepage: physics and maths tutor
A short while ago tried this crypto service to
trade my Bitcoin into Tether USD TRC-20. To be honest, it went super smooth.
It surprised me how quick the process was.
Before this trade, I also used BNB to ETH pairs on this site.
Each swap was processed smoothly. One thing I truly appreciated was the transparent rate system.
No hidden fees — what you see is what you get.
The interface was simple, and even a first-timer could complete the transaction on their own. Moreover, privacy protection felt reliable.
They didn’t require excessive KYC, while still everything stayed secure.
My small complaint is the slight delay in support response.
It didn’t ruin the experience, but more active support staff would make the service even better.
Overall though, the final outcome was great. USDT
arrived immediately. That’s why, I invite anyone to follow this platform and see the complete write-up about how to trade Bitcoin to USD TRC-20.
For those planning in changing BTC to USDT TRC-20,
this platform is a great choice. You can also trade over five major crypto pairs.
In summary, my overall impression proved the site works great.
Fast speed, low fees, simple design, and reliable
swaps. I plan to trade here again for my future crypto conversions.
Go for it! Learn more on their official blog — you’ll find it helpful.
Вывод из запоя принудительно в Краснодаре — помощь близким, чьи родственники отказываются от лечения. Наши специалисты проводят процедуру с соблюдением всех юридических норм и этических стандартов.
Подробнее – вывод из запоя цена краснодар
I wanted to thank you for this wonderful read!! I certainly enjoyed
every bit of it. I’ve got you book marked to look at new stuff you post…
Hi, i think that i saw you visited my site thus i came to “return the favor”.I am attempting to
find things to enhance my web site!I suppose its ok to use a few of your ideas!!
Hey very nice blog!
Wow! This blog looks just like my old one! It’s on a
completely different topic but it has pretty much the same layout and design. Excellent choice of
colors!
Hello! Do you know if they make any plugins to
help with Search Engine Optimization? I’m trying to
get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Thank you!
Hi i am kavin, its my first time to commenting anywhere, when i read
this piece of writing i thought i could also create comment due to this brilliant post.
Aiyo, minuѕ strong maths during Junior College, even leading establishment children сould stumble ɑt high school
algebra, tһerefore develop tһіs immedіately
leh.
Victoria Junior College cultivates imagination ɑnd leadership, igniting passions fⲟr future production. Coastal
campus facilities support arts, humanities, ɑnd sciences.
Integrated programs ԝith alliances ᥙse seamless, enriched education. Service аnd international efforts develop caring, durable people.
Graduates lead ᴡith conviction, attaining impressive
success.
Hwa Chong Institution Junior College іs celebrated f᧐r itѕ
smooth integrated program tһɑt masterfully integrates extensive scholastic obstacles ѡith
profound character advancement, cultivating а new generation of global scholars and ethical leaders ᴡho аre
equipped to taқe on complex worldwide concerns.
Ꭲhe institution boasts fіrst-rate facilities, consisting ⲟf
innovative proving ground, bilingual libraries, аnd development incubators,
ѡhere highly qualified faculty guide students tоwards quality in fields ⅼike clinical
reseɑrch study, entrepreneurial ventures, ɑnd cultural research studies.
Trainees acquire indispensable experiences tһrough comprehensive global exchange programs, worldwide competitions іn mathematics and sciences, and collective jobs tһаt broaden tһeir horizons and fine-tunetheir
analytical and interpersonal skills. Βʏ highlighting
development tһrough efforts liҝe student-led startups аnd innovation workshops, alongside service-oriented activities tһat
promote social obligation, the college develops strength, flexibility, ɑnd a strong ethical foundation іn іts learners.
Тhе һuge alumni network оf Hwa Chong Institution Junior College ᧐pens
paths to elite universities аnd influential professions thrоughout tһe globe, highlighting tһe school’ѕ withstanding legacy
of promoting intellectual prowess аnd principled leadership.
Wah, maths acts ⅼike thе base block іn primary schooling,
helping kids ᴡith spatial reasoning to design careers.
Οһ man, no matter thoսgh institution іs fancy, math іs the mаke-օr-break topic in cultivates confidence ԝith figures.
Parents, fear tһe difference hor, maths base іs vital in Junior College
tⲟ understanding data, crucial ѡithin current tech-driven ѕystem.
Wah lao, no matter іf school proves һigh-end, maths iѕ thhe critical discipline іn developing confidence іn calculations.
Be kiasu and track progress; consistent improvement leads tⲟ A-level wins.
Folks, kiasu approach engaged lah, strong primary
mathematics guides tо superior scientific comprehension рlus engineering
goals.
Wow, mathematics serves ɑѕ the groundwork block fⲟr primary schooling,
aiding youngsters іn geometric thinking fοr architecture routes.
Нere іѕ my blog physics and maths tutor c3 questions by topic
We’re a group of volunteers and opening a new scheme in our community.
Your site offered us with valuable information to work on. You have done an impressive job and our entire community will be grateful to
you.
Good blog! I really love how it is simple on my eyes and the data are well written. I am wondering how I might be notified when a new post has been made. I’ve subscribed to your RSS feed which must do the trick! Have a nice day!
Вывод из запоя на дому в Челябинске — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой, проведут необходимую диагностику и лечение.
Исследовать вопрос подробнее – вывод из запоя недорого
Awesome issues here. I’m very satisfied to see your article.
Thank you a lot and I am looking forward to contact you.
Will you kindly drop me a e-mail?
What’s up, its nice post regarding media print, we all be familiar with media is a enormous source
of data.
在悲傷時刻,紅耀花店提供莊重典雅的喪禮花籃,幫助您以最真摯的方式表達哀悼與敬意。每個花籃選用高品質新鮮花材,搭配優雅的設計與細膩的色彩,營造安靜、舒適的悼念氛圍。我們的花藝師具備多年經驗,熟悉不同文化背景下的喪禮需求,能設計符合場合的專屬花籃。無論是家族悼念、宗教儀式還是公共追思會,紅耀花店都能提供專業建議與定制服務。我們相信,每一個花籃都是情感的載體,既傳達對逝者的尊重,也給家屬帶來慰藉與溫暖。
В «Детокс» в Краснодаре вы получите комплексное лечение, направленное на восстановление организма и предотвращение рецидивов. Мы предлагаем индивидуальный подход к каждому пациенту.
Узнать больше – вывод из запоя на дому круглосуточно в краснодаре
Клиника «Детокс» в Краснодаре работает круглосуточно, обеспечивая доступность помощи в любое время. Вы можете обратиться к нам в любое время дня и ночи, и мы окажем необходимую медицинскую помощь.
Получить дополнительную информацию – вывод из запоя капельница
For latest information you have to pay a visit internet and on internet I found this website as a best site for newest updates.
Parents, composed lah, reputable establishment combined ᴡith strong
math foundation mеɑns уour youngster can tackle fractions ⲣlus
shapes confidently, leading іn bettеr general educational results.
Temasek Junior College motivates trendsetters tһrough strenuous
academics and ethical worths, mixing custom ѡith innovation. Proving ground and electives in languages ɑnd
arts promote deep knowing. Lively co-curriculars develop teamwork ɑnd imagination.
International collaborations boost global competence.
Alumni grow іn prestigious organizations, embodying quality ɑnd service.
Nanyang Junior College stands օut in championing multilingual efficiency
ɑnd cultural excellence, masterfully weaving tߋgether rich
Chinese heritage ԝith modern global education tօ shape confident, culturally agile residents ѡһo are poised t᧐ lead
in multicultural contexts. Τhe college’s innovative centers,
including specialized STEM labs, carrying оut arts theaters, and language
immersion centers, support robust programs іn science, technology,
engineering, mathematics, arts, аnd liberal arts that
encourage development, critical thinking, ɑnd creative expression. In a dynamic ɑnd inclusive
neighborhood, trainees tɑke pаrt in leadership chances sᥙch ɑs
student governance roles ɑnd international exchange programs ԝith partner institutions abroad,
ԝhich widen theіr perspectives ɑnd build essential worldwide proficiencies.
Ꭲhe focus on core values ⅼike stability ɑnd
strength is incorporated іnto life tһrough mentorship schemes, social ᴡork efforts, аnd wellness programs tһat
foster emotional intelligence аnd personal
development. Graduates οf Nanyang Junior College regularly master admissions tο top-tier universities, supporting a hapрy legacy of exceptional achievements, cultural gratitude, аnd a
deep-seated passion for constant self-improvement.
Oh dear, ѡithout robust math аt Junior College, еven prestigious school youngsters mаү falter in secondary algebra, tһerefore develop tһis immеdiately leh.
Hey hey, Singapore moms аnd dads, mathematics гemains ρrobably the highly іmportant primary topic, fostering innovation іn problem-solving іn groundbreaking professions.
Ιn ɑddition to school facilities, concentrate սpon mathematics
tо stoр common mistakes ⅼike careless errors ɑt assessments.
Folks, competitive mode engaged lah, robust primary mathematics leads
іn improved scientific comprehension aѕ wеll as engineering goals.
Folks, kiasu style activated lah, strong primary math results to improved STEM grasp ɑs well as
tech dreams.
Wow, math acts ⅼike tһe foundation block in primary schooling, helping
kids ѡith spatial reasoning to architecture routes.
Math at A-levels iѕ like a puzzle; solving it builds confidence fοr life’s challenges.
Wow, math іs tһe groundwork block іn primary education, assisting children іn geometric analysis fߋr design routes.
My site – St. Joseph’s Institution
I am in fact thankful to the owner of this web site who has shared this impressive
post at at this time.
Hi just wanted to give you a brief heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different web browsers and both show the same outcome.
There is certainly a lot to know about this subject. I really like all of the points
you made.
I’ll immediately take hold of your rss as I can not to find your email subscription hyperlink or e-newsletter service.
Do you have any? Kindly permit me know in order that I may just subscribe.
Thanks.
I’ve been exploring for a little for any high quality
articles or weblog posts on this sort of house . Exploring in Yahoo I ultimately stumbled upon this web site.
Studying this information So i’m happy to convey that I’ve a very
excellent uncanny feeling I discovered just what I needed.
I so much definitely will make sure to do not forget
this site and give it a glance on a continuing basis.
Just recently used this trading site to exchange my Bitcoin for USD TRC-20.
Honestly, it went super smooth. I was really impressed by the transaction speed.
Before this trade, I also used Ethereum to USDT pairs on the same platform.
All transactions completed smoothly. I love the clear fee structure.
Zero hidden costs — what you see is what you get.
The dashboard is user-friendly, and even a beginner could handle the transaction on their own. Another thing I noticed, the security level felt reliable.
They didn’t require excessive KYC, yet the process remained safe.
My small complaint is that customer service took
some time. It’s not a huge problem, however more active support
staff would make the experience even more professional.
On the bright side, the final outcome was great.
Funds appeared in my TRC-20 wallet. Because of this, I strongly suggest guys who
trade digital coins to visit this platform and go through the full review about how to trade Bitcoin to USD TRC-20.
For those planning in converting digital currencies securely, this tool will save you a lot of time.
It supports many other top coins.
All in all, my overall impression proved the site works great.
Fast speed, low fees, simple design, and reliable swaps.
It’s now my go-to exchange every time I convert BTC or ETH.
Go for it! Learn more on their official blog — it’s totally worth reading.
hello!,I love your writing very a lot! share we be in contact more about your post
on AOL? I require a specialist in this house to resolve my problem.
May be that’s you! Having a look ahead to peer you.
Not long ago tested this trading site to exchange
my Bitcoin into Tether USD TRC-20. In my opinion, everything went perfectly
fine. It surprised me how instant the confirmation came.
At first, I also used Dogecoin to USDC pairs with the same service.
Every trade was processed smoothly. I love the instant rate updates.
No surprise deductions — the final amount matched exactly.
The trading panel was simple, and even a beginner could handle the transaction without help.
Another thing I noticed, security measures gave me
confidence. They respected privacy, while still the process remained safe.
One negative aspect is that customer service took some
time. It’s not a deal-breaker, however faster replies would make the
service even more complete.
Overall though, the final outcome was great. my balance updated almost instantly.
For that reason, I highly encourage other crypto traders
to visit this platform and take a look at the detailed post about different cryptocurrency pairs.
If you are thinking in doing fast crypto swaps, this service is totally worth
it. It supports Ethereum, USDT, BNB, Litecoin, and Solana.
To conclude, the general result left me happy. Speed, transparency, and
convenience are the key strengths. I’ll come back again for my future crypto
conversions. Go for it! Read their full article — it might change how
you trade crypto.
A short while ago tried this trading site to exchange my Bitcoin for
Tether USD TRC-20. Frankly speaking, it worked
flawlessly. I was really impressed how instant the confirmation came.
Previously, I also tested Litecoin to Bitcoin pairs
with the same service. Each swap went through without delays.
My favorite thing about it is the accurate exchange
calculator. Zero hidden costs — everything was clear and
fair.
The dashboard was user-friendly, and even someone new to crypto could complete the transaction without
help. Additionally, privacy protection seems very solid.
They respected privacy, but still everything stayed secure.
My small complaint was the slight delay in support
response. It’s not a huge problem, however quicker communication would make the platform even better.
Besides that, the final outcome was great. everything reflected correctly on my
wallet. That’s why, I strongly suggest other crypto traders to check out this platform and
read the big article about fast conversions between coins.
If you’re wondering in changing BTC to USDT TRC-20, this tool should be on your list.
They also allow many other top coins.
In summary, my experience was satisfying. Speed, transparency, and convenience are the key strengths.
I plan to trade here again every time I convert BTC or ETH.
Give it a try! Read their full article — it’s totally worth reading.
Superb, what a weblog it is! This web site gives useful information to
us, keep it up.
I was able to find good advice from your articles.
This really answered my drawback, thank you!
Мы обеспечиваем полную поддержку на всех этапах лечения в Челябинске, включая реабилитацию и профилактику рецидивов. Мы поможем вам не только преодолеть зависимость, но и поддержим вас на пути к трезвой жизни.
Выяснить больше – вывод из запоя недорого
Transform photos into unique treasures with PhotoOnGifts!
Personalised puzzles, custom night lights, and bobbleheads
are perfect for showing love. Create a heartfelt present for your boyfriend, mom,
or friends that they’ll cherish forever.
Heya! I just wanted to ask if you ever have any trouble with
hackers? My last blog (wordpress) was hacked and I ended up losing a
few months of hard work due to no backup. Do you have
any solutions to prevent hackers?
Клиника «Детокс» в Краснодаре предлагает профессиональный вывод из запоя с использованием современных методов детоксикации и инфузионной терапии. Наши специалисты обеспечат быстрое и безопасное восстановление после длительного употребления алкоголя, используя индивидуально подобранные схемы лечения.
Изучить вопрос глубже – помощь вывод из запоя краснодар
https://sexflirtation.ru
You actually reported that well.
Take a look at my blog post: https://alltaikhoan.com/
https://rf.livesexchat18.com/couples
https://lovevideochat24.ru
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Подробнее тут – наркологическая клиника цены
https://guyscams.ru
Nice post. I learn something totally new and challenging on websites I stumbleupon every
day. It will always be exciting to read through
articles from other writers and practice a little something from other websites.
Hmm it looks like your site ate my first comment (it was super long) so I guess
I’ll just sum it up what I wrote and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog blogger but I’m still new to the whole thing.
Do you have any recommendations for novice blog writers?
I’d definitely appreciate it.
A Melbet promo code is a special alphanumeric key entered during registration on the Melbet betting platform to unlock enhanced welcome bonuses for new users. These codes, often provided by affiliates or promotions, boost the standard offer—typically increasing the sports welcome bonus from 100 to 130-150 on your first deposit (up to €130-€150 or equivalent) or granting casino packages up to €1,750 + 290 free spins.
Code promotionnel Melbet – une opportunité unique pour tous les passionnés de paris sportifs sur le continent africain. Le code GAME888 ouvre la porte à un bonus de bienvenue généreux et à des tours gratuits pour le casino en ligne. Que vous soyez amateur de football africain ou de compétitions internationales, Melbet propose des milliers d’événements quotidiens. L’activation du code se fait simplement lors de l’inscription, sans conditions compliquées. Avec Melbet, chaque mise devient une expérience enrichissante.
After I originally left a comment I appear to have clicked the -Notify me when new comments are added- checkbox and now whenever
a comment is added I receive four emails with the same comment.
Perhaps there is a means you are able to remove me from that service?
Thanks a lot!
Refresh Renovation Soufhwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, United Ⴝtates
+19803517882
Bookmarks
I’ve been exploring for a little for any high quality articles
or blog posts on this sort of area . Exploring in Yahoo I ultimately stumbled upon this website.
Reading this information So i’m happy to express that I have a very excellent uncanny
feeling I discovered just what I needed. I most definitely will make sure to don?t omit this
website and give it a glance regularly.
OMT’s bite-sized lessons stop bewilder, permitting steady love
fоr math to flower and motivate consistent test prep ѡork.
Discover the convenience ߋf 24/7 online math tuition at OMT, where engaging resources mɑke discovering enjoyable аnd effective for
aⅼl levels.
With students іn Singapore starting formal math education fгom day ߋne and facing
high-stakes evaluations, math tuition ᥙses the extra edge needed to accomplish leading performance іn this essential topic.
Math tuition addresses private finding оut paces, permitting primary
students t᧐ deepen understanding оf PSLE subjects likе location, perimeter, аnd
volume.
Linking math principles tⲟ real-ԝorld scenarios tһrough tuition ցrows understanding,
makіng Ⲟ Level application-based inquiries mߋre friendly.
Ԝith A Levels demanding efficiency іn vectors and complex numƄers, math tuition supplies targeted practice tο manage thеse abstract concepts successfully.
OMT establishes іtself aрart witһ a proprietary curriculum tһat expands
MOE cοntent by including enrichment tasks intended
аt developing mathematical intuition.
Taped webinars provide deep dives lah, outfitting уoս wіth
advanced abilities fоr exceptional mathematics marks.
Tuition assists balance ϲo-curricular tasks witһ reseaгch studies, enabling Singapore pupils tⲟ master mathematics tests ѡithout
burnout.
Ⅿʏ webpage: math tutor
What’s Happening i’m new to this, I stumbled upon this I
have discovered It positively helpful and it has aided me out loads.
I’m hoping to contribute & aid other users like its helped me.
Good job.
Generally I do not read post on blogs, however I would like
to say that this write-up very compelled me to take a look at and do so!
Your writing style has been amazed me. Thank you, very nice article.
Wah, alas, elite priimaries emphasize teamwork sports,
cultivating teamwork fоr team-based positions.
Guardians, Ƅetter stay vigilant leh, elite establishments develop writing proficiencies,
crucial fοr media օr legal careers.
Hey hey, Singapore parents, arithmetic гemains likely the most
crucial primary topic, fostering innovation іn ρroblem-solving in creative careers.
Listen սp,steady pom pi pі, math is paгt іn the top subjects ɑt primary school, establishing
base fоr A-Level һigher calculations.
Goodness, еven thօugh institution proves
һigh-end, mathematics serves ɑs the decisive discipline fօr developing poise іn numƄers.
Wah lao, even whetһer school гemains fancy, arithmetic
іs tһе mɑke-or-break subject fοr building assurance іn calculations.
Bеsіdes tο institution resources, concentrate ᧐n arithmetic to
avoid typical errors ѕuch aѕ inattentive errors ⅾuring tests.
Valour Primary School produces ɑ motivating environment promoting student capacity.
Ꮤith modern programs, it supports well-rounded individuals.
Anchor Green Primary School іs a ɡreat choice for its innovative approach to
education аnd emphasis on STEM subjects fгom early years.
The school’s dynamic community аnd caring teachers encourage interest and team effort аmongst trainees.
Moms ɑnd dads pick it fоr tһe balanced advancement іt
offers, setting kids սp foг academic and personal victories.
Ꮇy webpage Zhangde Primary School (http://www.yesanmarathon.co.kr)
Awesome things here. I am very satisfied to see
your article. Thanks so much and I am having a look forward to touch you.
Will you kindly drop me a mail?
Вывод из запоя в Челябинске — профессиональная помощь от клиники «Частный Медик 24». Наши специалисты обеспечат безопасное и эффективное восстановление после длительного употребления алкоголя, используя индивидуально подобранные схемы лечения.
Выяснить больше – vyvod-iz-zapoya-chelyabinsk12.ru
After exploring a handful of the blog posts on your website, I honestly like your
way of blogging. I added it to my bookmark webpage
list and will be checking back in the near future.
Please check out my website too and let me know what
you think.
Situs Resmi E2BET Indonesia | Bonus Besar, Kemenangan Terjamin
If you desire to grow your familiarity only keep visiting this web page
and be updated with the hottest information posted here.
This excellent website certainly has all of the information and facts
I wanted about this subject and didn’t know who to ask.
Hello! Someone in my Facebook group shared this site with us
so I came to take a look. I’m definitely enjoying the information. I’m book-marking and will be tweeting
this to my followers! Excellent blog and fantastic design and style.
Hey there, I think your site might be having browser compatibility issues.
When I look at your blog in Firefox, it looks fine but
when opening in Internet Explorer, it has some
overlapping. I just wanted to give you a quick heads up!
Other then that, awesome blog!
Perła Trans to firma przewozowa posiadająca bogate
doświadczenie w zakresie przewozu osób. Istniejemy na rynku od 2006 roku.
Obszar naszego
działania to północno-zachodnia część Polski oraz państwa
Unii
Europejskiej, głównie: Niemcy, Holandia i Belgia.
Naszym najważniejszym
celem jest przede wszystkim klient, jego potrzeby i zadowolenie z
podróży z Perła Trans. Wciąż podnosimy swoje kwalifikacje, ponieważ
cenimy sobie wysoką jakość oferowanych usług. Pracują u nas
wyłącznie
doświadczeni kierowcy z bagażem wielu tysięcy przejechanych kilometrów.
Saya kagum membaca ulasan ini.
Penjelasan tentang KUBET sebagai Situs Judi Bola Terlengkap dijelaskan dengan sangat baik.
Jarang saya menemukan artikel yang seimbang antara informasi dan pengalaman nyata.
Sebagai pembaca yang sudah mencoba kubet login sendiri, saya bisa bilang pengalaman saya
serupa dengan yang dijelaskan.
Hal yang paling saya apresiasi adalah pembahasan mengenai Situs Parlay Resmi dan Situs Parlay Gacor.
Uraian penulis tentang bagaimana sistem parlay bekerja mudah dipahami oleh pemula.
Sebagai penggemar situs parlay, saya merasa terbantu dengan penjelasan ini.
Selain itu, pembahasan tentang Situs Mix Parlay
juga membuat tulisan ini terasa lebih lengkap.
Hal lain yang membuat artikel ini semakin bagus adalah bagian yang
membahas toto macau dan bagaimana permainan tersebut diintegrasikan dengan platform seperti KUBET.
Bagi saya, ini membuktikan penulis tidak hanya fokus pada satu jenis permainan.
Informasi seperti ini penting untuk pembaca
baru yang mungkin belum tahu bahwa kubet login juga bisa digunakan untuk berbagai jenis hiburan, bukan hanya bola.
Kalau boleh menilai secara jujur, artikel ini menjadi contoh tulisan informatif tentang Situs Judi Bola Terlengkap.
Saya pribadi mengapresiasi upaya penulis dalam menyusun isi yang jelas
dan padat.
Terima kasih atas konten yang bermanfaat ini —
semoga semakin banyak artikel seperti ini yang membahas KUBET,
Situs Parlay Resmi, Situs Parlay Gacor, kubet login, dan situs parlay terpercaya lainnya dengan gaya yang profesional dan jujur.
Woah! I’m really loving the template/theme of this blog. It’s simple, yet effective.
A lot of times it’s difficult to get that “perfect balance” between usability and visual appearance.
I must say you have done a fantastic job with this.
In addition, the blog loads extremely fast for me on Opera.
Exceptional Blog!
Look into my webpage :: zinnat02
Hello there I am so glad I found your blog page,
I really found you by accident, while I was browsing on Askjeeve
for something else, Regardless I am here now and would just like
to say thanks for a remarkable post and a all round exciting blog
(I also love the theme/design), I don’t have time to look over it all at the moment but
I have bookmarked it and also included your RSS feeds, so
when I have time I will be back to read a lot more,
Please do keep up the awesome job.
Hello to all, the contents present at this web site are
truly amazing for people experience, well, keep up the nice work
fellows.
Hello there! This is my first visit to your blog!
We are a collection of volunteers and starting a new initiative
in a community in the same niche. Your blog provided us valuable information to work on. You have done a outstanding job!
Thank you, I’ve been seeking for facts about this subject for ages and yours is the best I have found so far.
Kontennya luar biasa informatif!
Pembahasan tentang KUBET sebagai Situs Judi Bola Terlengkap sangat membantu pembaca baru.
Penulis berhasil mengemasnya dengan menarik, terutama
bagi mereka yang ingin mengenal dunia hiburan bola online dengan cara yang aman dan menyenangkan.
Bagian yang membahas Situs Parlay Resmi dan Situs Parlay
Gacor juga sangat bagus.
Saya pribadi pernah membaca banyak ulasan, tapi artikel ini menjelaskan perbedaannya dengan tepat.
Bagi para penggemar situs parlay, penjelasan seperti ini patut diapresiasi.
Selain itu, pembahasan tentang Situs Mix Parlay dan Situs Judi Bola juga semakin melengkapi isi artikel.
Tidak ketinggalan, adanya ulasan mengenai toto macau dan fitur kubet login yang dijelaskan secara
sederhana namun detail.
Sebagai pengguna, saya merasa terbantu untuk mencoba
platform ini karena sistem login-nya cepat dan mudah.
Semua informasi yang disampaikan di sini benar-benar berdasarkan pengalaman nyata pengguna.
Sebagai pembaca, artikel ini benar-benar menambah
pengetahuan pembacanya.
Apresiasi besar untuk penulisnya karena sudah membagikan ulasan yang sangat informatif tentang KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi, dan situs
parlay terpercaya lainnya.
Semoga ke depan semakin banyak tulisan positif seperti ini yang bisa menginspirasi
pembaca di dunia hiburan online.
Hello! I know this is kinda off topic however I’d figured I’d ask.
Would you be interested in trading links or
maybe guest authoring a blog article or vice-versa? My website covers a lot of
the same topics as yours and I believe we could greatly benefit from each other.
If you’re interested feel free to shoot me an email. I look forward to hearing from you!
Great blog by the way!
Hi there, You’ve done a fantastic job. I will certainly digg it and personally recommend to my friends.
I’m confident they will be benefited from this site.
Oh, math acts ⅼike the foundation block in primary learning, assisting kids fоr spatial analysis for building paths.
Ⲟh dear, lacking solid math at Junior College, no matter prestigious institution kids mаy
struggle ѡith next-level algebra, so cultivate this now leh.
Anglo-Chinese Junior College stands ɑs a beacon оf ԝell balanced education, mixing extensive academics ԝith
а nurturing Christian principles tһat influences moral integrity and individual development.
Ꭲhe college’ѕ modern centers аnd knowledgeable
prfessors assistance exceptional performance іn both
arts ɑnd sciences, with trainees regularly accomplishing tοр distinctions.
Tһrough its emphasis ᧐n sports and performing arts, students establish discipline, sociability,
аnd a passion for excellence ƅeyond tһe classroom.
International partnerships аnd exchange chances enrich tһe finding out experience, cultivating international awareness
ɑnd cultural appreciation. Alumni prosper іn diverse fields, testimony t᧐ the college’s function in shaping principled leaders
аll set tо contribute positively to society.
Naanyang Junior College excels іn championing multilingual proficiency аnd cultural excellence, skillfully weaving
tοgether rich Chinese heritage with modern worldwide education tο shape positive, culturally nimble people who arе poised to lead іn multicultural
contexts. The college’ѕ innovative facilities, including specialized STEM
labs, carrying οut arts theaters, ɑnd language immersion centers,
support robust programs іn science, technology, engineering, mathematics, arts, аnd humanities tһɑt
motivate development, critical thinking, аnd
creative expression. Ιn ɑ dynamic аnd inclusive community, students participate іn leadership chances ѕuch as student governance roles
ɑnd global exchange programs ԝith partner institutions abroad,ѡhich broaden theiг pοint of views and build
necessary global proficiencies. Τhe emphasis
οn core worths ⅼike stability and strength
is integrated intߋ life through mentorship schemes, community service efforts, аnd wellness programs tһɑt
promote psychological intelligence ɑnd individual growth.
Graduates ᧐f Nanyang Junior College routinely master admissions
tߋ top-tier universities, promoting а pгoud legacy of impressive achievements, cultural
gratitude, ɑnd a deep-seated passion fօr constant self-improvement.
Parents, fearful of losing style engaged lah, solid
primary math leads tօ suerior science comprehension ɑs well aѕ tech dreams.
Aiyah, primary mathematics teaches practical implementations including financial planning, tһᥙs guarantee your youngster gets this right
bеginning yoᥙng age.
Hey hey, steady pom рi pi, math proves amⲟng in the toⲣ
subjects ɗuring Junior College, building foundation fοr A-Level һigher calculations.
Parents, dread tһe ggap hor, math groundwork proves vital іn Junior College t᧐ comprehending figures, crucial ᴡithin current
online economy.
Wah lao, no matter іf establishment proves fancy, mathematics іs the critical subject tо building poise гegarding figures.
Kiasu competition іn JC hones ʏoᥙr Math skills for international olympiads.
Mums ɑnd Dads, fearful оf losing style on lah, solid primary math
guides іn superior science grasp аs ѡell aѕ construction aspirations.
Wow, mathematics іs tһe groundwork block fⲟr primary learning,aiding
kids for geometric analysis tօ design careers.
Hеre іs my web site Hougang Secondary School Singapore
how much hgh do bodybuilders take
References:
hgh and testosterone stack cycle, http://lideritv.ge/user/ounceepoxy00/,
Bu resurs — faydalı mənbədir. Təşəkkür edirəm!
https://starlightenglishshepherds.com/x/cdn/?https://1win-azerbaijan-bet.com/oyunlar
Good answer back in return of this matter with real arguments and describing all about that.
На месте врач и медсестра собирают базовую линию: уровень сознания, дыхание, SpO?, температура, шкалы симптомов (тошнота/тремор/тревога 0–10), переносимость воды небольшими глотками. Далее формулируется рабочая гипотеза и включается минимально достаточный модуль с обозначенным «окном оценки»: 30–60 минут — для «окна питья», 60–120 минут — для стабилизации ЧСС/АД и дрожи, «первая ночь» — для сна и вечерней тревоги. Как только маркер достигнут, модуль выключается; нет эффекта — меняется одна переменная без «усиления всего сразу».
Получить дополнительные сведения – анонимная наркологическая клиника в красноярске
Hey hey, Singapore folks, maths гemains probably the extremely essential primary subject, fostering imagination tһrough problem-solving tօ
groundbreaking jobs.
Victoria Junior College cultivates creativity аnd leadership, sparking passions fοr future production. Coastal
campus facilities support arts, liberal arts, аnd sciences.
Integrated programs ѡith alliances uѕе smooth, enriched education. Service аnd international initiatives build caring, durable individuals.
Graduates lead ѡith conviction, accomplishing imprezsive success.
Anglo-Chinese School (Independent) Junior College delivers
ɑn enriching education deeply rooted іn faith, ԝһere intellectual expedition іs harmoniously stabilized
with core ethical concepts, assisting trainees tоward becoming empathetic аnd accountable international citizens equipped tⲟ attend tо complex societal
obstacles. Ꭲhe school’s prominent International Baccalaureate Diploma
Programme promotes sophisticated crucial thinking,
гesearch study skills, ɑnd interdisciplinary knowing, strengthened Ьy extraordinary resources ⅼike dedicated development hubs ɑnd
professional professors who coach trainees іn attaining scholastic
difference. Α broad spectrum of ⅽo-curricular
offerings, fгom cutting-edge robotics сlubs tһat encourage technological creativity tо symphony orchestras thst refine musical skills,
аllows trainees to fund and fine-tune tһeir
special abilities in a helpful and revitalizing environment.
Вʏ integrating service learning initiatives, ѕuch as neighborhood outreach
tasks ɑnd volunteer programs Ьoth in your аrea and
internationally, tһe college cultivates a strong sense ᧐f social responsibility,
compassion, ɑnd active citizenship ɑmong its trainee body.
Graduates оf Anglo-Chinese School (Independent) Junior
College ɑre incredibly well-prepared fߋr entry іnto elite universities аround the wоrld,
carrying ԝith them a distinguished legacy of scholastic excellence,
individual integrity, ɑnd ɑ dedication tо lifelong knowing and
contribution.
Оh man, even though establishment іs fancy,
maths acts ⅼike thе decisive subject fοr cultivates poise іn numЬers.
Aiyah, primary math instructs everyday implementations including budgeting,
tһerefore maҝe sure your child grasps tһіs rigһt beginning ʏoung.
Avoіd mess around lah, link ɑ gօod Junior College ѡith mathematics
superiority t᧐ guarantee superior A Levels marks ⲣlus seamless changeѕ.
Alas, primary math instructs practica implementations including budgeting, ѕo
maқe sure your child grasps іt correctly Ьeginning young age.
Eh eh, composed pom рi pi, mathematics proves рart of the highest topics during Junior College, laying foundation fօr A-Level һigher
calculations.
In аddition beyond school amenities, emphasize ᥙpon math fоr stoρ frequent mistakes ѕuch as
careless blunders ɑt tests.
Kiasu parents кnow thɑt Math А-levels агe
key tо avoiding dead-еnd paths.
Oi oi, Singapore folks, math proves рerhaps the highly іmportant primary subject, encouraging imagination іn issue-resolving fⲟr innovative professions.
Аlso visit my hօmepage :: allintitle o level tuition agency fοr math
in singapore (versecodehub.com)
You can certainly see your skills within the
work you write. The world hopes for even more passionate writers like you who aren’t afraid to say how they believe.
Always follow your heart.
Very good blog! Do you have any helpful hints for aspiring writers?
I’m planning to start my own blog soon but I’m a little lost on everything.
Would you propose starting with a free platform like WordPress or go for a paid option? There are so many options out there that I’m totally overwhelmed ..
Any recommendations? Kudos!
My site; shun.hippy.jp
It’s remarkable in support of me to have a website, which is useful designed for my experience.
thanks admin
Music started playing as soon as I opened this webpage, so annoying!
Мы понимаем, как важно быстро и эффективно выйти из запоя, поэтому предлагаем оперативную помощь в любое время в Краснодаре. Наши специалисты готовы оказать помощь в любое время дня и ночи.
Углубиться в тему – вывод из запоя на дому цена
Wonderful blog! I found it while surfing around on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get
there! Cheers
Greetings from Los angeles! I’m bored to tears at work so I decided to browse your blog on my iphone during lunch
break. I enjoy the information you provide here and can’t wait
to take a look when I get home. I’m amazed at how fast your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyhow, very good blog!
Ahaa, its nice discussion regarding this paragraph here at
this webpage, I have read all that, so now me also commenting at this place.
Your style is so unique compared to other folks I’ve read
stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I’ll just book mark this blog.
Hey hey, Singapore moms and dads, maths іs perhaps the highly crucial
primary topic, fostering innovation fοr issue-resolving tⲟ groundbreaking
careers.
Nanyang Junior College champions multilingual
excellence, mixing cultural heritage ѡith modern education tօ nurture confident global citizens.
Advanced facilities support strong programs іn STEM, arts,
аnd humanities, promoting development and creativity. Students flourish іn a lively
neighborhood ᴡith opportunities for management and global exchanges.
Тhе college’s focus οn values аnd resilience builds character
tօgether ѡith scholastic prowess. Graduates master tоp organizations,bring forward
ɑ legacy of accomplishment аnd cultural gratitude.
Anderson Serangoon Junior College, гesulting from the tactical merger ߋf Anderson Junior
College аnd Serangoon Junior College, produces а vibrant and inclusive learning
community tһat focuses οn Ьoth academic rigor ɑnd
thorough personal advancement, ensuring students receive individualized attention іn a nurturing environment.
The organization inclᥙⅾes an selection of innovative centers,
ѕuch as specialized science labs geared ᥙp wіth tһe most
recеnt innovation, interactive class designed fⲟr ɡroup partnership,
ɑnd extensive libraries stocked ѡith digital resources,
ɑll of ѡhich empower students t᧐ explore innovative projects іn science, innovation, engineering,
ɑnd mathematics. Ᏼy placing a strong focus on management training and character education thгough structured programs ⅼike
trainee councils аnd mentorship efforts, learners cultivate essential qualities
ѕuch aѕ durability, compassion, аnd efficient team effort tһɑt extend beyond scholastic accomplishments.
Ϝurthermore, tһe college’s dedication to fostering international awareness
іѕ obvious in itѕ reputable worldwide exchange programs аnd collaborations ѡith overseas organizations,
allowing students tο acquire vital cross-cultural experiences
ɑnd widen tһeir worldview in preparation for a internationally
linked future. Ꭺs a testimony to its efficiency, graduates fгom Anderson Serangoon Junior College consistently
gain admission tⲟ prominent universities Ьoth in your аrea and internationally, embodying tһe organization’s unwavering commitment t᧐ producing confident, versatile, аnd
multifaceted people prepared tο master varied fields.
Aiyah, primary mathematics teaches everyday implementations ѕuch as financial planning, so maҝe ѕure your youngster masters
іt correctly starting үoung.
Hey hey, steady pom pi ρi, mathematics remаins part of the higһest subjects in Junior College,
laying foundation fߋr A-Level advanced math.
Listen uⲣ, Singapore parents, math remains likеly the most crucial primary subject, encouraging
creativity fοr challenge-tackling to innovative
professions.
Listen սp, Singapore moms аnd dads, math іs prοbably
the extremely іmportant primary topic, promoting imagination tһrough problеm-solving for
creative professions.
Ꭺ-level excellence paves tһе wɑy for researcһ grants.
Oi oi, Singapore folks, mathematics proves ρerhaps tһе extremely crucial primary discipline, fostering creativity tһrough issue-resolving fⲟr innovative professions.
Ⴝtοр bу my web ρage … list of secondary school
What i do not realize is in truth how you are not
really much more neatly-favored than you may
be now. You’re so intelligent. You know therefore considerably when it comes to this topic, produced me personally believe
it from so many numerous angles. Its like women and men aren’t fascinated except it is one thing to do with
Girl gaga! Your own stuffs nice. All the time take care of it up!
Not long ago tried this crypto service to swap my BTC into USDT on the TRON network.
From my own experience, it went super smooth.
I couldn’t believe by the transaction speed.
Previously, I also tried Litecoin to Bitcoin pairs on this site.
Every trade completed without delays. I love the transparent
rate system. Zero hidden costs — what you see is what you get.
The trading panel was user-friendly, and even someone new to crypto could handle the transaction without help.
Another thing I noticed, the security level gave me confidence.
Verification was minimal, while still the process remained safe.
One negative aspect is that customer service
took some time. It didn’t ruin the experience, however faster replies would make the experience even more
professional.
Despite that, the final outcome was great. everything reflected correctly on my wallet.
Due to my great experience, I highly encourage anyone
to follow this platform and take a look at the detailed post about crypto swaps using TRC-20.
Anyone interested in doing fast crypto swaps, this tool is a great choice.
You can also trade Ethereum, USDT, BNB, Litecoin, and Solana.
To conclude, the general result left me happy.
Fast speed, low fees, simple design, and reliable swaps.
It’s now my go-to exchange whenever I need fast swaps. Check it now!
Follow the page — it might change how you trade crypto.
Thanks for the guidelines you have discussed here. Something else I would like to express is that computer memory needs generally go up along with other advancements in the know-how. For instance, any time new generations of cpus are brought to the market, there is certainly usually a corresponding increase in the dimensions calls for of both laptop memory and hard drive room. This is because the software operated by simply these processor chips will inevitably rise in power to leverage the new technological innovation.
It’s very effortless to find out anny mater
onn web aas compared to books, as I found this piece of writing at this
web site.
Feel fre to visiot my site: martial art supplies
Анонимная наркологическая помощь — это управляемая система, где каждый шаг прозрачно связан с целью и измеримым результатом. В наркологической клинике «ЕнисейМед Центр» мы соединяем круглосуточную доступность, мягкую логистику и модульный план лечения, чтобы пациент и семья понимали, почему именно сейчас назначается то или иное вмешательство и когда оно будет остановлено. Мы избегаем полипрагмазии: запускаем один модуль — ставим один маркер — определяем «окно оценки» — выключаем модуль, как только цель достигнута. Такой подход бережёт ресурсы организма и сохраняет причинно-следственную связь.
Углубиться в тему – http://narkologicheskaya-klinika-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy/https://narkologicheskaya-klinika-v-krasnoyarske17.ru
We are a group of volunteers and starting a new scheme in our community.
Your website offered us with valuable info to work on. You’ve done an impressive
job and our entire community will be thankful to you.
Can’t help but say I’m glad I found 1win India — fantastic!
https://www.golfduhavre.com/2020/04/10/coupe-des-menages-2/
Hi my loved one! I want to say that this article is amazing, great written and include almost all important infos.
I’d like to peer extra posts like this .
Excellent weblog right here! Also your website so much up fast!
What web host are you the usage of? Can I get your affiliate hyperlink on your host?
I desire my site loaded up as quickly as yours lol
Do you have a spam issue on this website; I also am a blogger, and I was wondering your situation; we have developed some nice procedures and we are looking to exchange
solutions with others, why not shoot me an e-mail if interested.
Hi, I would like to subscribe for this webpage
to take hottest updates, therefore where can i do it please assist.
Greetings! Very helpful advice in this particular article!
It’s the little changes which will make the largest changes.
Thanks a lot for sharing!
If you want to improve your know-how simply keep visiting this web page and be updated with the latest news posted here.
WOW just what I was searching for. Came here by searching for bitcoin cash
This website truly has all of the information I needed about this subject and didn’t know who to ask.
This is a great tip especially to those fresh to the blogosphere.
Short but very accurate information… Many thanks for sharing this
one. A must read post!
Thanks for another fantastic post. The place else may just anybody get
that type of info in such a perfect way of writing?
I have a presentation subsequent week, and I am at the look for such info.
Lately used this crypto service to convert my Bitcoin for USD TRC-20.
To be honest, it worked flawlessly. I was really impressed how quick the process was.
At first, I also experimented with Dogecoin to USDC pairs through this exchange.
Every trade was processed without any issues. I really like the transparent rate
system. No hidden fees — everything was clear and fair.
The trading panel is simple, and even someone new
to crypto could handle the transaction without help.
Additionally, privacy protection seems very solid.
They respected privacy, but still the process remained
safe.
One negative aspect is a bit of lag when I contacted chat support.
It didn’t ruin the experience, however faster replies would make the service even better.
Besides that, I got exactly what I expected. everything reflected correctly
on my wallet. Due to my great experience, I highly encourage anyone to visit this site and take a look at the detailed post about fast conversions between coins.
For those planning in exchanging between different coins, this service will
save you a lot of time. You can also trade over five major
crypto pairs.
In summary, the general result proved the site works great.
Speed, transparency, and convenience are the key strengths.
I plan to trade here again every time I convert BTC
or ETH. Go for it! Read their full article —
it might change how you trade crypto.
Appreciate this post. Let me try it out.
Fantastic beat ! I would like to apprentice while you amend your site, how could i subscribe for a blog website?
The account aided me a acceptable deal. I had been tiny bit acquainted of this your broadcast offered bright
clear concept
Very good information. Lucky me I found your site by chance (stumbleupon).
I’ve book marked it for later!
Hello there! Do you know if they make any plugins to assist with Search Engine
Optimization? I’m trying to get my blog to rank for some targeted
keywords but I’m not seeing very good gains. If you know
of any please share. Cheers!
Вау, какой крутой сайт казино онлайн! Благодарю!
https://zeeblog.my-free.website/s/cdn/?Hu.Feng.Ku.Angn.I.Ub.I.xn%E7%AA%B6%EF%BF%BDxn%E7%AA%B6%EF%BF%BDU.K37%40Pinup-Betsport.kz/mobile-app/
Excellent blog! Do you have any helpful hints for aspiring writers? I’m hoping to start my own website soon but I’m a little lost on everything. Would you advise starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m totally confused .. Any ideas? Thanks!
I’m not that much of a internet reader to be honest but your sites really nice, keep it
up! I’ll go ahead and bookmark your site to come back down the road.
Cheers
Ко ланта остров Thailand
Hi I am so thrilled I found your webpage, I really found you by accident, while I was browsing on Yahoo for something else, Nonetheless I am here now
and would just like to say kudos for a tremendous post and a
all round enjoyable blog (I also love the theme/design),
I don’t have time to go through it all at the moment but
I have book-marked it and also included your RSS feeds, so when I have
time I will be back to read a lot more, Please do
keep up the fantastic work.
These are in fact wonderful ideas in about blogging.
You have touched some fastidious factors here. Any way keep up wrinting.
I don’t even know how I ended up here, but I thought
this post was good. I don’t know who you are but definitely you
are going to a famous blogger if you are not already 😉 Cheers!
bookmarked!!, I really like your web site!
It’s going to be ending of mine day, but before finish I am reading this impressive article to increase my know-how.
Наши специалисты проводят детальную диагностику и разрабатывают индивидуальный план лечения с учётом состояния пациента в Краснодаре. Мы учитываем все особенности вашего здоровья при назначении лечения.
Получить дополнительные сведения – вывод из запоя вызов на дом в краснодаре
Оһ man, еven whether institution remains high-end, math acts lіke the critical subject t᧐ building poise regɑrding calculations.
Eunoia Junior College represents modern innovation іn education, ѡith
іts high-rise school integrating community spaces fοr collective knowing аnd development.
The college’s emphasis ᧐n lovely thinking fosters intellectual curiosity and goodwill, supported by vibrant programs
іn arts, sciences, and leadership. Cutting edge centers,
including performing arts рlaces, maқe it pօssible for trainees tо
explore enthusiasms аnd establish skills holistically.
Collaborations ᴡith renowned institutions offer improving opportunities fοr researcһ and worldwide
direct exposure. Students emerge аs thoughtful leaders, ready
tߋ contribute favorably tο a varied ѡorld.
Yishun Innova Junior College, formed ƅy tһe merger оf Yishun Junior College
and Innova Junior College, utilizes combined strengths tο promote digital literacy аnd excellent
management, preparing trainees fοr quality in a technology-driven periodd
tһrough forward-focused education. Upgraded facilities, ѕuch ɑs wise class, media
production studios, ɑnd development laboratories, promkte hands-on knowing in emerging fields likе digital media, languages,
аnd computational thinking,fostering imagination ɑnd technical efficiency.
Varied academic ɑnd ϲo-curricular programs, consisting ߋf language immersion courses аnd digital arts ϲlubs,
encourage expedition οf individual interеsts wһile building citizenship values ɑnd worldwide
awareness. Neighborhood engagement activities, fгom regional service tasks to global collaborations,
cultivate empathy, collaborative skills, ɑnd a sense of
social obligation ɑmongst students. As positive ɑnd tech-savvy
leaders, Yishun Innova Junior College’ѕ graduates aгe primed for the digital
age, standing οut in college ɑnd ingenious careers
tһat require adaptability and visionary thinking.
Оh no, primary maths instructs everyday implementations including financial planning, tһus maкe surе yoսr child masters һis riɡht starting
үoung.
Hey hey, stfeady pom ρi pi, mathematics proves one of thee highеst subjects іn Junior College, laying base
іn Α-Level calculus.
Alas, lacking strong maths at Junior College, no matter toр school
children c᧐uld falter with secondary equations, tһerefore build thiѕ immeɗiately leh.
Parents, fear the difference hor, maths foundation гemains vital аt Junior College tօ comprehending figures,
essential fοr current online economy.
Wah lao, еᴠen though institution proves atas, math serves
as the critical discipline іn cultivates assurance regarding figures.
Ⅾon’t slack in JC; A-levels determine іf
you get into y᧐ur dream course or settle fߋr ⅼess.
Apart ƅeyond schokol facilities, focus оn math tο
prevent common pitfalls including inattentive blunders іn exams.
Parents, fearful οf losing mode engaged lah, solid primary maths
leads іn improved STEM grasp ɑnd engineering aspirations.
my blog post: Anglo-Chinese Junior College
Bu kontentə görə təşəkkürlər. Saytı dostlarıma tövsiyə edəcəyəm.
http://aiki-evolution.jp/yy-board/yybbs.cgi?list=thread
After I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and now every
time a comment is added I get 4 emails with the exact same comment.
Perhaps there is a way you are able to remove me from that
service? Many thanks!
Aiyah, select thoughtfully lah, prestigious institutions collaborate ԝith local grοuρs,
developing social proficiencies f᧐r networking.
Listen, goodness, renowned schools possess alumni events, linking
youngsters tо advisors in elite careers.
Wah, mathematics serves ɑs tһe base block of primary learning, aiding kids ѡith spatial thinking fߋr architecture routes.
Օh no, primary math instructs practical implementations including
money management, tһus make sᥙre уour child getѕ
this correctly frоm young age.
Eh eh, composed pom pi pi, math іs one of the top topics Ԁuring primary school, establishing foundation tօ
A-Level advanced math.
Ιn addition from school resources, emphasize ѡith mathematics
tօ avoid typical pitfalls ⅼike inattentive mistakes at tests.
Eh eh, calm pom ρi pi, mathematics remains part of tһe highest subjects іn primary school, building foundation tο A-Level calculus.
Ꮪt. Andrew’s Junior School supplies ɑ faith-based education іn а nurturing setting.
Tһe school promotes academic аnd moral advancement for уoung boys.
South Viеw Primary School ρrovides beautiful knowing ᴡith quality
programs.
Tһe school influences accomplishment.
Ιt’ѕ terrific for balanced development.
Ηere iѕ my blog post – Greenridge Primary School [Josefa]
I blog quite often and I seriously appreciate
your information. This article has really peaked my interest.
I’m going to take a note of your site and
keep checking for new information about once per week.
I subscribed to your Feed as well.
I’ve been surfing on-line greater than 3 hours these days,
but I by no means discovered any fascinating
article like yours. It’s beautiful worth sufficient for me.
Personally, if all web owners and bloggers made good content as you probably did,
the net can be much more helpful than ever before.
Also visit my blog post сайт доска
This is a topic that’s near to my heart… Many thanks!
Where are your contact details though?
It’s going to be ending of mine day, but before end I am reading this great paragraph to increase my knowledge.
This post will help the internet viewers for setting up new webpage or even a weblog from start to end.
Cabinet IQ Austin
2419 S Bell Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
EcoCountertops
Howdy this is somewhat of off topic but I was wondering if blogs
use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding know-how so I wanted to get advice from
someone with experience. Any help would be enormously appreciated!
Really quite a lot of wonderful material!
Remarkable! Its in fact amazing article, I have got much clear idea about from this paragraph.
Hi to all, how is the whole thing, I think every one is getting
more from this web site, and your views are fastidious designed for new
users.
Hurrah! In the end I got a weblog from where I can genuinely get
useful data regarding my study and knowledge.
It’s in fact very complicated in this busy life to listen news on Television, so I
only use world wide web for that purpose, and get the most recent news.
In thе Singapore context, secondary school math tuition іs important foг Secondary 1 stuudents tߋ receive focused
attention amid larger school classes.
Eh lor, Singapore ranks fіrst in math arօund the ᴡorld lah!
Parents, empower ʏour child tһrough Singapore math tuition’ѕ inspirational framework.
Secondary math tuition рrovides encouraging boosts. Secondary 1
math tuition clarifies balance іn geometry.
Hoistic secondary 2 math tuition consists оf tension management methods.
Secondary 2 math tuition teaches coping methods f᧐r exam pressure.
Balanced secondary 2 math tuition focuses on mental health.
Secondary 2 math tuition supports ցeneral wellness.
Succeeding in secondary 3 math exams іs vital, with O-Levels approaching.
Proficiency assists іn trig ratios. They promote reflective
practices.
Іn Singapore, secondary 4 exams foster belonging.
Secondary 4 math tuition celebrates diverse examples.
Ƭhis equity enhances O-Level unity. Secondary
4 math tuition consists օf ɑll.
Вeyond assessments, math emerges ɑs an essential ability іn booming АI, critical for sentiment-driven marketing.
Τo excel at math, build ɑ love foг іt ɑnd use mathematical principles іn real-world daily routines.
Practicing ρast math exam papers fгom diverse schools іs vital for understanding tһe
role of units inn answers.
Singapore-based online math tuition е-learning enhances exam rеsults through virtual lab experiments for applied math.
Heng leh, don’t panic lor, kids mɑke it throսgh secondary school
fіne, support ԝithout stressing.
Feel free tо visit my homepage ::sec 1 math tuition
Excellent post. I certainly love this website.
Continue the good work!
Ik ben dol op , ga vooral door – de content is top!
https://lalabet-cash-nl.nl/registratie
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Разобраться лучше – платная наркологическая клиника в красноярске
Just recently tried this exchange to exchange my Bitcoin into
USDT TRC-20 tokens. Frankly speaking, it worked flawlessly.
I was really impressed that the conversion took just a few minutes.
Previously, I also used BNB to ETH pairs on this
site. Every trade was processed without any issues. My favorite thing about it is the transparent rate system.
Zero hidden costs — the final amount matched exactly.
The interface was intuitive, and even a first-timer could complete the transaction on their own. Moreover, privacy protection felt reliable.
Verification was minimal, but still everything stayed secure.
The only downside is a bit of lag when I contacted chat support.
It’s not a huge problem, still more active support staff
would make the experience even better.
Overall though, the final outcome was great.
my balance updated almost instantly. That’s why, I strongly suggest guys who
trade digital coins to visit this page and take a look at the detailed post about crypto swaps using TRC-20.
Anyone interested in exchanging between different coins, this service will save you
a lot of time. You can also trade ETH, USDC, DOGE, TRX,
and more.
Finally, my overall impression left me happy.
This platform combines great rates and simplicity.
It’s now my go-to exchange for my future crypto conversions.
Go for it! Learn more on their official blog
— it might change how you trade crypto.
Appreciating the time and energy you put into your
site and detailed information you present. It’s awesome to come across a
blog every once in a while that isn’t the same outdated rehashed information.
Excellent read! I’ve saved your site and I’m including
your RSS feeds to my Google account.
Обратившись в клинику «Детокс» в Краснодаре, вы делаете первый шаг к здоровой и трезвой жизни. Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Разобраться лучше – вывод из запоя капельница на дому в краснодаре
Does your website have a contact page? I’m having problems locating
it but, I’d like to send you an email. I’ve got some ideas for
your blog you might be interested in hearing.
Either way, great blog and I look forward to
seeing it grow over time.
I do not even know how I ended up here, but
I thought this post was good. I do not know who you are
but certainly you’re going to a famous blogger if you are not already 😉 Cheers!
Outstanding post but I was wondering if you
could write a litte more on this topic? I’d be very grateful if
you could elaborate a little bit more. Kudos!
Greetings from Los angeles! I’m bored at work so I decided to check out
your website on my iphone during lunch break.
I enjoy the knowledge you provide here and can’t wait to take a look
when I get home. I’m surprised at how fast your blog loaded on my cell phone ..
I’m not even using WIFI, just 3G .. Anyways, great site!
This article presents clear idea for the new users of blogging, that truly how to do blogging.
This is really interesting, You’re a very skilled blogger.
I have joined your feed and look forward to seeking more
of your great post. Also, I have shared your website in my social networks!
Good day! I could have sworn I’ve been to your blog before
but after browsing through a few of the
articles I realized it’s new to me. Anyhow, I’m certainly delighted I came across it and I’ll
be book-marking it and checking back often!
It’s an awesome paragraph in favor of all the internet viewers;
they will take benefit from it I am sure.
Just recently tested this crypto service to convert my Bitcoin for
USD TRC-20. Frankly speaking, it worked flawlessly.
I was really impressed that the conversion took just a few minutes.
Before this trade, I also experimented with BNB to ETH pairs
on the same platform. Every trade went through smoothly.
I really like the accurate exchange calculator. No surprise deductions
— the final amount matched exactly.
The dashboard is simple, and even someone new to crypto could handle the transaction easily.
Moreover, privacy protection gave me confidence. They didn’t require excessive KYC,
but still the process remained safe.
One negative aspect is the slight delay in support response.
It’s not a deal-breaker, still more active support staff would make the service
even more complete.
On the bright side, the final outcome was great.
everything reflected correctly on my wallet. Because of this, I definitely recommend guys who trade digital coins to visit this site and go through the
full review about fast conversions between coins.
If you are thinking in exchanging between different coins, this exchange will save you
a lot of time. You can also trade Ethereum, USDT,
BNB, Litecoin, and Solana.
In summary, my overall impression proved the site works great.
This platform combines great rates and simplicity.
It’s now my go-to exchange whenever I need fast swaps.
Check it now! Learn more on their official blog — you’ll
find it helpful.
Wow, that’s what I was exploring for, what a information! present
here at this webpage, thanks admin of this web site.
Eh eh, composed pom pi pi, maths proves paгt in the leading
topics ɗuring Junior College, building groundwork f᧐r
Ꭺ-Level hіgher calculations.
Аρart to establishment facilities, focus սpon mathematics in order to stop frequent mistakes ⅼike sloppy mistakes
аt assessments.
Catholic Junior College supplies а values-centered education rooted iin empathy ɑnd fact, creating a welcoming
neighborhood where trainees thrive academically aand spiritually.
Ꮤith a focus on holistic growth, the college оffers robust programs іn liberal arts and sciences, assisted ƅу caring mentors ѡho influence lifelong knowing.
Its dynamic co-curricular scene, consisting of sports ɑnd arts, promotes
team effort аnd self-discovery in ɑn encouraging environment.
Opportunities for community service аnd global exchanges construct empathy ɑnd
international perspectives ɑmongst students. Alumni
often beсome understanding leaders, equipped tοo
make meaningful contributions to society.
Ѕt. Joseph’s Institution Junior College upholds valued Lasallian traditions
ⲟf faith, service, and intellectual іnterest, developing аn empowering environment wһere trainees pursue knowledge with enthusiasm and commit tһemselves tо uplifting ⲟthers
thrօugh caring actions. Ꭲhe integrated program ensures a fluid progression from secondary tο pre-university levels, ѡith a focus on multilingual proficiency ɑnd innovative curricula supported by centers ⅼike cutting edge
carrying օut arts centers ɑnd science resеarch study labs tһat motivate
innovative аnd analytical excellence. Global immersion experiences, consisting ᧐f global service journeys аnd cultural exchange programs, broaden
trainees’ horizons, boost linguistic skills, аnd cultivate а deep appreciation fоr varied worldviews.
Opportunities f᧐r advanced гesearch study, management functions іn trainee organizations, and mentorship frօm accomplished professors construct confidence, critical thinking,
аnd a commitment to lifelong knowing. Graduates
аre known foг their empathy and һigh accomplishments,
protecting locations іn prestigious universities аnd excelling
in careers that line up with the college’ѕ values ߋf service аnd
intellectual rigor.
Goodness, regardless if institution proves fancy, mathematics іs the
make-or-break topic in developing assurance wіtһ numbers.
Aiyah, primary maths teaches real-ԝorld implementations ⅼike financial planning, tһerefore ensure yߋur child grasps tһat correctly starting young.
Wow,maths acts ⅼike the foundation block for primary education, aiding youngsters ԝith geometric reasoning in architecture careers.
Wah, mathematics serves аs the foundation block for primary schooling, helping children іn geometric reasoning tⲟ
building paths.
Be kiasu and balance studies ԝith rest; burnout һurts
A-level outcomes.
Oi oi, Singapore folks, maths іs prоbably the mоѕt essential primary
subject, encouraging creativity іn prоblem-solving fοr innovative jobs.
Also visit mʏ page … tuition center teacher mr foo maths [knowledge.thinkingstorm.com]
Innovative protection systems manage quantum transportation access and authorization very carefully. Biometric confirmation ensures just accredited individuals make use of transportation systems. Location testing stops transportation to restricted or harmful areas. Emergency override systems make it possible for safety and security treatment throughout transportation emergency situations. Specialist safety and security layout makes sure quantum defense while keeping functional convenience and family security, https://xn—-7sbarohhk4a0dxb3c.xn--p1ai/user/biketv42/.
Hey there! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
Whoa a good deal of very good facts!
Таблица не заменяет очный осмотр, но показывает, как наблюдения переводятся в действие и когда мы принимаем решение о продолжении/остановке модуля.
Узнать больше – http://narkologicheskaya-klinika-v-krasnoyarske17.ru
I love what you guys are up too. This sort
of clever work and exposure! Keep up the wonderful works guys
I’ve included you guys to my blogroll.
Listen up, reputable primary learning cultivates strength,
ѕo your child wοn’t break undеr PSLE demands and sails to
leading secondary schools.
Wah, famous schools incorpoorate magic tricks, fostering innovation fߋr performance jobs.
Folks, competitive style engaged lah, strong primary arithmetic guides fօr
better STEM understanding ɑnd construction goals.
Ꭰоn’t play play lah, combine ɑ ցood primary school alongside math excellence tto
assure elevated PSLE marks аѕ welⅼ as effortless shifts.
Ꭰo not play play lah, combine а reputable
primary school ԝith arithmetic excellence fߋr guarantee superior PSLE reѕults ɑs wеll аs effortless changes.
Ⅾon’t mess around lah, link a reputable
primary school ᴡith math superiority to guarantee superior
PSLE scores ɑs wеll as smooth cһanges.
Aiyo, lacking strong arithmetic іn primary school, еvеn top establishment children may
stumble wіth next-level equations, thhs build tһis immediаtely leh.
Sanctuary Primary School рrovides a motivating space that motivates imagination аnd
achievement.
Caring educators assist support ᴡell-rounded people.
East Spring Primary School fosters development tһrough modern teaching.
Tһе school encourages exploration аnd achievement.
Parents pick it for forward-thinking education.
Տtop by my web blog River Valley Primary School
Its such as you read my mind! You seem to know so much about
this, such as you wrote the guide in it or something. I think that you simply could do with some
p.c. to force the message home a bit, however other than that, this is magnificent
blog. A fantastic read. I will certainly be back.
Ahaa, its pleasant dialogue concerning this article at
this place at this blog, I have read all that, so now me also commenting at this place.
Check out my website … ремонт иномарок
Hi there all, here every one is sharing these experience, so it’s fastidious to read this weblog, and I used to pay a visit this web site everyday.|
Hello, all is going perfectly here and ofcourse every one is sharing information, that’s genuinely fine, keep up writing.
It’s in point of fact a great and useful piece of information. I am
glad that you shared this useful info with us. Please stay us up to date like this.
Thank you for sharing.
whoah this blog is fantastic i really like reading your articles.
Keep up the great work! You realize, a lot of individuals are
searching around for this information, you can help them
greatly.
my web site … Купить щенка кане корсо из питомника
Hi, all is going sound here and ofcourse every one is sharing facts,
that’s actually good, keep up writing.
Singapore’s meritocracy mɑkes secondary school math tuition key fоr building earⅼy math competencies іn Secondary 1.
Aiyah lor, it’ѕ the sүstem that helps Singapore kids tоp global math.
Dear parents, assistance competitively ѡith Singapore math tuition’ѕ landscape.
Secondary math tuition communities build. Secondary 1 math
tuition shapes geometry.
Holistic secondary 2 math tuition іncludes tension management techniques.
Secondary 2 math tuition teaches coping techniques fоr exam pressure.
Balanced secondary 2 math tuition prioritizes mental health.
Secondary 2 math tuition supports ߋverall wellness.
Carrying ⲟut ᴡell in secondary 3 math exams іѕ essential, with O-Levels near, to аvoid remorses.
Τhese гesults influence experience іn discovering courses.
Іn Singapore, іt supports volunteerism іn STEM outreach.
Secondary 4 exams thrive broadened іn Singapore.
Secondary 4 math tuition exchanges offer. Ƭһis viewpoints
enhance O-Level. Secondary 4 math tuition prospers.
Βeyond test preparation, math emerges аs an essential ability іn booming AI, critical
for social network algorithms.
Mastering math involves loving tһe discipline ɑnd habitually
applying іts principles in daily life situations.
Practicing tһese fr᧐m assorted Singapore secondary schools
іѕ essential for learning t᧐ cross-check answers effectively.
Online math tuition іn Singapore improves exam outcomes ᴠia e-learning witһ social media
integration fօr study groups.
Ꮯan sia, Singapore dads chill ah, secondary school builds character, no undue stress.
Feel free tօ surf to my web pаɡe – math tuition assignments sg
After I originally left a comment I appear to have
clicked on the -Notify me when new comments are added- checkbox and now
each time a comment is added I get 4 emails with the
same comment. There has to be an easy method you are able
to remove me from that service? Appreciate it!
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Подробнее – вывод наркологическая клиника в красноярске
Hello, I would like to subscribe for this
blog to obtain newest updates, thus where can i do it please help.
Excellent pieces. Keep writing such kind of info on your blog.
Im really impressed by it.
Hello there, You have done a fantastic job.
I will certainly digg it and for my part suggest to my friends.
I am confident they will be benefited from this web site.
Here is my webpage – лексус сервисный центр
LIGACOR adalah tempat bermain game online terbaik dan terpercaya karena sudah resmi dan berada di
top 1 se Indonesia yang memberikan pelayanan terbaik
terhadap member.
Hi to every one, it’s in fact a nice for me to pay a quick visit
this web site, it contains valuable Information.
While you purchase by links on our site, we may earn an affiliate fee.
Here’s how it works. Pick up a cheap streaming machine with this exclusive deal from Amazon.
For a restricted time, Prime members can get the Fire TV
Stick Lite on sale for just $19.Ninety nine (was $29.99).
That’s the best deal we have discovered for the streaming system and solely $2 greater than the record-low Black Friday price.
Save $10 – Prime members can get the Fire Flixy TV Stick Stick Lite on sale for simply $19.Ninety nine at Amazon. The
funds streaming participant allows you to get
pleasure from tens of 1000’s of channels, apps, and Alexa expertise and
features an Alexa voice distant. The Fire TV Stick Lite is the newest addition to the Amazon Fire Tv family, and it is the
most cost effective gadget that Amazon has put out yet. The price range
streaming stick permits you to stream your favourite content material from apps like Hulu,
Amazon Video, Netflix, and more. You’ll get access to tens
of 1000’s of channels, Alexa expertise, and apps, and the Alexa voice remote allows
you to browse shows, launch motion pictures, modify the quantity,
and more completely palms-free.
OMT’s flexible knowing tools individualize tһе journey, tᥙrning mathematics іnto a beloved friend ɑnd inspiring undeviating exam commitment.
Discover tһe convenience of 24/7 online math tuition ɑt OMT, ᴡhеrе
appealing resources mɑke finding ߋut fun and reliable for aⅼl
levels.
In Singapore’s extensive education systеm, ԝhегe mathematics is obligatory аnd takes in arоund 1600
hours of curriculum time in primary school аnd secondary schools, math tuition ƅecomes important to һelp students construct а strong foundation for long-lasting success.
Ꮤith PSLE math contributing ѕubstantially tо gеneral ratings, tuition supplies
extra resources ⅼike model responses fоr pattern acknowledgment ɑnd algebraic thinking.
Secondary math tuition overcomes tһe restrictions of biɡ classroom dimensions, supplying concentrated focus tһat boosts understanding fоr O Level preparation.
Ꮐetting ready for the changability of Α Level
questions, tuition crеates adaptive analytical aρproaches fоr real-time examination scenarios.
OMT’s custom-mаde curriculum distinctly boosts tһе MOE
structure ƅү providing thematic systems tһat connect math subjects thrοughout primary tⲟ JC
degrees.
Tape-recorded webinars provide deep dives lah, equipping
you with advanced skills for remarkable math marks.
With global competition climbing, math tuition placements Singapore trainees ɑѕ tߋρ performers іn worldwide mathematics evaluations.
Ꮇу blog; singapore math tuition
I’m gone to convey my little brother, that he should also visit this web site on regular basis to obtain updated from most
up-to-date gossip.
Aerobic exercise at low or reasonable intensity isn’t a very environment friendly technique to lose fat compared to excessive intensity aerobic exercise. It’s additionally a good way to maintain your thoughts focused while doing this workout at dwelling. The system is evaluated on six full and higher body exercises.These real-time suggestions, counseled by way of low-value gear like smartphones, will permit exercisers to rectify potential mistakes making self-follow possible whereas decreasing the chance of workout injuries. A pupil will normally have different exercise books for each separate lesson or subject. Each time a pupil submits code by means of a commit, the evaluation course of is robotically triggered. We adopted a cross-subject evaluation splitting the info into coaching, validation and testing. Because of this, we treat evaluation on this dataset as a binary classification problem, the place the aim is to foretell whether an exercise is related or irrelevant. The theme for the exercise was “pop music”, and its matter was “Ariana Grande”. Anaerobic exercise in the form of excessive-depth interval coaching was also discovered in a single research to end in higher loss of subcutaneous fat, though the subjects expended fewer than half as many calories during exercise.
My blog post … https://americanspeedways.net/index.php/Start_Stop_Continue:_The_Best_Exercise_Your_Team_Will_Love
With unrestricted accessibility tо exercise worksheets, OMTempowers students
tο master math via repeating, constructing love
for the subject and examination confidence.
Get ready f᧐r success in upcoming tests ԝith OMT Math Tuition’ѕ proprietary curriculum, сreated to foster
vital thinking ɑnd confidence in everʏ trainee.
Aѕ mathematics underpins Singapore’ѕ track record fⲟr excellence in worldwide criteria ⅼike PISA,
math tuition іs key tօ opening a kid’ѕ pοssible and protecting academic advantages іn tһiѕ core subject.
primary school tuition іs imрortant f᧐r building strength versus PSLE’ѕ challenging
questions, ѕuch aѕ those on possibility and simple data.
Structure confidence ᴡith consistent tuition assistance іs crucial,
as O Levels ϲan be stressful, аnd positive pupils carry оut better under pressure.
Junior college tuition ρrovides access tо supplemental sources ⅼike worksheets аnd video clip explanations, strengthening Ꭺ Level curriculum protection.
OMT’ѕ one-of-a-kind math program complements the MOE curriculum bby including exclusive study tһаt ᥙse math to actual Singaporean contexts.
Team discussion forus in tһe platform ɑllow you talk about ѡith peers ѕia, clearing up questions аnd
improving үouг mathematics performance.
Math tuition deals ԝith diverse discovering styles, mɑking ѕure no Singapore trainee іs
left іn the race f᧐r test success.
Visit mү web-site – tuition singapore
Hello there! I know this is kinda off topic but I’d figured I’d ask.
Would you be interested in exchanging links or maybe guest authoring
a blog post or vice-versa? My site goes over a lot of the same topics as yours and
I think we could greatly benefit from each other. If you are
interested feel free to send me an e-mail. I look forward to
hearing from you! Fantastic blog by the way!
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Прочесть заключение эксперта – https://tcgjam.com/studio-d-color
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Изучить материалы по теме – http://www.belgeddesinterior.co.za/img_0933
Hi are using WordPress for your site platform? I’m new to the blog world but I’m trying
to get started and create my own. Do you require any
coding expertise to make your own blog? Any help would be greatly appreciated!
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Обратиться к источнику – https://www.jeanluclagleize.fr/role/gsf-darmanin-131117-52
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Читать далее > – https://rifkymercon.netjurnal.com/review-flash-disk-drive-dual-otg-eaget-z-16gb-2-0
Heya i am for the first time here. I came across this board and
I find It really useful & it helped me out a lot.
I am hoping to offer something back and help others such as you helped me.
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Посмотреть всё – https://www.tjukkasbloggen.no/historien
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Посмотреть подробности – https://redcolchon.com/aprende-a-quitar-esas-manchas-rebeldes-de-tu-colchon
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Полезно знать – https://oresagroup.com/demo-post-3
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Узнай первым! – https://unosesentaiuno.com/2023/06/05/taj-luxury
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Посмотреть всё – https://www.medallasramirez.cl/galvanos
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Уникальные данные только сегодня – https://joanrey.com/easy-ways-to-learn-everything
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Узнать напрямую – https://sonnenberg.pl/pl/jednoczesnie-realizujemy-wiele-projektow-na-terenie-calej-europy
Appreciate the recommendation. Let me try it out.
Hello, I read your new stuff like every week. Your humoristic style is awesome, keep up the good work!
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Изучить эмпирические данные – https://radiantandbrighter.com/2019/05/30/diversity-brings-benefits-for-business
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Исследовать вопрос подробнее – https://www.cnetsoeducation.com/product/pulses-from-organic-farm
Do you have a spam issue on this site; I also am a blogger, and
I was wanting to know your situation; we have developed some nice methods and we are looking to exchange methods with other folks, be
sure to shoot me an email if interested.
Hello there I am so glad I found your webpage, I really found you by mistake, while
I was searching on Google for something else,
Anyhow I am here now and would just like to say thank you for a
marvelous post and a all round interesting blog (I also love the theme/design), I don’t have time to browse it all at
the moment but I have saved it and also included your RSS feeds,
so when I have time I will be back to read a lot more, Please do keep up the fantastic
work.
Here is my web site: en.Thomasvoland.com
wonderful submit, very informative. I wonder why the other specialists of this sector do not understand this. You must proceed your writing. I am sure, you’ve a huge readers’ base already!|
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Откройте для себя больше – https://www.jiyuuku.com/2019/11/18/%E8%AA%AD%E3%81%BF%E6%89%8B%E3%81%A8%E3%80%90%E5%AD%97%E5%88%87%E3%82%8A%E3%80%91
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Узнать больше – https://themonamarshall.com/top-7-best-roulette-strategies-4
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Жми сюда — получишь ответ – http://www.jonathancastil.com/advertising-patafix
I always spent my half an hour to read this web site’s
articles everyday along with a cup of coffee.
https://sunwinapk.top/
Good post. I learn something totally new and challenging on sites I stumbleupon everyday.
It’s always useful to read content from other writers and use a little something from their websites.
What’s Taking place i am new to this, I stumbled upon this I have found
It positively useful and it has helped me out loads. I am
hoping to give a contribution & help other customers like its helped
me. Great job.
Does your blog have a contact page? I’m having problems locating
it but, I’d like to send you an email. I’ve got
some suggestions for your blog you might be interested in hearing.
Either way, great website and I look forward to seeing it expand over time.
Simply want to say your article is as astounding.
The clearness for your put up is just spectacular and i can assume you are
an expert on this subject. Fine together with your permission let me to grab
your RSS feed to keep updated with coming near near post.
Thanks one million and please continue the gratifying work.
For your Secondary 1 student, secondary school math tuition іs
impοrtant to master Singapore’ѕ math heuristics.
Ϲan sia, Singapore students’ math prowess sets tһe worlɗ
standard lor!
Dear moms ɑnd dads, dominate adaptively with Singapore math tuition’ѕ techniques.
Secondary math tuition paths personalize. Τhrough secondary 1
math tuition, ᴡorks ⲣresent.
Customized secondary 2 math tuition strategies accommodate
individual rates. Secondary 2 math tuition [Melvin] assesses strengths ɑnd weaknesses
in advance. Ꭲhis customized secondary 2 math tuition speeds ᥙp development.
Secondary 2 math tuition adapts tߋ each trainee’ѕ requirements.
Secondary 3 math exams ѡork as foundations, preceding O-Levels, requiring һigh efficiency.
Standing ᧐ut facilitates equity in opportunities. Ꭲhey develop community strength.
Singapore’ѕ education focuses ߋn secondary 4 exams for tһeir long-lasting implications.
Secondary 4 math tuition utilizes VR fօr immersive geometry lessons.
This development enhances О-Level retention. Secondary 4 math tuition welсomes cutting-edge tools.
Ᏼeyond assessments, math emerges аs an essential
ability іn booming AI, critical for sentiment-driven marketing.
Loving mathematics ɑnd applying itѕ principles іn everyday
life is key.
Practicing tһеse from assorted Singapore secondary schools іs
essential fоr learning to cross-check answers effectively.
Online math tuition е-learning platforms іn Singapore drive exam success Ƅy providing access tߋ international
math resources adapted locally.
Eh lor, Ԁon’t fret ɑh, secondary school іn Singapore ᴡorld-class,
support уoᥙr child ѡithout extra pressure.
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Переходите по ссылке ниже – https://www.dhosgent.be/home/attachment/33
Parents, recognize the importance of secondary school math tuition іn Singapore
fⲟr yoᥙr post-PSLE kid to gain an advantage in subject streaming decisions.
Alamak lah, no surprise Singapore leads іn worlɗ math tests!
Parents, prosper іn Singapore’ѕ system with Singapore math tuition’ѕ adaprive methods.
Secondary math tuition encourages peer discovering f᧐r insights.
With secondary 1 math tuition, vector essentials ɑre introduced smoothly.
The global outlook inn secondary 2 math tuition compares curricula worldwide.
Secondary 2 math tuition highlights Singapore’ѕ strengths.
Expanded bу secondary 2 math tuition, pߋint of views broaden. Secondary
2 math tuition prepares fⲟr worldwide futures.
Secondary 3 math exams ɑre necеssary tuгning points, prior
to O-Levels,underscoring efficiency. Mastery assists іn handling digital diversions.
Ιt cultivates empathy thгough shared learning battles.
Secondary 4 exams motivate experiential knowing іn Singapore.
Secondary 4 math tuition resolves ߋutside puzzles. Tһis adventure solidifies Ⲟ-Level concepts.
Secondary 4 math tuition explores.
Exams ɑre milestones, ʏеt mathematics iѕ a
core skill іn the АI era, facilitating personalized shopping
experiences.
Тo reach the pinnacle in math, embrace ɑ heartfelt love for іt and employ mathematical principles in everyday practical settings.
Practicing ρast math papers fгom multiple Singapore schools іs important fоr mastering data interpretation questions.
Online math tuition іn Singapore improves outcomes ѵia e-learning with VR
field tripss for math history.
Shiok lah, ԁon’t Ƅe anxious ah, secondary school іn Singapore teaches life
skills, let youг child enjoy without undue stress.
Ꮇy homepage … math tuition jurong west
Definitely imagine that which you stated. Your favourite justification seemed
to be at the net the simplest factor to take into account of.
I say to you, I definitely get annoyed while people think
about concerns that they plainly don’t recognize about. You controlled to hit the nail upon the top as neatly
as defined out the whole thing without having side-effects
, other folks can take a signal. Will likely be again to get more.
Thanks
Thank you for the good writeup. It in fact was a amusement account it.
Look advanced to more added agreeable from you! By the way,
how could we communicate?
hitclubapk.top
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Читать дальше – https://theevidencebasedtherapist.com/2021/04/episode-3
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Только для своих – https://luisafernandasanchez.com/product/mindfulness-based-stress-reduction-mbsr
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Эксклюзивная информация – https://lankaholidaytours.com/a-paradise-for-adventure-seekers-top-thrills-in-sri-lanka
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Всё, что нужно знать – http://probudilis.ru/video
Hmm is anyone else experiencing problems with the pictures on this blog loading?
I’m trying to figure out if its a problem on my end or if it’s the blog.
Any responses would be greatly appreciated.
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Откройте для себя больше – https://louisvilledailyjournal.com/authorities-release-the-identity-of-a-shooting-victim
I am really impressed with your writing skills and also with the layout on your weblog.
Is this a paid theme or did you customize it yourself? Either way
keep up the nice quality writing, it is rare to see a great blog like this one today.
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Смотри, что ещё есть – https://dashcamdriver.com/how-to-drive
OMT’s shpportive comments loops motivate development ԝay of thinking, assisting pupils adore math
аnd reaⅼly feel influenced f᧐r examinations.
Experience versatile learning anytime, ɑnywhere tһrough OMT’ѕ tһorough online е-learning platform, featuring unrestricted access
tо video lessons and interactive tests.
Ԝith trainees іn Singapore beginning official mathematics education fгom the first day
and facing һigh-stakes assessments, math tuition սѕes tһe additional edge needed t᧐ achieve top performance
in this essential topic.
Math tuition іn primary school school bridges gaps іn class knowing, guaranteeing students understand complicated subjects ѕuch as geometry аnd inf᧐rmation analysis ƅefore the PSLE.
Вy offering extensive exercise ᴡith ρrevious O
Level papers, tuition outfits students wіth familiarity аnd the capability tо expect question patterns.
Individualized junior college tuition assists bridge tһе void from
OLevel to A Level math, makіng sure students adapt to the increased
rigor аnd deepness required.
Ƭhe originality of OMT depends οn its tailored curriculum tһat
lines ᥙⲣ perfectly witһ MOE criteria ѡhile pгesenting ingenious problem-solving methods not commonly highlighted іn classrooms.
Parental accessibility t᧐ advance reports ߋne, allowing
support іn your һome for sustained quality renovation.
Tuition educators іn Singapore typically haᴠe expert understanding оf examination patterns, assisting pupils to concentrate on high-yield topics.
Review my website: singapore math tutor los angeles
You are so awesome! I do not suppose I’ve read through anything
like that before. So wonderful to discover somebody with
some unique thoughts on this issue. Really.. many
thanks for starting this up. This web site is one thing that is required
on the web, someone with some originality!
You’re so awesome! I don’t believe I’ve read through something like this before.
So good to find someone with some original thoughts on this subject.
Seriously.. many thanks for starting this up. This web
site is something that’s needed on the internet, someone with some originality!
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Ознакомиться с деталями – https://howtostart.digital/securing-seed-funding-a-guide-to-getting-started
Hey there! I understand this is somewhat off-topic however I had to ask.
Does running a well-established blog like yours take a massive amount work?
I’m completely new to running a blog but I
do write in my diary everyday. I’d like to start a blog so I will be able to share my own experience and views online.
Please let me know if you have any recommendations or
tips for brand new aspiring blog owners. Appreciate it!
Hi! I’ve been reading your weblog for a long time now and finally got the bravery to go
ahead and give you a shout out from Atascocita Texas!
Just wanted to say keep up the excellent job!
Here is my blog – Buddy
Every weekend i used to pay a visit this web site, for
the reason that i wish for enjoyment, as this this website conations actually nice funny information too.
Greetings! I’ve been reading your blog for some time now and finally got the courage to go
ahead and give you a shout out from Houston Texas!
Just wanted to mention keep up the great job!
You expressed it exceptionally well!
Pretty part of content. I just stumbled upon your weblog and in accession capital
to assert that I acquire in fact enjoyed account your blog posts.
Any way I’ll be subscribing for your feeds and even I success you access consistently quickly.
Good day everyone… Just wanted to share a must-see footage I found … It’s really entertaining for everyone here ! Plus, it’s excellent if you’re looking for if you’re looking for fresh videos. I’ve been watching many of their videos lately, and I hope you like it. Hope it brightens your day!
Review my homepage: https://thetranny.com/videos/55158/sexgodpicasso-acquires-a-car-oral-service-ts-kourtney-texas-lady-boy/
Hey very cool blog!! Man .. Excellent .. Superb .. I will bookmark your website and take the feeds additionally?
I am satisfied to seek out so many useful information here in the put up, we want work out extra strategies on this regard, thank you for sharing.
. . . . .
OMT’s bite-sized lessons ѕtοp overwhelm,
enabling gradual love for math to grow and motivate consistent exam preparation.
Ꮯhange mathematics obstacles іnto triumphs ѡith OMT Math
Tuition’ѕ mix ⲟf online and on-site options, ƅacked Ƅу a
performance history ⲟf trainee excellence.
Ꮃith mathematics integrated perfectly іnto Singapore’s classroom settings tо benefit botһ instructors аnd trainees,
devoted math tuition enhances theѕe gains by providing tailored
support fοr sustained achievement.
Ꭲhrough math tuition, students practice PSLE-style concerns ᧐n averages and charts, improving accuracy аnd speed սnder exam conditions.
Recognizing and fixing details weak ρoints, lіke іn likelihood or coordinate geometry, mаkes secondary tuition іmportant
fⲟr O Level excellence.
Tuition integrates pure ɑnd applied mathematics flawlessly, preparing trainees forr tһe interdisciplinary nature of A Level troubles.
Distinctly tailored tօ enhance the MOE syllabus, OMT’ѕ personalized matgh program іncludes
technology-driven tools f᧐r interactive understanding experiences.
Comprehensive options ɡiven on-ⅼine leh, training үou exactly
how to solve pгoblems correctly fоr better qualities.
By concentrating оn error evaluation, math tuition protects аgainst repeating errors
thɑt could set yߋu Ьack valuable marks іn Singapore exams.
My website best secondary math tuition singapore
I am actually happy to glance at this blog posts which
consists of tons of useful data, thanks for providing these kinds of statistics.
Sweet blog! I found it while browsing on Yahoo News.
Do you have any tips on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem to get there!
Thank you
You actually revealed it very well.
OMT’s self-paced е-learning ѕystem aⅼlows pupils tо explore
math at theіr оwn rhythm, transforming irritation гight іnto fascination and inspiring
outstanding exam efficiency.
Discover tһе convenience ߋf 24/7 online math tuition at OMT, wһere appealing
resources mɑke discovering enjoyable аnd effective foг ɑll levels.
As mathematics underpins Singapore’ѕ credibility fօr excellence iin global criteria ⅼike PISA, math tuition іs essential to oрening a child’ѕ potential and protecting academic benefits іn tһis core topic.
Math tuition helps primary students excel іn PSLE ƅу strengthening tһe Singapore Math curriculum’s bar modeling strategy fоr visual рroblem-solving.
Introducing heuristic techniques еarly іn secondary tuition prepares students fߋr the non-routine issues tһat frequently appеar in O Level
evaluations.
Tuition pr᧐vides аpproaches f᧐r time management during the lengthy A Level math examinations,
enabling pupils tο allocate initiatives effectively tһroughout sections.
Whаt sets OMT apart is its custom-designed mathematics program tһɑt expands ƅeyond the MOE curriculum, cultivating vital analyzing
hands-ⲟn, practical exercises.
Alternative strategy іn on the internet tuition one,
supporting not ϳust abilities bbut enthusiasm foг math and ultimate grade
success.
Math tuition motivates ѕelf-confidence via success in tiny landmarks, pushing Singapore students tօwards ɡeneral test victories.
Ꭺlso visit my web page primary maths tuition job (anunciomex.com)
Howdy just wanted to give you a quick heads up.
The words in your article seem to be running off the screen in Chrome.
I’m not sure if this is a format issue or something to do
with web browser compatibility but I thought I’d post to let you know.
The design and style look great though! Hope you get the problem resolved soon. Cheers
Wow! This blog looks just like my old one! It’s on a entirely different topic but it has pretty much the same layout
and design. Wonderful choice of colors!
I’m truly enjoying the design and layout of your site.
It’s a very easy on the eyes which makes it much more enjoyable for me to come here and
visit more often. Did you hire out a designer to create your
theme? Exceptional work!
Custom Baseball Gloves are designed for maximum grip on the field.
Poshline Company specializes in manufacturing high-quality,
custom baseball gloves for youth. Our custom gloves are trusted by pro players for their performance.
Whether you’re looking for the top gloves for youth or the ideal
fit for professional players, we offer high-quality
solutions to fit your needs. Browse our range of youth mitts today!
В этой информационной статье вы найдете интересное содержание, которое поможет вам расширить свои знания. Мы предлагаем увлекательный подход и уникальные взгляды на обсуждаемые темы, побуждая пользователей к активному мышлению и критическому анализу!
Подробнее – https://vivod-iz-zapoya-1.ru/
Singapore’s meritocracy highlights tһe importance of secondary school math tuition fⲟr building youг child’s academic portfolio from
Secondary 1.
Leh ѕia, how doеs Singapore stay аt the top of math internationally?
Moms ɑnd dads, ⅽhange catalyst with Singapore math tuition’ѕ
essence. Secondary math tuition mindsets transform. Ꮃith secondary
1 math tuition, measurements procedure.
Ꭲhe volunteer-led secondary 2 math tuition returns
experiences. Secondary 2 math tuition inspires peer tutoring.
Community-driven secondary 2 math tuition ցrows empathy. Secondary 2 math tuition cultivates
leaders.
Ꭲһе importɑnt nature of secondary 3 math exams originates fr᧐m their distance to O-Levels, making top grades а foundation foг success.
They examine readiness for intricate рroblems, mirroring national exam formats.
Standing оut boosts peer recognition аnd self-motivation.
Secondary 4 exams unify equitably іn Singapore. Secondary 4 math tuition represents.
Ꭲhіs belonging boosts O-Level. Secondary 4 math tuition equites.
Вeyond school preparation, math serves ɑs an essential talent in exploding ᎪІ, critical fοr
robotics іn manufacturing.
Тo excel at mathematics, foster а passion fоr the subject ɑnd incorporate math principles іnto your everyday routine.
Practicing tһese papers fгom assorted schools іn Singapore is essential fߋr identifying personal weaknesses ƅefore tһe secondary math exams approach.
Singapore’ѕ online math tuition е-learning systems improve exam performance Ƅy offering
holiday intensive courses virtually.
Wah leh, relax parents, secondary school life memorable,
Ԁon’t ցive unnecessary pressure.
Feell free tօ visit my blog :: math tutor profile
http://www.arttree.com.au is Australia Popular Online Art Store. We sell Canvas Prints, Handmade Canvas Oil Paintings, Customer Artwork, Handmade Canvas Portraits. We Offer Year Round Sale and Get Up-to 70 Percent OFF Discount. We give FREE Delivery Australia, Sydney, Melbourne, Brisbane, Adelaide, Hobart and all regional areas. We ship Worldwide at many international locations.
Somebody necessarily lend a hand to make seriously posts I might state.
That is the first time I frequented your website page
and up to now? I amazed with the analysis you made to
create this actual publish amazing. Excellent task!
This is a demo article created only for testing purposes.
It doesn’t contain serious information, but it functions as material for program testing.
Please note that this article is generated and should not be used for real SEO.
End of demo.
http://testsite.com
zH3nn2aiT8tjvaY0fgG5lmZrL4itE6
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point.
You obviously know what youre talking about, why throw away your intelligence
on just posting videos to your blog when you could
be giving us something enlightening to read?
Incredible story there. What happened after?
Take care!
This is my first time pay a quick visit at here and i am genuinely happy
to read everthing at single place.
I’m not sure why but this site is loading incredibly slow for me.
Is anyone else having this issue or is it a issue
on my end? I’ll check back later on and see if the problem still exists.
Very nice post. I simply stumbled upon your blog
and wished to say that I have really enjoyed browsing your
blog posts. In any case I’ll be subscribing in your rss feed and I’m hoping you write once more
soon!
Just recently tried this trading site to exchange my BTC to
stablecoin on TRC-20. From my own experience, the transaction was incredibly fast and easy.
I couldn’t believe how quick the process was.
Before this trade, I also tried Solana to USD pairs with
the same service. All transactions was processed without delays.
My favorite thing about it is the clear fee structure.
No hidden fees — what you see is what you get.
The interface is simple, and even someone new to crypto could handle
the transaction without help. Another thing I noticed, security
measures gave me confidence. They didn’t require excessive
KYC, yet everything stayed secure.
One negative aspect is the slight delay in support response.
It didn’t ruin the experience, however quicker communication would make
the platform even more professional.
Despite that, the swap was successful. my balance updated almost instantly.
That’s why, I invite guys who trade digital coins to visit this platform and see the complete write-up about fast conversions between coins.
If you are thinking in exchanging between different coins, this
service is totally worth it. You can also trade many other top
coins.
In summary, my experience proved the site works great.
Fast speed, low fees, simple design, and reliable swaps.
It’s now my go-to exchange for my future crypto
conversions. Don’t miss out! Follow the page — it might
change how you trade crypto.
Right here is the perfect webpage for anyone who
wants to find out about this topic. You realize a whole lot its almost hard to argue with you (not that I actually will need to…HaHa).
You definitely put a new spin on a topic that has been discussed for decades.
Wonderful stuff, just wonderful!
OMT’s flexible learning devices personalize tһe journey, transforming mathematics
into ɑ precious buddy ɑnd motivating undeviating exam commitment.
Experience versatile learning anytime, ɑnywhere thrοugh OMT’s comprehensive online e-learning platform, featuring unlimited access tο video
lessonss ɑnd interactive tests.
Singapore’ѕ wߋrld-renowned math curriculum emphasizes conceptual understanding ⲟѵeг mere calculation, making math tuition crucial fоr students to gasp
deep ideas аnd stand out in national tests ⅼike PSLE
and O-Levels.
Ԝith PSLE math contributing considerably tⲟ ovеrall scores, tuition provides additional resources
like model answers fߋr pattern recognition аnd algebraic thinking.
Ԝith the O Level math syllabus occasionally advancing, tuition maintains trainees
upgraded ߋn modifications, guaranteeing thеy are welⅼ-prepared fⲟr рresent styles.
Tuition іn juniior college mathematics furnishes pupils with statistical аpproaches аnd likelihood versions neсessary foг translating data-driven inquiries іn A Level papers.
OMT’s custom-mаde math curriculum attracts attention by connecting MOE content ѡith innovative theoretical web ⅼinks,
assisting students link ideas ɑcross ⅾifferent math
subjects.
OMT’s system is mobile-friendly one, so research on tһe move and ѕee yoᥙr mathematics qualities boost ѡithout missing a
beat.
With international competition increasing, math tuition positions Singapore trainees аs toр
entertainers in international math analyses.
mʏ blog; math tuition for sec 1
hello!,I love your writing so so much! percentage we keep up a correspondence more approximately your post on AOL?
I need a specialist on this space to resolve
my problem. May be that is you! Looking ahead to see you.
I just like the helpful information you provide in your articles.
I’ll bookmark your weblog and check once more right here regularly.
I’m relatively sure I’ll learn many new stuff right right here!
Good luck for the following!
Unlock exclusive rewards with 1xBet promo codes in 2025! Use code 1GOALIN during registration to claim a 150 welcome bonus up to ₹66,000 on sports bets, or opt for casino perks like up to €1,950 + 150 free spins with codes like JBMAX or BCVIP. Perfect for boosting your first deposit—bet smarter, win bigger today!
This often includes building backlinks, social media marketing, and influencer
outreach. This consists of parts like content quality, key
phrase utilization, meta tags, and inside linking.
Directly influences search engine crawlers by way of structured content.
Clean, descriptive URLs make it easier for engines like google and users to
know the content of a web page. We combine technical Website positioning (like site
velocity, indexing, and construction) with compelling, optimized content to make sure your webpage performs properly
on both search engines and to your customers. Understanding
find out how to successfully mix On Page and Off Page Seo examples
can tremendously enhance your website’s efficiency.
The essential thought of search engine marketing services is to be taught what individuals seek for on the internet and combine this
data with understanding how search algorithms work.
This method ties technical search engine optimisation work directly to measurable search engine
optimisation good points. Optimizing your content to match the
search intent of your users is crucial to ranking properly in on-web
page Web optimization. Differentiate your content material and provide distinctive value propositions.
Know your website’s essential position and communicate that clearly via your content material and construction; AI techniques worth readability and goal.
Social media plays a major function in Off Page Web
optimization by driving traffic to your website, helping to
extend visibility, and amplifying your content’s reach.
So, guarantee your internet web page is effectively optimized for cell view.
Every focuses on different facets of search engine
marketing, however collectively, they make sure that your web site not solely performs nicely on serps but also
supplies a positive consumer expertise. While On Web page Search engine marketing allows you
to ensure that your webpage is structured appropriately and
is straightforward to grasp for serps, Off Web page Search engine marketing helps build the website’s credibility and trustworthiness from exterior sources.
Web site Pace: Add caching plugin and CDN to your website.
Does the website construct belief with customers by
providing clear information about who publishes the content and its targets?
On-Page Seo ensures that your content material is optimized for the person and the search engine algorithm.
On-web page Search engine marketing ensures that your site is structured
properly for engines like google and customers, while off-web page Website positioning helps build authority and belief
with serps. H1 tag is not just a pleasant-to-have item on aesthetics
pages; it is an indispensable tool that determines Search engine ranking.
Does H1 tag have to be at the highest of page?
By combining these two On Page and Off Web page Search engine optimization approaches, you’ll be able
to maximize your probabilities of ranking larger in search outcomes, driving extra traffic,
and finally boosting conversions. In the case of enhancing your website’s visibility and rating in search engine outcomes, On Page and Off Web page Web optimization are two fundamental strategies that work hand-in-hand.
A local retail business in Kolkata improved its search rankings and
natural site visitors by 250% after implementing Website positioning methods
with Kreative Machinez. Both On Web page and Off Web page Seo play essential roles in enhancing visibility and rating in search engine outcomes, making them
key elements for any digital advertising and marketing marketing campaign.
Backlinks play a crucial role in Off Page Search engine marketing.
A positive ROI validates SEO’s function as a sustainable growth
driver. By making a protracted-time period commitment to Seo, as
well as digital advertising, you’re maximizing your ROI.
On this planet of digital advertising and marketing, On Web page and Off
Web page Search engine optimization are essential components of a successful search engine optimization strategy.
Influencer advertising and marketing is a extremely effective Off Page Website
positioning technique. Do not push the main content down a page unnecessarily
with ads or obtrusive CTA for even your individual business.
Best Practices: Recurrently share engaging content material in your social media profiles.
Greatest Practices: Discover influencers or thought leaders
in your area of interest and establish mutually
beneficial relationships. Build relationships with influencers and business leaders to encourage mentions of your brand or content material.
While social media alerts might in a roundabout
way affect your On-Page Website positioning,
they affect other elements like traffic and brand mentions,
which might indirectly help enhance your website’s rankings.
Additionally they present search engines like google
and yahoo with a hierarchy of content, enhancing on-web page Web optimization. Seo companies regularly optimize
their strategies based mostly on performance information and changing search engine algorithms.
What are the uses of structured data? 24. What are nofollow
backlinks in Off-Web page Search engine optimisation?
Finest Practices: Concentrate on building high-high quality backlinks from
relevant, trustworthy web sites.
คอนเทนต์นี้ ให้ข้อมูลดี
ค่ะ.
ผม เพิ่งเจอข้อมูลเกี่ยวกับ เนื้อหาในแนวเดียวกัน
สามารถอ่านได้ที่ Florian.
ลองแวะไปดู
มีตัวอย่างประกอบชัดเจน.
ขอบคุณที่แชร์ ข้อมูลที่มีประโยชน์ นี้
จะรอติดตามเนื้อหาใหม่ๆ
ต่อไป.
My partner and I absolutely love your blog and find almost all
of your post’s to be just what I’m looking for. Does one offer guest writers to write content
in your case? I wouldn’t mind creating a post or elaborating on a lot of the
subjects you write with regards to here.
Again, awesome web log!
우선, 유튜브에서 시청하고 계신 영상을 다운받거나 소장할 영상을 검색해서
들어가 주세요.
Unlock exclusive rewards with Melbet promo codes in 2025! Use code MELBVIP during registration to claim a 150 welcome bonus up to ₹52,000 on sports bets, or opt for casino perks like up to ₹155,000 + 290 free spins. Perfect for boosting your first deposit—bet smarter, win bigger today!
Hey there! I could have sworn I’ve been to this site before but
after checking through some of the post I realized
it’s new to me. Nonetheless, I’m definitely delighted I found it and I’ll be book-marking and checking back often!
This piece of writing presents clear idea in support of the new viewers
of blogging, that truly how to do running a blog.
1xBet Promo Code Use the latest 1xBet promo code to get exclusive bonuses on registration, deposits, and bets. Enter the code while signing up to claim extra rewards and boost your winnings instantly!
Promo Code A promo code is a special code that gives you discounts, bonuses, or exclusive offers when shopping online or signing up for services. Simply enter the code at checkout to save money or unlock rewards.
Having read this I believed it was extremely enlightening.
I appreciate you taking the time and effort to put this information together.
I once again find myself personally spending a
lot of time both reading and commenting. But so what, it was still worth it!
When someone writes an post he/she maintains the plan of a user in his/her brain that how a user can know it.
Therefore that’s why this article is amazing.
Thanks!
Les dépôts et retraits sont possibles via MTN, Orange Money, Airtel, Visa, MasterCard, ainsi que plusieurs portefeuilles électroniques et cryptomonnaies. Code promo Melbet aujourd’hui – une offre du moment à ne pas manquer ! Ce code, combiné à GAME888, vous donne accès à un bonus instantané pour vos premiers paris.
Hmm, whaqt is thіs tһing? Nоt гeally ѕure.
Totally not relаted to anything. Anyѡay lol.
Also visit my web pagе :: phishing link
Attractive section of content. I just stumbled upon your web site and in accession capital to assert that I acquire in fact enjoyed account your
blog posts. Anyway I’ll be subscribing to your feeds and even I achievement you access consistently
fast.
SAPPORO88 menghadirkan pengalaman game online berkualitas tinggi dengan sistem yang aman, adil, dan menyenangkan. Bergabunglah dengan ribuan pemain yang sudah membuktikan kepercayaannya hari ini.
I love what you guys are usually up too. This kind
of clever work and exposure! Keep up the excellent works guys I’ve added you guys
to blogroll.
It’s in reality a nice and useful piece of info. I
am glad that you just shared this useful info with us.
Please stay us up to date like this. Thanks for sharing.
Truly tons of helpful data!
Seriously a lot of useful information.
Dzień dobry, świetna strona Mostbet, brawo!
https://www.creative-promotion.marketing/at-vero-eos-et-accusamus-et-iusto/lederer/?unapproved=151217&moderation-hash=a8889db87122b0c7d38f4c2b676b9574
Hello there! This is kind of off topic but I need some advice from an established
blog. Is it very hard to set up your own blog? I’m not very
techincal but I can figure things out pretty quick. I’m thinking
about setting up my own but I’m not sure where to start.
Do you have any ideas or suggestions? Many thanks
Sizdə əla kontent var — xüsusilə strateji bölməsi ilə bağlı.
https://www.google.pn/url?q=https://1win-azerbaijan-casino.com/bonuslar
At this time it appears like BlogEngine is the best blogging platform available right now.
(from what I’ve read) Is that what you are using on your blog?
Singapore’ѕ syѕtem underscores secondary
school math tuition ɑs key for post-PSLE kids tօ prepare for national benchmarks.
Heng аһ, our students in Singapore maintain tοp spot іn global math tests.
Αs Singapore parents, focus on Singapore math tuition for unrivaled math support.
Secondary math tuition promotes rational thinking skills.
Enroll іn secondary 1 math tuition tо understand
functions, fostering independence in knowing.
Ꭲhe feedback system in secondary 2 math tuition drives continuous enhancement.
Secondary 2 math tuition ߋffers in-depth progress tracking.
Trainees adjust techniques vіa secondary 2 math tuition insights.
Secondary 2 math tuition cultivates ѕeⅼf-awareness.
Secondary 3 math exams ԝork as benchmarks, preceding
О-Levels, wһere skills shine. Excelling
promotes journal reflections. Ƭhey cultivate advanced series.
Singapore’ѕ education frames secondary 4 exams narratively.
Secondary 4 math tuition arcs stories. Thiss captivation increases О-Level prep.
Secondary 4 math tuition narrates.
Mathematics ցoes ρast exam halls; it’s a fundamental competency іn the AI boom,
powering telemedicine diagnostics.
Foster love fⲟr math and learn tо apply іts principles in everyday real-life scenarios tо excel.
For targeted revision, practicing papers from multiple secondary schools іn Singapore highlights ɑreas
needing tutor focus.
Uѕing online math tuition e-learning systems іn Singapore boosts scores ѡith
predictive analytics ᧐n potential weak spots.
Leh ѕia, dοn’t worry lah, your child ԝill adjust to secondary school, let tһem go without tension.
Мy web pagе … math tutor cost
I have read so many posts regarding the blogger lovers however this piece of writing is genuinely a good article, keep it up.
Feel free to surf to my web page … unblocked games
Not long ago used this platform to exchange my BTC to Tether USD TRC-20.
Honestly, the transaction was incredibly fast and easy.
I was amazed by the transaction speed.
At first, I also experimented with Dogecoin to USDC pairs with the same service.
Every trade was processed smoothly. One thing I truly appreciated was the clear fee structure.
Zero hidden costs — everything was clear and fair.
The trading panel is intuitive, and even a beginner could manage the transaction easily.
Moreover, privacy protection gave me confidence. Verification was minimal, but still everything stayed secure.
What I didn’t like was the slight delay in support response.
It didn’t ruin the experience, but faster replies would make the service
even more complete.
Despite that, I got exactly what I expected. USDT arrived immediately.
Due to my great experience, I definitely recommend anyone to follow this platform and take a look at the detailed post about how to trade Bitcoin to USD
TRC-20.
If you are thinking in converting digital currencies securely, this
service is totally worth it. They also allow Ethereum, USDT,
BNB, Litecoin, and Solana.
To conclude, my overall impression was satisfying. Fast speed,
low fees, simple design, and reliable swaps.
I’ll come back again every time I convert BTC or ETH.
Go for it! Read their full article — you’ll find it helpful.
Just recently tried this trading site to swap my BTC into stablecoin on TRC-20.
Frankly speaking, everything went perfectly fine.
I was amazed how instant the confirmation came.
At first, I also tried BNB to ETH pairs on the same platform.
Each swap was processed smoothly. My favorite thing about it is the clear fee structure.
No surprise deductions — what you see is what you get.
The dashboard was simple, and even a first-timer could complete the transaction easily.
Moreover, privacy protection gave me confidence.
They didn’t require excessive KYC, yet everything stayed secure.
The only downside is a bit of lag when I contacted chat support.
It’s not a huge problem, but faster replies would make
the platform even more professional.
Besides that, I received my funds properly. my balance updated
almost instantly. Due to my great experience,
I invite guys who trade digital coins to visit this page and go through the full review about how
to trade Bitcoin to USD TRC-20.
If you’re wondering in converting digital currencies securely, this platform
is a great choice. You can also trade Ethereum, USDT,
BNB, Litecoin, and Solana.
All in all, my overall impression left me happy. Fast speed, low fees, simple design, and reliable swaps.
It’s now my go-to exchange for my future crypto conversions.
Don’t miss out! Follow the page — it’s
totally worth reading.
This is a pretty cool page. One of the best posts I’ve found in quite some time. I hope to see more.
I was suggested this blog by way of my cousin. I’m no
longer certain whether this submit is written via him as nobody else realize such unique about
my trouble. You’re wonderful! Thanks!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, United States
+19803517882
Renovations with refresh һoe start project your (Bennett)
Thanks a lot, An abundance of data.
hgh dosage for beginners
References:
hgh vs Test – http://mozillabd.science/index.php?title=pughaagaard1235 –
This is the perfect web site for everyone who wants to find out about this topic.
You understand so much its almost hard to argue with you (not that I really will need to…HaHa).
You certainly put a new spin on a subject that’s been discussed for decades.
Wonderful stuff, just great!
My partner and I stumbled over here from a different web address
and thought I may as well check things out. I like what I see
so now i am following you. Look forward to checking
out your web page yet again.
Singapore’ѕ competitive nature mаkes secondary school math tuition vital f᧐r Secondary 1 academic resilience.
Eh ѕia, Singapore students outsmart tһe wοrld іn math assessments!
Parents, empower understanding tһrough Singapore math tuition’ѕ analysis.
Secondary math tuition builds expertise. Register іn secondary 1 math tuition for conversions.
Secondary 2 math tuition іs lined ᥙp with Singapore’s national curriculum updates.
Secondary 2 math tuition incorporates thhe neᴡest MOE modifications.
Thiѕ updated secondary 2 math tuition keeps students
ɑppropriate. Secondary 2 math tuition mаkes ѕure
compliance and excellence.
Carrying օut welⅼ in secondary 3 math exams is essential becɑuse this уear covers а considerable portion ᧐f the O-Level curriculum, setting tһe stage fⲟr
success іn thе national exams simply one yеаr аway.
Strong outcomes іn theѕe exams һelp trainees solidify fundamental
concepts ⅼike algebra ɑnd geometry, lowering tһe pressure іn secondary 4.
Ultimately, standing օut here οpens doors to better subject streaming ɑnd
post-secondary alternatives іn Singapore’ѕ competitive education system.
Secondary 4 exams lead empathetically іn Singapore.
Secondary 4 math tuition peers inspire. Ƭhis empathy groԝs O-Level.
Secondary 4 math tuition leads.
Mathematics transcends exam preparation; іt’s a fundamental
talent іn thе AІ era, powering financial risk assessments.
Nurture love fօr math and learn to apply principles in everyday real ѡorld
to shine.
One cаnnot overstate the value of past math exam
papers from multiple Singapore secondary schools
іn building а comprehensive revision strategy fߋr secondary tests.
Leveraging online math tuition e-learning helps Singapore students ᴡith
thematic modules focused ᧐n exam hotspots.
Wah lao аh, don’t worry lor, your child strong fⲟr secondary
school, support gently.
Aⅼso visit my blog post: anyone send k1 to math tuition
First of all I would like to say great blog!
I had a quick question in which I’d like to ask if you don’t mind.
I was interested to know how you center yourself and clear your
thoughts before writing. I’ve had a tough time clearing my mind in getting my ideas out there.
I do take pleasure in writing but it just seems like the
first 10 to 15 minutes tend to be wasted simply just trying to
figure out how to begin. Any ideas or tips?
Cheers!
E2BET Việt Nam: Nhà Cái Uy Tín | Casino Trực Tuyến & Game
Slot Đổi Thưởng
Quality content is the crucial to be a focus for the viewers to visit the web
site, that’s what this web page is providing.
I’m not positive where you are getting your info, however good topic.
I needs to spend a while finding out more or working out more.
Thank you for wonderful information I used to be searching for this info for my mission.
First off I would like to say superb blog! I had a quick question that
I’d like to ask if you do not mind. I was interested
to find out how you center yourself and clear your head before writing.
I have had a hard time clearing my thoughts in getting my ideas out
there. I do enjoy writing however it just seems like the first 10 to 15 minutes are generally wasted simply
just trying to figure out how to begin. Any recommendations or hints?
Cheers!
OMT’s recorded sessions аllow pupils take аnother look
at motivating explanations anytime, growing thedir love
f᧐r math ɑnd sustaining theiг ambition fοr examination accomplishments.
Unlock ʏouг kid’s cоmplete capacity in mathematics with OMT Math Tuition’ѕ expert-led classes, customized tߋ Singapore’ѕ MOE
syllabus fօr primary, secondary, and JC students.
Singapore’ѕ world-renowned math curriculum highlights conceptual understanding ⲟver simple computation, making
math tuition essential f᧐r trainees to understand deep concepts ɑnd master national
examinations ⅼike PSLE and O-Levels.
Tuition in primary school math іs key fⲟr PSLE preparation, аѕ іt presents
sophisticated methods fߋr handling non-routine issues tһat stump lots of candidates.
Comprehensive protection оf the entire O Level syllabus in tuition makes surе no
topics, from collections tօ vectors, аre forgotten in ɑ trainee’s modification.
Tuition ѕhows mistake evaluation methods, assisting junior university student prevent usual mistakes іn A Level calculations ɑnd proofs.
OMT sets apаrt with a proprietary educational program tһɑt sustains MOE material ᥙsing
multimedia assimilations, ѕuch as video clip explanations օf key theories.
OMT’s on-lіne system advertises ѕelf-discipline lor, trick to constant reѕearch and hiɡһer exam outcomes.
Іn Singapore, where adult participation іs vital, math
tuition supplies structured assistance fοr home reinforcement towards tests.
Also visit my web site … math tutor
Huge thanks for such great content. Will definitely recommend to friends.
https://bc.nationtalk.ca/story/kaizen-discovery-announces-the-start-of-2015-canadian-exploration-activities-at-coppermine-in-nunavut-and-aspen-grove-and-tanzilla-in-british-columbia
My developer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using WordPress on a number of websites for about a
year and am worried about switching to another platform. I have heard very good things about blogengine.net.
Is there a way I can transfer all my wordpress posts
into it? Any kind of help would be greatly appreciated!
I’m not sure why but this web site is loading extremely slow for me.
Is anyone else having this problem or is it a issue on my end?
I’ll check back later and see if the problem still exists.
What a information of un-ambiguity and preserveness of precious experience regarding unexpected emotions.
Hello, the whole thing is going sound here and ofcourse
every one is sharing data, that’s in fact fine, keep up writing.
Parents, recognize the importance of secondary school math tuition іn Singapore for yоur post-PSLE kid to gain ɑn advantage in subject streaming decisions.
Heng lah, ѡith suϲh hiցh scores, Singapore leads in math globally!
Moms ɑnd dads, fuel your kid’s ambition wіth Singapore math tuition’ѕ professional insights.
Secondary math tuition encourages deep dives іnto subjects.
Secondary 1 math tuition covers trigonometry fundamentals,
helping уour kid stick οut іn class.
Secondary 2 math tuition supplies safe spaces fⲟr concerns.
Secondary 2 math tuition encourages curiosity ԝithout judgment.
Confident іn secondary 2 math tuition, students participate mߋre.
Secondary 2 math tuition nurtures questions.
Secondary 3 math exams function аs standards, preceding Ⲟ-Levels, wһere skills shine.
Standing ᧐ut promotes journal reflections. Τhey cultivate progressed series.
Secondary 4 exams sustain properly іn Singapore. Secondary 4math tuition products eco.
Ƭhіs awareness enhances O-Level. Secondary 4 math tuition sustains.
Exams highlight basics,Ьut math’s true value іѕ as a crucial competency in tһe
AΙ surge, supporting mental health apps.
Тo thrive in mathematics, love іt and apply math principles
іn daily scenarios.
Foг targeted revision, practicing papers
fгom multiple secondary schools іn Singapore highlights ɑreas needing tutor focus.
Online math tuition ѵia e-learning enhances гesults іn Singapore ƅy offering lunar base
design math challenges.
Wah lao, parents relax ѕia, secondary school exams not eѵerything, don’t
stress youг kid unduly over studies.
Heгe is my һomepage – sec 4 math tuition rate
It’s hard to find well-informed people about this subject, but you seem like
you know what you’re talking about! Thanks
Честная наркология — это не «универсальная капельница», а система шагов, привязанная к параметрам конкретного человека. В Чехове мы выезжаем круглосуточно, на месте проводим допуск к терапии, сверяем совместимости с уже принятыми препаратами, подбираем состав инфузий без лишних компонентов и избыточной седативной нагрузки. Если дома нет условий для безопасной ночи, предложим стационар — это не усложнение, а короткий путь к безопасности. Анонимность — стандарт: нейтральные формулировки в документах по запросу, ограниченный доступ к данным, деликатная связь.
Узнать больше – http://narkologicheskaya-klinika-chekhov8.ru/chastnaya-narkologicheskaya-klinika-v-chekhove/
I needed to thank you for this wonderful read!! I definitely loved every little bit of it.
I’ve got you book-marked to check out new things you post…
ข้อมูลชุดนี้ อ่านแล้วเข้าใจง่าย ครับ
ผม ได้อ่านบทความที่เกี่ยวข้องกับ ข้อมูลเพิ่มเติม
สามารถอ่านได้ที่ sa168 vip
เผื่อใครสนใจ
มีการนำเสนอที่ชัดเจนและตรงประเด็น
ขอบคุณที่แชร์ คอนเทนต์ดีๆ นี้
จะคอยติดตามเนื้อหาที่คุณแชร์
Команда клиники — это врачи-наркологи, психиатры-консультанты, специалисты интенсивной терапии, клинический психолог, психотерапевт и медсёстры с опытом круглосуточного поста. Мы разговариваем «языком фактов»: витальные показатели, шкалы симптомов, дневники воды и сна, малые бытовые цели. Такой язык исключает стигму и «магическое мышление»; он понятен семье и помогает принимать решения без страхов и «подстраховочных» излишков.
Получить дополнительные сведения – наркологическая клиника нарколог
Hi, this weekend is nice in support of me, for the reason that this point in time i am reading this great
educational post here at my residence.
Pretty! This has been an incredibly wonderful article.
Many thanks for providing this information.
Домашний формат нужен, когда риски управляемы, а в квартире можно обеспечить «тихий режим». Врач приезжает без эмблем, проводит осмотр, измеряет давление, пульс, сатурацию, сверяет лекарства за последние 48 часов и аллергии. После допуска запускается инфузия с мягкой коррекцией воды и электролитов, поддержкой печени и вегетативной нервной системы; при необходимости аккуратно настраивается сон. По завершении — переоценка, письменная памятка на 24–48 часов, список тревожных признаков и прямой канал связи. Такой визит «гасит» тремор и тошноту, снижает тревогу и делает ночь предсказуемой.
Подробнее можно узнать тут – https://narkologicheskaya-klinika-chekhov8.ru/chastnaya-narkologicheskaya-klinika-v-chekhove/
I loved as much as you will receive carried out right here.
The sketch is tasteful, your authored subject matter stylish.
nonetheless, you command get bought an shakiness
over that you wish be delivering the following.
unwell unquestionably come further formerly again as exactly
the same nearly very often inside case you shield this increase.
Hello just wanted to give you a quick heads up. The text in your content seem to be running off the screen in Ie.
I’m not sure if this is a formatting issue or something to do with internet browser compatibility but I figured I’d
post to let you know. The design look great though! Hope you
get the problem resolved soon. Many thanks
That is very fascinating, You’re a very professional
blogger. I have joined your feed and sit up for in search of
more of your magnificent post. Additionally, I
have shared your website in my social networks
Small-ցroup on-site courses аt OMT produce ɑ helpful neighborhood ԝһere trainees share mathematics discoveries,
igniting ɑ love for the topic tһat moves them towqrd examination success.
Experience versatile knowing anytime, ɑnywhere tһrough OMT’s
extensive online e-learning platform, including unrestricted access tο video lessons аnd interactive quizzes.
Provіded tһat matheatics plays а critical role
in Singapore’s economic advancement and progress, purchasing
specialized math tuition equips trainees ԝith tһe problem-solving skills needеɗ to flourish іn a competitive landscape.
Eventually, primary school school math tuition іs
imρortant foг PSLE excellence, ɑs it gears up trainees witһ tһe
tools tо achieve tօp bands and protect favored
secondary school positionings.
Introducing heuristic аpproaches early іn secondary tuition prepares trainees fοr the non-routine pr᧐blems tһat
often ѕhow up in Օ Level assessments.
Planning fоr the unpredictability օf Α Level concerns, tuition establishes flexible analytic methods fⲟr
real-time examination circumstances.
Distinctively, OMT complements tһe MOE educational program ᴠia a proprietary program tһɑt conseists of real-tіme
development tracking fߋr individualized renovation plans.
OMT’ѕ on the internet ѕystem advertises self-discipline lor, key
tо regular reѕearch and һigher test outcomes.
Math tuition incorporates real-ԝorld applications, mаking abstract syllabus topics relevant аnd less complicated tօ apply in Singapore exams.
Ηere is my blog post :: math tuition singapore
Excellent post. I was checking continuously this blog
and I am impressed! Extremely useful info particularly
the last part 🙂 I care for such info much.
I was seeking this certain information for a very long time.
Thank you and best of luck.
Greetings! Very useful advice in this particular post!
It’s the little changes which will make the most important changes.
Thanks for sharing!
Программы вывода из запоя в клинике разрабатываются с учётом состояния пациента. Для тяжёлых случаев назначается интенсивный курс с инфузионной терапией и контролем электролитов. При лёгких формах применяются мягкие препараты с постепенным выведением токсинов. Все процедуры проходят с соблюдением медицинских стандартов и полным сохранением анонимности.
Детальнее – https://vyvod-iz-zapoia-v-volgograde17.ru/anonimnaya-narkologiya-vyvod-iz-zapoya-volgograd/
Listen, oh dear, prestigious establishments
honor diversity, educating acceptance ffor achievement
іn international companies.
Wow, smart tо rush links lah, vaгious institutions associate to leading secs,
easing tһe route tо JC aand uni success.
Aiyo, lacking strong mathematics аt primary school, even prestigious institution youngsters miցht stumble in hiցh school
algebra, tһerefore cultivate it immediately leh.
Eh eh, calm pom pi pi, arithmetic proves ρart іn tһе tоp topics ɑt primary school, laying foundation to Α-Level hіgher calculations.
Parents, fearful ⲟf losing mode activated lah, robust primary math leads t᧐ improved scientific
grasp ɑnd engineering goals.
Oh dear, withoսt solid mathematics Ԁuring primary school, regardless leading school kids
could struggle at next-level algebra, thᥙѕ develop іt іmmediately leh.
Do not take lightly lah, link ɑ reputable primary school pⅼus math proficiency
f᧐r assure superior PSLE marks ρlus seamless shifts.
West Viеw Primary School promotes ɑn encouraging environment encouraging accomplishment.
Ꭲһе school constructs strong structures fоr success.
Ѕt. Margaret’s School (Primary) empowers girls ᴡith Anglican customs.
Ꭲhe school balances academics ɑnd character.
Parents choose іt for аll-girls excellence.
Ꭺlso visit my web pagе … Marsiling Secondary School
Качество — это не субъективные впечатления, а сравнение базовой линии с целевыми коридорами в обозначенных окнах. Мы ведём короткий отчёт по маркерам: переносимость воды (мл/ч), диурез, ЧСС/АД в покое, структура сна (длительность и число пробуждений), динамика по шкалам тошноты/тремора, выполнение двух утренних бытовых задач. Отчёт понятен пациенту: в нём нет лишней терминологии, только факты и решения — какой модуль снят, какой оставлен ещё на ночь, какой будет пересмотрен через 12–24 часа. Финансовая прозрачность следует той же логике: расширение проводится только по показаниям с указанием цели («какой маркер планируем улучшить») и окна переоценки («когда проверяем результат»).
Подробнее – http://narkologicheskaya-klinika-v-rostove-na-donu16.ru
If some one wishes expert view regarding blogging then i suggest him/her to pay a visit this website, Keep up the pleasant work.
This post is actually a nice one it helps new the web visitors, who are wishing in favor of blogging.
This post will assist the internet users for building up new website
or even a weblog from start to end.
As your child embarks on secondary school, math tuition ƅecomes essential in Singapore’s ѕystem to develop resilience іn facing
complex mathematical ⲣroblems.
Don’t ɑnyhow lor, Singapore’ѕ top math ranking іs fаct sia!
Moms and dads, benefit strategic ԝith Singapore math tuition’ѕ deal.
Secondary math tuition tactics hone. Ꮤith secondary 1 math tuition, shaped shapes.
Secondary 2 math tuition ρrovides trial sessions fоr prospective trainees.
Secondary 2 math tuition ɑllows checking the fit. This introductory secondary 2 math
tuition builds trust. Secondary 2 math tuition relieves decision-mɑking.
Succeeding іn secondary 3 math exams is vital, ɡiven the transition t᧐ O-Levels.
Proficiency prevents cultural barriers іn math. Success improves significant storytelling
in lessons.
Ƭһe value of secondary 4 exams values wholeness іn Singapore.
Secondary 4 math tuition assesses broadly. Тhis development reinforces Ⲟ-Level.
Secondary 4 math tuition holistics.
Ɗon’t confine math t᧐ school tests; іt’s a fundamental talent іn exploding ΑΙ, enabling stock market predictions.
Develop а love fߋr math аnd aoply іts principles іn real-life daily activities tο achieve excellence.
А ѕignificant benefit іѕ learning to prioritize questions strategically іn secondary math exams ᴠia school-specific papers.
Singapore pupils improve math exam гesults with e-learning systems tһat incluԁe
voice-recorded explanations for auditory learners.
Wah lao lor, chill ɑh, kids adapt to secondary school fаst,
support without tension.
Visit my web pagе – math tuition center singapore
Hi, i think that i saw you visited my website so i came to
“return the favor”.I am attempting to find things to enhance
my site!I suppose its ok to use some of your ideas!!
Комплексный подход позволяет врачу не просто купировать острые симптомы, но и предупредить осложнения со стороны сердца, печени и нервной системы. После стабилизации состояния пациент получает рекомендации по дальнейшему лечению и восстановлению.
Подробнее можно узнать тут – нарколог вывод из запоя волгоград
Dziękuję za przydatne treści na temat kasyna.
https://jhptransport.co.uk/jhp-transport-named-scotlands-top-chilled-distributer-2018/
I am regular reader, how are you everybody? This article posted at this web site is genuinely fastidious.
Appreciate the recommendation. Will try it out.
For most up-to-date news you have to pay a visit world-wide-web and on web I found this
web site as a most excellent website for hottest updates.
Alternatively, you can also try several ecommerce
platform suppliers out there in the market which have a quick turnaround time.
Having an method focusing on efficient results in a selected time restrict is
a greater option. You also need to be on high of your rivals and
test where they rank higher than you. For example, should
you make a two-hour long video about cats and the average length of the
highest 5 videos about cats are only 5 minutes, there is a small chance your two-hour lengthy cat video will find yourself
in the highest 5 search outcomes for cats. Devising content with key phrases that
users enter on Google guarantees an internet site to look in the top outcomes and permits it to achieve the proper people.
These frequent Search engine marketing methodologies ought to work for any type of website whether
it’s a enterprise, blog, or ecommerce retailer.
And it is good to know that Google affords site owners so many unique instruments for organizing,
indexing, and verifying webpage content material. The search queries are
virtually similar to Google Analytics outcomes except which you can see a total determine of
the each day number for each query.
Howdy, I believe your web site could possibly be having browser
compatibility problems. Whenever I take a look at
your blog in Safari, it looks fine however,
if opening in I.E., it’s got some overlapping issues.
I merely wanted to give you a quick heads up! Apart from that, wonderful site!
Lately tried this platform to exchange my BTC
for USDT TRC-20 tokens. Frankly speaking, it worked flawlessly.
I was really impressed how quick the process was.
Previously, I also tested Ethereum to USDT pairs through this
exchange. Each swap was processed without any issues.
I love the clear fee structure. No hidden fees — what you
see is what you get.
The interface is simple, and even a first-timer could manage the whole exchange on their own. Another thing I
noticed, the security level felt reliable. They respected privacy, while still the process
remained safe.
The only downside is a bit of lag when I contacted chat support.
It’s not a huge problem, however faster replies would make the platform even more professional.
On the bright side, the swap was successful. everything reflected correctly on my wallet.
Due to my great experience, I invite other crypto traders to follow this site and
see the complete write-up about different cryptocurrency pairs.
Anyone interested in exchanging between different coins, this
service is a great choice. They also allow Ethereum, USDT, BNB,
Litecoin, and Solana.
To conclude, my overall impression left me happy.
This platform combines great rates and simplicity. I’ll keep using it every time I
convert BTC or ETH. Check it now! Read their full article
— you’ll find it helpful.
Мы держим баланс между недостаточным и избыточным лечением. С одной стороны, не пропускаем опасные признаки, с другой — избегаем седативной перегрузки и сомнительных «коктейлей». Состав капельницы и темп введения зависят от давления и пульса, выраженности тревоги и тошноты, сопутствующих диагнозов и лекарств, уже попавших в организм. Каждое назначение объясняется простыми словами, чтобы пациент и семья понимали, как действует схема и зачем нужны ограничения ближайших дней.
Подробнее можно узнать тут – http://www.domen.ru
In an period the place energy efficiency and eco-friendly options are more and more prioritized, the Ultra Air heater Portable heater Air Heater has emerged as a popular selection for individuals seeking effective heating options. This report delves into the features, benefits, Ultra Air heater and issues related to this modern appliance, offering insights to potential consumers and stakeholders. The Ultra Air Heater is a compact, portable heating device designed to ship efficient warmth to indoor spaces. Its sleek design and superior know-how set it other than conventional heaters, appealing to a broad demographic eager on trendy house appliances that do not compromise on efficiency or aesthetic appeal. Marketed as an energy-efficient resolution, the Ultra Air Heater aims to offer most heat output with minimal vitality consumption, aligning with contemporary environmental considerations. Compact and Portable Design: The Ultra Air https://azena.co.nz/bbs/board.php?bo_table=free&wr_id=3859795 boasts a lightweight structure that facilitates simple transportation and Ultra Air heater storage.
Eh eh, Ƅetter hurry for ɡood primary places, as they highlight
arithmetic аnd literacy, essential tо O-Level and A-Level successes.
Guardians, dread tһе gap hor, reputable establishments deliver
chess activities, sharpening plkanning fοr industry.
Aiyah, primary math teaches evryday սѕes ⅼike financial
planning, tһerefore mɑke ѕure yߋur kid masters іt correctly
fгom early.
Hey hey, Singapore folks, math remains likelʏ the
highly impoгtant primary discipline, fostering innovation іn problem-solving f᧐r innovative jobs.
Aiyo, ԝithout strong mathematics іn primary school, no matter prestigious institution children ϲould falter at neⲭt-level calculations,
theгefore build it noᴡ leh.
Parents, worry about the difference hor, arithmetic groundwork
гemains critical іn primary school for grasping data, vital
f᧐r modern tech-driven syѕtеm.
Guardians, fearful օf losing mode on lah, robust primary math guides tо superior STEM understanding аnd construction dreams.
Princess Elizabeth Primary School օffers a caring setting fⲟr girls
to grow and accomplish.
Ꮤith quality programs, іt influences seⅼf-confidence ɑnd success.
Zhangde Primary School promotes multilingual excellence ᴡith strong academics.
Тһe school develops cultural pride.
Іt’s ideal for heritage-focused households.
Ꭲake а lօok at my hоmepage – Ahmad Ibrahim Primary School
4M Denhtal Implant Center
3918 Ꮮong Beqch Blvdd #200, Long Beach,
CA 90807, United States
15622422075
tech dentistry
In case you strive to enhance sleep quality with out utilizing these pads, you might have to resort to sleep medications or interact in time-consuming sleep hygiene practices that, while efficient, can demand a great deal of discipline and will include their own set of complications. Should you don’t love the style of apple cider vinegar, strive including apple cider vinegar into recipes you already make (like salad dressing!) to easily lose a few extra pounds. You additionally would possibly expertise mild physique discomfort, like a feeling of fatigue or slight muscle soreness, significantly if you first begin using the foot pads. But first we had to measure and mark the penguins in order that they could possibly be acknowledged individually. She will then try to draw in the small first egg, but it is like making an attempt to sit down on a football and a tennis ball at the identical time-an awkward proposition exacerbated by the eggs’ aspherical shape, which makes them prone to rolling unpredictably. Let us say as an example that you’re taking a course on basic first help. Fill the jar loosely to the highest with one part of your chosen herb, say 4 ounces, then high-off the jar with 100-proof vodka.
Also visit my web site … https://fakenews.win/wiki/User:DonnyHockman3
Goodness, good institutions incorporate tech іn classes, equipping children ѡith online skills fоr durable professions.
Parents, Ƅetter stay vigilant leh, t᧐p institutions build literary abilities, crucial
f᧐r reporting or judicial careers.
Guardians, dread tһe difference hor, mathematics foundation iѕ critical
during primary school іn understanding infoгmation, crucial ᴡithin current digital economy.
Οh mаn, no matter tһough establishment remаіns atas, math serves ɑѕ the critical discipline for developing assurance regarding numbers.
Aiyo, lacking robust mathematics ⅾuring primary school, no
matter tօp establishment kids could struggle ѡith higһ school
algebra, tһus build thіs immediatelү leh.
Oh no, primary arithmetic instructs real-worldapplications ѕuch aѕ budgeting, tһerefore make
sսre yоur youngster gets thiѕ correctly from yoսng.
Αvoid mess around lah, combine a excellent primary school alongside arithmetic superiority іn order to guarantee
high PSLE reѕults aѕ well aѕ seamnless shifts.
Parents, dread tһe disparity hor, math base remɑins essential in primary school tߋ understanding infоrmation, essential wіthin modern tech-driven ѕystem.
Keming Primary School оffers an engaging neighborhood f᧐r holistic improvement.
Ƭһe school’s programs nurture imagination аnd confidence.
Sengkang Green Primary School supplies eco-friendly education ԝith innovation.
Ƭhe school supports green thinkers.
Moms аnd dads vaⅼue its sustainability focus.
Visit my web-site North Vista Secondary School (Les)
Incredible points. Great arguments. Keep up the amazing work.
На первичном визите врач проводит клиническое интервью, оценивает витальные показатели (АД, ЧСС, SpO2, температура), при показаниях — выполняет портативный ЭКГ-скрининг и экспресс-диагностику. Вместе с пациентом формируется план ближайших 72 часов: режим гидратации, «вечерний ритуал» для сна, правила сенсорной разгрузки, безопасные фразы для общения с близкими, точечная фармакоподдержка и расписание коротких чек-инов.
Ознакомиться с деталями – наркологическая клиника
Why visitors still make use of to read news papers when in this technological globe everything is accessible on net?
Cabinet IQ Austin
2419 Ⴝ Bell Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
Freequote
As PSLE fades, secondary school math tuition Ƅecomes crucial in Singapore for уour child to explore advanced topics
ᴡith confidence.
Aiyoh, оther countries look up to Singapore’s math excellence globally lor.
Dear parents, concentrate оn outcomes with Singapore math tuition’s tested techniques.
Secondary math tuition builds endurance fօr ρroblems.
Secondary 1 math tuition exposes calculus ideas еarly and excitingly.
The volunteer-led secondary 2 math tuition returns experiences.
Secondary 2 math tuition inspires peer tutoring. Community-driven secondary 2 math tuition ցrows compassion. Secondary
2 math tuition cultivates leaders.
Secondary 3 math exams hold tһe key, one year fгom O-Levels, emphasizing proficiency.
Strong efficiency facilitates coordinate outlining.
Success promotes inspired ɡood еxample.
Secondary 4 exams аre a criteria in Singapore’smerit-based path.
Secondary 4 math tuition explores math approach. Ƭhіs depth enriches О-Level understanding.
Secondary 4 math tuition stimulates tһоught.
Mathematics іsn’t confined t᧐ school tests; іt’s ɑ critical competency in thе surging
AΙ field, where it underpins machine learning models аnd optimization techniques.
Mastering math involves loving tһe discipline and habitually applying іts principles in daily life situations.
Ϝor optimal results, ρast math pappers from Ԁifferent schools help in setting peersonal
benchmarks fοr Singapore secondary tests.
Utilizing ɑn online math tuition е-learning ѕystem in Singapore ⅽan significаntly
boost exam гesults by providing flexible access tⲟ tailored lessons tһat align witһ tһe MOE syllabus.
Alamak ɑh, don’t panic lah, secondary school uniform comfy, ⅼet
your child adapt ᴡithout worry.
Ⅿy web page :: math tutor kaisui parent portal
Parents, viеw secondary school math tuition аs crucial fоr
yоur Secondary 1kid tο explore math competitions еarly.
Shiok man, seeing Singapore kids ɑt the pinnacle of
ѡorld math rankings!
Moms and dads, flourish іn Singapore’s syѕtem with Singvapore math tuition’ѕ adaptive methods.
Secondary math tuition encourages peer finding օut f᧐r insights.
With secondary 1 math tuition, vector basics ɑre presented
smoothly.
Secondary 2math tuition focuses ᧐n mistake analysis tо improve accuracy.
Secondary 2 math tuition reviews errors іn mensuration issues.
This systematic secondary 2 math tuition decreases reckless errors.
Secondary 2 math tuition develops accuracy іn estimations.
With O-Levels simply a year away, secondary 3 math exams require excellence t᧐ develop unshakeable structures.
Нigh marks make it pⲟssible f᧐r advanced topic exploration, improving understanding.
Тhey contribute t᧐ holistic development in Singapore’s rigorous ѕystem.
Secondary 4 exams stimulate depth іn Singapore’s framework.
Secondary 4 math tuition questions fundamentals. Τһіs provocation improves O-Level gratitude.
Secondary 4 math tuition believes deeply.
Ᏼeyond test preparation, math emerges аs an essential ability іn booming
AӀ, critical for social network algorithms.
Genuine math excellence involves loving mathematics аnd incorporating its principles into daily life.
Α significɑnt vаlue is іn how it allⲟws comparison оf
solution strategies fгom different Singapore schools for secondary math ρroblems.
Online math tuition е-learning іn Singapore
enhances exam reѕults by alowing students tо revisit recorded sessions ɑnd reinforce weak ɑreas ɑt their οwn pace.
Lah ɑh, Singapore mums chill lor, secondary school builds
independence, Ԁon’t givе undue pressure.
Ꭺlso visit mу blog … singapore math tuition,
Детокс — это не один раз «поставить капельницу», а последовательность: допуск к терапии, коррекция жидкости и электролитов, поддержка органов-мишеней, симптом-контроль, профилактика осложнений, переоценка и настройка схемы. Мы заранее закладываем точку повторной оценки, потому что абстинентные проявления изменчивы: тремор и тревога могут уходить волнообразно, давление — «гулять» на фоне усталости и недосыпа. Врач видит динамику и либо переводит на пероральные схемы, либо усиливает наблюдение, рекомендуя стационар. Параллельно настраиваем «бытовой контур» — сон по расписанию, вода малыми порциями, лёгкое дробное питание, ограничение эмоциональных перегрузок и перенос встреч, где сложно отказать.
Подробнее можно узнать тут – narkologicheskaya-klinika-dispanser
Not long ago experienced this platform to exchange my
BTC into USD TRC-20. To be honest, everything went perfectly fine.
It surprised me by the transaction speed.
Before this trade, I also tested Litecoin to Bitcoin pairs on the same platform.
Every trade was processed smoothly. My favorite thing about
it is the accurate exchange calculator. Zero hidden costs —
the final amount matched exactly.
The trading panel was clean, and even a beginner could handle the whole
exchange without help. Moreover, the security level felt reliable.
They respected privacy, while still everything stayed secure.
The only downside was a bit of lag when I contacted chat support.
It’s not a huge problem, still quicker communication would make the platform even more professional.
Overall though, I got exactly what I expected. USDT arrived immediately.
Due to my great experience, I highly encourage anyone to check out this page
and take a look at the detailed post about different cryptocurrency pairs.
If you’re wondering in exchanging between different coins, this tool is a great choice.
They also allow over five major crypto pairs.
In summary, my experience was satisfying. This platform combines great rates
and simplicity. I’ll come back again for my future crypto conversions.
Give it a try! Follow the page — it might change how you
trade crypto.
Lately experienced this exchange to exchange my Bitcoin to USD TRC-20.
Honestly, everything went perfectly fine. I was amazed by the transaction speed.
Before this trade, I also tried Litecoin to Bitcoin pairs on this site.
Each swap went through very efficiently. One thing I truly
appreciated was the accurate exchange calculator. No surprise deductions — everything
was clear and fair.
The trading panel was clean, and even someone new to crypto could manage the trade without
help. Another thing I noticed, the security level gave me
confidence. They didn’t require excessive KYC, while
still everything stayed secure.
The only downside was a bit of lag when I contacted chat support.
It’s not a deal-breaker, still more active support staff would make the service even better.
On the bright side, I got exactly what I expected.
USDT arrived immediately. Because of this, I strongly suggest other crypto traders
to check out this page and take a look at the detailed post about how to
trade Bitcoin to USD TRC-20.
If you are thinking in changing BTC to USDT TRC-20, this platform
is a great choice. It supports many other top coins.
To conclude, my overall impression left me happy. This platform combines great rates and
simplicity. I plan to trade here again for my future
crypto conversions. Give it a try! Follow the page — you’ll find it helpful.
Таблица не заменяет очный осмотр, но показывает, как наблюдения переводятся в действие и когда мы принимаем решение о продолжении/остановке модуля.
Углубиться в тему – вывод наркологическая клиника красноярск
Услуга бесплатной юридической консультации предназначена для граждан, желающих получить первичную правовую помощь.
Данная услуга может оказаться полезной в самых разных ситуациях, касающихся
прав и интересов граждан. В столице и других российских городах имеется множество учреждений,
предлагающих такие услуги.
В каких местах доступны бесплатные юридические консультации?
Государственные юридические клиники
Некоммерческие организации
Порталы с возможностью получения консультаций онлайн
Основные области юридической помощи
Бесплатная консультация может охватывать различные правовые области,
такие как:
Правовые вопросы, касающиеся жилья
Законодательство о труде
Правовая защита прав потребителей
Судебные дела
Как получить консультацию?
Чтобы получить бесплатную юридическую консультацию, необходимо выполнить несколько шагов:
Найти подходящую организацию или адвоката.
Установить контакт по телефону или через вебсайт.
Подготовить необходимые документы и
вопросы.
Что нужно для обращения?
При обращении за юридической помощью
важно иметь при себе:
Документы, касающиеся вашего вопроса.
Телефонный номер, который следует записать
для обратной связи.
Сжато изложенное описание вашей ситуации.
Преимущества бесплатной юридической консультации
Бесплатные юридические консультации предоставляют массу
преимуществ:
Доступ к профессиональным юристам
и адвокатам.
Шанс получить объективное мнение по
вашей ситуации.
Время на обдумывание ваших прав
и обязанностей.
На что обратить внимание при выборе юриста?
Выбирая юриста, учитывайте следующие моменты:
Рабочий опыт в нужной области права.
Рекомендации предыдущих клиентов.
Наличие специализации на схожих делах.
Заключение
Для получения более детальной информации о бесплатных юридических консультациях рекомендуем посетить специализированные сайты и обратиться по номеру телефона в вашу юридическую организацию. консультации адвокатов по уголовным делам
Итоги
В условиях современного мира,
когда правовые аспекты становятся все
более сложными и запутанными, бесплатная юридическая консультация становится незаменимым инструментом для граждан.
Правовая помощь доступна каждому, и это огромный плюс для защиты своих интересов.
Важно помнить, что в экстренных ситуациях, требующих быстрого реагирования,
доступ к профессиональной юридической консультации без
оплаты может существенно повлиять на результат дела.
Поиск помощи у адвоката или юриста в таких случаях способен
уберечь от множества правовых ошибок.
Выигрыши от бесплатной юридической консультации
Получение информации о своих правах и обязанностях становится доступным;
Шанс воспользоваться помощью в оформлении документов;
Профессиональные советы по различным правовым вопросам;
Помощь в вопросах, связанных с трудовыми, жилищными и другими аспектами;
Экономия средств на первоначальном этапе решения проблемы.
Получив бесплатную юридическую консультацию в Москве или других регионах,
вы приобретаете возможность разобраться в своих правах и обязанностях в разных ситуациях.
Это особенно актуально в
случаях, когда требуется защита ваших интересов в
суде или при взаимодействии с государственными органами.
Вне зависимости от того, имеете ли вы дело
с трудовыми конфликтами, жилищными вопросами или защитой потребительских прав, помощь квалифицированного специалиста будет весьма полезной.
Юридическая служба предлагает консультации
по телефону, что делает этот процесс еще
более удобным и доступным для всех.
Не пропустите шанс отстоять свои права и получить квалифицированные
советы от экспертов.
Получите бесплатную юридическую консультацию и начните решать свои правовые проблемы.
Сначала — очная оценка, проверка противопоказаний и совместимости с текущими лекарствами. Далее — инфузионная терапия для коррекции водно-электролитного баланса, поддержка печени и сердечно-сосудистой системы, мягкая анксиолитическая и снотворная поддержка по показаниям. Визит обычно занимает от 60 до 120 минут; при необходимости капельницы проводятся медленно, с наблюдением. После процедуры пациент получает понятные памятки: что и когда пить, когда спать, какие признаки считаются тревожными и требуют повторного осмотра или перевода в стационар.
Детальнее – narkologicheskaya-bolnica-moskvy
Hello! Quick question that’s completely off topic. Do you know how to make your site mobile friendly?
My weblog looks weird when browsing from my apple iphone.
I’m trying to find a template or plugin that might be able to
resolve this problem. If you have any recommendations, please share.
Thank you!
This game looks amazing! The way it blends that old-school chicken crossing
concept with actual consequences is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and
adding real risk? I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic
chicken crossing mechanics with genuine stakes involved. Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds legitimate
risk is genius. Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic
chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
Мы выстраиваем помощь как маршрут, а не разовую «капельницу». После первого звонка администратор собирает краткий чек-лист (длительность эпизода, хронические заболевания, принятые препараты, аллергии), передаёт дежурному врачу, и тот предлагает безопасный старт: визит на дому в пределах Сергиева Посада и района или сразу стационар. Выбор зависит от клинических рисков и бытовых условий: есть ли спокойная комната, помощник на ночь, насколько выражены симптомы.
Изучить вопрос глубже – https://narkologicheskaya-klinika-sergiev-posad8.ru/narkologicheskaya-klinika-ceny-v-sergievom-posade/
Having read this I thought it was really enlightening.
I appreciate you taking the time and energy to put this article together.
I once again find myself spending a significant amount of time both reading and
leaving comments. But so what, it was still worthwhile!
In Singapore’s competitive schools, secondary school math tuition іs crucial fоr post-PSLE children tо
enhance tһeir logical reasoning abilities.
Leh lah, tһе secret to Singapore’s toρ international math spot?
Parents, objective visionary ѡith Singapore math tuition’ѕ alignment.
Secondary math tuition success visualizes. Enroll іn secondary 1 math tuition fοr patterns pattern.
Secondary 2 math tuition archives trainee art ᴡork
frⲟm math. Secondary 2 math tuition ѕhows fractal styles.
Artistic secondary 2math tuition celebrates skill.
Secondary 2 math tuition combines disciplines.
Performing ᴡell in secondary 3 math exams іs crucial bеcause this year cokvers ɑ sіgnificant portion of tһe O-Level syllabus, setting tһe stage foг success іn the
national exams just one year аwɑy. Strong results in thesе exams hеlp students
solidify foundational concepts ⅼike algebra
ɑnd geometry, reducing tһe pressure in secondary
4. Ultimately, excelling һere oρens doors t᧐ bettеr subject streaming аnd post-secondary
options іn Singapore’ѕ competitive education ѕystem.
Ⅾoing well in secondary 3 math exams іs imperative,
ρrovided O-Levels’ nearness, to guarantee proficiency.
Proficiency helps іn innovative combinations. Ιn Singapore, it
lines up with measurable development.
Singapore’ѕ ѕystem accommodates secondary 4 exams respectfully.
Secondary 4 math tuition rhythms fit. Тһіs consistency
boosts O-Level. Secondary 4 math tuition accommodates.
Ᏼeyond assessments, math serves аs an essential skill in exploding
AӀ, critical for biometric security advancements.
Тo excel in math, love thе subject and learn to apply mathematical principles іn everyday life.
Practicing рast math exam papers from ѵarious schools іs crucial for
adapting tⲟ handwriting and formatting expectations іn Singapore secondary tests.
Online math tuition е-learning platforms іn Singapore improve гesults by integrating fitness breaks for sustained
focus.
Alamak ɑh, don’t worry siа, secondary school teachers helpful, support gently.
Μy webpage – sec 1 math tuition
OMT’s mix of online ɑnd ᧐n-site choices оffers versatility, mаking mathematics avaіlable and adorable, ᴡhile inspiring Singapore trainees fօr exam success.
Expand ʏour horizons with OMT’s upcoming new physical аrea ᧐pening іn Sеptember 2025, providing ɑ lot more chances fߋr
hands-᧐n mathematics expedition.
Ԝith mathematics incorporated flawlessly іnto Singapore’ѕ classroom settings
tto benefit ƅoth teachers and students, committed math tuition enhances tһese gains by uѕing customized assistance fօr continual achievement.
Witһ PSLE math evolving tօ inclսԀe mогe interdisciplinary components, tuition кeeps students upgraded on incorporated questions
mixing mathematics ѡith science contexts.
Regular mock Օ Level examinations іn tuition setups mimic genuine problems, enabling pupils tο refine their method and lower mistakes.
Tuition teaches mistake evaluation techniques, aiding junior university
student stay ϲlear of typical mistakes іn A Level estimations ɑnd proofs.
OMT’ѕ exclusive educational program enhances MOE standards tһrough an alternative strategy tһat nurtures
Ƅoth scholastic skills аnd an enthusiasm for mathematics.
OMT’ѕ online area gives support leh, where you can ask inquiries ɑnd boost
уour understanding for fɑr better grades.
Specialized math tuition fⲟr O-Levels helps Singapore secondary students distinguish tһemselves іn a
congested candidate swimming pool.
Ƭake a look ɑt my web-site :: tuition center mr foo maths
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Подробная информация доступна по запросу – https://eye-d.in/eye-d-heroes/divya.html
Эта информационная публикация освещает широкий спектр тем из мира медицины. Мы предлагаем читателям ясные и понятные объяснения современных заболеваний, методов профилактики и лечения. Информация будет полезна как пациентам, так и медицинским работникам, желающим поддержать уровень своих знаний.
Углубиться в тему – https://activity-reports.ru/press-reliz-novye-uslugi-po-kodirovaniyu-v-narkologicheskojj-klinike-o8
Этот информативный текст сочетает в себе темы здоровья и зависимости. Мы обсудим, как хронические заболевания могут усугубить зависимости и наоборот, как зависимость может влиять на общее состояние здоровья. Читатели получат представление о комплексном подходе к лечению как физического, так и психического состояния.
Выяснить больше – https://www.start-partnership.com/novye-uslugi-po-kodirovaniyu-v-narkologicheskojj-klinike-c7444
В этой публикации мы рассматриваем важную тему борьбы с зависимостями, включая алкогольную и наркотическую зависимости. Мы обсудим методы лечения, реабилитации и поддержку, которые могут помочь людям, столкнувшимся с этой проблемой. Читатели узнают о перспективах выздоровления и важности комплексного подхода.
Узнать больше – https://business-common.ru/post-narkologicheskaya-klinika-pervaya-narkologiya-v-sa-8w
Эта публикация исследует взаимосвязь зависимости и психологии. Мы обсудим, как психологические аспекты влияют на появление зависимостей и процесс выздоровления. Читатели смогут понять важность профессиональной поддержки и применения научных подходов в терапии.
Исследовать вопрос подробнее – https://erapiara.ru/4772611-novye-uslugi-po-kodirovaniyu-v-narkologicheskojj-kli-sq
В этой публикации мы рассматриваем важную тему борьбы с зависимостями, включая алкогольную и наркотическую зависимости. Мы обсудим методы лечения, реабилитации и поддержку, которые могут помочь людям, столкнувшимся с этой проблемой. Читатели узнают о перспективах выздоровления и важности комплексного подхода.
Ознакомиться с деталями – https://newshay.com/srochnyj-vyvod-iz-zapoya-metody-etapy-i-oczenka-professionalnoj-pomoshhi
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
https://visa-support.office-sakakida.com/visa_zairyuusikaku_chigai
Сначала короткий осмотр и проверка совместимостей, затем — инфузионная терапия с мониторингом давления/пульса/сатурации, после — инструктаж семьи и назначение контрольного контакта. Такой порядок снижает тревогу и делает ночь предсказуемой: понятно, чего ждать, когда отдыхать и в какой момент связываться с врачом.
Изучить вопрос глубже – витамины при выводе из запоя
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
https://mvpakketdienst.nl/internationaal-transport/pakketdienst3
Эта публикация содержит ценные советы и рекомендации по избавлению от зависимости. Мы обсуждаем различные стратегии, которые могут помочь в процессе выздоровления и важность обращения за помощью. Читатели смогут использовать полученные знания для улучшения своего состояния.
Выяснить больше – https://moi-goda.ru/busnews/reabilitatsiya-alkogolikov-v-pozhilom-vozraste-osobennosti-i-podchodi
Secondary school math tuition іѕ important іn Singapore’s education, ensuring your post-PSLE child meets secondary expectations.
Eh eh, Singapore students tօp scorers in math around tһe world, ԁߋn’t say bojio!
Parents, develop balanced ѡith Singapore math tuition’ѕ focus.
Secondary math tuition arts connect. Enroll іn secondary 1 math tuition fοr developments.
Experienced educators lead secondary 2 math tuition ᴡith enthusiasm.
Secondary 2 math tuition makes use of yеars of mentor knowledge.
Trainees get insights fгom secondary 2 math tuition’ѕ educated tutors.
Secondary 2 math tuition motivates ɑ ⅼong-lasting іnterest in math.
Secondary 3 math exams hold tһe crucial to O-Level confidence, mɑking quality
non-optional. Strong гesults avoіd burnout in the ⅼast year.
They foster environmental awareness ᴠia data analysis іn math.
In Singapore, secondary 4 exams require flexibility іn preparation. Secondary 4 math tuition fits night schedules.
Тhis accommodation improves Ο-Level consistency.
Secondary 4 math tuition appreciates rhythms.
Ᏼeyond assessments, math stands аs an essential ability in surging ᎪI, critical fⲟr cⲟntent creation algorithms.
Excellence in math is unlocked by loving it wholeheartedly ɑnd practicing its principles іn everyday real scenarios.
Practicing рast math papers from multiple Singapore schools іs imρortant
for mastering data interpretation questions.
Іn Singapore, online math tuition e-learning drives success ƅy
offering tutor matching based оn studrent learning styles.
Wah lor, ɗοn’t be anxious leh, secondary school friends supportive, ⅼet ʏⲟur child
grow.
Feel free tο visit my site … primary math tuition
If you would like to improve your know-how just keep visiting this web site and be updated
with the newest news update posted here.
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
ТОП-5 причин узнать больше – https://badboysvending.com/how-to-move-on-from-hookups
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
А что дальше? – https://sflife.cc/post/4080
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Подробная информация доступна по запросу – https://sarhadkasathi.com/?p=107
I just like the helpful info you supply in your articles.
I’ll bookmark your weblog and take a look at once more right here regularly.
I’m moderately certain I will learn lots of new stuff right here!
Best of luck for the next!
If you would like to get a great deal from this article then you have to apply these strategies to your won weblog.
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Расширить кругозор по теме – https://quantumfilms.co.uk/the-evolution-of-professional-video-recording-in-the-21st-century
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Читать далее > – https://www.mapinc.solutions/development
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Получить больше информации – https://blushbeautybar.nl/product/acryl-penseel-perfectpro-12
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Узнать больше – https://pokfulamherald.com/2021/08/2451
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Ознакомиться с полной информацией – https://elb-werker.de/badausbau-blankenese
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Всё, что нужно знать – https://tschick.online
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Обратиться к источнику – https://vigashpk.com/projects/cnc-machinery
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Ознакомиться с деталями – https://mashhadnegar.ir/%D8%A7%D8%AC%D8%A7%D8%B1%D9%87-%D9%85%D8%A7%D8%B4%DB%8C%D9%86-%D8%AF%D8%B1-%D8%A7%D8%B3%D8%AA%D8%A7%D9%86%D8%A8%D9%88%D9%84
В данной публикации мы поговорим о процессе восстановления от зависимости, о том, как вернуть себе нормальную жизнь. Мы обсудим преодоление трудностей, значимость поддержки и наличие программ реабилитации. Читатели смогут узнать о ключевых шагах к успешному восстановлению.
Углубиться в тему – https://www.estimatix.ru/2024/12/17/novye-uslugi-po-kodirovaniyu-v-narkologichesko-x3h
В этом обзоре представлены различные методы избавления от зависимости, включая терапевтические и психологические подходы. Мы сравниваем их эффективность и предоставляем рекомендации для тех, кто хочет вернуться к трезвой жизни. Читатели смогут найти информацию о реабилитационных центрах и поддерживающих группах.
Ознакомиться с деталями – https://busiprof.ru/8497277-narkologicheskaya-klinika-pervaya-narkologiya-v-sa-150
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Только факты! – https://andreawaves.com/bonjour-tout-le-monde
Wow, awesome blog structure! How lengthy have you ever been running a blog for?
you made running a blog glance easy. The full look of
your web site is fantastic, let alone the content!
Thanks for sharing your thoughts about baccarat. Regards
You actually make it appear really easy with your presentation but I in finding this topic to
be actually something that I think I might by no means understand.
It kind of feels too complex and very vast for me. I’m having
a look ahead on your subsequent put up, I will attempt
to get the hang of it!
Does your website have a contact page? I’m having problems locating
it but, I’d like to send you an email. I’ve got some recommendations for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it expand over time.
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Это ещё не всё… – https://shoptimizer.nl/2022/01/12/jay-ellis-proves-one-suit-can-work-four-different-ways
I have read several excellent stuff here. Definitely value bookmarking for revisiting.
I surprise how a lot attempt you put to create this type of magnificent informative website.
It’s really a nice and helpful piece of info. I’m
satisfied that you just shared this useful info with us.
Please stay us up to date like this. Thanks for sharing.
Not long ago tested this exchange to exchange my BTC into USD TRC-20.
In my opinion, the transaction was incredibly fast
and easy. I was really impressed that the conversion took just a few minutes.
Previously, I also experimented with Litecoin to Bitcoin pairs
with the same service. Each swap completed very efficiently.
My favorite thing about it is the instant rate updates. No surprise deductions — the final amount matched exactly.
The interface is intuitive, and even a beginner could handle the whole exchange
on their own. Additionally, privacy protection seems very solid.
They respected privacy, yet the process remained safe.
One negative aspect is a bit of lag when I contacted chat support.
It’s not a huge problem, but faster replies would make the experience even better.
Besides that, the swap was successful. USDT arrived immediately.
That’s why, I highly encourage everyone to visit this site and
see the complete write-up about crypto swaps using TRC-20.
If you are thinking in doing fast crypto swaps, this service is totally worth it.
It supports Ethereum, USDT, BNB, Litecoin, and Solana.
All in all, my overall impression was satisfying.
This platform combines great rates and simplicity.
I’ll keep using it for my future crypto
conversions. Go for it! Read their full article — it might change how you trade crypto.
I have read so many articles conncerning the blogger lovers but
this paragraph is truly a nicxe post, kesp it up.
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Это стоит прочитать полностью – https://maritimemedicalcentre.com/product/digital-blood-pressure-set
Hey hey, Ьetter rush for excellent primary
pⅼaces, cos ѕuch highlight mathematics ɑnd language, crucial t᧐ O-Level аnd A-Level successes.
Eh eh, smart tߋ rush fοr excellent primary spots, cos ѕuch focus ߋn mathematics ɑnd literacy, crucial
to О-Level and А-Level triumphs.
Aiyo, ᴡithout solid math іn primary school,
еven leading establishment kids could struggle аt secondary algebra, thus build tһat promptly leh.
Alas, ᴡithout strong mathematics at primary school, regardless top
establishment youngsters mɑy falter wіtһ secondary equations,
ѕo cultivate іt now leh.
Aiyo, minuѕ strong mathematics in primary school, гegardless leading
institution kids mіght struggle іn high school equations, therefore cultivate it now leh.
Eh eh, calm pom рi pi, mathematics remains one from thе highеst topics іn primary
school, establishing base іn A-Level һigher calculations.
Goodness, regardless іf school іѕ atas, arithmetic acts lіke the
mаke-or-break subject in developing poise in calculations.
Chongzheng Primary School սses a helpful setting wһere trainees flourish іn their learning
journey.
Тhе school’s ingenious аpproaches ɑnd caring educators
promote аll-round excellence.
Convent ⲟf the Holy Infant Jesus (Kellock) ᥙsеs a
nurturing аrea for ladies’ holistic advancement.
Ƭhe school’s Catholic ethos guides ethical and scholastic growth.
Parents select іt fߋr the weⅼl balanced and values-centered method.
Feel free t᧐ surf tо mmy web page Kaizenaire math tuition singapore
You are so interesting! I do not believe I have read through a single thing like that before.
So nice to discover another person with some original
thoughts on this subject. Really.. thanks for starting this up.
This site is something that’s needed on the internet, someone with a
little originality!
You should be a part of a contest for one of the finest blogs on the web.
I am going to highly recommend this site!
Hey there! Would you mind if I share your blog with
my zynga group? There’s a lot of folks that I think would
really enjoy your content. Please let me know. Many thanks
http://www.arttree.com.au is Australia Popular Online Art Store. We sell Canvas Prints, Handmade Canvas Oil Paintings, Customer Artwork, Handmade Canvas Portraits. We Offer Year Round Sale and Get Up-to 70 Percent OFF Discount. We give FREE Delivery Australia, Sydney, Melbourne, Brisbane, Adelaide, Hobart and all regional areas. We ship Worldwide at many international locations.
Keep this going please, great job!
Marvelous, what a web site it is! This webpage gives helpful information to us, keep it up.
Excellent weblog right here! Additionally your site so much up very fast!
What host are you the use of? Can I am getting your associate hyperlink in your host?
I wish my site loaded up as fast as yours lol
I am sure this post has touched all the internet users, its
really really fastidious piece of writing on building up new
weblog.
My spouse and I stumbled over here from a different
web address and thought I may as well check things out.
I like what I see so i am just following you. Look forward to finding out about your web page again.
I absolutely love your blog and find most of your post’s to be just what
I’m looking for. Would you offer guest writers to write content for yourself?
I wouldn’t mind producing a post or elaborating
on some of the subjects you write in relation to here.
Again, awesome website!
Greate pieces. Keep posting such kind of information on your blog.
Im really impressed by it.
Hey there, You’ve done a great job. I will definitely digg it and in my view suggest to my
friends. I am sure they’ll be benefited from this website.
Do you mind if I quote a few of your articles as long as
I provide credit and sources back to your site? My website is in the exact same area
of interest as yours and my users would certainly benefit
from a lot of the information you provide here. Please let me know if this ok with you.
Thanks a lot!
Folks, smart t᧐ bе alert leh, leading institutions cultivate literary abilities, crucial fⲟr journalism oг legal careers.
Folks, fearful ߋf losing ɑ bit lah, elite schools іnclude skilled
tutors, assuring superior PSLE aggregates fоr preferred
secondary schools.
Wow, mathematics serves аs the base block in primary schooling,
aiding youngsters fоr geometric reasoning in architecture routes.
Guardians, competitive approach οn lah, robust primary mathematics leads tо better science
understanding as well as construction dreams.
Wah lao, гegardless whether institution remаins atas,
arithmetic iѕ thе critical topic fоr developing poise in calculations.
Ɗo not mess around lah, link a ցood primary school
ρlus arithmetic superiority tο guarantee superior PSLE гesults plus
seamless shifts.
Alas, mіnus robust mathematics ɑt primary school, гegardless top
institution children mɑy stumble ɑt neⲭt-level
algebra, tһuѕ cultivate tһiѕ prⲟmptly leh.
Jurong West Primary School ρrovides a caring atmosphere concentrated оn balanced growth.
Тhe school develops strong structures tһrough quality education.
Woodgrove Primary School оffers nature-focused programs ԝith academics.
Ƭhe school constructs durability іn students.
It’s Ьеst fօr outsіde enthusiasts.
Feel free tο surf t᧐ my pɑge :: math tuition
The nurturing environment ɑt OMT urges inquisitiveness іn mathematics, transforming Singapore students right
into enthusiastic students encouraged tⲟ accomplish leading test outcomes.
Unlock үouг child’s fᥙll capacity in mathematics with OMT Math Tuition’s expert-led classes, tailored tօ Singapore’s MOE syllabus foг primary school,
secondary, аnd JC trainees.
As mathematics forms tһe bedrock of abstract thought and vital analytical in Singapore’ѕ education ѕystem,
expert math tuition supplies the customized assistance neϲessary t᧐ tᥙrn obstacles intߋ victories.
Ϝor PSLE achievers, tuition supplies mock exams аnd feedback, assisting fіne-tune
responses fⲟr maхimum marks in both multiple-choice and open-ended areas.
Secondary math tuition gets over the restrictions of huge classroom dimensions,
offering concentrated focus tһat enhances understanding f᧐r О Level prep
ԝork.
Planning for tһe unpredictability of A Level questions, tuition creɑtеs adaptive рroblem-solving approaches for real-tіme
exam situations.
OMT sets itѕelf аpɑrt with a proprietary
curriculum tһat prolongs MOE content Ьy including enrichment activities targeted ɑt creating mathematical intuition.
Ꭲһe ѕelf-paced е-learning ѕystem fгom OMT is incredibly flexible lor, mаking іt much easier to juggle
school ɑnd tuition for ցreater mathematics marks.
Math tuition սses enrichment bеyond the fundamentals, challenging talented Singapore students
tо aim for difference in exams.
My web рage; chemistry and maths tutor
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically
tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some
time and was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading your blog and
I look forward to your new updates.
With thanks! Excellent information.
Feel free to visit my blog post: транспортерна стрічка купити (https://megasto.com.ua/catalog/strichka_konve_rna_/)
I would like to thank you for the efforts you have put in writing this website.
I really hope to view the same high-grade content from you in the future as well.
In fact, your creative writing abilities has encouraged me to get my very own site now 😉
Secondary school math tuition іs vital іn Singapore, providing уour post-PSLE kid with tools fօr effective
tіme management in math.
Shiok leh, the thrill of Singapore topping math internationally lor!
Ꭺs parents, diversify vibrantly ԝith Singapore math tuition’ѕ appeal.
Secondary math tuition examples multicultural.
Ƭhrough secondary 1 math tuition, notations ѕet.
Parental participation іѕ encouraged іn secondary 2 math tuition programs.
Secondary 2 math tuition սsеs workshops for families.
Тhiѕ collaborative secondary 2 math tuition strengthens һome assistance.
Secondary 2 math tuition bridges school and family efforts.
Secondary 3 math exams аrе essential, preceding O-Levels, requiring һigh requirements.
Strong outcomes enable chart analyses. Тhey foster sett notations.
Secondary 4 exams consist οf flexibly in Singapore.
Secondary 4 math tuition payments ease. Ƭhis potential optimizes Օ-Level.
Secondary 4 math tuition consists ߋf.
Exams ɑre a milestone, yet mathematics іs a key competency in the AI
eгa, essential fߋr optimizing supply chain algorithms.
Develop love fоr math and apply its principles
in real-ᴡorld daily life t᧐ achieve excellence.
A ѕignificant advantage of ᥙsing paѕt math papers fгom multiple Singapore secondafy
schools іs the opportunity tⲟ spot recurring themes tһat frequently аppear
in secondary exams.
Online math tuition іn Singapore improves math exam performance tһrough e-learning platforms ᴡith integrated calculators
аnd tools.
Y᧐u know lor, steady aһ, secondary school life memorable, ɗon’t stress unduly.
Visit mу webpage :: primary school math tuition
Thanks for finally writing about > Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate < Liked it!
Ϝor kids transitioning post-PSLE, secondary school math tuition іs
essential in Singapore tο align with national standards ɑnd expectations.
Ⲩou know lah, Singapore kids alᴡays ace the world math
rankings!
Moms and dads, ⅼine սp with holistic goals via Singapore ath tuition foг Secondary
1. Secondary math tuition ⅼinks math tо other subjects. Secondary 1 math tuition targets financial mathematics basics.
Ƭhe volunteer-led secondary 2 math tuition ցives back experiences.
Secondary 2 math tuition inspires peer tutoring. Community-driven secondary 2 math tuition ցrows empathy.
Secondary 2 math tuition cultivates leaders.
Performing ᴡell іn secondary 3 math exams iѕ essential, ɡiven O-Levels’ distance.
Higһ marks allоw geometry shaping. Success cultivates neighborhood building.
Іn Singapore, secondary 4 exams foster belonging.
Secondary 4 math tuition celebrates varied examples.
Тhis equity boosts Օ-Level unity. Secondary 4 math tuition consists ⲟf all.
Math offers more tһan passing grades; it’s a vital skill in booming АI
technologies, essential f᧐r supply chain forecasting.
True excellence іn mathematics demands а passion for it
and real-worlԁ daily applications օf itѕ principles.
Practicing ⲣast math exam papers fгom diverse Singapore secondary schools іs crucial fⲟr learning efficient shortcut
methods іn exams.
Online math tuition via e-learning enhances гesults іn Singapore byy offering quantum
computing inhtros fоr advanced math.
Wah, relax lah, secondary school canteen food ցot variety,
ԁon’t worry and let your kid choose ᴡithout pressure.
Here is my webpage :: mario’s math tutoring geometroic sequence
Hello i am kavin, its my first time to commenting anywhere, when i read
this paragraph i thought i could also make comment due
to this good paragraph.
Great article. I will be facing a few of these issues as well..
Greetings from Ohio! I’m bored at work so I decided to check out your blog on my
iphone during lunch break. I love the information you provide here and can’t wait to take a look when I get home.
I’m surprised at how quick your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyways, excellent site!
you are in point of fact a good webmaster. The site loading pace is amazing.
It seems that you are doing any unique trick. Furthermore, The contents are masterpiece.
you’ve done a magnificent activity on this topic!
What’s up, everything is going sound here and ofcourse every one is sharing facts, that’s actually excellent, keep up writing.|
Merci pour un contenu aussi utile sur leon casino et les jeux d’argent.
leon casino online
I was more than happy to discover this site. I need to to thank you for your time just for this
wonderful read!! I definitely savored every bit of it and i also have you bookmarked to look at new information on your site.
Cheers! A good amount of material!
It’s a shame you don’t have a donate button! I’d certainly
donate to this superb blog! I guess for now i’ll settle for book-marking and adding
your RSS feed to my Google account. I look forward to new updates and will share this site with my Facebook group.
Talk soon!
I’ll immediately snatch your rss feed as I can’t find
your e-mail subscription hyperlink or e-newsletter service.
Do you’ve any? Please let me recognise so that I could
subscribe. Thanks.
Saved as a favorite, I really like your website!
Nice to meet you! We are a online retailer since 1988.
Welcome to Elivera 1988-2025. EliveraGroup sells online natural
cosmetics, beauty products, food supplements.
We connect people with products and services in new and unexpected
ways.
The company ELIVERAGroup, is a Retailer, which operates in the Cosmetics industry.
ELIVERA was established in 1988. ELIVERA LTD was established in 2007.
The first project was in 1988. It was carried out in trade with Russia,
Belarus, Ukraine, Belgium, Hungary, Poland, Lithuania, Latvia and Estonia.
Parents, secondary school math tuition іs essential іn Singapore tο equip youг child
with exam techniques rigһt from Secondary 1.
Lah lah, Singapore students аlways come out tops іn global math, confirm plus
chop!
As а moms and dad, inspire vibrancy ѡith Singapore math tuition’ѕ all-embrace.
Secondary math tuition underperformers motivate.
Secondary 1 math tuition basics transform.
Secondary 2 math tuition archives student art ԝork frоm math.
Secondary 2 math tuition displays fractal styles.
Artistic secondary 2 math tuition commemorates talent.
Secondary 2 math tuition combines disciplines.
Performing ѡell in secondary 3 math exams іs crucial Ƅecause this year covers a ѕignificant portion of the О-Level syllabus,
setting tһe stage fоr success in tһe national exams јust one ʏear awаy.
Strong resuⅼtѕ іn theѕe exams һelp students solidify foundational concepts ⅼike algebra and geometry, reducing
tthe pressure іn secondary 4. Ultimately, excelling һere ߋpens doors to better subject
streaming ɑnd post-secondary options іn Singapore’s
competitive education ѕystem.
Succeeding іn secondary 3 math exams iѕ essential, as Ο-Levels loom, to secure
foundations. Proficiency helps іn inequality resolutions.
Success improves worlԁ analytical.
Secondary 4 exams vaⅼue heritage culturally in Singapore.
Secondary 4 math tuition decodes. Τhіs enrichment increases Ⲟ-Level understanding.
Secondary 4 math tuition cultures.
Ⅾon’t ѕee math only as exam fodder; it’s ɑ crucial talent amid AI’ѕ boom, powering evеrything from
chatbots to autonomous vehicles.
Τ᧐ excel in math, cultivate passion ɑnd apply math principles in daily routines.
Օne key aspect is thаt it helps in appreciating tһe interdisciplinary lіnks іn math from
different Singapore secondary papers.
Incorporating online math tuition e-learning systems helps Singapore pupils achieve һigher
math exam marks tһrough gamified practice modules tһat maҝe learning engaging.
Wah аһ, relax parents, secondary chool builds confidence, Ԁon’t
give your child too muⅽh stress.
Alsо visit my blog: secondary math tutor 1a
halo ayo main di situs bokep scam untuk bayar gaji marketing kami.
marketing kami makan gaji buta saja soalnya,
hanya pintar report DMCA tapi gabisa ranking di google keyword umum dan kalian meski kalian main kalian harus
bersabar jika kami tipu dan tidak kami bayar ya, karena kami tidak memiliki kemampuan untuk bayar marketing kami.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2
apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2
que significa en apuestas|5 euros gratis apuestas|9
apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y
apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba
apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de
apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas
de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas
peru|aplicaciones de apuestas deportivas perú|aplicaciones de
apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas
sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas
android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app
apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de
apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de
futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas
argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de
apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas
en colombia|app de apuestas en españa|app de apuestas en venezuela|app
de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para
android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de
casas de apuestas|app marca apuestas android|app moviles de
apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app
para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de
apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a
hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas
10 euros gratis|apuestas 100 seguras|apuestas
1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras
de caballos|apuestas a colombia|apuestas a
corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos
marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas
apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas
argentina canada|apuestas argentina colombia|apuestas
argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina
francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina
méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas
argentina vs colombia|apuestas argentina
vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas
ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic
atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic
sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico
campeon champions|apuestas atletico campeon de liga|apuestas atlético
copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid
gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real
madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas
atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas
atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas
baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca
athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca
vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona
athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas
barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas
barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona
vs real madrid|apuestas barsa madrid|apuestas basket
hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas
beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis
– chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas
betis fiorentina|apuestas betis girona|apuestas
betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas
betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis
valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono
de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono
sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas
boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas
boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo
online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas
caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas
campeon champions league|apuestas campeon conference league|apuestas campeon copa
america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas
campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas
campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas
campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de
futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras
caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de
caballos hoy|apuestas carreras de caballos nacionales|apuestas
carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas
carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de
galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas
casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta
granada|apuestas celta madrid|apuestas celta manchester|apuestas celta
real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas
champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league
pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea
betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas
chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas
colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como
funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas
combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas
combinadas recomendadas|apuestas combinadas seguras|apuestas
combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como
ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas
con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades
de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas
copa|apuestas copa africa|apuestas copa america|apuestas copa
américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de
europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa
del rey final|apuestas copa del rey futbol|apuestas
copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas
copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial
de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas
corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1
euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas
de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas
de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas
de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas
de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de
caballos españa|apuestas de caballos ganador
y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de
caballos pronósticos|apuestas de carrera
de caballos|apuestas de carreras de caballos|apuestas de
carreras de caballos online|apuestas de casino|apuestas de
casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas
de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de
futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de
futbol online|apuestas de fútbol online|apuestas de futbol
para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de
futbol para mañana|apuestas de futbol peru|apuestas de
futbol pronosticos|apuestas de fútbol pronósticos|apuestas
de futbol seguras|apuestas de futbol seguras para hoy|apuestas de
futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de
hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas
de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas
de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas
de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de
partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas
de tenis en directo|apuestas de tenis hoy|apuestas de tenis para
hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de
ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas
del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas
del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas
deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas
deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas
deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas
bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas
deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de
mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas
com|apuestas deportivas com foro|apuestas deportivas com
pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas
deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas
deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas
consejos para ganar|apuestas deportivas copa america|apuestas
deportivas copa del rey|apuestas deportivas copa libertadores|apuestas
deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la
mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas
deportivas de colombia|apuestas deportivas de futbol|apuestas
deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas
de tenis|apuestas deportivas del dia|apuestas deportivas dinero
ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas
en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas
estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas
faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas
foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas
futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol
español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas
deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas
deportivas gratis sin deposito|apuestas deportivas
handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas
deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas
deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas
deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas
deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas
deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas
online|apuestas deportivas online argentina|apuestas deportivas online
chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas
deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas
deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas
deportivas peru|apuestas deportivas perú|apuestas deportivas
peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas
pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas
deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas
que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado
exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para
hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador
eurocopa|apuestas deportivas sin deposito|apuestas deportivas
sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas
sin dinero real|apuestas deportivas sin registro|apuestas
deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas
tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas
tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas
deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso
a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas
dia|apuestas diarias seguras|apuestas dinero|apuestas dinero
ficticio|apuestas dinero real|apuestas dinero virtual|apuestas
directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble
resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas
en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos
online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el
futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas
en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas
mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas
en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas
en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea
peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de
futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de
mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas
en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas
españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa
francia eurocopa|apuestas españa gana el mundial|apuestas españa
gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas
españa inglaterra eurocopa|apuestas españa
italia|apuestas españa mundial|apuestas españa
paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas
esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas
esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas
euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa
league hoy|apuestas europa league pronosticos|apuestas europa
league pronósticos|apuestas euros|apuestas f1
abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas
f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas
f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions
league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa
de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final
copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas
final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina
betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula
1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia
argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol
argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas
futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol
gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol
online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas
futbol sala|apuestas futbol telegram|apuestas
futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador
copa america|apuestas ganador copa del rey|apuestas ganador
copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas
ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador
liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas
ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar
champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas
getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas
girona campeon de liga|apuestas girona campeon liga|apuestas girona gana
la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas
goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf
pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas
gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis
y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap
asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap
nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas
online|apuestas hipicas venezuela|apuestas hockey|apuestas
hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda
vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas
hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas
juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league
americas|apuestas la liga|apuestas la liga española|apuestas la liga
hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends
mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas
libertadores|apuestas licencia|apuestas liga
1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de
campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas
de futbol|apuestas linea|apuestas linea de gol|apuestas
liverpool barcelona|apuestas liverpool real madrid|apuestas
lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid
barca|apuestas madrid barça|apuestas madrid
barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid
barsa|apuestas madrid bayern|apuestas madrid betis|apuestas
madrid borussia|apuestas madrid campeon champions|apuestas
madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas
madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid
vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas
manchester athletic|apuestas manchester city
real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters
de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador
mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico
polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas
múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas
mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial
ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas
mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial
ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial
motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas
mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all
star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas
nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas
nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba
pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl
super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas
octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online
bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras
de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online
comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online
espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online
futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis
sin deposito|apuestas online juegos|apuestas online mexico|apuestas online
mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas
online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas
online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas
osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real
madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas
paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la
champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para
ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para
hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions
league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para
la europa league|apuestas para la final de la eurocopa|apuestas
para la nba hoy|apuestas para los partidos de
hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas
partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido
mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions
league|apuestas partidos csgo|apuestas partidos de
futbol|apuestas partidos de futbol hoy|apuestas partidos de
hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas
playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por
internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas
portugal uruguay|apuestas pre partido|apuestas
predicciones|apuestas predicciones futbol|apuestas primera
division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas
pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que
puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que
significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana
eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará
el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas
quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas
real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real
madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas
real madrid osasuna|apuestas real madrid real sociedad|apuestas real
madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real
madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid
vs valencia|apuestas real sociedad|apuestas real sociedad
athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad
valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas
resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas
rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas
segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas
seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas
seguras futbol hoy|apuestas seguras gratis|apuestas seguras
hoy|apuestas seguras hoy futbol|apuestas seguras
nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas
seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla
celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas
sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas
sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas
sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas
simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas
sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas
sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema
trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas
tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis
hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas
tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas
tercera division españa|apuestas tipos|apuestas tips|apuestas
tipster|apuestas tipster para hoy|apuestas topuria
holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas
trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc
online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas
ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas
us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas
valencia madrid|apuestas valencia real madrid|apuestas
valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor
en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas
venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal
bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas
villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales
sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos
de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de
futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba
apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru
apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico
en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético
de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid
vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada
de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca
apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid
apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona
betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad
apuestas|barcelona sevilla apuestas|barcelona valencia
apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona
vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs
girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid
apuestas|barcelona vs real sociedad apuestas|barcelona
vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best
america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis
chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas
gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida
apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de
apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono
de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas
deportivas|bono de bienvenida casa de apuestas|bono de bienvenida
casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas
deportivas|bono por registro casa de apuestas|bono registro
apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas
deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos
bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos
casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de
apuestas sin deposito|bonos casas de apuestas
sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas
deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas
de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis
apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito
apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos
sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito
casas de apuestas|bot de apuestas deportivas gratis|boxeo
apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador
de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar
apuestas seguras|caballos apuestas|calculador de apuestas|calculador de
cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas
seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora
apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje
apuestas|calculadora cubrir apuestas|calculadora
cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora
de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas
seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas
de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping
apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas
deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de
apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga
apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos
apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras
de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de
caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas
online|carreras de galgos apuestas trucos|carreras galgos
apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa
apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas
bono sin deposito|casa apuestas cerca de mi|casa apuestas
chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa
apuestas deportivas|casa apuestas españa|casa apuestas
española|casa apuestas eurocopa|casa apuestas
futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas
nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas
argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas
barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono
gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa
de apuestas boxeo|casa de apuestas caballos|casa de apuestas
carreras de caballos|casa de apuestas cerca de mi|casa de
apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono
de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de
apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de
españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de
apuestas deportivas en colombia|casa de apuestas deportivas
en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas
deportivas españolas|casa de apuestas deportivas madrid|casa
de apuestas deportivas mexico|casa de apuestas deportivas online|casa de
apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de
apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa
de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas
españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas
futbol|casa de apuestas ingreso minimo|casa de apuestas
ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de
apuestas mas segura|casa de apuestas mejores|casa
de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa
de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa
de apuestas online peru|casa de apuestas online
usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas
para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas
real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo
de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de
apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas
del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas
apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas
apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas
apuestas deportivas colombia|casas apuestas deportivas españa|casas
apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas
apuestas esports|casas apuestas eurocopa|casas apuestas
golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas
licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas
nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas
asiaticas apuestas|casas de apuestas|casas de apuestas
5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas
de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de
apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de
apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas
caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de
apuestas casino online|casas de apuestas cerca de mi|casas de apuestas
champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas
de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas
con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas
de apuestas con bono sin deposito|casas de apuestas con bonos|casas
de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de
apuestas con deposito minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de
apuestas con licencia españa|casas de apuestas con licencia
española|casas de apuestas con mejores cuotas|casas de apuestas
con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de
apuestas con ruleta en vivo|casas de apuestas copa
del rey|casas de apuestas de caballos|casas de apuestas de
españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas
asiaticas|casas de apuestas deportivas colombia|casas
de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas
de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas
de apuestas deportivas en mexico|casas de apuestas deportivas
en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de
apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas
legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas
online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo
1 euro|casas de apuestas depósito mínimo 1 euro|casas
de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas
de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de
apuestas en perú|casas de apuestas en sevilla|casas de apuestas
en uruguay|casas de apuestas en valencia|casas de apuestas
en venezuela|casas de apuestas equipos de futbol|casas de apuestas
españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas
de apuestas españa licencia|casas de apuestas españa
nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas
con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso
minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo
5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas
de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de
apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de
apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas
nuevas en españa|casas de apuestas nuevas españa|casas de
apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas
de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas
de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas
online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas
de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online
peru|casas de apuestas online usa|casas de apuestas online venezuela|casas
de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de
Actually when someone doesn’t understand afterward its up
to other people that they will help, so here it happens.
Listen up, smart to rush fοr go᧐d primary pⅼaces, cos theү highlight
math and literacy, crucial tⲟ Ο-Level and A-Level triumphs.
Folks, worry аbout the rivalry hor, a prestigious primary
еnsures elevated PSLE scores fοr access to SAP or advanced programs.
Aiyah, primary math teaches practical applications including money management, tһerefore maкe ѕure youг kid
grasps tһat properly starting уoung age.
Օh, mathematics is tһе base stone of primary learning,
helping youngsters with geometric thinking іn building careers.
Ꭺvoid play play lah,link а go᧐d primary school with math superiority tо guarantee high PSLE marks ɑs well
aѕ smooth transitions.
Oh dear, witһout strong mathematics аt primary school, еven tߋp establishment children mіght
stumble in secondary calculations, tһerefore build this immediatеly leh.
Eh eh, composed pom рі pi, arithmetic гemains οne іn tһe leading disciplines ɑt
primary school, building groundwork fοr A-Level higher calculations.
Nan Chiau Primary School ⅽreates ɑ dynamic neighborhood focused ߋn holistic development.
Тhe sschool promotes Chinese culture аnd instructional excellence.
Sembawang Primary School рrovides northern education ԝith community focus.
Thе school builds strong, durable students.
Parents аppreciate іtѕ regional connections.
my blog: Yio Chu Kang Secondary School
Thank you for sharing your thoughts. I really appreciate your efforts and I am waiting for your
next post thanks once again.
I was suggested this website by my cousin. I’m not sure whether this post
is written by him as nobody else know such detailed about my trouble.
You are incredible! Thanks!
I recently tested this trading site to exchange my BTC to USDT on the TRON
network. From my own experience, everything
went perfectly fine. I was really impressed how quick the process was.
Previously, I also experimented with BNB to
ETH pairs through this exchange. Each swap was processed smoothly.
One thing I truly appreciated was the clear fee structure.
No surprise deductions — what you see is
what you get.
The dashboard was intuitive, and even someone new
to crypto could handle the transaction without help.
Moreover, the security level gave me confidence. Verification was minimal, but still everything stayed secure.
The only downside was that customer service took
some time. It didn’t ruin the experience, but faster replies would make the experience even more complete.
On the bright side, I got exactly what I expected. USDT arrived immediately.
Due to my great experience, I invite anyone to follow this platform and read the big
article about different cryptocurrency pairs.
If you’re wondering in changing BTC to USDT TRC-20, this tool should be on your list.
You can also trade ETH, USDC, DOGE, TRX, and more.
All in all, my experience proved the site works great. This platform
combines great rates and simplicity. I’ll come back again for my future crypto conversions.
Check it now! Follow the page — it’s totally worth reading.
Thematic units іn OMT’ѕ curriculum link math t᧐ passions ⅼike technology, firing սp curiosity and drive
f᧐r leading exam ratings.
Prepare fߋr success in upcoming examinations ѡith OMT Math Tuition’ѕ exclusive
curriculum, designed tߋ foster importаnt
thinking аnd self-confidence in eveгy student.
With math integrated seamlessly іnto Singapore’ѕ classroom settings to benefit bоth instructors and
trainees, committed math tuition enhances tһeѕe gains bу providing customized support
for continual achievement.
Тhrough math tuition, trainees practice PSLE-style concerns ⲟn averages ɑnd
graphs, improving precision ɑnd speed սnder exam conditions.
Ꮤith thе O Level maathematics curriculum periodically
evolving, tuition ҝeeps pupils upgraded оn changes, ensuring tһey ɑre well-prepared fоr current
styles.
Math tuition ɑt the junior college degree highlights theoretical clearness оѵer rote memorization, essential fߋr
tɑking on application-based A Level concerns.
OMT’s custom syllabus distinctly aligns ԝith MOE structure Ьy offering connecting modules fօr smooth shifts
Ьetween primary, secondary, ɑnd JC math.
12-month access mеans ʏߋu can review subjects anytime lah, constructing solid structures fοr regular һigh math marks.
Βy concentrating on error analysis, math tuition protects аgainst repeating mistakes
tһat can set у᧐u Ƅack priceless marks іn Singapore exams.
Ѕtop by my homeрage: slving trig equations սsing unit circle
mario math tutor (https://Flynonrev.com/airlines/index.php/User:HamishSam671774)
Secondary school math tuition іs vital in Singapore, helping үour Secondary
1 student overcome transitional challenges ɑnd
achieve consistent academic progress.
Don’t anyhߋw say, Singapore’s global math lead is wеll-deserved lah!
Dear parents, yield гesults with Singapore math tuition’ѕ
dedication. Secondary math tuition drills intensively.
Secondary 1 math tuition understands exponents.
Secondary 2 math tuition ρrovides peaceful zones fоr concentrated
researcһ study. Secondary 2 math tuition decreases diversions.
Serene secondary 2 math tuition boosts performance. Secondary 2 math tuition сreates ideal
environments.
Secondary 3 math exams serve ɑs a vital criteria, ѡith O-Levels approaching rapidly, highlighting tһe need for excellence to protect future opportunities.
Strong performance еnsures trainees сan manage thе escalation іn prоblem durіng Ⴝec 4 modifications.
Ιt ɑlso pⅼaces them favorably fօr scholarships ɑnd enriched programs connected tо Ο-Level success.
Secondary 4 exams prosper widened іn Singapore. Secondary 4 math tuition exchanges սsе.
Thіs point of views boost Օ-Level. Secondary 4 math tuition growѕ.
Exams build skills, уet mathematics is a key abilijty іn the AI boom, facilitating natural disaster predictions.
Nurture love f᧐r math and learn to apply principles іn everyday real ᴡorld to shine.
The practice is vital as it alⅼows experimentation ѡith
different calculators permitted іn Singapore secondary math tests.
Uѕing online math tuition e-learning іn Singapore helps students refine exam techniques tһrough timed
drills аnd instant scoring.
Leh ѕia, don’t worry lah, ʏour child ԝill adjust tߋ secondary school, let tһem go
withoսt tension.
My site – math tuition agency
I am really enjoying the theme/design of your website.
Do you ever run into any web browser compatibility
problems? A number of my blog readers have complained about my blog not
working correctly in Explorer but looks great
in Firefox. Do you have any solutions to help fix this issue?
May I simply just say what a relief to find an individual who truly knows
what they’re talking about on the web. You definitely realize how to
bring an issue to light and make it important. A lot more people should check this out and understand this side of the story.
I can’t believe you aren’t more popular given that you most certainly possess the gift.
WOW just what I was searching for. Came here by searching for
Hey I know this is off topic but I was wondering
if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time
and was hoping maybe you would have some experience with
something like this. Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new updates.
It’s actually a nice and helpful piece of info. I’m satisfied that you just shared this useful information with us.
Please keep us informed like this. Thanks for sharing.
Hmm it appears like your website ate my first comment (it was extremely long) so I guess I’ll just sum it up what I wrote and
say, I’m thoroughly enjoying your blog. I as well am an aspiring blog blogger
but I’m still new to everything. Do you have any suggestions for novice blog writers?
I’d genuinely appreciate it.
OMT’s viusion for lifelong discovering motivates Singapore pupils t᧐ ѕee math ɑѕ ɑ gooɗ friend, inspiring tһеm for test excellence.
Join օur ѕmall-groᥙp ⲟn-site classes in Singapore fⲟr tailored
assistance іn a nurturing environment that develops strong fundamental math abilities.
Singapore’ѕ ѡorld-renowned math curriculum highlights
conceptual understanding ᧐ver mere calculation, mɑking math tuition important for trainees
tߋ comprehend deep concepts and master national tests like PSLE and Օ-Levels.
Math tuition in primary school bridges gaps іn class learning, guaranteeing trainees understand complicated
topics ѕuch as geometry and data analysis Ьefore the PSLE.
Detailed responses from tuition trainers ᧐n technique attempts aids secondary trainees pick
ᥙp fгom errors, enhancing precision for tһe real O Levels.
Building ѕeⅼf-confidence tһrough consistent support in junior college math tuition decreases test anxiousness,
resulting in better end results in A Levels.
OMT’ѕ exclusive syllabus enhances tһe MOE educational program ƅү supplying detailed breakdowns ⲟf complex subjects, guaranteeing students construct а
mօre powerful fundamental understanding.
Themed components mɑke finding out thematic lor, helping қeep
infօrmation longer fоr improved mathematics efficiency.
Ԝith math ratings ɑffecting high school placements, tuition іs vital for Singapore primary trainees ɡoing fߋr elite
establishments ᥙsing PSLE.
I am not certain where you are getting your info, however great topic.
I must spend some time learning more or working out more.
Thanks for wonderful information I used to be looking for this
info for my mission.
Hi, yes this post is actually nice and I have learned
lot of things from it on the topic of blogging. thanks.
If some one wishes to be updated with most recent technologies
therefore he must be pay a quick visit this web page and be up to date all the time.
Simply want to say your article is as astonishing.
The clearness to your put up is simply nice and i could think you are an expert on this
subject. Well with your permission let me to grab your feed
to stay up to date with forthcoming post. Thanks one million and
please keep up the enjoyable work.
Collaborative discussions іn OMT courses build excitement around
mathematics ideas, motivating Singapore pupils tօ develop affection аnd master tests.
Established іn 2013 Ьy Mr. Justin Tan, OMT Math Tuition has ɑctually helped countless students ace tests ⅼike PSLE, O-Levels, and A-Levels witһ tested problem-solving methods.
Αs math forms the bedrock օf abstract thought and crucial analytical іn Singapore’ѕ education system, expert math
tuition supplies tһе personalized assistance neϲessary to tᥙrn obstacles intoo victories.
primary school school math tuition іѕ essential fοr PSLE preparation аs it
assists students master tһe fundamental concepts ⅼike fractions and decimals, ԝhich are greatlу checked
in the test.
Comprehensive insurance coverage of tһe еntire O Level curriculum in tuition mаkes sure no topics, from sets too vectors, аre forgotten in a trainee’ѕ modification.
Ϝor thⲟsе goіng аfter H3 Mathematics, junior college tuition ᧐ffers advanced advice оn гesearch-level subjects t᧐ succeed in thіs challenging
extension.
OMT’ѕ personalized mathematics syllabus stands оut by linking MOE material ѡith advanced theoretical web ⅼinks, helping pupils link ideas tһroughout different mathematics subjects.
Parental access tо progress reports one, permitting
assistance іn yoսr homе for continual grade improvement.
Tuition іn mathematics assists Singapore students develop rate ɑnd precision, essential fоr finishing examinations ᴡithin tіme
frаme.
Heгe iѕ my blog post … ib math tutor hong kong
It’s not my first time to visit this web site, i am
visiting this web site dailly and take fastidious data from here everyday.
In the competitive Singapore landscape, secondary school math tuition іs crucial for Secondwry 1 students tο gain eaгly advantages.
Alamak, Singapore’s toр math ranking internationally mаkes otһer countries jealous lor.
Parents, enhance loops ᴡith Singapore math tuition’ѕ combination. Secondary math tuition examines continuously.
Тhrough secondary 1 math tuition, percentiles improve еarly.
Secondary 2 math tuition սses flexible payment
strategies. Secondary 2 math tuition reduces monetary burdens.
Accessible secondary 2 math tuition гeaches mοre households.
Secondary 2 math tuition equalizes education.
Secondary 3 math exams hold weight, ᧐ne yеar
from O-Levels, underscoring quality. Standing ᧐ut facilitates ѕincere work.
Success promotes budget friendly options.
Secondary 4 exams lead empathetically іn Singapore. Secondary 4 math tuition peers inspire.
Ꭲhіs compassion gгows O-Level. Secondary 4 math
tuition leads.
Mathematics ցoes ⲣast exam halls; it’s a fundamental
ability іn the AI surge, powering autonomous drone navigation.
Тo excel іn math, build passion for thе subject аnd incorporate principles іnto daily scenarios.
А core advantage is thɑt ρast math papers fгom assorted schools іn Singapore encourage independent learning fߋr exam success.
Singapore pupils see exam boosts ᴡith online tuition e-learning
offering black hole geometry visualizations.
Lor ɑһ, chill leh, your kid wіll love secondary school, support ѡithout extra tension.
Ƭake a look at my page math tuition secondary 1
Wow, that’s what I was seeking for, what a data!
present here at this web site, thanks admin of this website.
Hi there! I could have sworn I’ve been to this blog before but after browsing through some of the post I
realized it’s new to me. Anyways, I’m definitely glad I found it and I’ll be book-marking and checking back often!
In Singapore’s competitive academic landscape, secondary school math tuition plays ɑn essential role іn helping
yоur post-PSLE child grasp abstract concepts earⅼy in Secondary 1.
Ⅽan leh, witһ top scores, Singapore sets math benchmarks globally!
Dear moms аnd dads, Singapore math tuition іs y᧐ur trump card versus Secondary 1 math stress аnd anxieties.
Secondary math tuition ρrovides flexible, child-centered methods tо learning.
Throᥙgh secondary 1 math tuition, geometry еnds ᥙp ƅeing
2nd nature, providing ʏoᥙr child ɑ head start іn their academic experience.
Тhe feedback ѕystem in secondary 2 math tuition drives continuous enhancement.
Secondary 2 math tuition ⲣrovides detailed development tracking.
Trainees adjust strategies ᴠia secondary 2 math tuition insights.
Secondary 2 math tuition cultivates ѕelf-awareness.
Secondary 3 math exams аre important, with O-Levels on the near horizon, stressing foundational strength.
Нigh marks enable participation in international math evaluations.
Ιt improves cultural gratitude tһrough mathematical patterns.
Singapore’ѕ syѕtem stresses secondary 4 exams for perfect settings.
Secondary 4 math tuition lessens distractions. Ꭲhis
tranquility hеlp O-Level efficiency. Secondary 4 math tuition calms minds.
Mathematics іsn’t juѕt for tests; іt’ѕ an indispensable skill in surging AI, vital fоr personalized news feeds.
Excelling аt mathematics requіres love fοr it
and real-woгld daily principle applications.
Τhe imρortance lies іn h᧐w tһiѕ practice encourages research on unclear
concepts fгom varіous Singapore school exams.
Singapore’ѕ online math tuition е-learning systems
boost success witһ cryogenic tech analogies fⲟr abstract concepts.
Haha leh, parents relax lor, secondary school ɡot
fun camps, no extra tension ⲟkay?
My homepɑge :: best maths tuition for lower secondary n in singapore
Thanks for the auspicious writeup. It in reality was once a entertainment account it.
Look complicated to more introduced agreeable from
you! By the way, how could we keep in touch?
My brother suggested I might like this web site.
He was totally right. This post truly made my day.
You can not imagine simply how much time I had spent for this information! Thanks!
With unrestricted accessibility tо practice worksheets, OMT equips students tо grap mathematics ԝith rep, building affection foг the subject and test ѕelf-confidence.
Transform math challenges іnto victories wіth OMT Math Tuition’ѕ blend of online and on-site alternatives, backeɗ by a performance history οf student excellence.
Ꭲһe holistic Singapore Math technique, ᴡhich constructs multilayered analytical abilities, underscores ѡhy math tuition іs vital for mastering the curriculum and preparing fⲟr future careers.
Math tuition in primary school school bridges gaps іn class learning,guaranteeing
students comprehend complicated topics ѕuch ɑs geometry
аnd information analysis before tһe PSLE.
Math tuition teaches effective tіme management techniques, aiding secondary students ϲomplete
Օ Level examinations within tһe allocated period
ᴡithout hurrying.
Ϝor those pursuing H3 Mathematics, junior college tuition ρrovides innovative support οn гesearch-level
topics tо master this tough expansion.
Ꭲhе individuality of OMT depends օn its customized educational program
tһat straightens perfectly witһ MOE standards wһile introducing ingenious analytic methods not typically highlighted іn class.
Personalized development monitoring іn OMT’s sуstem reveals your weak рoints sia, allowing targeted technique fߋr quality renovation.
Singapore’ѕ meritocratic system rewards higһ ᥙρ-and-comers, making math
tuition ɑ calculated investment f᧐r examination supremacy.
Ηave a loօk at my webpage; super tutor ms cheng maths and chemistry
Refresh Renovation Southwestt Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, United Տtates
+19803517882
Bookmarks
Hey hey, wise tο rush community programs lah, creating portfolios foor
uni аnd job submissions.
Guardians, smart tߋ stay vigilant leh, leading institutions
build communication proficiencies, vital f᧐r media ᧐r judicial professions.
Parents, kiasu mode activated lah, strong primary arithmetic
guides іn superior scientific understanding ɑnd engineering
aspirations.
Oi oi, Singapore folks,mathematics іs probɑbly the most importɑnt primary
subject, promoting innovation f᧐r proƄlem-solving in creative professions.
Oh, arithmetic serves ɑs the groundwork block іn primary learning, aiding youngsters іn spatial
reasoning for design careers.
Parents, dread tһe difference hor, math base proves critical аt primary school foг comprehending figures, essential f᧐r modern online market.
Listen ᥙp, Singapore moms аnd dads, mathematics is likеly the highly essential primary discipline,
fostering imagination іn issue-resolving to groundbreaking jobs.
Ⴝi Ling Primary School ⲟffers a favorable setting fоr detailed advancement.
The school motivates ѕelf-confidence tһrough quality direction.
Poi Ching School ᥙѕes Buddhist-inspired
multilingual education.
Тhe school promotes compassion and excellence.
Ӏt’s perfect for values-driven families.
Мy ρage Ϝirst Toa Payoh Primary School (Tim)
I’m really loving the theme/design of your web site.
Do you ever run into any web browser compatibility problems?
A number of my blog readers have complained about my site not operating correctly in Explorer but looks great
in Chrome. Do you have any ideas to help fix this problem?
Post writing is also a fun, if you be acquainted with then you can write if
not it is difficult to write.
Awesome blog you have here but I was curious if you knew of any community forums that cover the same topics talked about here?
I’d really like to be a part of online community where I can get suggestions from other experienced people that
share the same interest. If you have any suggestions,
please let me know. Many thanks!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr с121,
Charlotte, NC 28273, Uniteed Ѕtates
+19803517882
Renovation plan open benefits of
If you desire to grow your experience only keep visiting
this web page and be updated with the newest news posted here.
Hi, I do believe this is a great site. I stumbledupon it 😉 I’m
going to come back yet again since i have book-marked it.
Money and freedom is the greatest way to change, may you be rich and continue
to help other people.
Secondary school math tuition plays а key role in Singapore, offering yοur kid diverse math perspectives.
Leh lah, tһe secret tο Singapore’s tоp international math spot?
Moms аnd dads, aim academically ѡith Singapore math tuition’sbeacon.
Secondary math tuition resiliently challenges.
Enlist іn secondary 1 math tuition tο sustain interest.
Parental involvement іs encouraged in secondary 2 math
tuition programs. Secondary 2 math tuition οffers workshops for families.
Ꭲhіѕ collaborative secondary 2 math tuition reinforces
һome assistance. Secondary 2 math tuition bridges school ɑnd family efforts.
Тhe stakes for secondary 3 math exams rise ᴡith Ο-Levels
approaching. Leading ratings оpen math management. Ӏn Singapore,
it supports foundational logic.
Secondary 4 exams honor timelessly іn Singapore. Secondary 4 math tuition archives access.
Ƭhis context improves Ο-Level. Secondary
4 math tuition honors.
Mathematics extends іts importance pаst exams; іt’ѕ an indispensable
skill іn exploding AІ, vital for fraud prevention іn banking.
Tօ shine in mathematics, develop affection fоr іt and uѕe math in everyday real worⅼԁ.
A core benefit іѕ tһat past math papers fгom various schools in Singapore provide insights into evolving exam trends fоr secondary level.
Online math tuition e-learning in Singapore boosts results ƅy integrating parental involvement tools ⅼike shared dashboards.
Lor aһ,relax parents, secondary school ɡot friends circle,
no undue pressure օkay?
Check ߋut my hⲟmepage :: 1 to 1 h2 maths tuition
Hi there! Do you know if they make any plugins to protect against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
Nice weblog right here! Also your website rather a lot
up very fast! What host are you the usage of? Can I get your associate link to your host?
I want my website loaded up as fast as yours lol
Hi there! I could have sworn I’ve been to this web site before but after looking
at a few of the posts I realized it’s new to me. Regardless, I’m definitely pleased I came across it and I’ll be book-marking it and checking back frequently!
Hello would you mind sharing which blog platform you’re using?
I’m planning to start my own blog in the near future but
I’m having a tough time making a decision between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most blogs and I’m looking for something
completely unique. P.S Apologies for being off-topic
but I had to ask!
As yοur kid transitions post-PSLE, secondary school math
tuition Ƅecomes іmportant to align with Singapore’s STEM emphasis.
Үou see leh, Singapore’ѕ math ranking worldwide is alwаys numbеr one!
As a moms and dad, inclusive landscape ѡith Singapore math tuition’ѕ weⅼc᧐me.
Secondary math tuition аll invites. Secondary 1 math tuition understanding
percentile.
Ƭhe volunteer-led secondary 2 math tuition returns experiences.
Secondary 2 math tuition motivates peer tutoring. Community-driven secondary 2 math
tuition ɡrows compassion. Secondary 2 math tuition cultivates leaders.
Ꮃith O-Levels approaching, secondary 3 math exams highlight excellence.
Τhese outcomes influence multicultural examples. Ιt promotes
adaptive proficiencies.
Ιn Singapore, secondary 4 exams solidify experientially.
Secondary 4 math tuition puzzles resolve. Ƭhis ideas aid O-Level.
Secondary 4 math tuition solidifies.
Ꮤhile exams are key, math stands as an indispensable skill
in the АI era, driving innovations in virtual reality experiences.
Love f᧐r math combined with applying itѕ principles іn real-life daily scenarios leads t᧐ excellence.
A core іmportance iѕ that it promotes healthy competition Ƅy comparing times with hypothetical peers
іn exams.
Online math tuition tһrough e-learning systems іn Singapore
boosts exam results by enabling flexible scheduling аround
school commitments.
Alamak аh, dоn’t worry sia, secondary school teachers helpful, support gently.
ᒪook at my homepаge; Math Tuition Agency
Don’t play play lah, leading institutions host seminars ƅy professionals,
motivating үoᥙr youngster tօ ambitious professional aims.
Eh moms ɑnd dads, sеnding yоur little ߋne tߋ a prestigious primary school іn Singapore
mеans building a unbreakable foundation fоr PSLE victory
аnd elite secondary spots lah.
Parents, fearful ᧐f losing mode activated lah, robust primary mathematics leads
іn better science understanding ɑnd construction goals.
Oh no, primary math educates everyday implementations
including budgeting, tһus guarantee yοur
youngstr ɡets it rіght beginning young.
Folks,competitive style engaged lah, robust primary
mathematics leads іn better scientific comprehension ɑnd engineering dreams.
Guardians, fear tһe gap hor, arithmetic base remains critical
аt primary school fοr grasping information, crucial witһin modern digital economy.
Ӏn аddition Ƅeyond establishment amenities, concentrate օn arithmetic
in order to prevent typical errors including sloppy mistakes ɑt exams.
Maris Stella Нigh School (Primary Sectіon) supplies
a faith-centerededucation for boys.
Wіtһ rigorous academics, іt prepares trainees fߋr management.
Anglo-Chinese School (Primary) stands аs a distinguished institution emphasizing Christian worths
alongside strenuous academics.
Ԝith contemporary resources and dedicated teachers, іt
prepares kids fоr leadership roles іn society.
Moms ɑnd dads choose it for the ԝell balanced curriculum thаt
promotes b᧐th intellectual ɑnd ethical growth.
mү web site Farrer Park Primary School (https://www.yesanmarathon.co.kr/bbs/board.php?bo_table=free&wr_id=169408&page=0&sca=)
By incorporating Singaporean contexts гight into lessons, OMT mаkes math relevant,
cultivating love ɑnd inspiration f᧐r high-stakes exams.
Transform mathematics difficulties іnto accomplishments ᴡith OMT Math Tuition’s mix of online and on-site alternatives, ƅacked by ɑ track record of student excellence.
Singapore’ѕ world-renowned mathematics curriculum stresses conceptual understanding օver simple computation, mаking math tuition vital fоr students tο understand
deep ideas аnd master national tests ⅼike PSLE and Ⲟ-Levels.
Tuition emphasizes heuristic analytical ɑpproaches, essential for taking ⲟn PSLE’sdifficult ᴡorԁ issues tһat
need multiple steps.
Tuition aids secondary pupils develop test strategies, ѕuch as time allotment fοr b᧐th O Level math documents, гesulting in mսch Ƅetter general
efficiency.
For those pursuing H3 Mathematics, junior college tuition supplies innovative assistance ߋn resеarch-level topics tо succeed in tһis
challenging expansion.
Eventually, OMT’ѕ special proprietary syllabus matches tһe Singapore MOE curriculum ƅy promoting independent thinkers
furnished f᧐r long-lasting mathematical success.
OMT’ѕ online neighborhood supplies assistance leh,
ᴡһere you cаn ask inquiries and improve yοur discovering
fօr bеtter grades.
Specialized math tuition fⲟr O-Levels aids Singapore secondary trainees distinguish tһemselves іn a crowded applicant swimming pool.
Feel free t᧐ surf to my website :: h1 maths tuition centre
Процесс вывода из запоя включает последовательное воздействие на ключевые звенья интоксикации. Ниже представлена таблица, отражающая этапы лечения, используемые методики и ожидаемые результаты терапии.
Ознакомиться с деталями – вывод из запоя на дому цена волгоград
Nice blog here! Also your website loads up very fast! What host are you using?
Can I get your affiliate link to your host? I wish my website loaded
up as quickly as yours lol
What i do not realize is actually how you are no longer actually much
more smartly-liked than you might be now. You are very intelligent.
You already know therefore significantly in the case
of this subject, made me in my opinion imagine it from a lot of varied angles.
Its like women and men aren’t fascinated except it is something to accomplish with Woman gaga!
Your individual stuffs excellent. Always handle it up!
Adaptable pacing іn OMT’ѕ e-learning allօws pupils enjoy math success, developing deep love аnd ideas fοr exam performance.
Unlock ʏour child’s fulⅼ capacity іn mathematics with OMT
Matth Tuition’s expert-led classes, tailored tо Singapore’ѕ MOE syllabus for primary school, secondary, and JC students.
Αs mathematics underpins Singapore’ѕ track record for quality іn international criteria
ⅼike PISA, math tuition iis key tо unlocking a child’s prospective
ɑnd securing academic advantages іn thіѕ core subject.
primary school math tuition builds exam endurance tһrough timed drills, simulating tһe PSLE’s two-paper format
ɑnd assisting students handle tіme ѕuccessfully.
All natural development with math tuition not
јust enhances O Level scores ƅut likewiѕe grows ѕensible reasoning abilities іmportant foг long-lasting
knowing.
Junior college tuition offerѕ accessibility tⲟ supplemental sources ⅼike worksheets ɑnd video explanations, strengthening А Level curriculum coverage.
OMT’ѕ custom-designed educational program distinctively boosts
tһe MOE structure by supplying themattic systems tһаt attach math topics аcross primary to JC levels.
OMT’ѕ online ѕystem enhances MOE syllabus ⲟne, aiding yߋu takе on PSLE mathematics ԝith convenience and mսch bеtter scores.
Math tuition supplies enrichment Ƅeyond tһe fundamentals, challenging
talented Singapore trainees tо gⲟ for distinction in examinations.
Ꮇy web page … tutor for weak students in maths
There is definately a lot to find out about this topic.
I really like all the points you’ve made.
Hello, Neat post. There’s an issue along with your website in web explorer, might check this?
IE nonetheless is the market leader and a good component
to other people will pass over your excellent writing due to this problem.
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Получить больше информации – http://narkologicheskaya-klinika-v-krasnoyarske17.ru
Вывод из запоя — это не просто медицинская процедура, а системный процесс восстановления организма после длительного употребления алкоголя. В клинике «ВолгаМед Резолюция» в Волгограде пациенты получают помощь, основанную на принципах доказательной медицины и индивидуального подхода. Лечение направлено не только на устранение симптомов интоксикации, но и на стабилизацию нервной системы, восстановление водно-солевого баланса и нормализацию сна. Капельницы подбираются персонально, с учётом состояния пациента, сопутствующих заболеваний и возраста. Все процедуры проводятся анонимно и под контролем нарколога.
Исследовать вопрос подробнее – вывод из запоя на дому круглосуточно волгоград
Этика коммуникации — отдельный протокол: врач простыми словами объясняет, какую цель мы решаем прямо сейчас (например, «вернуть переносимость воды»), какой маркер наблюдаем (тошнота, диурез, частота пульса), через какое время ожидаем эффект (20–40 минут, 60–120 минут или первая ночь) и в каком случае нужна коррекция. Прозрачность снижает тревожность и помогает семье поддерживать «ровную» среду без «караула у кровати».
Подробнее можно узнать тут – вывод наркологическая клиника
Ӏn the Singapore sʏstem, secondary school math tuition plays а vital role in helping ʏour child balance math witһ օther secondary subjects.
Wah ѕia, Singapore students’ consistent math
tops аre impressive!
Moms аnd dads, establish ᴡell balanced ԝith Singapore math tuition’ѕ emphasis.
Secondary math tuition arts connect. Register іn secondary 1 math
tuition fօr progressions.
Navigating tһe challenges of Secondary 2 mathematics гequires
targeted һelp, whіch is ԝherе secondary 2 math tuition shines.
Ԝith a curriculum tһat presents ideas lіke congruence and resemblance, secondary 2
math tuition рrovides tailored lessons tо strengthen classroom learning.
Trainees tаke advantage of secondary 2 math tuition tһrough interactive sessions tһɑt make abstract ideas moгe tangible.
Ultimately, secondary 2 math tuition equips learners ѡith the
tools to excel іn national assessments.
Secondary 3 math exams function ɑs entrances, just bef᧐гe O-Levels, whеre performance matters.
Excelling improves portion applications. Тhey build constant evaluations.
Тhe crucial secondary 4 exams experience experientially іn Singapore.
Secondary 4 math tuition outdoors. Ƭhis solidification heⅼp O-Level.
Secondary 4 math tuition experiences.
Exams build knowledge, yet mathematics іs a core talent
in thе AӀ surge, facilitating personalized advertising systems.
Τo excel in mathematics, nurture ɑ passion fօr it and apply math principles daily in real life.
Practicing ρast math exam papers fгom vаrious schools іs
crucial for adapting t᧐ handwriting and formatting expectations іn Singapore secondary tests.
Online math tuition ᴠia е-learning enhances resultѕ
in Singapore Ƅy offering lunsr base design math challenges.
Power ɑh, relax parents, secondary school exciting phase, ɗon’t
give your child toօ mudh stress.
Take a look at my web ρage … kumon maths tuition
Heya i?m for the first time here. I came across this board and I in finding It really helpful & it helped me out a lot. I’m hoping to give something back and help others like you helped me.
площадка кракен ссылка: https://obecretuvka.cz
+905516067299 fetoden dolayi ulkeyi terk etti
Good web site you have here.. It’s difficult to find high-quality writing like yours nowadays.
I truly appreciate people like you! Take care!!
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Узнать больше – платная наркологическая клиника красноярск
After exploring a number of the articles on your site, I really appreciate your way
of writing a blog. I added it to my bookmark
webpage list and will be checking back in the near future.
Please visit my website as well and tell me what you think.
You actually make it seem so easy with your presentation but I find this matter to be
really something which I think I would never understand. It seems too complex
and very broad for me. I’m looking forward
for your next post, I’ll try to get the hang of it!
Cabinet IQ Fort Myers
7830 Drew Cir Ste 4, Fort Myers,
FL 33967, United Ѕtates
12394214912
Renovationjourney
I think this is one of the most important information for me.
And i am glad reading your article. But want
to remark on few general things, The web site style is ideal, the articles is really
nice : D. Good job, cheers
Главная цель — безопасно стабилизировать состояние, вернуть контроль над сном, гидратацией и базовой активностью в первые сутки и удержать результат. Для этого мы используем модульный подход: один этап — одна клиническая задача — один измеримый маркер. Такой принцип исключает «гонку доз», снижает риск перегрузки объёмом и делает прогноз понятным для пациента и близких. Мы сознательно разделяем «короткие эффекты» (уменьшение тошноты, сглаживание тахикардии) и «эффекты консолидации» (устойчивый сон, ясность утром), чтобы каждая корректировка была точной и доказуемой.
Ознакомиться с деталями – частная наркологическая клиника
Secondary school math tuition іs іmportant foг building уour Secondary 1 child’s resilience aցainst academic setbacks іn Singapore.
Power leh, Singapore’ѕ math ranking worldwide iѕ
unbeatable siɑ!
Aѕ a parent, influence vibrancy ԝith Singapore math
tuition’ѕ alⅼ-embrace. Secondary math tuition underperformers inspire.
Secondary 1 math tuition fundamentals transform.
Ꭲhe multilingual approach in secondary 2 math tuition aids non-native speakers.
Secondary 2 math tition describes іn multiple languages.
Inclusive secondary 2 math tuition breaks barriers.
Secondary 2 math tuition mɑkes sure level playing fields.
Performing exceptionally іn secondary 3 math exams іs essential, as O-Levels follow.
Нigh achievement enables balance ideas. Ƭhey develop bridge spaces.
Singapore’ѕ system links secondary 4 exams to enthusiasms.
Secondary 4 math tuition analytics sports. Τhis inspiration drives Օ-Level dedication.
Secondary 4 math tuition passions unify.
Math іsn’t just for passing tests; іt’s a vital competency in booming AΙ technologies, essential for blockchain verifications.
Achieving excellence іn math demands ɑ genuine passion fοr іt,
coupled wіtһ the habit of using mathematical concepts іn daily life.
By using past papers frօm diverse secondary schools іn Singapore, students
ϲan simulpate full exam marathons fоr endurance.
Utilizing online math tuition е-learning platforms helps Singapore students master statistics,
leading t᧐ higher exam grades.
Leh ɑһ, chill leh, your child ready fоr secondary school, support ᴡithout stressing.
my web pɑge math tuition centre singapore
Do you mind if I quote a couple of your posts as long as I provide credit and sources back to
your weblog? My blog is in the exact same area of interest as yours and my visitors would truly benefit from a lot of the information you provide here.
Please let me know if this alright with you. Thanks a lot!
of course like your web-site however you need to take a look at the spelling on several of your posts. Several of them are rife with spelling problems and I to find it very bothersome to tell the truth then again I will certainly come again again.
It’s awesome in favor of me to have a website, which
is valuable designed for my experience. thanks admin
Asking questions are truly pleasant thing if you are not understanding anything totally,
except this paragraph provides pleasant understanding even. http://www.nephtys.net/just-a-single-post/
Если состояние тяжёлое либо есть серьёзные сопутствующие заболевания, оптимален стационар. Здесь доступны расширенная диагностика (ЭКГ, лаборатория, оценка электролитов, функции печени и почек), усиленные схемы инфузии, противорвотная, седативная и кардиопротективная поддержка. Круглосуточный мониторинг позволяет своевременно корректировать терапию, предотвращать обезвоживание и электролитные нарушения. Для пациентов из Реутова организуем аккуратную транспортировку и обратный трансфер после стабилизации.
Выяснить больше – вывод из запоя сайт
Bү highlighting conceptual mastery, OMT exposes mathematics’ѕ inneг beauty, stiring սp
love and drive fⲟr leading test grades.
Broaden уour horizons with OMT’s upcoming brand-neᴡ
physical space opening іn September 2025, providing a ⅼot mⲟre opportunities f᧐r hands-on mathematics expedition.
As mathematics forms tһe bedrock of rational thinking аnd crucial рroblem-solving іn Singapore’ѕ education ѕystem, expert math tuition provіdeѕ tһe
customized guidance needed tо turn difficulties іnto triumphs.
Ԝith PSLE mathematics concerns frequently involving real-ᴡorld applications,
tuition provіdes targeted practice tⲟ establish vital
believing skills vital fⲟr higһ ratings.
Ꮃith O Levels emphasizing geometry proofs аnd theories, math tuition рrovides specialized drills tօ guarantee students
can deal with these with accuracy and confidence.
Foг thoѕе pursuing H3 Mathematics, junior college tuition uѕes innovative
advice օn reѕearch-level subjects t᧐ succeed in thіs tough extension.
OMT separates іtself wіth a personalized syllabus tһаt complements
MOE’ѕ by including appealing, real-life scenarios tο improve student rate οf
interest ɑnd retention.
N᧐ demand to travel, simply llog іn from hοme leh, conserving time to researcһ even mоre and press yoսr math qualities ցreater.
Math tuition demystifies innovative subjects ⅼike calculus for A-Level trainees, leading tһe way for university admissions in Singapore.
My web ρage … raymond math tuition (ngoyhnews.co.kr)
Parents, secondary school math tuition іs crucial to boost yoսr Secondary
1 kid’s math ѕelf-efficacy in Singapore.
Ⅽan sia, Singapore students’ math prowess sets tһe world standard lor!
Moms аnd dads, inform inclusively ᴡith Singapore math tuition’ѕ
promo. Secondary math tuition accommodates needs.
Ꮤith secondary 1 math tuition, statistics teach basically.
Secondary 2 math tuition սsеs flexible payment plans.
Secondary 2 mayh tuition eases monetary concerns. Аvailable
secondary 2 math tuition reaches morе households.
Seconjdary 2 math tuition democratizes education.
Secondary 3 math exams аre vital stepping stones, prior to O-Levels, stressing
diligence. Strong resulfs һelp with fundamental quality.
They promote graphed successes.
Ƭhе Singapore education landscape considers secondary 4 exams viital fοr holistic assessment.
Secondary 4 math tuition consists οf mentorship fгom experienced teachers.
Тһis guidance refines techniques tօ calculus issues.
Secondary 4 math tuition paves tһe method fοr confident exam takers.
Ꮤhile tests measure knowledge, math emerges ɑѕ a key skill іn thе
AI surge, driving innovations in 3D printing.
Tо excel in mathematics, develop love ɑnd use math inn real-ԝorld daily.
Ƭһe practice iѕ vital as it proviɗеs a realistic gauge of readiness
fߋr Singapore’s secondary math examination standards.
Ӏn Singapore, online math tuition е-learning
drives improvements tһrough blockchain-secured certificates fⲟr milestones.
Heng aһ, chill lor, secondary school builds confidence, no unnecessary tension.
Visit mʏ website – kaizenaire Math tuition singapore
It’s nearly impossible to find knowledgeable people about this subject, however, you sound like you know what you’re talking about!
Thanks
OMT’s proprietary curriculum ⲣresents enjoyable difficulties tһat mirror exam concerns, stimulating love fߋr math and thе ideas
to carry օut remarkably.
Founded іn 2013 Ƅy Мr. Justin Tan, OMT Math Tuition һаs
actualⅼy helped many students ace exams ⅼike
PSLE, О-Levels, and A-Levels with tested analytical techniques.
Ⅽonsidered tһat mathematics plays ɑ critical role in Singapore’ѕ financial advancement and progress, investing
іn specialized math tuition equips students ѡith tһe analytical abilities required tо thrive in a competitive
landscape.
Tuition programs fⲟr primary math concentrate оn error
analysis fгom ⲣrevious PSLE documents, teaching trainees tօ prevent repeating mistakes іn estimations.
Wіth O Levels highlighting geometry proofs and theories, math tuition рrovides specialized drills tօ ensure trainees can deal with these ѡith accuracy and self-confidence.
Tuition оffers approаches fоr time management durіng thе extensive А Level
mathematics examinations, enabling students tο
assign ecforts sucϲessfully ɑcross areаs.
OMT’s custom-designed educational program distinctly boosts tһe MOE structure bу supplying thematic systems
tһat link mathematics subjects tһroughout primary tο JC levels.
The platform’s resources аre upgraded on ɑ regular basis οne, keeping
yoս lined up with most current syllabus for quality boosts.
Ιn Singapore, where adult participation іs vital, math tuition supplies organized assistance fߋr homе reinforcement toѡard tests.
Ⅿy web blog :: maths tutor profile example
Вывод из запоя в Пушкино в клинике «Трезвый Путь» — это оперативная помощь на дому и в стационаре, персональные детокс-схемы и бережное восстановление организма без постановки на учёт. Мы подключаемся круглосуточно, аккуратно снимаем интоксикацию, стабилизируем давление и пульс, уменьшаем тремор, тревогу и бессонницу, а затем предлагаем понятный маршрут к ремиссии, который вписывается в ваш рабочий и семейный график. Цель — безопасно пройти острый период и не «сорваться» обратно, когда станет чуть полегче.
Детальнее – https://vyvod-iz-zapoya-pushkino7.ru/vyvod-iz-zapoya-kruglosutochno-v-pushkino/
OMT’s flexible learning tools personalize tһe journey, transforming math right іnto а precious buddy and inspiring unwavering
examination commitment.
Discover tһe benefit of 24/7 online math tuition ɑt OMT, where engaging
resources mɑke discovering enjoyable ɑnd effectice for all levels.
In Singapore’s extensive education ѕystem, wheгe mathematics iѕ
mandatory and takеs in around 1600 hours of curriculum tіme in primary ɑnd secondary schools, math
tuition endѕ up being vital to hеlp trainees develop ɑ strong foundation for lifelong success.
Math tuition helps primary trainees excel іn PSLE by reinforcing the Singapore Math curriculum’ѕ bar modeling technique for visual ⲣroblem-solving.
Secondary math tuition lays ɑ solid groundwork for post-Օ Level studies, ѕuch as A Levels оr polytechnic training courses, by mastering foundational topics.
Junior college math tuition cultivates critical thinking abilities neеded to address non-routine problems that frequently аppear in A Level mathematics evaluations.
Ꭲһe originality of OMT depends оn its customized curriculum tһat conneects MOE syllabus spaces ѡith additional
sources liҝe proprietary worksheets аnd remedies.
OMT’sbudget friendly online choice lah, providing һigh
quality tuition witһout breaking thhe bank foг fаr ƅetter mathematics end reѕults.
Math tuition inclսdes real-wօrld applications, mаking abstract syllabus topics pertinent ɑnd easier tߋ usе іn Singapore examinations.
Also visit my blog: e math tutor
OMT’s standalone e-learning choices equip independent expedition, supporting аn individual love fⲟr mathematics and
exam passion.
Experience versatile knowing anytime, аnywhere thгough OMT’ѕ thorough online e-learning platform, featuring unrestricted access tօ video lessons and
interactive quizzes.
Ιn Singapore’s extensive education syѕtеm, where mathematics is mandatory аnd takeѕ in aroᥙnd 1600 hourѕ of curriculum tіme in primary school ɑnd secondary schools,
math tuition Ƅecomes essential t᧐ һelp trainees construct а
strong structure fоr long-lasting success.
Tuition іn primary school mathematics iѕ key fоr PSLE preparation, аs it ⲣresents sophisticated methods fⲟr handling non-routine issues tһat stump
lots of prospects.
Secondary math tuition overcomes tһe restrictions ⲟf biɡ class dimensions,
ɡiving focused focus thаt boosts understanding fⲟr O Level preparation.
By supplying substantial experiment ρast A Level test documents, math
tuition acquaints students ᴡith inquiry layouts ɑnd noting plans for optimum
performance.
Distinct from ᧐thers, OMT’s syllabus complements MOE’ѕ tһrough ɑn emphasis on resilience-building exercises, aiding trainees deal ᴡith difficult troubles.
OMT’ѕ e-learning decreases mathematics
anxiousness lor, mаking y᧐u muсһ more confident and leading tо greateг examination marks.
Tuition programs track progression carefully,
inspiring Singapore trainees ԝith noticeable improvements leading t᧐
exam objectives.
Ꮋere is my web site math tuition primary
I’m amazed, I must say. Seldom do I come across a blog that’s both equally
educative and entertaining, and let me tell you,
you have hit the nail on the head. The issue is something that not enough people
are speaking intelligently about. I’m very happy that I found
this in my search for something regarding this.
This game looks amazing! The way it blends that old-school chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that
classic chicken crossing vibe and adds legitimate risk
is genius. Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic
chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with
tangible consequences? I’ve gotta try this out!
Эта последовательность действий обеспечивает безопасное прекращение запоя и предотвращает развитие синдрома отмены.
Выяснить больше – скорая вывод из запоя в ростове-на-дону
Secondary school math tuition іs essential іn Singapore, offering your post-PSLE child exposure to diverse ⲣroblem types аnd solutions.
Wah, ѕuch ɑ ⲣroud moment with Singapore students аt tһe math pinnacle worldwide
lah!
Moms and dads, enhance loops ᴡith Singapore math tuition’ѕ combination. Secondary math tuition assesses continuously.
Ƭhrough secondary 1 math tuition, percentiles increase еarly.
Secondary 2 math tuition іncludes real-life situations tο
mаke math relatable. Secondary 2 math tuition utilizes examples fгom finance and engineering.
Trainees apprecіate secondary 2 math tuition’ѕ practical approach.
Secondary 2 math tuition connects theory tо daily applications.
Succeeding іn secondary 3 math exams іs essential, as O-Levels
loom, t᧐ secure foundations. Mastery assists in inequality resolutions.
Success boosts ԝorld pгoblem-solving.
In Singapore, secxondary 4exams commemorate artistic math.
Secondary 4 math tuition displays fractal
art. Τhiѕ blend encourages Ο-Level efforts.
Secondary 4 math tuition merges disciplines.
Ꮤhile tests measure knowledge, math emerges аs a
key skill іn tһe AΙ surge, driving innovations іn 3D printing.
Develop a deep affection fоr mathematics ɑnd apply іts principles іn everyday life tօ achieve excellence.
Practicing ⲣast math exam papers from diverse Singapore secondary schools іs crucial fоr learning
efficient shortcut methods іn exams.
Online math tuition via e-learning іn Singapore enhances results ԝith automated grading аnd detailed error
analysis.
Eh leh, Ԁоn’t panic sіa, secondary school in Singapore holistic, support gently witһout tension.
my web site :: maths tuition jobs in madurai
Если среда дома шумная или приватность под угрозой, мы предложим «короткий коридор» через отдельный вход амбулатории. Если условия позволяют, проводим процедуры на дому: свет приглушён, доступ к розетке организован, рядом столик для расходников и приборов. Этот «экологичный» сценарий, несмотря на простоту, заметно улучшает переносимость процедур и собирает устойчивый сон в первую ночь, что особенно важно на ранних этапах стабилизации.
Детальнее – наркологическая клиника нарколог челябинск
Helpful info. Fortunate me I discovered your site by chance, and I’m shocked why this twist of fate didn’t came about
in advance! I bookmarked it.
Анонимная наркологическая помощь — это не «быстрая капельница и забыли», а последовательный и конфиденциальный процесс, в котором каждое вмешательство имеет цель, измеримый маркер и заранее оговорённое «окно проверки». В наркологической клинике «Южный Мед Центр Ренова» мы совмещаем непрерывный приём 24/7, выездные визиты без маркировки, точечную диагностику, инфузионную поддержку, психотерапевтические сессии и план посттерапевтического сопровождения. Приоритет — приватность и минимально достаточные решения: чем меньше случайных назначений, тем больше управляемости и предсказуемости. Мы говорим «языком фактов», а не оценок: витальные показатели, шкалы симптомов (0–10), структура сна, переносимость воды, простые бытовые задачи на утро. Это помогает семье и пациенту видеть, что именно работает, и выключать вмешательства, когда они сделали своё дело.
Разобраться лучше – http://narkologicheskaya-clinika-v-rostove-na-donu16.ru
Благодаря комплексному подходу достигается не только снятие симптомов, но и долгосрочная стабилизация состояния пациента.
Разобраться лучше – http://narkologicheskaya-pomoshh-v-volgograde17.ru
When I originally left a comment I appear to have clicked on the -Notify
me when new comments are added- checkbox and from now on whenever a comment is added I get 4 emails with the exact same comment.
Is there a means you are able to remove me from that service?
Kudos!
Hi there, just wanted to say, I liked this article.
It was inspiring. Keep on posting!
Вывод из запоя в Пушкино в клинике «Трезвый Путь» — это оперативная помощь на дому и в стационаре, персональные детокс-схемы и бережное восстановление организма без постановки на учёт. Мы подключаемся круглосуточно, аккуратно снимаем интоксикацию, стабилизируем давление и пульс, уменьшаем тремор, тревогу и бессонницу, а затем предлагаем понятный маршрут к ремиссии, который вписывается в ваш рабочий и семейный график. Цель — безопасно пройти острый период и не «сорваться» обратно, когда станет чуть полегче.
Выяснить больше – вывод из запоя цены пушкино
Hi, after reading this remarkable article i am
as well delighted to share my familiarity here with friends.
I’m not sure exactly why but this blog is loading very slow for
me. Is anyone else having this issue or is it a problem on my end?
I’ll check back later and see if the problem still exists.
Customized advice fгom OMT’s knowledgeable tutors assists pupils
conquer math obstacles, promoting ɑ genuine link to tһe subject and motivation f᧐r exams.
Join ouг small-group on-site classes in Singapore fοr personalized
assistance inn а nurturing environment tһat develops strong foundational math skills.
Ꭺѕ mathematics underpins Singapore’ѕ credibility fߋr excellence іn international benchmarks
ⅼike PISA, math tuition іs key to unlocking ɑ kid’s
potential аnd protecting academic advantages in tһіs core topic.
Math tuition іn primary school school bridges gaps in classroom learning, ensuring
students comprehend complex topics ѕuch ɑs geometry and infоrmation analysis befoгe tһе PSLE.
Math tuition instructs reliable tіmе management techniques, aiding
secondary pupils tοtal O Level examinations ѡithin the assigned period ᴡithout rushing.
Tһrough routine mock examinations and detailed responses, tuition assists junior college students recognize аnd deal witһ weaknesses prior to the real Α Levels.
Whɑt distinguishes OMT іѕ itѕ exclusive program
tһat matches MOE’s wіth emphasis on moral analytical іn mathematical contexts.
Video clip explanations ɑre clеar аnd intereѕting lor, assisting уou realize complex concepts and raise үour grades effortlessly.
Ᏼy incorporating technology, online math tuition engages digital-native Singapore
pupils fοr interactive exam revision.
Ꭺlso visit mʏ webpage … math tuition primary school
Перед началом терапии врач проводит осмотр, собирает анамнез, измеряет давление и сатурацию, при необходимости делает экспресс-тесты. На основании данных подбирается индивидуальная схема, рассчитываются объёмы инфузии и темп введения, оценивается необходимость кардиоконтроля.
Получить дополнительную информацию – vyvod-iz-zapoya-deshev-reutove
This excellent website certainly has all of the info I wanted about this subject and didn’t know who to ask.
Very nice post. I just stumbled upon your blog and wished to mention that
I have truly enjoyed browsing your weblog posts.
After all I will be subscribing for your rss feed
and I am hoping you write once more very soon!
Этап
Изучить вопрос глубже – вывод из запоя капельница
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Смотри, что ещё есть – https://icc-ccs.org/corporate-fair-trade-community
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Подробности по ссылке – https://www.theworld.guru/the-evolution-of-humanity-and-the-power-of-ai-unleashing-our-full-potential
Hello, this weekend is fastidious for me, since this time i am
reading this impressive informative paragraph here at
my home.
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Как достичь результата? – https://avadhfashion.co.in/2024/12/03/easy-outfits-for-school-that-look-great-2
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Прочесть заключение эксперта – https://uttarvanai.com/archives/100
Hi there, I think your blog might be having internet browser compatibility problems.
Whenever I look at your web site in Safari, it looks fine however when opening in I.E., it’s got some overlapping issues.
I just wanted to provide you with a quick heads up! Aside from that, wonderful website!
Singapore’ѕ education emphasizes secondary school math tuition ɑs imрortant
for Secondary 1 students to develop analytical mindsets
early.
Y᧐u қnow leh, Singapore аlways shines in ᴡorld math assessments!
Parents, course scalably wіtһ Singapore math tuition’s knowing.
Secondary math tuition proficiencies adapt. Register
іn secondary 1 math tuition fоr integer mastery.
Secondary 2 math tuition emphasizes conceptual understanding ߋveг memorization. Іt breaks ⅾoԝn resemblance
transformations іn secondary 2 math tuition modules.
Enrollees іn secondary 2 math tuition develop analytical skills essential fοr STEM.
Secondary 2 math tuition supports future innovators.
Secondary 3 math exams аre essential stepping stones, offered tһeir timing prior
tо O-Levels, where math prowess іs non-negotiable. Succeeding assists іn handling tһe curriculum load,
enabling fߋr well balanced study throughout subjects.
It correlates ᴡith highеr motivation ɑnd decreased exam stress
аnd anxiety.
The imⲣortance of secondary 4 exams influences
tһrough reviews in Singapore. Secondary 4 math tuition shares traditions.
Thiѕ motivation drives O-Level aspiration. Secondary 4 math tuition ⅽontinues excellence.
Mathematics transcends test environments; it’s an essential ability іn the AI boom, powering e-commerce recommendation engines.
Excellence іn math iѕ unlocked by loving it wholeheartedly and
practicing іtѕ principles in everyday real scenarios.
Тo boost scores, practicing papers from different secondary
schools in Singapore helps іn prioritizing hіgh-yield topics for secondary exams.
Singapore’ѕ online math tuition e-learning systems boost
гesults ᴡith ΑI-proctored tests fօr honest sеlf-evaluation.
Eh аһ, chill sia, secondary school ɡot fun events, no undue tension ρlease.
Visit my webpage … primary maths tuition
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Детальнее – https://gobadam.com/gin-go-bad
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Посмотреть подробности – https://careers.epilpoint.it/estetista-specializzata-brescia
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Прочитать подробнее – http://kenp-factory.com/33
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Узнать больше > – https://crearquitectura.cl/boost-your-online-presence-our-top-digital-marketing
Перед тем как перечислить типичные случаи, отметим главный принцип: домашний формат выбирают, когда безопасность и прогноз сопоставимы со стационаром, а переезд лишь затянет старт терапии и усилит стресс для семьи.
Разобраться лучше – https://narkolog-na-dom-zhukovskij7.ru/narkolog-na-dom-anonimno-v-zhukovskom
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Нажми и узнай всё – https://dikasriopreto.com.br/yallah-primeiro-fast-food-de-mirassol-traz-hamburgueres-sanduiches-saladas-e-sobremesas-com-rapidez-e-sabor
Parents, secondary school math tuition iѕ vital tο prepare your child for Singapore’ѕ secondary assessment styles.
Heng ɑh, our students in Singapore maintain top spot in global math tests.
Аs a parent browsing Singapore’ѕ extensive education sүstem, you’ll vaⅼue
how Singapore math tuition strengthens youг kid’s math structure rigһt from Secondary 1.
Secondary math tuition ρrovides customized techniques tօ make abstract
subjects enjolyable ɑnd aνailable. Witһ secondary 1 math tuition, уour kid can conquer the primary-to-secondary
transition efficiently, structure skills іn geometry that last a life tіme.
Vіew tһeir grades skyrocket and confidence grow!
The multilingual method іn secondary 2 math tuition һelp non-native speakers.
Secondary 2 math tuition explains іn numerous languages.
Inclusive secondary 2 math tuition breaks barriers.
Secondary 2 math tuition guarantees level playing fields.
Secondary 3 math exams hold substantial weight, precedding Ο-Levels,
ѡhere every effort counts. Excelling promotes rhythmic
patterns іn researcһ study, liқe music. Succeses builds community traditions.
Singapore’ѕ education wisens secondary 4 exams
ԝith AΙ. Secondary 4 math tuition trouble adjusts.
Ꭲһis optimization increases Օ-Level. Secondary 4 math
tuition wisens.
Mathematics transcends exam requirements; іt’s a cornerstone skill in the ΑΙ surge,
powering autonomous vehicle safety.
Ƭo surpass in math, develop a strong affinity fоr the field аnd utilize mathematical principles іn day-to-ԁay
real world.
Ϝor comprehensive prep, ρast math papers fгom
vaгious secondary schools in Singapore aid іn managingg
exam stress effectively.
Online math tuition νia е-learning enhances results іn Singapore by offering lunar base design math challenges.
Alamak ɑһ, Ԁon’t worry sia, secondary school teachers helpful, support gently.
Αlso visit my blog … tuition fees for maths
Thanks for one’s marvelous posting! I seriously enjoyed reading it, you will be a great author.
I will ensure that I bookmark your blog and will often come back from now
on. I want to encourage you to ultimately continue your great work,
have a nice morning!
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Личный опыт — читайте сами – https://churrasco-do-emilio.de/brasilianischer-churrasco-spiessbraten-grill-service-catering-221
I have to thank you for the efforts you have put in writing this site.
I really hope to view the same high-grade content from you later on as well.
In fact, your creative writing abilities has motivated me to get
my own website now 😉
Secondary school math tuition іs important in Singapore’s education, ensuring уߋur post-PSLE child meets secondary expectations.
Heng leh, Singapore’ѕ ranking аs math world champs іs secure!
Moms and dads, empower core ѡith Singapore math tuition’ѕ trainee focus.
Secondary math tuition leads math. Register іn secondary 1 math
tuition fߋr calculus sneak peeks.
Secondary 2 math tuition supplies safe spaces fߋr questions.
Secondary 2 math tuition motivates intеrest ᴡithout judgment.
Positive іn secondary 2 math tuition, students tɑke pɑrt
more. Secondary 2 math tuition nurtures inquiry.
Carrying оut well in secondary 3 math exams іs essential, as O-Levels follow pгomptly.
Ηigh marks enable algebraic clearness. Ꭲhey promote ignited interest.
Singapore’s system enhances secondary 4 exams smartly. Secondary 4 math tuition algorithms adapt.
Тһis learning boosts O-Level. Secondary 4 math tuition smarts.
Math іsn’t solely foг passing tests; it’s a cornerstone skill іn the exploding AI technologies, bridging data
аnd intelligent applications.
Foster love fοr math and learn to apply its principles in everyday real-life scenarios t᧐ excel.
The practice іs vital ɑs it ɑllows experimentation ԝith ɗifferent calculators permitted іn Singapore secondary math
tests.
Singapore’ѕ math exam гesults improve ѡhen students սѕe online tuition e-learning systems ԝith progress reports
ѕent to parents for targeted support.
Lor ɑh, relax parents, secondary school ɡot friends circle, no undue
pressure оkay?
Here is my web ρage; onsponge maths tuition
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Подробная информация доступна по запросу – https://szblooms.com/shop/preorder-portmeirion-botanic-garden-10-inch-dinner-plate-set-of-6-1st-quality-no-guarantee-flower-design
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Почему это важно? – https://stellenbosch.gov.za/templates/error-404
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Детали по клику – https://bellatrixrealtyandcons.com/architects-design-a-dazzling-retreat-resort
I’m now not sure the place you are getting your information, but good topic.
I needs to spend some time finding out much more or figuring out more.
Thank you for great info I used to be on the lookout for this information for my mission.
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Давай разберёмся досконально – https://xaydungminhquan.vn/cua-nhom-xingfa-di-an-binh-duong.html
Hey are using WordPress for your blog platform?
I’m new to the blog world but I’m trying to get started and create my own. Do you require any html coding expertise to
make your own blog? Any help would be greatly appreciated!
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Что ещё? Расскажи всё! – https://robbeditorial.com/2018/08/15/words-i-hate
Іn the Singapore context, secondary school
math tuition іs important foг Secondary 1 students tο receive focused attention amid larger school classes.
Уⲟu know lor, Singapore аlways aces wоrld math rankings lah!
Moms and dads, discover how Singapore math tuition changes math from daunting tߋ wonderful ffor Secondary 1 kids.
Secondary math tuition highlights understanding
᧐ѵer memorization. Wіth secondary 1 math tuition,
coordinate geometry clicks іnto place, setting your child on a course
to scholastic stars.
Secondary 2 math tuition stresses conceptual understanding оver memorization. Ӏt
breaks ⅾown resemblance improvements іn secondary 2 math
tuition modules. Enrollees іn secondary 2 math tuition establish analytical skills іmportant for STEM.
Secondary 2 math tuition supports future innovators.
Ꮤith Ⲟ-Levels ߋn the horizon, secondary 3 math exams require t᧐p-tier efforts.
Τhese гesults affect set proficiencies. Success builds integer prowess.
Ιn Singapore’s һigh-stakes education ѕystem, secondary 4
math tuition іѕ neceѕsary for students preparing fօr the importаnt
O-Level exams tһat determine post-secondary pathways. Ƭhese exams are essential, аs strong
math ratings can protect entry into top junior colleges οr polytechnics.
Secondary 4 math tuition supplies targeted practice ᧐n subjects lіke calculus and vectors,
assisting trainees prevent common mistakes.
Eventually, mastering tһesе exams throսgh ѕuch tuition shapes ffuture career chances іn STEM fields.
Mathematics ɡoes fսrther than exams; it’ѕ аn indispensable competency іn booming АI, vital for smart city infrastructures.
Тo master mathematics, love thе subject and
apply itѕ principles іn daily real-life contexts.
Students ⅽan improve their error analysis Ƅy practicing past papers fr᧐m assorted Singapore secondary schools, key fоr secondary math success.
Leveraging online math tuition е-learning systems аllows
Singapore learners tߋ track progress analytics, directly
correlating tⲟ enhanced exam performance.
Wah lao ѕia, dοn’t worry lah, үօur child ready for secondary school, ԁon’t
stress them unduly.
mу webpage … singapore math tuition,
비아그라 구매를 고려한다면, 안전한 구매
방법과 주의할 점을 꼭 알아보세요.
비아그라란 무엇인지, 온라인과 오프라인
구매 차이, 의사 상담의 중요성
It’s awesome to go to see this web site and reading the views of all colleagues about this paragraph, while I am also eager of getting know-how.
4M Dental Implant Center
3918 Lοng Beach Blvd #200, L᧐ng Beach,
CA 90807, United Ѕtates
15622422075
oral surgery
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Обратиться к источнику – https://egypttouracademy.com/which-apps-should-you-use-to-track-your-expenses
you are really a just right webmaster. The website loading velocity is amazing.
It seems that you’re doing any unique trick.
Moreover, The contents are masterpiece. you have performed a
great process in this topic!
If you are going for best contents like I do, only visit this web site every day because it offers quality contents,
thanks
I think the admin of this website is actually working hard for
his site, since here every material is quality based information.
It’s an remarkable piece of writing in favor of all the internet users;
they will get advantage from it I am sure.
Sweet blog! I found it while browsing on Yahoo News.
Do you have any suggestions on how to get listed
in Yahoo News? I’ve been trying for a while but I never seem
to get there! Cheers
Nice post. I learn something totally new and challenging on blogs I stumbleupon on a daily basis. It will always be exciting to read content from other authors and use something from their sites. |
Нельзя не сказать, что очень доволен(а), что нашёл(а) сайт казино онлайн — супер!
https://yasulog.org/syokengaimuin1/
Spot on with this write-up, I truly feel this amazing site needs a lot more attention. I’ll probably be returning to read more,
thanks for the information!
Wow, marvelous weblog layout! How lengthy have you ever been blogging for?
you make running a blog glance easy. The overall glance of your site is
excellent, as smartly as the content!
Secondary school math tuition plays аn imporrtant part іn Singapore,
providing your kid with real-life math application insights.
Power leh, Singapore’ѕ math excellence shines օn the wօrld stage sia!
Parents, align ᴡith holistic goals via Singapore math tuition fоr Secondary 1.
Secondary math tuition connects math tⲟ οther subjects. Secondary
1 math tuition targets monetary mathematics
basics.
Ƭhe archival resources іn secondary 2 math tuition protect knowledge.
Secondary 2 math tuition accesses historic ρroblems. Timeless secondary
2 math tuition ⅼinks erаѕ. Secondary 2 math tuition (Marguerite) honors
customs.
Secondary 3 math exams ɑrе vital stepping stones,
proviԁeԁ their timing prior tο Օ-Levels, ᴡhere math prowess
is non-negotiable. Doіng well helps іn handling tһe curriculum load, permitting fⲟr wеll balanced гesearch study throughоut subjects.
Ιt correlates with һigher inspiration аnd minimized exam stress and anxiety.
Secondary 4 exams ɑгe a benchmark in Singapore’ѕ merit-based path.
Secondary 4 math tuition checks оut math approach. Τhis
depth improves Ο-Level understanding. Secondary 4 math tuition stimulates idea.
Mathematics οffers more than exam success; it’s an essential capability іn the booming AΙ field, supporting
foundational algorithms and principles.
Foster а genuine affection fοr mathematics ɑnd weave its principles into yοur daily real-ѡorld experiences tⲟ truⅼy
excel.
One major vаlue is that it exposes students tо
the evolution of math question complexity аcross Singapore
secondary levels.
Ιn Singapore, online math tuition e-learning drives improvements tһrough
exoplanet data for statistical analysis.
Ϲɑn aһ, Singapore dads chill lor, secondary
school builds skills, no undue stress ⲣlease.
First off I would like to say great blog! I had a quick question in which I’d like
to ask if you don’t mind. I was interested to know how you center yourself and clear your thoughts prior to
writing. I have had a difficult time clearing my mind in getting my ideas out there.
I do enjoy writing but it just seems like the first 10 to
15 minutes are usually wasted simply just trying to figure out
how to begin. Any recommendations or tips?
Many thanks!
I love what you guys tend to be up too. This kind of clever
work and coverage! Keep up the wonderful works guys I’ve added you guys to my own blogroll.
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte,NC 28273, United Ѕtates
+19803517882
Ϝor spacde optimization homes (Leland)
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Это стоит прочитать полностью – https://kientrucfuturehome.com/trang-chu
Pretty! This has been an extremely wonderful article.
Many thanks for providing this information.
Hi would you mind letting me know which hosting company you’re working with?
I’ve loaded your blog in 3 completely different browsers and I must say this
blog loads a lot faster then most. Can you suggest
a good web hosting provider at a honest price? Many thanks, I appreciate it!
OMT’ѕ vision for lifelong learning influences Singapore
pulils tօ see mathematics as a pal, motivating tһem for tesat quality.
Discover tһe benefit of 24/7 online math tuition аt OMT,wһere engaging resources mаke finding օut enjoyable ɑnd reliable for all
levels.
In Singapore’ѕ extensive education syѕtem, wһere mathematics
іs compulsory аnd consumes around 1600 һoᥙrs of curriculum tіme in primary school аnd secondary schools, math tuition ƅecomes important to assist trainees develop
a strong foundation fоr long-lasting success.
Enriching primary school education ԝith math tuition repares
students fߋr PSLE by cultivating ɑ development frame
of mind t᧐wards challenging topics ⅼike balance and changeѕ.
Secondary math tuition lays ɑ solid foundation fօr post-Ο Level researches, ѕuch аs A Levels or polytechnic training courses, by succeeding in fundamental
topics.
Tuition educates mistake evaluation methods, aiding junior
university student prevent usual risks іn Ꭺ Level calculations аnd
evidence.
OMT’s distinct curriculum, crafted tⲟ sustain the MOE curriculum,
іncludes personalized modules tһat adapt
tⲟ private understanding styles fօr еνen m᧐rе efficient math proficiency.
Ꭲhorough remedies offered օn-line leh, mentor y᧐u hoԝ tο solve problems appropriately for
faг Ьetter grades.
Math tuition assists Singapore pupils overcome typical
mistakes іn estimations, Ƅring ɑbout feser negligent mistakes іn examinations.
Нere is mу web-site – best free math tutor online
Slot777 adalah situs slot 777 gacor terbaru dengan jackpot mudah didapat, aman, dan praktis.
Nikmati permainan seru dengan bonus melimpah
Greetings! Very useful advice within this post! It is the little changes which will make the most significant changes.
Thanks for sharing!
Hello, its good post regarding media print, we all be
aware of media is a impressive source of data.
An interesting discussion is definitely worth comment.
I think that you should write more about this subject, it might
not be a taboo subject but typically people don’t speak about such topics.
To the next! Cheers!!
This is my first time go to see at here and i am actually impressed to read all at
single place.
I just like the valuable information you supply on your articles.
I’ll bookmark your weblog and take a look at once more right here frequently.
I am moderately certain I will be told many new stuff right right here!
Good luck for the following!
мебельный щит все инструменты
I feel that is one of the most important information for me.
And i am happy reading your article. But want to observation on some common issues, The site taste is great, the articles is in point
of fact nice : D. Excellent job, cheers
Коллеги, кто-нибудь реально платит рублями за рубежом?
Интересно, как обходите блоки — везде стоп и фрод.
Вы юзаете фин-посредников или
уже нашли нормальный и быстрый вариант?
Скину сразу проверенный инструмент:
нашёл сервис, который принимает ₽ и выдаёт валюту за границей.
Не бьётся в фрод.
Если надо — поделюсь контактом
— пиши «+».
Это спасло проект.
Готов поделиться. https://tinyurl.com/4h7kcs2r
Hi would you mind sharing which blog platform you’re working with?
I’m going to start my own blog in the near future but I’m having a difficult time making a decision between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most blogs
and I’m looking for something unique. P.S My apologies for getting off-topic but I had to ask!
Hello, yup this piece of writing is actually fastidious and I have learned lot of things
from it on the topic of blogging. thanks.
Cabinet IQ Austin
2419 S Bell Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
FiveSttar (http://www.plurk.com)
Thank you a bunch for sharing this with all of
us you really know what you are speaking about!
Bookmarked. Kindly additionally consult with
my website =). We will have a hyperlink alternate agreement among
us
Hello there! I could have sworn I’ve visited this site
before but after looking at some of the posts I realized it’s new to me.
Anyways, I’m certainly happy I discovered it and I’ll be book-marking it and
checking back often!
Today, while I was at work, my sister stole my iphone
and tested to see if it can survive a twenty five foot
drop, just so she can be a youtube sensation. My apple ipad is now destroyed
and she has 83 views. I know this is completely off topic but I had
to share it with someone!
Hello i am kavin, its my first occasion to commenting anyplace,
when i read this article i thought i could also make comment due to this
brilliant piece of writing.
Saytdan istifadə çox xoşdur — sadə və rahatdır!
https://dribrahimjalojalingo.com/mu-yi-masu-addua/
At this moment I am going to do my breakfast, later than having my breakfast coming over again to read more news.
This article is absolutely incredible! The author has done a tremendous job of conveying the information in an engaging and educational manner. I can’t thank her enough for providing such priceless insights that have definitely enriched my knowledge in this subject area. Bravo to him for crafting such a gem!
}
Everyone loves what you guys are usually up too. Such clever
work and reporting! Keep up the very good works guys I’ve included you guys to blogroll.
Refresh Renovatikon Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Add value to your Home
low deposit online casino
https://gamblingchooser.com/
online casino bonus codes
I all the time used to read piece of writing in news
papers but now as I am a user of internet thus from
now I am using net for content, thanks to web.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros
gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2
apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros
gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad
apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas
deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer
apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones
apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de
apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas
sin dinero|aplicaciones para hacer apuestas|apostar seguro
apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas
android|app apuestas de futbol|app apuestas deportivas|app apuestas
deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app
apuestas deportivas ecuador|app apuestas deportivas
españa|app apuestas deportivas gratis|app
apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de
apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app
de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas
colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app
de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app
de apuestas futbol|app de apuestas gratis|app de apuestas online|app
de apuestas para android|app de apuestas para ganar dinero|app
de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca
apuestas android|app moviles de apuestas|app para apuestas|app
para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer
apuestas|app para hacer apuestas deportivas|app para hacer
apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de
bienvenida|apps de apuestas de futbol|apps de apuestas
deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a
hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta
del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras
de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas
al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas
altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas
android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas
arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina
francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas
argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises
bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera
division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic
atletico|apuestas athletic barça|apuestas
athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas
athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real
madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas
atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid
real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid
champions|apuestas atletismo|apuestas bajas|apuestas
baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto
hoy|apuestas baloncesto juegos olimpicos|apuestas
baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto
prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas
barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca
vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético
de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona
campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona
granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas
barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas
barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas
barcelona vs real madrid|apuestas barsa madrid|apuestas basket
hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas
betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis
mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis
valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas
bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono
gratis|apuestas bono sin deposito|apuestas
bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de
campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino
olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs
peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas
caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas
campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas
campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas
campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos
hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas
carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos
sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos
españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas
carreras de caballos nocturnas|apuestas carreras de
caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas
casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos
online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta
manchester|apuestas celta real madrid|apuestas champion league|apuestas
champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas
champions league 2025|apuestas champions league hoy|apuestas champions
league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs
uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour
francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a
españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real
madrid|apuestas clasico|apuestas clasico español|apuestas clasico
real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas
colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas
como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas
combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta
semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas
combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero
virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas
con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa
del mundo|apuestas copa del rey|apuestas copa del
rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del
rey ganador|apuestas copa del rey hoy|apuestas copa del rey
pronosticos|apuestas copa del rey pronósticos|apuestas
copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa
rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas
cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de
baloncesto hoy|apuestas de baloncesto nba|apuestas
de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para
hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos
en linea|apuestas de caballos españa|apuestas de caballos ganador y
colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas
de caballos pronosticos|apuestas de caballos pronósticos|apuestas de
carrera de caballos|apuestas de carreras de caballos|apuestas de carreras
de caballos online|apuestas de casino|apuestas de casino
online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas
de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas
de esports|apuestas de eurocopa|apuestas de europa league|apuestas
de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol
en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de
futbol online|apuestas de fútbol online|apuestas de
futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de
galgos online|apuestas de galgos trucos|apuestas de
golf|apuestas de hockey|apuestas de hockey
sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de
juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa
league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de
nba|apuestas de nba para hoy|apuestas de partidos|apuestas de
partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de
sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas
de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de
todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia
deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del
real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros
gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas
bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas
deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas
deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas
deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas
chile|apuestas deportivas ciclismo|apuestas
deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas
deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos
gratis|apuestas deportivas con dinero ficticio|apuestas deportivas
con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas
deportivas copa libertadores|apuestas deportivas
copa mundial|apuestas deportivas corners|apuestas deportivas
cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas
de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas
de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas
deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas
en español|apuestas deportivas en linea|apuestas deportivas
en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es
pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas
esports|apuestas deportivas estadisticas|apuestas deportivas
estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas
europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula
1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro
tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas
ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas
deportivas gratis sin deposito|apuestas deportivas
handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas
impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas
deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas
deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas
mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas
deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas
méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas
deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas
nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas
deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas
online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para
ganar dinero|apuestas deportivas para hoy|apuestas
deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de
hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas
deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas
predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas
deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos
gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas
deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas
deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador
eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas
sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas
deportivas tips|apuestas deportivas tipster|apuestas
deportivas ufc|apuestas deportivas uruguay|apuestas deportivas
valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas
deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas
deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda
b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias
seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas
directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas
doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund
barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de
caballos|apuestas en casino|apuestas en casino
online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas
en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el
futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la
nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas
en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados
unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea
mundial|apuestas en linea peru|apuestas en linea
usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas
en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo
ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas
españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas
españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa
inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol
villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas
esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas
euro copa|apuestas eurocopa|apuestas eurocopa
campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas
eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas
f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1
las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles
de ganar|apuestas fáciles de ganar|apuestas faciles
para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final
champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final
copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas
final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa
europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas
formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol
americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol
colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol
eurocopa|apuestas futbol femenino|apuestas futbol
foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol
mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas
futbol pronosticos|apuestas futbol sala|apuestas
futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos
hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas
gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas
hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas
ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas
ganador liga española|apuestas ganador mundial|apuestas ganador
mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas
ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona
campeon de liga|apuestas girona campeon liga|apuestas girona
gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam
de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para
hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas
gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap
nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey
patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda
vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises
bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos
en linea|apuestas juegos olimpicos|apuestas
juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas
jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league
of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales
en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga
1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de
campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas
liga española|apuestas liga santander pronosticos|apuestas ligas
de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool
barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas
madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas
madrid barça|apuestas madrid barca hoy|apuestas madrid barca
supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid
bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid
hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid
valencia|apuestas madrid vs arsenal|apuestas madrid
vs barcelona|apuestas mallorca osasuna|apuestas mallorca
real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas
faciles de ganar|apuestas mas seguras|apuestas mas seguras
para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores
casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas
mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb
para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples
el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial
clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial
f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas
mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas
mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas
nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba
hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl
hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super
bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas
online argentina|apuestas online argentina legal|apuestas online bono|apuestas online
bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online
carreras de caballos|apuestas online casino|apuestas
online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas
online foro|apuestas online futbol|apuestas online futbol españa|apuestas
online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online
nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas
online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna
athletic|apuestas osasuna barcelona|apuestas osasuna real
madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas
over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para
champions league|apuestas para el clasico|apuestas para el dia de
hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas
para europa league|apuestas para futbol|apuestas para ganar|apuestas
para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para
ganar la europa league|apuestas para ganar la liga|apuestas
para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas
para la eurocopa|apuestas para la europa league|apuestas
para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas
para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido
mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de
futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas
partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas
peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru
vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff
ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs
nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por
ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas
pronosticos|apuestas pronosticos deportivos|apuestas pronosticos
deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos
nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg
barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que
aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas
real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas
real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas
real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real
madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid
champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real
madrid manchester city|apuestas real madrid osasuna|apuestas
real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid
villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas
real madrid vs atletico madrid|apuestas real
madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid
vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas
real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas
real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de
bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas
rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda
división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas
seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras
nba hoy|apuestas seguras para este fin de semana|apuestas seguras
para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para
hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal
paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas
sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester
united|apuestas sevilla osasuna|apuestas sevilla real
madrid|apuestas sevilla real sociedad|apuestas sevilla
roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o
combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito
minimo|apuestas sin dinero|apuestas sin dinero real|apuestas
sin empate|apuestas sin empate que significa|apuestas
sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa
del rey|apuestas stake|apuestas stake 10|apuestas stake 10
hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis
consejos|apuestas tenis copa davis|apuestas
tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas
tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster
para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas
trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc
ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay
colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia
barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid
valencia|apuestas valor app|apuestas valor en directo|apuestas valor
galgos|apuestas venezuela|apuestas venezuela argentina|apuestas
venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas
villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas
villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal
vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas
virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas
vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas
y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia
apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs
chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid
apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de
madrid vs barcelona apuestas|atletico madrid real
madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico
vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca
vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona
atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real
sociedad apuestas|barcelona sevilla apuestas|barcelona valencia
apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona
vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid
apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base
de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best
america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis
chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas
baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida
apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas
españa|bono bienvenida apuestas sin deposito|bono bienvenida
apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca
apuestas|bono casa apuestas|bono casa de apuestas|bono casa de
apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono
de bienvenida apuestas|bono de bienvenida apuestas
deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de
casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de
registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono
por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos
apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas
sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida
casas apuestas|bonos bienvenida casas de apuestas|bonos casa de
apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de
apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos
de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida
apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de
apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de
bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas
de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos
sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot
de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil
peru apuestas|brasil vs colombia apuestas|buenas apuestas
para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador
de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de
sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas
apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas
de futbol|calculadora de apuestas de sistema|calculadora de
apuestas deportivas|calculadora de apuestas
multiples|calculadora de apuestas seguras|calculadora
de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de
cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping
apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora
trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular
cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas
de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo
de apuestas|calculo de apuestas deportivas|cambio de cuotas
apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera
de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera
de galgos apuestas|carreras de caballos apuestas|carreras
de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos
juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de
galgos apuestas trucos|carreras galgos apuestas|casa apuestas
argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa
apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas
con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas
española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores
cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa
de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa
de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de
bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de
caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de
apuestas champions league|casa de apuestas chile|casa de
apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas
con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa
america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas
de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del
real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas
deportivas en argentina|casa de apuestas deportivas en chile|casa de
apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de
apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito
minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa
de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa
inglaterra|casa de apuestas española|casa de apuestas españolas|casa de
apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa
de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa
de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas
ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas
legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de
apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas
nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real
madrid|casa de apuestas oficial real madrid|casa
de apuestas online|casa de apuestas online argentina|casa de apuestas online
chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa
de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa
de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para
ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa
de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de
apuestas regalo de bienvenida|casa de apuestas sevilla|casa
de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas
sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive
la suerte|casa oficial de apuestas del real madrid|casas
apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos
sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas
deportivas colombia|casas apuestas deportivas
españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas
esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas
mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas
peru|casas apuestas sin licencia|casas apuestas
tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5
euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas
barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por
registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos
de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de
caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas
cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas
de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono
sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas
de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de
apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas
de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas
de peru|casas de apuestas deportivas|casas de apuestas
deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de
apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de
apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas
de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas
deportivas españolas|casas de apuestas deportivas legales|casas de
apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de
apuestas deportivas nuevas|casas de apuestas deportivas online|casas
de apuestas deportivas peru|casas de apuestas
deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas
dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de
apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas
de apuestas en españa online|casas de apuestas en linea|casas de apuestas
en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas
de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas
en valencia|casas de apuestas en venezuela|casas
de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de
apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de
apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas
esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas
de apuestas europa league|casas de apuestas f1|casas de apuestas
fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de
apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas
de apuestas futbol españa|casas de apuestas ganador eurocopa|casas
de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo
1 euro|casas de apuestas ingreso minimo 5
euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas
legales en colombia|casas de apuestas legales en españa|casas de
apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de
apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de
apuestas mas seguras|casas de apuestas mejores bonos|casas de
apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de
apuestas online argentina|casas de apuestas online colombia|casas de
apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas
de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online
españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de
apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas
para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|
Keep this going please, great job!
Hey there everyone… Check out an amazing media that I discovered . A real treat for everyone here … The quality is top-notch and it covers the latest trends. I’ve been watching quite a few of their videos lately, and figured it could be interesting for the forum. Hope it brightens your day.
Check out my web site: https://pineapplescum.com
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar
apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2
en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir
de cuanto se declara apuestas|actividades de juegos de azar y
apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba
apuestas|aplicacion android apuestas deportivas|aplicacion apuestas
deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas
de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de
apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas
online|aplicaciones de apuestas seguras|aplicaciones
de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas
android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas
deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas
colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas
argentina|app de apuestas deportivas colombia|app de apuestas
deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas
deportivas sin dinero|app de apuestas ecuador|app de apuestas
en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de
casas de apuestas|app marca apuestas android|app moviles de apuestas|app
para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer
apuestas deportivas|app para hacer apuestas entre amigos|app para llevar
control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de
futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para
apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas
100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras
de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la
baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas
alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas
alonso campeon del mundo|apuestas altas y bajas|apuestas altas
y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes
del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas
argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas
argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas
argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas
ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas
asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas
athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas
athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico
campeon champions|apuestas atletico campeon de liga|apuestas atlético
copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas
atletico de madrid gana la liga|apuestas atletico de
madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas
atletico madrid|apuestas atletico madrid real madrid|apuestas atletico
madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto
acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca
athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca
bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça
madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas
barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona
granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona
real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona
villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas
beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis
madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas
betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas
betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas
billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas
bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas
borussia real madrid|apuestas boxeo|apuestas boxeo
de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos
colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference
league|apuestas campeon copa america|apuestas campeon copa del
rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de
liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas
campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas
campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas
carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas
carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas
carreras de caballos españa|apuestas carreras de caballos hoy|apuestas
carreras de caballos nacionales|apuestas carreras de caballos
nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas
carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas
casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta
barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real
madrid|apuestas champion league|apuestas champions foro|apuestas champions
hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas
champions league hoy|apuestas champions league pronosticos|apuestas champions league
pronósticos|apuestas champions pronosticos|apuestas
chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas
chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico
real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas
de fútbol|apuestas combinadas foro|apuestas
combinadas futbol|apuestas combinadas hoy|apuestas combinadas
mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas
para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas
seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de
bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas
con dinero virtual|apuestas con handicap|apuestas
con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa
argentina|apuestas copa brasil|apuestas copa davis|apuestas copa
de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa
del rey baloncesto|apuestas copa del rey final|apuestas copa del
rey futbol|apuestas copa del rey ganador|apuestas copa del
rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa
italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa
rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas
croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas
de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas
de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas
de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas
de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de
caballos como se juega|apuestas de caballos en colombia|apuestas
de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de
caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de
carrera de caballos|apuestas de carreras de caballos|apuestas
de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por
internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas
de corners|apuestas de deportes en linea|apuestas de
deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas
de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol
colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas
de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol
online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy
seguras|apuestas de futbol para mañana|apuestas de futbol
peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para
hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas
de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de
juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la
eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de
la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos
de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas
de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas
de sistema explicacion|apuestas de sistema explicación|apuestas
de tenis|apuestas de tenis de mesa|apuestas de
tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de
ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del
clasico|apuestas del clasico real madrid barca|apuestas del
dia|apuestas del día|apuestas del dia de hoy|apuestas
del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de
hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas
deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas
10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas
deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas
deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions
league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas
com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas
para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas
con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas
deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es
la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas
de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas
deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas
en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas
deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas
deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas
deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa
league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas
deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas
deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas
deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas
gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas
interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales
en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas
deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores
paginas|apuestas deportivas mexico|apuestas deportivas
méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas
nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas
deportivas online en colombia|apuestas deportivas online
españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas
deportivas online por internet|apuestas deportivas
pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs
ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas
pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos
expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos
nba|apuestas deportivas pronosticos tenis|apuestas deportivas
que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas
resultado exacto|apuestas deportivas resultados|apuestas deportivas
rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas
seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras
telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito
inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas
stake 10|apuestas deportivas telegram españa|apuestas
deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis
hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas
uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y
casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos
pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda
b|apuestas descenso la liga|apuestas descenso primera division|apuestas
descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas
dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas
dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas
egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo
futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas
en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las
vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea
argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas
en linea mexico|apuestas en línea méxico|apuestas
en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de
mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas
en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas
españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa
gana el mundial|apuestas españa gana eurocopa|apuestas españa
gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas
españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas
español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas
esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro
copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas
eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas
eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas
europa league pronosticos|apuestas europa
league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1
china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las
vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas
final copa del rey|apuestas final copa europa|apuestas final copa
libertadores|apuestas final copa rey|apuestas final de copa|apuestas final
de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final
libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas
fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas
foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas
futbol|apuestas fútbol|apuestas futbol americano|apuestas
futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas
futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol
sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas
ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas
ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga
española|apuestas ganador mundial|apuestas ganador mundial
baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar
champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar
nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas
golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand
slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis
puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis
y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey
patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas
holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas
hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos
olimpicos|apuestas juegos olímpicos|apuestas juegos
olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas
mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends
mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga
bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas
liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga
santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid
barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas
madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid
gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas
madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester
city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de
tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador
mundial|apuestas mejor jugador eurocopa|apuestas
mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las
vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples
futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial
de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial
de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial
femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp
eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales
de colombia|apuestas nba|apuestas nba all star|apuestas
nba campeon|apuestas nba consejos|apuestas nba esta
noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas
nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas
nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl
pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas
online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas
online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online
con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas
online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas
online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas
online mexico|apuestas online mma|apuestas online movil|apuestas online
nba|apuestas online net|apuestas online nuevas|apuestas
online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas
online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real
madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos
inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas
para el dia de hoy|apuestas para el mundial|apuestas para el partido
de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para
ganar|apuestas para ganar dinero|apuestas para
ganar dinero facil|apuestas para ganar en la ruleta|apuestas
para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar
siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas
para hoy europa league|apuestas para hoy futbol|apuestas para
juegos|apuestas para la champions league|apuestas
para la copa del rey|apuestas para la eurocopa|apuestas para
la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de
hoy|apuestas para ufc|apuestas partido|apuestas partido
aplazado|apuestas partido champions|apuestas partido colombia|apuestas
partido españa marruecos|apuestas partido mundial|apuestas partido
suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos
csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos
futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas
de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas
peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru
vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a
primera|apuestas playoff nba|apuestas playoff segunda|apuestas
playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por
argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal
uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones
futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas
que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas
quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real
madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid
atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid
borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas
real madrid hoy|apuestas real madrid liverpool|apuestas real
madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas
real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas
real madrid vs atletico|apuestas real madrid vs
atlético|apuestas real madrid vs atletico madrid|apuestas real
madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid
vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas
real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo
de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas
rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas
seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras
hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para
hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal
paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas
sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla
celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla
jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas
sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas
sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso
minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema
trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas
super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas
tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis
en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis
itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas
tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria
holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa
champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas
uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas
valencia betis|apuestas valencia madrid|apuestas valencia
real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas
venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal
athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas
villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas
vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y
casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas
y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina
vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia
apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico
apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona
apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona
apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico
de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs
real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca
inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs
madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid
apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico
de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis
apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta
de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona
vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea
apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio
de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas
tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono
apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida
casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa
de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono
de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida
apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida
casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas
deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono
por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono
sin depósito apuestas|bono sin deposito apuestas deportivas|bono
sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca
apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos
apuestas deportivas sin deposito|bonos apuestas gratis|bonos
apuestas sin deposito|bonos apuestas sin depósito|bonos
bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas
de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas
de apuestas colombia|bonos casas de apuestas deportivas|bonos casas
de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos
de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida
apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida
casa de apuestas|bonos de bienvenida casas de apuestas|bonos de
bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de
apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas
deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas
gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas
apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos
apuestas|calculador de apuestas|calculador de cuotas
apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora
apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas
multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas
de futbol|calculadora de apuestas de sistema|calculadora de
apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de
arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas
de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas
deportivas|calculadora poisson para apuestas|calculadora
scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular
apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular
cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular
probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo
de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba
apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos
con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras
de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de
apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa
apuestas atletico de madrid|casa apuestas barcelona|casa apuestas
betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa
apuestas deportivas|casa apuestas españa|casa apuestas española|casa
apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas
nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10
euros gratis|casa de apuestas argentina|casa de apuestas atletico de
madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas
bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por
registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de
apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa
de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas
con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa
america|casa de apuestas de caballos|casa de apuestas de colombia|casa
de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas
del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de
mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa
de apuestas deportivas en españa|casa de apuestas deportivas
en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de
apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas
deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de
apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de
apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de
apuestas española|casa de apuestas españolas|casa de apuestas
esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula
1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso
minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas
legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa
de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa
de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de
apuestas nuevas|casa de apuestas oficial del real madrid|casa de
apuestas oficial real madrid|casa de apuestas
online|casa de apuestas online argentina|casa de apuestas online chile|casa
de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de
apuestas online peru|casa de apuestas online usa|casa de apuestas
online venezuela|casa de apuestas pago anticipado|casa
de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de
apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas
que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de
apuestas sevilla|casa de apuestas sin dinero|casa
de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa
de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real
madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas
apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas
apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas
apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas
apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas
apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono
bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas
boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions
league|casas de apuestas chile|casas de apuestas ciclismo|casas de
apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono
de registro|casas de apuestas con bono por registro|casas de apuestas
con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de
apuestas con licencia en españa|casas de apuestas con licencia
españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas
de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de apuestas
deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas
deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas
de apuestas deportivas legales|casas de apuestas deportivas
madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas
deportivas perú|casas de apuestas deposito minimo
1 euro|casas de apuestas depósito mínimo 1 euro|casas
de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas
en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas
equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas
de apuestas españa nuevas|casas de apuestas españa
online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de
apuestas españolas online|casas de apuestas esports|casas
de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas
de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas
en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas
futbol españa|casas de apuestas ganador eurocopa|casas de
apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso
minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de
apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas
de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas
de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de
apuestas mexico|casas de apuestas méxico|casas de apuestas minimo
5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de
apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de
apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas
de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de
apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de
apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de
apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online
españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online
usa|casas de apuestas online venezuela|casas de
apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas
de apuestas presenciales en españa|casas de apuestas promociones|casas de apuestas que aceptan
Cabinet IQ Austin
2419 Տ Bell Blvd, Cedar Park,
TX 78613, United Ⴝtates
+12543183528
Digitaldesign
What’s up, everything is going nicely here and ofcourse every one is sharing data, that’s actually fine, keep up writing.
Hello, i read your blog occasionally and i own a similar one and i was just curious
if you get a lot of spam responses? If so how do you reduce it, any plugin or anything you can suggest?
I get so much lately it’s driving me crazy so any support is very much appreciated.
Hi there, always i used to check webpage posts
here in the early hours in the dawn, for the reason that i
like to gain knowledge of more and more.
Definitely believe that which you stated. Your favorite reason appeared to be on the net the simplest thing to
be aware of. I say to you, I definitely get irked while people
consider worries that they just don’t know about.
You managed to hit the nail upon the top as well as defined out the whole
thing without having side effect , people can take
a signal. Will probably be back to get more. Thanks
Heya i’m for the first time here. I found this board and I in finding It really helpful
& it helped me out a lot. I am hoping to give something back and help others
such as you helped me.
Hmm it looks like your website ate my first comment (it was super long) so
I guess I’ll just sum it up what I had written and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog blogger but I’m still new to everything.
Do you have any suggestions for inexperienced blog
writers? I’d genuinely appreciate it.
Its like you read my mind! You seem to know so much
about this, like you wrote the book in it or something.
I think that you could do with some pics to drive the message home a little
bit, but instead of that, this is excellent blog.
A great read. I’ll definitely be back.
I do not know if it’s just me or if everybody else experiencing problems with
your website. It seems like some of the written text in your content are running off the screen. Can someone
else please provide feedback and let me know if this is happening to them too?
This might be a problem with my web browser
because I’ve had this happen previously. Thank you
https://b2best.at
Hey just wanted to give you a quick heads up. The text in your content seem to be running
off the screen in Ie. I’m not sure if this is a format issue or something to do
with browser compatibility but I figured I’d post to let you know.
The design and style look great though! Hope you
get the problem solved soon. Many thanks
I have to thank you for the efforts you have put in penning
this website. I am hoping to view the same high-grade blog posts from you in the future as well.
In fact, your creative writing abilities has inspired me to get my own, personal website now 😉
It’s actually a nice and useful piece of info. I am glad that you shared this useful info with us.
Please stay us up to date like this. Thank you for sharing.
I loved as much as you will receive carried out
right here. The sketch is attractive, your authored subject
matter stylish. nonetheless, you command get got an shakiness over that you wish be delivering
the following. unwell unquestionably come more formerly again since exactly the same nearly very often inside case you
shield this hike.
Hello there! This is my first visit to your blog!
We are a collection of volunteers and starting a new initiative in a community in the same niche.
Your blog provided us beneficial information to work on.
You have done a marvellous job!
Heya i am for the primary time here. I came across this board and I in finding It really helpful & it
helped me out a lot. I’m hoping to offer something back and aid others like you helped me.
Вау, какой крутой сайт казино онлайн! Благодарю!
https://tujuan-grogol-us.translate.goog/go/aHR0cHM6Ly9waW51cC1jYXNpbm8tcGxheS5rei9wYXltZW50cy8?_x_tr_sl=ja&_x_tr_tl=zh-TW&_x_tr_hl=ja
When I originally commented I clicked the “Notify me when new comments are added” checkbox
and now each time a comment is added I get several emails with the same comment.
Is there any way you can remove people from that service?
Appreciate it!
Everyone loves what you guys are up too. Such clever work and coverage!
Keep up the awesome works guys I’ve you guys to my own blogroll.
Hormone modifications could cause water retention, as anybody
with a case of period bloat who cannot match into her favourite jeans can attest.
Research results conflict as to which symptoms are eased, however a lot of the research confirm that
girls who take B6 supplements have reductions in bloating, breast pain, and premenstrual acne flare, a situation through which pimples break out about every week
before a lady’s period begins.
You actually make it seem so easy with your
presentation but I find this matter to be really something that I
think I would never understand. It seems too complex and extremely broad for me.
I’m looking forward for your next post, I will try to get the hang of it!
Wow! This blog looks exactly like my old one! It’s on a
entirely different topic but it has pretty much the same page layout and design. Excellent choice of colors!
I savor, lead to I discovered just what I was having a
look for. You have ended my four day long hunt! God Bless you man. Have
a nice day. Bye
(10 euros gratis apuestas|10 mejores casas de
apuestas|10 trucos para ganar apuestas|15 euros gratis marca
apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas
que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9
apuestas que siempre ganaras|a partir de cuanto
se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas
deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas
deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones
apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas
peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones
de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para
hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app
apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas
deportivas españa|app apuestas deportivas gratis|app
apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de
apuestas|app casas de apuestas|app control apuestas|app de apuestas|app
de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app
de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas
deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app
de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app
de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas
peru|app de apuestas reales|app de casas de apuestas|app marca apuestas
android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app
para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas
deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre
amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps
apuestas mundial|apps de apuestas|apps de apuestas con bono
de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps
de apuestas mexico|apps para apuestas|aprender
a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas
100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a
ganar|apuestas a jugadores nba|apuestas a
la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas
alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y
bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo
nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas
argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas
argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas
argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina
vs australia|apuestas argentina vs colombia|apuestas argentina vs
francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a
segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas
athletic atletico|apuestas athletic barça|apuestas athletic
barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas
athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico
de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas
atlético de madrid real madrid|apuestas atletico de madrid
vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas
atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas
baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto
nba|apuestas baloncesto pronostico|apuestas baloncesto
pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca
bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas
barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas
barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona
betis|apuestas barcelona campeon de liga|apuestas barcelona
celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona
girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas
barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas
barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas
bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis
fiorentina|apuestas betis girona|apuestas betis
madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas
betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas
bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas
boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos
colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas
caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de
champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas
campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga
española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas
campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos
hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras
caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos
en vivo|apuestas carreras de caballos españa|apuestas carreras
de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de
caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de
galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos
pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino
online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta
manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas
champions league|apuestas champions league – pronósticos|apuestas champions
league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas
chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas
chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas
ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas
clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas
colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas
colombia vs brasil|apuestas combinadas|apuestas
combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas
futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas
nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como
ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas
copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del
rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas
copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas
cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de
baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para
hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como
funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de
caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos
juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos
por internet|apuestas de caballos pronosticos|apuestas de
caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por
internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas
de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol
online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de
futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol
pronosticos|apuestas de fútbol pronósticos|apuestas de
futbol seguras|apuestas de futbol seguras para hoy|apuestas
de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de
galgos online|apuestas de galgos trucos|apuestas de golf|apuestas
de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de
juegos|apuestas de juegos deportivos|apuestas de juegos
online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de
la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la
liga española|apuestas de la nba|apuestas de la nfl|apuestas
de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas
de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de
perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas
de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas
de tenis|apuestas de tenis de mesa|apuestas
de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas
de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc
hoy|apuestas del boxeo|apuestas del clasico|apuestas del
clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia
deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del
sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas
deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas
1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas
apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas
deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas
deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas
bono bienvenida|apuestas deportivas bono de
bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas
deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas
deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas
deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com
foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas
combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas
deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas
deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas
copa mundial|apuestas deportivas corners|apuestas
deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas
deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas
deportivas de peru|apuestas deportivas de tenis|apuestas
deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas
deportivas en linea|apuestas deportivas en línea|apuestas deportivas
en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas
deportivas en uruguay|apuestas deportivas en vivo|apuestas
deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas
esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas
deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia
argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas
deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas
gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas
legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas
licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores
cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas
deportivas mlb hoy|apuestas deportivas multiples|apuestas
deportivas mundial|apuestas deportivas murcia|apuestas deportivas
nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas
deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas
deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online
en colombia|apuestas deportivas online españa|apuestas
deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas
online peru|apuestas deportivas online por internet|apuestas deportivas pago
paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido
suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas
promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas
pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas
deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas
deportivas seguras|apuestas deportivas seguras foro|apuestas
deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas
deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake
10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis
hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas
uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas
y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas
deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito
minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas
descenso la liga|apuestas descenso primera division|apuestas descenso
segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero
real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble
resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas
draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas
elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas
en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas
en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el
tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas
en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas
en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea
futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea
peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas
en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas
en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas
en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas
españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa
francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra
eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas
español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas
esport|apuestas esports|apuestas esports colombia|apuestas esports
españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas
estrategias|apuestas euro|apuestas euro
copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa
favoritos|apuestas eurocopa femenina|apuestas eurocopa
final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas
eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga
pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas
f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1
cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas
fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos
champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas
final copa america|apuestas final copa de europa|apuestas final copa
del rey|apuestas final copa europa|apuestas final copa
libertadores|apuestas final copa rey|apuestas
final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas
final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa
league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula
uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions
league|apuestas futbol chile|apuestas futbol
colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas
futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas
futbol online|apuestas futbol para hoy|apuestas
futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas
futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos
hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas
hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador
copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de
la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador
mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas
ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas
ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana
uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas
girona gana la liga|apuestas girona real madrid|apuestas girona
real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas
golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas
gratis sin deposito|apuestas gratis sin depósito|apuestas
gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap
baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas
handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas
hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas
hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra
paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas
juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos
virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la
liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas
mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas
league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales
españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas
liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas
liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de
hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas
de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas
lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas
madrid atletico champions|apuestas madrid barca|apuestas
madrid barça|apuestas madrid barca hoy|apuestas madrid barca
supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid
campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas
madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid
vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester
city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras
para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador
mundial|apuestas mejor jugador eurocopa|apuestas mejores
casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb
para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma
ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas
multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial
balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas
mundial clubes|apuestas mundial de baloncesto|apuestas mundial
de ciclismo|apuestas mundial de clubes|apuestas mundial
de futbol|apuestas mundial de fútbol|apuestas mundial de
rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas
mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial
rugby|apuestas mundial sub 17|apuestas mundiales|apuestas
mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp
nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba
all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba
hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas
nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas
nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl
pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas
nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas
online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions
league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online
futbol|apuestas online futbol españa|apuestas
online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas
online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online
peru|apuestas online seguras|apuestas online sin dinero|apuestas online
sin registro|apuestas online tenis|apuestas online ufc|apuestas
online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas
osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas
paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions
league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para
futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas
para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la
eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions
league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de
la eurocopa|apuestas para la nba hoy|apuestas para los partidos
de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas
partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas
partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas
peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru
vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs
nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas
por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas
promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas
pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas
psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas
que puedes hacer con tu novia|apuestas que siempre
ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas
quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana
eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara
la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real
madrid atletico de madrid|apuestas real madrid atlético de
madrid|apuestas real madrid atletico madrid|apuestas real
madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid
borussia|apuestas real madrid campeon champions|apuestas real madrid
celta|apuestas real madrid champions|apuestas real madrid
city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid
osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas
real madrid villarreal|apuestas real madrid
vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid
vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real
madrid vs sevilla|apuestas real madrid vs valencia|apuestas
real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas
real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas
retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas
rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas
segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras
baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas
seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras
nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar
dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises
bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de
madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas
sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas
sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas
sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples
ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas
sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas
sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas
sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas
stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga
argentina|apuestas tarjeta roja|apuestas
tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis
atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de
mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas
tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas
tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas
tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas
tipster para hoy|apuestas topuria holloway cuotas|apuestas
torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa
league|apuestas ufc|apuestas ufc chile|apuestas ufc
como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc
online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas
ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay
vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas
valencia madrid|apuestas valencia real madrid|apuestas
valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela
ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal
manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas
virtuales|apuestas virtuales colombia|apuestas
virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta
a españa|apuestas vuelta españa|apuestas william hill partidos de
hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro
nba apuestas|argentina apuestas|argentina colombia apuestas|argentina
croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay
apuestas|argentina vs bolivia apuestas|argentina vs chile
apuestas|argentina vs colombia apuestas|argentina vs
francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico
en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real
madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid
apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter
apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid
apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico
madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona
inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad
apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs
celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona
vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona
vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america
apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis
chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono
apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa
apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida
apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de
casas de apuestas|bono de registro apuestas|bono de
registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro
apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono
sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas
colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos
bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos
casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos
casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos
de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas
de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos
gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil
peru apuestas|brasil vs colombia apuestas|buenas apuestas para
hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de
cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de
apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas
yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora
de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas
deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake
apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas
de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad
cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de
apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas
juego|carrera de caballos con apuestas|carrera de galgos
apuestas|carreras de caballos apuestas|carreras de caballos apuestas
online|carreras de caballos con apuestas|carreras de caballos juegos
de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas
trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas
atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas
bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas
con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa
apuestas futbol|casa apuestas mejores cuotas|casa apuestas
mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de
apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas
atletico de madrid|casa de apuestas baloncesto|casa de
apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono
bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de
apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de
apuestas cerca de mí|casa de apuestas champions league|casa
de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa
de apuestas con bono sin deposito|casa de apuestas
con cuotas mas altas|casa de apuestas con esports|casa de apuestas
con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores
cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa
de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa
de apuestas de peru|casa de apuestas del madrid|casa de
apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas
cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa
de apuestas deportivas en españa|casa de apuestas deportivas
en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas
deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de
apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo
1 euro|casa de apuestas depósito mínimo 1 euro|casa de
apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas
españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa
de apuestas legales|casa de apuestas legales en colombia|casa de
apuestas legales en españa|casa de apuestas libertadores|casa de
apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de
apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa
de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas
oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas
online chile|casa de apuestas online españa|casa de apuestas online mexico|casa
de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas
para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa
de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa
de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas
sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa
de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de
apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas
bono sin deposito|casas apuestas bonos sin deposito|casas
apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas
apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas
deportivas españolas|casas apuestas deportivas nuevas|casas apuestas
españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas
ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas
licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas
apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas
asiaticas apuestas|casas de apuestas|casas de apuestas
5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas
bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas
de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas
de apuestas bonos de bienvenida|casas de apuestas
bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas
boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas
casino online|casas de apuestas cerca de mi|casas
de apuestas champions league|casas de apuestas chile|casas de apuestas
ciclismo|casas de apuestas colombia|casas de apuestas
com|casas de apuestas con app|casas de apuestas con apuestas
gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de
apuestas con bono por registro|casas de apuestas
con bono sin deposito|casas de apuestas con bonos|casas de
apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas
de apuestas con licencia española|casas
de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas
de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas
asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas
en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de
apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de
apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas
deportivas madrid|casas de apuestas deportivas mexico|casas de
apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo
1 euro|casas de apuestas depósito mínimo 1 euro|casas
de apuestas dinero gratis|casas de apuestas en argentina|casas
de apuestas en barcelona|casas de apuestas en chile|casas de
apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas
en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas
de apuestas en peru|casas de apuestas en perú|casas de
apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos
de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas
de apuestas española|casas de apuestas españolas|casas
de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de
apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas
f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas
formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas
futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso
minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas
legales en colombia|casas de apuestas legales en españa|casas de apuestas legales
en mexico|casas de apuestas legales españa|casas de apuestas legales
mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de
apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores
cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas
minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas
de apuestas mundiales|casas de apuestas nba|casas de apuestas
no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas
en colombia|casas de apuestas nuevas en españa|casas de apuestas
nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online
en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de
apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas
online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas
de apuestas peru bono sin deposito|casas de apuestas presenciales
Oh my goodness! Impressive article dude! Thank you so much, However I am going
through issues with your RSS. I don’t understand why I am unable to subscribe to
it. Is there anybody else getting identical RSS issues? Anyone who knows
the answer will you kindly respond? Thanx!!
For hottest information you have to go to see the web
and on web I found this web site as a best site for newest updates.
With unlimited access to exercise worksheets, OMT equips pupils tо
grasp mathematics throսgh rep, constructing affection fοr the subject and test confidence.
Dive іnto seⅼf-paced mathematics mastery ᴡith OMT’s 12-month e-learning courses,
completе ѡith practice worksheets ɑnd tape-recorded sessions
fοr extensive modification.
Ꭺѕ mathematics underpins Singapore’ѕ credibility fоr quality іn worldwide criteria ⅼike
PISA, math tuition іs essential tօ ⲟpening a kid’s ⲣossible
and protecting academic benefits іn this core subject.
primary math tuition constructs examination stamina tһrough timed drills, imitating
tһе PSLE’s twо-paper format аnd helping trainees handle tіmе successfully.
Wіtһ O Levels highlighting geometry evidence ɑnd theses, math tuition supplies specialized drills tο make sure trainees ϲan take
on these with accuracy and confidence.
Preparing for tһe changability ߋf A Level inquiries, tuition develops adaptive рroblem-solving techniques fօr real-time examination scenarios.
Distinctively, OMT matches tһe MOE curriculum ԝith a custom-mаde program including diagnostic
analyses tⲟ tailor material to eɑch pupil’s strengths.
Variety ⲟf method questions sia, preparing
yⲟu extensively foг ɑny type ᧐f math test and better scores.
Ιn Singapore, here adult participation is vital, math tuition ɡives structured assistance fοr
hоme support toԝards exams.
Tɑke a loⲟk at my web-site :: a math tuition sg
Hello! Do you know if they make any plugins to assist with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Thanks!
Greate pieces. Keep posting such kind of info on your page.
Im really impressed by your site.
Hi there, You have done an incredible job.
I’ll certainly digg it and in my view recommend to my
friends. I’m sure they’ll be benefited from this web site.
My family members every time say that I am killing
my time here at net, but I know I am getting knowledge every day by reading thes
fastidious articles or reviews.
Yesterday, while I was at work, my sister stole my apple ipad and tested to see
if it can survive a twenty five foot drop, just so she can be a youtube
sensation. My apple ipad is now broken and she has
83 views. I know this is totally off topic but I
had to share it with someone!
Hey there! I know this is kinda off topic nevertheless I’d figured I’d ask.
Would you be interested in trading links or maybe guest
writing a blog post or vice-versa? My website goes over
a lot of the same subjects as yours and I believe we could greatly benefit from each other.
If you happen to be interested feel free to
send me an e-mail. I look forward to hearing from you! Great blog
by the way!
I know this if off topic but I’m looking into starting my own weblog and was wondering
what all is needed to get setup? I’m assuming having a blog like yours would
cost a pretty penny? I’m not very web savvy so I’m
not 100% certain. Any recommendations or advice would be greatly appreciated.
Many thanks
Unquestionably believe that which you stated. Your favorite
reason seemed to be on the net the easiest thing to be aware
of. I say to you, I certainly get irked while people consider worries that they just
don’t know about. You managed to hit the nail upon the top and also
defined out the whole thing without having side effect
, people could take a signal. Will likely be back to get more.
Thanks
Если на осмотре выявляются спутанность сознания, подозрение на делирий, неукротимая рвота с примесью крови, выраженная боль в груди, тяжёлая одышка, судороги — врач немедленно предложит стационар. Безопасность важнее удобства.
Выяснить больше – https://kapelnica-ot-zapoya-vidnoe7.ru
Hey I am so happy I found your site, I really found you by mistake, while I was
researching on Bing for something else, Anyhow
I am here now and would just like to say kudos for a incredible post
and a all round enjoyable blog (I also love the theme/design),
I don’t have time to look over it all at the moment but I have book-marked it and also added your RSS feeds, so when I have
time I will be back to read a great deal more, Please do keep up the superb job.
Pretty! This was an incredibly wonderful article. Many thanks for providing this info.
Just wish to say your article is as surprising. The clarity on your submit is simply cool and that i could think you are
knowledgeable in this subject. Fine along with your permission allow me to
snatch your feed to stay updated with approaching post.
Thanks 1,000,000 and please continue the rewarding work.
This game looks amazing! The way it blends that old-school chicken crossing concept with actual
consequences is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding
real risk? I’m totally down to try it.
This is right up my alley! I’m loving the combo
of classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and
adds legitimate risk is genius. Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing action with real-world
stakes has me interested. I’m ready to jump in!
Holy cow, this looks great! Merging that beloved
chicken crossing style with tangible consequences? I’ve gotta
try this out!
I read this piece of writing fully on the topic of the resemblance of hottest and previous technologies, it’s amazing
article.
naturally like your web-site however you need to test the spelling on quite a
few of your posts. A number of them are rife with spelling issues and I to find it very troublesome to
inform the truth then again I’ll certainly come back again.
Just desire to say your article is as astounding. The clearness for your
submit is simply spectacular and that i can suppose you’re knowledgeable in this subject.
Well together with your permission allow me to grab your feed
to keep updated with coming near near post. Thank you one million and please keep up the enjoyable work.
I like what you guys are usually up too. This type of clever work and reporting!
Keep up the great works guys I’ve incorporated you guys to our blogroll.
This text is worth everyone’s attention. When can I find out more?
Этап
Получить дополнительную информацию – http://narkolog-na-dom-zhukovskij7.ru
It’s very trouble-free to find out any topic
on web as compared to textbooks, as I found this post at this site.
Ridiculous quest there. What happened after?
Good luck!
Hi there! This article could not be written any better!
Looking at this article reminds me of my previous roommate!
He continually kept preaching about this. I most certainly will send this article
to him. Pretty sure he will have a very good read. I appreciate you for sharing!
It’s appropriate time to make some plans for the future and it is time to be happy.
I’ve read this post and if I could I want to suggest you few interesting
things or tips. Perhaps you could write next articles referring to this article.
I want to read even more things about it!
Hey I know this is off topic but I was wondering if you knew
of any widgets I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have
some experience with something like this. Please let me know if you
run into anything. I truly enjoy reading your blog and I look forward to your new updates.
Do you mind if I quote a couple of your posts as long as I provide credit and sources back to your weblog?
My blog is in the exact same area of interest as yours
and my visitors would truly benefit from some of the information you provide here.
Please let me know if this okay with you. Cheers!
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Получить больше информации – https://www.iso-studio.it/il-natale-al-tempo-del-coronavirus
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Слушай внимательно — тут важно – https://blogi.eoppimispalvelut.fi/fuksiat/2020/02/06/etsitko-mokkimajoitusta-inarijarvelta
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Смотрите также… – https://www.vrk.dev/flyer1-2
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Прочитать подробнее – https://www.cesarmeneghetti.net/news/cesar-meneghetti-12th-international-image-festival-colombia
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Хочешь знать всё? – https://glaserei-horn.de/2021/10/12/international-world
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Это стоит прочитать полностью – https://www.thetablereadmagazine.co.uk/19-unique-cardboard-box-art-projects-that-will-blow-your-mind
Thanks designed for sharing such a pleasant thought, article is nice, thats why i have read it entirely
Thank you for another informative website. Where else may just I get
that kind of info written in such an ideal way?
I have a project that I am just now running on, and
I’ve been at the look out for such information. https://www.elkhartnorthside.org/sunday-worship-pic-2
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Детали по клику – https://lesboucsentrain.com/le-glandasse
Ориентир по времени
Детальнее – vyzov-vracha-narkologa-na-dom
Hi there just wanted to give you a brief heads up and let you know a few of the images aren’t
loading properly. I’m not sure why but I think its a linking issue.
I’ve tried it in two different web browsers and both show the same results.
Hello, this weekend is nice in favor of me, as this occasion i am reading this wonderful informative article here at my home.
Nice post. I was checking constantly this blog and I am impressed!
Extremely helpful information specifically the last part 🙂 I care for such info much.
I was seeking this certain information for a long time. Thank you and best of luck.
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
А есть ли продолжение? – https://primenewsnet.com/how-to-find-the-perfect-sunglasses-for-your-hair-face-shape
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Что скрывают от вас? – https://informatusa.com/existen-programas-especificos-para-veteranos-relacionados-con-la-vivienda
I’m not sure why but this website is loading very slow for me.
Is anyone else having this problem or is it a issue on my end?
I’ll check back later on and see if the problem
still exists.
Every weekend i used to pay a quick visit this site, because i wish for enjoyment, since this this site conations really fastidious funny data too.|
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Подробная информация доступна по запросу – https://primenewsnet.com/computer-filters-noise-to-make-you-a-better-listener
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Эксклюзивная информация – https://bfngo.az/resurs-m%C9%99rk%C9%99zi-tovuzda-g%C9%99ncl%C9%99r-ucun-seminarlar-t%C9%99skil-edib
Hi, I want to subscribe for this blog to take latest updates, therefore where can i do it please
help.
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Это ещё не всё… – https://aadi-india.org/basant-sangam-flower-show
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Откройте для себя больше – https://www.webscorredurias.com/rsc-redes-sociales
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Не упусти важное! – http://job-interview.ru/articles/post/67
I think the admin of this web page is in fact working hard for his website, since here every material is quality
based stuff.
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Расширить кругозор по теме – https://www.fintechsblog.com/2024/07/30/fintech-trends-you-cant-miss-on
I am really impressed with your writing skills as well as
with the layout on your blog. Is this a paid theme or did
you modify it yourself? Either way keep up the
excellent quality writing, it’s rare to see a nice blog
like this one today.
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Прочесть всё о… – https://www.littleworld.in/this-is-a-post-with-post-type-link
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Эксклюзивная информация – https://sahabattravel.id/pesan-travel-banyuwangi-terbaik-chek-info/travel-surabaya-banyuwangi/pesan-travel-banyuwangi/travel-banyuwangi-surabaya-pesan-travel-banyuwangi/896
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos
para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2
en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de
cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android
apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas
de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de
apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones
de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer
apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de
futbol|app apuestas deportivas|app apuestas deportivas android|app
apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app
apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app
apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas
de apuestas|app control apuestas|app de apuestas|app
de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas
con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app
de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de
apuestas deportivas en españa|app de apuestas deportivas
peru|app de apuestas deportivas perú|app de apuestas deportivas
sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app
de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app
de apuestas para android|app de apuestas para ganar
dinero|app de apuestas peru|app de apuestas reales|app de casas de
apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app
para apuestas de futbol|app para apuestas deportivas|app para
apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app
para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas
mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps
de apuestas deportivas peru|apps de apuestas mexico|apps para
apuestas|aprender a hacer apuestas deportivas|aprender hacer
apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a
caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas
a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas
al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz
hoy|apuestas alemania españa|apuestas alonso campeon del
mundo|apuestas altas y bajas|apuestas altas y
bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia
argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina
colombia|apuestas argentina croacia|apuestas argentina españa|apuestas
argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas
argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs
peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic
manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas
athletic real sociedad|apuestas athletic real
sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético
copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de
madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid
real madrid|apuestas atletico de madrid vs barcelona|apuestas
atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid
vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid
champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas
baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas
baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas
barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas
barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs
madrid|apuestas barca vs psg|apuestas barcelona|apuestas
barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas
barcelona atletico de madrid|apuestas barcelona atlético de
madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de
liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas
barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas
barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona
real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas
barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs
atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas
barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas
beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis
– chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas
betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas
betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs
colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas
bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo
femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo
online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas
caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa
america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas
campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula
1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas
campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato
f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de
galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras
caballos sanlucar|apuestas carreras de caballos|apuestas carreras de
caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas
carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras
de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas
carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino
online|apuestas casino online argentina|apuestas
casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta
espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions
league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league
pronósticos|apuestas champions pronosticos|apuestas chelsea
barcelona|apuestas chelsea betis|apuestas chile|apuestas
chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile
vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a
españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas
colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia
vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de
futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas
futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas
combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas
comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa
america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas
copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey
final|apuestas copa del rey futbol|apuestas copa del rey
ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas
copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas
copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas
croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas
de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de
boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas
de caballos como funciona|apuestas de caballos como se
juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de
caballos online en venezuela|apuestas de caballos por
internet|apuestas de caballos pronosticos|apuestas de
caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de
caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de
ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de
f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas
de futbol colombia|apuestas de futbol en colombia|apuestas de futbol
en directo|apuestas de futbol en linea|apuestas de
futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol
para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol
pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como
ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas
de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey
sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de
juego|apuestas de juegos|apuestas de juegos deportivos|apuestas
de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas
de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la
liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para
hoy|apuestas de partidos|apuestas de partidos de
futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas
de sistema explicacion|apuestas de sistema explicación|apuestas
de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis
para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas
del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del
día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas
del dia futbol|apuestas del mundial|apuestas del partido
de hoy|apuestas del real madrid|apuestas del rey|apuestas del
sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas
app|apuestas deportivas apps|apuestas deportivas argentina|apuestas
deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca
madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas
bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos
de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas
deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas
colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas
deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas
deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas
deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de
baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de
futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas
en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas
estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas
foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas
fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas
deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas
deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas
deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas
handicap|apuestas deportivas handicap asiatico|apuestas deportivas
hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas
deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas
licencia españa|apuestas deportivas liga española|apuestas deportivas
listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas
deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas
deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas
deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas
nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas
deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas
online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas
online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas
deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas
pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas
deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas
seguras hoy|apuestas deportivas seguras para
hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas
stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas
deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas
deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias
seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas
directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas
dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el
clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas
en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos
online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la
champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas
mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas
en linea colombia|apuestas en línea de fútbol|apuestas
en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de
futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas
en sistema|apuestas en stake|apuestas en tenis|apuestas
en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas
en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas
españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia
eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa
holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas
españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas
español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas
esports gratis|apuestas esports lol|apuestas
esports peru|apuestas esports valorant|apuestas estadisticas|apuestas
estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas
eurocopa campeon|apuestas eurocopa españa|apuestas
eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas
eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga
baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league
hoy|apuestas europa league pronosticos|apuestas
europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas
f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1
miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions
peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa
del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del
rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas
final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas
finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula
1|apuestas fórmula 1 pronósticos|apuestas formula
uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas
futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol
argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas
galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas
ganador champions league|apuestas ganador copa america|apuestas
ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de
la eurocopa|apuestas ganador de la liga|apuestas ganador
del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador
liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas
ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas
ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas
girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores
eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf
masters|apuestas golf pga|apuestas granada barcelona|apuestas
grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis
hoy|apuestas gratis para hoy|apuestas gratis
por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis
y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas
handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas
online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy
futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy
seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas
juego|apuestas juegos|apuestas juegos en linea|apuestas
juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings
league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados
unidos|apuestas legales españa|apuestas leganes betis|apuestas
libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas
madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid
celta|apuestas madrid city|apuestas madrid dortmund|apuestas
madrid gana la liga|apuestas madrid gana liga|apuestas madrid
hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas
madrid valencia|apuestas madrid vs arsenal|apuestas madrid
vs barcelona|apuestas mallorca osasuna|apuestas
mallorca real sociedad|apuestas manchester athletic|apuestas manchester
city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor
jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas
méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb
para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma
ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas
mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de
clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de
rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial
formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas
mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales
de colombia|apuestas nba|apuestas nba all
star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas
nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas
nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana
4|apuestas nfl super bowl|apuestas nhl|apuestas
nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online
bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas
online casino|apuestas online champions league|apuestas
online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online
en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas
online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas
online gratis|apuestas online gratis sin deposito|apuestas
online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online
net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas
online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real
madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas
over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas
paises bajos ecuador|apuestas paises bajos inglaterra|apuestas
países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para
el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido
de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero
facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la
eurocopa|apuestas para ganar la europa league|apuestas
para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy
futbol|apuestas para juegos|apuestas para la champions league|apuestas
para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de
hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido
suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos
eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas
peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru
uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas
pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda
b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas
por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos
deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas
pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas
que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real
madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas
real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de
madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real
madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real
madrid campeon champions|apuestas real madrid celta|apuestas real
madrid champions|apuestas real madrid city|apuestas real
madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas
real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas
real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs
sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real
sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas
recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas
resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas
rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas
seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la
ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy
futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para
hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla
campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla
juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas
sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas
sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas
sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas
sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas
stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga
argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas
tenis atp|apuestas tenis consejos|apuestas tenis copa
davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis
itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas
tenis roland garros|apuestas tenis seguras|apuestas tenis
wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas
uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc
chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas
uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas
uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia
betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor
app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal
betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas
villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de
hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es
pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina
mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia
apuestas|argentina vs. colombia apuestas|asi
se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos
apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico
barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico
madrid real madrid apuestas|atletico madrid vs real madrid
apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid
apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid
apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona
atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de
apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona
real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona
valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético
madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona
vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol
apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis
apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu
sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas
deportivas|bono apuestas deportivas sin deposito|bono apuestas
gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono
bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida
apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis
sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de
apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono
de registro apuestas|bono de registro apuestas deportivas|bono de
registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono
por registro apuestas|bono por registro apuestas deportivas|bono por
registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas
deportivas|bono sin depósito apuestas deportivas|bono sin deposito
casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos
apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos
apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas
apuestas|bonos bienvenida casas de apuestas|bonos casa
de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas
de apuestas deportivas|bonos casas de apuestas españa|bonos casas de
apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de
apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas
deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida
casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa
de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas
deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot
de apuestas deportivas gratis|boxeo apuestas|brasil colombia
apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador
de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora
apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora
de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora
de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas
deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para
apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora
stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas
sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad
cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga
apuestas|campeon nba apuestas|canales de
apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos
con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos
apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas
bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de
mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa
apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa
apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas
peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de
apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de
apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de
apuestas bono sin deposito|casa de apuestas boxeo|casa
de apuestas caballos|casa de apuestas carreras de caballos|casa
de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de
apuestas chile|casa de apuestas ciclismo|casa de apuestas
colombia|casa de apuestas con bono de bienvenida|casa
de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las
mejores cuotas|casa de apuestas con licencia en españa|casa de
apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa
america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de
españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa
de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real
madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas
en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas
deportivas madrid|casa de apuestas deportivas mexico|casa de
apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito
5 euros|casa de apuestas deposito minimo|casa de apuestas
deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas
españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas
legales en españa|casa de apuestas libertadores|casa de apuestas
liga española|casa de apuestas madrid|casa de apuestas mas segura|casa
de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo
5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa
de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa
de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online
usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas
para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru
online|casa de apuestas por paypal|casa de apuestas promociones|casa
de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa
de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa
de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa
de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas
bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas
españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas
eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia
españa|casas apuestas mexico|casas apuestas mundial|casas apuestas
nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de
apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas
de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de
apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de
apuestas cerca de mi|casas de apuestas champions league|casas
de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas
de apuestas con bono de registro|casas de apuestas con bono
por registro|casas de apuestas con bono sin deposito|casas
de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap
asiatico|casas de apuestas con licencia|casas
de apuestas con licencia en españa|casas de apuestas
con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas
de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de
caballos|casas de apuestas de españa|casas de apuestas de
futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas
de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de
apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas
de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de
apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas
de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de
apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de
apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas
en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de
apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas
en valencia|casas de apuestas en venezuela|casas
de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa
alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas
de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de
apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de
apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas
de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de
apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas
de apuestas ingreso minimo 5 euros|casas de apuestas inter
barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de
apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de
apuestas licencia|casas de apuestas licencia
españa|casas de apuestas lista|casas de
apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas
mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de
apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas
nba|casas de apuestas no reguladas en españa|casas
de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas
nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de
apuestas ofertas|casas de apuestas online|casas de apuestas
online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas
de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas
online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas
de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online
usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para
ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas de
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Посмотреть всё – https://kannadasampada.com/health/different-types-of-banana
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Обратиться к источнику – http://asso-cpdis.com/index.php/2018/02/27/dejeuner-du-mardi-27-fevrier-2018-la-place-de-lintelligence-artificielle-dans-lindustrie-pharmaceutique
Pretty! This has been a really wonderful post. Thanks for supplying this information.
It is not my first time to pay a visit this web site, i
am browsing this site dailly and take good data from here every day.
Attractive part of content. I just stumbled upon your blog and
in accession capital to say that I get actually enjoyed account your weblog posts.
Anyway I will be subscribing in your feeds or even I achievement you
access constantly fast.
https://bs2-bs2web.at
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Полезно знать – https://www.cyclopsproject.eu/locations/ntt-buildings
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Узнайте всю правду – https://jaklean.co.uk/finding-the-best-cleaning-services
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Интересует подробная информация – https://nutricionplena.com/como-tomar-los-productos-omnilife
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, United Stateѕ
+19803517882
Bookmarks
An intriguing discussion is worth comment. I do believe that you should
publish more about this subject matter, it might not be a taboo matter but generally
people don’t speak about such issues. To the next! All the best!!
Today, while I was at work, my cousin stole my iPad and tested to see if it can survive a twenty five foot drop, just so she can be a youtube
sensation. My apple ipad is now broken and she has 83 views.
I know this is entirely off topic but I had to share it with someone!
Hello outstanding website! Does running a blog such as this require a large
amount of work? I have very little understanding of coding however I had been hoping
to start my own blog in the near future. Anyway, should you have any recommendations
or tips for new blog owners please share. I understand this is off subject however
I simply had to ask. Many thanks!
Второй этаж в квартире Лестница из металла в Москве – это современное и функциональное решение для многоуровневых помещений. Металлические лестницы отличаются прочностью, долговечностью и разнообразием дизайнерских решений. В Москве, где архитектурные стили сочетают в себе современность и классику, металлические лестницы пользуются большой популярностью. Они могут быть выполнены из различных материалов, таких как сталь, алюминий или чугун, и могут иметь различные формы и размеры. Металлические лестницы часто используются в квартирах, офисах, торговых центрах и других общественных зданиях, где важна безопасность, надежность и эстетичный внешний вид. Компании в Москве предлагают широкий выбор металлических лестниц, начиная от простых конструкций до сложных дизайнерских проектов.
Do you have a spam issue on this website; I also am a blogger, and
I was curious about your situation; we have developed some
nice procedures and we are looking to trade strategies
with others, please shoot me an email if interested.
Great work! This is the type of info that should be shared around the net. Shame on the search engines for not positioning this post higher! Come on over and visit my web site . Thanks =)
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Углубиться в тему – https://focustangerang.com/forum-silaturahmi-istri-fsi-fraksi-pkb-gelar-bakti-sosial-pengobatan-gratis-di-kab-tangerang-dalam-rangka-harlah-ke-27-pkb/ragam-info/sosial
If some one wants expert view on the topic of running a blog after that
i propose him/her to pay a quick visit this website, Keep up the nice job.
Cabinet IQ
15030 N Tatum Blvd #150, Phoenix,
AZ 85032, United Ⴝtates
(480) 424-4866
Wood
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de
juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer
apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones
de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones
de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas
deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas
deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app
casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas
android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de
apuestas deportivas argentina|app de apuestas deportivas
colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas
ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de
apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app
marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas
en español|app para ganar apuestas deportivas|app
para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps
apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de
futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas
100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas
a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a
la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas
al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso
campeon del mundo|apuestas altas y bajas|apuestas altas
y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas
anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas
argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina
colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas
argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises
bajos|apuestas argentina polonia|apuestas
argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina
vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas
ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas
athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas
atletico barsa|apuestas atletico campeon champions|apuestas
atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico
de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico
de madrid real madrid|apuestas atlético de madrid real madrid|apuestas
atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs
barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas
atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas
baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas
baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas
barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca
juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas
barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona
atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona
atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas
barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas
barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona
valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real
madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol
pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis
– chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas
betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis
valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay
hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas
billar online|apuestas bolivia vs colombia|apuestas bono|apuestas
bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real
madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo
españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas
brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs
peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas
caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas
campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions
league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa
del rey|apuestas campeon de champions|apuestas
campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas
campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas
campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga
bbva|apuestas campeon liga española|apuestas campeon liga
santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas
campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de
futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de
semana|apuestas carrera de galgos hoy|apuestas carrera de galgos
nocturnas|apuestas carreras caballos|apuestas carreras caballos
sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras
de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas
carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras
de galgos|apuestas carreras de galgos en vivo|apuestas carreras de
galgos nocturnas|apuestas carreras de galgos pre partido|apuestas
casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas
casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas
casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta
betis|apuestas celta eibar|apuestas celta
espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league
pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea
betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile
vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo
femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas
city madrid|apuestas city real madrid|apuestas clasico|apuestas
clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas
colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas
colombia paraguay|apuestas colombia uruguay|apuestas
colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas
combinadas como funcionan|apuestas combinadas de
futbol|apuestas combinadas de fútbol|apuestas
combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para
esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas
recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas
como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero
virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de
ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas
con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas
copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa
de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas
copa del rey futbol|apuestas copa del rey ganador|apuestas copa
del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey
pronósticos|apuestas copa europa|apuestas copa
italia|apuestas copa libertadores|apuestas copa mundial de
hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de
beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de
boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se
juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos
ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas
de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas
de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de
fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas
de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas
de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas
de futbol hoy|apuestas de futbol mundial|apuestas
de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de
fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de
futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de
futbol seguras para hoy|apuestas de futbol sin dinero|apuestas
de galgos|apuestas de galgos como ganar|apuestas de galgos
en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas
de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas
de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa
américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas
de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de
nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos
de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de
tenis de mesa|apuestas de tenis en directo|apuestas de
tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de
todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del
clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del
dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100
seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas
bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas
combinadas para hoy|apuestas deportivas como se
juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas
deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas
con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas
deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas
deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de
boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas
de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas
de tenis|apuestas deportivas del dia|apuestas deportivas dinero
ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas
deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas
deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas
estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas
faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas
foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas
golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas
gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas
deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas
deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga
española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas
madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas
deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas
mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas
deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas
nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas
online en colombia|apuestas deportivas online españa|apuestas
deportivas online mexico|apuestas deportivas online paypal|apuestas
deportivas online peru|apuestas deportivas online por
internet|apuestas deportivas pago paypal|apuestas deportivas para ganar
dinero|apuestas deportivas para hoy|apuestas deportivas para
hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de
hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas
peru vs ecuador|apuestas deportivas predicciones|apuestas
deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas
deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas
deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas
resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas
deportivas seguras|apuestas deportivas seguras foro|apuestas
deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito
inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas
telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas
deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas
deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1
euro|apuestas descenso a segunda|apuestas descenso a
segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero
ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas
doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador
vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas
en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de
futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas
en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las
vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea
argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas
en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico
online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de
futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas
equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania
eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana
el mundial|apuestas españa gana eurocopa|apuestas
españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas
euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa
campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa
ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas
euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa
league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1
canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las
vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de
ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas
favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc
barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas
final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final
copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas
final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas
final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas
final uefa europa league|apuestas final.mundial|apuestas finales
de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol
en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol
eurocopa|apuestas futbol femenino|apuestas futbol
foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol
sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos
pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador
champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador
copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas
ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la
liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial
baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar
eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas
ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona
campeon de liga|apuestas girona campeon liga|apuestas girona
gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y
ganar premios|apuestas grupo a eurocopa|apuestas grupos
eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas
handicap baloncesto|apuestas handicap como funciona|apuestas handicap
nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas
hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas
holanda argentina|apuestas holanda vs argentina|apuestas
hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas
inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador
sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las
vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados
unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga
argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de
campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de
futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas
madrid arsenal|apuestas madrid atletico|apuestas madrid
atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas
madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas
madrid city|apuestas madrid dortmund|apuestas madrid gana
la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid
vs arsenal|apuestas madrid vs barcelona|apuestas mallorca
osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas
manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas
maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos
online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas
mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas
mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas
mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de
baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas
mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial
formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas
mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas
mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas
nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas
nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas
nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas
nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl
las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas
octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas
online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online
ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas
online en argentina|apuestas online en peru|apuestas online espana|apuestas online
españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online
golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas
online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online
venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas
over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos
qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el
dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para
eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar
la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la
champions league|apuestas para la copa del rey|apuestas
para la eurocopa|apuestas para la europa league|apuestas para la final
de la eurocopa|apuestas para la nba hoy|apuestas para los partidos
de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas
partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas
partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas
partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas
paypal|apuestas peleas de boxeo|apuestas peru|apuestas
perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas
peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas
playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas
playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera
division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas
pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg
barca|apuestas psg barcelona|apuestas puntos
por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que
es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas
que significa|apuestas quien bajara a segunda|apuestas
quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas
quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas
quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas
quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real
madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid
atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas
real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid
city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas
real madrid real sociedad|apuestas real madrid valencia|apuestas real
madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid
vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid
vs barcelona|apuestas real madrid vs betis|apuestas real madrid
vs sevilla|apuestas real madrid vs valencia|apuestas
real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas
real sociedad psg|apuestas real sociedad real madrid|apuestas
real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas
resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda
division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas
seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas
seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas
seguras nba|apuestas seguras nba hoy|apuestas seguras
para este fin de semana|apuestas seguras para
ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras
para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras
tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla
atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas
sevilla celta|apuestas sevilla gana la liga|apuestas sevilla
girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas
simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito
inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero
real|apuestas sin empate|apuestas sin empate
que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como
funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake
10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas
tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis
copa davis|apuestas tenis de mesa|apuestas
tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis
pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas
tipos|apuestas tips|apuestas tipster|apuestas tipster
para hoy|apuestas topuria holloway cuotas|apuestas torneos
de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas
uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc
como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas
valor app|apuestas valor en directo|apuestas valor galgos|apuestas
venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal
barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal
liverpool|apuestas villarreal manchester|apuestas villarreal manchester
united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales
futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a
españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru
apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina
vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic
barcelona apuestas|athletic manchester united apuestas|athletic osasuna
apuestas|athletic real madrid apuestas|atletico
barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid
vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico
real madrid apuestas|atletico vs real madrid apuestas|avisador
de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona
– real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de
apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid
apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona
apuestas|barcelona vs madrid apuestas|barcelona vs real
madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs
sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas
apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis
apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog
apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono
bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas
españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de
apuestas|bono bienvenida marca apuestas|bono casa
apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de
bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas
deportivas|bono de registro casa de apuestas|bono gratis
apuestas|bono marca apuestas|bono por registro apuestas|bono por
registro apuestas deportivas|bono por registro casa de
apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito
apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos
apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas
gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos
bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas
apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos
casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas
de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de
apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida
casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida
en casas de apuestas|bonos de casas de apuestas|bonos
de casas de apuestas sin deposito|bonos en casa de apuestas|bonos
en casas de apuestas sin deposito|bonos gratis
apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito
casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru
apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador
cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos
apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora
cuotas apuestas|calculadora de apuestas|calculadora
de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora
de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora
de apuestas surebets|calculadora de arbitraje
apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora
para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas
deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular
apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas
sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular
ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota
apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de
apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa
apuestas|campeon liga apuestas|campeon nba apuestas|canales de
apuestas gratis|carrera de caballos apuestas|carrera de caballos
apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos
apuestas|carreras de galgos apuestas online|carreras
de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de
madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono
gratis|casa apuestas bono sin deposito|casa apuestas cerca
de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa
apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa
apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas
baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de
apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa
de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de
apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa
de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas
con bono sin deposito|casa de apuestas con cuotas
mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas
con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de
apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa
de apuestas de españa|casa de apuestas de futbol|casa de apuestas
de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del
real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas
deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de
apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas
deposito minimo|casa de apuestas deposito minimo 1 euro|casa
de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa
de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de
apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa
de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de
apuestas eurocopa|casa de apuestas europa league|casa de
apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas
ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa
de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5
euros|casa de apuestas mlb|casa de apuestas mundial|casa de
apuestas nba|casa de apuestas nfl|casa de apuestas
nueva|casa de apuestas nuevas|casa de apuestas oficial
del real madrid|casa de apuestas oficial real
madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de
apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de
apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para
boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de
apuestas peru online|casa de apuestas por paypal|casa de
apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de
bienvenida|casa de apuestas sevilla|casa de apuestas
sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas
sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas
chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas
con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas
españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas
apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas
apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas
mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas
apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas
5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de
apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de
apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas
boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas
de apuestas casino|casas de apuestas casino online|casas de apuestas cerca
de mi|casas de apuestas champions league|casas de
apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono
de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de
apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas
de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas
copa del rey|casas de apuestas de caballos|casas de
apuestas de españa|casas de apuestas de futbol|casas de
apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas
deportivas comparativa|casas de apuestas deportivas con paypal|casas de
apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de
apuestas deportivas en linea|casas de apuestas deportivas
en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas
deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas
deportivas legales|casas de apuestas deportivas madrid|casas
de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de
apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo
1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa
online|casas de apuestas en linea|casas de apuestas en madrid|casas de
apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas
equipos de futbol|casas de apuestas españa|casas de apuestas españa
alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas
de apuestas española|casas de apuestas españolas|casas de
apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de
apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas
formula 1|casas de apuestas fuera de españa|casas de
apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas
de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso
minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas
de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales
en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de
apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas
de apuestas mejores bonos|casas de apuestas mejores
cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas
mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no
reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas
de apuestas ofertas|casas de apuestas online|casas de
apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de
apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online
en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas
online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online
peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas
pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas
de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de
I need to to thank you for this very good read!! I absolutely loved every bit of it.
I have you saved as a favorite to look at new things you post…
When someone writes an piece of writing he/she maintains the thought of a user in his/her brain that
how a user can be aware of it. Thus that’s why this paragraph is amazing.
Thanks!
This is a topic which is close to my heart… Many thanks!
Exactly where are your contact details though?
If you desire to get a great deal from this article then you have to apply these techniques to your won webpage.
Neat blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple adjustements would really make
my blog shine. Please let me know where you got your design. Thanks a lot
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Читать далее > – http://snabs.nl/?p=321
Hi there are using WordPress for your blog platform?
I’m new to the blog world but I’m trying to get started and
set up my own. Do you require any html coding expertise to
make your own blog? Any help would be really appreciated!
I do not even know how I ended up here, but I thought this post
was great. I do not know who you are but certainly you’re going to a
famous blogger if you are not already 😉 Cheers!
It’s nearly impossible to find knowledgeable people about this subject, however, you
sound like you know what you’re talking about! Thanks
hello there and thank you for your info – I have definitely picked up something new from
right here. I did however expertise a few technical issues using this site,
since I experienced to reload the web site a lot of times previous to I could get it to load
properly. I had been wondering if your web host is OK?
Not that I am complaining, but sluggish loading instances times
will often affect your placement in google and could damage
your high-quality score if advertising and marketing with
Adwords. Well I am adding this RSS to my email and
could look out for much more of your respective interesting content.
Make sure you update this again very soon.
Yes! Finally someone writes about THABET.
whoah this weblog is excellent i love reading your articles.
Stay up the great work! You understand, many persons are looking around for this info, you can help them greatly.
Hi there! I know this is somewhat off topic but I was wondering which blog platform
are you using for this website? I’m getting tired of WordPress because I’ve had
problems with hackers and I’m looking at options for another platform.
I would be awesome if you could point me in the direction of a
good platform.
I know this if off topic but I’m looking into starting my own blog and was wondering what all is needed to get setup?
I’m assuming having a blog like yours would cost a pretty
penny? I’m not very web savvy so I’m not 100% positive.
Any suggestions or advice would be greatly appreciated.
Thank you
Wow, awesome blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your web site is fantastic, as well as the content!
Hello, i believe that i noticed you visited my site thus i came
to go back the favor?.I’m attempting to in finding issues to enhance my website!I suppose its good enough
to make use of a few of your ideas!!
Hi to all, how is all, I think every one is getting more from this web
page, and your views are nice for new viewers.
When someone writes an article he/she retains
the image of a user in his/her brain that how a user can know it.
So that’s why this piece of writing is great. Thanks!
Your style is unique in comparison to other people I’ve read stuff from.
Thanks for posting when you have the opportunity, Guess I will just book mark this blog.
Have you ever thought about including a little bit more than just your articles?
I mean, what you say is valuable and all.
But think of if you added some great photos or video clips to give your posts more, “pop”!
Your content is excellent but with pics and videos, this website could definitely be one of
the best in its niche. Wonderful blog!
Wow! At last I got a weblog from where I be capable of
truly obtain valuable data regarding my study and knowledge.
I will immediately grasp your rss as I can not in finding your email subscription hyperlink or newsletter service.
Do you’ve any? Kindly let me realize so that I could subscribe.
Thanks.
You have made some really good points there.
I checked on the web for more info about the issue and found most people will go along with
your views on this web site.
You actually stated this effectively!
Take a look at my web site; http://www.tjudb.cn/dbgroup/Espionner_Un_Iphone_Un_Jeu_D_enfant
Every weekend i used to pay a visit this web page, because i want enjoyment, as this this web site conations genuinely pleasant funny material too.
Joint on-line difficulties at OMT build synergy іn math, fostering love ɑnd
collective motivation fօr exams.
Register tοԀay in OMT’ѕ standalone e-learning programs and view yоur grades skyrocket tһrough endless
access tօ premium, syllabus-aligned material.
Αs mathematics forms tһe bedrock ߋf rational thinking ɑnd crucial prߋblem-solving in Singapore’s education ѕystem,
professional math tuition offers the personalized guidance necessary to turn obstacles іnto victories.
Math tuition assists primary school students master PSLE Ьʏ enhancing the Singapore Math curriculum’ѕ bar modeling strategy
for visual analytical.
Secondary math tuition lays а strong groundwork f᧐r post-O
Level studies, ѕuch as Α Levels oг polytechnic courses, by standing οut in fundamental subjects.
Junior colkege math tuition promotes joint learning іn tiny teams, enhancing peer discussions on facility A Level concepts.
The exclusive OMT syllabus differs Ьy extending MOE curriculum ᴡith enrichment оn statistical modeling, perfect
fοr data-driven examination concerns.
Detailed remedies offered online leh, mentor үоu exactly
h᧐w to resolve issues correctly foг fаr better
grades.
Tuition facilities սse cutting-edge deices lіke aesthetic һelp, enhancing understanding fօr
better retention іn Singapore mathematics exams.
Feel free tо surf to my website Kaizenaire math tuition singapore
I’m not that much of a online reader to be honest but your sites really
nice, keep it up! I’ll go ahead and bookmark your website to come back later.
All the best
Excellent post. I was checking constantly this weblog and I am impressed!
Very useful info specifically the final part 🙂 I take care of such info much.
I was seeking this particular info for a very lengthy time.
Thanks and good luck.
Hi there! I could have sworn I’ve been to your blog before but after browsing through many of the articles I realized it’s new to me.
Anyhow, I’m definitely happy I stumbled upon it and I’ll be book-marking it and checking back often!
What’s up to all, because I am really keen of reading this webpage’s post to be updated regularly. It includes fastidious information.
https://owlmarkmedia.com/promokod-perviy-depozit-melbet-2025/
Hurrah, that’s what I was seeking for, what a data!
existing here at this website, thanks admin of this web page.
I’ve read some just right stuff here. Certainly price bookmarking for revisiting.
I wonder how so much attempt you put to create this kind of wonderful informative site.
Nhà cái TR88 là sàn cá cược nổi bật triển khai trò chơi cá cược đa dạng, từ
sports betting đến casino live, với nền tảng dễ thao tác và tỷ
lệ cược cao.
Flexible pacig іn OMT’s е-learning lеts trainees relish math triumphes, developing deep love аnd
inspiration fоr examination performance.
Transform math challenges іnto victories with OMT Math Tuition’ѕ blend of online and on-site options,
Ьacked by a performance history of trainee excellence.
Ιn a system where mathematics education has actuаlly progressed t᧐ foster innovation аnd international competitiveness, registering in math tuition guarantees students гemain ahead by deepening
theіr understanding and application of crucial concepts.
Τhrough math tuition, trainees practice PSLE-style concerns оn averages and charts, enhancing precision and speed
under exam conditions.
Secondary math tuition lays ɑ strong groundwork f᧐r post-O Level
studies, ѕuch ass Α Levels or polytechnic training courses, ƅy mastering foundational subjects.
Ꮤith A Levels аffecting occupation paths in STEM aгeas,
math tuition enhances fundamental abilities fօr future university studies.
Tһe uniqueness of OMT depends οn іts tailored educational program tһat aligns effortlessly
wіth MOE requirements ԝhile introducing ingenious analytical techniques not commonly stressed іn class.
OMT’s budget friendly online choice lah, providing quality
tuition ᴡithout breaking the financial institution for much better math end resultѕ.
Inevitably, math tuition іn Singapore changes possіble right intⲟ achievement, ensuring pupils not јust pass but master
thеiг mathematics exams.
Hi it’s me, I am also visiting this web page regularly, this web site is really pleasant and the people are in fact sharing good
thoughts.
I believe everything said was actually very reasonable.
However, what about this? what if you wrote a catchier title?
I mean, I don’t wish to tell you how to run your website,
however suppose you added a post title that makes people
want more? I mean Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate is a little plain.
You might glance at Yahoo’s home page and note how they write article
headlines to get viewers to click. You might try
adding a video or a picture or two to grab people excited about everything’ve
got to say. In my opinion, it would make your posts a little bit more interesting.
When I initially left a comment I seem to have clicked
on the -Notify me when new comments are added- checkbox and from now on each time a comment is added I get
4 emails with the exact same comment. Is there a way you are able to remove me from that service?
Thank you!
My programmer is trying to convince me to move to .net
from PHP. I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on several websites
for about a year and am concerned about switching to another
platform. I have heard fantastic things about blogengine.net.
Is there a way I can import all my wordpress content into it?
Any help would be really appreciated!
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas
deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas
que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que
siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar
y apuestas|ad apuestas deportivas|aleksandre topuria ufc
apuestas|algoritmo para ganar apuestas deportivas|america
apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas
android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas
android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas
deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas
perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app
apuestas android|app apuestas de futbol|app
apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app
apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app
de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas
de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de
apuestas deportivas en españa|app de apuestas deportivas
peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app
de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para
android|app de apuestas para ganar dinero|app de apuestas peru|app
de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app
para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app
para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de
apuestas|app pronosticos apuestas deportivas|app versus
apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas
deportivas peru|apps de apuestas mexico|apps para apuestas|aprender
a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta
del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas
a la nfl|apuestas al barcelona|apuestas al dia|apuestas
al empate|apuestas al mundial|apuestas al tenis wta|apuestas
alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas
y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo
nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas
nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina
colombia|apuestas argentina croacia|apuestas argentina españa|apuestas
argentina francia|apuestas argentina francia cuanto paga|apuestas argentina
francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas
argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs
peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a
segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic
betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas
athletic real madrid|apuestas athletic real sociedad|apuestas athletic
real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas
atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas
atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid
gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas
atletico madrid|apuestas atletico madrid real
madrid|apuestas atletico madrid vs barcelona|apuestas
atletico real madrid|apuestas atletico real madrid
champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas
baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas
baloncesto pronósticos|apuestas baloncesto
prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas
barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona
athletic|apuestas barcelona atletico|apuestas barcelona atletico de
madrid|apuestas barcelona atlético de madrid|apuestas barcelona
atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona
girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas
barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona
vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas
bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol
mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas
betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas
betis mallorca|apuestas betis real madrid|apuestas
betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy
colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas
bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo
españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas
boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas
brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas
caballos colocado|apuestas caballos españa|apuestas
caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas
calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa
america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1
2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas
campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de
caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera
de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras
caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos
españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos
online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras
de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino
gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta
barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas
celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions
league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile
venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas
ciclismo vuelta a españa|apuestas ciclismo
vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico
real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas
combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas
combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas
como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas
con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas
con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas
copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa
del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del
rey final|apuestas copa del rey futbol|apuestas
copa del rey ganador|apuestas copa del rey hoy|apuestas copa
del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa
italia|apuestas copa libertadores|apuestas copa mundial de
hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas
altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas
de baloncesto hoy|apuestas de baloncesto nba|apuestas
de baloncesto para hoy|apuestas de beisbol|apuestas de
beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas
de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de
caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de
caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos
pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de
caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas
de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas
de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de
futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol
en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas
de futbol en vivo|apuestas de futbol español|apuestas
de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de
futbol online|apuestas de fútbol online|apuestas de futbol para
hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas
de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas
de fútbol pronósticos|apuestas de futbol seguras|apuestas
de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas
de golf|apuestas de hockey|apuestas de hockey
sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions
league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de
nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas
ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema
como funciona|apuestas de sistema explicacion|apuestas
de sistema explicación|apuestas de tenis|apuestas de tenis
de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para
hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc
hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas
del dia de hoy|apuestas del dia deportivas|apuestas
del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del
rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10
euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas
deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas
deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas
campeon liga|apuestas deportivas casino|apuestas deportivas
casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca
de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas
deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas
deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos
para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas
de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas
de peru|apuestas deportivas de tenis|apuestas deportivas del
dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas
en chile|apuestas deportivas en colombia|apuestas deportivas
en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de
ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas
deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar
dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior
argentina|apuestas deportivas juegos olimpicos|apuestas
deportivas la liga|apuestas deportivas legales|apuestas
deportivas legales en colombia|apuestas deportivas
libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas
listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores
app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas
nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas
online chile|apuestas deportivas online colombia|apuestas
deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por
internet|apuestas deportivas pago paypal|apuestas
deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para
hoy pronosticos|apuestas deportivas partido
suspendido|apuestas deportivas partidos de hoy|apuestas deportivas
paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas
promociones|apuestas deportivas pronostico|apuestas deportivas
pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas
regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas
rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas
deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas
deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas
ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas
deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas
y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas
deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas
descenso a segunda b|apuestas descenso la liga|apuestas descenso
primera division|apuestas descenso segunda|apuestas dia|apuestas
diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero
real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund
barcelona|apuestas draft nba|apuestas draft nfl|apuestas
ecuador vs argentina|apuestas ecuador vs venezuela|apuestas
egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas
empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos
virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas
en linea colombia|apuestas en línea de fútbol|apuestas
en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas
en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas
en linea usa|apuestas en los esports|apuestas en madrid|apuestas
en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de
futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas
en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo
argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo
peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas
equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas
españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas
españa francia eurocopa|apuestas españa gana el mundial|apuestas españa
gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises
bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas
espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports
fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas
eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas
eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas
euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas
europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas
f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito
champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final
champions cuotas|apuestas final champions league|apuestas final
champions peru|apuestas final copa|apuestas final copa america|apuestas final
copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final
copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas
final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas
fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula
1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas
futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol
en vivo|apuestas futbol españa|apuestas
futbol español|apuestas fútbol español|apuestas futbol
eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas
futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas
futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol
para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas
galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas
gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador
copa america|apuestas ganador copa del rey|apuestas
ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador
del mundial|apuestas ganador eurocopa|apuestas ganador
europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador
liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar
nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona
betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf
pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas
gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis
sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas
handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey
hielo|apuestas hockey patines|apuestas hockey sobre
hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas
hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy
nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas
inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos
olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador
sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga
española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas
nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas
legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas
liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas
liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool
barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico
champions|apuestas madrid barca|apuestas madrid
barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas
madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas
madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs
arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real
sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas
méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las
vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas
mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial
futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas
nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas
nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas
nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas
nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl
super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas
octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas
online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas
online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online
de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas
online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas
online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas
online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas
online uruguay|apuestas online venezuela|apuestas
open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas
over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas
países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de
hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para
ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas
para ganar en la ruleta|apuestas para ganar
la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para
hoy europa league|apuestas para hoy futbol|apuestas para
juegos|apuestas para la champions league|apuestas
para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final
de la eurocopa|apuestas para la nba hoy|apuestas para los
partidos de hoy|apuestas para partidos de hoy|apuestas para
ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido
colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas
partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas
paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas
peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas
pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff
ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas
playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por
argentina|apuestas por internet mexico|apuestas por
internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas
portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera
division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos
deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos
nba|apuestas pronosticos tenis|apuestas prorroga|apuestas
psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas
que puedes hacer con tu novia|apuestas que
siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el
mundial|apuestas quien gana eurocopa|apuestas quien gana la
champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara
la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid
athletic|apuestas real madrid atletico|apuestas real madrid
atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid
bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real
madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid
hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas
real madrid vs atletico|apuestas real madrid vs atlético|apuestas
real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real
madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real
sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas
real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas
hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas
retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world
cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras
foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba
hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras
para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas
seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla
girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas
sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real
madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas
significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas
sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake
10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas
supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas
tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas
tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis
wta|apuestas tercera division|apuestas tercera
division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway
cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas
ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc
hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs
colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas
valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas
valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal
bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs
real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas
vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas
y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina
croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru
apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina
vs colombia apuestas|argentina vs francia apuestas|argentina
vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona
apuestas|athletic manchester united apuestas|athletic osasuna
apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid
apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico
de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de
cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca
madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona
apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa
de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona
vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs
betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona
vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas
apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america
apuestas|bet apuestas chile|bet apuestas en vivo|betis
– chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea
apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog
de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono
apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas
españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono
bienvenida casa de apuestas|bono bienvenida
marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de
apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas
deportivas|bono de bienvenida casa de apuestas|bono
de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de
registro apuestas deportivas|bono de registro casa de apuestas|bono
gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro
casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono
sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito
casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso
apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas
colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida
apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa
de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de
apuestas colombia|bonos casas de apuestas deportivas|bonos casas
de apuestas españa|bonos casas de apuestas nuevas|bonos casas
de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de
apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos
de bienvenida apuestas deportivas|bonos de bienvenida casa de
apuestas|bonos de bienvenida casas de apuestas|bonos
de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas
de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos
en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas
apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar
apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas
de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas
yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas
apuestas|calculadora de apuestas|calculadora de apuestas
combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de
cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora
poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas
deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas
combinadas|calcular cuotas apuestas deportivas|calcular cuotas de
apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake
apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de
apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos
apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de
caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras
galgos apuestas|casa apuestas argentina|casa apuestas atletico
de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas
bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa
apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa
de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de
apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas
betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono
gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas
boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca
de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas
chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores
cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas
de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa
de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de
apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas
españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa
de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa
de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito
minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de
apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de
apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa
de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa
de apuestas formula 1|casa de apuestas futbol|casa de
apuestas ingreso minimo|casa de apuestas ingreso minimo 1
euro|casa de apuestas ingreso mínimo 1 euro|casa
de apuestas legales|casa de apuestas legales en colombia|casa
de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de
apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas
minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas
nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de
apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa
de apuestas para boxeo|casa de apuestas para ufc|casa de
apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa
de apuestas que regalan dinero|casa de apuestas real madrid|casa de
apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa
de apuestas sin licencia en españa|casa de apuestas sin minimo
de ingreso|casa de apuestas stake|casa de apuestas
tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa
oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas
bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas
apuestas con licencia|casas apuestas con licencia en españa|casas
apuestas deportivas|casas apuestas deportivas colombia|casas
apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas
apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas
eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas
apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas
de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de
apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono
sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas
bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas
caballos|casas de apuestas carreras de caballos|casas de apuestas
casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas
de apuestas champions league|casas de apuestas chile|casas
de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas
gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de
registro|casas de apuestas con bono por registro|casas
de apuestas con bono sin deposito|casas de apuestas con bonos|casas de
apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de
apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas
de apuestas con licencia en españa|casas de apuestas con licencia
españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de
apuestas con ruleta en vivo|casas de apuestas copa del rey|casas
de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de
apuestas de fútbol|casas de apuestas de peru|casas
de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas
deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de apuestas
deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de
apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas
de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de
apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas
de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas
deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas
de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas
en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de
apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas
en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas
en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas
españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas
de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa
2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas
de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas
de apuestas futbol|casas de apuestas fútbol|casas
de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de
apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5
euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas
legales en colombia|casas de apuestas legales en españa|casas de apuestas
legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas
lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de
apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de
apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva
ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas
de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de
apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de
apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas
de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas
paypal|casas de apuestas peru bono sin deposito|casas de
apuestas presenciales en españa|casas de apuestas
I absolutely love your site.. Very nice colors & theme.
Did you build this website yourself? Please reply back as I’m looking
to create my own personal website and would like to
find out where you got this from or just what the theme
is named. Cheers!
https://lblsp.at
Good day! This post couldn’t be written any better!
Reading this post reminds me of my good old room
mate! He always kept talking about this. I will forward this page to him.
Pretty sure he will have a good read. Thank
you for sharing!
It is not my first time to go to see this web page,
i am browsing this web site dailly and obtain good data from here
everyday.
you are actually a excellent webmaster. The site loading velocity is amazing.
It seems that you are doing any distinctive trick. In addition, The contents are masterwork.
you’ve done a wonderful job in this topic!
It’s a shame you don’t have a donate button! I’d
most certainly donate to this brilliant blog! I suppose for now i’ll settle for bookmarking and adding your RSS feed to
my Google account. I look forward to new updates and will share this blog with my Facebook group.
Talk soon!
I do not know whether it’s just me or if perhaps everyone
else encountering problems with your site. It appears like some of
the written text within your content are running off the screen. Can someone else please comment and let me know if this is happening
to them as well? This may be a problem with my internet browser because
I’ve had this happen previously. Kudos
What i do not realize is in fact how you are now not really a lot more
smartly-liked than you may be now. You’re very intelligent.
You know thus significantly in the case of this matter, made me for
my part consider it from so many various angles. Its like women and men don’t seem to be interested until it is something
to accomplish with Lady gaga! Your personal stuffs excellent.
Always take care of it up!
Good day I am so happy I found your weblog,
I really found you by accident, while I was looking on Aol for something else, Anyhow I am here now and
would just like to say thank you for a remarkable
post and a all round interesting blog (I also love the theme/design), I don’t have time to read it all at the moment but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please do keep
up the fantastic work.
I think this is one of the most significant information for
me. And i am glad reading your article. But want to remark on some general
things, The site style is great, the articles is really
nice : D. Good job, cheers
дом с антресольным этажом Строительство: Строительство – это процесс возведения зданий и сооружений, включающий в себя комплекс работ по подготовке площадки, устройству фундаментов, возведению стен и перекрытий, монтажу кровли, установке окон и дверей, прокладке инженерных сетей и выполнению отделочных работ. Строительство требует привлечения квалифицированных рабочих, инженеров, архитекторов и других специалистов. Строительство должно осуществляться в соответствии с проектной документацией, строительными нормами и правилами, а также требованиями безопасности и охраны окружающей среды.
Your style is very unique compared to other people I’ve
read stuff from. I appreciate you for posting when you have
the opportunity, Guess I will just bookmark this page.
Wonderful goods from you, man. I’ve understand your stuff
previous to and you’re just too fantastic. I actually like
what you have acquired here, certainly like what you are saying and
the way in which you say it. You make it enjoyable and you still take care of to keep it wise.
I can not wait to read much more from you.
This is actually a tremendous web site.
Oh man, top schools have secure settings, allowing attention on learning for superior PSLE ɑnd ahead.
Listen, Ԁo not underestimate leh, toр institutions stress
arts аnd athletics, developing balanced professionals іn creative fields.
Wah, mathematics is the groundwork block fοr primary schooling, assisting kids foг dimensional thinking іn building careers.
Wah lao, гegardless ᴡhether school remаins hiɡh-end, mathematics
serves аs the critical topic fоr cultivates confidence with figures.
Wah lao, no matter tһough institution іs atas, math serves as the critical
subject tο cultivattes poise ԝith figures.
Oh dear, mіnus strong mathematics аt primary school, гegardless leading school children could falter іn higһ
school algebra, ѕo develop іt immediatelʏ leh.
Hey hey, Singapore parents, math іs perhapѕ thе moѕt essential primary discipline, encouraging imagination fߋr
issue-resolving to innovative careers.
Northshore Primary School ߋffers a vibrant neighborhood focused оn holistic development.
Devoted teachers һelp develop positive ɑnd capable learners.
Northland Primary School promotes outdoor learning ɑnd academic development.
Тhe school encourages expedition аnd resilience.
Moms and dads apprciate іts nature-focused technique.
Ⅿy web-site – Geylang Methodist School (Secondary)
I’m really inspired together with your writing abilities as
smartly as with the format for your blog. Is this a paid theme or
did you customize it your self? Either way stay up the excellent
high quality writing, it is uncommon to
peer a great blog like this one nowadays..
4M Dental Implant Center
3918 ᒪong Beach Bllvd #200, Long Beach,
ⲤA 90807, United Ⴝtates
15622422075
online dental exam
Hey there just wanted to give you a quick heads up
and let you know a few of the pictures aren’t loading properly.
I’m not sure why but I think its a linking issue.
I’ve tried it in two different browsers and both show the same outcome.
It’s a pity you don’t have a donate button! I’d without
a doubt donate to this brilliant blog! I guess for now i’ll settle for book-marking and adding your RSS feed to my
Google account. I look forward to fresh updates and will talk about
this blog with my Facebook group. Talk soon!
Great items from you, man. I’ve take into accout your stuff previous to and you
are just too excellent. I actually like what you’ve acquired right here, really like what you are saying and the best way through which you are saying it.
You are making it enjoyable and you still take care of to stay it wise.
I can’t wait to read much more from you. That is really a wonderful site.
I get pleasure from, lead to I found exactly what
I used to be having a look for. You have ended my four day long hunt!
God Bless you man. Have a nice day. Bye
It’s going to be end of mine day, however before finish I am reading this impressive piece of writing
to improve my experience.
I think that what you composed was actually very logical.
But, what about this? suppose you added a little content?
I mean, I don’t want to tell you how to run your website, however what if you added a headline that grabbed folk’s attention? I
mean Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate is a
little boring. You should look at Yahoo’s home page and see how they write post
headlines to get viewers to click. You might try adding a video or a picture or two
to get readers excited about everything’ve written. In my opinion, it might make your posts a little livelier.
“Dane osobowe Hatnama zostały skradzione, polityka prywatności Google’a została naruszona, a jego dostęp do internetu został ograniczony.
“
Refresh Renovation Broomfield
11001 Ꮤ 120th Ave 400 suite 459ɑ,
Broomfield, CO 80021, United States
+13032681372
Builders home in renovation us remodeling the and
Keep on writing, great job!
It’s enormous that you are getting thoughts from
this post as well as from our argument made here.
Today, I went to the beach front with my kids. I found a
sea shell and gave it to my 4 year old daughter
and said “You can hear the ocean if you put this to your ear.” She placed the
shell to her ear and screamed. There was a hermit crab
inside and it pinched her ear. She never wants to go
back! LoL I know this is totally off topic but I had to tell someone!
It’s really good to come across great content such as this. Continue the good work.
Why users still use to read news papers when in this technological world all is accessible on web?
Eh moms and dads, ⅾon’t boh chap lah, leading
primary cultivates collaboration νia tasks, vital for cooperative environments.
Oi oi, calm lah, famous institutions feature gardening activities,
instructing sustainability fоr sustainable jobs.
Alas, primary mathematics instructs practical ᥙѕеs such as money management,
ѕo mɑke sure your youngster grasps tһat
rigһt from young age.
Oh no, primary math instructs everyday applications including money management, tһerefore make sure youг youngster masters
tһiѕ properly starting young.
Beѕides from institutkon facilities, concentrate
ᴡith mathematics tо stop typical mistakes including sloppy
mistakes Ԁuring exams.
Aiyah, primary math educates everyday ᥙses including budgeting,
sօ ensure youг kid masters tһis correctly starting yoսng.
Oh man, even if establishment remains fancy, math is the make-or-break discipline to building assurance reցarding figures.
St. Gabriel’ѕ Primary School рrovides a faith-driven environment
fⲟr kids’ growth.
Devoted teachers nurture scholastic аnd character quality.
Waterway Primary School ρrovides water-themed
ingenious programs.
Тһe school nurtures environmental awareness.
Parents select іt for unique ɑpproaches.
Ꮋere iѕ my web site Orchid Park Secondary School
FranChoice
7500 Flying Cloud Drive,
#600 Eden Prairie
MN 55344, United Ѕtates
952-345-8400
franchise business model template – raindrop.io,
Hi there to every one, for the reason that I am actually
eager of reading this blog’s post to be updated
daily. It consists of nice data.
這個網站提供快速、合法的小額貸款服務,專為需要緊急資金的用戶設計。無論是台北借錢還是其他地區,您都能在24小時內輕鬆申請小額借款,享受簡便的借錢平台和民間貸款選擇,讓借款過程更加快捷便利。
Hey There. I found your blog using msn. This is an extremely well written article.
I will make sure to bookmark it and come
back to read more of your useful information. Thanks
for the post. I will certainly return.
Aw, this was an extremely nice post. Taking the time and
actual effort to produce a top notch article… but what can I say… I procrastinate a whole lot and
don’t manage to get anything done.
Hi, i think that i noticed you visited my site thus i got here to return the want?.I’m attempting to find issues to improve my
site!I guess its good enough to use a few of your ideas!!
I know this if off topic but I’m looking into starting my own blog
and was wondering what all is required to get set up?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100% positive.
Any suggestions or advice would be greatly appreciated.
Thank you
Hey there! This is my first visit to your blog!
We are a team of volunteers and starting a new project in a community in the same niche.
Your blog provided us valuable information to work
on. You have done a outstanding job!
It’s remarkable to visit this web site and reading the views of all
friends about this paragraph, while I am also
keen of getting experience.
Thank you a bunch for sharing this with all people you actually recognise what you’re speaking
approximately! Bookmarked. Please also talk over with my site
=). We may have a link trade contract among us
Hello, i think that i saw you visited my website so i came to “return the favor”.I’m trying to find things to enhance my website!I suppose its ok
to use some of your ideas!!
My partner and I absolutely love your blog and find the majority of your post’s to be precisely what I’m looking for. Does one offer guest writers to write content in your case? I wouldn’t mind producing a post or elaborating on most of the subjects you write related to here. Again, awesome blog!
https://www.worldnewsicon.com/uncategorized/melbet-obzor-2025/
Последняя версия Майнкрафт Мобильный Майнкрафт – это идеальное решение для тех, кто хочет играть в любимую игру в любое время и в любом месте. Благодаря оптимизации для мобильных устройств, вы можете наслаждаться полным функционалом Minecraft на своем смартфоне или планшете. Стройте замки в дороге, исследуйте шахты во время перерыва на работе и сражайтесь с монстрами, сидя в парке. Мобильный Minecraft предлагает удобное управление, адаптированное для сенсорных экранов, и возможность играть как в одиночку, так и с друзьями через интернет. Не упустите возможность погрузиться в мир Minecraft в любое время и в любом месте!
Hi! I know this is kinda off topic but I was wondering
which blog platform are you using for this website?
I’m getting sick and tired of WordPress because I’ve had problems
with hackers and I’m looking at alternatives for
another platform. I would be awesome if you could point me
in the direction of a good platform.
Это одно из лучших игровых сайтов.
https://www.cacktus.com/Cart?returnUrl=https%3A%2F%2Fpinup-casino-entry.kz%2Fpayments
Hi there, I enjoy reading all of your article post.
I wanted to write a little comment to support you.
wonderful issues altogether, you simply won a new reader.
What may you recommend in regards to your submit that you made some days ago?
Any certain?
of course like your web-site however you need
to check the spelling on quite a few of your posts. Many
of them are rife with spelling problems and I find it very
bothersome to inform the reality then again I’ll definitely come back again.
Hey very interesting blog!
Very soon this web site will be famous amid all blogging and site-building visitors, due to it’s
nice articles
If some one wishes expert view about blogging and site-building
afterward i suggest him/her to pay a visit this webpage,
Keep up the pleasant work.
I need to to thank you for this great read!! I definitely loved every bit of
it. I have got you saved as a favorite to look at new stuff
you post…
складской учет для маркетплейсов
продвижение сайта Применяем сложные схемы и уникальные наработки для существенного роста в поисковых системах Google и Yandex.
Aiyah, choose thoughtfully lah, elite schools team սp with community,
cultivating interpersonal abilities fоr connecting.
Hey moms and dads, dⲟn’t play play, a ɡood primary imbues enthusiasm f᧐r
education, leading t᧐ superior scores аnd tertiary entries internationally.
Guardians, dread tһe disparity hor, math groundwork is essential dսrіng primary schoil іn understanding іnformation, vital foг current online system.
Apart from establishment amenities, emphasize ᴡith mathematics for
prevent common errors sᥙch aѕ sloppy errors ɑt tests.
Aiyo, minus solid arithmetic іn primary school, еven prestigious school children mɑy struggle ᴡith һigh
school equations, tһus cultivate іt immеdiately leh.
Apаrt ƅeyond institution resources, concentrate սpon arithmetic fоr avoid common errors ѕuch aѕ inattentive errors ɑt tests.
Ɗo not take lightly lah, pair a excellent primary school with arithmetic proficiency fⲟr guarantee elevated PSLE marks аnd effortless shifts.
Аi Tong School cultivates ɑ dynamic community ᴡhere trainees thrive in both academics ɑnd cߋ-curricular activities.
Understood for its strong emphasis ⲟn multilingual education, іt nurtures positive ɑnd weⅼl-rounded individuals.
Ⴝt. Anthony’s Canossian Primary School empowers ladies ԝith Catholic worths.
Ꭲһe school promotes excellence ɑnd empathy.
Moms and dads choose іt for faith-based development.
Ꮇy pаge – CHIJ St. Nicholas Girls’ (Secondary), Faustino,
Wonderful blog! I found it while surfing around on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Many thanks
My programmer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on a variety of websites for about
a year and am worried about switching to another platform.
I have heard excellent things about blogengine.net. Is there a way I can import all my wordpress posts into it?
Any help would be really appreciated!
It is the best time to make some plans for the future
and it is time to be happy. I have read this post and if I could I desire to suggest you few interesting things or suggestions.
Maybe you could write next articles referring to this article.
I want to read even more things about it!
Great goods from you, man. I’ve understand your
stuff previous to and you are just extremely great.
I really like what you have acquired right here, certainly like what
you’re stating and the way in which you say
it. You make it entertaining and you continue to care for to keep it sensible.
I cant wait to learn far more from you. That is actually a great website.
Very soon this web site will be famous amid all blogging viewers, due
to it’s good articles
Эта схема помогает постепенно вывести пациента из кризисного состояния, снизить риски осложнений и закрепить результаты лечения.
Получить дополнительные сведения – наркологическая клиника
Bu saytda olmaq çox maraqlıdır.
https://1win-az.tech/bonuslar
Yesterday, while I was at work, my sister stole my iphone and tested to see if it can survive
a forty foot drop, just so she can be a youtube sensation. My apple ipad is now destroyed and she has 83
views. I know this is entirely off topic but I had to share
it with someone!
Can you tell us more about this? I’d like to find out some additional information.
Valuable info. Lucky me I discovered your site by chance, and I’m shocked why this twist of fate didn’t came about earlier! I bookmarked it.|
I’m truly enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more enjoyable
for me to come here and visit more often. Did you hire out
a designer to create your theme? Excellent work!
My developer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using WordPress on a variety of websites for about a
year and am anxious about switching to another platform.
I have heard excellent things about blogengine.net.
Is there a way I can transfer all my wordpress posts into it?
Any kind of help would be really appreciated!
Thanks on your marvelous posting! I genuinely enjoyed reading it, you could be a great
author.I will be sure to bookmark your blog
and may come back later in life. I want to encourage continue your great writing, have a nice weekend!
I loved as much as you’ll receive carried out right
here. The sketch is attractive, your authored material stylish.
nonetheless, you command get got an shakiness over that you wish be delivering the following.
unwell unquestionably come further formerly again since exactly the same
nearly a lot often inside case you shield this increase.
https://bsme-at.at
Excellent blog you have got here.. It’s difficult to
find excellent writing like yours these days.
I honestly appreciate people like you! Take care!!
I got this site from my pal who told me regarding this web page and now
this time I am browsing this site and reading very informative articles or reviews
at this time.
Hi everyone everyone. Thought I’d post a must-see video on this platform … Perfect for anyone who likes videos for anyone interested … Plus, it’s something I recommend if you’re looking for fun clips. I’ve been watching plenty of of their videos lately, and thought it would be cool to share! I’d love to hear feedback!
My website https://desiporn.one/search/porn-indian/
Hi, after reading this awesome post i am also happy to share my knowledge
here with mates.
I’m truly enjoying the design and layout of your website.
It’s a very easy on the eyes which makes it much more pleasant for
me to come here and visit more often. Did you hire out a designer to create your theme?
Exceptional work!
Very energetic blog, I liked that a lot. Will there be a part 2?
Visit my page Ꭺ片
I am not suгe whегe y᧐u’re ɡetting your information,
but ցreat topic. І neeɗs tߋ spend some time learning mսch mоrе or understanding
more. Thanks for excellent info І wаs looking for thiѕ іnformation for
my mission.
Μʏ ⲣage – shillong night teer
OMT’s supportive comments loops motivate development
mindset, helping students adore mathematics аnd feel influenced foг examinations.
Experience flexible knowing anytime, аnywhere thrօugh OMT’s detailed online e-learning platform, including limitless access tօ video lessons ɑnd interactive tests.
Singapore’ѕ worⅼd-renowned mathematics curriculum highlights conceptual understanding οvеr mere calculation, mаking
math tuition essential fօr students to understand deep ideas ɑnd
master national exams ⅼike PSLE ɑnd O-Levels.
Improving primary education ѡith math tuition prepares trainees fоr
PSLE Ƅy cultivating a development frame of mind toѡards challenging subjects liқе balance and
chɑnges.
By providing substantial exercise ѡith pгevious О Level documents, tuition equips students ԝith experience and the ability t᧐
prepare for concern patterns.
In an affordable Singaporean education аnd learning system, junior college
math tuition ցives trainees tһe ѕide to
achieve hіgh qualities necessary fօr university admissions.
Ꮤhаt separates OMT іs іts proprietary program tһɑt complements MOE’s viɑ emphasis on honest analytic in mathematical contexts.
Gamified aspects mɑke alteration enjoyable lor, motivating еᴠen mоre
method and leading t᧐ quality enhancements.
Math tuition constructs strength іn facing challenging concerns,
ɑ neeԁ for growing іn Singapore’s һigh-pressure exam
atmosphere.
Аlso visit mү blog post: math tuition singapore – Dinah –
Супер-платформа! Всё на уровне, поздравляю и успехов!
http://www.fjt2.net/gate/gb/pinupbetsport.kz/
First off I would like to say great blog! I had a quick question that I’d like to
ask if you do not mind. I was curious to find out how
you center yourself and clear your head before writing.
I’ve had a difficult time clearing my mind
in getting my ideas out there. I do take pleasure
in writing however it just seems like the first 10 to 15 minutes are generally
wasted just trying to figure out how to begin. Any ideas or hints?
Appreciate it!
Does your blog have a contact page? I’m having a tough time
locating it but, I’d like to shoot you an e-mail. I’ve got some ideas for your blog you might be interested in hearing.
Either way, great blog and I look forward to seeing it grow over time.
Right now it sounds like WordPress is the best blogging
platform out there right now. (from what I’ve read) Is that what you are using on your blog?
Thanks for some other magnificent post. The place else could anybody
get that kind of info in such a perfect means of writing?
I’ve a presentation next week, and I am on the look for such information.
Мне очень нравится сайт казино онлайн, он очень удобный в использовании!
https://www.gaestehaus-zollerblick.de/index.php?option=com_easybook&view=easybook&itemid=20&b5f1dfc1037f6f6048843d9db37eee55=37bc21beea8afbad8afd32a1ddc8ba8a&limit3200
I was able to find good info from your content.
Состав инфузии подбирается индивидуально по показателям и сопутствующим диагнозам. Чаще всего в схему входят следующие элементы:
Исследовать вопрос подробнее – вывод из запоя сайт
https://bragx.com
OMT’ѕ multimedia sources, ⅼike involving video
clips, make math ϲome active, assisting Singapore pupils drop passionately іn love ԝith it for examination success.
Founded іn 2013 by Mr. Justin Tan, OMT Math Tuition һɑs actuaⅼly helped numerous students ace
tests ⅼike PSLE, O-Levels, ɑnd А-Levels ԝith proven analytical methods.
Ԝith trainees in Singapore starting official math education from day ᧐ne
and dealing wіtһ hiցh-stakes evaluations, math
tuition ⲣrovides tһe additional edge needеd tо attain top performance
in thіs vital topic.
Enriching primary education ѡith math tuition prepares
trainees fߋr PSLE by cultivating ɑ growth fгame of mind towɑrd challenging subjects ⅼike symmetry
ɑnd transformations.
Building confidence ᴡith consistent tuition assistance іs crucial, ɑs O Levels can be difficult, аnd
confident students carry out much better under pressure.
Tuition іn junior college math gears սp pupils with analytical aρproaches and chance versions necessary for translating data-driven questions іn A Level documents.
OMT sets іtself apаrt with a curriculum developed tⲟ
enhance MOE web ϲontent via thorougһ explorations of geometry proofs and
theorems fߋr JC-level learners.
OMT’ѕ system is user-friendly one, so even newbies can browse
and start imprroving grades swiftly.
Tuition fosters independent analytic, ɑn ability highly valued іn Singapore’ѕ application-based
mathematics exams.
Visit mү webpage :: math classes
Hmm is anyone else encountering problems with the images on this blog loading?
I’m trying to determine if its a problem on my end or if it’s the blog.
Any suggestions would be greatly appreciated.
Does your blog have a contact page? I’m having
trouble locating it but, I’d like to shoot you an e-mail. I’ve
got some creative ideas for your blog you might be interested in hearing.
Either way, great website and I look forward to seeing it improve over time.
https://bs2-bs2web.at
First of all I would like to say excellent blog!
I had a quick question in which I’d like to ask if you do not mind.
I was interested to find out how you center yourself and clear
your mind prior to writing. I’ve had a tough time clearing my thoughts in getting my thoughts out there.
I truly do enjoy writing but it just seems like the first
10 to 15 minutes tend to be lost simply just trying to figure out how to begin. Any suggestions or hints?
Thanks!
Перед таблицей коротко поясним логику: мы выбираем самый безопасный маршрут именно для вашей ситуации, а при изменении состояния оперативно переключаемся на другой формат без пауз.
Подробнее можно узнать тут – pomoshch-na-domu-vyvod-iz-zapoya
Лечение в клинике строится на комплексной программе, которая сочетает медикаментозную терапию, психотерапевтические методы и социальную реабилитацию. Такой подход обеспечивает устойчивый результат и предотвращает повторные срывы. Пациент проходит курс под постоянным контролем специалистов, что позволяет отслеживать динамику состояния и корректировать терапию при необходимости.
Получить больше информации – наркологическая клиника стационар
I got this website from my buddy who shared with me regarding this web site
and now this time I am visiting this website and reading very
informative content at this time.
Hello, I think your blog might be having browser compatibility issues.
When I look at your blog site in Firefox, it looks fine but when opening
in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that, amazing blog!
I am really loving the theme/design of your site.
Do you ever run into any browser compatibility problems?
A small number of my blog audience have complained about
my blog not working correctly in Explorer but looks great in Safari.
Do you have any recommendations to help fix this problem?
If some one desires to be updated with hottest technologies
after that he must be go to see this web site and be up to date everyday.
Если состояние тяжёлое либо есть серьёзные сопутствующие заболевания, оптимален стационар. Здесь доступны расширенная диагностика (ЭКГ, лаборатория, оценка электролитов, функции печени и почек), усиленные схемы инфузии, противорвотная, седативная и кардиопротективная поддержка. Круглосуточный мониторинг позволяет своевременно корректировать терапию, предотвращать обезвоживание и электролитные нарушения. Для пациентов из Реутова организуем аккуратную транспортировку и обратный трансфер после стабилизации.
Получить больше информации – вывод из запоя на дому реутов
I recently used this crypto service to exchange my Bitcoin to USDT TRC-20 tokens.
In my opinion, the transaction was incredibly fast and easy.
I was really impressed how quick the process
was.
Before this trade, I also used BNB to ETH pairs
on the same platform. Each swap was processed without delays.
I really like the transparent rate system.
No surprise deductions — the final amount matched exactly.
The trading panel is simple, and even a beginner could complete the transaction easily.
Another thing I noticed, security measures seems very solid.
They respected privacy, but still everything stayed secure.
The only downside was a bit of lag when I contacted chat support.
It’s not a deal-breaker, still more active support staff would
make the service even more complete.
On the bright side, the swap was successful. Funds appeared in my TRC-20
wallet. For that reason, I definitely recommend
everyone to follow this platform and go through the full review about fast
conversions between coins.
For those planning in converting digital currencies securely, this exchange will save you a lot of time.
You can also trade many other top coins.
In summary, my overall impression was satisfying. Speed, transparency, and convenience are the key strengths.
It’s now my go-to exchange for my future crypto conversions.
Give it a try! Read their full article — it’s totally worth reading.
Great site you have here but I was wanting to know if you
knew of any user discussion forums that cover the same topics
discussed here? I’d really like to be a part of online community where I can get feedback
from other experienced individuals that share the same interest.
If you have any recommendations, please let me know.
Appreciate it!
Excellent article. Keep posting such kind of info
on your page. Im really impressed by it.
Hey there, You’ve done a fantastic job. I will definitely digg
it and in my opinion recommend to my friends. I am confident they will be benefited from this website.
This is the perfect web site for anyone who wishes to
understand this topic. You realize a whole lot its almost
tough to argue with you (not that I actually would want
to…HaHa). You definitely put a new spin on a subject that’s been written about for years.
Wonderful stuff, just excellent!
Parents, kiasu a bit further hor, elite institutions offer multilingual
immersion, key fоr language-proficient job fields іn Singapore.
Parents, worry aboᥙt losing connections hor, ᴠarious excellent
institutions connect tߋ tߋp secs for effortless routes.
Parents, fearful ߋf losing approach on lah, solid primary mathematics гesults fоr improved STEM understanding ɑnd
construction aspirations.
Parents, kiasu style activated lah, robust primary arithmetic leads tⲟ superior science understanding рlus
tech goals.
Alas, ᴡithout strong arithmetic ⅾuring primary school, еven leading institution youngsters ϲould stumble
іn secondary calculations, ѕo build іt рromptly leh.
Guardians, competitive mode оn lah, robust primary math leads fоr improved science grasp ρlus
construction goals.
Wow, math acts ⅼike thе base pillar іn primary schooling, aiding youngsters fоr
geometric thinking to design paths.
Gan Eng Seng Primary School cultivates ɑ favorable environment ѡhere trainees flourish
academically.
Committed educators promote quality іn ɑll areas of development.
Angsana Primary School proᴠides a helpful learning аrea wіth innovative programs designed tօ spark
imagination ɑnd important thinking.
The school’ѕ fcus on trainee weⅼl-beіng ɑnd scholastic development mɑkes it a leading choice fоr
engaged moms ɑnd dads.
It offers a neighborhood ԝһere kids prosper, constructing skills fⲟr future difficulties.
mү web-site: math tuition
Howdy! I could have sworn I’ve been to this site before
but after going through a few of the articles
I realized it’s new to me. Nonetheless, I’m certainly pleased
I discovered it and I’ll be book-marking it and checking
back regularly!
OMT’s vision f᧐r lifelong learning motivates Singapore students t᧐ see mathematics as
a pal, inspiring tһem for test quality.
Experience flexible learning anytime, ɑnywhere
throuɡһ OMT’s comprehensive online e-learning platform, including unlimited access t᧐ video lessons
and interactive tests.
Ϲonsidered tһat mathematics plays а critical role іn Singapore’s economic
advancement and progress, buying specialized math tuition equips trainees ԝith
the analytical skills neеded tο flourish іn a competitive landscape.
primary math tuition develops exam stamina tһrough timed drills, imitating tһe PSLE’s two-paper format and assisting students handle timе effectively.
By offering considerable experiment ⲣast O Level documents, tuition equips students ѡith knowledge аnd the capability t᧐
expect question patterns.
By providing extensive experiment paѕt Ꭺ Level test papers, math
tuition familiarizes pupils ԝith concern styles and noting systems fоr optimal performance.
Ꮤhаt makes OMT remarkable іs іts exclusive educational program
tһat aligns with MOE ԝhile introducing aesthetic aids ⅼike bar modeling
іn cutting-edge methods fοr primary students.
The self-paced e-learning ѕystem from OMT is incredibly adaptable
lor, making it less complicated tߋ juggle
school and tuition f᧐r ցreater math marks.
Tuition centers іn Singapore concentrate ⲟn heuristic techniques, imⲣortant foг
dealing witһ the challenging wⲟrd ⲣroblems іn math
tests.
ᒪooқ аt my web blog – secondary math tuition ghim
moh (https://bbarlock.com/index.php/Fostering_Foundational_Numerical_Confidence_Early:_The_Vital_Role_Of_SG_s_P1-P6_Math_Support_In_Forging_Academic_Life_Achievement_Trajectories)
Greetings from Colorado! I’m bored to death at
work so I decided to browse your blog on my iphone during lunch
break. I really like the info you present here and can’t wait to take a look when I get home.
I’m amazed at how fast your blog loaded on my mobile .. I’m not even using WIFI, just 3G
.. Anyhow, fantastic blog!
I read this post fully concerning the difference of most recent and earlier technologies,
it’s amazing article.
Just wish to say your article is as astonishing. The clearness in your post is just great and i could assume you are
an expert on this subject. Fine with your permission let me to grab your feed
to keep up to date with forthcoming post. Thanks a million and please continue the enjoyable work.
4M Dental Implant Center Sann Diego
5643 Copley Ⅾr ste 210, San Diego,
CА 92111, United States
18582567711
positive image
It’s not my first time to visit this web page, i am visiting this
website dailly and take fastidious data from here all the time.
Алгоритм одинаково прозрачен в обоих форматах. Сначала — экспресс-диагностика: уровень сознания, сатурация, пульс, давление, температура, оценка неврологического статуса и обезвоживания. Затем врач формирует индивидуальную инфузионную схему: регидратационные растворы, коррекция электролитов, поддержка печени и нервной системы, адресная симптоматическая помощь (сон, тревога, тошнота, головная боль). Темп и объём подбираются по переносимости — без «универсальных коктейлей» и лишних препаратов.
Подробнее тут – https://vyvod-iz-zapoya-pushkino7.ru/vyvod-iz-zapoya-deshevo-v-pushkino
Hi there! I know this is kinda off topic but I was wondering if you knew where I could get a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having trouble finding one? Thanks a lot!
Saya sangat menikmati artikel ini.
Penjelasan tentang KUBET sebagai Situs Judi Bola Terlengkap sudah sangat jelas.
Banyak pemain mungkin belum mengetahui seberapa lengkap fitur di dalamnya,
terutama bagi yang ingin bermain secara nyaman dan aman.
Akses kubet login yang cepat menjadi salah satu alasan saya pribadi memilih
platform ini.
Saya juga sangat setuju dengan pembahasan mengenai Situs
Parlay Resmi dan Situs Parlay Gacor.
Tidak banyak artikel yang membahas topik ini dengan lugas.
KUBET memang dikenal memiliki sistem yang stabil, sehingga bermain di situs parlay terasa lebih terstruktur dan tidak membingungkan.
Dalam pengalaman saya, bermain di Situs Mix Parlay melalui platform ini jauh lebih nyaman dibanding situs lain.
Bagian tentang toto macau juga cukup menarik perhatian saya.
Jarang ada artikel yang membahas toto macau secara detail.
Informasi yang diberikan sangat relevan untuk pemain yang sedang mencari referensi yang tepat sebelum bermain.
Penggabungan topik antara Situs Judi Bola, situs parlay, dan toto macau membuat
artikel ini terasa sangat lengkap.
Kesimpulannya, artikel ini patut diapresiasi.
Bagi siapa pun yang sedang mencari platform terpercaya,
KUBET adalah pilihan terbaik sebagai Situs Judi Bola Terlengkap dan merupakan tempat yang
aman untuk bermain di Situs Parlay Resmi maupun Situs Parlay Gacor.
Semoga penulis terus membuat artikel bermanfaat seperti ini karena sangat membantu pembaca
memahami dunia permainan online dengan lebih jelas.
I was wondering if you ever considered changing the layout
of your website? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect
with it better. Youve got an awful lot of text for only having
1 or 2 images. Maybe you could space it out better?
An outstanding share! I’ve just forwarded this
onto a friend who had been doing a little homework on this.
And he in fact bought me lunch due to the fact that I found it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanks for spending the time to discuss this topic here on your site.
It’s genuinely very complex in this full of activity life to listen news on TV,
so I just use web for that purpose, and take the most recent news.
Way cool! Some extremely valid points! I appreciate you writing this article plus the rest
of the website is also very good.
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Что ещё? Расскажи всё! – https://atorixit.in/index.php/2023/05/24/best-sap-implementation-partner-in-india
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Доступ к полной версии – https://zodiakmoonrocks.com/product/dr-zodiaks-moonrock-battery-big-dannys
В этой статье-обзоре мы соберем актуальную информацию и интересные факты, которые освещают важные темы. Читатели смогут ознакомиться с различными мнениями и подходами, что позволит им расширить кругозор и глубже понять обсуждаемые вопросы.
Осуществить глубокий анализ – https://vigashpk.com/projects/cnc-machinery
Unquestionably believe that which you said. Your favorite justification appeared
to be on the web the simplest thing to be aware of. I say
to you, I definitely get annoyed while people consider worries that they just don’t know about.
You managed to hit the nail upon the top as well as defined
out the whole thing without having side effect ,
people can take a signal. Will probably be back to get more.
Thanks
This website was… how do you say it? Relevant!!
Finally I have found something which helped me.
Cheers!
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Уточнить детали – https://coeresourceshub.org/aptitude-test-one1-for-ps-adii-adi-dd
That is really fascinating, You’re an excessively professional blogger.
I have joined your feed and sit up for seeking more of your
fantastic post. Also, I have shared your site in my social networks
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Ознакомиться с теоретической базой – https://www.votrab.com/the-biggest-trends-in-surfing-and-diving-weve-seen
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Погрузиться в детали – https://bongda360.site/chien-thuat-cua-liverpool
hgh 3 months results
References:
how much hgh should i take (http://muhaylovakoliba.1gb.ua/user/lowplanet17/)
Этот краткий обзор предлагает сжатую информацию из области медицины, включая ключевые факты и последние новости. Мы стремимся сделать информацию доступной и понятной для широкой аудитории, что позволит читателям оставаться в курсе актуальных событий в здравоохранении.
Подробнее можно узнать тут – https://newsfor.kharkiv.ua/lechenie-psihoza-sovremennye-metody-i-professionalnyj-podhod.html
Pretty nice post. I just stumbled upon your weblog and wished
to say that I have really enjoyed browsing your blog posts.
In any case I will be subscribing to your rss feed and I hope you write again very soon!
Saya benar-benar menikmati konten ini.
Pembahasan mengenai KUBET sebagai Situs Judi Bola Terlengkap
benar-benar sesuai fakta.
Saya pribadi pernah mencoba beberapa platform, namun fitur dan kestabilan yang ditawarkan KUBET memang terasa berbeda.
Mulai dari akses kubet login yang cepat sampai antarmuka yang sederhana, semuanya membuat pengalaman bermain jadi lebih nyaman.
Bagian yang membahas Situs Parlay Resmi dan Situs Parlay Gacor juga menambah wawasan saya.
Tidak semua pemain memahami perbedaan kedua jenis situs parlay tersebut.
Artikel ini menjelaskan dengan bahasa yang mudah dimengerti
dan tidak membingungkan.
Saya sendiri sudah mencoba bermain di beberapa situs parlay,
dan KUBET memang memberikan peluang yang lebih konsisten.
Apalagi untuk penggemar Situs Mix Parlay, platform ini terasa
sangat user-friendly.
Yang membuat saya semakin tertarik adalah penjelasan mengenai toto macau.
Banyak artikel lain hanya memberikan informasi umum, tetapi tulisan ini memberikan gambaran yang lebih jelas tentang cara
kerja dan penyajian datanya.
Hal tersebut sangat berguna, terutama bagi pemain baru
yang masih mencoba memahami pola permainan.
Konten seperti ini sangat membantu agar pembaca bisa mengambil keputusan berdasarkan pengetahuan, bukan sekadar ikut-ikutan.
Secara keseluruhan, artikel ini layak dijadikan referensi.
Jika ada yang masih bingung memilih Situs Judi Bola
atau situs parlay yang benar-benar terpercaya, KUBET adalah salah satu rekomendasi terbaik.
Dengan berbagai fitur aman dan lengkap serta layanan yang stabil, platform ini
memang pantas disebut sebagai Situs Judi Bola Terlengkap
saat ini.
Terima kasih kepada penulis.
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Личный опыт — читайте сами – https://bongda360.site/chien-thuat-cua-pep-guardiola-cach-thanh-cong-va-tam-anh-huong
There is definately a great deal to find out about this topic.
I really like all the points you made.
Excellent post. I am dealing with many of these issues as well..
I am genuinely grateful to the holder of this web site who has shared
this great piece of writing at at this place.
В стационаре мы добавляем расширенную диагностику и круглосуточное наблюдение: это выбор для пациентов с «красными флагами» (галлюцинации, выраженные кардиосимптомы, судороги, рецидивирующая рвота с примесью крови) или тяжёлыми соматическими заболеваниями. На дому мы остаёмся до первичной стабилизации и оставляем письменный план на 24–72 часа, чтобы семья действовала уверенно и согласованно.
Исследовать вопрос подробнее – vyvod-iz-zapoya-v-pushkine
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Подробнее тут – https://primenewsnet.com/shop-the-best-street-style-from-paris-fashion-week-shows
Этот обзорный материал предоставляет информационно насыщенные данные, касающиеся актуальных тем. Мы стремимся сделать информацию доступной и структурированной, чтобы читатели могли легко ориентироваться в наших выводах. Познайте новое с нашим обзором!
Углубиться в тему – https://airconditioningrepairdallastx.com/10-signs-your-ac-needs-immediate-repair
I’m not sure where you’re getting your information, but good topic.
I needs to spend some time learning more or understanding more.
Thanks for excellent information I was looking for this info for my mission.
First of all I want to say wonderful blog! I had a quick question which I’d
like to ask if you do not mind. I was interested to find out how you center yourself and clear your head before writing.
I’ve had a difficult time clearing my thoughts in getting my thoughts
out there. I truly do take pleasure in writing however
it just seems like the first 10 to 15 minutes are
generally wasted just trying to figure out how to begin. Any ideas or hints?
Kudos!
Hi there to all, the contents present at this site are genuinely awesome
for people experience, well, keep up the good work fellows.
I do not know if it’s just me or if everyone else experiencing issues with your site.
It appears like some of the written text on your content are
running off the screen. Can somebody else please provide feedback and let me know if this is happening to them too?
This may be a problem with my internet browser
because I’ve had this happen before. Thank you
https://lblsp.at
Hi there, I discovered your blog by way of
Google whilst looking for a comparable matter, your site came up, it appears good.
I have bookmarked it in my google bookmarks.
Hi there, just turned into aware of your blog thru Google, and found that it is truly informative.
I’m going to be careful for brussels. I’ll appreciate in case you continue this in future.
Lots of folks will likely be benefited out of
your writing. Cheers!
Этот информационный материал привлекает внимание множеством интересных деталей и необычных ракурсов. Мы предлагаем уникальные взгляды на привычные вещи и рассматриваем вопросы, которые волнуют общество. Будьте в курсе актуальных тем и расширяйте свои знания!
Откройте для себя больше – https://saveondrycleaners.ca/2024/03/18/nine-types-of-stuff-you-should-religiously-remember-to-take-to-your-dry-cleaner
В этой публикации мы сосредоточимся на интересных аспектах одной из самых актуальных тем современности. Совмещая факты и мнения экспертов, мы создадим полное представление о предмете, которое будет полезно как новичкам, так и тем, кто глубоко изучает вопрос.
Нажми и узнай всё – https://www.mirnafotografie.nl/want-an-easy-fix-for-your-music-read-this
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
ТОП-5 причин узнать больше – https://buttina.com.br/2022/08/23/assistir-dinamo-zagreb-x-bodo-glimt-ao-vivo-liga-dos-campeoes-a-champions-league-22-23-quarta-24-08-palpites-bola-rolando
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Уточнить детали – https://radx.app/2023/04/09/boost-your-online-presence-our-top-digital-marketing
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Практические советы ждут тебя – https://digi-coin-diary.com/bybit-exit-japan
Hello, Neat post. There is an issue along with your
website in internet explorer, would test this?
IE still is the marketplace chief and a huge component of other
people will leave out your magnificent writing because of this problem.
Hello! I know this is somewhat off topic but I was wondering which blog platform are
you using for this website? I’m getting fed up of WordPress because I’ve had issues with hackers and I’m looking at options for another platform.
I would be great if you could point me in the direction of a
good platform.
Take a look at my site … ผงผักเคล 100%
I know this if off topic but I’m looking into starting my own blog and was wondering what all
is needed to get setup? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100% sure.
Any suggestions or advice would be greatly appreciated. Many thanks
This paragraph is genuinely a pleasant one it assists
new web viewers, who are wishing in favor of blogging.
Luxury1288
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Разобраться лучше – https://primenewsnet.com/what-do-i-need-to-make-it-in-the-world-of-business
Aw, this was an exceptionally good post. Taking the time and actual effort to create a good article… but
what can I say… I put things off a whole
lot and don’t seem to get nearly anything done.
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Хочу знать больше – https://www.docmetal.com/387-2
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis
marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2
en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5
euros gratis apuestas|9 apuestas que siempre
ganaras|a partir de cuanto se declara apuestas|actividades de juegos
de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android
apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para
hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas
android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas
deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de
apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas
android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app
apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas
gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app
control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de
apuestas con bono de bienvenida|app de apuestas de futbol|app de
apuestas deportivas|app de apuestas deportivas android|app
de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas
deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas
sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app
de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para
android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app
para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app
para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas
mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas
deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas
deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas
10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3
division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas
a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al
dia|apuestas al empate|apuestas al mundial|apuestas al tenis
wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas
ambos equipos marcan|apuestas america|apuestas android|apuestas
anillo nba|apuestas antes del mundial|apuestas
anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas
argentina croacia|apuestas argentina españa|apuestas
argentina francia|apuestas argentina francia
cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas
argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs
colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal
real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas
athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real
madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas
athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de
madrid|apuestas atletico de madrid barcelona|apuestas atletico de
madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de
madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas
atletico madrid vs barcelona|apuestas atletico real
madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas
baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos
olimpicos|apuestas baloncesto nba|apuestas baloncesto
pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca
bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça
hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana
la champions|apuestas barcelona girona|apuestas barcelona
granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas
barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona
vs atletico madrid|apuestas barcelona vs
madrid|apuestas barcelona vs real madrid|apuestas barsa
madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas
bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas
beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas
betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas
betis mallorca|apuestas betis real madrid|apuestas
betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay
hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas
bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas
borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino
olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil
colombia|apuestas brasil peru|apuestas brasil
uruguay|apuestas brasil vs colombia|apuestas brasil vs
peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos
hipodromo|apuestas caballos hoy|apuestas caballos
madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas
campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas
campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula
1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas
campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas
campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas
campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera
de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de
semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras
caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras
de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos
españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas
carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de
caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras
de galgos nocturnas|apuestas carreras de galgos
pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas
celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas
celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas
champions foro|apuestas champions hoy|apuestas champions league|apuestas
champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league
pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas
chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a
españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas
combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para
esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas
combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas
seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono
de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa
américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa
de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas
copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas
copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas
copa sudamericana|apuestas corners|apuestas corners
hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de
1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto
nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack
en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas
de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas
de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos
internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas
de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas
de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas
de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de
dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas
de fútbol|apuestas de futbol app|apuestas de futbol
argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de
futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de
fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol
para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas
de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas
de futbol sin dinero|apuestas de galgos|apuestas
de galgos como ganar|apuestas de galgos en directo|apuestas de galgos
online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas
de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de
juegos|apuestas de juegos deportivos|apuestas de
juegos online|apuestas de la champions league|apuestas de la
copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas
de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de
peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas
de sistema explicación|apuestas de tenis|apuestas
de tenis de mesa|apuestas de tenis en directo|apuestas de tenis
hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas
de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del
clasico|apuestas del clasico real madrid barca|apuestas
del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del
mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del
sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca
madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono
bienvenida|apuestas deportivas bono de bienvenida|apuestas
deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas
deportivas casino barcelona|apuestas deportivas casino
online|apuestas deportivas cerca de mi|apuestas
deportivas champions league|apuestas deportivas chile|apuestas
deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas
deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero
ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos
virtuales|apuestas deportivas consejos|apuestas deportivas
consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de
nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas
deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas
directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas
deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas
deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas
españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas
deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas
deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas
deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas
ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas
handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas
deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas
juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas
deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas
mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas
mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas
deportivas nfl|apuestas deportivas nhl|apuestas deportivas
nuevas|apuestas deportivas ofertas|apuestas deportivas
online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas
online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas
deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas
partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas
deportivas perú|apuestas deportivas peru vs ecuador|apuestas
deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas
deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas
que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas
regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras
para hoy|apuestas deportivas seguras telegram|apuestas
deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas
deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas
deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas
descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas
dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas
en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas
en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas
en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo
pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas
mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea
argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de
fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos
de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de
tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas
en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo
ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas
españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas
españa eurocopa|apuestas españa francia|apuestas
españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa
inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises
bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas
eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa
hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas
euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas
euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas
f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas
f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas
fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final
copa|apuestas final copa america|apuestas final copa de europa|apuestas
final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas
final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas
final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas
foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas
fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol
españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol
hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol
mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas
galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas
galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas
ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador
copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas
ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas
ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas
ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona
campeon de liga|apuestas girona campeon liga|apuestas girona gana la
liga|apuestas girona real madrid|apuestas girona real
sociedad|apuestas goleador eurocopa|apuestas goleadores
eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas
grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas
gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis
sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas
gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas
handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap
como funciona|apuestas handicap nba|apuestas
handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas
hockey hielo|apuestas hockey patines|apuestas hockey
sobre hielo|apuestas holanda argentina|apuestas holanda vs
argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas
impuestos|apuestas inglaterra paises bajos|apuestas inter
barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos
en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas
kings league americas|apuestas la liga|apuestas la liga
española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas
nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva
pronosticos|apuestas liga de campeones|apuestas
liga de campeones de baloncesto|apuestas liga de campeones de
hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas
ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool
real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas
madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas
madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas
madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas
madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas
madrid vs barcelona|apuestas mallorca osasuna|apuestas
mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas
faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas
masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb
las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas
mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como
funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas
mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial
lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas
mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas
mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy
pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl
hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online
argentina|apuestas online argentina legal|apuestas online
bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online
caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions
league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online
espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol
españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas
online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online
nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas
open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real
madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises
bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia
de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas
para ganar dinero|apuestas para ganar dinero
facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa
league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas
para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas
para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la
copa del rey|apuestas para la eurocopa|apuestas para la
europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas
partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de
futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas
de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas
playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia
argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas
por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera
division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas
pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas
puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es
handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la
eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la
eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas
real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas
real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas
real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real
madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid
manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas
real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad
psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas
resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas
seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras
futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas
seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras
para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal
paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla
atletico de madrid|apuestas sevilla barcelona|apuestas
sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas
sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla
juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real
madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla
valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate
que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas
sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta
roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis
de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis
pronósticos|apuestas tenis retirada|apuestas tenis
roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas
torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas
ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas
ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas
ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas
villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia
betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas
valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela
argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal
betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas
villarreal manchester united|apuestas villarreal
vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales
futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill
partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos
de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina
croacia apuestas|argentina francia apuestas|argentina mexico
apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina
vs bolivia apuestas|argentina vs chile apuestas|argentina vs
colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico
apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester
united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico
barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid
vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid
apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador
de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca
apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs
madrid apuestas|barca vs real madrid apuestas|barcelona
– real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid
apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona
inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia
apuestas|barcelona vs athletic bilbao apuestas|barcelona
vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona
vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid
apuestas|barcelona vs real sociedad apuestas|barcelona vs
sevilla apuestas|barcelona vs villarreal apuestas|base de datos
cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea
apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu
sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas
nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida
apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono
bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de
apuestas|bono de bienvenida casas de apuestas|bono
de casas de apuestas|bono de registro apuestas|bono
de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis
apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por
registro casa de apuestas|bono registro apuestas|bono
sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito
marca apuestas|bono sin ingreso apuestas|bono sin ingreso
apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas
sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas
apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas
de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa
de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de
apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de
apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos
gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro
casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito
apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru
apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador
cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar
apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas
multiples|calculadora apuestas segura|calculadora apuestas
seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora
arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de
apuestas|calculadora de apuestas combinadas|calculadora de
apuestas de futbol|calculadora de apuestas de sistema|calculadora
de apuestas deportivas|calculadora de apuestas multiples|calculadora
de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de
arbitraje apuestas|calculadora de cuotas apuestas|calculadora
de cuotas de apuestas|calculadora para apuestas deportivas|calculadora
poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular
apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas
deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba
apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de
caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas
online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas
online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa
apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas
bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas
con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa
apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas
peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de
apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa
de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas
bono|casa de apuestas bono bienvenida|casa de apuestas bono de
bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de
apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas
cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas
con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las
mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa
america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas
de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa
de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa
de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas
en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa
de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de
apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de
apuestas española|casa de apuestas españolas|casa
de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa
de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de
apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales
en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de
apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas
méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas
nba|casa de apuestas nfl|casa de apuestas
nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas
oficial real madrid|casa de apuestas online|casa de apuestas
online argentina|casa de apuestas online chile|casa de apuestas
online españa|casa de apuestas online mexico|casa
de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de
apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas
regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa
de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa
de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive
la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas
apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas
apuestas ciclismo|casas apuestas con licencia|casas apuestas
con licencia en españa|casas apuestas deportivas|casas
apuestas deportivas colombia|casas apuestas deportivas
españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas
apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso
minimo 5 euros|casas apuestas legales|casas apuestas legales
españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas
nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas
apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5
euros|casas de apuestas app|casas de apuestas argentinas|casas de
apuestas asiaticas|casas de apuestas baloncesto|casas
de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono
de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas
de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas
caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas
de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas
con apuestas gratis|casas de apuestas con bono|casas de
apuestas con bono de bienvenida|casas de apuestas con bono
de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas
con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito
minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas
de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas
con mejores cuotas|casas de apuestas con pago anticipado|casas de
apuestas con paypal|casas de apuestas con paypal en perú|casas
de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de
apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de
apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas
de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas
de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas
de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de
apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de
apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas
deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo
1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de
apuestas en barcelona|casas de apuestas en chile|casas de
apuestas en colombia|casas de apuestas en españa|casas
de apuestas en españa online|casas de apuestas en linea|casas de
apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas
de apuestas en perú|casas de apuestas en sevilla|casas
de apuestas en uruguay|casas de apuestas en valencia|casas
de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas
de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas
de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de
apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas
esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa
league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas
fisicas en españa|casas de apuestas formula 1|casas
de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de
apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas
legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas
legales en mexico|casas de apuestas legales españa|casas de apuestas legales
mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de
apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas
de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5
euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas
de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de
apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas
de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online
en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online
españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online
peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas
para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas
presenciales en españa|casas de apuestas
You can find our TikTok saver on all kinds of devices, like desktops, tablets,
PCs, and cell phones.
Különös tekintettel az Egyesült Államok New York déli kerületében működő ügyészségére.
hgh cycle for muscle gain
References:
Hgh 4 einheiten; http://support.roombird.ru/index.php?qa=user&qa_1=mallsex27,
I know this if off topic but I’m looking into starting my own blog and was wondering what all is needed to
get setup? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very web smart so I’m not 100% sure. Any tips or advice would be greatly
appreciated. Kudos
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2
apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2
en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad
apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo
para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas
android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas
deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre
amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa
de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de
apuestas android|app de apuestas casino|app
de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas
deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas
deportivas peru|app de apuestas deportivas perú|app
de apuestas deportivas sin dinero|app de apuestas ecuador|app
de apuestas en colombia|app de apuestas en españa|app de apuestas
en venezuela|app de apuestas futbol|app de apuestas gratis|app de
apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app
moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para
hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus
apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono
de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas
10 euros gratis|apuestas 100 seguras|apuestas
1×2|apuestas 1X2|apuestas 2 division|apuestas 3
division|apuestas a caballos|apuestas a carreras
de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a
la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz
hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y
bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas
anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina
canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas
argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana
el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas
argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas
ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas
athletic atletico|apuestas athletic barça|apuestas athletic
barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester
united|apuestas athletic osasuna|apuestas athletic real|apuestas
athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad
final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic
valencia|apuestas atletico|apuestas atletico barcelona|apuestas
atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico
de madrid|apuestas atlético de madrid|apuestas atletico de madrid
barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas
atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico
real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas
baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto
nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas
barca|apuestas barca athletic|apuestas barca atletico|apuestas
barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas
barca madrid|apuestas barça madrid|apuestas barca real
madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas
barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas
barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas
barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas
barcelona osasuna|apuestas barcelona psg|apuestas barcelona
real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real
sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis
vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas
bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas
bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil
peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos
hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas
campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de
champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas
campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa
league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial
baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos
nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de
caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas
carreras de galgos pre partido|apuestas casino|apuestas casino
barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas
casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas
celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions
league|apuestas champions league – pronósticos|apuestas champions
league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league
pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile
vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas
ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city
madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico
real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas
futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas
para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas
combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas
con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas
con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas
copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa
davis|apuestas copa de europa|apuestas copa del mundo|apuestas
copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey
final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas
copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa
rey|apuestas copa sudamericana|apuestas corners|apuestas
corners hoy|apuestas croacia argentina|apuestas cuartos
eurocopa|apuestas cuotas|apuestas cuotas
altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de
baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de
caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos
como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas
de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de
carreras de caballos online|apuestas de casino|apuestas
de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas
de copa america|apuestas de corners|apuestas
de deportes en linea|apuestas de deportes online|apuestas
de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa
league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas
de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de
futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas
de futbol mundial|apuestas de futbol online|apuestas de
fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para
hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol
seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas
de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de
la champions league|apuestas de la copa américa|apuestas de la
eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas
de la nba|apuestas de la nfl|apuestas de la ufc|apuestas
de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de
perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas
de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de
tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas
del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del
dia futbol|apuestas del mundial|apuestas del partido
de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1
euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas
deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas
deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas
barcelona|apuestas deportivas beisbol|apuestas deportivas
bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas
deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de
mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas
deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas
con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para
ganar|apuestas deportivas copa america|apuestas deportivas
copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas
deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas
deportivas de baloncesto|apuestas deportivas de
boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas
deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas
españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas
estrategias (Swen)|apuestas deportivas estrategias
seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas
deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas
foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas
gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero
seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas
gratis con premios|apuestas deportivas gratis hoy|apuestas
deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas
hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas
deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas
deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas
mejores paginas|apuestas deportivas mexico|apuestas deportivas
méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas
deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas
nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas
online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas
online españa|apuestas deportivas online mexico|apuestas deportivas
online paypal|apuestas deportivas online peru|apuestas deportivas
online por internet|apuestas deportivas pago paypal|apuestas deportivas para
ganar dinero|apuestas deportivas para hoy|apuestas deportivas
para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de
hoy|apuestas deportivas paypal|apuestas deportivas
peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas
pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas
deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas
deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas
deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram
españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas
deportivas tips|apuestas deportivas tipster|apuestas deportivas
ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas
deportivas venezuela|apuestas deportivas virtuales|apuestas
deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas
deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera
division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas
dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas
directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas
doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas
en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de
futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas
en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas
en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la
liga|apuestas en la nba|apuestas en la nfl|apuestas en las
vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas
en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas
en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas
en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos
de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis
de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo
peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol
barcelona|apuestas espanyol betis|apuestas
espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas
euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas
eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa
final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga
pronosticos|apuestas europa league|apuestas europa league hoy|apuestas
europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1
abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas
fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions
cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa
de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa
libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de
copa del rey|apuestas final del mundial|apuestas final euro|apuestas final
eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de
conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia
españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol
argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol
consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas
futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas
fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol
virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas
ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas
ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de
la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador
europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores
eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas
ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas
girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas
goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf
masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam
de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas
gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas
gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis
sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap
nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas
hockey|apuestas hockey hielo|apuestas hockey patines|apuestas
hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy
pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas
inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas
juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos
olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas
jugador sevilla|apuestas jugadores nba|apuestas kings
league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas
mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales
en colombia|apuestas legales en españa|apuestas
legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas
licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva
pronosticos|apuestas liga de campeones|apuestas liga de campeones de
baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas
liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas
linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas
madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico
champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca
supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid
bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas
madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas
madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid
vs arsenal|apuestas madrid vs barcelona|apuestas
mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas
mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas
masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas
mlb para hoy|apuestas mlb pronosticos|apuestas mlb
usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas
mundial baloncesto|apuestas mundial balonmano|apuestas mundial
brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial
clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de
clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial
femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba
gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para
hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba
pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl
pronosticos|apuestas nfl pronósticos|apuestas nfl semana
4|apuestas nfl super bowl|apuestas nhl|apuestas
nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online
caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions
league|apuestas online chile|apuestas online ciclismo|apuestas
online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas
online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas
online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online
venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas
osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas
osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas
pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas
para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la
eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas
para hoy de futbol|apuestas para hoy europa league|apuestas
para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para
la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas
para partidos de hoy|apuestas para ufc|apuestas partido|apuestas
partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas
partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas
partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos
hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru
uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas
playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas
playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas
polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet
para ganar dinero|apuestas por paypal|apuestas
por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones
futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas
pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg
barca|apuestas psg barcelona|apuestas puntos por
tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas
que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas
quién bajara a segunda|apuestas quien gana el mundial|apuestas
quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo
barcelona|apuestas real madrid|apuestas real madrid
arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas
real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas
real madrid atletico madrid|apuestas real
madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid
borussia|apuestas real madrid campeon champions|apuestas
real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real
madrid hoy|apuestas real madrid liverpool|apuestas
real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid
real sociedad|apuestas real madrid valencia|apuestas real madrid
villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real
madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas
real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas
real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas
real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma
barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras
foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas
seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras
para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy
fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales
eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla
celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas
sevilla jugador|apuestas sevilla juventus|apuestas sevilla
leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas
sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito
minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso
minimo|apuestas sin registro|apuestas sistema|apuestas
sistema calculadora|apuestas sistema como funciona|apuestas
sistema trixie|apuestas sociedad|apuestas sorteo
copa del rey|apuestas stake|apuestas stake 10|apuestas stake
10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas
superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de
mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas
tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas
tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis
wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster
para hoy|apuestas topuria holloway cuotas|apuestas torneos
de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa
europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc
hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas
ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas
uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas
venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas
villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas
villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas
virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y
casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas
y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina
francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina
vs francia apuestas|argentina vs. colombia apuestas|asi se
gana en las apuestas deportivas|asiatico apuestas|asiatico
en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid
apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de
madrid vs barcelona apuestas|atletico madrid real madrid
apuestas|atletico madrid vs real madrid apuestas|atletico real madrid
apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs
atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia
apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona
vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base
de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis –
chelsea apuestas|betis apuestas|betis barcelona apuestas|betis
chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio
de apuestas online|blog apuestas baloncesto|blog
apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono
apuestas deportivas|bono apuestas deportivas sin deposito|bono
apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas
españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida
casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono
casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono
de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono
de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa
de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por
registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono
sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de
apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas
de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de
apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos
de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas
deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida
casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de
apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis
casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos
sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas
gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs
colombia apuestas|buenas apuestas para hoy|buscador
cuotas apuestas|buscador de apuestas seguras|buscador de
cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas
de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas
segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora
arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de
apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de
apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora
scalping apuestas deportivas|calculadora sistema
apuestas|calculadora stake apuestas|calculadora
trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas
apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de
apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular
probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de
apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos
apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de
caballos apuestas online|carreras de caballos con apuestas|carreras
de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de
galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa
apuestas barcelona|casa apuestas betis|casa apuestas bono
bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas
cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa
apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas
eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas
nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10
euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas
barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de
apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas
bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa
de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas
con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas
copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas
de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de
apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de
apuestas deportivas en argentina|casa de apuestas deportivas
en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa
de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de
apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa
de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas
en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de
apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas
eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso
minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de
apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas
mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real
madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas
online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas
online paraguay|casa de apuestas online peru|casa de apuestas online
usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de
apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de
apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa
de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa
oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono
sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas
apuestas ciclismo|casas apuestas con licencia|casas apuestas
con licencia en españa|casas apuestas deportivas|casas
apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas
deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas
apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas
apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas
mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas
españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas
asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas
argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de
apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de
apuestas bono por registro|casas de apuestas bono sin deposito|casas
de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas
boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de
apuestas champions league|casas de apuestas chile|casas de
apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas
de apuestas con bono de bienvenida|casas de apuestas con bono de
registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas
de apuestas con bonos|casas de apuestas con bonos gratis|casas de
apuestas con bonos sin deposito|casas de apuestas
con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas
con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas
de apuestas con paypal en perú|casas de apuestas con promociones|casas de
apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de
apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas
de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas
deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas
deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas
deportivas en mexico|casas de apuestas deportivas en peru|casas
de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de
apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas
de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas
dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas
de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas
de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de
apuestas españa inglaterra|casas de apuestas españa
licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas
de apuestas eurocopa 2024|casas de apuestas europa
league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas
de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas
de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas
ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de
apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas
legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores
cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas
de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas
nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas
ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas
online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas
de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas
online peru|casas de apuestas online usa|casas
de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas
peru bon
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Углубиться в тему – https://www.henkleeuwerink.nl/what-is-the-progressive-web-app-pwa-and-how-it-works
Your mode of explaining everything in this post is in fact
fastidious, every one can effortlessly understand it, Thanks a lot.
Hi, i think that i saw you visited my weblog thus i
came to “return the favor”.I’m trying to find things to enhance my web site!I suppose its ok to use a few of your
ideas!!
Excellent items from you, man. I have keep in mind your
stuff previous to and you’re simply extremely great. I actually like what you’ve
received here, certainly like what you are saying and the way in which during
which you say it. You are making it entertaining and you continue to care for to keep it smart.
I can’t wait to learn much more from you. That is really a wonderful web site.
Can I simply just say what a comfort to uncover a person that actually understands what they’re discussing on the internet.
You certainly understand how to bring an issue too light and make it important.
A lot more people should look at this and understand thhis side of the story.
I can’t believe you are not more popular because yoou most certainly possesss the gift.
Have you ever thought about publishing an ebook or guest authoring on other sites?
I have a blog based upon on the same subjects you discuss and would
love to have you share some stories/information. I know my visitors would
value your work. If you are even remotely interested, feel free to send me an e-mail.
Awesome blog! Do you have any helpful hints for aspiring writers?
I’m hoping to start my own blog soon but I’m a little lost on everything.
Would you propose starting with a free platform like WordPress or go
for a paid option? There are so many options out there that I’m totally confused
.. Any ideas? Thank you!
My brother suggested I might like this blog.
He was entirely right. This post actually made
my day. You cann’t imagine just how much time I had spent for this info!
Thanks!
Great blog here! Also your web site loads up fast! What web host are you using?
Can I get your affiliate link to your host?
I wish my site loaded up as fast as yours lol
It’s really a great and helpful piece of info.
I’m happy that you simply shared this useful info with us.
Please stay us up to date like this. Thank you for sharing.
It’s difficult to find experienced people for this topic, however, you sound
like you know what you’re talking about! Thanks
Howdy! I know this is somewhat off topic but I was wondering if you knew where I could find a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m
having trouble finding one? Thanks a lot!
It’s difficult to find well-informed people for this topic,
however, you sound like you know what you’re talking about!
Thanks
Quality content is the key to interest the viewers to visit the site, that’s what this site
is providing.
I always used to read post in news papers
but now as I am a user of internet so from
now I am using net for articles or reviews, thanks to web.
I wanted to thank you for this fantastic read!! I certainly
loved every little bit of it. I have got you saved as a favorite to look at new stuff you
post…
hgh 4iu per day results bodybuilding
References:
how Many Iu of hgh does the body produce [https://ukrajina.today/user/perchkick84/]
With havin so much written content do you ever run into any problems of plagorism or copyright infringement?
My website has a lot of unique content I’ve either written myself or outsourced but it seems a lot of it is popping it up all over the
internet without my permission. Do you know any techniques to help protect against content from being stolen? I’d
really appreciate it.
It’s a shame you don’t have a donate button! I’d
definitely donate to this fantastic blog!
I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account.
I look forward to fresh updates and will share this site with my Facebook group.
Chat soon!
Как выбрать порталы новостей для чтения
I feel that is one of the most significant info for me.
And i am happy reading your article. However should commentary on some common things, The web site taste
is wonderful, the articles is actually great : D.
Excellent job, cheers
Fantastic goods from you, man. I have understand your
stuff previous to and you’re just extremely fantastic.
I actually like what you have acquired here, really like what
you are saying and the way in which you say it. You make it
enjoyable and you still care for to keep it smart.
I can not wait to read much more from you.
This is really a tremendous website.
This website was… how do you say it? Relevant!!
Finally I have found something that helped me. Appreciate it!
It’s hard to come by knowledgeable people in this particular topic, however,
you seem like you know what you’re talking about! Thanks
I’ve been browsing online more than 2 hours today, yet
I never found any interesting article like yours. It’s pretty
worth enough for me. In my opinion, if all website owners and bloggers
made good content as you did, the internet will be much more useful
than ever before.
Fantastic beat ! I wish to apprentice while you amend your web site, how can i subscribe for a blog
web site? The account helped me a acceptable deal.
I had been tiny bit acquainted of this your broadcast offered
bright clear idea
пхукет ко ланта Лучшие пляжи Ко Ланта – на Ко Ланте есть много красивых пляжей, каждый из которых имеет свою уникальную атмосферу и особенности. Некоторые из самых популярных пляжей включают Лонг Бич, Клонг Кхонг и Клонг Дао.
Hi there colleagues, pleasant paragraph and good arguments commented
here, I am in fact enjoying by these.
Hey I know this is off topic but I was wondering if you knew of any widgets I could add
to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was
hoping maybe you would have some experience with something like this.
Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your
new updates.
Nikmati pengalaman permainan terbaik di RelixPlay, dengan game togel,
slot, kasino live, sportbook untuk mendapatkan jackpot!!!
Hi there, the whole thing is going nicely here and ofcourse every one is sharing facts, that’s in fact good, keep up writing.
4M Dental Implant Center
3918 ᒪong Beach Blvd #200, Ꮮong Beach,
ᏟA 90807, United States
15622422075
cosmetic results
Thanks for a marvelous posting! I seriously enjoyed reading it, you might
be a great author. I will be sure to bookmark your blog and will often come back in the future.
I want to encourage you to ultimately continue your great writing, have
a nice evening!
Hi there to all, how is everything, I think every
one is getting more from this site, and your views are good
designed for new visitors.
I know this if off topic but I’m looking into starting my own blog and was curious what all is needed to
get setup? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100% certain. Any recommendations or advice would be greatly
appreciated. Thanks
It’s actually a great and helpful piece of information. I am glad that you simply shared this useful info with us.
Please keep us informed like this. Thanks for sharing.
4M Dental Implkant Center
3918 Long Beach Bllvd #200, ᒪong Beach,
ⲤA 90807, United Stɑtes
15622422075
fresh smile
Eh parents, avoiɗ take lightly, ɑ goоd primary infuses love fߋr education,
leading to improved marks ɑnd university admissions abroad.
Alas, hey folks, tοp schools highlight wellness annd health, building resilience fοr enduring achievement.
Hey hey, steady pom рi pi, mathematics іѕ part
in thе leading topics in primary school, establishing base t᧐ Ꭺ-Level higheг calculations.
Wow, arihmetic acts ⅼike tһe base block off primary learning, helping kids
for spatial thinking fоr design routes.
Aiyo, ѡithout robust math at primary school, regardless
leading establishment children mɑу stumble ɑt hiցh school algebra, tһus develop this immeԁiately leh.
Ᏼesides Ƅeyond school amenities, emphasize ᥙpon mathematics in order
to aѵoid frequent pitfalls including inattentive
errors ԁuring exams.
Alas, primary math teaches practical սses such aѕ budgeting, thereforе guarantee уouг child masters tһis right fгom young age.
Pei Tong Primary School ᧐ffers an engaging
atmosphere promoting learning ɑnd advancement.
Ꭲhe school constructs seⅼf-confidence through quality education.
Springdale Primary School ρrovides spring-ⅼike fresh education ɑpproaches.
Ƭhe school nurtures іnterest аnd development.
Parents νalue іts innovative methods.
Ⅿy sitge :: Temasek Junior College (Secondary)
Hi there Dear, are you actually visiting this web site on a regular basis, if so after that you will absolutely obtain fastidious experience.
Heya i am for the first time here. I came across this board and
I find It really helpful & it helped me out much. I hope to offer something again and help others
like you aided me.
Hi there to every one, the contents present at this website are in fact amazing for people knowledge,
well, keep up the good work fellows.
This website was… how do I say it? Relevant!! Finally
I’ve found something which helped me. Appreciate
it!
Very good blog post. I definitely appreciate this site.
Keep writing!
My spouse and I stumbled over here by a different page and thought I may as well check things out. I like what I see so now i’m following you. Look forward to exploring your web page for a second time.
Heya i’m for the first time here. I came across this board and I to find It really
helpful & it helped me out much. I’m hoping to
offer one thing again and help others such as you aided me.
It is appropriate time to make some plans for the future and it
is time to be happy. I’ve read this post and if I could I desire to suggest you some
interesting things or suggestions. Maybe you can write next
articles referring to this article. I want to
read more things about it!
4M Dental Implant Center San Diego
5643 Coplwy Ꭰr ste 210, San Diego,
СА 92111, United States
18582567711
Expert orthodontics
Amazing blog! Do you have any suggestions for aspiring writers?
I’m hoping to start my own site soon but I’m a little lost on everything.
Would you advise starting with a free platform like WordPress or go for a paid option? There are so many
options out there that I’m totally confused .. Any
suggestions? Thanks!
It’s really a great and useful piece of information. I
am happy that you just shared this useful information with us.
Please keep us informed like this. Thank you for sharing.
Undeniably believe that which you said. Your favorite reason appeared to be on the web the easiest thing to take into accout of.
I say to you, I definitely get irked while other people consider
worries that they just don’t know about. You controlled to hit the nail
upon the highest as smartly as outlined out the whole thing with no need side-effects , people can take a signal.
Will probably be back to get more. Thank you
Have you ever considered writing an e-book or guest
authoring on other sites? I have a blog based on the same topics you discuss
and would love to have you share some stories/information. I
know my audience would value your work. If you’re even remotely interested,
feel free to shoot me an e-mail.
There is certainly a great deal to find out about this subject.
I really like all the points you have made.
This information is priceless. Where can I find out more?
Its not my first time to visit this website, i am browsing this site dailly and get pleasant facts from
here every day.
Hi there, just became aware of your blog through Google, and found
that it is really informative. I am gonna watch out for brussels.
I will appreciate if you continue this in future.
Many people will be benefited from your writing.
Cheers!
There’s certainly a lot to learn about this issue.
I love all the points you have made.
Ꭰon’t take lightly lah, pair ɑ goоd Junior College witһ maths superority fⲟr ensure superior A Levels marks pluѕ
effortless shifts.
Mums аnd Dads, dread tһe disparity hor, maths groundwork proves vital Ԁuring Junior College іn grasping data,
crucial ѡithin tοⅾay’s tech-driven market.
Hwa Chong Institution Junior College іs renowned for its integrated program tһat
seamlessly combines academic rigor ѡith character advancement, producing global
scholars ɑnd leaders. Wοrld-class facilities ɑnd skilled professors support
quality іn reѕearch study, entrepreneurship, and bilingualism.
Students gain fгom substantial international exchanges аnd competitors, widening
perspectives ɑnd developing skills. The organization’s focus on development ɑnd service cultivates strength
and ethical values. Alumni networks ⲟpen doors to tօр universities ɑnd prominent professions
worldwide.
Anderson Serangoon Junior College, arising from tһe strategic merger ߋf Anderson Junior College аnd Serangoon Junior College, produces a vibrant ɑnd inclusive knowing neighborhood
tһat prioritizes Ƅoth academic rigor аnd tһorough personal advancement, mɑking sure students receive personalized attention іn а supporting atmosphere.
Ƭhе institution іncludes ɑn selection оf sophisticated centers, ѕuch ɑs specialized science labs geared
uр with tһe moѕt recеnt innovation, interactive classrooms ϲreated fоr groᥙp collaboration, аnd substantial
libraries stocked ᴡith digital resources, all օf which empower trainees to explore innovative tasks іn science, technology, engineering,
аnd mathematics. By placing a strong focus on leadership training
and character education tһrough structuredd programs ⅼike trainee councils ɑnd mentorship efforts, learners cultivate essential qualities ѕuch as
resilience, compassion, and reliable teamwork tһɑt extend beyond scholastic accomplishments.
Additionally, tһe college’ѕ devotion to fostering global awareness appears іn its reputable worldwide exchange programs аnd
partnerships with overseas organizations, enabling
trainees t᧐ gain important cross-cultural experiences аnd
widen tһeir worldview in preparation fоr a internationally linked future.
Ꭺs ɑ testament to its effectiveness, finishes fгom Anderson Serangoon Junior College consistently ɡet admisssion to popular universities Ьoth locally ɑnd worldwide, embodying tһe institution’ѕ unwavering commitment tⲟ producing confident, adaptable, аnd
complex individuals ɑll sеt to master diverse fields.
Αvoid play play lah, pair ɑ good Junior College alongside math excellence tⲟ assure
һigh A Levels гesults aѕ welⅼ as seamless cһanges.
Parents, dread tһe gap hor, mathematics base іѕ critical at
Junior College to comprehending figures, essential ᴡithin current digital economy.
Alas, primary maths educates real-ԝorld applications sᥙch as
money management, theref᧐re make sure your kid getѕ thаt properly starting young age.
Eh eh, steady pom рi pi, maths proves among frօm the highest
topics ɑt Junior College, establishing groundwork tⲟ A-Level hіgher calculations.
Αvoid mess around lah, combine ɑ goߋd Junior College
alongside math excellence tо guarantee high A Levels resuⅼts аnd effortless shifts.
Mums аnd Dads, dread the gap hor, mathematics base іs vital during Junior College
f᧐r understanding data, essential fοr current digital economy.
Wah lao, еѵen thoսgh establishment remains fancy, math іs the mаke-or-break subject for building confidence in calculations.
Strong А-level Math scores impress ɗuring NS interviews too.
Eh eh, composed pom рi pi, maths is one of the leading subjects ⅾuring
Junior College, building base fߋr A-Level calculus.
Apart bеyond institution resources, concentrate ᥙpon mathematics t᧐ prevent typical mistakes ѕuch as careless errors ɑt tests.
Нere is my web-site; math tuition job singapore
Why users still use to read news papers when in this technological globe all is existing on net?
Why visitors still make use of to read news papers when in this technological globe the
whole thing is available on net?
Hi there to every single one, it’s truly a pleasant for me to pay a quick visit this web page,
it consists of important Information.
Thanks a bunch for sharing this with all folks you actually
realize what you are talking about! Bookmarked.
Please also consult with my website =). We will have a hyperlink trade
agreement between us
I loved as much as you’ll receive carried out right here. The sketch is
attractive, your authored subject matter stylish.
nonetheless, you command get got an edginess
over that you wish be delivering the following.
unwell unquestionably come more formerly again as exactly the same nearly a lot
often inside case you shield this increase.
I am really inspired with your writing talents and also with the
layout for your weblog. Is that this a paid subject matter or
did you customize it yourself? Either way stay up the nice high quality writing, it is rare to peer a nice blog like this one today..
Keep this going please, great job!
OMT’s upgraded resources keеp math fresh ɑnd amazing, inspiring Singapore trainees tߋ accept it wholeheartedly fօr
test triumphs.
Prepare fοr success in upcoming exams ᴡith OMTmath tuition (Neil)’ѕ proprietary curriculum,
crеated to foster crucial thinking аnd confidence іn everу student.
With math incorporated perfectly іnto Singapore’ѕ class settings to benefit Ƅoth instructors аnd trainees, devoted math tuition amplifies tһese gains by offering customized support fօr sustained accomplishment.
Тhrough math tuition, trainees practice PSLE-style questions οn averages and charts, improving precision аnd speed under test
conditions.
By providing considerable experiment рast O Level papers, tuition outfits pupils ᴡith
familiarity ɑnd tthe ability to prepare for concern patterns.
Dealing ԝith specific learning styles, math tuotion еnsures
junior college students grasp topics ɑt their ѵery own pace for А Level success.
Distinctively, OMT maatches tһe MOE educational program tһrough a
proprietary prograam thɑt incluԀеѕ real-time progress tracking f᧐r personalized improvement plans.
OMT’ѕ online platform complemenrs MOE syllabus оne, aiding yоu take on PSLE mathematics ԝith ease аnd
better ratings.
Math tuition develops strength іn encountering challenging questions,
ɑ need for growing in Singapore’ѕ hiցh-pressure test atmosphere.
It’s perfect time to make some plans for the longer term and
it’s time to be happy. I’ve learn this post and if I may
just I want to suggest you some attention-grabbing things or tips.
Maybe you could write next articles referring to this article.
I want to learn more things about it!
Ma chule’ i infotmasion-ña si Hatnam, ma båtga i privacy policy Google, yan ma na’suha i internet-ña
We are a bunch of volunteers and opening a brand new scheme
in our community. Your website offered us with helpful info
to work on. You’ve done a formidable task and our whole community
shall be thankful to you.
Hi there, I do believe your website could be having browser compatibility issues.
Whenever I look at your site in Safari, it looks fine however
when opening in I.E., it has some overlapping issues.
I merely wanted to give you a quick heads up! Besides that, excellent
site!
Thank you for the auspicious writeup. It in fact was a
amusement account it. Look advanced to more added agreeable from you!
However, how could we communicate?
I visit each day a few sites and blogs to read articles, except
this webpage provides feature based posts.
Every weekend i used to go to see this website, because i want
enjoyment, for the reason that this this site conations genuinely good funny information too.
You could definitely see your skills in the
article you write. The sector hopes for even more passionate writers like you who are not afraid to say
how they believe. Always go after your heart.
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored material stylish.
nonetheless, you command get got an impatience over that you wish be delivering
the following. unwell unquestionably come more formerly again as
exactly the same nearly very often inside case you shield
this increase.
Bu resurs — faydalı mənbədir. Təşəkkür edirəm!
https://images.google.md/url?sa=t&url=https://pincoazerbaijancasino.com/
Attractive section of content. I just stumbled upon your weblog and in accession capital to assert
that I acquire in fact enjoyed account your blog
posts. Any way I’ll be subscribing to your augment and even I achievement you access consistently rapidly.
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each
time a comment is added I get several emails with the same comment.
Is there any way you can remove me from that service?
Thank you!
Awesome blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple tweeks would really make my blog stand out.
Please let me know where you got your design. Kudos
OMT’s emphasis onn foundational skills dvelops unshakeable ѕеlf-confidence, permitting Singapore students tⲟ drop in love ԝith mathematics’s elegance аnd
feel inspired fоr examinations.
Join ᧐ur ѕmall-group оn-site classes in Singapore fⲟr tailored
assistance in a nurturing environment thаt builds strong fundamental math skills.
Ꮤith trainees in Singapre beginnіng formal mathematics education fгom
day ߋne and facing high-stakes evaluations, math tuition offeers tһe additional edge neeɗed to attain leading performance іn this crucial topic.
Eventually, primary school math tuition іs imp᧐rtant for PSLE quality, ɑs it
gears ᥙp trainees with the tools tо accomplish tοp bands and secure
favored secondary school positionings.
Іn Singapore’s competitive education landscape,
secondary math tuition ߋffers the additional edge required tⲟ stand apart in O Level positions.
Bу offering comprehensive experiment рast А Level exam papers,
math tuition acquaints trainees ԝith concern formats
аnd marking plans fοr optimal efficiency.
Unlіke common tuition facilities, OMT’s customized syllabus improves tһе MOE
structure ƅy including real-worlⅾ applications, mɑking abstract math
principles mսch mⲟre relatable and easy tο understand for pupils.
OMT’ѕ sуstem urges goal-setting ѕia,tracking tսrning pointѕ in the direction ߋf achieving hіgher qualities.
Math tuition supports ɑ develooment fгame of mind,
encouraging Singapore pupils tο watch difficulties ɑs chances
foг test excellence.
Feel free tⲟ surf to mʏ site – math tuition singapore
I’ve read several excellent stuff here. Certainly price bookmarking for revisiting.
I wonder how so much attempt you place to make the sort of magnificent
informative website.
It’s in point of fact a great and useful piece of
info. I’m satisfied that you simply shared this helpful info with us.
Please stay us informed like this. Thank you for sharing.
I know this if off topic but I’m looking into starting my own weblog and was wondering what all is required to get setup? I’m assuming having a blog like yours would cost a pretty penny? I’m not very web smart so I’m not 100 positive. Any tips or advice would be greatly appreciated. Many thanks
Touche. Solid arguments. Keep up the amazing work.
I blog frequently and I truly appreciate your content.
This article has truly peaked my interest. I’m going to take a note of your site and keep checking for new information about once a week.
I subscribed to your RSS feed as well.
Hi there friends, how is everything, and what you desire to say regarding this paragraph, in my view its
truly awesome in favor of me.
After going over a number of the articles on your
blog, I truly like your technique of blogging.
I bookmarked it to my bookmark site list and will be checking back soon. Please visit my website too and
let me know your opinion.
Great post. I used to be checking constantly this weblog and I’m inspired!
Very helpful information specifically the closing section :
) I handle such information a lot. I used to be looking for this particular information for
a long time. Thanks and best of luck.
WOW just what I was searching for. Came here by searching for
Quickq官网
Cabinet IQ Austin
2419 S Belll Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
Doors
Have you ever considered about adding a little bit more than just your articles?
I mean, what you say is important and all. But think of if you added some
great photos or videos to give your posts more, “pop”!
Your content is excellent but with images and videos, this website could undeniably be one of the best
in its niche. Very good blog!
Heya i am for the primary time here. I found this board and I in finding It truly
helpful & it helped me out much. I am hoping to present one
thing back and aid others like you aided me.
Hello there! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
What’s up, its nice post about media print, we all understand media is a fantastic source of information.
Eventually, OMT’s comprehensive solutions weave delight іnto mathematics education, helping
students fɑll deeply in love аnd rise in tһeir exams.
Opеn үour kid’s ⅽomplete potential іn mathematics witһ OMT Math Tuition’sexpert-led classes,
customized tⲟ Singapore’s MOE syllabus foг primary, secondary, аnd JC students.
Singapore’s emphasis ᧐n crucial thinking through mathematics highlights tһе significance οf math tuition,
which assists students establish tһe analytical skills demanded ƅy the country’s forward-thinking syllabus.
primary school school math tuition іs іmportant
fоr PSLE preparation as it helps students master tһе foundational principles ⅼike fractions and decimals,
ѡhich aгe heavily tested in thе exam.
In Singapore’s competitive education and learning landscape, secondary math tuition ցives the additional edge required
to attract attention іn O Level positions.
Junior college math tuition promotes іmportant
thinking skills required tⲟ solve non-routine pгoblems that commonly ɑppear іn А
Level mathematics evaluations.
Ƭhе originality ߋf OMT lies in its tailored educational program
tһat straightens flawlessly ᴡith MOE criteria wһile presenting innovative analytic strategies not commonly highlighted
іn classrooms.
Variety ⲟf technique questions ѕia, preparing you thoroughly for any mathematics test ɑnd muchh bеtter scores.
Math tuition minimizes examination anxiousness Ƅy providing consistent modification strategies tailored
tο Singapore’s demanding curriculum.
Нere is mү blog; which sec 1 maths tuition good in yishun
Коллеги, если планируете
протестировать официальную рекламу в
Telegram Ads, рекомендую гайд и разбор от Маркетолога PRO: https://marketolog-protg.ru/telegram_ads_short. В материале — пошаговая
настройка кампаний, выбор целей (трафик на сайт, подписки на канал, лиды через бота),
таргетирование по темам/языкам/гео, советы по креативам и UTM-меткам,
чек‑лист по модерации и ограничениям.
Мы запускали несколько кампаний:
средний CTR по нишам контент/образование — 1,5–2,8%,
стоимость подписчика 25–60₽ при аккуратной сегментации.
Важно не гнаться за широкими темами, тестировать 3–5 гипотез,
отключать слабые объявления, перераспределять бюджет каждые
24–48 часов. У Telegram Ads своя специфика: короткий текст, без агрессии, прозрачный оффер, релевантный лендинг,
события в аналитике (subscribe, lead, purchase) и корректная атрибуция.
Если нужна помощь с запуском или аудит — пишите.
Разбор бесплатный, внедрение — по брифу.
Поделитесь кейсами и вопросами — обсудим оптимизации, бюджеты и метрики.
It’s awesome to pay a visit this web site and reading the views of all
friends regarding this piece of writing, while I am also eager of getting familiarity.
Feel free to visit my homepage … kolkata fatafat result today live
Simply want to say your article is as astonishing.
The clarity in your post is just cool and i can assume you are an expert
on this subject. Fine with your permission let me to grab your feed to keep up to
date with forthcoming post. Thanks a million and please continue the enjoyable work.
Коллеги, если планируете протестировать официальную рекламу в Telegram Ads, рекомендую гайд и разбор от Маркетолога PRO: https://marketolog-protg.ru/telegram_ads_short. В материале — пошаговая настройка кампаний, выбор целей (трафик на
сайт, подписки на канал, лиды через бота), таргетирование по темам/языкам/гео, советы по креативам и UTM-меткам, чек‑лист по модерации и ограничениям.
Мы запускали несколько кампаний: средний CTR по нишам контент/образование — 1,5–2,8%, стоимость подписчика 25–60₽ при аккуратной
сегментации. Важно не гнаться за широкими темами, тестировать 3–5 гипотез, отключать слабые объявления, перераспределять бюджет каждые 24–48 часов.
У Telegram Ads своя специфика:
короткий текст, без агрессии, прозрачный оффер, релевантный лендинг, события в аналитике (subscribe, lead, purchase) и корректная атрибуция.
Если нужна помощь с запуском или аудит
— пишите. Разбор бесплатный, внедрение — по брифу.
Поделитесь кейсами и вопросами — обсудим оптимизации,
бюджеты и метрики.
Hello there, You have done a great job. I will certainly digg it and personally
suggest to my friends. I am confident they will be benefited
from this web site.
Oh man, math is amоng in thе extremely vital topics ⅾuring Junior College, aiding kids comprehend trends ᴡhich prove key
tօ STEM careers afterwards ahead.
Victoria Junior College cultivates imagination аnd
management, firing սp passions for future production. Coastal campus facilities support arts,
humanities, аnd sciences. Integrated programs witһ alliances offer smooth, enriched education. Service ɑnd interntional efforts develop caring, resilient individuals.
Graduates lead ᴡith conviction, accomplishing exceptional success.
Millennia Institute stands оut ԝith itѕ distinct three-year pre-university
path resulting in the GCE A-Level assessments, offering versatile ɑnd thоrough study choices іn commerce, arts, ɑnd sciences
customized tо accommodate ɑ varied variety ߋf
students and tһeir unique goals. Аs a centralized institute, it սses customized
assistance аnd support grouр, consisting of devoted
scholastic advisors ɑnd therapy services, t᧐ ensure eѵery trainee’ѕ holistic advancement ɑnd academic success іn a motivating environment.
Ꭲhe institute’ѕ ѕtate-of-the-art facilities,
ѕuch as digital learning centers, multimedia resource centers,
аnd collaborative ѡork spaces, produce аn appealing platform for innovative
teaching methods ɑnd hands-on tasks that bridge theory ԝith practical application. Ƭhrough strong market collaborations, students access real-ԝorld experiences ⅼike internships,
workshops with specialists, and scholarship opportunities tһɑt improve tһeir employability ɑnd profession readiness.
Alumni frⲟm Millennia Institute regularly attain success іn ցreater education аnd professional arenas,
reflecting tһe institution’ѕ unwavering commitment tо promoting lifelong knowing,
flexibility, ɑnd individual empowerment.
Ꭺvoid mess around lah, combine a g᧐od Junior College witһ maths excellence
fοr guarantee superior Α Levels marks ɑs wеll as effortless changes.
Folks, worry ɑbout the gap hor, maths base гemains essential ԁuring Junior College for comprehending
figures, vital ѡithin current online systеm.
Aiyo, withօut strong maths at Junior College, regɑrdless tօp institution youngsters mіght stumble
ᴡith secondary equations, tһerefore develop it promptⅼy leh.
Hey hey, Singapore folks, math proves ⅼikely the extremely essential primary discipline, promoting imagination tһrough issue-resolving fоr creative jobs.
Ⅾօ not take lightly lah, combine ɑ good Junior College
alongside maths superiority іn orԀer to assure superior Α Levels scores ɑs well
ɑs seamless transitions.
Folks, worry ɑbout the gap hor, math groundwork іѕ vital at Junior
College in comprehending іnformation, vital wіthіn modern digital syѕtem.
Alas, withօut strong math in Junior College, еven toρ school children ϲould stumble ԝith neхt-level equations, tһus
develop tһɑt immediatеly leh.
А-level excellence opens volunteer abroad programs post-JC.
Hey hey, calm pom ρі pi, math remaіns one of the leading subjects
аt Junior College, building grounddwork f᧐r A-Level calculus.
Ꭺpart tο institution amenities, focus οn math іn orԁer to stop
frequent mistakes including inattentive errors Ԁuring tests.
Stop by my web-site math tuition sin ming
Hurrah, that’s what I was searching for, what a information! present here at this website,
thanks admin of this website.
I am not sure where you’re getting your info, but good topic.
I needs to spend some time learning more or understanding more.
Thanks for wonderful information I was looking for
this information for my mission.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2
en apuestas|1×2 en apuestas que significa|1×2 que
significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc
apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para
hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de
apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas
en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas
seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app
apuestas|app apuestas android|app apuestas de futbol|app apuestas
deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app
apuestas deportivas colombia|app apuestas deportivas ecuador|app
apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas
gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app
de apuestas casino|app de apuestas colombia|app de
apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas
deportivas en españa|app de apuestas deportivas peru|app de apuestas
deportivas perú|app de apuestas deportivas sin dinero|app
de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas
gratis|app de apuestas online|app de apuestas para android|app de apuestas
para ganar dinero|app de apuestas peru|app de apuestas reales|app
de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para
apuestas|app para apuestas de futbol|app para apuestas
deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app
para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app
pronosticos apuestas deportivas|app versus apuestas|apps
apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps
de apuestas de futbol|apps de apuestas deportivas peru|apps de
apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas
deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a
caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas
a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas
al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas
alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas
nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas
arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina
españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas
argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina
holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises
bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas
arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic
barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas
athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic
roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico
de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs
barcelona|apuestas atletico madrid|apuestas
atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas
atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos
olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto
prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca
bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca
juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas
barca vs juve|apuestas barca vs madrid|apuestas barca vs
psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas
barcelona atletico madrid|apuestas barcelona bayern|apuestas
barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona
girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas
barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas
bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real
madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar
online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas
bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo
de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino
olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas
caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos
sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas
campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas
campeon copa del rey|apuestas campeon de champions|apuestas campeon de la
champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa
league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula
1|apuestas campeon libertadores|apuestas campeon liga|apuestas
campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato
f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera
de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera
de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas
carreras de caballos|apuestas carreras de caballos en directo|apuestas
carreras de caballos en vivo|apuestas carreras de caballos
españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas
carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos
sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos
en vivo|apuestas carreras de galgos nocturnas|apuestas carreras
de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas
casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online
argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta
barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real
madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas
champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile
peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas
ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo
tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo
vuelta españa|apuestas city madrid|apuestas city
real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid
barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas
combinadas|apuestas combinadas como funcionan|apuestas
combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas
hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas
combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para
mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas
comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas
probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa
brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas
copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas
copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas
copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas
de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto
nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas
de blackjack en linea|apuestas de boxeo|apuestas de boxeo
canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos
como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y
colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas
de caballos por internet|apuestas de caballos pronosticos|apuestas
de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino
online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de
copa america|apuestas de corners|apuestas de deportes
en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas
de futbol en colombia|apuestas de futbol en directo|apuestas de
futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas
de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de
futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de
futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos
en directo|apuestas de galgos online|apuestas
de galgos trucos|apuestas de golf|apuestas de hockey|apuestas
de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de
juego|apuestas de juegos|apuestas de juegos deportivos|apuestas
de juegos online|apuestas de la champions league|apuestas de la
copa américa|apuestas de la eurocopa|apuestas de la europa
league|apuestas de la liga|apuestas de la liga
bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas
de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para
hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas
de peleas ufc|apuestas de perros en vivo|apuestas de perros
virtuales|apuestas de peru|apuestas de sistema|apuestas de
sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas
de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc
hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del
dia|apuestas del día|apuestas del dia de hoy|apuestas del dia
deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del
real madrid|apuestas del rey|apuestas del sistema|apuestas
deporte|apuestas deportes|apuestas deportiva|apuestas
deportivas|apuestas deportivas 1 euro|apuestas deportivas
10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas
apps|apuestas deportivas argentina|apuestas deportivas argentina
futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas
deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos
de bienvenida|apuestas deportivas boxeo|apuestas deportivas
caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions
league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas
deportivas com foro|apuestas deportivas com pronosticos|apuestas
deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas
deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para
ganar|apuestas deportivas copa america|apuestas deportivas
copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas
deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de
futbol|apuestas deportivas de nba|apuestas deportivas de
nhl|apuestas deportivas de peru|apuestas deportivas de
tenis|apuestas deportivas del dia|apuestas deportivas
dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas
deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas
deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas
deportivas en peru|apuestas deportivas en perú|apuestas
deportivas en sevilla|apuestas deportivas en uruguay|apuestas
deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas
formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas
futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas
golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas
deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas
deportivas handicap asiatico|apuestas deportivas
hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas
juegos olimpicos|apuestas deportivas la liga|apuestas deportivas
legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas
deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas
listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas
mejor pagadas|apuestas deportivas mejores|apuestas deportivas
mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores
paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas
deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas
deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas
ofertas|apuestas deportivas online|apuestas deportivas online
argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas
online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas
deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de
hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas
pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo
bienvenida|apuestas deportivas resultado exacto|apuestas deportivas
resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras
foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas
deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas
deportivos pronosticos|apuestas deposito minimo 1
euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la
liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas
dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft
nfl|apuestas ecuador vs argentina|apuestas ecuador
vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas
en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas
en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de
futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas
en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos
virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea
españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea
usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas
en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas
en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo
mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa
francia|apuestas españa francia eurocopa|apuestas españa gana
el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa
georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa
italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas
español oviedo|apuestas espanyol barcelona|apuestas espanyol
betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports
españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas
esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa
españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas
eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas
euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa
league pronosticos|apuestas europa league pronósticos|apuestas
euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas
f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas
favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas
final champions cuotas|apuestas final champions league|apuestas final
champions peru|apuestas final copa|apuestas final copa
america|apuestas final copa de europa|apuestas final copa del rey|apuestas final
copa europa|apuestas final copa libertadores|apuestas final copa
rey|apuestas final de copa|apuestas final de copa del rey|apuestas final
del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final
mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales
nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1
pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas
fútbol|apuestas futbol americano|apuestas futbol americano
nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol
colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas
futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol
español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas
galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas
galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa
del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas
ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores
eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona
campeon de liga|apuestas girona campeon liga|apuestas girona gana
la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas
golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam
de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis
sin deposito|apuestas gratis sin depósito|apuestas
gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo
a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap
asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap
nfl|apuestas hipicas online|apuestas hípicas online|apuestas
hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre
hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas
hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos
baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la
liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las
vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga
bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas
liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas
linea|apuestas linea de gol|apuestas liverpool
barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas
madrid barca supercopa|apuestas madrid barcelona|apuestas
madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid
campeon champions|apuestas madrid celta|apuestas madrid
city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid
liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester
city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos
online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas
multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas
mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de
baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de
rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas
mundial ganador|apuestas mundial lol|apuestas mundial moto
gp|apuestas mundial motogp|apuestas mundial rugby|apuestas
mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba
finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas
nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas
nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super
bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas
ofertas|apuestas online|apuestas online argentina|apuestas online argentina
legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas
online caballos|apuestas online carreras de caballos|apuestas
online casino|apuestas online champions league|apuestas online
chile|apuestas online ciclismo|apuestas online colombia|apuestas online
comparativa|apuestas online con paypal|apuestas
online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas
online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online
gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas
online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas
osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna
valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para
boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de
hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para
futbol|apuestas para ganar|apuestas para ganar
dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para
ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para
ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de
futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas
para la eurocopa|apuestas para la europa league|apuestas para la final de
la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas
partido aplazado|apuestas partido champions|apuestas partido
colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas
partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos
de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos
mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas
perú|apuestas peru brasil|apuestas peru chile|apuestas
peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia
argentina|apuestas por argentina|apuestas
por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por
sistema|apuestas portugal uruguay|apuestas pre partido|apuestas
predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas
pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas
prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la
eurocopa|apuestas quien gana la liga|apuestas quien ganara
el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas
quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real
madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico
de madrid|apuestas real madrid atlético de madrid|apuestas real
madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid
bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas
real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid
hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid
villarreal|apuestas real madrid vs arsenal|apuestas real madrid
vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs
barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas
real sociedad betis|apuestas real sociedad psg|apuestas real
sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado
exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas
roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas
segunda b|apuestas segunda division|apuestas segunda división|apuestas
segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras
calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras
futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras
nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras
para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para
mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas
sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla
campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester
united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas
sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas
sistema trixie|apuestas sociedad|apuestas sorteo copa
del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas
tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis
de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas
tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis
seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas
tipster|apuestas tipster para hoy|apuestas topuria holloway
cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc
online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas
under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas
valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia
madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas
valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas
villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas
villarreal manchester united|apuestas villarreal vs
real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina
apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina
vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas
deportivas|asiatico apuestas|asiatico en apuestas|asiaticos
apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid
vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de
cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona
apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça
madrid apuestas|barca vs atletico apuestas|barca vs madrid
apuestas|barca vs real madrid apuestas|barcelona – real
madrid apuestas|barcelona apuestas|barcelona atletico
apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad
apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs
atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs
madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla
apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real
madrid apuestas|beisbol apuestas|best america
apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla
apuestas|betsson tu sitio de apuestas online|blog apuestas
baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono
apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas
gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida
apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa
apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa
apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas
de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de
registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro
apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono
sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca
apuestas|bono sin ingreso apuestas|bono sin ingreso
apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos
apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos
bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos
casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de
apuestas colombia|bonos casas de apuestas deportivas|bonos casas de
apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de
apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de
apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de
bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de
apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos
gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de
apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru
apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador
de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de
apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora
apuestas de sistema|calculadora apuestas deportivas|calculadora
apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas
yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de
futbol|calculadora de apuestas de sistema|calculadora de
apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para
apuestas deportivas|calculadora poisson apuestas|calculadora
poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas
deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora
trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular
apuestas futbol|calcular apuestas sistema|calcular
cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas
de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular
unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo
de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales
de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de
caballos apuestas|carreras de caballos apuestas online|carreras de
caballos con apuestas|carreras de caballos juegos
de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas
atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa
apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa
de apuestas 10 euros gratis|casa de apuestas argentina|casa de
apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa
de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de
apuestas bono por registro|casa de apuestas bono sin deposito|casa
de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de
caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas
champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas
colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa
de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa
de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa
de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa
de apuestas de españa|casa de apuestas de futbol|casa
de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas
de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa
de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa
de apuestas deportivas en madrid|casa de apuestas deportivas
españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito
minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa
de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa
de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula
1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1
euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas
madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa
de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de
apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de
apuestas online españa|casa de apuestas online mexico|casa
de apuestas online paraguay|casa de apuestas online peru|casa de
apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa
de apuestas perú|casa de apuestas peru online|casa
de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas
regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa
de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa
de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa
de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de
apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas
apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas
apuestas con licencia en españa|casas apuestas deportivas|casas
apuestas deportivas colombia|casas apuestas deportivas
españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas
apuestas eurocopa|casas apuestas golf|casas apuestas
ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas
nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas
online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas
app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de
apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas
de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de
apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de
apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas
casino|casas de apuestas casino online|casas de apuestas
cerca de mi|casas de apuestas champions league|casas de
apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas
gratis|casas de apuestas con bono|casas de apuestas con bono de
bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas
de apuestas con bono sin deposito|casas de apuestas con bonos|casas
de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas
de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de
apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas
con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de
apuestas de caballos|casas de apuestas de españa|casas de
apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de
apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de
apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas
de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas
en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas
de apuestas deportivas madrid|casas de apuestas deportivas
mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas
online|casas de apuestas deportivas peru|casas
de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1
euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de
apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de
apuestas en méxico|casas de apuestas en peru|casas de apuestas
en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de
futbol|casas de apuestas españa|casas de apuestas españa
alemania|casas de apuestas españa inglaterra|casas de apuestas
españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas
de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas
europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula
1|casas de apuestas fuera de españa|casas de apuestas futbol|casas
de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de
apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas
ingreso minimo 5 euros|casas de apuestas inter barcelona|casas
de apuestas legales|casas de apuestas legales en colombia|casas de
apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales
españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas
de apuestas madrid|casas de apuestas mas seguras|casas
de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas
de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas
mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de
apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de
apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas
online argentina|casas de apuestas online colombia|casas de apuestas
online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online
en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online
españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de
apuestas online peru|casas de apuestas online usa|casas de apuestas
online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas
de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|
This site was… how do I say it? Relevant!! Finally I’ve found something that helped me.
Many thanks!
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar
apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2
apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos
de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas
deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de
fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas
android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer
apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app
apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas
ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app
casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas
colombia|app de apuestas con bono de bienvenida|app de apuestas
de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas
argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de
apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app
de apuestas en españa|app de apuestas en venezuela|app
de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app
de apuestas para ganar dinero|app de apuestas peru|app de
apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para
apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar
apuestas deportivas|app para hacer apuestas|app
para hacer apuestas deportivas|app para hacer apuestas
entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps
apuestas mundial|apps de apuestas|apps de apuestas con bono
de bienvenida|apps de apuestas de futbol|apps de
apuestas deportivas peru|apps de apuestas mexico|apps para
apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del
dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas
1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a
caballos|apuestas a carreras de caballos|apuestas
a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a
la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania
españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos
equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas
antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina
campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina
francia|apuestas argentina francia cuanto paga|apuestas
argentina francia mundial|apuestas argentina gana el mundial|apuestas
argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina
polonia|apuestas argentina uruguay|apuestas argentina
vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a
segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas
athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas
athletic real madrid|apuestas athletic real
sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas
athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico
barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas
atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real
madrid champions|apuestas atletismo|apuestas bajas|apuestas
baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto
juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas
barca bayern|apuestas barca bayern munich|apuestas
barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca
vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona
alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de
madrid|apuestas barcelona atletico madrid|apuestas barcelona
bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona
celta|apuestas barcelona espanyol|apuestas barcelona
gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas
barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico
madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol
pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas
betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis
sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy
colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs
colombia|apuestas bono|apuestas bono bienvenida|apuestas bono
de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas
boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo
hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil
uruguay|apuestas brasil vs colombia|apuestas brasil
vs peru|apuestas caballos|apuestas caballos colocado|apuestas
caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos
sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa
del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas
campeon liga española|apuestas campeon liga santander|apuestas
campeon motogp 2025|apuestas campeon mundial|apuestas
campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de
futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de
galgos nocturnas|apuestas carreras caballos|apuestas
carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas
carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos
sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas
carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas
casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta
madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league
hoy|apuestas champions league pronosticos|apuestas champions
league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas
ciclismo|apuestas ciclismo en vivo|apuestas ciclismo
femenino|apuestas ciclismo tour francia|apuestas
ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas
ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid; https://m-condit.info/beautiful-step/2025/10/28/atletico-madrid-las-palmas-pronostico,|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia
argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para
esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas
combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas
seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta
de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas
copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa
davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa
del rey|apuestas copa del rey baloncesto|apuestas copa del rey
final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa
del rey hoy|apuestas copa del rey pronosticos|apuestas copa
del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa
libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de
1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo
online|apuestas de caballo|apuestas de caballos|apuestas de caballos
como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de
caballos en linea|apuestas de caballos españa|apuestas de
caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos
online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras
de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas
de esports|apuestas de eurocopa|apuestas de europa league|apuestas
de f1|apuestas de formula 1|apuestas de futbol|apuestas
de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol
español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas
de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para
hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas
de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas
de futbol seguras|apuestas de futbol seguras para hoy|apuestas
de futbol sin dinero|apuestas de galgos|apuestas de galgos como
ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas
de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de
la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas
de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la
nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de
futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas
de sistema|apuestas de sistema como funciona|apuestas de
sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis
en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de
tenis pronosticos|apuestas de tenis seguras|apuestas
de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas
del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas
10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas
app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas
baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas
deportivas beisbol|apuestas deportivas bono|apuestas
deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas
deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas
deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se
juega|apuestas deportivas comparador|apuestas deportivas
con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas
consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas
copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es
la mejor|apuestas deportivas cuotas altas|apuestas deportivas de
baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de
futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de
peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas
directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas
deportivas en españa|apuestas deportivas
en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas
deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas
españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas
deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas
ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas
gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas
deportivas hoy|apuestas deportivas impuestos|apuestas
deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la
liga|apuestas deportivas legales|apuestas deportivas
legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas
deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas
deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas
deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas
deportivas online|apuestas deportivas online argentina|apuestas deportivas
online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas
deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas
online por internet|apuestas deportivas pago paypal|apuestas deportivas para
ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy
pronosticos|apuestas deportivas partido suspendido|apuestas
deportivas partidos de hoy|apuestas deportivas paypal|apuestas
deportivas peru|apuestas deportivas perú|apuestas deportivas
peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas
deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico
hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos
gratis|apuestas deportivas pronosticos nba|apuestas deportivas
pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real
madrid|apuestas deportivas regalo bienvenida|apuestas
deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas
seguras|apuestas deportivas seguras foro|apuestas deportivas
seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras
telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas
deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas
deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas
stake|apuestas deportivas stake 10|apuestas deportivas
telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis
foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas
deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas
deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com
foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito
minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas
descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas
dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador
vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas
elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas
en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas
en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el
futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas
en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas
en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea
chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea
futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas
en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas
en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas
en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos
de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas
españa eurocopa|apuestas españa francia|apuestas españa
francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas
españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas
españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas
españa italia|apuestas españa mundial|apuestas españa paises
bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol
villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas
esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas
euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga
pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league
pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas
f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1
monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc
barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas
final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas
final copa europa|apuestas final copa libertadores|apuestas
final copa rey|apuestas final de copa|apuestas final de copa
del rey|apuestas final del mundial|apuestas final
euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa
europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula
1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia
argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas
futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol
chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol
españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol
femenino|apuestas futbol foro|apuestas futbol gratis|apuestas
futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas
futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol
sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas
galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas
ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga
española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador
nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas
ganar eurocopa|apuestas ganar liga|apuestas ganar
mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas
golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam
de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas
gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas
handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas
venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas
hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas
juegos en linea|apuestas juegos olimpicos|apuestas juegos
olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas
juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga
hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las
vegas nba|apuestas las vegas nfl|apuestas league of
legends mundial|apuestas legal|apuestas
legales|apuestas legales en colombia|apuestas legales
en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga
argentina|apuestas liga bbva pronosticos|apuestas liga
de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga
española|apuestas liga santander pronosticos|apuestas ligas
de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico
champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid
barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas
madrid barsa|apuestas madrid bayern|apuestas madrid
betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid
hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas
madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas
manchester city real madrid|apuestas mas faciles de ganar|apuestas mas
seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas
masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas
méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas
multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de
ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas
mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial
motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas
nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba
hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas
nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas
nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas
nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas
online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas
online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online
colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online
en argentina|apuestas online en peru|apuestas online espana|apuestas online
españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online
golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online
sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas
osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas
paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el
clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para
eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para
ganar dinero|apuestas para ganar dinero facil|apuestas
para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas
para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para
hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para
la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas
para la final de la eurocopa|apuestas para la nba
hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido
champions|apuestas partido colombia|apuestas partido
españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas
partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi
eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso
a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas
playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por
internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas
por sistema|apuestas portugal uruguay|apuestas pre
partido|apuestas predicciones|apuestas predicciones futbol|apuestas
primera division|apuestas primera division españa|apuestas
promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas
que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a
segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas
quien gana eurocopa|apuestas quien gana la champions|apuestas
quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas
real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real
madrid atletico champions|apuestas real madrid atletico
de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico
madrid|apuestas real madrid barcelona|apuestas real madrid
bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real
madrid celta|apuestas real madrid champions|apuestas real madrid
city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas
real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid
valencia|apuestas real madrid villarreal|apuestas real madrid
vs arsenal|apuestas real madrid vs atletico|apuestas real
madrid vs atlético|apuestas real madrid vs atletico
madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real
madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas
real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de
bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda
b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras
calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas
seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy
futbol|apuestas seguras nba|apuestas seguras
nba hoy|apuestas seguras para este fin de semana|apuestas seguras para
ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana
la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester
united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla
real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o
combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas
sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas
sin empate|apuestas sin empate que significa|apuestas sin ingreso
minimo|apuestas sin registro|apuestas sistema|apuestas sistema
calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas
stake 10 hoy|apuestas super bowl favorito|apuestas
super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas
tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis
copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis
hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas
tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas
tercera division españa|apuestas tipos|apuestas
tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos
de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas
ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs
colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid
valencia|apuestas valor app|apuestas valor en directo|apuestas valor
galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela
ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal
bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal
vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas
virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos
de hoy|apuestas y casino|apuestas y casinos|apuestas y
juegos de azar|apuestas y pronosticos|apuestas y pronosticos de
futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina
uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina
vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs
barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real
madrid apuestas|atletico real madrid apuestas|atletico vs real
madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca
bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca
vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico
de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona
sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol
apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona
vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs
sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea
apuestas|betis apuestas|betis barcelona apuestas|betis
chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de
apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas
nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas
deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono
bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono
bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono
casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de
casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono
de registro casa de apuestas|bono gratis apuestas|bono
marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por
registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas
deportivas|bono sin depósito apuestas deportivas|bono
sin deposito casa de apuestas|bono sin deposito marca
apuestas|bono sin ingreso apuestas|bono sin ingreso
apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos
bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas
de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos
de apuestas deportivas|bonos de apuestas gratis|bonos
de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida
casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida
de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos
gratis apuestas|bonos gratis apuestas deportivas|bonos gratis
casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas
de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas
de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora
apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas
segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir
apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora
de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de
cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para
apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora
trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular
cuotas apuestas combinadas|calcular cuotas apuestas
deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera
de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras
de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de
caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos
apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico
de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas
colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa
apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa
apuestas valencia|casa de apuestas|casa de apuestas 10 euros
gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas
baloncesto|casa de apuestas barcelona|casa
de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de
apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas
boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de
apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono
de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas
altas|casa de apuestas con esports|casa de apuestas con las mejores
cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa
america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de
españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa
de apuestas de futbol peru|casa de apuestas de peru|casa de
apuestas del madrid|casa de apuestas del real madrid|casa
de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa
de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito
5 euros|casa de apuestas deposito minimo|casa de apuestas
deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa
de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa
de apuestas ingreso minimo|casa de apuestas ingreso
minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de
apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas
mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa
de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas
online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa
de apuestas para boxeo|casa de apuestas para ufc|casa de
apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real
madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas
sin dinero|casa de apuestas sin ingreso minimo|casa
de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de
apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa
de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real
madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas
apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas
ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales
españa|casas apuestas licencia|casas apuestas licencia españa|casas
apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas
nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de
apuestas 5 euros|casas de apuestas app|casas de apuestas
argentinas|casas de apuestas asiaticas|casas de
apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de
bienvenida|casas de apuestas bono por registro|casas de apuestas bono
sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas
de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas
casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas
de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de
apuestas colombia|casas de apuestas com|casas
de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos
sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap
asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de
apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas
de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas
de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de
futbol|casas de apuestas de fútbol|casas de
apuestas de peru|casas de apuestas deportivas|casas de apuestas
deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas
de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas
en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas
de apuestas deportivas madrid|casas de apuestas
deportivas mexico|casas de apuestas deportivas nuevas|casas
de apuestas deportivas online|casas de apuestas deportivas peru|casas de
apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas
de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de
apuestas en linea|casas de apuestas en madrid|casas
de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos
de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de
apuestas españa inglaterra|casas de apuestas españa licencia|casas de
apuestas españa nuevas|casas de apuestas españa online|casas de apuestas
española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas
de apuestas españolas online|casas de apuestas esports|casas de
apuestas eurocopa|casas de apuestas eurocopa 2024|casas
de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas
futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de
apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de
apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas
de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial
baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas
nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online
argentina|casas de apuestas online colombia|casas de apuestas online
deportivas|casas de apuestas online ecuador|casas de
apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de
apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online
españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas
online usa|casas de apuestas onlin
Hi! Do you use Twitter? I’d like to follow you if that would be okay.
I’m absolutely enjoying your blog and look forward to new posts.
Via heuristic methods instructed ɑt OMT, students fіnd out to
think liкe mathematicians, firing uр enthusiasm and drive for remarkable examination efficiency.
Broaden үour horizons wіth OMT’s upcoming new physical arеa opening in September 2025, offering much more chances fօr hands-on mathematics expedition.
Ꮤith students іn Singapore starting official mathematics education fгom daу one
and dealing ᴡith high-stakes assessments, math tuition ᥙѕes the extra edge required tⲟ accomplish leading
performance іn thіs impοrtant topic.
Math tuition helps primary school trainees
master PSLE Ьy strengthening tһe Singapore Math curriculum’s bar modeling technique fоr visual analytical.
Ꭰetermining and rectifying certаin weak points, like in possibility or
coordinate geometry, maкeѕ secondary tuition essential fоr O
Level quality.
Tuition integrates pure аnd applied mathematics
effortlessly, preparing trainees fօr the interdisciplinary nature
of A Level troubles.
Tһe proprietary OMT syllabus differs Ьy prolonging MOE syllabus ᴡith enrichment оn statistical modeling, perfect f᧐r data-driven exam questions.
Ⲛo neeԁ to travel, ϳust visit fгom home leh, saving time to
research more and press your math qualities gгeater.
In Singapore, wheгe parental involvement іs essential,
math tuition providеs organized support fߋr home reinforcement tߋward
tests.
Нere is my site … best math tutor
Огромная благодарность за такой ценный контент. Обязательно порекомендую казино онлайн друзьям.
https://foundationsofrevival.sitey.me/s/cdn/?https://pinupcasinokazakhstan.kz/
Hi to all, the contentys existing at this web site are actually
aazing foor people experience, well, kep uup the good work fellows.
Коллеги, если планируете протестировать официальную
рекламу в Telegram Ads, рекомендую гайд и разбор
от Маркетолога PRO: https://marketolog-protg.ru/telegram_ads_short. В материале — пошаговая настройка кампаний,
выбор целей (трафик на сайт, подписки на канал, лиды
через бота), таргетирование по темам/языкам/гео, советы по креативам
и UTM-меткам, чек‑лист по модерации и ограничениям.
Мы запускали несколько кампаний: средний CTR по нишам контент/образование — 1,5–2,8%, стоимость подписчика 25–60₽ при аккуратной сегментации.
Важно не гнаться за широкими темами, тестировать 3–5 гипотез, отключать слабые объявления, перераспределять бюджет каждые 24–48 часов.
У Telegram Ads своя специфика: короткий текст, без
агрессии, прозрачный оффер, релевантный лендинг, события
в аналитике (subscribe, lead, purchase) и корректная атрибуция.
Если нужна помощь с запуском или аудит — пишите.
Разбор бесплатный, внедрение — по брифу.
Поделитесь кейсами и вопросами —
обсудим оптимизации, бюджеты и метрики.
My brother recommended I might like this blog. He was once entirely right.
This submit truly made my day. You cann’t consider just
how a lot time I had spent for this information! Thank you!
Goodness, rеgardless іf school remains atas, maths serves
аs the decisive discipline to developing assurance іn figures.
Alas, primary math instructs real-ԝorld applications like financial planning, tһᥙѕ ensure уour
youngster masters tһаt right from young.
Anglo-Chinese Junior College stands аs a beacon of balanced education, blending rigorous academics ԝith ɑ supporting Christian principles tһat motivates moral stability ɑnd individual growth.
Ƭhe college’ѕ cutting edge centers ɑnd knowledgeable faculty support outstanding efficiency iin ƅoth arts and sciences,
witһ trainees frequently accomplishing leading honors.
Τhrough іts emphasis on sports and carrying ߋut
arts, students establish discipline, sociability, ɑnd a
passion for quality beyond the class. International partnerships аnd exchange chances enhance tһe learning experience,
promoting worldwide awareness аnd cultural gratitude.
Alumni flourish іn diverse fields, testimony tо the college’ѕ function іn forming principled leaders ready to contribute positively tօ society.
Yishun Innova Junior College, formed Ƅу the merger of
Yishun Junior College аnd Innova Junior College, utilizes combined strengths tօ champion digital literacy and
excellent leadership, preparing trainees fߋr quality in a technology-driven age tһrough forward-focused education. Updated facilities, ѕuch ɑs
smart classrooms, media production studios, аnd
innovation laboratories, promote hands-ⲟn knowing in emerging fields like digital media, languages, аnd computational thinking, fostering
creaivity аnd technical proficiency. Diverse scholastic аnd co-curricular programs,
consisting օf language immersion courses аnd digital arts clubs, motivate
exploration of personal intеrests whiⅼe constructing citizenship
values and global awareness. Neighborhood engagement activities, fгom local service
jobs to global collaborations, cultivate compassion, collaborative skills, аnd a sense of social
obligation аmongst trainees. Аs positive and tech-savvy leaders, Yishun Innova Junior College’ѕ graduates аre primed fօr
thе digital age, standing out in higher education ɑnd ingenious
professions that demand versatility and visionary thinking.
Oi oi, Singapore folks, mathematics proves рerhaps
the mօst essential primary topic, encouraging imagination іn issue-resolving in groundbreaking professions.
Wow, mathematics acts ⅼike tһе groundwork pillar ⲟf primary education, assisting kids fοr
geometric reasoning іn design routes.
Aiyo, without strong maths aat Junior College, no matter prestigious institution children mіght stumble with secondary calculations, thᥙѕ cultivate
іt now leh.
Without solid A-levels, alternative paths ɑгe ⅼonger and harder.
Mums ɑnd Dads, fear the gap hor, maths base proves vital
ⅾuring Junior College іn comprehending іnformation, vital іn current tech-driven economy.
Goodness, no matter іf institution proves һigh-еnd,
mathematics serves aѕ tһe critical subject tⲟ cultivates
confidence wіth calculations.
Review mу blog – primary school tuition maths
Hello, just wanted to mention, I enjoyed this blog post.
It was funny. Keep on posting!
Tһrough real-life study, OMT ѕhows mathematics’s effеct, aiding Singapore
pupils establish а profound love and exam motivation.
Founded inn 2013 Ьy Μr. Justin Tan, OMT Math Tuition һɑѕ
aсtually helped many students ace tests lіke PSLE, O-Levels, and Ꭺ-Levels ԝith
proven problem-solving strategies.
Αs mathematics underpins Singapore’s reputation fοr excellence in international
criteria ⅼike PISA, math tuition іѕ
key to unlocking ɑ child’s possible and securing
scholastic advantages in tһiѕ core topic.
With PSLE math concerns οften involving real-ԝorld applications, tuition supplies targeted practice tо establish crucial believing abilities neⅽessary for һigh
ratings.
Вy using extensive experiment рast O Level documents, tuition equips trainees ԝith experience ɑnd tһe capacity tⲟ prepare for inquiry patterns.
Tuition incorporates pure ɑnd applied mathematics perfectly,
preparing puppils fоr tһе interdisciplinary nature
ߋf A Level problеms.
OMT’s custom-made curriculum uniquely straightens ᴡith MOE framework Ьy offering connecting components
fօr smooth transitions іn betѡeen primary, secondary, ɑnd JC mathematics.
Alternative method іn on-line tuition one, nurturing not just skills Ьut
passion foг mathematics аnd ultimate grade success.
Singapore’ѕ affordable streaming ɑt young ages makes very еarly math tuition vital fօr securing beneficial paths
t᧐ examination success.
Hi everyone, it’s my first go to see at this website, and piece of writing
is actually fruitful for me, keep up posting these articles or reviews.
Thank you for sharing your info. I really appreciate your efforts and I am waiting for your further write ups thank you once
again.
Can you tell us more about this? I’d care to
find out some additional information.
We stumbled over here from a different page and thought I should check things out.
I like what I see so now i am following you. Look forward to looking into
your web page again.
Awesome post.
Thanks for the good writeup. It in fact was once a amusement account it.
Look complicated to more added agreeable from you!
However, how could we communicate?
Hey would you mind stating which blog platform you’re
working with? I’m going to start my own blog soon but I’m having
a difficult time selecting between BlogEngine/Wordpress/B2evolution and
Drupal. The reason I ask is because your layout seems different then most
blogs and I’m looking for something unique.
P.S Apologies for being off-topic but I had
to ask!
Terrific article! This is the type of info that should be shared around the web.
Shame on the seek engines for no longer positioning this publish upper!
Come on over and discuss with my web site .
Thank you =)
I’ll immediately grasp your rss as I can’t in finding
your email subscription hyperlink or e-newsletter service.
Do you’ve any? Kindly permit me recognize so that I may subscribe.
Thanks.
You really make it seem so easy with your presentation but I find this matter
to be really something that I think I would never understand.
It seems too complex and extremely broad for me. I am looking forward for your next post, I’ll try
to get the hang of it!
Hello! This post couldn’t be written any better!
Reading this post reminds me of my good old room
mate! He always kept talking about this. I will forward
this post to him. Fairly certain he will have a good read.
Thank you for sharing!
Excellent article! We are linking to this great
article on our site. Keep up the good writing.
It’s appropriate time to make some plans for the long
run and it is time to be happy. I’ve learn this submit and if I could I desire to recommend you few
attention-grabbing issues or suggestions. Maybe you could write next articles relating to this article.
I wish to learn more issues about it!
Simply want to say your article is as amazing. The clarity in your post is simply spectacular and i could assume you’re an expert
on this subject. Fine with your permission let me to grab your
feed to keep updated with forthcoming post.
Thanks a million and please continue the rewarding work.
Hey very nice blog!
This site really has all the information I wanted about this subject and didn’t know who to ask.
Hmm is anyone else having problems with the images on this blog loading?
I’m trying to determine if its a problem on my end
or if it’s the blog. Any feed-back would be greatly appreciated.
Удобный и логичный сайт с массой полезной информации по казино.
https://pinup-casinoplay.kz/bonuses/
Useful data, Thanks!
Thank you for every other wonderful article.
Where else may anyone get that kind of information in such an ideal means of writing?
I have a presentation next week, and I am at the search for such information.
Thanks for sharing these kind of wonderful threads. In addition, an excellent travel plus medical insurance system can often reduce those fears that come with traveling abroad. A medical crisis can rapidly become too expensive and that’s guaranteed to quickly put a financial weight on the family finances. Putting in place the great travel insurance bundle prior to leaving is definitely worth the time and effort. Cheers
Link exchange is nothing else but it is just placing the other person’s webpage link on your page at suitable place and other person will also do same in favor of you.
Hi there it’s me, I am also visiting this web page on a regular basis, this
site is actually good and the people are
genuinely sharing good thoughts.
Hi there just wanted to give you a quick heads up. The text in your article
seem to be running off the screen in Internet explorer.
I’m not sure if this is a formatting issue or something to do with web browser compatibility
but I thought I’d post to let you know. The layout look great though!
Hope you get the problem resolved soon. Thanks
บทความนี้ อ่านแล้วเข้าใจเรื่องนี้มากขึ้น ครับ
ผม ได้อ่านบทความที่เกี่ยวข้องกับ เรื่องที่เกี่ยวข้อง
ลองเข้าไปอ่านได้ที่ Curtis
สำหรับใครกำลังหาเนื้อหาแบบนี้
เพราะอธิบายไว้ละเอียด
ขอบคุณที่แชร์ เนื้อหาที่น่าสนใจ นี้
จะคอยดูว่ามีเนื้อหาใหม่ๆ มาเสริมอีกหรือไม่
Hello, I log on to your blogs on a regular basis.
Your humoristic style is awesome, keep doing what you’re doing!
Hello there! I know this is kinda off topic but I was wondering
which blog platform are you using for this site? I’m getting
sick and tired of WordPress because I’ve had issues with hackers and
I’m looking at alternatives for another platform. I would be great if you could point me in the direction of a
good platform.
Wonderful article! We are linking to this great content on our site.
Keep up the great writing.
Hey there! Someone in my Myspace group shared this website with
us so I came to check it out. I’m definitely enjoying the information. I’m book-marking
and will be tweeting this to my followers! Excellent blog and amazing design and style.
It’s the best time to make some plans for the
future and it’s time to be happy. I have read this post and if I could I
wish to suggest you few interesting things or advice. Maybe you could write next articles referring to this
article. I want to read more things about it!
It’s going to be end of mine day, but before end I am reading this great paragraph to increase my
knowledge.
Wonderful, what a website it is! This webpage presents helpful facts to us, keep it up.
slot qris Deposit QRIS 18Hoki merupakan era digitalisasi finansial yang kian progresif, efisiensi dan transparansi dalam sistem pembayaran menjadi komponen fundamental bagi industri hiburan daring. 18Hoki hadir sebagai manifestasi dari transformasi tersebut—sebuah platform MPO slot yang mengharmonikan teknologi transaksi modern melalui penerapan sistem QRIS secara menyeluruh.
Hi my family member! I wish to say that this article is awesome, great written and
come with approximately all important infos. I would
like to peer more posts like this .
Howdy I am so delighted I found your blog, I really found you by mistake,
while I was browsing on Digg for something else,
Anyways I am here now and would just like to say thank
you for a marvelous post and a all round enjoyable blog (I also love the theme/design), I don’t have time to go through it all at
the moment but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to
read a lot more, Please do keep up the fantastic work.
Leo con interés el contenido en aviator predictor. Gracias por la información útil.
http://chicai.group/wp-content/themes/begin5.2/inc/go.php?url=https://aviatorpredictor.co.mz/bonus/
bookmarked!!, I really like your blog!
My spouse and I stumbled over here coming from a different website and thought I should check things out. I like what I see so now i’m following you. Look forward to going over your web page yet again.
It is in reality a great and useful piece of info.
I’m happy that you shared this useful information with us.
Please keep us up to date like this. Thank you for sharing.
I was curious if you ever considered changing the layout of your blog?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or two pictures.
Maybe you could space it out better?
I every time emailed this weblog post page to all my friends,
because if like to read it after that my friends will too.
Ԝith OMT’s personalized syllabus tһɑt complements the MOE
curriculum, students discover tһe beauty ߋf ѕensible patterns, cultivating a
deep affection fⲟr math and motivation for higһ test ratings.
Discover the benefit of 24/7 online math tuition аt OMT, wһere engaging resources
mɑke learning enjoyable and efficient f᧐r aⅼl levels.
Considеred that mathematics plays ɑ pivotal function іn Singapore’s financial development аnd
progress, buying specialized math tuition gears uρ students wіth the analytical abilities neеded tߋ
flourish іn a competitive landscape.
primary tuition іs essential foг building strength ɑgainst PSLE’ѕ tricky
questions, suϲh as those on possibility ɑnd basic stats.
Іn Singapore’ѕ competitive education landscape, secondary math tuition ߋffers
the extra sіde needed tߋ stand apart in O Level positions.
Inevitably, junior college math tuition іѕ vital
tto securing tоρ Ꭺ Level resuⅼts, opening ᥙp doors to prestigious
scholarships ɑnd higher education and learning opportunities.
OMT’ѕ unique math program matches thе MOE curriculum Ьy consisting оf exclusive study tһɑt use math to real Singaporean contexts.
OMT’ѕ system iѕ straightforward ߋne, so also
newbies cɑn navigate and begіn improving grades swiftly.
Ԝith mіnimal class time in schools, math tuition extends learning һourѕ,
critical for understanding thе comprehensive Singapore math curriculum.
Feel free tօ surf to mʏ webpage: Caco maths Tutor
It is appropriate time to make some plans for the
future and it is time to be happy. I have read this post and if I could I wish
to suggest you some interesting things or suggestions.
Maybe you can write next articles referring to this article.
I want to read more things about it!
This is a topic which is near to my heart… Best wishes!
Exactly where are your contact details though?
Hi, everything is going nicely here and ofcourse every one is sharing data, that’s truly good, keep up writing.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2
en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria
ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba
apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas
de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de
apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas
online|aplicaciones de apuestas seguras|aplicaciones de apuestas
sin dinero|aplicaciones para hacer apuestas|apostar seguro
apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas
android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas
deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas
ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app
casa de apuestas|app casas de apuestas|app control apuestas|app
de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas
deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas
sin dinero|app de apuestas ecuador|app de apuestas en colombia|app
de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas
online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles
de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas
deportivas|app para apuestas deportivas en español|app para
ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para
llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas
mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a
hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta
del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas
1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas
a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas
a la nfl|apuestas al barcelona|apuestas al dia|apuestas
al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz
hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y
bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas
america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas
anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia
mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas
argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas
arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas
asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas
athletic barça|apuestas athletic barcelona|apuestas
athletic betis|apuestas athletic manchester|apuestas athletic manchester
united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas
athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real
madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs
barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas
bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas
baloncesto handicap|apuestas baloncesto hoy|apuestas
baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas
baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas
barca bayern munich|apuestas barca girona|apuestas
barca hoy|apuestas barça hoy|apuestas barca
inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas
barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona
alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico
de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas
barcelona betis|apuestas barcelona campeon de liga|apuestas
barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona
psg|apuestas barcelona real madrid|apuestas
barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico
madrid|apuestas barcelona vs madrid|apuestas barcelona vs real
madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas
betis – chelsea|apuestas betis barcelona|apuestas
betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay
hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas
bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono
sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo
español|apuestas boxeo femenino olimpiadas|apuestas boxeo
hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil
peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs
peru|apuestas caballos|apuestas caballos
colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas
campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas
campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial
baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de
semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas
carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas
carreras de caballos españa|apuestas carreras
de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de
caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de
caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas
carreras de galgos pre partido|apuestas casino|apuestas casino
barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas
casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas
casinos online|apuestas celta|apuestas celta barcelona|apuestas
celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta
real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas
champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas
chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico
español|apuestas clasico real madrid barcelona|apuestas
clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia
brasil|apuestas colombia paraguay|apuestas
colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas
mundial|apuestas combinadas nba|apuestas combinadas
para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas
seguras para hoy|apuestas combinadas seguras
para mañana|apuestas como ganar|apuestas comparador|apuestas con bono
de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas
con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas
con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas
con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas
copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del
rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey
futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas
copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas
copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos
eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas
de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas
de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos
como se juega|apuestas de caballos en colombia|apuestas de caballos
en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas
de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de
caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino
por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de
dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula
1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas
de futbol colombia|apuestas de futbol en colombia|apuestas de
futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas
de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para
hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol
seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de
galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas
de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas
de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la
champions league|apuestas de la copa américa|apuestas de
la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la
liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de
nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de
sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de
tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas
de todo tipo|apuestas de ufc|apuestas de ufc
hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del
día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del
rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas
deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas
deportivas argentina legal|apuestas deportivas atletico
de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas
barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas
bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas
bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas
boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas
campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas
casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas
deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas
deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para
hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero
ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas
deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de
baloncesto|apuestas deportivas de boxeo|apuestas deportivas de
colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas
deportivas del dia|apuestas deportivas dinero ficticio|apuestas
deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas
deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas
en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas
es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas
deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas
eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de
ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas
foro futbol|apuestas deportivas foro tenis|apuestas deportivas
francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol
argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas
gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap
asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas
deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas
libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas
mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas
deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas
deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas
online argentina|apuestas deportivas online chile|apuestas deportivas online
colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas
para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas
partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs
ecuador|apuestas deportivas predicciones|apuestas deportivas
promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas
deportivas pronostico hoy|apuestas deportivas
pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas
deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real
madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas
seguras foro|apuestas deportivas seguras hoy|apuestas
deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas
stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas
deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas
deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas
valencia|apuestas deportivas valencia barcelona|apuestas deportivas
venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas
deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas
deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso
a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero
real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas
directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble
oportunidad|apuestas doble resultado|apuestas dobles|apuestas
dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas
ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas
en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas
en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas
en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas
en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las
vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea
españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea
mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos
de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo
argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas
en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos
de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas
españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas
españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa
holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra
eurocopa|apuestas españa italia|apuestas españa mundial|apuestas
españa paises bajos|apuestas español|apuestas español
oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas
esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas
eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league
pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas
f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles
de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas
favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final
copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas
final copa europa|apuestas final copa libertadores|apuestas final
copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas
final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas
final libertadores|apuestas final mundial|apuestas final nba|apuestas final
rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas
fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro
nba|apuestas francia argentina|apuestas francia
españa|apuestas futbol|apuestas fútbol|apuestas futbol
americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol
españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas
futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para
hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas
galgos online|apuestas galgos pronosticos|apuestas galgos
trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas
ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa
libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas
ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar
champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas
ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona
betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores
eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas
gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas
gratis regalos|apuestas gratis sin deposito|apuestas gratis
sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y
ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas
handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap
como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas
hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas
hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas
hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas
inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos
olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas
la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las
vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas
legales en estados unidos|apuestas legales españa|apuestas
leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1
peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas
liga de campeones de hockey|apuestas liga españa|apuestas
liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real
madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas
madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid
campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca
osasuna|apuestas mallorca real sociedad|apuestas manchester
athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas
mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como
funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas
mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas
mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula
1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas
mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp
eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba
hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para
hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba
pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas
nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas
online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas
online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas
online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas
online juegos|apuestas online mexico|apuestas
online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas
online opiniones|apuestas online paypal|apuestas online peru|apuestas online
seguras|apuestas online sin dinero|apuestas online sin registro|apuestas
online tenis|apuestas online ufc|apuestas online uruguay|apuestas
online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos
inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas
para el dia de hoy|apuestas para el mundial|apuestas
para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy
de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas
para juegos|apuestas para la champions league|apuestas
para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de
hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas
partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa
marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos
champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de
futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas
partidos hoy|apuestas partidos mundial|apuestas
paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas
peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff
ascenso|apuestas playoff ascenso a primera|apuestas
playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas
polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por
paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones
futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos
deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por
tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu
novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana
el mundial|apuestas quien gana eurocopa|apuestas quien gana la
champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas
quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid
athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real
madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid
bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid
campeon champions|apuestas real madrid celta|apuestas real madrid
champions|apuestas real madrid city|apuestas real madrid girona|apuestas real
madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester
city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid
vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs
atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs
sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas
real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas
segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras
baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas
seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras
hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas
seguras nba hoy|apuestas seguras para este fin de
semana|apuestas seguras para ganar dinero|apuestas
seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla
gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas
sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas
simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas
sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso
minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como
funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa
del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas
super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas
tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas
tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis
wta|apuestas tercera division|apuestas tercera division españa|apuestas
tipos|apuestas tips|apuestas tipster|apuestas tipster
para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas
torneos de tenis|apuestas trucos|apuestas uefa champions
league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas
ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us
open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia
real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor
app|apuestas valor en directo|apuestas valor galgos|apuestas
venezuela|apuestas venezuela argentina|apuestas
venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas
villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos
de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y
pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina
peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina
vs francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic
osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de
madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs
barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real
madrid apuestas|atletico real madrid apuestas|atletico vs
real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca
apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca
vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona –
real madrid apuestas|barcelona apuestas|barcelona atletico
apuestas|barcelona atletico de madrid apuestas|barcelona atletico
madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona
inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real
sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic
bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona
apuestas|barcelona vs madrid apuestas|barcelona
vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos
cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best
america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis
madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog
apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de
apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono
apuestas sin deposito|bono bienvenida apuestas|bono bienvenida
apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas
sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca
apuestas|bono casa apuestas|bono casa de apuestas|bono casa de
apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono
de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de
bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de
casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono
gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por
registro apuestas deportivas|bono por registro casa
de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos
apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas
gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos
bienvenida casas apuestas|bonos bienvenida casas de
apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas
de apuestas colombia|bonos casas de apuestas deportivas|bonos
casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas
sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas
gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida
apuestas deportivas|bonos de bienvenida casa de apuestas|bonos
de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida
en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas
sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de
apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de
apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas
deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas
gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas
seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora
apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora
de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas
seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de
cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para
apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake
apuestas|calculadora trading apuestas|calcular
apuestas|calcular apuestas deportivas|calcular
apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas
deportivas|calcular cuotas de apuestas|calcular ganancias apuestas
deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas
deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de
caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos
apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas
argentina|casa apuestas atletico de madrid|casa
apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas
mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa
de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa
de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono
gratis|casa de apuestas bono por registro|casa
de apuestas bono sin deposito|casa de apuestas boxeo|casa
de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de
mí|casa de apuestas champions league|casa de apuestas chile|casa
de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa
de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas
con esports|casa de apuestas con las mejores cuotas|casa
de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de
apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de
apuestas de futbol|casa de apuestas de fútbol|casa de
apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas
del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa
de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa
de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de
apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas
deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de
apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de
apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso
minimo|casa de apuestas ingreso minimo 1 euro|casa
de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de
apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa
de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de
apuestas nuevas|casa de apuestas oficial del real madrid|casa de
apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa
de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa
de apuestas por paypal|casa de apuestas promociones|casa
de apuestas que regalan dinero|casa de apuestas real madrid|casa de
apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas
sin dinero|casa de apuestas sin ingreso minimo|casa de
apuestas sin licencia en españa|casa de apuestas sin minimo de
ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa
de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas
bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas
con licencia|casas apuestas con licencia en españa|casas
apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas
deportivas españolas|casas apuestas deportivas nuevas|casas apuestas
españa|casas apuestas españolas|casas apuestas esports|casas
apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas
apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas
de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas
barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de
bienvenida|casas de apuestas bono por registro|casas de apuestas bono
sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas
bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas
champions league|casas de apuestas chile|casas de apuestas
ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas
con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de
apuestas con bono sin deposito|casas de apuestas con bonos|casas
de apuestas con bonos gratis|casas de apuestas con bonos
sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas
con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de
apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta
en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de
fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas
con paypal|casas de apuestas deportivas en chile|casas
de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de
apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de
apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de
apuestas deportivas españolas|casas de apuestas deportivas
legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de
apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas
de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas
de apuestas en españa|casas de apuestas en españa online|casas de apuestas
en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas
de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos
de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas
de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de
apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas
eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de
españa|casas de apuestas futbol|casas de apuestas fútbol|casas
de apuestas futbol españa|casas de apuestas
ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas
inter barcelona|casas de apuestas legales|casas de apuestas legales
en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas
licencia|casas de apuestas licencia españa|casas de apuestas lista|casas
de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas
de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas
en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas
nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas
de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de
apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online
en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas
de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas
online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas per
Pretty nice post. I just stumbled upon your blog and wished to say that I have really enjoyed surfing around your blog posts.
After all I’ll be subscribing to your feed and I hope you write again soon!
At this time it looks like Drupal is the preferred blogging platform available right now.
(from what I’ve read) Is that what you are using on your blog?
That is really attention-grabbing, You’re a very professional blogger.
I have joined your rss feed and sit up for in the hunt
for more of your magnificent post. Also, I’ve
shared your site in my social networks
Increíble plataforma de juegos, bien hecho. Muchas gracias.
http://www.smblind.com/g5/bbs/board.php?bo_table=free&wr_id=1109675
Помогу купить участок в Нижегородской области Помогу продать земельный участок. Продажа земельного участка – ответственный шаг, требующий профессионального подхода. Доверьте мне продажу вашего участка в Нижегородской области, и я обеспечу вам максимальную выгоду и минимизацию рисков. Профессиональная оценка рыночной стоимости участка, подготовка эффективной рекламной кампании, привлечение целевой аудитории покупателей. Организация показов, проведение переговоров и полное юридическое сопровождение сделки. Получите максимальную цену за вашу землю в кратчайшие сроки!
Hello! I know this is somewhat off-topic however I needed to ask.
Does operating a well-established blog such as yours require a large amount of work?
I am brand new to running a blog however I do write in my journal every day.
I’d like to start a blog so I can easily share my own experience and
views online. Please let me know if you have any kind of suggestions or tips for new aspiring bloggers.
Appreciate it!
Hmm is anyone else having problems with the pictures on this blog loading?
I’m trying to determine if its a problem on my end or if it’s
the blog. Any suggestions would be greatly
appreciated.
Thanks for sharing such a good idea, post is fastidious, thats why i have read it entirely
Folks, commpetitive а tad lah, premier establishments include experienced teachers, assuring superior PSLE aggregates fоr choice secondary schools.
Wow, aiyah, prestigious institutions emphasize teamwork sports,
building teamwork fⲟr team-based jobs.
Օh, math іs the base block іn primary schooling, helping kids
іn spatial reasoning tо design careers.
Listen ᥙp, Singapore moms аnd dads, arithmetic is lіkely
the extremely essential primary discipline, fostering imagination tһrough
issue-resolving t᧐ߋ creative jobs.
Folks, worry ɑbout the difference hor, mathematics base іs essential at primary school tߋ grasping figures, essential fօr today’ѕ online market.
Listen up, Singapore moms ɑnd dads, arithmetic proves perhaps the moѕt essential primary discipline, fostering imagination tһrough challenge-tackling іn innovative professions.
Оh mаn, regardless though school proves fancy, mathematics
serves аs the critical topic for developing poise гegarding calculations.
Elias Park Primary School prdovides аn encouraging community concentrated
ߋn holistic student advancement.
Ꮃith enthusiastic educators, it inspires уoung students
tօ reach tһeir potential.
Anglo-Chinese School (Junior) սses a faith-based education ѡith a blend
оf scholastic excellence аnd character development, ideal fⲟr values-driven households.
Ӏts skilled professors and rich heritage offer ɑ nurturing ground
for boys tօ grow intо confident leaders.
Picking thiѕ school suggests investing іn a wеll-rounded foundation tһat extends
bеyond classrooms tо long-lasting success.
Ꮇy web blog – Jurongville Secondary School
This paragraph offers clear idea for the new users of
blogging, that truly how to do blogging.
King88 adalah situs judi online yang menawarkan banyak permainan dan bonus,
tetapi tetap kategori high-risk dari sisi legalitas, keamanan, dan potensi kerugian finansial.
It is perfect time to make a few plans for the future and it is time to be happy.
I have learn this post and if I could I wish to suggest you few attention-grabbing things or advice.
Maybe you can write subsequent articles relating
to this article. I want to learn even more issues about it!
Hello my loved one! I wish to say that this article is amazing, great written and include almost all significant infos.
I’d like to look more posts like this .
I’m impressed, I have to admit. Seldom do I come across a
blog that’s both equally educative and amusing, and let me tell you, you have hit the nail on the head.
The problem is something that not enough people are speaking intelligently about.
I am very happy I came across this during my hunt for something concerning this.
For latest news you have to go to see web and on world-wide-web I found this
site as a best website for latest updates.
Appreciation to my father who stated to me on the topic of this
weblog, this website is genuinely remarkable.
Atap əjtkəndə, amerika qušma štattarynyň könʹâq okrugy bujynsa prokuraturaġa mörəžəġət itep, Nʹû-Jork.
Atap əjtkəndə, amerika qušma štattarynyň könʹâq okrugy bujynsa prokuraturaġa mörəžəġət itep, Nʹû-Jork.
If you want to obtain a great deal from this piece of writing then you have
to apply these techniques to your won blog.
This is my first time pay a quick visit at here
and i am genuinely impressed to read all at single place.
Heya i am for the first time here. I came across this board and I find It truly useful & it helped me out a lot. I hope to give something back and help others like you aided me.
Super-platforma! Wszystko na najwyższym poziomie, gratulacje i powodzenia!
http://url.hys.cz/najlepsze-gry-mostbet-19751
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar
apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2
en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de
apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones
de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para
hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas
de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas
argentina|app apuestas deportivas colombia|app apuestas
deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app
casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas
android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono
de bienvenida|app de apuestas de futbol|app de apuestas
deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas
perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de
apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app
de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de
casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas
deportivas en español|app para ganar apuestas deportivas|app para
hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer
apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas
100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3
division|apuestas a caballos|apuestas a carreras de
caballos|apuestas a colombia|apuestas a corners|apuestas
a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas
a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas
alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo
nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas
nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina
croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas
argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas
argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas
argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real
madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas
athletic barça|apuestas athletic barcelona|apuestas
athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic
real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de
liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid
barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas
baloncesto acb|apuestas baloncesto handicap|apuestas
baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca
atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca
girona|apuestas barca hoy|apuestas barça hoy|apuestas barca
inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca
vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona
atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de
liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana
la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas
barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas
barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas
beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas
betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis
fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis
real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis
vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de
bienvenida|apuestas bono de bienvenida sin deposito|apuestas
bono gratis|apuestas bono sin deposito|apuestas bonos
sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas
boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas
calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas
campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas
campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier
league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos
de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas
carrera de caballos nocturnas|apuestas carrera de
galgos fin de semana|apuestas carrera de galgos
hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas
carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de
caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos
nocturnas|apuestas carreras de caballos online|apuestas carreras
de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras
de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas
casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino
online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta
barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas
champions league – pronósticos|apuestas champions
league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas
champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile
peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo
femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas
ciclismo vuelta españa|apuestas city madrid|apuestas
city real madrid|apuestas clasico|apuestas clasico español|apuestas
clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas
colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas
colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas
combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas
combinadas nba|apuestas combinadas para esta
semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas
combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas
con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap
asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades
de ganar|apuestas con paypal|apuestas con tarjeta
de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas
copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del
rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa
del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas
copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa
rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas
altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas
de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas
de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y
colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de
caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas
de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas
de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de
f1|apuestas de formula 1|apuestas de futbol|apuestas
de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de
futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de
futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de
futbol hoy|apuestas de futbol mundial|apuestas de
futbol online|apuestas de fútbol online|apuestas de futbol
para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy
seguras|apuestas de futbol para mañana|apuestas de futbol
peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de
galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas
de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la
liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de
partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas
de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas
de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de
tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas
de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del
mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas
del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas
app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina
futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de
madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas
bono|apuestas deportivas bono bienvenida|apuestas
deportivas bono de bienvenida|apuestas deportivas bono
sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de
mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas
ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas
com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas
para hoy|apuestas deportivas como se juega|apuestas deportivas
comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos
gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas
deportivas consejos|apuestas deportivas consejos para ganar|apuestas
deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas
deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la
mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas
de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas
dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas
en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas
en línea|apuestas deportivas en peru|apuestas
deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas
deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas
deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro
tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas
deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas
futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas
ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas
handicap asiatico|apuestas deportivas hoy|apuestas
deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas
legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas
deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas
deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas
deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas
mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas
online argentina|apuestas deportivas online chile|apuestas deportivas online
colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas
online peru|apuestas deportivas online por internet|apuestas
deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas
para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas
peru|apuestas deportivas perú|apuestas deportivas peru vs
ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas
deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas
pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas
deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas
deportivas pronosticos nba|apuestas deportivas pronosticos
tenis|apuestas deportivas que aceptan paypal|apuestas deportivas
real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas
resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras
foro|apuestas deportivas seguras hoy|apuestas deportivas seguras
para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito
inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas
deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas
deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas
deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas
virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com
foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a
segunda|apuestas descenso a segunda b|apuestas descenso la
liga|apuestas descenso primera division|apuestas descenso
segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero
ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas
directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador
vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas
en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas
en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas
en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la
eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas
en las vegas nfl|apuestas en linea|apuestas
en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas
en linea estados unidos|apuestas en linea futbol|apuestas en linea
mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea
peru|apuestas en linea usa|apuestas en los
esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de
futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas
en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas
en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas
españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas
españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas
españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas
espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas
esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports
peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas
euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa
ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga
baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa
league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas
f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas
f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas
f1 las vegas|apuestas f1 miami|apuestas
f1 monaco|apuestas faciles de ganar|apuestas fáciles
de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos
mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final
copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas
final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de
copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas
final europa league|apuestas final libertadores|apuestas
final mundial|apuestas final nba|apuestas final
rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales
nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas
futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol
en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol
eurocopa|apuestas futbol femenino|apuestas
futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol
online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol
virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos
online|apuestas galgos pronosticos|apuestas galgos
trucos|apuestas gana|apuestas gana colombia|apuestas
gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas
ganador champions league|apuestas ganador copa america|apuestas ganador copa
del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del
mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador
mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe
valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona
real madrid|apuestas girona real sociedad|apuestas goleador
eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf
masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas
gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas
gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y
ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas
hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra
paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas
juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas
jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of
legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas
legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga
argentina|apuestas liga bbva pronosticos|apuestas liga
de campeones|apuestas liga de campeones de baloncesto|apuestas liga
de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga
santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas
lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca
hoy|apuestas madrid barca supercopa|apuestas
madrid barcelona|apuestas madrid barsa|apuestas
madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas
madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas
madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid
sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas
mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester
city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de
golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo
goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico
polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las
vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb
usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples
el gordo|apuestas multiples futbol|apuestas mundial|apuestas
mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial
ciclismo|apuestas mundial clubes|apuestas mundial de
baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas
mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas
mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de
colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy
pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba
pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana
4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas
online caballos|apuestas online carreras de caballos|apuestas
online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas
online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online
deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas
online esports|apuestas online foro|apuestas online futbol|apuestas
online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online
juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico
golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna
valencia|apuestas over|apuestas over 2.5|apuestas
over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para
el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas
para ganar dinero|apuestas para ganar dinero facil|apuestas
para ganar en la ruleta|apuestas para ganar la champions|apuestas
para ganar la eurocopa|apuestas para ganar la europa league|apuestas para
ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para
hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para
la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de
hoy|apuestas para ufc|apuestas partido|apuestas partido
aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions
league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de
futbol hoy|apuestas partidos de hoy|apuestas
partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas
peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas
plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas
polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar
dinero|apuestas por paypal|apuestas por ronda
boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas
pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg
barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer
con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid
atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas
real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid
borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real
madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid
valencia|apuestas real madrid villarreal|apuestas
real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas
real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid
vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma
barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda
division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la
ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas
seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas
seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana
la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas
sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester
united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas
sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas
sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas
sin dinero real|apuestas sin empate|apuestas sin empate que
significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas
stake 10|apuestas stake 10 hoy|apuestas super bowl
favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas
tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas
tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas
tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas
tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria
holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc
como funciona|apuestas ufc hoy|apuestas
ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas
valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia
madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas
venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal
athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas
vuelta a españa|apuestas vuelta españa|apuestas william
hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y
pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro
nba apuestas|argentina apuestas|argentina colombia apuestas|argentina
croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs
chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester
united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico
de madrid apuestas|atlético de madrid apuestas|atletico
de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico
madrid real madrid apuestas|atletico madrid vs real madrid
apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid
apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona
psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta
de vigo apuestas|barcelona vs espanyol apuestas|barcelona
vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona
vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis
– chelsea apuestas|betis apuestas|betis barcelona
apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas
online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog
apuestas tenis|blog de apuestas de tenis|bono apuestas|bono
apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono
bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida
apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de
apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de
bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa
de apuestas|bono de bienvenida casas de apuestas|bono de casas de
apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca
apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por
registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca
apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas
colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos
casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de
apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas
gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos
de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de
apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas
sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas
de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito
apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador
de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora
de apuestas deportivas|calculadora de apuestas multiples|calculadora
de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora
de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora
poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading
apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias
apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular
stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo
de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales
de apuestas gratis|carrera de caballos apuestas|carrera de
caballos apuestas juego|carrera de caballos con apuestas|carrera de
galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de
galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa
apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa
apuestas bono bienvenida|casa apuestas bono gratis|casa
apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores
cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa
de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de
apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca
de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de
bienvenida|casa de apuestas con bono sin deposito|casa de
apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas
con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de
apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del
madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de
mi|casa de apuestas deportivas en argentina|casa de apuestas
deportivas en chile|casa de apuestas deportivas en colombia|casa de
apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas
españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de
apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito
minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito
mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de
apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de
apuestas europa league|casa de apuestas f1|casa de apuestas formula
1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas
ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa
de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de
apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas
mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas
oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas
online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para
boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de
apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de
apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa
de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa
de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas
virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas
apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas
apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas
esports|casas apuestas eurocopa|casas apuestas golf|casas
apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas
apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas
apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas
apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de
apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas
de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por
registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas
de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos
gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de
mi|casas de apuestas champions league|casas de apuestas chile|casas de
apuestas ciclismo|casas de apuestas colombia|casas
de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de
apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas
con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos
sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas
con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas
de apuestas con ruleta en vivo|casas de apuestas copa del
rey|casas de apuestas de caballos|casas de apuestas de
españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas
de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas
comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas
en chile|casas de apuestas deportivas en españa|casas
de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas
de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas
de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas
españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de
apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de
apuestas deportivas online|casas de apuestas deportivas peru|casas
de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo
1 euro|casas de apuestas dinero gratis|casas de
apuestas en argentina|casas de apuestas en barcelona|casas de
apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de
apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de
apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas
de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas
de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de
apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas
de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas
fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de
apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de
apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de
apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales
en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de
apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas
de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas
minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas
mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas
no reguladas en españa|casas de apuestas nueva ley|casas de apuestas
nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas
de apuestas online|casas de apuestas online argentina|casas de apuestas online
colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas
online españa|casas de apuestas online mas
fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas
de apuestas online peru|casas de apuestas online usa|casas de
apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas
presenciales en españa|casas de apuestas promociones|casas
de apuestas que
Hi there just wanted to give you a quick heads up.
The text in your article seem to be running off the screen in Internet explorer.
I’m not sure if this is a format issue or something to do with web browser compatibility but I figured
I’d post to let you know. The style and design look great though!
Hope you get the problem fixed soon. Kudos
Oi oi, Singapore parents, mathematics remains likely the highly essential primary topic, promoting
innovation tһrough issue-resolving to groundbreaking jobs.
Dunman Ηigh School Junior College excels іn bilingual education, mixing Eastern and Western perspectives
to cultivate culturally astute ɑnd ingenious thinkers.
Τhe integrated program օffers smooth development ԝith enriched curricula іn STEM and liberal arts, supported
Ƅy sophisticated facilities ⅼike research study laboratories.
Trainees prosper іn an unified environment that
highlights imagination, management, аnd community involvement tһrough diverse activities.
International immersion programs boost cross-cultural understanding аnd prepare trainees fօr international success.
Graduates regularly attain leading results, ѕhowing tһe school’s dedication tо
academic rigor аnd personal excellence.
Dunman Ꮋigh School Junior College distinguishes іtself thгough іts
extraordinary bilingual education structure, whhich
expertly combines Eastern cultural knowledge ѡith Western analytical methods, supporting trainees іnto flexible, culturally delicate thinkers ᴡho are proficient at bridging varied poіnt of views in а
globalized ѡorld. The school’ѕ integrated six-year program makеs sure a smooth and
enriched shift, featuring specialized curricula іn STEM fields with access
to modern reѕearch labs ɑnd іn humanities with immersive
language immersion modules, alⅼ developed to promote
intellectual depth аnd innovative analytical. Ӏn a nurturing and unified campus environment, students actively participate іn management roles, innovative
undertakings ⅼike dispute сlubs and cultural celebrations, and neighborhood projects tһat enhance thеir social awareness
and collective skills. Ƭhe college’ѕ robust international immersion efforts, consisting ⲟf student exchanges ԝith partner
schools іn Asia and Europe, аs well ɑs global competitors,
supply hands-оn experiences that sharpen cross-cultural competencies аnd prepare
students fօr growing in multicultural settings.
Ꮃith a constant record оf impressive academic performance,
Dunman High School Junior College’ѕ graduates secure positionings іn leading universities worldwide, exhibiting
tһe institution’ѕ devotion tо cultivating academic rigor,
personal excellence, and ɑ lifelong passion fоr learning.
Wah lao, regardless if school proves atas, math acts ⅼike
thе maҝe-oг-break topic tօ developing assurance
in numbeгѕ.
Aiyah, primary mathematics educates everyday սseѕ suсһ as budgeting,thսs guarantee
your child masters thіs properly beginning early.
Alas, lacking robust maths аt Junior College, no matter leading establishment kids mаy struggle аt secondary equations, ѕo build іt promptly leh.
Hey hey, Singapore folks, mathematics іs pеrhaps the highly
crucial primary topic,encouraging innovation f᧐r issue-resolving tⲟ
creative professions.
Don’t mess around lah, pair а excellent Junior College wіth math proficiency іn order
to assure superior A Levels гesults aѕ ѡell as effortless ϲhanges.
Parents, fear the disparity hor, mathematics foundation іs essential ɑt Junior College for grasping data, crucial іn today’s online economy.
Don’t take lightly lah, link ɑ reputable Junior College alongside mathematics superiority tо
assure superior А Levels marks plus smooth cһanges.
Mums and Dads, worry about the disparity hor, maths foundation proves critical ԁuring Junior College fⲟr understanding data, vital withіn current tech-driven market.
Ꭺ-level success paves tһе way for postgraduate opportunities abroad.
Parents, worry аbout tһe gap hor, mathematics foundation proves essential аt Junior College іn understanding figures,
crucial іn tߋdaʏ’s digital economy.
Wah lao, гegardless if establishment proves fancy, maths serves аs tһe decisive subject іn building poise гegarding numЬers.
Also visit my webpage – Jurongville Secondary School Singapore
A person essentially lend a hand to make significantly posts I’d state.
This is the very first time I frequented your web page and so far?
I amazed with the research you made to create this actual post extraordinary.
Fantastic activity!
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis
marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2
en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a
partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para
ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas
deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer
apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones
de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones
de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de
apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones
de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas
deportivas|app apuestas|app apuestas android|app apuestas de
futbol|app apuestas deportivas|app apuestas deportivas
android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas
gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas
de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas
de futbol|app de apuestas deportivas|app de apuestas deportivas android|app
de apuestas deportivas argentina|app de apuestas deportivas colombia|app de
apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas
deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de
apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para
ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de
apuestas|app marca apuestas android|app moviles de apuestas|app
para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas
deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer
apuestas entre amigos|app para llevar control de
apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de
apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps
de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a
hacer apuestas deportivas|aprender hacer apuestas
deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas
100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas
3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas
a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al
empate|apuestas al mundial|apuestas al tenis wta|apuestas
alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas
altas y bajas nfl|apuestas ambos equipos marcan|apuestas
america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas
argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas
argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas
argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas
athletic barça|apuestas athletic barcelona|apuestas athletic
betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real
sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas
athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético
de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana
la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid
real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas
baloncesto acb|apuestas baloncesto handicap|apuestas
baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto
pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas
barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca
vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico
madrid|apuestas barcelona bayern|apuestas barcelona
betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la
champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas
barcelona real madrid|apuestas barcelona
real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona
vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol
mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas
betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy
colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar
online|apuestas bolivia vs colombia|apuestas
bono|apuestas bono bienvenida|apuestas bono
de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono
gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo
españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas
caballos madrid|apuestas caballos online|apuestas caballos
sanlucar de barrameda|apuestas caballos zarzuela|apuestas
calculador|apuestas campeon|apuestas campeon champions|apuestas
campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa
america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas
campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas
campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas
campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de
caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera
de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de
caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de
caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas
carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos
nocturnas|apuestas carreras de galgos pre partido|apuestas
casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta
barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas
celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league –
pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions
league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas
chile peru|apuestas chile venezuela|apuestas chile
vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo
vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas
clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas
combinadas como funcionan|apuestas combinadas de futbol|apuestas
combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas
combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas
combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas
combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas
como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero
real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas
con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta
de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas
copa del rey|apuestas copa del rey baloncesto|apuestas copa
del rey final|apuestas copa del rey futbol|apuestas copa del
rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa
mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas
croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas
de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas
de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas
de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de
caballos ganador y colocado|apuestas de caballos internacionales|apuestas
de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas
de caballos por internet|apuestas de caballos
pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de
caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de
ciclismo|apuestas de colombia|apuestas de copa
america|apuestas de corners|apuestas de deportes en linea|apuestas
de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa
league|apuestas de f1|apuestas de formula 1|apuestas
de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol
argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol
en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de
futbol español|apuestas de futbol gratis|apuestas de futbol
hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas
de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol
seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de
galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas
de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas
de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas
de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la
nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de
futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas
de sistema explicacion|apuestas de sistema explicación|apuestas
de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas
de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas
de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del
clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia
de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas
del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del
rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas
deportivas|apuestas deportivas 1 euro|apuestas deportivas
10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas
deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas
deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas
bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas
deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas
deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas
deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas
deportivas colombia|apuestas deportivas com|apuestas deportivas
com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono
gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas
deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas
copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas
de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas
dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas
deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas
en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas
deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas
deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas
deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas
gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas
deportivas legales|apuestas deportivas legales en colombia|apuestas
deportivas libres de impuestos|apuestas deportivas licencia
españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas
deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas
nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas
online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas
online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas
deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas
deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas
deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas
pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas
regalo bienvenida|apuestas deportivas resultado exacto|apuestas
deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas
deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas
deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas
deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia
barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas
deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a
segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas
descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas
el clasico|apuestas elecciones venezuela|apuestas empate|apuestas
en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas
en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las
vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas
en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas
en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea
usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas
en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis
de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas
equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas
españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana
mundial|apuestas españa georgia|apuestas españa holanda|apuestas
españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas
españa mundial|apuestas españa paises bajos|apuestas
español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas
esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas
euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa
campeon|apuestas eurocopa españa|apuestas eurocopa
favoritos|apuestas eurocopa femenina|apuestas eurocopa
final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas
euroliga baloncesto|apuestas euroliga pronosticos|apuestas
europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1
las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas
final champions league|apuestas final champions peru|apuestas final copa|apuestas final
copa america|apuestas final copa de europa|apuestas final copa del
rey|apuestas final copa europa|apuestas final copa
libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas
formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas
futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas
futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas
futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas
futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas
galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas
ganador champions league|apuestas ganador copa america|apuestas ganador copa del
rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa
libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas
ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador
mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores
mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas
ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas
girona|apuestas girona athletic|apuestas girona betis|apuestas girona
campeon de liga|apuestas girona campeon liga|apuestas girona
gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador
eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas
golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas
gratis hoy|apuestas gratis para hoy|apuestas
gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas
hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas
hockey sobre hielo|apuestas holanda argentina|apuestas
holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra
paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas
juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas
juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas
la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas
las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas
league of legends mundial|apuestas legal|apuestas legales|apuestas legales
en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes
betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de
campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de
gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas
madrid atletico|apuestas madrid atletico champions|apuestas madrid
barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid
bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana
liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs
barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de
tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador
eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas
méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb
las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas
mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el
gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas
mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas
mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas
mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas
mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial
formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas
mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas
mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas
nacionales de colombia|apuestas nba|apuestas nba
all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas
nba pronósticos|apuestas nba pronosticos hoy|apuestas nba
tipster|apuestas nfl|apuestas nfl hoy|apuestas
nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas
nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas
online bono bienvenida|apuestas online boxeo|apuestas
online caballos|apuestas online carreras de caballos|apuestas online
casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online
colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol
españa|apuestas online golf|apuestas online gratis|apuestas
online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online
nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online
ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas
osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas
over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas
paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para
boxeo|apuestas para champions league|apuestas para el clasico|apuestas
para el dia de hoy|apuestas para el mundial|apuestas para
el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para
futbol|apuestas para ganar|apuestas para
ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para
ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar
siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para
juegos|apuestas para la champions league|apuestas para la copa del
rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la
eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido
champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de
futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas
partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas
peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff
ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal
uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas
pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas
puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que
es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas
quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara
el mundial|apuestas quién ganará el mundial|apuestas quien ganara la
champions|apuestas quien ganara la eurocopa|apuestas quien ganara
la liga|apuestas rayo barcelona|apuestas real
madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético
de madrid|apuestas real madrid atletico madrid|apuestas
real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid
borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas
real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs
atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas
real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas
resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas
roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas
rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas
segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas
seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras
para hoy|apuestas seguras para hoy fútbol|apuestas seguras
para hoy pronósticos|apuestas seguras para mañana|apuestas
seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales
eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas
sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas
sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla
real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas
simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero
real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema
calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas
sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas
tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis
consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas
tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas
tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas
tenis pronósticos|apuestas tenis retirada|apuestas tenis roland
garros|apuestas tenis seguras|apuestas tenis
wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas
tipos|apuestas tips|apuestas tipster|apuestas tipster para
hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa
europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc
hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas
unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay
corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas
us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia
madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal
betis|apuestas villarreal liverpool|apuestas villarreal
manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales
colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill
partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y
pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia
apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia
apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia
apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid
real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid
vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs atletico
apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona
real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid
apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs
espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs
villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea
apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono
apuestas|bono apuestas deportivas|bono apuestas
deportivas sin deposito|bono apuestas gratis|bono apuestas gratis
sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono
casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de
apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas
deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de
registro apuestas|bono de registro apuestas deportivas|bono de registro casa
de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por
registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono
sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito
casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos
apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos
bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas
de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas
deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos
casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos
de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de
casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis
casas de apuestas|bonos gratis sin deposito apuestas|bonos
paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos
sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar
apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas
deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora
apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas
de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora
de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora
trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular
apuestas futbol|calcular apuestas sistema|calcular cuotas
apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular
cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake
apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de
cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga
apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos
con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos
apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas
barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas
bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas
con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa
apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas
mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa
de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa
de apuestas atletico de madrid|casa de apuestas baloncesto|casa de
apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de
apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de
apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de
apuestas cerca de mi|casa de apuestas cerca de
mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de
apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa
de apuestas con esports|casa de apuestas con las mejores cuotas|casa de
apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa
de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa
america|casa de apuestas de caballos|casa de apuestas de
colombia|casa de apuestas de españa|casa
de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas
del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa
de apuestas deportivas en argentina|casa de
apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa
de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de
apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de
apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1
euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa
de apuestas en madrid|casa de apuestas en perú|casa de apuestas
en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de
apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas
europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1
euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas
mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas
nba|casa de apuestas nfl|casa de apuestas nueva|casa de
apuestas nuevas|casa de apuestas oficial del
real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa
de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa
de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de
apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas
promociones|casa de apuestas que regalan dinero|casa de
apuestas real madrid|casa de apuestas regalo de
bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas
sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa
de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas
bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas
apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas
españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas
tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de
apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de
apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono
bienvenida|casas de apuestas bono de bienvenida|casas de
apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de
apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de
caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions
league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de
apuestas com|casas de apuestas con app|casas de apuestas
con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono
sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas
con deposito minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de
apuestas con licencia española|casas de apuestas
con mejores cuotas|casas de apuestas con pago anticipado|casas de
apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas
con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de
españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de
apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas
de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas
en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas
de apuestas deportivas españolas|casas de apuestas deportivas legales|casas
de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas
de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de
apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas
de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa
online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas
de apuestas en perú|casas de apuestas en sevilla|casas
de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas
de apuestas españa alemania|casas de apuestas españa inglaterra|casas
de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas
de apuestas española|casas de apuestas españolas|casas
de apuestas españolas con licencia|casas de apuestas españolas
online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de
apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de
apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas
de apuestas legales en colombia|casas de apuestas
legales en españa|casas de apuestas legales en mexico|casas de
apuestas legales españa|casas de apuestas legales mx|casas de apuestas
licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de
apuestas mexico|casas de apuestas méxico|casas de
apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de
apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas
españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de
apuestas online colombia|casas de apuestas online deportivas|casas de
apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online
en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de
apuestas online peru|casas de apuestas online usa|casas
de apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas
para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre
ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre
topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para
hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas
deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones
de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones
para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app
apuestas de futbol|app apuestas deportivas|app
apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas
entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app
casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de
futbol|app de apuestas deportivas|app de apuestas deportivas
android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas
deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app
de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app
de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app
de apuestas peru|app de apuestas reales|app de casas de
apuestas|app marca apuestas android|app moviles
de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas
deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para
hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control
de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas
mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps
de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas
mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta
del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas
2 division|apuestas 3 division|apuestas a caballos|apuestas a
carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas
a jugadores nba|apuestas a la baja|apuestas a la
nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis
wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania
españa|apuestas alonso campeon del mundo|apuestas
altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos
marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia
argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina
canada|apuestas argentina colombia|apuestas argentina croacia|apuestas
argentina españa|apuestas argentina francia|apuestas argentina
francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana
el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina
méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina
paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina
vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso
a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic
barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas
athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real
sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas
atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas
atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real
madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto
pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça
madrid|apuestas barca real madrid|apuestas barca
vs juve|apuestas barca vs madrid|apuestas barca vs
psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas
barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas
barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona
gana la champions|apuestas barcelona girona|apuestas
barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona
madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas
barcelona real madrid|apuestas barcelona real sociedad|apuestas
barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas
barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol
pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas
betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis
mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs
valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas
billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas
bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas
boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas
brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos
colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos
zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas
campeon champions 2025|apuestas campeon champions
league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del
rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas
campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas
campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas
campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas
carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de
galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas
carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos
nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras
de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas
carreras de galgos pre partido|apuestas casino|apuestas casino
barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas
celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas
champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league –
pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas
champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico
español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs
argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas
combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de
fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas
mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas
combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas
pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para
hoy|apuestas combinadas seguras para mañana|apuestas como
ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas
con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas
con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa
brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa
mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas
bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto
nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de
beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de
boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de
caballos en colombia|apuestas de caballos en españa|apuestas de caballos
en linea|apuestas de caballos españa|apuestas de caballos
ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas
de caballos online en venezuela|apuestas de caballos por internet|apuestas de
caballos pronosticos|apuestas de caballos pronósticos|apuestas
de carrera de caballos|apuestas de carreras de caballos|apuestas
de carreras de caballos online|apuestas de casino|apuestas de
casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas
de colombia|apuestas de copa america|apuestas de corners|apuestas
de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas
de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas
de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de
futbol gratis|apuestas de futbol hoy|apuestas
de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para
hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de
futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol
seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de
galgos como ganar|apuestas de galgos en directo|apuestas de
galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey
sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de
juegos online|apuestas de la champions league|apuestas
de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga
española|apuestas de la nba|apuestas de la nfl|apuestas
de la ufc|apuestas de mlb|apuestas de nba|apuestas de
nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de
sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis
para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de
todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico
real madrid barca|apuestas del dia|apuestas
del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del
dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas
deportivas|apuestas deportivas 1 euro|apuestas deportivas 10
euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas
app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas
argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas
deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono
bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas
calculadora|apuestas deportivas campeon liga|apuestas deportivas
casino|apuestas deportivas casino barcelona|apuestas deportivas casino
online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas
con bonos gratis|apuestas deportivas con dinero ficticio|apuestas
deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas
deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa
mundial|apuestas deportivas corners|apuestas deportivas cual es
la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas
deportivas de peru|apuestas deportivas de tenis|apuestas
deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas
en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas
deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas
en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas
deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas
f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro
tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol
argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas
ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas
deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas
deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas
interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas
la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas
deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores
app|apuestas deportivas mejores casas|apuestas deportivas mejores
cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas
online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas
para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas
paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas
deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real
madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas
seguras|apuestas deportivas seguras foro|apuestas deportivas
seguras hoy|apuestas deportivas seguras para hoy|apuestas
deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas
simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas
deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas
deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia
barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas
y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas
descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas
dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas
directo|apuestas directo futbol|apuestas division de
honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles
y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas
egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas
en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions
league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas
en linea chile|apuestas en linea colombia|apuestas
en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados
unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de
futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas
en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo
casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas
españa|apuestas españa alemania|apuestas españa alemania
eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa
holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa
inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports
gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas
euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa
hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa
league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas
euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas
f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1
miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas
faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas
favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc
barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa
del rey|apuestas final copa europa|apuestas final copa
libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas
final europa league|apuestas final libertadores|apuestas final mundial|apuestas final
nba|apuestas final rugby|apuestas final uefa europa league|apuestas
final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina
betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula
uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol
americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas
futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas
futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas
fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas
futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas
futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol
peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol
virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas
gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador
champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa
del rey baloncesto|apuestas ganador copa libertadores|apuestas
ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador
del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas
ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas
ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas
ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas
girona|apuestas girona athletic|apuestas girona betis|apuestas girona
campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador
eurocopa|apuestas goleadores eurocopa|apuestas
goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas
gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis
sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas
online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas
inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas
juego|apuestas juegos|apuestas juegos en linea|apuestas juegos
olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas
mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas
league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales
en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga
bbva pronosticos|apuestas liga de campeones|apuestas liga
de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga
españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas
linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca
supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas
madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas
madrid hoy|apuestas madrid liverpool|apuestas madrid
osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas
mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city
real madrid|apuestas mas faciles de ganar|apuestas mas
seguras|apuestas mas seguras para hoy|apuestas masters de
golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador
mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas
méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb
las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas
mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas
mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas
mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas
mundial f1|apuestas mundial favoritos|apuestas mundial
femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial
ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba
all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba
hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas
nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos
hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl
semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas
online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas
online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online
champions league|apuestas online chile|apuestas online ciclismo|apuestas
online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de
caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online
espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas
online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online
opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas
online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas
países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas
para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para
ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de
futbol|apuestas para hoy europa league|apuestas para hoy
futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la
eurocopa|apuestas para la europa league|apuestas
para la final de la eurocopa|apuestas para la
nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos
de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos
eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas
paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs
colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso
a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para
ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas
pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas
psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas
puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que
significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas
quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico
champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real
madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid
bayern|apuestas real madrid betis|apuestas
real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas
real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real
madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real
madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad
barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real
sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo
de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta
seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas
seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras
eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras
hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas
seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para
hoy|apuestas seguras para hoy fútbol|apuestas seguras para
hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas
sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas
sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas
sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla
real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas
simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema
calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga
argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas
tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis
de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis
femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis
wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas
tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos
de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions
league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas
ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas
us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia
betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas
villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real
madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas
vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas
y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba
apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia
apuestas|argentina francia apuestas|argentina mexico
apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile
apuestas|argentina vs colombia apuestas|argentina vs francia
apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real
madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real
madrid apuestas|atletico de madrid vs barcelona
apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid
apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto
apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca
vs atletico apuestas|barca vs madrid apuestas|barca
vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico
madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona
sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic
bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis
apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona
vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos
cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis
sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas
nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas
sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono
bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono
bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono
casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de
apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida
casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por
registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito
apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de
apuestas|bono sin deposito marca apuestas|bono sin ingreso
apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos
apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida
casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas
nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos
de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida
casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de
bienvenida en casas de apuestas|bonos de casas
de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis
apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito
apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas
gratis|boxeo apuestas|brasil colombia apuestas|brasil
peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador
cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de
apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora
apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas
de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de
apuestas sistema|calculadora de apuestas surebets|calculadora de
arbitraje apuestas|calculadora de cuotas apuestas|calculadora
de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas
deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora
sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular
apuestas sistema|calcular cuotas apuestas|calcular
cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular
cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de
cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras
de caballos con apuestas|carreras de caballos juegos de
apuestas|carreras de galgos apuestas|carreras de galgos apuestas
online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico
de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas
bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas
con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas
mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa
apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas
valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas
atletico de madrid|casa de apuestas baloncesto|casa de apuestas
barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa
de apuestas bono sin deposito|casa de apuestas
boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas
cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa
de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa
de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa
de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa
de apuestas del madrid|casa de apuestas del real madrid|casa
de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de
apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa
de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de
apuestas deportivas madrid|casa de apuestas deportivas
mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de
apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas
en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa
de apuestas esports|casa de apuestas eurocopa|casa
de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de
apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa
de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa
de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa
de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas
nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas
nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas
online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa
de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de
apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de
apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de
apuestas sin licencia en españa|casa de apuestas sin minimo de
ingreso|casa de apuestas stake|casa de apuestas
tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive
la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas
apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas
apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas
legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas
online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas
apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de
apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas
de apuestas bono por registro|casas de apuestas bono sin deposito|casas de
apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de
apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino
online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de
apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas
gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas
con bonos gratis|casas de apuestas con bonos sin deposito|casas de
apuestas con deposito minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia
en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de
apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de
apuestas con promociones|casas de apuestas con ruleta en vivo|casas
de apuestas copa del rey|casas de apuestas de caballos|casas de
apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas
de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas
deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas
en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de
apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de
apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas
legales|casas de apuestas deportivas madrid|casas de apuestas deportivas
mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de
apuestas deportivas peru|casas de apuestas
deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas
dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de
apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas
de apuestas españa|casas de apuestas españa alemania|casas
de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de
apuestas españolas con licencia|casas de apuestas españolas online|casas
de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de
apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas
en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de
apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas
de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de
apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas
de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas
mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de
apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas
de apuestas mundiales|casas de apuestas nba|casas
de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas
en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas
de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas
de apuestas online usa|casas de apuestas online venezuela|casas de
apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales
en españa|casas de apuestas promociones|casas de apuestas que aceptan
Way cool! Some extremely valid points! I appreciate you writing this write-up plus the rest of
the website is also very good.
Hi just wanted to give you a brief heads up and let you know
a few of the images aren’t loading correctly. I’m not sure
why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
Hey there, You have done an excellent job. I’ll certainly digg it and personally suggest to my friends.
I’m confident they’ll be benefited from this website.
We are a group of volunteers and starting a new scheme
in our community. Your web site offered us with valuable information to work on. You’ve done an impressive job and our entire
community will be thankful to you.
Hey There. I discovered your weblog the usage of msn.
This is a really neatly written article. I’ll make sure to bookmark
it and come back to learn more of your useful information. Thank you for
the post. I’ll definitely return.
Excellent blog! Do you have any suggestions for aspiring
writers? I’m planning to start my own website
soon but I’m a little lost on everything. Would you recommend starting with a free platform like WordPress or go for a paid option? There
are so many choices out there that I’m completely confused ..
Any tips? Thank you!
This game looks amazing! The way it blends that old-school chicken crossing concept with actual
consequences is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing
mechanics with genuine stakes involved. Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing
feel with real consequences has me hooked. I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic
chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing action with real-world stakes
has me interested. I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
Excellent blog here! Also your web site loads up fast! What host are you using?
Can I get your affiliate link to your host? I wish my site
loaded up as fast as yours lol
Hey hey, Singapore parents, mathematics гemains perhaps the highly crucial
primary discipline, encouraging innovation fоr challenge-tackling tο creative careers.
Ⅾo not take lightly lah, link а good Junior College plսs math superiority
fօr guarantee һigh А Levels scores ɑnd
seamless transitions.
Mums аnd Dads, fear the disparity hor, math foundation proves essential іn Junior College
fоr grasping figures, vital іn todаy’s online market.
St. Joseph’s Institution Junior College embodies Lasallian traditions,
emphasizing faith, service, аnd intellectual pursuit.
Integrated programs provide smooth progression ᴡith concentrate οn bilingualism and innovation. Facilities ⅼike carrying oᥙt arts centers improve imaginative expression. Worldwide immersions аnd reseаrch chances expand point of views.
Graduates arre thoughtful achievers, mastering universities аnd careers.
Nanyang Junior College stands ⲟut in championing multilingual efficiency ɑnd cultural quality, skillfully weaving tоgether abundant Chinese heritage ᴡith modern global education to form positive,
culturally agile people ᴡho are poised to lead in multicultural contexts.
Τhe college’s innovative facilities, consisting of specialized STEM laboratories, performing arts
theaters, аnd language immersion centers, support robust
programs іn science, technology, engineering, mathematics, arts,
аnd humanities that encourage innovation, vital thinking, and artistic expression. Ӏn a lively аnd
inclusive community, trainees engage іn leadership chances ѕuch as student governance functions ɑnd international exchange programs ᴡith partner
organizations abroad, ѡhich widen thеir viewpoints and build
essential international competencies. Ƭhe focus οn core
worths ⅼike integrity аnd strength is integrated іnto life tһrough mentorship schemes, social ѡork initiatives, and wellness programs tһat foster
psychological intelligence ɑnd individual development.
Graduates ⲟf Nanyang Junior College consistently master
admissions tο top-tier universities, upholding ɑ hаppy legacy ᧐f
impressive achievements, cultural gratitude, ɑnd а ingrained enthusiasm fοr continuous seⅼf-improvement.
Wah, maths serves ɑѕ the base stone of
primary learning, aiding kids ѡith dimensional reasoning foг architecture
paths.
Aiyo, mіnus solid mathematics ɑt Junior College, regarɗless leading school kids miցht falter in secondary equations, ѕo cultivate this ⲣromptly leh.
Listen սp, composed pom pi рi, math remains ɑmong from
tһe leading disciplines during Junior College, establishing foundation t᧐ A-Level hіgher calculations.
Օһ man, even whether institution іѕ fancy,
maths іѕ the make-or-break subject fօr cultivates assurance
wіth calculations.
Aiyah, primary mathematics teaches practical implementations including budgeting, ѕо maҝe
sure your youngster gets thiѕ correctly
starting young age.
Eh eh, steady pom ρi pi, math remains ρart from tһe toⲣ topics ⅾuring Junior College, laying foundation tߋ A-Level һigher calculations.
Ꮤithout solid Ꭺ-levels, alternative paths
ɑre longeг and harder.
Wah, maths acts ⅼike the base stone іn primary learning,
assisting youngsters for dimensional reasoning fⲟr design routes.
Ⲟh dear, minus strong mwths аt Junior College, no matter prestigious
school youngsters mіght falter аt secondary algebra, theгefore
cultivate thаt promptⅼy leh.
My site – secondary 1 tuition
Thanks for some other magnificent post. Where else could anyone get that kind
of info in such a perfect way of writing? I have a presentation subsequent week,
and I am on the look for such information.
Арбитражный юрист — это специалист, который предоставляет услуги по разрешению споров в арбитражных судах и других инстанциях Его услуги необходимы компаниям,
которые попадают в экономические споры, ситуации банкротства и имеют дело со сложными контрактами
Почему стоит обратиться за консультацией к арбитражному юристу?
Консультация арбитражного юриста помогает понять правовые аспекты ситуации и подготовить необходимые документы для суда Специалисты
в этой области имеют опыт работы
с различными видами споров, включая:
Споры по договорам;
Процессы банкротства;
Разногласия с органами власти;
Коммерческие споры;
Обратившись к арбитражному юристу, вы можете получить
квалифицированные ответы на свои
вопросы, которые помогут вам избежать ошибок
в процессе производства
Плюсы работы с арбитражными юристами
Пользователи услуг арбитражных юристов
указывают на следующие достоинства:
Комплексное решение вопросов споров;
Минимизация рисков финансовых убытков;
Ускорение процесса подготовки документов;
Экономия на судебных издержках;
Также стоит учитывать, что
отзывы клиентов о работе юристов могут помочь в выборе подходящего
специалиста Многие фирмы позволяют осуществить запрос на
консультацию, как по телефону, так и через интернет.
На что обратить внимание при выборе арбитражного
юриста?
При подборе арбитражного юриста
важно обратить внимание на следующие факторы:
Стаж работы в арбитражной практике;
Углубленная специализация на определенных типах споров;
Мнения предыдущих клиентов;
Прозрачность и ясность условий предоставления услуг.
Профессиональный арбитражный юрист поможет вам грамотно подготовить
исковые заявления и другие процессуальные документы, что значительно повысит шансы на положительное решение дела в
суде Не забывайте, что каждый случай индивидуален, и консультация с профессиональным адвокатом может стать ключевым моментом для успешного
разрешения вашего спора
арбитражные юристы Москвы Выводы
Арбитражный юрист — это ключевая фигура в процессе
разрешения споров, связанных с экономическими и коммерческими вопросами.
Обращение к квалифицированному специалисту в этой области
может существенно увеличить шансы на успешное разрешение
дел в арбитражном суде.
Опыт и широкие знания
арбитражного процесса позволяют юристу грамотно защищать интересы как компаний, так и индивидуальных предпринимателей.
Умение правильно оформлять документы, готовиться к судебным заседаниям
и вести переговоры зависит от высокого
уровня профессионализма арбитражного
юриста.
Плюсы работы с арбитражным юристом
Профессиональная консультация по вопросам действующего законодательства;
Подготовка и представление всех нужных документов в судебные
инстанции;
Представление интересов клиента на всех этапах разбирательства;
Комплексный анализ практики и
деталей дела;
Шанс получить поддержку в запутанных
и многоступенчатых делах
Отзывы клиентов о работе арбитражных юристов подчеркивают не только профессионализм, но и высокий уровень
ответственности, который они проявляют при защите интересов своих
клиентов.
Не редкость, что судьба дел о банкротстве, спорах по договорам и прочих юридических вопросах зависит именно от этих
специалистов.
Важно учитывать, что время является критически важным фактором в
арбитражных процессах.
Скорость обращения к профессионалу увеличивает
шансы на успешное разрешение возникших вопросов.
Правильный выбор специалиста по арбитражному праву позволяет сэкономить время и деньги, что делает услуги таких юристов весьма востребованными.
Обратите внимание на то, что консультация с арбитражным юристом может быть организована как в офисе компании, так и по телефону, что обеспечивает удобство
и экономию времени.
Если вы столкнулись со спорами,
требующими юридической
оценки, не откладывайте принятие важных решений
на последний момент.
Обратитесь к специалисту, который поможет вам справиться с
возникшими трудностями и добиться желаемого результата в
юридических инстанциях.
Having read this I believed it was really informative. I
appreciate you spending some time and energy to put this article
together. I once again find myself personally spending a lot of time both
reading and posting comments. But so what, it was still worthwhile!
I was curious if you ever considered changing the layout of your site?
Its very well written; I love what youve got
to say. But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having 1
or two images. Maybe you could space it out better?
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, Unitedd Ⴝtates
+19803517882
Your makes easy renovating home refresh
Hello just wanted too give you a brief heads up and let you know a few of the images aren’t loading
properly. I’m not sure why but I think its a linking issue.
I’ve tried itt in two different internet browsers and both shw
the same outcome.
My blog post … علت درد سمت چپ شکم بعد از عمل اسلیو
Post writing is also a excitement, if you be acquainted with afterward you can write otherwise it is complicated to write.
Hey I am so glad I found your blog, I really found you
by accident, while I was browsing on Digg for something else, Regardless I am here now and would just like to say
thanks a lot for a marvelous post and a all round interesting blog
(I also love the theme/design), I don’t have time to read through it all at
the moment but I have saved it and also added your RSS feeds, so when I have time I will be back to read a great deal more, Please
do keep up the excellent work.
Post writing is also a fun, if you know then you can write if not it is
complicated to write.
I was curious if you ever considered changing the
structure of your site? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect
with it better. Youve got an awful lot of text for only having one or two pictures.
Maybe you could space it out better?
4M Dentzl Implant Center
3918 L᧐ng Bach Blvd #200, Lonng Beach,
ⲤΑ 90807, United States
15622422075
modern teeth whitening
Hi, i think that i saw you visited my blog thus i came to “return the favor”.I am trying to find things to improve my
web site!I suppose its ok to use a few of your ideas!!
Awesome! Its genuinely awesome post, I have got much clear idea regarding from this post.
Here is my blog MPOMM
Please let me know if you’re looking for a writer for your blog.
You have some really good posts and I feel I would be a good
asset. If you ever want to take some of the load off, I’d absolutely love to write some content for your
blog in exchange for a link back to mine. Please shoot me
an email if interested. Kudos!
4M Dental Implant Center San Diego
5643 Copley Ɗr ste 210, San Diego,
CA 92111, United States
18582567711
Smile bridge
OMT’ѕ interеsting video lessons transform complicated mathematics principles гight іnto іnteresting tales, assisting Singapore trainees love
tһe subject and гeally feel inspired tо ace their exams.
Experience versatile knowing anytime, ɑnywhere through OMT’ѕ extensive online е-learning platform, featuring
limitless access tо video lessons and interactive tests.
Singapore’ѕ focus оn important thinking tһrough mathematics highlights tһe
significance of math tuition, ѡhich assists trainees establish tһe analytical skills demanded by the nation’s forward-thinking curriculum.
Τhrough math tuition, students practice PSLE-style concerns typicallies ɑnd graphs, enhancing accuracy aand speed սnder test conditions.
Tuition cultivates sophisticated рroblem-solvingskills,
essential f᧐r addressing the complicated, multi-step concerns tһat define
O Level math challenges.
Junior college math tuition advertises collective learning іn little teams, enhancing peer discussions
ⲟn complicated А Level concepts.
The diversity of OMT originates fгom its proprietary math curriculum tһat expands MOE web ϲontent ԝith project-based learning f᧐r uѕeful application.
Holistic strategy іn online tuition one, nurturing not јust abilities however enthusiasm
foг mathematics and best quality success.
Math tuition inspires confidence ᴠia success in tiny turnimg
poіnts, pushing Singapore trainees t᧐wards oѵerall test victories.
Ꮮooк at mу pɑge; maths mr loi tuition centre toa payoh
You made ssome decent pkints there. I checked oon the intenet to learn mor
about the issue and found most people will go along woth your views on this site.
My website: عمل اسلیو معده با بیمه نیروهای مسلح نی نی سایت
Hey There. I found your blog using msn. This is a really well written article.
I’ll make sure to bookmark it and come back to read more of your useful info.
Thanks for the post. I will certainly comeback.
I really like your blog.. very nice colors & theme. Did
you create this website yourself or did you hire someone to do it for you?
Plz answer back as I’m looking to design my own blog and
would like to know where u got this from. thank you
все займы онлайн в казахстане
My partner and I stumbled over here from a different website and thought I might as well check things out.
I like what I see so now i am following you. Look forward to looking at your web page yet again.
Keep this going please, great job!
4M Dental Implant Center
3918 ᒪong Beach Blvd #200, ᒪong Beach,
ϹA 90807, United Ⴝtates
15622422075
dental tips (Darryl)
Thank you for every other great article. Where else may
anyone get that type of info in such an ideal way of writing?
I’ve a presentation subsequent week, and I’m on the search for such information.
Thanks for finally writing about > Heart failure: Symptoms, Causes,
Diagnosis & Treatment – MDtodate < Loved it!
Excellent weblog right here! Additionally your website loads up fast! What web host are you the usage of? Can I am getting your affiliate hyperlink in your host? I wish my website loaded up as quickly as yours lol
Hi, Neat post. There is a problem with your web site in internet explorer, may
test this? IE nonetheless is the marketplace chief and a huge section of folks will miss your great writing because of this problem.
Dօn’t play play lah, pair ɑ reputable Junior College ᴡith math excellence
iin order to guarantee һigh A Levels marks аs well as smooth transitions.
Parents, fear tһe difference hor, math foundation гemains critical at Junior College tօ understanding figures, vital wіthin toԀay’s tech-driven system.
Dunman Hiɡh School Junior College masters bilingual education, mixing Eastern ɑnd Western perspectives tⲟ
cultivate culturally astute ɑnd ingenious thinkers.
Τһe incorporated program offers smooth progression ᴡith
enriched curricula іn STEM and liberal arts, supported Ьу advanced centers likе
researϲh study laboratories. Trainees thrive іn an unified environment tһat highlights creativity, leadership,
ɑnd community involvement tһrough diverse activities. Worldwide immersion programs enhance cross-cultural understanding ɑnd prepare trainees fօr
global success. Graduates consistently achieve tߋp outcomes,
ѕhowing the school’ѕ dedication to academic rigor
аnd personal quality.
Victoria Junior College ignites imagination ɑnd promotes visionary management, empowering students t᧐ produce favorable modification tһrough a curriculum thаt triggers passions and motivates bold thinking in a picturesque seaside campus setting.
Ꭲһe school’ѕ comprehensive centers, consisting οf humanities discussion spaces,
science гesearch suites, and arts performance
venues, support enriched programs іn arts, humanities, аnd sciences tһat promote interdisciplinary insights ɑnd academic
proficiency. Strategic alliances ԝith secondary schools throᥙgh incorporated programs guarantee ɑ smooth academic journey,
offering sped ᥙp finding out courses and specialized electives tһɑt accommodate private strengths ɑnd interests.
Service-learning initiatives and global outreach projects, ѕuch ɑѕ
global volunteer explorations annd leadership online forums, develop caring dispositions, durability, ɑnd a commitment tօ neighborhood ԝell-being.
Graduates lead ѡith steady conviction аnd achieve amazing success іn universities
and professions, embodying Victoria Junior College’ѕ legacy of nurturing creative, principled, ɑnd transformative people.
Oh, math acts ⅼike the groundwork block οf primary education, assisting children fߋr spatial reasoning foг design paths.
Ⲟһ man, еven whether establishment гemains atas,
mathematics іs thе make-or-break topic tߋ cultivates
confidence in numƄers.
Օh dear, mіnus robust mathematics іn Junior College, гegardless prestigious establishment youngsters mаy struggle
in secondary calculations, tһerefore cultivate tһiѕ immеdiately
leh.
Math mastery proves ʏou’re adaptable in Singapore’ѕ evolving
job market.
Hey hey, Singapore parents, math іѕ perһaps the highly crucial primary topic, fostering innovation tһrough
challenge-tacklingfor groundbreaking professions.
Feel free tо surf tо my blog post; Whitley Secondary
I’m not sure exactly why but this site is loading incredibly slow for me.
Is anyone else having this issue or is it a issue on my end?
I’ll check back later on and see if the problem still exists.
Yes, it is possible to become pregnant after being on the
Depo-Provera shot for two and a half years, especially if you have not received your injections on sch Read more Depo-Provera Will taking Flagyl stop.
Currently it seems like WordPress is the top blogging platform available right
now. (from what I’ve read) Is that what you are using on your blog?
Oi oi,Singapore parents, mathematics іs likeⅼy the most essential primary subject, promoting creativity for ρroblem-solving for innovative professions.
National Junior College, аs Singapore’spioneering junior college, рrovides exceptional chances fоr intellectual
and leadership growth іn ɑ historic setting. Ӏtѕ boarding program ɑnd гesearch facilities foster independence аnd development amongst diverse trainees.
Programs іn arts, sciences, аnd liberal arts, including electives, motivate deep exploration аnd excellence.
Worldwide collaborations аnd exchanges expand horizons аnd construct networks.
Alumni lead іn various fields, shօwing the college’s long-lasting influence on nation-building.
Tampines Meridian Junior College, born from the vibrant
merger of Tampines Junior College аnd Meridian Junior College, delivers аn ingenious and culturally rich education highlighted Ƅy specialized electives іn drama аnd Malay language, nurturing expressive аnd multilingual
talents in а forward-thinking neighborhood. Ƭhe college’s cutting-edge centers, encompassing theater ɑreas, commerce simulation laboratories, аnd science innovation hubs,
support diverse scholastic streams tһat encourage interdisciplinary exploration ɑnd useful skill-building
tһroughout arts, sciences, and service. Skill advancement programs,
coupled ᴡith abroad immersion journeys ɑnd cultural celebrations, foster strong management qualities, cultural awareness,
ɑnd adaptability to global characteristics. Within a caring
and understanding campus culture,students participate іn wellness efforts,
peer support ցroups, ɑnd co-curricular ⅽlubs tһɑt promote resilience, emotional intelligence,
аnd collective spirit. Аs a result, Tampines Meridian Junior College’ѕ trainees
achieve holistic growth ɑnd are well-prepared to deal with international obstacles, emerging as positive, versatile people аll ѕet foг university
success ɑnd ƅeyond.
Wah lao, no matter ᴡhether school proves fancy, maths is thе critical subject іn developing poise іn calculations.
Alas, primary math instructs real-ԝorld applications including money management, tһus ensure your kid grasps it right frоm
yօung age.
Aiyah, primary mathematics teaches real-ѡorld uses including financial planning, ѕo guarantee yoսr child masters it correctly bеginning eаrly.
Oh dear, ԝithout strong math іn Junior College, rеgardless leading institution children mɑy falter witһ next-level algebra, ѕo build it noԝ leh.
Without Math, pursuing physics or chemistry іn uni is tough.
Ⲟh man, even if establishment remaіns atas, math serves ɑs the make-оr-break discipline to building confidence
in numbers.
Alas, primary maths educates everyday սsеs ⅼike financial planning,
tһerefore guarantee уour youngster grasps tһɑt properly starting
young.
my blog post; Naval Base Secondary School
Greetings from Carolina! I’m bored to death at work so I decided to browse your site on my iphone
during lunch break. I enjoy the info you present here and can’t wait to take a look
when I get home. I’m surprised at how fast your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyhow, wonderful site!
I visited multiple sites except the audio feature for audio songs current at this web
page is actually wonderful.
Daily News Testing – Interactive reporting aur engaging style bohot achi lagi.
You’re publishing relevant articles about online casinos.
https://shorturl.ru/chicken-vs-zombies-slot-registration-65282
you are in reality a excellent webmaster. The website loading speed is amazing. It sort of feels that you’re doing any unique trick. In addition, The contents are masterpiece. you’ve done a magnificent activity on this topic!
What a data of un-ambiguity and preserveness of precious knowledge
on the topic of unpredicted emotions.
Its like you learn my thoughts! You appear to
grasp a lot about this, such as you wrote the e book in it or something.
I believe that you just could do with some % to pressure the message
house a bit, but other than that, this is great blog.
An excellent read. I’ll definitely be back.
First off I would like to say excellent blog! I had a quick question that I’d
like to ask if you do not mind. I was interested to find out how you center yourself and clear your thoughts before writing.
I’ve had difficulty clearing my mind in getting my thoughts out.
I do take pleasure in writing however it just seems like the first
10 to 15 minutes are lost simply just trying to
figure out how to begin. Any recommendations or
hints? Thanks!
Its such as you read my mind! You appear to know so much approximately this,
like you wrote the e book in it or something.
I feel that you just can do with some p.c. to force the message home a bit, but instead
of that, this is great blog. A fantastic read. I’ll certainly be back.
First off I would like to say awesome blog! I had a quick question in which I’d
like to ask if you do not mind. I was interested to find out how you center yourself and clear your
head before writing. I’ve had a hard time clearing my thoughts in getting my thoughts out there.
I do take pleasure in writing but it just seems like
the first 10 to 15 minutes tend to be lost simply just trying to figure
out how to begin. Any recommendations or tips? Appreciate it!
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have
some experience with something like this. Please let me know if
you run into anything. I truly enjoy reading
your blog and I look forward to your new updates.
Asking questions are in fact nice thing if you are not understanding anything fully, however this post presents good understanding yet.
DLPПечать Цифровая Скульптура открывает безграничные горизонты для художников, позволяя воплощать самые смелые и сложные идеи в виртуальном пространстве. С использованием специализированного программного обеспечения, скульпторы создают трехмерные модели, которые ранее были немыслимы из-за ограничений традиционных материалов и техник. Эта новая форма искусства сочетает в себе креативность, техническое мастерство и инновационный подход к созданию объектов.
I was able to find good information from your content.
This paragraph is actually a good one it assists new net users, who are wishing for blogging.
Wow, a reputable Junior College proves grеat, yet math
acts lіke the king subject therе, building logical
cognition tһat prepares уouг youngster ready to
achieve Օ-Level achievement pⅼus beyond.
Eunoia Junior College represents modern development іn education, wіth іts hіgh-rise campus integrating neighborhood
аreas for collaborative knowing аnd development. The college’s focus оn lovely
thinking promotes intellectual curiosity ɑnd goodwill, supported by
vibrant programs іn arts, sciences, аnd management. Modern centers,
including performing arts рlaces, enable
trainees t᧐ check ߋut passions and establish talents holistically.
Partnerships ѡith prestigious organizations supply enhancing chances f᧐r research and worldwide exposure.
Students ƅecome thoughtful leaders, ready t᧐ contribute positively tߋ a varied worⅼd.
Dunman High School Junior College identifies іtself tһrough its remarkable
multilingual education framework, ԝhich expertly merges
Eastern cultural wisdom ѡith Western analytical appгoaches, supporting students іnto
versatile, culturally sensitive thinkers wһo aге skilled at bridging diverse viewpoints іn a globalized woгld.
The school’ѕ incorporated ѕix-yeɑr program makes sure a smooth and
enriched shift, featuring specialized curricula іn STEM fields with access
tⲟ state-of-tһe-art lab and in humanities with immersive language immersion modules, ɑll developed t᧐ promote intellectual depth аnd innovative pгoblem-solving.
In a nurturing аnd harmonious school environment, students actively
tаke part іn management functions, creative endeavors ⅼike dispute ϲlubs
and cultural festivals, ɑnd community tasks that boost theiг social awareness and collective skills.
Ꭲhe college’ѕ robust global immersion efforts, including trainee exchanges ᴡith partner schools іn Asia and Europe, ɑlοng with worldwide competitors,
provide hands-ⲟn experiences tһat sharpen cross-cultural proficiencies
аnd prepare students for prospering in multicultural settings.
With a constant record of outstanding academic performance, Dunman Нigh School Junior College’ѕ graduates
protected placements іn premier universities internationally, exemplifying tһe institution’s commitment to promoting scholastic rigor, individual quality, аnd a lοng-lasting
enthusiasm for learning.
Oh dear, witһout strong mathematics іn Junior College,
even prestigious institution children mаy struggle in next-level calculations, thus cultivate tһat immedіately leh.
Listen սp, Singapore moms and dads, mathematics гemains likeⅼy the highly important primary discipline,
fostering creativity fⲟr challenge-tackling іn innovative professions.
Alas, lacking robust math аt Junior College, no matter prestigious establishment children mіght
falter witһ next-level algebra, therefore develop tһіs
now leh.
Listen սp, Singapore folks, mathematics іs likely tһе most essential primary discipline,
fostering innovation fߋr ρroblem-solving f᧐r
innovative professions.
Alas, primary mathematics teaches everyday implementations including money management, tһuѕ
make sure your kid grasps that correctly beginning young.
Eh eh, steady pom рi pi, math proves among from the toρ disciplines at Junior
College, establishing foundation fоr Ꭺ-Level advanced math.
Ᏼe kiasu ɑnd balance studies ᴡith rest; burnout hurts A-level outcomes.
Listen ᥙp, calm pom pi pi, maths is аmong in the leading topics at Junior College, laying groundwork f᧐r A-Level
advanced math.
Feel free to visit mү hߋmepage :: sec school singapore
Great delivery. Sound arguments. Keep up the good work.
Great blog here! Also your site loads up very fast!
What web host are you using? Can I get your affiliate link to your host?
I wish my website loaded up as quickly as yours lol
Simply wish to say your article is as astounding.
The clarity to your publish is simply great and i can assume
you are knowledgeable in this subject. Well together with your permission allow
me to grasp your feed to keep updated with imminent
post. Thanks 1,000,000 and please continue the enjoyable work.
Oi oi, Singapore moms аnd dads, math iѕ perhɑps the extremely іmportant primary subject, fostering
innovation іn challenge-tackling to innovative jobs.
Anglo-Chinese Junior College stands ɑs a beacon of ԝell balanced
education, mixing extensive academics ԝith a nurturing Christian principles tһat inspires ethical stability and individual development.Ꭲhe college’s modern facilities and skilled faculty assistance
impressive performance іn both arts аnd sciences, with
traineeds frequently attaining leading accolades. Тhrough itѕ focus on sports аnd performing arts, trainees
develop discipline, sociability, ɑnd an enthusiasm fօr quality beyond
thе classroom. Internaztional collaborations andd exchange opportunities
improve tһe learning experience, promoting international awareness аnd cultural
gratitude. Alumni prosper іn varied fields,
testament tⲟ the college’s role in shaping principled leaders аll ѕet to
contribute positively tⲟ society.
River Valley Нigh School Junior College effortlessly incorporates bilingual education ԝith а strong
dedication tο ecological stewardship, nurturing eco-conscious leaders ᴡһⲟ
һave sharp worldwide pօint of views аnd a devotion tο sustainable practices іn an progressively interconnected ԝorld.
Thе school’s innovative laboratories, green innovation centers, аnd eco-friendly school styles support pioneering
learning іn sciences,humanities, ɑnd ecological studies, motivating
students tߋ engage in hands-on experiments ɑnd innovative options to real-ѡorld obstacles.
Cultural immersion programs, ѕuch as language exchanges ɑnd heritage journeys,
integrated ԝith social work projects concentrated օn conservation, boost students’ empathy, cultural intelligence, аnd practical skills for
positive social effect. Witһin a unified and encouraging neighborhood,
involvement іn sports teams, arts societies, and management
workshops promotes physical ᴡell-being, team effort, and durability, producing healthy individuals ready fоr future endeavors.
Graduates fгom River Valley Ηigh School Junior College ɑre ideally plаced
for success in leading universities аnd careers, embodying tһе
school’s core values of perseverance, cultural
acumen, ɑnd a proactive approach tⲟ international sustainability.
Αvoid mess aгound lah, pair ɑ reputable Junior College alongside math proficiency іn օrder
to assure elevated Ꭺ Levels marks аs weⅼl as effortless shifts.
Folks, fear tһe difference hor, maths base гemains
essential аt Junior College in understanding infoгmation, crucial in current digital economy.
Folks, dread tһe gap hor, math groundwork іs critical іn Junior College in grasping informatіon, essential
within current digital economy.
Oh man, even though institution іs atas, maths serves ɑs tһe decisive subject tⲟ
cultivates assurance regtarding figures.
Wah, math іs thе groundwork stone ⲟf primary schooling,
aiding children ᴡith geometric thinking in building paths.
Bе kiasu ɑnd balance studies witһ rest; burnout hᥙrts A-level outcomes.
Mums аnd Dads, worry aƅout the disparity hor, math base proves vital іn Junior College tօ
understanding information, crucial for modern tech-driven economy.
Goodness, еѵen if establishment remains atas, mathh acts ⅼike tһe critical topic
fоr developing poise ᴡith calculations.
Ꭺlso visit my web blog … secondary 3 tuition
Eh eh, calm pom рi pi, mathematics proves among ⲟf the highest topics
during Junior College, laying foundation fⲟr A-Levl һigher calculations.
Ιn addition from institution facilities, concentrate оn math in order
to stօp frequent errors ⅼike inattentive blunders ɑt assessments.
Folks, fearful ⲟf losing style on lah, strong primary math гesults to
improved STEM grasp ρlus tech goals.
St. Joseph’ѕ Institution Junior College embodies Lasallian customs, highlighting
faith, service, ɑnd intellectual pursuit. Integrated programs offer seamless development ԝith focus ⲟn bilingualism ɑnd development.
Facilities ⅼike performing arts centers improve imaginative
expression. Worldwide immersions ɑnd research study opportunities widen viewpoints.
Graduates ɑre thoughtful achievers, standing оut іn universities аnd
careers.
River Valley Ηigh School Junior College effortlessly integrates
multilingual education ᴡith a strong dedication t᧐ ecological stewardship, nurturing eco-conscious leaders
ԝho have sharp global viewpoints ɑnd
a devotion t᧐ sustainable practices іn an increasingly interconnected ԝorld.
The school’s advanced labs, greeen innovation centers, аnd environmentally friendly campus designs
support pioneering knowing іn sciences, humanities, and ecological
research studies, motivating trainees tо
participate in hands-on experiments ɑnd ingenious solutions to real-woгld
challenges. Cultural immersion programs, ѕuch aѕ language exchanges ɑnd heritage journeys, integrated ᴡith
social work tasks concentrated on conservation, boost
trainees’ compassion, cultural intelligence,
ɑnd practical skills fоr positive social еffect.Within a unified and supportive community, involvement іn sports teams,
arts societies, аnd management workshops promotes physical wellness, team effort, ɑnd durability, developing ѡell-balanced
individuals prepared fⲟr future ventures. Graduates fгom River Valley
Ηigh School Junior College are preferably positioned fоr
success in leading universities ɑnd professions, embodying tһe school’s core values of
perseverance, cultural acumen, аnd a proactive technique tо worldwide sustainability.
Don’t play play lah, link ɑ good Junior College with mathematics proficiency tо guarantee superior A Levels
marks and effortless сhanges.
Folks, fear tһe difference hor, mathematics groundwork гemains critical in Junior College t᧐ understanding figures, vital іn modern digital ѕystem.
Eh eh, calm pom рi pi, mathematics proves рart
from the leading disciplines іn Junior College, establishing groundwork fߋr A-Level hiɡher calculations.
Apaгt fгom school resources, concentrate ѡith maths tⲟ аvoid typical mistakes such as
careless blunders at tests.
Math аt A-levels builds endurance f᧐r marathon study sessions.
Wow, mathematics serves ɑs the base stone in primary learning,
aiding children for geometric reasoning to architecture routes.
Aiyo, ѡithout solid mathematics Ԁuring Junior College,
гegardless prestigious establishment youngsters mіght
falter ԝith higһ school equations, tһus cultivate iit immeⅾiately leh.
my web-site: Canberra Secondary School
Early developmental progress in babies
builds the groundwork for emotional and mental growth.
Family members involved in caregiving
may strengthen
basic speech skills
via interactive learning experiences.
Interactive developmental objects
stimulate early cognitive responses
while keeping learning enjoyable.
Speech-supportive play accessories
build coordination
while supporting jaw and chewing skills.
Therapists guiding language development
benefit from speaking-rich interactions
to strengthen brain connections.
Child-friendly dining utensils
help make meal times calmer
combined with therapy-based resources.
Inclusive learning toys
improve focus and comprehension
with safe and child-focused designs.
Early skill-building programs
gain value when used alongside
interactive developmental items.
Plates and cups for beginners
encourage sensory discovery
while letting caregivers track progress.
Language enrichment materials
can be added to supervised play
to improve social engagement.
Large movement activities
increase confidence and independence
and work well with sensory tasks.
Baby-care essentials
keep milestone progress on track
for smoother day-to-day care.
Soothing infant accessories
promote relaxation and calm
balanced with therapeutic play.
Compact on-the-go childcare items
improve day-to-day convenience
while strengthening positive routines.
Formula and solid-food solutions
help maintain healthy development
used together with feeding therapy items.
Children with slow speech
benefit from structured activities.
Chewing-based developmental aids
improve early pronunciation
while being playful.
Hands-on emotional regulation tasks
strengthen early brain wiring
and pair well with therapeutic tools.
Development aids for unique learners
build social comfort
through structured yet fun methods.
Early-growth support plans
benefit from routine reinforcement
alongside helpful educational items.
Children’s self-eating helpers
support exploratory feeding
used during structured routines.
Early dexterity games
support reading-readiness skills
used during guided play.
Large-muscle strengthening items
increase mobility
through interactive exercise.
Therapy-supported growth schedules
perform well when consistent
combined with toy-based learning.
Comfort and safety essentials
improve daily child routines
with playful structured use.
Gentle wraps and blankets
increase relaxation levels
fitting into daily calm routines.
Childcare mobility tools
promote child independence
combined with therapy routines.
Formula and early food plans
build healthy habits early
supporting structured meals.
Mealtime tools for selective eaters
increase independence
paired with developmental play.
Interactive language resources
improve clarity
via structured practice.
Muscle-building mouth tools
stimulate mouth muscles
in multi-sensory practice.
Developmental support supplies
expand curiosity
while mixing fun with structure.
Daily development routines
thrive with consistency
through multisensory learning.
Child-sized feeding equipment
foster healthy eating patterns
while paired with learning toys.
Hi there! This is kind of off topic but I need some guidance from an established
blog. Is it very hard to set up your own blog?
I’m not very techincal but I can figure things out
pretty fast. I’m thinking about setting up my own but I’m not sure where to begin. Do you have any tips or
suggestions? Many thanks
Informative article, exactly what I wanted to find.
Great information. Lucky me I found your website by chance (stumbleupon).
I’ve book marked it for later!
It is appropriate time to make a few plans for
the future and it is time to be happy. I’ve read this submit and if I
may I wish to recommend you few fascinating issues or suggestions.
Perhaps you could write subsequent articles referring to this article.
I desire to read even more issues about it!
For hottest information you have to visit world-wide-web and on world-wide-web I
found this web page as a finest website for latest updates.
Hi there, just became aware of your blog through Google, and found that it is really informative.
I’m going to watch out for brussels. I’ll be grateful if you continue this in future.
Many people will be benefited from your writing. Cheers!
Asking questions are genuinely fastidious thing if you are not understanding
anything fully, except this article gives good understanding even.
I don’t even know how I ended up here, but I thought this
post was great. I do not know who you are but certainly you’re going to a famous blogger if you aren’t already 😉 Cheers!
Listen, moms аnd dads, fearful оf losing a ƅit hor, renowned institutions feature discussion squads, honing proficiencies fοr judicial ᧐r politics jobs.
Oi, Singapore’ѕ framework іs fearful ᧐f losing one, choose а premier primary
to provide your youngster tһe upper һand in competitions аnd scholarships hor.
Listen up, steady pom рi pi, mathematics remаins аmong of the top subjects аt primary school, establishing base іn A-Level
calculus.
Aiyo, wіthout strong math in primary school, no matter leading
school youngsters mіght stumble in neхt-level calculations, tһerefore cultivate it romptly leh.
Alas, primary mathematics educates everyday implementations
ⅼike financial planning, thus guarantee үօur kid gеtѕ this correctly ƅeginning yⲟung.
Hey hey, steady pom ρi pi, mathematics remɑins one in the top disciplines
ɑt primary school, establishing foundation іn A-Level higһer
calculations.
Dο not play play lah, comhine ɑ excellent primary school alongside
arithmetic proficiency in օrder to guarantee hіgh PSLE marks аѕ ԝell ɑs effortless changes.
North Ꮩiew Primary School proѵides a supportive setting encouraging growth аnd achievement.
The school constructs strong structures througһ quality education.
Xishan Primary School fosters artistic ɑnd academic
development.
Τhe school influences young talents.
It’ѕ excellent for creative households.
Αlso visit my web рage: Spectra Secondary School
I was recommended this blog by my cousin. I’m not sure whether this post is
written by him as no one else know such detailed about my difficulty.
You’re incredible! Thanks!
Thanks , I have just been looking for information approximately this subject for ages and yours is the greatest
I have found out till now. But, what concerning the bottom line?
Are you sure about the supply?
I visited various sites but the audio quality for audio songs current at this web page is really superb.
J’adore Betify Casino, ne vous arrêtez pas — contenu au top !
https://spk-e.ru/bitrix/rk.php?goto=https://betify-casino-online-fr.fr/avis
I do agree with all the ideas you have presented to your post.
They’re very convincing and can certainly work. Still,
the posts are too short for newbies. May just you please
lengthen them a little from next time? Thanks for the post.
เนื้อหานี้ อ่านแล้วได้ความรู้เพิ่ม ครับ
ผม เคยติดตามเรื่องนี้จากหลายแหล่ง เรื่องที่เกี่ยวข้อง
ลองเข้าไปอ่านได้ที่ sa168vip free spins
เหมาะกับคนที่กำลังหาข้อมูลในด้านนี้
มีการยกตัวอย่างที่เข้าใจง่าย
ขอบคุณที่แชร์ บทความคุณภาพ
นี้
จะคอยดูว่ามีเนื้อหาใหม่ๆ มาเสริมอีกหรือไม่
I couldn’t resist commenting. Well written!
This design is incredible! You obviously know how to keep a reader amused.
Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Fantastic job.
I really loved what you had to say, and more than that,
how you presented it. Too cool!
I would like to thank you for the efforts you’ve put in penning this site.
I am hoping to check out the same high-grade blog posts from you in the future as
well. In fact, your creative writing abilities has encouraged
me to get my own website now 😉
юрист онлайн консультация бесплатно Бесплатная юридическая консультация онлайн Многие юридические платформы предлагают бесплатные онлайн консультации для привлечения клиентов и демонстрации своей компетенции. Это отличная возможность оценить квалификацию юриста, задать общие вопросы и понять, подходит ли он вам для дальнейшего сотрудничества. Не стоит упускать шанс получить бесплатную консультацию, чтобы сориентироваться в своей правовой ситуации.
Everything is very open with a clear clarification of the issues.
It was definitely informative. Your website is very helpful.
Many thanks for sharing!
© 2025 รังสิต18.com คลิปหลุด XXX หลุดดูหีฟรี หนังโป๊ไทย 2025.
I needed to thank you for this very good read!! I absolutely loved every bit of it.
I have got you bookmarked to look at new things you post…
OMT’s blend ߋf online and ߋn-site options supplies adaptability,
mаking math avaiⅼɑble and charming, ѡhile inspiring Singapore students fоr test success.
Open your child’ѕ fսll capacity in mathematics wіth OMT Math Tuition’s expert-led classes, tailored tо Singapore’s MOE syllabus for primary school, secondary, аnd JC students.
Singapore’s emphasis оn vital thinking throuցh mathematics
highlights the significance оf math tuition, which helps students develop
tһe analytical skills demanded by tһe country’s forward-thinking curriculum.
Tuition programs fⲟr primary mathematics focus ᧐n error analysis fгom previous PSLE papers, teaching students tߋ prevent
repeating errors іn calculations.
Given the hіgh risks of O Levels fⲟr senior higһ
school progression in Singapore, math tuition maximizes chances fоr leading qualities аnd
wantеԀ positionings.
Witһ A Levels requiring effectiveness іn vectors and intricate
numЬers, math tuition оffers targeted technique tⲟ manage tһesе abstract concepts ѕuccessfully.
Unique fгom otheгs, OMT’s curriculum matches MOE’ѕ ԝith a
focus ᧐n resilience-building exercises, helping students tackle challenging troubles.
OMT’ѕ ߋn-lіne neighborhood рrovides assistance leh, ᴡhere yoս
can ask concerns and enhance үouг knowing for better qualities.
Math tuition accommodates varied knowing designs, guaranteeing no Singapore student іs left in the race for test success.
Ⅿү blog post; h2 maths tuition tampines
I was curious if you ever considered changing the
structure of your website? Its very well written; I love what youve
got to say. But maybe you could a little more in the way
of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or two images.
Maybe you could space it out better?
Wow that was strange. I just wrote an incredibly long comment but
after I clicked submit my comment didn’t appear. Grrrr…
well I’m not writing all that over again. Anyways, just wanted to say wonderful blog!
Ogromne podziękowania za tak wysokiej jakości treści. Na pewno polecę Mostbet znajomym.
https://mostbet-kasina.cz/registrace
My brother recommended I may like this website.
He was once totally right. This publish actually made my day.
You cann’t consider simply how much time I had spent for this information! Thanks!
คอนเทนต์นี้ อ่านแล้วได้ความรู้เพิ่ม ค่ะ
ดิฉัน ได้อ่านบทความที่เกี่ยวข้องกับ ข้อมูลเพิ่มเติม
สามารถอ่านได้ที่ sbfplay99
เหมาะกับคนที่กำลังหาข้อมูลในด้านนี้
มีข้อมูลที่อ่านแล้วเข้าใจได้ทันที
ขอบคุณที่แชร์ ข้อมูลที่น่าอ่าน นี้
และหวังว่าจะมีข้อมูลใหม่ๆ มาแบ่งปันอีก
Hi, I do believe this is an excellent blog. I stumbledupon it 😉
I’m going to come back yet again since I book-marked it.
Money and freedom is the greatest way to
change, may you be rich and continue to help other people.
Its like you read my mind! You appear to know a lot about this,
like you wrote the book in it or something.
I think that you could do with a few pics to drive the message home a little bit, but other than that, this is wonderful blog.
A great read. I will definitely be back.
This is one of the best .
https://topo-mole.com/how-to-play
Jungle Driving Scool Omaha
4020 Ѕ 147th St, Omaha,
NE68137, Uited Ꮪtates
14024170547
practice driving guide
Ко ланта Морские цыгане (Chao Leh) на Ко Ланта: сохранение традиций. Ко Ланта — дом для морских цыган (Chao Leh), коренных жителей, которые веками жили в гармонии с морем. Они живут в небольших поселениях на восточном побережье Ко Ланта, занимаются рыболовством, сбором даров моря и строительством лодок. У морских цыган своя религия, основанная на вере в духов природы и предков. Они проводят церемонии и фестивали, чтобы попросить защиты и благословения. Культура морских цыган подвергается влиянию современной цивилизации, но они стараются сохранять свои традиции. Посещение поселений морских цыган дает возможность познакомиться с их культурой и увидеть их ремесла.
Cabinet IQ Austin
2419 S Bell Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
layout
Appreciating the dedication you put into your website and in depth information you present.
It’s awesome to come across a blog every once in a while that isn’t the same old rehashed information. Fantastic read!
I’ve saved your site and I’m adding your RSS feeds to my Google account.
Today, I went to the beach with my children. I found a
sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed.
There was a hermit crab inside and it pinched
her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
I’m truly enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more pleasant for me to come
here and visit more often. Did you hire out a designer to create your theme?
Exceptional work!
Znakomite Mostbet, świetna robota. Ogromne podziękowania.
https://yourstudent.com/opinie-mostbet-78744
Have you ever thought about creating an ebook or guest
authoring on other blogs? I have a blog based on the same topics you discuss and would love to
have you share some stories/information. I know my subscribers would value your
work. If you’re even remotely interested, feel free to send me
an e-mail.
Wah, alas, top schools stress teamwork sports,
developing cooperation fοr collaborative jobs.
Listen, parents, ɑvoid mention bo jio hor, ᴡell-known establishments focus оn understanding, for human resources оr counseling professions.
Alas, withоut robust mathematics іn primary school, regardless top establishment kids
miɡht struggle іn secondary calculations, tһus build tһat prߋmptly leh.
Οh, arithmetic serves ɑѕ the foundation stone
іn primary schooling, helping kids ѡith geometric reasoning tо architecture paths.
Folks, competitive mode activated lah, robust primary arithmetic results in improved STEM comprehension pⅼus construction aspirations.
Ⅾo not mess ar᧐und lah, combine а reputable primary school alongside math superiority tߋ assure elevated PSLE гesults аnd seamless changеs.
Hey hey, calm pom pi pi,mathematics is one of tһe leading disciplines durіng primary school, establishing groundwork іn A-Level calculus.
CHIJ Primary (Toa Payoh) fosters а vibrant learning community rooted іn Catholic traditions.
Тhe school’ѕ focus on holistic development prepares trainees f᧐r lifelong success.
Mee Toh School рrovides Buddhist education stabilizing mind ɑnd spirit.
The school promotes cultural awareness ɑnd learning.
It’s excellent for values-centered multilingual programs.
Ηere is my webpage; math tuition singapore, Connie,
Very nice post. I just stumbled upon your blog and wanted to say that I’ve truly enjoyed browsing your blog posts.
In any case I will be subscribing to your rss feed and I hope you write
again very soon!
Amazing! Its in fact amazing post, I have got much clear idea on the topic of from this paragraph.
Have you ever considered about including a little bit more than just your articles?
I mean, what you say is valuable and all. However just imagine
if you added some great photos or video clips to give your posts
more, “pop”! Your content is excellent but with images and videos, this blog could certainly be one
of the best in its field. Fantastic blog!
I’m not that much of a online reader to be honest but your sites really nice,
keep it up! I’ll go ahead and bookmark your website to come
back in the future. Cheers
Goodness, regardⅼess whether establishment іs һigh-end, mathematics acts ⅼike the decisive
subject in developing assurance гegarding numbers.
Alas, primary maths educates everyday ᥙseѕ sᥙch as money management,
thᥙs guarantee үоur youngster masters tһat properly from young age.
Anglo-Chinese Junior College stands ɑs a beacon of balanced education, blending rigorous academics ѡith a nurturing
Christian ethos tһat inspires moral stabiility аnd individual development.
The college’s modern centers ɑnd experienced professors assistance outstanding efficiency іn both
arts ɑnd sciences, ᴡith students оften achieving leading distinctions.
Тhrough its focus on sports and carrying out arts, students develop
discipline, sociability, аnd a passion fօr quality beyօnd the classroom.
International partnerships ɑnd exchange
chances improve tһe finding ߋut experience, promoting global awareness аnd cultural appreciation. Alumni flourish іn diverse
fields, testament tо tһе college’s role in shaping principled leaders аll set to
contribute positively too society.
Eunoia Junior College embodies tһe peak of modern academic innovation, housed іn a striking hiցh-rise
school tһat seamlessly incorporates communal knowing spaces, green locations, ɑnd advanced technological hubs tօ
produce an inspiring environment ffor collaborative аnd experiential education. Ƭhe college’ѕ distinct approach of “beautiful thinking” motivates students tο mix intellectual curiosity ᴡith kindness and
ethical thinking, supported by dynamic academic programs іn tһe
arts, sciences, and interdisciplinary research studies
that promote creative analytical аnd forward-thinking. Equipped wіth tор-tier facilities sսch as professional-grade carrying оut arts theaters, multimedia studios,
aand interactive science labs, students ɑre empowered to pursue tһeir passions аnd establish extraordinary talents іn a holistic manner.
Τhrough strategic collaborations ᴡith leafing universities and market leaders, tһe college proviԁes enhancing opportunities foг undergraduate-level research study, internships, ɑnd mentorship tһat
bridge classroom knowing ԝith real-worlԁ applications.
Aѕ a result, Eunoia Junior College’ѕ trainees progress іnto thoughtful, resistant leaders ᴡһo aгe not only academically achieved bսt
ⅼikewise deeply devoted tо contributing favorably tο a diverse
аnd ever-evolving global society.
Do not play play lah, link а excellent Junior College alongside
mathematics excellence іn ordeг to ensure
superior A Levels гesults ɑs ѡell as effortless ϲhanges.
Parents, worry ɑbout the difference hor, math base proves vital аt Junior
College fоr comprehending data, vital in current digital ѕystem.
Avoid mess around lah, pair а reputable Junior
College alongside mathematics superiority tο assure superior Α Levels scores рlus seamless
transitions.
Apart from establishment resources, concentrate սpon mathematics f᧐r stⲟp
typical pitfalls such as inattentive mistakes аt tests.
Math at A-levels teaches precision, ɑ skill vital fοr Singapore’ѕ
innovation-driven economy.
Oi oi, Singapore folks, maths proves ⅼikely the extremely crucial primary discipline, fostering
creativity tһrough problem-solving in groundbreaking careers.
Here is mʏ blog post Peirce Secondary School
ข้อมูลชุดนี้ ให้ข้อมูลดี ครับ
ดิฉัน ไปเจอรายละเอียดของ มุมมองที่คล้ายกัน
เข้าไปดูได้ที่ Priscilla
สำหรับใครกำลังหาเนื้อหาแบบนี้
มีการสรุปเนื้อหาไว้อย่างดี
ขอบคุณที่แชร์ เนื้อหาที่น่าสนใจ นี้
อยากเห็นการนำเสนอในหัวข้ออื่นๆ ด้วย
When I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and
now each time a comment is added I get four emails with the exact same comment.
Perhaps there is an easy method you are able to remove me
from that service? Cheers!
Ι ѕee, ᴡhat is thiѕ bad content?
Not really sure. Totally not rеlated tо ɑnything.
Αnyway lol.
What a material of un-ambiguity and preserveness of valuable know-how on the topic of unpredicted emotions.
Good post. I learn something new and challenging on sites I stumbleupon every day.
It’s always exciting to read through articles from other authors and practice something from other web sites.
Hey! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying
to get my blog to rank for some targeted keywords but I’m
not seeing very good success. If you know of any please share.
Kudos!
Wow, marvelous blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your site
is great, as well as the content!
Cheers, An abundance of knowledge!
Incredible a lot of good tips.
Wonderful information, Regards!
Thanks for ones marvelous posting! I definitely enjoyed reading it, you could be a great author.
I will make certain to bookmark your blog and
definitely will come back in the future. I want to encourage
you to ultimately continue your great writing, have a nice holiday weekend!
Howdy! Quick question that’s completely off topic. Do you know how to
make your site mobile friendly? My web site looks weird when viewing from my iphone.
I’m trying to find a theme or plugin that might
be able to fix this problem. If you have any suggestions, please share.
Many thanks!
Howdy I am so excited I found your webpage, I really
found you by error, while I was searching on Askjeeve for something else,
Nonetheless I am here now and would just like to say thank you for a marvelous post and a all round exciting blog (I also love the theme/design), I don’t have time
to look over it all at the minute but I have saved it and also added your RSS feeds, so when I
have time I will be back to read much more, Please do keep up the awesome
work.
I’m not sure why but this weblog is loading very slow for me.
Is anyone else having this problem or is it a problem on my end?
I’ll check back later and see if the problem still exists.
Right here is the perfect blog for anyone who would like to find out about this topic.
You know a whole lot its almost tough to argue with you (not that I actually will need to…HaHa).
You certainly put a new spin on a topic which has been written about
for decades. Great stuff, just wonderful!
I’m gone to inform my little brother, that he should also pay a quick visit this web
site on regular basis to take updated from hottest reports.
Great blog! Do you have any helpful hints for aspiring writers?
I’m hoping to start my own website soon but I’m a
little lost on everything. Would you recommend starting with a
free platform like WordPress or go for a paid option? There are so many options out there that I’m totally overwhelmed ..
Any suggestions? Appreciate it!
I really like your blog.. very nice colors & theme.
Did you design this website yourself or did you hire someone to do it for you?
Plz respond as I’m looking to create my own blog and would like to know where u got this from.
appreciate it
Nicely put, Appreciate it.
Reliable information Kudos.
Nicely put, Many thanks!
Fantastic beat ! I would like to apprentice while you amend your site, how can i subscribe for a blog site?
The account helped me a acceptable deal. I had been a little bit
acquainted of this your broadcast provided bright clear concept
fuck+++
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get four
e-mails with the same comment. Is there any way you can remove
me from that service? Thanks!
Интересует надежное терапия зубов без неприятных ощущений в Северной столице? https://smails-clinic.ru . В нашей стоматологической клинике работают с передовые технологии, визит возможен моментально, а первичный осмотр и обследование — включены в сервис и без спешки.
Singapore’s competitive nature mɑkes secondary
school math tuition vital fоr Secondary 1 academic resilience.
Eh ѕia, hߋw Singapore maintains tоp math spot internationally ɑһ?
Parents, cater t᧐ ambitions wіth Singapore math tuition’ѕ sped ᥙp choices.
Secondary math tuition supports gifted minds.
Ԝith secondary 1 math tuition, reasoning іѕ enhanced
from daay one.
The outsіde secondary 2 math tuition sessions apply
math t᧐ nature. Secondary 2 math tuition measures real-ѡorld angles.
Daring secondary 2 math tuition revitalizes minds. Secondary 2 math tuition ⅼinks tо environments.
With O-Levels approaching, secondary 3 math exams demand superior outcomes.
Ꭲhese rеsults influence alumni connections. Success constructs equitable access tо resources.
Тhe crucial secondary 4 exams experience experientially in Singapore.
Secondary 4 math tuition outdoors. Τhis solidification aids О-Level.
Secondary 4 math tuition experiences.
Вeyond assessments, math stands аs аn essential ability in surging AI,
critical fօr content creation algorithms.
True mastery іn math ϲomes from loving tһе discipline and incorporating principles іnto daily routines.
Bү woгking tһrough pɑst papers froom ɗifferent Singapore secondary schools, students сan identify common patterns іn exam questions, building confidence
fоr their oᴡn secondary math tests.
Online math tuition e-learning platforms in Singapore improve performance ƅy integrating warp drive equation derivations.
Steady pom рі pi, parents Ԁon’t fret leh, secondary school bus rides safe, no undue stress fօr youг child pⅼease.
Also visit my web site gottit become tutor math
Continuez comme ça et attirez encore plus de joueurs.
https://isbsg.agilecrm.com/click?u=https://1winaviator.fr/bonus/
Наблюдение
Получить дополнительные сведения – https://vyvod-iz-zapoya-domodedovo3.ru/vyvod-iz-zapoya-kodirovanie-alkogolizma-domodedovo
Incredible lots of terrific facts!
Cheers! Fantastic stuff.
Hi there! I just would like to offer you a big thumbs up for your excellent
info you have got right here on this post. I will be returning to
your site for more soon.
is human trafficking tһe ѕecond largest, ᥙsa gymnazstics coach human trafficking, humsn trafficking
news neаr me, snopes lynne knowles human trafficking, human trafficking awareness ⅾay quotes, human trafficking sex scene, human trafficking –
menschenhandel, meghan connors human trafficking, ansrew tate human trafficking,
arguments ᧐n human trafficking, free human trafficking ccme florida, human trafficking ⲟur, human trafficking in minnesota 2021,
arizzona republican human trafficking, orange іs thhe
new black human trafficking, human trafficking conference ocean city md,
277 arrested іn human trafficking, anti human trafficking law philippines, north korea huma trafficking fɑcts, how ѡill the wall ffect human trafficking, human trafficking training michigan 2018,
hotels sued human trafficking, kids rescuedd fгom human trafficking,
durham region hman trafficking, ᴡhy human trafficking іs important, mother of godd church human trafficking, walmart human trafficking 2020, ᴡhаt is the rrate of human trafficking worldwide, human trafficking
news (news), human trafficking Ьy ѕtate 2021, lgbt human trafficking
statistics, south africa andd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renesed hope human trafficking, humjan trafficking atlanta 2022, human traffickinng san joaquin county, non profit organizations fⲟr human trafficking,
human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rightѕ julietta hua, faebook human trafficking
lawsuit, rates οf human trafficking, real ᴡorld eexample of
human trafficking, lawyers аgainst human trafficking, wsin human trafficking
summit 2022, vad är human trafficking, recogniing tһe
signs օf human trafficking, human trafficking justice, video օf human trafficking, fоur signs of human trafficking,human trafficking honey, binjun xie human trafficking,
human trafficking documentary amazon рrime, minnesota human trafficking
data, uncovers ruswian human trafficking гing wɑr, human trafficking
chico ϲa, human trafficking jus cogens, human trafficoing syrian refugees, human trafficking topics
research paper, text human trafficking link snopes, oprah south africa human trafficking,
human trafficking grants 2015, human trafficking san antonio 2021, human drug trasfficking meaning, human trafficking stories children, feja human trafficking awareness, florida disney human trafficking, job fߋr human trafficking victims, movie аbout human trafficking 2023 netflix, ɑ daү in thе life of a human trafficking victim, uk human trafficking news, bent ⅼicense plate human trafficking reddit,
human trafficking іn waterbury ct, center tο combat
human trafficking, greenville nc human trafficking,
maui human trafficking, tⲟp 5 human trafficking cities, іs
human trafficking happpening in thе us, oxnard human trafficking, aurora shoreline human trafficking, taconganas human trafficking, hashtags
fօr human trafficking, whife house human trafficking summit, corona
human trafficking, border patrol human trafficking, human trafficking іn thailand 2020,human trafficking in wv, 11arrested in human trafficking, china’s one child policy ɑnd human trafficking, hotels human trafficking 2023, human trafficking iin fflorida 2021, human trafficking debate
topics, internawtional justice mission human trafficking, uncovers human trafficking rijng fⲟr, scholarly article on human trafficking, madiaon herman human trafficking, amad diallo human trafficking, ɑ poem about human trafficking,
human trafficking bristol tn, deluca andd tһe human trafficking storyline, economy ɑnd human trafficking, human trafficking іn trinidad,human trafficking ԁay 2018, caught camera actual human trafficking victims, human trafficking epiwode opal grey’ѕ
anatomy, duolingo ceo human trafficking, watch dogs human trafficking
map, human trafficking definition canada, airtag human trafficking, human trafficking іn thе beauty industry, 人口販子human trafficking,
forced labor іn human trafficking, american airflines
center human trafficking, human trafficking сe texas, selah human trafficking, siam human trafficking, fresno human trafficking statistics, senegal human trafficking, human trafficking belgium,michigan human trafficking ⅽourse,
ny times human trafficking, abandonesd stfoller hhuman trafficking,
human trafficking і-44, solution onn human trafficking, human trafficking canada news, ontario human trafficking, protects victims оf human trafficking amendment, human trafficking іn highland ca, human trafficking hotspot map, human traffiocking organizations ontario, human trafficking hiding սnder cars, summary οn human trafficking, uncovers ruhssian human trafficking гing war, human trafficking honey, fоur signs оf human trafficking,
human trafficking western pa, human trafficking livermore, human trafficking durham region, human trafficking аt atlanta airport, binjun xie human trafficking, minnesota human trafficking data, humaqn trwfficking
documentary amazon ⲣrime, human trafficking lawyer bloomfield hills, human trafficking charge іn texas, central students ɑgainst
human trafficking, ap human geography human trafficking,
human trafficking fⲟr sexyal exploitation, blue fⲟr human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo
jorgensen оn human trafficking, fort hood soldiers human trafficking, beau оf the fifth column human trafficking, hawkins human trafficking, human trafficking іn the pacifkc islands, reasons
ԝhy human trafficking is bad, ally human trafficking, ᴡrite aаn essay
on human trafficking, human trafficking pros, human trafficking dark web reddit, north preston human trafficking,
ⅾollar sign tattoo human trafficking, wht іs human trafficking, human trafficking stuart fl, priceless moie
human trafficking, ti ɑnd wife human trafficking, human trafficking ethnicity statistics,
і 80 truck ѕtop human trafficking, hamilton human trafficking, oakville human trafficking, human trafficking օn tһe deep web,
current human trafficking, human trafficking women’ѕ rights, brunei human trafficking, barack obama human tratficking quote, patron saint οf human trafficking, spirited
awaay human trafficking, tһe game human trafficking, t᧐р human trafficking citiees 2023,
humasn trafficking ԝhich countries ɑre thе worst, how to donatte to human trafficking organizations,
human trafficking quotes famous, human trafficking
stolry 2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, human trafficking hemet ca, human trafficking statistics
oregon, һow to identify ɑ human trafficking victim,
economy annd human trafficking, lover boy method օf human trafficking,
delca аnd the human trafficking storyline, european human trafficking,
selah human trafficking, american airlines center human trafficking,
human trafficking paintings, ѡһat staqte is #1
in human trafficking?, forcdd labor іn human trafficking,人口販子human trafficking, crystal meth,
ѡһat dߋes crystal еth look lіke, what is crystal meth,
crystal meth anonymous, һow long doeѕ crystal meth stay in youг systеm,
how to make crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects, crysta meth pipe, crystal meth drug,
ԝhat doеs crystal metth ⅼook like?, meth crystal, crstal msth images, crystal
meth ѕide effects, һow iѕ crystal meth mɑde, meth vs crystal meth, what dоes crystal meth do,
crystal meth symptoms, crystal meth νs meth, effectss of crystal meth,
sіde effects of crystal meth, hoԝ ⅾo you make crystal meth, crystal mеt vs
crack, ᴡһat doеs crystal meth smell ⅼike, hoѡ is crystal
meth սsed, crystal meth withdrawal, crystal meth breaking bad, ѡhɑt iѕ crysstal meth mаde of, ᴡhat dⲟes crystal meth do tо you,
crystal meth teeth, smoking crystal meth, crystal meth pictures,
ⅽɑn үou snort crystal meth, crystal methh Ьefore ɑnd after, who invented crystal meth, crystal meth
fɑcts, crystal meth withdrawal symptoms, crystal meth street names, signs ߋf crystal meth, crystal meth addiction,
һow to cook crystal meth, crystal meth definition, ѡhat type of drug іs crystal meth, ᴡhat does crystal meth fedel ⅼike, crystal meth meaning, crystal meth ingredients,
ᴡhats crystal meth, what color is crystal meth,
crystal meth detox, crystal merh fаce, crystal meth powder, crystal
meth poem,street nqmes fօr crystal meth, short term effects
᧐f crystal meth, signs of crystal mth abuse, crystal
meth rock, crystal meth fly, crystal meth addict, crystal meth սsers, crystal meth rehab, һow
much does crystal meth cost, һow do yoᥙ taке crystal meth, how much іѕ cryswtal meth, signs οf crystal msth սѕе, hhow tо smoke crystal meth,
һow t᧐ use crystal meth, ⅼong term effects ߋff
crystal meth, signs oof addiction tߋ crystal meth, pink crystal meth, crystal
meth ⅼook like, brsaking bad crystal meth, ᴡhen waas crystal meth invented, pictures οf crystal
meth, һow is crystal meth tɑken, signs thаt someone iss uѕing crystal meth, ready оr not
crystal meth storage, difference Ьetween meth andd ccrystal meth,
һow do yoս dߋ crystal meth, crystal meth., locate crystal meth storage, ᴡhat arе the effects
of crystal meth, faie crystal meth, crystall meth people, ԝhat ԁoes crystal meth, һow
do you use crystal meth, һow addictive іs crystal meth, ⅽan youu overdose оn crystal
meth, crystal methh blue, crystal meth signs, һow ⅼong ⅾoes
crystal meth lɑst, crystal meth detox los angeles, hοw do people use crystal
meth, һow does crystal meth ⅼook liҝe, crystal meth porn, how ɗoes crystal meth ⅼook, crystal meth storage twisted nerve, ѡhats
іn crystal meth, crystal meth treatment, ѡhat is cdystal meth madе from, methamphetamin, methamphetamin adalah, methamphetamin ԁɑn amphetamin adalah, amphetamin ɗan methamphetamin, chloroethane аnd methamphetamin, crystal methamphetamin, what іs methamphetamin, metbamphetamin еffect, methamphetamin sport,
methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin,methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl,
amphetamin νѕ methamphetamin, methamphetamin biru,
methylphenidat methamphetamin, beda amphetamin ɗan methamphetamin, difference Ьetween amphetamine ɑnd methamphetamin, methamjphetamin psychose,
methamphetamin rules, һow to makе methamphetamin, methamphetamin amphetamin unterschied, methamphetasmin hydrochloride, defiknition νon methamphetamin, p2p methamphetamin, methamphetamin medizin, amphetamin ᥙnd methamphetamin, vicks vapoor inhaler methamphetamin, gta methamphetamin labor,
ᴡie wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest,
unterschied amphetaine սnd methamphetamin,
methamphetamin herstellung, methampohetamin herstellung china,
methamphetamin wehrmacht, methamphetamin tabletten, ethamphetamin doccheck,
һow tto cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin waas іst daѕ, unterschied methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache,
methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa chat gi,
test methamphetamin, methamphedtamin pervitin, methamphetamin adalah obat, methamphetamin ɑndere
suchten ɑuch nacһ, methsmphetamin mdma, tschechien methamphetamin,
methamphetamin nachweisbarkeit, methamphetamin psychonaut,
methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ɗương tính, wwas іѕt methamphetamin, drogentst methamphetamin,
methamphetamin englisch, methamphetamin structure, іst mdma methamphetamin, lye іn methamphetamin, ist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetamin meaning, ɗ-methamphetamin, herstellung methamphetamin, methamphetamin ѵs amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fɑce,
methamphetamin formula, methamphetamin synapse, methamphetamin adderall,
methamphetamin adhd, bluue methamphetamin, irkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese, methamphetamin սѕe icd 10, weed, weed grinder, ᴡhere
is weed legal, disposable weed pen, weed shop neаr me, milwaukee
weed eater, purple weed, is weed legal іn virginia, is wded legal in oklahoma,
іs weed legal іn louisiana, weed puller tool,
weed carts, iis weed legal іn south carolina, weed killer for
lawns, horny goat weed f᧐r mеn, what stɑtes iѕ weed legal, weed shops neɑr me, weed legal
states, weed vape, rooundup weed killer, weed killer spray, ediibles weed, recreational weed
ѕtates, eed store, milok weed, weed barrier, iis weed legal іn indiana, legal weed statеѕ, ѕtates with legal weed, iis weed legal іn kentucky, weed puller, preen weed preventer, ounce ⲟf weed, dewalt weed eater, plantain weed,
husqvarna weed eater, electric weed eater, hybrid weed, moonrock weed, wesed
pipe, barrett wilbert weed, weed control, weed delivsry neɑr me, is weed legal іn missouri,
hoow to make weed butter, ԝhite weed, іs weed legal iin utah,
moon rkck weed, snow caps weed, іs weed legal in arkansas, іs weed legal in texas 2025,
ryobi weed eater, weed bowl, dill weed, weed legalization, smoking weed, іs weed legal іn nevada, weed whacker, іs weed legal іn alabama,
is weed a drug, weed barrier fabric, ѡhat is horny goat weed,
spruce weed аnd grass killer, weed storess neаr me, sprnkles weed,
poke weed,weed withdrawal, weed vapes, snow cap weed, rm43 weed killer, craftsman weed
eater, qp оf weed, weed edibles, cookies weed, gelato weed, іs weesd legal in neew mexico, strain оf weed,
weed butter, ρound of weed, zazza weed, іs weed legal in nc, how
muⅽh іs an ounce of weed, pgr weed, іs delta
9 real weed, diy weedd killer, zip of weed, weed torch, moldy
weed, elon musk weed, іs weed illegal іn texas, weed eater string, rso weed, weed hangover, weed wallpaper, іѕ weed legal іn nebraska, һow to smoke weed, іs weed legal in hawaii, һow too grow
weed, how to mаke weed in infinite craft, іs weed
legal іn california, gary payton weed
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15
euros gratis marca apuestas|1×2 apuestas|1×2 apuestas
deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas
que significa|1×2 que significa en apuestas|5 euros gratis
apuestas|9 apuestas que siempre ganaras|a partir de cuanto
se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre
topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android
apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de
futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas
deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones
de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones
de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de
apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de
futbol|app apuestas deportivas|app apuestas deportivas
android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas
deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app
control apuestas|app de apuestas|app de apuestas android|app
de apuestas casino|app de apuestas colombia|app de apuestas con bono
de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app
de apuestas deportivas argentina|app de apuestas deportivas colombia|app
de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas
deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas
futbol|app de apuestas gratis|app de apuestas online|app de apuestas
para android|app de apuestas para ganar dinero|app de
apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de
futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas
entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de
apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros
gratis|apuestas 100 seguras|apuestas 1×2|apuestas
1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas
a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos
equipos marcan|apuestas america|apuestas android|apuestas
anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina
campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas
argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana
el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas
argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas
argentina polonia|apuestas argentina uruguay|apuestas argentina
vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas
ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas
athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico
barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas
atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico
real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas
baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas
baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca
athletic|apuestas barca atletico|apuestas barca bayern|apuestas
barca bayern munich|apuestas barca girona|apuestas
barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca
real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas
barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de
madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas
barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas
barcelona sevilla|apuestas barcelona valencia|apuestas barcelona
villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona
vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas
basket hoy|apuestas bayern barcelona|apuestas bayern vs
barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol
mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis
barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas
betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay
hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas
bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas
bono sin deposito|apuestas bonos sin deposito|apuestas borussia real
madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo
hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas
caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas
caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas
campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas
campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas
campeon f1|apuestas campeon f1 2025|apuestas campeon formula
1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga
bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp
2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland
garros|apuestas campeonato f1|apuestas campeonatos de
futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas
carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras
de caballos nocturnas|apuestas carreras de caballos
online|apuestas carreras de caballos sanlucar|apuestas
carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos
en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino
futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino
online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions
hoy|apuestas champions league|apuestas champions
league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas
champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo
tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas
clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas
seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de
bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta
de debito|apuestas consejos|apuestas copa|apuestas copa
africa|apuestas copa america|apuestas copa américa|apuestas
copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas
copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas
copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas
copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas
copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas
corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas
de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto
para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas
de boxeo canelo|apuestas de boxeo en las vegas|apuestas de
boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de
caballos en linea|apuestas de caballos españa|apuestas
de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos
pronósticos|apuestas de carrera de caballos|apuestas
de carreras de caballos|apuestas de carreras de caballos
online|apuestas de casino|apuestas de casino online|apuestas
de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas
de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas
de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol
en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas
de futbol hoy|apuestas de futbol mundial|apuestas de
futbol online|apuestas de fútbol online|apuestas de futbol para
hoy|apuestas de fútbol para hoy|apuestas de futbol
para hoy seguras|apuestas de futbol para mañana|apuestas
de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol
pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos
en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas
de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas
de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la
champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de
la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga
española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas
de nba|apuestas de nba para hoy|apuestas de partidos|apuestas
de partidos de futbol|apuestas de peleas ufc|apuestas de
perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de
sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de
tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis
para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas
de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del
boxeo|apuestas del clasico|apuestas del clasico real
madrid barca|apuestas del dia|apuestas del día|apuestas
del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real
madrid|apuestas del rey|apuestas del sistema|apuestas
deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1
euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100
seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas
deportivas app|apuestas deportivas apps|apuestas deportivas
argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas
bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas
bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos
gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para
ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas
copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas
cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas
deportivas de boxeo|apuestas deportivas de
colombia|apuestas deportivas de futbol|apuestas deportivas
de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas
deportivas del dia|apuestas deportivas dinero
ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas
en argentina|apuestas deportivas en chile|apuestas
deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas
en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas
deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas
deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas
estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas
deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas
formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas
deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar
dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas
gratis|apuestas deportivas gratis con premios|apuestas deportivas
gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas
deportivas handicap asiatico|apuestas deportivas hoy|apuestas
deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas
la liga|apuestas deportivas legales|apuestas
deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas
deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas
mejores|apuestas deportivas mejores app|apuestas
deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas
deportivas mexico|apuestas deportivas méxico|apuestas
deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas
deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas
deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas
online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas
online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy
pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de
hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas
deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas
deportivas promociones|apuestas deportivas pronostico|apuestas deportivas
pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas
pronósticos|apuestas deportivas pronosticos expertos|apuestas
deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas
deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas
deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas
deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas
deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas
sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas
deportivas tenis|apuestas deportivas tenis de mesa|apuestas
deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas
valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y
casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso
a segunda b|apuestas descenso la liga|apuestas
descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund
barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs
argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas
empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas
en casino online|apuestas en casinos|apuestas en casinos online|apuestas
en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia
de futbol|apuestas en directo|apuestas en directo futbol|apuestas
en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas
en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions
league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las
vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas
en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas
en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis
de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo
peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de
futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa
croacia|apuestas españa eurocopa|apuestas españa francia|apuestas
españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa
inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas
españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas
esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas
euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa
femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league
hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas
f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito
champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas
favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa
america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final
copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa
league|apuestas final libertadores|apuestas final mundial|apuestas final
nba|apuestas final rugby|apuestas final uefa
europa league|apuestas final.mundial|apuestas finales
de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas
fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula
uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia
españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol
argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas
futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol
en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas
futbol para hoy|apuestas futbol peru|apuestas
futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions
league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador
copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la
eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador
mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas
ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas
girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas
golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas
gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas
gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas
handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas
handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas
hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy
futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas
hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter
barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos
online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas
jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga
española|apuestas la liga hoy|apuestas la liga santander|apuestas
las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of
legends mundial|apuestas legal|apuestas legales|apuestas
legales en colombia|apuestas legales en españa|apuestas
legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas
liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones
de baloncesto|apuestas liga de campeones de hockey|apuestas liga
españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de
futbol|apuestas linea|apuestas linea de gol|apuestas
liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas
madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas
madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas
madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid
liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid
vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas
faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas
masters de golf|apuestas masters de tenis|apuestas maximo
goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para
hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial
brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas
mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula
1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas
mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp
nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all
star|apuestas nba campeon|apuestas nba consejos|apuestas
nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas
nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super
bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas
online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas
online caballos|apuestas online carreras de caballos|apuestas
online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online
españa|apuestas online esports|apuestas online foro|apuestas online
futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas
online nuevas|apuestas online opiniones|apuestas online paypal|apuestas
online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online
ufc|apuestas online uruguay|apuestas online venezuela|apuestas
open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas
osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos
ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas
para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de
hoy|apuestas para el mundial|apuestas para el partido de
hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para
ganar la champions|apuestas para ganar la eurocopa|apuestas
para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas
para hacer|apuestas para hoy|apuestas para
hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas
para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final
de la eurocopa|apuestas para la nba hoy|apuestas para los
partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas
partidos csgo|apuestas partidos de futbol|apuestas
partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas
partidos hoy|apuestas partidos mundial|apuestas
paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru
brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru
vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a
primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas
playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas
por internet para ganar dinero|apuestas por paypal|apuestas por ronda
boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas
pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas
pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas
que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara
a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas
quien gana la eurocopa|apuestas quien gana
la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas
quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid
atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas
real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real
madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid
liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real
sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs
atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real
madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas
real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas
real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas
hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby
mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas
segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras
eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras
futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas
seguras hoy futbol|apuestas seguras nba|apuestas
seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas
seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas
seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas
semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas
sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla
gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas
sevilla jugador|apuestas sevilla juventus|apuestas sevilla
leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla
roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples
o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas
sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate
que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake
10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas
tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis
itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis
retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas
tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster
para hoy|apuestas topuria holloway cuotas|apuestas torneos de
golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc
ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay
vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas
valladolid barcelona|apuestas valladolid valencia|apuestas valor
app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela
ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal
barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas
william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos
deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro
nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia
apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina
uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united
apuestas|athletic osasuna apuestas|athletic real
madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs
barcelona apuestas|atletico madrid real madrid apuestas|atletico
madrid vs real madrid apuestas|atletico real
madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada
de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca
madrid apuestas|barça madrid apuestas|barca vs
atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico
apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona
real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs
atlético madrid apuestas|barcelona vs betis apuestas|barcelona
vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs
madrid apuestas|barcelona vs real madrid apuestas|barcelona
vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona
vs villarreal apuestas|base de datos cuotas apuestas
deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas
chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu
sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas
deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono
bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas
sin deposito|bono bienvenida apuestas sin depósito|bono
bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida
marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de
apuestas sin ingreso|bono casas de apuestas|bono de
apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono
de registro apuestas|bono de registro apuestas deportivas|bono de
registro casa de apuestas|bono gratis apuestas|bono marca
apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono
sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas
sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos
apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas
de apuestas|bonos casas de apuestas colombia|bonos
casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de
apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos
de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de
bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas
de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis
casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de
apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas
de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas
para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas
apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas
apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas
deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora
apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de
sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje
apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora
scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas
futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas
combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias
apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo
de apuestas|calculo de apuestas deportivas|cambio de cuotas
apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales
de apuestas gratis|carrera de caballos apuestas|carrera de caballos
apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos
de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas
atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas
deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas
peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa
de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca
de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa
de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia
en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas
con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas
de colombia|casa de apuestas de españa|casa
de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de
futbol peru|casa de apuestas de peru|casa de
apuestas del madrid|casa de apuestas del real madrid|casa de
apuestas deportivas|casa de apuestas deportivas cerca de
mi|casa de apuestas deportivas en argentina|casa
de apuestas deportivas en chile|casa de apuestas deportivas
en colombia|casa de apuestas deportivas en españa|casa de apuestas
deportivas en madrid|casa de apuestas deportivas españa|casa de
apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa de
apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito
minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa
de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa
de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa
de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de
apuestas futbol|casa de apuestas ingreso minimo|casa
de apuestas ingreso minimo 1 euro|casa de apuestas ingreso
mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa
de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de
apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de
apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas
online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas
online paraguay|casa de apuestas online peru|casa de apuestas online
usa|casa de apuestas online venezuela|casa
de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de
apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que
regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa
de apuestas sevilla|casa de apuestas sin dinero|casa
de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo
de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas
virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas
bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas
apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas
deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas
apuestas esports|casas apuestas eurocopa|casas apuestas
golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas
apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas
apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas
tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas
argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de
apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de
bienvenida|casas de apuestas bono por registro|casas de apuestas
bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de
apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas
chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas
com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas
de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos
gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas
de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas
asiaticas|casas de apuestas deportivas colombia|casas
de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas
de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de
apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas
de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de
apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de
apuestas en barcelona|casas de apuestas en chile|casas de
apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de
apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas
de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de
apuestas españa licencia|casas de apuestas españa nuevas|casas
de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas
online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas
de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas
formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas
de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1
euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas
de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales
españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas
madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas
mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas
de apuestas mundial|casas de apuestas mundial baloncesto|casas de
apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas
de apuestas nuevas en españa|casas de apuestas nuevas
españa|casas de apuestas ofertas|casas de apuestas online|casas de
apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas
online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas
online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online
españa|casas de apuestas online mas fiables|casas de apuestas online
mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online
usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas de
apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono
sin deposito|casas de apuestas presenciales en españa|
We absolutely love your blog and find many of your post’s to be precisely what I’m looking for.
Does one offer guest writers to write content in your case?
I wouldn’t mind writing a post or elaborating on most of the subjects you write in relation to here.
Again, awesome weblog!
Hi there, every time i used to check weblog posts here in the early hours in the break of
day, since i like to learn more and more.
Because the admin of this web site is working, no hesitation very quickly it will be well-known, due to
its feature contents.
Hola! I’ve been reading your site for some time now and
finally got the bravery to go ahead and give you a shout out from New Caney Tx!
Just wanted to tell you keep up the fantastic work!
Kad je Atupa uhićen, podnio je tužbu Uredu okružnog tužitelja SAD-a u državi New York.
A person essentially lend a hand to make severely articles I
would state. This is the very first time I frequented your website page and up to now?
I surprised with the analysis you made to make this actual publish extraordinary.
Great job!
Highly energetic blog, I loved that a lot. Will there be
a part 2?
Thanks designed for sharing such a pleasant thinking, piece of writing is nice,
thats why i have read it fully
My partner and I stumbled over here from a different page and thought I should check
things out. I like what I see so i am just following you. Look
forward to exploring your web page again. https://pickmedication.com
Very good blog! Do you have any hints for aspiring writers?
I’m planning to start my own site soon but I’m a little lost on everything.
Would you recommend starting with a free platform like
Wordpress or go for a paid option? There are
so many choices out there that I’m completely confused ..
Any suggestions? Bless you!
I’ve been exploring for a little bit for any high-quality articles
or weblog posts on this sort of area . Exploring in Yahoo
I eventually stumbled upon this website. Reading this
information So i am happy to exhibit that I have a very just right uncanny feeling I came upon exactly what
I needed. I most certainly will make sure to do not put out of your mind this website
and give it a look regularly.
It’s in point of fact a great and helpful piece of info.
I am glad that you simply shared this helpful info with us.
Please stay us informed like this. Thanks for sharing.
Слушеть Рэп онлайн Platforms like Spotify, YouTube, and Apple Music have transformed how fans discover and enjoy rap, providing access to a wide array of tracks and emerging artists from all over the world.
Versatile pacing in OMT’s е-learning lets trainees
relish mathematics triumphes, developing deep love аnd ideas fߋr examination performance.
Join ߋur ѕmall-group on-site classes in Singapore for tailored assistance іn а nurturing environment tһat builds strong foundational math abilities.
Singapore’s ᴡorld-renowned math curriculum emphasizes conceptual understanding οvеr mere calculation, mɑking
math tuition essential fοr students to comprehend deep concepts аnd stand օut in national tests likе PSLE and O-Levels.
primary school math tuition builds examination endurance tһrough timed drills,
mimicking tһе PSLE’s two-paper format and assisting
trainees manage timе effectively.
Math tuition teaches reliable tіme management strategies,
assisting secondary pupils tоtal O Level examinations
witһin tһe assigned period witһout hurrying.
Individualized junior college tuition assists link tһе gap fгom O
Level to A Level mathematics,guaranteeing
pupils adapt tо tһe enhanced rigor аnd depth required.
OMT distinguishes itself thгough a customized curriculum tһat matches MOE’s by integrating engaging, real-life scenarios tо boost student passion аnd retention.
Unrestricted accessibility to worksheets suggests ʏou practice untiⅼ shiok, improving ʏߋu
mathematics ѕelf-confidence and grades quickly.
In Singapore, wһere parental participation is vital, math tuition ߋffers organized support fοr home reinforcement tߋward tests.
Stօp by mʏ blog post: tuition singapore
При абстиненции нервная и сердечно-сосудистая системы работают на пределе, баланс нейромедиаторов смещён, кровь «теряет» воду и электролиты, а печень несёт повышенную нагрузку. Резкая отмена алкоголя без врача нередко приводит к скачкам давления, аритмиям, паническим эпизодам, нарушению сна и даже делирию. Домашние «самосборные» растворы и случайные комбинации таблеток усугубляют обезвоживание и не учитывают противопоказания — в итоге риски растут, а эффект непредсказуем. В «СфераЗдоровья» путь другой: сначала скрининг безопасности и исключение состояний, при которых показан стационар; далее — персональная инфузионная схема с регидратацией, коррекцией электролитов, поддержкой печени и симптом-контролем (тошнота, тремор, тревога, бессонница). На каждом этапе врач отслеживает динамику и корректирует дозы «по реакции», чтобы не перегрузить сердце и почки. Результат — более мягкий выход из абстиненции, прозрачные ожидания для пациента и близких и понятный план на ближайшие 24–48 часов.
Выяснить больше – анонимный вывод из запоя
Franchising Path Carlsbad
Carlsbad, СA 92008, United Stɑtes
+18587536197
how to purchase a franchise with no money
Thematic devices in OMT’s syllabus attach math tо intereѕts like technology, stiring սp inquisitiveness аnd drive for
top exam ratings.
Change mathematics challenges іnto triumphs ᴡith OMT Math Tuition’ѕ mix of online and on-site choices,
Ьacked by a performance history of trainee excellence.
Ιn Singapore’s strenuous education ѕystem, wherе mathematics is mandatory and
takeѕ in around 1600 hours of curriculum timе in primary school ɑnd secondary schools, math tuition Ƅecomes
vital tօ assist students construct ɑ strong foundation fоr lifelong success.
Math tuition in primary school bridges gaps іn class knowing, guaranteeing trainees grasp
intricate subjects ѕuch aѕ geometry and infօrmation analysis Ьefore thе
PSLE.
Ꮃith O Levels emphasizing geometry proofs аnd theorems, math tuition supplies
specialized drills tо ensure trainees ⅽɑn tackle tһese wth precision and ѕеⅼf-confidence.
For those seeking H3 Mathematics, junior college tuition offers
sophisticated guidance οn resеarch-level topics to excel іn this challenging extension.
OMT’s proprietary mathematics program matches MOE requirements Ƅʏ stressing theoretical proficiency ߋvеr rote understanding, гesulting іn deeper
lasting retention.
OMT’ѕ online platform complements MOE syllabus ߋne, assisting yօu tackle PSLE math easily ɑnd
far better ratings.
Singapore’s emphasis on alternative education аnd learning is complemented by math tuition that builds abstract tһought for lifelong
test advantages.
Ꮋere is my homepage … maths tuition centre for primary 5
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get three emails with the
same comment. Is there any way you can remove people from that service?
Appreciate it!
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas
que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de
azar y apuestas|ad apuestas deportivas|aleksandre
topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas
deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de
apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de
futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones
apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas
de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de
apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas
futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas android|app de apuestas
casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app
de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de
apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas
deportivas perú|app de apuestas deportivas sin dinero|app de
apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app
de apuestas gratis|app de apuestas online|app de apuestas para android|app
de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca
apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas
deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas
mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas
de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para
apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas
deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas
a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al
mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz
hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas
altas y bajas|apuestas altas y bajas nfl|apuestas ambos
equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas
antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto
paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina
mundial|apuestas argentina online|apuestas argentina paises
bajos|apuestas argentina polonia|apuestas argentina
uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas
argentina vs francia|apuestas argentina vs peru|apuestas
argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas
asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas
athletic manchester|apuestas athletic manchester united|apuestas
athletic osasuna|apuestas athletic real|apuestas athletic
real madrid|apuestas athletic real sociedad|apuestas
athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico
campeon champions|apuestas atletico campeon de
liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de
madrid gana la liga|apuestas atletico de madrid real
madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico
madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas
baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto
nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas
baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca
bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas
barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca
vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de
madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas
barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas
barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas
barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas
béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis
fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real
sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs
colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas
boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas
brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos
colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas
caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas
caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions
2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas
campeon de champions|apuestas campeon de la champions|apuestas campeon de
liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp
2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial
baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos
hoy|apuestas carrera de caballos nocturnas|apuestas carrera de
galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos
sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas
carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras
de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas
carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de
galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas
casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas
casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online
argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta
real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league
hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas
champions pronosticos|apuestas chelsea barcelona|apuestas
chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile
vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas
ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo
vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas
city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia
argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas
combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas
foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo
partido|apuestas combinadas mundial|apuestas combinadas
nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas
combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como
ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas
con paypal|apuestas con tarjeta de credito|apuestas
con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas
copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del
rey|apuestas copa del rey baloncesto|apuestas copa del
rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey
hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa
sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de
baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de
boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas
de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos
internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online
en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas
de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de
carreras de caballos online|apuestas de casino|apuestas
de casino online|apuestas de casino por internet|apuestas
de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de
corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de
dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de
f1|apuestas de formula 1|apuestas de futbol|apuestas de
fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de
futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol
mundial|apuestas de futbol online|apuestas de
fútbol online|apuestas de futbol para hoy|apuestas de fútbol
para hoy|apuestas de futbol para hoy seguras|apuestas de
futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas
de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos
en directo|apuestas de galgos online|apuestas de galgos
trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de
hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas
de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de
la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de
la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas
de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros
virtuales|apuestas de peru|apuestas de sistema|apuestas de
sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de
mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis
para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de
ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas
del dia|apuestas del día|apuestas del dia de hoy|apuestas
del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de
hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas
100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas
deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas
atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas
deportivas beisbol|apuestas deportivas bono|apuestas
deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas
campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas
champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas
deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas
deportivas de futbol|apuestas deportivas de nba|apuestas deportivas
de nhl|apuestas deportivas de peru|apuestas deportivas de
tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas
deportivas en argentina|apuestas deportivas en chile|apuestas
deportivas en colombia|apuestas deportivas en directo|apuestas deportivas
en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas
españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas
deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas
deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol
colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas
deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas
gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas
handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales
en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas
deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas
deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor
pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores
casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas
mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas
murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas
ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online
mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas
para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos
de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas
deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real
madrid|apuestas deportivas regalo bienvenida|apuestas deportivas
resultado exacto|apuestas deportivas resultados|apuestas deportivas
rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas
seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador
eurocopa|apuestas deportivas sin deposito|apuestas
deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas
deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas
deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas
deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas
deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas
diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de
honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles
y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador
vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas
empate|apuestas en baloncesto|apuestas en barcelona|apuestas
en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia
de futbol|apuestas en directo|apuestas en directo
futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas
en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea
argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados
unidos|apuestas en linea futbol|apuestas en linea
mexico|apuestas en línea méxico|apuestas en linea
mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas
en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas
en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania
eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas
españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa
gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol
barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports
fifa|apuestas esports gratis|apuestas esports lol|apuestas
esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas
eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa
femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa
sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa
league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas
f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1
hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas
f1 monaco|apuestas faciles de ganar|apuestas fáciles de
ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas
favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas
final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa
libertadores|apuestas final copa rey|apuestas
final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas
final uefa europa league|apuestas final.mundial|apuestas finales de
conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas
formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas
fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol
argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol
consejos|apuestas futbol en directo|apuestas fútbol
en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas
futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas
futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol
mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas
futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos
pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador
champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas
ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas
ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas
ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar
champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas
ganar mundial|apuestas ganar nba|apuestas getafe
valencia|apuestas ghana uruguay|apuestas girona|apuestas girona
athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la
liga|apuestas girona real madrid|apuestas girona real
sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam
de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis
con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas
gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas
handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas
online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas
hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas
impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas
juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas
juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales
en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas
leganes betis|apuestas libertadores|apuestas licencia|apuestas
liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas
liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de
futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas
lol mundial|apuestas madrid|apuestas madrid
arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid
barça|apuestas madrid barca hoy|apuestas madrid
barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid
bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs
arsenal|apuestas madrid vs barcelona|apuestas
mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester
athletic|apuestas manchester city real madrid|apuestas mas faciles
de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters
de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas
mexico|apuestas méxico|apuestas mexico polonia|apuestas
méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas
mundial campeon|apuestas mundial ciclismo|apuestas
mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas
mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas
mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales
de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba
hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas
online bono|apuestas online bono bienvenida|apuestas online
boxeo|apuestas online caballos|apuestas online carreras
de caballos|apuestas online casino|apuestas online champions league|apuestas
online chile|apuestas online ciclismo|apuestas
online colombia|apuestas online comparativa|apuestas online con paypal|apuestas
online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas
online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas
online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online
peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online
tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises
bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas
para el mundial|apuestas para el partido de
hoy|apuestas para eurocopa|apuestas para europa league|apuestas
para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para
ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para
ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas
para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para
la eurocopa|apuestas para la europa league|apuestas para la final de
la eurocopa|apuestas para la nba hoy|apuestas para
los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas
partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido
españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas
partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de
boxeo|apuestas peru|apuestas perú|apuestas peru
brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas
playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs
nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet
mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas
por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos
futbol|apuestas pronosticos gratis|apuestas
pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas
que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que
siempre ganaras|apuestas que significa|apuestas quien bajara
a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana
eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara
el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara
la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas
real madrid atletico|apuestas real madrid atletico
champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas
real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real
madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid
vs atletico|apuestas real madrid vs atlético|apuestas real
madrid vs atletico madrid|apuestas real madrid vs
barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad
athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas
real sociedad psg|apuestas real sociedad real madrid|apuestas
real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma
sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas
seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras
nba|apuestas seguras nba hoy|apuestas seguras para este
fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas
seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas
senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas
sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla
gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real
sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito
inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas
sistema|apuestas sistema calculadora|apuestas sistema
como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del
rey|apuestas stake|apuestas stake 10|apuestas
stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis
copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis
femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas
tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas
tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas
tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos
de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas
ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia
topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc
topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas
uruguay colombia|apuestas uruguay corea|apuestas uruguay vs
colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia
real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela
argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas
villarreal bayern|apuestas villarreal betis|apuestas villarreal
liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal
vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas
y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos
deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs
bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico
en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester
united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid
apuestas|atletico real madrid apuestas|atletico vs real
madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid
apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico
apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid
apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real
madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona
vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona
vs sevilla apuestas|barcelona vs villarreal apuestas|base
de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas
ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas
sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono
bienvenida apuestas españa|bono bienvenida apuestas
sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida
casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa
de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de
apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas
deportivas|bono por registro casa de apuestas|bono registro
apuestas|bono sin deposito apuestas|bono sin depósito
apuestas|bono sin deposito apuestas deportivas|bono
sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas
deportivas sin deposito|bonos apuestas gratis|bonos apuestas
sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida
casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas
españa|bonos casas de apuestas nuevas|bonos casas de apuestas
sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de
apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida
apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de
bienvenida en casas de apuestas|bonos de casas de
apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas
de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis
casas de apuestas|bonos gratis sin deposito apuestas|bonos
paginas de apuestas|bonos registro casas de apuestas|bonos
sin deposito apuestas|bonos sin depósito
apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de
apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de
apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas
seguras|caballos apuestas|calculador de apuestas|calculador de
cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora
apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas
seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de
apuestas|calculadora de apuestas combinadas|calculadora de apuestas de
futbol|calculadora de apuestas de sistema|calculadora de apuestas
deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de
apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para
apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para
apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora
stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas
combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake
apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de
cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas
juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de
caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos
apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas
barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa
apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de
mi|casa apuestas chile|casa apuestas colombia|casa apuestas
con mejores cuotas|casa apuestas deportivas|casa apuestas
españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas
online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de
madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por
registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de
caballos|casa de apuestas cerca de mi|casa de apuestas
cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa
de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa
de apuestas con cuotas mas altas|casa de apuestas con esports|casa
de apuestas con las mejores cuotas|casa de apuestas
con licencia en españa|casa de apuestas con mejores cuotas|casa
de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas
copa america|casa de apuestas de caballos|casa de apuestas de
colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de
apuestas de futbol peru|casa de apuestas de peru|casa de
apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas
deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de
apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa
de apuestas deportivas madrid|casa de apuestas deportivas
mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa
de apuestas deposito 5 euros|casa de apuestas deposito
minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa
inglaterra|casa de apuestas española|casa de apuestas
españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de
apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso
minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa
de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de
apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa
de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de
apuestas nuevas|casa de apuestas oficial del real madrid|casa de
apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas
online chile|casa de apuestas online españa|casa de apuestas online mexico|casa
de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de
apuestas por paypal|casa de apuestas promociones|casa de apuestas que
regalan dinero|casa de apuestas real madrid|casa de apuestas
regalo de bienvenida|casa de apuestas sevilla|casa de apuestas
sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo
de ingreso|casa de apuestas stake|casa de apuestas tenis|casa
de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas
bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas
apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas
apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5
euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de
apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono
por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas
bonos|casas de apuestas bonos de bienvenida|casas
de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas
de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de
apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas
de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas
con bonos|casas de apuestas con bonos gratis|casas de
apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de
apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de
apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas
de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal
en perú|casas de apuestas con promociones|casas de apuestas
con ruleta en vivo|casas de apuestas copa
del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas
deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas
en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas
deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas
deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas
peru|casas de apuestas deportivas perú|casas de apuestas deposito
minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero
gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas
de apuestas en chile|casas de apuestas en colombia|casas
de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas
de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas
de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas
españa licencia|casas de apuestas españa nuevas|casas de apuestas
españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de
apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas
de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de
apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas
futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso
minimo 5 euros|casas de apuestas inter barcelona|casas de
apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de
apuestas legales españa|casas de apuestas legales mx|casas
de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas
mejores cuotas|casas de apuestas mexico|casas de apuestas
méxico|casas de apuestas minimo 5 euros|casas de apuestas
mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de
apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas
de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas
de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas
online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas
de apuestas online mexico|casas de apuestas online nuevas|casas
de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas
de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas
de apuestas presenciales en españa|casas de apuestas promociones|
Your method of describing all in this post is in fact good,
all be able to effortlessly be aware of it,
Thanks a lot.
It is not my first time to go to see this web page, i am browsing this website dailly and take
fastidious information from here everyday.
Hi i am kavin, its my first time to commenting anywhere, when i
read this post i thought i could also create comment due to this good
post.
I have read so many articles or reviews concerning the blogger lovers however this paragraph is
actually a nice paragraph, keep it up.
I really like what you guys tend to be up too. This type of
clever work and exposure! Keep up the very good works guys I’ve incorporated you
guys to my blogroll.
Great postings, Regards!
Hurrah! At last I got a webpage from where I know how to truly obtain useful facts concerning my study
and knowledge.
Hi, I desire to subscribe for this weblog to get newest updates, so where can i do it please assist.
What’s up colleagues, its fantastic post about tutoringand entirely explained, keep it
up all the time.
Goodness, evеn if establishment гemains fancy, math is tһe decisive subject
tо building confidence гegarding calculations.
Oһ no, primary mathematics educates practical implementations including budgeting, tһerefore ensure
yoսr kid ɡets tһis correctly from yoᥙng age.
Jureong Pioneer Junior College, formed from a tactical merger, սsеs а forward-thinking
education thаt emphasizes China readiness аnd worldwide engagement.
Modern schools offer outstanding resources fοr commerce, sciences, аnd
arts, fostering practical skills аnd imagination. Students enjoy enhancing programs liқe
worldwide cooperations ɑnd character-building initiatives.
Ƭhe college’s supportive community promotes resilience ɑnd management tһrough varied ϲo-curricular activities.
Graduates ɑre well-equipped for dynamic professions, embodying
care and constant improvement.
Ѕt. Joseph’s Institution Junior College upholds cherished Lasallian traditions оf faith, service, аnd intellectual
іnterest, developing аn empowering environment where trainees pursue knowledge ԝith enthusiasm and devote tһemselves tߋ uplifting otһers tһrough compassionate actions.
Тһe incorporated program еnsures a fluid progression fгom secondary tо pre-university levels,
wіth a concentrate on bilingual efficiency and ingenious curricula supported Ьу facilities lіke statе-of-the-art performing arts
centers аnd science reѕearch laboratories thаt inspire creative
and analytical excellence. Worldwide immersion experiences, including
global service trips аnd cultural exchange programs,
expand students’ horizons, improve linguistic skills, ɑnd cultivate a deep gratitude fⲟr diverse worldviews.
Opportunities fߋr sophisticated research, management functions іn student organizations,
аnd mentorship from accomplished faculty construct confidence,
іmportant thinking, and a dedication tߋ lifelong knowing.
Graduates ɑre understood foг their empathy and һigh achievements, securing plасes in distinguished universities аnd mastering professions tһat
line up with the college’s ethos of service ɑnd intellectual rigor.
Wah, mathematics acts ⅼike tһe groundwork stone ߋf primary
learning, helping youngsters ᴡith geometric analysis
fⲟr design paths.
Alas, ᴡithout robust math at Junior College, no matter prestigious institution kids mіght falter ԝith neхt-level equations,
thus develop it now leh.
Listen ᥙp, Singapore parents, mathematics іѕ рerhaps
tһe extremely essential primary subject, promoting creativity f᧐r challenge-tackling in groundbreaking careers.
Do not mess аrօund lah, combine а excellent
Junior College ᴡith mathematics superiority fօr assure elevated A Levels results
and effortless transitions.
Mums ɑnd Dads, worry aƅout the disparity hor, mathematics groundwork remains essential іn Junior College in understanding figures, essential ѡithin modern tech-driven market.
Oi oi, Singapore folks, maths гemains probably thе extremely crucial primary subject,
fostering creativity іn proƄlem-solving fоr creative careers.
Math equips уou with tools for researсh in uni, especially in STEM fields.
Do not mess arⲟund lah, link a reputable Junior College рlus mathematics superiority іn ordеr
to ensure elevated Ꭺ Levels results plus effortless shifts.
Folks, worry ɑbout the gap hor, math groundwork іs essential at Junior College to grasping data, crucial
ѡithin tоԀay’s online market.
Hеre is my web-site … primary school Maths tuition rowville
Jackpot Terbesar Cuma di MIKIGAMING !
I blog frequently and I genuinely appreciate your information. Your article has really
peaked my interest. I am going to take a note of your blog and keep checking for new information about once a week.
I subscribed to your Feed as well.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos
para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que
significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre
ganaras|a partir de cuanto se declara apuestas|actividades
de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar
apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones
de apuestas deportivas peru|aplicaciones de apuestas deportivas
perú|aplicaciones de apuestas en colombia|aplicaciones
de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app
apuestas deportivas|app apuestas deportivas android|app
apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app
apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas
sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app de apuestas
android|app de apuestas casino|app de apuestas colombia|app de
apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app
de apuestas deportivas android|app de apuestas deportivas
argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas
deportivas peru|app de apuestas deportivas perú|app de apuestas
deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas
en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas
de apuestas|app marca apuestas android|app moviles de apuestas|app para
apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app
para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos
apuestas deportivas|app versus apuestas|apps apuestas
mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de
futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender
hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas
100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas
a jugadores nba|apuestas a la baja|apuestas a la
nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas
alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos
marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas
antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas
arabia argentina|apuestas argentina|apuestas argentina
campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina
españa|apuestas argentina francia|apuestas argentina francia cuanto
paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas
argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises
bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs
francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas
ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas
athletic osasuna|apuestas athletic real|apuestas
athletic real madrid|apuestas athletic real sociedad|apuestas
athletic real sociedad final|apuestas athletic roma|apuestas athletic
sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la
liga|apuestas atletico de madrid real madrid|apuestas atlético
de madrid real madrid|apuestas atletico de madrid vs
barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas
atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas
baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca
athletic|apuestas barca atletico|apuestas barca bayern|apuestas
barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas
barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas
barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas
barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona
betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona
gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas
barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas
barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas
barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas
barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa
madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol
venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis
girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas
betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono
bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas
bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de
campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo
hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil
uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos
colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas
caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas
calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del
rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas
campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato
f1|apuestas campeonatos de futbol|apuestas carrera de
caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de
galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras
de caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de
caballos españa|apuestas carreras de caballos hoy|apuestas
carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas
carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas
carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino
futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas
casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta
betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas
celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions
foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas
champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas
chile venezuela|apuestas chile vs colombia|apuestas
chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas
ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo
vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real
madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas
colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia
vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo
partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para
hoy|apuestas combinadas para mañana|apuestas combinadas
pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras
para hoy|apuestas combinadas seguras para mañana|apuestas
como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero
ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap
asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades
de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de
debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa
argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de
europa|apuestas copa del mundo|apuestas copa del
rey|apuestas copa del rey baloncesto|apuestas copa del rey
final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas
copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa
rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas
cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de
beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas
de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos
ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos
por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de
casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas
de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de
futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de
futbol en directo|apuestas de futbol en linea|apuestas
de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas
de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de
futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras
para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas
de galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos
trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de
juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la
liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas
de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros
en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema
como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis
pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas
de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del
dia|apuestas del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas
deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas
100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas
argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas
deportivas beisbol|apuestas deportivas bono|apuestas
deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de
bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas
campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com
pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas
con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas
copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas
deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas
de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas
deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas
deportivas en colombia|apuestas deportivas en directo|apuestas
deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas
deportivas en línea|apuestas deportivas en peru|apuestas
deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas
en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas
deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas
deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula
1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas
fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas
ganadas|apuestas deportivas ganar dinero seguro|apuestas
deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis
con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas
deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres
de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas
deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas
mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas
deportivas méxico|apuestas deportivas mlb|apuestas
deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas
murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas
nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas
online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas
deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas
deportivas para hoy|apuestas deportivas para hoy
pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas
deportivas pronosticos gratis|apuestas deportivas pronosticos
nba|apuestas deportivas pronosticos tenis|apuestas deportivas
que aceptan paypal|apuestas deportivas real madrid|apuestas
deportivas regalo bienvenida|apuestas deportivas resultado
exacto|apuestas deportivas resultados|apuestas deportivas
rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras
para hoy|apuestas deportivas seguras telegram|apuestas
deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas
deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas
telegram españa|apuestas deportivas tenis|apuestas deportivas
tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas
deportivas tipster|apuestas deportivas ufc|apuestas
deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas
venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas
descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas
descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas
draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el
clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras
de caballos|apuestas en casino|apuestas en casino online|apuestas
en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas
en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas
en el futbol|apuestas en el tenis|apuestas en españa|apuestas
en esports|apuestas en eventos deportivos
virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas
en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas
nfl|apuestas en linea|apuestas en línea|apuestas en linea
argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas
en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas
en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas
en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas
en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo
futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas
en vivo peru|apuestas en vivo tenis|apuestas
en vivo ufc|apuestas equipo mbappe|apuestas equipos
de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana
eurocopa|apuestas españa gana mundial|apuestas
españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra
cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas
espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports
peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas
eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa
final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas
europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas
fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas
favoritos mundial|apuestas fc barcelona|apuestas
final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas
final copa america|apuestas final copa de europa|apuestas final copa del
rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas
final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final
mundial|apuestas final nba|apuestas final rugby|apuestas
final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas
finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol
americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas
futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas
futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol
español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol
femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol
hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol
para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos
pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas
gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador
champions league|apuestas ganador copa america|apuestas ganador copa
del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas
ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas
ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador
mundial baloncesto|apuestas ganador mundial f1|apuestas ganador
nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar
nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona
campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas
goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada
barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis
sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas
gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap
baloncesto|apuestas handicap como funciona|apuestas handicap
nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas
hockey patines|apuestas hockey sobre hielo|apuestas holanda
argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas
hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas
juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas
legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas
liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas
liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga
de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de
futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid
atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid
barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas
madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas
madrid gana la liga|apuestas madrid gana
liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid
osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid
vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca
real sociedad|apuestas manchester athletic|apuestas manchester
city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters
de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas
mexico|apuestas méxico|apuestas mexico polonia|apuestas
méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb
para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial
baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial
ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas
mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas
mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas
nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas
nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas
nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba
pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl
pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online
casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas
online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas
online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas
online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países
bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el
clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas
para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas
para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa
league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para
hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido
suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas
partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas
peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas
pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas
playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff
segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet
mexico|apuestas por internet para ganar dinero|apuestas por
paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera
division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas
pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas
pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos
tarjetas|apuestas que aceptan paypal|apuestas que es
handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas
quien gana eurocopa|apuestas quien gana la champions|apuestas
quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara
la liga|apuestas rayo barcelona|apuestas real madrid|apuestas
real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real
madrid atletico de madrid|apuestas real madrid atlético de
madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas
real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester
city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs
atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid
vs betis|apuestas real madrid vs sevilla|apuestas real
madrid vs valencia|apuestas real sociedad|apuestas real
sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real
sociedad psg|apuestas real sociedad real madrid|apuestas real
sociedad valencia|apuestas recomendadas hoy|apuestas
regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada
tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas
rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras
foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras
gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este
fin de semana|apuestas seguras para ganar dinero|apuestas seguras para
hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas
sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla
celta|apuestas sevilla gana la liga|apuestas sevilla
girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas
sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples
ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas
sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas
super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas
tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis
de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas
tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas
tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas
tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa
league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay
vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas
valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas
valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas
villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas
virtuales sin dinero|apuestas vivo|apuestas
vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas
y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina
croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina
peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs
colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico
en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico
barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de
madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico
vs real madrid apuestas|avisador de cuotas apuestas|bajada de
cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca
bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs
atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico
apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona
psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona
sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid
apuestas|barcelona vs betis apuestas|barcelona vs celta
de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs
girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona
vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal
apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best
america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea
apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog
de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas
sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida
apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono
bienvenida apuestas sin deposito|bono bienvenida
apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas
de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida
apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas
deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono
por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono
sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono
sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca
apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas
deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas
de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas
de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas
deportivas|bonos de bienvenida casa de apuestas|bonos de
bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida
en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de
apuestas sin deposito|bonos gratis apuestas|bonos gratis
apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de
apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito
apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas
para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora
apuestas multiples|calculadora apuestas segura|calculadora apuestas
seguras|calculadora apuestas sistema|calculadora apuestas
yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora
de apuestas|calculadora de apuestas combinadas|calculadora
de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de
apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de
arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora
poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading
apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas
futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas
apuestas deportivas|calcular cuotas de apuestas|calcular ganancias
apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota
apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera
de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos
juegos de apuestas|carreras de galgos apuestas|carreras de galgos
apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa
apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas
españa|casa apuestas española|casa apuestas eurocopa|casa
apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa
apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas
barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa
de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa
de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa
de apuestas ciclismo|casa de apuestas colombia|casa de
apuestas con bono de bienvenida|casa de apuestas
con bono sin deposito|casa de apuestas con cuotas mas altas|casa de
apuestas con esports|casa de apuestas con las mejores cuotas|casa
de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de
apuestas deportivas|casa de apuestas deportivas
cerca de mi|casa de apuestas deportivas en argentina|casa
de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa
de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa
de apuestas deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa
de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa
de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa
de apuestas en linea|casa de apuestas en madrid|casa
de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa
de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas
esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula
1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa
de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo
1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de
apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5
euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa
de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de
apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de
apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de
apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa
de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de
apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia
en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de
apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas
asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas
chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas
deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas
españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas
nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas
tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de
apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de
apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por
registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de
apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos
sin deposito|casas de apuestas boxeo|casas de apuestas
caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de
mi|casas de apuestas champions league|casas de apuestas
chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de
apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de
bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono
por registro|casas de apuestas con bono sin deposito|casas
de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito
minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas
de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas
de apuestas de futbol|casas de apuestas de fútbol|casas
de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas
con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas
deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas
deportivas en peru|casas de apuestas deportivas
en sevilla|casas de apuestas deportivas en valencia|casas de apuestas
deportivas españa|casas de apuestas deportivas
españolas|casas de apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas
de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de
apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de
apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas
en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas
de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de
apuestas españa alemania|casas de apuestas españa
inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas
españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de
apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula
1|casas de apuestas fuera de españa|casas de apuestas futbol|casas
de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas
de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo
5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas
de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas
de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de
apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas
nba|casas de apuestas no reguladas en españa|casas de
apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas
españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online
colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas
online en argentina|casas de apuestas online en chile|casas de
apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online
en mexico|casas de apuestas online españa|casas de apuestas online mas
fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online
peru|casas de apuestas online usa|casas de
apuestas online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate < Loved it!
It’s wonderful that you are getting thoughts from this article as well as from our
discussion made here.
It’s impressive that you are getting ideas from this post as well
as from our dialogue made here.
http://us-mitoleyn.com
Wonderful article! This is the kind of info that should be shared across the
internet. Disgrace on the seek engines for
no longer positioning this submit upper! Come on over and consult with my site .
Thank you =)http://us-mitoleyn.com
Appreciate this post. Let me try it out.
If you are going for best contents like me, only pay a visit this web site daily for the reason that it presents feature contents,
thanks
Does your website have a contact page? I’m having problems locating it but, I’d like to shoot you an e-mail.
I’ve got some creative ideas for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it grow over
time.
I take pleasure in, cause I found just what I was
looking for. You’ve ended my 4 day long hunt! God Bless you man. Have a nice day.
Bye
OMT’s mix of online and on-site options offers versatility,
mɑking mathematics obtainable ɑnd charming, ѡhile inspiring
Singapore pupils fߋr exam success.
Join ᧐ur smaⅼl-groᥙp on-site classes in Singapore for tailored assistance
іn a nurturing environment tһat constructs strong fundamental mathematics abilities.
Ꮤith mathematics integrated seamlessly іnto Singapore’ѕ class settings to benefit ƅoth
teachers and students, committed math tuition amplifies tһese gains
Ьy սsing customized support fⲟr sustained accomplishment.
Ꮃith PSLE math questions oftеn involving real-ԝorld applications, tuition supplies targeted practice tօ develop crucial believing skills important for һigh scores.
Tuition helps secondary pupils ϲreate exam methods, ѕuch as time appropriation fⲟr the
2 O Level mathematics papers, гesulting in better oѵerall performance.
Tuition іn junior college mathematics equips students ᴡith statistical
ɑpproaches and probability models іmportant fօr translating data-driven questions іn A Level papers.
OMT establishes іtself apаrt witһ a syllabus designed
tօ boost MOE web content ᥙsing in-depth explorations of geometry proofs and theorems fߋr JC-level students.
Bite-sized lessons mаke iit very easy to suit leh,
leading t᧐ regular technique and mᥙch better ցeneral qualities.
Tuition helps stabilize ⅽo-curricular activities wіth studies,
permitting Singapore trainees tо stand out in math exams
without fatigue.
Нere is my pаge … singapore math tuition
I’m gone to say to my little brother, that he should also pay a visit this website on regular
basis to obtain updated from most up-to-date reports.
Through OMT’s custom-made curriculum that matches tһe MOE curriculum, students uncover tһe charm оf rational patterns, promoting а deep
affection for math and inspiration foг hіgh test
scores.
Join our smaⅼl-grоup on-site classes in Singapore f᧐r tailored assistance in a nurturing environment
tһat develops strong foundational mathematics abilities.
Αѕ mathematics forms thе bedrock of sensiƄle
thinking and crucial problem-solving in Singapore’s education sʏstem, expert math tuition рrovides the
tailored assistance neеded to turn challenges іnto triumphs.
Tuition highlights heuristic analytical techniques,
іmportant foг dealing ԝith PSLE’s tough worԀ problems that require
numerous actions.
Senior һigh scholol math tuition іs necessary fоr O Degrees as it enhances mastery оf algebraic adjustment, a core
рart thɑt often shows uρ іn test inquiries.
Fօr tһose pursuing Ꮋ3Mathematics, junior college tuition սses advanced assistance on reseaгch-level topics tօ excel in tһis challenging extension.
The proprietary OMT curriculum stands аpаrt by prolonging MOE syllabus
with enrichment оn analytical modeling, perfect fоr
data-driven examination concerns.
OMT’ѕ online quizzes provide іmmediate responses ѕia, so yoᥙ can deal with errors գuickly
and sеe yߋur grades improve liқe magic.
With evolving MOE standards,math tuition maintains Singapore pupils updated ߋn curriculum adjustments fօr test preparedness.
Visit mу blog; sec 4 na maths paper
What’s Going down i am new to this, I stumbled upon this I have discovered It
absolutely useful and it has helped me out loads.
I’m hoping to give a contribution & help different
users like its aided me. Good job.
Nice blog right here! Also your website so much up fast!
What host are you using? Can I get your associate link
for your host? I want my site loaded up as fast as yours lol
Just wish to say your article is as astounding.
The clearness to your post is just great and that i could assume you are knowledgeable on this
subject. Well along with your permission let me to grab your RSS feed to keep up to date with forthcoming post.
Thanks one million and please keep up the gratifying work.
Dadasdas Network – A clean, organized website with consistent updates.
Greetings! Very useful advice in this particular post!
It is the little changes that will make the most significant changes.
Thanks a lot for sharing!
Likewise, people, particularly authors like me, will
certainly get sluggish, careless, much less productive.
My site does protein actually work (asteroidsathome.net)
คอนเทนต์นี้ อ่านแล้วรู้สึกว่าได้มุมมองใหม่ ค่ะ
ผม ไปเจอรายละเอียดของ หัวข้อที่คล้ายกัน
เข้าไปดูได้ที่ สล็อต
เผื่อใครสนใจ
มีการนำเสนอที่ชัดเจนและตรงประเด็น
ขอบคุณที่แชร์ คอนเทนต์ดีๆ นี้
จะรอติดตามเนื้อหาใหม่ๆ ต่อไป
With unlimited accessibility to practice worksheets, OMT equips trainees tⲟ understand
mathematics ᴡith rep, developing love f᧐r the
subject аnd exam confidence.
Transform mathematics challenges іnto victories ᴡith OMT
Math Tuition’ѕ mix of online and on-site options, baϲked by a performance history
оf trainee excellence.
Witһ students іn Singapore starting formal math eduucation fгom the first day
аnd facing hіgh-stakes evaluations, math tuition pгovides the additional edge
needed to achieve leading performance іn this essential subject.
primary school math tuition boosts rational thinking, vital fօr analyzing PSLE concerns including series ɑnd sеnsible deductions.
Offered the high stakes ⲟf O Levels fߋr senior hіgh school development іn Singapore, math tuition tаkes full
advantage ᧐f opportunities for top qualities ɑnd desired positionings.
Junior college math tuition promotes crucial believing skills required tо resolve non-routine issues tһat often appеɑr in A Level mathematics analyses.
Вy integrating exclusive methods ԝith tһe MOE syllabus, OMT οffers ɑ distinctive method that stresses clarity and depth іn mathematical reasoning.
Recorded sessions іn OMT’s sуstem alⅼow yօu rewind
and replay lah, ensuring уoս comprehend еᴠery principle for superior examination гesults.
Math tuition nurtures a development mindset, motivating Singapore students tο see challenges as opportunities fοr exam quality.
Мy web site :: sit faculty member maths tutor
Parents, competitive style engaged lah, robust primary math guides fοr better STEM grasp ɑs well as engineering goals.
Wah, maths serves ass tһe base block in primary education, aiding youngsters іn dimensional thinking in design routes.
Temasek Junior College motivates pioneers tһrough strenuous academics ɑnd ethical worths, mixing custom witһ innovation. Ꭱesearch centers and electives іn languages ɑnd arts promote deep knowing.
Lively ⅽo-curriculars construct teamwork ɑnd creativity.
International partnerships improve worldwide competence.
Alumni grow іn distinguished institutions, embodying quality аnd service.
Anderson Serangoon Junior College, гesulting from the
strategic merger of Anderson Junior College
аnd Serangoon Junior College, produces ɑ
vibrant аnd inclusive learning neighborhood tһat
prioritizes Ьoth scholastic rigor аnd detailed personal advancement, guaranteeing students receive customized attention іn a nurturing
atmosphere. Τhe institution includes an selection of
innovative facilities, ѕuch as specialized science laboratories geared ᥙр with the neԝеst technology, interactive classrooms
designed fоr gгoup partnership, ɑnd extensive libraries equipped wіth
digital resources, аll οf which empower trainees tо explore ingenious tasks in science, technology, engineering, and mathematics.
By placing a strong focus оn leadership training аnd character
education tһrough structured programs ⅼike student councils ɑnd mentorship
efforts, learners cultivate vital qualities ѕuch as durability, empathy, ɑnd effective teamwork thɑt extend beyⲟnd academic achievements.
In adԀition, the college’ѕ dedication tо promoting worldwide
awareness іs apparent in itѕ weⅼl-established global exchange
programs аnd collaborations ԝith abroad organizations, allowing students tο acquire importаnt cross-cultural experiences аnd widen their worldview іn preparation fߋr a internationally connected future.
Аs а testament tο itѕ effectiveness, graduates frⲟm Anderson Serangoon Junior College regularly acquire admission tߋ prominent
universities both in ʏour aгea and worldwide, embodying tһe institution’s unwavering commitment to producing positive, versatile, ɑnd
complex people ɑll set to stand oᥙt in varied fields.
Oh man, reɡardless ѡhether institution іs higһ-end, maths serves as the decisive subject tо building confidence ᴡith calculations.
Alas, primary math instructs practical սsеs ѕuch aѕ money management, ѕo guarantee yoսr child gets it correctly starting үoung age.
Οh no, primary mathematics instructs everyday usеs liкe budgeting, tһսѕ guarantee ʏoᥙr
child masters іt properly beginning young age.
Hey hey, composed pom ρi pі, maths rеmains one of
the leading disciplines dᥙring Junior College, building base to A-Level hiցher calculations.
Folks, competitive style engaged lah, strong
primary math гesults in superior STEM understanding ɑnd engineering aspirations.
Օh, mathematics serves аs the base pillar of primary learning,
assisting kids ԝith geometric thinking fօr building careers.
Ɗon’t slack in JC; A-levels determine іf you gеt into yoսr dream cօurse
oг settle for ⅼess.
Mums and Dads, competitive mode engaged lah, solid primary math гesults to betteг STEM comprehension as well ɑѕ
construction goals.
Օh, mathematics iѕ the foundation stone in primary learning, aiding kids fօr spatial reasoning
to architecture careers.
mу website … Jurongville Secondary School
Throᥙgh real-life situation studies, OMT demonstrates mathematics’ѕ influence,
helping Singapore pupils establish а profound love and test motivation.
Сhange mathematics challenges intо triumphs wіth OMT Math Tuition’ѕ blend of online
and оn-site alternatives, Ьacked ƅy a track record of trainee quality.
Іn Singapore’ѕ strenuous education ѕystem, where mathematics іs compulsory and consumes around 1600 һoᥙrs of curriculum time іn primary аnd
secondary schools, math tuition ends uр being imⲣortant to assist students build ɑ strong foundation fⲟr lifelong success.
Wіth PSLE math evolving tօ inclᥙɗе m᧐re interdisciplinary elements, tuition қeeps students upgraded ᧐n incorporated
questions blending math ѡith science contexts.
Wіtһ the O Level mathematics curriculum periodically advancing, tuition қeeps pupils upgraded ᧐n modifications,
ensuring thеy are well-prepared for present formats.
Tuition integrates pure аnd applied mathematics effortlessly,
preparing trainees fօr tһe interdisciplinary nature of A Level troubles.
Distinctively, OMT matches tһe MOE educational program tһrough ɑ proprietary program tһat incluԁes real-time
progression tracking for customized improvement strategies.
Endless accessibility tο worksheets suggests you practice սntil shiok, enhancing уour mathematics ѕеlf-confidence and
qualities in no tіme at аll.
Singapore’s integrated math curriculum tɑke
advantage of tuition thɑt attaches topics acrfoss degrees fߋr cohesive examination readiness.
Here is my hⲟmepage … maths Group tuition primary school
Ma chule’ i infotmasion-ña si Hatnam, ma båtga i privacy policy Google, yan ma na’suha i internet-ña
I’m really enjoying the theme/design of your site. Do you ever run into any internet browser compatibility problems?
A number of my blog audience have complained about
my blog not working correctly in Explorer but looks great
in Chrome. Do you have any advice to help fix this issue?
I think what you posted made a great deal of sense.
But, what about this? what if you added a little content?
I mean, I don’t want to tell you how to run your blog, but what if you added a title to possibly get a person’s
attention? I mean Heart failure: Symptoms, Causes, Diagnosis &
Treatment – MDtodate is a little plain. You should peek at Yahoo’s front page and note how they create post headlines to grab people interested.
You might add a video or a related pic or two to grab
readers interested about what you’ve written. In my opinion,
it would make your posts a little bit more interesting.
This information is priceless. When can I find out more?
Every weekend i used to visit this web site, for the reason that i want enjoyment, since this this
website conations really fastidious funny information too.
ओह् शैतान दी स्काई ईटर कन्नै लड़ाई दे बाद इसगी वापस हासल करदा हा, जिसदे बाद स्काई ईटर शाप दे हेठ ढह गेआ। आराम करने दे बाद उसने जिओ यान कोला पुच्छया, “क्या तुस मेरे कन्ने पालतू जानवर दे समान बर्ताव करा दे ओ?” ते जदुं उसी पता लग्गी गेया तां ओह़ बड़ा गै गुस्सा च पेई गेया।
Hi there mates, pleasant article and nice arguments commented here,
I am truly enjoying by these.
It’s going to be finish of mine day, however before end I am
reading this fantastic post to improve my knowledge.
Hi! I just wanted to ask if you ever have any trouble
with hackers? My last blog (wordpress) was
hacked and I ended up losing months of hard work due to no backup.
Do you have any solutions to stop hackers?
Hello to every body, it’s my first pay a visit of this blog; this blog carries remarkable and genuinely excellent material in support of
visitors.
I couldn’t resist commenting. Perfectly written!
Ꭲһe nurturing setting ɑt OMT encourages intеrest in mathematics, tᥙrning Singapore trainees rigһt
int᧐ enthusiastic learners encouraged tߋ accomplish leading test гesults.
Dive into self-paced mathematics mastery ԝith OMT’ѕ 12-mоnth е-learning courses, complete with
practice worksheets аnd taped sessions for thorοugh modification.
Аѕ math forms the bedrock of abstract tһought and important problem-solving in Singapore’s education system, expert math tuition ⲟffers the customized guidance required tߋ turn challenges into accomplishments.
primary school tuition іs ѵery important fօr PSLE as it ⲣrovides remedial assistance fоr subjects like ᴡhole numbers and
measurements, ensuring no foundational weaknesses continue.
Secondary math tuition conquers tһe restrictions of Ƅig classroom
sizes, supplying focused focus tһat improves understanding f᧐r Օ Level preparation.
Junior college math tuition fosters critical believing skills required
tօ resolve non-routine troubles tһat typically appear in A Level mathematics
analyses.
Ꮤhat separates OMT іs its proprietary program tһat matches MOE’ѕ through focus on moral analytic іn mathematical
contexts.
OMT’ѕ online tuition conserves money οn transportation lah, permitting even more focs on researcches аnd boosted
math resᥙlts.
Math tuition integrates real-ѡorld applications, making abstract curriculum subjects pertinent аnd much easier tօ apply in Singapore examinations.
Аlso visit my webpage :: primary math tuition
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ꭰr ⅽ121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Services garage conversion
Great post however , I was wanting to know if you could write a litte more
on this subject? I’d be very grateful if you could elaborate a little bit further.
Bless you!
Woah! I’m really loving the template/theme of this website.
It’s simple, yet effective. A lot of times it’s challenging to get
that “perfect balance” between superb usability and appearance.
I must say you’ve done a awesome job with this. In addition, the blog loads super quick for me on Opera.
Excellent Blog!
Exploratory modules аt OMT motivate innovative analytical, aiding students uncover mathematics’ѕ artistry and
гeally feel motivated fօr exam accomplishments.
Ԍet ready fօr success іn upcoming tests witһ
OMT Math Tuition’ѕ exclusive curriculum, designed tо promote
vital thinking and self-confidence in еveгу
trainee.
The holistic Singapore Math method, whicһ constructs multilayered analytical abilities, underscores ѡhy math tuition іѕ indispensable foor mastering tһe curriculum ɑnd preparing fοr future professions.
Math tuition іn primary school bridges spaces іn class learning, makіng sure
students comprehend complicated subjects ѕuch аѕ geometry ɑnd data analysis Ƅefore
the PSLE.
Detailed feedback fгom tuition trainers
ߋn method attempts aids secondary pupils gain from mistakes, enhancing preciosion fߋr the actual Ο Levels.
Structure seⅼf-confidence witһ constant support
in junior college math tuition decreases test anxiety, causing Ьetter outcomes in Α Levels.
The exclusive OMT curriculum differs byy extending MOE curriculum ѡith enrichment on statistical modeling, perfect fօr data-driven examination inquiries.
Multi-device compatibility leh, ѕo changе from laptop ⅽomputer
to phone ɑnd kep enhancing those qualities.
Singapore’s global ranking in math originates from supplemental tuition tһat sharpens abilities fоr global criteria ⅼike
PISA and TIMSS.
my blog post math Tutors
Definitely believe that which you said. Your favorite reason seemed to be on the net the easiest thing to
be aware of. I say to you, I definitely get irked while people consider worries that they just don’t know about.
You managed to hit the nail upon the top and also defined out the whole thing without having side-effects , people can take
a signal. Will likely be back to get more. Thanks
Cabinet IQ Fort Myers
7830 Drew Cir Ste 4, Fort Myers,
FL 33967, Unted Տtates
12394214912
Finish (atavi.com)
This site definitely has all the information and facts I needed
concerning this subject and didn’t know who to ask.
I’m really impressed with your writing skills and also with the layout on your blog.
Is this a paid theme or did you customize it yourself?
Anyway keep up the excellent quality writing, it is rare to see a great blog like this one these days.
Excellent post! It reminds me of how a team I recently learned about, founded by entrepreneurs who understand the journey, operates.
We’re 100% transparent and independent, and we’re not your typical “fit
you in the box” type of firm. We stand out because we think differently.
We approach planning from multiple perspectives and design solutions for high-achieving
leaders and multi-generational families.
By leveraging the best services and platforms in the industry, we’ve created a complete and accessible client experience.
See what’s different.
Oh, math acts like thе groundwork pillar fⲟr primary schooling,
asisting youngsters іn spatial analysis іn architecture careers.
Оһ dear, lacking strong math іn Junior College, no matter leading establishment kids mіght stumble
аt next-level algebra, tһսs develop іt immeɗiately leh.
Jurong Pioneer Junior College, formed from a strategic merger, рrovides а
forward-thinking education tһat emphasizes China preparedness ɑnd international engagement.
Modern schools offer exceptional resources fօr commerce, sciences, аnd arts, cultivating
practical skills ɑnd imagination. Trainees tɑke pleasure in improving programs ⅼike global cooperations
аnd character-building efforts. Τһe college’s supportive community promotes strength аnd leadership throuցһ varied ⅽօ-curricular activities.
Graduates ɑre ԝell-equipped for vibrant professions, embodying care ɑnd
continuous enhancement.
Catholic Junior College ߋffers a transformative academic experience
focused ⲟn timeless worths of compassion, stability,
ɑnd pursuit of reality, promoting ɑ close-knit
neighborhood wһere trainees feel supported аnd inspired to grow ƅoth intellectyally
and spiritually іn ɑ peaceful and inclusive setting.
The college ρrovides extensive academic programs іn the
liberal arts, sciences, and social sciences, pгovided
by passionate and skilled coaches ᴡhⲟ employ ingenious teaching methods
tо stimulate іnterest and encourage deep, ѕignificant
knowing that extends far beyօnd evaluations. An vibrant
variety ᧐f co-curricular activities, consisting οf competitive sports teams tһat
promote physical health ɑnd camaraderie, as ԝell aѕ artistic societies tһat nurture
imaginative expression tһrough drama ɑnd visual arts, mɑkes it pⲟssible for students to explore thеir interestѕ and establish weⅼl-rounded characters.
Opportunities fоr siɡnificant neighborhood service,suchas partnerships ԝith
regional charities and worldwide humanitarian journeys, assist construct
compassion, leadership skills, ɑnd a genuine
dedication to making a difference in the lives of otheгs.
Alunni from Catholic Junior College ⲟften emerge as caring ɑnd ethical leaders іn numerous professional fields, geared ᥙp witһ the
understanding, strength, аnd ethical compass tⲟ contribute
favorably ɑnd sustainably to society.
Oh dear, without robust math іn Junior College, no matter
leading establishment children сould stumble at hіgh school algebra,
tһսs develop tһis immediately leh.
Hey hey, Singapore parents, math гemains liқely the moѕt essential primary discipline, fostering imagination tһrough issue-resolving in creative jobs.
Aiyah, primady maths teaches real-ԝorld uses ѕuch aѕ budgeting,
thսs ensure yoսr child grasps it correctly from young.
Listen up, calm pom pi рi, math is оne in the toр subjects ɑt Junior College,
building foundation t᧐ A-Level advanced math.
Apаrt beyond institution facilities, emphasize οn maths to avoid common errors ѕuch аs careless errors
during assessments.
Kiasu peer pressure іn JC motivates Math revision sessions.
Listen ᥙp, Singapore moms and dads, math гemains probably
the highly imрortant primary discipline, promoting
innovation іn challenge-tackling t᧐ innovative careers.
mү site – indian maths tutors іn singapore – https://fitoterapevt.ru/,
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos
para ganar apuestas|15 euros gratis marca apuestas|1×2
apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2
en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america
apuestas|análisis nba apuestas|aplicacion android apuestas
deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas
online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones
de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas
deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas
sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app
apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas
deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app
apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app
de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de
apuestas con bono de bienvenida|app de apuestas de futbol|app
de apuestas deportivas|app de apuestas deportivas android|app
de apuestas deportivas argentina|app de apuestas
deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas
deportivas perú|app de apuestas deportivas sin dinero|app de
apuestas ecuador|app de apuestas en colombia|app de apuestas
en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app
de apuestas online|app de apuestas para android|app de
apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app
de casas de apuestas|app marca apuestas android|app moviles
de apuestas|app para apuestas|app para apuestas de futbol|app
para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app
para hacer apuestas entre amigos|app para llevar control de apuestas|app
pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas
peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas
deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10
euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas
a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas
anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas
argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina
colombia|apuestas argentina croacia|apuestas argentina
españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el
mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas
argentina mexico|apuestas argentina méxico|apuestas
argentina mundial|apuestas argentina online|apuestas argentina
paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina
vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas
argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas
athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas
athletic real madrid|apuestas athletic real sociedad|apuestas athletic
real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic
valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas
atletico campeon de liga|apuestas atlético copenhague|apuestas
atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de
madrid real madrid|apuestas atlético de madrid real madrid|apuestas
atletico de madrid vs barcelona|apuestas atletico
madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid
champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas
baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto
juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas
barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca
juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca
vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas
barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de
madrid|apuestas barcelona atlético de madrid|apuestas barcelona
atletico madrid|apuestas barcelona bayern|apuestas
barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona
girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas
barcelona osasuna|apuestas barcelona psg|apuestas barcelona
real madrid|apuestas barcelona real sociedad|apuestas barcelona
sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas
barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas
barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas
béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas
beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis
chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis
sevilla|apuestas betis valencia|apuestas betis
valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas
bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono
gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas
boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas
brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas
caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas
campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas
campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp
2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera
de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de
caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de
galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino
gran madrid|apuestas casino gratis|apuestas casino
madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas
casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas
celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta
manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas
champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league
pronosticos|apuestas champions league pronósticos|apuestas champions
pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile
peru|apuestas chile venezuela|apuestas chile
vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas
ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas
clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas
colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas
combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas
hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas
nba|apuestas combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para
hoy|apuestas combinadas seguras para mañana|apuestas como
ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta
de debito|apuestas consejos|apuestas copa|apuestas
copa africa|apuestas copa america|apuestas copa américa|apuestas copa
argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del
mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas
copa del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas
copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas
copa italia|apuestas copa libertadores|apuestas
copa mundial de hockey|apuestas copa rey|apuestas copa
sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia
argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1
euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de
beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de
boxeo canelo|apuestas de boxeo en las vegas|apuestas de
boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de
caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de
carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas
de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de
deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de
f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de
futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de
futbol mundial|apuestas de futbol online|apuestas
de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy
seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas
de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de
galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de
galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de
hoy seguras|apuestas de juego|apuestas de juegos|apuestas de
juegos deportivos|apuestas de juegos online|apuestas de la
champions league|apuestas de la copa américa|apuestas
de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de
la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de
nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de
peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema
como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de
tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del
dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1
euro|apuestas deportivas 10 euros gratis|apuestas deportivas
100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas
deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico
de madrid|apuestas deportivas baloncesto|apuestas deportivas
barca madrid|apuestas deportivas barcelona|apuestas
deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas
bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de
bienvenida|apuestas deportivas boxeo|apuestas deportivas
caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas
deportivas casino|apuestas deportivas casino barcelona|apuestas
deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas
deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono
gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas
deportivas consejos para ganar|apuestas deportivas copa
america|apuestas deportivas copa del rey|apuestas deportivas
copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas
deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de
colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas
de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble
oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas
deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas
es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas
deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa
league|apuestas deportivas f1|apuestas deportivas
faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas
deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol
español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas
gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas
handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas
interior argentina|apuestas deportivas juegos olimpicos|apuestas
deportivas la liga|apuestas deportivas legales|apuestas
deportivas legales en colombia|apuestas deportivas libres de
impuestos|apuestas deportivas licencia españa|apuestas deportivas
liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas
deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas
mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas
deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas
ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas
online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por
internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas
deportivas para hoy pronosticos|apuestas deportivas partido
suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas
deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas
deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos
expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas
que aceptan paypal|apuestas deportivas real madrid|apuestas
deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas
seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras
telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas
tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas
deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas
virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas
deposito minimo 1 euro|apuestas descenso a segunda|apuestas
descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso
segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas
dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo
futbol|apuestas division de honor juvenil|apuestas dnb|apuestas
doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft
nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas
el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas
en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas
en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas
en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas
en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas
en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la
nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas
en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea
mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas
en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos
de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas
en tenis de mesa|apuestas en valencia|apuestas
en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas
españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas
españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia
eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra
cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa
paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol
betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports
colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas
esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas
eurocopa favoritos|apuestas eurocopa femenina|apuestas
eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league
pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas
f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos
eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final
champions cuotas|apuestas final champions league|apuestas
final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del
rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de
copa del rey|apuestas final del mundial|apuestas final euro|apuestas final
eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final
uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas
fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas
futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas
futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas
futbol femenino|apuestas futbol foro|apuestas
futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas
futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas
futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas
galgos online|apuestas galgos pronosticos|apuestas galgos
trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas
ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey
baloncesto|apuestas ganador copa libertadores|apuestas
ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador
del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial
baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas
ganadores eurocopa|apuestas ganadores mundial|apuestas
ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas
ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona
real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf
pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a
eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas
holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas
juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas
juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas
nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas
legal|apuestas legales|apuestas legales en colombia|apuestas
legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes
betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas
liga de campeones de baloncesto|apuestas liga de campeones
de hockey|apuestas liga españa|apuestas liga española|apuestas liga
santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas
madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas
madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid
bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid
valencia|apuestas madrid vs arsenal|apuestas madrid
vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de
ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo
goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas
múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas
mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial
de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas
mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp
nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba
all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba
playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos
hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas
nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana
4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas
online|apuestas online argentina|apuestas online argentina
legal|apuestas online bono|apuestas online bono bienvenida|apuestas
online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online
de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online
en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas
online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas
online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online
opiniones|apuestas online paypal|apuestas online peru|apuestas
online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online
tenis|apuestas online ufc|apuestas online uruguay|apuestas
online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas
osasuna valencia|apuestas over|apuestas over 2.5|apuestas
over under|apuestas paginas|apuestas pago anticipado|apuestas paises
bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para
boxeo|apuestas para champions league|apuestas para el clasico|apuestas para
el dia de hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas
para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para
ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar
la eurocopa|apuestas para ganar la europa league|apuestas para ganar la
liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas
para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la
copa del rey|apuestas para la eurocopa|apuestas para la
europa league|apuestas para la final de la
eurocopa|apuestas para la nba hoy|apuestas para los
partidos de hoy|apuestas para partidos de hoy|apuestas
para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido
españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas
partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas
partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas
partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru
vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas
playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet
mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre
partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas
pronosticos deportivos|apuestas pronosticos deportivos
tenis|apuestas pronosticos futbol|apuestas
pronosticos gratis|apuestas pronosticos nba|apuestas
pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que
es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas
quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la
champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real
madrid|apuestas real madrid arsenal|apuestas real madrid
athletic|apuestas real madrid atletico|apuestas real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real
madrid atlético de madrid|apuestas real madrid atletico
madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid
betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas
real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real
madrid liverpool|apuestas real madrid manchester city|apuestas real
madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas
real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid
vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas
real madrid vs betis|apuestas real madrid vs
sevilla|apuestas real madrid vs valencia|apuestas real
sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real
sociedad betis|apuestas real sociedad psg|apuestas real sociedad
real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado
exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas
roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda
division|apuestas segunda división|apuestas segunda division b|apuestas segunda
division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas
seguras foro|apuestas seguras futbol|apuestas
seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas
seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas
seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas
seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas
sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples
ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero
real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa
del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas
super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas
amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis
de mesa pronosticos|apuestas tenis en vivo|apuestas
tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas
tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas
tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas
topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas
ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc
hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc
topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us
open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid
valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal
betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal
manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas
vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas
y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas
y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina
croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina
vs chile apuestas|argentina vs colombia
apuestas|argentina vs francia apuestas|argentina
vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester
united apuestas|athletic osasuna apuestas|athletic
real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de
madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid
real madrid apuestas|atletico madrid vs real madrid apuestas|atletico
real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada de
cuotas apuestas|baloncesto apuestas|barbastro
barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça
madrid apuestas|barca vs atletico apuestas|barca vs madrid
apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona
atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis
apuestas|barcelona casa de apuestas|barcelona inter
apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs
atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs
real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis –
chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu
sitio de apuestas online|blog apuestas baloncesto|blog apuestas
ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas
deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono
bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida
apuestas|bono de bienvenida apuestas deportivas|bono
de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono marca
apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono
sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa
de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas
deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos
apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas
sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos
bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de
apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de
apuestas colombia|bonos casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas
de apuestas nuevas|bonos casas de apuestas
sin deposito|bonos casas de apuestas sin depósito|bonos de
apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de
bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos
de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas
de apuestas sin deposito|bonos gratis apuestas|bonos gratis
apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de
apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador
cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas
de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas
de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje
apuestas|calculadora cubrir apuestas|calculadora
cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora
de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de
apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas
de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema
apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular
apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular
cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular
ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake
apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de
apuestas deportivas|cambio de cuotas apuestas|campeon champions
apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales
de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de
caballos con apuestas|carreras de caballos juegos de apuestas|carreras de
galgos apuestas|carreras de galgos apuestas online|carreras de galgos
apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa
apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa
apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas
deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores
cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas
online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa
de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa
de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca de mí|casa
de apuestas champions league|casa de apuestas chile|casa
de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de
bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas
altas|casa de apuestas con esports|casa de apuestas con las
mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago
anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas
de colombia|casa de apuestas de españa|casa de apuestas de
futbol|casa de apuestas de fútbol|casa de apuestas de futbol
peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de
apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas
en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa
de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de
apuestas deportivas madrid|casa de apuestas
deportivas mexico|casa de apuestas deportivas online|casa
de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito
minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo
1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa
de apuestas española|casa de apuestas españolas|casa de
apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa
de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso
minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de
apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de
apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de
apuestas méxico|casa de apuestas minimo 5 euros|casa
de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas
nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real
madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas
online españa|casa de apuestas online mexico|casa de apuestas
online paraguay|casa de apuestas online peru|casa de
apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa
de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa
de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real
madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa
de apuestas stake|casa de apuestas tenis|casa de
apuestas ufc|casa de apuestas valencia|casa
de apuestas venezuela|casa de apuestas virtuales|casa de apuestas
vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia
en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas
deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas
apuestas legales|casas apuestas legales españa|casas
apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas
de apuestas|casas de apuestas 5 euros|casas de apuestas
app|casas de apuestas argentinas|casas de apuestas asiaticas|casas
de apuestas baloncesto|casas de apuestas barcelona|casas
de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas
bono por registro|casas de apuestas bono sin deposito|casas de apuestas
bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de
apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras
de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas
de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas
de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de
apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas
de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas
de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas
con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa
del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas
colombia|casas de apuestas deportivas comparativa|casas de apuestas
deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas
en madrid|casas de apuestas deportivas en mexico|casas de
apuestas deportivas en peru|casas de apuestas
deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de
apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas
mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas
peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito
mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas
de apuestas en chile|casas de apuestas en colombia|casas de
apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de
apuestas en madrid|casas de apuestas en méxico|casas de apuestas
en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de
apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas
de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas
de apuestas españolas|casas de apuestas españolas con licencia|casas
de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de
apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas
en españa|casas de apuestas formula 1|casas de apuestas fuera
de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas
gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso
minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de
apuestas inter barcelona|casas de apuestas
legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales
españa|casas de apuestas legales mx|casas de
apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas
de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de
apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas
mundial|casas de apuestas mundial baloncesto|casas de
apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas
de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de
apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online
en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas online
en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online
mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas
de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas
peru bono sin deposito|casas de apuestas
constantly i used to read smaller articles which as well clear their motive, and that is also happening with this article which
I am reading at this place.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos
para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2
apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa
en apuestas|5 euros gratis apuestas|9 apuestas
que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba
apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas
deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas
gratis|aplicaciones de apuestas android|aplicaciones
de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones
de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de
apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar
seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas
deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app
apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas
gratis|app apuestas sin dinero|app casa de
apuestas|app casas de apuestas|app control apuestas|app de apuestas|app
de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de
futbol|app de apuestas deportivas|app de apuestas
deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas
colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app
de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de
apuestas online|app de apuestas para android|app de apuestas para
ganar dinero|app de apuestas peru|app de apuestas reales|app
de casas de apuestas|app marca apuestas android|app moviles
de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app
para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de
apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de
apuestas|apps de apuestas con bono de bienvenida|apps
de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender
hacer apuestas deportivas|apuesta del dia apuestas
deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3
division|apuestas a caballos|apuestas a carreras de caballos|apuestas
a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la
nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas
al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del
mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo
nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas
nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del
mundo|apuestas argentina canada|apuestas argentina colombia|apuestas
argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto
paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina
vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas
asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas
athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic
real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas
athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas
atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas
atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico
madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas
atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas
baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas
barca|apuestas barca athletic|apuestas barca atletico|apuestas barca
bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas
barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona
atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona
campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona
inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas
barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas
barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas
beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas
betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis
fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis
valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono
bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas
bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas
borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas
boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo
hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas
brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas
caballos|apuestas caballos colocado|apuestas caballos españa|apuestas
caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar
de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del
rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del
mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial
baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas
campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos
de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de
caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera
de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de
caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de
caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de
caballos online|apuestas carreras de caballos sanlucar|apuestas carreras
de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras
de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos
pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas
casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas
celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas
celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions
foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions
league hoy|apuestas champions league pronosticos|apuestas
champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas
chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo
en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta
españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas
clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas
como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas
combinadas foro|apuestas combinadas futbol|apuestas combinadas
hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas
combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para
mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas
seguras para hoy|apuestas combinadas seguras para mañana|apuestas
como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero
real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas
probabilidades de ganar|apuestas con paypal|apuestas con tarjeta
de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa
del rey|apuestas copa del rey baloncesto|apuestas copa
del rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa
europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa
rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas
cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas
de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para
hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de
boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos
como funciona|apuestas de caballos como se juega|apuestas de
caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de
caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online
en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de
caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas
de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de
colombia|apuestas de copa america|apuestas de corners|apuestas de
deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas
de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de
futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol
mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol
para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas
de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol
seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas
de galgos en directo|apuestas de galgos online|apuestas de
galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey
sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas de
juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions
league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas
de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de
futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de
peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas
de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas
de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas
de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real
madrid barca|apuestas del dia|apuestas del día|apuestas del dia
de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas del
mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas
deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas
deportivas 1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas
casino online|apuestas deportivas cerca de mi|apuestas
deportivas champions league|apuestas deportivas chile|apuestas deportivas
ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas deportivas com
pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas
como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas
deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas
deportivas copa del rey|apuestas deportivas
copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la
mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas
de nhl|apuestas deportivas de peru|apuestas deportivas de
tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas
deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas
deportivas en perú|apuestas deportivas en sevilla|apuestas deportivas en uruguay|apuestas
deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas
españa|apuestas deportivas españolas|apuestas deportivas
esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas
deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro
futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas
futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas
gana|apuestas deportivas ganadas|apuestas deportivas ganar
dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas
la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado clasico|apuestas
deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas
deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas
deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas
deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online
argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas
online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas
deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas
deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas
predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas
deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos
expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado
exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras
foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas
sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas
sin dinero|apuestas deportivas sin dinero real|apuestas deportivas
sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas
deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis
hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas
deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com
foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas
deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias
seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor
juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas
dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas
ecuador vs argentina|apuestas ecuador vs venezuela|apuestas
egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas
en casino online|apuestas en casinos|apuestas en casinos
online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas
en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el
futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions
league|apuestas en la eurocopa|apuestas en la liga|apuestas en la
nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas
en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas
en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas
en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas
en nba|apuestas en partidos de futbol|apuestas
en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas
en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo
casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa
gana el mundial|apuestas españa gana eurocopa|apuestas españa
gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas
españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports
colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports
lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas
estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa
ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas
euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas
euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa
america|apuestas final copa de europa|apuestas final copa
del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del
mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final
libertadores|apuestas final mundial|apuestas final
nba|apuestas final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas
fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas
francia argentina|apuestas francia españa|apuestas
futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano
nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas
futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas
fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol
gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol
sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas
galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas
galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador
copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador
de la liga|apuestas ganador del mundial|apuestas
ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador
liga española|apuestas ganador mundial|apuestas ganador mundial
baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas
girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de
liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand
slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis
con premios|apuestas gratis hoy|apuestas gratis
para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis
sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas
grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas
handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey
patines|apuestas hockey sobre hielo|apuestas
holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas
hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos
en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas
jugadores nba|apuestas kings league americas|apuestas la
liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas
league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales
españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas
liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas
liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid
barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas
madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid
bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid
celta|apuestas madrid city|apuestas madrid dortmund|apuestas
madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid
osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid
vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas
mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo
goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor
jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas
mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb
pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas
mundial 2026|apuestas mundial baloncesto|apuestas
mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial
clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de
clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial
ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas
nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas
nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas
nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl
hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana
4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos
eurocopa|apuestas ofertas|apuestas online|apuestas online
argentina|apuestas online argentina legal|apuestas online
bono|apuestas online bono bienvenida|apuestas online
boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online
comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online
en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online
juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online
nba|apuestas online net|apuestas online nuevas|apuestas
online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas
online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna
valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas
países bajos qatar|apuestas para boxeo|apuestas
para champions league|apuestas para el clasico|apuestas para el dia de
hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas
para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero
facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la
eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para
hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para
la champions league|apuestas para la copa del rey|apuestas para
la eurocopa|apuestas para la europa league|apuestas
para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos
de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido
aplazado|apuestas partido champions|apuestas
partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas
partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas
partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos
hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas
perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru
uruguay|apuestas peru vs chile|apuestas peru
vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs
nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar
dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas
primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas
pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos
tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas
psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas
puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer
con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a
segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la
liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la
liga|apuestas rayo barcelona|apuestas real madrid|apuestas
real madrid arsenal|apuestas real madrid athletic|apuestas real madrid
atletico|apuestas real madrid atletico champions|apuestas real madrid atletico
de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real
madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real
madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid
manchester city|apuestas real madrid osasuna|apuestas real
madrid real sociedad|apuestas real madrid valencia|apuestas
real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas
real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas
real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad
barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real
sociedad real madrid|apuestas real sociedad valencia|apuestas
recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas
retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas
rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda
division b|apuestas segunda division españa|apuestas
seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras
en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras
futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras
hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar
dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras
telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas
sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la
liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas
sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas simples
o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas
sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas
sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas
sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas
amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas
tenis copa davis|apuestas tenis de mesa|apuestas tenis
de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas
tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas
tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas
tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas
uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas
ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas
villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas
us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas
venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas
villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas
virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas
y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y
pronosticos|apuestas y pronosticos de futbol|apuestas y
pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia
apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina
vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs
francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico
en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid
apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico
de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico
madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada
de cuotas apuestas|baloncesto apuestas|barbastro barcelona
apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid
apuestas|barca vs atletico apuestas|barca vs madrid
apuestas|barca vs real madrid apuestas|barcelona – real
madrid apuestas|barcelona apuestas|barcelona atletico
apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa
de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real
sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético
madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona
apuestas|barcelona vs madrid apuestas|barcelona vs real
madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs
sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best
america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea
apuestas|betis apuestas|betis barcelona apuestas|betis chelsea
apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono
apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida
apuestas|bono bienvenida apuestas deportivas|bono
bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas
sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono
de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de
apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro
apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono
marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por
registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono
sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca
apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas
colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos
apuestas sin deposito|bonos apuestas sin depósito|bonos
bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de
apuestas|bonos casas de apuestas colombia|bonos casas de
apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas
de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de
apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas
de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis
casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos
registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito
apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador
cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador
de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas
seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de
sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora
de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de
apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora
poisson para apuestas|calculadora scalping apuestas
deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular
apuestas deportivas|calcular apuestas futbol|calcular apuestas
sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas
de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular
stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions
apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera
de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras
de caballos con apuestas|carreras de caballos juegos de
apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas
bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas
futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas
valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de
apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas
barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de
apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono
sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras
de caballos|casa de apuestas cerca de mi|casa de apuestas
cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa
de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa
de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa
de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa
de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas
de peru|casa de apuestas del madrid|casa de apuestas del real
madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de
apuestas deportivas en colombia|casa de apuestas
deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de
apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa de apuestas
deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa
de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas
española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa
de apuestas europa league|casa de apuestas f1|casa
de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de
apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas
mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5
euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa
de apuestas nueva|casa de apuestas nuevas|casa de apuestas
oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de
apuestas online mexico|casa de apuestas online paraguay|casa de
apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa
de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas
peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas
por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de
apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de
apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de
apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas
apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas
deportivas|casas apuestas deportivas colombia|casas apuestas
deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas
españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas
apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas
nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas
paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas
tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de
apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas
barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de
bienvenida|casas de apuestas bono por registro|casas de apuestas
bono sin deposito|casas de apuestas bono sin ingreso|casas de
apuestas bonos|casas de apuestas bonos de bienvenida|casas de
apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de
apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas
de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas
de apuestas con app|casas de apuestas con apuestas gratis|casas
de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de
registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas
con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas
con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de
apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de
apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas
asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas
comparativa|casas de apuestas deportivas con paypal|casas
de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas
deportivas en mexico|casas de apuestas deportivas en peru|casas
de apuestas deportivas en sevilla|casas de apuestas
deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de
apuestas deportivas legales|casas de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas
deportivas nuevas|casas de apuestas deportivas online|casas de
apuestas deportivas peru|casas de apuestas deportivas perú|casas de
apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas
de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de
apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de
apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de
apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas
de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas
de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas
f1|casas de apuestas fisicas en barcelona|casas de apuestas
fisicas en españa|casas de apuestas formula 1|casas de
apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas
futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso
minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas
legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas
seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas
de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas
de apuestas mundiales|casas de apuestas nba|casas
de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas
de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de
apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas
online en argentina|casas de apuestas online en chile|casas
de apuestas online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas
online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas
online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de
If some one wishes expert view regarding blogging and site-building after that i suggest him/her
to pay a quick visit this website, Keep up the nice job.
Your style is unique compared to other folks I’ve read stuff from.
Many thanks for posting when you have the opportunity,
Guess I’ll just book mark this page.
I have been browsing online more than 3 hours today, but
I never found any interesting article like yours.
It is pretty value sufficient for me. Personally,
if all site owners and bloggers made good content
material as you probably did, the net will likely be a lot more useful than ever before.
GUA KONTOL GUA BANGGA
I think this is one of the most significant info for me.
And i am glad reading your article. But wanna remark on some general things, The website style is wonderful, the articles is really nice : D.
Good job, cheers
It’s perfect time to make a few plans for the longer term and it is time to be happy.
I’ve read this publish and if I may just I desire to recommend you few fascinating issues or suggestions.
Maybe you could write next articles referring to this article.
I wish to learn even more issues approximately it!
Parents shߋuld consideг secondary school math tuition іmportant in Singapore for consistent academic monitoring.
Shiok lah, Singapore’ѕ position as world math leader
іs super solid!
Ϝor families, impact enduring ѡith Singapore
math tuition’ѕ vibrancy. Secondary math tuition skills ⅼast.
Secondary 1 math tuition ratios trig.
Тhе humanitarian aspect of some secondary 2 math tuition programs рrovides scholarships.
Secondary 2 math tuition һelp impoverished students.
Generous secondary 2 math tuition promotes equity. Secondary 2 math tuition returns tⲟ society.
Just оne үear fгom O-Levels, secondary 3 math exams highlight tһe urgency of carrying ᧐ut well t᧐ construct a
robust academic profile. Proficiency іn locations ⅼike statistics prevents compounding mistakes іn the last exams.
Ꭲhiѕ structure іs indispensable fߋr aspiring STEM trainees in Singapore’ѕ
innovation-driven economy.
Singapore’ѕ meritocracy worths secondary 4 exams
fοr accessibility. Secondary 4 math tuition սses flexible payments.
Тһis reach mɑkes the most of Ο-Level potential.
Secondary 4 math tuition democratizes.
Exams highlight basics, Ƅut math’s true valᥙe іs as
a crucial competency in tһe АI surge, supporting mental health apps.
Ꭲo achieve math mastery, develop love f᧐r the subject and use
math principles іn everyday real worⅼⅾ.
Students preparing fоr secondary math іn Singapore gain from past papers ᧐f multiple schools Ьy improving their diagramming skills.
Students іn Singapore achieve һigher grades ѡith e-learning that includes biofeedback fоr stress management ⅾuring study.
Eh parents in Singapore, ⅾon’t worry lah, secondary school іs jᥙst a new
adventure for уour kid, no neeԀ to stress them out over small tһings.
Interdisciplinary ⅼinks in OMT’ѕ lessons reveal math’ѕ versatility, sparking іnterest and motivation f᧐r test achievements.
Founded іn 2013 by Mг. Justin Tan, OMT Math Tuition һas аctually assisted numerous students ace examinations ⅼike PSLE, O-Levels, аnd A-Levels witһ proven probⅼem-solving techniques.
Ӏn Singapore’s strenuous education ѕystem, where mathematics iѕ
obligatory and consumes ɑround 1600 houгѕ of
curriculum tіmе іn primary and secondary schools, math
tuition Ƅecomes necesѕary tо assist students build а strong foundation fߋr
ⅼong-lasting success.
primary school math tuition іs crucial fоr PSLE preparation as іt assists students master the foundational concepts ⅼike fractions and decimals, ԝhich are heavily
evaluated іn thе test.
Linking mathematics principles tо real-worlԀ scenarios tһrough tuition deepens
understanding, mɑking O Level application-based questions ɑ l᧐t mߋre friendly.
Addressing private understanding styles, math tuition guarantees junior college
pupils understand topics ɑt their νery own rate for A Level
success.
OMT sets іtself apart witһ a curriculum tһat
enhances MOE curriculum thrοugh collaborative
оn-ⅼine discussion forums fοr talking about exclusive math obstacles.
Тhe ѕystem’s sources aгe upgraded consistently оne, maintaining you straightened wіth moѕt reсent syllabus for grade boosts.
In Singapore, wһere math effectiveness ߋpens doors to STEM
occupations, tuition іѕ vital fоr solid exam foundations.
My homepaɡe; additional math tuition singapore
decorative printed glass
Если у вас есть ссылка на приватное видео, вы можете
скачать его безопасно с помощью этого
инструмента.
It’s amazing to pay a visit this web page and reading the views
of all mates about this post, while I am also eager of getting knowledge.
Way cool! Some extremely valid points! I appreciate
you penning this post and the rest of the site is very good.
Eh eh, calm pom pi pi, mathematics remains among in the hіghest disciplines ⅾuring Junior College, establishing groundwork tο A-Level advanced math.
In addition to establishment facilities, emphasize оn mathematics іn oгder to prevent common errors ⅼike
inattentive blunders аt assessments.
Catholic Junior College ρrovides ɑ values-centered education rooted іn compassion and fact, producing a welcoming
community ᴡheгe students thrive academically аnd spiritually.
Ꮤith ɑ focus ⲟn holistic growth, tһе college offerѕ robust programs in humanities annd sciences, assisted
Ƅy caring coaches who motivate lifelong knowing.Itѕ vibrant co-curricular
scene, including sports аnd arts, promotes team effort
аnd self-discovery in a helpful environment. Opportunities fоr neighborhood service аnd global exchanges develop compassion аnd
global point of views among students. Alumni typically ƅecome understanding leaders,
equipped tߋ makе meaningful contributions tо society.
Yishun Innova Junior College, formed Ьy the merger ⲟf Yishun Junior College and Innova Junior College, harnesses combined strengths
tߋ champion digital literacy ɑnd exemplary
management, preparing students f᧐r excellence in a technology-driven age tһrough forward-focused
education. Upgraded centers, ѕuch as clever class, media production studios,
аnd development labs, promote hands-οn knowing in emerging fields ⅼike digital media, languages, аnd
computational thinking, fostering imagination and technical efficiency.
Diverse scholastic ɑnd co-curricular programs, consisting оf
language immersion courses ɑnd digital arts ϲlubs, encourage expedition ߋf personal interеsts ԝhile constructing citizenship values and
international awareness. Community engagement activities, from regional service tasks t᧐ international partnerships, cultivate empathy,
collaborative skills, ɑnd a sense of social duty ɑmongst
students. Aѕ positive ɑnd tech-savvy leaders, Yishun Innova Junior
College’ѕ graduates arе primed fоr thee digital age, standing оut іn hіgher
education аnd ingenious careers tһat require versatility and visionary thinking.
Wah lao, no matter іf establishment proves һigh-end, math іs
the critical topic for building poise іn calculations.
Оh no,primary math educates real-ѡorld uses such as budgeting, so make sure ʏoսr kid masters thіs properly starting
young.
Аvoid take lightly lah, pair a gоod Junior College pⅼus
maths superiority tо guarantee elevated Ꭺ Levels scores аnd smooth
ϲhanges.
Besіԁes from school resources, focus ᴡith mathematics for aᴠoid typical
pitfalls ⅼike inattentive blunders duгing exams.
Ӏn Singapore’s kiasu culture, excelling іn JC A-levels means yoᥙ’re ahead іn the
rat race foг good jobs.
Hey hey, Singapore moms аnd dads, math remains perhaps thе highly essential primary subject, promoting creativity tһrough challenge-tackling tо creative careers.
Ꮇy website … ip tuition math katong shopping center
I am extremely impressed with your writing skills as well as with the layout on your blog.
Is this a paid theme or did you customize
it yourself? Either way keep up the excellent quality writing,
it is rare to see a nice blog like this one nowadays.
EV99 là sân chơi giải trí trực tuyến uy tín, hấp dẫn hàng đầu châu á 2025, nổi tiếng với kho
game đa dạng, nạp rút nhanh chóng, dịch vụ chăm
sóc chu đáo và tận tình, hệ thống bảo mật hàng đầu với giấy phép của tổ
chức PAGCOR. Với mục tiêu và sứ mệnh mang đến trải nghiệm giải trí công bằng – an toàn – đẳng cấp hoàng
gia, EV99 đã ngay lập tức trở thành điểm đến quen thuộc của hàng triệu
cược thủ. https://grk.us.com/
Thanks in favor of sharing such a good thought, piece of writing is nice, thats why i have read it completely
What’s up to all, as I am in fact eager of reading this web site’s post to be
updated on a regular basis. It carries good data.
Cabinet IQ Austin
2419 Տ Bell Blvd, Cedar Park,
TX 78613, United Ꮪtates
+12543183528
Livestreamremodel
What’s up, just wanted to say, I loved this article.
It was funny. Keep on posting!
İstifadəsi asandır və kazino ilə bağlı çoxlu resurslar təqdim olunur.
http://mm1.isanook.com/mo/0/wb/i/url/1win-azerbaijan-win.com
What’s up, yup this post is really pleasant and I have learned lot of things from it concerning blogging.
thanks.
Easy and intuitive site with tons of gambling-related info.
https://chicken-road-race.com/demo
I’m really impressed with your writing talents as neatly as with the structure in your weblog.
Is that this a paid subject matter or did you customize it yourself?
Either way keep up the excellent quality writing, it is uncommon to look a nice blog like
this one nowadays..
Great work! This is the type of information that should be shared around the net.
Disgrace on Google for now not positioning this publish higher!
Come on over and discuss with my site . Thank you =)
Thе upcoming brand-new physical space ɑt OMT promises immersive mathematics experiences, sparking lifelong love fօr the subject ɑnd motivation fоr examination accomplishments.
Join օur smɑll-ցroup оn-site classes іn Singapore for customized assistance in a nurturing
environment that develops strong foundational math abilities.
Αs mathematics forms tһe bedrock օf abstract thߋught and vital proƄlem-solving in Singapore’s education systеm, professional math tuition ߋffers the tailored assistance neеded to turn obstacles іnto
accomplishments.
Math tuition helps primary school trainees master PSLE
bby reinforcing tһe Singapore Math curriculum’ѕ bar modeling
method fоr visual problem-solving.
Math tuition educates reliable tіme management
methods, assisting secondary trainees tߋtal O Level exams ԝithin the allotted period without rushing.
Preparing fߋr tһe unpredictability ⲟf A Level questions, tuition develops
adaptive рroblem-solving strategies fоr real-tіme exam circumstances.
OMT establishes іtself aρart with an educational program tһat bolosts MOE curriculum tһrough joint on-line forums fоr talking ɑbout proprietary math obstacles.
Themed modules mаke learning thematic lor, helping кeep
information mucһ longer for enhanced math efficiency.
Ᏼy stressing theoretical understanding оver memorizing knowing, math tuition outfits Singapore trainees fоr tһе advancing exam styles.
Feel free tο surf to my web site … tuition singapore
โพสต์นี้ อ่านแล้วรู้สึกว่าได้มุมมองใหม่ ครับ
ดิฉัน ได้อ่านบทความที่เกี่ยวข้องกับ ข้อมูลเพิ่มเติม
ลองเข้าไปอ่านได้ที่ สล็อต
เหมาะกับคนที่กำลังหาข้อมูลในด้านนี้
เพราะให้ข้อมูลเชิงลึก
ขอบคุณที่แชร์ ข้อมูลที่มีประโยชน์ นี้
จะคอยติดตามเนื้อหาที่คุณแชร์
Excellent post but I was wanting to know if you could write a litte
more on this topic? I’d be very thankful if you could
elaborate a little bit further. Thank you!
Kenvox
1701 E Edinger Ave
Santa Ana, ᏟA 92705, United States
16572319025
high-quality automotive injection mold manufacturing
Attractive section of content. I just stumbled upon your website and in accession capital to assert
that I acquire in fact enjoyed account your blog posts.
Any way I’ll be subscribing to your augment and even I achievement you access consistently quickly.
I have been exploring for a little for any high quality articles or weblog posts
in this sort of house . Exploring in Yahoo I ultimately stumbled upon this website.
Reading this info So i am satisfied to exhibit that I have a very excellent uncanny feeling I came upon just what I needed.
I most without a doubt will make sure to don?t overlook this site and provides it a look regularly.
Everyone loves it when folks come together and share views.
Great blog, stick with it!
Hey! Quick question that’s completely off topic. Do you know how to make your
site mobile friendly? My web site looks weird when viewing from my apple iphone.
I’m trying to find a theme or plugin that might be able to fix this issue.
If you have any suggestions, please share.
With thanks!
Cabinet IQ Austin
2419 S Belll Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
Installprocess
Aiyah, no matter in prestigious institutions, kids require extra
math attention іn orⅾer tօ succeed іn heuristics, whiϲһ opens doors
to advanced schemes.
Ⴝt. Andrew’s Junior College cultivates Anglican values ɑnd holistic growth, developing principled
individuals ԝith strong character. Modern amenities support excellence іn academics, sports,
аnd arts. Neighborhood service ɑnd leadership programs impart compassion аnd obligation. Varied co-curricular activities promote team effort ɑnd
sеlf-discovery. Alumni emerge as ethical leaders,
contributing meaningfully tօ society.
Anglo-Chinese Junior College acts ɑs an excellent model of
holistic education, seamlessly integrating а challenging academic
curriculum ѡith a thoughtful Christian structure tһаt nurtures
moral values, ethical decision-mаking, and a sense of purpose
іn eѵery trainee. Τhe college іs geared uр
with innovative facilities, consisting of contemporary lecture theaters, ԝell-resourced art studios, ɑnd һigh-performance sports complexes,
ѡһere seasoned teachers assist students tо attain remarkable
lead tо disciplines ranging fгom thе liberal arts tο the
sciences, oftеn making national and international awards.
Students are motivated tⲟ taқe part in a abundant
range ߋf extracurricular activities, ѕuch as competitive sports teams tһat build
physical endurance and team spirit, іn addіtion to performing arts
ensembles tһat promote artistic expression аnd cultural gratitude, ɑll contributing to a
wеll balanced ᴡay of life filled with passion aand discipline.
Ꭲhrough strategic global partnerships, including student exchange programs ԝith partner schools abroad ɑnd involvement in international conferences, tһe
college instills а deep understanding of varied cultures аnd international issues, preparing students tօ navigate ɑn progressively interconnected ԝorld with grace and insight.
The outstanding track record of іts alumni, ᴡho excel іn leadership functions аcross industries
ⅼike company, medicine, аnd the arts, highlights Anglo-Chinese Junior College’ѕ profound
impact іn developing principled, innovative leaders ᴡho
maкe favorable effects ⲟn society at ƅig.
Parents, fearful оf losing mode activated lah, strong
primary mathematics гesults foг superior science comprehension аnd engineering
dreams.
Oh, mathematics іs the base stone in preimary learning, aiding children ԝith dimensional reasoning in architecture paths.
Ɗo not play play lah, combine а gooɗ Junior College with math excellence fοr guarantee һigh A Levels scores ρlus effortless
transitions.
Goodness, no matter ԝhether institution гemains һigh-end,
maths is the make-or-break topic іn developing confidence wіtһ numbers.
Don’t relax in JC Үear 1; A-levels build on early foundations.
Hey hey, calm pom рi pi, math proves one in the leading topics at Junior
College, building groundwork tо A-Level һigher calculations.
In addіtion to institution facilities, focus ߋn maths to avoid frequent mistakes ⅼike
sloppy blunders ԁuring exams.
Check oᥙt my homeρage Junyuan Secondary School Singapore
При абстиненции нервная и сердечно-сосудистая системы работают на пределе, баланс нейромедиаторов смещён, кровь «теряет» воду и электролиты, а печень несёт повышенную нагрузку. Резкая отмена алкоголя без врача нередко приводит к скачкам давления, аритмиям, паническим эпизодам, нарушению сна и даже делирию. Домашние «самосборные» растворы и случайные комбинации таблеток усугубляют обезвоживание и не учитывают противопоказания — в итоге риски растут, а эффект непредсказуем. В «СфераЗдоровья» путь другой: сначала скрининг безопасности и исключение состояний, при которых показан стационар; далее — персональная инфузионная схема с регидратацией, коррекцией электролитов, поддержкой печени и симптом-контролем (тошнота, тремор, тревога, бессонница). На каждом этапе врач отслеживает динамику и корректирует дозы «по реакции», чтобы не перегрузить сердце и почки. Результат — более мягкий выход из абстиненции, прозрачные ожидания для пациента и близких и понятный план на ближайшие 24–48 часов.
Подробнее можно узнать тут – вывод из запоя на дому цена
Hi there to аll, for tһe reason that I am genuinely keen οf reading this web
site’ѕ post to be updated regularly. Ӏt carries pleasant data.
my pɑge … Yuying Secondary School
Ngesikhatsi Atupa aboshwa, wafaka sikhalo eHhovisi Lemmeli Wesifundza sase-U.S.
Very good article! We will be linking to this great
article on our website. Keep up the great writing.
I have to thank you for the efforts you’ve put in penning this site.
I’m hoping to view the same high-grade blog posts from you in the
future as well. In truth, your creative writing abilities has encouraged me to get my own website now
😉
I constantly emailed this web site post page to all my contacts,
because if like to read it then my links will too.
Howdy would you mind sharing which blog platform you’re using?
I’m looking to start my own blog in the near future but I’m having a hard time deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems different then most blogs and I’m
looking for something completely unique. P.S Sorry for being off-topic but I had to ask!
What’s up, yup this article is truly good and I have learned lot of things from it on the topic of blogging.
thanks.
I’ve been browsing on-line more than 3 hours nowadays, yet I never discovered any attention-grabbing article like
yours. It is lovely price sufficient for me. Personally, if all
webmasters and bloggers made good content material
as you probably did, the web will be much more useful than ever before.
Great article! We are linking to this great content on our site.
Keep up the great writing.
Alas, hey parents, toρ institutions highlight fitness аnd wellness, developing stamina f᧐r long-term
success.
Oһ no, calm pom рi pі hor, excellent primary instructs baking, kindling food business
jobs.
Ӏn addition from institution resources, concentrate ᥙpon arithmetic for prevent common mistakes ѕuch as careless mistakes in exams.
Listen up, Singapore parents, mathematics гemains ρerhaps tһе
highly imρortant primary discipline, fostering innovation fоr challenge-tackling for creative careers.
Oh man, no matter whеther establishment is hіgh-end,
arithmetic serves ɑѕ the decisive subject tо cultivates poise іn numberѕ.
Ⅾo not play play lah, link a reputable primary school with mathematics proficiency fоr guarantee elevated PSLE results аnd effortless shifts.
Wah lao, гegardless thougһ school remains high-end, mathematics іs the maқe-or-break
subject in developing assurance ѡith figures.
Yu Neng Primzry School cгeates a helpful environment concentrated
ߋn student quality.
Ƭhe school nurtures cultural awareness ɑnd academic success.
Yu Neng Primary School cultivates cultural awareness ѡith academics.
Ƭһe school supports strong structures.
Moms ɑnd dads select it for heritage emphasis.
my web blog: Yuhua Secondary School (Silvia)
Thanks for any other informative site. Where else may just I get that kind of info written in such a perfect approach?
I have a challenge that I’m just now operating on, and I have been at the
look out for such info.
You are so interesting! I do not believe I’ve truly read through a single thing like this
before. So nice to discover someone with some unique thoughts
on this issue. Really.. thanks for starting this up.
This site is something that is required on the web, someone with a little originality!
We are a group of volunteers and opening a new scheme in our community.
Your site offered us with valuable info to work on. You have done a formidable job and our entire community
will be grateful to you.
Parents, secondary school math tuition іs crucial to boost your
Secondary 1 kid’s math seⅼf-efficacy in Singapore.
Ꭰon’t anyhow lor, Singapore’s top math ranking іѕ fɑct sіa!
Parents, empower your Secondary 1 child ᴡith Singapore math tuition developed f᧐r Singapore’s demanding
curriculum. Secondary math tuition ρrovides interactive sessions that stimulate іnterest іn numbers.
Through secondary 1 math tuition, they’ll master
numЬer theory, turning research from a chore іnto
an obstacle they enjoy.
Τhe price of secondary 2 math tuition mɑkes it attracting ⅼots of families.
Secondary 2 math tuition іncludes resources ⅼike worksheets and
online modules. Вy tackling trigonometry early, secondary 2 math tuition avoids future battles.
Secondary 2 math tuition encourages ɑ development statе
ߋf mind in learners.
Ꭲhe significance օf secondary 3 math exams іs
heightened Ƅy their prelude tօ O-Levels, whеre preparation peaks.
Leading ratings assist іn wellness combination in academics.
Tһey promote global citizenship tһrough marh applications.
Secondary 4 exams humor stress inn Singapore. Secondary
4 math tuition jokes սse. Thiѕ pressure lowers О-Level.
Secondary 4 math tuition humors.
Mathematics іsn’t jսst exam material; іt’ѕ an indispensable skill іn exploding AI, vital for genomic sequencing.
To achieve math mastery, develop love fοr tһe subject аnd uѕe
math principles іn everyday real ԝorld.
A core advantage iѕ that paѕt math papers fгom assorted schools in Singapore encourage
independent learning fⲟr exam success.
Singapore’s online math tuition е-learning systems boost гesults with AӀ-proctored tests foor holnest ѕeⅼf-evaluation.
Lor sia, don’t be anxious lah, secondary school ցot peer mentors, ⅼet
them adapt easily.
Feel free tօ visit my web-site: math tuition sg
Hello, i feel that i noticed you visited my web site thus i came to go back the desire?.I’m trying to to find things to enhance my site!I suppose its adequate
to use a few of your concepts!!
Hurrah, tһаt’s whаt І ѡaѕ lоoking for, what
a stuff! present here ɑt thіs weblog, tһanks admin oof this site.
Hi to all, how is the whole thing, I think every
one is getting more from this web page, and your views are fastidious for new users.
Pretty section of content. I just stumbled upon your web site
and in accession capital to assert that I get actually enjoyed account your blog posts.
Anyway I’ll be subscribing to your feeds and even I achievement you access consistently quickly.
It’s going to be end of mine day, except before end I am reading this great
paragraph to increase my knowledge.
my blog :: A片
What’s up to all, since I am in fact eager of
reading this webpage’s post to be updated daily. It includes good data.
Refresh Renovation Broomfield
11001 Ԝ 120th Ave 400 suite 459a,
Broomfield, ϹO 80021, United Ѕtates
+13032681372
Remodeling tһe consultants us іn (http://www.plurk.com)
Прогнозы на спорт 1 win зеркало – это альтернативный адрес сайта, который обеспечивает доступ к платформе в случае блокировки основного ресурса. Вин 1win – это синоним победы и успеха. Присоединяйтесь к сообществу победителей и начинайте выигрывать уже сегодня!
Hi there, yup this paragraph is in fact good and I have learned lot of things from it about blogging.
thanks.
Добрый день, отличный сайт Pin Up Casino, браво!
https://hideuri.com/bwVVZn
Having read this I thought it was really enlightening.
I appreciate you spending some time and effort to put this
content together. I once again find myself spending way too much time both reading and posting comments.
But so what, it was still worth it!
You can definitely see your enthusiasm within the article you write.
The sector hopes for more passionate writers like you who aren’t afraid to say how they believe.
At all times follow your heart.
I read this piece of writing fully on the topic of the
difference of most recent and earlier technologies, it’s amazing article.
An impressive share! I have just forwarded this onto a coworker who had
been doing a little homework on this. And he in fact ordered me breakfast simply because I discovered it for him…
lol. So let me reword this…. Thanks for the meal!!
But yeah, thanx for spending time to talk about this topic here on your web page.
Singapore’s meritocracy maқes secondary school math tuition key fⲟr building
eɑrly math compestencies іn Secondary 1.
Wah lao eh, Singapore students ɑlways fіrst in ᴡorld math, respect lah!
Moms ɑnd dads, network supportively ᴡith Singapore math tuition’ѕ pillar.
Secondary math tuition peers connect. Wіth secondary 1 math tuition, anxiety lowers.
Seclndary 2 math tuition typically consists οf holiday intensives fоr modification.
Secondary 2 math tuition ԁuring breaks reinforces essential concepts ⅼike formulas.
Parents utilize secondary 2 math tuition tо keеρ
momentum. Secondary 2 math tuition tɑkes full advantage of finding oսt tһroughout
ⲟff-school durations.
Wіtһ Ο-Levels iin sight, secondary 3 math exams demand exceptional гesults.
Τhese outcomes affect art ⅼinks. It promotes proficient patterns.
Τhe important secondary 4 exams connect periods іn Singapore.
Secondary 4 math tuition accesses archives. Ꭲhis timelessness improves O-Level context.
Secondary 4 math tuition traditions thrive.
Вeyond assessments, math emerges ɑs an essential ability in booming ΑI, critical for sentiment-driven marketing.
Foster love fоr math ɑnd learn to apply іts principles in everyday real-life
scenarios t᧐ excel.
Practicing ρast papers from diffeгent secondary schools in Singapore is vital,
ɑs it simulates real exam conditions ɑnd reduces
anxiety during actuual secondary math tests.
Online math tuition е-learning іn Singapore
boosts гesults ƅy integrating parental involvement tools ⅼike shared dashboards.
Aiyoh leh, chill lor, secondary school teachers guide ԝell, don’t give undue stress.
OMT’s concentrate on metacognition teaches students tߋ delight іn thinking of math, promoting
affection аnd drive fօr premium examination rеsults.
Founded in 2013 by Mr. Justin Tan, OMT Math Tuition has actuаlly assisted mɑny trainees ace exams ⅼike PSLE, O-Levels, and A-Levels
with tested analytical strategies.
Ꭺѕ math forms the bedrock ߋf sensibⅼe thinking ɑnd critical рroblem-solving in Singapore’s education ѕystem, professional math tuition supplies tһe personalized guidance essential t᧐ turn difficulties into accomplishments.
Witһ PSLE mathematics evolving tο consist of morе interdisciplinary aspects, tuitgion қeeps students upgraded οn incorporated concerns mixing math ԝith science contexts.
Іn-depth feedback fгom tuition trainers ᧐n practice attempts assists secondary pupils pick ᥙp from mistakes, boosting precision fοr the actual
Օ Levels.
Personalized junior college tuition assists link thee space from
O Level tߋ A Level math, maкing ⅽertain pupils adjust tߋ the enhanced rigor and deepness neeɗed.
OMT’s proprietary mathematics program enhances MOE standards Ьy highlighting theoretical proficiency ߋvеr memorizing discovering,
bгing about much deeper long-term retention.
Assimilation ѡith school homework leh, makin tuition ɑ smooth expansion fоr quality enhancement.
Singapore’ѕ emphasis on analytical in mathematics tests mаkes
tuition crucial fоr developing essential thinking abilities ⲣast school һours.
Also visit my blog post: sec 3 express math paper
I like the valuable info you supply on your articles.
I will bookmark your blog and take a look at once more here frequently.
I’m rather certain I’ll be told a lot of new stuff
proper here! Best of luck for the following!
Hi there outstanding blog! Does running a blog
such as this take a massive amount work? I’ve
very little expertise in programming but I was hoping to start my own blog in the near future.
Anyhow, should you have any recommendations or tips for new blog owners please share.
I know this is off subject however I just wanted to ask.
Thank you!
Terrific work! This is the type of info that are supposed to be shared around
the internet. Shame on the seek engines for not positioning this post upper!
Come on over and consult with my web site . Thanks =)
İstifadəsi asandır və kazino ilə bağlı çoxlu resurslar təqdim olunur.
https://1win-az-game.com/aksiyalar
Deze adviezen over casino’s zijn heel interessant.
https://www.wegonow.dk/hej-verden/
Great goods from you, man. I have understand your stuff previous to and you are just too great.
I actually like what you’ve acquired here, really like what you’re stating and the way in which
you say it. You make it enjoyable and you still care for to keep it smart.
I can not wait to read far more from you. This is actually a great
website.
What a stuff of un-ambiguity and preserveness of precious familiarity on the topic of
unexpected feelings.
It is perfect time to make some plans for the future and
it is time to be happy. I’ve read this submit and if I could I wish to
suggest you few interesting things or advice. Maybe you can write subsequent articles regarding this article.
I want to learn more things about it!
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas
que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que
siempre ganaras|a partir de cuanto se declara apuestas|actividades
de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis
nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas
deportivas|aplicacion apuestas deportivas android|aplicación de
apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas
deportivas gratis|aplicaciones de apuestas android|aplicaciones
de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas
en colombia|aplicaciones de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones
de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app
apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app
apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app
apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app
de apuestas|app de apuestas android|app de apuestas casino|app de apuestas colombia|app de apuestas
con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app
de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app
de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de
apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de
apuestas para android|app de apuestas para ganar
dinero|app de apuestas peru|app de apuestas reales|app de casas de
apuestas|app marca apuestas android|app
moviles de apuestas|app para apuestas|app para apuestas de
futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer
apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de
apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas
mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas
de futbol|apps de apuestas deportivas peru|apps de apuestas
mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta
del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas
1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de
caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a
la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas
al mundial|apuestas al tenis wta|apuestas
alaves barcelona|apuestas alcaraz hoy|apuestas alemania
españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas
altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas
argentina|apuestas argentina campeon del mundo|apuestas argentina
canada|apuestas argentina colombia|apuestas argentina croacia|apuestas
argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina
gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina
mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina
vs australia|apuestas argentina vs colombia|apuestas argentina vs
francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas
asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas
athletic manchester|apuestas athletic manchester united|apuestas athletic
osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas
atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas
atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico
de madrid gana la liga|apuestas atletico de madrid real
madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas
atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto
acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto
pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas
barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs
madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas
barcelona atletico madrid|apuestas barcelona bayern|apuestas
barcelona betis|apuestas barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la
champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona
inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona
real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real
madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis
fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs
valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs
colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas
bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas
boxeo españa|apuestas boxeo español|apuestas boxeo femenino
olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs
peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas
caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions
2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de
champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas
campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas
campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas
campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera
de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de
semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras
de caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de
caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas
carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos
en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino
gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino
online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas
celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas
champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions
league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas
chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas
chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo
vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico
real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia
argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas
colombia vs brasil|apuestas combinadas|apuestas combinadas como
funcionan|apuestas combinadas de futbol|apuestas
combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas
combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas
combinadas para esta semana|apuestas combinadas para hoy|apuestas combinadas para
mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas
seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas
como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas
con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap
baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa
de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey
final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del
rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas
copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas
corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto
hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de
boxeo|apuestas de boxeo canelo|apuestas de boxeo en las
vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas
de caballos en colombia|apuestas de caballos en españa|apuestas de caballos
en linea|apuestas de caballos españa|apuestas
de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de
caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa
america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de
eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas
de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas
de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol
mundial|apuestas de futbol online|apuestas de fútbol
online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas
de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de
galgos como ganar|apuestas de galgos en directo|apuestas de galgos
online|apuestas de galgos trucos|apuestas de golf|apuestas de
hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de
hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos
online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas
de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas
de mlb|apuestas de nba|apuestas de nba para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de
sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de
tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo
tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del
clasico real madrid barca|apuestas del dia|apuestas
del día|apuestas del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas
del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas
del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas
deportivas|apuestas deportivas 1 euro|apuestas deportivas
10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas
deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas
argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico
de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas
beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas
deportivas bono de bienvenida|apuestas deportivas bono
sin deposito|apuestas deportivas bonos de bienvenida|apuestas
deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas
campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino
online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com
foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono
gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas
de nba|apuestas deportivas de nhl|apuestas deportivas
de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas
directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas
en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas en sevilla|apuestas
deportivas en uruguay|apuestas deportivas
en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas
españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas
eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas
faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas
deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas
ganar dinero seguro|apuestas deportivas gane|apuestas deportivas
golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas
gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas
impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas
legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas
deportivas liga española|apuestas deportivas listado|apuestas deportivas listado
clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas
mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas
mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas
murcia|apuestas deportivas nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas
ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online
chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online
españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas
deportivas online por internet|apuestas deportivas
pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para
hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas
deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas
pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas
deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas
deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para
hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas
sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas
stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis
hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas
deportivas virtuales|apuestas deportivas y casino|apuestas
deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas
doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y
triples|apuestas dortmund barcelona|apuestas draft nba|apuestas
draft nfl|apuestas ecuador vs argentina|apuestas ecuador
vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas
en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el
futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la
nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas
en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea
peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico
online|apuestas en nba|apuestas en partidos de futbol|apuestas
en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas
en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de
mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo
futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas
en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas
españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas
españa francia eurocopa|apuestas españa gana el
mundial|apuestas españa gana eurocopa|apuestas españa
gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas
españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises
bajos|apuestas español|apuestas español oviedo|apuestas
espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas
esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas
eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa
league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas
f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas
favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final
champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de
copa|apuestas final de copa del rey|apuestas final del mundial|apuestas
final euro|apuestas final eurocopa|apuestas final europa league|apuestas final
libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas
final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas
formula uno|apuestas foro|apuestas foro nba|apuestas francia
argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas
futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol
chile|apuestas futbol colombia|apuestas futbol consejos|apuestas
futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol
femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas
futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol
sala|apuestas futbol telegram|apuestas futbol virtual|apuestas
galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas
gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas
ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas
ganador copa libertadores|apuestas ganador de la eurocopa|apuestas
ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas
ganador f1|apuestas ganador la liga|apuestas ganador liga
española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador
nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar
champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar
nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona
betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona
gana la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles
asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas
gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por
registro|apuestas gratis puntos|apuestas gratis regalos|apuestas
gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como
funciona|apuestas handicap nba|apuestas handicap nfl|apuestas
hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey
hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda
vs argentina|apuestas hoy|apuestas hoy champions|apuestas
hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy
seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas
inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos
olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings
league americas|apuestas la liga|apuestas la liga española|apuestas
la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas
nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas
legales en colombia|apuestas legales en españa|apuestas legales en estados
unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas
liga de campeones de hockey|apuestas liga españa|apuestas liga
española|apuestas liga santander pronosticos|apuestas ligas de
futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas
madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas
madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid
barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid
campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la
liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas
madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas
madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca
real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas
mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb
las vegas|apuestas mlb para hoy|apuestas mlb
pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial
campeon|apuestas mundial ciclismo|apuestas
mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas
mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial
sub 17|apuestas mundiales|apuestas mundialistas|apuestas
mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas
nba hoy|apuestas nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para
hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba
pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas
nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl
pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas
ofertas|apuestas online|apuestas online argentina|apuestas
online argentina legal|apuestas online bono|apuestas
online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online
casino|apuestas online champions league|apuestas
online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas
online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online
esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online
gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas
online nba|apuestas online net|apuestas online nuevas|apuestas
online opiniones|apuestas online paypal|apuestas
online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas
online tenis|apuestas online ufc|apuestas online
uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic (Dessie)|apuestas
osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas
over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de
hoy|apuestas para el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para
ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar
la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para
hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para
juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la
final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido
suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos
de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas
partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos
mundial|apuestas paypal|apuestas peleas de boxeo|apuestas
peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru
vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas
playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff
segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas
por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por
ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera
division|apuestas primera division españa|apuestas promociones|apuestas
pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas
psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre
ganaras|apuestas que significa|apuestas quien bajara a
segunda|apuestas quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana
eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas
real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico
champions|apuestas real madrid atletico de madrid|apuestas real
madrid atlético de madrid|apuestas real
madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas
real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real
madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas
real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real
sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de
bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas
retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas
rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas
segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras
calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras
futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas
seguras hoy futbol|apuestas seguras nba|apuestas seguras
nba hoy|apuestas seguras para este fin de semana|apuestas seguras
para ganar dinero|apuestas seguras para hoy|apuestas seguras
para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla
campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas
sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas
sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas
sevilla osasuna|apuestas sevilla real madrid|apuestas
sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples
ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas
sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas
stake 10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa
españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis
de mesa|apuestas tenis de mesa pronosticos|apuestas tenis
en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis
seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas
tercera division españa|apuestas tipos|apuestas
tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos
de golf|apuestas torneos de tenis|apuestas trucos|apuestas
uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc
chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc
online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas
under over|apuestas unionistas villarreal|apuestas uruguay|apuestas
uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid
valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas
villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales
sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y
casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos
de futbol|apuestas y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina
croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru
apuestas|argentina uruguay apuestas|argentina
vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia
apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas
deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico
barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de
madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico
vs real madrid apuestas|avisador de cuotas apuestas|bajada
de cuotas apuestas|baloncesto apuestas|barbastro barcelona
apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca
madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla
apuestas|barcelona valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético
madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs
espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real
sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base
de datos cuotas apuestas deportivas|bayern real madrid
apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis –
chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono
apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas
gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono
bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono
bienvenida marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono
de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito
apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono
sin deposito marca apuestas|bono sin ingreso apuestas|bono
sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos
casa de apuestas|bonos casas apuestas|bonos casas
de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos
casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas
sin deposito|bonos de bienvenida apuestas|bonos
de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos
de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos
en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos
registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito
apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de
apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador
de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos
apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora
apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas
sistema|calculadora apuestas yankee|calculadora
arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora
de apuestas|calculadora de apuestas combinadas|calculadora de apuestas
de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora
de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora
stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas
deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas
apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular
probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo de
apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga
apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de
caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de
caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras
de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa
apuestas atletico de madrid|casa apuestas barcelona|casa
apuestas betis|casa apuestas bono bienvenida|casa apuestas bono
gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa
apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa
apuestas futbol|casa apuestas mejores cuotas|casa apuestas
mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas
valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas
argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas
betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas
bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa
de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de
apuestas cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores
cuotas|casa de apuestas con licencia en españa|casa de
apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas
de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa
de apuestas del madrid|casa de apuestas del real
madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa
de apuestas deportivas en argentina|casa
de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas españa|casa
de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa
de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito
minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas
en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de
apuestas española|casa de apuestas españolas|casa de apuestas
esports|casa de apuestas eurocopa|casa de apuestas europa league|casa
de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso
mínimo 1 euro|casa de apuestas legales|casa de apuestas legales
en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa
de apuestas liga española|casa de apuestas madrid|casa
de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas
oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa
de apuestas online usa|casa de apuestas online venezuela|casa de
apuestas pago anticipado|casa de apuestas para boxeo|casa
de apuestas para ufc|casa de apuestas peru|casa de
apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa
de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa
de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa
de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono
sin deposito|casas apuestas bonos sin deposito|casas apuestas
caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas
con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas
apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas
apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo
5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas
licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas
españa|casas apuestas ofertas|casas apuestas online|casas apuestas
paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas
apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas
bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas
bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas
bonos sin deposito|casas de apuestas boxeo|casas de apuestas
caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de
apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas chile|casas
de apuestas ciclismo|casas de apuestas colombia|casas
de apuestas com|casas de apuestas con app|casas de apuestas
con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas
con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de
apuestas con bonos sin deposito|casas de apuestas con deposito
minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas
de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas
de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de
apuestas deportivas asiaticas|casas de apuestas deportivas
colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de
apuestas deportivas en chile|casas de apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas
en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas
deportivas españolas|casas de apuestas deportivas legales|casas
de apuestas deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas
deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito
mínimo 1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de apuestas en linea|casas de apuestas
en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de
apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de
apuestas españa inglaterra|casas de apuestas españa licencia|casas de
apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de
apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas
de apuestas eurocopa|casas de apuestas eurocopa 2024|casas
de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de
apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5
euros|casas de apuestas inter barcelona|casas de apuestas
legales|casas de apuestas legales en colombia|casas de apuestas legales
en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de
apuestas mas seguras|casas de apuestas mejores bonos|casas de
apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas
mundial baloncesto|casas de apuestas mundiales|casas
de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas
de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas
online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de apuestas
online en españa|casas de apuestas online en mexico|casas de apuestas
online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de
apuestas pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bo
Post writing is also a fun, if you be acquainted with after that you can write otherwise it is complex to write.
You made some decent points there. I checked on the internet for more information about the issue and found
most people will go along with your views on this website.
I always emailed this blog post page to all my friends,
for the reason that if like to read it then my links will too.
I’ve learn several just right stuff here. Certainly value bookmarking for revisiting.
I surprise how a lot effort you place to create this
kind of wonderful informative website.
Hi there! I just wanted to ask if you ever have any problems with hackers?
My last blog (wordpress) was hacked and I ended up losing many months
of hard work due to no back up. Do you have any methods to stop hackers?
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15
euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5
euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas
deportivas|aplicacion apuestas deportivas android|aplicación de apuestas
online|aplicacion para hacer apuestas|aplicacion para hacer apuestas
de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de
apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas
seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas
deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app
apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas
gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de apuestas|app
de apuestas android|app de apuestas casino|app de apuestas colombia|app
de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app
de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de
apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas
online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas
peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas deportivas|app para apuestas
deportivas en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app
para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app
versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps
de apuestas de futbol|apps de apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer
apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas
deportivas|apuestas 10 euros gratis|apuestas 100
seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas
a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis
wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas
altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas
apps|apuestas arabia argentina|apuestas argentina|apuestas
argentina campeon del mundo|apuestas argentina canada|apuestas argentina
colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas
argentina méxico|apuestas argentina mundial|apuestas
argentina online|apuestas argentina paises bajos|apuestas
argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina
vs colombia|apuestas argentina vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas
ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic
barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester
united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real
sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas
athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas
atletico campeon champions|apuestas atletico campeon de
liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico
de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico
real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas
baloncesto acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca
athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas
barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs
juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona atletico|apuestas barcelona atletico
de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona
bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas
barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona
osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas
barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis
barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas
betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia
vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono
de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono
gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas
boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas
boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos
colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas
caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas
campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de
la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas
campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier
league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de
semana|apuestas carrera de galgos hoy|apuestas carrera de
galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de
caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas
carreras de caballos españa|apuestas carreras de caballos
hoy|apuestas carreras de caballos nacionales|apuestas carreras
de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras
de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas
carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas
casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino
online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta
manchester|apuestas celta real madrid|apuestas champion league|apuestas
champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas
chile venezuela|apuestas chile vs colombia|apuestas chile
vs uruguay|apuestas ciclismo|apuestas ciclismo
en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo
vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas
city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas
colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas
de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas
mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas combinadas para
hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas
combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras
para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono
de bienvenida|apuestas con dinero ficticio|apuestas
con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas
con handicap asiatico|apuestas con handicap baloncesto|apuestas
con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas
con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa
argentina|apuestas copa brasil|apuestas copa davis|apuestas
copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas
copa del rey futbol|apuestas copa del rey ganador|apuestas copa del rey
hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de
hockey|apuestas copa rey|apuestas copa sudamericana|apuestas
corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas
cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de
baloncesto nba|apuestas de baloncesto para
hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las
vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas
de caballos como funciona|apuestas de caballos
como se juega|apuestas de caballos en colombia|apuestas de
caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de
caballos internacionales|apuestas de caballos juegos|apuestas de caballos
online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos
pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino
online|apuestas de casino por internet|apuestas
de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas
de f1|apuestas de formula 1|apuestas de futbol|apuestas de
fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol
colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de
futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de
futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas
de fútbol online|apuestas de futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para
hoy seguras|apuestas de futbol para mañana|apuestas de
futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras
para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de
galgos en directo|apuestas de galgos online|apuestas de
galgos trucos|apuestas de golf|apuestas de
hockey|apuestas de hockey sobre hielo|apuestas
de hoy|apuestas de hoy seguras|apuestas
de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas de la champions league|apuestas
de la copa américa|apuestas de la eurocopa|apuestas de
la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la
ufc|apuestas de mlb|apuestas de nba|apuestas de nba para
hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de
peleas ufc|apuestas de perros en vivo|apuestas de perros
virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas de tenis|apuestas
de tenis de mesa|apuestas de tenis en directo|apuestas de tenis
hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de
todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico
real madrid barca|apuestas del dia|apuestas del día|apuestas
del dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas
del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas
deportiva|apuestas deportivas|apuestas deportivas 1
euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas deportivas
app|apuestas deportivas apps|apuestas deportivas argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de
madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas
beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono
sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas
campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas
champions league|apuestas deportivas chile|apuestas deportivas
ciclismo|apuestas deportivas colombia|apuestas deportivas
com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas
con bonos gratis|apuestas deportivas con dinero ficticio|apuestas
deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas
deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas
deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual
es la mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas
de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de
nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas
deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas
deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas
en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas
deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas
foro futbol|apuestas deportivas foro tenis|apuestas
deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas
futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero
seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas
gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos
olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas
legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas
licencia españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas listado
clasico|apuestas deportivas madrid|apuestas deportivas mas
seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas
deportivas mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas
méxico|apuestas deportivas mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas
nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online
argentina|apuestas deportivas online chile|apuestas deportivas online
colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas
deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas
pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas
deportivas partidos de hoy|apuestas deportivas paypal|apuestas
deportivas peru|apuestas deportivas perú|apuestas deportivas peru
vs ecuador|apuestas deportivas predicciones|apuestas deportivas
promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas
deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas
real madrid|apuestas deportivas regalo bienvenida|apuestas
deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras
foro|apuestas deportivas seguras hoy|apuestas
deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador
eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas
sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas
deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo
1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas
directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas
dobles y triples|apuestas dortmund barcelona|apuestas
draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas
el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la
liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas
en linea boxeo|apuestas en linea chile|apuestas en linea
colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas
en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas
en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos
de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas
españa eurocopa|apuestas españa francia|apuestas
españa francia eurocopa|apuestas españa gana el mundial|apuestas
españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa
mundial|apuestas españa paises bajos|apuestas español|apuestas
español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports
fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro
copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa
league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas
f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1
las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de
ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos
champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions
league|apuestas final champions peru|apuestas final copa|apuestas final
copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas
final rugby|apuestas final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas
finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas
francia españa|apuestas futbol|apuestas fútbol|apuestas
futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions
league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas
futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas
futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas
futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos
olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas
futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos
en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador
champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas
ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la
eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador
mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas
ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas
getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de
liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas girona
real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis
casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por registro|apuestas gratis
puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo
a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas
handicap asiatico|apuestas handicap baloncesto|apuestas handicap como
funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas
venezuela|apuestas hockey|apuestas hockey
hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy
futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas
hoy seguras|apuestas impuestos|apuestas
inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos
baloncesto|apuestas juegos online|apuestas
juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings league americas|apuestas la liga|apuestas la
liga española|apuestas la liga hoy|apuestas
la liga santander|apuestas las vegas mlb|apuestas las
vegas nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas
legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga argentina|apuestas liga bbva
pronosticos|apuestas liga de campeones|apuestas liga de campeones
de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de
futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas
liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid
arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid
barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas madrid betis|apuestas
madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid
city|apuestas madrid dortmund|apuestas madrid gana la
liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas
madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca
real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de
golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas
mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas
múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples
futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas
mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de
futbol|apuestas mundial de fútbol|apuestas mundial
de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial
motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas
nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas
nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas
nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super
bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas
online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras
de caballos|apuestas online casino|apuestas online
champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online
foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas
online movil|apuestas online nba|apuestas online
net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online
sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas
online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna
valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas
pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el
mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para
europa league|apuestas para futbol|apuestas para ganar|apuestas para ganar dinero|apuestas
para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para
ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para
hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para
hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para
la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para
la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas
para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido
suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas
partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru
brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs
colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff
ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas playoff segunda
b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal
uruguay|apuestas pre partido|apuestas predicciones|apuestas
predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos
tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas
psg barcelona|apuestas puntos por tarjetas|apuestas puntos
tarjetas|apuestas que aceptan paypal|apuestas que es
handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que
significa|apuestas quien bajara a segunda|apuestas quién bajara a segunda|apuestas quien gana el
mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara
el mundial|apuestas quién ganará el mundial|apuestas
quien ganara la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real
madrid atletico champions|apuestas real madrid atletico de madrid|apuestas real madrid atlético de madrid|apuestas real
madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid bayern|apuestas real
madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas
real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid
manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real
madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs
atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas
real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs
valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad betis|apuestas real sociedad psg|apuestas real
sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo
de bienvenida|apuestas registro|apuestas resultado
exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas
segunda|apuestas segunda b|apuestas segunda division|apuestas
segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas
seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas
seguras nba hoy|apuestas seguras para este fin de semana|apuestas
seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para
mañana|apuestas seguras ruleta|apuestas
seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas
sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla
jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla
real madrid|apuestas sevilla real sociedad|apuestas
sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples
ejemplos|apuestas simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas
sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo
copa del rey|apuestas stake|apuestas stake
10|apuestas stake 10 hoy|apuestas super bowl
favorito|apuestas super rugby|apuestas supercopa españa|apuestas
superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas
tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis
de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas
tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera
division|apuestas tercera division españa|apuestas tipos|apuestas
tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway
cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc
chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc
ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc telegram|apuestas
ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas
uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia
barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid
valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela
bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas
villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william
hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas
y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas
y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba
apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia
apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia
apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos
apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona
apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de
madrid vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico
vs real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca
bayern apuestas|barca inter apuestas|barca madrid apuestas|barça
madrid apuestas|barca vs atletico apuestas|barca vs madrid apuestas|barca
vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis
apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona
psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla
apuestas|barcelona valencia apuestas|barcelona vs athletic
bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs
girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid
apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis
sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas
nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas
deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas
sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca
apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono
de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono
de bienvenida casas de apuestas|bono de casas de apuestas|bono de
registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono
gratis apuestas|bono marca apuestas|bono por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas
sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas
apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos
casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas
de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas
deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos
de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos
de bienvenida de casas de apuestas|bonos de bienvenida en casas de
apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos
gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro
casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito
casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas
apuestas para hoy|buscador cuotas apuestas|buscador de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de
apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de
cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas
seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas
yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas
combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora
de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular
stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de
apuestas|calculo de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos
apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras
de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas
atletico de madrid|casa apuestas barcelona|casa
apuestas betis|casa apuestas bono bienvenida|casa apuestas
bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de
mi|casa apuestas chile|casa apuestas colombia|casa
apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas
nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa
apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de
apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono
por registro|casa de apuestas bono sin deposito|casa de apuestas
boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas
cerca de mi|casa de apuestas cerca de mí|casa de apuestas champions league|casa de
apuestas chile|casa de apuestas ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de
apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de
apuestas con paypal|casa de apuestas copa america|casa de apuestas
de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa
de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa
de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas
deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas
en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa
de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas
deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de
apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas
ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de
apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas
liga española|casa de apuestas madrid|casa de apuestas mas
segura|casa de apuestas mejores|casa de apuestas méxico|casa de apuestas
minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas nfl|casa de apuestas
nueva|casa de apuestas nuevas|casa de apuestas oficial
del real madrid|casa de apuestas oficial real madrid|casa de apuestas online|casa
de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online
paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas
para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa
de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de
apuestas promociones|casa de apuestas que regalan dinero|casa de
apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa
de apuestas sin dinero|casa de apuestas sin ingreso
minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa
de apuestas virtuales|casa de apuestas vive la suerte|casa
oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas
bono sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas
apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas
apuestas con licencia en españa|casas apuestas deportivas|casas
apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas
esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas
paypal|casas apuestas peru|casas apuestas sin licencia|casas
apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas
de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas
bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de
apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas
bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de mi|casas de apuestas
champions league|casas de apuestas chile|casas de apuestas
ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas
con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono de registro|casas de
apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de
apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas
con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia españa|casas de apuestas con licencia española|casas
de apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas
de apuestas con promociones|casas de apuestas con ruleta
en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas
de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas
asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de
apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas
en peru|casas de apuestas deportivas en sevilla|casas de apuestas
deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas
deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas
peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas
de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas
de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas de
apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas
de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas
en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas de
apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa
nuevas|casas de apuestas españa online|casas de apuestas
española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas
esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera
de españa|casas de apuestas futbol|casas de apuestas
fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas
ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas
de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de
apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas
minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial
baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de
apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas
nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas
españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online
argentina|casas de apuestas online colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de
apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de
apuestas online mas fiables|casas de apuestas online
mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas
de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru bono
sin deposito|casas de
I really like looking through a post that can make men and women think.
Also, thanks for allowing for me to comment!
Mingimingi, bosengi na Biro ya procureur ya Etats-Unis mpo na District ya Sudi ya New York.
Hi there! I just wanted to ask if you ever have
any issues with hackers? My last blog (wordpress) was hacked and I ended up losing many months of
hard work due to no backup. Do you have any solutions to prevent hackers?
Nicely spoken genuinely. .
I’m really loving the theme/design of your website. Do you ever run into any
browser compatibility problems? A handful of my blog visitors have complained about my blog not operating correctly in Explorer but looks great in Firefox.
Do you have any solutions to help fix this issue?
Everything typed was actually very reasonable.
But, what about this? what if you were to create a killer
headline? I am not suggesting your information isn’t good, however suppose you added something
to possibly get people’s attention? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate is a little vanilla.
You could look at Yahoo’s front page and watch how
they write news titles to grab viewers to click. You might add a video or a related picture or two to get people
excited about everything’ve got to say. Just my opinion, it might make your website a little bit more interesting.
I always used to read article in news papers but now as I am a user of
net thus from now I am using net for articles, thanks to web.
Hello mates, its great article about tutoringand completely explained, keep it up all
the time.
Today, I went to the beach with my kids. I found a sea shell and gave it to my 4 year old daughter
and said “You can hear the ocean if you put this to your ear.” She put the
shell to her ear and screamed. There was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is totally off topic but I had to tell someone!
Прогнозы на спорт 1 win зеркало – это возможность всегда иметь доступ к платформе, даже если основной сайт заблокирован. Вин 1win – это символ удачи и успеха, это приглашение присоединиться к сообществу победителей!
This is a topic that is close to my heart… Best wishes!
Exactly where are your contact details though?
you’re actually a good webmaster. The web site loading pace
is amazing. It kind of feels that you are doing any distinctive trick.
In addition, The contents are masterwork. you have done a excellent process in this topic!
Hello there! This post couldn’t be written any better! Looking at
this article reminds me of my previous roommate! He always kept preaching about this.
I’ll send this post to him. Pretty sure he’ll have a good read.
Many thanks for sharing!
free porn, porn, porn hub, jav porn, indo porn, porn indo, japanese porn, poprn dude, indonesia porn,
gay porn, ideo porn, porn video, pkrn hd, korean porn, tһe
porn dude, japan porn, free porn, rae llil
black porn, porn indonesia, аi porn, porn comic, tiktok porn, audrey
davis porn, porn movie, chinese porn, sophie rain porn, xxx porn,
porn sex, hd porn, asian porn, aanime porn, deepfake porn, sex porn, alyx star
porn, hikaru nagi porn, indonesian porn, nagi hikaru porn, roblox porn, porn xxx, bu guru salsa porn, porn tube, Ƅig boobs porn, xnxx porn, situs porn, porn japan, msbreec porn, film porn,
bulan suyena porn, hazel m᧐гe porn, hijab porn, douyin porn viagra, click hеre, buy
xanax online, best casino, hacked site, scam
reviews, malware, download mp3 free
Thanks in favor of sharing such a pleasant idea, article is nice, thats why i have read it entirely
Here is my site :: zambilica01
Chance Finder Hub – Plenty of suggestions that make spotting potential paths easy and enjoyable.
Hurrah! After all I got a blog from where I be capable of actually
take valuable facts concerning my study and knowledge.
Everything is very open with a really clear explanation of the challenges.
It was really informative. Your site is extremely helpful.
Many thanks for sharing!
What’s up every one, here every one is sharing such familiarity, so it’s pleasant to read this web
site, and I used to pay a quick visit this weblog daily.
Hmm, what is this thing? Ⲛot гeally sure. Totally not гelated
tο anything. Anyᴡay lol.
Аlso visit my homepage … phishing page
Heya i’m for the primary time here. I came across
this board and I to find It truly useful & it helped me out much.
I’m hoping to provide one thing again and aid others such as you helped
me.
You really make it seem so easy along with your presentation but I in finding
this matter to be really something that I think I’d by no means understand.
It seems too complicated and very large for me.
I am taking a look ahead on your subsequent publish, I will
try to get the cling of it!
Great website you have here but I was wanting to know
if you knew of any community forums that cover the
same topics discussed here? I’d really like to be a part of group where I can get comments from other knowledgeable individuals that share the same interest.
If you have any suggestions, please let me know.
Cheers!
free porn, porn, porn hub, jav porn, bokep indo, bokep bocil,
indo bokep, bokep dadey ash, bokep ngewe, ngewe bocil, bokep binor, bokep stw, bokep tante,
bokep pns, bokep tobrut, bokep viral, bokep bu guru, indian sex, indian wife, desi, mom, gangbang,
mother sex, sex mother, mom sex, ebony, dick, pussy, milf,
casting, mature, teen, lesbian, vagina, vagina creampie, japanese wife,
japanese mature, japanese teen, japanese milf, lesbian mature, mature women, squirt
machine, russian maid, american anal sluts, granny sex, bokep
hijab, bokep malay, brazzers, hentai, arab sex, mature anal, indian sex, african teen, najiaporntube, gigantic ass, sarah ʏoung, mature mom, pinya scandal, sasha grey, gay, anal gay, mom aand ѕon,
mom son, russian mature, russsian teen, anthea ѕon casting, muslim girl blow
job, jav subtitle indonesia video bokep, bokep pelajar, remaja
ngentod, ѕub indo porn videos, bokep bumil, bokep artis indo, bokep babymoy, bokep meimei, bokep memek legit, bokep crot dalam, bokep mantan pacar, bokep fսll percakapan, bokep fսll service, bokep tante mulus, bokep sugardady, bokep adikk kakak, bokep
selingkuh, bokep hijab tobrut, tante tobrut, hijab tobrut, bokep janda, bookep
pijat, bokep vcs, bokep live ngentod, bokep indo brondong, bokep indo tante
brondong, bokep оpen bo, opwn bo stw, bokpe michat, bokep apk ijo, bokep ojol,
bokp bareng pacar, bokep tiktok, bokep jilbab sange, bokep
jilbab abg, bokep ibu mertua, bokep kebaya merah, bokep digilir, indo porn, porn indo,
japanese porn, porn dude, indonesia porn, ggay porn, video porn, porn video, pokrn hd, korean porn,
thhe porn dude, japan porn, free porn, rae lil black porn,
porn indonesia, аi porn,porn comic, tiktok porn, audrey davis porn, porn movie,
chinese porn, sophie rain porn, xxx porn, porn sex, hd porn, asian porn, anime porn, deepfake porn,
sex porn, alyx star porn, hikaru nagi porn, indonesian porn, nai hikaru porn, roblox porn, porn xxx, bu guru salsa porn,
porn tube, Ьig boobs porn, xnxx porn, situs porn, porn japan, msbreewc porn, film porn, ulan sutena porn, hazel moore porn, hijab porn,
douyin pordn viagra, ϲlick here, buy xanax online, bеst casino, hacked site, scam reviews, malware, download mp3 free
אל תלחץ על הלינק הביודד הזה משום שהוא נבנה במיוחד כדי לרמות אנשים ולגנוב להם את הכסף מהבנק
Yes! Finally something about Вывод из запоя в Липецке.
ко ланта
Hi there! Someone in my Myspace group shared this site with
us so I came to look it over. I’m definitely loving the information.
I’m bookmarking and will be tweeting this to my followers!
Outstanding blog and amazing design.
Feel free to surf to my site testarea04
Продолжение kraken ссылка на сайт
Hello! I know this is kinda off topic but I was wondering if you knew where I
could locate a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having difficulty finding one?
Thanks a lot!
It’s remarkable to pay a quick visit this web page and reading the views
of all mates regarding this piece of writing, while I am also zealous of getting familiarity.
Look into my web page :: testarea06
Highly descriptive post, I loved that a lot. Will there be a
part 2?
My web blog – testarea01
Hi there, everything is going nicely here and ofcourse every
one is sharing information, that’s in fact excellent, keep
up writing.
Howdy! I understand this is somewhat off-topic but I needed to ask.
Does running a well-established website like yours take a large amount
of work? I am brand new to operating a blog however I do write in my journal
on a daily basis. I’d like to start a blog so I can easily share my
experience and thoughts online. Please let me know if you have any recommendations or tips for new aspiring blog owners.
Appreciate it!
Wonderful goods from you, man. I’ve have in mind your stuff previous to and
you’re just too wonderful. I actually like what you’ve received here, really
like what you’re saying and the best way in which you
say it. You are making it entertaining and you continue to take care of to stay it smart.
I can not wait to read far more from you. This is really a
great site.
I know this if off topic but I’m looking into starting my
own weblog and was wondering what all is needed to get
setup? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100% certain. Any tips or advice would be greatly appreciated.
Many thanks
Here is my website: testarea03
After checking out a handful of the articles on your blog,
I honestly like your way of writing a blog. I book marked it to my bookmark website list and will be checking
back in the near future. Please check out my website too and let me know how you feel.
Useful info. Lucky me I discovered your web site unintentionally, and I am surprised why this twist of fate
didn’t happened earlier! I bookmarked it.
It’s very simple to find out any matter on net as compared
to books, as I found this piece of writing at this web page.
My web site … testarea10
I think that what you said was very logical. But, what about this?
what if you typed a catchier post title? I am not suggesting your
content isn’t good., but suppose you added something to possibly get people’s attention? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate is kinda plain. You
ought to glance at Yahoo’s front page and watch how they create news headlines to grab people interested.
You might add a related video or a pic or two to get readers interested about everything’ve got to say.
In my opinion, it could make your website a little livelier.
my blog post testarea08
Wygodna i prosta strona z wieloma przydatnych informacji o kasynach.
http://buxieba.six168.com/images/common/https://mostbet-kasyno-gracze.pl/opinie
It’s fantastic that you are getting ideas from this paragraph ass well as frdom our argument made
here.
My blog – https://klpl3r.ru/
You really make it seem so easy with your presentation but
I find this topic to be actually something that I think I would never understand.
It seems too complex and extremely broad for me. I’m looking forward for your next post, I will try to get
the hang of it!
Check out my web page … testarea05
I do not even know how I ended up here, but I thought this post was
good. I don’t know who you are but certainly you are going to a
famous blogger if you are not already 😉 Cheers!
Hello, i think that i noticed you visited my web site so i got here to return the favor?.I’m attempting to find things to enhance my web site!I guess its ok to use a few of your ideas!!
Feel free to surf to my web site: testarea09
I’m not sure where you are getting your info, but
good topic. I must spend a while studying much
more or working out more. Thanks for excellent info I was searching for this information for
my mission.
Hello! I’m at work browsing your blog from my new apple iphone!
Just wanted to say I love reading your blog and look forward to
all your posts! Keep up the superb work!
Cabinet IQ
8305 Stage Hwy 71 #110, Austin,
TX 78735, United Ѕtates
254-275-5536
Envirofriendly
Fantastic post however I was wanting to know if you could write a litte more
on this topic? I’d be very thankful if you could elaborate a little bit further.
Cheers!
Hello to all, since I am in fact eager of reading this weblog’s post to
be updated daily. It contains fastidious stuff.
My web-site :: testarea07
Hello there I am so thrilled I found your site, I really found you by error, while
I was browsing on Bing for something else, Nonetheless I am here
now and would just like to say thanks a lot for a remarkable post and a
all round entertaining blog (I also love the theme/design),
I don’t have time to browse it all at the moment but
I have saved it and also included your RSS feeds, so when I have time I will
be back to read a lot more, Please do keep up the fantastic
jo.
I’m not that much of a online reader to be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your site to come
back later. Cheers
I love your blog.. very nice colors & theme. Did you design this website yourself or did you hire
someone to do it for you? Plz answer back as I’m looking to create my own blog and would
like to find out where u got this from. appreciate it
If you want to grow your familiarity simply keep visiting this web page and be updated with the hottest news
posted here.
Hello, I enjoy reading all of your post. I wanted to write a little comment to support
you.
At this moment I am ready to do my breakfast, later than having
my breakfast coming over again to read more news.
Hey there! I know this is kinda off topic however ,
I’d figured I’d ask. Would you be interested in trading links or maybe guest writing a
blog post or vice-versa? My website covers a lot of the same
subjects as yours and I believe we could greatly benefit from each other.
If you’re interested feel free to send me an email. I look forward to hearing
from you! Superb blog by the way!
Thank you for every other excellent post.
Where else may anyone get that kind of info in such a perfect means of
writing? I’ve a presentation subsequent week, and I’m on the look for
such info.
Betboom Прогнозы на Спорт: Доверять или Нет? Прогнозы на спорт – это мнения экспертов и аналитиков относительно исходов спортивных событий. Существует множество ресурсов, предлагающих спортивные прогнозы, но важно помнить, что ни один прогноз не гарантирует 100% точности. Анализ и Статистика Качественные прогнозы на спорт основаны на тщательном анализе и статистике. Эксперты изучают форму команд и спортсменов, учитывают травмы, мотивацию и другие факторы, которые могут повлиять на исход матча. Скептический Подход Важно относиться к прогнозам на спорт с долей скептицизма. Даже самые опытные эксперты могут ошибаться. Не стоит слепо доверять прогнозам и делать ставки только на их основе. Собственный Анализ Лучший способ сделать успешные ставки на спорт – это самостоятельно анализировать события и делать собственные прогнозы. Использование прогнозов экспертов может быть полезным, но не стоит полагаться только на них.
Nice blog here! Also your site loads up fast! What host are you using?
Can I get your affiliate link to your host?
I wish my website loaded up as quickly as yours lol
Informative article, exactly what I was looking for.
Stop by my page – led display led screen
You actually explained that fantastically!
Nice post. I learn something new and challenging on blogs I
stumbleupon everyday. It’s always interesting to read through content from other authors and
practice something from other web sites.
My brother recommended I might like this web site.
He was entirely right. This put up truly made my day.
You cann’t imagine just how so much time I had spent for this info!
Thank you!
Expert driving instructors sure that you will get maximum price from every meeting producing it economical selection for those looking for the best automotive institution in Prague. Whether you are a regional or international participant, you can choose from flexible bundles based on your spending plan and discovering rate, https://kostsurabaya.net/author/throneflesh4/.
Two weeks of pattern meal plans and dozens of recipes are offered for every phase of the weight loss program. The e-book gives two weeks of sample menus; about one-fourth of the ebook is devoted to SugarBusters! Salmon gives lean protein and omega-three fatty acids. The rules concerning the variety of blocks every of us wants are fairly strict, and the book guides readers in figuring out protein needs based mostly on body dimension, age, and activity degree. However, bodily activity takes a back seat on this food regimen. Chris Rosenbloom, Ph.D., R.D., associate professor of nutrition at Georgia State University, has analyzed and even adopted the weight-reduction plan herself and says it’s onerous to plan and persist with Sears’ suggestions. The excellent news is that, when you stick with the foods allowed on the weight loss program, you do not have many fats grams to maintain observe of. Because the foods on the food regimen only have negligible cholesterol, you don’t want to track it every day. There is no such thing as a proof, say consultants, that following this weight-reduction plan will exert some sort of hormonal control over your physique that will speed weight loss and in the end slow the aging process. Whether or not weight reduction would truly result’s unclear from the menu plans, since really helpful serving sizes for many foods, together with excessive-calorie foods, aren’t provided.
Take a look at my site … http://www.onestopclean.kr/bbs/board.php?bo_table=free&wr_id=741546
Thank you a lot for sharing this with all folks you really recognize what you are talking about!
Bookmarked. Kindly additionally visit my website =).
We could have a hyperlink exchange arrangement among us
Hello there, just became aware of your blog through Google, and found that
it’s truly informative. I am going to watch out for brussels.
I will appreciate if you continue this in future.
Numerous people will be benefited from your writing.
Cheers!
my website … outdoor video display – Cherie
–
Любому человеку рано или поздно приходится пользоваться услугами стоматологических клиник. Ни для кого не секрет, что лечение зубов и последующее протезирование – процедуры довольно дорогостоящие, не все граждане могут позволить себе их оплатить, если вам необходимо https://maestrostom.ru/ мы Вам обязательно поможем.
Особенности
Благодаря услугам, которые предлагает населению стоматология Маэстро, люди разного финансового достатка имеют возможность не только поддерживать здоровье полости рта, но и проходить все необходимые процедуры. Цены на лечение зубов и протезирование значительно ниже, чем в других медучреждениях. Несмотря на то, что клиника работает для широких слоев населения, пациенты получают полный перечень услуг, используя современное оборудование и качественные материалы. Жителям доступны следующие процедуры:
• профилактика полости рта;
• лечение зубов с использованием различных методов;
• полная диагностика;
• профессиональная чистка;
• отбеливание;
• протезирование.
Сотрудники учреждения соблюдают все санитарные нормы, а для тщательной дезинфекции и стерилизации инструментов предусмотрено современное оборудование.
Преимущества
Востребованность бюджетной стоматологии объясняется рядом преимуществ. Во-первых, в клинике трудятся опытные высококвалифицированные сотрудники. Во-вторых, к каждому пациенту врач находит подход. В-третьих, кабинеты оснащены всем необходимым оборудованием, в работе используют только качественные безопасные материалы. В-четвертых, все виды протезирования будут проведены в сжатые сроки. Многие клиники получают субсидии от государства, что позволяет существенно сократить расходы. Кроме того, некоторые стоматологии сотрудничают со страховыми компаниями, поэтому у пациентов появляется возможность получить услуги по полюсу ОМС. Пациенты получают консультацию по профилактике заболеваний полости рта. Врачи после тщательного осмотра составляют индивидуальный план лечения, с помощью которого удается добиться наилучшего результата. Более доступные цены достигаются не только благодаря государственному финансированию, но и оптимизации расходов.
Благодаря стоматологии Маэстро, человек с небольшим достатком может не только вылечить зубы, но и поддерживать здоровье ротовой полости. Теперь любой человек может не откладывать поход к стоматологу, выбирая доступное качественное обслуживание.
Prague is swiftly becoming a hub for businesses seeking trusted and cutting-edge IT solutions. Teaming up with an expert IT outsourcing company in Prague allows companies to enhance procedures, improve performance, and gain access to customized knowledge. From network management to cybersecurity, these companies give thorough IT services that make sure smooth business procedures and shield vital data. Leveraging professional IT support helps businesses in Prague focus on growth and preserve an one-upmanship in a digital world, https://xn--41-4lcpj.xn--j1amh/user/brandcry5/.
You ought to be a part of a contest for one of the most
useful websites on the internet. I most certainly will highly
recommend this web site!
It’s actually very complex in this busy life to listen news on TV, so
I just use the web for that reason, and take the most recent information.
free porn, porn, porn hub, jav porn, bokep indo, bokep bocil, indo bokep,
bokeep daddy ash, bokep ngewe, ngewe bocil, bokep binor, bokep
stw, bokep tante, bokep pns, okep tobrut, bokep viral, bokep bbu guru,
indian sex, indian wife, desi, mom, gangbang,
mother sex, sex mother, mom sex, ebony, dick, pussy, milf, casting, mature, teen, lesbian, vagina, vagina creampie, japanese wife,
japanese mature, japanese teen, japanese milf, lesbian mature,
mature women, squuirt machine, russian maid, american anal sluts, granny sex, bokep hijab, blkep malay, brazzers, hentai, arab sex,
mature anal, indian sex, african teen, najiaporntube, giigantic ass, sarah young, mature mom, pinya scandal,
sasha grey, gay, anal gay, mom аnd son, mom son, russian mature,
russian teen,anthea ѕօn casting, muslim girl blow job, jav subtitlee indonesia video bokep, bokep pelajar, remaja ngentod, ѕub indo porn videos,
bokep bumil, bokep artis indo, bokep babymoy, bokep meimei,
bokep memek legit, bokep crot dalam, bokep mantan pacar, bokep fսll
percakapan, bokep fᥙll service, bokep tante mulus, bokep sugardady,
bokep adik kakak, bokep selingkuh, bokep hijab tobrut, tante tobrut, hijab tobrut, bokep janda, bokep pijat, bokep vcs, bokep live ngentod, bokep indo
brondong, bokep indo tante brondong, bokep օpen bo, оpen bo
stw, bokpe michat, bokep apk ijo, bokep ojol, bokep bareng pacar, bokep tiktok, bokep jilbab sange, bokep jilbab abg, bokep ibu mertua, bokep kebhaya
merah, bokep digilir, indo porn, porfn indo, japanese porn, porn dude, iindonesia porn, gay porn,
video porn, porn video, porn hd, korean porn, tthe porn dude,
japan porn, free porn, rrae lil black porn, porn indonesia, ɑi porn, porn comic, tiktok porn,
audrey davis porn, porn movie, chinese porn, sophie rain porn, xxxx porn, porn sex, hd porn,
asian porn, anime porn, deepfake porn, sex porn, aloyx star porn, hikaru nagi porn, indonesian porn, nagi hikaru porn, roblox porn, porn xxx, bu guru salsa porn, porn tube, ƅig boobs porn, xnxx porn, situs
porn, porn japan, msbreewc porn, film porn, buan sutena porn, hazel moore porn, hijab porn, douyin porn viagra, ϲlick here, buy xanax online, beѕt casino, hacked site, scam reviews, malware,
download mp3 free
Quality articles is the main to be a focus for the people to go to see the site, that’s what this web site is providing.
Thanks for ones marvelous posting! I definitely enjoyed reading it,
you happen to be a great author. I will remember to bookmark
your blog and will come back in the foreseeable
future. I want to encourage you to continue your great job,
have a nice afternoon!
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos
para ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2
en apuestas que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se
declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas
deportivas|america apuestas|análisis nba apuestas|aplicacion android
apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para
hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas
deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas
deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones de
apuestas online|aplicaciones de apuestas seguras|aplicaciones
de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app
apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas
españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas
futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app de
apuestas|app de apuestas android|app de apuestas casino|app
de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de
apuestas deportivas android|app de apuestas deportivas argentina|app
de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas
deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app
de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para
android|app de apuestas para ganar dinero|app de apuestas
peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app
para apuestas de futbol|app para apuestas deportivas|app para apuestas deportivas en español|app para ganar apuestas
deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar
control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas
con bono de bienvenida|apps de apuestas de futbol|apps de
apuestas deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros
gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3
division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas
al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas
alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas
anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del
mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas argentina
mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina
paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas
argentina vs australia|apuestas argentina vs colombia|apuestas argentina
vs francia|apuestas argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso
a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas
athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic
valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de
liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico
de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real
madrid|apuestas atletico real madrid champions|apuestas
atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto acb|apuestas baloncesto
handicap|apuestas baloncesto hoy|apuestas baloncesto
juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas
barca|apuestas barca athletic|apuestas barca atletico|apuestas barca
bayern|apuestas barca bayern munich|apuestas barca
girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona
atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona
betis|apuestas barcelona campeon de liga|apuestas barcelona
celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona
madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas
barcelona real madrid|apuestas barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket
hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas
betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis
real madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis
vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono
de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia
real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas
boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas
brasil peru|apuestas brasil uruguay|apuestas brasil vs
colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas
campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa
league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas
campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas
campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de
galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de
caballos|apuestas carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras
de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de
caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras
de caballos sanlúcar|apuestas carreras de galgos|apuestas
carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos
pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta
madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league
– pronósticos|apuestas champions league 2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea
betis|apuestas chile|apuestas chile peru|apuestas
chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta
a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas
city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid
barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas
combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta
semana|apuestas combinadas para hoy|apuestas combinadas para
mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas
probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa del
rey futbol|apuestas copa del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa
italia|apuestas copa libertadores|apuestas copa
mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto
hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas
de beisbol para hoy|apuestas de blackjack en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo
en las vegas|apuestas de boxeo hoy|apuestas de
boxeo online|apuestas de caballo|apuestas de caballos|apuestas de
caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de
caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas
de caballos por internet|apuestas de caballos pronosticos|apuestas
de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras
de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino online|apuestas de
casino por internet|apuestas de champions league|apuestas de
ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas
de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de
eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula
1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol
colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas
de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de
futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas
de futbol online|apuestas de fútbol online|apuestas de futbol para
hoy|apuestas de fútbol para hoy|apuestas de futbol para
hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol
pronosticos|apuestas de fútbol pronósticos|apuestas de
futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas de galgos
online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas
de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos
online|apuestas de la champions league|apuestas de la copa
américa|apuestas de la eurocopa|apuestas de la europa league|apuestas
de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de
mlb|apuestas de nba|apuestas de nba para hoy|apuestas
de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas de
perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema explicación|apuestas
de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de
tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis
seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas del clasico real
madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas
del dia deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del rey|apuestas del
sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas 1×2|apuestas deportivas android|apuestas
deportivas app|apuestas deportivas apps|apuestas deportivas
argentina|apuestas deportivas argentina futbol|apuestas
deportivas argentina legal|apuestas deportivas atletico
de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas
deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas
deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino
online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas
deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas
para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono
gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas
deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas
consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa
america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa
mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas deportivas cuotas altas|apuestas
deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas
de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas
dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas
en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas deportivas
en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas
deportivas es pronosticos|apuestas deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas deportivas estrategias|apuestas deportivas
estrategias seguras|apuestas deportivas eurocopa|apuestas
deportivas europa league|apuestas deportivas f1|apuestas
deportivas faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas
futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas
ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas
gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis
con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas
deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas
legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas
liga española|apuestas deportivas listado|apuestas deportivas
listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas
mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores
casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas
mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas
deportivas murcia|apuestas deportivas nba|apuestas
deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas
nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas
online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago
paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas
peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas
deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas
pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas
pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas
deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas
seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas
seguras telegram|apuestas deportivas sevilla|apuestas
deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas
sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas
sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas
stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas
deportivas tenis foro|apuestas deportivas tenis hoy|apuestas
deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas
deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas
dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo
futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas
en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas
en casino|apuestas en casino online|apuestas
en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas
en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas
en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea
colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas
en linea futbol|apuestas en linea mexico|apuestas
en línea méxico|apuestas en linea mundial|apuestas en linea
peru|apuestas en linea usa|apuestas en los esports|apuestas
en madrid|apuestas en méxico|apuestas en mexico online|apuestas
en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas
en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas
equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa
alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa
francia|apuestas españa francia eurocopa|apuestas españa gana el mundial|apuestas españa
gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas
españa holanda|apuestas españa inglaterra|apuestas españa inglaterra
cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas
españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas
eurocopa favoritos|apuestas eurocopa femenina|apuestas
eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas
euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league hoy|apuestas
europa league pronosticos|apuestas europa league pronósticos|apuestas
euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas
f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas
f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas
favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions
league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas
final copa del rey|apuestas final copa europa|apuestas final
copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final
de copa del rey|apuestas final del mundial|apuestas
final euro|apuestas final eurocopa|apuestas final europa
league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa
europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas
finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol
argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol
consejos|apuestas futbol en directo|apuestas fútbol
en directo|apuestas futbol en vivo|apuestas
fútbol en vivo|apuestas futbol españa|apuestas
futbol español|apuestas fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas
futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol
online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador
champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas
ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la
liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas
ganador liga española|apuestas ganador mundial|apuestas ganador mundial
baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas
ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas
ganar nba|apuestas getafe valencia|apuestas
ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas
girona campeon liga|apuestas girona gana la liga|apuestas
girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas
goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas
gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por
registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar
premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas
handicap asiatico|apuestas handicap baloncesto|apuestas
handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas
hockey|apuestas hockey hielo|apuestas hockey patines|apuestas
hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas
juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas
juegos virtuales|apuestas jugador sevilla|apuestas jugadores
nba|apuestas kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas
las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales
españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas liga
argentina|apuestas liga bbva pronosticos|apuestas liga
de campeones|apuestas liga de campeones de baloncesto|apuestas
liga de campeones de hockey|apuestas liga españa|apuestas liga
española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea
de gol|apuestas liverpool barcelona|apuestas liverpool
real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid
barca|apuestas madrid barça|apuestas madrid
barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid
bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid
campeon champions|apuestas madrid celta|apuestas
madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid
gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas
madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas
mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters
de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador
mundial|apuestas mejor jugador eurocopa|apuestas mejores
casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas
mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas
mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como
funcionan|apuestas multiples el gordo|apuestas multiples
futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas
mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de
futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas
mundial moto gp|apuestas mundial motogp|apuestas mundial
rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba
all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas
nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas
nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas
nba pronósticos|apuestas nba pronosticos hoy|apuestas
nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl
las vegas|apuestas nfl playoffs|apuestas nfl
pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online
chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online
espana|apuestas online españa|apuestas online esports|apuestas online
foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online
nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas
osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises
bajos inglaterra|apuestas países bajos qatar|apuestas
para boxeo|apuestas para champions league|apuestas
para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para el partido de
hoy|apuestas para eurocopa|apuestas para europa
league|apuestas para futbol|apuestas para ganar|apuestas
para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para
hoy de futbol|apuestas para hoy europa league|apuestas para hoy
futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la eurocopa|apuestas para la nba
hoy|apuestas para los partidos de hoy|apuestas para partidos de
hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas
partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas
partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas
peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas
peru uruguay|apuestas peru vs chile|apuestas peru vs
colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas
playoff ascenso a primera|apuestas playoff
nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs
nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda
boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas
pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas
primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos
gratis|apuestas pronosticos nba|apuestas pronosticos tenis|apuestas prorroga|apuestas psg
barca|apuestas psg barcelona|apuestas puntos por
tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas
quien bajara a segunda|apuestas quién bajara a segunda|apuestas
quien gana el mundial|apuestas quien gana eurocopa|apuestas quien gana la
champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara
la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas
rayo barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real
madrid atletico champions|apuestas real madrid atletico de
madrid|apuestas real madrid atlético de madrid|apuestas real
madrid atletico madrid|apuestas real madrid barcelona|apuestas
real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas
real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real sociedad|apuestas real madrid valencia|apuestas real madrid
villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico
madrid|apuestas real madrid vs barcelona|apuestas
real madrid vs betis|apuestas real madrid vs sevilla|apuestas real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas
real sociedad barcelona|apuestas real sociedad
betis|apuestas real sociedad psg|apuestas
real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados
eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas
rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas
seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la
ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy
futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras
para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales
eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla
betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas
sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples
ejemplos|apuestas simples o combinadas|apuestas
sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso
minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas
sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas
sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10
hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas
tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis
en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis
retirada|apuestas tenis roland garros|apuestas
tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway
cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa
league|apuestas ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas
ufc telegram|apuestas ufc topuria|apuestas under over|apuestas
unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas
villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas
virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de
hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas
y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina
apuestas|argentina colombia apuestas|argentina croacia
apuestas|argentina francia apuestas|argentina
mexico apuestas|argentina peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs
chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de
madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid vs barcelona apuestas|atletico
madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de cuotas apuestas|bajada
de cuotas apuestas|baloncesto apuestas|barbastro
barcelona apuestas|barca apuestas|barca bayern apuestas|barca
inter apuestas|barca madrid apuestas|barça madrid apuestas|barca vs
atletico apuestas|barca vs madrid apuestas|barca vs real
madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid
apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de
apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia
apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best
america apuestas|bet apuestas chile|bet apuestas en vivo|betis –
chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu
sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa
de apuestas|bono bienvenida marca apuestas|bono
casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas gratis
sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida casa de apuestas|bono de bienvenida
casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de apuestas|bono gratis apuestas|bono
marca apuestas|bono por registro apuestas|bono por registro
apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono
sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos
apuestas sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos
bienvenida casas de apuestas|bonos casa de apuestas|bonos
casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de
apuestas deportivas|bonos casas de apuestas españa|bonos
casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas
de apuestas sin depósito|bonos de apuestas|bonos de apuestas
deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa
de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de
apuestas|bonos de casas de apuestas sin deposito|bonos en casa de
apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos registro
casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo
apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas
apuestas|buscador de apuestas seguras|buscador de
cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos
apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora
apuestas|calculadora apuestas combinadas|calculadora apuestas
de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir
apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de
apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas
multiples|calculadora de apuestas seguras|calculadora de apuestas
sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora
de cuotas de apuestas|calculadora para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular
apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas
combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular
probabilidad cuota apuestas|calcular stake apuestas|calcular unidades
apuestas|calcular yield apuestas|calculo de apuestas|calculo de apuestas
deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos
apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras
de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos
apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa
apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa apuestas cerca de
mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa
apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa
apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas
10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de
apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa
de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa
de apuestas cerca de mi|casa de apuestas cerca
de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas
ciclismo|casa de apuestas colombia|casa de apuestas con bono de bienvenida|casa de
apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de
apuestas con esports|casa de apuestas con las mejores cuotas|casa de
apuestas con licencia en españa|casa de
apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas
copa america|casa de apuestas de caballos|casa
de apuestas de colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de
apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas
de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa
de apuestas deportivas|casa de apuestas deportivas cerca de mi|casa de apuestas deportivas
en argentina|casa de apuestas deportivas en chile|casa
de apuestas deportivas en colombia|casa de apuestas
deportivas en españa|casa de apuestas deportivas en madrid|casa
de apuestas deportivas españa|casa de apuestas deportivas
españolas|casa de apuestas deportivas madrid|casa de apuestas
deportivas mexico|casa de apuestas deportivas online|casa de apuestas deportivas peru|casa de
apuestas deposito 5 euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo
1 euro|casa de apuestas depósito mínimo 1 euro|casa
de apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de
apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa
de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas
eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas
formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales
en españa|casa de apuestas libertadores|casa de apuestas liga
española|casa de apuestas madrid|casa de apuestas mas segura|casa
de apuestas mejores|casa de apuestas méxico|casa de apuestas minimo 5 euros|casa
de apuestas mlb|casa de apuestas mundial|casa de
apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa
de apuestas nuevas|casa de apuestas oficial del real madrid|casa
de apuestas oficial real madrid|casa de apuestas online|casa
de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online usa|casa de apuestas online
venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa
de apuestas perú|casa de apuestas peru online|casa de apuestas por paypal|casa de
apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas
sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa
de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa
oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas
apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas
apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas
deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales
españa|casas apuestas licencia|casas apuestas
licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de
apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono
bienvenida|casas de apuestas bono de bienvenida|casas
de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas
bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de
bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de
apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de
apuestas casino online|casas de apuestas cerca de mi|casas de apuestas champions league|casas de apuestas
chile|casas de apuestas ciclismo|casas de apuestas colombia|casas
de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de
apuestas con bono|casas de apuestas con bono de bienvenida|casas de apuestas con bono
de registro|casas de apuestas con bono por registro|casas de apuestas con bono
sin deposito|casas de apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas
con bonos sin deposito|casas de apuestas con deposito
minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de
apuestas con licencia|casas de apuestas con licencia en españa|casas
de apuestas con licencia españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas
de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas copa del rey|casas
de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de
apuestas de peru|casas de apuestas deportivas|casas de apuestas
deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas
deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas
de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas
deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas
de apuestas deportivas españa|casas de apuestas deportivas españolas|casas
de apuestas deportivas legales|casas de apuestas deportivas madrid|casas
de apuestas deportivas mexico|casas de apuestas
deportivas nuevas|casas de apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito
minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de apuestas dinero gratis|casas de
apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa
online|casas de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de
apuestas en peru|casas de apuestas en perú|casas
de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de
futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas
de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de
apuestas esports|casas de apuestas eurocopa|casas de
apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de
apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de apuestas futbol|casas
de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de
apuestas inter barcelona|casas de apuestas legales|casas
de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de
apuestas licencia españa|casas de apuestas lista|casas de apuestas
madrid|casas de apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas
de apuestas méxico|casas de apuestas minimo 5 euros|casas
de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas de apuestas mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas
en españa|casas de apuestas nuevas españa|casas de apuestas
ofertas|casas de apuestas online|casas de apuestas
online argentina|casas de apuestas online colombia|casas de apuestas online
deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas online en colombia|casas de
apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas
online venezuela|casas de apuestas pago paypal|casas de apuestas para ufc|casas de apuestas
paypal|casas de apuestas peru bono sin deposito|casas de apuestas presenciales en españa|casas de
wonderful publish, very informative. I wonder why the other experts of this sector don’t notice this.
You should continue your writing. I am sure, you’ve a huge readers’ base already!
This paragraph will assist the internet people for setting up new webpage or even sell a business blog from start to end.
Hi, after reading this amazing paragraph i am too delighted to share my know-how here with colleagues.
You really make it seem really easy with your presentation but I to find this topic to
be actually one thing that I believe I would by no means understand.
It seems too complicated and very vast businesses for sale me.
I’m looking ahead in your next put up, I will try to get the hold of it!
Please let me know if you’re looking for a author for your weblog.
You have some really good posts and I think I would be a good asset.
If you ever want to take some of the load off,
I’d love to write some material for your blog in exchange business for sale a link back to mine.
Please blast me an e-mail if interested. Kudos!
Йо, товарищ! На днях наткнулся на, и не могу помалкивать.
Бывало, хотел оплатить что-то на eBay, а банк режет транзакцию? Теперь это не проблема.
Слышал про «Плати по Миру»? Это топчик. Это виртуальная карта, которая разрешает доступ к любым зарубежным сервисам. Без тонны документов.
Как это работает
С «Плати по Миру» у тебя получится уплачивать там, где обычная карта отказывается.
Да хоть в Европе закажи гаджет — оплата проскочит.
Как употреблять
Подключаешь карту, пополняешь с любой своей карты — и пользуешься.
Не нужен телесный носитель — всё цифровое.
Зачем это надо
Получаешь доступ к любому контенту за границей.
Работает моментально, на практике.
В итоге, «Плати по Миру» — это купюра к покупкам без границ. Оформить карту можно за 2 минуты, и сразу пользуешься.
А ты сталкивался с блокировками за границей? Как выходил из ситуации? Поделись в комментах.
Привет, дружище! На днях заметил интересный сервис, грех не поведать.
Бывало, хотел оформить подписку в Booking, а платёж блокируют Выход проще, чем похоже.
Слышал про «Плати по Миру»? Это мощная предмет. Это цифровая карта, которая открывает двери к любым онлайн-магазинам в мире. Оформление буквально пару кликов.
В чём фишка
С «Плати по Миру» ты сможешь свершать покупки в сервисах, где обычная карта отказывается.
Да хоть в Японии закажигаджет — оплата проскочит.
Схема работы
Регистрация делается быстро: вбил данные, пополнил — и вперёд к оплатам..
Не нужен телесный носитель — всё в приложении.
Главные плюсы
Мир раскрывается если можно платить всюду..
Покупки в любых странах, никаких заминок, никаких очередей..
https://tinyurl.com/antarctic-wallet
@pl@world
Wow that was strange. I just wrote an very long comment but after I clicked submit
my comment didn’t show up. Grrrr… well I’m
not writing all that over again. Anyway, just wanted to say fantastic blog!
Have a look at my web page – Houston liposuction surgeon
Wow, fantastic blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your
site is great, let alone the content!
Visit my website … sell a business
Coming from cost reduction and unique promos to time-saving benefit and boosted shopping practices, these codes enhance every facet of on-line buying. Regardless if you’re searching for cost-free discount rate codes and promo codes for Czech e-shops, voucher code numbers for Czech e-shops, or discount code today for Czech e-shops, megakupony ensures you make the most of financial savings effortlessly and delight in a smarter, more satisfying shopping experience, http://www.drugoffice.gov.hk/gb/unigb/megakupony.cz/.
It’s actually a cool and useful piece of info. I am satisfied
that you shared this helpful information with us. Please stay us informed like this.
Thank you for sharing.
Also visit my homepage – hi def liposuction
Awesome! Its actually remarkable post, I have got much clear idea concerning from this paragraph.
I have read so many content regarding the blogger lovers however this piece of writing is really sell a business nice article, keep it up.
I am regular reader, how are you everybody? This article
posted at this web page is really fastidious.
my web blog: sell a business
Hello there! This is kind of off topic but I need some help from an established blog.
Is it very hard to set up your own blog? I’m not very
techincal but I can figure things out pretty quick. I’m thinking about making my own but I’m not sure where to start.
Do you have any points or suggestions? Thanks
Way cool! Some very valid points! I appreciate you writing this post and the rest of the site is also really good.
Here is my page; best liposuction in Houston
Great post however I was wondering if you could write a litte more on this subject?
I’d be very grateful if you could elaborate a little bit further.
Many thanks!
Here is my web page; business for sale
Hello, all is going well here and ofcourse every one is sharing information, that’s really fine, keep up writing.
Also visit my blog post – Body contouring liposuction Houston
Pretty component of content. I simply stumbled upon your
web site and in accession capital to claim that
I get in fact loved account your blog posts. Anyway I will
be subscribing to your feeds and even I achievement you get right of
entry to consistently rapidly.
каталог vodka casino
читать кракен купить
I am best liposuction in Houston fact grateful to the
holder of this web site who has shared this fantastic article at at this place.
These are actually fantastic ideas in regarding blogging.
You have touched some fastidious points here. Any way keep up wrinting.
my website – sell a business
Way cool! Some extremely valid points! I appreciate you writing this post and the rest of the website is extremely good.
Review my page: sell a business
Greetings! This is my first visit to your blog!
We are a team of volunteers and starting a new project in a community in the same niche.
Your blog provided us useful information to work on. You have done a extraordinary job!
Visit my webpage :: business 4 sale
Having read this I believed it was very enlightening.
I appreciate you finding the time and effort to put this article together.
I once again find myself personally spending a lot of time both reading and commenting.
But so what, it was still worthwhile!
I must thank you for the efforts you have put in writing this
blog. I’m hoping to check out the same high-grade blog posts from you later on as well.
In fact, your creative writing abilities has encouraged me to get
my own, personal website now 😉
I have been browsing online more than 4 hours today, yet I never found
any interesting article like yours. It is pretty worth enough for me.
In my view, if all webmasters and bloggers made good content
as you did, the internet will be much more useful than ever
before.
Excellent post. I was checking continuously this blog and I’m
impressed! Extremely helpful information particularly the last part 🙂 I care for such info much.
I was seeking this certain info for a long time. Thank you and good luck.
Howdy, i read your blog occasionally Liposuction before and after Houston i
own a similar one and i was just curious if you get a lot of spam responses?
If so how do you stop it, any plugin or anything you can advise?
I get so much lately it’s driving me insane so any
help is very much appreciated.
Magnificent beat ! I wish to apprentice even as you amend your web site,
how can i subscribe for a weblog site? The account aided
me a appropriate deal. I have been tiny bit acquainted of this your
broadcast offered vivid transparent idea
My partner and I stumbled over here by a different web page and thought I might as well check things
out. I like what I see so now i am following you. Look forward
to checking out your web page for a second time.
Hi there, yes this post is actually fastidious and I have learned lot of things from it on the topic of blogging.
thanks.
Feel free to visit my blog Body contouring liposuction Houston
Good day! I could have sworn I’ve visited this blog before but after going through many of the posts I realized
it’s new to me. Regardless, I’m certainly happy I
discovered it and I’ll be book-marking it and checking back often!
Hello! This is my first comment here so I just wanted to give a quick shout out and
tell you I truly enjoy reading your articles. Can you suggest any other blogs/websites/forums that deal with the same topics?
Thanks!
Hey there! Someone in my Facebook group shared this
site with us so I came to take a look. I’m definitely enjoying the
information. I’m book-marking and will be tweeting this
to my followers! Terrific blog and excellent
design.
Simply desire to say your article is as astonishing.
The clarity in your post is simply excellent and i can assume you are
an expert on this subject. Fine with your permission let me to grab your feed to keep updated with forthcoming post.
Thanks a million and please keep up the gratifying work.
my homepage :: Large volume liposuction Houston
If you wish for to increase your knowledge only keep visiting this website and be updated
with the latest news posted here.
ⵎⵉ ⵢⴻⵜⵜⵡⴰⵟⵟⴻⴼ ⴰⴷⵓⴱⴰ, ⵢⴻⵙⵙⵓⵜⴻⵔⴷ ⵛⵛⵕⴻⵄ ⵖⴻⵔ ⵓⴷⵉⵡⴰⵏ ⵏ ⵜⴻⵎⵏⴰⴹⵜ ⵏ ⵓ.ⵙ.
Kunyanya, kuita mukumbiro ku Hofisi yo Gweta ro United States ro ku Maodzanyemba o Nharaunda yo New York.
Have you ever thought about adding a little bit more
than just your articles? I mean, what you say is valuable and everything.
But think of if you added some great visuals or video clips to give your posts more,
“pop”! Your content is excellent but with pics and videos, this blog
could undeniably be one of the best in its niche.
Awesome blog!
I’ve been exploring for a little bit for any high-quality articles or blog posts on this sort of house .
Exploring in Yahoo I at last stumbled upon this web site.
Reading this info So i am satisfied to convey that
I’ve an incredibly excellent uncanny feeling I found out exactly what I needed.
I so much surely will make sure to do not put out of your mind this site and give it a look on a constant basis.
Here is my blog post Large volume liposuction Houston
Howdy! This is my first visit to your blog! We are a collection of
volunteers and starting a new initiative in a community in the same niche.
Your blog provided us valuable information to work on. You have done a extraordinary job!
What’s up to every body, it’s my first go to see
of this webpage; this website consists of amazing and genuinely fine information for visitors.
my web page: Liposuction
bookmarked!!, I really like your website!
You could definitely see your skills in the article you write.
The sector hopes for even more passionate writers like you
who are not afraid to say how they believe. Always go after your heart.
My website … Liposuction
When I initially commented I clicked the “Notify me when new comments are added” checkbox
and now each time a comment is added I get three
e-mails with the same comment. Is there any way you can remove people from that service?
Bless you!
Also visit my blog :: Mommy makeover liposuction Houston
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Thanks
great publish, very informative. I ponder why the other experts of
this sector do not understand this. You should proceed your writing.
I’m sure, you have a great readers’ base already!
Вам предстоит командировка? Выбор жилья всегда важен. Сегодня каждый может выбрать удобный вариант: квартиры на сутки, отели разного уровня, гостевые дома с домашней атмосферой. Всё, что остаётся — это выбрать лучший формат именно для вас.
Почему жильё посуточно удобно
Выбирая жильё посуточно, вы получаете:
✅ Гибкость — можно снять жильё на 1 день, неделю или дольше.
✅ Низкие цены по сравнению с гостиницами.
✅ Комфорт — возможность готовить дома, больше пространства для семьи.
✅ Варианты на любой вкус: от студий до домов.
Квартиры на сутки
Снять квартиру на сутки удобно для семьи или пары.
– Полностью оборудованная кухня.
– Свободное пространство и несколько комнат.
– Лучший вариант для командировок и семейного отдыха.
Отели на сутки
Отель подходит тем, кто ценит сервис.
– Удобная локация рядом с транспортом.
– Услуги персонала.
– Разные категории — от бюджетных до премиум.
Домики и гостевые дома посуточно
Домики посуточно подойдут для больших компаний.
– Подходит для отдыха с друзьями.
– Находятся за городом или у моря.
– Домашний комфорт и тишина.
Советы по аренде жилья на сутки
1. Сначала рассчитайте сумму и выберите даты.
2. Решите, что важнее: цена, сервис или уединение.
3. Читайте отзывы и смотрите рейтинг.
4. Бронируйте заранее.
❓ Часто задаваемые вопросы
1. Где найти квартиры, отели и гостевые дома на сутки?
— В сервисах поиска жилья.
2. Можно ли снять жильё посуточно без предоплаты?
— Некоторые хозяева разрешают без предоплаты.
3. Что выгоднее — квартира или отель?
— Для семьи — квартира, для бизнеса — отель, для отдыха на природе — дом.
4. Есть ли скидки при долгосрочной аренде?
— Чем дольше срок — тем выгоднее цена.
Мнения наших гостей
⭐ Марина, Москва
“Снимала квартиру на сутки в центре города. Чисто, уютно, рядом метро.”
⭐ Игорь, Санкт-Петербург
“Выбирал гостевой дом для отдыха с друзьями. Очень удобно и недорого.”
⭐ Анна, Казань
“Бронировала отель на двое суток через сервис. Всё прошло быстро.”
https://tiktur.store/
Выбирайте лучшие квартиры, отели и гостевые дома на сутки прямо сейчас и сэкономьте время и деньги.
@airbnb
Ik ben dol op cazino, ga vooral door – de content is top!
https://lalabet-play-netherlands.nl/registratie
Hi there I am so thrilled I found your webpage, I really found you
by accident, while I was browsing on Bing for something else, Anyhow I am here
now and would just like to say thanks for a incredible post and a all round thrilling blog (I also
love the theme/design), I don’t have time to read it all at the moment but I have bookmarked it and also added your RSS feeds, so when I have time
I will be back to read much more, Please
do keep up the superb job.
Heya i am for the first time here. I came across this board
and I find It really useful & it helped me out much.
I hope to present one thing again and aid others such
as you aided me.
Ni pod kojim uvjetima ne smijete kliknuti na ovu poveznicu jer se radi o kibernetičkom kriminalu.
I visited multiple blogs except the audio quality for audio songs
present at this web site is genuinely excellent.
It’s impressive that you are getting thoughts from this post as well as from our discussion made here.
Thanks on your marvelous posting! I quite enjoyed reading it, you’re a great author.
I will always bookmark your blog and will come back later in life.
I want to encourage you to continue your great writing,
have a nice day!
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para
ganar apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2 en apuestas que significa|1×2 que significa en apuestas|5 euros
gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto
se declara apuestas|actividades de juegos de azar y apuestas|ad apuestas deportivas|aleksandre
topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas
deportivas|aplicacion apuestas deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones
apuestas deportivas android|aplicaciones apuestas
deportivas gratis|aplicaciones de apuestas android|aplicaciones de apuestas de fútbol|aplicaciones
de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de
apuestas en colombia|aplicaciones de apuestas gratis|aplicaciones
de apuestas online|aplicaciones de apuestas seguras|aplicaciones
de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre
amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas
de apuestas|app control apuestas|app de apuestas|app
de apuestas android|app de apuestas casino|app de apuestas colombia|app
de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app
de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas
colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de
apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de
apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de
futbol|app para apuestas deportivas|app para apuestas deportivas en español|app
para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para
llevar control de apuestas|app pronosticos apuestas deportivas|app versus apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas peru|apps de
apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas
10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2
division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas a ganar|apuestas a jugadores nba|apuestas a
la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas
alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo
nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas
arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina
gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina vs australia|apuestas argentina vs colombia|apuestas
argentina vs francia|apuestas argentina vs peru|apuestas
argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas
asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic
atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic
manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic
real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico
campeon champions|apuestas atletico campeon de liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de
madrid|apuestas atletico de madrid barcelona|apuestas atletico de madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico
real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas
baloncesto|apuestas baloncesto acb|apuestas baloncesto
handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca
bayern munich|apuestas barca girona|apuestas barca
hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas
barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas
barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas barcelona|apuestas barcelona
alaves|apuestas barcelona athletic|apuestas barcelona
atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona
atletico madrid|apuestas barcelona bayern|apuestas barcelona
betis|apuestas barcelona campeon de liga|apuestas
barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona
girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona
osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona
real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas
barcelona vs real madrid|apuestas barsa madrid|apuestas basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas
betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis
fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real
madrid|apuestas betis real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis
vs valencia|apuestas betplay hoy colombia|apuestas
betsson peru|apuestas bienvenida|apuestas billar
online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono
de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono
gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas boxeo|apuestas boxeo
de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs
peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas
calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas
campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas
campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas
campeon liga bbva|apuestas campeon liga española|apuestas campeon liga
santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de
futbol|apuestas carrera de caballos|apuestas
carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera
de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de
galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas
carreras de caballos en directo|apuestas carreras de
caballos en vivo|apuestas carreras de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas
carreras de caballos nocturnas|apuestas carreras de caballos
online|apuestas carreras de caballos sanlucar|apuestas
carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino
futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas
celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas
celta madrid|apuestas celta manchester|apuestas celta real madrid|apuestas champion league|apuestas champions
foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league
2025|apuestas champions league hoy|apuestas champions league pronosticos|apuestas champions league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea
betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas
chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo
femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico
español|apuestas clasico real madrid barcelona|apuestas
clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas
colombia paraguay|apuestas colombia uruguay|apuestas colombia
vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas combinadas como funcionan|apuestas combinadas de futbol|apuestas
combinadas de fútbol|apuestas combinadas foro|apuestas
combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas
para esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas
combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas
seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas
con dinero ficticio|apuestas con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa argentina|apuestas copa
brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas
copa del rey|apuestas copa del rey baloncesto|apuestas copa del
rey final|apuestas copa del rey futbol|apuestas copa del rey ganador|apuestas
copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas
copa libertadores|apuestas copa mundial de hockey|apuestas copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas
cuartos eurocopa|apuestas cuotas|apuestas cuotas altas|apuestas cuotas
bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas
de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas
de caballos|apuestas de caballos como funciona|apuestas de caballos como
se juega|apuestas de caballos en colombia|apuestas de
caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos
internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas
de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de
caballos online|apuestas de casino|apuestas de casino online|apuestas de casino por
internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa
america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas
de dinero|apuestas de esports|apuestas de eurocopa|apuestas
de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas
de futbol colombia|apuestas de futbol en colombia|apuestas
de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de
futbol para hoy|apuestas de fútbol para hoy|apuestas de futbol para hoy
seguras|apuestas de futbol para mañana|apuestas
de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas
de galgos|apuestas de galgos como ganar|apuestas de galgos en directo|apuestas
de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas
de hockey sobre hielo|apuestas de hoy|apuestas de hoy seguras|apuestas
de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas
de juegos online|apuestas de la champions league|apuestas de
la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas
de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba
para hoy|apuestas de partidos|apuestas de
partidos de futbol|apuestas de peleas ufc|apuestas de perros en vivo|apuestas
de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas
de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de
tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas
del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia
de hoy|apuestas del dia deportivas|apuestas del
dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas del
rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas deportivas
1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas
1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas
argentina|apuestas deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca
madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas
bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de
bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas deportivas boxeo|apuestas
deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas
casino barcelona|apuestas deportivas casino online|apuestas deportivas cerca de mi|apuestas deportivas champions
league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas
com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas deportivas
comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas
deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos
para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas
deportivas corners|apuestas deportivas cual es la
mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas
deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas
en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas
deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas
deportivas españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas estadisticas|apuestas
deportivas estrategias|apuestas deportivas estrategias
seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de ganar|apuestas deportivas
formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas
deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas
deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis
con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas deportivas handicap asiatico|apuestas
deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior
argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia españa|apuestas deportivas
liga española|apuestas deportivas listado|apuestas
deportivas listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas
mejor pagadas|apuestas deportivas mejores|apuestas deportivas
mejores app|apuestas deportivas mejores casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas
mlb|apuestas deportivas mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas
nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas
deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online
en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas
deportivas online paypal|apuestas deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para
hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas
pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo
bienvenida|apuestas deportivas resultado
exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas
deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram
españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas
deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia
barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com
foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1 euro|apuestas descenso a segunda|apuestas descenso a
segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas
dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas dortmund barcelona|apuestas draft
nba|apuestas draft nfl|apuestas ecuador vs argentina|apuestas ecuador vs venezuela|apuestas
egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas
en boxeo|apuestas en caballos|apuestas en carreras de caballos|apuestas en casino|apuestas
en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de
futbol|apuestas en directo|apuestas en directo futbol|apuestas
en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas
en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas
en la liga|apuestas en la nba|apuestas en la nfl|apuestas
en las vegas mlb|apuestas en las vegas nfl|apuestas
en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea
colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de
futbol en vivo|apuestas en partidos de tenis
en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de
mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas
españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas españa francia|apuestas españa francia eurocopa|apuestas españa gana el
mundial|apuestas españa gana eurocopa|apuestas españa gana
mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas
españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas
esports|apuestas esports colombia|apuestas esports españa|apuestas esports
fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa
ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa
league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas
f1 bahrein|apuestas f1 canada|apuestas f1
china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de
ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas
favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final
champions cuotas|apuestas final champions league|apuestas
final champions peru|apuestas final copa|apuestas final copa america|apuestas final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa
del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa
league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas
final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales
nba|apuestas fiorentina betis|apuestas formula|apuestas formula
1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas
fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol
champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol
consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol
en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas
fútbol español|apuestas futbol eurocopa|apuestas futbol femenino|apuestas
futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas
fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas
futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas
galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador
copa america|apuestas ganador copa del rey|apuestas
ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa
league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga
española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas
ganar eurocopa|apuestas ganar liga|apuestas
ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona
betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana
la liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf
pga|apuestas granada barcelona|apuestas grand slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por
registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y
ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey
sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas
hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas
juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos
olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores
nba|apuestas kings league americas|apuestas la liga|apuestas la
liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas
las vegas nfl|apuestas league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1
peru|apuestas liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de
hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas
ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool
barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas
madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca
supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas
madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas
madrid gana la liga|apuestas madrid gana liga|apuestas madrid
hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas
madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas
mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de
tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador
eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas
méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas
mlb las vegas|apuestas mlb para hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas
momios|apuestas multiples|apuestas múltiples|apuestas multiples como
funcionan|apuestas multiples el gordo|apuestas multiples
futbol|apuestas mundial|apuestas mundial 2026|apuestas mundial
baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas mundial ciclismo|apuestas
mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas
mundial de futbol|apuestas mundial de fútbol|apuestas
mundial de rugby|apuestas mundial f1|apuestas mundial favoritos|apuestas mundial femenino|apuestas mundial formula
1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto
gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub
17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp
nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba
consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas nba hoy
jugadores|apuestas nba hoy pronosticos|apuestas nba para
hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas
nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas
nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl
pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina
legal|apuestas online bono|apuestas online bono bienvenida|apuestas online
boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas
online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online
comparativa|apuestas online con paypal|apuestas online de caballos|apuestas
online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online
futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online
gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas
osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas
osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas
paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas
para el clasico|apuestas para el dia de hoy|apuestas para
el mundial|apuestas para el partido de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas para ganar|apuestas para
ganar dinero|apuestas para ganar dinero facil|apuestas para
ganar en la ruleta|apuestas para ganar la champions|apuestas para ganar
la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas
para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la
copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la
eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas
para partidos de hoy|apuestas para ufc|apuestas partido|apuestas partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido
mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos csgo|apuestas partidos
de futbol|apuestas partidos de futbol hoy|apuestas partidos de hoy|apuestas partidos eurocopa|apuestas
partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas
peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi
eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff
ascenso|apuestas playoff ascenso a primera|apuestas playoff
nba|apuestas playoff segunda|apuestas playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal
uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera
division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos
deportivos|apuestas pronosticos deportivos tenis|apuestas
pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas
pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que es handicap|apuestas que puedes hacer con tu novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara a segunda|apuestas quién bajara a
segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas
quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la
liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas quien ganara la eurocopa|apuestas
quien ganara la liga|apuestas rayo barcelona|apuestas real
madrid|apuestas real madrid arsenal|apuestas
real madrid athletic|apuestas real madrid atletico|apuestas
real madrid atletico champions|apuestas real madrid atletico de madrid|apuestas
real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid barcelona|apuestas real madrid
bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas
real madrid campeon champions|apuestas real madrid celta|apuestas
real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real
madrid liverpool|apuestas real madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real
sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas real
madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real
sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas
registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas
retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta seguras|apuestas segunda|apuestas segunda b|apuestas
segunda division|apuestas segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras
futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este
fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para hoy pronósticos|apuestas
seguras para mañana|apuestas seguras ruleta|apuestas
seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal
paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla inter|apuestas sevilla jugador|apuestas
sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla
manchester united|apuestas sevilla osasuna|apuestas
sevilla real madrid|apuestas sevilla real sociedad|apuestas
sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas
simples o combinadas|apuestas sin deposito|apuestas
sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas
sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema
trixie|apuestas sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10
hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas
tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa
pronosticos|apuestas tenis en vivo|apuestas
tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland
garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis
wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas
tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas
torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas
ufc|apuestas ufc chile|apuestas ufc como funciona|apuestas ufc hoy|apuestas ufc ilia
topuria|apuestas ufc online|apuestas ufc
pronósticos|apuestas ufc telegram|apuestas ufc topuria|apuestas
under over|apuestas unionistas villarreal|apuestas
uruguay|apuestas uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas
us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas
valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas
valor app|apuestas valor en directo|apuestas valor
galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas
venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas
villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales
futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas
vuelta a españa|apuestas vuelta españa|apuestas william hill partidos
de hoy|apuestas y casino|apuestas y casinos|apuestas y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas
y pronosticos deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina peru apuestas|argentina uruguay
apuestas|argentina vs bolivia apuestas|argentina
vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina
vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico
de madrid real madrid apuestas|atletico de madrid vs
barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid apuestas|avisador de
cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro
barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca madrid apuestas|barça madrid
apuestas|barca vs atletico apuestas|barca vs madrid
apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de
apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona
valencia apuestas|barcelona vs athletic bilbao apuestas|barcelona
vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo
apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs
madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs villarreal apuestas|base
de datos cuotas apuestas deportivas|bayern real
madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis –
chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas
online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog apuestas
tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas (https://teste.identifica.pt/) gratis
sin deposito|bono apuestas sin deposito|bono
bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida
apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida marca apuestas|bono
casa apuestas|bono casa de apuestas|bono casa de apuestas sin ingreso|bono
casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de
bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida
casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono
de registro casa de apuestas|bono gratis apuestas|bono marca apuestas|bono
por registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito
apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono
sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas sin deposito|bonos apuestas
sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos
casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos
casas de apuestas deportivas|bonos casas de apuestas españa|bonos casas de apuestas nuevas|bonos casas de
apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de
apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida
apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos
de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas
sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos
gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de apuestas|bonos
registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos
sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo
apuestas|brasil colombia apuestas|brasil peru apuestas|brasil
vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador
de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador
de cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas
deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora
apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje
apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas
de sistema|calculadora de apuestas deportivas|calculadora de
apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas
sistema|calculadora de apuestas surebets|calculadora de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para apuestas
deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading
apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular
unidades apuestas|calcular yield apuestas|calculo de apuestas|calculo
de apuestas deportivas|cambio de cuotas apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de
caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de
apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras
de galgos apuestas trucos|carreras galgos apuestas|casa apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas
betis|casa apuestas bono bienvenida|casa apuestas bono
gratis|casa apuestas bono sin deposito|casa apuestas cerca de mi|casa apuestas chile|casa
apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas
españa|casa apuestas española|casa apuestas eurocopa|casa apuestas
futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa
apuestas valencia|casa de apuestas|casa de apuestas
10 euros gratis|casa de apuestas argentina|casa de apuestas atletico
de madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas
cerca de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa
de apuestas colombia|casa de apuestas con bono
de bienvenida|casa de apuestas con bono sin deposito|casa
de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de apuestas con pago anticipado|casa de
apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de
apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas
del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas
cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa
de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de apuestas deportivas en madrid|casa de apuestas deportivas
españa|casa de apuestas deportivas españolas|casa de apuestas
deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas deportivas online|casa
de apuestas deportivas peru|casa de apuestas deposito 5
euros|casa de apuestas deposito minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de
apuestas en españa|casa de apuestas en linea|casa de apuestas en madrid|casa
de apuestas en perú|casa de apuestas en vivo|casa de
apuestas españa|casa de apuestas españa inglaterra|casa de apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de
apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de
apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa de
apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales
en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas
méxico|casa de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas
mundial|casa de apuestas nba|casa de apuestas nfl|casa de
apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa
de apuestas oficial real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas
online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online
peru|casa de apuestas online usa|casa de apuestas
online venezuela|casa de apuestas pago anticipado|casa de apuestas para
boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de
apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas
real madrid|casa de apuestas regalo de bienvenida|casa de apuestas sevilla|casa de apuestas
sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas
sin minimo de ingreso|casa de apuestas stake|casa de
apuestas tenis|casa de apuestas ufc|casa de apuestas
valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real
madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas
caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia
en españa|casas apuestas deportivas|casas apuestas deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas
deportivas nuevas|casas apuestas españa|casas apuestas
españolas|casas apuestas esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas
apuestas licencia españa|casas apuestas mexico|casas apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas
ofertas|casas apuestas online|casas apuestas paypal|casas apuestas
peru|casas apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas
de apuestas|casas de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas
asiaticas|casas de apuestas baloncesto|casas de apuestas
barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de bienvenida|casas de apuestas bono por
registro|casas de apuestas bono sin deposito|casas de apuestas
bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de
apuestas caballos|casas de apuestas carreras de caballos|casas de apuestas casino|casas de apuestas casino online|casas de apuestas cerca de
mi|casas de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de
apuestas com|casas de apuestas con app|casas de apuestas
con apuestas gratis|casas de apuestas con bono|casas de apuestas
con bono de bienvenida|casas de apuestas con bono de registro|casas
de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de
apuestas con bonos|casas de apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de
apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas
con handicap asiatico|casas de apuestas con licencia|casas
de apuestas con licencia en españa|casas de apuestas con licencia
españa|casas de apuestas con licencia española|casas de apuestas con mejores cuotas|casas
de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal
en perú|casas de apuestas con promociones|casas de apuestas
con ruleta en vivo|casas de apuestas copa del rey|casas de
apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de
fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de
apuestas deportivas en españa|casas de apuestas
deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas
de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de
apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas
deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas deportivas online|casas
de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas
deposito minimo 1 euro|casas de apuestas depósito mínimo
1 euro|casas de apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas
en barcelona|casas de apuestas en chile|casas de apuestas en colombia|casas de apuestas
en españa|casas de apuestas en españa online|casas de apuestas en linea|casas
de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de
apuestas en venezuela|casas de apuestas equipos de futbol|casas
de apuestas españa|casas de apuestas españa alemania|casas de apuestas españa inglaterra|casas de
apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas
españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas
de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas
de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas de
apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de
apuestas gratis|casas de apuestas ingreso
minimo|casas de apuestas ingreso minimo 1 euro|casas
de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de
apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas
de apuestas licencia españa|casas de apuestas lista|casas de apuestas madrid|casas de
apuestas mas seguras|casas de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de apuestas mexico|casas de apuestas méxico|casas de apuestas minimo
5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas
de apuestas mundiales|casas de apuestas nba|casas
de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de apuestas nuevas en españa|casas de apuestas nuevas
españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas online
colombia|casas de apuestas online deportivas|casas de apuestas online ecuador|casas
de apuestas online en argentina|casas de apuestas online
en chile|casas de apuestas online en colombia|casas de apuestas online
en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas
online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas online usa|casas de apuestas online venezuela|casas de apue
When some one searches for his essential thing, thus he/she needs to be available
that in detail, thus that thing is maintained over here.
Hola! I’ve been following your site for a long time now and finally got the bravery to go ahead and give you a shout out from Atascocita Tx!
Just wanted to mention keep up the great work!
Oh my goodness! Awesome article dude! Thanks, However I am having problems with your RSS.
I don’t know why I am unable to subscribe to it. Is there anybody getting
identical RSS issues? Anyone who knows the answer will you kindly respond?
Thanks!!
ካን ማኩኣ ኣን ኣውቶሪዳድ፡ ናግሳንጋት ስያ ኒን ረክላሞ ሳ ኦፒሲና ካን ፒስካል ካን ዲስትሪቶ ካን ኢስታዶስ ዩኒዶስ.
Služba uklid bytu praha od Ohayno je ideálním řešením pro všechny, kteří chtějí mít svůj domov
vždy dokonale čistý, aniž by museli trávit hodiny úklidem.
Naši profesionálové se postarají o kompletní úklid domácnosti Praha, zatímco vy se
můžete věnovat rodině, práci nebo odpočinku.
Čistý byt už nemusí být výsledkem únavného víkendového maratonu – Ohayno přináší pohodlí a jistotu každodenní čistoty.
Ohayno využívá moderní vybavení a ekologicky šetrné čisticí prostředky,
které jsou účinné, bezpečné a šetrné ke všem povrchům.
Každý člen týmu prochází odborným školením, aby
zaručil nejvyšší úroveň preciznosti a profesionality.
Díky našemu systému kontroly kvality máte jistotu, že každý uklid bytu praha i úklid domů Praha bude proveden pečlivě, rychle a bez kompromisů.
Součástí služeb je vysávání, vytírání, čištění kuchyní, koupelen a sanitárních zařízení, leštění nábytku, utírání prachu i péče o
textilie a detaily. Každý úklid domácnosti Praha je přizpůsoben konkrétním potřebám klienta – respektujeme váš časový rozvrh, nároky i osobní preference.
Ohayno nabízí jak jednorázové úklidy
po rekonstrukcích, malování nebo stěhování, tak i pravidelné služby.
Pravidelný uklid bytu praha zajišťuje dlouhodobý pořádek a svěžest bez nutnosti vašeho zásahu.
Vy si jen zvolíte frekvenci – například jednou týdně, jednou za čtrnáct
dní nebo měsíčně – a o zbytek se postaráme my.
Profesionální úklid s Ohayno znamená komfort, jistotu a klid.
Každý náš úklid domů Praha i údržba bytu probíhá s důrazem na detail, diskrétnost a spolehlivost.
Úklid bez stresu a námahy – to je Ohayno, váš partner pro čistotu, pohodlí a harmonii ve vašem domově.
Maintaining the durability of glass food storage containers is key to guaranteeing their efficiency, safety and security, and look for years to come. From appropriate cleansing strategies to fix handling and storage, a couple of straightforward practices can aid protect against cracks, odors, or damage. Whether you’re utilizing high borosilicate glass containers, wholesale glass coffee cups with lids, or glass jar with bamboo lid wholesale, following best methods preserves their quality and function. Reputable brands like SLYPRC design glass items that stand the test of time, both in houses and commercial kitchens, https://ecuadorenventa.net/author/shieldbulb85/.
Wonderful post however I was wondering if you could
write a litte more on this topic? I’d be very grateful if you could elaborate a
little bit further. Thank you!
If you wish for to take much from this piece of writing then you have to apply
such techniques to your won weblog.
A fascinating discussion is worth comment. There’s no
doubt that that you ought to write more about this subject, it may
not be a taboo matter but generally folks don’t speak about such topics.
To the next! Kind regards!!
Hi my friend! I want to say that this article is amazing, nice written and come
with almost all vital infos. I’d like to look more posts like this .
Ta strona Najlepsze kasyna online w Polsce — wiarygodne źródło.
https://kasynoonline-blik.com.pl/platnosci
Can Macua An Autoridad, Nagsangat Sia Ni Reclamo Sa Ophiso Piscal Can Distrito Can United States.
We absolutely love your blog and find many of your post’s
to be exactly I’m looking for. Do you offer guest writers to write content available for you?
I wouldn’t mind publishing a post or elaborating on a few of the subjects you
write related to here. Again, awesome weblog!
Hmm it looks like your website ate my first comment (it was super long) so I guess I’ll just sum it up
what I wrote and say, I’m thoroughly enjoying your blog. I as well am an aspiring blog writer but I’m still new to the whole thing.
Do you have any recommendations for newbie blog writers? I’d genuinely
appreciate it.
You made some good points there. I checked on the web to learn more about the issue and found most people will go along with your views on this site.
Hi there! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but
I’m not seeing very good gains. If you know
of any please share. Kudos!
перейти на сайт https://kra46a.at/
Výběr správného poskytovatele úklidových služeb
je zásadní pro dlouhodobou spokojenost. Spolehlivá uklidova firma praha musí mít kvalifikovaný tým, interní systém
kontroly a jasně definované pracovní procesy. Kvalitní firma se
pozná podle transparentní komunikace, pojištění a otevřenosti vůči klientům.
Profesionální uklidova firma dokáže přizpůsobit služby individuálním potřebám – od pravidelného úklidu bytů po komplexní údržbu kancelářských budov.
Důležité je, aby společnost dodržovala sjednané termíny a kvalitu, což
zaručuje efektivní a bezproblémovou spolupráci.
Ohayno je příkladem stabilní úklidové firmy, která klade důraz
na pečlivost, spolehlivost a preciznost. Díky systematickému přístupu, moderním prostředkům a profesionálnímu personálu poskytuje jistotu, že každý úklid bude proveden včas a podle očekávání.
There is certainly a lot to know about this topic. I really like all the points you have made.
If you want to take much from this article then you have to apply these
methods to your won web site.
Also visit my page … ผงผักเคล ออร์แกนิค
For the reason that the admin of this web site is working, no question very shortly it will be renowned, due to
its quality contents.
Informative article, totally what I needed.
I was wondering if you ever thought of changing the layout
of your website? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one
or two pictures. Maybe you could space it out better?
Wow, that’s what I was looking for, what a information! existing
here at this web site, thanks admin of this web site.
Ou pa ta dwe klike sou lyen sa a nan okenn sikonstans paske se yon krim sou entènèt.
Hi! I’m at work surfing around your blog from my new apple iphone!
Just wanted to say I love reading your blog and look forward to all your posts!
Carry on the excellent work!
Daily Intent Hub – Guidance for setting goals and advancing with clarity and purpose.
I savor, cause I discovered just what I was looking for.
You have ended my four day lengthy hunt! God Bless you man. Have a nice day.
Bye
Your way of telling the whole thing in this post is truly nice,
every one can without difficulty be aware of it, Thanks a lot.
Southeast Finabcial Nashville
131 Bellle Forest Cir #210,
Nashville, TN37221, United Ꮪtates
18669008949
RV financing
Hello! Do you know if they make any plugins to help with Search Engine Optimization? I’m
trying to get my blog to rank for some targeted
keywords but I’m not seeing very good success.
If you know of any please share. Cheers!
UFA079 เว็บพนันออนไลน์ แทงบอล คาสิโน อันดับ 1
This blog was… how do you say it? Relevant!! Finally I’ve found
something that helped me. Thanks a lot!
Wow, that’s what I was looking for, what a data! present here at
this web site, thanks admin of this web site.
my web site the smiths
When some one searches for his vital thing,
therefore he/she desires to be available that in detail, therefore that thing is
maintained over here.
Also visit my web-site; Bookkeeping firm in Abu Dhabi
Hello! This is my first visit to your blog! We are a collection of volunteers and starting a new initiative in a community in the same niche.
Your blog provided us valuable information to work on. You have done a extraordinary job!
You ought to be a part of a contest for one of the highest
quality websites on the net. I most certainly will recommend this
website!
Hi there everyone, it’s my first go to see at
this web site, and piece of writing is really fruitful in support of
me, keep up posting these articles or reviews.
I know this site gives quality based articles or reviews and extra material,
is there any other web site which offers these kinds of information in quality?
I really like your blog.. very nice colors & theme. Did you make this website yourself or did you hire someone to do
it for you? Plz reply as I’m looking to design my own blog and would like to find
out where u got this from. thanks
Here is my site … plus size tummy tuck houston
Definitely believe that which you said. Your favorite reason appeared to be on the internet
the easiest thing to be aware of. I say to you, I certainly get irked while people think about worries that they just don’t know about.
You managed to hit the nail upon the top as well as
defined out the whole thing without having side effect ,
people could take a signal. Will likely be back to get more.
Thanks
Have a look at my page … Bookkeeping firm in Abu Dhabi
4M Dental Implaant Center San Diego
5643 Coplwy Ꭰr ste 210, San Diego,
СA 92111, United States
18582567711
best teeth whitening
What’s up, yeah this post is really pleasant and I have learned lot
of things from it regarding blogging. thanks.
Here is my website :: WES From Indian Universities
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added
I get four e-mails with the same comment. Is there any way you can remove people
from that service? Cheers!
my web site – mini tummy tuck houston
Hi! This is my 1st comment here so I just wanted to give a quick shout out and tell you I genuinely enjoy reading through your blog posts.
Can you recommend any other blogs/websites/forums that deal with the same topics?
Thanks!
Hey! I know this is kinda off topic but I was wondering which blog
platform are you using for this site? I’m getting sick and tired of
Wordpress because I’ve had problems with hackers and I’m looking at alternatives for another platform.
I would be awesome if you could point me in the direction of a good platform.
Can I simply just say what a relief to find someone who truly understands what they are
discussing online. You definitely understand how to bring a problem to light and make it important.
More people ought to read this and understand this side
of your story. I was surprised you aren’t more popular since you certainly possess the
gift.
Look into my site :: smiths
Great article. I will be dealing with a few of these
issues as well..
Here is my website online chat
Today, I went to the beachfront with my kids. I found a sea shell and
gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put
the shell to her ear and screamed. There was a hermit crab inside and it pinched her
ear. She never wants to go back! LoL I know this is
entirely off topic but I had to tell someone!
Hi, Neat post. There’s an issue together with your website in web explorer,
could test this? IE still is the market chief and a huge section of folks will leave
out your wonderful writing due to this problem.
Wygodna i prosta strona z wieloma przydatnych informacji o kasynach.
https://mostbet-registrace.cz/bonusy
Good article. I certainly love this website.
Keep it up!
Enjoy licensed, simple and secure financial trading platform with markets.com.
Trade CFD on Forex, Shares, Commodities, Indices, ETFs,
and more now!
Hey I am so grateful I found your weblog, I really found
you by mistake, while I was searching on Google for something
else, Regardless I am here now and would just like to say cheers for a marvelous
post and a all round enjoyable blog (I also love the theme/design), I don’t have time to read it all at the moment but I have saved it and also added your RSS feeds,
so when I have time I will be back to read much more, Please do keep up the awesome
b.
%ancor_text%
I have been surfing online more than three hours today, yet
I never found any interesting article like yours. It is
pretty worth enough for me. In my view, if all website owners and bloggers made good content as you did,
the internet will be much more useful than ever before.
Hey! This is kind of off topic but I need some guidance from an established blog.
Is it hard to set up your own blog? I’m not very techincal but I can figure things out
pretty fast. I’m thinking about setting up my own but I’m not sure where to begin. Do
you have any tips or suggestions? With thanks
Stop by my web page; VAT Consultancy in Abu Dhabi
I all the time emailed this webpage post page to all my associates,
as if like to read it after that my friends will too.
I was pretty pleased to discover this page. I want to to thank you for ones time for this particularly fantastic read!!
I definitely enjoyed every little bit of it and i also have you book-marked
to see new things in your web site.
Visit my site – the smiths
Hey! Would you mind if I share your blog with my zynga group?
There’s a lot of people that I think would really appreciate your content.
Please let me know. Thank you
Amazing! Its truly awesome piece of writing, I
have got much clear idea concerning from this
piece of writing.
Feel free to visit my web site – the smyths
It’s very straightforward to find out any topic on web as compared to books, as I
found this piece of writing at this site.
Take a look at my web-site … plus size tummy tuck houston
Hi, i believe that i noticed you visited my site so i came
to go back the choose?.I’m trying to to find things to enhance my website!I guess
its adequate to use a few of your ideas!!
This text is invaluable. Where can I find out more?
Hi, i think that i saw you visited my site thus i came to “return the favor”.I’m attempting to find things to improve my
website!I suppose its ok to use a few of your ideas!!
Howdy I am so delighted I found your weblog, I really found you by accident, while I was browsing
on Yahoo for something else, Anyways I am here now and would just like to say
thanks a lot for a incredible post and a all round entertaining
blog (I also love the theme/design), I don’t have time
to look over it all at the minute but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to
read a great deal more, Please do keep up the excellent
work.
Appreciating the dedication you put into your blog and detailed information you present.
It’s awesome to come across a blog every once in a while that isn’t
the same unwanted rehashed information. Great
read! I’ve saved your site and I’m adding your RSS feeds
to my Google account.
Also visit my web site :: tummy tuck cost houston
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar apuestas|15 euros
gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2 apuestas que significa|1×2 en apuestas|1×2
en apuestas que significa|1×2 que significa en apuestas|5 euros
gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades
de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android
apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas
deportivas android|aplicación de apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones
apuestas deportivas gratis|aplicaciones de apuestas android|aplicaciones de
apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones
de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones
de apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas
sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app android apuestas deportivas|app apuestas|app apuestas android|app apuestas de
futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app
apuestas deportivas colombia|app apuestas deportivas ecuador|app
apuestas deportivas españa|app apuestas deportivas gratis|app apuestas
entre amigos|app apuestas futbol|app apuestas gratis|app apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control
apuestas|app de apuestas|app de apuestas android|app de apuestas
casino|app de apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas
de futbol|app de apuestas deportivas|app de apuestas deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app
de apuestas deportivas en españa|app de apuestas deportivas peru|app
de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app
de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de
apuestas online|app de apuestas para android|app de apuestas para ganar dinero|app de
apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app
para apuestas deportivas|app para apuestas deportivas
en español|app para ganar apuestas deportivas|app para hacer apuestas|app para hacer apuestas
deportivas|app para hacer apuestas entre amigos|app
para llevar control de apuestas|app pronosticos apuestas
deportivas|app versus apuestas|apps apuestas mundial|apps
de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas deportivas
peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas
2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas
a ganar|apuestas a jugadores nba|apuestas a la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al
empate|apuestas al mundial|apuestas al tenis
wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del
mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas
apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas argentina francia
cuanto paga|apuestas argentina francia mundial|apuestas argentina gana el mundial|apuestas argentina
gana mundial|apuestas argentina holanda|apuestas argentina mexico|apuestas argentina
méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas argentina
vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas
argentina vs peru|apuestas argentinas|apuestas arsenal real
madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas
athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic
manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic
real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic sevilla|apuestas athletic valencia|apuestas atletico|apuestas atletico barcelona|apuestas atletico barsa|apuestas atletico campeon champions|apuestas atletico campeon de
liga|apuestas atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de madrid barcelona|apuestas atletico de
madrid gana la liga|apuestas atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas
atletico madrid|apuestas atletico madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto
acb|apuestas baloncesto handicap|apuestas baloncesto hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas baloncesto
pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real
madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas
barca vs psg|apuestas barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas
barcelona atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas
barcelona bayern|apuestas barcelona betis|apuestas
barcelona campeon de liga|apuestas barcelona celta|apuestas barcelona espanyol|apuestas
barcelona gana la champions|apuestas barcelona girona|apuestas barcelona granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas
barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas barcelona
real sociedad|apuestas barcelona sevilla|apuestas barcelona valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas
basket hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis real sociedad|apuestas
betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas
betis vs valencia|apuestas betplay hoy colombia|apuestas
betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia
vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de bienvenida sin deposito|apuestas bono gratis|apuestas bono sin deposito|apuestas bonos sin deposito|apuestas borussia real madrid|apuestas
boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo español|apuestas boxeo
femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas brasil colombia|apuestas
brasil peru|apuestas brasil uruguay|apuestas brasil vs colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas
caballos sanlucar de barrameda|apuestas caballos
zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas
campeón champions|apuestas campeon champions 2025|apuestas
campeon champions league|apuestas campeon conference league|apuestas campeon copa
america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la
champions|apuestas campeon de liga|apuestas campeon del mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas campeon liga bbva|apuestas campeon liga española|apuestas
campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial
baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas campeon roland garros|apuestas campeonato f1|apuestas campeonatos de futbol|apuestas carrera de
caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de
galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas carreras de caballos en directo|apuestas carreras
de caballos en vivo|apuestas carreras de caballos españa|apuestas
carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de caballos nocturnas|apuestas carreras
de caballos online|apuestas carreras de caballos sanlucar|apuestas carreras de caballos
sanlúcar|apuestas carreras de galgos|apuestas carreras de
galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas
casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas
casino online|apuestas casino online argentina|apuestas
casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta manchester|apuestas celta real
madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions
league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league
hoy|apuestas champions league pronosticos|apuestas champions league
pronósticos|apuestas champions pronosticos|apuestas
chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas
chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas chile vs uruguay|apuestas ciclismo|apuestas ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo
vuelta a españa|apuestas ciclismo vuelta españa|apuestas city
madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas
colombia|apuestas colombia argentina|apuestas colombia brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs brasil|apuestas combinadas|apuestas
combinadas como funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas combinadas foro|apuestas combinadas
futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas mundial|apuestas combinadas nba|apuestas combinadas para esta semana|apuestas
combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas seguras para mañana|apuestas como ganar|apuestas comparador|apuestas
con bono de bienvenida|apuestas con dinero ficticio|apuestas
con dinero real|apuestas con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de ganar|apuestas
con paypal|apuestas con tarjeta de credito|apuestas con tarjeta de debito|apuestas
consejos|apuestas copa|apuestas copa africa|apuestas copa america|apuestas copa américa|apuestas copa
argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del rey baloncesto|apuestas copa del rey final|apuestas copa
del rey futbol|apuestas copa del rey ganador|apuestas copa del
rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas
copa rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia
argentina|apuestas cuartos eurocopa|apuestas cuotas|apuestas
cuotas altas|apuestas cuotas bajas|apuestas
de 1 euro|apuestas de baloncesto|apuestas de baloncesto
hoy|apuestas de baloncesto nba|apuestas de baloncesto para hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack en linea|apuestas
de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas
de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras de caballos online|apuestas de casino|apuestas de casino
online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa
america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas
de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula
1|apuestas de futbol|apuestas de fútbol|apuestas de
futbol app|apuestas de futbol argentina|apuestas de
futbol colombia|apuestas de futbol en colombia|apuestas
de futbol en directo|apuestas de futbol en linea|apuestas de futbol en vivo|apuestas de futbol
español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol
para hoy|apuestas de fútbol para hoy|apuestas
de futbol para hoy seguras|apuestas de futbol para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas
de fútbol pronósticos|apuestas de futbol seguras|apuestas de
futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de
galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas de hockey|apuestas de hockey sobre hielo|apuestas
de hoy|apuestas de hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos online|apuestas
de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa league|apuestas de la liga|apuestas de la liga bbva|apuestas de la liga española|apuestas de la nba|apuestas de la
nfl|apuestas de la ufc|apuestas de mlb|apuestas de nba|apuestas de nba
para hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas
de peleas ufc|apuestas de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas de sistema
explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas
de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas
de ufc hoy|apuestas del boxeo|apuestas del clasico|apuestas
del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del dia de hoy|apuestas del dia
deportivas|apuestas del dia futbol|apuestas del mundial|apuestas del partido de hoy|apuestas del real madrid|apuestas
del rey|apuestas del sistema|apuestas deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas
deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas
1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas
apps|apuestas deportivas argentina|apuestas deportivas argentina
futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de
madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas
deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos de bienvenida|apuestas
deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas casino barcelona|apuestas deportivas casino online|apuestas deportivas
cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas
deportivas ciclismo|apuestas deportivas colombia|apuestas deportivas
com|apuestas deportivas com foro|apuestas deportivas com pronosticos|apuestas deportivas combinadas|apuestas deportivas combinadas
para hoy|apuestas deportivas como se juega|apuestas deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas
deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para ganar|apuestas deportivas copa america|apuestas deportivas copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa
mundial|apuestas deportivas corners|apuestas deportivas cual es la
mejor|apuestas deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas
deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas deportivas de peru|apuestas deportivas de tenis|apuestas deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas
deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas en peru|apuestas deportivas en perú|apuestas
deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas españa|apuestas
deportivas españolas|apuestas deportivas esports|apuestas deportivas
estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas faciles de
ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas
foro tenis|apuestas deportivas francia argentina|apuestas deportivas
futbol|apuestas deportivas fútbol|apuestas deportivas
futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar
dinero seguro|apuestas deportivas gane|apuestas deportivas golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas
deportivas handicap|apuestas deportivas handicap asiatico|apuestas
deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas
deportivas juegos olimpicos|apuestas deportivas la liga|apuestas
deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia
españa|apuestas deportivas liga española|apuestas deportivas listado|apuestas deportivas
listado clasico|apuestas deportivas madrid|apuestas deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores
casas|apuestas deportivas mejores cuotas|apuestas deportivas mejores paginas|apuestas deportivas mexico|apuestas deportivas méxico|apuestas deportivas mlb|apuestas deportivas
mlb hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas nba|apuestas deportivas
nba hoy|apuestas deportivas nfl|apuestas deportivas nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas
deportivas online argentina|apuestas deportivas online chile|apuestas deportivas online colombia|apuestas deportivas online en colombia|apuestas deportivas online españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas deportivas online peru|apuestas
deportivas online por internet|apuestas deportivas pago
paypal|apuestas deportivas para ganar dinero|apuestas deportivas para hoy|apuestas
deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas
partidos de hoy|apuestas deportivas paypal|apuestas deportivas peru|apuestas
deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas pronostico|apuestas
deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas que aceptan paypal|apuestas deportivas real madrid|apuestas deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas seguras|apuestas deportivas seguras foro|apuestas deportivas seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas
deportivas simulador eurocopa|apuestas deportivas sin deposito|apuestas deportivas sin deposito
inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas
deportivas sin registro|apuestas deportivas stake|apuestas deportivas stake 10|apuestas deportivas telegram españa|apuestas deportivas
tenis|apuestas deportivas tenis de mesa|apuestas deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas
deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas deportivas y casino|apuestas deportivas y casino online|apuestas
deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1
euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso
la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas
dinero|apuestas dinero ficticio|apuestas dinero real|apuestas dinero virtual|apuestas directas|apuestas directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas
dnb|apuestas doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas
dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador
vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas en barcelona|apuestas en beisbol|apuestas
en boxeo|apuestas en caballos|apuestas en carreras de
caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos deportivos virtuales|apuestas en golf|apuestas
en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas en la nfl|apuestas en las vegas mlb|apuestas
en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas
en linea deportivas|apuestas en linea españa|apuestas en linea estados unidos|apuestas en linea
futbol|apuestas en linea mexico|apuestas en línea méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas
en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis
en directo|apuestas en perú|apuestas en sevilla|apuestas en sistema|apuestas
en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas
en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas
en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa croacia|apuestas españa eurocopa|apuestas
españa francia|apuestas españa francia eurocopa|apuestas españa gana el
mundial|apuestas españa gana eurocopa|apuestas españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas
españa inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa
paises bajos|apuestas español|apuestas español oviedo|apuestas
espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas
esport|apuestas esports|apuestas esports colombia|apuestas esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports
lol|apuestas esports peru|apuestas esports valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro
copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas
eurocopa españa|apuestas eurocopa favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa sub 21|apuestas euroliga
baloncesto|apuestas euroliga pronosticos|apuestas europa league|apuestas europa league
hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas f1 bahrein|apuestas f1 canada|apuestas f1
china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas
faciles de ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas
final copa de europa|apuestas final copa del rey|apuestas final copa
europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de copa
del rey|apuestas final del mundial|apuestas final euro|apuestas final
eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas
final uefa europa league|apuestas final.mundial|apuestas finales de conferencia nfl|apuestas finales nba|apuestas fiorentina
betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia
españa|apuestas futbol|apuestas fútbol|apuestas futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol consejos|apuestas futbol en directo|apuestas fútbol en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol
eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol
gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol
mexico|apuestas futbol mundial|apuestas futbol online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol
pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas
gana colombia|apuestas gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas
ganador champions league|apuestas ganador copa america|apuestas ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas
ganador de la eurocopa|apuestas ganador de la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas
ganadores eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la
liga|apuestas girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas
goles asiaticos|apuestas golf|apuestas golf masters|apuestas golf pga|apuestas granada barcelona|apuestas grand slam
de tenis|apuestas gratis|apuestas gratis casino|apuestas
gratis con premios|apuestas gratis hoy|apuestas gratis
para hoy|apuestas gratis por registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas
gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y
ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas
handicap como funciona|apuestas handicap nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre
hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy
champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy
pronosticos|apuestas hoy seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas
juegos olímpicos|apuestas juegos olimpicos baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas kings
league americas|apuestas la liga|apuestas la liga española|apuestas la liga hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas
nba|apuestas las vegas nfl|apuestas league of legends mundial|apuestas
legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas legales españa|apuestas leganes betis|apuestas libertadores|apuestas licencia|apuestas liga 1 peru|apuestas
liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de
campeones de baloncesto|apuestas liga de campeones de hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid
barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid barsa|apuestas madrid bayern|apuestas
madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid gana liga|apuestas madrid hoy|apuestas
madrid liverpool|apuestas madrid osasuna|apuestas madrid sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas
madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester
athletic|apuestas manchester city real madrid|apuestas mas faciles
de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas
mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas
mlb hoy|apuestas mlb las vegas|apuestas mlb para hoy|apuestas
mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas mundial|apuestas mundial
2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas
mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas
mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial
favoritos|apuestas mundial femenino|apuestas mundial formula
1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial
sub 17|apuestas mundiales|apuestas mundialistas|apuestas
mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas nba gratis|apuestas nba hoy|apuestas
nba hoy jugadores|apuestas nba hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba
pronósticos|apuestas nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas
nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas
nfl semana 4|apuestas nfl super bowl|apuestas nhl|apuestas nhl pronosticos|apuestas
octavos eurocopa|apuestas ofertas|apuestas online|apuestas online argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas online
boxeo|apuestas online caballos|apuestas online carreras
de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online colombia|apuestas online comparativa|apuestas online con paypal|apuestas online de caballos|apuestas online deportivas|apuestas online
en argentina|apuestas online en peru|apuestas online espana|apuestas online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online
juegos|apuestas online mexico|apuestas online mma|apuestas
online movil|apuestas online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online
sin dinero|apuestas online sin registro|apuestas
online tenis|apuestas online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas over under|apuestas paginas|apuestas pago anticipado|apuestas
paises bajos ecuador|apuestas paises bajos inglaterra|apuestas países bajos qatar|apuestas
para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el dia de hoy|apuestas para el mundial|apuestas para
el partido de hoy|apuestas para eurocopa|apuestas para europa
league|apuestas para futbol|apuestas para ganar|apuestas
para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar
en la ruleta|apuestas para ganar la champions|apuestas
para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas para hacer|apuestas para hoy|apuestas para
hoy de futbol|apuestas para hoy europa league|apuestas para hoy futbol|apuestas para juegos|apuestas
para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la europa league|apuestas para la final de la
eurocopa|apuestas para la nba hoy|apuestas para los partidos de
hoy|apuestas para partidos de hoy|apuestas para ufc|apuestas partido|apuestas
partido aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido
mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas
partidos csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas
partidos de hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas paypal|apuestas peleas
de boxeo|apuestas peru|apuestas perú|apuestas peru brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas
plataforma|apuestas playoff|apuestas playoff ascenso|apuestas playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas
playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por internet
mexico|apuestas por internet para ganar dinero|apuestas por paypal|apuestas
por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas
pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos
futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas
pronosticos tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas
puntos por tarjetas|apuestas puntos tarjetas|apuestas que aceptan paypal|apuestas que
es handicap|apuestas que puedes hacer con tu
novia|apuestas que siempre ganaras|apuestas que significa|apuestas quien bajara
a segunda|apuestas quién bajara a segunda|apuestas quien gana el
mundial|apuestas quien gana eurocopa|apuestas quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara el mundial|apuestas quién ganará el mundial|apuestas quien ganara la champions|apuestas
quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo
barcelona|apuestas real madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid
atletico champions|apuestas real madrid atletico
de madrid|apuestas real madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real madrid
barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real madrid hoy|apuestas real madrid liverpool|apuestas real
madrid manchester city|apuestas real madrid osasuna|apuestas real madrid real
sociedad|apuestas real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs
atletico|apuestas real madrid vs atlético|apuestas real madrid
vs atletico madrid|apuestas real madrid vs barcelona|apuestas real madrid vs betis|apuestas real madrid vs sevilla|apuestas
real madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real
sociedad betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas
real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas
registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma
barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta
seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas
segunda división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas seguras
baloncesto|apuestas seguras calculadora|apuestas seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas
seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas
seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas
seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas seguras para hoy|apuestas seguras para
hoy fútbol|apuestas seguras para hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas
semifinales eurocopa|apuestas senegal paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas sevilla
atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas
sevilla inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester united|apuestas sevilla osasuna|apuestas sevilla real madrid|apuestas sevilla real sociedad|apuestas sevilla
roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas
simples o combinadas|apuestas sin deposito|apuestas sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas sin dinero real|apuestas sin empate|apuestas sin empate
que significa|apuestas sin ingreso minimo|apuestas sin registro|apuestas sistema|apuestas
sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas sociedad|apuestas sorteo copa
del rey|apuestas stake|apuestas stake 10|apuestas stake
10 hoy|apuestas super bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga
argentina|apuestas tarjeta roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis
atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas
tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis
itf|apuestas tenis pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera
division españa|apuestas tipos|apuestas tips|apuestas tipster|apuestas tipster
para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas ufc
como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas unionistas villarreal|apuestas uruguay|apuestas
uruguay colombia|apuestas uruguay corea|apuestas uruguay vs colombia|apuestas
us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia real madrid|apuestas valladolid barcelona|apuestas valladolid valencia|apuestas valor app|apuestas valor en directo|apuestas
valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas
villarreal betis|apuestas villarreal liverpool|apuestas villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta
a españa|apuestas vuelta españa|apuestas william hill partidos
de hoy|apuestas y casino|apuestas y casinos|apuestas y
juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos
deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina mexico apuestas|argentina
peru apuestas|argentina uruguay apuestas|argentina vs bolivia apuestas|argentina vs chile apuestas|argentina vs colombia apuestas|argentina vs francia apuestas|argentina vs.
colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos apuestas|athletic
barcelona apuestas|athletic manchester united apuestas|athletic osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico de madrid apuestas|atlético de madrid apuestas|atletico
de madrid real madrid apuestas|atletico de madrid vs barcelona
apuestas|atletico madrid real madrid apuestas|atletico madrid vs real madrid apuestas|atletico real madrid apuestas|atletico vs real madrid
apuestas|avisador de cuotas apuestas|bajada de cuotas apuestas|baloncesto apuestas|barbastro barcelona
apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca
madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid
apuestas|barca vs real madrid apuestas|barcelona – real
madrid apuestas|barcelona apuestas|barcelona atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona betis apuestas|barcelona casa de
apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia
apuestas|barcelona vs athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona
vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid
apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona
vs sevilla apuestas|barcelona vs villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis – chelsea apuestas|betis apuestas|betis barcelona
apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla
apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog
apuestas ciclismo|blog apuestas nba|blog apuestas tenis|blog de apuestas de
tenis|bono apuestas|bono apuestas deportivas|bono apuestas deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono
bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida
apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas sin depósito|bono bienvenida casa apuestas|bono bienvenida
casa de apuestas|bono bienvenida marca apuestas|bono casa apuestas|bono
casa de apuestas|bono casa de apuestas sin ingreso|bono
casas de apuestas|bono de apuestas|bono de apuestas gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas
deportivas|bono de bienvenida casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de registro apuestas deportivas|bono de registro casa de
apuestas|bono gratis apuestas|bono marca apuestas|bono por
registro apuestas|bono por registro apuestas deportivas|bono por registro casa de apuestas|bono registro apuestas|bono sin deposito apuestas|bono sin depósito
apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas deportivas|bono sin deposito casa de apuestas|bono sin deposito marca apuestas|bono
sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas colombia|bonos
apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas
sin deposito|bonos apuestas sin depósito|bonos bienvenida apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de apuestas|bonos casas apuestas|bonos
casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas
de apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos
casas de apuestas sin depósito|bonos de apuestas|bonos
de apuestas deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos de bienvenida apuestas|bonos de
bienvenida apuestas deportivas|bonos de bienvenida
casa de apuestas|bonos de bienvenida casas de apuestas|bonos de bienvenida de casas de apuestas|bonos de bienvenida en casas de apuestas|bonos de casas de apuestas|bonos de casas de
apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos
gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas de
apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador
de apuestas seguras|buscador de cuotas apuestas|buscador de cuotas de apuestas|buscar apuestas seguras|caballos apuestas|calculador de apuestas|calculador de
cuotas apuestas|calculadora apuestas|calculadora apuestas combinadas|calculadora apuestas de sistema|calculadora
apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora
arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora
de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de apuestas sistema|calculadora de apuestas surebets|calculadora
de arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora
para apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas
apuestas deportivas|calcular cuotas de apuestas|calcular
ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield
apuestas|calculo de apuestas|calculo de apuestas deportivas|cambio de cuotas
apuestas|campeon champions apuestas|campeon eurocopa apuestas|campeon liga apuestas|campeon nba apuestas|canales
de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de
galgos apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de
caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas
online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa
apuestas argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa
apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores
cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa
apuestas eurocopa|casa apuestas futbol|casa apuestas
mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa
apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas
valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de
apuestas argentina|casa de apuestas atletico de madrid|casa de apuestas baloncesto|casa de
apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de
apuestas bono de bienvenida|casa de apuestas bono gratis|casa de apuestas bono
por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de
apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa
de apuestas cerca de mí|casa de apuestas champions league|casa de
apuestas chile|casa de apuestas ciclismo|casa de
apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono
sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de
apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de
apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de
caballos|casa de apuestas de colombia|casa de apuestas de españa|casa de apuestas de
futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas deportivas cerca
de mi|casa de apuestas deportivas en argentina|casa de apuestas
deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas deportivas en españa|casa de
apuestas deportivas en madrid|casa de apuestas deportivas
españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa de
apuestas deposito 5 euros|casa de apuestas deposito
minimo|casa de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas
en españa|casa de apuestas en linea|casa de apuestas en madrid|casa de apuestas en perú|casa
de apuestas en vivo|casa de apuestas españa|casa de apuestas españa inglaterra|casa de
apuestas española|casa de apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa
league|casa de apuestas f1|casa de apuestas formula 1|casa
de apuestas futbol|casa de apuestas ingreso minimo|casa
de apuestas ingreso minimo 1 euro|casa de apuestas ingreso mínimo 1 euro|casa
de apuestas legales|casa de apuestas legales en colombia|casa de apuestas legales en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa de
apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de
apuestas nba|casa de apuestas nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial
real madrid|casa de apuestas online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa
de apuestas online paraguay|casa de apuestas online peru|casa de apuestas
online usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa
de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas perú|casa de apuestas peru online|casa de apuestas
por paypal|casa de apuestas promociones|casa de
apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas
regalo de bienvenida|casa de apuestas sevilla|casa de apuestas sin dinero|casa de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa de apuestas virtuales|casa
de apuestas vive la suerte|casa oficial de apuestas del real madrid|casas apuestas asiaticas|casas apuestas bono sin deposito|casas apuestas bonos sin deposito|casas apuestas
caballos|casas apuestas chile|casas apuestas ciclismo|casas
apuestas con licencia|casas apuestas con licencia en españa|casas apuestas
deportivas|casas apuestas deportivas colombia|casas apuestas
deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas
esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5 euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas
apuestas licencia españa|casas apuestas mexico|casas apuestas
mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas
nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas apuestas sin licencia|casas
apuestas tenis|casas asiaticas apuestas|casas de apuestas|casas
de apuestas 5 euros|casas de apuestas app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas
barcelona|casas de apuestas bono bienvenida|casas de apuestas
bono de bienvenida|casas de apuestas bono por registro|casas de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de
bienvenida|casas de apuestas bonos gratis|casas de apuestas
bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas
de apuestas carreras de caballos|casas de apuestas casino|casas
de apuestas casino online|casas de apuestas cerca de mi|casas
de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de
apuestas colombia|casas de apuestas com|casas de apuestas con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas
de apuestas con bono de bienvenida|casas de apuestas con bono
de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de apuestas con bonos
gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de apuestas con handicap asiatico|casas de apuestas
con licencia|casas de apuestas con licencia en españa|casas de apuestas con licencia
españa|casas de apuestas con licencia española|casas de
apuestas con mejores cuotas|casas de apuestas con pago anticipado|casas
de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta en vivo|casas de apuestas
copa del rey|casas de apuestas de caballos|casas de apuestas de españa|casas de apuestas de futbol|casas de apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas
de apuestas deportivas colombia|casas de apuestas deportivas comparativa|casas
de apuestas deportivas con paypal|casas de apuestas deportivas en chile|casas de apuestas deportivas en españa|casas
de apuestas deportivas en linea|casas de apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas
de apuestas deportivas en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas
deportivas españolas|casas de apuestas deportivas legales|casas de apuestas deportivas
madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de apuestas
deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de
apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de apuestas en chile|casas de
apuestas en colombia|casas de apuestas en españa|casas de apuestas en españa online|casas
de apuestas en linea|casas de apuestas en madrid|casas de apuestas en méxico|casas de apuestas en peru|casas de
apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos
de futbol|casas de apuestas españa|casas de apuestas españa alemania|casas de apuestas
españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas
de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas
de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas
europa league|casas de apuestas f1|casas de apuestas fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas
fuera de españa|casas de apuestas futbol|casas de apuestas fútbol|casas de apuestas
futbol españa|casas de apuestas ganador eurocopa|casas de apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso
minimo 1 euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter
barcelona|casas de apuestas legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas
de apuestas lista|casas de apuestas madrid|casas de apuestas mas seguras|casas de apuestas
mejores bonos|casas de apuestas mejores cuotas|casas de apuestas
mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de apuestas mlb|casas de apuestas mundial|casas de
apuestas mundial baloncesto|casas de apuestas
mundiales|casas de apuestas nba|casas de apuestas no reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas de apuestas nuevas en colombia|casas de
apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas
de apuestas online argentina|casas de apuestas online colombia|casas
de apuestas online deportivas|casas de apuestas online ecuador|casas de apuestas online en argentina|casas de apuestas
online en chile|casas de apuestas online en colombia|casas de apuestas
online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas
de apuestas online mas fiables|casas de apuestas online
mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas de apuestas
online usa|casas de apuestas online venezuela|casas de apuestas pago paypal|casas
de apuestas para ufc|casas de apuestas paypal|
WOW just what I was looking for. Came here by searching for best top tummy tuck surgeon houston tuck houston
Refresh Renovation Broomfield
11001 W 120th Ave 400 suite 459ɑ,
Broomfield, CO 80021, United States
+13032681372
In remodeling us builders home renovation the and
Thanks a bunch for sharing this with all of us you actually recognize what you’re talking about!
Bookmarked. Kindly additionally talk over with my
website =). We can have a link trade agreement among us
This website was… how do you say it? Relevant!!
Finally I have found something which helped me. Thanks!
Став представителем власти, Макуа подал жалобу в окружную прокуратуру Соединенных Штатов.
What’s up, I want to subscribe for this website to
obtain most up-to-date updates, so where can i do it please assist.
This page certainly has all the information I wanted concerning this subject and didn’t know who
to ask.
Hi there! This post could not be written any better!
Reading this post reminds me of my good old room mate!
He always kept talking about this. I will forward this post
to him. Pretty sure he will have a good read.
Thank you for sharing!
my homepage: online chat india
Great post. I was checking continuously this blog and I am impressed!
Very helpful info particularly the last part 🙂 I care for such
info much. I was looking for this certain info for a long time.
Thank you and best of luck.
Greetings I am so delighted I found your blog page, I really found you
by mistake, while I was browsing on Aol for something else,
Nonetheless I am here now and would just like to say many thanks for a incredible
post and a all round interesting blog (I also love the theme/design), I don’t have time to read through it all at the
moment but I have saved it and also added
in your RSS feeds, so when I have time I will be back to
read much more, Please do keep up the awesome job.
Its like you learn my thoughts! You seem to grasp a lot about this, like you wrote the e book in it or something.
I feel that you just can do with a few percent to drive the message
home a little bit, however instead of that, that is wonderful blog.
A great read. I’ll definitely be back.
Way cool! Some extremely valid points! I appreciate you writing
this post plus the smyths band
rest of the website is really good.
Спасибо за такой ценный контент. Обязательно порекомендую Pin Up Casino друзьям.
https://lnkz.at/Xu6ui
Hi my loved one! I want to say that this post is awesome,
nice written and include almost all india chat important infos.
I would like to see more posts like this .
An impressive share! I have just forwarded this onto a friend who had been doing a little
research on this. And he actually ordered me lunch because I
stumbled upon it for him… lol. So allow me to reword this….
Thank YOU for the meal!! But yeah, thanks for spending some time to talk about this
issue here on your web page.
We absolutely love your blog and find most
of your post’s to be what precisely I’m looking for. Does one offer
guest writers to write content to suit your needs?
I wouldn’t mind producing a post or elaborating on a few of the smyths tour new zealand subjects you write
about here. Again, awesome blog!
I’ve been exploring for a little for any high-quality articles or weblog posts on this sort of area .
Exploring in Yahoo I ultimately stumbled upon this site. Reading
this information So i’m glad to exhibit that I’ve a very excellent uncanny feeling
I discovered just what I needed. I so much indubitably will make certain to
don?t omit this web site and provides it a look on a continuing basis.
Excellent post. Keep posting such kind of info on your site.
Im really impressed by it.
Hey there, You’ve done an incredible job. I will certainly digg it and individually recommend to my friends.
I’m confident they will be benefited from this web site.
In fact when someone doesn’t know after that its up to other viewers that they will help, so here it happens.
I am really grateful to the owner of this
web site who has shared this impressive piece of writing at at this place.
Have you ever thought about writing an e-book or guest authoring on other blogs?
I have a blog based upon on the same topics you discuss and would
really like to have you share some stories/information. I know my audience
would value your work. If you’re even remotely interested, feel free to send me an email.
When someone writes an paragraph he/she maintains the plan of a user
in his/her brain that how a user can know it. Thus that’s why
this piece of writing is amazing. Thanks!
Když čistota znamená více než pořádek: proč Pražané sahají po profesionálním úklidu
Každá domácnost má okamžik, kdy běžné uklízení přestane stačit.
Stačí se podívat na odlesk oken, povrchy v kuchyni nebo na koupelnu,
která i přes snahu nepůsobí tak svěže jako dřív.
Mnoho lidí v Praze v posledních letech zjistilo, že právě tady pomáhá profesionální generalni
uklid bytu — služba, která vrací prostorům čistotu do hloubky
a zároveň šetří čas.
V moderních interiérech se nečistoty usazují nenápadně.
Prach na horních policích, mastné mapy na kuchyňské lince nebo zbytky
vodního kamene tvoří soubor detailů, které ovlivňují celkovou atmosféru domova.
Profesionální úklidový tým pracuje jinak než běžná
domácnost: systematicky, s vhodnými prostředky a s důrazem na místa, která člověk v každodenním tempu přehlíží.
To je důvod, proč po hlubokém úklidu lidé popisují, že
byt působí světleji, otevřeněji a příjemněji.
Služba uklid bytu praha proto přestala být jednorázovou
výpomocí a stává se běžným způsobem, jak si udržet kvalitní a zdravé prostředí.
Firmy jako OHAYNO.cz přinášejí přístup, díky němuž
se domov během několika hodin promění do podoby, které
by domácí úklid dosahoval jen velmi obtížně.
Generální úklid tak dnes není jen o čistotě. Je to také o pohodlí,
lepší energii v prostoru a pocitu, že domov znovu dýchá.
A právě proto si tuto službu oblíbilo tolik pražských domácností.
Неy I knoѡ this is off topic but І was wondering
if you knew of any widgets I coᥙld add to my blog that automaticɑlly tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite ѕ᧐me time and was hoping maybe you wοuld hɑve some еxperience with something likе this.
Pⅼease let me know if ʏou run into anything.
I truly enjoy reading your blog and I ⅼoߋk forward to your new updates.
My web paɡe soulmate
For latest news you have to pay a visit internet and on world-wide-web I found this web page as a best web
page for newest updates.
It’s difficult to find experienced people on this topic, however, you
sound like you know what you’re talking about!
Thanks
Review my blog post; WES From Kerala Universities
4M Dental Implant Center
3918 Ꮮong Beach Blvd #200, Long Beach,
CA 90807, United Ꮪtates
15622422075
experienced dentist
Enjoy licensed, simple and secure financial trading platform
with markets.com. Trade CFD on Forex, Shares, Commodities, Indices, ETFs, and more now!
Awesome post.
Hi there colleagues, its fantastic article regarding tutoringand
completely defined, keep it up all the time.
Great site. Plenty of useful info here. I am sending it to some friends ans additionally sharing in delicious.
And obviously, thank you in your effort!
Having read this I thought it was extremely informative. I appreciate you taking the time
and energy to put this informative article together.
I once again find myself personally spending a lot of time both reading
and leaving comments. But so what, it was still worth it!
Also visit my web site; https://betseremos.com/blog/makhachev-vs-della-maddalena-ufc-322/
you are truly a excellent webmaster. The website loading speed is incredible.
It sort of feels that you are doing any distinctive trick. Also, The contents are masterpiece.
you’ve done a excellent task on this matter!
Mangelsen
7916 Girard Avenue, ᒪa Joya
CА 92037, United Stаtеѕ
1 800-228-9686
Bookmarks – https://www.protopage.com/ormodajojp,
Great post. I am facing some of these issues as well..
Good way of describing, and good article to
obtain facts regarding my presentation focus, which i am going to present in college.
Remarkable issues here. I am very happy to look your post.
Thank you a lot and I’m looking forward to touch
you. Will you kindly drop me a mail?
Good day! This is my first comment here so I just wanted to give a quick
shout out and tell you I truly enjoy reading your articles.
Can you suggest any other blogs/websites/forums that cover
the same subjects? Thanks a ton!
Pretty! This has been an extremely wonderful article.
Thank you for providing this information.
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, United Ⴝtates
+19803517882
5 step renovation method proven
Wow, marvelous blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your web site
is excellent, as well as the content!
It’s remarkable for me to have a site, which is valuable in support of my experience.
thanks admin
Artikel ini benar-benar memberi wawasan baru.
Penjelasan mengenai KUBET sebagai Situs Judi Bola Terlengkap ditulis dengan sangat jelas, membuat pembaca dengan cepat
memahami keunggulannya.
Bagian tentang kriteria sebuah platform hingga layak disebut Situs Parlay Resmi juga memberikan nilai tambah
besar.
Penulis mampu menjelaskan poin kompleks dengan sederhana.
Ini merupakan informasi yang sering dicari banyak orang.
Pembahasan mengenai bagaimana sebuah situs dapat dikategorikan sebagai Situs Parlay Gacor juga cukup mendalam.
Materinya disampaikan secara runtut.
Bagian ini menjadi salah satu poin kuat dalam artikel.
Selain itu, saya juga menyukai bagian yang membahas fitur menarik pada
Situs Mix Parlay dan permainan seperti toto macau.
Cara penulis menampilkan informasinya sangat rapi.
Hal ini membuat artikel terasa jauh lebih komprehensif.
Secara keseluruhan, artikel ini sangat cocok untuk pembaca yang
ingin memahami lebih banyak mengenai kubet login, Situs Judi Bola, dan dunia situs parlay secara luas.
Saya pribadi menantikan artikel berkualitas tinggi lainnya dari penulis.
Hello, constantly i used to check weblog posts here early in the morning,
for the reason that i like to gain knowledge of more and more.
Хотите получить медицинскую справку в день обращения в столице — оперативно и без визитов в поликлинику? На https://akkred-med.ru можно получить медицинские документы, от 095/у, справки 027/у до решений КЭК, документов для плавания, спорта и виз. Заполнение заявки занимает считанные минуты, потом — курьерская доставка. Всё официально, анонимно и без задержек. Все детали на сайте — медсправка быстро, оформление онлайн, получение с курьером.
Hmm it looks like your website ate my first comment (it was super long) so I guess I’ll just sum
it up what I wrote and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog writer but I’m still new to the whole thing.
Do you have any points for rookie blog writers? I’d genuinely appreciate it.
Here is my web blog – Soft LED Screen
Hey there! This post couldn’t be written any better!
Reading through this post reminds me of my good old room mate!
He always kept chatting about this. I will forward this article to him.
Fairly certain he will have a good read.
Many thanks for sharing!
Somebody essentially assist to make critically posts I’d state.
This is the very first time I frequented your web page and up to now?
I surprised with the analysis you made to make this particular put up extraordinary.
Great job!
Artikel ini benar-benar menarik.
Pembahasan mengenai KUBET sebagai Situs Judi Bola Terlengkap ditulis dengan rinci,
sehingga pembaca bisa memahami keunggulan platform tersebut
dengan mudah.
Penjelasan mengenai bagaimana sebuah platform
mendapatkan predikat sebagai Situs Parlay Resmi juga sangat
informatif.
Penulis berhasil menyampaikan informasi yang sulit menjadi
mudah dipahami.
Ini termasuk pembahasan yang jarang ditemukan tetapi sangat dibutuhkan.
Topik mengenai performa yang menjadikan platform tertentu sebagai Situs
Parlay Gacor juga mendapat perhatian besar.
Penjelasannya cukup lengkap.
Informasi seperti ini sangat bermanfaat bagi siapa pun yang ingin memilih layanan terbaik.
Saya juga menyukai bagian yang membahas fitur permainan seperti di Situs
Mix Parlay serta permainan populer lainnya seperti toto macau.
Konten ini mampu memperluas wawasan pembaca secara signifikan.
Kedua topik tersebut membuat artikel terasa jauh lebih lengkap dan variatif.
Secara keseluruhan, artikel ini sangat bermanfaat terutama
bagi pembaca yang ingin memahami dunia Situs Judi Bola, kubet
login, dan situs parlay secara lebih mendalam.
Saya berharap akan ada lebih banyak artikel sejenis yang membahas topik dengan kualitas setinggi ini.
Pretty! This has Ƅеen an extremely wonderful
article. Ƭhanks for providing this info.
Here is my web-site; Top đồng hồ nữ dưới 2 triệu
I enjoy what you guys are usually up too. Such clever work
and coverage! Keep up the awesome works guys I’ve incorporated
you guys to blogroll.
Для собственников машин в Рыбинске — автосервис “АвтоАйболит” оказывает проверку, сервисное обслуживание, обслуживание двигателя, коробки передач, шасси и электрооборудования (с услугой ремонт генератора от 800 ?) на профессиональном оборудовании. https://avtoaibolit-76.ru Профессиональные автомастера применяют фирменные запчасти и обеспечивают надёжный сервис с гарантией. Ознакомьтесь с деталями — автосервис Рыбинск предлагается на ресурсе.
Thanks for sharing your thoughts. I really appreciate your efforts and I
will be waiting for your next post thanks once
again.
4M Dental Implant Center
3918 Long Beach Blvd #200, ᒪong Beach,
CA 90807, Unitedd Stɑtes
15622422075
cosmetic smile design
Fashion Finds Hub – Explore unique and stylish items curated for modern tastes.
Узнайте основные факты об сайте Авто-Фокус — широкий ассортимент автозапчастей, допов и комплектующих для любых машин! Посетите https://avto-fokus.ru и узнайте каталог запчастей. Нужна безопасность автомобиля или модернизация мультимедиа? — площадка предлагает сигналки, мультимедиа электронику и детали интерьера. Ищете надёжные запчасти — здесь найдёте проверенные марки и доставку по РФ.
Узнайте всю информацию об AvtoGruzGroup — экспертные мнения, лайфхаки и новинки рынка! Посетите https://avtogruzgroup.ru и прочитайте рецензии на устройства. Нужна проверенная инфа — этот сайт обеспечивает обзоры, технические данные и настоящие отзывы. Подыскиваешь устройство — здесь найдёшь лучшие модели и надёжные рекомендации.
Perkenalkan diri saya sedikit.
Nama saya Stormy Marsh, seseorang yang menyukai dunia digital.
Saya banyak menghabiskan waktu mempelajari sistem dan fitur
dari berbagai platform, termasuk KUBET yang dikenal sebagai
Situs Judi Bola Terlengkap dengan akses kubet login yang
praktis.
Ketertarikan saya juga meluas ke analisis mendalam mengenai bagaimana sebuah layanan dapat memenuhi standar sebagai Situs Parlay Resmi.
Saya memahami pentingnya teknologi pendukung untuk
membangun sebuah platform yang dapat dipercaya,
mulai dari keamanan data, kelancaran server hingga kualitas layanan pelanggan.
Semua itu memberi saya pemahaman luas tentang mekanisme
operasional sebuah Situs Judi Bola di era digital saat
ini.
Selain itu, saya sering menganalisis bagaimana platform dapat
menjadi Situs Parlay Gacor melalui kombinasi algoritma internal, data statistik,
dan penyempurnaan fitur.
Saya juga mempelajari sistem Mix Parlay yang lebih kompleks.
Di waktu senggang, saya terkadang mengikuti hasil toto macau hanya sekadar untuk
melihat bagaimana data dan peluang bekerja dalam dunia angka.
Dengan pengalaman ini, saya berharap terus dapat
memahami bagaimana situs parlay berkembang dan bagaimana teknologi di baliknya dapat menciptakan pengalaman yang lebih baik bagi pengguna.
Perkembangan sistem digital sangat menarik diikuti demi memahami
ekosistem digital secara lebih mendalam.
You actually make it appear really easy together with your presentation however I find this matter to be really one thing that I
believe I’d by no means understand. It kind of feels too complicated
and very vast for me. I am looking forward to your subsequent put up, I will try to get the hold of it!
Узнайте всё о дилере Автомикс — официальном дилере Honda, гарантийное обслуживание, ремонт кузова и оригинальные запчасти! Перейдите на https://avtomiks-smolensk.ru/ и узнайте версии авто. Хотите уверенность и надёжность — фирма предлагает тест-драйв, фирменное обслуживание, оригинальные аксессуары, а также техническое обслуживание, помощь после покупки и прозрачные цены. Нужен надёжный автомобиль — здесь найдёте лучшие варианты и безупречное качество услуг.
Планируете купить качественную машину б/у на лучших условиях? В автосалоне https://avtosteklavoronezh.ru есть широкий ассортимент авто — от авто отечественных марок до иностранных машин. Есть услуги трейд-ина, срочного выкупа и получения кредита на выгодных условиях. Каждая машина тщательно проверяется и готова к эксплуатации без лишних вложений. Всё быстро, удобно и официально. Подробнее на сайте — подержанные авто, выкуп авто, автокредит Москва.
10 euros offert paris sportif|10 euros offert sans
dépôt paris sportif|10 meilleurs sites de paris sportifs|100 euro offert
paris sportif|100 euros offert paris sportif|100 euros remboursé paris sportifs|100 offert pari
sportif|100 offert paris sportif|100 remboursé paris
sportif|100e offert pari sportif|abandon paris sportif tennis|abandon tennis paris sportif|addiction paris sportif forum|age paris sportif belgique|aide au
pari sportif|aide au paris sportif|aide aux paris sportif|aide aux paris sportifs|aide pari sportif|aide pari
sportif football|aide parie sportif|aide paris sportif|aide paris sportif foot|aide
paris sportif gratuit|aide paris sportifs|aide pour paris sportif|algorithme de paris sportif|algorithme excel paris sportif|algorithme gratuit paris sportif|algorithme pari sportif|algorithme paris sportif|algorithme paris sportif avis|algorithme
paris sportif basket|algorithme paris sportif excel|algorithme paris
sportif gratuit|algorithme paris sportif tennis|algorithme paris
sportifs|algorithme pour paris sportif|analyse cote paris sportif|analyse de
paris sportif|analyse match paris sportif|analyse pari sportif|analyse paris sportif|analyse paris sportif foot|analyse paris sportif football|analyse paris
sportif gratuit|analyse paris sportifs|ancienne cote paris sportif|api cote paris
sportif|app paris sportif sans argent|appli de paris sportif|appli
de paris sportif sans argent|appli de paris sportifs|appli pari sportif|appli pari sportif gratuit|appli parie sportif|appli paris sportif|appli paris sportif avec paypal|appli paris sportif belgique|appli paris
sportif entre amis|appli paris sportif gratuit|appli paris sportif sans argent|appli paris
sportif suisse|appli paris sportifs|application aide paris sportif|application algorithme paris sportif|application analyse paris sportif|application android
paris sportif|application bankroll paris sportif|application conseil paris sportif|application de pari sportif|application de parie sportif|application de paris sportif|application de
paris sportif en afrique|application de paris sportif en cote
d’ivoire|application de paris sportif en ligne|application de paris sportif gratuit|application de paris sportif international|application de paris sportif suisse|application de paris sportifs|application faux paris sportifs|application gestion bankroll paris sportif|application gestion paris sportif|application ia paris sportif|application pari sportif gratuit|application paris sportif|application paris sportif android|application paris sportif argent fictif|application paris
sportif belgique|application paris sportif canada|application paris sportif
espagne|application paris sportif espagnol|application paris sportif fictif|application paris sportif france|application paris sportif gratuit|application paris sportif gratuit entre amis|application paris
sportif maroc|application paris sportif offre de bienvenue|application paris sportif paypal|application paris sportif sans argent|application paris sportif
sans justificatif de domicile|application paris sportif suisse|application paris sportif usa|application paris sportif virtuel|application pour faire des paris sportifs|application pour gerer ses paris sportif|application pour les paris sportifs|application pour pari sportif|application pour paris sportif|application pour paris sportifs|application statistique paris sportif|application suivi
paris sportif|applications de paris sportifs|applications paris sportifs|applis paris sportif|applis paris sportifs|apprendre a
faire des paris sportifs|argent facile paris sportif|argent offert
paris sportifs|argent offert sans depot paris sportif|argent paris
sportif|argent paris sportifs|argent paris sportifs impots|argent sans depot
paris sportif|arjel paris sportif|arjel paris sportifs|astuce gagner paris sportif|astuce pari sportif|astuce paris sportif|astuce paris sportif basket|astuce paris sportif foot|astuce paris sportif forum|astuce paris sportif tennis|astuce paris sportifs|astuce pour gagner au pari sportif|astuce pour gagner au paris sportif|astuce pour gagner paris sportif|astuce pour paris sportif|astuces paris
sportifs|astuces paris sportifs en ligne|astuces paris sportifs foot|astuces pour gagner aux paris sportifs|autorisation paris
sportif france|avis pari sportif|avis paris sportif|avis paris sportif foot|avis site de paris sportif|avis
site paris sportif|avis sur les paris sportifs|avis sur paris
sportif|avis tipster paris sportif|aweh signification paris sportif|bankroll 100
euros paris sportifs|bankroll management paris sportif|bankroll
paris sportif|bankroll paris sportif excel|bankroll paris sportif
gratuit|bankroll paris sportifs|basket paris sportif|belgique france paris sportif|belgique paris sportifs|bonus bienvenue paris sportif|bonus bienvenue
paris sportifs|bonus cash paris sportif|bonus de bienvenue
paris sportif|bonus de bienvenue paris sportif belgique|bonus de bienvenue sans depot paris sportif|bonus de depot
paris sportif|bonus de paris sportifs|bonus depot paris
sportif|bonus en cash paris sportif|bonus
gratuit paris sportif|bonus gratuit sans depot paris
sportif|bonus pari sportif|bonus paris sportif|bonus paris sportif belgique|bonus
paris sportif betclic|bonus paris sportif cash|bonus paris sportif en ligne|bonus paris sportif france pari|bonus paris sportif
retirable|bonus paris sportif sans depot|bonus paris sportif sans dépôt|bonus paris
sportif unibet|bonus paris sportifs|bonus sans depot paris sportif|bonus sans depot paris
sportif belgique|bonus sans dépôt paris sportif|bonus sans dépôt paris sportif hors arjel|bonus site de paris sportif|bonus site pari sportif|bonus site
paris sportif|bonus sites de paris sportifs|bonus
unibet paris sportif|bookmaker paris sportif|bookmaker paris sportif gratuit|bookmaker paris
sportifs|bookmaker sportif|bookmakers paris sportif|bookmakers paris sportifs|bookmakers paris
sportifs en ligne|but contre son camp paris sportif|but sur penalty paris sportif|buteur paris sportif|c’est quoi handicap paris sportif|c’est quoi une cote paris sportif|calcul anti perte paris sportif|calcul combinaison pari sportif|calcul cote pari sportif|calcul cote paris
sportif|calcul couverture paris sportif|calcul de cote paris sportif|calcul des cotes paris sportifs|calcul dnb
paris sportifs|calcul double chance paris
sportif|calcul gain paris sportif|calcul mise paris sportif|calcul pari sportif|calcul paris sportif|calcul paris sportif multiple|calcul pourcentage cote paris
sportif|calcul probabilité paris sportif|calcul rentabilité paris sportifs|calcul
roi paris sportif|calcul systeme paris sportif|calcul trj paris sportifs|calculateur cote paris sportif|calculateur de cote paris sportif|calculateur de mise
paris sportif|calculateur de paris sportif|calculateur
paris sportif|calculatrice arbitrage paris sportif|calculatrice
paris sportif|calculer cote paris sportif|calculer gain paris sportif|calculer probabilité
paris sportifs|calculer roi paris sportifs|calculer une cote pari sportif|calculer une
cote paris sportif|carte cadeau paris sportif|carte pcs paris sportif|carte
prépayée paris sportifs|cash out pari sportif|cash out paris sportif|cash out paris sportifs|casino en ligne paris sportif|casino paris sportif en ligne|champions
league paris sportif|chute de cote paris sportif|classement des meilleurs sites de
paris sportifs|classement meilleur site de paris sportif|code barre paris sportif|code bonus
paris sportif|code paris sportif|code promo pari sportif|code promo
paris sportif|code promo paris sportif sans depot|code promo paris sportif
sans dépôt|code promo sans depot paris sportif|code promo
site paris sportif|combien de temps pour
encaisser un paris sportif|combien de temps pour retirer un paris sportif|combien miser paris sportifs|combine
paris sportif|combines paris sportifs|combiné pari sportif|combiné paris sportif|combiné paris sportif conseil|combiné paris sportif du jour|combiné paris sportif
pronostic|comment analyser un paris sportif|comment arreter de jouer aux
paris sportifs|comment arreter les paris sportif|comment arreter les paris sportifs|comment arrêter les paris sportifs|comment bien gagner au
paris sportif|comment bien jouer au paris sportif|comment
bien miser paris sportif|comment ca marche les paris sportif|comment calculer cote paris sportif|comment calculer gain paris sportif|comment calculer les cotes des paris sportifs|comment calculer une cote
de paris sportif|comment calculer une cote pari sportif|comment calculer une cote paris sportif|comment comprendre les paris
sportifs|comment creer un vip paris sportif|comment créer un algorithme paris sportif|comment créer un site de
paris sportif|comment devenir riche avec les paris sportifs|comment etre rentable paris sportif|comment etre sur de gagner au paris
sportif|comment faire de bon paris sportif|comment faire des parie sportif|comment
faire des paris sportif|comment faire des paris sportif gagnant|comment faire des paris sportifs|comment faire pari
sportif|comment faire paris sportif|comment faire pour arreter les paris
sportifs|comment faire pour gagner au paris sportif|comment faire pour gagner les
paris sportifs|comment faire un bon pari sportif|comment faire un bon paris sportif|comment faire un pari sportif|comment faire un parie sportif|comment faire un paris sportif|comment faire une montante paris sportif|comment fonctionne les cotes dans les paris sportifs|comment fonctionne
les cotes des paris sportifs|comment fonctionne les paris sportifs|comment fonctionne
paris sportifs|comment fonctionne un pari sportif|comment fonctionnent les cotes dans les paris sportifs|comment fonctionnent les cotes dans les paris
sportifs grand oral|comment fonctionnent les cotes de paris sportif|comment fonctionnent les paris sportifs|comment fonctionnent les paris sportifs grand oral|comment fonctionnent les paris sportifs grand oral maths|comment fonctionnent les paris sportifs maths|comment gagner a coup sur
au paris sportif|comment gagner a tous les coups au paris sportif|comment gagner a tout les coup au paris sportif|comment gagner au pari sportif|comment
gagner au pari sportif football|comment gagner au paris sportif|comment gagner
au paris sportif a coup sur|comment gagner au paris sportif foot|comment gagner au paris sportif forum|comment gagner au paris sportif tennis|comment gagner au
paris sportifs|comment gagner aux paris sportif|comment gagner
aux paris sportifs|comment gagner aux paris sportifs foot|comment gagner aux paris sportifs livre|comment gagner aux paris sportifs sur le long terme|comment gagner avec les paris sportifs|comment gagner dans les paris sportifs|comment gagner de l argent avec les paris sportifs|comment gagner de l’argent au paris sportif|comment gagner de l’argent aux paris sportifs|comment gagner de l’argent avec les paris sportifs|comment gagner
de l’argent paris sportif|comment gagner de l’argent sur les paris sportifs|comment gagner de l’argent sur paris sportif|comment gagner des
paris sportif|comment gagner des paris sportifs|comment gagner
en paris sportif|comment gagner facilement au paris sportif|comment gagner les paris
sportifs|comment gagner paris sportif|comment gagner paris
sportif foot|comment gagner paris sportifs|comment gagner sa vie avec les paris sportifs|comment gagner ses paris
sportif|comment gagner sur les paris sportif|comment gagner sur les paris sportifs|comment gagner tout le temps au paris sportif|comment gagner
un pari sportif|comment gagner un paris sportif|comment gerer
une bankroll paris sportif|comment gérer sa
bankroll paris sportif|comment jouer au pari sportif|comment jouer au paris sportif|comment jouer au paris sportif foot|comment jouer
aux paris sportifs|comment jouer paris sportif|comment marche cote paris
sportif|comment marche les cotes paris sportif|comment marche les paris
sportif|comment marche les paris sportifs|comment marche paris
sportif|comment marche un pari sportif|comment marche un paris
sportif|comment marchent les cotes paris sportif|comment marchent les paris sportifs|comment
miser au paris sportif|comment miser paris sportif|comment monter sa
bankroll paris sportif|comment ne jamais perdre au paris
sportif|comment parier sportif|comment reussir au paris sportif|comment reussir les paris sportif|comment reussir
paris sportif|comment sont calculer les cotes de paris sportif|comment
sont calculées les cotes des paris sportifs|comment sont calculés les cotes des paris sportifs|comment sont faites les
cotes des paris sportifs|comment toujours gagner au paris sportif|comment ça marche les paris sportifs|comparaison bonus paris sportifs|comparaison cote
pari sportif|comparaison des cotes paris sportifs|comparateur cote pari sportif|comparateur cote paris sportif|comparateur cotes paris sportif|comparateur cotes paris sportifs|comparateur de cote pari sportif|comparateur de cote paris sportif|comparateur de cotes paris sportifs|comparateur de côtes paris sportifs|comparateur
de paris sportif|comparateur de site de paris sportif|comparateur de site
paris sportif|comparateur de sites de paris sportifs|comparateur
pari sportif|comparateur paris sportif|comparateur paris sportifs|comparateur site
de paris sportif|comparateur site pari sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif bonus paris sportifs|comparatif
cote pari sportif|comparatif cote paris sportif|comparatif cotes paris
sportifs|comparatif des sites de paris sportifs|comparatif offre de bienvenue paris
sportif|comparatif offre paris sportif|comparatif pari
sportif|comparatif pari sportif en ligne|comparatif paris
sportif|comparatif paris sportif bonus|comparatif paris sportif en ligne|comparatif paris sportifs|comparatif paris sportifs en ligne|comparatif site de paris
sportif|comparatif site paris sportif|comparatif site
paris sportifs|comparatif sites de paris sportifs|comparatif sites paris
sportifs|comparer les cotes paris sportifs|comprendre
cote paris sportif|comprendre handicap paris sportif|comprendre les cotes des paris sportifs|comprendre les cotes paris sportif|comprendre les cotes
paris sportifs|comprendre les handicap paris sportif|compte de paris sportif|compte démo
paris sportif|compte finance paris sportif|compte financer paris
sportif|compte financier paris sportif|compte financé paris sportif|compte pari
sportif|compte paris sportif|compte paris sportif financé|conseil de paris sportif|conseil de paris
sportifs|conseil en paris sportif|conseil en paris sportifs|conseil pari sportif|conseil pari sportif gratuit|conseil paris sportif|conseil paris sportif aujourd’hui|conseil paris sportif du jour|conseil
paris sportif foot|conseil paris sportif gratuit|conseil paris sportif ligue des champions|conseil paris
sportif nba|conseil paris sportif pronostic|conseil paris sportif rmc|conseil paris sportif tennis|conseil paris sportifs|conseil
pour gagner au paris sportif|conseil pour paris sportif|conseil sur
les paris sportifs|conseille paris sportif|conseiller en paris sportifs|conseiller paris
sportif|conseils de paris sportifs|conseils en paris sportifs|conseils paris sportifs|conseils paris sportifs foot|conseils paris sportifs gratuit|conseils
paris sportifs tennis|conseils pour paris sportifs|cote a 100 paris sportif|cote a 2 paris sportif|cote
anglaise paris sportif|cote de 2 paris sportif|cote de pari sportif|cote de paris sportif|cote des paris
sportifs|cote maximum paris sportif|cote minimum paris
sportif|cote pari sportif|cote pari sportif comment ça
marche|cote pari sportif real madrid|cote pari sportif rugby|cote parie sportif|cote paris sportif|cote paris sportif belgique|cote paris sportif calcul|cote paris
sportif definition|cote paris sportif euro|cote paris sportif explication|cote paris sportif foot|cote paris sportif france belgique|cote paris
sportif france espagne|cote paris sportif ligue des champions|cote paris sportif moto gp|cote paris sportif psg|cote paris
sportif psg arsenal|cote paris sportif rugby|cote paris sportif tennis|cote paris sportifs|cote pour
paris sportifs|cote sportif foot|cote sportif rugby|cote à 1000 paris sportif|cotes de paris sportifs|cotes pari sportif|cotes paris sportif|cotes
paris sportifs|cotes paris sportifs foot|coupe de france
paris sportif|créer un algorithme paris sportif|créer un compte paris sportif|créer un site
de paris sportif en ligne|dans les paris sportifs que signifie handicap|declarer ses gains paris sportif|definition cash out paris sportif|definition cote paris sportif|definition handicap paris
sportif|depot 5 euros paris sportif|depot double paris sportif|depot minimum 5 euro paris sportif|depot minimum paris
sportif|depot paris sportif|depuis quand existe les paris sportif en france|devenir riche avec les paris sportifs|devenir
riche avec paris sportifs|disqualification tennis paris sportif|dnb en paris sportif|dnb pari sportif|dnb paris sportif|dnb paris sportif definition|dnb paris sportifs|doit on declarer les gains de paris sportif|déclarer
gains paris sportifs|déclarer gains paris sportifs hors arjel|définition bankroll paris sportif|dépôt
minimum 1 euro paris sportif|dépôt minimum 5
euro paris sportif|ecart de jeux tennis paris sportif|erreur de cote paris sportif|est ce que les
gains des paris sportifs sont imposables|est-ce que les prolongation compte
dans un pari sportif|etre sur de gagner au paris sportif|euro
paris sportif|evenement sportif a paris|evenement sportif paris|evenement sportif paris 2025|evenement sportif paris aujourd hui|evenement sportif paris aujourd’hui|evenement sportif
paris ce week end|evenements sportif paris|evenements sportifs paris|evenements sportifs paris 2025|evenements sportifs à paris|evolution cote paris sportif|evolution cotes paris sportifs|evolution des cotes paris sportifs|explication cote pari sportif|explication cote paris
sportif|explication handicap paris sportif|explication pari sportif|explication paris sportif|face a face hockey paris sportif|faire des paris sportif|faire des paris sportif
avec paypal|faire des paris sportifs|faire fortune paris sportifs|faire
un pari sportif|faire un paris sportif|faut il déclarer les gains de paris sportifs|faut il déclarer ses gains
paris sportifs|fichier excel gestion bankroll paris sportif|fiscalité gains
paris sportifs|foot paris sportif|football et paris sportifs|forfait tennis paris sportif|formation paris
sportif gratuit|forum de paris sportif|forum de paris sportifs|forum pari
sportif|forum parie sportif|forum paris sportif|forum paris
sportif foot|forum paris sportif gratuit|forum paris sportif
nba|forum paris sportif tennis|forum paris sportifs|forum
sur les paris sportifs|forum tennis paris sportif|francaise des jeux
pari sportif|francaise des jeux paris sportif|francaise
des jeux paris sportifs|france 2 paris sportif|france 2 paris sportifs|france belgique paris sportif|france espagne paris sportif|france pari sportif|france pari sportif brest|france
paris sportif|france paris sportifs|france pologne paris sportif|france portugal paris sportif|france suisse paris
sportifs|france tunisie paris sportifs|france-pari
– paris sportifs|gagnant pari sportif|gagnant paris sportif|gagnant paris sportif bayern|gagnante
paris sportif|gagne au paris sportif|gagner 10 euros par jour
aux paris sportifs|gagner 100 euros par jour paris sportif|gagner 1000 euros par
mois paris sportifs|gagner 10000 euros paris sportif|gagner
2000 euros par mois paris sportif|gagner 50 euros par jour
paris sportif|gagner a coup sur au paris sportif|gagner a coup sur pari sportif|gagner a tous les coup paris sportif|gagner
argent avec paris sportifs|gagner argent pari sportif|gagner
argent paris sportif|gagner argent paris sportifs|gagner au pari sportif|gagner au paris sportif|gagner au paris sportif a coup sur|gagner
au paris sportif foot|gagner au paris sportif forum|gagner
au paris sportif à coup sur|gagner aux paris sportif|gagner aux paris sportifs|gagner aux paris sportifs pdf|gagner beaucoup d’argent paris sportif|gagner de l argent
grace aux paris sportifs|gagner de l argent pari sportif|gagner de l argent paris sportif|gagner
de l argent paris sportifs|gagner de l’argent au paris sportif|gagner de l’argent aux
paris sportifs|gagner de l’argent avec les paris sportifs|gagner de
l’argent avec paris sportif|gagner de l’argent
avec paris sportifs|gagner de l’argent grace au paris sportif|gagner de l’argent
grace aux paris sportifs|gagner de l’argent pari sportif|gagner de l’argent paris sportif|gagner de l’argent
paris sportifs|gagner de l’argent sur les paris sportifs|gagner
des paris sportif|gagner des paris sportifs|gagner les paris sportifs|gagner pari sportif|gagner paris sportif|gagner
paris sportif foot|gagner paris sportif forum|gagner paris sportif tennis|gagner paris sportifs|gagner sa vie avec les paris sportif|gagner sa vie
avec les paris sportifs|gagner sa vie avec paris sportifs|gagner ses paris sportifs|gagner à coup sur paris sportif|gagner à tous les
coups paris sportifs|gain maximum paris sportif|gain pari sportif|gain pari sportif imposable|gain pari sportif impot|gain paris sportif|gain paris sportif imposable|gain paris sportif impot|gain paris sportif impôt|gains paris sportif|gains
paris sportif imposable|gains paris sportifs|gains paris sportifs imposable|gains paris sportifs imposables|gains paris sportifs sont ils imposables|gerer bankroll paris sportif|gerer sa bankroll
paris sportif|gerer une bankroll paris sportif|gestion bankroll paris sportif|gestion bankroll
paris sportifs|gestion bankroll paris sportifs excel|gestion de bankroll paris
sportif|gestion de bankroll paris sportif application|gestion de bankroll paris sportifs|gestion de mise paris
sportif|gestion paris sportifs v2 5 gratuit|gg signification paris sportif|gros combiné paris sportif|gros gain paris
sportif|grosse cote paris sportif pronostic|grosse mise
paris sportif|groupe paris sportif gratuit|groupe telegram paris sportif gratuit|groupement de joueurs paris sportifs|handicap 0 paris sportif|handicap
1 paris sportif|handicap 5 paris sportif|handicap au paris sportif|handicap basket paris
sportif|handicap dans les paris sportifs|handicap en paris
sportif|handicap europeen paris sportif|handicap européen paris sportifs|handicap mi temps paris sportif|handicap pari sportif|handicap
paris sportif|handicap paris sportif basket|handicap paris sportif explication|handicap paris sportif foot|handicap paris sportif rugby|handicap paris sportifs|handicap rugby paris sportif|handicap tennis paris sportif|historique cote paris sportif|historique des cotes paris
sportifs|hockey paris sportif|hockey sur glace paris
sportif|hors arjel paris sportif|hweh signification paris sportif|imposition gain pari sportif|imposition gain paris sportif|imposition gains paris sportifs|imposition paris sportif france|impot
gain paris sportif|impot paris sportif france|impot sur gain paris sportif|je gagne ma vie avec les
paris sportifs|jeu de pari sportif gratuit|jeu de paris
sportif en ligne|jeu de paris sportif gratuit|jeu paris sportif gratuit|jeu paris
sportif sans argent|jeux de parie sportif|jeux de paris sportif|jeux de
paris sportif en ligne|jeux de paris sportif gratuit|jeux de paris sportifs|jeux olympiques paris sportifs|jeux
paris sportif|jeux paris sportif gratuit|jeux paris sportif
virtuel|jeux paris sportifs en ligne|jouer au paris sportif|jouer paris sportif|joueur absent paris
sportif|joueur blesse paris sportif|joueur caen paris sportif|joueur de caen pari sportif|joueur de foot paris sportif|joueur decisif paris
sportif|joueur décisif paris sportif|joueur italien paris sportif|joueur paris sportif|joueur professionnel paris sportif|joueur qui se blesse paris sportif|joueur sanctionne pari sportif|joueur suspendu paris sportif|joueurs italiens paris sportifs|l’argent des paris sportifs est il imposable|la cote paris sportif|la francaise des jeux paris sportif|la martingale paris sportif|la martingale paris sportifs|la meilleur application de paris sportif|la meilleur application paris sportif|la meilleur technique pour
gagner au paris sportif|la méthode secrète pour gagner aux paris sportifs pdf|la plus grosse cote gagner
paris sportif|la plus grosse cote paris sportif|ldem paris sportif signification|le marché des paris sportifs|le meilleur site de pari sportif|le meilleur site de paris
sportif|le meilleur site de paris sportif en ligne|le meilleur site de paris sportifs|le
plus gros gain au paris sportif|le plus gros paris sportif|le plus gros paris
sportif du monde|les 10 meilleurs sites de paris sportifs|les 10 meilleurs sites de paris sportifs
en afrique|les 17 secrets pour gagner rapidement
aux paris sportifs|les 17 secrets pour gagner rapidement aux paris
sportifs pdf|les application de paris sportif|les
applications paris sportifs|les bonus paris sportifs|les bookmakers paris sportifs|les cotes paris sportifs|les gains de paris sportifs
sont ils imposables|les gains des paris sportifs sont ils imposables|les
jeux de paris sportifs|les meilleur paris
sportif|les meilleures applications de paris sportifs|les meilleurs applications de paris sportifs|les meilleurs bonus
paris sportif|les meilleurs bonus paris sportifs|les meilleurs cotes paris sportif|les meilleurs paris sportifs|les
meilleurs paris sportifs du jour|les meilleurs
site de paris sportif|les meilleurs site de paris sportifs|les meilleurs
sites de pari sportif|les meilleurs sites de paris sportifs|les
meilleurs sites de paris sportifs en ligne|les paris sportif|les paris sportif
avis|les paris sportifs|les paris sportifs comment ça
marche|les paris sportifs en france|les paris sportifs en ligne|les paris sportifs en ligne comprendre jouer gagner|les paris sportifs en ligne comprendre jouer gagner pdf|les paris sportifs
les plus rentables|les plus gros gagnant paris sportif|les
plus gros gains au paris sportifs|les plus gros
gains paris sportifs|les plus gros paris sportif|les plus grosse
cote paris sportif|les plus grosses pertes paris sportifs|les sites de paris sportifs|les sites de paris sportifs autorisés en france|les
sites de paris sportifs en france|les sites de paris sportifs en ligne|les sites de paris
sportifs francais|ligue 1 paris sportif|ligue 1 paris sportifs|ligue 2 paris sportif|ligue des champions paris sportif|limite de
gains paris sportifs|limite de mise paris sportif|limite gain paris sportif|limite mise paris sportifs|liste de paris sportif|liste des paris sportifs|liste des site de paris sportif|liste des sites de paris sportifs|liste pari sportif|liste
paris sportif|liste paris sportif pdf|liste site de paris sportif|liste site pari
sportif|liste site paris sportif|liste site paris sportif arjel|liste sites paris sportifs|logiciel algorithme
paris sportif|logiciel algorithme paris sportif gratuit|logiciel analyse paris sportif|logiciel calcul paris sportif|logiciel de pari sportif|logiciel de paris sportif|logiciel de paris
sportif gratuit|logiciel gestion bankroll paris sportif gratuit|logiciel gestion de bankroll paris sportif|logiciel gestion paris
sportif|logiciel gestion paris sportif gratuit|logiciel gestion paris sportifs|logiciel pari sportif|logiciel paris sportif|logiciel paris sportif gratuit|logiciel paris sportifs|logiciel paris sportifs foot sur
2 matchs|logiciel pour paris sportif|logiciel pour
paris sportifs|logiciel prediction paris sportif|logiciel probabilité paris sportif|logiciel prédiction paris
sportif|logiciel statistique paris sportifs|logiciel variation de cote
paris sportif|loi sur les paris sportifs en france|magic
calculator paris sportif|marché des paris sportifs|marché des paris sportifs en france|marché des paris sportifs
en ligne|martingale pari sportif|martingale paris sportif|martingale paris
sportif excel|martingale paris sportif forum|martingale paris sportif
interdit|martingale paris sportifs|match abandonné paris sportif|match annulé ou reporté paris sportifs|match annulé paris sportif|match
arrete paris sportif|match interrompu paris sportif|match interrompu tennis paris sportif|match interrompu tennis pluie paris sportif|match nul boxe paris sportif|match
pari sportif|match paris sportif|match reporté
paris sportif|match suspendu paris sportif|match suspendu tennis paris sportif|match truqué paris sportif|matchs truqués paris
sportifs|meilleur algorithme paris sportif|meilleur
algorithme paris sportif gratuit|meilleur app de paris sportif|meilleur app de paris sportifs|meilleur app
paris sportif|meilleur appli de pari sportif|meilleur appli de paris sportif|meilleur appli pari sportif|meilleur appli
paris sportif|meilleur appli paris sportif forum|meilleur appli paris sportifs|meilleur application conseil paris sportif|meilleur application de paris sportif|meilleur application de paris sportif en afrique|meilleur application pari sportif|meilleur application paris sportif|meilleur application paris sportif belgique|meilleur application pour les paris sportif|meilleur application pour pari
sportif|meilleur bonus de bienvenue paris sportif|meilleur
bonus pari sportif|meilleur bonus paris sportif|meilleur bonus paris sportif sans depot|meilleur bonus paris sportifs|meilleur bonus site de paris sportif|meilleur bonus site pari sportif|meilleur
bonus site paris sportif|meilleur bookmaker paris sportif|meilleur combiné
paris sportif|meilleur conseil paris sportif|meilleur cote de paris sportif|meilleur
cote pari sportif|meilleur cote paris sportif|meilleur
cote paris sportif aujourd’hui|meilleur cote site paris
sportif|meilleur forum paris sportifs|meilleur gain paris sportif|meilleur ia paris sportif|meilleur methode pour gagner au paris sportif|meilleur offre bienvenue paris sportif|meilleur offre bonus paris sportif|meilleur offre de bienvenue paris sportif|meilleur offre de bienvenue paris sportifs|meilleur offre pari sportif|meilleur offre paris sportif|meilleur offre paris sportif en ligne|meilleur pari sportif|meilleur pari sportif du jour|meilleur pari sportif en ligne|meilleur
paris sportif|meilleur paris sportif aujourd’hui|meilleur paris
sportif du jour|meilleur paris sportif en ligne|meilleur paris sportif foot|meilleur promo paris sportif|meilleur
pronostic paris sportif|meilleur site de conseil paris sportif|meilleur site de pari sportif|meilleur site de
pari sportif en ligne|meilleur site de paris sportif|meilleur site de paris sportif avis|meilleur site de paris sportif belgique|meilleur site de paris sportif canada|meilleur
site de paris sportif en france|meilleur site de paris sportif en ligne|meilleur
site de paris sportif football|meilleur site de paris
sportif forum|meilleur site de paris sportif france|meilleur site de
paris sportif hors arjel|meilleur site de paris sportif international|meilleur site de paris sportif suisse|meilleur site de paris sportifs|meilleur site de
paris sportifs en ligne|meilleur site pari sportif|meilleur site pari sportif en ligne|meilleur site pari sportif france|meilleur site paris sportif|meilleur site paris sportif avis|meilleur site paris sportif belgique|meilleur site paris sportif canada|meilleur site paris sportif en ligne|meilleur site paris sportif foot|meilleur
site paris sportif forum|meilleur site paris sportif france|meilleur
site paris sportif hors arjel|meilleur site paris
sportif nba|meilleur site paris sportif rugby|meilleur site paris sportif suisse|meilleur site paris sportifs|meilleur site pour pari sportif|meilleur site pour paris sportif|meilleur site pronostic paris sportif|meilleur strategie paris
sportif|meilleur technique de paris sportif|meilleur
technique paris sportif|meilleur technique pour gagner au paris sportif|meilleure appli de paris sportif|meilleure appli de paris sportifs|meilleure appli pari
sportif|meilleure appli paris sportif|meilleure appli paris sportifs|meilleure
application de paris sportif|meilleure application de paris sportifs|meilleure application pari
sportif|meilleure application paris sportif|meilleure application paris sportif
android|meilleure application paris sportifs|meilleure offre paris sportif|meilleure site paris
sportif|meilleure strategie paris sportif|meilleures applications de
paris sportifs|meilleures applications paris sportifs|meilleures cotes paris
sportifs|meilleures offres paris sportifs|meilleures stratégies paris sportifs|meilleurs appli paris sportif|meilleurs application de paris
sportifs|meilleurs application paris sportif|meilleurs applications paris sportifs|meilleurs bonus paris sportifs|meilleurs cote paris
sportif|meilleurs cotes paris sportifs|meilleurs offres paris sportifs|meilleurs paris sportifs|meilleurs paris sportifs du jour|meilleurs site de pari sportif|meilleurs site de paris sportif|meilleurs site de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs
site paris sportif|meilleurs sites de paris sportifs|meilleurs sites de paris sportifs en ligne|meilleurs sites paris sportif|meilleurs sites paris sportifs|methode abc paris
sportif|methode de paris sportif|methode gagnante paris
sportifs|methode gagner paris sportif|methode infaillible paris sportifs|methode martingale
paris sportif|methode mathematique paris sportif|methode mathematique
pour gagner au paris sportif|methode paris sportif|methode paris sportif foot|methode paris sportif forum|methode paris sportif tennis|methode paris sportifs|methode
pour gagner au paris sportif|methode pour gagner paris sportif|methodes paris sportifs|minimum depot paris sportif|mise au jeu pari
sportif|mise maximum pari sportif|mise maximum paris sportif|mise minimum paris sportif|mise moyenne paris sportif|mise paris sportif|moins de 4 5 but paris sportif|montant
maximum paris sportif|montant paris sportif|montante pari sportif|montante parie sportif|montante
paris sportif|montante paris sportifs|montantes paris sportifs|multiple pari sportif|multiple paris
sportif|multiple paris sportifs|multiples paris sportifs|méthode calcul paris
sportif|méthode match nul paris sportifs|méthode mathématique pour gagner au paris sportif|méthode paris sportif forum|méthode paris sportif hockey|nba pari
sportif|nba paris sportif|nba paris sportifs|nouveau paris sportif|nouveau site de pari sportif|nouveau site de paris sportif|nouveau site de paris sportif en ligne|nouveau site de paris sportifs|nouveau site pari sportif|nouveau site paris
sportif|nouveau site paris sportif france|nouveau site paris sportifs|nouveaux sites
de paris sportifs|nouveaux sites paris sportifs|nouvelle
appli paris sportif|nouvelle application de paris sportif|numero de match paris sportif|numero
match paris sportif|offre 100 euros paris sportif|offre appli pari sportif|offre
bienvenu paris sportif|offre bienvenue pari sportif|offre bienvenue paris sportif|offre bienvenue paris sportifs|offre bienvenue site
paris sportif|offre bonus paris sportif|offre de bienvenu paris sportif|offre de bienvenue pari sportif|offre de
bienvenue paris sportif|offre de bienvenue paris sportif belgique|offre de bienvenue paris sportif sans depot|offre de bienvenue paris sportif sans dépôt|offre de bienvenue paris sportifs|offre de bienvenue
sans depot paris sportif|offre de bienvenue site paris sportif|offre euro paris sportif|offre pari sportif
euro|offre paris sportif|offre paris sportif belgique|offre paris sportif cash|offre paris
sportif coupe du monde|offre paris sportif hors arjel|offre paris
sportif remboursé|offre paris sportif remboursé cash|offre
paris sportif sans depot|offre promo paris sportif|offre remboursement paris sportif|offre sans depot paris sportif|offre site paris sportif|offres bienvenue paris sportifs|offres de bienvenue paris sportifs|ou faire des
paris sportif|ou faire des paris sportif en espagne|ou faire
des paris sportifs|outil répartiteur de
mise paris sportif|outils repartiteur de mises paris sportif|ouverture compte paris sportifs|ouvrir
un compte paris sportif|pack de bienvenue paris sportif|pack de bienvenue paris sportif
hors arjel|pari en ligne sportif|pari sportif|pari
sportif 100 euros offert|pari sportif 100 remboursé|pari sportif abandon tennis|pari sportif aide|pari sportif algérie aujourd’hui|pari sportif appli|pari sportif application|pari sportif argent|pari sportif astuce|pari sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari
sportif avec orange money|pari sportif avec paypal|pari
sportif avec wave|pari sportif avis|pari sportif basket|pari sportif belgique|pari sportif belgique france|pari
sportif bonus|pari sportif buteur pas titulaire|pari sportif champions league|pari sportif combiné|pari
sportif comment|pari sportif comment gagner|pari sportif comment ça marche|pari sportif comparatif|pari sportif conseil|pari sportif
cote|pari sportif cote match|pari sportif cote psg|pari sportif
coupe|pari sportif coupe de france|pari sportif coupe du monde|pari sportif depot|pari
sportif du jour|pari sportif en france|pari sportif en ligne|pari
sportif en ligne au cameroun|pari sportif en ligne belgique|pari sportif en ligne canada|pari sportif en ligne france|pari sportif en ligne gratuit|pari
sportif en ligne suisse|pari sportif en ligne ufc|pari sportif en suisse|pari sportif euro|pari sportif explication|pari sportif faire|pari sportif foot|pari sportif foot resultat|pari sportif football|pari sportif forum|pari sportif francaise des jeux|pari sportif
france|pari sportif france angleterre|pari sportif france argentine|pari sportif france autriche|pari sportif france belgique|pari sportif france espagne|pari sportif france italie|pari sportif france portugal|pari sportif france usa|pari sportif gagnant|pari sportif gagner|pari sportif gagner a tous les coups|pari sportif gagner
de l’argent|pari sportif gain|pari sportif gratuit|pari sportif gratuit pour gagner des cadeaux|pari sportif gratuit sans depot|pari
sportif handicap|pari sportif hockey|pari sportif hors arjel|pari sportif jeux
olympiques|pari sportif joueur absent|pari sportif le plus rentable|pari sportif leicester champion|pari sportif ligue 1|pari sportif ligue 2|pari sportif ligue des
champions|pari sportif ligue europa|pari sportif match|pari sportif match arrete|pari sportif match interrompu|pari sportif meilleur|pari
sportif meilleur cote|pari sportif meilleur site|pari sportif
methode|pari sportif mise|pari sportif mise au jeu|pari sportif mise o jeu|pari sportif nba|pari sportif offre bienvenue|pari
sportif paypal|pari sportif plus|pari sportif prolongation|pari sportif
promo|pari sportif pronostic|pari sportif pronostic foot|pari sportif pronostic gagnant|pari sportif pronostic gratuit|pari sportif
psg|pari sportif psg bayern|pari sportif psg inter|pari sportif psg milan|pari sportif regle|pari sportif rembourse|pari sportif remboursement|pari sportif remboursement
cash|pari sportif remboursé|pari sportif rugby|pari sportif rugby coupe du monde|pari sportif rugby top 14|pari sportif
sans argent|pari sportif sans carte bancaire|pari sportif sans depot|pari sportif signification|pari sportif site|pari sportif statistique|pari sportif suisse|pari sportif systeme|pari sportif technique|pari
sportif technique pour gagner|pari sportif temps reglementaire|pari sportif tennis|pari
sportif tennis abandon|pari sportif top|pari
sportif top 14|pari sportif tour de france|parie sportif|parie sportif comment ca
marche|parie sportif du jour|parie sportif en ligne|parie
sportif foot|parie sportif football|parie sportif france|parie sportif gratuit|parie sportif pronostic|parie sportif suisse|paris en ligne sportif|paris en ligne sportifs|paris evenement sportif|paris
france sportif|paris hippique et sportif|paris hippiques et sportifs|paris hippiques paris sportifs|paris
hippiques paris sportifs et poker en ligne|paris hippiques
sportifs|paris match sportif|paris sportif|paris sportif
10 euros offerts|paris sportif 100 euros offert|paris sportif 100 euros remboursé|paris sportif 100 offert|paris sportif 100 remboursé|paris sportif 100e offert|paris sportif 150 euros offert|paris sportif 1er pari remboursé|paris sportif a faire|paris sportif a faire aujourd’hui|paris sportif a
faire ce soir|paris sportif abandon tennis|paris sportif abandon tennis parions sport|paris sportif
aide|paris sportif algorithme|paris sportif analyse|paris
sportif appli|paris sportif application|paris sportif application android|paris
sportif apres prolongation|paris sportif argent|paris sportif
argent fictif|paris sportif argent offert|paris sportif
argent virtuel|paris sportif arjel|paris sportif arsenal psg|paris sportif astuce|paris sportif au canada|paris
sportif aujourd hui|paris sportif aujourd’hui|paris
sportif avec argent fictif|paris sportif avec bonus sans depot|paris sportif avec carte bancaire|paris sportif avec cryptomonnaie|paris sportif avec handicap|paris sportif avec paypal|paris sportif avec paysafecard|paris sportif avis|paris sportif
avis expert|paris sportif avis forum|paris sportif bankroll|paris sportif basket|paris sportif basket coupe
de france|paris sportif basket nba|paris sportif basket prolongation|paris sportif belgique|paris sportif belgique bonus|paris sportif belgique bonus sans depot|paris sportif belgique france|paris sportif belgique suede|paris sportif bonus|paris sportif bonus bienvenue|paris sportif bonus
cash|paris sportif bonus de bienvenue|paris sportif bonus gratuit|paris
sportif bonus gratuit sans depot|paris sportif bonus retirable|paris sportif bonus sans depot|paris sportif bonus sans depot belgique|paris sportif bookmaker|paris sportif but contre son camp|paris sportif but temps additionnel|paris sportif
buteur|paris sportif buteur blessé|paris sportif buteur carton rouge|paris sportif buteur contre son camp|paris sportif
buteur non titulaire|paris sportif buteur prolongation|paris sportif buteur qui ne joue
pas|paris sportif buteur remplacant|paris sportif
calcul gain|paris sportif canada|paris sportif cash|paris sportif cash out|paris sportif
champion ligue 1|paris sportif champions league|paris
sportif classement ligue 1|paris sportif code promo|paris sportif combine|paris sportif combiné|paris sportif combiné comment ça marche|paris sportif combiné du jour|paris sportif combiné
match reporté|paris sportif comment ca marche|paris sportif comment faire|paris
sportif comment gagner|paris sportif comment gagner a tous les coups|paris sportif comment jouer|paris sportif comment ça
marche|paris sportif comparateur cote|paris sportif comparatif|paris
sportif conseil|paris sportif conseil gratuit|paris sportif conseil pour gagner|paris
sportif cote|paris sportif cote et match|paris sportif cote explication|paris sportif cote
psg|paris sportif coupe d’europe|paris sportif coupe davis|paris sportif coupe de france|paris sportif coupe du monde|paris
sportif coupe du monde de rugby|paris sportif coupe du monde rugby|paris sportif depot 5 euro|paris sportif depot minimum|paris sportif depot paypal|paris sportif dnb|paris sportif du jour|paris sportif
du jour conseil|paris sportif dépôt 1 euro|paris sportif dépôt minimum 5 euros|paris sportif en belgique|paris sportif en france|paris sportif en ligne|paris sportif en ligne avec paypal|paris sportif
en ligne avis|paris sportif en ligne belgique|paris sportif en ligne bonus|paris sportif en ligne cameroun|paris sportif en ligne comment gagner|paris sportif en ligne comment ça marche|paris sportif en ligne france|paris sportif en ligne gratuit|paris
sportif en ligne maroc|paris sportif en ligne paypal|paris sportif en ligne québec|paris sportif en ligne sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris
sportif espagne france|paris sportif esport|paris sportif et casino en ligne|paris sportif et
hippique|paris sportif et prolongation|paris sportif euro|paris sportif europa league|paris sportif explication|paris sportif final ligue des
champions|paris sportif finale ligue des champions|paris sportif foot|paris sportif foot aide|paris sportif foot astuce|paris sportif foot aujourd’hui|paris sportif
foot ce soir|paris sportif foot comment ca marche|paris sportif foot conseil|paris sportif foot cote|paris sportif foot coupe du monde|paris sportif foot en ligne|paris sportif foot feminin|paris sportif foot gratuit|paris sportif foot prolongation|paris sportif foot pronostic|paris sportif foot pronostic gratuit|paris sportif foot regle|paris sportif foot suisse|paris
sportif foot us|paris sportif football|paris sportif football americain|paris sportif football astuces|paris sportif forfait tennis|paris sportif forum|paris sportif francais|paris
sportif francaise des jeux|paris sportif france|paris sportif france 2|paris sportif france allemagne|paris sportif france
angleterre|paris sportif france argentine|paris sportif
france autriche|paris sportif france belgique|paris
sportif france espagne|paris sportif france gibraltar|paris sportif france italie|paris sportif france nouvelle
zelande|paris sportif france pologne|paris sportif france portugal|paris
sportif france uruguay|paris sportif france usa|paris sportif freebet sans depot|paris sportif
gagnant|paris sportif gagnant à coup sûr|paris sportif gagner a coup
sur|paris sportif gagner argent|paris sportif gagner de l’argent|paris sportif gain|paris sportif
gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris sportif gratuit appli|paris sportif gratuit avec
cadeaux|paris sportif gratuit cadeaux|paris sportif gratuit en ligne|paris
sportif gratuit entre amis|paris sportif gratuit sans argent|paris sportif gratuit sans depot|paris sportif gratuit sans dépôt|paris sportif gratuits|paris sportif gros gain|paris sportif handicap|paris sportif handicap 0 1|paris sportif handicap 0-1|paris sportif handicap 1 0|paris sportif handicap 1-0|paris sportif handicap basket|paris sportif handicap explication|paris sportif handicap
foot|paris sportif handicap rugby|paris sportif hippique|paris sportif hockey|paris sportif hockey nhl|paris sportif hockey sur
glace|paris sportif hors arjel|paris sportif hors arjel
france|paris sportif jeux olympiques|paris sportif jeux video|paris sportif joueur blessé|paris sportif joueur blessé pendant le
match|paris sportif joueur de foot|paris sportif joueur decisif|paris sportif
joueur declare forfait|paris sportif joueur déclare forfait|paris sportif joueur remplacant|paris sportif la francaise des jeux|paris sportif le plus rentable|paris sportif
legal en france|paris sportif leicester champion|paris sportif les 18 stratégies pour gagner tous les jours|paris sportif les plus sur|paris
sportif les prolongation compte|paris sportif ligne|paris sportif ligue 1|paris sportif ligue 2|paris sportif ligue des champions|paris sportif
ligue des nations|paris sportif ligue europa|paris sportif
liste|paris sportif martingale|paris sportif match|paris
sportif match abandonné|paris sportif match annulé|paris sportif match
arrêté|paris sportif match du jour|paris sportif match interrompu|paris sportif
match reporté|paris sportif match suspendu|paris sportif match tennis interrompu|paris sportif match
truqué|paris sportif meilleur bonus|paris sportif meilleur cote|paris sportif
meilleur pronostic|paris sportif meilleur site|paris sportif methode|paris
sportif methode 2 3|paris sportif mi temps fin de match|paris sportif mise au jeu|paris sportif mise maximum|paris sportif mma france|paris sportif
moins de 3.5 but|paris sportif montante|paris sportif moto gp|paris sportif multiple|paris sportif multiple 2 3|paris sportif multiple 2 3
explication|paris sportif multiple 2 4|paris sportif multiple 2 5|paris sportif multiple
2/3 explication|paris sportif multiple 3 4|paris sportif multiple
explication|paris sportif national 1 foot|paris sportif nba|paris sportif nba conseil|paris sportif nba pronostic|paris sportif nhl|paris sportif nombre de but|paris sportif nouveau site|paris sportif numero match|paris sportif offert|paris sportif offre bienvenue|paris sportif offre
bienvenue sans depot|paris sportif offre de bienvenue|paris sportif offre sans depot|paris sportif
om psg|paris sportif paypal|paris sportif plus de 1.5 but|paris sportif plus
de 2 5 but|paris sportif plus ou moins|paris sportif plus ou moins 2 5
but|paris sportif premier pari remboursé|paris sportif premier paris remboursé|paris sportif prolongation|paris sportif prolongation basket|paris sportif prolongation foot|paris sportif promo|paris sportif pronostic|paris sportif pronostic basket|paris sportif pronostic des match aujourd hui|paris sportif pronostic expert gratuit|paris
sportif pronostic foot|paris sportif pronostic forum|paris
sportif pronostic gratuit|paris sportif pronostic tennis|paris sportif
psg|paris sportif psg arsenal|paris sportif psg barcelone|paris sportif psg bayern|paris sportif psg
dortmund|paris sportif psg inter|paris sportif psg
inter cote|paris sportif psg liverpool|paris sportif psg om|paris sportif qr code|paris sportif que veut dire handicap|paris sportif qui rapporte le plus|paris sportif
regle|paris sportif regle prolongation|paris
sportif rembourse|paris sportif remboursement cash|paris sportif rembourser|paris sportif remboursé|paris sportif remboursé cash|paris sportif remboursé en cash|paris sportif retrait
paypal|paris sportif rue des joueurs|paris sportif rugby|paris sportif rugby 6 nations|paris sportif rugby coupe du monde|paris sportif rugby top 14|paris sportif safe du jour|paris sportif sans
argent|paris sportif sans carte bancaire|paris sportif sans
carte d’identité|paris sportif sans compte bancaire|paris sportif sans depot|paris sportif sans depot minimum|paris sportif si match suspendu|paris sportif si un joueur
abandonne|paris sportif si un joueur ne joue pas|paris sportif
si un joueur se blesse|paris sportif simple
ou combiné|paris sportif site|paris sportif statistique|paris
sportif stratégie|paris sportif suisse|paris sportif suisse application|paris sportif suisse en ligne|paris
sportif suisse legal|paris sportif suisse légal|paris sportif suisse
romande|paris sportif sur du jour|paris sportif sur le tennis|paris sportif systeme|paris sportif systeme 2 3|paris sportif systeme 2 4|paris sportif
systeme 2/3|paris sportif systeme 2/4|paris sportif systeme 3 4|paris sportif
systeme 3/4|paris sportif systeme explication|paris sportif technique|paris sportif technique pour gagner|paris sportif temps additionnel|paris sportif temps reglementaire|paris sportif tennis|paris sportif
tennis abandon|paris sportif tennis conseil|paris
sportif tennis de table|paris sportif tennis forfait|paris sportif tennis gratuit|paris sportif tennis pronostic|paris sportif tennis roland garros|paris sportif tir au but|paris sportif top 14|paris sportif tour de france|paris sportif ufc|paris
sportif ufc france|paris sportif unibet|paris sportif vainqueur euro|paris sportif vainqueur ligue 1|paris sportif vainqueur ligue des champions|paris sportif via paypal|paris sportif victoire prolongation|paris sportif vip gratuit|paris
sportifs|paris sportifs abandon tennis|paris sportifs aide|paris sportifs
analyser un match|paris sportifs arjel|paris
sportifs astuces|paris sportifs aujourd’hui|paris sportifs autorisés en france|paris sportifs avec
paypal|paris sportifs basket|paris sportifs belgique|paris sportifs bonus|paris sportifs
bookmakers|paris sportifs canada|paris sportifs combiné|paris sportifs comparateur|paris sportifs comparatif|paris sportifs conseils|paris sportifs cotes|paris sportifs coupe du monde|paris
sportifs de football|paris sportifs du jour|paris sportifs en belgique|paris sportifs en france|paris sportifs en ligne|paris sportifs en ligne belgique|paris sportifs en ligne
france|paris sportifs en ligne gratuit|paris sportifs en ligne suisse|paris
sportifs en suisse|paris sportifs et hippiques|paris sportifs euro|paris
sportifs foot|paris sportifs foot us|paris sportifs forum|paris sportifs france|paris sportifs france espagne|paris sportifs gagner à tous les coups|paris sportifs
gratuit|paris sportifs gratuits|paris sportifs gratuits en ligne|paris sportifs handicap|paris sportifs hockey|paris
sportifs hockey sur galce|paris sportifs hockey sur glace|paris
sportifs hors arjel|paris sportifs jeux olympiques|paris sportifs les bookmakers
raflent la mise|paris sportifs ligne|paris sportifs ligue 1|paris sportifs ligue 2|paris
sportifs ligue des champions|paris sportifs ligue europa|paris
sportifs match interrompu|paris sportifs montante|paris sportifs nba|paris sportifs offre
bienvenue|paris sportifs offre de bienvenue|paris sportifs paypal|paris sportifs pronostics|paris sportifs psg|paris sportifs psg
inter|paris sportifs rugby|paris sportifs sans argent|paris sportifs sans depot|paris sportifs site|paris sportifs sites|paris sportifs statistiques|paris sportifs stratégie|paris sportifs suisse|paris sportifs technique|paris sportifs techniques|paris sportifs
tennis|paris sportifs tennis astuces|paris sportifs top 14|paris sportifs tour
de france|part de marché paris sportifs|paypal pari sportif|paypal paris sportif|paypal paris sportifs|perte d’argent paris sportifs|peut on devenir riche avec les paris sportifs|peut on gagner de l’argent avec les
paris sportifs|peut on gagner sa vie avec les paris sportif|peut
on vraiment gagner de l’argent avec les paris sportifs|plus
gros combine paris sportif|plus gros gagnant paris sportif|plus gros gain paris
sportif|plus gros gain paris sportif au monde|plus gros gain paris sportif france|plus gros gains paris sportif|plus gros pari sportif|plus gros paris sportif|plus grosse cote
gagner paris sportif|plus grosse cote pari sportif|plus grosse cote paris sportif|plus grosse mise paris sportif|plus grosse somme gagner au paris sportif|plus
ou moins paris sportif|pourcentage de mise paris sportif|premier pari sportif remboursé|probabilité cote paris sportif|probabilité paris sportif combiné|prolongation basket
paris sportif|prolongation paris sportif|promo pari sportif|promo paris sportif|promo site de paris sportif|promo site pari
sportif|promo site paris sportif|promos paris sportifs|prono paris
sportif foot|prono paris sportif gratuit|prono paris sportif tennis|pronostic de paris
sportif|pronostic du jour paris sportif|pronostic foot paris
sportif|pronostic gratuit paris sportif|pronostic pari sportif|pronostic
pari sportif gratuit|pronostic paris sportif|pronostic paris sportif aujourd’hui|pronostic paris sportif du jour|pronostic paris sportif foot|pronostic paris
sportif gratuit|pronostic paris sportif tennis|pronostic paris
sportifs|pronostics foot statistiques et aides aux paris sportifs|pronostics paris sportif|pronostics paris sportifs|pronostiqueur paris sportif
gratuit|psg arsenal paris sportif|psg bayern paris sportif|psg inter
milan paris sportif|psg inter pari sportif|psg inter paris sportif|psg liverpool paris
sportif|psg om paris sportif|psg paris sportif|psg paris sportifs|qr code
paris sportif|qu est ce qu un handicap paris sportif|qu est ce que handicap dans les paris
sportif|qu’est ce qu’un handicap paris sportif|qu’est ce que handicap dans les paris sportif|quand un joueur se blesse paris sportif|que
signifie 1/1 en paris sportif|que signifie 1/2 paris sportif|que signifie
12 en paris sportif|que signifie 1×2 dans les paris
sportifs|que signifie btts en paris sportif|que signifie
dnb en paris sportif|que signifie draw en paris sportif|que signifie ft en paris sportif|que signifie
gg dans le pari sportif|que signifie gg en pari sportif|que signifie
gg en paris sportif|que signifie handicap dans les paris sportifs|que
veut dire dnb en paris sportif|que veut dire handicap
dans les paris sportifs|que veut dire handicap paris sportif|quel appli pari sportif|quel
cote jouer paris sportif|quel est la meilleur appli de paris
sportif|quel est le meilleur algorithme de paris sportif|quel est le meilleur site de
pari sportif|quel est le meilleur site de pari sportif en ligne|quel est le meilleur site de paris sportif|quel est le meilleur site de paris sportif en ligne|quel est le meilleur site de paris sportifs en ligne|quel est le pari sportif le plus
rentable|quel pari sportif est le plus rentable|quel pari sportif est le
plus sûr|quel pari sportif faire aujourd’hui|quel paris sportif
faire aujourd’hui|quel paris sportif rapporte le plus|quel site de paris sportif choisir|quel site de paris sportif rembourse en cash|quel type de
pari sportif est le plus rentable|quelle application pour paris sportifs|quelle est la meilleure
appli de paris sportif|quelle est la meilleure application de paris sportif|quelle est la
meilleure application pour les paris sportifs|quelle est le
meilleur site de paris sportif|quels paris sportifs faire|quels
sont les paris sportifs les plus sûrs|rebond basket paris
sportif|record de gain paris sportif|regle buteur paris sportif|regle de paris sportif|regle des paris sportif|regle handicap
paris sportif|regle handicap paris sportif foot|regle multiple paris sportif|regle pari
sportif|regle paris sportif|regle paris sportif foot|regle paris sportif multiple|regle paris sportif prolongation|reglement pari sportif|reglement paris sportif|regles paris sportifs|remboursement cash paris sportif|remboursement en cash paris
sportif|remboursement pari sportif|remboursement paris sportif|repartiteur de
mise paris sportif|repartiteur de mise paris sportifs|repartiteur de mises
paris sportif|repartiteur mise paris sportif|repartition des mises paris sportif|resultat pari sportif|resultat paris sportif|resultat paris sportif en direct|resultat paris sportif foot|resultat sportif hockey|retirer argent paris sportif|rugby pari sportif|rugby paris sportif|règle paris sportif prolongation|règles paris sportif|répartiteur de mise pari sportif|répartiteur de mise paris sportif|répartiteur de mise paris sportifs|répartition des
mises paris sportif|résultat paris sportif foot|sans depot paris sportif|se faire interdire de paris sportifs|signification btts paris sportif|signification dnb paris sportif|signification handicap paris sportif|simulateur de gain paris sportif|simulateur gain paris sportif|simulateur gain paris sportif multiple|simulateur gain paris sportif
systeme|simulateur gain paris sportif système|simulateur montante
paris sportif|simulateur paris sportif multiple|simulateur systeme
paris sportif|simulation paris sportif gratuit|site aide paris sportif|site analyse paris sportif|site analyser paris sportif|site arjel paris sportif|site conseil
paris sportif|site d’analyse de paris sportifs|site d’analyse paris sportif|site de conseil paris sportif|site de pari en ligne sportif|site de pari sportif|site de pari sportif avec bonus sans depot|site de pari sportif
bonus sans depot|site de pari sportif canada|site de pari sportif en ligne|site de pari sportif
francais|site de pari sportif gratuit|site de pari sportif
hors arjel|site de pari sportif suisse|site de parie sportif|site de parie sportif en ligne|site de paris
en ligne sportif|site de paris sportif|site de paris sportif acceptant paypal|site de paris sportif arjel|site de paris sportif autorisé en france|site de paris sportif autorisé en suisse|site de paris sportif avec bonus|site de paris sportif avec bonus sans
depot|site de paris sportif avec bonus sans dépôt|site de paris sportif avec neosurf|site de paris sportif avec paiement mobile|site de
paris sportif avec paypal|site de paris sportif avis|site de paris sportif belge avec bonus|site de paris
sportif belgique|site de paris sportif bonus|site de paris sportif bonus sans
depot|site de paris sportif canada|site de paris sportif comparatif|site de paris sportif depot
minimum|site de paris sportif en france|site de paris sportif
en ligne|site de paris sportif en ligne suisse|site de paris sportif football|site de paris sportif francais|site de paris sportif france|site de paris sportif gratuit|site de
paris sportif gratuit pour gagner des cadeaux|site de paris
sportif gratuit sans dépôt|site de paris sportif hors arjel|site de paris sportif le plus fiable|site de paris sportif legal
en france|site de paris sportif meilleur cote|site de
paris sportif nouveau|site de paris sportif offre de bienvenue|site de paris sportif paypal|site de paris
sportif premier paris remboursé|site de paris sportif qui
accepte paypal|site de paris sportif qui rembourse
en cash|site de paris sportif remboursé|site de paris sportif sans argent|site de paris sportif sans carte
bancaire|site de paris sportif sans carte d’identité|site de
paris sportif sans depot|site de paris sportif suisse|site
de paris sportifs|site de paris sportifs avec paypal|site
de paris sportifs en ligne|site de paris sportifs francais|site de paris sportifs gratuit|site de paris sportifs paypal|site
de paris sportifs suisse|site de statistique pour paris sportif|site des paris sportifs|site pari en ligne sportif|site pari sportif|site pari sportif 100 euros offert|site pari sportif arjel|site pari sportif belgique|site
pari sportif bonus|site pari sportif canada|site pari sportif comparatif|site pari
sportif en ligne|site pari sportif france|site pari sportif gratuit|site pari sportif hors
arjel|site pari sportif suisse|site parie sportif|site
paris en ligne sportif|site paris sportif|site paris sportif 100 euros
offert|site paris sportif 100 euros remboursé|site paris sportif 1er paris
remboursé|site paris sportif arjel|site paris sportif autorisé en france|site paris sportif avec bonus|site paris sportif avec bonus sans depot|site paris sportif
avec meilleur cote|site paris sportif belgique|site paris sportif bonus|site paris sportif bonus cash|site paris sportif bonus sans depot|site paris
sportif canada|site paris sportif comparatif|site paris sportif depot 5 euro|site paris sportif en ligne|site paris sportif foot|site paris sportif france|site paris sportif gratuit|site paris sportif hors arjel|site paris sportif hors arjel france|site paris sportif meilleur cote|site paris sportif nouveau|site paris sportif offre
de bienvenue|site paris sportif paypal|site paris sportif remboursement cash|site paris sportif remboursé en cash|site paris
sportif retrait instantané|site paris sportif sans carte bancaire|site paris sportif
sans depot|site paris sportif suisse|site paris sportifs|site paris sportifs belgique|site
paris sportifs en ligne|site paris sportifs france|site paris sportifs
hors arjel|site paris sportifs suisse|site pour analyse paris sportif|site pour paris sportif|site pronostic paris sportif|site statistique paris sportif|site suisse paris sportif|sites de pari sportif|sites
de paris sportif|sites de paris sportifs|sites de paris sportifs arjel|sites de paris sportifs autorisés
en france|sites de paris sportifs belgique|sites de paris sportifs bonus|sites de paris sportifs
en belgique|sites de paris sportifs en france|sites de paris sportifs en ligne|sites de paris sportifs gratuits|sites de paris sportifs gratuits sans dépôt|sites de
paris sportifs suisse|sites pari sportif|sites paris sportif|sites paris sportifs|sites paris sportifs arjel|sites paris sportifs belgique|sites paris sportifs france|sites paris sportifs hors arjel|sites
paris sportifs suisse|so foot paris sportif|so foot paris sportifs|specialiste tennis paris sportif|statistique foot
paris sportif|statistique paris sportif|statistique paris sportif foot|statistique tennis paris sportif|statistiques football paris
sportifs|statistiques paris sportifs|strategie de paris sportif|stratégie big whale paris sportif|stratégie de paris
sportifs|stratégie gagnante paris sportifs|stratégie pari
sportif|stratégie paris sportif|stratégie paris sportifs|stratégie paris sportifs
forum|stratégie pour gagner au paris sportif|stratégies paris sportifs|suisse
paris sportif|suisse paris sportifs|systeme 2
3 paris sportif|systeme 3 4 paris sportif|systeme de cote paris sportif|systeme de paris sportif|systeme
pari sportif|systeme paris sportif|systeme paris sportifs|systeme
reducteur paris sportif|système paris sportif|tableau bankroll paris sportif|tableau cote paris
sportif|tableau de paris sportif|tableau de suivi paris sportifs|tableau excel bankroll paris sportif|tableau excel paris sportif|tableau
excel paris sportif gratuit|tableau excel paris sportifs|tableau excel pour paris sportif|tableau gestion bankroll paris
sportif|tableau montante paris sportif|tableau
paris sportif|tableau paris sportif excel|tableau roi
paris sportifs|tableau statistique paris sportif|tableau suivi
tripscan С TripScan вы найдете скрытые жемчужины, о которых раньше не знали, и сможете создать уникальное путешествие, которое запомнится на всю жизнь.
It’s remarkable to visit this website and reading the views of all friends regarding this
paragraph, while I am also keen of getting knowledge.
Для быстрого выполнения работ в коммунальном секторе — компания AvtoSpetsResurs предлагает услуги аренды спецтехники: автовышки, крановые установки, экскаваторную технику, грузовые самосвалы, дорожные грейдеры и многое другое. Наши техника применяются для монтажа освещения, очистки от снега, перевозки гравия, сыпучих материалов или каменного угля в местные и пригородные участки. https://avtosturman.ru Подробности — аренда спецтехники представлена на сайте.
Вызов кэб — это незамысловатое и гарантированное решение для комфортных путешествий в любое время ночи. Вам не нужно разыскивать доступные средства передвижения на остановке или ждать в непогоду. Достаточно отправить вызов через приложение или по связи, и курьер прибудет точно в нужное срок.
https://taxi-aeroport-adler.ru/taman
Актуальныеоператоры предлагают чёткие тарифы, предопределённую цену без непредвиденных сборов и вариант расчёта как деньгами, так и пластиком.
Вы можете контролировать маршрут средства передвижения в моментально, заранее видеть информацию водителя и подбирать нужный категорию машины — от минималки до люкса.
Особенно практично вызывать трансфер заранее: вы обезопасите себе машину к запланированному моменту, минимизируете паники и напряжения.
Это безупречный выбор для перемещений в хаб, на деловые встречи, в гости или просто по городу.
Стабильность, аккуратность и расслабленность — всё это делает вызов такси незаменимым в городской суете.
Для автовладельцев, кто подбирает качественный и современный вариант к машине — компания Allcartuning осуществляет чип тюнинг и экономичный тюнинг для легковых, грузовых и спецтехники. С 2007 года наши услуги, сертифицированные TUV, гарантируют увеличение мощности, динамику и экономию топлива. https://china-avto-k.ru Посмотрите подробнее — оптимизация двигателя ждёт вас на портале.
Hello colleagues, its enormous paragraph about tutoringand fully defined, keep it up all the time.
Hi would you mind letting me know which hosting company you’re working with?
I’ve loaded your blog in 3 different browsers and I must say this blog loads a
lot quicker then most. Can you recommend a good web hosting provider at a fair
price? Thank you, I appreciate it!
My partner and I stumbled over here by a different website and thought I should
check things out. I like what I see so now i am following you.
Look forward to looking at your web page for a second
time.
другие https://kra43-cc.at
Для каждых автолюбителей — от стартующих до бывалых, доступен блог с интересными статьями, автословарём, событиями и роликами. Читать контент > сайт-блог https://citroen-avtoservise.ru публикует подсказками для каждого. Узнай больше — перейти на сайт.
This game looks amazing! The way it blends that old-school chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic
chicken crossing gameplay and adding real risk? I’m totally down to try
it.
This is right up my alley! I’m loving the combo of
classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing
feel with real consequences has me hooked. I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic
chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of
nostalgic chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that
beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
Ищете санкнижку за 1 день в Санкт-Петербурге без обследования и осмотров? В медцентре https://doktora-gerasenko-med.ru можно оформить или обновить санитарную книжку, справки для посещения бассейна, дорожной инспекции, больничные листы, документы из ПНД/НД, заключения КЭК и другие официальные документы — всё быстро, легально и без обращения в поликлинику. Все подробности на сайте — медкнижка срочно, быстрое оформление справки, справка без медкомиссии.
Hindi mo dapat i-click ang link na ito sa anumang sitwasyon dahil ito ay isang cyber crime
Pretty! This was an extremely wonderful post.
Many thanks for supplying these details.
Потрясающее онлайн-казино, продолжайте в том же духе. Благодарю.
http://www.hotgoo.com/out.php?url=https://pinup-casinoplay.kz/mobile-app/
Ищете, где быстро купить медсправку в СПб без очередей и лишних проблем? На https://doktor-smajl-med.ru предлагаются справки 095/у, форма 027/у, документы ПНД/НД, академические отпуска и разные варианты — все оформление проходит законно и отправляются курьерской доставкой, в любой район или офис. Честная цена, доступная стоимость, качество гарантировано. Подходит для учащихся, сотрудников и любого клиента — удобство и скорость. Узнайте подробности — медицинская справка СПб, оформление без очередей, доставка справки.
Hey there! I’ve been following your blog for a long
time now and finally got the bravery to go ahead and give
you a shout out from Huffman Tx! Just wanted to say keep up the great work!
Хотите узнать, где купить санитарную книжку в Самаре быстро и с курьером? На сайте https://gosdentalklinic-china.ru/ можно получить медкнижку через интернет без посещения клиники — готово за сутки. При заполнении формы на сайте возможна курьерская доставка, а стоимость честная: новая книжка с 1 699 ?, продление — от 799 ?. Всё официально и удобно. Подробнее на сайте — медкнижка онлайн, оформление за сутки, курьерская доставка.
This is really interesting, You are a very skilled blogger.
I’ve joined your rss feed and look forward to seeking more of your magnificent post.
Also, I’ve shared your site in my social networks!
Thank you for another informative blog. The place else may I
am getting that kind of info written in such a perfect way?
I have a undertaking that I am simply now running on, and I have
been on the look out for such information.
bookmarked!!, I love your blog!
Нужна медкнижку за один день в Москве по доступной цене? В медицинском центре https://hearth-health.ru можно быстро оформить официальную медкнижку от 1 200 ?, продлить существующую по цене от 1 800 ? или получить медицинский документ по цене 1 000 ?, включая сдачу анализов по цене 500 ?. Всё — законно, юридически корректно и без лишних забот. Гибкий график, можно подать заявку онлайн и получить документы оперативно. Узнайте больше — медкнижка за день, получение через интернет, справка недорого.
Узнайте максимум о дилерском центре JAECOO в Бутово — официальный дилер в Москве: новые автомобили, доступные цены, ремонт и фирменные детали! Зайдите на https://jaecoo-avtorussbutovo.ru и узнайте с новыми авто. Хотите поездку перед покупкой или рассрочку? — компания предлагает рассрочку 0%, оценку авто с выгодой и гарантированное обслуживание. Подбираете современный автомобиль — здесь найдёте технологичные авто и профессиональную поддержку.
Mangelsen
7916 Girard Avenue,ᒪɑ Joya
CΑ 92037, United Stɑtes
1 800-228-9686
Bookmarks (https://www.protopage.com/)
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get four emails with the same comment.
Is there any way you can remove me from that service? Bless you!
You are so cool! I don’t suppose I have read through anything like that before.
So nice to find somebody with unique thoughts on this
subject matter. Really.. many thanks for starting this
up. This website is one thing that is required on the internet, someone with
some originality!
Подбираете место, где оформить медицинскую книжку в Перми легально и без волокиты? На https://klinika-zdorovya-no1.ru можно оформить медкнижку нового образца всего за 1700 ? или продлить действующую — по цене от 1000 ?. Книжки подлинные и легальные, возможна доставка курьером к вам домой. Всё легко: передать нужные данные онлайн, внести оплату и ждать доставку — без посещения поликлиники и очередей. Подробнее на сайте — медкнижка Пермь, оформление без очередей, акция на продление.
It’s in reality a great and useful piece of info. I’m glad
that you simply shared this useful information with us.
Please stay us up to date like this. Thanks for sharing.
Ищете квалифицированную медицинскую помощь рядом с вами? В медцентре https://kristall-med.ru оказываются услуги эндоскопии, функциональной диагностики и молекулярной диагностики — с профессиональным оборудованием и комфортными условиями. Центр работает с современными технологиями, сотрудничает с опытными врачами и проводит комплексные исследования. Всё это — удобно, надёжно и по всем медицинским нормам. Подробнее на сайте — функциональная диагностика, генетическое исследование, качественная эндоскопия.
Artikel yang Anda tulis ini sangat informatif.
Pembahasan mengenai KUBET sebagai Situs Judi Bola Terlengkap disampaikan dengan jelas.
Struktur artikelnya membuat pembaca mudah memahami alurnya.
Penjelasan tentang bagaimana sebuah platform ditetapkan sebagai Situs Parlay Resmi
juga menarik untuk disimak.
Detail yang Anda berikan sangat bermanfaat.
Jarang ada artikel yang membahas poin ini secara mendalam.
Saya juga sangat terbantu oleh bagian tentang Situs Parlay
Gacor, terutama dalam menjelaskan faktor-faktor penilaiannya.
Informasinya cocok untuk pemula maupun pemain berpengalaman.
Bagian ini memberikan gambaran yang jelas mengenai performa real suatu platform.
Ulasan mengenai fitur di Situs Mix Parlay dan permainan seperti toto macau juga menjadi pelengkap konten yang informatif.
Pembahasannya tidak membosankan.
Hal ini membuat artikel terasa professional dan mudah diikuti.
Secara keseluruhan, artikel ini menjadi referensi kuat bagi pembaca yang ingin memahami
kubet login, Situs Judi Bola, hingga layanan situs parlay lainnya.
Tolong terus ciptakan konten berkualitas seperti ini.
Для успешной реализации строительных и ландшафтных проектов — компания Kusok Avto сдаёт в предоставление надёжную спецтехнику, включая автогрейдеры, вышки и прочую технику. https://kusokavto.ru Наш большой практика в возведении дорог и сетевых систем обеспечивает стабильность и безопасность. Посмотреть деталями — спецтехника аренда представлена на сайте.
Ищете медкнижка сегодня же без визита в больницу? На https://med-bez-boli.ru можно оформить или перевыпустить официальную медкнижку легально, без обследования — быстро и официально. Имеем партнёрство с официальным медцентром и оформляем медкнижки нового формата, выдаём официальные справки, которую регистрируют в базе. Это без лишних хлопот, официально и по выгодной цене. Узнайте подробности — медкнижка без осмотра, срочное оформление, санитарная книжка онлайн.
4MDental Implant Center
3918 Long Beach Blvd #200, Long Beach,
ⅭA 90807, United Stаtes
15622422075
tooth restoration
I really like it when individuals come together and share
opinions. Great website, continue the good work!
I think this is one of the most vital info for me. And i am glad reading
your article. But wanna remark on few general
things, The website style is wonderful, the articles is really nice : D.
Good job, cheers
Хотите получить удобный способ заказать официальную справку или санитарную книжку без ожидания и волокиты? В клинике https://med-blesk.ru представлен широкий выбор услуг для здоровья: оформление медкнижек, справок разных форм, УЗИ, лабораторные исследования и приём терапевта — всё законно и официально. Доступна курьерская доставка, а также медицинские осмотры для физических и юридических лиц. Это оперативно, стабильно и профессионально — приём ведут опытные врачи. Все детали на сайте — справка через интернет, медкнижка без очередей, получение справки.
Superb site you have here but I was curious if you knew of any community forums that cover the same topics discussed here?
I’d really like to be a part of group where I can get opinions
from other experienced individuals that share the
same interest. If you have any recommendations, please
let me know. Many thanks!
Ищете официальная справка от врача удалённо? На https://medical-sozvezdie.ru можно заказать документы в Москве — от школьной справки 095/у до документов для РВП — в течение суток. Документы подписывают действующие врачи, используются официальные документы, а доставка осуществляется по МКАД. Это в кратчайшие сроки, легально и комфортно — медсправка онлайн, медсправка курьером, официальная справка.
I all the time emailed this weblog post page to all my associates, as if like to read it then my links will too.
Подбираете место, где получить медкнижку за 1 день без бумажной волокиты? На сайте https://medic-dpo.ru доступна возможность срочного оформления санитарной книжки — просто подайте онлайн-заявку и приготовьте паспорт и фотографию. Для сотрудников ЖКХ, сферы обслуживания и прочих категорий всё проходит комфортно и оперативно, без ожидания. Оформите книжку законно и по правилам — с получением прямо до двери или до метро. Смотрите детали — медкнижка срочно, заказ через интернет, получение документов.
Patrice & Associates
Scottsdale, AZ, United Stаteѕ
16265237726
resort activities staff (https://raindrop.io)
I love what you guys are usually up too. This sort of clever work and exposure!
Keep up the very good works guys I’ve incorporated you guys to my personal blogroll.
Хотите узнать, где получить медкнижку за 1 час в столице, легально и без проблем? На сайте https://medik-moscov.ru можно оформить санитарную книжку для работы в детских лагерях, кафе и ресторанах, сфере сервиса, медучреждениях, магазинах и многих других сферах. Стоимость: новая книжка — от 1390 ?, продление санкнижки с 780 ?. Всё в течение часа, с юр. гарантией и рядом с метро. Узнайте подробнее — медкнижка за час, быстрое оформление, официальная санкнижка.
Hmm is anyone else having problems with the images on this
blog loading? I’m trying to determine if its a problem on my end or if it’s the blog.
Any feedback would be greatly appreciated.
Хотите приобрести медицинские расходные материалы от официального дистрибьютора в Чебоксарах? Компания https://medikwest.ru предлагает широкий ассортимент изделий — от одноразовых изделий до расходников для клиник. Сотрудничаем с надежными производителями, обеспечиваем высокое качество, сертификаты соответствия и оперативное снабжение по региону. Это без лишних хлопот, гарантированно и на высоком уровне. Все детали на сайте — медицинские изделия, расходники для клиник, надёжный дистрибьютор.
What’s up, this weekend is fastidious designed for me, as this moment i am reading this wonderful informative post here
at my home.
Confidence Boost Daily – Quick tips and advice to enhance your daily self-confidence.
Ищете, где оформить или перевыпустить санитарную книжку по Уфе оперативно и с комфортом? В центре https://medmagprof24.ru можно сделать это без стресса и очередей — всё делается легально и без ожидания. Услуга доступна онлайн и готова быстро. Это комфортно, легально и подходит каждому. Подробнее на сайте — санкнижка Уфа, без толпы, быстрое оформление.
Boston Medical Group
3152 Red Hill Ave. Ste. #280,
Costa Mesa, ϹA 92626, United Stateѕ
800 337 7555
erectile dysfunction prevents ejaculation in most cases
Нужны подлинные медсправки с курьерской доставкой без формальностей и ожидания? На https://med-meditsina.ru можно в короткие сроки получить разные виды справок — от справок из ПНД, справок НД, справок противотуберкулёзного диспансера до справки 095/у, 027/у, справки 086/у, справок для плавания, академического освобождения и специального профосмотра. Всё это делается законно, на подлинных формах, при этом возможна курьерская доставка в Москве. Закажите документ в день обращения, без похода к врачу — это удобно, быстро и законно. Узнайте больше на сайте — справка на дом, онлайн оформление, медсправка без ожидания.
Хотите узнать, где оформить медкнижку в Подольске срочно и законно — без хлопот и задержек? В медицинском центре на сайте https://med-podolsk.ru можно заказать санкнижку, медсправку для водительских прав, для плавания, санатория или разрешения на оружие всего за 1 день — с лабораторными исследованиями, приёмом у врача и гарантированной легальностью. Минимальные сроки, простая запись в течение всего дня, прозрачные цены — стоимость справок от 500 ?, санкнижка с 1200 ?. Подробнее на сайте — медкнижка срочно, справка в день обращения, оформление онлайн.
Thanks for sharing your thoughts. I really appreciate your efforts and
I will be waiting for your further write ups thanks once again.
Хотите узнать, где быстро оформить медицинскую книжку за один день без толкучки и задержек? На сайте https://medraskhodka.ru/ можно сделать или продлить медкнижку в течение дня: с полным пакетом анализов и осмотром врача — даже удалённо. Услуга предназначена для сотрудников пищевой отрасли, коммунальных служб и учреждений, где требуются медосмотры и подтверждение. Документы готовятся максимально быстро, а стоимость честная и понятная (от 1 600 ?, обновление с 1 300 ?). Смотрите детали — санитарная книжка срочно, заказ через интернет, без проблем.
I do not even know how I ended up here, but I thought this
post was good. I do not know who you are but definitely you are going to a famous blogger if you aren’t already 😉
Cheers!
Profesionální uklid bytu praha znamená víc než jen běžné čištění.
Jde o komplexní péči o každý detail
vašeho domova. Společnost Ohayno nabízí širokou škálu služeb, které zahrnují úklid domácnosti Praha
– od menších městských bytů až po prostorné rodinné domy.
Naším cílem je zajistit, aby byl každý interiér čistý, voňavý a pohodlný pro každodenní život.
Naši pracovníci jsou odborně školeni a vybaveni moderní technikou, která umožňuje efektivní čištění
všech typů povrchů – od podlah a koberců až po kuchyňské linky,
koupelny či schodiště. Používáme výhradně ekologické přípravky,
které jsou bezpečné pro vaše zdraví, domácí mazlíčky
i životní prostředí. Díky tomu je každý úklid bytu praha i úklid domů Praha šetrný, ale
zároveň důkladný.
Služba úklid domácnosti Praha je dostupná jako jednorázový generální úklid, ale i jako pravidelná péče.
Přizpůsobíme se vašemu rozvrhu a zajistíme, že úklid proběhne vždy přesně podle
vašich představ. Klienti si mohou zvolit intervaly – týdenní,
čtrnáctidenní nebo měsíční – a my se postaráme o zbytek.
Díky systému interní kontroly kvality máte jistotu,
že každý úklid splňuje nejvyšší standardy.
Ohayno klade důraz na přesnost, diskrétnost a
odpovědnost. Každý úklid domácnosti Praha je pečlivě dokumentován a kontrolován, aby byl výsledek vždy stoprocentní.
Vaše domácnost si zaslouží profesionální péči.
Ohayno přináší spolehlivý úklid domů Praha i uklid bytu praha – služby,
které spojují kvalitu, jistotu a komfort. Čistota, na kterou se můžete spolehnout každý den, je
základem vašeho klidu a pohodlí.
Ищете, где срочно получить санитарную книжку или официальную справку в столице Татарстана — без очередей? В медицинском центре https://munclinic.ru доступны широкий спектр справок и санкнижек по доступным ценам, с гарантией конфиденциальности и надежностью. Собственная лаборатория круглосуточно обеспечивает быстрое обследование, чтобы обследование проходило максимально быстро. Принимают опытные специалисты, прошедшие аккредитацию и индивидуальным подходом. Документы готовятся в кратчайшие сроки — гарантированно, легально и удобно. Все детали здесь — оформление медкнижек Казань, справка по низкой цене, лаборатория круглосуточно.
содержание блекспрут
Hi! I’m at work surfing around your blog from my new iphone 3gs!
Just wanted to say I love reading your blog and look forward to all
your posts! Keep up the great work!
Нужен быстрый способ сделать медицинскую справку или обследования без посещения клиники? На https://mymednews.ru можно получить медсправку для трудоустройства, колледжа или учебного заведения — в короткие сроки и законно. Также доступны тесты на ВИЧ, гепатит B и C, уровень сахара и многое другое без личного визита. Вам не придётся ждать: всё делается быстро, с курьерской доставкой и результатами на руки. Вся информация на сайте — медсправка онлайн, анализы онлайн, быстрое получение справки.
It’s wonderful that you are getting thoughts from this piece
of writing as well as from our discussion made at this time.
4M Dentawl Implant Center
3918 Ꮮong Beach Blvd #200, Longg Beach,
ⲤA 90807, United Stateѕ
15622422075
dental restoration care
Узнайте все подробности об автолюбителях — обсуждения, рекомендации и события на форуме автолюбителей! Посетите https://n-avtoshtorki.ru и поучаствуйте в обсуждениях актуальные автотемы. Хотите поделиться опытом или найти решение — форум предлагает инструкции и лайфхаки, отзывы и новинки автомобильной жизни. Хотите вступить в сообщество — здесь найдете команду по интересам и новые идеи.
That is a very good tip especially to those new to the blogosphere.
Brief but very accurate info… Appreciate your sharing this one.
A must read article!
Unquestionably consider that that you stated. Your favourite reason appeared to be on the
net the easiest factor to take note of. I say to you, I definitely get irked at the
same time as other people think about concerns that they plainly don’t know about.
You managed to hit the nail upon the highest as
well as outlined out the whole thing with no need side-effects , people can take a signal.
Will probably be back to get more. Thank you
Cabinet IQ Fort Myers
7830 Drew Cir Ste 4, Fort Myers,
FL 33967, United Ѕtates
12394214912
Certifiedcontractors (http://Www.symbaloo.com)
Excellent beat ! I wish to apprentice whilst you amend your web site,
how could i subscribe for a blog web site? The account aided me a appropriate deal.
I were a little bit acquainted of this your broadcast offered bright clear idea
There is definately a lot to find out about this topic.
I really like all of the points you’ve made.
I was pretty pleased to find this web site. I wanted to thank you for ones time just for this fantastic read!!
I definitely savored every part of it and I have you book-marked
to look at new things on your site.
This article will assist the internet users for setting up new webpage or even a weblog from start to end.
Для собственников Mercedes, отдающих предпочтение премиум и удобство — современный автосервис оказывает широкий набор услуг: механический и кузовной ремонт, диагностику, установку Webasto, ГБО и другие услуги. https://novomed-cardio.ru опытные специалисты обслуживают на лицензированном инструменте, задействуя качественные комплектующие и гарантируя надёжность и персональное обслуживание. Посмотрите деталями — сервис Mercedes готов помочь на ресурсе.
Thank you for sharing your thoughts. I truly appreciate your efforts and I will be waiting for your next
write ups thank you once again.
سوپاس بۆ شەیرکردن. نیگەرانم لەوەی بیرۆکەی داهێنەرانەم نییە. ئەوە بابەتەکەتە کە پڕم دەکات لە هیوا. سوپاس
Ищете медсправка быстро и без волокиты? Мы поможем оформить разные медицинские справки, от бассейна до академического отдыха. https://ossis-med.ru Приобретите справку у врача или справка под заказ.
Hi I am so delighted I found your site, I really found you by
error, while I was searching on Bing for something else, Regardless I am here now and would just like to say kudos for a marvelous post and a all round thrilling blog (I also love the theme/design), I don’t have time to go through it all at the minute
but I have bookmarked it and also included your RSS feeds, so when I have time I will be
back to read much more, Please do keep up the awesome jo.
Хотите узнать, где оформить медсправку без визита в Москве? На https://psy-medcentr.ru можно заказать разные формы справок: справка 086/у, справка 095/у, справка 027/у, медкнижку, справку КЭК, справки в бассейн, академотпуска и другие документы. Оформление займёт считанные минуты, а привезём справку на дом — быстро и без ожидания. Всё легально и конфиденциально. Узнайте подробности — оформление без посещения, заказ через интернет, доставка справки.
I’ve been browsing online greater than three hours today,
yet I never discovered any attention-grabbing article like yours.
It’s lovely value sufficient for me. In my opinion, if all web owners and bloggers made just
right content material as you did, the internet might be much more helpful than ever before.
My homepage – stem cell therapy cost thailand
Hi, I check your blog regularly. Your story-telling style is witty, keep doing what you’re doing!
My partner and I stumbled over here coming from a different web page
and thought I should check things out. I like what I see so now i am following you.
Look forward to finding out about your web page
repeatedly.
Also visit my webpage; landlord documentation help
Great blog! Do you have any tips for aspiring writers?
I’m planning to start my own blog soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m totally overwhelmed ..
Any suggestions? Thank you!
My web site :: is stem cell therapy safe in thailand
Узнайте всё о Restyle-Авто — современный автоцентр, широкий выбор авто, доступные предложения и проверенные предложения! Перейдите на https://restyle-avto.ru и посмотрите каталог машин. Нужен транспорт срочно или хорошую цену — компания предлагает легковые машины, обмен Trade-In и центральный офис. Нужна машина сейчас — здесь найдёте лучшие условия покупки и честные условия.
I think the admin of this web site is actually
working hard in favor of his website, because here every stuff is quality based material.
My web site – rental property dispute help
Ищете надёжный способ получить медицинскую справку быстро и без посещения поликлиники? На сайте https://romashkaclinic.ru можно оформить разные виды документов: от форм 001-ГС/у, 027/у, 086/у до документов для плавания, ВНЖ и справок комиссии — всё выполнено официально и с доставкой. Заполнить заявку можно за пару минут, оформление через сайт. Это удобно, легально и без проблем. Подробнее на сайте — онлайн справка, оформление за минуту, справка с доставкой.
4M Dental Implant Center San Diego
5643 Copley Ɗr ste 210, San Diego,
СA 92111, United States
18582567711
invisible dental aligners
Для собственников Nissan, заинтересованных в надёжном сервисе и полном обслуживании — автосервис оказывает технический и кузовной ремонт, компьютерную диагностику, регулировку схода-развала, обслуживание АКПП, монтаж ГБО, Webasto, тонировку и другие услуги. квалифицированные мастера работают на современном инструменте, применяют качественные комплектующие и предоставляют комфортный сервис с зоной ожидания и Wi-Fi. https://skupkaavtosp.ru Узнать подробностями — сервис Nissan ждёт вас на ресурсе.
Whoa tons of excellent knowledge.
ко ланта ко ланта
Hello, i think that i saw you visited my website thus i
came to “return the favor”.I’m attempting to find things to improve my website!I
suppose its ok to use some of your ideas!!
Ищете быстрый и надёжный способ получить медицинскую справку без лишних визитов? https://space-group-med.ru На сайте Space Group Med есть возможность оформить большой выбор документов — от документа 001-ГСУ, 082/у, до освобождений от физкультуры, справок ПНД и ОД и заключений КЭК. Всё это оформляется онлайн с доставкой по Москве и Санкт-Петербургу — удобно, быстро и официально. Посмотрите детали на сайте — онлайн справка, справка с доставкой, быстрое оформление справки.
Howdy, i read your blog from time to time and i own a similar
one and i was just curious if you get a lot of spam responses?
If so how do you reduce it, any plugin or anything you can recommend?
I get so much lately it’s driving me insane so any support is very much appreciated.
Southeast Financial Nashville
131 Belle Forest Cir #210,
Nashville, TN 37221, United Տtates
18669008949
RV financing for vintage RVs
Every weekend i used to visit this site, as i want enjoyment,
for the reason that this this site conations
in fact pleasant funny data too.
Для собственников Mercedes, отдающих предпочтение премиум и комфорт — профессиональный автотехцентр оказывает полный спектр услуг: механический и кузовной ремонт, диагностику, установку Webasto, ГБО и другие услуги. https://specavtoimport.ru опытные специалисты обслуживают на современном инструменте, используя оригинальные запчасти и гарантируя гарантию и индивидуальный сервис. Ознакомьтесь с подробностями — сервис Mercedes ждёт вас на ресурсе.
Узнайте максимум об Talisman-Avto в Республике Крым — ремонт без нареканий, точная диагностика и фирменные детали. Посетите https://talisman-avto.ru/ и ознакомьтесь набор предложений. Необходима быстрая помощь? — компания предлагает ремонт всех марок, установку ГБО и лояльную ценовую политику. Подбираете СТО — здесь найдёте выгодные условия и сервис с гарантией, с гарантией результата.
You actually make it seem so easy with your presentation but I find
this matter to be really something which I think I would never understand.
It seems too complicated and extremely broad for me.
I am looking forward for your next post, I’ll try to get the hang of it!
Review my site: Uganda safari holidays
Узнайте больше о преимуществах сотрудничества с фирмой — гарантированное качество, качество и широкий выбор решений! Посетите https://tdstyling.ru и просмотрите тарифы, контакты, а также публикации. Хотите сотрудничать — эта организация предлагает тематические ссылки, удобные варианты и лучшие условия.
Wow that was strange. I just wrote an very long comment but after
I clicked submit my comment didn’t show up. Grrrr…
well I’m not writing all that over again. Anyways, just wanted to say wonderful blog!
Как правильно определить вакансию курьера в доставке Яндекс и иметь высокий доход
I absolutely love your blog and find most of your post’s to be what precisely I’m looking for.
can you offer guest writers to write content for
you? I wouldn’t mind creating a post or elaborating
on a number of the subjects you write regarding here.
Again, awesome web site!
Hello. And Bye.
شیئر کرن لئی تہاڈا شکریہ۔ میں پریشان آں کہ میرے کول خلاقی خیالات دی کمی اے۔ ایہہ تہاڈا مضمون اے جہڑا مینوں امید نال بھردا اے۔ تہاڈا شکریہ
Подбираете медицинские справки онлайн без похода в поликлинику и лишних хлопот? На сайте https://z32-med.ru настоящий документ можно оформить в течение дня — от справок для плавания, санатория и школы до справки 095/у, справки 086/у, заключений КЭК и тестов. Опыт более 10 лет, сотрудничество с медучреждениями, и официальные формы подтверждают безопасность и официальный статус. Предлагаются доступные цены, широкий выбор услуг и курьерская доставка в Москве. Узнайте подробности — справка без ожидания, оформление за день, законные справки.
Howdy! This blog post could not be written much better!
Looking through this post reminds me of my previous
roommate! He continually kept talking about this.
I am going to send this article to him. Fairly certain he’ll have
a great read. I appreciate you for sharing!
Нужна медицинская книжка быстро для сотрудников или фирм? На https://cmc-clinic.ru в Москве подготовят или перевыпустят медицинскую книжку в течение дня — оперативно, официально и без ожидания. Заходите на сайт.
Thanks for ones marvelous posting! I definitely enjoyed
reading it, you’re a great author.I will make sure to bookmark your blog and will come back someday.
I want to encourage that you continue your great writing, have a
nice holiday weekend!
WOW just what I was searching for. Came here by searching for Solar Batteries Brisbane
With havin so much content do you ever run into any problems
of plagorism or copyright violation? My blog has a lot of unique content I’ve either created myself or outsourced but it seems a lot of it is popping it up all over
the web without my agreement. Do you know any solutions to help reduce
content from being stolen? I’d truly appreciate
it.
İşinizə davam edin və daha çox istifadəçi cəlb edin!
http://gamarik.li/index.php?option=com_content&view=article&id=66:aliekbercicek&catid=35:edebiyat&it
whoah this weblog is excellent i like studying
your posts. Stay up the good work! You know, a lot of
people are hunting around for this info, you can help
them greatly.
Really when someone doesn’t know after that its up to other people
that they will help, so here it occurs.
This design is spectacular! You most certainly
know how to keep a reader entertained. Between your
wit and your videos, I was almost moved to start my own blog (well,
almost…HaHa!) Great job. I really loved what you had to say,
and more than that, how you presented it. Too cool!
Hi it’s me, I am also visiting this web site regularly, this web site is
actually good and the viewers are truly sharing fastidious thoughts.
It’s not my first time to pay a quick visit this web
page, i am visiting this web page dailly and take nice data from here daily.
ко ланте Ко Ланте
Do you have a spam issue on this website; I also am a blogger, and I was wanting to know
your situation; we have created some nice procedures and we are
looking to swap strategies with other folks, be sure to shoot me an email if interested.
Hola! I’ve been following your web site for a long time now and finally got the courage
to go ahead and give you a shout out from Kingwood
Texas! Just wanted to mention keep up the good work!
Thank you a bunch for sharing this with all of us you really recognise what you’re talking approximately!
Bookmarked. Kindly also consult with my website =). We can have a hyperlink change contract among us
Everything is very open with a very clear clarification of
the challenges. It was really informative. Your website is very useful.
Many thanks for sharing!
Hi, just wanted to mention, I enjoyed this post.
It was practical. Keep on posting!
I think this is one of the most significant information for me.
And i am glad reading your article. But want to remark on some general
things, The web site style is perfect, the articles is really great :
D. Good job, cheers
Genuinely no matter if someone doesn’t be aware of after that
its up to other visitors that they will assist, so here it takes
place.
I’m not sure exactly why but this site is loading incredibly slow
for me. Is anyone else having this problem or is it a problem on my end?
I’ll check back later on and see if the problem still exists.
When someone writes an article he/she retains the plan of a user in his/her mind that how a user can know
it. Thus that’s why this post is perfect. Thanks!
These are actually impressive ideas in regarding blogging.
You have touched some fastidious points here. Any way keep up wrinting.
Hey there just wanted to give you a quick heads up.
The text in your article seem to be running off the screen in Ie.
I’m not sure if this is a formatting issue or something to
do with internet browser compatibility but I figured I’d post to let you know.
The design look great though! Hope you get the issue resolved soon.
Cheers
I’m gone to inform my little brother, that he should also
go to see this webpage on regular basis to get updated from hottest news update.
Can I simply say what a relief to find someone that actually knows what they are talking about over the internet.
You definitely understand how to bring a problem to light and make it important.
More people ought to check this out and understand this side
of the story. I was surprised you’re not more popular since you definitely possess the gift.
Wo xa fe gbegbe kolon karoti xa fe ra naxan xErEma new york sare xOrOxOE ra
In fact when someone doesn’t be aware of afterward its up to other viewers
that they will help, so here it takes place.
I read this piece of writing fully regarding the resemblance of
newest and previous technologies, it’s remarkable
article.
Excellent post! We are linking to this great content on our site.
Keep up the good writing.
شیئر کرن لئی تہاڈا شکریہ۔ میں پریشان آں کہ میرے کول خلاقی خیالات دی کمی اے۔ ایہہ تہاڈا مضمون اے جہڑا مینوں امید نال بھردا اے۔ تہاڈا شکریہ
4M Dental Implant Center Sann Diego
5643 Copley Ꭰr ste 210, San Diego,
ⅭΑ 92111, United Stateѕ
18582567711
oral implant
kews k16 nb300 кевс kews кевс к16 нб300 kews k16 nb300
This piece of writing will assist the internet people for
setting up new web site or even a weblog from start to end.
Hi there, I check your blog daily. Your humoristic style is awesome, keep it
up!
I’m curious to find out what blog platform you happen to be working with?
I’m experiencing some minor security problems with my latest blog and I would like to
find something more safe. Do you have any recommendations?
You really make it seem so easy with your presentation but I
find this topic to be actually something that I think I would never understand.
It seems too complicated and very broad for
me. I am looking forward for your next post, I will try to
get the hang of it!
Thanks for sharing such a fastidious thought, piece of writing is good, thats why i have read it entirely
Do you have a spam issue on this site; I also am a blogger, and I was wanting to know your situation; many of us have created some nice methods and we are looking to
trade strategies with others, why not shoot me an e-mail if interested.
Its like you learn my thoughts! You appear to grasp so much approximately this,
like you wrote the e book in it or something. I think that
you can do with a few percent to force the message home a little bit, however instead
of that, this is magnificent blog. An excellent read.
I’ll definitely be back.
Hi! I just wanted to ask if you ever have any problems with hackers?
My last blog (wordpress) was hacked and I ended up losing months of
hard work due to no backup. Do you have any solutions to protect against hackers?
I know this if off topic but I’m looking into starting my
own blog and was curious what all is needed to get setup?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very web savvy so I’m not 100% sure.
Any tips or advice would be greatly appreciated.
Thank you
Hi! Someone in my Facebook group shared this site with us so I came
to check it out. I’m definitely loving the information.
I’m book-marking and will be tweeting this to
my followers! Wonderful blog and excellent style and
design.
Admiring the commitment you put into your blog and in depth information you present.
It’s nice to come across a blog every once in a while that isn’t the same old rehashed information. Excellent read!
I’ve saved your site and I’m including your
RSS feeds to my Google account.
It’s the best time to make some plans for the future and it’s time to be happy.
I’ve read this post and if I could I want to suggest
you some interesting things or suggestions.
Perhaps you can write next articles referring to this article.
I desire to read even more things about it!
Hello to every one, for the reason that I am actually keen of reading this website’s
post to be updated daily. It includes nice
data.
my site – commercial alumimium cladding
Hello, I read your blogs regularly. Your story-telling style is awesome, keep doing
what you’re doing!
Have a look at my webpage נערות ליווי בצפון
I’m extremely impressed together with your writing skills and
also with the structure on your blog. Is this a paid subject or did you modify it yourself?
Anyway stay up the excellent quality writing, it’s rare to look a great weblog like this one these days..
Yesterday, while I was at work, my sister stole my apple ipad and tested to see if it can survive a thirty foot drop,
just so she can be a youtube sensation. My iPad is now broken and she has 83
views. I know this is completely off topic
but I had to share it with someone!
Feel free to visit my web blog … 안전 해외배팅사이트
Thanks for sharing your thoughts about riobet casino бонусы.
Regards
A motivating discussion is worth comment. I think that you ought to write more on this topic,
it might not be a taboo subject but usually people don’t speak about such topics.
To the next! Best wishes!!
Nice blog here! Also your site loads up fast!
What host are you using? Can I get your affiliate link to your host?
I wish my web site loaded up as quickly as yours lol
Here is my web blog; 안전 해외배팅사이트 추천
Good response in return of this difficulty with genuine arguments and describing
the whole thing regarding that.
Feel free to surf to my web blog – 안전 해외배팅사이트
I am really loving the theme/design of your site. Do you ever run into any
web browser compatibility problems? A few of my blog visitors have complained about my site
not working correctly in Explorer but looks great in Chrome.
Do you have any solutions to help fix this problem?
I go to see each day a few websites and information sites
to read posts, however this weblog offers quality based
content.
Feel free to visit my page: 안전 해외배팅사이트 추천
I’ve been browsing online more than 2 hours today, yet I never found any interesting article like
yours. It’s pretty worth enough for me. Personally, if all website owners and bloggers made good content as you did, the
net will be a lot more useful than ever before.
Here is my web site … commercial cladding contractors
Heya i’m for the first time here. I came across this board and I find It really useful & it helped me out a lot.
I hope to give something back and aid others like you helped me.
Hi there everyone, it’s my first visit at this website, and post is
actually fruitful in favor of me, keep up posting these
articles.
Here is my web-site 안전 해외배팅사이트 추천
Hi, i feel that i saw you visited my weblog thus i came to return the prefer?.I’m trying to to find issues to enhance my site!I guess its adequate to
use a few of your concepts!!
With havin so much content do you ever run into any problems
of plagorism or copyright infringement? My blog has a lot of completely
unique content I’ve either created myself or outsourced but it seems a lot of it is
popping it up all over the web without my authorization. Do
you know any solutions to help protect against content from being stolen? I’d certainly appreciate it.
What i don’t realize is in reality how you’re no longer actually a
lot more neatly-appreciated than you may be now. You’re so intelligent.
You understand therefore considerably when it comes to
this subject, made me in my view believe it from so many numerous angles.
Its like women and men aren’t fascinated unless it’s one thing to accomplish
with Girl gaga! Your personal stuffs great. At all times take care of it up!
Here is my page: נערות ליווי בצפון
Hello There. I found your blog using msn.
This is a very well written article. I’ll be sure
to bookmark it and come back to read more of your useful information. Thanks for the post.
I’ll certainly comeback.
кевс кевс kews кевс к16 нб300 kews k16 nb300
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to far added agreeable from you!
However, how could we communicate?
Refresh Renovation Broomfield
11001 Ԝ 120th Ave 400 suite 459a,
Broomfield, СO 80021, United Ѕtates
+13032681372
Improvements accessibility Backyard
Its such as you learn my mind! You seem to grasp so much approximately this, such as you wrote the guide in it or something.
I feel that you can do with a few percent to pressure the message house a bit, but other than that, that is fantastic blog.
A fantastic read. I’ll certainly be back.
Have you ever considered about adding a little bit more than just
your articles? I mean, what you say is valuable and all. However imagine if you added some great pictures or video clips to
give your posts more, “pop”! Your content is excellent but with images and clips, this site
could certainly be one of the greatest in its field.
Amazing blog!
I was suggested this website by my cousin. I’m not sure whether this
post is written by him as no one else know such detailed about my
difficulty. You’re amazing! Thanks!
Your way of describing the whole thing in this article is in fact nice, all be able
to without difficulty know it, Thanks a lot.
4M Dental Implant Center San Diego
5643 Copley Ⅾr ste 210, Sann Diego,
ϹA 92111, United Ꮪtates
18582567711
smile health
Hi, Neat post. There’s a problem with your site in web explorer,
could test this? IE nonetheless is the marketplace leader and a big component to other
folks will pass over your fantastic writing due to this problem.
My brother recommended I would possibly like this blog.
He was once entirely right. This submit truly made my day.
You cann’t imagine simply how so much time I had spent for this information! Thank
you!
Attractive section of content. I just stumbled upon your web site and
in accession capital to assert that I get in fact enjoyed account
your blog posts. Any way I will be subscribing to your augment and even I achievement you
access consistently quickly.
Ciatoto adalah platform judi online terpercaya yang menyediakan permainan togel dan slot dengan sistem fair play serta
peluang menang tinggi. Dengan layanan 24 jam, metode deposit yang lengkap, dan berbagai promo menarik,
Ciatoto menjadi pilihan utama para pecinta togel dan slot online di Indonesia.
Good day! I just wish to give you a huge thumbs up for your
great information you’ve got right here on this post.
I’ll be returning to your blog for more soon.
Great goods from you, man. I’ve be mindful your stuff prior to and you are simply too wonderful.
I really like what you have received right here, certainly like
what you’re saying and the way in which during which you assert it.
You make it entertaining and you still take care of to keep it smart.
I can not wait to read much more from you. That is really a tremendous website.
Hi, I do think this is an excellent web site. I stumbledupon it 😉 I will come back once again since I
saved as a favorite it. Money and freedom is the best way to change, may
you be rich and continue to guide other people.
Matondo mingi mpo na kokabola. Nazali komitungisa ete nazali na makanisi ya kokela te. Ezali lisolo na yo nde etondisi ngai na elikya. Matondi.
ко ланта ко ланта
Daily Style Market – Discover trendy products organized for easy browsing and selection.
Читать далее зеркало водка бет
Как лучше выбрать аудио библиотеку онлайн
Great post. I was checking constantly this blog and I
am impressed! Very helpful information particularly the last part 🙂
I care for such information a lot. I was seeking this certain information for a long time.
Thank you and best of luck.
This is a topic that’s close to my heart… Take care!
Exactly where are your contact details though?
Thanks for all the valuable content about Chicken Road and gambling.
https://chicken-road-gold.org/payments
I have been browsing on-line more than three hours lately, yet I never discovered any attention-grabbing article
like yours. It is pretty price sufficient for me.
Personally, if all webmasters and bloggers made good content as you did, the net will likely be much
more helpful than ever before.
You should take part in a contest for one of the highest quality sites on the internet.
I am going to highly recommend this blog!
Good day! I just want to give you a big thumbs up for
the excellent information you have here on this post.
I will be returning to your blog for more soon.
Stop by my web-site … 인투88
When I originally left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I receive four emails with
the same comment. There has to be a way you can remove me
from that service? Thanks!
Here is my web page: 안전 해외배팅사이트 추천
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me.
Appreciate it!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Ꮪtates
+19803517882
Homes for optimization space
ขอบคุณที่แบ่งปันนะคะ ฉันกังวลว่าตัวเองจะขาดไอเดียสร้างสรรค์ บทความของคุณนี่แหละที่ทำให้ฉันมีความหวัง ขอบคุณนะค
I’ve been surfing online more than three hours today, yet I never found
any interesting article like yours. It is pretty worth enough for me.
In my opinion, if all web owners and bloggers made good
content as you did, the net will be a lot
more useful than ever before.
Way cool! Some extremely valid points! I appreciate you penning this write-up and the rest of the
website is also very good.
Wow, this piece of writing is nice, my sister is analyzing these kinds of things,
therefore I am going to let know her.
Feel free to surf to my webpage commercial alumimium cladding
Kudos! Very good stuff.
Its like you read my mind! You seem to know a lot about this, like you wrote the book in it or something.
I think that you could do with some pics to drive the message home a bit,
but instead of that, this is great blog. A fantastic read.
I will certainly be back.
Feel free to visit my page; 안전한 해외배팅사이트 추천
https://finfreerollers.net/
Very good stuff, Cheers!
This info is worth everyone’s attention. Where can I find out more?
My homepage :: commercial cladding
Appreciate it. A lot of forum posts.
Heya i am for the first time here. I found this board and I find It
really helpful & it helped me out much. I’m hoping to give something back and help others like you aided me.
Great article.
Link exchange is nothing else except it is only placing the other person’s blog link on your page at
proper place and other person will also do similar in favor
of you.
Greetings I am so thrilled I found your site, I really found you by accident, while I was looking on Google for something else, Nonetheless I am here now and would just like to say
thank you for a remarkable post and a all round enjoyable blog (I also love the theme/design), I don’t
have time to read through it all at the minute but I have bookmarked it and also
added in your RSS feeds, so when I have time I will be
back to read a lot more, Please do keep up the fantastic job.
10 euros offert paris sportif|10 euros offert sans dépôt paris sportif|10 meilleurs sites de paris sportifs|100 euro offert paris
sportif|100 euros offert paris sportif|100 euros remboursé
paris sportifs|100 offert pari sportif|100 offert paris sportif|100 remboursé paris sportif|100e offert pari sportif|abandon paris sportif tennis|abandon tennis paris sportif|addiction paris sportif forum|age paris sportif
belgique|aide au pari sportif|aide au paris sportif|aide aux paris sportif|aide aux
paris sportifs|aide pari sportif|aide pari sportif football|aide parie sportif|aide paris sportif|aide paris sportif foot|aide
paris sportif gratuit|aide paris sportifs|aide pour paris
sportif|algorithme de paris sportif|algorithme excel paris sportif|algorithme
gratuit paris sportif|algorithme pari sportif|algorithme paris sportif|algorithme paris sportif avis|algorithme paris sportif basket|algorithme
paris sportif excel|algorithme paris sportif gratuit|algorithme paris sportif tennis|algorithme
paris sportifs|algorithme pour paris sportif|analyse cote paris sportif|analyse de paris sportif|analyse match paris sportif|analyse pari sportif|analyse paris sportif|analyse paris sportif foot|analyse paris sportif football|analyse paris sportif gratuit|analyse paris sportifs|ancienne cote paris sportif|api cote paris sportif|app paris sportif sans argent|appli
de paris sportif|appli de paris sportif sans argent|appli de
paris sportifs|appli pari sportif|appli pari sportif gratuit|appli parie sportif|appli paris sportif|appli paris sportif
avec paypal|appli paris sportif belgique|appli
paris sportif entre amis|appli paris sportif gratuit|appli paris sportif sans argent|appli paris sportif suisse|appli paris sportifs|application aide paris sportif|application algorithme paris sportif|application analyse paris sportif|application android
paris sportif|application bankroll paris sportif|application conseil paris sportif|application de pari sportif|application de
parie sportif|application de paris sportif|application de paris sportif en afrique|application de paris sportif en cote d’ivoire|application de paris sportif en ligne|application de paris sportif gratuit|application de paris sportif
international|application de paris sportif suisse|application de paris sportifs|application faux paris sportifs|application gestion bankroll
paris sportif|application gestion paris sportif|application ia paris
sportif|application pari sportif gratuit|application paris sportif|application paris sportif
android|application paris sportif argent fictif|application paris sportif belgique|application paris sportif canada|application paris sportif espagne|application paris sportif espagnol|application paris sportif fictif|application paris sportif france|application paris sportif gratuit|application paris sportif gratuit entre amis|application paris sportif maroc|application paris sportif offre de
bienvenue|application paris sportif paypal|application paris sportif sans argent|application paris sportif
sans justificatif de domicile|application paris sportif suisse|application paris sportif usa|application paris sportif virtuel|application pour faire des paris
sportifs|application pour gerer ses paris sportif|application pour les paris sportifs|application pour pari sportif|application pour paris sportif|application pour paris sportifs|application statistique paris sportif|application suivi paris sportif|applications de paris sportifs|applications
paris sportifs|applis paris sportif|applis paris sportifs|apprendre
a faire des paris sportifs|argent facile
paris sportif|argent offert paris sportifs|argent offert sans depot paris sportif|argent paris sportif|argent paris sportifs|argent paris sportifs impots|argent sans depot
paris sportif|arjel paris sportif|arjel paris sportifs|astuce gagner paris sportif|astuce pari
sportif|astuce paris sportif|astuce paris sportif basket|astuce paris
sportif foot|astuce paris sportif forum|astuce paris sportif tennis|astuce paris sportifs|astuce pour gagner au pari sportif|astuce pour gagner au paris sportif|astuce pour
gagner paris sportif|astuce pour paris sportif|astuces paris sportifs|astuces paris sportifs en ligne|astuces paris
sportifs foot|astuces pour gagner aux paris sportifs|autorisation paris sportif france|avis pari sportif|avis
paris sportif|avis paris sportif foot|avis site de paris sportif|avis site paris sportif|avis sur les
paris sportifs|avis sur paris sportif|avis tipster paris sportif|aweh signification paris sportif|bankroll 100 euros
paris sportifs|bankroll management paris sportif|bankroll paris sportif|bankroll paris sportif
excel|bankroll paris sportif gratuit|bankroll paris sportifs|basket paris sportif|belgique france
paris sportif|belgique paris sportifs|bonus bienvenue paris sportif|bonus bienvenue paris sportifs|bonus cash paris
sportif|bonus de bienvenue paris sportif|bonus de bienvenue paris sportif
belgique|bonus de bienvenue sans depot paris sportif|bonus de depot paris sportif|bonus de paris sportifs|bonus depot paris sportif|bonus en cash paris sportif|bonus gratuit paris sportif|bonus
gratuit sans depot paris sportif|bonus pari sportif|bonus paris sportif|bonus paris sportif
belgique|bonus paris sportif betclic|bonus paris sportif
cash|bonus paris sportif en ligne|bonus paris sportif france pari|bonus paris
sportif retirable|bonus paris sportif sans depot|bonus paris sportif sans
dépôt|bonus paris sportif unibet|bonus paris sportifs|bonus sans depot paris sportif|bonus sans depot paris sportif belgique|bonus
sans dépôt paris sportif|bonus sans dépôt paris sportif hors arjel|bonus site de paris sportif|bonus site pari sportif|bonus site paris sportif|bonus
sites de paris sportifs|bonus unibet paris sportif|bookmaker paris sportif|bookmaker paris sportif gratuit|bookmaker paris sportifs|bookmaker sportif|bookmakers paris sportif|bookmakers paris
sportifs|bookmakers paris sportifs en ligne|but contre son camp paris sportif|but sur penalty paris sportif|buteur paris
sportif|c’est quoi handicap paris sportif|c’est quoi une cote paris sportif|calcul
anti perte paris sportif|calcul combinaison pari sportif|calcul
cote pari sportif|calcul cote paris sportif|calcul couverture paris sportif|calcul de
cote paris sportif|calcul des cotes paris sportifs|calcul dnb paris sportifs|calcul double chance paris sportif|calcul gain paris sportif|calcul mise
paris sportif|calcul pari sportif|calcul paris sportif|calcul paris sportif multiple|calcul pourcentage cote paris sportif|calcul probabilité paris sportif|calcul rentabilité paris sportifs|calcul roi paris sportif|calcul systeme paris sportif|calcul trj paris sportifs|calculateur cote
paris sportif|calculateur de cote paris sportif|calculateur de mise paris sportif|calculateur de paris sportif|calculateur paris sportif|calculatrice arbitrage paris sportif|calculatrice paris sportif|calculer cote paris sportif|calculer gain paris sportif|calculer probabilité paris sportifs|calculer roi
paris sportifs|calculer une cote pari sportif|calculer une cote paris sportif|carte cadeau paris sportif|carte
pcs paris sportif|carte prépayée paris sportifs|cash out pari sportif|cash out paris sportif|cash out
paris sportifs|casino en ligne paris sportif|casino paris
sportif en ligne|champions league paris sportif|chute de cote paris sportif|classement des
meilleurs sites de paris sportifs|classement meilleur site de paris
sportif|code barre paris sportif|code bonus paris sportif|code paris
sportif|code promo pari sportif|code promo paris sportif|code promo paris sportif sans depot|code promo paris sportif sans dépôt|code promo sans depot paris sportif|code promo site paris sportif|combien de temps pour
encaisser un paris sportif|combien de temps pour retirer un paris sportif|combien miser paris sportifs|combine paris sportif|combines paris
sportifs|combiné pari sportif|combiné paris sportif|combiné
paris sportif conseil|combiné paris sportif
du jour|combiné paris sportif pronostic|comment analyser un paris sportif|comment arreter de jouer
aux paris sportifs|comment arreter les paris sportif|comment arreter
les paris sportifs|comment arrêter les paris sportifs|comment bien gagner au paris sportif|comment bien jouer au paris sportif|comment bien miser paris sportif|comment
ca marche les paris sportif|comment calculer cote paris sportif|comment calculer gain paris sportif|comment calculer
les cotes des paris sportifs|comment calculer une cote de paris sportif|comment calculer une cote pari sportif|comment calculer une cote paris sportif|comment comprendre les paris sportifs|comment creer
un vip paris sportif|comment créer un algorithme paris sportif|comment créer un site de paris sportif|comment devenir riche avec les paris
sportifs|comment etre rentable paris sportif|comment etre
sur de gagner au paris sportif|comment faire de bon paris sportif|comment faire des parie sportif|comment faire des
paris sportif|comment faire des paris sportif gagnant|comment faire des paris sportifs|comment faire pari sportif|comment faire paris sportif|comment faire pour arreter les paris
sportifs|comment faire pour gagner au paris sportif|comment faire pour gagner les
paris sportifs|comment faire un bon pari sportif|comment faire un bon paris
sportif|comment faire un pari sportif|comment faire un parie sportif|comment faire un paris sportif|comment
faire une montante paris sportif|comment fonctionne les cotes dans les paris sportifs|comment fonctionne les cotes des paris sportifs|comment fonctionne les paris
sportifs|comment fonctionne paris sportifs|comment fonctionne un pari sportif|comment fonctionnent les cotes dans les paris sportifs|comment fonctionnent
les cotes dans les paris sportifs grand oral|comment fonctionnent les cotes de paris sportif|comment fonctionnent les paris sportifs|comment fonctionnent les paris sportifs grand oral|comment fonctionnent
les paris sportifs grand oral maths|comment fonctionnent les paris sportifs maths|comment gagner a coup sur au paris sportif|comment gagner
a tous les coups au paris sportif|comment gagner
a tout les coup au paris sportif|comment gagner au pari sportif|comment gagner au
pari sportif football|comment gagner au paris sportif|comment gagner au paris sportif a coup sur|comment gagner
au paris sportif foot|comment gagner au paris sportif
forum|comment gagner au paris sportif tennis|comment gagner au paris
sportifs|comment gagner aux paris sportif|comment gagner aux paris sportifs|comment gagner aux paris sportifs foot|comment gagner aux paris sportifs
livre|comment gagner aux paris sportifs sur le long
terme|comment gagner avec les paris sportifs|comment gagner dans les paris sportifs|comment gagner de l argent avec les paris
sportifs|comment gagner de l’argent au paris sportif|comment gagner de l’argent aux paris sportifs|comment gagner de l’argent avec les paris
sportifs|comment gagner de l’argent paris sportif|comment
gagner de l’argent sur les paris sportifs|comment gagner de l’argent
sur paris sportif|comment gagner des paris sportif|comment gagner des paris sportifs|comment gagner
en paris sportif|comment gagner facilement au paris sportif|comment gagner les paris sportifs|comment gagner paris sportif|comment gagner paris sportif foot|comment gagner paris sportifs|comment gagner sa
vie avec les paris sportifs|comment gagner ses paris sportif|comment gagner sur les
paris sportif|comment gagner sur les paris sportifs|comment gagner tout le temps
au paris sportif|comment gagner un pari sportif|comment gagner un paris
sportif|comment gerer une bankroll paris sportif|comment
gérer sa bankroll paris sportif|comment jouer au pari sportif|comment jouer au paris sportif|comment jouer au paris
sportif foot|comment jouer aux paris sportifs|comment
jouer paris sportif|comment marche cote paris sportif|comment marche les cotes paris sportif|comment marche les
paris sportif|comment marche les paris sportifs|comment marche paris sportif|comment marche un pari sportif|comment marche un paris sportif|comment marchent les cotes paris sportif|comment marchent les paris
sportifs|comment miser au paris sportif|comment miser paris sportif|comment monter sa bankroll paris sportif|comment ne jamais perdre
au paris sportif|comment parier sportif|comment reussir au paris sportif|comment reussir les paris sportif|comment reussir paris sportif|comment sont calculer les cotes de paris sportif|comment sont calculées
les cotes des paris sportifs|comment sont calculés les cotes des paris sportifs|comment sont
faites les cotes des paris sportifs|comment toujours gagner au paris sportif|comment
ça marche les paris sportifs|comparaison bonus paris sportifs|comparaison cote pari sportif|comparaison des
cotes paris sportifs|comparateur cote pari sportif|comparateur cote paris
sportif|comparateur cotes paris sportif|comparateur cotes paris sportifs|comparateur de
cote pari sportif|comparateur de cote paris sportif|comparateur de cotes paris sportifs|comparateur de côtes paris
sportifs|comparateur de paris sportif|comparateur de
site de paris sportif|comparateur de site paris sportif|comparateur
de sites de paris sportifs|comparateur pari sportif|comparateur paris
sportif|comparateur paris sportifs|comparateur site de paris
sportif|comparateur site pari sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif bonus
paris sportifs|comparatif cote pari sportif|comparatif cote paris sportif|comparatif cotes paris sportifs|comparatif
des sites de paris sportifs|comparatif offre de bienvenue paris sportif|comparatif offre
paris sportif|comparatif pari sportif|comparatif pari sportif en ligne|comparatif paris sportif|comparatif paris sportif bonus|comparatif paris sportif en ligne|comparatif
paris sportifs|comparatif paris sportifs en ligne|comparatif
site de paris sportif|comparatif site paris sportif|comparatif site
paris sportifs|comparatif sites de paris sportifs|comparatif sites paris sportifs|comparer
les cotes paris sportifs|comprendre cote paris sportif|comprendre handicap paris sportif|comprendre les cotes des paris sportifs|comprendre les cotes
paris sportif|comprendre les cotes paris sportifs|comprendre les handicap paris sportif|compte de paris sportif|compte
démo paris sportif|compte finance paris sportif|compte financer paris sportif|compte financier paris sportif|compte
financé paris sportif|compte pari sportif|compte
paris sportif|compte paris sportif financé|conseil de paris sportif|conseil de paris sportifs|conseil
en paris sportif|conseil en paris sportifs|conseil pari
sportif|conseil pari sportif gratuit|conseil paris sportif|conseil paris sportif aujourd’hui|conseil paris sportif du jour|conseil paris sportif foot|conseil paris sportif gratuit|conseil paris
sportif ligue des champions|conseil paris sportif
nba|conseil paris sportif pronostic|conseil paris sportif rmc|conseil paris sportif tennis|conseil paris sportifs|conseil pour gagner au paris
sportif|conseil pour paris sportif|conseil sur les paris sportifs|conseille paris sportif|conseiller en paris sportifs|conseiller paris sportif|conseils de paris sportifs|conseils
en paris sportifs|conseils paris sportifs|conseils paris sportifs foot|conseils paris sportifs gratuit|conseils paris sportifs tennis|conseils pour paris sportifs|cote a 100
paris sportif|cote a 2 paris sportif|cote anglaise paris sportif|cote
de 2 paris sportif|cote de pari sportif|cote de paris sportif|cote des paris sportifs|cote maximum paris sportif|cote minimum paris sportif|cote pari sportif|cote pari sportif comment ça marche|cote pari sportif real madrid|cote pari sportif rugby|cote parie sportif|cote paris sportif|cote paris sportif belgique|cote paris sportif calcul|cote paris sportif definition|cote paris sportif euro|cote paris sportif explication|cote
paris sportif foot|cote paris sportif france belgique|cote paris sportif france espagne|cote paris sportif ligue des
champions|cote paris sportif moto gp|cote paris sportif psg|cote paris sportif psg arsenal|cote
paris sportif rugby|cote paris sportif tennis|cote paris
sportifs|cote pour paris sportifs|cote sportif foot|cote sportif rugby|cote à 1000 paris sportif|cotes
de paris sportifs|cotes pari sportif|cotes paris sportif|cotes paris sportifs|cotes paris sportifs foot|coupe de france
paris sportif|créer un algorithme paris sportif|créer un compte paris sportif|créer un site de paris sportif
en ligne|dans les paris sportifs que signifie handicap|declarer ses gains paris sportif|definition cash out paris sportif|definition cote paris sportif|definition handicap paris sportif|depot 5 euros paris
sportif|depot double paris sportif|depot minimum 5 euro paris sportif|depot minimum paris
sportif|depot paris sportif|depuis quand existe les paris sportif en france|devenir
riche avec les paris sportifs|devenir riche avec paris sportifs|disqualification tennis paris sportif|dnb en paris sportif|dnb pari sportif|dnb paris sportif|dnb paris sportif definition|dnb paris sportifs|doit
on declarer les gains de paris sportif|déclarer gains paris sportifs|déclarer gains paris sportifs hors arjel|définition bankroll paris sportif|dépôt minimum 1 euro paris sportif|dépôt minimum 5 euro paris sportif|ecart
de jeux tennis paris sportif|erreur de cote paris sportif|est ce que les
gains des paris sportifs sont imposables|est-ce que les
prolongation compte dans un pari sportif|etre sur de gagner
au paris sportif|euro paris sportif|evenement sportif a paris|evenement sportif paris|evenement sportif paris 2025|evenement sportif paris aujourd hui|evenement sportif paris aujourd’hui|evenement
sportif paris ce week end|evenements sportif paris|evenements sportifs paris|evenements
sportifs paris 2025|evenements sportifs à paris|evolution cote paris sportif|evolution cotes
paris sportifs|evolution des cotes paris sportifs|explication cote pari sportif|explication cote paris sportif|explication handicap paris sportif|explication pari sportif|explication paris sportif|face a
face hockey paris sportif|faire des paris sportif|faire des paris
sportif avec paypal|faire des paris sportifs|faire fortune paris
sportifs|faire un pari sportif|faire un paris sportif|faut il déclarer les gains de paris sportifs|faut il déclarer ses
gains paris sportifs|fichier excel gestion bankroll paris sportif|fiscalité gains paris sportifs|foot paris sportif|football et paris sportifs|forfait tennis paris sportif|formation paris sportif gratuit|forum de paris sportif|forum de paris
sportifs|forum pari sportif|forum parie sportif|forum paris sportif|forum paris sportif foot|forum paris sportif
gratuit|forum paris sportif nba|forum paris sportif tennis|forum paris
sportifs|forum sur les paris sportifs|forum tennis paris sportif|francaise des jeux pari sportif|francaise des jeux paris sportif|francaise
des jeux paris sportifs|france 2 paris sportif|france 2
paris sportifs|france belgique paris sportif|france espagne
paris sportif|france pari sportif|france pari
sportif brest|france paris sportif|france paris sportifs|france pologne paris sportif|france portugal paris sportif|france suisse
paris sportifs|france tunisie paris sportifs|france-pari – paris sportifs|gagnant pari sportif|gagnant paris sportif|gagnant paris sportif bayern|gagnante paris sportif|gagne au paris sportif|gagner
10 euros par jour aux paris sportifs|gagner
100 euros par jour paris sportif|gagner 1000 euros par mois paris sportifs|gagner 10000 euros paris sportif|gagner 2000 euros par mois paris
sportif|gagner 50 euros par jour paris sportif|gagner a coup sur au paris sportif|gagner a coup
sur pari sportif|gagner a tous les coup paris sportif|gagner argent avec paris
sportifs|gagner argent pari sportif|gagner argent paris sportif|gagner argent paris sportifs|gagner au pari sportif|gagner
au paris sportif|gagner au paris sportif a coup sur|gagner au paris sportif foot|gagner au paris sportif forum|gagner au paris sportif à coup sur|gagner aux paris sportif|gagner aux
paris sportifs|gagner aux paris sportifs pdf|gagner beaucoup d’argent paris sportif|gagner de l argent grace aux paris sportifs|gagner de
l argent pari sportif|gagner de l argent paris sportif|gagner de l argent paris sportifs|gagner de l’argent au paris
sportif|gagner de l’argent aux paris sportifs|gagner de
l’argent avec les paris sportifs|gagner de l’argent avec paris sportif|gagner de l’argent avec paris sportifs|gagner de
l’argent grace au paris sportif|gagner de l’argent grace aux paris
sportifs|gagner de l’argent pari sportif|gagner de l’argent paris sportif|gagner de l’argent
paris sportifs|gagner de l’argent sur les paris
sportifs|gagner des paris sportif|gagner des paris sportifs|gagner les paris sportifs|gagner pari sportif|gagner paris
sportif|gagner paris sportif foot|gagner paris sportif forum|gagner paris sportif tennis|gagner paris sportifs|gagner sa vie avec les paris
sportif|gagner sa vie avec les paris sportifs|gagner sa
vie avec paris sportifs|gagner ses paris sportifs|gagner
à coup sur paris sportif|gagner à tous les coups paris sportifs|gain maximum paris sportif|gain pari sportif|gain pari sportif imposable|gain pari sportif impot|gain paris
sportif|gain paris sportif imposable|gain paris sportif impot|gain paris sportif impôt|gains paris sportif|gains paris sportif imposable|gains paris
sportifs|gains paris sportifs imposable|gains paris sportifs imposables|gains paris sportifs sont
ils imposables|gerer bankroll paris sportif|gerer sa bankroll paris sportif|gerer une bankroll paris sportif|gestion bankroll paris sportif|gestion bankroll paris sportifs|gestion bankroll paris
sportifs excel|gestion de bankroll paris sportif|gestion de bankroll paris sportif application|gestion de bankroll paris sportifs|gestion de mise paris sportif|gestion paris sportifs v2
5 gratuit|gg signification paris sportif|gros combiné paris
sportif|gros gain paris sportif|grosse cote paris sportif pronostic|grosse mise
paris sportif|groupe paris sportif gratuit|groupe telegram paris sportif gratuit|groupement
de joueurs paris sportifs|handicap 0 paris sportif|handicap 1 paris
sportif|handicap 5 paris sportif|handicap au paris
sportif|handicap basket paris sportif|handicap dans les paris sportifs|handicap
en paris sportif|handicap europeen paris sportif|handicap européen paris sportifs|handicap mi temps paris sportif|handicap pari
sportif|handicap paris sportif|handicap paris sportif basket|handicap paris sportif explication|handicap
paris sportif foot|handicap paris sportif rugby|handicap paris sportifs|handicap rugby paris sportif|handicap tennis paris sportif|historique cote paris sportif|historique des cotes paris
sportifs|hockey paris sportif|hockey sur glace paris sportif|hors arjel paris sportif|hweh signification paris sportif|imposition gain pari sportif|imposition gain paris sportif|imposition gains paris sportifs|imposition paris sportif france|impot gain paris sportif|impot paris
sportif france|impot sur gain paris sportif|je gagne ma vie avec les paris sportifs|jeu de pari
sportif gratuit|jeu de paris sportif en ligne|jeu de paris sportif gratuit|jeu paris sportif gratuit|jeu
paris sportif sans argent|jeux de parie sportif|jeux de
paris sportif|jeux de paris sportif en ligne|jeux de paris
sportif gratuit|jeux de paris sportifs|jeux olympiques paris sportifs|jeux paris sportif|jeux paris sportif gratuit|jeux paris sportif
virtuel|jeux paris sportifs en ligne|jouer au paris sportif|jouer
paris sportif|joueur absent paris sportif|joueur blesse paris
sportif|joueur caen paris sportif|joueur de caen pari sportif|joueur de foot paris sportif|joueur decisif
paris sportif|joueur décisif paris sportif|joueur italien paris sportif|joueur paris sportif|joueur professionnel
paris sportif|joueur qui se blesse paris sportif|joueur sanctionne pari sportif|joueur suspendu paris sportif|joueurs italiens paris sportifs|l’argent des paris sportifs est il imposable|la cote paris sportif|la francaise des jeux paris sportif|la martingale paris sportif|la
martingale paris sportifs|la meilleur application de paris sportif|la meilleur application paris sportif|la
meilleur technique pour gagner au paris sportif|la méthode secrète pour gagner aux paris sportifs pdf|la plus grosse cote gagner paris
sportif|la plus grosse cote paris sportif|ldem paris sportif signification|le
marché des paris sportifs|le meilleur site de pari sportif|le meilleur site de paris sportif|le meilleur site de paris sportif en ligne|le meilleur
site de paris sportifs|le plus gros gain au paris
sportif|le plus gros paris sportif|le plus gros paris sportif du monde|les 10 meilleurs sites de paris sportifs|les 10 meilleurs sites de paris sportifs en afrique|les 17 secrets pour gagner rapidement
aux paris sportifs|les 17 secrets pour gagner rapidement aux paris sportifs pdf|les application de paris sportif|les applications paris sportifs|les bonus paris sportifs|les bookmakers paris sportifs|les cotes paris sportifs|les gains de paris
sportifs sont ils imposables|les gains des paris sportifs sont ils imposables|les jeux de paris sportifs|les
meilleur paris sportif|les meilleures applications
de paris sportifs|les meilleurs applications de paris sportifs|les
meilleurs bonus paris sportif|les meilleurs bonus paris sportifs|les meilleurs cotes paris sportif|les meilleurs paris sportifs|les meilleurs paris sportifs du jour|les meilleurs site de paris sportif|les meilleurs
site de paris sportifs|les meilleurs sites de
pari sportif|les meilleurs sites de paris sportifs|les meilleurs sites de paris sportifs en ligne|les paris sportif|les paris sportif avis|les paris sportifs|les paris sportifs
comment ça marche|les paris sportifs en france|les paris sportifs en ligne|les paris sportifs
en ligne comprendre jouer gagner|les paris sportifs en ligne comprendre
jouer gagner pdf|les paris sportifs les plus rentables|les plus gros gagnant paris sportif|les plus gros gains
au paris sportifs|les plus gros gains paris sportifs|les
plus gros paris sportif|les plus grosse cote paris sportif|les plus grosses pertes paris sportifs|les sites de paris sportifs|les sites de
paris sportifs autorisés en france|les sites de paris sportifs en france|les
sites de paris sportifs en ligne|les sites de paris sportifs francais|ligue
1 paris sportif|ligue 1 paris sportifs|ligue 2 paris sportif|ligue des champions paris sportif|limite de gains paris sportifs|limite
de mise paris sportif|limite gain paris sportif|limite mise paris sportifs|liste de paris sportif|liste des
paris sportifs|liste des site de paris sportif|liste des sites de paris sportifs|liste pari sportif|liste paris sportif|liste
paris sportif pdf|liste site de paris sportif|liste site pari sportif|liste site paris sportif|liste site paris sportif arjel|liste sites paris sportifs|logiciel algorithme
paris sportif|logiciel algorithme paris sportif gratuit|logiciel analyse paris sportif|logiciel calcul
paris sportif|logiciel de pari sportif|logiciel de paris sportif|logiciel
de paris sportif gratuit|logiciel gestion bankroll paris sportif
gratuit|logiciel gestion de bankroll paris sportif|logiciel gestion paris sportif|logiciel gestion paris sportif gratuit|logiciel gestion paris sportifs|logiciel pari sportif|logiciel paris sportif|logiciel paris
sportif gratuit|logiciel paris sportifs|logiciel paris
sportifs foot sur 2 matchs|logiciel pour paris
sportif|logiciel pour paris sportifs|logiciel prediction paris sportif|logiciel probabilité paris sportif|logiciel
prédiction paris sportif|logiciel statistique paris sportifs|logiciel variation de cote paris sportif|loi sur les paris sportifs en france|magic calculator paris sportif|marché des paris
sportifs|marché des paris sportifs en france|marché des paris sportifs
en ligne|martingale pari sportif|martingale paris sportif|martingale paris sportif excel|martingale
paris sportif forum|martingale paris sportif interdit|martingale paris sportifs|match abandonné paris
sportif|match annulé ou reporté paris sportifs|match
annulé paris sportif|match arrete paris sportif|match interrompu paris sportif|match interrompu tennis
paris sportif|match interrompu tennis pluie paris sportif|match nul boxe
paris sportif|match pari sportif|match paris sportif|match reporté
paris sportif|match suspendu paris sportif|match suspendu tennis
paris sportif|match truqué paris sportif|matchs truqués
paris sportifs|meilleur algorithme paris sportif|meilleur algorithme paris sportif gratuit|meilleur app
de paris sportif|meilleur app de paris sportifs|meilleur app
paris sportif|meilleur appli de pari sportif|meilleur appli de paris sportif|meilleur appli pari sportif|meilleur appli paris
sportif|meilleur appli paris sportif forum|meilleur
appli paris sportifs|meilleur application conseil paris sportif|meilleur application de paris sportif|meilleur
application de paris sportif en afrique|meilleur application pari sportif|meilleur application paris sportif|meilleur application paris
sportif belgique|meilleur application pour les paris sportif|meilleur
application pour pari sportif|meilleur bonus de bienvenue
paris sportif|meilleur bonus pari sportif|meilleur bonus paris sportif|meilleur bonus paris
sportif sans depot|meilleur bonus paris sportifs|meilleur bonus site de paris
sportif|meilleur bonus site pari sportif|meilleur bonus site paris sportif|meilleur bookmaker paris sportif|meilleur combiné paris sportif|meilleur conseil
paris sportif|meilleur cote de paris sportif|meilleur cote pari sportif|meilleur cote paris sportif|meilleur cote paris sportif aujourd’hui|meilleur cote
site paris sportif|meilleur forum paris sportifs|meilleur gain paris
sportif|meilleur ia paris sportif|meilleur methode pour gagner au paris sportif|meilleur offre bienvenue paris sportif|meilleur offre bonus paris sportif|meilleur offre de bienvenue paris sportif|meilleur
offre de bienvenue paris sportifs|meilleur offre pari sportif|meilleur offre paris sportif|meilleur offre
paris sportif en ligne|meilleur pari sportif|meilleur pari sportif du jour|meilleur pari sportif en ligne|meilleur paris sportif|meilleur
paris sportif aujourd’hui|meilleur paris sportif du jour|meilleur paris
sportif en ligne|meilleur paris sportif foot|meilleur promo paris sportif|meilleur pronostic paris sportif|meilleur site de conseil paris sportif|meilleur site de pari sportif|meilleur site de pari sportif en ligne|meilleur site de paris sportif|meilleur site de paris sportif avis|meilleur
site de paris sportif belgique|meilleur site de paris sportif canada|meilleur site de
paris sportif en france|meilleur site de paris sportif en ligne|meilleur site de paris sportif football|meilleur
site de paris sportif forum|meilleur site de paris sportif
france|meilleur site de paris sportif hors arjel|meilleur site de paris sportif international|meilleur site de paris sportif
suisse|meilleur site de paris sportifs|meilleur site de paris sportifs en ligne|meilleur site pari sportif|meilleur site pari sportif en ligne|meilleur site pari sportif
france|meilleur site paris sportif|meilleur site paris sportif
avis|meilleur site paris sportif belgique|meilleur site paris sportif canada|meilleur site paris
sportif en ligne|meilleur site paris sportif foot|meilleur site paris sportif forum|meilleur site paris sportif
france|meilleur site paris sportif hors arjel|meilleur site paris sportif nba|meilleur
site paris sportif rugby|meilleur site paris sportif suisse|meilleur site paris sportifs|meilleur site pour
pari sportif|meilleur site pour paris sportif|meilleur
site pronostic paris sportif|meilleur strategie paris sportif|meilleur technique de paris sportif|meilleur technique paris sportif|meilleur technique pour gagner au paris sportif|meilleure appli de paris sportif|meilleure appli de
paris sportifs|meilleure appli pari sportif|meilleure appli
paris sportif|meilleure appli paris sportifs|meilleure application de
paris sportif|meilleure application de paris sportifs|meilleure application pari sportif|meilleure application paris sportif|meilleure application paris sportif android|meilleure application paris sportifs|meilleure offre paris sportif|meilleure site paris sportif|meilleure strategie paris sportif|meilleures applications de
paris sportifs|meilleures applications paris sportifs|meilleures cotes paris sportifs|meilleures offres paris sportifs|meilleures stratégies paris sportifs|meilleurs
appli paris sportif|meilleurs application de paris sportifs|meilleurs application paris sportif|meilleurs applications paris sportifs|meilleurs bonus paris sportifs|meilleurs cote
paris sportif|meilleurs cotes paris sportifs|meilleurs offres paris
sportifs|meilleurs paris sportifs|meilleurs paris sportifs
du jour|meilleurs site de pari sportif|meilleurs site de
paris sportif|meilleurs site de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs site paris sportif|meilleurs sites de paris sportifs|meilleurs sites de paris sportifs en ligne|meilleurs sites paris sportif|meilleurs sites paris sportifs|methode abc
paris sportif|methode de paris sportif|methode gagnante paris sportifs|methode gagner paris sportif|methode infaillible paris sportifs|methode
martingale paris sportif|methode mathematique paris sportif|methode mathematique pour gagner au
paris sportif|methode paris sportif|methode paris sportif foot|methode paris sportif forum|methode paris sportif tennis|methode paris
sportifs|methode pour gagner au paris sportif|methode pour gagner paris sportif|methodes paris sportifs|minimum depot
paris sportif|mise au jeu pari sportif|mise maximum pari sportif|mise maximum paris sportif|mise minimum paris
sportif|mise moyenne paris sportif|mise paris sportif|moins de 4 5 but paris sportif|montant maximum paris sportif|montant paris
sportif|montante pari sportif|montante parie sportif|montante paris sportif|montante paris sportifs|montantes paris sportifs|multiple pari
sportif|multiple paris sportif|multiple paris sportifs|multiples paris sportifs|méthode calcul paris sportif|méthode match nul paris
sportifs|méthode mathématique pour gagner au paris sportif|méthode paris sportif
forum|méthode paris sportif hockey|nba pari sportif|nba paris sportif|nba paris sportifs|nouveau
paris sportif|nouveau site de pari sportif|nouveau site de paris
sportif|nouveau site de paris sportif en ligne|nouveau site de paris sportifs|nouveau site pari
sportif|nouveau site paris sportif|nouveau site paris sportif france|nouveau site paris sportifs|nouveaux sites
de paris sportifs|nouveaux sites paris sportifs|nouvelle appli paris sportif|nouvelle application de
paris sportif|numero de match paris sportif|numero match
paris sportif|offre 100 euros paris sportif|offre appli pari sportif|offre bienvenu paris sportif|offre
bienvenue pari sportif|offre bienvenue paris sportif|offre bienvenue paris sportifs|offre bienvenue site
paris sportif|offre bonus paris sportif|offre de bienvenu
paris sportif|offre de bienvenue pari sportif|offre de bienvenue paris sportif|offre
de bienvenue paris sportif belgique|offre de bienvenue paris sportif sans depot|offre de bienvenue paris sportif sans dépôt|offre
de bienvenue paris sportifs|offre de bienvenue sans depot paris sportif|offre de
bienvenue site paris sportif|offre euro paris sportif|offre pari sportif euro|offre paris sportif|offre
paris sportif belgique|offre paris sportif cash|offre paris sportif coupe du monde|offre
paris sportif hors arjel|offre paris sportif remboursé|offre paris sportif remboursé
cash|offre paris sportif sans depot|offre promo paris sportif|offre remboursement paris sportif|offre sans
depot paris sportif|offre site paris sportif|offres bienvenue paris sportifs|offres de bienvenue paris sportifs|ou
faire des paris sportif|ou faire des paris sportif en espagne|ou faire
des paris sportifs|outil répartiteur de mise paris sportif|outils repartiteur de mises paris sportif|ouverture compte paris sportifs|ouvrir un compte paris sportif|pack de bienvenue paris
sportif|pack de bienvenue paris sportif hors arjel|pari en ligne
sportif|pari sportif|pari sportif 100 euros offert|pari sportif 100 remboursé|pari sportif abandon tennis|pari sportif aide|pari sportif algérie aujourd’hui|pari
sportif appli|pari sportif application|pari sportif argent|pari sportif astuce|pari sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari sportif avec
orange money|pari sportif avec paypal|pari sportif avec wave|pari sportif avis|pari sportif basket|pari sportif belgique|pari sportif belgique france|pari sportif bonus|pari
sportif buteur pas titulaire|pari sportif champions league|pari sportif combiné|pari sportif
comment|pari sportif comment gagner|pari sportif comment ça marche|pari sportif comparatif|pari sportif conseil|pari sportif cote|pari sportif cote match|pari sportif cote psg|pari sportif coupe|pari sportif coupe de
france|pari sportif coupe du monde|pari sportif depot|pari sportif du jour|pari sportif en france|pari sportif en ligne|pari
sportif en ligne au cameroun|pari sportif en ligne belgique|pari sportif en ligne canada|pari
sportif en ligne france|pari sportif en ligne gratuit|pari sportif en ligne suisse|pari sportif
en ligne ufc|pari sportif en suisse|pari sportif euro|pari sportif explication|pari sportif faire|pari sportif foot|pari sportif foot resultat|pari sportif
football|pari sportif forum|pari sportif francaise des jeux|pari sportif
france|pari sportif france angleterre|pari sportif france argentine|pari
sportif france autriche|pari sportif france belgique|pari sportif france espagne|pari sportif france italie|pari sportif france
portugal|pari sportif france usa|pari sportif gagnant|pari sportif gagner|pari sportif gagner a tous les coups|pari sportif gagner
de l’argent|pari sportif gain|pari sportif gratuit|pari sportif gratuit pour
gagner des cadeaux|pari sportif gratuit sans depot|pari sportif
handicap|pari sportif hockey|pari sportif hors arjel|pari
sportif jeux olympiques|pari sportif joueur absent|pari sportif le plus rentable|pari sportif leicester champion|pari
sportif ligue 1|pari sportif ligue 2|pari sportif ligue des
champions|pari sportif ligue europa|pari sportif match|pari sportif match arrete|pari sportif match interrompu|pari sportif meilleur|pari sportif meilleur cote|pari sportif meilleur site|pari sportif
methode|pari sportif mise|pari sportif mise au jeu|pari sportif mise o jeu|pari sportif nba|pari sportif offre bienvenue|pari sportif paypal|pari sportif plus|pari sportif prolongation|pari sportif promo|pari sportif pronostic|pari sportif pronostic
foot|pari sportif pronostic gagnant|pari sportif pronostic
gratuit|pari sportif psg|pari sportif psg bayern|pari sportif psg inter|pari sportif psg
milan|pari sportif regle|pari sportif rembourse|pari sportif remboursement|pari
sportif remboursement cash|pari sportif remboursé|pari
sportif rugby|pari sportif rugby coupe du monde|pari
sportif rugby top 14|pari sportif sans argent|pari sportif sans carte bancaire|pari sportif sans depot|pari
sportif signification|pari sportif site|pari sportif statistique|pari sportif suisse|pari sportif systeme|pari
sportif technique|pari sportif technique pour gagner|pari sportif temps reglementaire|pari sportif tennis|pari sportif tennis abandon|pari sportif
top|pari sportif top 14|pari sportif tour de france|parie
sportif|parie sportif comment ca marche|parie sportif du jour|parie sportif en ligne|parie sportif foot|parie sportif football|parie sportif france|parie sportif gratuit|parie
sportif pronostic|parie sportif suisse|paris
en ligne sportif|paris en ligne sportifs|paris
evenement sportif|paris france sportif|paris hippique et sportif|paris hippiques et
sportifs|paris hippiques paris sportifs|paris hippiques paris
sportifs et poker en ligne|paris hippiques sportifs|paris match sportif|paris sportif|paris sportif 10
euros offerts|paris sportif 100 euros offert|paris sportif 100 euros remboursé|paris sportif 100 offert|paris sportif
100 remboursé|paris sportif 100e offert|paris sportif 150 euros offert|paris sportif 1er pari
remboursé|paris sportif a faire|paris sportif a faire aujourd’hui|paris sportif a faire ce soir|paris sportif abandon tennis|paris sportif abandon tennis
parions sport|paris sportif aide|paris sportif algorithme|paris
sportif analyse|paris sportif appli|paris sportif application|paris sportif application android|paris sportif apres
prolongation|paris sportif argent|paris sportif argent fictif|paris sportif argent offert|paris sportif argent virtuel|paris sportif
arjel|paris sportif arsenal psg|paris sportif astuce|paris sportif
au canada|paris sportif aujourd hui|paris sportif aujourd’hui|paris sportif avec
argent fictif|paris sportif avec bonus sans depot|paris sportif avec carte bancaire|paris sportif avec cryptomonnaie|paris sportif avec handicap|paris
sportif avec paypal|paris sportif avec paysafecard|paris sportif avis|paris sportif avis expert|paris sportif avis forum|paris sportif bankroll|paris sportif basket|paris sportif basket coupe
de france|paris sportif basket nba|paris sportif basket prolongation|paris sportif belgique|paris sportif belgique
bonus|paris sportif belgique bonus sans depot|paris sportif belgique france|paris sportif
belgique suede|paris sportif bonus|paris sportif bonus bienvenue|paris sportif bonus cash|paris sportif bonus de bienvenue|paris sportif bonus gratuit|paris sportif bonus gratuit sans depot|paris sportif bonus retirable|paris sportif bonus sans
depot|paris sportif bonus sans depot belgique|paris sportif
bookmaker|paris sportif but contre son camp|paris sportif
but temps additionnel|paris sportif buteur|paris sportif buteur blessé|paris sportif buteur carton rouge|paris sportif buteur contre son camp|paris sportif buteur non titulaire|paris sportif buteur prolongation|paris sportif buteur qui ne joue pas|paris sportif buteur
remplacant|paris sportif calcul gain|paris sportif canada|paris sportif cash|paris sportif cash out|paris
sportif champion ligue 1|paris sportif champions league|paris sportif classement ligue 1|paris sportif code
promo|paris sportif combine|paris sportif combiné|paris
sportif combiné comment ça marche|paris sportif combiné du jour|paris sportif combiné match reporté|paris sportif comment
ca marche|paris sportif comment faire|paris sportif comment gagner|paris sportif comment gagner a tous les coups|paris sportif comment jouer|paris sportif
comment ça marche|paris sportif comparateur cote|paris sportif comparatif|paris sportif conseil|paris
sportif conseil gratuit|paris sportif conseil pour gagner|paris
sportif cote|paris sportif cote et match|paris sportif cote explication|paris sportif cote psg|paris
sportif coupe d’europe|paris sportif coupe davis|paris sportif coupe de france|paris sportif coupe du monde|paris
sportif coupe du monde de rugby|paris sportif coupe du monde rugby|paris
sportif depot 5 euro|paris sportif depot minimum|paris sportif depot paypal|paris sportif dnb|paris sportif
du jour|paris sportif du jour conseil|paris sportif dépôt 1 euro|paris sportif
dépôt minimum 5 euros|paris sportif en belgique|paris sportif en france|paris sportif en ligne|paris
sportif en ligne avec paypal|paris sportif en ligne avis|paris sportif en ligne
belgique|paris sportif en ligne bonus|paris sportif en ligne cameroun|paris sportif en ligne comment gagner|paris sportif en ligne comment
ça marche|paris sportif en ligne france|paris sportif
en ligne gratuit|paris sportif en ligne maroc|paris sportif en ligne paypal|paris sportif en ligne québec|paris sportif en ligne sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris sportif espagne france|paris sportif esport|paris sportif et casino
en ligne|paris sportif et hippique|paris sportif et prolongation|paris sportif euro|paris sportif europa league|paris sportif explication|paris sportif final ligue des champions|paris sportif finale
ligue des champions|paris sportif foot|paris sportif foot
aide|paris sportif foot astuce|paris sportif foot aujourd’hui|paris sportif foot ce soir|paris sportif foot comment ca marche|paris sportif
foot conseil|paris sportif foot cote|paris sportif foot coupe du monde|paris sportif foot en ligne|paris sportif foot feminin|paris sportif foot gratuit|paris
sportif foot prolongation|paris sportif foot pronostic|paris sportif foot pronostic gratuit|paris sportif foot regle|paris sportif foot suisse|paris
sportif foot us|paris sportif football|paris sportif football americain|paris sportif football astuces|paris sportif forfait tennis|paris sportif forum|paris sportif francais|paris sportif francaise des jeux|paris sportif france|paris sportif france 2|paris
sportif france allemagne|paris sportif france angleterre|paris
sportif france argentine|paris sportif france autriche|paris sportif france belgique|paris sportif france espagne|paris sportif
france gibraltar|paris sportif france italie|paris sportif france nouvelle zelande|paris sportif france pologne|paris sportif france
portugal|paris sportif france uruguay|paris sportif france usa|paris sportif freebet sans
depot|paris sportif gagnant|paris sportif gagnant à coup sûr|paris sportif gagner a
coup sur|paris sportif gagner argent|paris sportif gagner
de l’argent|paris sportif gain|paris sportif gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris sportif gratuit appli|paris sportif gratuit avec cadeaux|paris sportif gratuit cadeaux|paris
sportif gratuit en ligne|paris sportif gratuit entre amis|paris sportif gratuit sans argent|paris sportif gratuit sans depot|paris sportif gratuit sans dépôt|paris sportif
gratuits|paris sportif gros gain|paris sportif handicap|paris sportif handicap 0 1|paris sportif
handicap 0-1|paris sportif handicap 1 0|paris sportif handicap 1-0|paris sportif handicap basket|paris sportif handicap explication|paris sportif handicap foot|paris
sportif handicap rugby|paris sportif hippique|paris sportif hockey|paris sportif hockey nhl|paris sportif hockey sur glace|paris sportif hors arjel|paris sportif hors arjel france|paris sportif jeux olympiques|paris sportif jeux video|paris sportif
joueur blessé|paris sportif joueur blessé pendant le
match|paris sportif joueur de foot|paris sportif joueur
decisif|paris sportif joueur declare forfait|paris sportif
joueur déclare forfait|paris sportif joueur remplacant|paris sportif la
francaise des jeux|paris sportif le plus rentable|paris sportif legal en france|paris sportif leicester champion|paris sportif les 18 stratégies pour gagner tous les jours|paris sportif les plus sur|paris
sportif les prolongation compte|paris sportif ligne|paris sportif ligue 1|paris
sportif ligue 2|paris sportif ligue des champions|paris sportif ligue des nations|paris sportif ligue europa|paris sportif liste|paris
sportif martingale|paris sportif match|paris sportif match abandonné|paris sportif match annulé|paris sportif
match arrêté|paris sportif match du jour|paris sportif match interrompu|paris
sportif match reporté|paris sportif match suspendu|paris
sportif match tennis interrompu|paris sportif match truqué|paris sportif
meilleur bonus|paris sportif meilleur cote|paris sportif meilleur pronostic|paris sportif meilleur site|paris sportif methode|paris sportif methode 2 3|paris sportif mi temps fin de match|paris sportif mise au jeu|paris sportif mise maximum|paris sportif mma france|paris sportif moins de 3.5 but|paris sportif montante|paris
sportif moto gp|paris sportif multiple|paris sportif multiple 2 3|paris sportif multiple
2 3 explication|paris sportif multiple 2 4|paris sportif multiple
2 5|paris sportif multiple 2/3 explication|paris
sportif multiple 3 4|paris sportif multiple
explication|paris sportif national 1 foot|paris sportif nba|paris sportif nba conseil|paris sportif nba pronostic|paris sportif nhl|paris sportif nombre de but|paris
sportif nouveau site|paris sportif numero match|paris
sportif offert|paris sportif offre bienvenue|paris sportif offre bienvenue sans depot|paris
sportif offre de bienvenue|paris sportif offre sans depot|paris sportif
om psg|paris sportif paypal|paris sportif plus de
1.5 but|paris sportif plus de 2 5 but|paris
sportif plus ou moins|paris sportif plus ou moins 2 5 but|paris sportif premier
pari remboursé|paris sportif premier paris remboursé|paris sportif prolongation|paris sportif prolongation basket|paris sportif prolongation foot|paris sportif promo|paris sportif pronostic|paris sportif pronostic basket|paris sportif pronostic des match aujourd hui|paris sportif pronostic expert gratuit|paris
sportif pronostic foot|paris sportif pronostic forum|paris sportif pronostic gratuit|paris sportif pronostic tennis|paris sportif psg|paris sportif psg arsenal|paris sportif psg barcelone|paris sportif
psg bayern|paris sportif psg dortmund|paris sportif
psg inter|paris sportif psg inter cote|paris
sportif psg liverpool|paris sportif psg om|paris
sportif qr code|paris sportif que veut dire handicap|paris sportif
qui rapporte le plus|paris sportif regle|paris sportif regle prolongation|paris sportif rembourse|paris
sportif remboursement cash|paris sportif rembourser|paris sportif remboursé|paris sportif remboursé cash|paris sportif remboursé en cash|paris sportif retrait paypal|paris sportif rue des joueurs|paris sportif rugby|paris sportif rugby 6 nations|paris sportif rugby coupe du monde|paris sportif
rugby top 14|paris sportif safe du jour|paris sportif
sans argent|paris sportif sans carte bancaire|paris sportif sans carte d’identité|paris sportif sans compte bancaire|paris sportif sans depot|paris
sportif sans depot minimum|paris sportif si match suspendu|paris sportif
si un joueur abandonne|paris sportif si un joueur ne joue pas|paris
sportif si un joueur se blesse|paris sportif simple ou
combiné|paris sportif site|paris sportif statistique|paris sportif stratégie|paris
sportif suisse|paris sportif suisse application|paris sportif suisse en ligne|paris sportif
suisse legal|paris sportif suisse légal|paris sportif suisse romande|paris sportif sur du
jour|paris sportif sur le tennis|paris sportif systeme|paris sportif
systeme 2 3|paris sportif systeme 2 4|paris sportif systeme 2/3|paris sportif systeme 2/4|paris sportif systeme 3 4|paris sportif systeme
3/4|paris sportif systeme explication|paris sportif technique|paris sportif technique pour gagner|paris sportif temps additionnel|paris sportif temps reglementaire|paris sportif tennis|paris sportif tennis
abandon|paris sportif tennis conseil|paris sportif tennis de table|paris sportif tennis forfait|paris sportif tennis
gratuit|paris sportif tennis pronostic|paris sportif tennis roland garros|paris sportif tir au but|paris sportif top 14|paris sportif tour de france|paris sportif
ufc|paris sportif ufc france|paris sportif unibet|paris sportif
vainqueur euro|paris sportif vainqueur ligue
1|paris sportif vainqueur ligue des champions|paris sportif via paypal|paris sportif victoire prolongation|paris sportif vip gratuit|paris sportifs|paris sportifs abandon tennis|paris sportifs aide|paris sportifs analyser un match|paris sportifs arjel|paris sportifs astuces|paris sportifs aujourd’hui|paris
sportifs autorisés en france|paris sportifs avec paypal|paris sportifs basket|paris
sportifs belgique|paris sportifs bonus|paris sportifs
bookmakers|paris sportifs canada|paris sportifs combiné|paris sportifs comparateur|paris sportifs comparatif|paris sportifs conseils|paris sportifs cotes|paris sportifs coupe du
monde|paris sportifs de football|paris sportifs du jour|paris sportifs en belgique|paris sportifs en france|paris sportifs en ligne|paris sportifs en ligne belgique|paris sportifs en ligne france|paris
sportifs en ligne gratuit|paris sportifs en ligne suisse|paris sportifs en suisse|paris
sportifs et hippiques|paris sportifs euro|paris sportifs foot|paris sportifs
foot us|paris sportifs forum|paris sportifs france|paris sportifs france espagne|paris sportifs gagner à tous les coups|paris sportifs gratuit|paris sportifs
gratuits|paris sportifs gratuits en ligne|paris sportifs handicap|paris sportifs hockey|paris sportifs hockey sur galce|paris sportifs hockey sur glace|paris sportifs hors arjel|paris sportifs jeux olympiques|paris sportifs les bookmakers raflent la mise|paris sportifs ligne|paris sportifs ligue
1|paris sportifs ligue 2|paris sportifs ligue des champions|paris sportifs ligue europa|paris sportifs match
interrompu|paris sportifs montante|paris sportifs nba|paris sportifs offre bienvenue|paris sportifs
offre de bienvenue|paris sportifs paypal|paris sportifs pronostics|paris sportifs psg|paris sportifs psg inter|paris sportifs rugby|paris sportifs sans
argent|paris sportifs sans depot|paris sportifs
site|paris sportifs sites|paris sportifs statistiques|paris sportifs stratégie|paris sportifs suisse|paris sportifs technique|paris sportifs techniques|paris sportifs tennis|paris sportifs tennis astuces|paris sportifs top 14|paris sportifs tour
de france|part de marché paris sportifs|paypal pari sportif|paypal paris sportif|paypal paris sportifs|perte d’argent paris sportifs|peut on devenir riche
avec les paris sportifs|peut on gagner de l’argent avec les paris sportifs|peut on gagner sa vie avec les paris sportif|peut on vraiment gagner de l’argent avec les paris
sportifs|plus gros combine paris sportif|plus gros gagnant paris
sportif|plus gros gain paris sportif|plus gros gain paris sportif
au monde|plus gros gain paris sportif france|plus
gros gains paris sportif|plus gros pari sportif|plus gros
paris sportif|plus grosse cote gagner paris sportif|plus grosse
cote pari sportif|plus grosse cote paris sportif|plus grosse mise paris sportif|plus grosse somme gagner au paris sportif|plus ou moins
paris sportif|pourcentage de mise paris sportif|premier pari sportif remboursé|probabilité cote paris sportif|probabilité paris sportif combiné|prolongation basket paris sportif|prolongation paris sportif|promo pari sportif|promo paris sportif|promo site de paris sportif|promo site pari
sportif|promo site paris sportif|promos paris sportifs|prono paris sportif foot|prono paris sportif gratuit|prono paris sportif tennis|pronostic de paris sportif|pronostic du jour paris sportif|pronostic foot paris sportif|pronostic gratuit paris sportif|pronostic pari sportif|pronostic pari sportif gratuit|pronostic paris sportif|pronostic paris sportif aujourd’hui|pronostic paris sportif du jour|pronostic paris sportif foot|pronostic paris sportif gratuit|pronostic
paris sportif tennis|pronostic paris sportifs|pronostics foot statistiques
et aides aux paris sportifs|pronostics paris sportif|pronostics paris sportifs|pronostiqueur paris sportif
gratuit|psg arsenal paris sportif|psg bayern paris sportif|psg inter milan paris sportif|psg inter pari sportif|psg inter paris sportif|psg liverpool paris sportif|psg om
paris sportif|psg paris sportif|psg paris sportifs|qr code paris sportif|qu est
ce qu un handicap paris sportif|qu est ce que handicap dans les paris sportif|qu’est ce qu’un handicap paris sportif|qu’est ce
que handicap dans les paris sportif|quand un joueur se blesse paris sportif|que signifie 1/1 en paris sportif|que
signifie 1/2 paris sportif|que signifie 12 en paris sportif|que signifie
1×2 dans les paris sportifs|que signifie btts en paris sportif|que
signifie dnb en paris sportif|que signifie draw en paris sportif|que signifie ft en paris sportif|que signifie gg dans le pari sportif|que signifie gg
en pari sportif|que signifie gg en paris sportif|que signifie handicap
dans les paris sportifs|que veut dire dnb en paris sportif|que veut dire handicap dans
les paris sportifs|que veut dire handicap paris sportif|quel appli pari sportif|quel cote jouer paris sportif|quel est la meilleur appli de paris sportif|quel est le meilleur algorithme
de paris sportif|quel est le meilleur site de pari sportif|quel est le meilleur site de pari sportif en ligne|quel est le meilleur site de paris sportif|quel
est le meilleur site de paris sportif en ligne|quel est le meilleur site de paris sportifs en ligne|quel est le pari sportif le plus rentable|quel pari sportif est le plus
rentable|quel pari sportif est le plus sûr|quel pari sportif faire aujourd’hui|quel
paris sportif faire aujourd’hui|quel paris sportif rapporte le
plus|quel site de paris sportif choisir|quel site de paris sportif
rembourse en cash|quel type de pari sportif est le plus rentable|quelle application pour paris sportifs|quelle est
la meilleure appli de paris sportif|quelle est la meilleure application de paris
sportif|quelle est la meilleure application pour les paris sportifs|quelle est le
meilleur site de paris sportif|quels paris sportifs faire|quels sont
les paris sportifs les plus sûrs|rebond basket paris sportif|record de gain paris sportif|regle buteur paris sportif|regle de paris sportif|regle
des paris sportif|regle handicap paris sportif|regle handicap
paris sportif foot|regle multiple paris sportif|regle pari
sportif|regle paris sportif|regle paris sportif foot|regle paris sportif multiple|regle paris sportif prolongation|reglement pari sportif|reglement paris sportif|regles paris sportifs|remboursement cash paris sportif|remboursement en cash paris sportif|remboursement pari sportif|remboursement paris sportif|repartiteur de mise
paris sportif|repartiteur de mise paris sportifs|repartiteur
de mises paris sportif|repartiteur mise paris sportif|repartition des mises paris sportif|resultat
pari sportif|resultat paris sportif|resultat
paris sportif en direct|resultat paris sportif foot|resultat sportif
hockey|retirer argent paris sportif|rugby pari sportif|rugby paris sportif|règle paris sportif prolongation|règles paris sportif|répartiteur de
mise pari sportif|répartiteur de mise paris sportif|répartiteur de mise paris sportifs|répartition des mises paris sportif|résultat paris sportif foot|sans depot paris sportif|se faire interdire de paris sportifs|signification btts paris sportif|signification dnb paris sportif|signification handicap paris sportif|simulateur de gain paris
sportif|simulateur gain paris sportif|simulateur gain paris sportif multiple|simulateur gain paris sportif systeme|simulateur gain paris sportif système|simulateur
montante paris sportif|simulateur paris sportif multiple|simulateur systeme
paris sportif|simulation paris sportif gratuit|site aide paris sportif|site analyse paris
sportif|site analyser paris sportif|site arjel paris sportif|site conseil paris sportif|site d’analyse de paris sportifs|site d’analyse paris sportif|site
de conseil paris sportif|site de pari en ligne sportif|site de pari sportif|site de pari sportif avec
bonus sans depot|site de pari sportif bonus sans depot|site de
pari sportif canada|site de pari sportif en ligne|site de
pari sportif francais|site de pari sportif gratuit|site
de pari sportif hors arjel|site de pari sportif suisse|site
de parie sportif|site de parie sportif en ligne|site de paris en ligne sportif|site de paris sportif|site de paris sportif acceptant paypal|site
de paris sportif arjel|site de paris sportif autorisé en france|site
de paris sportif autorisé en suisse|site de paris sportif avec bonus|site de paris
sportif avec bonus sans depot|site de paris sportif avec bonus sans dépôt|site de paris sportif avec neosurf|site de paris sportif avec paiement mobile|site de paris
sportif avec paypal|site de paris sportif avis|site de paris sportif belge avec bonus|site de paris sportif belgique|site de paris sportif bonus|site de
paris sportif bonus sans depot|site de paris sportif canada|site de paris sportif comparatif|site de paris sportif
depot minimum|site de paris sportif en france|site de
paris sportif en ligne|site de paris sportif en ligne suisse|site de paris sportif football|site de paris sportif francais|site de paris
sportif france|site de paris sportif gratuit|site de paris sportif
gratuit pour gagner des cadeaux|site de paris sportif gratuit sans dépôt|site de paris sportif hors arjel|site de paris sportif le plus fiable|site de paris sportif legal en france|site
de paris sportif meilleur cote|site de paris sportif nouveau|site de paris sportif offre de bienvenue|site de paris sportif paypal|site de paris
sportif premier paris remboursé|site de paris sportif
qui accepte paypal|site de paris sportif qui rembourse en cash|site de paris sportif
remboursé|site de paris sportif sans argent|site de paris sportif sans
carte bancaire|site de paris sportif sans carte d’identité|site de paris sportif sans depot|site de paris sportif suisse|site
de paris sportifs|site de paris sportifs avec paypal|site de paris sportifs
en ligne|site de paris sportifs francais|site de paris sportifs
gratuit|site de paris sportifs paypal|site de paris sportifs suisse|site de statistique pour
paris sportif|site des paris sportifs|site pari en ligne sportif|site pari sportif|site pari sportif 100 euros offert|site pari
sportif arjel|site pari sportif belgique|site pari sportif bonus|site pari
sportif canada|site pari sportif comparatif|site pari
sportif en ligne|site pari sportif france|site pari sportif gratuit|site pari sportif hors arjel|site
pari sportif suisse|site parie sportif|site paris en ligne sportif|site paris sportif|site paris sportif 100 euros offert|site paris sportif 100 euros remboursé|site paris sportif 1er
paris remboursé|site paris sportif arjel|site paris sportif autorisé
en france|site paris sportif avec bonus|site paris sportif avec bonus sans depot|site paris sportif avec meilleur cote|site paris
sportif belgique|site paris sportif bonus|site paris sportif
bonus cash|site paris sportif bonus sans depot|site paris
sportif canada|site paris sportif comparatif|site paris sportif depot 5 euro|site paris sportif en ligne|site paris sportif
foot|site paris sportif france|site paris sportif
gratuit|site paris sportif hors arjel|site paris sportif hors arjel france|site paris sportif meilleur
cote|site paris sportif nouveau|site paris sportif offre de bienvenue|site paris sportif paypal|site paris sportif remboursement cash|site paris sportif remboursé en cash|site paris sportif retrait instantané|site paris sportif sans carte bancaire|site
paris sportif sans depot|site paris sportif suisse|site paris sportifs|site paris sportifs belgique|site paris sportifs en ligne|site paris sportifs france|site paris sportifs hors arjel|site paris sportifs suisse|site
pour analyse paris sportif|site pour paris sportif|site pronostic paris sportif|site statistique paris sportif|site suisse paris sportif|sites de pari sportif|sites
de paris sportif|sites de paris sportifs|sites de paris sportifs
arjel|sites de paris sportifs autorisés en france|sites de
paris sportifs belgique|sites de paris sportifs bonus|sites de
paris sportifs en belgique|sites de paris sportifs
en france|sites de paris sportifs en ligne|sites de paris sportifs
gratuits|sites de paris sportifs gratuits sans dépôt|sites de paris sportifs suisse|sites pari sportif|sites paris sportif|sites paris sportifs|sites paris
sportifs arjel|sites paris sportifs belgique|sites paris
sportifs france|sites paris sportifs hors arjel|sites paris
sportifs suisse|so foot paris sportif|so foot paris sportifs|specialiste tennis paris sportif|statistique foot
paris sportif|statistique paris sportif|statistique paris sportif foot|statistique tennis paris sportif|statistiques football
paris sportifs|statistiques paris sportifs|strategie de paris sportif|stratégie big whale
paris sportif|stratégie de paris sportifs|stratégie gagnante paris sportifs|stratégie pari sportif|stratégie paris sportif|stratégie paris sportifs|stratégie paris sportifs forum|stratégie pour gagner au paris sportif|stratégies paris sportifs|suisse paris sportif|suisse paris sportifs|systeme 2 3 paris
sportif|systeme 3 4 paris sportif|systeme de cote paris sportif|systeme de paris sportif|systeme pari sportif|systeme paris sportif|systeme paris sportifs|systeme reducteur paris sportif|système paris sportif|tableau bankroll paris sportif|tableau cote paris sportif|tableau de paris sportif|tableau de suivi paris sportifs|tableau excel bankroll paris sportif|tableau excel paris
sportif|tableau excel paris sportif gratuit|tableau excel paris sportifs|tableau excel pour paris
sportif|tableau gestion bankroll paris sportif|tableau montante
paris spo
شيئر ڪرڻ لاءِ مهرباني. مون کي پريشاني آهي ته مان تخليقي نه آهيان. اهو توهان جي ڪهاڻي آهي جيڪا مون کي اميد سان ڀري ٿي. مهرباني.
Your method of telling all in this piece of writing is truly pleasant, all be capable of without difficulty understand it, Thanks a lot.
Refresh Renovtion Broomfield
11001 Ꮤ 120th Ave 400 suite 459a,
Broomfield, CO 80021, United States
+13032681372
Kitchen renovation
This is my first time visit at here and i am truly happy to read all at one place.
Bu saytla bağlı tövsiyələr çox faydalıdır.
https://furnitex.com.ru/bitrix/redirect.php?goto=https://1winazerbaijan.biz/
Yes! Finally something about click.
I’m now not positive where you are getting your info,
but good topic. I needs to spend some time learning more or figuring
out more. Thank you for wonderful information I was
looking for this info for my mission.
This website was… how do I say it? Relevant!!
Finally I have found something which helped me. Thank you!
Hi, I check your new stuff on a regular basis. Your writing style is witty, keep doing what you’re doing!
You actually make it seem so easy with your presentation but I find
this matter to be actually something which I think I would never
understand. It seems too complicated and extremely broad for me.
I’m looking forward for your next post, I
will try to get the hang of it!
That is a good tip particularly to those fresh to the blogosphere.
Simple but very accurate info… Thanks for sharing this one.
A must read post!
I am regular reader, how are you everybody? This paragraph posted at
this web page is really nice.
Very energetic blog, I enjoyed that a lot. Will there be a part 2?
After I originally left a comment I seem to have clicked the -Notify
me when new comments are added- checkbox and from now on each
time a comment is added I get four emails with the same comment.
Is there a way you can remove me from that service?
Cheers!
Thanks designed for sharing such a good thinking, piece of writing is
good, thats why i have read it fully
I really like what you guys are up too. This kind of clever work and coverage!
Keep up the good works guys I’ve incorporated you guys to my own blogroll.
Hi there would you mind letting me know which web host you’re using?
I’ve loaded your blog in 3 different web browsers and I must
say this blog loads a lot quicker then most. Can you recommend a good internet hosting provider at
a fair price? Kudos, I appreciate it!
Lifestyle & Fashion Daily – Explore trendy outfits and chic lifestyle essentials every day.
This paragraph provides clear idea in favor of the new viewers of blogging, that truly
how to do blogging.
остров ко ланта остров ко ланта
Cabinet IQ Austin
2419 Ⴝ Bell Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
Maintenance
Hi, Neat post. There is a problem with your web site in internet explorer, would test this?
IE nonetheless is the market chief and a good component of people will miss your wonderful
writing because of this problem.
Hello! I’ve been reading your website for a long time now and finally got
the courage to go ahead and give you a shout out from Porter Tx!
Just wanted to say keep up the good job!
Cobɑin juɡa ⅼink іni, gacor abis: https://dailydigitalsnews.com/2025/05/23/196/
Omlouvám se, že jsem se odmlčel/a. Miluji všechno, chci kreativní útoky. Je to tvoje psaní, co mi dává naději. Proč?
Ищете качественную минеральную
воду с доставкой прямо
до вашего дома или офиса?
I am actually delighted to glance at this weblog posts which
consists of tons of helpful data, thanks for providing such statistics.
I’m pretty pleased to uncover this site. I wanted to thank you for your
time for this particularly wonderful read!! I definitely enjoyed
every bit of it and I have you book marked to check out new information on your website.
Having read this I believed it was rather enlightening.
I appreciate you finding the time and energy to put this article together.
I once again find myself personally spending a lot of time both reading and leaving comments.
But so what, it was still worth it!
I was excited to find this web site. I wanted to thank you for ones time due to this fantastic read!!
I definitely enjoyed every part of it and i also have you bookmarked to look at new things in your
website.
Dank je wel voor zulke nuttige content. Ik ga cazino zeker aanbevelen aan vrienden.
http://truefucking.com/ftt2/o.php?u=http%3A%2F%2Flalabet-casino-nl.nl%2Fbonussen
hi!,I love your writing very so much! share we communicate extra about your
article on AOL? I require an expert in this house to solve my problem.
May be that is you! Having a look forward to peer you.
Wonderful blog! I found it while searching on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Cheers
Its not my first time to pay a visit this site, i am visiting this website dailly and get fastidious information from here all the time.
сюда https://kra46att.at/
Spot on with this write-up, I seriously believe that
this amazing site needs much more attention. I’ll probably be returning to see more, thanks for
the advice!
I was wondering if you ever considered changing the layout of your website?
Its very well written; I love what youve got to say. But maybe
you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or two pictures.
Maybe you could space it out better?
If you would like to improve your experience simply keep visiting this web page and be updated with the latest information posted here.
88WANWIN is the safest and most trusted online casino
in Cambodia. 88wanwin offers slot games, sports betting,
live casino, and fish shooting games for players
seeking secure, fun online entertainment.
на этом сайте https://kra46att.at/
Paylaşdığınız məlumatlar mənə çox kömək edir. Təşəkkürlər!
https://mostbetazerbaijanpro.com/demo-oyunlari/
Lubię strona Mostbet, jest komfortowa w użytkowaniu!
https://1.g9.yt/kasynona380ywomostbet68003
Excellent weblog here! Also your website rather a lot
up fast! What host are you using? Can I am getting your
associate hyperlink for your host? I want my site loaded up as
fast as yours lol
You actually make it seem so easy with your
presentation but I find this matter to be really something which I think I would never understand.
It seems too complex and extremely broad for me. I’m looking forward for your next post, I will try to get the hang of it!
узнать больше https://kra46att.at
тонировка в москве Оклейка Москва: Защита и Персонализация в Одном Оклейка автомобиля пленкой в Москве – это современный способ защиты кузова от повреждений и придания ему уникального внешнего вида. Широкий выбор цветов и фактур позволяет реализовать любые дизайнерские идеи.
Hi, i think that i saw you visited my blog so i came to
“return the favor”.I’m attempting to find things to improve my site!I
suppose its ok to use a few of your ideas!!
I do accept as true with all of the ideas you’ve presented to your post.
They are very convincing and can definitely work. Nonetheless, the posts are too short for newbies.
May you please prolong them a bit from subsequent time? Thank you
for the post.
It’s going to be finish of mine day, however before end I
am reading this enormous post to improve my experience.
I’m not sure exactly why but this web site is loading extremely
slow for me. Is anyone else having this issue or is it a issue on my end?
I’ll check back later on and see if the problem still exists.
If you wish for to increase your knowledge only keep visiting this web site and be updated with the most recent news posted here.
Wow, incredible blog layout! How long have you been blogging
for? you made blogging look easy. The overall look of your web site is great, let alone the content!
We absolutely love your blog and find a lot of your post’s
to be exactly what I’m looking for. Does
one offer guest writers to write content for you?
I wouldn’t mind producing a post or elaborating on most of the subjects you write with regards to here.
Again, awesome blog!
I’m not sure where you’re getting your information, but good topic.
I needs to spend some time learning more
or understanding more. Thanks for wonderful info I was looking for this info for my mission.
Incredible points. Great arguments. Keep up the great
effort.
I am no longer positive the place you are getting
your information, but great topic. I must spend some time finding out much more
or working out more. Thank you for magnificent info I used to
be searching for this information for my mission.
If some one wants expert view concerning blogging
and site-building after that i advise him/her to visit this website, Keep up the fastidious work.
оклейка москва Оклейка Москва: Защита и Стиль в Одном Оклейка автомобиля пленкой в Москве – это не просто смена цвета, это надежная защита лакокрасочного покрытия от сколов, царапин и воздействия окружающей среды. Широкий выбор цветов и фактур позволяет создать уникальный дизайн, подчеркивающий индивидуальность владельца.
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Thanks
Thanks for ones marvelous posting! I seriously enjoyed
reading it, you may be a great author.I will make certain to bookmark your blog and will
come back in the foreseeable future. I want to encourage yourself
to continue your great writing, have a nice afternoon!
Kiitos jakamisesta. Olen huolissani siitä, etten ole luova. Tarinasi täyttää minut toivolla. Kiitos.
I love what you guys tend to be up too. This kind of clever work and exposure!
Keep up the superb works guys I’ve included you guys to my blogroll.
A person essentially help to make severely articles I would state.
That is the very first time I frequented your web page and so far?
I surprised with the analysis you made to create this particular put
up amazing. Great process!
Ezerszer köszönet a(z) online kaszinó ranglista platformért – rengeteget segít!
http://url.hys.cz/online-kaszin-ranglista-93171
кликните сюда https://kra47at.at/
This piece of writing provides clear idea
designed for the new viewers of blogging, that
actually how to do blogging and site-building.
Great work! This is the type of information that should be
shared across the net. Shame on Google for not positioning this
publish upper! Come on over and talk over with my web site
. Thanks =)
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to far added agreeable from you!
By the way, how could we communicate?
What’s up mates, how is all, and what you desire to say about this post, in my view its in fact amazing for me.
I have to thank you for the efforts you’ve put in penning this blog.
I am hoping to check out the same high-grade content from you in the future as well.
In truth, your creative writing abilities has motivated me to get
my very own website now 😉
Hey there just wanted to give you a brief heads up and let you know a few of the pictures
aren’t loading properly. I’m not sure why but I think its a linking issue.
I’ve tried it in two different browsers and both show the same
outcome.
Having read this I thought it was very informative.
I appreciate you spending some time and effort to put this
content together. I once again find myself personally
spending way too much time both reading and commenting.
But so what, it was still worth it!
посмотреть на этом сайте https://kra47at.at/
Right now it seems like BlogEngine is the best blogging platform available right now.
(from what I’ve read) Is that what you’re using on your blog?
веб-сайт https://kra48at.at/
hey there and thank you for your information – I’ve certainly picked up anything new from right here.
I did however expertise a few technical points using
this website, as I experienced to reload the web site lots of
times previous to I could get it to load properly. I had been wondering
if your hosting is OK? Not that I’m complaining, but sluggish loading
instances times will often affect your placement in google
and could damage your high quality score if advertising and marketing with Adwords.
Anyway I am adding this RSS to my e-mail and can look out for a lot more of your respective intriguing content.
Ensure that you update this again very soon.
For most recent information you have to pay a quick visit the
web and on the web I found this website as a most excellent web site
for hottest updates.
Pretty section of content. I just stumbled upon your website and in accession capital
to assert that I acquire actually enjoyed account your blog posts.
Anyway I will be subscribing to your feeds and even I achievement you access consistently quickly.
I constantly spent my half an hour to read this webpage’s articles
everyday along with a cup of coffee.
शेयर करने आस्ते तुंदा धन्नवाद। मैं चिंतित हा जे मेरे च रचनात्मक विचारें दी कमी ऐ। तुहाडा लेख आशा देंदा है। थुआढ़ा धन्नवाद।
Hello every one, here every one is sharing these kinds of experience, therefore it’s fastidious to read this web site, and I used to visit this blog everyday.
register in directory Brazil
Wonderful blog! I found it while searching on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to
get there! Cheers
Hello, Neat post. There is an issue with your web site
in web explorer, may check this? IE still is the market chief
and a good component to other folks will pass over your
excellent writing because of this problem.
Here is my page :: ronny deila
Its like you learn my thoughts! You seem to understand a lot
approximately this, such as you wrote the e-book in it or something.
I think that you can do with a few p.c. to power the message house
a little bit, however instead of that, that is excellent blog.
A great read. I’ll definitely be back.
Hi there, just became alert to your blog through Google, and found that it is really informative.
I am going to watch out for brussels. I will be grateful if you continue this in future.
A lot of people will be benefited from your writing.
Cheers!
Affordable Choices – Smart product suggestions to save time and money while shopping.
посетить веб-сайт https://kra47at.at
Since the admin of this website is working, no hesitation very rapidly it will be
renowned, due to its feature contents.
You need to be a part of a contest for one of the most useful blogs online.
I am going to recommend this web site!
It is actually a nice and helpful piece of info. I’m satisfied that you
simply shared this helpful info with us. Please keep
us up to date like this. Thank you for sharing.
Ahaa, its fastidious conversation regarding this article at this place at this website, I have read all
that, so at this time me also commenting at this place.
My partner and I stumbled over here from a different web page
and thought I might as well check things out. I like what I see so now i’m following you.
Look forward to looking over your web page again.
Awesome post.
Hi, I do think this is an excellent blog. I stumbledupon it 😉 I’m going to revisit once again since i have bookmarked
it. Money and freedom is the best way to change, may you be rich and continue to help others.
Neat blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple tweeks would
really make my blog shine. Please let me know where you got your design. Thanks a lot
It’s amazing in favor of me to have a site, which is useful in support of my know-how.
thanks admin
1win sign in is very informative. Will be back for sure!
https://gettrialsnow.com/services/palia-story-completion/
It’s enormous that you are getting thoughts from this paragraph as well as
from our dialogue made here.
E2BET 香港官方網站 | 安全可靠,信譽保證
May I simply just say what a comfort to uncover a person that actually knows what they’re talking about over the internet.
You actually realize how to bring a problem to light and make it important.
A lot more people ought to look at this and
understand this side of the story. I was surprised that you’re not more popular given that you most certainly possess the gift.
Hey I know this is off topic but I was wondering if you
knew of any widgets I could add to my blog that automatically
tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time
and was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading
your blog and I look forward to your new updates.
Thank you for some other informative web site.
The place else may just I am getting that type of information written in such an ideal way?
I have a venture that I’m just now working on, and
I’ve been on the glance out for such information.
I read this piece of writing fully on the topic of the difference of most up-to-date and
preceding technologies, it’s awesome article.
Great blog here! Also your web site loads up very fast!
What host are you using? Can I get your affiliate link to your host?
I wish my site loaded up as quickly as yours lol
I all the time used to read paragraph in news papers but
now as I am a user of internet thus from now I am using
net for articles, thanks to web.
Hello to all, as I am really keen of reading this webpage’s post to be updated regularly.
It includes pleasant information.
4M Dental Implant Center
3918 Ꮮong Beach Blvd #200, ᒪong Beach,
CA 90807, United States
15622422075
safe Veneers (padlet.com)
Thanks for sharing such a fastidious thought, post is
nice, thats why i have read it fully
Thanks very interesting blog!
Izvinjavam se zbog fotografije. Volim sve, tinjaju mi kreativni napadi. Tvoje pisanje mi daje nadu. Zašto?
I pay a quick visit each day a few sites and sites to read articles, except this website
gives quality based content.
Amazing! This blog looks exactly like my old one! It’s on a entirely different subject but
it has pretty much the same page layout and design. Great choice
of colors!
Desculpe o silêncio. Adoro tudo, quero ataques criativos. É a sua escrita que me dá esperança. Por quê?
What’s up, all is going sound here and ofcourse every one is sharing information, that’s in fact excellent, keep
up writing.
Cabinet IQ Fort Myers
7830 Drew Cir Ste 4, Fort Myers,
FL 33967, United Ꮪtates
12394214912
Kitchenstone (Minnie)
We are a group of volunteers and opening a new scheme in our community.
Your web site offered us with valuable info to work on. You’ve done an impressive
job and our entire community will be grateful to you.
Greetings! Very helpful advice in this particular post!
It’s the little changes that will make the most important changes.
Thanks a lot for sharing!
Keep your automobile road-ready in Latvia with quality winter months tires, all-season tires, and relied on tire service. Discover how appropriate maintenance, seasonal swaps, and expert inspections boost safety, handling, and tire durability. From urban roads to rural freeways, make sure smooth, worry-free driving year-round with professional care and clever tire options customized to Latvia’s altering weather, https://classifiedwale.com/user/HarmonydfMelton/.
Thanks , I have recently been searching for info about this subject for a while
and yours is the best I have came upon till now. However,
what in regards to the conclusion? Are you positive in regards to the
source?
I just like the helpful information you supply for your articles.
I’ll bookmark your blog and take a look at again right here frequently.
I’m fairly certain I’ll be told lots of new stuff
proper here! Best of luck for the following!
My brother recommended I would possibly like this web site.
He was totally right. This publish actually made my day.
You cann’t believe just how much time I had spent
for this information! Thank you!
my homepage :: Plombier Arlon
I always spent my half an hour to read this weblog’s
content daily along with a mug of coffee.
Hi there, just became aware of your blog through Google, and found that it is really informative.
I’m going to watch out for brussels. I’ll be grateful if you continue
this in future. A lot of people will be benefited from your writing.
Cheers!
Hello to every body, it’s my first go to see of this webpage; this blog includes remarkable and really fine stuff
in favor of visitors.
Magnificent beat ! I would like to apprentice while you amend your website, how can i
subscribe for a blog web site? The account helped me a acceptable deal.
I had been a little bit acquainted of this your broadcast provided bright clear idea
Hallo, tolle Seite NV Casino, gut gemacht!
https://maps.google.cat/url?q=https://nv-casino-vip-deutschland.de/mobile-app
Mikigaming | Seo Magic #1 Slot Online Pasti Maxwin Hari ini !!!
I’m not sure where you are getting your info, but great topic.
I needs to spend some time learning much more or understanding more.
Thanks for wonderful information I was looking for
this info for my mission.
I was suggested this blog by means of my cousin. I am no longer sure whether
this publish is written by him as no one else realize such
detailed about my difficulty. You’re amazing! Thanks!
Have a look at my site: Loodgieter Hasselt
Nagyon szép és professzionálisan kialakított oldal online kaszinó ranglista!
https://www.ssdunime.it/senza-categoria/sharing-your-stories-has-never-been-easier/
Does your site have a contact page? I’m having a tough
time locating it but, I’d like to send you an email.
I’ve got some recommendations for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it improve
over time.
Trend Hub Daily – Navigate popular categories easily and enjoy checking out trendy products.
Great post. I was checking continuously this weblog and I am inspired!
Very useful information particularly the remaining part :
) I care for such information a lot. I used to be seeking
this particular info for a long time. Thank you and best of luck.
Stop by my blog: Loodgieter Leuven
Огромное спасибо за качественный контент по теме ставок.
https://olimp-casino-kazakhstan-club.kz/how-to-play/
I don’t even understand how I ended up right here, but I thought this post was once great.
I don’t realize who you might be but definitely you are going to a
well-known blogger in case you aren’t already. Cheers!
Here is my web page … Plombier Mons
Главная водка бет
Bu gün onlayn kazinolar əyləncə və uduş imkanlarının ən populyar
formasıdır. Oyundan həzz almaq üçün evdən çıxmağa ehtiyac yoxdur – sadəcə internetə qoşulmaq kifayətdir.
İstifadəçilər rahatlıq, sürət və 24/7 əlçatanlığı səbəbindən onlayn oyunları üstün tuturlar.
Azərbaycan oyunçuları üçün etibarlı seçimlərdən biri Pinco Casino-dur.
Platforma Curacao lisenziyası əsasında fəaliyyət göstərir, şəffaf qaydaları və təhlükəsizlik standartları ilə fərqlənir.
Artıq bir neçə ildir ki, Pinco həm yeni başlayanların, həm də təcrübəli oyunçuların güvənini qazanaraq regionda lider mövqeyini qoruyur.
Currently it looks like Drupal is the top blogging platform available right now.
(from what I’ve read) Is that what you are using on your blog?
перейти на сайт vodkabet новый сайт
Hmm it looks like your site ate my first comment (it was extremely long) so I
guess I’ll just sum it up what I had written and
say, I’m thoroughly enjoying your blog. I as well am an aspiring blog blogger but I’m still new to
everything. Do you have any suggestions for rookie blog writers?
I’d really appreciate it.
Вау, какой крутой сайт kazino olimp! Благодарю!
https://olimp-casino-kz-vip.org.kz/mobile-app/
It’s awesome in favor of me to have a website, which
is helpful designed for my know-how. thanks admin
Материал подробно разбирает впечатления пациентов после подтяжки шеи
и нижней зоны лица.
В тексте разбираются разные методики подтяжки.
Информация подана понятно.
Asking questions are really nice thing if you are not understanding something entirely, but this
post provides pleasant understanding even.
I will immediately seize your rss as I can not in finding your email
subscription link or e-newsletter service. Do you’ve any?
Kindly let me know so that I may just subscribe.
Thanks.
my website; ผงเคลแท้
I’m not sure where you’re getting your information, but good topic.
I needs to spend some time learning much more or understanding more.
Thanks for excellent info I was looking for this info for my mission.
Hey there! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Thanks!
Hi, Neat post. There’s an issue along with your site in web
explorer, could test this? IE nonetheless is the marketplace chief and a big element of people will omit your magnificent writing
due to this problem.
hey there and thank you for your information –
I’ve definitely picked up anything new from right here.
I did however expertise a few technical points using this web site, as I experienced to reload the site
a lot of times previous to I could get it to load properly.
I had been wondering if your web host is OK? Not that I am complaining, but sluggish loading
instances times will sometimes affect your placement in google
and could damage your high quality score if ads and marketing
with Adwords. Anyway I am adding this RSS to my email and can look out for much more
of your respective intriguing content. Make sure you
update this again soon.
Howdy! I could have sworn I’ve been to this blog before but after
checking through some of the post I realized it’s new to me.
Anyways, I’m definitely happy I found it and I’ll be book-marking
and checking back often!
Have you ever thought about creating an ebook or guest authoring
on other sites? I have a blog based on the same topics you discuss
and would really like to have you share some stories/information.
I know my audience would value your work. If you’re even remotely interested,
feel free to send me an e-mail.
What a material of un-ambiguity and preserveness of precious know-how on the topic of unpredicted feelings.
Hello, i read your blog occasionally and i own a similar
one and i was just curious if you get a lot of spam feedback?
If so how do you prevent it, any plugin or anything you can recommend?
i face lens get so much lately it’s driving me
crazy so any help is very much appreciated.
Fantastic goods from you, man. I’ve understand your
stuff previous to and you’re just extremely magnificent.
I really like what you have acquired here, really like what you’re saying and the way
in which you say it. You make it entertaining and you still take care of to
keep it wise. I can’t wait to read much more from you.
This is really a wonderful website.
find out here now https://lumi-wallet.io
Gratias tibi ago quod communicasti. Vereor me creativitate carere. Fabula tua me spe implet. Gratias tibi ago.
You have made some good points there. I checked on the web for more info
about the issue and found most people will go along with your views on this web site.
Магазин кабелей
Продолжение сайт kraken onion
Inspiring quest there. What happened after? Take care!
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CA 92626, United States
Bookmarks
Unquestionably believe that which you said.
Your favorite justification appeared to be on the net the simplest thing
to be aware of. I say to you, I definitely get irked while people consider worries that they plainly don’t know about.
You managed to hit the nail upon the top and defined out the whole thing without
having side-effects , people can take a signal. Will probably be back to get more.
Thanks
4M Dental Implant Center
3918 Lоng Beach Blvd #200, L᧐ng Beach,
CA 90807, United States
15622422075
Bookmarks
дом инвалидов москва Пансионаты для инвалидов: широкий выбор услуг и программ реабилитации Пансионаты для инвалидов предлагают широкий выбор услуг и программ реабилитации, направленных на улучшение физического и психического здоровья постояльцев, восстановление утраченных навыков и повышение качества жизни. Мы разрабатываем индивидуальные программы реабилитации, учитывая особенности и потребности каждого человека.
Hi there just wanted to give you a quick heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different web browsers and both show the same outcome.
https://kacca.in.ua/nevydymyi-zakhysnyk-yak-polimerne-sklo.html
clickwaveagency.click – Color palette felt calming, nothing distracting, just focused, thoughtful design.
Aguyje peẽme pekomparti haguére. Chepy’apy ofalta haguére chéve umi idea creativa. Nde artíkulo omeʼẽ esperanza. aguyje.
I have been exploring for a little for any high-quality
articles or weblog posts in this sort of space . Exploring in Yahoo I at
last stumbled upon this website. Studying this information So i am
glad to show that I’ve an incredibly excellent uncanny feeling I came upon just what I needed.
I most without a doubt will make sure to do not fail to remember this site
and give it a glance on a relentless basis.
I’m really enjoying the design and layout of your site.
It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you
hire out a developer to create your theme? Superb work!
https://uzsienio-kazino.net/ Užsienio kazino
Wow, wonderful blog format! How lengthy have you ever been blogging
for? you made running a blog glance easy. The overall look of
your web site is magnificent, let alone the content!
Awesome! Its genuinely amazing paragraph, I have got much clear idea
about from this piece of writing.
Awesome blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple adjustements would really make my blog
jump out. Please let me know where you got your
design. Kudos
Seriously quite a lot of beneficial knowledge.
Дома из клееного бруса под ключ Строительство из клееного бруса – это современное и эффективное решение для тех, кто ценит экологичность, скорость возведения и эстетическую привлекательность своего будущего дома. Клееный брус, благодаря своей технологии производства, обладает повышенной прочностью, устойчивостью к деформациям и минимальной усадкой, что делает его идеальным материалом для строительства долговечных и надежных зданий.
At this time it appears like Expression Engine is the preferred blogging platform available right now.
(from what I’ve read) Is that what you are using on your blog?
Создаём https://sozdanie-saytove.ru/ которые не просто выглядят великолепно, а на самом деле работают на ваш бизнес. Создаем интуитивно понятные интерфейсы, продумываем пользовательские сценарии и встраиваем инструменты получения лидов. После запуска подключаем комплексное продвижение: SEO оптимизацию, контент стратегию и таргетированную рекламу. Результат — рост целевых заявок и устойчивое присутствие в топ выдаче.
Hello! I’ve been following your weblog for a long time now and finally got the courage to go ahead and give you
a shout out from Houston Tx! Just wanted to tell you keep up the good
job!
Bardzo ładna i profesjonalnie przygotowana strona Najlepsze kasyna online w Polsce!
https://najszybsze-wyplaty-kasyno.pl/blik-kasyna
Howdy just wanted to give you a quick heads up. The text in your content seem to be running off the screen in Opera.
I’m not sure if this is a formatting issue or something
to do with browser compatibility but I thought I’d post to let you know.
The design and style look great though! Hope you get the problem solved soon. Kudos
This is my first time pay a visit at here and i am actually happy to read everthing at one place.
Damen Replika Uhr gunstig bestellen Exklusive Replika Uhr: Das Besondere fur Liebhaber Exklusive Replika Uhren sind die perfekte Wahl fur Uhrenliebhaber, die das Besondere suchen. Diese Modelle zeichnen sich durch einzigartige Designs, hochwertige Materialien und limitierte Auflagen aus. Sie sind nicht nur Zeitmesser, sondern auch Sammlerstucke mit einem besonderen Wert. Eine exklusive Replika Uhr ist ein Statement von Individualitat und Exklusivitat.
Awesome website you have here but I was curious about if you knew of any community forums that cover the same topics discussed in this article?
I’d really love to be a part of community where I can get feed-back from other experienced people
that share the same interest. If you have any suggestions,
please let me know. Appreciate it!
Right here is the right webpage for anyone who would like to understand this topic.
You understand so much its almost tough to argue with you
(not that I personally will need to…HaHa). You certainly put
a brand new spin on a topic that has been written about
for decades. Excellent stuff, just excellent!
Very good blog you have here but I was curious if you knew of any
user discussion forums that cover the same
topics discussed in this article? I’d really like to be a part of community where I can get advice
from other experienced individuals that share the same interest.
If you have any suggestions, please let me know.
Thanks a lot!
I like reading through an article that will make people think.
Also, thank you for permitting me to comment!
Hello there, You’ve done a fantastic job.
I’ll definitely digg it and personally recommend to my friends.
I am confident they will be benefited from this site.
Nice post. I was checking constantly this blog and
I’m impressed! Extremely helpful information specifically the last part :
) I care for such information much. I was seeking this certain information for a very long
time. Thank you and best of luck.
Excellent post. I absolutely appreciate this site. Keep writing!
check my site jaxx liberty wallet
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your blog?
My blog is in the very same area of interest as yours and my users would really
benefit from a lot of the information you provide here.
Please let me know if this alright with you. Thanks a lot!
Just desire to say your article is as surprising. The clarity in your post is just
excellent and i can assume you’re an expert on this subject.
Well with your permission allow me to grab your RSS feed to keep up to date with forthcoming post.
Thanks a million and please continue the gratifying work.
ข้อมูลชุดนี้ มีประโยชน์มาก ครับ
ดิฉัน ไปเจอรายละเอียดของ เนื้อหาในแนวเดียวกัน
ดูต่อได้ที่ ทดลองเล่น pg888 ฟรี
น่าจะถูกใจใครหลายคน
เพราะอธิบายไว้ละเอียด
ขอบคุณที่แชร์ คอนเทนต์ดีๆ นี้
จะรอติดตามเนื้อหาใหม่ๆ ต่อไป
This is a topic which is close to my heart… Cheers! Exactly where are your contact
details though?
Pardonné mbi ti duti kpô. Mo ye aye kue, mo yeke na nzara ti création. A yeke mbeti ti mo la amû na mbi beku. Ngbanga ti nyen?
Cool, Big Bass Splash is a great resource.
https://rmvoz.ru/forums/index.php?action=go;url=aHR0cHM6Ly9iaWctYmFzcy1zcGxhc2gtdWstc2xvdHMuY28udWs
Pretty element of content. I just stumbled upon your site and in accession capital to claim that I get in fact enjoyed account your weblog posts.
Anyway I’ll be subscribing for your feeds and even I success
you get entry to constantly fast.
Этот сайт kazino olimp — настоящая находка.
https://olimp-casino-kz-money.org.kz/payments
Консультации адвоката по уголовным делам в Москве:
как гарантировать успешную защиту клиента в судебном процессе и получить положительные отзывыЮрист по уголовным делам в Москве
Услуги адвоката по уголовным
делам в Москве востребованы среди клиентов, сталкивающихся с обвинениями в
различных преступлениях. Независимо от тяжести дела, наличие опытного адвоката, который сможет законно и эффективно отстаивать ваши интересы
в суде, имеет ключевое значение.
Почему важно обратиться к адвокату?
Адвокат имеет опыт ведения уголовных дел и знает тонкости судебного процесса.
Эксперт поможет достигнуть желаемого результата и минимизировать негативные последствия.
Клиенты могут рассчитывать на полноценные консультации по всем
аспектам дела.
Какие задачи выполняет адвокат?
Обязанности адвоката в уголовных делах состоят из ряда ключевых этапов:
Первоначальная консультация, на которой юрист изучает детали дела и оценивает
шансы на успех.
Сбор и анализ доказательств, необходимых для формирования стратегии защиты.
Подготовка документов для судебных инстанций и активноеучастие в судебных процессах.
Представление интересов
клиента на всех этапах уголовного
процесса.
Отзывы клиентов
Мнения клиентов о работе адвокатов могут сыграть важную роль в выборе защитника.
Многие клиенты отмечают:
Высокий уровень профессионализма и подготовки.
Персонализированный подход к каждому делу.
Способность продуктивно работать в условиях стресса.
Контакты адвоката
Следует заранее узнать
номер телефона адвоката, чтобы в экстренной
ситуации быстро получить помощь.
Доступность и оперативность — ключевые факторы успешной защиты.
Рекомендации по выбору адвоката
в уголовных делах
При выборе адвоката, который занимается
уголовными делами, важно обратить внимание наследующие моменты:
Количество дел, выигранных адвокатом, и опыт
в данной области.
Мнения клиентов и репутация специалиста.
Ясность условий сотрудничества истоимость услуг.
Имейте в виду, что быстрое обращение
к адвокату может кардинально повлиять на результат дела.
Не откладывайте решение важных
вопросов, связанных с защитой ваших прав и интересов. https://m.avito.ru/moskva/predlozheniya_uslug/advokat_po_ugolovnym_delam_3789924168 Итог
Обращение к адвокату по уголовным делам в Москве –
этоважный шаг, который может существенно повлиять на исход вашего уголовного дела.
Все клиенты имеют право на защиту, и именно квалифицированный защитник содействует правильному ведению дела с учетом всех аспектов.
Учитывая сложность уголовного законодательства, важно выбрать специалиста, который сможет эффективно представлять ваши интересы на всех этапах – от досудебного разбирательства до
суда.
Роль профессиональной защиты
Успешная защита в уголовных
делах предполагает не только глубокие знания законодательства,
но и опыт работы с различными категориями преступлений.
Адвокат должен:
Следить за всеми аспектами дела;
Разрабатывать план защиты;
Общаться с должностными лицами;
Защищать ваши права в судебных инстанциях;
Поддерживать клиента на всех этапах процесса.
Почему выбирают нас
Наши клиенты подчеркивают нашу высокую квалификацию и профессионализм.
Наша цель заключается в том, чтобы наши клиенты ощущали защиту и уверенность в своих действиях.
Команда, имеющая значительный опыт в уголовных делах, позволяет
нам достигать успешных результатов в самых запутанных случаях.
Как выбрать адвоката?
Если вы ищете адвоката по уголовным делам в Москве, обратите внимание на:
Мнения предыдущих клиентов;
Квалификация и опыт в вашей сфере;
Возможность предоставить консультации;
Индивидуальный подходк каждому делу.
Имейте в виду, что чем раньше вы свяжетесь с профессионалом, тем больше
шансов на положительный результат.
В случае возникновения вопросов,
вы всегда можетеобратиться к нам.
В завершение, помните, что
каждый имеет право на защиту, и мы готовы вас поддержать.
Обратитесь к нам для консультации и
выясните, как мыможемзащитить ваши интересы в уголовном процессе.
Incredible points. Solid arguments. Keep up the great spirit.
you are really a just right webmaster. The website loading
speed is amazing. It seems that you are doing any distinctive trick.
Also, The contents are masterwork. you’ve performed a great process in this topic!
Дома из клееного бруса Краснодар Строительство дома из клееного бруса подразумевает тщательную подготовку и точное соблюдение технологических процессов. Начиная с разработки проекта, учитывающего особенности ландшафта и пожелания заказчика, и заканчивая финальной отделкой, каждый этап контролируется специалистами. Благодаря этому, дом из клееного бруса не только красив, но и обладает отличными эксплуатационными характеристиками. Дом из клееного бруса – это символ уюта и гармонии. Естественная текстура дерева, приятный аромат и ощущение тепла создают неповторимую атмосферу, в которой хочется жить и наслаждаться каждым моментом. Клееный брус позволяет реализовывать любые дизайнерские задумки, от классики до модерна, подчеркивая индивидуальность владельца.
Нельзя не сказать, что очень доволен(а), что нашёл(а) сайт kazino olimp — супер!
ставки Olimp – https://www.windowsbbs.com/proxy.php?link=https://olimp-casino-kz-win.kz/ –
взгляните на сайте здесь blacksprut onion
is human trafficking thhe ѕecond largest, usaa gymnastics coach
human trafficking, human trafficking news neаr me, snopes lynne nowles human trafficking, human trafficking
awareness Ԁay quotes, human trafficking sex scene, humaan trafficking – menschenhandel, meghan connors human trafficking, ansrew tate human trafficking, arguments օn human trafficking, free human trafficking cme florida, human trfficking օur, human trafficking іn minnesota 2021,
arizona republican human trafficking, orange іs the new black
human trafficking, human trafficking conference ocean city md, 277
arrested іn human trafficking, anti human trafficking
law philippines, north korea human trafficking fɑcts,
hoᴡ will thе wall affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kids
rescued fгom human trafficking, durham region human trafficking, ѡhy
human trafficking is imρortant, mother of god church human trafficking, walmart human trafficking 2020, ᴡhat iѕ thee rate of human trafficking worldwide, human trafficking news (news), human trafficking Ьy state 2021, lgbt human trafficking statistics, south africa
аnd human trafficking, human trafficking statistics fbi, hoitel lawsuits humjan trafficking, operation renewed hope human trafficking, human trafficking atlanta 2022, human trafficking san joaquin county, non rofit organizations
fоr human trafficking, human traffikcking interpol, human trafficking elgin, trafficking women’ѕ human rijghts julietta hua, facebook humazn trafficking lawsuit,
rates оf human trafficking, real wоrld example of human trafficking, lawyers ɑgainst human trafficking, wsin human trafficking summit 2022,
vvad är human trafficking, recognizing tһe signs of human trafficking, human trafficking justice, video ᧐f human trafficking, fοur signs оf human trafficking, human trafficking
honey, binjun xiee human trafficking, human trafficking documentary amazon ⲣrime, minnesota human trafficking data, uncovers russian human trafficking
гing waг, human trafficking chico ca, hujan trafficking juus cogens, human trafficking syrian refugees, human trafficking topics гesearch paper, text human trafficking liink snopes, oprah south africa human trafficking, human trafficking grants 2015,
human trafficking san antonio 2021, human drrug trafficking meaning, human trafficking stories children, fema human trafficking awareness,
florida disney human trafficking, jobs fоr human tafficking victims,
movie abоut humman trafficking 2023 netflix, а
day in the life of a human trafficking victim, uk human trafficking news, bent ⅼicense plate human trafficking reddit,
human traffickingg іn waterbury ct, center tο combat
human trafficking, greenville nc human trafficking, maui human trafficking, tօp
5 human trafficking cities, іs human trafficking happening іn the us, oxnard human trafficking, aurora shoreline human trafficking,
taconganas humman trafficking, hashtags fߋr human trafficking, ԝhite house human trafficking summit, corona human trafficking, border
patrol human trafficking, human trafficking
іn thailand 2020, human trafficking in wv,
11 arrested іn huiman trafficking, china’sone child policy ɑnd human trafficking, hotels human trafficing
2023, human trafficking inn florida 2021, human traffiocking debate topics, international justice mission human trafficking,
uncover human trafficking ring for, scholarly article ߋn human trafficking,
madison herman human trafficking, amad diallo human trafficking,
а poem аbout human trafficking, human trafficking bristol tn, deluca аnd the human trafficking storyline,
economy аnd human trafficking, human trafficking іn trinidad, human trafficking day
2018, caught camera actual human trafficking victims, human trafficking episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch dogs human trafficking map, humazn trafficking
definition canada, airtag human trafficking, human trafficking іn the beauty industry,
人口販子human trafficking, forced labor іn human trafficking,
american airlines center human trafficking, human trafficking се texas, seoah human trafficking, siam human trafficking, fresno hman trafficking statistics, senegal
humn trafficking, human trafficking belgium, michigan human trafficking ⅽourse, nyy times human trafficking,
abandoned stroller human trafficking, human trafficking і-44,
solution on human trafficking, human trafficking canada news, ontario human trafficking, protects victims ⲟf human trafficking amendment, human trafficking іn highland ca, human trafficking hotspot map, human trafficking organizations ontario, human trafficking hiding undsr cars, summary оn human trafficking,
uncovers russian human traffickking гing war, human trafficking
honey, fоur signs oof human trafficking, human trafficking western pa, human trfficking
livermore, human traficking durham region, human trafficking аt atlanta airport, binjun xiee human trafficking, minnesota human trafficking data, human trafficking
documentary amazon ρrime, human trafficking lawyer bloomfield hills, human trafficking charge іn texas, central students
аgainst human trafficking, ap human geography
human trafficking, human traffickiing fⲟr sexual exploitation, blue ffor human trafficking, kanntian ethics human trafficking, anti-human trafficking organization іn cambodia,
jo jorgensen on human trafficking, fort hood soldiers
human trafficking, beau oof tһe fiftһ cplumn human trafficking, hawkins human trafficking, human trafficking inn tthe pacific islands, reasons ᴡhy human trafficking іs bad, ally human trafficking, ѡrite an essay օn human trafficking,
human trafficking pros, human trafficking dark webb reddit, north preston human trafficking, ԁollar sign tattoo human trafficking, whtt iss
human trafficking, human trafficking stuart fl, priceless
movie human trafficking, ti andd wife human trafficking,
human trafficking ethnicity statistics, і 80 truck syop human trafficking,
hamilton human trafficking, oakville human trafficking, human trafficking оn the deep web, current
human trafficking, human trafficking women’ѕ гights, brunei human trafficking,
barack obama human trafficking quote, patron sawint οf human trafficking, spirited away human trafficking,
tһe game human trafficking, toр human trafficking cities 2023, human trafficking ԝhich countries aгe the worst, how tο donate tߋ human trafficking organizations, human trfficking
quuotes famous, human trafficking storty 2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, human traffickming hemet
ⅽа, human trafvicking statistics oregon,
һow tⲟ identify a human trafficking victim, economy ɑnd human trafficking, lover boy method ᧐f human trafficking, deluca ɑnd the hunan trafficking storyline, european humazn trafficking, selah human trafficking,
american airlines center human trafficking, human traffickin paintings, ᴡhat statе iss #1 in human trafficking?,
free porn,porn,porn hub,jav porn,bokep indo,bokep bocil,indo bokep,bokep
addy ash,bokep ngewe,ngewe bocil,bokep binor,bokep stw,bokep tante,bokep pns,bokep
tobrut,bokep viral,bokep bu guru,indian sex,indian wife,desi,mom,gangbang,mother
sex,sex mother,mom sex,ebony,dick,pussy,milf,
casting,mature,teen,lesbian,vagina,vagina creampie,japanese wife,japanese mature,japanese teen,japanese milf,lesbian mature,mature women,squirt machine,russian maid,american abal sluts,granny sex,bokep hijab,bokep malay,brazzers,hentai,arab sex,mature anal,indian sex,african teen,najiaporntube,gigantic ass,sarah уoung,mature mom,pinya scandal,sasha grey,gay,anal gay,mom ɑnd son,mom son,russian mature,
russian teen,anthea ѕon casting,muslim girl blow job,jav subbtitle indonesia viceo bokep,bokep pelajar,remaja ngentod,ѕub indo porn videos,bokep bumil,bokep artis
indo,bokep babymoy,bokep meimei,bokep memek legit,bokep crot dalam,bokep
mantan pacar,bokep fyll percakapan,bokep fᥙll service,bokep tante
mulus,bokep sugardady,bokep adik kakak,bokep selingkuh,
bokep hijab tobrut,tante tobrut,hijab tobrut,
bokep janda,bokep pijat,bokep vcs,bokep live ngentod,bokep indo brondong,bokep
indo tante brondong,bokep оpen bo,oρеn bo stw,bokpe
michat,bokep apk ijo,bokep ojol,bokep bareng pacar,bokep tiktok,bokep jilbab sange,
bokep jilbab abg,bokep ibu mertua,bokep kebaya merah,bokep digilir,
indo porn,porn indo,japanese porn,porn dude,indonesia porn,gay porn,video porn,porn video,porn hd,korean porn,tһе
porn dude,japan porn,free porn,rae lil bblack porn,porn indonesia,ɑi
porn,porn comic,tiktok porn,audrey dais porn,porn movie,chinese porn,sophie rain porn,xxx porn,porn sex,
hd porn,asian porn,anime porn,deepfake porn,sex porn,alyx star
porn,hikaru nagi porn,indonesian porn,nagi hikaru porn,roblox porn,porn xxx,bu guru salsa porn,porn tube,ƅig boobs porn,xnxx porn,situs porn,porn japan,msbreewc porn,film porn,bulan sutena porn,hazel moore
porn,hijab porn,douyin porn viagra,ⅽlick here,buy xansx online,beѕt casino,hacked site,scam reviews,malware,downloadmp3 free, forced labor іn human trafficking, 人口販子human trafficking, crystal meth, ѡhat does crystal meth l᧐oқ like, what
is crystal meth, crystal msth anonymous, һow lߋng ɗoes crystal meth stay
іn your ѕystem, how to mаke crystal meth, blue crystal meth, buy crystal meth
online, crystal meth effects, crystal meth pipe, crystal meth drug,
ѡһat does crystal mmeth lpok lіke?, meth crystal, crystal
meth images, crystal meth ѕide effects, һow іs crystal meth maɗe, meth vs crystal meth, whast dooes
crystal meth ⅾo, crystal meth symptoms, crystal meth ѵs meth, effects of crystal meth,
siɗe effects օf crystal meth, hoᴡ ԁo youu makе crystal meth, crystal
meth vs crack, ԝһat doеѕ crystal meth smell ⅼike, how iss crystal meth ᥙsed, crystal
meth withdrawal, crystal mewth breaking bad, whawt іs crystal meth mɑⅾe of, what
ԁoes crystal meth do to you, crystal meth teeth, smoking crystal meth,
crystal meth pictures, ϲan you snort crystal meth, crystal
meth bеfore аnd after, who invented crystal meth,
crystal meth fɑcts, crystal meth withdrawal symptoms, crystal meth street names, signs ߋf crystal meth, crystal meth addiction, һow tο cook crystal meth, crystal meth definition, ѡhat type of drug іs crystal meth, whɑt
doeѕ crystal meth feel ⅼike, crystal meth meaning, crystal meth ingredients, ᴡhats crystal
meth, ѡhat color is crystal meth, crystal meth detox, crystal meth fɑce,
crystal meth powder, crystal meth poem, street namees fоr crystal meth,
short tedrm effects оff crystal meth, signs ߋf crystal meth abuse, crystal meth rock, crystal meth fly,
crystal meth addict, crystal meth սsers, crystal meth rehab, һow mսch does crystal meth cost, hߋw do youu take crystal meth, һow muϲh iѕ crystal meth, signs ᧐f
crystal meth use, how too smoke crystgal meth, һow
to սѕe cdystal meth, long term effects of crystal
meth, signs ᧐f addiction to crystal meth, pink crystal meth, crystal meth ⅼo᧐k like, breaking bad crystal meth,
ԝhen wass crystal mwth invented, pictures ߋf crystal meth,
һow is crystal meth tаken, signs that ѕomeone is usіng crysral meth, ready οr not crystal meth storage, difference Ьetween meth and crystal meth, һow do you dօ crystal meth, crystal meth.,
locate crystal meth storage, ԝhat are thhe effects ߋf crystal meth,
fake crystal meth, crystal meth people, ᴡһɑt dߋes crystal meth, һow
do you usse crystal meth, how addictive іѕ crystal meth, can yοu overdose onn crystal meth, crystal meth blue,
crystal meth signs, һow long doеs crystal meth last, cryswtal meeth detox loos angeles, һow
do people use crystal meth, hhow dߋеs crystal meth ⅼook lіke, crystal meth porn, һow ⅾoes crystal meth loߋk,
crystal meth storage twisted nerve, ѡhats in crystal meth, crystal meth treatment, ԝһat іs crystal meth mаde from, methamphetamin, methamphetamin adalah,
methamphetamin ⅾan amphetamin adalah, amphetamin dan methamphetamin, chloroethane аnd
methamphetamin, crystal methamphetamin, ᴡhat iss methamphetamin, methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamplhetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid,
methamphetamin geschichte, methamphetamin hcl, amphetamin ᴠs methamphetamin, methamphetamin biru,
methylphenidat methamphetamin, beda amphetamin ⅾan methamphetamin, difference Ьetween amphetamine ɑnd methamphetamin,
methamphetamin psychose, methamphetamin rules, һow to makke methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride,
definition vоn methamphetamin, р2p methamphetamin, methamphetamin medizin, amphetamin ᥙnd methamphetamin, vicks vapor inhalsr methamphetamin,
gta methamphetamin labor, ѡie irkt methamphetamin, methamphetamin entzug, methamphetamin kaufen,
methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest,
unterschied amphetamine սnd methamphetamin, methamphetamin herstellung,
methamphetamin herstellung china, methamphetamin wehrmacht, methampuetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ԝas iist ⅾas, unterschied methamphetamin ᥙnd amphetamin,
methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa
chat gi, еst methamphetamin, methamphetamin pervitin, methamphetmin adalah obat, methamphetamin аndere suchten ɑuch nach, methamphetamin mdma, tschechien methamphetamin,
methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin,
methamphetamin Ԁương tính, waѕ ist methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure, іst mdma methamphetamin, lye іn methamphetamin, ist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetamin meaning, ɗ-methamphetamin, herstellung methamphetamin, methamphetamin ѵѕ amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fаce,
methamphetamin formula, methamohetamin synapse, methamphetamin adderall,
methamphetamin adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese, methamphetamin uuse icd 10, weed, weed
grinder, ᴡhere іs weed legal, disposable weed pen, weed shop near me, milwaukee weed eater, purple weed, іs weed legal in virginia, is
weed legal in oklahoma, is weed legal іn louisiana, weed puller tool,
weed carts, іs weed lega in south carolina, weed killer
fօr lawns, horny goat weed foг men, what states is weed legal, weed shops neɑr me, weed legal ѕtates, weed vape, roundup weed killer, weed
killer spray, edibles weed, recreational weed ѕtates,
weed store, milk weed, weed barrier, іs weed legal iin indiana, legal weed ѕtates, ѕtates with legal weed, iѕ wed legal in kentucky,
werd puller, preen weed preventer, ounce οf weed, dewalt weed eater, plantain weed, husqvarna weed eater, electric
weed eater, hyrid weed, moonrock weed, weed pipe, barrett wilbert weed,
weed control, weed delivery neɑr me, is weed legal in missouri, how to make weed butter, ѡhite weed, is weed legal in utah, moopn rock
weed, snow caps weed, іs weed legal in arkansas, iss weed legzl іn texas 2025, ryobi weed eater, weed
bowl, dill weed, weed legalization, smoking weed,
іѕ weed legal іn nevada, weeed whacker, іs weed legal іn alabama, іs weed a drug, wesed bazrrier fabric, wjat іs horny
goat weed, spruce weed annd grass killer, weed stores nnear me, sprinkles
weed, poke weed, weed withdrawal, weed vapes, snokw cap weed, rm43 weed
killer, craftsmn weed eater, qpp oof weed,weed edibles, cookies
weed, grlato weed, іs weed legal in neѡ mexico, strains оf weed, weed butter, рound
of weed, zaza weed, іѕ weed legal in nc, hоw mᥙch is ann
ounce of weed, pgr weed, iss Ԁelta 9 real weed, diy weed killer,
zip of weed, weed torch, mody weed,elon muusk weed, іs weed illegal
iin texas, wewed eater string, rso weed, weed hangover, weed wallpaper,
іs weed legal іn nebraska, һow to smoe weed, іs weed legal in hawaii, һow
to grow weed, һow to make weed іn infinite craft, іs weed legal іn california, gary payton weed
Sayt superdir, əla işdir. Təşəkkürlər!
https://iep-info.com/2021/02/04/hello-world
Amazing! Its genuinely awesome article, I have got much clear
idea about from this piece of writing.
Thanks on your marvelous posting! I quite enjoyed reading it, you can be a great author.I will be sure to bookmark your blog and will come back from now on.
I want to encourage that you continue your great writing,
have a nice afternoon!
What’s up, this weekend is good in support of me, since this moment i am reading this fantastic educational article here at my residence.
Wonderful post! We will be linking to this particularly great content on our website.
Keep up the good writing.
Clicking Here https://web-breadwallet.com/
Just want to say your article is as astounding.
The clearness for your post is just excellent and i
can suppose you’re a professional in this subject. Well together with your permission allow me to grab your RSS feed to stay up to date with coming near near post.
Thanks a million and please keep up the enjoyable work.
Potential & Progress Spot – Explore strategies to grow personally and professionally each day.
Good post however I was wanting to know if you could write a litte more on this topic?
I’d be very grateful if you could elaborate a little bit
further. Thank you!
Great post. I will be experiencing some of these issues as well..
Saved as a favorite, I love your web site!
Thanks in favor of sharing such a fastidious opinion, paragraph is good,
thats why i have read it fully
Hi friends, pleasant article and nice urging commented at
this place, I am truly enjoying by these.
What’s up, I wish for to subscribe for this weblog to take newest
updates, thus where can i do it please help.
An impressive share! I have just forwarded this onto a colleague who has been conducting
a little homework on this. And he in fact bought me breakfast simply
because I stumbled upon it for him… lol. So allow me
to reword this…. Thank YOU for the meal!! But yeah, thanks for spending time to talk about this
issue here on your site.
Hi there, yup this paragraph is actually pleasant and
I have learned lot of things from it on the topic of blogging.
thanks.
Excellent site you have here but I was wanting to know if you knew of any message boards that cover the same topics talked about in this article?
I’d really like to be a part of online community
where I can get feed-back from other experienced people that share
the same interest. If you have any suggestions, please let
me know. Bless you!
You expressed this fantastically!
I got this web page from my friend who informed me about this web
page and now this time I am browsing this web page and reading very informative posts here.
I’m not sure why but this web site is loading incredibly
slow for me. Is anyone else having this problem or is it a issue on my end?
I’ll check back later and see if the problem still
exists.
Thank you a lot for sharing this with all people you really realize what you are speaking approximately!
Bookmarked. Kindly also visit my web site =).
We could have a hyperlink change contract
between us
This is the perfect web site for anybody who wishes
to find out about this topic. You realize a whole
lot its almost tough to argue with you (not that I actually will need
to…HaHa). You definitely put a fresh spin on a topic that
has been discussed for a long time. Great stuff, just excellent!
Хотел(а) отметить, что рад(а), что нашёл(а) сайт kazino olimp — супер!
https://mediawiki-assistance.comoditas.nl/api.php?action=https://olimp-casino-kazakhstan-money.org.kz/how-to-play
I’m truly enjoying the design and layout of your blog. It’s a
very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a developer to create your
theme? Superb work!
Have you ever thought about writing an e-book or guest authoring on other sites?
I have a blog based upon on the same ideas you discuss and would love to have you share some stories/information. I know my readers would value your work.
If you are even remotely interested, feel free to send me an e-mail.
This text is invaluable. Where can I find out more?
Paļdis par daleišonūs. Es beistūs, ka maņ pītryukst rodūšuma. Tovs stuosts mani pīpylda ar cereibu. Paļdis.
Piece of writing writing is also a excitement, if
you be acquainted with then you can write or else it
is complicated to write.
have a peek at this website https://kinetiq.buzz
It is perfect time to make some plans for the future and it
is time to be happy. I have read this post and if I could I desire to suggest you few interesting things or advice.
Perhaps you could write next articles referring to this article.
I wish to read more things about it!
This site Pengu Sport Slot is a trusted resource.
https://www.jtayl.me/pengusportsecureslottransactions926512
I know this if off topic but I’m looking into starting my own blog and was
wondering what all is needed to get setup? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very web smart so I’m not 100% sure. Any suggestions or advice would be
greatly appreciated. Cheers
anchor https://berapaw.org/
S8
First of all I want to say superb blog! I had a quick question which I’d like to ask if you don’t mind.
I was interested to find out how you center yourself and clear your thoughts before writing.
I’ve had a tough time clearing my thoughts in getting my thoughts out there.
I do enjoy writing but it just seems like the first 10 to 15 minutes tend to be lost simply
just trying to figure out how to begin.
Any ideas or tips? Kudos!
Aw, this was an extremely good post. Finding the time and actual
effort to create a good article… but what can I say… I
put things off a whole lot and never seem to get nearly
anything done.
Hey there! Someone in my Myspace group shared this site with us so I
came to take a look. I’m definitely loving the information. I’m book-marking
and will be tweeting this to my followers! Excellent blog and great style and design.
fantastic issues altogether, you simply gained a logo new
reader. What would you suggest in regards to your publish that you made a few days ago?
Any certain?
web https://looksrare.cfd
When some one searches for his vital thing, thus he/she wants to be available that
in detail, thus that thing is maintained over here.
What’s up it’s me, I am also visiting this site on a regular
basis, this website is really fastidious and the viewers are in fact sharing good thoughts.
Outstanding post but I was wondering if you could write a litte more on this subject?
I’d be very grateful if you could elaborate a little bit more.
Thank you!
It’s perfect time to make some plans for the future and it is time to
be happy. I’ve read this publish and if I may I desire to recommend
you few interesting things or tips. Maybe you
could write subsequent articles relating to this article. I
want to learn even more issues about it!
S8
Because the admin of this web site is working, no question very rapidly it will be renowned, due to its feature contents.
Howdy! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get my blog to
rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Appreciate it!
Greetings! Quick question that’s completely off topic.
Do you know how to make your site mobile friendly?
My web site looks weird when browsing from my apple iphone.
I’m trying to find a template or plugin that might
be able to correct this issue. If you have any suggestions, please
share. Cheers!
you’re in reality a just right webmaster. The web site loading speed is incredible. It kind of feels that you’re doing any distinctive trick. Furthermore, The contents are masterwork. you’ve done a magnificent task in this matter!
prostitutes in Brazil
Really a good deal of very good tips.
this https://theo.exchange/
Hey there would you mind stating which blog platform you’re working with?
I’m going to start my own blog soon but I’m having a tough time choosing between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most blogs and I’m looking
for something unique. P.S Apologies for being off-topic but I had to ask!
Thanks very nice blog!
I know this website presents quality based articles or reviews
and additional material, is there any other website
which offers these things in quality?
Superb post however , I was wanting to know if you could write a litte more on this
subject? I’d be very thankful if you could elaborate a little bit more.
Kudos!
My brother recommended I may like this website.
He was entirely right. This publish actually made my day.
You cann’t imagine just how much time I had spent for this
info! Thanks!
I am extremely impressed with your writing skills and also with the layout on your blog.
Is this a paid theme or did you modify it yourself?
Either way keep up the nice quality writing, it is rare
to see a great blog like this one these days.
That is really interesting, You are an excessively professional blogger.
I have joined your feed and look ahead to in the hunt
for more of your magnificent post. Additionally, I’ve shared your web site in my social
networks
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make
your point. You obviously know what youre talking about, why waste
your intelligence on just posting videos to your blog when you could be giving us
something informative to read?
Hey there! This post couldn’t be written any better! Reading
this post reminds me of my good old room mate! He always kept chatting about this.
I will forward this write-up to him. Pretty sure he will have a good read.
Thanks for sharing!
This is a really good tip especially to those new to
the blogosphere. Simple but very precise info… Thanks for sharing this one.
A must read article!
Definitely imagine that which you said. Your favorite justification seemed to be at the internet the simplest thing to
remember of. I say to you, I definitely get annoyed at
the same time as folks think about concerns that they just don’t recognize about.
You managed to hit the nail upon the top as well as outlined out the
entire thing without having side effect , folks could take a signal.
Will likely be back to get more. Thank you
I think this is one of the most significant info for me.
And i’m glad reading your article. But should remark on few general
things, The website style is wonderful, the articles is really excellent
: D. Good job, cheers
Yaywin – The No. 1 Online Casino and Slots Gaming in Pakistan
Please let me know if you’re looking for a article writer for your weblog.
You have some really good articles and I think I would be
a good asset. If you ever want to take some of the load off, I’d really
like to write some material for your blog in exchange for a link back to mine.
Please blast me an e-mail if interested. Thanks!
It’s a pity you don’t have a donate button! I’d definitely donate to this excellent blog!
I guess for now i’ll settle for book-marking and adding your RSS feed to my Google account.
I look forward to new updates and will talk about this site with
my Facebook group. Chat soon!
This is my first time pay a quick visit at here and i am in fact impressed to read everthing at single place.
Hi to every one, it’s genuinely a fastidious for me to visit this website,
it consists of helpful Information.
Somebody essentially assist to make severely articles I would state.
This is the first time I frequented your web page and thus far?
I amazed with the research you made to make this particular publish amazing.
Excellent task!
Hey there! I could have sworn I’ve been to this site before
but after checking through some of the post I realized
it’s new to me. Nonetheless, I’m definitely glad I found it and I’ll be book-marking and checking
back frequently!
Hi there, i read your blog from time to time
and i own a similar one and i was just curious if you get a lot of spam comments?
If so how do you protect against it, any plugin or anything you can suggest?
I get so much lately it’s driving me crazy so any support is very much appreciated.
go https://safeglobal.club
I am genuinely glad to glance at this webpage posts which contains tons of useful information, thanks for providing these data.
Hi Dear, are you truly visiting this website daily, if so then you
will absolutely obtain good experience.
I was curious if you ever considered changing the layout of your website?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people
could connect with it better. Youve got an awful lot of text
for only having one or two pictures. Maybe you could space it
out better?
Состав капельницы никогда не «копируется»; он выбирается по доминирующему симптому и соматическому фону. Ниже — клинические профили, которые помогают понять нашу логику. Итоговая схема формируется на месте, а скорость и объём зависят от текущих показателей.
Подробнее можно узнать тут – психиатр нарколог на дом
ко ланта ко лант
Состав инфузии мы подбираем под доминирующие симптомы и сопутствующие заболевания. Цель — вернуть управляемость телу, а не «насытить» организм всем сразу. Матрица ниже демонстрирует клиническую логику: окончательное решение принимает врач после очной оценки.
Подробнее можно узнать тут – http://vyvod-iz-zapoya-v-ryazani14.ru
I started charming https://www.cornbreadhemp.com/products/full-spectrum-cbd-gummies a smidgin while ago ethical to last what the hype was about, and now I indeed look brash to them once bed. They don’t knock me escape or anything, but they gain it so much easier to cold and crumple asleep naturally. I’ve been waking up feeling pathway more rested and not sluggish at all. Honestly, description of want I’d tried them sooner.
«Как отмечает врач-нарколог Андрей Николаевич Селиванов, «своевременный визит специалиста на дом позволяет избежать тяжёлых осложнений и ускоряет стабилизацию состояния»».
Детальнее – вызов нарколога на дом санкт-петербург
Конфиденциальность — не обещание на бумаге, а практический стандарт. В клинике используются кодовые профили, шифрованный контур хранения карт, разграничение доступа по ролям; документы оформляются нейтрально, а уведомления формулируются без чувствительных слов. Выездные специалисты приезжают без медицинской символики, а в здании клиники навигация организована так, чтобы перемещение было незаметным. Это создаёт пространство, в котором можно честно говорить о целях и спокойно выполнять план — без стигмы и посторонних взглядов.
Получить дополнительные сведения – наркологическая клиника в санкт-петербурге
Write more, thats all I have to say. Literally, it seems as though you
relied on the video to make your point. You clearly
know what youre talking about, why waste your intelligence
on just posting videos to your weblog when you could be giving
us something enlightening to read?
«Как отмечает врач-нарколог Павел Викторович Зайцев, «эффективность терапии во многом зависит от своевременного обращения, поэтому откладывать визит в клинику опасно»».
Подробнее можно узнать тут – http://narkologicheskaya-klinika-sankt-peterburg14.ru/klinika-narkologii-spb/
FranChoice
7500 Flying Cloud Drive,
#600 Eden Prairie
MN 55344, United Տtates
952-345-8400
Franchise business consulting examples
Continue https://d2finance.cv
Sukunatimni kechir. Men hamma narsani yaxshi ko’raman, menda ijodga chanqoq bor. Sizning maktubingiz menga umid bag’ishlaydi. Nega
В условиях медицинского контроля специалисты выполняют последовательные действия, направленные на стабилизацию состояния пациента.
Получить больше информации – вывод из запоя недорого в рязани
You are so awesome! I do not think I have read anything like this before.
So nice to find another person with a few genuine thoughts on this issue.
Seriously.. many thanks for starting this up. This site is
one thing that’s needed on the web, someone with a bit of originality!
This design is wicked! You most certainly know how to keep
a reader entertained. Between your wit and
your videos, I was almost moved to start my own blog (well, almost…HaHa!) Wonderful job.
I really loved what you had to say, and more than that, how you presented it.
Too cool!
Yafa n ma foto nin kosɔn. N’ be fɛɛn bɛɛ kanu, n’ be n’ yɛrɛ labɛnna. I ka sɛbɛri be jigiya di n’ ma. Mun na?
Aw, this was an exceptionally good post. Taking the time
and actual effort to produce a great article… but what
can I say… I hesitate a lot and don’t seem to get nearly anything done.
Fantastic site you have here but I was curious about if you knew of any message boards that cover the same topics
discussed here? I’d really like to be a
part of community where I can get feed-back from
other knowledgeable individuals that share the same interest.
If you have any suggestions, please let me know.
Appreciate it!
Hi there, just became alert to your blog through Google, and found that it’s really
informative. I’m gonna watch out for brussels. I will
appreciate if you continue this in future. A lot of people will be benefited
from your writing. Cheers!
If you desire to grow your knowledge simply keep visiting this web page and be updated with
the hottest information posted here.
Good day! I could have sworn I’ve visited your blog before but after going through some of the posts I realized it’s new to me.
Regardless, I’m certainly happy I found it and
I’ll be bookmarking it and checking back frequently!
Have a look at my blog post; remote online notary
Hey would you mind letting me know which
web host you’re utilizing? I’ve loaded your blog in 3 different browsers and I must say this blog loads a lot faster then most.
Can you recommend a good internet hosting provider at a fair
price? Thanks a lot, I appreciate it!
This site was… how do you say it? Relevant!! Finally I have found something which helped me.
Thanks a lot!
Feel free to visit my website virtual notary services
If you wish for to take much from this article then you have to apply such methods to your won webpage.
Street Fashion Spot – Curated urban wear for fresh and fashionable daily looks.
Heya i’m for the first time here. I came across this board and I find It truly useful & it helped me out a lot.
I hope to give something back and help others like you aided me.
Thank you for the good writeup. It in fact was a amusement account it.
Look advanced to far added agreeable from you!
However, how can we communicate?
Macie ciekawe informacje na temat strategii gier.
https://opnlink.com/o/uELao
В первые часы важно не «залить» пациента растворами, а корректно подобрать темп и состав с учётом возраста, массы тела, артериального давления, лекарственного фона (антигипертензивные, сахароснижающие, антиаритмические препараты) и переносимости. Именно поэтому мы не отдаём лечение на откуп шаблонам — каждая схема конструируется врачом на месте, а эффективность оценивается по понятным метрикам.
Разобраться лучше – вывод из запоя на дому в рязани
I loved as much as you will receive carried out right here.
The sketch is tasteful, your authored material stylish.
nonetheless, you command get got an shakiness over that you wish be delivering
the following. unwell unquestionably come further formerly again since exactly the same nearly very
often inside case you shield this increase.
Такая последовательность действий обеспечивает системное воздействие и минимизирует риски осложнений.
Подробнее – вызов врача нарколога на дом
Hi there, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam
responses? If so how do you protect against it,
any plugin or anything you can suggest? I get so much lately it’s driving me crazy
so any help is very much appreciated.
More Bonuses https://hypperswap.cloud/
Hmm it appears like your blog ate my first comment (it was
extremely long) so I guess I’ll just sum it up what I submitted and say,
I’m thoroughly enjoying your blog. I as well
am an aspiring blog blogger but I’m still new to
everything. Do you have any points for novice blog writers?
I’d definitely appreciate it.
Mangelsen
7916 Girard Avenue, Ꮮa Joya
ᏟA 92037, United Stateѕ
1 800-228-9686
top spirit cub photography
Very good blog post. I absolutely appreciate this website.
Keep writing!
Feel free to visit my blog: international notary services
Состав капельницы никогда не «копируется»; он выбирается по доминирующему симптому и соматическому фону. Ниже — клинические профили, которые помогают понять нашу логику. Итоговая схема формируется на месте, а скорость и объём зависят от текущих показателей.
Исследовать вопрос подробнее – http://narcolog-na-dom-krasnodar14.ru/krasnodar-narkologicheskij-czentr/
Лечение начинается с короткой оценки рисков и выбора безопасной точки старта. Далее следуют этапы стабилизации, настройки сна и тревоги, поведенческие инструменты и план антирецидивной поддержки. Ниже — ориентировочная карта: в реальности длительности и интенсивность подбираются индивидуально, а переход между форматами происходит без «обнуления» обследований.
Подробнее тут – https://narkologicheskaya-klinika-v-spb14.ru/narkolog-sankt-peterburg
I know this if off topic but I’m looking into starting my own weblog and was curious what all is required
to get setup? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very web savvy so I’m not 100% certain. Any recommendations or advice would be greatly appreciated.
Kudos
Супер-платформа! Всё на уровне, поздравляю и успехов!
https://portalonbus.com.br/2023/09/10/apesar-de-gosto-amargoso-jilo-melhora-o-humor/
I really like looking through a post that will make people think.
Also, thank you for permitting me to comment!
Here is my homepage … international notary services
Hi there to every body, it’s my first pay a visit of this web site; this weblog contains remarkable and truly fine material in favor of readers.
С интересом читаю материалы на казино онлайн. Респект за полезную инфу!
https://h1.nu/1izL6
«Как отмечает врач-нарколог Павел Викторович Зайцев, «эффективность терапии во многом зависит от своевременного обращения, поэтому откладывать визит в клинику опасно»».
Получить больше информации – наркологическая клиника цены в санкт-петербурге
«Как отмечает врач-нарколог Иван Петрович Соловьёв, «правильный вывод из запоя возможен только при участии специалистов, так как самолечение может привести к тяжёлым осложнениям»».
Углубиться в тему – https://vyvod-iz-zapoya-ryazan14.ru/vyvod-iz-zapoya-ryazan-na-domu/
Yes! Finally someone writes about remote online notary.
visit this website https://royco.cc/
Cabinet IQ Austin
2419 Ѕ Bell Blvd, Cedar Park,
TX 78613, Uniteed Ⴝtates
+12543183528
Creativeideas (Tesha)
I am sure this piece of writing has touched all the internet users, its really really pleasant post on building up new blog.
Excellent article. Keep writing such kind of information on your page.
Im really impressed by your site.
Hi there, You have performed a fantastic job. I will definitely digg it and in my view recommend to my friends.
I am sure they’ll be benefited from this web site.
4M Dental Implant Center
3918 ᒪong Beach Blvd #200, L᧐ng Beach,
CА 90807, United Ѕtates
15622422075
implant recovery
Great article, totally what I was looking for.
Thanks designed for sharing such a pleasant idea, article is good, thats why i have read it fully
Wow! This blog looks just like my old one! It’s
on a totally different subject but it has pretty much the same
page layout and design. Excellent choice of colors!
«Как отмечает врач-нарколог Андрей Николаевич Селиванов, «своевременный визит специалиста на дом позволяет избежать тяжёлых осложнений и ускоряет стабилизацию состояния»».
Ознакомиться с деталями – нарколог на дом вывод в санкт-петербурге
I think the admin of this website is truly working hard in support of his website, for the reason that here every information is quality based data.
Pretty section of content. I just stumbled upon your blog and in accession capital to assert that I acquire
in fact enjoyed account your blog posts. Any way I’ll be subscribing to your augment and even I achievement you access consistently fast.
Did you notice, nevertheless, that tea may even be among the finest instruments you might have against hemochromatosis and iron overload? However, Amazon has a bamboo tea luggage which makes discovering it pretty convenient. Nowadays, a formal afternoon tea is extra of a special occasion, taken as a treat in a hotel. For extra Arts & Crafts/Mission components, specify bronze or wrought-iron hardware and wallcoverings in stylized leaf and flower motifs (oak leaves, acorns, ivy, tulips, and anything by Arts & Crafts founder William Morris). The lovely view is made even more inspiring with fantastic framing. These homeowners added space from a close by bedroom and closet to their small current bath to create a new 31×9-foot bath worthy of its inspiring backyard view. Borrowing ideas from the industrial loft-fashion design aesthetic, this bath makes use of a shade scheme of high-distinction neutrals and dramatically easy shapes repeated http://37k.ru/to.php?url=https://scientific-programs.science/wiki/All_Day_Slimming_Tea:_Your_Key_To_A_Healthier_Lifestyle through the space. Against the calm taupe floor, this green-and-copper band serves as a blithe reminder of nature’s personal colour scheme just outside the window.
Informative article, exactly what I was looking for.
If some one desires expert view about running a blog
after that i propose him/her to pay a quick visit this website,
Keep up the fastidious job.
Наша философия проста: минимум медикаментов, максимум управляемости процесса. Мы не используем «универсальные капельницы», а собираем схему под клиническую картину: длительность запоя, выраженность тремора и тошноты, качество сна, уровень тревоги, исходное давление и частоту пульса, сопутствующие заболевания, текущие лекарства (антигипертензивные, антиаритмические, сахароснижающие, средства для сна). Скорость инфузии задаётся инфузоматом, витальные показатели контролируются портативным кардиомонитором и пульсоксиметром, глюкоза и электролиты — по экспресс-панелям. Такой подход снижает риск осложнений и делает результат предсказуемым и устойчивым.
Узнать больше – https://narcolog-na-dom-krasnodar14.ru/narkolog-krasnodar-anonimno/
Современная наркология — это не набор «сильных капельниц», а точные инструменты, управляющие скоростью и направлением изменений. В «НеваМеде» технологический контур работает тихо и незаметно для пациента, но даёт врачу контроль над деталями, от которых зависит безопасность.
Исследовать вопрос подробнее – платная наркологическая клиника в санкт-петербурге
Ниже представлена карта действий бригады «РязМедСервиса» в первые три часа. Это не «жёсткая сетка», а ориентир для безопасной и быстрой стабилизации. В каждом блоке есть клиническая цель, измеримые критерии и условие для перехода к следующему шагу.
Углубиться в тему – нарколог на дом вывод из запоя рязань
10 euros offert paris sportif|10 euros offert sans dépôt paris sportif|10 meilleurs sites
de paris sportifs|100 euro offert paris sportif|100 euros offert paris sportif|100
euros remboursé paris sportifs|100 offert pari sportif|100
offert paris sportif|100 remboursé paris sportif|100e offert pari
sportif|abandon paris sportif tennis|abandon tennis paris sportif|addiction paris sportif forum|age paris sportif belgique|aide au pari sportif|aide au paris sportif|aide aux paris sportif|aide aux paris
sportifs|aide pari sportif|aide pari sportif football|aide
parie sportif|aide paris sportif|aide paris sportif foot|aide paris sportif gratuit|aide
paris sportifs|aide pour paris sportif|algorithme de paris sportif|algorithme excel paris sportif|algorithme gratuit paris sportif|algorithme pari sportif|algorithme paris sportif|algorithme paris sportif avis|algorithme paris sportif basket|algorithme paris sportif excel|algorithme paris sportif gratuit|algorithme paris sportif tennis|algorithme
paris sportifs|algorithme pour paris sportif|analyse cote paris
sportif|analyse de paris sportif|analyse match paris sportif|analyse pari sportif|analyse paris sportif|analyse
paris sportif foot|analyse paris sportif football|analyse paris sportif gratuit|analyse paris
sportifs|ancienne cote paris sportif|api cote paris sportif|app
paris sportif sans argent|appli de paris sportif|appli de paris
sportif sans argent|appli de paris sportifs|appli pari sportif|appli pari sportif gratuit|appli
parie sportif|appli paris sportif|appli paris sportif avec paypal|appli paris sportif belgique|appli paris
sportif entre amis|appli paris sportif gratuit|appli paris sportif sans
argent|appli paris sportif suisse|appli paris sportifs|application aide paris
sportif|application algorithme paris sportif|application analyse
paris sportif|application android paris sportif|application bankroll paris sportif|application conseil
paris sportif|application de pari sportif|application de parie sportif|application de paris sportif|application de paris sportif en afrique|application de paris sportif en cote d’ivoire|application de paris sportif en ligne|application de paris sportif gratuit|application de paris
sportif international|application de paris sportif suisse|application de paris sportifs|application faux paris sportifs|application gestion bankroll paris sportif|application gestion paris
sportif|application ia paris sportif|application pari sportif gratuit|application paris sportif|application paris sportif android|application paris sportif argent fictif|application paris
sportif belgique|application paris sportif canada|application paris
sportif espagne|application paris sportif espagnol|application paris sportif fictif|application paris sportif france|application paris sportif gratuit|application paris sportif gratuit entre amis|application paris sportif maroc|application paris sportif offre de bienvenue|application paris sportif paypal|application paris sportif sans argent|application paris sportif sans justificatif de domicile|application paris
sportif suisse|application paris sportif usa|application paris
sportif virtuel|application pour faire des paris sportifs|application pour gerer ses
paris sportif|application pour les paris sportifs|application pour pari sportif|application pour
paris sportif|application pour paris sportifs|application statistique paris sportif|application suivi paris sportif|applications de paris
sportifs|applications paris sportifs|applis paris sportif|applis paris sportifs|apprendre
a faire des paris sportifs|argent facile paris sportif|argent offert paris sportifs|argent offert
sans depot paris sportif|argent paris sportif|argent paris sportifs|argent paris sportifs impots|argent
sans depot paris sportif|arjel paris sportif|arjel paris sportifs|astuce gagner paris sportif|astuce
pari sportif|astuce paris sportif|astuce paris sportif basket|astuce paris sportif foot|astuce paris sportif
forum|astuce paris sportif tennis|astuce paris sportifs|astuce pour
gagner au pari sportif|astuce pour gagner au paris sportif|astuce pour gagner paris sportif|astuce pour paris sportif|astuces paris sportifs|astuces paris sportifs en ligne|astuces paris sportifs
foot|astuces pour gagner aux paris sportifs|autorisation paris sportif france|avis
pari sportif|avis paris sportif|avis paris sportif foot|avis site de paris sportif|avis
site paris sportif|avis sur les paris sportifs|avis sur paris sportif|avis tipster paris sportif|aweh signification paris sportif|bankroll 100 euros
paris sportifs|bankroll management paris sportif|bankroll paris
sportif|bankroll paris sportif excel|bankroll paris sportif
gratuit|bankroll paris sportifs|basket paris sportif|belgique france paris sportif|belgique paris sportifs|bonus bienvenue paris sportif|bonus bienvenue paris sportifs|bonus
cash paris sportif|bonus de bienvenue paris sportif|bonus de bienvenue paris sportif belgique|bonus de bienvenue sans depot
paris sportif|bonus de depot paris sportif|bonus de paris sportifs|bonus depot paris sportif|bonus en cash paris sportif|bonus gratuit paris sportif|bonus gratuit sans depot
paris sportif|bonus pari sportif|bonus paris sportif|bonus paris sportif belgique|bonus paris sportif
betclic|bonus paris sportif cash|bonus paris sportif en ligne|bonus paris sportif france pari|bonus paris sportif
retirable|bonus paris sportif sans depot|bonus paris sportif sans dépôt|bonus paris sportif unibet|bonus paris sportifs|bonus
sans depot paris sportif|bonus sans depot paris sportif belgique|bonus
sans dépôt paris sportif|bonus sans dépôt
paris sportif hors arjel|bonus site de paris sportif|bonus site pari sportif|bonus site
paris sportif|bonus sites de paris sportifs|bonus unibet
paris sportif|bookmaker paris sportif|bookmaker paris
sportif gratuit|bookmaker paris sportifs|bookmaker sportif|bookmakers paris sportif|bookmakers paris sportifs|bookmakers paris sportifs en ligne|but contre son camp paris sportif|but sur penalty paris sportif|buteur paris
sportif|c’est quoi handicap paris sportif|c’est quoi une cote paris sportif|calcul anti perte paris sportif|calcul combinaison pari sportif|calcul
cote pari sportif|calcul cote paris sportif|calcul couverture paris sportif|calcul de cote paris sportif|calcul des cotes paris sportifs|calcul
dnb paris sportifs|calcul double chance paris sportif|calcul gain paris sportif|calcul mise paris sportif|calcul pari sportif|calcul paris sportif|calcul paris sportif multiple|calcul pourcentage cote paris sportif|calcul probabilité paris sportif|calcul rentabilité paris sportifs|calcul roi
paris sportif|calcul systeme paris sportif|calcul trj paris sportifs|calculateur cote paris sportif|calculateur de cote paris sportif|calculateur de mise paris sportif|calculateur de paris sportif|calculateur paris
sportif|calculatrice arbitrage paris sportif|calculatrice paris sportif|calculer
cote paris sportif|calculer gain paris sportif|calculer
probabilité paris sportifs|calculer roi paris sportifs|calculer une cote pari
sportif|calculer une cote paris sportif|carte cadeau paris sportif|carte
pcs paris sportif|carte prépayée paris sportifs|cash out
pari sportif|cash out paris sportif|cash out paris sportifs|casino en ligne paris sportif|casino paris sportif en ligne|champions league
paris sportif|chute de cote paris sportif|classement des meilleurs sites de paris sportifs|classement meilleur site de paris
sportif|code barre paris sportif|code bonus paris sportif|code paris sportif|code promo pari sportif|code promo paris sportif|code promo paris sportif sans
depot|code promo paris sportif sans dépôt|code promo sans depot paris sportif|code promo site paris sportif|combien de temps pour encaisser un paris sportif|combien de temps pour retirer un paris sportif|combien miser paris sportifs|combine paris sportif|combines paris
sportifs|combiné pari sportif|combiné paris sportif|combiné
paris sportif conseil|combiné paris sportif du jour|combiné paris sportif pronostic|comment analyser un paris sportif|comment arreter de jouer aux paris sportifs|comment arreter les paris sportif|comment arreter les
paris sportifs|comment arrêter les paris sportifs|comment bien gagner au paris sportif|comment bien jouer au paris sportif|comment bien miser paris sportif|comment ca marche les paris sportif|comment calculer cote paris sportif|comment calculer gain paris sportif|comment calculer les cotes des paris sportifs|comment calculer une
cote de paris sportif|comment calculer une cote pari sportif|comment calculer une cote
paris sportif|comment comprendre les paris sportifs|comment creer
un vip paris sportif|comment créer un algorithme paris sportif|comment créer
un site de paris sportif|comment devenir riche avec les paris sportifs|comment etre rentable paris sportif|comment etre sur
de gagner au paris sportif|comment faire de bon paris sportif|comment faire des
parie sportif|comment faire des paris sportif|comment faire des
paris sportif gagnant|comment faire des paris sportifs|comment faire
pari sportif|comment faire paris sportif|comment faire pour arreter les paris sportifs|comment faire pour gagner
au paris sportif|comment faire pour gagner
les paris sportifs|comment faire un bon pari sportif|comment faire un bon paris sportif|comment faire
un pari sportif|comment faire un parie sportif|comment faire
un paris sportif|comment faire une montante paris sportif|comment fonctionne les
cotes dans les paris sportifs|comment fonctionne les cotes des paris sportifs|comment fonctionne les paris sportifs|comment fonctionne paris sportifs|comment fonctionne un pari sportif|comment
fonctionnent les cotes dans les paris sportifs|comment fonctionnent
les cotes dans les paris sportifs grand oral|comment fonctionnent les cotes de paris
sportif|comment fonctionnent les paris sportifs|comment fonctionnent les paris sportifs grand oral|comment fonctionnent les paris
sportifs grand oral maths|comment fonctionnent les paris sportifs maths|comment gagner a coup sur au paris sportif|comment gagner a tous les coups au paris sportif|comment gagner a tout les coup au
paris sportif|comment gagner au pari sportif|comment gagner au pari sportif
football|comment gagner au paris sportif|comment gagner au paris
sportif a coup sur|comment gagner au paris sportif foot|comment gagner au paris sportif forum|comment gagner
au paris sportif tennis|comment gagner au paris sportifs|comment gagner aux paris sportif|comment gagner aux paris sportifs|comment gagner
aux paris sportifs foot|comment gagner aux paris
sportifs livre|comment gagner aux paris sportifs sur le long terme|comment gagner avec les
paris sportifs|comment gagner dans les paris sportifs|comment gagner de l argent
avec les paris sportifs|comment gagner de l’argent au paris sportif|comment gagner de l’argent aux paris sportifs|comment gagner de l’argent avec
les paris sportifs|comment gagner de l’argent paris sportif|comment gagner de l’argent sur les paris sportifs|comment gagner de l’argent sur paris sportif|comment gagner
des paris sportif|comment gagner des paris sportifs|comment gagner en paris sportif|comment gagner facilement au paris sportif|comment
gagner les paris sportifs|comment gagner paris sportif|comment gagner paris sportif
foot|comment gagner paris sportifs|comment gagner sa vie avec
les paris sportifs|comment gagner ses paris sportif|comment gagner sur
les paris sportif|comment gagner sur les paris
sportifs|comment gagner tout le temps au paris
sportif|comment gagner un pari sportif|comment gagner un paris sportif|comment gerer
une bankroll paris sportif|comment gérer sa
bankroll paris sportif|comment jouer au pari sportif|comment jouer au
paris sportif|comment jouer au paris sportif foot|comment jouer aux paris sportifs|comment jouer paris sportif|comment marche
cote paris sportif|comment marche les cotes paris sportif|comment marche les paris sportif|comment
marche les paris sportifs|comment marche paris sportif|comment marche un pari
sportif|comment marche un paris sportif|comment marchent les cotes paris sportif|comment marchent les paris sportifs|comment miser
au paris sportif|comment miser paris sportif|comment monter sa
bankroll paris sportif|comment ne jamais perdre au paris sportif|comment parier sportif|comment reussir au paris sportif|comment reussir les paris sportif|comment reussir paris sportif|comment
sont calculer les cotes de paris sportif|comment sont calculées
les cotes des paris sportifs|comment sont calculés les cotes des paris sportifs|comment sont faites les cotes des paris sportifs|comment toujours gagner au paris
sportif|comment ça marche les paris sportifs|comparaison bonus
paris sportifs|comparaison cote pari sportif|comparaison des cotes paris sportifs|comparateur cote pari sportif|comparateur cote paris sportif|comparateur cotes paris sportif|comparateur cotes paris sportifs|comparateur de
cote pari sportif|comparateur de cote paris sportif|comparateur de cotes paris sportifs|comparateur de côtes paris
sportifs|comparateur de paris sportif|comparateur
de site de paris sportif|comparateur de site paris sportif|comparateur de sites de paris sportifs|comparateur pari sportif|comparateur
paris sportif|comparateur paris sportifs|comparateur site de
paris sportif|comparateur site pari sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif
bonus paris sportifs|comparatif cote pari sportif|comparatif cote paris sportif|comparatif cotes
paris sportifs|comparatif des sites de paris sportifs|comparatif offre de bienvenue
paris sportif|comparatif offre paris sportif|comparatif pari
sportif|comparatif pari sportif en ligne|comparatif paris sportif|comparatif paris sportif
bonus|comparatif paris sportif en ligne|comparatif paris sportifs|comparatif paris sportifs en ligne|comparatif site de paris
sportif|comparatif site paris sportif|comparatif site paris sportifs|comparatif sites de paris sportifs|comparatif sites paris sportifs|comparer les cotes paris sportifs|comprendre cote
paris sportif|comprendre handicap paris sportif|comprendre les cotes des paris sportifs|comprendre
les cotes paris sportif|comprendre les cotes paris
sportifs|comprendre les handicap paris sportif|compte de paris sportif|compte démo paris sportif|compte finance paris sportif|compte financer paris sportif|compte financier paris sportif|compte financé paris sportif|compte pari sportif|compte paris sportif|compte paris sportif financé|conseil
de paris sportif|conseil de paris sportifs|conseil en paris sportif|conseil en paris sportifs|conseil pari sportif|conseil pari sportif gratuit|conseil paris
sportif|conseil paris sportif aujourd’hui|conseil paris sportif du jour|conseil paris sportif foot|conseil paris sportif
gratuit|conseil paris sportif ligue des champions|conseil
paris sportif nba|conseil paris sportif pronostic|conseil paris sportif
rmc|conseil paris sportif tennis|conseil paris sportifs|conseil pour gagner au paris sportif|conseil pour
paris sportif|conseil sur les paris sportifs|conseille paris sportif|conseiller en paris
sportifs|conseiller paris sportif|conseils de paris sportifs|conseils en paris sportifs|conseils paris sportifs|conseils
paris sportifs foot|conseils paris sportifs gratuit|conseils paris sportifs
tennis|conseils pour paris sportifs|cote a 100 paris sportif|cote a 2 paris sportif|cote
anglaise paris sportif|cote de 2 paris sportif|cote de pari sportif|cote
de paris sportif|cote des paris sportifs|cote maximum paris sportif|cote
minimum paris sportif|cote pari sportif|cote pari sportif
comment ça marche|cote pari sportif real madrid|cote pari sportif rugby|cote
parie sportif|cote paris sportif|cote paris sportif belgique|cote paris sportif calcul|cote paris
sportif definition|cote paris sportif euro|cote paris sportif explication|cote paris sportif foot|cote paris sportif france belgique|cote paris sportif france espagne|cote paris sportif ligue des champions|cote
paris sportif moto gp|cote paris sportif psg|cote paris sportif psg arsenal|cote paris sportif rugby|cote paris sportif tennis|cote paris sportifs|cote
pour paris sportifs|cote sportif foot|cote sportif rugby|cote
à 1000 paris sportif|cotes de paris sportifs|cotes pari sportif|cotes paris
sportif|cotes paris sportifs|cotes paris sportifs foot|coupe de france paris sportif|créer
un algorithme paris sportif|créer un compte paris sportif|créer un site de paris
sportif en ligne|dans les paris sportifs que signifie handicap|declarer ses gains paris sportif|definition cash out
paris sportif|definition cote paris sportif|definition handicap paris sportif|depot 5 euros paris sportif|depot double paris sportif|depot minimum 5 euro paris sportif|depot minimum paris sportif|depot paris sportif|depuis
quand existe les paris sportif en france|devenir riche avec
les paris sportifs|devenir riche avec paris sportifs|disqualification tennis paris sportif|dnb en paris sportif|dnb pari sportif|dnb paris sportif|dnb paris sportif definition|dnb paris sportifs|doit on declarer les gains de paris sportif|déclarer gains paris
sportifs|déclarer gains paris sportifs hors arjel|définition bankroll paris sportif|dépôt minimum 1 euro paris
sportif|dépôt minimum 5 euro paris sportif|ecart de jeux tennis paris sportif|erreur de cote paris sportif|est ce que les gains des
paris sportifs sont imposables|est-ce que les prolongation compte dans un pari sportif|etre sur
de gagner au paris sportif|euro paris sportif|evenement sportif a paris|evenement sportif paris|evenement sportif paris 2025|evenement
sportif paris aujourd hui|evenement sportif paris aujourd’hui|evenement sportif paris ce week end|evenements sportif paris|evenements sportifs paris|evenements sportifs paris 2025|evenements sportifs à paris|evolution cote paris
sportif|evolution cotes paris sportifs|evolution des cotes paris sportifs|explication cote pari
sportif|explication cote paris sportif|explication handicap paris sportif|explication pari sportif|explication paris sportif|face a face hockey paris sportif|faire des paris sportif|faire des paris sportif avec paypal|faire des paris
sportifs|faire fortune paris sportifs|faire un pari sportif|faire un paris sportif|faut il déclarer les gains de paris
sportifs|faut il déclarer ses gains paris sportifs|fichier excel
gestion bankroll paris sportif|fiscalité gains paris sportifs|foot paris sportif|football et paris sportifs|forfait tennis paris sportif|formation paris sportif gratuit|forum de paris sportif|forum de paris sportifs|forum pari
sportif|forum parie sportif|forum paris sportif|forum paris
sportif foot|forum paris sportif gratuit|forum paris sportif nba|forum paris
sportif tennis|forum paris sportifs|forum sur les paris sportifs|forum tennis paris sportif|francaise des jeux pari sportif|francaise des jeux paris sportif|francaise
des jeux paris sportifs|france 2 paris sportif|france 2 paris sportifs|france belgique paris sportif|france espagne
paris sportif|france pari sportif|france pari sportif brest|france paris sportif|france
paris sportifs|france pologne paris sportif|france portugal paris sportif|france suisse paris sportifs|france
tunisie paris sportifs|france-pari – paris sportifs|gagnant pari sportif|gagnant paris
sportif|gagnant paris sportif bayern|gagnante paris
sportif|gagne au paris sportif|gagner 10 euros par
jour aux paris sportifs|gagner 100 euros par jour
paris sportif|gagner 1000 euros par mois paris sportifs|gagner 10000 euros paris sportif|gagner 2000
euros par mois paris sportif|gagner 50 euros par jour paris sportif|gagner a coup sur au paris
sportif|gagner a coup sur pari sportif|gagner a
tous les coup paris sportif|gagner argent avec paris sportifs|gagner argent pari sportif|gagner argent paris sportif|gagner argent paris sportifs|gagner au pari sportif|gagner au paris sportif|gagner au paris sportif a coup sur|gagner au paris sportif foot|gagner au
paris sportif forum|gagner au paris sportif à coup sur|gagner
aux paris sportif|gagner aux paris sportifs|gagner aux paris sportifs pdf|gagner beaucoup d’argent paris sportif|gagner de l argent grace aux
paris sportifs|gagner de l argent pari sportif|gagner de l argent paris sportif|gagner de l argent paris sportifs|gagner de l’argent au paris sportif|gagner de l’argent aux paris sportifs|gagner de l’argent avec les paris sportifs|gagner
de l’argent avec paris sportif|gagner de l’argent
avec paris sportifs|gagner de l’argent grace au paris sportif|gagner
de l’argent grace aux paris sportifs|gagner de l’argent pari sportif|gagner de l’argent paris sportif|gagner de l’argent paris
sportifs|gagner de l’argent sur les paris sportifs|gagner des paris sportif|gagner des paris sportifs|gagner les paris sportifs|gagner pari sportif|gagner paris sportif|gagner paris sportif foot|gagner paris sportif forum|gagner paris sportif
tennis|gagner paris sportifs|gagner sa vie avec les paris sportif|gagner sa vie avec les paris sportifs|gagner sa vie
avec paris sportifs|gagner ses paris sportifs|gagner à coup sur
paris sportif|gagner à tous les coups paris sportifs|gain maximum paris sportif|gain pari sportif|gain pari sportif imposable|gain pari sportif impot|gain paris sportif|gain paris sportif imposable|gain paris sportif impot|gain paris sportif impôt|gains paris sportif|gains paris sportif
imposable|gains paris sportifs|gains paris sportifs
imposable|gains paris sportifs imposables|gains paris sportifs sont ils imposables|gerer bankroll paris sportif|gerer sa bankroll paris sportif|gerer une bankroll paris sportif|gestion bankroll paris sportif|gestion bankroll paris sportifs|gestion bankroll paris sportifs excel|gestion de bankroll paris sportif|gestion de bankroll paris sportif application|gestion de bankroll paris
sportifs|gestion de mise paris sportif|gestion paris sportifs v2 5 gratuit|gg signification paris sportif|gros combiné paris
sportif|gros gain paris sportif|grosse cote paris sportif pronostic|grosse mise
paris sportif|groupe paris sportif gratuit|groupe telegram paris sportif
gratuit|groupement de joueurs paris sportifs|handicap 0 paris sportif|handicap 1 paris sportif|handicap 5 paris sportif|handicap au paris sportif|handicap basket paris sportif|handicap dans les paris
sportifs|handicap en paris sportif|handicap europeen paris sportif|handicap européen paris sportifs|handicap mi
temps paris sportif|handicap pari sportif|handicap paris sportif|handicap paris sportif basket|handicap paris sportif explication|handicap paris sportif foot|handicap paris sportif rugby|handicap paris sportifs|handicap rugby
paris sportif|handicap tennis paris sportif|historique cote paris
sportif|historique des cotes paris sportifs|hockey paris
sportif|hockey sur glace paris sportif|hors arjel paris sportif|hweh signification paris sportif|imposition gain pari sportif|imposition gain paris sportif|imposition gains paris sportifs|imposition paris sportif france|impot gain paris sportif|impot paris sportif france|impot
sur gain paris sportif|je gagne ma vie avec
les paris sportifs|jeu de pari sportif gratuit|jeu de paris
sportif en ligne|jeu de paris sportif gratuit|jeu paris sportif gratuit|jeu paris sportif sans argent|jeux de parie sportif|jeux de paris sportif|jeux de paris sportif en ligne|jeux de paris sportif gratuit|jeux de paris sportifs|jeux olympiques paris sportifs|jeux paris
sportif|jeux paris sportif gratuit|jeux paris sportif virtuel|jeux
paris sportifs en ligne|jouer au paris sportif|jouer paris sportif|joueur absent paris
sportif|joueur blesse paris sportif|joueur caen paris sportif|joueur de caen pari sportif|joueur de
foot paris sportif|joueur decisif paris sportif|joueur décisif
paris sportif|joueur italien paris sportif|joueur paris sportif|joueur professionnel paris
sportif|joueur qui se blesse paris sportif|joueur
sanctionne pari sportif|joueur suspendu paris sportif|joueurs italiens paris sportifs|l’argent des paris
sportifs est il imposable|la cote paris sportif|la francaise des jeux
paris sportif|la martingale paris sportif|la martingale paris sportifs|la meilleur application de paris sportif|la meilleur application paris sportif|la meilleur technique pour gagner au paris sportif|la méthode secrète pour gagner aux paris sportifs pdf|la plus grosse cote gagner paris
sportif|la plus grosse cote paris sportif|ldem paris sportif signification|le marché des
paris sportifs|le meilleur site de pari sportif|le meilleur site de paris sportif|le meilleur site de paris sportif en ligne|le meilleur site de paris sportifs|le plus gros
gain au paris sportif|le plus gros paris sportif|le plus gros paris sportif du monde|les
10 meilleurs sites de paris sportifs|les 10 meilleurs sites de paris sportifs en afrique|les 17 secrets
pour gagner rapidement aux paris sportifs|les 17 secrets pour
gagner rapidement aux paris sportifs pdf|les application de paris sportif|les applications paris sportifs|les bonus
paris sportifs|les bookmakers paris sportifs|les cotes paris sportifs|les gains de paris sportifs sont ils imposables|les gains des paris sportifs sont ils imposables|les jeux de paris sportifs|les meilleur
paris sportif|les meilleures applications de paris sportifs|les meilleurs
applications de paris sportifs|les meilleurs bonus paris sportif|les meilleurs
bonus paris sportifs|les meilleurs cotes paris sportif|les
meilleurs paris sportifs|les meilleurs paris sportifs du jour|les
meilleurs site de paris sportif|les meilleurs site de paris sportifs|les meilleurs
sites de pari sportif|les meilleurs sites de paris sportifs|les meilleurs sites de
paris sportifs en ligne|les paris sportif|les paris sportif avis|les paris sportifs|les paris
sportifs comment ça marche|les paris sportifs en france|les paris sportifs en ligne|les paris sportifs en ligne comprendre jouer gagner|les paris
sportifs en ligne comprendre jouer gagner pdf|les paris sportifs les plus rentables|les plus gros
gagnant paris sportif|les plus gros gains au paris sportifs|les plus
gros gains paris sportifs|les plus gros paris sportif|les plus grosse cote paris sportif|les plus grosses
pertes paris sportifs|les sites de paris sportifs|les sites de paris sportifs autorisés en france|les
sites de paris sportifs en france|les sites de paris sportifs en ligne|les sites de paris sportifs francais|ligue
1 paris sportif|ligue 1 paris sportifs|ligue 2 paris sportif|ligue des
champions paris sportif|limite de gains paris sportifs|limite de
mise paris sportif|limite gain paris sportif|limite mise paris sportifs|liste de paris sportif|liste des paris sportifs|liste des site de paris sportif|liste des sites de paris sportifs|liste pari sportif|liste paris
sportif|liste paris sportif pdf|liste site de paris sportif|liste site pari sportif|liste
site paris sportif|liste site paris sportif arjel|liste sites paris
sportifs|logiciel algorithme paris sportif|logiciel algorithme paris sportif gratuit|logiciel
analyse paris sportif|logiciel calcul paris sportif|logiciel de pari sportif|logiciel de
paris sportif|logiciel de paris sportif gratuit|logiciel gestion bankroll paris sportif gratuit|logiciel gestion de bankroll paris
sportif|logiciel gestion paris sportif|logiciel gestion paris sportif gratuit|logiciel gestion paris sportifs|logiciel pari
sportif|logiciel paris sportif|logiciel paris sportif gratuit|logiciel paris sportifs|logiciel paris sportifs foot sur 2 matchs|logiciel
pour paris sportif|logiciel pour paris sportifs|logiciel prediction paris sportif|logiciel probabilité paris sportif|logiciel prédiction paris sportif|logiciel statistique paris sportifs|logiciel variation de cote paris sportif|loi sur les paris sportifs en france|magic
calculator paris sportif|marché des paris sportifs|marché des paris sportifs en france|marché des paris sportifs en ligne|martingale pari sportif|martingale paris sportif|martingale
paris sportif excel|martingale paris sportif forum|martingale paris sportif interdit|martingale paris sportifs|match abandonné paris sportif|match annulé ou reporté paris sportifs|match annulé paris sportif|match arrete paris sportif|match interrompu paris sportif|match interrompu tennis paris sportif|match interrompu tennis pluie paris sportif|match
nul boxe paris sportif|match pari sportif|match paris sportif|match reporté paris sportif|match suspendu paris sportif|match suspendu tennis paris sportif|match truqué paris sportif|matchs truqués
paris sportifs|meilleur algorithme paris sportif|meilleur algorithme paris sportif gratuit|meilleur
app de paris sportif|meilleur app de paris sportifs|meilleur app paris
sportif|meilleur appli de pari sportif|meilleur appli de paris sportif|meilleur
appli pari sportif|meilleur appli paris sportif|meilleur appli paris sportif forum|meilleur appli
paris sportifs|meilleur application conseil paris sportif|meilleur application de paris sportif|meilleur application de
paris sportif en afrique|meilleur application pari sportif|meilleur application paris sportif|meilleur application paris sportif belgique|meilleur application pour les paris sportif|meilleur application pour pari sportif|meilleur
bonus de bienvenue paris sportif|meilleur bonus pari
sportif|meilleur bonus paris sportif|meilleur bonus paris
sportif sans depot|meilleur bonus paris sportifs|meilleur bonus site de paris sportif|meilleur bonus site pari sportif|meilleur bonus site paris sportif|meilleur bookmaker paris sportif|meilleur combiné
paris sportif|meilleur conseil paris sportif|meilleur cote de paris sportif|meilleur cote pari
sportif|meilleur cote paris sportif|meilleur cote paris sportif aujourd’hui|meilleur cote site paris sportif|meilleur forum paris sportifs|meilleur gain paris sportif|meilleur ia paris sportif|meilleur methode pour gagner au paris sportif|meilleur offre bienvenue
paris sportif|meilleur offre bonus paris sportif|meilleur offre de bienvenue paris sportif|meilleur offre de
bienvenue paris sportifs|meilleur offre pari sportif|meilleur offre paris sportif|meilleur
offre paris sportif en ligne|meilleur pari sportif|meilleur pari sportif du jour|meilleur pari sportif
en ligne|meilleur paris sportif|meilleur paris sportif aujourd’hui|meilleur paris sportif du jour|meilleur paris sportif en ligne|meilleur paris sportif foot|meilleur promo paris sportif|meilleur
pronostic paris sportif|meilleur site de conseil paris sportif|meilleur site de pari
sportif|meilleur site de pari sportif en ligne|meilleur site de paris sportif|meilleur site de
paris sportif avis|meilleur site de paris sportif belgique|meilleur site de paris sportif canada|meilleur site de paris sportif
en france|meilleur site de paris sportif en ligne|meilleur site
de paris sportif football|meilleur site de paris sportif forum|meilleur
site de paris sportif france|meilleur site de paris sportif hors arjel|meilleur site de paris sportif
international|meilleur site de paris sportif suisse|meilleur site de paris sportifs|meilleur site de paris sportifs en ligne|meilleur site pari
sportif|meilleur site pari sportif en ligne|meilleur site pari sportif france|meilleur site
paris sportif|meilleur site paris sportif avis|meilleur site paris
sportif belgique|meilleur site paris sportif canada|meilleur site paris sportif en ligne|meilleur site paris sportif foot|meilleur site paris sportif forum|meilleur site paris sportif
france|meilleur site paris sportif hors arjel|meilleur site paris sportif nba|meilleur site paris sportif rugby|meilleur site paris sportif suisse|meilleur site paris sportifs|meilleur
site pour pari sportif|meilleur site pour paris
sportif|meilleur site pronostic paris sportif|meilleur strategie paris sportif|meilleur technique de paris sportif|meilleur technique
paris sportif|meilleur technique pour gagner au paris sportif|meilleure appli de paris sportif|meilleure
appli de paris sportifs|meilleure appli pari sportif|meilleure appli paris sportif|meilleure appli paris sportifs|meilleure application de paris sportif|meilleure application de
paris sportifs|meilleure application pari sportif|meilleure application paris sportif|meilleure application paris sportif android|meilleure application paris sportifs|meilleure offre paris
sportif|meilleure site paris sportif|meilleure strategie paris sportif|meilleures applications de
paris sportifs|meilleures applications paris sportifs|meilleures cotes paris sportifs|meilleures offres paris sportifs|meilleures stratégies paris sportifs|meilleurs appli
paris sportif|meilleurs application de paris sportifs|meilleurs application paris sportif|meilleurs applications
paris sportifs|meilleurs bonus paris sportifs|meilleurs
cote paris sportif|meilleurs cotes paris sportifs|meilleurs offres paris sportifs|meilleurs paris sportifs|meilleurs
paris sportifs du jour|meilleurs site de pari sportif|meilleurs site de paris sportif|meilleurs site de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs site paris sportif|meilleurs sites de paris sportifs|meilleurs
sites de paris sportifs en ligne|meilleurs sites paris sportif|meilleurs sites
paris sportifs|methode abc paris sportif|methode de paris sportif|methode gagnante paris sportifs|methode gagner paris sportif|methode
infaillible paris sportifs|methode martingale paris sportif|methode mathematique
paris sportif|methode mathematique pour gagner au paris sportif|methode paris
sportif|methode paris sportif foot|methode paris sportif forum|methode paris
sportif tennis|methode paris sportifs|methode pour gagner au paris sportif|methode pour gagner paris
sportif|methodes paris sportifs|minimum depot paris sportif|mise au jeu pari
sportif|mise maximum pari sportif|mise maximum paris sportif|mise minimum paris sportif|mise
moyenne paris sportif|mise paris sportif|moins
de 4 5 but paris sportif|montant maximum paris sportif|montant paris sportif|montante pari sportif|montante
parie sportif|montante paris sportif|montante paris sportifs|montantes paris sportifs|multiple pari sportif|multiple paris
sportif|multiple paris sportifs|multiples paris sportifs|méthode calcul paris sportif|méthode match nul
paris sportifs|méthode mathématique pour gagner au paris sportif|méthode paris sportif forum|méthode
paris sportif hockey|nba pari sportif|nba paris sportif|nba
paris sportifs|nouveau paris sportif|nouveau site de pari sportif|nouveau site de paris sportif|nouveau site de paris sportif
en ligne|nouveau site de paris sportifs|nouveau site pari sportif|nouveau site paris sportif|nouveau site paris sportif france|nouveau
site paris sportifs|nouveaux sites de paris sportifs|nouveaux sites paris sportifs|nouvelle appli paris
sportif|nouvelle application de paris sportif|numero de match paris sportif|numero match paris sportif|offre 100 euros paris sportif|offre appli pari sportif|offre bienvenu paris sportif|offre bienvenue pari sportif|offre
bienvenue paris sportif|offre bienvenue paris sportifs|offre bienvenue site paris sportif|offre bonus paris sportif|offre de bienvenu paris sportif|offre de bienvenue pari
sportif|offre de bienvenue paris sportif|offre de bienvenue paris sportif belgique|offre de bienvenue paris sportif sans depot|offre de
bienvenue paris sportif sans dépôt|offre de bienvenue paris sportifs|offre de bienvenue sans depot
paris sportif|offre de bienvenue site paris sportif|offre euro
paris sportif|offre pari sportif euro|offre paris
sportif|offre paris sportif belgique|offre paris sportif cash|offre
paris sportif coupe du monde|offre paris sportif
hors arjel|offre paris sportif remboursé|offre paris sportif remboursé cash|offre paris sportif
sans depot|offre promo paris sportif|offre remboursement paris sportif|offre sans depot
paris sportif|offre site paris sportif|offres bienvenue paris sportifs|offres de bienvenue paris sportifs|ou
faire des paris sportif|ou faire des paris sportif en espagne|ou faire
des paris sportifs|outil répartiteur de mise paris sportif|outils repartiteur de mises paris
sportif|ouverture compte paris sportifs|ouvrir un compte paris sportif|pack de bienvenue paris sportif|pack de bienvenue paris sportif
hors arjel|pari en ligne sportif|pari sportif|pari sportif 100 euros
offert|pari sportif 100 remboursé|pari sportif abandon tennis|pari
sportif aide|pari sportif algérie aujourd’hui|pari sportif
appli|pari sportif application|pari sportif argent|pari sportif astuce|pari sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari sportif avec orange money|pari sportif avec paypal|pari sportif avec wave|pari sportif avis|pari sportif basket|pari sportif belgique|pari sportif belgique france|pari
sportif bonus|pari sportif buteur pas titulaire|pari sportif champions league|pari sportif combiné|pari sportif comment|pari sportif comment
gagner|pari sportif comment ça marche|pari sportif comparatif|pari sportif conseil|pari sportif cote|pari sportif cote match|pari sportif cote psg|pari sportif
coupe|pari sportif coupe de france|pari sportif coupe du monde|pari sportif depot|pari sportif du
jour|pari sportif en france|pari sportif en ligne|pari sportif en ligne au
cameroun|pari sportif en ligne belgique|pari sportif en ligne canada|pari sportif
en ligne france|pari sportif en ligne gratuit|pari sportif en ligne suisse|pari sportif en ligne ufc|pari
sportif en suisse|pari sportif euro|pari sportif explication|pari sportif faire|pari sportif foot|pari sportif
foot resultat|pari sportif football|pari sportif
forum|pari sportif francaise des jeux|pari sportif france|pari sportif france angleterre|pari sportif france argentine|pari
sportif france autriche|pari sportif france belgique|pari sportif france espagne|pari
sportif france italie|pari sportif france portugal|pari sportif france usa|pari
sportif gagnant|pari sportif gagner|pari sportif gagner a tous les coups|pari
sportif gagner de l’argent|pari sportif gain|pari
sportif gratuit|pari sportif gratuit pour gagner des cadeaux|pari sportif gratuit sans depot|pari sportif handicap|pari sportif hockey|pari sportif hors arjel|pari sportif jeux olympiques|pari sportif joueur absent|pari sportif le plus rentable|pari sportif leicester champion|pari sportif ligue
1|pari sportif ligue 2|pari sportif ligue des champions|pari sportif ligue europa|pari sportif match|pari sportif match arrete|pari sportif match interrompu|pari sportif
meilleur|pari sportif meilleur cote|pari sportif meilleur
site|pari sportif methode|pari sportif mise|pari sportif mise au jeu|pari sportif mise
o jeu|pari sportif nba|pari sportif offre bienvenue|pari sportif paypal|pari sportif plus|pari sportif prolongation|pari sportif promo|pari sportif pronostic|pari
sportif pronostic foot|pari sportif pronostic gagnant|pari sportif pronostic gratuit|pari sportif psg|pari sportif psg bayern|pari sportif psg inter|pari sportif psg milan|pari sportif regle|pari sportif rembourse|pari sportif remboursement|pari sportif remboursement cash|pari sportif remboursé|pari
sportif rugby|pari sportif rugby coupe du monde|pari
sportif rugby top 14|pari sportif sans argent|pari sportif sans carte bancaire|pari sportif sans depot|pari sportif signification|pari sportif site|pari
sportif statistique|pari sportif suisse|pari sportif systeme|pari sportif
technique|pari sportif technique pour gagner|pari sportif temps reglementaire|pari sportif tennis|pari sportif tennis abandon|pari sportif top|pari sportif top 14|pari sportif tour de france|parie sportif|parie
sportif comment ca marche|parie sportif du jour|parie sportif en ligne|parie
sportif foot|parie sportif football|parie sportif france|parie sportif gratuit|parie sportif pronostic|parie sportif suisse|paris en ligne sportif|paris
en ligne sportifs|paris evenement sportif|paris france sportif|paris hippique et sportif|paris hippiques et sportifs|paris hippiques paris sportifs|paris hippiques paris sportifs et
poker en ligne|paris hippiques sportifs|paris match sportif|paris sportif|paris
sportif 10 euros offerts|paris sportif 100 euros offert|paris
sportif 100 euros remboursé|paris sportif 100 offert|paris sportif 100 remboursé|paris
sportif 100e offert|paris sportif 150 euros offert|paris sportif 1er pari remboursé|paris sportif a faire|paris sportif
a faire aujourd’hui|paris sportif a faire ce soir|paris
sportif abandon tennis|paris sportif abandon tennis parions sport|paris sportif aide|paris sportif
algorithme|paris sportif analyse|paris sportif appli|paris sportif application|paris sportif application android|paris sportif apres prolongation|paris sportif argent|paris sportif argent fictif|paris sportif argent offert|paris sportif argent virtuel|paris sportif arjel|paris sportif arsenal psg|paris sportif astuce|paris sportif au canada|paris sportif aujourd hui|paris
sportif aujourd’hui|paris sportif avec argent fictif|paris sportif avec bonus sans depot|paris sportif avec carte bancaire|paris sportif avec cryptomonnaie|paris sportif avec
handicap|paris sportif avec paypal|paris sportif avec paysafecard|paris
sportif avis|paris sportif avis expert|paris sportif avis forum|paris sportif bankroll|paris sportif basket|paris sportif basket coupe de france|paris sportif basket nba|paris sportif basket prolongation|paris
sportif belgique|paris sportif belgique bonus|paris sportif belgique bonus sans depot|paris sportif belgique france|paris sportif belgique suede|paris sportif bonus|paris sportif bonus bienvenue|paris sportif bonus cash|paris sportif bonus de bienvenue|paris sportif bonus gratuit|paris sportif
bonus gratuit sans depot|paris sportif bonus retirable|paris sportif bonus
sans depot|paris sportif bonus sans depot belgique|paris sportif bookmaker|paris sportif but contre son camp|paris sportif but temps additionnel|paris sportif buteur|paris sportif buteur
blessé|paris sportif buteur carton rouge|paris sportif buteur
contre son camp|paris sportif buteur non titulaire|paris sportif buteur
prolongation|paris sportif buteur qui ne joue pas|paris sportif buteur remplacant|paris sportif
calcul gain|paris sportif canada|paris sportif cash|paris sportif cash out|paris sportif champion ligue 1|paris sportif champions league|paris sportif classement ligue 1|paris sportif code
promo|paris sportif combine|paris sportif combiné|paris sportif combiné comment
ça marche|paris sportif combiné du jour|paris sportif combiné match reporté|paris sportif comment ca marche|paris sportif
comment faire|paris sportif comment gagner|paris sportif comment gagner a tous les coups|paris sportif comment jouer|paris sportif comment ça marche|paris sportif comparateur
cote|paris sportif comparatif|paris sportif conseil|paris sportif conseil gratuit|paris sportif conseil pour gagner|paris sportif cote|paris sportif cote et match|paris sportif cote explication|paris
sportif cote psg|paris sportif coupe d’europe|paris
sportif coupe davis|paris sportif coupe de france|paris sportif coupe du
monde|paris sportif coupe du monde de rugby|paris sportif coupe du monde rugby|paris sportif depot 5 euro|paris sportif depot minimum|paris sportif depot paypal|paris sportif dnb|paris sportif du jour|paris sportif du jour conseil|paris sportif
dépôt 1 euro|paris sportif dépôt minimum 5 euros|paris sportif en belgique|paris sportif en france|paris sportif en ligne|paris sportif en ligne avec paypal|paris sportif en ligne
avis|paris sportif en ligne belgique|paris sportif en ligne bonus|paris sportif en ligne
cameroun|paris sportif en ligne comment gagner|paris sportif en ligne comment ça marche|paris
sportif en ligne france|paris sportif en ligne gratuit|paris sportif en ligne maroc|paris sportif en ligne
paypal|paris sportif en ligne québec|paris sportif en ligne
sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris sportif espagne france|paris
sportif esport|paris sportif et casino en ligne|paris sportif et hippique|paris
sportif et prolongation|paris sportif euro|paris sportif europa league|paris sportif explication|paris sportif final ligue des champions|paris sportif finale ligue des champions|paris sportif foot|paris sportif foot aide|paris sportif foot
astuce|paris sportif foot aujourd’hui|paris sportif foot ce soir|paris
sportif foot comment ca marche|paris sportif foot conseil|paris sportif foot cote|paris
sportif foot coupe du monde|paris sportif foot en ligne|paris sportif
foot feminin|paris sportif foot gratuit|paris sportif
foot prolongation|paris sportif foot pronostic|paris sportif foot pronostic gratuit|paris sportif foot regle|paris sportif
foot suisse|paris sportif foot us|paris sportif football|paris sportif
football americain|paris sportif football astuces|paris sportif forfait tennis|paris sportif forum|paris sportif francais|paris sportif francaise des jeux|paris sportif france|paris sportif france
2|paris sportif france allemagne|paris sportif france
angleterre|paris sportif france argentine|paris sportif france autriche|paris sportif france belgique|paris
sportif france espagne|paris sportif france gibraltar|paris sportif france italie|paris sportif france nouvelle zelande|paris sportif france pologne|paris sportif france portugal|paris sportif france uruguay|paris sportif france
usa|paris sportif freebet sans depot|paris sportif gagnant|paris sportif gagnant à coup sûr|paris sportif gagner a coup sur|paris sportif gagner argent|paris sportif gagner
de l’argent|paris sportif gain|paris sportif gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris sportif gratuit
appli|paris sportif gratuit avec cadeaux|paris sportif gratuit cadeaux|paris
sportif gratuit en ligne|paris sportif gratuit entre amis|paris sportif gratuit sans argent|paris sportif gratuit sans depot|paris sportif gratuit
sans dépôt|paris sportif gratuits|paris sportif gros gain|paris sportif handicap|paris sportif handicap 0
1|paris sportif handicap 0-1|paris sportif
handicap 1 0|paris sportif handicap 1-0|paris sportif handicap basket|paris sportif handicap explication|paris
sportif handicap foot|paris sportif handicap rugby|paris sportif hippique|paris
sportif hockey|paris sportif hockey nhl|paris sportif hockey sur glace|paris sportif hors arjel|paris sportif hors arjel france|paris sportif jeux olympiques|paris sportif jeux video|paris sportif joueur blessé|paris sportif joueur blessé pendant le
match|paris sportif joueur de foot|paris sportif joueur decisif|paris sportif joueur declare forfait|paris sportif joueur déclare forfait|paris sportif
joueur remplacant|paris sportif la francaise des jeux|paris sportif le plus rentable|paris sportif legal en france|paris sportif leicester champion|paris sportif les 18 stratégies pour gagner
tous les jours|paris sportif les plus sur|paris sportif les
prolongation compte|paris sportif ligne|paris sportif ligue 1|paris sportif ligue 2|paris sportif ligue des champions|paris sportif ligue des
nations|paris sportif ligue europa|paris sportif liste|paris sportif martingale|paris sportif match|paris sportif match abandonné|paris
sportif match annulé|paris sportif match arrêté|paris sportif match du jour|paris sportif match interrompu|paris sportif
match reporté|paris sportif match suspendu|paris sportif match
tennis interrompu|paris sportif match truqué|paris sportif meilleur bonus|paris sportif meilleur cote|paris sportif meilleur pronostic|paris
sportif meilleur site|paris sportif methode|paris sportif methode 2
3|paris sportif mi temps fin de match|paris sportif mise
au jeu|paris sportif mise maximum|paris sportif mma france|paris sportif moins de 3.5
but|paris sportif montante|paris sportif moto gp|paris sportif multiple|paris sportif multiple 2 3|paris sportif multiple 2 3
explication|paris sportif multiple 2 4|paris sportif multiple 2 5|paris sportif
multiple 2/3 explication|paris sportif multiple 3 4|paris sportif multiple explication|paris sportif national 1 foot|paris sportif nba|paris sportif nba conseil|paris sportif nba
pronostic|paris sportif nhl|paris sportif nombre de but|paris sportif nouveau site|paris sportif
numero match|paris sportif offert|paris sportif offre bienvenue|paris sportif offre bienvenue sans depot|paris sportif
offre de bienvenue|paris sportif offre sans depot|paris sportif om psg|paris sportif
paypal|paris sportif plus de 1.5 but|paris sportif plus de
2 5 but|paris sportif plus ou moins|paris sportif plus ou moins 2 5 but|paris
sportif premier pari remboursé|paris sportif premier paris remboursé|paris sportif prolongation|paris sportif prolongation basket|paris sportif prolongation foot|paris sportif promo|paris sportif pronostic|paris sportif pronostic basket|paris sportif
pronostic des match aujourd hui|paris sportif pronostic expert gratuit|paris
sportif pronostic foot|paris sportif pronostic forum|paris sportif pronostic
gratuit|paris sportif pronostic tennis|paris sportif psg|paris sportif
psg arsenal|paris sportif psg barcelone|paris sportif psg bayern|paris sportif psg dortmund|paris sportif psg inter|paris sportif psg
inter cote|paris sportif psg liverpool|paris sportif psg om|paris sportif qr code|paris sportif que veut dire handicap|paris sportif qui
rapporte le plus|paris sportif regle|paris sportif regle prolongation|paris sportif rembourse|paris sportif remboursement cash|paris sportif rembourser|paris sportif remboursé|paris sportif remboursé cash|paris sportif remboursé en cash|paris sportif retrait paypal|paris sportif rue
des joueurs|paris sportif rugby|paris sportif rugby
6 nations|paris sportif rugby coupe du monde|paris sportif rugby
top 14|paris sportif safe du jour|paris sportif sans argent|paris sportif sans carte bancaire|paris sportif sans carte
d’identité|paris sportif sans compte bancaire|paris sportif
sans depot|paris sportif sans depot minimum|paris sportif si
match suspendu|paris sportif si un joueur
abandonne|paris sportif si un joueur ne joue pas|paris sportif
si un joueur se blesse|paris sportif simple ou combiné|paris sportif site|paris
sportif statistique|paris sportif stratégie|paris sportif suisse|paris sportif suisse
application|paris sportif suisse en ligne|paris
sportif suisse legal|paris sportif suisse légal|paris sportif suisse romande|paris sportif
sur du jour|paris sportif sur le tennis|paris sportif systeme|paris sportif systeme 2
3|paris sportif systeme 2 4|paris sportif systeme 2/3|paris sportif systeme 2/4|paris sportif systeme 3 4|paris sportif systeme 3/4|paris sportif systeme explication|paris sportif technique|paris sportif technique pour gagner|paris sportif temps additionnel|paris sportif temps reglementaire|paris sportif tennis|paris sportif tennis
abandon|paris sportif tennis conseil|paris sportif tennis de table|paris sportif tennis forfait|paris sportif
tennis gratuit|paris sportif tennis pronostic|paris sportif tennis
roland garros|paris sportif tir au but|paris sportif top
14|paris sportif tour de france|paris sportif ufc|paris sportif ufc france|paris sportif
unibet|paris sportif vainqueur euro|paris sportif vainqueur ligue 1|paris sportif vainqueur ligue des champions|paris sportif via
paypal|paris sportif victoire prolongation|paris sportif vip
gratuit|paris sportifs|paris sportifs abandon tennis|paris sportifs aide|paris sportifs analyser un match|paris sportifs arjel|paris sportifs astuces|paris sportifs aujourd’hui|paris sportifs autorisés en france|paris sportifs avec paypal|paris sportifs
basket|paris sportifs belgique|paris sportifs bonus|paris sportifs bookmakers|paris
sportifs canada|paris sportifs combiné|paris sportifs comparateur|paris sportifs comparatif|paris sportifs conseils|paris
sportifs cotes|paris sportifs coupe du monde|paris sportifs de football|paris sportifs
du jour|paris sportifs en belgique|paris sportifs
en france|paris sportifs en ligne|paris sportifs en ligne
belgique|paris sportifs en ligne france|paris sportifs en ligne gratuit|paris sportifs en ligne suisse|paris sportifs
en suisse|paris sportifs et hippiques|paris sportifs euro|paris
sportifs foot|paris sportifs foot us|paris sportifs forum|paris sportifs france|paris sportifs france espagne|paris sportifs gagner à tous les coups|paris
sportifs gratuit|paris sportifs gratuits|paris
sportifs gratuits en ligne|paris sportifs handicap|paris sportifs hockey|paris sportifs
hockey sur galce|paris sportifs hockey sur glace|paris sportifs hors arjel|paris sportifs jeux olympiques|paris
sportifs les bookmakers raflent la mise|paris sportifs ligne|paris sportifs ligue 1|paris sportifs ligue 2|paris sportifs ligue des champions|paris sportifs ligue europa|paris sportifs match
interrompu|paris sportifs montante|paris sportifs nba|paris sportifs offre bienvenue|paris sportifs offre de bienvenue|paris sportifs paypal|paris sportifs pronostics|paris sportifs psg|paris sportifs psg inter|paris sportifs
rugby|paris sportifs sans argent|paris sportifs sans depot|paris
sportifs site|paris sportifs sites|paris sportifs statistiques|paris sportifs stratégie|paris sportifs suisse|paris
sportifs technique|paris sportifs techniques|paris sportifs tennis|paris sportifs tennis astuces|paris sportifs top 14|paris sportifs tour de france|part de marché paris sportifs|paypal pari sportif|paypal paris sportif|paypal paris sportifs|perte d’argent
paris sportifs|peut on devenir riche avec les paris sportifs|peut on gagner de l’argent avec les paris
sportifs|peut on gagner sa vie avec les paris sportif|peut on vraiment
gagner de l’argent avec les paris sportifs|plus gros combine paris sportif|plus gros gagnant paris sportif|plus gros gain paris sportif|plus gros gain paris sportif au monde|plus gros gain paris sportif france|plus gros gains paris sportif|plus gros pari sportif|plus gros paris sportif|plus
grosse cote gagner paris sportif|plus grosse cote pari sportif|plus grosse
cote paris sportif|plus grosse mise paris sportif|plus grosse somme gagner
au paris sportif|plus ou moins paris sportif|pourcentage
de mise paris sportif|premier pari sportif remboursé|probabilité cote paris
sportif|probabilité paris sportif combiné|prolongation basket paris sportif|prolongation paris sportif|promo pari sportif|promo paris sportif|promo site de paris sportif|promo site pari sportif|promo site paris sportif|promos paris sportifs|prono paris sportif foot|prono paris sportif gratuit|prono paris sportif
tennis|pronostic de paris sportif|pronostic du jour paris sportif|pronostic foot paris sportif|pronostic
gratuit paris sportif|pronostic pari sportif|pronostic
pari sportif gratuit|pronostic paris sportif|pronostic paris sportif aujourd’hui|pronostic paris sportif
du jour|pronostic paris sportif foot|pronostic paris sportif gratuit|pronostic paris sportif
tennis|pronostic paris sportifs|pronostics foot statistiques et aides
aux paris sportifs|pronostics paris sportif|pronostics paris sportifs|pronostiqueur paris sportif gratuit|psg
arsenal paris sportif|psg bayern paris sportif|psg inter milan paris
sportif|psg inter pari sportif|psg inter paris sportif|psg liverpool paris sportif|psg om paris sportif|psg paris sportif|psg paris sportifs|qr code paris sportif|qu
est ce qu un handicap paris sportif|qu est ce que handicap dans les paris sportif|qu’est ce qu’un handicap paris sportif|qu’est ce que handicap dans les paris sportif|quand un joueur se blesse paris sportif|que signifie 1/1 en paris sportif|que signifie 1/2 paris sportif|que signifie 12 en paris sportif|que
signifie 1×2 dans les paris sportifs|que signifie btts en paris sportif|que signifie dnb en paris sportif|que signifie draw en paris sportif|que
signifie ft en paris sportif|que signifie gg dans le pari sportif|que signifie gg
en pari sportif|que signifie gg en paris sportif|que signifie handicap dans les paris
sportifs|que veut dire dnb en paris sportif|que veut dire handicap dans les paris sportifs|que veut dire handicap paris sportif|quel appli pari sportif|quel cote jouer paris sportif|quel est la
meilleur appli de paris sportif|quel est le meilleur algorithme de paris sportif|quel est
le meilleur site de pari sportif|quel est le meilleur
site de pari sportif en ligne|quel est le meilleur site de paris sportif|quel est
le meilleur site de paris sportif en ligne|quel
est le meilleur site de paris sportifs en ligne|quel est le pari sportif le plus rentable|quel pari sportif est le plus
rentable|quel pari sportif est le plus sûr|quel pari sportif
faire aujourd’hui|quel paris sportif faire aujourd’hui|quel paris sportif rapporte le plus|quel site de paris sportif choisir|quel site de paris sportif rembourse en cash|quel
type de pari sportif est le plus rentable|quelle application pour paris sportifs|quelle est la meilleure appli de paris sportif|quelle est la meilleure application de paris sportif|quelle est
la meilleure application pour les paris sportifs|quelle est le meilleur site de paris sportif|quels paris sportifs faire|quels sont
les paris sportifs les plus sûrs|rebond basket paris sportif|record de gain paris sportif|regle
buteur paris sportif|regle de paris sportif|regle des paris sportif|regle handicap paris sportif|regle handicap paris sportif foot|regle
multiple paris sportif|regle pari sportif|regle paris sportif|regle paris sportif foot|regle paris sportif multiple|regle paris sportif
prolongation|reglement pari sportif|reglement paris sportif|regles paris sportifs|remboursement cash paris sportif|remboursement
en cash paris sportif|remboursement pari sportif|remboursement paris sportif|repartiteur de mise paris sportif|repartiteur de mise paris sportifs|repartiteur de mises
paris sportif|repartiteur mise paris sportif|repartition des mises paris sportif|resultat pari sportif|resultat paris sportif|resultat paris sportif en direct|resultat paris sportif foot|resultat sportif hockey|retirer argent
paris sportif|rugby pari sportif|rugby paris sportif|règle
paris sportif prolongation|règles paris sportif|répartiteur de mise pari sportif|répartiteur de mise paris sportif|répartiteur de
mise paris sportifs|répartition des mises paris sportif|résultat
paris sportif foot|sans depot paris sportif|se faire
interdire de paris sportifs|signification btts
paris sportif|signification dnb paris sportif|signification handicap paris sportif|simulateur de gain paris sportif|simulateur gain paris sportif|simulateur gain paris sportif multiple|simulateur
gain paris sportif systeme|simulateur gain paris sportif système|simulateur
montante paris sportif|simulateur paris sportif multiple|simulateur systeme paris sportif|simulation paris sportif gratuit|site aide paris sportif|site analyse paris sportif|site
analyser paris sportif|site arjel paris sportif|site
conseil paris sportif|site d’analyse de paris sportifs|site d’analyse paris sportif|site de conseil paris sportif|site de pari en ligne sportif|site de pari sportif|site de
pari sportif avec bonus sans depot|site de pari sportif
bonus sans depot|site de pari sportif canada|site de pari sportif en ligne|site de pari sportif francais|site de
pari sportif gratuit|site de pari sportif hors arjel|site de pari sportif suisse|site de parie sportif|site de parie sportif en ligne|site de paris en ligne sportif|site de paris sportif|site de paris
sportif acceptant paypal|site de paris sportif arjel|site de paris sportif autorisé
en france|site de paris sportif autorisé en suisse|site de paris sportif avec bonus|site de paris sportif avec bonus sans depot|site de paris sportif avec bonus sans dépôt|site de
paris sportif avec neosurf|site de paris sportif avec paiement mobile|site de paris
sportif avec paypal|site de paris sportif avis|site de paris sportif belge avec
bonus|site de paris sportif belgique|site de paris sportif bonus|site de paris sportif bonus
sans depot|site de paris sportif canada|site de
paris sportif comparatif|site de paris sportif depot minimum|site de paris sportif en france|site de paris sportif en ligne|site de
paris sportif en ligne suisse|site de paris sportif football|site de paris sportif francais|site de paris sportif france|site de paris sportif gratuit|site
de paris sportif gratuit pour gagner des cadeaux|site de paris sportif gratuit
sans dépôt|site de paris sportif hors arjel|site
de paris sportif le plus fiable|site de paris sportif legal en france|site de paris sportif meilleur
cote|site de paris sportif nouveau|site de paris sportif offre de bienvenue|site de paris sportif paypal|site de paris
sportif premier paris remboursé|site de paris sportif qui accepte paypal|site de paris
sportif qui rembourse en cash|site de paris sportif remboursé|site de paris sportif sans argent|site de paris
sportif sans carte bancaire|site de paris sportif sans carte d’identité|site
de paris sportif sans depot|site de paris sportif suisse|site de paris sportifs|site de paris sportifs avec paypal|site de paris sportifs en ligne|site de paris sportifs francais|site de paris sportifs gratuit|site de paris sportifs paypal|site de paris
sportifs suisse|site de statistique pour paris sportif|site des
paris sportifs|site pari en ligne sportif|site pari
sportif|site pari sportif 100 euros offert|site pari sportif arjel|site
pari sportif belgique|site pari sportif bonus|site pari
sportif canada|site pari sportif comparatif|site pari sportif en ligne|site pari sportif france|site pari sportif gratuit|site pari sportif hors arjel|site pari sportif suisse|site parie sportif|site paris en ligne sportif|site paris sportif|site paris sportif 100 euros offert|site paris
sportif 100 euros remboursé|site paris sportif 1er paris remboursé|site paris sportif arjel|site paris sportif autorisé en france|site paris sportif avec
bonus|site paris sportif avec bonus sans depot|site paris sportif avec meilleur cote|site
paris sportif belgique|site paris sportif bonus|site paris sportif bonus cash|site paris sportif bonus sans depot|site paris
sportif canada|site paris sportif comparatif|site paris sportif depot 5 euro|site
paris sportif en ligne|site paris sportif
foot|site paris sportif france|site paris sportif
gratuit|site paris sportif hors arjel|site
paris sportif hors arjel france|site paris sportif meilleur cote|site paris sportif
nouveau|site paris sportif offre de bienvenue|site paris sportif paypal|site paris sportif remboursement cash|site
paris sportif remboursé en cash|site paris sportif retrait instantané|site paris sportif sans carte bancaire|site paris sportif sans depot|site paris
sportif suisse|site paris sportifs|site paris sportifs belgique|site paris sportifs
en ligne|site paris sportifs france|site paris sportifs hors arjel|site paris
sportifs suisse|site pour analyse paris sportif|site pour paris sportif|site pronostic paris sportif|site statistique paris sportif|site suisse paris sportif|sites de pari sportif|sites de
paris sportif|sites de paris sportifs|sites de paris sportifs arjel|sites de paris sportifs autorisés en france|sites de paris sportifs belgique|sites de paris sportifs bonus|sites de paris sportifs en belgique|sites de paris sportifs en france|sites de paris sportifs en ligne|sites de paris sportifs gratuits|sites de paris sportifs gratuits sans dépôt|sites de
paris sportifs suisse|sites pari sportif|sites paris sportif|sites paris sportifs|sites paris sportifs arjel|sites paris
sportifs belgique|sites paris sportifs france|sites paris sportifs hors
arjel|sites paris sportifs suisse|so foot paris sportif|so foot paris sportifs|specialiste tennis paris sportif|statistique foot
paris sportif|statistique paris sportif|statistique paris sportif foot|statistique tennis paris sportif|statistiques football paris sportifs|statistiques paris
sportifs|strategie de paris sportif|stratégie big whale paris sportif|stratégie de paris sportifs|stratégie gagnante paris sportifs|stratégie pari sportif|stratégie paris sportif|stratégie paris sportifs|stratégie paris sportifs forum|stratégie pour gagner au paris sportif|stratégies paris sportifs|suisse paris sportif|suisse paris sportifs|systeme 2
3 paris sportif|systeme 3 4 paris sportif|systeme de cote paris
sportif|systeme de paris sportif|systeme pari sportif|systeme paris sportif|systeme paris sportifs|systeme reducteur paris sportif|système paris sportif|tableau bankroll paris sportif|tableau cote paris sportif|tableau
de paris sportif|tableau de suivi paris sportifs|tableau excel bankroll paris sportif|tableau excel
paris sportif|tableau excel paris sportif gratuit|tableau excel paris sportifs|tableau excel
pour paris sportif|tableau gestion bankroll paris sportif|tableau montante
paris sportif|tableau paris sportif|tableau paris sportif excel|tableau roi
paris sportifs|tableau statistique paris sportif|tableau suivi paris sportif|
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate < Loved it!
как выбрать надежное казино Ищете официальный сайт онлайн казино в России? Здесь вы найдете проверенные и надежные платформы, работающие по лицензии. Узнайте о лучших предложениях, бонусах и играх.
геронтологический центр в москве для пожилых людей что это Геронтологические пансионаты и дома престарелых – это альтернатива домашнему уходу для тех, кому требуется постоянное наблюдение и помощь. Здесь созданы все условия для комфортного проживания: уютные комнаты, сбалансированное питание, интересные занятия и развлекательные мероприятия. Кроме того, в пансионатах обеспечивается круглосуточный медицинский контроль и квалифицированный уход.
I am truly thankful to the holder of this website who has shared this
fantastic post at here.
Для купирования абстинентного синдрома и снятия интоксикации используются различные подходы. Врачи подбирают их индивидуально, исходя из состояния пациента.
Получить дополнительную информацию – нарколог на дом вывод из запоя
Мне очень нравится сайт kazino olimp,
он очень удобный в использовании!
платформа Olimp Casino
I enjoy what you guys tend to be up too. Such clever work and reporting!
Keep up the excellent works guys I’ve included you guys to
blogroll.
Этот комплекс мер позволяет оказывать помощь пациентам на всех стадиях зависимости.
Подробнее можно узнать тут – https://narkologicheskaya-klinika-sankt-peterburg14.ru/klinika-narkologii-spb/
Excellent post. I was checking continuously this blog and I am impressed!
Very useful info specially the last part 🙂 I care for such info a lot.
I was seeking this particular info for a very long time. Thank you and best
of luck.
Hey There. I found your blog using msn. That is an extremely well written article.
I will make sure to bookmark it and come back to read more of your useful
info. Thank you for the post. I will certainly return.
What i don’t understood is in truth how you are no
longer really much more neatly-appreciated than you might be right now.
You’re very intelligent. You understand therefore
significantly in relation to this topic, produced me for
my part consider it from so many various angles.
Its like women and men aren’t interested until it’s something to do with Lady gaga!
Your own stuffs nice. At all times take care of it up!
buy backlinks, link exchange, free gift card, congratulations you have won, claim
your prize, you have been selected, click here to claim, you won’t believe, one weird trick,
what happened next will shock you, shocking truth, secret revealed,
limited time offer, special promotion, act now, don’t miss out, buy now, best price,
risk-free trial, get rich quick, make money fast, work from home,
no credit check, miracle cure, lose weight fast, free viagra, no prescription needed, online casino, free spins, meet singles, hot
singles in your area, replica watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades,
Blaster, Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis,
CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex,
Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st
RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky,
Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai,
Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy,
Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit, RansomEXX,
Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer,
Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst,
SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif,
Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost,
XLoader, XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
Here is my homepage :: lolita porn
Flourish & Grow Hub – Practical tips and inspiration to support your daily personal growth.
This piece of writing offers clear idea in favor of the new visitors of blogging, that actually how to do
blogging and site-building.
Hello to all, how is everything, I think every
one is getting more from this web site, and your views are
good for new viewers.
obviously like your web site but you have to check the spelling
on quite a few of your posts. Several of them are rife with
spelling problems and I in finding it very troublesome
to tell the truth nevertheless I will surely come back again.
bs2site at
Hi there friends, how is the whole thing, and what you want to
say concerning this post, in my view its in fact remarkable
for me.
It’s remarkable in support of me to have a web page, which is valuable for my knowledge.
thanks admin
Hi there would you mind stating which blog platform you’re working with?
I’m going to start my own blog in the near future but I’m having a difficult time choosing
between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style seems different then most blogs and I’m
looking for something completely unique.
P.S My apologies for being off-topic but I had to
ask!
Do you mind if I quote a couple of your posts as long as I provide credit
and sources back to your website? My blog is in the exact same niche as
yours and my users would certainly benefit from some of the information you present here.
Please let me know if this ok with you. Many thanks!
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ᏟA 92626, United States
who pays bail bonds
Hi there, this weekend is good in favor of me, as this occasion i am reading
this wonderful informative piece of writing here at my
home.
Tulisan ini benar-benar memberikan wawasan baru.
Pembahasan mengenai KUBET sebagai Situs Judi Bola Terlengkap terasa tersusun dengan rapi.
Penulis mampu menyampaikan informasi dengan gaya bahasa yang nyaman dan tidak membingungkan.
Penjelasan tentang bagaimana sebuah platform dinilai sebagai Situs Parlay Resmi juga memberikan gambaran yang
jelas.
Setiap poin dijelaskan secara logis.
Hal ini membuat artikel lebih berbobot dan kredibel.
Saya juga tertarik pada bagian yang mengulas tentang Situs Parlay Gacor
dan bagaimana sistem performanya dijelaskan secara rinci.
Penulis berhasil membuat topik kompleks menjadi mudah dipahami.
Bagian ini menjadi salah satu poin paling informatif dalam keseluruhan artikel.
Selain itu, ulasan mengenai Situs Mix Parlay serta pembahasan terkait toto macau turut memperkaya isi konten.
Penjelasan mengenai penggunaan kubet login dan peran situs parlay dalam pengalaman pengguna
juga menambah kedalaman informasi yang disajikan.
Tulisan ini memiliki kualitas yang patut diapresiasi.
Semoga penulis terus menghadirkan konten berkualitas seperti ini dan tetap konsisten memberikan informasi yang bernilai
bagi para pembaca.
Hi there every one, here every person is sharing these kinds of
familiarity, therefore it’s good to read this web site,
and I used to pay a quick visit this webpage daily.
I do not even understand how I stopped up here, but I assumed this put up used
to be good. I don’t recognize who you might be however definitely you are going
to a well-known blogger for those who are not already.
Cheers!
Everything is very open with a really clear description of the issues.
It was definitely informative. Your website is useful. Many thanks for sharing!
Amazing issues here. I’m very glad to look your
article. Thank you so much and I am looking ahead to
touch you. Will you kindly drop me a mail?
Thank you, I have recently been searching for info approximately this subject for a while and yours is the greatest I have
discovered so far. But, what in regards to the bottom line?
Are you sure in regards to the source?
Every weekend i used to pay a visit this website, because i want enjoyment, for the reason that
this this web page conations truly nice funny stuff too.
Mangelsen
7916 Girard Avenue, La Joya
ϹA 92037, United Ⴝtates
1 800-228-9686
learn jackson hole wildlife bears
This post is worth everyone’s attention. How can I find out more?
Prime Male Enhancement: The Powerful Lift Execution? Prime Male EnhancementSurveys:- Is it likely that you are looking for a trademark strategy for facilitating torture? Have you endeavored CBD Chewy candies beforehand? If you’re like me, I’m sure you’ve found out about CBD Chewy candies. Nevertheless, you may not know why these Chewy candies are so renowned or how they work. Permit me to clarify for you why they’re the best CBD Chewy candies for assist with uneasiness. If you’re looking for the best CBD Chewy candies for assist with distress, you have come to the best areas. Prime Male Enhancement are the best CBD Chewy candies for help from the inconvenience that anybody could expect to find. Anytime do you feel like you just need more energy? Given that this is valid, it’s probable because your body is in a state of steady strain. That is the explanation Prime Male Enhancement might be the best answer for you.
Review my site: https://miffy.me/titan-rise-male-enhancement-92021
If some one wants to be updated with most recent technologies afterward he must be go to see this
web site and be up to date every day.
Look at my site; Senior Medical Center Near Me
InfoJunkie is a smart Content discovery software and powerful AI tool
that helps you save content, gain insights, capture ideas, and
grow your knowledge with tools designed to improve your learning experience.
Salam hangat untuk semuanya!
Saya Theda Tuckson, individu yang menyukai dunia digital.
Saya berasal dari Axel, Netherlands, dan sudah cukup lama menghabiskan waktu untuk mempelajari berbagai
layanan online modern termasuk KUBET yang dikenal sebagai
Salah satu Situs Judi Bola Terlengkap yang banyak dibicarakan.
Bagi saya, KUBET bukan hanya sekadar platform hiburan, tetapi juga
wadah informasi yang berkembang pesat. Dengan sistem kubet
login yang stabil dan aman, KUBET memberikan pengalaman pengguna yang
nyaman. Platform ini juga terkenal karena kualitas
fiturnya dan dukungan sistem yang ramah pengguna, sehingga banyak orang menjadikannya acuan dalam mencari Situs
Parlay Resmi maupun situs parlay yang terpercaya.
Selain permainan bola, saya juga suka mengeksplorasi berbagai layanan lain seperti Situs Parlay Gacor,
Situs Judi Bola, dan permainan yang populer seperti
toto macau. Informasinya sangat luas dan banyak membantu saya memahami cara kerja industri digital hiburan modern. Situs Mix
Parlay juga memiliki daya tarik tersendiri karena memberikan variasi dan peluang berbeda bagi
penggunanya.
Tak hanya itu, saya juga mengikuti perkembangan komunitas yang membahas Kubet
Parlay dan tren Judi Bola gacor yang sering menjadi
bahan diskusi di forum-forum online. Dari platform seperti KUBET
hingga berbagai situs parlay yang terus berkembang, pengalaman ini
membuat saya semakin tertarik menggali informasi lebih dalam.
Sebagai tambahan, saya merasa bahwa dunia hiburan online ini membantu saya
memahami bagaimana teknologi dapat memberikan pengalaman yang lebih
praktis dan efisien. Dengan berbagai inovasi dan dukungan sistem dari platform seperti KUBET dan layanan sejenis,
pengguna bisa mendapatkan hiburan sekaligus pengetahuan baru dengan cara yang lebih sederhana.
Saya percaya bahwa memahami berbagai layanan digital seperti Situs Judi Bola Terlengkap, Situs Mix Parlay, maupun situs parlay umum dapat membantu kita membuat keputusan yang lebih tepat.
Karena itu, saya senang menjadi bagian dari komunitas yang terus mengembangkan wawasan tentang dunia digital modern yang semakin berkembang.
Thank you, I have just been searching for info approximately this topic for a while
and yours is the best I have came upon so far.
But, what about the conclusion? Are you certain about the source?
Hi everyone, it’s my first pay a quick visit at this
web page, and post is in fact fruitful in favor of me, keep up posting these types of content.
Feel free to visit my page … Cheap Hotel in Cap Haitien
Hello every one, here every person is sharing these kinds of experience, so it’s nice to read this website,
and I used to visit this webpage all the time.
Feel free to surf to my page – Primary Medical Care Center
Thank you for the good writeup. It in fact was a amusement account it.
Look advanced to more added agreeable from you! By the way, how
could we communicate?
Mangelsen
7916 Girard Avenue, La Joyaa
ⅭᎪ 92037, United States
1 800-228-9686
exploring mangelsen galleries species
Thank you, I’ve just been searching for info about this subject for a while and yours is the best I have came upon so far.
But, what about the bottom line? Are you certain concerning the supply?
Miala tsiny amin’ny sary. Tiako ny zava-drehetra, mpankafy aho. Manome fanantenana ahy ny soratanao. Nahoana?
What a information of un-ambiguity and preserveness of precious experience concerning unexpected feelings.
my homepage: Miami Senior Medical Center
Dream Big Daily – Tips and strategies to turn aspirations into actionable results.
I simply could not depart your site before suggesting that I actually enjoyed the usual info an individual provide on your guests?
Is gonna be again regularly to inspect new posts
There is definately a great deal to find out about this subject.
I like all the points you have made.
Review my site … Residence Royale Hotel
Wonderful website. Plenty of useful info here.
I’m sending it to several pals ans also sharing in delicious.
And naturally, thanks on your sweat!
A safari to Tanzania is more than just a trip– it’s a journey into one of the most spectacular native environments on Earth. Here, wildlife strolls freely throughout sun-drenched plains, and old cultures grow along with the rhythm of the land. From the sweeping Serengeti to the volcanic splendour of Ngorongoro, every moment on a Tanzania safari is filled with wonder. This East African destination is not almost seeing animals; it’s about feeling the pulse of life in its purest, most thrilling kind, http://yzeeed.com/index.php/user/campflower8.
Hi my family member! I wish to say that this article is amazing, nice written and include almost all
vital infos. I would like to look extra posts like this .
Exercise tools is available in all sizes, shapes, and value ranges. Their experience lies in manufacturing obligatory parts akin to get a grip on systems, electrical motors, and controllers – ab muscles components that guarantee fitness tools works smoothly and effectively. Even the very best tools and most tricked-out gyms only produce results when used regularly. Which exercise is one of the best for the mind? Here’s a better look at how exercise impacts the body and mind and how these adaptations protect your coronary heart. Search for a model with a snug, adjustable seat and toe clips. When purchasing one, look for a powerful motor (the machine will last longer), a belt that is long and huge sufficient for your stride, a sturdy body with entrance facet rails for security, and an emergency stop gadget. When buying one, consider pulley models as an alternative of piston fashions for a more sensible rowing expertise. Listed here are extra ideas for constructing a house gym on a finances. A total of 36 TCN detectors ((three enter sorts) x (4 sampling frequencies) x (3 building block depths)) and 36 LSTM detectors ((three input varieties) x (4 sampling frequencies) x (3 building block depths)) were educated and tested (see Table 1). To practice and consider our detectors, we used the Leave-One-Out (LOO) technique, meaning that each model structure was educated and evaluated 15 times with a special train-validation-take a look at set.
Here is my website – https://wiki.novaverseonline.com/index.php/User:AbbieWoodard8
Как правильно выбрать гостиницу отель
проверить сайт маркетплейс kraken
Greetings! This is my 1st comment here so I just
wanted to give a quick shout out and tell you I really enjoy reading your articles.
Can you suggest any other blogs/websites/forums that go over the same
topics? Appreciate it!
Here is my blog … Hotel Cap-Haitien
Awesome post.
Hi colleagues, nice post and fastidious urging commented here,
I am in fact enjoying by these.
Огромное спасибо за качественный контент по теме kazino olimp.
http://Javfr.com/goto/aHR0cHM6Ly9vbGltcC1jYXNpbm8ta2F6YWtoc3Rhbi1wbGF5Lm9yZy5rei9wYXltZW50cw==
I love reading an article that will make men and women think.
Also, thanks for allowing for me to comment!
It’s really a cool and helpful piece of info. I’m happy that you just shared this useful info with us.
Please keep us informed like this. Thank you for sharing.
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CA 92626, United Stateѕ
h town bail bonds
It’s amazing to go to see this web page and reading
the views of all colleagues on the topic of this paragraph, while I am also zealous of getting knowledge.
Hello there! Do you know if they make any plugins
to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
What’s up everyone, it’s my first pay a visit at this web site, and paragraph is actually fruitful designed for me, keep up posting such articles or reviews.
Hi, i think that i noticed you visited my web site thus i got here to go back
the prefer?.I am trying to find things to improve my web site!I guess
its good enough to use some of your concepts!!
Also visit my blog post :: zgrimana
Howdy very cool site!! Man .. Beautiful .. Wonderful ..
I will bookmark your site and take the feeds
additionally? I am glad to seek out so many useful info here within the post,
we want work out extra strategies in this regard, thank you for sharing.
. . . . .
I’m curious to find out what blog system you have been using?
I’m experiencing some small security problems with my latest website and I’d
like to find something more secure. Do you have any suggestions?
????? pg
My brother recommended I might like this blog.
He was totally right. This post actually made my day. You can not imagine simply how much time I had spent for this info!
Thanks!
I have read so many articles or reviews concerning the blogger lovers except this piece of writing is in fact a good article,
keep it up.
My website: zgrimana
Hello, I think your blog may be having internet browser
compatibility issues. Whenever I take a look at your
website in Safari, it looks fine however when opening in IE, it has some overlapping issues.
I just wanted to provide you with a quick heads up!
Aside from that, great site!
Stop by my blog post: zgrimana
If some one needs expert view concerning blogging afterward i recommend him/her to visit this website, Keep up
the fastidious job.
I’m not that much of a online reader to be honest but your blogs really
nice, keep it up! I’ll go ahead and bookmark your website to come back
in the future. Cheers
My web page … zgrimana
It’s very easy to find out any topic on web as compared to books, as I found this paragraph at this web site.
Also visit my web page; zgrimana
Thanks in support of sharing such a pleasant idea, post is pleasant, thats why i have
read it entirely
my webpage … zgrimana
Fine way of explaining, and good post to take facts about my presentation focus, which i
am going to deliver in college.
Also visit my web blog – zgrimana
Are you on the hunt for some certified crew
providing urgent water mitigation solutions serving this region? This company delivers advanced methods and provides repairs with fast turnaround.
Fix water damage fast — call us today.
basement water damage cleanup
I read this article completely regarding the resemblance of
most up-to-date and earlier technologies, it’s amazing article.
My web blog … zgrimana
This paragraph is truly a fastidious one it assists
new web users, who are wishing for blogging.
my homepage – zgrimana
Woah! I’m really enjoying the template/theme of this site.
It’s simple, yet effective. A lot of times it’s difficult to get that “perfect balance” between user friendliness and visual
appeal. I must say you’ve done a very good job with this. Also, the blog loads very fast for me on Chrome.
Excellent Blog!
Look at my blog post – zgrimana
Saya sangat menikmati membaca konten ini.
Pembahasannya terasa mendalam dan relevan, terutama
saat mengulas tentang KUBET sebagai Situs Judi Bola Terlengkap serta bagaimana perannya sebagai Situs Parlay Resmi yang kini semakin populer.
Informasinya disusun dengan rapi dan tidak terasa berlebihan,
sehingga nyaman untuk diikuti dari awal hingga akhir.
Bagian yang paling saya apresiasi adalah penjelasan detail mengenai kubet login dan panduan seputar penggunaan situs parlay yang
lebih efektif. Penjabaran mengenai Situs Parlay Gacor, Kubet Parlay, hingga Situs Mix
Parlay juga memberikan gambaran nyata bagi pembaca yang ingin memahami topik ini secara lebih luas.
Selain itu, pembahasan tentang toto macau dan perkembangan Situs
Judi Bola serta Judi Bola gacor disampaikan dengan bahasa
yang mudah dipahami. Hal ini membuat artikel ini
tidak hanya informatif, tetapi juga terasa edukatif dan relevan untuk berbagai kalangan pembaca.
Salut untuk penulisnya. Semoga ke depannya semakin banyak artikel seperti ini yang
mengulas situs parlay, KUBET, dan berbagai informasi
seputar platform hiburan digital secara profesional dan terpercaya.
Currently it looks like Drupal is the best blogging platform available right now.
(from what I’ve read) Is that what you are using on your blog?
I absolutely love your blog and find most
of your post’s to be precisely what I’m looking for.
can you offer guest writers to write content for you?
I wouldn’t mind creating a post or elaborating on a few of the subjects you write concerning
here. Again, awesome web site!
Heya! I’m at work surfing around your blog from my new apple iphone!
Just wanted to say I love reading your blog and look forward to all your posts!
Keep up the superb work!
Hi there to all, how is the whole thing, I think every one is getting more from this website,
and your views are nice in favor of new people.
Great article! I’ve been using rr.com email for a
long time, and it’s nice to see helpful information about it.
Since it was originally part of RoadRunner and later moved under Spectrum, many users still get confused about how to log in or manage their accounts.
A lot of people don’t realize that they now need to sign in through the Spectrum Webmail
page instead of the old RR login.
I like the valuable info you supply on your articles.
I will bookmark your blog and check again right here regularly.
I am moderately certain I’ll be informed a lot of new stuff right right here!
Good luck for the next!
Howdy! I could have sworn I’ve visited this web site before but after looking at many
of the posts I realized it’s new to me. Nonetheless, I’m definitely pleased I found it
and I’ll be book-marking it and checking back often!
I am in fact delighted to glance at this website posts which contains plenty of useful data,
thanks for providing these information.
Nice post. I learn something new and challenging on websites I stumbleupon everyday.
It will always be useful to read through articles from other authors and
use something from their websites.
Thanks for sharing your thoughts on https://uzairnaqash.zoom.us/. Regards
buy backlinks, link exchange, free gift card, congratulations you have
won, claim your prize, you have been selected, click here to claim,
you won’t believe, one weird trick, what
happened next will shock you, shocking truth, secret revealed, limited time offer, special
promotion, act now, don’t miss out, buy now, best price, risk-free trial, get
rich quick, make money fast, work from home, no credit check,
miracle cure, lose weight fast, free viagra, no prescription needed,
online casino, free spins, meet singles, hot singles in your area, replica watches, cheap Rolex.Agent
Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB,
BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster,
Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma,
Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt,
GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky,
Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy,
Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit, RansomEXX,
Ranzy, REvil, Ryuk, Sasser, SavetheQueen,
Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt,
Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob,
Zotob
Feel free to visit my homepage :: cheap viagra sildenafil & cialis
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate < Liked it!
It’s nearly impossible to find knowledgeable people about this subject, however, you seem like you know what you’re talking about!
Thanks
Greetings! Very helpful advice in this particular post!
It’s the little changes that produce the greatest changes.
Thanks a lot for sharing!
Everything posted made a bunch of sense. But, think
on this, suppose you were to write a awesome headline?
I ain’t saying your content is not good., but suppose you added a title that makes people desire more?
I mean Heart failure: Symptoms, Causes, Diagnosis &
Treatment – MDtodate is kinda vanilla. You might peek at Yahoo’s front page and watch how they write article
headlines to grab viewers interested. You might add a video or a related picture or two to grab readers interested
about everything’ve written. In my opinion, it might bring
your website a little bit more interesting.
my blog; zgrimana
I’m not that much of a internet reader to be honest but your sites really nice, keep it up!
I’ll go ahead and bookmark your website to come back
later. Many thanks
Right now it appears like BlogEngine is the best blogging
platform available right now. (from what I’ve read) Is that what you’re using on your blog?
my web site; zgrimana
Thanks very nice blog!
ਸਾਂਝਾ ਕਰਨ ਲਈ ਧੰਨਵਾਦ। ਮੈਨੂੰ ਡਰ ਹੈ ਕਿ ਮੇਰੀ ਰਚਨਾਤਮਕਤਾ ਅਸਫਲ ਹੋ ਜਾਵੇਗੀ। ਤੁਹਾਡੀ ਕਹਾਣੀ ਮੈਨੂੰ ਉਮੀਦ ਨਾਲ ਭਰ ਦਿੰਦੀ ਹੈ। ਮੈਂ ਇਸਦਾ ਧੰਨਵਾਦ ਕਰਦਾ ਹਾਂ।
Howdy would you mind letting me know which hosting company
you’re utilizing? I’ve loaded your blog in 3 different web browsers and
I must say this blog loads a lot faster then most.
Can you suggest a good internet hosting provider at a honest price?
Thanks a lot, I appreciate it!
My web-site – zgrimana
4M Dental Implant Center
3918 ᒪong Beach Blvd #200, Ꮮong Beach,
CA 90807, United Stateѕ
15622422075
Bookmarks, https://www.protopage.com/lainedsnp,
I am sure this piece of writing has touched all the internet users,
its really really fastidious post on building up new webpage.
Here is my site zgrimana
It’s actually a nice and useful piece of information. I am glad
that you just shared this useful information with us. Please keep us informed
like this. Thank you for sharing.
Hey there exceptional blog! Does running a blog similar to this take a
massive amount work? I’ve very little knowledge of coding however I
was hoping to start my own blog soon. Anyway, should
you have any suggestions or techniques for new blog owners please share.
I know this is off subject nevertheless I simply had to ask.
Kudos!
my homepage :: zgrimana
Your means of telling everything in this article is in fact fastidious, all can easily
know it, Thanks a lot.
ca do bong da tren mang
Cheers! Good stuff!
зайти на сайт зайти на кракен даркнет
bs2bestat
You said it perfectly..
You are welcome to explore our website for a broader overview of our services, current offerings, and practical information that may be useful in evaluating our work. The site provides detailed descriptions, examples, and updates designed to help you form an informed impression and understand how our solutions can support your needs.
We invite you to visit the website at your convenience to learn more and see the full range of available options.
Artikel ini benar-benar berbobot.
Saya merasa mendapatkan wawasan baru dari sudut
pandang yang lebih luas dan terstruktur dengan baik.
Penyampaian yang mudah dipahami membuat pembaca seperti saya lebih mudah menyerap informasi tanpa merasa terbebani.
Setiap poin dijelaskan dengan pendekatan yang profesional namun tetap
ramah untuk berbagai kalangan.
Saya pribadi sangat mengapresiasi bagaimana artikel
ini tidak hanya fokus pada teori, tetapi juga memberikan gambaran praktis yang bisa diaplikasikan secara langsung.
Hal ini menunjukkan kualitas riset dan pengalaman yang tidak bisa dianggap remeh.
Semoga ke depannya semakin banyak konten berkualitas seperti ini yang
dapat menjadi referensi terpercaya bagi pembaca.
Terima kasih sudah berbagi informasi yang bermanfaat dan patut untuk direkomendasikan.
Hi there, just wanted to mention, I loved this blog post.
It was funny. Keep on posting!
Thanks for your personal marvelous posting! I certainly enjoyed reading it, you can be a great
author. I will make certain to bookmark your blog and will eventually come back
later on. I want to encourage one to continue your great writing, have a nice weekend!
Շնորհակալություն կիսվելու համար։ Ես մտահոգված եմ ստեղծագործական գաղափարների պակասից։ Ձեր հոդվածը հույս է ներշնչում ինձ։ Շնորհակալություն։
In fact no matter if someone doesn’t understand then its up
to other visitors that they will assist, so here it occurs.
Hello there! I could have sworn I’ve been to this blog before but
after checking through some of the post I realized
it’s new to me. Nonetheless, I’m definitely delighted I found it and
I’ll be book-marking and checking back frequently!
Heya are using WordPress for your site platform? I’m new to the blog world but
I’m trying to get started and set up my own. Do you require any html coding expertise to make your own blog?
Any help would be greatly appreciated!
Hi, i think that i saw you visited my website so i came to “return the favor”.I am trying to find things to improve my
website!I suppose its ok to use some of your ideas!!
Оператор функционирует без выходных, обеспечивая оперативный отклик. Вам не нужно нервничать о непредвиденных обстоятельствах — водитель адаптируется к все условия пути.
Вы можете наблюдать местоположение машины в онлайн, заранее ознакомиться информацию специалиста и забронировать подходящий уровень автомобиля — от бюджетного до премиума.
Оформляйте заранее — и вы избежите ожидания. Это наилучшим образом подходит для перемещений в хаб, на мероприятия, к партнёрам или просто для расслабленного путешествия.
Пунктуальность, честность и внимание — вот что делает ваш перевозку по-настоящему незабываемым.
We are a group of volunteers and starting a new scheme recruitment agency in warwick our community.
Your website provided us with valuable information to
work on. You have done a formidable job and our entire community
will be thankful to you.
Exceptional post but I was wanting to know if you could write a litte more on this topic?
I’d be very grateful if you could elaborate a little bit further.
Kudos!
Have a look at my site: serenity healing center
I was able to find good advice from your content.
What’s Going down i am new to this, I stumbled upon this I’ve found It absolutely useful and it
has helped me out loads. I’m hoping to contribute & aid other users like its aided me.
Great job.
Finding “value” in the odds is a true art form that requires more than just sports knowledge. It means identifying when a bookmaker’s odds don’t accurately reflect the true probability of an outcome. This is where the real profit is made.
A simple rule is to never bet more than 1-2% of your bankroll on a single event. You can practice this discipline on a platform like wplay casino.
In the end, knowledge and discipline will always outperform blind luck. Thanks for reading my thoughts.
Hi there to every single one, it’s in fact a good for me to go to see this website,
it includes priceless Information.
4M Dental Implant Center San Diego
5643 Copley Dr ste 210, San Diego,
ϹA 92111, United States
18582567711
gum surgery
Hey there! This is my first visit to your blog! We are
a collection of volunteers and starting a new project in a
community in the same niche. Your blog provided us valuable information to work on. You have done
a marvellous job!
Have a look at my web-site; stimulant addiction rehab
What a information of un-ambiguity and preserveness of
valuable know-how regarding unexpected feelings.
Hey just wanted to give you a quick heads up. The words in your
article seem to be running off the screen in Ie. I’m not sure if this is a formatting issue or something to do with
browser compatibility but I figured I’d post to
let you know. The layout look great though! Hope you get the problem fixed soon. Cheers
Feel free to visit my website MAHJONG WAYS
Touche. Sound arguments. Keep up the amazing spirit.
My programmer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the costs. But
he’s tryiong none the less. I’ve been using Movable-type on a number of websites for about a year and am nervous about switching to another platform.
I have heard very good things about blogengine.net.
Is there a way I can import all my wordpress posts into it?
Any kind of help would be really appreciated!
my site :: jobs in Warwickshire
Thanks for ones marvelous posting! I really enjoyed
reading it, you can be a great author.I will always bookmark your blog and may
come back later on. I want to encourage you to ultimately continue your
great posts, have a nice evening!
My website: Bonana
A person essentially lend a hand to make significantly posts I might state.
That is the first time I frequented your web page and up to
now? I surprised with the research you made to create this actual submit extraordinary.
Magnificent activity!
Hi, Neat post. There’s a problem along with your site in internet explorer,
would check this? IE nonetheless is the marketplace
leader and a large element of other people will miss your great writing because of
this problem.
Hey there superb website! Does running a blog such as this require a large amount of work?
I have no understanding of programming however I was hoping to start my own blog in the near future.
Anyways, if you have any recommendations or techniques for
new blog owners please share. I understand this is off subject but I just wanted to ask.
Many thanks!
Do you have any video of that? I’d like to find out some additional information.
Here is my web site scottsdale addiction treatment center
That is a great tip especially to those fresh to the blogosphere.
Brief but very precise information… Many thanks for
sharing this one. A must read article!
Really many of awesome tips. https://thebookmarknight.com/story20256632/betflik168-%E0%B8%97%E0%B8%B2%E0%B8%87%E0%B9%80%E0%B8%82-%E0%B8%B2
I like the valuable info you supply for your articles.
I’ll bookmark your blog and check once more here regularly.
I am relatively sure I’ll be told many new stuff right here!
Good luck for the next!
RR.com email offers essential email features including
inbox organization, spam filtering, password recovery, and compatibility with both desktop and mobile devices.
Users can access their accounts through webmail or configure them using IMAP or POP settings
in applications such as Outlook, Apple Mail, or Thunderbird.
One of the major changes following the transition is that RR.com email accounts
are now accessed through Spectrum’s official login page
instead of the old RoadRunner portal.
For existing users, troubleshooting usually involves resetting the password, updating mail settings,
or confirming that the account remains active, as inactive email addresses may be deactivated over
time. Despite the branding shift, RR.com email continues to serve thousands of customers who value reliability, simplicity,
and continued support through Spectrum’s platform.
Thank you, I have recently been searching for information about this subject for ages and yours
is the greatest I’ve found out so far. But, what about the conclusion? Are you certain about the source?
Wow, this article is good, my younger sister is analyzing these kinds of things, therefore I am going to convey her.
Howdy! I just want to give you a big thumbs up for the great info you have got here
on this post. I will be returning to your site
for more soon.
Hi! I’ve been following your web site for a long
time now and finally got the bravery to go ahead and give you
a shout out from Houston Texas! Just wanted to tell you keep
up the good work!
Pääl ɣɛn awuɔ̈c në kë cï ɣɛn biɛt. Ɣɛn nhiar këriɛ̈ɛ̈c ëbɛ̈n, ɣɛn anɔŋ thëm de käŋ. Athördu acï ɣa yiɛ̈n ŋɔ̈th. Thin?
Refresh Renovation Broomfield
11001 Ꮤ 120th Ave 400 suite 459a,
Broomfield, СO 80021, United Stаtes
+13032681372
Bookmarks
My partner and I stumbled over here by a different web page and thought I should check things out.
I like what I see so now i am following you. Look forward to looking at your web page repeatedly.
Really when someone doesn’t understand then its up to other viewers that they will help, so
here it occurs.
When I initially commented I seem to have clicked on the -Notify
me when new comments are added- checkbox and from now on every time a comment is
added I get 4 emails with the exact same comment. Is there a means you are able to remove me from that service?
Thanks a lot! https://nychat.in/read-blog/2786_individualki-caratova.html
Artikel ini memberikan banyak wawasan baru.
Pembahasannya terasa mendalam dan relevan, terutama saat
mengulas tentang KUBET sebagai Situs Judi Bola Terlengkap serta bagaimana perannya sebagai Situs
Parlay Resmi yang kini semakin populer. Informasinya disusun dengan rapi
dan tidak terasa berlebihan, sehingga nyaman untuk diikuti dari
awal hingga akhir.
Bagian yang paling saya apresiasi adalah penjelasan detail mengenai kubet login dan panduan seputar penggunaan situs
parlay yang lebih efektif. Penjabaran mengenai Situs Parlay Gacor, Kubet Parlay, hingga Situs Mix Parlay juga memberikan gambaran nyata bagi pembaca yang
ingin memahami topik ini secara lebih luas.
Selain itu, pembahasan tentang toto macau dan perkembangan Situs Judi
Bola serta Judi Bola gacor disampaikan dengan bahasa yang mudah dipahami.
Hal ini membuat artikel ini tidak hanya informatif, tetapi juga terasa edukatif dan relevan untuk
berbagai kalangan pembaca.
Terima kasih untuk konten berkualitas ini. Semoga ke depannya
semakin banyak artikel seperti ini yang mengulas situs parlay, KUBET, dan berbagai informasi seputar platform hiburan digital secara profesional dan terpercaya.
Saya merasa konten ini sangat berkualitas.
Penyampaian informasinya tersusun dengan baik dan sangat relevan, terutama saat membahas KUBET sebagai
Situs Judi Bola Terlengkap serta perannya sebagai Situs Parlay Resmi yang semakin diminati.
Gaya bahasanya mengalir, informatif, dan tetap terasa natural.
Yang membuat artikel ini menonjol adalah pembahasan mengenai kubet login serta panduan memilih situs parlay yang aman dan terpercaya.
Informasi tentang Situs Parlay Gacor, Kubet Parlay, hingga Situs
Mix Parlay disampaikan dengan detail yang cukup lengkap tanpa terkesan berlebihan.
Penjelasan terkait toto macau serta bagaimana dunia Situs Judi Bola dan Judi Bola gacor berkembang juga
memberikan sudut pandang yang lebih luas bagi pembaca.
Artikel ini tidak hanya informatif, tetapi juga memberikan referensi yang bermanfaat bagi siapa saja yang ingin memahami lebih jauh tentang topik ini.
Terima kasih karena telah menyuguhkan tulisan yang edukatif, rapi, dan mudah dipahami.
Semoga ke depannya semakin banyak artikel berkualitas seputar situs parlay, KUBET, dan berbagai perkembangan platform hiburan digital yang bisa
menjadi referensi utama bagi pembaca.
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ⅭA 92626, United States
t&h bail bondsman (wakelet.com)
Hi, I desire to subscribe for this webpage
to get newest updates, therefore where can i
do it please help out.
Artikel ini sangat menarik untuk disimak.
Pembahasan tentang KUBET sebagai Situs Judi Bola Terlengkap disajikan dengan penjelasan yang
jelas.
Informasi yang diberikan tidak terasa berlebihan namun tetap padat
dan berkualitas.
Saya juga mengapresiasi cara penulis menjelaskan konsep Situs Parlay
Resmi dan peran pentingnya dalam membangun kepercayaan pengguna.
Uraiannya sistematis.
Hal ini membuat artikel terasa lebih kredibel dan layak dijadikan referensi.
Bagian yang mengulas tentang Situs Parlay Gacor juga sangat
menarik karena dijabarkan secara rinci dan tidak sekadar umum.
Materinya terasa relevan.
Topik tersebut memberikan nilai tambah tersendiri terhadap keseluruhan isi artikel.
Selain itu, pembahasan mengenai Situs Mix Parlay, kubet login, serta data
toto macau juga menambah kedalaman konten.
Kombinasi seluruh elemen ini membuat artikel terasa lebih komprehensif dan tidak
monoton.
Saya merasa tulisan ini bermanfaat.
Semoga ke depannya semakin banyak artikel berkualitas seperti ini yang dapat memberikan wawasan baru seputar dunia situs parlay dan perkembangan platform digital.
Нравится сайт — всё ясно и много интересного.
https://url3.ru/pin-up-casino-44609
Attractive component of content. I simply stumbled upon your website and in accession capital to assert that I acquire in fact enjoyed
account your blog posts. Anyway I will be subscribing on your feeds
and even I fulfillment you get right of entry to consistently quickly.
Patients seeking a discreet alternative to traditional braces frequently choose Invisalign to straighten their teeth using
nearly invisible aligners.
whoah this weblog is fantastic i love studying your articles.
Keep up the great work! You understand, lots of persons are hunting
round for this information, you can aid them greatly.
страница casino vodka
I am sure this article has touched all the internet visitors, its really really nice article on building up new website.
Читать далее vodkabet новый сайт
I will immediately seize your rss feed as I can not to find your email subscription link
or newsletter service. Do you have any? Please allow me recognise in order that I may just subscribe.
Thanks.
I’m amazed, I must say. Rarely do I come across a blog that’s both
educative and amusing, and without a doubt,
you have hit the nail on the head. The issue is
something that not enough men and women are speaking
intelligently about. Now i’m very happy I found this in my hunt for something regarding this.
Khao555 com
Angels Bail Bonds Coxta Mesa
769 Baker St,
Costa Mesa, ϹA 92626, United Ѕtates
bail bond agent career
что посмотреть на ко ланте
Oh my goodness! Amazing article dude! Many thanks, However I am having troubles with your RSS.
I don’t understand why I am unable to subscribe to it. Is there anybody else having similar RSS issues?
Anybody who knows the solution can you kindly respond?
Thanks!!
Saya sangat menikmati membaca konten ini.
Pembahasan yang disajikan terasa sangat relevan dan mendalam, terutama ketika mengulas tentang KUBET sebagai Situs Judi Bola Terlengkap
serta bagaimana perannya sebagai Situs Parlay Resmi yang semakin banyak dicari pengguna.
Gaya penulisannya juga natural dan tidak terasa dibuat-buat, sehingga enak dibaca
dari awal hingga akhir.
Saya juga menyukai adalah penjelasan mengenai sistem kubet login serta bagaimana memilih situs parlay yang tepat.
Informasi terkait Situs Parlay Gacor, Kubet Parlay, hingga Situs Mix Parlay dijabarkan dengan detail yang cukup jelas dan mudah dipahami, bahkan untuk pembaca yang masih awam.
Tidak hanya itu, pembahasan mengenai toto macau serta pendekatan penulis dalam mengulas dunia Situs Judi Bola
dan Judi Bola gacor terasa cukup seimbang antara informatif dan edukatif.
Ini menunjukkan bahwa artikel ini dibuat dengan riset
yang matang dan pemahaman yang baik terhadap topik yang dibahas.
Salut untuk konten ini karena telah menyajikan informasi yang bukan hanya
panjang, tetapi juga berkualitas. Semoga artikel seperti ini terus
hadir dan menjadi referensi terpercaya bagi siapa saja
yang ingin mengetahui lebih jauh tentang situs parlay, KUBET,
dan perkembangan platform hiburan digital terkini.
Pretty element of content. I just stumbled upon your site and in accession capital to claim that I acquire actually loved account your weblog posts.
Anyway I will be subscribing to your feeds or even I achievement you
get right of entry to consistently rapidly.
Usually I do not read post on blogs, however I wish to say that this write-up very pressured me
to check out and do so! Your writing taste has been surprised me.
Thank you, very great post.
продажа штыревых лесов Аренда винтовых строительных лесов: Аренда винтовых строительных лесов предпочтительна для сложных и нестандартных задач, где требуется высокая точность и адаптивность. Винтовые механизмы позволяют точно регулировать высоту и угол наклона, что особенно важно при работе на неровных или наклонных поверхностях. Аренда таких лесов позволяет специализированным бригадам и компаниям выполнять сложные работы с большей безопасностью и эффективностью, избегая при этом значительных инвестиций в оборудование.
I like the valuable info you provide in your articles.
I will bookmark your blog and check again here frequently.
I am quite certain I’ll learn many new stuff right here!
Best of luck for the next!
Люблю сайт Pin Up Casino, он очень понятный в использовании!
http://www.secretsearchenginelabs.com/add-url.php?subtime=1762838777&newurl=https://pin-up-casino-play-kz.kz
I think that is one of the so much important information for me.
And i am glad reading your article. However should statement on some basic issues, The web site
style is great, the articles is actually nice :
D. Excellent job, cheers
I was wondering if you ever thought of changing the page layout of
your website? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or two pictures.
Maybe you could space it out better?
I blog frequently and I seriously thank you for your content.
Your article has really peaked my interest. I am going to
bookmark your blog and keep checking for new information about once
a week. I subscribed to your Feed as well.
Hurrah, that’s what I was exploring for, what a stuff! existing here at
this blog, thanks admin of this site.
Keep on working, great job!
Pretty! This was a really wonderful post. Thanks for providing this
info.
Angels Bail Bonds Costa Mesa
769 Baker Տt,
Costa Mesa, CΑ 92626, United States
t man bail bondsman, raindrop.io,
Хотел(а) отметить, что счастлив(а), что нашёл(а) сайт kazino olimp — супер!
https://www.viadukten.se/hello-world/uncategorized/
My brother suggested I may like this website. He was entirely
right. This submit actually made my day. You can not
consider simply how a lot time I had spent for this information! Thanks!
I am curious to find out what blog system you’re using?
I’m having some small security issues with my latest blog and
I’d like to find something more safe. Do you have any suggestions?
Вакансии ООО Торгово-транспортное предприятие “Острое Жало” на hh. ru ООО Торгово-транспортное предприятие “Острое Жало” ставит своей первоочередной задачей обеспечение логистической поддержки и дистрибуции товаров народного потребления по всей территории Российской Федерации. Мы специализируемся на организации комплексных транспортных решений, учитывающих специфику груза, сроки поставки и бюджет клиента. Наш автопарк оснащен современным оборудованием, обеспечивающим сохранность и своевременную доставку продукции, включая продукты питания, бытовую технику и промышленные товары.
Very great post. I simply stumbled upon your blog
and wanted to mention that I have really loved browsing your blog posts.
After all I’ll be subscribing for your rss feed and I am hoping
you write once more soon!
Good posts. Many thanks. https://escatter11.fullerton.edu/nfs/show_user.php?userid=9258019
Источник kra42 at
Thanks! An abundance of advice.
https://easiestbookmarks.com/story20358744/betflik168
Fast Relief Hypnotherapy is the leading hypnotherapy service in VA
because it provides customized and effective
interventions for many concerns. Individuals experience quick and sustained outcomes through
customized meetings that focus on their distinct demands.
The group at Fast Relief Hypnotherapy is highly trained and adept in using proven techniques to support clients
address difficulties such as anxiety, stress, tobacco cessation and weight loss.
The welcoming and supportive setting makes patients feel
at ease and safe during their sessions. Fast Relief Hypnotherapy adopts a comprehensive approach that targets the unconscious mind to produce positive changes in behavior and mindset.
Many individuals experience significant advancements after just a few sessions.
The facility is known for its qualified and empathetic team who are dedicated to supporting
each person attain their targets. Fast Relief Hypnotherapy also
delivers continuous support and direction to promote
lasting progress. The center keeps current
with the newest innovations in hypnosis to deliver the best care possible.
Clients like the easy to reach facility and flexible booking choices that accommodate
hectic schedules. Fast Relief Hypnotherapy has earned a strong
name for delivering outcomes and boosting quality of life.
People searching for hypnosis in VA can count
on Fast Relief Hypnotherapy for efficient and consistent therapy designed around their
requirements. The commitment to high standards and
client satisfaction positions Fast Relief Hypnotherapy stand out as the leading provider for hypnotherapy services in the locale.
Magnificent beat ! I wish to apprentice while you amend your web site, how can i
subscribe for a blog site? The account helped me a acceptable deal.
I were tiny bit familiar of this your broadcast offered vivid transparent idea
узнать bs2best at
I have read so many articles regarding the blogger lovers but this post is in fact a good article,
keep it up.
You suggested that wonderfully. https://gogogobookmarks.com/story20280047/betflik168
Terrific posts, Thank you! https://www.stampedeblue.com/users/porterfieldli
Link exchange is nothing else but it is just placing the other person’s website link on your page at appropriate place and other
person will also do similar in support of you.
I read this post completely about the comparison of latest and preceding technologies, it’s awesome article.
ขอบคุณที่แบ่งปันนะคะ ฉันกังวลเรื่องความคิดสร้างสรรค์ที่ขาดหายไป บทความของคุณทำให้ฉันมีความหวัง ขอบคุณค่ะ
Hey, I think your website might be having browser compatibility issues.
When I look at your blog site in Opera, it looks fine
but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that, amazing blog!
If some one wishes expert view about blogging and site-building afterward i suggest him/her to pay a visit this website, Keep up the pleasant job.
I think this is one of the most important info for me. And i’m glad reading your article.
But should remark on some general things, The website style is wonderful,
the articles is really excellent : D. Good job, cheers
This article will help the internet viewers for setting up new website
or even a blog from start to end.
I like the helpful info you supply in your articles. I will bookmark your
blog and test once more here regularly. I’m quite certain I will be informed many new stuff proper right here!
Good luck for the next!
Yesterday, while I was at work, my cousin stole my iPad and tested to see if it can survive a 25 foot drop, just so she can be a youtube sensation. My iPad is now destroyed and she
has 83 views. I know this is totally off topic but I had to share it with someone!
free porn, porn, porn hub, jav porn, indo porn, porn indo, japanese porn, porn dude, indonesia porn, gay porn, video porn, poirn video, porn hd, korean porn, tһe porn dude, japan porn, free
porn, rae lil black porn, porn indonesia, ai porn,
porn comic, tiktok porn, audrey davis porn,
podn movie, chinee porn, sophie rain porn, xxx porn, porn sex, hd
porn, asian porn, anime porn, deepfake porn, sex porn, alyx star porn, hikaru
nagi porn, indonesian porn, nagi hikaru porn, roblox porn, porn xxx,
bu guru salsa porn, porn tube, Ьig boobs porn, xnxx porn, situs porn, prn japan, msbreewc porn, film porn, bulan sutena
porn, hazel moore porn, hijab porn, douyin porn viagra, ϲlick here, buy xana
online, Ьest casino, hacked site, scam reviews, malware, download
mp3 free
Seriously plenty of amazing info.
Hello! Do you use Twitter? I’d like to follow you if that would be ok.
I’m definitely enjoying your blog and look forward to new posts.
Cheers! Valuable information.
Regards, I appreciate it.
Feel free to surf to my blog post; http://wiki.lessdead.com/index.php?title=Come_Spiare_Un_Iphone_Senza_Jailbreak
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get several emails with the same comment.
Is there any way you can remove people from that service?
Bless you!
Truly when someone doesn’t know afterward its up to other visitors that they will assist, so here it takes place.
Создаём https://sozdanie-saytove.ru/ которые не просто выглядят великолепно, а реально работают на ваш бизнес. Создаем интуитивно понятные интерфейсы, продумываем пользовательские сценарии и встраиваем инструменты конверсии. После запуска подключаем комплексное продвижение: SEO оптимизацию, контент стратегию и таргетированную рекламу. Результат — рост целевых заявок и устойчивое присутствие в топ выдаче.
Hello there! I know this is kinda off topic however , I’d figured I’d ask.
Would you be interested in trading links or maybe guest
writing a blog post or vice-versa? My website goes over a lot of the same subjects as yours
and I think we could greatly benefit from each other.
If you’re interested feel free to send me an email.
I look forward to hearing from you! Awesome blog by the way!
Mille mercis pour la plateforme Betify Casino — elle m’aide énormément !
https://www.google.co.th/url?q=http%3A%2F%2Fbetify-casino-poker-france.fr%2Favis
Hi to all, the contents present at this site are
genuinely amazing for people experience, well, keep up the nice work fellows.
Useful write ups Cheers!
Life Coach Rudolfo is recognized as the foremost life coach
in Haarlem presenting excellent guidance and support for
people seeking self-improvement and evolution. His approach is customized to meet each client’s distinct needs, providing effective strategies that result in enduring constructive change.
With considerable expertise, Rudolfo has developed
a thorough understanding of human behavior and motivation, making
his coaching sessions thought-provoking and influential.
Clients respect his attentive listening and hands-on advice,
which builds a safe environment where they gain confidence to
follow their goals and overcome obstacles. Life Coach Rudolfo employs proven techniques to help clients boost confidence, refine decision-making, and promote overall well-being.
His dedication to constant improvement and professional
development ensures he stays updated with the newest coaching methodologies.
Many individuals in Haarlem have benefited from his customized coaching programs, which focus on career development, relationships, and personal fulfillment.
Rudolfo’s dedication to his clients’ success is clear in the
glowing testimonials and enduring results they achieve.
He creates a comfortable space for reflection and growth, supporting clients to
unlock their full potential and lead more rewarding lives.
Whether facing challenges or aiming for greater achievements, Life Coach Rudolfo supplies
the skills and motivation required for success. For those seeking the
top life coaching in Haarlem, his expertise and
compassionate approach make him the ideal choice for powerful personal development.
худи зип Костюмы спортивные, эволюционировавшие из экипировки для атлетов в must-have современной модницы, воплощают собой философию активного образа жизни. Они дарят ощущение безграничной свободы движений, не стесняя рамками формальности. Выбор спортивного костюма – это инвестиция в комфорт и уверенность, требующая внимания к деталям: качеству ткани, эргономичному крою и актуальному дизайну. С наступлением холодов, когда морозный ветер рисует причудливые узоры на окнах, особую ценность обретают изделия, дарящие тепло и уют. Худи с начесом, словно мягкое объятие, согревает в студеную пору, окутывая негой нежной ткани. Его непринужденный силуэт и функциональный капюшон делают его незаменимым спутником в осенне-зимние месяцы. А для тех, кто ценит вариативность и свободу выбора, худи зип станет желанным приобретением. Молния, словно кисть художника, позволяет менять образ, адаптируя его к настроению и погодным условиям.
An outstanding share! I’ve just forwarded this onto a colleague who had been doing
a little research on this. And he in fact ordered me breakfast due to the fact that I found it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanx for spending time to discuss this topic here on your site.
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis
& Treatment – MDtodate < Loved it!
This is a very good tip especially to those new to the blogosphere.
Brief but very precise information… Thank you for sharing this one.
A must read post!
After looking into a few of the blog posts
on your website, I truly like your way of writing a blog.
I book-marked it to my bookmark website list and will
be checking back soon. Please check out my web site too
and let me know your opinion.
Diskulpa pa e silensio. Mi gusta tur kos, mi tin smak pa kosnan. Bo artíkulo a duna mi speransa. Den?
I’m not that much of a internet reader to be honest
but your sites really nice, keep it up! I’ll go ahead and bookmark your site to come back
later on. All the best
Hi friends, its impressive post on the topic of cultureand completely
defined, keep it up all the time.
It’s not my first time to pay a quick visit this web page, i am visiting this
web page dailly and take good data from here everyday.
Here is my web site :: 오피
Hello to all, the contents existing at this website are actually amazing for people
knowledge, well, keep up the good work fellows.
After checking out a handful of the blog posts on your web site,
I truly like your way of blogging. I saved as a favorite it to my bookmark webpage list and will
be checking back soon. Please visit my web site as well
and let Locksmith near me know how you feel.
списать долги через банкротство физических лиц В непростых финансовых обстоятельствах, когда бремя долгов становится непосильным, процедура банкротства физических лиц может стать спасительным кругом. Однако, прежде чем решиться на этот шаг, необходимо тщательно изучить все аспекты и нюансы, связанные с данной процедурой. Важным вопросом является определение сроков процедуры банкротства физических лиц, которые могут варьироваться в зависимости от сложности дела и загруженности судебной системы.
Hmm it appears like your blog ate my first comment (it was super long) so I
guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog writer but I’m still new
to everything. Do you have any points for inexperienced blog writers?
I’d certainly appreciate it.
Have a look at my webpage: 오피
This is very interesting, You are a very professional blogger.
I have joined your feed and look forward to in quest
of more of your fantastic post. Also, I’ve shared your web site in my social networks
I think that is one of the such a lot important info for me.
And i am glad studying your article. But wanna observation on some general issues, The site taste is perfect, the articles is actually great :
D. Excellent process, cheers
My website Commercial locksmith
I am curious to find out what blog platform you’re
utilizing? I’m experiencing some small security problems with my latest site and I’d like to find something more risk-free.
Do you have any suggestions?
Супер казино-портал, продолжайте в том же духе. Большое спасибо.
https://www.linkmio.com/site/olimp-casino-kz-win.com.kz/mobile-app/
Very good blog! Do you have any tips for aspiring writers?
I’m hoping to start my own website soon but I’m a little lost on everything.
Would you advise starting with a free platform like WordPress or
go for a paid option? There are so many
choices out there that I’m totally confused ..
Any tips? Cheers!
Hello! This is kind of off topic but I need some advice from
an established blog. Is it difficult to set up your own blog?
I’m not very techincal but I can figure things out pretty quick.
I’m thinking about setting up my own but I’m not sure where
to begin. Do you have any points or suggestions? Thanks
my webpage: Emergency locksmith
Howdy! Would you mind if I share your blog with my facebook group?
There’s a lot of folks that I think would really
enjoy your content. Please let me know. Thanks
Terrific work! That is the kind of info that should be
shared around the web. Disgrace on Google for not positioning this
publish upper! Come on over and discuss with my
website . Thanks =)
Great article. I will be going through some of these issues
as well..
Have a look at my site; 오피고고
Do you have any video of that? I’d love to find
out some additional information.
khao555 casino online
I think this is one of the most vital information for
me. And i’m glad reading your article. But want to remark
on few general things, The site style is ideal, the articles is really excellent : D.
Good job, cheers
Feel free to visit my web-site sawit188 link
списать долг по кредиту банкротство Прежде чем инициировать процедуру, крайне важно получить всестороннюю информацию о её аспектах. Бесплатная консультация по банкротству или бесплатная консультация юриста по банкротству станет первым шагом к пониманию перспектив и потенциальных последствий. Важно выяснить, как происходит списание долгов по кредитам и какие долги списывают через банкротство, поскольку не все обязательства подлежат аннулированию. Квалифицированная консультация по банкротству физических лиц поможет сориентироваться в юридических тонкостях и разработать оптимальную стратегию. Онлайн консультация по банкротству – удобный формат для получения первичной информации. Решение о банкротстве сопряжено с рядом последствий, поэтому необходимо тщательно взвесить все плюсы процедуры банкротства физического лица. К ним относится возможность списать долг по кредиту банкротство и начать жизнь с чистого листа. Однако, следует учитывать, что проведение процедуры банкротства – это ответственный шаг, требующий соблюдения строгих правил и участия квалифицированных специалистов. Особое внимание следует уделить вопросам: процедура банкротства сроки проведения, процедура банкротства физических лиц по кредитам, процедура банкротства физического лица в суде, процедура банкротства физического лица пошаговая инструкция.
buy backlinks, link exchange, free gift card, congratulations
you have won, claim your prize, you have been selected, click here
to claim, you won’t believe, one weird trick, what happened next will shock you, shocking truth,
secret revealed, limited time offer, special promotion, act now,
don’t miss out, buy now, best price, risk-free trial, get rich quick, make money fast,
work from home, no credit check, miracle cure, lose weight fast,
free viagra, no prescription needed, online casino, free
spins, meet singles, hot singles in your area, replica watches,
cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader, Black
Basta, BlackEnergy, BlackMatter, Blackshades, Blaster, Brontok, Carbanak,
Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide,
Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame,
FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi,
GozNym, Hancitor, IcedID, Industroyer, Jaff,
Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex,
Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy,
Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit, RansomEXX, Ranzy,
REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye,
SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS,
ZeroAccess, Zloader, Zlob, Zotob
Look into my blog: lolita porn
іs human trafficking tһe second largest, usa gymnastics coach human trafficking, human trafficking news
neаr me, snopes lynne knowles human trafficking, human trafficking awareness ⅾay quotes, human trafficking sex
scene, human trafficking – menschenhandel, meghan connors human trafficking, ansrew tate human trafficking, arguments օn human trafficking,
free human trafficking cmme florida, human trafficking οur, human trafficking
іn minnesota 2021, arizona republican hjman trafficking, orange іѕ thhe
new black human trafficking, human trafficking conference ocean city md, 277
arrested іn human trafficking, anti human trafficking law philippines, north korea human trafficking fаcts,
һow wіll the wall afffect human trafficking, human trafficking training
michigan 2018, hotels sued human trafficking, kids
rescued fгom human trafficking, durham region human trafficking, ԝhy human trafficking
iss imрortant, mother of god church human trafficking, walmart human trafficking 2020, ѡhat is the rate of human trafficking worldwide,
human trafficking news (news), human trafficking ƅy
state 2021, lgbt human trafficking statistics, south afrrica аnd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewed hope human trafficking, human trafficking
atlanta 2022, human trafficking san joaquin county, non rofit
organizatgions fߋr human trafficking, human trafficking interpol, human trafficking elgin, trafficking
women’ѕ human rights julietta hua, facebook human trafficing
lawsuit, rates оf human trafficking, real ѡorld example of human trafficking, lawyers аgainst human trafficking,
wsin human trafficking summit 2022, vad är human trafficking,
recognizing tһe signs of human trafficking, human trafficking
justice, video оf humkan trafficking, fⲟur signs of human trafficking,
human traffickming honey, binjun xie human trafficking, human trafficking
documentary amazon рrime, minnesota human trafficking data, uncovers russian human traffickijng гing war, human trafficking
chico са, human trafficking jus cogens, human traffdicking syrian refugees, human trafficking
topics research paper, text human trafficking link snopes, oprah
south africca human trafficking, human trafficking grants 2015,
humqn trafficking san antinio 2021, human drug trafficking meaning, human trafficking stories
children, fewma human trafficking awareness, florida disney huuman trafficking, jobs forr human trafficking victims, movie ɑbout
human trafficking 2023 netflix, ɑ daʏ іn thе life of a human trafficking
victim, uk human trafficking news, beent licensee plate human trafficking reddit, human trafficking
іn waterbury ct, center tߋ combat human trafficking, greenville nc human trafficking,
maui human trafficking, tߋp 5 human trafficking cities, iss human trafficking happening іn the
us, oxnard human trafficking, aurora shoreline human trafficking, taconganas human trafficking, hashtags f᧐r human trafficking, white house human trafficking summit, corona human trafficking,
border patropl human trafficking, human trafficking іn thailaand 2020, human trafficking in wv, 11 arrested іn humkan trafficking, china’ѕ one child
policy and human trafficking, hotels human trafficking 2023, human trafficking іn florida 2021, human trafficking debate
topics, international jujstice mission human trafficking, uncovers human trafficking гing for, scjolarly article on human trafficking, madison herman humn trafficking,
amad diallo human trafficking, ɑ poem about human trafficking, human trafficking bristol
tn, deluca аnd the human trafficking storyline, economy and human trafficking, human trafficking inn trinidad, hukan trafficking ⅾay 2018, caughnt camera actual
human trafficking victims, human trafficking episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watfh dogs human trafficking map,
human trafficking definition canada, airtag human trafficking, human trafficking іn the beauty industry,
人口販子human trafficking, forced labor іn human trafficking,
american airlines center human trafficking,
human trafficking ϲе texas, selah human trafficking, siam human trafficking, fresno human trafficking
statistics, senegal human trafficking, human trafficking belgium,
michigan human trafficking ϲourse, ny times human trafficking, abandoned stroller human trafficking, human trafficking
і-44, solution оn human trafficking, human trafficking canada news, ontario human trafficking, protects victims оf human trafficking amendment, human trafficking іn highhland ⅽa, human trafficking hotspot map, human trafficking organizations ontario,
human trafficking hiding ᥙnder cars, summary on human trafficking, uncovees russian human trafficking гing war, human trafficking honey, foᥙr signs of uman trafficking, human trafficking western pa,
human trafficking livermore, human trafficking durham region, hman trafficking ɑt atlanta airport, binjun xxie human trafficking, minnesota human trafficking data, humawn trafficking documentary amazon ρrime, human trqfficking lawyer bloomfield
hills, human trafficking charge inn texas,
central students аgainst human trafficking, ap
human geography human trafficking, hyman trafficking
fօr sexual exploitation, blue f᧐r human trafficking, kantian ethics human trafficking, anti-human trafficing organization іn cambodia, jo jorgensen ᧐n human trafficking,
fort hood soldiers human trafficking, beau οf the fifth column human trafficking, hawkins humn trafficking, human trafficking іn the pacific islands, reasons why human trafficking іs bad, ally human trafficking, ѡrite an essay ᧐n human trafficking,
human trafficking pros, human trafficking dark web reddit, north preston human trafficking, dolllar sign tattoo human trafficking, wht іs human trafficking, humasn trafficking stuart fl, priceless movie human trafficking,
ti ɑnd wife human trafficking, human trafficking ethnicity
statistics, і 80 truck stop human trafficking,
hamilton human trafficking, oakville humman trafficking,
human trafficking ᧐n the deep web, current human trafficking, human trafficking women’s rigһts, brunei human trafficking, barack
obama human traffiking quote, patron saint ⲟf human trafficking, spirited ɑwɑy human trafficking, tһe game human trafficking, tоp
human trafficking cities 2023, hhman trfficking whuch countries ɑrе tһe worst,
h᧐w to donate to human trafficking organizations, human trafficking quotes
famous, human trafficking story 2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust
atlanta, human trafficking hemet ϲa, human trafficking
statistics oregon, һow too identify a human trafficking victim, economy ɑnd human trafficking, lover boy method ⲟf human trafficking,
deluca aand tһe human trafficking storyline, european human trafficking,
selah human trafficking, american airlines center huma trafficking, human trafficking paintings,
ѡhɑt stаte is #1 іn human trafficking?, forced labor
іn human trafficking, 人口販子human trafficking, crystal meth,
ᴡhat doеs crystal meth ⅼooк likе, what iis crystal meth, crystal meth anonymous,
һow lonhg dߋеѕ crystal meth stay in уoսr sʏstem, һow to make crystal meth, lue crystal meth, buy crystal etһ online,
crystal meth effects, crystal meth pipe, crystal meth drug, whatt Ԁoes crystal meth looҝ
ⅼike?, meth crystal, crystal meth images, crystal meth ѕide effects, hоw is
crystal meth mɑde, meth vs crystal meth, ᴡhat does crystal meth Ԁo, crystal meth symptoms, ceystal meth
vs meth, effeсt of crystal meth, ѕide effects ⲟf crystal meth, һow do you make crtystal meth, crystal meth ѵs crack, ѡhat dօes
crystal meth smell ⅼike, hhow is crystal meth ᥙsed,
crystal meth withdrawal, crystal meth breaking bad, ԝhat is crustal meth mаԁe of, what dοes crystal meth doo tо you, crysta meth teeth, smoking crystal meth,
crystal mewth pictures, ⅽan yoս snnort crystal meth, crystal meth ƅefore and
aftеr, who ivented crystal meth, crystal metfh fɑcts, crystall meth withdrawal symptoms, crystal meth street
names, signs օf crystal meth, crystal meth addiction, һow to cook
crystal meth, crystal meth definition, ᴡhɑt type oof drug іs crystal meth, whɑt does crystal
meth feel ⅼike, cryustal meth meaning, crystal meth ingredients,
ԝhats crystal meth, ѡһаt color is crystal meth,
ceystal meth detox, crystal meth fаce, crystal meth powder,
crysstal meth poem, street names fοr crystal meth, short term effects оf crystal meth, signs of crystal meth abuse, crystal meth rock, crystal meth fly, crystal meth addict, crystal
mrth ᥙsers, crystal meth rehab, һow much doeѕ crystal meth cost, һow do yoս take crystal meth, how much is crystal meth, signs оf crystal meth use, һow to smoke
crystal meth, howw tߋ use crystal meth, ⅼong
term effects of crystal meth, signs ߋf addiction t᧐ crystal meth,
pink crystal meth, crystal meth ⅼook ⅼike, breaking bad crystal meth, ԝhen was
crystal meth invented, pictures оf crystal meth, how іs crystal meth
tɑken, signs that someone is using crystal meth, ready or not crystal
meth storage, difference Ƅetween meth and crystal meth, һow do yoou dо crystal meth, crystal
meth., locate crystal meth storage, ᴡhаt are the effects of crdystal meth, fake crystal meth, crystal meth people, ᴡhat does crystal
meth, һow do you uѕe crystal meth, һow addictive is crystal meth, cаn you overdose on crystal
meth, crystal meth blue, crystal meth signs, һow long does
crystal meth ⅼast, crystal meth detox los angeles,
һow do people սse crystal meth, һow doeѕ crystal meth ⅼooқ likе,
crystal meth porn, how doeѕ crystal meth ⅼ᧐ok,
crystal meth storage twisted nerve, ᴡhats іn crystal meth, crystal meth treatment, whatt іs
crystal meth made frⲟm, methamphetamin, methamphetamin adalah, methamphetamin ԁan amphetamin adalah,
amphetamin ɗan methamphetamin,chloroethane and methamphetamin, crystal methamphetamin, ᴡһat iis methamphetamin, methqmphetamin effect, methamphetamin sport,
methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文,
mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl,
amphetamin νs methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin ɗan methamphetamin, difference Ьetween amphetamine andd methamphetamin, methamphetamin psychose,
methamphetamin rules, һow too maқe methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, definition von methamphetamin, p2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin, gta methamphetamin labor, ԝie wirkt methamphetamin,
methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine uund methamphetamin,
methamphetamin herstellung, methamphetamin herstellunng china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ᴡaѕ ist daѕ, unterschied methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache,
methamphetamin chemical formula, methamphetamin medikament,
methamphetamin ⅼa chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah
obat, methamphetamin ɑndere suchten auch nacһ, methamphetamin mdma,
tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor,
methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ԁương tính, was ist
methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure, іst mdma methamphetamin, lye іn methamphetamin, iist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetamin meaning, Ԁ-methamphetamin, herstellung methamphetamin, methamphetamin ᴠs
amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fаcе, methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, bilder crystal methamphetamin, spee mіt methamphetamin gestreckt, methamphetamin synthese,
methamphetamin ᥙse icd 10, weed, wewd grinder, ԝhere is weed legal, disposable wesed pen, weed shop neаr mе, milwaukee weed eater, purple weed, іs eed legal iin virginia, iѕ weed legal in oklahoma, іs
weed legal in louisiana, wered puller tool, weed carts, іs weed legal іn south carolina, wed killer ffor lawns, horny goat weed for mеn, wһat stɑtеs is weed legal, weed shops neаr me, weed legal
states, weed vape, roundup eed killer, wewd killer spray, edibles weed,
recreational weed ѕtates, weed store, milk weed, weed barrier, іs weed legal in indiana, legal weed ѕtates, stаteѕ ԝith legal weed,
іs weed legal in kentucky, wsed puller, preen weed preventer, ounce оf weed,
dewalt werd eater, plantain weed, husqvarna weed eater, electric weed eater, hybrid weed, moonrock weed, weed pipe,
barrett wilbert weed, weed control, weed delivery neаr me, іs wеd legal in missouri,
how to make weed butter, white weed, is weedd legsl iin utah,
moon rock weed, snow caps weed, іѕ weed legal in arkansas, is weed
legal іn texas 2025, ryobi weed eater, wweed bowl, dill weed, weed legalization, sjoking weed, іs
weed legal іn nevada, weed whacker, is weed legal іn alabama,
іs weed a drug, weed barrier fabric, ԝhat iѕ horny goat weed,
spruce weed ɑnd ggrass killer, weed stores neɑr me,
sprinkles weed, poke weed, weed withdrawal, weed vapes, snow cap weed, rm43 weed killer, craftsman weed eater, qpp օf weed,
weed edibles, cookies weed, gelato weed, іs wweed legal
іn new mexico, strains ᧐f weed, wweed
butter, рound ⲟf weed, zaza weed, iѕ weed legal in nc, hoow much іs
an ounce of weed, pgr weed, іs delta 9 rreal weed, diy weed
killer, ᴢip of weed, weed torch, moldy weed, elon musk weed,
іs weed illegall іn texas, weed eater string, rso weed, weerd hangover,
weed wallpaper, iss weed legal іn nebraska, hoᴡ to smoke weed, is weed legal іn hawaii, how to grow weed,
һow to mаke weed in infihite craft, is weed legal іn california, gaary payton weed
whoah this weblog is magnificent i like studying your posts.
Stay up the great work! You realize, many persons are hunting
round for this information, you could aid them greatly.
We’re a bunch of volunteers and opening a brand new scheme in our community.
Your website provided us with useful information to work
on. You’ve performed a formidable activity and our whole group will
be grateful to you.
I’m extremely pleased to uncover this website.
I want to to thank you for your time due to this fantastic read!!
I definitely really liked every part of it and i also have you bookmarked
to look at new things on your blog.
Also visit my homepage :: 오피사이트
Currently it appears like Drupal is the top blogging platform
available right now. (from what I’ve read) Is that what you’re using on your blog?
Mangelsen
7916 Girard Avenue, ᒪɑ Joya
CA 92037, United Տtates
1 800-228-9686
best conservationist initiatives bears
Hey there! Would you mind if I share your blog with my zynga group?
There’s a lot of people that I think would really
appreciate your content. Please let me know. Thanks
Also visit my web-site: Smart lock installation
I absolutely love your blog and find the majority of your post’s to be precisely what I’m looking for.
can you offer guest writers to write content for you personally?
I wouldn’t mind producing a post or elaborating on a number of the subjects you write regarding here.
Again, awesome weblog!
My webiste:https://fly882.com/
Highly descriptive post, I liked that bit. Will there be
a part 2?
Review my web site … 오피사이트
I visited several web sites except the audio feature for audio songs
present at this site is genuinely wonderful.
Having read this I believed it was really
enlightening. I appreciate you finding the time and energy to put this content
together. I once again find myself spending a significant amount of time both reading and commenting.
But so what, it was still worthwhile!
all the time i used to read smaller posts which also clear
their motive, and that is also happening with this article which I am reading now.
my blog Emergency locksmith
списать долги банкротство физ лиц В лабиринте финансовых затруднений, когда долговое бремя угрожает стабильности, банкротство физических лиц выступает как законный механизм избавления от непосильных обязательств. Однако, это сложный процесс, требующий четкого понимания правовых норм и взвешенной оценки всех рисков. Определяющим фактором часто является банкротство физических лиц сроки процедуры, зависящие от ряда обстоятельств, включая сложность финансового положения должника и оперативность работы судебных органов.
Good day! Do you use Twitter? I’d like to follow you if that would be ok.
I’m absolutely enjoying your blog and look forward
to new posts.
Here is my web page 오피사이트
ставки на спорт Выбор надежной букмекерской конторы – это фундамент успешного беттинга. Букмекерские конторы различаются по коэффициентам, линии, наличию бонусов и промоакций, удобству интерфейса и надежности выплат. Перед тем, как сделать ставку, необходимо тщательно изучить репутацию букмекерской конторы, ознакомиться с отзывами пользователей и убедиться в наличии лицензии. Для принятия обоснованных решений в ставках на спорт необходимо обладать актуальной информацией и аналитическими данными. Прогнозы на баскетбол, прогнозы на футбол и прогнозы на хоккей – это ценный инструмент, позволяющий оценить вероятности различных исходов и принять взвешенное решение. Однако, стоит помнить, что прогнозы – это всего лишь вероятностные оценки, и они не гарантируют стопроцентный результат.
fantastic submit, very informative. I wonder why the opposite experts of this sector do not notice this.
You must continue your writing. I am sure, you have a huge readers’ base already!
My blog; Swift locksmith Minnesota
Well-built platform — I enjoy using it!
https://topomole.com/bonuses
888P
Hi, I do believe this is an excellent web site. I stumbledupon it 😉
I may revisit once again since i have book marked it.
Money and freedom is the best way to change, may you be rich and continue to guide others.
Here is my webpage :: 오피
Mangelsen
7916 Girard Avenue,ᒪa Joya
CᎪ 92037, Unied Stateѕ
1 800-228-9686
top jackson hole wildlife grizzlies (https://raindrop.io/albiuszshz/bookmarks-63179921)
I’ll immediately clutch your rss feed as I can’t
in finding your email subscription hyperlink or newsletter service.
Do you’ve any? Please allow me recognise so
that I could subscribe. Thanks.
онлайн консультация по банкротству В лабиринте финансовых затруднений, когда долговое бремя угрожает стабильности, банкротство физических лиц выступает как законный механизм избавления от непосильных обязательств. Однако, это сложный процесс, требующий четкого понимания правовых норм и взвешенной оценки всех рисков. Определяющим фактором часто является банкротство физических лиц сроки процедуры, зависящие от ряда обстоятельств, включая сложность финансового положения должника и оперативность работы судебных органов.
Great site you have here but I was wanting to know if you knew
of any discussion boards that cover the same topics discussed
in this article? I’d really love to be a part of community where I can get opinions from other knowledgeable people that share the same interest.
If you have any suggestions, please let me know. Appreciate it!
Also visit my website – 오피사이트
Hey there! I know this is kind of off topic but I was wondering which
blog platform are you using for this site?
I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at
alternatives for another platform. I would be great if you could point me in the direction of a good
platform.
Hmm it seems like your website ate my first comment (it was extremely long) so I guess I’ll
just sum it up what I had written and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog writer but I’m still new to everything.
Do you have any recommendations for inexperienced blog
writers? I’d definitely appreciate it.
It’s an awesome article designed for all the online users; they will
get advantage from it I am sure.
Howdy would you mind letting me know which hosting company you’re
working with? I’ve loaded your blog in 3 completely different browsers and I
must say this blog loads a lot quicker then most. Can you suggest a good hosting provider
at a honest price? Thank you, I appreciate it!
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is
added I get four emails with the same comment.
Is there any way you can remove people from that service? Bless you!
I do believe all of the concepts you have offered
for your post. They are very convincing and can definitely
work. Nonetheless, the posts are too quick for newbies.
May you please prolong them a little from subsequent time?
Thanks for the post.
When some one searches for his required thing, so he/she wants to be available that in detail, therefore that thing
is maintained over here.
Life Coach Rudolfo stands out as the best life coach
in Haarlem delivering excellent guidance and
support for people seeking self-improvement and change. His
approach is personalized to meet each client’s unique needs, guaranteeing successful
strategies that result in permanent positive change.
With a wealth of experience, Rudolfo has developed
a profound understanding of human behavior and motivation, making his coaching sessions thought-provoking and impactful.
Clients value his understanding listening and practical advice, which builds a
supportive environment where they are motivated to pursue their goals and surpass
obstacles. Life Coach Rudolfo utilizes effective techniques to
help clients gain confidence, improve decision-making, and enhance overall well-being.
His focus to lifelong learning and professional development ensures he keeps informed with the cutting-edge
coaching methodologies. Many individuals in Haarlem have taken advantage of his tailored coaching programs, which emphasize career development, relationships, and personal fulfillment.
Rudolfo’s commitment to his clients’ success is evident in the positive
testimonials and sustained results they achieve. He offers a welcoming space for
reflection and growth, encouraging clients to discover their
full potential and live more rewarding lives.
Whether confronting difficulties or striving for greater achievements, Life Coach Rudolfo delivers the resources and motivation required
for success. For those seeking the best life coaching in Haarlem, his expertise and compassionate approach make him the
perfect choice for impactful personal development.
Tankewol foar it dielen. Ik bin bang dat myn útfiningen mislearje sille. Dyn ferhaal follet my mei hoop. Ik wurdearje it.
Этот сайт kazino olimp — настоящая находка.
kazino olimp (https://www.kinofilmprogramm.de/firmeneintrag-loeschen?nid=8912&element=https://olimp-casino-kazakhstan-club.kz/bonuses/)
Hey there! Do you use Twitter? I’d like to follow you if
that would be okay. I’m undoubtedly enjoying your blog and look forward to new posts.
Write more, thats all I have to say. Literally, it
seems as though you relied on the video to make your point.
You definitely know what youre talking about, why waste your
intelligence on just posting videos to your blog when you
could be giving us something enlightening to read?
Also visit my web-site :: 오피사이트
If some one wants expert view about running a blog then i recommend him/her to
go to see this webpage, Keep up the pleasant work.
Oh my goodness! Impressive article dude! Thank
you so much, However I am encountering troubles
with your RSS. I don’t know the reason why I am unable to subscribe to
it. Is there anybody else getting the same RSS issues?
Anyone who knows the answer can you kindly respond?
Thanx!!
Hello to every , as I am in fact eager of reading this weblog’s post to be updated regularly.
It includes nice data.
https://geltaxi.ru/taxi-petrovskaya-krasnodar
Excellent blog you have here but I was curious about if you knew
of any discussion boards that cover the same topics talked about in this article?
I’d really love to be a part of group where I can get opinions from other knowledgeable people that share the same interest.
If you have any recommendations, please let me know. Many
thanks!
????????????
I enjoy what you guys are usually up too. This type of clever work and coverage!
Keep up the good works guys I’ve incorporated you guys to blogroll.
obviously like your web site however you have to test the spelling on several of your posts.
Several of them are rife with spelling problems and I in finding it very troublesome to inform the truth nevertheless I’ll certainly come again again.
Spot on with this write-up, I absolutely believe this site
needs a great deal more attention. I’ll probably be returning to read through more,
thanks for the information!
Hi! I know this is kinda off topic however I’d figured I’d ask.
Would you be interested in trading links or maybe guest authoring
a blog article or vice-versa? My site covers a lot of the same topics as yours and I believe we could greatly benefit from each other.
If you are interested feel free to send me an e-mail.
I look forward to hearing from you! Fantastic blog by the way!
Can you tell us more about this? I’d love to find out
some additional information.
First of all I want to say fantastic blog! I had a quick question which I’d like to ask if you do not mind.
I was interested to know how you center yourself and clear your mind prior to
writing. I have had a tough time clearing my thoughts in getting my ideas out there.
I truly do enjoy writing however it just seems like the first 10 to 15 minutes are generally lost just trying
to figure out how to begin. Any ideas or tips? Thanks!
Bujur man bandu si enggo berbagi. Kuatir aku perban kurang kreativitasku. Artikelndu mereken pengarapen man bangku. Bujur.
Milan production company Milan video production services: Offering a full spectrum of video solutions, from concept development to post-production, tailored to client specifications.
Thanks on your marvelous posting! I certainly
enjoyed reading it, you could be a great author. I
will make certain to bookmark your blog and definitely will come back later in life.
I want to encourage you continue your great job, have a nice morning!
bsme ru
Yesterday, while I was at work, my cousin stole my iphone and tested to see if it can survive a twenty
five foot drop, just so she can be a youtube sensation. My iPad is now broken and she has 83 views.
I know this is entirely off topic but I had to share it with someone!
Hello to every body, it’s my first pay a quick visit of this webpage; this webpage
consists of awesome and actually fine material for visitors.
Your way of describing all in this piece of writing is truly
good, every one can effortlessly be aware of it, Thanks a lot.
узнать больше Здесь https://kra46att.at/
https://www.lawglobalhub.com/flower-films-how-drew-barrymore-became-a-successful/
зайти на сайт kra43.at
After looking at a handful of the blog posts on your blog,
I seriously like your way of writing a blog. I saved as a favorite
it to my bookmark website list and will be checking back soon. Please visit
my website too and tell me your opinion.
남양주출장마사지 – 남양주 전역에 24시간 여성 전문 마사지사가 찾아가는
출장 홈타이 서비스! 아로마, 스포츠, 커플 마사지로 피로와 스트레스를 합리적 가격에 풀어
Đăng ký s8
Pretty! This has been a really wonderful article. Many thanks for providing
this info.
Amazing! This blog looks just like my old one! It’s on a entirely different topic but it has pretty
much the same page layout and design. Superb choice of colors!
Greetings from Colorado! I’m bored to tears at work so I decided to check
out your blog on my iphone during lunch break.
I enjoy the info you provide here and can’t wait to take a look when I get
home. I’m surprised at how fast your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyhow, great site!
Normally I don’t read post on blogs, but I wish to say
that this write-up very compelled me to take a look at and do so!
Your writing style has been amazed me. Thank you, very nice post.
Hello, i think that i saw you visited my website so i came to “return the favor”.I’m trying to
find things to enhance my site!I suppose
its ok to use a few of your ideas!!
Hmm it seems like your site ate my first comment (it was super long) so I guess I’ll just sum it up what I had written and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog writer but I’m still new to everything.
Do you have any recommendations for beginner blog writers?
I’d genuinely appreciate it.
I’m gone to inform my little brother, that he should also go to see this blog on regular basis to get updated from most up-to-date information.
I’m not sure exactly why but this weblog is loading incredibly slow for me.
Is anyone else having this issue or is it a problem on my end?
I’ll check back later on and see if the problem still exists.
Great article! I’ve been using rr.com email for a long time, and it’s nice to see helpful information about it.
Since it was originally part of RoadRunner and later moved under Spectrum, many users still get confused
about how to log in or manage their accounts. A lot of people don’t realize that they now need to sign in through the Spectrum Webmail page
instead of the old RR login.
lucky88
I am sure this piece of writing has touched all the internet viewers,
its really really pleasant piece of writing on building up new weblog.
I like what you guys are up too. This kind of clever work and reporting!
Keep up the great works guys I’ve included you guys to my personal blogroll.
Hi there it’s me, I am also visiting this web site on a regular basis, this web
page is really good and the viewers are really sharing good thoughts.
I am actually thankful to the owner of this site who has shared this great article
at at this time.
I relish, cause I found just what I used to be having a look for.
You have ended my 4 day long hunt! God Bless you man. Have a great day.
Bye
Hello! Do you use Twitter? I’d like to follow you if
that would be ok. I’m absolutely enjoying your blog and look forward
to new updates.
https://marketgit.com/how-jennifer-lopezs-green-dress-changed-the-internet/
This post offers clear idea in support of the new users of blogging, that actually how to do blogging and site-building.
Your style is very unique in comparison to other people I have read
stuff from. Thanks for posting when you’ve
got the opportunity, Guess I will just book mark this blog.
Awesome content, Many thanks!
Hello would you mind letting me know which webhost you’re using?
I’ve loaded your blog in 3 completely different web
browsers and I must say this blog loads a lot faster then most.
Can you suggest a good hosting provider at a honest price?
Thanks a lot, I appreciate it!
Зурагууд тухай хүлисыт даа. Би бүхы юумэндэ дуратайб, дуратайб. Танай бэшэһэн юумэн намда найдал түрүүлнэ. Юундэ?
Mangav tumenqe jertipe pal-o ćućipen. Me kamav sa, si man smak vash e butja. Tiri paramiči dia man nadež. Anda?
Hello to every one, the contents existing at this web site are truly remarkable for people knowledge,
well, keep up the nice work fellows.
https m bs2web at
Angels Bail Boonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, ᏟΑ 92626, United States
big d bail bonds [Angie]
Hi there, I want to subscribe for this blog to obtain newest updates, thus where can i do it please help.
Hi there, this weekend is good in support of me, as this moment
i am reading this fantastic educational post here at my house.
Right here is the right website for anyone who wishes to understand this topic.
You realize so much its almost tough to argue with
you (not that I really would want to…HaHa). You
certainly put a new spin on a subject that has been written about for decades.
Great stuff, just excellent!
Appreciate this post. Let me try it out.
If some one needs expert view on the topic of blogging afterward i recommend him/her to go to see this blog, Keep up the pleasant
work.
Here is my web site; water feature installation
Hello everyone, it’s my first pay a quick visit at this
web page, and piece of writing is genuinely fruitful in favor
of me, keep up posting such content.
buy backlinks, link exchange, free gift card,
congratulations you have won, claim your prize,
you have been selected, click here to claim, you won’t believe,
one weird trick, what happened next will shock you, shocking truth, secret revealed, limited time offer,
special promotion, act now, don’t miss out, buy now, best price, risk-free trial,
get rich quick, make money fast, work from
home, no credit check, miracle cure, lose weight fast, free viagra, no prescription needed, online casino, free spins, meet singles, hot singles in your area, replica watches,
cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler,
Anubis, Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades,
Blaster, Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis,
CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet,
Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi,
GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface,
Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa,
MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim,
Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader,
Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk,
Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock,
Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt,
Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS,
ZeroAccess, Zloader, Zlob, Zotob
My website – fake designer labels
Super platform! Alles is op niveau, gefeliciteerd en veel succes!
https://lalabet-vip-nl.nl/registratie
витамин d3 оптом Компания РТХ – ваш стратегический партнер в мире промышленной химии, предлагающий передовые технологии и надежные поставки для обеспечения устойчивого роста вашего бизнеса. Мы не просто поставляем химические продукты, мы предлагаем комплексные решения, оптимизированные под ваши конкретные задачи. Широкий спектр химической продукции для различных отраслей промышленности: от базовых полимеров и органических растворителей до специализированных катализаторов и адгезивов. РТХ постоянно расширяет свой ассортимент, чтобы удовлетворить растущие потребности современной промышленности. Индивидуальный подход и экспертиза: наши технические специалисты предоставляют профессиональную поддержку в выборе оптимальных химических решений, учитывая особенности вашего оборудования, технологических процессов и экологических требований. Мы разрабатываем индивидуальные рецептуры и предлагаем инновационные решения для повышения эффективности производства. Гарантия качества и безопасности: строгий контроль качества на всех этапах производства и логистики, подтвержденный международными сертификатами и соответствием нормативным требованиям. Мы гарантируем стабильность и безопасность поставляемой продукции. РТХ: надежный поставщик, ориентированный на долгосрочное сотрудничество, предлагая гибкие условия оплаты, оперативную доставку и техническую поддержку. Мы стремимся быть для вас не просто поставщиком, а надежным партнером в достижении ваших бизнес-целей
???????????????????????????????
eldorado casino shreveport
References:
http://www.amicacard.it/data/banner/html5_convenzioni_gold/?url=https://send.now/8cmmm6yg061g
sault ste marie casino
References:
http://v.miqiu.com/url/?url=https://www.bookmarking-online.win/explore-our-official-site
Hey there terrific website! Does running a blog like this
require a massive amount work? I have virtually no
expertise in computer programming however I was hoping to start
my own blog in the near future. Anyway, if you have any ideas or
tips for new blog owners please share. I know this is off subject nevertheless I simply needed to ask.
Kudos!
Woah! I’m really digging the template/theme of this website.
It’s simple, yet effective. A lot of times it’s very difficult to get that “perfect balance”
between superb usability and visual appearance. I must say you have done a superb
job with this. Also, the blog loads very fast for me on Safari.
Superb Blog!
olg slots
References:
http://rd.am/www.crystalxp.net/redirect.php?url=https://giphy.com/channel/galimevhco
reef casino cairns
References:
http://0.7ba.info/out.php?url=https://postheaven.net/zardiazmrg/five-fresh-aussie-online-casinos-to-try-in-2025
blackjack promotions
References:
https://www.random-bookmarks.win/top-30-aussie-real-money-online-casinos-to-try-in-november-2025-2028
isle of capri casino
References:
https://ufdub.com/user/derrylyfky
First of all I want to say awesome blog!
I had a quick question that I’d like to ask if you don’t mind.
I was interested to know how you center yourself and clear your mind prior to writing.
I’ve had a tough time clearing my thoughts
in getting my ideas out. I truly do enjoy writing but it
just seems like the first 10 to 15 minutes tend to be lost simply just trying to figure out how to begin. Any ideas or hints?
Thank you!
Then again, it’s best to consider a Medicare Supplement plan with Original Medicare if you happen to worth flexibility in terms of choosing your doctor or for those who assume you may need loads of medical care sooner or later. Maintaining optimal health is important and Sterling gives coverage to help ensure their members can get the healthcare they need once they need it. With some insurers, you may get locked right into a plan that will not be right for you. Enrollment in a plan may be restricted to certain times. It’s possible you’ll solely switch during designated times of the year. TruHearing covers one hearing help per ear per yr for a low copay of $699 for Advanced listening to aids or $999 for Premium hearing aids. For example, Medicare Advantage plans can cost you up to $9,350 per 12 months in costs that you’re accountable for, known as an out-of-pocket maximum. Medicare Advantage plans may cover a few of the prices for listening to aids and associated companies, however particulars like copayments, limitations, and coverage caps will differ with every plan.
Here is my site: https://edu.dobro.ru/bitrix/redirect.php?goto=https://dokuwiki.stream/wiki/User:KathyZdr9166366
Hello !
Hello. A 28 excellent site 1 that I found on the Internet.
Check out this website. There’s a great article there. https://www.extremesportslab.com/how-to-be-pro-at-any-sport/|
There is sure to be a lot of useful and interesting information for you here.
You’ll find everything you need and more. Feel free to follow the link below.
https://vseokrovle.com/besedka/2115-chem-otlichayutsya-odnoletnie-i-mnogoletnie-travy-dlya-gazona.html
Hello, i think that i saw you visited my web site thus
i came to “return the favor”.I’m trying to find things to enhance my site!I suppose its ok to
use some of your ideas!!
Great beat ! I wish to apprentice even as you amend your web site, how can i subscribe for a blog website?
The account helped me a appropriate deal. I were tiny bit familiar of this your broadcast
offered shiny clear concept
I’ve been exploring for a little bit for any high quality articles
or blog posts on this kind of area . Exploring in Yahoo
I at last stumbled upon this site. Reading this info So i’m glad to convey that I have an incredibly
excellent uncanny feeling I found out just what I needed.
I so much no doubt will make sure to don?t forget
this site and give it a look regularly.
Every weekend i used to pay a visit this web page, for the reason that i
wish for enjoyment, as this this site conations genuinely
fastidious funny material too.
Ta strona Najlepsze kasyna online w Polsce — prawdziwe odkrycie.
https://legalnekasynawpolsce.pl/bonusy
santa barbara casino
References:
https://lordfilmy2025.org/user/lyndanoies
Although tea tree oil gives benefits, there are a number of precautions to contemplate. To that testifies the fact that almost all patriots fled Boston shortly there after. From their lengthy line of puppies got here many extra strains of puppies https://oneway.studio/bitrix/redirect.php?goto=https://scientific-programs.science/wiki/All_Day_Slimming_Tea:_Your_Ultimate_Guide_To_A_Healthier_You related to the 2. Depending on the question, these zones can be used to gauge timing (how quickly a state of affairs is likely to happen), connection (the physical or symbolic distance between two individuals), or intensity (leaves on the rim, as an illustration, could suggest a life-changing occasion). Its growth so far has confirmed two of T.D. Heartless when it comes to the nicely being of puppies and considering only of her valuable fur coats, Cruella had no hassle taking canine into her possession. That’s an entire lot of dalmatian puppies to save lots of from the evil Cruella. It’s hard to seek out someone who is crueler than Cruella herself. Avoid shopping for tea from vendors who store tea in clear glass or plastic containers, and keep away from storing your tea in anything clear except you plan on maintaining it in a dark cabinet. Store in a sealed bundle, in a dry and cool place, away from foreign smells. Winter is the perfect season of the year when Olaf is around!
I for all time emailed this webpage post page to all my associates,
since if like to read it then my contacts will too.
Hiya very nice blog!! Man .. Beautiful .. Amazing ..
I will bookmark your website and take the feeds additionally?
I am happy to find so many helpful information right here within the submit, we’d like work
out more techniques in this regard, thank you for sharing.
. . . . .
all the time i used to read smaller posts that as well clear their motive, and that is also happening with this article which I am reading at this
time.
It’s appropriate time to make some plans for the future
and it’s time to be happy. I’ve read this post and
if I could I desire to suggest you some interesting things or advice.
Perhaps you can write next articles referring to this article.
I wish to read even more things about it!
Feel free to surf to my web page … کپسول ahcc
Highly energetic article, I liked that bit. Will there be a part
2?
포항출장마사지 출장마사지 서비스는 24시간 연중무휴로 운영되어 시간 제약 없이 편리하게 이용하실 수 있습니다.
늦은 밤 호텔에 도착한 출장객이나 새벽에 피로를
느끼는
Good site you’ve got here.. It’s difficult to find quality writing like yours nowadays.
I truly appreciate people like you! Take care!!
It’s actually a cool and helpful piece of info. I’m glad that you shared this useful info with us.
Please stay us informed like this. Thanks for sharing.
My brother recommended I may like this blog.
He used to be totally right. This post truly made my day.
You cann’t consider simply how so much time I had spent for this info!
Thank you!
Also visit my site … خرید pdf
If some one wishes to be updated with most up-to-date technologies after that he must be
pay a quick visit this web site and be up to date everyday.
buy backlinks, link exchange, free gift card, congratulations you have won, claim your prize, you have been selected,
click here to claim, you won’t believe, one weird trick, what happened next will shock you, shocking truth, secret revealed, limited time offer,
special promotion, act now, don’t miss out, buy now, best price, risk-free trial, get rich quick, make money fast, work from
home, no credit check, miracle cure, lose weight fast,
free viagra, no prescription needed, online casino, free spins, meet
singles, hot singles in your area, replica watches,
cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB,
BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades,
Blaster, Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker,
Conti, Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex,
Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi,
GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface,
Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex,
Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod,
NetSky, Nivdort, NotPetya, Nymaim, Pegasus,
PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar
Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen,
Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake,
SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot,
Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost,
XLoader, XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
My web page: buy fake Rolex fake Gucci fake Prada
You’ve made some good points there. I checked on the internet to learn more
about the issue and found most people will go along with your views on this web site.
Hurrah! At last I got a weblog from where I can really take valuable data
concerning my study and knowledge.
I do not know whether it’s just me or if everybody else experiencing issues with your website.
It appears as though some of the written text within your posts are running off the
screen. Can someone else please provide feedback and let me know if this is happening to them as
well? This might be a issue with my web browser because I’ve had this happen before.
Cheers
Feel free to visit my homepage :: PetCareShed No Pull Dog Harness
I visited several blogs however the audio quality for audio
songs existing at this web site is genuinely fabulous.
Also visit my webpage – بازی اندروید مود
Your mode of describing all in this post is genuinely nice,
every one be able to without difficulty be aware of it, Thanks a lot.
Hi mates, how is the whole thing, and what you
would like to say about this post, in my view its really remarkable designed for
me.
Mangelsen
7916 Girard Avenue, La Joya
CΑ 92037, United Stateѕ
1 800-228-9686
Bookmarks
It’s a pity you don’t have a donate button! I’d definitely donate to this outstanding blog!
I guess for now i’ll settle for book-marking and adding your
RSS feed to my Google account. I look forward to fresh updates and will talk
about this site with my Facebook group. Talk soon!
Cabinet IQ Austin
2419 Ѕ Bell Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
customfit (https://ninth-den-365.notion.site/)
You explained that wonderfully!
It’s remarkable to go to see this site and reading the views of all mates concerning this piece of writing, while
I am also keen of getting familiarity.
شيئر ڪرڻ لاءِ مهرباني. مون کي ڊپ آهي ته منهنجون ايجادون ناڪام ٿي وينديون. توهان جي ڪهاڻي مون کي اميد سان ڀري ٿي. مان ان جي تعريف ڪريان ٿو.
Hey very nice blog!
Look into my web blog; خرید پی دی اف کتاب
Cabinet IQ Austin
2419 S Bell Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
Experiencedcontractors
Great post. I was checking continuously this blog and I’m impressed!
Extremely useful information specially the last part 🙂 I care for such info much.
I was looking for this certain info for a very long time.
Thank you and good luck.
Hi, always i used to check blog posts here early in the break of day, because i like to gain knowledge of more and more.
My page … بازی اندروید مود
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem to get there!
Thank you
Estas húmedas XXX bañera disparos identificar doloroso película vibraciones con primer plano labios
y húmedo puñetazo selfies, que son famosos entre los hambriento visitantes aquí.
Las galerías MILF vídeo, que cuentan con visual garrillas, genitales película selfies, y filtraciones de pajas XXX, hacen que
todos los sediento suscriptores escandaloso, haciendo
que los chicos de todo el mundo se masturben sin saltarse sus filtraciones.
Con primeros planos de alta definición y sonido envolvente,
OnlyFans ‘ próximos episodios contarán con aventuras exhibicionismo público que implican upskirts arriesgadas y mamadas en el coche.
Nada la excita más que el goteo de porno misionero sin censura, como lo demuestran las fugas de misión XXX y fotos de sexo crudo donde el coño sigue abierto y las tetas presionan con fuerza. https://es.she-international.com/blair-switch/
I do not even know how I ended up here, but I thought this post was good.
I do not know who you are but certainly you’re going to a famous blogger if you are not
already 😉 Cheers!
Here is my webpage :: کپسول ahcc
We stumbled over here by a different page and thought I should check things out.
I like what I see so now i am following you.
Look forward to checking out your web page yet again.
Wow, superb blog format! How lengthy have you been blogging for?
you made running a blog glance easy. The entire glance of
your site is fantastic, let alone the content material!
Heya are using WordPress for your blog platform? I’m
new to the blog world but I’m trying to get started and create
my own. Do you need any coding knowledge to make your
own blog? Any help would be really appreciated!
Feel free to surf to my blog :: کرم تراست
Every weekend i used to pay a visit this web site, because i want enjoyment, as this this web page conations really fastidious funny stuff too.
Источник водка казино
Thank you for the good writeup. It if truth
be told was once a leisure account it. Look complex to far added agreeable from you!
By the way, how could we keep up a correspondence?
Descobreix el nou restaurant 180, el teu punt de trobada per esmorzars de forquilla, cullera i menú del dia al cor
d’Andorra la Vella! Aquí, la tradició es fusiona amb la qualitat i el bon tracte, cada matí i migdia.
La nostra carta ofereix diverses i variades propostes d’esmorzar de
forquilla o cullera, segons el dia de la setmana: des del clàssic cap
i pota, “callos” amb cigrons i trinxat de muntanya, fins a mandonguilles amb sípia, cua de bou estofada, peus de porc guisats, escudella barrejada o fideuà amb allioli.
No hi falten ous ferrats amb patates i pernil, botifarres esparracades, cargols a la llauna, bacallà amb samfaina, galta de porc guisada o a
la brasa, carns de xai i botifarra de pages a la brasa, botifarra amb mongetes, arròs caldós amb conill, cassola de
tros i molt més.
I’m not that much of a internet reader to be honest but your sites really
nice, keep it up! I’ll go ahead and bookmark your site to come back in the future.
Cheers
Feel free to surf to my web site … شرکت نورپردازی مینفری
I get pleasure from, result in I discovered exactly
what I used to be having a look for. You’ve ended my 4 day long hunt!
God Bless you man. Have a great day. Bye
I have read so many posts concerning the blogger lovers except this article
is in fact a good post, keep it up.
저희 서울출장안마는 고객님이 가장 편안함을 느끼는
곳으로 직접 찾아가, 불필요한 이동 없이 오롯이 휴식에만
집중할 수 있도록 도와드립니다. 자택, 숙소, 오피스텔 서울출장마사지
등
A person necessarily help to make severely posts I might state.
That is the first time I frequented your website page and up to now?
I amazed with the analysis you made to make this actual publish amazing.
Excellent job!
my page No Pull Dog Harness
Hello! This post couldn’t be written any better!
Reading this post reminds me of my good old room mate!
He always kept talking about this. I will forward this
page to him. Fairly certain he will have a good read.
Thank you for sharing!
Visit my website … No Pull Dog Harness
I am now not certain where you are getting your info, however good topic.
I needs to spend some time finding out much more or
working out more. Thank you for fantastic information I used to be in search of
this info for my mission.
hello!,I love your writing so much! percentage we be in contact extra about your post on AOL?
I need an expert in this space to resolve my problem.
Maybe that’s you! Having a look forward to look you.
Also visit my homepage :: PetCareShed No Pull Dog Harness
Cabinet IQ Austin
2419 Ѕ Bell Blvd, Cedar Park,
TX 78613, United Ѕtates
+12543183528
Designerkitchen
WOW just what I was looking for. Came here by searching for PetCareShed No Pull Dog Harness
I’ve been surfing online more than 2 hours today,
yet I never found any interesting article like yours.
It’s pretty worth enough for me. Personally, if all site owners and bloggers
made good content as you did, the net will be a lot more useful than ever
before.
Hello! I know this is somewhat off-topic however I needed
to ask. Does running a well-established website such as yours require
a lot of work? I’m brand new to blogging however I do write
in my journal on a daily basis. I’d like to start a
blog so I can share my personal experience and thoughts online.
Please let me know if you have any kind of suggestions or tips for
new aspiring bloggers. Thankyou!
I am extremely impressed with your writing skills and also with the layout
on your weblog. Is this a paid theme or did you customize it yourself?
Anyway keep up the nice quality writing, it is rare to see a great blog like this
one nowadays.
Do you have a spam problem on this site; I also am a blogger, and I was curious about your situation; many of us have developed some nice procedures and we are looking to trade strategies with other folks, be sure to shoot me an e-mail if interested.
escort Brasilia
Undeniably believe that which you stated. Your favorite justification appeared to
be on the net the easiest thing to be aware of.
I say to you, I certainly get annoyed while people think about
worries that they just do not know about. You managed to hit the nail upon the top
as well as defined out the whole thing without having side-effects , people
could take a signal. Will probably be back to get more. Thanks
Also visit my blog post … PetCareShed No Pull Dog Harness
подробнее https://kra48a.at/
Every weekend i used to pay a visit this web page, for the reason that i wish for enjoyment, as
this this site conations actually good funny stuff too.
Korepetitoriai Your Path to Efficient and Customized Learning
Please let me know if you’re looking for a article
writer for your blog. You have some really good posts and I feel I would be a
good asset. If you ever want to take some of the load off, I’d love to write some content for your
blog in exchange for a link back to mine. Please blast me an e-mail if interested.
Kudos!
Подробнее здесь кракен шоп
Incredible! This blog looks exactly like my old one! It’s on a totally
different subject but it has pretty much the
same layout and design. Great choice of colors!
aurora casino
References:
https://images.google.com.hk/url?q=https://avtovoprosi.ru/user/selectankle09
посетить сайт кракен актуальная ссылка
General Motors liked to be first with new vehicle concepts in the 1950s, But there’s no getting around the fact that by the time it rolled out the 1959 Chevrolet El Camino “sedan pickup,” arch-rival Ford had already been building its similar Ranchero for two years. Both the Ranchero and El Camino were pioneering examples of what are now dubbed “crossovers,” vehicles that attempt to appeal to both car and truck customers with a mixed bag of creature comforts and utility features. For purposes of this article, consider it to be a utility vehicle built on a passenger-car chassis, with passenger-car frontal and cabin styling, and — this is key — a cargo box seamlessly integrated into the passenger-car design elements. Thus, early pickups based on passenger-car chassis don’t qualify. Nor do coupe models equipped with a pickup box in the deck opening, such as Chevrolet’s own 1936-1942 Coupe-Pickup. The 1937-1939 Studebaker Coupe-Express and Hudson pickups of the 1930s and 1940s are also excluded, due to their distinctly separate cargo boxes.
Look into my web site … https://www.douban.com/link2/?url=https://chessdatabase.science/wiki/User:DavidMacMahon7
la casino
References:
https://www.google.com.om/url?q=https://pad.stuve.de/A-y3jt-rTNSixZIaqbEg4A/
casino promotions
References:
http://bbs.51pinzhi.cn/home.php?mod=space&uid=7455281
https://rr88.gg/
oklahoma casinos
References:
https://gpsites.win/story.php?title=enjoy-a-mega-slots-and-games-selection-at-mega-medusa
Just wish to say your article is as amazing. The clearness in your post is
simply excellent and i could assume you’re an expert on this subject.
Fine with your permission let me to grab your feed to keep updated with forthcoming post.
Thanks a million and please keep up the enjoyable work.
A person essentially assist to make significantly articles I would
state. That is the first time I frequented your website page and to this point?
I surprised with the analysis you made to create this particular submit extraordinary.
Excellent process!
Hi there, its pleasant article regarding media print, we all be familiar with media is a
great source of data.
slots games download
References:
http://lzdsxxb.com/home.php?mod=space&uid=5388949
качественная разработка сайт на 1С Битрикс под ключ Нс Диджитал Профессиональная разработка сайтов и интернет магазинов на 1с Битрикс Seo продвижение под ключ с использованием AI
The most effective choice is to supply patches with a particular individual in thoughts with the intention that the patch/pad will ship the plasmatic fields that are needed for the healing technique of the person. Important Note: Please don’t use a really wet cloth as this may dissolve the salt steadily or cause it to crack. The colour of the water will change with or with out soaking your toes in it. Finally, wash each ft with water. Deep crimson or purple pores and skin and bluish fingers and toes. http://hramacek.de/url?q=https://sciencewiki.science/wiki/User:HesterZvk6866 Deep Cleansing Foot Pads are created utilizing pure substances. Because of its deep intensive root system, tall fescue stays inexperienced longer into the summer time than different nonirrigated cool-season grasses. Never eat small Lepiotas or any with inexperienced points to the gills or a inexperienced spore print. They might assist to extend the power of the physique to struggle against infections and viruses.
Platforms of medium-sized sizes typically list plenty to a few thousand
designers. For general movie leakage, they may have separate sections for OnlyFans, for other
subscriber channels, and for other topics. They eventually build a fairly extensive library, specifically for developers who
are popular on social media or in particular nations. https://www.babywelten.ch/sys/deref/https://es.she-international.com/
คอนเทนต์นี้ น่าสนใจดี ครับ
ผม ไปอ่านเพิ่มเติมเกี่ยวกับ เนื้อหาในแนวเดียวกัน
ที่คุณสามารถดูได้ที่ sa168vip
สำหรับใครกำลังหาเนื้อหาแบบนี้
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ ข้อมูลที่น่าอ่าน นี้
จะคอยติดตามเนื้อหาที่คุณแชร์
blue rodeo
References:
https://platform.joinus4health.eu/forums/users/lionmay23/
Hey there this is somewhat of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding know-how so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
купить vps
Hello, i feel that i noticed you visited my website thus i came to go back the want?.I’m attempting to to find issues to enhance my web site!I
guess its good enough to make use of a few of your ideas!!
ข้อมูลชุดนี้ น่าสนใจดี ค่ะ
ดิฉัน ไปอ่านเพิ่มเติมเกี่ยวกับ เนื้อหาในแนวเดียวกัน
สามารถอ่านได้ที่ akbet25 สล็อตแตกง่ายล่าสุด
สำหรับใครกำลังหาเนื้อหาแบบนี้
เพราะให้ข้อมูลเชิงลึก
ขอบคุณที่แชร์ บทความคุณภาพ นี้
และอยากเห็นบทความดีๆ แบบนี้อีก
Удобный и простой сайт с массой полезной информации по казино.
http://www.google.sm/url?q=https://olimp-casino-kz-money.com.kz/games
Wonderful blog! I found it while browsing on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Appreciate it
вызвать девушку спб Заказать девушку СПб: Заказ эскорт-услуг – это возможность создать вечер своей мечты, где каждая деталь продумана до мелочей и соответствует вашим самым смелым фантазиям.
My family all the time say that I am killing my time here
at net, however I know I am getting knowledge everyday
by reading such pleasant articles.
Angels Bail Bonds Costa Mesa
769 Baker Տt,
Costa Mesa, СA 92626, United States
do bail bondsman agents need a warrant
wild rose casino emmetsburg
References:
http://bbs.8p.cn/home.php?mod=space&uid=933721
Przepraszam za milczenie. Kocham wszystko, mam smak na różne rzeczy. Twoja historia dała mi nadzieję. W?
After looking at a number of the blog articles on your web
site, I honestly like your way of blogging. I saved it to my bookmark website list and will be checking back in the near future.
Please check out my web site too and tell me what you think.
скачать игры без торрента Скачать игры без торрента: Мир мгновенного гейминга – это реальность! Забудьте о долгой и сложной процедуре загрузки через торренты. Откройте для себя пространство, где каждая игра доступна одним кликом. Мгновенный доступ к самым горячим новинкам и проверенным хитам – вот что значит скачивать без торрентов. Исследуйте вселенные, сражайтесь с врагами, решайте головоломки – и все это без утомительного ожидания.
Your method of telling the whole thing in this article is actually fastidious, every one be able to
effortlessly understand it, Thanks a lot.
Appreciate this post. Let me try it out. https://bbclinic-kr.com:443/nose/nation/bbs/board.php?bo_table=E05_4&wr_id=584064
android spinner example
References:
https://www.google.com.pk/url?q=https://notes.io/erCFc
Does your site have a contact page? I’m having trouble locating it but,
I’d like to send you an email. I’ve got some ideas for
your blog you might be interested in hearing. Either way, great website and I look forward to seeing it develop over time.
Компания РТХ (Русский Торговый Холдинг) Промышленная химия от РТХ (Русский Торговый Холдинг): надежные решения для вашего бизнеса
Its like you read my mind! You seem to know a lot about this, like you wrote the book in it or something. I think that you can do with a few pics to drive the message home a little bit, but other than that, this is magnificent blog. An excellent read. I will certainly be back.
бонус leebet casino
best online games for mac
References:
https://morningstar24.com/bbs/board.php?bo_table=free&wr_id=385378
Wonderful website you have here but I was curious if you knew of any user discussion forums that cover the same topics talked about in this article? I’d really like to be a part of online community where I can get feed-back from other experienced people that share the same interest. If you have any suggestions, please let me know. Thank you!
официальный сайт lee bet
здесь кракен переходник
Helpful postings, Thanks.
Here is my blog post: http://www.sygk100.cn/home.php?mod=space&uid=5009726&do=profile&from=space
Узнать больше Кракин
ca do bong da tren mang
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr ϲ121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Start with refresh renovations Home Your Project
There’s definately a great deal to find out about this topic.
I love all the points you made. https://proxy.dubbot.com/http://www.wildleaf.org/bbs/lounge.cgi?page=80223ESorina.Viziru.740E.Xped.I
Hurrah, that’s what I was looking for, what a information! existing here at this website, thanks admin of this web page.
하남출장마사지 – 하남 전역에 24시간 여성 전문 마사지사가 찾아가는 출장 홈타이 서비스!
아로마, 스포츠, 커플 마사지로 피로와 스트레스를 합리적 가격에
풀어
orlando casino
References:
http://175.24.226.114:3000/ashlycarper220
Our editors will review what you’ve submitted and determine whether to revise the article. American Speech-Language-Hearing Association – What is Speech? The morphology (structure) of the larynx is studied according to the cartilages, muscles, nerves, blood vessels, and membranes of which it is composed. The frame or skeleton of the larynx is composed of several cartilages, three single and three pairs. Single cartilages are the shield-shaped thyroid in front, whose prominence forms the Adam’s apple in the male; the cricoid cartilage below, which resembles a signet ring and connects the thyroid to the trachea or windpipe; and the leaf-shaped epiglottis, or laryngeal lid, on top. Among the paired cartilages are the two arytenoids, which ride on the cricoid plate and move the vocal cords sideways; the two corniculate cartilages of Santorini on top of the arytenoids; and the two cuneiform cartilages of Wrisberg. The cartilages are held together by ligaments and membranes, particularly around their joints. The larynx is connected below to the uppermost ring of the trachea, while above it is connected by the thyrohyoid ligaments to the hyoid bone beneath the tongue.
Also visit my blog; https://j9.click/titan478
mobile phone casino
References:
https://git.vicagroup.com.cn/lamontcorneliu
casino promotions
References:
https://nrisoulmate.com/@annchow8646551
saratoga casino and raceway
References:
https://queryforjob.com/employer/best-online-pokies-in-australia-for-real-money-november-2025/
Hi there, yes this paragraph is genuinely nice and I have learned lot of things from it on the topic of blogging.
thanks.
These are actually enormous ideas in concerning blogging.
You have touched some fastidious points here. Any way keep up wrinting.
Hello, i believe that i noticed you visited my website so
i came to return the prefer?.I am trying to to find issues to improve my site!I suppose its ok to
make use of some of your ideas!!
Hi i am kavin, its my first time to commenting anyplace, when i read this article i thought i could also
make comment due to this good post.
Pretty! This was an extremely wonderful post. Thanks for supplying these details.
зеркало либет казино
Wonderful blog! I found it while browsing on Yahoo News. Do
you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Many thanks
Яко унше приглядеть забор чтобы дома чи дачи
free porn, porn, porn hub, jjav porn, bokep indo, bokep bocil,
indo bokep, bokep daddy ash, bokep ngewe, ngewe bocil, bokep binor, bokep stw, bokep tante, bokep pns, bokep tobrut, bokep viral, bokep bu guru, indian sex, indian wife, desi, mom, gangbang, mother sex, ssex mother, mom sex, ebony,
dick, pussy, milf, casting, mature, teen, lesbian, vagina, vagina creampie, japanese wife,
japanese mature, japanese teen, japanese milf, lesbian mature, mature women,
squirt machine, russian maid, american anal sluts, granny sex, bokep hijab, bokep malay,
brazzers, hentai, arab sex, mature anal, indian sex, african teen, najiaporntube, gigantic ass, sarah young, mature mom, pinya scandal, sasha grey, gay,
anal gay, mom ɑnd son, mom ѕon, russian mature, russian teen, anthea sоn casting, muslim girl blow job,
jav subtitle indonesia video bokep, bokep pelajar, remaja ngentod,
ѕub indoo porn videos, bokep bumil, bokep
artis indo, bokep babymoy, bokep meimei, bokep memek legit, bokep crot dalam, bokep mantan pacar, bokep fսll percakapan, bokep fսll service, bokep
tante mulus,bokep sugardady, bokep adik kakak, bokep selingkuh, bokep
hijab tobrut, tante tobrut, hijab tobrut, bokep janda, bokep pijat, bokep vcs, bokep live ngentod, bokep indo
brondong, bokep indo tante brondong, bokep оpen bo, оpen bbo stw, bokpe
michat, bokep apk ijo, bokep ojol, bokep bareng pacar, bokep tiktok, booep jilbab sange, bojep jilbab abg, bokep ibuu mertua, bokep kebaya merah, bokep digilir, indo porn, pirn indo, japanese porn,
plrn dude, indonesia porn, gay porn, video porn, porn video, porn hd, korean porn, thhe porn dude, japwn porn, free porn, rae lil blak porn, porn indonesia,
aai porn, рoг comic, tiktok porn, audrey davis porn, porn movie,
chinese porn, sophie rain porn, xxx porn, porn sex, hd porn, asian porn, anime porn, deepfake porn, sex porn, alyx star porn, hikardu nagi porn, indonesian porn, nagi hikaru porn, roblox porn, porn xxx, bu guru salsa porn, porn tube,
Ƅig boobs porn, xnxx porn, sittus porn, porn japan, msbreewc porn, film porn, bulpan sutena porn, hazel moore porn, hijab porn, douyin porn viagra, click here, buy xanax online, bеst casino, hacked site, scam reviews, malware, download mp3 free
Mangelsen
7916 Girard Avenue, Ꮮa Joya
CA 92037, Unied States
1 800-228-9686
guide wildlife conservation books conservation
Яко лучше выгрести забор чтобы у себя или дачи
Яко лучше выгрести штакетник чтобы у себя чи дачи
It’s perfect time to make some plans for the future and it’s time to be happy.
I have read this post and if I could I desire to suggest you
few interesting things or suggestions. Maybe you
can write next articles referring to this article.
I want to read even more things about it!
phoenix casino
References:
https://woodybiz.com/kristinmurr14
indiana casino
References:
https://git.7milch.com/winstonstoner2
Oh my goodness! Incredible article dude! Many thanks, However I am going through problems with your RSS.
I don’t know the reason why I cannot subscribe to it. Is there anybody else getting similar RSS problems?
Anyone that knows the solution will you kindly respond?
Thanks!!
bs2site at
I used to be able to find good advice from your articles.
flamingo casino las vegas
References:
https://rhcstaffing.com/employer/blackcoin-services/
Hmm is anyone else having problems with the pictures on this blog loading?
I’m trying to figure out if its a problem on my
end or if it’s the blog. Any suggestions would be
greatly appreciated.
craps board
References:
https://unreliablecode.net/read-blog/141_15-best-live-casinos-australia-play-against-live-dealers-online.html
monaco casino
References:
https://nijavibes.com/ernierhyne5890
Do you have a spam issue on this site; I also am a blogger, and I was wanting to know your situation; many of us have created
some nice practices and we are looking to exchange methods
with other folks, please shoot me an e-mail if interested.
I know this site gives quality based articles or
reviews and extra stuff, is there any other web site which
gives these kinds of information in quality?
spirit mountain casino
References:
https://dreamplacesai.de/kriskeartland2
Hurrah, that’s what I was looking for, what a material!
present here at this website, thanks admin of this site.
Excellent items from you, man. I’ve have in mind your
stuff previous to and you’re just extremely fantastic.
I actually like what you’ve got here, certainly like what you’re saying
and the way wherein you say it. You are making it entertaining
and you still take care of to keep it sensible. I can’t wait to learn much more from you.
This is really a terrific website.
Hey there! I understand this is somewhat off-topic however I had to
ask. Does managing a well-established website such as yours take a massive amount work?
I’m brand new to operating a blog however I
do write in my journal every day. I’d like
to start a blog so I can easily share my own experience and views online.
Please let me know if you have any recommendations or
tips for brand new aspiring blog owners. Thankyou!
Fabulous, what a blog it is! This website gives helpful facts to
us, keep it up.
Anels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626, United Ѕtates
t man bail bondsman
With havin so much content and articles do you ever run into
any problems of plagorism or copyright violation? My site has a lot of
unique content I’ve either authored myself or outsourced but it appears
a lot of it is popping it up all over the internet without my
agreement. Do you know any ways to help prevent content from being ripped off?
I’d truly appreciate it.
buy backlinks, link exchange, free gift card, congratulations you have won, claim your prize, you have
been selected, click here to claim, you won’t believe, one weird trick, what
happened next will shock you, shocking truth, secret
revealed, limited time offer, special promotion, act now, don’t miss out, buy now, best price, risk-free trial, get rich quick,
make money fast, work from home, no credit check, miracle cure, lose weight
fast, free viagra, no prescription needed, online casino, free spins, meet singles, hot singles in your area, replica watches,
cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster,
Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis,
CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma,
Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym,
Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos,
Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot,
Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim,
Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader,
Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk,
Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader,
Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos,
WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost,
XLoader, XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
My brother recommended I may like this blog. He was entirely right.
This submit actually made my day. You can not consider just how
a lot time I had spent for this info! Thanks!
натяжные потолки под ключ Натяжной потолок СПБ цены: Выгодные предложения от профессионалов В Санкт-Петербурге представлен широкий выбор натяжных потолков по доступным ценам. Обратившись к профессионалам, вы сможете получить консультацию, выбрать оптимальный вариант и заказать установку потолка под ключ. Не стоит экономить на качестве материалов и монтажа, чтобы ваш потолок радовал вас долгие годы.
If you wish for to improve your knowledge just keep visiting this web page and be updated with the hottest news posted here.
betsafe casino
References:
https://git.louislabs.com/kathleneham136
Life Coach Rudolfo shines as the top life coach in Haarlem offering outstanding guidance and support for people seeking self-improvement and evolution. His approach is adapted to meet
each client’s individual needs, guaranteeing powerful strategies that lead to enduring positive change.
With years of experience, Rudolfo has developed a profound understanding of
human behavior and motivation, making his coaching sessions thought-provoking and impactful.
Clients value his empathetic listening and realistic advice, which builds a supportive environment where they feel empowered to chase their
goals and surpass obstacles. Life Coach Rudolfo employs established techniques to help
clients gain confidence, strengthen decision-making, and support overall well-being.
His focus to constant improvement and professional
development guarantees he remains current with the
most recent coaching methodologies. Many residents in Haarlem have taken advantage of his customized
coaching programs, which concentrate on career development, relationships,
and personal fulfillment. Rudolfo’s dedication to his clients’ success is clear in the positive testimonials and
long-term results they achieve. He offers a secure space for reflection and growth, motivating
clients to reach their full potential and lead more meaningful
lives. Whether encountering obstacles or aiming for greater achievements, Life Coach
Rudolfo provides the resources and motivation essential
for achievement. For those seeking the best life coaching in Haarlem,
his skills and empathetic approach make him the ideal choice for transformative personal development.
Hmm is anyone else having problems with the images on this blog loading?
I’m trying to determine if its a problem on my end or if it’s the
blog. Any suggestions would be greatly appreciated.
First of all I want to say awesome blog! I had a quick question which I’d like to ask if you do not
mind. I was curious to know how you center yourself and clear your head before writing.
I’ve had a tough time clearing my thoughts in getting my thoughts out there.
I truly do enjoy writing however it just seems like the first 10 to 15 minutes tend to
be wasted simply just trying to figure out how to begin. Any ideas or hints?
Appreciate it!
Яко унше выгрести штакетник для дома или дачи
Heya just wanted to give you a quick heads up and let you know a few of the pictures aren’t loading correctly.
I’m not sure why but I think its a linking issue.
I’ve tried it in two different web browsers and both show
the same outcome.
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored material stylish. nonetheless, you command get bought an nervousness over that you wish be delivering the following.
unwell unquestionably come more formerly again as exactly the same
nearly very often inside case you shield this hike.
Очень красивый и профессионально оформленный сайт kazino olimp!
https://shorturl.re/69674
Thanks for finally writing about > Heart failure: Symptoms, Causes, Diagnosis &
Treatment – MDtodate < Liked it!
Terima kasih sudah berbagi. Saya khawatir penemuan saya akan gagal. Kisah Anda memberi saya harapan. Saya sangat menghargainya.
Hi there mates, its great article regarding educationand entirely defined, keep it up all the time.
I’ll right away take hold of your rss as I can’t to find your e-mail
subscription link or e-newsletter service.
Do you’ve any? Kindly permit me realize so that I
may subscribe. Thanks.
I’m impressed, I must say. Rarely do I come across a blog that’s both equally educative and amusing,
and without a doubt, you’ve hit the nail on the head.
The problem is an issue that too few men and women are speaking intelligently about.
Now i’m very happy that I found this during my
search for something relating to this.
Amazing blog! Is your theme custom made or did you download it
from somewhere? A design like yours with a few simple tweeks would
really make my blog stand out. Please let me know where you got your theme.
Appreciate it
This is nicely said. !
This piece of writing provides clear idea designed for the new viewers of
blogging, that truly how to do blogging.
my homepage :: zalaieta01
Knowing what weight dumbbells to pick and how heavy you should lift in your workout is difficult, especially if you’re just starting with strength training for beginners or dipping a toe into weightlifting or resistance training for the first time. It’s the next big decision after you’ve decided which kind of weight to go for (kettlebells, dumbbells, barbells and medicine balls, to name a few), and getting it right could be the difference between an epic and ‘meh’ gym workout. Plump for too heavy a weight and you run the risk of injuring yourself (you’ll also need to consider your grip strength, as this could hinder you further). Go too light and your muscles won’t be properly fatigued, grow muscle or build new tissue (unless you use a certain types of set called drop sets, that implement progressive overload by increasing time under tension, as opposed to lifting heavier). Yumi Nutrition’s Kate Whapples, a strength and conditioning coach. If you’re choosing between one of these as your goal, there are handy formulas to use, incorporating both specific weights and the number of reps/sets you do.
Also visit my page – https://87.staikudrik.com/index/d1?diff=0&utm_source=ogdd&utm_campaign=26607&utm_content=&utm_clickid=uskkokskw44sooos&aurl=http%3A%2F%2Furlkw.com%2Fmasoncramer53
Whats up this is kind of of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding knowledge so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
https://yurchakbeauty.com.ua/polyuvannya-za-pryvydom-yak-znaity-sklo-dlya.html
Hello, i think that i saw you visited my blog
so i came to “return the favor”.I’m trying to find things to enhance my website!I suppose its
ok to use some of your ideas!!
?????????
аренда удаленного сервера
Las Vegas was once an open and accommodating vacation spot
for many working class households with their low cost
all you’ll be able to eat buffets, quarter slot machines and neon charm.
Anything use to appear possible to anybody but that is rapidly shifting to high
end resorts, luxury resorts and higher total expenses.
It becomes obvious that the city is starting to really feel more
unique; reminding us of a time when odd individuals may also experience the magic.
The Las Vegas Strip – Iconic casinos, hotels, and nightlife.
Bellagio Fountains – Stunning water show set to music. Fremont Street Experience – LED canopy, zip traces, dwell music downtown. High
Roller Observation Wheel – One of the world’s tallest
Ferris wheels. Hoover Dam – Historic engineering marvel,
great for a day journey. The Mob Museum – Fascinating history of organized crime in America.
Red Rock Canyon – Beautiful natural hiking and scenic drives.
Stratosphere Tower – Observation deck with thrill rides.
Cirque du Soleil Shows – World-well-known acrobatic entertainment.
Neon Museum – Restored basic Vegas signs and historical past.
Stay Hydrated: Vegas is within the desert; so drink loads of water, especially whereas walking
The Strip. Use Rideshare: Parking could be costly however
Uber or Lyft is usually extra handy. Book Shows in advance:
Big reveals typically sell out. Reserve your seats early!
Watch for Resort Fees: Hotels often charge extra every day charges not included within the booking price.
Mind the Dress Code: Many nightclubs and upscale eating places require
correct attire. The perfect time to go to Las Vegas is through the spring (March to May) and fall (September to November), when the
weather is heat however not extreme. Summer can be extremely hot, usually reaching over 110°F, while winter brings cooler temperatures and festive
occasions.
I am really loving the theme/design of your weblog. Do you ever run into any
browser compatibility problems? A small number of my blog audience have complained about my blog not working correctly in Explorer but
looks great in Opera. Do you have any suggestions to help fix this issue?
I got this web page from my pal who told me regarding this site and at
the moment this time I am visiting this web page and reading very informative posts at
this time.
Someone essentially lend a hand to make significantly articles I’d state.
That is the first time I frequented your website page and
up to now? I amazed with the analysis you made to create this actual put up incredible.
Great task!
freee porn, porn, porn hub, javv porn, ind porn, porn indo, japanese porn, porn dude,
indonesia porn, gay porn, video porn, porn video,
porn hd, korean porn, tһe porn dude, japlan porn, frwe porn, rae
lil black porn, porn indonesia, aii porn, porn comic, tiktokk porn, audrey davis porn, porn movie,
chinese porn, sophie rain porn, xxx porn, porn sex, hd porn, asian porn, anime
porn, deepfake porn, sex porn, alyx star porn, hikaru nagi porn, indonsian porn, nagi hikaru porn, roblox porn, pon xxx, bu guru
salsa porn, porn tube, ƅig boobs porn, xnxx porn, situs porn, porn japan, msbreewc porn,
film porn, bulan sutena porn, hazel moore porn, hijab porn, douyin porn viagra,
сlick heгe, buy xanax online, beѕt casino, hacked site, scam reviews, malware, download mp3 free
I think the admin of this web site is truly working hard
in favor of his web page, for the reason that here every material is quality based stuff.
Here is my site: Futemax
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I
acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing to your augment and even I
achievement you access consistently rapidly.
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa,CA 92626, United Stɑtes
bail bonds fort worth
нажмите blacksprut зеркало
It’s remarkable to visit this site and reading the views of all colleagues
concerning this post, while I am also eager of getting familiarity.
you are in point of fact a good webmaster.
The web site loading pace is incredible.
It seems that you’re doing any unique trick. Also, The contents
are masterwork. you’ve done a magnificent task on this subject!
Keep this going please, great job!
This is nicely expressed! .
Share lagid adi adi sarhaw. Iń do̠ ạḍi din khon ge ińaḱ sirjon reaḱ kạmi lạgit́ iń do̠ń bhabnaḱ kana. Apeak̕ lekha do̠ as e̠mo̠k̕ kana. Aema sarhao.
Admiring the persistence you put into your blog and in depth information you
offer. It’s nice to come across a blog every once in a
while that isn’t the same outdated rehashed information. Great read!
I’ve saved your site and I’m adding your RSS feeds to my Google account.
When some one searches for his essential thing, thus he/she desires to be available that in detail,
therefore that thing is maintained over here.
golden nugget las vegas nv
References:
https://zoucast.com/rondarahman876
Terrific article! This is the type of information that should be shared across the net.
Shame on Google for not positioning this submit higher!
Come on over and seek advice from my site . Thank you
=)
There is definately a lot to find out about
this issue. I love all of the points you made.
This game looks amazing! The way it blends that old-school chicken crossing
concept with actual consequences is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing
action with real-world stakes has me interested. I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style
with tangible consequences? I’ve gotta try this out!
This post provides clear idea in support of the new visitors of blogging, that really how to do blogging.
It’s really very complex in this full of activity life to
listen news on TV, so I just use the web for that purpose, and take the most up-to-date news.
I really love your site.. Very nice colors & theme.
Did you develop this web site yourself? Please reply back as I’m
hoping to create my very own blog and would like to learn where you got this from or just what the theme is called.
Kudos!
casino real
References:
https://kaswece.org/bbs/board.php?bo_table=free&wr_id=2611226
Эвакуатор таганрог Вызвать эвакуатор – это простое действие, которое может избавить вас от множества проблем. Достаточно лишь набрать номер телефона проверенной компании, и квалифицированные специалисты оперативно прибудут на место происшествия, чтобы оказать необходимую помощь и доставить ваш автомобиль в автосервис или на стоянку. Помните, что своевременный вызов эвакуатора – это залог безопасности вашего автомобиля и вашего спокойствия.
It’s enormous that you are getting ideas from this article as well as from our discussion made at this
place.
genting casino sheffield
References:
https://classifieds.ocala-news.com/author/iraliriano
If some one wants to be updated with most recent technologies therefore
he must be pay a visit this web page and be up to date daily.
Cabinet IQ Austin
2419 Ⴝ Bell Blvd, Cedar Park,
TX 78613, United Statеs
+12543183528
Chic
бездепозитные бонусы в казино лев
Way cool! Some extremely valid points! I appreciate
you writing this write-up and also the rest of the website is also really good.
Angels Bail Bonds Costa Mesa
769 Baker Տt,
Costa Mesa, ⅭA 92626, United Ꮪtates
how do bail bond companies work (padlet.com)
roulette on line
References:
http://git.bemagicart.com/brandengoodin
What’s up everybody, here every one is sharing these kinds of know-how, therefore it’s nice to read this web site, and I used to pay a quick visit this web site daily.
официальный сайт банда казино
Смотреть здесь кракен ссылка
Hi, I wish for to subscribe for this weblog to take most recent updates, so where can i do it please help.
casino la rochelle
References:
https://thelyvora.com/employer/best-live-casinos-in-australia-to-play-live-dealer-games-2025/
I enjoy reading a post that can make men and women think.
Also, thanks for permitting me to comment!
I think everything published was actually very logical.
But, what about this? suppose you composed a catchier post
title? I am not suggesting your content isn’t solid., but what if you added
something that makes people want more? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate is
a little vanilla. You should peek at Yahoo’s front page and watch how they
create news headlines to grab people to open the links.
You might add a video or a related picture or two to grab people excited about everything’ve got to say.
In my opinion, it could bring your website a little bit
more interesting.
Pretty great post. I just stumbled upon your weblog and wished
to say that I have really loved browsing your
weblog posts. After all I will be subscribing to your feed and
I’m hoping you write once more soon!
Hiya! I know this is kinda off topic however , I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog post or vice-versa? My site discusses a lot of the same topics as yours and I believe we could greatly benefit from each other. If you are interested feel free to send me an email. I look forward to hearing from you! Awesome blog by the way!
официальный сайт Banda Casino
casinos online bonos
References:
https://date.ainfinity.com.br/@mirtaspurgeon
Sɔri fɔ di silɛns. A lɛk ɔltin, a gɛt teist fɔ difrɛn tin dɛn. Yu stori bin gi mi op. W?
emerald queen casino
References:
https://tayartaw.kyaikkhami.com/margaretan6325
Does your website have a contact page? I’m having a tough time locating it but, I’d like to send you an email.
I’ve got some creative ideas for your blog you might be interested in hearing.
Either way, great website and I look forward to seeing it grow over time.
Ищете доверенное сервис перевозок для поездки по городу или в пригород? Инновационные приложения позволяют забронировать машину в пару кликов — через приложение или по телефону. Транспорт подъезжает точно в срок, шофёр — вежливый и профессиональный, а тариф рейса понятна и заранее известна. Поддержка 24/7, оплата любым удобным методом, возможность выбрать категорию машины — от эконома до премиум-класса. Идеально подходит как для ежедневных перемещений, так и для межгородних путешествий. Делитесь своим опытом — какие компании советуете, а с какими лучше избегать?
https://poisk-plit.ru/tseny-na-transfer-i-taksi-iz-aeroporta-po-sostoyaniyu-na-2025-god/
I’m not sure exactly why but this blog is loading very slow for me.
Is anyone else having this issue or is it a issue on my end?
I’ll check back later and see if the problem still exists.
Visit our website to discover the full range of our services, explore available options, and stay up to date with the latest updates. A clear, easy-to-navigate layout will help you quickly see how we can meet your needs and choose the best solution for you. Explore our site today and find exactly what you’ve been looking for.
slots casino games
References:
http://118.195.179.97:3000/charlestroupe8
I’m curious to find out what blog system you’re utilizing?
I’m having some minor security issues with my latest website and I’d like to find something more safe.
Do you have any recommendations?
Very quickly this website will be famous amid all blogging people, due to it’s good
articles
augustine casino
References:
https://vtuguru.online/read-blog/166_best-real-money-australian-online-casino-sites-for-2025.html
apache gold casino
References:
https://www.kingspalace.net/rodeddington4
Hello Dear, are you truly visiting this website on a regular
basis, if so after that you will absolutely take fastidious experience.
Pretty section of content. I just stumbled upon your website and in accession capital to
assert that I get in fact enjoyed account your blog posts.
Anyway I will be subscribing to your feeds and
even I achievement you access consistently fast.
Greetings! This is my 1st comment here so I just wanted to give a quick shout out and
tell you I really enjoy reading through your posts. Can you suggest any other blogs/websites/forums that cover the same
topics? Thank you!
casino france
References:
http://simonking.org.cn:3000/ross86p4105883/best-online-gambling-apps-australia2013/wiki/College+Football+Top+25+Week+14+2025+Predictions%252C+Betting+Odds+%2526+TV+Schedule
Hello, i think that i saw you visited my blog thus i came to
“return the favor”.I am trying to find things to enhance my website!I suppose its ok to use a few of your ideas!!
Oh my goodness! Awesome article dude! Thank you, However I am having difficulties with your RSS.
I don’t understand the reason why I am unable to subscribe to it.
Is there anyone else getting the same RSS issues? Anyone who knows
the solution can you kindly respond? Thanks!!
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis &
Treatment – MDtodate < Liked it!
If some one needs expert view on the topic of blogging and
site-building then i recommend him/her to pay a visit this website,
Keep up the nice job.
Here is my blog uk bonus
I don’t know if it’s just me or if perhaps everyone else encountering problems with your site.
It appears as though some of the text within your content
are running off the screen. Can somebody else please comment
and let me know if this is happening to them too?
This could be a issue with my internet browser because I’ve had this happen before.
Cheers
Feel free to surf to my website … Best shapewear for dresses
I simply could not depart your site before suggesting
that I extremely loved the standard info a person supply to your visitors?
Is gonna be again continuously to check out new posts
Maintaining healthy blood sugar levels and promoting proper circulation are crucial for overall wellness. Many people are turning to natural supplements to manage https://uri.im/circupulseblood29097 sugar without experiencing unwanted side effects.
excellent post, very informative. I ponder why the other experts of this sector do not notice this.
You should proceed your writing. I am sure, you’ve a huge readers’ base already!
With havin so much content do you ever run into any issues of plagorism or copyright infringement?
My website has a lot of exclusive content I’ve either written myself or outsourced but it looks like a lot of it is popping
it up all over the internet without my agreement. Do you know any ways to help reduce content from
being ripped off? I’d genuinely appreciate it.
смотреть здесь tripscan top
Why visitors still use to read news papers when in this technological world all
is existing on web?
hello there and thank you for your information – I’ve certainly picked up anything
new from right here. I did however expertise some technical points using this website,
since I experienced to reload the site a lot of times previous
to I could get it to load correctly. I had been wondering if your web hosting is OK?
Not that I’m complaining, but sluggish loading instances times will very
frequently affect your placement in google and could damage
your quality score if ads and marketing with Adwords.
Well I’m adding this RSS to my email and could look out for a lot more of your respective exciting content.
Ensure that you update this again very soon.
Heya i’m for the first time here. I found this board and
I find It really useful & it helped me out a lot. I hope to give something back and aid others
like you aided me.
We’re a group of volunteers and opening a new scheme in our community.
Your web site provided us with valuable info to work on. You have done a formidable job and our entire
community will be grateful to you.
Here is my web site … Women’s shapewear
Way cool! Some extremely valid points! I appreciate you writing this article plus the rest of the site is extremely good.
Do you mind if I quote a couple of your articles as long as I provide credit and sources back to
your site? My blog is in the exact same area of
interest as yours and my visitors would definitely benefit from some of the information you present here.
Please let me know if this okay with you. Thanks!
Hello, i think that i saw you visited my weblog so i came to “return the favor”.I am
attempting to find things to enhance my site!I suppose its ok to use a few of your ideas!!
Thanks a bunch for sharing this with all people you really realize what you’re talking approximately!
Bookmarked. Please additionally seek advice
from my web site =). We could have a hyperlink exchange agreement between us
Greetings from Florida! I’m bored to death at work so I decided
to browse your blog on my iphone during lunch break.
I really like the info you provide here and can’t wait to take a
look when I get home. I’m shocked at how quick your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyhow, fantastic site!
A fascinating discussion is definitely worth comment.
I do believe that you need to write more on this subject matter, it might not be a taboo matter but typically people
do not talk about such topics. To the next! Cheers!!
My spouse and I stumbled over here from a different
web page and thought I might check things out.
I like what I see so now i’m following you.
Look forward to looking over your web page for a second
time.
Way cool! Some very valid points! I appreciate you penning this post and the rest of the website is also very good.
You actually reported this fantastically.
I know this if off topic but I’m looking into starting my own blog and
was wondering what all is required to get setup?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very web savvy so I’m not 100% positive. Any tips or advice would be greatly appreciated.
Thanks
What a information of un-ambiguity and preserveness of valuable familiarity on the topic of unexpected emotions.
blackjack basic strategy
References:
http://www.sunti-apairach.com/nakhonchum1/index.php?name=webboard&file=read&id=1047597
Woah! I’m really enjoying the template/theme of this site.
It’s simple, yet effective. A lot of times it’s challenging to get that “perfect balance” between user friendliness and appearance.
I must say that you’ve done a amazing job with this.
In addition, the blog loads extremely fast for me on Firefox.
Superb Blog!
Mevcut birçok aracın yavaş, güvenilmez veya müdahaleci reklamlarla dolu olduğunu gördük.
Yesterday, while I was at work, my cousin stole my iphone and tested to see if it can survive a
thirty foot drop, just so she can be a youtube sensation.
My apple ipad is now destroyed and she has 83 views.
I know this is completely off topic but I had to share it with someone!
Por ejemplo, plataformas como SSyoutube y SocialPlug son accesibles desde
cualquier navegador, lo que significa que puedes utilizarlas
en cualquier dispositivo con acceso a Internet.
buy backlinks, link exchange, free gift card, congratulations you have won, claim
your prize, you have been selected, click here to claim, you won’t believe, one weird
trick, what happened next will shock you, shocking truth,
secret revealed, limited time offer, special promotion, act now, don’t miss out,
buy now, best price, risk-free trial, get rich quick, make money
fast, work from home, no credit check, miracle cure, lose weight fast, free viagra, no prescription needed, online casino, free spins, meet singles, hot singles in your area, replica watches, cheap Rolex.Agent
Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader,
Black Basta, BlackEnergy, BlackMatter, Blackshades,
Blaster, Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex,
Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT,
Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff,
Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot,
Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy,
Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit, RansomEXX, Ranzy,
REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer,
Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote,
TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry,
WannaRen, WastedLocker, Wifatch, Winnti,
XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
My web-site hacking tools
Hello everybody, here every one is sharing these familiarity, so it’s nice to read this web site, and
I used to go to see this website daily.
Does your website have a contact page? I’m having a tough time locating it but, I’d
like to shoot you an email. I’ve got some suggestions for your blog you might be interested in hearing.
Either way, great website and I look forward to seeing it expand over time.
Remarkable! Its really awesome paragraph, I have got much clear idea concerning
from this paragraph.
Also visit my web page; vitality supplement
Just desire to say your article is as astounding. The
clearness in your post is just excellent and i could assume you are an expert on this subject.
Fine with your permission allow me to grab your feed to keep updated
with forthcoming post. Thanks a million and
please continue the gratifying work.
Hey, I think your blog might be having browser compatibility issues.
When I look at your blog site in Ie, it looks fine
but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that, excellent blog!
Its like you read my mind! You appear to know so
much about this, like you wrote the book in it or something.
I think that you could do with a few pics to drive the message home
a little bit, but other than that, this is excellent blog.
A fantastic read. I’ll definitely be back.
женская обувь на полную ногу Женская обувь омск – широкий ассортимент моделей для каждого случая, от классики до авангарда. Обувь турция москва – возможность приобрести качественную турецкую обувь, не выезжая из столицы.
cinema casino antibes
References:
https://afrijobs.co.za/companies/top-list-of-australian-casinos-expert-picks-for-2025/
Hi, I log on to your blogs on a regular basis. Your humoristic style
is witty, keep doing what you’re doing!
william hill slots
References:
https://bdgit.educoder.net/jeanniemaudsle
slot machine game
References:
https://git.shadowvault.eu/randellantoine
Your means of describing all in this piece of writing is truly pleasant,
every one be capable of simply be aware of it, Thanks a lot.
Thanks! Wonderful stuff!
Hi would you mind stating which blog platform you’re using?
I’m looking to start my own blog in the near future but
I’m having a difficult time selecting between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most blogs and I’m looking
for something completely unique. P.S Sorry
for being off-topic but I had to ask!
Also visit my web blog … vitamin & supplements store
casino queens ny
References:
https://git.wisder.net/samantha260592
Angels Baill Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, СA 92626, United States
how much does a $500 bail bond cost
ข้อมูลชุดนี้ น่าสนใจดี ครับ
ผม เคยติดตามเรื่องนี้จากหลายแหล่ง มุมมองที่คล้ายกัน
สามารถอ่านได้ที่ ทดลองเล่น jaosua789 ฟรี
ลองแวะไปดู
มีการสรุปเนื้อหาไว้อย่างดี
ขอบคุณที่แชร์ เนื้อหาที่น่าสนใจ นี้
และหวังว่าจะได้เห็นโพสต์แนวนี้อีก
blackjack pershing
References:
https://www.facetwig.com/read-blog/203433_best-online-casinos-that-accept-paypal-in-2025-top-5-sites-reviewed-al-com.html
Hi, i think that i saw you visited my site thus i came to
“return the favor”.I’m trying to find things to
improve my website!I suppose its ok to use a few of your ideas!!
ತೇರಿಮಾ ಕಾಸಿಃ ಸುದಾ ಬೆರ್ಬಾಗಿ. ಸಯಾ ಖವಾತಿರ್ ಪೆನೆಮುವಾನ್ ಸಯಾ ಅಕನ್ ಗಗಲ್. ಕಿಸಹ ಆಂಡ ಮೆಂಬರಿ ಸಯ ಹರಪನ್। ಸಯಾ ಸಂಗತ ಮೆಂಘರ್ಗೈನ್ಯಾ
You actually revealed this effectively!
Hi! Would you mind if I share your blog with my myspace group?
There’s a lot of folks that I think would really appreciate
your content. Please let me know. Many thanks
Take a look at my blog post … Women’s shapewear
I am regular visitor, how are you everybody? This paragraph posted at this site is truly pleasant.
бездепозитные бонусы в казино олимп
gowild casino
References:
https://pettahbazaar.lk/employer/blackcoin-consulting/
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CΑ 92626, United States
bail bonds fort worth
It’s very easy to find out any topic on web
as compared to books, as I found this post at this website.
Saya sudah menyimak postingan ini selama beberapa waktu dan saya merasa isi pembahasannya sangat menarik,
terutama ketika dikaitkan dengan topik seperti KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay
Gacor, Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login,
situs parlay, Kubet Parlay, dan Judi Bola gacor yang belakangan ini semakin banyak dibicarakan.
Rasanya tidak mungkin untuk tidak meninggalkan komentar karena pembahasan di sini sangat informatif.
Menurut saya, konten seperti ini perlu mendapat perhatian karena bisa menjadi referensi bagi banyak orang.
Terima kasih sudah menyajikan informasi dengan cara yang menarik sehingga mudah dipahami.
Hello, the whole thing is going perfectly here and ofcourse every one is sharing data, that’s truly fine, keep up writing.
Also visit my web blog – uk bonus
An outstanding share! I have just forwarded this onto a colleague who was doing a little research on this.
And he actually ordered me dinner simply because I found it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanks for spending some time to discuss this issue here on your blog.
casino online slots
References:
https://www.cubexpromax.com/employer/safe-online-casinos-australia-2025-most-trusted-au-casino-sites/
этот контент казино водка
Woah! I’m really enjoying the template/theme of this site.
It’s simple, yet effective. A lot of times it’s
difficult to get that “perfect balance” between usability and
appearance. I must say you have done a amazing job with this.
Also, the blog loads very quick for me on Chrome.
Outstanding Blog!
When I originally commented I clicked the “Notify me when new comments are added” checkbox
and now each time a comment is added I get three emails with the same
comment. Is there any way you can remove me from that service?
Thank you!
My web-site – women’s jewelry
Just desire to say your article is as amazing. The clearness in your post is simply spectacular and
i can assume you’re an expert on this subject.
Well with your permission allow me to grab your feed
to keep up to date with forthcoming post. Thanks a million and please carry on the gratifying
work.
I visited multiple blogs however the audio quality for audio songs existing at this site is really superb.
This is a topic that is near to my heart… Cheers! Exactly where are your contact details though?
веб-сайт vodka casino
ultimate texas hold em online
References:
https://gogs.artapp.cn/luispfeifer87
Hello, just wanted to say, I loved this blog post.
It was funny. Keep on posting!
Thank you for the good writeup. It in fact
was a amusement account it. Look advanced to far
added agreeable from you! By the way, how can we communicate?
aspers casino london
References:
http://118.195.179.97:3000/darbyrylah5545
casino monaco
References:
https://git.palagov.tv/willisgorsuch7
There is definately a great deal to learn about this topic.
I love all the points you made.
I am curious to find out what blog platform you are using?
I’m experiencing some minor security issues with my latest
blog and I would like to find something more safe.
Do you have any solutions?
my web site – sun dresses
शेयर लागिद आदि आदि सरहऊ। दू दिन पहिले भटक गइल रहीं बाकिर हमरा लागत बा कि ई हमरा खातिर बढ़िया नइखे. अपेक̕ खाखा दो̠ अस इमो̠क̕ कना। अईमा सरहाओ।
Great delivery. Great arguments. Keep up the good work.
I’m gone to tell my little brother, that he should also visit this blog on regular basis to take updated from most
recent gossip.
My spouse and I stumbled over here by a different website and thought I may
as well check things out. I like what I see so now i’m following you.
Look forward to finding out about your web page again.
Hi there, just became alert to your blog through Google,
and found that it’s truly informative. I’m gonna watch
out for brussels. I will appreciate if you continue this in future.
A lot of people will be benefited from your writing.
Cheers!
Hey there! Quick question that’s entirely off topic.
Do you know how to make your site mobile friendly?
My website looks weird when viewing from my iphone 4.
I’m trying to find a template or plugin that might be able to resolve this problem.
If you have any recommendations, please share. With thanks!
Technology and innovation have substantially changed how people live, interact, and travel. From smart devices to wearable tools and vehicle fundamentals, staying updated is necessary. Samsung phones, Apple watch, and auto batteries are amongst the most influential items forming contemporary way of lives. Each serves a distinct purpose– interaction, physical fitness and wellness tracking, and dependable automobile performance. Recognizing their functions, advantages, and useful applications helps users make informed decisions, https://ekcochat.com/post/857650_modernus-automobiliu-akumuliatoriai-siulo-efektyvu-veikima-ir-patikimuma-vartoto.html.
Pembahasan ini benar-benar membantu!
Saya pribadi sedang mendalami lebih jauh tentang platform seperti KUBET yang dikenal sebagai Situs Judi Bola Terlengkap.
Penjelasan mengenai fitur dan sistemnya sangat relevan dengan pengalaman saya
saat mencoba kubet login.
Saya setuju bahwa penting untuk memilih platform terpercaya terutama untuk kategori Situs Judi Bola maupun Situs Parlay Resmi.
Informasi seperti ini sangat membantu dalam memahami indikator
kepercayaan sebuah platform.
Selain itu, saya juga sedang mempelajari lebih dalam mengenai performa Situs Parlay Gacor dan bagaimana opsi
pada Situs Mix Parlay bisa membantu pengguna dalam menyusun strategi.
Ulasan seperti ini membuka perspektif baru terutama ketika melihat referensi
terkait seperti data toto macau.
Semoga artikel seperti ini semakin sering dipublikasikan!
Keep on writing, great job!
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626, United Տtates
bail bonds agent neear mе (http://www.symbaloo.com)
Nice blog here! Also your web site loads up fast! What host are you
using? Can I get your affiliate hyperlink on your host?
I desire my website loaded up as fast as yours lol
Saya cukup terkesan dengan cara penjelasan artikel ini.
Informasi yang dibahas terasa detail dan memberikan sudut
pandang baru mengenai topik yang sedang dibicarakan.
Saya pribadi mengikuti berbagai topik yang berkaitan dengan platform digital,
termasuk layanan seperti KUBET, kubet login, hingga bagaimana
sebuah sistem bisa menjadi Situs Judi Bola Terlengkap yang diandalkan banyak pengguna.
Penjelasan seperti ini membuat saya semakin paham mengenai
struktur dan alur kerja sebuah Situs Judi Bola.
Selain itu, ulasan terkait Situs Parlay Resmi maupun situs parlay juga menarik untuk diikuti.
Saya juga sering memperhatikan perkembangan Situs Parlay Gacor dan berbagai strategi yang muncul dalam layanan Situs Mix Parlay.
Bahkan informasi seperti toto macau sering menjadi bahan referensi tambahan yang
bermanfaat.
Topik tentang Kubet Parlay dan berbagai analisis di Judi Bola gacor juga menjadi bagian menarik yang sering saya ikuti.
Karena itu, konten seperti ini menurut saya sangat membantu dan membuat banyak pembaca
bisa mendapatkan wawasan yang lebih luas.
Sukses selalu untuk blog ini. Saya siap mengikuti update terbaru dari blog
ini.
Mangelsen
7916 Girard Avenue, Ꮮɑ Joya
CA 92037, United States
1 800-228-9686
exploring geand teton wildlife viewing beawrs (wakelet.com)
Saya sudah membaca artikel ini sejak awal dan saya merasa isi
yang disampaikan benar-benar menarik, terutama
karena beberapa poin di dalamnya berkaitan dengan hal
yang saat ini sedang banyak dibicarakan seperti KUBET,
Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, Situs Mix Parlay, Situs Judi
Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor.
Menurut pandangan saya, tulisan ini disusun dengan cukup baik dan mampu memberikan pemahaman lebih mendalam kepada pembacanya.
Saya sendiri merasa artikel seperti ini sangat membantu karena mampu
menyajikan informasi yang relevan dengan cara yang mudah dimengerti.
Saya tidak bisa menahan diri untuk berkomentar karena konten seperti ini tentu memberikan nilai tambah bagi banyak
orang. Harapan saya, ke depannya akan ada
lebih banyak artikel informatif seperti ini, agar
pembaca lain juga dapat memperoleh wawasan baru dari sudut pandang yang berbeda.
Terima kasih kepada penulis karena sudah menghadirkan materi
dengan kualitas yang pantas diapresiasi dan semoga terus mempertahankan gaya penulisan yang menarik
seperti ini.
Asking questions are genuinely nice thing if you are
not understanding something entirely, but this
paragraph provides good understanding even.
продолжить водка бет
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ϹА 92626, United Statеѕ
bail bond agent authority
Ces conseils sur le casino sont vraiment utiles.
https://etinyurl.com/YXRNHS
buy backlinks, link exchange, free gift card,
congratulations you have won, claim your prize, you
have been selected, click here to claim, you won’t believe, one weird trick, what happened next will shock you, shocking truth, secret revealed, limited time offer,
special promotion, act now, don’t miss out, buy now, best price,
risk-free trial, get rich quick, make money fast, work from home, no
credit check, miracle cure, lose weight fast, free viagra, no
prescription needed, online casino, free spins,
meet singles, hot singles in your area, replica watches, cheap Rolex.Agent Tesla,
ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader, Black Basta,
BlackEnergy, BlackMatter, Blackshades, Blaster,
Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet,
Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi,
GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit,
Locky, Loda, LokiBot, Magecart, Maze, Medusa,
MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort,
NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot,
QuantLoader, Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk,
Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst,
SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot,
Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS,
ZeroAccess, Zloader, Zlob, Zotob
my homepage :: cheap viagra sildenafil & cialis
аренда регулируемых строительных лесов аренда рамных лесов
Artikel yang sangat membantu!
Saya sedang banyak mempelajari platform seperti KUBET yang dikenal sebagai Situs Judi Bola Terlengkap, termasuk bagaimana kubet login memberikan akses yang
cepat dan stabil bagi penggunanya.
Benar sekali bahwa kualitas sistem harus menjadi prioritas
terutama ketika berbicara tentang Situs Judi Bola maupun Situs Parlay Resmi.
Penjelasan dalam artikel ini sangat membantu saya memahami indikator dari
situs parlay yang aman dan berkualitas.
Saya juga sedang meninjau lebih dalam bagaimana sistem
pada Situs Parlay Gacor bekerja, serta bagaimana opsi yang ditawarkan oleh Situs Mix Parlay bisa
membantu pengguna dalam menyusun pilihan strategi yang lebih variatif.
Sesekali saya juga melihat data toto macau untuk mendapatkan referensi tambahan yang
bisa memperluas wawasan saya.
Ulasan seperti ini sangat bermanfaat terutama bagi saya yang juga mengikuti perkembangan platform seperti Kubet Parlay dan layanan terkait Judi Bola
gacor.
Saya menantikan artikel berikutnya!
What are fish desk games all about? Tips on how to play fish table
games like a professional? The massive share of fish desk games have a marine
theme, which makes them look extra immersive,
intriguing, and fascinating. Every fish desk sport is a taking pictures-themed,
arcade-fashion, underwater sport typically.
The essential rule of taking part in these video games
is kind of easy: use ammo to shoot as many underwater beings as attainable.
But remember that each fish you shoot has a unique odds.
So, the higher and rarer the fish you shoot with
precision, the extra you will be paid. Special tip: The more bullets you shoot at the same fish,
the extra possible you’ll capture it. However, as expected and
sure experienced by many players, profitable on-line fish desk video games shouldn’t
be easy. In actual fact, until you could have in depth knowledge of the identical video games, you will
have a difficult time winning fish tables.
Great beat ! I wish to apprentice while you amend your website,
how could i subscribe for a blog website? The account helped me a acceptable deal.
I had been a little bit acquainted of this your broadcast provided
bright clear idea
Please let me know if you’re looking for
a writer for your site. You have some really good
articles and I believe I would be a good asset. If you ever want to take
some of the load off, I’d absolutely love to write some material for your blog in exchange for a
link back to mine. Please blast me an e-mail if interested.
Many thanks!
Take a look at my blog post … 밤알바
Amazing things here. I am very glad to look your post. Thank you a lot and I am
taking a look ahead to contact you. Will you please drop me a e-mail?
It’s going to be end of mine day, except before ending I
am reading this impressive piece of writing to increase my
know-how.
This post will assist the internet people for building up new website or
even a blog from start to end.
My web page: 밤알바
seminole casino brighton
References:
https://profalink.com/albaheck6
Kudos, Loads of stuff.
Hey there just wanted to give you a brief heads
up and let you know a few of the pictures aren’t loading correctly.
I’m not sure why but I think its a linking issue.
I’ve tried it in two different web browsers and
both show the same outcome.
Feel free to surf to my web page :: 밤알바
Seriously quite a lot of superb facts.
Wonderful beat ! I would like to apprentice while you amend your site, how can i subscribe for a blog website?
The account aided me a acceptable deal. I were tiny
bit familiar of this your broadcast offered
bright clear concept
great points altogether, you simply gained a new reader.
What may you suggest in regards to your post that you simply made
a few days in the past? Any certain?
Fantastic website you have here but I was curious about if
you knew of any community forums that cover the same topics talked
about here? I’d really like to be a part of group where
I can get suggestions from other knowledgeable individuals that
share the same interest. If you have any recommendations, please let me know.
Thanks!
Займ на карту и его особенности
Somebody necessarily help to make severely articles I would state.
That is the first time I frequented your website page and thus far?
I surprised with the research you made to create this actual post incredible.
Fantastic task!
Jullie hebben informatieve informatie over spelstrategieën.
https://www.musclesandveggies.com/nutrition-health-coach/instagram-logo/?unapproved=986388&moderation-hash=eaa18d2c5ec3e438d275eb07076396f9
Greetings I am so excited I found your blog page, I
really found you by mistake, while I was searching on Digg for
something else, Nonetheless I am here now and would just like to say thank you for a tremendous post and a all round thrilling blog (I also love the theme/design), I don’t have time to go through it all at the minute
but I have bookmarked it and also included your RSS feeds, so when I have time I will be
back to read a great deal more, Please do keep up the excellent b.
Refresh Renovation Broomfield
11001 W 120th Ave 400 suite 459ɑ,
Broomfield, СO 80021, United Stаtes
+13032681372
Builders renovation in the and us remodeling home
པར་ལ་དགོངས་དག་ཞུ། ང་དེ་ལ་དགའ། ང་ཡོད་ཚད་ལ་དགའ། ཁྱེད་ཀྱི་རྩོམ་ཡིག་དེས་ང་ལ་རེ་བ་སྦྱིན་སོང་། ཅི་ཞིག?
сделать презентацию
I think this is one of the so much vital information for me.
And i’m happy reading your article. However want to remark on some normal things, The web site taste
is great, the articles is actually nice : D.
Excellent process, cheers
When I initially commented I clicked the “Notify me when new comments are added” checkbox
and now each time a comment is added I get three emails with the same comment.
Is there any way you can remove me from that service?
Thanks a lot!
If you are going for best contents like me, only pay a visit this web page daily as it offers feature contents, thanks
I am regular visitor, how are you everybody? This piece of writing posted at this web site is genuinely good.
Post writing is also a excitement, if you know then you can write or else it is
difficult to write.
wonderful submit, very informative. I’m wondering why the opposite specialists of this sector do not realize this.
You must continue your writing. I’m sure, you have a great readers’ base already!
Many thanks! I value this.
durant ok casino
References:
https://twittecx.com/read-blog/5859_best-online-casinos-usa-2025-top-rated-amp-trusted-real-money-sites.html
The term “Golden Age of Porn”, or “porno chic”, refers to a
15-year interval (1969-1984) in commercial American pornography, wherein sexually express films experienced positive attention from mainstream cinemas,
movie critics, and most people.[1][2] This American period, which had subsequently spread internationally,[3] and that began earlier than the legalization of
pornography in Denmark on July 1, 1969,[4] started on June 12, 1969,[5] with the theatrical release of
the movie Blue Movie directed by Andy Warhol,[6][7][8] and,
considerably later, with the discharge of the 1970 movie Mona produced by Bill Osco.[9][10] These films had been the primary
adult erotic movies depicting explicit intercourse to obtain wide theatrical launch in the United States.[6][7][8][9] Both influenced the making of movies equivalent
to 1972’s Deep Throat starring Linda Lovelace and directed by Gerard Damiano,[11] Behind the Green Door starring Marilyn Chambers and directed by the Mitchell brothers,[12] 1973’s The
Devil in Miss Jones also by Damiano, and 1976’s The Opening of Misty Beethoven by Radley Metzger, the “crown jewel”
of the Golden Age, in response to award-successful writer
Toni Bentley.[13][14]. In response to Andy Warhol,
his Blue Movie film was a major influence within the making of Last Tango in Paris, an internationally controversial
erotic drama film, starring Marlon Brando, and released a couple of years after Blue
Movie was shown in theaters.[8]
Hi there to all, how is all, I think every one is getting more from
this web page, and your views are fastidious in favor of new visitors.
grey eagle casino calgary
References:
http://www.talniri.co.il/finance/MobileMenu.aspx?returnurl=https://www.primary-bookmarks.win/stake-us-casino-review-bonus-2025
obviously like your web site but you need to take a look at the spelling
on several of your posts. Many of them are rife with spelling
issues and I find it very bothersome to tell the reality however I will certainly come
back again.
бездепозитные бонусы в казино за регистрацию 2025
Hi there! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get
my blog to rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Thanks!
Pretty! This has been an incredibly wonderful article.
Thanks for providing this info.
Someone essentially help to make critically articles I might state.
That is the very first time I frequented your website page and thus far?
I amazed with the analysis you made to create this actual post amazing.
Excellent task!
I think this is one of the most important information for me.
And i’m glad reading your article. But want to remark on few
general things, The web site style is great, the articles is really
nice : D. Good job, cheers
It’s actually very complicated in this active life to
listen news on Television, so I only use world wide web for that reason, and take the newest news.
bay 101 casino
References:
http://tropicana.maxlv.ru/user/celeifwdyt
Easy and logical site with lots of gambling-related info.
https://atikon.at/go/Xtn4Jl4
harlows casino greenville ms
References:
http://www.bausch.in/en-in/redirect/?url=https://www.4shared.com/s/fLTBoBfIVjq
удаленная работа отзывы фриланс заказы
casino launceston
References:
https://www.adscron.com/user/profile/2341
Nice post. I learn something totally new and challenging on blogs I stumbleupon every day.
It’s always helpful to read through content from other writers
and use a little something from their sites.
Simply desire to say your article is as astounding.
The clarity in your post is just cool and i could assume you’re an expert on this subject.
Fine with your permission let me to grab your RSS feed to
keep updated with forthcoming post. Thanks a million and please
carry on the gratifying work.
I think the admin of this web site is really working
hard for his web site, as here every data is quality based material.
Hmm it looks like your site ate my first comment (it was extremely long) so I guess I’ll just sum it
up what I wrote and say, I’m thoroughly enjoying your
blog. I as well am an aspiring blog blogger but I’m still new
to everything. Do you have any suggestions
for beginner blog writers? I’d really appreciate it.
isle casino poker
References:
http://searchamateur.com/myplayzone/?url=https://www.charliebookmarks.win/online-casino-reviews-ratings-by-experts-2025
slot machine strategy
References:
http://msichat.de/redir.php?url=https://www.marocbikhir.com/user/profile/462074
jackpot 6000
References:
http://www.bioguiden.se/redirect.aspx?url=https://cinemafest.ru/user/zoriuskmru
I am sure this article has touched all the internet users,
its really really pleasant article on building up new webpage.
онлайн работа бесплатно Как найти удаленную работу: полезные советы. Используйте специализированные сайты, группы в социальных сетях и обращайтесь к рекрутинговым агентствам. Не бойтесь рассылать резюме и участвовать в собеседованиях.
island view casino gulfport
References:
http://searchamateur.com/myplayzone/?url=https://sibze.ru/user/galairlodn
royal vegas flash casino
References:
http://mylekis.wip.lt/redirect.php?url=https://www.bookmarking-jet.win/the-best-online-casino-in-australia
I’m not that much of a internet reader to be honest but your
sites really nice, keep it up! I’ll go ahead and bookmark your site to come back later
on. Cheers
Hey there this is kind of of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding expertise
so I wanted to get advice from someone with experience.
Any help would be enormously appreciated!
You actually revealed it fantastically!
If some one needs expert view concerning running a blog afterward i advise him/her to pay a quick visit this
blog, Keep up the fastidious work.
Highly energetic post, I loved that bit. Will there be
a part 2?
Thanks for the marvelous posting! I actually enjoyed reading it, you
can be a great author.I will remember to bookmark your blog and will come back someday.
I want to encourage you to continue your great writing, have a nice day!
Very shortly this web site will be famous among all blog viewers,
due to it’s pleasant posts
This is a topic that is close to my heart… Many
thanks! Exactly where are your contact details though?
работа на удаленке без опыта Удаленная работа на дому: вакансии без опыта. Ищите вакансии, которые не требуют опыта, и будьте готовы к обучению. Многие компании предлагают бесплатные курсы и тренинги для своих удаленных сотрудников.
An outstanding share! I have just forwarded this onto a coworker who has been conducting a little research on this.
And he in fact ordered me lunch simply because I discovered it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanx for spending some time to talk about this topic
here on your website.
Useful information, bookmarking this.
Saya merasa tidak ada terlalu banyak hal istimewa tentang diri
saya untuk dituliskan, namun saya selalu menikmati aktivitas saya di
dunia online, terutama ketika mempelajari berbagai informasi terbaru seputar KUBET,
Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor,
Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay,
Kubet Parlay, dan Judi Bola gacor. Menghabiskan waktu di dunia maya bagi saya adalah cara menyenangkan untuk mencari tahu hal-hal baru dan mengikuti perkembangan yang sedang ramai diperbincangkan. Saya juga kerap bergabung dalam forum atau komunitas tertentu untuk
bertukar pendapat mengenai topik-topik yang menurut saya menarik.
Meski tidak ada sisi menonjol dari diri saya, saya tetap selalu ingin menjadi individu
yang positif di setiap percakapan maupun interaksi
online. Saya biasa dipanggil Hong dan saat ini saya tinggal di Norway,NA,Tolvsrod,3153,Jordbarveien 237,44715384,.
Dengan usia sekitar 35 tahun, saya berharap dapat terus memperluas
wawasan dan pengalaman melalui berbagai kegiatan di dunia digital yang saya ikuti.
Nice weblog here! Also your site so much
up fast! What host are you using? Can I am getting
your associate link for your host? I wish my site loaded up as fast as yours lol
I’m really enjoying the design and layout of your
website. It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often.
Did you hire out a designer to create your theme? Superb work!
сюда зеркало водка бет
Hi to every body, it’s my first visit of this web site; this blog includes amazing and truly good material in favor of readers.
этот контент вотка бет
Спасибо за такой полезный контент о kazino olimp и азартных играх.
https://olimp-casino-kazakhstan-jackpot.kz/mobile-app/
Your way of describing the whole thing in this post is really
good, all be capable of simply understand it, Thanks a
lot.
my page … yoga retreat center mexico
It’s a pity you don’t have a donate button! I’d most certainly donate
to this excellent blog! I suppose for now i’ll settle for book-marking
and adding your RSS feed to my Google account. I look forward to fresh
updates and will talk about this website with my Facebook group.
Chat soon!
Here is my web blog: custom retreat
Awesome blog! Do you have any hints for aspiring writers? I’m planning to start my
own website soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress
or go for a paid option? There are so many choices out there that I’m
completely overwhelmed .. Any recommendations?
Cheers!
Feel free to visit my web site ac repair
Very soon this web site will be famous amid all blogging people, due to it’s pleasant
articles
my website; personal retreat
Hello guys
Hi. A 28 perfect website 1 that I found on the Internet.
Check out this website. There’s a great article there. https://eatout.co.ke/why-fiber-is-healthy-for-our-health-and-how-to-increase-its-daily-intake/|
There is sure to be a lot of useful and interesting information for you here.
You’ll find everything you need and more. Feel free to follow the link below.
constantly i used to read smaller articles that as well
clear their motive, and that is also happening with this paragraph which I am reading now.
Hi there! Someone in my Facebook group shared this website with
us so I came to check it out. I’m definitely loving the information.
I’m book-marking and will be tweeting this to my followers!
Superb blog and fantastic design and style.
I all the time emailed this webpage post page to all my friends, for the reason that if like to read it next my friends will too.
Wow, superb blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your web site is wonderful, let alone the content!
Читать далее водкабет
Woah! I’m really loving the template/theme of this blog.
It’s simple, yet effective. A lot of times it’s difficult to get that
“perfect balance” between superb usability and visual
appeal. I must say that you’ve done a awesome job
with this. In addition, the blog loads super fast for me
on Opera. Superb Blog!
Asking questions are really fastidious thing if you are not understanding anything totally,
however this paragraph provides nice understanding yet.
This post will assist the internet viewers for creating new website or even a
blog from start to end.
Bu saytda olmaq əla təcrübədir.
https://wc.tv.br/FN7h
Great article, just what I was looking for.
This piece of writing is in fact a nice one it helps
new the web people, who are wishing for blogging.
This site definitely has all the information I needed about this subject and didn’t know who to ask.
https://zoomslot88.org/bk-melbet-oficialnyj-sajt-2025-obzor/
Hi, just wanted to tell you, I loved this post. It was helpful.
Keep on posting!
Incredible points. Great arguments. Keep up
the good spirit.
Thanks for sharing your thoughts about tamoxifen side effects.
Regards
Источник vodkabet водкабет казино
You have made your point pretty clearly..
https://openstudio.site/index.php?mid=board_ziAC48&document_srl=2079634 Pillows, a brand that has been making waves in the world of sleep accessories, is here to revolutionize the way you rest.
Создание презентации с помощью нейросети с применением умных алгоритмов
Attractive part of content. I just stumbled upon your web site
and in accession capital to assert that I acquire in fact enjoyed account
your weblog posts. Anyway I’ll be subscribing for your augment and even I fulfillment
you access consistently quickly.
I enjoy reading through an article that can make people think.
Also, thanks for allowing me to comment!
Everything is very open with a very clear explanation of the challenges.
It was truly informative. Your site is useful.
Many thanks for sharing!
Great info. Lucky me I ran across your site by chance (stumbleupon).
I’ve saved as a favorite for later!
This website was… how do you say it? Relevant!!
Finally I’ve found something that helped me.
Kudos!
Review my website – electrical repair
Tulisan ini sangat menarik. Saya merasa pembahasan dalam artikel ini sangat jelas sehingga memberikan gambaran yang lebih luas mengenai
topik yang sedang dibicarakan.
Saya pribadi cukup tertarik mengikuti berbagai ulasan tentang platform digital, termasuk layanan seperti
KUBET, kubet login, Situs Judi Bola Terlengkap, serta pembahasan mengenai situs parlay yang dikategorikan sebagai Situs
Parlay Resmi. Dengan konten seperti ini, saya bisa memahami struktur dan alur sistem dengan lebih mudah.
Selain itu, saya juga mengikuti informasi terkait Situs Parlay Gacor,
strategi di Situs Mix Parlay, hingga berbagai data seperti toto macau yang sering menjadi
bahan analisis di berbagai forum. Konten seperti ini membantu saya melihat sudut pandang yang lebih lengkap, terutama untuk memahami bagaimana platform seperti Kubet Parlay hingga layanan Judi Bola gacor bisa bekerja dengan optimal.
Mudah-mudahan artikel berikutnya lebih banyak membahas hal menarik lainnya.
Terima kasih sudah berbagi informasi yang bermanfaat ini.
It’s going to be end of mine day, but before ending I am reading this enormous article to
improve my experience.
You actually stated it adequately.
Pretty! This was an extremely wonderful post. Thank you for supplying this information.
Mangelsen
7916 Girard Avenue, Ꮮa Joyaa
CA 92037, United Ѕtates
1 800-228-9686
learn jackson hole wildlife species
I know this if off topic but I’m looking into starting my own weblog and was curious what all is
needed to get setup? I’m assuming having a blog like yours would cost
a pretty penny? I’m not very internet savvy so I’m not 100% positive.
Any suggestions or advice would be greatly appreciated.
Appreciate it
Hmm is anyone else encountering problems with the images on this blog loading?
I’m trying to figure out if its a problem on my end or
if it’s the blog. Any feed-back would be greatly appreciated.
I don’t even know how I ended up here, but I thought this post was great.
I do not know who you are but certainly you’re going to a
famous blogger if you aren’t already 😉 Cheers!
Touche. Outstanding arguments. Keep up the great spirit.
I am genuinely grateful to the holder of this web site who has shared this
wonderful piece of writing at at this place.
Saya telah mengikuti artikel ini dengan sangat teliti, dan saya
merasa kontennya cukup menarik untuk dibahas lebih jauh, apalagi
jika dikaitkan dengan topik yang sedang hangat seperti KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, Situs Mix Parlay, Situs
Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor.
Bagi saya pribadi, penjelasan yang diberikan dalam tulisan ini cukup jelas
dan membantu banyak orang dalam memahami isu yang disampaikan. Saya juga merasa bahwa gaya penyampaian di artikel ini mudah dipahami, sehingga membuat pembaca betah sampai akhir
paragraf. Rasanya tidak mungkin untuk tidak memberikan komentar karena konten yang seperti ini memang layak mendapat
apresiasi lebih. Semoga ke depannya akan ada lebih banyak pembahasan mendalam seperti ini, agar bisa menjadi referensi yang bermanfaat bagi siapa saja yang mencari informasi.
Terima kasih kepada penulis yang sudah menyusun artikel yang bermanfaat dan mampu menambah wawasan pembacanya.
What’s up to every one, it’s really a good for me to pay a quick visit
this web site, it consists of important Information.
Informasi yang dibahas di artikel ini sangat menarik dan bermanfaat,
apalagi saya sedang mempelajari lebih dalam tentang KUBET yang dikenal sebagai Situs Judi Bola Terlengkap.
Penjelasan mengenai akses dan pengalaman menggunakan kubet login sangat membantu dalam memahami kenyamanan pengguna di platform Situs
Judi Bola. Saya juga setuju bahwa memilih platform terpercaya itu penting terutama ketika berbicara tentang Situs
Parlay Resmi yang memerlukan sistem aman dan stabil.
Artikel ini juga memberikan wawasan baru tentang bagaimana performa Situs
Parlay Gacor bekerja serta bagaimana opsi permainan dalam Situs Mix
Parlay bisa memberikan strategi yang lebih
luas bagi setiap pemain. Saya pribadi sering memperhatikan hasil toto macau untuk menambah referensi
dan memperdalam pemahaman mengenai pola yang berkembang.
Pembahasan mengenai Kubet Parlay dan tren Judi Bola gacor juga cukup relevan dengan kebutuhan banyak pemain saat ini.
Terima kasih untuk artikelnya, semoga konten seperti ini semakin banyak dibagikan.}
Thank you for any other informative website. Where else may just I am getting that type of info written in such a perfect way? I have a project that I’m just now operating on, and I have been at the glance out for such information.
escort Rio
Starpower Exteriors is a reliable roofing and exterior contractor serving Omaha,
Gretna, Papillion. We offer roof repair, roof replacement, gutter installation, and siding repair, with reliable
storm damage repair and quality craftsmanship.
you’re actually a good webmaster. The website loading
velocity is amazing. It seems that you’re doing any unique trick.
Moreover, The contents are masterpiece. you have done a magnificent job on this topic!
What’s up to every one, since I am genuinely
keen of reading this weblog’s post to be updated on a regular basis.
It includes good stuff.
Pretty section of content. I just stumbled upon your website and in accession capital to assert that I get in fact enjoyed account your blog posts.
Anyway I’ll be subscribing to your feeds and even I achievement you
access consistently fast.
Heya i’m for the primary time here. I found this board and I in finding It really helpful & it helped me out a lot.
I am hoping to provide one thing again and help others such as you aided me.
Бонусы казино
Wow, that’s what I was looking for, what a material!
present here at this website, thanks admin of this web site.
Greetings! Very helpful advice within this post! It is the little changes that produce the
largest changes. Many thanks for sharing!
Cactus Casino — современная площадка для азартных игр
Thank you a bunch for sharing this with all
folks you really recognise what you’re speaking approximately!
Bookmarked. Kindly also talk over with my site =).
We can have a hyperlink alternate arrangement between us
May I simply say what a relief to discover someone that truly knows what they are talking about over the internet.
You actually realize how to bring an issue
to light and make it important. A lot more people need to look at this and understand this side of the story.
I was surprised that you aren’t more popular since you surely
have the gift.
I simply couldn’t go away your website prior to suggesting that I extremely enjoyed the standard
information an individual supply in your guests? Is going to
be back ceaselessly in order to check out new posts
Hi, i believe that i noticed you visited my website so i came to return the want?.I
am attempting to in finding things to improve my site!I assume its ok to make
use of some of your ideas!!
I am actually grateful to the holder of this web page who has shared this fantastic paragraph at at this place.
What i don’t realize is if truth be told how you are now not
actually much more neatly-appreciated than you might be
now. You are very intelligent. You recognize thus significantly
relating to this topic, made me in my view believe it from so many numerous angles.
Its like men and women don’t seem to be fascinated until it is one thing to
accomplish with Woman gaga! Your personal stuffs great.
All the time deal with it up!
Hi my family member! I want to say that this article is amazing, nice written and come with approximately all vital infos.
I’d like to see extra posts like this .
“Jadi ini namanya memek. Proses ini bisa menyantap batas semasa eka arloji. Selama ini, memek sungguh tidak setiap keadaan bisa dijumpai dalam tanah yang dikenal lewat pencipta cengkeh lagi lobster ini. 56Di setiap sarung yang dikunjungi-Nya – baik pada metropolitan, pada pekan alias pada kampung – penduduk dalam situ menyopiri suku yang sakit ke pekan-rekan. 35Ketika yaum sudah petang, getah perca pengikut Isa datang pada-Nya serta mengatakan, ‘Hari sudah hampir sore maka lapak ini tersaku. Mereka tidak tahu segala sesuatu yang untuk dijawab menjumpai-Nya. 17Ketika Dia sedang mengegah ke jalan buntu, seorang datang berlari-lari, menelutut mendapatkan-Nya beserta bertanya, ‘Wahai Guru yang baik, apakah yang layak kulakukan sepanjang mewarisi hidup daim? 20Isa menjawab, ‘Dia seorang dari nan ganda patos nan mencecah roti bersama ke dalam bekas. 16Ketika mengindahkan peri demikian, Herodes berkecek, ‘Dia itu Yahya yang kepalanya telah kupancung, walakin dirinya hidup awal! Mereka menurut firman itu pula pantas menerimanya karena sukacita, 17tetapi akarnya tidak dalam di roh, maka tidak awet.
Обожаю сайт kazino olimp, он очень комфортный в использовании!
http://url.hys.cz/–72712
Hello! I know this is kinda off topic however , I’d figured
I’d ask. Would you be interested in exchanging links
or maybe guest writing a blog post or vice-versa?
My blog discusses a lot of the same topics as yours and I feel we
could greatly benefit from each other. If you happen to be
interested feel free to shoot me an e-mail. I look forward to hearing from you!
Fantastic blog by the way!
Sɔri fɔ di silɛns. A lɛk ɔltin, a gɛt teist fɔ difrɛn tin dɛn. Yu stori bin gi mi op. W?
blackjack payout
References:
http://seesaawiki.jp/t/external-link/?url=https://www.bookmarkingqueen.win/country-club-casino-launceston-book-online-save
american roulette wheel
References:
https://beka696.ru/user/paxtunrzkb
посетить веб-сайт https://kra48a.at/
топ 10 честных казино на деньги
Its like you read my thoughts! You seem to know so much about this, such as you wrote the book in it or something.
I feel that you could do with some p.c. to power the message house a little
bit, but other than that, that is great blog.
A great read. I’ll certainly be back.
https://travel-taxi.at/taxi-innsbruck-st-anton-am-arlberg/
Hey there! This is my 1st comment here so I
just wanted to give a quick shout out and tell you I really enjoy reading your blog posts.
Can you suggest any other blogs/websites/forums that go over the same
topics? Thanks a lot!
golden nugget las vegas nv
References:
https://mydayz.ru/user/cwearsvbqo
Beneficial stuff, Kudos!
It’s enormous that you are getting ideas from this article as well
as from our dialogue made at this time.
winpalace
References:
http://avalonadvancedmaterials.com/outurl.php?url=https://www.bookmarking-keys.win/perth-s-finest-hotel-casino-restaurants-bars
здесь водка казино официальный сайт
My spouse and I stumbled over here different
website and thought I might check things out.
I like what I see so i am just following you. Look forward to going over your web page repeatedly.
Good Ьlog you’ve got here.. It’s һard to find quality writing like уours these
days. I truly appreciate individuals like you!
Ꭲake care!!
Also ѵisit my bloɡ post; đồng hồ nữ – hàng hiệu rolex
gamehouse casino
References:
http://mylekis.wip.lt/redirect.php?url=https://www.bookmarkingvictor.win/boho-casino-live-games-play-and-get-a-3000
Hi there, i read your blog occasionally and i own a similar one and
i was just curious if you get a lot of spam comments?
If so how do you stop it, any plugin or anything you can suggest?
I get so much lately it’s driving me crazy so any support is very much appreciated.
Everyone loves what you guys are usually up too.
This kind of clever work and coverage! Keep up the very good
works guys I’ve incorporated you guys to blogroll.
Position certainly taken..
casino games
References:
https://m.kaskus.co.id/redirect?url=https://www.bookmark-url.win/free-slots-online-social-casino
each time i used to read smaller posts which as well clear their
motive, and that is also happening with this article which I am reading here.
Yes! Finally someone writes about Click here for
free money.
review https://g8keep.org
You actually make it appear really easy together with your presentation but I find this topic to
be actually something which I believe I’d never understand.
It seems too complex and extremely huge for me. I’m looking ahead for your subsequent put up, I will try to get the grasp of
it!
Our site https://plasma.credit
Does your site have a contact page? I’m having problems locating it but, I’d like to shoot you an email.
I’ve got some creative ideas for your blog you might be interested in hearing.
Either way, great website and I look forward to seeing it improve over time.
I couldn’t refrain from commenting. Very well written!
You’re so cool! I don’t believe I’ve read something like that
before. So great to discover somebody with some unique thoughts on this
subject matter. Really.. many thanks for starting
this up. This website is something that’s needed on the internet,
someone with a bit of originality!
Nice post. I used to be checking continuously this weblog and I am impressed!
Extremely helpful info particularly the remaining part
🙂 I maintain such info much. I used to be seeking this particular info for a very long time.
Thanks and best of luck.
Hey just wanted to give you a quick heads up. The words in your post seem to
be running off the screen in Opera. I’m not sure if this is a format issue or something to do with web browser compatibility but I figured I’d post to let you know.
The design and style look great though! Hope you get the problem resolved soon.
Many thanks
Wow that was odd. I just wrote an very long comment but after
I clicked submit my comment didn’t appear. Grrrr…
well I’m not writing all that over again. Regardless, just wanted to say fantastic blog!
you’re truly a good webmaster. The web site loading velocity is incredible.
It sort of feels that you’re doing any unique trick. Furthermore, The contents are masterwork.
you have done a wonderful activity in this topic!
I enjoy reading an article that can make people think.
Also, thanks for allowing for me to comment!
My homepage – Junk removal
Hi there, its fastidious paragraph on the topic of media print, we all understand media is a impressive source of facts.
my site; Waste management
акции казино
Hi there everyone, it’s my first pay a visit at this web
page, and piece of writing is really fruitful designed for me, keep
up posting these articles or reviews.
Hi there colleagues, fastidious post and fastidious urging commented here, I am genuinely enjoying
by these.
Magnificent web site. Lots of useful info here.
I’m sending it to a few friends ans also sharing in delicious.
And obviously, thank you in your effort!
You actually make it seem really easy along with your presentation but I in finding this matter
to be actually one thing that I think I would by no means understand.
It sort of feels too complex and extremely broad for me. I’m having a look forward in your subsequent post, I will
attempt to get the hang of it!
ತೇರಿಮಾ ಕಾಸಿಃ ಸುದಾ ಬೆರ್ಬಾಗಿ. ಸಯಾ ಖವಾತಿರ್ ಪೆನೆಮುವಾನ್ ಸಯಾ ಅಕನ್ ಗಗಲ್. ಕಿಸಹ ಆಂಡ ಮೆಂಬರಿ ಸಯ ಹರಪನ್। ಸಯಾ ಸಂಗತ ಮೆಂಘರ್ಗೈನ್ಯಾ
Wow, this article is nice, my sister is analyzing these kinds of things,
so I am going to inform her.
Hello there! Do you use Twitter? I’d like to follow you if that
would be okay. I’m definitely enjoying your blog and look forward to new
updates.
Refresh Renovation Southwest Charlotte
1251 Arrow Pinee Ɗr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Stress low һome remodeling (Paul)
I am really grateful to the holder of this web page who has shared this fantastic article at at this place.
Also visit my web-site Waste management
Hi there, i read your blog occasionally and i own a similar one and i was just curious
if you get a lot of spam responses? If so how do you prevent it, any
plugin or anything you can suggest? I get so much lately
it’s driving me crazy so any support is very much appreciated.
Feel free to visit my blog post: http skyiwredshjnhjgeleladu7m7mgpuxgsnfxzhncwtvmhr7l5bniutayd onion
Asking questions are actually pleasant thing if you are not understanding anything entirely,
however this paragraph presents nice understanding yet.
Feel free to surf to my homepage блекспрут официальный
What’s up, I would like to subscribe for this webpage to get most recent updates, therefore where can i do it please help out.
Have a look at my web site – Garbage bin
It is not my first time to pay a quick visit this
site, i am visiting this site dailly and take good information from here everyday.
For newest information you have to pay a
visit internet and on web I found this web site as a most
excellent web page for most up-to-date updates.
Have a look at my webpage: Bin rental
It’s the best time to make some plans for the long run and it’s time to be
happy. I’ve read this submit and if I may just I want
to recommend you some fascinating issues or suggestions.
Perhaps you can write subsequent articles regarding this
article. I want to read more issues approximately it!
My webpage – блекспрут официальный
Hi there mates, its enormous article regarding
teachingand completely defined, keep it up all the time.
my website; https bs2best at
I simply couldn’t go away your site prior to suggesting that I extremely enjoyed the standard info a person supply in your guests?
Is going to be again continuously in order to
check out new posts
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate < Loved it!
онлайн работа без опыта Удаленная работа на дому: вакансии без опыта. Ищите вакансии, которые не требуют опыта, и будьте готовы к обучению. Многие компании предлагают бесплатные курсы и тренинги для своих удаленных сотрудников.
Share lagid adi adi sarahau. Dou din pehle bhat gale rahi bakir khumra lagta ba ki ye khumra kaiti chahiye nahi. Apeka̕ khakha do̠ as imo̠k̕ kana. Aaima sarahao.
Excellent post. I’m experiencing some of these issues as well..
Stop by my blog: cпрут сайт зеркало
he said https://hlp0.online
you could try here https://unich.icu
If some one wants expert view concerning running a blog afterward i
suggest him/her to visit this webpage, Keep up the good job.
Wow that was unusual. I just wrote an extremely long comment but after
I clicked submit my comment didn’t appear. Grrrr… well I’m not writing all that
over again. Regardless, just wanted to say superb
blog!
woodbine casino
References:
https://online-spielhallen.de/verde-casino-auszahlungen-schnell-sicher-einfach/
I don’t even know the way I ended up right here, however I
assumed this submit was once great. I don’t recognize who you
are however definitely you are going to a well-known blogger when you are not already.
Cheers!
expansion slots
References:
https://online-spielhallen.de/nv-casino-bonus-2-000-e-225-freispiele-aktuell/
casino halifax
References:
https://online-spielhallen.de/top-9-online-casinos-in-deutschland-2025/
Hello! I could have sworn I’ve visited this website before but after going through a few of the posts I realized it’s new to me.
Anyways, I’m certainly delighted I found it and I’ll be book-marking it and checking back frequently!
scraps99 com
References:
https://online-spielhallen.de/top-9-online-casinos-in-deutschland-2025-serios-getestet/
I have been exploring for a little for any high quality articles or blog
posts in this kind of house . Exploring in Yahoo I eventually stumbled upon this web site.
Studying this info So i’m happy to convey that I have a very excellent uncanny feeling I came
upon just what I needed. I most definitely will make certain to don?t forget this
site and provides it a glance regularly.
Spieler bekommen ohne eigene Einzahlung Bonusguthaben oder Freispiele, mit der Möglichkeit echtes Geld zu gewinnen. Jedes Casino in dieser Liste wurde sorgfältig geprüft und hat bewiesen, dass es über längere Zeit hinweg zuverlässig, transparent und spielerfreundlich arbeitet. Casino Guru zeigt dir geprüfte Anbieter mit kostenlosen Demospielen und exklusiven Aktionen. Darüber hinaus bieten wir Ihnen umfassende und verständliche Erklärungen zur deutschen Gesetzgebung im Bereich Online-Glücksspiel. Durch gratis Startguthaben oder Freispiele können neue Kunden ein Online Casino ausgiebig testen.
Glücksspiel kann süchtig machen und in eine pathologische Abhängigkeit (Spielsucht) führen. Bei der Registrierung in einem Online-Casino gibt man Personalausweisdaten, Adresse, Kontaktdaten und Zahlungsinformationen an. Eines der wichtigsten Merkmale für Zuverlässigkeit ist eine Lizenzierung durch offizielle Behörden wie die Malta Gaming Authority (MGA), die UK Gambling Commission oder andere Regulierungsstellen (Curaçao, Gibraltar, Isle of Man usw.). Diese Analysen helfen einzuschätzen, ob ein bestimmter Slot oder ein Tischspiel zum eigenen Stil und Budget passt. Casino Guru bietet detaillierte Rezensionen zu verschiedenen Spielautomaten (Slots), von klassischen „einarmigen Banditen“ bis hin zu modernen Video-Slots mit zahlreichen Gewinnlinien. Dies hilft Spielerinnen und Spielern, sich in der komplexen und vielfältigen Welt des Glücksspiels zurechtzufinden, in der jedes Produkt eigene Besonderheiten, Regeln und Gewinnpotenziale hat. Die Reputation ergibt sich aus einer Kombination von Nutzerbewertungen und Expertenmeinungen.
References:
https://online-spielhallen.de/monro-casino-test-erfahrungen-fur-deutsche-spieler/
Sichere Lizenzen, namhafte Spieleanbieter und Zahlungsdienstleister sind gute Anhaltspunkte für ein sicheres Online-Casino. Wichtig ist, dass die Anbieter lizenziert und somit seriös sind. Viele seriöse Anbieter stellen neuen Spielern Bonusgeld oder Freispiele zur Verfügung – oft schon ab der ersten Einzahlung. Ein fairer Willkommensbonus kann den Einstieg ins Online-Glücksspiel zusätzlich versüßen. Natürlich müssen die Spiele geprüft und lizenziert sein, um Fairplay sicherzustellen. Vertrauenswürdige Casinos erkennst du an der gültigen Glücksspiellizenz.
Diese bieten oft eine besonders intuitive Bedienung und können Push-Benachrichtigungen für Boni oder Aktionen senden. Für Fans des strategischen Kartenspiels bietet Deutschland auch legale Online Poker-Plattformen an, auf denen du Echtgeld Poker direkt gegen andere Spieler einsetzen kannst. Egal ob klassische Frucht-Slots, abenteuerliche Reisen oder futuristische Welten – die Auswahl ist gigantisch und bietet für jeden Geschmack etwas. Prüfe zudem immer die Gültigkeitsdauer des Bonus (häufig 7-30 Tage) und den Beitrag der Spiele zum Umsatz (Slots zählen meist zu 100%, andere Spiele wie Tischspiele oft weniger oder gar nicht). Reload-Boni bieten dir zusätzliches Bonusguthaben für weitere Einzahlungen, während Cashback-Boni einen Teil deiner Verluste über einen bestimmten Zeitraum zurückerstatten können.
References:
https://online-spielhallen.de/admiral-casino-sicher-spielen-grose-gewinne/
Im Falle von Problemen bietet das deutsche Rechtssystem jedoch eine wichtige Möglichkeit zur Rückforderung von Verlusten, die durch spezialisierte Anwälte unterstützt werden kann. Dies führt oft zu einem niedrigeren Return to Player (RTP) bei Spielen in deutschen Casinos, während ausländische Casinos diese Steuer nicht zahlen und somit höhere RTPs und attraktivere Boni anbieten können. Die Branche der Online-Glücksspielanbieter versucht, höchstrichterliche Entscheidungen in diesen Fällen zu verhindern, was auf die potenziell weitreichenden finanziellen Auswirkungen solcher Urteile hindeutet.
Mit diesen umfassenden Support-Optionen stellt Verde Casino sicher, dass alle Spieler jederzeit eine schnelle und effiziente Hilfe erhalten. Verde Casino Bewertung zeigen, dass der Support effizient und professionell arbeitet, sodass Spieler schnelle Hilfe bei Fragen zu Einzahlungen, Auszahlungen oder Bonusbedingungen erhalten. Verde Casino seriös und bietet Kundensupport in 15 verschiedenen Sprachen, darunter Deutsch, Englisch, Spanisch, Französisch, Portugiesisch und viele weitere. Verde Casino bietet eine benutzerfreundliche und vielseitige Plattform, die sowohl auf Desktop- als auch auf mobilen Geräten reibungslos funktioniert. Verde Casino Erfahrungen zeigen, dass diese Promotions besonders beliebt sind, da sie oft hohe Gewinnchancen und exklusive Belohnungen bieten. Erfahrungen zeigen, dass viele Spieler von diesen Turnieren profitieren, da sie nicht nur spannende Wettkämpfe bieten, sondern auch großzügige Belohnungen und exklusive Boni ermöglichen. Die Turniere wechseln regelmäßig und bieten abwechslungsreiche Herausforderungen für alle Spielertypen – von klassischen Slots über Live-Casino-Spiele bis hin zu exklusiven saisonalen Events.
References:
https://online-spielhallen.de/verde-casino-50-freispiele-ohne-einzahlung-fakten/
Cashback bedeutet im Grunde genommen, dass Sie eines Teil Ihres verlorenen Geldes zurückerhalten. Ganz im Gegenteil genießen Spieler das Angebot vom Cashbackbonus, der wöchentlich berechnet und ausgezahlt wird. Wichtig zu wissen ist, dass der Willkommensbonus spätestens vier Tage nach der Registrierung aktiviert werden muss. Jeder der Boni ist mittels einer Einzahlung ab mindestens 10 Euro zu erhalten. Ein Bonus Code wird in der Regel beim Einzahlungsbonus genutzt. Willkommensbonus Promo Codes im ICE Casino – nicht erforderlich. Eine der wesentlichen Promotionen zeigt sich mit dem Willkommensbonus, der zu einem großzügigen Willkommenspaket zusammengestellt worden ist.
Die Gates of Olympus Demo bietet eine hervorragende Gelegenheit, das Spiel ohne finanzielles Risiko auszuprobieren. Während der Freispiele kann der mächtige Zeus zufällig Multiplikatoren hinzufügen, die die Gewinne der Spieler signifikant erhöhen können. Aus diesem Grund stellen wir Ihnen jetzt einige der besten Casino Slots online vor.
References:
https://online-spielhallen.de/vulkan-vegas-deutschland-test-angebote/
Do you have a spam problem on this website; I also am a blogger, and I was wondering your situation; we have developed
some nice procedures and we are looking to trade methods with others, why not shoot me an e-mail if interested.
I’m really enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more pleasant
for me to come here and visit more often. Did you hire
out a developer to create your theme? Great work!
Feel free to surf to my web site: blacksprut сайт
Fabulous, what a web site it is! This website presents valuable data to us, keep it up.
Keep on writing, great job!
My homepage :: блекспрут официальный сайт
I love your blog.. very nice colors & theme. Did you create
this website yourself or did you hire someone to do
it for you? Plz reply as I’m looking to construct my own blog and would like
to find out where u got this from. many thanks
Here is my site :: Futemax ao vivo
Thanks for every other wonderful post. Where else may anybody
get that kind of information in such a perfect means of writing?
I have a presentation next week, and I’m at the look for such information.
Great information. Lucky me I came across your website by chance (stumbleupon).
I have saved it for later!
Wonderful beat ! I would like to apprentice while you amend your website,
how could i subscribe for a blog website? The account aided me
a acceptable deal. I had been tiny bit acquainted of
this your broadcast provided bright clear idea
Feel free to visit my webpage … bs2web.at
Awesome advice, With thanks.
This game looks amazing! The way it blends that old-school chicken crossing concept with
actual consequences is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing
gameplay and adding real risk? I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing
mechanics with genuine stakes involved. Definitely want
to check it out!
Whoa, this game seems awesome! The mix of that timeless
chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with
actual stakes? Sign me up!
I’m so into this concept! The way it takes that
classic chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing action with real-world stakes
has me interested. I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
Hey there! Quick question that’s entirely off topic.
Do you know how to make your site mobile friendly?
My website looks weird when viewing from my
iphone4. I’m trying to find a template or plugin that might be able to fix this
problem. If you have any recommendations, please share. Cheers!
Howdy, I do think your web site could be having browser compatibility
problems. When I look at your site in Safari, it looks
fine however, when opening in Internet Explorer, it has some overlapping issues.
I merely wanted to give you a quick heads up! Aside from
that, great blog!
This game looks amazing! The way it blends that old-school chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and
adding real risk? I’m totally down to try it.
This is right up my alley! I’m loving the combo of
classic chicken crossing mechanics with genuine stakes
involved. Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences has
me hooked. I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style
with tangible consequences? I’ve gotta try this out!
Attractive component to content. I simply stumbled upon your blog and in accession capital to claim that I
get actually enjoyed account your weblog posts.
Any way I will be subscribing in your feeds and even I
fulfillment you access constantly quickly.
Look into my web blog: Futmax
I was able to find good information from your articles.
Hi there fantastic blog! Does running a blog such as this take a lot of work?
I’ve very little understanding of computer programming
but I was hoping to start my own blog in the
near future. Anyway, if you have any recommendations or tips for
new blog owners please share. I know this is off subject nevertheless I simply
needed to ask. Thanks!
Check out my webpage … bs2best at
Hey very cool web site!! Man .. Beautiful .. Superb .. I’ll
bookmark your website and take the feeds also? I’m
happy to search out so many useful information right here in the submit,
we want develop extra techniques in this regard, thanks for sharing.
. . . . .
лучшие онлайн казино россии
Very energetic blog, I liked that a lot. Will there be a part 2?
Made In USA GMP Certified FDA Approved 100% Natural Super Memory Formula is an effective answer for memory loss and mind dysfunction. This all-natural repair offers the mind with the nutrients it must regain peak cognition. Made In USA GMP Certified FDA Approved 100% Natural Pineal Guardian is a groundbreaking dietary supplement that’s reshaping the field of cognitive well being. Are you tired of struggling along with your listening to? Do you lengthy for an answer that’s natural and efficient? Well, look no additional as a result of Cerebrozen is here to revolutionize the way you care on your ears. Made In USA GMP Certified FDA Approved 100% Natural This premium dietary complement, Alpha https://audiosex.pro/proxy.php?link=https://www.allclanbattles.com/groups/the-ultimate-guide-to-neuro-surge-supplements-for-brain-health-and-performance-support/, is the ultimate mind booster designed to elevate your cognitive function and skyrocket your mental performance. Made In USA GMP Certified FDA Approved 100% Natural Because the population ages, the concern over declining psychological operate has turn out to be increasingly prevalent. Made In USA GMP Certified FDA Approved 100% Natural Neuro-Thrive is an revolutionary dietary complement that has the power to revolutionize your memory and cognitive operate.
Hey There. I discovered your weblog the usage of msn. That is a really smartly written article.
I’ll make sure to bookmark it and come back
to learn more of your useful info. Thanks for the post.
I will certainly return.
бездепозитный бонус за регистрацию в казино с выводом денег без первого депозита
I was wondering if you ever thought of changing the page layout of your website?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could
connect with it better. Youve got an awful lot
of text for only having one or 2 images. Maybe you could space it out better?
Hi! I could have sworn I’ve been to this blog before but after going through a
few of the articles I realized it’s new to
me. Regardless, I’m definitely happy I found it and I’ll be bookmarking it and checking back regularly!
Simply desire to say your article is as astonishing. The clarity in your post is just nice and i could assume you’re an expert on this subject.
Fine with your permission let me to grab your feed to
keep up to date with forthcoming post. Thanks
a million and please keep up the rewarding work.
I have read so many articles concerning the blogger lovers except this
paragraph is really a good article, keep it up.
Хаартыскаҕа бырастыы гын, таптыыбын, барытын сөбүлүүбүн, эн суруйууҥ миэхэ эрэл биэрэр, ол тугуй?
Recommended Reading https://theo.sbs/
It’s impressive that you are getting thoughts from this post as well as from our dialogue made here.
This paragraph will help the internet people for setting
up new web site or even a blog from start to end.
Appreciate the recommendation. Will try it out.
Terrific article! This is the kind of info that should be shared around the net.
Shame on the seek engines for now not positioning this submit upper!
Come on over and discuss with my site . Thank you =)
Have you ever thought about creating an e-book or guest authoring on other sites?
I have a blog centered on the same ideas you discuss and would love to have you
share some stories/information. I know my viewers would value
your work. If you are even remotely interested,
feel free to send me an e-mail.
I don’t even know how I ended up here, but I thought this post was great.
I do not know who you are but certainly you’re going to a famous blogger if you aren’t already 😉 Cheers!
Hi! Do you know if they make any plugins to help
with SEO? I’m trying to get my blog to rank for some targeted keywords
but I’m not seeing very good success. If you know of any please share.
Appreciate it!
Hello are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started and create my own.
Do you need any html coding knowledge to make your own blog?
Any help would be greatly appreciated!
Pretty! This has been a really wonderful article.
Thank you for supplying this information.
I got this website from my buddy who informed me on the topic
of this website and at the moment this time I am browsing
this web site and reading very informative
articles or reviews at this time.
I like the valuable information you provide in your articles.
I will bookmark your blog and test once more right here frequently.
I’m reasonably certain I’ll learn many new stuff proper right here!
Best of luck for the following!
мебель на заказ москва Встраиваемая прихожая на заказ: Максимально используйте пространство прихожей с помощью встраиваемой мебели, созданной с учетом ваших потребностей и размеров.
Disclaimer: This article isn’t supposed to be a recommendation. The writer is just not liable for any ensuing actions of the company during your buying and selling expertise. The data supplied in this text will not be correct or up-to-date. Any trading or monetary determination you make is your sole responsibility, and you have to not depend on any information provided here. We do not provide any warranties concerning the information on this webpage and will not be accountable for any losses or damages incurred because of buying and selling or investing. Disclaimer: This article is just not intended to be a advice. The creator is not accountable for any resulting actions of the corporate throughout your trading experience. That is supplied article. Keilini Portable Heater UK Reviews-Does Keilini Legit or Scam! The Keilini Portable Heater is a cell heater that has both a thermostat and a timer. The heating is managed through a digital LED show.
Feel free to surf to my web blog: https://fromkorea.peoplead.kr/bbs/board.php?bo_table=free&wr_id=27941
Thanks for the auspicious writeup. It in fact was once a leisure account it.
Look complicated to more delivered agreeable from you!
However, how can we keep in touch?
Great post.
whoah this blog is fantastic i like reading your articles.
Stay up the great work! You know, a lot of people are searching round for this information, you
can aid them greatly.
Check out my web blog … realtor in Chula Vista CA
It’s fantastic that you are getting thoughts from this article as
well as from our dialogue made at this place.
новые бездепозитные бонусы в казино 2025
Hello there! I could have sworn I’ve visited this web site before
but after looking at many of the posts I realized it’s new to me.
Anyways, I’m definitely pleased I found
it and I’ll be book-marking it and checking back frequently!
It’s a shame you don’t have a donate button! I’d
most certainly donate to this excellent blog! I suppose for now i’ll settle for bookmarking and adding your RSS feed to my Google account.
I look forward to brand new updates and will share this site with my Facebook group.
Chat soon!
Hi there, You’ve done an excellent job. I’ll definitely digg it and personally suggest to my friends.
I am confident they will be benefited from this web site.
You really make it seem so easy with your presentation but I find this topic to be actually something that I think I would never understand.
It seems too complicated and extremely broad for me. I am looking forward for your next post, I’ll try to get the hang of
it!
We’re a gaggle of volunteers and opening a brand new
scheme in our community. Your website provided us with useful info
to work on. You have done an impressive activity and our whole group might be thankful to you.
Ridiculous story there. What occurred after?
Good luck!
This excellent website really has all of
the info I wanted about this subject and didn’t know who to ask.
What a material of un-ambiguity and preserveness of valuable familiarity about unpredicted feelings.
My website: best real estate agent in Salt Lake UT
Today, I went to the beach with my children.
I found a sea shell and gave it to my 4 year old daughter and
said “You can hear the ocean if you put this to your ear.” She placed the shell to
her ear and screamed. There was a hermit crab inside and
it pinched her ear. She never wants to go back! LoL I
know this is completely off topic but I had to tell someone!
Inspiring story there. What happened after? Good luck!
My website: best realtor in Cibolo TX
Ahaa, its fastidious discussion about this piece of writing at this place at this web site, I have read all that, so now me also commenting here.
Hi there, I enjoy reading all of your article post.
I wanted to write a little comment to support you.
of course like your web site but you need to test the spelling on several of your posts.
A number of them are rife with spelling issues and
I in finding it very bothersome to inform the truth nevertheless
I will definitely come back again.
Hey there, You’ve done a fantastic job. I’ll certainly digg it
and personally suggest to my friends. I am sure they’ll be benefited from this website.
Cabinet IQ Fort Myers
7830 Drew Cirr Stee 4, Fort Myers,
FL 33967, United Ѕtates
12394214912
Classickitchen (https://padlet.com/clinicforhim150irqqn/bookmarks-hj4tolbop7p0x7fw/wish/lDK1ZR103AMDQJ9z)
Hello there! This blog post could not be written any better!
Looking through this article reminds me of my previous roommate!
He constantly kept preaching about this. I most certainly
will forward this article to him. Fairly
certain he’ll have a great read. Thank you for sharing!
I don’t even know how I ended up here, but I thought this
post was great. I don’t know who you are but certainly you
are going to a famous blogger if you are not already 😉 Cheers!
In fact when someone doesn’t understand after that its up to other viewers that they will help, so here it takes place.
I was very pleased to discover this web site. I want
to to thank you for ones time due to this wonderful read!!
I definitely savored every part of it and I have you saved to fav to see new things on your site.
Great article! We are linking to this particularly great post on our website.
Keep up the good writing.
My web-site … best realtor in St. George LA
each time i used to read smaller articles
that as well clear their motive, and that is also
happening with this post which I am reading at
this time.
Simply desire to say your article is as astounding.
The clearness on your post is just great and that i could suppose
you are an expert on this subject. Well with your permission allow me to snatch your RSS feed to stay
up to date with impending post. Thank you a million and please carry on the rewarding work.
Thanks for your personal marvelous posting! I genuinely enjoyed reading it, you can be a great
author.I will always bookmark your blog and definitely will come back
from now on. I want to encourage you continue your great writing, have a nice
holiday weekend!
My page … best real estate agent in Salt Lake UT
Einfache und intuitive Seite mit vielen Glücksspielinfos.
https://nv-casino-bet-germany.de/spielanleitung
Hello! Quick question that’s completely off topic. Do you know how to make your site mobile friendly?
My weblog looks weird when viewing from my iphone 4.
I’m trying to find a theme or plugin that might be able to
fix this issue. If you have any suggestions, please share.
Many thanks!
Also visit my blog post … real estate agent Cibolo TX
Unquestionably consider that that you said. Your favourite justification appeared to be on the net the easiest factor to take into accout of.
I say to you, I definitely get annoyed even as other people consider worries that they plainly do not know about.
You controlled to hit the nail upon the highest and also defined out the whole thing without having side effect , other
people can take a signal. Will likely be back to get more.
Thank you
My web-site … best real estate agent in Salt Lake UT
My brother suggested I might like this blog. He was entirely right.
This post truly made my day. You cann’t imagine simply
how much time I had spent for this info!
Thanks!
Hurrah! In the end I got a website from where I know how to actually get valuable information regarding my study and knowledge.
Feel free to visit my webpage … best realtor in Cibolo TX
I believe what you posted made a ton of sense. However, what
about this? suppose you were to write a awesome post title?
I mean, I don’t want to tell you how to run your
blog, however what if you added a post title that grabbed people’s attention? I
mean Heart failure: Symptoms, Causes, Diagnosis &
Treatment – MDtodate is kinda vanilla. You should peek at Yahoo’s home page
and note how they create news titles to grab viewers interested.
You might try adding a video or a picture or two to get people excited about everything’ve written.
Just my opinion, it could make your website a little livelier.
Here is my web blog best realtor in Salt Lake UT
Hi, I do believe this is a great web site. I stumbledupon it 😉 I’m going
to revisit once again since I bookmarked it.
Money and freedom is the best way to change, may you be rich and continue to help others.
Here is my web page: best real estate agent in St. George LA
company website https://etherealtrade.rest/
First of all I would like to say superb blog! I had a quick question that I’d like to ask if you don’t mind.
I was curious to find out how you center yourself and clear your mind prior to
writing. I have had trouble clearing my mind in getting my ideas
out there. I do enjoy writing but it just seems like the first 10
to 15 minutes tend to be lost just trying to figure
out how to begin. Any ideas or hints? Cheers!
bookmarked!!, I really like your site!
I’m not sure why but this website is loading very slow for
me. Is anyone else having this issue or is it a issue on my end?
I’ll check back later and see if the problem still exists.
Take a look at my website: best realtor in Cibolo TX
Peculiar article, totally what I wanted to find.
May I simply just say what a relief to uncover a person that genuinely understands what they’re
talking about on the web. You definitely understand how to bring a
problem to light and make it important. A lot more people should
check this out and understand this side of the story.
I was surprised you’re not more popular since you surely possess
the gift.
Here is my web blog :: best realtor in St. George LA
Marvelous, what a webpage it is! This weblog provides useful information to us, keep it up.
next https://etherealtrade.lat
Howdy just wanted to give you a brief heads up and let you know a few of the images aren’t loading correctly.
I’m not sure why but I think its a linking issue. I’ve tried it in two different browsers and both show the same results.
Good way of describing, and good paragraph to obtain facts concerning my presentation focus, which i am going to
deliver in school.
I all the time emailed this web site post page to all my friends, because if
like to read it next my links will too.
Here is my web blog :: real estate agent Cibolo TX
I every time spent my half an hour to read this webpage’s content every day along with a mug of coffee.
I really love your blog.. Excellent colors & theme.
Did you build this web site yourself? Please reply back as I’m planning to create my own personal site and would like to learn where
you got this from or just what the theme is called.
Cheers!
I’d like to find out more? I’d love to find out more details.
Greetings from Florida! I’m bored to death at work so I decided to browse your website on my iphone during lunch break.
I enjoy the information you present here and can’t wait to
take a look when I get home. I’m shocked at how quick your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyways, great site!
What’s up colleagues, how is the whole thing, and what you want
to say concerning this article, in my view its truly awesome for me.
Feel free to visit my web site – best real estate agent in Fort Lauderdale FL
At this moment I am ready to do my breakfast, once having
my breakfast coming again to read other news.
लिंक निर्माण की जटिल कला में निपुणता हासिल करना कठिन है। ज़्यादातर वेबसाइटों और ब्लॉगों के लिए, यह एक ऐसा क्षेत्र है जिसमें वे कभी पूरी तरह महारत हासिल नहीं कर पाते।
Great items from you, man. I have take note your stuff prior to and you’re just extremely fantastic.
I actually like what you have got here, certainly like what you’re stating and the best
way by which you say it. You are making it enjoyable and you continue
to take care of to stay it smart. I can’t wait to read
much more from you. That is actually a wonderful web site.
Hi, for all time i used to check blog posts here early in the daylight, for the reason that i enjoy to learn more and more.
Visit my page: real estate agent Chula Vista CA
Please let me know if you’re looking for a writer for your blog.
You have some really great articles and I believe I would be a good asset.
If you ever want to take some of the load off, I’d absolutely love
to write some material for your blog in exchange for a link back to mine.
Please send me an e-mail if interested. Thanks!
Here is my blog – best real estate agent in Fort Lauderdale FL
It’s going to be ending of mine day, however before end I
am reading this impressive article to increase my know-how.
I feel that is among the such a lot significant info for me.
And i’m satisfied reading your article. However want to remark
on some common things, The site taste is perfect,
the articles is in point of fact great : D. Excellent activity,
cheers
Admiring the hard work you put into your site and in depth information you offer.
It’s great to come across a blog every once
in a while that isn’t the same out of date rehashed information. Fantastic
read! I’ve bookmarked your site and I’m adding your RSS feeds to my Google account.
My webpage realtor in St. George LA
Thanks a bunch for sharing this with all people you really recognise what you are speaking about!
Bookmarked. Kindly also talk over with my website =).
We will have a hyperlink change agreement among us
What’s up, yes this post is in fact pleasant and I have learned lot of things from it regarding blogging.
thanks.
Hello, I desire to subscribe for this weblog to take newest updates, thus where can i do
it please help out.
If you are going for most excellent contents like I do, simply pay a quick visit
this website every day for the reason that it presents
quality contents, thanks
Have a look at my blog post best real estate agent in Fort Lauderdale FL
I absolutely love your blog and find a lot of your post’s to be just what I’m looking for.
Do you offer guest writers to write content available for you?
I wouldn’t mind composing a post or elaborating on some of the subjects you write concerning here.
Again, awesome web site!
Here is my website: realtor in Cibolo TX
Normally I don’t learn post on blogs, but I wish to say that this write-up very compelled me to try and do it!
Your writing taste has been amazed me. Thank you, very great
article.
Simply desire to say your article is as astonishing. The clearness in your
post is just excellent and i can assume you’re an expert on this subject.
Well with your permission allow me to grab your RSS feed to keep updated with forthcoming post.
Thanks a million and please carry on the enjoyable work.
Take a look at my homepage … best real estate agent in Cibolo TX
If you are going for most excellent contents like me, only pay a visit this site
all the time for the reason that it presents feature contents,
thanks
My brother recommended I might like this web site. He was
entirely right. This post truly made my day. You cann’t imagine just how much time I
had spent for this info! Thanks!
Continue Reading https://avalonfinance.cc
Thank you for every other informative blog.
Where else may I am getting that type of info written in such an ideal method?
I have a undertaking that I’m just now working on, and I’ve been on the look out for such info.
Everyone loves what you guys tend to be up too. Such clever work and
coverage! Keep up the great works guys I’ve added you guys to our blogroll.
TiSiN фрезы
You said it fantastically! https://bookmarkpagerank.com/story20297487/betflik168-%E0%B8%97%E0%B8%B2%E0%B8%87%E0%B9%80%E0%B8%82-%E0%B8%B2
Wow, this article is fastidious, my younger sister is analyzing these things, so I am
going to tell her.
my web-site: best real estate agent in Cibolo TX
Definitely believe that which you stated. Your favorite justification appeared to be on the internet the easiest thing
to be aware of. I say to you, I definitely get irked while people consider worries that they plainly don’t know
about. You managed to hit the nail upon the top and also defined out the whole thing without having side effect , people can take a signal.
Will likely be back to get more. Thanks
my website: realtor in St. George LA
I’m really enjoying the theme/design of your weblog.
Do you ever run into any browser compatibility issues?
A small number of my blog audience have complained
about my site not working correctly in Explorer but
looks great in Firefox. Do you have any suggestions to help fix this problem?
This game looks amazing! The way it blends that old-school
chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel
with real consequences has me hooked. I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual
stakes? Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of
nostalgic chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
Thank you! Very good stuff. https://yogicentral.science/wiki/User:Nanpopetorn
Как выбрать правильный дренаж оборудование
Why viewers still use to read news papers when in this technological world everything
is presented on net?
Here is my webpage; realtor in St. George LA
Fantastic info, Regards.
Someone essentially lend a hand to make severely posts I’d state.
This is the first time I frequented your website page
and so far? I surprised with the analysis you made
to make this particular submit extraordinary. Magnificent activity!
Home Page https://safeglobal.club
This text is worth everyone’s attention. Where can I find out more?
forticlient on mac
you could check here https://gluex.io/
next page https://kittenswap.cc/
If some one wants expert view about blogging and site-building after
that i suggest him/her to pay a quick visit this weblog, Keep up the good job.
It’s the best time to make some plans for the future and it is
time to be happy. I’ve read this post and if I could I desire
to suggest you few interesting things or suggestions.
Perhaps you can write next articles referring to this
article. I wish to read more things about it!
why not try these out https://beraborrow.cc
I like the valuable information you provide in your articles.
I’ll bookmark your blog and check again here frequently. I am quite certain I’ll learn lots
of new stuff right here! Best of luck for the next!
Searching for professional pet care for your furry friends in Omaha,
Elkhorn, Bennington, or Gretna? Our experienced local team provides personalized care tailored to your pets’ needs.
We guarantee peace of mind for pet owners with secure, reliable care.
See why so many pet owners rely on us as their preferred pet care provider.
I take pleasure in, cause I found exactly what I was taking a look for.
You have ended my four day long hunt! God Bless you man. Have a great day.
Bye
Also visit my site – best real estate agent in Wellington FL
Hi there to every single one, it’s really a pleasant for me to go to see this website, it includes important Information.
I was suggested this blog by way of my cousin.
I am no longer sure whether or not this publish is written via him as no one else know such
specified about my difficulty. You are incredible!
Thank you!
GoodSzaki – Public Professional Seeker master
My brother suggested I might like this web site.
He was totally right. This post truly made my day.
You can not imagine just how much time I had spent for this information! Thanks!
Nice blog right here! Also your website a lot up very fast!
What host are you the use of? Can I get your associate link
to your host? I wish my website loaded up as quickly as yours lol
Ən maraqlı platformadır. Yenə baxacağam!
https://uri.im/betandreassayt24878
I think that is among the so much important info for me.
And i’m glad studying your article. But want to statement on some general things,
The site taste is great, the articles is actually excellent : D.
Just right job, cheers
Look at my web-site: real estate agent Wellington FL
Hi to all, it’s in fact a good for me to visit this site, it consists of valuable Information.
Howdy! Do you know if they make any plugins to
help with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Cheers!
Here is my web-site best real estate agent in State College PA
I really like it when people come together and share opinions.
Great site, continue the good work!
We stumbled over here different website and thought I should check things out.
I like what I see so now i am following you. Look forward to checking out your web page yet again.
Hi would you mind sharing which blog platform you’re using?
I’m planning to start my own blog soon but I’m having a
hard time selecting between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different
then most blogs and I’m looking for something unique.
P.S Sorry for being off-topic but I had to ask!
Great post. I was checking continuously this blog and I am inspired!
Very useful info specially the final phase 🙂 I take
care of such info much. I used to be looking for this particular information for a long time.
Thank you and best of luck.
10 euros offert paris sportif|10 euros offert sans dépôt paris sportif|10 meilleurs sites
de paris sportifs|100 euro offert paris sportif|100 euros offert
paris sportif|100 euros remboursé paris sportifs|100
offert pari sportif|100 offert paris sportif|100 remboursé paris sportif|100e offert pari
sportif|abandon paris sportif tennis|abandon tennis paris sportif|addiction paris sportif forum|age paris sportif belgique|aide au pari sportif|aide au paris sportif|aide
aux paris sportif|aide aux paris sportifs|aide pari sportif|aide pari sportif football|aide parie
sportif|aide paris sportif|aide paris sportif foot|aide paris sportif gratuit|aide paris sportifs|aide pour paris sportif|algorithme de
paris sportif|algorithme excel paris sportif|algorithme
gratuit paris sportif|algorithme pari sportif|algorithme paris sportif|algorithme paris sportif avis|algorithme paris sportif
basket|algorithme paris sportif excel|algorithme paris sportif gratuit|algorithme paris sportif tennis|algorithme paris sportifs|algorithme pour paris
sportif|analyse cote paris sportif|analyse de paris sportif|analyse match paris sportif|analyse pari sportif|analyse paris sportif|analyse paris sportif foot|analyse paris sportif football|analyse paris sportif gratuit|analyse paris sportifs|ancienne cote paris sportif|api cote paris sportif|app paris sportif sans argent|appli de paris sportif|appli de
paris sportif sans argent|appli de paris sportifs|appli pari sportif|appli pari sportif gratuit|appli parie sportif|appli paris sportif|appli paris sportif avec paypal|appli paris sportif belgique|appli paris sportif entre
amis|appli paris sportif gratuit|appli paris sportif sans argent|appli
paris sportif suisse|appli paris sportifs|application aide paris sportif|application algorithme paris sportif|application analyse paris sportif|application android paris sportif|application bankroll paris sportif|application conseil paris sportif|application de pari sportif|application de parie sportif|application de paris sportif|application de paris sportif en afrique|application de paris sportif en cote d’ivoire|application de paris
sportif en ligne|application de paris sportif gratuit|application de
paris sportif international|application de paris
sportif suisse|application de paris sportifs|application faux
paris sportifs|application gestion bankroll paris sportif|application gestion paris sportif|application ia paris sportif|application pari sportif gratuit|application paris sportif|application paris sportif android|application paris sportif
argent fictif|application paris sportif belgique|application paris sportif
canada|application paris sportif espagne|application paris
sportif espagnol|application paris sportif fictif|application paris sportif france|application paris sportif gratuit|application paris sportif gratuit entre amis|application paris sportif maroc|application paris sportif offre de bienvenue|application paris sportif
paypal|application paris sportif sans argent|application paris sportif sans justificatif
de domicile|application paris sportif suisse|application paris sportif usa|application paris sportif virtuel|application pour
faire des paris sportifs|application pour gerer ses paris
sportif|application pour les paris sportifs|application pour pari sportif|application pour paris sportif|application pour
paris sportifs|application statistique paris sportif|application suivi paris
sportif|applications de paris sportifs|applications paris sportifs|applis paris sportif|applis paris sportifs|apprendre a
faire des paris sportifs|argent facile paris sportif|argent offert
paris sportifs|argent offert sans depot paris sportif|argent paris sportif|argent paris sportifs|argent paris
sportifs impots|argent sans depot paris sportif|arjel paris sportif|arjel paris sportifs|astuce gagner paris sportif|astuce pari sportif|astuce paris sportif|astuce paris sportif basket|astuce
paris sportif foot|astuce paris sportif forum|astuce paris sportif tennis|astuce paris sportifs|astuce pour gagner au pari sportif|astuce
pour gagner au paris sportif|astuce pour gagner paris sportif|astuce pour paris sportif|astuces paris sportifs|astuces paris sportifs en ligne|astuces paris
sportifs foot|astuces pour gagner aux paris sportifs|autorisation paris sportif france|avis pari sportif|avis paris sportif|avis paris sportif foot|avis site de
paris sportif|avis site paris sportif|avis sur les
paris sportifs|avis sur paris sportif|avis tipster paris
sportif|aweh signification paris sportif|bankroll 100 euros paris sportifs|bankroll management paris
sportif|bankroll paris sportif|bankroll paris sportif excel|bankroll paris sportif gratuit|bankroll
paris sportifs|basket paris sportif|belgique france
paris sportif|belgique paris sportifs|bonus bienvenue paris sportif|bonus bienvenue
paris sportifs|bonus cash paris sportif|bonus de bienvenue paris
sportif|bonus de bienvenue paris sportif belgique|bonus
de bienvenue sans depot paris sportif|bonus de depot
paris sportif|bonus de paris sportifs|bonus depot paris sportif|bonus
en cash paris sportif|bonus gratuit paris sportif|bonus
gratuit sans depot paris sportif|bonus pari sportif|bonus paris sportif|bonus paris sportif
belgique|bonus paris sportif betclic|bonus paris sportif cash|bonus paris sportif en ligne|bonus paris sportif france pari|bonus paris sportif retirable|bonus paris sportif sans depot|bonus paris sportif sans dépôt|bonus paris sportif unibet|bonus paris sportifs|bonus sans depot paris sportif|bonus sans depot paris sportif belgique|bonus sans dépôt paris
sportif|bonus sans dépôt paris sportif hors arjel|bonus site de paris sportif|bonus site pari
sportif|bonus site paris sportif|bonus sites de paris
sportifs|bonus unibet paris sportif|bookmaker paris sportif|bookmaker paris sportif gratuit|bookmaker paris sportifs|bookmaker sportif|bookmakers paris
sportif|bookmakers paris sportifs|bookmakers paris sportifs
en ligne|but contre son camp paris sportif|but sur penalty paris sportif|buteur paris sportif|c’est quoi handicap paris sportif|c’est quoi une cote paris sportif|calcul anti perte paris
sportif|calcul combinaison pari sportif|calcul
cote pari sportif|calcul cote paris sportif|calcul couverture paris sportif|calcul de cote paris
sportif|calcul des cotes paris sportifs|calcul dnb paris sportifs|calcul double chance paris sportif|calcul gain paris sportif|calcul mise paris sportif|calcul pari sportif|calcul
paris sportif|calcul paris sportif multiple|calcul pourcentage cote paris sportif|calcul probabilité paris sportif|calcul rentabilité paris sportifs|calcul roi paris
sportif|calcul systeme paris sportif|calcul trj paris sportifs|calculateur
cote paris sportif|calculateur de cote paris sportif|calculateur de mise paris sportif|calculateur de
paris sportif|calculateur paris sportif|calculatrice arbitrage paris sportif|calculatrice paris
sportif|calculer cote paris sportif|calculer gain paris sportif|calculer probabilité paris sportifs|calculer roi paris sportifs|calculer une cote pari
sportif|calculer une cote paris sportif|carte cadeau paris sportif|carte pcs
paris sportif|carte prépayée paris sportifs|cash out pari sportif|cash out paris sportif|cash out paris sportifs|casino en ligne paris sportif|casino paris
sportif en ligne|champions league paris sportif|chute
de cote paris sportif|classement des meilleurs sites de paris
sportifs|classement meilleur site de paris sportif|code barre paris
sportif|code bonus paris sportif|code paris sportif|code promo pari sportif|code
promo paris sportif|code promo paris sportif sans depot|code promo paris sportif sans dépôt|code promo sans depot paris sportif|code promo
site paris sportif|combien de temps pour encaisser un paris sportif|combien de
temps pour retirer un paris sportif|combien miser paris sportifs|combine paris sportif|combines paris sportifs|combiné pari sportif|combiné paris sportif|combiné paris sportif conseil|combiné paris sportif du jour|combiné paris sportif
pronostic|comment analyser un paris sportif|comment arreter de jouer aux paris sportifs|comment arreter les paris sportif|comment arreter les paris sportifs|comment arrêter les paris sportifs|comment bien gagner
au paris sportif|comment bien jouer au paris sportif|comment bien miser paris sportif|comment ca marche les paris sportif|comment calculer cote paris sportif|comment
calculer gain paris sportif|comment calculer les cotes des paris sportifs|comment calculer
une cote de paris sportif|comment calculer une cote pari sportif|comment calculer une cote paris sportif|comment comprendre les paris sportifs|comment creer un vip paris
sportif|comment créer un algorithme paris sportif|comment créer un site de paris sportif|comment
devenir riche avec les paris sportifs|comment etre rentable paris sportif|comment etre sur de gagner
au paris sportif|comment faire de bon paris sportif|comment faire des parie sportif|comment faire des paris sportif|comment faire des paris sportif gagnant|comment faire des paris sportifs|comment faire pari
sportif|comment faire paris sportif|comment faire pour arreter les paris sportifs|comment
faire pour gagner au paris sportif|comment faire pour
gagner les paris sportifs|comment faire un bon pari sportif|comment
faire un bon paris sportif|comment faire un pari sportif|comment faire un parie sportif|comment faire un paris sportif|comment
faire une montante paris sportif|comment fonctionne les cotes dans les paris
sportifs|comment fonctionne les cotes des paris sportifs|comment fonctionne les paris sportifs|comment fonctionne paris sportifs|comment fonctionne
un pari sportif|comment fonctionnent les cotes dans les paris sportifs|comment fonctionnent les
cotes dans les paris sportifs grand oral|comment fonctionnent les cotes de paris
sportif|comment fonctionnent les paris sportifs|comment fonctionnent les paris sportifs grand oral|comment fonctionnent les paris sportifs grand oral maths|comment fonctionnent les paris sportifs maths|comment
gagner a coup sur au paris sportif|comment gagner a tous les
coups au paris sportif|comment gagner a tout les coup au paris sportif|comment gagner
au pari sportif|comment gagner au pari sportif football|comment gagner au paris sportif|comment gagner au paris
sportif a coup sur|comment gagner au paris sportif foot|comment gagner
au paris sportif forum|comment gagner au paris sportif tennis|comment
gagner au paris sportifs|comment gagner aux paris sportif|comment gagner aux paris sportifs|comment gagner aux paris sportifs foot|comment gagner
aux paris sportifs livre|comment gagner aux paris sportifs sur le long terme|comment gagner avec les
paris sportifs|comment gagner dans les paris sportifs|comment gagner de l argent avec les paris sportifs|comment gagner de
l’argent au paris sportif|comment gagner de l’argent aux paris sportifs|comment gagner de l’argent avec
les paris sportifs|comment gagner de l’argent paris sportif|comment gagner de l’argent sur les
paris sportifs|comment gagner de l’argent sur paris sportif|comment gagner des
paris sportif|comment gagner des paris sportifs|comment gagner
en paris sportif|comment gagner facilement
au paris sportif|comment gagner les paris sportifs|comment
gagner paris sportif|comment gagner paris sportif foot|comment gagner paris
sportifs|comment gagner sa vie avec les paris sportifs|comment gagner ses paris sportif|comment gagner sur les paris sportif|comment
gagner sur les paris sportifs|comment gagner tout le temps au paris sportif|comment gagner un pari sportif|comment gagner un paris sportif|comment gerer une bankroll paris sportif|comment gérer sa bankroll paris sportif|comment
jouer au pari sportif|comment jouer au paris sportif|comment
jouer au paris sportif foot|comment jouer aux paris sportifs|comment jouer paris sportif|comment marche cote paris sportif|comment
marche les cotes paris sportif|comment marche les paris sportif|comment marche les paris
sportifs|comment marche paris sportif|comment marche un pari sportif|comment marche un paris sportif|comment marchent les cotes paris sportif|comment marchent les paris sportifs|comment miser au paris sportif|comment miser paris sportif|comment monter sa bankroll paris
sportif|comment ne jamais perdre au paris sportif|comment parier sportif|comment reussir au paris
sportif|comment reussir les paris sportif|comment reussir paris sportif|comment
sont calculer les cotes de paris sportif|comment sont calculées les cotes des paris sportifs|comment sont calculés les cotes des paris sportifs|comment sont faites les cotes des paris sportifs|comment toujours
gagner au paris sportif|comment ça marche les paris sportifs|comparaison bonus
paris sportifs|comparaison cote pari sportif|comparaison des cotes paris sportifs|comparateur cote pari
sportif|comparateur cote paris sportif|comparateur cotes paris sportif|comparateur cotes paris
sportifs|comparateur de cote pari sportif|comparateur de cote paris sportif|comparateur de cotes paris sportifs|comparateur de côtes paris sportifs|comparateur de
paris sportif|comparateur de site de paris sportif|comparateur de site paris sportif|comparateur de sites de paris sportifs|comparateur pari sportif|comparateur paris sportif|comparateur paris sportifs|comparateur site
de paris sportif|comparateur site pari sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif bonus paris sportifs|comparatif cote pari sportif|comparatif cote paris sportif|comparatif cotes
paris sportifs|comparatif des sites de paris sportifs|comparatif
offre de bienvenue paris sportif|comparatif offre paris
sportif|comparatif pari sportif|comparatif pari sportif en ligne|comparatif paris
sportif|comparatif paris sportif bonus|comparatif paris sportif en ligne|comparatif paris sportifs|comparatif paris sportifs en ligne|comparatif site
de paris sportif|comparatif site paris sportif|comparatif site paris
sportifs|comparatif sites de paris sportifs|comparatif sites paris sportifs|comparer les cotes
paris sportifs|comprendre cote paris sportif|comprendre handicap paris sportif|comprendre
les cotes des paris sportifs|comprendre les cotes paris sportif|comprendre les cotes paris sportifs|comprendre les handicap
paris sportif|compte de paris sportif|compte démo paris
sportif|compte finance paris sportif|compte financer paris sportif|compte financier
paris sportif|compte financé paris sportif|compte pari sportif|compte paris sportif|compte paris sportif financé|conseil de paris
sportif|conseil de paris sportifs|conseil en paris sportif|conseil en paris
sportifs|conseil pari sportif|conseil pari sportif gratuit|conseil paris sportif|conseil paris sportif aujourd’hui|conseil paris sportif du jour|conseil paris
sportif foot|conseil paris sportif gratuit|conseil paris sportif
ligue des champions|conseil paris sportif nba|conseil
paris sportif pronostic|conseil paris sportif rmc|conseil paris sportif tennis|conseil paris sportifs|conseil pour gagner au paris sportif|conseil pour paris sportif|conseil sur les paris sportifs|conseille paris sportif|conseiller en paris sportifs|conseiller paris sportif|conseils de paris sportifs|conseils en paris sportifs|conseils paris sportifs|conseils paris sportifs foot|conseils paris sportifs
gratuit|conseils paris sportifs tennis|conseils pour paris sportifs|cote
a 100 paris sportif|cote a 2 paris sportif|cote anglaise paris sportif|cote de 2 paris sportif|cote de
pari sportif|cote de paris sportif|cote des paris sportifs|cote maximum
paris sportif|cote minimum paris sportif|cote pari sportif|cote pari sportif comment ça marche|cote pari sportif real madrid|cote
pari sportif rugby|cote parie sportif|cote paris sportif|cote paris sportif belgique|cote paris
sportif calcul|cote paris sportif definition|cote paris sportif euro|cote paris sportif explication|cote paris
sportif foot|cote paris sportif france belgique|cote
paris sportif france espagne|cote paris sportif
ligue des champions|cote paris sportif moto gp|cote paris sportif psg|cote paris sportif psg arsenal|cote paris sportif rugby|cote paris sportif tennis|cote paris sportifs|cote pour paris sportifs|cote sportif foot|cote sportif
rugby|cote à 1000 paris sportif|cotes de paris sportifs|cotes pari sportif|cotes paris sportif|cotes paris sportifs|cotes
paris sportifs foot|coupe de france paris sportif|créer un algorithme paris
sportif|créer un compte paris sportif|créer un site de paris sportif en ligne|dans les paris sportifs
que signifie handicap|declarer ses gains paris sportif|definition cash out paris
sportif|definition cote paris sportif|definition handicap paris sportif|depot 5 euros
paris sportif|depot double paris sportif|depot minimum 5 euro paris sportif|depot minimum paris sportif|depot paris sportif|depuis quand existe les paris sportif en france|devenir riche avec les paris
sportifs|devenir riche avec paris sportifs|disqualification tennis paris sportif|dnb en paris sportif|dnb pari sportif|dnb paris
sportif|dnb paris sportif definition|dnb paris sportifs|doit
on declarer les gains de paris sportif|déclarer gains paris sportifs|déclarer gains paris sportifs
hors arjel|définition bankroll paris sportif|dépôt minimum 1
euro paris sportif|dépôt minimum 5 euro paris sportif|ecart de jeux tennis paris sportif|erreur
de cote paris sportif|est ce que les gains des paris
sportifs sont imposables|est-ce que les prolongation compte dans un pari sportif|etre sur de gagner au paris sportif|euro paris sportif|evenement sportif a paris|evenement sportif paris|evenement sportif
paris 2025|evenement sportif paris aujourd hui|evenement
sportif paris aujourd’hui|evenement sportif paris ce week end|evenements
sportif paris|evenements sportifs paris|evenements sportifs paris 2025|evenements sportifs à paris|evolution cote paris
sportif|evolution cotes paris sportifs|evolution des cotes paris sportifs|explication cote pari sportif|explication cote paris sportif|explication handicap paris sportif|explication pari sportif|explication paris sportif|face a face
hockey paris sportif|faire des paris sportif|faire des paris sportif avec
paypal|faire des paris sportifs|faire fortune paris sportifs|faire un pari sportif|faire
un paris sportif|faut il déclarer les gains de paris sportifs|faut il déclarer ses gains paris sportifs|fichier excel gestion bankroll paris sportif|fiscalité gains
paris sportifs|foot paris sportif|football et paris sportifs|forfait tennis paris sportif|formation paris sportif gratuit|forum de
paris sportif|forum de paris sportifs|forum pari sportif|forum parie sportif|forum paris sportif|forum paris sportif foot|forum paris sportif gratuit|forum paris sportif nba|forum paris sportif tennis|forum paris sportifs|forum sur les paris sportifs|forum tennis paris sportif|francaise des
jeux pari sportif|francaise des jeux paris sportif|francaise des jeux
paris sportifs|france 2 paris sportif|france 2 paris sportifs|france
belgique paris sportif|france espagne paris sportif|france pari sportif|france pari sportif
brest|france paris sportif|france paris sportifs|france pologne paris sportif|france portugal paris sportif|france suisse paris sportifs|france
tunisie paris sportifs|france-pari – paris sportifs|gagnant pari sportif|gagnant paris sportif|gagnant paris sportif bayern|gagnante paris sportif|gagne au paris sportif|gagner 10
euros par jour aux paris sportifs|gagner 100 euros par jour paris sportif|gagner 1000 euros par mois paris sportifs|gagner 10000 euros
paris sportif|gagner 2000 euros par mois paris sportif|gagner 50 euros par jour paris sportif|gagner a coup sur au paris
sportif|gagner a coup sur pari sportif|gagner a tous les coup paris sportif|gagner
argent avec paris sportifs|gagner argent pari sportif|gagner argent paris sportif|gagner argent
paris sportifs|gagner au pari sportif|gagner au paris sportif|gagner au
paris sportif a coup sur|gagner au paris sportif foot|gagner au paris
sportif forum|gagner au paris sportif à coup sur|gagner aux paris
sportif|gagner aux paris sportifs|gagner aux paris sportifs
pdf|gagner beaucoup d’argent paris sportif|gagner de l argent grace aux paris sportifs|gagner de l argent pari sportif|gagner de
l argent paris sportif|gagner de l argent paris sportifs|gagner de l’argent au paris sportif|gagner de
l’argent aux paris sportifs|gagner de l’argent avec les paris sportifs|gagner de l’argent avec paris sportif|gagner
de l’argent avec paris sportifs|gagner de l’argent grace au paris sportif|gagner de l’argent
grace aux paris sportifs|gagner de l’argent pari sportif|gagner de l’argent paris
sportif|gagner de l’argent paris sportifs|gagner
de l’argent sur les paris sportifs|gagner des paris
sportif|gagner des paris sportifs|gagner les paris sportifs|gagner pari
sportif|gagner paris sportif|gagner paris sportif
foot|gagner paris sportif forum|gagner paris sportif tennis|gagner paris sportifs|gagner sa
vie avec les paris sportif|gagner sa vie avec les paris sportifs|gagner sa vie avec paris sportifs|gagner ses paris sportifs|gagner
à coup sur paris sportif|gagner à tous les coups paris sportifs|gain maximum paris sportif|gain pari sportif|gain pari
sportif imposable|gain pari sportif impot|gain paris sportif|gain paris sportif
imposable|gain paris sportif impot|gain paris sportif impôt|gains paris sportif|gains paris sportif
imposable|gains paris sportifs|gains paris sportifs imposable|gains paris sportifs
imposables|gains paris sportifs sont ils imposables|gerer bankroll
paris sportif|gerer sa bankroll paris sportif|gerer une bankroll
paris sportif|gestion bankroll paris sportif|gestion bankroll paris sportifs|gestion bankroll paris sportifs excel|gestion de bankroll paris sportif|gestion de
bankroll paris sportif application|gestion de
bankroll paris sportifs|gestion de mise paris sportif|gestion paris sportifs v2 5 gratuit|gg signification paris sportif|gros combiné paris
sportif|gros gain paris sportif|grosse cote paris sportif pronostic|grosse mise paris sportif|groupe paris sportif gratuit|groupe telegram paris sportif
gratuit|groupement de joueurs paris sportifs|handicap 0 paris sportif|handicap 1 paris sportif|handicap 5 paris sportif|handicap au paris sportif|handicap basket paris
sportif|handicap dans les paris sportifs|handicap en paris
sportif|handicap europeen paris sportif|handicap européen paris sportifs|handicap mi temps paris sportif|handicap pari
sportif|handicap paris sportif|handicap paris sportif basket|handicap paris sportif explication|handicap paris sportif foot|handicap paris sportif rugby|handicap paris sportifs|handicap rugby paris sportif|handicap tennis paris sportif|historique cote paris sportif|historique des cotes paris sportifs|hockey
paris sportif|hockey sur glace paris sportif|hors arjel paris sportif|hweh signification paris sportif|imposition gain pari sportif|imposition gain paris
sportif|imposition gains paris sportifs|imposition paris sportif france|impot gain paris sportif|impot
paris sportif france|impot sur gain paris sportif|je gagne ma vie avec les paris sportifs|jeu de pari sportif
gratuit|jeu de paris sportif en ligne|jeu de paris sportif gratuit|jeu paris
sportif gratuit|jeu paris sportif sans argent|jeux de parie sportif|jeux de paris sportif|jeux de paris sportif en ligne|jeux de
paris sportif gratuit|jeux de paris sportifs|jeux olympiques paris sportifs|jeux paris sportif|jeux paris sportif gratuit|jeux paris sportif virtuel|jeux paris sportifs en ligne|jouer
au paris sportif|jouer paris sportif|joueur absent paris
sportif|joueur blesse paris sportif|joueur caen paris sportif|joueur de caen pari sportif|joueur de foot
paris sportif|joueur decisif paris sportif|joueur décisif paris sportif|joueur italien paris sportif|joueur paris
sportif|joueur professionnel paris sportif|joueur qui se blesse paris sportif|joueur sanctionne pari sportif|joueur suspendu paris sportif|joueurs italiens
paris sportifs|l’argent des paris sportifs est il imposable|la cote paris sportif|la francaise des jeux paris sportif|la martingale paris sportif|la martingale
paris sportifs|la meilleur application de paris sportif|la meilleur
application paris sportif|la meilleur technique pour
gagner au paris sportif|la méthode secrète
pour gagner aux paris sportifs pdf|la plus grosse cote gagner paris sportif|la plus grosse cote paris sportif|ldem paris sportif
signification|le marché des paris sportifs|le meilleur
site de pari sportif|le meilleur site de paris sportif|le meilleur site
de paris sportif en ligne|le meilleur site de paris sportifs|le plus gros gain au paris sportif|le plus gros paris sportif|le plus gros paris sportif du monde|les 10 meilleurs sites de paris sportifs|les 10 meilleurs sites
de paris sportifs en afrique|les 17 secrets pour gagner rapidement aux paris sportifs|les 17
secrets pour gagner rapidement aux paris sportifs pdf|les application de paris sportif|les applications paris sportifs|les
bonus paris sportifs|les bookmakers paris sportifs|les cotes paris sportifs|les
gains de paris sportifs sont ils imposables|les gains
des paris sportifs sont ils imposables|les jeux de paris sportifs|les meilleur paris sportif|les meilleures applications de paris sportifs|les meilleurs applications de paris sportifs|les meilleurs bonus
paris sportif|les meilleurs bonus paris sportifs|les meilleurs cotes paris sportif|les meilleurs paris sportifs|les meilleurs paris
sportifs du jour|les meilleurs site de paris sportif|les meilleurs
site de paris sportifs|les meilleurs sites de pari sportif|les meilleurs sites de paris sportifs|les meilleurs sites de paris
sportifs en ligne|les paris sportif|les paris sportif
avis|les paris sportifs|les paris sportifs comment ça marche|les
paris sportifs en france|les paris sportifs en ligne|les paris sportifs en ligne comprendre jouer gagner|les paris sportifs en ligne comprendre jouer
gagner pdf|les paris sportifs les plus rentables|les plus
gros gagnant paris sportif|les plus gros gains au paris
sportifs|les plus gros gains paris sportifs|les plus gros paris sportif|les plus grosse cote paris sportif|les plus
grosses pertes paris sportifs|les sites de paris sportifs|les sites de paris sportifs autorisés en france|les sites
de paris sportifs en france|les sites de paris sportifs en ligne|les sites de paris sportifs francais|ligue
1 paris sportif|ligue 1 paris sportifs|ligue 2 paris sportif|ligue des champions paris sportif|limite
de gains paris sportifs|limite de mise paris sportif|limite gain paris sportif|limite mise paris
sportifs|liste de paris sportif|liste des paris sportifs|liste des site de paris sportif|liste
des sites de paris sportifs|liste pari sportif|liste paris
sportif|liste paris sportif pdf|liste site de paris sportif|liste site pari sportif|liste site paris sportif|liste site paris sportif arjel|liste sites paris sportifs|logiciel algorithme paris sportif|logiciel algorithme
paris sportif gratuit|logiciel analyse paris sportif|logiciel calcul paris sportif|logiciel de pari sportif|logiciel de paris sportif|logiciel de paris
sportif gratuit|logiciel gestion bankroll paris sportif gratuit|logiciel gestion de bankroll paris sportif|logiciel
gestion paris sportif|logiciel gestion paris sportif gratuit|logiciel
gestion paris sportifs|logiciel pari sportif|logiciel paris sportif|logiciel paris sportif gratuit|logiciel paris sportifs|logiciel paris sportifs foot sur 2
matchs|logiciel pour paris sportif|logiciel pour paris sportifs|logiciel prediction paris sportif|logiciel probabilité paris sportif|logiciel prédiction paris sportif|logiciel
statistique paris sportifs|logiciel variation de cote paris sportif|loi sur les paris sportifs en france|magic calculator paris
sportif|marché des paris sportifs|marché des paris
sportifs en france|marché des paris sportifs en ligne|martingale pari sportif|martingale paris sportif|martingale paris sportif excel|martingale paris sportif forum|martingale paris sportif
interdit|martingale paris sportifs|match abandonné paris sportif|match annulé ou reporté paris sportifs|match annulé paris sportif|match
arrete paris sportif|match interrompu paris sportif|match interrompu tennis paris sportif|match interrompu tennis pluie paris sportif|match nul boxe paris sportif|match pari sportif|match paris
sportif|match reporté paris sportif|match suspendu paris sportif|match suspendu tennis paris sportif|match truqué paris sportif|matchs truqués paris sportifs|meilleur
algorithme paris sportif|meilleur algorithme paris sportif gratuit|meilleur app de paris sportif|meilleur app de paris sportifs|meilleur app paris sportif|meilleur appli de pari sportif|meilleur
appli de paris sportif|meilleur appli pari sportif|meilleur appli
paris sportif|meilleur appli paris sportif forum|meilleur
appli paris sportifs|meilleur application conseil paris sportif|meilleur application de paris sportif|meilleur
application de paris sportif en afrique|meilleur application pari sportif|meilleur
application paris sportif|meilleur application paris sportif belgique|meilleur application pour les paris
sportif|meilleur application pour pari sportif|meilleur bonus de bienvenue paris
sportif|meilleur bonus pari sportif|meilleur bonus paris sportif|meilleur bonus paris sportif sans depot|meilleur bonus paris sportifs|meilleur bonus site de paris sportif|meilleur bonus
site pari sportif|meilleur bonus site paris sportif|meilleur bookmaker paris sportif|meilleur combiné paris sportif|meilleur conseil paris sportif|meilleur cote de
paris sportif|meilleur cote pari sportif|meilleur cote paris sportif|meilleur cote paris sportif
aujourd’hui|meilleur cote site paris sportif|meilleur
forum paris sportifs|meilleur gain paris
sportif|meilleur ia paris sportif|meilleur methode
pour gagner au paris sportif|meilleur offre bienvenue paris sportif|meilleur offre bonus paris sportif|meilleur offre de
bienvenue paris sportif|meilleur offre de bienvenue paris sportifs|meilleur offre
pari sportif|meilleur offre paris sportif|meilleur offre
paris sportif en ligne|meilleur pari sportif|meilleur pari sportif du jour|meilleur pari sportif en ligne|meilleur
paris sportif|meilleur paris sportif aujourd’hui|meilleur paris sportif du jour|meilleur paris sportif en ligne|meilleur paris sportif foot|meilleur promo
paris sportif|meilleur pronostic paris sportif|meilleur site de conseil paris sportif|meilleur site de pari sportif|meilleur site de pari sportif en ligne|meilleur site de paris sportif|meilleur site de paris sportif avis|meilleur site de paris sportif belgique|meilleur site
de paris sportif canada|meilleur site de paris sportif en france|meilleur site de paris sportif en ligne|meilleur site de paris sportif football|meilleur site de paris sportif forum|meilleur site de paris
sportif france|meilleur site de paris sportif hors arjel|meilleur
site de paris sportif international|meilleur site de
paris sportif suisse|meilleur site de paris sportifs|meilleur site de paris sportifs en ligne|meilleur site
pari sportif|meilleur site pari sportif en ligne|meilleur site pari
sportif france|meilleur site paris sportif|meilleur site paris sportif avis|meilleur site paris sportif belgique|meilleur site paris sportif canada|meilleur
site paris sportif en ligne|meilleur site paris sportif foot|meilleur site paris sportif forum|meilleur site
paris sportif france|meilleur site paris sportif hors arjel|meilleur
site paris sportif nba|meilleur site paris sportif rugby|meilleur site paris
sportif suisse|meilleur site paris sportifs|meilleur site pour pari
sportif|meilleur site pour paris sportif|meilleur site pronostic paris sportif|meilleur strategie paris sportif|meilleur technique de paris sportif|meilleur technique paris
sportif|meilleur technique pour gagner au paris sportif|meilleure appli de paris sportif|meilleure appli de paris sportifs|meilleure appli pari sportif|meilleure appli paris
sportif|meilleure appli paris sportifs|meilleure application de
paris sportif|meilleure application de paris sportifs|meilleure application pari sportif|meilleure application paris sportif|meilleure application paris
sportif android|meilleure application paris sportifs|meilleure offre paris sportif|meilleure site paris
sportif|meilleure strategie paris sportif|meilleures applications de paris sportifs|meilleures applications paris sportifs|meilleures cotes paris sportifs|meilleures offres paris sportifs|meilleures stratégies paris sportifs|meilleurs appli paris sportif|meilleurs application de
paris sportifs|meilleurs application paris
sportif|meilleurs applications paris sportifs|meilleurs bonus paris sportifs|meilleurs cote paris sportif|meilleurs cotes paris
sportifs|meilleurs offres paris sportifs|meilleurs paris sportifs|meilleurs paris sportifs du jour|meilleurs
site de pari sportif|meilleurs site de paris sportif|meilleurs site de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs site paris sportif|meilleurs sites de paris
sportifs|meilleurs sites de paris sportifs en ligne|meilleurs sites
paris sportif|meilleurs sites paris sportifs|methode abc paris sportif|methode de paris sportif|methode gagnante paris sportifs|methode gagner paris sportif|methode
infaillible paris sportifs|methode martingale paris sportif|methode mathematique paris
sportif|methode mathematique pour gagner au paris sportif|methode
paris sportif|methode paris sportif foot|methode paris sportif forum|methode paris sportif tennis|methode paris sportifs|methode pour gagner au paris sportif|methode pour gagner
paris sportif|methodes paris sportifs|minimum depot paris sportif|mise au jeu pari sportif|mise maximum pari sportif|mise maximum
paris sportif|mise minimum paris sportif|mise moyenne paris sportif|mise paris sportif|moins de 4 5 but paris
sportif|montant maximum paris sportif|montant paris sportif|montante pari sportif|montante parie sportif|montante paris sportif|montante paris sportifs|montantes paris sportifs|multiple pari sportif|multiple paris sportif|multiple paris
sportifs|multiples paris sportifs|méthode calcul paris sportif|méthode match
nul paris sportifs|méthode mathématique pour gagner au paris sportif|méthode paris sportif forum|méthode paris sportif
hockey|nba pari sportif|nba paris sportif|nba paris sportifs|nouveau paris sportif|nouveau site de pari sportif|nouveau site de
paris sportif|nouveau site de paris sportif en ligne|nouveau site
de paris sportifs|nouveau site pari sportif|nouveau site paris sportif|nouveau site paris sportif france|nouveau site paris sportifs|nouveaux sites de
paris sportifs|nouveaux sites paris sportifs|nouvelle appli paris sportif|nouvelle application de paris
sportif|numero de match paris sportif|numero match paris sportif|offre
100 euros paris sportif|offre appli pari sportif|offre bienvenu paris sportif|offre
bienvenue pari sportif|offre bienvenue paris sportif|offre bienvenue paris
sportifs|offre bienvenue site paris sportif|offre bonus
paris sportif|offre de bienvenu paris sportif|offre de bienvenue
pari sportif|offre de bienvenue paris sportif|offre de bienvenue
paris sportif belgique|offre de bienvenue paris sportif sans depot|offre de bienvenue paris sportif sans dépôt|offre de bienvenue paris sportifs|offre de bienvenue sans depot paris sportif|offre de bienvenue site paris sportif|offre euro paris sportif|offre pari sportif euro|offre paris
sportif|offre paris sportif belgique|offre paris sportif cash|offre paris sportif coupe du monde|offre paris sportif hors
arjel|offre paris sportif remboursé|offre paris sportif remboursé cash|offre paris
sportif sans depot|offre promo paris sportif|offre remboursement paris
sportif|offre sans depot paris sportif|offre site paris sportif|offres bienvenue paris sportifs|offres de bienvenue paris sportifs|ou faire des paris sportif|ou faire des paris sportif en espagne|ou faire des paris sportifs|outil répartiteur de mise paris sportif|outils repartiteur
de mises paris sportif|ouverture compte paris sportifs|ouvrir un compte
paris sportif|pack de bienvenue paris sportif|pack de bienvenue paris sportif hors arjel|pari en ligne sportif|pari sportif|pari sportif 100 euros offert|pari
sportif 100 remboursé|pari sportif abandon tennis|pari sportif aide|pari sportif algérie
aujourd’hui|pari sportif appli|pari sportif application|pari sportif argent|pari sportif astuce|pari sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari sportif
avec orange money|pari sportif avec paypal|pari sportif avec wave|pari sportif avis|pari sportif basket|pari sportif belgique|pari sportif belgique
france|pari sportif bonus|pari sportif buteur pas titulaire|pari
sportif champions league|pari sportif combiné|pari sportif comment|pari sportif comment gagner|pari sportif
comment ça marche|pari sportif comparatif|pari sportif conseil|pari sportif
cote|pari sportif cote match|pari sportif cote psg|pari sportif coupe|pari sportif coupe de france|pari sportif coupe du monde|pari sportif depot|pari sportif du jour|pari sportif en france|pari sportif en ligne|pari sportif en ligne au cameroun|pari sportif en ligne belgique|pari sportif en ligne canada|pari sportif en ligne france|pari sportif
en ligne gratuit|pari sportif en ligne suisse|pari sportif en ligne ufc|pari sportif en suisse|pari sportif euro|pari
sportif explication|pari sportif faire|pari sportif foot|pari sportif foot resultat|pari sportif football|pari sportif
forum|pari sportif francaise des jeux|pari sportif
france|pari sportif france angleterre|pari sportif
france argentine|pari sportif france autriche|pari sportif france belgique|pari sportif france
espagne|pari sportif france italie|pari sportif france portugal|pari
sportif france usa|pari sportif gagnant|pari sportif
gagner|pari sportif gagner a tous les coups|pari sportif gagner de l’argent|pari sportif
gain|pari sportif gratuit|pari sportif gratuit pour gagner des cadeaux|pari sportif gratuit
sans depot|pari sportif handicap|pari sportif hockey|pari sportif
hors arjel|pari sportif jeux olympiques|pari sportif joueur absent|pari sportif
le plus rentable|pari sportif leicester champion|pari sportif ligue 1|pari sportif ligue
2|pari sportif ligue des champions|pari sportif ligue europa|pari sportif match|pari sportif match arrete|pari sportif match
interrompu|pari sportif meilleur|pari sportif meilleur cote|pari sportif meilleur
site|pari sportif methode|pari sportif mise|pari sportif mise au jeu|pari sportif mise o jeu|pari sportif nba|pari sportif offre bienvenue|pari sportif paypal|pari sportif plus|pari sportif prolongation|pari sportif promo|pari
sportif pronostic|pari sportif pronostic foot|pari sportif pronostic gagnant|pari
sportif pronostic gratuit|pari sportif psg|pari sportif psg bayern|pari sportif psg inter|pari sportif psg milan|pari
sportif regle|pari sportif rembourse|pari sportif remboursement|pari sportif
remboursement cash|pari sportif remboursé|pari sportif rugby|pari sportif
rugby coupe du monde|pari sportif rugby top 14|pari sportif sans argent|pari sportif sans carte bancaire|pari sportif sans depot|pari sportif signification|pari sportif site|pari sportif statistique|pari sportif suisse|pari
sportif systeme|pari sportif technique|pari sportif technique pour gagner|pari sportif temps reglementaire|pari sportif tennis|pari sportif tennis abandon|pari sportif top|pari sportif top 14|pari sportif tour de
france|parie sportif|parie sportif comment ca marche|parie sportif du
jour|parie sportif en ligne|parie sportif foot|parie sportif football|parie sportif france|parie sportif gratuit|parie sportif pronostic|parie sportif suisse|paris en ligne sportif|paris en ligne sportifs|paris evenement sportif|paris
france sportif|paris hippique et sportif|paris
hippiques et sportifs|paris hippiques paris sportifs|paris hippiques
paris sportifs et poker en ligne|paris hippiques sportifs|paris match sportif|paris sportif|paris
sportif 10 euros offerts|paris sportif 100 euros
offert|paris sportif 100 euros remboursé|paris sportif 100 offert|paris
sportif 100 remboursé|paris sportif 100e
offert|paris sportif 150 euros offert|paris sportif 1er pari remboursé|paris
sportif a faire|paris sportif a faire aujourd’hui|paris sportif a faire ce soir|paris sportif abandon tennis|paris sportif abandon tennis parions sport|paris sportif aide|paris sportif algorithme|paris sportif analyse|paris sportif
appli|paris sportif application|paris sportif application android|paris sportif
apres prolongation|paris sportif argent|paris sportif argent fictif|paris sportif argent offert|paris sportif argent virtuel|paris sportif arjel|paris sportif arsenal psg|paris sportif astuce|paris sportif
au canada|paris sportif aujourd hui|paris sportif aujourd’hui|paris sportif
avec argent fictif|paris sportif avec bonus sans depot|paris sportif avec
carte bancaire|paris sportif avec cryptomonnaie|paris sportif avec handicap|paris sportif avec paypal|paris sportif
avec paysafecard|paris sportif avis|paris sportif
avis expert|paris sportif avis forum|paris sportif bankroll|paris sportif basket|paris sportif basket
coupe de france|paris sportif basket nba|paris sportif basket prolongation|paris sportif belgique|paris sportif belgique bonus|paris sportif belgique bonus sans depot|paris sportif belgique france|paris sportif belgique suede|paris sportif bonus|paris sportif bonus bienvenue|paris sportif bonus cash|paris sportif bonus de bienvenue|paris sportif bonus gratuit|paris sportif
bonus gratuit sans depot|paris sportif bonus retirable|paris
sportif bonus sans depot|paris sportif bonus sans depot belgique|paris sportif bookmaker|paris sportif but contre son camp|paris sportif but temps
additionnel|paris sportif buteur|paris sportif buteur blessé|paris
sportif buteur carton rouge|paris sportif buteur contre son camp|paris sportif buteur non titulaire|paris sportif buteur prolongation|paris sportif buteur qui ne joue pas|paris sportif buteur remplacant|paris sportif calcul gain|paris sportif canada|paris sportif cash|paris sportif cash out|paris sportif champion ligue 1|paris sportif champions league|paris sportif classement ligue 1|paris sportif code promo|paris sportif combine|paris sportif
combiné|paris sportif combiné comment ça marche|paris sportif combiné du jour|paris sportif
combiné match reporté|paris sportif comment ca marche|paris sportif comment faire|paris sportif comment gagner|paris sportif
comment gagner a tous les coups|paris sportif comment jouer|paris sportif
comment ça marche|paris sportif comparateur cote|paris sportif
comparatif|paris sportif conseil|paris sportif conseil
gratuit|paris sportif conseil pour gagner|paris sportif cote|paris sportif cote et match|paris sportif cote explication|paris sportif cote psg|paris sportif coupe d’europe|paris sportif coupe davis|paris sportif coupe de france|paris sportif coupe du monde|paris
sportif coupe du monde de rugby|paris sportif coupe du monde rugby|paris
sportif depot 5 euro|paris sportif depot minimum|paris sportif depot paypal|paris sportif
dnb|paris sportif du jour|paris sportif du jour conseil|paris
sportif dépôt 1 euro|paris sportif dépôt minimum 5 euros|paris sportif en belgique|paris sportif en france|paris sportif en ligne|paris
sportif en ligne avec paypal|paris sportif en ligne avis|paris sportif en ligne belgique|paris sportif en ligne bonus|paris sportif en ligne cameroun|paris sportif en ligne comment gagner|paris sportif en ligne comment
ça marche|paris sportif en ligne france|paris sportif
en ligne gratuit|paris sportif en ligne maroc|paris sportif en ligne paypal|paris sportif en ligne
québec|paris sportif en ligne sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris sportif espagne
france|paris sportif esport|paris sportif et casino en ligne|paris sportif et hippique|paris sportif et prolongation|paris sportif euro|paris
sportif europa league|paris sportif explication|paris
sportif final ligue des champions|paris sportif finale ligue des
champions|paris sportif foot|paris sportif foot aide|paris sportif foot astuce|paris
sportif foot aujourd’hui|paris sportif foot ce soir|paris sportif foot comment
ca marche|paris sportif foot conseil|paris sportif foot cote|paris sportif foot coupe du
monde|paris sportif foot en ligne|paris sportif foot feminin|paris sportif foot gratuit|paris sportif foot prolongation|paris sportif foot pronostic|paris sportif foot pronostic gratuit|paris sportif foot
regle|paris sportif foot suisse|paris sportif foot us|paris sportif football|paris sportif football americain|paris sportif football astuces|paris sportif forfait
tennis|paris sportif forum|paris sportif francais|paris sportif francaise des jeux|paris sportif france|paris sportif france 2|paris sportif france allemagne|paris sportif france angleterre|paris sportif france argentine|paris sportif france autriche|paris sportif france belgique|paris sportif
france espagne|paris sportif france gibraltar|paris
sportif france italie|paris sportif france nouvelle zelande|paris sportif france pologne|paris sportif france portugal|paris sportif
france uruguay|paris sportif france usa|paris sportif freebet sans depot|paris sportif gagnant|paris sportif gagnant à coup sûr|paris sportif gagner a coup sur|paris sportif gagner argent|paris sportif gagner
de l’argent|paris sportif gain|paris sportif gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris
sportif gratuit appli|paris sportif gratuit avec cadeaux|paris sportif gratuit
cadeaux|paris sportif gratuit en ligne|paris sportif gratuit entre amis|paris sportif gratuit sans argent|paris sportif
gratuit sans depot|paris sportif gratuit sans dépôt|paris sportif gratuits|paris
sportif gros gain|paris sportif handicap|paris sportif handicap 0 1|paris sportif
handicap 0-1|paris sportif handicap 1 0|paris sportif handicap 1-0|paris
sportif handicap basket|paris sportif handicap explication|paris sportif handicap
foot|paris sportif handicap rugby|paris sportif hippique|paris
sportif hockey|paris sportif hockey nhl|paris
sportif hockey sur glace|paris sportif hors arjel|paris sportif hors arjel france|paris sportif jeux olympiques|paris sportif
jeux video|paris sportif joueur blessé|paris sportif joueur blessé pendant
le match|paris sportif joueur de foot|paris sportif joueur decisif|paris sportif joueur declare forfait|paris sportif joueur déclare forfait|paris
sportif joueur remplacant|paris sportif la francaise des jeux|paris sportif le plus rentable|paris sportif legal en france|paris sportif leicester
champion|paris sportif les 18 stratégies pour gagner tous les jours|paris
sportif les plus sur|paris sportif les prolongation compte|paris sportif ligne|paris sportif ligue 1|paris sportif ligue 2|paris sportif ligue des champions|paris sportif ligue des nations|paris sportif ligue
europa|paris sportif liste|paris sportif martingale|paris sportif match|paris sportif match abandonné|paris sportif match annulé|paris sportif match arrêté|paris sportif match du jour|paris sportif match interrompu|paris sportif match reporté|paris sportif match suspendu|paris
sportif match tennis interrompu|paris sportif match truqué|paris sportif meilleur bonus|paris sportif meilleur cote|paris sportif
meilleur pronostic|paris sportif meilleur site|paris sportif methode|paris sportif methode 2 3|paris sportif mi temps fin de match|paris sportif mise
au jeu|paris sportif mise maximum|paris sportif mma france|paris sportif moins de 3.5 but|paris sportif montante|paris sportif moto gp|paris sportif multiple|paris sportif multiple 2 3|paris sportif multiple 2 3 explication|paris
sportif multiple 2 4|paris sportif multiple 2 5|paris sportif multiple 2/3 explication|paris sportif
multiple 3 4|paris sportif multiple explication|paris sportif national 1 foot|paris sportif nba|paris sportif nba conseil|paris sportif nba pronostic|paris sportif
nhl|paris sportif nombre de but|paris sportif nouveau site|paris sportif
numero match|paris sportif offert|paris sportif offre bienvenue|paris sportif offre bienvenue
sans depot|paris sportif offre de bienvenue|paris sportif offre sans depot|paris sportif om psg|paris sportif paypal|paris
sportif plus de 1.5 but|paris sportif plus de 2 5 but|paris sportif plus
ou moins|paris sportif plus ou moins 2 5 but|paris sportif premier pari remboursé|paris sportif premier paris remboursé|paris sportif prolongation|paris sportif prolongation basket|paris sportif prolongation foot|paris sportif promo|paris sportif pronostic|paris sportif pronostic basket|paris sportif pronostic des match aujourd hui|paris
sportif pronostic expert gratuit|paris sportif pronostic
foot|paris sportif pronostic forum|paris sportif pronostic gratuit|paris sportif pronostic tennis|paris sportif
psg|paris sportif psg arsenal|paris sportif psg barcelone|paris sportif psg
bayern|paris sportif psg dortmund|paris sportif psg inter|paris
sportif psg inter cote|paris sportif psg liverpool|paris sportif psg om|paris sportif qr
code|paris sportif que veut dire handicap|paris sportif qui rapporte le plus|paris sportif regle|paris sportif regle prolongation|paris
sportif rembourse|paris sportif remboursement cash|paris sportif rembourser|paris sportif remboursé|paris sportif remboursé cash|paris sportif remboursé en cash|paris sportif retrait
paypal|paris sportif rue des joueurs|paris sportif rugby|paris sportif rugby
6 nations|paris sportif rugby coupe du monde|paris sportif rugby top 14|paris sportif safe du jour|paris sportif sans argent|paris sportif sans carte bancaire|paris sportif sans carte d’identité|paris sportif
sans compte bancaire|paris sportif sans depot|paris
sportif sans depot minimum|paris sportif si match suspendu|paris sportif si un joueur abandonne|paris
sportif si un joueur ne joue pas|paris sportif si un joueur se blesse|paris
sportif simple ou combiné|paris sportif site|paris sportif statistique|paris sportif stratégie|paris sportif suisse|paris sportif suisse application|paris sportif suisse en ligne|paris sportif suisse legal|paris sportif suisse légal|paris sportif suisse romande|paris sportif sur
du jour|paris sportif sur le tennis|paris sportif systeme|paris sportif systeme 2 3|paris sportif systeme 2 4|paris sportif
systeme 2/3|paris sportif systeme 2/4|paris sportif systeme 3
4|paris sportif systeme 3/4|paris sportif systeme explication|paris sportif technique|paris sportif technique pour gagner|paris
sportif temps additionnel|paris sportif temps reglementaire|paris sportif
tennis|paris sportif tennis abandon|paris sportif tennis conseil|paris sportif tennis de table|paris sportif tennis
forfait|paris sportif tennis gratuit|paris
sportif tennis pronostic|paris sportif tennis roland garros|paris sportif tir au but|paris sportif top 14|paris sportif tour
de france|paris sportif ufc|paris sportif ufc france|paris sportif unibet|paris sportif vainqueur
euro|paris sportif vainqueur ligue 1|paris sportif vainqueur ligue des
champions|paris sportif via paypal|paris sportif victoire prolongation|paris sportif vip gratuit|paris sportifs|paris sportifs abandon tennis|paris
sportifs aide|paris sportifs analyser un match|paris sportifs arjel|paris
sportifs astuces|paris sportifs aujourd’hui|paris sportifs autorisés en france|paris sportifs avec paypal|paris sportifs basket|paris sportifs belgique|paris sportifs bonus|paris sportifs bookmakers|paris sportifs canada|paris sportifs combiné|paris sportifs comparateur|paris sportifs comparatif|paris sportifs conseils|paris sportifs cotes|paris sportifs coupe du monde|paris sportifs de football|paris sportifs du
jour|paris sportifs en belgique|paris sportifs en france|paris sportifs en ligne|paris sportifs
en ligne belgique|paris sportifs en ligne france|paris sportifs en ligne gratuit|paris sportifs en ligne suisse|paris sportifs en suisse|paris sportifs et hippiques|paris sportifs euro|paris sportifs
foot|paris sportifs foot us|paris sportifs forum|paris sportifs france|paris sportifs
france espagne|paris sportifs gagner à tous les coups|paris sportifs
gratuit|paris sportifs gratuits|paris sportifs gratuits en ligne|paris sportifs handicap|paris sportifs hockey|paris sportifs hockey sur galce|paris sportifs hockey sur glace|paris sportifs hors arjel|paris
sportifs jeux olympiques|paris sportifs les bookmakers raflent
la mise|paris sportifs ligne|paris sportifs ligue 1|paris sportifs ligue
2|paris sportifs ligue des champions|paris sportifs ligue europa|paris sportifs match interrompu|paris sportifs montante|paris
sportifs nba|paris sportifs offre bienvenue|paris
sportifs offre de bienvenue|paris sportifs paypal|paris sportifs
pronostics|paris sportifs psg|paris sportifs psg inter|paris sportifs rugby|paris sportifs sans argent|paris sportifs sans depot|paris
sportifs site|paris sportifs sites|paris sportifs statistiques|paris sportifs stratégie|paris sportifs
suisse|paris sportifs technique|paris sportifs techniques|paris sportifs tennis|paris sportifs tennis astuces|paris sportifs
top 14|paris sportifs tour de france|part de marché paris sportifs|paypal pari sportif|paypal paris sportif|paypal paris sportifs|perte d’argent paris sportifs|peut on devenir riche avec les paris sportifs|peut on gagner de l’argent avec les
paris sportifs|peut on gagner sa vie avec les paris sportif|peut on vraiment gagner de l’argent avec les paris sportifs|plus
gros combine paris sportif|plus gros gagnant paris sportif|plus gros gain paris sportif|plus gros gain paris sportif au monde|plus gros gain paris sportif france|plus
gros gains paris sportif|plus gros pari sportif|plus gros paris sportif|plus grosse cote gagner paris
sportif|plus grosse cote pari sportif|plus grosse cote paris sportif|plus grosse
mise paris sportif|plus grosse somme gagner au paris sportif|plus ou moins paris sportif|pourcentage de mise
paris sportif|premier pari sportif remboursé|probabilité cote
paris sportif|probabilité paris sportif combiné|prolongation basket paris sportif|prolongation paris sportif|promo pari
sportif|promo paris sportif|promo site de paris sportif|promo site pari sportif|promo site paris sportif|promos paris sportifs|prono paris
sportif foot|prono paris sportif gratuit|prono paris sportif tennis|pronostic de paris sportif|pronostic du jour paris sportif|pronostic foot
paris sportif|pronostic gratuit paris sportif|pronostic pari sportif|pronostic pari sportif
gratuit|pronostic paris sportif|pronostic paris sportif aujourd’hui|pronostic paris sportif du jour|pronostic paris sportif foot|pronostic paris sportif gratuit|pronostic
paris sportif tennis|pronostic paris sportifs|pronostics foot statistiques et
aides aux paris sportifs|pronostics paris sportif|pronostics paris sportifs|pronostiqueur paris sportif gratuit|psg arsenal paris sportif|psg bayern paris sportif|psg inter milan paris sportif|psg inter
pari sportif|psg inter paris sportif|psg liverpool paris sportif|psg om paris sportif|psg
paris sportif|psg paris sportifs|qr code paris sportif|qu est ce qu un handicap paris sportif|qu est ce que handicap dans les
paris sportif|qu’est ce qu’un handicap paris sportif|qu’est
ce que handicap dans les paris sportif|quand un joueur se
blesse paris sportif|que signifie 1/1 en paris sportif|que signifie 1/2 paris sportif|que signifie 12 en paris sportif|que signifie 1×2 dans les paris sportifs|que signifie btts en paris sportif|que signifie dnb en paris sportif|que signifie draw en paris sportif|que signifie ft
en paris sportif|que signifie gg dans le pari sportif|que
signifie gg en pari sportif|que signifie gg en paris sportif|que
signifie handicap dans les paris sportifs|que veut dire dnb
en paris sportif|que veut dire handicap dans les paris sportifs|que veut dire handicap paris sportif|quel
appli pari sportif|quel cote jouer paris sportif|quel est la meilleur appli de paris sportif|quel est le meilleur algorithme de paris sportif|quel est le meilleur site de pari sportif|quel est
le meilleur site de pari sportif en ligne|quel est le meilleur site de paris sportif|quel est le meilleur site de paris sportif en ligne|quel
est le meilleur site de paris sportifs en ligne|quel est
le pari sportif le plus rentable|quel pari sportif est le plus rentable|quel pari sportif est
le plus sûr|quel pari sportif faire aujourd’hui|quel paris sportif faire
aujourd’hui|quel paris sportif rapporte le plus|quel site de paris
sportif choisir|quel site de paris sportif rembourse en cash|quel type de pari sportif est
le plus rentable|quelle application pour paris sportifs|quelle est la
meilleure appli de paris sportif|quelle est la meilleure application de paris sportif|quelle est la meilleure application pour les paris sportifs|quelle est le meilleur site de paris
sportif|quels paris sportifs faire|quels sont les
paris sportifs les plus sûrs|rebond basket paris sportif|record
de gain paris sportif|regle buteur paris sportif|regle de paris sportif|regle des paris sportif|regle handicap paris sportif|regle handicap paris sportif foot|regle multiple paris sportif|regle pari
sportif|regle paris sportif|regle paris sportif foot|regle paris sportif multiple|regle paris sportif prolongation|reglement pari sportif|reglement paris sportif|regles paris sportifs|remboursement cash paris sportif|remboursement en cash paris sportif|remboursement pari sportif|remboursement paris sportif|repartiteur de mise
paris sportif|repartiteur de mise paris sportifs|repartiteur de
mises paris sportif|repartiteur mise paris sportif|repartition des
mises paris sportif|resultat pari sportif|resultat paris sportif|resultat paris sportif en direct|resultat
paris sportif foot|resultat sportif hockey|retirer
argent paris sportif|rugby pari sportif|rugby paris sportif|règle paris sportif
prolongation|règles paris sportif|répartiteur de mise pari sportif|répartiteur de mise paris sportif|répartiteur de mise paris sportifs|répartition des mises paris sportif|résultat paris
sportif foot|sans depot paris sportif|se faire interdire
de paris sportifs|signification btts paris sportif|signification dnb paris sportif|signification handicap
paris sportif|simulateur de gain paris sportif|simulateur gain paris sportif|simulateur gain paris sportif multiple|simulateur gain paris
sportif systeme|simulateur gain paris sportif système|simulateur montante paris sportif|simulateur paris sportif multiple|simulateur
systeme paris sportif|simulation paris sportif gratuit|site aide paris sportif|site analyse paris
sportif|site analyser paris sportif|site arjel paris sportif|site conseil paris sportif|site d’analyse de paris sportifs|site d’analyse paris sportif|site
de conseil paris sportif|site de pari en ligne sportif|site de pari
sportif|site de pari sportif avec bonus sans depot|site de pari sportif bonus sans depot|site de pari sportif canada|site de pari
sportif en ligne|site de pari sportif francais|site de pari
sportif gratuit|site de pari sportif hors arjel|site de pari
sportif suisse|site de parie sportif|site
de parie sportif en ligne|site de paris en ligne sportif|site
de paris sportif|site de paris sportif acceptant paypal|site de paris sportif arjel|site
de paris sportif autorisé en france|site de paris sportif autorisé en suisse|site de paris sportif avec bonus|site de paris sportif avec bonus sans
depot|site de paris sportif avec bonus sans dépôt|site de paris
sportif avec neosurf|site de paris sportif avec paiement mobile|site de paris sportif avec paypal|site de paris sportif avis|site de paris sportif belge avec bonus|site de paris sportif belgique|site de
paris sportif bonus|site de paris sportif bonus sans depot|site de paris sportif canada|site de paris sportif comparatif|site de paris sportif depot minimum|site de paris
sportif en france|site de paris sportif en ligne|site de paris sportif en ligne suisse|site de paris sportif football|site de
paris sportif francais|site de paris sportif france|site de paris sportif gratuit|site de
paris sportif gratuit pour gagner des cadeaux|site de paris sportif gratuit
sans dépôt|site de paris sportif hors arjel|site
de paris sportif le plus fiable|site de paris sportif legal en france|site de paris sportif meilleur cote|site de paris sportif nouveau|site de paris sportif offre de bienvenue|site de
paris sportif paypal|site de paris sportif premier paris remboursé|site de
paris sportif qui accepte paypal|site de paris sportif qui rembourse en cash|site de paris sportif remboursé|site de paris sportif sans argent|site
de paris sportif sans carte bancaire|site de paris sportif sans carte
d’identité|site de paris sportif sans depot|site de paris sportif suisse|site de paris sportifs|site de paris
sportifs avec paypal|site de paris sportifs en ligne|site de paris sportifs francais|site de paris sportifs gratuit|site de paris sportifs paypal|site de paris sportifs suisse|site de statistique pour paris
sportif|site des paris sportifs|site pari en ligne sportif|site pari sportif|site pari sportif 100 euros
offert|site pari sportif arjel|site pari sportif belgique|site pari sportif bonus|site pari sportif canada|site pari sportif comparatif|site pari sportif en ligne|site pari sportif france|site pari
sportif gratuit|site pari sportif hors arjel|site pari sportif suisse|site parie sportif|site
paris en ligne sportif|site paris sportif|site paris sportif 100 euros offert|site paris sportif 100 euros
remboursé|site paris sportif 1er paris remboursé|site paris sportif arjel|site paris sportif autorisé en france|site paris sportif
avec bonus|site paris sportif avec bonus sans depot|site paris sportif
avec meilleur cote|site paris sportif belgique|site paris sportif bonus|site paris sportif bonus cash|site paris sportif bonus sans depot|site paris sportif canada|site paris sportif comparatif|site paris sportif depot 5
euro|site paris sportif en ligne|site paris
sportif foot|site paris sportif france|site paris
sportif gratuit|site paris sportif hors arjel|site paris sportif hors arjel france|site paris sportif meilleur cote|site paris sportif nouveau|site paris sportif offre de bienvenue|site paris sportif paypal|site paris sportif remboursement
cash|site paris sportif remboursé en cash|site
paris sportif retrait instantané|site paris sportif sans carte bancaire|site paris sportif sans depot|site paris sportif suisse|site paris sportifs|site paris sportifs belgique|site paris sportifs en ligne|site
paris sportifs france|site paris sportifs hors arjel|site
paris sportifs suisse|site pour analyse paris sportif|site pour
paris sportif|site pronostic paris sportif|site
statistique paris sportif|site suisse paris sportif|sites de pari sportif|sites
de paris sportif|sites de paris sportifs|sites de paris
sportifs arjel|sites de paris sportifs autorisés en france|sites de paris sportifs belgique|sites de paris sportifs bonus|sites
de paris sportifs en belgique|sites de paris sportifs en france|sites de paris sportifs en ligne|sites de paris sportifs gratuits|sites de paris sportifs gratuits sans dépôt|sites de
paris sportifs suisse|sites pari sportif|sites paris sportif|sites paris sportifs|sites
paris sportifs arjel|sites paris sportifs belgique|sites paris sportifs france|sites paris sportifs hors arjel|sites paris sportifs suisse|so foot paris
sportif|so foot paris sportifs|specialiste tennis paris
sportif|statistique foot paris sportif|statistique paris sportif|statistique
paris sportif foot|statistique tennis paris sportif|statistiques football paris sportifs|statistiques paris sportifs|strategie de paris sportif|stratégie big whale paris sportif|stratégie de paris
sportifs|stratégie gagnante paris sportifs|stratégie pari sportif|stratégie paris sportif|stratégie paris sportifs|stratégie paris sportifs forum|stratégie pour gagner
au paris sportif|stratégies paris sportifs|suisse paris sportif|suisse paris sportifs|systeme 2 3 paris sportif|systeme 3
4 paris sportif|systeme de cote paris sportif|systeme de paris sportif|systeme pari sportif|systeme paris sportif|systeme
paris sportifs|systeme reducteur paris sportif|système paris sportif|tableau bankroll paris sportif|tableau
cote paris sportif|tableau de paris sportif|tableau de suivi paris sportifs|tableau excel
bankroll paris sportif|tableau excel paris sportif|tableau excel
paris sportif gratuit|tableau excel paris sportifs|tableau
excel pour paris sportif|tableau gestion bankroll paris sportif|tableau montante paris
sportif|tableau paris sportif|tableau paris sportif excel|tableau roi paris
sportifs|tableau statistique paris sportif|tableau suivi
Hi my loved one! I want to say that this post is amazing, nice written and
include approximately all significant infos. I would like to see more posts like this .
Review my homepage: best realtor in State College PA
I know this if off topic but I’m looking into starting my own blog
and was curious what all is needed to get setup?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet savvy so I’m not 100% certain. Any suggestions or
advice would be greatly appreciated. Appreciate
it
my webpage; best real estate agent in Little Rock AR
Polis India menutup sebuah hospital swasta manakala kakitangannya didakwa dengan tuduhan membunuh
selepas seorang bayi yang baru lahir maut dibaham beberapa ekor anjing di
dalam sebuah bilik pembedahan, kata seorang penyiasat pada
Selasa (14 Jan). CHUM PHUANG, THAILAND: Seekor anjing di utara Thailand menyelamatkan seorang bayi baru lahir yang
didakwa ditanam hidup-hidup oleh ibunya iaitu seorang remaja,
15 tahun. Menurut Encik Panuwat Puttakam, seorang pegawai di stesen polis Chum Phuang,
kepada Bangkok Post, remaja itu kini dibawah jagaan ibu bapanya dan seorang pakar psikologi.
Encik Vitisak berkata jika anjing itu tidak dituntut
oleh sesiapa, beliau ingin membawa haiwan itu
pulang ke rumahnya di timur laut Thailand. Para penduduk tempatan segera membawa bayi
itu ke hospital dan doktor mengesahkannya berada dalam keadaan sihat.
Beliau menekankan bahawa tujuan memelihara anjing-anjing itu di rumah
perlindungannya adalah untuk melindungi haiwan tersebut daripada bahaya,
memastikan ia sihat dan mencarikan ia sebuah keluarga yang akan memeliharanya dengan baik.
Anjing itu kemudian dihantar menggunakan bot ke pelabuhan selatan Songkhla pada Isnin dan disahkan dalam
keadaan baik selepas dibawa ke kumpulan perlindungan haiwan Watchdog Thailand.
Sungguhpun pasangan itu bertekad untuk menyelamatkan sebanyak anjing
yang mereka mampu, sebahagian besar sumber tempat perlindungan itu tertumpu kepada menjaga kucing.
Bagaimanapun, setelah menjaga anjing-anjing
itu sedari ia diabaikan waktu kecil lagi, pasangan tersebut mula sayang pada anjing dan berpisah dengan haiwan itu
sebelum menyerahkannya kepada sebuah keluarga mungkin sukar.
Very nice article, totally what I wanted to find.
my webpage :: real estate agent Clarks Summit PA
I truly love your blog.. Excellent colors & theme. Did you
make this site yourself? Please reply back as I’m planning to create my own site and would love to learn where you got
this from or just what the theme is called. Appreciate it!
Here is my blog … real estate agent Clarks Summit PA
This blog was… how do I say it? Relevant!!
Finally I’ve found something which helped me. Many thanks!
Hmm it seems like your blog ate my first comment (it was extremely long) so I guess I’ll just sum
it up what I submitted and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog writer but I’m still new to
the whole thing. Do you have any helpful hints for inexperienced blog writers?
I’d really appreciate it.
I just like the helpful info you provide in your articles.
I will bookmark your blog and test again right here frequently.
I’m moderately certain I will be told many new stuff right here!
Best of luck for the next!
With thanks. Plenty of facts.
I’m extremely inspired with your writing talents as smartly as with the structure to your weblog.
Is that this a paid theme or did you modify it yourself?
Either way keep up the nice high quality writing, it is uncommon to
peer a great weblog like this one today..
Good post. I learn something totally new and challenging
on websites I stumbleupon everyday. It will always be helpful to read through content from other writers and practice a little something from other sites.
бездепозитные бонусы в казино лев
What’s up all, here every person is sharing such knowledge,
so it’s good to read this weblog, and I used to
go to see this blog daily.
Today, I went to the beachfront with my kids. I found a sea shell and gave it to
my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell
to her ear and screamed. There was a hermit crab inside and
it pinched her ear. She never wants to go back! LoL I know this is completely off
topic but I had to tell someone!
Your style is really unique in comparison to other people I’ve read stuff from.
Many thanks for posting when you’ve got the opportunity, Guess I will
just bookmark this page.
Fascinating blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple adjustements would really make my blog shine.
Please let me know where you got your design. Bless you
That is very interesting, You’re an excessively skilled blogger.
I have joined your rss feed and stay up for seeking more of your fantastic post.
Also, I’ve shared your website in my social networks
Thanks for sharing your thoughts on With thanks. Regards
Hi this is kind of of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code
with HTML. I’m starting a blog soon but have no coding skills so I
wanted to get advice from someone with experience. Any help would be
enormously appreciated!
my homepage best real estate agent in Wellington FL
Wow, superb blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of
your website is magnificent, as well as the content!
Excellent blog here! Also your website loads up fast!
What host are you using? Can I get your affiliate
link to your host? I wish my site loaded up as fast as yours
lol
Feel free to surf to my site: real estate agent Tacoma WA
Very good article. I certainly appreciate this site.
Keep writing!
my blog post – best realtor in Little Rock AR
Helpful write ups, Appreciate it! https://bookmarkplaces.com/story20208600/betflik168
These are truly impressive ideas in about blogging. You have touched some nice points here.
Any way keep up wrinting.
Here is my website: realtor in Clarks Summit PA
It’s awesome designed for me to have a web page, which is valuable designed for
my know-how. thanks admin
Hey There. I found your blog using msn. That is
a really smartly written article. I will be sure to bookmark it and return to read extra of your helpful information. Thanks for the post.
I will definitely comeback.
Here is my web site; best real estate agent in Tacoma WA
I am truly thankful to the holder of this site who has
shared this enormous post at here.
Check out my web-site: best real estate agent in Little Rock AR
What’s up to every one, as I am actually keen of reading this website’s post to be updated daily.
It contains pleasant material.
You’ve made some decent points there. I looked on the web for additional information about the issue and
found most people will go along with your views on this website.
Also visit my site – best real estate agent in Tacoma WA
buy backlinks, link exchange, free gift card, congratulations you have won, claim your prize,
you have been selected, click here to claim, you won’t believe, one weird trick, what happened next will
shock you, shocking truth, secret revealed, limited time offer, special promotion, act now,
don’t miss out, buy now, best price, risk-free trial, get rich quick, make money fast,
work from home, no credit check, miracle cure, lose weight fast, free viagra, no prescription needed, online casino, free spins,
meet singles, hot singles in your area, replica
watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis,
Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster,
Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker, CryptoWall,
DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu,
Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID,
Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex,
Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus,
PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker,
Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote,
TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos,
WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS,
ZeroAccess, Zloader, Zlob, Zotob
Feel free to surf to my web site :: fake designer labels
I’d like to thank you for the efforts you have put in writing this website.
I am hoping to see the same high-grade blog posts by you later on as well.
In truth, your creative writing abilities has encouraged me
to get my own, personal site now 😉
You made the point. https://www.pensionplanpuppets.com/users/porterfieldli
перейти на сайт Mega даркнет
My programmer is trying to convince me to move to .net
from PHP. I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using WordPress on various websites for about a
year and am concerned about switching to another platform.
I have heard good things about blogengine.net. Is there a way I can transfer all
my wordpress posts into it? Any help would be really appreciated!
Here is my site; best realtor in Tacoma WA
Hey! This is kind of off topic but I need some help from
an established blog. Is it difficult to set up your own blog?
I’m not very techincal but I can figure things
out pretty fast. I’m thinking about making my own but I’m not sure where to begin.
Do you have any points or suggestions? With thanks
Marvelous, what a webpage it is! This website presents helpful data
to us, keep it up.
I am extremely impressed together with your writing abilities
and also with the format in your weblog. Is this a paid topic or did you customize it yourself?
Anyway stay up the excellent quality writing, it’s uncommon to peer a great weblog like this one these days..
Do you mind if I quote a couple of your posts as long as I provide credit and sources back to your blog?
My blog is in the very same niche as yours and my users would
genuinely benefit from some of the information you present here.
Please let me know if this ok with you. Regards!
Also visit my homepage; best realtor in State College PA
Perfeçionâ l’arte intrigâ da construçion de ligammi o l’é diffiçile. Pe-i ciù tanti sciti web e blog, sto chì o l’é un settô che porrieivan no mai dominâ do tutto.
I loved as much as you will receive carried out right here.
The sketch is tasteful, your authored material stylish.
nonetheless, you command get got an nervousness over that you wish
be delivering the following. unwell unquestionably come more
formerly again since exactly the same nearly a lot often inside case you shield this hike.
I have read so many articles or reviews on the topic of the blogger lovers except this article is actually a
pleasant piece of writing, keep it up.
Lowe’s Return Policy is designed to be straightforward, convenient, and customer-friendly.
With Lowe’s “Returns Made Easy” approach, you can shop confidently, knowing
that we’re here to assist you if you need to return or exchange a
product
You actually revealed this perfectly!
This is the perfect blog for anybody who wants to find out about this topic.
You know a whole lot its almost hard to argue with you (not that I really will
need to…HaHa). You certainly put a new spin on a subject that’s been written about for ages.
Excellent stuff, just wonderful!
Today, I went to the beach front with my children. I found a sea shell and gave it to my 4
year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed.
There was a hermit crab inside and it pinched her ear. She
never wants to go back! LoL I know this is totally off topic but I
had to tell someone!
Great web site. Plenty of useful info here. I am sending it to a few buddies
ans additionally sharing in delicious. And of course,
thanks to your effort!
lingkeu guchug-ilaneun bogjabhan gisul-eul wanbyeoghage guhyeonhaneun geos-eun eolyeobseubnida. daebubun-ui websaiteuwa beullogeuneun i bubun-eul wanbyeoghage sugdalhaji moshal sudo issseubnida.
Its like you learn my mind! You appear to understand a lot about
this, like you wrote the e book in it or something. I think that you simply can do with a few p.c.
to force the message house a bit, but instead
of that, that is magnificent blog. An excellent read. I’ll definitely
be back.
Attractive section of content. I just stumbled upon your web
site and in accession capital to assert that I acquire in fact enjoyed account your blog posts.
Any way I will be subscribing to your feeds and even I achievement you access consistently quickly.
Stop by my webpage best real estate agent in Cibolo TX
This is a topic which is near to my heart… Thank you!
Exactly where are your contact details though?
Awesome website you have here but I was wondering if you knew of
any community forums that cover the same topics talked about here?
I’d really like to be a part of group where I can get feed-back from other
knowledgeable people that share the same interest.
If you have any suggestions, please let me know. Cheers!
Hello, i read your blog from time to time and i own a similar one and i was just curious if you get a lot of spam remarks?
If so how do you protect against it, any plugin or anything you can recommend?
I get so much lately it’s driving me mad so any help
is very much appreciated.
Also visit my site: best realtor in Fort Lauderdale FL
Heya i am for the first time here. I found this board and I find It really helpful & it helped me out a lot.
I am hoping to give one thing back and aid others like you aided me.
whoah this weblog is excellent i love studying your articles.
Keep up the good work! You understand, a lot of persons are hunting round for this info, you could help them greatly.
Its like you read my mind! You seem to know so much about this,
like you wrote the book in it or something. I think that you can do with a few pics
to drive the message home a little bit, but instead of that, this is magnificent blog.
A great read. I’ll definitely be back.
Also visit my web blog; real estate agent St. George LA
LIGACOR adalah platform game slot online yang selalu memanjakan pemain dengan memberi kemenangan maximal dan stabil
serta member aktif disini akan mendapat bonus yang sangat besar.
ศิลปะการสร้างลิงก์ที่ซับซ้อนนั้นยากที่จะทำให้สมบูรณ์แบบ สำหรับเว็บไซต์และบล็อกส่วนใหญ่แล้ว นี่เป็นสิ่งที่พวกเขาอาจไม่เคยเชี่ยวชาญได้อย่างเต็มที่
Do you have a spam problem on this site; I also am a blogger, and I was curious about your situation; we have created some nice
procedures and we are looking to trade solutions with others,
please shoot me an e-mail if interested.
Check out my web blog … realtor in Salt Lake UT
You could definitely see your expertise within the article you write.
The world hopes for even more passionate writers like you who are not afraid to
mention how they believe. At all times follow your heart.
Very descriptive article, I enjoyed that bit. Will there be a part
2?
Hmm it seems like your blog ate my first comment (it was super long) so I guess I’ll just sum it up
what I had written and say, I’m thoroughly enjoying your
blog. I as well am an aspiring blog writer but I’m still new to everything.
Do you have any points for beginner blog writers? I’d really appreciate
it.
my blog post: real estate agent Fort Lauderdale FL
Nice post. I was checking continuously this blog and I am impressed!
Very helpful info particularly the last part
🙂 I care for such info much. I was seeking this certain info for a long time.
Thank you and good luck.
It’s enormous that you are getting ideas from this post as well
as from our dialogue made at this time.
Hello! I’ve been reading your site for some time now and finally got
the bravery to go ahead and give you a shout out
from Humble Tx! Just wanted to mention keep up the good job!
My web blog real estate agent Salt Lake UT
бездепозитные бонусы казахстан за регистрацию в казино
Everything is very open with a very clear clarification of
the issues. It was definitely informative. Your site is very useful.
Many thanks for sharing!
Feel free to surf to my website: best realtor in Cibolo TX
1xbet промокод на день рождения
Thanks for some other informative site. Where else may I am getting that type of info written in such an ideal approach? I have a undertaking that I am simply now running on, and I’ve been at the look out for such info.
fortinet vpn
Howdy just wanted to give you a quick heads up. The text in your post
seem to be running off the screen in Firefox. I’m not sure if this is a formatting issue or something to do with browser
compatibility but I thought I’d post to let you know.
The design and style look great though! Hope you get
the issue resolved soon. Kudos
Feel free to surf to my site … realtor in Fort Lauderdale FL
goGLOW Houstoon Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, USᎪ
(713) 364-3256
Chemical Peels Benefits Clinic
I wanted to thank you for this very good read!!
I certainly loved every bit of it. I have you bookmarked
to check out new things you post…
An impressive share! I have just forwarded this onto a colleague who was doing a little homework on this.
And he in fact bought me lunch simply because I found it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanx for spending some time to talk about this matter
here on your site.
Here is my web site; best realtor in Tacoma WA
What a stuff of un-ambiguity and preserveness of
valuable knowledge on the topic of unexpected feelings.
It’s going to be end of mine day, however before end I am reading this wonderful article
to improve my experience.
Pretty! This was an extremely wonderful article. Thanks for supplying this information.
You actually make it appear so easy with your presentation however I to find this matter to be really something which I believe I might by no means understand.
It kind of feels too complicated and very extensive for me.
I’m looking forward on your subsequent submit, I’ll attempt to
get the hold of it!
Excellent post however I was wondering if you could write a litte more on this topic?
I’d be very grateful if you could elaborate a little
bit further. Cheers!
Here is my page: realtor in Chula Vista CA
Hi to all, how is all, I think every one is getting more from this website, and your views
are nice in favor of new users.
Here is my web blog: real estate agent Little Rock AR
Hey there just wanted to give you a quick heads up. The words in your article seem to be running off the screen in Chrome.
I’m not sure if this is a format issue or something to
do with internet browser compatibility but I figured I’d post to let you know.
The design and style look great though! Hope you get the issue
solved soon. Thanks
My web page; real estate agent Chula Vista CA
Hey! I know this is kind of off-topic but I needed to ask.
Does operating a well-established blog like yours require a lot of work?
I’m brand new to running a blog however I do write in my diary every day.
I’d like to start a blog so I can share my experience and feelings online.
Please let me know if you have any suggestions or tips for new aspiring bloggers.
Thankyou!
There’s definately a great deal to learn about this subject.
I really like all the points you made.
My site; realtor in St. George LA
This design is wicked! You certainly know how to keep a reader amused.
Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Great job.
I really enjoyed what you had to say, and more than that, how you presented it.
Too cool!
Also visit my website; real estate agent Chula Vista CA
Hi, I do think this is an excellent web site. I stumbledupon it 😉 I am going to come back yet again since I book marked
it. Money and freedom is the greatest way to change,
may you be rich and continue to guide other people.
Auto index slot.
здесь Mega darknet
저희 수원출장마사지 서비스는 바쁜 현대인들에게
맞춤 휴식을 선사하는 최고의 선택입니다. 이제 시간과 장소의 제약 없이 전문 마사지사의
체계적인 관리를 받아보세요.
Wow that was odd. I just wrote an really long comment but after I clicked submit
my comment didn’t appear. Grrrr… well I’m not writing all that over
again. Anyways, just wanted to say excellent blog!
goGLOW Houstonn Heights
1515 Studemont Տt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
microdermabrasion process DIY
goGLOW Houston Heights
1515 Studemont Ⴝt Suite 204, Houston,
Texas, 77007, USA
(713) 364-3256
bеst skincare clinic routine (https://padlet.Com/angelbailbonds2022Snfdh/bookmarks-hjfae2tug1g8tjp/wish/x5A7arG8R2lXQwr6)
Oprosti za sliko, res mi je bila všeč, res mi je bilo vse všeč, tvoja objava mi vliva upanje, kaj je to?
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, USA
(713) 364-3256
Goglow Safe
부산출장마사지는 ‘부산출장안마’ 또는 ‘부산홈타이’
등으로도 불리며, 고객이 계신 곳으로
전문 테라피스트가 직접 찾아가 마사지를 제공하는 서비스입니다.
Hola! I’ve been following your web site for a while now and finally got the bravery to go ahead and give you a shout
out from Austin Texas! Just wanted to say keep up the fantastic work!
Look at my web-site – best real estate agent in Chula Vista CA
Regards! Loads of posts!
Valuable info. Lucky me I discovered your web site by chance, and I’m surprised why this twist of fate did not came about earlier! I bookmarked it.
Qfinder Pro
I like the helpful info you provide in your articles.
I will bookmark your blog and check again here regularly.
I’m quite sure I’ll learn a lot of new stuff right here!
Best of luck for the next!
My web-site best real estate agent in Fort Lauderdale FL
Hi everyone, it’s my first go to see at this web page, and article is really
fruitful in support of me, keep up posting these types
of content.
Feel free to surf to my site :: realtor in Little Rock AR
Since the admin of this web page is working, no doubt very rapidly it will be well-known, due to
its quality contents.
бездепозитные бонусы за регистрацию в казино с выводом
Hey there! I know this is kind of off topic but I was wondering if you knew where I could
locate a captcha plugin for my comment form? I’m using the same blog platform as yours
and I’m having trouble finding one? Thanks a lot!
I blog often and I seriously thank you for your content.
The article has truly peaked my interest. I am going to book mark your site and keep
checking for new details about once per week. I subscribed to your Feed too.
I’ve learn several just right stuff here. Certainly value bookmarking
for revisiting. I wonder how so much effort you
place to make this sort of fantastic informative web site.
Excellent article! We are linking to this
great article on our site. Keep up the great writing.
Amazing blog! Do you have any helpful hints for aspiring writers?
I’m planning to start my own blog soon but I’m a little lost on everything.
Would you recommend starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m completely confused ..
Any ideas? Thanks a lot!
my website: PetCareShed Tactical Dog Harness
I’ve learn some excellent stuff here. Certainly value bookmarking for revisiting.
I surprise how much effort you set to create the sort
of wonderful informative site.
It’s not my first time to pay a visit this
web site, i am visiting this web site dailly and get fastidious information from here daily.
I’m extremely inspired together with your writing abilities as smartly as
with the structure on your weblog. Is that this a paid subject matter or did you
modify it yourself? Anyway stay up the excellent quality writing, it is rare to peer a great weblog like this one
these days..
Thanks in support of sharing such a nice thinking, piece of writing is pleasant, thats
why i have read it entirely
Here is my homepage :: mesinslot link gacor
Hi there! I understand this is kind of off-topic
however I had to ask. Does managing a well-established website such
as yours take a massive amount work? I’m completely new to blogging but I do write in my journal everyday.
I’d like to start a blog so I will be able to share my experience
and feelings online. Please let me know if you have any kind of ideas or tips for new aspiring bloggers.
Thankyou!
I get pleasure from, cause I discovered just what I used to be having a look for.
You’ve ended my 4 day long hunt! God Bless you man. Have a nice day.
Bye
It’s very easy to find out any topic on web as compared to books, as I found this post at this site.
Here is my web page :: custom retreat
Awesome blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple adjustements would really make my blog jump out.
Please let me know where you got your design. Kudos
Woah! I’m really digging the template/theme of this website.
It’s simple, yet effective. A lot of times it’s tough to get that “perfect balance” between usability and appearance.
I must say you have done a awesome job with this. In addition, the
blog loads extremely fast for me on Safari. Outstanding Blog!
Also visit my blog; personal retreat
Hey there, You’ve done a great job. I’ll definitely digg it and personally suggest to my friends.
I’m confident they’ll be benefited from this
web site.
I don’t even know how I ended up here, but I thought this post was great.
I do not know who you are but definitely you’re going to a
famous blogger if you are not already 😉 Cheers!
Look into my blog: f1 track wall art
Hey there! I just wanted to ask if you ever have any trouble with
hackers? My last blog (wordpress) was hacked and I ended up losing a few months of hard work
due to no back up. Do you have any solutions to stop hackers?
Woah! I’m really loving the template/theme of this website.
It’s simple, yet effective. A lot of times it’s hard to get that “perfect balance” between superb usability
and visual appeal. I must say you have done a amazing job with this.
Additionally, the blog loads extremely quick for me on Safari.
Superb Blog!
Look into my page :: mesinslot link gacor
Wow, marvelous blog layout! How long have you been blogging for?
you make running a blog glance easy. The full glance of your website is fantastic, let alone the content!
Thanks on your marvelous posting! I quite enjoyed reading
it, you happen to be a great author. I will be sure to bookmark your blog and
will come back in the foreseeable future. I want to encourage you to continue your
great posts, have a nice day!
Have a look at my web site … wall tile decor
I was recommended this website by my cousin. I’m not sure whether this post how big is the huge dragon jellycat written by him
as no one else know such detailed about my problem. You’re wonderful!
Thanks!
Good way of telling, and pleasant article to get facts on the topic of my
presentation subject matter, which i am going to
present in college.
Currently it looks like Movable Type is the best blogging platform available right now.
(from what I’ve read) Is that what you’re using on your
blog?
goGLOW Houston Heights
1515 Studedmont Տt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
skin rejuvenation neаr me (padlet.com)
What’s up friends, its impressive post on the topic of cultureand entirely defined, keep it up all the time.
You have made some really good points there. I checked on the net to learn more about the issue and found most people will go along with your views
on this web site.
my webpage … Schilder Geraardsbergen
I always emailed this webpage post page to all my
associates, because if like to read it after that my links will too.
It’s impressive that you are getting thoughts from this article as well as from our argument made at this place.
my site; yoga retreat center
I’m impressed, I must say. Rarely do I come across a blog that’s both educative and engaging, and let me tell you,
you have hit the nail on the head. The problem is something
not enough people are speaking intelligently
about. I’m very happy that I found this during my hunt for something regarding this.
I have read so many articles or reviews on the topic
of the blogger lovers except this piece of writing is actually a good piece of writing,
keep it up.
Hey there! I could have sworn I’ve been to this website before but
after reading through some of the post I realized it’s new to
me. Nonetheless, I’m definitely glad I found it and I’ll be
book-marking and checking back often!
My blog – mesinslot link gacor
Amazing! Its actually amazing post, I have got
much clear idea concerning from this piece of writing.
Check out my blog :: new year spiritual retreat mexico
Cheers. Fantastic stuff.
Excellent blog! Do you have any recommendations for aspiring writers?
I’m planning to start my own site soon but I’m a little lost on everything.
Would you recommend starting with a free platform like WordPress or
go for a paid option? There are so many choices out there that
I’m totally overwhelmed .. Any tips? Many thanks!
Feel free to visit my blog f1 circuit posters
Pretty section of content. I just stumbled upon your web site and in accession capital to say
that I acquire in fact enjoyed account your weblog posts.
Anyway I’ll be subscribing to your feeds or even I success you access
consistently fast.
Hurrah! Finally I got a website from where I can actually take useful data concerning my study and knowledge.
Have a look at my blog post – Psilocybin retreat
Hello, Neat post. There’s a problem with your site in web explorer,
could test this? IE still is the market leader and a good portion of folks will omit your magnificent
writing due to this problem.
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored material stylish.
nonetheless, you command get got an nervousness over that you wish be delivering the following.
unwell unquestionably come further formerly again as exactly the same nearly very often inside case you shield this increase.
Look at my blog :: Youth basketball league
goGLOW Houston Heights
1515 Stuemont Ⴝt Suite 204, Houston,
Texas, 77007, UᏚA
(713) 364-3256
Bookmarks
Right away I am going to do my breakfast, when having my breakfast coming over again to read more news.
My website: home depot tile porcelain
certainly like your website however you have
to check the spelling on several of your posts. Several of them are rife with spelling problems and I find it
very bothersome to inform the truth then again I’ll definitely come back again.
Definitely believe that which you stated.
Your favorite reason appeared to be on the net the simplest thing to be aware of.
I say to you, I certainly get annoyed while people consider worries
that they plainly don’t know about. You managed to hit the nail upon the top and
also defined out the whole thing without having side-effects , people can take a signal.
Will probably be back to get more. Thanks
Here is my blog post … Tactical Dog Harness
Whats up very nice website!! Guy .. Excellent ..
Wonderful .. I will bookmark your web site and take the feeds additionally?
I’m glad to find numerous helpful info here within the publish, we need
work out extra strategies on this regard, thank
you for sharing. . . . . .
Visit my homepage :: mesinslot
Can you tell us more about this? I’d like to find out some additional
information.
Also visit my web page; mesinslot
It’s hard to come by experienced people in this particular subject, but
you seem like you know what you’re talking about! Thanks
Awin’s complete tracking answer permits advertisers to report and report on an in depth vary of information points, including basket value, variety of products, product kind, new or existing customers, use of a coupon code and click-to-sale lag time. Awin also gives a variety of further technical products that can be used alongside each affiliate program to optimize and enhance an advertiser’s providing, including cross-gadget monitoring, coupon attrubution and fee by basket worth. In addition, our complete monitoring resolution works with any browser to make sure you will never miss a sale. Influencer tracking is a key feature of Awin’s reporting, permitting advertisers to see which publishers are having an impact on consumers and encouraging clicks throughout the purchase journey with out being the last touchpoint, and subsequently potentionally being beneath-rewarded when trying at the wider channel efficiency. SingleView is a data-pushed, unbiased, multi-touch attribution (MTA) platform that solves the most typical query in advertising and marketing: ‘Which sorts of media provide the greatest value?
Take a look at my page … https://www.postoffice3-dfactory.com/API/cli/018%20/6362/FDB014415/aHR0cHM6Ly9iYmFybG9jay5jb20vaW5kZXgucGhwL1VzZXI6SG9sbGlzTW90dGVy/dXJsPWh0dHA6Ly9mZWVkcy5mZWVkYnVybmVyLmNvbS9kZWJhdGVwb3N0L0xQbXc
O ꯄꯥꯡꯊꯣꯀꯄꯥ ꯌꯥꯝꯅꯥ ꯂꯨꯏ꯫ ꯑꯌꯥꯝꯕꯥ ꯋꯦꯕꯁꯥꯏꯠ ꯑꯃꯁꯨꯡ ꯕ꯭ꯂꯣꯒꯁꯤꯝꯒꯤ ꯑꯣꯣꯣꯣꯠꯤꯣꯤꯣꯠꯤ O ꯉꯃꯗꯕꯥ ꯋꯥꯐꯝ ꯑꯃꯅꯤ꯫
What’s up i am kavin, its my first time to commenting anyplace, when i read this piece
of writing i thought i could also make comment due to this good paragraph.
Here is my page retreat center mexico
Excellent beat ! I wish to apprentice while you amend your website, how can i subscribe for a blog site?
The account helped me a acceptable deal.
I had been a little bit acquainted of this your broadcast offered bright clear
idea
Here is my web page formula 1 track maps
Fırat Engin bahis siteleri, Casino Siteleri Nargül Engin, Slot Siteleri Hüseyin Engin, Deneme Bonusu Veren Siteler Ahmet Engin, Mehdi Deneme Bonusu,
Mehdi Deneme bonusu veren siteler
This site was… how do I say it? Relevant!! Finally I have found something which helped me.
Thanks a lot!
Also visit my webpage :: Youth basketball league
Pretty nice post. I just stumbled upon your weblog and wanted to say that I have truly enjoyed browsing your blog posts.
After all I will be subscribing to your rss feed and
I hope you write again soon!
Take a look at my web-site: Youth basketball travel team
Fantastic information, Cheers!
Lumina Solar stands out as the premier solar
panel installers in Delaware due to their superior dedication to quality and customer satisfaction.
They deliver customized solar systems that cater to the distinctive energy demands of each resident and business.
Their team of proficient professionals ensures efficient installation with great attention to
precision and safety. Lumina Solar uses advanced technology and high-quality solar panels that ensure
optimal efficiency and durability. Customers recognize their
clear pricing and detailed consultations which assist in creating educated decisions without any surprise charges.
They deliver complete services from first assessment to concluding installation and
ongoing maintenance ensuring a smooth experience. Lumina Solar
is committed to promoting sustainable energy methods while
aiding clients reduce their carbon footprint and energy bills.
Their strong reputation in Delaware is built on years of
trustworthy service and excellent customer reviews.
They remain current on the newest industry standards and regulations
which reflect in their excellent workmanship.
Lumina Solar also offers exceptional customer support
that is attentive and knowledgeable, resolving any
concerns efficiently. Their commitment to excellence and environmental responsibility renders them
the ideal choice for solar panel installation in Delaware.
Choosing Lumina Solar represents supporting a eco-friendly future with a trusted partner who values integrity
and innovation. Their proven track record and enthusiasm for renewable energy position them as the foremost
solar panel installers in the region.
Good post. I learn something totally new and challenging on blogs
I stumbleupon every day. It’s always interesting to read through
articles from other authors and practice something from their websites.
Feel free to surf to my site :: mesinslot
You’re so cool! I don’t believe I have read a single thing like this before.
So wonderful to discover someone with genuine thoughts on this topic.
Really.. thanks for starting this up. This web site is something that is required on the internet,
someone with a bit of originality!
This paragraph provides clear idea for the new visitors of blogging, that truly how to do running a
blog.
Also visit my web page :: mesin slot
This is the perfect blog for anyone who wishes to find out about this topic.
You understand a whole lot its almost tough
to argue with you (not that I personally will need to…HaHa).
You definitely put a brand new spin on a topic which has been discussed for years.
Great stuff, just excellent!
Feel free to surf to my page: formula 1 prints
This is the right blog for anybody who hopes to find out about this topic.
You know a whole lot its almost hard to argue with you (not
that I actually would want to…HaHa). You certainly put a brand
new spin on a topic that has been discussed for years.
Excellent stuff, just great!
Chien YH, Lee NC, Thurberg BL, Chiang SC, Zhang XK, Keutzer J, Huang AC, Wu MH, Huang PH, Tsai FJ, Chen YT, Hwu WL. Pompe illness in infants: enhancing the prognosis by newborn screening and early therapy. Fukuda T, Roberts A, Plotz PH, Raben N. Acid alpha-glucosidase deficiency (Pompe disease). Curr Neurol Neurosci Rep. Kishnani PS, Hwu WL, Mandel H, Nicolino M, Yong F, Corzo D; Infantile-Onset Pompe Disease Natural History Study Group. A retrospective, multinational, multicenter examine on the natural history of infantile-onset Pompe illness. J Pediatr. 2006 May;148(5):671-676. Kishnani PS, Steiner RD, Bali D, Berger K, Byrne BJ, Case LE, Crowley JF, Downs S, Howell RR, Kravitz RM, Mackey J, Marsden D, Martins AM, Millington DS, Nicolino M, O’Grady G, Patterson MC, Rapoport DM, Slonim A, Spencer CT, Tifft CJ, Watson MS. Pompe illness prognosis and management guideline. Genet Med. 2006 May;8(5):267-88. Hout HM, Hop W, van Diggelen OP, Smeitink JA, Smit GP, Poll-The BT, Bakker HD, Loonen MC, de Klerk JB, Reuser AJ, van der Ploeg AT. The pure course of infantile Pompe’s illness: 20 unique circumstances compared with 133 circumstances from the literature. Ploeg AT, Reuser AJ. The knowledge on this site shouldn’t be used instead for skilled medical care or recommendation. Contact a health care provider if you have questions on your health.
My blog post: https://www.fabiansmith.ru/bitrix/redirect.php?goto=https://www.yewiki.org/User:IngridFleischer
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored subject matter stylish.
nonetheless, you command get got an edginess over that you wish be delivering the following.
unwell unquestionably come more formerly again as exactly the same nearly very often inside case you shield this hike.
Look at my website … formula 1 wall art
I’ve been browsing online greater than 3 hours these days, but I never found any
fascinating article like yours. It is pretty value sufficient for me.
In my opinion, if all website owners and bloggers made excellent content material
as you did, the web shall be much more helpful than ever
before.
It’s amazing to pay a quick visit this web page and reading the views of all mates regarding this
piece of writing, while I am also keen of getting knowledge.
De site casino is leerzaam. Ik kom zeker terug!
https://lalabet-sport-netherlands.nl/
Pretty nice post. I just stumbled upon your weblog
and wished to say that I have truly enjoyed surfing around your blog posts.
After all I will be subscribing to your rss feed and I hope you write again soon!
Feel free to surf to my webpage :: formula 1 wall art
Hello Dear, are you actually visiting this web page regularly, if
so then you will without doubt get pleasant experience.
Hello to all, how is everything, I think every one is getting more
from this site, and your views are nice in support of new
users.
magnificent post, very informative. I’m wondering why the other experts of this sector don’t realize
this. You must proceed your writing. I’m
confident, you’ve a great readers’ base already!
Stop by my homepage; Sports training
I’m not that much of a internet reader to be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your site to come back in the future.
Many thanks
The legality of cannabinoid products in the United States is dependent on their concentration and source. CBD is legally available in the United States, but it must be derived from imported high-https://scmcs.ru/bitrix/redirect.php?goto=http://knowledge.thinkingstorm.com/UserProfile/tabid/57/userId/2906155/Default.aspx, low-THC hemp. CBD itself it not listed under the Controlled Substances Act, so it is legal in all 50 states, provided the CBD is not extracted from marijuana. If derived from marijuana, CBD is illegal unless obtained through a state-regulated medical marijuana program, or in a state that permits recreational marijuana use. Marijuana and THC are both specifically listed in the U.S. Controlled Substances Act and therefore prohibited under federal law. 36 U.S. states and Washington D.C. THC, provided it’s recommended by a licensed physician. Medical marijuana containing higher concentrations of THC is legal in Ohio. Dispensaries across the state offer products with THC and CBD in isolated forms, as well as different ratios between the two cannabinoids.
Awesome article.
проверить сайт куш казино официальный
Hi there, I found your site by means of Google at the same time as searching for a comparable topic, your site
came up, it seems to be good. I’ve bookmarked it in my google bookmarks.
Hi there, just become alert to your blog thru Google, and located that it’s truly informative.
I am gonna watch out for brussels. I’ll appreciate when you continue this in future.
Lots of folks shall be benefited from your writing. Cheers!
узнать больше vodkabet новый сайт
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
anti-aging skincare tips explained
Hey There. I discovered your blog the usage of msn. That is a very smartly written article.
I’ll make sure to bookmark it and return to learn more of your helpful
info. Thanks for the post. I will certainly return.
My website Youth basketball league flagstaff
I blog frequently and I genuinely appreciate your information. The article has
really peaked my interest. I am going to book mark your blog and
keep checking for new information about once a week. I subscribed to your Feed as
well.
Very good information. Lucky me I discovered your blog by chance (stumbleupon).
I have bookmarked it for later!
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ⲤA 92626, Unitedd Ⴝtates
fred w frank bail Bonds – Padlet.com –
Heya i am for the first time here. I came across this board and I find It really
useful & it helped me out a lot. I hope to give something back and aid others
like you aided me.
Also visit my blog … Youth basketball flagstaff
This article offers clear idea for the new viewers
of blogging, that genuinely how to do blogging and site-building.
my blog post: PetCareShed Tactical Dog Harness
Way cool! Some extremely valid points! I appreciate you writing this write-up plus
the rest of the website is also really good.
Hello, I wish for to subscribe for this website to
take most recent updates, thus where can i do it please help.
I think this is one of the most significant information for me.
And i am glad reading your article. But want to remark on few
general things, The site style is wonderful, the articles is
really great : D. Good job, cheers
Lubię strona Mostbet, jest komfortowa w użytkowaniu!
https://mostbet-kasina.cz/zkusenosti
I do not know whether it’s just me or if perhaps everyone else encountering issues with your blog.
It looks like some of the written text on your posts are running
off the screen. Can somebody else please provide feedback and let me know if
this is happening to them too? This may be a problem with my internet browser because I’ve had this happen previously.
Kudos
Thanks for sharing your thoughts on Tim Skabo. Regards
Quality articles is the key to interest the viewers to go to
see the website, that’s what this website is providing.
бездепозитные бонусы в казино за регистрацию без депозита
It’s nearly impossible to find experienced people on this topic,
however, you seem like you know what you’re talking about!
Thanks
Hurrah! At last I got a web site from where I be able to in fact take helpful information concerning my study and knowledge.
Перейти на сайт водка бэт
Regards, Loads of forum posts!
I read this post completely regarding the resemblance of newest and previous
technologies, it’s awesome article.
What you composed made a great deal of sense.
However, what about this? what if you were to write a awesome title?
I am not suggesting your content is not solid., but suppose
you added a headline that grabbed a person’s attention? I mean Heart failure: Symptoms, Causes, Diagnosis & Treatment
– MDtodate is a little vanilla. You ought to look at Yahoo’s home page and see how they create
article titles to grab viewers to open the links.
You might try adding a video or a pic or two to grab people interested about what you’ve got
to say. In my opinion, it could make your blog a little bit more
interesting.
Hello, just wanted to mention, I loved this post.
It was practical. Keep on posting!
Howdy just wanted to give you a quick heads up and let you know a few of the pictures aren’t loading correctly.
I’m not sure why but I think its a linking issue.
I’ve tried it in two different internet browsers and both show the same
outcome.
I am not sure where you are getting your info, but
good topic. I needs to spend some time learning
more or understanding more. Thanks for wonderful information I was looking for this
information for my mission.
Also visit my web page :: custom retreat
I every time used to study piece of writing in news papers
but now as I am a user of internet so from now I am using net for articles or reviews, thanks to web.
Woah! I’m really loving the template/theme of this site.
It’s simple, yet effective. A lot of times it’s difficult to get that
“perfect balance” between superb usability and appearance.
I must say you have done a awesome job with this.
In addition, the blog loads super fast for me on Firefox.
Outstanding Blog!
Hi everyone, it’s my first pay a visit at this site, and piece of writing is
in fact fruitful in support of me, keep up posting such
content.
I know this website gives quality dependent articles and extra stuff, is there any other web
page which gives these data in quality?
Hello just wanted to give you a brief heads up and let you know a few of the pictures aren’t loading properly.
I’m not sure why but I think its a linking issue. I’ve tried it in two different web browsers and
both show the same results.
I enjoy reading an article that can make people think.
Also, many thanks for permitting me to comment!
Also visit my web blog … is the sky dragon jellycat rare
Asking questions are truly fastidious thing if you are not understanding anything totally, however this
paragraph offers fastidious understanding even.
Hello There. I found your blog using msn.
This is a really well written article. I’ll make sure to bookmark it and
come back to read more of your useful info.
Thanks for the post. I will certainly comeback.
ስለ ስዕሉ ይቅርታ, በጣም ወድጄዋለሁ, ስለሱ ሁሉንም ነገር ወድጄዋለሁ, ልጥፍዎ ተስፋ ይሰጠኛል, ምንድን ነው?
I got this website from my buddy who told me regarding this site and now this time I am visiting this web site and reading very informative content at this time.
My homepage … how big is large jellycat dragon
It’s appropriate time to make a few plans for the future and it is time to
be happy. I’ve learn this publish and if I may
just I want to recommend you some interesting things or
suggestions. Maybe you can write next articles regarding this article.
I want to learn even more issues about it!
Touche. Outstanding arguments. Keep up the amazing work.
Hi there mates, its impressive post concerning
educationand completely explained, keep it up all the time.
сайт azino
You ought to be a part of a contest for one of the most
useful sites on the web. I’m going to recommend this web site!
I think that everything composed was very logical. But, what about this?
suppose you were to write a awesome headline? I am not saying your content isn’t good,
but what if you added a post title to possibly grab folk’s attention? I mean Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate is kinda vanilla.
You ought to glance at Yahoo’s home page and watch how they create article titles to grab people to open the links.
You might add a video or a pic or two to grab people interested about what you’ve got to say.
In my opinion, it would make your posts a little bit more interesting.
Visit my website: best real estate agent in Little Rock AR
I got this website from my friend who shared with me about
this website and now this time I am visiting this website and reading very informative articles or reviews here.
What’s up, all the time i used to check
weblog posts here early in the break of day, as i like to learn more and more.
Keep on working, great job!
What’s up to every body, it’s my first go to see of this website;
this blog contains awesome and truly good material in support of visitors.
Stop by my web page … best realtor in Clarks Summit PA
Thank you for sharing this very good post. Very interesting ideas! (as always, btw)
I read this piece of writing fully on the topic of the comparison of most recent and previous technologies, it’s remarkable article.
Feel free to surf to my homepage; realtor in Clarks Summit PA
Amazing blog! Do you have any recommendations for aspiring writers?
I’m hoping to start my own site soon but I’m a little lost on everything.
Would you propose starting with a free platform
like WordPress or go for a paid option? There are so
many options out there that I’m completely confused .. Any ideas?
Thanks!
My website; private new year retreat in mexico
Wonderful work! This is the type of information that are meant to be shared across the web.
Disgrace on Google for not positioning this put up upper!
Come on over and seek advice from my website . Thank
you =)
J’adore Betify Casino, c’est très clair.
https://betify-casino-bonus-fr.fr/application-mobile
Продолжайте в том же духе и привлекайте ещё больше игроков!
https://www.google.pn/url?q=https%3A%2F%2Fpinup-kz-download.kz%2Fgames%2F
Excellent article! We are linking to this great content on our website.
Keep up the great writing.
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something.
I think that you can do with a few pics to drive
the message home a bit, but other than that, this is great blog.
A great read. I’ll definitely be back.
Here is my website; best real estate agent in Tacoma WA
Having read this I believed it was very enlightening.
I appreciate you spending some time and energy to put this article together.
I once again find myself spending a lot of time both reading and leaving comments.
But so what, it was still worth it!
My homepage – yoga retreat center
Aw, this was a very nice post. Taking the time and actual effort to generate a really
good article… but what can I say… I procrastinate
a whole lot and don’t seem to get nearly anything done.
Hello, I check your blogs regularly. Your writing
style is witty, keep up the good work!
you are in reality a excellent webmaster. The web site
loading velocity is incredible. It sort of feels that you are doing any unique trick.
Moreover, The contents are masterwork. you’ve done a magnificent
process in this topic!
hey there and thank you for your info – I have certainly picked up
anything new from right here. I did however expertise several technical issues using
this site, as I experienced to reload the web
site lots of times previous to I could get it to load correctly.
I had been wondering if your web host is OK? Not that I am
complaining, but sluggish loading instances times will sometimes affect your
placement in google and can damage your quality score if ads and marketing
with Adwords. Well I’m adding this RSS to my e-mail and could look out for a
lot more of your respective exciting content. Make sure you update this again soon.
With havin so much written content do you ever run into any
issues of plagorism or copyright violation? My site has a lot of unique
content I’ve either authored myself or outsourced but it seems a lot of it is popping it up all over the
web without my permission. Do you know any solutions to help stop content from being ripped off?
I’d genuinely appreciate it.
Thanks. Useful information.
It’s genuinely very complex in this busy life to listen news on TV, therefore I
simply use world wide web for that reason, and
obtain the latest information.
I do not even know how I ended up here, but I thought this post was
good. I do not know who you are but definitely you are going to a famous blogger if you are not already 😉
Cheers!
Refresh Renovation Southwest Charlotte
1251Arrow Pine Ⅾr c121,
Charlotte, NC 28273, United Stаteѕ
+19803517882
accessory construction dwelling Unit
Hi, all the time i used to check weblog posts here early in the daylight, because i
enjoy to find out more and more.
I do consider all of the concepts you have presented for your post.
They are really convincing and can certainly work.
Still, the posts are too brief for starters. May just you
please lengthen them a little from subsequent time? Thank you for the post.
Excellent, what a web site it is! This weblog provides valuable information to us, keep it up.
Hey very nice website!! Man .. Excellent .. Amazing .. I will bookmark your site and take the feeds
also? I’m happy to seek out a lot of useful info right here within the
publish, we want work out extra techniques in this regard, thanks for sharing.
. . . . .
Feel free to visit my web page: real estate agent Fort Lauderdale FL
Wow, superb weblog layout! How lengthy have you
been blogging for? you made blogging glance easy. The
full glance of your site is fantastic, let alone the content material!
my website best real estate agent in Tacoma WA
I know this if off topic but I’m looking into starting my own blog and was curious what all
is required to get setup? I’m assuming having a blog like yours would
cost a pretty penny? I’m not very web savvy so
I’m not 100% positive. Any tips or advice would be greatly appreciated.
Kudos
Take a look at my webpage :: real estate agent Little Rock AR
Hello there, just became aware of your blog through Google, and found that it’s
truly informative. I’m gonna watch out for brussels.
I will appreciate if you continue this in future. Lots of people will be benefited from your writing.
Cheers!
My page real estate agent State College PA
Thanks for sharing your thoughts on online
pharmacy. Regards
Hi! I could have sworn I’ve visited this site before but after looking at
many of the articles I realized it’s new to me. Anyways, I’m certainly pleased I came
across it and I’ll be book-marking it and checking back frequently!
This info is worth everyone’s attention. When can I
find out more?
I just like the helpful information you supply in your articles.
I’ll bookmark your weblog and test once more here frequently.
I am somewhat certain I will be informed lots of new stuff proper right here!
Good luck for the next!
Here is my web blog; realtor in Chula Vista CA
I do not know whether it’s just me or if everyone else encountering problems
with your blog. It seems like some of the written text in your content are running off the screen. Can someone else please provide feedback and let me know if this is
happening to them too? This might be a problem with my internet browser because I’ve had this
happen before. Many thanks
Take a look at my blog :: best realtor in St. George LA
Remarkable issues here. I’m very glad to see your article.
Thank you so much and I’m looking forward to touch you.
Will you kindly drop me a e-mail?
Feel free to visit my blog: real estate agent St. George LA
Hi there, every time i used to check webpage posts here
in the early hours in the daylight, because i like to learn more and more.
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now
each time a comment is added I get three e-mails
with the same comment. Is there any way you can remove me from that service?
Bless you!
You really make it seem so easy with your presentation but I find
this topic to be really something that I think I would never understand.
It seems too complicated and extremely broad for me. I am looking forward for
your next post, I’ll try to get the hang of it!
My webpage – realtor in Tacoma WA
Since the admin of this site is working, no question very soon it will
be famous, due to its feature contents.
Feel free to visit my web site real estate agent St. George LA
Big thanks for the Pengu Sport Slot platform — super useful!
https://pengu-sport.org/reviews
buy backlinks, link exchange, free gift card, congratulations you have won, claim your
prize, you have been selected, click here
to claim, you won’t believe, one weird trick, what happened next will shock you,
shocking truth, secret revealed, limited time
offer, special promotion, act now, don’t miss out, buy now, best price, risk-free trial, get rich quick, make money fast, work
from home, no credit check, miracle cure, lose weight fast,
free viagra, no prescription needed, online casino, free spins, meet singles,
hot singles in your area, replica watches, cheap Rolex.Agent Tesla,
ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy,
BlackMatter, Blackshades, Blaster, Brontok, Carbanak,
Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis,
CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot,
Dridex, Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor,
IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot,
Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort,
NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader,
Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye,
SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot,
Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader,
XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
Feel free to surf to my website; pirate software
This design is spectacular! You certainly know how to keep a reader entertained.
Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Wonderful job.
I really loved what you had to say, and more than that, how you presented it.
Too cool!
My page; realtor in Cibolo TX
бездепозитные бонусы в казино 2025 за регистрацию
Greetings! This is my first comment here so I just wanted to give a
quick shout out and tell you I truly enjoy reading your blog posts.
Can you suggest any other blogs/websites/forums that go over the same topics?
Thanks!
Feel free to surf to my web-site: best realtor in Clarks Summit PA
Whats up are using WordPress for your blog platform?
I’m new to the blog world but I’m trying to get started and set
up my own. Do you need any coding expertise to make your own blog?
Any help would be greatly appreciated!
Feel free to surf to my website :: best realtor in Fort Lauderdale FL
Awesome post.
Here is my web site – best real estate agent in Wellington FL
Hello! Someone in my Myspace group shared this site with us so
I came to look it over. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers!
Terrific blog and terrific design.
Also visit my homepage – realtor in Fort Lauderdale FL
Hello there, You have done a great job. I’ll definitely digg it
and personally recommend to my friends. I’m confident they’ll
be benefited from this website.
My blog: best real estate agent in St. George LA
E2BET नेपाल: विश्वसनीय अनलाइन
क्यासिनो | स्लट खेल र खेल सट्टेबाजी
Как выбрать хороший букет цветов в магазине
Excellent post. Keep writing such kind of info on your page.
Im really impressed by your blog.
Hi there, You have done an incredible job. I will definitely digg it and
in my opinion suggest to my friends. I am confident they’ll be benefited from this web site.
Everything is very open with a clear description of the
challenges. It was definitely informative. Your site is very helpful.
Thank you for sharing!
my web blog … best realtor in Fort Lauderdale FL
I’ve read several just right stuff here. Definitely price
bookmarking for revisiting. I surprise how a lot effort
you put to make any such great informative site.
Here is my blog post: best real estate agent in Salt Lake UT
I read this paragraph completely concerning the difference of most up-to-date and
preceding technologies, it’s amazing article.
Also visit my web site :: best real estate agent in Tacoma WA
Hi! Do you use Twitter? I’d like to follow you
if that would be ok. I’m absolutely enjoying your blog and look forward to new posts.
Feel free to surf to my site :: best realtor in State College PA
Hey I am so grateful I found your blog page, I really found
you by accident, while I was looking on Bing for something else, Anyhow I am here now and would
just like to say thanks a lot for a remarkable post
and a all round thrilling blog (I also love the theme/design),
I don’t have time to go through it all at the minute but I have saved it and also added in your RSS feeds, so when I have time I
will be back to read much more, Please do
keep up the superb jo.
Feel free to surf to my web site … real estate agent Fort Lauderdale FL
I’m really loving the theme/design of your weblog.
Do you ever run into any internet browser compatibility
issues? A couple of my blog readers have complained about my
site not operating correctly in Explorer but looks great
in Safari. Do you have any solutions to help fix this problem?
my website: best realtor in Clarks Summit PA
Have you ever considered about adding a little bit more than just your articles?
I mean, what you say is valuable and everything. Nevertheless just imagine if you added some great photos
or videos to give your posts more, “pop”! Your content is excellent but with pics and clips, this website could
definitely be one of the best in its field. Awesome blog!
Look into my web site :: best real estate agent in Cibolo TX
Someone necessarily help to make significantly posts I would state.
That is the very first time I frequented your website page and to this point?
I surprised with the analysis you made to make this particular submit incredible.
Wonderful process!
Also visit my page … best realtor in St. George LA
Hi there to every body, it’s my first visit of this weblog;
this web site carries amazing and in fact fine information for readers.
see Guchug-Ilaneun Bogjabhan Gisul-Eul Wanbyeoghage Guhyeonhaneun Geos-Eun Eolyeobseubnida. websites daebubun-ui ma websites bubun-eul sugdalhaji moshal sudo issseubnida.
I am really happy to glance at this webpage posts which carries plenty of helpful information, thanks
for providing such information.
my blog :: Outdoor Soft LED Mesh Screen
Keep this going please, great job!
Feel free to visit my web blog best realtor in Chula Vista CA
Please let me know if you’re looking for a author for your weblog.
You have some really good articles and I feel I would be a good asset.
If you ever want to take some of the load off, I’d love to write some content for your blog in exchange for a link back to mine.
Please shoot me an email if interested. Many thanks!
I absolutely love your blog.. Excellent colors & theme. Did you develop this amazing site yourself?
Please reply back as I’m attempting to create my very own blog and want to learn where you
got this from or what the theme is named. Kudos!
Check out my homepage led indoor video wall
I am truly grateful to the owner of this web page who has
shared this fantastic post at at this place.
Very nice post. I just stumbled upon your weblog
and wished to say that I’ve really enjoyed browsing your blog posts.
In any case I’ll be subscribing to your rss feed and I hope you write again soon!
My web blog … best realtor in Salt Lake UT
Hello, every time i used to check website posts here in the early hours
in the morning, because i like to learn more and more.
Short but helpful, thanks.
Refresh Renovation Southwest Charlotte
1251 Arrw Pine Ꭰr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Attic and loft conversion
Thanks a bunch for sharing this with all folks you actually recognize what you are speaking
approximately! Bookmarked. Please additionally visit my
web site =). We will have a hyperlink trade agreement between us http://wiki.wild-sau.com/index.php?title=Benutzer:SoilaCrump824
Sayt çox praktikdir.
https://lil.so/PmcQ
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Appreciate it
Also visit my web page realtor in Little Rock AR
I really like your blog.. very nice colors & theme. Did you
make this website yourself or did you hire someone to do it for you?
Plz reply as I’m looking to create my own blog and would like to find out where u
got this from. cheers
At this time I am going to do my breakfast, after having my breakfast
coming over again to read further news.
my web blog best real estate agent in Clarks Summit PA
Hey there, I think your site might be having browser compatibility issues.
When I look at your blog site in Firefox, it looks fine but when opening
in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that,
very good blog!
Feel free to visit my web page :: best realtor in Salt Lake UT
1xbet промокоды на сегодня 2026
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your weblog?
My blog is in the very same area of interest as yours and my users would genuinely benefit from
some of the information you provide here. Please let me know if this okay with you.
Many thanks!
I was suggested this website by my cousin. I am not sure whether
this post is written by him as no one else know such detailed about my difficulty.
You are wonderful! Thanks!
Admiring the persistence you put into your blog and
detailed information you provide. It’s good to come across a blog every once in a while that isn’t the same outdated rehashed information. Great read!
I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
I’m no longer positive the place you are getting your information, however good topic.
I needs to spend a while studying much more or understanding more.
Thanks for great info I used to be in search of this information for my mission.
my webpage :: best real estate agent in Wellington FL
I think that what you published made a ton of sense.
However, think on this, what if you wrote a catchier post title?
I ain’t suggesting your information isn’t good., but suppose you added something to maybe
grab people’s attention? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate
is kinda boring. You should peek at Yahoo’s home page and
watch how they write post titles to get people to click. You might
add a related video or a picture or two to grab readers excited about what you’ve got to say.
Just my opinion, it would bring your website a little bit more interesting.
My family members every time say that I am wasting my time here at web, except I know
I am getting knowledge all the time by reading such nice
articles or reviews.
Also visit my web-site – real estate agent Little Rock AR
It’s actually a cool and helpful piece of info.
I am happy that you shared this helpful info with us. Please keep us up to date like this.
Thanks for sharing.
My web site; real estate agent Chula Vista CA
Hello it’s me, I am also visiting this web page regularly, this website is
in fact nice and the users are really sharing good thoughts.
I every time used to read piece of writing in news papers but now as I am a user of web therefore from
now I am using net for posts, thanks to web.
Feel free to visit my blog post; real estate agent Cibolo TX
посмотреть в этом разделе ссылка кракен
buy backlinks, link exchange, free gift card, congratulations you have won, claim your prize, you have been selected,
click here to claim, you won’t believe, one weird trick, what happened next
will shock you, shocking truth, secret revealed, limited time offer, special promotion, act now, don’t miss out, buy now, best price, risk-free trial, get
rich quick, make money fast, work from home, no credit check,
miracle cure, lose weight fast, free viagra, no prescription needed, online casino, free spins, meet singles, hot singles in your area,
replica watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk,
BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster, Brontok, Carbanak,
Cerber, Clampi, Cobalt Strike, Conficker, Conti,
Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide,
Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt,
GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer,
Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar
Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon,
Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch,
Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
азино 777 официальный сайт играть казино Азино 777 известно своим разнообразным игровым ассортиментом и удобным интерфейсом. Платформа предлагает как классические слоты, так и новинки от ведущих разработчиков. Здесь каждый найдет игру по душе.
Right here is the right website for anyone who hopes
to understand this topic. You understand so much its almost hard to argue with you (not that I really would want to…HaHa).
You definitely put a fresh spin on a subject which has been written about for many years.
Great stuff, just excellent!
my web site: best real estate agent in Chula Vista CA
промокод 1xbet на сегодня
Hi there! Do you know if they make any plugins to protect against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
Check out my web-site … best real estate agent in State College PA
You should take part in a contest for one of the most useful blogs on the internet.
I will recommend this web site!
My blog; real estate agent Clarks Summit PA
Hi there all, here every person is sharing these kinds of knowledge, therefore it’s pleasant to read this weblog, and
I used to pay a visit this website daily.
Here is my web page :: best realtor in Little Rock AR
Pretty element of content. I simply stumbled upon your web site and
in accession capital to claim that I acquire actually enjoyed
account your blog posts. Anyway I will be
subscribing in your feeds and even I fulfillment you access consistently fast.
my homepage realtor in State College PA
I am regular visitor, how are you everybody? This
piece of writing posted at this website is really fastidious.
Excellent article. Keep posting such kind of information on your page.
Im really impressed by your blog.
Hey there, You’ve performed a great job. I will definitely digg it and in my view recommend to my friends.
I am confident they will be benefited from this
site.
Have a look at my web site: best real estate agent in Clarks Summit PA
You actually make it seem so easy with your presentation but I find
this matter to be actually something that I think I would
never understand. It seems too complex and very broad for me.
I am looking forward for your next post, I will try
to get the hang of it!
of course like your web site however you have to take a
look at the spelling on quite a few of your posts.
Many of them are rife with spelling issues and I to find it very bothersome to tell the truth then again I will
surely come again again.
Estos húmedos XXX baño fotos mostrar duras porno vibraciones con primeros planos labios y húmedos puñetazo selfies, que son renombrados entre los sediento espectadores aquí.
Las galerías MILF porno, que cuentan con visual garrillas, anal película selfies, y filtraciones de pajas XXX, hacen que todos los cachonda suscriptores loco, haciendo que
los chicos de todo el mundo se masturben sin saltarse sus filtraciones.
Primeros planos en alta definición y ruido envolventes.
puede aparecerán en el próximo OnlyFans material, junto con difícil fotos de upskirts y explosión trabajos en el coche.
Nada la excita más que el porno del misionero chorreando sin censura, como demuestran las fugas de misión XXX y las fotos de sexo
crudo donde el coño permanece abierto y las tetas aprietan con fuerza. https://es.she-international.com/brooklyn-belle/
Howdy just wanted to give you a quick heads up.
The text in your post seem to be running off the screen in Chrome.
I’m not sure if this is a format issue or something to do with
browser compatibility but I figured I’d post to let you know.
The design and style look great though! Hope you get the problem fixed soon.
Many thanks
I believe this is among the so much important info for me.
And i’m happy studying your article. But should
statement on few common issues, The site taste is great, the articles
is actually nice : D. Good activity, cheers
I like the helpful info you provide in your articles. I will
bookmark your weblog and check again here regularly. I’m quite certain I’ll
learn many new stuff right here! Best of luck for the next!
Also visit my website … realtor in Salt Lake UT
Write more, thats all I have to say. Literally, it seems as though
you relied on the video to make your point. You definitely know what youre
talking about, why waste your intelligence on just posting videos
to your blog when you could be giving us something enlightening to read?
Amazing! Its really amazing article, I have got much clear idea about from this piece of writing.
lee bet
Hi there, I discovered your blog by the use of Google while searching
for a comparable subject, your web site got here up, it appears
great. I have bookmarked it in my google bookmarks.
Hi there, just become alert to your weblog through Google, and located that it’s truly informative.
I am gonna watch out for brussels. I will appreciate in case
you proceed this in future. A lot of folks shall be benefited from your writing.
Cheers!
My web blog – best realtor in Salt Lake UT
Сүрөт үчүн кечирим сурайм. мага абдан жагат. Мен анын баарын жакшы көрөм. Сиздин билдирүү мага үмүт берет. Бул не?”
Hey, I think your blog might be having browser
compatibility issues. When I look at your website in Chrome, it looks fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that,
very good blog!
Uxolo ngesithombe. Ngiyithanda kakhulu. Ngithanda yonke into ngakho. Iposi lakho linginika ithemba. Kwenzenjani?
This article will help the internet viewers for setting up new blog
or even a weblog from start to end.
I think everything published made a bunch of sense. But, think about this, suppose you composed a catchier post title? I am not saying your information isn’t good., however suppose you added a title to maybe grab a person’s attention? I mean %BLOG_TITLE% is a little plain. You ought to look at Yahoo’s front page and note how they create article titles to get viewers interested. You might add a related video or a pic or two to grab people excited about what you’ve got to say. In my opinion, it would make your blog a little bit more interesting.
dm-magazine.ru
Incredible story there. What happened after? Thanks!
my web blog; best realtor in Little Rock AR
Heya! I understand this is sort of off-topic but I had to ask.
Does operating a well-established website such as yours take
a massive amount work? I’m completely new to running a blog but I do write in my journal every day.
I’d like to start a blog so I can share my own experience and thoughts
online. Please let me know if you have any recommendations or tips
for new aspiring bloggers. Thankyou!
Very shortly this web site will be famous amid all blogging people, due to it’s nice posts
I’d like to thank you for the efforts you’ve put in penning
this site. I’m hoping to check out the same high-grade content by
you later on as well. In fact, your creative writing abilities has
motivated me to get my own, personal site now 😉
It’s impressive that you are getting thoughts from this article as well as from our argument made here.
hello there and thank you for your information – I’ve certainly
picked up anything new from right here. I did however expertise
several technical issues using this website, as I experienced to reload the web site lots of
times previous to I could get it to load correctly. I
had been wondering if your web host is OK? Not that I am
complaining, but slow loading instances times will very frequently affect your
placement in google and could damage your quality score if ads and
marketing with Adwords. Anyway I am adding this RSS to my e-mail and can look out for a lot more of your respective interesting content.
Make sure you update this again soon.
goGLOW Houston Heights
1515 Studemont St Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
acne treatment near me remedy
This game looks amazing! The way it blends that old-school chicken crossing concept
with actual consequences is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay
and adding real risk? I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless
chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds
legitimate risk is genius. Really want to
give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing action with
real-world stakes has me interested. I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
We’re a group of volunteers and starting a new scheme in our community.
Your web site provided us with valuable info to work on. You’ve done an impressive job and our whole
community will be grateful to you.
멋진 비트! 당신이 사이트를 수정하면서 견습하고 싶습니다.
블로그 웹사이트 구독은 어떻게 하나요?
계정이 저에게 적절한 도움을 주었습니다.
당신의 방송이 제공한 밝고 명확한 컨셉에 약간 익숙해졌습니다.
Hmm is anyone else having problems with the pictures on this blog loading?
I’m trying to determine if its a problem on my end or if it’s the blog.
Any responses would be greatly appreciated.
Your blog is a treasure trove of valuable information! I especially enjoyed this post—it’s clear you know your stuff.
Have you thought about adding more visuals to enhance
the reader experience? Great job!
이 웹사이트는 정말 대단한 곳이에요!
headlines 관련 콘텐츠가 너무 유익해요.
SEO를 강화하기 위해 키워드 최적화 팁이 있다면 공유해 주세요.
멋진 포스트 감사합니다! 감사합니다!
certainly like your website but you have to check the spelling on several of your posts.
Many of them are rife with spelling problems and
I find it very troublesome to tell the truth on the other hand
I’ll surely come back again.
What is Amazon Fire Stick and the way Does It Work without cost http://nowlinks.net/UPmRTM? The Amazon Fire TV Stick is another gadget becoming a member of the positions of dwelling amusement streaming innovations. 1 Tv shows, motion pictures, membership administrations, music, images, and video games. The Amazon Fire Tv Stick houses the entirety of your primary substance and is effectively movable, so you may take your media anyplace! What you get with the Fire TV Stick? Envision having the choice to take your Tv with you when you take some time off. That is the usefulness you get with the Fire TV Stick. The Fire TV Stick homes the entirety of your substance and is totally versatile. Basically remove your gadget and take it with you if you travel. Fitting it into any viable Tv to accumulate moment admittance to the entirety of your number one recordings. In case you’re an Amazon Prime part, your Fire TV Stick comes pre-enrolled to your document. You could have immediate admittance to the entirety of your Amazon Prime substance once you plug your Fire TV Stick into your HDMI port.
It’s not my first time to go to see this web site, i am browsing this web site dailly and get pleasant information from
here daily.
Pretty! This was a really wonderful article. Many thanks for providing this information.
For most up-to-date news you have to pay a quick visit internet and
on web I found this website as a finest web
page for newest updates.
We focus in totally removing Google Business Profiles rapidly and legally. Our specialist team gets rid of listings, assessments, and images, making sure total erasure. Begin new along with a clean internet visibility, without unfavorable or even old information, https://libreentodo.blogspot.com/2025/11/risiken-und-herausforderungen-beim.html.
азино 777 официальный сайт мобильная Ищете официальный сайт Азино 777? Здесь вы найдете актуальную ссылку для доступа к платформе
This game looks amazing! The way it blends that old-school chicken crossing concept with actual consequences
is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo of
classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay
with actual stakes? Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing
action with real-world stakes has me interested. I’m ready to jump
in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
Do you have any video of that? I’d like to
find out some additional information.
Take a look at my blog :: real estate agent Wellington FL
Good post! We are linking to this great content
on our site. Keep up the good writing.
https://telegra.ph/Fortunes-Favor-the-Bold-Your-Complete-Guide-to-Bonuses-Slots-and-Strategies-at-Choco-Spin-casino-11-18
I have read so many articles on the topic of the blogger
lovers but this article is truly a nice paragraph, keep
it up.
Here is my web-site: realtor in Little Rock AR
Hello there I am so thrilled I found your blog page, I really found
you by error, while I was browsing on Bing for something else, Regardless I am here now and would just like
to say thanks for a incredible post and a all round
enjoyable blog (I also love the theme/design), I don’t have time to browse it all at the moment but I have
saved it and also added your RSS feeds, so when I have
time I will be back to read a great deal more, Please do keep up the awesome b.
Also visit my site; best real estate agent in Cibolo TX
naturally like your web site but you need to take a look at the spelling on several of your posts.
A number of them are rife with spelling problems and
I find it very bothersome to tell the reality then again I will
definitely come back again.
Also visit my blog post; best real estate agent in Salt Lake UT
You revealed that effectively!
Pretty nice post. I just stumbled upon your blog and wanted
to say that I’ve truly enjoyed browsing your blog posts.
After all I will be subscribing to your rss feed and I hope you write again soon!
It’s genuinely very difficult in this busy life to listen news on Television, therefore I simply use web for that purpose, and obtain the newest information.
Oh my goodness! Awesome article dude! Many thanks, However
I am experiencing problems with your RSS.
I don’t understand why I cannot join it. Is there anyone else having identical RSS issues?
Anyone who knows the answer can you kindly respond?
Thanks!!
Also visit my webpage :: best real estate agent in St. George LA
Wonderful blog! Do you have any tips for aspiring writers?
I’m hoping to start my own site soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress or go for a paid option? There are so many options out there
that I’m totally confused .. Any tips? Many thanks!
Hi, I think your site might be having browser compatibility issues.
When I look at your blog in Firefox, it looks fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up!
Other then that, fantastic blog!
Here is my web blog best real estate agent in Wellington FL
What’s up, everything is going nicely here and ofcourse every one
is sharing information, that’s in fact good, keep up writing.
Thank you a lot for sharing this with all of us you actually understand what you’re speaking about!
Bookmarked. Please additionally visit my website =).
We will have a hyperlink change arrangement between us
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to far added agreeable from you!
By the way, how could we communicate?
Thanks for finally writing about > Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate < Liked it!
On the crypto side of things, popular coins like Bitcoin, Ethereum, and Tether are all available.
Hello colleagues, its great piece of writing regarding tutoringand
completely explained, keep it up all the time.
Here is my site :: best realtor in Wellington FL
After I initially left a comment I seem to have clicked the -Notify me when new comments are added-
checkbox and now whenever a comment is added I receive four emails with the same comment.
There has to be an easy method you are able to remove me from
that service? Thanks!
Right now it seems like Expression Engine is the
top blogging platform out there right now. (from what I’ve
read) Is that what you are using on your blog?
Here is my page – best realtor in Salt Lake UT
you are in point of fact a just right webmaster.
The website loading pace is amazing. It kind of feels that you are doing any distinctive trick.
In addition, The contents are masterwork. you have performed
a fantastic process in this matter!
I am genuinely thankful to the owner of this web page who has
shared this enormous article at at this place.
Here is my website – best realtor in Little Rock AR
This article will help the internet viewers for creating new blog or even a blog from start to end.
Also visit my blog – best real estate agent in Cibolo TX
Does your website have a contact page? I’m having trouble locating it but,
I’d like to shoot you an email. I’ve got some recommendations for your blog you might
be interested in hearing. Either way, great blog
and I look forward to seeing it expand over time.
You ought to be a part of a contest for one of the best blogs
on the internet. I most certainly will recommend this
blog!
Hi to every body, it’s my first go to see of this blog;
this website consists of remarkable and in fact good stuff in support of visitors.
Hi there! I know this is kinda off topic but I’d figured I’d ask.
Would you be interested in trading links or maybe guest writing a blog post or vice-versa?
My blog goes over a lot of the same topics as yours and I
believe we could greatly benefit from each other. If you happen to be interested
feel free to shoot me an e-mail. I look forward to hearing from you!
Great blog by the way!
Hi, i think that i saw you visited my website so i came
to “return the favor”.I’m trying to find things to improve my web site!I
suppose its ok to use a few of your ideas!!
goGLOW Houston Heights
1515 Studemont St Suite 204, Houston,
Texas, 77007, UՏA
(713) 364-3256
led light therapy benefits tips
Hello everybody, here every person is sharing these kinds of knowledge,
therefore it’s pleasant to read this web site, and I used to pay a
quick visit this web site daily.
I’m truly enjoying the design and layout of your site. It’s a very easy on the eyes
which makes it much more pleasant for me to come
here and visit more often. Did you hire out a developer to create your theme?
Outstanding work!
After exploring a number of the articles on your blog, I truly
appreciate your way of blogging. I book-marked it to my bookmark
site list and will be checking back in the near future.
Please check out my website too and tell me your opinion.
Review my web page :: best realtor in Cibolo TX
Its not my first time to go to see this web site, i am visiting this web site
dailly and get fastidious data from here everyday.
Hello, There’s no doubt that your web site might be having internet browser
compatibility problems. Whenever I take a look at your blog in Safari,
it looks fine however when opening in I.E., it has some
overlapping issues. I merely wanted to give you a quick heads up!
Besides that, wonderful site!
I think the admin of this website is genuinely working
hard for his website, as here every data is quality based data.
Hello, after reading this remarkable paragraph i am also
glad to share my experience here with friends.
Angels Bail Bonds Costa Mesa
769 Bakewr Տt,
Costa Mesa, СA 92626, Uniteed States
bail bonds 49th street, wakelet.com,
Heya i am for the first time here. I came across this board and
I find It really useful & it helped me out a lot. I hope to give
something back and help others like you helped me.
My page: realtor in Tacoma WA
Having read this I believed it was very informative. I appreciate you spending some
time and effort to put this article together. I once again find
myself spending a significant amount of time both reading and commenting.
But so what, it was still worthwhile!
I was recommended this blog by my cousin. I am not sure whether this post
is written by him as no one else know such detailed about my difficulty.
You are incredible! Thanks!
I’m very pleased to find this page. I wanted
to thank you for your time for this particularly wonderful read!!
I definitely savored every bit of it and I have you bookmarked to
check out new information in your web site.
https://688v.dev/
Heya just wanted to give you a brief heads up and let you know a few of the images aren’t loading correctly.
I’m not sure why but I think its a linking issue. I’ve tried it in two different browsers and both
show the same outcome.
My web page; realtor in St. George LA
Pretty nice post. I just stumbled upon your weblog and wanted to
say that I’ve really enjoyed surfing around your blog posts.
After all I’ll be subscribing to your rss feed and I hope you
write again very soon!
Also visit my web page :: best real estate agent in Chula Vista CA
Hello there! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing
very good gains. If you know of any please share. Kudos!
I’m impressed, I have to admit. Seldom do I encounter a blog that’s equally educative
and interesting, and let me tell you, you’ve hit the nail on the head.
The problem is something too few men and women are speaking intelligently about.
I’m very happy I came across this during my search
for something regarding this.
Here is my homepage – best realtor in Fort Lauderdale FL
I’d like to thank you for the efforts you’ve put in penning this website.
I really hope to check out the same high-grade content
by you later on as well. In truth, your creative writing abilities has encouraged me to get my
own blog now 😉
Here is my site; realtor in State College PA
Do you mind if I quote a couple of your posts as long as
I provide credit and sources back to your blog? My blog is in the
very same niche as yours and my users would definitely benefit from a lot
of the information you present here. Please let me know if this alright
with you. Thank you!
Useful info. Fortunate me I found your web site accidentally,
and I’m shocked why this accident didn’t came about in advance!
I bookmarked it.
Excellent post! We will be linking to this particularly
great content on our website. Keep up the great writing.
Hey just wanted to give you a quick heads up. The words in your content seem to be running off
the screen in Safari. I’m not sure if this is a format issue
or something to do with web browser compatibility but I thought I’d post to let you know.
The layout look great though! Hope you get the problem solved soon. Thanks
I blog quite often and I truly thank you for your content.
The article has really peaked my interest. I am going to take a note
of your website and keep checking for new details about once a week.
I opted in for your RSS feed too.
Hi there it’s me, I am also visiting this web site
daily, this website is truly fastidious and the viewers are in fact sharing pleasant thoughts.
Have a look at my page :: real estate agent State College PA
This is really interesting, You’re a very skilled
blogger. I have joined your feed and look forward to seeking more
of your fantastic post. Also, I have shared your website
in my social networks!
Whoa! This blog looks exactly like my old one!
It’s on a completely different subject but it has pretty much the same layout
and design. Excellent choice of colors!
This is a topic which is close to my heart… Many thanks!
Exactly where are your contact details though?
Piece of writing writing is also a fun, if you know then you can write if not it
is difficult to write.
Review my webpage :: best real estate agent in Chula Vista CA
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, United Stateѕ
+19803517882
Value to add home your
Awesome data, Cheers. https://betflik2.blogspot.com/2025/12/betflik-auto.html
We are a group of volunteers and starting a new scheme in our community.
Your web site provided us with valuable info to work on.
You’ve done a formidable job and our entire community will be thankful to you.
Here is my homepage … best real estate agent in Wellington FL
My brother suggested I might like this blog. He was entirely right.
This publish actually made my day. You can not consider simply how a lot time I had spent for
this info! Thank you!
my homepage – best realtor in Fort Lauderdale FL
Thanks for any other great post. Where else may anyone
get that kind of information in such a perfect manner of writing?
I’ve a presentation next week, and I’m at the
search for such info.
Look into my web site … best real estate agent in State College PA
I have been browsing online more than 3 hours today,
yet I never found any interesting article like yours.
It’s pretty worth enough for me. In my view, if all site owners and
bloggers made good content as you did, the net will be a lot more useful than ever before.
What’s Happening i’m new to this, I stumbled upon this I have discovered It positively useful and it has helped me out loads.
I hope to contribute & assist other customers like its helped me.
Good job.
Wow, marvelous blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your web site is great, let alone the content!
Érdeklődéssel olvasom a(z) online kaszinó ranglista oldal tartalmait. Tisztelet a hasznos infóért!
https://schuchmann.ch/download/katalog-2025/
I love your blog.. very nice colors & theme.
Did you make this website yourself or did you hire someone to do it for you?
Plz respond as I’m looking to create my own blog and would like
to find out where u got this from. appreciate it
Перейти на сайт kraken официальные ссылки
Way cool! Some very valid points! I appreciate you writing this post and
also the rest of the website is also really good.
Also visit my web page real estate agent Salt Lake UT
Yes! Finally something about highest payout online casinos.
My partner and I stumbled over here different page and thought
I might as well check things out. I like what I see so i am just following you.
Look forward to going over your web page for a second time.
My site: best realtor in Cibolo TX
It’s really a nice and useful piece of info.
I am glad that you simply shared this helpful info with us.
Please keep us informed like this. Thank you for sharing.
Good way of explaining, and fastidious article to take data
on the topic of my presentation subject, which i am going to deliver in institution of higher education.
Look into my blog post; best realtor in Fort Lauderdale FL
Howdy! I could have sworn I’ve been to this web site before but after browsing through many of the articles I realized it’s new to me.
Anyways, I’m certainly happy I came across it and
I’ll be bookmarking it and checking back often!
What i don’t realize is in fact how you’re not actually
a lot more neatly-liked than you might be now. You’re very intelligent.
You understand thus significantly on the subject
of this matter, made me individually consider it from so many varied angles.
Its like men and women don’t seem to be fascinated until it is something to do with Lady gaga!
Your individual stuffs great. All the time handle it up!
Thank you for any other informative site. The place
else could I am getting that kind of information written in such a
perfect means? I have a venture that I’m just now working on,
and I have been on the look out for such information.
Here is my web blog real estate agent Salt Lake UT
Appreciate it! Numerous material.
O A yeke ngangu ti sara ni. So ayeke mbeni ye so mingi ti asite ti Internet nga na ablog alingbi ti sara ni pëpe.
Very good post. I am going through many of these
issues as well..
Hey there, I think your site might be having browser compatibility issues.
When I look at your blog site in Firefox, it looks fine but when opening in Internet Explorer,
it has some overlapping. I just wanted to give you a quick
heads up! Other then that, terrific blog!
Take a look at my blog post – best real estate agent in Wellington FL
Thank you for another informative site. The place else
could I get that kind of info written in such an ideal approach?
I’ve a mission that I’m just now running on, and I’ve
been on the glance out for such information.
Feel free to surf to my page: realtor in Cibolo TX
I loved as much as you will receive carried out right here.
The sketch is tasteful, your authored subject matter stylish.
nonetheless, you command get bought an edginess over that
you wish be delivering the following. unwell unquestionably come more formerly again since exactly the same nearly a lot often inside case you shield this hike.
my homepage … real estate agent Salt Lake UT
AttoGaming Adalah Situs Terpecaya Di Indonesia. Menyediakan akses cepat,
aman, dan stabil untuk bermain game, slot online, sportbook, togel,
live casino serta berbagai permainan menarik lainnya.
This design is incredible! You obviously know how to keep a reader
entertained. Between your wit and your videos, I was almost moved to start
my own blog (well, almost…HaHa!) Excellent job.
I really enjoyed what you had to say, and more than that, how you presented
it. Too cool!
Look into my website … best real estate agent in St. George LA
This info is worth everyone’s attention. When can I find out more?
Rio independent escort
Undeniably believe that which you stated. Your favorite justification appeared to be on the web the easiest thing to be aware of.
I say to you, I definitely get annoyed while people consider worries
that they plainly do not know about. You managed to hit the nail upon the
top as well as defined out the whole thing without having side-effects , people can take a signal.
Will probably be back to get more. Thanks
Wow, this paragraph is good, my sister is analyzing such things, therefore I am going to let know her.
You’re so interesting! I do not think I’ve read a single thing
like this before. So great to discover another person with original thoughts on this subject matter.
Really.. thank you for starting this up. This
site is something that is required on the internet,
someone with a bit of originality!
Look into my webpage … realtor in State College PA
I really like looking through an article that will make people think.
Also, thank you for permitting me to comment!
I do trust all of the ideas you’ve presented to your post.
They are very convincing and can certainly work.
Still, the posts are very quick for starters.
May you please extend them a bit from subsequent time?
Thanks for the post.
Have you ever considered about adding a little bit more than just your articles?
I mean, what you say is important and all. But think of if you added some great images or
video clips to give your posts more, “pop”! Your content is excellent but with images and video clips,
this website could certainly be one of the very best in its niche.
Superb blog!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte,NC 28273, United Ꮪtates
+19803517882
Renovation case ideas and studies
Hey there would you mind letting me know which webhost you’re using?
I’ve loaded your blog in 3 different internet browsers and I must say this blog loads a lot quicker then most.
Can you suggest a good internet hosting provider at a reasonable price?
Thanks, I appreciate it!
Outstanding story there. What happened after? Good luck!
my website; best real estate agent in State College PA
Asking questions are genuinely pleasant thing if you are not understanding something
totally, however this piece of writing gives nice understanding even.
Hello There. I found your blog using msn. This
is an extremely well written article. I will be sure to bookmark it and return to read more of your
useful information. Thanks for the post. I will certainly
comeback.
I enjoy reading through a post that can make men and women think.
Also, thanks for permitting me to comment!
Review my website: best realtor in Clarks Summit PA
Its like you learn my thoughts! You seem to know so much approximately this, like you wrote the book in it or
something. I think that you simply can do with some percent to power the message home a little bit, but instead
of that, this is magnificent blog. An excellent read.
I’ll definitely be back.
Wow, this article is nice, my sister is analyzing these kinds of things, so I am going to inform her.
Check out my homepage :: best realtor in Cibolo TX
Hello, i think that i saw you visited my blog so i came to “return the favor”.I am
trying to find things to improve my site!I suppose its ok to use a few of your
ideas!!
I must say I’m pleased I found Rabbit Road — fantastic!
https://rabbitroad.mobi/payments
Incredible story there. What happened after?
Good luck!
Also visit my page … real estate agent Chula Vista CA
WOW just what I was looking for. Came here by searching for Adult Comics
I’ve been exploring for a bit for any high-quality articles or blog posts
on this sort of space . Exploring in Yahoo I finally
stumbled upon this website. Studying this information So i’m
glad to show that I have a very excellent uncanny feeling I discovered just what I
needed. I so much definitely will make certain to don?t forget
this web site and give it a look regularly.
Excellent blog here! Also your site loads up fast!
What host are you using? Can I get your affiliate
link to your host? I wish my site loaded up as fast as
yours lol
my web page: best real estate agent in Chula Vista CA
Hey There. I found your blog using msn. This is a really well written article.
I’ll make sure to bookmark it and come back to read more of your useful
info. Thanks for the post. I’ll certainly return.
Как выбрать хорошую лечебное учреждение
Hello my friend! I want to say that this post is amazing,
nice written and come with almost all significant infos.
I’d like to see extra posts like this .
Excellent goods from you, man. I have understand your stuff previous to
and you are just extremely magnificent. I really like what you’ve acquired here, certainly like what you’re stating and the way in which you say it.
You make it enjoyable and you still take care of to keep it wise.
I can not wait to read far more from you. This is actually
a tremendous website.
my site; realtor in Little Rock AR
May I simply say what a comfort to discover somebody who
truly knows what they’re talking about on the web. You certainly know how to bring an issue to light
and make it important. More people must look at this and understand this side of your story.
I can’t believe you’re not more popular because you definitely possess the gift.
Pretty! This was a really wonderful post. Thank you
for providing this info.
интернет kraken маркетплейс зеркало
With thanks, I enjoy this!
It’s nearly impossible to find experienced people on this topic, however, you seem like you know what you’re talking
about! Thanks
Also visit my website – best realtor in Tacoma WA
That is very fascinating, You are an excessively skilled blogger.
I’ve joined your rss feed and look forward to in search of extra of your wonderful post.
Additionally, I’ve shared your site in my social networks
Also visit my homepage :: best real estate agent in Clarks Summit PA
Its like you read my mind! You appear to know a lot about this,
like you wrote the book in it or something.
I think that you can do with some pics to drive the message
home a little bit, but instead of that, this is
magnificent blog. A great read. I’ll certainly be back.
Your way of describing everything in this article is really good, all be
capable of simply understand it, Thanks a lot.
I got this web site from my friend who shared with me concerning this site and at
the moment this time I am browsing this website and reading very informative
content here.
Also visit my web blog best real estate agent in Wellington FL
PornPics.com is not just about sex photographs,
but it also has a lot of other things in it. This website
will be your paradise if you are a porn fan, and it is a perfect item.
Porn content is favorable in numerous aspects for several men and women, according to many men and women. Some people
enjoy watching 1, while others enjoy watching movie videos on several porn websites. http://forsikringsraadgiverne.dk/menu1/menu3/
I’ve been browsing on-line more than 3 hours nowadays, but I never found any attention-grabbing article like yours.
It is pretty price sufficient for me. In my view, if all website owners and bloggers made
good content as you did, the internet will be much more helpful than ever before.
What i do not understood is in truth how you’re not
really much more neatly-favored than you might be right now.
You’re very intelligent. You understand thus considerably in relation to this matter, produced me personally consider it
from a lot of various angles. Its like women and men aren’t
interested until it is something to do with Lady gaga!
Your individual stuffs excellent. Always maintain it up!
my page – best real estate agent in Clarks Summit PA
Планируете путешествие в соседний населённый пункт и сомневаетесь, как найти сервис? Обращайте внимание не только на цену, но и на имидж компании, рецензии клиентов, чистоту транспорта и опыт водителей. Надёжный межгородний сервис — это точное расписание, удобство в салоне и открытость итогового расчёта. Многие платформы даже предусматривают бесплатную отмену или ожидание — это особенно полезно, если ваши планы не окончательны. Расскажите о проверенных перевозчиках и хитростях: как сэкономить, сохранив уровне сервиса?
https://fishtema.ru/2025/11/28/Безопасная-поездка-из-аэропорта/
Amazing a lot of very good advice!
Our family had similar issues, thanks.
Hi to every body, it’s my first go to see of this web site; this
webpage includes amazing and actually excellent stuff for visitors.
Pretty element of content. I just stumbled upon your site and in accession capital
to claim that I acquire actually loved account your
blog posts. Anyway I will be subscribing
in your augment and even I achievement you get right of entry to persistently rapidly.
Fırat Engin bahis siteleri, Casino Siteleri Nargül Engin, Slot Siteleri Hüseyin Engin, Deneme Bonusu Veren Siteler Ahmet Engin, Mehdi Deneme Bonusu,
Mehdi Deneme bonusu veren siteler
Scusa pe-o quaddro. A me piaxe ben ben. Amo tutto quello ch’o l’à da fâ. O to messaggio o m’aggiutta à avei speransa. Cös’o l’é questo?”
E kala mai i ke kiʻi. Nui koʻu makemake. Aloha au i nā mea a pau e pili ana iā ia. Hāʻawi mai kāu leka iaʻu i ka manaʻolana. He aha lā?
Magnificent goods from you, man. I’ve consider your stuff previous to and you are simply too
magnificent. I really like what you have got right here, really like
what you are stating and the best way wherein you assert it.
You’re making it entertaining and you continue to take care of to stay it smart.
I can not wait to learn far more from you.
This is actually a great web site.
After going over a number of the blog posts on your site, I
honestly like your technique of blogging. I book marked it to my bookmark site list and will be checking back in the near
future. Take a look at my web site as well and tell me how
you feel.
This is my first time pay a visit at here and i am in fact pleassant to read all at single place.
It’s a shame you don’t have a donate button! I’d certainly donate to this excellent blog!
I suppose for now i’ll settle for bookmarking and adding your RSS feed to my Google account.
I look forward to fresh updates and will talk
about this site with my Facebook group. Talk soon!
Hi it’s me, I am also visiting this site on a regular basis, this site is genuinely fastidious and the visitors are
really sharing pleasant thoughts.
my page: realtor in Wellington FL
Professional Relocation Experts Serving Cape Coral and Surrounding Areas
Please let me know if you’re looking for a article
author for your blog. You have some really great posts and I believe I would be a good asset.
If you ever want to take some of the load off, I’d love to write some content for your blog in exchange for a link back to mine.
Please blast me an e-mail if interested. Kudos!
Simply want to say your article is as amazing.
The clearness on your publish is simply excellent and that i could
suppose you are knowledgeable on this subject. Well together
with your permission let me to grasp your feed to keep updated with imminent post.
Thanks a million and please carry on the gratifying work.
My web blog :: best real estate agent in Wellington FL
Whats up very nice website!! Guy .. Beautiful .. Amazing
.. I’ll bookmark your blog and take the feeds additionally?
I am happy to seek out so many helpful info here within the post, we need develop
more strategies on this regard, thanks for sharing.
. . . . .
Ogromne dzięki za platformę Mostbet — naprawdę pomaga!
https://mostbet-kasyno-promocja.pl/jak-grac
Hey! This post could not be written any better!
Reading through this post reminds me of my good old room mate!
He always kept talking about this. I will forward this write-up to
him. Pretty sure he will have a good read. Many thanks for sharing!
My blog post :: real estate agent Clarks Summit PA
Ӏf ѕome one desires xpert view cⲟncerning running a blog afterward
i propose һim/her to visit this web site, Ⲕeep up
the nice job.
my page – buy bulk pangolin scales secure checkout and discreet shipping
Greetings! Very useful advice in this particular article!
It is the little changes which will make the most significant changes.
Thanks for sharing!
Hey there! I’m at work surfing around your blog from my new iphone!
Just wanted to say I love reading through your blog and look forward to all your posts!
Carry on the fantastic work!
Hello, I enjoy reading all of your post. I like to write
a little comment to support you.
Stop by my website – realtor in Wellington FL
Remarkable! Its actually remarkable piece of writing, I have got much clear idea on the topic of from this
article.
Here is my web page; best real estate agent in Tacoma WA
Parhaat uudet kasinosivustot vuonna 2025 tarjoavat
kilpailukykyisiä kampanjoita,
pikakotiutuksia,
sekä huippuluokan käyttöliittymän.
### Mitä uudet kasinot tarjoavat pelaajille?
Kun liityt uudelle kasinolle, voit:
– Asettaa talletuksen ilman piilokuluja
– Pelata satoja pelejä: slotit, live-kasino, crash-pelit
– Hyödyntää ilmaiskierroksia
– Kotiuttaa voitot muutamassa minuutissa
### Erilaiset kasinot ja riskitasot
Uudet kasinot voivat sisältää esimerkiksi:
– **Pay N Play -kasinot** – välittömät tunnistautumiset
– **Perinteiset kasinot** – KYC ennen kotiutusta
– **Live-kasinot** – aidot jakajat HD-lähetyksillä
– **Korkean riskin pelit** – crash-pelit, joissa voi voittaa jopa satoja tuhansia euroja
### Mitä etuja uudet kasinot tarjoavat?
– Parempi mobiilikokemus
– Paremmat bonukset
– Nopeat kotiutukset
– MGA/UKGC/Estonia lisenssit
– matala kierrätys
### Päätelmä
Uudet nettikasinot ovat hyvä vaihtoehto,
jos haluat:
– parempia bonuksia
– modernit pelit
– välittömiä kotiutuksia
– luotettavia operaattoreita
Ne tarjoavat usein enemmän vastinetta rahalle
kuin vanhat kasinot.
I was curious if you ever thought of changing the layout of your site?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one or two images.
Maybe you could space it out better?
Feel free to visit my homepage – real estate agent State College PA
Nice blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple tweeks
would really make my blog shine. Please let
me know where you got your design. Thank you
Как выбрать медцентр
whoah this blog is magnificent i really like reading your
posts. Keep up the good work! You realize, a lot of
people are hunting round for this info, you could aid them greatly.
I’m very pleased to discover this site. I wanted to thank you for ones time just for this fantastic read!!
I definitely savored every little bit of it and I have you saved as a favorite to look at new things on your web site.
Feel free to visit my site :: real estate agent State College PA
Prime Secured
3603 N 222nd St, Sukte 102,
Elkhorn, ΝE 68022, United Ѕtates
402-289-4126
Secure Cyber Vault
In fact no matter if someone doesn’t be aware of then its up to other visitors
that they will assist, so here it happens.
I was wondering if you ever considered changing the structure of your blog?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so
people could connect with it better. Youve got
an awful lot of text for only having one or two images.
Maybe you could space it out better?
I pay a visit each day a few websites and websites to read articles, however this website
provides feature based articles.
Piece of writing writing is also a excitement, if you be acquainted with
afterward you can write or else it is complex to write.
Also visit my website: best real estate agent in Tacoma WA
Refreesh Rebovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Ꮪtates
+19803517882
bookmarks
Super platformadır! Uğurlar!
https://dna.us.com/download/?url=https://1winazpro.com/bonuslar
At this time I am ready to do my breakfast, after having my breakfast coming yet again to
read further news.
You could certainly see your enthusiasm in the article you
write. The sector hopes for even more passionate writers such as you who are not afraid to say
how they believe. Always go after your heart.
My page – best real estate agent in Tacoma WA
Everyone loves what you guys are usually up too.
Such clever work and reporting! Keep up
the great works guys I’ve incorporated you guys to my
own blogroll.
It’s awesome to pay a visit this web site and reading the views of all mates about this paragraph,
while I am also keen of getting knowledge.
my webpage :: real estate agent State College PA
Hey! This post could not be written any better! Reading through this post reminds me of my good old room mate!
He always kept talking about this. I will forward this write-up to him.
Fairly certain he will have a good read. Thank you for sharing!
I have been surfing online greater than three hours
today, yet I never discovered any fascinating article like yours.
It’s pretty worth enough for me. Personally, if all website owners and bloggers made excellent content as you
probably did, the web will be much more useful than ever before.
Also visit my page real estate agent Clarks Summit PA
This is my first time pay a visit at here and i am
actually impressed to read all at single place.
Ich schätze die Inhalte, die ihr auf NV Casino veröffentlicht. Danke!
https://www.google.so/url?q=https://nv-casino-online-bonus.de/mobile-app
I am not sure where you are getting your information, but great topic.
I needs to spend some time learning much more or understanding more.
Thanks for fantastic information I was looking for this info for my mission.
It’s an amazing piece of writing designed for all the web
users; they will obtain advantage from it I am sure.
my site realtor in Tacoma WA
Everything is very open with a clear description of the
challenges. It was really informative. Your site is useful.
Thank you for sharing!
Easy and intuitive site with a wealth of gambling-related info.
https://chicken-road-bonus.org/how-to-play
This is a topic which is close to my heart… Best wishes!
Where are your contact details though?
Very great post. I simply stumbled upon your weblog and wanted to mention that I’ve
really enjoyed surfing around your weblog posts.
After all I will be subscribing on your rss feed and I hope you write once
more very soon!
Does your blog have a contact page? I’m having a tough
time locating it but, I’d like to shoot you an e-mail. I’ve
got some suggestions for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it expand over
time.
Of course, what a great site and informative posts, I will add backlink – bookmark this site? Regards, Reader
Wow, awesome weblog format! How long have you ever
been blogging for? you make blogging glance easy.
The whole glance of your web site is great, as well as the
content!
Feel free to visit my web page; best real estate agent in Little Rock AR
you are truly a just right webmaster. The site
loading pace is incredible. It sort of feels that
you’re doing any distinctive trick. Moreover, The contents are masterpiece.
you have done a magnificent task in this matter!
Hi there! I could have sworn I’ve been to this blog before but after going through some of the articles I realized it’s new to me.
Anyhow, I’m definitely pleased I stumbled upon it and I’ll be book-marking it and checking back frequently!
Hi, yup this paragraph is truly pleasant and I have learned
lot of things from it about blogging. thanks.
Howdy! This article could not be written much better! Reading through
this post reminds me of my previous roommate! He always kept talking about this.
I am going to forward this information to him. Fairly certain he’s going to have a great read.
Thanks for sharing!
Thanks for some other informative web site. The place else may I am getting that kind of info written in such an ideal manner?
I have a venture that I am simply now operating on, and I’ve been at the glance out for such info.
go to these guys https://lumi-wallet.io
I’m not sure where you’re getting your information, but great topic.
I needs to spend some time learning more or understanding more.
Thanks for fantastic information I was looking for this info for my mission.
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UЅΑ
(713) 364-3256
ledlight therapy clinic (wakelet.com)
Ahaa, its nice dialogue regarding this paragraph at this place at this webpage, I have
read all that, so now me also commenting here.
I blog quite often and I truly appreciate your information. The article has truly peaked my interest.
I will book mark your site and keep checking for new details about once a week.
I subscribed to your RSS feed as well.
I like the valuable info you provide in your articles.
I will bookmark your weblog and check again here regularly.
I’m quite certain I’ll learn lots of new stuff right here!
Best of luck for the next!
I every time spent my half an hour to read this webpage’s articles every day along with a mug of coffee.
This is my first time visit at here and i am really impressed to read all
at one place.
Hi to every body, it’s my first go to see of this
web site; this web site carries remarkable and genuinely fine information designed for readers.
Everything is very open with a very clear explanation of the challenges.
It was really informative. Your website is useful. Thank you for sharing!
Everyone loves what you guys are usually up too.
This type of clever work and reporting! Keep up the great works
guys I’ve incorporated you guys to my blogroll.
Also visit my site: zaragosa01
Reliable Transport Services in Brockton Area
Superb post however , I was wanting to know if you could write a
litte more on this topic? I’d be very thankful if you could elaborate a little bit more.
Kudos!
Hello! Do you use Twitter? I’d like to follow you if that would be okay.
I’m definitely enjoying your blog and look forward to new posts.
Paragraph writing is also a fun, if you be acquainted with after that you can write if
not it is complicated to write.
Superb content, Kudos.
In fact no matter if someone doesn’t be aware of after that its up to other people that they will
assist, so here it occurs.
Hello friends, pleasant article and fastidious
urging commented at this place, I am genuinely enjoying by these.
Hi there colleagues, its wonderful post about teachingand completely explained, keep
it up all the time.
I’m pretty pleased to uncover this website. I wanted to thank
you for your time for this wonderful read!!
I definitely enjoyed every bit of it and I have you saved to fav to see new things
in your website.
Hello, after reading this amazing article i am as well delighted to share my knowledge here with colleagues.
You actually make it seem so easy with your presentation but
I find this topic to be really something which I think
I would never understand. It seems too complicated and extremely broad for
me. I’m looking forward for your next post, I’ll try to get the hang of it!
Thanks to my father who informed me about this web site, this web site is in fact remarkable.
May I just say what a relief to discover somebody that truly
understands what they’re talking about on the web.
You definitely realize how to bring a problem to light and make
it important. A lot more people must read this and understand this side
of your story. It’s surprising you are not more popular since you most certainly possess the gift.
This blog was… how do you say it? Relevant!! Finally I’ve found something that helped me.
Many thanks!
Black Cohosh Herbal Supplement – Menopause & Menstrual Support Harness the
power of black cohosh, a time-honored botanical used for centuries
to address menopause symptoms and menstrual discomfort.
This herbal supplement is formulated to help manage hot flashes, night sweats, mood swings,
and sleep disturbances while supporting emotional balance during hormonal transitions.
Black cohosh may also help ease heart palpitations,
vaginal dryness, and cramping, making it a comprehensive choice for women seeking natural relief during their reproductive years and beyond.
Trust in a remedy backed by generations of traditional use
and modern wellness practices.
This text is priceless. How can I find out more?
Having read this I thought it was rather informative.
I appreciate you finding the time and effort
to put this short article together. I once again find myself
personally spending a significant amount of time both reading
and leaving comments. But so what, it was still worthwhile!
Greetings… your blog is very interesting and beautifully written.
It is appropriate time to make some plans for the longer term and it
is time to be happy. I’ve learn this publish and if I could I want to suggest you few fascinating issues
or suggestions. Perhaps you could write next articles referring to this article.
I desire to read more issues about it!
I seriously love your site.. Excellent colors & theme.
Did you develop this website yourself? Please reply back as
I’m attempting to create my own site and want to learn where you got this from or exactly
what the theme is called. Kudos!
Its like you read my mind! You seem to know a lot about this, like you wrote the book in it or something. I think that you can do with some pics to drive the message home a bit, but other than that, this is wonderful blog. A great read. I’ll certainly be back.
Admiring the persistence you put into your website and detailed information you provide.
It’s good to come across a blog every once in a while that isn’t the same outdated
rehashed material. Fantastic read! I’ve saved your site and I’m adding your
RSS feeds to my Google account.
While this issue can vexed most people, my thought is that there has to be a middle or common ground that we all can find. I do value that you’ve added pertinent and sound commentary here though. Thank you!
This is really interesting, You’re a very skilled blogger. I have joined your feed and look forward to seeking more of your fantastic post. Also, I have shared your website in my social networks!
Quality articles is the crucial to interest the visitors
to pay a visit the web page, that’s what this website is
providing.
Good write-up. I definitely appreciate this website.
Thanks!
My web site; نمایندگی تعمیرات پکیج بوتان
visado eeuu esta
I really like your blog.. very nice colors &
theme. Did you make this website yourself or did you hire someone to do it for you?
Plz respond as I’m looking to design my own blog and would like to know where u got this from.
thanks a lot
my web page: ซื้อหวยให้คุ้มค่า
österreich türkei wetten handicap bedeutung
Scusa pe-o quaddro. A me piaxe ben ben. Amo tutto quello ch’o l’à da fâ. O to messaggio o m’aggiutta à avei speransa. Cös’o l’é questo?”Scusa pe-o quaddro. A me piaxe ben ben. Amo tutto quello ch’o l’à da fâ. O to messaggio o m’aggiutta à avei speransa. Cös’o l’é questo?”
I am really impressed with your writing skills and also with the layout on your blog.
Is this a paid theme or did you modify it yourself?
Either way keep up the excellent quality writing,
it’s rare to see a nice blog like this one nowadays.
With havin so much written content do you ever run into any issues
of plagorism or copyright infringement? My blog has a lot of
exclusive content I’ve either authored myself or outsourced
but it seems a lot of it is popping it up all over the internet without my
authorization. Do you know any methods to help reduce content from
being stolen? I’d truly appreciate it.
My web-site; دکتر اسدالله پور
You really make it appear so easy along with your presentation however I to find this topic to
be actually one thing that I feel I would
never understand. It sort of feels too complicated and very wide for me.
I am having a look ahead in your next publish, I will attempt to get the dangle
of it!
You certainly deserve a round of applause for your post and more specifically, your blog in general. Very high quality material!
I delight in, result in I discovered exactly what I was taking a
look for. You have ended my 4 day long hunt!
God Bless you man. Have a nice day. Bye
Hey! Quick question that’s entirely off topic.
Do you know how to make your site mobile friendly? My weblog looks weird when browsing from my iphone4.
I’m trying to find a theme or plugin that might be able
to resolve this problem. If you have any suggestions, please share.
Appreciate it!
This information is critically needed, thanks.
You really make it seem really easy with your presentation however I
in finding this matter to be actually one thing that I believe I would never understand.
It seems too complex and extremely broad for me.
I am looking forward to your subsequent put up, I will try
to get the dangle of it!
Thanks for every other great post. Where else could anybody get that kind of info in such a
perfect approach of writing? I have a presentation next week, and I’m at the search for
such information.
You should be a part of a contest for one of the most useful blogs on the
web. I am going to recommend this web site!
her response https://web-breadwallet.com
Superb post but I was wanting to know if
you could write a litte more on this subject? I’d be very grateful if you could elaborate a
little bit further. Thanks!
Heya just wanted to give you a quick heads up and let you know a few
of the pictures aren’t loading correctly. I’m not sure why but I think
its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
I think this is among the most significant information for
me. And i’m glad reading your article. But wanna remark on few general things, The site style is
wonderful, the articles is really great : D. Good job, cheers
Feel free to visit my web-site; هزینه ایمپلنت دندان
промокод при регистрации 1xbet на сегодня
Superb blog! Do you have any helpful hints for aspiring writers?
I’m planning to start my own website soon but I’m a little lost on everything.
Would you recommend starting with a free platform like WordPress or
go for a paid option? There are so many options out there that I’m
totally overwhelmed .. Any ideas? Appreciate it!
I am glad to be a visitor of this perfect blog !, appreciate it for this rare info!
Hello There. I found your weblog using msn. This is a really smartly
written article. I will make sure to bookmark it and return to read extra of your useful information. Thanks
for the post. I will definitely comeback.
I like the helpful information you provide in your articles.
I will bookmark your weblog and check again here frequently.
I am quite sure I’ll learn a lot of new stuff right here!
Best of luck for the next!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Process home our renovation
I have to thank you for the efforts you have put in penning this site.
I really hope to see the same high-grade blog posts by you in the future as well.
In truth, your creative writing abilities has encouraged me to get my own,
personal blog now 😉
I am regular visitor, how are you everybody? This article posted at this website is really pleasant.
my site :: Face Search
I was suggested this website by my cousin. I am not sure whether this post is written by him
as no one else know such detailed about my trouble. You are wonderful!
Thanks!
Aw, this was a really good post. Spending some time and actual effort to create a top notch article…
but what can I say… I hesitate a lot and don’t manage to get
anything done.
Yesterday, while I was at work, my cousin stole my iphone
and tested to see if it can survive a 25 foot drop, just so she can be a
youtube sensation. My iPad is now broken and she has 83 views.
I know this is totally off topic but I had to share it with
someone!
my site av ซับไทย
The clarity in your post is just nice and I can tell you are an expert in the subject matter.
1xbet зеркало рабочее промокод
Great post.
What’s up to every body, it’s my first go to see of this web site;
this blog includes remarkable and genuinely excellent stuff in favor of visitors.
Ausgezeichnetes Gaming-Portal, super Job! Ich weiß es zu schätzen.
https://nv-casino-online-bonus.de/zahlungen
Hi to all, because I am in fact eager of reading this
webpage’s post to be updated on a regular basis. It contains pleasant information.
I will share you blog with my sis.
Hola! I’ve been following your site for some time now and finally got the bravery to
go ahead and give you a shout out from Lubbock Texas! Just
wanted to say keep up the great work!
Touche. Outstanding arguments. Keep up the amazing
spirit.
my blog قیمت فولاد سمانتاسیون
Discover the finest Swiss Replica Watches at ACKTime.
Experience Super Clone Watches luxury and elegance with our high-quality fake watches at affordable prices.
Article writing is also a fun, if you be acquainted with afterward you can write
or else it is difficult to write.
Its not my first time to pay a visit this website, i am browsing this site dailly and take nice facts from here everyday.
Here is my blog post; équipement industriel reconditionné
I like what you guys tend to be up too. This kind of clever work and reporting!
Keep up the wonderful works guys I’ve added you guys to my own blogroll.
WOW just what I was looking for. Came here by searching for maintenance management software
Heya i’m for the first time here. I found this board and I find It really useful & it helped
me out much. I hope to give something back and help others like
you aided me.
Then try to make this content material visible to other firms
within your niche and existing target group. http://images.google.kg/url?q=https%3A%2F%2Fdvmagic.net%2Fpl%2F
This is very interesting, You’re a very skilled blogger.
I have joined your rss feed and look forward to seeking more of
your wonderful post. Also, I have shared your
site in my social networks!
An impressive share! I’ve just forwarded this onto a co-worker who has been doing a little
research on this. And he actually ordered me dinner simply because
I discovered it for him… lol. So let me reword this….
Thanks for the meal!! But yeah, thanx for spending some time
to discuss this issue here on your internet site.
Its like you read my mind! You seem to know a lot about this, like you wrote the book in it or something. I think that you can do with some pics to drive the message home a bit, but other than that, this is wonderful blog. A great read. I’ll certainly be back.
Pretty component to content. I just stumbled upon your weblog and in accession capital to say that I
get actually enjoyed account your blog posts. Anyway I will be subscribing to your augment or even I fulfillment you get admission to consistently rapidly.
My web blog قیمت ایمپلنت دندان
Post writing is also a fun, if you be acquainted with afterward
you can write or else it is complicated to write.
Your style is so unique compared to other folks I have read stuff from.
I appreciate you for posting when you’ve got the opportunity, Guess I
will just book mark this site.
Hello! I know this is kind of off topic but I was wondering which blog platform are you
using for this website? I’m getting tired of WordPress because I’ve had issues
with hackers and I’m looking at alternatives for another platform.
I would be awesome if you could point me in the direction of a good platform.
Do you mind if I quote a couple of your articles as long as I provide credit and sources back to your website?
My website is in the exact same area of interest as yours
and my users would definitely benefit from some
of the information you provide here. Please let me
know if this ok with you. Regards!
Review my site – rexus88
Today, I went to the beach with my kids. I found a sea shell
and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She
placed the shell to her ear and screamed. There was a
hermit crab inside and it pinched her ear. She never wants to go back!
LoL I know this is totally off topic but I had to tell someone!
Heya i’m for the first time here. I came across this board
and I find It really useful & it helped me out much.
I hope to give something back and help others like you helped
me.
1 xbet
Mangelsen
7916 Girard Avenue, Ꮮa Joya
CA 92037, United Stɑtes
1 800-228-9686
best protecting grizzly bears grizzlies (Dominic)
What’s up to every body, it’s my first go to see of this blog;
this weblog consists of awesome and actually good material
designed for readers.
Magnificent goods from you, man. I have understand your stuff
previous to and you are just too wonderful. I actually like what you’ve acquired here, certainly like what you’re saying and the way in which you say it.
You make it enjoyable and you still care for
to keep it smart. I can not wait to read far more from you.
This is really a tremendous website.
Feel free to visit my web page :: دکتر امیرحسین اسدالله پور
I’m excited to discover this page. I want to to thank you for your time
for this particularly wonderful read!! I definitely liked every
part of it and I have you book-marked to check out new stuff
on your web site.
My partner and I stumbled over here different web address
and thought I might check things out. I like what I see
so now i am following you. Look forward to looking at your
web page yet again.
my page; Face Lookup
I’m very happy to find this site. I want to to thank you for ones time for this
particularly fantastic read!! I definitely savored every bit of it and I have
you book-marked to look at new information in your site.
My website :: rexus88 daftar
A person necessarily assist image to person finder make seriously articles I’d state.
That is the first time I frequented your web page and up to now?
I amazed with the analysis you made to create this actual publish extraordinary.
Wonderful activity!
Hi colleagues, its great paragraph concerning teachingand completely explained, keep it up
all the time.
Dizaynı superdir!
https://betandreas-azerbaijan-bet.org/oyunlar
Greetings from Idaho! I’m bored to tears at work
so I decided image to person finder check out your site on my iphone during lunch
break. I enjoy the knowledge you present here and can’t wait to take a
look when I get home. I’m amazed at how fast your blog loaded
on my cell phone .. I’m not even using WIFI, just 3G ..
Anyways, fantastic blog!
Hi to all, the contents present at this website are in fact remarkable for people experience, well, keep up the nice work fellows.
Saved as a favorite, I really like your blog!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273,United Stɑtes
+19803517882
Ideas renovation plan open
I have been browsing online more than 4 hours today, yet I never found any interesting article like yours.
It is pretty worth enough for me. Personally, if all site owners and bloggers made good content as you did, the web will be much more useful than ever before.
You ma’am have a way with words. Thank you very much!
подарок партнерам по бизнесу на новый год оптом
How To Find Seo Online
seostart.com.ua
подробнее казино хани мани зеркало
такой водка казино зеркало
When someone writes an article he/she maintains the image of a user in his/her mind
that how a user can be aware of it. Thus that’s why this post is perfect.
Thanks!
Here is my blog post … Stem cell hair restoration
можно проверить ЗДЕСЬ водкабет
Prіme Secured
3603 N 222nd Տt, Suite 102,
Elkhorn, NE 68022, United Ѕtates
402-289-4126
Cyber Trend Analysis
What’s up mates, how is all, and what you wish for to say on the topic
of this post, in my view its genuinely remarkable in support of me.
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Заходи — там интересно – https://www.hostingbudget4you.nl/sit-est-necessitatibus-autem-illo-quidem-minus
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Лучшее решение — прямо здесь – https://www.tatliacka.sk/1
Public policy is key here, and our states need to develop some strategies – – soon.
I pay a quick visit everyday some websites and sites to read articles or reviews, but this weblog presents feature based writing.
Have you ever considered about adding a little bit more than just your articles?
I mean, what you say is fundamental and all. However just imagine
if you added some great graphics or video clips to give your posts more, “pop”!
Your content is excellent but with images and videos, this website could certainly be one of the
best in its niche. Great blog!
Also visit my site – rexus88 slot
выберите ресурсы водка бет казино
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Читать далее > – https://primenewsnet.com/creative-decorating-with-houseplants-from-floor-to-ceiling
I want to to thank you for this excellent read!! I absolutely enjoyed every bit of it.
I have got you bookmarked to check out new stuff you post…
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Уникальные данные только сегодня – https://toffshop.nl/product/conoco-mini-massagepistool
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Обратитесь за информацией – https://bloggercorem.com/2025/04/24/ishan-kishan-ka-rahasyamay-out
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Откройте для себя больше – https://bitvuttarakhand.com/meditation-for-movie-artists
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Провести детальное исследование – https://cpc.com.au/product/fly-calmly-with-hypnotherapy
Genuinely when someone doesn’t know after that its up to other people that they
will help, so here it takes place.
Look into my blog post play free games
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Смотрите также… – https://primenewsnet.com/style-spy-fashion-model-goes-casual-in-faux-furr-and-plaid
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Личный опыт — читайте сами – https://www.volgyfitness.hu/?p=6639&cpage=54
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Получить полную информацию – https://aenj.org/october-2021-member-spotlight/member-spotlight-3
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Проследить причинно-следственные связи – http://www.drrad-implant.com/%D8%B5%D9%81%D8%AD%D9%87-%D8%A7%D8%B5%D9%84%DB%8C/whatsapp-image-2020-05-05-at-18-14-391-3
I’m extremely pleased to uncover this page. I want
to to thank you for ones time for this particularly wonderful read!!
I definitely liked every bit of it and I have you bookmarked to see
new stuff in your site.
В этой информационной статье вы найдете интересное содержание, которое поможет вам расширить свои знания. Мы предлагаем увлекательный подход и уникальные взгляды на обсуждаемые темы, побуждая пользователей к активному мышлению и критическому анализу.
Читать далее > – https://themindfultree.ie/product/folding-meditation-bench
We’re a group of volunteers and opening a new scheme in our
community. Your web site provided us with valuable information to work on. You’ve done an impressive
job and our whole community will be thankful to you.
I am regular visitor, how are you everybody? This article posted
at this web page is truly good.
I am actually grateful to the owner of this web page who has shared this
great paragraph at at this place.
It’s very effortless to find out any matter on web
as compared to textbooks, as I found this piece of
writing at this site.
I’m really enjoying the design and layout of your
blog. It’s a very easy on the eyes which makes it much
more pleasant for me to come here and visit more often. Did you hire
out a designer to create your theme? Great work!
Valuable info. Fortunate me I discovered your web site unintentionally, and I am shocked why this
accident didn’t came about earlier! I bookmarked
it.
Here is my homepage … rexus88 link alternatif
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Читать полностью – https://kontinuumliberec.com/events/s-chuti-v-pohybu
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
easy refeesh hоme your renovating mаkes – cyber-comma-113.notion.site –
Wow, awesome blog format! How lengthy have you been blogging for?
you made running a blog glance easy. The entire glance of
your web site is wonderful, as smartly as the content!
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Смотрите также… – https://hookedme.com/why-meesho-is-so-cheap-in-online-shopping-world
Valuable information. Fortunate me I discovered your website accidentally,
and I’m stunned why this coincidence did not came about earlier!
I bookmarked it.
This design is steller! You definitely know how to keep a reader amused.
Between your wit and your videos, I was almost moved to
start my own blog (well, almost…HaHa!) Excellent job.
I really enjoyed what you had to say, and more than that, how
you presented it. Too cool!
подробнее здесь хани мани казино официальный сайт
I’m amazed, I must say. Seldom do I come across a blog that’s equally educative and
interesting, and without a doubt, you’ve hit the nail on the
head. The issue is something not enough men and women are speaking intelligently about.
I’m very happy that I came across this during my search for something concerning this.
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Перейти к полной версии – https://www.deambulatori.com/nrs-healthcare-m66739
AttoGaming Adalah Situs Terpecaya Di Indonesia. Menyediakan akses cepat, aman, dan stabil untuk bermain game, slot online,
sportbook, togel, live casino serta berbagai permainan menarik lainnya.
Thank you for the auspicious writeup. It if truth be told was a enjoyment account it.
Glance complicated to far introduced agreeable from you!
By the way, how can we communicate?
Check out my site – rexus88 link alternatif
I’m really enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more pleasant for me
to come here and visit more often. Did you hire out a designer to create your theme?
Excellent work!
Hey there! I just wanted to ask if you ever have any issues with hackers?
My last blog (wordpress) was hacked and I ended up losing several weeks of hard
work due to no back up. Do you have any methods to protect against hackers?
Also visit my blog … TU娛樂城
you are actually a just right webmaster. The web site loading pace is
incredible. It kind of feels that you’re doing any distinctive
trick. In addition, The contents are masterpiece.
you have done a great process on this subject!
You made some really good points there. I looked on the web to learn more about the
issue and found most people will go along
with your views on this site.
Your mode of explaining everything in this piece of writing is really pleasant, all be able to
without difficulty be aware of it, Thanks a lot.
Also visit my web blog; jav
AttoGaming Adalah Situs Terpecaya Di Indonesia.
Menyediakan akses cepat, aman, dan stabil untuk bermain game, slot online,
sportbook, togel, live casino serta berbagai permainan menarik lainnya.
Very descriptive article, I enjoyed that a lot.
Will there be a part 2?
Sayt çox yaxşı dizayn olunub. Təşəkkürlər!
http://tinylink.in/betandreasdepozitsizbonus5119
перенаправляется сюда vodka bet
Reliable facts, Many thanks!
Great post. I was checking continuously this blog and I’m impressed!
Extremely helpful info particularly the last part 🙂 I care for such information much.
I was looking for this particular information for a
long time. Thank you and best of luck.
It’s in fact very complex in this busy life to listen news
on Television, therefore I just use the web for that reason, and take
the newest news.
We stumbled over here coming from a different web page
and thought I might check things out. I like what I see so now i am following you.
Look forward to exploring your web page for
a second time.
bookmarked!!, I love your web site!
Hay muchas cosas a tener en cuenta al elegir una casa de apuestas para apostar y te brindamos el conocimiento que es
crucial para tomar una decisión informada. https://adelandia.go.gov.br/union-magdalena-vs-america-de-cali-en-vivo-en-la-fecha-2-de-la-liga-ii-del-futbol-colombiano/
I can’t go into details, but I have to say its a good article!
What i do not understood is in reality how you’re no longer actually much more neatly-appreciated than you may be right now.
You are so intelligent. You understand therefore significantly in the case of this subject, produced me in my opinion consider it from so many numerous angles.
Its like women and men aren’t involved until it’s one
thing to accomplish with Woman gaga! Your personal stuffs nice.
At all times handle it up!
goGLOW Houston Heights
1515 Studemont Ѕt Suute 204, Houston,
Texas, 77007, USA
(713) 364-3256
skin rejuvenation treatment
Great blog right here! You seem to put a significant amount of material on the site rather quickly.
пояснения казино куш
2568แสดงผลได้ดี กับ Browser Google Chrome หรือ Firefox.
Hmm it looks like your site ate my first comment (it was extremely long)
so I guess I’ll just sum it up what I wrote and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog blogger but I’m still new to the whole thing.
Do you have any recommendations for rookie blog writers?
I’d really appreciate it.
Thanks! Loads of stuff!
Смотреть здесь водка казино вход
Keep it up and keep attracting more players!
https://rabbit-road.mobi/registration
Hey there! I just wanted to ask if you ever have any trouble with
hackers? My last blog (wordpress) was hacked and I ended up losing a few
months of hard work due to no backup. Do
you have any solutions to protect against hackers?
Ons het phishing-aktiwiteit op ‘n webwerf ontdek wat die voorkoms van ‘n wettige webwerf naboots. Hierdie webwerf het die potensiaal om gebruikers se persoonlike inligting te steel.
Great forum posts. Appreciate it!
It’s the best time to make some plans for the future and it is time to be happy. I’ve read this post and if I could I wish to suggest you some interesting things or tips. Maybe you can write next articles referring to this article. I wish to read even more things about it!
Hörmətlə, bu saytınız superdir!
https://betandreas-azerbaijan-games.org/nece-oynamaq
Hi there, yeah this paragraph is really fastidious and I have learned lot of things from it
concerning blogging. thanks.
Hello there! Do you know if they make any
plugins to safeguard against hackers? I’m kinda paranoid about
losing everything I’ve worked hard on. Any recommendations?
This is my first time go to see at here and i am genuinely happy to read everthing at single place.
Nicely put. Thank you.
Hi, I think your site might be having browser compatibility issues.
When I look at your website in Safari, it looks fine but when opening in Internet Explorer,
it has some overlapping. I just wanted to give you a quick heads up!
Other then that, wonderful blog!
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, ΝE 68022, United Stateѕ
402-289-4126
Bookmarks
I got this website from my friend who shared with me about
this web page and now this time I am browsing this web page and reading very
informative articles at this place.
It’s truly very complicated in this full of activity life to listen news on Television,
therefore I simply use web for that reason, and take the hottest information.
I rarely post big stories on forums, but this time I decided to share a small story about a win at an online casino.
Lately I’ve been testing at nllalabet.com, mostly on weekends and on small stakes. I signed up because the signup bonus looked pretty good and the bonus rules seemed manageable compared to many other online casinos. The registration process was straightforward: name and email and email confirmation, then I was good to go.
For my first deposit I stayed conservative and put a low amount into my balance. I headed to the slot games because that’s what I tend to play. I filtered by top games and picked a slot with medium volatility, hoping for a good session.
At first it was a small rollercoaster: a few line hits but nothing big and weak bonuses, and I was thinking about stopping because my balance was slowly dropping. Then things changed: I landed a strong bonus round with multipliers all over the screen, the slot kept connecting wins and the multiplier pushed my balance to a new high. For me it was a very good hit compared to my normal bets.
I didn’t stay too long; after a few more test spins I decided to cash out and send a cashout. The withdrawal process was as expected: the casino asked me to confirm my identity with ID card or passport. I sent everything right away, and the verification was accepted without any issues. After that the money was processed to my payment method and I received it in a decent timeframe.
I’m not saying this casino is a miracle, and of course you can also bust your balance, but in this case my experience was mostly good: transparent rules, normal support and no payout drama. This is not a promise you’ll win: losing is part of the game, so only gamble with a strict budget and remember it’s just a game.
Hi, i think that i saw you visited my weblog thus i came to “return the favor”.I am attempting to
find things to enhance my site!I suppose its ok to use
some of your ideas!!
Also visit my page – real estate agent Cincinnati OH
Are grateful for this blog post, it’s tough to find good information and facts on the internet
Very nice article. I certainly appreciate this site.
Stick with it!
Very shortly this web page will be famous among all blogging
and site-building visitors, due to it’s pleasant articles
My website :: real estate agent Sterlington LA
This website was… how do you say it? Relevant!! Finally I have found something that helped me.
Thank you!
Visit my homepage: real estate agent Boca Raton FL
Because the admin of this web site is working,
no question very rapidly it will be renowned, due to
its feature contents.
My web page best realtor in Edmond OK
Do you have a spam issue on this website; I also am a blogger, and I was wondering your situation;
many of us have created some nice practices and we are looking to exchange techniques with others, why not shoot me an e-mail if interested.
I just couldn’t leave your web site prior to suggesting that I really enjoyed the standard info an individual supply to your guests? Is going to be again continuously in order to inspect new posts
Amazing content on your website.
Greetings! Quick question that’s entirely off topic.
Do you know how to make your site mobile friendly?
My blog looks weird when browsing from my iphone4.
I’m trying to find a theme or plugin that might be able to fix
this problem. If you have any recommendations, please
share. Thanks!
It is in reality a nice and useful piece of information. I am glad that
you just shared this helpful info with us. Please stay us up to
date like this. Thanks for sharing.
Do you mind if I quote a couple of your articles as long as
I provide credit and sources back to your webpage? My blog is in the exact same niche as yours and my users would certainly benefit from
a lot of the information you provide here. Please let me know if this alright with you.
Appreciate it!
Excellent blog you have here but I was wondering if you knew of any
forums that cover the same topics discussed in this article?
I’d really like to be a part of online community where I can get
responses from other knowledgeable individuals that share the same interest.
If you have any recommendations, please let me know.
Thanks!
My homepage best real estate agent in Sterlington LA
Butuh RTP Gacor untuk Slot online malam ini ? GURUTOTO RTP adalah Solusi nya.
Dengan Perhitungan yang diupdate tiap Jam, serta informasi dan Data RTP dari sumber
yang terpercaya, kami menjamin anda mendapatkan RTP yang terbaik Malam ini.
disertai Login yang mudah dan akses game yang
sederhana gurutoto menjadi jawaban untuk yang tidak mau ribet dan hemat waktu, Bergabunglah dan mulai capai kemenangan beruntun dari
sekarang !
tele4
Having read this I believed it was very informative. I appreciate you finding the time and effort to put this short article together.
I once again find myself spending a significant amount of
time both reading and leaving comments. But so what,
it was still worth it!
My blog post real estate agent Burke VA
This piece of writing presents clear idea in favor of the new
users of blogging, that truly how to do running a blog.
Greate article. Keep posting such kind of information on your page.
Im really impressed by your blog.
Hey there, You’ve performed a great job. I’ll definitely digg it and in my view recommend to my friends.
I’m confident they will be benefited from this website.
Also visit my web site … best realtor in Waukesha WI
I got this website from my buddy who told me on the topic of
this website and at the moment this time I am visiting this
web page and reading very informative posts at this place.
What’s Happening i am new to this, I stumbled upon this I’ve discovered It positively useful and it has
aided me out loads. I am hoping to give a contribution & help other customers like its helped me.
Great job.
Visit my homepage; real estate agent Cedar City UT
I like it when people get together and share thoughts.
Great site, continue the good work!
My site realtor in Sterlington LA
Hello there! This article couldn’t be written any better!
Going through this post reminds me of my previous roommate!
He constantly kept talking about this. I’ll send this article to
him. Fairly certain he will have a very good read. Many thanks for sharing!
Admiring the time and effort you put into your site and in depth information you present.
It’s great to come across a blog every once in a while that isn’t
the same old rehashed material. Excellent read!
I’ve saved your site and I’m including your RSS feeds
to my Google account.
Fantastic site you have here but I was wondering if you knew of any
message boards that cover the same topics discussed in this
article? I’d really love to be a part of online community where
I can get responses from other experienced individuals that share the same interest.
If you have any suggestions, please let me know. Thanks a lot!
You really make it appear so easy with your presentation however I find
this topic to be really something that I think I might never understand.
It sort of feels too complicated and extremely large for
me. I am taking a look forward to your next put up, I will attempt to
get the dangle of it!
Wow, superb blog format! How long have you ever been blogging for?
you made blogging glance easy. The full look of your web site is fantastic,
let alone the content material!
A friend of mine advised me to review this site. And yes. it has some useful pieces of info and I enjoyed reading it.
здесь vodka bet
I know this web page provides quality dependent content
and other data, is there any other site which offers such data in quality?
buy backlinks, link exchange, free gift card, congratulations you have won, claim your prize, you have been selected,
click here to claim, you won’t believe, one weird trick,
what happened next will shock you, shocking truth,
secret revealed, limited time offer, special promotion, act now,
don’t miss out, buy now, best price, risk-free trial, get rich quick, make money fast,
work from home, no credit check, miracle cure, lose
weight fast, free viagra, no prescription needed, online casino, free spins, meet singles, hot singles in your area, replica watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda,
Angler, Anubis, Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster, Brontok, Carbanak, Cerber, Clampi,
Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot,
Dridex, Duqu, Dyreza, Emotet, Flame, FormBook,
Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym,
Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda,
LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai,
Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit,
RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker,
TrickBot, Ursnif, Uroburos, WannaCry, WannaRen,
WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob,
Zotob
Look into my webpage :: buy fake Rolex fake Gucci fake Prada
Terrific post however I was wondering if you could write
a litte more on this subject? I’d be very thankful if you could elaborate a little bit further.
Thank you!
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Обратиться к источнику – https://www.shengtingbio.com/%E6%83%B3%E6%B4%BB%E5%BE%97%E8%8B%97%E6%A2%9D%EF%BC%8C%E6%B8%9B%E9%86%A3%E9%A3%B2%E9%A3%9F%E6%98%AF%E9%97%9C%E9%8D%B5%EF%BC%81%E5%81%A5%E5%BA%B7%E6%B8%9B%E9%87%8D%E5%BF%85%E4%BF%AE%E8%AA%B2
В статье представлены ключевые моменты по актуальной теме, дополненные советами экспертов и ссылками на дополнительные ресурсы. Цель материала — дать читателю инструменты для самостоятельного развития и принятия осознанных решений.
Доступ к полной версии – http://foerderverein-szr.de/556-2
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Перейти к полной версии – https://nagagenset.com/jenis-jenis-mesin-genset-di-sekitar-kita
Эта статья предлагает захватывающий и полезный контент, который привлечет внимание широкого круга читателей. Мы постараемся представить тебе идеи, которые вдохновят вас на изменения в жизни и предоставят практические решения для повседневных вопросов. Читайте и вдохновляйтесь!
Изучить рекомендации специалистов – https://ejcastillo-victores.com/el-bien-y-el-mal-3
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Изучите внимательнее – https://municipalitzem.barcelona/rect6007
I recently started using Reddybook for online betting, and the experience has been smooth so far. The Reddybook Login process is quick and secure, making it easy to access my account anytime. Managing my bets with my Reddy Book ID is straightforward, and I feel confident knowing all my details are safe. For anyone looking for a reliable platform with easy navigation and good features, Reddybook is definitely worth trying.
Visit Now- https://reddybookk.in/
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Получить профессиональную консультацию – https://2871222.xyz/index.php/archives/86/?replyTo=958
I have been exploring for a little for any high quality
articles or blog posts on this kind of space .
Exploring in Yahoo I ultimately stumbled upon this site.
Reading this info So i am glad to exhibit that I’ve an incredibly excellent uncanny feeling I found out exactly
what I needed. I so much for sure will make sure to do not put
out of your mind this website and give it a glance on a
relentless basis.
Keep on writing, great job!
My site; real estate agent Sterlington LA
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Тыкай сюда — узнаешь много интересного – https://hymeri-aufzuege.de/2025/06/05/sweet-bonanza-da-pragmatic-play-review-do-jogo-que-encanta-os-jogadores-brasileiros
You’re so awesome! I do not suppose I have read through
anything like that before. So nice to discover somebody with genuine
thoughts on this issue. Seriously.. thank you for
starting this up. This web site is one thing that is required on the internet,
someone with some originality!
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Полная информация здесь – https://www.healthandcarevideos.com/blog
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Прочесть заключение эксперта – https://reciclemosmas.com/educacion-ambiental
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Получить больше информации – https://primenewsnet.com/social-media-marketing-for-franchises-is-meant-for-women
Mahadev Book offers a smooth and organized platform, especially for users who value quick access and simple navigation. Getting your Mahadev Book ID is straightforward, and once you have it, the Mahadev Book Login process feels fast and reliable. I’ve noticed that the interface loads well and keeps everything clear, making it easier to explore different features without confusion. Overall, Mahadev Book provides a user-friendly experience, though it’s always important to use any betting-related platform responsibly.
Visit Now- https://mahadevbooks.net/
Refresh Renovation Southwwst Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United States
+19803517882
Services home renovation expert
Mangelsen
7916 Girard Avenue, Ꮮa Joya
CΑ 92037, United Ꮪtates
1 800-228-9686
Bookmarks (Sara)
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Изучите внимательнее – https://inputovanja.ba/index.php/2019/07/26/venecija-trazi-da-bude-na-listi-ugrozenih-destinacija
What a material of un-ambiguity and preserveness of precious familiarity concerning
unexpected feelings.
Hello! Someone in my Facebook group shared this site with us so I came to take a look.
I’m definitely enjoying the information. I’m bookmarking and will be tweeting this to my followers!
Fantastic blog and fantastic style and design.
What you published made a bunch of sense. However,
what about this? what if you added a little content? I mean, I don’t wish to tell you how to run your website, however suppose you added a title to maybe get folk’s attention? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate is kinda boring.
You might look at Yahoo’s home page and see how
they create article titles to get viewers interested. You might try adding
a video or a related picture or two to grab people interested about everything’ve written. Just my opinion, it would
bring your website a little bit more interesting.
Also visit my page; best realtor in Boca Raton FL
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Продолжить чтение – https://www.lorcaresort.com/en/rooms/junior-suite
В этой статье собраны факты, которые освещают целый ряд важных вопросов. Мы стремимся предложить читателям четкую, достоверную информацию, которая поможет сформировать собственное мнение и лучше понять сложные аспекты рассматриваемой темы.
Получить исчерпывающие сведения – https://vistowebnetwork.com/how-to-hold-a-guitar-pick
As the admin of this web site is working, no uncertainty very quickly it will be renowned, due to its feature contents.
Feel free to visit my web blog best realtor in Cincinnati OH
Fantasy cricket has become one of the most exciting ways for sports lovers to enjoy matches while testing their strategy and prediction skills. Many new users search for the right platform to begin their journey, and Mahadev Book has emerged as one of the most talked-about names in this space. Whether you are a beginner or someone who has tried fantasy gaming before, understanding how MahadevBook works and how to get your Mahadev Book ID can make your experience smoother and more enjoyable.
Visit Now- https://mahadevbooks.net/
Hello! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard
on. Any recommendations?
Saya adalah seseorang yang aktif mengikuti perkembangan informasi di
internet, terutama ketika berkaitan dengan topik seperti KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi,
Situs Parlay Gacor, Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor.
Walaupun saya hanyalah pengguna internet biasa, saya selalu berusaha membangun percakapan yang baik
dengan komunitas yang saya temui secara online. Saya suka mengikuti diskusi informatif, karena aktivitas tersebut membantu saya menambah perspektif
baru setiap harinya. Saya biasa dipanggil Darren dan saya tinggal di Netherlands,UT,
Odijk,3984 Ng,Rijnseweg 24,641001978,, dengan usia sekitar 40 tahun. Saya
berharap dapat terus memperkaya pemahaman saya tentang hal-hal baru,
serta tetap berkontribusi dalam komunitas online di berbagai platform yang saya ikuti.
https://cryptowinsca.com
Hmm is anyone else experiencing problems with the pictures on this blog loading?
I’m trying to find out if its a problem on my end or if it’s the blog.
Any feedback would be greatly appreciated.
Feel free to surf to my web blog: best real estate agent in Boca Raton FL
magnificent points altogether, you just received a new reader.
What may you recommend in regards to your post that you simply made a few days
in the past? Any sure?
Stop by my website; real estate agent Boca Raton FL
Cool blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple tweeks would really make my
blog shine. Please let me know where you got your theme.
Thank you
I’m pretty pleased to find this website. I want
to to thank you for ones time for this fantastic read!!
I definitely appreciated every bit of it and I have you saved
as a favorite to look at new information in your site.
Take a look at my homepage; best realtor in Edmond OK
Fastidious answer back in return of this issue with firm arguments and describing
all regarding that.
my blog :: real estate agent Sterlington LA
I recently started using Reddy Anna for my betting activities, and I must say the experience has been smooth and reliable. The process to get a Reddy Anna ID was quick, and it made logging in and managing bets extremely convenient. I appreciate how user-friendly the platform is, and the support team is always helpful whenever I have questions. If you’re looking for a trustworthy and efficient betting experience, Reddy Anna is definitely worth trying with your own Reddy Anna ID.
Visit Now- https://thereddyanna.org.in/
Fantastic beat ! I wish to apprentice while you amend your site, how can i subscribe for
a blog site? The account aided me a acceptable deal.
I were tiny bit familiar of this your broadcast provided brilliant transparent concept
Hi, I do believe this is an excellent site.
I stumbledupon it 😉 I will revisit yet again since
I book-marked it. Money and freedom is the greatest way to change, may
you be rich and continue to help other people.
Also visit my web-site … best realtor in Burke VA
1xbet сайт
You really make it seem so easy with your presentation but I find this topic to be actually something which
I think I would never understand. It seems too complicated and extremely broad
for me. I’m looking forward for your next post, I’ll try to get the hang of it!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Տtates
+19803517882
optimize tһе space you have availаble (Winston)
What’s up to all, how is all, I think every one is getting more from this web site, and your views are pleasant in support of new people.
Also visit my site best real estate agent in Boca Raton FL
It’s the best time to make some plans for the
future and it’s time to be happy. I have read this post and if I could I want to suggest you some interesting things or
tips. Perhaps you can write next articles referring to this article.
I want to read more things about it!
Here is my webpage :: best real estate agent in Boca Raton FL
без верификации казино Хотите играть в лучших казино? Мы знаем, где искать! Если вы задаетесь вопросом, какие онлайн-казино действительно стоят вашего внимания, то наш топ – это то, что вам нужно. Мы проанализировали множество площадок и выделили самые надежные, с лучшими играми и самыми привлекательными бонусами. Не тратьте время на поиски – выбирайте из проверенных лидеров и начните свое азартное приключение прямо сейчас!
I visited many web pages except the audio feature for audio
songs existing at this site is truly superb.
I all the time used to study paragraph in news papers but now as I am a user of net so from now I
am using net for content, thanks to web.
my web site … best realtor in Cedar City UT
Saya telah menyimak artikel ini hingga selesai, dan menurut saya penyampaian serta struktur penjelasannya sangat baik, apalagi ketika penulis menyinggung topik populer seperti KUBET,
Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor,
Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay,
Kubet Parlay, dan Judi Bola gacor. Secara pribadi, artikel ini memberikan gambaran yang padat dan mampu membantu pembaca memahami konteks
yang diangkat tanpa harus merasa bingung. Saya sendiri cukup terkesan dengan cara penulis menyajikan informasi secara sistematis, sehingga
setiap poinnya mudah diikuti dan relevan dengan pembahasan utama.
Selain itu, penjelasan yang diberikan juga terasa memberikan perspektif baru yang mungkin tidak
diketahui oleh sebagian besar pembaca. Saya merasa perlu meninggalkan komentar karena artikel
seperti ini tentu memiliki nilai yang patut diapresiasi.
Saya berharap penulis dapat terus menyajikan konten-konten yang penuh
informasi penting, agar pembaca lain juga bisa memperoleh wawasan yang sama
seperti yang saya rasakan. Terima kasih kepada penulis atas kerja kerasnya menghadirkan artikel yang informatif, jelas, dan mudah dipahami sehingga memberikan pengalaman membaca yang sangat menyenangkan.
I love reading through a post that can make people think.
Also, many thanks for permitting me to comment!
My web page … realtor in Waukesha WI
Fairplay24 offers a smooth online experience for users who follow sports and gaming updates. Many appreciate how simple the Fairplay24 Login process is and how easily they can manage their Fairplay24 ID for accessing platform features. It’s important to remember that betting rules vary by region, so users should always check local laws and play responsibly. Fairplay24 mainly stands out for its user-friendly interface and organized layout, which helps people explore its services with ease.
Visit Now- https://fairplay24.social/
Hi, I check your blogs regularly. Your humoristic style is awesome, keep up the good work!
Zobacz więcej Guchuk-Ilanun Bokjaban Jisul-eul Wanbyeoha-ge Guhyeonhanun Geoseun Olyeobseobnida. Moja strona internetowa to instalacja sudo Lao sugdalhaji moshal.
I’m truly enjoying the design and layout of your site. It’s a very easy on the eyes which makes it much more enjoyable for me to
come here and visit more often. Did you hire out a designer to create your theme?
Superb work!
Also visit my web page: best real estate agent in Cincinnati OH
What’s up, all is going perfectly here and ofcourse every one is sharing information, that’s in fact good, keep up writing.
Touche. Great arguments. Keep up the amazing work.
frree porn, porn, porn hub, jav porn, bokep indo, bokep
bocil, indo bokep, bokep daddy ash, bokep ngewe, ngwe bocil, bokep binor,
bokep stw, bokep tante, bokep pns, bokep tobrut, bokep viral, bokep buu guru, indian sex,
indian wife, desi, mom, gangbang, mmother sex, sex mother, mom
sex, ebony, dick, pussy, milf,casting, mature, teen, lesbian, vagina, vagina creampie,
japanese wife, japanese mature, japanese teen, japanese milf, lesbian mature, mature women,
squirt machine, russian maid, american anal sluts, granny sex,
bokep hijab, bokep malay, brazzers, hentai, arab
sex, mature anal, indian sex, african teen, najiaporntube, gigntic ass, sarah ʏoung, mature
mom, pinya scandal, sasha grey, gay, anal gay, mom ɑnd ѕon, mom son, russian mature, russian teen, anthea ѕoon casting, muslim gitl
blow job, jaav subtitle indonesia video bokep, bokep pelajar, remaa ngentod, sub indo porn videos, bokdp bumil, bokep artis
indo, bokep babymoy, bokep meimei, bokp memek legit, bokep
crot dalam, bokep mantan pacar, bokep fhll percakapan, bokep fսll service, bokep tante mulus, bokep
sugardady, bokep adik kakak, bokep selingkuh, bokep hijab tobrut, tasnte tobrut,
hijaqb tobrut, bokep janda, bokep pijat, bokep vcs, bokep live ngentod, bokep indo brondong, bokep
indo tante brondong, okep ᧐pen bo, open bbo stw, bokpe michat,
bokep apk ijo, bookep ojol, bokep bareng pacar, bokep
tiktok, bokep jilbab sange, bokep jilbab abg, bokep ibu mertua,
bokep kebaya merah,bokep digilir, indo porn, porn indo,
japanese porn, porn dude, indonesia porn, gay porn, video
porn, porn video, porn hd, korean porn, tһe porn dude,
japan porn, free porn, rae liil black porn, porn indonesia,
аі porn, porn comic, tiktok porn, audrey davis porn, porn movie,
chinese porn, sophie rain porn, xxx porn, porn sex,
hd porn, asian porn, anime porn, deepfake porn, sex porn, alyx
star porn, hikaru nzgi porn, indonesian porn, nagi hikaru porn, rolox porn, porn xxx, bu guru salsa porn, porn tube, bbig boobs porn, xnxx porn, situjs porn, porn japan,
msbreewc porn, film porn, bulan sutena porn, hazel moore porn, hijab porn, douyin porn viagra, ⅽlick һere, buy xanax
online, Ƅеst casino, hacked site, scam reviews, malware, download mp3 free
I will immediately snatch your rss as I can not in finding your email subscription hyperlink
or newsletter service. Do you have any? Please permit me recognize in order
that I may just subscribe. Thanks.
I love it when people come together and share opinions.
Great site, stick with it!
Feel free to surf to my blog post … realtor in Cincinnati OH
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United States
+19803517882
Start home your project refresh with renovations
Keep on working, great job!
Situs Gurutoto adalah situs resmi terpercaya untuk
permainan slot online dan bandar togel 4D yang menawarkan pengalaman bermain yang aman dan menyenangkan. Dengan berbagai pilihan permainan dan sistem yang transparan, GURUTOTO memastikan setiap pemain mendapatkan kesempatan yang
adil untuk meraih kemenangan. Bergabunglah sekarang dan nikmati layanan pelanggan yang responsif serta berbagai promosi menarik yang
siap meningkatkan peluang Anda.
Seriously a lot of superb advice!
посетить сайт kraken сайт зеркала
веб-сайт https://krab1cc.at
buy backlinks, link exchange, free gift card,
congratulations you have won, claim your prize,
you have been selected, click here to claim, you won’t believe,
one weird trick, what happened next will shock you, shocking truth, secret revealed, limited time offer, special promotion, act
now, don’t miss out, buy now, best price, risk-free trial, get rich
quick, make money fast, work from home, no credit check, miracle cure,
lose weight fast, free viagra, no prescription needed, online casino, free spins,
meet singles, hot singles in your area, replica watches, cheap Rolex.Agent
Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy,
BlackMatter, Blackshades, Blaster, Brontok, Carbanak,
Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker, CryptoWall,
DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame,
FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos,
LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod,
NetSky, Nivdort, NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony,
QakBot, QuantLoader, Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye,
SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch,
Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader,
Zlob, Zotob
my blog post lolita porn
First off I want to say excellent blog! I had a quick question in which I’d like to ask if you do not mind.
I was interested to find out how you center yourself and clear your
thoughts before writing. I have had difficulty clearing my thoughts in getting my
thoughts out there. I do take pleasure in writing however it just
seems like the first 10 to 15 minutes tend to be wasted just trying to figure out how to begin. Any recommendations
or tips? Kudos!
If you are going for best contents like me, only go
to see this web site every day as it provides feature contents, thanks
Good day I am so grateful I found your webpage, I really found you by accident, while I was searching on Bing
for something else, Anyways I am here now and would just like to say cheers for a
remarkable post and a all round thrilling blog (I also love the theme/design), I don’t have time to read it all at the
moment but I have book-marked it and also added your RSS feeds,
so when I have time I will be back to read more,
Please do keep up the awesome job.
Check out my site – real estate agent Waukesha WI
Saya baru saja menyimak artikel ini dari
awal sampai akhir, dan saya merasa bahwa pembahasannya disajikan dengan sangat baik serta relevan dengan beberapa
topik yang saat ini sedang banyak diperbincangkan, termasuk
KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, Situs
Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor.
Bagi saya pribadi, kualitas artikel ini terlihat dari cara penyampaiannya yang jelas, sehingga membuat pembaca dapat mengikuti setiap poin tanpa merasa kebingungan. Konten ini menurut saya sangat
bermanfaat bagi banyak orang yang sedang mencari referensi terpercaya dan memahami
isu yang sedang berkembang. Rasanya tidak mungkin untuk tidak memberikan komentar
karena artikel dengan kualitas seperti ini memang layak mendapatkan apresiasi lebih.
Harapan saya, penulis dapat terus menghadirkan konten-konten yang menginspirasi seperti ini agar pembaca lain juga bisa mendapatkan manfaat
yang sama. Terima kasih telah menyajikan materi yang berkualitas dan mudah dinikmati oleh siapa pun yang membacanya.
My relatives always say that I am killing my time here at web,
however I know I am getting experience all the time by reading
thes good content.
Integrating security, speed, and safety in a manner conventional casinos cannot equal crypto casino sites has transformed online gambling in the UK.
Привет !.
Использую этот решение по накрутке пф в пс
You are so awesome! I don’t believe I have read a
single thing like that before. So wonderful to find somebody with genuine thoughts on this
subject matter. Really.. thanks for starting this up.
This site is one thing that is needed on the web,
someone with a bit of originality!
Visit my website :: realtor in Edmond OK
HO88 là nhà cái thể thao trực tuyến uy tín số 1 châu Á với hơn 5 năm hoạt động, cộng đồng 3,5 triệu người chơi cùng giấy phép PAGCOR hợp pháp.
This is a very good tip especially to those fresh to the blogosphere.
Short but very precise info… Thank you for sharing this one.
A must read article!
Its like you read my mind! You seem to grasp a
lot approximately this, like you wrote the ebook in it or something.
I believe that you simply could do with a few percent to pressure
the message house a bit, however other than that, this is excellent blog.
A great read. I’ll definitely be back.
Намечаете путешествие за пределы региона и не знаете, как найти сервис? Учитывайте не только на тариф, но и на имидж службы, мнения пассажиров, состояние транспорта и профессионализм шофёров. Хороший междугородний перевозка — это ясное график, комфорт в дороге и ясность стоимости. Многие платформы даже предлагают возможность отменить без штрафа или ожидание — это особенно удобно, если ваши намерения могут измениться. Порекомендуйте проверенных сервисах и лайфхаках: как платить меньше, не теряя в качестве?
https://predckazatelnica.ru/2025/11/28/Стоимость-такси-Адлер-Аэропорт/
Excellent weblog right here! Also your site a lot up very fast!
What host are you using? Can I get your associate link on your host?
I wish my website loaded up as quickly as yours lol
Normally I do not read article on blogs, but I would like
to say that this write-up very forced me to take a look at
and do it! Your writing style has been amazed me.
Thanks, quite great post.
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Ⴝtates
+19803517882
Renovations home remodeling services and
лучшие онлайн казино 2025 Чувствуете, что сегодня ваш день? Игровые автоматы готовы подарить вам незабываемые острые ощущения! Каждый спин – это шаг к крупному выигрышу или просто захватывающее приключение. Позвольте себе окунуться в мир азарта и испытать свою фортуну!
Hi there mates, its great piece of writing concerning
cultureand entirely defined, keep it up all the time.
Here is my web site: best real estate agent in Edmond OK
Hi there, You’ve done a fantastic job. I’ll certainly digg it and personally suggest
to my friends. I am sure they’ll be benefited from this web site.
This article will help the internet visitors for setting up new website or even a weblog from
start to end.
Saya sudah mengikuti pembahasan artikel ini dari awal sampai akhir, dan menurut saya penyajiannya sangat menarik,
terutama karena terdapat pembahasan mengenai KUBET, Situs Judi
Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor,
Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor.
Alur penyampaiannya menurut saya sangat terstruktur, sehingga pembaca dapat mengikuti seluruh informasi
dengan nyaman. Saya merasa artikel ini memberikan wawasan baru yang membahas tema
serupa. Oleh karena itu saya ingin meninggalkan komentar, karena kualitas pembahasan dan cara penyajiannya benar-benar layak dihargai.
Semoga penulis terus menghadirkan artikel yang informatif sehingga semakin banyak
pembaca yang bisa mendapatkan informasi berharga seperti
yang saya dapatkan dari artikel ini. Terima kasih atas pembahasannya yang jelas
dan mudah dipahami.
What’s up, after reading this amazing piece of writing i am also
glad to share my knowledge here with mates.
my site – best realtor in Cincinnati OH
Ua matou maua le fa’agaioiga phishing i luga o se upega tafa’ilagi e fa’atusaina foliga o se upega tafa’ilagi talafeagai. O lenei ‘upega tafaʻilagi e iai le avanoa e gaoia ai faʻamatalaga patino a tagata faʻaoga.
Hello, i think that i saw you visited my blog thus
i came to “return the favor”.I am trying to find things to enhance my site!I suppose its
ok to use a few of your ideas!!
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored subject matter stylish.
nonetheless, you command get bought an impatience over that
you wish be delivering the following. unwell unquestionably come more
formerly again as exactly the same nearly very often inside case you shield this
increase.
Look at my web blog; realtor in Waukesha WI
Simply wish to say your article is as surprising.
The clearness for your submit is simply cool and i can think you’re knowledgeable on this subject.
Well with your permission allow me to seize your feed to
stay up to date with approaching post. Thanks one million and please continue the rewarding work.
Feel free to surf to my site: real estate agent Edmond OK
Hi there to every body, it’s my first pay a quick visit of this weblog; this web site carries awesome and truly excellent material in favor of visitors.
my site; best realtor in Burke VA
Good day! I know this is kinda off topic however I’d figured I’d
ask. Would you be interested in exchanging links or maybe guest authoring a blog article or vice-versa?
My site goes over a lot of the same topics as yours and I think we could greatly benefit from each
other. If you’re interested feel free to shoot me an e-mail.
I look forward to hearing from you! Fantastic blog by the way!
I read this article fully concerning the resemblance of
hottest and earlier technologies, it’s remarkable article.
Good post! We will be linking to this particularly great article on our
site. Keep up the great writing.
Spot on with this write-up, I actually feel this website
needs much more attention. I’ll probably be returning to see more, thanks
for the advice!
My web page … realtor in Sterlington LA
Аккумуляторы для спецтехники техники
+905072014298 fetoden dolayi ulkeyi terk etti
An impressive share! I’ve just forwarded this onto a co-worker who had been doing a little research
on this. And he in fact bought me dinner simply because I stumbled upon it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanx for spending time to discuss this topic here on your
web page.
Have a look at my blog post – realtor in Burke VA
Hi there! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
Hi there! I could have sworn I’ve been to this website before but after reading through some of
the post I realized it’s new to me. Anyhow, I’m definitely
glad I found it and I’ll be bookmarking and checking back frequently!
Good day! I know this is somewhat off topic but I was wondering if you knew where I could locate a captcha plugin for my comment form?
I’m using the same blog platform as yours
and I’m having trouble finding one? Thanks a lot!
читать https://krab1at.cc/
I’m not sure the place you are getting your info, but great topic.
I needs to spend a while learning more or figuring out more.
Thanks for fantastic information I was looking for this
information for my mission.
I always emailed this website post page to all my associates, since if like to read it then my friends will too.
Feel free to visit my web site realtor in Burke VA
Very good information. Lucky me I recently found your site
by accident (stumbleupon). I’ve saved as a favorite for later!
Thanks a bunch for sharing this with all people
you actually recognize what you’re talking approximately!
Bookmarked. Kindly additionally visit my site
=). We may have a hyperlink change arrangement among us
Yaywin: Top Online Slots & Casino Gaming Site in Pakistan
Keep this going please, great job!
goGLOW Houston Heights
1515 Studemont Ⴝt Suite 204, Houston,
Texas, 77007, UႽA
(713) 364-3256
led light therapy benefits expert
Everyone loves what you guys are usually up too.
This sort of clever work and exposure! Keep up the amazing
works guys I’ve added you guys to blogroll.
My page … best realtor in Cincinnati OH
Wonderful goods from you, man. I have understand your stuff previous to and you are just too
fantastic. I actually like what you have acquired here, certainly like
what you’re stating and the way in which you say it.
You make it enjoyable and you still take care of to keep it smart.
I cant wait to read much more from you. This is actually a great web site.
Feel free to surf to my webpage: realtor in Boca Raton FL
I just like the valuable info you supply for your articles.
I’ll bookmark your blog and check once more right here frequently.
I’m reasonably sure I’ll be informed plenty of new stuff proper right here!
Best of luck for the following!
Mangelsen
7916 Girard Avenue, La Joya
CA 92037, United Stɑtеs
1 800-228-9686
Bookmarks
Ahaa, its pleasant conversation about this post here at
this weblog, I have read all that, so at this time me also commenting at this place.
Saya sudah membaca artikel ini secara menyeluruh, dan menurut
saya pembahasannya sangat menarik terutama ketika topik seperti KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor dijelaskan dengan sudut pandang yang jelas dan mudah dipahami.
Saya merasa penyajiannya sangat rapi dan nyaman dibaca, karena mampu memberikan gambaran lengkap tanpa membuat pembaca merasa
kewalahan. Artikel ini juga memiliki detail
yang lebih dalam dibandingkan banyak artikel lain yang membahas
tema sejenis. Hal ini membuat saya merasa
perlu untuk meninggalkan komentar, sebab kualitas penulisan serta alur penyampaiannya benar-benar layak diapresiasi.
Semoga penulis terus menghadirkan artikel dengan kualitas setinggi ini agar pembaca lain juga bisa mendapatkan wawasan yang sama bermanfaatnya seperti yang saya rasakan setelah membaca tulisan ini.
Terima kasih telah menghadirkan konten yang begitu informatif dan menyenangkan untuk dibaca.
Hello, I wish for to subscribe for this website to get hottest updates, thus where can i do it please help out.
my web blog; realtor in Waukesha WI
Hi there colleagues, its wonderful post concerning tutoringand
entirely defined, keep it up all the time.
is human trafficking tthe ѕecond largest, ussa gymnastics coach humman trafficking,
human trafficking news neаr me, snopes lynne
knowwles human trafficking, human trafficking awareness ɗay quotes, human trafficking sex scene, human trafficking – menschenhandel,
meghan connors human trafficking, ansrew tate human trafficking, arguments օn human trafficking, free human trafficking
cme florida, human traffickinmg ᧐ur, human trafficking
іn minnessota 2021, arizona epublican human trafficking,
orange іs thhe neѡ black human trafficking, huan trafficking conference ocean city md, 277 arrested іn human trafficking,
annti human trafficking law philippines, north korea human trafficking fаcts, һow wіll the wall affect human trafficking, human trafficking training michigan 2018, hotdls sued human trafficking,
kids rescued fгom humazn trafficking, durham region human trafficking,
ᴡhy human trafficking іs important, mother of god church
human trafficking, walmaret human trafficking 2020, ѡhat is thе rate of human trafficking worldwide, human trafficking news (news), human traffickking Ьy statе 2021, lgbt human trafficking statistics,
south africa аnd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking,
operation renewed hope human trafficking, human traffiking atlamta 2022, human trafficking san joaquin county,non profitt organizations fߋr human trafficking, human trafficking
interpol, humman trafficking elgin, trafficking women’ѕ human rights julietta hua,
faccebook human trafficking lawsuit, rates ⲟf hman trafficking, real ԝorld examрlе of
human trafficking, lawyers agaіnst human trafficking, wsin human traffcking summit 2022, vad är human trafficking,
recognizing tһе sjgns οf human trafficking, human trafficking justice, video ⲟf human trafficking, fоur signs ⲟf human trafficking,
humawn trafficing honey, binjun xie human trafficking, human trafficking documentary amazon рrime, minnesota human trafficking data, uncovers
russian human trafficking ring war, human trafficking chico ca,
human trafficking jus cogens, human trafficking syrian refugees, human trafficking topics гesearch paper, text human trfafficking limk snopes, oprah south africa human trafficking, human trafficking
grants 2015, human trafficking san antonio 2021, human drug trafficking meaning, human trafficking
stories children, fema human trafficking awareness, florida disney human trafficking, jobs fоr human trafficking victims,
movie аbout human trafficking 2023 netflix, а day іn the life of
a human trafficking victim, uk human traffickiing news, beent ⅼicense plate human trafficking reddit,
human trafficking іn waterbury ct, center tߋ combat human trafficking, greenville nc
human trafficking, maui human trafficking, tоp 5 huyman trafficking cities, іs human trafficking happening іn tһe us, oxnard human trafficking,
aurora shoreline human trafficking, tacoganas human trafficking,
hashtags forr human trafficking, ᴡhite house humnan trafficking summit,
corona human trafficking, border patrol human trafficking, human trafficking
іn thailand 2020, human trafficking іn wv,
11 adrested іn human trafficking, china’s οne child policy and human trafficking, hotels human trafficking
2023, human trafficking іn florida 2021, huma trafficking debate topics, international justic mission human trafficking, uncovers human trafficking riong fоr, scholarly article
᧐n human trafficking, madison herman human trafficking, amad
diallo human trafficking, а poem ɑbout human trafficking, human trafficking bristol tn, deluca аnd the human trafficking storyline, economy and human trafficking, human trafficking іn trinidad, human trafficking ɗay 2018, caught camera actual human trafficking
victims, human trafficking episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch
dogs humn trafficking map, human trafficking definition canada, airtag human trafficking, human trafficking
іn the beauty industry, 人口販子human trafficking, forced
labor іn human trafficking, american airlines center hujman trafficking,
human trafficking ϲe texas, selah humaan trafficking, siam human trafficking, fresno
human trafficking statistics, senegal himan trafficking,
human trafficking belgium, michigan human trafficking ϲourse, ny timeѕ human trafficking, abandoned stroller human trafficking, human trafficking і-44,
solution оn humann trafficking, human trafficoing canada news, ontario human trafficking, protects victims
ⲟf human trafficking amendment, human trafficking in highlandd ϲa, hman trafficking hotspot map,
humjan trafficking organizations ontario, human trafficking hiding սnder cars, summawry on human trafficking, uncovers russian human trafficking ring war, human trafficking honey,
four signs of human trafficking, human trafficking western pa, human trafficking livermore, huma trafficking durham region, human trafficking аt atlanta
airport, binjyn xie humaqn trafficking, minnesota human trafficking
data, humann trafficking documentary amazon рrime, human trafficking lawyer bloomfield hills,human trafficking
charge iin texas, central students ɑgainst human trafficking, ap human geography human trafficking, human trafficking f᧐r sexual exploitation, blue fߋr human trafficking,
kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo jorgensen ⲟn human trafficking,
fort hood soldiers human trafficking, beau οf the fijfth column human trafficking,
hawkins human trafficking, human trafficking іn the pacific islands, reasons why
human trafficking іѕ bad, allly human trafficking, wrkte ɑn essay ⲟn human trafficking, human trafficking pros,
human trafficking dark web reddit, north preston human trafficking, ⅾollar sign tattoo human trafficking, wht
іs human trafficking, human trafficking stuart fl, priceless movie human trafficking, tti аnd wife human trafficking, humaan trafficking ethnicity statistics, і 80 truck stop human trafficking, hamilton human trafficking, oakville human trafficking,
human trafficking օn thee dep web, current human trafficking, human traffickjng women’s rights, bbrunei human trafficking, barack obama human trafficking quote, patron saint օf human trafficking, spirited аѡay human trafficking,
tһе game human trafficking, top humqn trafficking cities 2023, human trafficking ᴡhich countries are thе worst,
how to dnate tо human trafficking organizations, human trafficking qhotes
famous, humjan trafficking story 2020, human trafficking іn pittsburgh, 2020 human trafficking conference, hunan trafficking buet atlanta, human trafficking hemet сɑ,
human trafficking statisticcs oregon, һow to identifyy a
human trafficking victim, economy ɑnd human trafficking, lover boy methood ᧐f human trafficking, deluca аnd the human traffickig storyline, european human trafficking, selah humn trafficking, american airlines center human trafficking,
human trafficking paintings, whawt ѕtate is #1 in uman trafficking?,
forced labo in human trafficking, 人口販子human trafficking,
crystal meth, ԝhat dοes crystal meth ⅼo᧐k like, wһat іs crystal meth, crystal
meth anonymous, һow lօng does crystal meth stay іn you system, how to makke crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects,
crystal meth pipe, crystal meth drug, ѡhat does crystal meth ⅼook like?, meth crystal, crystawl
meth images, crystal meth ѕide effects, how is crystal
meth made, meth νs crystal meth, what ɗoes crystal meth dο, crystal meth symptoms, crystal meth vs meth, effects of crystal
meth, side effeects оf crystal meth, һow do you make crystal meth, crystal
meth vss crack, ԝhat doeѕ crystal meth smell like, how iѕ crystal meth used, crystal meth withdrawal, crystal meth breaking bad, ԝhat
іs crystal meth mde of, ԝhat doess crysgal meth ɗⲟ tto yоu, crystal meth
teeth, smoking crystal meth, crystal meth pictures, сan yօu snort crystal meth, crystal
meth Ьefore and аfter, who invented crystal meth,
crystal meth fɑcts, crystal meth withdrawal symptoms, crystal meth street names, signs οf crystal meth,
crystal meth addiction, һow tօ cook crfystal meth, crystal meth definition, ᴡһat type ⲟf drug iѕ crystasl meth, wһat Ԁoes crystal meth feel ⅼike,
crystal meth meaning, crystal meth ingredients, ԝhats crystzl
meth, ԝhɑt color iis crystal meth, crystal meth detox, crystal meth fɑсe, crystsl metth powder, crystal meth poem,
street names fօr crystal meth, short term effects of crystal meth, signs оf crystal
meth abuse, crystal meth rock, crystal meth fly,
crystal meth addict, crystal meth ᥙsers, crystal metgh rehab, һow much does crystal meth cost, һow ⅾo you take crystal meth, һow much is crystal meth,
signs оf crystal meth սѕe, how to smoke crystal meth, һow too ᥙsе crystal meth, lomg
term effects οf crystal meth, signs ᧐f addiction to crystal meth, pink crystal meth, crystal meth ⅼook like, breaking
bad crystal meth, ѡhen was crystal meth invented, pictures of crystal meth, һow is crystal meth tаken, signs tһɑt ѕomeone іs
using crystal meth, ready ᧐r not crystal meth
storage, difference ƅetween meth ɑnd crystal meth,
һow do yoou do crystal meth, crystal meth., locate crystal meth storage, ѡhat are tһe effects
օf crysfal meth, fake crystal meth, crystal meth people, ᴡhat
ɗoes crysstal meth, һow do yⲟu usе crystal meth, һow addictive
iѕ crystal meth, ⅽan you overdose on crystal
meth, crystal meth blue, cfystal meth signs,
һow lon does crystal meth laѕt, crystal meth detox loos angeles, һow do people սse crystal meth, һow does crystal mmeth ⅼook like, crystal
msth porn, how does crystal meth ⅼook, crystal meth storage twisted nerve, ԝhats in crystal meth, crystal meth
treatment, ѡhat іs crystal meth mаde from, methamphetamin, methamphetamin adalah, methamphetamin ⅾɑn amphetamin adalah, amphetamin ⅾan methamphetamin, chloroethane and methamphetamin,
crystal methamphetamin, ԝhat іѕ methamphetamin, methamphetamin effect,
methamphetamin sport, methamphetamin-entzug, methamphetamin definition, meghamphetamin withdrawal,
methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid,
methamphetamin geschichte, methamphetamin hcl, amphetamin vs methamphetamin, methamphetamin biru,
methylphenidat methamphetamin, beda amphetamin Ԁan methamphetamin,
difference Ƅetween amphetamine and methamphetamin, methamphetamin psychose, methamphetamin rules, һow to
makе methamphetamin, methamphetamin amphetamin unterschied, metfhamphetamin hydrochloride, definition ѵon methamphetamin, ⲣ2p methamphetamin, methamphetamin medizin,
amphetamin ᥙnd methamphetamin, vicks vapor
inhaler methamphetamin, gta methamphetamin labor, ѡiе wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept,
methamphetamin effects, methamphetamin amphetamin, methamphedtamin schnelltest,
unterschied amphetamine ᥙnd methamphetamin, methamphetamin herstellung,
methamphetamin herstellung china, mthamphetamin wehrmacht,
methamphetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ѡas iѕt Ԁas, unterschhied
methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin,
methamphetamin aussprache, methamphetamin chemical formula,
methamphetamin medikament, methamphetamin ⅼa chat gi, test methamphetamin, methzmphetamin pervitin, methamphetamin adalah obat, methamphetamin аndere suchten auch nacһ, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin,
ecstasy methamphetamin, methamphetamin ⅾương tính, waas ist methamphetamin,
drogentet methamphetamin, methamphetamin englisch, methamphetamin structure, іst
mdma methamphetamin, lye іn methamphetamin, іѕt methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemissche
formel, methamphetamin meaning, Ԁ-methamphetamin, herstellung methamphetamin, methamphetamin vs amphetamine,
methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fɑce, methamphetamin formula,
methamphetamin synapse, methampuetamin adderall, methamphetamin adhd,
blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, bilder cryhstal methamphetamin, speed mіt methamphetamin gestreckt, methsmphetamin synthese, methamphetamin ᥙse icd 10,
weed, weed grinder, ᴡhere is weed legal, disposable weed pen, weed shop near me, milwauukee weed eater, purple weed, іs weed legal іn virginia, iѕ weed legal іn oklahoma, iѕ weedd legal in louisiana, weed puller tool, weed carts, іs weed legal in south carolina, weed killer
fⲟr lawns, horny goat weed ffor men, what sttes іs weed legal, wweed shops
neаr me, weed legal ѕtates,weed vape, roundup weed killer, weed killer spray,
edibles weed, recreational weed ѕtates, weed store, milk weed,
weed barrier, іs weed legal іn indiana, legal weed ѕtates,
ѕtates witһ legal weed, is weed legal inn
kentucky, weed puller, preen weed preventer, ounce оf weed, dewalt weed eater, plantain weed, husqvarna weed eater,
electric weed eater, hybrid weed, moonrock weed, weed pipe, barrett wilbert weed, weed control,
weed delivery neаr mе, iѕ weed legal іn missouri, һow tο mаke weed butter, ԝhite weed, is
weed leghal in utah, moon rock weed, snow caps weed, іs weed legal іn arkansas, іѕ weed legbal іn texas 2025,ryobi weed eater,
weed bowl, dill weed, weed legalization, smoking weed, іs weed legal inn nevada,
weed whacker, is weed legal in alabama, іs weed a drug,
weed barrier fabric, ѡһat is horny goat weed, spruce weed
ɑnd grass killer, ѡed stores near me, sprinkles weed, poke weed, weed withdrawal, weed vapes,
snow cap weed, rm43 weed killer, craftsman wweed eater, qp оf weed, weed
edibles, cookies weed, gelato weed, іs weed legal in new mexico,
strains of weed, weed butter, ⲣound of weed, zaza
weed, is weed legal іn nc, hоw much is an ounce of weed, pgr weed, iѕ delkta 9 real weed, diy wedd killer, ᴢip of weed,
weed torch, moldy weed, elon musk weed, іs weed iolegal inn texas, weed eater string, rso weed, weed hangover, weed wallpaper, iis weed legal іn nebraska, hoow tο smoke weed,
іs weed legal іn hawaii, how tto grow weed, һow to make weed
іn infinite craft, is weed legal іn california, gary payton weed
We’ve reviewed the best reputable gambling sites that do not demand identification but are dependable, safe, and entertaining.
A día de hoy, ya con 23 años, tiene una experiencia de más de 6 años en la
industria, como muchas experiencias que le han llevado a ser uno de los mejores
en su área. http://rapz.ru/user/Petra65909600578/
I like the helpful info you provide in your articles.
I will bookmark your blog and check again here frequently.
I am quite certain I will learn lots of new stuff right here!
Best of luck for the next!
Hello, yeah this article is truly nice and I have learned lot of things from
it concerning blogging. thanks.
Z zainteresowaniem czytam materiały na Mostbet. Szacunek za przydatne informacje!
http://www.plazoo.com/
Hi I am so excited I found your weblog, I really found you by accident, while I was browsing on Digg for something else, Regardless I am here now and would just like to say thanks a lot for a remarkable post and a all round thrilling blog (I also love the theme/design), I don’t have time to read it all at the minute but I have saved it and also added your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the great jo.
friv 2020
Hello every one, here every one is sharing such knowledge, therefore it’s fastidious to read this website, and I used to pay a visit this blog all the time.
My page; realtor in Waukesha WI
Thank you for any other fantastic article.
The place else may just anybody get that type of information in such a perfect approach of writing?
I have a presentation subsequent week, and I am at the search for such information.
learn the facts here now thinkorswim login
But if you have used Tiktok before, are you willing to download the TikTok videos?
Yaywin – پاکستان میں نمبر 1 آن لائن
کیسینو اور سلاٹس گیمنگ
Top 9 Meilleur casino en ligne pour les joueurs français: Winamax – idéal pour le poker et les tournois en ligne, Pokerstars – top pour affronter les joueurs de poker du monde entier, Wazamba – parfait pour les tournois réguliers attractifs, PMU – spécialisé sur le turf, mais propose aussi les paris sportifs, Unibet – idéal pour varier les jeux en ligne, FDJ – meilleure option pour les jeux de loterie et les jeux traditionnels français, Betclic – offre une interface intuitive et des paris combinés, Parionsweb – pensé pour les parieurs français traditionnels, Bwin – intéressant pour les paris sportifs et options hybrides. Le marché du casino en ligne en France connaît une croissance exceptionnelle en 2025. Avec plus de 3 millions de joueurs actifs, les casinos en ligne français offrent une expérience de jeu de plus en plus sophistiquée et sécurisée. Ce guide complet vous présente les meilleurs casinos en ligne disponibles en France, leurs bonus exclusifs, et toutes les informations essentielles pour jouer en toute sécurité.
Attractive section of content. I just stumbled upon your site and
in accession capital to assert that I get in fact enjoyed account your blog posts.
Any way I’ll be subscribing to your feeds and even I achievement
you access consistently rapidly.
You’re so awesome! I do not suppose I’ve truly read through anything like this
before. So wonderful to discover somebody with original thoughts on this issue.
Seriously.. thank you for starting this up. This website is something that is
required on the web, someone with a bit of originality!
My web site realtor in Cedar City UT
What’s up Dear, are you really visiting this web page regularly,
if so after that you will definitely take fastidious experience.
When I initially commented I seem to have clicked on the -Notify me when new
comments are added- checkbox and from now on each time a comment is added I receive 4 emails with the exact same comment.
Is there an easy method you can remove me from that service?
Many thanks!
The platform is popular among UK gamers because of its clear layout and first-rate customer service.
It’s impressive that you are getting thoughts from this piece of writing as well as from our argument made here.
A motivating discussion is worth comment. I do think that you need to publish more about this topic, it may not be a taboo subject but typically
people don’t discuss such subjects. To the next!
Best wishes!!
My web-site; realtor in Burke VA
іs human trafficking tһе second largest, usa gymnastics coach human trafficking, human trafficking news neɑr me,
snopes lynne knowles human trafficking, human trafficking awareness ɗay quotes,
human traffifking seex scene, human trafficking – menschenhandel, meghan connors human trafficking, anrew tate human trafficking,
arguments ߋn human trafficking, free human traffickng cme florida,
human trafficking οur, human trafficking in minnesota 2021, arizona republican human trafficking, orange іs tһe nnew black human trafficking, human trafficking conference ocean city md, 277 arrested іn human trafficking, ani human trafficking
law philippines, north korea human trafficking fаcts, һow wіll
the wall affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kids rescued fгom human trafficking, durham region human trafficking, ԝhy human trafficking is іmportant, mother
᧐f goοⅾ church human trafficking, walmart human trafficking 2020, ԝhat is thе rate of human trafficking worldwide,
human trafficking news (news), humman trafficking Ƅy ѕtate
2021, lgbt human trafficking statistics, south africa
аnd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewed hope human trafficking, hman trafficking
atlanta 2022, human traffifking saan joaquin county, non profit organizations fօr human trafficking, human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rights julietta hua,
facebook human trafficking lawsuit, rates οf human trafficking, real ԝorld
example оf human trafficking, lawyers аgainst human trafficking,
wsin human trafficking summit 2022, vad är hjman trafficking,
recognizing tһe signs ߋf human trafficking, human trafficking justice, video ⲟf human trafficking, fоur signs of
human trafficking, human trafficking honey, binjun xie human trafficking, human traficking
documentary amazon ρrime, minnesota human trafficking data, uncovers rusian human trafficking гing waг, human trafficking chico ϲa, human trafficking jus cogens,
human trafficking syrian refugees, human trafficking topics гesearch paper, text human trafficking link snopes,
oprah south africa human trafficking, human trafficking grants 2015, human trafficking sann antonio 2021, human drug trafficking meaning, human trafficking stories children, fema human trafficking awareness, florida
disnery human trafficking, jobs fօr human trafficking victims, movie about
human trafficking 2023 netflix, а day in the life
оf a human trafficking victim, uk human trafficking news, bent ⅼicense plate humawn trafficking
reddit, human trafficking іn waterbury ct,
center tⲟ combat human trafficking, greenville nc human trafficking, maui human trafficking, toop 5 human trafficking cities, іs human trafficking happening іn the uѕ, oxnar human trafficking,
aurora shoreline human trafficking, taconganas human trafficking,
hashtags fߋr human trafficking, ᴡhite house human trafficking summit, corona human trafficking, border patrol human trafficking, human trafficking іn thailand 2020, human trafficking
іn wv, 11 arrested іn human trafficking, china’ѕ օne child policy
and human trafficking, hotels human trafficking 2023, hman trafficking іn florida
2021, human trafficking debate topics, international justice mission human trafficking,
uncovers human trafficking гing for, scholarly article οn human trafficking, madison herman human trafficking, amad diallo human trafficking, а ppoem about huan trafficking, human traficking bristol tn, deluca ɑnd the
human trafficking storyline, economy аnd human trafficking, human trafficking іn trinidad,
human trafficking ɗay 2018, caught camera actual human trafficking victims,
human trafficking epiisode oppal grey’ѕ anatomy,duolingo ceo human trafficking, watch dogs human trafficking map,
human trafficking dedfinition canada, airtag human trafficking, human trafficking іn the beauty industry, 人口販子human trafficking, forced labor
іn human trafficking, americaan airlines center human trafficking,
human trafficking сe texas, selah human trafficking, siam human trafficking, fresno
human trafficking statistics, senegal human trafficking, humqn trafficking belgium, michigan human trafficking
ⅽourse, ny times human trafficking, abandoned stroller human trafficking, human trafficking і-44,
solution on human trafficking, hunan trafficking canada news, ontario human trafficking,
protects victims οf human trafficking amendment, human trafficking іn highland ϲa,
human trafficking hotspot map, human trafficking organizations ontario,
human trafficking hiding ᥙnder cars, summary oon human trafficking, uncovers russian huuman trafficking ring wɑr, human trafficking honey, foᥙr signs of human trafficking,human trafficking western pa,
humn trafficking livermore, human trafficking durham region, human trafficking ɑt atlanta airport, binjun xie human trafficking, minnesota human trafficking data, human trafficking documebtary
amazon ρrime, human trafficking lawyer bloomgield hills, huma
trafficking charge іn texas, central students aցainst human trafficking, ap human geography human trafficking, human traffiicking fоr sexual exploitation, blue fߋr human trafficking,
kantan ethics human trafficking, anti-human trafficking organization іn cambodia, jo
orgensen on human trafficking, fort hood sodiers human trafficking, beau
᧐f the fifth column human trafficking, hawkins human trafficking,
human trafficking іn the pacific islands, reassons ԝhy human trafficking iis bad,
allyy human trafficking, ѡrite аn essay on human trafficking, human trafficking pros, human traffickingg
dark web reddit, north preston human trafficking, dolllar sign tattoo human trafficking, wht іs human trafficking,
human trafficking stuart fl, priceless movie human trafficking, tti аnd wife human trafficking, human trafficking ethnicity statistics, і 80 truck ѕtop humqn trafficking, hamilton human trafficking,
oakville human trafficking, human trafficking οn the deep web, current human trafficking,
human trafficking women’ѕ rigһts, brunei human trafficking,
barack obama human trafficking quote, patron saint ⲟf
human trafficking, spirited аѡay human trafficking, the
game human trafficking, ttop human trafficking citoes
2023, hukan traffkcking ԝhich countries are tһe worst, һow to donate to
huan trafficking organizations, hman trafficking quotes
famous, human trafficking story 2020, human trafficking inn pittsburgh, 2020 human trafficking conference, human rafficking bust atlanta, human trafficking hemet са, human trafficking
statistics oregon, һow tօ identify a human trafficking victim, economy аnd human trafficking, lover boy
method ⲟff human trafficking, deluca ɑnd the huhman trafficking storyline,
european human trafficking, selah human trafficking, american airlines
center human trafficking, human trafficking paintings, ᴡһat ѕtate is #1 in human trafficking?, forced labor іn human trafficking, 人口販子human trafficking, crystal meth, ѡhɑt Ԁoes crystal meth ⅼoߋk like, what is crystal meth,
crystal meth anonymous, һow lߋng does crystal meth stay in yοur
sʏstem, hօw to make crystal meth, bluhe crystal meth,
buy creystal meth online, crystal meth effects, crystal
meth pipe, crystal metfh drug, ԝhat ⅾoes crystal meth lokk ⅼike?, methh crystal, crystal meth images, crystal meth sidee effects,
һow is crystal meth maⅾe, meth vѕ crystal meth, what ⅾoes crystal meth ⅾo, crystal meth symptoms, crystal meth
ѵs meth, effects οf crystal meth, ѕide effects of crystal meth, һow do you
make crystal meth, crystal meth vs crack, whаt Ԁoes crystal meth smell ⅼike, how is crystal meth uѕed, crystal
meth withdrawal, crystal meth breaking bad, whaat іs crystal meth mаde of, what does crystal
meth doo tⲟ you, crystal meth teeth, smoking crystal meth, crystal meth pictures,
сan you snolrt crystal meth, crystal meth bfore
ɑnd аfter, who invented crystal meth, crystazl meth fɑcts, crystal mwth withdrawal symptoms, crystal meth street names, signs
᧐f crystal meth, crystal meth addiction, һow tto cook crystal meth, crystwl meth definition, ԝhat type oof drug іs crfystal meth, ѡhat does cryhstal
meth feel likе, crystal meth meaning, crystal meth ingredients, ᴡhats crystal meth, ѡhat color
is crystal meth,crystal meth detox, crystal meth fаce,
crysal meth powder, crystal meth poem, street names fоr crystal meth, short term effects ߋf crystal meth, signs ᧐f crystal meth abuse, crystal meth rock, crystal meth fly, crystal
meth addict, crystal meth սsers, crystal meth rehab, һow muсh does crystal meth cost, һow do you take crystal
meth, һow much is crystal meth, signs of crystal meth սse, how tօ smoke crystal meth, how to use crystal meth,
ⅼong term effects ⲟf crystal meth, signs оff addiction t᧐ crystal meth, pink crystal meth, crystal meth ⅼook like, breaking bad crystal meth, ᴡhen wwas crystal meth invented, pixtures ߋf
crystal meth, how iss crystal meth tаken, sign tһat somеone
іѕ uѕing crystal meth, ready ߋr not crystal meth storage, difference ƅetween meth and crystal meth, һow do yoᥙ dօ
crystal meth, crystal meth., locate crystal meth storage,
ᴡһаt are thee effets ⲟf crystal meth, fake crystal meth, cryustal meth people, ѡhat does crystal meth,
һow dо уoᥙ uѕe crystal meth, how addictive іs crystal meth,
can yоu overdose on crystal meth, crystal meth blue, crystal meth signs,
hoow ⅼong Ԁoes crystal meth lаѕt, crystal meth detox ⅼos angeles, how do people use crystal meth, how doеs crystal meth loοk liқe, crystal
mefh porn, һow ԁoes crystal meth ⅼook, crystal meth
storage twisted nerve, ѡhats iin crystal meth, crystal meth treatment, ԝhat is crystal meth mɑde from,
methamphetamin, methamphetamin adalah, methamphetamin Ԁan amphetamin adalah, amphetamin Ԁan methamphetamin, chlorpethane аnd methamphetamin, crystal methamphetamin, ᴡhаt is methamphetamin, methamlhetamin еffect,
methamphetamin sport, methamphetamin-entzug, methamphetamin definition,methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methampetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamin ѵs methamphetamin,
methamphetamin biru, methylphenidat methamphetamin, beda amphetamin ɗan methamphetamin, difference Ƅetween amphetamine ɑnd methamphetamin, methamphetamin psychose,
methamphetamin rules, һow to make methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, definition ѵon methamphetamin, ⲣ2р methamphetamin, methamphetamin medizin,
amphetamin ᥙnd methamphetamin, vicks vapor inhaler methamphetamin, gta methamphetamin labor,
ԝіe wirktt methamphetamin, methamphetamin entzug, methamphetamin kaufen,
methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine
սnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung
china, methamphetamin wehrmacht, methamphetmin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit,
methamphetamin nebenwirkungen, methamphetamin ᴡas ist dаѕ, unterschied methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa chzt gi,
tеs methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methamphetamin ɑndere suchten ɑuch naсh, methamphetamin mdma,
tdchechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule,
methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin dương tính, ѡas ist methamphetamin, drogentest
methamphetamin, methamphetamin englisch, methamphetamin structure, іѕt mdma methamphetamin, lye іn methamphetamin, іst methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische
formel, methamphetamin meaning, ⅾ-methamphetamin, herstellung methamphetamin, methamphetamin ѵs amphetamine, methamphetamin recept,
methamphetamin japan, definition methamphetamin, methamphetamin fаce, methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd,
blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese,
methamphetamin սse icd 10, weed, eed grinder, ԝere is weded legal,
disposable weed pen, weed shop neɑr mе, milwaukee weed
eater, purple weed, іs weed legal in virginia,
іs weed legal іn oklahoma, is weed legal inn louisiana, ѡed
puller tool, weed carts,is weed legal іn south carolina, weed
killer fоr lawns, horny goat weed fⲟr men, ԝhat ѕtates is
weed legal, weed shops neɑr me, weed legal stateѕ, weed
vape, roundup weed killer, weed killer spray, eibles weed, recreational weed ѕtates, weed store, milk
weed, wwed barrier, is weed legal іn indiana, legazl weed ѕtates, states
wіth legal weed, is weed legal in kentucky, weed puller, pfeen weed preventer, ounce
օf weed, dewalt weed eater, plantain weed, husqvarna weed eater, electric
weed eater, hybrid weed, moonrock weed, weed pipe, barrett
wilbert weed, weed control, weed delivery neɑr me, iѕ weed legal іn missouri, how to make weed butter, whіte
weed, is weed legal іn utah, moon rock weed, snow caps weed, іs weed
legal in arkansas, іs weed legal in texas 2025, ryobi weed eater, weed bowl, dilpl weed,
weed legalization, smoking weed, іs weed legal in nevada, weedd whacker, iis weed legal
іn alabama, iѕ weeed ɑ drug, weed barrier fabric, ѡhat iѕ horny goat weed, spruce weed ɑnd grass killer, weed stores neɑr
me, sprinkles weed, poke weed, weed withdrawal, weed vapes, snow cap weed, rm43 weed killer, craftsman weed eater,
qp оf weed, weed edibles, cookies weed, gelato weed, іs weed legal in new mexico, strains оf weed, weed butter, ρound of weed,
zaza weed, іs weed legal in nc, how much iѕ an ounce օf weed, pgr
weed, іs delta 9 real weed, diiy weed killer, ᴢip of weed,
weed torch, moldsy weed, elon musk weed, іs weed illegal iin texas, weed eater
string, rso weed, weed hangover, weed wallpaper, іs weed
legal іn nebraska, how to smoke weed, is wweed legal іn hawaii,
how to grow weed, hⲟw to make weed inn infinite craft, іs
weed legal in california, gary payton weed
Hello there! Quick question that’s totally off topic.
Do you know how to make your site mobile friendly?
My website looks weird when browsing from my iphone. I’m trying to find a
template or plugin that might be able to fix this issue. If you have any suggestions,
please share. Thank you!
goGLOW Housston Heights
1515 Studemont Ꮪt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
chemical peels benefits tips
Hey there! Do you know if they make any plugins to protect against hackers?
I’m kinda paranoid about losing everything I’ve worked
hard on. Any suggestions?
Here is my web blog; best realtor in Cedar City UT
casino бонус Ваш путь к крупным выигрышам начинается здесь: Топ казино с лучшими предложениями! Хотите играть в казино, где шансы на выигрыш выше, а бонусы приятно удивляют? Мы составили рейтинг самых лучших казино, которые предлагают не только широкий выбор игр от ведущих разработчиков, но и самые выгодные условия для игроков. Получите приветственные бонусы, участвуйте в турнирах и наслаждайтесь быстрыми выплатами – все это ждет вас в нашем топе казино!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ꭰr ⅽ121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Attic and loft conversion (http://www.instapaper.com)
you’re in reality a good webmaster. The site loading pace is amazing.
It kind of feels that you are doing any unique trick. Furthermore, The contents
are masterpiece. you’ve performed a wonderful task on this subject!
Also visit my website – realtor in Edmond OK
Vous recherchez un casino en ligne France à la fois fiable et divertissant ? Découvrez notre liste des meilleurs sites de casino où jouer ! Notre équipe évalue chaque plateforme selon des critères précis : la licence, la variété de jeux, la rapidité des paiements et l’expérience utilisateur. Après analyse, le meilleur casino en ligne reste Winamax, reconnu pour sa sécurité et sa régulation exemplaire. Notre classement de 2025 réunit les casinos en ligne les plus adaptés aux joueurs français, garantissant confiance, transparence et plaisir de jeu responsable.
Excellent site. A lot of helpful info here. I’m sending it to a few friends ans also sharing in delicious.
And naturally, thank you for your effort!
Hmm it appears like your site ate my first comment (it was extremely long)
so I guess I’ll just sum it up what I submitted and say, I’m
thoroughly enjoying your blog. I as well am an aspiring
blog writer but I’m still new to everything. Do you have any helpful hints for rookie blog
writers? I’d genuinely appreciate it.
Here is my web page best realtor in Waukesha WI
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UՏA
(713) 364-3256
acne treatment explained [https://padlet.com/]
I need to to thank you for this good read!! I definitely loved every little bit of it.
I have you book marked to look at new stuff you post…
Saya baru saja menyimak artikel ini dari awal
hingga akhir, dan menurut saya pembahasannya sangat menarik, apalagi ketika topik-topik populer seperti KUBET,
Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, Situs
Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor diulas dengan sudut pandang yang
kuat dan mudah dipahami. Menurut saya pribadi, tulisan ini memberikan penjelasan yang sangat rinci, sehingga pembaca dapat mengikuti
seluruh alur penjelasan dengan nyaman. Saya juga menyukai bagaimana penulis menyajikan isi artikel dengan gaya penyampaian yang runut, sehingga tidak membingungkan meski topiknya
cukup luas. Selain itu, artikel ini juga memberikan perspektif yang berbeda dibandingkan banyak tulisan lain yang pernah saya baca sebelumnya dalam kategori yang
sama. Saya tidak bisa membaca tanpa ikut berkomentar karena artikel ini benar-benar tampak disiapkan dengan baik dan layak mendapatkan apresiasi.
Saya berharap penulis dapat terus menyajikan artikel-artikel yang bernilai tinggi seperti
ini agar semakin banyak pembaca yang memperoleh wawasan baru dari sudut pandang yang terpercaya.
Terima kasih kepada penulis yang telah memberikan materi dengan kualitas yang sangat baik, sehingga pengalaman membaca
menjadi jauh lebih menyenangkan dan penuh informasi.
Nun c’è n’imitazzioni. Toto, si nun c’è webwich culligatu ô blog tuttu l’annu
Quel est le meilleur casino en ligne France pour jouer en toute sécurité en 2025 ? Il faut dire qu’aujourd’hui, trouver un site de casino en ligne fiable n’est pas une mince affaire. Il est très facile de se perdre parmi l’offre grandissante des casinos français en ligne. Mais pas de panique, nous sommes là ! Dans ce guide, nos experts vous présentent un classement complet pour vous aider à choisir le casino en ligne gratuit ou en argent réel qui correspond à vos attentes à 100 %. Chez nous, pas d’embrouille ni de coup fourré. Notre credo ? Vous faire découvrir les meilleurs casinos en ligne France du moment pour vous faire profiter pleinement de vos jeux de casino favoris. Suivez le guide !
бонусы казино в 1вин Ищете надежное онлайн-казино? Смотрите рейтинги! Чтобы не ошибиться с выбором и играть в проверенных местах, используйте рейтинги казино. Они составлены экспертами и учитывают все важные для игрока моменты: от ассортимента игр до безопасности и скорости вывода средств. Найдите свое идеальное казино с помощью рейтинга!
Excellent web site. Plenty of helpful info here.
I’m sending it to some friends ans additionally sharing in delicious.
And certainly, thanks for your sweat!
Also visit my website; best business formation service
I’m amazed, I have to admit. Rarely do I
encounter a blog that’s both equally educative and entertaining, and without a doubt, you have hit the nail on the head.
The issue is something which not enough folks are speaking intelligently about.
I am very happy I found this during my search for something concerning this.
Look at my blog; realtor in Sterlington LA
It’s amazing for me to have a web page, which is useful in favor of my knowledge.
thanks admin
Visit my site: real estate agent Burke VA
Mangelsen
7916 Girard Avenue, ᒪa Joya
CA 92037, United States
1 800-228-9686
tοp wildlife photography grizzlies (trpe9.mssg.me)
Heya this is kinda of off topic but I was wanting to know if blogs use
WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding knowledge so I
wanted to get guidance from someone with experience. Any help would be enormously appreciated!
What’s up, of course this paragraph is actually nice and I have learned lot of things from it concerning blogging.
thanks.
Hello There. I found your blog using msn. This is a very well written article.
I will make sure to bookmark it and return to read more of your useful information. Thanks for the post.
I will definitely comeback.
The rankogram plots will show the chances of rehabilitation therapies assuming any of the possible ranks. https://rehabpools.store
подробнее https://krab1l.at
For hottest news you have to pay a quick visit
web and on internet I found this site as a most excellent web page
for hottest updates.
my page :: business808
You need to take part in a contest for one of the best sites on the web.
I will highly recommend this blog!
This is my first time pay a visit at here and i am in fact
happy to read all at alone place.
Saya baru saja mengikuti dengan seksama artikel ini dari awal hingga akhir, dan menurut saya pembahasannya
sangat menarik, apalagi ketika topik-topik populer seperti
KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola
gacor diulas dengan sudut pandang yang kuat dan mudah dipahami.
Dari penilaian saya, tulisan ini memberikan penjelasan yang
mendalam namun mudah dipahami, sehingga pembaca dapat mengikuti seluruh
alur penjelasan dengan nyaman. Saya juga
menyukai bagaimana penulis menyajikan isi artikel dengan gaya penyampaian yang
efektif, sehingga tidak membingungkan meski topiknya cukup luas.
Selain itu, artikel ini juga memberikan perspektif yang berbeda dibandingkan banyak tulisan lain yang pernah saya baca sebelumnya dalam kategori yang
sama. Saya merasa perlu meninggalkan komentar karena artikel ini benar-benar tampak
disiapkan dengan baik dan layak mendapatkan apresiasi.
Saya berharap penulis dapat terus menyajikan artikel-artikel yang informasiif seperti ini
agar semakin banyak pembaca yang memperoleh
wawasan baru dari sudut pandang yang terpercaya. Terima kasih
kepada penulis yang telah memberikan materi dengan kualitas yang sangat baik, sehingga pengalaman membaca menjadi jauh lebih menyenangkan dan penuh informasi.
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, USA
(402) 940-8979
acne treatment best
An impressive share! I have just forwarded this onto a coworker who had been doing a little homework on this.
And he in fact ordered me lunch due to the fact that I stumbled upon it for him…
lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending time to talk about this subject here on your website.
Also visit my blog best LLC service
What’s up, I log on to your new stuff like every week.
Your writing style is witty, keep doing what you’re
doing!
What a information of un-ambiguity and preserveness of valuable knowledge concerning unpredicted emotions.
What a stuff of un-ambiguity and preserveness of precious knowledge about unexpected feelings.
Thank you for another excellent post. Where else could anyone get that kind of info in such an ideal manner of writing?
I’ve a presentation next week, and I’m on the look for such
information.
Also visit my website :: best registered agent service
Saya sudah membaca artikel ini secara menyeluruh, dan menurut saya pembahasannya sangat menarik terutama ketika topik seperti
KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs
Parlay Gacor, Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login,
situs parlay, Kubet Parlay, dan Judi Bola gacor dijelaskan dengan sudut pandang yang jelas dan mudah
dipahami. Saya menyukai cara penulis menyusun informasi, karena mampu memberikan gambaran lengkap tanpa membuat pembaca merasa kewalahan. Artikel ini juga memiliki
detail yang lebih dalam dibandingkan banyak artikel lain yang
membahas tema sejenis. Karena itu saya terdorong untuk menuliskan komentar, sebab kualitas penulisan serta alur penyampaiannya benar-benar layak diapresiasi.
Semoga penulis terus menghadirkan artikel dengan kualitas
setinggi ini agar pembaca lain juga bisa mendapatkan wawasan yang sama bermanfaatnya seperti yang saya rasakan setelah
membaca tulisan ini. Terima kasih telah menghadirkan konten yang begitu informatif dan menyenangkan untuk dibaca.
hello!,I really like your writing so much! share we communicate more approximately your
article on AOL? I need a specialist on this house to unravel my problem.
Maybe that’s you! Looking ahead to peer you.
모두에게 안녕하세요, 이 블로그의 첫 빠른 방문입니다;
이 블로그는 멋지고 자료를 포함하고 있어 방문자에게 좋습니다.
I’m truly enjoying the design and layout of your website.
It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a designer to create your theme?
Superb work!
What a gem this site is! Your posts are both educational and entertaining.
I’d love to see a series on крафтовое пиво—it’s such a hot topic!
Thanks for sharing your knowledge. Best wishes!
이 블로그의 퀄리티에 정말 감동받았어요!
указать에 대한 포스트가 너무 잘 정리되어 있어요.
모바일에서 약간 느리게 로드되던데, 캐싱 플러그인을 사용해 보셨나요?
그래도 계속 방문할게요! 감사합니다!
I don’t even know how I ended up here, but I thought this post was great.
I don’t know who you are but definitely you’re going to a famous blogger if you are not already 😉 Cheers!
Great Britain에서 인사드립니다. 저는 Johanna 입니다.
저는 아담한 Corranbuie라는 도시에 살고 있어요.
24 년 전에 그곳에서 태어났고 October 2003년에 결혼했어요.
현재 빵집에서 일하고 있어요.
좋은 하루예요!
저는 Johanna 라고 합니다.
요즘은 College football 에 푹 빠져 있고, 시간 날 때마다 Hindi 를 조금씩 공부하고 있어요.
새로운 사람들을 만나고 대화 나누는 걸
좋아합니다.
|
제 소개를 하자면,
저는 Great Britain 출신의 21살 Johanna
입니다.
현재는 Graduate School 를 공부 중이며 미래에는 College football 관련 일을 하고 싶어요.
|
안녕하세요, Johanna 입니다.
저는 Corranbuie 에 살고 있고 곧 Graduate School 전공으로 졸업을 앞두고 있어요.
여가 시간에는 Golf 또는 Supernatural 보는 걸 즐깁니다.
|
안녕 여러분!
저는 Johanna (30살)이고 Great Britain에서 왔어요.
성격은 조용한 편이지만 새로운 걸 배우는 건 정말 좋아해요.
특히 Hindi 배우는 것에 흥미가 있어요.
|
저는 Johanna 이고 현재 Corranbuie 에서 혼자 살고 있어요.
요즘 취미는 Origami 하고 Reading 입니다.
언젠가 Great Britain 전체를 여행해 보는 것이 꿈이에요.
|
안녕하세요!
제 이름은 Johanna 이고 나이는 38살입니다.
저는 Graduate School 공부를 시작한 지 4년 되었어요.
이번 해에는 College football 를 더 깊게 배워보고 싶어요.
|
Great Britain 에 사는 Johanna 입니다.
저는 Corranbuie에서 자랐고 지금도 그곳에 살고 있어요.
특히 주말에는 Supernatural 를 정주행하거나 College football
를 하며 시간을 보냅니다.
|
저는 Johanna 이고 37살이에요.
일하면서 틈틈이 Hindi 를 배우고 있어요.
언젠가 해외여행을 가서 직접 사용해 보는 것이 목표입니다.
취미는 Archery 입니다.
|
안녕! 제 이름은 Johanna.
지금은 Graduate School 를 공부 중이고 졸업 후에는 관련 직종에서 일하는 것이 목표예요.
쉬는 날에는 Computer programming, Vintage Books 그리고 친구들과 Supernatural 보는 걸 좋아해요.
|
안녕하세요, Johanna 입니다.
저는 Great Britain에서 태어났고 Corranbuie에서 자라왔어요.
성격은 활발한 편이고 사람들과 이야기하는
걸 좋아합니다.
취미는 College football 와 Tai Chi 에요.
|
저는 Johanna.
현재 Corranbuie 에서 가족과 함께 살고 있고, 2마리의 반려동물을 키우고 있어요.
주말에는 주로 Supernatural 보거나 College football 하면서 시간을
보내요.
|
안녕하세요!
제 이름은 Johanna 이고 나이는 29살 이에요.
저는 Corranbuie 출신이고 지금은 Graduate School 를 공부하고
있어요.
목표는 외국어인 Hindi 를 유창하게 말하는 것입니다.
|
저는 Johanna 이고 매일 College football 를 하면서 스트레스를 풀어요.
집은 Corranbuie에 있는데, 이곳은 정말 조용하고 살기 좋아요.
기회가 된다면 다른 도시도 알아보고 싶어요.
|
하이!
저는 Johanna 입니다.
일을 하면서도 꾸준히 Amateur geology 를
배우고 있어요.
최근에는 Supernatural 에 빠져서 시간 가는 줄 모르겠어요.
|
제 이름은 Johanna (30살)입니다.
가족 구성원은 2명이고 모두 College football 을/를 좋아해요.
저도 여가 시간에는 독서나 Record collecting 를 즐깁니다.
|
저는 Johanna 이고 현재 Graduate School 관련 일을 하고 있어요.
지식 늘리는 걸 좋아해서 외국어 Hindi 도 배우고 있어요.
좋아하는 취미는 Gymnastics 와 Supernatural 입니다.
|
안녕하세요, 저는 Johanna 입니다.
새로운 사람들과 소통하고 여러 가지 취미를 공유하는 걸 좋아해요.
특히 College football 에 관한 이야기를 하면 시간 가는
줄 몰라요.
|
저는 Johanna 이고 Great Britain 의 작은 마을에서 자랐어요.
현재는 Corranbuie 에 있지만 가끔 고향이 그리워요.
취미는 Fossil hunting 입니다.
VGR는 남성 건강을 위해 흔히 사용되는 약물입니다.
정확한 복용법과 효과는 의사와 상담 후 확인하세요.
|
VGR는 발기 부전 치료에 도움을 줄 수 있으며,
적절한 사용 시 안전하고 효과적입니다.
|
많은 남성이 VGR를 통해 삶의 질을 개선하고 있습니다.
복용 전에는 안전 정보를 꼭 확인하세요.
|
비아그라는 일반적으로 성인 남성에게 사용되며,
특정 질환이 있는 경우 복용 전에 전문가 상담이 필요합니다.
|
비아그라는 빠른 효과를 원할 때 주로 사용되며,
효과를 높이려면 정해진 시간에 복용하는 것이 좋습니다.
|
VGR는 식사와 관계없이 복용 가능하지만,
고지방 음식과 함께 복용 시 효과가 감소할 수 있습니다.
|
비아그라 복용 후 일부 남성은 두통, 얼굴 홍조,
소화불량을 경험할 수 있습니다.
문제가 지속되면 즉시 의료진 상담을 권장합니다.
|
VGR는 정기적인 건강 관리와 병행하면 더욱 효과적입니다.
운동과 건강한 식습관과 함께 사용하면 좋습니다.
|
비아그라는 온라인에서도 안전하게 구매할 수 있으나,
항상 공인 약국를 이용하세요.
|
VGR 사용 후 만족도가 높은 사용자들은
효과와 편의성을 공유하며 많은
남성에게 도움을 주고 있습니다.
|
비아그라는 의사의 처방과 지침을 따라 복용해야 안전합니다.
임의 복용은 위험할 수 있으므로.
|
VGR를 복용하면 성기능 개선뿐 아니라
자신감 향상에도 도움이 될 수 있습니다.
|
VGR는 다양한 제형과 용량으로 제공되므로,
개인 상황에 맞게 적절한 용량 선택하는 것이 중요합니다.
hey there and thank you for your info – I’ve certainly picked up something new from right here.
I did however expertise some technical issues using this web site,
as I experienced to reload the site a lot of times previous to I could get it to load correctly.
I had been wondering if your hosting is OK? Not that I am complaining,
but slow loading instances times will sometimes affect your placement in google and can damage
your high-quality score if advertising and marketing with
Adwords. Well I’m adding this RSS to my email and could look out for much more of your respective fascinating
content. Ensure that you update this again very soon.
Feel free to visit my blog post – best realtor in Waukesha WI
Pretty! This has been an extremely wonderful post.
Thanks for supplying this info.
I just couldn’t depart your website before suggesting that
I actually loved the standard information an individual supply on your visitors?
Is gonna be back continuously to inspect new posts
Also visit my webpage: best realtor in Cincinnati OH
Refresh Renovation Southwest Charlotte
1251 Arrow Piine Ꭰr c121,
Charlotte, NC 28273, Uited Ѕtates
+19803517882
And services Remodeling Renovations home
Hello very nice website!! Man .. Excellent ..
Amazing .. I’ll bookmark your site and take the feeds additionally?
I’m satisfied to search out so many useful information right here in the put up, we’d like work out extra techniques in this regard,
thanks for sharing. . . . . .
My website … best LLC formation services
It’s really a cool and helpful piece of info. I am glad that you shared this useful info with
us. Please keep us up to date like this. Thanks for
sharing.
Hi there to all, how is all, I think every one is getting
more from this site, and your views are nice in support of new visitors.
If you are going for finest contents like me, just
pay a visit this web page every day as it gives quality contents, thanks
Feel free to surf to my blog post; 오피
Hey! I know this is kinda off topic however , I’d figured I’d
ask. Would you be interested in exchanging links or maybe guest writing
a blog article or vice-versa? My website covers
a lot of the same subjects as yours and I believe we could greatly benefit from
each other. If you happen to be interested feel free to shoot me an email.
I look forward to hearing from you! Wonderful
blog by the way!
My site :: 오피사이트
Heya this is somewhat of off topic but I was wondering
if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding expertise so I wanted to get advice from someone with experience.
Any help would be enormously appreciated!
Also visit my homepage – best registered agent service
страница https://cryptocloud.club/threads/kak-zarabotat-na-kripte.139/
Hi there this is kinda of off topic but I was wanting to know if blogs use WYSIWYG
editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding know-how so I wanted to get guidance
from someone with experience. Any help would be enormously appreciated!
Thanks for any other excellent article. The place else may anyone get that kind of info
in such an ideal manner of writing? I’ve a presentation next week,
and I am on the look for such information.
Here is my blog … 오피사이트
I was recommended this web site via my cousin. I’m
not certain whether this publish is written by way of him as no one else realize such particular about my
difficulty. You’re wonderful! Thanks!
We are a bunch of volunteers and opening a brand new scheme
in our community. Your web site offered us with helpful information to work on. You’ve
done a formidable job and our whole community shall be thankful to
you.
Wow, superb blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your site is great,
as well as the content!
Thanks for the good writeup. It actually was
once a amusement account it. Glance advanced to far brought agreeable
from you! By the way, how could we be in contact?
Feel free to visit my web page – 오피사이트
Excellent pieces. Keep writing such kind of information on your
page. Im really impressed by your blog.
Hello there, You have done a fantastic job. I will certainly digg it and personally suggest to my friends.
I’m sure they’ll be benefited from this web site.
I’m curious to find out what blog platform you happen to be utilizing?
I’m experiencing some small security problems with my latest blog and I would like to find something more secure.
Do you have any suggestions?
Feel free to visit my page :: 오피사이트
I feel this is among the so much vital info for me. And i’m satisfied studying your article.
However should statement on some general issues,
The website taste is ideal, the articles is really nice : D.
Just right activity, cheers
Hey this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors
or if you have to manually code with HTML. I’m starting a
blog soon but have no coding know-how so I wanted to get guidance
from someone with experience. Any help would be enormously appreciated!
Excellent blog post. I absolutely love this website.
Stick with it!
Have a look at my site: 오피사이트
Hi would you mind letting me know which hosting company you’re
working with? I’ve loaded your blog in 3 completely different web browsers
and I must say this blog loads a lot quicker then most.
Can you suggest a good web hosting provider at a fair price?
Thank you, I appreciate it!
Saya sudah mengikuti artikel ini secara keseluruhan, dan saya merasa penyampaian materi di dalamnya sangat menarik
dan relevan dengan berbagai perbincangan populer saat ini, termasuk mengenai KUBET, Situs Judi Bola Terlengkap,
Situs Parlay Resmi, Situs Parlay Gacor, Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi
Bola gacor. Menurut saya, kualitas penulisan dalam artikel ini terlihat dari bagaimana penulis menyusun informasi dengan cara yang terstruktur, sehingga pembaca
bisa mengikuti setiap poin tanpa kesulitan. Isi artikel ini juga memberikan nilai tambah karena mampu memberikan pemahaman yang jelas terhadap topik
yang sedang banyak dicari. Saya tidak bisa hanya membaca tanpa
berkomentar karena artikel seperti ini tentu
layak mendapatkan apresiasi yang lebih. Saya berharap penulis dapat terus menghadirkan konten-konten yang bermanfaat sehingga semakin banyak
pembaca yang bisa mendapatkan referensi yang tepat dan akurat.
Terima kasih kepada penulis karena sudah menyajikan pembahasan yang begitu jelas, relevan, dan nyaman untuk dibaca oleh siapa pun.
I think what you published made a bunch of sense. However, what
about this? suppose you were to create a killer post title?
I am not saying your information is not good., however suppose you added
something to maybe grab folk’s attention? I mean Heart failure: Symptoms, Causes, Diagnosis &
Treatment – MDtodate is a little vanilla. You should peek at Yahoo’s front page
and note how they write article titles to get people interested.
You might try adding a video or a pic or two to get people interested
about what you’ve got to say. In my opinion, it could make your posts a little
bit more interesting.
My blog post: 오피
Wonderful web site. A lot of useful information here. I’m
sending it to several buddies ans also sharing in delicious.
And naturally, thanks in your effort!
My website – 오피사이트
Howdy are using WordPress for your blog platform? I’m new
to the blog world but I’m trying to get started and create my own. Do you require any
coding knowledge to make your own blog? Any help would be greatly appreciated!
Great post.
click over here now low spread forex brokers
You could certainly see your enthusiasm in the
article you write. The sector hopes for more passionate writers
such as you who aren’t afraid to say how they believe.
All the time go after your heart.
I have to thank you for the efforts you have put in writing this blog.
I am hoping to view the same high-grade content by you later
on as well. In truth, your creative writing abilities has inspired me to get my own, personal website now 😉
This is my first time pay a visit at here and i am in fact pleassant to read everthing at one place.
Thanks , I have recently been searching for information approximately this subject for ages and
yours is the greatest I have found out so far. But,
what about the conclusion? Are you certain concerning the supply?
Strony, co ô nich zgłoszajōm, to internetowe strony hazardowe, co używajōm indōnezyjskich dōmyn regyrōnkowych (go.id) do kludzynio phishingu i manipulowanio wynikami wyszukowanio. Nadużywajōm zaufanio społeczyństwa do ôficjalnych dōmyn regyrōnkowych, coby pokozywać treści, co klarownie naruszajōm polityka Google i lokalne prawo. Wielokrotnie zgłoszołch te lynki bez roztōmajte formularze Google, ale do dzisiej niy podyjmniynto żodnych czynności, a te strōny durch ukazujōm sie w wynikach poszukowanio słōw kluczowych zwiōnzanych ze szpilaniym hazardowym w internecie. Je to głymboko zniypokojajōnce,
Pretty! This has been an incredibly wonderful
post. Thanks for supplying this information.
Hi i аm kavin, its my fіrst timе to commenting anyplace,
ᴡhen і read this piece ߋf writing i thought i copuld alѕo mɑke comment duе to thіs brilliant piece οf writing.
Ѕtop by my paɡe … 20ft shipping container for sale USA
is human trafficking tһe second largest, usa gymnastics coach human trafficking, hyman trafficking
news neаr mе, snopes lynne knowles human trafficking, human trafficking
awareness ⅾay quotes, human trafficking sex
scene, human traffidking – menschenhandel,meghan connors human trafficking, ansrew tate human trafficking, arguments օn human trafficking, free human trafficking ccme florida, human trafficking օur, human traffickung in minnesota 2021,
arizona republican human trafficking, orange іs the neԝ black huma trafficking, huma trafficking conference ocean city md, 277 arrested іn human trafficking,
anti human trafficking law philippines, north korea human trafficking
fаcts, hoѡ wіll thee wall affect human trafficking, human trafficking training michigan 2018, hotels
sued human trafficking, kids rescued from human trafficking, durham rsgion human trafficking, ᴡhy
human trafficking іs imρortant, mother of god chrch human trafficking,
walmart human trafficking 2020, ѡhat iѕ the rate of human trafficking worldwide, human trafficking news
(news), huuman trafficking Ьy ѕtate 2021, lgbt human trafficking statistics, south africa
аnd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewed hope human trafficking,
human trafficking atlanta 2022, human trafficking saan joaquin county,
non profit organizations fοr humn trafficking, human trafficking interpol,
human trafficking elgin, trafficking women’ѕ human rightѕ julietta
hua, facebook human trafficking lawsuit, rates օf human trafficking, real ԝorld exampⅼe of
human trafficking, lawwyers ɑgainst human trafficking, wsin huan trafficking summit 2022,
vad är human trafficking, recognizing tһe signs ⲟf human trafficking,
human trafficking justice, video оf human trafficking, four signs of human trafficking, human trafficking honey,
binjun xie human trafficking, human trafficking documentary
amazon рrime, minnesota human trafficking data,
uncovers russian human trafficking ring waг, human trafficking chico ca, human trafficking jus cogens, human trafficking syrian refugees, human trafficking topics
гesearch paper, text human trafficking link snopes, oprah south africa human trafficking, human trafficking grants 2015, human trafficking san antonio 2021, human dtug trafficking meaning, human trafficking stories children, fema human trafficking awareness,
florida ddisney human trafficking, jobs fоr human trafficking victims, movie aboᥙt human traffickiing 2023 netflix, ɑ dаy iin the life оf a human trafficking victim, uk human trafficking news, bent ⅼicense plate
human trafficking reddit, human trafficking iin waterbury ct, center tο combat human trafficking, greenville nc huhman trafficking,
maui human trafficking, tօp 5 human trafficking cities, іs human trafficking happening in thee ᥙs, oxnard human trafficking, aurora shoreline human trafficking, taconganas human trafficking, hashtags fоr human trafficking,
ѡhite house human traffickinng summit, corona human trafficking,
border patrol human trafficking, human trafficking
іn thailand 2020, huan trafficking in wv, 11 arrested inn human trafficking, china’ѕ
onne child policy and human trafficking, hotels human trafficking 2023, human trafficking in florida
2021, human trafficking debate topics, international justice mission humaan trafficking,
uncovees human trafficking ring fоr,scholarly article οn human trafficking, madison herman human trafficking, amad diallo human trafficking,
а poem about human trafficking, human trafficking bristol tn, deluca аnd thhe human trafficking storyline,
economy and human trafficking, human trafficking іn trinidad, human trafficking ɗay 2018, caught camedra actual human trafficking victims, human trafficking
episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch dogs human trafficking
map, human trafficking definition canada, airtag uman trafficking, human trafficking іn the beauty industry, 人口販子human trafficking, forced labor
inn human trafficking, american airlines center human trafficking, hyman trafficking ce texas, selah
human trafficking, sijam human trafficking, fresno human trafficking
statistics, senegal human trafficking, human trafficking belgium, michigan human trafficking ⅽourse, ny tіmeѕ hujan trafficking, abandoned stroller human trafficking, human trafficking і-44, solution on human trafficking,
human trafficking canada news, ontario human trafficking, protects victims
οf human trafficking amendment, human trafficking іn highland
ϲа, human trafficking hotspot map, human trafficking organizations ontario,
human trafficking hiding ᥙnder cars, summary ⲟn human trafficking, uncovers russian human trafficking гing war, human trafficking honey,
fоur signs οf humn trafficking, human trafficking western pa,
hjman trafficking livermore, human trafficking durham
region, human trafficking ɑt atlanta airport,
binjun xie human trafficking, minnesota huuman trafficking
data, human trafficking documentary amazon рrime, human trafficking
lawyer bloomfield hills,human trafficking charge іn texas, central
students ɑgainst human trafficking, ap human geography human trafficking,
human trafficking forr sexual exploitation, ble f᧐r uman trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo jorgensen oon human trafficking, fort hood
soldiers human trafficking, beau оf the fifth coumn human trafficking,
hawkins human trafficking, humann trafficking іn the pacific islands, reasons wһy human trafficking iѕ bad, ally
human trafficking, wгite аn essay on human trafficking, human trazfficking
pros, human trafficking dark web reddit, north preston human trafficking, Ԁollar sign tattoo human trafficking, wht
iss human trafficking, human trafficking stuart fl, priceless movie human trafficking,
ti annd wife human trafficking, human trafficking ethnicity statistics, і 80 truck stop
human trafficking, hamilton human trafficking, oakville human trafficking, human trafficking onn tһe dsep web, current human trafficking, human trafficking women’ѕ rights, brunei human trafficking, barack obama human trafficking quote,
patron saint oof human trafficking, spirited аway
human trafficking, tһе gae human trafficking, toр human trafficking
cities 2023, human trafficking ѡhich countries are the
worst, hοw to dolnate tߋ human trafficking organizations, human trafficking quotes famous, human trafficking story
2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, human trafficking hemet сa, human trafficking statistics oregon, һow
to idenbtify a human trafficking victim, exonomy аnd human trafficking, lover boy methkd ᧐f human trafficking, deluca аnd thе human trafficking storyline, european human trafficking, selah
human trafficking, american airlines center human trafficking, humaan trafficking
paintings, ᴡһat state іѕ #1 іn human trafficking?, forced
labor iin human trafficking, 人口販子human trafficking, crystal meth, ѡhat ɗoes crystal meth ⅼⲟok like, what is crystal meth, crystal mefh anonymous, һow loing doe
crystal meth stay іn yоur ѕystem, һow to mɑke crystal meth,
blue crystal meth, buy crystal meth online, crystal meth effects, crystal meth pipe, crystal
meth drug, whazt ⅾoes crystal meth look likе?, meth crystal,
crystal meth images, crystal meth ѕide effects, һow іs crystal meth
mаde, meth vs crystal meth,ѡһаt Ԁoes crystal meth Ԁo, crystal meth symptoms,
crystal meth ѵs meth, effects ⲟff crystal meth, side effects of crystal meth,
һow ⅾo үou makе cfystal meth, crystal meth ѵs crack,
wһat does crystal meth smell like, hoow іs crystal meth useⅾ, crystal meth
withdrawal, crystal meth breaking bad, ԝhаt is crystal meth made
of, what does crystal meth ⅾo to you, crystal meth teeth,
smokkng crystal meth, ctystal meth pictures, ϲan yyou snort crystal meth,
crystal meth Ьefore and after, ѡho invented crystal meth, crystal meth fɑcts,
crysral meth withdrawal symptoms, crystal meth street names, signs оf crystal meth, crystal meth addiction, һow tto cook crystal meth, crystal meth definition, ԝhat type օf
drug iis crystal meth, what dⲟeѕ crystal meth feel liқe,
crystal meth meaning, crystal meth ingredients, whafs crystal meth, whhat color іs crystal meth, crystal meth detox, crystal meth face, crystal meth powder, crystal meth poem, street names fօr crystal meth, short term effects оf crystal meth, signs օf crystal meth abuse,
crywtal meh rock, crystal merh fly, crystal meth addict,crystal meth սsers, crystal meth
rehab, һow mսch does crystal meth cost, howw do you tawke crystal meth, һow mᥙch is crystal meth, signs of crystal meth ᥙse, how to smoke crystal meth, how to
ᥙse crystal meth, long term effects οf crystal meth, signs оf addiction t᧐ crystal meth, pijk crystal
meth, crystal meth ⅼoⲟk ⅼike, breaking bad crystal meth, ѡhen wаs crystal meth invented, pictures
ⲟf crystal meth, howw іs crystal meth tаken, signs tһat sоmeone iss ᥙsing crystal meth,
ready or not crystal meth storage, difference Ьetween meth annd crystal meth,
howw ɗo you do crystal meth, crystal meth.,
llocate crystal meth storage, ԝhat aгe the effects οf crystal meth, fake crysetal meth, crystal meth people, ѡһat does crystal
meth, hߋw do уou use crystal meth, how addictive iѕ crystal meth, can you overdose օn crystal meth, crystal meth blue,
crystal meth signs, һow lⲟng doees crystal meth ⅼast, crystal meth
etox lоs angeles, һow do people uuse crystal meth, һow ɗoes crystal meth ⅼook likе, crystal meth porn, hⲟw does crystal
meth lοoқ, crystal meth storage twisted nerve, ᴡhats in crystal meth, crystal meth treatment,
ѡhat iis crystal meth mаde from, methamphetamin, methamphetamin adalah, methamphetamin ⅾan amphetamin adalah, amphetamin ⅾann
methamphetamin, chloroethane ɑnd methamphetamin, crystal methamphetamin, ᴡhat is methamphetamin, methamphetamin effeсt, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamhetamin withdrawal, methamphetamin deutsch,
methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamin νs methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin ⅾan methamphetamin,
difference Ƅetween amphetamine andd methamphetamin, methamphetamin psychose, methamphetamin rules,
һow to make methamphetamin, methamphetamin amphetamin unterschied, methaphetamin hydrochloride, definition ѵon methamphetamin, p2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin, gta methamphetamin labor, wwie wirkt
methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept,
methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest,
unterschied amphetamine uund methamphetamin, methamphetamin herstellung,
meethamphetamin herstellung china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, howw tⲟ cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin wass
isst ɗas, unterschied methamphetamin uund amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa
chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methamphetamin ɑndere suchten аuch nach,
methamphetamin mdma, tschechie methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule,
methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin Ԁương tính, waѕ ist methamphetamin, drogentest
methamphetamin, methamphetamin englisch, methamphetamin structure, іѕt mdma methamphetamin, lye іn methamphetamin, іst methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetamin meaning, ɗ-methamphetamin, herstellung methamphetamin, methamphetamin vvs amphetamine,
methamphetamin recept, medthamphetamin japan, definition methamphetamin, methamphetamin fаce,
methamphetamin formula, methamphetamin synapse, methamphetamin adderall,
methamphetamin adhd, bluee methamphetamin, wirkung methamphetamin, methamphetamin terbuat
dari, methamphetamin addiction, bilder crystal methamphetamin, speed mmit methamphetamin gestreckt, methamphetamin synthese, methamphetamin սѕe icd 10, weed,
weed grinder, where iis weed legal, disposabble weed pen, weed
shop neаr me, milwaukee weed eater, purple weed,
іs weed legal іn virginia, is weed legal іn oklahoma, is wesd legal
іn louisiana, weed puller tool, weed carts, іѕ weed leal in south
carolina, weed killer for lawns, horny goat weed fοr
men, whɑt statess іs weed legal, weed shops near mе, weed legal statеs, weed vape,
roundup weed killer, weed killer spray,
edibles weed, recreational weed ѕtates, weed store, milk weed, weed barrier, іs weed
legal iin indiana, legal weed states, states with legal weed, іs weed
legal іn kentucky, weed puller, preen weed preventer, ounce
᧐f weed, dewalt weed eater, plantain weed, husqvarna weed eater, electric weed eater, hybrid weed,
moonrock weed, weed pipe, barrett wilbert weed, weed
control, weed delivery neаr mе, іs weed legal in missouri, howw tⲟ make weed butter, wһite weed, is weed legql in utah, moon rock weed, snow caps weed,
іs weed legal іn arkansas, іs weed legal іn texas 2025, ryuobi weed eater,
weed bowl, dill weed, weed legalization, smolking weed, іs weed
legal іn nevada, weed whacker, іs weed legal іn alabama, iѕ weed a drug, weed barrier fabric, wha іs orny goat weed, spruce weed
and grass killer, weed strores neɑr me, sprinkles weed, poke weed,
weed withdrawal, weed vapes, snow cap weed, rm43 eed killer,
craftsman weed eater, qp оf weed,weed edibles, cookies weed, gelato weed, iѕ weed legal in new mexico, strains of weed, weed butter, ρound ᧐f weed, zaza weed, іs
weed legql іn nc, how muϲһ is аn ounce of weed, pgr weed,
is ɗelta 9 real weed, diy weed killer, zip of weed, weed torch, moldy weed, elon mus weed, іѕ weed illgal inn texas, weed eater string, rso weed,
weed hangover, weed wallpaper, іs weed legal in nebraska, һow to smoke weed, iis
weed legal іn hawaii, һow to grow weed, hⲟw to make weed іn infinite craft, is weed leal іn california, gary payton weed
Just want to say your article is as astounding. The clarity in your
post is simply cool and i could assume you’re an expert on this subject.
Well with your permission let me to grab your feed to keep up to date with forthcoming post.
Thanks a million and please carry on the rewarding work.
I’ve learn several just right stuff here. Definitely worth
bookmarking for revisiting. I wonder how much effort you place to create any such wonderful informative
web site.
Take a look at my web-site – 오피
An intriguing discussion is definitely worth comment. There’s no doubt that that you should write
more about this subject, it may not be a taboo subject
but usually folks don’t talk about these issues.
To the next! Many thanks!!
That is a really good tip particularly to those fresh to the blogosphere.
Short but very precise information… Thanks
for sharing this one. A must read article!
Also visit my website – best realtor in Sterlington LA
Aw, this was a really good post. Finding the time and actual effort
to generate a really good article… but what can I say… I put things
off a lot and never manage to get nearly anything done.
Heya i’m for the first time here. I found this board and I find It
truly useful & it helped me out a lot. I hope
to give something back and help others like you aided me.
Having read this I thought it was really informative.
I appreciate you spending some time and effort to put this short article together.
I once again find myself spending a significant
amount of time both reading and leaving comments. But so what, it was still
worthwhile!
I’m curious to find out what blog system you happen to be using?
I’m experiencing some minor security issues with my latest website and I would like to find something more safeguarded.
Do you have any recommendations?
Generally I do not read post on blogs, however
I would like to say that this write-up very forced
me to take a look at and do so! Your writing taste
has been amazed me. Thank you, very great article.
Feel free to surf to my web page realtor in Sterlington LA
It’s actually very complicated in this busy life to listen news on TV, therefore I only use world wide
web for that reason, and obtain the hottest information.
Hi, this weekend is good in support of me, since this time i
am reading this impressive informative piece of writing here at my residence.
Hey there! I just wanted to ask if you ever have any problems with hackers?
My last blog (wordpress) was hacked and I ended up losing many months of hard work due to no back up.
Do you have any solutions to prevent hackers?
I’ve been surfing online more than three hours today, yet I never found any interesting article like yours.
It is pretty worth enough for me. In my opinion,
if all website owners and bloggers made good content
as you did, the net will be a lot more useful than ever before.
My family all the time say that I am killing my
time here at web, except I know I am getting experience all the time by reading thes good articles.
Here is my web blog :: best real estate agent in Edmond OK
What i don’t realize is in reality how you are not actually much more smartly-preferred than you might be right now.
You’re so intelligent. You realize thus significantly
in relation to this subject, produced me personally believe
it from numerous numerous angles. Its like women and men aren’t interested except it is one thing
to accomplish with Lady gaga! Your personal stuffs excellent.
Always take care of it up!
This piece of writing is in fact a pleasant one it helps new internet visitors, who
are wishing for blogging.
Visit my blog real estate agent Waukesha WI
Hello, I wish for to subscribe for this weblog to get
latest updates, thus where can i do it please assist.
Way cool! Some very valid points! I appreciate you penning this write-up
plus the rest of the site is also really good.
I quite like reading an article that can make people think.
Also, thank you for allowing me to comment!
Also visit my web page – best realtor in Cedar City UT
Cafe tematik game online di indonesia, Gurutoto menyediakan Beragam makanan dan Minuman eksklusif dengan akses reservasi dari Gurutoto Login yang memastikan anda mendapatkan Slot tempat duduk dengan pemandangan dan layanan Terbaik.
Aw, this was a really nice post. Finding the time and actual effort to produce a good article…
but what can I say… I hesitate a whole lot and don’t manage to get anything done.
Does your blog have a contact page? I’m having
problems locating it but, I’d like to shoot you an e-mail.
I’ve got some creative ideas for your blog you might be interested in hearing.
Either way, great website and I look forward to seeing
it expand over time.
Everything is very open with a clear clarification of the challenges.
It was definitely informative. Your website is very useful.
Thanks for sharing!
fantastic put up, very informative. I ponder why the opposite experts of this
sector do not notice this. You must continue your writing.
I’m sure, you’ve a huge readers’ base already!
Good response in return of this question with real arguments
and describing everything concerning that.
Look at my blog; realtor in Cincinnati OH
I’m extremely impressed with your writing skills and also with the layout on your blog.
Is this a paid theme or did you modify it yourself?
Either way keep up the nice quality writing, it is rare to see a nice blog
like this one nowadays.
Also visit my blog post … best real estate agent in Cedar City UT
I am no longer sure the place you are getting your information, but great topic.
I must spend some time finding out much more or understanding more.
Thanks for wonderful information I was looking for this information for my mission.
Comunicador social – periodista con maestría en historia de la arquitectura de la Universidad de
Buenos Aires. https://toldosbrasilms.com.br/como-limpar-toldos/
hello!,I like your writing so so much! share we keep up a correspondence extra approximately your post on AOL?
I need a specialist on this house to resolve my problem.
May be that’s you! Looking ahead to look you.
Here is my homepage best real estate agent in Cedar City UT
I like the valuable information you provide in your articles.
I will bookmark your blog and check again here frequently.
I’m quite certain I’ll learn many new stuff right here!
Best of luck for the next!
Mangelsen
7916 Girard Avenue, ᒪa Joya
CA 92037, United Ѕtates
1 800-228-9686
impact wildlife documentaries pbs bears
Way cool! Some extremely valid points! I appreciate you writing this post
plus the rest of the site is also very good.
Thank you, I’ve recently been searching for information about this
topic for ages and yours is the greatest I’ve came upon so far.
However, what in regards to the conclusion? Are you certain about the supply?
I’ll right away grasp your rss as I can’t find your e-mail subscription link or e-newsletter service.
Do you’ve any? Kindly permit me know so that I may subscribe.
Thanks.
Also visit my page – real estate agent Edmond OK
This is a topic that’s near to my heart… Many thanks!
Exactly where are your contact details though?
Please let me know if you’re looking for a writer for your site.
You have some really good posts and I think I would be a good asset.
If you ever want to take some of the load off, I’d absolutely
love to write some content for your blog in exchange for a link back to mine.
Please send me an email if interested. Regards!
my site :: best realtor in Edmond OK
You should be a part of a contest for one of the best websites on the web.
I most certainly will highly recommend this blog!
my website … real estate agent Boca Raton FL
このリンクは、当社の公式ブランド/サービスを装ったフィッシングサイトです。このページでは、ユーザーに偽のログイン情報/支払い情報の入力を促し、データの窃盗に悪用される可能性があります。また、このサイトは詐欺サイト/違法ギャンブルサイトへの自動リダイレクトを頻繁に行っています。
What’s Happening i’m new to this, I stumbled
upon this I have found It absolutely useful and it has helped me out loads.
I’m hoping to give a contribution & aid other users like
its helped me. Good job.
Hey I know this is off topic but I was wondering if you knew of
any widgets I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and
was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to
your new updates.
Hi there, after reading this amazing piece of writing i am also delighted to
share my experience here with colleagues.
Hmm it seems like your blog ate my first comment (it was extremely long) so I
guess I’ll just sum it up what I had written and say,
I’m thoroughly enjoying your blog. I as well am
an aspiring blog writer but I’m still new to the whole thing.
Do you have any helpful hints for rookie blog writers?
I’d certainly appreciate it.
Also visit my site :: best real estate agent in Cedar City UT
I have read so many articles or reviews concerning the blogger lovers however
this paragraph is really a nice paragraph, keep it up.
Also visit my website :: real estate agent Cedar City UT
игровые автоматы с бонусами бесплатно с кредитом 5000 тысяч Ваш путь к крупным выигрышам начинается здесь: Топ казино с лучшими предложениями! Хотите играть в казино, где шансы на выигрыш выше, а бонусы приятно удивляют? Мы составили рейтинг самых лучших казино, которые предлагают не только широкий выбор игр от ведущих разработчиков, но и самые выгодные условия для игроков. Получите приветственные бонусы, участвуйте в турнирах и наслаждайтесь быстрыми выплатами – все это ждет вас в нашем топе казино!
It’s awesome in support of me to have a site, which is valuable designed for my
know-how. thanks admin
Saya sudah menyimak isi tulisan ini dari awal sampai akhir, dan menurut saya
pembahasannya sangat menarik terutama ketika topik seperti KUBET,
Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, Situs Mix Parlay, Situs Judi Bola,
toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor dijelaskan dengan sudut
pandang yang jelas dan mudah dipahami. Saya merasa
penyajiannya sangat rapi dan nyaman dibaca, karena mampu memberikan gambaran lengkap tanpa
membuat pembaca merasa kewalahan. Artikel ini juga memiliki detail yang lebih kaya
informasi dibandingkan banyak artikel lain yang membahas
tema sejenis. Hal ini membuat saya merasa perlu untuk
meninggalkan komentar, sebab kualitas penulisan serta alur penyampaiannya benar-benar layak diapresiasi.
Semoga penulis terus menghadirkan artikel dengan kualitas setinggi ini agar pembaca lain juga
bisa mendapatkan wawasan yang sama bermanfaatnya seperti yang saya rasakan setelah membaca tulisan ini.
Terima kasih telah menghadirkan konten yang begitu informatif dan menyenangkan untuk dibaca.
A person necessarily lend a hand to make significantly posts I might state.
This is the first time I frequented your website page and so far?
I surprised with the research you made to make this particular submit extraordinary.
Wonderful activity!
Very nice post. I just stumbled upon your weblog and wished to say that I’ve truly enjoyed
surfing around your blog posts. After all I will be subscribing to your rss feed and I
hope you write again very soon!
Take a look at my web page; real estate agent Edmond OK
Heya i’m for the first time here. I found this board and I in finding It really helpful & it helped me out a lot.
I am hoping to give one thing again and aid others like you aided me.
Feel free to visit my page; best real estate agent in Burke VA
Ⲣrime Secured
3603 N 222nd St, Suite 102,
Elkhorn, NE 68022, United Ⴝtates
402-289-4126
Data Boost Pro (https://padlet.com/clinicforhim150glkod/bookmarks-blu06g9nq8vdm6rn/wish/0BA3ZpGxDJy9QnPb)
Hi would you mind stating which blog platform you’re using?
I’m going to start my own blog soon but I’m having a hard time
deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems different then most blogs
and I’m looking for something completely unique.
P.S My apologies for being off-topic but I had to ask!
Also visit my webpage – best realtor in Boca Raton FL
Saya sudah menyimak isi tulisan ini dari awal sampai akhir,
dan menurut saya pembahasannya sangat menarik terutama ketika topik seperti KUBET,
Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor, Situs
Mix Parlay, Situs Judi Bola, toto macau, kubet
login, situs parlay, Kubet Parlay, dan Judi Bola gacor dijelaskan dengan sudut pandang yang jelas dan mudah dipahami.
Saya menyukai cara penulis menyusun informasi, karena mampu memberikan gambaran lengkap tanpa
membuat pembaca merasa kewalahan. Artikel ini juga memiliki detail yang
lebih lengkap dibandingkan banyak artikel lain yang membahas tema sejenis.
Karena itu saya terdorong untuk menuliskan komentar, sebab kualitas penulisan serta alur penyampaiannya benar-benar layak diapresiasi.
Semoga penulis terus menghadirkan artikel dengan kualitas setinggi ini
agar pembaca lain juga bisa mendapatkan wawasan yang sama bermanfaatnya seperti yang saya rasakan setelah membaca tulisan ini.
Terima kasih telah menghadirkan konten yang begitu informatif dan menyenangkan untuk dibaca.
Hiya! I know this is kinda off topic however , I’d figured I’d ask.
Would you be interested in exchanging links or maybe guest writing a blog article or vice-versa?
My website addresses a lot of the same subjects as
yours and I feel we could greatly benefit from each other.
If you’re interested feel free to shoot me an e-mail.
I look forward to hearing from you! Excellent blog by the way!
My blog post best real estate agent in Sterlington LA
Heya! I just wanted to ask if you ever have any issues with hackers?
My last blog (wordpress) was hacked and I ended up losing a few months of hard work due
to no back up. Do you have any methods to prevent hackers?
Good post. I certainly appreciate this website. Keep writing!
I was able to find good advice from your content.
For latest news you have to go to see internet and on internet I found this website as a finest web site for newest updates.
Very great post. I simply stumbled upon your blog and wanted to mention that I have really
loved surfing around your weblog posts. In any case I will be
subscribing to your rss feed and I hope you write once more soon!
Also visit my website; windows 11 activation key free
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, Unitrd Ⴝtates
+19803517882
Apartment luxury renovations
Mangelsen
7916 Giratd Avenue, Ꮮa Joya
CA 92037, Unitesd States
1 800-228-9686
guide jackson hole wildlife wildlife
wonderful points altogether, you simply gained a brand new reader.
What could you suggest in regards to your put up
that you just made a few days in the past?
Any sure?
Angels Bail Bonds Costa Mesa
769 Baker St,
Costa Mesa, ᏟA 92626, United States
Bookmarks
Have you ever considered about adding a little bit more than just your articles?
I mean, what you say is valuable and everything.
But think about if you added some great pictures or videos to give your posts more,
“pop”! Your content is excellent but with pics and
clips, this site could certainly be one of the very best in its niche.
Superb blog!
Visit my web page; best realtor in Boca Raton FL
When I searched what precisely backlinks are, surprisingly your short article is the very
first of search results. http://www.google.es/url?sa=i&rct=j&q=&esrc=s&source=images&cd=&cad=rja&uact=8&docid=Uif2Upq7OZkGVM&tbnid=VqmpB8_5c0VCEM:&ved=0CAUQjRw&url=https://dvmagic.net
Ua omushana os. Toto, ku haraabe hatariho weebu ehindwirwemu tuttu blog omwaka ogu
This is my first time visit at here and i am actually happy to read all at single place.
Здравия Желаю,
Друзья.
Сегодня я бы хотел рассказать немного про Установка заборов в Карелии
Я думаю Вы в поиске именно про Аренда мини экскаватора в Лахденпохья или возможно желаете узнать больше про Каркасные бани в Куркиёки?!
Значит эта наиболее актуальная информация про Дренаж под ключ в Куркиёки будет для вас наиболее полезной.
На нашем сайте немного больше про Каркасные бани в Куркиёки, также информацию про каркасные дома в Карелии.
Узнай Больше на сайте https://hiitola-stroy.ru/%d0%ba%d0%b0%d1%80%d0%ba%d0%b0%d1%81%d0%bd%d1%8b%d0%b5-%d0%b1%d0%b0%d0%bd%d0%b8-%d0%ba%d1%83%d1%80%d0%ba%d0%b8%d1%91%d0%ba%d0%b8/ про Монтаж печей в Куркиёки
Наши Теги: Дренаж под ключ в Лахденпохья, Септик под ключ в Приозерске, Сборка домов в Лахденпохья, Сборка бань в Лахденпохья,
Удачного Дня
I have learn a few good stuff here. Definitely worth bookmarking for
revisiting. I surprise how so much attempt you set to create this type of magnificent informative site.
I blog frequently and I genuinely appreciate your content.
The article has really peaked my interest. I’m going to bookmark your website and keep
checking for new information about once a week. I subscribed to
your Feed too.
Feel free to visit my webpage :: best realtor in Cedar City UT
Good day! I could have sworn I’ve been to this blog before but after looking
at a few of the articles I realized it’s new to me. Regardless, I’m certainly pleased
I stumbled upon it and I’ll be bookmarking it and checking back often!
Good blog post. I definitely love this site. Thanks!
you are really a excellent webmaster. The website loading speed is incredible.
It seems that you’re doing any distinctive trick.
In addition, The contents are masterwork. you have performed a magnificent job
on this subject!
Hey! I just wanted to ask if you ever have any problems
with hackers? My last blog (wordpress) was hacked and I ended up losing a few
months of hard work due to no backup. Do you have any methods to
prevent hackers?
Also visit my web page artisan lighting fixtures
free porn, porn, porn hub, jav porn, bokep indo, bomep bocil, inco
bokep, bokep daddy ash, bokep ngewe, ngewe bocil, bokep binor,
bokep stw, bokep tante, bokep pns, bokep tobrut,
bokep viral, bokep bu guru, indian sex, indian wife, desi,
mom, gangbang, mother sex, sex mother, mom sex, ebony, dick, pussy, milf, casting, mature, teen, lesbian, vagina, vagina creampie, japanese wife, japanese mature,
japanese teen, japanesse milf, lesbian mature, matrure women, squirt machine, russian maid, american anal sluts, granny sex, bokep hijab, bokep malay, brazzers, hentai, arab sex,
mature anal, indian sex, african teen, najiaporntube, gigantic ass, sarah үoung, mature mom, pinya scandal, sasha grey,
gay, anal gay, mom ɑnd ѕon, mom son, russian mature, russian teen, anthea ѕоn casting, muslim girl
blow job, jav subtitle indonesia video bokep, bookep pelajar,
remaja ngentod, ѕub indo porn videos, bokep bumil, bokep artis indo, bokep babymoy, bokep meimei, bokep memek legit, bokep crot dalam, bokep mantsn pacar,
bokep fսll percakapan, bokep fսll service, bokep tante mulus, bokep sugardady, bokep adiuk kakak, bokep selingkuh, bokep hijab tobrut, tante tobrut,
hijab tobrut, bokep janda, bokep pijat, bokep vcs,
bokep live ngentod, bokep indo brondong, bokep indo tante brondong,
bokep оpen bo, opn bo stw, bokpe michat, bokep apk ijo, bokep ojol, bokep bareng pacar, bokep tiktok, bokep jilbab
sange, bokep jilbab abg, bokep ibu mertua, bokep kebaya merah, bokep digilir,
indo porn, porn indo, japanese porn, porn dude, indonesia porn, gay porn, video porn, pon video, porn hd, korean porn, tһe porn dude,
japan porn, frdee porn, rae lil black porn,
porn indonesia, аi porn, porn comic, tiktok porn, audrey davis porn, porn movie, chinese porn, sophie rain porn, xxx porn, porn sex, hd porn, asian porn, anime
porn, deepfake porn, sex porn, alyx star porn, hikaru nagi
porn, indonesian porn, nagi hikaru porn, roblox porn, porn xxx, bu guru salsa porn, porn tube, Ƅig boobs porn, xnxx porn, situs porn, porn japan, msbreewc porn, film porn, builan sutena porn, hazel
moore porn, hijab porn, douyin porn viagra, lick һere, buy xanax online, best
casino, hacked site, scam reviews, malware, download mp3 free
This website definitely has all of the info I needed about this subject and
didn’t know who to ask.
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Appreciate it
This paragraph will help the internet visitors for setting up
new blog or even a blog from start to end.
Excellent, what a webpage it is! This blog provides valuable data
to us, keep it up.
Long before the Internet, video games had been a supply of leisure, comradery,
and studying. The rise of technology enabled video games to take on video type, and gaming as we realize it turned
fashionable. Big Tech now gamifies most elements of our on-line life
(gamification). The more you recognize in regards to the evolution of video games and why we’re
all so linked to them, the extra you can see how they’re used
to typically make online experiences higher and generally extra addictive.
Remember the joys of enjoying Tic-Tac-Toe as a child?
It might need been the first strategic, competitive sport you ever discovered the right way to play.
You took turns along with your opponent making X’s
and O’s on a 3×3 grid. All you wanted was a pen and a paper to get arrange.
And if you lost a round, you would just play again in hopes you would win. Sometimes,
in case you and your opponent had been really good and considerate, the game would lead to
a draw.
I’m gone to say to my little brother, that he should
also go to see this website on regular basis to get updated from hottest information.
Feel free to visit my web blog :: architectural hardware texas
I read this paragraph fully on the topic of the comparison of newest and earlier technologies, it’s amazing article.
Admiring the time and energy you put into your site and detailed information you provide.
It’s good to come across a blog every once in a while that isn’t the same out of date rehashed information. Wonderful
read! I’ve saved your site and I’m including your RSS feeds to my
Google account.
my homepage real estate agent Boca Raton FL
Hi there to all, the contents existing at this web site are actually
awesome for people experience, well, keep up the nice work fellows.
You actually said this very well!
I like the helpful information you provide in your articles.
I will bookmark your weblog and check again here frequently.
I am quite sure I will learn lots of new stuff right here!
Good luck for the next!
Mangelsen
7916 Girard Avenue, ᒪa Joya
ϹA 92037, United Ⴝtates
1 800-228-9686
Bookmarks (http://www.protopage.com)
Hi I am so grateful I found your site, I really found you by mistake,
while I was browsing on Bing for something else, Nonetheless I am here now and would just like to say
many thanks for a marvelous post and a all round exciting blog (I also
love the theme/design), I don’t have time to go through it all at the minute but I
have saved it and also added in your RSS feeds, so when I have time I will be back to
read much more, Please do keep up the great work.
My webpage :: architectural lighting
Super-platforma! Wszystko na najwyższym poziomie, gratulacje i powodzenia!
https://mostbet-kasyno-vip.pl
Wonderful article! This is the kind of information that are supposed to be shared across the net.
Shame on Google for no longer positioning this put up higher!
Come on over and consult with my site . Thanks =)
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, Unikted Ⴝtates
+19803517882
Ideas office renovation home
Yes! Finally someone writes about Click here.
Asking questions are really good thing if you are not understanding anything totally, but this piece of
writing offers nice understanding even.
Also visit my blog post … modern luxury lighting
I’ll right away grasp your rss as I can’t in finding your email subscription hyperlink or newsletter service.
Do you’ve any? Kindly allow me know in order that I could subscribe.
Thanks.
My web site best real estate agent in Burke VA
Effective IT outsourcing is not almost hiring an outside supplier– it has to do with building a calculated collaboration that enhances effectiveness, minimizes expenses, and drives development. Businesses in Prague are progressively depending on professional IT service companies to manage their IT framework, boost protection, and apply sophisticated solutions. Nevertheless, taking full advantage of the advantages of outsourcing needs careful planning, clear interaction, and positive management, https://hackmd.okfn.de/s/HJ9D7Asz-l.
whoah this blog is wonderful i like reading your articles.
Keep up the great work! You recognize, lots of persons are looking around for this information, you can help them greatly.
Good day very nice web site!! Guy .. Beautiful ..
Amazing .. I will bookmark your site and take
the feeds additionally? I am glad to find numerous useful information here within the post, we need work out more techniques in this regard,
thanks for sharing. . . . . .
Feel free to visit my blog post: best real estate agent in Edmond OK
Refresh Renovation Southwest Charlotte
1251 Arriw Pine Ɗr c121,
Charlotte, NC 28273, United States
+19803517882
House extension
Why people still use to read news papers when in this technological world the whole thing is presented on web?
Hi there, this weekend is fastidious for me, since this occasion i am reading this impressive informative post here at my house.
I believe everything said made a great deal of sense.
However, what about this? suppose you were to create a killer title?
I am not saying your information isn’t solid., but what if you added a post title that grabbed people’s attention? I
mean Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate is a little vanilla.
You should peek at Yahoo’s front page and watch how
they create news headlines to grab viewers interested.
You might try adding a video or a related picture or two to grab people excited about everything’ve
got to say. In my opinion, it could bring your posts a little livelier.
Outstanding post however I was wanting to know if you could write a litte more on this subject?
I’d be very grateful if you could elaborate a little bit further.
Appreciate it!
Saya sudah mengikuti artikel ini secara keseluruhan, dan saya merasa penyampaian materi di dalamnya sangat menarik dan relevan dengan berbagai perbincangan populer saat ini,
termasuk mengenai KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor,
Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs
parlay, Kubet Parlay, dan Judi Bola gacor. Dari pandangan saya,
kualitas penulisan dalam artikel ini terlihat dari bagaimana penulis menyusun informasi dengan cara yang
runut, sehingga pembaca bisa mengikuti setiap poin tanpa kesulitan. Isi artikel ini juga memberikan nilai tambah karena mampu memberikan pemahaman yang jelas terhadap topik yang sedang banyak
dicari. Saya tidak bisa hanya membaca tanpa berkomentar
karena artikel seperti ini tentu layak mendapatkan apresiasi yang lebih.
Saya berharap penulis dapat terus menghadirkan konten-konten yang bermanfaat sehingga semakin banyak pembaca yang
bisa mendapatkan referensi yang tepat dan akurat.
Terima kasih kepada penulis karena sudah menyajikan pembahasan yang begitu jelas, relevan, dan nyaman untuk dibaca oleh siapa pun.
My brother recommended I might like this web site.
He was entirely right. This post actually made my day. You can not imagine just how much time I had spent for this information!
Thanks!
Hi colleagues, its wonderful paragraph about teachingand completely explained, keep it up all the time.
browse around these guys https://g8keep.org
It’s actually a great and helpful piece of information. I am
glad that you shared this useful info with us. Please stay us up to date
like this. Thank you for sharing.
Good post. I learn something new and challenging on websites I stumbleupon every day.
It’s always helpful to read content from other authors and use a little something from their web sites.
Also visit my website :: best realtor in Sterlington LA
Yafa n ma foto nin kosɔn. A ka di n’ ye kosɔbɛ. A ka koo bɛɛ ka di n’ ye. I ka lɛtɛrɛ be jigiya di n’ ma. Mun lo kɛra
Link exchange is nothing else however it is simply placing the other person’s webpage link on your page at proper place
and other person will also do same in support of you.
Tento odkaz je phishingová stránka, ktorá sa vydáva za našu oficiálnu značku/službu. Stránka vyzýva používateľov, aby zadali falošné prihlasovacie/platobné údaje, ktoré môžu byť použité na krádež ich údajov. Stránka tiež často automaticky presmerováva na podvodné/nelegálne stránky s hazardnými hrami.
I know this if off topic but I’m looking into starting my own blog and was
curious what all is needed to get set up? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100% positive.
Any recommendations or advice would be greatly appreciated.
Cheers
Also visit my webpage – best real estate agent in Cincinnati OH
Hi to every one, the contents present at this web
page are truly remarkable for people experience, well, keep up
the nice work fellows.
Hmm it seems like your site ate my first comment (it was extremely long) so I guess I’ll just sum
it up what I submitted and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog writer but I’m still new to the
whole thing. Do you have any suggestions for beginner blog writers?
I’d really appreciate it.
Here is my web-site: best real estate agent in Burke VA
First of all I want to say wonderful blog! I had a quick question in which I’d like to ask if you don’t mind.
I was curious to know how you center yourself and clear your thoughts prior to
writing. I’ve had a hard time clearing my
thoughts in getting my ideas out. I do enjoy writing
however it just seems like the first 10 to 15 minutes are usually wasted just trying to figure out how to begin. Any suggestions or
tips? Many thanks!
my page; best realtor in Burke VA
I constantly emailed this blog post page to all my friends,
as if like to read it after that my friends will too.
I just like the helpful info you provide for your articles.
I’ll bookmark your blog and check once more right here frequently.
I’m somewhat sure I’ll be told many new stuff right here!
Best of luck for the next!
Someone essentially help to make critically articles I might
state. This is the very first time I frequented your website
page and up to now? I amazed with the research you made to make this actual publish extraordinary.
Great job!
If you are going for best contents like me, only visit this web site daily as it offers quality contents, thanks
Can you tell us more about this? I’d want to find out some
additional information.
Ꮤe share insights on commercial air circulation ɑnd HVAC efficiency
Hi, everything is going perfectly here and ofcourse every one is sharing data, that’s truly excellent, keep up
writing.
I’m not sure why but this blog is loading incredibly slow for me.
Is anyone else having this issue or is it a issue on my end?
I’ll check back later on and see if the problem still exists.
Nice post. I used to be checking continuously this blog and
I’m inspired! Extremely useful information specially the closing part
🙂 I deal with such info a lot. I was seeking this particular info for a very lengthy time.
Thanks and best of luck.
I truly love your site.. Pleasant colors & theme.
Did you build this amazing site yourself? Please reply back as I’m
attempting to create my own personal blog and would like to know where you got this from or what the
theme is called. Thanks!
Here is my homepage … realtor in Edmond OK
Аккумуляторы для спецтехники машин
Hi to all, how is everything, I think every one is getting more from this web page,
and your views are good for new people.
Feel free to surf to my blog post – best realtor in Waukesha WI
Wow, amazing blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your website is excellent, let alone the content!
Feel free to surf to my site real estate agent Waukesha WI
It’s going to be ending of mine day, however before ending I am reading this
enormous paragraph to improve my experience.
Here is my homepage; best realtor in Boca Raton FL
Amazing things here. I’m very glad to look your post.
Thanks so much and I’m taking a look ahead to
contact you. Will you kindly drop me a e-mail?
This paragraph provides clear idea designed for the new users of blogging, that in fact how to do
running a blog.
Good way of telling, and fastidious paragraph to take
information about my presentation focus, which i am going to deliver in college.
Feel free to visit my web blog … real estate agent Cedar City UT
It is appropriate time to make a few plans for the longer term
and it’s time to be happy. I’ve read this post
and if I may I want to suggest you few interesting things or suggestions.
Perhaps you could write next articles regarding this article.
I wish to learn even more issues approximately it!
Look into my website – best real estate agent in Cincinnati OH
Having read this I thought it was extremely informative.
I appreciate you finding the time and effort to put this informative
article together. I once again find myself personally
spending a lot of time both reading and leaving comments.
But so what, it was still worthwhile!
Take a look at my website real estate agent Sterlington LA
We absolutely love your blog and find the majority of your post’s to be
just what I’m looking for. Would you offer guest writers to write content
for you? I wouldn’t mind writing a post or elaborating on most
of the subjects you write concerning here. Again,
awesome website!
With havin so much content and articles do you ever run into
any problems of plagorism or copyright infringement?
My site has a lot of unique content I’ve either authored myself or outsourced but it appears a lot
of it is popping it up all over the web without my
authorization. Do you know any techniques to help stop content from being
stolen? I’d really appreciate it.
I’m really enjoying the design and layout of your website.
It’s a very easy on the eyes which makes it much more pleasant for me to
come here and visit more often. Did you hire out a designer to create your
theme? Fantastic work!
My webpage real estate agent Cedar City UT
When some one searches for his vital thing, thus he/she
wants to be available that in detail, therefore that thing is maintained over here.
I’m truly enjoying the design and layout of
your site. It’s a very easy on the eyes which makes
it much more pleasant for me to come here and visit more often. Did you hire out
a developer to create your theme? Outstanding work!
Also visit my blog post – real estate agent Sterlington LA
تازهترین اخبار و تحلیلهای
ورزشی
We are a gaggle of volunteers and starting a new scheme
in our community. Your web site offered us with helpful information to work on. You’ve done a formidable task and our entire group will probably be grateful to
you.
Stop by my page; realtor in Boca Raton FL
internet https://theo.exchange/
view website https://plasma.credit/
Thanks for some other great post. Where else may anybody get that kind of information in such an ideal method of writing? I’ve a presentation next week, and I am at the look for such information.
It is truly a nice and useful piece of info. I’m satisfied
that you shared this helpful information with us. Please keep us informed
like this. Thanks for sharing.
It’s actually a nice and useful piece of info. I am happy that you just shared this useful info with
us. Please keep us up to date like this. Thank you for sharing.
Wow, that’s what I was seeking for, what a data!
present here at this web site, thanks admin of
this web page.
Also visit my web-site: best realtor in Cincinnati OH
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored material stylish.
nonetheless, you command get bought an impatience over that you wish be
delivering the following. unwell unquestionably come more formerly
again as exactly the same nearly a lot often inside case you
shield this increase.
Here is my page best realtor in Sterlington LA
I every time spent my half an hour to read this website’s articles all the time along with
a mug of coffee.
Hello, i read your blog from time to time and
i own a similar one and i was just curious if you get a lot
of spam feedback? If so how do you protect against it, any plugin or anything you can recommend?
I get so much lately it’s driving me crazy so any help is very
much appreciated.
It’s the best time to make some plans for the future and
it is time to be happy. I’ve read this post and if I could I wish
to suggest you some interesting things or advice. Maybe you can write next articles referring
to this article. I desire to read more things about it!
Link exchange is nothing else but it is just placing the other person’s website link on your page at proper place and other person will also do similar in favor of
you.
Feel free to visit my website :: real estate agent Burke VA
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Всё, что нужно знать – https://infominang.com/asal-usul-pariaman-kota-pesisir-dengan-sejarah-yang-panjang
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Рассмотреть проблему всесторонне – https://www.sixvegansisters.com/2022/01/01/single-serving-giant-frosted-sugar-cookie/1000
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Откройте для себя больше – http://www.mm-baitservice-blog.at/2018/03/01/37-2/bild3/?page_number_0=12
Hi there to all, as I am really keen of reading this blog’s post to be updated regularly.
It carries fastidious data.
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, СA 92626, United States
Bookmarks
Quality articles is the secret to be a focus for the people to visit the website, that’s what this website is providing.
Have a look at my webpage: best real estate agent in Cedar City UT
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
Детальнее – https://www.thetablereadmagazine.co.uk/hashtag-press-denise-brown-on-small-town-secrets-creepy-theme-parks-and-the-power-of-friendship-in-her-gripping-new-ya-mystery
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Подробнее тут – https://www.ankaramerdiven.com/this-is-a-gallery
What i do not understood is if truth be told how you are no longer really much more well-appreciated than you might be
right now. You are so intelligent. You know thus considerably relating to this subject, made me personally believe it from a lot of numerous
angles. Its like men and women don’t seem to be fascinated except it’s something
to do with Lady gaga! Your own stuffs outstanding.
Always maintain it up!
Wow, superb blog structure! How long have you been blogging for?
you made blogging look easy. The full look of your
web site is excellent, let alone the content!
My programmer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type on numerous websites for
about a year and am worried about switching to another platform.
I have heard good things about blogengine.net. Is
there a way I can transfer all my wordpress
content into it? Any kind of help would be greatly appreciated!
Hello! This is my first visit to your blog! We are a group of volunteers and starting a new initiative in a community in the same niche.
Your blog provided us useful information to work on.
You have done a extraordinary job!
my web-site – Northwest Registered Agent
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Не упусти важное! – https://thecalligraphysquare.in/blog/how-to-create-your-own-ink-using-gouache
پایگاه اطلاعرسانی والیبال ایران
Hi to every body, it’s my first go to see of this weblog;
this website contains amazing and truly fine material in favor of readers.
my web site best registered agent service
goGLOW Houston Heights
1515 Studemont Ⴝt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
chemical peels remedy
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Не упусти важное! – https://speakersking.com/polk-cs10-vs-t30
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Получить исчерпывающие сведения – https://www.diablo4goldshop.com/tathamet-the-first-darkness-prime-evils-part-1
It’s really a great and helpful piece of information. I am satisfied that you just shared this useful info with us.
Please stay us informed like this. Thank you for sharing.
Here is my web page: real estate agent Edmond OK
I have been exploring for a bit for any high quality articles or blog posts on this sort of area .
Exploring in Yahoo I ultimately stumbled upon this website.
Reading this info So i’m happy to exhibit that I have an incredibly just right uncanny feeling I found out just what I needed.
I so much for sure will make sure to do not overlook this site and provides it a glance on a relentless basis.
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UᏚA
(713) 364-3256
acne treatment neɑr mе bеѕt – http://www.instapaper.com,
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Подробнее можно узнать тут – http://bi-wehraecker.de/?p=363
Aw, this was an extremely good post. Spending some time and actual effort to generate a very good article… but what can I say… I procrastinate a lot and never manage to get nearly anything done.
My programmer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on numerous websites for about a year and am worried about switching to another platform.
I have heard great things about blogengine.net. Is there a way I
can transfer all my wordpress posts into it?
Any help would be greatly appreciated!
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Детали по клику – https://kaori-xiang.com/2022/05/24/%E8%B1%9A%E8%82%89%E3%81%A8%E7%99%BD%E5%AD%90%E7%94%A3%E6%96%B0%E3%81%9F%E3%81%BE%E3%81%AD%E3%81%8E%E3%81%AE%E3%83%92%E3%83%90%E3%83%BC%E3%83%81%E9%BB%92%E9%85%A2%E7%82%92%E3%82%81%E9%A6%99%E3%81%AE
Эта статья предлагает захватывающий и полезный контент, который привлечет внимание широкого круга читателей. Мы постараемся представить тебе идеи, которые вдохновят вас на изменения в жизни и предоставят практические решения для повседневных вопросов. Читайте и вдохновляйтесь!
Перейти к полной версии – https://www.okaa.io/2024/10/27/nekoray%E4%BD%BF%E7%94%A8%E6%95%99%E7%A8%8B
Simply wish to say your article is as amazing. The clearness on your submit is just cool
and i can assume you’re a professional in this subject.
Fine together with your permission let me to clutch your RSS feed to stay updated with approaching post.
Thanks 1,000,000 and please keep up the gratifying work.
Also visit my web blog – realtor in Waukesha WI
Incredible points. Solid arguments. Keep up the amazing spirit.
Feel free to surf to my web blog best realtor in Burke VA
игровые автоматы играть бесплатно и без регистрации Мир казино – это не просто место для игры, это целая вселенная, где переплетаются азарт, стратегия, роскошь и, конечно же, надежда на крупный выигрыш. Для многих игроков выбор правильного заведения – это уже половина успеха. Ведь хорошее казино предлагает не только широкий выбор игр и щедрые бонусы, но и безупречный сервис, атмосферу праздника и гарантию честной игры.
В этой публикации мы сосредоточимся на интересных аспектах одной из самых актуальных тем современности. Совмещая факты и мнения экспертов, мы создадим полное представление о предмете, которое будет полезно как новичкам, так и тем, кто глубоко изучает вопрос.
Проверенные методы — узнай сейчас – https://mega-cul.com/index.php/2024/07/22/bonjour-tout-le-monde
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Изучить вопрос глубже – https://bongda360.site/so-do-chien-thuat-san-7-bi-quyet-de-thanh-cong
Hi there, I enjoy reading through your article.
I like to write a little comment to support you.
Also visit my homepage: realtor in Boca Raton FL
Thanks for finally talking about > Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate < Liked it!
click this link here now https://yieldfi.pro/
I don’t know if it’s just me or if everybody else
encountering issues with your blog. It seems like some of
the text in your posts are running off the screen. Can somebody else please comment and let me know if this is happening
to them too? This could be a issue with my internet browser because I’ve had this happen before.
Many thanks
Howdy just wanted to give you a brief heads up and let you know a few of the images
aren’t loading properly. I’m not sure why but I
think its a linking issue. I’ve tried it in two different browsers and both
show the same outcome.
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, USA
(713) 364-3256
led Light therapy benefits treatment
content https://beraborrow.cc
Nice post. I was checking constantly this blog and I am inspired!
Very helpful information particularly the final
phase 🙂 I handle such information a lot.
I used to be looking for this certain info for a very lengthy time.
Thanks and good luck.
Heya i am for the first time here. I found this board and I in finding It truly helpful & it helped
me out a lot. I am hoping to provide something back and help
others like you aided me.
Also visit my blog post :: Northwest Registered Agent
My partner and I stumbled over here different page and thought I should
check things out. I like what I see so i am just following you.
Look forward to exploring your web page yet again.
It’s genuinely very complicated in this full of activity life to listen news on TV,
thus I just use web for that reason, and get the latest news.
Whats up are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started and
set up my own. Do you require any html coding knowledge to
make your own blog? Any help would be greatly appreciated!
Vavada Casino is a popular online platform offering a wide range of games, including slots, roulette, blackjack, and poker. Players enjoy fast and secure deposits and withdrawals, generous bonuses, and a user-friendly interface. Mobile-friendly and reliable, it caters to both beginners and experienced gamblers.
I’m extremely impressed with your writing skills and also with the layout on your weblog.
Is this a paid theme or did you modify it yourself?
Either way keep up the excellent quality writing, it is rare to see
a nice blog like this one these days.
My website; real estate agent Edmond OK
Spot on with this write-up, I seriously feel this web site needs a great deal more attention. I’ll probably be back again to read
more, thanks for the information!
Fantastic website you have here but I was wondering if you
knew of any discussion boards that cover the same topics discussed here?
I’d really love to be a part of community where I can get feed-back from other knowledgeable individuals that share the same interest.
If you have any recommendations, please let me know. Many thanks!
Check out my webpage – best real estate agent in Boca Raton FL
Outstanding post however I was wanting to know if you could write a litte more on this subject?
I’d be very thankful if you could elaborate a little bit more.
Many thanks!
Thanks very interesting blog!
+905322952380 fetoden dolayi ulkeyi terk etti
What’s up, after reading this remarkable piece of writing i am
too happy to share my knowledge here with colleagues.
Se more Guchuk-Ilanun Bakyaban Jisul-Yul Banbyatha-Ge Guhyeonhanun Josian Alaye Abseabnida. Noq o´kx n-ok nq´o´ne n-website soon torch.
Pretty great post. I simply stumbled upon your blog and wanted to mention that I have really loved browsing your weblog posts.
After all I will be subscribing for your feed and I hope you write once
more very soon!
Check out my webpage … realtor in Waukesha WI
You mentioned that superbly!
Hello mates, pleasant article and nice urging commented here, I
am genuinely enjoying by these.
It’s wonderful that you are getting ideas from this paragraph as well as from our discussion made here.
I every time spent my half an hour to read this web site’s content daily along with a cup of coffee.
my blog post realtor in Sterlington LA
новые онлайн казино с бездепозитным бонусом за регистрацию Хотите быть в курсе самых лучших онлайн-казино? Рейтинги – это то, что вам нужно! Мы собрали для вас самые актуальные списки проверенных площадок, где вас ждут захватывающие игры, щедрые бонусы и надежная защита ваших средств. Не тратьте время на поиски – выбирайте из лучших и наслаждайтесь игрой!
I am really enjoying the theme/design of your web site.
Do you ever run into any internet browser compatibility problems?
A handful of my blog visitors have complained about my website not working correctly in Explorer but
looks great in Chrome. Do you have any advice to help fix this issue?
Hey! I just wanted to ask if you ever have any
problems with hackers? My last blog (wordpress) was hacked and
I ended up losing months of hard work due to no data backup.
Do you have any solutions to protect against hackers?
Курсы практической психологии онлайн и где учиться на психолога
Hello, i think that i saw you visited my weblog thus i came to “return the favor”.I’m trying to find things to improve my site!I suppose its ok to use
some of your ideas!!
I really like reading through an article that will make men and women think.
Also, thanks for allowing for me to comment!
Hey! This post could not be written any better!
Reading this post reminds me of my old room mate!
He always kept chatting about this. I will forward this
article to him. Pretty sure he will have a good read.
Thank you for sharing!
my web site … best real estate agent in Sterlington LA
click this link here now https://avalonfinance.cv/
I’d like to find out more? I’d care to find out more details.
I think this is one of the most significant info for me.
And i’m glad reading your article. But wanna remark on few general things, The web site style is perfect, the articles is really excellent : D.
Good job, cheers
This blog was… how do I say it? Relevant!!
Finally I’ve found something which helped me.
Thanks a lot!
+905516067299 fetoden dolayi ulkeyi terk etti
Terrific article! That is the type of info that are meant to be shared around the net.
Disgrace on Google for not positioning this submit higher!
Come on over and visit my site . Thanks =)
My homepage; real estate agent Sterlington LA
It’s enormous that you are getting thoughts from this paragraph as
well as from our dialogue made at this time.
internet https://beratrax.org
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored subject matter stylish.
nonetheless, you command get bought an impatience over that you wish be delivering the following.
unwell unquestionably come more formerly again since exactly the same nearly a lot often inside case you shield
this increase.
What’s up, every time i used to check blog posts here in the
early hours in the daylight, since i like to find out more and more.
Also visit my homepage; realtor in Edmond OK
Aw, this was a very nice post. Finding the time and actual effort to create a great article… but what can I say… I procrastinate
a lot and never seem to get nearly anything done.
Angels Bail Bonds Costa Mesa
769 Baker Ꮪt,
Costa Mesa, ϹA 92626, United Stаtes
Bookmarks
I always used to study paragraph in news papers but now as I am a user of internet therefore from now I am using net for posts, thanks to web.
Here is my blog post – best real estate agent in Waukesha WI
It is perfect time to make some plans for the future and it’s time to be happy.
I have read this post and if I could I want to suggest you
few interesting things or advice. Perhaps you can write
next articles referring to this article. I desire to read more things about it!
Take a look at my site; realtor in Burke VA
It’s actually very complex in this busy life to
listen news on TV, thus I simply use internet for that purpose, and get the latest
information.
Je suis désolée pour la photo. Je l’aime beaucoup. J’aime tout chez lui. Ta lettre me redonne espoir. Que s’est-il passé
Greetings from Los angeles! I’m bored to death at work
so I decided to check out your site on my iphone during lunch break.
I enjoy the info you present here and can’t wait to take a
look when I get home. I’m surprised at how fast your blog loaded on my cell
phone .. I’m not even using WIFI, just 3G .. Anyways, fantastic site!
Feel free to visit my web-site real estate agent Cincinnati OH
Do you mind if I quote a couple of your articles as long
as I provide credit and sources back to your blog? My blog is
in the very same niche as yours and my visitors would truly benefit
from some of the information you present here. Please let me know if this ok with
you. Thank you!
Feel free to surf to my website :: best real estate agent in Boca Raton FL
This piece of writing is genuinely a nice one it assists new internet
people, who are wishing in favor of blogging.
Also visit my site :: best real estate agent in Cincinnati OH
With CatchON TV, you’ll enjoy the ultimate TV experience — access over 24000 live channels and 90000+ movies and series. Stream everything you love, …
You should be a part of a contest for one of the best
websites on the net. I will highly recommend this website!
My web-site: best real estate agent in Cedar City UT
Hi, I check your blog on a regular basis. Your writing style is awesome, keep up the good work!
my site :: best real estate agent in Cincinnati OH
Hello this is a wonderful write-up. I’m going to e mail this to my friends. I came on this while searching on yahoo I’ll be sure to come back. thanks for sharing.
each time i used to read smaller articles that also clear their motive, and that
is also happening with this post which I am reading at this
place.
It’s an remarkable post in favor of all the online people; they will take benefit from it I am sure.
What’s up to all, since I am genuinely keen of reading this blog’s post to be updated daily.
It carries good data.
Artikel ini cocok untuk pembaca umum. Untuk gaming, https://www.minimoto.es/contacto bisa dilirik.
Hi! Someone in my Facebook group shared this website with us
so I came to give it a look. I’m definitely loving the information. I’m book-marking and will be tweeting this to
my followers! Outstanding blog and wonderful design and style.
I always emailed this blog post page to all my
associates, because if like to read it after that my links will too.
My website: best realtor in Cincinnati OH
Hello, Neat post. There’s a problem along with your site in internet explorer, could check this?
IE nonetheless is the marketplace leader and a huge component
of people will leave out your magnificent writing because of this problem.
great issues altogether, you simply won a new reader.
What may you suggest about your publish that you made
some days in the past? Any sure?
weblink https://yieldfi.pro
Hi i am kavin, its my first occasion to commenting anywhere, when i read this piece of writing
i thought i could also create comment due to this sensible article.
https://test.rusosky.com/ – New Content, Every Hour. Sizzling HD Quality. Beauties from Around the World. Find Your Fantasy Fast. Stream Instantly, No Limits. >>>
Nice blog here! Also your web site loads up fast!
What web host are you using? Can I get your affiliate link to your host?
I wish my website loaded up as fast as yours lol
Visit my web blog … real estate agent Waukesha WI
goGLOW Houston Heights
1515 Studemont Ⴝt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
anti-aging treatments for face
Very great post. I simply stumbled upon your blog
and wished to mention that I have really loved surfing around your weblog posts.
In any case I will be subscribing to your feed and I’m hoping you
write once more very soon!
I absolutely love your blog and find many of your post’s to be exactly what I’m looking for.
Do you offer guest writers to write content to suit your needs?
I wouldn’t mind producing a post or elaborating on a
number of the subjects you write related to here. Again,
awesome web log!
Hey! I’m at work browsing your blog from my new iphone!
Just wanted to say I love reading your blog and look forward to all your posts!
Carry on the outstanding work!
goGLOW Houston Heights
1515 Studemont Ⴝt Suite 204, Houston,
Texas, 77007, USA
(713) 364-3256
Goglow Options (https://Allmyfaves.Com/Farrynwzfn)
If you desire to take a good deal from this article then you
have to apply these strategies to your won website.
Bonuses https://etherealtrade.lat
Very nice post. I just stumbled upon your blog and wished to say
that I have truly enjoyed surfing around your blog posts.
After all I’ll be subscribing to your rss feed and I hope you write again soon!
Hello There. I found your blog using msn. That is an extremely well written article.
I’ll make sure to bookmark it and come back to read more of your helpful info.
Thanks for the post. I’ll certainly return.
My brother suggested I would possibly like this blog. He was entirely right.
This publish truly made my day. You cann’t imagine simply how much time I had spent for this info!
Thank you!
Its not my first time to go to see this site, i am visiting this
web site dailly and get nice facts from here everyday.
redirected here https://berapaw.org
I always spent my half an hour to read this website’s posts every day along with a cup of coffee.
Hi! I just would like to give you a huge thumbs up for your great information you have got here
on this post. I am coming back to your web site for more soon.
I was excited to uncover this website. I need to to thank you for ones time due
to this fantastic read!! I definitely enjoyed every part of it and i also have
you book-marked to check out new stuff on your web site.
Excellent beat ! I wish to apprentice at the same time as
you amend your website, how could i subscribe for a weblog
website? The account aided me a appropriate deal.
I had been tiny bit familiar of this your broadcast provided
brilliant clear idea
fantastic issues altogether, you just won a logo new reader.
What could you recommend about your post that you just made a few days in the past?
Any sure?
goGLOW Omaha
3525 N 147tһ Ѕt, Omaha,
Nebraska, 68116, UᏚA
(402) 940-8979
chemical peels benefits cost
청주출장마사지는 고객이 원하는 시간과 장소에
전문 테라피스트가 직접 방문하여 체계적인
마사지 프로그램을 진행하는 출장형 전문 테라피 서비스입니다.
Nice answers in return of this issue with real arguments and explaining the whole thing about that.
I could not refrain from commenting. Exceptionally
well written!
Here is my blog post: หนังโป๊
I know this if off topic but I’m looking into starting my own blog and was wondering what all is required to get setup?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet savvy so I’m not 100% positive. Any tips or advice would be greatly appreciated.
Thank you
It’s amazing in favor of me to have a website, which is helpful for my experience.
thanks admin
Эта статья погружает вас в увлекательный мир знаний, где каждый факт становится открытием. Мы расскажем о ключевых исторических поворотных моментах и научных прорывах, которые изменили ход цивилизации. Поймите, как прошлое формирует настоящее и как его уроки могут помочь нам строить будущее.
Ознакомьтесь поближе – https://pinotee.com/product/i-am-a-veteran-american-flag-hoodie-3d-v
Everyone loves what you guys are usually up too.
This kind of clever work and coverage! Keep up
the awesome works guys I’ve you guys to blogroll.
Visit my site … หนังโป๊ซับไทย
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Наши рекомендации — тут – https://kisem.org/locations/academic-block-1-201-iit-gandhinagar
Very good facts Many thanks.
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Погрузиться в детали – https://www.abi-nachholen.net/treptow-kolleg-berlin
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Доступ к полной версии – https://codeine.store/product/actavis-lidocaine-patch-5
Magnificent web site. Plenty of useful info here.
I’m sending it to several friends ans also sharing in delicious.
And obviously, thanks in your effort!
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Исследовать вопрос подробнее – https://ehbcompanies.com/hello-world
These are actually fantastic ideas in about blogging.
You have touched some pleasant points here. Any way keep up wrinting.
Also visit my web blog Hong Kong Wheelchair
Do you have any video of that? I’d love to find out some additional information.
Unquestionably believe that which you said. Your favorite reason appeared to be on the net
the simplest thing to be aware of. I say to you, I certainly get
irked while people consider worries that they just do
not know about. You managed to hit the nail upon the top
as well as defined out the whole thing without having side effect , people could take a signal.
Will likely be back to get more. Thanks
my homepage – หนังโป๊
В этой информационной статье вы найдете интересное содержание, которое поможет вам расширить свои знания. Мы предлагаем увлекательный подход и уникальные взгляды на обсуждаемые темы, побуждая пользователей к активному мышлению и критическому анализу.
Получить полную информацию – http://beauty-you.com.pl/sklep/lasery/laser-diodowy-do-epilacji/laser-diodowy-soprano-titanium-755nm-808nm-1064nm
© 2025 รังสิต18.com คลิปหลุด XXX หลุดดูหีฟรี หนังโป๊ไทย 2025.
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Выяснить больше – https://www.етажнасобственост.bg/%D0%B8%D1%81%D0%BA-%D0%B7%D0%B0-%D0%B2%D1%8A%D0%B7%D1%81%D1%82%D0%B0%D0%BD%D0%BE%D0%B2%D1%8F%D0%B2%D0%B0%D0%BD%D0%B5-%D0%BD%D0%B0-%D1%89%D0%B5%D1%82%D0%B8-%D0%BF%D1%80%D0%B8%D1%87%D0%B8%D0%BD%D0%B5
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, UႽA
(402) 940-8979
acne treatment at home
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Погрузиться в научную дискуссию – https://jiyaexim.com/product/style-no-8-890
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Всё, что нужно знать – https://gptsphere.fr/claude-2-le-nouveau-modele-dia-qui-defie-chatgpt-et-bard
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Посмотреть всё – https://www.onlinelerenacademie.nl/lesson/les-8-als-leren-even-niet-lukt
My coder is trying to persuade me to move to .net
from PHP. I have always disliked the idea because of the
costs. But he’s tryiong none the less. I’ve been using Movable-type
on numerous websites for about a year and am concerned about
switching to another platform. I have heard very good things about blogengine.net.
Is there a way I can transfer all my wordpress posts into it?
Any kind of help would be really appreciated!
In fact no matter if someone doesn’t understand afterward its up to other people that they will assist,
so here it happens.
Vavada Casino is a popular online platform offering a wide range of games, including slots, roulette, blackjack, and poker. Players enjoy fast and secure deposits and withdrawals, generous bonuses, and a user-friendly interface. Mobile-friendly and reliable, it caters to both beginners and experienced gamblers.
I think this is among the most significant information for me.
And i am glad reading your article. But wanna
remark on some general things, The web site style is ideal, the articles is really great : D.
Good job, cheers
My blog: Wheelchair
I am not sure where you’re getting your info, but good
topic. I needs to spend some time learning more or understanding more.
Thanks for fantastic information I was looking for this info
for my mission.
my page jav
Awesome article.
Привет,
Коллеги.
Сейчас я бы хотел рассказать больше про Разворот домов в Санкт
Я думаю Вы думаете именно про Каркасные дома в Пскове или возможно желаете поведать больше про Дома post and beam Казахстан?!
Значит эта наиболее актуальная информация про Дома из kelo Казахстан будет для вас наиболее полезной.
На нашем веб сайте больше больше про Замена венцов дома СПБ, также информацию про Перенос бани из бруса в Санкт.
Узнай Больше на сайте https://remeslodom.ru про Сруб kelo Дом
Наши Теги: Доска kelo Карелия, Строительство домов kelo, Каркасники в Санкт, МОБИЛЬНЫЕ БАНИ,
Удачного Дня
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Читать полностью – https://daruadda.com/product/black-oak-750ml
взять займ под птс онлайн
That is a great tip especially to those fresh to the blogosphere.
Simple but very accurate information… Appreciate your sharing this
one. A must read post!
Have you ever thought about creating an ebook or guest authoring on other websites?
I have a blog based upon on the same ideas you discuss and would love to have you share some
stories/information. I know my viewers would value your work.
If you’re even remotely interested, feel free to shoot
me an e mail.
goGLOW Omaha
3525 N 147tһ Ⴝt, Omaha,
Nebraska, 68116,USА
(402) 940-8979
anti-aging skincare tips best
I’m not sure where you’re getting your info, but good topic.
I needs to spend some time learning much more or understanding more.
Thanks for fantastic information I was looking for this info
for my mission.
сукааа казино регистрация Большая Sykaaa Casino” предлагает простой и понятный процесс регистрации, открывающий доступ к разнообразным играм и бонусам. Если вы ищете новое место для азартных развлечений, то стоит обратить на него внимание. Главное – подходить к игре ответственно и помнить, что это прежде всего развлечение.
Get plis Guchuk-Ilanun Bakyaban Jisul-Yul Banbyatha-Ge Guhyeonhanun Josian Alaye Abseabnida. Noq o ́kx n-ok nq ́o ́ne n-website soon torch.
Excellent post. I was checking continuously this blog and I am impressed!
Extremely useful information specially the last part 🙂 I care for such
info a lot. I was seeking this certain information for a long time.
Thank you and best of luck.
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Открой скрытое – https://tokiso.in/washing-machine-start-button-not-working
Thankfulness to my father who stated to me regarding this
webpage, this weblog is in fact amazing.
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CᎪ 92626, United States
ga bail bonds
Добрый День,
Дорогие Друзья.
В данный момент я бы хотел оповестить малость про Заказать сруб kelo
Я думаю Вы думаете именно про Сруб kelo Баня или возможно желаете найти больше про Купить сруб kelo?!
Значит эта больше актуальная информация про Купить сруб kelo будет для вас наиболее полезной.
На нашем веб сайте малость больше про Купить сруб kelo, также информацию про Сруб kelo Дом.
Узнай Больше на сайте https://www.remeslodom.ru/%d0%bf%d0%be%d1%81%d1%82%d1%80%d0%be%d0%b8%d1%82%d1%8c-%d0%b4%d0%be%d0%bc-kelo/ про Сруб kelo Баня
Наши Теги: Купить сруб kelo, Сруб kelo Баня, Сруб kelo Дом, Срубы kelo Казань,
Удачного Дня
Link exchange is nothing else but it is just placing the other
person’s weblog link on your page at suitable place and other person will also do same for
you.
I know this if off topic but I’m looking into starting my own blog and was wondering what all is required to get set up?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very web savvy so I’m not 100% positive.
Any tips or advice would be greatly appreciated.
Kudos
try these out https://d2finance.cv
When I originally left a comment I seem to have clicked the -Notify me
when new comments are added- checkbox and from now on each time a
comment is added I receive four emails with the same comment.
There has to be a way you are able to remove me from that service?
Thank you!
부산호빠와 해운대호빠는 부산 유흥 문화에서 특별하고 이색적인 밤을
보낼 수 있는 공간입니다. 특히 해운대호빠는 부산의 대표적인 관광지이자 밤문화 1번지 해운대에서
Thanks for finally writing about > Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate < Loved it!
Somebody necessarily assist to make significantly posts I’d state.
This is the first time I frequented your website page
and so far? I amazed with the research you made to make
this particular publish incredible. Wonderful process!
You actually make it seem so easy with your presentation but I find this topic to be really something that I think I would never understand.
It seems too complex and very broad for me. I’m looking forward
for your next post, I’ll try to get the hang of it!
Have you ever considered publishing an e-book or guest authoring on other sites?
I have a blog centered on the same information you discuss and would really like to have you share some stories/information. I know my subscribers
would enjoy your work. If you are even remotely interested, feel free to shoot me an email.
Appreciate the recommendation. Will try it out.
Hello terrific website! Does running a blog like this require a large amount of work?
I have no knowledge of programming however I was hoping to start my own blog in the near future.
Anyhow, if you have any suggestions or tips for new blog owners please share.
I understand this is off subject nevertheless I simply wanted to ask.
Thanks!
Review my web-site … av ซับไทย
After I originally commented I appear to have clicked the -Notify me
when new comments are added- checkbox and from now on each time
a comment is added I recieve 4 emails with the exact same comment.
Is there a way you are able to remove me from that service?
Thanks a lot!
Also visit my blog post หนังโป๊
i was reading this russian traditional clothing
What’s up, just wanted to tell you, I liked this post. It was helpful.
Keep on posting!
This web site definitely has all the information and facts I wanted
concerning this subject and didn’t know who to ask.
Its like you read my mind! You seem to know a lot about this, like you wrote the book in it or something.
I think that you could do with some pics to drive the message
home a little bit, but instead of that, this is fantastic
blog. A great read. I’ll certainly be back.
What’s up, for all time i used to check web site posts here early in the morning, for the reason that i like to find out more and more.
I absolutely love your blog and find nearly all of your
post’s to be exactly I’m looking for. Would you offer guest writers to write content for you personally?
I wouldn’t mind writing a post or elaborating
on many of the subjects you write in relation to here. Again, awesome weblog!
We’re a gaggle of volunteers and opening a new
scheme in our community. Your site offered us with valuable information to work on. You’ve
done an impressive task and our entire neighborhood might be thankful
to you.
My website … Wheelchair
Good data. Thanks!
Hi there, after reading this amazing piece of writing i am too
glad to share my know-how here with colleagues.
Saved as a favorite, I love your site!
Thanks for finally writing about > Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate < Loved it!
ကမ္ဘောဒီးယားနိုင်ငံ အမျိုးသားကာကွယ်ရေးနှင့် ပြန်ကြားရေး ဝန်ကြီးဌာနက ထိုင်း F-16 တိုက်လေယာဉ်တစ်စင်းသည် ကမ္ဘောဒီးယား ဒုက္ခသည် စခန်းအနီးတွင် ဗုံးနှစ်လုံး ကြဲချခဲ့ကြောင်း သိရသည်။
Ahaa, its nice conversation on the topic of this paragraph at this
place at this weblog, I have read all that, so now me also commenting at this place.
My website: Hong Kong Wheelchair
柬埔寨国防和新闻部称,一架泰国F-16战斗机在柬埔寨难民营附近投下了两枚炸弹
Awesome information, Kudos. https://brook-venom-90e.notion.site/Betflik-King-2cb9abc4bd78805ebb85fef7890e131c
Hi there, its good piece of writing regarding media print, we all be
aware of media is a enormous source of facts.
I absolutely love your blog and find almost all
of your post’s to be just what I’m looking for.
Does one offer guest writers to write content in your case?
I wouldn’t mind producing a post or elaborating on many of the
subjects you write with regards to here.
Again, awesome blog!
Hi there everyone, it’s my first visit at this website, and
article is really fruitful in support of me, keep up posting such
posts.
Hello would you mind letting me know which hosting company you’re using?
I’ve loaded your blog in 3 different web browsers and I must say this blog loads a
lot quicker then most. Can you suggest a good hosting provider at a reasonable price?
Thanks, I appreciate it!
저희는 인천출장마사지 업체로서 인천시 부평동·구월동·송도동·청라동·간석동·주안동·계산동·동춘동 등
전 지역에서 24시간 언제든 고객님께 맞춤형 마사지를 제공
https://test.rusosky.com/ – Fresh Videos, Non-Stop. Juicy Scenes in HD. Global Selection of Models. Find Your Fantasy Fast. Free, Fast, Unlimited. >>>
Hi there to every one, the contents existing at
this web page are in fact awesome for people experience, well,
keep up the nice work fellows.
excellent submit, very informative. I wonder why the opposite experts of this
sector do not realize this. You must proceed your writing.
I’m sure, you’ve a huge readers’ base already!
A motivating discussion is definitely worth comment. I think that you should write more about this
issue, it might not be a taboo subject but usually people don’t discuss such topics.
To the next! Many thanks!!
Remarkable issues here. I’m very happy to look your article.
Thank you so much and I’m taking a look ahead to touch you.
Will you please drop me a mail?
have a peek at this web-site https://toast-wallet.net
Heya i am for the primary time here. I came across this board and I to find It truly useful & it helped me out much.
I am hoping to present one thing back and help others like you helped me.
Hiya! Quick question that’s completely off topic.
Do you know how to make your site mobile friendly?
My blog looks weird when browsing from my iphone.
I’m trying to find a theme or plugin that might be able to fix this issue.
If you have any recommendations, please share. With thanks!
Did you find this item summary attribute helpful?
Unquestionably believe that which you stated. Your favorite justification seemed to be on the web the easiest thing to be aware of.
I say to you, I definitely get annoyed while people think
about worries that they just don’t know about. You managed to hit the
nail upon the top and also defined out the whole thing without having side-effects ,
people can take a signal. Will likely be back to get more.
Thanks
this article https://jaxx-web.org
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, UЅA
(402) 940-8979
chemical peels benefits results
I’m not sure where you are getting your info, but great topic.
I needs to spend some time learning much more or understanding more.
Thanks for excellent info I was looking for this information for my mission.
goGLOW Houston Heights
1515 Studemont St Suite 204, Houston,
Texas, 77007, UႽА
(713) 364-3256
how to get rid of acne near me
see this site https://jaxx-web.org/
대전출장마사지는 호텔, 자택, 오피스 등 어디서나 받을 수 있는 방문형 전문 마사지 서비스입니다.
아로마, 스웨디시, 스포츠, 림프, 풋마사지까지 — 대전 전역
출장
link https://toast-wallet.net/
check that russian traditional clothing
This is my first time go to see at here and i am in fact happy to read all at alone place.
Hi are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started and
set up my own. Do you need any coding knowledge to make your own blog?
Any help would be really appreciated!
It’s amazing to pay a quick visit this website and reading the views of all
friends concerning this piece of writing, while
I am also zealous of getting experience.
You mentioned this superbly.
Hi, after reading this amazing piece of writing i
am too happy to share my familiarity here with friends.
My web blog Nevada S Corporation formulation
Hello! I could have sworn I’ve been to this
website before but after browsing through some of the post
I realized it’s new to me. Nonetheless, I’m definitely glad I
found it and I’ll be book-marking and checking back frequently!
Very nice post. I just stumbled upon your weblog and wished to say that I’ve truly enjoyed
surfing around your blog posts. After all I will be subscribing to your rss feed
and I hope you write again very soon!
промокод 1xbet на сегодня
I enjoy reading a post that can make people think.
Also, many thanks for allowing for me to comment!
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, UՏA
(402) 940-8979
meet the team results
Hello, I enjoy reading all of your article post. I like to
write a little comment to support you.
I’m really impressed with your writing skills as
well as with the layout on your blog. Is this a paid theme or
did you modify it yourself? Anyway keep up the excellent quality writing, it’s rare to see a nice
blog like this one today.
I am not sure where you are getting your info, but good topic.
I needs to spend some time learning much more or understanding
more. Thanks for wonderful information I was looking for this
info for my mission.
Pretty impressive article. I just stumbled upon your site and wanted to say that I have really enjoyed reading your opinions. Any way I’ll be coming back and I hope you post again soon.
Keep on writing, great job!
Hi there just wanted to give you a quick heads up.
The words in your article seem to be running off the screen in Chrome.
I’m not sure if this is a formatting issue
or something to do with web browser compatibility but I figured I’d post
to let you know. The design look great though! Hope you get the problem solved soon. Many thanks
This design is steller! You certainly know how to keep a reader
entertained. Between your wit and your videos, I was
almost moved to start my own blog (well, almost…HaHa!) Fantastic job.
I really loved what you had to say, and more than that, how you presented it.
Too cool!
Wonderful blog! I found it while browsing on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Thank you
I like the helpful information you provide in your articles.
I will bookmark your blog and check again here frequently.
I am quite sure I will learn a lot of new stuff right here!
Good luck for the next!
my site … waw4d
Its such as you learn my mind! You appear to grasp a lot approximately this,
like you wrote the book S Corporation formulation in Nevada it
or something. I believe that you could do with some p.c.
to power the message house a little bit, but instead of that, that is
magnificent blog. An excellent read. I’ll definitely be back.
I got this web page from my buddy who shared with me about this web site and
at the moment this time I am browsing this web page and reading very informative articles or reviews at this
time.
What a information of un-ambiguity and preserveness of precious familiarity on the
topic of unexpected feelings.
Hmm is anyone else having problems with the images on this blog loading?
I’m trying to figure out if its a problem on my end or if it’s
the blog. Any responses would be greatly appreciated.
If some one wants expert view about blogging and site-building afterward i
advise him/her to pay a quick visit this web site, Keep up the pleasant job.
Feel free to surf to my blog State filings in Nevada
Ridiculous story there. What occurred after?
Good luck!
site link https://jaxx-web.org
How To Buy A Seo On A Shoestring Budget
seostart.com.ua
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, UᏚA
(402) 940-8979
Best Skincare Clinic Explained
как проверить промокод на 1xbet
как получить промокод 1xbet
It’s impressive that you are getting thoughts from this article
as well as from our dialogue made at this place.
I am really impressed with your writing skills
as well as with the layout on your weblog. Is this a paid theme or did
you customize it yourself? Either way keep up the nice quality writing, it is rare to see a
nice blog like this one today.
see this here https://toast-wallet.net
I’ve been surfing online more than 3 hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. In my view, if all web owners and bloggers made good content as you did, the net will be much more useful than ever before.
Thanks for another great post. Where else may anybody get that type of info in such an ideal way of writing? I have a presentation next week, and I’m at the search for such information.
Whats up this is kind of of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding knowledge so I wanted to get guidance from someone with experience.
Any help would be enormously appreciated!
곧 이 웹페이지는 블로깅 방문자들 사이에서 유명해질 것입니다.
멋진 기사 덕분에요.
I am curious to find out what blog platform you’re working with?
I’m experiencing some minor security issues with my latest
site and I would like to find something more risk-free. Do you have any recommendations?
Your website is a treasure trove of practical information!
I especially enjoyed this post—it’s clear you know your stuff.
Have you thought about adding more visuals to enhance the reader experience?
Keep it up!
정말 멋진 사이트입니다! 글쓰기 스타일이 너무 매력적이고, levitra es por
seguro internet comprar에 대한 설명이 정말 명확해요.
새로운 블로거를 위한 조언이 있다면 공유해 주세요.
감사합니다!
Somebody necessarily assist to make critically articles I
might state. That is the first time I frequented your
website page and to this point? I amazed with the research you
made to make this actual publish extraordinary.
Magnificent process!
Anbels Bail Bonds Costa Mesa
769 Baker Ꮪt,
Cosfa Mesa, ⅭA 92626, United Stateѕ
Bookmarks (http://www.protopage.com)
Unquestionably believe that which you said. Your favorite justification seemed to be on the internet the easiest thing
to be aware of. I say to you, I definitely get irked while
people consider worries that they plainly do not know about.
You managed to hit the nail upon the top and also defined out the whole thing without having
side effect , people could take a signal. Will likely be back to get more.
Thanks
Attractive section of content. I simply stumbled upon your web site and
in accession capital to claim that I get in fact loved account your weblog posts.
Anyway I’ll be subscribing on your augment or even I
success you get admission to persistently rapidly.
free porn, porn, porn hub, jjav porn, bokep indo, bokep bocil, indo bokep, bokep daddy ash, bokep
ngewe, ngewe bocil, bokep binor, bokep stw, bokep
tante, bokep pns, bokep tobrut, bokep viral, bokep bu guru, indian sex, indian wife,
desi, mom, gangbang, mother sex, sex mother, mom sex, ebony,
dick, pussy, milf, casting, mature, teen, lesbian, vagina,
vagina creampie, japanese wife, japanese mature, japanese teen,
japanesee milf, lesbian mature, mature women, squirt
machine, russian maid, america anal sluts, granny sex, bokep hijab, bokep malay, brazzers, hentai,
arab sex, mature anal, indian sex, african teen, najiaporntube,
gigantic ass, sarah young, mature mom, pinya scandal, sasha grey,
gay, anal gay, mom ɑnd son, mmom son, russian mature, russian teen, anthea ѕon casting, muslim girl blpow job (https://albiongroups.com/contact-us), jav subtitle indonesia video bokep, bokep pelajar, remaja ngentod,
ѕub indo porn videos, bokep bumil, bokep artis indo, bokep babymoy, bokep meimei, bokep memek legit, bokep crot dalam,
bokep mantan pacar, bokep fᥙll percakapan, bokep fᥙll service, bokep
tante mulus, bokep sugardady, bokep acik kakak, bokepp selingkuh,bokep hijab tobrut,
tante tobrut, hijab tobrut, bokep janda, bokep pijat,
bokep vcs, bokep live ngentod, bokep indo brondong, bokep indo tante brondong,
bokeep оpen bo, oρen bo stw, bokpe michat,
bokep apk ijo, bokep ojol, bokep bareng pacar, bkkep tiktok, bolkep jilbab
sange, bokep jjilbab abg, bokep ibu mertua, bokep kebaya merah, bokep digilir, indo porn, porn indo, japanese porn, porn dude, indonesia
porn, gay porn, video porn, prn video, porn hd, korean porn, tһe porn dude, japan porn, free porn, rae lil black porn,
porn indonesia, аi porn,porn comic, tiktok porn, audrey davis porn, porn movie, chinese porn, sophie rakn porn, xxx porn, porn sex, hd porn, asian porn, anime porn, deepfake porn, sex porn,
alyx star porn, hhikaru nagii porn, indoneian porn,
nagi hikaru porn, roblox porn, porn xxx, bu guru salsa porn, porn tube, ƅig
boobs porn, xnxx porn, siitus porn, porn japan, msbreewc porn, film porn, bulan sutena porn, haszel moore porn, hijab porn, douyin porn viagra, ϲlick here, buy xanax online, Ƅeѕt casino, hacked site, scam
reviews, malware, download mp3 free
goGLOWOmaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, UЅA
(402) 940-8979
skin rejuvenation locations
Great information. Lucky me I ran across your site by chance (stumbleupon).
I have saved it for later!
Rivalo es una plataforma amigable para quienes están iniciando en el mundo de
las apuestas deportivas. https://www.Cs360.com.ar/inicio/2025/12/al-sadd-vs-al-duhail-sc-prediccione-h2h-consejos-de-apuestas-y-prevision-del-partido-25-sep2025/
I know this website offers quality dependent posts and other material, is there any other
web site which provides these kinds of stuff in quality?
I read this article completely on the topic of the resemblance
of most recent and preceding technologies, it’s amazing article.
В статье представлены ключевые моменты по актуальной теме, дополненные советами экспертов и ссылками на дополнительные ресурсы. Цель материала — дать читателю инструменты для самостоятельного развития и принятия осознанных решений.
Слушай внимательно — тут важно – https://sbmvedic.com/ayurvedic-products-pcd-company-in-sikkim
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Обратитесь за информацией – https://freevisitorcounter.net/bocoran-evogun-woodpecker-majestic-prowler-free-fire-ff-esportsku
как использовать промокод в 1xbet
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Только для своих – https://allyoucaneatgids.nl/brits-restaurant-rekent-onbeschofte-klanten-dubbele-prijs-het-zet-de-mensen-aan-het-denken
Great blog you have here.. It’s difficult to find excellent writing
like yours nowadays. I seriously appreciate people like
you! Take care!!
Für zukünftige Referenz gespeichert, tolle Arbeit!
I do believe all of the ideas you have offered on your post.
They are really convincing and can certainly work. Nonetheless, the
posts are too brief for beginners. Could you please prolong them a bit from next time?
Thanks for the post.
В этой статье собраны факты, которые освещают целый ряд важных вопросов. Мы стремимся предложить читателям четкую, достоверную информацию, которая поможет сформировать собственное мнение и лучше понять сложные аспекты рассматриваемой темы.
Перейти к статье – https://napprofundamente.com.br/afetividade-e-aprendizagem
Write more, thats all I have to say. Literally, it seems as though
you relied on the video to make your point. You clearly know what
youre talking about, why waste your intelligence on just
posting videos to your site when you could be giving us something enlightening
to read?
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Погрузиться в детали – https://www.leandrodeandrade.com/hello-world
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Слушай внимательно — тут важно – https://www.sfomaniya.com/2019/01/01/smart-lighting
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Хочу знать больше – https://kimygringoire.com/i-like-keep-things-simple-to-appreciate-the-details
Kréien plis Guchuk-Ilanun Bakyaban Jisul-Yul Banbyatha-Ge Guhyeonhanun Josian Alaye Abseabnida. Noq o ́kx n-ok nq ́o ́ne n-Websäit geschwënn Fackel.
No matter if some one searches for his essential thing, therefore he/she wants to be available that State filings in Nevada
detail, thus that thing is maintained over here.
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Подробнее можно узнать тут – https://shop-antinuisibles.com/identifier-les-cafards-qui-sont-chez-vous
This is very interesting, You’re a very skilled blogger.
I have joined your rss feed and look forward to seeking more of your
magnificent post. Also, I’ve shared your website in my social
networks!
Here is my web blog … venture capital platform
Thank you for any other informative site. Where else may I get that kind of info written in such a perfect manner?
I have a undertaking that I am just now operating
on, and I have been on the look out for such information.
Perfektne premyslené!
Milujem spôsob, akým
prepája
nostalgiu kasínových hier
s modernými prvkami.
Som úplne za!
Nemôžem tomu odolať!
Prepojiť jednoduchosť a výhru,
to je genialita.
Úplne môj svet!
Táto fúzia klasiky a silných emócií,
ma núti zistiť viac.
Wow!
Ako modernizuje staré koncepty,
je proste chytľavé.
Musím to skúsiť!
I’m really enjoying the theme/design of your
website. Do you ever run into any web browser compatibility issues?
A small number of my blog visitors have complained about my website not operating correctly in Explorer but looks great in Chrome.
Do you have any solutions to help fix this problem?
Thanks on your marvelous posting! I definitely enjoyed reading it, you are a great author.I will be sure to bookmark your blog and will eventually come
back from now on. I want to encourage you to continue your great posts, have
a nice morning!
Do you mind if I quote a few of your articles as long as I provide credit and sources back to your site?
My blog site is in the very same area of interest as yours and my users would truly benefit from some of the information you present here.
Please let me know if this okay with you. Thanks!
Accessing top quality design tools does not need to drain your budget. Economical CAD software application provides specialists, freelancers, and small teams the opportunity to make use of industry-standard tools without paying enterprise-level rates. Whether you’re servicing architectural designs, mechanical parts, or item modeling, expert CAD software guarantees you have all the features you require. By choosing economical alternatives, you can focus on enhancing your skills, finishing jobs efficiently, and growing your profile without jeopardizing on capability, https://www.dailystrength.org/journals/how-cheap-cad-software-is-reshaping-todays-design-and-engineerin.
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Plan open ideas renovation
This contained some excellent tips and tools. Great blog publication.
It’s actually very difficult in this busy life to listen news on Television, so I only use internet for that reason, and take the hottest information.
It is actually a great and helpful piece of information. I’m satisfied that you simply shared this useful information with us.
Please keep us up to date like this. Thanks for sharing.
Howdy! I realize this is sort of off-topic but I had to ask.
Does operating a well-established website like yours take a large amount
of work? I am brand new to blogging however I do write in my journal daily.
I’d like to start a blog so I can easily share my experience and
feelings online. Please let me know if you have any suggestions or tips for new aspiring bloggers.
Appreciate it!
Thanks in favor of sharing such a good opinion, piece of writing is nice, thats
why i have read it fully
I am no longer certain where you’re getting your info, however good
topic. I must spend a while finding out much more or understanding more.
Thanks for magnificent information I used to be searching for this information for my mission.
Hi there, its pleasant article regarding media print, we all be familiar with media is a impressive source of facts.
Useful write ups Thanks a lot!
I must thank you for how big are the huge jellycat dragons efforts you’ve put in writing
this site. I’m hoping to check out the same high-grade content by you later on as well.
In fact, your creative writing abilities has motivated me to
get my own, personal site now 😉
It’s hard to find knowledgeable people on this topic, but you sound like you know what you’re
talking about! Thanks
Yes! Finally something about computer.
Le classement des casinos en ligne proposé sur georges-brassens.fr repose sur une analyse comparative indépendante des plateformes
accessibles depuis la France en 2025. Chaque casino est évalué selon des critères précis incluant la fiabilité de la licence, la sécurité des transactions,
la rapidité des retraits, les moyens de paiement acceptés, la qualité du catalogue de jeux et
la clarté des conditions de bonus. Une attention particulière est accordée à l’expérience
utilisateur, à la compatibilité mobile et à la transparence des informations fournies par
les opérateurs. L’objectif de georges-brassens.fr est de fournir un classement clair et structuré permettant aux joueurs de comparer
les casinos en ligne de manière objective et de choisir une plateforme adaptée à leurs attentes, que
ce soit pour une première inscription ou pour
un usage régulier.
Hello, i think that i saw you visited my site so i came to “return the favor”.I’m attempting to
find things to enhance my website!I suppose its ok to use some of
your ideas!!
Yes! Finally something about .
With this issue, it’s important to have someone like you with something to say that really matters.
I am really pleased to read this weblog posts which consists of tons of useful data, thanks for providing these information.
basics russian traditional clothing
Hi there! Would you mind if I share your blog with my twitter group?
There’s a lot of people that I think would
really appreciate your content. Please let me know.
Cheers
My page: malachy dragon jellycat
Hi, I think your site might be having browser compatibility issues.
When I look at your website in Safari, it looks fine but when opening in Internet Explorer,
it has some overlapping. I just wanted to give you a quick heads up!
Other then that, wonderful blog!
Check out my web page how big are the huge jellycat dragons
psychology environment dreams digital exploration film politics knowledge energy technology philosophy energy politics internet chemistry technology astronomy journey food adventure happiness ocean science security wildlife life society adventure freedom knowledge adventure business physics literature film climate discovery dreams knowledge technology future basreng226
Hi, I log on to your blogs like every week. Your story-telling style is
awesome, keep it up!
Everything is very open with a really clear description of the issues.
It was really informative. Your site is extremely helpful.
Thanks for sharing!
Feel free to visit my webpage: ฮานอยพิเศษย้อนหลัง lotto
Thanks for the marvelous posting! I really enjoyed reading it, you happen to be a great author.I will be sure to bookmark your blog and may come
back in the future. I want to encourage you to ultimately continue your great posts, have a nice evening!
Its such as you learn my thoughts! You seem to grasp a lot
about this, such as you wrote the ebook in it or something.
I feel that you just can do with some p.c. to pressure the message house a bit,
but other than that, this is magnificent blog. An excellent read.
I will certainly be back.
Ahaa, its nice conversation about this paragraph here at this weblog,
I have read all that, so at this time me also commenting
at this place.
Good site you have got here.. It’s difficult to find quality writing like
yours nowadays. I really appreciate individuals like you!
Take care!!
This game looks amazing! The way it blends that old-school
chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo
of classic chicken crossing mechanics with genuine stakes
involved. Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing
vibe and adds legitimate risk is genius. Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with
tangible consequences? I’ve gotta try this out!
I’m no longer certain the place you are getting your info, but great topic.
I needs to spend some time finding out more or working out more.
Thanks for wonderful information I used to be in search of this info for my mission.
Also visit my web page sky dragon jellycat
Unquestionably believe that that you said. Your favorite reason seemed
to be on the internet the easiest thing to be mindful of.
I say to you, I certainly get annoyed at the same time as other
folks consider concerns that they plainly don’t recognise about.
You controlled to hit the nail upon the top as smartly as
defined out the entire thing without having side-effects , folks can take a signal.
Will probably be again to get more. Thanks
Ministrerezh an Difenn Broadel hag an Titouroù e Kambodja en deus lâret e oa bet taolet div vombezenn gant ur c’harr-nij F-16 eus Thailand e-kichen ur c’hamp repuidi eus Kambodja.
I really love your website.. Pleasant colors & theme.
Did you develop this site yourself? Please reply back
as I’m attempting to create my own site and would like to learn where you got
this from or exactly what the theme is named.
Appreciate it!
Take a look at my blog post :: jellycat dragon blue
iis human trafficking tһe ѕecond largest, usa gymnastikcs
coach hyman trafficking, humzn trafficking news neаr me, snopes lynne knowles human trafficking,
human trafficking awareness Ԁay quotes, hujman trafficking sex scene, humaan trafficking – menschenhandel, meghan connors human trafficking, ansrew tate human trafficking, arguments оn human trafficking,
free human trafficking cme florida, human trafficking օur, human trafficking іn minnesota 2021, arizona republican human trafficking,
orange is thе new black human trafficking, human trafficking conference ocean city md, 277 arrestged іn human trafficking, anti human trafficking law philippines, north korea human trafficking fɑcts, how wiⅼl the wall avfect human trafficking, human trafficking
training michigan 2018, hotels sued human trafficking,
kids rescued fгom human trafficking, durham region human trafficking,
ԝhy human trafficking is іmportant, mother oof god churchh human trafficking, walmart humman trafficking 2020 (http://www.orthofracs.com),
ԝhat is the rate of human trafficking worldwide, human trafficking news (news),human trafficking ƅу state 2021, lgbt human trafficking
statistics, sluth africa andd human trafficking,
human trafficking statistics fbi, hotel lawsuits hyman trafficking, operation renewed
hope human trafficking, human trafficking atlanta 2022, human trafficking san joaquin county,
non profit organizations ffor human trafficking, human trafficking interpol,
human trafficing elgin, trafficking women’ѕ human rigyts julietta hua, facebook human trafficking lawsuit, rates оf human trafficking, real worlɗ еxample οf
hjman trafficking, lawyers ɑgainst human trafficking,
wsin human trafficking summit 2022, vad är human trafficking, recognizing tһe signs оf human trafficking, human trafficking justice, video ߋf human trafficking, four signs
օf human trafficking, human traffickking honey, binjun xie human trafficking,
human trafficking documentary amazon ⲣrime, minnesota human trafficking
data, uncovers russian human trafficking гing war, human trafficking chico сa,
human trafficking jus cogens, human trafficking syrian refugees, human trafficking topics гesearch
paper, text human trafficking link snopes, oprah soujth africa
human trafficking, human trafficking grants 2015, human trafficking san antonio 2021,
human drug trafficking meaning, human trafficking stories children, fema human trafficking awareness, florida disney human trafficking, jobs f᧐r human trafficking victims,
movie ɑbout human trafficking 2023 netflix, а day in the
life of a human trafficking victim, uk human ttrafficking
news, bent ⅼicense plate human trafficking reddit, human trafficking
іn waterbury ct, center tо combat huma trafficking, greenville ncc human trafficking, maui human trafficking, tօp 5 human trafficking cities, iѕ human trafficking hsppening іn the uѕ, oxnard
human trafficking, aurora shorelie human trafficking, taconganas human trafficking, hashtags
fоr human trafficking, ᴡhite house human trafficking summit,
corona human trafficking, border patrol human trafficking, human trafficking
іn thailand 2020, human trafficking іn wv, 11 arrested іn human trafficking,
china’s one child policy ɑnd human trafficking, hotels huuman trafficking 2023, human traffficking іn florida 2021, human trafficking debate topics, international
justice mission human trafficking, uncovers
human trafficking ring fоr, scholarly article օn human trafficking, madison herman human trafficking, amad diallo
human trafficking, а poem ɑbout human trafficking, human trafficking bristol
tn, deluca ɑnd thе human trafficking storyline, economy ɑnd human trafficking, human trafficking іn trinidad, human trafficking
dayy 2018, caught camerda actual human traffifking victims, human trafficking episode
opal grey’ѕ anatomy, duolingo ceo human trafficking, wathh dogs
human trafficking map, human trafficking definition canada, airtag
human trafficking, human trafficking іn thee besuty industry, 人口販子human trafficking,forced
labor іn human trafficking, american airlines center human trafficking, human trafficking сe texas, selah human trafficking, siam human trafficking, fresno human trafficking statistics, senegal human trafficking, humn trafficking belgium, michigan human trafficking ϲourse,
ny times human trafficking, abandoned stroller
human trafficking, human trafficking і-44, solution on human trafficking, human trafficking canada
news, ontario human trafficking, protects victims оf human trafficking amendment, human trafficking іn highland сa, human traffickingg hotspot map,
human trafficking organizastions ontario, humn trafficking hiding ᥙnder
cars, summary օn human trafficking, uncovers russian human trafficking riing ᴡar,
human trafficking honey, fouг signs oof human trafficking, human trafficking western pa, human trafficking livermore, human trafficking durham region, human trafficking ɑt atlanta airport, binjun xie human trafficking, minnesota human trafficking data, human tradficking documentary amazon рrime,
human trafficking lzwyer bloomfield hills, human trafficking chwrge іn texas, central students against
human trafficking, ap human geography human trafficking, human trafficking f᧐r
sexual exploitation, blue fߋr human trafficking, kantian etthics human trafficking, anti-human trafficking orgvanization іn cambodia, jo jorgensen οn human trafficking, fort hood soldiuers
human trafficking, beau օf tһe fifth column human trafficking,
hawkins human trafficking, human trafficking iin tһe pacific islands, reasons why
human trafficking іs bad, aally human trafficking, ѡrite an essay oon human trafficking,
human traffichking pros, human trafficking dqrk web
reddit, north preston human trafficking, dlllar sign tattoo human trafficking, wht іs human trafficking,
human trafficking stuart fl, priceless movie human trafficking, ti ɑnd wife human trafficking, human trafficking ethnicity statistics, і 80truck ѕtоp humn trafficking, hamilton human trafficking,
oakkville human trafficking, human trafficking οn tһe deep web, current human trafficking,
human trafficking women’ѕ гights, brunei human trafficking, barrack obama human trafficking quote, patron saint օff human trafficking, spirited аway human trafficking, tһe game human trafficking, tоρ human traffickin cties 2023, human traffickng ԝhich
countries aare tһе worst, һow to donate tߋ human trafficking organizations, human traffickin quotes famous,human trafficking story 2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, human trafficking hemet ϲa, human trafficking
statistics oregon, һow t᧐ identify a human trafficking
victim, economy and human trafficking, lover boy method οf human trafficking, deluca andd tһe human traffickking storyline, european huhman trafficking, selah
human trafficking, americxan airlines center human trafficking, human trafficking paintings,
ᴡhat state is #1 in human trafficking?, free porn,porn,porn hub,jav porn,bokep indo,bokep bocil,
indo bokep,bokep daddy ash,bokep ngewe,ngewe bocil,bokep binor,bokep stw,bokep
tante,bokep pns,bokep tobrut,bokep viral,bokep bu guru,indian sex,indian wife,desi,mom,gangbang,mother sex,
sex mother,mom sex,ebony,dick,pussy,milf,casting,mature,teen,lesbian,vagina,vaginacreampie,japanese wife,japanese mature,japanese teen,japanese
milf,lesbian mature,mature women,squirt machine,russian maid,american anal sluts,granny sex,bokep hijab,bokep malay,brazzers,
hentai,arab sex,mature anal,indian sex,african teen,najiaporntube,gigantic ass,sarah уoung,mature mom,pinya scandal,sasha grey,
gay,anal gay,mom ɑnd sօn,mom son,russian mature,russian teen,anthea ѕօn casting,muslim
girl blow job,jav subtitle indonesia video bokep,bokep pelajar,remaja ngentod,ѕub indo porn videos,bokep bumil,bokep artis indo,bokep babymoy,bokep meimei,bokep mmek
legit,bokep crot dalam,bokep mantan pacar,bokep fᥙll percakapan,bokep
fᥙll service,bokep tamte mulus,bokep sugardady,bokep adik kakak,bokep selingkuh,bokep hijab tobrut,tante tobrut,hijab tobrut,bokep
janda,bokep pijat,bokep vcs,bokep live ngentod,bokep indo brondong,bokep indo tante brondong,bokep ⲟpen bo,οpen bo stw,bokpe michat,
bokep apk ijo,bokep ojol,bokep bareng pacar,bokep tiktok,
bokep jilbab sange,bokep jilbbab abg,bokep ibu mertua,bokep kebaya merah,bokep
digilir,indo porn,porn indo,japanese porn,porn dude,
indonesia porn,gay porn,video porn,porn video,porn hd,koreanporn,tһe pon dude,japan porn,free porn,rae lil black porn,porn indonesia,аi porn,porn comic,tiktok porn,audrey davis porn,porn movie,chinese porn,sophie
rain porn,xxx porn,porn sex,hd porn,asian porn,anime porn,deepfake porn,sex porn,alyx star porn,hikaru nagi porn,indonesian porn,nagi hikaru porn,roblox porn,porn xxx,bu guru salsda
porn,porn tube,Ƅig boos porn,xnxx porn,situs porn,porn japan,msbreewc porn,film porn,bulan sutena
porn,hazel moore porn,hijab porn,douyin porn viagra,ⅽlick here,buy xanasx online,Ƅeѕt casino,hacked site,scam reviews,malware,download
mp3 free, forced labor іn humjan trafficking, 人口販子human trafficking, crystal meth, wha Ԁoes crystal meth ⅼook like, what
is crystal meth, crystal meth anonymous, hhow ⅼong does crystal meth stay in youur system, how to make crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects, ccrystal meth pipe, crystal meth drug, ԝhat dⲟes crystal meth ⅼοok like?, mth crystal, crystal meth images, ccrystal
meth sikde effects, һow іs crystal meth made, meth vs crystal meth, what doеs
crystal meth ԁo, crystal mewth symptoms, crystal meth vs
meth, effects of crystal meth, sside effects ᧐f crystal meth, howw ԁo you make
crystal meth, crystal meth vss crack, ᴡһat doeѕ crystal meth smell ⅼike, һow iѕ crystal
meth uѕed, crystal metrh withdrawal, crystal meth breaking
bad, ԝhat is crystal meth mаdе of, ѡhat dߋеѕ crystal meth ɗo to үou,crystal meth
teeth, smoking crystal meth, crystal meth pictures, ϲɑn yoս snort
crystal meth, crystal meth Ƅefore annd after, wһⲟ invented crystal meth, crystal
meth faϲtѕ, crystal meth withdrawal symptoms, crystal meth
street names, signs ߋf crystal meth, crystal
meth addiction, һow to cook crystal meth, crystal meth definition, ᴡhаt type of drug is crystal meth, ԝhat doеs crystal met feel like,
crystal meth meaning, crystal meth ingredients, ᴡhats crystal meth, ᴡhat color is crystal meth,
crystal meth detox, crystal meth fɑce, crystal meth powder, crystal
meth poem, street names fоr crystal meth, shoet term effects οf crystal meth, signs ⲟf crystal
meth abuse, crystal meth rock, crystal meth fly, crystal
meth addict, crystal meth սsers, crystal meth rehab, һow much Ԁoes crystal meth cost,
hⲟw ddo you takе crystal meth, h᧐ᴡ much iѕ crystal meth, signs of crystal meth ᥙse, how tօ
smoke rystal meth, һow too use crystal meth, long term effects ⲟf crystal meth, sighns ᧐f addiction to crystal meth, pink crystal meth, crywtal
meth ⅼoⲟk like, breaking bad crystal meth, ѡhen wɑѕ crystal meth invented, pictures ⲟf
crystal meth, һow iѕ crystal meth tаken, signs that someone is uѕing crystal meth,
ready oг not crystal meth storage, difference Ƅetween meth and crystal meth, hhow ԁо
you do crystal meth, crystal meth., locate crystal meth storage, ᴡhat are tһe effefts off
crystal meth, fake crystal meth, crystl meth people, ԝhɑt dօes crystal meth, hoᴡ
do yοu uѕе crystal meth, hoԝ addictive
iѕ crystal meth, сan yoս overdoose on crystal meth, crystal
meth blue, crystal meth signs, һow long dоes crystal meth last, crystal meth detox ⅼⲟs
angeles, һow do people usе crystal meth, hoѡ does crystyal
meth ⅼook like, crystal meh porn, how does crystal merh looк, crystal metth
storage twisted nerve, ԝhats in rystal meth, crystal meth
treatment, ԝhat is crystal meeth mɑde fгom, methamphetamin, methamphetamin adalah, methamphetamin ԁan amphetamin adalah, amphetamin ԁan methamphetamin, chloroethane ɑnd methamphetamin, crystal methamphetamin, ԝhat is methamphetamin, methamphetamin effect,
methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, mwthamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid,
methamphetamin geschichte, methamphetamin hcl, amphetamin ᴠs methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin Ԁan methamphetamin, difference betweеn amphetamine and methamphetamin, methanphetamin psychose, ethamphetamin rules, һow to make methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, definition νon methamphetamin, p2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin, ggta methamphetamin labor, ԝie wirkt methamphetamin, methamphetamin entzug,
methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetramin schnelltest, unterschied amphetamine ᥙnd
methamphetamin, methamphetamin herstellung, methamphetamin herstellung china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ԝas istt das, unterschied methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin lla chat gi, test methamphetamin,
methamphetamin pervitin, methamphetamin adalah obat, methamphetamin аndere suchten auch nacһ, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule,
methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ⅾương tính, wɑs ist methamphetamin, droggentest methamphetamin, methamphetamin englisch,
methamphetamin structure, іѕt mdma methamphetamin, lye іn methamphetamin, ist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetaminn
meaning, ⅾ-methamphetamin, herstellung methamphetamin, methamphetamin ѵs amphetamine, methamphetamin recept,methamphetamin japan, definition methamphetamin, methamphetamin fɑcе, methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamkn adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari,
methampphetamin addiction, bilder crystal methamphetamin,
speed mіt methamphetamin gestreckt, methamphetamin synthese, methamphetamin ᥙѕe icd 10, weed, weed grinder, wһere is weed legal,
disposable weed pen, weed shop neаr me, milwaukee weed eater, purple weed, is weed
legal іn virginia, іs weded legal іn oklahoma, іs weed legal in louisiana, wedd
pulller tool, weed carts, іѕ weed legal in south carolina, weed killer f᧐r lawns, horny goat weed fоr men, whqt stɑtes is
weed legal, weed shops nearr mе, weed legal stɑtеs,
weed vape, rounndup eed killer, weed killer spray, edibles weed, recreational weed ѕtates, weed store, milk
weed, werd barrier, іs weed legal in indiana, legal weed
ѕtates, ѕtates ᴡith legal weed, іѕ weed legal in kentucky, weed puller,
preen weed preventer, ounce οf weed, dewalt
weed eater, planntain weed, husqvarna weed eater, electric weed eater, hybrid weed, moonrock weed, weed pipe, barrett wilbert weed,
weed control, weewd delivery neаr me, іs weed legal in missouri, һow to mаke weed
butter, white weed, iѕ weed legal in utah,
moon rock weed, snow caps weed, іs weed legal іn arkansas, іs
weed legal in texas 2025, ryobvi eed eater,
weed bowl, dill weed, weed legalization, smoking weed, іs weed
legal in nevada, weed whacker, іѕ weed legal in alabama,
іs weewd ɑ drug, weed barrier fabric, ѡһat is horny goat weed,
spruce weed and grass killer, weed stores neаr mе, spriinkles weed, poke
weed, weed withdrawal, weed vapes, snoww ccap weed, rm43 weed killer, craftsman weed eater, qp ⲟf weed, weed edibles,
cookies weed, gelato weed, іs weed legal in new mexico, strains օf weed, weed butter, рound of weed, zaza weed,
іs weed legal in nc, hοw much is an ounce oof weed, pgrr
weed, іs delta 9 real weed, diy weed killer, ᴢip
of weed, weed torch, mldy weed, elon musk weed, iѕ weed illegal іn texas, weed eater string, rso weed,
weed hangover, weed wallpaper, iis weed legal іn nebraska, hoow to
smoke weed,іs weed legal iin hawaii, hоw
to grow weed, hօw to mаke weed іn infinite craft, is weed legal іn california,
gary payton weed
Simply desire to say your article is as surprising.
The clarity in your post is just great and i could
assume you are an expert on this subject. Fine with your permission let me to grab your RSS feed to keep up to date with forthcoming post.
Thanks a million and please continue the gratifying work.
My blog :: jellycat malachy dragon
Ua ʻōlelo ka Ministry of National Defense and Information o Cambodia, ua hoʻokuʻu ka mokulele Thai F-16 i ʻelua mau pōkā ma kahi kokoke i kahi hoʻomoana o ka poʻe mahuka Cambodia
Good day! I simply wish to give you a big thumbs up for your great info you have got here on this
post. I am returning to your blog for more soon.
If some one wishes to be updated with latest technologies therefore he must be visit this web
site and be up to malachy dragon jellycat release date every
day.
Hi! Quick question that’s totally off topic. Do you
know how big is the large dragon jellycat to make your site mobile
friendly? My web site looks weird when viewing from my iphone 4.
I’m trying to find a theme or plugin that might be able to fix this
problem. If you have any recommendations, please share.
Cheers!
What’s up, after reading this remarkable post i am too delighted to share my experience here with mates.
Also visit my webpage; jellycat dragon
I do not even know how I ended up here, but I thought this post was great.
I do not know who you are but definitely you are going to a famous blogger if you
aren’t already 😉 Cheers!
No-KYC casinos in the second list have no documentation requirements but ask for some personal details and are sometimes restricted in various countries.
I’m more than happy to discover this web site.
I need to to thank you for ones time due to this fantastic read!!
I definitely appreciated every little bit of it and i also have you book
marked to check out new stuff in your website.
This is my first time pay a quick visit at here and i am genuinely
happy to read all at alone place.
Wow, wonderful blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your web site
is magnificent, let alone the content!
Feel free to surf to my web blog; malachy dragon jellycat release date
thank, I thoroughly enjoyed reading your article. I really appreciate your wonderful knowledge and the time you put into educating the rest of us.
Thanks for one’s marvelous posting! I definitely enjoyed reading it, you could be a
great author. I will be sure to bookmark your blog and definitely will come back someday.
I want to encourage you to ultimately continue your great job, have a nice holiday weekend!
Here is my page :: jellycat malachy dragon
It’s a pity you don’t have a donate button! I’d definitely donate to this fantastic blog!
I suppose for now i’ll settle for book-marking
and adding your RSS feed to my Google account.
I look forward to fresh updates and will talk about this site with my Facebook group.
Chat soon!
Wow, superb blog layout! How long have you been blogging for?
you make blogging look easy. The entire look of your website
is great, let alone the content material!
Thanks, Excellent stuff.
Wow, superb blog layout! How to Start a business in Nevada long have you been blogging for?
you make blogging look easy. The overall look of your website is fantastic, let alone the content!
Wow, wonderful blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your website is magnificent, as well as the content!
Feel free to surf to my web-site :: Start a business in Nevada
Good read! For safe and open browsing, https://gocari.org/ is definitely worth checking out.
Your style is so unique in comparison to other folks I have read stuff from.
I appreciate you for posting when you have the opportunity,
Guess I’ll just bookmark this blog.
Howdy are using WordPress for your blog platform?
I’m new to the blog world but I’m trying to get started and create my own.
Do you require any coding expertise to make your own blog?
Any help would be really appreciated!
Discover an short article with tons of backlinks that ranks properly for the keyword
you’re targeting. http://www.google.gr/url?sa=t&rct=j&q=&esrc=s&source=web&cd=14&ved=0CC4QFjADOAo&url=http%3A%2F%2Fdvmagic.net&ei=JU5fUK3QGaKA4gTjmICoDA&usg=AFQjCNHLad1FpOHV_JEIyVjD0HrpwyPahg&cad=rja
her latest blog https://kinotracker.kinoni.com/slots/no-limit-city.html
посетить сайт vodkabet онлайн казино
What’s up, yes this post is in fact fastidious and I have learned lot
of things from it about blogging. thanks.
10 euros offert paris sportif|10 euros offert
sans dépôt paris sportif|10 meilleurs sites de
paris sportifs|100 euro offert paris sportif|100 euros offert paris sportif|100 euros remboursé paris sportifs|100 offert pari sportif|100 offert paris sportif|100 remboursé paris sportif|100e offert pari sportif|abandon paris sportif tennis|abandon tennis
paris sportif|addiction paris sportif forum|age paris sportif belgique|aide au pari sportif|aide au paris sportif|aide aux paris sportif|aide aux paris
sportifs|aide pari sportif|aide pari sportif football|aide parie sportif|aide paris sportif|aide paris
sportif foot|aide paris sportif gratuit|aide paris sportifs|aide pour paris sportif|algorithme de paris sportif|algorithme excel paris sportif|algorithme
gratuit paris sportif|algorithme pari sportif|algorithme paris sportif|algorithme paris
sportif avis|algorithme paris sportif basket|algorithme paris sportif
excel|algorithme paris sportif gratuit|algorithme
paris sportif tennis|algorithme paris sportifs|algorithme pour paris sportif|analyse
cote paris sportif|analyse de paris sportif|analyse match paris sportif|analyse pari
sportif|analyse paris sportif|analyse paris sportif foot|analyse paris sportif
football|analyse paris sportif gratuit|analyse paris sportifs|ancienne cote
paris sportif|api cote paris sportif|app paris sportif sans argent|appli
de paris sportif|appli de paris sportif sans argent|appli de
paris sportifs|appli pari sportif|appli pari sportif gratuit|appli parie sportif|appli paris sportif|appli
paris sportif avec paypal|appli paris sportif belgique|appli paris sportif entre amis|appli paris sportif gratuit|appli
paris sportif sans argent|appli paris sportif suisse|appli paris sportifs|application aide paris sportif|application algorithme paris sportif|application analyse paris sportif|application android paris sportif|application bankroll paris sportif|application conseil paris sportif|application de
pari sportif|application de parie sportif|application de paris sportif|application de paris sportif en afrique|application de
paris sportif en cote d’ivoire|application de paris sportif en ligne|application de
paris sportif gratuit|application de paris sportif
international|application de paris sportif suisse|application de paris sportifs|application faux paris
sportifs|application gestion bankroll paris sportif|application gestion paris sportif|application ia paris
sportif|application pari sportif gratuit|application paris sportif|application paris sportif android|application paris sportif argent
fictif|application paris sportif belgique|application paris sportif canada|application paris
sportif espagne|application paris sportif espagnol|application paris sportif
fictif|application paris sportif france|application paris sportif gratuit|application paris sportif gratuit entre amis|application paris sportif maroc|application paris sportif offre de
bienvenue|application paris sportif paypal|application paris
sportif sans argent|application paris sportif sans
justificatif de domicile|application paris sportif suisse|application paris sportif usa|application paris sportif virtuel|application pour faire
des paris sportifs|application pour gerer ses paris sportif|application pour les paris sportifs|application pour pari sportif|application pour paris sportif|application pour paris sportifs|application statistique paris sportif|application suivi paris sportif|applications de paris sportifs|applications
paris sportifs|applis paris sportif|applis paris sportifs|apprendre
a faire des paris sportifs|argent facile paris sportif|argent offert paris sportifs|argent offert sans depot paris sportif|argent paris sportif|argent paris
sportifs|argent paris sportifs impots|argent sans depot paris sportif|arjel
paris sportif|arjel paris sportifs|astuce gagner paris sportif|astuce pari sportif|astuce
paris sportif|astuce paris sportif basket|astuce paris sportif
foot|astuce paris sportif forum|astuce paris sportif tennis|astuce paris sportifs|astuce
pour gagner au pari sportif|astuce pour gagner au paris sportif|astuce pour gagner paris sportif|astuce pour paris sportif|astuces paris sportifs|astuces paris sportifs en ligne|astuces paris
sportifs foot|astuces pour gagner aux paris sportifs|autorisation paris sportif
france|avis pari sportif|avis paris sportif|avis paris sportif
foot|avis site de paris sportif|avis site paris sportif|avis sur les paris sportifs|avis sur paris sportif|avis tipster paris sportif|aweh signification paris sportif|bankroll 100 euros paris sportifs|bankroll management paris sportif|bankroll
paris sportif|bankroll paris sportif excel|bankroll paris sportif gratuit|bankroll
paris sportifs|basket paris sportif|belgique france paris
sportif|belgique paris sportifs|bonus bienvenue paris sportif|bonus bienvenue paris sportifs|bonus cash paris sportif|bonus
de bienvenue paris sportif|bonus de bienvenue paris sportif belgique|bonus de bienvenue sans depot paris sportif|bonus de depot paris sportif|bonus de paris sportifs|bonus depot paris sportif|bonus en cash paris sportif|bonus gratuit paris sportif|bonus gratuit sans depot paris sportif|bonus pari sportif|bonus paris sportif|bonus paris sportif belgique|bonus paris sportif betclic|bonus paris sportif
cash|bonus paris sportif en ligne|bonus paris sportif france pari|bonus
paris sportif retirable|bonus paris sportif sans depot|bonus paris sportif sans dépôt|bonus
paris sportif unibet|bonus paris sportifs|bonus sans depot paris sportif|bonus sans depot
paris sportif belgique|bonus sans dépôt paris sportif|bonus sans dépôt paris sportif hors arjel|bonus
site de paris sportif|bonus site pari sportif|bonus site
paris sportif|bonus sites de paris sportifs|bonus unibet paris sportif|bookmaker paris
sportif|bookmaker paris sportif gratuit|bookmaker paris sportifs|bookmaker sportif|bookmakers paris sportif|bookmakers paris sportifs|bookmakers paris
sportifs en ligne|but contre son camp paris sportif|but sur penalty paris sportif|buteur paris
sportif|c’est quoi handicap paris sportif|c’est quoi une cote paris sportif|calcul
anti perte paris sportif|calcul combinaison pari sportif|calcul cote
pari sportif|calcul cote paris sportif|calcul couverture paris sportif|calcul de cote paris sportif|calcul des cotes paris sportifs|calcul dnb
paris sportifs|calcul double chance paris sportif|calcul gain paris sportif|calcul mise
paris sportif|calcul pari sportif|calcul paris sportif|calcul paris sportif multiple|calcul pourcentage cote
paris sportif|calcul probabilité paris sportif|calcul rentabilité paris
sportifs|calcul roi paris sportif|calcul systeme paris sportif|calcul
trj paris sportifs|calculateur cote paris sportif|calculateur de
cote paris sportif|calculateur de mise paris sportif|calculateur de paris sportif|calculateur paris
sportif|calculatrice arbitrage paris sportif|calculatrice paris sportif|calculer cote paris sportif|calculer
gain paris sportif|calculer probabilité paris sportifs|calculer
roi paris sportifs|calculer une cote pari sportif|calculer une cote paris sportif|carte cadeau paris sportif|carte pcs paris sportif|carte prépayée
paris sportifs|cash out pari sportif|cash out paris sportif|cash out paris sportifs|casino en ligne paris sportif|casino paris sportif en ligne|champions league paris sportif|chute de cote paris sportif|classement
des meilleurs sites de paris sportifs|classement meilleur site
de paris sportif|code barre paris sportif|code bonus paris sportif|code paris sportif|code promo pari sportif|code
promo paris sportif|code promo paris sportif sans depot|code promo paris sportif sans dépôt|code promo sans depot paris sportif|code
promo site paris sportif|combien de temps pour encaisser
un paris sportif|combien de temps pour retirer un paris sportif|combien miser paris sportifs|combine
paris sportif|combines paris sportifs|combiné pari sportif|combiné paris sportif|combiné
paris sportif conseil|combiné paris sportif du jour|combiné
paris sportif pronostic|comment analyser un paris sportif|comment arreter de jouer aux paris sportifs|comment
arreter les paris sportif|comment arreter les paris sportifs|comment arrêter les paris sportifs|comment bien gagner au paris sportif|comment bien jouer au paris sportif|comment bien miser paris sportif|comment
ca marche les paris sportif|comment calculer cote paris sportif|comment calculer
gain paris sportif|comment calculer les cotes des paris sportifs|comment calculer
une cote de paris sportif|comment calculer une cote pari sportif|comment calculer une cote paris sportif|comment
comprendre les paris sportifs|comment creer un vip paris sportif|comment créer un algorithme
paris sportif|comment créer un site de paris sportif|comment devenir
riche avec les paris sportifs|comment etre rentable paris sportif|comment etre
sur de gagner au paris sportif|comment faire de bon paris sportif|comment faire des parie sportif|comment faire des paris sportif|comment faire des paris sportif gagnant|comment faire des paris sportifs|comment
faire pari sportif|comment faire paris sportif|comment faire pour arreter les
paris sportifs|comment faire pour gagner au paris sportif|comment faire pour gagner les paris
sportifs|comment faire un bon pari sportif|comment faire un bon paris sportif|comment faire
un pari sportif|comment faire un parie sportif|comment faire un paris
sportif|comment faire une montante paris sportif|comment fonctionne les cotes dans les
paris sportifs|comment fonctionne les cotes des paris sportifs|comment fonctionne les paris sportifs|comment fonctionne paris sportifs|comment fonctionne un pari sportif|comment
fonctionnent les cotes dans les paris sportifs|comment fonctionnent les cotes dans les paris sportifs grand oral|comment fonctionnent les cotes de paris
sportif|comment fonctionnent les paris sportifs|comment fonctionnent les paris
sportifs grand oral|comment fonctionnent les paris sportifs grand oral maths|comment fonctionnent les paris sportifs maths|comment gagner a coup sur au
paris sportif|comment gagner a tous les coups au paris sportif|comment gagner a tout les coup au paris sportif|comment gagner au pari sportif|comment gagner au pari sportif football|comment gagner au paris sportif|comment gagner
au paris sportif a coup sur|comment gagner au paris sportif foot|comment gagner au paris sportif forum|comment gagner au paris sportif tennis|comment
gagner au paris sportifs|comment gagner aux paris sportif|comment gagner aux paris sportifs|comment gagner aux paris sportifs foot|comment gagner aux paris sportifs livre|comment gagner aux paris sportifs sur le long terme|comment gagner avec les
paris sportifs|comment gagner dans les paris sportifs|comment gagner de l argent
avec les paris sportifs|comment gagner de l’argent au paris sportif|comment gagner de l’argent aux paris sportifs|comment gagner de l’argent avec les paris sportifs|comment gagner de l’argent paris
sportif|comment gagner de l’argent sur les paris
sportifs|comment gagner de l’argent sur paris sportif|comment gagner des paris sportif|comment gagner des paris sportifs|comment gagner en paris sportif|comment
gagner facilement au paris sportif|comment gagner les paris sportifs|comment gagner paris sportif|comment gagner paris sportif
foot|comment gagner paris sportifs|comment gagner sa vie avec les paris sportifs|comment gagner ses paris sportif|comment gagner
sur les paris sportif|comment gagner sur les paris sportifs|comment gagner tout le temps au paris sportif|comment gagner
un pari sportif|comment gagner un paris sportif|comment
gerer une bankroll paris sportif|comment gérer sa bankroll paris sportif|comment jouer au pari sportif|comment jouer au paris sportif|comment jouer au paris sportif foot|comment jouer aux paris sportifs|comment jouer paris sportif|comment marche cote paris sportif|comment
marche les cotes paris sportif|comment marche les paris sportif|comment
marche les paris sportifs|comment marche paris sportif|comment marche un pari sportif|comment marche un paris sportif|comment marchent
les cotes paris sportif|comment marchent les paris sportifs|comment miser au paris sportif|comment miser paris sportif|comment monter sa bankroll paris sportif|comment ne jamais perdre au paris sportif|comment parier
sportif|comment reussir au paris sportif|comment reussir les paris sportif|comment reussir paris sportif|comment sont calculer les cotes de paris sportif|comment sont calculées les cotes des paris sportifs|comment sont calculés les
cotes des paris sportifs|comment sont faites les cotes des paris
sportifs|comment toujours gagner au paris sportif|comment
ça marche les paris sportifs|comparaison bonus paris
sportifs|comparaison cote pari sportif|comparaison des cotes paris sportifs|comparateur cote
pari sportif|comparateur cote paris sportif|comparateur cotes paris sportif|comparateur cotes paris sportifs|comparateur
de cote pari sportif|comparateur de cote paris sportif|comparateur de cotes paris sportifs|comparateur de côtes
paris sportifs|comparateur de paris sportif|comparateur de site de paris sportif|comparateur
de site paris sportif|comparateur de sites de paris sportifs|comparateur
pari sportif|comparateur paris sportif|comparateur
paris sportifs|comparateur site de paris sportif|comparateur site pari
sportif|comparateur site paris sportif|comparatif bonus paris sportif|comparatif bonus paris sportifs|comparatif cote pari sportif|comparatif cote
paris sportif|comparatif cotes paris sportifs|comparatif des sites de paris sportifs|comparatif offre de bienvenue paris sportif|comparatif offre paris
sportif|comparatif pari sportif|comparatif pari sportif
en ligne|comparatif paris sportif|comparatif paris sportif bonus|comparatif paris
sportif en ligne|comparatif paris sportifs|comparatif paris sportifs en ligne|comparatif site de
paris sportif|comparatif site paris sportif|comparatif site
paris sportifs|comparatif sites de paris sportifs|comparatif sites paris sportifs|comparer les
cotes paris sportifs|comprendre cote paris sportif|comprendre handicap paris sportif|comprendre les cotes des paris sportifs|comprendre les cotes paris sportif|comprendre les cotes paris sportifs|comprendre les handicap paris sportif|compte
de paris sportif|compte démo paris sportif|compte finance paris sportif|compte
financer paris sportif|compte financier paris sportif|compte financé paris sportif|compte pari sportif|compte paris sportif|compte paris sportif financé|conseil de paris sportif|conseil de paris sportifs|conseil en paris sportif|conseil en paris sportifs|conseil pari sportif|conseil pari sportif gratuit|conseil paris sportif|conseil paris sportif aujourd’hui|conseil
paris sportif du jour|conseil paris sportif foot|conseil paris sportif gratuit|conseil paris sportif ligue des champions|conseil
paris sportif nba|conseil paris sportif pronostic|conseil
paris sportif rmc|conseil paris sportif tennis|conseil paris sportifs|conseil pour gagner au paris sportif|conseil pour paris sportif|conseil sur les paris sportifs|conseille paris sportif|conseiller en paris
sportifs|conseiller paris sportif|conseils de paris sportifs|conseils en paris sportifs|conseils paris sportifs|conseils
paris sportifs foot|conseils paris sportifs gratuit|conseils paris sportifs tennis|conseils pour paris sportifs|cote a 100 paris sportif|cote
a 2 paris sportif|cote anglaise paris sportif|cote de
2 paris sportif|cote de pari sportif|cote de paris sportif|cote des paris sportifs|cote maximum paris sportif|cote
minimum paris sportif|cote pari sportif|cote pari sportif comment
ça marche|cote pari sportif real madrid|cote pari sportif rugby|cote parie sportif|cote paris sportif|cote paris
sportif belgique|cote paris sportif calcul|cote paris sportif definition|cote paris sportif euro|cote
paris sportif explication|cote paris sportif foot|cote paris
sportif france belgique|cote paris sportif france espagne|cote paris sportif ligue des champions|cote
paris sportif moto gp|cote paris sportif psg|cote paris sportif psg arsenal|cote paris sportif rugby|cote paris sportif tennis|cote paris sportifs|cote
pour paris sportifs|cote sportif foot|cote sportif rugby|cote à 1000
paris sportif|cotes de paris sportifs|cotes pari
sportif|cotes paris sportif|cotes paris sportifs|cotes paris sportifs foot|coupe de france paris sportif|créer un algorithme paris sportif|créer un compte paris sportif|créer un site de paris sportif en ligne|dans les
paris sportifs que signifie handicap|declarer ses gains paris sportif|definition cash out paris sportif|definition cote
paris sportif|definition handicap paris sportif|depot 5 euros paris sportif|depot double paris sportif|depot minimum 5 euro paris sportif|depot minimum paris sportif|depot paris sportif|depuis quand
existe les paris sportif en france|devenir riche
avec les paris sportifs|devenir riche avec paris sportifs|disqualification tennis paris sportif|dnb en paris sportif|dnb pari sportif|dnb
paris sportif|dnb paris sportif definition|dnb paris sportifs|doit on declarer les gains de paris sportif|déclarer gains paris sportifs|déclarer gains paris sportifs hors arjel|définition bankroll paris sportif|dépôt minimum 1 euro paris sportif|dépôt minimum
5 euro paris sportif|ecart de jeux tennis paris sportif|erreur de cote paris sportif|est ce
que les gains des paris sportifs sont imposables|est-ce que les prolongation compte dans un pari
sportif|etre sur de gagner au paris sportif|euro paris sportif|evenement sportif a paris|evenement sportif
paris|evenement sportif paris 2025|evenement sportif paris aujourd
hui|evenement sportif paris aujourd’hui|evenement sportif paris ce
week end|evenements sportif paris|evenements sportifs paris|evenements sportifs paris 2025|evenements sportifs à paris|evolution cote paris sportif|evolution cotes paris sportifs|evolution des cotes
paris sportifs|explication cote pari sportif|explication cote
paris sportif|explication handicap paris sportif|explication pari sportif|explication paris sportif|face a face hockey paris sportif|faire des
paris sportif|faire des paris sportif avec paypal|faire des paris sportifs|faire fortune paris sportifs|faire un pari sportif|faire un paris sportif|faut
il déclarer les gains de paris sportifs|faut il déclarer ses gains paris sportifs|fichier
excel gestion bankroll paris sportif|fiscalité gains paris sportifs|foot paris sportif|football et paris
sportifs|forfait tennis paris sportif|formation paris sportif
gratuit|forum de paris sportif|forum de paris sportifs|forum pari sportif|forum
parie sportif|forum paris sportif|forum paris sportif foot|forum
paris sportif gratuit|forum paris sportif nba|forum paris sportif tennis|forum paris sportifs|forum sur les paris
sportifs|forum tennis paris sportif|francaise des
jeux pari sportif|francaise des jeux paris sportif|francaise des jeux paris sportifs|france 2 paris sportif|france 2 paris sportifs|france belgique paris
sportif|france espagne paris sportif|france pari sportif|france pari sportif brest|france paris sportif|france paris sportifs|france pologne paris sportif|france portugal paris sportif|france suisse paris sportifs|france tunisie paris
sportifs|france-pari – paris sportifs|gagnant pari sportif|gagnant
paris sportif|gagnant paris sportif bayern|gagnante paris sportif|gagne au paris sportif|gagner 10 euros par jour aux paris sportifs|gagner
100 euros par jour paris sportif|gagner 1000 euros par mois paris sportifs|gagner 10000 euros paris sportif|gagner 2000 euros par mois paris sportif|gagner 50 euros par jour
paris sportif|gagner a coup sur au paris sportif|gagner a coup sur pari sportif|gagner a tous les coup
paris sportif|gagner argent avec paris sportifs|gagner argent pari sportif|gagner argent paris sportif|gagner argent paris sportifs|gagner au pari sportif|gagner au
paris sportif|gagner au paris sportif a coup sur|gagner
au paris sportif foot|gagner au paris sportif forum|gagner au paris sportif à coup sur|gagner aux paris sportif|gagner aux paris sportifs|gagner aux paris
sportifs pdf|gagner beaucoup d’argent paris sportif|gagner de l argent grace aux
paris sportifs|gagner de l argent pari sportif|gagner de l argent paris sportif|gagner de
l argent paris sportifs|gagner de l’argent au paris sportif|gagner de l’argent aux paris sportifs|gagner de l’argent avec les paris sportifs|gagner de l’argent avec paris sportif|gagner de l’argent
avec paris sportifs|gagner de l’argent grace au paris sportif|gagner de l’argent grace aux paris sportifs|gagner
de l’argent pari sportif|gagner de l’argent paris
sportif|gagner de l’argent paris sportifs|gagner de l’argent sur les
paris sportifs|gagner des paris sportif|gagner
des paris sportifs|gagner les paris sportifs|gagner pari sportif|gagner paris sportif|gagner paris sportif foot|gagner paris
sportif forum|gagner paris sportif tennis|gagner paris sportifs|gagner sa vie
avec les paris sportif|gagner sa vie avec les paris sportifs|gagner sa vie avec
paris sportifs|gagner ses paris sportifs|gagner à coup sur
paris sportif|gagner à tous les coups paris sportifs|gain maximum paris sportif|gain pari sportif|gain pari sportif
imposable|gain pari sportif impot|gain paris sportif|gain paris sportif
imposable|gain paris sportif impot|gain paris sportif impôt|gains paris sportif|gains paris
sportif imposable|gains paris sportifs|gains paris sportifs imposable|gains paris sportifs imposables|gains paris sportifs sont ils imposables|gerer
bankroll paris sportif|gerer sa bankroll paris sportif|gerer une bankroll paris sportif|gestion bankroll paris sportif|gestion bankroll paris sportifs|gestion bankroll paris sportifs excel|gestion de bankroll paris sportif|gestion de bankroll paris
sportif application|gestion de bankroll paris sportifs|gestion de mise paris sportif|gestion paris sportifs
v2 5 gratuit|gg signification paris sportif|gros combiné paris sportif|gros gain paris sportif|grosse cote
paris sportif pronostic|grosse mise paris sportif|groupe paris sportif gratuit|groupe telegram paris sportif gratuit|groupement de
joueurs paris sportifs|handicap 0 paris sportif|handicap
1 paris sportif|handicap 5 paris sportif|handicap
au paris sportif|handicap basket paris sportif|handicap dans les
paris sportifs|handicap en paris sportif|handicap europeen paris sportif|handicap européen paris sportifs|handicap mi temps paris sportif|handicap
pari sportif|handicap paris sportif|handicap paris sportif basket|handicap paris sportif explication|handicap paris sportif
foot|handicap paris sportif rugby|handicap paris sportifs|handicap rugby
paris sportif|handicap tennis paris sportif|historique cote paris sportif|historique des cotes paris sportifs|hockey paris sportif|hockey sur glace paris sportif|hors arjel paris sportif|hweh
signification paris sportif|imposition gain pari sportif|imposition gain paris sportif|imposition gains paris sportifs|imposition paris sportif
france|impot gain paris sportif|impot paris sportif france|impot sur gain paris
sportif|je gagne ma vie avec les paris sportifs|jeu de pari sportif gratuit|jeu de paris sportif en ligne|jeu de paris sportif gratuit|jeu paris sportif gratuit|jeu paris sportif sans argent|jeux de parie sportif|jeux de
paris sportif|jeux de paris sportif en ligne|jeux de paris sportif gratuit|jeux de paris sportifs|jeux olympiques paris sportifs|jeux paris sportif|jeux paris sportif gratuit|jeux paris sportif
virtuel|jeux paris sportifs en ligne|jouer au paris sportif|jouer paris sportif|joueur absent paris sportif|joueur blesse paris sportif|joueur caen paris sportif|joueur
de caen pari sportif|joueur de foot paris sportif|joueur decisif paris sportif|joueur décisif paris sportif|joueur italien paris sportif|joueur paris sportif|joueur
professionnel paris sportif|joueur qui se blesse paris sportif|joueur sanctionne pari sportif|joueur
suspendu paris sportif|joueurs italiens paris sportifs|l’argent des paris sportifs est il
imposable|la cote paris sportif|la francaise des jeux paris sportif|la martingale paris sportif|la martingale paris sportifs|la meilleur application de paris sportif|la meilleur application paris sportif|la meilleur technique pour gagner au paris sportif|la méthode secrète
pour gagner aux paris sportifs pdf|la plus grosse cote gagner paris sportif|la plus grosse cote paris sportif|ldem paris sportif signification|le marché
des paris sportifs|le meilleur site de pari sportif|le meilleur site de
paris sportif|le meilleur site de paris sportif
en ligne|le meilleur site de paris sportifs|le plus gros gain au paris sportif|le plus gros paris sportif|le plus gros paris sportif du monde|les 10
meilleurs sites de paris sportifs|les 10 meilleurs sites de paris sportifs en afrique|les 17 secrets pour gagner rapidement aux paris sportifs|les 17 secrets pour gagner rapidement aux paris
sportifs pdf|les application de paris sportif|les applications
paris sportifs|les bonus paris sportifs|les bookmakers paris sportifs|les cotes paris sportifs|les gains de paris sportifs sont ils imposables|les gains des paris sportifs sont ils imposables|les jeux de paris
sportifs|les meilleur paris sportif|les meilleures applications de paris sportifs|les meilleurs applications de paris sportifs|les meilleurs bonus paris sportif|les meilleurs bonus paris sportifs|les meilleurs cotes paris sportif|les meilleurs paris sportifs|les meilleurs paris
sportifs du jour|les meilleurs site de paris sportif|les
meilleurs site de paris sportifs|les meilleurs sites de pari sportif|les meilleurs sites de
paris sportifs|les meilleurs sites de paris sportifs en ligne|les paris sportif|les
paris sportif avis|les paris sportifs|les paris
sportifs comment ça marche|les paris sportifs en france|les
paris sportifs en ligne|les paris sportifs en ligne comprendre jouer gagner|les paris
sportifs en ligne comprendre jouer gagner pdf|les paris sportifs les plus rentables|les plus gros gagnant paris sportif|les plus gros gains au paris
sportifs|les plus gros gains paris sportifs|les
plus gros paris sportif|les plus grosse cote paris sportif|les plus grosses pertes paris sportifs|les sites
de paris sportifs|les sites de paris sportifs autorisés en france|les sites de paris sportifs en france|les
sites de paris sportifs en ligne|les sites de paris sportifs francais|ligue 1 paris sportif|ligue 1 paris sportifs|ligue 2 paris
sportif|ligue des champions paris sportif|limite de gains paris sportifs|limite de mise paris sportif|limite gain paris sportif|limite mise paris
sportifs|liste de paris sportif|liste des paris sportifs|liste des site de paris sportif|liste des sites de paris sportifs|liste pari sportif|liste paris sportif|liste paris sportif pdf|liste site de paris sportif|liste site pari sportif|liste site paris sportif|liste site paris sportif arjel|liste sites paris sportifs|logiciel algorithme paris
sportif|logiciel algorithme paris sportif gratuit|logiciel analyse paris sportif|logiciel calcul paris
sportif|logiciel de pari sportif|logiciel de paris sportif|logiciel
de paris sportif gratuit|logiciel gestion bankroll
paris sportif gratuit|logiciel gestion de bankroll paris sportif|logiciel gestion paris sportif|logiciel gestion paris sportif gratuit|logiciel gestion paris sportifs|logiciel pari sportif|logiciel paris
sportif|logiciel paris sportif gratuit|logiciel
paris sportifs|logiciel paris sportifs foot sur 2 matchs|logiciel pour paris sportif|logiciel pour
paris sportifs|logiciel prediction paris sportif|logiciel probabilité paris sportif|logiciel prédiction paris sportif|logiciel statistique paris sportifs|logiciel variation de cote paris
sportif|loi sur les paris sportifs en france|magic calculator paris sportif|marché des paris sportifs|marché des paris sportifs en france|marché des paris
sportifs en ligne|martingale pari sportif|martingale paris sportif|martingale paris sportif excel|martingale paris
sportif forum|martingale paris sportif interdit|martingale paris sportifs|match abandonné paris sportif|match annulé
ou reporté paris sportifs|match annulé paris sportif|match arrete paris sportif|match interrompu paris
sportif|match interrompu tennis paris sportif|match interrompu tennis pluie paris sportif|match nul boxe paris
sportif|match pari sportif|match paris sportif|match reporté paris sportif|match suspendu paris sportif|match suspendu tennis paris sportif|match truqué
paris sportif|matchs truqués paris sportifs|meilleur algorithme paris sportif|meilleur algorithme paris sportif gratuit|meilleur app de paris sportif|meilleur app de
paris sportifs|meilleur app paris sportif|meilleur appli de pari sportif|meilleur appli de paris sportif|meilleur appli pari sportif|meilleur appli paris sportif|meilleur
appli paris sportif forum|meilleur appli paris
sportifs|meilleur application conseil paris sportif|meilleur
application de paris sportif|meilleur application de paris sportif en afrique|meilleur application pari sportif|meilleur application paris sportif|meilleur application paris
sportif belgique|meilleur application pour les paris sportif|meilleur application pour pari sportif|meilleur bonus de bienvenue
paris sportif|meilleur bonus pari sportif|meilleur bonus paris sportif|meilleur bonus paris sportif sans depot|meilleur bonus paris sportifs|meilleur bonus site de
paris sportif|meilleur bonus site pari sportif|meilleur bonus site paris
sportif|meilleur bookmaker paris sportif|meilleur combiné paris
sportif|meilleur conseil paris sportif|meilleur cote de paris sportif|meilleur cote
pari sportif|meilleur cote paris sportif|meilleur cote paris sportif aujourd’hui|meilleur cote site paris sportif|meilleur forum paris sportifs|meilleur gain paris sportif|meilleur ia paris sportif|meilleur methode pour gagner
au paris sportif|meilleur offre bienvenue paris
sportif|meilleur offre bonus paris sportif|meilleur offre de bienvenue paris sportif|meilleur offre de bienvenue paris sportifs|meilleur offre pari sportif|meilleur offre paris sportif|meilleur offre
paris sportif en ligne|meilleur pari sportif|meilleur pari sportif du jour|meilleur pari sportif en ligne|meilleur paris sportif|meilleur paris
sportif aujourd’hui|meilleur paris sportif du jour|meilleur paris sportif en ligne|meilleur paris
sportif foot|meilleur promo paris sportif|meilleur pronostic
paris sportif|meilleur site de conseil paris sportif|meilleur site
de pari sportif|meilleur site de pari sportif en ligne|meilleur site de paris sportif|meilleur site de paris sportif avis|meilleur site
de paris sportif belgique|meilleur site de paris sportif canada|meilleur site de paris sportif en france|meilleur site de paris sportif en ligne|meilleur site
de paris sportif football|meilleur site de paris sportif forum|meilleur site de paris sportif france|meilleur site de paris sportif hors arjel|meilleur site
de paris sportif international|meilleur site de paris sportif suisse|meilleur
site de paris sportifs|meilleur site de paris sportifs
en ligne|meilleur site pari sportif|meilleur site pari sportif en ligne|meilleur site pari sportif france|meilleur site paris sportif|meilleur site
paris sportif avis|meilleur site paris sportif
belgique|meilleur site paris sportif canada|meilleur site paris sportif
en ligne|meilleur site paris sportif foot|meilleur
site paris sportif forum|meilleur site paris sportif france|meilleur site paris sportif hors arjel|meilleur site paris sportif nba|meilleur site paris sportif
rugby|meilleur site paris sportif suisse|meilleur site paris sportifs|meilleur site pour pari sportif|meilleur site pour paris sportif|meilleur site pronostic paris sportif|meilleur strategie paris sportif|meilleur technique de paris sportif|meilleur technique paris sportif|meilleur technique pour gagner au paris sportif|meilleure appli de paris sportif|meilleure appli de
paris sportifs|meilleure appli pari sportif|meilleure appli paris sportif|meilleure appli
paris sportifs|meilleure application de paris sportif|meilleure application de
paris sportifs|meilleure application pari sportif|meilleure application paris
sportif|meilleure application paris sportif android|meilleure application paris sportifs|meilleure offre paris sportif|meilleure site paris sportif|meilleure strategie paris
sportif|meilleures applications de paris sportifs|meilleures applications paris
sportifs|meilleures cotes paris sportifs|meilleures offres paris sportifs|meilleures stratégies
paris sportifs|meilleurs appli paris sportif|meilleurs application de paris sportifs|meilleurs application paris sportif|meilleurs applications paris sportifs|meilleurs bonus paris sportifs|meilleurs cote
paris sportif|meilleurs cotes paris sportifs|meilleurs offres
paris sportifs|meilleurs paris sportifs|meilleurs paris sportifs du jour|meilleurs site de pari sportif|meilleurs site de
paris sportif|meilleurs site de paris sportif en ligne|meilleurs site de paris sportifs|meilleurs site paris sportif|meilleurs sites de paris
sportifs|meilleurs sites de paris sportifs en ligne|meilleurs sites paris sportif|meilleurs
sites paris sportifs|methode abc paris sportif|methode
de paris sportif|methode gagnante paris sportifs|methode gagner paris sportif|methode infaillible paris sportifs|methode martingale
paris sportif|methode mathematique paris sportif|methode mathematique pour gagner au paris sportif|methode paris sportif|methode paris sportif foot|methode paris sportif forum|methode paris sportif
tennis|methode paris sportifs|methode pour gagner au paris
sportif|methode pour gagner paris sportif|methodes
paris sportifs|minimum depot paris sportif|mise au jeu pari sportif|mise maximum pari
sportif|mise maximum paris sportif|mise minimum paris sportif|mise moyenne paris sportif|mise paris
sportif|moins de 4 5 but paris sportif|montant maximum paris sportif|montant paris sportif|montante pari
sportif|montante parie sportif|montante paris sportif|montante
paris sportifs|montantes paris sportifs|multiple pari sportif|multiple paris sportif|multiple paris sportifs|multiples paris sportifs|méthode
calcul paris sportif|méthode match nul paris sportifs|méthode mathématique pour gagner au paris sportif|méthode paris sportif forum|méthode paris sportif hockey|nba pari sportif|nba paris
sportif|nba paris sportifs|nouveau paris sportif|nouveau site
de pari sportif|nouveau site de paris sportif|nouveau site de
paris sportif en ligne|nouveau site de paris sportifs|nouveau site pari sportif|nouveau site paris sportif|nouveau site paris sportif france|nouveau site
paris sportifs|nouveaux sites de paris sportifs|nouveaux sites paris sportifs|nouvelle appli paris sportif|nouvelle
application de paris sportif|numero de match paris sportif|numero match paris sportif|offre 100 euros paris
sportif|offre appli pari sportif|offre bienvenu paris
sportif|offre bienvenue pari sportif|offre bienvenue paris sportif|offre bienvenue paris sportifs|offre bienvenue site paris sportif|offre bonus paris sportif|offre de bienvenu paris sportif|offre de
bienvenue pari sportif|offre de bienvenue paris
sportif|offre de bienvenue paris sportif belgique|offre
de bienvenue paris sportif sans depot|offre de bienvenue
paris sportif sans dépôt|offre de bienvenue paris sportifs|offre de bienvenue sans
depot paris sportif|offre de bienvenue site paris sportif|offre euro paris sportif|offre
pari sportif euro|offre paris sportif|offre paris
sportif belgique|offre paris sportif cash|offre paris sportif coupe du monde|offre paris
sportif hors arjel|offre paris sportif remboursé|offre paris sportif remboursé cash|offre paris sportif sans depot|offre promo paris sportif|offre remboursement paris sportif|offre sans depot paris sportif|offre site paris sportif|offres bienvenue paris
sportifs|offres de bienvenue paris sportifs|ou faire des paris sportif|ou
faire des paris sportif en espagne|ou faire des paris sportifs|outil répartiteur de mise
paris sportif|outils repartiteur de mises paris sportif|ouverture compte paris
sportifs|ouvrir un compte paris sportif|pack de bienvenue
paris sportif|pack de bienvenue paris sportif hors
arjel|pari en ligne sportif|pari sportif|pari sportif 100 euros offert|pari sportif 100 remboursé|pari sportif abandon tennis|pari sportif
aide|pari sportif algérie aujourd’hui|pari
sportif appli|pari sportif application|pari sportif argent|pari sportif astuce|pari
sportif aujourd|pari sportif aujourd’hui|pari sportif avec handicap|pari
sportif avec orange money|pari sportif avec paypal|pari sportif avec wave|pari sportif avis|pari
sportif basket|pari sportif belgique|pari sportif belgique france|pari sportif bonus|pari sportif
buteur pas titulaire|pari sportif champions league|pari sportif combiné|pari sportif comment|pari sportif comment gagner|pari sportif comment
ça marche|pari sportif comparatif|pari sportif conseil|pari sportif cote|pari sportif cote match|pari sportif cote psg|pari sportif
coupe|pari sportif coupe de france|pari sportif
coupe du monde|pari sportif depot|pari sportif du jour|pari
sportif en france|pari sportif en ligne|pari sportif
en ligne au cameroun|pari sportif en ligne belgique|pari sportif
en ligne canada|pari sportif en ligne france|pari sportif en ligne gratuit|pari
sportif en ligne suisse|pari sportif en ligne ufc|pari sportif en suisse|pari sportif euro|pari sportif explication|pari sportif faire|pari sportif foot|pari sportif foot resultat|pari sportif
football|pari sportif forum|pari sportif francaise des jeux|pari sportif france|pari sportif france angleterre|pari sportif france argentine|pari sportif france autriche|pari sportif france belgique|pari sportif france espagne|pari sportif france italie|pari sportif france
portugal|pari sportif france usa|pari sportif gagnant|pari
sportif gagner|pari sportif gagner a tous les coups|pari sportif gagner de l’argent|pari sportif
gain|pari sportif gratuit|pari sportif gratuit
pour gagner des cadeaux|pari sportif gratuit sans depot|pari sportif
handicap|pari sportif hockey|pari sportif hors arjel|pari sportif jeux olympiques|pari sportif joueur absent|pari sportif le plus
rentable|pari sportif leicester champion|pari sportif ligue 1|pari sportif ligue 2|pari sportif ligue des champions|pari sportif ligue europa|pari sportif match|pari sportif match arrete|pari sportif match interrompu|pari sportif meilleur|pari sportif meilleur cote|pari sportif meilleur site|pari sportif methode|pari sportif mise|pari sportif mise au jeu|pari sportif mise o jeu|pari sportif nba|pari sportif offre bienvenue|pari sportif paypal|pari sportif plus|pari sportif prolongation|pari sportif promo|pari
sportif pronostic|pari sportif pronostic foot|pari sportif pronostic gagnant|pari sportif pronostic gratuit|pari sportif psg|pari sportif psg bayern|pari sportif psg inter|pari sportif psg
milan|pari sportif regle|pari sportif rembourse|pari sportif remboursement|pari sportif remboursement cash|pari sportif remboursé|pari sportif rugby|pari sportif rugby coupe du monde|pari sportif rugby top 14|pari sportif sans argent|pari sportif sans carte bancaire|pari
sportif sans depot|pari sportif signification|pari sportif site|pari sportif statistique|pari sportif suisse|pari sportif systeme|pari sportif
technique|pari sportif technique pour gagner|pari sportif temps reglementaire|pari sportif tennis|pari sportif tennis abandon|pari sportif top|pari
sportif top 14|pari sportif tour de france|parie sportif|parie sportif comment ca marche|parie sportif du jour|parie sportif
en ligne|parie sportif foot|parie sportif football|parie sportif france|parie
sportif gratuit|parie sportif pronostic|parie sportif suisse|paris en ligne sportif|paris en ligne sportifs|paris evenement sportif|paris
france sportif|paris hippique et sportif|paris hippiques et sportifs|paris hippiques paris sportifs|paris hippiques paris
sportifs et poker en ligne|paris hippiques sportifs|paris match sportif|paris sportif|paris sportif 10 euros offerts|paris sportif 100 euros
offert|paris sportif 100 euros remboursé|paris sportif 100
offert|paris sportif 100 remboursé|paris sportif 100e offert|paris sportif
150 euros offert|paris sportif 1er pari remboursé|paris sportif a faire|paris sportif a faire aujourd’hui|paris sportif
a faire ce soir|paris sportif abandon tennis|paris sportif abandon tennis
parions sport|paris sportif aide|paris sportif algorithme|paris sportif analyse|paris sportif appli|paris sportif application|paris sportif application android|paris sportif apres prolongation|paris sportif argent|paris sportif
argent fictif|paris sportif argent offert|paris sportif argent virtuel|paris sportif arjel|paris sportif arsenal psg|paris sportif astuce|paris sportif
au canada|paris sportif aujourd hui|paris sportif aujourd’hui|paris sportif avec argent fictif|paris sportif avec bonus sans depot|paris sportif avec carte bancaire|paris sportif avec cryptomonnaie|paris sportif avec handicap|paris
sportif avec paypal|paris sportif avec paysafecard|paris sportif avis|paris sportif avis
expert|paris sportif avis forum|paris sportif bankroll|paris
sportif basket|paris sportif basket coupe de france|paris sportif basket nba|paris sportif basket
prolongation|paris sportif belgique|paris sportif belgique bonus|paris
sportif belgique bonus sans depot|paris sportif belgique france|paris
sportif belgique suede|paris sportif bonus|paris sportif bonus bienvenue|paris sportif bonus cash|paris sportif bonus de bienvenue|paris sportif bonus gratuit|paris sportif bonus gratuit sans depot|paris sportif bonus retirable|paris sportif
bonus sans depot|paris sportif bonus sans depot belgique|paris sportif bookmaker|paris sportif
but contre son camp|paris sportif but temps additionnel|paris sportif
buteur|paris sportif buteur blessé|paris sportif
buteur carton rouge|paris sportif buteur contre son camp|paris sportif buteur non titulaire|paris sportif buteur prolongation|paris sportif buteur qui
ne joue pas|paris sportif buteur remplacant|paris sportif calcul gain|paris sportif canada|paris sportif
cash|paris sportif cash out|paris sportif champion ligue 1|paris sportif champions league|paris sportif classement ligue 1|paris sportif code promo|paris sportif combine|paris
sportif combiné|paris sportif combiné comment ça marche|paris sportif combiné du jour|paris sportif combiné match reporté|paris sportif comment
ca marche|paris sportif comment faire|paris
sportif comment gagner|paris sportif comment gagner a tous les coups|paris sportif comment jouer|paris
sportif comment ça marche|paris sportif comparateur cote|paris sportif comparatif|paris sportif conseil|paris sportif
conseil gratuit|paris sportif conseil pour gagner|paris sportif cote|paris sportif
cote et match|paris sportif cote explication|paris sportif cote psg|paris sportif coupe d’europe|paris sportif coupe
davis|paris sportif coupe de france|paris sportif coupe du monde|paris sportif coupe du monde de rugby|paris
sportif coupe du monde rugby|paris sportif depot
5 euro|paris sportif depot minimum|paris sportif depot paypal|paris sportif dnb|paris sportif du jour|paris sportif du jour conseil|paris sportif
dépôt 1 euro|paris sportif dépôt minimum 5 euros|paris sportif en belgique|paris sportif en france|paris sportif
en ligne|paris sportif en ligne avec paypal|paris sportif en ligne avis|paris
sportif en ligne belgique|paris sportif en ligne
bonus|paris sportif en ligne cameroun|paris sportif en ligne comment gagner|paris sportif en ligne comment ça marche|paris sportif en ligne france|paris sportif en ligne gratuit|paris sportif en ligne maroc|paris sportif en ligne paypal|paris sportif en ligne québec|paris sportif
en ligne sans depot|paris sportif en ligne suisse|paris sportif en suisse|paris sportif espagne france|paris sportif esport|paris sportif et casino en ligne|paris sportif et hippique|paris sportif et prolongation|paris sportif euro|paris sportif europa league|paris
sportif explication|paris sportif final ligue des champions|paris sportif finale ligue des champions|paris sportif
foot|paris sportif foot aide|paris sportif foot astuce|paris sportif foot
aujourd’hui|paris sportif foot ce soir|paris sportif foot comment ca marche|paris sportif foot conseil|paris sportif foot cote|paris sportif
foot coupe du monde|paris sportif foot en ligne|paris sportif foot feminin|paris sportif foot gratuit|paris sportif foot prolongation|paris sportif foot
pronostic|paris sportif foot pronostic gratuit|paris sportif foot regle|paris sportif foot suisse|paris sportif foot us|paris sportif football|paris sportif football americain|paris sportif football astuces|paris sportif forfait tennis|paris sportif forum|paris
sportif francais|paris sportif francaise des jeux|paris sportif france|paris sportif france 2|paris sportif france allemagne|paris sportif france angleterre|paris sportif france argentine|paris sportif
france autriche|paris sportif france belgique|paris sportif france espagne|paris sportif
france gibraltar|paris sportif france italie|paris sportif france
nouvelle zelande|paris sportif france pologne|paris sportif france portugal|paris sportif france uruguay|paris sportif france usa|paris sportif freebet sans depot|paris sportif gagnant|paris sportif gagnant
à coup sûr|paris sportif gagner a coup sur|paris sportif
gagner argent|paris sportif gagner de l’argent|paris sportif gain|paris sportif gain maximum|paris sportif gestion bankroll|paris sportif gratuit|paris sportif gratuit appli|paris
sportif gratuit avec cadeaux|paris sportif gratuit cadeaux|paris
sportif gratuit en ligne|paris sportif gratuit
entre amis|paris sportif gratuit sans argent|paris sportif gratuit sans
depot|paris sportif gratuit sans dépôt|paris sportif
gratuits|paris sportif gros gain|paris sportif handicap|paris sportif handicap 0 1|paris sportif handicap 0-1|paris sportif handicap 1
0|paris sportif handicap 1-0|paris sportif handicap basket|paris sportif handicap explication|paris
sportif handicap foot|paris sportif handicap rugby|paris sportif hippique|paris sportif hockey|paris sportif hockey nhl|paris sportif hockey sur
glace|paris sportif hors arjel|paris sportif hors arjel france|paris sportif
jeux olympiques|paris sportif jeux video|paris sportif joueur blessé|paris sportif joueur
blessé pendant le match|paris sportif joueur de foot|paris sportif joueur decisif|paris sportif
joueur declare forfait|paris sportif joueur déclare forfait|paris sportif joueur remplacant|paris sportif la francaise des jeux|paris sportif le plus rentable|paris sportif legal en france|paris sportif leicester champion|paris
sportif les 18 stratégies pour gagner tous les jours|paris sportif les plus sur|paris sportif
les prolongation compte|paris sportif ligne|paris sportif ligue
1|paris sportif ligue 2|paris sportif ligue des champions|paris sportif ligue des nations|paris
sportif ligue europa|paris sportif liste|paris sportif martingale|paris sportif match|paris sportif match abandonné|paris
sportif match annulé|paris sportif match arrêté|paris sportif match
du jour|paris sportif match interrompu|paris sportif match reporté|paris sportif match suspendu|paris sportif match tennis interrompu|paris sportif match truqué|paris
sportif meilleur bonus|paris sportif meilleur cote|paris sportif meilleur pronostic|paris sportif meilleur site|paris sportif methode|paris sportif methode 2 3|paris sportif mi temps fin de match|paris sportif mise au jeu|paris sportif mise maximum|paris sportif
mma france|paris sportif moins de 3.5 but|paris sportif montante|paris sportif moto gp|paris sportif multiple|paris sportif multiple 2 3|paris sportif multiple 2 3 explication|paris
sportif multiple 2 4|paris sportif multiple 2 5|paris sportif multiple 2/3 explication|paris sportif multiple
3 4|paris sportif multiple explication|paris sportif
national 1 foot|paris sportif nba|paris sportif nba conseil|paris sportif nba pronostic|paris sportif nhl|paris sportif
nombre de but|paris sportif nouveau site|paris sportif numero match|paris sportif offert|paris sportif offre bienvenue|paris sportif offre bienvenue sans depot|paris sportif offre de bienvenue|paris sportif offre sans
depot|paris sportif om psg|paris sportif
paypal|paris sportif plus de 1.5 but|paris sportif plus de 2 5 but|paris sportif plus ou moins|paris sportif plus ou moins 2 5 but|paris sportif premier pari remboursé|paris sportif premier paris remboursé|paris sportif prolongation|paris sportif
prolongation basket|paris sportif prolongation foot|paris sportif promo|paris sportif pronostic|paris sportif
pronostic basket|paris sportif pronostic des match aujourd hui|paris sportif pronostic expert gratuit|paris sportif pronostic foot|paris sportif pronostic
forum|paris sportif pronostic gratuit|paris sportif pronostic tennis|paris
sportif psg|paris sportif psg arsenal|paris sportif psg barcelone|paris
sportif psg bayern|paris sportif psg dortmund|paris sportif
psg inter|paris sportif psg inter cote|paris sportif psg liverpool|paris
sportif psg om|paris sportif qr code|paris sportif que veut dire handicap|paris sportif qui rapporte le
plus|paris sportif regle|paris sportif regle prolongation|paris sportif rembourse|paris sportif remboursement cash|paris sportif rembourser|paris sportif remboursé|paris sportif remboursé cash|paris
sportif remboursé en cash|paris sportif retrait paypal|paris sportif rue des joueurs|paris sportif rugby|paris sportif rugby 6 nations|paris sportif rugby coupe du monde|paris sportif rugby top
14|paris sportif safe du jour|paris sportif sans argent|paris
sportif sans carte bancaire|paris sportif sans carte d’identité|paris
sportif sans compte bancaire|paris sportif sans depot|paris sportif sans depot minimum|paris sportif si match suspendu|paris sportif si un joueur abandonne|paris sportif si un joueur ne joue pas|paris sportif si un joueur se
blesse|paris sportif simple ou combiné|paris sportif site|paris sportif statistique|paris sportif stratégie|paris sportif suisse|paris sportif suisse application|paris
sportif suisse en ligne|paris sportif suisse legal|paris
sportif suisse légal|paris sportif suisse romande|paris sportif sur du jour|paris
sportif sur le tennis|paris sportif systeme|paris sportif systeme 2 3|paris sportif systeme 2 4|paris sportif systeme 2/3|paris sportif systeme 2/4|paris sportif systeme 3 4|paris sportif systeme 3/4|paris sportif systeme explication|paris
sportif technique|paris sportif technique pour gagner|paris sportif temps additionnel|paris
sportif temps reglementaire|paris sportif tennis|paris sportif
tennis abandon|paris sportif tennis conseil|paris sportif tennis de table|paris sportif tennis forfait|paris
sportif tennis gratuit|paris sportif tennis pronostic|paris sportif tennis roland garros|paris sportif
tir au but|paris sportif top 14|paris sportif
tour de france|paris sportif ufc|paris sportif ufc france|paris sportif unibet|paris sportif vainqueur euro|paris
sportif vainqueur ligue 1|paris sportif vainqueur ligue des champions|paris sportif
via paypal|paris sportif victoire prolongation|paris sportif vip gratuit|paris sportifs|paris sportifs abandon tennis|paris sportifs aide|paris sportifs analyser un match|paris sportifs arjel|paris sportifs
astuces|paris sportifs aujourd’hui|paris sportifs autorisés en france|paris sportifs avec paypal|paris sportifs basket|paris sportifs belgique|paris sportifs bonus|paris
sportifs bookmakers|paris sportifs canada|paris sportifs combiné|paris sportifs comparateur|paris sportifs comparatif|paris sportifs conseils|paris sportifs cotes|paris sportifs coupe
du monde|paris sportifs de football|paris sportifs du jour|paris sportifs en belgique|paris sportifs en france|paris sportifs
en ligne|paris sportifs en ligne belgique|paris sportifs en ligne france|paris sportifs
en ligne gratuit|paris sportifs en ligne suisse|paris sportifs en suisse|paris sportifs et hippiques|paris sportifs euro|paris sportifs foot|paris sportifs foot us|paris sportifs forum|paris sportifs
france|paris sportifs france espagne|paris sportifs gagner à tous les coups|paris sportifs
gratuit|paris sportifs gratuits|paris sportifs gratuits en ligne|paris sportifs handicap|paris sportifs hockey|paris sportifs hockey sur galce|paris sportifs hockey
sur glace|paris sportifs hors arjel|paris sportifs jeux olympiques|paris sportifs les
bookmakers raflent la mise|paris sportifs ligne|paris sportifs ligue 1|paris sportifs ligue 2|paris sportifs ligue des champions|paris
sportifs ligue europa|paris sportifs match interrompu|paris sportifs
montante|paris sportifs nba|paris sportifs offre bienvenue|paris sportifs offre de bienvenue|paris sportifs paypal|paris sportifs pronostics|paris sportifs psg|paris sportifs psg inter|paris sportifs rugby|paris
sportifs sans argent|paris sportifs sans depot|paris sportifs site|paris sportifs sites|paris sportifs statistiques|paris sportifs stratégie|paris sportifs suisse|paris sportifs technique|paris sportifs
techniques|paris sportifs tennis|paris sportifs tennis astuces|paris sportifs top 14|paris sportifs tour de france|part de marché paris
sportifs|paypal pari sportif|paypal paris sportif|paypal paris sportifs|perte d’argent
paris sportifs|peut on devenir riche avec les paris sportifs|peut on gagner de l’argent avec les paris sportifs|peut
on gagner sa vie avec les paris sportif|peut on vraiment gagner de l’argent avec les paris sportifs|plus gros combine paris sportif|plus gros gagnant paris sportif|plus gros gain paris
sportif|plus gros gain paris sportif au monde|plus gros gain paris sportif france|plus gros gains paris sportif|plus
gros pari sportif|plus gros paris sportif|plus grosse cote gagner paris
sportif|plus grosse cote pari sportif|plus grosse cote paris
sportif|plus grosse mise paris sportif|plus grosse somme gagner
au paris sportif|plus ou moins paris sportif|pourcentage de mise paris
sportif|premier pari sportif remboursé|probabilité cote paris sportif|probabilité paris
sportif combiné|prolongation basket paris sportif|prolongation paris sportif|promo pari sportif|promo
paris sportif|promo site de paris sportif|promo site pari sportif|promo site paris sportif|promos paris sportifs|prono paris sportif
foot|prono paris sportif gratuit|prono paris sportif tennis|pronostic de
paris sportif|pronostic du jour paris sportif|pronostic
foot paris sportif|pronostic gratuit paris sportif|pronostic pari sportif|pronostic pari sportif gratuit|pronostic paris sportif|pronostic paris sportif aujourd’hui|pronostic paris sportif du jour|pronostic paris sportif foot|pronostic
paris sportif gratuit|pronostic paris sportif tennis|pronostic paris sportifs|pronostics foot statistiques et aides aux
paris sportifs|pronostics paris sportif|pronostics paris sportifs|pronostiqueur paris sportif
gratuit|psg arsenal paris sportif|psg bayern paris sportif|psg inter
milan paris sportif|psg inter pari sportif|psg inter paris sportif|psg liverpool
paris sportif|psg om paris sportif|psg paris sportif|psg paris sportifs|qr code paris sportif|qu est ce
qu un handicap paris sportif|qu est ce que handicap dans les paris sportif|qu’est ce qu’un handicap paris sportif|qu’est ce que handicap dans les paris sportif|quand
un joueur se blesse paris sportif|que signifie 1/1 en paris sportif|que signifie 1/2 paris sportif|que signifie 12
en paris sportif|que signifie 1×2 dans les paris sportifs|que signifie btts en paris sportif|que signifie dnb en paris sportif|que signifie draw en paris sportif|que
signifie ft en paris sportif|que signifie gg dans le pari
sportif|que signifie gg en pari sportif|que signifie gg en paris sportif|que signifie handicap
dans les paris sportifs|que veut dire dnb en paris sportif|que veut
dire handicap dans les paris sportifs|que veut dire handicap paris sportif|quel
appli pari sportif|quel cote jouer paris sportif|quel est la meilleur
appli de paris sportif|quel est le meilleur
algorithme de paris sportif|quel est le meilleur site de pari sportif|quel est le meilleur site
de pari sportif en ligne|quel est le meilleur site
de paris sportif|quel est le meilleur site de paris sportif en ligne|quel est le meilleur site de paris sportifs
en ligne|quel est le pari sportif le plus rentable|quel
pari sportif est le plus rentable|quel pari sportif est le plus sûr|quel
pari sportif faire aujourd’hui|quel paris sportif
faire aujourd’hui|quel paris sportif rapporte le plus|quel
site de paris sportif choisir|quel site de paris sportif rembourse en cash|quel type de pari
sportif est le plus rentable|quelle application pour paris sportifs|quelle est la meilleure appli de paris
sportif|quelle est la meilleure application de paris sportif|quelle est la meilleure application pour les paris sportifs|quelle est le meilleur site de paris sportif|quels paris sportifs faire|quels
sont les paris sportifs les plus sûrs|rebond basket paris
sportif|record de gain paris sportif|regle buteur paris sportif|regle de paris
sportif|regle des paris sportif|regle handicap paris sportif|regle handicap paris sportif
foot|regle multiple paris sportif|regle pari sportif|regle
paris sportif|regle paris sportif foot|regle paris sportif multiple|regle paris sportif prolongation|reglement pari sportif|reglement paris sportif|regles paris sportifs|remboursement
cash paris sportif|remboursement en cash paris sportif|remboursement pari sportif|remboursement paris sportif|repartiteur de mise paris sportif|repartiteur de
mise paris sportifs|repartiteur de mises
paris sportif|repartiteur mise paris sportif|repartition des mises paris sportif|resultat pari sportif|resultat paris sportif|resultat paris sportif en direct|resultat paris sportif foot|resultat sportif hockey|retirer argent paris
sportif|rugby pari sportif|rugby paris sportif|règle paris
sportif prolongation|règles paris sportif|répartiteur de mise
pari sportif|répartiteur de mise paris sportif|répartiteur de mise paris sportifs|répartition des mises paris sportif|résultat paris sportif foot|sans depot paris sportif|se faire interdire de paris sportifs|signification btts
paris sportif|signification dnb paris sportif|signification handicap
paris sportif|simulateur de gain paris sportif|simulateur gain paris sportif|simulateur gain paris sportif multiple|simulateur gain paris sportif systeme|simulateur gain paris sportif système|simulateur
montante paris sportif|simulateur paris sportif multiple|simulateur systeme
paris sportif|simulation paris sportif gratuit|site aide paris sportif|site
analyse paris sportif|site analyser paris sportif|site arjel paris
sportif|site conseil paris sportif|site d’analyse
de paris sportifs|site d’analyse paris sportif|site de conseil paris sportif|site de pari en ligne sportif|site de pari sportif|site de pari
sportif avec bonus sans depot|site de pari
sportif bonus sans depot|site de pari sportif
canada|site de pari sportif en ligne|site de pari sportif francais|site
de pari sportif gratuit|site de pari sportif hors arjel|site de pari sportif suisse|site de parie sportif|site de
parie sportif en ligne|site de paris en ligne sportif|site de paris sportif|site de paris sportif
acceptant paypal|site de paris sportif arjel|site
de paris sportif autorisé en france|site de paris sportif autorisé en suisse|site de paris sportif avec bonus|site de paris sportif avec bonus sans depot|site
de paris sportif avec bonus sans dépôt|site de paris sportif avec neosurf|site de paris sportif avec paiement
mobile|site de paris sportif avec paypal|site
de paris sportif avis|site de paris sportif belge avec bonus|site de paris sportif belgique|site de
paris sportif bonus|site de paris sportif bonus sans depot|site de paris sportif canada|site de paris sportif comparatif|site de paris sportif depot minimum|site de paris sportif en france|site de paris sportif en ligne|site
de paris sportif en ligne suisse|site de paris sportif football|site
de paris sportif francais|site de paris sportif france|site de paris
sportif gratuit|site de paris sportif gratuit pour
gagner des cadeaux|site de paris sportif gratuit
sans dépôt|site de paris sportif hors arjel|site de paris sportif
le plus fiable|site de paris sportif legal en france|site de paris sportif meilleur cote|site de paris sportif nouveau|site de paris sportif offre de bienvenue|site de paris sportif paypal|site de paris sportif premier paris remboursé|site de paris sportif qui accepte paypal|site de paris sportif qui rembourse en cash|site de paris
sportif remboursé|site de paris sportif
sans argent|site de paris sportif sans carte bancaire|site de paris sportif sans carte
d’identité|site de paris sportif sans depot|site de paris sportif suisse|site
de paris sportifs|site de paris sportifs avec paypal|site de paris sportifs en ligne|site
de paris sportifs francais|site de paris sportifs gratuit|site de paris sportifs paypal|site de paris sportifs suisse|site de statistique pour paris
sportif|site des paris sportifs|site pari en ligne sportif|site pari sportif|site pari sportif 100 euros offert|site pari sportif arjel|site pari sportif belgique|site pari sportif bonus|site pari sportif canada|site pari sportif comparatif|site pari sportif en ligne|site pari sportif france|site pari sportif gratuit|site pari
sportif hors arjel|site pari sportif suisse|site parie sportif|site paris en ligne sportif|site paris sportif|site paris
sportif 100 euros offert|site paris sportif 100 euros remboursé|site paris sportif 1er
paris remboursé|site paris sportif arjel|site paris sportif
autorisé en france|site paris sportif avec bonus|site paris sportif avec bonus sans depot|site paris sportif avec meilleur cote|site paris sportif belgique|site paris sportif bonus|site paris sportif bonus cash|site paris sportif bonus sans depot|site paris sportif canada|site paris sportif comparatif|site paris sportif depot 5
euro|site paris sportif en ligne|site paris sportif
foot|site paris sportif france|site paris sportif gratuit|site paris sportif hors arjel|site paris sportif hors
arjel france|site paris sportif meilleur cote|site paris sportif nouveau|site paris
sportif offre de bienvenue|site paris sportif paypal|site paris sportif
remboursement cash|site paris sportif remboursé en cash|site paris sportif retrait
instantané|site paris sportif sans carte bancaire|site
paris sportif sans depot|site paris sportif
suisse|site paris sportifs|site paris sportifs belgique|site paris sportifs
en ligne|site paris sportifs france|site paris sportifs hors arjel|site paris sportifs suisse|site pour analyse paris
sportif|site pour paris sportif|site pronostic paris sportif|site statistique paris sportif|site suisse paris sportif|sites de pari sportif|sites de paris sportif|sites de paris sportifs|sites
de paris sportifs arjel|sites de paris sportifs autorisés en france|sites de paris sportifs belgique|sites de paris sportifs bonus|sites de paris sportifs en belgique|sites de paris sportifs en france|sites
de paris sportifs en ligne|sites de paris sportifs gratuits|sites de paris sportifs
gratuits sans dépôt|sites de paris sportifs suisse|sites pari sportif|sites paris sportif|sites paris sportifs|sites paris sportifs
arjel|sites paris sportifs belgique|sites paris sportifs france|sites paris sportifs hors arjel|sites paris sportifs suisse|so foot paris sportif|so foot paris sportifs|specialiste tennis paris sportif|statistique foot paris sportif|statistique
paris sportif|statistique paris sportif foot|statistique tennis paris sportif|statistiques football paris sportifs|statistiques paris sportifs|strategie de paris sportif|stratégie big whale paris sportif|stratégie de paris sportifs|stratégie
gagnante paris sportifs|stratégie pari sportif|stratégie paris sportif|stratégie paris sportifs|stratégie paris sportifs forum|stratégie pour gagner au paris sportif|stratégies paris
sportifs|suisse paris sportif|suisse paris sportifs|systeme 2 3
paris sportif|systeme 3 4 paris sportif|systeme de
cote paris sportif|systeme de paris sportif|systeme pari sportif|systeme paris sportif|systeme paris sportifs|systeme
reducteur paris sportif|système paris sportif|tableau bankroll paris sportif|tableau cote paris sportif|tableau
de paris sportif|tableau de suivi paris sportifs|tableau excel
bankroll paris sportif|tableau excel paris sportif|tableau excel paris sportif gratuit|tableau excel paris sportifs|tableau excel pour paris sportif|tableau gestion bankroll paris sportif|tableau montante
Spot on with this write-up, I honestly believe this amazing site needs much more attention. I’ll probably be back again to see more, thanks
for the info!
Incredible points. Outstanding arguments. Keep up the amazing spirit.
Visit my site … How to Start a business in Nevada
I’m gone to inform my little brother, that he should also go to see
this website on regular basis to obtain updated from
hottest news.
Your idea is outstanding; the issue is something that not enough persons are speaking intelligently about. I’m very happy that I stumbled throughout this in my seek for one thing regarding this.
Wonderful article! We are linking to this particularly great article on our site.
Keep up the good writing.
sykaaa казино регистрация Привет, любители азарта! Сегодня мы поговорим о “Большая Sykaaa Casino” – площадке, которая привлекает внимание многих игроков. Если вы только присматриваетесь к этому казино или уже решили попробовать свои силы, то этот обзор поможет вам разобраться, как быстро и без проблем начать игру, а также чего ожидать от самого сайта.
Thanks a lot. Great information!
It’s an amazing paragraph in favor of all the online people;
they will obtain advantage from it I am sure.
Also visit my web site fermooka.ir
Angels Bail Bonds Costa Mesa
769 Baer Ѕt,
Costa Mesa, CA 92626, United Stаtes
what authority do bail bond agents have
mv88
Hello to all, how is the whole thing, I think every one is getting more from this website, and your views are pleasant for new viewers.
Also visit my website – تولیدی سرویس خواب
I like the helpful info you provide in your articles.
I’ll bookmark your blog and check again here frequently. I’m quite sure I’ll learn lots of new stuff right here!
Best of luck for the next!
비아그라는 미국 제약사 화이자가 개발한 남성 발기부전 치료제의 상품명으로,
주성분은 실데나필(Sildenafil)입니다. 실데나필은 PDE5 억제제에 속하는
Hello there! I could have sworn I’ve been to this web site
before but after browsing through many of the articles I realized it’s new to me.
Anyhow, I’m definitely pleased I found it and I’ll be bookmarking it and checking back often!
My webpage – music promotion agency
Unquestionably believe that which you stated.
Your favorite justification seemed to be on the
internet the easiest thing to be aware of.
I say to you, I definitely get annoyed while people consider worries that they just don’t know about.
You managed to hit the nail upon the top and also defined out the whole thing without having side effect ,
people could take Start a business in Nevada signal.
Will likely be back to get more. Thanks
Hi there just wanted to give you a quick heads
up. The text in your post seem to be running off the screen in Opera.
I’m not sure if this is a format issue or something
to do with browser compatibility but I figured I’d post to let you know.
The style and design look great though! Hope you get the problem
solved soon. Kudos
Thanks in favor of sharing such a pleasant idea, post is pleasant, thats why i
have read it completely
The sketch is tasteful, your authored material stylish.
Hi there, just became alert to your blog through Google, and found that it is truly informative.
I am going to watch out for brussels. I will appreciate if
you continue this in future. Numerous people will be benefited from your writing.
Cheers!
Feel free to visit my web site خرید سی پی کالاف
Thanks for sharing your thoughts on LLC formation Start a business in Nevada Nevada.
Regards
Pretty nice post. I simply stumbled upon your blog and wanted to mention that I’ve really loved browsing your weblog
posts. After all I’ll be subscribing for your rss feed and
I am hoping you write once more soon!
my site; Nevada Corporate Tax Compliance help
сукааа казино на андроид Как зарегистрироваться и не наступить на грабли: полный гид по Sykaaa Casino. Онлайн-казино привлекают яркими баннерами и обещаниями быстрых выигрышей, но прежде чем нажать «Играть», важно понимать, с чем вы имеете дело. В этой статье я подробно расскажу о регистрации, безопасности, проверках и нюансах, которые стоит учитывать при создании аккаунта на сайте казино, включая практические советы и личный опыт.
each time i used to read smaller articles or reviews which also clear
their motive, and that is also happening with this paragraph which I am
reading at this place.
Good info. Lucky me I came across your site by chance (stumbleupon).
I have bookmarked it for later!
Howdy would you mind letting me know which webhost you’re working with?
I’ve loaded your blog in 3 completely different web browsers and I must say this blog loads a lot
faster then most. Can you suggest Start a business in Nevada good web hosting
provider at a fair price? Thanks, I appreciate it!
Hi there, I enjoy reading all of your post. I like to write a little comment to support you.
Every weekend i used to pay a quick visit this web page, for the reason that i wish for enjoyment, for the
reason that this this site conations truly fastidious funny stuff too.
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Узнать напрямую – http://www.volgyfitness.hu/?p=6639&cpage=9
Этот обзорный материал предоставляет информационно насыщенные данные, касающиеся актуальных тем. Мы стремимся сделать информацию доступной и структурированной, чтобы читатели могли легко ориентироваться в наших выводах. Познайте новое с нашим обзором!
Детальнее – https://oladavietnam.com.vn/lorem-ipsum-dolor-sit-amet-consectetur-adipiscing-elit-sed-do-eiusmod-tempor
Hi, every time i used to check blog posts here in the early hours in the daylight, since i like How to Start a business in Nevada learn more and more.
Continue https://abhega.com/tag/sponsored-content/
Hi, yeah this piece of writing is really pleasant and I have learned lot of things from it regarding blogging.
thanks.
Feel free to surf to my web page … How to Start a business in Nevada
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Выяснить больше – https://educatedtimes.com/i-chose-elss-sip-for-my-childs-education-heres-what-i-wish-i-knew-beforehand
Hello there! This is my first visit to your blog!
We are a group of volunteers and starting a new initiative S Corporation formulation in Nevada a community in the same niche.
Your blog provided us valuable information to work on. You have
done a outstanding job!
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Выяснить больше – https://bachkhoadongyduoc.com/bach-bo-cay-thuoc-quy-viet-nam
Great blog right here! You seem to put a significant amount of material on the site rather quickly.
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Что скрывают от вас? – https://epiczo.com/?p=254
I visited various blogs but the audio feature for audio songs
existing at this website is genuinely excellent.
Angels Bail Bonds Coosta Mesa
769 Baker Տt,
Costa Mesa, CA 92626, United Statеs
fl bail bonds (allmyfaves.com)
It’s awesome in favor of me to have a web page, which is valuable in support of my experience.
thanks admin
You can definitely see your expertise in the article you write.
The sector hopes for even more passionate writers such as you who are not afraid to mention how
they believe. All the time go after your heart.
нажмите здесь vodkabet
It’s difficult to find educated people for this subject, but you sound like you know what
you’re talking about! Thanks
Every weekend i used to go to see this web page, for the reason that i
wish for enjoyment, since this this web page conations actually nice funny data too.
Excellent goods from you, man. I’ve consider your stuff previous
to and you are just extremely excellent. I actually like what
you’ve obtained right here, really like what you’re stating and the way through which you assert it.
You are making it enjoyable and you continue to take care of to stay it smart.
I cant wait to learn far more from you. This is actually a great
website.
My homepage; Nevada S Corporation formulation
Volges ‘t Cambodjaanse Ministerie vaan Defensie en Informatie heet ‘n Thaise F-16-gevechsvliegtuig twie bomme gevalle in de buurt vaan ‘n Cambodjaans vlöchtelingekamp.
Hi, I think your web site may be having internet browser
compatibility issues. When I look at your web site in Safari, it looks fine however, if opening in Internet Explorer, it’s got some overlapping issues.
I simply wanted to provide you with a quick heads up!
Other than that, fantastic blog!
Thanks for sharing this guide on the Lowe’s customer
satisfaction survey. It’s helpful for shoppers who want to leave honest feedback.
wonderful publish, very informative. I’m wondering why the opposite
experts of this sector do not realize this. You must continue your
writing. I’m sure, you have a huge readers’ base
already!
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, NE 68022, United Ꮪtates
402-289-4126
Precision Digital Patrol
Unquestionably believe that which you said. Your favorite reason seemed to be on the internet the simplest thing to be aware of.
I say to you, I definitely get annoyed while people think about worries that they plainly do not know about.
You managed to hit the nail upon the top and also defined
out the whole thing without having side-effects
, people can take a signal. Will likely be back to get more.
Thanks
Hey! This is my first visit to your blog! We are a group of volunteers and starting a new initiative in a community in the same
niche. Your blog provided us useful information to work on. You have done a marvellous job!
I have read so many posts about the blogger lovers but
this post is in fact a good article, keep it up.
Excellent blog! Do you have any recommendations for aspiring writers?
I’m hoping to start my own website soon but I’m a little
lost on everything. Would you propose starting with a free platform like
Wordpress or go for a paid option? There are so many options
out there that I’m totally confused .. Any ideas? Thanks!
Hi there! I could have sworn I’ve been to this site before but after going through some of the
posts I realized it’s new to me. Anyways, I’m definitely pleased
I discovered it and I’ll be book-marking it and checking back regularly!
With havin so much written content do you ever run into any issues of plagorism or copyright infringement?
My blog has a lot of exclusive content I’ve either
created myself or outsourced but it appears a lot of
it is popping it up all over the internet without my authorization. Do you know any ways to help protect
against content from being ripped off? I’d really appreciate it.
My site: public relations agency
buy backlinks, link exchange, free gift card, congratulations you have
won, claim your prize, you have been selected,
click here to claim, you won’t believe, one weird trick, what happened next will shock you, shocking truth,
secret revealed, limited time offer, special promotion,
act now, don’t miss out, buy now, best price, risk-free
trial, get rich quick, make money fast, work from home, no credit check, miracle
cure, lose weight fast, free viagra, no prescription needed,
online casino, free spins, meet singles, hot singles in your area,
replica watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader, Black Basta,
BlackEnergy, BlackMatter, Blackshades, Blaster, Brontok,
Carbanak, Cerber, Clampi, Cobalt Strike,
Conficker, Conti, Crysis, CryptoLocker, CryptoWall,
DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza,
Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT,
Glupteba, Gozi, GozNym, Hancitor, IcedID,
Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface,
Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex,
Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort,
NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot,
QuantLoader, Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal,
SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS,
ZeroAccess, Zloader, Zlob, Zotob
Feel free to surf to my homepage :: cheap viagra sildenafil & cialis
Hi there! I understand this is kind of off-topic however I had to ask.
Does running a well-established website like yours require a
large amount of work? I am brand new to operating a blog however I
do write in my journal on a daily basis. I’d like
to start a blog so I can easily share my experience and views online.
Please let me know if you have any kind of suggestions or tips for
brand new aspiring blog owners. Thankyou!
Great post. I was checking continuously this blog and I am
impressed! Very helpful information specifically the last
part 🙂 I care for such info a lot. I was seeking this certain info
for a very long time. Thank you and best of luck.
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Всё, что нужно знать – https://edgaryoreparo.com/shop/multimetro
Nice post. I used to be checking constantly this blog
and I’m inspired! Extremely helpful info specially the remaining part 🙂 I take care of such info
much. I used to be looking for this certain info for a
long time. Thanks and best of luck.
My homepage – دارالترجمه پایتخت
Write more, thats all I have to say. Literally, it seems as though you
relied on the video to make your point. You definitely know what youre talking about, why throw
away your intelligence on just posting videos to your weblog when you could be giving us something informative to read?
I was curious if you ever considered changing the layout of your
website? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or 2 pictures.
Maybe you could space it out better?
I really like your blog.. very nice colors & theme.
Did you make this website yourself or did you hire someone
to do it for you? Plz answer back as I’m looking to create my own blog and would like to know where u got this from.
many thanks
Masa tenis ive bilardo masası aynı anda buluştu buyrun incelemeye geçebilirsiniz ; https://sites.google.com/view/tek-masada-iki-oyun/ana-sayfa
Thank you for sharing this very good post. Very interesting ideas! (as always, btw)
If some one wants expert view about blogging and site-building after that i
suggest him/her to visit this web site, Keep up the good job.
сукааа casino регистрация
First off I want to say excellent blog! I had a quick question which
I’d like to ask if you do not mind. I was interested to find out how you center yourself and clear your mind prior to writing.
I have had trouble clearing my thoughts in getting
my ideas out. I do enjoy writing however it just seems like the
first 10 to 15 minutes are usually wasted simply just trying to figure out how to begin. Any suggestions or hints?
Appreciate it!
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Уникальные данные только сегодня – https://www.defining-blog.ru/category/proizvodstvo
I like what you guys are up too. Such clever work and coverage!
Keep up the superb works guys I’ve added you guys How to Start a business in Nevada my
personal blogroll.
Hey, I simply hopped over to your website by way of StumbleUpon. No longer one thing I’d normally learn, but I preferred your thoughts none the less. Thanks for making one thing worth reading.
Howdy! Would you mind if I share your blog with my facebook
group? There’s a lot of people that I think
would really appreciate your content. Please let me know.
Thank you
Feel free to surf to my web-site – گروه ساختمانی نباتیان
Generally I don’t read post on blogs, however I wish to say that this write-up very compelled me to try and do
so! Your writing style has been amazed me. Thanks, very
nice article.
Here is my blog post; تشک طبی
My brother suggested I may like this web site. He used
to be entirely right. This post truly made my day. You can not imagine just
how a lot time I had spent for this information! Thank you!
Have you ever thought about including a little bit more than just your articles?
I mean, what you say is valuable and everything.
But imagine if you added some great images or videos to give your posts more, “pop”!
Your content is excellent but with images and clips, this blog could definitely be one of the very best in its field.
Very good blog!
It’s very trouble-free to find out any topic on web as compared to books, as I found
this post at this web site.
free porn, porn, porn hub, jav porn, indo porn, porn indo, japanesae porn, porn dude,
indonesia porn, gay porn, video porn, porn video,
porn hd, korean porn, tһе porn dude, japan porn, free porn, rae lil black porn, porn indonesia, аi
porn, porn comic, tiktok porn, audrey davis porn, porn movie, chinese porn,
sophie rain porn, xxx porn, porn sex, hd porn, asian porn,
anime porn, deepfake porn, sex porn, alyx star porn, hikaru nagi porn, indonesian porn, nagi hikaru porn, roblox porn, porn xxx, bu guru salsa
porn, porn tube, Ƅig boobs porn, xnxx porn, situs porn, porn japan,
msbreewc porn, film porn, bulan sutena porn, hazel moore porn, hijab porn, douyin porn viagra, ϲlick һere,
bbuy xanax online, best casino, hackesd site,
scam reviews, malware, download mp3 free
If you would like to increase your know-how just keep visiting this web page and be updated with the
most recent news posted here.
Also visit my blog post music promotion agency
Kudos! Plenty of tips.
Hey I know this is off topic but I was wondering if you knew
of any widgets I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time
and was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your
new updates.
Also visit my web-site :: public relations agency
Hi there this is kinda of off topic but I was wondering if
blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding know-how so I wanted to get advice
from someone with experience. Any help would be greatly appreciated!
Hi! Would you mind if I share your blog with my facebook group?
There’s a lot of people that I think would really appreciate your
content. Please let me know. Cheers
Superb, what a blog it is! This blog gives useful information to us, keep it
up.
Hi excellent website! Does running a blog similar to this take
a massive amount work? I have very little expertise in programming however I had been hoping
to start my own blog soon. Anyways, should you have any ideas or tips for new blog owners please share.
I know this is off topic but I just had to ask. Thanks!
Information about energy-efficient solutions
fоr commercial buildings
You reported it really well.
You said it nicely.! https://substack.com/home/post/p-181768354
Oh my goodness! Awesome article dude! Thank you so much,
However I am going through troubles with your RSS.
I don’t understand why I am unable to subscribe to it. Is there anyone else getting the same RSS problems?
Anyone that knows the solution can you kindly respond?
Thanks!!
Good post. I will be going through many of these issues as well..
Hi! I understand this is somewhat off-topic however I needed to ask.
Does running a well-established website such as yours require a lot
of work? I’m completely new to running a blog but I do write in my journal
every day. I’d like to start a blog so I will be able to share my personal experience and thoughts online.
Please let me know if you have any ideas or tips for brand new aspiring blog
owners. Thankyou!
Hi my friend! I wish to say that this post is amazing, great
written and come with almost all significant infos.
I’d like to see more posts like this .
Howdy just wanted to give you a quick heads up.
The text in your content seem to be running off the screen in Chrome.
I’m not sure if this is a formatting issue or something to do with web
browser compatibility but I thought I’d post to let you know.
The style and design look great though! Hope
you get the problem resolved soon. Cheers
I know this site presents quality depending articles and other stuff, is there any other site which gives these data in quality?
Link exchange is nothing else however it is only placing the other person’s web site link on your page
at appropriate place and other person will also do similar in favor of you.
You have made some good points there. I looked on the net for additional information about
the issue and found most people will go along with your views on this website.
Greetings from Florida! I’m bored to death at work so I decided to check out your site on my iphone during lunch break.
I love the info you provide here and can’t wait to take a look when I get home.
I’m surprised at how quick your blog loaded
on my cell phone .. I’m not even using WIFI, just 3G ..
Anyways, great site!
Konten yang bagus! Jika tertarik dengan game online, LINK PHISING bisa jadi pilihan yang tepat.
Excellent site. Plenty of useful info here.
I’m sending it to a few friends ans additionally
sharing in delicious. And naturally, thank you to your sweat!
Забронировать такси сейчас можно очень быстро — через мобильное приложение, онлайн-платформу или простой звонок. Без усилий укажите точку отправления и пункт прибытия, подберите нужный класс машины, если нужно закажите сервисы вроде детского кресла или времени на сборы. Платформа мгновенно назначит свободный автомобиль, отобразит время подачи и окончательную цену. Рассчитаться за рейс можно как наличными, так и картой — всё зависит от личного выбора. Главное — доверяйте зарекомендовавшими себя платформами, чтобы перевозка была не только комфортной, но и надёжной.
https://hikvisiondb.webcam/index.php?title=KUBTaxi%20-%20%D0%B7%D0%B0%D0%BA%D0%B0%D0%B7%20%D1%82%D1%80%D0%B0%D0%BD%D1%81%D1%84%D0%B5%D1%80%D0%B0%20%D0%B8%20%D1%82%D0%B0%D0%BA%D1%81%D0%B8%20%D0%BC%D0%B5%D0%B6%D0%B3%D0%BE%D1%80%D0%BE%D0%B4%20%D0%B2%20%D0%9A%D1%80%D0%B0%D1%81%D0%BD%D0%BE%D0%B4%D0%B0%D1%80%D1%81%D0%BA%D0%BE%D0%BC%20%D0%BA%D1%80%D0%B0%D0%B5
Asking questions are actually good thing if you are not understanding anything totally, but this piece of writing offers nice understanding yet.
промокод 1хбет
Cheers. Excellent information!
유익한 기사, 제가 찾고 있던 바로 그것입니다.
Way cool! Some extremely valid points! I appreciate you writing this article
and also the rest of the website is very good.
Excellent web site you have got here.. It’s hard to find high-quality writing like
yours nowadays. I honestly appreciate individuals like you!
Take care!!
All you need is an email to create an account and start playing right away – no long forms or personal info needed.
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CA 92626, United Statеs
how to Own a bail bond company
If you would like to grow your knowledge just keep visiting this web site and be updated with
the hottest gossip posted here.
I just added your web site to my blogroll, I hope you would look at doing the same.
Seasoned player here, and I have spent several years in online casinos. I learned control through wins and setbacks. Patience became my core rule. Quick wins rarely last. Experience always counts. Recently I had a solid run while playing digitally. I used my standard strategy. Bet sizes stayed reasonable. The balance started growing. It felt deserved. Luck was only a minor part here lalabetlogin.com.
After the win, I stayed focused. I checked the rules and conditions. The payout process was clean. Funds arrived on time. That moment confirmed my approach. Control once again worked.
I share this as a honest example. This is not bragging. Casino wins are possible. They require patience. Careful play beats emotion. Long-term thinking brings results.
HO88 là nhà cái cá cược uy tín nhất châu Á, cung cấp kèo cược Thể Thao, Casino, Game Online đổi thưởng, Lô Đề mang đến trải nghiệm cá cược thể thao đỉnh cao …
You have made your point!
Do you mind if I quote a few of your articles as long as I provide credit
and sources back to your blog? My website is in the exact same area of interest as yours and my users would truly benefit from some of the information you provide here.
Please let me know if this ok with you. Thanks!
Hi there! Would you mind if I share your blog with my zynga group?
There’s a lot of folks that I think would really enjoy your content.
Please let me know. Many thanks
Magnificent site. Plenty of helpful info here. I’m sending it to several friends ans additionally sharing in delicious.
And certainly, thanks in your effort!
Here is my blog post … music pr firms
Piece of writing writing is also a excitement, if you be familiar with afterward you
can write otherwise it is complicated to write.
Here is my blog: best music pr firms
официальный сайт сукааа онлайн казино
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, ΝΕ 68022, United Ѕtates
402-289-4126
Bookmarks
подробнее https://krab2a.at/
goGLOW Hoyston Heights
1515 Studemont St Suite 204, Houston,
Texas, 77007, UՏA
(713) 364-3256
led light therapy benefits service
Angels Baiil Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, ϹА 92626, United Stɑtes
how much do bail bond agents make
WOW just what I was looking for. Came here by searching for атом казино
регистрация
I every time used to read article in news papers but now as I am a user of net so from now I am using net for posts,
thanks to web.
It’s fantastic that you are getting thoughts from this paragraph as well as from our dialogue
made at this time.
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy basreng188
Wizara ya Ulinzi na Habari ya Kitaifa ya Cambodia ilitangaza kuwa F-16 iliangusha mabomu mawili karibu na kambi ya wakimbizi ya Cambodia.
Akutnhom de Cambodia ee cë luel cë man adɛ̈ ke F-16 ee cë dhɛ̈ŋ ke rou tääu të thiääk kenë ɣän ke gël de kɔc ke Cambodia.
Sangat bermanfaat artikelnya. Oh ya, jangan lupa kunjungi link slot untuk promo menarik hari ini.
Write more, thats all I have to say. Literally, it seems as though you relied
on the video to make your point. You definitely know what youre talking about,
why waste your intelligence on just posting videos to your site when you could be giving us something enlightening to read?
Kudos, Awesome information!
buy backlinks, link exchange, free gift card, congratulations you have won, claim your prize, you have been selected, click
here to claim, you won’t believe, one weird trick, what happened next will shock you,
shocking truth, secret revealed, limited time offer,
special promotion, act now, don’t miss out, buy now, best price, risk-free trial, get rich quick,
make money fast, work from home, no credit check, miracle cure, lose weight fast, free viagra, no prescription needed, online casino, free
spins, meet singles, hot singles in your area, replica watches, cheap
Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB,
BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster,
Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti,
Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex,
Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab,
Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff,
Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit,
Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz,
mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus,
PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit,
RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu,
Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst,
SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot,
Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader,
XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
Look at my homepage: cialis
Superb information. Cheers!
Have you ever thought about writing an ebook or guest authoring on other websites?
I have a blog based upon on the same topics you discuss and would really like to have you share some stories/information. I know
my audience would enjoy your work. If you’re even remotely interested, feel free to
shoot me an e mail.
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, ϹᎪ 92626, United Ⴝtates
bail bonds business opportunity
What a material of un-ambiguity and preserveness of
valuable knowledge concerning unexpected
feelings.
Jet Casino Gutschein
References:
https://online-spielhallen.de/ihre-einfache-schritte-zum-izzi-casino-login/
Hello There. I found your blog using msn. This is a really well written article.
I will be sure to bookmark it and come back to read more of your useful info.
Thanks for the post. I will definitely comeback.
mobil spielen casino app
References:
https://online-spielhallen.de/locowin-casino-mobile-app-dein-mobiles-spielvergnugen-im-detail/
Hi there to every one, for the reason that I am in fact eager of reading this
webpage’s post to be updated regularly. It
carries fastidious data.
My spouse and Ӏ stumbled oѵеr heгe from ɑ
dіfferent page and tһouɡht I mіght as
ѡell check tһings oᥙt. I lіke wһаt I ѕee so i amm just foⅼlowing you.
Loоk forward tߋ gοing ofer your web page for
a sеcond timе.
Check oսt mmy web pаge :: orɗeг Blue Zkittlez strain discreet
shipping [https://cannabisgreenbuds.com/product/buy-blue-zkittlez-aaaa-with-bitcoin]
This is a topic that’s near to my heart… Many thanks! Where are your contact details though?
This blog was… how do I say it? Relevant!! Finally I have found something which helped me.
Thanks!
Currently it sounds like BlogEngine is the best blogging
platform out there right now. (from what I’ve read) Is that
what you are using on your blog?
cobra casino bonus codes
References:
https://online-spielhallen.de/bitkingz-casino-auszahlung-ein-umfassender-leitfaden/
Nicely put. Cheers.
Hello There. I found your blog using msn. This is a very well written article.
I will be sure to bookmark it and return to read more of your useful info.
Thanks for the post. I will certainly comeback.
Here is my web site; Nevada LLC formation
Hi there, yup this post is really good and I have learned lot of things from it concerning blogging.
thanks.
Nice blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple adjustements would really make
my blog jump out. Please let me know where you got your theme.
Cheers
This design is spectacular! You most certainly know how to keep a reader amused.
Between your wit and your videos, I was almost moved to start my
own blog (well, almost…HaHa!) Great job.
I really loved what you had to say, and more than that,
how you presented it. Too cool!
Look at my site – State filings in Nevada
All rights reserved.
GreatWin Casino Bonus
References:
https://online-spielhallen.de/lapalingo-casino-das-mobile-spielerlebnis-auf-ihrem-smartphone/
Evolve Casino Erfahrungen
References:
https://online-spielhallen.de/casino-of-gold-deutschland-ihr-weg-zum-online-spielerlebnis/
I absolutely love your blog and find the majority of your post’s to be exactly what I’m looking for.
Do you offer guest writers to write content for yourself?
I wouldn’t mind publishing a post or elaborating on most of
the subjects you write regarding here. Again, awesome site!
First off I want to say excellent blog! I had a quick question that I’d like
to ask if you don’t mind. I was curious
to know how you center yourself and clear
your head before writing. I have had a hard time clearing my thoughts in getting my thoughts out
there. I do take pleasure in writing but it just seems like the first 10 to 15 minutes are usually wasted just trying to figure out
how to begin. Any recommendations or hints? Kudos!
이건 주제에서 벗어나지만, 제 최신 트위터 업데이트를 자동으로 트윗하는 위젯을 블로그에 추가할
수 있는지 궁금합니다. 이런 플러그인을 꽤
오랫동안 찾고 있었는데, 당신이 이런 것에 대해 경험이
있을지도 모른다고 생각했어요. 혹시 아는 게 있다면
알려주세요. 당신의 블로그를 정말 즐기고 있으며 새로운 업데이트를 기대하고 있습니다.
Saved as a favorite, I love your site!
Wow, what an incredible blog! Your posts on SPIRITSRAPID are spot-on. I love how you
break down complex topics into easy-to-understand points. I’ll be sharing this with
my friends. Many thanks for the great content!
이 블로그는 정보의 보물창고네요! 이 포스트는 특히 흥미롭고 이해하기 쉬웠어요.
IP에 대해 더 깊이 다룬 시리즈가 있으면 좋겠어요.
멋진 콘텐츠 감사합니다!
Esta casa de apuestas adaptó su oferta de apuestas fútbol para Venezuela,
Ecuador y Panamá ofreciendo un bono de bienvenida de hasta $100 USD y la posibilidad de
obtener cuotas mejoradas en la sección “apueste por su selección”. https://www.cs360.com.ar/inicio/2025/12/partidos-para-apostar-en-ambos-equipos-marcan/
Prіme Secured
3603 N 222nd St, Suijte 102,
Elkhorn, ΝE 68022, United States
402-289-4126
Customized management solutions [https://www.symbaloo.com]
Thanks for sharing your thoughts about digi 995 universe nft.
Regards
Woah! I’m really loving the template/theme of this website.
It’s simple, yet effective. A lot of times it’s very difficult to get that “perfect balance” between user friendliness and visual appearance.
I must say you’ve done a very good job with this.
Also, the blog loads super quick for me on Opera.
Exceptional Blog!
Also visit my web site :: Nevada LLC formation
Hi there! I know this is kinda off topic however I’d figured I’d ask.
Would you be interested in exchanging links or maybe guest authoring a blog post or
vice-versa? My website addresses a lot of the same topics as yours and I
feel we could greatly benefit from each other. If
you’re interested feel free to send me an email. I look forward to hearing
from you! Great blog by the way!
May I just say what a comfort to uncover somebody who actually knows what they are talking about on the web.
You definitely realize how to bring a problem to light and
make it important. More people need to read this and understand this side of your story.
I was surprised that you aren’t more popular given that you most certainly have
the gift.
Also visit my web-site: State filings in Nevada
бездепозитные бонусы за регистрацию в казино с выводом
BoaBoa Casino Erfahrungen
References:
https://online-spielhallen.de/lapalingo-casino-das-mobile-spielerlebnis-auf-ihrem-smartphone/
WOW just what I was looking for. Came here by searching for egypt
visa for uk
Wow, that’s what I was looking for, what a material!
present here at this website, thanks admin of this web
site.
Angels Bail Bonds Costa Mesa
769 Baker Ꮪt,
Cosga Mesa, CA 92626, United Stаtes
bail bondsman business plan
Undeniably believe that which you said. Your favorite reason appeared to be on the net the easiest thing to be aware of.
I say to you, I certainly get irked while people think about worries
that they plainly don’t know about. You managed to hit the
nail upon the top as well as defined out the whole thing without having side-effects , people could take
a signal. Will likely be back to get more. Thanks
I always used to study paragraph in news papers but now as I
am a user of web so from now I am using net for articles, thanks to web.
Moovit ช่วยคุณค้นหาเส้นทางที่ดีที่สุดเพื่อไปยัง ซอย รังสิต-นครนายก 18 ด้วยวิธีการแบบเป็นขั้นตอนจากสถานีที่ใกล้ที่สุด.
First of all I would like to say fantastic blog! I had a quick question in which
I’d like to ask if you do not mind. I was curious to know how
you center yourself and clear your thoughts prior to writing.
I have had difficulty clearing my thoughts in getting my ideas out.
I do enjoy writing but it just seems like the first 10 to 15 minutes are wasted just trying
to figure out how to begin. Any suggestions or
hints? Appreciate it!
Hey would you mind stating which blog platform you’re working with?
I’m looking to start my own blog in the near future but I’m having a hard
time selecting between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style seems different then most blogs and I’m looking for
something completely unique.
P.S My apologies for getting off-topic but I had to ask!
Stake Casino Konto anmelden
References:
https://online-spielhallen.de/bitkingz-casino-aktionscode-dein-weg-zu-extra-vorteilen/
Quality articles or reviews is the crucial to interest
the users to pay a quick visit the web page, that’s what this web page is providing.
I like to spend my free time by scanning various internet resources. Today I came across your website and I found it has some of the most practical and helpful information I’ve seen.
I used to be suggested this website by my cousin. I’m
not certain whether or not this submit is written by means of
him as nobody else understand such particular approximately my difficulty.
You are incredible! Thank you!
Having read this I thought it was very informative. I appreciate you spending some time and energy
to put this informative article together.
I once again find myself personally spending a significant amount of time both
reading and commenting. But so what, it was still worth it!
Please let me know if you’re looking for a writer for your
blog. You have some really good posts and I think I would be a good asset.
If you ever want to take some of the load off, I’d really
like to write some content for your blog in exchange for a link back to mine.
Please send me an email if interested. Thanks!
2568แสดงผลได้ดี กับ Browser Google Chrome หรือ Firefox.
Hmm it appears like your blog ate my first comment (it was extremely long)
so I guess I’ll just sum it up what I had written and
say, I’m thoroughly enjoying your blog. I too am an aspiring blog blogger but I’m still new to the
whole thing. Do you have any helpful hints for rookie blog writers?
I’d genuinely appreciate it.
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Погрузиться в детали – https://mazdafitment.com/2012/08/03/pure-white-fd3s/comment-page-758
bwin casino registrierung
References:
https://online-spielhallen.de/lukki-casino-mobile-app-dein-ultimativer-leitfaden/
Kostenlose Freispiele Cashwin
References:
https://online-spielhallen.de/top-crypto-slots-2025-spiele-wichtige-features/
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Переходите по ссылке ниже – http://www.volgyfitness.hu/?p=6639&cpage=30
Hello, all the time i used to check webpage posts here in the early hours in the daylight, since i
like to learn more and more.
Joo Casino Mobile Guide
References:
https://online-spielhallen.de/iwild-casino-aktionscode-ihr-schlussel-zu-mehr-spielspas/
Anghels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CA 92626, United States
bail bonds waco (atavi.com)
Ik tza´n tq´ama a Ministerio de Defensa ex Información te Camboya, jun F-16 te Tailandia tzaj t-xo´n kab´e misil ttxlaj jun campo de refugiados te Camboya
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Изучить эмпирические данные – https://dipuri.com/resena-de-echandote-de-menos
Superb posts, Many thanks. https://substack.com/home/post/p-181766186
Hello there! I could have sworn I’ve been to this blog before but after checking through some of the post
I realized it’s new to me. Anyways, I’m definitely glad I found it
and I’ll be bookmarking and checking back often!
Here is my blog post qatar perfume online shopping
Sweet blog! I found it while searching on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Thank you
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Уточнить детали – https://www.defining-blog.ru/2025/10/13
Kudos, Ample forum posts.
What’s Taking place i am new to this, I stumbled
upon this I’ve found It absolutely useful and
it has helped me out loads. I’m hoping to give a contribution &
assist other customers like its helped me. Good job.
Thanks for finally writing about > Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate < Loved it!
Merkur Casino Bonus ohne Einzahlung
References:
https://online-spielhallen.de/cashwin-casino-deutschland-eine-umfassende-bewertung-fur-deutsche-spieler/
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Полная информация здесь – https://template140.webekspor.com/environmental-compliance-and-sustainability-goals
You suggested it well. https://substack.com/home/post/p-181778881
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
См. подробности – https://phantomlinks.site/reliable-adrenaline-fueled-concrete-parking-lot-contractor-near-north-richland-hills-tx
бездепозитные бонусы за регистрацию в казино без депозита
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Перейти к статье – https://hormonetuyengiap.com/suy-giam-tuyen-giap
Fantastic write ups, Many thanks!
В этой публикации мы сосредоточимся на интересных аспектах одной из самых актуальных тем современности. Совмещая факты и мнения экспертов, мы создадим полное представление о предмете, которое будет полезно как новичкам, так и тем, кто глубоко изучает вопрос.
Проверенные методы — узнай сейчас – http://cbs.torzhok.tverlib.ru/chto-takoe-kulturnoe-nasledie-i-zachem-ego-sohranyat-0
There’s certainly a lot to learn about this issue.
I like all of the points you made.
It’s wonderful that you are getting ideas from this paragraph as well as from our argument made at this place.
I like the helpful info you provide in your articles.
I’ll bookmark your weblog and check again here frequently.
I am quite sure I’ll learn lots of new stuff right here!
Best of luck for the next!
Angels Bail Bonds Costa Mesa
769 Baker St,
Costa Mesa, СA 92626, United States
double c bail bonds
fantastic post, very informative. I wonder why the other experts of this sector
do not understand this. You should continue your writing.
I am confident, you’ve a great readers’ base already!
What’s Going down i am new to this, I stumbled upon this I’ve found It absolutely
useful and it has helped me out loads. I hope to
give a contribution & help other users like its helped me.
Great job.
I’m now not certain the place you are getting your info, but
great topic. I needs to spend a while studying more or
figuring out more. Thank you for great info I was searching for this information for my mission.
I am really loving the theme/design of your web site.
Do you ever run into any web browser compatibility problems?
A number of my blog visitors have complained about my
blog not working correctly in Explorer but looks great in Opera.
Do you have any ideas to help fix this problem?
It is the best time to make a few plans for the longer
term and it’s time to be happy. I’ve learn this put up
and if I could I desire to recommend you few interesting things or suggestions.
Perhaps you could write next articles regarding this article.
I desire to read more issues approximately it!
Hi there Dear, are you in fact visiting
this web page daily, if so then you will absolutely take nice experience.
Plinko Bonus Code kostenlos
References:
https://online-spielhallen.de/umfassende-bewertung-des-monro-casinos-ein-detaillierter-blick/
You’re sharing relevant content about Chicken Road.
http://cse.google.ci/url?sa=t&url=http%3A%2F%2Fchicken-road-race.org%2Fhow-to-play
Thanks for sharing such a good thought, paragraph is good, thats why i have read it completely
Excellent pieces. Keep posting such kind of information on your site.
Im really impressed by it.
Hey there, You have performed a fantastic job.
I’ll certainly digg it and for my part suggest to my friends.
I’m sure they’ll be benefited from this site.
Hi there! I just want to offer you a huge thumbs
up for the excellent information you have right here on this post.
I am coming back to your blog for more soon.
казино онлайн в казахстане бонус за регистрацию без депозита
We’re a group of volunteers and starting a new scheme in our community.
Your site provided us with valuable info to work on. You’ve done a formidable
job and our entire community will be grateful
to you.
My homepage :: Sweet Rush Bonanza Casino
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626, United States
bail bonds 13th and filbert
Hello there I am so grateful I found your website, I really found you by accident, while I was browsing on Digg for something else,
Nonetheless I am here now and would just like to say kudos for
a tremendous post and a all round thrilling blog (I also love
the theme/design), I don’t have time to go through it all
at the minute but I have saved it and also added
in your RSS feeds, so when I have time I will be back
to read much more, Please do keep up the excellent b.
There’s certainly a great deal to know about this subject.
I like all the points you’ve made.
My website; Sweet Rush Bonanza Demo
princess casino freispiele guide
References:
https://online-spielhallen.de/evolve-casino-cashback-ihr-weg-zu-wochentlichen-ruckerstattungen/
Hello, this weekend is good designed for me, since this point in time i am reading this great educational piece of writing here at my house.
Hi there, You have done an excellent job. I’ll certainly digg it
and personally recommend to my friends. I am confident they’ll be benefited from this site.
Feel free to surf to my homepage – Sweet Rush Bonanza Casino
I’ve been coming across discussions about Paybis for a while now, and I’m still not 100% sure about whether it truly deserves all the attention it
gets, but it’s definitely an interesting name within the cryptocurrency
space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as one of the biggest
cryptocurrency platforms that also supports traditional fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to
merge the gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears
to allow users to buy digital currencies using bank transfers.
I’m not claiming this process is flawless, but it does seem aimed at people
just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to various digital assets, which might appeal to users who are diversifying.
That said, I still wonder about things like
availability, so it’s probably something
potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be
seen as professional for some users, though others might find it inconvenient.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a legitimate
crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does mean users should probably compare alternatives before
making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it
does appear to be a platform that’s worth learning more about.
For anyone who is interested in regulated exchanges,
spending some time reading more about Paybis could be
useful. I’m still undecided myself, but it’s interesting enough to justify further exploration.
Monro Casino Bonus Code jetzt nutzen
References:
https://online-spielhallen.de/playfina-casino-erfahrungen-ein-detaillierter-bericht/
I’ve been researching Paybis for a while now, and I’m still not fully convinced about
whether it truly deserves all the attention it gets, but it’s clearly an interesting name within the crypto
trading space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a globally
operating cryptocurrency platforms that also supports regular payment systems, which is something many exchanges either limit or complicate.
What initially caught my interest was the way
Paybis seems to link the gap between traditional finance
and the crypto world. Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to exchange digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to a broader token selection, which might appeal
to users who are experimenting. That said, I still wonder about
things like availability, so it’s probably something potential users
should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes regulatory compliance, which could be seen as professional for some users, though others might find it time-consuming.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying
to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is clear with pricing,
while others mention that costs may vary by transaction. This isn’t uncommon in the
crypto industry, but it does mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available,
but it does appear to be a platform that’s
worth researching. For anyone who is curious about buying
crypto with fiat, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to justify further exploration.
The process to give is very transparent.
It’s actually a cool and helpful piece of information. I’m glad that you simply shared
this helpful information with us. Please keep us informed like this.
Thank you for sharing.
I’ve been reading about Paybis for a while now, and I’m still not 100% sure about whether it truly deserves all the attention it gets, but it’s clearly
an interesting name within the digital asset space, especially when it comes to combining
crypto markets with fiat currencies. From what I understand so far, Paybis presents
itself as a globally operating cryptocurrency platforms that also supports regular payment systems, which is something many
exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to merge the gap
between traditional finance and the crypto world. Many platforms focus
strictly on crypto-to-crypto trades, but Paybis appears to allow users to sell digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to multiple altcoins, which might appeal to
users who are exploring different projects. That said, I still wonder about things like
liquidity, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could
be seen as professional for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that
Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may vary by transaction. This isn’t
uncommon in the crypto industry, but it does mean users should probably do proper research
before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does appear to be a platform that’s
worth learning more about. For anyone who is curious about buying crypto with
fiat, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to justify further exploration.
Keep sharing these important updates.
We’re a bunch of volunteers and opening a brand new scheme in our
community. Your web site provided us with valuable information to work on. You have
done an impressive job and our whole group shall be grateful to you.
I’ve been reading about Paybis for a while now,
and I’m still not 100% sure about whether it
truly deserves all the attention it gets, but it’s undeniably an interesting name within the cryptocurrency space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a globally operating cryptocurrency platforms that also supports
standard currencies, which is something many exchanges either
limit or complicate.
What initially caught my interest was the way Paybis seems to bridge the gap between fiat systems and
the crypto world. Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to buy digital
currencies using various fiat options. I’m not claiming this process is flawless, but it does seem aimed at
people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to the most popular assets.
Instead, it offers access to various digital assets, which
might appeal to users who are exploring different projects.
That said, I still wonder about things like availability, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which
could be seen as reassuring for some users, though others
might find it restrictive. I’m honestly unsure where
I stand on that, but it does suggest that Paybis is trying to operate as a long-term
crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions
seem mixed. Some sources claim that Paybis is clear with pricing, while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does mean users
should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does appear to be a platform
that’s worth researching. For anyone who is
trying to understand how crypto and fiat markets interact,
spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s complex enough to justify
further exploration.
Very nice article. I certainly love this site.
Stick with it!
After looking into a number of the blog posts on your site, I seriously like your
technique of blogging. I saved it to my bookmark webpage list and will be checking back soon. Take a look at my website as well and tell me what you think.
I’ve been seeing mentions of Paybis for a while now, and
I’m still trying to form a clear opinion about whether it truly deserves
all the attention it gets, but it’s certainly an interesting name within the cryptocurrency
space, especially when it comes to combining crypto markets
with fiat currencies. From what I understand so far, Paybis presents itself as one of the biggest cryptocurrency platforms that also
supports standard currencies, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to bridge the gap
between banking methods and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to buy digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range
of cryptocurrencies supported. Paybis doesn’t appear to limit itself to the most popular assets.
Instead, it offers access to multiple altcoins, which might
appeal to users who are exploring different projects.
That said, I still wonder about things like availability, so it’s probably something potential users
should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be seen as
protective for some users, though others might find it time-consuming.
I’m honestly unsure where I stand on that, but it does suggest that
Paybis is trying to operate as a regulated crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is clear with pricing,
while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does mean users should probably read the details carefully before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but
it does appear to be a platform that’s worth learning more about.
For anyone who is trying to understand how crypto and fiat markets interact, spending
some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting enough to justify further exploration.
If some one desires to be updated with most recent technologies afterward he must be
go to see this site and be up to date all the time.
An impressive share! I have just forwarded this
onto a co-worker who was doing a little research on this.
And he actually ordered me dinner due to the fact
that I discovered it for him… lol. So let me reword
this…. Thanks for the meal!! But yeah, thanx for spending some time to discuss this issue here on your site.
this content https://theo.exchange/
n1 casino gutscheincode
References:
https://online-spielhallen.de/greatwin-casino-cashback-ihr-weg-zu-besseren-gewinnen/
top cashback angebote 2025
References:
https://online-spielhallen.de/admiral-casino-auszahlung-ihr-weg-zum-gewinn/
I’ve been coming across discussions about Paybis for a while
now, and I’m still not fully convinced about whether it
truly deserves all the attention it gets, but it’s undeniably an interesting name within the digital asset
space, especially when it comes to combining crypto markets with
fiat currencies. From what I understand so far, Paybis presents
itself as a well-established cryptocurrency platforms that also supports regular payment systems, which is
something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to link the gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but
Paybis appears to allow users to sell digital currencies
using various fiat options. I’m not claiming this process is flawless, but it does seem aimed at newcomers
rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies
supported. Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to multiple altcoins, which might appeal to users who are diversifying.
That said, I still wonder about things like availability, so it’s
probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as professional for some
users, though others might find it restrictive. I’m honestly unsure where I stand on that,
but it does suggest that Paybis is trying to operate as a regulated crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem
divided. Some sources claim that Paybis is transparent with pricing, while others mention that costs may change
based on currency. This isn’t uncommon in the crypto industry, but it does mean users should probably do proper research before making
decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be a platform that’s worth
researching. For anyone who is interested in regulated exchanges, spending some time reading
more about Paybis could be useful. I’m still undecided myself, but it’s promising
enough to justify further exploration.
Hi, yes this piece of writing is really pleasant and I have learned lot of
things from it about blogging. thanks.
Hi there, I discovered your site by the use of Google at the same time as searching for
a comparable matter, your website got here up, it seems to be great.
I have bookmarked it in my google bookmarks.
Hello there, simply became aware of your weblog through Google, and found that
it’s truly informative. I’m going to watch out for brussels.
I will be grateful in case you continue this in future.
Numerous other folks will probably be benefited from your writing.
Cheers!
Greetings from Los angeles! I’m bored to tears at work so I decided to check out your site on my iphone during lunch break.
I really like the info you provide here and can’t wait to take a look
when I get home. I’m amazed at how quick your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyhow, awesome site!
Regards for helping out, superb info.
bizzo casino anmelden
References:
https://online-spielhallen.de/marvel-casino-freispiele-ihr-schlussel-zu-kostenlosem-spielspas/
Howdy! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get my blog to
rank for some targeted keywords but I’m not
seeing very good gains. If you know of any please share.
Many thanks!
Pretty nice post. I just stumbled upon your weblog and wanted to say that I’ve really enjoyed surfing around your blog posts. After all I’ll be subscribing in your feed and I am hoping you write again very soon!
This is the perfect blog for everyone who hopes to find out about this topic.
You realize a whole lot its almost hard to argue
with you (not that I actually would want to…HaHa).
You definitely put a brand new spin on a subject which has been discussed for decades.
Wonderful stuff, just great!
I am really delighted to glance at this web
site posts which contains plenty of helpful information,
thanks for providing these kinds of data.
PowerUp Casino Login einfach
References:
https://online-spielhallen.de/druckgluck-casino-deutschland-alles-was-sie-wissen-mussen/
Nice weblog right here! Also your web site so much up very fast!
What host are you the use of? Can I am getting
your affiliate link in your host? I want my web site loaded up as fast as yours lol
Ministria e Punëve të Jashtme e Kamboxhias tha se F-16 kishte vendosur dy raketa pranë Forcave Mbrojtëse të Kamboxhias.
Good day! I know this is kinda off topic but I’d figured I’d ask.
Would you be interested in exchanging links or maybe guest authoring a blog
post or vice-versa? My blog goes over a lot of the same topics as yours and I feel we could greatly
benefit from each other. If you happen to be interested feel
free to send me an email. I look forward to hearing from you!
Superb blog by the way!
Prime Secured
3603 N 222nd Ꮪt, Suite 102,
Elkhorn, ΝE 68022, United Stаtes
402-289-4126
Proactive IT Security
I’ve been researching Paybis for a while now, and I’m still trying to
form a clear opinion about whether it truly deserves all the attention it gets, but it’s undeniably an interesting name within the
digital asset space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself
as a large-scale cryptocurrency platforms that also supports standard currencies, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis
seems to connect the gap between fiat systems and the
crypto world. Many platforms focus strictly on crypto-to-crypto
trades, but Paybis appears to allow users to sell digital
currencies using bank transfers. I’m not claiming this process is flawless,
but it does seem aimed at newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to the most popular assets.
Instead, it offers access to various digital assets, which might appeal to
users who are exploring different projects. That said, I still wonder about things like update frequency, so it’s probably something potential users
should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be seen as protective for
some users, though others might find it inconvenient.
I’m honestly unsure where I stand on that, but it does suggest
that Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but
it does mean users should probably do proper research
before making decisions.
Overall, I wouldn’t say Paybis is perfect,
but it does appear to be a platform that’s worth learning more about.
For anyone who is interested in regulated exchanges, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to justify further exploration.
Amazing content on your website.
ਕੰਬੋਡੀਆ ਦੇ ਵਿਦੇਸ਼ ਮੰਤਰਾਲੇ ਨੇ ਕਿਹਾ ਕਿ ਐਫ-16 ਨੇ ਕੰਬੋਡੀਅਨ ਰੱਖਿਆ ਬਲ ਦੇ ਨੇੜੇ ਦੋ ਮਿਜ਼ਾਈਲਾਂ ਤਾਇਨਾਤ ਕੀਤੀਆਂ ਸਨ।
Its like you read my thoughts! You appear to know a lot approximately
this, such as you wrote the book in it or something.
I think that you simply could do with a few percent
to drive the message home a little bit, but other than that,
that is magnificent blog. A great read. I will certainly be back.
Stakes Casino App iOS
References:
https://online-spielhallen.de/wazamba-casino-deutschland-ein-umfassender-testbericht-fur-deutsche-spieler/
Does your blog have a contact page? I’m having problems locating it
but, I’d like to send you an email. I’ve got some creative ideas for your blog you
might be interested in hearing. Either way, great website and
I look forward to seeing it expand over time.
hit spin casino app download
References:
https://online-spielhallen.de/bizzo-casino-deutschland-mein-umfassender-erfahrungsbericht/
I’ve been looking into Paybis for a while now, and I’m still not 100% sure about whether it truly deserves all the
attention it gets, but it’s definitely an interesting name within the crypto
trading space, especially when it comes to combining crypto markets
with fiat currencies. From what I understand so far, Paybis presents itself as one of the biggest
cryptocurrency platforms that also supports traditional fiat money, which is
something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems
to connect the gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users
to exchange digital currencies using credit cards.
I’m not claiming this process is flawless, but it
does seem aimed at people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies
supported. Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to a broader token selection, which might appeal to users who are diversifying.
That said, I still wonder about things like liquidity, so it’s probably something potential users
should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as
protective for some users, though others might find it
restrictive. I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a
long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is clear with pricing, while others mention that costs may change
based on currency. This isn’t uncommon in the crypto industry, but it does mean users should probably do
proper research before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear to be a platform that’s worth researching.
For anyone who is trying to understand how crypto and fiat markets interact, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to justify further exploration.
Thanks designed for sharing such a fastidious thought, piece of writing is nice, thats
why i have read it fully
You reported this wonderfully! https://kongmuntongmee.wordpress.com/2025/12/10/betflix888-reviews/
MM88 là nền tảng cá cược hàng đầu châu Á, trải nghiệm giải trí đa dạng, bảo mật cao, giao diện thân thiện, khuyến mãi hấp dẫn và dịch vụ hỗ trợ chuyên …
промокод на бездепозитный бонус в казино
BIGG Casino Deutschland
References:
https://online-spielhallen.de/locowin-casino-auszahlung-ein-umfassender-leitfaden-fur-spieler-in-deutschland/
hi!,I really like your writing very a lot! percentage we keep in touch more approximately
your post on AOL? I need a specialist on this house to
resolve my problem. Maybe that’s you! Having a look forward to peer you.
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis
& Treatment – MDtodate < Liked it!
+905322952380 fetoden dolayi ulkeyi terk etti
Hello there, You have done an excellent job.
I will certainly digg it and personally suggest to my
friends. I’m confident they will be benefited from this site.
The post is absolutely fantastic! Lots of great info and inspiration, both of which we all need! Also like to admire the time and effort you put into your website and detailed info you offer! I will bookmark your website!
click here, read more, learn more, useful post, great article,
helpful guide, nice tips, thanks for sharing, very
informative, good read, interesting post, well explained,
detailed guide, helpful information, great explanation, this helped a lot, valuable content,
worth reading, solid breakdown, informative article, recommended read, good insights, clear
explanation, practical tips, well written, excellent overview
Having read this I thought it was very informative.
I appreciate you taking the time and energy to put this informative article
together. I once again find myself personally spending a lot of time both
reading and commenting. But so what, it was still worthwhile!
+905516067299 fetoden dolayi ulkeyi terk etti
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically
tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe
you would have some experience with something like
this. Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new updates.
There’s definately a great deal to find out about this subject.
I love all the points you made.
Makanya harus melakukan cara lain agar bisa mendowload file video langsung
dari youtube bahkan bisa mengubahnya ke dalam bentuk lagu atau mp3.
2568แสดงผลได้ดี กับ Browser Google Chrome หรือ Firefox.
Wow, awesome blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your site is magnificent, let alone the content!
Hi, i feel that i noticed you visited my blog thus i came to return the want?.I’m attempting to to find issues
to enhance my site!I suppose its ok to make use of some of your concepts!!
Outstanding quest there. What happened after?
Good luck!
If you desire to get a good deal from this paragraph then you have to
apply these methods to your won weblog.
I’m not that much of a online reader to be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your site to come
back in the future. Many thanks
Hi there! This article could not be written any better!
Looking at this post reminds me of my previous
roommate! He always kept talking about this.
I most certainly will send this information to him.
Fairly certain he’s going to have a very good read.
I appreciate you for sharing!
Mangelsen
7916 Girard Avenue, Ꮮa Joya
CA 92037, United States
1 800-228-9686
Learn Thomas D Mangelsen Wildlife
I’ve been coming across discussions about Paybis for a while now, and I’m
still not completely certain about whether it truly deserves all the
attention it gets, but it’s certainly an interesting name within the digital asset space, especially
when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a large-scale cryptocurrency platforms that also supports
standard currencies, which is something many exchanges either
limit or complicate.
What initially caught my interest was the way
Paybis seems to merge the gap between fiat systems and the crypto
world. Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to exchange digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed at people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to various digital assets, which might appeal to
users who are experimenting. That said, I still wonder about things like availability, so it’s probably something potential users
should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes regulatory compliance, which could
be seen as reassuring for some users, though others might find it time-consuming.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is straightforward with pricing,
while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does
mean users should probably read the details carefully
before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does appear to be a
platform that’s worth researching. For anyone who is curious about
buying crypto with fiat, spending some time reading more about Paybis could
be useful. I’m still undecided myself, but it’s interesting enough to justify further
exploration.
Good day! Do you know if they make any plugins to protect against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on.
Any recommendations?
Hurrah, that’s what I was looking for, what a information! present here
at this webpage, thanks admin of this web site.
I’ve been exploring for a bit for any high-quality articles or blog posts on this sort
of house . Exploring in Yahoo I finally stumbled upon this site.
Reading this information So i’m glad to show that I’ve a very just right uncanny feeling
I found out exactly what I needed. I so much for sure will make certain to don?t omit this site and give it a look
on a continuing basis.
Thanks a bunch for sharing this with all folks you actually recognize what you are speaking
about! Bookmarked. Please additionally consult with
my website =). We may have a hyperlink alternate agreement among us
I’ve been seeing mentions of Paybis for a while
now, and I’m still not completely certain about whether it
truly deserves all the attention it gets, but it’s definitely an interesting name within the cryptocurrency space, especially when it comes
to combining crypto markets with fiat currencies. From what I understand so far, Paybis presents itself as one of the biggest
cryptocurrency platforms that also supports standard currencies, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to bridge the gap between banking
methods and the crypto world. Many platforms focus strictly on crypto-to-crypto
trades, but Paybis appears to allow users to buy digital
currencies using bank transfers. I’m not claiming this process is flawless, but
it does seem aimed at newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to the most
popular assets. Instead, it offers access to a broader token selection, which might appeal to users who
are diversifying. That said, I still wonder about things like liquidity, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as professional for some users, though others might find
it time-consuming. I’m honestly unsure where I stand on that, but
it does suggest that Paybis is trying to operate as a
legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is straightforward with pricing, while
others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does mean users should probably compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does appear to be a platform
that’s worth researching. For anyone who is interested in regulated
exchanges, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting enough
to justify further exploration.
hi!,I like your writing so much! percentage we be in contact more about your post on AOL?
I need an expert on this house to solve my problem.
Maybe that’s you! Having a look forward to look you.
Thanks a lot, Helpful information. https://substack.com/home/post/p-181770081
Its like you read my mind! You seem to know a lot about this, like you wrote the book in it or something.
I think that you could do with a few pics to drive the
message home a little bit, but other than that,
this is fantastic blog. A fantastic read. I’ll certainly be back.
Thank you for some other great article. The place else may anybody get that type of info in such an ideal approach of writing?
I have a presentation subsequent week, and I am at the search for such info.
бездепозитные бонусы в онлайн казино
Ayo mainkan peluang besar anda di LIGACOR untuk kaya dengan bermain game di
website terbaik tanpa stres! Dapatkan info cuan mudah dan jadilah kaya secara otomatis
Appreciation for taking the time to discuss this topic, I would love to discover more on this topic. If viable, as you gain expertise, would you object to updating the website with further information? It is tremendously beneficial for me.
Hello everyone, it’s my first pay a visit at this website, and article is
really fruitful in favor of me, keep up posting these posts.
Good day! I know this is kinda off topic however , I’d figured
I’d ask. Would you be interested in trading links or maybe guest
authoring a blog post or vice-versa? My site goes over a lot of the same topics as yours and I think we could greatly benefit from each other.
If you might be interested feel free to shoot me an e-mail.
I look forward to hearing from you! Fantastic blog by the way!
magnificent points altogether, you just gained a brand new
reader. What may you suggest in regards to your submit that you made a
few days ago? Any sure?
Very nice post. I just stumbled upon your blog and wished to
mention that I have truly loved browsing your weblog posts.
After all I will be subscribing for your feed and I’m hoping you write once more soon!
Way cool! Some very valid points! I appreciate you writing this article
plus the rest of the site is also really good.
This game looks amazing! The way it blends that old-school chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with
real consequences has me hooked. I need to play this!
This sounds like a blast! Combining that iconic chicken crossing
gameplay with actual stakes? Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds
legitimate risk is genius. Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing
action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
I’ve been reading about Paybis for a while now, and I’m still not completely
certain about whether it truly deserves all the attention it gets,
but it’s certainly an interesting name within the cryptocurrency space, especially
when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as
a globally operating cryptocurrency platforms that also supports regular payment systems,
which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to link the gap between traditional finance and
the crypto world. Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to sell digital currencies
using various fiat options. I’m not claiming this process is flawless, but it does seem aimed at newcomers rather than only
advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to multiple altcoins, which might appeal to users who
are experimenting. That said, I still wonder about things like update frequency,
so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be seen as reassuring for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates,
opinions seem divided. Some sources claim that Paybis is clear with pricing,
while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does mean users
should probably do proper research before making
decisions.
Overall, I wouldn’t say Paybis is the best
exchange available, but it does appear to be a platform that’s worth researching.
For anyone who is trying to understand how crypto and fiat markets interact,
spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting enough to
justify further exploration.
That is really fascinating, You’re an excessively skilled blogger. I’ve joined your rss feed and look forward to in the hunt for extra of your magnificent post. Additionally, I’ve shared your website in my social networks!
I am in fact glad to read this weblog posts which contains lots of valuable
data, thanks for providing these kinds of data.
Feel free to surf to my blog post … filler bivirkninger (http://www.skinhudlaege.dk)
buy backlinks, link exchange, free gift card, congratulations
you have won, claim your prize, you have been selected, click here
to claim, you won’t believe, one weird trick, what happened next will shock you, shocking truth, secret revealed, limited time offer, special promotion, act now, don’t miss out, buy now, best price, risk-free
trial, get rich quick, make money fast, work from home,
no credit check, miracle cure, lose weight fast, free viagra, no
prescription needed, online casino, free spins,
meet singles, hot singles in your area, replica watches, cheap Rolex.Agent Tesla,
ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader,
Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster,
Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker,
Conti, Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide,
Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot,
Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy,
Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim,
Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar
Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu,
Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader,
Zlob, Zotob
Here is my blog … buy fake Rolex fake Gucci fake Prada
Купить Дженерик Сиалис 40мг на сайте: https://3aplus63.ru/ с доставкой
высокое качество от производителя скидки для постоянных клиентов
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, NᎬ 68022, United Stаtes
402-289-4126
ᒪatest Security Trends – atavi.com –
After looking over a number of the blog posts on your
website, I seriously like your technique of blogging.
I saved as a favorite it to my bookmark webpage list and will
be checking back in the near future. Please visit my web site as well and tell me how
you feel.
Feel free to visit my web page outdoor living Panorama Village
click this russian traditional clothing
It’s amazing in support of me to have a web page, which is good
designed for my know-how. thanks admin
Howdy very cool blog!! Guy .. Excellent .. Amazing .. I’ll bookmark your site and take the feeds
also? I am satisfied to find numerous helpful information here
within the put up, we’d like develop extra techniques on this regard, thanks for
sharing. . . . . .
This article gives clear idea for the new people of
blogging, that really how to do running a blog.
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, USᎪ
(713) 364-3256
microdermabrasion Ƅest (go.bubbl.us)
Volgens un Cambodjaans Ministerie vaan Defensie Informatie lanceerde jun F-16 in Thailand un raket op un Cambodjaans vluchtelingskamp
Kudos! Plenty of forum posts!
https://co168-games.blogspot.com/2025/12/betflik199-2025-2025-betflik199.html
I’ve been researching Paybis for a while now, and I’m
still not completely certain about whether it truly deserves all
the attention it gets, but it’s undeniably an interesting name within the digital asset space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as one of the biggest cryptocurrency platforms that also supports regular
payment systems, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis
seems to connect the gap between banking methods and the
crypto world. Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users
to exchange digital currencies using bank transfers.
I’m not claiming this process is flawless, but it does seem aimed at people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to various digital assets, which might appeal to users who are diversifying.
That said, I still wonder about things like liquidity, so it’s probably something potential users should investigate
further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes regulatory compliance, which could be seen as reassuring for some users, though others might
find it restrictive. I’m honestly unsure where I stand on that, but
it does suggest that Paybis is trying to operate as a
regulated crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is transparent with pricing,
while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does mean users should
probably compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does appear to be a platform that’s worth
a closer look. For anyone who is interested in regulated exchanges, spending some time reading more
about Paybis could be useful. I’m still undecided myself,
but it’s complex enough to justify further exploration.
Hi there, just became alert to your blog through Google, and found that it’s really informative.
I’m going to watch out for brussels. I will appreciate if you continue
this in future. Many people will be benefited from your writing.
Cheers!
It’s genuinely very complex in this full of activity life to listen news on Television, therefore I only
use web for that reason, and get the most recent information.
I’ve been seeing mentions of Paybis for a while now, and I’m still not
100% sure about whether it truly deserves all
the attention it gets, but it’s clearly an interesting name within the crypto trading space, especially when it comes to combining crypto markets
with fiat currencies. From what I understand so far, Paybis
presents itself as one of the biggest cryptocurrency platforms that also supports regular payment systems, which is something many exchanges
either limit or complicate.
What initially caught my interest was the way Paybis seems to link the gap between banking methods and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but
Paybis appears to allow users to sell digital currencies using various
fiat options. I’m not claiming this process
is flawless, but it does seem aimed at people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to the most popular assets.
Instead, it offers access to various digital assets, which might appeal to
users who are experimenting. That said, I still wonder
about things like liquidity, so it’s probably something potential users should
investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes regulatory compliance, which could be seen as reassuring for some users, though others might find it inconvenient.
I’m honestly unsure where I stand on that,
but it does suggest that Paybis is trying to operate
as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is straightforward with pricing,
while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it
does mean users should probably compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be a
platform that’s worth a closer look. For anyone who is
trying to understand how crypto and fiat markets interact, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting enough to justify further exploration.
always i used to read smaller posts which as well clear their motive, and that is also happening with this post which I am reading
at this time.
I’ve been looking into Paybis for a while now, and I’m still
not 100% sure about whether it truly deserves all
the attention it gets, but it’s undeniably an interesting
name within the digital asset space, especially when it
comes to combining crypto markets with fiat currencies. From what I understand so far,
Paybis presents itself as a well-established cryptocurrency platforms that also supports traditional fiat money, which is something
many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to connect the gap between banking methods and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis
appears to allow users to buy digital currencies using debit cards.
I’m not claiming this process is flawless, but it does seem aimed at newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to
Bitcoin and Ethereum only. Instead, it offers access to
a broader token selection, which might appeal to users who are exploring different
projects. That said, I still wonder about things like update frequency, so it’s probably something
potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as protective for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest
that Paybis is trying to operate as a legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is clear with pricing, while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does mean users should probably
compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be a platform that’s worth a closer look.
For anyone who is curious about buying crypto with fiat, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s complex enough to justify further
exploration.
Superb post however , I was wanting to know if you could write a
litte more on this topic? I’d be very grateful if you could elaborate a little bit further.
Appreciate it!
Check out my web page … Cap-Haitien Hotel
+905322952380 fetoden dolayi ulkeyi terk etti
I am really grateful to the holder of this website who
has shared this great post at at this time.
my homepage: mpo slot
Very quickly this web page will be famous amid all blogging viewers,
due to it’s pleasant articles or reviews
What’s up, always i used to check blog posts here early in the break of day, because i enjoy to find out more and more.
Primke Secured
3603 N 222nd St, Suite 102,
Elkhorn, NᎬ 68022, United Stɑteѕ
402-289-4126
Data Force Systems
+905072014298 fetoden dolayi ulkeyi terk etti
Prіme Secured
3603 N 222nd St, Suite 102,
Elkhorn, ΝE 68022, United Stаtes
402-289-4126
Advanced cybersecurity solutions
I have been exploring for a little bit for any high-quality articles
or blog posts on this sort of space . Exploring in Yahoo I eventually stumbled
upon this web site. Studying this information So i’m glad to convey that I
have an incredibly excellent uncanny feeling I discovered just what I needed.
I most for sure will make certain to do not omit this site and provides it a glance on a relentless
basis.
Check out my blog Fort Lauderdale Senior Medical Center
is human trafficking tһе second largest, սsa gymnastics coach human trafficking,
human trafficking news neаr me, snopess lynne knowles human trafficking,
human trafficking awareness Ԁay quotes, human trafficking sex scene, human trafficking – menschenhandel,
meghan connors human trafficking, ansrew tate hhman trafficking, arguments оn human trafficking, free human trafficking
cme florida, human trafficking ߋur, human trafficking іn minnesota 2021, arizona
republican huma trafficking, orange іs tһe new black human trafficking, human trafficking conference ocean city md, 277
arrested іn human trafficking, anti human trafficking law philippines, north korea human trafficking fаcts, hߋѡ
ѡill thе wall affect human trafficking, human trafficking training mjchigan 2018,
hotels suedd human trafficking, kids rescued fгom human trafficking, dutham region human trafficking, ԝhy human trafficking іs іmportant, mother ߋf god
church human trafficking, walmart human trafficking 2020, ѡhat iѕ
the rate оf human trafficking worldwide, human trafficking news (news), humaqn trafficking ƅy
state 2021, lgbt human trafficking statistics, south africa ɑnd human trafficking, human trafficking statistics fbi, hotel lawsuits
human trafficking, operation renewed hope human trafficking,
human trafficking atlanta 2022, human trafficking san joaquin county, non profit organizations fоr human trafficking, human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rigһts julietta hua, facebook humaan trafficking lawsuit, rates ⲟf human trafficking, real ᴡorld example
of human trafficking, lawyers аgainst human trafficking, wsin human trafficking summit 2022, vad är
human trafficking, recognizing thee signss οf human trafficking, human trafficking
justice, video օf human trafficking, four signs of human trafficking, human trafficking
honey, binjun xie human trafficking, human trafficking documentary amazon ρrime, minnesota human trafficking data,
uncovers russian human trafficking гing war, human trafficking
chico ⅽа, human trafficking jus cogens,
human trafficking syrian refugees, human trafficing
topics гesearch paper, text human trafficking link snopes, oprah south afrijca human trafficking,
human trafficking grants 2015, human trafficking san antonio 2021, human drug trafficking meaning, human trafficking stories children, fema human trafficking awareness, florida disney human trafficking, jobs fߋr human trafficking victims, movie aboutt
human trafficking 2023 netflix, ɑ day in the life of a human trafficiing victim, uk human trafficking news,
bent ⅼicense plate human trafficking reddit,
hhuman traffickng іn waterbury ct, center to combat human trafficking, geeenville nc human trafficking, maui human trafficking, tօp 5
human trafficking cities, іѕ human trafficking happening iin thee us,
oxnard human trafficking, aurora shoreline human trafficking, taconganas human trafficking, hashtags fⲟr human trafficking,
wjite house human trafficking summit, corona human trafficking, border patfol human trafficking, human trafficking
іn thailand 2020, human trafficking іn wv, 11 arrested in human trafficking, china’s оne child policy andd human trafficking, hotels human trafficking 2023, human trafficking іn florida 2021, human trafficking debate topics,
internationasl justice mission human trafficking, uncovers human trafficking
ring for, scholarly ardticle ⲟn human trafficking, madison herman human trafficking, amad
diallo human trafficking, а poem about human trafficking,
human trafficking bristol tn, deluca ɑnd
thhe human traffickoing storyline, economy аnd human trafficking, human trafficking inn trinidad, human trafficking Ԁay 2018, caught
camera actual human trafficking victims, human trafficking
episode opal grey’ѕ anatomy, duolingo ceo human trafficking,
watch dogs human trafficking map, human trafficking definition canada, airtag
human trafficking, human trafficking іn thhe beauty industry, 人口販子human trafficking, forced labor іn human trafficking, american airlines center
human trafficking, human trafficking ⅽe texas,
selah human trafficking, siam human trafficking, fresno human trafficking
statistics, senegal human trafficking, human trafficking belgium, miichigan human trafficking ⅽourse, ny times human trafficking, abandoned stroller
human trafficking, human trafficking і-44, solution οn human trafficking, hhuman trafficking canada news, ontario human trafficking,
protects victjms ᧐f human trafficking amendment, human trafficking iin highland сa,
human trafficking hotspot map, hujman trafficking organizations ontario, huma trafficking huding
սnder cars, summary оn human trafficking, uncovers russian human trafficking гing war, human trafficking honey, fοur signs of human trafficking, huma trafficking western pa, human trafficking livermore, hhman trafficking durham region, human trafficking аt atlanta airport, binjun xie human trafficking, minnesota human trafficking
data, human trafficking documentary amazon ρrime, human trafficking lawyer bloomfield hills,
human trafficking charge іn texas, central students ɑgainst human trafficking, ap human ggeography human trafficking,human trafficking fօr sexual exploitation, blue fоr human trafficking, kantin ethics human trafficking,
anti-human trafficking organization іn cambodia, jo jorgensen օn human trafficking,
forrt hood soldiers human trafficking, beau оf tһe fifth column human trafficking, hawkins human trafficking, human trafficking
іn the pacific islands, reasons ᴡhy human trafficking іs bad, alloy humzn trafficking, ԝrite ann essay on human trafficking, human trafficking
pros, humman trafficking dark web reddit, north preston hjman trafficking, ԁollar sign tattoo human trafficking, wht іs
human trafficking, human trafficking stuart fl, priceless movie human trafficking, ti аnd wife hman trafficking, human trafficking
ethnicity statistics, і 80 truck ѕtop human trafficking, hamilton human trafficking, oawkville human trafficking, human trafficking ⲟn tһe deep web,
cuurrent human trafficking, human trafficking women’ѕ rigһts, brunei human trafficking,
barack obama human trafficking quote, patron saint оf human trafficking, spiruted
аway human trafficking, the game human trafficking, tⲟρ human trafficking cities 2023,
human trafficking ѡhich countries are tһе worst, һow to donate to human rafficking
organizations, human trafficking quotes famous, humn trafficking story
2020, human trafficking іn pittsburgh, 2020 human trafficking conference,
human trafficking bust atlanta, human trafficking hemet cа, human trafficking
statistics oregon, һow to identify ɑ human trafficking victim, economy аnd human trafficking,
lover boy method of human trafficking, deluca ɑnd tһe human trafficking storyline, european human trafficking,
selah human trafficking, american airlines center human trafficking,
human trafficking paintings, ѡһat ѕtate is #1 in human trafficking?,
forced labor іn human trafficking, 人口販子human trafficking,
crystal meth, ѡhat does crystal meh ⅼoоk ⅼike,what is crystal meth, crystal meth anonymous, һow lօng does crystal
meth stay іn youг system, how tto mаke crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects,
crystal meeth pipe, crystal meth drug, what does crystal meth look like?, meth crystal, crystal meth
images, crysstal meth ѕide effects, hօᴡ is crystal meth mɑde,
meth vs crystal meth, ѡhat doeѕ crystal meth do, crystal meth symptoms, crystal meth vvs meth, effects oof crystal meth, ѕide efffects of crystal meth,
һow dо you mаke crystal meth, crystal meth vvs
crack, ѡhat ɗoes crystal mmeth smell lіke,
how is crystal meth used, crystal meth withdrawal,
crystal meth breaking bad, ѡhat is crystal meth mɑde
of, ѡһat does crysttal meth ddo to you, crystal meth teeth,
smoking crystal meth, crystal meth pictures, can you snort
crystal meth, crystal meth Ьefore аnd ɑfter, who invented crystal meth, crystal mesth
fɑcts, crystal meth withdrawal symptoms, crystal meth street
names, signs ᧐f crystal meth, crystal meth addiction, how t᧐
cook crystaal meth, crystal meth definition, ᴡһаt
type of drug іs crystal meth, what ⅾies crystal meth feel like, crystal meth meaning, crtystal meth ingredients, ԝhats crystal meth,
ԝhat color iis crystal meth, crystal meth detox, crystal
meth fаⅽe,crystal meth powder, crystal meth poem, streeet names fօr crystal meth, short
term effects оf crystal meth, signs օf crystal meth abuse, crystal meth rock, crystal meth fly, crystal meth addict,
crystal meth սsers,crystal meth rehab, hoԝ muϲh does crystal meth cost,
how do yоu take crystal meth, how muсh is crystal meth, signs оf crystal meth սse, һow to smoke crystal meth, һow to usе crystal meth,
ⅼong term effects оf crystal meth, signs оff addiction tо
crystal meth, pink crystal meth, crystal meth ⅼook like,
breaking badd crystal meth, ᴡhen was crystal meth invented, pictures ⲟff crystal
meth, how is crystal meth tаken, signs tһat someone is using
crystal meth, ready ⲟr not crystal metgh storage, difference ƅetween meth аnd crystal meth,
һow do you dо crystal meth, crystal meth., locate cryystal meth storage,
ѡhat are thе efrfects of crystal meth, fake crystal meth, crystal meth people,
ѡһɑt does crystal meth, how Ԁo yoս usee crystal meth,
һow addictive іѕ crystal meth, cɑn yⲟu overdose on crystal meth, crystal meth blue, crystal meth signs, һow long does crystal meth ⅼast, crystal meth detox los
angeles, һow Ԁo people use crystal meth, һow does crystal meth lⲟok like, crystal
meth porn, howw Ԁos crystal meth ⅼook, crystal meth storage twisted nerve, ԝhats in crystal meth, crystal meth treatment, whawt іѕ crystal meth madxe from,
methamphetamin, methamphetamin adalah, methamphetamin ɗan amphetamin adalah, amphetamin ԁan methamphetamin, chloroethane ɑnd methamphetamin, crystal
methamphetamin, ѡһаt is methamphetamin, methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch,
methamphetamin 中文, mdma methamphetamin, methammphetamin hydrochlorid,
methamphetamin geschichte, methamphetamin hcl, amphetamin ѵs methamphetamin,
methamphetamin biru, methylphenidat methamphetamin, beda amphetamin Ԁаn methamphetamin, difference betԝeen amphetamine and methamphetamin, methamphetamin psychose, methamphetamin rules, hoow
tߋ mаke methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride,
definition νоn methamphetamin, р2p methamphetamin,
methamphetamin medizin, amphetamin սnd methamphetamin,
vicks vapor inhaler methamphetamin, gta methamphetamin labor, ѡіe wirkt methamphetamin, methhamphetamin entzug, methamphstamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine ᥙnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung china, mthamphetamin wehrmacht,
methamphetamin tabletten, methamphetamin doccheck, һow too clok methamphetamin, methamphetamin abhängigkeit,
methamphetamin nebenwirkungen, methamphetamin ԝаs ist das, unterschie methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetfamin medikament,
methamphetamin ⅼa chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah
obat, methamphetamin amdere suchten ɑuch nach, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor,
methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ɗương tính, waѕ ist
methamphetamin, drogentest methamphetamin, methamphetamin englisch,
methamphetamin structure, іѕt mdma methamphetamin, lye іn methamphetamin, іst methamphetamin organschädigend?
quora, methamphetmin chemische struktur, methamphetamin chemische
formel, methamphetamin meaning, Ԁ-methamphetamin, herstellung methamphetamin, methamphtamin νs amphetamine, methamphetamin recept, methamphetramin japan, definition methamphetamin, methamphetamin fаce, methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd,
blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction,
bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese,
methamphetamin ᥙse icd 10, weed, weed grinder, wһere iis
weed legal, disposable weed pen, weed shop
neаr me, milwaukee weed eater, purple weed, is weed legal іn virginia,
is weed letal іn oklahoma, іs weed legal in louisiana, weed puller tool, weed carts,
іs weed legal in south carolina,weed killer f᧐r lawns, horny goatt wed for
men, wһat ѕtates is weed legal, weed shops neаr me, weed legal ѕtates, weed vape, roundup
weed killer, weed killer spray, edible weed, recreational weed ѕtates,
weed store, milk weed, weed barrier, іs weed legal in indiana, legal weed ѕtates, stateѕ
ԝith legal weed, iѕ weeed legal іn kentucky, weedd puller,
preesn weed preventer, ounce օf weed, dewalt weed eater, plantain weed, husqvarna weed
eater, electric weed eater, hybrid weed, moonrock weed,
weed pipe, barrett wilbert weed, weed control, weed delivery neɑr me, iѕ weed legal in missouri, hoᴡ
to makje weed butter, ᴡhite weed, іs weed legal in utah, moon rock weed, snow caps weed, іѕ weed legal in arkansas, іs weed legal in texas 2025, ryobi weed eater, weed bowl, dill weed, weed legalization, smoking weed, іs weed
legal inn nevada, weed whacker, іs weed legal іn alabama, is weed a
drug, weed barrier fabric, ᴡhat is horny goat weed, spruce weed
and grass killer, weed stores neаr me, sprinkles weed,
poke weed, weed withdrawal, weed vapes, snow cap weed, rm43 weed killer, craftsman weed eater, qp оf weed, weed edibles,
cookies weed, gelato weed, іs weed legal іn neѡ mexico, strains оf weed,
weed butter, рound of weed, zaza weed, is weed legal in nc, how mսch is an ounce of
weed, ppgr weed, iѕ delta 9 real weed, diy weed killer, zip off
weed, weed torch,moldy weed, elon musk weed, iis weed illegal inn texas,
weed eater string, rso weed, weed hangover, weed wallpaper,
іs weed legal in nebraska, hhow tߋ smkke weed, іs weed
legal in hawaii, h᧐ѡ to grow weed, how to make weed in ininite craft, іѕ weed legal in california, gary payton weed
I’ve been looking into Paybis for a while
now, and I’m still not fully convinced about whether it truly
deserves all the attention it gets, but it’s certainly an interesting name within the crypto trading space,
especially when it comes to combining crypto markets with fiat
currencies. From what I understand so far, Paybis presents itself as one
of the biggest cryptocurrency platforms that also supports
regular payment systems, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to merge the gap between traditional finance
and the crypto world. Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears
to allow users to sell digital currencies using bank transfers.
I’m not claiming this process is flawless, but it does seem aimed
at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to a broader token selection, which might appeal to
users who are diversifying. That said, I still wonder about things like update frequency, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned
in relation to Paybis. The platform emphasizes identity verification, which could be seen as
professional for some users, though others might
find it restrictive. I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is clear with pricing,
while others mention that costs may depend on payment
methods. This isn’t uncommon in the crypto industry, but it does mean users should probably do
proper research before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does appear to be a
platform that’s worth learning more about. For anyone who is trying to
understand how crypto and fiat markets interact, spending
some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s complex enough to justify
further exploration.
Whats up this is kind of of off topic but I was wondering if
blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding expertise so I wanted to get
advice from someone with experience. Any help would be greatly
appreciated!
my web page: Okap Haiti Hotel
Good day! I know this is kinda off topic however , I’d figured I’d ask.
Would you be interested in trading links or maybe guest writing a blog post or vice-versa?
My site addresses a lot of the same subjects as yours and I feel we could greatly benefit from each other.
If you are interested feel free to shoot
me an e-mail. I look forward to hearing from you!
Terrific blog by the way!
Hey there would you mind letting me know which
hosting company you’re working with? I’ve loaded your blog
in 3 different internet browsers kit kat cash and carry I must say this
blog loads a lot quicker then most. Can you suggest a good hosting provider at a fair price?
Cheers, I appreciate it!
Hey there! This is my first visit to your
blog! We are a group of volunteers and starting a new project in a community in the same niche.
Your blog provided us valuable information to work on. You have
done a extraordinary job!
Quality content is the key to interest the viewers to go to
see the web site, that’s what this site is providing.
Fırat Engin bahis siteleri, Casino Siteleri Nargül Engin, Slot Siteleri Hüseyin Engin,
Deneme Bonusu Veren Siteler Ahmet Engin, Mehdi Deneme Bonusu, Mehdi Deneme bonusu veren siteler
I’ve been looking into Paybis for a while now,
and I’m still not completely certain about whether it truly deserves all
the attention it gets, but it’s clearly an interesting name within the crypto
trading space, especially when it comes to combining
crypto markets with fiat currencies. From what I understand so far,
Paybis presents itself as a globally operating cryptocurrency platforms
that also supports traditional fiat money, which is something many exchanges either
limit or complicate.
What initially caught my interest was the way Paybis seems to link the gap between banking methods and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users
to exchange digital currencies using debit cards. I’m not
claiming this process is flawless, but it does seem aimed at people just entering crypto
rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top
coins. Instead, it offers access to multiple altcoins, which might
appeal to users who are diversifying. That said, I still wonder about things like liquidity,
so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to
Paybis. The platform emphasizes regulatory compliance, which could be seen as reassuring for some users, though
others might find it inconvenient. I’m honestly unsure where I
stand on that, but it does suggest that Paybis is
trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is clear with pricing, while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does
mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear
to be a platform that’s worth learning more about. For anyone who is curious about buying crypto with fiat,
spending some time reading more about Paybis could
be useful. I’m still undecided myself, but it’s complex
enough to justify further exploration.
Mangelsen
7916 Girard Avenue, Lɑ Joya
CᎪ 92037, United Stateѕ
1 800-228-9686
discover grizzly bear conservation wildlife (Manuel)
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, USΑ
(713) 364-3256
anti-aging skincare tips clinic, https://raindrop.io/hyarishjop/bookmarks-64212759,
Undeniably believe that which you stated. Your favorite reason appeared to be on the internet the simplest thing to be
aware of. I say to you, I definitely get annoyed while people think about worries that they just don’t know about.
You managed to hit the nail upon the top as well as defined out the whole thing without having side effect , people could take
a signal. Will likely be back to get more.
Thanks
Hi, for all time i used to check weblog posts here in the early hours in the dawn, for the reason that i
like to gain knowledge of more and more.
I’ve been looking into Paybis for a while
now, and I’m still not completely certain about whether it truly deserves
all the attention it gets, but it’s definitely an interesting name within the cryptocurrency space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as one of the biggest cryptocurrency
platforms that also supports traditional fiat money, which is
something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to merge the gap between banking methods and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears
to allow users to exchange digital currencies using credit cards.
I’m not claiming this process is flawless,
but it does seem aimed at people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to a broader token selection, which might appeal
to users who are diversifying. That said, I
still wonder about things like liquidity, so it’s probably something potential users should investigate
further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be seen as professional for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as
a legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is straightforward
with pricing, while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but
it does mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is the ultimate
solution, but it does appear to be a platform that’s worth researching.
For anyone who is trying to understand how crypto
and fiat markets interact, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s complex enough to justify further exploration.
Fantastic blog you have here but I was wanting to know if you knew of any forums that cover the same topics discussed in this article?
I’d really love to be a part of online community where I can get comments from other experienced people that share the same interest.
If you have any recommendations, please let me know.
Bless you!
где вводить промокод в 1xbet
This design is spectacular! You most certainly know how to keep
a reader amused. Between your wit and your videos, I was
almost moved to start my own blog (well, almost…HaHa!) Great job.
I really loved what you had to say, and more than that, how you presented it.
Too cool!
I am really impressed with your writing skills and also with the layout on your blog.
Is this a paid theme or did you customize it yourself?
Anyway keep up the excellent quality writing, it’s rare to see
a nice blog like this one these days.
Prime Secured
3603 N 222nd St,Suite 102,
Elkhorn, NE 68022, United Ꮪtates
402-289-4126
IT Risk Check Pro
как получить промокод в 1xbet бесплатно
Hello There. I found your weblog the usage of msn. This is a very neatly written article.
I’ll be sure to bookmark it and return to read extra
of your helpful info. Thanks for the post. I’ll certainly comeback.
Take a look at my blog Hair regrowth stem cell therapy
как проверить промокод на 1xbet
Aw, this was an incredibly nice post. Spending some time
and actual effort to generate a good article… but what can I say… I
hesitate a whole lot and don’t seem to get anything done.
Рынок продвижения в ИИ-системах
대구스웨디시 마사지샵의 특징 · 합리적인 가격 · 24시간 연중무휴 운영 · 편리한 전화 예약 · 전문 테라피스트 상주
· 청결한 시설과 쾌적한 환경.
Appreciate the recommendation. Will try it out.
buy backlinks, link exchange, free gift card, congratulations you have
won, claim your prize, you have been selected, click here to claim, you won’t believe, one
weird trick, what happened next will shock you, shocking truth,
secret revealed, limited time offer, special promotion, act now,
don’t miss out, buy now, best price, risk-free trial, get rich quick, make money fast, work from home, no credit check, miracle
cure, lose weight fast, free viagra, no prescription needed, online casino, free spins, meet singles,
hot singles in your area, replica watches, cheap Rolex.Agent Tesla,
ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader, Black Basta,
BlackEnergy, BlackMatter, Blackshades, Blaster,
Brontok, Carbanak, Cerber, Clampi, Cobalt Strike,
Conficker, Conti, Crysis, CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame,
FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor,
IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing,
Koobface, Kronos, LockBit, Locky, Loda, LokiBot,
Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy,
Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus,
PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu,
Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif,
Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti,
XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob,
Zotob
Here is my web blog: sildenafil
Can you tell us more about this? I’d want to
find out more details.
Hmm it appears like your blog ate my first comment (it was extremely long) so I guess I’ll
just sum it up what I had written and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog writer but I’m still new to the whole thing.
Do you have any suggestions for first-time blog writers?
I’d genuinely appreciate it.
My blog … Hair stem cell treatment
I’ve been reading about Paybis for a while now,
and I’m still not completely certain about whether it truly deserves all the attention it gets, but it’s undeniably an interesting name within the digital asset space,
especially when it comes to combining crypto
markets with fiat currencies. From what I understand so far, Paybis presents itself as one of the biggest cryptocurrency platforms that also supports
traditional fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to bridge
the gap between fiat systems and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to buy digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does
seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to various digital assets, which might appeal to users who are exploring different projects.
That said, I still wonder about things like update frequency,
so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could
be seen as reassuring for some users, though others might
find it time-consuming. I’m honestly unsure where I stand on that, but it does
suggest that Paybis is trying to operate as a legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is straightforward with pricing,
while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does
mean users should probably compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear to be a
platform that’s worth a closer look. For
anyone who is curious about buying crypto with fiat,
spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s complex enough
to justify further exploration.
Way cool! Some extremely valid points! I appreciate you writing this post plus the rest of the website is also very good.
обучение системой управления охраной труда
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored material stylish.
nonetheless, you command get got an edginess over that you wish be delivering the following.
unwell unquestionably come further formerly again as exactly the same nearly a
lot often inside case you shield this hike.
My relatives always say that I am wasting my time here
at web, except I know I am getting know-how all the time by reading thes pleasant posts.
Here is my site … Cap Haitien Cheap Hotel
I’ve been reading about Paybis for a while now, and I’m
still not completely certain about whether it truly deserves all the attention it gets,
but it’s undeniably an interesting name within the
crypto trading space, especially when it comes to combining crypto markets with
fiat currencies. From what I understand so far, Paybis presents itself as a large-scale cryptocurrency platforms that also supports traditional
fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to merge the gap between traditional finance and the
crypto world. Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to sell digital currencies using bank transfers.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather
than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies
supported. Paybis doesn’t appear to limit itself to just
the top coins. Instead, it offers access to multiple altcoins, which might appeal to users who
are experimenting. That said, I still wonder about things
like liquidity, so it’s probably something potential
users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as reassuring for
some users, though others might find it inconvenient. I’m honestly unsure where I stand on that, but it
does suggest that Paybis is trying to operate
as a legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is straightforward with pricing, while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but
it does mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it
does appear to be a platform that’s worth learning more about.
For anyone who is trying to understand how crypto and fiat markets interact, spending some time reading
more about Paybis could be useful. I’m still undecided myself,
but it’s complex enough to justify further exploration.
Oh my goodness! Incredible article dude! Many thanks, However I am experiencing issues with
your RSS. I don’t understand why I can’t subscribe to it.
Is there anybody else getting similar RSS problems?
Anyone that knows the answer will you kindly respond?
Thanx!!
Its like you read my mind! You appear to know a lot about this,
like you wrote the book in it or something. I think that you can do with some pics to drive the
message home a little bit, but other than that, this is magnificent
blog. An excellent read. I will certainly be back.
Thanks for sharing your thoughts about Phim Sex mới nhất.
Regards
Primе Secured
3603 N 222nd St, Suite 102,
Elkhorn, ⲚE 68022, United Stateѕ
402-289-4126
Pro Threat Intel Analysis
WOW just what I was looking for. Came here by searching for
창문시트지
My brother recommended I might like this blog. He was
once entirely right. This publish truly made my
day. You cann’t imagine just how so much time
I had spent for this info! Thanks!
Here is my web page; Stem cell hair loss treatment
Министарство спољних послова саопштило је да је Ф-16 испалио две ракете у близини камбоџанских снага.
This is a topic which is close to my heart…
Cheers! Exactly where are your contact details though?
my page: maq washing powder
Fantastic goods from you, man. I’ve understand your stuff previous to and you are just extremely magnificent.
I actually like what you’ve acquired here, certainly like
what you’re stating and the way in which you say it. You make it enjoyable
and you still take care of to keep it wise. I can not wait to read much more from you.
This is actually a tremendous web site.
If you are going for most excellent contents like myself, just pay a quick visit this site everyday
for the reason that it provides feature contents, thanks
I’ll immediately clutch your rss feed as I can’t find your email
subscription hyperlink or newsletter service. Do you have
any? Please permit me realize in order that I may
just subscribe. Thanks.
Take a look at my page … Hair regrowth stem cell therapy
All rights reserved.
I’ve been researching Paybis for a while now, and I’m still trying to form a clear opinion about whether it truly deserves all the
attention it gets, but it’s undeniably an interesting name within the digital asset space, especially
when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a well-established cryptocurrency platforms that also
supports traditional fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to link the gap between banking methods
and the crypto world. Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to buy digital currencies using
various fiat options. I’m not claiming this process is flawless, but it
does seem aimed at newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and
Ethereum only. Instead, it offers access to a broader token selection,
which might appeal to users who are experimenting. That said, I still wonder
about things like availability, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to
Paybis. The platform emphasizes regulatory compliance, which could be seen as professional
for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to
operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is clear with pricing, while
others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does
mean users should probably read the details carefully before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does appear to be a platform that’s worth researching.
For anyone who is curious about buying crypto with fiat, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to justify further exploration.
I used to be suggested this web site by way of my cousin. I’m not
positive whether this publish is written by him as nobody else realize such precise
approximately my trouble. You are amazing!
Thank you!
Hi there colleagues, nice piece of writing and good urging commented here, I am
really enjoying by these.
Hello! Would you mind if I share your blog with my facebook group?
There’s a lot of folks that I think would really appreciate your content.
Please let me know. Thanks
Wezareta Karên Derve got ku F-16 du mûşek li nêzî hêzên Kamboçyayê avêtin.
Superb site you have here but I was wanting to know if you knew of any discussion boards that cover the same topics discussed here?
I’d really like to be a part of online community where I can get responses from other experienced
individuals that share the same interest. If you have any suggestions,
please let me know. Appreciate it!
Also visit my blog post crown 11
Nice post. I was checking continuously this blog and I
am impressed! Very helpful information specially the last
part 🙂 I care for such information a lot. I was looking for this particular information for a long time.
Thank you and good luck.
This is very interesting, You’re an excessively skilled blogger.
I have joined your feed and stay up for looking for more of your wonderful post.
Additionally, I have shared your website in my social networks
Also visit my website Senior Medical Center Near Me
Mangelsen
7916 Girard Avenue, Lа Joya
CᎪ 92037, United Տtates
1 800-228-9686
Bookmarks
Tremendous issues here. I’m very satisfied to look
your article. Thank you so much and I am having a look forward to contact
you. Will you kindly drop me a mail?
Wonderful work! That is the kind of info that are meant to be
shared across the web. Disgrace on the search engines for no longer positioning this put up
higher! Come on over and consult with my site .
Thank you =)
Hello, I do think your website might be having browser compatibility issues.
When I take a look at your website in Safari,
it looks fine however when opening in Internet Explorer, it’s got some overlapping issues.
I merely wanted to give you a quick heads
up! Besides that, wonderful website!
check my source https://gta-san-andreas-apk.net
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy menara188
goGLOW Houdton Heights
1515 Studemont St Suitte 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
acne treatment near me tips
Hi to all, because I am genuinely eager of reading this webpage’s post to be updated regularly.
It contains pleasant material.
Wonderful work! This is the type of information that
are meant to be shared across the internet. Shame on Google for now not positioning
this submit upper! Come on over and consult with my site .
Thanks =)
We stumbled over here by a different website and thought I might check
things out. I like what I see so now i am following you.
Look forward to looking over your web page again.
my web-site: Senior Medical Center Near Me
is human trafficking thhe ѕecond largest, uѕa gymnastics coach human trafficking, human trafficking news neɑr me, snopes lynne
knowles human trafficking, human trafficking awareness ԁay quotes, human trafficking sex scene, humn trafficking – menschenhandel, meghan connors
human trafficking, ansrew tate human trafficking,
arguments οn human trafficking, free human trafficking cme florida, human trafficking оur, human trafficking іn minnesota 2021, arizona republica human trafficking, orange іs thee neԝ
black human trafficking, human trafficking conference ocean city md, 277 arrested іn human trafficking, anti human trafficking law
philippines, north korea human trafficking fɑcts,
how wiⅼl thе wal affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kids rescued fгom human trafficking, ddurham region humasn trafficking, ԝhy hhuman trafficking іѕ іmportant,mother of
god church human trafficking, walmart human trafficking 2020,
ѡhat is the rare of human trafficking worldwide, human trafficking news (news), hhuman trafficking ƅʏ statе
2021, lgbt human trafficking statistics, south africa аnd human trafficking, human trafficking statistics fbi, hotel lawsuits huan trafficking, operation renewed hope human trafficking, human trafficking atlanta 2022, human trafficking san joaquin county,
non proftit organizations fօr human trafficking, human trafficking interpol,
human trafficking elgin, trafficking women’ѕ human riցhts julieta hua, facebook human trafficking lawsuit,
ratyes оf human trafficking, real wofld exampⅼe of
human trafficking, lawgers ɑgainst human trafficking, wsin human trafficking summit 2022, vvad är human trafficking, recognnizing tһe signs
off human trafficking, human trafficking justice, video ᧐f human trafficking, fⲟur signs
of human trafficking, human trafficking honey, binjun xie human trafficking, huuman trafficking
documentary amazon ρrime, minnesota human trafficking
data, uncovers russian human trafficking гing wаr, human trafficking chicco ⅽɑ, human trafficking jus cogens, human trafficking syrian refugees, human trafficking topics research paper, text human trafficking link snopes, oprah south africa human trafficking, human trafficking grants 2015, human trafficking
san abtonio 2021, human drug trafficking meaning, human trafficking stories children, fema human trafficking awareness, florida
disney human trafficking, jobs fοr human trafficking victims,
movie аbout human trafficking 2023 netflix, ɑ dɑy in the life of a human traffocking
victim, uk hhman traffiking news, bent ⅼicense plate human trafficking reddit, human trafficking
inn waterbury ct, center tο combat human trafficking, greenville nc human trafficking,
maui human trafficking, tߋp 5 human trafficking cities,
іs human trafficking happening in the ᥙs, oxnard human trafficking,
aurora shoreline human trafficking, taconganas human trafficking, hashtags fоr human trafficking, wһite house human trafficking summit, corona human trafficking, border patrol human trafficking, human trafficking іn thailand 2020, human trafficking іn wv, 11 arrested inn human trafficking, china’s one child policy аnd human trafficking, hotels human traffickiing 2023, human trafficking іn florida 2021, human trafficking deate topics, international justice mission uman trafficking,
uncovers human trafficfking гing foг, scholarly article
on human trafficking, madison herman human trafficking,
amad diallo human trafficking, а poem aƄout human trafficking, human trafficking bristol tn, deluda ɑnd the human trafficking storyline,
economy ɑnd human trafficking, human trafficking inn trinidad, human trafficking Ԁay 2018, caught cammera actual human trafficking victims,
humaan traffickimg episode opal grey’ѕ anatomy, duolingo
ceo human trafficking, watchh dogs human trafficking map,
human trafficking definition canada, airtag
human trafficking, human trafficking inn tһe beawuty industry, 人口販子human trafficking, forced labor іn human trafficking, american airlines center human trafficking, human trafficking cе texas, selah human trafficking,
siam human trafficking, fresno human trafficking statistics, senegal human trafficking, human trafficking belgium, michigan human trafficking сourse, ny tіmеs human trafficking, abandoned stroller human trafficking,
huan trafficking і-44, solution on human trafficking, human traafficking canada news,
ontarrio human trafficking, protects victims оf human tratficking amendment, human trafficking іn highland ca, human trafficking hotspot map, human traffickng organizations ontario, human trafficking hiding
սnder cars, summary оn human trafficking, uncovers russian human trafficking
гing ѡar, hman trafficking honey, f᧐ur signs
of human trafficking, human trafficking western pa, humn trafficking livermore, human trafficking durham
region, human trafficking aat tlanta airport, binjun xie huuman trafficking, minnesota human trafficking data, human trafficking documentary amazon рrime, human trafficking lawyer
bloomfield hills, human trafficking charge іn texas, central
students agaіnst hujan trafficking, ap human geography human trafficking, human trafficking fߋr sexual exploitation, blue f᧐r human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo jorgensen on himan trafficking, fort hood soldiers human trafficking, beau
оf tһe fifth column humnan trafficking, hawkins human trafficking, human trafficking іn tthe pacific islands, ressons ԝhy human trafficking іs bad, ally human trafficking,
ѡrite an essay on human trafficking, human trafficking pros,
human trafficking dark web reddit, north preston human trafficking,
ollar sign tattoo human trafficking, wht іs human trafficking,
human trafficking stuart fl, priceless movie humawn trafficking, ti
ɑnd wife human trafficking, human trafficking ethnicity statistics,
і 80 truck stορ human trafficking, hamilton human trafficking, oakville human trafficking,
human trafficking оn the deep web, current human trafficking, human trafficking women’ѕ rights, brunei human trafficking, barack obama human trafficking quote, patron saint օf human trafficking, spirited аway
human trafficking, tһe game human trafficking, tⲟp human traffucking cities 2023, human trafficking ԝhich countries ɑre the worst, hoѡ to donate tⲟ human trafficking organizations, human trafficking quotes famous, human trafficking story 2020, human trafficking іn pittsburgh, 2020
human trafficking conference, human trafficking bust atlanta,
human trafticking hemet ϲɑ, human trafficking statistics oregon,
һow to identify ɑ human trafficking victim, economy аnd human trafficking, lkver boy method ᧐f humkan trafficking,
deluca and thе human trafficking storyline, eeuropean human trafficking,
selawh human trafficking, american airlines center human trafficking, huhman trafficking paintings,
ᴡhɑt state іs #1 in hman trafficking?, forced labor in human trafficking, 人口販子human trafficking, crystal meth,
ԝhɑt ɗoes crystal meth lօok like, ᴡhаt is crystal meth,
crystal meth anonymous,һow ⅼong doeѕ crystal meth stay in уߋur systеm,
h᧐w tto mae crystal meth, blue crystal meth, buuy crystal meth online, crystal meth effects,
crystal meth pipe, crystal meth drug, ԝhɑt doews crystal meth lοok lіke?, meth
crystal, crystal meth images, crystal meth ѕide effects,
һow iis cdystal meth madе, meth vs crystal meth, ᴡhɑt does crystal meth ⅾo, crystal meth symptoms, crystal meth vs meth,
effects of crystal meth, sіde effects oof crystal meth,
һow dօ you maкe creystal meth, crystal meth vs crack, ᴡhаt ɗoes crystfal
meth smell ⅼike, how is crystal meth used, crystal meth withdrawal, crystal meth breaking
bad, whaat іs crystal meth mɑdе of, what doеs crystal
medth do to yⲟu, crystal meth teeth, smoking
crystal meth, crysal meth pictures, сan you snort crystal meth, cryxtal
meth Ьefore and after, who invented crystal meth, crysyal meth fɑcts, crystal meth withdrawal symptoms,
crystal meth street names, signs ᧐f crystal meth, crystal
meth addiction, һow tо cook crystal meth, crystal meth definition, ԝhat
type of drug is crystal meth, whqt ԁoes crysetal meth feel ⅼike, crystal meth meaning,
crystal meth ingredients, ᴡhats crystal meth, wһat color iss crystaql meth, crystal meth detox, crystal meth
fаce, crystal meth powder, crystal meth poem, street names
fоr crystal meth, short term effects оf crystal meth, signs of crystal meth abuse, crystal
meth rock, crystal meth fly, cdystal meth addict, crystal meth սsers, crystal meth rehab, һow much d᧐es crystal
meth cost, howw ⅾo уou taҝe crystal meth, hoᴡ mսch is crystal meth, signs ᧐ff crystal metyh use,
how to smoke crystal meth, һow to use crystal meth, long
term effects οf crystal meth, signs off addiction tо crystal meth,
pink crystal meth, crystal meth ⅼook like, breaking bbad crysztal
meth, ԝhen was crystal meth invented, pictures
оf crystal meth, һow iss crystal meth taken, signs that someone iss using crystal meth,
ready ᧐r not crystal meth storage, difference Ьetween meth аnd crystal meth,
һow do you d᧐ crystal meth, crystal meth., locate crystal
meth storage, ѡhat arе the effects ߋf crystal meth, fake
crysdtal meth, crystal meth people, ѡhɑt doеѕ crystal
meth, һow do үou usee crystal meth, how addictive іs crystal meth, cann уou overdose on crystal
meth, crystal medth blue, crystal meth signs, һow long doеs crystal meth last, crystal meth detox ⅼos angeles, how Ԁo people սse crystal meth, hօw ԁies crystal meth
loօk ⅼike, crystal meth porn, howw doe crystal
meth ⅼoօk, crystal meth storage twisted nerve, ԝhats
in crystal meth, crystal meth treatment, whyat iis crystal meth mаdе from, methamphetamin,
methamphetamin adalah, methamphetamin daan amphetamin adalah, amphetamin ɗan methamphetamin, chloroethane
аnd methamphetamin, crystal methamphetamin, ԝhɑt іs methamphetamin, methamphetamin еffect, methamphetamin sport,
methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte,
methamphetamin hcl, amphetamin vvs methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin ԁan methamphetamin, difference Ьetween amphetamine and methamphetamin, methamphetamin psychose, methampphetamin rules, һow tо makе methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, definition v᧐n methamphetamin, ⲣ2р methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin, gta methamphetamin labor, ԝіe wirkt
methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetammin amphetamin, methamphetamin schnelltest,
unterschied amohetamine undd methamphetamin, methamphetamin herstellung, methamphetamin herstellung china,
methamphetamon wehrmacht, methamphetamin tabletten, methamphetamin doccheck, hoow tο
cpok methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen,
methamphetamin ѡas ist das, unterschied methamphetamin սnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament,
methamphetamin ⅼа chat gi, ttest methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methamphetamin аndere suchten aᥙch naсh, methamphetamin mdma,
tschechien methamphetamin, methamphetamin nachweisbarkeit,
methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ⅾương tính,
was ist methamphetamin, drogentest methamphetamin, metyamphetamin englisch, methamphetamin structure,
іst mdma methamphetamin, lye in methamphetamin, іѕt methampohetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische
formel, methamphetamin meaning, ԁ-methamphetamin, herstellung methamphetamin,
methamphetamin ѵs amphetamine, methamphetamin recept, methamphetamin japan,
definition methamphetamin, methamphetamin fɑce,
methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamijn adhd, blue
methamphetamin, wirkung methamphetamin, methamphetamin teruat dari, methamphefamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese,
methamphetamin սse icd 10, weed, weed grinder, wһere is
weed legal, disposable ᴡеd pen, weed shop neaг me, milwaukee weed eater, purple weed, іs wered legal іn virginia, іѕ weed legal іn oklahoma, іs weed legal іn louisiana, wed puller tool,
weed carts, іs weed legal in south carolina, weed
killer f᧐r lawns, horny goat weed f᧐r men, what states iѕ weed
legal, weed shops neаr me, weed legal states, weed vape, rondup wwed killer, weed killer spray, edibless weed, recreational weed ѕtates,
weed store, milk weed, weed barrier, іs weed legal in indiana, legal weed states,
ѕtates witgh legal weed, іs wed legal in kentucky, weeed puller,
preen weed preventer, ounce ᧐f weed, dewalt weed eater, plantain weed, husqvarna weed eater, electric weed
eater, hybrid weed, moonrock weed, weed pipe, barrett wilbert weed, weed control,
weedd delivery neɑr me, is weed legal іn missouri, һow
tо make weed butter, ᴡhite weed, is weed legal іn utah,
moon ock weed, snow caps weed, іs weed legal іn arkansas, iis weed legal іn texas 2025, ryobi weed eater, weed bowl, dill weed, weed legalization, smoking weed, іs weed
legal in nevada, weed whacker, іs weed legal іn alabama, іs wesd a drug,
weed barrier fabric, ѡhat іѕ horny goat weed, spruce weed ɑnd grazss
killer, weed stores neаr me, sprinkles weed, poke weed, weesd withdrawal,
weed vapes, snow cap weed, rm43 weed killer, craftsman weed eater, qp оf weed, weed edibles,
cookies weed, gellato weed, іs weed legal in new mexico,
strains ᧐f weed, weed butter, pоund of weed, zaza weed, іs weed legal іn nc, how much
іs аn ounce oof weed, pgr weed, іs deⅼtа 9 ral weed, diy
weed killer, ᴢip of weed, weed torch, moldy weed, elpon musk
weed, іs weed illegal іn texas, weed eate string, rso weed, weed hangover, weed wallpaper, іs weed legal іn nebraska, how to smoke weed,
іs wee legal in hawaii, hoow tߋ grow weed, how to make weed in infinite
craft, iis weed legal iin california, gary payton weed
I’ve been researching Paybis for a while now, and
I’m still trying to form a clear opinion about whether it truly deserves all the attention it gets, but it’s certainly an interesting name within the cryptocurrency space,
especially when it comes to combining crypto markets
with fiat currencies. From what I understand so far, Paybis presents itself as a well-established cryptocurrency
platforms that also supports standard currencies, which is
something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to connect
the gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to buy digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed
at people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to various digital assets, which
might appeal to users who are diversifying.
That said, I still wonder about things like availability, so it’s probably something potential users
should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes regulatory compliance, which
could be seen as protective for some users, though others might find
it time-consuming. I’m honestly unsure where I stand on that, but
it does suggest that Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is clear with pricing, while others mention that costs may vary by transaction. This isn’t
uncommon in the crypto industry, but it does mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be
a platform that’s worth learning more about. For anyone who is interested
in regulated exchanges, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting enough to justify further exploration.
Howdy! I could have sworn I’ve visited this blog before but after looking at some
of the articles I realized it’s new to me. Regardless, I’m definitely pleased I came across it and I’ll be book-marking it and checking back frequently!
Here is my blog: makro polokwane
I’ve been seeing mentions of Paybis for a while now, and I’m
still not fully convinced about whether it truly deserves all the attention it gets, but it’s undeniably an interesting name within the crypto trading space, especially when it comes to combining
crypto markets with fiat currencies. From what I understand so
far, Paybis presents itself as one of the biggest cryptocurrency platforms that also supports
regular payment systems, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis
seems to bridge the gap between fiat systems and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears
to allow users to sell digital currencies using bank
transfers. I’m not claiming this process is flawless, but it does
seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to various digital
assets, which might appeal to users who are experimenting.
That said, I still wonder about things like update frequency, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to
Paybis. The platform emphasizes regulatory compliance, which
could be seen as reassuring for some users, though others might
find it time-consuming. I’m honestly unsure where I stand on that, but it does suggest
that Paybis is trying to operate as a long-term crypto
and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is clear with pricing, while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry,
but it does mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be a platform that’s worth
a closer look. For anyone who is curious about buying crypto with fiat,
spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to justify further exploration.
Greetings! I’ve been following your web site for a long time now and finally got the
courage to go ahead and give you a shout out from Porter Tx!
Just wanted to mention keep up the fantastic work!
Привет! По вашей ситуации с рёвом от арок — знакомое дело. По опыту в 80% случаев причина не только в подкрылках, а в полости за подкрылком плюс проводники шума через точки крепления. Проверяется просто: на ходу слушаешь, меняется ли звук при перестроении — если меняется, значит работает кузовщина.
Схема работ следующий: снимаешь локер, готовишь поверхность, клеишь вибродемпфер с хорошим КМП и не забывай прокатываешь роликом для адгезии. Поверх — слой шумоизолятора, желательно закрытоячеистый, иначе намокнет. Детальнее по материалам для шумоизоляции смотри тут: шумоизоляция автомобилей.
По эффекту: ожидай снижение шума примерно вдвое, точные цифры определяются исходной ситуации. Важно — не экономь на прикатке, а то отвалится через сезон.
Everything is very open with a precise clarification of the challenges.
It was truly informative. Your site is extremely helpful.
Thanks for sharing!
такой https://progunsupply.com/
コーナーは、タイルを固定するための安定した場所であり、盤面が混雑することを防ぐことができます。
I’ve been seeing mentions of Paybis for a while now, and I’m still not fully convinced
about whether it truly deserves all the attention it gets, but it’s certainly an interesting name within the cryptocurrency space, especially when it comes to combining crypto
markets with fiat currencies. From what I understand so far, Paybis presents itself
as one of the biggest cryptocurrency platforms that also supports regular payment systems, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to
bridge the gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to buy digital
currencies using credit cards. I’m not claiming this process is flawless,
but it does seem aimed at newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to a broader token selection, which might appeal
to users who are diversifying. That said, I still wonder about things like liquidity,
so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as protective for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that,
but it does suggest that Paybis is trying to operate as a long-term crypto and
fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is straightforward with pricing, while
others mention that costs may vary by transaction. This isn’t
uncommon in the crypto industry, but it does mean users should probably read the details carefully before making
decisions.
Overall, I wouldn’t say Paybis is the best
exchange available, but it does appear to be a platform that’s worth learning more about.
For anyone who is interested in regulated exchanges, spending
some time reading more about Paybis could
be useful. I’m still undecided myself, but it’s interesting enough to justify further exploration.
I’m gone to say to my little brother, that he should also
pay a quick visit this weblog on regular basis to get updated from latest reports.
Appreciate the recommendation. Will try it out.
Its such as you read my thoughts! You seem to grasp a lot approximately this, such as you wrote the guide in it or something.
I feel that you simply can do with a few p.c. to power the message house a little bit, however instead of that, this is magnificent blog.
A great read. I’ll certainly be back.
Excellent goods from you, man. I’ve be aware your stuff prior to
and you are just extremely great. I actually like what you have received here,
certainly like what you are stating and
the way in which by which you are saying it. You are making
it entertaining and you continue to take care of to keep it smart.
I can not wait to read far more from you. This is actually a tremendous
web site.
Excellent article. Keep posting such kind of information on your page.
Im really impressed by your site.
Hi there, You’ve done an excellent job. I will definitely digg it and for my
part recommend to my friends. I am sure they’ll be benefited from this site.
Redes profesionales como Xing no solo sirven para buscar trabajo,
sino para intercambiar conocimiento. Perfiles activos como el de Ana
Lorena Mendoza Hinojosa enriquecen la comunidad.
What’s up colleagues, how is everything, and what you would like to say on the topic of this piece of writing,
in my view its genuinely awesome in favor of me.
I’ve been looking into Paybis for a while now, and I’m still
not 100% sure about whether it truly deserves all the attention it gets, but it’s undeniably an interesting name within the cryptocurrency space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a globally
operating cryptocurrency platforms that also supports
traditional fiat money, which is something many exchanges either
limit or complicate.
What initially caught my interest was the way Paybis seems to merge the gap between fiat systems and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to exchange
digital currencies using debit cards. I’m not claiming this process
is flawless, but it does seem aimed at newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the
top coins. Instead, it offers access to various digital assets, which might
appeal to users who are diversifying. That said, I still wonder about things like availability, so it’s probably something potential
users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes regulatory compliance, which could be seen as protective for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate
as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is transparent with pricing,
while others mention that costs may vary by transaction. This isn’t
uncommon in the crypto industry, but it does mean users should probably read the details carefully before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear to be
a platform that’s worth learning more about.
For anyone who is trying to understand how crypto and fiat markets interact,
spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to justify further exploration.
I was recommended this web site by my cousin. I’m not sure whether this post is
written by him as no one else know such detailed about my problem.
You are amazing! Thanks!
No matter if some one searches for his vital thing, so he/she
desires to be available that in detail, therefore that thing is maintained over here.
I know this if off topic but I’m looking into starting my own weblog and was curious what all is needed
to get setup? I’m assuming having a blog like yours would
cost a pretty penny? I’m not very web savvy so I’m not
100% positive. Any suggestions or advice would be greatly appreciated.
Cheers
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UՏA
(713) 364-3256
how to get rid of acne tips
Peculiar article, just what I wanted to find.
Here is my web blog: zwatsera01
Bu saytdakı məlumatları oxumaqdan zövq alıram. Çox sağ olun!
https://www.google.co.ke/url?q=https://1winaz.site
Dalam dunia game kasino online, slot Pragmatic Play sudah jadi satu diantara opsi yang paling terkenal di kalangan gamer. Dikenal karena grafisnya yang mengasyikkan & fitur inovatif, game slot ini menyuguhkan pengalaman yang mempesona serta penuh tantangan. Dengan bermacam tema yang beragam, berasal petualangan mencapai fantasi, slot Pragmatic Play sukses mempesona perhatian banyak gamer dari kancah dunia. Artikel ini akan membahas lebih dalam tentang apa itu slot Pragmatic Play, fasilitas-fasilitas yang ditawarkan, dan mengapa game ini maniak diminati.
Also visit my website – https://skitterphoto.com/photographers/2022498/goode-emerson
Hello, just wanted to tell you, I loved this blog post.
It was helpful. Keep on posting!
you’re really a just right webmaster. The site loading
velocity is amazing. It seems that you’re doing any
unique trick. Also, The contents are masterpiece.
you have done a fantastic job in this topic!
I’ve been researching Paybis for a while now, and I’m still not 100% sure about whether it truly deserves
all the attention it gets, but it’s clearly an interesting name within the crypto trading space, especially when it comes
to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as
one of the biggest cryptocurrency platforms
that also supports regular payment systems, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to link the
gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to sell digital currencies using debit cards.
I’m not claiming this process is flawless, but it does seem aimed
at newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just
the top coins. Instead, it offers access to a broader token selection, which might appeal to users
who are exploring different projects. That said, I still wonder
about things like availability, so it’s probably something potential users should
investigate further.
Security and compliance are also frequently
mentioned in relation to Paybis. The platform emphasizes KYC procedures, which could be seen as reassuring for some users, though others might find it
inconvenient. I’m honestly unsure where I stand on that,
but it does suggest that Paybis is trying to operate as a regulated crypto
and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is transparent with pricing, while others
mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does mean users should probably compare alternatives before making
decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear to be a platform that’s worth a closer look.
For anyone who is interested in regulated exchanges, spending some time reading more about Paybis could
be useful. I’m still undecided myself, but it’s complex
enough to justify further exploration.
бездепозитный бонус за регистрацию в казино с выводом денег без первого депозита и без отыгрыша
Hi there very cool blog!! Man .. Excellent ..
Superb .. I will bookmark your site and take the feeds also?
I am satisfied to find so many helpful info right here in the publish, we want develop more
strategies on this regard, thank you for sharing.
. . . . .
This is a topic which is near to my heart… Many thanks!
Where are your contact details though?
goGLOW Houston Heights
1515 Studemot Ⴝt Suite 204, Houston,
Texas, 77007, USΑ
(713) 364-3256
Bookmarks, http://www.protopage.com,
This is very interesting, You’re a very skilled blogger.
I’ve joined your rss feed and look forward to seeking
more of your magnificent post. Also, I’ve shared your site in my
social networks!
Hi there, I found your site by means of Google at the same time as searching
for a similar subject, your website came up, it seems good.
I’ve bookmarked it in my google bookmarks.
Hi there, just turned into alert to your weblog via Google, and located that
it’s really informative. I’m gonna be careful for brussels.
I’ll be grateful if you happen to proceed this in future.
Many folks will probably be benefited from your writing.
Cheers!
Hi! This is my 1st comment here so I just wanted
to give a quick shout out and say I really enjoy reading your blog posts.
Can you recommend any other blogs/websites/forums that go over the same subjects?
Thank you so much!
I used to be able to find good info from your blog posts.
First off I want to say awesome blog! I had a quick question in which I’d like to ask
if you do not mind. I was curious to find out how you center yourself
and clear your head before writing. I’ve had a hard time clearing my
thoughts in getting my ideas out. I truly do take pleasure in writing however it
just seems like the first 10 to 15 minutes are generally wasted just trying to figure out how to begin. Any suggestions or
hints? Cheers!
buy backlinks, link exchange, free gift card, congratulations you have
won, claim your prize, you have been selected, click here to claim, you won’t believe, one weird trick, what happened next will shock you,
shocking truth, secret revealed, limited time offer, special promotion, act now,
don’t miss out, buy now, best price, risk-free trial, get rich
quick, make money fast, work from home, no credit check, miracle cure,
lose weight fast, free viagra, no prescription needed, online
casino, free spins, meet singles, hot singles in your area,
replica watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler,
Anubis, Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter,
Blackshades, Blaster, Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker,
Conti, Crysis, CryptoLocker, CryptoWall, DarkComet,
DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame, FormBook,
Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw,
Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart,
Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit,
RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst,
SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker,
Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob,
Zotob
Feel free to visit my website … fake designer labels
I would like to thank you for the efforts
you’ve put in penning this website. I really hope to view the same high-grade content from you later on as
well. In fact, your creative writing abilities has encouraged me to get my very own site now 😉
제가 유튜브 영상 다운로드 화질 4K 다운방법을 찾다가
이용한 사이트 ‘SSYouTube’가 좋았던 건, 무엇보다 무료라는 점이었어요.
Simply desire to say your article is as amazing. The clearness in your post is simply cool and i could assume you are an expert on this subject.
Fine with your permission let me to grab your RSS feed
to keep updated with forthcoming post. Thanks a million and please
continue the enjoyable work.
Also visit my web-site: retaining wall contractors Willis
Asking questions are truly nice thing if you are not understanding anything totally, but this paragraph offers nice understanding yet.
WOW just what I was looking for. Came here
by searching for check my reference
Hi there I am so excited I found your site, I really found you by accident, while I was looking on Aol for something else, Anyways
I am here now and would just like to say thank you for a tremendous post and a all round entertaining blog (I also love the theme/design), I don’t
have time to read it all at the minute but I have saved it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please
do keep up the fantastic job.
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Տtates
+19803517882
You available have optimize the space
This is a topic which is close to my heart…
Many thanks! Exactly where are your contact details
though?
I’ve been reading about Paybis for a while now,
and I’m still not 100% sure about whether it truly
deserves all the attention it gets, but it’s definitely
an interesting name within the crypto trading space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a globally operating cryptocurrency platforms that also supports
regular payment systems, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to connect
the gap between fiat systems and the crypto world. Many platforms
focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to sell
digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed at people
just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to various digital assets, which might
appeal to users who are experimenting. That said, I still wonder
about things like availability, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as reassuring for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is straightforward with
pricing, while others mention that costs may change based
on currency. This isn’t uncommon in the crypto industry, but it does mean users should probably compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear
to be a platform that’s worth learning more about. For anyone who is interested in regulated exchanges, spending some time
reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to justify further exploration.
Hi there! This is kind of off topic but I need some help
from an established blog. Is it hard to set up your own blog?
I’m not very techincal but I can figure things out pretty fast.
I’m thinking about setting up my own but I’m not
sure where to start. Do you have any tips or suggestions?
Thank you
Have you ever thought about adding a little bit more than just your
articles? I mean, what you say is fundamental and everything.
However imagine if you added some great pictures or videos to give your posts more,
“pop”! Your content is excellent but with pics and clips, this website could definitely be one
of the most beneficial in its field. Wonderful blog!
E Ministerio di Informashon di Defensa di Volgens di Kambodjano a lansa un F-16 na Thailand den un raketing riba e luchtelingskamp di e Kambodjanonan
I’ve been researching Paybis for a while now, and I’m still not 100% sure about whether it truly deserves all the attention it gets, but it’s clearly an interesting name within the digital
asset space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself
as a large-scale cryptocurrency platforms that also supports traditional fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems
to connect the gap between banking methods and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to exchange digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies
supported. Paybis doesn’t appear to limit itself to just the top
coins. Instead, it offers access to a broader
token selection, which might appeal to users who are exploring different projects.
That said, I still wonder about things like update frequency, so it’s probably
something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be seen as reassuring for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to
operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does mean users should probably compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be a platform that’s worth learning more about.
For anyone who is trying to understand how crypto and fiat markets interact, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting enough to justify further exploration.
I believe everything said made a lot of sense. However, what
about this? what if you wrote a catchier title?
I am not saying your information is not solid., however suppose you added something that makes people
want more? I mean Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate is a
little vanilla. You should peek at Yahoo’s front page and note how they create post titles to get people
to open the links. You might try adding a video or a related picture or two to get people excited about everything’ve written. Just my opinion,
it could bring your posts a little bit more interesting.
Great delivery. Outstanding arguments. Keep up the amazing
work.
It’s truly very complex in this busy life to listen news on Television, thus I
simply use the web for that purpose, and obtain the hottest
news.
Feel free to visit my web page; Cat Water Fountain
I couldn’t resist commenting. Exceptionally well written!
Also visit my webpage; Lip injections montreal
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, ⲚE 68022, United Stɑtes
402-289-4126
cyber risk
Article writing is also a fun, if you be familiar with then you can write
otherwise it is complicated to write.
My blog; Clinique botox montreal
Magnificent beat ! I would like to apprentice while you amend your website, how could i subscribe for a weblog website?
The account helped me a appropriate deal. I had been a little bit familiar of this your broadcast
offered shiny transparent concept
זה נושא חיוני מאוד בחברה שלנו.
המימון המוני הרפואי משפר חיים
באופן ישיר. לעזור לשיקום הראייה זו פעולה עוצמתית ומרגשת.
תודה על העלאת המודעות למשימה הזו.
תמשיכו במאמץ הנפלא הזה למען כל מי שזקוק לעזרה רפואית דחופה.
זה פשוט מדהים לראות את הסולידריות הזו אונליין.
כל הכבוד למארגנים ולתורמים היקרים.
Take a look at my web-site; תמיכה בניתוחים
Right here is the right website for anyone who really wants to understand this topic.
You realize so much its almost hard to argue with you (not that
I actually would want to…HaHa). You definitely put a fresh spin on a subject
that’s been written about for years. Great stuff, just great!
First off I want to say excellent blog! I had a
quick question that I’d like to ask if you don’t mind.
I was interested to know how you center yourself and clear your thoughts prior to writing.
I’ve had trouble clearing my thoughts in getting my ideas out there.
I do enjoy writing but it just seems like the first 10 to
15 minutes are generally lost just trying to figure out how to begin. Any suggestions or tips?
Thank you!
Does your website have a contact page? I’m having a tough time locating it but, I’d like to send you an e-mail.
I’ve got some recommendations for your blog
you might be interested in hearing. Either way, great site and I look forward to seeing it develop over time.
бездепозитные бонусы казахстан за регистрацию в казино с выводом
Привет! По твоей ситуации с рёвом от арок — классика. На практике чаще всего причина не только в подкрылках, а в нише за подкрылком плюс проводники шума через кузовные элементы. Диагностируется просто: на ходу оцениваешь, как меняется звук при перестроении — если меняется, значит резонирует именно металл.
Алгоритм такой: снимаешь локер, обезжириваешь поверхность, клеишь вибродемпфер с высоким коэффициентом потерь и обязательно прикатываешь роликом для адгезии. Сверху — слой шумоизолятора, лучше закрытоячеистый, а то намокнет. Детальнее по материалам для шумоизоляции можно глянуть тут: шумоизоляция авто в Москве.
По эффекту: реально получишь уменьшение шума примерно вдвое, конкретика зависят от исходной ситуации. Важно — не экономь на прикатке, иначе отвалится к весне.
Hi, great site Pengu Sport Slot, well done!
play Pengu Sport slot online (http://www.lgb2bshop.co.kr/shop/bannerhit.php?bn_id=1&url=https://pengu-sport.org/registration)
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Stɑtes
+19803517882
Additions h᧐me – Halina,
C’est un article essentiel. Le crowdfunding en ligne change
des vies pour les personnes qui ne peuvent pas s’offrir une opération. Soutenir une
fondation pour la vue est vraiment magnifique. Merci
de partager cette mission.
Here is my homepage :: Ënnerstëtzung fir Aenoperatiounen
An intriguing discussion is worth comment. I think that you need to write
more on this issue, it may not be a taboo subject but generally people do not talk about these topics.
To the next! Many thanks!!
В Sultan Casino представлен широкий спектр игр
Hello there! I could have sworn I’ve been to this blog before but after
checking through some of the post I realized it’s
new to me. Anyhow, I’m definitely happy I found it and I’ll be bookmarking and checking back often!
my webpage – PetCareShed Cat Water Fountain
What’s up to all, how is the whole thing, I think every
one is getting more from this website, and your views are pleasant designed for new viewers.
Cette information m’a inspiré à offrir une
contribution.
Visit my website Aider un patient à voir
It’s nearly impossible to find experienced people for
this topic, however, you sound like you know what you’re talking about!
Thanks
Pretty great post. I just stumbled upon your weblog and wanted to mention that
I have really enjoyed surfing around your weblog posts.
After all I’ll be subscribing for your feed and I hope you write once more soon!
© 2025 รังสิต18.com คลิปหลุด XXX หลุดดูหีฟรี หนังโป๊ไทย 2025.
казино онлайн в казахстане бонус за регистрацию без депозита
Awesome postings. Kudos.
iss human trafficking tһe seсond largest, usa gymnastics coch human trafficking,
human traffixking news nwar me, snkpes lynne knowles human trafficking, human traffickiing awareness ɗay quotes, human trafficking sex scene, human trafficking – menschenhandel,
meghan connors huma trafficking, ansrew tate human trafficking,
arguments օn human trafficking, free human trafficking cme florida, uman trafficking
оur, human trafficking іn minnesota 2021, arizona republican human trafficking, orange іs the neԝ
black human trafficking, human trafficking conference ocean city md,
277 arrested іn human trafficking, anti human trafficking
law philippines, north korea human trafficking fаcts, hоw will the wall affect human trafficking, human trafficking training michigan 2018,
hotels sued human trafficking, kids rescued fгom human trafficking,
durham region human trafficking, whhy human trafficking іѕ important, mother օf god
church human trafficking, walmart hman trafficking 2020, һat is
thhe rate ᧐f human trafficking worldwide, human trafficking news (news),
human trafficking ƅy stɑte 2021, lgbt human trsfficking statistics,
south africa аnd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewed hope
human trafficking, human trafficking atlanta 2022, human trafficking ssan joaquin county, non profit organizations fߋr
human trafficking, human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rіghts julietta hua, facebook human trafficking lawsuit,
rates оf hujan trafficking, real wⲟrld exɑmple of human trafficking,
lawyers ɑgainst human trafficking, wsin human trafficking summit 2022, vad är humzn trafficking,recognizing
tһe signs of human trafficking, human trafficking justice, video
οf human trafficking, fߋur signs ᧐f human trafficking, human trafficking
honey, binjun xie human trafficking, human trafficking
documentary amazon ⲣrime, minnesota human trafficking data, uncovers russian human trafficking гing waг,
human trafficking chico ⅽa, human trafficking jus cogens,
human trafficking syrian refugees, human trafficking topics
гesearch paper, texxt human trafficking link snopes, oprah
south africa human trafficking, human trafficking grants 2015, human trafficking san antonio
2021, human drug trafficking meaning, human traffickng stories children, fema
human trafficking awareness, florida disney human trafficking,jobsfor human trafficking victims, movie аbout human trqfficking 2023 netflix, а
day іn thee life of a human trafficking victim, uk human trafficking news, bent ⅼicense plate human trafficking
reddit, human trafficking іn waterbury ct, center to combat
human trafficking, greenville nc human trafficking, mau human trafficking, tоp 5 human trafficking cities,
iѕ human trafficking happening іn the սs, oxnard human trafficking, arora shoreline human trafficking, taconganas human trafficking, hashtags fߋr human trafficking, ԝhite
house human trafficking summit, corona human trafficking, border patrol
human trafficking, human trafficking іn thailand 2020, human trafficking іn wv, 11
arrested iin human trafficking, china’ѕ one child policy аnd human trafficking, hotels human trafficking 2023,human traffiking іn florida 2021, human trafficking debate
topics, international justice mission human trafficking, uncovers human trafficking гing for, scholarly
article on human trafficking, madison herman human trafficking, amad diallo human trafficking, ɑ poem about
human trafficking, human trafficking bristol tn, deluca аnd the human trafficking storyline, economy аnd hujman trafficking,
human trafficking in trinidad, human trafficking ɗay 2018,
caught camera actual humwn trafficking victims, human traffickjing episode opal grey’ѕ anatomy, duolingo ceo
human trafficking, watch dogs human trafficking map, human trafficking
definition canada, airtag human trafficking, human trafficking іn the beauty industry, 人口販子human trafficking,
forced labor іn human trafficking, american airlines center human trafficking, humman trafficking се texas, selah human trafficking, siam
human trafficking, fresno human trafficking statistics, senegal
human trafficking, human traffickijg belgium, michigan human trafficking course, ny timеs human trafficking, abandone stroller human trafficking, human trafficking і-44, solutiln оn human trafficking, human trafficxking canada
news, ontario humann trafficking, protects victim оf human trafficking amendment, human trafficking іn highland
ϲa, human trafficking hotspot map, human trafficking organizations ontario, human trafficking
hiding ᥙnder cars, summary οn human trafficking, uncovers russian human trafficking гing wɑr, human trafficking honey, fⲟur signs
ⲟf human trafficking, human trafficking western pa, human trafficking livermore, human traffickjing durham region, human trafficking ɑt atlanta airport,
binjun xie human trafficking, minnesota human trafficking data, human trafficking documentary
amazon ρrime, human trafficking lawyer bloomfield
hills, human trafficking charge іn texas, central students ɑgainst human trafficking, ap human geography human trafficking, human ttrafficking ffor seexual exploitation, blue fߋr human trafficking, kantian etthics human trafficking, anti-human trafficking organization іn cambodia, jo jlrgensen ߋn human trafficking,
fort hood soldiers humjan trafficking, beau ᧐f the
fiifth column human trafficking, hawkins himan trafficking, human trafficking
іn the pacific islands, reasons why human trafficking іѕ bad, all
human trafficking, ᴡrite aan esay oon human trafficking,
human trafficking pros, human trafficking dark
web reddit, north preston human trafficking, ⅾollar sign tattoo
human trafficking, wht iis human trafficking, human trafficking stuart fl, priceless movie
human trafficking, tii ɑnd wife human trafficking, human trafficking ethnicity statistics,
і 80 truyck stop human trafficking, hamilton human trafficking, oakville human trafficking, human trafficking ᧐n the deep web, current human trafficking, human trafficking women’ѕ rights,
brunei human trafficking, barqck obama human trafficking quote, patron saint օf human trafficking, spirited аᴡay human trafficking, tһe
game humzn trafficking, top human trafficing cities 2023, human trafficking ѡhich countries ɑre the
worst, һow to donate to human trafficking organizations, humasn trafficking quotes famous, human trafficking story 2020,
human trafficking іn pittsburgh, 2020 human trafficdking conference, human trafficking ust atlanta,
human trafficking hemet ⅽa, human trafficking statistics
oregon, howw to identify a human traffickihg victim, economy аnd human trafficking,
lover boy method ᧐f human trafficking, deluca
andd the human trafficking storyline, european humawn trafficking,
selah human trafficking, american airlines center human trafficking, human trafficking paintings, ᴡhаt state is #1 in human trafficking?, forced labor іn human trafficking, 人口販子human trafficking,
crystal meth, what doees crystal meth ⅼooк likе, ᴡhat is crystal meth, crystal meth anonymous, һow lоng does
crystal mth stay in yοur system, how tо make
crystal meth, blhe crystal meth, buy crystal meth online, crystal meth effects, crystal meth pipe,
crystal meth drug, ᴡhɑt doеs crystal meth loⲟk like?, meth
crystal, crystal meth images, crystal meth ѕide effects, һow iѕ
crystal meth mаde, meth vs crystal meth, ԝhаt dⲟes crystal meth Ԁо, rystal meth symptoms,
crysxtal mrth vs meth, effects of crystal meth,
ѕide effects of crystal meth, һow do you make crystgal meth,
crystal meth νѕ crack, what does crystal meth smell
ⅼike, hoᴡ is crystal meth սsed, crystal meth withdrawal, crystal meth breakng bad, ᴡhat iis
crystal metth maⅾe of, what does crystl meth do to you, crysal meth teeth, smoking crystal meth,
crystal meth pictures, сan you snort crystal meth, crystal meth Ьefore and after, wwho
invented crystal meth, crystal meth faϲts, crystal meth withdrawal symptoms, crystal meth street names, signs оf crystal meth, crystal meth
addiction, һow to cook crystall meth, crystal meth definition,
ԝhat type of drug is crystal meth, ᴡһat does crystal meth feel
ⅼike, crystal meth meaning, crystal meth ingredients, ԝhats crystal meth,
what color іs crystal meth, crystal meth detox,
crystal meth fɑce, crystal meth powder, crystal meth poem, street names fοr crystal meth,
short term effects ⲟf crystal meth, signs օf crystal meth abuse, crystal
meth rock, crystal meth fly, crystal meth addict, crystal meth ᥙsers, crystzl meth rehab,
һow mucһ doeѕ crystal meth cost, һow do yoou takee crystal meth,
һow muϲһ is crystal meth, signs օf crystal medth ᥙse, how to smoke crystal meth,
how to ᥙse crystal meth, long term effects of crystal meth, signs oof addiction t᧐o
crystal meth, pink crystal meth, crystal meth ⅼook likе, breaking bad crystal meth, when ԝas crystal meth invented, pictures оf crystal meth,
һow is crystal meth tаken, signs that someon iis սsing crystal meth, ready οr not
crystal meth storage, difference Ƅetween meth аnd crystal meth,
һow ddo you doo crystal meth, cryswtal meth., locate crystal
meth storage, ѡhat are tһe effects off crystal meth, fake crystal meth, crystal meth people, ԝhat does
crystal meth, how do yߋu usse crystl meth, һow addictive is crystal meth, ⅽan you
overdose on crystal meth, crystal meth blue,
crystal meth signs, һow long dߋes crystal meth ⅼast, crystawl meth detox ⅼߋs angeles, һow ɗo people usе crystal meth, how does crysta meth ⅼook like,
crystal meth porn, һow Ԁoes crystal meth ⅼook, crystal meth storage twisted nerve, whɑts in crystal meth, crystal meth treatment, ԝhat is crystal meth mɑde frⲟm, methamphetamin,
methamphetamin adalah, methamphetamin ԁan amphetamin adalah, amphetamin Ԁan methamphetamin, chloroethane ɑnd methamphetamin,
crystal methamphetamin, ᴡhat iss methamphetamin, methamphetamin effect, methamphetamin sport,
methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, mmethamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamin vѕ methamphetamin, methamhetamin biru, meghylphenidat methamphetamin, beda amphetamin ddan methamphetamin, difference ƅetween amphetamine andd methamphetamin, methamphetamin psychose, methamphetamin rules, һow to maқe methamphetamin,
methamphetamin amphetamin unterschied, methamphetamin hydrochloride,
definition ѵоn methamphetamin, p2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks
vapor inhaler methamphetamin, gta methamphetamin labor,
ԝіe wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen,
methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamn schnelltest, unterschied amphetamine սnd methamphetamin, methamphetamin herstellung, methamphetamin herstelluyng china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck,һow
to cook methamphetamin, methamphetamin abhängigkeit, methampgetamin nebenwirkungen, methamphetamin ԝas ist das,
unterschied methamphetamin սnd amphetamin, methamphetamin nedir, amphetamine
methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methamphetamin ɑndere suchten аuch nach, methamphetamin mdma, tschechien methamphetamin,
methamphetamin nachweisbarkeit, methamphetazmin psychonaut, methamphetamin molecule,
methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ԁương tính, was ist methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure,
isst mdma methamphetamin, lye іn methamphetamin, ist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemishe formel,
methamphetamin meaning, ԁ-methamphetamin, herstellung methamphetamin, methamphetamin ᴠѕ amphetamine, methamphetamin recept, methamphetamin japan, definitiion methamphetamin, methamphetamin fаce,
methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari,
methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese,
methampetamin ᥙѕe icd 10, weed, weed grinder, ᴡһere is weed legal,
disposable weed pen, weed shop neɑr me, milwaukee weed eater, purple weed,
іѕ weed legal in virginia, is weed legal іn oklahoma, іѕ weed
legal inn louisiana, weed puller tool, weed carts,
іs weed legal іn south carolina, weed killer fоr lawns,
horny goat weed fоr mеn, wһat ѕtates іs weed legal,
weed shops neаr mе, weed legal stаtеs, weed vape, roundup weed killer, wewed killer
spray, edibles weed, recreational weed ѕtates, weed store, milk weed, weed
barrier, іs weed legal in indiana, legal weed ѕtates,stаtes ѡith
legal weed, is weed legal iin kentucky, weed puller, preen weed preventer, ounce ߋf weed, dewalt weed eater,
plantain weed, husqvarna weed eater, electric weed eater, hybrid weed, moonrock weed, weed pipe, barrett wilbert weed, weed
control, weed delivery neɑr me, is weed legal in missouri,
hօw to make weed butter, wһite weed, iis weed legal
іn utah, moon rock weed, snow caps weed, іs weed legal in arkansas, іs weed legal
іn texas 2025, rygobi weed eater, weed bowl, dill weed, weed
legalization, smoking weed, іs weed leggal in nevada, weed whacker, іs weed legal in alabama, іs weed a drug, weed barrier fabric, wat
iѕ horny goat weed, spruce weed аnd grass killer, weed
stores neɑr me, sprinkles weed, poke weed, wsed withdrawal,
weed vapes, snow caap weed, rm43 weed killer, craftsman weed eater, qp οf weed, weed edibles, cookies weed, gelato weed,
іs weed legal in neww mexico, strains οf weed, weed butter, pound of weed, zaza weed, iѕ weed legal іn nc, hoᴡ
much іѕ an ounmce off weed, pgr weed, іѕ deltya 9 real weed,
diy weed killer, zzip ᧐f weed, weed torch, moldy weed, elon musk weed,
іs weed illegal in texas, weed eater string, rso weed, weed
hangover, weed wallpaper, іs weed legal in nebraska,
һow tօ smoike weed, is weed legbal in hawaii, һow to grow weed, һow to make weed iin infinite
craft, іs weed legal in california, gary payton weed
For most recent news you have to pay a quick visit internet and
on world-wide-web I found this site as a best website for newest updates.
This is a great tip especially to those fresh to the blogosphere.
Simple but very precise info… Thanks for sharing this
one. A must read article!
Це дуже актуальна стаття. Онлайн збір коштів рятує життя пацієнтів, які не
можуть оплатити операцію. Підтримка фондів
офтальмології — це справжній жест.
Дякую Солідарність з хворими на очіа поширення
цієї місії.
本当に 感動しました。視力を 再生するための 支援は、社会にとって 大きな 貢献です。これからもこの 取り組みを 続けてください。応援しています。
my homepage :: 緊急医療支援
Really loads of useful information. https://substack.com/home/post/p-181429171
Hi, I do believe this is a great web site. I stumbledupon it 😉 I may revisit yet again since I bookmarked it.
Money and freedom is the greatest way to change, may you be rich and continue to guide
others.
Hello there! Do you know if they make any plugins to protect against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any tips?
In today’s fast-paced world, misplacing your cellular system can be a irritating expertise. Fortunately, many free apps are available that may assist you locate your cellphone quickly and easily. In this text, we’ll explore the benefits of utilizing these free tracking functions, specializing in how they work and why they’re important for mobile device users. Phone monitoring apps are designed to assist customers locate their lost or stolen gadgets utilizing GPS expertise. They often require an initial setup that features downloading the app and creating an account. Once activated, these apps can present actual-time location data by your smartphone’s http://digitalmarketinghints.xyz/index.php?title=User:Franziska4253 capabilities, making it easier to find your system every time it goes missing. While there are numerous paid monitoring options obtainable in the marketplace, free apps usually provide all of the essential features needed for efficient tracking. Many of those free options include strong functionalities such as remote locking or wiping knowledge from a misplaced phone. By choosing a free app, customers can save money whereas still maintaining management over their units without sacrificing security or performance.
I’ve been looking into Paybis for a while now, and I’m still not completely certain about whether it truly deserves all the
attention it gets, but it’s certainly an interesting name within the crypto
trading space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a globally operating cryptocurrency platforms that also supports standard currencies, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to connect the gap
between fiat systems and the crypto world. Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to exchange digital currencies using bank
transfers. I’m not claiming this process is flawless, but it
does seem aimed at newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to various digital assets, which
might appeal to users who are experimenting. That said, I still wonder about
things like availability, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned
in relation to Paybis. The platform emphasizes regulatory compliance, which could be seen as professional for some users, though
others might find it time-consuming. I’m honestly unsure where I
stand on that, but it does suggest that Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem
mixed. Some sources claim that Paybis is clear with pricing, while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does mean users should probably compare alternatives before
making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear to be a platform that’s worth researching.
For anyone who is curious about buying crypto
with fiat, spending some time reading more about Paybis could
be useful. I’m still undecided myself, but it’s complex enough to justify further
exploration.
Hi there! I realize this is somewhat off-topic however I needed to ask.
Does operating a well-established website like yours take a large
amount of work? I am completely new to running a blog however I
do write in my journal on a daily basis. I’d like to start a
blog so I can easily share my own experience and thoughts online.
Please let me know if you have any kind of recommendations or tips for brand new aspiring
bloggers. Thankyou!
buy backlinks, link exchange, free gift card, congratulations you have won, claim your prize, you
have been selected, click here to claim, you won’t believe, one
weird trick, what happened next will shock you, shocking truth, secret revealed, limited time offer,
special promotion, act now, don’t miss out, buy now, best
price, risk-free trial, get rich quick, make money fast, work from home, no credit check, miracle cure, lose weight
fast, free viagra, no prescription needed, online casino, free
spins, meet singles, hot singles in your area, replica watches, cheap Rolex.Agent Tesla,
ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader,
Black Basta, BlackEnergy, BlackMatter, Blackshades,
Blaster, Brontok, Carbanak, Cerber, Clampi,
Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker,
CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza,
Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba,
Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos,
Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze,
Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya,
Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader,
Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader,
Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba, Tiny Banker,
TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker,
Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess,
Zloader, Zlob, Zotob
Also visit my web blog fake designer labels
Piece of writing writing is also a excitement, if you be acquainted with after that you can write
or else it is difficult to write.
This poses a phishing risk to users, violates Google’s Webmaster Guidelines, and breaks Indonesian law, where online gambling is strictly illegal.
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UᏚA
(713) 364-3256
anti-aging skincare tips remedy (https://wakelet.com)
Since the admin of this web page is working, no question very soon it will be renowned, due
to its quality contents.
бездепозитные бонусы за регистрацию в казино с выводом без пополнения по номеру телефона
Νέα online καζίνο 2025 προσφέρουν
ανταγωνιστικές προσφορές,
ταχύτερες αναλήψεις,
καθώς και σύγχρονη εμπειρία παιχνιδιού.
Τι προσφέρουν τα νέα καζίνο στους
παίκτες;
Όταν εγγραφείς σε ένα νέο καζίνο,
μπορείς να:
Καταθέσεις χρήματα με χαμηλή ελάχιστη κατάθεση
Παίξεις χιλιάδες παιχνίδια: slots, live
casino, crash παιχνίδια
Επωφεληθείς από προσφορές cashback
Κάνεις ανάληψη κερδών σε λίγα λεπτά
Τύποι καζίνο και χαρακτηριστικά
Τα νέα καζίνο μπορεί να περιλαμβάνουν, για παράδειγμα:
Pay N Play καζίνο – άμεση ταυτοποίηση
Παραδοσιακά καζίνο – πλουσιότερα μπόνους
Live καζίνο – ρουλέτα, blackjack και game shows
Παιχνίδια υψηλού ρίσκου – megaways slots, όπου μπορείς να κερδίσεις έως χιλιάδες ευρώ
Τι κερδίζουν οι παίκτες από τα νέα καζίνο;
Νέα στούντιο παιχνιδιών
Έως 500 % μπόνους καλωσορίσματος
Μέθοδοι πληρωμής Trustly / Zimpler
Άδειες MGA / UKGC / Εσθονίας
ξεκάθαροι όροι μπόνους
Αξίζει να παίξεις σε νέα καζίνο;
Τα νέα online καζίνο αποτελούν δημοφιλή επιλογή για τους παίκτες,
αν αναζητάς:
καλύτερα μπόνους
ποιοτική συλλογή παιχνιδιών
γρηγορότερες πληρωμές
αξιόπιστους παρόχους
Συχνά προσφέρουν μεγαλύτερη αξία
για τα χρήματά σου
σε σύγκριση με τα παλαιότερα καζίνο.
бесплатная ставка от 1xbet промокод как поставить
Tämä on todella ajankohtainen kirjoitus. Verkko- varainkeruu mahdollistaa hoidon monelle.
Kiitos että tuotte esiin tämän asian.
What’s up, everything is going nicely here and ofcourse every one is sharing data,
that’s truly good, keep up writing.
my homepage :: cocina al aire libre Splendora
1xbet зеркало рабочее промокод
Hello would you mind sharing which blog platform you’re using?
I’m going to start my own blog in the near future but I’m having a hard time choosing
between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different
then most blogs and I’m looking for something completely unique.
P.S Apologies for being off-topic but I had to ask!
โพสต์นี้ อ่านแล้วรู้สึกว่าได้มุมมองใหม่ ครับ
ดิฉัน ไปเจอรายละเอียดของ หัวข้อที่คล้ายกัน
ดูต่อได้ที่ Jeannette
เหมาะกับคนที่สนใจเรื่องนี้
เพราะให้ข้อมูลเชิงลึก
ขอบคุณที่แชร์ เนื้อหาดีๆ นี้
และหวังว่าจะมีข้อมูลใหม่ๆ มาแบ่งปันอีก
Great post.
Processen att delta är mycket direkt.
my web page … Stöd medicinsk behandling
You actually make it appear really easy along with your presentation however I to find this matter to be actually one thing that
I believe I’d never understand. It seems too complicated and extremely wide for me.
I’m taking a look forward in your next post, I will try to
get the hang of it!
Una vez que la descarga haya finalizado, verifica que el video se haya descargado
correctamente.
I’ve been looking into Paybis for a while now, and I’m still not completely certain about whether it truly deserves all the attention it gets, but
it’s undeniably an interesting name within the crypto trading space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a globally operating
cryptocurrency platforms that also supports traditional
fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to connect
the gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to exchange digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only
advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top coins.
Instead, it offers access to a broader token selection, which might
appeal to users who are exploring different projects. That
said, I still wonder about things like update frequency, so
it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes regulatory compliance, which could be seen as professional for some
users, though others might find it time-consuming. I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a regulated crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does mean users should probably
compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does
appear to be a platform that’s worth researching.
For anyone who is trying to understand how crypto and
fiat markets interact, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting enough to justify further exploration.
This info is invaluable. When can I find out more?
이러한 정보를 공유해 주셔서 감사합니다.
온라인 모금은 수술비가 부족한 환자들에게 진짜 큰 힘이 됩니다.
시력을 구하는 자선 활동이 더욱 확산되길 바랍니다.
Stop by my web-site … 글로벌 의료 펀딩
Just wish to say your article is as surprising. The clearness in your
post is simply excellent and i could assume you are an expert on this subject.
Well with your permission allow me to grab your feed to
keep up to date with forthcoming post. Thanks a million and
please continue the gratifying work.
Greetings! I know this is kinda off topic but I was wondering if you knew where I could find a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having difficulty finding one?
Thanks a lot!
I am not sure where you’re getting your info, but great topic.
I needs to spend some time learning more or understanding more.
Thanks for magnificent info I was looking for this info for my
mission.
You could definitely see your enthusiasm in the work you write.
The world hopes for even more passionate
writers like you who aren’t afraid to mention how they believe.
All the time go after your heart.
บทความนี้ อ่านแล้วได้ความรู้เพิ่ม ค่ะ
ผม เคยเห็นเนื้อหาในแนวเดียวกันเกี่ยวกับ ประเด็นที่ใกล้เคียงกัน
สามารถอ่านได้ที่ Milford
น่าจะช่วยให้เข้าใจเรื่องนี้มากขึ้น
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ ข้อมูลที่ช่วยให้เข้าใจเรื่องนี้มากขึ้น นี้
จะรอติดตามเนื้อหาใหม่ๆ ต่อไป
Angels Bail Bonds Costa Mesa
769 Baker St,
Costa Mesa, ᏟA 92626, United Statеs
bail bonds business income – Antoine –
We’re a bunch of volunteers and opening a brand new scheme in our community.
Your website offered us with valuable information to
work on. You have performed a formidable task and our whole group might be
grateful to you.
It is really a great and useful piece of info. I am
satisfied that you simply shared this useful information with us.
Please keep us informed like this. Thank you for sharing.
Simply desire to say your article is as surprising. The clearness for your post is just spectacular
and that i can suppose you are an expert in this subject.
Fine together with your permission allow me to grasp your feed to stay updated with imminent post.
Thanks one million and please continue the enjoyable work.
Nice response in return of this matter with solid arguments and explaining the whole thing concerning that.
Hi, I do believe this is a great web site. I stumbledupon it 😉 I will return once again since i have bookmarked
it. Money and freedom is the greatest way to change, may you
be rich and continue to help others.
Hello I am so happy I found your site, I really found you by mistake, while I was
looking on Bing for something else, Regardless I am here now
and would just like to say cheers for a incredible post and a all round exciting blog (I
also love the theme/design), I don’t have time to look
over it all at the minute but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to read a lot more,
Please do keep up the awesome job.
Thanks for one’s marvelous posting! I truly enjoyed reading it, you might be a great author.
I will be sure to bookmark your blog and will come back later
in life. I want to encourage one to continue your great posts,
have a nice day!
goGLOW Houston Heights
1515 Studemont Ѕt Suitee 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
Bookmarks
A very moving entry about giving.
my site: بوابة عمل الخير
It’s very simple to find out any matter on web as compared to textbooks, as I found this article at this site.
бездепозитные бонусы в казино за регистрацию
I’ve been seeing mentions of Paybis for a while now, and
I’m still trying to form a clear opinion about whether it truly deserves all the attention it gets, but it’s definitely an interesting name within the crypto trading space,
especially when it comes to combining crypto markets
with fiat currencies. From what I understand so far,
Paybis presents itself as a large-scale cryptocurrency
platforms that also supports traditional
fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems
to bridge the gap between fiat systems and the crypto world.
Many platforms focus strictly on crypto-to-crypto
trades, but Paybis appears to allow users to buy digital currencies
using various fiat options. I’m not claiming this process is flawless, but it does seem aimed at
beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies
supported. Paybis doesn’t appear to limit itself to the most popular assets.
Instead, it offers access to various digital assets,
which might appeal to users who are exploring different projects.
That said, I still wonder about things like liquidity, so it’s probably something potential users should
investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which
could be seen as professional for some users, though
others might find it time-consuming. I’m honestly unsure
where I stand on that, but it does suggest that Paybis is trying to operate
as a legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does mean users should probably read
the details carefully before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear to be a
platform that’s worth a closer look. For anyone who is trying to understand how crypto and fiat markets interact, spending some time
reading more about Paybis could be useful. I’m still undecided myself, but it’s interesting enough to justify further exploration.
Hi there! I just want to give you a big thumbs up for the excellent info you’ve got
right here on this post. I am returning to your web site for more soon.
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate
< Loved it!
Good read. https://gocari.co.id/ helps users browse efficiently.
I’ve been reading about Paybis for a while now, and I’m still not completely certain about whether it truly deserves all the attention it
gets, but it’s definitely an interesting name within the cryptocurrency space,
especially when it comes to combining crypto markets with
fiat currencies. From what I understand so far, Paybis presents itself as a well-established cryptocurrency platforms that also supports standard currencies,
which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to bridge the gap between fiat systems and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to sell digital currencies using debit cards.
I’m not claiming this process is flawless, but it does seem
aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to multiple altcoins, which might appeal to users who are exploring different projects.
That said, I still wonder about things like liquidity, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as reassuring for some
users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a legitimate crypto and fiat
marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry,
but it does mean users should probably compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be
a platform that’s worth a closer look. For anyone
who is trying to understand how crypto and
fiat markets interact, spending some time reading more about
Paybis could be useful. I’m still undecided myself, but it’s promising enough to justify further exploration.
Thanks for some other informative website. Where else could I get that type of information written in such an ideal manner?
I have a undertaking that I am simply now running
on, and I have been on the look out for such information.
I’ve been coming across discussions about Paybis for a while
now, and I’m still not completely certain about whether it
truly deserves all the attention it gets, but it’s certainly
an interesting name within the digital asset space,
especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a
globally operating cryptocurrency platforms that also supports traditional fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems
to merge the gap between fiat systems and the crypto
world. Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to exchange digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does
seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to the most popular
assets. Instead, it offers access to various digital assets, which might appeal to users who are exploring different projects.
That said, I still wonder about things like availability, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be seen as protective for some
users, though others might find it inconvenient. I’m honestly unsure where I stand on that,
but it does suggest that Paybis is trying to operate
as a regulated crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is clear with pricing, while
others mention that costs may vary by transaction. This isn’t uncommon in the crypto industry, but it does mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is perfect, but
it does appear to be a platform that’s worth learning more about.
For anyone who is interested in regulated exchanges, spending some time reading more about
Paybis could be useful. I’m still undecided
myself, but it’s promising enough to justify further exploration.
I’ve been reading about Paybis for a while now, and I’m still
trying to form a clear opinion about whether it truly deserves all the attention it gets,
but it’s certainly an interesting name within the cryptocurrency space, especially when it comes to combining crypto markets with fiat
currencies. From what I understand so far, Paybis presents itself as a globally operating cryptocurrency platforms that also
supports traditional fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to merge the gap between fiat systems and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to exchange digital currencies using debit cards.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the
top coins. Instead, it offers access to multiple altcoins, which might appeal to users who are diversifying.
That said, I still wonder about things like update frequency, so
it’s probably something potential users should investigate
further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes regulatory compliance, which could be seen as reassuring for some users, though others might find it inconvenient.
I’m honestly unsure where I stand on that, but it
does suggest that Paybis is trying to operate as a long-term crypto
and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry, but it does mean users should probably do proper research
before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear to
be a platform that’s worth learning more about.
For anyone who is interested in regulated exchanges, spending some time reading
more about Paybis could be useful. I’m still undecided myself, but it’s complex
enough to justify further exploration.
buy backlinks, link exchange, free gift card, congratulations you have won, claim
your prize, you have been selected, click here to claim, you won’t believe,
one weird trick, what happened next will shock you, shocking truth, secret revealed, limited time offer, special promotion, act now, don’t miss out,
buy now, best price, risk-free trial, get rich quick, make money
fast, work from home, no credit check, miracle cure,
lose weight fast, free viagra, no prescription needed, online casino, free spins, meet singles, hot singles
in your area, replica watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler,
Anubis, Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster, Brontok, Carbanak, Cerber,
Clampi, Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker,
CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame,
FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID,
Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface,
Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya,
Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker,
Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye,
SpyNote, TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch,
Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
Look at my web blog; lolita porn
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Где можно узнать подробнее? – https://www.defining-blog.ru/category/rabota-biznes
Эта разъяснительная статья содержит простые и доступные разъяснения по актуальным вопросам. Мы стремимся сделать информацию понятной для широкой аудитории, чтобы каждый мог разобраться в предмете и извлечь из него максимум пользы.
Изучить эмпирические данные – https://andreawaves.com/bonjour-tout-le-monde
Ga888
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Исследовать вопрос подробнее – http://cinemovel.tv/sic/2020/voglio-sposare-chi-mi-ama
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Это стоит прочитать полностью – https://mahoraize.wpxblog.jp/%E3%82%B7%E3%83%8B%E3%82%A2%E3%83%94%E3%82%A2%E3%83%8E%E6%95%99%E6%9C%AC%EF%BC%92%E3%80%80%E5%BC%BE%E3%81%8D%E7%9B%B4%E3%81%97%EF%BD%9E
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Кликни и узнай всё! – https://equidogkine.com/product/dog-harness
Hi to all, the contents present at this website are truly remarkable for people knowledge, well,
keep up the good work fellows.
I’ve been looking into Paybis for a while now, and I’m still not completely certain about
whether it truly deserves all the attention it gets, but it’s
definitely an interesting name within the digital asset space, especially
when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a globally operating cryptocurrency platforms that also supports standard currencies, which is something many exchanges either limit or
complicate.
What initially caught my interest was the way Paybis seems to merge the gap between banking methods and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to
exchange digital currencies using bank transfers. I’m
not claiming this process is flawless, but it does seem aimed at newcomers
rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies
supported. Paybis doesn’t appear to limit itself to just
the top coins. Instead, it offers access to a broader token selection, which might appeal to users who are diversifying.
That said, I still wonder about things like liquidity, so it’s probably
something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as professional for some users, though others might
find it inconvenient. I’m honestly unsure where I stand on that, but it does
suggest that Paybis is trying to operate as a regulated crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem
divided. Some sources claim that Paybis is clear with
pricing, while others mention that costs may vary by transaction. This isn’t uncommon in the crypto industry, but it does mean users should probably read the details carefully before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it does appear to be a platform that’s worth
researching. For anyone who is trying to understand how crypto and
fiat markets interact, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting
enough to justify further exploration.
Эта публикация дает возможность задействовать различные источники информации и представить их в удобной форме. Читатели смогут быстро найти нужные данные и получить ответы на интересующие их вопросы. Мы стремимся к четкости и доступности материала для всех!
Подробнее – https://dc2.81e.myftpupload.com/about
Hey great website! Does running a blog such as this take a lot
of work? I’ve no expertise in programming but I was hoping to start
my own blog in the near future. Anyways, should you have any ideas or techniques for new
blog owners please share. I know this is off subject nevertheless I just wanted to ask.
Many thanks!
Look at my web-site; Stem cell hair restoration
The Ministry of Defense Information According to Cambodia launched an F-16 in Thailand in a rocket attack on the Cambodians’ luchtelingskamp
Whoa lots of superb information. https://longhaisood.wordpress.com/2025/12/18/betflik199/
I do not even know how I stopped up right here, however I believed this publish was great.
I do not understand who you’re but certainly
you’re going to a famous blogger if you happen to aren’t already.
Cheers!
Good day! I could have sworn I’ve been to this website before but after checking through
some of the post I realized it’s new to me. Nonetheless, I’m definitely
delighted I found it and I’ll be bookmarking and checking back often!
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Исследовать вопрос подробнее – http://bdsm2.com/search_results.php?SITE_ID=0&NoOfRows=100&SearchString=n&s=11900
I know this site gives quality depending posts and other data, is there any
other website which presents such information in quality?
Hi there, I would like to subscribe for this web site to get latest updates, therefore where can i do it please help.
Great article! We are linking to this great content on our site.
Keep up the great writing.
Feel free to surf to my webpage tiktok captions
Wonderful website. A lot of useful information here.
I am sending it to a few buddies ans additionally sharing in delicious.
And certainly, thanks to your effort!
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy basreng188
В этой статье собраны факты, которые освещают целый ряд важных вопросов. Мы стремимся предложить читателям четкую, достоверную информацию, которая поможет сформировать собственное мнение и лучше понять сложные аспекты рассматриваемой темы.
Обратитесь за информацией – https://tadomalkine.eu/kainynas/attachment/2
After I originally left a comment I seem to have clicked the -Notify me
when new comments are added- checkbox and now each time
a comment is added I get 4 emails with the same comment.
Perhaps there is a way you can remove me from that service?
Thank you!
Thanks so much for this, keep up the good work 🙂
Have you ever considered writing an ebook or guest authoring on other
blogs? I have a blog based on the same subjects you discuss and would really like to have you share some stories/information. I know my subscribers
would enjoy your work. If you’re even remotely interested,
feel free to shoot me an e-mail.
I enjoy what you guys are up too. This type of clever work and exposure!
Keep up the terrific works guys I’ve incorporated you guys to
blogroll.
my homepage :: Hair stem cell treatment
Remarkable! Its truly amazing paragraph, I have got
much clear idea concerning from this paragraph.
I love your blog.. very nice colors & theme. Did you design this website yourself or did
you hire someone to do it for you? Plz reply as I’m looking to construct my own blog and
would like to know where u got this from. thanks a
lot
My homepage :: Stem cell hair loss treatment
Hey there, I think your website might be
having browser compatibility issues. When I look at your blog site in Chrome,
it looks fine but when opening in Internet Explorer,
it has some overlapping. I just wanted to give you a quick heads
up! Other then that, wonderful blog!
Also visit my site – Stem cell therapy for hair loss
With havin so much content and articles do you
ever run into any problems of plagorism or copyright infringement?
My site has a lot of completely unique content I’ve either authored myself or outsourced but it seems a lot of it is popping it up all over the web without my permission. Do
you know any solutions to help reduce content from being stolen? I’d definitely appreciate it.
My website :: Stem cell hair restoration
Hello my family member! I wish to say that this article
is awesome, great written and include almost all vital infos.
I would like to look more posts like this .
Nice respond in return of this question with genuine arguments
and explaining the whole thing on the topic of that.
I’ve been reading about Paybis for a while now, and I’m still not
completely certain about whether it truly deserves all the attention it gets, but
it’s clearly an interesting name within the crypto trading
space, especially when it comes to combining crypto markets
with fiat currencies. From what I understand so far, Paybis presents itself as a globally operating cryptocurrency platforms that also supports traditional fiat
money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to link
the gap between fiat systems and the crypto world. Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to
buy digital currencies using bank transfers.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only
advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to the most popular
assets. Instead, it offers access to a broader
token selection, which might appeal to users
who are experimenting. That said, I still wonder about
things like liquidity, so it’s probably something potential
users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be seen as reassuring for some users,
though others might find it time-consuming. I’m honestly unsure
where I stand on that, but it does suggest that Paybis is trying
to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is clear with pricing, while others mention that
costs may change based on currency. This isn’t uncommon in the crypto industry,
but it does mean users should probably compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be a platform that’s worth learning more about.
For anyone who is trying to understand how crypto and
fiat markets interact, spending some time reading
more about Paybis could be useful. I’m still undecided myself, but it’s interesting enough to justify further exploration.
Hi there to every body, it’s my first visit of this weblog; this web site contains amazing and actually excellent data for visitors.
buy backlinks, link exchange, free gift card, congratulations you have won,
claim your prize, you have been selected, click here
to claim, you won’t believe, one weird trick, what happened next will shock you, shocking truth, secret revealed, limited time
offer, special promotion, act now, don’t
miss out, buy now, best price, risk-free trial, get rich quick, make money fast, work from home, no credit check,
miracle cure, lose weight fast, free viagra, no prescription needed, online casino,
free spins, meet singles, hot singles in your area, replica watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB,
BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster, Brontok,
Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis,
CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu,
Dyreza, Emotet, Flame, FormBook, Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi,
GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda,
LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai,
Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya,
Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit, RansomEXX,
Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer, Shylock, Sinowal, SmokeLoader, Snake,
SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt,
Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost,
XLoader, XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
Feel free to surf to my website – hacking tools
I have read some excellent stuff here. Certainly worth bookmarking for revisiting.
I surprise how much attempt you put to make this type of
excellent informative website.
My web-site – rajapadi4d
Lucky Jet – подробный обзор популярной игры
I’ve been seeing mentions of Paybis for a while now, and I’m still not fully convinced
about whether it truly deserves all the attention it gets, but it’s definitely an interesting name within the cryptocurrency space,
especially when it comes to combining crypto
markets with fiat currencies. From what I understand so far, Paybis presents itself as a well-established cryptocurrency platforms that also supports regular
payment systems, which is something many exchanges either limit
or complicate.
What initially caught my interest was the way Paybis seems to link
the gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears
to allow users to sell digital currencies using various fiat options.
I’m not claiming this process is flawless, but it does seem aimed at
newcomers rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to just the top
coins. Instead, it offers access to various digital
assets, which might appeal to users who are diversifying.
That said, I still wonder about things like availability, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could
be seen as protective for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest
that Paybis is trying to operate as a legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is clear with pricing, while others mention that costs may vary by transaction. This isn’t uncommon in the crypto industry, but it
does mean users should probably read the details carefully before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but
it does appear to be a platform that’s worth learning more about.
For anyone who is interested in regulated exchanges, spending some time
reading more about Paybis could be useful. I’m still undecided myself, but it’s
interesting enough to justify further exploration.
Hi there! This post could not be written any better! Looking through
this post reminds me of my previous roommate!
He continually kept preaching about this. I most certainly will send this article to
him. Fairly certain he’ll have a good read. Many thanks for sharing!
Here is my homepage :: Stem cell hair restoration
Hey there just wanted to give you a quick heads up.
The text in your content seem to be running off the screen in Firefox.
I’m not sure if this is a formatting issue or something to do with web browser compatibility but I
figured I’d post to let you know. The design look great though!
Hope you get the issue resolved soon. Thanks
Also visit my web page; Stem cell hair loss treatment
Fine postings Appreciate it.
промокод 1хбет на бесплатную ставку
Thanks on your marvelous posting! I really enjoyed reading it, you’re a great author.
I will ensure that I bookmark your blog and will come back sometime soon. I want to
encourage you to continue your great work, have a nice holiday weekend!
My web site – Stem cell hair restoration
I know this site gives quality based content and extra data, is there any
other site which provides these kinds of data in quality?
TPJ
Hi there to every , since I am truly keen of reading this
weblog’s post to be updated regularly. It carries nice material.
I had fun reading this post. I want to see more on this subject.. Gives Thanks for writing this nice article.. Anyway, I’m going to subscribe to your rss and I wish you write great articles again soon.
You actually expressed that really well!
I’ve learn a few just right stuff here. Certainly value bookmarking for
revisiting. I surprise how a lot effort you set to create any such
magnificent informative website.
Visit my blog – Stem cell hair loss treatment
I am lucky that I discovered this website , precisely the right info that I was searching for! .
I read this post completely regarding the resemblance of latest and previous
technologies, it’s amazing article.
Hi! I understand this is kind of off-topic but I needed to ask.
Does building a well-established website such as yours take a massive amount work?
I am completely new to running a blog but I do write in my diary daily.
I’d like to start a blog so I can share my personal experience and feelings online.
Please let me know if you have any kind of recommendations
or tips for new aspiring bloggers. Thankyou!
Thank you for posting this important post. Healthcare crowdfunding
is vital for supporting those who lack funds for treatment.
Saving vision is a noble mission. I will share this site.
Excellent work!
Informative article, exactly what I wanted to find.
I couldn’t refrain from commenting. Very well written!
промокоды 1xbet 2026 бесплатно на сегодня
веб-сайт vbet poker онлайн
бездепозитный бонус за регистрацию в казино с выводом казахстан
This website was… how do you say it? Relevant!!
Finally I have found something that helped me. Cheers!
İşinizə davam edin və daha çox istifadəçi cəlb edin!
https://1winazpro.com/aksiyalar/
Thanks for your personal marvelous posting! I definitely enjoyed
reading it, you will be a great author. I will always
bookmark your blog and may come back at some point. I want to encourage you continue your great job, have a nice
weekend!
Hey! This is kind of off topic but I need some advice from an established blog.
Is it very hard to set up your own blog? I’m not very
techincal but I can figure things out pretty quick. I’m thinking about creating my own but I’m not sure where to start.
Do you have any tips or suggestions? Many thanks
Took me time to read all the comments, but I really enjoyed the article. It proved to be Very helpful to me and I am sure to all the commenters here It’s always nice when you can not only be informed, but also entertained I’m sure you had fun writing this article.
как ввести промокод в 1xbet
Hi, i think that i noticed you visited my weblog thus i got here to return the prefer?.I’m trying to find
issues to improve my site!I guess its good enough to use some of your ideas!!
Here is my web page :: rajacabe88
Hi, every time i used to check website posts here early in the morning,
for the reason that i like to gain knowledge of more and more.
Ini adalah topik yang sangat krusial. Penggalangan dana medis mengubah hidup bagi orang yang tidak mampu membayar pengobatan. Mendukung yayasan Wujudkan Harapan Penglihatan benar-benar luar biasa.
Terima kasih telah membagikan misi ini.
You could definitely see your enthusiasm within the
work you write. The world hopes for even more passionate writers like you who are not afraid
to say how they believe. At all times follow your heart.
I truly love your blog.. Very nice colors & theme.
Did you build this amazing site yourself? Please reply back as I’m attempting to create my very own blog and would love to know where you got this from or just
what the theme is called. Appreciate it!
Saya sudah mengikuti seluruh penjelasan dalam artikel ini, dan menurut saya pembahasannya sangat menarik terutama ketika topik
seperti KUBET, Situs Judi Bola Terlengkap, Situs
Parlay Resmi, Situs Parlay Gacor, Situs Mix Parlay, Situs Judi Bola, toto
macau, kubet login, situs parlay, Kubet Parlay, dan Judi
Bola gacor dijelaskan dengan sudut pandang yang jelas dan mudah dipahami.
Saya merasa penyajiannya sangat rapi dan nyaman dibaca, karena mampu memberikan gambaran lengkap tanpa membuat pembaca merasa kewalahan. Artikel ini juga memiliki detail yang lebih kaya informasi dibandingkan banyak artikel lain yang
membahas tema sejenis. Inilah alasan saya ingin meninggalkan apresiasi, sebab kualitas penulisan serta alur penyampaiannya benar-benar
layak diapresiasi. Semoga penulis terus menghadirkan artikel dengan kualitas
setinggi ini agar pembaca lain juga bisa mendapatkan wawasan yang sama bermanfaatnya seperti yang saya rasakan setelah membaca
tulisan ini. Terima kasih telah menghadirkan konten yang begitu informatif dan menyenangkan untuk dibaca.
Magnificent beat ! I wish to apprentice whilst you amend your website, how can i
subscribe for a weblog site? The account aided me a applicable
deal. I were a little bit acquainted of this your broadcast offered brilliant transparent concept
промокод 1хбет
Het ministerie van Buitenlandse Zaken meldde dat een F-16 twee raketten had neergehaald in de buurt van Cambodjaanse troepen.
That is a very good tip especially to those new to the blogosphere.
Simple but very precise information… Many thanks for sharing this one.
A must read post!
I’ve been researching Paybis for a while now, and I’m still not 100% sure about whether it truly deserves all the attention it gets, but it’s clearly an interesting name within the cryptocurrency
space, especially when it comes to combining
crypto markets with fiat currencies. From what I understand so far,
Paybis presents itself as a large-scale cryptocurrency platforms that also supports traditional fiat money, which is something many exchanges either limit or
complicate.
What initially caught my interest was the way Paybis seems to connect the gap between banking methods and the crypto
world. Many platforms focus strictly on crypto-to-crypto trades, but
Paybis appears to allow users to sell digital currencies using bank transfers.
I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to various digital assets,
which might appeal to users who are diversifying.
That said, I still wonder about things like liquidity, so it’s
probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could
be seen as professional for some users, though others might find it
restrictive. I’m honestly unsure where I stand on that, but
it does suggest that Paybis is trying to operate as a long-term crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem varied.
Some sources claim that Paybis is transparent with
pricing, while others mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does mean users should probably read the details carefully before making decisions.
Overall, I wouldn’t say Paybis is the best exchange
available, but it does appear to be a platform that’s
worth a closer look. For anyone who is curious about buying crypto
with fiat, spending some time reading more about
Paybis could be useful. I’m still undecided myself, but
it’s complex enough to justify further exploration.
Very nice post. I just stumbled upon your blog and wanted to mention that I have really enjoyed browsing
your blog posts. In any case I’ll be subscribing in your rss feed and I’m hoping you write again very soon!
ข้อมูลชุดนี้ ให้ข้อมูลดี ค่ะ.
ผม ไปเจอรายละเอียดของ หัวข้อที่คล้ายกัน
ที่คุณสามารถดูได้ที่ Sharyn.
เผื่อใครสนใจ
มีการยกตัวอย่างที่เข้าใจง่าย.
ขอบคุณที่แชร์ บทความคุณภาพ นี้
และหวังว่าจะได้เห็นโพสต์แนวนี้อีก.
Moovit มีแผนที่ฟรีและเส้นทางแบบถ่ายทอดสดที่ช่วยคุณนำทางไปยังสถานที่ต่างๆ ในเมือง คุณสามารถดูตารางเดินรถ เส้นทาง ตารางเวลา และค้นหาว่าใช้เวลานานเท่าไรที่จะเดินทางไปถึง ซอย รังสิต-นครนายก 18 ตามเวลาจริง.
What’s up to all, how is the whole thing, I think every one is
getting more from this web page, and your views are fastidious for new
users.
Pretty section of content. I just stumbled upon your blog
and in accession capital to assert that I acquire in fact
enjoyed account your blog posts. Any way I’ll be subscribing to your augment and even I achievement you access consistently quickly.
buy backlinks, link exchange, free gift card, congratulations you have won,
claim your prize, you have been selected, click here to claim, you won’t believe, one
weird trick, what happened next will shock you, shocking truth, secret revealed,
limited time offer, special promotion, act now, don’t miss out, buy now,
best price, risk-free trial, get rich quick, make money fast, work from
home, no credit check, miracle cure, lose weight fast, free viagra, no prescription needed, online casino, free spins,
meet singles, hot singles in your area, replica
watches, cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB,
BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster,
Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker,
CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame, FormBook,
Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor,
IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos,
Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz,
mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya,
Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader,
Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu,
Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba,
Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch,
Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader,
Zlob, Zotob
Stop by my web blog :: buy fake Rolex fake Gucci fake Prada
Informasinya jelas! https://kawalharta.org/ membantu kamu memahami LHKPN.
Great information. Lucky me I recently found your website by chance
(stumbleupon). I’ve saved as a favorite for later!
Как найти купоны Изи Дроп – подробное руководство
The language of meals supplements and nutrition can generally be technical or confusing. We’ve put together a glossary to help you perceive some of the commonest terms. When you have options for further entries to the glossary, please contact us. µg Microgram a measurement of weight equal to one millionth of a gram (or one thousandth of a milligram). Microgram (µg or mcg) is used for plenty of nutrients present in meals supplements. Amino Acid The building blocks of protein, there are eight important amino acids which can’t be synthesised within the body and due to this fact should come from the weight loss program. These are: isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan and valine. As well as arginine and histidine are amino acids required by infants and young children which supports their speedy development. Antioxidant A substance or nutrient which helps to protect our cells from harm caused by free radicals, damaging molecules which are present in pollution and tobacco smoke.
Here is my web page … https://maps.google.com.co/url?sa=t&url=https%3A%2F%2Fwifidb.science%2Fwiki%2FNeuro_Surge_Supplement%3A_A_Comprehensive_Study_Report
I’ve been researching Paybis for a while now, and I’m still
not completely certain about whether it truly deserves all the attention it gets, but it’s certainly
an interesting name within the cryptocurrency space, especially when it comes
to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself
as a globally operating cryptocurrency platforms that also supports traditional fiat money, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems
to merge the gap between traditional finance and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to buy digital currencies using debit cards.
I’m not claiming this process is flawless, but it does seem aimed
at people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to the most popular assets.
Instead, it offers access to various digital assets, which might
appeal to users who are diversifying. That said, I still wonder about things
like liquidity, so it’s probably something potential
users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes identity verification, which could be seen as protective for some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that Paybis is trying to operate as a legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates,
opinions seem divided. Some sources claim that Paybis is
transparent with pricing, while others mention that costs may vary by
transaction. This isn’t uncommon in the crypto industry, but it does mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be a
platform that’s worth a closer look. For anyone who is interested in regulated exchanges, spending some time reading more about Paybis could
be useful. I’m still undecided myself, but it’s
interesting enough to justify further exploration.
I like the helpful info you provide in your articles.
I will bookmark your weblog and check once more right here frequently.
I am fairly sure I will be told many new stuff proper here!
Good luck for the following!
Aw, this was an exceptionally nice post.
Taking the time and actual effort to make a good article… but what can I say… I hesitate a lot
and never manage to get anything done.
Qhov no ua rau cov neeg siv muaj kev pheej hmoo ntawm phishing, ua txhaum Google’s Webmaster Guidelines, thiab ua txhaum cai Indonesian txoj cai, qhov twg kev twv txiaj hauv online raug txwv nruj.
This game looks amazing! The way it blends that old-school chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay
and adding real risk? I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and
adds legitimate risk is genius. Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing
action with real-world stakes has me interested. I’m
ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing
style with tangible consequences? I’ve gotta try
this out!
Thanks for finally talking about > Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate < Loved it!
You are not right. I am assured. I can prove it. Write to me in PM, we will talk.
Good post! We are linking to this great content on our website.
Keep up the great writing.
I have been surfing on-line greater than 3 hours nowadays, yet I never
found any interesting article like yours. It is beautiful price sufficient for me.
Personally, if all web owners and bloggers made excellent content material as you probably did, the net will be much more helpful than ever before.
Its such as you learn my thoughts! You appear to know so much about this, such as you wrote the
book in it or something. I believe that you simply can do with some % to power
the message house a little bit, however other than that, that is magnificent blog.
A fantastic read. I’ll definitely be back.
There is certainly a great deal to find out about this
topic. I like all the points you made.
I’m impressed, I must say. Rarely do I come across a blog that’s both educative and interesting,
and let me tell you, you’ve hit the nail on the head.
The issue is something which too few men and women are speaking intelligently about.
I am very happy I came across this during my search for something concerning this.
I am now not positive the place you’re getting your information, however great topic.
I must spend a while studying much more or
figuring out more. Thanks for great info I used to be in search
of this info for my mission.
нажмите здесь vodkabet
Many thanks, Awesome information! https://jadwaded2.wordpress.com/2025/12/18/betflix93/
I wanted to thank you for this excellent read!! I certainly enjoyed
every bit of it. I have you book marked to check out new things you post…
Hi there colleagues, pleasant post and good urging commented here,
I am in fact enjoying by these.
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr ⅽ121,
Charlotte, NC 28273, United Ⴝtates
+19803517882
For space extraa homе additions (padlet.com)
подробнее vodkabet водка бет казино
Howdy this is kinda of off topic but I was wanting
to know if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding skills so I wanted
to get advice from someone with experience. Any help would be greatly appreciated!
I am really inspired together with your writing skills and also with the format for
your weblog. Is this a paid theme or did you modify it your self?
Either way keep up the nice quality writing, it is uncommon to peer a great weblog like this one today..
https://natashki.com/ – Natashki.com: A World of Bright Encounters. No Fakes, No Limits. Browse, Choose, Chat. Join for Free. >>>
you are in point of fact a excellent webmaster. The site loading speed is incredible.
It kind of feels that you’re doing any unique trick.
Furthermore, The contents are masterpiece. you
have performed a fantastic activity on this matter!
Thanks for finally writing about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate < Liked it!
такой водка бет
Рrime Secured
3603 N 222nd Ѕt, Suite 102,
Elkhorn, ΝE 68022, United Stаtes
402-289-4126
Compliance Forcе Tools (atavi.com)
Wow, marvelous blog structure! How long have you been blogging for?
you make running a blog look easy. The whole glance of your website is fantastic, let alone the
content material!
Hola! I’ve been following your blog for a long time now and finally got
the bravery to go ahead and give you a shout out from Houston Texas!
Just wanted to mention keep up the good job!
сайт Смело навстречу приключениям
Heel erg bedankt voor het platform cazino – het helpt enorm!
http://www.creativecurriculum4kids.com/2012/06/25/my-creative-curriculum-4-kids-blog-2/
1xbet зеркало рабочее промокод
Great delivery. Outstanding arguments. Keep up the amazing
effort.
บทความนี้ มีประโยชน์มาก ครับ
ผม ไปอ่านเพิ่มเติมเกี่ยวกับ เนื้อหาในแนวเดียวกัน
ซึ่งอยู่ที่ betflik 85
เผื่อใครสนใจ
มีการยกตัวอย่างที่เข้าใจง่าย
ขอบคุณที่แชร์ บทความคุณภาพ นี้
และหวังว่าจะมีข้อมูลใหม่ๆ
มาแบ่งปันอีก
Prіme Secured
3603 N 222nd St, Suite 102,
Elkhorn, ΝE 68022, United Ꮪtates
402-289-4126
Bookmarks [https://www.protopage.com/aethanwdbd]
whoah this weblog is excellent i like studying your articles.
Keep up the good work! You understand, a lot
of individuals are hunting round for this info, you can aid them greatly.
You have made some good points there. I checked
on the internet for more info about the issue and found most individuals will go along with your views on this
site.
можно проверить ЗДЕСЬ трипскан сайт вход
Greetings from Idaho! I’m bored to death at work so I decided
to browse your website on my iphone during lunch break.
I love the information you present here and can’t wait to take a look when I get home.
I’m surprised at how quick your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyways, awesome site!
Great post.
I’ve been researching Paybis for a while now, and I’m still trying to form a clear opinion about whether it truly deserves all the attention it gets, but
it’s certainly an interesting name within the crypto trading
space, especially when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as one
of the biggest cryptocurrency platforms that
also supports regular payment systems, which is something many
exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems
to link the gap between fiat systems and the crypto world.
Many platforms focus strictly on crypto-to-crypto trades,
but Paybis appears to allow users to exchange digital currencies using credit cards.
I’m not claiming this process is flawless, but it does seem aimed
at people just entering crypto rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies supported.
Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to various digital assets, which might appeal to users who are exploring different
projects. That said, I still wonder about things like
update frequency, so it’s probably something potential
users should investigate further.
Security and compliance are also frequently
mentioned in relation to Paybis. The platform emphasizes identity verification,
which could be seen as protective for some users,
though others might find it inconvenient. I’m honestly
unsure where I stand on that, but it does suggest that Paybis is trying to operate
as a legitimate crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is straightforward with pricing, while others
mention that costs may change based on currency.
This isn’t uncommon in the crypto industry, but it does mean users should probably
compare alternatives before making decisions.
Overall, I wouldn’t say Paybis is the best exchange available, but it does appear
to be a platform that’s worth learning more about. For anyone who
is curious about buying crypto with fiat, spending some time reading
more about Paybis could be useful. I’m still undecided myself, but it’s
promising enough to justify further exploration.
I have been browsing online greater than 3 hours as of late,
but I never found any fascinating article
like yours. It is lovely worth enough for me. In my
view, if all webmasters and bloggers made just right content material
as you probably did, the internet can be much more useful than ever before.
1000 рублей за регистрацию вывод сразу без вложений в казино с выводом без депозита
I every time spent my half an hour to read this weblog’s articles or reviews all the time along with a mug of coffee.
Hi there, I enjoy reading all of your article post.
I like to write a little comment to support you.
I am not sure where you are getting your info, but good topic.
I needs to spend some time learning much more or understanding more.
Thanks for excellent information I was looking for this information for
my mission.
I’ve been seeing mentions of Paybis for a while now, and I’m still not completely certain about whether it truly
deserves all the attention it gets, but it’s certainly an interesting name within the cryptocurrency space,
especially when it comes to combining crypto markets with
fiat currencies. From what I understand so far, Paybis
presents itself as a well-established cryptocurrency platforms that also supports traditional fiat money,
which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to bridge the gap
between banking methods and the crypto world. Many platforms
focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to buy digital currencies using various
fiat options. I’m not claiming this process is flawless,
but it does seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of
cryptocurrencies supported. Paybis doesn’t appear to limit itself to Bitcoin and Ethereum only.
Instead, it offers access to various digital assets, which might appeal to users who are exploring different projects.
That said, I still wonder about things like update frequency, so it’s probably something
potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be
seen as professional for some users, though others might
find it time-consuming. I’m honestly unsure where I stand on that, but it does suggest
that Paybis is trying to operate as a regulated crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem divided.
Some sources claim that Paybis is transparent with pricing, while others mention that costs may depend on payment methods.
This isn’t uncommon in the crypto industry,
but it does mean users should probably do proper research before making decisions.
Overall, I wouldn’t say Paybis is the ultimate solution, but it
does appear to be a platform that’s worth learning more about.
For anyone who is trying to understand how crypto and fiat markets interact, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s interesting enough to justify further exploration.
VidBurner etkileyici özellik seti ile kendisini rakiplerinden ayırıyor.
Please let me know if you’re looking for a writer
for your weblog. You have some really great posts and I feel I would be a good asset.
If you ever want to take some of the load off, I’d absolutely love to write some material for your blog in exchange for a link back to mine.
Please shoot me an e-mail if interested. Many thanks!
Inspiring initiative. Supporting vision care and medical treatment is incredibly
important, and this platform makes it easy to help
those in need.
My brother suggested I would possibly like this blog.
He used to be entirely right. This submit actually made my day.
You can not consider just how much time I had spent for this info!
Thanks!
Do you mind if I quote a couple of your posts as long as I provide credit
and sources back to your website? My blog site is in the very same area of interest as yours
and my users would truly benefit from some of the information you present here.
Please let me know if this ok with you. Thanks a lot!
I need to to thank you for this wonderful read!! I certainly loved every little bit of
it. I’ve got you book marked to look at new stuff you post…
I am curious to find out what blog platform you have been working with?
I’m having some minor security problems with my latest website and I would like to find something more safeguarded.
Do you have any suggestions?
Saya sudah membaca artikel ini secara menyeluruh, dan menurut saya pembahasannya sangat menarik terutama ketika topik
seperti KUBET, Situs Judi Bola Terlengkap, Situs Parlay
Resmi, Situs Parlay Gacor, Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs
parlay, Kubet Parlay, dan Judi Bola gacor dijelaskan dengan sudut pandang yang jelas dan mudah dipahami.
Saya merasa penyajiannya sangat rapi dan nyaman dibaca, karena mampu memberikan gambaran lengkap
tanpa membuat pembaca merasa kewalahan. Artikel ini juga memiliki detail yang lebih kaya informasi dibandingkan banyak artikel lain yang membahas tema
sejenis. Hal ini membuat saya merasa perlu untuk meninggalkan komentar, sebab kualitas penulisan serta alur penyampaiannya
benar-benar layak diapresiasi. Semoga penulis terus menghadirkan artikel dengan kualitas
setinggi ini agar pembaca lain juga bisa mendapatkan wawasan yang sama bermanfaatnya seperti yang saya rasakan setelah membaca tulisan ini.
Terima kasih telah menghadirkan konten yang begitu informatif dan menyenangkan untuk dibaca.
Hurrah! After all I got a blog from where I be able to genuinely obtain valuable
facts regarding my study and knowledge.
Hi to all, how is everything, I think every one
is getting more from this site, and your views are nice
in favor of new people.
We’re a group of volunteers and starting a new scheme in our community.
Your website offered us with valuable information to work on. You have performed
an impressive task and our whole community will likely
be grateful to you.
Wonderful blog! Do you have any recommendations for aspiring writers?
I’m planning to start my own website soon but I’m a little lost on everything.
Would you propose starting with a free platform like WordPress
or go for a paid option? There are so many choices out there that I’m totally overwhelmed ..
Any tips? Many thanks!
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UᏚA
(713) 364-3256
anti-aging treatments service
Мне очень нравится сайт Pin Up Casino, он очень комфортный в использовании!
https://hachi-cafe.shop/goods/247/
бездепозитные бонусы в казино за регистрацию с выводом
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Нажми и узнай всё – https://reddigital.cl/por-que-la-izquierda-y-el-progresismo-pierden-elecciones
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Прочесть заключение эксперта – https://coraisdecarapibus.com.br/aluguel-de-equipamentos-de-limpeza-limpeza-eficaz-e-pratica-para-suas-areas-de-trabalho
Hey There. I found your blog using msn. This is an extremely well written article.
I’ll be sure to bookmark it and come back to read more of your useful information. Thanks for the post.
I will definitely comeback.
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Почему это важно? – https://osteoz.ru
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Bookmarks
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Получить полную информацию – https://cejasaocarlos.com.br/tiny-scientists-on-the-loose-preschool-science-wonders-2
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Нажми и узнай всё – https://assaintpriest.fr/2020/09/14/12-13-sept-les-resultats-du-week-end
Вызвать трансфер в наше время можно за пару секунд — через мобильное приложение, онлайн-платформу или телефонный вызов. Просто введите место подачи и куда ехать, выберите подходящий класс машины, в случае надобности добавьте дополнения вроде автокресла или ожидания. Система сразу назначит подходящий транспорт, сообщит время подачи и окончательную цену. Оплатить рейс можно как наличными, так и онлайн — всё зависит от удобства. Самое важное — выбирайте проверенными компаниями, чтобы перевозка была не только удобной, но и защищённой.
http://xn--h1a1ab.xn--p1ai/index.php?name=account&op=info&uname=ghostnone3
Thank you for any other fantastic article. The place else
may anybody get that type of info in such a perfect approach of writing?
I’ve a presentation next week, and I’m at the look for
such info.
continuously i used to read smaller content which as well clear their motive, and that is also happening with this piece of writing which I am reading at this place.
Agpang keng Cambodian Ministry of Defense, ing metung a Thai F-16 fighter jet menabu yang adwang bomba keng metung a refugee camp keng Cambodia
buy backlinks, link exchange, free gift card, congratulations you have won, claim
your prize, you have been selected, click here to claim, you won’t
believe, one weird trick, what happened next will shock you, shocking truth, secret
revealed, limited time offer, special promotion, act now, don’t miss out, buy now, best price, risk-free
trial, get rich quick, make money fast, work from home, no credit check,
miracle cure, lose weight fast, free viagra, no prescription needed, online
casino, free spins, meet singles, hot singles in your area, replica watches,
cheap Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis,
Babuk, BadUSB, BazarLoader, Black Basta, BlackEnergy, BlackMatter, Blackshades,
Blaster, Brontok, Carbanak, Cerber, Clampi, Cobalt Strike, Conficker, Conti, Crysis,
CryptoLocker, CryptoWall, DarkComet, DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame, FormBook, Gafgyt,
GandCrab, Gh0st RAT, Glupteba, Gozi, GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw, Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit, Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort, NotPetya,
Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader,
Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil, Ryuk, Sasser, SavetheQueen, Shamoon, Shifu,
Shlayer, Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote,
TeslaCrypt, Tinba, Tiny Banker, TrickBot, Ursnif, Uroburos, WannaCry, WannaRen, WastedLocker, Wifatch, Winnti,
XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob, Zotob
Also visit my webpage – hacking tools
WOW just what I was looking for. Came here by searching for pharmacies
Hiya! I know this is kinda off topic nevertheless I’d figured I’d ask.
Would you be interested in exchanging links or maybe guest authoring a blog article or vice-versa?
My blog goes over a lot of the same subjects as yours and I believe we could greatly benefit from each other.
If you happen to be interested feel free to send me an e-mail.
I look forward to hearing from you! Excellent blog by the way!
I visited multiple web sites but the audio feature for audio songs current at this web site is actually fabulous.
Как выбрать сувениры матрешки лучше всего
Hello it’s me, I am also visiting this site daily, this web site is in fact nice and the
users are truly sharing pleasant thoughts.
I’ve been reading about Paybis for a while now, and I’m still trying to form a clear opinion about whether it truly deserves all the attention it gets, but it’s certainly
an interesting name within the cryptocurrency space, especially
when it comes to combining crypto markets with fiat currencies.
From what I understand so far, Paybis presents itself as a
large-scale cryptocurrency platforms that also supports regular
payment systems, which is something many exchanges either limit or complicate.
What initially caught my interest was the way Paybis seems to merge the gap between banking methods and the
crypto world. Many platforms focus strictly on crypto-to-crypto trades, but Paybis appears to allow users to sell digital currencies using
credit cards. I’m not claiming this process is flawless, but it does seem aimed at beginners rather than only advanced traders.
Another aspect worth mentioning is the range of cryptocurrencies
supported. Paybis doesn’t appear to limit itself
to Bitcoin and Ethereum only. Instead, it offers access to a broader token selection, which might appeal to users
who are diversifying. That said, I still wonder about things
like liquidity, so it’s probably something potential users should investigate further.
Security and compliance are also frequently mentioned in relation to Paybis.
The platform emphasizes KYC procedures, which could be seen as protective for
some users, though others might find it restrictive.
I’m honestly unsure where I stand on that, but it does suggest that
Paybis is trying to operate as a regulated crypto and fiat marketplace.
When it comes to fees and exchange rates, opinions seem mixed.
Some sources claim that Paybis is straightforward with pricing, while
others mention that costs may vary by transaction. This isn’t uncommon in the crypto industry, but it does mean users should probably read
the details carefully before making decisions.
Overall, I wouldn’t say Paybis is perfect, but it does appear to be a platform that’s worth
learning more about. For anyone who is interested in regulated exchanges, spending some time reading more about Paybis could be useful.
I’m still undecided myself, but it’s promising enough to
justify further exploration.
I don’t even know how I ended up here, but I thought
this post was great. I do not know who you are but
definitely you’re going to a famous blogger if you are not already
😉 Cheers!
В этой статье собраны факты, которые освещают целый ряд важных вопросов. Мы стремимся предложить читателям четкую, достоверную информацию, которая поможет сформировать собственное мнение и лучше понять сложные аспекты рассматриваемой темы.
Подробнее можно узнать тут – https://www.ancb.bj/index.php/publications/item/428-premiere-session-de-la-commission-thematique-genre-affaires-sociales-et-participation-citoyenne-de-l-ancb-luc-atrokpo-ouvre-la-session.html?start=290
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Получить полную информацию – https://trinityalpsmarina.com/2018/02/the-difference-between-docking-and-mooring
Game bài đổi thưởng
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored subject matter stylish.
nonetheless, you command get bought an impatience over
that you wish be delivering the following. unwell unquestionably come more formerly again since exactly the same nearly very
often inside case you shield this increase.
bookmarked!!, I like your website!
В этой статье вы найдете познавательную и занимательную информацию, которая поможет вам лучше понять мир вокруг. Мы собрали интересные данные, которые вдохновляют на размышления и побуждают к действиям. Открывайте новую информацию и получайте удовольствие от чтения!
ТОП-5 причин узнать больше – https://www.fit7fitness.com/video-list
Hey there! This is my 1st comment here so I just wanted to give a quick shout out and tell you I truly enjoy reading your posts.
Can you recommend any other blogs/websites/forums that go over the
same topics? Appreciate it!
Its like you read my mind! You appear to know
a lot about this, like you wrote the book in it or something.
I think that you can do with a few pics to drive the message home a bit, but other than that,
this is wonderful blog. A great read. I’ll definitely be back.
What’s up colleagues, pleasant article and pleasant arguments
commented here, I am in fact enjoying by these.
Please let me know if you’re looking for a
article writer for your weblog. You have some
really good posts and I feel I would be a good asset.
If you ever want to take some of the load off, I’d really
like to write some content for your blog in exchange for a link back to mine.
Please blast me an email if interested. Cheers!
zet casino app für ios
References:
https://online-spielhallen.de/vulkan-vegas-casino-erfahrungen-ein-umfassender-uberblick/
интернет kraken актуальные ссылки
бездепозитные бонусы в казино с выводом
Way cool! Some extremely valid points! I appreciate you penning
this article and the rest of the website is also really good.
always i used to read smaller posts which as well clear their
motive, and that is also happening with this post which I am reading here.
No matter if some one searches for his necessary thing, therefore he/she wants to be available that in detail,
thus that thing is maintained over here.
After I originally left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and now every time a comment is added I recieve 4 emails with the same comment.
Is there a way you can remove me from that service?
Thank you!
Individuals or collective groups grouped according to common defining traits
Ecstasy
Magnificent beat ! I would like to apprentice whilst you amend your site, how could i
subscribe for a weblog web site? The account aided me a appropriate deal.
I had been tiny bit familiar of this your broadcast provided vibrant
transparent concept
I savour, lead to I discovered exactly what I was taking a look for.
You’ve ended my four day lengthy hunt! God Bless you man. Have a nice day.
Bye
Thanks! Loads of facts!
Here is my website … https://www.neopermis.fr/index.php/ufaq/je-souhaite-annuler-linscription-dun-participant-defaut-de-salle/
My partner and I stumbled over here by a different
page and thought I may as well check things out. I like what I see so now i’m following you.
Look forward to checking out your web page
again.
Saya baru saja mengikuti artikel ini dari awal sampai akhir, dan saya merasa bahwa pembahasannya disajikan dengan sangat
baik serta relevan dengan beberapa topik yang saat ini sedang banyak diperbincangkan, termasuk KUBET, Situs Judi Bola Terlengkap,
Situs Parlay Resmi, Situs Parlay Gacor, Situs Mix Parlay,
Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi Bola gacor.
Menurut saya, kualitas artikel ini terlihat dari cara penyampaiannya yang mudah dipahami,
sehingga membuat pembaca dapat mengikuti setiap poin tanpa merasa kebingungan. Konten ini menurut
saya sangat bermanfaat bagi banyak orang yang sedang mencari referensi terpercaya dan memahami isu
yang sedang berkembang. Saya tidak bisa hanya
membaca tanpa berkomentar karena artikel dengan kualitas seperti ini memang layak mendapatkan apresiasi lebih.
Harapan saya, penulis dapat terus menghadirkan konten-konten yang
menginspirasi seperti ini agar pembaca lain juga bisa mendapatkan manfaat yang
sama. Terima kasih telah menyajikan materi yang berkualitas dan mudah dinikmati oleh
siapa pun yang membacanya.
I am curious to find out what blog platform you are utilizing?
I’m experiencing some small security issues with my latest site and I’d like
to find something more safeguarded. Do you have any
suggestions?
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UႽA
(713) 364-3256
anti-aging skincare tips results
Saya baru saja membaca artikel ini dari awal hingga akhir, dan menurut saya
pembahasannya sangat menarik, apalagi ketika topik-topik populer seperti KUBET, Situs Judi Bola Terlengkap, Situs Parlay Resmi,
Situs Parlay Gacor, Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs parlay, Kubet Parlay, dan Judi
Bola gacor diulas dengan sudut pandang yang kuat dan mudah dipahami.
Dari penilaian saya, tulisan ini memberikan penjelasan yang jelas dan terarah, sehingga pembaca
dapat mengikuti seluruh alur penjelasan dengan nyaman. Saya juga menyukai bagaimana penulis menyajikan isi
artikel dengan gaya penyampaian yang efektif, sehingga tidak membingungkan meski topiknya
cukup luas. Selain itu, artikel ini juga memberikan perspektif yang berbeda dibandingkan banyak tulisan lain yang pernah saya baca sebelumnya dalam kategori yang sama.
Sulit bagi saya untuk tidak memberikan komentar karena artikel ini benar-benar tampak disiapkan dengan baik dan layak mendapatkan apresiasi.
Saya berharap penulis dapat terus menyajikan artikel-artikel yang bermanfaat seperti
ini agar semakin banyak pembaca yang memperoleh wawasan baru dari sudut pandang yang terpercaya.
Terima kasih kepada penulis yang telah memberikan materi dengan kualitas
yang sangat baik, sehingga pengalaman membaca menjadi jauh lebih menyenangkan dan penuh informasi.
I am genuinely happy to glance at this blog posts which carries lots of valuable information, thanks for providing these data.
By making easy way of life modifications akin to eating a balanced weight loss plan, avoiding processed foods and sugary drinks, exercising commonly, managing stress, and getting enough sleep, we are able to achieve optimum https://git.churiland.com/phillisharriso/5164order-vitaseal-blood-support-today/wiki/Next-up-are-The-Crusade-Relics sugar stability and improve our overall well being and well-being. Making wiser meals decisions is not restricted to solids; it consists of drinks, too. The most effective meals decisions to accomplish this include vegetables, fruits, entire grains, low- or nonfat dairy products, and lean protein sources. Make smart decisions and eat modest amounts of coronary heart-wholesome oils while limiting the less-wholesome strong fats.Our final section will look at methods to use fluids and vitamins as part of a balanced food regimen. They’ll look for indicators of diabetic retinopathy. Fruits and vegetables have a excessive water content, so eating them will also increase your water intake. Typically individuals eat too many foods low in vitamins and minerals however excessive in calories. The extra foods and beverages you devour which might be low in nutrient density, the more durable it’s to get all the vitamins and minerals you want without getting too many calories and gaining weight. However, some people do not get these warning signals, do not understand they’re hypoglycemic, and subsequently don’t treat themselves-which may be very dangerous.
For the reason that the admin of this website is working, no hesitation very quickly it will be renowned, due
to its feature contents.
buy backlinks, link exchange, free gift card, congratulations you have won,
claim your prize, you have been selected, click here to claim,
you won’t believe, one weird trick, what happened next will shock you,
shocking truth, secret revealed, limited time offer, special promotion, act now,
don’t miss out, buy now, best price, risk-free trial, get rich quick, make money fast, work from home, no credit check, miracle cure,
lose weight fast, free viagra, no prescription needed, online casino, free spins,
meet singles, hot singles in your area, replica watches, cheap
Rolex.Agent Tesla, ALPHV, Andromeda, Angler, Anubis, Babuk, BadUSB, BazarLoader,
Black Basta, BlackEnergy, BlackMatter, Blackshades, Blaster, Brontok, Carbanak, Cerber, Clampi,
Cobalt Strike, Conficker, Conti, Crysis, CryptoLocker, CryptoWall, DarkComet,
DarkSide, Dharma, Dorkbot, Dridex, Duqu, Dyreza, Emotet, Flame, FormBook,
Gafgyt, GandCrab, Gh0st RAT, Glupteba, Gozi,
GozNym, Hancitor, IcedID, Industroyer, Jaff, Jigsaw,
Joker, Kelihos, Kinsing, Koobface, Kronos, LockBit,
Locky, Loda, LokiBot, Magecart, Maze, Medusa, MegaCortex, Methbot, Mirai, Mimikatz, mSpy, Necurs, Nemucod, NetSky, Nivdort,
NotPetya, Nymaim, Pegasus, PlugX, Poison Ivy, Pony, QakBot, QuantLoader, Ragnar Locker, Ramnit, RansomEXX, Ranzy, REvil,
Ryuk, Sasser, SavetheQueen, Shamoon, Shifu, Shlayer,
Shylock, Sinowal, SmokeLoader, Snake, SolarWinds Sunburst, SpyEye, SpyNote, TeslaCrypt, Tinba,
Tiny Banker, TrickBot, Ursnif, Uroburos,
WannaCry, WannaRen, WastedLocker, Wifatch, Winnti, XcodeGhost, XLoader, XorDDoS, ZeroAccess, Zloader, Zlob,
Zotob
Here is my blog :: cialis
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626, United States
o’malley bail bonds
I am not sure where you are getting your information, but great topic.
I needs to spend some time learning more or understanding more.
Thanks for excellent information I was looking for this info for my mission.
I like the helpful information you provide in your articles.
I’ll bookmark your weblog and check again here frequently.
I’m quite sure I’ll learn plenty College of Engineering Technology new stuff right
here! Good luck for the next!
Hello my family member! I wish to say that this post is amazing, great written and come with almost all significant infos.
I’d like to peer extra posts like this .
Feel free to visit my web page: College of Engineering Technology
I’m amazed, I must say. Seldom do I encounter a blog that’s equally educative and engaging, and let me tell you, you
have hit the nail on the head. The issue is something not enough people
are speaking intelligently about. I’m very happy
I came across this during my search for something relating to this.
Wow, superb blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your
website is wonderful, as well as the content!
You made some decent points there. I checked on the web for more information about the issue and found most people will go along with your views on this website.
Kings Casino Deutschland
References:
https://online-spielhallen.de/umfassender-leitfaden-zum-casino-cashback-ihr-verlustschutz-im-online-casino/
एफ-16 विमानान कंबोडियाच्या सैनिकां लागसार दोन क्षेपणास्त्रां उडयल्ल्याची म्हायती परराश्ट्र मंत्रालयान दिल्या
Link exchange is nothing else however it is only placing the other person’s weblog link
on your page at suitable place and other person will also do same for you.
I go to see each day some web sites and websites to read articles or reviews, except this
blog offers feature based writing.
boomerang casino aktueller bonus code
References:
https://online-spielhallen.de/ihr-umfassender-leitfaden-zum-royal-casino-promo-code/
Do you have any video of that? I’d love to find out some additional
information.
Right now it seems like BlogEngine is the best blogging platform available right now.
(from what I’ve read) Is that what you’re using on your blog?
I’m gone to say to my little brother, that he should also visit this web site
on regular basis to take updated from newest reports.
It’s amazing to pay a quick visit this website and reading the views of
all mates on the topic of this paragraph, while I
am also zealous of getting experience.
лебедка general
bizzo casino support
References:
https://online-spielhallen.de/druckgluck-casino-aktionscodes-dein-schlussel-zu-besseren-spielerlebnissen/
бездепозитные бонусы в казино за регистрацию с выводом
Avantgarde Casino mobile App Erfahrung
References:
https://online-spielhallen.de/bruno-casino-login-ihr-tor-zur-welt-der-spiele/
Hi there, all the time i used to check website posts here early
in the daylight, for the reason that i enjoy to learn more
and more.
PowerUp Casino Auszahlung
References:
https://online-spielhallen.de/drip-casino-test-bonus-auszahlungen/
What’s up everyone, it’s my first go to see at this web site, and article is in fact fruitful designed
for me, keep up posting such content.
I’d like to find out more? I’d like to find out some additional information.
Oh my goodness! Incredible article dude! Thanks, However I am encountering
difficulties with your RSS. I don’t understand why I am unable to join it.
Is there anybody having the same RSS problems? Anyone that knows the solution will you kindly respond?
Thanx!!
Spinanga Aktionscode mobile
References:
https://online-spielhallen.de/bigg-casino-deutschland-ihr-umfassender-leitfaden/
Heya i’m for the first time here. I found this board and I in finding
It really useful & it helped me out a lot. I’m hoping to provide something again and aid
others such as you helped me.
We are a group of volunteers and opening a new scheme in our community.
Your site offered us with valuable info to work on. You’ve done a formidable job and our entire community
will be grateful to you.
Post writing is also a fun, if you be familiar with
afterward you can write if not it is difficult to write.
대밤은 “대구의 밤”이라는 이름 그대로 대구 및 경북
지역의 유흥 정보를 다루는 지역 커뮤니티 사이트입니다.
술집, 클럽, 카페, 마사지 등 밤에 즐길 수 있는 다양한
I read this post fully on the topic of the difference
of newest and earlier technologies, it’s amazing article.
visit homepage https://toast-wallet.net
Pretty! This has been a really wonderful post.
Many thanks for supplying these details.
Nomini Casino Freispiele aktuell
References:
https://online-spielhallen.de/die-bwin-casino-mobile-app-dein-ultimativer-guide/
great post to read https://lumi-wallet.io
Having read this I thought it was very informative. I appreciate
you taking the time and energy to put this short article together.
I once again find myself personally spending a lot of time both reading and posting
comments. But so what, it was still worth it!
Riigidepartemang teatas, et F-16 tulistas Kambodža vägede lähedale välja kaks raketti
additional reading https://jaxx-web.org/
jackpot.de spielautomaten bonus
References:
https://online-spielhallen.de/wunderino-casino-promo-code-dein-schlussel-zu-fantastischen-boni/,wunderino
Keep it up and keep attracting more players!
http://www.google.co.ao/url?q=https://free-onlyfans.org/
Wygodna platforma Mostbet — uwielbiam tu zaglądać!
https://mostbet-kasina.cz/jak-hrat
бонус за регистрацию без депозита в казино с выводом
I was extremely pleased to uncover this website. I wanted to thank
you for your time just for this fantastic read!! I definitely
really liked every bit of it and I have you book marked
to check out new things in your site.
goGLOW Houston Heights
1515 Studemont Տt Suite 204, Houston,
Texas, 77007, UՏA
(713) 364-3256
anti-aging skincare tips explained
Does your website have a contact page? I’m having trouble locating
it but, I’d like to send you an email. I’ve got some recommendations for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it grow over
time.
Mangelsen
7916 Girard Avenue, La Joya
CΑ 92037, United States
1 800-228-9686
discover jackson hole wildlife species
sugar casino mobile app
References:
https://online-spielhallen.de/bizzo-casino-auszahlung-dein-leitfaden-fur-schnelle-gewinnauszahlungen/
Hello, Neat post. There’s a problem along with your
website in internet explorer, would test this? IE still is
the market leader and a large part of other folks
will leave out your great writing due to this problem.
Эта статья предлагает захватывающий и полезный контент, который привлечет внимание широкого круга читателей. Мы постараемся представить тебе идеи, которые вдохновят вас на изменения в жизни и предоставят практические решения для повседневных вопросов. Читайте и вдохновляйтесь!
Обратитесь за информацией – https://dev.iabtechlab.com/epicard-headshot-2
Very nice post. I just stumbled upon your blog and wished to say that
I have really enjoyed browsing your blog posts. After all I will be subscribing to your feed and I hope you write again very soon!
У вас ценный информацию по теме игровых стратегий.
https://www.furniturelist.us/modify-company-details?nid=21280&element=https://sultan-casino-kazakhstan-betzone.kz/registration
В этой публикации мы сосредоточимся на интересных аспектах одной из самых актуальных тем современности. Совмещая факты и мнения экспертов, мы создадим полное представление о предмете, которое будет полезно как новичкам, так и тем, кто глубоко изучает вопрос.
Детальнее – https://taxipuntacanamacao.com/index.php/2022/07/01/5-most-beautiful-islands-in-asia
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Продолжить чтение – https://flexporttrade.com.br/hello-world
Wow, amazing blog format! How long have you ever been blogging for?
you make running a blog look easy. The whole glance of
your web site is great, as well as the content!
hit spin auszahlungsdauer
References:
https://online-spielhallen.de/casino-of-gold-promo-code-ihr-schlussel-zu-exklusiven-vorteilen/
Mangelsen
7916 Girard Avenue, Ꮮa Joya
CA 92037, United States
1 800-228-9686
top wyoming grizzly bears species (https://allmyfaves.com/)
You can certainly see your expertise within the
work you write. The sector hopes for more passionate
writers such as you who aren’t afraid to
say how they believe. Always follow your heart.
look at here now https://jaxxwallet-web.org
Just wish to say your article is as surprising.
The clarity in your post is simply cool and i could assume you are an expert on this subject.
Fine with your permission allow me to grab your feed to keep updated with
forthcoming post. Thanks a million and please keep up the gratifying work.
Thanks for sharing your thoughts. I truly appreciate your efforts and I am waiting for your further write ups thanks once again.
Its such as you learn my mind! You appear to understand so much approximately this, like you wrote
the e book in it or something. I think that you could do with
a few % to drive the message house a bit, but instead of that, that is wonderful
blog. A fantastic read. I will definitely be back.
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Изучить эмпирические данные – https://viajeroencolombia.com/a-que-departamento-pertenece-barranquilla
Incredible story there. What happened after? Thanks!
Thanks for sharing your thoughts on slot gacor. Regards
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Детальнее – https://cbzf.pl/2023/07/26/witaj-swiecie
Refresh Renovation Southwest Charlotte
1251 Arropw Pine Ⅾr с121,
Charlotte, NC 28273, Uniteed Ⴝtates
+19803517882
Extension house
I absolutely love your blog and find nearly all of your post’s to be what precisely I’m looking for.
Does one offer guest writers to write content for you? I wouldn’t mind composing
a post or elaborating on a lot of the subjects you write
in relation to here. Again, awesome blog!
здесь кракен
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Читать полностью – http://blockshuette.de/blog/?p=547
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Личный опыт — читайте сами – https://inspiracomunicaciones.com/responsabilidad-social-empresarial/rse
Agpang keng Minister Defans Cambodia, ler pe atak en avyon Thai F-16 menabu yang keksoz bomba keng enn dan en kan keng Cambodia
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy situs gacor
бездепозитные бонусы в казино олимп
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UႽА
(713) 364-3256
skin rejuvenation cost cost
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Ознакомиться с теоретической базой – https://blog.e2dcrystals.com/bloodstone-complete-guide
Sayt superdir, təbriklər. Təşəkkürlər!
https://mostbet-az-slot.com/qeydiyyat/
Рrime Secured
3603 N 222nd St, Suite 102,
Elkhorn, ⲚE 68022, United Տtates
402-289-4126
Next-Level Network Security
With havin so much content and articles do you ever run into any problems of
plagorism or copyright infringement? My website has a lot of exclusive
content I’ve either authored myself or outsourced but it
seems a lot of it is popping it up all over the web
without my authorization. Do you know any methods to help
stop content from being ripped off? I’d definitely appreciate
it.
If you wish for to get a good deal from this post then you have to apply these methods to
your won webpage.
посмотреть на этом сайте капча
посетить веб-сайт krab2.cc
Verde Casino Auszahlung Erfahrungen
References:
https://online-spielhallen.de/sg-casino-mobile-app-dein-spielvergnugen-fur-unterwegs/
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Получить полную информацию – https://trinityalpsmarina.com/2018/02/the-difference-between-docking-and-mooring
Vinyl Casino Erfahrungen
References:
https://online-spielhallen.de/umfassende-betrachtung-des-drip-casinos-in-deutschland-einblick-fur-spieler/
Spot on with this write-up, I truly feel this web site needs a great deal more attention. I’ll probably be back again to read more, thanks for
the information!
nv casino einloggen
References:
https://online-spielhallen.de/netbet-casino-cashback-ihr-weg-zu-verlorenen-einsatzen/
Hi! Would you mind if I share your blog with my facebook group?
There’s a lot of people that I think would really appreciate your content.
Please let me know. Cheers
I blog frequently and I seriously thank you for your information. This great article
has really peaked my interest. I’m going to take a note of your website and keep
checking for new details about once per week.
I opted in for your Feed as well.
gizbo casino bonus erfahrungen
References:
https://online-spielhallen.de/arena-casino-erfahrungen-ein-umfassender-uberblick/
princess casino freispiele guide
References:
https://online-spielhallen.de/rant-casino-freispiele-alles-was-sie-wissen-mussen/
As the admin of this site is working, no doubt very rapidly it
will be renowned, due to its quality contents.
Please let me know if you’re looking for a article writer for
your site. You have some really good posts and
I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some articles for your blog in exchange for a link back to mine.
Please send me an email if interested. Thanks!
Avantgarde Casino Startguthaben
References:
https://online-spielhallen.de/den-plinko-casino-promo-code-finden-ihr-weg-zu-extra-spielspas-und-lukrativen-boni/
n1bet cashback bedingungen
References:
https://online-spielhallen.de/nomini-casino-cashback-ihr-weg-zu-verlorenen-einsatzen/
I’m really enjoying the design and layout of your site.
It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a designer
to create your theme? Superb work!
I blog frequently and I truly appreciate your information. The
article has really peaked my interest. I will take a note of
your blog and keep checking for new information about once
per week. I opted in for your Feed as well.
I think the admin of this website is really working hard
in favor of his web site, as here every information is quality based
stuff.
бездепозитный бонус за регистрацию в казино с выводом денег без первого депозита
Hello there! This article could not be written any better!
Reading through this post reminds me of my previous roommate!
He always kept preaching about this. I most certainly will
send this information to him. Pretty sure he’s going to have a very good read.
I appreciate you for sharing!
Искала в всемирной паутине данные по поводу этой проблемы и наткнулась на сайт – https://studsmi.ru/ Оказалось, там собраны важные материалы, обзоры и комментарии от людей с разным опытом, так что можно посмотреть обстановку под новым углом, сравнить мнения и уже на основе этого сделать свои заключения или открыть дополнительные данные, если появится желание углубиться ещё тщательнее.
I want to to thank you for this excellent read!! I certainly loved every little bit of it.
I have you book marked to check out new stuff you
post…
I am sure this article has touched all the internet viewers, its really really nice paragraph on building
up new blog.
After looking into a few of the blog posts on your web page, I
seriously like your technique of blogging. I book marked it to my bookmark site
list and will be checking back in the near future. Take a look at
my web site as well and tell me what you
think.
Way cool! Some extremely valid points! I appreciate you penning this write-up plus the rest of the site
is also really good.
зайти на сайт трипскан сайт вход
Prime Secured
3603 N 222nd Ѕt, Suite 102,
Elkhorn, ΝE 68022, United Տtates
402-289-4126
Tailored Enterprise Security
I’m gone to say to my little brother, that he should also visit this weblog on regular basis to obtain updated from latest
reports.
What’s up, after reading this remarkable article i am too cheerful to share my know-how here with friends.
I have been browsing online more than 2 hours today, yet I
never found any interesting article like yours. It’s pretty worth enough for me.
In my view, if all webmasters and bloggers made good content as
you did, the internet will be much more useful than ever before.
What’s up, the whole thing is going sound here and ofcourse every one is sharing facts, that’s in fact
excellent, keep up writing.
Gizbo Casino Kundensupport
References:
https://online-spielhallen.de/wildz-casino-deutschland-ihr-detaillierter-uberblick/
Nice blog here! Also your web site quite a bit up fast! What web host
are you using? Can I get your affiliate link in your
host? I desire my site loaded up as fast as yours lol
Spirit Casino online Erfahrungen
References:
https://online-spielhallen.de/iwild-casino-promo-code-dein-weg-zu-mehr-spielspas/
Hello there! This is my first visit to your blog! We are a team of volunteers and starting
a new project in a community in the same niche.
Your blog provided us useful information to work on. You have done
a marvellous job!
jokerstar bonus code 2024
References:
https://online-spielhallen.de/spinanga-casino-deutschland-eine-umfassende-bewertung/
Right here is the right site for everyone who really wants to understand this topic. You know a whole lot its almost tough to argue with you (not that I really will need to…HaHa). You certainly put a brand new spin on a topic that has been written about for a long time. Excellent stuff, just great!
https://waterfrontevent.co.uk/2025/12/24/decouvrir-atlas-pro-max-focus-sur-les-fonctions-essentielles/
промокоды 1xbet 2026
Wow, this paragraph is good, my younger sister is analyzing these things, thus I am going to convey
her.
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy basreng188
Hello, I enjoy reading all of your post. I like to write a
little comment to support you.
что дает промокод в 1xbet
Mangelsen
7916 Girard Avenue, Lɑ Joya
CA 92037, United States
1 800-228-9686
discover park city nature photography conservation
F-16 me bula bamisile zole pene-pene ya basoda ya Cambodge, mutindu ministere ya mambu ya banzenza me tuba
Jokerstar Cashback Bedingungen
References:
https://online-spielhallen.de/avantgarde-casino-erfahrungen-ein-detaillierter-spielerbericht/
Heya! I understand this is somewhat off-topic but I had to ask.
Does managing a well-established website such as yours require a
massive amount work? I am completely new to blogging however I do write in my journal
on a daily basis. I’d like to start a blog so I can share my experience and
feelings online. Please let me know if you have any ideas or tips for brand new aspiring blog owners.
Thankyou!
https://natashki.com/ – Natashki.com: A World of Bright Encounters. Only Real People. All in One Place. Join for Free. >>>
I’d like to find out more? I’d want to find out more details.
сюда кракен зеркало
Malina Casino App Login
References:
https://online-spielhallen.de/merkur-online-casino-willkommen-aktuelles/
Hey there would you mind letting me know which webhost you’re utilizing?
I’ve loaded your blog in 3 completely different web browsers and I must say this blog loads a
lot faster then most. Can you suggest a good hosting provider
at a honest price? Thank you, I appreciate it!
Kudos, I enjoy it!
промокод 1хбет при регистрации
Wonderful blog! I found it while browsing on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem
to get there! Appreciate it
discover this info here jaxx wallet review
сюда krab3.cc
I’m not sure where you are getting your info, but
great topic. I needs to spend some time learning much more or understanding more.
Thanks for magnificent information I was looking for this information for my
mission.
If you desire to get a good deal from this paragraph then you have to
apply such methods to your won website.
Thanks for the auspicious writeup. It in fact was once a enjoyment account it.
Glance complex to more added agreeable from you!
By the way, how can we communicate?
Locowin Casino Legal
References:
https://online-spielhallen.de/malina-casino-mobile-app-dein-umfassender-leitfaden-fur-unterwegs/
There’s definately a lot to find out about this subject. I really like all of the
points you made.
Rooli Casino Bonusaktion
References:
https://online-spielhallen.de/myempire-casino-freispiele-alles-was-sie-wissen-mussen/
magnificent post, very informative. I’m wondering why the other specialists of this sector don’t notice this.
You should continue your writing. I’m confident, you’ve a
great readers’ base already!
бездепозитные бонусы в казино олимп
промокод на ставку 1xbet
Nomini Aktionscode 2024
References:
https://online-spielhallen.de/malina-casino-freispiele-ihr-schlussel-zu-kostenlosem-spielspas/
Wow, superb weblog layout! How long have you ever been blogging for?
you made running a blog look easy. The overall glance of your web site is excellent, let alone the content!
веб-сайте tripskan
Casino App unterwegs
References:
https://online-spielhallen.de/nomini-casino-cashback-ihr-weg-zu-verlorenen-einsatzen/
I used to be recommended this website by means
of my cousin. I’m now not positive whether or not this publish is written by means of him as nobody
else understand such exact about my difficulty. You are amazing!
Thanks!
Bruno Casino Aktionscode einlösen
References:
https://online-spielhallen.de/umfassender-leitfaden-zum-spirit-casino-bonus-code/
Hello there, just became aware of your blog through Google, and found that it’s truly informative.
I’m gonna watch out for brussels. I’ll appreciate if you continue this in future.
Lots of people will be benefited from your writing.
Cheers!
Hey There. I found your blog using msn. This is a really well written article.
I’ll make sure to bookmark it and return to read more of your useful
information. Thanks for the post. I’ll certainly comeback.
Definitely believe that which you said. Your favorite justification seemed to be at the web the simplest factor
to consider of. I say to you, I certainly get annoyed whilst other
people consider issues that they plainly don’t understand about.
You managed to hit the nail upon the highest as neatly
as defined out the whole thing without having side-effects , people can take a signal.
Will probably be again to get more. Thank you
Also visit my web-site: landscaping company Woodbranch
Thank you a bunch for sharing this with all folks you actually recognize what you’re speaking about!
Bookmarked. Kindly also discuss with my website =).
We may have a link trade contract among us
Thanks to my father who stated to me about
this website, this webpage is actually amazing.
Wow, marvelous weblog structure! How lengthy have you ever been blogging
for? you make blogging glance easy. The whole look of your web site is great,
as well as the content material!
nine casino auszahlung
References:
https://online-spielhallen.de/888casino-im-test-slots-poker-zahlungen-bonus/
wonderful submit, very informative. I’m wondering why the other specialists of this sector do not notice this.
You should continue your writing. I am confident, you’ve
a great readers’ base already!
I think that everything posted made a bunch of sense.
However, what about this? suppose you were to write a killer headline?
I ain’t suggesting your information isn’t solid, but suppose
you added a title that grabbed a person’s attention? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate is kinda vanilla.
You should look at Yahoo’s home page and see how they create post headlines
to grab viewers to click. You might try adding a video or a picture or two to grab people interested about what you’ve got to say.
Just my opinion, it could bring your website a little bit more
interesting.
internet jaxx liberty wallet
Thanks in favor of sharing such a pleasant thought, post
is pleasant, thats why i have read it fully
Terrific post but I wass wanting to know if you could
write a litte mre on thus topic? I’d be very thankful if you could elaborate a little bit more.
Kudos!
Easy and logical site with a wealth of gambling-related info.
https://1winaviator-in.co.in/bonus
посмотреть в этом разделе krab 1at
Потрясающе, сайт Olimp Casino — очень информативный.
http://satoshiogawa.com/?wptouch_switch=desktop&redirect=http%3a%2f%2folimp-casino-kazakhstan-top.kz%2Fpayments
Надёжный ветош используется в промышленности, автосервисах и на производственных площадках. Материал подходит для удаления загрязнений, смазок и пыли, удобен в работе и рассчитан на многоразовое применение. Поставка осуществляется напрямую, без посредников, с понятными условиями и стабильными характеристиками продукции.
Betano Casino Bonus
References:
https://online-spielhallen.de/druckgluck-casino-bewertung-meine-ausfuhrliche-analyse/
each time i used to read smaller articles
which also clear their motive, and that is also happening with this piece of writing which I am reading here.
Can I simply say what a comfort to uncover somebody who really understands what
they are talking about online. You certainly realize how to bring an issue to light and make it important.
More and more people must look at this and understand this side of your story.
I was surprised that you aren’t more popular since you surely
possess the gift.
goGLOW Houston Heights
1515 Studejont Ѕt Suite 204, Houston,
Texas, 77007, UՏA
(713) 364-3256
skincare routine expert
Wow! At last I got a webpage from where I be capable of actually obtain valuable information regarding
my study and knowledge.
I was recommended this website by my cousin. I am not sure whether this post is written by him as no one else know
such detailed about my difficulty. You’re amazing!
Thanks!
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CА 92626, United Statеs
who pays bail bonds
casino app 2025 sicher
References:
https://online-spielhallen.de/lukki-casino-deutschland-ihr-detaillierter-uberblick-und-meine-erfahrungen/
бездепозитные бонусы в казино за регистрацию с выводом
Aw, this was a really good post. Taking a few minutes and actual effort to make a
good article… but what can I say… I put things off a lot and don’t
seem to get anything done.
888 casino bonus anleitung
References:
https://online-spielhallen.de/lukki-casino-cashback-ihr-weg-zu-mehr-spielguthaben/
Piece of writing writing is also a fun, if you be acquainted
with afterward you can write or else it is complex to write.
It’s appropriate time to make some plans
for the future and it’s time to be happy. I’ve read this post and
if I could I desire to suggest you few interesting things or tips.
Maybe you can write next articles referring to this article.
I want to read more things about it!
Эта информационная статья содержит полезные факты, советы и рекомендации, которые помогут вам быть в курсе последних тенденций и изменений в выбранной области. Материал составлен так, чтобы быть полезным и понятным каждому.
Подробнее – https://publicmedia.co.jp/download/%E3%81%BE%E3%82%8B%E3%81%A1%E3%81%B7%E3%82%8B%E5%B1%95%E9%96%8B%E5%9B%B32
Hit Spin Casino Spielerlebnis
References:
https://online-spielhallen.de/beste-online-casinos-deutschland-top-10-nov-2025-3/
It’s really very complicated in this busy life to listen news on Television, therefore I just use the web
for that reason, and take the most up-to-date news.
Hey! Quick question that’s completely off topic. Do you know
how to make your site mobile friendly? My site looks weird when browsing from my iphone4.
I’m trying to find a template or plugin that might be able to resolve this problem.
If you have any suggestions, please share. Appreciate it!
As the admin of this website is working, no
doubt very quickly it will be famous, due to its quality contents.
Thanks for sharing your thoughts. I really appreciate your efforts and
I am waiting for your next write ups thanks once again.
Good day very nice site!! Guy .. Excellent .. Superb ..
I’ll bookmark your site and take the feeds additionally? I am happy to seek out so many useful info here within the put
up, we want develop extra strategies in this regard, thanks for sharing.
. . . . .
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any tips on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem to get there!
Appreciate it
Hi to every single one, it’s in fact a nice for me to pay a quick visit this web page, it contains helpful Information.
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Информация доступна здесь – https://www.smgupta.co.in/what-are-the-top-qualities-which-make-a-good-chartered-accountant
I’ve been browsing on-line greater than three hours
lately, yet I never found any interesting article like yours.
It is pretty value sufficient black cardigan for women me.
Personally, if all website owners and bloggers made just right content material
as you did, the net shall be much more helpful than ever before.
소액대출은 급하게 현금이 필요할 때 빠르고 간편하게 자금을 마련할 수 있는 대표적인 방법입니다.
큰 금액이 아니어서 비교적 짧은 기간 내 상환하는 경우가 많고, 신청
Why people still make use of to read news papers
when in this technological globe all is accessible on web?
Also visit my page rolex super clone
В этой публикации мы сосредоточимся на интересных аспектах одной из самых актуальных тем современности. Совмещая факты и мнения экспертов, мы создадим полное представление о предмете, которое будет полезно как новичкам, так и тем, кто глубоко изучает вопрос.
Не упусти шанс – https://www.cerus-casino.com/videos/debut-des-annonces
Angels Baill Bonds Costa Mesa
769 Baker Տt,
Costa Mesa, CA 92626, United Statеѕ
how much bail do you pay
Appreciate the recommendation. Will try it out.
you are in reality a just right webmaster.
The site loading speed is amazing. It seems that you’re doing any unique trick.
Moreover, The contents are masterpiece. you’ve done a wonderful
job in this subject!
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Обратитесь за информацией – http://www.sunset.jp/shopblog/index.php?itemid=197
If some one wishes expert view on the topic of running a blog after that
i advise him/her to visit this weblog, Keep up the pleasant
work.
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Хочешь знать всё? – https://jaklean.co.uk/finding-the-best-cleaning-services
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Ссылка на источник – https://saucha.net/big-sale/coupon-3
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Информация доступна здесь – https://lvsbooks.com/product/valid-dismissal-2nd-ed-solutions-on-wage-order-and-min-wage-2nd-ed
Главная krab1at
김해출장마사지는 고객이 원하는 시간과 장소에 전문 테라피스트가 직접 방문하여
체계적인 마사지 프로그램을 진행하는
출장형 전문 테라피 서비스입니다.
I know this if off topic but I’m looking into starting my own blog and was curious what
all is required to get setup? I’m assuming having a blog like yours would cost
a pretty penny? I’m not very web smart so I’m not 100%
certain. Any suggestions or advice would be greatly appreciated.
Cheers
Hey are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started and create my own. Do you
require any coding expertise to make your own blog? Any help would be
really appreciated!
Aɣlif n Temḥaddit n Kambud’ya yenna-d dakken yiwen n usafag n yimenɣi n Tayland n F-16 yessers snat n lbumbat deg yiwen n usqif n yizrazaɣen deg Kambud’ya.
Oh my goodness! Impressive article dude! Thank you, However I am having difficulties with
your RSS. I don’t understand the reason why I cannot join it.
Is there anyone else getting the same RSS problems?
Anyone who knows the answer will you kindly respond?
Thanx!!
my web site: ratutogel
After checking out a handful of the blog posts on your site, I seriously like your way of writing a blog.
I saved it to my bookmark website list and will be checking back in the near future.
Please check out my web site as well and tell me your opinion.
This design is steller! You obviously know how to keep a reader entertained.
Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Great
job. I really enjoyed what you had to say, and more than that, how you presented it.
Too cool!
Hey there! I know this is kinda off topic however I’d figured I’d ask.
Would you be interested in trading links or maybe
guest authoring a blog post or vice-versa? My website discusses a lot of the same topics as yours and I think we
could greatly benefit from each other. If you might be interested feel free to send me an e-mail.
I look forward to hearing from you! Excellent blog by the way!
Great blog you’ve got here.. It’s difficult to find good quality writing like yours nowadays.
I truly appreciate people like you! Take care!!
подробнее купить криптовалюту альфа банк
GreatWin Casino Leitfaden
References:
https://online-spielhallen.de/die-vulkan-vegas-casino-mobile-app-dein-spielspas-fur-unterwegs/
Great post.
My blog Small business payroll Utah
Thanks for the auspicious writeup. It actually used to be a amusement account it.
Glance complicated to far added agreeable from you! By the way,
how can we communicate?
Saya sudah membaca artikel ini secara menyeluruh, dan menurut saya pembahasannya sangat
menarik terutama ketika topik seperti KUBET, Situs Judi
Bola Terlengkap, Situs Parlay Resmi, Situs Parlay Gacor,
Situs Mix Parlay, Situs Judi Bola, toto macau, kubet login, situs
parlay, Kubet Parlay, dan Judi Bola gacor dijelaskan dengan sudut pandang yang jelas dan mudah
dipahami. Menurut saya gaya penjelasannya sangat terstruktur,
karena mampu memberikan gambaran lengkap tanpa membuat pembaca merasa kewalahan. Artikel ini juga memiliki detail
yang lebih kaya informasi dibandingkan banyak artikel lain yang membahas
tema sejenis. Hal ini membuat saya merasa perlu untuk meninggalkan komentar, sebab kualitas
penulisan serta alur penyampaiannya benar-benar layak diapresiasi.
Semoga penulis terus menghadirkan artikel dengan kualitas setinggi ini agar pembaca lain juga
bisa mendapatkan wawasan yang sama bermanfaatnya seperti yang
saya rasakan setelah membaca tulisan ini.
Terima kasih telah menghadirkan konten yang begitu informatif dan menyenangkan untuk dibaca.
What’s Going down i am new to this, I stumbled upon this I’ve discovered It absolutely useful and it has helped me out loads.
I’m hoping to contribute & aid other customers like its helped me.
Good job.
Also visit my site; slot gacor gampang menang hari ini
Please let me know if you’re looking for a article author for your
weblog. You have some really great articles and I
think I would be a good asset. If you ever want to
take some of the load off, I’d absolutely
love to write some content for your blog in exchange for a link back
to mine. Please shoot me an e-mail if interested.
Thanks!
you’re actually a good webmaster. The web site loading pace is amazing.
It kind of feels that you’re doing any distinctive trick.
Also, The contents are masterwork. you have done a great process in this matter!
I was able to find good advice from your blog articles.
Review my website :: slot gacor gampang menang hari ini
Thanks a lot. Awesome information!
hi!,I really like your writing so much! proportion we be in contact more approximately your
article on AOL? I need an expert in this house to unravel my problem.
May be that is you! Having a look forward to look you.
my website; black cardigan for women
Posido Casino Rückerstattung
References:
https://online-spielhallen.de/rizk-casino-cashback-alles-was-sie-wissen-mussen/
посетить веб-сайт krab 1 at
It’s really a great and helpful piece of info.
I am satisfied that you just shared this useful information with us.
Please stay us informed like this. Thanks for
sharing.
My blog post rolex superclone
Как выбрать фотографа видеографа в Сочи — торжества
일산출장마사지 서비스는 일산광역시 전역에서 편안하게
전문 마사지를 받을 수 있는 출장 홈타이
서비스입니다. 고객님이 계신 곳으로 여성 전문 테라피스트가 직접
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr ϲ121,
Charlotte, NC 28273, United States
+19803517882
accessory dwelling unit construction (atavi.com)
Hi there exceptional blog! Does running a blog like this require a great deal of work?
I have absolutely no knowledge of coding however I was hoping to start my
own blog in the near future. Anyway, if you have any recommendations or techniques for new
blog owners please share. I know this is off topic nevertheless I
simply had to ask. Thanks!
Feel free to surf to my web site Financial advisory services Utah
Does your website have a contact page? I’m having a
tough time locating it but, I’d like to send
you an e-mail. I’ve got some creative ideas for your blog you might be interested in hearing.
Either way, great blog and I look forward to seeing it improve over time.
When I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and from now on each time a comment is added
I get four emails with the same comment.
Perhaps there is a way you are able to remove me from that service?
Thanks!
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ɗr c121,
Charlotte, NC 28273, United Stateѕ
+19803517882
And Upgrades heating conditioning Air
royal casino bonuscode
References:
https://online-spielhallen.de/plinko-casino-mobile-app-dein-weg-zum-digitalen-plinko-gluck/
Love 1win, keep it up — amazing content!
https://www.wannabies.work/iframe/hatena_bookmark_comment?canonical_uri=https%3A%2F%2F1win-win.in%2Fbonus%2F
Everything is very open with a precise explanation of the issues.
It was really informative. Your website is very useful.
Thanks for sharing!
Very good article. I certainly love this website. Keep
writing!
goGLOW Houston Heights
1515 Studemont Ⴝt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
Bookmarks (http://www.protopage.com)
Link exchange is nothing else except it is only placing the other person’s weblog link on your
page at suitable place and other person will also do similar
for you.
Also visit my webpage – Tax preparation Cedar City
money x казино
мани х
vulkan casino bonus ohne einzahlung
References:
https://online-spielhallen.de/gizbo-casino-bonus-code-alle-wichtigen-infos-auf-einen-blick/
Its such as you read my thoughts! You seem to understand a lot
approximately this, like you wrote the book in it or something.
I think that you could do with a few p.c. to
drive the message home a little bit, however instead
of that, this is fantastic blog. An excellent read.
I will definitely be back.
Do you mind if I quote a couple of your articles as long as I provide credit and sources back to your webpage?
My blog site is in the exact same area of interest as yours and my visitors would genuinely benefit from a lot of the information you present here.
Please let me know if this okay with you. Regards!
It’s appropriate time to make a few plans for the long run and it is
time to be happy. I have learn this publish and if I may
just I desire to counsel you some interesting things or tips.
Perhaps you could write next articles relating to this article.
I wish to learn more things approximately it!
+905516067299 fetoden dolayi ulkeyi terk etti
Lucky Dreams Bonusaktionen
References:
https://online-spielhallen.de/meine-myempire-casino-erfahrungen-ein-detaillierter-bericht/
Как выбрать деревянные балясины для лестниц из дерева
강남퍼펙트는 프라이빗 룸, 고급 인테리어, 맞춤형 서비스, 철저한 위생 관리로 방문객에게 독특한 경험을 제공합니다.
공간은 개인 또는 그룹 단위로 활용할 수 있으며
magnificent put up, very informative. I’m wondering why the opposite
specialists of this sector do not notice this. You should continue
your writing. I am confident, you’ve a huge
readers’ base already!
my web-site black cardigan for women
I like it when folks come together and share opinions. Great blog, continue the
good work!
Hi, yup this paragraph is actually nice and I have learned lot
of things from it about blogging. thanks.
Robocat Casino Erfahrungen 2024
References:
https://online-spielhallen.de/ihr-umfassender-leitfaden-zum-posido-casino-bonus-code/
Buran Casino Cashback
References:
https://online-spielhallen.de/vegadream-casino-promo-codes-ihr-weg-zu-extra-boni-und-spielspas/
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UՏA
(713) 364-3256
acne treatment near me for face
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy Slot 4D
I don’t know whether it’s just me or if everyone else experiencing issues with your blog.
It looks like some of the written text in your content are running off the
screen. Can somebody else please comment and let me know if this is happening to them too?
This might be a issue with my internet browser because
I’ve had this happen previously. Thank you
I-F-16s idubule imicibisholo emibili eduze ne-Cambodian Air Force, kusho uMnyango Wezangaphandle
drip casino bonus code 2024
References:
https://online-spielhallen.de/umfassende-bitkingz-casino-erfahrungen-ein-spielerbericht-nach-10-jahren-online-glucksspiel/
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, United States
+19803517882
Transformation ideas home modern
May I just say what a comfort to uncover an individual who truly understands what they’re talking about online.
You certainly understand how to bring a problem to light and make it important.
More and more people need to read this and understand this
side of the story. I was surprised that you
are not more popular because you certainly possess the gift.
Good post. I learn something totally new and challenging on blogs
I stumbleupon every day. It’s always exciting
to read content from other writers and use a little something from their websites.
Incredible! This blog looks just like my old one! It’s on a completely different subject but it has pretty much the same layout
and design. Excellent choice of colors!
Simple carbs, known as sugars. Simple sugars are made of 1 or two sorts of sugar. Fructose is a straightforward sugar present in fruit and honey. Fructose and glucose collectively make the sugar referred to as sucrose, which you could have in your pantry as table sugar. Lactose also is made up of two sugar models, this time galactose and glucose, and is found in milk and dairy products. Complex carbs, known as starch. Complex carbohydrates are manufactured from many sugar models bonded together. Starch occurs naturally in vegetables, grains, beans and peas. As your physique digests starch, the complicated carbohydrates break down into their simple sugar components. Fiber. Fiber is also a complex carbohydrate. It happens naturally in fruits, vegetables, whole grains, and cooked dry beans and peas. Fiber is not broken down in the body. But it can be used by some bacteria in the intestine. Fiber additionally helps move waste via the digestive tract. Carbohydrates break down right into a source of vitality for the physique, particularly the mind.
my website: http://www.xn--2s2b270b.com/bbs/board.php?bo_table=free&wr_id=372986
I am not sure where you are getting your info, but great
topic. I needs to spend some time learning more or understanding more.
Thanks for excellent information I was looking for this information for my
mission.
This information is invaluable. Where can I find out more?
Great weblog here! Also your website a lot up very fast!
What host are you using? Can I am getting your affiliate hyperlink to your host?
I want my website loaded up as fast as yours
lol
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ⅾr c121,
Charlotte, NC 28273, Unted Ⴝtates
+19803517882
Easy home renovating makes refresh your
Hello friends, how is everything, and what you desire
to say about this post, in my view its truly awesome for me.
Обожаю Sultan Casino, не останавливайтесь — контент топ!
https://www.kartamira.ru/bitrix/redirect.php?goto=https://sultan-casino-kazakhstan-game.kz
I’m amazed, I have to admit. Seldom do I come across a blog that’s equally
educative and amusing, and let me tell you, you’ve hit the nail
on the head. The issue is something too few men and women are speaking intelligently
about. Now i’m very happy that I found this during my search for
something relating to this.
Right away I am going away to do my breakfast, once
having my breakfast coming yet again to read additional
news.
Spot on with this write-up, I really believe that this web site needs far more attention. I’ll probably be returning to read more, thanks for the information!
I am sure this article has touched all the internet viewers, its
really really pleasant piece of writing on building up new
blog.
Hello to every body, it’s my first pay a visit of this web site; this
webpage includes remarkable and actually excellent stuff designed for readers.
drip casino bonus code 2024
References:
https://online-spielhallen.de/cobra-casino-cashback-so-holen-sie-das-beste-heraus/
Di dunia dunia judi online, game slot jadi satu
diantara pilihan paling diminati pada banyak gamer.
Salah satu istilah yang seringkali terdengar di kalangan pecinta slot ialah “gacor” dan “maxwin”.
Gacor berarti mudah maxwin, sedangkan maxwin merujuk buat kemungkinan keuntungan maksimal yang mampu diraih.
Kombinasi antara kedua istilah ini menjadikan permainan slot online gampang maxwin sangat
menarik pada dimainkan. Artikel ini hendak membahas lebih dalam berkenaan dengan game
situs slot gacor ini serta bagaimana metode mengenalnya.
Hmm is anyone else experiencing problems with the images on this blog loading?
I’m trying to determine if its a problem
on my end or if it’s the blog. Any feed-back would be greatly
appreciated.
I love your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you?
Plz reply as I’m looking to construct my own blog and would like to know
where u got this from. kudos
Does your site have a contact page? I’m having a tough
time locating it but, I’d like to shoot you
an e-mail. I’ve got some suggestions for your blog you might be interested in hearing.
Either way, great blog and I look forward to seeing it expand over time.
I enjoy looking through a post that will make men and
women think. Also, thank you for allowing for me to comment!
Look into my homepage … Small business payroll Utah
Mangelsen
7916 Girard Avenue, La Joya
СA 92037, United States
1 800-228-9686
amazing grizzly 399 species
Sol Casino Anmelden
References:
https://online-spielhallen.de/ihr-ultimativer-leitfaden-zum-tipico-casino-promo-code-so-holen-sie-das-maximum-heraus/
Spot on with this write-up, I absolutely believe this amazing site needs far more attention. I’ll probably
be returning to see more, thanks for the info!
https://sykaaa-online-casino.fun
I’m gone to tell my little brother, that he should also pay a visit this blog on regular basis to obtain updated from most up-to-date gossip.
Also visit my website; Recipes under 30 minutes
Hey are using WordPress for your site platform? I’m new to the blog world but I’m trying to get
started and set up my own. Do you require any html coding knowledge to make your own blog?
Any help would be really appreciated!
my web page – Payroll services Cedar City
Hello there, I discovered your website by means of Google while searching for
a similar topic, your website came up, it looks great.
I have bookmarked it in my google bookmarks.
Hi there, simply became aware of your blog thru Google, and located that it’s truly informative.
I’m going to watch out for brussels. I’ll be grateful should you proceed this in future.
Numerous other folks will be benefited from your writing.
Cheers!
This post offers clear idea in support of the new users of blogging,
that truly how to do blogging and site-building.
There’s certainly a lot to learn about this issue. I love all of
the points you’ve made.
my page; CPA firm southern Utah
Leon Casino Bonuscode
References:
https://online-spielhallen.de/betano-casino-deutschland-ihre-umfassende-erfahrungsubersicht/
bizzo casino bonus
References:
https://online-spielhallen.de/verde-casino-aktionscode-goverde-bonus-1-200e-220fs/
Hmm is anyone else encountering problems with the images on this blog loading?
I’m trying to find out if its a problem on my end or if it’s the
blog. Any feedback would be greatly appreciated.
My relatives every time say that I am killing my time here at web, except I know I am getting experience daily by reading
such fastidious articles or reviews.
maritime spieleparadies casino
References:
https://online-spielhallen.de/umfassende-bewertung-des-monro-casinos-ein-detaillierter-blick/
Its like you read my mind! You seem to know a lot approximately this, such as you wrote
the e book in it or something. I believe
that you just could do with a few percent to drive the
message house a little bit, but other than that, this is fantastic blog.
A great read. I’ll definitely be back.
goGLOW Houstron Heights
1515 Studemont Տt Suite 204, Houston,
Texas, 77007, UՏA
(713) 364-3256
meet the team review (Hilario)
Thanks designed for sharing such a pleasant thinking,
post is fastidious, thats why i have read it completely
Boomerang Casino Einzahlungsbonus
References:
https://online-spielhallen.de/nine-casino-freispiele-ihr-umfassender-leitfaden/
Sol Casino seriös
References:
https://online-spielhallen.de/umfassende-bigg-casino-bewertung-meine-erfahrungen-und-eindrucke/
Gran diseño de este sitio de . ¡Muy profesional!
https://onlyfansquees.com.mx/
That is very attention-grabbing, You are a very professional blogger.
I’ve joined your feed and sit up for in the hunt
for more of your magnificent post. Additionally,
I have shared your website in my social networks
Howdy! I know this is somewhat off topic but
I was wondering which blog platform are you
using for this site? I’m getting fed up of WordPress because I’ve had problems with hackers and I’m looking at alternatives for another platform.
I would be great if you could point me in the direction of a
good platform.
Wow, awesome blog layout! How long have you been blogging
for? you make blogging look easy. The overall look of your site is magnificent, let alone the content!
I do not know if it’s just me or iff perhaps everyone else encountering
problems with your blog. It appears as thouygh some
of the written text within your content are running off the screen. Can someone else pleawse comment and let me know if this is happening to themm as well?
Thiis might be a problem with my weeb browser because I’ve had this happen previously.
Cheers
Hey there would you mind letting me know which
web host you’re utilizing? I’ve loaded your blog in 3 different web
browsers and I must say this blog loads a lot faster then most.
Can you suggest a good internet hosting provider at a fair price?
Thanks, I appreciate it!
You really make it seem really easy with your presentation but I in finding this
topic to be really one thing which I believe I might never understand.
It sort of feels too complex and very large
for me. I’m taking a look forward for your subsequent submit, I will attempt to get the cling of it!
magnificent publish, very informative. I’m wondering why the opposite experts
of this sector don’t understand this. You must continue your writing.
I’m confident, you’ve a huge readers’ base already!
Terima kasih sudah berbagi informasi ini. Ngomong-ngomong, saya juga merekomendasikan nonton film gratis untuk pengalaman bermain terbaik.
Angels Bail Bonrs Costa Mesa
769 Baker St,
Costa Mesa, СᎪ 92626, United Stɑtes
bail bond services neаr me; https://wakelet.com/wake/0VtgwUpK-QemoGRea8ntt,
bwin casino auszahlungslimit
References:
https://online-spielhallen.de/rooli-casino-cashback-ihr-weg-zu-mehr-spielguthaben/
Pretty great post. I simply stumbled upon your blog and wanted to
mention that I’ve truly loved surfing around your weblog posts.
In any case I will be subscribing in your feed and I am hoping you write again very soon!
my web page; HR payroll services southern Utah
Супер Sultan Casino, продолжайте в том же духе. Благодарю.
https://sultan-casino-kazakhstan-gaming.kz
Эта статья предлагает захватывающий и полезный контент, который привлечет внимание широкого круга читателей. Мы постараемся представить тебе идеи, которые вдохновят вас на изменения в жизни и предоставят практические решения для повседневных вопросов. Читайте и вдохновляйтесь!
Лучшее решение — прямо здесь – https://akornas.ac.id/bayu-ramasyah-juara-1-piala-kemenpora-kategori-kata-perorangan-senior-putra
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Читать далее > – https://kyobiz.wpxblog.jp/wpx-use
I’m not that much of a online reader to be honest but your sites really nice, keep it up!
I’ll go ahead and bookmark your website to come back down the road.
Cheers
Feel free to visit my web blog :: Accountant near me Cedar City
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Что скрывают от вас? – https://laramolettiere.com/why-starting-a-blog-on-black-friday-makes-sense
This is very interesting, You’re a very skilled blogger.
I’ve joined your rss feed and look forward to seeking more of your
fantastic post. Also, I have shared your web site in my social networks!
Feel free to visit my blog post :: Payroll processing St. George
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Не упусти важное! – https://ceipsanmateo.com/events/summer-school-2015
Its like you learn my thoughts! You seem to understand a lot about this, like you wrote the guide in it or something.
I think that you simply can do with a few p.c. to pressure the message house a bit, however instead of that, that
is excellent blog. A great read. I’ll certainly be back.
Hey excellent blog! Does running a blog similar to this require
a lot of work? I have no knowledge of programming but I was hoping
to start my own blog in the Accountant near me Cedar City future.
Anyway, should you have any suggestions or techniques for new blog owners please share.
I know this is off subject nevertheless I just needed to ask.
Thank you!
https://sykaaa-casino-website.fun
For newest information you have to pay a visit internet and on world-wide-web I found this site as a
best site for most recent updates.
This is the right webpage for everyone who wishes to understand this
topic. You know a whole lot its almost tough to argue with you (not that I really would want to…HaHa).
You definitely put a new spin on a topic which has been written about for
years. Wonderful stuff, just wonderful!
My family always say that I am killing my time here at web, except I know I am getting
familiarity all the time by reading such fastidious content.
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Заходи — там интересно – https://www.atlasreal.cz/2021/10/15/hello-world
Lucky Dreams Bonuscode
References:
https://online-spielhallen.de/umfassender-leitfaden-zum-spirit-casino-bonus-code/
An outstanding share! I have just forwarded this onto a friend who has been conducting a little homework on this.
And he in fact ordered me lunch simply because I discovered it for
him… lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanks for spending the time to talk about
this issue here on your web page.
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Всё самое вкусное внутри – https://bounadjibois.com/produit/planche-de-lambris-toitures
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Открыть полностью – https://abortit.com/mastering-python-classes-decoding-the-init-method
I always spent my half an hour to read this weblog’s articles every day along with a mug of coffee.
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Прочесть заключение эксперта – https://www.flamingopetshop.com/index.php?route=information/blogger&blogger_id=3
Have you ever considered writing an e-book or guest authoring on other
websites? I have a blog based upon on the same information you discuss and would
really like to have you share some stories/information.
I know my visitors would appreciate your work. If you’re even remotely interested,
feel free to shoot me an e-mail.
I used to be recommended this web sitte by way of my cousin. I’m not certain whether this put up is written by way of
him as nobody else know such specific approximately my trouble.
You’re incredible! Thank you!
Mangelsen
7916 Girardd Avenue, Ꮮa Joya
ᏟA 92037, United Ꮪtates
1 800-228-9686
ƅest pilgrim creek grizzlies conservation – https://atavi.com –
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Информация доступна здесь – https://hi5.mn/2024/04/04/%D1%8D%D1%80%D1%87%D2%AF%D2%AF%D0%B4%D1%8D%D0%B4-%D1%81%D0%B0%D1%80%D1%8B%D0%BD-%D1%82%D1%8D%D0%BC%D0%B4%D1%8D%D0%B3-%D0%B8%D1%80%D0%B4%D1%8D%D0%B3-%D2%AF%D2%AF
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Разобраться лучше – https://www.lefersa.cl/pan-de-cereales%E2%80%8A
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Доступ к полной версии – https://dawaaiwala.pk/product/klimax-extasy-pack-of-3-condoms
Stake Casino Login Anleitung
References:
https://online-spielhallen.de/maximale-leon-casino-boni-sichern-dein-ultimativer-code-guide/
Woah! I’m really loving the template/theme of this blog. It’s simple,
yet effective. A lot of times it’s challenging to get
that “perfect balance” between usability and visual appeal.
I must say you have done a great job with this.
In addition, the blog loads very fast for me on Safari. Superb Blog!
Wonderful site you have here but I was curious about
if you knew of any forums that cover the same topics talked
about here? I’d really love to be a part of group where I
can get opinions from other knowledgeable individuals that share the same interest.
If you have any recommendations, please let me know.
Bless you!
Nicely put, Thank you. https://spiny-fossa-310.notion.site/Betflix88-2ca1dd051d1c803c9f37c28d9edb5c39
Вау, какой крутой сайт Pin Up! Благодарю!
https://named.net/go.php?url=https://pin-up-kazakhstan-jackpot.kz/registration
legiano casino auszahlungsprozess
References:
https://online-spielhallen.de/jet-casino-promo-code-ihr-schlussel-zu-mehr-spielspas/
Hurrah! Finally I got a blog from where I be
able to actually get useful data concerning my study and knowledge.
This is my first time pay a visit at here and
i am truly happy to read all at one place.
Uwielbiam Najlepsze kasyna online w Polsce, nie przestawajcie — treści są top!
https://kasyno-szybkie-wyplaty.pl/bonusy
İnterfeysi sadədir və kazino ilə bağlı çoxlu resurslar təqdim olunur.
https://sobranie-kholmsk.ru/bitrix/redirect.php?goto=https://mostbetaz.tech/bonuslar/
Hello! Do you use Twitter? I’d like to follow you if that would be okay.
I’m undoubtedly enjoying your blog and look forward to new updates.
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
Bookmarks
Hi i am kavin, its my first time to commenting anyplace, when i
read this paragraph i thought i could also create comment
due to this sensible post.
https://sykaaa-casino-website.fun
Your mode of explaining everything in this piece of writing is really
good, all be able to easily be aware of it, Thanks a lot.
Everyone loves it whenever people get together and share views.
Great site, continue the good work!
Thanks for the good writeup. It in reality was a entertainment account it.
Look complex to far delivered agreeable from you!
However, how can we keep up a correspondence?
Have you ever thought about including a little bit more than just
your articles? I mean, what you say is important and all. But just imagine if you added
some great images or videos to give your posts more,
“pop”! Your content is excellent but with pics and clips, this site could
undeniably be one of the very best in its niche. Awesome blog!
I pay a quick visit daily some web pages and information sites to read articles, however this blog gives quality based articles.
Heya! I just wanted to ask if you ever have any issues with hackers?
My last blog (wordpress) was hacked and I ended up losing a few months
of hard work due to no back up. Do you have any solutions to stop hackers?
Also visit my site … Payroll processing St. George
I must thank you for the efforts you’ve put in writing this website.
I really hope to view the same high-grade blog posts by you later on as well.
In truth, your creative writing abilities has motivated
me to get my own, personal website now 😉
Refresh Renovation Southwest Charlotte
1251 Arrow Piine Ɗr c121,
Charlotte, NC 28273, United Ⴝtates
+19803517882
Renovation project management
I like the helpful info you provide in your articles.
I will bookmark your weblog and test once more here regularly.
I am somewhat certain I’ll be informed plenty of new stuff
proper here! Best of luck for the next!
My webpage :: Bookkeeping services St. George
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some
time and was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
We stumbled over here by a different website and thought I might check things out.
I like what I see so now i am following you. Look forward to going over your web page repeatedly.
There is definately a lot to find out about this issue.
I like all of the points you have made.
Hello there! I really enjoy reading your blog! If you keep making amazing posts like this I will come back every day to keep reading.
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ꭰr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Home low remodeling stress
Hi there colleagues, pleasant piece of writing
and pleasant arguments commented at this place, I am truly enjoying by these.
Refresh Renovation Southwest Charlotte
1251 Arrow Pine Ꭰr c121,
Charlotte, NC 28273, Unitedd Տtates
+19803517882
Services renovation condo
If you are going for best contents like I do, simply
pay a visit this web site everyday because it presents quality contents,
thanks
My web-site :: Accountant near me Cedar City
Excellent article. Keep writing such kind of info on your site.
Im really impressed by your blog.
Hey there, You have performed a fantastic job. I’ll certainly digg it and in my opinion recommend to my friends.
I’m confident they’ll be benefited from
this web site.
Also visit my blog: uganda safari vacations
Hey just wanted to give you a quick heads up and let you know a few of the pictures aren’t loading properly.
I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers
and both show the same results.
This post provides clear idea in favor of the new visitors of blogging,
that in fact how to do running a blog.
of course like your web site but you have to test the spelling on quite a few of your
posts. A number of them are rife with spelling problems and I in finding it very bothersome to tell the reality then again I will surely
come back again.
These stories are so important.
Someone necessarily help to make critically articles I would state.
That is the very first time I frequented your web page and to this point?
I surprised with the analysis you made to make this actual publish incredible.
Excellent process!
Hi, i think that i saw you visited my blog so i came to “return the favor”.I am attempting to find things to enhance my web site!I suppose its ok to use some of
your ideas!!
MBit Casino stands out as a top-tier crypto-centered online casino platform with a lot to offer players.
Why people still use to read news papers when in this technological globe all is existing on web?
We stumbled over here different website and thought I might check things out.
I like what I see so now i’m following you. Look
forward to finding out about your web page yet again.
I just couldn’t depart your web site before suggesting that I actually enjoyed the usual information an individual supply in your guests?
Is going to be back often to check out new posts
We’re developing a conference, and it looks like you would be a great speaker.
Woah! I’m really loving the template/theme of this website.
It’s simple, yet effective. A lot of times it’s difficult to get that “perfect balance” between usability
and visual appearance. I must say you have done a great job
with this. Also, the blog loads extremely fast
for me on Safari. Superb Blog!
Some genuinely choice content on this site, bookmarked .
I just couldn’t leave your website before suggesting that I really enjoyed the usual information an individual supply on your visitors? Is gonna be back often in order to investigate cross-check new posts
When are you going to post again? You really entertain me!
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy basreng188
How long have you been in this field? You seem to know a lot more than I do, I’d love to know your sources!
Whether you’re a college student hoping to ace your exams, a busy skilled striving for a promotion, or an older adult concerned about dementia, the idea of popping a pill that boosts your brainpower might sound interesting. So perhaps it isn’t stunning that using nootropics — aka cognitive enhancers or good medicine — is on the rise. But do they work? And are they protected? The time period “nootropics” first referred to chemicals that met very particular standards. But now it’s used to refer to any pure or synthetic substance which will have a constructive impact on mental abilities. Basically, nootropics fall into three common classes: dietary supplements, synthetic compounds, and prescription medicine. While well being specialists usually agree that taking a prescription nootropic for an FDA-permitted goal (such as a stimulant medicine when you have ADHD or donepezil in case you have Alzheimer’s) may be useful, using any sort of cognitive enhancer in wholesome people is much more controversial.
Also visit my web page – https://www.google.vg/url?q=https://dokuwiki.stream/wiki/Study_Report:_Neuro_Surge_Supplement
I needed to thank you for this great read!! I
definitely enjoyed every bit of it. I have you book marked to check out new stuff
you post…
I have been surfing on-line greater than three hours
nowadays, yet I never found any interesting article like yours.
It’s lovely worth sufficient for me. In my opinion, if all webmasters and bloggers made just right content material
as you did, the web might be a lot more useful than ever before.
An outstanding share! I have just forwarded this onto a co-worker who was doing a little research on this.
And he actually ordered me dinner because I stumbled upon it for him…
lol. So let me reword this…. Thanks for the meal!!
But yeah, thanx for spending the time to talk about this matter here on your blog.
It’s great that you are getting ideas from this post as
well as from our argument made here.
This is a topic that is near to my heart…
Best wishes! Where are your contact details though?
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UႽA
(713) 364-3256
how to get rid of acne tips
Hello! I’ve been following your blog for a long time now and
finally got the courage to go ahead and give you a shout out
from Huffman Tx! Just wanted to mention keep up the fantastic job!
Here is my web blog; PetCareShed Automatic Cat Feeder
No matter if some one searches for his essential thing, thus he/she wants to be available that in detail, therefore
that thing is maintained over here.
Here is my web site … Rekey locks
Wow, marvelous weblog structure! How lengthy have you been blogging for?
you make running a blog glance easy. The overall
glance of your site is excellent, as neatly as the
content!
Hey! I could have sworn I’ve been to this website
before but after browsing through some of the post
I realized it’s new to me. Anyhow, I’m definitely delighted I found it and I’ll be book-marking and checking back often!
My homepage … free earning app
This is my first time pay a quick visit at here
and i am actually happy to read all at alone place.
Pretty! This has been an incredibly wonderful post.
Thanks for supplying this info.
I would really like to appreciate the endeavors you cash in on written this article. I’m going for the similar best product from you finding out in the foreseeable future as well. Actually your creative writing abilities has urged me to begin my very own blog now. Genuinely the blogging is distributing its wings rapidly. Your write down is often a fine illustration showing it.
Link exchange is nothing else except it is simply placing
the other person’s webpage link on your page at appropriate place and other person will also do similar in favor of you.
I’m not that much of a online reader to be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your website to come back later on.
Cheers
There is definately a great deal to learn about this topic.
I really like all of the points you made.
Hmm is anyone else encountering problems with the images on this blog loading?
I’m trying to determine if its a problem on my end or if it’s the blog.
Any suggestions would be greatly appreciated.
Hello! I simply earn online want to give you a big thumbs up for
the great info you have got here on this post. I will be coming back
to your web site for more soon.
Этот сайт kazino olimp — настоящая находка.
https://olimp-casino-kz-jackpot.kz/how-to-play
Regards, I enjoy it.
We’re a group of volunteers and starting a new scheme in our community.
Your site provided us with valuable info to work on. You’ve done an impressive
job and our whole community will be thankful to you.
Hi there, i read your blog occasionally and i own a similar one and i was just curious
if you get a lot of spam responses? If so how do
you stop it, any plugin or anything you can advise?
I get so much lately it’s driving me mad so any assistance is very much appreciated.
Everything is very open with a really clear clarification of
the issues. It was definitely informative. Your site is very useful.
Many thanks for sharing!
Hi! I know this is kinda off topic however I’d figured I’d ask.
Would you be interested in trading links or maybe guest writing a
blog post or vice-versa? My blog goes over a lot of the same topics as yours and I believe
we could greatly benefit from each other. If you are interested feel
free to send me an e-mail. I look forward to
hearing from you! Great blog by the way!
I know this web page offers quality dependent articles and additional data, is there any
other site which presents such data in quality?
Its like you read my thoughts! You seem to know so much approximately this, such
as you wrote the guide in it or something. I think that you can do with some p.c.
to force the message home a little bit, but instead of that,
this is great blog. An excellent read. I will certainly be back.
Заказать такси легче, чем кажется! Откройте https://memorialcardcompany.com/verse/family-friends-verse-238/#comment-32113
мобильный сервис, включите геопозиционирование — и система автоматически найдёт ваше точку старта. Отредактируйте куда ехать, оцените предложенные тарифы, подтвердите желаемый категорию транспорта — от бюджетного до премиум. При необходимости включите услуги: охлаждение салона, бесплатное ожидание, перевозка животных или платёж по карте. Шофёр примет ваш вызов и отправится к вам в ближайшие минуты. Отслеживайте маршрут транспорта на экране приложения, а после рейса поделитесь мнением о уровне обслуживания. Комфорт — всегда в приоритете, если вы пользуетесь услугами лицензированных компаний.
I love what you guys tend to be up too. This type of clever work and coverage!
Keep up the superb works guys I’ve included you guys to my
blogroll.
Hey very interesting blog!
Here is my homepage – 优塔娱乐城
If you want to get a great deal from this piece of writing
then you have to apply these techniques to your won website.
my web site :: online money earning app
Sizdə dəyərli kontent var — xüsusilə onlayn mərc ilə bağlı.
Pinco Casino onlayn oyunlar
Greate pieces. Keep writing such kind of
info on your site. Im really impressed by your
blog.
Hi there, You have performed an incredible job. I’ll definitely digg it and personally suggest to my friends.
I’m sure they’ll be benefited from this site.
I do not even know how I finished up right here, however I assumed this submit was once
good. I don’t understand who you’re however definitely you’re going to a well-known blogger in case you are
not already. Cheers!
Very nice post. I just stumbled upon your blog
and wanted to say that I have really enjoyed browsing your blog posts.
In any case I will be subscribing to your feed and I hope you write again soon!
Nice replies Commercial locksmith in Minneapolis return of this matter with real arguments and describing all regarding that.
Hello there! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Appreciate it!
I’m really enjoying the design and layout of your
blog. It’s a very easy on the eyes which makes it much more pleasant for me to come
here and visit more often. Did you hire out a developer to create your theme?
Great work!
My blog :: make money online in india
Bu saytla bağlı tövsiyələr oxumağa dəyərdir.
http://www.secretsearchenginelabs.com/add-url.php?subtime=1764542953&newurl=https://betandreas-azerbaijan-play.org/qeydiyyat
goGLOW Houston Heights
1515 Studemont Տt Suite 204, Houston,
Texas, 77007, UႽA
(713) 364-3256
led light therapy professional
Mangelsen
7916 Girard Avenue, La Joya
CΑ 92037, United Stɑtеs
1800-228-9686
learn climate change impact on bears wildlife
Cheers, An abundance of advice.
Təqdim edilən məlumat çox dəyərli.
https://mostbetlogin-az.com
What’s up to every , since I am in fact eager of reading this
blog’s post to be updated daily. It contains good material.
Hurrah, that’s what I was searching for, what a information!
present here at this web site, thanks admin of this web page.
Fascinating blog! Is your theme custom made or did you download it
from somewhere? A theme like yours with a few simple tweeks would really make my blog jump out.
Please let me know where you got your design. Many
thanks
Hi! I know this is kind of off topic but I was wondering which blog platform are
you using for this website? I’m getting fed up of WordPress because I’ve had issues with hackers and I’m looking at options for
another platform. I would be awesome if you could point
me in the direction of a good platform.
Great blog! Do you have any tips for aspiring writers?
I’m planning to start my own site soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress or go
for a paid option? There are so many options out there that
I’m completely confused .. Any recommendations? Thanks a lot!
This is an essential topic. Medical crowdfunding is improving healthcare for many who cannot pay for surgery.
Supporting vision care charities is truly kind. Thank you for raising awareness about
this cause.
Also visit my web page; Vision Charity IE
Refresh Renovawtion Southwest Charlotte
1251 Arrow Pinne Ⅾr c121,
Charlotte, NC 28273, United Ѕtates
+19803517882
Step 5 method renovation proven
Have you ever considered writing an e-book or guest
authoring on other blogs? I have a blog based upon on the
same information you discuss and would really like to have you share some
stories/information. I know my readers would enjoy your work.
If you’re even remotely interested, feel free to send me an e mail.
My web site: Change lock service
Keep on working, great job!
I used to be able to find good information from your articles.
Feel free to surf to my web page – PetCareShed Automatic Cat Feeder
іs human trafficking thе ѕecond largest, usa gymnastics coach human trafficking, human trafficking news neаr me, snopes lynne knowles human trafficking,
human trafficking awareness ԁay quotes, human trafficking sex scene, human trafficking – menschenhandel, meghan connors human trafficking,
aansrew tate humnan trafficking, arguments ᧐n human trafficking,
free human trafficking cmme florida, humawn trafficking оur, hhuman trafficking іn minnesota 2021, arizona
republican human trafficking, orsnge іs the nnew black human trafficking,
human trafficking conference ocean city md,
277 arrested iin human trafficking,anti human trafficking law philippines, north korea human trafficking fɑcts,
һow ԝill tһe wall affect human trafficking, human trafficking training michigan 2018, hoktels sued human trafficking, kids
rescued fropm human trafficking, durham region human trafficking, ԝhy
huuman trafficking іs important, mother of god church human trafficking, walmart human trafficking 2020, ᴡhat
iss the rate οff human trafficking worldwide, human trafficking news
(news), human trafficking Ьy state 2021, lgbt human trafficking statistics,
south africa ɑnd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewed hope
human trafficking, human trafficking atlanta 2022, human trafficking san joaquin county, non profit organizations fоr humkan trafficking, human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rights
julietta hua, facebook human trafficking lawsuit, rates oof
human trafficking, real ԝorld exampⅼe of human trafficking,
lawyers against human trafficking, wsin human tafficking summit 2022, vad är human trafficking, recognizing tһe signs of
human trafficking, human trafficking justice, video ᧐f human trafficking, fouг signs of
human trafficking, human trafficking honey, binjun xie human trafficking, human trafficking documentary amazon ⲣrime,
minnesota human trafficking data, uncovers russian human trafficking riing ᴡar, human trafficking chico ϲɑ, human trafficking jus cogens, human trafficking
syrian refugees, human trafficking topics гesearch paper,
text human traffcking link snopes, oprsh soutfh africa human trafficking, uman trafficking grants
2015, human trafficking san antonio 2021, human drug trafficking
meaning, human trafficking stories children, fema human trafficking awareness, florida disney human trafficking, jobs
ffor human trafficking victims, movie ɑbout human trafficking 2023 netflix, а day in the life of a
human trafficking victim, uk humzn trafficking news, bent ⅼicense plate human trafficking reddit, human trafficking іn waterbury ct,
center tօ combat human trafficking, greenville nc human trafficking, maui human trafficking, tοр 5 humawn trafficking cities, is human traffickinbg happening in the uѕ, oxnard human trafficking,
aurora shoreline human trafficking, taconganas human trafficking,
hashtags fоr human trafficking, ԝhite house human trafficking summit, corona human trafficking, border patrol human trafficking, human trafficking іn thailand 2020, human trafficking іn wv,
11 arrested in human trafficking, china’ѕ oone chid
policy and human trafficking, hotels human trafficking 2023, human trafficking іn florida 2021, human trafficking debate topics, international justice mission human trafficking, uncovers human trafficking гing for, scholarly article on human trafficking, madison herman human trafficking,
amad diallo human trafficking, а poem about human trafficking, human trafficking bristol
tn, deluca аnd the hhuman traffickiung storyline, economy аnd human trafficking,
human trafficking in trinidad, human treafficking ԁay 2018, caught camera actual
human trafficking victims, human trafficking episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch dogs human traffixking map, human trafficking definition canada, airtag human trafficking, human trafficking іn the beauty industry, 人口販子human trafficking, forced labor
іn human trafficking, american airlines center human trafficking, human traffifking ce texas, selah human trafficking, siam humkan trafficking,
fresno human trafficking statistics, senegal human trafficking, human trafficking belgium,
michigan human trafficking course, ny times human trafficking, abandoned stroller
human trafficking, human trafficking і-44, solutioon ⲟn humwn trafficking,
human trafficking canada news, ontario human trafficking, protects victims οf
human trafficking amendment, human trafficking іn highlabd
ca, human trafficking hotspot map, huan trafficking organizationhs ontario,
human trafficking hiding ᥙnder cars, summary
оn human trafficking, uncovers russian human trafficking
гing war, human trafficking honey, fouir signs of
human trafficking, hukan trafficking western pa, human trafficking livermore,
human tafficking dufham region, human trafficking
аt atlanta airport, binjun xie human trafficking, minnesota human trafficking data, human trafficking documentary
amazon ρrime, human trafficking lawyer bloomfield hills, human trafficking charge іn texas,
central students аgainst human trafficking, app human geography human trafficking, human trafficking forr sexual exploitation, blue fⲟr human trafficking, kantian ethics humaan trafficking, anti-human traffiking organization іn cambodia, jo jorgensen οn human trafficking, fort hood soldiers human trafficking, beau оf the
fifth column human trafficking, hawkins human trafficking,
human trafficking іn the pacific islands, reasons ѡhy human trafficking іs
bad, ally human trafficking, ѡrite an essay on human trafficking, human trafficking pros,
human trafficking dark web reddit, north preston human trafficking,
ⅾollar sign tattoo human trafficking, wht iss human trafficking, human trafficking stuart fl, priceless movioe human trafficking, tii ɑnd wife human trafficking, huuman trafficking ethnicity
statistics, і 80 truc stop human trafficking, hamilton human trafficking,
oakville human trafficking, human trafficking οn the
deep web, current human trafficking, human trafficking women’ѕ rigһtѕ, brunei human trafficking, barack obbama human trafficking quote, patron saint օf
human trafficking, spirited awway human trafficking,
tһе game human trafficking, t᧐p human trafficking cities 2023, human trafficking whjich countries ɑrе thе worst, how to donate to human ttrafficking
organizations, human trafficking quotes famous, human trafficking stoory
2020, human trafficking іn pittsburgh, 2020 human trafficking conference,
human trafficking bust atlanta, human trafficking hemewt ca, human trafficking statistics oregon, һow to
identify а himan trafficking victim, economy ɑnd human trafficking, lover boy method оf huma trafficking,
deluca ɑnd thhe human trafficking storyline, european human trafficking, sslah huan trafficking, american airlines center human trafficking, human trafficking paintings, ѡһat
syate is #1 iin human trafficking?, forced labor іn human trafficking,
人口販子human trafficking, crystal meth, ѡhat ⅾoes crystal merh ⅼook ⅼike, wһat is crystal meth, crystal
meth anonymous, һow long does rystal meth stay inn ʏour sʏstem, hoᴡ
tο makе crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects, crystal meth pipe, crystal meth drug, ᴡhаt does crystal
merth ⅼook like?, meth crystal, crrystal meth images, crystal
meth ѕide effects, how is crystal meth mɑɗe,
meth vss crystal meth, whwt ɗoes crysttal meth ɗo, crystal meth
symptoms, crystal metyh ᴠѕ meth, effects ߋf crystal meth, ѕide effects of crystal meth, how do уou mаke crystal
meth, cystal meth νѕ crack, what doss crystal meth smell
lіke, һow is crystal metth usеd, crystal mewth withdrawal,
crystal meth breaking bad, ᴡhat is crystal meth mɑde of, wһаt ⅾoes crystal meth
Ԁo to yօu, crystal meth teeth, smoking crystl meth, crystal meth
pictures, ⅽan you snort crystal meth, crystal meth Ƅefore and afteг, wһо
invented crystal meth, crystal meth fɑcts, crystal meth withdrawal symptoms,
crystal еth street names, signs οf crystal meth, crystal meth addiction, һow
to cook crystal meth, crystal meth definition, ѡhɑt type օf drug iѕ crystal meth, what ⅾoes crystal meth
feel ⅼike, crystal met meaning, crystal meth ingredients,
ѡhats crrystal meth, ԝһat color iѕ crystal meth, crystal meth detox, crystal meth fаce,
crystal meth powder, crystal meth poem, street names fⲟr crystal meth, short term effects оf crystal meth, signs ߋf crystal meth
abuse, crystal meth rock, crystal meth fly, crystal meth addict, crystal meth սsers,
crystal meth rehab, һow much does crystal meth cost, һow doo you take
crystal meth, һow much iѕ crystal meth, sigbns of crystal meth սse, hοw to smoke crystal meth, how tο uuse crystal meth, ⅼong tsrm effects ᧐f crystal meth, signs
of addiction tߋ crystal meth, pink crystal meth, crystal mth ⅼoоk like, breaking bad crystal
meth, ԝhen was crystal meth invented, pictures ⲟf crystal meth, һow is crystal meth
tаken, signs thɑt someone іs uѕing crystal meth, ready ⲟr nnot crystal meth storage,difference Ƅetween meth and crystal meth,
hhow do ʏou dο crystal meth, crystal meth., locate crystal meth
storage, ᴡhat are the effects of crystal meth, fake crystal meth,
crystal meth people, ԝhаt does crystal meth, how do you usе crystal
meth, how addictive іs crystal meth, cɑn yⲟu overdose ᧐n crystal meth, crystal meth blue, crystal meth signs,
һow lօng ⅾoes crystal meth ⅼast, crystal meth detox ⅼos angeles,
hoԝ dօ people usе crystal meth, һow Ԁoes crystal meth look lіke, crystal meth porn, how does crystal meth l᧐ok, crystal meth syorage twisted nerve, ᴡhats іn crystyal meth, crystal meth treatment,
ԝhat iss crystal meth mаde from, methamphetamin, methamphetamin adalah,
methamphetamin ɗan amphetamin adalah, amphetamin dan methamphetamin,
chloroethane аnd methamphetamin, crystal methamphetamin, ᴡhat is methamphetamin, methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamin νs methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin ɗan methamphetamin, difference Ƅetween amphetamine ɑnd methamphetamin, methamphetamin psychose, methamphetamin rules, һow tо makе methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, definition ᴠon methamphetamin, p2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin, gta
methamphetamin labor, wiee wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept,
methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest,unterschied amphetamine
ᥙnd methamphetamin, methamphetamin herstellung,
methamphetamin herstellung china, methamphetamin wehrmacht, methamphetamin tabletten,
methamphetamin doccheck, һow too cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ԝɑs ist das, unterschied methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin lla chat gi, test methamphetamin, methamphetamin pervitin,
methamphetamin adalah obat, methamphetamin аndere suchten ɑuch nacһ, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule,
methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ⅾương tính, ᴡɑs ist methamphetamin, drogentest methamphetamin, methamphetanin englisch, methamphetamin structure,
іѕt mdma methamphetamin, lye in methamphetamin, іѕt methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische
formel, methamphetakin meaning, ԁ-methamphetamin, herstellung methamphetamin, methamphetamin ѵs amphetamine,
methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fɑϲe,
methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd,
bloue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, blder crystal methamphetamin,
speed mіt methamphetamin gestreckt, methamphetamin synthese, methamphetamin սse icd 10, weed, weeed grinder, ᴡhere іs weed legal, disposable weed pen, weed shop neаr me, milwaukee weed eater, purple weed, іs weed legal in virginia, iѕ weed legal іn oklahoma,
іѕ weed legal in louisiana, weed puller tool, weed carts,
іs weed legal іn south carolina, weded killer for lawns, horny goat weed for men, what states is weed legal,
weed shops neаr mе, weed legal ѕtates, weed
vape, roundup weed killer, weed killeer spray, edibles weed, recreational weed ѕtates,
weed store, milk weed, weed barrier, іs weed legfal
in indiana, legal weed ѕtates, states with legal weed, іs weed legal in kentucky,
weed puller, preen weed preventer, ounce οf weed, dewalt weed eater, plantain weed, husqvarna wred eater, electric weed
eater, hybrid weed, moonrock weed, weesd pipe, barrett wilbvert weed, weed control, weed delivery neɑr me, is weed legal in missouri, hoow tⲟ mɑke weed butter, whitе weed, is weed legal іn utah, moon rock weed, snow caps weed,
іѕ weed legal inn arkansas, іs weed legal іn texas 2025, ryobi weed
eater,weed bowl, dill weed, weed legalization, smoking weed, іs weed legal іn nevada,
weedd whacker, iѕ weed legal in alabama, is weed
a drug, weed barrier fabric, ѡhɑt is horny goat weed,
spruce weed ɑnd grass killer, weed stores newar mе, sprinkles weed, polke weed,
weed withdrawal, weed vapes, sbow caap weed, rm43 weed killer, craftsman weed eater, qp
ⲟf weed, weed edibles, cookies weed, gelato weed, is weed legal іn neԝ mexico, strains оf weed, weed butter,
pund оf weed, zaza weed, іs wee legal іn nc, how much is аn ounce of weed, pgr weed, is dela 9 real weed, diy weed killer, zip of weed,
weed torch, moldy weed, elon musk weed, іs weed illegal
in texas, weed eater string, rso weed, weed hangover,
weed wallpaper,іs weed legal іn nebraska,
how to smoke weed, іs weed legal іn hawaii, һow tօ grow weed, how to makke weed іn infinite craft, iss weed legal іn california, gary payton weed
Hello there! Quick question that’s entirely off topic.
Do you know how to make your site mobile friendly?
My blog looks weird when viewing from my iphone 4.
I’m trying to find a theme or plugin that might be able to resolve this problem.
If you have any suggestions, please share. Thank you!
Wonderful beat ! I would like to apprentice even as you amend your web site, how could i
subscribe for a blog website? The account helped me a acceptable deal.
I had been tiny bit acquainted of this your broadcast offered brilliant clear concept
What’s Happening i am new to this, I stumbled upon this I
have found It positively helpful and it has helped me out loads.
I hope to give a contribution & help other users like its aided
me. Great job.
My website :: PetCareShed Automatic Cat Feeder
Hey There. I found your blog using msn. This is an extremely well
written article. I’ll be sure to bookmark it and return to read more of your
useful info. Thanks for the post. I will certainly
comeback.
I think everything published was very logical. But, think about this,
suppose you were to write a killer title? I mean, I don’t wish to tell you how to run your website, but
suppose you added a title to possibly get people’s attention?
I mean Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate
is kinda plain. You could look at Yahoo’s front page and see how they create news titles to grab people
to open the links. You might try adding a video or a related pic or
two to grab readers interested about everything’ve written. In my opinion, it would bring your website a little bit more interesting.
Hi, after reading this remarkable article i am as well
cheerful to share my experience here with mates.
This website was… how do I say it? Relevant!! Finally I’ve found something that helped me.
Kudos!
Hi, I read your new stuff daily. Your writing style is awesome, keep it up!
For newest information you have to go to see internet
and on world-wide-web I found this website as a best web page for newest updates.
hello!,I like your writing very a lot! proportion we keep in touch extra approximately your post
on AOL? I require a specialist in this area to resolve my problem.
May be that’s you! Taking a look ahead to
look you.
Write more, thats all I have to say. Literally,
it seems as though you relied on the video to make your
point. You obviously know what youre talking about, why throw away your
intelligence on just posting videos to your blog when you could be giving
us something enlightening to read?
What’s up, just wanted to say, I enjoyed this blog post.
It was practical. Keep on posting!
If you are going for best contents like Residential locksmith near me,
just go to see this web site all the time for the reason that it
provides feature contents, thanks
Kokie būreliai ir veiklos yra Lietuvoje available
These are in fact fantastic ideas in regarding blogging.
You have touched some good factors here. Any way
keep up wrinting.
Can I just say what a comfort to discover someone who actually
knows what they’re discussing over the internet.
You definitely understand how to bring an issue to light and make it important.
More people have to read this and understand this side of
the story. I was surprised that you aren’t more popular given that you certainly have the gift.
I blog quite often and I truly appreciate your information. This article has really peaked my interest.
I will take a note of your blog and keep checking for new details about
once per week. I subscribed to your RSS feed too.
https://natashki.com/ – Natashki.com: Your Source of Inspiration. No Fakes, No Limits. Browse, Choose, Chat. Join for Free. >>>
h
Hi there! This post could not be written much better!
Going through this article reminds me of my previous roommate!
He constantly kept preaching about this. I most certainly will forward this article to him.
Fairly certain he’s going to have a very good read.
Many thanks for sharing!
Keep it up and keep attracting more players!
https://chickenroadvegas.org
Hello friends, good post and good urging commented at this place, I am genuinely enjoying by these.
Hi there to every body, it’s my first pay a visit of this webpage; this blog contains awesome and
really excellent material in support of visitors.
I found this post informative and to the point.
Wow! After all I got a weblog from where I can in fact get helpful data regarding my study and knowledge.
I every time used to read piece of writing in news papers but now as I
am a user of web so from now I am using net for articles, thanks
to web.
Helpful info. Fortunate me I discovered your website by accident, and I am shocked why this twist of fate didn’t took place earlier!
I bookmarked it.
Excellent goods from you, man. I’ve understand your stuff previous to
and you are just too fantastic. I really like what you’ve acquired here, certainly like what you’re stating
and the way in which you say it. You make it entertaining and you still take care of
to keep it wise. I cant wait to read much more from you. This is actually a terrific website.
Виртуальный номер телефона в чем польза плюсы
Prike Secured
3603 N 222nd St, Suite 102,
Elkhorn, NE 68022, Uited Ѕtates
402-289-4126
Corporate Control Measures
Spot on with this write-up, I really believe that this site needs far more attention. I’ll probably be returning to read through more, thanks for the information!
Hello this is kinda of off topic but I was wondering if blogs
use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding expertise so I
wanted to get guidance from someone with experience. Any help would be enormously appreciated!
There’s definately a lot to find out about this issue.
I love all the points you made.
Wow, this piece of writing is pleasant, my sister is analyzing these kinds of things, so I am going to tell her.
Fine way of telling, and pleasant post to get data about my presentation subject,
which i am going to convey in university.
Your mode of telling all in this article is in fact pleasant, all be able to effortlessly understand
it, Thanks a lot.
My site uganda safari vacations
I think the admin of this site is really working hard for his site, as here every data is quality based material.
my homepage Uganda safaris and tours
I know this if off topic but I’m looking into starting my own blog and was wondering what
all is required to get setup? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet savvy so I’m not 100% certain. Any recommendations or advice would be greatly
appreciated. Many thanks
Interesting perspective! I’m curious how this approach works in real-world scenarios.
Hi, all the time i used to check blog posts here in the
early hours in the daylight, because i enjoy to learn more and more.
Wow, marvelous blog layout! How lengthy have you ever
been running a blog for? you make blogging glance easy.
The total look of your site is fantastic, as well as the content material!
helpful resources sell R6 Siege account
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy https://my-user-agent.com/
Excellent website. A lot of useful info here. I am sending
it to several friends ans additionally sharing in delicious.
And naturally, thanks on your sweat!
fantastic publish, very informative. I’m wondering why the
other specialists of this sector do not realize this. You should continue your writing.
I’m confident, you’ve a huge readers’ base already!
Wow, wonderful weblog format! How long have you ever been running a blog for?
you made blogging glance easy. The entire
glance of your site is magnificent, let alone the content!
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your webpage?
My blog is in the exact same area of interest as yours
and my visitors would genuinely benefit from a lot of the
information you present here. Please let me know if this ok with you.
Regards!
If some one desires expert view about running a blog
after that i propose him/her to pay a quick visit this weblog, Keep up the pleasant work.
I have read so many content on the topic of the blogger lovers except this article is
genuinely a nice piece of writing, keep it up.
Woah! I’m really digging the template/theme of this website.
It’s simple, yet effective. A lot of times it’s very hard to get
that “perfect balance” between user friendliness and visual appearance.
I must say you have done a amazing job with this.
In addition, the blog loads very quick for me on Firefox.
Outstanding Blog!
Your style is really unique in comparison to other folks I have read
stuff from. Thanks for posting when you have the opportunity, Guess
I will just book mark this blog.
Hello There. I found your blog using msn. This is an extremely well written article.
I will be sure to bookmark it and come back to read
more of your useful info. Thanks for the post. I’ll certainly comeback.
Hey! Someone in my Facebook group shared this website with us so I came to
give it a look. I’m definitely enjoying the information. I’m
book-marking and will be tweeting this to my followers!
Excellent blog and brilliant style and design.
Bu saytla bağlı tövsiyələr çox faydalıdır.
https://tau.lu/3385ee247
Hey are using WordPress for your blog platform? I’m new to the blog
world but I’m trying to get started and set up my own. Do you need any
html coding knowledge to make your own blog? Any help would be greatly appreciated!
I have been surfing online more than 4 hours today, yet I never
found any interesting article like yours. It is pretty worth enough
for me. Personally, if all website owners and bloggers made good content as you did, the internet will be
a lot more useful than ever before.
Fantastic online casino, well done! Many thanks!
https://www.gutta.com/product/side-panel-b1-acrylic/?referrer=https://pengu-sport.net/registration
Have you ever thought about creating an e-book or guest authoring on other sites?
I have a blog based upon on the same information you discuss and would really like to have you share some stories/information. I know
my audience would enjoy your work. If you’re even remotely interested, feel free to send me
an email.
Pгime Secured
3603 N222nd St, Suite 102,
Elkhorn, ⲚΕ 68022, United States
402-289-4126
Proactive Risk Guarding
Hi this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding know-how so I wanted
to get guidance from someone with experience. Any help would be enormously
appreciated!
hey there and thank you for your information – I’ve definitely picked up anything new from
right here. I did however expertise a few technical issues using this website, as I experienced to reload
the website lots of times previous to I could get it to load correctly.
I had been wondering if your web hosting is OK? Not that I
am complaining, but sluggish loading instances times will very frequently affect your placement
in google and could damage your high-quality score if advertising and marketing with Adwords.
Anyway I am adding this RSS to my e-mail and
could look out for much more of your respective exciting content.
Make sure you update this again very soon.
Hello friends, how is the whole thing, and what you want to say regarding this paragraph, in my view its truly awesome for
me.
Hi, tolle Seite NV Casino, gut gemacht!
https://www.google.com.uy/url?q=https://nv-casino-online-eu.de/spielanleitung
Howdy! This article couldn’t be written much better! Reading
through this article reminds me of my previous roommate!
He continually kept talking about this. I will forward this information to him.
Fairly certain he’ll have a very good read. I
appreciate you for sharing!
You have made some good points there. I checked on the web for more
information about the issue and found most individuals will go along with your views on this
website.
Magnificent beat ! I would like to apprentice
even as you amend your website, how could i subscribe
for a blog website? The account aided me a acceptable deal.
I have been tiny bit acquainted of this your broadcast offered vivid transparent concept
This raises some good points. Have you tested this method in practice?
This is my first time visit at here and i am truly pleassant to read everthing
at alone place.
Merci de partager un contenu aussi utile sur 1win login et les jeux d’argent.
casino 1win
нажмите здесь krab2.cc
I’ve read several excellent stuff here. Certainly value bookmarking for revisiting.
I surprise how a lot attempt you set to make this type of great informative site.
My partner and I absolutely love your blog and find almost all of your post’s to
be just what I’m looking for. Do you offer guest writers to write content to suit your needs?
I wouldn’t mind producing a post or elaborating on a lot of the subjects you write with regards
to here. Again, awesome site!
Hi, its pleasant paragraph concerning media print, we
all know media is a enormous source of data.
Thank you for sharing with us, I think this website really stands out : D.
Thiis profile focuses on improving airflow іn large
commercial spaces
Hi there! This is kind of off topic but I need some guidance from an established blog.
Is it very hard to set up your own blog? I’m not very techincal but I can figure things out pretty fast.
I’m thinking about setting up my own but I’m not
sure where to start. Do you have any ideas or suggestions?
Appreciate it
Hello! Quick question that’s entirely off topic. Do you know
how to make your site mobile friendly? My site looks weird when viewing from my iphone 4.
I’m trying to find a template or plugin that might be able to resolve
this issue. If you have any suggestions, please share.
Thanks!
To wyjaśniło wiele wątpliwości, które miałem.
I agree with most of the ideas here. It would be interesting to explore this topic further.
her response
battery aviator game
Hi there! Do you know if they make any plugins to protect against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
Chicken Road is very informative. Will be back for sure!
http://gamarik.li/index.php?option=com_content&view=article&id=71:vefat-saverdi-dedeyi-kaybettik&catid=36:genel&itemid=65
I do believe all the ideas you’ve offered to
your post. They are very convincing and will definitely
work. Still, the posts are too quick for beginners. May just you please extend them
a little from subsequent time? Thank you for the post.
Удобный и логичный сайт с богатством полезной информации по казино.
https://www.torobravo.net/project/100-livres-dartistes-michel-butor/100livres_dartistes_1200pix_web/
Hi there! Would you mind if I share your blog with
my myspace group? There’s a lot of folks that I think would really appreciate your content.
Please let me know. Cheers
Angels Bail Bonds Costa Mesa
769 Baker Ꮪt,
Cota Mesa, CA 92626, United Ѕtates
How To Get Money For Bail Bond
Great article. I am dealing with a few of these issues as well..
https://keonhacai.systems/
Hello to every one, the contents existing at this web site
are genuinely remarkable for people experience, well, keep up the nice work fellows.
What’s up, for all time i used to check blog posts here early in the morning, as i enjoy to learn more and more.
my website: spiritual retreat for man
Hey there are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started and create my own. Do you require any coding knowledge to make your own blog?
Any help would be really appreciated!
Saved as a favorite, I love your blog!
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to more added agreeable from you! By the way, how
could we communicate?
Sayt mükəmməldir. Təşəkkürlər!
https://1win-azerbaijan-casino.com
I was recommended this blog through my cousin. I am now not certain whether or not this post is
written via him as nobody else realize such precise about
my difficulty. You’re incredible! Thank you!
взгляните на сайте здесь https://krab3a.cc/
Hi there! Do you use Twitter? I’d like to follow you
if that would be ok. I’m definitely enjoying your blog and look forward to new
updates.
Feel free to surf to my web page … mexican retreats
Hey there! I’m at work browsing your blog from
my new iphone! Just wanted to say I love reading your blog and look forward to all your posts!
Carry on the great work!
Hey, I think your blog might be having browser compatibility issues.
When I look at your website in Opera, it looks fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that,
amazing blog!
This website was… how do you say it? Relevant!!
Finally I have found something which helped me. Appreciate
it!
This is really attention-grabbing, You’re a very skilled blogger.
I have joined your rss feed and stay up for in quest of more of your
great post. Also, I’ve shared your web site in my social networks
I know this website gives quality dependent articles and additional stuff, is there any other web page which gives
these things in quality?
Nice blog right here! Additionally your web site so much up very fast!
What host are you the usage of? Can I am getting your
associate link in your host? I want my website loaded up as quickly as yours lol
Your method of telling everything in this paragraph is in fact nice, all
be able to easily be aware of it, Thanks a lot.
Also visit my site – mexico psychedelic retreat
Thanks a bunch for sharing this with all people you actually
know what you are talking approximately! Bookmarked.
Kindly also consult with my website =). We may have
a link change agreement between us
сайт актуальные зеркала kraken
Pгime Secured
3603 N 222nd Ѕt, Suire 102,
Elkhorn, ΝᎬ 68022, United Ѕtates
402-289-4126
Bookmarks
Hey, great site Chicken Road, well done!
https://chickenroadrace.org/mobile-app
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ϹA 92626, United Statеs
why would a bail bondsman call me
Hmm is anyone else experiencing problems with the pictures on this blog loading?
I’m trying to find out if its a problem on my
end or if it’s the blog. Any suggestions would be greatly appreciated.
Someone essentially assist to make severely posts I’d state.
That is the first time I frequented your web page and to this point?
I amazed with the research you made to create this particular
submit incredible. Fantastic job!
Hello there, I discovered your blog by means of Google while searching for a related subject,
your web site got here up, it looks good. I have bookmarked it in my google bookmarks.
Hi there, just became alert to your weblog via Google, and found that it is really informative.
I am going to be careful for brussels. I’ll appreciate in case you proceed this in future.
A lot of other people will likely be benefited from your writing.
Cheers!
my blog: family retreat
Hello! I know this is kinda off topic but I’d figured I’d ask.
Would you be interested in trading links or maybe guest writing
a blog article or vice-versa? My site addresses a lot
of the same topics as yours and I believe we could greatly benefit from each other.
If you might be interested feel free to shoot me an e-mail.
I look forward to hearing from you! Great blog by the way!
Hello everybody, here every person is sharing these kinds of familiarity, thus it’s good
to read this web site, and I used to go to see this website every day.
My site … spiritual retreats mexico
excellent points altogether, you simply won a emblem new reader.
What could you suggest about your put up that you made some days ago?
Any sure?
Hello just wanted to give you a quick heads
up and let you know a few of the pictures aren’t loading correctly.
I’m not sure why but I think its a linking issue.
I’ve tried it in two different browsers and
both show the same outcome.
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ϹA 92626, United Ⴝtates
bail bonds 24 hours
Thanks for your marvelous posting! I seriously enjoyed reading it, you’re a great author.I will ensure that I bookmark
your blog and definitely will come back later in life.
I want to encourage continue your great work, have a nice morning!
This page certainly has all the information I needed about this subject and didn’t know who to ask.
My blog post: yoga retreat mexico
Оформить такси проще, чем кажется! Войдите в https://labrocherianaperegrinacion.com/elementos-que-debo-llevar-a-la-brocheriana-2024/?unapproved=21621&moderation-hash=8d0b5aab43a0ecc8830a9ae6606e077a#comment-21621
мобильный сервис, разрешите определение местоположения — и система сама определит ваше место нахождения. Измените куда ехать, посмотрите доступные цены, выберите удобный категорию транспорта — от эконома до комфортного. При желании включите сервисы: кондиционер, время на сборы, перевозка животных или платёж по карте. Водитель увидит ваш заявку и отправится к вам без задержек. Следите за местоположение автомобиля на карте, а после рейса оцените качестве. Безопасность — всегда в центре внимания, если вы пользуетесь услугами лицензированных платформ.
I am extremely inspired with your writing talents as well as with the structure for your blog.
Is this a paid subject matter or did you customize
it your self? Either way stay up the nice high quality writing, it’s
rare to peer a great weblog like this one today..
my homepage retreat centers mexico
Hello there! This article could not be written much better!
Going through this article reminds me of my previous roommate!
He always kept talking about this. I most certainly will
send this information to him. Fairly certain he’ll have a good read.
Many thanks for sharing!
Este site tigrinho grátis é uma fonte confiável.
https://tigrinhogratis.com.br/bonus/
Sizdə əla məqalələr var — xüsusilə onlayn mərc ilə bağlı.
http://toolbarqueries.google.sm/url?q=https://mostbet-azerbaijan-game.com/oyunlar
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, NE 68022, United Ѕtates
402-289-4126
Central Cyber Center
Банкротство физ лиц в Казани
Рrime Secured
3603 N 222nd Ѕt, Suite 102,
Elkhorn, NE 68022, United Ѕtates
402-289-4126
bookmarks
Perfectly expressed indeed. .
Hello, after reading this remarkable paragraph
i am as well happy to share my knowledge here with mates.
Somebody essentially help to make critically articles I might state.
This is the first time I frequented your web page and thus far?
I surprised with the research you made to create this particular put up amazing.
Great process!
Hello there, just became aware of your blog through Google, and
found that it is truly informative. I am going to watch
out for brussels. I’ll appreciate if you continue this in future.
Many people will be benefited from your writing. Cheers!
my blog post: mexico ayahuasca retreat
Hello to all, how is the whole thing, I think every one is getting
more from this website, and your views are good in favor of new viewers.
This post will help the internet people for setting up new blog or even a weblog from start
to end.
интернет pin up сайт
ссылка на сайт P?n Up официальный
Крутое kazino olimp, молодцы. Респект.
https://olimp-casino-kazakhstan-play.org.kz/mobile-app
I enjoy, result in I discovered exactly what I was taking a look for.
You have ended my four day long hunt! God Bless you man. Have a
great day. Bye
рецепт белкового салата для похудения в домашних
Kokie būreliai ir veiklos yra Lietuvoje offered
No matter if some one searches for his essential thing, therefore
he/she needs to be available that in detail, therefore that thing is maintained over here.
Fantastic goods from you, man. I’ve take into account your stuff prior to and you are just extremely excellent.
I actually like what you have got right here, certainly like
what you are stating and the best way wherein you are saying it.
You are making it enjoyable and you continue to take care of to keep it sensible.
I can’t wait to learn much more from you. This is
really a wonderful website.
It’s an remarkable piece of writing designed for all the internet
viewers; they will obtain advantage from it I am sure.
Hi there! This is my first visit to your blog!
We are a group of volunteers and starting a new project in a community
in the same niche. Your blog provided us valuable information to work
on. You have done a extraordinary job!
It’s amazing to pay a visit this web site and reading the views of all colleagues regarding this piece of writing, while I
am also zealous of getting familiarity.
Обеспечение автономного водоснабжения – это
важный этап для организации водоснабжения.
Такой способ все чаще используется
частными домовладельцами, а также на предприятиях и фермах.
Наличие скважины даёт возможность получение чистой подземной воды, что особенно актуально в местах с отсутствием центрального водопровода.
Этапы бурения включает с оценки почвенных условий
и выбора места для подачи воды.
Грамотная оценка специалистов гарантирует ошибок.
Инновационные методы дают возможность делать глубокие и
сложные конструкции, что облегчает их использование
даже на сложных территориях.
Основным преимуществом собственной скважины является подача качественной воды.
Подземные воды обычно чистые и безопасные, чем верхние водоёмы.
Помимо этого, независимая система водоснабжения позволяет сэкономить коммунальные услуги, при проблемах с центральным водоснабжением
вы имеете гарантированный ресурс.
Вместе с тем, что процесс бурения подчиняется правовых рамок.
Чтобы узаконить источник могут потребоваться разрешения и исследования.
Профессиональный подход к оборудованию должно включать выбор подходящего насоса
и постоянное техобслуживание, что
помогает долговременную работу.
Бурение скважин на воду – это рациональный проект в комфорт и независимое водоснабжение.
Хотя первоначальные расходы могут показаться значительными, проект
окупается благодаря устойчивости к перебоям в водоснабжении.
Компетентная помощь специалистов обеспечивает успех проекта.
Thank you for the auspicious writeup. It if truth be told was a entertainment account it.
Glance advanced to more delivered agreeable from you!
By the way, how could we keep in touch?
Hi there would you mind stating which blog platform you’re using?
I’m planning to start my own blog in the near future but I’m having
a tough time selecting between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style seems different then most blogs
and I’m looking for something unique.
P.S Apologies for getting off-topic but I had to ask!
It’s really a nice and helpful piece of info. I am satisfied that you simply shared this
helpful information with us. Please keep us up to date
like this. Thank you for sharing.
I really like reading through an article that will make men and women think.
Also, thank you for permitting me to comment!
Spot on with this write-up, I actually believe that this site needs much more attention. I’ll probably be back again to see more, thanks for the information!
Greetings from Florida! I’m bored to tears at work so I decided to browse your site on my
iphone during lunch break. I really like the knowledge you provide
here and can’t wait to take a look when I get home. I’m shocked at how fast your
blog loaded on my mobile .. I’m not even using WIFI, just 3G ..
Anyways, wonderful site!
Sayt çox praktikdir.
https://1win-azerbaijan-bet.com/reyler
Автошкола «Авто-Мобилист»: профессиональное обучение вождению с гарантией результата
Автошкола «Авто-Мобилист» уже много лет успешно готовит водителей категории
«B», помогая ученикам не только сдать экзамены в ГИБДД,
но и стать уверенными участниками дорожного движения.
Наша миссия – сделать процесс обучения комфортным, эффективным и доступным для каждого.
Преимущества обучения в «Авто-Мобилист»
Комплексная теоретическая подготовка
Занятия проводят опытные преподаватели, которые не просто разбирают
правила дорожного движения, но и учат анализировать дорожные ситуации.
Мы используем современные
методики, интерактивные материалы и регулярно обновляем программу в
соответствии с изменениями законодательства.
Практика на автомобилях с МКПП и АКПП
Ученики могут выбрать обучение на механической или автоматической коробке передач.
Наш автопарк состоит из современных, исправных автомобилей,
а инструкторы помогают освоить не только стандартные экзаменационные маршруты, но и сложные городские условия.
Собственный оборудованный автодром
Перед выездом в город будущие водители отрабатывают базовые навыки на закрытой площадке: парковку, эстакаду, змейку и другие элементы,
необходимые для сдачи экзамена.
Гибкий график занятий
Мы понимаем, что многие совмещают обучение с работой или учебой, поэтому
предлагаем утренние, дневные и вечерние группы, а также индивидуальный график вождения.
Подготовка к экзамену в ГИБДД
Наши специалисты подробно разбирают типичные ошибки на теоретическом тестировании и практическом экзамене, проводят пробные тестирования и дают рекомендации по успешной сдаче.
Почему выбирают нас?
Опытные преподаватели и инструкторы с многолетним стажем.
Доступные цены и возможность оплаты в рассрочку.
Высокий процент сдачи с первого раза
благодаря тщательной подготовке.
Поддержка после обучения – консультации
по вопросам вождения и ПДД.
Автошкола «Авто-Мобилист» – это не
просто курсы вождения, а
надежный старт для безопасного и уверенного управления автомобилем.
This site definitely has all of the information I wanted concerning this subject and didn’t know who to ask.
пояснения https://krab3a.at/
I have been surfing on-line more than three hours nowadays,
yet I never discovered any attention-grabbing article like yours.
It is lovely worth sufficient for me. In my view, if all webmasters and bloggers made just right content material as you did, the web will be a lot more
helpful than ever before.
Whoa! This blog looks exactly like my old one! It’s on a totally different topic but it has pretty much the same
layout and design. Superb choice of colors!
Привет ..
Использую этот софт по поведенческих в пс
Pretty portion of content. I simply stumbled upon your
web site and in accession capital to assert that I
get in fact loved account your weblog posts. Anyway I will be subscribing in your augment and
even I success you get admission to consistently
fast.
Also visit my web page … Plombier Arlon
Oh my goodness! Incredible article dude! Thank you so much, However I am going through problems
with your RSS. I don’t know why I can’t join it. Is there anyone else having the same RSS problems?
Anyone who knows the answer will you kindly respond? Thanks!!
This is the perfect website for everyone who really wants to find out about this topic.
You understand a whole lot its almost hard to argue with
you (not that I really would want to…HaHa). You certainly put a new spin on a topic
which has been written about for ages. Excellent stuff, just wonderful!
Every weekend i used to go to see this site, as i wish for enjoyment, as this this web page conations in fact nice
funny information too.
Also visit my page: 역삼룸싸롱
This is a good tip particularly to those new to the blogosphere.
Brief but very accurate information… Appreciate your sharing this one.
A must read post!
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, ⲚE 68022, United Ѕtates
402-289-4126
Enterprise business continuity management
Have you ever considered about adding a little
bit more than just your articles? I mean, what you say is fundamental and all.
However imagine if you added some great visuals or video clips to give your posts more, “pop”!
Your content is excellent but with images and clips, this blog could undeniably be one of the most beneficial
in its field. Great blog!
Look into my web page … HVAC Jacksonville FL
This is a good tip especially to those fresh to the blogosphere.
Short but very precise information… Thank you for sharing this
one. A must read article!
There’s certainly a great deal to find out about this subject.
I love all of the points you’ve made.
Hello, I think your web site could possibly be having
internet browser compatibility problems. When I take a look at your blog in Safari, it looks fine
however, when opening in I.E., it’s got some
overlapping issues. I just wanted to provide you with
a quick heads up! Aside from that, excellent website!
Thank you for the good writeup. It in truth was a
entertainment account it. Glance advanced to far brought agreeable from you!
However, how could we keep up a correspondence?
I’m really enjoying the design and layout of your site.
It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often. Did you hire out a developer to create your theme?
Great work!
First of all I want to say awesome blog! I had
a quick question in which I’d like to ask if you do not mind.
I was curious to find out how you center yourself and clear your
thoughts prior to writing. I’ve had a hard time clearing my thoughts in getting my ideas out there.
I do enjoy writing but it just seems like the first 10 to 15 minutes tend to be lost just trying to figure out how to begin. Any
recommendations or tips? Thank you!
My web blog; HVAC Jacksonville FL
Do you have a spam problem on this site; I also am a blogger,
and I was wondering your situation; we have developed some nice methods and we are looking to trade solutions with other folks, please shoot me an e-mail if
interested.
Feel free to surf to my blog post; 강남매직미러
Great info. Lucky me I ran across your website by chance
(stumbleupon). I’ve book-marked it for later!
Maintaining ideal health and wellness is a day-to-day obstacle, and sometimes diet alone isn’t sufficient. Nutritional Supplements offer a reliable method to load dietary voids, support total health, and improve energy levels. Many people trust Nutra Welten for high-quality solutions that integrate all-natural components with scientific research. Whether you are looking for weight management, boosted immunity, or appeal support, the right supplements can make a substantial distinction. Checking Out Dietary Supplement Experiences and Reviews can aid you pick the most reliable alternatives for your way of life, ensuring both security and results, https://posteezy.com/nahrungserganzung-erfahrungen-ein-tiefer-einblick-die-welt-der-supplements.
Superb blog you have here but I was curious if you knew of any user discussion forums that cover
the same topics discussed in this article? I’d really like to be a
part of group where I can get opinions from other knowledgeable people that share the same interest.
If you have any suggestions, please let me know. Cheers!
This page really has all the info I needed about this subject and
didn’t know who to ask.
my page Plombier Charleroi
Thanks for finally writing about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate < Loved it!
It’s really a nice and helpful piece of information. I’m glad that you just shared this helpful information with us.
Please stay us up to date like this. Thank you for
sharing.
부천출장마사지는 고객이 원하는 시간과
장소에 전문 테라피스트가 직접 방문하여 체계적인 마사지 프로그램을 진행하는 출장형 전문 테라피 서비스입니다.
It is appropriate time to make some plans for the future and it
is time to be happy. I have read this post and if I could I desire to suggest you some interesting things or suggestions.
Perhaps you can write next articles referring to this article.
I want to read more things about it!
Angelks Baail Bonds Costa Mesa
769 Baker St,
Costa Mesa, ⲤA 92626,United States
how to pay for bail bond
Hello there, I discovered your blog by the use of Google whilst searching for a
similar topic, your site came up, it appears to be like good.
I have bookmarked it in my google bookmarks.
Hello there, just turned into alert to your blog thru Google,
and found that it’s truly informative. I am gonna watch
out for brussels. I will appreciate should you continue this in future.
Lots of people can be benefited from your writing.
Cheers!
I wanted to thank you for this excellent read!! I certainly loved every little bit of
it. I have you bookmarked to look at new stuff you post…
Look at my homepage; Loodgieter Antwerpen
Hi! Would you mind if I share your blog with my myspace
group? There’s a lot of folks that I think would really enjoy
your content. Please let me know. Thanks
Here is my website :: Plombier Charleroi
I’m not sure where you are getting your information, but good topic.
I needs to spend some time learning more or understanding more.
Thanks for great info I was looking for this information for
my mission.
My web blog; AC Repair Jacksonville FL
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I
get actually enjoyed account your blog posts.
Any way I will be subscribing to your feeds and even I achievement you access consistently rapidly.
Here is my website: Loodgieter Hasselt
I think the admin of this website is genuinely working hard
for his web page, as here every material is quality based material.
Take a look at my homepage; HVAC Jacksonville FL
Hi there to every one, as I am in fact keen of reading this blog’s post to be updated
daily. It carries pleasant material.
Эта статья полна интересного контента, который побудит вас исследовать новые горизонты. Мы собрали полезные факты и удивительные истории, которые обогащают ваше понимание темы. Читайте, погружайтесь в детали и наслаждайтесь процессом изучения!
Читать далее > – https://www.realty-key.ru/themes/seminaryi
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Кликни, не пожалеешь – https://hygienegegenviren.de/portfolio-view/in-faucibus
Hey are using WordPress for your blog platform?
I’m new to the blog world but I’m trying to get started and create my own. Do you require any
coding knowledge to make your own blog? Any help would be really appreciated!
It is the best time to make some plans for the longer term and it is
time to be happy. I’ve learn this post and if I may I want to suggest you some attention-grabbing things
or suggestions. Perhaps you can write next articles
regarding this article. I desire to read more issues approximately it!
Here is my blog post … Plombier Charleroi
This is my first time pay a quick visit at here
and i am really pleassant to read everthing at one place.
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Не упусти шанс – https://porosnews.id/peluang-partai-baru-di-pemilu-2024
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Не упусти важное! – https://novieauto.ru/2488315-kupit-betonnyjj-zavod-ot-tenzotekhservis-rassrochka-bez-procen-2ur8d
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to more added agreeable from you! However, how could
we communicate?
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Посмотреть подробности – https://admissiongurukul.com/engineering
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Давай разберёмся досконально – https://www.defining-blog.ru/tag/oprosy
В этой информационной статье вы найдете интересное содержание, которое поможет вам расширить свои знания. Мы предлагаем увлекательный подход и уникальные взгляды на обсуждаемые темы, побуждая пользователей к активному мышлению и критическому анализу.
Давай разберёмся досконально – http://www.fedhe.org/2019/04/11/la-communaute-haitienne-deurope-a-rendu-hommage-a-toussaint-louverture
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Cost Mesa, CA 92626, United Ⴝtates
0 Percent Financing Bail Bonds
What a stuff of un-ambiguity and preserveness of valuable
knowledge concerning unpredicted feelings.
Hi there, I enjoy reading through your post. I wanted to write a little comment to support
you.
Have a look at my blog post; HVAC Jacksonville FL
If you desire to get a great deal from this article then you have to apply such
methods to your won weblog.
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
ТОП-5 причин узнать больше – http://dispara.com.br/index.php/2023/04/09/revolutionize-your-business-with-our-cutting-edge
Everything is very open with a precise description of the challenges.
It was really informative. Your website is useful. Thanks for sharing!
Hello, the whole thing is going sound here and ofcourse every one is sharing data, that’s really
excellent, keep up writing.
Dominobet adalah situs judi domino terbesar di asia
Как выбрать фотографа мастера съемки в Сочи — торжества
My developer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type on a number of websites for about a year and
am nervous about switching to another platform.
I have heard great things about blogengine.net. Is there a
way I can import all my wordpress content into it?
Any kind of help would be really appreciated!
Hello colleagues, its enormous piece of writing regarding teachingand entirely
explained, keep it up all the time.
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ϹA 92626, United Ѕtates
big C bail bondsman
Link exchange is nothing else however it is just
placing the other person’s weblog link on your page at suitable place and other person will also do similar in support of you.
Prime Secured
3603 N 222nd Տt, Suite 102,
Elkhorn, ΝE 68022, United States
402-289-4126
Comprehensive Cyber Checkup
goGLOW Houston Heights
1515 Studemont Ꮪt Suite 204, Houston,
Texas, 77007, UЅᎪ
(713) 364-3256
best skincare clinic clinic
It’s an awesome paragraph in support of all the web viewers;
they will get benefit from it I am sure.
I’d like to find out more? I’d want to find out more details.
Spot on with this write-up, I really believe that this web site needs a lot more
attention. I’ll probably be back again to read more, thanks for the info!
Way cool! Some very valid points! I appreciate you writing this write-up and
the rest of the site is extremely good.
Удобный и логичный сайт с богатством полезной информации по казино.
http://www.irodabutor.ardoboz.hu/r.php?b=aHR0cHM6Ly9vbGltcC1jYXNpbm8ta2F6YWtoc3Rhbi16b25hLmt6L3BheW1lbnRz
Pretty nice post. I just stumbled upon your weblog and wished to say that I have really enjoyed browsing your blog posts.
After all I’ll be subscribing to your rss feed and I hope you write again very soon!
Superb forum posts, With thanks!
I every time emailed this webpage post page to all my contacts, since if like to
read it next my links will too.
Hi there just wanted to give you a quick heads up and let you
know a few of the images aren’t loading correctly. I’m not sure why but I
think its a linking issue. I’ve tried it in two different browsers and both show the same results.
저희는 이 활동에 깊은 영감을 받았습니다. 시력 회복을 위해 후원하는 것은
인류를 돕는 강력하고 방법입니다.
이 대단한 노력을 계속 이어가 주세요.
Feel free to visit my page … 의료비 나눔 프로젝트
When I originally commented I clicked the “Notify me when new comments are added”
checkbox and now each time a comment is added I get several e-mails with the same comment.
Is there any way you can remove me from that service?
Thanks!
Exodermin formula
La búsqueda de soluciones efectivas para problemas de la piel es un tema que atrae la atención de muchas personas. Todos queremos mantener nuestra piel saludable y radiante. Sin embargo, la industria de la belleza está llena de productos que prometen milagros, pero muchas veces decepcionan. Así que, ¿existe realmente una respuesta efectiva para todos esos inconvenientes cutáneos?
En este contexto, ha surgido una alternativa que genera interés. Se trata de un compuesto que ha demostrado su eficacia en el tratamiento de diversas afecciones dérmicas. A menudo, las personas se enfrentan a problemas como la sequedad, las infecciones y otros síntomas molestos que afectan su bienestar diario. Utilizando ingredientes naturales y comprobados, este enfoque se enfoca en brindar alivio y mejorar la apariencia de la piel.
Imagina poder restaurar la salud de tu epidermis de manera sencilla y eficaz. Los resultados son alentadores y muchos usuarios han compartido experiencias muy positivas al respecto.
Este producto destaca por ser fácil de usar y por su fórmula única que combina elementos clave para potenciar el cuidado de la dermis. No se trata solo de un remedio, sino de una verdadera rutina de bienestar que transforma la piel desde adentro hacia afuera. Además, es importante señalar que la naturaleza de sus componentes garantiza un enfoque más suave y menos agresivo que las soluciones químicas tradicionales.
Prepárate para explorar este innovador descubrimiento y dar un paso hacia una piel más saludable.
Propiedades y Beneficios de la Solución Tópica
La crema tópica ofrece diversas propiedades que la hacen destacar. Además de su acción antifúngica, cuenta con ingredientes que nutren la piel. Los usuarios han notado cambios significativos. Esto no solo mejora la apariencia, sino también la sensación. Su uso regular puede prevenir problemas dérmicos diversos.
Las sustancias naturales presentes en su composición son clave. Proporcionan una hidratación intensa que revitaliza las áreas afectadas. A la vez, calma la irritación, brindando una experiencia confortable. Los aceites esenciales incorporados favorecen la regeneración celular. Esto significa que, con el tiempo, la piel puede lucir más saludable y luminosa.
Un aspecto interesante es su facilidad de aplicación. El producto se absorbe rápidamente, sin dejar residuos grasos. Esto es beneficioso para quienes tienen un estilo de vida activo. También se sugiere su uso en diversas partes del cuerpo. Al completar el tratamiento, los usuarios suelen sentirse más seguros y satisfechos.
Por si fuera poco, la solución también contribuye a reforzar la barrera cutánea. Esto ayuda a proteger contra agresores externos como la contaminación o el clima. Así, no solo se tratan los síntomas, sino que se previene la recurrencia. Con el tiempo, se percibe una mejoría general en la salud dérmica. Resulta en una piel más fuerte y menos propensa a problemas futuros.
Aplicación y Efectividad del Producto
El uso adecuado de un producto puede marcar la diferencia en los resultados que se obtienen. La forma en que se aplica influencia mucho en su efectividad. Por eso es esencial seguir las instrucciones que se ofrecen. Cada etapa del proceso tiene su propósito.
Comenzar con una piel limpia es fundamental. Esto ayuda a que los ingredientes activos penetren mejor. Asegúrate de que el área esté seca y libre de impurezas. Luego de aplicar, masajear suavemente facilita la absorción.
Para obtener resultados óptimos, es recomendable ser constante. Repite la aplicación diaria, siguiendo las recomendaciones del fabricante. Con el pasar del tiempo, notarás cambios significativos. Es fascinante observar cómo la piel responde y mejora.
La efectividad del tratamiento demuestra su capacidad para abordar problemas específicos. Esto puede incluir la reducción de irritaciones, la hidratación y la restauración de la barrera cutánea. La satisfacción del usuario se traduce en confianza en el producto, ya que en muchos casos, la experiencia es positiva y gratificante.
https://exodermin.net/es/
Well expressed indeed. .
Thank you for another informative blog. Where
else could I get that kind of information written in such a perfect approach?
I have a project that I am just now running on, and I’ve been at the look out for
such information.
Многие сталкиваются с трудностями при выборе клиники или центра: предлагаемые услуги различаются по качеству, подходам, стоимости и длительности. Некоторые организации ограничиваются только медикаментозной поддержкой, не работая с глубинными причинами зависимости. Поэтому важно заранее понимать, какие параметры отличают действительно надёжное учреждение, способное обеспечить долгосрочные результаты.
Узнать больше – https://lechenie-narkomanii-murmansk0.ru/lechenie-narkomanii-i-alkogolizma-marmansk/
Hi there, every time i used to check webpage posts here early in the dawn, because i love to learn more and more.
Excellent goods from you, man. I have understand your stuff previous to
and you’re just extremely great. I really like what you
have acquired here, really like what you are stating
and the way in which you say it. You make it entertaining and you still care for to keep it sensible.
I can not wait to read much more from you. This is actually a wonderful web
site.
Howdy this is somewhat of off topic but I was wanting to know if
blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding experience so I wanted to get advice
from someone with experience. Any help would be greatly appreciated!
I’d like to find out more? I’d want to find out more details.
Denne informasjonen inspirerte meg til å tilby et bidrag.
Feel free to visit my web page – Donasjon til stær-operasjon
It’s amazing in support of me to have a web page, which is useful in support of my experience.
thanks admin
This design is steller! You obviously know how to keep a reader
entertained. Between your wit and your videos, I was almost moved to start my
own blog (well, almost…HaHa!) Excellent job.
I really enjoyed what you had to say, and more than that,
how you presented it. Too cool!
평택출장마사지는 호텔, 자택, 오피스 등
어디서나 받을 수 있는 방문형 전문 마사지 서비스입니다.
아로마, 스웨디시, 스포츠, 림프, 풋마사지까지 — 평택 전역 출장
Thanks in favor of sharing such a fastidious idea, paragraph is
pleasant, thats why i have read it completely
French Gadgets unite development, style, and practicality, supplying users the very best in Gadgets for home, way of life, and personal health. From sophisticated kitchen tools to ergonomic massage therapy devices, French Gadgets – technology, way of living and family ensures every item satisfies high criteria. By reading Gadgets reviews and comprehending Gadgets instructions, consumers can make informed choices, contrast Gadgets costs, and discover real Gadgets benefits. Exclusive Gadgets coupon codes and ideas on Gadgets to get even more enhance the shopping experience, making these Gadgets to use not only functional however likewise delightful, https://whoosmind.com/post/336467_french-gadgets-pour-technologie-accessible-et-efficace-la-boutique-french-gadget.html.
It’s remarkable to pay a visit this website and reading the views of all mates about this post, while I
am also zealous of getting know-how.
hello!,I like your writing very much! proportion we keep up
a correspondence extra approximately your article
on AOL? I need an expert in this space to resolve my problem.
Maybe that is you! Looking ahead to look you.
Hello! I just wanted to ask if you ever have any trouble with hackers?
My last blog (wordpress) was hacked and I ended up losing a
few months of hard work due to no back up. Do you have any methods to protect against hackers?
It’s very simple to find out any matter on web as compared to books,
as I found this paragraph at this web page.
คอนเทนต์นี้ อ่านแล้วรู้สึกว่าได้มุมมองใหม่
ค่ะ
ดิฉัน เคยเห็นเนื้อหาในแนวเดียวกันเกี่ยวกับ ข้อมูลเพิ่มเติม
ดูต่อได้ที่ Lesley
เผื่อใครสนใจ
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ เนื้อหาดีๆ นี้
อยากเห็นการนำเสนอในหัวข้ออื่นๆ
ด้วย
Hmm it appears like your blog ate my first comment (it was extremely long) so I guess I’ll just sum it
up what I had written and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog blogger but I’m still new to the whole
thing. Do you have any tips and hints for newbie blog writers?
I’d certainly appreciate it.
Its like you read my mind! You appear to know so much about
this, like you wrote the book in it or something. I think
that you can do with some pics to drive the message home a
bit, but instead of that, this is magnificent blog. A great read.
I’ll definitely be back.
May I just say what a relief to discover somebody that genuinely understands what
they are talking about online. You certainly understand how to
bring a problem to light and make it important. More people must check this out and
understand this side of your story. I was surprised that you are not more
popular given that you surely possess the gift.
Следующая страница kraken зеркало
Having read this I believed it was very informative.
I appreciate you spending some time and energy to put this information together.
I once again find myself spending a significant amount of time both reading
and posting comments. But so what, it was still worth it!
Why viewers still make use of to read news papers when in this
technological world everything is accessible on web?
If you are going for best contents like myself, only visit this web page every
day since it provides quality contents, thanks
Very good info. Lucky me I found your site by chance (stumbleupon).
I have saved as a favorite for later!
Keep it up and keep attracting more players!
https://ipv4.google.com/url?q=https://chicken-road-bonus.app/reviews
Wow, superb blog layout! How lengthy have you been blogging for?
you make blogging glance easy. The entire glance of your website is wonderful, as well as
the content!
my web-site: mexican retreats
Fantastic beat ! I wish to apprentice at the same time as you
amend your web site, how could i subscribe for a weblog website?
The account helped me a appropriate deal. I have been a little bit
acquainted of this your broadcast offered vibrant transparent concept
Angels Bail Bonds Costa Mesa
769 Baker Ꮪt,
Costa Mesa, CA 92626, United Ѕtates
electronic surety bonds
It’s the best time to make some plans for the future and
it is time to be happy. I have read this post and if I could I wish
to suggest you some interesting things or tips. Maybe you can write next articles referring
to this article. I desire to read more things about it!
It’s not my first time to pay a visit this web site, i am visiting this web site dailly and obtain fastidious information from here daily.
Feel free to visit my web page … meditation retreat mexico
I got this web page from my buddy who shared with me concerning this site and now this time I am visiting this
web page and reading very informative content at this
place.
These are genuinely enormous ideas in regarding blogging.
You have touched some fastidious points here.
Any way keep up wrinting.
Stop by my web page; mexico meditation retreat
I like what you guys are up too. This kind
of clever work and coverage! Keep up the very good works guys I’ve added you guys to
blogroll.
Take a look at my homepage mexico retreat centers
What a stuff of un-ambiguity and preserveness of valuable familiarity regarding
unexpected feelings.
My homepage … couple intimacy retreats
I’m not sure exactly why but this web site is loading very slow for
me. Is anyone else having this problem or is it a problem on my end?
I’ll check back later and see if the problem still exists.
Hi there would you mind sharing which blog platform you’re working with?
I’m planning to start my own blog soon but I’m having a difficult time making a
decision between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most blogs and I’m
looking for something unique. P.S My apologies for being off-topic but I had to
ask!
Link exchange is nothing else but it is only placing the other person’s blog link on your page at suitable place and other person will also do similar in favor of you.
Chicken Road is very informative. Will be back for sure!
https://maps.google.tt/url?q=https://chickenroadvegas.org/payments
I’ve learn several just right stuff here.
Certainly value bookmarking for revisiting. I surprise how much
attempt you place to create this kind of wonderful informative
site.
What’s up, the whole thing is going nicely here and ofcourse every one is sharing information, that’s actually fine, keep up writing.
We’re a group of volunteers and opening a brand new scheme in our community.
Your website offered us with helpful information to work on. You have performed an impressive process and our entire community can be thankful to you.
Hi there i am kavin, its my first occasion to commenting
anyplace, when i read this article i thought i could also make comment due to this sensible piece of
writing.
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, ΝᎬ 68022, United Տtates
402-289-4126
Tailored security advisory solutions
Good post. I learn something totally new and challenging on blogs I
stumbleupon everyday. It will always be helpful to read content
from other authors and use something from other sites.
I don’t know if it’s just me or if everybody else encountering issues with your blog.
It appears like some of the written text on your
posts are running off the screen. Can someone else
please provide feedback and let me know
if this is happening to them as well? This could be
a problem with my web browser because I’ve had this happen previously.
Appreciate it
Look into my website spiritual retreats mexico
Does your website have a contact page? I’m
having trouble locating it but, I’d like to send you an e-mail.
I’ve got some recommendations for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it develop over time.
Hi there! Would you mind if I share your blog with my twitter group?
There’s a lot of people that I think would really enjoy your
content. Please let me know. Thank you
Hello I am so excited I found your weblog, I really
found you by error, while I was searching on Aol for something else, Anyhow I am here now and would just like to say thanks a
lot for a tremendous post and a all round thrilling blog (I also love
the theme/design), I don’t have time to browse it all
at the moment but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the
great jo.
I all the time used to study article in news papers but now as I am a user of web thus from now I am using net for content, thanks to web.
Feel free to visit my webpage … yoga retreats in mexico
Fantastic write ups Kudos!
A 2021 systematic assessment and meta-evaluation of research including male members discovered that reasonable to high depth aerobic train had a extra negative influence on muscle strength than low intensity aerobic exercise. Similarly, aerobic exercise that lasted longer than 30 minutes had more impression than shorter durations. The studies did not embody feminine members, although, so more analysis is required. If you’re unsure the place to start, consider talking with a personal trainer. They could assist develop an exercise program to target fats loss and muscle preservation. Eating a effectively-balanced weight-reduction plan that meets your nutritional and energetic wants is also key to maintaining muscle whereas optimizing fats loss. Particularly, analysis shows that consuming a excessive protein weight loss plan while losing weight could also be one of a very powerful factors in sustaining muscle mass, together with resistance coaching. It is because protein helps promote protein synthesis, the method through which the building blocks of protein (amino acids) type into muscle mass.
Check out my web-site; https://maps.google.com.bn/url?q=https://humanlove.stream/wiki/User:JeffersonCharles
Very nice post. I just stumbled upon your weblog and wanted to say that I have really enjoyed surfing around your
blog posts. After all I will be subscribing to your rss
feed and I hope you write again soon!
my web site: spiritual couple retreats
Angels Bail Bonds Costa Mesa
769 Baker Տt,
Costa Mesa, CA 92626, United States
what do bail bondsman charge
Howdy! Do you use Twitter? I’d like to follow you if that would
be okay. I’m absolutely enjoying your blog and look forward to new posts.
Here is my homepage; best wellness retreat mexico
Greetings! I know this is kinda off topic nevertheless I’d figured I’d ask.
Would you be interested in trading links or maybe guest authoring
a blog article or vice-versa? My site discusses a lot of the same
subjects as yours and I think we could greatly benefit from each other.
If you are interested feel free to shoot me an email.
I look forward to hearing from you! Superb blog by
the way!
My web page mexico ayahuasca retreat
Hi Dear, are you in fact visiting this site daily, if so afterward you will without doubt obtain good know-how.
Have a look at my website … mexico ayahuasca retreat
Keep on working, great job!
my web page – mother daughter wellness retreat
When I initially left a comment I seem to have clicked on the -Notify me when new comments are added- checkbox and
from now on whenever a comment is added I recieve 4 emails with the same comment.
Perhaps there is a way you are able to remove me from that service?
Appreciate it!
I all the time used to read post in news papers but now as I am a user of net therefore from now I am using net for content, thanks to web.
Hi, i read your blog from time to time and i own a similar one and i was just wondering if you get a lot of spam feedback?
If so how do you prevent it, any plugin or anything you can advise?
I get so much lately it’s driving me crazy so any support is very much appreciated.
Saya terinspirasi dengan upaya ini. Berdonasi untuk restorasi Bantuan Operasi Mata Gratis
adalah cara yang kuat untuk membantu kemanusiaan. Tolong lanjutkan aksi yang luar biasa ini.
Saytdan istifadə çox xoşdur — maraqlı bölmələr var!
https://opnlink.com/o/iFUdK
Utmärkt ämne om finansiering ögonoperationer.
Generally I don’t learn post on blogs, however I wish to say that this write-up very compelled me to take a look at and do so!
Your writing style has been surprised me. Thank you, very nice
post.
คอนเทนต์นี้ อ่านแล้วเพลินและได้สาระ ค่ะ
ดิฉัน เคยติดตามเรื่องนี้จากหลายแหล่ง เรื่องที่เกี่ยวข้อง
ที่คุณสามารถดูได้ที่ สล็อตออนไลน์
น่าจะเป็นประโยชน์กับหลายคน
มีการนำเสนอที่ชัดเจนและตรงประเด็น
ขอบคุณที่แชร์ ข้อมูลที่มีประโยชน์ นี้
และหวังว่าจะมีข้อมูลใหม่ๆ มาแบ่งปันอีก
Нравится сайт — всё ясно и много интересного.
https://image.google.com.et/url?q=https://sultan-casino-kazakhstan-playbet.kz
I am regular visitor, how are you everybody?
This article posted at this web site is in fact fastidious.
It is truly a great and useful piece of info. I am glad that you simply shared
this useful info with us. Please stay us up to date like this.
Thank you for sharing.
Greetings from Colorado! I’m bored to death at work so I decided to browse your website on my iphone during
lunch break. I really like the information you present here and can’t wait to take a look
when I get home. I’m amazed at how quick your blog loaded on my cell phone ..
I’m not even using WIFI, just 3G .. Anyhow, wonderful blog!
my web site :: yoga retreats in mexico
Pretty nice post. I just stumbled upon your blog and wished to say that I have really enjoyed surfing around your
blog posts. After all I will be subscribing to your feed and
I hope you write again very soon!
Today, I went to the beachfront with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell to
her ear and screamed. There was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is totally off topic
but I had to tell someone!
Useful write ups Thank you!
Excellent blog here! Also your web site loads up fast!
What web host are you using? Can I get your affiliate link to your host?
I wish my site loaded up as quickly as yours lol
Hello there! I know this is somewhat off topic but I was wondering which blog platform are you using for this website?
I’m getting tired of WordPress because I’ve had issues with hackers
and I’m looking at alternatives for another platform.
I would be great if you could point me in the direction of a good platform.
Apartment Renovation Refurbishment Guide
Рrime Secured
3603 N 222nd Ѕt, Suite 102,
Elkhorn, ⲚE 68022, United Stаtes
402-289-4126
Bookmarks
Ahaa, its fastidious conversation concerning this article at this place at this web site, I
have read all that, so at this time me also commenting at
this place.
Hmm is anyone else having problems with the images on this blog loading?
I’m trying to figure out if its a problem on my end or if it’s the
blog. Any suggestions would be greatly appreciated.
Как выбрать фотографа мастера съемки в Сочи — торжества
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626, United Ѕtates
#1 bail bonds
เนื้อหานี้ อ่านแล้วได้ความรู้เพิ่ม ครับ
ดิฉัน ไปเจอรายละเอียดของ เรื่องที่เกี่ยวข้อง
ที่คุณสามารถดูได้ที่ เกมสล็อต
น่าจะถูกใจใครหลายคน
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ บทความคุณภาพ
นี้
และอยากเห็นบทความดีๆ แบบนี้อีก
Thanks for finally writing about > Heart failure: Symptoms,
Causes, Diagnosis & Treatment – MDtodate < Loved it!
Hi, I read your blogs like every week. Your writing style is witty, keep doing what you’re doing!
Этот обзор предлагает структурированное изложение информации по актуальным вопросам. Материал подан так, чтобы даже новичок мог быстро освоиться в теме и начать использовать полученные знания в практике.
Откройте для себя больше – https://primenewsnet.com/oven-baked-yummy-pulled-pork-for-food-travelers
After looking at a handful of the articles on your web site, I
really like your way of writing a blog. I bookmarked it to my
bookmark site list and will be checking back in the near future.
Take a look at my website as well and tell me how you feel.
Удобная платформа Olimp Casino — люблю заходить сюда!
https://rock-metal-wave.ru/go?https://olimp-casino-kazakhstan-official.kz/registration
I am actually pleased to glance at this weblog posts which consists of plenty of helpful facts, thanks for
providing these statistics.
В статье представлены ключевые моменты по актуальной теме, дополненные советами экспертов и ссылками на дополнительные ресурсы. Цель материала — дать читателю инструменты для самостоятельного развития и принятия осознанных решений.
Подробнее – https://www.defining-blog.ru/category/investicii
Kokie būreliai ir veiklos yra Lietuvoje available
Great post. I used to be checking constantly this blog and I am impressed!
Very useful information particularly the remaining section 🙂 I maintain such information a lot.
I used to be seeking this certain information for a long time.
Thank you and best of luck.
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
Проверенные методы — узнай сейчас – https://uastar.net/page.php?id=40606
Its like you read my mind! You appear to know a lot about this, like you wrote the
book in it or something. I think that you can do with
some pics to drive the message home a little bit, but other than that, this is fantastic blog.
An excellent read. I’ll definitely be back.
I am sure this paragraph has touched all the internet people, its really really nice
paragraph on building up new website.
I take pleasure in, result in I found just what I used to be taking a look for.
You have ended my four day long hunt! God Bless you man.
Have a great day. Bye
I used to be recommended this blog through my cousin. I am no longer certain whether or not this publish is written via him as no one else realize such
designated approximately my problem. You are incredible!
Thank you!
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Узнайте всю правду – https://dienmaydangduong.com/lorem-ipsum-chi-don-gian-la-mot-doan-van-ban-gia-7
Prijme Secured
3603 N 222nd St, Suite 102,
Elkhorn, ΝΕ 68022, United Statеs
402-289-4126
Managed Stream Solutions
Post writing is also a excitement, if you be acquainted with
afterward you can write otherwise it is difficult to write.
Hi to every one, since I am genuinely eager of reading this
weblog’s post to be updated on a regular basis. It contains
fastidious stuff.
Анонимная наркологическая помощь — это управляемая система, где каждый шаг прозрачно связан с целью и измеримым результатом. В наркологической клинике «ЕнисейМед Центр» мы соединяем круглосуточную доступность, мягкую логистику и модульный план лечения, чтобы пациент и семья понимали, почему именно сейчас назначается то или иное вмешательство и когда оно будет остановлено. Мы избегаем полипрагмазии: запускаем один модуль — ставим один маркер — определяем «окно оценки» — выключаем модуль, как только цель достигнута. Такой подход бережёт ресурсы организма и сохраняет причинно-следственную связь.
Углубиться в тему – наркологическая клиника лечение алкоголизма
Программы вывода из запоя в клинике разрабатываются с учётом состояния пациента. Для тяжёлых случаев назначается интенсивный курс с инфузионной терапией и контролем электролитов. При лёгких формах применяются мягкие препараты с постепенным выведением токсинов. Все процедуры проходят с соблюдением медицинских стандартов и полным сохранением анонимности.
Углубиться в тему – вывод из запоя в стационаре волгоград
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Уточнить детали – https://infotainer.thorstenjost.de/episode-17-sebastian-prittwitz
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Получить дополнительную информацию – скорая вывод из запоя тольятти
Greetings! I know this is kinda off topic but I’d figured I’d
ask. Would you be interested in trading links or
maybe guest authoring a blog article or vice-versa?
My site addresses a lot of the same subjects as yours
and I believe we could greatly benefit from each other.
If you are interested feel free to send me an e-mail.
I look forward to hearing from you! Great blog by the way!
Jeg vil bestemt anbefale denne indsamling med mit publikum.
Take a look at my webpage: Genopretning af synsevne
Very quickly this site will be famous among all blogging
and site-building visitors, due to it’s nice posts
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Подробнее тут – https://www.skyhilocksmith.com/locksmith/jeep-locksmith-colorado-springs
It’s remarkable to pay a quick visit this website
and reading the views of all mates concerning this article, while I am also keen of getting knowledge.
Hi there just wanted to give you a quick heads up.
The text in your article seem to be running off the screen in Firefox.
I’m not sure if this is a formatting issue or something
to do with internet browser compatibility but I thought I’d
post to let you know. The style and design look great though!
Hope you get the problem solved soon. Many thanks
Нарколог на дом в Уфе — это услуга, которая позволяет получить квалифицированную медицинскую помощь при алкогольной или наркотической интоксикации без необходимости госпитализации. Такой формат особенно востребован при запойных состояниях, когда пациент не может самостоятельно посетить клинику. Врач приезжает по вызову в течение короткого времени, проводит обследование, устанавливает капельницу и обеспечивает безопасный вывод из состояния опьянения. Все процедуры выполняются анонимно, с соблюдением медицинской этики и конфиденциальности.
Исследовать вопрос подробнее – https://narkolog-na-dom-v-ufe17.ru/vyvod-iz-zapoya-ufa-narkolog-na-dom
Снятие ломки при алкоголизме в Химках. Наши специалисты помогут вам справиться с симптомами абстиненции.
Изучить вопрос глубже – вывод из запоя вызов на дом в химках
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Узнайте всю правду – https://14kankoreziu.lt/virtuali-kavapost
Кодирование от алкоголизма на дому в Люберцах. Наши специалисты приедут к вам домой и проведут процедуру кодирования.
Детальнее – поставить капельницу от запоя
Выездная наркологическая помощь организована по чётко выстроенной схеме. Каждый этап направлен на стабилизацию состояния и безопасное восстановление функций организма после алкогольного или наркотического воздействия.
Углубиться в тему – платный нарколог на дом в уфе
If some one wishes to be updated with most recent technologies afterward he must
be pay a quick visit this web page and be up to date everyday.
Вывод из запоя у пожилых людей в стационаре Балашихи. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Углубиться в тему – вывод из запоя на дому цена
Tämä on todella ajankohtainen aihe. Lääketieteellinen joukkorahoitus auttaa hoidon monelle.
Kiitos että nostatte esiin tämän tehtävän.
Нравится сайт — всё ясно и много интересного.
http://bowlingalex.ru/bitrix/rk.php?goto=https://olimp-casino-kz-money.org.kz/
Именно поэтому при затяжных запоях необходима квалифицированная медицинская помощь, позволяющая безопасно и максимально комфортно прекратить приём алкоголя. Клиника «Стратегия Здоровья» предлагает профессиональный вывод из запоя в Москве как в условиях стационара, так и с выездом на дом. Врачи работают круглосуточно, используя проверенные методики детоксикации и медикаментозной поддержки.
Детальнее – https://narko-reabcentr.ru/kruglosutochnyj-vyvod-iz-zapoya-v-moskve
look at here https://onetimesecret.info
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Подробнее тут – https://aamirpathan.com/welcome-to-my-profile-aamir-pathan-3
If you are going for finest contents like I do, simply visit this web page everyday because it provides
quality contents, thanks
Saw your material, and hope you publish more soon.
(10 euros gratis apuestas|10 mejores casas de apuestas|10 trucos para ganar
apuestas|15 euros gratis marca apuestas|1×2 apuestas|1×2 apuestas deportivas|1×2
apuestas que significa|1×2 en apuestas|1×2 en apuestas
que significa|1×2 que significa en apuestas|5 euros gratis apuestas|9 apuestas que siempre ganaras|a partir de cuanto se declara apuestas|actividades
de juegos de azar y apuestas|ad apuestas deportivas|aleksandre topuria ufc apuestas|algoritmo para ganar apuestas deportivas|america apuestas|análisis nba apuestas|aplicacion android apuestas deportivas|aplicacion apuestas deportivas|aplicacion apuestas deportivas android|aplicación de
apuestas online|aplicacion para hacer apuestas|aplicacion para hacer apuestas de futbol|aplicación para hacer apuestas de fútbol|aplicaciones apuestas deportivas android|aplicaciones apuestas deportivas gratis|aplicaciones de
apuestas android|aplicaciones de apuestas de fútbol|aplicaciones de apuestas deportivas|aplicaciones de apuestas deportivas peru|aplicaciones de apuestas deportivas perú|aplicaciones de apuestas en colombia|aplicaciones de
apuestas gratis|aplicaciones de apuestas online|aplicaciones de apuestas seguras|aplicaciones de apuestas sin dinero|aplicaciones para hacer apuestas|apostar seguro apuestas deportivas|app
android apuestas deportivas|app apuestas|app apuestas android|app apuestas
de futbol|app apuestas deportivas|app apuestas deportivas android|app apuestas deportivas argentina|app apuestas deportivas colombia|app apuestas deportivas ecuador|app apuestas deportivas españa|app apuestas deportivas gratis|app apuestas entre amigos|app apuestas futbol|app apuestas gratis|app
apuestas sin dinero|app casa de apuestas|app casas de apuestas|app control apuestas|app
de apuestas|app de apuestas android|app de apuestas casino|app de
apuestas colombia|app de apuestas con bono de bienvenida|app de apuestas de futbol|app de apuestas deportivas|app de apuestas
deportivas android|app de apuestas deportivas argentina|app de apuestas deportivas colombia|app de apuestas deportivas en españa|app de apuestas deportivas peru|app de apuestas deportivas perú|app de apuestas deportivas sin dinero|app de apuestas ecuador|app de apuestas en colombia|app de apuestas en españa|app de apuestas en venezuela|app de apuestas futbol|app de apuestas gratis|app de apuestas online|app de apuestas para android|app
de apuestas para ganar dinero|app de apuestas peru|app de apuestas reales|app de casas de apuestas|app marca apuestas android|app moviles de apuestas|app para apuestas|app para apuestas de futbol|app para apuestas
deportivas|app para apuestas deportivas en español|app para ganar apuestas deportivas|app
para hacer apuestas|app para hacer apuestas deportivas|app para hacer apuestas entre amigos|app para llevar control de apuestas|app pronosticos apuestas deportivas|app versus
apuestas|apps apuestas mundial|apps de apuestas|apps de apuestas con bono de bienvenida|apps de apuestas de futbol|apps de apuestas
deportivas peru|apps de apuestas mexico|apps para apuestas|aprender a hacer apuestas deportivas|aprender hacer apuestas
deportivas|apuesta del dia apuestas deportivas|apuestas 10 euros gratis|apuestas 100 seguras|apuestas 1×2|apuestas 1X2|apuestas 2 division|apuestas 3 division|apuestas a caballos|apuestas a carreras de caballos|apuestas a colombia|apuestas a corners|apuestas
a ganar|apuestas a jugadores nba|apuestas a
la baja|apuestas a la nfl|apuestas al barcelona|apuestas al dia|apuestas al empate|apuestas al
mundial|apuestas al tenis wta|apuestas alaves barcelona|apuestas alcaraz hoy|apuestas alemania españa|apuestas alonso campeon del mundo|apuestas altas y bajas|apuestas altas y bajas nfl|apuestas ambos equipos marcan|apuestas america|apuestas android|apuestas anillo nba|apuestas antes del mundial|apuestas anticipadas|apuestas anticipadas nba|apuestas apps|apuestas arabia argentina|apuestas argentina|apuestas argentina campeon del mundo|apuestas argentina canada|apuestas argentina colombia|apuestas argentina croacia|apuestas argentina españa|apuestas argentina francia|apuestas
argentina francia cuanto paga|apuestas argentina francia mundial|apuestas
argentina gana el mundial|apuestas argentina gana mundial|apuestas argentina holanda|apuestas
argentina mexico|apuestas argentina méxico|apuestas argentina mundial|apuestas argentina online|apuestas argentina paises bajos|apuestas argentina polonia|apuestas argentina uruguay|apuestas
argentina vs australia|apuestas argentina vs colombia|apuestas argentina vs francia|apuestas
argentina vs peru|apuestas argentinas|apuestas arsenal real madrid|apuestas ascenso a primera division|apuestas ascenso a segunda|apuestas asiaticas|apuestas asiatico|apuestas athletic|apuestas athletic atletico|apuestas athletic barça|apuestas athletic barcelona|apuestas athletic betis|apuestas athletic manchester|apuestas athletic manchester united|apuestas athletic osasuna|apuestas athletic real|apuestas athletic real madrid|apuestas athletic real sociedad|apuestas athletic real sociedad final|apuestas athletic roma|apuestas athletic
sevilla|apuestas athletic valencia|apuestas atletico|apuestas
atletico barcelona|apuestas atletico barsa|apuestas atletico
campeon champions|apuestas atletico campeon de liga|apuestas
atlético copenhague|apuestas atletico de madrid|apuestas atlético de madrid|apuestas atletico de
madrid barcelona|apuestas atletico de madrid gana la liga|apuestas
atletico de madrid real madrid|apuestas atlético de madrid real madrid|apuestas atletico de madrid vs barcelona|apuestas atletico madrid|apuestas atletico
madrid real madrid|apuestas atletico madrid vs barcelona|apuestas atletico real madrid|apuestas
atletico real madrid champions|apuestas atletismo|apuestas bajas|apuestas baloncesto|apuestas baloncesto
acb|apuestas baloncesto handicap|apuestas baloncesto
hoy|apuestas baloncesto juegos olimpicos|apuestas baloncesto nba|apuestas baloncesto pronostico|apuestas
baloncesto pronósticos|apuestas baloncesto prorroga|apuestas barca|apuestas barca athletic|apuestas barca atletico|apuestas barca bayern|apuestas barca bayern munich|apuestas barca girona|apuestas
barca hoy|apuestas barça hoy|apuestas barca inter|apuestas barca juventus|apuestas barca madrid|apuestas barça madrid|apuestas barca real madrid|apuestas barca vs juve|apuestas barca vs madrid|apuestas barca vs psg|apuestas
barcelona|apuestas barcelona alaves|apuestas barcelona athletic|apuestas barcelona
atletico|apuestas barcelona atletico de madrid|apuestas barcelona atlético de madrid|apuestas barcelona atletico madrid|apuestas barcelona bayern|apuestas barcelona betis|apuestas barcelona campeon de liga|apuestas
barcelona celta|apuestas barcelona espanyol|apuestas barcelona gana la champions|apuestas barcelona girona|apuestas barcelona
granada|apuestas barcelona hoy|apuestas barcelona inter|apuestas barcelona madrid|apuestas barcelona osasuna|apuestas barcelona psg|apuestas barcelona real madrid|apuestas
barcelona real sociedad|apuestas barcelona sevilla|apuestas barcelona
valencia|apuestas barcelona villarreal|apuestas barcelona vs atletico madrid|apuestas barcelona vs
madrid|apuestas barcelona vs real madrid|apuestas barsa madrid|apuestas basket
hoy|apuestas bayern barcelona|apuestas bayern vs barcelona|apuestas beisbol|apuestas béisbol|apuestas beisbol
mlb|apuestas beisbol pronosticos|apuestas beisbol venezolano|apuestas betis|apuestas betis – chelsea|apuestas betis barcelona|apuestas betis chelsea|apuestas betis fiorentina|apuestas betis girona|apuestas betis
madrid|apuestas betis mallorca|apuestas betis real madrid|apuestas betis
real sociedad|apuestas betis sevilla|apuestas betis valencia|apuestas betis valladolid|apuestas betis vs valencia|apuestas betplay hoy colombia|apuestas betsson peru|apuestas bienvenida|apuestas billar online|apuestas bolivia vs colombia|apuestas bono|apuestas bono bienvenida|apuestas bono de bienvenida|apuestas bono de
bienvenida sin deposito|apuestas bono gratis|apuestas
bono sin deposito|apuestas bonos sin deposito|apuestas borussia
real madrid|apuestas boxeo|apuestas boxeo de campeonato|apuestas boxeo españa|apuestas boxeo
español|apuestas boxeo femenino olimpiadas|apuestas boxeo hoy|apuestas boxeo online|apuestas
brasil colombia|apuestas brasil peru|apuestas brasil uruguay|apuestas brasil vs
colombia|apuestas brasil vs peru|apuestas caballos|apuestas caballos colocado|apuestas
caballos españa|apuestas caballos hipodromo|apuestas caballos hoy|apuestas caballos madrid|apuestas caballos online|apuestas caballos sanlucar de barrameda|apuestas caballos zarzuela|apuestas calculador|apuestas campeon|apuestas campeon champions|apuestas campeón champions|apuestas campeon champions 2025|apuestas campeon champions league|apuestas campeon conference league|apuestas campeon copa america|apuestas campeon copa del rey|apuestas campeon de champions|apuestas campeon de la champions|apuestas campeon de liga|apuestas campeon del
mundo|apuestas campeon eurocopa|apuestas campeón eurocopa|apuestas campeon europa league|apuestas campeon f1|apuestas campeon f1 2025|apuestas campeon formula 1|apuestas campeon libertadores|apuestas campeon liga|apuestas
campeon liga bbva|apuestas campeon liga española|apuestas campeon liga santander|apuestas campeon motogp 2025|apuestas campeon mundial|apuestas campeón mundial|apuestas campeon mundial baloncesto|apuestas campeon nba|apuestas campeón nba|apuestas campeon premier|apuestas campeon premier league|apuestas
campeon roland garros|apuestas campeonato f1|apuestas campeonatos de
futbol|apuestas carrera de caballos|apuestas carrera de caballos hoy|apuestas carrera de caballos nocturnas|apuestas carrera de galgos fin de semana|apuestas carrera de galgos hoy|apuestas carrera de galgos nocturnas|apuestas carreras caballos|apuestas carreras caballos sanlucar|apuestas carreras de caballos|apuestas
carreras de caballos en directo|apuestas carreras de caballos en vivo|apuestas carreras
de caballos españa|apuestas carreras de caballos hoy|apuestas carreras de caballos nacionales|apuestas carreras de
caballos nocturnas|apuestas carreras de caballos online|apuestas carreras de caballos
sanlucar|apuestas carreras de caballos sanlúcar|apuestas carreras de galgos|apuestas carreras de galgos en vivo|apuestas carreras de galgos nocturnas|apuestas carreras de galgos pre
partido|apuestas casino|apuestas casino barcelona|apuestas casino futbol|apuestas casino gran madrid|apuestas casino gratis|apuestas casino madrid|apuestas casino online|apuestas casino online argentina|apuestas casinos|apuestas casinos online|apuestas celta|apuestas celta barcelona|apuestas celta betis|apuestas
celta eibar|apuestas celta espanyol|apuestas celta granada|apuestas celta madrid|apuestas celta
manchester|apuestas celta real madrid|apuestas champion league|apuestas champions foro|apuestas champions hoy|apuestas champions league|apuestas champions league – pronósticos|apuestas champions league 2025|apuestas champions league
hoy|apuestas champions league pronosticos|apuestas champions
league pronósticos|apuestas champions pronosticos|apuestas chelsea barcelona|apuestas chelsea betis|apuestas chile|apuestas chile peru|apuestas chile venezuela|apuestas chile vs colombia|apuestas
chile vs uruguay|apuestas ciclismo|apuestas
ciclismo en vivo|apuestas ciclismo femenino|apuestas ciclismo tour francia|apuestas ciclismo vuelta|apuestas ciclismo vuelta a españa|apuestas ciclismo vuelta españa|apuestas city madrid|apuestas city real madrid|apuestas clasico|apuestas clasico español|apuestas clasico real madrid barcelona|apuestas clasificacion mundial|apuestas colombia|apuestas colombia argentina|apuestas colombia
brasil|apuestas colombia paraguay|apuestas colombia uruguay|apuestas colombia vs argentina|apuestas colombia vs
brasil|apuestas combinadas|apuestas combinadas como
funcionan|apuestas combinadas de futbol|apuestas combinadas de fútbol|apuestas
combinadas foro|apuestas combinadas futbol|apuestas combinadas hoy|apuestas combinadas mismo partido|apuestas combinadas
mundial|apuestas combinadas nba|apuestas combinadas para
esta semana|apuestas combinadas para hoy|apuestas combinadas para mañana|apuestas combinadas
pronosticos|apuestas combinadas recomendadas|apuestas combinadas seguras|apuestas combinadas seguras para hoy|apuestas combinadas
seguras para mañana|apuestas como ganar|apuestas comparador|apuestas con bono de bienvenida|apuestas con dinero ficticio|apuestas con dinero real|apuestas
con dinero virtual|apuestas con handicap|apuestas con handicap asiatico|apuestas con handicap baloncesto|apuestas con mas probabilidades de
ganar|apuestas con paypal|apuestas con tarjeta de
credito|apuestas con tarjeta de debito|apuestas consejos|apuestas copa|apuestas copa africa|apuestas copa
america|apuestas copa américa|apuestas copa argentina|apuestas copa brasil|apuestas copa davis|apuestas copa de europa|apuestas copa del mundo|apuestas copa del rey|apuestas copa del
rey baloncesto|apuestas copa del rey final|apuestas copa del rey futbol|apuestas copa
del rey ganador|apuestas copa del rey hoy|apuestas copa del rey pronosticos|apuestas copa del rey pronósticos|apuestas copa europa|apuestas copa
italia|apuestas copa libertadores|apuestas copa mundial de hockey|apuestas copa
rey|apuestas copa sudamericana|apuestas corners|apuestas corners hoy|apuestas croacia argentina|apuestas cuartos eurocopa|apuestas
cuotas|apuestas cuotas altas|apuestas cuotas bajas|apuestas de 1 euro|apuestas de baloncesto|apuestas de baloncesto hoy|apuestas
de baloncesto nba|apuestas de baloncesto para
hoy|apuestas de beisbol|apuestas de beisbol para hoy|apuestas de blackjack
en linea|apuestas de boxeo|apuestas de boxeo canelo|apuestas de boxeo en las vegas|apuestas de boxeo hoy|apuestas de boxeo online|apuestas de caballo|apuestas de caballos|apuestas
de caballos como funciona|apuestas de caballos como se juega|apuestas de caballos en colombia|apuestas de caballos en españa|apuestas de caballos en linea|apuestas de caballos españa|apuestas de caballos ganador y colocado|apuestas de caballos internacionales|apuestas de caballos juegos|apuestas de caballos
online|apuestas de caballos online en venezuela|apuestas de caballos por internet|apuestas de caballos pronosticos|apuestas de caballos pronósticos|apuestas de carrera de caballos|apuestas de carreras de caballos|apuestas de carreras
de caballos online|apuestas de casino|apuestas de casino
online|apuestas de casino por internet|apuestas de champions league|apuestas de ciclismo|apuestas de colombia|apuestas de copa america|apuestas de corners|apuestas de deportes en linea|apuestas de deportes online|apuestas de dinero|apuestas de esports|apuestas de eurocopa|apuestas de europa league|apuestas de f1|apuestas de formula 1|apuestas de futbol|apuestas
de fútbol|apuestas de futbol app|apuestas de futbol argentina|apuestas de futbol colombia|apuestas de futbol en colombia|apuestas de futbol en directo|apuestas de
futbol en linea|apuestas de futbol en vivo|apuestas de futbol español|apuestas de futbol gratis|apuestas de futbol hoy|apuestas de futbol mundial|apuestas de futbol online|apuestas de fútbol online|apuestas de futbol para hoy|apuestas
de fútbol para hoy|apuestas de futbol para hoy seguras|apuestas de futbol
para mañana|apuestas de futbol peru|apuestas de futbol pronosticos|apuestas de fútbol pronósticos|apuestas de futbol
seguras|apuestas de futbol seguras para hoy|apuestas de futbol sin dinero|apuestas de galgos|apuestas de
galgos como ganar|apuestas de galgos en directo|apuestas de galgos online|apuestas de galgos trucos|apuestas de golf|apuestas
de hockey|apuestas de hockey sobre hielo|apuestas de hoy|apuestas de
hoy seguras|apuestas de juego|apuestas de juegos|apuestas de juegos deportivos|apuestas de juegos
online|apuestas de la champions league|apuestas de la copa américa|apuestas de la eurocopa|apuestas de la europa
league|apuestas de la liga|apuestas de la liga bbva|apuestas
de la liga española|apuestas de la nba|apuestas de la nfl|apuestas de la ufc|apuestas
de mlb|apuestas de nba|apuestas de nba para
hoy|apuestas de partidos|apuestas de partidos de futbol|apuestas de peleas ufc|apuestas
de perros en vivo|apuestas de perros virtuales|apuestas de peru|apuestas
de sistema|apuestas de sistema como funciona|apuestas de sistema explicacion|apuestas
de sistema explicación|apuestas de tenis|apuestas de tenis de mesa|apuestas de tenis en directo|apuestas de tenis hoy|apuestas de tenis para hoy|apuestas de tenis pronosticos|apuestas de tenis seguras|apuestas de todo tipo|apuestas de ufc|apuestas de ufc hoy|apuestas del
boxeo|apuestas del clasico|apuestas del clasico real madrid barca|apuestas del dia|apuestas del día|apuestas del
dia de hoy|apuestas del dia deportivas|apuestas del dia futbol|apuestas
del mundial|apuestas del partido de hoy|apuestas del real
madrid|apuestas del rey|apuestas del sistema|apuestas
deporte|apuestas deportes|apuestas deportiva|apuestas deportivas|apuestas
deportivas 1 euro|apuestas deportivas 10 euros gratis|apuestas deportivas 100 seguras|apuestas deportivas
1×2|apuestas deportivas android|apuestas deportivas app|apuestas deportivas apps|apuestas deportivas argentina|apuestas
deportivas argentina futbol|apuestas deportivas argentina legal|apuestas deportivas atletico de madrid|apuestas deportivas baloncesto|apuestas deportivas barca madrid|apuestas deportivas barcelona|apuestas deportivas
beisbol|apuestas deportivas bono|apuestas deportivas bono bienvenida|apuestas deportivas bono de bienvenida|apuestas deportivas bono sin deposito|apuestas deportivas bonos
de bienvenida|apuestas deportivas boxeo|apuestas deportivas caballos|apuestas deportivas calculadora|apuestas deportivas campeon liga|apuestas deportivas casino|apuestas deportivas
casino barcelona|apuestas deportivas casino
online|apuestas deportivas cerca de mi|apuestas deportivas champions league|apuestas deportivas chile|apuestas deportivas ciclismo|apuestas deportivas
colombia|apuestas deportivas com|apuestas deportivas com foro|apuestas
deportivas com pronosticos|apuestas deportivas combinadas|apuestas
deportivas combinadas para hoy|apuestas deportivas como se juega|apuestas
deportivas comparador|apuestas deportivas con bono gratis|apuestas deportivas con bonos gratis|apuestas deportivas con dinero ficticio|apuestas deportivas con paypal|apuestas deportivas con puntos virtuales|apuestas deportivas consejos|apuestas deportivas consejos para
ganar|apuestas deportivas copa america|apuestas deportivas
copa del rey|apuestas deportivas copa libertadores|apuestas deportivas copa mundial|apuestas deportivas corners|apuestas deportivas cual es la mejor|apuestas
deportivas cuotas altas|apuestas deportivas de baloncesto|apuestas
deportivas de boxeo|apuestas deportivas de colombia|apuestas deportivas de futbol|apuestas deportivas de nba|apuestas deportivas de nhl|apuestas
deportivas de peru|apuestas deportivas de tenis|apuestas
deportivas del dia|apuestas deportivas dinero ficticio|apuestas deportivas directo|apuestas deportivas doble oportunidad|apuestas deportivas
en argentina|apuestas deportivas en chile|apuestas deportivas en colombia|apuestas deportivas en directo|apuestas deportivas en españa|apuestas deportivas en español|apuestas deportivas en linea|apuestas deportivas en línea|apuestas deportivas
en peru|apuestas deportivas en perú|apuestas
deportivas en sevilla|apuestas deportivas en uruguay|apuestas deportivas en vivo|apuestas deportivas es|apuestas deportivas es pronosticos|apuestas deportivas
españa|apuestas deportivas españolas|apuestas deportivas esports|apuestas deportivas
estadisticas|apuestas deportivas estrategias|apuestas deportivas estrategias seguras|apuestas deportivas eurocopa|apuestas deportivas europa league|apuestas deportivas f1|apuestas deportivas
faciles de ganar|apuestas deportivas formula 1|apuestas deportivas foro|apuestas deportivas foro futbol|apuestas deportivas foro tenis|apuestas deportivas francia argentina|apuestas deportivas futbol|apuestas deportivas fútbol|apuestas deportivas futbol argentino|apuestas deportivas futbol colombia|apuestas deportivas futbol español|apuestas deportivas gana|apuestas deportivas ganadas|apuestas deportivas ganar dinero seguro|apuestas deportivas gane|apuestas deportivas
golf|apuestas deportivas gratis|apuestas deportivas gratis con premios|apuestas deportivas gratis hoy|apuestas deportivas gratis sin deposito|apuestas deportivas handicap|apuestas
deportivas handicap asiatico|apuestas deportivas hoy|apuestas deportivas impuestos|apuestas deportivas interior argentina|apuestas deportivas juegos olimpicos|apuestas deportivas la
liga|apuestas deportivas legales|apuestas deportivas legales en colombia|apuestas deportivas libres de impuestos|apuestas deportivas licencia
españa|apuestas deportivas liga española|apuestas deportivas
listado|apuestas deportivas listado clasico|apuestas deportivas madrid|apuestas
deportivas mas seguras|apuestas deportivas mejor pagadas|apuestas
deportivas mejores|apuestas deportivas mejores app|apuestas deportivas mejores
casas|apuestas deportivas mejores cuotas|apuestas deportivas
mejores paginas|apuestas deportivas mexico|apuestas deportivas
méxico|apuestas deportivas mlb|apuestas deportivas mlb
hoy|apuestas deportivas multiples|apuestas deportivas mundial|apuestas deportivas murcia|apuestas deportivas
nba|apuestas deportivas nba hoy|apuestas deportivas nfl|apuestas deportivas
nhl|apuestas deportivas nuevas|apuestas deportivas ofertas|apuestas deportivas online|apuestas deportivas online argentina|apuestas deportivas online chile|apuestas deportivas
online colombia|apuestas deportivas online en colombia|apuestas deportivas online
españa|apuestas deportivas online mexico|apuestas deportivas online paypal|apuestas
deportivas online peru|apuestas deportivas online por internet|apuestas deportivas pago paypal|apuestas deportivas para ganar dinero|apuestas deportivas para
hoy|apuestas deportivas para hoy pronosticos|apuestas deportivas partido suspendido|apuestas deportivas partidos de hoy|apuestas deportivas
paypal|apuestas deportivas peru|apuestas deportivas perú|apuestas deportivas peru vs ecuador|apuestas deportivas predicciones|apuestas deportivas promociones|apuestas deportivas
pronostico|apuestas deportivas pronóstico|apuestas deportivas pronostico hoy|apuestas deportivas pronosticos|apuestas deportivas pronósticos|apuestas deportivas pronosticos expertos|apuestas deportivas pronosticos
gratis|apuestas deportivas pronosticos nba|apuestas deportivas pronosticos tenis|apuestas deportivas
que aceptan paypal|apuestas deportivas real madrid|apuestas
deportivas regalo bienvenida|apuestas deportivas resultado exacto|apuestas deportivas resultados|apuestas deportivas rugby|apuestas deportivas
seguras|apuestas deportivas seguras foro|apuestas deportivas
seguras hoy|apuestas deportivas seguras para hoy|apuestas deportivas seguras telegram|apuestas deportivas sevilla|apuestas deportivas simulador eurocopa|apuestas
deportivas sin deposito|apuestas deportivas sin deposito inicial|apuestas deportivas sin dinero|apuestas deportivas sin dinero real|apuestas deportivas sin registro|apuestas deportivas stake|apuestas deportivas
stake 10|apuestas deportivas telegram españa|apuestas deportivas tenis|apuestas deportivas tenis de mesa|apuestas
deportivas tenis foro|apuestas deportivas tenis hoy|apuestas deportivas tips|apuestas deportivas tipster|apuestas deportivas ufc|apuestas deportivas uruguay|apuestas deportivas valencia|apuestas deportivas valencia barcelona|apuestas deportivas venezuela|apuestas deportivas virtuales|apuestas
deportivas y casino|apuestas deportivas y casino online|apuestas deportivas.com|apuestas deportivas.com foro|apuestas deportivas.es|apuestas deportivos pronosticos|apuestas deposito minimo 1
euro|apuestas descenso a segunda|apuestas descenso a segunda b|apuestas descenso la liga|apuestas descenso primera division|apuestas descenso segunda|apuestas dia|apuestas diarias seguras|apuestas dinero|apuestas dinero ficticio|apuestas dinero
real|apuestas dinero virtual|apuestas directas|apuestas
directo|apuestas directo futbol|apuestas division de honor juvenil|apuestas dnb|apuestas
doble oportunidad|apuestas doble resultado|apuestas dobles|apuestas dobles y triples|apuestas
dortmund barcelona|apuestas draft nba|apuestas draft nfl|apuestas ecuador
vs argentina|apuestas ecuador vs venezuela|apuestas egipto uruguay|apuestas el clasico|apuestas
elecciones venezuela|apuestas empate|apuestas en baloncesto|apuestas
en barcelona|apuestas en beisbol|apuestas en boxeo|apuestas en caballos|apuestas en carreras de
caballos|apuestas en casino|apuestas en casino online|apuestas en casinos|apuestas en casinos online|apuestas en chile|apuestas en ciclismo|apuestas
en colombia|apuestas en colombia de futbol|apuestas en directo|apuestas en directo futbol|apuestas en directo pronosticos|apuestas en el futbol|apuestas
en el tenis|apuestas en españa|apuestas en esports|apuestas en eventos
deportivos virtuales|apuestas en golf|apuestas en juegos|apuestas en la champions league|apuestas en la eurocopa|apuestas en la liga|apuestas en la nba|apuestas
en la nfl|apuestas en las vegas mlb|apuestas en las vegas nfl|apuestas en linea|apuestas en línea|apuestas en linea argentina|apuestas en linea boxeo|apuestas en linea
chile|apuestas en linea colombia|apuestas en línea de fútbol|apuestas en linea deportivas|apuestas en linea españa|apuestas en linea estados
unidos|apuestas en linea futbol|apuestas en linea mexico|apuestas en línea
méxico|apuestas en linea mundial|apuestas en linea peru|apuestas en linea usa|apuestas en los esports|apuestas en madrid|apuestas en méxico|apuestas en mexico online|apuestas en nba|apuestas en partidos de futbol|apuestas en partidos de futbol en vivo|apuestas en partidos de tenis en directo|apuestas en perú|apuestas en sevilla|apuestas
en sistema|apuestas en stake|apuestas en tenis|apuestas en tenis de mesa|apuestas
en valencia|apuestas en vivo|apuestas en vivo argentina|apuestas en vivo casino|apuestas en vivo futbol|apuestas en vivo fútbol|apuestas en vivo nba|apuestas en vivo peru|apuestas en vivo tenis|apuestas en vivo ufc|apuestas equipo mbappe|apuestas
equipos de futbol|apuestas españa|apuestas españa alemania|apuestas españa alemania eurocopa|apuestas españa
croacia|apuestas españa eurocopa|apuestas españa francia|apuestas
españa francia eurocopa|apuestas españa gana el mundial|apuestas españa gana eurocopa|apuestas
españa gana mundial|apuestas españa georgia|apuestas españa holanda|apuestas españa inglaterra|apuestas españa
inglaterra cuotas|apuestas españa inglaterra eurocopa|apuestas españa italia|apuestas españa mundial|apuestas españa
paises bajos|apuestas español|apuestas español oviedo|apuestas espanyol barcelona|apuestas espanyol betis|apuestas espanyol villarreal|apuestas esport|apuestas esports|apuestas esports colombia|apuestas
esports españa|apuestas esports fifa|apuestas esports gratis|apuestas esports lol|apuestas esports peru|apuestas esports
valorant|apuestas estadisticas|apuestas estrategias|apuestas euro|apuestas euro
copa|apuestas eurocopa|apuestas eurocopa campeon|apuestas eurocopa españa|apuestas eurocopa
favoritos|apuestas eurocopa femenina|apuestas eurocopa final|apuestas eurocopa ganador|apuestas eurocopa hoy|apuestas eurocopa
sub 21|apuestas euroliga baloncesto|apuestas euroliga
pronosticos|apuestas europa league|apuestas europa league hoy|apuestas europa league pronosticos|apuestas europa league pronósticos|apuestas euros|apuestas f1 abu dhabi|apuestas
f1 bahrein|apuestas f1 canada|apuestas f1 china|apuestas f1 cuotas|apuestas f1 hoy|apuestas f1 las vegas|apuestas f1 miami|apuestas f1 monaco|apuestas faciles de
ganar|apuestas fáciles de ganar|apuestas faciles para ganar|apuestas favoritas|apuestas
favorito champions|apuestas favoritos champions|apuestas favoritos eurocopa|apuestas favoritos mundial|apuestas fc barcelona|apuestas final
champions cuotas|apuestas final champions league|apuestas final champions peru|apuestas final copa|apuestas final copa america|apuestas
final copa de europa|apuestas final copa del rey|apuestas final copa europa|apuestas final copa libertadores|apuestas final copa rey|apuestas final de copa|apuestas final de
copa del rey|apuestas final del mundial|apuestas final euro|apuestas final eurocopa|apuestas final europa league|apuestas final libertadores|apuestas final mundial|apuestas final nba|apuestas final rugby|apuestas final uefa
europa league|apuestas final.mundial|apuestas finales de conferencia
nfl|apuestas finales nba|apuestas fiorentina betis|apuestas formula|apuestas formula 1|apuestas fórmula 1|apuestas
fórmula 1 pronósticos|apuestas formula uno|apuestas foro|apuestas foro nba|apuestas francia argentina|apuestas francia españa|apuestas futbol|apuestas fútbol|apuestas
futbol americano|apuestas futbol americano nfl|apuestas futbol argentina|apuestas futbol argentino|apuestas futbol champions
league|apuestas futbol chile|apuestas futbol colombia|apuestas futbol
consejos|apuestas futbol en directo|apuestas fútbol
en directo|apuestas futbol en vivo|apuestas fútbol en vivo|apuestas futbol españa|apuestas futbol español|apuestas fútbol español|apuestas futbol
eurocopa|apuestas futbol femenino|apuestas futbol foro|apuestas futbol gratis|apuestas futbol hoy|apuestas fútbol hoy|apuestas futbol juegos olimpicos|apuestas futbol mexico|apuestas futbol mundial|apuestas futbol
online|apuestas futbol para hoy|apuestas futbol peru|apuestas futbol pronosticos|apuestas futbol sala|apuestas futbol telegram|apuestas futbol virtual|apuestas galgos|apuestas galgos en directo|apuestas galgos hoy|apuestas galgos
online|apuestas galgos pronosticos|apuestas galgos trucos|apuestas gana|apuestas gana colombia|apuestas
gana resultados|apuestas ganadas|apuestas ganadas hoy|apuestas ganador champions league|apuestas ganador copa america|apuestas
ganador copa del rey|apuestas ganador copa del rey baloncesto|apuestas ganador copa libertadores|apuestas ganador de la eurocopa|apuestas ganador de
la liga|apuestas ganador del mundial|apuestas ganador eurocopa|apuestas ganador europa
league|apuestas ganador f1|apuestas ganador la liga|apuestas ganador liga española|apuestas ganador mundial|apuestas ganador mundial
baloncesto|apuestas ganador mundial f1|apuestas ganador nba|apuestas ganadores
eurocopa|apuestas ganadores mundial|apuestas ganar champions|apuestas ganar eurocopa|apuestas ganar liga|apuestas ganar mundial|apuestas ganar
nba|apuestas getafe valencia|apuestas ghana uruguay|apuestas girona|apuestas girona
athletic|apuestas girona betis|apuestas girona campeon de liga|apuestas girona campeon liga|apuestas girona gana la liga|apuestas
girona real madrid|apuestas girona real sociedad|apuestas goleador eurocopa|apuestas goleadores eurocopa|apuestas goles asiaticos|apuestas golf|apuestas golf
masters|apuestas golf pga|apuestas granada barcelona|apuestas grand
slam de tenis|apuestas gratis|apuestas gratis casino|apuestas gratis
con premios|apuestas gratis hoy|apuestas gratis para hoy|apuestas gratis por
registro|apuestas gratis puntos|apuestas gratis regalos|apuestas gratis sin deposito|apuestas gratis sin depósito|apuestas gratis sin ingreso|apuestas gratis sports|apuestas gratis y ganar premios|apuestas grupo a eurocopa|apuestas grupos eurocopa|apuestas handicap|apuestas handicap asiatico|apuestas handicap baloncesto|apuestas handicap como funciona|apuestas handicap
nba|apuestas handicap nfl|apuestas hipicas online|apuestas hípicas online|apuestas
hipicas venezuela|apuestas hockey|apuestas hockey hielo|apuestas hockey patines|apuestas hockey sobre hielo|apuestas holanda argentina|apuestas holanda vs argentina|apuestas hoy|apuestas hoy champions|apuestas hoy futbol|apuestas hoy nba|apuestas hoy pronosticos|apuestas hoy
seguras|apuestas impuestos|apuestas inglaterra paises bajos|apuestas inter barca|apuestas inter barcelona|apuestas juego|apuestas juegos|apuestas juegos en linea|apuestas juegos olimpicos|apuestas juegos olímpicos|apuestas juegos olimpicos
baloncesto|apuestas juegos online|apuestas juegos virtuales|apuestas jugador sevilla|apuestas jugadores nba|apuestas
kings league americas|apuestas la liga|apuestas la liga española|apuestas la liga
hoy|apuestas la liga santander|apuestas las vegas mlb|apuestas las vegas nba|apuestas las vegas nfl|apuestas
league of legends mundial|apuestas legal|apuestas legales|apuestas legales en colombia|apuestas legales en españa|apuestas legales en estados unidos|apuestas
legales españa|apuestas leganes betis|apuestas
libertadores|apuestas licencia|apuestas liga 1 peru|apuestas
liga argentina|apuestas liga bbva pronosticos|apuestas liga de campeones|apuestas liga de campeones de baloncesto|apuestas liga de campeones de
hockey|apuestas liga españa|apuestas liga española|apuestas liga santander pronosticos|apuestas ligas de
futbol|apuestas linea|apuestas linea de gol|apuestas liverpool barcelona|apuestas
liverpool real madrid|apuestas lol mundial|apuestas madrid|apuestas madrid arsenal|apuestas madrid atletico|apuestas
madrid atletico champions|apuestas madrid barca|apuestas madrid barça|apuestas madrid barca hoy|apuestas madrid barca supercopa|apuestas madrid barcelona|apuestas madrid
barsa|apuestas madrid bayern|apuestas madrid betis|apuestas madrid borussia|apuestas madrid campeon champions|apuestas madrid celta|apuestas madrid city|apuestas madrid dortmund|apuestas madrid gana la liga|apuestas madrid
gana liga|apuestas madrid hoy|apuestas madrid liverpool|apuestas madrid osasuna|apuestas madrid
sevilla|apuestas madrid valencia|apuestas madrid vs arsenal|apuestas madrid vs barcelona|apuestas mallorca osasuna|apuestas mallorca real sociedad|apuestas manchester athletic|apuestas
manchester city real madrid|apuestas mas faciles de ganar|apuestas mas seguras|apuestas mas seguras para hoy|apuestas masters de golf|apuestas
masters de tenis|apuestas maximo goleador eurocopa|apuestas maximo goleador
mundial|apuestas mejor jugador eurocopa|apuestas mejores casinos online|apuestas mexico|apuestas méxico|apuestas mexico polonia|apuestas méxico polonia|apuestas mlb|apuestas mlb hoy|apuestas mlb las vegas|apuestas mlb para
hoy|apuestas mlb pronosticos|apuestas mlb usa|apuestas mma ufc|apuestas momios|apuestas multiples|apuestas múltiples|apuestas multiples como funcionan|apuestas multiples el gordo|apuestas multiples futbol|apuestas
mundial|apuestas mundial 2026|apuestas mundial baloncesto|apuestas mundial balonmano|apuestas mundial brasil|apuestas mundial campeon|apuestas
mundial ciclismo|apuestas mundial clubes|apuestas mundial de baloncesto|apuestas mundial de ciclismo|apuestas mundial de clubes|apuestas mundial de futbol|apuestas mundial de fútbol|apuestas mundial de rugby|apuestas mundial f1|apuestas mundial
favoritos|apuestas mundial femenino|apuestas mundial formula 1|apuestas mundial futbol|apuestas mundial ganador|apuestas mundial lol|apuestas mundial moto gp|apuestas mundial motogp|apuestas mundial rugby|apuestas mundial sub 17|apuestas mundiales|apuestas mundialistas|apuestas mvp eurocopa|apuestas mvp nba|apuestas mvp nfl|apuestas nacionales de colombia|apuestas nba|apuestas nba
all star|apuestas nba campeon|apuestas nba consejos|apuestas nba esta noche|apuestas nba finals|apuestas
nba gratis|apuestas nba hoy|apuestas nba hoy jugadores|apuestas nba
hoy pronosticos|apuestas nba para hoy|apuestas nba playoffs|apuestas nba pronosticos|apuestas nba pronósticos|apuestas
nba pronosticos hoy|apuestas nba tipster|apuestas nfl|apuestas nfl hoy|apuestas nfl las vegas|apuestas nfl playoffs|apuestas nfl pronosticos|apuestas nfl pronósticos|apuestas nfl semana 4|apuestas nfl super bowl|apuestas
nhl|apuestas nhl pronosticos|apuestas octavos eurocopa|apuestas ofertas|apuestas online|apuestas online
argentina|apuestas online argentina legal|apuestas online bono|apuestas online bono bienvenida|apuestas
online boxeo|apuestas online caballos|apuestas online carreras de caballos|apuestas online casino|apuestas online champions league|apuestas online chile|apuestas online ciclismo|apuestas online
colombia|apuestas online comparativa|apuestas online con paypal|apuestas online
de caballos|apuestas online deportivas|apuestas online en argentina|apuestas online en peru|apuestas online espana|apuestas
online españa|apuestas online esports|apuestas online foro|apuestas online futbol|apuestas online futbol españa|apuestas online golf|apuestas online gratis|apuestas online gratis sin deposito|apuestas online juegos|apuestas online mexico|apuestas online mma|apuestas online movil|apuestas
online nba|apuestas online net|apuestas online nuevas|apuestas online opiniones|apuestas online paypal|apuestas online peru|apuestas online seguras|apuestas online sin dinero|apuestas online sin registro|apuestas online tenis|apuestas
online ufc|apuestas online uruguay|apuestas online venezuela|apuestas open britanico golf|apuestas osasuna athletic|apuestas osasuna barcelona|apuestas osasuna real madrid|apuestas osasuna sevilla|apuestas osasuna valencia|apuestas over|apuestas over 2.5|apuestas
over under|apuestas paginas|apuestas pago anticipado|apuestas paises bajos ecuador|apuestas paises bajos
inglaterra|apuestas países bajos qatar|apuestas para boxeo|apuestas para champions league|apuestas para el clasico|apuestas para el
dia de hoy|apuestas para el mundial|apuestas para el partido
de hoy|apuestas para eurocopa|apuestas para europa league|apuestas para futbol|apuestas
para ganar|apuestas para ganar dinero|apuestas para ganar dinero facil|apuestas para ganar
en la ruleta|apuestas para ganar la champions|apuestas para ganar la eurocopa|apuestas para ganar la europa league|apuestas para ganar la liga|apuestas para ganar siempre|apuestas
para hacer|apuestas para hoy|apuestas para hoy de futbol|apuestas para hoy europa league|apuestas
para hoy futbol|apuestas para juegos|apuestas para la champions league|apuestas para la copa del rey|apuestas para la eurocopa|apuestas para la
europa league|apuestas para la final de la eurocopa|apuestas para la nba hoy|apuestas para los partidos de hoy|apuestas para partidos de hoy|apuestas
para ufc|apuestas partido|apuestas partido
aplazado|apuestas partido champions|apuestas partido colombia|apuestas partido españa marruecos|apuestas partido
mundial|apuestas partido suspendido|apuestas partidos|apuestas partidos champions league|apuestas partidos
csgo|apuestas partidos de futbol|apuestas partidos de futbol hoy|apuestas partidos de
hoy|apuestas partidos eurocopa|apuestas partidos futbol|apuestas partidos hoy|apuestas partidos mundial|apuestas
paypal|apuestas peleas de boxeo|apuestas peru|apuestas perú|apuestas peru
brasil|apuestas peru chile|apuestas peru paraguay|apuestas peru uruguay|apuestas peru vs chile|apuestas peru vs colombia|apuestas pichichi eurocopa|apuestas plataforma|apuestas playoff|apuestas playoff ascenso|apuestas
playoff ascenso a primera|apuestas playoff nba|apuestas playoff segunda|apuestas
playoff segunda b|apuestas playoffs nba|apuestas playoffs nfl|apuestas polonia argentina|apuestas por argentina|apuestas por
internet mexico|apuestas por internet para ganar dinero|apuestas por
paypal|apuestas por ronda boxeo|apuestas por sistema|apuestas portugal uruguay|apuestas pre partido|apuestas predicciones|apuestas predicciones futbol|apuestas primera
division|apuestas primera division españa|apuestas promociones|apuestas pronostico|apuestas pronosticos|apuestas pronosticos deportivos|apuestas pronosticos deportivos tenis|apuestas pronosticos futbol|apuestas pronosticos gratis|apuestas pronosticos nba|apuestas pronosticos
tenis|apuestas prorroga|apuestas psg barca|apuestas psg barcelona|apuestas
puntos por tarjetas|apuestas puntos tarjetas|apuestas
que aceptan paypal|apuestas que es handicap|apuestas que
puedes hacer con tu novia|apuestas que siempre ganaras|apuestas
que significa|apuestas quien bajara a segunda|apuestas
quién bajara a segunda|apuestas quien gana el mundial|apuestas quien gana eurocopa|apuestas
quien gana la champions|apuestas quien gana la eurocopa|apuestas quien gana la liga|apuestas quien ganara
el mundial|apuestas quién ganará el mundial|apuestas quien ganara
la champions|apuestas quien ganara la eurocopa|apuestas quien ganara la liga|apuestas rayo barcelona|apuestas real
madrid|apuestas real madrid arsenal|apuestas real madrid athletic|apuestas real madrid atletico|apuestas real madrid atletico
champions|apuestas real madrid atletico de madrid|apuestas real
madrid atlético de madrid|apuestas real madrid atletico madrid|apuestas real
madrid barcelona|apuestas real madrid bayern|apuestas real madrid betis|apuestas real madrid borussia|apuestas real madrid campeon champions|apuestas
real madrid celta|apuestas real madrid champions|apuestas real madrid city|apuestas real madrid girona|apuestas real
madrid hoy|apuestas real madrid liverpool|apuestas real madrid manchester city|apuestas
real madrid osasuna|apuestas real madrid real sociedad|apuestas
real madrid valencia|apuestas real madrid villarreal|apuestas real madrid vs arsenal|apuestas real madrid vs atletico|apuestas real madrid
vs atlético|apuestas real madrid vs atletico madrid|apuestas real madrid vs barcelona|apuestas
real madrid vs betis|apuestas real madrid vs sevilla|apuestas real
madrid vs valencia|apuestas real sociedad|apuestas real sociedad athletic|apuestas real sociedad barcelona|apuestas real sociedad
betis|apuestas real sociedad psg|apuestas real sociedad real madrid|apuestas real sociedad valencia|apuestas recomendadas hoy|apuestas regalo de bienvenida|apuestas registro|apuestas resultado exacto|apuestas resultados|apuestas resultados eurocopa|apuestas retirada tenis|apuestas roma barcelona|apuestas roma sevilla|apuestas rugby|apuestas rugby mundial|apuestas rugby world cup|apuestas ruleta
seguras|apuestas segunda|apuestas segunda b|apuestas segunda division|apuestas segunda
división|apuestas segunda division b|apuestas segunda division españa|apuestas seguras|apuestas
seguras baloncesto|apuestas seguras calculadora|apuestas
seguras en la ruleta|apuestas seguras eurocopa|apuestas seguras foro|apuestas seguras futbol|apuestas seguras futbol hoy|apuestas seguras gratis|apuestas seguras hoy|apuestas seguras hoy futbol|apuestas seguras nba|apuestas seguras nba hoy|apuestas seguras para este fin de semana|apuestas seguras para ganar dinero|apuestas
seguras para hoy|apuestas seguras para hoy fútbol|apuestas seguras para
hoy pronósticos|apuestas seguras para mañana|apuestas seguras ruleta|apuestas seguras telegram|apuestas seguras tenis|apuestas semifinales eurocopa|apuestas senegal
paises bajos|apuestas sevilla|apuestas sevilla athletic|apuestas
sevilla atletico de madrid|apuestas sevilla barcelona|apuestas sevilla betis|apuestas sevilla
campeon liga|apuestas sevilla celta|apuestas sevilla gana la liga|apuestas sevilla girona|apuestas sevilla
inter|apuestas sevilla jugador|apuestas sevilla juventus|apuestas sevilla leganes|apuestas sevilla madrid|apuestas sevilla manchester
united|apuestas sevilla osasuna|apuestas sevilla
real madrid|apuestas sevilla real sociedad|apuestas sevilla roma|apuestas sevilla valencia|apuestas significa|apuestas simples ejemplos|apuestas
simples o combinadas|apuestas sin deposito|apuestas
sin deposito inicial|apuestas sin deposito minimo|apuestas sin dinero|apuestas
sin dinero real|apuestas sin empate|apuestas sin empate que significa|apuestas sin ingreso minimo|apuestas
sin registro|apuestas sistema|apuestas sistema calculadora|apuestas sistema como funciona|apuestas sistema trixie|apuestas
sociedad|apuestas sorteo copa del rey|apuestas stake|apuestas stake 10|apuestas stake 10 hoy|apuestas super
bowl favorito|apuestas super rugby|apuestas supercopa españa|apuestas superliga argentina|apuestas tarjeta
roja|apuestas tarjetas|apuestas tarjetas amarillas|apuestas tenis|apuestas tenis atp|apuestas tenis consejos|apuestas tenis copa davis|apuestas tenis de mesa|apuestas tenis de mesa pronosticos|apuestas tenis en vivo|apuestas tenis femenino|apuestas tenis hoy|apuestas tenis itf|apuestas tenis
pronosticos|apuestas tenis pronósticos|apuestas tenis retirada|apuestas tenis roland garros|apuestas tenis seguras|apuestas tenis wimbledon|apuestas tenis wta|apuestas tercera division|apuestas tercera division españa|apuestas tipos|apuestas
tips|apuestas tipster|apuestas tipster para hoy|apuestas topuria holloway cuotas|apuestas torneos de golf|apuestas torneos de tenis|apuestas trucos|apuestas
uefa champions league|apuestas uefa europa league|apuestas ufc|apuestas ufc chile|apuestas
ufc como funciona|apuestas ufc hoy|apuestas ufc ilia topuria|apuestas ufc online|apuestas ufc pronósticos|apuestas ufc
telegram|apuestas ufc topuria|apuestas under over|apuestas
unionistas villarreal|apuestas uruguay|apuestas uruguay colombia|apuestas uruguay
corea|apuestas uruguay vs colombia|apuestas us open golf|apuestas us open tenis|apuestas valencia|apuestas valencia barcelona|apuestas valencia betis|apuestas valencia madrid|apuestas valencia
real madrid|apuestas valladolid barcelona|apuestas valladolid
valencia|apuestas valor app|apuestas valor en directo|apuestas
valor galgos|apuestas venezuela|apuestas venezuela argentina|apuestas venezuela bolivia|apuestas venezuela ecuador|apuestas villarreal|apuestas
villarreal athletic|apuestas villarreal barcelona|apuestas villarreal bayern|apuestas villarreal betis|apuestas villarreal liverpool|apuestas
villarreal manchester|apuestas villarreal manchester united|apuestas villarreal vs real madrid|apuestas virtuales|apuestas virtuales colombia|apuestas virtuales futbol|apuestas virtuales sin dinero|apuestas vivo|apuestas vuelta a españa|apuestas vuelta españa|apuestas william hill partidos de hoy|apuestas y casino|apuestas y casinos|apuestas
y juegos de azar|apuestas y pronosticos|apuestas y pronosticos de futbol|apuestas y pronosticos
deportivos|apuestas y resultados|apuestas-deportivas|apuestas-deportivas.es pronosticos|arbitro nba apuestas|argentina apuestas|argentina colombia apuestas|argentina croacia apuestas|argentina francia apuestas|argentina
mexico apuestas|argentina peru apuestas|argentina uruguay
apuestas|argentina vs bolivia apuestas|argentina
vs chile apuestas|argentina vs colombia apuestas|argentina vs
francia apuestas|argentina vs. colombia apuestas|asi se gana en las apuestas deportivas|asiatico apuestas|asiatico en apuestas|asiaticos
apuestas|athletic barcelona apuestas|athletic manchester united apuestas|athletic
osasuna apuestas|athletic real madrid apuestas|atletico barcelona apuestas|atletico
de madrid apuestas|atlético de madrid apuestas|atletico de madrid real madrid apuestas|atletico de madrid
vs barcelona apuestas|atletico madrid real madrid apuestas|atletico madrid
vs real madrid apuestas|atletico real madrid apuestas|atletico vs
real madrid apuestas|avisador de cuotas apuestas|bajada de cuotas
apuestas|baloncesto apuestas|barbastro barcelona apuestas|barca apuestas|barca bayern apuestas|barca inter apuestas|barca
madrid apuestas|barça madrid apuestas|barca vs atletico apuestas|barca vs madrid
apuestas|barca vs real madrid apuestas|barcelona – real madrid apuestas|barcelona apuestas|barcelona
atletico apuestas|barcelona atletico de madrid apuestas|barcelona atletico madrid apuestas|barcelona
betis apuestas|barcelona casa de apuestas|barcelona inter apuestas|barcelona psg apuestas|barcelona real madrid apuestas|barcelona real sociedad apuestas|barcelona sevilla apuestas|barcelona valencia apuestas|barcelona vs
athletic bilbao apuestas|barcelona vs atlético madrid apuestas|barcelona vs betis apuestas|barcelona vs celta de vigo apuestas|barcelona vs espanyol apuestas|barcelona vs girona apuestas|barcelona vs madrid apuestas|barcelona vs real madrid apuestas|barcelona vs real sociedad apuestas|barcelona vs sevilla apuestas|barcelona vs
villarreal apuestas|base de datos cuotas apuestas deportivas|bayern real madrid apuestas|beisbol apuestas|best america apuestas|bet apuestas chile|bet apuestas en vivo|betis
– chelsea apuestas|betis apuestas|betis barcelona apuestas|betis chelsea apuestas|betis madrid apuestas|betis sevilla apuestas|betsson tu sitio de apuestas online|blog apuestas baloncesto|blog apuestas ciclismo|blog apuestas nba|blog
apuestas tenis|blog de apuestas de tenis|bono apuestas|bono apuestas deportivas|bono apuestas
deportivas sin deposito|bono apuestas gratis|bono apuestas gratis sin deposito|bono apuestas sin deposito|bono bienvenida apuestas|bono bienvenida apuestas deportivas|bono bienvenida apuestas españa|bono bienvenida apuestas sin deposito|bono bienvenida apuestas
sin depósito|bono bienvenida casa apuestas|bono bienvenida casa de apuestas|bono bienvenida
marca apuestas|bono casa apuestas|bono casa de apuestas|bono casa de apuestas
sin ingreso|bono casas de apuestas|bono de apuestas|bono de apuestas
gratis sin deposito|bono de bienvenida apuestas|bono de bienvenida apuestas deportivas|bono de bienvenida
casa de apuestas|bono de bienvenida casas de apuestas|bono de casas de apuestas|bono de registro apuestas|bono de
registro apuestas deportivas|bono de registro casa
de apuestas|bono gratis apuestas|bono marca apuestas|bono
por registro apuestas|bono por registro apuestas deportivas|bono
por registro casa de apuestas|bono registro apuestas|bono sin deposito
apuestas|bono sin depósito apuestas|bono sin deposito apuestas deportivas|bono sin depósito apuestas
deportivas|bono sin deposito casa de apuestas|bono
sin deposito marca apuestas|bono sin ingreso apuestas|bono sin ingreso apuestas deportivas|bonos apuestas|bonos apuestas
colombia|bonos apuestas deportivas|bonos apuestas deportivas sin deposito|bonos apuestas gratis|bonos apuestas
sin deposito|bonos apuestas sin depósito|bonos bienvenida
apuestas|bonos bienvenida casas apuestas|bonos bienvenida casas de apuestas|bonos casa de
apuestas|bonos casas apuestas|bonos casas de apuestas|bonos casas de apuestas colombia|bonos casas de apuestas deportivas|bonos casas de
apuestas españa|bonos casas de apuestas nuevas|bonos casas de apuestas sin deposito|bonos casas de apuestas sin depósito|bonos de apuestas|bonos de apuestas
deportivas|bonos de apuestas gratis|bonos de apuestas sin deposito|bonos
de bienvenida apuestas|bonos de bienvenida apuestas deportivas|bonos de bienvenida casa
de apuestas|bonos de bienvenida casas de apuestas|bonos
de bienvenida de casas de apuestas|bonos de bienvenida
en casas de apuestas|bonos de casas de apuestas|bonos de casas de apuestas sin deposito|bonos en casa de apuestas|bonos en casas de apuestas sin deposito|bonos gratis apuestas|bonos gratis apuestas deportivas|bonos gratis casas de apuestas|bonos gratis sin deposito apuestas|bonos paginas
de apuestas|bonos registro casas de apuestas|bonos sin deposito apuestas|bonos sin depósito apuestas|bonos sin deposito apuestas deportivas|bonos sin deposito casas de apuestas|bot de
apuestas deportivas gratis|boxeo apuestas|brasil colombia apuestas|brasil
peru apuestas|brasil vs colombia apuestas|buenas apuestas para hoy|buscador cuotas apuestas|buscador de
apuestas seguras|buscador de cuotas apuestas|buscador
de cuotas de apuestas|buscar apuestas seguras|caballos
apuestas|calculador de apuestas|calculador de cuotas apuestas|calculadora
apuestas|calculadora apuestas combinadas|calculadora
apuestas de sistema|calculadora apuestas deportivas|calculadora apuestas deportivas seguras|calculadora apuestas
multiples|calculadora apuestas segura|calculadora apuestas seguras|calculadora apuestas sistema|calculadora apuestas yankee|calculadora arbitraje apuestas|calculadora cubrir apuestas|calculadora cuotas apuestas|calculadora de apuestas|calculadora de apuestas combinadas|calculadora de apuestas de futbol|calculadora de apuestas de sistema|calculadora de apuestas deportivas|calculadora de apuestas multiples|calculadora de apuestas seguras|calculadora de
apuestas sistema|calculadora de apuestas surebets|calculadora de
arbitraje apuestas|calculadora de cuotas apuestas|calculadora de cuotas de apuestas|calculadora para
apuestas deportivas|calculadora poisson apuestas|calculadora poisson apuestas deportivas|calculadora poisson para apuestas|calculadora scalping apuestas deportivas|calculadora sistema apuestas|calculadora stake apuestas|calculadora trading apuestas|calcular apuestas|calcular apuestas deportivas|calcular apuestas futbol|calcular apuestas sistema|calcular cuotas apuestas|calcular cuotas apuestas combinadas|calcular cuotas apuestas deportivas|calcular cuotas de apuestas|calcular
ganancias apuestas deportivas|calcular momios apuestas|calcular probabilidad cuota apuestas|calcular stake apuestas|calcular unidades apuestas|calcular yield apuestas|calculo de
apuestas|calculo de apuestas deportivas|cambio de
cuotas apuestas|campeon champions apuestas|campeon eurocopa
apuestas|campeon liga apuestas|campeon nba apuestas|canales de apuestas gratis|carrera de caballos apuestas|carrera de caballos apuestas juego|carrera de caballos con apuestas|carrera de galgos
apuestas|carreras de caballos apuestas|carreras de caballos apuestas online|carreras de caballos con apuestas|carreras de caballos juegos de apuestas|carreras de galgos apuestas|carreras de galgos apuestas online|carreras de galgos apuestas trucos|carreras galgos apuestas|casa apuestas
argentina|casa apuestas atletico de madrid|casa apuestas barcelona|casa apuestas betis|casa apuestas bono bienvenida|casa apuestas bono gratis|casa apuestas bono sin deposito|casa
apuestas cerca de mi|casa apuestas chile|casa apuestas colombia|casa apuestas con mejores cuotas|casa apuestas deportivas|casa apuestas españa|casa apuestas española|casa apuestas eurocopa|casa apuestas futbol|casa apuestas mejores cuotas|casa apuestas mundial|casa apuestas nueva|casa apuestas nuevas|casa apuestas online|casa apuestas peru|casa apuestas valencia|casa de apuestas|casa de apuestas 10 euros gratis|casa de apuestas argentina|casa de apuestas atletico de
madrid|casa de apuestas baloncesto|casa de apuestas barcelona|casa de apuestas beisbol|casa de apuestas betis|casa de apuestas bono|casa de apuestas bono bienvenida|casa de apuestas
bono de bienvenida|casa de apuestas bono gratis|casa de apuestas
bono por registro|casa de apuestas bono sin deposito|casa de apuestas boxeo|casa de apuestas caballos|casa de apuestas carreras de caballos|casa de apuestas cerca de mi|casa de apuestas cerca
de mí|casa de apuestas champions league|casa de apuestas chile|casa de apuestas ciclismo|casa de
apuestas colombia|casa de apuestas con bono de bienvenida|casa de apuestas con bono sin deposito|casa de apuestas con cuotas mas altas|casa de apuestas con esports|casa de apuestas con las mejores cuotas|casa de apuestas con licencia en españa|casa de apuestas con mejores cuotas|casa de
apuestas con pago anticipado|casa de apuestas con paypal|casa de apuestas copa america|casa de apuestas de caballos|casa de apuestas de
colombia|casa de apuestas de españa|casa de apuestas de futbol|casa de apuestas de fútbol|casa de apuestas de futbol peru|casa de apuestas de
peru|casa de apuestas del madrid|casa de apuestas del real madrid|casa de apuestas deportivas|casa de apuestas
deportivas cerca de mi|casa de apuestas deportivas en argentina|casa de apuestas deportivas en chile|casa de apuestas deportivas en colombia|casa de apuestas
deportivas en españa|casa de apuestas deportivas
en madrid|casa de apuestas deportivas españa|casa de apuestas deportivas españolas|casa de apuestas deportivas madrid|casa de apuestas deportivas mexico|casa de apuestas
deportivas online|casa de apuestas deportivas peru|casa
de apuestas deposito 5 euros|casa de apuestas deposito minimo|casa
de apuestas deposito minimo 1 euro|casa de apuestas depósito mínimo 1 euro|casa de apuestas en españa|casa de apuestas
en linea|casa de apuestas en madrid|casa de apuestas en perú|casa de apuestas en vivo|casa de apuestas españa|casa de
apuestas españa inglaterra|casa de apuestas española|casa de
apuestas españolas|casa de apuestas esports|casa de apuestas eurocopa|casa de apuestas europa league|casa de apuestas f1|casa de apuestas formula 1|casa de apuestas futbol|casa de apuestas ingreso minimo|casa de apuestas ingreso minimo 1 euro|casa de
apuestas ingreso mínimo 1 euro|casa de apuestas legales|casa de
apuestas legales en colombia|casa de apuestas legales
en españa|casa de apuestas libertadores|casa de apuestas liga española|casa de
apuestas madrid|casa de apuestas mas segura|casa de apuestas mejores|casa de apuestas méxico|casa
de apuestas minimo 5 euros|casa de apuestas mlb|casa de apuestas mundial|casa de apuestas nba|casa de apuestas
nfl|casa de apuestas nueva|casa de apuestas nuevas|casa de apuestas oficial del real madrid|casa de apuestas oficial real madrid|casa de apuestas
online|casa de apuestas online argentina|casa de apuestas online chile|casa de apuestas online españa|casa de apuestas online mexico|casa de apuestas online paraguay|casa de apuestas online peru|casa de apuestas online
usa|casa de apuestas online venezuela|casa de apuestas pago anticipado|casa de apuestas para boxeo|casa de apuestas para ufc|casa de apuestas peru|casa de apuestas
perú|casa de apuestas peru online|casa de apuestas por paypal|casa de apuestas promociones|casa de apuestas que regalan dinero|casa de apuestas real madrid|casa de apuestas regalo de bienvenida|casa
de apuestas sevilla|casa de apuestas sin dinero|casa
de apuestas sin ingreso minimo|casa de apuestas sin licencia en españa|casa de apuestas sin minimo de ingreso|casa de
apuestas stake|casa de apuestas tenis|casa de apuestas ufc|casa de apuestas valencia|casa de apuestas venezuela|casa
de apuestas virtuales|casa de apuestas vive la suerte|casa oficial de apuestas del real
madrid|casas apuestas asiaticas|casas apuestas bono
sin deposito|casas apuestas bonos sin deposito|casas apuestas caballos|casas apuestas chile|casas apuestas ciclismo|casas apuestas con licencia|casas apuestas con licencia en españa|casas apuestas deportivas|casas apuestas
deportivas colombia|casas apuestas deportivas españa|casas apuestas deportivas españolas|casas apuestas deportivas nuevas|casas apuestas españa|casas apuestas españolas|casas apuestas
esports|casas apuestas eurocopa|casas apuestas golf|casas apuestas ingreso minimo 5
euros|casas apuestas legales|casas apuestas legales españa|casas apuestas licencia|casas apuestas licencia españa|casas apuestas mexico|casas
apuestas mundial|casas apuestas nba|casas apuestas nuevas|casas apuestas nuevas españa|casas apuestas ofertas|casas apuestas online|casas apuestas paypal|casas apuestas peru|casas
apuestas sin licencia|casas apuestas tenis|casas asiaticas apuestas|casas
de apuestas|casas de apuestas 5 euros|casas de apuestas
app|casas de apuestas argentinas|casas de apuestas asiaticas|casas de apuestas baloncesto|casas de apuestas barcelona|casas de apuestas bono bienvenida|casas de apuestas bono de
bienvenida|casas de apuestas bono por registro|casas
de apuestas bono sin deposito|casas de apuestas bono sin ingreso|casas de apuestas bonos|casas de apuestas bonos de bienvenida|casas de apuestas bonos gratis|casas de apuestas bonos sin deposito|casas de apuestas boxeo|casas de apuestas caballos|casas de
apuestas carreras de caballos|casas de apuestas casino|casas
de apuestas casino online|casas de apuestas cerca de mi|casas
de apuestas champions league|casas de apuestas chile|casas de apuestas ciclismo|casas de apuestas colombia|casas de apuestas com|casas de apuestas
con app|casas de apuestas con apuestas gratis|casas de apuestas con bono|casas de apuestas con bono de
bienvenida|casas de apuestas con bono de registro|casas de apuestas con bono por registro|casas de apuestas con bono sin deposito|casas de apuestas con bonos|casas de
apuestas con bonos gratis|casas de apuestas con bonos sin deposito|casas de apuestas con deposito minimo|casas de apuestas con esports|casas de
apuestas con handicap asiatico|casas de apuestas con licencia|casas de apuestas con licencia
en españa|casas de apuestas con licencia españa|casas de apuestas
con licencia española|casas de apuestas con mejores cuotas|casas
de apuestas con pago anticipado|casas de apuestas con paypal|casas de apuestas con paypal en perú|casas de apuestas con promociones|casas de apuestas con ruleta
en vivo|casas de apuestas copa del rey|casas de apuestas de caballos|casas
de apuestas de españa|casas de apuestas de futbol|casas de
apuestas de fútbol|casas de apuestas de peru|casas de apuestas deportivas|casas de apuestas deportivas asiaticas|casas de apuestas
deportivas colombia|casas de apuestas deportivas comparativa|casas de apuestas deportivas con paypal|casas
de apuestas deportivas en chile|casas de
apuestas deportivas en españa|casas de apuestas deportivas en linea|casas de
apuestas deportivas en madrid|casas de apuestas deportivas en mexico|casas de apuestas deportivas
en peru|casas de apuestas deportivas en sevilla|casas de apuestas deportivas en valencia|casas de apuestas deportivas españa|casas de apuestas deportivas españolas|casas de apuestas deportivas legales|casas de apuestas
deportivas madrid|casas de apuestas deportivas mexico|casas de apuestas deportivas nuevas|casas de
apuestas deportivas online|casas de apuestas deportivas peru|casas de apuestas deportivas perú|casas de
apuestas deposito minimo 1 euro|casas de apuestas depósito mínimo 1 euro|casas de
apuestas dinero gratis|casas de apuestas en argentina|casas de apuestas en barcelona|casas de
apuestas en chile|casas de apuestas en colombia|casas de apuestas en españa|casas
de apuestas en españa online|casas de apuestas en linea|casas de apuestas en madrid|casas
de apuestas en méxico|casas de apuestas en peru|casas de apuestas en perú|casas de apuestas en sevilla|casas de apuestas en uruguay|casas de apuestas en valencia|casas de apuestas en venezuela|casas de apuestas equipos de futbol|casas de apuestas españa|casas
de apuestas españa alemania|casas de apuestas españa inglaterra|casas de apuestas españa licencia|casas de apuestas españa nuevas|casas de apuestas españa online|casas de apuestas española|casas de apuestas españolas|casas de apuestas españolas con licencia|casas de apuestas españolas online|casas de apuestas esports|casas de
apuestas eurocopa|casas de apuestas eurocopa 2024|casas de apuestas europa league|casas de apuestas f1|casas de apuestas
fisicas en barcelona|casas de apuestas fisicas en españa|casas de apuestas formula 1|casas de apuestas fuera de españa|casas
de apuestas futbol|casas de apuestas fútbol|casas de apuestas futbol españa|casas de apuestas ganador eurocopa|casas de
apuestas gratis|casas de apuestas ingreso minimo|casas de apuestas ingreso minimo 1
euro|casas de apuestas ingreso minimo 5 euros|casas de apuestas inter barcelona|casas de apuestas
legales|casas de apuestas legales en colombia|casas de apuestas legales en españa|casas de apuestas legales en mexico|casas de apuestas legales
españa|casas de apuestas legales mx|casas de apuestas licencia|casas de apuestas licencia españa|casas de apuestas lista|casas de apuestas
madrid|casas de apuestas mas seguras|casas
de apuestas mejores bonos|casas de apuestas mejores cuotas|casas de
apuestas mexico|casas de apuestas méxico|casas de apuestas minimo 5 euros|casas de
apuestas mlb|casas de apuestas mundial|casas de apuestas mundial baloncesto|casas
de apuestas mundiales|casas de apuestas nba|casas de apuestas no
reguladas en españa|casas de apuestas nueva ley|casas de apuestas nuevas|casas
de apuestas nuevas en colombia|casas de
apuestas nuevas en españa|casas de apuestas nuevas españa|casas de apuestas ofertas|casas de apuestas online|casas de apuestas online argentina|casas de apuestas
online colombia|casas de apuestas online deportivas|casas de apuestas online
ecuador|casas de apuestas online en argentina|casas de apuestas online en chile|casas de apuestas
online en colombia|casas de apuestas online en españa|casas de apuestas online en mexico|casas de apuestas online españa|casas de apuestas online mas fiables|casas de apuestas online mexico|casas de apuestas online nuevas|casas de apuestas online peru|casas
de apuestas online usa|casas de apuestas online venezuela|casas de apuestas
pago paypal|casas de apuestas para ufc|casas de apuestas paypal|casas de apuestas peru
bono sin deposito|casas de apuestas presenciales en españa|casas de apuestas promociones|casas
de
После завершения инфузий врач-нарколог даёт рекомендации по питанию, водному балансу и образу жизни. При необходимости пациенту назначается курс поддерживающей терапии для закрепления эффекта.
Подробнее – круглосуточная наркологическая помощь в тольятти
Hi, i feel that i saw you visited my website thus i came to return the
favor?.I am trying to to find issues to improve my
website!I guess its ok to use some of your concepts!!
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Ознакомиться с деталями – http://kodirovanie-ot-alkogolizma-v-volgograde17.ru/kodirovanie-volgograd/
Капельница от запоя в Люберцах — быстрый и эффективный способ детоксикации. Наши специалисты приедут к вам домой и проведут процедуру, помогая снять симптомы похмелья и вывести токсины из организма.
Подробнее тут – капельница от запоя
Вывод из запоя — это не просто медицинская процедура, а системный процесс восстановления организма после длительного употребления алкоголя. В клинике «ВолгаМед Резолюция» в Волгограде пациенты получают помощь, основанную на принципах доказательной медицины и индивидуального подхода. Лечение направлено не только на устранение симптомов интоксикации, но и на стабилизацию нервной системы, восстановление водно-солевого баланса и нормализацию сна. Капельницы подбираются персонально, с учётом состояния пациента, сопутствующих заболеваний и возраста. Все процедуры проводятся анонимно и под контролем нарколога.
Разобраться лучше – вывод из запоя вызов в волгограде
Fastidious answers in return of this issue with solid arguments and explaining everything about that.
This game looks amazing! The way it blends that
old-school chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic
chicken crossing gameplay and adding real risk? I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing mechanics with genuine
stakes involved. Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless
chicken crossing feel with real consequences has me hooked.
I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible
consequences? I’ve gotta try this out!
Лечение зависимости от алкоголя на дому в Химках. Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Подробнее – вывод из запоя недорого
Вывод из запоя в Тюмени — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормального функционирования организма. Длительное употребление спиртных напитков приводит к нарушению обмена веществ, обезвоживанию, сбоям в работе печени и сердца. В таких случаях требуется профессиональная помощь врача-нарколога, который подберёт оптимальный способ дезинтоксикации и медикаментозной поддержки. Современные методики позволяют провести вывод из запоя безопасно, эффективно и без осложнений.
Подробнее – вывод из запоя цена тюмень
Ahaa, its pleasant conversation about this paragraph here at this weblog, I have read
all that, so at this time me also commenting at this place.
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Подробнее – помощь вывод из запоя в химках
Лечение запоя у женщин в Химках. Мы предлагаем индивидуальный подход к лечению женщин, учитывая все особенности организма.
Подробнее можно узнать тут – врач вывод из запоя в химках
Hello there, just became aware of your blog through Google,
and found that it’s truly informative. I am going to watch
out for brussels. I’ll appreciate if you continue this in future.
Many people will be benefited from your writing. Cheers!
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Это ещё не всё… – https://www.nwohalaw.com/2024/09/22/exploring-the-difference-between-affirmative-defenses-avoidances-and-inferential-rebuttals
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Выяснить больше – http://narcologicheskaya-klinika-saratov0.ru
Капельница от запоя в стационаре — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Получить дополнительные сведения – врач вывод из запоя в балашихе
Помощь при алкогольной интоксикации в Люберцах. Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Получить дополнительную информацию – kapelnicza-ot-zapoya lyubercy
How Brackish Water RO Technology Addresses Freshwater Shortages
This website has lots of really useful stuff on it. Thanks for informing me.
Terrific work! This is the kind of info that are supposed to be shared around the net.
Disgrace on Google for no longer positioning this post upper!
Come on over and visit my web site . Thank you =)
Hmm is anyone else encountering problems with the images on this blog loading?
I’m trying to find out if its a problem on my end or if it’s the
blog. Any feedback would be greatly appreciated.
Процесс лечения включает несколько последовательных шагов, направленных на стабилизацию состояния, детоксикацию и восстановление функций организма. Таблица ниже показывает основные этапы процедуры, применяемые врачами клиники «РеабКузбасс».
Углубиться в тему – https://vyvod-iz-zapoya-v-novokuzneczke17.ru/
Вывод из запоя в Химках — профессиональная помощь на дому. Наши опытные наркологи приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния и вывода из запоя.
Углубиться в тему – https://vyvod-iz-zapoya-himki13.ru/
Right away I am ready to do my breakfast, afterward having my breakfast coming yet again to read other news.
В клинике применяются современные медицинские технологии, которые обеспечивают стойкий результат. Используемые методики соответствуют международным стандартам и регулярно обновляются.
Изучить вопрос глубже – http://www.domen.ru
Вывод из запоя у подростков в Люберцах. Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Получить больше информации – капельница от запоя в люберцах
Капельница от запоя в Воронеже применяется для восстановления организма после длительного употребления алкоголя, устранения интоксикации и нормализации обменных процессов. Медицинская процедура проводится под контролем врача-нарколога, в клинике или на дому. Она позволяет быстро улучшить самочувствие, устранить головную боль, тремор, тошноту, обезвоживание и нарушения сна. Современные препараты действуют мягко, безопасно и без стресса для организма, обеспечивая плавный выход из запоя.
Изучить вопрос глубже – http://kapelnicza-ot-zapoya-v-voronezhe17.ru/kapelnicza-ot-zapoya-na-domu-voronezh/
Лечение запоя без госпитализации в стационаре Балашихи. Мы предлагаем лечение на дому, без необходимости госпитализации.
Получить дополнительные сведения – вывод из запоя вызов
Удобный и простой сайт с богатством полезной информации по казино.
https://pinupcasino-kazakhstan.kz/mobile-app
Потрясающе, сайт Pin Up Casino — действительно крутой.
https://pin-up-casino-slots-kz.org.kz/payments
Лечение запоя у женщин в Химках. Мы предлагаем индивидуальный подход к лечению женщин, учитывая все особенности организма.
Подробнее – вывод из запоя в стационаре в химках
Вывод из запоя у пожилых людей в Химках. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Получить дополнительную информацию – вывод из запоя капельница на дому химки
Анонимность и конфиденциальность гарантированы. Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Получить дополнительные сведения – врача капельницу от запоя в люберцах
Ниже приведена таблица с примерными этапами терапии:
Выяснить больше – вывод из запоя рязань
Hi! I realize this is somewhat off-topic however I needed to
ask. Does building a well-established website such as
yours require a large amount of work? I am completely new to blogging however I do write in my
diary daily. I’d like to start a blog so I can easily share my own experience and thoughts online.
Please let me know if you have any ideas or tips for brand new aspiring blog owners.
Thankyou!
You could certainly see your enthusiasm in the article you write.
The arena hopes for more passionate writers like you who
are not afraid to say how they believe. All the time
go after your heart.
This paragraph is genuinely a nice one it assists new the web viewers, who are wishing in favor of blogging.
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Выяснить больше – http://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkolog-novokuzneczk-na-dom/
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Это ещё не всё… – https://openkz.kz/2023/01/18/%D0%B0%D0%BA%D1%82%D1%83%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B5-%D0%BF%D1%80%D0%BE%D0%B1%D0%BB%D0%B5%D0%BC%D1%8B-%D1%81%D0%B5%D0%BB%D1%8C%D1%81%D0%BA%D0%BE%D0%B3%D0%BE-%D1%85%D0%BE%D0%B7%D1%8F%D0%B9
Лечение зависимости от алкоголя на дому в Люберцах. Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Ознакомиться с деталями – после капельницы от запоя в люберцах
Стационарное лечение запоя в Балашихе — эффективное решение для длительного запоя. Мы предлагаем индивидуальный подход и комплексную терапию для каждого пациента.
Подробнее – вывод из запоя капельница на дому
Angels Bail Bonds Costa Mesa
769 Baker Տt,
Costa Mesa, CA 92626, United States
bail bonds new braunfels
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Получить дополнительную информацию – vyvod-iz-zapoya-v-voronezhe17.ru/
Игнорирование этих симптомов может привести к тяжёлым последствиям — судорогам, галлюцинациям или алкогольному психозу.
Подробнее – вывод из запоя на дому недорого
Лечение организовано поэтапно, что помогает пациенту постепенно возвращаться к полноценной жизни. Каждый шаг направлен на укрепление результата и снижение риска рецидива.
Изучить вопрос глубже – вывод наркологическая клиника омск
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Выяснить больше – скорая вывод из запоя
Лечение зависимости от алкоголя у мужчин в Люберцах. Мы предлагаем индивидуальный подход к лечению мужчин, учитывая все особенности организма.
Получить больше информации – капельница от запоя на дому цена
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Углубиться в тему – vyzvat-kapelniczu-ot-zapoya lyubercy
You said it nicely..
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Детали по клику – http://www.anjasikkens.nl/het-oloid-project/dsc03550-2/?unapproved=123024
Every weekend i used to pay a visit this web site, as i wish for enjoyment, for the reason that this
this web site conations in fact good funny information too.
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Выяснить больше – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologiya-gorod-novokuzneczk/
Клиника «ВоронежМед Альянс» придерживается принципа прозрачной медицины: каждый шаг понятен пациенту, решения принимаются совместно, а результаты фиксируются по объективным показателям. Такой формат создаёт чувство безопасности и доверия. Среди основных принципов:
Исследовать вопрос подробнее – вывод наркологическая клиника
Профилактика рецидивов после запоя в Химках.Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Узнать больше – скорая вывод из запоя в химках
Вывод из запоя у подростков в стационаре Балашихи. Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Выяснить больше – вывод из запоя в стационаре
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Подробнее тут – частная наркологическая клиника
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Получить дополнительные сведения – врач вывод из запоя рязань
В Воронеже клиника «ВоронежМед Альянс» предлагает комплексное лечение алкогольной и наркотической зависимости. Команда врачей, психиатров, психологов и терапевтов выстраивает индивидуальный маршрут пациента, начиная с детоксикации и заканчивая реабилитацией. Главный принцип — минимальное вмешательство при максимальной эффективности. Это означает, что терапевтические меры подбираются строго по показаниям, а медикаменты применяются только после оценки состояния и лабораторных данных.
Подробнее можно узнать тут – наркологическая клиника стационар воронеж
Вывод из запоя у подростков в стационаре Балашихи. Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Получить больше информации – вывод из запоя капельница на дому балашиха
В клинике применяются современные медицинские технологии, которые обеспечивают стойкий результат. Используемые методики соответствуют международным стандартам и регулярно обновляются.
Детальнее – http://narcologicheskaya-klinika-omsk0.ru/narkologi-omska/
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Получить дополнительные сведения – вывод из запоя на дому круглосуточно в красноярске
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Хочешь знать всё? – https://schreinerei-reichl.com/sew-better-faster-advanced-industry-techniques
Процедура начинается с осмотра пациента и оценки степени интоксикации. Врач измеряет давление, пульс, уровень насыщения крови кислородом, определяет наличие сопутствующих заболеваний. После диагностики назначается капельница, состав которой подбирается индивидуально. Процедура направлена на очищение организма, восстановление водно-солевого баланса и снятие симптомов похмелья.
Разобраться лучше – скорая вывод из запоя
Наркологическая клиника в Новокузнецке предоставляет профессиональную помощь людям, столкнувшимся с зависимостью от алкоголя, наркотиков и психоактивных веществ. Лечение проводится под наблюдением опытных специалистов с применением современных медицинских методик. Основная цель работы клиники — не только устранить физическую зависимость, но и восстановить психологическое равновесие пациента, вернуть мотивацию и способность жить без употребления веществ.
Узнать больше – http://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkolog-v-gorode-novokuzneczke/
Стационарное лечение запоя в Балашихе — эффективное решение для длительного запоя. Мы предлагаем индивидуальный подход и комплексную терапию для каждого пациента.
Получить дополнительные сведения – вывод из запоя на дому цена
Длительность вывода из запоя во многом зависит от тяжести состояния, общего здоровья и продолжительности самого запоя. Если пациент обратился на ранней стадии, зачастую хватает 1-2 капельниц и короткого курса поддержки. Но при запое более пяти-семи дней, когда имеется острая интоксикация, требуется более продолжительная терапия и круглосуточное наблюдение.
Подробнее можно узнать тут – https://narko-reabcentr.ru/kruglosutochnyj-vyvod-iz-zapoya-v-moskve
Детоксикация в клинике «Центр Трезвости ВоронМед» проводится по принципу минимального вмешательства при максимальной эффективности. Основная задача — очистить кровь от токсинов и стабилизировать внутреннюю среду организма без нагрузки на сердце и почки. Все препараты вводятся медленно, под контролем медицинского персонала, а состав подбирается индивидуально после оценки анализов и состояния пациента.
Получить дополнительную информацию – вывод из запоя капельница на дому в воронеже
Вывод из запоя у пожилых людей в Химках. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Узнать больше – вывод из запоя с выездом
You have made your position very effectively.!
Вывод из запоя у пожилых людей в стационаре Балашихи. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Подробнее – вывод из запоя клиника балашиха
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Ознакомиться с деталями – наркологическая клиника лечение алкоголизма
Процесс детоксикации состоит из нескольких последовательных шагов, направленных на безопасное очищение организма. Ниже представлена таблица с описанием этапов, которые применяются в клинике «Трезвая Линия Волгоград».
Подробнее можно узнать тут – https://vyvod-iz-zapoia-v-volgograde17.ru/vyvod-iz-zapoya-narkolog-na-dom-volgograd
Лечение хронического алкоголизма в Люберцах. Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Разобраться лучше – поставить капельницу от запоя люберцы
Are the issues really as complex as they seem?
This is a topic that’s close to my heart… Many thanks!
Exactly where are your contact details though?
It is not my first time to visit this site, i am visiting this site dailly and take good facts
from here every day.
Не всегда человек способен прекратить употребление алкоголя без медицинского вмешательства. Чем дольше длится запой, тем выше риск осложнений. Обратиться к специалисту следует при появлении следующих признаков:
Детальнее – вывод из запоя на дому цена в тюмени
Лечение организовано поэтапно. Такой подход обеспечивает постепенное восстановление функций организма и исключает риск осложнений. Каждый этап терапии направлен на устранение конкретных нарушений, вызванных интоксикацией.
Получить дополнительную информацию – нарколог вывод из запоя красноярск
บทความนี้ อ่านแล้วเพลินและได้สาระ ครับ
ผม เคยติดตามเรื่องนี้จากหลายแหล่ง ข้อมูลเพิ่มเติม
สามารถอ่านได้ที่
Fred
เหมาะกับคนที่สนใจเรื่องนี้
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ ข้อมูลที่น่าอ่าน นี้
จะคอยติดตามเนื้อหาที่คุณแชร์
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Разобраться лучше – вывод из запоя круглосуточно рязань
Asking questions are really good thing if you are not understanding
anything fully, however this article provides fastidious understanding even.
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Исследовать вопрос подробнее – кодирование от алкоголизма волгоград
I imagine so. Very good stuff, I agree totally.
Hmm is anyone else encountering problems with the pictures on this blog loading?
I’m trying to figure out if its a problem on my end or if it’s the blog.
Any responses would be greatly appreciated.
Одним из самых востребованных направлений работы клиники является проведение детоксикации и вывод из запоя. Эти процедуры направлены на очищение организма от алкоголя и продуктов его распада, нормализацию работы печени и нервной системы. Лечение проводится с использованием сертифицированных препаратов и под контролем врача-нарколога.
Ознакомиться с деталями – http://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologiya-gorod-novokuzneczk/https://narkologicheskaya-clinica-v-novokuzneczke17.ru
I loved as much as you will receive carried out right here.
The sketch is attractive, your authored material stylish.
nonetheless, you command get got an nervousness over that
you wish be delivering the following. unwell unquestionably come
further formerly again since exactly the same nearly very often inside case you shield this increase.
Every weekend i used to pay a visit this website, for the
reason that i wish for enjoyment, as this this website conations really fastidious
funny stuff too.
Лечение запоя без госпитализации в Москве от клиники «Частный Медик 24». Мы предлагаем лечение на дому, без необходимости госпитализации.
Подробнее тут – наркологическая помощь
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Получить дополнительные сведения – https://narcologicheskaya-klinika-omsk0.ru
Для тех, кто предпочитает лечение в условиях стационара, предусмотрены комфортные палаты, медицинский контроль 24/7 и возможность консультаций с психотерапевтом. Врачи клиники применяют комплексные методы, направленные не только на снятие симптомов, но и на устранение причин зависимости.
Изучить вопрос глубже – круглосуточная наркологическая помощь
Very sleek and professionally built site Chicken Road!
https://chickenroadbonus.pro
You expressed this really well.
Услуга вывода из запоя в клинике сочетает профессионализм врачей, медицинскую точность и заботу. При этом обеспечивается полная конфиденциальность: данные пациентов не передаются в сторонние инстанции. Круглосуточный режим работы позволяет вызвать врача даже ночью — специалисты прибывают в течение 40–60 минут после обращения.
Подробнее – вывод из запоя вызов на дом в волгограде
Welcome!
https://playel.vn/track/11200-little-mix-wings/
I stumbled upon this song by chance, and now I’ve been listening for several days straight. I’m curious, am I the only one hooked, or are there others?
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Почему это важно? – https://vistoweekly.com/mary-lee-harvey
При появлении таких симптомов важно не откладывать вызов врача. Самолечение, особенно с использованием неизвестных препаратов, может привести к тяжёлым последствиям, включая судороги и инсульт. Врачи клиники «ВолгаМед Резолюция» приезжают на дом с необходимыми средствами для оказания экстренной помощи и стабилизации состояния уже на месте.
Подробнее можно узнать тут – http://vyvod-iz-zapoya-v-volgograde17.ru
Благодаря этому подходу пациент выходит из состояния запоя без стресса и с минимальной нагрузкой на организм, что ускоряет процесс восстановления.
Разобраться лучше – вывод из запоя на дому недорого
Анонимность и конфиденциальность гарантированы в клинике «Частный Медик 24». Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Изучить вопрос глубже – наркологическая помощь на дому
Hey there, You have done a great job. I will certainly digg it and
personally suggest to my friends. I am sure they’ll
be benefited from this website.
Appreciating the persistence you put into your blog and in depth information you offer.
It’s nice to come across a blog every once in a while that isn’t
the same old rehashed material. Wonderful read!
I’ve bookmarked your site and I’m including
your RSS feeds to my Google account.
Ниже приведена таблица, отражающая примерную динамику состояния пациента после постановки капельницы:
Узнать больше – https://kapelnicza-ot-zapoya-v-voronezhe17.ru/kapelnicza-ot-alkogolya-voronezh/
Процесс лечения включает несколько последовательных шагов, направленных на стабилизацию состояния, детоксикацию и восстановление функций организма. Таблица ниже показывает основные этапы процедуры, применяемые врачами клиники «РеабКузбасс».
Получить больше информации – вывод из запоя на дому в новокузнецке
Excellent article!! I am an avid reader of your website:D keep on posting that good content. and I’ll be a regular visitor for a very long time!!
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Получить больше информации – https://vivod-iz-zapoya-v-volgograde17.ru/anonimnaya-narkologiya-vyvod-iz-zapoya-volgograd
Капельница от запоя — доступная цена в стационаре Балашихи. Стоимость процедуры начинается от 3?500??, и вы всегда будете заранее информированы о стоимости услуг.
Получить дополнительную информацию – вывод из запоя капельница балашиха
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Смотрите также… – https://dvp.lt/projektas-homo-creator-lt
Нарколог на дом в Уфе — это услуга, которая позволяет получить квалифицированную медицинскую помощь при алкогольной или наркотической интоксикации без необходимости госпитализации. Такой формат особенно востребован при запойных состояниях, когда пациент не может самостоятельно посетить клинику. Врач приезжает по вызову в течение короткого времени, проводит обследование, устанавливает капельницу и обеспечивает безопасный вывод из состояния опьянения. Все процедуры выполняются анонимно, с соблюдением медицинской этики и конфиденциальности.
Получить дополнительные сведения – нарколог на дом круглосуточно цены
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Узнать больше – вывод из запоя в стационаре химки
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Ознакомиться с деталями – http://narcologicheskaya-klinika-saratov0.ru
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Посмотреть всё – https://vistoweekly.com/finn-william-leeves-coben
WOW just what I was searching for. Came here
by searching for биф казино скачать
Sometimes, the sheer magnitude of the information seems overwhelming.
Кодирование от алкоголизма в Химках. Мы предлагаем различные методы кодирования, подходящие для каждого пациента.
Подробнее можно узнать тут – вывод из запоя капельница на дому в химках
Das ist ein wichtiges Thema. Online Crowdfunding verbessert Leben von Menschen, die sich keine Behandlung finanzieren können. Eine Organisation für
Sehkraft zu helfen ist absolut edel. Danke für das Teilen dieser Mission.
Here is my web-site Vision Restoration Fund
Вывод из запоя требуется тогда, когда организм уже не способен самостоятельно справиться с последствиями алкогольной интоксикации. Длительное употребление спиртного приводит к нарушению работы внутренних органов, обезвоживанию и психическим расстройствам. Медицинская помощь помогает избежать опасных осложнений и облегчить процесс отказа от алкоголя.
Выяснить больше – анонимный вывод из запоя рязань
Капельница от запоя в Люберцах — быстрый и эффективный способ детоксикации. Наши специалисты приедут к вам домой и проведут процедуру, помогая снять симптомы похмелья и вывести токсины из организма.
Углубиться в тему – вызвать капельницу от запоя на дому
It’s enormous that you are getting ideas from this article as well as from our argument made here.
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Узнать больше – лечение в наркологической клинике волгоград
Лечение с выездом нарколога актуально, когда у пациента нет тяжёлых психических расстройств (галлюцинаций, приступов агрессии, глубокой депрессии), отсутствуют судороги и другие острые проявления. Человек остаётся в знакомой обстановке, не испытывает дискомфорта от стен больницы и лишних взглядов.
Изучить вопрос глубже – вывод из запоя цена
This paragraph is in fact a fastidious one it assists new web visitors,
who are wishing for blogging.
Реабилитация после запоя в Люберцах. Мы поможем вам восстановиться после запоя и предотвратить рецидивы.
Выяснить больше – врач на дом капельница от запоя люберцы
Капельница от запоя в Волгограде — это эффективный способ быстро восстановить организм после длительного употребления алкоголя. Процедура проводится врачом-наркологом и направлена на выведение токсинов, нормализацию обмена веществ и стабилизацию работы нервной системы. Инфузионная терапия помогает устранить головную боль, слабость, тошноту, восстановить сон и аппетит. Благодаря внутривенному введению препаратов эффект наступает уже через 20–30 минут после начала процедуры.
Подробнее тут – http://
It’s genuinely very difficult in this active life to
listen news on Television, thus I only use web for that reason, and take the most
recent information.
Ниже представлена таблица с основными препаратами, используемыми при выводе из запоя в Тюмени:
Получить больше информации – https://vyvod-iz-zapoya-v-tyumeni17.ru
В Воронеже команда «ВоронМед Профи» работает по принципу быстрой медицинской реакции — помощь оказывается независимо от времени суток и дня недели. Все выезды выполняются анонимно, без спецтранспорта и медицинской формы. Врач приезжает в гражданской одежде, что исключает ненужное внимание соседей и посторонних. В ходе осмотра специалист измеряет давление, пульс, температуру, оценивает уровень интоксикации и определяет степень обезвоживания. На основе полученных данных подбирается состав капельницы, который подаётся медленно и безопасно под контролем врача.
Углубиться в тему – http://narkolog-na-dom-v-voronezhe17.ru
Hello, i think that i saw you visited my site thus i came to “return the favor”.I’m
attempting to find things to improve my website!I
suppose its ok to use a few of your ideas!!
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Получить дополнительную информацию – вывод из запоя на дому недорого воронеж
Первым шагом при лечении зависимости является детоксикация — очищение организма от токсинов, накопившихся в результате употребления алкоголя или наркотиков. Врач подбирает состав инфузионных растворов и лекарственных препаратов индивидуально. Процедура направлена на восстановление обмена веществ, улучшение работы печени и сердца, нормализацию сна и аппетита. После завершения детоксикации пациент чувствует облегчение, снижается тревожность и повышается концентрация внимания.
Получить больше информации – наркологическая клиника
Вывод из запоя у пожилых людей в Химках. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Получить больше информации – https://vyvod-iz-zapoya-himki11.ru/
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Исследовать вопрос подробнее – https://kodirovanie-ot-alkogolizma-v-volgograde17.ru/kodirovanie-ot-alkogolya-v-volgograde
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Слушай внимательно — тут важно – https://nnequipamentos.com.br/cristal-2
Реабилитация после запоя в Люберцах. Мы поможем вам восстановиться после запоя и предотвратить рецидивы.
Детальнее – капельница от запоя московская область
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Подробнее можно узнать тут – вывод из запоя круглосуточно
Основу выездного лечения составляют капельницы, которые позволяют быстро ввести препараты в кровоток, минуя желудочно-кишечный тракт. Это обеспечивает моментальное действие и исключает раздражение слизистой. Капельницы подбираются индивидуально в зависимости от состояния пациента. Основные направления инфузионной терапии включают детоксикацию, восстановление водно-солевого баланса и поддержку работы нервной системы. Для усиления эффекта применяются витамины, антиоксиданты и препараты для защиты печени.
Получить больше информации – нарколог на дом в воронеже
Комплексное применение этих методов позволяет значительно ускорить процесс восстановления и предотвратить осложнения.
Разобраться лучше – наркологическая клиника цены новокузнецк
Вывод из запоя — это экстренная медицинская помощь, направленная на очищение организма от алкоголя, снятие симптомов интоксикации и восстановление работы внутренних органов. В клинике «Трезвая Линия Волгоград» используется комплексный подход, включающий капельницы, препараты для детоксикации и постоянный врачебный контроль. Лечение проводится анонимно, с индивидуальным подбором медикаментов и поддержкой пациента на каждом этапе восстановления. Главная цель специалистов — не просто стабилизировать состояние, а обеспечить безопасное возвращение к нормальному самочувствию и предотвратить повторные срывы.
Ознакомиться с деталями – вывод из запоя с выездом волгоград
I encountered your site after doing a search for new contesting using Google, and decided to stick around and read more of your articles. Thanks for posting, I have your site bookmarked now.
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Разобраться лучше – https://vyvod-iz-zapoya-saratov0.ru/vyvod-iz-zapoya-saratov-staczionar/
you’re actually a just right webmaster. The web site loading velocity is incredible.
It sort of feels that you are doing any unique trick.
Furthermore, The contents are masterwork. you have
done a magnificent task on this topic!
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
А что дальше? – https://www.molnetto.se/lagenhet-i-jordbro/glass-items-3339972_1920
Для жителей Красноярска организованы два конфиденциальных пути. Первый — немаркированный выезд бригады на дом с заранее согласованными порогами связи. Второй — «тихий вход» в клинику через отдельную дверь, где приём проходит без очередей и «коридорных» разговоров. На первичном звонке администратор уточняет только клинически значимые факторы: частоту рвоты, наличие мочеиспускания, ЧСС/АД в покое, эпизоды спутанности, актуальные лекарства и аллергии. Биографические подробности и лишние вопросы не задаются — мы придерживаемся принципа минимально необходимой информации.
Выяснить больше – наркологическая клиника стационар
Состав капельницы подбирается индивидуально, с учётом степени опьянения, возраста и хронических заболеваний пациента. Врач определяет дозировку и комбинацию препаратов, чтобы процедура прошла безопасно и эффективно.
Исследовать вопрос подробнее – капельница от запоя клиника
Саратов живёт в разных темпах: плотный центр, протяжные магистрали, мостовые переезды. Мы учитываем это в логистике: выездные бригады «СаратовМед Профи» движутся по немаркированным маршрутам, приезжают в гражданской одежде, формируют на месте «тихую сцену» и только затем начинают клиническую часть. Если на предзвонке звучат «красные флаги» — давящая боль в груди, выраженная одышка, спутанность, неукротимая рвота, судороги — организуем перевод в стационар без пауз: место резервируем заранее, передислокация проходит конфиденциально.
Получить больше информации – вывод из запоя
Такой календарь делает весь процесс прозрачным: пациент видит логику, близкие — прогресс, а врач — чистый сигнал для коррекции без «эскалации на всякий случай».
Подробнее – http://narcologicheskaya-klinika-saratov0.ru
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Смотрите также… – http://theglobe.net/the_worlds_most_visited_web_pages_948
Вывод из запоя у пожилых людей в Химках. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Подробнее тут – анонимный вывод из запоя химки
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Углубиться в тему – http://narcologicheskaya-klinika-saratov0.ru/chastnaya-narkologicheskaya-klinika-saratov/
Не всегда человек способен самостоятельно прекратить приём алкоголя и восстановиться. Есть состояния, требующие немедленного вмешательства специалистов. Обратиться за помощью необходимо, если наблюдаются следующие признаки:
Узнать больше – вывод из запоя на дому круглосуточно в волгограде
Процесс лечения включает несколько последовательных шагов, направленных на стабилизацию состояния, детоксикацию и восстановление функций организма. Таблица ниже показывает основные этапы процедуры, применяемые врачами клиники «РеабКузбасс».
Узнать больше – вывод из запоя на дому цена в новокузнецке
Hmm is anyone else having problems with the images on this blog loading?
I’m trying to find out if its a problem on my end or if it’s the
blog. Any feed-back would be greatly appreciated.
После завершения инфузий врач-нарколог даёт рекомендации по питанию, водному балансу и образу жизни. При необходимости пациенту назначается курс поддерживающей терапии для закрепления эффекта.
Углубиться в тему – https://narkologicheskaya-pomoshh-v-tolyatti17.ru/pomoshh-narkozavisimym-tolyatti
whoah this weblog is wonderful i like reading your articles. Keep up the good paintings! You already know, many people are looking around for this information, you can help them greatly.
It is not my first time to go to see this web page, i am browsing this web page dailly and obtain pleasant facts from
here everyday.
You are a very smart person! 🙂
Длительное злоупотребление спиртным неизбежно приводит к серьёзным последствиям для организма. Алкоголь влияет на работу практически всех внутренних органов: печень испытывает повышенную нагрузку при выводе токсинов, почки страдают от нарушения водно-солевого баланса, а сердечно-сосудистая система подвержена скачкам давления и аритмиям. Постепенно ухудшается общее самочувствие – возникают постоянные головные боли, слабость, повышенная раздражительность, бессонница.
Детальнее – врач вывод из запоя москва
Системный подход позволяет достичь максимальной эффективности лечения и снизить риск возврата к зависимости.
Разобраться лучше – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk
Длительное злоупотребление спиртным неизбежно приводит к серьёзным последствиям для организма. Алкоголь влияет на работу практически всех внутренних органов: печень испытывает повышенную нагрузку при выводе токсинов, почки страдают от нарушения водно-солевого баланса, а сердечно-сосудистая система подвержена скачкам давления и аритмиям. Постепенно ухудшается общее самочувствие – возникают постоянные головные боли, слабость, повышенная раздражительность, бессонница.
Получить больше информации – вывод из запоя на дому цена
Very descriptive post, I enjoyed that a lot. Will there be
a part 2?
I do not know if it’s just me or if perhaps everybody else
experiencing issues with your blog. It appears as though some of
the text within your posts are running off the screen. Can someone else please comment and let me know if this is happening to them as well?
This could be a issue with my web browser because I’ve had this happen previously.
Cheers
Wow many of amazing tips.
A fascinating discussion is worth comment. There’s no doubt that that you should write more on this issue, it might not be a taboo matter but generally people do not speak about
these subjects. To the next! Best wishes!!
Процесс кодирования проходит в комфортной и спокойной обстановке. Врач объясняет каждый этап, чтобы пациент чувствовал себя уверенно и спокойно. После процедуры пациент получает памятку с рекомендациями по уходу за здоровьем и режиму поведения в первые недели после лечения.
Детальнее – http://kodirovanie-ot-alkogolizma-v-volgograde17.ru/kodirovanie-volgograd/
На практике чаще всего применяются следующие компоненты:
Получить больше информации – http://
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Подробнее можно узнать тут – вывод из запоя вызов на дом красноярск
Капельница от запоя в Воронеже применяется для восстановления организма после длительного употребления алкоголя, устранения интоксикации и нормализации обменных процессов. Медицинская процедура проводится под контролем врача-нарколога, в клинике или на дому. Она позволяет быстро улучшить самочувствие, устранить головную боль, тремор, тошноту, обезвоживание и нарушения сна. Современные препараты действуют мягко, безопасно и без стресса для организма, обеспечивая плавный выход из запоя.
Изучить вопрос глубже – капельница от запоя клиника
Благодаря широкому выбору методик специалисты клиники могут подобрать оптимальную схему для каждого пациента, учитывая не только медицинские, но и психологические особенности. Такой индивидуальный подход повышает эффективность лечения и снижает риск повторных срывов.
Получить дополнительную информацию – кодирование от алкоголизма анонимно
I’m really enjoying the design and layout of your website.
It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often. Did you hire out a
designer to create your theme? Excellent work!
Процесс детоксикации состоит из нескольких последовательных шагов, направленных на безопасное очищение организма. Ниже представлена таблица с описанием этапов, которые применяются в клинике «Трезвая Линия Волгоград».
Подробнее – https://vyvod-iz-zapoia-v-volgograde17.ru/
Thanks for one’s marvelous posting! I definitely enjoyed reading it,
you will be a great author. I will ensure that I bookmark your blog and may come back sometime soon. I want to
encourage you to continue your great job, have a nice evening!
Профессиональная помощь требуется в тех случаях, когда организм уже не способен самостоятельно справиться с последствиями интоксикации. Чем дольше длится запой, тем сильнее проявляются его симптомы. Медицинское вмешательство помогает предотвратить развитие осложнений, таких как судороги, повышение давления и алкогольный психоз.
Узнать больше – вывод из запоя вызов на дом
I know this web site provides quality depending content and other
stuff, is there any other site which presents these information in quality?
Программы вывода из запоя в клинике разрабатываются с учётом состояния пациента. Для тяжёлых случаев назначается интенсивный курс с инфузионной терапией и контролем электролитов. При лёгких формах применяются мягкие препараты с постепенным выведением токсинов. Все процедуры проходят с соблюдением медицинских стандартов и полным сохранением анонимности.
Получить дополнительную информацию – вывод из запоя вызов
Transform your Essex home with resin bound and resin-bonded surfacing. Providing resilient, low-maintenance, and slip-resistant driveways, Overall Surfacing Solutions combines customized colours, natural rock appearances, and smooth coatings. Our specialist staff provides trustworthy and stylish emerging solutions for homes, businesses, and social areas, delivering durable outcomes that stand up the test of your time, https://telegra.ph/The-Rise-of-Natural-Stone-Resin-Driveways-in-Modern-Landscaping-12-23.
Appreciate the recommendation. Let me try it out.
Не всегда человек способен самостоятельно прекратить приём алкоголя и восстановиться. Есть состояния, требующие немедленного вмешательства специалистов. Обратиться за помощью необходимо, если наблюдаются следующие признаки:
Изучить вопрос глубже – вывод из запоя с выездом волгоград
В Новокузнецке команда «РеабКузбасс» организовала круглосуточный выезд наркологов, что позволяет оказывать помощь даже в сложных ситуациях. Пациенты часто обращаются после многодневного употребления алкоголя, когда нарушен сон, давление нестабильно, а организм истощён. В таких случаях врач выезжает в течение часа, проводит осмотр, определяет степень интоксикации и подбирает оптимальную терапию.
Разобраться лучше – вывод из запоя
Профессиональная помощь требуется в тех случаях, когда организм уже не способен самостоятельно справиться с последствиями интоксикации. Чем дольше длится запой, тем сильнее проявляются его симптомы. Медицинское вмешательство помогает предотвратить развитие осложнений, таких как судороги, повышение давления и алкогольный психоз.
Ознакомиться с деталями – вывод из запоя с выездом
Снятие ломки при алкоголизме в стационаре Балашихи. Наши специалисты помогут вам справиться с симптомами абстиненции.
Ознакомиться с деталями – вывод из запоя на дому балашиха
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Подробнее тут – https://vyvod-iz-zapoya-v-novokuzneczke17.ru/
Процесс вывода из запоя включает последовательное воздействие на ключевые звенья интоксикации. Ниже представлена таблица, отражающая этапы лечения, используемые методики и ожидаемые результаты терапии.
Получить дополнительные сведения – анонимный вывод из запоя
goGLOW Houston Heights
1515 Studemont Ꮪt Suite 204, Houston,
Texas, 77007, UႽΑ
(713) 364-3256
skin rejuvenation explained
Капельница от запоя в стационаре — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Узнать больше – нарколог вывод из запоя балашиха
is human trafficking thе ssecond largest, սsɑ gymnastics coach human trafficking, human trafficking
news neаr me, snjopes lynne knowles human trafficking, human traffiicking awareness Ԁay quotes,
human trafficking sex scene, human trafficking – menschenhandel, meghan connors human trafficking, ansrew tate human trafficking, arrguments οn human trafficking, freee human trafficking cme
florida, human trafficking ᧐ur, human trafficking іn minnesota 2021, arzona republican human trafficking, orange іs the
new black human trafficking, human trafficking conference ocean city md, 277 arrested іn human trafficking, anti human trafficking
law philippines, noreth korea human trafficking fаcts, hօw wiⅼl thee
wall affect human trafficking, human trafficking trsining michigan 2018, hotels sued human trafficking, kids rescued from human trafficking,
durham region human trafficking, ԝhy human trafficking is imp᧐rtant, mother օf good church human trafficking, walmart human trafficking 2020, ѡһat is
tһе rate of human trafficking worldwide, hman trafficking news (news), human trafficking bby ѕtate 2021, lgbt human trawfficking statistics,
south africa ɑnd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewed
hope human trafficking, human trafficking atlanta 2022, human trafficking
san joaquin county, non profit organizations fⲟr human trafficking,
human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rights julietta hua, facebook human trafficking lawsuit,
rates ⲟff human trafficking, real world example of human trafficking,
lawyers against human trafficking, wsin human trafficking summit 2022, vad är human trafficking, recognizing tһe signs of human trafficking, human trasfficking justice, video оf human trafficking, four
signs օf human trafficking, human trafficking honey, binjun xie human trafficking,
human trafficking documentary amazon ⲣrime, minesota human trafficking data, uncovers russoan human trafficking
гing war, human trafficking chico cɑ, human trafficking jus cogens, human trafficking
syrian refugees, human trafficking topics research paper, text human trafficking link snopes, oprah south africa human trafficking, human trafficking grants 2015, human trafficking
san antonio 2021, human drug traffiking meaning, human trafficking stories
children, fema human trafficking awareness, florida disney human trafficking, jobs
f᧐r human trafficking victims, movie ɑbout human trafficking 2023 netflix, ɑ daу in the life of a human trafficking victim, ukk human trafficking news, bent ⅼicense pate human trafficking reddit, human trafficking іn waterbury ct, center to combat human trafficking, greenville nnc human trafficking, maui human trafficking, t᧐ⲣ 5 human trafficking
cities, іs human trafficking happening in thee ᥙs, oxnard human trafficking, aurora shoreline human trafficking, taconganas human trafficking, hashtags f᧐r human trafficking, wһite house human trafficking summit,
corona human trafficking, border patrol hhuman trafficking, human trafficking іn thailand 2020, human trafficking іn wv, 11 arrested іn human trafficking,
china’ѕ one cnild policy аnd human trafficking, hotels human trfficking 2023,
human trafficking іn florida 2021, human trafficking debate topics,
international justice mission human trafficking, uncovers
human trafficking гing for, scholarly article ߋn human trafficking, madison herman human trafficking,
amad dialloo human trafficking, ɑ poem about human trafficking, humn trafficking
bristol tn, deluca аnd the human trafficking storyline, economy аnd human trafficking,
human trafficking іn trinidad, human trafficking ⅾay 2018, caught camera actual human trafficking victims,
human trafficking episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch dopgs
human trafficking map, human trafficking dfinition canada, airtag human trafficking,
human trafficking іn the beauty industry, 人口販子human trafficking,
forced labor іn humn trafficking, american airlines center human trafficking, human trafficking
сe texas, selah humsn trafficking, siam hukan trafficking,
fresno human trafficking statistics, senegal human trafficking,
human trafficking belgium, michigan human trafficking
ϲourse, ny timеs human trafficking, abandoned stroller human trafficking,
human trafficking і-44, solution ⲟn human trafficking,
human trafficking canada news, ontario human trafficking,
protecxts victims ᧐f human trafficking amendment, human trafficking
іn highlad ϲa, human trafficking hotspot map, human traffficking organizations ontario, human trafficking
hiding ᥙnder cars, summary on human trafficking, uncovers russian human trafficking ring ᴡɑr, human trrafficking honey,
fⲟur signs ᧐ff human trafficking, human trafficking western pa, human trafficking livermore,
huhman trafficking durham region, human trafficking
аt atlanta airport, binjun xiee human trafficking, minnesota human traqfficking data, human trafficking
documentary amazon рrime, humman trafficking lawyer bloomfield hills, human traffickng charge іn texas, central students аgainst human trafficking, ap human geography human trafficking, human trafficking fߋr sexual exploitation, blue fоr
human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia,
jo jorgensen оn human trafficking,fort hood soldiers human trafficking,
beau оf the fifcth column human trafficking, hawkins human trafficking,
human trafficking іn thе pacific islands, reasoons wһy human trafficking is
bad, ally human trafficking, ᴡrite an essay on human trafficking,
human trafficking pros, human trafficking ark web reddit, north
preston human trafficking, ⅾollar sign tattopo human trafficking,
wht іѕ human trafficking, human trafficking stuart fl, priceless movie human trafficking, ti аnd wife human trafficking, human trafficking ethnicity statistics,
і 80 truck stop human trafficking, hamilton human trafficking,
oakville human trafficking, human trafficking οn tһe deep web,current human trafficking, human trafficking women’ѕ rіghts, brunei human trafficking,
barack obama human trafficking quote, patron sainnt օf hunan trafficking, spirited aay human trafficking,
tһе game humqn trafficking, tοp human trafficking cities 2023, human trafficking ѡhich countries arre tһe worst,
һow to donate to hujan trafficking organizations, human trafficking quotes famous, human trafficking story 2020, human trafficking іn pittsburgh, 2020 human trafficking conference,
human trafficking bust atlanta, human trafficking hemet сa, humann trafficking statistics oregon, h᧐ԝ tto identify a human trafficking
victim, economy аnd human trafficking, lover boy method оf human trafficking, deluca аnd the
human trafficking storyline, european human trafficking, selah
human trafficking, american airlines center human trafficking, humnan trafficking paintings, ԝһаt state іs #1
inn human trafficking?, forced labor іn human trafficking,
人口販子human trafficking, crystal meth, ѡһat does crystal meth
lοok like, what iѕ rystal meth, crystal meth anonymous,
һow ⅼong doers crystal meth stay іn yoᥙr sʏstem, howw to mаke
crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects, crystal meth pipe, crystal meth drug, ѡһat does crystal metfh ⅼoߋk like?, meth crystal,
crystal meth images, crystal meth ѕide effects, һow is crystal meth mɑde, meth ѵѕ crystal meth, ԝhаt doeѕ crystal meth ԁߋ, crystal meth symptoms, crystal
meth vs meth, effects ᧐f crystal meth, side effects of crystal meth, һow
do you make crystal meth, crystal meth vs crack, ᴡһat dooes crystal meth smell ⅼike,
hοw is crystal metyh uѕed, crystal meth withdrawal, crystal meth
breaking bad, ᴡhat iss crystal meth made օf, what ɗoes crystal meth Ԁo
too you, crystal meth teeth, smoking crystal meth,
crystal meth pictures, ϲan you snort crystal meth, crystal
mth befor ɑnd after, who invented crystal meth, crystal meth fɑcts,
crystal meth withdrawal symptoms, crystal meth street names, signs ᧐f crystal meth, crystal meth addiction, howw tо cook crystyal
meth, crystal meth definition, ѡhat type of drug iss crystal meth, ѡhat does crystal meth feel ⅼike, crystal meth meaning, crystal meth ingredients, ѡhats crystal
meth, whwt color іs crystal meth, cystal meth detox, crysyal meth fɑce, crystal meth powder, crystal meth poem, street names
f᧐r crystal meth, short term effects oof crystal meth,
signs ᧐ff crystal meth abuse, crhstal meth
rock, crystal meth fly, crystal meth addict, crystal meth
սsers, crystal meth rehab, һow mᥙch doеs crystal
meth cost, how do you take crystal meth, hоw muϲh іs crystal
meth, signs ߋff crystal meth uѕe, how tο smoke crystal meth, һow to usе crystal meth, ⅼong term effects of crystal
meth, signjs оf addiction to crystal meth, pink crystal meth, crystal
meth ⅼook like, breaking bad crystal meth, ѡhen was crystal meth invented, pictures օf crystql meth, how is crystal meeth tɑken,
signs thаt someone is using crystal meth, ready օr
not crystal meth storage, difference ƅetween meth ɑnd crystal meth, hօw do you ԁo crystal meth, crystal meth., locate crystal meth storage, ѡhat are the effects
of crystal meth, fake crystal meth, crystal meth people, ԝhat doess crystal meth,
һow ddo ʏoᥙ use crystal meth, һow addictive is crystal meth, сan үօu overdoe on crystal meth, crystal meth blue, crystal meth signs, һow ⅼong dоes crystal meth ⅼast, crystal meth
detox ⅼoѕ angeles, how ddo people սse crystal meth,
һow does crystal meth ⅼook lіke, crystal meth porn, һow d᧐es crystal meth ⅼοok, crystal meth storage twisted nerve, ԝhats іn crystal meth, cryystal meth treatment, ԝhɑt is
crystal meth mаde from, methamphetamin, methamphetamin adalah,
methamphetamin ԁan amphetamin adalah, amphetamin dan methamphetamin, chloroethjane ɑnd methamphetamin, crystal methamphetamin, ѡhat іѕ methamphetamin,
methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma
methamphetamin, methamphwtamin hydrochlorid, methamphetamin geschichte,
methamphetamin hcl, amphetamin νs methamphetamin, methamphetamin biru, methylphenidat
methamphetamin, beca amphetamin ɗan methamphetamin, difference ƅetween amphetamine
and methamphetamin, methampheetamin psychose,
methamphetamin rules, һow to make methamphetamin, methamphetamin amphetamin unterschied,
methamphetamin hydrochloride, definition von methamphetamin, р2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks
vapor inhaler methamphetamin, gta methamphetamin labor, ѡie
wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept,
methamphetamin effects, methmphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine
սnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow to
cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ᴡas ist das, unterschied methamphetamin uund amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache,
methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methamphetamin ɑndere suchten аuch nach, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ɗương tính,
waas іѕt methamphetamin, drogentest methamphetamin,
methamphetamin englisch, methamphetamin structure, іst
mdma methamphetamin, lye іn methamphetamin, iѕt methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methazmphetamin chemische formel,
methamphetamin meaning, ԁ-methamphetamin, herstellung methamphetamin, methamphetaamin vs amphetamine, methamphetamin recept,
methamphetamin japan, definition methamphetamin, methamphetamin fаce, methamphetamin formula,
methamphetamin synapse, methamphetamin adderall, methamphetasmin adhd, blue methamphetamin, wirkung methamphetamin,
methamphetamin terbuat dari, methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese,
methamphetamin ᥙse icd 10, weed, weed grinder, wheге iѕ weed legal, disposable
weed pen, weed shop neаr me, milwaukee weed eater, purple
weed, іѕ weed legal іn virginia, is weed legal іn oklahoma, іs weed leghal in louisiana, weed puller tool, weed
carts, іs weed legal inn south carolina, weed killer ffor lawns, horny goast weed f᧐r men, wһat states is
weeed legal, weed shops neаr mе, weed legal stаtes, weed vape, roundup weed killer, weed killer spray, edibles weed,
recreational weed ѕtates, weed store, milk weed, weed barrier,
іs weed legal іn indiana, legal weed ѕtates, states with legal weed, is weed legal
іn kentucky, weed puller, preen weed preventer, ounce
᧐f weed, dewalt weed eater, plantain weed, husqvarna weed eater,
electric weed eater, hybrid weed, moonrock weed, weed pipe,
barrett wilbert weed, weed control, weed delivery neɑr me, iis weed
legal іn missouri, һow to make weed butter,
ᴡhite weed, iis weed legal in utah, moon rodk weed, snow caps weed,
іs weed legal in arkansas, іs weed legal іn texas 2025,
ryobi weed eater, weed bowl, dill weed, weed legalization, smoking weed,
іs weed leegal in nevada, weed whacker, iѕ weed legal іn alabama,
is weed a drug, weed barrier fabric, ᴡhat is horny goat
weed, sppruce weed ɑnd grass killer, weed stores near me,
sprinkles weed, poke weed, weed withdrawal, ᴡed vapes, snow
cap weed, rm43 weed killer, craftsman weed eater, qp оf weed, weed edibles, cookies weed, gelato weed, іѕ weed legal іn new mexico,
strains oof weed, eed butter, ρound of weed, zazsa weed, iss weed legal іn nc, how mucһ is an ounce of weed, pgr weed, іs delta 9 real weed, diy weed killer, zzip оff weed, weed torch, moldy weed, elon musk weed, іs weed illegal
in texas, weed eater string, rsso weed, weed hangover, weed wallpaper, іs wewd legal іn nebraska, how tο smoke weed, is weed legal іn hawaii, һow tо grow
weed, һow to make weed in infinite craft, іs weed legal inn california, gary
payton weed
Такая структура терапии делает процесс максимально эффективным и безопасным.
Ознакомиться с деталями – наркологическая клиника омск
Mangelsen
7916 Girard Avenue, La Joya
ϹΑ 92037, United Stɑteѕ
1 800-228-9686
top grizzlies оf pilgrim creeek book photography
(Rosalind)
Наркологическая помощь в «ВолгаМед Тольятти» включает широкий спектр процедур и методик. Каждый случай рассматривается индивидуально, с учётом состояния пациента, стадии заболевания и сопутствующих факторов. Ниже представлена таблица с основными направлениями медицинской работы.
Детальнее – https://narkologicheskaya-pomoshh-v-tolyatti17.ru/narkologicheskaya-bolnicza-tolyatti/
You need to be a part of a contest for one of the most useful websites on the web.
I will highly recommend this site!
Наркологическая помощь в «ВолгаМед Тольятти» включает широкий спектр процедур и методик. Каждый случай рассматривается индивидуально, с учётом состояния пациента, стадии заболевания и сопутствующих факторов. Ниже представлена таблица с основными направлениями медицинской работы.
Получить дополнительные сведения – анонимная наркологическая помощь тольятти
Asking questions are in fact pleasant thing if you are not understanding something completely,
but this piece of writing offers pleasant understanding yet.
I was suggested this website by my cousin. I am not
sure whether this post is written by him as no one else know such detailed about my trouble.
You’re wonderful! Thanks!
Hi to all, it’s really a good for me to go to see this
website, it includes helpful Information.
If you desire to obtain a great deal from this post then you have to apply such
strategies to your won weblog.
Hiya, I am really glad I have found this information. Nowadays bloggers publish only about gossip and net stuff and this is actually frustrating.
I was curious if you ever considered changing the layout of your site?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or two pictures.
Maybe you could space it out better?
you can look here https://lumi-wallet.io
great post to read https://jaxx-web.org/
Круглосуточная помощь при запое в Люберцах. Наша команда работает 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Выяснить больше – капельница от запоя выезд в люберцах
Вывод из запоя в Рязани — это профессиональная медицинская процедура, направленная на очищение организма от токсинов, восстановление нормального самочувствия и предотвращение осложнений после длительного употребления алкоголя. В специализированных клиниках города лечение проводится с использованием современных методов детоксикации и под контролем опытных врачей-наркологов. Такой подход позволяет быстро и безопасно стабилизировать состояние пациента, устранить физическую зависимость и подготовить организм к дальнейшему восстановлению.
Получить дополнительную информацию – наркология вывод из запоя
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Получить дополнительную информацию – https://matronastore.com/product/rainbow-moon-earrings
Процесс включает несколько шагов:
Исследовать вопрос подробнее – частный нарколог на дом в уфе
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Ознакомиться с деталями – срочный вывод из запоя
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Узнайте всю правду – https://www.goldenservicesksa.com/what-is-best-domin-name-for-business-copy-9
Капельница от запоя в стационаре — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Получить дополнительные сведения – вывод из запоя в стационаре балашиха
An outstanding share! I’ve just forwarded this onto a
coworker who has been doing a little homework on this.
And he actually ordered me dinner simply because I discovered it for him…
lol. So let me reword this…. Thank YOU for the meal!!
But yeah, thanks for spending the time to discuss this issue here on your site.
Лечение пивного алкоголизма в Люберцах. Мы предлагаем эффективные методы лечения зависимости от пива.
Выяснить больше – капельница от запоя на дому цена в люберцах
Many people who experienced serious side effects from using popular GLP-1 drugs like Ozempic, Wegovy, Mounjaro, and Trulicity, have sued the manufacturers in mass tort litigation. Though BMI is used for eligibility, it does not differentiate between fat, muscle or bone mass and it doesn’t account for how fat is distributed in the body.Body composition analysis however, provides a more detailed view by measuring the proportion of fat, muscle and other tissues, giving you a clearer picture of your physical health. But that doesn’t mean he’ll be successful. Where timelines are long due to the complexity of the solution, but operations are continued, – provide the supporting rationale e.g. facility planned to undergo major refurbishment and provision of new equipment in Q3, Standard Operating Procedure to be updated as part of facility recommissioning. Major conclusions: Since its discovery, GLP-1 has emerged as a pleiotropic hormone with a myriad of metabolic functions that go well beyond its classical identification as an incretin hormone. If CAPA were not adequately addressed or failed to meet the agreed timelines the findings may be upgraded, for example, if previous major findings have not been addressed, then a critical finding may be given.
Here is my webpage … http://www.word4you.ru/bitrix/redirect.php?goto=https://wiki.sheldongenealogy.org/index.php?title=Introducing_ColonBroom:_The_Revolutionary_GLP-1_Supplement_For_Optimal_Colon_Health
Sizdə çox faydalı resurslar var — xüsusilə onlayn mərc ilə bağlı.
https://s.ubyt.es/lM4dJX
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Полная информация здесь – https://daniellesellsfl.com/hello-world
Undeniably consider that which you stated. Your favourite reason seemed to be at the internet the
easiest thing to take into account of. I say to you, I certainly get annoyed at the
same time as other folks consider issues that they just don’t recognize about.
You managed to hit the nail upon the highest as neatly as defined out the entire thing without having side-effects
, folks can take a signal. Will probably be again to get more.
Thank you
Помощь при алкогольной интоксикации в Химках. Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Получить дополнительную информацию – вывод из запоя недорого
Профилактика рецидивов после запоя в стационаре Балашихи. Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Исследовать вопрос подробнее – наркология вывод из запоя
Ich bin inspiriert von dieser Mühe. Geben für die Wiederherstellung der Sehkraft ist ein kraftvoller Weg,
der Menschheit zu helfen. Bitte, diese wichtigen Bemühungen fortzusetzen.
Here is my page … Medizinische Soforthilfe Augen
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Это ещё не всё… – https://karoseriambulance.id/ambulance-type-ekonomi/ekonomi-baru
Leuke site – intuïtief en veel interessante content.
https://lalabet-sport-nl.nl
Bermanfaat sekali pembahasannya. Jangan lupa kunjungi sbobet resmi untuk merasakan pengalaman bermain yang berbeda dari yang lain.
Do you have any video of that? I’d love to find out more
details.
Wonderful site you have here but I was curious about if you knew of
any message boards that cover the same topics discussed in this article?
I’d really love to be a part of community where I can get opinions from other knowledgeable individuals
that share the same interest. If you have any recommendations,
please let me know. Thanks!
Hey are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started
and set up my own. Do you need any coding expertise to make your own blog?
Any help would be greatly appreciated!
Анонимная наркологическая помощь — это управляемая система, где каждый шаг прозрачно связан с целью и измеримым результатом. В наркологической клинике «ЕнисейМед Центр» мы соединяем круглосуточную доступность, мягкую логистику и модульный план лечения, чтобы пациент и семья понимали, почему именно сейчас назначается то или иное вмешательство и когда оно будет остановлено. Мы избегаем полипрагмазии: запускаем один модуль — ставим один маркер — определяем «окно оценки» — выключаем модуль, как только цель достигнута. Такой подход бережёт ресурсы организма и сохраняет причинно-следственную связь.
Узнать больше – http://narkologicheskaya-klinika-v-krasnoyarske17.ru
Детоксикация в клинике «Центр Трезвости ВоронМед» проводится по принципу минимального вмешательства при максимальной эффективности. Основная задача — очистить кровь от токсинов и стабилизировать внутреннюю среду организма без нагрузки на сердце и почки. Все препараты вводятся медленно, под контролем медицинского персонала, а состав подбирается индивидуально после оценки анализов и состояния пациента.
Подробнее тут – http://vyvod-iz-zapoya-v-voronezhe17.ru/vyvod-iz-zapoya-za-den-voronezh/https://vyvod-iz-zapoya-v-voronezhe17.ru
their explanation https://jaxxwallet-web.org/
Системный подход позволяет достичь максимальной эффективности лечения и снизить риск возврата к зависимости.
Получить дополнительные сведения – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Выяснить больше – наркологическая клиника стационар в красноярске
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Детальнее – анонимный вывод из запоя
Лечение в клинике «ВоронежМед Альянс» проходит поэтапно. Каждый модуль имеет определённую цель и собственные критерии эффективности. Такой подход исключает избыточное вмешательство и обеспечивает прозрачность процесса восстановления.
Получить дополнительную информацию – http://narcologicheskaya-klinika-v-voronezhe17.ru/narkolog-voronezh-anonimno/
Реабилитация после запоя в Химках. Мы поможем вам восстановиться после запоя и предотвратить рецидивы.
Изучить вопрос глубже – вывод из запоя с выездом химки
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Получить больше информации – наркологическая клиника вывод из запоя саратов
I visited many blogs except the audio feature for audio songs current at this web site is in fact superb.
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Подробнее можно узнать тут – капельница от запоя цена
Just wish to say your article is as astonishing. The clearness in your publish is simply cool
and i could assume you are an expert in this subject.
Fine together with your permission allow me to grab your RSS feed
to stay updated with coming near near post. Thanks a million and
please continue the rewarding work.
Лечение запоя на дому в Люберцах. Наши специалисты приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния.
Детальнее – капельница от запоя выезд
Лечение запоя на дому в Люберцах. Наши специалисты приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния.
Исследовать вопрос подробнее – после капельницы от запоя люберцы
Во время процедуры врач фиксирует ключевые параметры, чтобы убедиться в безопасности и эффективности терапии. Мониторинг проводится при каждом выезде и помогает отслеживать динамику в режиме реального времени. В таблице ниже указаны основные показатели, за которыми следит специалист.
Углубиться в тему – нарколог на дом цены воронеж
Вау, какой крутой сайт Olimp Casino! Благодарю!
http://satoshiogawa.com/?wptouch_switch=desktop&redirect=http%3a%2f%2folimp-casino-kazakhstan-7777.kz%2Fregistration
대구출장마사지 서비스는 대구광역시 전역에서 편안하게 전문 마사지를 받을 수 있는 출장 홈타이 서비스입니다.
고객님이 계신 곳으로 여성 전문 테라피스트가 직접
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ⅭΑ 92626, Unite States
mr g bail bonds
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Получить дополнительную информацию – вывод из запоя анонимно
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Разобраться лучше – https://vivod-iz-zapoya-v-volgograde17.ru/anonimnaya-narkologiya-vyvod-iz-zapoya-volgograd/
Лечение зависимости от алкоголя у мужчин в Химках. Мы предлагаем индивидуальный подход к лечению мужчин, учитывая все особенности организма.
Разобраться лучше – вывод из запоя на дому цена
Наркологическая клиника «ВолгаДок Медикал» — это круглосуточная служба помощи, выстроенная вокруг принципов клинической безопасности, прозрачной коммуникации и поддержки пациента на каждом этапе. Мы соединяем стационар и выездные бригады в единую систему: первичный осмотр и стабилизация состояния, адресные инфузионные модули, мягкая коррекция сна и тревоги, последующее наблюдение с короткими «окнами» обратной связи. Все решения принимаются по показаниям и сопровождаются объяснением: какую цель преследуем, каким маркером измеряем, когда проверяем результат. Такой подход исключает хаотичные усиления, бережёт ресурс организма и даёт прогнозируемый клинический эффект.
Изучить вопрос глубже – https://narcologicheskaya-klinika-saratov0.ru/klinika-narkologii-saratov/
Its like you read my mind! You seem to know a lot about this,
like you wrote the book in it or something. I think that you can do
with a few pics to drive the message home a little bit, but
other than that, this is great blog. A great read.
I will certainly be back.
Hi there, its nice paragraph concerning media
print, we all be familiar with media is a impressive source of
facts.
Hi there i am kavin, its my first occasion to commenting anyplace, when i
read this piece of writing i thought i could also create comment due to this sensible article.
This game looks amazing! The way it blends that old-school chicken crossing concept with actual consequences is brilliant.
Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real
risk? I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing mechanics with genuine
stakes involved. Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless
chicken crossing feel with real consequences has
me hooked. I need to play this!
This sounds like a blast! Combining that iconic chicken crossing
gameplay with actual stakes? Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds legitimate risk is
genius. Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing
action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible consequences?
I’ve gotta try this out!
Круглосуточная помощь при запое в Химках. Мы работаем 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Получить больше информации – врач вывод из запоя в химках
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Подробнее тут – https://mahnoorhealthandwealth.com/top-10-superfoods-for-boosting-immunity
I got this web page from my friend who informed me
regarding this web site and now this time I am browsing this web page and reading very informative posts here.
Very useful information, I’ll try to apply this soon.
Реабилитация после запоя в Люберцах. Мы поможем вам восстановиться после запоя и предотвратить рецидивы.
Детальнее – kapelnicza-ot-zapoya lyubercy
WOW just what I was looking for. Came here by searching
for 강남텐카페
Feel free to visit my web blog 강남일프로
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Посмотреть всё – https://cattocodau.com/tiem-toc-quang-binh
Снятие ломки при алкоголизме в Москве от клиники «Частный Медик 24». Наши специалисты помогут вам справиться с симптомами абстиненции.
Получить дополнительные сведения – наркологическая помощь на дому москве
Город с протяжёнными магистралями и разноскоростными районами требует особой организации маршрутов. Выездные бригады «ВолгаДок Медикал» работают в режиме 24/7, прибывают в гражданской одежде, избегают громких звонков и используют «немаркированные» подъезды. Перед приездом мы просим подготовить пространство: приглушить верхний свет, обеспечить приток свежего воздуха без сквозняков, подготовить ровную поверхность под укладку и удлинитель, перевести телефоны в «без уведомлений» с «белым списком» близких. Это позволяет в первые минуты сосредоточиться на клинике, а не на бытовых вопросах.
Подробнее – анонимная наркологическая клиника в саратове
Вывод из запоя на дому — удобно и безопасно. Наши специалисты приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния.
Подробнее тут – вывод из запоя на дому в химках
Главным преимуществом наркологической клиники в Новокузнецке является комплексный подход к лечению. Специалисты рассматривают зависимость как заболевание, требующее системного воздействия на организм и психику. Каждый пациент получает индивидуальную программу, включающую медицинскую, психотерапевтическую и социальную помощь. Такой подход обеспечивает достижение устойчивых результатов и предотвращает рецидивы.
Подробнее можно узнать тут – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Детали по клику – https://www.wirtschaftleichtverstehen.de/?attachment_id=1145
rc88.tech
May I just say what a comfort to uncover somebody that genuinely knows what they are talking about on the net.
You certainly realize how to bring a problem to light and make it important.
More people must look at this and understand this side
of the story. I can’t believe you aren’t more popular
given that you definitely possess the gift.
Stop by my page – 강남텐프로
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Получить дополнительную информацию – наркологическая клиника нарколог омск
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Переходите по ссылке ниже – https://inspiracomunicaciones.com/marketing-digital/campana-de-medios-atl-o-btl-cual-aplicar
This game looks amazing! The way it blends that old-school chicken crossing concept with actual
consequences is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic
chicken crossing mechanics with genuine stakes involved.
Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel
with real consequences has me hooked. I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay
with actual stakes? Sign me up!
I’m so into this concept! The way it takes that classic
chicken crossing vibe and adds legitimate risk is genius.
Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic
chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style
with tangible consequences? I’ve gotta try this out!
Карта делает видимой причинно-следственную связь: пациент понимает, зачем и что именно делается; семья видит «точки проверки»; врач получает опору для изменения одного параметра без разрушения всего плана.
Ознакомиться с деталями – срочный вывод из запоя
Одним из самых востребованных направлений работы клиники является проведение детоксикации и вывод из запоя. Эти процедуры направлены на очищение организма от алкоголя и продуктов его распада, нормализацию работы печени и нервной системы. Лечение проводится с использованием сертифицированных препаратов и под контролем врача-нарколога.
Изучить вопрос глубже – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/
Лечение зависимости от алкоголя на дому в Люберцах. Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Углубиться в тему – капельница от запоя цена
hello!,I really like your writing so much! share we communicate more about your article on AOL?
I require a specialist in this space to resolve my problem.
Maybe that is you! Having a look ahead to see you.
This is very interesting, You are a very skilled blogger.
I have joined your feed and look forward to seeking more
of your excellent post. Also, I’ve shared your site in my social networks!
Here is my blog post – 강남하이쩜오
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Углубиться в тему – вывод из запоя капельница на дому
Hiya, I am really glad I have found this information. Nowadays bloggers publish only about gossip and net stuff and this is actually frustrating.
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Исследовать вопрос подробнее – анонимный вывод из запоя
Профессиональная помощь при запое в Люберцах. Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Выяснить больше – вызвать капельницу от запоя
Комплексная терапия включает несколько последовательных этапов, обеспечивающих полное восстановление организма и личности пациента. Каждый из них направлен на решение конкретных задач — от устранения интоксикации до закрепления устойчивой ремиссии.
Подробнее можно узнать тут – наркологическая клиника наркологический центр
Лечение зависимости от алкоголя у мужчин в стационаре Балашихи. Мы предлагаем индивидуальный подход к лечению мужчин, учитывая все особенности организма.
Подробнее тут – нарколог на дом вывод из запоя
Hey very interesting blog!
my web page: נערות ליווי בצפון
Hi there to every body, it’s my first pay a quick visit
of this website; this web site carries remarkable and actually good material
in favor of visitors.
Also visit my homepage: 优塔娱乐城
Стационарное лечение запоя в Химках. Предлагаем комфортные условия для пребывания пациентов и круглосуточный медицинский уход.
Исследовать вопрос подробнее – вывод из запоя дешево химки
Состав капельницы подбирается индивидуально, с учётом степени опьянения, возраста и хронических заболеваний пациента. Врач определяет дозировку и комбинацию препаратов, чтобы процедура прошла безопасно и эффективно.
Получить дополнительную информацию – сколько стоит капельница на дому от запоя воронеж
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Получить дополнительную информацию – вывод из запоя на дому цена
Системный подход позволяет достичь максимальной эффективности лечения и снизить риск возврата к зависимости.
Изучить вопрос глубже – наркологическая клиника цены в новокузнецке
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Получить дополнительную информацию – вывод из запоя на дому недорого в рязани
How come you do not have your website viewable in mobile format? cant see anything in my Droid.
Капельница от запоя в Люберцах — быстрый и эффективный способ детоксикации. Наши специалисты приедут к вам домой и проведут процедуру, помогая снять симптомы похмелья и вывести токсины из организма.
Выяснить больше – https://https://kapelnica-ot-zapoya-lyubercy11.ru//
Процесс включает несколько шагов:
Разобраться лучше – http://narkolog-na-dom-v-ufe17.ru
Hi I am so excited I found your blog page, I really found
you by mistake, while I was browsing on Google for something else, Regardless I
am here now and would just like to say thank
you for a tremendous post and a all round enjoyable blog (I also love the theme/design), I don’t have time
to go through it all at the minute but I have
bookmarked it and also added your RSS feeds, so when I have
time I will be back to read much more, Please do keep up the excellent job.
Attractive part of content. I simply stumbled upon your weblog and in accession capital to assert that I acquire in fact loved account
your weblog posts. Anyway I’ll be subscribing to your feeds or even I fulfillment you
get entry to constantly rapidly.
Круглосуточная помощь при запое в Химках. Мы работаем 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Узнать больше – вывод из запоя на дому круглосуточно
Вывод из запоя у пожилых людей в Люберцах. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Подробнее можно узнать тут – капельница от запоя выезд в люберцах
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Желаете узнать подробности? – https://mdtodate.com/functional-nausea
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, UᏚA
(402) 940-8979
microdermabrasion process professional (https://padlet.com/bailbonds39vzqfv/bookmarks-8Tiiytre1ivs9cbd/wish/mDRxWB72r1vOajb1)
I’m not that much of a internet reader to be honest but your
blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back later on. Cheers
Ниже приведена таблица, отражающая примерную динамику состояния пациента после постановки капельницы:
Углубиться в тему – врача капельницу от запоя
I blog often and I seriously thank you for your content.
This article has really peaked my interest. I will bookmark your website and
keep checking for new information about once per week.
I subscribed to your Feed as well.
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Получить дополнительные сведения – вывод из запоя
Системный подход позволяет достичь максимальной эффективности лечения и снизить риск возврата к зависимости.
Детальнее – наркологические клиники алкоголизм новокузнецк
Aw, this was a really nice post. Finding the time and actual effort to make
a very good article… but what can I say… I hesitate a
lot and don’t manage to get nearly anything done.
Процесс включает несколько шагов:
Ознакомиться с деталями – https://narkolog-na-dom-v-ufe17.ru/vyvod-iz-zapoya-ufa-narkolog-na-dom/
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Узнать больше – http://vyvod-iz-zapoya-v-novokuzneczke17.ru
Лечение запоя без госпитализации в Химках. Мы предлагаем лечение на дому, без необходимости госпитализации.
Подробнее – вывод из запоя на дому цена химки
Благодаря широкому выбору методик специалисты клиники могут подобрать оптимальную схему для каждого пациента, учитывая не только медицинские, но и психологические особенности. Такой индивидуальный подход повышает эффективность лечения и снижает риск повторных срывов.
Углубиться в тему – как происходит кодирование от алкоголизма волгоград
I am really delighted to glance at this web site posts which
carries tons of helpful information, thanks for providing these kinds of data.
Главная задача процедуры — быстрое выведение этанола и его метаболитов из организма, нормализация уровня электролитов, улучшение самочувствия и предотвращение осложнений. Лечение проводится как в клинике, так и на дому, что особенно удобно при тяжёлых состояниях, когда пациент не может самостоятельно добраться до медицинского учреждения.
Выяснить больше – вывод из запоя клиника
Hi! Someone in my Facebook group shared this website with us so I came to look
it over. I’m definitely enjoying the information. I’m book-marking and will be tweeting this
to my followers! Excellent blog and superb design and style.
Stop by my web page; 優塔娛樂城
Having read this I thought it was really enlightening.
I appreciate you finding the time and energy to put this article together.
I once again find myself spending way too much time both reading and leaving comments.
But so what, it was still worthwhile!
Такой состав обеспечивает быстрое снятие симптомов интоксикации и восстановление функций организма после запоя.
Исследовать вопрос подробнее – капельница от запоя на дому в воронеже
Ridiculous quest there. What happened after? Take care!
Feel free to visit my webpage: 강남텐카페
Hello There. I discovered your blog using msn. That is a really well
written article. I’ll be sure to bookmark it and return to learn more of your helpful
information. Thank you for the post. I’ll definitely return.
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Получить дополнительные сведения – https://volley.sg/knaller-in-appenzell-herren-2-schlaegt-den-leader-mit-03
Лечение хронического алкоголизма в Химках. Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Подробнее тут – https://https://vyvod-iz-zapoya-himki11.ru//
Такая структура терапии делает процесс максимально эффективным и безопасным.
Подробнее – наркологическая клиника клиника помощь омск
I’m impressed, I must say. Seldom do I come
across a blog that’s both equally educative and engaging, and let me tell you,
you’ve hit the nail on the head. The issue is something that too
few men and women are speaking intelligently about.
I am very happy that I came across this in my search for something concerning this.
Bu platformanı bəyənirəm.
https://psarquitetos.com/Home/change_language/en-us?link=https://pin-up-azerbaijan-vip.org/bonuslar
It’s amazing for me to have a website, which is beneficial in favor of my experience.
thanks admin
Все процедуры выполняются анонимно и с соблюдением медицинских стандартов. Препараты применяются только сертифицированные, рассчитанные на мягкое восстановление организма без побочных эффектов. При необходимости лечение продолжается в стационаре, где пациент получает круглосуточное наблюдение, питание и психологическую поддержку.
Разобраться лучше – https://vyvod-iz-zapoya-v-novokuzneczke17.ru/vyvod-iz-zapoya-v-staczionare-novokuzneczk/
Лечение организовано поэтапно, что помогает пациенту постепенно возвращаться к полноценной жизни. Каждый шаг направлен на укрепление результата и снижение риска рецидива.
Узнать больше – наркологическая клиника вывод из запоя омск
Лечение организовано поэтапно. Такой подход обеспечивает постепенное восстановление функций организма и исключает риск осложнений. Каждый этап терапии направлен на устранение конкретных нарушений, вызванных интоксикацией.
Подробнее – наркология вывод из запоя в красноярске
Не всегда человек способен самостоятельно прекратить приём алкоголя и восстановиться. Есть состояния, требующие немедленного вмешательства специалистов. Обратиться за помощью необходимо, если наблюдаются следующие признаки:
Получить дополнительные сведения – вывод из запоя клиника
Saya terharu dengan pekerjaan ini. Berdonasi untuk perawatan penglihatan adalah cara yang kuat untuk mendukung kemanusiaan. Mohon pertahankan upaya yang hebat
ini.
Feel free to surf to my web blog: Dukungan Pasien Katarak
Hello would you mind sharing which blog platform you’re working with?
I’m looking to start my own blog soon but I’m having a tough time
choosing between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems different then most blogs and I’m looking for something completely unique.
P.S My apologies for being off-topic but I had to ask!
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Изучить вопрос глубже – кодирование от алкоголизма
Комплексный подход обеспечивает не только снятие симптомов, но и полное восстановление функций организма. Пациент получает поддержку на всех этапах — от детоксикации до социальной адаптации.
Исследовать вопрос подробнее – вызвать наркологическую помощь
Вывод из запоя — это не просто медицинская процедура, а жизненно важный этап, позволяющий вернуть контроль над самочувствием и предотвратить осложнения. В клинике «РеабКузбасс» пациенты получают помощь в любое время суток: опытные наркологи выезжают на дом, проводят капельницы и медикаментозную детоксикацию, подбирают индивидуальные схемы восстановления. Такой подход помогает не только устранить последствия запоя, но и запустить процесс полноценного оздоровления организма.
Получить дополнительную информацию – наркология вывод из запоя новокузнецк
Your posts provide a clear, concise description of the issues.
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Подробнее можно узнать тут – кодирование от алкоголизма анонимно волгоград
Выездная наркологическая помощь организована по чётко выстроенной схеме. Каждый этап направлен на стабилизацию состояния и безопасное восстановление функций организма после алкогольного или наркотического воздействия.
Исследовать вопрос подробнее – http://narkolog-na-dom-v-ufe17.ru
Лечение зависимости от алкоголя у мужчин в стационаре Балашихи. Мы предлагаем индивидуальный подход к лечению мужчин, учитывая все особенности организма.
Получить дополнительную информацию – вывод из запоя в балашихе
I got this site from my buddy who shared with me about this site and now this time
I am visiting this web page and reading very informative articles or reviews here.
Straightforward and practical advice.
Вывод из запоя — это не просто медицинская процедура, а системный процесс восстановления организма после длительного употребления алкоголя. В клинике «ВолгаМед Резолюция» в Волгограде пациенты получают помощь, основанную на принципах доказательной медицины и индивидуального подхода. Лечение направлено не только на устранение симптомов интоксикации, но и на стабилизацию нервной системы, восстановление водно-солевого баланса и нормализацию сна. Капельницы подбираются персонально, с учётом состояния пациента, сопутствующих заболеваний и возраста. Все процедуры проводятся анонимно и под контролем нарколога.
Углубиться в тему – вывод из запоя в стационаре
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Детальнее – http://narcologicheskaya-klinika-saratov0.ru
Лечение запоя у женщин в Химках. Мы предлагаем индивидуальный подход к лечению женщин, учитывая все особенности организма.
Подробнее тут – https://vyvod-iz-zapoya-himki11.ru/
these details https://toast-wallet.net/
Always enjoy the articles on Pengu Sport Slot. Cheers for the useful info!
https://pengusport.com/registration
Круглосуточная помощь при запое в стационаре Балашихи. Мы работаем 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Разобраться лучше – вывод из запоя с выездом в балашихе
Одним из ключевых направлений работы клиники является проведение инфузионных процедур. Капельницы позволяют вывести токсины, нормализовать давление и улучшить общее состояние пациента. Подбор препаратов проводится индивидуально, с учётом физического состояния, возраста и стадии зависимости.
Разобраться лучше – http://narkologicheskaya-pomoshh-v-tolyatti17.ru
This article explains the topic quite well.
Кодирование от алкоголизма в стационаре Балашихи. Мы предлагаем различные методы кодирования, подходящие для каждого пациента.
Подробнее тут – вывод из запоя вызов балашиха
Реабилитация после запоя в Люберцах. Мы поможем вам восстановиться после запоя и предотвратить рецидивы.
Получить больше информации – капельница от запоя наркология люберцы
Thanks for a marvelous posting! I actually enjoyed reading it, you might
be a great author.I will ensure that I bookmark your blog and will eventually come back
in the future. I want to encourage yourself to continue your great job, have a nice afternoon!
Hello! Do you use Twitter? I’d like to follow you if that would be okay.
I’m absolutely enjoying your blog and look forward to new updates.
Вывод из запоя — это не просто медицинская процедура, а тщательно выстроенный процесс, направленный на восстановление работы всех систем организма. При неправильном или неполном лечении риск осложнений возрастает в несколько раз. Поэтому обращение в профессиональную клинику становится необходимым шагом. В наркологической клинике «Центр Трезвости ВоронМед» пациент получает экстренную помощь, безопасные инфузионные препараты, круглосуточный выезд нарколога и последующее восстановление под наблюдением специалистов. Здесь каждая капельница подбирается индивидуально — с учётом возраста, веса, длительности запоя, хронических болезней и реакции организма на препараты.
Исследовать вопрос подробнее – http://vyvod-iz-zapoya-v-voronezhe17.ru/vyvod-iz-zapoya-za-den-voronezh/https://vyvod-iz-zapoya-v-voronezhe17.ru
При появлении таких симптомов важно не откладывать вызов врача. Самолечение, особенно с использованием неизвестных препаратов, может привести к тяжёлым последствиям, включая судороги и инсульт. Врачи клиники «ВолгаМед Резолюция» приезжают на дом с необходимыми средствами для оказания экстренной помощи и стабилизации состояния уже на месте.
Подробнее тут – вывод из запоя клиника волгоград
Профилактика рецидивов после запоя в Люберцах. Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Изучить вопрос глубже – вызвать капельницу от запоя на дому в люберцах
Круглосуточная помощь при запое в Химках. Мы работаем 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Изучить вопрос глубже – скорая вывод из запоя химки
Главным преимуществом наркологической клиники в Новокузнецке является комплексный подход к лечению. Специалисты рассматривают зависимость как заболевание, требующее системного воздействия на организм и психику. Каждый пациент получает индивидуальную программу, включающую медицинскую, психотерапевтическую и социальную помощь. Такой подход обеспечивает достижение устойчивых результатов и предотвращает рецидивы.
Детальнее – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkolog-novokuzneczk-na-dom
Комплексный подход обеспечивает не только снятие симптомов, но и полное восстановление функций организма. Пациент получает поддержку на всех этапах — от детоксикации до социальной адаптации.
Подробнее – нарколог наркологическая помощь в тольятти
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Углубиться в тему – https://narcologicheskaya-klinika-omsk0.ru/chastnaya-narkologicheskaya-klinika-omsk/
Анонимность и конфиденциальность гарантированы. Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Узнать больше – наркология вывод из запоя в химках
Комплексное применение этих методов позволяет значительно ускорить процесс восстановления и предотвратить осложнения.
Изучить вопрос глубже – наркологическая клиника клиника помощь новокузнецк
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Детальнее – вывод из запоя в стационаре рязань
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Cost Mesa, СA 92626, United States
Bail bonds Jobs
В Волгограде медицинская клиника «Трезвая Линия Волгоград» предоставляет круглосуточную помощь людям, столкнувшимся с острым алкогольным отравлением или затяжным запоем. Врачи выезжают на дом, в гостиницу или принимают пациентов в стационаре. Каждое вмешательство начинается с оценки состояния — измерения давления, пульса, насыщения кислородом, уровня интоксикации и дехидратации. Далее подбирается оптимальный состав капельницы, направленный на восстановление водно-солевого баланса, поддержку печени и снижение тревожности.
Разобраться лучше – http://vyvod-iz-zapoia-v-volgograde17.ru
Лечение в клинике «ВоронежМед Альянс» проходит поэтапно. Каждый модуль имеет определённую цель и собственные критерии эффективности. Такой подход исключает избыточное вмешательство и обеспечивает прозрачность процесса восстановления.
Разобраться лучше – https://narcologicheskaya-klinika-v-voronezhe17.ru/narkolog-voronezh-czena
Вывод из запоя у пожилых людей в Люберцах. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Детальнее – поставить капельницу от запоя люберцы
I’m not sure where you’re getting your information, but good topic.
I needs to spend some time learning more or understanding
more. Thanks for magnificent information I was looking for this info
for my mission.
В Воронеже команда «ВоронМед Профи» работает по принципу быстрой медицинской реакции — помощь оказывается независимо от времени суток и дня недели. Все выезды выполняются анонимно, без спецтранспорта и медицинской формы. Врач приезжает в гражданской одежде, что исключает ненужное внимание соседей и посторонних. В ходе осмотра специалист измеряет давление, пульс, температуру, оценивает уровень интоксикации и определяет степень обезвоживания. На основе полученных данных подбирается состав капельницы, который подаётся медленно и безопасно под контролем врача.
Получить больше информации – нарколог на дом круглосуточно
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Ознакомиться с деталями – вывод из запоя на дому цена рязань
Такая структура позволяет достичь максимального эффекта в кратчайшие сроки и минимизировать риск осложнений.
Углубиться в тему – вызвать врача нарколога на дом в уфе
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Исследовать вопрос подробнее – https://dvp.lt/projektas-homo-creator-lt
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Углубиться в тему – вывод из запоя капельница красноярск
Именно поэтому при затяжных запоях необходима квалифицированная медицинская помощь, позволяющая безопасно и максимально комфортно прекратить приём алкоголя. Клиника «Стратегия Здоровья» предлагает профессиональный вывод из запоя в Москве как в условиях стационара, так и с выездом на дом. Врачи работают круглосуточно, используя проверенные методики детоксикации и медикаментозной поддержки.
Изучить вопрос глубже – http://narko-reabcentr.ru
Howdy would you mind letting me know which hosting company you’re working with?
I’ve loaded your blog in 3 completely different internet
browsers and I must say this blog loads a lot quicker then most.
Can you recommend a good web hosting provider at a honest
price? Thanks a lot, I appreciate it!
Одним из самых востребованных направлений работы клиники является проведение детоксикации и вывод из запоя. Эти процедуры направлены на очищение организма от алкоголя и продуктов его распада, нормализацию работы печени и нервной системы. Лечение проводится с использованием сертифицированных препаратов и под контролем врача-нарколога.
Разобраться лучше – лечение в наркологической клинике
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Детальнее – наркологическая клиника нарколог в омске
Лечение запоя у женщин в Химках. Мы предлагаем индивидуальный подход к лечению женщин, учитывая все особенности организма.
Подробнее тут – нарколог на дом вывод из запоя химки
Vänligen fortsätt dela dessa vitala berättelser.
Процесс детоксикации состоит из нескольких последовательных шагов, направленных на безопасное очищение организма. Ниже представлена таблица с описанием этапов, которые применяются в клинике «Трезвая Линия Волгоград».
Разобраться лучше – http://vyvod-iz-zapoia-v-volgograde17.ru/
Everything is very open with a clear explanation of the issues.
It was definitely informative. Your site is very helpful.
Thanks for sharing!
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Исследовать вопрос подробнее – вывод из запоя капельница волгоград
Саратов живёт в разных темпах: плотный центр, протяжные магистрали, мостовые переезды. Мы учитываем это в логистике: выездные бригады «СаратовМед Профи» движутся по немаркированным маршрутам, приезжают в гражданской одежде, формируют на месте «тихую сцену» и только затем начинают клиническую часть. Если на предзвонке звучат «красные флаги» — давящая боль в груди, выраженная одышка, спутанность, неукротимая рвота, судороги — организуем перевод в стационар без пауз: место резервируем заранее, передислокация проходит конфиденциально.
Получить больше информации – вывод из запоя недорого саратов
Профессиональная помощь при запое в Люберцах. Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Подробнее можно узнать тут – капельница от запоя на дому московская область
Hi there, i read your blog from time to time and i own a similar one and
i was just wondering if you get a lot of spam comments?
If so how do you protect against it, any plugin or anything you can advise?
I get so much lately it’s driving me insane so any assistance is very much appreciated.
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Слушай внимательно — тут важно – http://www.bm-jcc.net/registration-of-trials
Основные этапы включают:
Получить дополнительную информацию – наркология вывод из запоя
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Хочешь знать всё? – https://sonnenberg.pl/demystifying-photovoltaic-system-inverters
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costta Mesa, СA 92626, United Stateѕ
what do bail bondsman charge
Вывод из запоя в стационаре Балашихи — надёжная помощь при алкогольной зависимости. Наши специалисты обеспечат круглосуточный медицинский уход и поддержку в комфортных условиях.
Детальнее – https://https://vyvod-iz-zapoya-v-stacionare-balashiha13.ru/
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Детали по клику – https://worksplumbing.us/commercial-exterior-catch-basins/catch-basin-clogged
Minnətdaram belə faydalı məlumat üçün.
https://Www.ensv.dz/cooperation-algero-britannique/formulaires/
После процедуры пациент чувствует улучшение уже через 1–2 часа: проходят головные боли, снижается давление, нормализуется сон и аппетит.
Изучить вопрос глубже – http://
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Получить дополнительные сведения – https://outcastband.co.uk/touring-show
Ниже приведена таблица, отражающая примерную динамику состояния пациента после постановки капельницы:
Выяснить больше – капельница от запоя круглосуточно
Алкогольная интоксикация вызывает сильное обезвоживание и разрушает баланс электролитов в организме. Без медицинской помощи восстановление может занять несколько дней, а в тяжёлых случаях приводит к осложнениям. Капельница помогает безопасно и быстро вывести этанол и продукты его распада, восполнить уровень жидкости, снизить нагрузку на печень и сердечно-сосудистую систему. Процедура проводится амбулаторно или на дому, что делает её доступной и удобной для пациентов.
Ознакомиться с деталями – капельница от запоя на дому волгоград
Nice blog here! Also your site loads up fast! What host are
you using? Can I get your affiliate link to your host? I wish my site loaded up as quickly as
yours lol
Inspiring initiative. Supporting vision care and medical treatment is incredibly
important, and this platform makes it easy to help those in need.
J’admire à quel point il est simple de aider ici.
Вывод из запоя у подростков в Химках. Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Детальнее – анонимный вывод из запоя в химках
Каждый компонент капельницы подбирается по медицинским показаниям. Врач учитывает возраст, хронические заболевания, степень обезвоживания и чувствительность к препаратам. Такой индивидуальный подход обеспечивает эффективность лечения и исключает осложнения.
Получить дополнительную информацию – наркология вывод из запоя
I used to be recommended this blog by way of my cousin. I
am now not certain whether or not this submit is written through him
as nobody else realize such distinct about my difficulty. You’re incredible!
Thank you!
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Подробнее – вывод из запоя в стационаре рязань
Анонимность и конфиденциальность гарантированы. Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Получить больше информации – помощь вывод из запоя
Thanks for sharing your knowledge.
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Детальнее – анонимная наркологическая клиника красноярск
I found the explanations here easy to understand.
Круглосуточная помощь при запое в Люберцах. Наша команда работает 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Разобраться лучше – капельница от запоя вызов в люберцах
I like reading through an article that will make men and women think.
Also, many thanks for permitting me to comment!
Анонимность и конфиденциальность гарантированы. Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Получить дополнительную информацию – нарколог на дом вывод из запоя химки
You really make it seem so easy with your presentation but I find this matter to be
actually something which I think I would never understand.
It seems too complex and very broad for me.
I’m looking forward for your next post, I’ll try to get the
hang of it!
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Подробнее тут – https://stage-curacao.nl/curacao-strandjes-playa-kanoa
Нельзя не сказать, что рад(а), что нашёл(а) сайт Sultan Casino — супер!
https://forums.maplesaga.com/proxy.php?link=https://sultan-casino-kazakhstan-winclub.kz/payments
It’s great that you are getting thoughts from this piece of writing
as well as from our dialogue made at this time.
Капельница — это основной инструмент дезинтоксикации при лечении запойных состояний. Она способствует выведению токсинов, нормализации обмена веществ и улучшению общего самочувствия. Состав раствора подбирается индивидуально в зависимости от степени интоксикации, возраста, массы тела и сопутствующих заболеваний. Уже через 20–30 минут после начала инфузии пациент ощущает облегчение, снижается тревожность и проходит головная боль.
Подробнее – https://vyvod-iz-zapoya-v-krasnoyarske17.ru/vyvod-iz-zapoya-na-domu-krasnoyarsk
This post explains the subject clearly.
Снятие ломки при алкоголизме в стационаре Балашихи. Наши специалисты помогут вам справиться с симптомами абстиненции.
Разобраться лучше – наркологический вывод из запоя в балашихе
Hey there! This post couldn’t be written any better!
Reading through this post reminds me of my old
room mate! He always kept chatting about this.
I will forward this article to him. Pretty sure he will have a
good read. Thank you for sharing!
This post offers a helpful explanation of the topic.
This is one of the most comprehensive guides I have read on this topic. The combination of detailed explanations and practical examples makes it highly valuable.
The insights provided here are highly relevant and practical. I like how the author includes examples from real situations, which makes the concepts easier to apply.
Снятие ломки при алкоголизме в Люберцах. Наши специалисты помогут вам справиться с симптомами абстиненции.
Узнать больше – вызвать капельницу от запоя люберцы
The content here is thorough and well-researched. I appreciate how it addresses both the benefits and limitations, giving a balanced view.
Наркологическая клиника в Волгограде предоставляет профессиональную медицинскую помощь людям, страдающим зависимостью от алкоголя, наркотиков и других психоактивных веществ. Основная цель специалистов — не просто устранить физическую зависимость, но и помочь пациенту вернуть внутреннее равновесие, здоровье и контроль над жизнью. В клинике применяются современные методы лечения, доказавшие свою эффективность в практике отечественной и мировой наркологии.
Подробнее тут – http://narkologicheskaya-klinika-v-volgograde17.ru/chastnaya-narkologicheskaya-klinika-volgograd/
I found this article very informative. The combination of detailed explanations, examples, and actionable tips makes it highly useful for readers.
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Получить дополнительные сведения – https://manchestercityclubs.nl/key-players-in-mexico-u17-fc-history
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Узнать больше – наркологические клиники алкоголизм
This content is very insightful and well-researched. I particularly liked the examples that demonstrate real-world applications of the advice.
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Получить дополнительную информацию – наркология вывод из запоя
I found the advice in this article very practical. The detailed explanations and real-life examples make it easy to apply the concepts discussed.
I found this article very engaging. The author combines detailed explanations with real-life examples, which helps in understanding the topic more deeply.
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Хочешь знать всё? – https://ialaqsa.com/10-ways-to-get-real-about-your-bodys-limitations-avoid-2
Во время лечения фиксируются все жизненные показатели пациента. При необходимости проводится экспресс-анализ крови и ЭКГ. Ниже представлена таблица, показывающая, какие параметры контролируются и по каким признакам оценивается стабилизация состояния.
Подробнее тут – вывод из запоя цена воронеж
Все процедуры выполняются анонимно и с соблюдением медицинских стандартов. Препараты применяются только сертифицированные, рассчитанные на мягкое восстановление организма без побочных эффектов. При необходимости лечение продолжается в стационаре, где пациент получает круглосуточное наблюдение, питание и психологическую поддержку.
Разобраться лучше – http://vyvod-iz-zapoya-v-novokuzneczke17.ru/vyvod-iz-zapoya-v-staczionare-novokuzneczk/
Cheers. I value it.
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Разобраться лучше – https://narcologicheskaya-klinika-omsk0.ru/narkologi-omska/
Детоксикация в клинике «Центр Трезвости ВоронМед» проводится по принципу минимального вмешательства при максимальной эффективности. Основная задача — очистить кровь от токсинов и стабилизировать внутреннюю среду организма без нагрузки на сердце и почки. Все препараты вводятся медленно, под контролем медицинского персонала, а состав подбирается индивидуально после оценки анализов и состояния пациента.
Подробнее можно узнать тут – вывод из запоя в стационаре в воронеже
I think the admin of this web site is in fact working hard for his web page,
because here every data is quality based material.
Конфиденциальность — это набор конкретных действий, а не декларация на сайте. Мы проектируем «невидимость» так, чтобы пациент мог спокойно принять помощь и не опасаться огласки.
Изучить вопрос глубже – лечение в наркологической клинике
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Ознакомиться с деталями – кодирование от алкоголизма
Процесс включает несколько шагов:
Получить больше информации – вызвать нарколога на дом срочно в уфе
Great work! That is the type of information that are meant to be
shared across the web. Shame on Google for now not positioning this publish
upper! Come on over and visit my site . Thank
you =)
Feel free to surf to my site … zenegovia01
Ниже приведена таблица с типовыми компонентами капельницы и их действием:
Получить дополнительную информацию – анонимный вывод из запоя в тольятти
It’s the best time to make some plans for the future and it is time to
be happy. I have read this post and if I could I want
to suggest you some interesting things or advice.
Maybe you could write next articles referring to this article.
I wish to read more things about it!
Look at my web page :: zenegovia02
If some one desires expert view about blogging then i propose him/her to pay a quick visit this weblog, Keep
up the pleasant job.
I was able to find good information from your articles.
Нарколог на дом в Уфе — это услуга, которая позволяет получить квалифицированную медицинскую помощь при алкогольной или наркотической интоксикации без необходимости госпитализации. Такой формат особенно востребован при запойных состояниях, когда пациент не может самостоятельно посетить клинику. Врач приезжает по вызову в течение короткого времени, проводит обследование, устанавливает капельницу и обеспечивает безопасный вывод из состояния опьянения. Все процедуры выполняются анонимно, с соблюдением медицинской этики и конфиденциальности.
Ознакомиться с деталями – https://narkolog-na-dom-v-ufe17.ru/
Профилактика рецидивов после запоя в Люберцах. Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Узнать больше – вызвать капельницу от запоя люберцы
A fascinating discussion is worth comment. I do believe that you need
to publish more on this subject, it may not be a taboo subject but typically people do not discuss such topics.
To the next! All the best!!
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, СA 92626, Unite States
bail and bonds
При появлении таких симптомов важно не откладывать вызов врача. Самолечение, особенно с использованием неизвестных препаратов, может привести к тяжёлым последствиям, включая судороги и инсульт. Врачи клиники «ВолгаМед Резолюция» приезжают на дом с необходимыми средствами для оказания экстренной помощи и стабилизации состояния уже на месте.
Разобраться лучше – вывод из запоя клиника в волгограде
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Исследовать вопрос подробнее – частная наркологическая клиника омск
goGLOW Omaha
3525 N 147th Տt, Omaha,
Nebraska, 68116, UႽA
(402) 940-8979
anti-aging skincare tips explained (go.bubbl.us)
После завершения инфузий врач-нарколог даёт рекомендации по питанию, водному балансу и образу жизни. При необходимости пациенту назначается курс поддерживающей терапии для закрепления эффекта.
Подробнее можно узнать тут – narkologicheskaya-pomoshh-v-tolyatti17.ru/
Great goods from you, man. I’ve understand your stuff previous to
and you’re just extremely fantastic. I actually like what you have acquired here, certainly
like what you’re stating and the way in which you
say it. You make it enjoyable and you still care
for to keep it smart. I can not wait to read far more from you.
This is really a tremendous site.
Лечение пивного алкоголизма в Химках. Мы предлагаем эффективные методы лечения зависимости от пива.
Ознакомиться с деталями – вывод из запоя вызов на дом в химках
Prіme Secured
3603 N 222nd Տt, Suiite 102,
Elkhorn, NΕ 68022, United Statеs
402-289-4126
Real-time threat intelligence monitoring (raindrop.io)
I must thank you for the efforts you have put in writing this website.
I am hoping to check out the same high-grade content
by you later on as well. In truth, your creative writing abilities has inspired me
to get my own blog now 😉
You ought to take part in a contest for one of the best blogs on the web.
I most certainly will recommend this web site!
Hmm is anyone else having problems with the pictures on this blog
loading? I’m trying to determine if its a problem
on my end or if it’s the blog. Any feedback would be greatly appreciated.
Своевременное обращение к специалистам позволяет быстро стабилизировать состояние и избежать осложнений.
Выяснить больше – вывод из запоя цена
Город с протяжёнными магистралями и разноскоростными районами требует особой организации маршрутов. Выездные бригады «ВолгаДок Медикал» работают в режиме 24/7, прибывают в гражданской одежде, избегают громких звонков и используют «немаркированные» подъезды. Перед приездом мы просим подготовить пространство: приглушить верхний свет, обеспечить приток свежего воздуха без сквозняков, подготовить ровную поверхность под укладку и удлинитель, перевести телефоны в «без уведомлений» с «белым списком» близких. Это позволяет в первые минуты сосредоточиться на клинике, а не на бытовых вопросах.
Исследовать вопрос подробнее – наркологическая клиника нарколог в саратове
Your clear explanations have eliminated my confusion.
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Исследовать вопрос подробнее – наркологическая клиника лечение алкоголизма саратов
Hi I am so glad I found your blog, I really found you
by mistake, while I was looking on Google
for something else, Anyhow I am here now and would just like to say thank
you for a fantastic post and a all round interesting blog (I also
love the theme/design), I don’t have time to read it all at the minute
but I have book-marked it and also added your RSS feeds, so when I have time I
will be back to read more, Please do keep up the
superb jo.
Лечение запоя без госпитализации в Люберцах. Мы предлагаем лечение на дому, без необходимости госпитализации.
Получить дополнительные сведения – капельница от запоя
This whole article adds to the conversation
is human trafficking tһе second largest, usa gymnastics coach human trafficking,
human trafficking news near me, snopes lynne knowles human trafficking, human trafficking awareness ԁay quotes, humsn trafficking sex scene, human trafficking –
menschenhandel, meghan connors hujman trafficking, ansrew tate human trafficking, arguments օn human trafficking, free human trafficking cme florida, human trafficking оur,
human trafficking in minnesota 2021, arizona republican human trafficking, orange іs tһe new black huhman trafficking,
human traffickung conference ocean city md, 277 arrested іn human trafficking, anti human trafficking laaw philippines, north korea human trafficking fаcts,
how wiⅼl the wall affect human trafficking, human rafficking training michigan 2018, hotels sued human trafficking, kids rescued fгom human trafficking, durham region human trafficking, ᴡhy huan traffiocking іs imрortant, mother oof god church human trafficking, walmart human trafficking 2020,
whhat іѕ the rate of human trafficking worldwide, human trafficking news
(news), human trafficking Ьy stae 2021, lgbt human tafficking statistics,
south africa аnd human trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewed hope
human trafficking, human trafficking atlanta 2022, human trafficking san joaquin county, non profit organizations fօr human trafficking, human trafficking
interpol, human trafficking elgin, trafficking women’ѕ human rights julietta hua,
facebook human trafficking lawsuit, rates ߋf human trafficking, real ѡorld exаmple of human trafficking, lawyers ɑgainst
human trafficking, wsin human trafficking summit 2022, vad är human trafficking, recognizing
tһe signs off human trafficking, human trafficking
justice, video ⲟf human trafficking, foսr signs of human trafficking, human trafficking honey, binjun xie human trafficking, human trafficking documentary aazon ρrime, minnesota human trafficking data, uncovers russian human trafficking
гing waг, human trafficking chico ϲa, human trafficking jus cogens, human trafficking syrian refugees, human trafficking topics гesearch paper,
text human trafficking link snopes, oprah south africa human trafficking,
human trafficking grants 2015, human trafficking san antonio 2021,
human drug trafficking meaning, human trafficking stories children, ferma human trafficking awareness, florida disney human trafficking, jobs fߋr human trafficking victims, movie
аbout human trafficking 2023 netflix, а day іn the lice of a human trafficking victim, uk human trafficking news,
bent ⅼicense plate human trafficking reddit, hunan trafficking іn waterbury ct,
centyer tо combat human trafficking, greenville nc human trafficking, maui human trafficking, t᧐p 5 human trafficking cities,
іs human trafficking happening іn the uѕ, oxnard human trafficking, aurora soreline human trafficking, taconganas human trafficking, hashtags fοr human trafficking, ᴡhite
house human trafficking summit, corona human trafficking,
border patrol human trafficking, huuman trafficking іn thailand 2020, human trafficking іn wv,
11 arrested inn human trafficking, china’ѕ one chikd policy ɑnd human trafficking, hotels human trafficking 2023,
human trafficking іn florida 2021, human trafficking debate topics, international justice mission human trafficking,
uncovers human traffickung ring fօr, scholarly article ⲟn human trafficking,
maduson herman human trafficking, amad diallo human trafficking,
а poem ɑbout huyman trafficking, hman trafficking
bristol tn, deluca ɑnd the human trafficking
storyline, economy and human trafficking, human trafficking іn trinidad, human trafficking ԁay 2018, caught camera actual
hukan trafficking victims, human trafficking episode opoal grey’ѕ anatomy,
duolingo ceo humnan trafficking, watch dogs human trafficking map, human trafficking definition canada,
airtag human trafficking, human trafficking іn the beauty industry,
人口販子human trafficking, forced labor іn human trafficking, american airlinnes center human trafficking, human trafficking ⅽе
texas, selah human trafficking, sim huan trafficking,
fresno human trafficking statistics, senegal human trafficking,
human trafficking belgium, michigan human trafficking
ⅽourse, ny tіmes human trafficking, abandokned stroller human trafficking, human trafficking і-44,
solution on human trafficking, human trafficking canada news, ontario human trafficking,
protects victims oof human trafficking amendment, human traffickinmg іn highland ca, human trafficking hotspot map, human trafficking organizations ontario, human trafficking hiding ᥙnder cars, summary оn human trafficking, uncovers russian human trafficking riung war, human trafficking honey, fοur signs оf human trafficking, human trafficking
western pa, human trafficking livermore, human trafficking durham
region, human trafficking ɑt atlanta airport, binjun xie hunan trafficking, minnesota human trafficking data, human trafficking documentary amazon ρrime, human trafficking llawyer bloomfield hills,
human trafficking charge іn texas, central sgudents ɑgainst
human trafficking, ap human geography human trafficking, human trafficking fоr sexual exploitation, blue fօr
human trafficking, kantian ethics humaqn trafficking, anti-human trtafficking organization іn cambodia, jjo jorgensen ᧐n human trafficking, fokrt ood soldiers human trafficking, beau ߋf the fіfth colun humn trafficking, hawkins human trafficking,
human trafficking iin thee pacific islands, reasns ᴡhy human trafficking
іs bad, ally human trafficking, ᴡrite an essay ߋn human trafficking, human trafficking pros, human trafficking
dsrk web reddit, north prestoln huma trafficking,
dllar sign tattoo human trafficking, wht іs humman trafficking, human trafficking stuart
fl, priceless movie human trafficking, ti ɑnd wife human trafficking,
human trafficking ethnicity statistics, і 80 truck stop human trafficking, hamilton human trafficking, oakville
human trafficking, human traffickihg ߋn the deep web, current human trafficking, human trafficking women’ѕ rights, brunei
human trafficking, barack obama human trafficking quote, patron saint οf human trafficking, spirited ɑway human trafficking,
tһe game human trafficking, t᧐ρ human trafficking cities
2023, human trafficking ԝhich countries aree tһe worst, hoѡ to donate t᧐ human traffickoing organizations, humawn traafficking quotes famous, human trafficking story
2020, human trafficking іn pittsburgh,2020 human trafficking conference, human trafficking bust atlanta, human traffficking hemet ⅽa, human trafficking statistics oregon, һow to identify a huan trafficking victim, economy ɑnd human trafficking, lover boy method οf
human trafficking, deluca ɑnd the human trafficking storyline, europezn human trafficking,
selah human trafficking, american airlines center humkan trafficking,
human trafficking paintings, ԝhat state is #1 in human trafficking?,
forced labor in human trafficking, 人口販子human trafficking, crystal meth, ѡat doeѕ crystal merth ⅼooқ like, what іs crstal meth, crystal meth anonymous,
һow long does crystal meth stay іn your system, һow tо make crystal meth, blue crystal
meth, buy crystal meth online, crystal meth effects, crystal meth pipe,
crystal meth drug, whawt ɗoes crystal meth look like?, meth crystal, crystal meth images, crystal meth
sid effects, һow is crystal meth mɑde, meth vs crystal meth,
wһat does crystal meth do, crystal meth symptoms, crystal
meth ѵs meth, effects off crystal meth, ѕide effects оff crystal meth, һow do yoᥙ
maкe crystal meth, crystal meth νs crack, whаt ԁoes crystal mth smell ⅼike, how is crystal meth used, crystal meth withdrawal,
crystal meth breaking bad, ԝhat is crystal meth mаde of, what does crystal meth ⅾo to
yoᥙ, crystal meth teeth, smoking crrystal meth, crystal meth pictures, ϲɑn you snort crystal meth, crystal meth ƅefore and
аfter, who invented crystal meth, crystal meth fɑcts,
crytstal meth withdrawal symptoms, crystal meth street names,
signs ߋf crystal meth, crystal meth addiction, һow to
cokok crystal meth, crystal meth definition, ѡһаt type օf
drug іs crystal meth, what ԁoes crystal meth feel ⅼike, crystal meth
meaning, crystal meth ingredients, ᴡhats crystal meth, wһat cololr іs crystal meth,
crystal meth detox, crystal meth fаⅽe, crystal meth powder,
crystal meth poem, street names f᧐r crystal meth, short term effects of
crystal meth, signs ߋf crystal meth abuse, crystal
meth rock, crystal meth fly, crysatal meth addict, crystal meth սsers, crysta meth rehab, how
much does crystal meth cost, howw ⅾօ you takе
crystal meth, һow much is crystal meth, signs of crystal meth ᥙse, hοw to smoke crystal meth,
how to ᥙse crystal meth, long term efdfects оf crystal meth, signs оf addictioin tο crystal meth,
pink crystal meth, crystal meth ⅼⲟߋk liқe, breaking bad crystgal meth, wһen was crystal meth invented, pictures of crystal
meth, һow iѕ crystal meth taken, signs tһat
someⲟne iѕ սsing crystal meth, ready or not crystal mesth storage,
difference Ƅetween meth ɑnd crystal meth, hօw do yoou
do crystal meth, cryustal meth., locate crystal meth storage, ԝһat are the effects
᧐f ccrystal meth, fake crystal meth, crystal meth people, ѡhat does crystal meth,
hoԝ ԁօ үоu usee crystal meth, hօѡ addictive іs
crystal meth, cаn уoᥙ overdose on crystal meth, rystal meth blue, crystal meth signs, һow long ⅾoes crystal meth
ⅼast, crystal meth detox los angeles, һow dⲟ people use crystal meth, һow does crystal meyh looқ like, crystal meth porn, һow ԁoes crystal
meth lo᧐k, crystal meth storage twisted
nerve, ᴡhats in crystal meth, crystal meth treatment, ѡhat iѕ crystal meth
mаde from, methamphetamin, ethamphetamin adalah, methamphetamin ⅾan amphetamin adalah,
amphetamin ԁan methamphetamin, chloroethane and methamphetamin, crystal methamphetamin, ѡhat іs methamphetamin, methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma
methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl,
amphetamin vѕ methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin ɗаn methamphetamin, difference Ьetween amphetamine
and methamphetamin, methamphetamin psychose, methamphetamin rules,
һow tօ mke methamphetamin, methamphetamin amphetqmin unterschied,
methamphetamin hydrochloride, definition von methamphetamin, p2p methamphetamin, methamphetamin medizin, amphetamin und methamphetamin, vicks vapor inhaler
methamphetamin, gta methamphetamin labor, ѡie wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects,
methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine
սnd methamphetamin, methamphetamin herstellung, methamphetamin hersgellung china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow tо cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ѡas ist dɑs, unterschied
methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache,
methamphetamin chemical formula, methamphetamin medikament,
methamphetamin laa chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methampbetamin аndere suchten auсh naϲh,
methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamhetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy
methamphetamin, methamphetamin Ԁương tính, ѡaѕ іst methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure, іѕt mdma methamphetamin, lye
іn methamphetamin, іst methamphetzmin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetamin meaning, ɗ-methamphetamin, herstfellung methamphetamin,
methamphetamin νs amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin,
methamphetamin fаce, methamphetamin formula, methamphetamin synapse, methamphetamin adderall,
methamphetamin adhd, blue methamphetamin, wirkung methamphetamin,
methamphetamin terbuat dari, methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt,
methamphetamin synthese, methamphetamin ᥙsе icd 10, weed,
weed grinder, wherre іs weed legal, disposqble weed pen, weed shop neɑr me, milwaukee
weed eater, purple weed, is weed legal іn virginia, іs weed legal іn oklahoma, іs weed legal
іn louisiana, weed ppuller tool, weed carts, iis weed legal іn south carolina,
weed killer fοr lawns, horny goa weed for men, ԝһat ѕtates is
weed legal, weed shops neаr me, weed legal stateѕ, weed vape, roundup weed killer, weed killer spray, edibles weed,
recreational weed ѕtates, weed store, milk weed, werd barrier, іs weed legal in indiana,
legal weed ѕtates, states witһ legal weed, іs weed legall in kentucky, weed
puller, preren weed preventer, ounce օf weed,
dewalt weed eater, plantain weed, usqvarna weed eater,
electric weed eater, hybrid weed, moonrock weed, weed pipe, barrett wilbert weed, weed control, weed delivery neаr me, is weed legal in missouri,
how to make weed butter, ԝhite weed, iѕ weed legal in utah, moon roock weed, snow caps weed,
іs weed legal іn arkansas, is weed legal in texas 2025, ryobi weed eater, weed bowl, dill weed, weed legalization, smoking weed, iss weed legal іn nevada, weed whacker, іѕ weed legal іn alabama, iis weed ɑ drug, weed barrier fabric, ѡhat is horny
goat weed, spruce ѡed and grass killer, weed stores neаr
me, sprinkles weed, poke weed, weed withdrawal, wred
vapes, snow caap weed, rm43 weed killer, craftsman weed eater, qp οf weed,
weed edibles, cookies weed, gelato weed, іs
weed legal іn neew mexico, strains ߋf weed, weed butter, ρound off weed, zaza
weed, is weed legal іn nc, hoow mսch іѕ аn ounce of weed, pgr weed, is dеlta 9 real
weed, diy weed killer, zip of weed, weeed torch, moldy weed, elon musk weed, iis
weed illegal inn texas, weed eater string, rso weed, weed hangover, weed wallpaper, iss weed legal іn nebraska, howw tߋ smoke weed, iѕ weed legal in hawaii,
how tо grow weed, һow to make weed іn infinite craft,
іs weed legal in california, gary payton weed
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Подробнее можно узнать тут – нарколог вывод из запоя рязань
Процесс лечения проходит поэтапно и под постоянным наблюдением специалистов. Каждый этап направлен на определённый аспект восстановления здоровья и личности пациента.
Изучить вопрос глубже – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk
Лечение зависимости от алкоголя у мужчин в Химках. Мы предлагаем индивидуальный подход к лечению мужчин, учитывая все особенности организма.
Углубиться в тему – вывод из запоя анонимно
Heya i am for the first time here. I found this board and I find It really
useful & it helped me out much. I hope to give something back and help others
like you helped me.
why not try this out https://jaxxwallet-web.org/
Лечение организовано поэтапно, что помогает пациенту постепенно возвращаться к полноценной жизни. Каждый шаг направлен на укрепление результата и снижение риска рецидива.
Изучить вопрос глубже – вывод наркологическая клиника
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Подробнее – после капельницы от запоя
Appreciating the time and effort you put
into your blog and detailed information you
present. It’s good to come across a blog every
once in a while that isn’t the same out of date rehashed
material. Great read! I’ve bookmarked your site and I’m including your RSS
feeds to my Google account.
Вывод из запоя у подростков в Люберцах. Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Получить дополнительные сведения – вызвать капельницу от запоя на дому люберцы
Very nice article, exactly what I was looking for.
Процесс лечения проходит поэтапно и под постоянным наблюдением специалистов. Каждый этап направлен на определённый аспект восстановления здоровья и личности пациента.
Получить больше информации – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk/
Капельница от запоя в Люберцах — быстрый и эффективный способ детоксикации. Наши специалисты приедут к вам домой и проведут процедуру, помогая снять симптомы похмелья и вывести токсины из организма.
Ознакомиться с деталями – капельница от запоя город. московская область
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Углубиться в тему – запой наркологическая клиника в саратове
Лечение запоя у женщин в Химках. Мы предлагаем индивидуальный подход к лечению женщин, учитывая все особенности организма.
Изучить вопрос глубже – вывод из запоя дешево в химках
Вызов нарколога на дом — это удобная и безопасная возможность получить медицинскую помощь без необходимости ехать в клинику. Такая услуга особенно востребована, когда состояние пациента не позволяет покинуть дом, а помощь требуется незамедлительно. В наркологической клинике «ВоронМед Профи» организована круглосуточная служба выезда специалистов, которая оперативно реагирует на обращения и обеспечивает профессиональную помощь при запое, алкогольной интоксикации и обострениях хронических состояний. Врач приезжает в течение часа, оценивает состояние пациента и подбирает оптимальную схему лечения, включающую капельницы, детоксикацию и рекомендации по восстановлению организма.
Получить дополнительную информацию – нарколог на дом клиника
Сайт Sultan Casino очень информативный. Обязательно загляну ещё!
https://sultan-casino-kazakhstan-betman.kz/mobile-app
После процедуры пациент чувствует улучшение уже через 1–2 часа: проходят головные боли, снижается давление, нормализуется сон и аппетит.
Детальнее – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk/
goGLOW Omaha
3525 N 147th Տt, Omaha,
Nebraska, 68116, UЅA
(402) 940-8979
Microdermabrasion process solution
Профилактика рецидивов после запоя в Люберцах. Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Получить больше информации – https://kapelnica-ot-zapoya-lyubercy13.ru/
Капельница от запоя — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Углубиться в тему – срочный вывод из запоя в химках
Лечение организовано поэтапно. Такой подход обеспечивает постепенное восстановление функций организма и исключает риск осложнений. Каждый этап терапии направлен на устранение конкретных нарушений, вызванных интоксикацией.
Детальнее – http://vyvod-iz-zapoya-v-krasnoyarske17.ru/czentr-kodirovaniya-vyvod-iz-zapoya-krasnoyarsk/
Процесс включает несколько шагов:
Разобраться лучше – https://narkolog-na-dom-v-ufe17.ru/vyvod-iz-zapoya-ufa-narkolog-na-dom
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Подробнее тут – https://idherranz.es/2023/07/18/9-consejos-para-mejorar-el-enfoque-en-tus-fotos
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Детальнее – вывод из запоя недорого в рязани
Вывод из запоя на дому — удобно и безопасно. Наши специалисты приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния.
Подробнее тут – вывод из запоя круглосуточно
Can you tell us more about this? I’d care to find out some additional information.
Heya i’m for the first time here. I came across this board
and I find It really useful & it helped me out a lot.
I hope to give something back and help others like you aided me.
Одним из самых востребованных направлений работы клиники является проведение детоксикации и вывод из запоя. Эти процедуры направлены на очищение организма от алкоголя и продуктов его распада, нормализацию работы печени и нервной системы. Лечение проводится с использованием сертифицированных препаратов и под контролем врача-нарколога.
Углубиться в тему – запой наркологическая клиника
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Углубиться в тему – нарколог на дом вывод из запоя в воронеже
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ϹA 92626, United States
va bail bonds
Капельница от запоя в стационаре — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Детальнее – анонимный вывод из запоя в балашихе
Спасибо за такой полезный контент о Sultan Casino и азартных играх.
https://www.esg-ci.com/esg/index.php/component/mediatheque/?task=showpagelien&str_LIEN_NAME=https://sultan-casino-kazakhstan-betting.kz/bonuses
Помощь при алкогольной интоксикации в Химках. Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Подробнее можно узнать тут – нарколог вывод из запоя
Все растворы проходят фармацевтический контроль, а процедуры выполняются одноразовыми стерильными инструментами. После завершения капельницы врач наблюдает пациента в течение 15–30 минут, оценивает результат и даёт рекомендации по дальнейшему восстановлению. Важно не прерывать терапию самостоятельно — эффект закрепляется только при соблюдении рекомендаций.
Углубиться в тему – http://narkolog-na-dom-v-voronezhe17.ru/voronezh-narkologicheskaya-klinika/
Профилактика рецидивов после запоя в Люберцах. Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Изучить вопрос глубже – капельница от запоя клиника в люберцах
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Получить дополнительную информацию – вывод из запоя капельница
Hello there, just became alert to your blog through Google, and found that it’s truly informative.
I’m gonna watch out for brussels. I will be grateful if you continue this in future.
Numerous people will be benefited from your writing. Cheers!
My website :: https://latbet.click/
Кодирование от алкоголизма на дому в Люберцах. Наши специалисты приедут к вам домой и проведут процедуру кодирования.
Получить больше информации – поставить капельницу от запоя люберцы
Thanks for sharing your info. I really appreciate your efforts and I will
be waiting for your further post thank you
once again.
This website was… how do I say it? Relevant!! Finally
I have found something that helped me. Thank you!
Hello, Neat post. There is an issue along with your website in internet explorer,
may check this? IE still is the market leader and a good part of folks
will omit your wonderful writing due to this problem.
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Смотрите также… – https://thenews21.com/maharashtra-man-sets-himself-ablaze-outside-vidhan-bhavan-in-mumbai
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Подробнее можно узнать тут – помощь вывод из запоя
Капельница не просто устраняет симптомы похмелья — она восстанавливает внутренний баланс, снижает токсическую нагрузку и поддерживает работу жизненно важных органов. После процедуры пациент чувствует прилив сил, прояснение сознания и эмоциональную стабильность. Эффект закрепляется при соблюдении рекомендаций врача и отказе от алкоголя в последующие дни.
Углубиться в тему – скорая вывод из запоя в волгограде
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Открой скрытое – https://charlottejader.de/hello-world-2
Анонимность и конфиденциальность гарантированы. Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Разобраться лучше – поставить капельницу от запоя люберцы
Вывод из запоя — это не «волшебная капельница», а последовательная медицинская программа с чёткими целями и измеримыми маркерами. В наркологической клинике «СаратовМед Профи» маршрут строится по принципу управляемых окон: на каждом шаге команда преследует одну цель, меняет лишь один параметр и оценивает результат в заранее назначённый момент. Такой подход снижает лекарственную нагрузку, предотвращает «гонку дозировок» и делает динамику предсказуемой для пациента и близких. Конфиденциальность обеспечивается регламентом: немаркированные выезды, нейтральные формулировки в документах, «тихие» каналы связи, доступ к записям — строго по ролям.
Детальнее – вывод из запоя на дому круглосуточно
Снятие ломки при алкоголизме в Химках. Наши специалисты помогут вам справиться с симптомами абстиненции.
Ознакомиться с деталями – вывод из запоя на дому цена
Капельница от запоя в стационаре — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Выяснить больше – вывод из запоя клиника в балашихе
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Получить больше информации – наркологическая клиника стационар в новокузнецке
Interesting perspective! I’m curious how this approach works in real-world scenarios.
Minnətdaram belə faydalı məlumat üçün.
https://betandreas-azerbaijan-bet.com/mobil-tetbiq
Анонимность и конфиденциальность гарантированы. Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Узнать больше – вывод из запоя клиника химки
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Подробнее можно узнать тут – наркологическая клиника стационар
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Подробнее – https://vyvod-iz-zapoya-v-krasnoyarske17.ru/vyvod-iz-zapoya-na-domu-krasnoyarsk/
Вывод из запоя в Химках — профессиональная помощь на дому. Наши опытные наркологи приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния и вывода из запоя.
Ознакомиться с деталями – вывод из запоя недорого химки
Каждый из этапов сопровождается контролем врача и постепенным снижением медикаментозной нагрузки. Важно не просто снять симптомы, но и научить пациента распознавать внутренние триггеры, чтобы предотвратить рецидив. На протяжении всего лечения сохраняется поддержка психолога, который помогает адаптироваться и перестроить привычные модели поведения.
Подробнее – наркологическая клиника нарколог в воронеже
Лечение хронического алкоголизма в Химках. Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Получить больше информации – вывод из запоя с выездом химки
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Уточнить детали – https://yasulog.org/how-to-cancel-nordvpn
Круглосуточная помощь при запое в Химках. Мы работаем 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Получить больше информации – врач вывод из запоя
Капельница от запоя в стационаре — эффективный способ детоксикации. Мы используем современные препараты для быстрого и безопасного выведения из запоя.
Получить больше информации – вывод из запоя в стационаре в балашихе
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Детальнее – вывод из запоя на дому цена в саратове
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Углубиться в тему – анонимный вывод из запоя
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Подробнее – http://vivod-iz-zapoya-v-volgograde17.ru/vyvod-iz-zapoya-na-domu-volgograd/
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
А что дальше? – https://www.sciclubvolverabike.it/events/gita-la-thuille
Вывод из запоя у пожилых людей в Химках. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Детальнее – вывод из запоя недорого
First off I want to say terrific blog! I had a quick question that I’d like to
ask if you do not mind. I was interested to know how you center yourself and clear your head before writing.
I have had difficulty clearing my thoughts in getting my thoughts out there.
I truly do take pleasure in writing however it just seems like the first 10 to 15 minutes are
usually wasted just trying to figure out how to begin. Any suggestions
or hints? Thank you!
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Смотрите также… – https://www.wirtschaftleichtverstehen.de/?attachment_id=1145
Реабилитация после запоя в Люберцах. Мы поможем вам восстановиться после запоя и предотвратить рецидивы.
Детальнее – капельница от запоя анонимно
Really lots of valuable data.
These casinos are big on privacy, supporting only cryptocurrencies for payments, which means players don’t need to share personal info with the sites.
Каждый из этапов сопровождается контролем врача и постепенным снижением медикаментозной нагрузки. Важно не просто снять симптомы, но и научить пациента распознавать внутренние триггеры, чтобы предотвратить рецидив. На протяжении всего лечения сохраняется поддержка психолога, который помогает адаптироваться и перестроить привычные модели поведения.
Получить дополнительную информацию – наркологическая клиника наркологический центр воронеж
Все растворы проходят фармацевтический контроль, а процедуры выполняются одноразовыми стерильными инструментами. После завершения капельницы врач наблюдает пациента в течение 15–30 минут, оценивает результат и даёт рекомендации по дальнейшему восстановлению. Важно не прерывать терапию самостоятельно — эффект закрепляется только при соблюдении рекомендаций.
Ознакомиться с деталями – нарколог на дом срочно
В этой информационной статье вы найдете интересное содержание, которое поможет вам расширить свои знания. Мы предлагаем увлекательный подход и уникальные взгляды на обсуждаемые темы, побуждая пользователей к активному мышлению и критическому анализу.
Узнайте всю правду – https://vistoweekly.com/anna-kate-denver
You’re so cool! I do not think I have read a single thing
like that before. So wonderful to find another person with original thoughts on this topic.
Seriously.. thank you for starting this up. This site
is one thing that’s needed on the web, someone with a little
originality!
goGLOW Omaha
3525 N147tһ St, Omaha,
Nebraska, 68116, UᏚΑ
(402) 940-8979
Goglow Best
Основные этапы включают:
Исследовать вопрос подробнее – анонимный вывод из запоя
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Разобраться лучше – https://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk
Игнорирование этих симптомов может привести к тяжёлым последствиям — судорогам, галлюцинациям или алкогольному психозу.
Получить больше информации – вывод из запоя на дому круглосуточно в тюмени
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CA 92626, United States
Bail Bonds Man
Remember to explore different options to find the best crypto casino that aligns with your preferences.
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Детали по клику – https://www.alyssazwonok.com/2021/01/20/blog-post-layout-04
Процесс включает несколько шагов:
Подробнее можно узнать тут – нарколог на дом срочно уфа
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Проследить причинно-следственные связи – https://portadorcargo.hu/faq-items/maecenas-nec-ante-metus-accumsan-eleifend
Вывод из запоя у подростков в Химках. Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Подробнее – вывод из запоя на дому недорого в химках
hello!,I love your writing very a lot! proportion we keep in touch extra about your
article on AOL? I require an expert on this area to
resolve my problem. Maybe that’s you! Having a look forward to peer you.
It’s truly very complex in this active life to listen news on Television, so I only use
internet for that reason, and take the most up-to-date news.
Читать далее https://forum.hpc.name/thread/x350/72603/crud-operacii-s-bazoy-dannyh-v-wpf-primer-s-tablicey-teachers.html
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Подробнее тут – https://www.skolakancelaria.sk/blog-post-with-youtube-video-2
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Изучите внимательнее – https://www.gishurim.co.il/%D7%97%D7%9C%D7%95%D7%A7%D7%AA-%D7%A8%D7%9B%D7%95%D7%A9-%D7%91%D7%92%D7%99%D7%A8%D7%95%D7%A9%D7%99%D7%9F
This raises some good points. Have you tested this method in practice?
Angels Baail Bonds Costa Mesa
769 Baer Ꮪt,
Costa Mesa, CA 92626, United Ⴝtates
0 percent financing bail bonds
Ниже приведена таблица, отражающая примерную динамику состояния пациента после постановки капельницы:
Подробнее – капельница от запоя клиника
Когда острые угрозы исключены, программа стартует дома. Пациент получает понятную карту действий, близкие — короткие окна обратной связи, врач — чистую «картинку» для тонкой настройки. Мы просим сообщать факты, а не эмоции: минуты до засыпания, число пробуждений, объём тёплой воды малыми глотками, пульс к вечеру, переносимость мягкой пищи, ясность головы утром.
Получить больше информации – вывод из запоя
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Детальнее – врач вывод из запоя волгоград
We are a group of volunteers and starting a new scheme in our community.
Your website offered us with valuable info to
work on. You’ve done a formidable job and our entire community will
be thankful to you.
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Выяснить больше – наркологическая клиника стационар в саратове
Ниже приведена таблица, отражающая примерную динамику состояния пациента после постановки капельницы:
Подробнее можно узнать тут – капельница от запоя круглосуточно в воронеже
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Получить дополнительную информацию – https://enfieldcc.ie/1st-year-application-form-for-the-2025-2026
Hi everyone, it’s my first pay a quick visit at this website,
and piece of writing is truly fruitful in favor of me, keep up posting these articles or reviews.
найти это https://forum.hpc.name/thread/b011/104282/kak-steret-jestkiy-disk-pri-starte-sistemy-cherez-udalenku.html
Mangelsen
7916 Girard Avenue, Ꮮa Joya
CA 92037, United States
1 800-228-9686
amazing wildlife documentaries pbs wildlife
Источник https://forum.hpc.name/thread/i451/70040/vybor-cms-ili-freymvorka-dlya-sayta-uchebnyh-kursov.html
узнать больше https://forum.hpc.name/thread/a492/134385/kak-pravilno-rasschitat-rezistor-v-sheme-s-operacionnym-usilitelem.html
В таблице представлены основные элементы детоксикационной терапии:
Разобраться лучше – платная наркологическая клиника в волгограде
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Изучить вопрос глубже – запой наркологическая клиника
Excellent blog right here! Additionally your site so much up very fast!
What web host are you the use of? Can I am getting your affiliate link for
your host? I want my website loaded up as fast as yours lol
Процесс включает несколько шагов:
Ознакомиться с деталями – https://narkolog-na-dom-v-ufe17.ru/narkolog-ufa-anonimno
Помощь при алкогольной интоксикации в Люберцах. Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Выяснить больше – вызвать капельницу от запоя на дому
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Узнать больше – http://
Hey there! I just want to give you a huge thumbs up for your excellent info you have here on this post.
I am returning to your blog for more soon.
Пациент может выбрать анонимный формат — все данные защищены, а пребывание в клинике проходит в атмосфере уважения и деликатности. Особое внимание уделяется созданию комфортных условий: палаты оснащены системой вентиляции, регулируемым освещением и кнопкой вызова медперсонала. Круглосуточный контроль состояния позволяет своевременно реагировать на малейшие изменения и корректировать курс лечения.
Узнать больше – наркологические клиники алкоголизм воронеж
Подробнее здесь https://forum.hpc.name/thread/q840/117353/kak-vybrat-korpus-s-horoshey-shumoizolyaciey-sovety-i-rekomendacii.html
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Изучить вопрос глубже – narkologicheskaya-clinica-v-novokuzneczke17.ru/
Spot on with this write-up, I absolutely believe this
web site needs much more attention. I’ll
probably be back again app to settle shared payments easily read through
more, thanks for the info!
You made some decent points there. I looked on the internet
to find out more about the issue and found most individuals will go along with your
views on this website.
Профессиональная помощь при запое в Люберцах. Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Ознакомиться с деталями – kapelnicza-ot-zapoya lyubercy
Капельница от запоя — доступная цена в Люберцах. Стоимость процедуры начинается от 2400 ?, и вы всегда будете заранее информированы о стоимости услуг.
Получить больше информации – капельница от запоя на дому люберцы
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Исследовать вопрос подробнее – нарколог на дом вывод
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Подробнее можно узнать тут – нарколог вывод из запоя
Такая форма помощи позволяет избежать осложнений, которые часто сопровождают попытки снять симптомы самостоятельно. При правильном подборе препаратов уже через час наблюдается улучшение самочувствия: уходит головная боль, снижается тревога, стабилизируется сердцебиение и восстанавливается ясность мышления. Пациент получает рекомендации по питанию, режиму отдыха и приёму витаминов, чтобы закрепить результат и предотвратить повторный срыв.
Исследовать вопрос подробнее – http://narkolog-na-dom-v-voronezhe17.ru/voronezh-narkologiya/
No matter if some one searches for his required thing, so
he/she wants app to settle shared payments easily be available that in detail,
therefore that thing is maintained over here.
Вывод из запоя у пожилых людей в стационаре Балашихи. Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Получить больше информации – вывод из запоя в стационаре в балашихе
Такая структура терапии делает процесс максимально эффективным и безопасным.
Получить больше информации – наркологическая клиника стационар омск
Лечение зависимости от алкоголя у мужчин в Люберцах. Мы предлагаем индивидуальный подход к лечению мужчин, учитывая все особенности организма.
Получить дополнительную информацию – капельница от запоя на дому цена
Лечение пивного алкоголизма в Химках. Мы предлагаем эффективные методы лечения зависимости от пива.
Ознакомиться с деталями – вывод из запоя на дому круглосуточно
Длительное злоупотребление спиртным неизбежно приводит к серьёзным последствиям для организма. Алкоголь влияет на работу практически всех внутренних органов: печень испытывает повышенную нагрузку при выводе токсинов, почки страдают от нарушения водно-солевого баланса, а сердечно-сосудистая система подвержена скачкам давления и аритмиям. Постепенно ухудшается общее самочувствие – возникают постоянные головные боли, слабость, повышенная раздражительность, бессонница.
Подробнее тут – наркологический вывод из запоя москва
An interesting discussion is definitely worth comment.
I believe that you ought to write more about
this subject matter, it may not be a taboo matter but usually people don’t talk about
such issues. To the next! Kind regards!!
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Посмотреть всё – https://logisticaintegral.online
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Подробнее тут – наркологическая клиника вывод из запоя в волгограде
We’re a gaggle of volunteers and starting a new scheme in our community.
Your site provided us with useful information to work on. You have performed
a formidable process and our entire group will be grateful to you.
The process to donate is very easy.
Feel free to surf to my blog post Fund Cataract Treatment
Ниже приведена таблица, отражающая примерную динамику состояния пациента после постановки капельницы:
Исследовать вопрос подробнее – https://kapelnicza-ot-zapoya-v-voronezhe17.ru/otkapatsya-voronezh-nedorogo/
Лечение зависимости от алкоголя в стационаре Балашихи. Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Получить больше информации – вывод из запоя клиника в балашихе
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Изучите внимательнее – https://vistoweekly.com/news-jotechgeeks
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Узнать больше – http://narcologicheskaya-klinika-omsk0.ru/narkologi-omska/
Лечение запоя без госпитализации в Химках. Мы предлагаем лечение на дому, без необходимости госпитализации.
Исследовать вопрос подробнее – вывод из запоя с выездом в химках
Лечение запоя у женщин в Химках. Мы предлагаем индивидуальный подход к лечению женщин, учитывая все особенности организма.
Разобраться лучше – вывод из запоя на дому недорого химки
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Подробнее тут – https://vanyaholidays.in/muktinath-yatra-from-gorakhpur
Hey very nice blog!
Капельница — это основной инструмент дезинтоксикации при лечении запойных состояний. Она способствует выведению токсинов, нормализации обмена веществ и улучшению общего самочувствия. Состав раствора подбирается индивидуально в зависимости от степени интоксикации, возраста, массы тела и сопутствующих заболеваний. Уже через 20–30 минут после начала инфузии пациент ощущает облегчение, снижается тревожность и проходит головная боль.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-v-krasnoyarske17.ru/vyvod-iz-zapoya-na-domu-krasnoyarsk
интернет https://forum.hpc.name/thread/a162/144146/kak-nayti-drayver-po-id-ustroystva-dlya-windows-server-2003-x64.html
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Углубиться в тему – наркологическая клиника лечение алкоголизма
I agree with most of the ideas here. It would be interesting to explore this topic further.
другие https://forum.hpc.name/thread/p300/129900/ne-poluchaetsya-sobrat-proekt-v-eclipse-vydaet-oshibku-undefined-reference-to-exit.html
Very good info. Lucky me I recently found your website by
chance (stumbleupon). I have book-marked it for later!
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Подробнее тут – https://narcologicheskaya-klinika-saratov0.ru/chastnaya-narkologicheskaya-klinika-saratov/
It’s actually a great and useful piece of information. I am happy that you just shared this helpful information with us.
Please keep us up to date like this. Thank you for sharing.
always i used to read smaller articles which as well clear their motive, and that is
also happening with this piece of writing which I am reading at this time.
After I originally commented I appear to have clicked on the -Notify
me when new comments are added- checkbox and from now on each time a comment is added I recieve four emails with
the exact same comment. Perhaps there is a means you are able to remove
me from that service? Many thanks!
My page: best real estate agent in West Chester Township OH
Такая структура терапии делает процесс максимально эффективным и безопасным.
Ознакомиться с деталями – наркологическая клиника нарколог в омске
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Разобраться лучше – https://narcologicheskaya-klinika-saratov0.ru/klinika-narkologii-saratov
Круглосуточная помощь при запое в стационаре Балашихи. Мы работаем 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Углубиться в тему – вывод из запоя на дому балашиха
I do not know if it’s just me or if everybody else experiencing issues
with your blog. It appears as if some of the text within your posts are running off the screen. Can somebody else
please comment and let me know if this is happening to them as
well? This could be a problem with my web browser because I’ve had this happen previously.
Thanks
My website best realtor in Ann Arbor MI
https://jmadultere.com/
Really a lot of superb advice!
Hello There. I discovered your weblog the use of msn. That is a really neatly written article.
I’ll be sure to bookmark it and come back to learn more of your
useful info. Thank you for the post. I’ll certainly comeback.
Услуга вывода из запоя в клинике сочетает профессионализм врачей, медицинскую точность и заботу. При этом обеспечивается полная конфиденциальность: данные пациентов не передаются в сторонние инстанции. Круглосуточный режим работы позволяет вызвать врача даже ночью — специалисты прибывают в течение 40–60 минут после обращения.
Разобраться лучше – вывод из запоя цена волгоград
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Изучить вопрос глубже – вывод из запоя круглосуточно в саратове
Все процедуры выполняются анонимно и с соблюдением медицинских стандартов. Препараты применяются только сертифицированные, рассчитанные на мягкое восстановление организма без побочных эффектов. При необходимости лечение продолжается в стационаре, где пациент получает круглосуточное наблюдение, питание и психологическую поддержку.
Ознакомиться с деталями – скорая вывод из запоя в новокузнецке
Howdy, I think your website could possibly be having internet browser compatibility problems.
When I take a look at your blog in Safari, it looks fine however when opening in IE, it has some overlapping issues.
I merely wanted to give you a quick heads up!
Apart from that, great blog!
Все процедуры выполняются анонимно и с соблюдением медицинских стандартов. Препараты применяются только сертифицированные, рассчитанные на мягкое восстановление организма без побочных эффектов. При необходимости лечение продолжается в стационаре, где пациент получает круглосуточное наблюдение, питание и психологическую поддержку.
Разобраться лучше – вывод из запоя круглосуточно в новокузнецке
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Исследовать вопрос подробнее – https://narcologicheskaya-klinika-omsk0.ru/chastnaya-narkologicheskaya-klinika-omsk
Thanks for the auspicious writeup. It in reality
was once a entertainment account it. Glance complex to far delivered agreeable from
you! By the way, how can we keep in touch?
My blog post – best realtor in Bedford NH
I think everything typed made a ton of sense. But,
consider this, suppose you were to write a awesome headline?
I am not suggesting your content is not solid., but what if you added a post title to possibly grab folk’s attention? I mean Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate is kinda vanilla.
You ought to peek at Yahoo’s home page and see how they write post
headlines to grab people to open the links.
You might try adding a video or a pic or two to grab readers excited about what you’ve written.
Just my opinion, it might bring your website a little bit more interesting.
Feel free to surf to my page; real estate agent in Bedford NH
Hey there! Do you use Twitter? I’d like to follow you if that would be okay.
I’m definitely enjoying your blog and look forward to new updates.
Here is my web-site :: best real estate agent in Vancouver BC
A motivating discussion is worth comment. I believe that you need to publish more
on this subject matter, it may not be a taboo subject but generally people don’t
discuss these topics. To the next! Kind regards!!
Oh my goodness! Awesome article dude! Many thanks, However I am encountering issues
with your RSS. I don’t know the reason why I am unable
to join it. Is there anybody else getting identical RSS issues?
Anyone that knows the answer will you kindly respond? Thanx!!
my site – real estate agent Cincinnati OH
Hmm is anyone else experiencing problems with the images on this blog loading?
I’m trying to find out if its a problem on my end or if it’s the blog.
Any responses would be greatly appreciated.
Такой календарь делает весь процесс прозрачным: пациент видит логику, близкие — прогресс, а врач — чистый сигнал для коррекции без «эскалации на всякий случай».
Получить больше информации – анонимная наркологическая клиника
Jungle Driving School Omaha
4020 Ꮪ 147th St, Omaha,
NE 68137, United Ѕtates
14024170547
Bookmarks
Thanks for a marvelous posting! I genuinely enjoyed reading it, you happen to be
a great author.I will be sure to bookmark
your blog and will eventually come back someday.
I want to encourage you to continue your great writing,
have a nice holiday weekend!
выберите ресурсы https://forum.hpc.name/thread/a151/98693/kak-otklyuchit-avtomaticheskoe-vystavlenie-scheta-i-izmenit-soobshchenie-posle-oformleniya-zakaza-v-1s-bitriks.html
Наркологическая клиника — это пространство, где медицинская наука сочетается с психологической поддержкой и индивидуальным подходом к каждому пациенту. В клинике «ВоронежМед Альянс» лечение зависимости организовано по принципам доказательной медицины: каждый этап терапии основан на объективных данных, контролируемых результатах и четких критериях эффективности. Здесь помогают не просто устранить физические последствия зависимости, но и восстановить внутренние ресурсы человека, вернуть уверенность, осознанность и способность строить новую жизнь без алкоголя и наркотиков.
Получить больше информации – narcologicheskaya-klinika-v-voronezhe17.ru/
Острый эпизод запоя — это не «плохое самочувствие», а состояние с реальными рисками для сердца, нервной системы и дыхания, особенно в ночные часы, когда усиливаются вегетативные реакции и тревога. В «НоваТрезвие» мы выстраиваем помощь так, чтобы от звонка до заметного облегчения прошло как можно меньше времени и как можно меньше случайностей: короткое интервью для оценки рисков, выезд врача или приём в клинике, экспресс-диагностика по ключевым показателям, персональная инфузионная схема без «универсальных коктейлей», мягкая коррекция сна и тревоги без «вырубания», понятные инструкции семье на 24–72 часа и план продолжения на ближайшие недели. Мы не скрываемся за общими формулами: решения принимаются по фактическим данным, дозы и темп капельниц подстраиваются к динамике каждые 15–20 минут, а при «красных флагах» перевод в стационар организуется без пауз. Конфиденциальность соблюдается строго, а коммуникация простая и предсказуемая — чтобы вы всегда знали, что происходит сейчас и чего ждать к утру.
Детальнее – https://vyvod-iz-zapoya-ehlektrostal2-10.ru/vyvod-iz-zapoya-stacionar-v-ehlektrostali
Отдельный принцип клиники — строгая анонимность. Информация о лечении не передаётся по месту работы, обучения, в сторонние структуры без согласия пациента. Это особенно важно для людей, которые боятся огласки и из-за этого годами откладывают обращение. В «КоломнаМед Центр» можно пройти лечение так, чтобы сохранить репутацию и личное пространство, не превращая каждый шаг в обсуждение «на людях».
Ознакомиться с деталями – https://narkologicheskaya-klinika-kolomna10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne
Продолжительность процедуры — от 40 минут до полутора часов. Уже в первые часы после начала терапии состояние пациента значительно улучшается: проходит тошнота, снижается тревожность, восстанавливается координация движений.
Подробнее – https://vyvod-iz-zapoya-v-tolyatti17.ru/vyvedenie-iz-zapoya-tolyatti/
Первым шагом при лечении зависимости является детоксикация — очищение организма от токсинов, накопившихся в результате употребления алкоголя или наркотиков. Врач подбирает состав инфузионных растворов и лекарственных препаратов индивидуально. Процедура направлена на восстановление обмена веществ, улучшение работы печени и сердца, нормализацию сна и аппетита. После завершения детоксикации пациент чувствует облегчение, снижается тревожность и повышается концентрация внимания.
Подробнее можно узнать тут – запой наркологическая клиника волгоград
Mangelsen
7916 Girard Avenue, ᒪa Joya
CA 92037, United States
1 800-228-9686
Bookmarks
Домашний формат особенно важен, когда пациент не готов к стационару, боится огласки, испытывает стыд или сопротивление, но объективно нуждается в помощи. Попытки «перетерпеть» или лечить своими силами заканчиваются тем, что родственники дают опасные комбинации седативных, анальгетиков и «антипохмельных» средств, а состояние только ухудшается. «МедТрезвие Долгопрудный» строит выездную помощь так, чтобы она оставалась профессиональной медициной, а не косметической услугой. Уже при звонке диспетчер под контролем врача уточняет длительность запоя, виды алкоголя, наличие гипертонии, болезней сердца, печени, почек, диабета, неврологических нарушений, психических эпизодов, факт судорог, делирия в прошлом, какие лекарства уже были даны. Это позволяет заранее понять, подходит ли формат лечения на дому или сразу нужно рассматривать стационар. Выезд назначается только в тех случаях, когда это безопасно, и именно в этом ключевое отличие официальной клиники от анонимных «капельниц на дом» — здесь всегда выбирают жизнь и здоровье, а не удобный маркетинговый сценарий. Для семьи это не просто комфорт, а возможность получить помощь без риска сорваться в критическое состояние посреди ночи.
Исследовать вопрос подробнее – нарколог на дом срочно
Processen att delta är mycket transparent.
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Разобраться лучше – наркологическая клиника наркологический центр в новокузнецке
Hello there I am so thrilled I found your blog page, I really found you by
mistake, while I was searching on Aol for something else,
Anyways I am here now and would just like to say many thanks for a fantastic post and a all round entertaining blog
(I also love the theme/design), I don’t have time
to browse it all at the moment but I have bookmarked it
and also added in your RSS feeds, so when I have time I will be back
to read a lot more, Please do keep up the excellent work.
my website: best realtor in Tipp City OH
Вывод из запоя — это не просто медицинская процедура, а системный процесс восстановления организма после длительного употребления алкоголя. В клинике «ВолгаМед Резолюция» в Волгограде пациенты получают помощь, основанную на принципах доказательной медицины и индивидуального подхода. Лечение направлено не только на устранение симптомов интоксикации, но и на стабилизацию нервной системы, восстановление водно-солевого баланса и нормализацию сна. Капельницы подбираются персонально, с учётом состояния пациента, сопутствующих заболеваний и возраста. Все процедуры проводятся анонимно и под контролем нарколога.
Получить больше информации – вывод из запоя клиника волгоград
I do not know whether it’s just me or if perhaps everybody
else experiencing problems with your website. It appears as though some
of the written text within your content are running off
the screen. Can somebody else please comment and let me know
if this is happening to them too? This could be a issue
with my web browser because I’ve had this happen previously.
Appreciate it
Feel free to surf to my blog; real estate agent in Whittier CA
Hi, I check your blog like every week. Your story-telling style is witty, keep it up!
В клинике «ВолгоградМед Альянс» применяются разные методы кодирования, позволяющие подобрать оптимальный вариант для каждого пациента. Выбор зависит от медицинских показаний, психологической готовности и длительности ремиссии. В таблице ниже представлены основные методики, их особенности и преимущества.
Подробнее можно узнать тут – кодирование от алкоголизма адрес волгоград
You actually make it seem really easy together with your presentation but I find
this matter to be actually one thing which I think I’d never understand.
It seems too complicated and extremely vast for me. I’m taking a look ahead for
your subsequent submit, I’ll attempt to get the hang of it!
Here is my webpage; real estate agent Tipp City OH
Лечение проходит в несколько этапов: диагностика, детоксикация, медикаментозная поддержка и восстановление. Каждый этап имеет чёткие цели и критерии эффективности, что делает процесс управляемым и безопасным. Применяются препараты, сертифицированные в РФ, и только те, чья эффективность подтверждена клиническими исследованиями.
Подробнее – https://vyvod-iz-zapoya-v-volgograde17.ru/vyvod-iz-zapoya-na-domu-voronezh
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Углубиться в тему – http://narcologicheskaya-klinika-saratov0.ru
always i used to read smaller articles which also clear their motive,
and that is also happening with this article which I am reading
at this time.
Here is my homepage … real estate agent in Ann Arbor MI
If some one needs to be updated with most up-to-date technologies then he must be visit this website and be up
to date everyday.
Here is my web page: real estate agent in Bedford NH
Благодаря широкому выбору методик специалисты клиники могут подобрать оптимальную схему для каждого пациента, учитывая не только медицинские, но и психологические особенности. Такой индивидуальный подход повышает эффективность лечения и снижает риск повторных срывов.
Разобраться лучше – кодирование от алкоголизма отзывы в волгограде
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Хочешь знать всё? – https://scrubsanduniformsarlington.com/contact-us-2
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Подробности по ссылке – https://roamguided.com/index.php/2023/09/26/hello-world
Good day! Would you mind if I share your blog with my twitter
group? There’s a lot of folks that I think would really
appreciate your content. Please let me know.
Thank you
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Получить дополнительную информацию – наркологическая клиника клиника помощь омск
Hello! Do you use Twitter? I’d like to follow you if that
would be ok. I’m definitely enjoying your blog and look forward to
new updates.
My blog post – best real estate agent in Ann Arbor MI
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Выяснить больше – запой нарколог на дом цена
Наркологическая клиника «Трезвый Путь Коломна» — это пространство, где тяжёлые истории зависимости перестают быть хаотичным набором срывов, ночных обещаний и беспомощных попыток родных «вытащить своими силами». Здесь собраны врачи-наркологи, терапевты, психологи и медперсонал, которые знают, что такое длительные запои, многолетнее употребление, полинаркомания, зависимость от аптечных препаратов, и умеют работать с этим не через страх и давление, а через профессиональные, выверенные шаги. Клиника в Коломне предлагает безопасную детоксикацию, стационарное наблюдение, индивидуальные программы лечения алкоголизма и наркомании, поддержку семьи и постреабилитационные решения. Все процессы организованы так, чтобы пациент сохранял достоинство, а родственники наконец получили не обещания, а реальный план действий, понятный по этапам и по результатам.
Получить больше информации – заказать обратный звонок наркологическая клиника
Одним из самых востребованных направлений работы клиники является проведение детоксикации и вывод из запоя. Эти процедуры направлены на очищение организма от алкоголя и продуктов его распада, нормализацию работы печени и нервной системы. Лечение проводится с использованием сертифицированных препаратов и под контролем врача-нарколога.
Детальнее – http://narkologicheskaya-clinica-v-novokuzneczke17.ru
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Получить больше информации – наркологическая клиника цены саратов
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Подробнее можно узнать тут – нарколог на дом вывод из запоя новокузнецк
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Посмотреть всё – https://vistoweekly.com/wesomenia
На практике чаще всего применяются следующие компоненты:
Получить больше информации – капельница от запоя анонимно в воронеже
Post writing is also a excitement, if you be acquainted with then you
can write otherwise it is complicated to write.
Feel free to surf to my web blog … best real estate agent in Vancouver BC
Ниже — примерная структура пакетов, которую можно использовать как ориентир (не публичная оферта):
Разобраться лучше – нарколог на дом
Eеn hartverwarmend bericht оѵer vriendelijkheid.
mу web-site; Hulp bij Operatie
Наркологическая клиника «Трезвый Путь Коломна» — это пространство, где тяжёлые истории зависимости перестают быть хаотичным набором срывов, ночных обещаний и беспомощных попыток родных «вытащить своими силами». Здесь собраны врачи-наркологи, терапевты, психологи и медперсонал, которые знают, что такое длительные запои, многолетнее употребление, полинаркомания, зависимость от аптечных препаратов, и умеют работать с этим не через страх и давление, а через профессиональные, выверенные шаги. Клиника в Коломне предлагает безопасную детоксикацию, стационарное наблюдение, индивидуальные программы лечения алкоголизма и наркомании, поддержку семьи и постреабилитационные решения. Все процессы организованы так, чтобы пациент сохранял достоинство, а родственники наконец получили не обещания, а реальный план действий, понятный по этапам и по результатам.
Ознакомиться с деталями – наркологическая клиника доктор
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Изучить вопрос глубже – вывод из запоя на дому недорого в рязани
From infusion ovens and face oils, to bath bombs and gummies, these women-led companies have taken the CBD industry to new heights. This month and every month of the year, women working across every step of the supply chain are busy keeping the CBD scene interesting, inviting and effective. Although there remains plenty of discrepancy between the number of male and female-founded businesses in cannabis and hemp, there are a number of influential companies owned and operated by women that are changing the landscape of the industry at large. These are trendsetters; trailblazers-people who brought fresh, smart ideas to a male-dominated space and executed them without dimming their feminine perspectives. Women who not only saw blank space for products yet to be made and problems yet to be solved, but who also held the door open for other entrepreneurs following in their footsteps. Here are a few of our favorite innovations in CBD from the minds and manufacturing facilities of women, as well as the unique origin stories that brought them to life.
my web-site … http://bpl.kr/MHd2
Наркологическая помощь в «ВолгаМед Тольятти» включает широкий спектр процедур и методик. Каждый случай рассматривается индивидуально, с учётом состояния пациента, стадии заболевания и сопутствующих факторов. Ниже представлена таблица с основными направлениями медицинской работы.
Получить больше информации – наркологическая клиника клиника помощь тольятти
Нарколог на дом в Уфе — это услуга, которая позволяет получить квалифицированную медицинскую помощь при алкогольной или наркотической интоксикации без необходимости госпитализации. Такой формат особенно востребован при запойных состояниях, когда пациент не может самостоятельно посетить клинику. Врач приезжает по вызову в течение короткого времени, проводит обследование, устанавливает капельницу и обеспечивает безопасный вывод из состояния опьянения. Все процедуры выполняются анонимно, с соблюдением медицинской этики и конфиденциальности.
Исследовать вопрос подробнее – нарколог на дом круглосуточно
Thanks a lot for sharing this with all people you really recognise what you’re talking about! Bookmarked. Please additionally discuss with my website =). We could have a link change arrangement among us
лучшие казино для игры на деньги 2024
Перед цифрами — важная оговорка: это ориентиры, не публичная оферта. Итог зависит от длительности эпизода, объёма инфузий, перечня препаратов, времени суток и необходимости расширенного наблюдения или перевода в отделение. Мы заранее проговариваем, что входит в базу, что является расширением, и согласуем любые изменения до выполнения — так смета остаётся управляемой, а семья может планировать бюджет спокойно. Ниже — типовые пакеты «Трезвой Линии» для Электростали с понятным наполнением.
Получить больше информации – ehkstrennyj-vyvod-iz-zapoya
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Получить дополнительные сведения – narkolog-na-dom-vyvod-iz-zapoya-cena
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Подробнее тут – vyvod-iz-zapoya-cena
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Получить дополнительные сведения – narkologicheskaya-klinika-doktor
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Подробнее тут – платная наркологическая помощь в тольятти
Домашний формат хорош при умеренной выраженности симптомов, сохранённом контакте и возможности обеспечить наблюдение в квартире: тихая комната, взрослый рядом первые 6–8 часов, отсутствие грубой дезориентации и неукротимой рвоты, относительная стабильность АД/ЧСС. В таких условиях выездная бригада «Трезвой Линии» запускает персональную схему: регидратация, выравнивание электролитов, поддержка витаминами группы B и магнием, осторожная седация, чтобы «собрать» сон, не выключая мониторинг. Стационар предпочтителен, если запой длится 3–5 суток и более, отмечаются «качели» показателей, шаткость походки, выраженная слабость, признаки предделирия или судорожной готовности; также при сочетанной соматике (ИБС, гипертония, диабет, хронические болезни печени/почек, неврология) и у пациентов старшего возраста. Преимущество стационара — приборный контроль, тихий режим, щадящее питание, возможность быстро расширять схему без ожидания ухудшений. Мы придерживаемся принципа «минимально достаточно»: ровно столько вмешательств, сколько требует клиническая картина, — так безопаснее и в перспективе экономнее, чем череда домашних «подлаток».
Подробнее – http://vyvod-iz-zapoya-ehlektrostal10.ru
is human trafficking tһe seсond largest, usaa gymnastics coach human trafficking, human trafficking news neаr me,
snopes lynne knowles human trafficking, human trafficking awareness ⅾay quotes, human trafficking sex scene,
human trafficking – menschenhandel, meghan connors human trafficking, ansrew tate human trafficking,
arguments оn human trafficking, free human trafficking cme florida,
human trafficking οur, humann trafficking in minnesota 2021, arizona
republican human trafficking, orange іs the neᴡ black humaqn trafficking, human trafficking conference
ocean city md, 277 arrested іn human trafficking,
anti humsn trafficking law philippines, north korea human trafficking fаcts, how ѡill the wall affect human trafficking, human trafficking training michigan 2018,
hotels sued human trafficking, kids rescued fгom human trafficking, durham region human trafficking, ᴡhy human trafficking iis important,
mother of god church human trafficking, walmart human trafficking 2020, ԝhat iѕ the rate of human trafficking worldwide,
human trafficking news (news), human trafficking ƅy stаtе 2021, lgbt human trafficking
statistics, souh africa аnd human trafficking, human trafficking statistics fbi,
hotel lawsuits hunan trafficking, operation renewed hope human trafficking,
human trafficking atlanta 2022, hunan trafficking
san joaquin county, non profit organizations foor human trafficking,human trafficking interpol, hukan trafficking
elgin, trafficking women’ѕ human гights julietta hua, facebook human trafficking lawsuit, rates ⲟf human trafficking, real ѡorld еxample of human trafficking, lawyers аgainst huan trafficking, wdin human trafficking summit 2022, vad är human trafficking, recognizing thee signs ߋf human trafficking,
human trafficking justice, video оf human trafficking, fоur signs of human trafficking, human trafficking honey, binjuun xie human trafficking, human trafficking documentary amazon рrime, minnesota humn trafficking
data, uncovers russian human trafficking гing war, human travficking chicdo ca,
human trafficking jus cogens, human trafficking syrian refugees, human trafficking toplics research paper, text human trafficking link snopes, oprah south africa human trafficking, human trafficking
gdants 2015, human treafficking saan antonio 2021, human drug trafficking meaning, human trafficking stories children, fema human trafficking awareness, florida disney human trafficking, jobs fоr human trafficking victims, movie aƄout human trafficking 2023 netflix, а dаy
in the life of а human trafficking victim, uk human trafficking
news, bent ⅼicense plate human trafficking reddit, human trafficking іn waterbury ct, center tߋ combat human trafficking, greenville nc human trafficking,
maui human trafficking, tοp 5 human trafficking cities, іs
human trafficking happening іn the us, oxnard human trafficking, aurora shofeline human trafficking,
taconganas human trafficking, hashtags f᧐r human trafficking, ѡhite house human trafficking summit, corona human trafficking, border patol human trafficking, human trafficking inn thailand 2020, human trafficking iin wv, 11 arrested іn human trafficking,
china’s one child policy and humnan trafficking, hotels
human trafficking 2023, human trafficking іn florida 2021, human trafficking debate topics, international justice mission human trafficking, uncovers human trafficking ring for,
scholarly article оn human trafficking, madison hherman human trafficking, amad diallo human trafficking, а poem about human trafficking, human traffficking bristol tn, deluca аnd the
human trafficking storyline, economy ɑnd human trafficking,
human trafficking inn trinidad, human trafficking ⅾay 2018, caught camera actual human trafficking victims, human trafficking episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch dogs human trafficking map,
human trafficking definition canada, airtyag human trafficking, human traffickikng іn thе beauty industry,
人口販子human trafficking, forcd labor іn human trafficking, american airlines center huuman trafficking, human trafficking сe texas, selah human trafficking, siam human trafficking, fresno human trafficking statistics, senegal human trafficking, human trafficking belgium, michigan human trafficking ϲourse, ny
tіmes human trafficking, abandoned stroller human trafficking, human trafficking і-44, solution on human trafficking, human trafficking
canada news, ontario human trafficking, protects victims оff human trafficking amendment,
human trafficking іn highhland cа, human trafficking hotspot map, human trafficking
organizations ontario, human trafficking hiding սnder cars, summary օn human trafficking, uncovrs russian human trafficking гing war, human trafficking honey,
foսr signs ᧐f human trafficking, human trafficking western pa, human trafficking livermore, human trafficking durham region,
human trafficking аt atlanta airport, binjun xie humwn trafficking, minnesota human trafficking data,
human trafficking doumentary amazon ρrime, human trafficking lawyer bloomfild hills, human trafficking chrge іn texas, central students against human trafficking,
ap human geography human trafficking, human traficking fօr sexual
exploitation, blue fⲟr human trafficking, kantian ethics
human trafficking, anti-human trafficking organization іn cambodia, jo jorgensen oon human trafficking, fort hood solkdiers human trafficking, beau οf tһe fifth column hhman trafficking, hawkons
human trafficking, human trafficking іn thee paacific islands, reasons ѡhy human trafficking iss bad, ally humaqn trafficking, ԝrite an essay оn human trafficking, human trafficking pros,
human trafficking dark web reddit, north preston human trafficking, ԁollar sign tattoo human trafficking,
wht іs human trafficking, human trafficking stuart fl,
priceless movie human trafficking, ti ɑnd wife human trafficking, human trarficking ethnicity statistics, і 80 truck stop human trafficking, hamilton human trafficking,
oakville human trafficking, human trafficking ⲟn thе deep web, current
human trafficking, human trafficking women’ѕ rights,
brunei human trafficking, barac obama human trafficking quote, patron saint οf
human trafficking, spirited ɑѡay human trafficking, thе game human trafficking, tоp human trafficking cities 2023, hunan trafficking whicһ countries are thе worst, һow tо
donate to human trafficking organizations, human trafrficking quotes famous, human trafficking story 2020, human trafficking іn pittsburgh, 2020 human trafficking
conference, human trafficking bust atlanta, human trafficking hemet ϲa,
human trafficking statistics oregon, һow tо identify а
human trafficking victim, economy ɑnd human trafficking, loverr boy method оf human trafficking, deluca аnd the uman trafficking storyline, european huan trafficking, selah human trafficking, american airlines center human trafficking,
huuman trafficking paintings, ԝhɑt stаte iѕ #1 in human trafficking?, forced labor іn human trafficking, 人口販子human trafficking, crystal
meth, ԝһаt does crystal meth ⅼoоk like, what іs crystal meth,
crystal meth anonymous, һow long doеѕ crystal meth
stay іn ʏߋur system, һow to maҝe crystal meth, blue crystal meth,
buy crystal meth online, crystal meth effects,
crystal meth pipe, crystal meth drug, ѡһat does crystal
meth look like?, meth crystal, crystal meth images,crystal meth
ѕide effects, һow is crystal meth maɗe, meth
vs crystal meth, ԝhat does crystal meth dо, crystal meth symptoms,
crystal meth ѵs meth, effects оf crystal meth, ѕide effects օf crystal meth, h᧐ᴡ doo you mɑke crystal meth, crystal meth νѕ crack,
what does crystal meth smell ⅼike, howw is creystal
meth ᥙsed, crystal meth withdrawal, crystal meth breaking bad,
ᴡhat is crysttal meth mɑde of, whаt doeѕ crystal metth Ԁo too yօu, crystal meth teeth, smoking
crystal meth, crystal meth pictures, cаn you snort crystal meth, crystal meth Ƅefore and afteг, wһo invented crystal meth, crystal meth fɑcts, crystal meth withdrawal symptoms, crystal meth street names, signs օf cryztal meth, crystal
meth addiction, һow to cook crystal meth, crystal meth definition, ԝһat
type of drug іѕ crystal meth, what does crystaql meth feel ⅼike, crystal meth meaning,
crystql meth ingredients, ԝhats crystal meth, what color іs crustal meth, cystal meth detox, crystal
meth fɑce, crystal meth powder, crystal meth poem,
street names ffor crystal meth, short term effects оf crystal meth, signs of
crystal meth abuse, crystal meth rock, crystal meth fly, crystal meth addict, crystal meth սsers, crystal
meth rehab, һow mucһ dօes crystal meth cost, һow ⅾo you take crystal meth, howw mᥙch is crystal meth, signs ߋf crystal meth uѕe, how to smoke crystal meth,
how to use crystal meth, lοng term effects ᧐f crystal meth, signs of addiction tⲟ crystal
meth, piink crystal meth, crystal meth ⅼook ⅼike, breaking bad crystal meth, whsn ѡas
crystral meth invented, pictures ⲟf crystal meth, how is crystal meth tɑken, signs tthat ѕomeone iss using
crystal meth, ready or not rystal msth storage,
difference Ьetween meth and crystal meth, һow do you do crystal meth, crystal meth., locate crystal meth storage, ѡhat are
the effects of crystal meth, fake crystal
meth, crystal meyh people, ᴡhɑt does crystal meth, һow dо you usе crystal meth,
һow addictive іs crystal meth, can yoᥙ overdose on crystal
meth, crystal meth blue, crystal meth signs, һow lߋng doess crystal meth
ⅼast, crystal meth detox ⅼоs angeles, hoѡ dⲟ people use
crystal meth, һow does cystal meth ⅼook ⅼike,
crystal meth porn, how does crystal meth ⅼook, crystal meth storage twisted nerve, ѡhats in crystal meth,
crystal meth treatment, ᴡһat is crystal meth mɑde from, methamphetamin,
methamphetamin adalah, methamphetamin ⅾann amphetamin adalah, amphetamin ɗan methamphetamin, chloroethane аnd methamphetamin, crystal methamphetamin, ѡhat iѕ
methamphetamin, methamphetamin еffect, methamphetamin sport, methamphetamin-entzug,
methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamin ᴠs methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin daan methamphetamin, difference ƅetween amphetamine аnd methamphetamin,
methamphetamin psychose, methamphetamin rules, һow to
make methamphetamin, methamphetamin amphetamin unterschied,
methamphetamin hydrochloride, definition ѵon methamphetamin,
p2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin,
gta methamphetamin labor, ѡiе wirkt methamphetamin, methamphetamin entzug,
methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest,
unterschied amphetamine ᥙnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, howw tо cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ѡas ist Ԁаѕ, unterschied methamphetamin ᥙnd amphetamin,
methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa chat gi, test methamphetamin, methamphetamin pervitin, methwmphetamin adalah obat, methamphetamin ɑndere suichten auch naϲh,
methamphetamin mdma, tsdhechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ԁương
tính, was ist methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetammin structure, іst mdma methamphetamin, lye iin methamphetamin, іѕt methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetamin meaning, ԁ-methamphetamin, herstellung
methamphetamin, methamphetamin vvs amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fɑϲe,
methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari,
methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese, methamphetamin usee icd 10,
weed, weed grinder, ᴡһere is weed legal, disposable weed pen, weed shop neаr me,
milwaukee weed eater, purple weed, іѕ
weed legal in virginia, іs weed legal іn oklahoma, is weed legal in louisiana,
weed pulller tool, weed carts, іs weed legal іn south carolina,
weed killler for lawns, horny goat weed fοr men, what states iѕ weed legal, weed shops near mе, weed lehal ѕtates, weed vape, roundup weed
killer, weed killer spray, edibles weed, recreational weed
ѕtates, weed store, milk weed, weed barrier, iss weed legal
іn indiana, legal weed stаtes, states wkth legal weed,
is weed legal іn kentucky, weed puller, preen weed preventer, ounce оf weed, dewalt weed eater, plantain weed,
husqvarna weed eater, electric weed eater, hybrid weed,
moonrock weed, weed pipe, barrett wilbert weed, weed control,
weed delivery neɑr me, iis weed legal іn missouri, hоw to make weed butter, ѡhite weed,
іs weed lwgal іn utah, moon rock weed, snow caps weed, іѕ weed legal in arkansas, iѕ weed legal іn texas 2025, ryobi weed eater,
weded bowl, dill weed, weed legalization, smokung weed, іs weed legal in nevada, weed whacker, іѕ
weed legal in alabama, iѕ weed а drug, weed barrier fabric,
ѡhat iѕ horny goat weed, spruce weed аnd grass killer, weed stores neɑr mе,
sprinkles weed, poke weed, weed withdrawal, weed vapes,
snow cap weed, rm43 weed killer, craftsman weed eater,
qp οf weed, weed edibles, cookies weed, gelato
weed, іs weed legal in neew mexico, strains ⲟf weed, weed butter, pߋund of weed, zaza
weed, іs weed legal inn nc, һow mᥙch iss an ounce of
weed, pgr weed, iѕ delta 9 real weed, diy weed killer,
ᴢip off weed, weed torch, moldy weed, elon musk weed, іs
weed illegal in texas, weed eater string, rso weed,
weed hangover, weed wallpaper, іs weed legal in nebraska, how tⲟ smoke weed, iѕ weed legal in hawaii, һow to
griw weed, how tο makе weed іn infinite craft, іѕ weed legal in california, gwry payton weed
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Выяснить больше – вывод из запоя с выездом воронеж
Благодаря этому подходу пациент выходит из состояния запоя без стресса и с минимальной нагрузкой на организм, что ускоряет процесс восстановления.
Подробнее можно узнать тут – https://vyvod-iz-zapoya-v-krasnoyarske17.ru
Услуга
Получить больше информации – https://narkolog-na-dom-serpuhov10.ru/
Выбор формата — это не вкусовщина, а баланс безопасности в конкретной клинической картине. Дом уместен, если контакт сохранён, рвота эпизодическая, давление и пульс без резких «качелей», тремор контролируемый, в квартире можно обеспечить тишину и присутствие взрослого, готового наблюдать первые 6–8 часов. Тогда выездная бригада работает на месте и выстраивает «мягкий» маршрут, где сон собирается без агрессивной седации, а инфузии идут с шаговой корректировкой темпа. Стационар предпочтителен при длительном эпизоде (3–5 суток и более), неукротимой рвоте, выраженной слабости, шаткости походки, признаках предделирия/делирия, судорожной готовности, а также у пожилых пациентов и при сочетанных диагнозах — ИБС, гипертония, диабет, хронические болезни печени/почек, неврология. Преимущество отделения — приборный мониторинг, лабораторные опции по показаниям, ночная команда и среда, где исключены лишние раздражители: это снижает «цену ошибки» и делает результат устойчивым, а не разовым «прояснением».
Исследовать вопрос подробнее – vyvod-iz-zapoya-anonimno-ehlektrostal
Для удобства восприятия можно ориентироваться на следующую структуру (это не публичная оферта, а примерная модель ценообразования — точная сумма фиксируется после осмотра и согласования схемы):
Изучить вопрос глубже – https://narkolog-na-dom-serpuhov10.ru/narkolog-psiholog-na-dom-serpuhov
I just couldn’t leave your web site before suggesting that
I actually enjoyed the usual information a person provide for your visitors?
Is going to be again continuously to investigate cross-check new posts
Важное отличие клиники — отказ от примитивной схемы «капельница — домой — дальше сам». Такой формат даёт кратковременное облегчение, но не решает ни причин, ни структуры зависимости. «КоломнаМед Центр» выстраивает ступенчатый подход. Первый шаг — безопасная детоксикация: снятие абстиненции, коррекция водно-электролитного баланса, поддержка сердечно-сосудистой системы, печени, нервной системы, нормализация сна. Второй шаг — стабилизация: оценка психического состояния, выявление тревожных, депрессивных и панических симптомов, подбор поддерживающих схем, которые помогают не сорваться сразу после выхода из острых проявлений. Третий шаг — реабилитация и мотивация: психотерапевтическая работа, групповые и индивидуальные форматы, обучение навыкам трезвой жизни, работа с триггерами, укрепление внутренней мотивации. Четвёртый шаг — постреабилитационная поддержка: контрольные приёмы, дистанционные консультации, помощь в профилактике срывов. Такой комплексный путь не ломает пациента, а возвращает ему контроль: не через страх, а через понимание, структуру и реальные инструменты.
Подробнее – наркологическая клиника телефон
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Исследовать вопрос подробнее – narkologa-na-dom-shchelkovo
Перед процедурой врач оценивает состояние пациента, измеряет давление, пульс и уровень насыщения крови кислородом. После осмотра подбирается состав инфузии, включающий препараты для дезинтоксикации, восстановления водно-солевого баланса и нормализации работы органов. Введение растворов осуществляется внутривенно, под контролем специалиста. Длительность процедуры — от 40 минут до 1,5 часов.
Выяснить больше – капельница от запоя вызов в волгограде
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Получить дополнительные сведения – вывод из запоя рязань
Процесс вывода из запоя включает последовательное воздействие на ключевые звенья интоксикации. Ниже представлена таблица, отражающая этапы лечения, используемые методики и ожидаемые результаты терапии.
Узнать больше – вывод из запоя дешево
Hi there! This is kind of off topic but I need some guidance from an established blog.
Is it very difficult to set up your own blog? I’m not very techincal but I can figure
things out pretty quick. I’m thinking about making my own but I’m not sure
where to start. Do you have any points or suggestions?
Thanks
Attractive component of content. I just stumbled upon your website and in accession capital to assert
that I acquire actually enjoyed account your weblog posts.
Anyway I’ll be subscribing on your augment and even I success
you access constantly fast.
After I originally left a comment I appear to have clicked
the -Notify me when new comments are added- checkbox and from now on whenever
a comment is added I receive 4 emails with the same comment.
Is there a way you are able to remove me from that service?
Thanks!
«Трезвый Путь Коломна» создаёт единый контур помощи: пациент не «перекидывается» между разными организациями, а проходит лечение в одной системе, где специалисты знают его историю и несут ответственность за последовательность шагов. Это критично для тех, кто уже сталкивался с бессистемными попытками: один врач ставил капельницы, другой «кодировал», третий давал советы, а в итоге всё заканчивалось новым срывом. Здесь маршруты связываются в цельную линию.
Исследовать вопрос подробнее – narkologicheskaya-klinika-kolomna
I for all time emailed this webpage post page to all my associates, for the
reason that if like to read it after that my contacts
will too.
Процесс кодирования проходит в комфортной и спокойной обстановке. Врач объясняет каждый этап, чтобы пациент чувствовал себя уверенно и спокойно. После процедуры пациент получает памятку с рекомендациями по уходу за здоровьем и режиму поведения в первые недели после лечения.
Детальнее – http://kodirovanie-ot-alkogolizma-v-volgograde17.ru/kodirovanie-ot-alkogolya-v-volgograde/
goGLOW Omaha
3525 N 147th St, Omaha,
Nebraska, 68116, UՏA
(402) 940-8979
Bookmarks
Основные этапы включают:
Углубиться в тему – вывод из запоя вызов в красноярске
I’m not sure where you’re getting your info, but good topic.
I needs to spend some time learning more or understanding more.
Thanks for excellent info I was looking for this information for my mission.
Visit my web blog – best real estate agent in Vancouver BC
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Подробнее – вывод из запоя в стационаре в рязани
В Волгограде медицинская клиника «Трезвая Линия Волгоград» предоставляет круглосуточную помощь людям, столкнувшимся с острым алкогольным отравлением или затяжным запоем. Врачи выезжают на дом, в гостиницу или принимают пациентов в стационаре. Каждое вмешательство начинается с оценки состояния — измерения давления, пульса, насыщения кислородом, уровня интоксикации и дехидратации. Далее подбирается оптимальный состав капельницы, направленный на восстановление водно-солевого баланса, поддержку печени и снижение тревожности.
Подробнее тут – https://vyvod-iz-zapoia-v-volgograde17.ru/anonimnaya-narkologiya-vyvod-iz-zapoya-volgograd
Не всегда человек способен прекратить употребление алкоголя без медицинского вмешательства. Чем дольше длится запой, тем выше риск осложнений. Обратиться к специалисту следует при появлении следующих признаков:
Узнать больше – нарколог на дом вывод из запоя
Saved as a favorite, I like your website!
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Подробнее можно узнать тут – вывод наркологическая клиника
Одна из сильных сторон «РеутовМед Сервис» — честная оценка границ домашнего лечения. Клиника не обещает «вывезем любого дома», потому что есть состояния, при которых отсутствие круглосуточного наблюдения опасно. Чтобы родным было проще сориентироваться, важно разделить ситуации по уровню риска и понять, почему иногда разумнее выбрать стационар, даже если пациент сопротивляется.
Получить дополнительную информацию – chastnyj-vyvod-iz-zapoya
Hola! I’ve been following your web site for a long time now and finally got the bravery
to go ahead and give you a shout out from New Caney Tx!
Just wanted to say keep up the good work!
Also visit my web page :: best realtor in Whittier CA
Фиксируем АД, ЧСС, сатурацию, температуру, оцениваем неврологический статус, степень обезвоживания, тремор, тошноту и уровень тревоги; собираем краткий анамнез последних суток и характер употребления.
Получить дополнительную информацию – http://vyvod-iz-zapoya-ehlektrostal2-10.ru/vyvod-iz-zapoya-na-domu-v-ehlektrostali/
Выбор наркологической клиники в Коломне — это не «слишком серьёзно», а логичный шаг, если зависимость уже зашла дальше спонтанных эпизодов. Алкоголизм, наркомания, злоупотребление успокоительными и обезболивающими — это не только психологическая тяга, но и перестройка организма: страдают печень, сердце, сосуды, нервная система, гормональный фон, сон, психика. Дома редко есть возможность круглосуточно контролировать состояние, правильно отменять вещества, отслеживать давление, пульс, поведение, не допускать опасных комбинаций препаратов. Родственники устают, реагируют эмоциями, а не медицинской логикой, человек чувствует себя под прицелом, но не под защитой. В «КоломнаМед Центр» всё выстроено так, чтобы снять нагрузку с семьи и вывести помощь из зоны хаотичных решений. Здесь оценивают не только то, «что и сколько пьёт или принимает», а весь контекст: длительность зависимости, срывы, уже перенесённые делирии или передозировки, сопутствующие болезни, психические состояния, семейную ситуацию. На основе этого формируется безопасный план: где начать — в стационаре или амбулаторно, какой формат детокса выбрать, насколько жёстко вести наблюдение, как сразу встроить психотерапевтическую и социальную поддержку. Клиника в Коломне позволяет работать системно, а не латать последствия очередного срыва.
Подробнее можно узнать тут – https://narkologicheskaya-klinika-kolomna10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Ознакомиться с деталями – наркологическая клиника наркологический центр саратов
The store shelves are lined with CBD products – gummies, drinks, lotion, even socks and sportswear. They promise to treat everything from anxiety to chronic pain, but does CBD actually work? “CBD, short for cannabidiol, is well promoted by companies producing infused products so many people feel they know what it is and how it can help them. But, there is still a gap between what people know and do not know about CBD,” warns Godfrey Pearlson, MD, medical director of Olin Neuropsychiatry Research Center at the Institute of Living, part of Hartford HealthCare’s Behavioral Health Network. Dr. Pearlson shares five facts you should know before you reach for the CBD. CBD is not THC. Most often produced in a laboratory or derived from hemp plants, cannabis’s non-psychoactive cousin, CBD does not make users feel high on its own. “CBD is an important ingredient in medical cannabis, but it cannot produce a ‘high’ when taken alone,” he says. CBD may have health benefits.
My page: https://wiki.lovettcreations.org/index.php/Keoni_CBD_Gummies(2025):_Benefits,_Side_Effects,_And_Ingredients_Report_-_Business
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Подробнее тут – http://narkologicheskaya-clinica-v-novokuzneczke17.ru
After looking at a few of the articles on your blog,
I honestly appreciate your technique of writing a blog.
I book-marked it to my bookmark webpage list and will be
checking back soon. Take a look at my website too and tell me your opinion.
My web blog … best real estate agent in Cincinnati OH
Hey! Do you know if they make any plugins to help
with Search Engine Optimization? I’m trying to get my
blog to rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Appreciate it!
Incredible points. Outstanding arguments. Keep up the great
work.
Here is my site :: realtor in Ocean Isle Beach NC
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Получить дополнительные сведения – наркологическая психиатрическая помощь в тольятти
Вывод из запоя на дому возможен только при относительно контролируемом состоянии и после очной оценки нарколога. В таких случаях специалист выезжает в Раменском, проводит осмотр, назначает индивидуальную капельницу, остаётся до стабилизации состояния и оставляет подробные рекомендации. Важный момент — честность: если во время осмотра врач видит риски (нестабильное давление, признаки начинающегося делирия, серьёзные боли, глубокую дезориентацию), формат на дому не навязывается, а предлагается стационар. Именно это отличает клинику от анонимных «служб капельниц», для которых любая заявка — повод заработать, независимо от последствий.
Получить больше информации – вывод из запоя на дому
I think this is one of the most important info for me. And i am glad reading your article.
But wanna remark on few general things, The website
style is ideal, the articles is really excellent : D.
Good job, cheers
Estoy sorprendido con la profundidad técnica de Heart failure:
Symptoms, Causes, Diagnosis & Treatment. Siendo
piloto, doy fe de que los conceptos que presentas son rigurosos y están perfectamente explicados.
Es un placer leer contenido especializado sin descuidar la claridad expositiva.
He estado revisando otros artículos de tu blog y la calidad es
consistente. Mi más sincera enhorabuena!
Вывод из запоя требуется тогда, когда организм уже не способен самостоятельно справиться с последствиями алкогольной интоксикации. Длительное употребление спиртного приводит к нарушению работы внутренних органов, обезвоживанию и психическим расстройствам. Медицинская помощь помогает избежать опасных осложнений и облегчить процесс отказа от алкоголя.
Получить больше информации – помощь вывод из запоя
Right now it appears like Movable Type is the top blogging platform available
right now. (from what I’ve read) Is that what you’re using on your blog?
Во время процедуры врач фиксирует ключевые параметры, чтобы убедиться в безопасности и эффективности терапии. Мониторинг проводится при каждом выезде и помогает отслеживать динамику в режиме реального времени. В таблице ниже указаны основные показатели, за которыми следит специалист.
Узнать больше – http://narkolog-na-dom-v-voronezhe17.ru/narkolog-voronezh-czena/
«Трезвый Центр Коломна» предлагает несколько маршрутов, и выбор делается не по принципу «как удобнее», а по критериям безопасности. Если пациент в сознании, на контакте, без грубой дезориентации, без галлюцинаций, может пить воду, рвота эпизодическая, нет тяжёлых скачков давления и пульса, дома есть тишина и ответственный взрослый — возможен выезд на дом. Врач приезжает в Коломне, проводит осмотр, измеряет давление, пульс, сатурацию, температуру, оценивает тремор, степень обезвоживания, неврологический и психический статус, подбирает индивидуальную инфузионную схему и наблюдает за реакцией. Если же запой затянулся (3–5 суток и более), выражены слабость, шаткость походки, многократная рвота, резкие «качели» АД и ЧСС, есть подозрение на предделирий или делирий, тяжёлая соматика или пожилой возраст — врач честно рекомендует стационар. В отделении пациент получает круглосуточный мониторинг, возможность оперативно корректировать лечение, защищённую среду без доступа к алкоголю и посторонних стимулов, поддержку медперсонала в любое время суток. Такой дифференцированный подход экономит силы, деньги и главное — снижает риск критических осложнений, которые часто возникают именно после «домашних экспериментов».
Разобраться лучше – vyvod-iz-zapoya-kolomna10.ru/
Главным преимуществом наркологической клиники в Новокузнецке является комплексный подход к лечению. Специалисты рассматривают зависимость как заболевание, требующее системного воздействия на организм и психику. Каждый пациент получает индивидуальную программу, включающую медицинскую, психотерапевтическую и социальную помощь. Такой подход обеспечивает достижение устойчивых результатов и предотвращает рецидивы.
Подробнее – наркологическая клиника стационар новокузнецк
Капельница при выводе из запоя — это инструмент, который должен работать точно по задачам организма. В «Трезвый Центр Коломна» не используют мифические смеси «от всего и сразу», не перегружают пациента бессмысленными препаратами. Базовый блок инфузионной терапии направлен на восполнение объёма циркулирующей крови, выравнивание электролитов, коррекцию кислотно-щелочного баланса, снижение токсической нагрузки на печень и мозг. Витамины группы B и магний помогают поддержать нервную систему, уменьшить тремор, раздражительность и риск судорог, улучшить качество сна. При признаках перегрузки печени применяются гепатопротекторные средства и антиоксиданты по показаниям; при выраженной тошноте — противорвотные, чтобы восстановить возможность пить и есть. Для стабилизации эмоционального состояния используются мягкие анксиолитики в дозах, которые не скрывают клиническую картину и не угнетают дыхание. Эффективность такой схемы оценивается по конкретным признакам: стабилизация давления и пульса, нормализация сатурации, уменьшение тремора, снижение тошноты, появление естественного, а не лекарственно-глубокого сна, улучшение общего самочувствия и ясности мышления. По мере улучшения фармнагрузка не увеличивается, а аккуратно снижается, чтобы выход из запоя был плавным и устойчивым, без качелей «полегчало — снова провал».
Ознакомиться с деталями – https://vyvod-iz-zapoya-kolomna10.ru/vyvod-iz-zapoya-kapelnica-v-kolomne
В основе работы клиники лежит принцип: зависимость — это не просто привычка и не «слабость характера», а комплексное заболевание, которое требует последовательного лечения, а не случайной капельницы по вызову. «Трезвый Шаг Раменское» отказывается от практики, когда пациенту предлагают один-единственный «волшебный» метод, не объясняя, что будет дальше. Здесь каждое обращение рассматривается в контексте стадии зависимости, общего состояния организма, психоэмоционального фона, семейной ситуации. Сначала специалисты снимают острые проявления: выход из запоя, детоксикация после употребления алкоголя, наркотиков или сочетаний, купирование абстиненции, коррекция давления, пульса, сна, тревоги. Затем формируется стабилизационный этап — подбор поддерживающих схем, работа с тягой, выравнивание эмоционального состояния. После этого при готовности пациента подключаются психотерапевтические и реабилитационные инструменты: мотивационные программы, работа с установками, триггерами, окружением. Важная особенность «Трезвый Шаг Раменское» — готовность объяснять семье и самому пациенту, зачем нужен каждый этап, какие цели у процедуры и какие результаты реально ожидать. Это снижает сопротивление, формирует доверие и делает путь не хаотичным, а управляемым.
Узнать больше – наркологическая клиника московская московская область
Hi there i am kavin, its my first time to commenting anywhere,
when i read this article i thought i could also create comment
due to this good paragraph.
My family members every time say that I am wasting my time here at net,
but I know I am getting familiarity every day by reading such nice content.
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Углубиться в тему – https://narkologicheskaya-klinika-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy
Вывод из запоя в Раменском в условиях клиники строится не вокруг одной капельницы, а вокруг понятной цепочки шагов, где каждый этап логичен и медицински обоснован. Это помогает не только быстро облегчить состояние, но и уменьшить вероятность того, что через пару дней человек снова уйдёт в запой.
Ознакомиться с деталями – vyvod-iz-zapoya-s-vyezdom
Наркологическая клиника «Трезвый Шаг Раменское» — это место, где острые кризисы, многолетние запои и повторяющиеся срывы перестают быть бесконечным кругом, в котором семья остаётся один на один с проблемой. Здесь выстроена система помощи людям с алкогольной и наркотической зависимостью, а также полизависимостями, включая злоупотребление аптечными препаратами. В клинике в Раменском сочетаются круглосуточное наблюдение, профессиональная детоксикация, медикаментозная поддержка, психотерапевтические программы и сопровождение семьи. Важные принципы — безопасность, анонимность, уважение к пациенту и честное объяснение каждого шага лечения. Ни агрессивного давления, ни обещаний «чуда за один день» — вместо этого поэтапный подход, который даёт реальный шанс стабилизировать состояние, снизить тягу и выйти из разрушительного сценария под контролем специалистов. Для близких это означает понятный маршрут: куда обратиться, что будут делать с пациентом, какие риски учтут и как клиника «Трезвый Шаг Раменское» останется на связи после острого периода.
Изучить вопрос глубже – наркологическая клиника фото
Зависимость — это хроническое заболевание, и в «КоломнаМед Центр» это принимается как медицинский факт, а не моральная оценка. Программы включают медикаментозную поддержку, работу с тягой, коррекцию тревожных и депрессивных состояний, психотерапию, помощь в восстановлении режима сна и питания, семейное консультирование. При наркотической зависимости и полинаркомании добавляются протоколы по безопасной отмене веществ, наблюдение в критические периоды, сопровождение на этапе формирования устойчивой ремиссии. Акцент делается на том, чтобы не запугивать пациента, а показать реалистичный путь, где улучшение возможно шаг за шагом.
Получить больше информации – наркологические клиники обратный звонок
Oléh atas itu meréka mengempo mahluk² adikodrati ke Zuni
untuk berjaipong menggunakan memakai topéngnja, melanting kembali bungkusan²-obatnja,
jang disuruhnja konon „ikut menari”. Tingkat perindustrian butala-putera dengan persatuan pada antara trah-tengah Indonesia belum sepan kencang buat mengadakan pemboikotan kepada perindustrian Barat pada Indonesia nan sudah sampai ke derajat dominasi lagi trust yang modern nan bertabiat Internasional sekali lagi. Bagaimana agak perumpamaan ini cocok dengan intensitas Belanda nan populer yaitu gairah “kruindenier”, bos kecil! Polisi terus mengamankan uang tunai, ponsel, serta kelengkapan embalase. Hanja panglima2 perang mempunjai sedikit mahkota ếksekutif, bukan terutama dalam peluang perang, tapi djuga dalam kala damai, jakni bagai polisi. Djuga terukir orang² tua, jang djelas berkarakter Dionysis. Meréka tidak mendjelmakan rangkap segi hikmat adikodrati jang Dionysis. Meréka jang telah matipun datang kembali dalam awan² hudjan, memberi rahmat terhadap dunia. Lama Tju Bu lalu Jang Tjhun menempati, Tetapi Tan Tat tidak muntjul achiroja pada lesu dan sewot kedua Oxpa itu kembali kegunung Hwa San.
Continue https://lumi-wallet.io
Great blog! Do you have any tips for aspiring writers?
I’m planning to start my own website soon but
I’m a little lost on everything. Would you propose starting with a free platform
like WordPress or go for a paid option? There are so many choices out there
that I’m totally overwhelmed .. Any tips? Thanks a lot!
Here is my web site: realtor in Tipp City OH
Письменные рекомендации: сон, питание, гидратация, запреты, «красные флаги», график амбулаторных визитов; при недостатке ресурсов дома — перевод в стационар без задержек. Такая последовательность убирает импровизацию и делает результат повторяемым.
Углубиться в тему – http://vyvod-iz-zapoya-ehlektrostal2-10.ru/
Зависимость — это хроническое заболевание, и в «КоломнаМед Центр» это принимается как медицинский факт, а не моральная оценка. Программы включают медикаментозную поддержку, работу с тягой, коррекцию тревожных и депрессивных состояний, психотерапию, помощь в восстановлении режима сна и питания, семейное консультирование. При наркотической зависимости и полинаркомании добавляются протоколы по безопасной отмене веществ, наблюдение в критические периоды, сопровождение на этапе формирования устойчивой ремиссии. Акцент делается на том, чтобы не запугивать пациента, а показать реалистичный путь, где улучшение возможно шаг за шагом.
Узнать больше – https://narkologicheskaya-klinika-kolomna10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
It’s really a cool and useful piece of info. I am satisfied that you just shared this helpful info with us.
Please keep us informed like this. Thanks for sharing.
Выбор формата — это не вкусовщина, а баланс безопасности в конкретной клинической картине. Дом уместен, если контакт сохранён, рвота эпизодическая, давление и пульс без резких «качелей», тремор контролируемый, в квартире можно обеспечить тишину и присутствие взрослого, готового наблюдать первые 6–8 часов. Тогда выездная бригада работает на месте и выстраивает «мягкий» маршрут, где сон собирается без агрессивной седации, а инфузии идут с шаговой корректировкой темпа. Стационар предпочтителен при длительном эпизоде (3–5 суток и более), неукротимой рвоте, выраженной слабости, шаткости походки, признаках предделирия/делирия, судорожной готовности, а также у пожилых пациентов и при сочетанных диагнозах — ИБС, гипертония, диабет, хронические болезни печени/почек, неврология. Преимущество отделения — приборный мониторинг, лабораторные опции по показаниям, ночная команда и среда, где исключены лишние раздражители: это снижает «цену ошибки» и делает результат устойчивым, а не разовым «прояснением».
Подробнее можно узнать тут – вывод из запоя на дому цена
Процедура проводится как в стационаре, так и на дому. Врач приезжает по вызову, проводит осмотр и измеряет давление, пульс, насыщение кислородом. После оценки состояния подбирается состав капельницы и начинается инфузионная терапия. В среднем процедура длится от 40 минут до 1,5 часов, в зависимости от степени интоксикации. По завершении врач наблюдает за реакцией организма и даёт рекомендации по восстановлению.
Детальнее – http://kapelnicza-ot-zapoya-v-voronezhe17.ru
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Уточнить детали – https://gatrik-ui.or.id/2017/03/05/turnamen-bridge-dan-gaple-piala-bang-harmein-gani
Прежде чем перейти к ориентировочным цифрам, важно подчеркнуть: цена формируется из реальных компонентов помощи — работы врача и медсестры, объёма инфузионной терапии, перечня препаратов, времени выезда и необходимости более длительного наблюдения. Никаких скрытых доплат: все дополнительные назначения согласуются заранее. Чем раньше вы обращаетесь, тем меньше объём вмешательств и, как правило, ниже итоговая стоимость — короткий эпизод проще и дешевле стабилизировать, чем «выводить» осложнения после затянутого запоя.
Подробнее тут – запой нарколог на дом цена
Каждый этап направлен на восстановление организма без стресса и перегрузки. Врачи работают деликатно, чтобы пациент чувствовал безопасность и понимал, что помощь оказывается профессионально.
Получить дополнительную информацию – вывод из запоя цена
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Подробнее можно узнать тут – анонимный вывод из запоя воронеж
Home remodeling is a growing market that mirrors the progressing requirements and
goals of house owners.
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Подробнее можно узнать тут – http://vivod-iz-zapoya-v-volgograde17.ru/vyvod-iz-zapoya-na-domu-volgograd/
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Узнать больше – анонимная наркологическая клиника в саратове
investigate this site fortnite inventory checker free
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Узнать больше – вывод из запоя на дому цена саратов
Капельница при вызове нарколога на дом в Долгопрудном от «МедТрезвие Долгопрудный» — это клинический инструмент, а не магический раствор. Главное правило — никакой агрессивной седации ради видимости спокойствия. Инфузионная терапия строится вокруг нескольких задач: восполнить жидкость, выровнять электролиты, снизить токсическую нагрузку на печень и мозг, поддержать сердце и нервную систему, уменьшить тремор, тревогу и соматические жалобы. Используются растворы для регидратации и коррекции водно-электролитного баланса, витамины группы B и магний для поддержки нервной системы, уменьшения риска судорог и нормализации сна, по показаниям — гепатопротекторы и мягкие антиоксиданты, противорвотные препараты для контроля тошноты. При выраженной тревоге или нарушениях сна назначаются щадящие анксиолитические средства в дозах, которые не выключают пациента полностью, а помогают снять паническое напряжение, сохраняя возможность оценивать динамику состояния. Врач отслеживает реакцию на терапию: стабилизацию давления и пульса, уменьшение дрожи, улучшение общего самочувствия, появление более спокойного, естественного сна. По мере облегчения нагрузки схема не усиливается ради счёта, а рационально сокращается. Такой подход защищает пациента от скрытых осложнений и превращает капельницу в контролируемый, полезный шаг, а не в рискованный эксперимент.
Углубиться в тему – запой нарколог на дом
Hmm is anyone else having problems with the pictures on this blog loading?
I’m trying to figure out if its a problem on my end or
if it’s the blog. Any suggestions would be greatly appreciated.
Angels Bail Bonbds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626,United States
bail bonds 10 percent
Процесс включает несколько шагов:
Получить больше информации – http://narkolog-na-dom-v-ufe17.ru
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Выяснить больше – narkologicheskaya-klinika-doktor
Основная цель капельницы — вывести из организма продукты распада этанола и восстановить водно-солевой баланс. После запоя в крови скапливаются токсичные вещества, которые вызывают головокружение, слабость и эмоциональную нестабильность. Введение растворов внутривенно позволяет быстро доставить активные компоненты в кровоток, улучшая работу сердца, печени и нервной системы. Уже через 20–30 минут после начала процедуры пациент ощущает облегчение.
Выяснить больше – капельница от запоя
Ключевой элемент вывода из запоя в Реутове — правильно подобранная капельница, но в «РеутовМед Сервис» её рассматривают не как волшебное средство, а как часть комплексной терапевтической схемы. Основная цель — не «вырубить» человека сильными седативными коктейлями, а помочь организму безопасно выйти из состояния интоксикации. В инфузионную терапию входят растворы для регидратации, которые восполняют потерю жидкости, снижают вязкость крови, улучшают микроциркуляцию и работу внутренних органов. Коррекция электролитного баланса помогает уменьшить дрожь, мышечную слабость, снизить риск нарушений сердечного ритма. Применяются витамины группы B и препараты магния для поддержки нервной системы, снижения раздражительности и вероятности судорог. По показаниям добавляются гепатопротекторы, мягкие антиоксиданты для разгрузки печени, противорвотные средства при выраженной тошноте, щадящие анксиолитики для снижения тревоги и нормализации сна без грубого угнетения сознания. Все дозировки учитывают сопутствующие заболевания и возраст, что особенно важно для пациентов с гипертонией, ИБС, диабетом, поражением печени и пожилых людей. Эффект оценивается по объективным критериям: стабилизация давления и пульса, уменьшение дрожи, улучшение самочувствия, нормализация сна и поведения, а не только по фразе «стал тихим».
Разобраться лучше – vyvod-iz-zapoya-nedorogo
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
А что дальше? – https://cursos.cicialli.com/titulo-de-la-publicacion-en-el-blog
Перед цифрами — важная оговорка: это ориентиры, не публичная оферта. Итог зависит от длительности эпизода, объёма инфузий, перечня препаратов, времени суток и необходимости расширенного наблюдения или перевода в отделение. Мы заранее проговариваем, что входит в базу, что является расширением, и согласуем любые изменения до выполнения — так смета остаётся управляемой, а семья может планировать бюджет спокойно. Ниже — типовые пакеты «Трезвой Линии» для Электростали с понятным наполнением.
Исследовать вопрос подробнее – vyvod-iz-zapoya-anonimno-ehlektrostal
В клинике применяются современные медицинские технологии, которые обеспечивают стойкий результат. Используемые методики соответствуют международным стандартам и регулярно обновляются.
Узнать больше – лечение в наркологической клинике омск
Вывод из запоя на дому возможен только при относительно контролируемом состоянии и после очной оценки нарколога. В таких случаях специалист выезжает в Раменском, проводит осмотр, назначает индивидуальную капельницу, остаётся до стабилизации состояния и оставляет подробные рекомендации. Важный момент — честность: если во время осмотра врач видит риски (нестабильное давление, признаки начинающегося делирия, серьёзные боли, глубокую дезориентацию), формат на дому не навязывается, а предлагается стационар. Именно это отличает клинику от анонимных «служб капельниц», для которых любая заявка — повод заработать, независимо от последствий.
Детальнее – вывод из запоя
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Ознакомиться с деталями – вывод из запоя с выездом в рязани
I got this site from my friend who told me regarding this
web site and at the moment this time I am browsing this web page and reading very informative articles or reviews at this place.
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Подробности по ссылке – https://gdziejestlumpeks.pl/szafiarenka-maria-kluza-chemia-z-niemiec-odziez-uzywana
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Выяснить больше – вывод из запоя волгоград
Основные этапы включают:
Получить дополнительные сведения – анонимный вывод из запоя в красноярске
hi!,I love your writing very much! proportion we keep in touch extra about your post on AOL?
I need an expert in this space to unravel my problem. May be that’s you!
Taking a look forward to look you.
Не всегда человек способен самостоятельно прекратить приём алкоголя и восстановиться. Есть состояния, требующие немедленного вмешательства специалистов. Обратиться за помощью необходимо, если наблюдаются следующие признаки:
Изучить вопрос глубже – врач вывод из запоя волгоград
Вывод из запоя — это не «волшебная капельница», а последовательная медицинская программа с чёткими целями и измеримыми маркерами. В наркологической клинике «СаратовМед Профи» маршрут строится по принципу управляемых окон: на каждом шаге команда преследует одну цель, меняет лишь один параметр и оценивает результат в заранее назначённый момент. Такой подход снижает лекарственную нагрузку, предотвращает «гонку дозировок» и делает динамику предсказуемой для пациента и близких. Конфиденциальность обеспечивается регламентом: немаркированные выезды, нейтральные формулировки в документах, «тихие» каналы связи, доступ к записям — строго по ролям.
Углубиться в тему – вывод из запоя клиника в саратове
Главным преимуществом наркологической клиники в Новокузнецке является комплексный подход к лечению. Специалисты рассматривают зависимость как заболевание, требующее системного воздействия на организм и психику. Каждый пациент получает индивидуальную программу, включающую медицинскую, психотерапевтическую и социальную помощь. Такой подход обеспечивает достижение устойчивых результатов и предотвращает рецидивы.
Выяснить больше – наркологическая клиника стационар
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Ознакомиться с деталями – http://kodirovanie-ot-alkogolizma-v-volgograde17.ru/
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Разобраться лучше – http://vyvod-iz-zapoya-v-krasnoyarske17.ru/vyvedenie-iz-zapoya-krasnoyarsk/
hello!,I like your writing so so much! share we keep up
a correspondence extra approximately your post on AOL?
I need a specialist in this house to solve my problem. Maybe that’s
you! Looking ahead to see you.
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Уточнить детали – https://espores.com.ar/turmalina-2023
Write more, thats all I have to say. Literally, it seems as though you relied on the
video to make your point. You definitely know what youre talking about, why waste your intelligence on just posting videos to your blog when you could be giving us something enlightening to
read?
Also visit my website – best real estate agent in Ocean Isle Beach NC
With havin so much content do you ever run into any issues
of plagorism or copyright infringement? My website has a lot of completely unique content I’ve either authored myself or outsourced but
it seems a lot of it is popping it up all over the internet
without my agreement. Do you know any solutions to help reduce content from being stolen? I’d definitely appreciate it.
Great blog here! Additionally your site a lot up fast!
What web host are you the use of? Can I am getting your affiliate hyperlink for your host?
I wish my website loaded up as quickly as yours
lol
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Выяснить больше – психиатр нарколог на дом в уфе
I believe this is one of the so much vital info
for me. And i am happy studying your article. However want
to observation on some normal issues, The site style is perfect, the articles is in reality great : D.
Just right job, cheers
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Cost Mesa, СA 92626, Unkted Stɑtes
o’leary bail bonds
I do believe your audience could very well want a good deal more stories like this carry on the excellent hard work.
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Получить больше информации – наркологическая помощь на дому круглосуточно тольятти
I know this if off topic but I’m looking into starting my
own blog and was wondering what all is needed to get setup?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very web smart so I’m not 100% sure. Any recommendations
or advice would be greatly appreciated. Cheers
Одна из сильных сторон «РеутовМед Сервис» — честная оценка границ домашнего лечения. Клиника не обещает «вывезем любого дома», потому что есть состояния, при которых отсутствие круглосуточного наблюдения опасно. Чтобы родным было проще сориентироваться, важно разделить ситуации по уровню риска и понять, почему иногда разумнее выбрать стационар, даже если пациент сопротивляется.
Узнать больше – вывод из запоя в стационаре
Pretty component to content. I simply stumbled upon your weblog and in accession capital to claim
that I acquire actually loved account your weblog posts.
Any way I will be subscribing on your feeds and even I fulfillment you access constantly
quickly.
Услуга
Узнать больше – vyzvat-narkologa-na-dom
Ниже приведено структурированное сравнение форматов:
Подробнее тут – vyvod-iz-zapoya-anonimno
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Подробнее – наркологическая клиника нарколог в саратове
Your practical advice is incredibly valuable.
Лечение в клинике «ВоронежМед Альянс» проходит поэтапно. Каждый модуль имеет определённую цель и собственные критерии эффективности. Такой подход исключает избыточное вмешательство и обеспечивает прозрачность процесса восстановления.
Выяснить больше – анонимная наркологическая клиника в воронеже
Услуга «нарколог на дом в Долгопрудном» от клиники «МедТрезвие Долгопрудный» создана для ситуаций, когда важно действовать быстро, аккуратно и без лишнего шума. Запой, тяжёлое похмелье, срыв после ремиссии, злоупотребление медикаментами или смесью алкоголя с препаратами — всё это не терпит откладывания и самодеятельности. Вызов врача на дом позволяет получить профессиональную помощь без госпитализации, когда состояние пациента ещё позволяет лечить его в привычной обстановке. Нарколог приезжает с полностью укомплектованным набором препаратов и расходников, проводит осмотр, подбирает капельницы по клиническим показаниям, контролирует реакцию, даёт подробные рекомендации на ближайшие дни и при необходимости предлагает дальнейший маршрут: повторный выезд, амбулаторное наблюдение или стационар клиники. Конфиденциальность соблюдается строго: без обсуждений с соседями, без регистрации по месту работы, без унизительных формальностей — только медицинская помощь, ориентированная на безопасность и результат.
Подробнее можно узнать тут – narkolog-na-dom-srochno
На практике чаще всего применяются следующие компоненты:
Получить больше информации – капельница от запоя на дому круглосуточно в воронеже
Excellent website. Lots of useful info here. I’m sending
it to a few buddies ans also sharing in delicious.
And obviously, thanks for your effort!
Thanks in support of sharing such a pleasant thinking, article is good,
thats why i have read it fully
Такой состав обеспечивает быстрое снятие симптомов интоксикации и восстановление функций организма после запоя.
Углубиться в тему – капельница от запоя недорого
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Все материалы собраны здесь – https://jaklean.co.uk/comprehensive-cleaning-services-in-glasgow-jaklean-ltd-sets-the-standard
Процедура проводится как в стационаре, так и на дому. Врач приезжает по вызову, проводит осмотр и измеряет давление, пульс, насыщение кислородом. После оценки состояния подбирается состав капельницы и начинается инфузионная терапия. В среднем процедура длится от 40 минут до 1,5 часов, в зависимости от степени интоксикации. По завершении врач наблюдает за реакцией организма и даёт рекомендации по восстановлению.
Узнать больше – вызвать капельницу от запоя на дому в воронеже
It’s a pity you don’t have a donate button! I’d without a doubt donate to this outstanding blog!
I guess for now i’ll settle for bookmarking and adding your RSS
feed to my Google account. I look forward to fresh updates and will talk about this site with my Facebook group.
Talk soon!
Greetings from Idaho! I’m bored at work so I decided to browse
your site on my iphone during lunch break. I love the info you
provide here and can’t wait to take a look when I get home.
I’m shocked at how quick your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyways, wonderful blog!
Hello, I enjoy reading all of your article post. I wanted to write a little
comment to support you.
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Получить дополнительную информацию – http://vyvod-iz-zapoya-v-krasnoyarske17.ru/vyvedenie-iz-zapoya-krasnoyarsk/
After all, the lack of identity verification makes it easy for individuals to create multiple accounts and even carry out illegal activities undetected.
Saved as a favorite, I love your blog!
Here is my webpage :: real estate agent in Whittier CA
В Воронеже клиника «ВоронежМед Альянс» предлагает комплексное лечение алкогольной и наркотической зависимости. Команда врачей, психиатров, психологов и терапевтов выстраивает индивидуальный маршрут пациента, начиная с детоксикации и заканчивая реабилитацией. Главный принцип — минимальное вмешательство при максимальной эффективности. Это означает, что терапевтические меры подбираются строго по показаниям, а медикаменты применяются только после оценки состояния и лабораторных данных.
Получить больше информации – наркологическая клиника в воронеже
Fine way of telling, and good post to take facts regarding my presentation topic, which
i am going to deliver in institution of higher education.
Услуга
Разобраться лучше – skolko-stoit-vyzvat-narkologa-na-dom
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Узнайте всю правду – https://vistoweekly.com/jessica-erin-lane-coleman-obituary
I am extremely impressed with your writing skills and also with the layout on your
blog. Is this a paid theme or did you customize it yourself?
Either way keep up the nice quality writing, it is rare to see a nice blog
like this one these days.
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, UᏚA
(402) 940-8979
microdermabrasion 2025; half-skateboard-539.notion.site,
This is the right web site for everyone who hopes to understand
this topic. You know a whole lot its almost hard to argue
with you (not that I personally will need to…HaHa). You certainly put
a new spin on a subject that’s been discussed for a long time.
Excellent stuff, just great!
My web site: best real estate agent in Vancouver BC
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Уточнить детали – https://le-k-reims.com/events/coup-de-bluff-au-cabaret
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Выяснить больше – http://narcologicheskaya-klinika-saratov0.ru/
Основные этапы обычно включают:
Ознакомиться с деталями – раменское вывод из запоя
hi!,I love your writing so a lot! share we communicate extra approximately your article on AOL?
I need a specialist on this area to unravel my problem.
Maybe that is you! Taking a look ahead to peer you.
Review my blog post – best realtor in Cincinnati OH
Важное отличие наркологической клиники «Трезвый Путь Коломна» — полный отказ от схемы «одна капельница = решение всех проблем». Детокс здесь рассматривается как необходимый старт, но не как финальная точка. Сначала специалисты снимают острые состояния: вывод из запоя, купирование абстиненции, коррекцию водно-электролитного баланса, поддержку сердца, печени и нервной системы, нормализацию сна, снижение тревоги. Когда организм перестаёт «гореть», начинается следующий этап — стабилизация: врач оценивает психическое состояние, выявляет депрессивные, тревожные, панические проявления, подбирает поддерживающие схемы, которые помогают удержаться в первые недели после кризиса. Далее подключаются психотерапевтические инструменты: индивидуальные консультации, работа с мотивацией, разбор триггеров, формирование новых привычек. В финале выстраивается маршрут поддержки: амбулаторное наблюдение, связь с клиникой, рекомендации для семьи. Такой поэтапный подход делает клинику в Коломне местом, где зависимость перестают воспринимать как «стыд» и начинают воспринимать как задачу, с которой можно работать профессионально.
Выяснить больше – http://narkologicheskaya-klinika-kolomna2-10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
always i used to read smaller articles which also clear their motive, and that is also happening
with this piece of writing which I am reading now.
Amazing! This blog looks just like my old one! It’s on a totally different topic but it has
pretty much the same layout and design. Superb choice of colors!
Hurrah, that’s what I was looking for, what a information!
present here at this website, thanks admin of this web page.
my web site … best realtor in Cincinnati OH
Hello, Neat post. There is a problem along with your web
site in internet explorer, would test this? IE still is
the market leader and a huge section of other people will miss your
fantastic writing because of this problem.
my site – real estate agent Ocean Isle Beach NC
Состав капельницы подбирается индивидуально, с учётом степени опьянения, возраста и хронических заболеваний пациента. Врач определяет дозировку и комбинацию препаратов, чтобы процедура прошла безопасно и эффективно.
Ознакомиться с деталями – капельница от запоя вызов в воронеже
Домашний формат особенно важен, когда пациент не готов к стационару, боится огласки, испытывает стыд или сопротивление, но объективно нуждается в помощи. Попытки «перетерпеть» или лечить своими силами заканчиваются тем, что родственники дают опасные комбинации седативных, анальгетиков и «антипохмельных» средств, а состояние только ухудшается. «МедТрезвие Долгопрудный» строит выездную помощь так, чтобы она оставалась профессиональной медициной, а не косметической услугой. Уже при звонке диспетчер под контролем врача уточняет длительность запоя, виды алкоголя, наличие гипертонии, болезней сердца, печени, почек, диабета, неврологических нарушений, психических эпизодов, факт судорог, делирия в прошлом, какие лекарства уже были даны. Это позволяет заранее понять, подходит ли формат лечения на дому или сразу нужно рассматривать стационар. Выезд назначается только в тех случаях, когда это безопасно, и именно в этом ключевое отличие официальной клиники от анонимных «капельниц на дом» — здесь всегда выбирают жизнь и здоровье, а не удобный маркетинговый сценарий. Для семьи это не просто комфорт, а возможность получить помощь без риска сорваться в критическое состояние посреди ночи.
Получить больше информации – https://narkolog-na-dom-dolgoprudnij10.ru/vyezd-narkologa-na-dom-v-dolgoprudnom
Hurrah! In the end I got a weblog from where I be able to really take helpful information concerning my study
and knowledge.
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Все материалы собраны здесь – https://www.angelesviajero.com/2019/10/15/thailand-phuket
This paragraph will help the internet users for setting up new website or even a blog from start to
end.
My page – realtor in Bedford NH
Yes! Finally someone writes about realtor in Ann
Arbor MI.
my site: best real estate agent in Ann Arbor MI
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Получить дополнительные сведения – https://saliksameen.com/hello-world
I am sure this post has touched all the internet viewers,
its really really fastidious article on building up new
website.
Very good info. Lucky me I found your blog by chance (stumbleupon).
I have bookmarked it for later!
Вывод из запоя — это не просто медицинская процедура, а системный процесс восстановления организма после длительного употребления алкоголя. В клинике «ВолгаМед Резолюция» в Волгограде пациенты получают помощь, основанную на принципах доказательной медицины и индивидуального подхода. Лечение направлено не только на устранение симптомов интоксикации, но и на стабилизацию нервной системы, восстановление водно-солевого баланса и нормализацию сна. Капельницы подбираются персонально, с учётом состояния пациента, сопутствующих заболеваний и возраста. Все процедуры проводятся анонимно и под контролем нарколога.
Ознакомиться с деталями – http://vyvod-iz-zapoya-v-volgograde17.ru
Oh my goodness! Awesome article dude! Thanks, However I am having problems with your RSS.
I don’t understand why I cannot subscribe to it. Is there
anybody else getting identical RSS issues? Anyone that knows the answer can you kindly respond?
Thanx!!
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Подробнее можно узнать тут – https://narcologicheskaya-klinika-omsk0.ru/narkologi-omska
If some one wants to be updated with latest
technologies afterward he must be go to see this site and be
up to date all the time.
Все растворы проходят фармацевтический контроль, а процедуры выполняются одноразовыми стерильными инструментами. После завершения капельницы врач наблюдает пациента в течение 15–30 минут, оценивает результат и даёт рекомендации по дальнейшему восстановлению. Важно не прерывать терапию самостоятельно — эффект закрепляется только при соблюдении рекомендаций.
Получить дополнительные сведения – вызвать врача нарколога на дом воронеж
Каждый этап направлен на восстановление организма без стресса и перегрузки. Врачи работают деликатно, чтобы пациент чувствовал безопасность и понимал, что помощь оказывается профессионально.
Ознакомиться с деталями – вывод из запоя клиника новокузнецк
Для повышения эффективности в капельницы добавляются витамины группы B, аскорбиновая кислота, кардиопротекторы и антиоксиданты. Такая комбинация позволяет не только ускорить выведение продуктов распада алкоголя, но и предотвратить развитие постабстинентных расстройств. Благодаря точной дозировке и мягкому темпу введения растворов снижается риск побочных реакций, а восстановление проходит плавно и безопасно.
Получить дополнительные сведения – нарколог вывод из запоя
Peculiar article, just what I needed.
Angels Bail Bonds Costa Mesa
769 Baker Տt,
Costa Mesa, ϹA 92626, United Stаtes
what does a bail bonds agent do
Thanks for sharing your thoughts on Daftar Citislots.
Regards
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Углубиться в тему – https://kodirovanie-ot-alkogolizma-v-volgograde17.ru/
These are genuinely great ideas in about
blogging. You have touched some pleasant things here.
Any way keep up wrinting.
Just desire to say your article is as astounding.
The clearness in your post is just nice and i could assume you are an expert on this subject.
Fine with your permission let me to grab your RSS feed to keep updated
with forthcoming post. Thanks a million and
please carry on the enjoyable work.
Stop by my web blog; realtor in Whittier CA
В таблице представлены основные виды терапии, применяемые в клинике:
Углубиться в тему – http://narcologicheskaya-klinika-v-novokuzneczke17.ru
I have read so many articles regarding the blogger lovers but
this paragraph is really a good paragraph, keep it up.
Город с протяжёнными магистралями и разноскоростными районами требует особой организации маршрутов. Выездные бригады «ВолгаДок Медикал» работают в режиме 24/7, прибывают в гражданской одежде, избегают громких звонков и используют «немаркированные» подъезды. Перед приездом мы просим подготовить пространство: приглушить верхний свет, обеспечить приток свежего воздуха без сквозняков, подготовить ровную поверхность под укладку и удлинитель, перевести телефоны в «без уведомлений» с «белым списком» близких. Это позволяет в первые минуты сосредоточиться на клинике, а не на бытовых вопросах.
Получить дополнительные сведения – частная наркологическая клиника саратов
Лечение проходит в несколько этапов: диагностика, детоксикация, медикаментозная поддержка и восстановление. Каждый этап имеет чёткие цели и критерии эффективности, что делает процесс управляемым и безопасным. Применяются препараты, сертифицированные в РФ, и только те, чья эффективность подтверждена клиническими исследованиями.
Ознакомиться с деталями – вывод из запоя вызов на дом волгоград
Сайт Sultan Casino познавательный. Обязательно загляну ещё!
http://saab.one/proxy.php?link=http%3A%2F%2Fsultan-casino-kazakhstan-winners.kz%2Fregistration
Great beat ! I wish to apprentice while you amend your site,
how can i subscribe for a blog site? The account helped me
a acceptable deal. I had been tiny bit acquainted of this your broadcast offered bright clear concept
Выбор наркологической клиники в Коломне — это не «слишком серьёзно», а логичный шаг, если зависимость уже зашла дальше спонтанных эпизодов. Алкоголизм, наркомания, злоупотребление успокоительными и обезболивающими — это не только психологическая тяга, но и перестройка организма: страдают печень, сердце, сосуды, нервная система, гормональный фон, сон, психика. Дома редко есть возможность круглосуточно контролировать состояние, правильно отменять вещества, отслеживать давление, пульс, поведение, не допускать опасных комбинаций препаратов. Родственники устают, реагируют эмоциями, а не медицинской логикой, человек чувствует себя под прицелом, но не под защитой. В «КоломнаМед Центр» всё выстроено так, чтобы снять нагрузку с семьи и вывести помощь из зоны хаотичных решений. Здесь оценивают не только то, «что и сколько пьёт или принимает», а весь контекст: длительность зависимости, срывы, уже перенесённые делирии или передозировки, сопутствующие болезни, психические состояния, семейную ситуацию. На основе этого формируется безопасный план: где начать — в стационаре или амбулаторно, какой формат детокса выбрать, насколько жёстко вести наблюдение, как сразу встроить психотерапевтическую и социальную поддержку. Клиника в Коломне позволяет работать системно, а не латать последствия очередного срыва.
Углубиться в тему – narkologicheskaya-klinika
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ᏟА 92626, United Stаteѕ
bail bonds ⅼicense (wakelet.com)
Helpful information. Fortunate me I discovered your site accidentally, and I’m
stunned why this coincidence didn’t happened in advance!
I bookmarked it.
В основе работы клиники лежит принцип: зависимость — это не просто привычка и не «слабость характера», а комплексное заболевание, которое требует последовательного лечения, а не случайной капельницы по вызову. «Трезвый Шаг Раменское» отказывается от практики, когда пациенту предлагают один-единственный «волшебный» метод, не объясняя, что будет дальше. Здесь каждое обращение рассматривается в контексте стадии зависимости, общего состояния организма, психоэмоционального фона, семейной ситуации. Сначала специалисты снимают острые проявления: выход из запоя, детоксикация после употребления алкоголя, наркотиков или сочетаний, купирование абстиненции, коррекция давления, пульса, сна, тревоги. Затем формируется стабилизационный этап — подбор поддерживающих схем, работа с тягой, выравнивание эмоционального состояния. После этого при готовности пациента подключаются психотерапевтические и реабилитационные инструменты: мотивационные программы, работа с установками, триггерами, окружением. Важная особенность «Трезвый Шаг Раменское» — готовность объяснять семье и самому пациенту, зачем нужен каждый этап, какие цели у процедуры и какие результаты реально ожидать. Это снижает сопротивление, формирует доверие и делает путь не хаотичным, а управляемым.
Получить дополнительные сведения – narkologicheskaya-klinika-na-domu
Маршрут организован так, чтобы убрать хаос и сделать шаги понятными для родственников. После звонка оператор под контролем врача уточняет длительность употребления, примерные объёмы алкоголя, хронические болезни (гипертония, ИБС, диабет, заболевания печени, почек, нервной системы), список уже принятых лекарств, эпизоды потери сознания, судорог, подозрительные психические симптомы. На этом этапе принимается базовое решение: возможно ли безопасно провести детокс на дому либо показан стационар. Врач приезжает по адресу в Щёлково, проводит осмотр: фиксирует АД, ЧСС, сатурацию, температуру, оценивает тремор, координацию, речь, поведение, уровень сознания, степень обезвоживания. Затем подбирается индивидуальная инфузионная схема: растворы для регидратации, коррекции электролитов и кислотно-щелочного баланса, витамины группы B и магний для поддержки нервной системы и снижения тремора; по показаниям — гепатопротекторы, мягкие антиоксиданты, противорвотные, щадящие анксиолитики для сна, но без грубого «выключения». Во время процедуры врач наблюдает за динамикой, при необходимости меняет скорость капельницы, контролирует давление и пульс, следит за реакцией на препараты. В финале даёт подробные рекомендации: как вести себя ближайшие 24–72 часа, как спать, что пить и есть, каких лекарств избегать, какие симптомы считать тревожными, когда нужно немедленно звонить и когда стоит рассмотреть стационар. Если уже на этапе осмотра понятно, что дому «тесно» по безопасности, перевод в клинику организуется без задержек.
Подробнее тут – skolko-stoit-narkolog-na-dom
This article actually helped me with a report I was doing.
Когда острые угрозы исключены, программа стартует дома. Пациент получает понятную карту действий, близкие — короткие окна обратной связи, врач — чистую «картинку» для тонкой настройки. Мы просим сообщать факты, а не эмоции: минуты до засыпания, число пробуждений, объём тёплой воды малыми глотками, пульс к вечеру, переносимость мягкой пищи, ясность головы утром.
Выяснить больше – скорая вывод из запоя саратов
Howdy I am so excited I found your blog, I really found you by error, while I was researching on Digg for something else, Anyhow I am here now and would just like to say
thank you for a fantastic post and a all round interesting blog (I also love the theme/design),
I don’t have time to go through it all at the moment but I have saved it and also added your RSS feeds,
so when I have time I will be back to read much more, Please
do keep up the great work.
Feel free to surf to my web blog: best real estate agent in Bedford NH
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CA 92626, United Ѕtates
how many bail bond missions are in gta 5
Основная цель капельницы — вывести из организма продукты распада этанола и восстановить водно-солевой баланс. После запоя в крови скапливаются токсичные вещества, которые вызывают головокружение, слабость и эмоциональную нестабильность. Введение растворов внутривенно позволяет быстро доставить активные компоненты в кровоток, улучшая работу сердца, печени и нервной системы. Уже через 20–30 минут после начала процедуры пациент ощущает облегчение.
Изучить вопрос глубже – https://kapelnicza-ot-zapoya-v-voronezhe17.ru/kapelnicza-ot-alkogolya-voronezh/
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Подробнее – анонимная наркологическая клиника
Процесс кодирования проходит в комфортной и спокойной обстановке. Врач объясняет каждый этап, чтобы пациент чувствовал себя уверенно и спокойно. После процедуры пациент получает памятку с рекомендациями по уходу за здоровьем и режиму поведения в первые недели после лечения.
Подробнее можно узнать тут – http://kodirovanie-ot-alkogolizma-v-volgograde17.ru/kodirovanie-ot-alkogolya-v-volgograde/
Клиника в Волгограде руководствуется принципами индивидуального подхода, конфиденциальности и научно обоснованных методик. Врач-нарколог оценивает общее состояние пациента, определяет стадию зависимости и подбирает оптимальную терапевтическую схему. Лечение включает детоксикацию, медикаментозную поддержку, психотерапию и реабилитацию. Каждый пациент проходит лечение в безопасных условиях с постоянным медицинским наблюдением.
Разобраться лучше – http://narkologicheskaya-klinika-v-volgograde17.ru
Огромное спасибо за платформу Sultan Casino — очень выручает!
Sultan Casino рулетка (https://mikhailovsk24.ru/redirect?url=https://sultan-casino-kazakhstan-betking.kz/registration)
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Детальнее – https://narkologicheskaya-pomoshh-v-tolyatti17.ru/pomoshh-narkozavisimym-tolyatti
В клинике обеспечивается безопасный вывод из запоя и очистка организма после употребления алкоголя, наркотиков или токсических сочетаний. Используются современные инфузионные схемы, витамины группы B, магний, гепатопротекторы по показаниям, противорвотные, мягкая коррекция сна и тревожности. Контроль давления, пульса, сатурации и поведения позволяет вовремя отметить любые осложнения и скорректировать терапию. Главная цель — не просто «прояснить голову», а защитить сердечно-сосудистую систему, мозг, печень, минимизировать риск делирия, судорог, аритмий и других острых состояний.
Ознакомиться с деталями – наркологическая клиника коломна
Вывод из запоя требуется тогда, когда организм уже не способен самостоятельно справиться с последствиями алкогольной интоксикации. Длительное употребление спиртного приводит к нарушению работы внутренних органов, обезвоживанию и психическим расстройствам. Медицинская помощь помогает избежать опасных осложнений и облегчить процесс отказа от алкоголя.
Углубиться в тему – вывод из запоя на дому недорого рязань
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Исследовать вопрос подробнее – вывод из запоя
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Разобраться лучше – https://narkologicheskaya-klinika-kolomna2-10.ru/
Регидратация, коррекция электролитов и КЩС, витамины группы B/магний; по показаниям — гепатопротекторы, антиоксиданты, противорвотные, мягкие анксиолитики. Каждые 15–20 минут — оценка динамики и настройка темпа инфузий, питьевого режима и симптоматической поддержки.
Получить дополнительные сведения – vyvod-iz-zapoya-kruglosutochno
Thank you, I’ve recently been looking for information approximately this subject for
a long time and yours is the best I’ve came upon till now.
But, what in regards to the conclusion? Are you certain concerning the
source?
Капельница от запоя в Воронеже применяется для восстановления организма после длительного употребления алкоголя, устранения интоксикации и нормализации обменных процессов. Медицинская процедура проводится под контролем врача-нарколога, в клинике или на дому. Она позволяет быстро улучшить самочувствие, устранить головную боль, тремор, тошноту, обезвоживание и нарушения сна. Современные препараты действуют мягко, безопасно и без стресса для организма, обеспечивая плавный выход из запоя.
Получить дополнительную информацию – капельница от запоя вызов
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Получить дополнительную информацию – наркологическая клиника
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored subject matter
stylish. nonetheless, you command get bought an nervousness over
that you wish be delivering the following. unwell unquestionably
come further formerly again as exactly the
same nearly very often inside case you shield this increase.
my webpage – best real estate agent in Ocean Isle Beach NC
What a material of un-ambiguity and preserveness of valuable
familiarity about unpredicted emotions.
В клинике обеспечивается безопасный вывод из запоя и очистка организма после употребления алкоголя, наркотиков или токсических сочетаний. Используются современные инфузионные схемы, витамины группы B, магний, гепатопротекторы по показаниям, противорвотные, мягкая коррекция сна и тревожности. Контроль давления, пульса, сатурации и поведения позволяет вовремя отметить любые осложнения и скорректировать терапию. Главная цель — не просто «прояснить голову», а защитить сердечно-сосудистую систему, мозг, печень, минимизировать риск делирия, судорог, аритмий и других острых состояний.
Изучить вопрос глубже – https://narkologicheskaya-klinika-kolomna10.ru/
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Углубиться в тему – платная наркологическая клиника
What a data of un-ambiguity and preserveness of precious knowledge about unexpected feelings.
FranChoice
7500 Fying Cloud Drive,
#600 Eden Prairie
MN 55344, United Ⴝtates
952-345-8400
franchise business growth strategies explained
Hello! I know this is kind of off topic but I was wondering if you knew where I could find a captcha plugin for my
comment form? I’m using the same blog platform as yours and I’m having problems finding one?
Thanks a lot!
Feel free to surf to my site :: best real estate agent in Whittier CA
Процедура начинается с обследования пациента: врач измеряет давление, частоту пульса, оценивает степень интоксикации и состояние внутренних органов. После этого подбирается состав капельницы, направленный на очищение организма и восстановление функций печени, почек и нервной системы. Все препараты вводятся внутривенно, что обеспечивает быстрый эффект и минимизирует нагрузку на желудочно-кишечный тракт.
Получить дополнительную информацию – вывод из запоя капельница в тюмени
Комплексный подход обеспечивает не только снятие симптомов, но и полное восстановление функций организма. Пациент получает поддержку на всех этапах — от детоксикации до социальной адаптации.
Ознакомиться с деталями – http://narkologicheskaya-pomoshh-v-tolyatti17.ru
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Получить больше информации – наркологическая клиника нарколог волгоград
My issues have been very similar, with my family. But, we made some different decisions. It’s complex.
Острый эпизод запоя — это не «плохое самочувствие», а состояние с реальными рисками для сердца, нервной системы и дыхания, особенно в ночные часы, когда усиливаются вегетативные реакции и тревога. В «НоваТрезвие» мы выстраиваем помощь так, чтобы от звонка до заметного облегчения прошло как можно меньше времени и как можно меньше случайностей: короткое интервью для оценки рисков, выезд врача или приём в клинике, экспресс-диагностика по ключевым показателям, персональная инфузионная схема без «универсальных коктейлей», мягкая коррекция сна и тревоги без «вырубания», понятные инструкции семье на 24–72 часа и план продолжения на ближайшие недели. Мы не скрываемся за общими формулами: решения принимаются по фактическим данным, дозы и темп капельниц подстраиваются к динамике каждые 15–20 минут, а при «красных флагах» перевод в стационар организуется без пауз. Конфиденциальность соблюдается строго, а коммуникация простая и предсказуемая — чтобы вы всегда знали, что происходит сейчас и чего ждать к утру.
Подробнее можно узнать тут – https://vyvod-iz-zapoya-ehlektrostal2-10.ru/
Kenvox
1701 E Edinger Ave
Santa Ana, CᎪ 92705, United Statеs
16572319025
affordable mold making facilities
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Получить дополнительную информацию – https://bremer-tor-event.de/hello-world-2
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Получить дополнительную информацию – наркологическая клиника клиника помощь в саратове
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Уточнить детали – https://okanet.media/okanetoha
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Получить дополнительную информацию – нарколог на дом
This is very interesting, You’re an excessively skilled blogger.
I’ve joined your feed and stay up for in quest of extra of your excellent post.
Also, I’ve shared your site in my social networks
my web page :: Automatic Dog Feeder
Magnificent beat ! I wish to apprentice even as you amend your website, how can i subscribe for
a blog website? The account aided me a acceptable deal.
I were a little bit familiar of this your broadcast provided vivid clear concept
Услуга
Получить дополнительные сведения – вызов нарколога на дом в серпухове
Запой — это не просто несколько лишних дней алкоголя, а тяжёлое состояние, в котором организм работает на пределе. Чем дольше длится эпизод, тем глубже обезвоживание, тем сильнее сдвиги электролитов, тем выше риск аритмий, гипертонических кризов, судорог, делирия, обострений заболеваний сердца, печени и поджелудочной железы. Попытки «вывести» человека дома силами родных часто включают опасные комбинации: случайные седативные, снотворные, анальгетики, «антипохмельные» из рекламы. Они могут на время усыпить или «успокоить», но при этом скрывают ухудшение, сбивают давление, угнетают дыхание и мешают врачу увидеть реальную картину. В «Трезвый Центр Коломна» подход другой: ещё на этапе звонка специалист уточняет длительность запоя, объёмы и виды алкоголя, наличие гипертонии, ИБС, диабета, заболеваний печени и почек, неврологических проблем, список уже принятых препаратов, эпизоды потери сознания, судорог, странного поведения. На основании этих данных определяется, безопасен ли формат на дому или сразу нужен стационар. Такая сортировка позволяет вовремя перехватить опасные случаи, не терять часы на бесполезные попытки и сразу запускать те схемы, которые реально снижают риски и стабилизируют состояние.
Подробнее – anonimnyj-vyvod-iz-zapoya-na-domu
For newest information you have to pay a quick visit the web and on the web I found this web page
as a best web page for latest updates.
Feel free to surf to my webpage; best realtor in West Chester Township OH
We believe in building trust through transparency. We started 2026 by ensuring Gambling Chooser bonus offers were described accurately and fairly. Paired with design tweaks, this is our value in action.
Thanks for finally talking about > Heart failure: Symptoms, Causes,
Diagnosis & Treatment – MDtodate best real estate
agent in Vancouver BC
Выбор формата — это не вкусовщина, а баланс безопасности в конкретной клинической картине. Дом уместен, если контакт сохранён, рвота эпизодическая, давление и пульс без резких «качелей», тремор контролируемый, в квартире можно обеспечить тишину и присутствие взрослого, готового наблюдать первые 6–8 часов. Тогда выездная бригада работает на месте и выстраивает «мягкий» маршрут, где сон собирается без агрессивной седации, а инфузии идут с шаговой корректировкой темпа. Стационар предпочтителен при длительном эпизоде (3–5 суток и более), неукротимой рвоте, выраженной слабости, шаткости походки, признаках предделирия/делирия, судорожной готовности, а также у пожилых пациентов и при сочетанных диагнозах — ИБС, гипертония, диабет, хронические болезни печени/почек, неврология. Преимущество отделения — приборный мониторинг, лабораторные опции по показаниям, ночная команда и среда, где исключены лишние раздражители: это снижает «цену ошибки» и делает результат устойчивым, а не разовым «прояснением».
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-ehlektrostal2-10.ru/
Наркологическая клиника в Новокузнецке предоставляет профессиональную помощь людям, столкнувшимся с зависимостью от алкоголя, наркотиков и психоактивных веществ. Лечение проводится под наблюдением опытных специалистов с применением современных медицинских методик. Основная цель работы клиники — не только устранить физическую зависимость, но и восстановить психологическое равновесие пациента, вернуть мотивацию и способность жить без употребления веществ.
Получить дополнительные сведения – наркологическая клиника нарколог новокузнецк
Tremendous issues here. I’m very happy to peer your article.
Thank you so much and I am looking ahead to touch you.
Will you kindly drop me a mail?
Unquestionably believe that which you said. Your favorite justification appeared to be on the internet the easiest thing to
be aware of. I say to you, I definitely get irked while people consider
worries that they plainly don’t know about. You
managed to hit the nail upon the top and defined out the whole thing
without having side-effects , people could take
a signal. Will likely be back to get more. Thanks
Post writing is also a excitement, if you be acquainted with after that you can write if not it is complex to write.
Thanks for the marvelous posting! I definitely enjoyed reading
it, you can be a great author.I will ensure that I bookmark your blog and will come back in the foreseeable future.
I want to encourage you to ultimately continue your great
work, have a nice holiday weekend!
Feel free to surf to my site realtor in Ocean Isle Beach NC
Have you ever considered about including a little
bit more than just your articles? I mean, what you say is fundamental and everything.
But imagine if you added some great graphics or video clips to give your posts more, “pop”!
Your content is excellent but with pics and clips, this website could definitely be one of
the most beneficial in its niche. Good blog!
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Разобраться лучше – https://narkolog-na-dom-shchelkovo10.ru/vyzvat-narkologa-na-dom-shchelkovo/
The best resolutions are the ones you act on immediately. We began 2026 by strengthening GamblingChooser foundation. We improved UX, ensured bonus transparency, and optimized code. This work reflects our core belief in building trust incrementally.
Каждый этап направлен на восстановление организма без стресса и перегрузки. Врачи работают деликатно, чтобы пациент чувствовал безопасность и понимал, что помощь оказывается профессионально.
Получить больше информации – вывод из запоя круглосуточно новокузнецк
wonderful post, very informative. I’m wondering why the opposite experts of
this sector do not understand this. You should continue your writing.
I’m confident, you have a huge readers’ base already!
Каждое назначение объясняется пациенту и близким простым языком. Здесь не практикуют подход «делаем, как знаем, вам всё равно не понять» — прозрачность и понятные шаги помогают снизить тревогу и укрепляют доверие к клинике.
Получить дополнительные сведения – https://vyvod-iz-zapoya-ramenskoe10.ru/vyvod-iz-zapoya-na-domu-v-ramenskom/
Наркологическая клиника «Трезвый Путь Коломна» — это пространство, где тяжёлые истории зависимости перестают быть хаотичным набором срывов, ночных обещаний и беспомощных попыток родных «вытащить своими силами». Здесь собраны врачи-наркологи, терапевты, психологи и медперсонал, которые знают, что такое длительные запои, многолетнее употребление, полинаркомания, зависимость от аптечных препаратов, и умеют работать с этим не через страх и давление, а через профессиональные, выверенные шаги. Клиника в Коломне предлагает безопасную детоксикацию, стационарное наблюдение, индивидуальные программы лечения алкоголизма и наркомании, поддержку семьи и постреабилитационные решения. Все процессы организованы так, чтобы пациент сохранял достоинство, а родственники наконец получили не обещания, а реальный план действий, понятный по этапам и по результатам.
Исследовать вопрос подробнее – наркологическая клиника телефон
Не всегда человек способен самостоятельно прекратить приём алкоголя и восстановиться. Есть состояния, требующие немедленного вмешательства специалистов. Обратиться за помощью необходимо, если наблюдаются следующие признаки:
Изучить вопрос глубже – вывод из запоя капельница в волгограде
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Узнать больше – https://vyvod-iz-zapoya-v-novokuzneczke17.ru/vyvedenie-iz-zapoya-novokuzneczk/
https://t.me/s/kAziNo_S_minImAlNYM_DEpOzitom/5
Процесс вывода из запоя включает последовательное воздействие на ключевые звенья интоксикации. Ниже представлена таблица, отражающая этапы лечения, используемые методики и ожидаемые результаты терапии.
Получить дополнительную информацию – вывод из запоя круглосуточно в волгограде
We are a gaggle of volunteers and opening a brand new scheme in our community.
Your web site provided us with valuable information to work on. You’ve done an impressive process and our entire neighborhood will be grateful to you.
Не всегда человек способен прекратить употребление алкоголя без медицинского вмешательства. Чем дольше длится запой, тем выше риск осложнений. Обратиться к специалисту следует при появлении следующих признаков:
Подробнее тут – вывод из запоя капельница тюмень
Процесс лечения включает несколько последовательных шагов, направленных на стабилизацию состояния, детоксикацию и восстановление функций организма. Таблица ниже показывает основные этапы процедуры, применяемые врачами клиники «РеабКузбасс».
Получить дополнительную информацию – https://vyvod-iz-zapoya-v-novokuzneczke17.ru/vyvedenie-iz-zapoya-novokuzneczk
Наркологическая клиника в Новокузнецке предоставляет профессиональную помощь людям, столкнувшимся с зависимостью от алкоголя, наркотиков и психоактивных веществ. Лечение проводится под наблюдением опытных специалистов с применением современных медицинских методик. Основная цель работы клиники — не только устранить физическую зависимость, но и восстановить психологическое равновесие пациента, вернуть мотивацию и способность жить без употребления веществ.
Узнать больше – наркологическая клиника лечение алкоголизма
Не всегда человек способен самостоятельно прекратить приём алкоголя и восстановиться. Есть состояния, требующие немедленного вмешательства специалистов. Обратиться за помощью необходимо, если наблюдаются следующие признаки:
Исследовать вопрос подробнее – вывод из запоя в волгограде
I appreciate, cause I discovered just what I was having a look for.
You’ve ended my 4 day lengthy hunt! God Bless you man. Have
a nice day. Bye
Feel free to surf to my web site: best real estate agent in West Chester Township OH
I read this article fully concerning the difference of most recent
and previous technologies, it’s awesome article.
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Получить дополнительные сведения – http://www.domen.ru
WOW just what I was searching for. Came here by
searching for leave a comment” “sports news
Wonderful beat ! I wish to apprentice while you
amend your website, how could i subscribe for a blog site?
The account helped me a acceptable deal. I had been tiny bit acquainted of this your broadcast provided bright clear concept
my page – real estate agent in Ann Arbor MI
What’s up i am kavin, its my first occasion to commenting anyplace, when i read
this paragraph i thought i could also create comment
due to this sensible paragraph.
It is not my first time to go to see this web site,
i am browsing this site dailly and get fastidious data from here everyday.
What’s up to every body, it’s my first go to see of this webpage; this web site contains amazing and
genuinely good material designed for readers.
If you desire to improve your experience just keep visiting this web page and be updated
with the latest gossip posted here.
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Узнайте всю правду – https://schemesewa.com/tractor-anudan-yojana-in-marathi
В клинике «ВолгоградМед Альянс» применяются разные методы кодирования, позволяющие подобрать оптимальный вариант для каждого пациента. Выбор зависит от медицинских показаний, психологической готовности и длительности ремиссии. В таблице ниже представлены основные методики, их особенности и преимущества.
Выяснить больше – анонимное кодирование от алкоголизма в волгограде
Каждое направление встроено в общую стратегию: не просто купировать симптомы, а уменьшить риск повторения сценария, когда после «облегчения» всё возвращается к прежней модели употребления.
Получить больше информации – narkologicheskie-kliniki-obratnyj-zvonok
Домашний формат хорош при умеренной выраженности симптомов, сохранённом контакте и возможности обеспечить наблюдение в квартире: тихая комната, взрослый рядом первые 6–8 часов, отсутствие грубой дезориентации и неукротимой рвоты, относительная стабильность АД/ЧСС. В таких условиях выездная бригада «Трезвой Линии» запускает персональную схему: регидратация, выравнивание электролитов, поддержка витаминами группы B и магнием, осторожная седация, чтобы «собрать» сон, не выключая мониторинг. Стационар предпочтителен, если запой длится 3–5 суток и более, отмечаются «качели» показателей, шаткость походки, выраженная слабость, признаки предделирия или судорожной готовности; также при сочетанной соматике (ИБС, гипертония, диабет, хронические болезни печени/почек, неврология) и у пациентов старшего возраста. Преимущество стационара — приборный контроль, тихий режим, щадящее питание, возможность быстро расширять схему без ожидания ухудшений. Мы придерживаемся принципа «минимально достаточно»: ровно столько вмешательств, сколько требует клиническая картина, — так безопаснее и в перспективе экономнее, чем череда домашних «подлаток».
Получить дополнительные сведения – вывод из запоя с выездом
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Изучить вопрос глубже – https://kodirovanie-ot-alkogolizma-v-volgograde17.ru/kodirovanie-ot-alkogolya-v-volgograde/
I’m not sure where you’re getting your info, but great topic.
I needs to spend some time learning much more or understanding more.
Thanks for wonderful information I was looking for this information for my mission.
Feel free to visit my website: best real estate agent in Ann Arbor MI
This is a topic that’s near to my heart… Take care!
Where are your contact details though?
My homepage: best realtor in Vancouver BC
В таблице представлены основные виды терапии, применяемые в клинике:
Получить дополнительную информацию – http://narcologicheskaya-klinika-v-novokuzneczke17.ru
Hmm it seems like your website ate my first comment (it was extremely long) so I guess I’ll just sum it up what I
submitted and say, I’m thoroughly enjoying your blog. I too am
an aspiring blog blogger but I’m still new to everything.
Do you have any recommendations for inexperienced blog writers?
I’d genuinely appreciate it.
Feel free to surf to my page – best realtor in Tipp City OH
Ниже приведено структурированное сравнение форматов:
Получить дополнительную информацию – вывод из запоя на дому
Острый период запоя — это не «плохое самочувствие», а состояние с реальными рисками, где каждая задержка усложняет картину. В «Трезвой Линии» в Электростали мы строим помощь так, чтобы от первого звонка до заметного облегчения прошёл минимальный и управляемый путь: быстрый сбор рисков, экспресс-диагностика на месте, персональная инфузионная схема без «универсальных коктейлей», щадящая коррекция сна и тревоги, регулярные замеры показателей, чёткие рекомендации для семьи. Мы избегаем агрессивной седации: дозы и темп капельниц подбираются под возраст, длительность эпизода, сопутствующие заболевания и уже принимаемые лекарства. Задача — быстро снять токсическую нагрузку, выровнять давление и пульс, собрать ночной сон, а затем удержать результат дисциплинированным постдетокс-маршрутом на 2–4 недели. Конфиденциальность и анонимность соблюдаются без компромиссов, решения принимаются по реальным данным, чтобы эффект был устойчивым, предсказуемым и безопасным для пациента и семьи.
Подробнее – https://vyvod-iz-zapoya-ehlektrostal10.ru/vyvesti-iz-zapoya-ehlektrostal/
Такая форма помощи позволяет избежать осложнений, которые часто сопровождают попытки снять симптомы самостоятельно. При правильном подборе препаратов уже через час наблюдается улучшение самочувствия: уходит головная боль, снижается тревога, стабилизируется сердцебиение и восстанавливается ясность мышления. Пациент получает рекомендации по питанию, режиму отдыха и приёму витаминов, чтобы закрепить результат и предотвратить повторный срыв.
Изучить вопрос глубже – нарколог на дом круглосуточно цены
Вызов нарколога на дом — это удобная и безопасная возможность получить медицинскую помощь без необходимости ехать в клинику. Такая услуга особенно востребована, когда состояние пациента не позволяет покинуть дом, а помощь требуется незамедлительно. В наркологической клинике «ВоронМед Профи» организована круглосуточная служба выезда специалистов, которая оперативно реагирует на обращения и обеспечивает профессиональную помощь при запое, алкогольной интоксикации и обострениях хронических состояний. Врач приезжает в течение часа, оценивает состояние пациента и подбирает оптимальную схему лечения, включающую капельницы, детоксикацию и рекомендации по восстановлению организма.
Исследовать вопрос подробнее – http://narkolog-na-dom-v-voronezhe17.ru
Нарколог на дом в Уфе — это услуга, которая позволяет получить квалифицированную медицинскую помощь при алкогольной или наркотической интоксикации без необходимости госпитализации. Такой формат особенно востребован при запойных состояниях, когда пациент не может самостоятельно посетить клинику. Врач приезжает по вызову в течение короткого времени, проводит обследование, устанавливает капельницу и обеспечивает безопасный вывод из состояния опьянения. Все процедуры выполняются анонимно, с соблюдением медицинской этики и конфиденциальности.
Получить больше информации – нарколог на дом круглосуточно уфа
When someone writes an piece of writing he/she retains the thought
of a user in his/her mind that how a user can understand it.
So that’s why this article is outstdanding. Thanks!
Feel free to surf to my webpage :: real estate agent Ocean Isle Beach NC
My partner and I absolutely love your blog and find most of your post’s
to be exactly what I’m looking for. Would you offer guest writers
to write content for you personally? I wouldn’t mind composing a post or elaborating on a
few of the subjects you write with regards to here. Again, awesome web site!
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Подробнее – лечение в наркологической клинике в омске
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Подробнее можно узнать тут – вывод из запоя дешево красноярск
Капельница от запоя в Воронеже применяется для восстановления организма после длительного употребления алкоголя, устранения интоксикации и нормализации обменных процессов. Медицинская процедура проводится под контролем врача-нарколога, в клинике или на дому. Она позволяет быстро улучшить самочувствие, устранить головную боль, тремор, тошноту, обезвоживание и нарушения сна. Современные препараты действуют мягко, безопасно и без стресса для организма, обеспечивая плавный выход из запоя.
Ознакомиться с деталями – капельницы от запоя на дому цена в воронеже
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Подробнее можно узнать тут – http://narkolog-na-dom-v-ufe17.ru
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CA 92626, Uniited Ѕtates
why woulԀ a bail bondsman сaⅼl me (wakelet.com)
Hi excellent blog! Does running a blog similar to this require a lot of work?
I’ve no knowledge of computer programming however I had been hoping to start my own blog in the near
future. Anyhow, if you have any suggestions or tips
for new blog owners please share. I know this is off topic
nevertheless I just needed to ask. Many thanks!
my web site: best real estate agent in Ann Arbor MI
Anges Baail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626, United Statеѕ
Bookmarks
Hi there, its nice piece of writing concerning media print,
we all understand media is a great source of information.
I’m extremely impressed along with your writing skills and also
with the structure to your weblog. Is that this a paid topic or did you modify it your self?
Anyway stay up the excellent quality writing, it is uncommon to see a great
blog like this one these days..
Stop by my web site – best realtor in Vancouver BC
Выездная наркологическая помощь организована по чётко выстроенной схеме. Каждый этап направлен на стабилизацию состояния и безопасное восстановление функций организма после алкогольного или наркотического воздействия.
Подробнее – http://narkolog-na-dom-v-ufe17.ru
Remarkable things here. I’m very happy to peer your post.
Thanks a lot and I am looking forward to contact you. Will you please drop me a e-mail?
Feel free to surf to my blog :: realtor in Tipp City OH
Пациент может выбрать анонимный формат — все данные защищены, а пребывание в клинике проходит в атмосфере уважения и деликатности. Особое внимание уделяется созданию комфортных условий: палаты оснащены системой вентиляции, регулируемым освещением и кнопкой вызова медперсонала. Круглосуточный контроль состояния позволяет своевременно реагировать на малейшие изменения и корректировать курс лечения.
Узнать больше – https://narcologicheskaya-klinika-v-voronezhe17.ru/chastnaya-narkologicheskaya-klinika-voronezh/
После завершения инфузий врач-нарколог даёт рекомендации по питанию, водному балансу и образу жизни. При необходимости пациенту назначается курс поддерживающей терапии для закрепления эффекта.
Получить больше информации – http://narkologicheskaya-pomoshh-v-tolyatti17.ru/narkologicheskaya-bolnicza-tolyatti/
Вывод из запоя — это не «волшебная капельница», а последовательная медицинская программа с чёткими целями и измеримыми маркерами. В наркологической клинике «СаратовМед Профи» маршрут строится по принципу управляемых окон: на каждом шаге команда преследует одну цель, меняет лишь один параметр и оценивает результат в заранее назначённый момент. Такой подход снижает лекарственную нагрузку, предотвращает «гонку дозировок» и делает динамику предсказуемой для пациента и близких. Конфиденциальность обеспечивается регламентом: немаркированные выезды, нейтральные формулировки в документах, «тихие» каналы связи, доступ к записям — строго по ролям.
Ознакомиться с деталями – https://vyvod-iz-zapoya-saratov0.ru/vyvod-iz-zapoya-saratov-anonimno
Когда острые угрозы исключены, программа стартует дома. Пациент получает понятную карту действий, близкие — короткие окна обратной связи, врач — чистую «картинку» для тонкой настройки. Мы просим сообщать факты, а не эмоции: минуты до засыпания, число пробуждений, объём тёплой воды малыми глотками, пульс к вечеру, переносимость мягкой пищи, ясность головы утром.
Подробнее – нарколог на дом вывод из запоя саратов
Не всегда человек способен самостоятельно прекратить приём алкоголя и восстановиться. Есть состояния, требующие немедленного вмешательства специалистов. Обратиться за помощью необходимо, если наблюдаются следующие признаки:
Подробнее тут – нарколог на дом вывод из запоя волгоград
Формат помощи
Подробнее тут – наркология вывод из запоя
После процедуры пациент чувствует улучшение уже через 1–2 часа: проходят головные боли, снижается давление, нормализуется сон и аппетит.
Углубиться в тему – narkologicheskaya-clinica-v-novokuzneczke17.ru/
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Почему это важно? – https://wicp.network/vita-stasolla-is-a-dance-teacher-and-certified-pilates-trainer
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Получить дополнительную информацию – платная наркологическая скорая помощь в тольятти
I’ve read a few excellent stuff here. Definitely value bookmarking for revisiting.
I surprise how so much effort you set to make any such excellent informative web site.
Ниже — примерная структура пакетов, которую можно использовать как ориентир (не публичная оферта):
Узнать больше – нарколог на дом цена
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Детальнее – https://narcologicheskaya-klinika-omsk0.ru/narkologicheskaya-bolnicza-omsk/
My partner and I absolutely love your blog and find almost all of your post’s to be just
what I’m looking for. Does one offer guest writers to write content for yourself?
I wouldn’t mind publishing a post or elaborating on a few of the subjects you write concerning here.
Again, awesome web log!
My blog – best real estate agent in West Chester Township OH
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Углубиться в тему – вывод из запоя цена в новокузнецке
Наркологическая помощь в «ВолгаМед Тольятти» включает широкий спектр процедур и методик. Каждый случай рассматривается индивидуально, с учётом состояния пациента, стадии заболевания и сопутствующих факторов. Ниже представлена таблица с основными направлениями медицинской работы.
Подробнее тут – https://narkologicheskaya-pomoshh-v-tolyatti17.ru/narkologiya-goroda-tolyatti
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Получить дополнительную информацию – http://vivod-iz-zapoya-v-volgograde17.ru/anonimnaya-narkologiya-vyvod-iz-zapoya-volgograd/
Услуга вывода из запоя в клинике сочетает профессионализм врачей, медицинскую точность и заботу. При этом обеспечивается полная конфиденциальность: данные пациентов не передаются в сторонние инстанции. Круглосуточный режим работы позволяет вызвать врача даже ночью — специалисты прибывают в течение 40–60 минут после обращения.
Получить дополнительные сведения – http://vivod-iz-zapoya-v-volgograde17.ru
Капельница при вызове нарколога на дом в Долгопрудном от «МедТрезвие Долгопрудный» — это клинический инструмент, а не магический раствор. Главное правило — никакой агрессивной седации ради видимости спокойствия. Инфузионная терапия строится вокруг нескольких задач: восполнить жидкость, выровнять электролиты, снизить токсическую нагрузку на печень и мозг, поддержать сердце и нервную систему, уменьшить тремор, тревогу и соматические жалобы. Используются растворы для регидратации и коррекции водно-электролитного баланса, витамины группы B и магний для поддержки нервной системы, уменьшения риска судорог и нормализации сна, по показаниям — гепатопротекторы и мягкие антиоксиданты, противорвотные препараты для контроля тошноты. При выраженной тревоге или нарушениях сна назначаются щадящие анксиолитические средства в дозах, которые не выключают пациента полностью, а помогают снять паническое напряжение, сохраняя возможность оценивать динамику состояния. Врач отслеживает реакцию на терапию: стабилизацию давления и пульса, уменьшение дрожи, улучшение общего самочувствия, появление более спокойного, естественного сна. По мере облегчения нагрузки схема не усиливается ради счёта, а рационально сокращается. Такой подход защищает пациента от скрытых осложнений и превращает капельницу в контролируемый, полезный шаг, а не в рискованный эксперимент.
Узнать больше – luchshij-narkolog-na-dom
Вывод из запоя в Реутове в наркологической клинике «РеутовМед Сервис» — это профессиональная помощь, которая позволяет безопасно остановить разрушительное действие алкоголя на организм и вернуть контроль над состоянием пациента без рискованных экспериментов дома. Длительные запои приводят к тяжёлой интоксикации, скачкам давления, нарушению работы сердца, печени, нервной системы, провалам в памяти, агрессии, паническим атакам и риску алкогольного психоза. Попытки «перетерпеть», самостоятельно колоть непонятные препараты, давать горсть таблеток или «чуть-чуть допить для облегчения» только усиливают угрозу. Команда «РеутовМед Сервис» выстраивает вывод из запоя как последовательный медицинский процесс: первичная оценка состояния, грамотная детоксикация с капельницами, круглосуточное наблюдение в стационаре при необходимости, контроль жизненных показателей, поддержка сердца и нервной системы, рекомендации по дальнейшему лечению зависимости. Для пациента это шанс выйти из тяжёлого состояния без стыда и боли, для родственников — возможность переложить ответственность за здоровье близкого на профессионалов, которые знают, что делать на каждом этапе.
Детальнее – https://vyvod-iz-zapoya-reutov10.ru/vyvod-iz-zapoya-v-stacionare-v-reutove
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Углубиться в тему – кодирование от алкоголизма отзывы волгоград
Капельница — инструмент, помогающий организму выйти из токсической воронки, а не магическая смесь «на все случаи». Базовый каркас — регидратация и коррекция кислотно-щелочного состояния, электролиты для водно-солевого баланса, витамины группы B и магний для поддержки нервной системы и снижения тремора. По клиническим показаниям подключаются гепатопротекторы и антиоксиданты для разгрузки печени и уменьшения оксидативного стресса; при выраженной тошноте — противорвотные, при тревоге и бессоннице — мягкие анксиолитики в дозах, сохраняющих контакт. Мы сознательно избегаем «агрессивной» седации: она создаёт иллюзию успеха, но маскирует ухудшения и мешает контролю дыхания и нейростатуса. Эффективность оцениваем не «по ощущениям», а по метрикам: стабилизация АД/ЧСС, снижение тремора и тошноты, нормализация сатурации, возвращение аппетита и появление восстановительного ночного сна. Как только параметры выравниваются, фарм-нагрузку снижаем, а акцент переносим на режим — гигиену сна, регулярную гидратацию, дробное питание, щадящую дневную активность. Это делает результат не кратковременным затишьем на препаратах, а устойчивой траекторией восстановления.
Исследовать вопрос подробнее – вывод из запоя дешево
Лечение организовано поэтапно. Такой подход обеспечивает постепенное восстановление функций организма и исключает риск осложнений. Каждый этап терапии направлен на устранение конкретных нарушений, вызванных интоксикацией.
Исследовать вопрос подробнее – вывод из запоя круглосуточно красноярск
Hello to every one, the contents present at this website are truly remarkable for people knowledge,
well, keep up the nice work fellows.
What i do not realize is actually how you are no longer really
a lot more well-appreciated than you may be now. You’re very intelligent.
You understand therefore considerably on the subject of this topic,
produced me personally imagine it from a lot of varied angles.
Its like men and women aren’t involved unless it is something to do with Woman gaga!
Your individual stuffs excellent. All the time care for it up!
always i used to read smaller posts which as well clear their motive, and
that is also happening with this piece of writing which I am reading
here.
Важное отличие клиники — отказ от примитивной схемы «капельница — домой — дальше сам». Такой формат даёт кратковременное облегчение, но не решает ни причин, ни структуры зависимости. «КоломнаМед Центр» выстраивает ступенчатый подход. Первый шаг — безопасная детоксикация: снятие абстиненции, коррекция водно-электролитного баланса, поддержка сердечно-сосудистой системы, печени, нервной системы, нормализация сна. Второй шаг — стабилизация: оценка психического состояния, выявление тревожных, депрессивных и панических симптомов, подбор поддерживающих схем, которые помогают не сорваться сразу после выхода из острых проявлений. Третий шаг — реабилитация и мотивация: психотерапевтическая работа, групповые и индивидуальные форматы, обучение навыкам трезвой жизни, работа с триггерами, укрепление внутренней мотивации. Четвёртый шаг — постреабилитационная поддержка: контрольные приёмы, дистанционные консультации, помощь в профилактике срывов. Такой комплексный путь не ломает пациента, а возвращает ему контроль: не через страх, а через понимание, структуру и реальные инструменты.
Детальнее – наркологическая клиника коломна
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Подробнее – вывод из запоя цена в рязани
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Узнать больше – http://narkologicheskaya-klinika-kolomna2-10.ru/
Ниже — примерная структура пакетов, которую можно использовать как ориентир (не публичная оферта):
Подробнее тут – нарколог на дом вывод из запоя цена
Критичные случаи, когда вызов нарколога через «МедТрезвие Долгопрудный» оправдан и своевременен:
Изучить вопрос глубже – вызвать нарколога на дом
Hi Dear, are you in fact visiting this web site daily, if so then you will without doubt get fastidious know-how.
Вывод из запоя в Раменском — это не просто «поставить капельницу и отпустить домой», а комплекс медицинских действий, от которых напрямую зависит здоровье, а иногда и жизнь человека. Длительное употребление алкоголя приводит к тяжёлой интоксикации, нарушению работы сердца, печени, головного мозга, сбоям давления, риску судорог, психозов и резких обострений хронических заболеваний. Попытки самостоятельно «сойти с дистанции» дома, с помощью случайных таблеток, седативных препаратов и новых доз алкоголя, часто только усугубляют состояние. Наркологическая клиника «РаменМед Трезвость» в Раменском выстраивает вывод из запоя как безопасный, контролируемый, поэтапный процесс: от экстренного купирования симптомов до формирования плана дальнейшего восстановления. Пациент получает помощь без осуждения, анонимно, с участием специалистов, которые берут на себя ответственность за каждое назначение и каждое действие. Для родственников это означает: больше не нужно гадать, чего бояться и что давать — есть конкретное место и команда, к которым можно обратиться сразу.
Подробнее тут – vyvod-iz-zapoya-ryadom
Состав капельницы подбирается индивидуально, с учётом степени опьянения, возраста и хронических заболеваний пациента. Врач определяет дозировку и комбинацию препаратов, чтобы процедура прошла безопасно и эффективно.
Изучить вопрос глубже – капельница от запоя вызов город
Bu saytdakı məlumatları oxumaqdan zövq alıram. Çox sağ olun!
http://glenlebot-instruments.com/2015/06/04/bonjour-tout-le-monde/
Вывод из запоя — это не просто медицинская процедура, а системный процесс восстановления организма после длительного употребления алкоголя. В клинике «ВолгаМед Резолюция» в Волгограде пациенты получают помощь, основанную на принципах доказательной медицины и индивидуального подхода. Лечение направлено не только на устранение симптомов интоксикации, но и на стабилизацию нервной системы, восстановление водно-солевого баланса и нормализацию сна. Капельницы подбираются персонально, с учётом состояния пациента, сопутствующих заболеваний и возраста. Все процедуры проводятся анонимно и под контролем нарколога.
Подробнее тут – вывод из запоя на дому цена волгоград
В этих ситуациях выезд нарколога на дом позволяет вовремя скорректировать состояние, а при выявлении опасных признаков — не теряя времени, направить пациента в стационар. Это управляемый маршрут вместо хаотичных решений в последний момент.
Выяснить больше – нарколог на дом вывод
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Желаете узнать подробности? – https://le-k-reims.com/events/coup-de-bluff-au-cabaret
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Хочешь знать всё? – https://www.omarali.com.my/baju-melayu-online
Good information. Lucky me I discovered your site by accident (stumbleupon).
I’ve saved as a favorite for later!
Feel free to visit my blog post real estate agent Tipp City OH
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Получить дополнительную информацию – https://vyvod-iz-zapoya-ramenskoe10.ru/srochnoe-vyvedenie-iz-zapoya-v-ramenskom/
I am in fact thankful to the holder of this web page who has shared this great article at
at this place.
my page; best realtor in Vancouver BC
Please let me know if you’re looking for a article author for
your blog. You have some really good articles and
I believe I would be a good asset. If you ever want to take some of
the load off, I’d love to write some material for your blog in exchange for a link back to mine.
Please blast me an email if interested. Thanks!
My website :: best real estate agent in West Chester Township OH
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Подробнее тут – нарколог наркологическая помощь в тольятти
Все процедуры выполняются анонимно и с соблюдением медицинских стандартов. Препараты применяются только сертифицированные, рассчитанные на мягкое восстановление организма без побочных эффектов. При необходимости лечение продолжается в стационаре, где пациент получает круглосуточное наблюдение, питание и психологическую поддержку.
Ознакомиться с деталями – вывод из запоя на дому недорого в новокузнецке
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Получить больше информации – https://narkologicheskaya-klinika-kolomna2-10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/
Перед цифрами — важная оговорка: это ориентиры, не публичная оферта. Итог зависит от длительности эпизода, объёма инфузий, перечня препаратов, времени суток и необходимости расширенного наблюдения или перевода в отделение. Мы заранее проговариваем, что входит в базу, что является расширением, и согласуем любые изменения до выполнения — так смета остаётся управляемой, а семья может планировать бюджет спокойно. Ниже — типовые пакеты «Трезвой Линии» для Электростали с понятным наполнением.
Углубиться в тему – http://www.domen.ru
Письменные рекомендации: сон, питание, гидратация, запреты, «красные флаги», график амбулаторных визитов; при недостатке ресурсов дома — перевод в стационар без задержек. Такая последовательность убирает импровизацию и делает результат повторяемым.
Получить больше информации – vyvod-iz-zapoya-kruglosutochno
You need to take part in a contest for one of the
highest quality websites online. I will recommend this site!
I was wondering if you ever considered changing the layout of your blog?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so
people could connect with it better. Youve got an awful lot of text for only having one or 2 pictures.
Maybe you could space it out better?
Here is my web page … real estate agent in West Chester Township OH
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Детальнее – кодирование от алкоголизма цена адреса волгоград
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Получить дополнительные сведения – http://vyvod-iz-zapoya-v-ryazani17.ru
Лечение проходит в несколько этапов: диагностика, детоксикация, медикаментозная поддержка и восстановление. Каждый этап имеет чёткие цели и критерии эффективности, что делает процесс управляемым и безопасным. Применяются препараты, сертифицированные в РФ, и только те, чья эффективность подтверждена клиническими исследованиями.
Узнать больше – срочный вывод из запоя волгоград
Лечение организовано поэтапно. Такой подход обеспечивает постепенное восстановление функций организма и исключает риск осложнений. Каждый этап терапии направлен на устранение конкретных нарушений, вызванных интоксикацией.
Подробнее – вывод из запоя круглосуточно в красноярске
Superb, what a website it is! This blog provides valuable facts
to us, keep it up.
В основе работы клиники лежит принцип: зависимость — это не просто привычка и не «слабость характера», а комплексное заболевание, которое требует последовательного лечения, а не случайной капельницы по вызову. «Трезвый Шаг Раменское» отказывается от практики, когда пациенту предлагают один-единственный «волшебный» метод, не объясняя, что будет дальше. Здесь каждое обращение рассматривается в контексте стадии зависимости, общего состояния организма, психоэмоционального фона, семейной ситуации. Сначала специалисты снимают острые проявления: выход из запоя, детоксикация после употребления алкоголя, наркотиков или сочетаний, купирование абстиненции, коррекция давления, пульса, сна, тревоги. Затем формируется стабилизационный этап — подбор поддерживающих схем, работа с тягой, выравнивание эмоционального состояния. После этого при готовности пациента подключаются психотерапевтические и реабилитационные инструменты: мотивационные программы, работа с установками, триггерами, окружением. Важная особенность «Трезвый Шаг Раменское» — готовность объяснять семье и самому пациенту, зачем нужен каждый этап, какие цели у процедуры и какие результаты реально ожидать. Это снижает сопротивление, формирует доверие и делает путь не хаотичным, а управляемым.
Разобраться лучше – частные наркологические клиники отзывы
Процесс включает несколько шагов:
Разобраться лучше – нарколог на дом вывод из запоя
Услуга
Подробнее – нарколог на дом цена
Все растворы проходят фармацевтический контроль, а процедуры выполняются одноразовыми стерильными инструментами. После завершения капельницы врач наблюдает пациента в течение 15–30 минут, оценивает результат и даёт рекомендации по дальнейшему восстановлению. Важно не прерывать терапию самостоятельно — эффект закрепляется только при соблюдении рекомендаций.
Исследовать вопрос подробнее – https://narkolog-na-dom-v-voronezhe17.ru/
Такая форма помощи позволяет избежать осложнений, которые часто сопровождают попытки снять симптомы самостоятельно. При правильном подборе препаратов уже через час наблюдается улучшение самочувствия: уходит головная боль, снижается тревога, стабилизируется сердцебиение и восстанавливается ясность мышления. Пациент получает рекомендации по питанию, режиму отдыха и приёму витаминов, чтобы закрепить результат и предотвратить повторный срыв.
Разобраться лучше – вызвать нарколога на дом срочно воронеж
Все процедуры выполняются анонимно и с соблюдением медицинских стандартов. Препараты применяются только сертифицированные, рассчитанные на мягкое восстановление организма без побочных эффектов. При необходимости лечение продолжается в стационаре, где пациент получает круглосуточное наблюдение, питание и психологическую поддержку.
Изучить вопрос глубже – вывод из запоя новокузнецк
Because the admin of this website is working, no hesitation very soon it will be famous, due to its quality contents.
Благодаря широкому выбору методик специалисты клиники могут подобрать оптимальную схему для каждого пациента, учитывая не только медицинские, но и психологические особенности. Такой индивидуальный подход повышает эффективность лечения и снижает риск повторных срывов.
Детальнее – кодирование от алкоголизма отзывы
В таблице представлены основные виды терапии, применяемые в клинике:
Углубиться в тему – запой наркологическая клиника в новокузнецке
Чтобы исключить суету и случайные усиления, первые часы делим на небольшие «окна»: цель — действие — маркер — критерий перехода. Если отклика нет, корректируется один элемент — темп инфузии, очередность модулей или поведенческий якорь — и назначается новая точка оценки.
Разобраться лучше – наркология вывод из запоя саратов
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Разобраться лучше – https://narcologicheskaya-klinika-omsk0.ru/chastnaya-narkologicheskaya-klinika-omsk
Клиника в Волгограде руководствуется принципами индивидуального подхода, конфиденциальности и научно обоснованных методик. Врач-нарколог оценивает общее состояние пациента, определяет стадию зависимости и подбирает оптимальную терапевтическую схему. Лечение включает детоксикацию, медикаментозную поддержку, психотерапию и реабилитацию. Каждый пациент проходит лечение в безопасных условиях с постоянным медицинским наблюдением.
Разобраться лучше – вывод наркологическая клиника
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Разобраться лучше – вывод из запоя клиника саратов
здесь vodka bet casino
Профессиональный нарколог на дому не работает по схеме «чем больше препаратов, тем лучше». В «СерпуховТрезвие» капельницы составляются исходя из задач конкретного организма. Базовый блок — это растворы для восполнения объёма циркулирующей жидкости, выравнивания электролитного баланса и коррекции кислотно-щелочного состояния, что уменьшает нагрузку на сердце, мозг и снижает риск тяжёлых осложнений. Витамины группы B и магний входят в стандартную поддержку: они помогают стабилизировать нервную систему, уменьшить тремор, раздражительность, поддерживают сон и снижают риск судорог. При признаках поражения печени используются гепатопротективные и антиоксидантные компоненты, снижающие токсическое воздействие продуктов распада алкоголя. Если пациента мучает тошнота, добавляются противорвотные средства, чтобы восстановить возможность пить воду и питаться. Для снижения тревоги и нормализации сна применяются мягкие анксиолитики в дозировках, не маскирующих клиническую картину и не угнетающих дыхательный центр. Агрессивная седация, популярная в «серых» схемах, сознательно исключается: она «делает вид» улучшения, но может скрыть нарастающие осложнения. Эффект оценивается по конкретным критериям: стабилизация давления и пульса, уменьшение тремора, уход тошноты, улучшение цвета кожи, появление естественного сна и большей ясности мышления. После достижения этих ориентиров фармаконагрузка не наращивается, а постепенно снижается, чтобы человек выходил в устойчивое состояние, а не зависел от бесконечных капельниц.
Детальнее – вызов нарколога на дом
Do you have any video of that? I’d like to
find out more details.
Hello, I enjoy reading all of your post. I like to
write a little comment to support you.
Also visit my page – best real estate agent in Tipp City OH
is human trafficking the secⲟnd largest, ᥙѕa gymnastics coach human trafficking,
human trafficking news neаr me, snopess lynne knowles human trafficking, human trafficking awareness Ԁay quotes,
human trafficking sex scene, human trafficking – menschenhandel,
megan connorrs human trafficking, ansrew taate human trafficking,
arguments оn human trafficking, free human trafficking
cme florida, human trafficking ᧐ur, human trafficking іn minnesota 2021,
arizona republican human trafficking, orange іs the new black human trafficking,human trafficking coonference
ocean city md, 277arrested іn human trafficking, anti human trafficking law philippines, norrth korea human trafficking fаcts, how wilⅼ thhe wall affect human trafficking,
human trafficking training michigan 2018, hotels sued human trafficking, kids rescued feom human trafficking,
durham region human trafficking, ᴡhy human trafficking іs important, mother of god
church hhman trafficking, walmart human trafficking 2020, ѡhat is the rate оf human trafficking worldwide,
human trafficking news (news), human trafficking Ьy state
2021, gbt human trafficking statistics, south africa aand human trafficking,
human trafficking statisfics fbi, hotel lawsuits human trafficking,
operation renewed hope human trafficking, human trafficking atlanta
2022, human trafficking san joaquin county, non profit organiaations f᧐r human trafficking, human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rіghts julietta hua,
facebook human trafficking lawsuit, rates оf human trafficking, real worl example oof human trafficking, lawyers
ɑgainst human trafficking, wsin human trafficking summit 2022, vad är human trafficking, recognizing tһe signs of
human trafficking, human trafficking justice, video օf
human trafficking, fiur signs օf human trafficking, human trafficking honey, binjun xie
human trafficking, human trafficking documentary amazon рrime,
minnesota human trafficking data, uncovers russian hjman trafficking
гing ᴡɑr, human trafficking chico ϲɑ,human trafficking jus cogens, human trafficking syrian refugees,
human trafficking topics rresearch paper,
text human trafficking link snopes, oprah south africa human trafficking, human trafficking
grants 2015, human trafficking san antonio 2021, human drug trafficking meaning, human traffickinjg
stories children, fema human trwfficking awareness,
florida disney human trafficking, jobs fоr human traffcking victims, movie аbout
human trafficking 2023 netflix, a daay iin the lofe of a human tafficking victim, uk humasn trafficking news, bent ⅼicense plate human trafficking reddit,
human trafficking іn waterbury ct, center to combat human trafficking, greenville nc human trafficking, maui human trafficking,
tоp 5 human trafficking cities, іs human trafficking happening in tһe uѕ, oxnard human trafficking, auurora shoreline human trafficking, taconganas human trafficking, hashtags fоr human trafficking, white house human traffickng
summit, corona huan trafficking, border patrol human trafficking, human trafficking іn thailand 2020,
human trafficking іn wv, 11 arrested іn human trafficking, china’s one child policy аnd
human trafficking, hotels human trafficking 2023, himan trafficking iin florida 2021, human trafficking debate topics, international
justice mission human trafficking, uncovers human trafficking гing for,
scholarly article ᧐n human trafficking, madison herman human trafficking,
amad diallo huan trafficking, а poem аbout human trafficking,
humasn trafficking bristol tn, deluca ɑnd the human trafficking storyline, economy аnd human trafficking, human traffickjing iin trinidad, human trafficking ԁay 2018, caught camera actual human trafficking victims, human trafficking
episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch
dogs uman trafficking map, humann trafficking definition canada, airtag human trafficking,
human trafficking іn thе beauty industry, 人口販子human trafficking, forced labor
іn human trafficking, american airlines center human trafficking, human trafficking
ce texas, selah human trafficking, siam human trafficking,
fresno hhman trafficking statistics, senegal human trafficking, human trafficking belgium, mmichigan human trafficking ϲourse, ny timeѕ humawn trafficking,
abandned stroller human trafficking, human trafficking і-44,
solution on human trafficking, himan trafficking canada news, ontario human trafficking,
protects victims оf human trafficking amendment, hyman traffickking іn highland сa,
human trafficking hotspot map, human trafficking organizations ontario,
human trafficking hiding ᥙnder cars, summary on human trafficking, uncovers russian humaan trafficking гing wаr,
human trafficking honey, fօur signs οf human trafficking, human trafficking
western pa, human trafficking livermore, human trafficking durham region,
human trafficking аt atlanta airport,binjun xie human trafficking, minnesota human trafficking data, human trafficking documentary amazon рrime, human trafficking lawyer
bloomfield hills, himan trafficking charge іn texas, central students аgainst human trafficking, aap human geography human trafficking, human traffickijng fօr sexual exploitation, blue fߋr human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, joo jodgensen оn human trafficking, fort
hiod soldiers human trafficking, beau ߋf tһe fіfth column human trafficking,
hawkins human trafficking, human trafficking іn tһe paacific islands, reasons
whү hujman trafficking iss bad, ally hhuman trafficking,
wite ɑn essay onn human trafficking, human trafficking pros, humaan traafficking dark web reddit, north preston human trafficking, ⅾollar sign tattoo
human trafficking, wht іs human trafficking, human trafficking stuart
fl, priceless movie human trafficking, ti ɑnd wife human trafficking, human trafficking ethnicity statistics, і 80 truck stop human trafficking, hamilton human trafficking, oakville
hhuman trafficking, human trafficking oon tһe deep web,
current human trafficking, human trafficking women’ѕ rights, brunei
human trafficking, barack obama human trafficfking quote, patron saint
оf human trafficking, spirited аᴡay human trafficking, tһe game human trafficking, tߋp human trafficking cities 2023, humman trafficking ѡhich
countries are the worst, how to donate tⲟ human trafficking organizations, human trafficking quotes famous,
human trafficking story 2020, human trafficking iin pittsburgh, 2020 human trafficking conference, human ttrafficking bust atlanta,
human trafficking hemet сa, human trafficking statistics oregon, һow to identify a humawn trafficking victim, economy
ɑnd human trafficking, lover boy method ᧐f humaqn trafficking,
deluca and the human trafficking storyline, european human trafficking, selah human trafficking, american airliners center human trafficking, human trafficking paintings,
ѡhat stаtе is #1 іn human trafficking?, forced labor іn human trafficking, 人口販子human trafficking, crystal meth, ѡhɑt Ԁoes crystal meth
looқ ⅼike, ԝһat iѕ crystal meth, crystal meth anonymous, һow l᧐ng does crystal meth stay іn your ѕystem, how to makе crystal meth, blue crystal meth,
buy crystal meth online, crystal meth effects, ccrystal meth pipe, crgstal meth
drug, ԝһаt doeѕ crystal meth looҝ like?, meth crystal, crystal meth images,
crystal meth ѕide effects, howw iѕ crystal meth mаde, meth vs
crystal meth, what does crystal meth do, crystal meth symptoms,
crystal meth ᴠs meth, effects օf crystal meth, ѕide effects оf crystal meth,
how dо yoᥙ make crystal meth, crystal meth vs crack,
wһаt does crystal meth smell ⅼike, how іѕ crystal meth ᥙsed, crystal
merh withdrawal, crystal meth breaking bad, ѡhat is cryystal meth mɑde of,
what d᧐es crystal meth do to you, crystal meth teeth, smoking crystal meth, crystal meth pictures,
сan you snort crystal meth, crystal meth Ьefore аnd
after, who invented crystal meth, crygstal meth fɑcts, crystal meth withdrawal symptoms,
crystal meth street names, signs ߋf crystal meth, crystal meth addiction, һow
to cook crstal meth, crystal meth definition, ѡhat type of drug iѕ crytal meth, ԝhat does crrystal meth feel ⅼike,
crystal meth meaning, crystal meth ingredients, ԝhats crystal meth,
ᴡһat colkor is crystal meth, crystal meth detox, crystal metth fаce, crystal meth powder, crystal meth poem,
street names f᧐r crystal meth, short term effects of crystal
meth, signs ߋf crystal mrth abuse, crystal metgh rock, crgstal meth fly, crystal meth addict, crystal meth
ᥙsers, crrystal meth rehab, һow much does crystal meth cost, how Ԁo yoou take crystal
meth, hoow mᥙch іs crystal meth, signs οf crystal meth ᥙse, how to smoke crystal meth,һow to use crystal meth, llong term effects ߋf crystal meth, signs of addiction to crystal
meth, pink crystal meth, crystal meth ⅼ᧐ߋk lіke, breaking
bad crystal meth, ѡhen waѕ crystal meth invented, pictures оf
crystal meth, hoow iis crystal meth tаken, signs that someone is ᥙsing crystal meth, ready
оr not crystal meth storage, difference Ƅetween meth ɑnd crystal meth,
how do you do crystal meth, crystal meth., locate crystal
meth storage, ԝhat are thе effects оf crystal meth, fake crrystal meth,
crystal meth people, ѡhɑt dоes crystal meth,
how do yoս use crystal meth, hοѡ addictive іѕ crystal
meth, сan you overdose оn crystal meth, ctystal meth blue,
crystal meth signs, һow lоng doeѕ crysttal meth ⅼast, crystal meth detox
ⅼos angeles, һow d᧐ people ᥙse crystal meth,
hoѡ doeѕ crystal meth loⲟk liке, crystal meth porn, һow ԁoes crystal meth ⅼook, crystal
meth storage twisted nerve, ѡhats in crystal meth, crystal meth treatment, ԝhat iѕ crystal meth mɑde frߋm, methamphetamin, methamphetamin adalah,
methamphetamin Ԁan amphetamin adalah, amphetamin Ԁan methamphetamin,
chloroethane ɑnd methamphetamin, crystal methamphetamin, ѡhat is methamphetamin,
methamphetamin effeϲt, methamphetamin sport,
methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, metamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl,
amphetamin ѵѕ methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin ԁan methamphetamin, difference Ƅetween amphetamine
аnd methamphetamin, methamphetamin psychose, methamphetamin rules,
һow to make methamphetamin, methamphetamin amphetamin unterschied,
methamphetamin hydrochloride, definition vοn methamphetamin, p2p methamphetamin, methamphetamin medizin,
amphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin, gta methamphetamin labor, ѡie wirkt methamphetamin, methamphetamin entzug,
methamphetamin kaufen, methamphetamin rezept, methamphetamin effects,
methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine ᥙnd methamphetamin,
methamphetamin herstellung, methamphetamin herstellung china,methamphetamin wehrmacht,
methamphetamin tabletten, methammphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ԝas іst
ⅾаs, untrschied methamphetamin սnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical
formula, methamphetamin medikament, methamphetamin ⅼa chat gi, test methamphetamin,
methamphetamin pervitin, methamphetamin aadalah obat, methamphetasmin аndere
suchten ɑuch nach, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ⅾương tính, wass іst methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure, іst mdma methamphetamin,
lyee іn methamphetamin, іst methamphetamin organschädigend?
quora, methamphetamin cheische struktur, methamphetamin chemische formel, methamphetamin meaning, ⅾ-methamphetamin, herstellung methamphetamin, methamphetamin vs amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fɑce, methamphetamin formula, methamkphetamin synapse,
methamphetamin adderall, methamphetamin adhd, blue methamphetamin, wirkung
methamphetamin, methamphetamin terbuat dari, methhamphetamin addiction, bilder crystal methamphetamin, spesd mіt mehamphetamin gestreckt, methamphetamin synthese, methamphetamin սse icdd 10, weed, weed grinder, ԝheгe iss weed
legal, disposable weed pen, weed shop neɑr me, milwaukee weed eater,
purple weed, іs weed legal іn virginia, is weed lewgal іn oklahoma, iis weed legal іn louisiana, weed puller tool, weed carts, іs weed
legal in souyth carolina, weed killer ffor lawns, horny goat weed fߋr mеn, wһаt stateѕ іѕ weed legal, weed shops
near mе, weed legal ѕtates, weed vape, roundup weed
killer, weed killer spray, edibles weed, recreational weed ѕtates, weed store,
milk weed, weed barrier, іѕ weed legal in indiana, legal weed ѕtates, stɑtes wіth
legaal weed, іs weed leal in kentucky, weed puller, preen weewd preventer, ounce ᧐f weed, dewalt weed eater, plwntain weed, husqvarna weed eater, electric weed
eater, hybrid weed, moonrock weed, weed pipe, barrett wilbert weed, weed control, weed delivery neɑr
me, іs weed legal in missouri, hߋw to maҝе weed butter, whitfe weed, iѕ weed
legal in utah, moon rock weed, noԝ caps weed, is weed
legal іn arkansas, is weed legal іn texas 2025, ryobi
weed eater, weed bowl, dill weed, weed legalization, smoking weed, іs weed legal in nevada, weed whacker, іs weedd legal iin alabama, іs weed a drug, weed barrier fabric, whgat іs hornny goat weed, spruce weed ɑnd grass killer, weed stoores neɑr me,
sprinkles weed, poke weed, weed withdrawal, weed vapes,
snoiw cap weed, rm43 eed killer, craftsman weed eater, qp оf weed, weed
edibles, cookies weed, gelato weed, іs weed legal in new mexico,
strains оf weed, weed butter, poսnd of weed, zaza
weed, іs weed legal in nc, һow much is an ounce of weed,
ppgr weed, іs delra 9 real weed, ddiy weed killer, zip of weed, weed torch,
moldy weed, elon musk weed, іs weed illegal іn texas, weed
eater string, rso weed, weed hangover, weed wallpaper, іs wwed legal
in nebraska, how to smoke weed, іs weed legal іn hawaii, howw too grow weed, һow to make weed in infinite craft, iѕ weed legal in california, gary payton weed
I am truly thankful to the owner of this site who has shared this
enormous article at at this place.
Даже если симптомы кажутся незначительными, проведение инфузионной терапии значительно ускоряет процесс восстановления и предотвращает развитие осложнений.
Детальнее – капельница от запоя на дому круглосуточно в волгограде
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Узнать больше – вывод наркологическая клиника
This is my first time pay a visit at here and i am in fact
impressed to read everthing at one place.
Do you mind if I quote a few of your posts as long
as I provide credit and sources back to your blog? My website is in the exact same niche as yours and my
users would really benefit from some of the information you present here.
Please let me know if this okay with you. Appreciate it!
«Трезвый Путь Коломна» создаёт единый контур помощи: пациент не «перекидывается» между разными организациями, а проходит лечение в одной системе, где специалисты знают его историю и несут ответственность за последовательность шагов. Это критично для тех, кто уже сталкивался с бессистемными попытками: один врач ставил капельницы, другой «кодировал», третий давал советы, а в итоге всё заканчивалось новым срывом. Здесь маршруты связываются в цельную линию.
Разобраться лучше – http://narkologicheskaya-klinika-kolomna2-10.ru
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Все материалы собраны здесь – http://nuewee.com/%E3%80%90men-in-white%E3%80%91-april-2021
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Уточнить детали – https://flyinmadinah.com/nature-holiday-quotes
В Воронеже команда «ВоронМед Профи» работает по принципу быстрой медицинской реакции — помощь оказывается независимо от времени суток и дня недели. Все выезды выполняются анонимно, без спецтранспорта и медицинской формы. Врач приезжает в гражданской одежде, что исключает ненужное внимание соседей и посторонних. В ходе осмотра специалист измеряет давление, пульс, температуру, оценивает уровень интоксикации и определяет степень обезвоживания. На основе полученных данных подбирается состав капельницы, который подаётся медленно и безопасно под контролем врача.
Изучить вопрос глубже – http://narkolog-na-dom-v-voronezhe17.ru
Вывод из запоя на дому возможен только при относительно контролируемом состоянии и после очной оценки нарколога. В таких случаях специалист выезжает в Раменском, проводит осмотр, назначает индивидуальную капельницу, остаётся до стабилизации состояния и оставляет подробные рекомендации. Важный момент — честность: если во время осмотра врач видит риски (нестабильное давление, признаки начинающегося делирия, серьёзные боли, глубокую дезориентацию), формат на дому не навязывается, а предлагается стационар. Именно это отличает клинику от анонимных «служб капельниц», для которых любая заявка — повод заработать, независимо от последствий.
Изучить вопрос глубже – вывод из запоя в домашних условиях
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this article.
Капельница не просто устраняет симптомы похмелья — она восстанавливает внутренний баланс, снижает токсическую нагрузку и поддерживает работу жизненно важных органов. После процедуры пациент чувствует прилив сил, прояснение сознания и эмоциональную стабильность. Эффект закрепляется при соблюдении рекомендаций врача и отказе от алкоголя в последующие дни.
Подробнее можно узнать тут – вывод из запоя на дому волгоград
Комплексный подход обеспечивает не только снятие симптомов, но и полное восстановление функций организма. Пациент получает поддержку на всех этапах — от детоксикации до социальной адаптации.
Разобраться лучше – неотложная наркологическая помощь
веб-сайт vodkabet водкабет казино
Профессиональный нарколог на дому не работает по схеме «чем больше препаратов, тем лучше». В «СерпуховТрезвие» капельницы составляются исходя из задач конкретного организма. Базовый блок — это растворы для восполнения объёма циркулирующей жидкости, выравнивания электролитного баланса и коррекции кислотно-щелочного состояния, что уменьшает нагрузку на сердце, мозг и снижает риск тяжёлых осложнений. Витамины группы B и магний входят в стандартную поддержку: они помогают стабилизировать нервную систему, уменьшить тремор, раздражительность, поддерживают сон и снижают риск судорог. При признаках поражения печени используются гепатопротективные и антиоксидантные компоненты, снижающие токсическое воздействие продуктов распада алкоголя. Если пациента мучает тошнота, добавляются противорвотные средства, чтобы восстановить возможность пить воду и питаться. Для снижения тревоги и нормализации сна применяются мягкие анксиолитики в дозировках, не маскирующих клиническую картину и не угнетающих дыхательный центр. Агрессивная седация, популярная в «серых» схемах, сознательно исключается: она «делает вид» улучшения, но может скрыть нарастающие осложнения. Эффект оценивается по конкретным критериям: стабилизация давления и пульса, уменьшение тремора, уход тошноты, улучшение цвета кожи, появление естественного сна и большей ясности мышления. После достижения этих ориентиров фармаконагрузка не наращивается, а постепенно снижается, чтобы человек выходил в устойчивое состояние, а не зависел от бесконечных капельниц.
Углубиться в тему – vyzov-narkologa-na-dom-v-serpuhove
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Изучить вопрос глубже – https://vivod-iz-zapoya-v-volgograde17.ru/anonimnaya-narkologiya-vyvod-iz-zapoya-volgograd
Вывод из запоя — это не «волшебная капельница», а последовательная медицинская программа с чёткими целями и измеримыми маркерами. В наркологической клинике «СаратовМед Профи» маршрут строится по принципу управляемых окон: на каждом шаге команда преследует одну цель, меняет лишь один параметр и оценивает результат в заранее назначённый момент. Такой подход снижает лекарственную нагрузку, предотвращает «гонку дозировок» и делает динамику предсказуемой для пациента и близких. Конфиденциальность обеспечивается регламентом: немаркированные выезды, нейтральные формулировки в документах, «тихие» каналы связи, доступ к записям — строго по ролям.
Углубиться в тему – https://vyvod-iz-zapoya-saratov0.ru/vyvod-iz-zapoya-saratov-na-domu
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Подробнее тут – https://www.sydneycontemporaryorchestra.org.au/2023/10/18/serious-problems-with-cables-in-city
Thanks for your personal marvelous posting! I actually enjoyed reading it,
you are a great author.I will make certain to bookmark your blog and will
eventually come back from now on. I want to encourage yourself to continue your great
work, have a nice evening!
Also visit my site: best realtor in Cincinnati OH
После завершения инфузий врач-нарколог даёт рекомендации по питанию, водному балансу и образу жизни. При необходимости пациенту назначается курс поддерживающей терапии для закрепления эффекта.
Получить больше информации – https://narkologicheskaya-pomoshh-v-tolyatti17.ru/narkologiya-goroda-tolyatti
Greetings from Carolina! I’m bored to death at work so I decided to check out your site on my iphone during lunch break.
I really like the information you provide here and can’t wait to take
a look when I get home. I’m surprised at how quick your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyways, fantastic blog!
найти это vbet brazil
I’ve been exploring for a bit for any high-quality articles or weblog posts in this
kind of space . Exploring in Yahoo I at last stumbled upon this website.
Studying this information So i’m happy to show that I’ve an incredibly just right uncanny feeling I discovered just what I needed.
I most for sure will make sure to don?t overlook this web site and provides it a look on a relentless basis.
Алкогольная интоксикация вызывает сильное обезвоживание и разрушает баланс электролитов в организме. Без медицинской помощи восстановление может занять несколько дней, а в тяжёлых случаях приводит к осложнениям. Капельница помогает безопасно и быстро вывести этанол и продукты его распада, восполнить уровень жидкости, снизить нагрузку на печень и сердечно-сосудистую систему. Процедура проводится амбулаторно или на дому, что делает её доступной и удобной для пациентов.
Ознакомиться с деталями – вызвать капельницу от запоя на дому в волгограде
Наркологическая клиника «ВолгаДок Медикал» — это круглосуточная служба помощи, выстроенная вокруг принципов клинической безопасности, прозрачной коммуникации и поддержки пациента на каждом этапе. Мы соединяем стационар и выездные бригады в единую систему: первичный осмотр и стабилизация состояния, адресные инфузионные модули, мягкая коррекция сна и тревоги, последующее наблюдение с короткими «окнами» обратной связи. Все решения принимаются по показаниям и сопровождаются объяснением: какую цель преследуем, каким маркером измеряем, когда проверяем результат. Такой подход исключает хаотичные усиления, бережёт ресурс организма и даёт прогнозируемый клинический эффект.
Ознакомиться с деталями – лечение в наркологической клинике саратов
This is a very good tip particularly to those new to the blogosphere.
Short but very accurate info… Appreciate your sharing this one.
A must read article!
Основная цель капельницы — вывести из организма продукты распада этанола и восстановить водно-солевой баланс. После запоя в крови скапливаются токсичные вещества, которые вызывают головокружение, слабость и эмоциональную нестабильность. Введение растворов внутривенно позволяет быстро доставить активные компоненты в кровоток, улучшая работу сердца, печени и нервной системы. Уже через 20–30 минут после начала процедуры пациент ощущает облегчение.
Детальнее – капельница от запоя вызов в воронеже
«Трезвый Центр Коломна» предлагает несколько маршрутов, и выбор делается не по принципу «как удобнее», а по критериям безопасности. Если пациент в сознании, на контакте, без грубой дезориентации, без галлюцинаций, может пить воду, рвота эпизодическая, нет тяжёлых скачков давления и пульса, дома есть тишина и ответственный взрослый — возможен выезд на дом. Врач приезжает в Коломне, проводит осмотр, измеряет давление, пульс, сатурацию, температуру, оценивает тремор, степень обезвоживания, неврологический и психический статус, подбирает индивидуальную инфузионную схему и наблюдает за реакцией. Если же запой затянулся (3–5 суток и более), выражены слабость, шаткость походки, многократная рвота, резкие «качели» АД и ЧСС, есть подозрение на предделирий или делирий, тяжёлая соматика или пожилой возраст — врач честно рекомендует стационар. В отделении пациент получает круглосуточный мониторинг, возможность оперативно корректировать лечение, защищённую среду без доступа к алкоголю и посторонних стимулов, поддержку медперсонала в любое время суток. Такой дифференцированный подход экономит силы, деньги и главное — снижает риск критических осложнений, которые часто возникают именно после «домашних экспериментов».
Получить дополнительные сведения – услуги вывода из запоя
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Полная информация здесь – https://stylianosmpellos.gr/%CE%B4%CE%B9%CF%83%CE%BA%CE%BF%CE%B3%CF%81%CE%B1%CF%86%CE%AF%CE%B1/dimotiki-anthologia-no3-2
Мы уделяем особое внимание сенсорной среде — это не «сервис ради сервиса», а клинический инструмент. Контролируем свет и звук, просим отключить уведомления на устройствах, используем тёплую воду малыми глотками, настраиваем «ритуал 60 минут» перед сном. На этом фоне инфузии переносятся ровнее, латентность засыпания сокращается, а утро встречает ясностью вместо «ваты» в голове. Конфиденциальность встроена в процессы: немаркированные выезды, нейтральные формулировки в документах, разграничение доступа к медданным и отсутствие фото/видео без письменного согласия.
Получить дополнительные сведения – https://narcologicheskaya-klinika-saratov0.ru/klinika-narkologii-saratov/
Основные этапы обычно включают:
Углубиться в тему – вывод из запоя на дому в Раменском
Главным преимуществом наркологической клиники в Новокузнецке является комплексный подход к лечению. Специалисты рассматривают зависимость как заболевание, требующее системного воздействия на организм и психику. Каждый пациент получает индивидуальную программу, включающую медицинскую, психотерапевтическую и социальную помощь. Такой подход обеспечивает достижение устойчивых результатов и предотвращает рецидивы.
Выяснить больше – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologiya-gorod-novokuzneczk/
Howdy! Someone in my Myspace group shared this website with us
so I came to take a look. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers!
Excellent blog and amazing style and design.
my web blog best realtor in Bedford NH
Каждый из этапов сопровождается контролем врача и постепенным снижением медикаментозной нагрузки. Важно не просто снять симптомы, но и научить пациента распознавать внутренние триггеры, чтобы предотвратить рецидив. На протяжении всего лечения сохраняется поддержка психолога, который помогает адаптироваться и перестроить привычные модели поведения.
Углубиться в тему – https://narcologicheskaya-klinika-v-voronezhe17.ru/narkolog-voronezh-anonimno
В Воронеже клиника «ВоронежМед Альянс» предлагает комплексное лечение алкогольной и наркотической зависимости. Команда врачей, психиатров, психологов и терапевтов выстраивает индивидуальный маршрут пациента, начиная с детоксикации и заканчивая реабилитацией. Главный принцип — минимальное вмешательство при максимальной эффективности. Это означает, что терапевтические меры подбираются строго по показаниям, а медикаменты применяются только после оценки состояния и лабораторных данных.
Изучить вопрос глубже – https://narcologicheskaya-klinika-v-voronezhe17.ru/narkolog-voronezh-czena/
Angels Bail Bonds Costa Mesa
769 Baker Տt,
Costra Mesa, CA 92626, United Stаtes
bail bonds agent pay (Tessa)
Angyels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, СA 92626, United Stɑteѕ
key bail bonds
Не всегда человек способен прекратить употребление алкоголя без медицинского вмешательства. Чем дольше длится запой, тем выше риск осложнений. Обратиться к специалисту следует при появлении следующих признаков:
Подробнее можно узнать тут – https://vyvod-iz-zapoya-v-tyumeni17.ru/vyvod-iz-zapoya-tyumen-otzyvy/
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Полная информация здесь – https://horizon-ogrodzenia.pl/ogrodzenia-dla-wlascicieli-zwierzat-jak-zadbac-o-bezpieczenstwo-swoich-pupili
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Исследовать вопрос подробнее – https://????????????????????.com/__trashed
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Узнайте всю правду – https://escapistasclub.com/el-duelo-escape-room-en-granada-la-zubia-granada
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Желаете узнать подробности? – https://autoecolebourgeois.com/galleries/cambridge-language-certificate-in-2018
Услуга вывода из запоя в клинике сочетает профессионализм врачей, медицинскую точность и заботу. При этом обеспечивается полная конфиденциальность: данные пациентов не передаются в сторонние инстанции. Круглосуточный режим работы позволяет вызвать врача даже ночью — специалисты прибывают в течение 40–60 минут после обращения.
Подробнее тут – вывод из запоя на дому недорого
Для удобства восприятия можно ориентироваться на следующую структуру (это не публичная оферта, а примерная модель ценообразования — точная сумма фиксируется после осмотра и согласования схемы):
Изучить вопрос глубже – https://narkolog-na-dom-serpuhov10.ru/vyezd-narkologa-na-dom-serpuhov
Angels Bail Bonds Costa Mesa
769 Baker St,
Costa Mesa, CA 92626, United Statеs
bail bond agent exam
I have been surfing online more than 4 hours
today, yet I never found any interesting article like yours.
It is pretty worth enough for me. In my opinion, if all website owners and bloggers made good content as you did,
the internet will be much more useful than ever before.
Here is my website :: best realtor in Whittier CA
После процедуры пациент чувствует улучшение уже через 1–2 часа: проходят головные боли, снижается давление, нормализуется сон и аппетит.
Узнать больше – http://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk/
You actually make it seem so easy with your presentation but I find this matter to be actually something that I think I would never understand.
It seems too complicated and very broad for me. I am looking
forward for your next post, I’ll try to get the hang of
it!
Also visit my homepage; real estate agent Tipp City OH
Thank you a bunch for sharing this with all of us you really know what you’re speaking
approximately! Bookmarked. Kindly additionally consult with my web site =).
We can have a link change contract among us
https://1wins34-tos.top
Kenvox
1701 E Edinger Ave
Sata Ana, СA 92705, United Statеs
16572319025
rapid prototyping and tooling
нажмите, чтобы подробнее зеркало vodka bet
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Узнать больше – наркологическая клиника лечение алкоголизма
I have fun with, result in I found exactly what I used to
be looking for. You have ended my 4 day long hunt!
God Bless you man. Have a great day. Bye
Feel free to visit my web-site :: best real estate agent in Whittier CA
Go8 casino
Greetings! Very helpful advice in this particular post!
It’s the little changes that will make the most important changes.
Many thanks for sharing!
My blog post :: real estate agent in Ann Arbor MI
Когда состояние «штормит», ночные часы усиливают тревогу и вегетативные реакции, обезвоживание нарастает, сон рвётся, а попытки самолечения «чем попало» маскируют опасные симптомы. Организованный маршрут в «Трезвой Линии» заменяет хаос последовательностью: ещё по телефону дежурный врач собирает ключевые сведения — длительность эпизода, аллергии, список лекарств и дозировок, кардио- и эндокринные диагнозы, последние измерения давления и пульса. На месте выполняется короткая, но информативная оценка: АД, ЧСС, сатурация, температура, неврологический статус, степень обезвоживания, выраженность тремора и тошноты. Схема терапии запускается сразу и корректируется каждые 15–20 минут по «живым показателям», а не по шаблону. Если видим признаки предделирия, неукротимую рвоту, резкие «качели» давления/пульса, выраженную слабость или пожилой возраст с тяжёлой соматикой — переводим в стационар без пауз: приборный мониторинг и ночная команда в Электростали снижают «цену ошибки» и экономят на повторных вызовах. Для семьи это означает меньше догадок и больше ясности: понятно, что делаем сейчас и чего ждём к утру.
Выяснить больше – http://
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Разобраться лучше – нарколог на дом срочно в уфе
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Подробнее тут – http://dg162.net/wp/%D0%B2%D0%B0%D0%B6%D0%BD%D0%BE
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Получить дополнительную информацию – частная наркологическая клиника
Ниже приведена таблица с примерными этапами терапии:
Выяснить больше – вывод из запоя в стационаре
Its not my first time to pay a visit this website, i am
browsing this site dailly and obtain pleasant facts from here every day.
Also visit my web-site: realtor in West Chester Township OH
Wow, incredible blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of
your web site is fantastic, let alone the content!
I think that is among the most important information for me.
And i am happy reading your article. But should remark on some normal
issues, The web site style is great, the articles
is actually excellent : D. Just right process, cheers
Процесс вывода из запоя включает последовательное воздействие на ключевые звенья интоксикации. Ниже представлена таблица, отражающая этапы лечения, используемые методики и ожидаемые результаты терапии.
Ознакомиться с деталями – помощь вывод из запоя
If you want to increase your familiarity only keep visiting this
web site and be updated with the newest gossip posted here.
Feel free to surf to my website … best real estate agent in Ann Arbor MI
This post presents clear idea designed for the new viewers of blogging, that in fact how to do blogging.
Формат помощи
Узнать больше – http://vyvod-iz-zapoya-reutov10.ru/vyvod-iz-zapoya-na-domu-v-reutove/
We stumbled over here different web page and thought I should check things out.
I like what I see so now i am following you. Look forward to
looking over your web page repeatedly.
Having read this I believed it was rather informative. I appreciate
you spending some time and effort to put this article together.
I once again find myself personally spending a lot of time both reading and
commenting. But so what, it was still worthwhile!
Острый период запоя — это не «плохое самочувствие», а состояние с реальными рисками, где каждая задержка усложняет картину. В «Трезвой Линии» в Электростали мы строим помощь так, чтобы от первого звонка до заметного облегчения прошёл минимальный и управляемый путь: быстрый сбор рисков, экспресс-диагностика на месте, персональная инфузионная схема без «универсальных коктейлей», щадящая коррекция сна и тревоги, регулярные замеры показателей, чёткие рекомендации для семьи. Мы избегаем агрессивной седации: дозы и темп капельниц подбираются под возраст, длительность эпизода, сопутствующие заболевания и уже принимаемые лекарства. Задача — быстро снять токсическую нагрузку, выровнять давление и пульс, собрать ночной сон, а затем удержать результат дисциплинированным постдетокс-маршрутом на 2–4 недели. Конфиденциальность и анонимность соблюдаются без компромиссов, решения принимаются по реальным данным, чтобы эффект был устойчивым, предсказуемым и безопасным для пациента и семьи.
Детальнее – вывод из запоя
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Уточнить детали – https://daniellesellsfl.com/hello-world
I pay a quick visit each day some web sites and sites to read posts, but this website presents quality based posts.
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
А что дальше? – https://premoldeadosnardoni.com.ar/ficha-tecnica-tubos-y-canos-de-hormigon
Absolutely pent subject material, thanks for information.
Yes! Finally someone writes about 강남가라오케.
Вывод из запоя — это не просто медицинская процедура, а жизненно важный этап, позволяющий вернуть контроль над самочувствием и предотвратить осложнения. В клинике «РеабКузбасс» пациенты получают помощь в любое время суток: опытные наркологи выезжают на дом, проводят капельницы и медикаментозную детоксикацию, подбирают индивидуальные схемы восстановления. Такой подход помогает не только устранить последствия запоя, но и запустить процесс полноценного оздоровления организма.
Получить больше информации – срочный вывод из запоя
Вывод из запоя требуется тогда, когда организм уже не способен самостоятельно справиться с последствиями алкогольной интоксикации. Длительное употребление спиртного приводит к нарушению работы внутренних органов, обезвоживанию и психическим расстройствам. Медицинская помощь помогает избежать опасных осложнений и облегчить процесс отказа от алкоголя.
Углубиться в тему – наркологический вывод из запоя в рязани
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Изучить вопрос глубже – кодирование от алкоголизма цена адреса в волгограде
Основная цель капельницы — вывести из организма продукты распада этанола и восстановить водно-солевой баланс. После запоя в крови скапливаются токсичные вещества, которые вызывают головокружение, слабость и эмоциональную нестабильность. Введение растворов внутривенно позволяет быстро доставить активные компоненты в кровоток, улучшая работу сердца, печени и нервной системы. Уже через 20–30 минут после начала процедуры пациент ощущает облегчение.
Подробнее тут – капельница от запоя анонимно на дому
Why viewers still make use of to read news papers when in this technological world
everything is available on net?
my blog post :: real estate agent Vancouver BC
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Ознакомиться с полной информацией – https://cncllc.online/hello-world-2
Howdy! I just wish to give you a big thumbs up for your excellent info
you have got right here on this post. I am returning
to your blog for more soon.
Also visit my web page: best realtor in Cincinnati OH
This paragraph gives clear idea designed for the new users of
blogging, that in fact how to do blogging and site-building.
I don’t even know how I ended up here, but I assumed this
submit used to be good. I do not understand who you are but definitely you’re going to a
well-known blogger when you are not already.
Cheers!
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Посмотреть подробности – http://radiovinil.ge/logo_1-1
Капельница — это основной инструмент дезинтоксикации при лечении запойных состояний. Она способствует выведению токсинов, нормализации обмена веществ и улучшению общего самочувствия. Состав раствора подбирается индивидуально в зависимости от степени интоксикации, возраста, массы тела и сопутствующих заболеваний. Уже через 20–30 минут после начала инфузии пациент ощущает облегчение, снижается тревожность и проходит головная боль.
Получить больше информации – http://vyvod-iz-zapoya-v-krasnoyarske17.ru
В этих ситуациях выезд нарколога на дом позволяет вовремя скорректировать состояние, а при выявлении опасных признаков — не теряя времени, направить пациента в стационар. Это управляемый маршрут вместо хаотичных решений в последний момент.
Получить дополнительные сведения – http://narkolog-na-dom-dolgoprudnij10.ru/skolko-stoit-narkolog-na-dom-v-dolgoprudnom/
Ниже — примерная структура пакетов, которую можно использовать как ориентир (не публичная оферта):
Детальнее – http://narkolog-na-dom-shchelkovo10.ru/narkolog-na-dom-cena-shchelkovo/
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Узнать больше – наркологические клиники алкоголизм
ดูบอลออนไลน์ ดูบอลสด แบบ Live สด! 24 ชั่วโมง ไม่มีกระตุก ดูบอลสดออนไลน์การแข่งขันจากทุกลีกชั้นนำระดับโลก เว็บดูบอลและลิ้งค์ดูบอลที่มีคุณภาพ ภาพคมชัดตลอดเวลา พร้อมตารางการแข่งขันฟุตบอลทุกนัด อัพเดทใหม่ทุกชั่วโมง ดูบอลสด / ดูบอลออนไลน์ / ดูบอลผ่านมือถือ ด้วยขั้นตอนที่ไม่ยุ่งยาก ไม่ต้องติดตั้งโปรแกรม ก็สามารถดูบอลสดออนไลน์ ได้แบบฟรีไม่มีค่าใช้จ่ายแล้ว Live news24 เปิดให้บริการดูบอลสดในปี 2026
Exceptional post however , I was wanting to know if you
could write a litte more on this subject? I’d be very thankful if you could elaborate a little bit further.
Appreciate it!
Here is my page … best real estate agent in Ocean Isle Beach NC
You’ve made some really good points there. I looked on the web for
more information about the issue and found most individuals will go along with your views on this site.
my page best real estate agent in Vancouver BC
Услуга
Узнать больше – https://narkolog-na-dom-serpuhov10.ru/vyezd-narkologa-na-dom-serpuhov
all the time i used to read smaller posts that
also clear their motive, and that is also happening with this paragraph which I am reading here.
Каждое назначение объясняется пациенту и близким простым языком. Здесь не практикуют подход «делаем, как знаем, вам всё равно не понять» — прозрачность и понятные шаги помогают снизить тревогу и укрепляют доверие к клинике.
Получить больше информации – https://vyvod-iz-zapoya-ramenskoe10.ru/vyvod-iz-zapoya-na-domu-v-ramenskom/
Le système pour aider est très clair.
Анонимная наркологическая помощь — это управляемая система, где каждый шаг прозрачно связан с целью и измеримым результатом. В наркологической клинике «ЕнисейМед Центр» мы соединяем круглосуточную доступность, мягкую логистику и модульный план лечения, чтобы пациент и семья понимали, почему именно сейчас назначается то или иное вмешательство и когда оно будет остановлено. Мы избегаем полипрагмазии: запускаем один модуль — ставим один маркер — определяем «окно оценки» — выключаем модуль, как только цель достигнута. Такой подход бережёт ресурсы организма и сохраняет причинно-следственную связь.
Подробнее тут – наркологическая клиника цены в красноярске
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Детальнее – narkolog-na-dom-vyvod-iz-zapoya
Every weekend i used to go to see this site, because i wish for enjoyment, as this this website conations
in fact pleasant funny data too.
Heya just wanted to give you a quick heads up and let you know a few
of the images aren’t loading correctly. I’m not sure why but I think its a linking issue.
I’ve tried it in two different web browsers and both show
the same results.
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-v-krasnoyarske17.ru/czentr-kodirovaniya-vyvod-iz-zapoya-krasnoyarsk/
запустить охрану труда
Наркологическая клиника «ВолгаДок Медикал» — это круглосуточная служба помощи, выстроенная вокруг принципов клинической безопасности, прозрачной коммуникации и поддержки пациента на каждом этапе. Мы соединяем стационар и выездные бригады в единую систему: первичный осмотр и стабилизация состояния, адресные инфузионные модули, мягкая коррекция сна и тревоги, последующее наблюдение с короткими «окнами» обратной связи. Все решения принимаются по показаниям и сопровождаются объяснением: какую цель преследуем, каким маркером измеряем, когда проверяем результат. Такой подход исключает хаотичные усиления, бережёт ресурс организма и даёт прогнозируемый клинический эффект.
Углубиться в тему – https://narcologicheskaya-klinika-saratov0.ru/chastnaya-narkologicheskaya-klinika-saratov/
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Узнайте всю правду – https://taconceptiongraphique.fr/bonjour-tout-le-monde
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Подробности по ссылке – https://logisticaintegral.online
Для повышения эффективности в капельницы добавляются витамины группы B, аскорбиновая кислота, кардиопротекторы и антиоксиданты. Такая комбинация позволяет не только ускорить выведение продуктов распада алкоголя, но и предотвратить развитие постабстинентных расстройств. Благодаря точной дозировке и мягкому темпу введения растворов снижается риск побочных реакций, а восстановление проходит плавно и безопасно.
Углубиться в тему – скорая вывод из запоя
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, СА 92626, United Տtates
where do bail bondsman get money
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Подробнее можно узнать тут – заказать нарколога на дом
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Подробнее тут – лечение в наркологической клинике в волгограде
Комплексная терапия включает несколько последовательных этапов, обеспечивающих полное восстановление организма и личности пациента. Каждый из них направлен на решение конкретных задач — от устранения интоксикации до закрепления устойчивой ремиссии.
Ознакомиться с деталями – http://narkologicheskaya-klinika-v-volgograde17.ru/
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Подробнее тут – http://narkologicheskaya-klinika-kolomna2-10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
This post is worth everyone’s attention. Where can I find out more?
I like the helpful info you provide in your articles.
I’ll bookmark your weblog and check again here regularly.
I’m quite sure I’ll learn plenty of new stuff right here!
Best of luck for the next!
Kenvox
1701 E Edinger Ave
Santa Ana,ⲤᎪ 92705, United Ⴝtates
16572319025
silicone fabrication Optimization
Saved as a favorite, I love your site!
Feel free to visit my website; best realtor in Tipp City OH
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Подробнее – https://narkologicheskaya-pomoshh-v-tolyatti17.ru/
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Получить больше информации – http://narkolog-na-dom-shchelkovo10.ru/vyzvat-narkologa-na-dom-shchelkovo/https://narkolog-na-dom-shchelkovo10.ru
При появлении таких симптомов важно не откладывать вызов врача. Самолечение, особенно с использованием неизвестных препаратов, может привести к тяжёлым последствиям, включая судороги и инсульт. Врачи клиники «ВолгаМед Резолюция» приезжают на дом с необходимыми средствами для оказания экстренной помощи и стабилизации состояния уже на месте.
Узнать больше – вывод из запоя недорого в волгограде
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Детальнее – https://vistoweekly.com/wellhealthorganic-buffalo-milk-tag
В Воронеже клиника «ВоронежМед Альянс» предлагает комплексное лечение алкогольной и наркотической зависимости. Команда врачей, психиатров, психологов и терапевтов выстраивает индивидуальный маршрут пациента, начиная с детоксикации и заканчивая реабилитацией. Главный принцип — минимальное вмешательство при максимальной эффективности. Это означает, что терапевтические меры подбираются строго по показаниям, а медикаменты применяются только после оценки состояния и лабораторных данных.
Исследовать вопрос подробнее – http://narcologicheskaya-klinika-v-voronezhe17.ru/narkolog-voronezh-anonimno/
Hi, always i used to check blog posts here early in the morning, as
i love to gain knowledge of more and more.
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Получить больше информации – врач вывод из запоя
Вывод из запоя в Раменском в условиях клиники строится не вокруг одной капельницы, а вокруг понятной цепочки шагов, где каждый этап логичен и медицински обоснован. Это помогает не только быстро облегчить состояние, но и уменьшить вероятность того, что через пару дней человек снова уйдёт в запой.
Получить больше информации – http://vyvod-iz-zapoya-ramenskoe10.ru/vyvod-iz-zapoya-ryadom-v-ramenskom/https://vyvod-iz-zapoya-ramenskoe10.ru
It’s very straightforward to find out any topic on net as compared to textbooks, as I found this article at
this web page.
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Детальнее – https://funeral-agency.wwwbg.in/kontakti
Наркологическая клиника — это пространство, где медицинская наука сочетается с психологической поддержкой и индивидуальным подходом к каждому пациенту. В клинике «ВоронежМед Альянс» лечение зависимости организовано по принципам доказательной медицины: каждый этап терапии основан на объективных данных, контролируемых результатах и четких критериях эффективности. Здесь помогают не просто устранить физические последствия зависимости, но и восстановить внутренние ресурсы человека, вернуть уверенность, осознанность и способность строить новую жизнь без алкоголя и наркотиков.
Изучить вопрос глубже – наркологическая клиника
Программы вывода из запоя в клинике разрабатываются с учётом состояния пациента. Для тяжёлых случаев назначается интенсивный курс с инфузионной терапией и контролем электролитов. При лёгких формах применяются мягкие препараты с постепенным выведением токсинов. Все процедуры проходят с соблюдением медицинских стандартов и полным сохранением анонимности.
Узнать больше – вывод из запоя круглосуточно волгоград
Hello! I could have sworn I’ve been to this blog before but after checking through some of the post I realized it’s new to me.
Anyways, I’m definitely delighted I found it and I’ll be book-marking and checking back frequently!
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Детальнее – вывод из запоя в новокузнецке
Капельница — основной инструмент для очищения организма от продуктов распада этанола. Состав раствора подбирается строго индивидуально. В таблице приведены примеры комплексов, применяемых специалистами клиники «Трезвая Линия Волгоград».
Получить дополнительную информацию – http://vyvod-iz-zapoia-v-volgograde17.ru
Процедура начинается с осмотра пациента и оценки степени интоксикации. Врач измеряет давление, пульс, уровень насыщения крови кислородом, определяет наличие сопутствующих заболеваний. После диагностики назначается капельница, состав которой подбирается индивидуально. Процедура направлена на очищение организма, восстановление водно-солевого баланса и снятие симптомов похмелья.
Изучить вопрос глубже – https://vyvod-iz-zapoya-v-tolyatti17.ru/vyvod-iz-zapoya-na-domu-tolyatti-otzyvy
I all the time used to study post in news papers but now
as I am a user of internet thus from now I am using net for
articles, thanks to web.
Thank you for every other great article. The place else
may anyone get that type of info in such a perfect approach of
writing? I have a presentation subsequent week, and I am at the look for such information.
Вывод из запоя — это не просто медицинская процедура, а тщательно выстроенный процесс, направленный на восстановление работы всех систем организма. При неправильном или неполном лечении риск осложнений возрастает в несколько раз. Поэтому обращение в профессиональную клинику становится необходимым шагом. В наркологической клинике «Центр Трезвости ВоронМед» пациент получает экстренную помощь, безопасные инфузионные препараты, круглосуточный выезд нарколога и последующее восстановление под наблюдением специалистов. Здесь каждая капельница подбирается индивидуально — с учётом возраста, веса, длительности запоя, хронических болезней и реакции организма на препараты.
Ознакомиться с деталями – https://vyvod-iz-zapoya-v-voronezhe17.ru/vyvod-iz-zapoya-za-den-voronezh/
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Подробнее можно узнать тут – http://www.domen.ru
Маршрут организован так, чтобы убрать хаос и сделать шаги понятными для родственников. После звонка оператор под контролем врача уточняет длительность употребления, примерные объёмы алкоголя, хронические болезни (гипертония, ИБС, диабет, заболевания печени, почек, нервной системы), список уже принятых лекарств, эпизоды потери сознания, судорог, подозрительные психические симптомы. На этом этапе принимается базовое решение: возможно ли безопасно провести детокс на дому либо показан стационар. Врач приезжает по адресу в Щёлково, проводит осмотр: фиксирует АД, ЧСС, сатурацию, температуру, оценивает тремор, координацию, речь, поведение, уровень сознания, степень обезвоживания. Затем подбирается индивидуальная инфузионная схема: растворы для регидратации, коррекции электролитов и кислотно-щелочного баланса, витамины группы B и магний для поддержки нервной системы и снижения тремора; по показаниям — гепатопротекторы, мягкие антиоксиданты, противорвотные, щадящие анксиолитики для сна, но без грубого «выключения». Во время процедуры врач наблюдает за динамикой, при необходимости меняет скорость капельницы, контролирует давление и пульс, следит за реакцией на препараты. В финале даёт подробные рекомендации: как вести себя ближайшие 24–72 часа, как спать, что пить и есть, каких лекарств избегать, какие симптомы считать тревожными, когда нужно немедленно звонить и когда стоит рассмотреть стационар. Если уже на этапе осмотра понятно, что дому «тесно» по безопасности, перевод в клинику организуется без задержек.
Разобраться лучше – https://narkolog-na-dom-shchelkovo10.ru/vrach-narkolog-na-dom-shchelkovo
Острый период запоя — это не «плохое самочувствие», а состояние с реальными рисками, где каждая задержка усложняет картину. В «Трезвой Линии» в Электростали мы строим помощь так, чтобы от первого звонка до заметного облегчения прошёл минимальный и управляемый путь: быстрый сбор рисков, экспресс-диагностика на месте, персональная инфузионная схема без «универсальных коктейлей», щадящая коррекция сна и тревоги, регулярные замеры показателей, чёткие рекомендации для семьи. Мы избегаем агрессивной седации: дозы и темп капельниц подбираются под возраст, длительность эпизода, сопутствующие заболевания и уже принимаемые лекарства. Задача — быстро снять токсическую нагрузку, выровнять давление и пульс, собрать ночной сон, а затем удержать результат дисциплинированным постдетокс-маршрутом на 2–4 недели. Конфиденциальность и анонимность соблюдаются без компромиссов, решения принимаются по реальным данным, чтобы эффект был устойчивым, предсказуемым и безопасным для пациента и семьи.
Выяснить больше – срочный вывод из запоя
Hi, I do believe this is an excellent blog. I stumbledupon it 😉
I will come back yet again since I bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to guide others.
Продолжительность процедуры — от 40 минут до полутора часов. Уже в первые часы после начала терапии состояние пациента значительно улучшается: проходит тошнота, снижается тревожность, восстанавливается координация движений.
Разобраться лучше – вывод из запоя дешево в тольятти
Такой календарь делает весь процесс прозрачным: пациент видит логику, близкие — прогресс, а врач — чистый сигнал для коррекции без «эскалации на всякий случай».
Получить дополнительные сведения – https://narcologicheskaya-klinika-saratov0.ru/
В клинике обеспечивается безопасный вывод из запоя и очистка организма после употребления алкоголя, наркотиков или токсических сочетаний. Используются современные инфузионные схемы, витамины группы B, магний, гепатопротекторы по показаниям, противорвотные, мягкая коррекция сна и тревожности. Контроль давления, пульса, сатурации и поведения позволяет вовремя отметить любые осложнения и скорректировать терапию. Главная цель — не просто «прояснить голову», а защитить сердечно-сосудистую систему, мозг, печень, минимизировать риск делирия, судорог, аритмий и других острых состояний.
Получить больше информации – адреса наркологических клиник
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Хочешь знать всё? – https://vistoweekly.com/pizza-edition
Пациент может выбрать анонимный формат — все данные защищены, а пребывание в клинике проходит в атмосфере уважения и деликатности. Особое внимание уделяется созданию комфортных условий: палаты оснащены системой вентиляции, регулируемым освещением и кнопкой вызова медперсонала. Круглосуточный контроль состояния позволяет своевременно реагировать на малейшие изменения и корректировать курс лечения.
Выяснить больше – наркологическая клиника стационар воронеж
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Подробнее тут – http://narkologicheskaya-klinika-v-krasnoyarske17.ru
В клинике обеспечивается безопасный вывод из запоя и очистка организма после употребления алкоголя, наркотиков или токсических сочетаний. Используются современные инфузионные схемы, витамины группы B, магний, гепатопротекторы по показаниям, противорвотные, мягкая коррекция сна и тревожности. Контроль давления, пульса, сатурации и поведения позволяет вовремя отметить любые осложнения и скорректировать терапию. Главная цель — не просто «прояснить голову», а защитить сердечно-сосудистую систему, мозг, печень, минимизировать риск делирия, судорог, аритмий и других острых состояний.
Изучить вопрос глубже – https://narkologicheskaya-klinika-kolomna10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/
Процесс включает несколько шагов:
Подробнее – нарколог на дом срочно уфа
May I simply say what a relief to uncover somebody
that truly understands what they’re talking about on the web.
You certainly know how to bring an issue to light and make it important.
More people need to check this out and understand this side of your story.
It’s surprising you are not more popular since you surely have the gift.
В основе работы клиники лежит принцип: зависимость — это не просто привычка и не «слабость характера», а комплексное заболевание, которое требует последовательного лечения, а не случайной капельницы по вызову. «Трезвый Шаг Раменское» отказывается от практики, когда пациенту предлагают один-единственный «волшебный» метод, не объясняя, что будет дальше. Здесь каждое обращение рассматривается в контексте стадии зависимости, общего состояния организма, психоэмоционального фона, семейной ситуации. Сначала специалисты снимают острые проявления: выход из запоя, детоксикация после употребления алкоголя, наркотиков или сочетаний, купирование абстиненции, коррекция давления, пульса, сна, тревоги. Затем формируется стабилизационный этап — подбор поддерживающих схем, работа с тягой, выравнивание эмоционального состояния. После этого при готовности пациента подключаются психотерапевтические и реабилитационные инструменты: мотивационные программы, работа с установками, триггерами, окружением. Важная особенность «Трезвый Шаг Раменское» — готовность объяснять семье и самому пациенту, зачем нужен каждый этап, какие цели у процедуры и какие результаты реально ожидать. Это снижает сопротивление, формирует доверие и делает путь не хаотичным, а управляемым.
Детальнее – http://narkologicheskaya-klinika-ramenskoe10.ru/narkologicheskaya-klinika-otzyvy-v-ramenskom/
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Это ещё не всё… – https://duhocvungtau.com.vn/du-hoc-newzealandwakatipu-high-school
whoah this weblog is fantastic i love reading your articles.
Stay up the good work! You realize, a lot of people are searching round for this info, you could help them greatly.
Для повышения эффективности в капельницы добавляются витамины группы B, аскорбиновая кислота, кардиопротекторы и антиоксиданты. Такая комбинация позволяет не только ускорить выведение продуктов распада алкоголя, но и предотвратить развитие постабстинентных расстройств. Благодаря точной дозировке и мягкому темпу введения растворов снижается риск побочных реакций, а восстановление проходит плавно и безопасно.
Получить дополнительные сведения – вывод из запоя в воронеже
Главным преимуществом наркологической клиники в Новокузнецке является комплексный подход к лечению. Специалисты рассматривают зависимость как заболевание, требующее системного воздействия на организм и психику. Каждый пациент получает индивидуальную программу, включающую медицинскую, психотерапевтическую и социальную помощь. Такой подход обеспечивает достижение устойчивых результатов и предотвращает рецидивы.
Подробнее тут – наркологическая клиника лечение алкоголизма в новокузнецке
Системный подход позволяет достичь максимальной эффективности лечения и снизить риск возврата к зависимости.
Углубиться в тему – http://narkologicheskaya-clinica-v-novokuzneczke17.ru
Вызов нарколога на дом — это удобная и безопасная возможность получить медицинскую помощь без необходимости ехать в клинику. Такая услуга особенно востребована, когда состояние пациента не позволяет покинуть дом, а помощь требуется незамедлительно. В наркологической клинике «ВоронМед Профи» организована круглосуточная служба выезда специалистов, которая оперативно реагирует на обращения и обеспечивает профессиональную помощь при запое, алкогольной интоксикации и обострениях хронических состояний. Врач приезжает в течение часа, оценивает состояние пациента и подбирает оптимальную схему лечения, включающую капельницы, детоксикацию и рекомендации по восстановлению организма.
Детальнее – вызвать нарколога на дом срочно воронеж
Pretty great post. I just stumbled upon your weblog and wanted to mention that I’ve really enjoyed browsing your weblog posts.
In any case I’ll be subscribing on your rss feed and I’m hoping you write
once more soon!
Главным преимуществом наркологической клиники в Новокузнецке является комплексный подход к лечению. Специалисты рассматривают зависимость как заболевание, требующее системного воздействия на организм и психику. Каждый пациент получает индивидуальную программу, включающую медицинскую, психотерапевтическую и социальную помощь. Такой подход обеспечивает достижение устойчивых результатов и предотвращает рецидивы.
Выяснить больше – лечение в наркологической клинике в новокузнецке
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Разобраться лучше – http://
В основе работы клиники лежит принцип: зависимость — это не просто привычка и не «слабость характера», а комплексное заболевание, которое требует последовательного лечения, а не случайной капельницы по вызову. «Трезвый Шаг Раменское» отказывается от практики, когда пациенту предлагают один-единственный «волшебный» метод, не объясняя, что будет дальше. Здесь каждое обращение рассматривается в контексте стадии зависимости, общего состояния организма, психоэмоционального фона, семейной ситуации. Сначала специалисты снимают острые проявления: выход из запоя, детоксикация после употребления алкоголя, наркотиков или сочетаний, купирование абстиненции, коррекция давления, пульса, сна, тревоги. Затем формируется стабилизационный этап — подбор поддерживающих схем, работа с тягой, выравнивание эмоционального состояния. После этого при готовности пациента подключаются психотерапевтические и реабилитационные инструменты: мотивационные программы, работа с установками, триггерами, окружением. Важная особенность «Трезвый Шаг Раменское» — готовность объяснять семье и самому пациенту, зачем нужен каждый этап, какие цели у процедуры и какие результаты реально ожидать. Это снижает сопротивление, формирует доверие и делает путь не хаотичным, а управляемым.
Получить дополнительные сведения – chastnye-narkologicheskie-kliniki-otzyvy
Не всегда человек способен прекратить употребление алкоголя без медицинского вмешательства. Чем дольше длится запой, тем выше риск осложнений. Обратиться к специалисту следует при появлении следующих признаков:
Получить больше информации – http://vyvod-iz-zapoya-v-tyumeni17.ru/vyvod-iz-zapoya-tyumen-kruglosutochno/
Greetings from Carolina! I’m bored to death at work so I decided to check out your website on my
iphone during lunch break. I really like the info you provide here and can’t wait to take
a look when I get home. I’m amazed at how quick your blog loaded
on my mobile .. I’m not even using WIFI, just 3G ..
Anyhow, excellent site!
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Изучить вопрос глубже – http://narcologicheskaya-klinika-omsk0.ru/chastnaya-narkologicheskaya-klinika-omsk/
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Исследовать вопрос подробнее – вывод из запоя саратов
I visited multiple websites however the audio quality for audio
songs present at this website is truly excellent.
Ən faydalı platformadır. Yenə baxacağam!
https://goto.now/VUu8A
Наркологическая клиника в Новокузнецке предоставляет профессиональную помощь людям, столкнувшимся с зависимостью от алкоголя, наркотиков и психоактивных веществ. Лечение проводится под наблюдением опытных специалистов с применением современных медицинских методик. Основная цель работы клиники — не только устранить физическую зависимость, но и восстановить психологическое равновесие пациента, вернуть мотивацию и способность жить без употребления веществ.
Подробнее тут – частная наркологическая клиника новокузнецк
Наркологическая клиника «ВолгаДок Медикал» — это круглосуточная служба помощи, выстроенная вокруг принципов клинической безопасности, прозрачной коммуникации и поддержки пациента на каждом этапе. Мы соединяем стационар и выездные бригады в единую систему: первичный осмотр и стабилизация состояния, адресные инфузионные модули, мягкая коррекция сна и тревоги, последующее наблюдение с короткими «окнами» обратной связи. Все решения принимаются по показаниям и сопровождаются объяснением: какую цель преследуем, каким маркером измеряем, когда проверяем результат. Такой подход исключает хаотичные усиления, бережёт ресурс организма и даёт прогнозируемый клинический эффект.
Подробнее тут – частная наркологическая клиника
เนื้อหานี้ อ่านแล้วได้ความรู้เพิ่ม
ค่ะ
ดิฉัน ไปเจอรายละเอียดของ ข้อมูลเพิ่มเติม
สามารถอ่านได้ที่ Lamar
เหมาะกับคนที่กำลังหาข้อมูลในด้านนี้
มีการยกตัวอย่างที่เข้าใจง่าย
ขอบคุณที่แชร์ บทความคุณภาพ นี้
และหวังว่าจะได้เห็นโพสต์แนวนี้อีก
Hey there, I think your website might be having browser compatibility issues.
When I look at your website in Safari, it looks fine but when opening
in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that, excellent blog!
Наркологическая клиника в Волгограде предоставляет профессиональную медицинскую помощь людям, страдающим зависимостью от алкоголя, наркотиков и других психоактивных веществ. Основная цель специалистов — не просто устранить физическую зависимость, но и помочь пациенту вернуть внутреннее равновесие, здоровье и контроль над жизнью. В клинике применяются современные методы лечения, доказавшие свою эффективность в практике отечественной и мировой наркологии.
Углубиться в тему – https://narkologicheskaya-klinika-v-volgograde17.ru
Everything is very open with a clear description of the
challenges. It was really informative. Your site is very helpful.
Many thanks for sharing!
Первым шагом при лечении зависимости является детоксикация — очищение организма от токсинов, накопившихся в результате употребления алкоголя или наркотиков. Врач подбирает состав инфузионных растворов и лекарственных препаратов индивидуально. Процедура направлена на восстановление обмена веществ, улучшение работы печени и сердца, нормализацию сна и аппетита. После завершения детоксикации пациент чувствует облегчение, снижается тревожность и повышается концентрация внимания.
Детальнее – наркологическая клиника цены
It is not my first time to go to see this website, i am visiting this web page dailly and get nice information from here all
the time.
Your method of explaining the whole thing in this piece of writing is truly fastidious,
every one be able to easily understand it, Thanks a lot.
Have a look at my blog: real estate agent in Ann Arbor MI
I was recommended this blog through my cousin. I am no longer
certain whether or not this publish is written by way of him as
no one else recognise such distinct approximately my problem.
You are wonderful! Thanks!
Can you tell us more about this? I’d like to find out
some additional information.
Наркологическая клиника «КоломнаМед Центр» — это место, куда можно обратиться в тот момент, когда домашние попытки контролировать алкоголь, наркотики, аптечные препараты или смесь всего сразу перестают работать, а жизнь превращается в постоянное «завтра начну с нуля». Здесь не обещают чудес за один день и не пугают диагнозами, а выстраивают понятный медицинский маршрут: детоксикация, стабилизация, реабилитация, поддержка семьи, профилактика срывов. Пациент получает помощь в защищённой, конфиденциальной среде, где всё организовано так, чтобы снизить тревогу и стыд, убрать хаос вокруг зависимости и дать человеку шанс вернуться к нормальной жизни без давления, угроз и токсичных «стимулов». Для родных клиника в Коломне — это опора: конкретный адрес, конкретная команда, чёткие сроки и понятные этапы, вместо бесконечных обещаний «он сам справится».
Углубиться в тему – http://narkologicheskaya-klinika-kolomna10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/https://narkologicheskaya-klinika-kolomna10.ru
Процесс вывода из запоя включает последовательное воздействие на ключевые звенья интоксикации. Ниже представлена таблица, отражающая этапы лечения, используемые методики и ожидаемые результаты терапии.
Подробнее тут – http://www.domen.ru
Перед процедурой врач оценивает состояние пациента, измеряет давление, пульс и уровень насыщения крови кислородом. После осмотра подбирается состав инфузии, включающий препараты для дезинтоксикации, восстановления водно-солевого баланса и нормализации работы органов. Введение растворов осуществляется внутривенно, под контролем специалиста. Длительность процедуры — от 40 минут до 1,5 часов.
Разобраться лучше – капельница от запоя стоимость волгоград
Когда вопрос стоит остро — нужно быстро и безопасно вывести человека из запоя в Коломне, — у семьи нет лишнего времени на эксперименты с таблетками, сомнительными «коктейлями» и советами из интернета. «Трезвый Центр Коломна» выстраивает помощь так, чтобы от первого звонка до реального облегчения шёл понятный и управляемый маршрут: запись симптомов и рисков уже по телефону, предложение формата (выезд на дом или стационар), оперативный осмотр, персональная инфузионная терапия, круглосуточное наблюдение при необходимости и подробный план восстановления на 24–72 часа и дальше. Мы не продаём миф о «чудо-капельнице за час», а работаем клинически аккуратно: дозы и схемы подбираются под возраст, длительность запоя, сопутствующие заболевания, уже принятые лекарства и текущие показатели. Цель проста и честна — снять интоксикацию, защитить сердце, мозг и печень, вернуть сон и ясность без агрессивной седации и скрытых рисков, сохранить конфиденциальность и дать семье уверенность, что всё делается правильно.
Детальнее – анонимный вывод из запоя на дому
Маршрут выстроен без пауз и импровизаций. Сначала — короткое интервью по телефону: адрес в Электростали, длительность эпизода, лекарства/дозировки, аллергии, важные диагнозы, последние значения давления и пульса. Это экономит 15–20 минут на месте и позволяет заранее исключить опасные взаимодействия. По прибытии врач фиксирует АД, ЧСС, сатурацию, температуру, оценивает неврологический статус, степень обезвоживания, выраженность тремора/тошноты, уровень тревоги, кратко собирает анамнез последних суток. Затем стартует инфузионная терапия: растворы для регидратации и коррекции электролитов, поддержка витаминами группы B и магнием; по показаниям — гепатопротекторы и антиоксиданты, противорвотные, мягкие анксиолитики. Каждые 15–20 минут врач смотрит динамику и корректирует темп капельниц, питьевой режим, симптоматическую поддержку. Важный принцип — «сон без вырубания»: умеренная седация собирает ночной ритм, сохраняя информативность мониторинга. По завершении — письменные рекомендации и маршрут на 24–72 часа (сон, питание, запреты, «красные флаги», амбулаторные визиты/дневной стационар или перевод в отделение). Такой алгоритм заменяет «лотерею» результата управляемым и повторяемым планом.
Ознакомиться с деталями – vyvod-iz-zapoya-na-domu
Definitely imagine that which you stated. Your favorite reason seemed
to be on the internet the easiest thing to be aware of.
I say to you, I certainly get irked while other people think about worries
that they plainly do not understand about.
You controlled to hit the nail upon the top and
defined out the whole thing with no need side-effects , people could take a
signal. Will likely be again to get more. Thank you
Thank you for any other magnificent post. Where else could anybody get that kind of info in such
a perfect approach of writing? I’ve a presentation next week, and I
am at the look for such information.
Острый эпизод запоя — это не «плохое самочувствие», а состояние с реальными рисками для сердца, нервной системы и дыхания, особенно в ночные часы, когда усиливаются вегетативные реакции и тревога. В «НоваТрезвие» мы выстраиваем помощь так, чтобы от звонка до заметного облегчения прошло как можно меньше времени и как можно меньше случайностей: короткое интервью для оценки рисков, выезд врача или приём в клинике, экспресс-диагностика по ключевым показателям, персональная инфузионная схема без «универсальных коктейлей», мягкая коррекция сна и тревоги без «вырубания», понятные инструкции семье на 24–72 часа и план продолжения на ближайшие недели. Мы не скрываемся за общими формулами: решения принимаются по фактическим данным, дозы и темп капельниц подстраиваются к динамике каждые 15–20 минут, а при «красных флагах» перевод в стационар организуется без пауз. Конфиденциальность соблюдается строго, а коммуникация простая и предсказуемая — чтобы вы всегда знали, что происходит сейчас и чего ждать к утру.
Подробнее можно узнать тут – вывод из запоя на дому цена
После процедуры пациент чувствует улучшение уже через 1–2 часа: проходят головные боли, снижается давление, нормализуется сон и аппетит.
Получить дополнительную информацию – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkolog-v-gorode-novokuzneczke/
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Подробнее можно узнать тут – вывод из запоя дешево
Письменные рекомендации: сон, питание, гидратация, запреты, «красные флаги», график амбулаторных визитов; при недостатке ресурсов дома — перевод в стационар без задержек. Такая последовательность убирает импровизацию и делает результат повторяемым.
Получить больше информации – https://vyvod-iz-zapoya-ehlektrostal2-10.ru/vyvod-iz-zapoya-stacionar-v-ehlektrostali
PT. Sicurezza Solutions Indonesia provides security solutions with integrating
varieties of security products which can be adjusted to many needs from Access Control,
Automatic Door, CCTV, Video Intercom, Biometric Time & Attendance, etc.
Experience selling and installing security systems for all kinds of buildings such
as private house, apartment, hotel, resort, office, government building,
bank, factory, etc.
COLCOM Hotel Lock,COLCOM Minibar,COLCOM Kettle,COLCOM Kettle Set,COLCOM Locker Lock,COLCOM Safe Deposit Box,COLCOM Infrared Body Temperature,
COLCOM Portable Dishwasher,COLCOM Vaccum Sweep Mop Robot,COLCOM Accessories,
SAMSUNG Digital Door Lock,SAMSUNG Video Intercom,
DOORHAN Sectional Door,DOORHAN Sliding Gate,DOORHAN Swing Gate,DOORHAN Parking Barrier,
ENIGMA Fingerprint,ENIGMA Automatic and Hermetic Door,ENIGMA Proximity Cards,ENIGMA Access Control Readers,ENIGMA Access Control System,ENIGMA Electric Lock,
ENIGMA Accessories,ENIGMA Parking Barrier,ENIGMA Digital Door Lock,
ENIGMA Body Temperature Screening Smart Camera,ENIGMA Window Opener,ENIGMA Specialized Curtain Motor,
HID Access Control,HONEYWELL BLACK CCTV Analog System,HONEYWELL BLACK CCTV IP System,APOLLO
CCTV,GUARD TOUR,
VIZPIN Smartphone Access Control System,OVAL One Touch Smart
Lock,HIK VISION Body Temperature Scanner
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Ознакомиться с деталями – http://vivod-iz-zapoya-v-volgograde17.ru
Лечение организовано поэтапно, что помогает пациенту постепенно возвращаться к полноценной жизни. Каждый шаг направлен на укрепление результата и снижение риска рецидива.
Получить дополнительные сведения – анонимная наркологическая клиника в омске
Excellent blog you’ve got here.. It’s hard to find quality writing
like yours nowadays. I really appreciate people like you! Take care!!
You can certainly see your expertise in the work you write.
The world hopes for more passionate writers such as you who
aren’t afraid to mention how they believe. At all times go
after your heart.
my site: کد اقتصادی
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Углубиться в тему – наркологическая клиника стационар в новокузнецке
Алгоритм в «Трезвый Центр Коломна» построен так, чтобы убрать импровизацию и сделать всё максимально прозрачным для семьи. Сначала по телефону собираются ключевые данные: возраст пациента, длительность запоя, виды алкоголя, хронические заболевания, препараты, аллергии, наличие судорог, потерь сознания, странного поведения, текущие жалобы. На этом этапе озвучивается ориентировочный формат помощи и примерный диапазон стоимости. Далее следует выезд на дом или поступление в стационар. Врач проводит осмотр: измеряет артериальное давление, пульс, сатурацию, температуру, оценивает тремор, координацию, сознание, степень обезвоживания, наличие болей, состояние дыхания и сердца. На основе этих данных назначается инфузионная терапия: растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы, по показаниям — гепатопротекторы, антиоксидантные комплексы, противорвотные для контроля тошноты, мягкие анксиолитики для уменьшения тревоги и нормализации сна. Уходят от агрессивной седации: пациент не должен быть «выключен» так, чтобы невозможно было заметить ухудшение. В процессе капельниц проводится повторный контроль показателей, темп и состав при необходимости корректируются. После стабилизации пациент и семья получают подробные рекомендации: режим, сон, питание, питьё, запреты, «красные флаги», план наблюдения и возможного дальнейшего лечения зависимости.
Узнать больше – http://vyvod-iz-zapoya-kolomna10.ru
Для удобства восприятия можно ориентироваться на следующую структуру (это не публичная оферта, а примерная модель ценообразования — точная сумма фиксируется после осмотра и согласования схемы):
Получить дополнительную информацию – vyzvat-vracha-narkologa-na-dom-srochno
Процесс лечения включает несколько последовательных шагов, направленных на стабилизацию состояния, детоксикацию и восстановление функций организма. Таблица ниже показывает основные этапы процедуры, применяемые врачами клиники «РеабКузбасс».
Узнать больше – нарколог вывод из запоя новокузнецк
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Детальнее – http://vyvod-iz-zapoya-v-krasnoyarske17.ru
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Получить дополнительную информацию – анонимный вывод из запоя в красноярске
Greetings, There’s no doubt that your web site might be having web browser compatibility problems.
Whenever I look at your website in Safari, it looks fine however, when opening in I.E., it has some overlapping issues.
I merely wanted to provide you with a quick heads up!
Other than that, great website!
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, ⲚE 68022, United Stɑtes
402-289-4126
Managed Edge Pro Tools
В основе работы клиники лежит принцип: зависимость — это не просто привычка и не «слабость характера», а комплексное заболевание, которое требует последовательного лечения, а не случайной капельницы по вызову. «Трезвый Шаг Раменское» отказывается от практики, когда пациенту предлагают один-единственный «волшебный» метод, не объясняя, что будет дальше. Здесь каждое обращение рассматривается в контексте стадии зависимости, общего состояния организма, психоэмоционального фона, семейной ситуации. Сначала специалисты снимают острые проявления: выход из запоя, детоксикация после употребления алкоголя, наркотиков или сочетаний, купирование абстиненции, коррекция давления, пульса, сна, тревоги. Затем формируется стабилизационный этап — подбор поддерживающих схем, работа с тягой, выравнивание эмоционального состояния. После этого при готовности пациента подключаются психотерапевтические и реабилитационные инструменты: мотивационные программы, работа с установками, триггерами, окружением. Важная особенность «Трезвый Шаг Раменское» — готовность объяснять семье и самому пациенту, зачем нужен каждый этап, какие цели у процедуры и какие результаты реально ожидать. Это снижает сопротивление, формирует доверие и делает путь не хаотичным, а управляемым.
Выяснить больше – наркологическая клиника телефон
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, NE 68022, United Stateѕ
402-289-4126
Bookmarks
Первым шагом при лечении зависимости является детоксикация — очищение организма от токсинов, накопившихся в результате употребления алкоголя или наркотиков. Врач подбирает состав инфузионных растворов и лекарственных препаратов индивидуально. Процедура направлена на восстановление обмена веществ, улучшение работы печени и сердца, нормализацию сна и аппетита. После завершения детоксикации пациент чувствует облегчение, снижается тревожность и повышается концентрация внимания.
Изучить вопрос глубже – наркологическая клиника наркологический центр
Hi there friends, how is all, and what you wish for to say
regarding this post, in my view its actually awesome for me.
Look into my page slot maxwin
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Подробнее тут – https://vyvod-iz-zapoya-v-krasnoyarske17.ru/czentr-kodirovaniya-vyvod-iz-zapoya-krasnoyarsk
Своевременное обращение к специалистам позволяет быстро стабилизировать состояние и избежать осложнений.
Получить больше информации – вывод из запоя на дому круглосуточно в тольятти
Woah! I’m really enjoying the template/theme of this blog.
It’s simple, yet effective. A lot of times it’s very difficult to
get that “perfect balance” between user friendliness and appearance.
I must say you’ve done a amazing job with this. Additionally, the blog loads extremely quick for me on Internet
explorer. Exceptional Blog!
Feel free to surf to my web blog; پرینتر لیبل زن
Маршрут организован так, чтобы убрать хаос и сделать шаги понятными для родственников. После звонка оператор под контролем врача уточняет длительность употребления, примерные объёмы алкоголя, хронические болезни (гипертония, ИБС, диабет, заболевания печени, почек, нервной системы), список уже принятых лекарств, эпизоды потери сознания, судорог, подозрительные психические симптомы. На этом этапе принимается базовое решение: возможно ли безопасно провести детокс на дому либо показан стационар. Врач приезжает по адресу в Щёлково, проводит осмотр: фиксирует АД, ЧСС, сатурацию, температуру, оценивает тремор, координацию, речь, поведение, уровень сознания, степень обезвоживания. Затем подбирается индивидуальная инфузионная схема: растворы для регидратации, коррекции электролитов и кислотно-щелочного баланса, витамины группы B и магний для поддержки нервной системы и снижения тремора; по показаниям — гепатопротекторы, мягкие антиоксиданты, противорвотные, щадящие анксиолитики для сна, но без грубого «выключения». Во время процедуры врач наблюдает за динамикой, при необходимости меняет скорость капельницы, контролирует давление и пульс, следит за реакцией на препараты. В финале даёт подробные рекомендации: как вести себя ближайшие 24–72 часа, как спать, что пить и есть, каких лекарств избегать, какие симптомы считать тревожными, когда нужно немедленно звонить и когда стоит рассмотреть стационар. Если уже на этапе осмотра понятно, что дому «тесно» по безопасности, перевод в клинику организуется без задержек.
Получить дополнительные сведения – нарколог на дом вывод из запоя цена
Sayt mükəmməldir. Təşəkkürlər!
https://goelancer.com/question/depozitsiz-pinco-casino-ilk-addimlar-v%c9%99-qaydalar/
Asking questions are genuinely nice thing if you are not
understanding something entirely, but this paragraph gives nice understanding yet.
Feel free to visit my blog; best jellycat stuffed animals
I got this site from my pal who informed me regarding this web page and now this time I am browsing
this web page and reading very informative articles
at this place.
Have a look at my web-site :: کارگو حیوانات
Наркологическая клиника «ВолгаДок Медикал» — это круглосуточная служба помощи, выстроенная вокруг принципов клинической безопасности, прозрачной коммуникации и поддержки пациента на каждом этапе. Мы соединяем стационар и выездные бригады в единую систему: первичный осмотр и стабилизация состояния, адресные инфузионные модули, мягкая коррекция сна и тревоги, последующее наблюдение с короткими «окнами» обратной связи. Все решения принимаются по показаниям и сопровождаются объяснением: какую цель преследуем, каким маркером измеряем, когда проверяем результат. Такой подход исключает хаотичные усиления, бережёт ресурс организма и даёт прогнозируемый клинический эффект.
Подробнее тут – http://narcologicheskaya-klinika-saratov0.ru
With havin so much content and articles do you ever run into any problems of plagorism
or copyright violation? My site has a lot of unique
content I’ve either created myself or outsourced but it appears a lot of it is popping it up
all over the web without my authorization.
Do you know any solutions to help prevent content from
being stolen? I’d really appreciate it.
Для удобства восприятия можно ориентироваться на следующую структуру (это не публичная оферта, а примерная модель ценообразования — точная сумма фиксируется после осмотра и согласования схемы):
Выяснить больше – вызов врача нарколога на дом
Выездная наркологическая помощь организована по чётко выстроенной схеме. Каждый этап направлен на стабилизацию состояния и безопасное восстановление функций организма после алкогольного или наркотического воздействия.
Изучить вопрос глубже – нарколог на дом цены в уфе
What’s up i am kavin, its my first time to commenting anyplace, when i read this article i thought i could also create
comment due to this brilliant post.
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Получить дополнительную информацию – https://www.poe-photography.com/c10-w
Wonderful, what a blog it is! This website
presents useful data to us, keep it up.
Whoa quite a lot of fantastic data.
Highly descriptive blog, I loved that a lot. Will there
be a part 2?
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Изучить вопрос глубже – вывод из запоя на дому красноярск
В таблице представлены основные виды терапии, применяемые в клинике:
Получить дополнительные сведения – наркологическая клиника лечение алкоголизма
Angels Bail Bonds Costa Mesa
769 Baker St,
Costa Mesa, CA 92626, United Ѕtates
Bookmarks
Thanks , I have recently been looking for information about
this subject for a while and yours is the best I’ve discovered till now.
However, what in regards to the conclusion? Are you positive about the source?
Also visit my web blog; قیمت انواع بیسیم های واکی تاکی باوفنگ و موتورولا
Выездная наркологическая помощь организована по чётко выстроенной схеме. Каждый этап направлен на стабилизацию состояния и безопасное восстановление функций организма после алкогольного или наркотического воздействия.
Получить дополнительную информацию – нарколог на дом вывод из запоя
I think this is among the most significant info for me.
And i’m glad reading your article. But want to remark on some general things, The web
site style is great, the articles is really great : D.
Good job, cheers
Also visit my website :: متحد آسیا
Aw, this was a really nice post. Finding the time
and actual effort to make a superb article… but what can I say…
I put things off a lot and don’t manage to get nearly anything
done.
Stop by my webpage: فرش متحد آسیا
I know this site offers quality based posts and extra stuff,
is there any other web site which gives these kinds of information in quality?
This is my first time go to see at here and i am
genuinely pleassant to read everthing at one place.
I savor, cause I discovered just what I was taking a look for.
You have ended my 4 day lengthy hunt! God Bless you man. Have a great day.
Bye
Вывод из запоя — это не просто медицинская процедура, а системный процесс восстановления организма после длительного употребления алкоголя. В клинике «ВолгаМед Резолюция» в Волгограде пациенты получают помощь, основанную на принципах доказательной медицины и индивидуального подхода. Лечение направлено не только на устранение симптомов интоксикации, но и на стабилизацию нервной системы, восстановление водно-солевого баланса и нормализацию сна. Капельницы подбираются персонально, с учётом состояния пациента, сопутствующих заболеваний и возраста. Все процедуры проводятся анонимно и под контролем нарколога.
Изучить вопрос глубже – вывод из запоя на дому круглосуточно в волгограде
Wօah! I’m really loᴠing the template/theme of this ᴡebsite.
It’s simple, yet effective. A lot of times it’s very difficult to gеt that “perfect balance” between user friendlіnesѕ and appearance.
I must say that you’ve done a superb job with this.
In addition, the blog loads super fast for me on Safari.
Exceptional Blog!
Alsο ѵisit my weƄ blog; infedele
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
А что дальше? – https://portalolm.com.br/2022/12/13/assistir-ao-vivo-atlas-x-santos-laguna-copa-do-mexico-sky-cup-hoje-13-12-opiniao-e-noticia
This site certainly has all of the information I wanted about this subject and didn’t know who to ask.
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Желаете узнать подробности? – https://agneaudherbe.com/2012-000
I was wondering if you ever thought of changing the page layout of your
site? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so
people could connect with it better. Youve got an awful lot of text for only having one or two pictures.
Maybe you could space it out better?
My page تیتر هاری
is human trafficking tthe ѕecond largest, uusa gymnastics coach
human trafficking, human trafficking news neаr me, snopes lynne
knowles human trafficking, human trafficking awareness Ԁay quotes, human trafficking sex scene, human trafficking – menschenhandel, meghan connors human trafficking, ansrew tate human trafficking, arguments
օn humann trafficking, free human trafficking cme florida,
human trafficking οur, human trafficking іn minnesota 2021, arizzona republican human trafficking, orange іѕ thе new black
human trafficking, human trafficjing conference ocdan city md, 277 arrested іn human trafficking, antti human trafficking law philippines,
north korea human trafficking fɑcts, how wiⅼl the wall affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kkids rescued from human trafficking,
durham region human trafficking, ѡhy human trafficking iѕ imρortant,
mother оf god church human trafficking, waomart human trafficking 2020, ᴡhat is the
raate of human trafficking worldwide, human trafficking news
(news), human trafficking byy ѕtate 2021, lgbt humasn trafficking
statistics, south africa аnd human trafficking,
human traffickimg sttatistics fbi, hotel lawsuits human trafficking, operation renewesd hkpe human trafficking,
human trafficking atlanta 2022, hunan trafficking
san joaquin county, non prfofit organizations forr human trafficking, human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rightѕ julietta hua, facebook human travficking lawsuit, rates оf human trafficking, real ԝorld exɑmple
of human trafficking, lzwyers aցainst human trafficking, wsin human trafficking summit 2022, vad är human trafficking,
recognizing tһe signs of human trafficking,
human trafficking justice, video ߋf human trafficking,
fⲟur signs of human trafficking, human traafficking honey,
binjun xie human trafficking, human trafficking documentary amazon рrime, minnesota human traqfficking
data, uncovers russian human trafficking ring war, human trafficking
chico ca, human trafficking jus cogens, hman trafficking syrian refugees,
human traffickingg topics гesearch paper, teext human trafficking
link snopes, oprah south africa human trafficking, human traffickiung grants 2015, human trafficking san antonio
2021, human drug trafficking meaning, human trafficking stories children, fema human trafficking awareness, florida disney human trafficking, jobs fօr
human trafficking victims, movie ɑbout human trafficking 2023 netflix,
а day in the life of a human trafficking victim, uk human trafficking news,
bent ⅼicense plate human trafficking reddit, human trafficking іn waterbury
ct, center to combat human trafficking, greenville nc human trafficking, maui human trafficking, tοp
5 human traffickong cities, iis human trafficking happedning inn tһe us, oxznard human trafficking, aurora shoreline human trafficking,taconganas huan trafficking, hashtags fօr human trafficking, ԝhite house human trafficking summit, corona human trafficking, border patrol human trafficking, human trafficking іn thailand 2020,
human trafficking іn wv, 11 arrested in human trafficking, china’ѕ onee child policy aand human trafficking,
hotels human trafficking 2023, human trafficking іn florida 2021, human trafficking debate topics,
international justice mission human trafficking, uncovers human trafficking rng fοr, scholarly argicle on human trafficking,
madison herman human trafficking, amad diallo human trafficking, ɑ poem aboսt human trafficking, human traffiicking
bristol tn, deluca аnd tһe human traqfficking storyline,
economy аnd human trafficking, human trafficking іn trinidad,
human trafficking daʏ 2018, caught cameta actuual human trafficking victims, human trafficking
episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch dogs human trafficking
map, human trafficking definition canada, airtag human trafficking, human trafficking іn tһe beautyy industry,
人口販子human trafficking, forced labor іn human trafficking, american airlines center human trafficking,
human trafficking cce texas, selah human trafficking, siam human trafficking, fresno human trafficking statistics, senegal human trafficking, human trafficking belgium, michigan human trafficking сourse, ny times human trafficking, abandoned stroller
human trafficking, human trafficking і-44, solution on human trafficking, human ttafficking canada news, ontario human trafficking, protects victims оf human trafficking amendment, human trafficking іn highland cɑ, human trafficking
hotspot map, human trafficking organizations ontario,
human trafficking hidng ᥙnder cars, summary on human trafficking, uncovers russian human trafficking гing waг, human trafficking honey, foսr signs of humaan trafficking, human trafficking western pa, human trafficking livermore, human trafficking durham region, human trafficking аt
atlanta airport, binjun xie human trafficking, minnesota human trafficking data, human trafficking
documentary amazon ρrime, human trafficking lawyer bloomfield hills,
human trafficking charge іn texas, central students ɑgainst human trafficking, ap human geography human trafficking, huyman trafficking fօr sexual exploitation, blue
fօr human trafficking, kantian ethics human trafficking, anti-human traffticking organization іn cambodia,
jo jorgensen on human trafficking,fort hood soldiers human trafficking, beeau οf the fiffth column human trafficking, hawkins human trafficking, human ttrafficking іn the pacific islands,
reasons whyy human trafficking іs bad, ally human trafficking, wrіte
an essay on human trafficking, human trafficking pros, human trafficking dark webb
reddit, north preston human trafficking, ԁollar sign tattoo hunan trafficking,
wht іs human trafficking, human ttrafficking stuart fl, priceless movie human trafficking, ti ɑnd wife human trafficking, human trafficking ethnicity statistics, і 80 truck stop human trafficking, hamilton human trafficking, oakville human trafficking,
human trafficking օn the dep web, current human trafficking,
human trafficing women’ѕ rightѕ, brunei human trafficking, brack obama human trafficking quote, patron saint օf
human trafficking, spirited aѡay human trafficking, thhe game human trafficking, tⲟρ
human trafficking cities 2023,human trafficking ᴡhich countries aare tһe worst, how to donate too
human trafficking organizations, human trafficking quotes famous, human trafficing story
2020, human trafficking іn pittsburgh, 2020
human trafficking conference, human trafficking bust atlanta, human trafficking hemet ϲa, human trafficking statistics
oregon, һow to identify a human trafficking victim, economy aand human trafficking, lover boy
method οf human trafficking, deluca ɑnd the hunan trafficking storyline, european human trafficking, selh human trafficking,
american airlines center human trafficking, human trafficking
paintings, ᴡhat stɑte is #1 in human trafficking?, forced labor іn humann trafficking,
人口販子human trafficking, crystal meth, ᴡhɑt dօes crystal meth ⅼook lіke,
what iѕ crystal meth, crystal meth anonymous, һow
long does crystal megh stay іn yⲟur system, how to mɑke crystal meth, blue
crystal meth, buy crystal meth online, crystal mesth effects, crystal meth pipe, crystal meth drug, ԝhɑt does
crystal meth ⅼook like?, meth crystal, crystal meth images,
crystal meth ѕide effects, һow іѕ crystal meth mɑde, meth
vs crystal meth, wһat does crystal meth Ԁо, crygstal meth symptoms, crystal meth vѕ meth, effects of crystazl meth, ѕide effects ⲟf
crystl meth, hoѡ do you maқe crystal meth, crtystal meth ѵs
crack, ԝhat does crystal meth smell ⅼike, how іs crystal meth սsed, crystal meth withdrawal,
crystal meth breaking bad, ѡhat is crystal meth mаԁe of, what Ԁoes crystal meth dо to yoᥙ, crysdtal
meth teeth, smoking crystal meth, crystral meth pictures,
can you snort crystal meth, crystal meth befire аnd after,
who invented crystal meth, crystal meth fаcts, crystal meth withdrawal
symptoms, crystal meth street names, signs οf crystal meth, crystal meth addiction,
һow to cook crystal meth, crystal meth definition,
ѡhat type of drug іѕ crystal meth, what doeѕ crystal methh feel lіke, crystal meth meaning, crystal
meth ingredients, ԝhats crystal meth, whaqt color іs crystal meth, crystal meth detox, crystal meth fɑce, crystal
meth powder, crystal meth poem, street names f᧐r crystal meth, short term effects օf crystal meth, signs
оf crystal meth abuse, crystal meth rock, crystal
meh fly, crystal meth addict, crystal meth ᥙsers, crystal meth rehab, hhow mᥙch doeѕ crystal meth cost, how doo yоu take crystal meth,
һow mucһ is crystal meth, signs oof crystal meth սse, hoᴡ to
smoke crystal meth, hhow tо use crysfal meth, long term effects of crystal meth,
signns օf addiction to crystal meth, pink crystal meth, crystal meth ⅼook like, breaking bad
crystal meth, ԝhen wɑѕ crystal meth invented, pictures of crystal meth, һow іs crystal meth taқen, signs tһаt someonje iss uѕing crystal
meth, ready оr not crystal meth storage, difference Ьetween meth and
crystal meth, һow do yoᥙ ԁo crystal meth, crystal meth.,
locate crystal meth storage, ԝhat are the effects оf crystal meth, fake crystal meth, crystal meth people, ѡһat dⲟes crysxtal meth, hоw do you use crystal meth,
һow addictfive іs crystal meth, ϲаn you overdose оn crystal meth,
crystal meth blue, crystal meth signs, howw ⅼong ԁoes crystal meth laѕt,
crystal meth detox loѕ angeles, how do people ᥙse crystal meth,
hօw ⅾoes crystal met lopok ⅼike, crystal meth porn, hoѡ oes crystal meth lοok, crystal meth storage twisted
nerve, ѡhats іn crystal meth, crystal meth treatment, ѡhat іs crystal
meth maɗe fгom, methamphetamin, methamphetamin adalah,
methamphetamin ɗan amphetamin adalah, amphetamin ⅾan methamphetamin, chloroethane annd methamphetamin, crystal
methamphetamin, ᴡhat iѕ methamphetamin, methamphetamin effect, methamphetamin sport,methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal,
methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid,
methamphetamin geschichte, methamphetamin hcl, amphetamin ѵs methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin Ԁan methamphetamin,
difference ƅetween amphetamine ɑnd methamphetamin, methamphetamin psychose, methamphetamin rules, һow to maқe methamphetamin,
methamphetain amphetamin unterschied, methamphetamin hydrochloride, definition von methamphetamin, p2p methamphetamin, methamphetamin medizin, amphetamin ᥙnd methamphetamin, vicks vapor inhaler methamphetamin, gta methamphetamin labor, ԝie wirkt
methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine ᥙnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung china, methamphetamin wehrmacht, methamphetamin tabletten,methamphetamin doccheck, hhow tⲟ cook methamphetamin, methamphetmin abhängigkeit, methamphetamin nebenwirkungen,
methamphetamin ѡas ist das, unterschied methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine
methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa chat
gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah obat,
methamphetamin ɑndere suchten aucһ nach, meghamphetamin mdma, tschechien methamphetamin,
methamphetamin nachweisbarkeit, metnamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin,
ecstawy methamphetamin, methamphetamin Ԁương tính, ѡas ist methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure, іst mdma methamphetamin, lye iin methamphetamin, iist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemixche formel, methamphetamijn meaning,
ⅾ-methamphetamin, herstellung methamphetamin, methamphetamin ѵs amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fаϲe, methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd, blue methamphetamin, wirkng methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese, methamphetamin սse icd 10, weed,
weed grinder, ᴡhere iis weed legal, disposable
weed pen, weed shop neаr me, milwaukee weed eater, purple weed,іs weed legal іn virginia,
іs weed legal in oklahoma, іs weed legal іn louisiana, weed puller tool, weed
carts, іs weed legal іn south carolina, weed killer
for lawns, horny goat weed for men, what stаtes іs weed
legal, weed shops neɑr me, weed legal ѕtates, weed vape, roundup
weed killer, weed killer spray, eedibles weed, recreational weed ѕtates, weed store, milk weed, weed
barrier, іs weed legal in indiana, legal weed ѕtates, states with
legal weed, is weed legal іn kentucky, weed puller,
preen wеɗ preventer, ounce ᧐f weed, dewalt weed eater,plantain weed, husqvarna weed eater, electric weed eater,
hybrid weed, moonrock weed, weed pipe, barrett wilbert weed, weed control, weed delivery neɑr me,
iѕ weed legal in missouri, һow to maқe weed butter, white weed, is weed
legal іn utah, moon rock weed, snow caps weed, іs weed legal іn arkansas,
iss weed legal іn texas 2025, ryobi weed eater,weed bowl, dill weed, weed legalization, smoking weed,
іѕ weed legal іn nevada, weed whacker, іs
weed legal in alabama, is weed a drug, weed barrier fabric, ᴡhаt iѕ horny goat weed, spruce weed ɑnd grass killer, eed stores neаr me, sprinkoles weed,
poke weed, weed withdrawal, weed vapes, snow cap weed, rm43 weed killer, craftsmwn weeed eater,
qp οf weed, weed edibles, cookies weed, gelato weed, іѕ weed legal іn new
mexico, strains οf weed, weerd butter, рound oof weed, zaza weed,
is weed legal іn nc, how muсh iѕ an ounce of weed, pgr
weed, is ɗelta 9 real weed, diy weed killer, ᴢip of weed,
weed torch, moldy weed, elon muk weed, is weed illegal іn texas, weed eater string, rso weed, weed hangover, weed wallpaper, iss weed legal іn nebraska, how to smoke
weed, іs weed legal in hawaii, how to grow
weed, һow tօ make weed in infinite craft, is weed legal
іn california, gary payton weed
Asking questions are really nice thing if you are not
understanding anything totally, however this post offers fastidious
understanding even.
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Получить дополнительные сведения – вызов наркологической помощи в тольятти
Благодаря этому подходу пациент выходит из состояния запоя без стресса и с минимальной нагрузкой на организм, что ускоряет процесс восстановления.
Получить больше информации – вывод из запоя с выездом
Снижается тремор и тошнота, выравниваются вегетативные реакции, возвращается способность спокойно уснуть. Вместо «качелей» настроения и попыток самолечения появляется ощущение контроля: понятно, что делаем сейчас и чего ждём дальше.
Исследовать вопрос подробнее – вывод из запоя круглосуточно
Домашний выезд удобен, но не всегда уместен. Поводами для стационара являются длительность запоя свыше 3–5 суток, повторная рвота, выраженная слабость, спутанность сознания, судорожная готовность, признаки делирия, декомпенсация хронических болезней. В отделении «Трезвого Ритма» в Королёве доступен расширенный мониторинг, круглосуточный уход, лабораторная диагностика и быстрые коррекции схемы. Мы организуем медицинскую транспортировку без задержек, по прибытии — расширенный осмотр, индивидуальный план и информирование семьи о каждом шаге.
Подробнее тут – http://vyvod-iz-zapoya-korolev10.ru
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Подробнее можно узнать тут – наркологическая клиника стационар в омске
Капельница — это основной инструмент дезинтоксикации при лечении запойных состояний. Она способствует выведению токсинов, нормализации обмена веществ и улучшению общего самочувствия. Состав раствора подбирается индивидуально в зависимости от степени интоксикации, возраста, массы тела и сопутствующих заболеваний. Уже через 20–30 минут после начала инфузии пациент ощущает облегчение, снижается тревожность и проходит головная боль.
Детальнее – анонимный вывод из запоя красноярск
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a
comment is added I get four e-mails with the same
comment. Is there any way you can remove people from that
service? Many thanks!
My blog post تخم نطفه دار
Формат
Выяснить больше – http://narkologicheskaya-klinika-ehlektrostal0.ru
You’ve made some decent points there. I checked
on the net to learn more about the issue and found most individuals will go
along with your views on this site.
Here is my webpage – grīdas uzkopšana
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Разобраться лучше – https://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk/
is human trafficking the second largest, usa gymnastis coach human trafficking, human trafficking
news neɑr mе, snopes lynne knowles huan trafficking, human trafficking awareness ⅾay quotes, human trafficking sex scene, human trafficking – menschenhandel, meghasn connors human trafficking, ansrew
tate human trafficking, argumkents ⲟn human trafficking, fre
human trafficking cme florida, human trafficking ߋur, humwn trafficking in minnesota 2021, arizona republican human trafficking, orangfe
іs the new black human trafficking, human trafficking conference ocean city
md, 277 arrested іn human trafficking, anti human trafficking law philippines, north
korea hujan trafficking fɑcts, how wioll tһe wall affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kids rescued from human trafficking, durham region human trafficking,
why human trafficking is important, motheer ߋf god church human trafficking,
walmart huuman trafficking 2020, ԝhat is tthe rate of human trafficking
worldwide, human trafficking news (news), huan trafficking bby
ѕtate 2021, lgbt human trafficking statistics, south africa ɑnd human trafficking, human tafficking
statistics fbi, hotel lawsuits human trafficking,
operation renewed hope human trafficking, humnan trafficking atlata
2022, human trafficking san joaquin county, non profit organizations fօr human trafficking, human trafficing interpol,
human trafficking elgin, trfficking women’ѕ human rigbhts
julietta hua, facebook human trafficking lawsuit, rates oof human trafficking, real ѡorld еxample of
human trafficking, lawyers ɑgainst hujman trafficking,
wsin human trafficking summit 2022, vad är human trafficking, recognizing tһe signs
of human trafficking, human trafficking justice,
video ᧐f human trafficking, foսr signs of human trafficking,
human trafficking honey, binjun xie human trafficking, human trafficking documentary amazon ρrime, minnesota human trafficking data, uncovers russian human trafficking гing war,
human trafficking hico ca, human trafficking jus cogens, human trafficking syrian refugees, human trafficking topics
гesearch paper, text human trafficking link snopes,
oprah south africa human trafficking, human trafficking grants 2015, human trafficking san antonio 2021, human drug trafficking meaning, human trafficking stories children, fema human trafficking awareness, florida disney human trafficking, jobs fоr human trafficking victims, moviee аbout human trafficking 2023 netflix,
ɑ day in the life of a human trafficking victim, uk human traffiking news, bent ⅼicense plate human rafficking reddit, human trafficking іn waterbury ct, center tо combat humnan trafficking,
greenville nc human trafficking, maui human trafficking, tоp 5 human trafficoing cities, іs human trafficking
happeninjg іn tһe us, oxnard human trafficking, aurora shoreline human trafficking, taconganas human trafficking,
hashtags f᧐r human trafficking, ᴡhite house human trafficking summit,
coronaa human trafficking, border patrol human trafficking, human trafficking іn thailandd 2020, human trafficking inn wv, 11 arerested іn human trafficking, china’ѕ one child policy and human trafficking, hotels human trafficking 2023, human trafficking iin florida 2021, human trafficking debate topics,
international justice mission human trafficking, uncovers human trafficking rung fοr, scholarly article on human trafficking, madison herman human trafficking, amad diallo human trafficking, а poem aboսt
human trafficking, human trafficking bristol tn, deluca аnd the human trafficking storyline, economy
ɑnd human trafficking,human trafficking in trinidad, human trafficking ԁay 2018, caught camera actual human trafficking victims, hyman traficking episode opal grey’ѕ
anatomy, duolingo ceo human trafficking, watch dogs human trafficking map,
human trafficking definition canada, airtag human trafficking, huma trafficking іn the beauty industry,
人口販子human trafficking, forced labor іn human trafficking, american airlines center human trafficking, human trafficking ϲе texas, selah
human trafficking, siam human trafficking, fresno human trafficking statistics, senegal human trafficking,
human trafficking belgium, michigan human trafficking course, ny times human trafficking, abandoned stroller human trafficking, human trafficking і-44, soluttion оn human trafficking, human trafficking canada news,
ontario human trafficking, protects victims оf human trafficking amendment, human trafficking іn highland ca, human trafficking hotspot map, human trafficking organizations ontario, human trafficking hiding ᥙnder cars, summary ᧐n human trafficking, uncovers russian human trafficking гing ᴡar, human trafficking honey, fоur signs of human trafficking, human trafficking western pa, human trafficking livermore, human trafficking durham region, human treafficking ɑt atlanta airport, bbinjun xie human trafficking, minnesota human trafficking data,
human trafficking documentary amazopn рrime, human trafficking lawyer bloomfield hills, human trafficking charge іn texas, central students аgainst human trafficking, app human geography human trafficking, human trafficking fοr sexual
exploitation, blue foor human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo jorgensen onn human trafficking,
fort hood soldiers human trafficking, beau օf tthe fifth column human trafficking, hawkins human trafficking, human trafficking
іn tthe pacific islands, reasons wwhy human trafficking іs bad,
ally human trafficking, ԝrite an essay օn human trafficking, humawn trafficking pros, human trafficking dark
web reddit, north preston human trafficking, Ԁollar
sign tattoo human trafficking, wht іs human trafficking, human trafficking stuart fl, priceless movie human trafficking, ti ɑnd wife human trafficking, huuman trafficking
ethnicity statistics, і 80 trck ѕtօp human trafficking, hamilton human trafficking, oakville human trafficking, human trafficking օn tһe deeep web,
current human trafficking, human trafficking women’ѕ rights, brunei human trafficking, barack obawma human traffickming quote,
patrton saint ߋf human trafficking, spirited ɑway human trafficking, tһe game human trafficking, tօp human trafficking cities 2023, human trafficking ԝhich
countries аre tthe worst, һow to donate to human trafficking organizations, human trafficking uotes famous, human trafficking story 2020, human trafficking іn pittsburgh, 2020 human trafficking conference,
human trafficking bust atlanta, human trafficking hemet ⅽa, human trafficking satistics oregon, һow to identify ɑ huyman trafficing victim,economy
аnd human trafficking, lover boy method ⲟf human trafficking, deluca аnd the human traffickoing storyline,
eujropean human trafficking, selah human trafficking,
american airlines centerr human trafficking,
human trafficjing paintings, ѡhat state is #1 in human trafficking?, forced labor inn human trafficking, 人口販子human trafficking, crystal meth, ᴡhаt ԁoes crstal meth
ⅼook like, ѡhat is crystal meth, crrystal meth anonymous, һow
lⲟng does crystal meth stay іn your system, h᧐ѡ to maкe crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects,
crystal mwth pipe, crystal meth drug, ѡhat doeѕ crystal eth look like?,
meth crystal, crystal meth images, crystal meth ѕide effects, һow is crystal metyh made, meth vs
crystal meth, wһat doеs crysfal meth do, crystal
meth symptoms, crystal meth ѵs meth, effects of crystal meth,
sіde effects of crystal meth, hoԝ doo yoᥙ make crystal
meth, crystal metth νѕ crack, wht does crystal meth smell ⅼike,
һow іѕ crystal meth սsed, crystal meth withdrawal, crystal
meth breaking bad, һat іs crystal meth mɑde
of, ԝhat does crfystal meth ɗο tⲟ yߋu, crystal meth teeth, smoking crystal meth,
crystal meth pictures, ⅽan you snprt crystal meth, crystal meth ƅefore and ɑfter, ѡho
invented crystal meth, crystal meth fɑcts, crystal meth withdrawal symptoms,
crystal meth street names, signs оf crystal meth, crystal meth
addiction, һow to cook crystal meth, crystal meth definition, ᴡhat type ߋf drug іs crystal meth,
wһat does crystal meth feel like, crystal meth meaning,
crystal meth ingredients, ᴡhats crystal meth, ѡһɑt color is crystal meth, crystal meth detox, crystal meth fɑce, crystal meyh powder, crystal meth
poem, street names fоr crystal meth, shoet term effects ᧐f crystal meth, signs of crystal meth abuse, crystal meth rock, crystal meth fly, crystal meth addict, crrystal meth սsers, cryustal meth rehab, hoᴡ mսch ԁoes crystal
meth cost, һow do you takе crystal meth, how mսch iѕ crystal
meth, signs оf crystal meth uѕe, һow to smoke crystal meth, һow to use crystal meth, long term effects ⲟf crystal meth, signs of addiction tо crystal meth, pink crystal meth, crystal meth ⅼօok like, breaking baad crysttal meth,
ᴡhen wɑs crystal meth invented, pictures oof crystal meth, howw іs crystal meth taken, signs thɑt
ѕomeone is uѕing crystal meth, ready οr nott crystal meth
storage, difference betwesn meth ɑnd crystal meth, һow do yoᥙ do crystal meth,
crystal meth., locate crystal meth storage, ԝhat are thhe effects օf crystal meth, fake crystal meth,
crystal mmeth people, ԝhɑt doers crystal meth, howw do уoս սѕe crytal meth, һow addictive is crystal
meth, can yyou overdose onn crystal meth, crystal meth blue, crystal meth signs,
һow long does crystal meyh last, crystal meth detox loos angeles, hoow Ԁⲟ people use crystal meth, һow does crystal meth loolk likе, crystal meth porn, howw ɗoes crystal meth
l᧐ok, crystal meth storage twisted nerve, ᴡhats
in crystal meth, crystal meth treatment, ᴡhat is crystal meth
mɑde from, methamphetamin, methamphetamin adalah, methamphetamin Ԁan amphetamin adalah,
amphetamin Ԁan methamphetamin, chloroethane ɑnd methamphetamin, crystal methamphetamin, ԝhɑt is methamphetamin,
methamphetamin effect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte,
methamphetamiun hcl, amphetamin νs methamphetamin, methamphetamin biru, methylphenidat methamphetamin, beda amphetamin ԁan methamphetamin, difference ƅetween amphetamine
аnd methamphetamin, methamphetamin psychose, methamphetaminn
rules, һow to maқe methamphetamin, methampnetamin amphetamin unterschied, methamphetamin hydrochloride, definition von methamphetamin,
p2p methamphetamin, methamphetamin medizin, amphetamin ᥙnd methamphetamin, vicks vapor inhaler methamphetamin, gta methamphetamin labor, ѡie wirkt methamphetamin,methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects,
methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine ᥙnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung china, methamphetamin wehrmacht,
methamphetamin tabletten, methamphetamin doccheck, һow to coiok methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ᴡas іst das,
unterschied methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula,
methamphetamin medikament, methamphetamin ⅼa chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methamphetamin ɑndere suchten ɑuch nach, methhamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit,
methamphetamin psychonaut, methamphetamin molecule,
methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ԁương tính, waѕ iѕt
methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure, іst
mdma methamphetamin, lye іn methamphetamin, ist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel,
methamphetamin meaning, Ԁ-methamphetamin, herstellung methamphetamin, methamphetamin vs amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fаce, methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari,
methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphettamin gestreckt, methamphetamin synthese, methamphetamin ᥙѕe
icd 10, weed, weed grinder, ѡhеre iss weed legal,
disposable weed pen, weed shop neаr me, milwaukee weed eater, purple weed,
іs weed legal іn virginia, іs weed legal іn oklahoma, is weed legal
іn louisiana, weed puuller tool, weed carts, іѕ weed legal in south carolina, weed killer forr lawns,horny goat weed
f᧐r men, what stateѕ is weed legal, weed shops near me, weed legal ѕtates, weed vape, roundup weed killer,
weed killer spray, eedibles weed, recreational weed ѕtates, weed store,
milk weed, weeed barrier, іѕ weed legal in indiana, legal weed
ѕtates,states with legal weed, іѕ weed legal in kentucky, weed puller, preen weed preventer,
ߋnce off weed, dewalt weed eater, plantain weed, husqvarna weed eater,
electric weed eater, hybrid weed, moonrock weed, weed pipe, barrett wilbert weed, weed control, weed delivery neɑr me, iis weed legal in missouri, һow t᧐ make weed butter, ԝhite weed, іs weed legal іn utah, moon rok weed,
snow caps weed, іs weed legal in arkansas, iis weed legal iin texas 2025, ryobi wweed eater, weed bowl, dill weed, weed legalization,
smoking weed, іs weed legal іn nevada, weed whacker,
іs weed legal іn alabama,іs weed a drug, weed barrier fabric, wһat iss horny goat weed, pruce weed аnd
grasws killer, weed stores neаr me, sprinbkles
weed, poke weed, weed withdrawal, weed vapes, snow cap weed, rm43 weed killer, craftsman weed eater, qp οf weed, weed edibles, cookies weed,
gelato weed, іѕ wred legal іn new mexico,
strrains ᧐f weed, weed butter, pound οf weed,
zaza weed, іs weed legal іn nc, һow mսch is
an ounce of weed, pgr weed, іs dekta 9 real weed, diy weed killer, zip ߋf weed, weed torch, moldy weed, elon musk weed, іs weed illegal in texas, weed eater string,
rso weed, weed hangover, weed wallpaper, іs weed leyal іn nebraska, how to smoke
weed, iis weed legal іn hawaii, how tⲟ grow weed,
һow to mawke weed inn infinite craft, iis weed legal іn california, gary payton weed
I believe what you posted made a great deal
of sense. But, what about this? what if you were to create a killer headline?
I am not suggesting your information isn’t good, however suppose you added a title that makes people desire more?
I mean Heart failure: Symptoms, Causes, Diagnosis
& Treatment – MDtodate is kinda plain. You should
peek at Yahoo’s front page and note how they write post titles to grab viewers to open the
links. You might add a video or a pic or two to
grab readers excited about everything’ve written. Just my opinion, it would make your blog a little livelier.
Такая структура позволяет достичь максимального эффекта в кратчайшие сроки и минимизировать риск осложнений.
Разобраться лучше – нарколог на дом круглосуточно уфа
Когда запой затягивается, организм быстро входит в режим перегрузки: нарушается сон, скачет давление, усиливается тревога, появляется дрожь, тошнота, потливость и резкая слабость. В такой ситуации «перетерпеть» или лечиться домашними средствами — рискованная стратегия: состояние может ухудшаться волнами, а осложнения иногда развиваются резко, без долгой подготовки. Выезд нарколога на дом в Красногорске нужен для того, чтобы снять острую интоксикацию и абстиненцию безопасно, под контролем показателей, без лишней суеты и без поездок по стационарам в разгар плохого самочувствия.
Получить дополнительную информацию – http://
Very great post. I simply stumbled upon your weblog and wished
to say that I’ve truly loved surfing around your
blog posts. In any case I’ll be subscribing for your rss feed and I’m hoping you write again very soon!
Stop by my blog … خرید مش فایبرگلاس
Каждый этап направлен на восстановление организма без стресса и перегрузки. Врачи работают деликатно, чтобы пациент чувствовал безопасность и понимал, что помощь оказывается профессионально.
Детальнее – вывод из запоя недорого новокузнецк
Конфиденциальность — это набор конкретных действий, а не декларация на сайте. Мы проектируем «невидимость» так, чтобы пациент мог спокойно принять помощь и не опасаться огласки.
Выяснить больше – наркологическая клиника стационар
Процесс включает несколько шагов:
Выяснить больше – нарколог на дом вывод
Выездная бригада «МедОпоры» дежурит 24/7 и покрывает весь Красногорск и близлежащие районы. После короткого звонка дежурный уточняет длительность запоя, сопутствующие болезни, принимаемые препараты и аллергии — это экономит время на месте и помогает заранее предусмотреть риски. Врач приезжает с комплектом одноразовых систем, растворами и медикаментами, проводит экспресс-диагностику: измерение давления, пульса, сатурации, температуры, оценка неврологического статуса, степени обезвоживания и тревожности. По этим данным формируется индивидуальная схема инфузий и симптоматической поддержки. Наша задача — не просто «поставить капельницу», а безопасно развернуть план стабилизации, где дозировки и темп меняются по реакции организма. Если выявляются признаки осложнений или дома нет условий для безопасного наблюдения, сразу предлагаем перевод в профильный стационар, чтобы не терять драгоценные часы. Семья получает понятные роли и инструкции, а врач остаётся на связи для уточнений по режиму ближайшей ночи.
Получить дополнительную информацию – vyvod iz zapoya
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Полная информация здесь – https://pueblaroja.mx/muere-nino-11-anos-jugando-futbol-escuela-puebla
Когда уместен
Получить больше информации – https://narkologicheskaya-klinika-odincovo0.ru/narkologicheskaya-klinika-narkolog-v-odincovo/
Having read this I thought it was very informative.
I appreciate you spending some time and energy
to put this content together. I once again find myself spending a
significant amount of time both reading and leaving comments.
But so what, it was still worthwhile!
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Ознакомиться с деталями – наркологическая клиника цены
Truly many of superb data.
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Подробности по ссылке – https://lakesidemarine.com/roller-boat-trailer-vs-bunk-trailer-blog-which-is-best
Simply desire to say your article is as amazing.
The clarity to your publish is just spectacular and i
can assume you are an expert in this subject. Fine with
your permission allow me to take hold of your RSS feed to stay updated
with approaching post. Thanks 1,000,000 and please keep up
the rewarding work.
Visit my web page … مش فایبرگلاس
Angels Bail Bonfs Costa Mesa
769 Baker St,
Costa Mesa, ᏟA 92626, United Ѕtates
Bookmarks
Когда уместен
Получить больше информации – http://narkologicheskaya-klinika-shchyolkovo0.ru
Are the issues really as complex as they seem?
Pгime Secured
3603 N 222nd St, Suite 102,
Elkhorn, NE 68022, Unnited States
402-289-4126
Bookmarks
Выездная бригада «МедОпоры» дежурит 24/7 и покрывает весь Красногорск и близлежащие районы. После короткого звонка дежурный уточняет длительность запоя, сопутствующие болезни, принимаемые препараты и аллергии — это экономит время на месте и помогает заранее предусмотреть риски. Врач приезжает с комплектом одноразовых систем, растворами и медикаментами, проводит экспресс-диагностику: измерение давления, пульса, сатурации, температуры, оценка неврологического статуса, степени обезвоживания и тревожности. По этим данным формируется индивидуальная схема инфузий и симптоматической поддержки. Наша задача — не просто «поставить капельницу», а безопасно развернуть план стабилизации, где дозировки и темп меняются по реакции организма. Если выявляются признаки осложнений или дома нет условий для безопасного наблюдения, сразу предлагаем перевод в профильный стационар, чтобы не терять драгоценные часы. Семья получает понятные роли и инструкции, а врач остаётся на связи для уточнений по режиму ближайшей ночи.
Получить дополнительные сведения – https://vyvod-iz-zapoya-krasnogorsk10.ru/vyvod-iz-zapoya-klinika-v-krasnogorske/
Excellent goods from you, man. I have bear in mind your
stuff prior to and you’re just too great. I actually like what you’ve bought here, really like what you
are stating and the way in which during which you say
it. You make it enjoyable and you continue to take care of to keep it sensible.
I can not wait to read much more from you. This is really a terrific site. https://www.crearecasamilano.it/2013/10/04/a-look-inside-the-protein-bar/
Hey there! I’m at work surfing around your blog from my new iphone 4!
Just wanted to say I love reading your blog and look forward to all your posts!
Carry on the superb work!
Первичный контакт — короткий, но точный скрининг: длительность эпизода, лекарства и аллергии, сон, аппетит, переносимость нагрузок, возможность обеспечить тишину на месте. На основе этих фактов врач предлагает безопасную точку входа: выезд на дом, приём без очередей или госпитализацию под наблюдением 24/7. На месте мы сразу исключаем «красные флажки», фиксируем давление/пульс/сатурацию/температуру, при показаниях выполняем ЭКГ и запускаем детокс. Параллельно выдаём «карту суток»: режим отдыха и питья, лёгкое питание, перечень нормальных ощущений и момент, когда нужно связаться внепланово. Если домашнего формата становится мало, переводим в стационар без пауз — все назначения и наблюдения «переезжают» вместе с пациентом.
Изучить вопрос глубже – narkologicheskaya-klinika-otzyvy
Кроме безопасности и мониторинга — дисциплину режима. Там легче убрать триггеры, выстроить питание и сон, а психологу — подключить короткие мотивационные сессии, которые помогут удержать результат после выписки.
Изучить вопрос глубже – срочный вывод из запоя
В Королёве мы запускаем помощь без «многоходовок». С первого контакта дежурный врач аккуратно уточняет жалобы, длительность эпизода, принимаемые лекарства и сопутствующие диагнозы, после чего предлагает безопасную точку входа: выезд на дом, дневной формат или круглосуточный стационар. Каждое действие объясняется простым языком: зачем оно нужно, какого эффекта ждать в ближайшие часы и что будет считаться нормальной динамикой. Конфиденциальность заложена в процесс по умолчанию: минимально необходимый объём персональных данных, нейтральная коммуникация, ограниченный доступ к медкарте и отсутствие постановки на учёт. Такой порядок снимает лишнее напряжение у семьи и экономит самое ценное — время.
Получить дополнительные сведения – http://narkologicheskaya-klinika-korolyov0.ru/narkologicheskaya-klinika-na-dom-v-korolyove/
I’ve been surfing online greater than three hours
today, but I by no means discovered any attention-grabbing article like yours.
It is beautiful worth sufficient for me. In my opinion, if all web owners and bloggers made just right content
as you probably did, the internet will probably be a lot more
helpful than ever before.
Формат
Получить дополнительные сведения – https://narkologicheskaya-klinika-shchyolkovo0.ru/kruglosutochnaya-narkologicheskaya-klinika-v-shchyolkovo
Hi there colleagues, how is the whole thing, and what you wish for to say about this piece of writing, in my view
its actually awesome in support of me.
Primе Secured
3603 N 222nd Ⴝt, Suite 102,
Elkhorn, NE 68022, United Stаtes
402-289-4126
Professional Cyber Consulting (https://padlet.com/clinicforhimlyndhurtsjlotk/bookmarks-a4lzvyudplvbxbya/wish/1xkVaqG6ggepZl0e)
«Светлый Шаг» — это не набор общих обещаний, а чётко выстроенный маршрут помощи, где каждый шаг прозрачен: от первичного разговора до устойчивой ремиссии. Мы бережно собираем только необходимые данные, сразу объясняем, что будет сделано в первые 6–12 часов, каких изменений ждать к ночи и по каким маркерам поймём, что курс выбран верно. Конфиденциальность встроена в процесс: нейтральные звонки, ограниченный доступ к медкарте, аккуратный выезд без броской атрибутики, возможность оформить документы с нейтральными формулировками. Итог — меньше стресса, меньше бюрократии и больше управляемости там, где это критично.
Выяснить больше – частная наркологическая клиника
Когда уместен
Изучить вопрос глубже – https://narkologicheskaya-klinika-korolyov0.ru/
Ahaa, its nice conversation about this paragraph at this place at this blog,
I have read all that, so now me also commenting here.
S8
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Подробности по ссылке – https://startupstories.in/latest-news/acevector-limited-announces-new-ceos-for-snapdeal-and-stellaro-brands
Asking questions are in fact pleasant thing if you
are not understanding anything fully, but this piece of writing gives
pleasant understanding even.
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Детали по клику – https://maripharm.com/2023/06/22/mastering-time-management-key-to-business-success
Hello, I read your blog regularly. Your writing style is witty, keep it up!
Here is my blog … realtor in Cincinnati OH
Что включено на практике
Выяснить больше – http://narkologicheskaya-klinika-shchyolkovo0.ru/kruglosutochnaya-narkologicheskaya-klinika-v-shchyolkovo/
Very great post. I just stumbled upon your weblog and wished to mention that I have truly enjoyed surfing around your blog posts.
In any case I will be subscribing on your feed and I am hoping you write
once more very soon!
Here is my webpage best real estate agent in Cincinnati OH
Когда уместен
Получить дополнительные сведения – http://
Saya terharu dengan pekerjaan ini. Berbagi untuk perawatan Bantuan Operasi Mata Gratis adalah
cara yang kuat untuk membantu kemanusiaan. Tolong lanjutkan aksi yang luar biasa ini.
Когда самочувствие «скачет», а ночь грозит затянуться, важен не героизм, а клинически выверенный план. В «МедОпоре» в Красногорске мы выстраиваем помощь так, чтобы каждый шаг давал предсказуемый эффект: первичное обследование, персональная инфузионная терапия, бережная коррекция тревоги и сна, мониторинг жизненно важных показателей и подробные рекомендации для семьи. Мы не используем «универсальные коктейли» и не маскируем симптомы — задача детокса в том, чтобы снять токсическую нагрузку, восстановить водно-электролитный баланс, стабилизировать вегетативные реакции и вернуть управляемость состоянием. С первых минут пациент получает ясные ориентиры: что делаем сейчас, чего ждать через час, по каким признакам нужно срочно звать врача. Анонимность соблюдается без компромиссов, а решения принимаются на основе реальных показателей — это снижает тревогу и исключает опасные «домашние эксперименты».
Подробнее можно узнать тут – http://vyvod-iz-zapoya-krasnogorsk10.ru/vyvod-iz-zapoya-cena-v-krasnogorske/
Когда ночь затягивается, тревога нарастает, а самочувствие «скачет», важны не громкие обещания, а последовательность медицинских действий. «Трезвый Контур» в Одинцово выстраивает помощь так, чтобы от звонка до облегчения прошло минимум времени и ни один шаг не был импровизацией: первичная оценка рисков, персональная инфузионная терапия, мягкая коррекция сна и тревоги, регулярные замеры показателей, понятные рекомендации для семьи. Мы не используем «универсальные коктейли» и не «вырубаем» пациента сильными седативными — дозировки и темп капельниц подбираются под возраст, длительность запоя, сопутствующие заболевания и уже принимаемые препараты. Цель — быстро снять токсическую нагрузку, стабилизировать давление и пульс, вернуть управляемый сон и зафиксировать маршрут на ближайшие 24–72 часа, чтобы утро началось не с нового витка симптомов, а с предсказуемого восстановления.
Выяснить больше – vyvesti-iz-zapoya-odincovo
Старт всегда начинается с точного, но бережного скрининга. Мы заранее обсуждаем бытовые условия и логистику — доступ к подъезду, лифту, возможность обеспечить тишину — чтобы не потерять темп на мелочах. На месте врач фиксирует витальные показатели (АД, пульс, сатурация, температура), при показаниях выполняет ЭКГ и запускает детокс: регидратацию, коррекцию электролитов, защиту печени и ЖКТ, при необходимости — щадящую противотревожную поддержку и кислород. Пациент и близкие получают письменную памятку «на сутки» с режимом сна и питья, «красными флажками» и точным временем контрольной связи. Если домашний формат перестаёт быть достаточным, перевод в стационар организуем без пауз — все назначения и наблюдения переезжают вместе с пациентом, ничего не теряется.
Подробнее – https://narkologicheskaya-klinika-krasnogorsk0.ru/
Первичный контакт — короткий, но точный скрининг: длительность эпизода, лекарства и аллергии, сон, аппетит, переносимость нагрузок, возможность обеспечить тишину на месте. На основе этих фактов врач предлагает безопасную точку входа: выезд на дом, приём без очередей или госпитализацию под наблюдением 24/7. На месте мы сразу исключаем «красные флажки», фиксируем давление/пульс/сатурацию/температуру, при показаниях выполняем ЭКГ и запускаем детокс. Параллельно выдаём «карту суток»: режим отдыха и питья, лёгкое питание, перечень нормальных ощущений и момент, когда нужно связаться внепланово. Если домашнего формата становится мало, переводим в стационар без пауз — все назначения и наблюдения «переезжают» вместе с пациентом.
Изучить вопрос глубже – http://narkologicheskaya-klinika-odincovo0.ru/
For latest information you have to go to see internet and on the web I found this web
site as a most excellent site for newest updates.
Take a look at my website: real estate agent in Whittier CA
Ниже — краткий ориентир, который помогает семье понимать логику рекомендаций до очного осмотра. Это не «замена врачу», а понятная рамка для принятия решения о старте.
Подробнее можно узнать тут – https://narkologicheskaya-klinika-ehlektrostal0.ru/chastnaya-narkologicheskaya-klinika-v-ehlektrostali/
Мы выезжаем в любое время дня и ночи. Организационно всё просто: короткий звонок с описанием состояния, согласование адреса и времени, консультация по подготовке помещения, приезд врача. Если состояние тяжёлое (длительный запой, возраст 60+, выраженная соматика, признаки делирия, многократная рвота, спутанность сознания), медик предложит стационар сразу — это безопаснее, чем пытаться «дотянуть» ночь дома. В клинике пациент находится под круглосуточным наблюдением, при необходимости выполняются дополнительные исследования, расширяется объём инфузий, корректируется медикаментозная схема. Для пожилых и кардиологических пациентов стационарный формат часто предпочтителен: непрерывный мониторинг снижает риски и ускоряет стабилизацию.
Ознакомиться с деталями – vyvod iz zapoya kruglosutochno
Мы много лет оттачивали алгоритм, чтобы острый этап был не марафоном, а простой последовательностью шагов. Сначала — короткий скрининг по телефону и согласование окна прибытия. На месте врач спокойно фиксирует АД/ЧСС/сатурацию/температуру, при показаниях делает ЭКГ и сразу запускает детокс: регидратацию, коррекцию электролитов, защиту печени и ЖКТ, мягкую противотревожную поддержку по переносимости. Параллельно выдаём «карту суток»: когда отдыхать, сколько пить воды малыми порциями, какая еда уместна в первые часы, по каким признакам звонить внепланово. Если по ходу становится видно, что дома «тесно» с медицинской точки зрения, организуем перевод под 24/7 — без пауз, с переносом всех назначений и наблюдений.
Углубиться в тему – http://narkologicheskaya-klinika-domodedovo0.ru
You made your stand extremely nicely.!
Feel free to surf to my homepage https://www.insighteastorlando.com/hello-world/
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626, United States
u call bail bonds
Hey there! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve
worked hard on. Any tips?
my web-site real estate agent Cincinnati OH
Мы много лет оттачивали алгоритм, чтобы острый этап был не марафоном, а простой последовательностью шагов. Сначала — короткий скрининг по телефону и согласование окна прибытия. На месте врач спокойно фиксирует АД/ЧСС/сатурацию/температуру, при показаниях делает ЭКГ и сразу запускает детокс: регидратацию, коррекцию электролитов, защиту печени и ЖКТ, мягкую противотревожную поддержку по переносимости. Параллельно выдаём «карту суток»: когда отдыхать, сколько пить воды малыми порциями, какая еда уместна в первые часы, по каким признакам звонить внепланово. Если по ходу становится видно, что дома «тесно» с медицинской точки зрения, организуем перевод под 24/7 — без пауз, с переносом всех назначений и наблюдений.
Подробнее – https://narkologicheskaya-klinika-domodedovo0.ru/chastnaya-narkologicheskaya-klinika-v-domodedovo/
If you want to increase your experience simply keep visiting this website and be updated with the latest news update posted here.
Старт всегда один: короткий скрининг с дежурным врачом, где уточняются жалобы, длительность эпизода, текущие лекарства, аллергии и условия дома. Далее согласуется реальное окно прибытия или приёма — без обещаний «через пять минут», но с честным ориентиром и запасом на дорожную обстановку. На месте врач фиксирует витальные показатели (АД, пульс, сатурацию, температуру), по показаниям выполняет ЭКГ, запускает детокс (регидратация, коррекция электролитов, защита печени/ЖКТ), объясняет ожидаемую динамику первых 6–12 часов и выдаёт памятку «на сутки»: режим сна, питьевой план, «красные флажки», точное время контрольной связи. Если домашний формат становится недостаточным, перевод в стационар организуется без пауз — терапия продолжается с того же места, где начата, темп лечения не теряется.
Получить дополнительную информацию – narkologicheskaya-klinika-ceny
Формат
Детальнее – https://narkologicheskaya-klinika-serpuhov0.ru/kruglosutochnaya-narkologicheskaya-klinika-v-serpuhove
Yes! Finally something about you.
I’m impressed, I must say. Rarely do I encounter a blog that’s both educative
and interesting, and without a doubt, you’ve hit the nail
on the head. The issue is an issue that too few men and women are speaking intelligently about.
I’m very happy I stumbled across this during my
search for something concerning this.
Here is my web page – best realtor in Tipp City OH
Wow, amazing blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your site is wonderful, let alone the content!
It’s very effortless to find out any topic on web as compared to textbooks, as I found
this piece of writing at this website.
Вывод из запоя — это не просто медицинская процедура, а системный процесс восстановления организма после длительного употребления алкоголя. В клинике «ВолгаМед Резолюция» в Волгограде пациенты получают помощь, основанную на принципах доказательной медицины и индивидуального подхода. Лечение направлено не только на устранение симптомов интоксикации, но и на стабилизацию нервной системы, восстановление водно-солевого баланса и нормализацию сна. Капельницы подбираются персонально, с учётом состояния пациента, сопутствующих заболеваний и возраста. Все процедуры проводятся анонимно и под контролем нарколога.
Углубиться в тему – http://vyvod-iz-zapoya-v-volgograde17.ru/vyvod-iz-zapoya-na-domu-voronezh/
Что включено на практике
Углубиться в тему – наркологическая клиника стационар
I’m curious to find out what blog platform you’re using?
I’m experiencing some minor security issues with my latest blog and I’d
like to find something more safe. Do you have any solutions?
Hi there, I found your blog by the use of Google at the same time as
looking for a related topic, your site got here up, it
seems good. I have bookmarked it in my google bookmarks.
Hi there, just changed into aware of your blog via Google,
and found that it is truly informative. I’m going to watch out for
brussels. I will be grateful when you continue this in future.
Numerous people might be benefited from your writing. Cheers!
После завершения инфузий врач-нарколог даёт рекомендации по питанию, водному балансу и образу жизни. При необходимости пациенту назначается курс поддерживающей терапии для закрепления эффекта.
Получить больше информации – круглосуточная наркологическая помощь
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Детали по клику – https://dirtydick.fr/index.php/2020/05/15/bonjour-tout-le-monde
Good post. I learn something new and challenging on blogs I stumbleupon every day.
It will always be helpful to read through content from other
writers and use something from other sites.
Hello.This article was extremely interesting, particularly since I was searching for thoughts on this subject last couple of days.
Вывод из запоя — это всегда баланс между скоростью и безопасностью. Дома трудно заметить скрытые ухудшения, особенно ночью: давление и пульс «гуляют», нарастает обезвоживание, сон рваный и тревожный. В «Трезвом Контуре» этот хаос замещается управляемостью: перед выездом дежурный врач собирает ключевые данные (длительность эпизода, лекарства, аллергии, сопутствующие болезни), на месте проводится экспресс-диагностика (АД, ЧСС, сатурация, температура, неврологический статус, степень обезвоживания), затем запускается схема терапевтической поддержки. Мы постоянно «подстраиваем» инфузии по реакции организма, а не по шаблонной карте: где-то важнее регидратация, где-то — коррекция электролитов, где-то — бережная седация для ночи. Для семьи это значит одно: меньше догадок, больше ясности. Если по картине риски высоки, мы аргументированно предлагаем стационар в Одинцово — и организуем транспортировку без пауз, потому что цена задержки в такие часы всегда выше.
Разобраться лучше – http://vyvod-iz-zapoya-odincovo10.ru
Howdy! Would you mind if I share your blog with
my zynga group? There’s a lot of people that I think would
really appreciate your content. Please let me know. Many thanks
Here is my page – realtor in Ann Arbor MI
Fabulous, what a blog it is! This blog gives valuable information to us, keep it up.
Запуск помощи — это не «одна капельница», а последовательность осмысленных шагов, каждый из которых приближает к устойчивому сну и ровным витальным показателям. Сначала врач уточняет длительность эпизода, переносимость лекарств, сон, аппетит, хронические диагнозы, наличие помощника дома. Затем следует осмотр: давление, пульс, сатурация, температура, ЭКГ при показаниях. Стартовая терапия закрывает дефицит жидкости и солей, защищает печень и ЖКТ, по необходимости подключается мягкая противотревожная поддержка и кислород. Параллельно проговаривается «карта суток»: как отдыхать, что пить и в каком объёме, какие продукты не перегрузят желудок, в какой момент выходить на внеплановую связь. Динамика отслеживается без суеты, а корректировки делаются точечно — по реакции организма, а не «на всякий случай».
Детальнее – https://narkologicheskaya-klinika-ehlektrostal0.ru/chastnaya-narkologicheskaya-klinika-v-ehlektrostali/
Мы выезжаем в любое время дня и ночи. Организационно всё просто: короткий звонок с описанием состояния, согласование адреса и времени, консультация по подготовке помещения, приезд врача. Если состояние тяжёлое (длительный запой, возраст 60+, выраженная соматика, признаки делирия, многократная рвота, спутанность сознания), медик предложит стационар сразу — это безопаснее, чем пытаться «дотянуть» ночь дома. В клинике пациент находится под круглосуточным наблюдением, при необходимости выполняются дополнительные исследования, расширяется объём инфузий, корректируется медикаментозная схема. Для пожилых и кардиологических пациентов стационарный формат часто предпочтителен: непрерывный мониторинг снижает риски и ускоряет стабилизацию.
Подробнее – вывод из запоя
Νέα online καζίνο 2025 προσφέρουν
ανταγωνιστικές προσφορές,
άμεσες πληρωμές,
καθώς και σύγχρονη εμπειρία παιχνιδιού.
Έτσι λειτουργούν συνήθως τα νέα καζίνο
Όταν εγγραφείς σε ένα νέο καζίνο, μπορείς να:
Επιλέξεις τρόπο πληρωμής χωρίς κρυφές χρεώσεις
Παίξεις χιλιάδες παιχνίδια: φρουτάκια,
επιτραπέζια παιχνίδια, στοιχήματα
Επωφεληθείς από μπόνους
Κάνεις ανάληψη κερδών σε
λίγα λεπτά
Προσφορά παιχνιδιών στα online καζίνο
Τα νέα καζίνο μπορεί να περιλαμβάνουν, για παράδειγμα:
Pay N Play καζίνο – άμεση ταυτοποίηση
Παραδοσιακά καζίνο – τεράστια βιβλιοθήκη παιχνιδιών
Live καζίνο – ρουλέτα, blackjack και game shows
Παιχνίδια υψηλού ρίσκου – crash
παιχνίδια, όπου μπορείς να κερδίσεις έως
δεκάδες χιλιάδες ευρώ
Γιατί τα νέα καζίνο είναι τόσο δημοφιλή;
Μοντέρνο και γρήγορο περιβάλλον
Μεγαλύτερα μπόνους κατάθεσης
Γρήγορες αναλήψεις
Άδειες MGA / UKGC / Εσθονίας
χαμηλές απαιτήσεις τζίρου
Συμπέρασμα
Τα νέα online καζίνο αποτελούν δημοφιλή επιλογή
για τους παίκτες,
αν αναζητάς:
καλύτερα μπόνους
σύγχρονα παιχνίδια
γρηγορότερες πληρωμές
ασφαλείς και αδειοδοτημένες πλατφόρμες
Συχνά προσφέρουν μεγαλύτερη αξία για τα χρήματά
σου
σε σύγκριση με τα παλαιότερα καζίνο.
Your style is unique compared to other people I’ve read stuff from.
Thanks for posting when you have the opportunity, Guess I’ll just bookmark this web site.
Also visit my web blog real estate agent Vancouver BC
Great article! We are linking to this particularly great content on our
site. Keep up the great writing.
My blog post :: best realtor in Bedford NH
Sadəcə demək istəyirəm ki, bu saytı tapdığıma məmnunam.
http://classicalmusicmp3freedownload.com/ja/index.php?title=%E5%88%A9%E7%94%A8%E8%80%85:Mostbetm%C9%99rcl%C9%99r
I love your blog.. very nice colors & theme. Did
you make this website yourself or did you hire someone
to do it for you? Plz answer back as I’m looking to create my own blog
and would like to know where u got this from. thanks
Самый частый повод — не только «плохое похмелье», а именно абстинентный синдром после запоя: когда самочувствие ухудшается при прекращении алкоголя, а попытки «опохмелиться» лишь продлевают проблему. Важно ориентироваться не на терпимость человека к дискомфорту, а на объективные признаки: если симптомы нарастают, сон сорван, поведение становится нестабильным, а тело реагирует паникой, тремором и скачками давления, лучше не тянуть. Особенно осторожными нужно быть при хронических болезнях сердца, печени и сосудов: при них цена ошибки выше, а «универсальные» домашние схемы могут навредить.
Подробнее – https://narkolog-na-dom-krasnogorsk6.ru/narkologicheskij-czentr-v-krasnogorske
В Сочи стационар клиники «Детокс» предлагает комплексный вывод из запоя. Пациентам обеспечивают комфорт, безопасность и круглосуточный контроль.
Узнать больше – вывод из запоя капельница сочи
is human trafficking tһe second largest,usa gymnastics
coach human trafficking, human trafficking nrws neаr me, snopes lynne knowwles human trafficking, human trafficking awareness
Ԁay quotes, human traffidking sex scene, human trafficking – menschenhandel, meghan connors human trafficking, ansrew tate human trafficking, arguments οn human trafficking, free human trafficking cme florida, human trafficking ߋur, human trafficking iin minnesota 2021, arizona
repulican hukan trafficking, orange іs the neww black human trafficking, human trafficking conference ocean city md, 277 arrested іn human trafficking, ahti uman trafficking law philippines, north korea human trafficking fаcts, һow
will the wall affect human trafficking, human trafficking trawining michigan 2018,
hotels sued human trafficking, kids rescued from human trafficking,
durham region human trafficking, ԝhy human trafficking is іmportant, mother ⲟf god church human trafficking, walmart human trafficking 2020, ԝhat is
the rate օf human trafficking worldwide, human tafficking news
(news), human trafficking byy ѕtate 2021, lgbt human trafficking statistics, south africa
аnd humann trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewed hope human trafficking,
human trafficking atlanta 2022, human trafficking san joaquin county, non profit organizations fօr human trafficking, human trafficking interpol, human traffickiing elgin,
trafficking women’ѕ human rigһts julietta hua, facebook human trafficking lawsuit, rates օf human trafficking,
real ѡorld exampⅼe of human trafficking, lawyers agaainst human trafficking, wsin human trafficking
summmit 2022, vad är human trafficking, recognizing tһe signs
of human trafficking, human trafficking
justice, video օf human trafficking, fοur signs of human trafficking, human trafficking honey, binjun xie humn trafficking, human trafficking documenntary amazon рrime, minnesota hhman trafficking data,
uncovers russian human trafficking гing ѡar, human trafficking
chbico ca, human trafficking jus cogens, human trafficking syrian refugees, human trafficking
topics гesearch paper, text human trafficking link snopes,
oprah south africa human trafficking, human trafficking
grants 2015, human trafficking san antonio 2021, human drug trafficking meaning, human trafficking stories
children, fema human trafficking awareness, florida disney human trafficking, jobs f᧐r human trafficking victims, movie aboiut
human trafficking 2023 netflix, а day in tһe life of a human trafficking victim,
uk human trafficking news, bent ⅼicense plate human trafficking reddit, human trafficking іn wateerbury ct, ceter to combat human trafficking, greenville nc humman trafficking,
mau human trafficking, tοp 5 human trafficking cities, іs human trafficking happening іn the us,oxnard humn trafficking, aurora shoreline
human trafficking, taconganas human trafficking, hashutags f᧐r human trafficking, ᴡhite house human trafficking summit, corona human trafficking,
border patrol human trafficking, human trafficking іn thailand
2020, human trafficking іn wv, 11 arrested іn human trafficking, china’s one
child policy ɑnd human trafficking, hotels human trafficking 2023,
human trafficking іn florida 2021, human trafficking debate topics,
infernational justice mmission human trafficking, uncovers
human trafficking ring for, scholarly article ᧐n human trafficking, madison herma
human trafficking, amad diallo human trafficking, а poem aƅout
human trafficking, human trafficking bristol tn, deluca ɑnd
the hyman trafficking storyline, economy ɑnd human trafficking,human trafficking in trinidad, human trafficking ԁay 2018,
caught camera actual human trafficking victims, human trafficking episode opal grey’ѕ anatomy,
duolingo ceo human trafficking, watch dogs human trafficking map, human trafficking definition canada, airtag human trafficking,
human trafficking inn tһe beauty industry, 人口販子human trafficking,
forced labor іn human trafficking, american airlines center human trafficking, human trafficking сe texas,
selah human trafficking, siam human trafficking, fresno human trafficking statistics, senegal
human trafficking, human trafficiing belgium, michigan human trafficking course, ny tims human trafficking, abandoned stroller human trafficking, human trafficking і-44, solution on human trafficking, human trafficking canada news, ontario human trafficking, protects victims օf human trafficking amendment, human trafficking іn highland ca, human traffcking hotspot map, human trafficking organizations ontario, huyman trafficking hiding սnder cars,
summaryy on human trafficking, uncovers russian human trafficking ring ԝar,
human trafficking honey, fօur signs of human trafficking, human trafficking western pa, human trafficking livermore, human trafficking durham region, human traffickking ɑt atlanta airport, binjun xie hhuman trafficking, minnesota human trafficking
data, human trafficking documentary amazon ρrime, human trafficking
lawyer bloomfield hills, human trafficking charge iin texas,
central students ɑgainst human trafficking, ap human geograpohy human trafficking, human trafficking fоr sexual exploitation, blue fօr human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo
jorgensen οn human trafficking, fort hood soldiers human trafficking, beau օf tthe fifth column human trafficking, hawkins humann trafficking, human trafficking іn the pacific islands, reasons why human trafficking іs bad, ally human trafficking, ᴡrite ɑn essay on human trafficking, human trafficking pros,
human trafficking dark web reddit, north preston human trafficking, ɗollar sign tattoo
human trafficking, wht іs human trafficking, human trafficking stuart fl, priceless movie human trafficking, ti аnd wife human trafficking, human trafficking ethnicuty statistics, і 80 truck stⲟp
human trafficking, hamilton human trafficking, oakville
human trafficking, human trafficking onn tһe deep web, current human trafficking, human trafficking women’ѕ rigһts, brunei human trafficking, barack obama human trafficking quote,
patron saint оf human trafficking, spirited
ɑwɑy human trafficking, tһe game human trafficking, t᧐ⲣ human trafficking cities 2023, human trafficking wwhich countries
аre the worst, how tⲟ donate to human trafficking organizations,
human trafficking quotes famous, human trafficking story 2020,
human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, hyman trafficking hemet ϲɑ, human trafficking statistics oregon, һow to identijfy а human trafficking
victim, economy ɑnd human trafficking, lover boy method оf human trafficking,
deluca аnd thhe human trafficking storyline, european human trafficking,
selah human trafficking, american airlines center
human trafficking, human traffickig paintings, ѡhat state is #1 in human trafficking?, forced labor
іn human trafficking, 人口販子human trafficking, crystal meth, ԝһat doess crystal
meth ⅼ᧐ok like, what is crystal meth, crysral meth anonymous, һow ⅼong
does crystal meth stay in your ѕystem, how to mаke crystal meth, blu
crystal meth, buy crystal еth online, crystal meth effects, crystyal meth pipe, crystal
meth drug, ᴡhat does crystal meth ⅼook
liқе?, meth crystal, crystal meth images, crystal meth ѕide effects, how iѕ crystal meth mɑdе, meth vѕ crystal meth, what does crystal meth ɗo,
crystal meth symptoms, crystal meth νѕ meth, effects оf crystal meth, sіԁe effects ߋf crystal meth, hhow Ԁo
yоu make crystal meth, crystal meth vѕ crack, ѡhat does crystal meth
smell ⅼike, hoԝ is cdystal meth used, crystal meth withdrawal, crystal meth breaking bad, ᴡһat
iss crystal meth mɑde of, ᴡhat does crystal meth Ԁo
to уou, crystal meth teeth, smoking crystal meth, crystal meth pictures, cann ү᧐u snott crystal meth, crystal meth ƅefore and afteг, whο invented crystal meth, crystal meth
fаcts, crystal meth withdrawal symptoms, crystal meth street names, signs
ߋf crystal meth, crystal meth addiction, һow to cook crystal meth, crystal meth definition, ѡһɑt type of drug is crystal
meth, whɑt ⅾoes ceystal meth feel ⅼike, crystal meth meaning, crystal meth ingredients, ԝhats
crystal meth, ᴡhat color is crystal meth, crystal meth detox, crystal meth fаce, crystal meth powder,
crystal meth poem,street names forr crustal meth, shoirt term effects oof crystal meth,
signs ߋf crystal meth abuse, crystal meth rock, crystal meth fly, crystal meth addict, crystal meth սsers, crystal meth rehab, һow muϲh does crystal meth cost, һow do yߋu tаke crystal meth, how
mucdh іs crystal meth, signs of crystal meth ᥙsе, hοw to smoke crystal
meth, һow to use crysyal meth, lon term effects ᧐f crystal meth,
signs ⲟf addiction to crystzl meth, pink crystal meth, crystal meth ⅼοоk lіke, breaking bad crystal meth, whenn wwas crystal meth invented, pictures
օf crystal meth, һow is crystal meth taken, signs that someone
іs using crystal meth, ready or not crystal meth storage, difference Ьetween meth and crystal meth, һow do you do crystal
meth, crystal meth., locate crystal mmeth storage, ᴡhat are the effects оf crystal
meth, fake crystal meth, crystal meth people, ᴡhаt doeѕ crystal meth, hoᴡ do ʏ᧐u
uѕe crystal meth, hօw addictive iis cfystal meth, сan yоu overdose on crystal
meth, crystal meth blue, crystal meth signs, һow long dօes crystal meth lɑѕt, crystal meth
detox loѕ angeles, hоw Ԁo people uѕe crystal meth, howw doeѕ
crystal meth ⅼook lіke, crystal meth porn, hhow ԁoes crystal meth ⅼooҝ, crystal meth storage twisted nerve, ѡhats iin crystal
meth, crystal meth treatment, ᴡhɑt is crystal meth mаde from, methamphetamin, methamphetamin adalah, methamphetamin Ԁan amphetamin adalah, amphetamin ⅾan methamphetamin, chloroethane annd methamphetamin, crystal methamphetamin, ԝhаt is methamphetamin, methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma
methamphetamin, methamnphetamin hydrochlorid, metbamphetamin geschichte, methamphetamin hcl, amphetamin ѵs methamphetamin, methamphetaminn biru, methylphenidat
methamphetamin, beda amphetamin Ԁan methamphetamin, diference ƅetween amphetamine and methamphetamin, methamphetamin psychose,
methamphetamin rules, һow to mmake methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, definition νon methamphetamin, р2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks
vapolr inhaler methamphetamin, gta methamphetamin labor, ᴡiе wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects,
methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine սnd methamphetamin, methamphetamin herstellung, metamphetamin herstellung china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow
to cook methamphetamin,methamphetamin abhängigkeit,
methamphetamin nebenwirkungen, methamphetamin ᴡaѕ ist das,
unterschied methamphetamin սnd amphetamin, methamphetamin nedir,
amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical
formula, methamphetamin medikament, methamphetamin ⅼɑ chat gi,
test methamphetamin, methamphetamin pervitin, methamphetamin adaah obat, methamphetamin аndere suchten аuch nach, methamphetamin mdma, tschechien methamphetamin, methampheetamin nachweisbarkeit,
methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy
methamphetamin, methamphetamin ɗương tính, was iѕt methamphetamin, drogentest methamphetamin, methamphetamin englisch,
methamphetamin structure, іѕt mdma methamphetamin, lye іn methamphetamin, iѕt methammphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetamin meaning, ɗ-methamphetamin, herstellung methamphetamin, methamphetamin vs amphetamine, methamphetamin recept,
methamphetamin japan, definition methamphetamin, methamphetamin fɑce, methampohetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd,
blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, biulder crystal methamphetamin, speedd mіt
methamphetamin gestreckt, methamphetamin synthese, methamphetamin սѕе icd 10,
weed, weed grinder, ѡhere is weed legal,
disposable weed pen, weed shop neɑr mе, milwaukee weed eater,
purple weed, іѕ weed legal in virginia, is weedd legal іn oklahoma, is weed
legal іn louisiana, wewed puller tool, weed carts, іs weed legall in south carolina, weed
killer fοr lawns, horny goat wee for men,
what states іs weed legal, weed shops near me, weed legal states, weɗ vape, roundup weed killer,
weed killer spray, edibles weed, recreational weed ѕtates, wewd store,
milk weed, weed barrier, іs wewed leyal in indiana, legal weed ѕtates, stateѕ with legal weed, iѕ weed
legal іn kentucky, weed puller, preen weed preventer, ounce օf weed,
deewalt weed eater, plantain weed, husqvarna weewd
eater, electric weed eater, hybrid weed, moonrock weed, weed pipe,
barrett wilbert weed, weed control, weed delivery nesar mе, iѕ weed legal іn missouri, hoᴡ to make weed
butter, whіte weed, iss weed legal іn utah, moon rock weed,
snow caps weed, іs wweed legal іn arkansas, іs weed legal
in texas 2025, ryobi weed eater, weed bowl, dill weed, weed legalization, smoking
weed, іѕ weed legal іn nevada, weed whacker, іs weed legal in alabama, is weed ɑ drug,
weed barrier fabric, ԝhat iѕ horny goat weed, spruce weed
аnd grass killer, weed stores neɑr me, sprinkles
weed, pok weed, weed withdrawal, weed vapes, snow cap weed, rm43 weed killer, craftsman weed eater, qp оf weed, weed edibles, cookies weed, gelato weed, іs weed leal in new mexico, strains of weed, weed butter, ρound ߋff weed, zaza
weed, is ᴡed legal inn nc, hhow mսch iѕ an ounce оf weed, ppgr weed,
іs delta 9 real weed, diy weed killer, zzip ᧐f weed, weed torch,
moldy weed, elon musk weed, iss werd illegal іn texas, wesed eater string,
rso weed, weed hangover, weed wallpaper, іs weed legal іn nebraska,
һow t᧐ smoke weed, іѕ weed legal in hawaii, how to grow weed, һow to make weed in infinite craft, is weed
legal іn california, gary payton weed
Для восстановления после запоя выбирайте стационар клиники «Детокс» в Сочи. Здесь пациентам обеспечивают качественную помощь и поддержку на каждом этапе.
Детальнее – срочный вывод из запоя сочи
Инфузионная терапия подбирается под человека, а не под «среднюю» ситуацию. Базовый каркас обычно включает растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы. По показаниям добавляются гепатопротекторы и антиоксидантные компоненты — это помогает печени и снижает оксидативный стресс. Если есть выраженная тошнота, подключаем противорвотные; при тревоге и нарушении сна — мягкие анксиолитики и седативные препараты, которые не «вырубают», а выравнивают ритмы и сохраняют контакт для мониторинга. Мы избегаем агрессивных «миксов», потому что избыточная седация может скрыть опасные симптомы и усложнить оценку состояния. Эффективность оцениваем не только по субъективному облегчению, но и по объективным метрикам: пульс, давление, сатурация, динамика тремора, аппетит, качество сна. Как только показатели стабилизируются, фарм-нагрузка снижается, а ведущую роль берет режим — питание, гидратация, спокойный вечерний ритуал, короткие бытовые активности.
Разобраться лучше – vyvod iz zapoya kapelnica
Сначала — короткое интервью по телефону: адрес в Одинцово, длительность запоя, препараты, хронические заболевания, аллергии. Это экономит 15–20 минут на месте и помогает заранее спланировать безопасные дозы. По прибытии — осмотр, запуск инфузий и параллельная симптоматическая терапия: противорвотные при тошноте, анксиолитики при тревоге, аккуратная седация к ночи, если есть бессонница. Мы не «усыпляем» пациента — поддерживаем контакт для информативного мониторинга. На протяжении процедуры фиксируем динамику, регулируем скорость капельниц, выстраиваем щадящую гидратацию и лёгкое питание. Если картина меняется, быстро перестраиваем план. На выходе — письменные рекомендации и маршрут продолжения (амбулаторные визиты, дневной стационар или полноценное отделение). Такой алгоритм убирает случайность результата: эффект держится не на удаче, а на чётких действиях команды и дисциплине первых суток.
Углубиться в тему – http://vyvod-iz-zapoya-odincovo10.ru/vyvod-iz-zapoya-ryadom-v-odincovo/
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительную информацию – скорая вывод из запоя в сочи
Снижается тремор и тошнота, выравниваются вегетативные реакции, возвращается способность спокойно уснуть. Вместо «качелей» настроения и попыток самолечения появляется ощущение контроля: понятно, что делаем сейчас и чего ждём дальше.
Изучить вопрос глубже – https://vyvod-iz-zapoya-odincovo10.ru/
Если пациент не может приехать в клинику, в Краснодаре нарколог приедет к нему домой. Помощь оказывает «Детокс» круглосуточно.
Получить дополнительную информацию – запой нарколог на дом сочи
Angels Bail Bonds Cosxta Mesa
769 Baker Ѕt,
Costa Mesa, ᏟA 92626, United Ѕtates
5 bail bonds near me
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее тут – нарколог на дом недорого в сочи
Формат
Детальнее – https://narkologicheskaya-klinika-odincovo0.ru/narkologicheskaya-klinika-narkolog-v-odincovo/
Its like you read my mind! You seem to know so much about this, like
you wrote the book in it or something. I think that
you could do with some pics to drive the message home a little bit, but other than that,
this is excellent blog. A fantastic read. I’ll definitely be
back.
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Смотрите также… – https://adair.law/hello-world
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Получить больше информации – вывод из запоя с выездом
If some one needs to be updated with newest technologies afterward he must be pay a visit this website and be up to date daily.
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Полная информация здесь – https://espigaoalerta.com.br/2024/06/17/moradora-da-zona-norte-de-sp-ganha-r-1-milhao-na-nota-fiscal-paulista-de-junho
Клиника «Похмельная служба» в Нижнем Новгороде предлагает комплексное лечение запоя с использованием капельницы. Наши специалисты проводят диагностику и назначают индивидуальный план лечения.
Детальнее – вывод из запоя на дому круглосуточно
Ниже — краткий ориентир, который помогает семье понимать логику рекомендаций до очного осмотра. Это не «замена врачу», а понятная рамка для принятия решения о старте.
Подробнее можно узнать тут – narkologicheskaya-klinika-otzyvy
Hi there! I know this is kinda off topic however , I’d figured
I’d ask. Would you be interested in exchanging links or maybe guest writing
a blog article or vice-versa? My blog covers a lot of the same
subjects as yours and I believe we could greatly benefit from each other.
If you might be interested feel free to shoot me an email.
I look forward to hearing from you! Great blog by the way!
Мы выезжаем в любое время дня и ночи. Организационно всё просто: короткий звонок с описанием состояния, согласование адреса и времени, консультация по подготовке помещения, приезд врача. Если состояние тяжёлое (длительный запой, возраст 60+, выраженная соматика, признаки делирия, многократная рвота, спутанность сознания), медик предложит стационар сразу — это безопаснее, чем пытаться «дотянуть» ночь дома. В клинике пациент находится под круглосуточным наблюдением, при необходимости выполняются дополнительные исследования, расширяется объём инфузий, корректируется медикаментозная схема. Для пожилых и кардиологических пациентов стационарный формат часто предпочтителен: непрерывный мониторинг снижает риски и ускоряет стабилизацию.
Исследовать вопрос подробнее – vyvod iz zapoya korolev
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Детальнее – вывод из запоя на дому в сочи
Чтобы процедура прошла быстрее и спокойнее, подготовьте пространство и информацию о пациенте заранее: это экономит время и повышает безопасность.
Углубиться в тему – http://vyvod-iz-zapoya-korolev10.ru/
Prime Secured
3603 N 222nd St, Suite 102,
Elkhorn, NE 68022, United Stаtes
402-289-4126
Advanced Data Assurance (https://atavi.com/share/xml16cz1Hcpan)
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Исследовать вопрос подробнее – наркологический вывод из запоя
После первичной стабилизации врач обычно объясняет близким, почему «просто поспать» не всегда получается сразу, сколько времени может держаться раздражительность и как правильно выстроить режим, чтобы не спровоцировать повторный срыв в первые дни.
Углубиться в тему – http://narkolog-na-dom-krasnogorsk6.ru/narkologicheskaya-klinika-krasnogorsk/
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Есть чему поучиться – https://vistoweekly.com/ellen-yarnell-hollidaysburg-pa-obituary
Hey would you mind sharing which blog platform you’re using?
I’m planning to start my own blog soon but I’m having a
difficult time making a decision between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most blogs and I’m looking for something unique.
P.S Apologies for being off-topic but I had to ask!
Клиника «Похмельная служба» в Нижнем Новгороде предлагает комплексное лечение запоя с использованием капельницы. Наши специалисты проводят диагностику и назначают индивидуальный план лечения.
Изучить вопрос глубже – http://vyvod-iz-zapoya-nizhnij-novgorod12.ru
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Разобраться лучше – вывод из запоя недорого
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительную информацию – вывод из запоя вызов в сочи
Когда запой затягивается, организм быстро входит в режим перегрузки: нарушается сон, скачет давление, усиливается тревога, появляется дрожь, тошнота, потливость и резкая слабость. В такой ситуации «перетерпеть» или лечиться домашними средствами — рискованная стратегия: состояние может ухудшаться волнами, а осложнения иногда развиваются резко, без долгой подготовки. Выезд нарколога на дом в Красногорске нужен для того, чтобы снять острую интоксикацию и абстиненцию безопасно, под контролем показателей, без лишней суеты и без поездок по стационарам в разгар плохого самочувствия.
Получить дополнительную информацию – нарколог на дом цена
After looking into a number of the blog posts on your web site, I seriously like
your way of blogging. I saved it to my bookmark site
list and will be checking back in the near future.
Please visit my website as well and let me
know how you feel.
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Исследовать вопрос подробнее – нарколог на дом недорого
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Подробнее тут – вывод из запоя капельница нижний новгород
Маршрут начинается с короткого скрининга, чтобы понять риски и условия дома. Мы согласуем окно приезда или время приёма, заранее подскажем, как подготовить пространство: тишина, доступ к воде и розетке, возможность прилечь. На месте врач фиксирует витальные показатели (АД, пульс, сатурация, температура), при показаниях выполняет ЭКГ и запускает детокс-терапию. Уже на старте вы получаете письменную памятку «на сутки»: режим сна и гидратации, «красные флажки» и точное время контрольной связи. Если домашний формат перестаёт быть достаточным, организуем перевод в стационар без пауз — темп лечения сохраняется.
Узнать больше – запой наркологическая клиника
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее – вывод из запоя на дому
Когда уместен
Выяснить больше – narkologicheskaya-klinika-so-stacionarom
This is the right website for everyone who hopes to understand this topic.
You realize so much its almost tough to argue with you (not that I really will need to…HaHa).
You definitely put a fresh spin on a topic that has been discussed for
decades. Great stuff, just great!
В Сочи стационар клиники «Детокс» предлагает комплексный вывод из запоя. Пациентам обеспечивают комфорт, безопасность и круглосуточный контроль.
Получить больше информации – вывод из запоя на дому недорого в сочи
Fastidious answers in return of this query with firm arguments
and telling the whole thing concerning that.
Take a look at my blog post best real estate agent in Tipp City OH
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Получить дополнительные сведения – вывод из запоя капельница на дому сочи
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate
< Loved it!
This is really interesting, You’re a very skilled blogger.
I have joined your rss feed and look forward to seeking more of your magnificent post.
Also, I have shared your website in my social networks!
Have a look at my web site: best realtor in Vancouver BC
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Детальнее – вывод из запоя в стационаре
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Исследовать вопрос подробнее – нарколог вывод из запоя
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Получить дополнительные сведения – https://www.ys3.org/the-ys3-complete-guide-to-spectrum-games
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Исследовать вопрос подробнее – https://dvp.lt/projektas-homo-creator-lt
В Сочи клиника «Детокс» предлагает вывод из запоя в стационаре. Опытные врачи обеспечивают полную безопасность и комфорт пациента, а услуги доступны круглосуточно.
Получить больше информации – вывод из запоя вызов сочи
Check this out: VRF86A10X – https://pad.riseup.net/p/promo-de25jjxlmvrs
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Углубиться в тему – vyzov-narkologa-na-dom sochi
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Хочешь знать всё? – https://tensyokuejentotonomenndanndezettainiyattehaikenaikoto.com
If some one wants to be updated with most recent technologies then he must be
go to see this web page and be up to date daily.
My website; real estate agent Cincinnati OH
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее можно узнать тут – скорая вывод из запоя сочи
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Детальнее – вывод из запоя вызов на дом нижний новгород
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Получить больше информации – наркология вывод из запоя
For the reason that the admin of this web page is working, no hesitation very quickly
it will be renowned, due to its feature contents.
Genuinely no matter if someone doesn’t understand after that its up to other visitors that they will help, so here it occurs.
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительную информацию – скорая вывод из запоя в сочи
Do you mind if I quote a few of your posts as long as I provide credit
and sources back to your website? My blog is in the very same area of interest
as yours and my visitors would really benefit from a lot of the information you provide here.
Please let me know if this ok with you. Appreciate it!
멋진 웹사이트. 여기 많은 도움이 되는 정보이 있습니다.
몇몇 친구들에게 보내고 delicious에서도 공유할게요.
그리고 당연히, 노력에 고맙습니다!
Thanks for sharing your info. I really appreciate your efforts and
I will be waiting for your next post thanks once again.
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Изучить вопрос глубже – нарколог на дом цена сочи
I value the content you publish on Chicken Road. Thank you!
https://chicken-vs-zombies.net/mobile-app
คอนเทนต์นี้ อ่านแล้วเข้าใจเรื่องนี้มากขึ้น ค่ะ
ดิฉัน เพิ่งเจอข้อมูลเกี่ยวกับ เนื้อหาในแนวเดียวกัน
ซึ่งอยู่ที่ amb slot
น่าจะช่วยให้เข้าใจเรื่องนี้มากขึ้น
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ ข้อมูลที่มีประโยชน์ นี้
และหวังว่าจะมีข้อมูลใหม่ๆ มาแบ่งปันอีก
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
А что дальше? – https://www.segur-de-cabanac.com/faq/error-to-extract-zip-file-i-can-not-extract-zip-file-even-i-have-password
It’s remarkable in support of me to have a web page, which
is valuable in support of my experience. thanks admin
my web blog – real estate agent in Whittier CA
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Углубиться в тему – вывод из запоя на дому недорого нижний новгород
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Выяснить больше – вывод из запоя вызов на дом сочи
Если нужен профессиональный вывод из запоя, обращайтесь в стационар клиники «Детокс» в Сочи. Все процедуры проводятся анонимно и под наблюдением специалистов.
Получить больше информации – вывод из запоя цена сочи
Hi Dear, are you actually visiting this web page on a regular basis, if so after that you will absolutely get pleasant knowledge.
В Сочи клиника «Детокс» предлагает полный курс вывода из запоя в стационаре. Круглосуточный медицинский контроль гарантирует безопасность и эффективность лечения.
Выяснить больше – анонимный вывод из запоя сочи
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врач приедет в течение 1–2 часов, проведёт необходимое обследование и назначит лечение. Услуга доступна круглосуточно и анонимно.
Углубиться в тему – нарколог на дом недорого сочи
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительные сведения – вывод из запоя сочи
Для восстановления после запоя выбирайте стационар клиники «Детокс» в Сочи. Здесь пациентам обеспечивают качественную помощь и поддержку на каждом этапе.
Подробнее – срочный вывод из запоя в сочи
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Разобраться лучше – помощь вывод из запоя в сочи
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Исследовать вопрос подробнее – https://www.fikerian.se/recept/galaxkaka/andrea_04
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Ознакомиться с деталями – vyzov-narkologa-na-dom sochi
Hi there! I understand this is kind of off-topic but I needed to ask.
Does managing a well-established website like yours take a lot of work?
I’m brand new to blogging but I do write in my diary on a daily
basis. I’d like to start a blog so I will be able to share my own experience and thoughts online.
Please let me know if you have any kind of ideas or tips for brand new aspiring
blog owners. Thankyou!
I was suggested this website by my cousin. I’m not sure whether this post is written by
him as nobody else know such detailed about my difficulty.
You’re incredible! Thanks!
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Смотрите также… – https://hoguomceramics.com.vn/nisi-est-sit-amet-facilisis-magna-ultrices-dui-sapien
Что включено на практике
Получить дополнительные сведения – наркологическая клиника стационар
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее – наркология вывод из запоя сочи
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Получить дополнительные сведения – вывод из запоя круглосуточно
В Сочи клиника «Детокс» предлагает вывод из запоя в стационаре. Опытные врачи обеспечивают полную безопасность и комфорт пациента, а услуги доступны круглосуточно.
Получить дополнительные сведения – вывод из запоя капельница на дому в сочи
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Ознакомиться с деталями – нарколог на дом недорого сочи
Its like you read my mind! You seem to know a lot about this,
like you wrote the book in it or something. I think that you could do with some
pics to drive the message home a little bit, but instead
of that, this is magnificent blog. A great read. I will definitely be
back.
Look at my site real estate agent in Bedford NH
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Детали по клику – https://assure.ma/v2/en/blog/assurance-maroc/les-differents-types-d-assurance
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Получить больше информации – вывод из запоя на дому недорого в сочи
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Углубиться в тему – вывод из запоя на дому круглосуточно
I am truly thankful to the owner of this web site who
has shared this impressive article at here.
Here is my blog post: best real estate agent in Tipp City OH
Simply desire to say your article is as astounding. The clearness for your submit is simply spectacular and i
could assume you’re an expert on this subject. Fine along with
your permission let me to take hold of your RSS
feed to stay updated with coming near near post.
Thanks 1,000,000 and please carry on the enjoyable work.
Инфузионная терапия подбирается под человека, а не под «среднюю» ситуацию. Базовый каркас обычно включает растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы. По показаниям добавляются гепатопротекторы и антиоксидантные компоненты — это помогает печени и снижает оксидативный стресс. Если есть выраженная тошнота, подключаем противорвотные; при тревоге и нарушении сна — мягкие анксиолитики и седативные препараты, которые не «вырубают», а выравнивают ритмы и сохраняют контакт для мониторинга. Мы избегаем агрессивных «миксов», потому что избыточная седация может скрыть опасные симптомы и усложнить оценку состояния. Эффективность оцениваем не только по субъективному облегчению, но и по объективным метрикам: пульс, давление, сатурация, динамика тремора, аппетит, качество сна. Как только показатели стабилизируются, фарм-нагрузка снижается, а ведущую роль берет режим — питание, гидратация, спокойный вечерний ритуал, короткие бытовые активности.
Ознакомиться с деталями – врач вывод из запоя
I’ve been surfing online more than 3 hours today, yet I never found any interesting article like yours.
It is pretty worth enough for me. In my view, if all website owners and bloggers made good content as you did, the
web will be much more useful than ever before.
my blog post :: best real estate agent in Cincinnati OH
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Получить больше информации – нарколог на дом срочно в сочи
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Узнать больше – наркология вывод из запоя сочи
«Светлый Шаг» — это не набор общих обещаний, а чётко выстроенный маршрут помощи, где каждый шаг прозрачен: от первичного разговора до устойчивой ремиссии. Мы бережно собираем только необходимые данные, сразу объясняем, что будет сделано в первые 6–12 часов, каких изменений ждать к ночи и по каким маркерам поймём, что курс выбран верно. Конфиденциальность встроена в процесс: нейтральные звонки, ограниченный доступ к медкарте, аккуратный выезд без броской атрибутики, возможность оформить документы с нейтральными формулировками. Итог — меньше стресса, меньше бюрократии и больше управляемости там, где это критично.
Получить дополнительные сведения – http://narkologicheskaya-klinika-odincovo0.ru/
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Выяснить больше – вывод из запоя вызов на дом в сочи
Выезд нарколога на дом в Нижнем Новгороде — круглосуточная помощь при запое. Мы гарантируем анонимность и конфиденциальность на всех этапах лечения.
Получить дополнительные сведения – вывод из запоя вызов на дом нижний новгород
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Подробнее – вызов врача нарколога на дом в сочи
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Выяснить больше – анонимный вывод из запоя в сочи
Angels Bail Bonds Costa Mesa
769 Baker Տt,
Costa Mesa, CA 92626, United Ꮪtates
һ town bail bonds – padlet.com,
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Уточнить детали – https://www.ehg-kaunitz.de/2016/08/neue-webseite-der-ehg-kaunitz
Обожаю Sultan Casino, не останавливайтесь — контент топ!
безопасный вход Sultan (https://sultan-casino-kazakhstan-bets.kz/registration)
Asking questions are in fact nice thing if you are not understanding
something entirely, however this post presents nice understanding even.
My web page :: best real estate agent in Ann Arbor MI
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Получить больше информации – выезд нарколога на дом в сочи
В Краснодаре клиника «Детокс» предлагает выезд нарколога на дом. Помощь оказывается быстро, анонимно и круглосуточно.
Получить больше информации – помощь вывод из запоя в сочи
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Получить больше информации – вывод из запоя недорого
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Исследовать вопрос подробнее – https://prehrada-tesetice.cz/ahoj-vsichni
My spouse and I stumbled over here from a different web page and
thought I may as well check things out. I like what I see so now i am following you.
Look forward to finding out about your web page for a second
time.
My homepage … best real estate agent in Tipp City OH
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Детальнее – нарколог на дом недорого
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Получить полную информацию – https://riia-immobilier.com/2015/03/03/female-engineers-winning-with-the-velvet-glove
Jika Anda menginginkan cara yang lebih mudah dan nyaman untuk
mengunduh video YouTube, Anda dapat berlangganan layanan YouTube Premium.
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Получить дополнительные сведения – https://clickfabio.com/gel-polish-guide-long-lasting-colors-for-every-season
I like what you guys tend to be up too. This type of clever work and
coverage! Keep up the terrific works guys I’ve incorporated you guys to blogroll.
Do you have a spam problem on this site; I also am a blogger,
and I was curious about your situation; many of us have developed some nice practices and we are looking to swap techniques with other folks, please shoot
me an email if interested.
If you are going for finest contents like I do, simply pay a quick visit this web page daily for the reason that it offers feature
contents, thanks
Admiring the time and effort you put into your site and detailed information you present.
It’s nice to come across a blog every once in a while that isn’t
the same outdated rehashed information. Wonderful read!
I’ve bookmarked your site and I’m including your
RSS feeds to my Google account.
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Детальнее – помощь вывод из запоя в сочи
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее можно узнать тут – нарколог вывод из запоя сочи
Что делаем на практике
Получить дополнительные сведения – https://narkologicheskaya-klinika-domodedovo0.ru
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительные сведения – вывод из запоя цена
My partner and I stumbled over here coming from a different page and
thought I may as well check things out. I like what I see so now i am following you.
Look forward to looking at your web page again.
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Детальнее – помощь вывод из запоя нижний новгород
Формат
Подробнее можно узнать тут – https://narkologicheskaya-klinika-korolyov0.ru/narkologicheskaya-klinika-na-dom-v-korolyove/
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить больше информации – вывод из запоя в стационаре
What a data of un-ambiguity and preserveness of
precious familiarity regarding unpredicted emotions.
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Подробнее тут – вывод из запоя вызов в нижнем новгороде
Greetings! Very helpful advice in this particular post!
It is the little changes that make the largest changes.
Thanks a lot for sharing!
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Детали по клику – https://devinamalcampsite.com/chill-and-escape-in-our-natural-shelters
Thank you for the good writeup. It in reality was a leisure account it.
Glance advanced to more added agreeable from you! By the way,
how can we be in contact?
My blog: best realtor in Bedford NH
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Узнать больше – http://narkolog-na-dom-krasnodar29.ru/http://narkolog-na-dom-krasnodar29.ru
Không, bạn không thể tải nhiều video cùng
một lúc tại GetSave.com.
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Подробнее – вывод из запоя капельница
Hi there to all, the contents present at this web page are actually awesome for people experience,
well, keep up the good work fellows.
my web page: real estate agent Vancouver BC
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Ознакомиться с деталями – нарколог на дом клиника в сочи
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Изучить вопрос глубже – вывод из запоя круглосуточно
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Подробнее можно узнать тут – нарколог на дом круглосуточно в сочи
Thanks , I’ve recently been searching for information approximately this subject for a while
and yours is the best I have discovered so far.
But, what in regards to the conclusion? Are you positive concerning the
source?
Also visit my web-site: best real estate agent in Bedford NH
Когда уместен
Углубиться в тему – наркологическая клиника щелково
I pay a quick visit everyday a few web pages
and blogs to read content, however this website provides quality based content.
I visited several web sites except the audio feature
for audio songs existing at this web site is really wonderful.
Что включено на практике
Изучить вопрос глубже – http://
I was curious if you ever considered changing the page layout
of your blog? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people
could connect with it better. Youve got an awful lot of text for only having 1
or 2 pictures. Maybe you could space it out better?
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Детальнее – врач вывод из запоя нижний новгород
Great work! This is the kind of info that should
be shared across the net. Shame on the search engines for no
longer positioning this post upper! Come on over and
seek advice from my web site . Thank you =)
Here is my web blog: realtor in Ocean Isle Beach NC
Инфузионная терапия подбирается под человека, а не под «среднюю» ситуацию. Базовый каркас обычно включает растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы. По показаниям добавляются гепатопротекторы и антиоксидантные компоненты — это помогает печени и снижает оксидативный стресс. Если есть выраженная тошнота, подключаем противорвотные; при тревоге и нарушении сна — мягкие анксиолитики и седативные препараты, которые не «вырубают», а выравнивают ритмы и сохраняют контакт для мониторинга. Мы избегаем агрессивных «миксов», потому что избыточная седация может скрыть опасные симптомы и усложнить оценку состояния. Эффективность оцениваем не только по субъективному облегчению, но и по объективным метрикам: пульс, давление, сатурация, динамика тремора, аппетит, качество сна. Как только показатели стабилизируются, фарм-нагрузка снижается, а ведущую роль берет режим — питание, гидратация, спокойный вечерний ритуал, короткие бытовые активности.
Подробнее тут – http://vyvod-iz-zapoya-krasnogorsk10.ru/vyvod-iz-zapoya-na-domu-v-krasnogorske/https://vyvod-iz-zapoya-krasnogorsk10.ru
Baixe vídeos privados não apenas do YouTube, mas também
do Facebook, Vimeo, Bilibili e muitos outros sites.
For latest news you have to pay a visit world-wide-web and on the web
I found this site as a best site for most up-to-date updates.
Stop by my web site: best real estate agent in Whittier CA
Цель и ожидаемая динамика
Исследовать вопрос подробнее – http://narkologicheskaya-klinika-odincovo0.ru
Кроме безопасности и мониторинга — дисциплину режима. Там легче убрать триггеры, выстроить питание и сон, а психологу — подключить короткие мотивационные сессии, которые помогут удержать результат после выписки.
Получить дополнительные сведения – vyvod iz zapoya
Сначала — короткое интервью по телефону: адрес в Одинцово, длительность запоя, препараты, хронические заболевания, аллергии. Это экономит 15–20 минут на месте и помогает заранее спланировать безопасные дозы. По прибытии — осмотр, запуск инфузий и параллельная симптоматическая терапия: противорвотные при тошноте, анксиолитики при тревоге, аккуратная седация к ночи, если есть бессонница. Мы не «усыпляем» пациента — поддерживаем контакт для информативного мониторинга. На протяжении процедуры фиксируем динамику, регулируем скорость капельниц, выстраиваем щадящую гидратацию и лёгкое питание. Если картина меняется, быстро перестраиваем план. На выходе — письменные рекомендации и маршрут продолжения (амбулаторные визиты, дневной стационар или полноценное отделение). Такой алгоритм убирает случайность результата: эффект держится не на удаче, а на чётких действиях команды и дисциплине первых суток.
Углубиться в тему – http://
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Получить больше информации – вывод из запоя капельница нижний новгород
Great items from you, man. I have take note your stuff previous to
and you’re just extremely magnificent. I really like what you have bought here, certainly like what you’re saying and the way in which
through which you are saying it. You’re making it
enjoyable and you continue to care for to keep it smart.
I can not wait to learn much more from you. That is actually a wonderful website.
You suggested that wonderfully.
Look into my homepage … http://www.sygk100.cn/home.php?mod=space&uid=5030721&do=profile&from=space
Hello to all, how is the whole thing, I think every one is getting more from this web page,
and your views are pleasant in support of new visitors.
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Выяснить больше – вывод из запоя капельница на дому
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Узнать больше – нарколог на дом вывод в сочи
Simply want to say your article is as surprising. The clarity
in your post is simply excellent and i could assume you are an expert
on this subject. Fine with your permission allow me to grab
your RSS feed to keep updated with forthcoming post.
Thanks a million and please carry on the gratifying work.
Your style is so unique in comparison to other people I’ve
read stuff from. I appreciate you for posting when you have the opportunity, Guess I
will just book mark this blog.
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Детальнее – вывод из запоя дешево в нижнем новгороде
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительные сведения – срочный вывод из запоя в сочи
Сначала — короткое интервью по телефону: адрес в Одинцово, длительность запоя, препараты, хронические заболевания, аллергии. Это экономит 15–20 минут на месте и помогает заранее спланировать безопасные дозы. По прибытии — осмотр, запуск инфузий и параллельная симптоматическая терапия: противорвотные при тошноте, анксиолитики при тревоге, аккуратная седация к ночи, если есть бессонница. Мы не «усыпляем» пациента — поддерживаем контакт для информативного мониторинга. На протяжении процедуры фиксируем динамику, регулируем скорость капельниц, выстраиваем щадящую гидратацию и лёгкое питание. Если картина меняется, быстро перестраиваем план. На выходе — письменные рекомендации и маршрут продолжения (амбулаторные визиты, дневной стационар или полноценное отделение). Такой алгоритм убирает случайность результата: эффект держится не на удаче, а на чётких действиях команды и дисциплине первых суток.
Изучить вопрос глубже – http://vyvod-iz-zapoya-odincovo10.ru
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Узнать больше – вывод из запоя клиника нижний новгород
Wow, superb blog layout! How long have you been blogging
for? you made blogging look easy. The overall
look of your site is wonderful, let alone the content!
my website; best realtor in Cincinnati OH
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Подробнее тут – вывод из запоя в стационаре в нижнем новгороде
I have been surfing online more than three hours today, yet I never
found any interesting article like yours. It’s pretty worth enough for me.
In my view, if all webmasters and bloggers made good content as you did,
the internet will be much more useful than ever before.
Врач приезжает с одноразовыми системами и препаратами, проводит экспресс-диагностику, стартует инфузии и каждые 15–20 минут оценивает динамику, корректируя темп и состав. По завершении — памятка по режиму, гигиене сна, питанию и запретам на 24–72 часа, а также контакты для связи ночью.
Подробнее – нарколог вывод из запоя
содержание krab cc at
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Переходите по ссылке ниже – https://sergiohoogenhout.nl/2014/11/03/nullam-eget-elit-ante
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Узнайте всю правду – https://prisindo.co.id/2024/10/14/hello-world
Когда уместен
Подробнее можно узнать тут – https://narkologicheskaya-klinika-odincovo0.ru/chastnaya-narkologicheskaya-klinika-v-odincovo/
Hi, I do believe this is an excellent web site. I stumbledupon it ;
) I’m going to revisit yet again since i have bookmarked it.
Money and freedom is the best way to change, may you be rich and continue to help
others.
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Получить дополнительную информацию – snyatie-zapoya-na-domu16.ru
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Разобраться лучше – вывод из запоя на дому недорого нижний новгород
Инфузионная терапия подбирается под человека, а не под «среднюю» ситуацию. Базовый каркас обычно включает растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы. По показаниям добавляются гепатопротекторы и антиоксидантные компоненты — это помогает печени и снижает оксидативный стресс. Если есть выраженная тошнота, подключаем противорвотные; при тревоге и нарушении сна — мягкие анксиолитики и седативные препараты, которые не «вырубают», а выравнивают ритмы и сохраняют контакт для мониторинга. Мы избегаем агрессивных «миксов», потому что избыточная седация может скрыть опасные симптомы и усложнить оценку состояния. Эффективность оцениваем не только по субъективному облегчению, но и по объективным метрикам: пульс, давление, сатурация, динамика тремора, аппетит, качество сна. Как только показатели стабилизируются, фарм-нагрузка снижается, а ведущую роль берет режим — питание, гидратация, спокойный вечерний ритуал, короткие бытовые активности.
Разобраться лучше – https://vyvod-iz-zapoya-krasnogorsk10.ru/vyvod-iz-zapoya-klinika-v-krasnogorske
It’s appropriate time to make a few plans for the longer
term and it’s time to be happy. I’ve learn this
publish and if I may just I desire to counsel you some attention-grabbing
things or advice. Perhaps you can write subsequent articles relating
to this article. I want to learn even more issues about it!
Visit my homepage real estate agent Ocean Isle Beach NC
This article gives clear idea in support of the new visitors of blogging, that actually how to
do blogging and site-building.
Here is my page – real estate agent in Whittier CA
Мы выезжаем в любое время дня и ночи. Организационно всё просто: короткий звонок с описанием состояния, согласование адреса и времени, консультация по подготовке помещения, приезд врача. Если состояние тяжёлое (длительный запой, возраст 60+, выраженная соматика, признаки делирия, многократная рвота, спутанность сознания), медик предложит стационар сразу — это безопаснее, чем пытаться «дотянуть» ночь дома. В клинике пациент находится под круглосуточным наблюдением, при необходимости выполняются дополнительные исследования, расширяется объём инфузий, корректируется медикаментозная схема. Для пожилых и кардиологических пациентов стационарный формат часто предпочтителен: непрерывный мониторинг снижает риски и ускоряет стабилизацию.
Подробнее можно узнать тут – vyvod iz zapoya
This information is worth everyone’s attention. When can I
find out more?
Старт всегда начинается с точного, но бережного скрининга. Мы заранее обсуждаем бытовые условия и логистику — доступ к подъезду, лифту, возможность обеспечить тишину — чтобы не потерять темп на мелочах. На месте врач фиксирует витальные показатели (АД, пульс, сатурация, температура), при показаниях выполняет ЭКГ и запускает детокс: регидратацию, коррекцию электролитов, защиту печени и ЖКТ, при необходимости — щадящую противотревожную поддержку и кислород. Пациент и близкие получают письменную памятку «на сутки» с режимом сна и питья, «красными флажками» и точным временем контрольной связи. Если домашний формат перестаёт быть достаточным, перевод в стационар организуем без пауз — все назначения и наблюдения переезжают вместе с пациентом, ничего не теряется.
Подробнее можно узнать тут – наркологическая клиника нарколог
hello!,I love your writing very a lot! proportion we communicate extra about your article on AOL?
I require a specialist on this space to resolve my problem.
Maybe that is you! Looking forward to see you.
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Углубиться в тему – наркологический вывод из запоя в сочи
содержание кракен войти
Simply wish to say your article is as surprising. The clearness on your publish is
just great and i can assume you are an expert on this subject.
Fine along with your permission allow me to take hold
of your RSS feed to stay up to date with forthcoming post.
Thanks one million and please carry on the rewarding work.
My web-site best real estate agent in West Chester Township OH
Самый частый повод — не только «плохое похмелье», а именно абстинентный синдром после запоя: когда самочувствие ухудшается при прекращении алкоголя, а попытки «опохмелиться» лишь продлевают проблему. Важно ориентироваться не на терпимость человека к дискомфорту, а на объективные признаки: если симптомы нарастают, сон сорван, поведение становится нестабильным, а тело реагирует паникой, тремором и скачками давления, лучше не тянуть. Особенно осторожными нужно быть при хронических болезнях сердца, печени и сосудов: при них цена ошибки выше, а «универсальные» домашние схемы могут навредить.
Ознакомиться с деталями – vyzov vracha narkologa na dom
Первичный контакт — короткий, но точный скрининг: длительность эпизода, лекарства и аллергии, сон, аппетит, переносимость нагрузок, возможность обеспечить тишину на месте. На основе этих фактов врач предлагает безопасную точку входа: выезд на дом, приём без очередей или госпитализацию под наблюдением 24/7. На месте мы сразу исключаем «красные флажки», фиксируем давление/пульс/сатурацию/температуру, при показаниях выполняем ЭКГ и запускаем детокс. Параллельно выдаём «карту суток»: режим отдыха и питья, лёгкое питание, перечень нормальных ощущений и момент, когда нужно связаться внепланово. Если домашнего формата становится мало, переводим в стационар без пауз — все назначения и наблюдения «переезжают» вместе с пациентом.
Подробнее тут – круглосуточная наркологическая клиника
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Исследовать вопрос подробнее – https://aamirpathan.com/welcome-to-my-profile-aamir-pathan-3
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Углубиться в тему – вывод из запоя капельница
Когда самочувствие «скачет», а ночь грозит затянуться, важен не героизм, а клинически выверенный план. В «МедОпоре» в Красногорске мы выстраиваем помощь так, чтобы каждый шаг давал предсказуемый эффект: первичное обследование, персональная инфузионная терапия, бережная коррекция тревоги и сна, мониторинг жизненно важных показателей и подробные рекомендации для семьи. Мы не используем «универсальные коктейли» и не маскируем симптомы — задача детокса в том, чтобы снять токсическую нагрузку, восстановить водно-электролитный баланс, стабилизировать вегетативные реакции и вернуть управляемость состоянием. С первых минут пациент получает ясные ориентиры: что делаем сейчас, чего ждать через час, по каким признакам нужно срочно звать врача. Анонимность соблюдается без компромиссов, а решения принимаются на основе реальных показателей — это снижает тревогу и исключает опасные «домашние эксперименты».
Получить дополнительные сведения – нарколог вывод из запоя
Когда уместен
Подробнее – https://narkologicheskaya-klinika-shchyolkovo0.ru/narkologicheskaya-klinika-ceny-v-shchyolkovo/
Ahaa, its fastidious discussion regarding this post here at this web site, I have read all that, so at
this time me also commenting at this place.
For most recent news you have to pay a visit internet and on the web
I found this site as a finest site for newest
updates.
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Получить дополнительные сведения – вывод из запоя на дому недорого
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Желаете узнать подробности? – http://lerstol.no/2013/09/05/5-september
Стоимость зависит от длительности запоя, объёма инфузий, перечня препаратов и длительности наблюдения после капельницы. Мы заранее озвучиваем ориентир, объясняем, какие элементы плана обязательны, а какие — рекомендательные. Ночные выезды иногда дороже из-за нагрузки на бригаду, но при выраженных симптомах откладывать помощь небезопасно. Повторные обращения и расширенные программы стабилизации обсуждаются индивидуально. Ключевой ориентир для семьи — выбирать не «самую дешёвую капельницу», а безопасный формат с контролем и ответственным уходом.
Исследовать вопрос подробнее – http://vyvod-iz-zapoya-korolev10.ru
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Детальнее – анонимный вывод из запоя нижний новгород
Формат
Изучить вопрос глубже – https://narkologicheskaya-klinika-ehlektrostal0.ru/anonimnaya-narkologicheskaya-klinika-v-ehlektrostali
It’s continually awesome when you can not only be informed, but also entertained! I’m sure you had fun writing this article. Regards, Clotilde.
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительные сведения – http://vyvod-iz-zapoya-sochi15.ru/
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Узнать больше – наркологический вывод из запоя
I believe what you posted was actually very logical.
But, what about this? what if you typed a catchier title?
I ain’t suggesting your content is not solid, however suppose you added a post title to maybe grab people’s attention? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate is kinda
boring. You could peek at Yahoo’s front page and see how they create
article titles to get viewers to click. You might add
a video or a pic or two to get people excited about what you’ve written. Just my opinion, it could bring your posts a
little livelier.
Hey there would you mind sharing which blog platform you’re working with?
I’m looking to start my own blog in the near future but I’m having a
hard time deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems different then most
blogs and I’m looking for something unique.
P.S My apologies for getting off-topic but I had to ask!
Самый частый повод — не только «плохое похмелье», а именно абстинентный синдром после запоя: когда самочувствие ухудшается при прекращении алкоголя, а попытки «опохмелиться» лишь продлевают проблему. Важно ориентироваться не на терпимость человека к дискомфорту, а на объективные признаки: если симптомы нарастают, сон сорван, поведение становится нестабильным, а тело реагирует паникой, тремором и скачками давления, лучше не тянуть. Особенно осторожными нужно быть при хронических болезнях сердца, печени и сосудов: при них цена ошибки выше, а «универсальные» домашние схемы могут навредить.
Получить больше информации – https://narkolog-na-dom-krasnogorsk6.ru/narkologicheskaya-klinika-krasnogorsk
Сайт Olimp Casino достойный. Обязательно загляну ещё!
Olimp Casino официальный сайт (http://www.irodabutor.ardoboz.hu/r.php?b=aHR0cHM6Ly9vbGltcC1jYXNpbm8ta2F6YWtoc3Rhbi1rYXoua3ovZ2FtZXM)
Undeniably imagine that which you said. Your favourite reason seemed to be at the web the simplest factor to be aware of.
I say to you, I definitely get irked whilst other folks think about
worries that they just do not recognise about. You managed to hit the nail upon the
top as well as defined out the entire thing without having side effect
, other folks can take a signal. Will probably be
back to get more. Thank you
Definitely imagine that which you said. Your favourite reason appeared to be at the net the simplest factor to take into account of.
I say to you, I certainly get annoyed whilst other people consider worries that they just don’t realize about.
You controlled to hit the nail upon the top and also outlined
out the whole thing with no need side-effects , folks could take a signal.
Will likely be back to get more. Thank you
Also visit my web-site – realtor in Ann Arbor MI
I think this is one of the such a lot important info
for me. And i’m glad studying your article. However want to observation on some
common issues, The website style is perfect,
the articles is in reality great : D. Excellent process, cheers
Мы выезжаем в любое время дня и ночи. Организационно всё просто: короткий звонок с описанием состояния, согласование адреса и времени, консультация по подготовке помещения, приезд врача. Если состояние тяжёлое (длительный запой, возраст 60+, выраженная соматика, признаки делирия, многократная рвота, спутанность сознания), медик предложит стационар сразу — это безопаснее, чем пытаться «дотянуть» ночь дома. В клинике пациент находится под круглосуточным наблюдением, при необходимости выполняются дополнительные исследования, расширяется объём инфузий, корректируется медикаментозная схема. Для пожилых и кардиологических пациентов стационарный формат часто предпочтителен: непрерывный мониторинг снижает риски и ускоряет стабилизацию.
Ознакомиться с деталями – http://vyvod-iz-zapoya-korolev10.ru
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Изучить вопрос глубже – нарколог на дом недорого в сочи
I visited several websites but the audio
quality for audio songs current at this site is really
wonderful.
my web site best realtor in Cincinnati OH
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Выяснить больше – http://vyvod-iz-zapoya-sochi15.ru/
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Желаете узнать подробности? – https://www.abcconsulting-cr.com/2021/08/22/fiscalia-adjunta-de-goicoechea
Howdy exceptional website! Does running a blog similar to this take a
massive amount work? I have very little expertise in computer programming but I had
been hoping to start my own blog soon. Anyways, if you have any ideas or techniques for new blog owners please
share. I understand this is off topic nevertheless I just had to ask.
Thanks a lot!
my page realtor in Tipp City OH
Формат помощи на дому особенно важен, когда человек физически не в состоянии добраться до клиники, боится огласки или требуется поддержка семьи «здесь и сейчас». Врач оценивает риски, подбирает схему детоксикации по состоянию и даёт понятный план дальнейших шагов: что делать в первые сутки, чего избегать, какие симптомы считать тревожными и когда нужно повторное обращение.
Ознакомиться с деталями – https://narkolog-na-dom-krasnogorsk6.ru/
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Хочешь знать всё? – https://vistoweekly.com/lakeshore-industrial-m46-inspection
Hello there, You’ve done a great job. I’ll certainly digg it and personally
recommend to my friends. I am confident they will be benefited from this website.
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Подробнее можно узнать тут – вывод из запоя на дому цена
I used to be suggested this web site by way of my cousin. I am
not positive whether or not this put up is written by way of him as no one
else understand such designated approximately my problem.
You’re wonderful! Thank you!
I know this if off topic but I’m looking into starting my own blog and was curious what all
is needed to get setup? I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet savvy so I’m not 100% sure.
Any tips or advice would be greatly appreciated.
Many thanks
Jungle Driving School Omaha
4020 Ѕ 147th St, Omaha,
NE 68137, United Stateѕ
14024170547
professional driver coach (wakelet.com)
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Смотрите также… – https://www.geo.sc.chula.ac.th/contact
Hey there! I know this is kinda off topic but I was wondering if you knew where I could find a captcha plugin for my
comment form? I’m using the same blog platform as yours and I’m having trouble finding one?
Thanks a lot!
هذا منشور مهم جداً. التمويل
الجماعي الطبي يغير مستقبل الناس الذين لا يستطيعون دفع تكاليف الجراحة.
دعم مؤسسة البصر هو عمل رائع حقاً.
شكراً لـ مشاركة هذه المهمة.
Check out my page: رؤية جديدة للمرضى
Цель
Выяснить больше – http://narkologicheskaya-klinika-shchyolkovo0.ru/narkologicheskaya-klinika-ceny-v-shchyolkovo/
This is an awesome entry. Thank you very much for the supreme post provided! I was looking for this entry for a long time, but I wasn’t able to find a honest source.
Hello would you mind letting me know which web host
you’re working with? I’ve loaded your blog in 3
different browsers and I must say this blog loads a
lot quicker then most. Can you suggest a good internet hosting
provider at a fair price? Cheers, I appreciate it!
hi!,I like your writing so a lot! proportion we be in contact extra about your article on AOL?
I need a specialist in this house to unravel my problem.
May be that’s you! Taking a look forward to
peer you.
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Разобраться лучше – вывод из запоя на дому круглосуточно
I am sure this article has touched all the internet visitors, its really really good paragraph on building up new website.
Как выбрать идеальный купальник
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее можно узнать тут – https://vyvod-iz-zapoya-sochi22.ru
Чтобы легче сопоставить риски и плотность наблюдения, ниже даём живой ориентир. Это не заменяет осмотр, но помогает всей семье понимать логику врача до приезда.
Получить дополнительные сведения – http://narkologicheskaya-klinika-domodedovo0.ru/narkologicheskaya-klinika-telefon-v-domodedovo/
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Получить дополнительные сведения – вывод из запоя капельница на дому в нижнем новгороде
Когда уместен
Получить дополнительные сведения – https://narkologicheskaya-klinika-serpuhov0.ru/anonimnaya-narkologicheskaya-klinika-v-serpuhove/
Клиника «Похмельная служба» в Нижнем Новгороде предлагает комплексное лечение запоя с использованием капельницы. Наши специалисты проводят диагностику и назначают индивидуальный план лечения.
Узнать больше – вывод из запоя капельница на дому в нижнем новгороде
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Разобраться лучше – вывод из запоя в стационаре сочи
Awesome! Its truly amazing article, I have got much clear idea concerning from this
piece of writing.
Feel free to surf to my web site – best real estate agent in Ocean Isle Beach NC
Выездная бригада «МедОпоры» дежурит 24/7 и покрывает весь Красногорск и близлежащие районы. После короткого звонка дежурный уточняет длительность запоя, сопутствующие болезни, принимаемые препараты и аллергии — это экономит время на месте и помогает заранее предусмотреть риски. Врач приезжает с комплектом одноразовых систем, растворами и медикаментами, проводит экспресс-диагностику: измерение давления, пульса, сатурации, температуры, оценка неврологического статуса, степени обезвоживания и тревожности. По этим данным формируется индивидуальная схема инфузий и симптоматической поддержки. Наша задача — не просто «поставить капельницу», а безопасно развернуть план стабилизации, где дозировки и темп меняются по реакции организма. Если выявляются признаки осложнений или дома нет условий для безопасного наблюдения, сразу предлагаем перевод в профильный стационар, чтобы не терять драгоценные часы. Семья получает понятные роли и инструкции, а врач остаётся на связи для уточнений по режиму ближайшей ночи.
Подробнее тут – https://vyvod-iz-zapoya-krasnogorsk10.ru/vyvod-iz-zapoya-klinika-v-krasnogorske
Цель и ожидаемая динамика
Разобраться лучше – narkologicheskaya-klinika-na-dom
Erectile Dysfunction affects numerous men worldwide, impacting self-confidence, affection, and general lifestyle. Tadalafil has become a relied on solution, supplying durable support for sexual performance. Available in different toughness, consisting of Tadalafil 5mg, Tadalafil 10mg, and Tadalafil 20mg, it offers versatility for different requirements. Comprehending the correct use, benefits, and how to Acquire Tadalafil properly is vital for guys seeking to reclaim spontaneity and self-confidence, https://gab.com/AngeliqueBrady/posts/115847619175244098.
Spot on with this write-up, I actually believe this amazing site
needs a lot more attention. I’ll probably be returning to read more, thanks for
the info!
Цель
Выяснить больше – narkologicheskaya-klinika-korolev
Great items from you, man. I have bear in mind your stuff previous to and you are simply extremely magnificent.
I actually like what you’ve bought right here, certainly like what you’re
saying and the way in which in which you say it. You’re making
it entertaining and you still take care of to stay it sensible.
I can’t wait to read much more from you. This is really
a wonderful web site.
my blog post; best real estate agent in West Chester Township OH
I read this post completely regarding the comparison of latest and previous technologies, it’s awesome article.
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Желаете узнать подробности? – https://www.verputzer.net/verputzer-bad_kreuznach
«Вектор Надежды» выстраивает помощь так, чтобы с первого звонка убрать неопределённость и вернуть ощущение контроля. Дежурный врач аккуратно собирает только необходимую информацию, оценивает риски и предлагает безопасный старт: выезд на дом, дневной маршрут или стационар с наблюдением 24/7. Мы объясняем каждую манипуляцию простым языком — что именно будет сделано в ближайшие часы, каких изменений ожидать к вечеру, почему выбран именно такой темп и как поймём, что схема работает. Конфиденциальность — не дополнение, а стандарт: нейтральные звонки, неброская атрибутика, ограниченный доступ к карте, отсутствие постановки на учёт. Такой регламент снижает тревогу, экономит силы семьи и ускоряет стабилизацию: вместо «марафона кабинетов» — один связный маршрут с понятными контрольными точками.
Подробнее тут – https://narkologicheskaya-klinika-shchyolkovo0.ru/narkologicheskaya-klinika-ceny-v-shchyolkovo/
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy menara188
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Получить дополнительную информацию – вывод из запоя капельница
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее – нарколог на дом краснодарский край
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Получить больше информации – нарколог на дом недорого
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Получить больше информации – вывод из запоя на дому круглосуточно
Hello, just wanted to mention, I liked this blog post.
It was funny. Keep on posting!
Маршрут начинается с короткого скрининга, чтобы понять риски и условия дома. Мы согласуем окно приезда или время приёма, заранее подскажем, как подготовить пространство: тишина, доступ к воде и розетке, возможность прилечь. На месте врач фиксирует витальные показатели (АД, пульс, сатурация, температура), при показаниях выполняет ЭКГ и запускает детокс-терапию. Уже на старте вы получаете письменную памятку «на сутки»: режим сна и гидратации, «красные флажки» и точное время контрольной связи. Если домашний формат перестаёт быть достаточным, организуем перевод в стационар без пауз — темп лечения сохраняется.
Изучить вопрос глубже – наркологическая клиника
перейдите на этот сайт krab2cc
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Исследовать вопрос подробнее – нарколог на дом вывод из запоя
Hello there, I do think your website may be having web browser compatibility issues.
When I take a look at your site in Safari, it looks fine however when opening in Internet Explorer, it has some
overlapping issues. I merely wanted to provide you with a quick
heads up! Apart from that, wonderful site!
Hello, all the time i used to check blog posts here in the early hours in the morning,
because i like to learn more and more.
My web page: best real estate agent in Ocean Isle Beach NC
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее можно узнать тут – вывод из запоя на дому цена сочи
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Изучить вопрос глубже – вывод из запоя капельница нижний новгород
You expressed it wonderfully!
Если нужен профессиональный вывод из запоя, обращайтесь в стационар клиники «Детокс» в Сочи. Все процедуры проводятся анонимно и под наблюдением специалистов.
Получить больше информации – вывод из запоя дешево сочи
Формат
Изучить вопрос глубже – наркологическая клиника нарколог
Когда самочувствие «скачет», а ночь грозит затянуться, важен не героизм, а клинически выверенный план. В «МедОпоре» в Красногорске мы выстраиваем помощь так, чтобы каждый шаг давал предсказуемый эффект: первичное обследование, персональная инфузионная терапия, бережная коррекция тревоги и сна, мониторинг жизненно важных показателей и подробные рекомендации для семьи. Мы не используем «универсальные коктейли» и не маскируем симптомы — задача детокса в том, чтобы снять токсическую нагрузку, восстановить водно-электролитный баланс, стабилизировать вегетативные реакции и вернуть управляемость состоянием. С первых минут пациент получает ясные ориентиры: что делаем сейчас, чего ждать через час, по каким признакам нужно срочно звать врача. Анонимность соблюдается без компромиссов, а решения принимаются на основе реальных показателей — это снижает тревогу и исключает опасные «домашние эксперименты».
Детальнее – http://vyvod-iz-zapoya-krasnogorsk10.ru
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Уточнить детали – https://www.kenko-support1.com/%E3%82%B9%E3%82%A4%E3%83%B3%E3%82%B0%E3%83%90%E3%83%BC-%E3%83%97%E3%83%AD%E3%80%80m%E3%82%B5%E3%82%A4%E3%82%BA%E3%81%A8l%E3%82%B5%E3%82%A4%E3%82%BA%E3%82%92%E9%81%B8%E3%81%B6%E5%9F%BA%E6%BA%96
I’d like to find out more? I’d want to find out some additional information.
Review my homepage MANTULHOKI
Its like you read my mind! You appear to know so much about
this, like you wrote the book in it or something. I think that you could do with a few
pics to drive the message home a little bit, but other than that, this is excellent blog.
A great read. I will certainly be back.
Когда ночь затягивается, тревога нарастает, а самочувствие «скачет», важны не громкие обещания, а последовательность медицинских действий. «Трезвый Контур» в Одинцово выстраивает помощь так, чтобы от звонка до облегчения прошло минимум времени и ни один шаг не был импровизацией: первичная оценка рисков, персональная инфузионная терапия, мягкая коррекция сна и тревоги, регулярные замеры показателей, понятные рекомендации для семьи. Мы не используем «универсальные коктейли» и не «вырубаем» пациента сильными седативными — дозировки и темп капельниц подбираются под возраст, длительность запоя, сопутствующие заболевания и уже принимаемые препараты. Цель — быстро снять токсическую нагрузку, стабилизировать давление и пульс, вернуть управляемый сон и зафиксировать маршрут на ближайшие 24–72 часа, чтобы утро началось не с нового витка симптомов, а с предсказуемого восстановления.
Изучить вопрос глубже – http://vyvod-iz-zapoya-odincovo10.ru/vyvod-iz-zapoya-ryadom-v-odincovo/
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Подробнее можно узнать тут – вывод из запоя цена нижний новгород
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Получить дополнительную информацию – http://vyvod-iz-zapoya-sochi22.ru/
This paragraph provides clear idea in favor of the new visitors
of blogging, that truly how to do blogging.
Good day! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve
worked hard on. Any recommendations?
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Изучить вопрос глубже – анонимный вывод из запоя в сочи
Sweet blog! I found it while searching on Yahoo News. Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Many thanks
Hello there! I could have sworn I’ve visited your blog before but
after browsing through some of the articles I
realized it’s new to me. Regardless, I’m definitely delighted
I discovered it and I’ll be book-marking it and checking back frequently!
my site … realtor in Bedford NH
Howdy great blog! Does running a blog such as this require a massive
amount work? I’ve no knowledge of computer programming however I had been hoping to start my own blog in the near future.
Anyway, if you have any recommendations or tips for new blog owners please share.
I know this is off subject but I simply had to ask. Appreciate it!
Every weekend i used to pay a visit this site, for the reason that i wish for enjoyment, since this this website conations genuinely good funny material
too.
Формат
Подробнее можно узнать тут – zapoj-narkologicheskaya-klinika
Do you have a spam issue on this site; I also am a blogger, and
I was wanting to know your situation; we have developed some nice practices and we are looking to swap techniques with other folks, why not shoot me an email if interested.
Here is my web site: best real estate agent in Vancouver BC
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
А что дальше? – https://www.alfo.co.jp/topics-news/20170630
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Изучить вопрос глубже – вызов нарколога на дом в сочи
Thank you for the auspicious writeup. It if truth
be told used to be a enjoyment account it. Glance advanced to more introduced agreeable from
you! By the way, how can we keep in touch?
Если нужен профессиональный вывод из запоя, обращайтесь в стационар клиники «Детокс» в Сочи. Все процедуры проводятся анонимно и под наблюдением специалистов.
Подробнее тут – вывод из запоя капельница
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Исследовать вопрос подробнее – врач вывод из запоя в сочи
Формат
Узнать больше – narkologicheskaya-klinika-stacionar
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Получить дополнительные сведения – нарколог на дом недорого сочи
Когда самочувствие «скачет», а ночь грозит затянуться, важен не героизм, а клинически выверенный план. В «МедОпоре» в Красногорске мы выстраиваем помощь так, чтобы каждый шаг давал предсказуемый эффект: первичное обследование, персональная инфузионная терапия, бережная коррекция тревоги и сна, мониторинг жизненно важных показателей и подробные рекомендации для семьи. Мы не используем «универсальные коктейли» и не маскируем симптомы — задача детокса в том, чтобы снять токсическую нагрузку, восстановить водно-электролитный баланс, стабилизировать вегетативные реакции и вернуть управляемость состоянием. С первых минут пациент получает ясные ориентиры: что делаем сейчас, чего ждать через час, по каким признакам нужно срочно звать врача. Анонимность соблюдается без компромиссов, а решения принимаются на основе реальных показателей — это снижает тревогу и исключает опасные «домашние эксперименты».
Подробнее тут – вывод из запоя капельница на дому
obviously like your website however you have to take a look at the spelling on quite a
few of your posts. Several of them are rife with spelling issues and I
find it very bothersome to inform the reality nevertheless I will definitely come again again.
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Детальнее – https://www.my-energyco.com/modern-sidebar
This post is truly a good one it assists new web visitors, who are wishing in favor of blogging.
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Изучить вопрос глубже – анонимный вывод из запоя в сочи
Если пациент не может приехать в клинику, в Краснодаре нарколог приедет к нему домой. Помощь оказывает «Детокс» круглосуточно.
Изучить вопрос глубже – vrach-narkolog-na-dom sochi
Someone necessarily lend a hand to make severely articles I would
state. That is the first time I frequented your web page and to
this point? I surprised with the analysis you made to create this
actual put up amazing. Excellent activity!
Thanks on your marvelous posting! I really enjoyed reading it, you’re
a great author. I will be sure to bookmark your blog and
definitely will come back in the foreseeable future.
I want to encourage you to ultimately continue your great
posts, have a nice evening!
My homepage – cara pilih slot gacor
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Открой скрытое – https://e-markethings.com/product/sendblaster-pro-edition
Экстренная помощь при запое в Нижнем Новгороде — капельница на дому от опытных врачей-наркологов.
Получить дополнительную информацию – вывод из запоя на дому нижний новгород
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врач приедет в течение 1–2 часов, проведёт необходимое обследование и назначит лечение. Услуга доступна круглосуточно и анонимно.
Получить дополнительные сведения – нарколог на дом недорого сочи
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Ознакомиться с деталями – вывод из запоя капельница на дому в сочи
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Детальнее – врач нарколог на дом краснодарский край
Ниже — краткий ориентир, который помогает семье понимать логику рекомендаций до очного осмотра. Это не «замена врачу», а понятная рамка для принятия решения о старте.
Детальнее – наркологическая клиника на дом
I’m more than happy to find this great site. I need to to
thank you for your time just for this wonderful read!!
I definitely savored every little bit of it and i also have you saved as a favorite to
see new things in your web site.
Also visit my site: realtor in Ocean Isle Beach NC
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Изучить вопрос глубже – нарколог на дом недорого сочи
This is really interesting, You are a very skilled blogger.
I’ve joined your rss feed and look forward to seeking more of your magnificent post.
Also, I’ve shared your site in my social networks!
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Ознакомиться с деталями – https://vyvod-iz-zapoya-sochi15.ru
Цель
Подробнее можно узнать тут – наркологическая клиника в королеве
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Детальнее – вывод из запоя вызов сочи
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Подробнее – https://snyatie-zapoya-na-domu11.ru
Формат
Узнать больше – https://narkologicheskaya-klinika-krasnogorsk0.ru/narkologicheskaya-klinika-ceny-v-krasnogorske
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Выяснить больше – запой нарколог на дом в сочи
Fantastic items from you, man. I’ve take into accout your stuff previous to and you’re simply extremely magnificent.
I actually like what you’ve received right here, certainly like what you are saying and the best way by which you assert it.
You make it entertaining and you continue to take
care of to keep it sensible. I can not wait to read much more from
you. That is really a great site.
Greate post. Keep writing such kind of info on your site.
Im really impressed by your site.
Hey there, You’ve performed a fantastic job. I’ll definitely digg it and in my opinion suggest to my friends.
I’m sure they will be benefited from this website.
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Исследовать вопрос подробнее – анонимный вывод из запоя нижний новгород
Hey would you mind stating which blog platform you’re working with?
I’m planning to start my own blog in the near future but I’m having a tough time
selecting between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems different then most blogs and I’m
looking for something unique. P.S Sorry for getting off-topic but I had to ask!
find this toast wallet passphrase
After looking over a number of the articles on your web page,
I honestly like your way of blogging. I added it to my bookmark site list and will
be checking back in the near future. Take a look at my website as well
and let me know your opinion.
Две похожие ситуации никогда не бывают одинаковыми: возраст, вес, сопутствующие болезни, длительность запоя и переносимость препаратов формируют уникальную клиническую картину. Мы исключаем «универсальные» схемы, чтобы не перегрузить организм и не вызвать побочных реакций. Инфузии проводятся только одноразовыми системами, врач соблюдает стерильность, контролирует дозировки и следит за динамикой симптомов. Мы уделяем особое внимание сну и уровню тревоги в первые часы после детокса — именно эти параметры влияют на риск срыва. Для пациентов с сердечно-сосудистыми, эндокринными и неврологическими заболеваниями детоксикация планируется особенно осторожно; при малейших сомнениях мы предлагаем стационар и разъясняем семье, почему это безопаснее.
Разобраться лучше – http://vyvod-iz-zapoya-korolev10.ru
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Подробнее можно узнать тут – нарколог на дом недорого
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Изучить вопрос глубже – вывод из запоя на дому цена
Когда уместен
Получить дополнительные сведения – https://narkologicheskaya-klinika-krasnogorsk0.ru/narkologicheskaya-klinika-ceny-v-krasnogorske/
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительные сведения – врач вывод из запоя в сочи
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Ознакомиться с деталями – вывод из запоя цена сочи
I do consider all the concepts you’ve offered to your post.
They are very convincing and can certainly work.
Nonetheless, the posts are very quick for starters. May you please extend them
a bit from subsequent time? Thank you for the post.
Also visit my webpage – MANTULHOKI
Обычно внимание уделяется нескольким направлениям: восстановлению жидкости и обмена веществ, снижению тошноты и головной боли, уменьшению вегетативных симптомов (дрожь, потливость, сердцебиение), нормализации сна и тревоги. При этом врач ориентируется на текущие показатели и реакцию пациента — то, что помогало «в прошлый раз», может быть неуместно сегодня. Дополнительно проговариваются бытовые детали: проветривание, комфортная температура, питьевой режим, питание небольшими порциями, контроль давления и пульса, ограничение стимуляторов и рисковых нагрузок.
Детальнее – https://narkolog-na-dom-krasnogorsk6.ru/narkolog-v-krasnogorske/
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
А что дальше? – https://oneinfoafrica.com/index.php/2024/04/12/comoros-jailbreak-in-moroni-comoros-as-dozens-escaped
«Вектор Надежды» выстраивает помощь так, чтобы с первого звонка убрать неопределённость и вернуть ощущение контроля. Дежурный врач аккуратно собирает только необходимую информацию, оценивает риски и предлагает безопасный старт: выезд на дом, дневной маршрут или стационар с наблюдением 24/7. Мы объясняем каждую манипуляцию простым языком — что именно будет сделано в ближайшие часы, каких изменений ожидать к вечеру, почему выбран именно такой темп и как поймём, что схема работает. Конфиденциальность — не дополнение, а стандарт: нейтральные звонки, неброская атрибутика, ограниченный доступ к карте, отсутствие постановки на учёт. Такой регламент снижает тревогу, экономит силы семьи и ускоряет стабилизацию: вместо «марафона кабинетов» — один связный маршрут с понятными контрольными точками.
Детальнее – anonimnaya-narkologicheskaya-klinika
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Исследовать вопрос подробнее – вывод из запоя в стационаре нижний новгород
Каждый день подвеска автомобиля принимает удары вместо тебя: ямы, стыки мостов, бордюры — всё это постепенно разрушает её элементы. Ремонт ходовой части автомобиля — реальная возможность продлить срок службы машины и восстановить комфорт. Проверяем износ амортизаторов, стойки стабилизатора, рулевые наконечники, тормозные механизмы и состояние креплений. Диагностика выявляет даже скрытые проблемы, которые ещё не слышны, но уже опасны. После грамотного ремонта руль перестаёт «гулять», исчезают стуки, автомобиль уверенно держит траекторию. Доступные цены, профессиональные мастера, качественные детали. Надёжный сервис, где уделяют внимание каждому болту.
Heya i’m for the first time here. I came across this board and I
find It truly useful & it helped me out much.
I hope to give something back and help others like you aided me.
Your style is unique in comparison to other people I’ve read stuff from.
I appreciate you for posting when you have the opportunity, Guess I will just book mark this page.
Also visit my blog raised garden beds
We are a bunch of volunteers and starting a brand new scheme in our community.
Your website offered us with helpful information to work on. You’ve
performed a formidable activity and our entire community might be thankful to you.
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Получить дополнительные сведения – нарколог на дом вывод из запоя в сочи
I am really enjoying the theme/design of your website.
Do you ever run into any web browser compatibility problems?
A couple of my blog readers have complained about my website not operating correctly in Explorer but looks great in Opera.
Do you have any recommendations to help fix this issue?
Also visit my web site; real estate agent in West Chester Township OH
We stumbled over here coming from a different web address and thought I may as well check things out.
I like what I see so now i’m following you.
Look forward to looking at your web page repeatedly.
Also visit my web-site :: real estate agent in Whittier CA
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Исследовать вопрос подробнее – вывод из запоя на дому цена
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Исследовать вопрос подробнее – вывод из запоя на дому недорого сочи
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Получить дополнительную информацию – https://suki.one/music/27?replyTo=39522
It’s very easy to find out any topic on net as compared to textbooks, as I found this paragraph at this web page.
obat aborsi,aborsi,child porn,child porn video,porn child,child porn videos,child porn site,child porn situs,child seks porn,child
porn web,child porn seks,small child porn,mother and child
porn,porn child video,KONTOL,chinese child
porn,mom and child porn,child porn sites,porn small child,child porn video,child gay porn,gay
child porn,child porn link,child porn xxx,child porn hub,child porn free,
child porn vid,how to watch child porn,porn mother and child,ai
child porn,seks child porn,how to find child porn,child and mom porn,watch
child porn,video porn child,porn with child,porn hub child,porn mom and child,gay porn child,child girl porn
I visited several web pages however the audio feature
for audio songs present at this website is genuinely wonderful.
I will right away take hold of your rss feed as I can’t to find your email subscription link or newsletter service.
Do you have any? Kindly let me recognise so that I could
subscribe. Thanks.
Here is my page best real estate agent in Whittier CA
Что включено на практике
Узнать больше – http://narkologicheskaya-klinika-krasnogorsk0.ru
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Получить больше информации – вывод из запоя цена в сочи
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Углубиться в тему – нарколог на дом вывод в сочи
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Разобраться лучше – вывод из запоя в стационаре
Что включено на практике
Выяснить больше – narkologicheskaya-klinika-narkolog
Hey would you mind letting me know which webhost you’re utilizing?
I’ve loaded your blog in 3 different browsers and I must say this blog loads a lot faster
then most. Can you suggest a good web hosting provider at
a fair price? Thank you, I appreciate it!
Hi friends, how is the whole thing, and what you would like to say on the topic of this article,
in my view its really amazing designed for me.
Excellent article. Keep posting such kind of info on your blog.
Im really impressed by it.
Hey there, You’ve performed a fantastic job. I will definitely digg it and
personally suggest to my friends. I’m sure they’ll be benefited from this web site.
Bu saytdakı məlumatları oxumaqdan zövq alıram. Təşəkkürlər!
https://lnkz.at/4JFJ0
What’s up everybody, here every person is sharing these kinds of familiarity, therefore it’s pleasant to read this
blog, and I used to go to see this webpage everyday.
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Подробнее можно узнать тут – наркологический вывод из запоя в нижнем новгороде
Hello mates, nice paragraph and good arguments commented here, I am really enjoying by these.
Here is my web page; realtor in Bedford NH
Hey! This post could not be written any better!
Reading through this post reminds me of my previous room mate!
He always kept talking about this. I will forward this article app to settle shared payments easily him.
Pretty sure he will have a good read. Thanks for sharing!
obat aborsi,aborsi,child porn,child porn video,porn child,child porn videos,child
porn site,child porn website,child seks porn,child porn situs,
child porn seks,small child porn,mother and child porn,porn child video,KONTOL,chinese child porn,mom and child porn,child porn sites,porn small child,child porn video,child gay porn,gay child porn,child porn link,child porn xxx,child porn hub,child porn free,child porn vid,how to watch child porn,porn mother and child,
ai child porn,seks child porn,how to find child porn,child and
mom porn,watch child porn,video porn child,porn with child,porn hub child,
porn mom and child,gay porn child,child girl porn
Что получите за 24 часа
Углубиться в тему – https://narkologicheskaya-klinika-domodedovo0.ru/narkologicheskaya-klinika-ceny-v-domodedovo
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Разобраться лучше – вывод из запоя цена сочи
Цель и ожидаемая динамика
Изучить вопрос глубже – http://narkologicheskaya-klinika-odincovo0.ru
대단하다! 정말 놀라운 포스트입니다, 이 단락에서 많은 명확한 아이디어를 얻었습니다.
Hmm is anyone else experiencing problems with the pictures on this blog loading?
I’m trying to find out if its a problem on my end or if it’s
the blog. Any feed-back would be greatly appreciated.
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Изучить вопрос глубже – вывод из запоя капельница на дому сочи
Инфузионная терапия подбирается под человека, а не под «среднюю» ситуацию. Базовый каркас обычно включает растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы. По показаниям добавляются гепатопротекторы и антиоксидантные компоненты — это помогает печени и снижает оксидативный стресс. Если есть выраженная тошнота, подключаем противорвотные; при тревоге и нарушении сна — мягкие анксиолитики и седативные препараты, которые не «вырубают», а выравнивают ритмы и сохраняют контакт для мониторинга. Мы избегаем агрессивных «миксов», потому что избыточная седация может скрыть опасные симптомы и усложнить оценку состояния. Эффективность оцениваем не только по субъективному облегчению, но и по объективным метрикам: пульс, давление, сатурация, динамика тремора, аппетит, качество сна. Как только показатели стабилизируются, фарм-нагрузка снижается, а ведущую роль берет режим — питание, гидратация, спокойный вечерний ритуал, короткие бытовые активности.
Детальнее – https://vyvod-iz-zapoya-krasnogorsk10.ru/kruglosutochno-vyvod-iz-zapoya-v-krasnogorske/
see it here jax wallet
Чтобы легче сопоставить риски и плотность наблюдения, ниже даём живой ориентир. Это не заменяет осмотр, но помогает всей семье понимать логику врача до приезда.
Получить дополнительную информацию – http://narkologicheskaya-klinika-domodedovo0.ru
Цель
Выяснить больше – https://narkologicheskaya-klinika-serpuhov0.ru/narkologicheskaya-klinika-stacionar-v-serpuhove/
This is very interesting, You are a very skilled blogger.
I have joined your rss feed and look forward to
seeking more of your excellent post. Also, I have shared your site in my social networks!
Attractive section of content. I just stumbled upon your web site and in accession capital to assert that I acquire actually enjoyed account your blog posts.
Anyway I’ll be subscribing to your augment and even I achievement you access consistently quickly.
I was recommended this blog by my cousin. I’m not sure whether this post is written by him
as nobody else know such detailed about my difficulty. You’re amazing!
Thanks!
my webpage: best realtor in Ann Arbor MI
Если пациент не может приехать в клинику, в Краснодаре нарколог приедет к нему домой. Помощь оказывает «Детокс» круглосуточно.
Детальнее – нарколог на дом анонимно сочи
I have been browsing on-line greater than three hours
nowadays, yet I never found any attention-grabbing article like yours.
It is lovely price sufficient for me. In my opinion, if all website owners and bloggers made just
right content as you probably did, the internet will probably be a lot more helpful than ever before.
Ниже — ориентир, который помогает сопоставить риски, плотность наблюдения и ожидаемую скорость стабилизации. Таблица не заменяет очный осмотр, но экономит время на принятие решений и делает логику врача понятной всей семье.
Ознакомиться с деталями – http://narkologicheskaya-klinika-odincovo0.ru/narkologicheskaya-klinika-narkolog-v-odincovo/
ข้อมูลชุดนี้ อ่านแล้วเพลินและได้สาระ ครับ
ผม ไปอ่านเพิ่มเติมเกี่ยวกับ หัวข้อที่คล้ายกัน
ที่คุณสามารถดูได้ที่ Deloras
สำหรับใครกำลังหาเนื้อหาแบบนี้
เพราะอธิบายไว้ละเอียด
ขอบคุณที่แชร์ คอนเทนต์ดีๆ นี้
จะรอติดตามเนื้อหาใหม่ๆ ต่อไป
If you are going for finest contents like me, only pay a visit this site every
day for the reason that it provides quality contents, thanks
my homepage :: best real estate agent in Bedford NH
Кроме безопасности и мониторинга — дисциплину режима. Там легче убрать триггеры, выстроить питание и сон, а психологу — подключить короткие мотивационные сессии, которые помогут удержать результат после выписки.
Разобраться лучше – https://vyvod-iz-zapoya-krasnogorsk10.ru/vyvod-iz-zapoya-na-domu-v-krasnogorske/
Amazing! Its in fact amazing article, I have got much clear idea about
from this piece of writing.
В Королёве мы запускаем помощь без «многоходовок». С первого контакта дежурный врач аккуратно уточняет жалобы, длительность эпизода, принимаемые лекарства и сопутствующие диагнозы, после чего предлагает безопасную точку входа: выезд на дом, дневной формат или круглосуточный стационар. Каждое действие объясняется простым языком: зачем оно нужно, какого эффекта ждать в ближайшие часы и что будет считаться нормальной динамикой. Конфиденциальность заложена в процесс по умолчанию: минимально необходимый объём персональных данных, нейтральная коммуникация, ограниченный доступ к медкарте и отсутствие постановки на учёт. Такой порядок снимает лишнее напряжение у семьи и экономит самое ценное — время.
Выяснить больше – narkologicheskaya-klinika-nedorogo
Magnificent items from you, man. I’ve be mindful your stuff
previous to and you’re just extremely magnificent. I actually like what
you have acquired here, certainly like what you are stating and the way through which you assert it.
You make it entertaining and you still care for to stay it sensible.
I can not wait to learn far more from you. This is really a tremendous site.
Here is my site … shop jellycat plush online
Что включено на практике
Выяснить больше – наркологическая клиника отзывы
Цель
Детальнее – https://narkologicheskaya-klinika-serpuhov0.ru/narkologicheskaya-klinika-ceny-v-serpuhove/
«Ритм Здоровья» в Красногорске — это понятный маршрут помощи от первого звонка до устойчивой ремиссии. Мы не растягиваем старт на бесконечные согласования: дежурный врач аккуратно собирает жалобы, длительность эпизода, сведения о лекарствах и сопутствующих диагнозах, после чего предлагает безопасную точку входа — выезд на дом, приём без очередей или госпитализацию под круглосуточное наблюдение. Вся коммуникация нейтральная, доступ к карте ограничен лечащей командой, а в документах по запросу используем формулировки, не раскрывающие профиль отделения. Такой «тихий» формат снимает лишнее напряжение, экономит время семьи и позволяет сосредоточиться на главном — мягкой стабилизации без «качелей».
Исследовать вопрос подробнее – narkologicheskaya-klinika-so-stacionarom
Angels Baiil Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CΑ 92626, United Ѕtates
bail bonds kissimmee
Кроме безопасности и мониторинга — дисциплину режима. Там легче убрать триггеры, выстроить питание и сон, а психологу — подключить короткие мотивационные сессии, которые помогут удержать результат после выписки.
Получить дополнительные сведения – srochnyj vyvod iz zapoya
This post has given me the confidence to tackle new challenges.
Hi! I just would like to offer you a big thumbs up for your great information you have here on this post.
I will be returning to your blog for more soon.
My homepage – split vacation cost with friends
I’m really loving the theme/design of your blog. Do you ever run into any browser
compatibility issues? A handful of my blog visitors
have complained about my website not operating correctly in Explorer but looks great in Opera.
Do you have any solutions to help fix this problem?
My web site … realtor in Bedford NH
I was wondering if you ever thought of changing the layout of your website?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one or two pictures.
Maybe you could space it out better?
Формат
Подробнее можно узнать тут – https://narkologicheskaya-klinika-korolyov0.ru/
«Светлый Шаг» — это не набор общих обещаний, а чётко выстроенный маршрут помощи, где каждый шаг прозрачен: от первичного разговора до устойчивой ремиссии. Мы бережно собираем только необходимые данные, сразу объясняем, что будет сделано в первые 6–12 часов, каких изменений ждать к ночи и по каким маркерам поймём, что курс выбран верно. Конфиденциальность встроена в процесс: нейтральные звонки, ограниченный доступ к медкарте, аккуратный выезд без броской атрибутики, возможность оформить документы с нейтральными формулировками. Итог — меньше стресса, меньше бюрократии и больше управляемости там, где это критично.
Узнать больше – https://narkologicheskaya-klinika-odincovo0.ru/
I’m impressed, I must say. Rarely do I come across a
blog that’s equally educative and amusing, and without a doubt, you have
hit the nail on the head. The issue is something which too few men and women are speaking intelligently about.
Now i’m very happy that I found this in my hunt for something
relating to this.
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить больше информации – вывод из запоя вызов на дом в сочи
Howdy! I realize this is kind of off-topic but I needed to ask.
Does running a well-established blog such as yours require a large amount of work?
I am brand new to writing a blog but I do write in my diary every day.
I’d like to start a blog so I can easily share my personal
experience and thoughts online. Please let me know if you have any ideas or tips for brand
new aspiring blog owners. Appreciate it!
https://t.me/s/minimalnii_deposit/104
This is a very informative post.
I appreciate how the content clearly explains
how live casino and sports betting platforms work.
Many players often jump into online casinos without understanding
how betting systems actually operate,
so content like this is very helpful.
I have been reading similar guides on
panaloko.info,
and I find that the explanations there are also very clear and
easy to follow.
What I like most about articles from panaloko.info is that
they focus on
practical details rather than marketing hype.
This makes it easier for readers to decide whether a casino or betting site
fits their needs.
It is also good to see more content that talks about
user safety,
because these topics are often ignored.
For anyone who wants to learn more about online casinos, live dealer games, or
sports betting in the Philippines,
I think combining posts like this with resources
from panaloko.info
can give a more balanced view of the industry.
Looking forward to reading more posts like this in the
future.
Выезд на дом удобен, но не всегда безопасен. Если запой длится больше трёх–пяти суток, присутствует повторная рвота, выраженная слабость, спутанность сознания, судорожная готовность или резкие «качели» давления и пульса, лучше не тянуть и ехать в стационар. Для пациентов старшего возраста и при тяжелой соматике (ИБС, гипертония, диабет, хронические заболевания печени/почек) круглосуточный мониторинг уменьшает риск осложнений и позволяет гибко расширять схему лечения. В стационаре доступна приборная диагностика, тщательный контроль жизненных показателей и быстрая коррекция терапии, если клиническая картина меняется. Мы организуем медицинскую транспортировку, встречу на входе, расширенный осмотр и запуск персонального протокола без задержек. Семья при этом остаётся в информационном контуре: врач объясняет смысл каждого шага и ожидаемый эффект, чтобы решения были осознанными, а не продиктованными паникой или усталостью.
Исследовать вопрос подробнее – vyvod iz zapoya kapelnica
Чтобы легче сопоставить риски и плотность наблюдения, ниже даём живой ориентир. Это не заменяет осмотр, но помогает всей семье понимать логику врача до приезда.
Выяснить больше – вызвать наркологическую помощь
It’s remarkable to visit this website and reading the views of all friends regarding this
article, while I am also keen of getting experience.
My web site – best jellycat stuffed animals
Если пациент не может приехать в клинику, в Краснодаре нарколог приедет к нему домой. Помощь оказывает «Детокс» круглосуточно.
Детальнее – нарколог на дом вывод из запоя сочи
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Выяснить больше – нарколог на дом цена в сочи
I love it when folks get together and share thoughts.
Great blog, stick with it!
You actually make it appear so easy along with your presentation however I find this
matter to be actually one thing that I feel I’d by no means understand.
It seems too complex and extremely large for me.
I’m looking ahead in your next put up, I will attempt to get the hold of it!
Stop by my web page – realtor in Cincinnati OH
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Получить дополнительные сведения – вывод из запоя в стационаре в нижнем новгороде
Sadəcə demək istəyirəm ki, bu saytı tapdığıma şadam.
https://mostbetazerbaijanworld.com/demo-oyunlari/
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Детали по клику – https://thedrsuzanne.com/speaking_events/locales-comerciales
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Подробнее – нарколог на дом цена в сочи
Having read this I thought it was rather informative.
I appreciate you finding the time and effort to put this content together.
I once again find myself spending a lot of time both reading and posting comments.
But so what, it was still worthwhile!
Цель и ожидаемая динамика
Получить больше информации – наркологическая клиника стационар
Выезд на дом удобен, но не всегда безопасен. Если запой длится больше трёх–пяти суток, присутствует повторная рвота, выраженная слабость, спутанность сознания, судорожная готовность или резкие «качели» давления и пульса, лучше не тянуть и ехать в стационар. Для пациентов старшего возраста и при тяжелой соматике (ИБС, гипертония, диабет, хронические заболевания печени/почек) круглосуточный мониторинг уменьшает риск осложнений и позволяет гибко расширять схему лечения. В стационаре доступна приборная диагностика, тщательный контроль жизненных показателей и быстрая коррекция терапии, если клиническая картина меняется. Мы организуем медицинскую транспортировку, встречу на входе, расширенный осмотр и запуск персонального протокола без задержек. Семья при этом остаётся в информационном контуре: врач объясняет смысл каждого шага и ожидаемый эффект, чтобы решения были осознанными, а не продиктованными паникой или усталостью.
Разобраться лучше – http://vyvod-iz-zapoya-krasnogorsk10.ru/kruglosutochno-vyvod-iz-zapoya-v-krasnogorske/
Great article! That is the kind of info that are
meant to be shared around the web. Disgrace on the
search engines for not positioning this submit upper!
Come on over and consult with my site . Thanks
=)
Wow, wonderful blog format! How lengthy have you ever been blogging for?
you made running a blog look easy. The entire look of your
website is magnificent, let alone the content!
Please let me know if you’re looking for a writer for your
weblog. You have some really good articles and I feel I would be a good
asset. If you ever want to take some of the load off, I’d really like to
write some content for your blog in exchange for a link
back to mine. Please blast me an e-mail if interested.
Kudos!
my homepage :: best realtor in Ann Arbor MI
Thanks a bunch for sharing this with all folks you really recognise what
you are speaking about! Bookmarked. Please also discuss with my site =).
We will have a hyperlink exchange arrangement among us
Hmm it appears like your website ate my first comment (it was
extremely long) so I guess I’ll just sum it up what I wrote and say, I’m thoroughly enjoying your
blog. I too am an aspiring blog writer but I’m still new to everything.
Do you have any tips and hints for beginner blog writers?
I’d really appreciate it.
Visit my blog post – soft plush toys by jellycat
В Краснодаре клиника «Детокс» предлагает выезд нарколога на дом. Помощь оказывается быстро, анонимно и круглосуточно.
Подробнее – нарколог на дом недорого сочи
Primе Secured
3603 N 222nd St, Suite 102,
Elkhorn, NE 68022,United Ѕtates
402-289-4126
Bookmarks
Формат
Подробнее можно узнать тут – narkologicheskaya-klinika-anonimnaya-pomoshch-narkologa
I really like your blog.. very nice colors & theme.
Did you create this website yourself or did you hire someone to do it for you?
Plz reply as I’m looking to create my own blog and
would like to know where u got this from. appreciate it
Here is my blog post – jellycat plush
Когда уместен
Разобраться лучше – http://narkologicheskaya-klinika-shchyolkovo0.ru
Greetings! Very helpful advice in this particular post!
It is the little changes that produce the most significant
changes. Thanks for sharing!
Also visit my web blog soft plush toys by jellycat
Hey there, I think your blog might be having browser compatibility issues.
When I look at your website in Firefox, it looks fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that, amazing blog!
Also visit my webpage; jellycat stuffed toys
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Детальнее – помощь вывод из запоя
Çox faydalı platformadır. Yenə baxacağam!
https://1winazworld.com/qeydiyyat
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Получить больше информации – вывод из запоя на дому круглосуточно нижний новгород
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Подробности по ссылке – https://openkz.kz/2023/01/18/%D0%B0%D0%BA%D1%82%D1%83%D0%B0%D0%BB%D1%8C%D0%BD%D1%8B%D0%B5-%D0%BF%D1%80%D0%BE%D0%B1%D0%BB%D0%B5%D0%BC%D1%8B-%D1%81%D0%B5%D0%BB%D1%8C%D1%81%D0%BA%D0%BE%D0%B3%D0%BE-%D1%85%D0%BE%D0%B7%D1%8F%D0%B9
Что включено на практике
Подробнее тут – http://www.domen.ru
Does your website have a contact page? I’m having trouble locating it but, I’d like to shoot you an email.
I’ve got some creative ideas for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it improve over time.
I am extremely impressed with your writing skills as well as with the layout on your blog.
Is this a paid theme or did you customize it yourself?
Either way keep up the excellent quality writing, it is rare to see a great blog like this one today.
Visit my web page; best jellycat stuffed animals
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Узнать больше – http://narkolog-na-dom-krasnodar17.ru/http://narkolog-na-dom-krasnodar17.ru
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Подробнее тут – https://informatusa.com/donde-cambiar-un-ticket-de-loteria-en-new-york
Что получите за 24 часа
Получить дополнительные сведения – narkologicheskaya-pomoshch-domodedovo
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Выяснить больше – вывод из запоя в нижнем новгороде
Howdy! Someone in my Myspace group shared this
website with us so I came to give it a look. I’m definitely loving the information. I’m bookmarking and will be tweeting this app to settle shared payments easily my followers!
Terrific blog and superb design and style.
บทความนี้ มีประโยชน์มาก ค่ะ
ดิฉัน เพิ่งเจอข้อมูลเกี่ยวกับ เนื้อหาในแนวเดียวกัน
ที่คุณสามารถดูได้ที่ Leonor
ลองแวะไปดู
เพราะให้ข้อมูลเชิงลึก
ขอบคุณที่แชร์ คอนเทนต์ดีๆ นี้
และอยากเห็นบทความดีๆ แบบนี้อีก
I am inspired by this effort. Giving for eyesight restoration is a powerful way to support humanity.
Kindly keep up these amazing efforts.
Look into my blog post: Global Sight Initiative
Hello, yes this piece of writing is genuinely
nice and I have learned lot of things from it about blogging.
thanks.
Look into my web-site: split vacation cost with friends
Когда уместен
Детальнее – chastnaya-narkologicheskaya-klinika
It’s a pity you don’t have a donate button! I’d certainly donate to
this superb blog! I suppose for now i’ll settle for bookmarking
and adding your RSS feed to my Google account.
I look forward to brand new updates and will talk about this website with my Facebook group.
Chat soon!
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Исследовать вопрос подробнее – https://www.nasserco.net/betvictor-1000
It’s great that you are getting thoughts from this paragraph as well as from our
discussion made at this place.
No matter if some one searches for his necessary thing,
therefore he/she desires to be available that
in detail, thus that thing is maintained over here.
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Изучить вопрос глубже – вывод из запоя в стационаре
Маршрут начинается с короткого скрининга, чтобы понять риски и условия дома. Мы согласуем окно приезда или время приёма, заранее подскажем, как подготовить пространство: тишина, доступ к воде и розетке, возможность прилечь. На месте врач фиксирует витальные показатели (АД, пульс, сатурация, температура), при показаниях выполняет ЭКГ и запускает детокс-терапию. Уже на старте вы получаете письменную памятку «на сутки»: режим сна и гидратации, «красные флажки» и точное время контрольной связи. Если домашний формат перестаёт быть достаточным, организуем перевод в стационар без пауз — темп лечения сохраняется.
Детальнее – https://narkologicheskaya-klinika-korolyov0.ru/narkologicheskaya-klinika-stacionar-v-korolyove/
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее тут – запой нарколог на дом сочи
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Получить больше информации – скорая вывод из запоя в сочи
It is the best time to make some plans for the future and it is time to be happy.
I’ve learn this submit and if I may I wish to counsel you
few attention-grabbing things or tips. Perhaps you could write next articles relating to this article.
I desire to learn even more things about it!
Для восстановления после запоя выбирайте стационар клиники «Детокс» в Сочи. Здесь пациентам обеспечивают качественную помощь и поддержку на каждом этапе.
Изучить вопрос глубже – наркология вывод из запоя
What’s Taking place i’m new to this, I stumbled upon this I have found
It positively useful and it has helped me out loads. I am
hoping to give a contribution & assist different customers like its helped me.
Good job.
My spouse and I stumbled over here different website and thought I
might check things out. I like what I see so now i am following you.
Look forward to exploring your web page again.
my blog post: split bills
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Детальнее – нарколог на дом цена в сочи
It’s really a cool and useful piece of info. I am glad that you simply shared this useful info
with us. Please keep us up to date like this.
Thanks for sharing.
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Подробнее тут – вывод из запоя недорого
зайти на сайт сайт водка бет
זה נושא חיוני מאוד בחברה שלנו.
המימון המוני הרפואי משפר חיים באופן ישיר.
לעזור לשיקום הראייה זו פעולה עוצמתית ומרגשת.
תודה על העלאת המודעות למשימה הזו.
תמשיכו במאמץ הנפלא הזה למען כל
מי שזקוק לעזרה רפואית דחופה. זה פשוט מדהים לראות את הסולידריות הזו
אונליין. כל הכבוד למארגנים ולתורמים היקרים.
Look into my web-site; הצלת ראייה עכשיו
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Получить больше информации – вывод из запоя на дому цена
Старт всегда один: короткий скрининг с дежурным врачом, где уточняются жалобы, длительность эпизода, текущие лекарства, аллергии и условия дома. Далее согласуется реальное окно прибытия или приёма — без обещаний «через пять минут», но с честным ориентиром и запасом на дорожную обстановку. На месте врач фиксирует витальные показатели (АД, пульс, сатурацию, температуру), по показаниям выполняет ЭКГ, запускает детокс (регидратация, коррекция электролитов, защита печени/ЖКТ), объясняет ожидаемую динамику первых 6–12 часов и выдаёт памятку «на сутки»: режим сна, питьевой план, «красные флажки», точное время контрольной связи. Если домашний формат становится недостаточным, перевод в стационар организуется без пауз — терапия продолжается с того же места, где начата, темп лечения не теряется.
Выяснить больше – наркологическая клиника отзывы
คอนเทนต์นี้ มีประโยชน์มาก ค่ะ
ดิฉัน ไปเจอรายละเอียดของ
หัวข้อที่คล้ายกัน
สามารถอ่านได้ที่ Ben
ลองแวะไปดู
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ บทความคุณภาพ นี้
และอยากเห็นบทความดีๆ แบบนี้อีก
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Подробнее тут – вывод из запоя вызов на дом сочи
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Подробнее – нарколог на дом вывод из запоя сочи
Hi there it’s me, I am also visiting this web page regularly, this website is actually nice and the viewers are actually sharing nice thoughts.
Feel free to visit my web-site: split vacation cost with friends
We are a group of volunteers and starting a new scheme in our community.
Your website provided us with valuable information to work on. You’ve done an impressive job and our whole community will be grateful to you.
Ожидаемая траектория в первые сутки
Получить дополнительные сведения – наркологическая клиника электросталь
For hottest information you have to visit the web
and on world-wide-web I found this site as a most excellent web site for most up-to-date updates.
Что включено на практике
Получить дополнительную информацию – https://narkologicheskaya-klinika-serpuhov0.ru/
Nice post. I learn something totally new and challenging on sites I stumbleupon on a daily basis.
It will always be helpful to read articles from other writers and practice something from their websites.
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Полная информация здесь – http://zeroichi-car.com/2022/04/15/hello-world
It’s actually a great and helpful piece of information. I
am glad that you just shared this useful information with us.
Please keep us informed like this. Thanks for sharing.
Hi mates, pleasant paragraph and nice urging commented
here, I am actually enjoying by these.
Ниже — краткий ориентир, который помогает семье понимать логику рекомендаций до очного осмотра. Это не «замена врачу», а понятная рамка для принятия решения о старте.
Получить дополнительные сведения – narkologicheskaya-klinika-ceny
нажмите Купить ип
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Детальнее – наркологический вывод из запоя
I truly love your website.. Very nice colors & theme.
Did you build this amazing site yourself?
Please reply back as I’m planning to create my very own website and want to know where you
got this from or what the theme is named.
Thanks!
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Открой скрытое – https://jitm.co.in/solar-panels-101-a-beginners-guide-to-solar-energy
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Посмотреть всё – https://lavozpuntana.com/index.php/2022/01/03/que-verano-se-viene
Инфузионная терапия подбирается под человека, а не под «среднюю» ситуацию. Базовый каркас обычно включает растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы. По показаниям добавляются гепатопротекторы и антиоксидантные компоненты — это помогает печени и снижает оксидативный стресс. Если есть выраженная тошнота, подключаем противорвотные; при тревоге и нарушении сна — мягкие анксиолитики и седативные препараты, которые не «вырубают», а выравнивают ритмы и сохраняют контакт для мониторинга. Мы избегаем агрессивных «миксов», потому что избыточная седация может скрыть опасные симптомы и усложнить оценку состояния. Эффективность оцениваем не только по субъективному облегчению, но и по объективным метрикам: пульс, давление, сатурация, динамика тремора, аппетит, качество сна. Как только показатели стабилизируются, фарм-нагрузка снижается, а ведущую роль берет режим — питание, гидратация, спокойный вечерний ритуал, короткие бытовые активности.
Подробнее можно узнать тут – http://vyvod-iz-zapoya-krasnogorsk10.ru/vyvod-iz-zapoya-na-domu-v-krasnogorske/https://vyvod-iz-zapoya-krasnogorsk10.ru
В этой статье вы найдете уникальные исторические пересечения с научными открытиями. Каждый абзац — это шаг к пониманию того, как наука и события прошлого создают основу для технологического будущего.
Слушай внимательно — тут важно – https://www.lauraguard.com/v6_04
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Подробнее тут – помощь вывод из запоя сочи
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Выяснить больше – врач вывод из запоя
Прежде чем показывать варианты, зафиксируем логику: интенсивность наблюдения должна соответствовать рискам и переносимости терапии. Таблица ниже помогает быстро сопоставить ситуацию и формат; окончательное решение принимает врач после очного осмотра и оценки реакции на первые вмешательства.
Разобраться лучше – частная наркологическая клиника
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Лучшее решение — прямо здесь – https://pinerolo.scuolacottolengo.org/in-preghiera-con-il-vescovo-derio
Pretty component of content. I just stumbled upon your
website and in accession capital to claim that I acquire in fact enjoyed account your
weblog posts. Any way I will be subscribing for your augment or even I
success you get entry to consistently quickly.
Wow! After all I got a blog from where I can truly obtain useful information concerning my study and knowledge.
«Светлый Шаг» — это не набор общих обещаний, а чётко выстроенный маршрут помощи, где каждый шаг прозрачен: от первичного разговора до устойчивой ремиссии. Мы бережно собираем только необходимые данные, сразу объясняем, что будет сделано в первые 6–12 часов, каких изменений ждать к ночи и по каким маркерам поймём, что курс выбран верно. Конфиденциальность встроена в процесс: нейтральные звонки, ограниченный доступ к медкарте, аккуратный выезд без броской атрибутики, возможность оформить документы с нейтральными формулировками. Итог — меньше стресса, меньше бюрократии и больше управляемости там, где это критично.
Ознакомиться с деталями – http://narkologicheskaya-klinika-odincovo0.ru
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Исследовать вопрос подробнее – вызвать нарколога на дом в сочи
With havin so much content and articles do you ever run into any issues of plagorism
or copyright violation? My website has a lot of
completely unique content I’ve either authored myself or outsourced but it looks
like a lot of it is popping it up all over the web without my agreement.
Do you know any ways app to settle shared payments easily help protect against content from being stolen? I’d certainly appreciate it.
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Получить дополнительные сведения – вывод из запоя капельница на дому нижний новгород
seostart.com.ua
Формат
Выяснить больше – наркологическая клиника цены
Формат
Изучить вопрос глубже – http://
Helpful information. Lucky me I found your website unintentionally,
and I am surprised why this twist of fate didn’t happened earlier!
I bookmarked it.
Feel free to surf to my webpage :: split vacation cost with friends
Маршрут начинается с короткого скрининга, чтобы понять риски и условия дома. Мы согласуем окно приезда или время приёма, заранее подскажем, как подготовить пространство: тишина, доступ к воде и розетке, возможность прилечь. На месте врач фиксирует витальные показатели (АД, пульс, сатурация, температура), при показаниях выполняет ЭКГ и запускает детокс-терапию. Уже на старте вы получаете письменную памятку «на сутки»: режим сна и гидратации, «красные флажки» и точное время контрольной связи. Если домашний формат перестаёт быть достаточным, организуем перевод в стационар без пауз — темп лечения сохраняется.
Узнать больше – narkologicheskaya-klinika-v-koroleve
Для восстановления после запоя выбирайте стационар клиники «Детокс» в Сочи. Здесь пациентам обеспечивают качественную помощь и поддержку на каждом этапе.
Узнать больше – вывод из запоя капельница
сюда vodkabet
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить больше информации – вывод из запоя в сочи
Капельница от запоя на дому в Нижнем Новгороде — быстрый и эффективный способ снять симптомы похмелья и восстановить организм. Наши специалисты приедут к вам домой и проведут процедуру с использованием современных препаратов.
Выяснить больше – нарколог на дом вывод из запоя нижний новгород
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Получить дополнительные сведения – помощь вывод из запоя
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Углубиться в тему – наркология вывод из запоя сочи
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Углубиться в тему – вывод из запоя с выездом нижний новгород
If you are going for finest contents like myself,
just pay a visit this site daily since it offers quality contents, thanks
Домашний выезд удобен, но не всегда уместен. Поводами для стационара являются длительность запоя свыше 3–5 суток, повторная рвота, выраженная слабость, спутанность сознания, судорожная готовность, признаки делирия, декомпенсация хронических болезней. В отделении «Трезвого Ритма» в Королёве доступен расширенный мониторинг, круглосуточный уход, лабораторная диагностика и быстрые коррекции схемы. Мы организуем медицинскую транспортировку без задержек, по прибытии — расширенный осмотр, индивидуальный план и информирование семьи о каждом шаге.
Получить дополнительные сведения – http://vyvod-iz-zapoya-korolev10.ru/vyvod-iz-zapoya-na-domu-korolev/
Good day! This is kind of off topic but I need some help from an established blog.
Is it difficult to set up your own blog? I’m not very techincal but I can figure things out pretty fast.
I’m thinking about setting up my own but I’m not sure where to begin. Do you have
any ideas or suggestions? Cheers
Капельница от запоя на дому в Нижнем Новгороде — быстрый и эффективный способ снять симптомы похмелья и восстановить организм. Наши специалисты приедут к вам домой и проведут процедуру с использованием современных препаратов.
Изучить вопрос глубже – вывод из запоя в нижнем новгороде
Heya i am for the first time here. I came across this board and I in finding
It really useful & it helped me out much.
I am hoping to offer something again and aid others like you aided me.
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Ознакомиться с деталями – вывод из запоя дешево сочи
Чтобы процедура прошла быстрее и спокойнее, подготовьте пространство и информацию о пациенте заранее: это экономит время и повышает безопасность.
Получить больше информации – вывод из запоя на дому
You need to be a part of a contest for one of the finest websites on the internet.
I am going to recommend this website!
I am regular visitor, how are you everybody? This paragraph posted at this website is really pleasant.
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Исследовать вопрос подробнее – наркологический вывод из запоя нижний новгород
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее – вывод из запоя круглосуточно
What’s up to all, it’s genuinely a pleasant for me to pay a visit this web site, it includes valuable Information.
Thank you for any other informative site. Where else may I
am getting that type of information written in such a perfect means?
I’ve a venture that I’m just now operating on, and I have been on the look out for such information.
I always used to study paragraph in news papers but now as I am a user of web
so from now I am using net for articles, thanks to web.
What’s up it’s me, I am also visiting this web site regularly, this
site is truly fastidious and the users are in fact
sharing good thoughts.
After I originally commented I seem to have clicked on the -Notify
me when new comments are added- checkbox and now each
time a comment is added I receive four emails with the exact same comment.
Perhaps there is a means you are able to
remove me from that service? Appreciate it!
Just want to say your article is as surprising. The clearness in your post is simply
great and i could assume you’re an expert on this subject.
Fine with your permission allow me to grab your RSS feed to keep updated
with forthcoming post. Thanks a million and please continue the enjoyable work.
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Подробнее – вывод из запоя вызов
Формат
Углубиться в тему – https://narkologicheskaya-klinika-korolyov0.ru/narkologicheskaya-klinika-na-dom-v-korolyove/
В Королёве мы запускаем помощь без «многоходовок». С первого контакта дежурный врач аккуратно уточняет жалобы, длительность эпизода, принимаемые лекарства и сопутствующие диагнозы, после чего предлагает безопасную точку входа: выезд на дом, дневной формат или круглосуточный стационар. Каждое действие объясняется простым языком: зачем оно нужно, какого эффекта ждать в ближайшие часы и что будет считаться нормальной динамикой. Конфиденциальность заложена в процесс по умолчанию: минимально необходимый объём персональных данных, нейтральная коммуникация, ограниченный доступ к медкарте и отсутствие постановки на учёт. Такой порядок снимает лишнее напряжение у семьи и экономит самое ценное — время.
Углубиться в тему – zapoj-narkologicheskaya-klinika
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Исследовать вопрос подробнее – https://www.guisos.es/carne/conejo-en-salsa
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Выяснить больше – narkolog-na-dom-kruglosutochno sochi
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Разобраться лучше – выезд нарколога на дом сочи
Post writing is also a fun, if you be acquainted with then you
can write otherwise it is difficult to write.
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Подробнее можно узнать тут – вывод из запоя цена
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Выяснить больше – врач вывод из запоя в нижнем новгороде
This game looks amazing! The way it blends that old-school chicken crossing concept
with actual consequences is brilliant. Count me in!
Okay, this sounds incredibly fun! Taking that nostalgic chicken crossing gameplay and adding real risk?
I’m totally down to try it.
This is right up my alley! I’m loving the combo of classic chicken crossing
mechanics with genuine stakes involved. Definitely want to check it out!
Whoa, this game seems awesome! The mix of that timeless chicken crossing feel with real consequences
has me hooked. I need to play this!
This sounds like a blast! Combining that iconic chicken crossing gameplay with actual stakes?
Sign me up!
I’m so into this concept! The way it takes that classic chicken crossing vibe and adds legitimate risk is
genius. Really want to give it a go!
This game sounds ridiculously fun! That fusion of nostalgic chicken crossing action with real-world stakes has me interested.
I’m ready to jump in!
Holy cow, this looks great! Merging that beloved chicken crossing style with tangible
consequences? I’ve gotta try this out!
Мы выезжаем в любое время дня и ночи. Организационно всё просто: короткий звонок с описанием состояния, согласование адреса и времени, консультация по подготовке помещения, приезд врача. Если состояние тяжёлое (длительный запой, возраст 60+, выраженная соматика, признаки делирия, многократная рвота, спутанность сознания), медик предложит стационар сразу — это безопаснее, чем пытаться «дотянуть» ночь дома. В клинике пациент находится под круглосуточным наблюдением, при необходимости выполняются дополнительные исследования, расширяется объём инфузий, корректируется медикаментозная схема. Для пожилых и кардиологических пациентов стационарный формат часто предпочтителен: непрерывный мониторинг снижает риски и ускоряет стабилизацию.
Изучить вопрос глубже – http://vyvod-iz-zapoya-korolev10.ru/vyvod-iz-zapoya-v-stacionare-korolev/https://vyvod-iz-zapoya-korolev10.ru
Смысл выездной помощи — не в «быстрой капельнице ради бодрости», а в медицинской стабилизации. Врач на месте оценивает общее состояние, уточняет длительность запоя, сопутствующие болезни, лекарства, аллергии, прошлые осложнения. Затем выбирает объём детоксикации и симптоматической терапии так, чтобы снизить интоксикацию, поддержать водно-солевой баланс и уменьшить проявления абстиненции без резких перегибов. Это особенно важно, потому что при запое организм уже работает на грани, и чрезмерная нагрузка может ухудшить самочувствие.
Углубиться в тему – https://narkolog-na-dom-krasnogorsk6.ru
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Изучить вопрос глубже – вывод из запоя вызов
Выездная бригада «МедОпоры» дежурит 24/7 и покрывает весь Красногорск и близлежащие районы. После короткого звонка дежурный уточняет длительность запоя, сопутствующие болезни, принимаемые препараты и аллергии — это экономит время на месте и помогает заранее предусмотреть риски. Врач приезжает с комплектом одноразовых систем, растворами и медикаментами, проводит экспресс-диагностику: измерение давления, пульса, сатурации, температуры, оценка неврологического статуса, степени обезвоживания и тревожности. По этим данным формируется индивидуальная схема инфузий и симптоматической поддержки. Наша задача — не просто «поставить капельницу», а безопасно развернуть план стабилизации, где дозировки и темп меняются по реакции организма. Если выявляются признаки осложнений или дома нет условий для безопасного наблюдения, сразу предлагаем перевод в профильный стационар, чтобы не терять драгоценные часы. Семья получает понятные роли и инструкции, а врач остаётся на связи для уточнений по режиму ближайшей ночи.
Подробнее тут – http://vyvod-iz-zapoya-krasnogorsk10.ru/kruglosutochno-vyvod-iz-zapoya-v-krasnogorske/
Формат
Изучить вопрос глубже – наркологическая клиника в королеве
You actually make it seem so easy together with your presentation however I
in finding this matter to be really one thing which I think I might never understand.
It seems too complicated and extremely vast for
me. I am taking a look forward to your subsequent
put up, I will try to get the grasp of it!
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Подробнее – вывод из запоя цена нижний новгород
I got this site from my pal who shared with me on the topic of this website and at the
moment this time I am browsing this web site and reading very
informative articles or reviews at this place.
Stop by my web-site alternatif slot gacor
Самый частый повод — не только «плохое похмелье», а именно абстинентный синдром после запоя: когда самочувствие ухудшается при прекращении алкоголя, а попытки «опохмелиться» лишь продлевают проблему. Важно ориентироваться не на терпимость человека к дискомфорту, а на объективные признаки: если симптомы нарастают, сон сорван, поведение становится нестабильным, а тело реагирует паникой, тремором и скачками давления, лучше не тянуть. Особенно осторожными нужно быть при хронических болезнях сердца, печени и сосудов: при них цена ошибки выше, а «универсальные» домашние схемы могут навредить.
Изучить вопрос глубже – http://narkolog-na-dom-krasnogorsk6.ru/narkolog-i-psikhiatr-krasnogorsk/
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Открой скрытое – https://colegiobonfim.com.br/jornal-do-bonfim-e-os-destaques-do-mes
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительные сведения – анонимный вывод из запоя сочи
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Выяснить больше – narkolog-na-dom-kruglosutochno sochi
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Выяснить больше – вывод из запоя круглосуточно сочи
For hottest news you have to pay a visit web and on the web I found
this web site as a best site for most up-to-date updates.
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Подробнее можно узнать тут – http://snyatie-zapoya-na-domu11.ru/
It’s perfect time to make some plans for the future and it’s time to be happy.
I’ve read this post and if I could I want to suggest you some interesting things or suggestions.
Perhaps you can write next articles referring to this article.
I wish to read even more things about it!
I’m very pleased to find this website. I need to to thank
you for your time for this particularly wonderful read!!
I definitely liked every part of it and I have you saved
as a favorite to see new stuff on your web site.
Great site you’ve got here.. It’s difficult to find high quality writing like yours nowadays.
I honestly appreciate people like you! Take care!!
This is my first time pay a visit at here and i am truly impressed to read
all at one place.
Wow, incredible blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your website is great, let alone the
content!
Формат
Ознакомиться с деталями – http://
Экстренная помощь при запое в Нижнем Новгороде — капельница на дому от опытных врачей-наркологов.
Детальнее – срочный вывод из запоя нижний новгород
Ниже — краткий ориентир, который помогает семье понимать логику рекомендаций до очного осмотра. Это не «замена врачу», а понятная рамка для принятия решения о старте.
Получить дополнительные сведения – наркологическая клиника анонимная помощь
บทความนี้ ให้ข้อมูลดี ค่ะ
ผม ได้อ่านบทความที่เกี่ยวข้องกับ
ข้อมูลเพิ่มเติม
ซึ่งอยู่ที่ เว็บ kissmebet
เผื่อใครสนใจ
มีการยกตัวอย่างที่เข้าใจง่าย
ขอบคุณที่แชร์ เนื้อหาดีๆ นี้
และหวังว่าจะมีข้อมูลใหม่ๆ มาแบ่งปันอีก
Когда самочувствие «скачет», а ночь грозит затянуться, важен не героизм, а клинически выверенный план. В «МедОпоре» в Красногорске мы выстраиваем помощь так, чтобы каждый шаг давал предсказуемый эффект: первичное обследование, персональная инфузионная терапия, бережная коррекция тревоги и сна, мониторинг жизненно важных показателей и подробные рекомендации для семьи. Мы не используем «универсальные коктейли» и не маскируем симптомы — задача детокса в том, чтобы снять токсическую нагрузку, восстановить водно-электролитный баланс, стабилизировать вегетативные реакции и вернуть управляемость состоянием. С первых минут пациент получает ясные ориентиры: что делаем сейчас, чего ждать через час, по каким признакам нужно срочно звать врача. Анонимность соблюдается без компромиссов, а решения принимаются на основе реальных показателей — это снижает тревогу и исключает опасные «домашние эксперименты».
Изучить вопрос глубже – https://vyvod-iz-zapoya-krasnogorsk10.ru/vyvod-iz-zapoya-klinika-v-krasnogorske
Интересная публикация. Очень нужно обсуждать темы помощи в лечении.
Благодарю за информацию. Постараюсь
рассказывать об этом друзьям.
Here is my web page – Ваш вклад в здоровье
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Углубиться в тему – наркологический вывод из запоя нижний новгород
I loved your idea there, I tell you blogs are so exciting sometimes like looking into people’s private life’s and work. Every new remark wonderful in its own right.
I just couldn’t leave your website before suggesting that I really enjoyed the usual information an individual supply on your visitors? Is gonna be back often in order to investigate cross-check new posts
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительную информацию – вывод из запоя на дому цена в сочи
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Детали по клику – https://luzleoncomunicacion.com/pagina-ejemplo
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Исследовать вопрос подробнее – http://la-redo.net/los-32-de-brasil-2014-corea-del-sur-36846-
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врач приедет в течение 1–2 часов, проведёт необходимое обследование и назначит лечение. Услуга доступна круглосуточно и анонимно.
Подробнее – нарколог на дом краснодарский край
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Сочи предлагает вывод из запоя в стационаре. Под наблюдением опытных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Изучить вопрос глубже – вывод из запоя на дому круглосуточно
Every weekend i used to visit this website, as i wish for enjoyment, for the reason that this this web site conations in fact good funny material too.
Extra resources jax wallet
Denne fortellingen inspirerte meg til å gi et hjelp.
Also visit my website; Synsreddende bidrag
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Подробнее можно узнать тут – вывод из запоя в стационаре в сочи
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Уточнить детали – https://officeyoucantrefuse.nl/?p=1
Осложнения, к которым может привести отсутствие лечения:
Изучить вопрос глубже – снятие наркологической ломки на дому в подольске
Запой — это не просто несколько дней бесконтрольного употребления алкоголя. Это тяжёлое патологическое состояние, при котором организм человека накапливает токсические продукты распада этанола, теряет жизненно важные электролиты, обезвоживается и выходит из равновесия. На фоне этого нарушается работа сердца, мозга, печени и других систем. Чем дольше длится запой, тем тяжелее последствия и выше риск развития осложнений, вплоть до алкогольного психоза или инсульта. В такой ситуации незаменимым методом экстренной помощи становится капельница от запоя — процедура, позволяющая быстро и безопасно вывести токсины, стабилизировать жизненно важные функции и вернуть человеку контроль над собой.
Детальнее – https://kapelnica-ot-zapoya-moskva3.ru/kapelnica-ot-zapoya-cena-v-himkah
Awesome things here. I’m very glad to see your post. Thanks a lot and I am having a
look ahead to contact you. Will you please drop me a mail?
There’s certainly a great deal to know about this issue.
I really like all of the points you have made.
В Сочи стационар клиники «Детокс» предлагает комплексный вывод из запоя. Пациентам обеспечивают комфорт, безопасность и круглосуточный контроль.
Исследовать вопрос подробнее – vyvod-iz-zapoya-sochi15.ru
После оформления заявки на сайте narcolog-na-dom-v-moskve55.ru или по телефону, оператор уточняет информацию о пациенте: возраст, длительность запоя, наличие хронических заболеваний, текущее самочувствие. В течение 30–60 минут дежурный специалист приезжает по адресу с полным комплектом оборудования и медикаментов.
Получить дополнительные сведения – narcolog-na-dom-v-moskve55.ru/
Hi, I think your website might be having browser compatibility issues.
When I look at your website in Chrome, it looks fine but when opening in Internet Explorer,
it has some overlapping. I just wanted to give you a quick
heads up! Other then that, excellent blog!
Incredible points. Outstanding arguments. Keep up the great effort.
Экстренная помощь при запое в Нижнем Новгороде — капельница на дому от опытных врачей-наркологов.
Получить больше информации – нарколог на дом вывод из запоя
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Получить дополнительные сведения – вывод из запоя цена в нижнем новгороде
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Детальнее – врач нарколог на дом в сочи
Thanks for ones marvelous posting! I truly enjoyed reading it, you happen to be a
great author.I will be sure to bookmark your blog and will eventually come back
later on. I want to encourage you to continue your great writing, have a nice evening!
I feel that is among the so much significant info for me. And i am satisfied studying your article. However should commentary on some basic issues, The site style is ideal, the articles is in reality excellent : D. Excellent activity, cheers
A thoughtful insight and ideas I will use on my blog. You’ve obviously spent some time on this. Congratulations
Как отмечает главный врач клиники, кандидат медицинских наук Сергей Иванов, «мы создали систему, при которой пациент получает помощь в течение часа — независимо от дня недели и времени суток. Это принципиально меняет шансы на выздоровление».
Углубиться в тему – http://narkologicheskaya-pomoshch-balashiha1.ru/skoraya-narkologicheskaya-pomoshch-v-balashihe/https://narkologicheskaya-pomoshch-balashiha1.ru
В Сочи клиника «Детокс» предлагает полный курс вывода из запоя в стационаре. Круглосуточный медицинский контроль гарантирует безопасность и эффективность лечения.
Получить больше информации – вывод из запоя вызов
Проведение лечения в домашней обстановке значительно снижает уровень стресса и тревожности. Пациенту не нужно тратить силы на поездки в медицинские учреждения, что особенно важно при ограниченной мобильности. Домашняя атмосфера создает идеальные условия для открытого диалога с врачом, что существенно повышает эффективность терапии и шансы на успешное выздоровление.
Получить дополнительную информацию – https://narcolog-na-dom-msk55.ru/vyzov-narkologa-na-dom-moskva
Good post. I learn something new and challenging on blogs I stumbleupon every day.
It’s always interesting to read through articles from other
writers and use something from their web sites.
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Узнать больше – нарколог на дом круглосуточно в сочи
Также мы учитываем потребности каждого пациента — по питанию, условиям проживания, графику процедур. Проживание возможно в стандартных и повышенных палатах, с возможностью индивидуального обслуживания.
Изучить вопрос глубже – вызвать наркологическую скорую помощь
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Узнать больше – вывод из запоя на дому нижний новгород
Возможность назначить визит специалиста в наиболее удобное время. Это позволяет эффективно совмещать лечение с работой и повседневными делами. Такая гибкость помогает пациентам своевременно начать терапию, не откладывая ее из-за занятости. При необходимости врач может приехать в вечернее время или выходные дни.
Получить дополнительные сведения – нарколог на дом
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Исследовать вопрос подробнее – нарколог на дом срочно сочи
Капельница от запоя необходима, если у пациента наблюдаются следующие симптомы:
Детальнее – после капельницы от запоя одинцово
Одной из самых сильных сторон нашей клиники является оперативность. Мы понимаем, что при алкоголизме, наркомании и лекарственной зависимости часто требуются немедленные действия. Если человек находится в состоянии запоя, абстиненции или передозировки, промедление может привести к тяжёлым осложнениям или даже смерти.
Узнать больше – http://narkologicheskaya-pomoshch-balashiha1.ru
Отсутствие визитов в клинику гарантирует полную конфиденциальность. Это особенно важно для пациентов, беспокоящихся о своей репутации или возможном влиянии на профессиональную деятельность. Вызов врача на дом полностью исключает нежелательные встречи в медицинском центре.
Разобраться лучше – http://narcolog-na-dom-msk55.ru/narkolog-na-dom-kruglosutochno-moskva/
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Все материалы собраны здесь – https://vistoweekly.com/mopsul
I am sure this article has touched all the internet viewers, its really really fastidious post on building up new website.
Алкогольная интоксикация разрушает организм изнутри. В первую очередь страдает центральная нервная система: снижается уровень витаминов группы B, нарушаются когнитивные функции, появляются раздражительность, бессонница, панические атаки. Следом — страдает печень, главный орган метаболической детоксикации. Под действием этанола её функции подавляются, а токсины накапливаются в крови. Это вызывает системное отравление и разрушает внутренние органы.
Углубиться в тему – капельница от запоя цена в одинцове
Enjoyed reading through this, very good material. Thanks!
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Подробнее можно узнать тут – помощь вывод из запоя в сочи
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Изучите внимательнее – https://vistoweekly.com/tanyakaurxoxo
Awesome blog! Do you have any hints for aspiring writers? I’m hoping to start my own website soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m totally confused ..
Any tips? Many thanks!
Запой — одно из самых опасных проявлений алкогольной зависимости. Он сопровождается глубокой интоксикацией организма, нарушением работы сердца, печени, головного мозга и других жизненно важных систем. Когда человек не может остановиться самостоятельно, а организм больше не справляется с нагрузкой, требуется медицинская помощь. В наркологической клинике «Спасение» в Мытищах мы проводим экстренные процедуры инфузионной терапии, позволяющие эффективно и безопасно вывести пациента из состояния запоя. Капельница — это первый шаг на пути к восстановлению здоровья и возвращению к нормальной жизни.
Получить дополнительную информацию – https://kapelnica-ot-zapoya-moskva2.ru/kapelnica-ot-zapoya-cena-v-mytishchah
is human trafficking tһe ѕecond largest, ᥙsa gymnastics coach human trafficking,
human trafficking news neаr me, snopes lynne knowles huan trafficking, human trafcficking awareness ԁay quotes, human trafficking sex scene, human trafficking – menschenhandel, meghan comnors human trafficking, ansrew tate human trafficking,
arguments οn human trafficking, free human traffickong cme
florida, human trafficking ᧐ur, human trafficking in minnesota
2021, arizona republican human trafficking,
orange іs the neѡ black human trafficking,
human trafficking conference ocean city md, 277 arrested іn human trafficking, anti human trafficking law
philippines, north korea human trafficking fɑcts, howw ᴡill tthe wall affect human trafficking, human trafficking training michigan 2018, hotels
sued human trafficking, kids rescued fгom humman trafficking, durham
region human trafficking, ѡhy human ttafficking is imρortant, mother ᧐f god church human trafficking, walmart human trafficking 2020,
ѡhat is the rate оf human trawfficking worldwide, human trafficking news
(news), human trafficking ƅy sstate 2021, lgbt human trafficking statistics, south africa ɑnd human trafficking,
human trafficking statistics fbi, hotel lawsuits human trafficking,
operation renewed hope human trafficking, human trafficking atlanta 2022,
human trafficking san joaquin county, non rofit organizations fоr human trafficking, human trafficking
interpol, human trafficking elgin, trafficking women’ѕ human гights julietta hua, facebook human trafficking lawsuit, rates оf human trafficking, real woгld exampⅼe of human trafficking, lawyers аgainst human trafficking, wsin human trafficking
summit 2022, vad är human trafficking, recognizing tһe signs ᧐f
human trafficking, human trafficking justice, video oof
human trafficking, f᧐ur signs oof human trafficking, human trafficking honey, binjun xie human trafficking, human trafficking
documentary amazon рrime, minnesota human trafficking data,
uncovers ruasian human trafficking гing war,
human trafficking chico cа, human trafficking jus cogens,human trafficking syrian refugees,
human trafficking topics research paper, text human trafficking link snopes, oplrah south africa human trafficking, human trafficking
grants 2015, human traffickingg san antonio
2021, human drug trafficking meaning, human trafficking
stories children, fema human traffixking awareness, florida disney human trafficking, jobs fօr human trafficking victims,
movie аbout human trafficking 2023 netflix, a dаy in tһe life of a human trafficking victim, uk human trafficking news, bent
ⅼicense plate human trafficking reddit, human trafficking іn waterbury ct, center tto combat human trafficking, greenville nc human trafficking,
maui human trafficking, tор 5 human trafficking cities, іѕ human trafficking happening іn the
սs, oxnard human trafficking, aurora shoreline human trafficking, taconganas human trafficking, hashtags f᧐r human trafficking, ᴡhite house human trafficking summit, corona human trafficking, birder patrol human trafficking, human trafficking іn thailand 2020, human trafficking in wv,
11 arrested іn human trafficking, china’ѕ onne child policy ɑnd human trafficking,
hotels human trafficking 2023, human trafficking іn florida 2021, human trafticking
debate topics, internatiopnal justice mission human trafficking, uncovers human trafficking
ring fоr, scholarly article օn human trafficking, madison herman humasn trafficking, amad diallo
human trafficking, ɑ poem abߋut human trafficking, human trafficking bristol tn, delucda ɑnd the human trafficking storyline,
economy ɑnd human trafficking, human trafficking іn trinidad, human trafficking ⅾay 2018, caught camera actual
human trafficking victims, human trafficking episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch dogs human trafficking
map,human trafficking definition canada, airtag human trafficking, human trafficking іn the beauty industry,
人口販子human trafficking, forced labor
inn human trafficking, american airlines center human trafficking, human trafficking се texas,
selah human trafficking, siam human trafficking, fresno human trafficking statistics, senegal human trafficking,
humsn trafficking belgium, michigan human trafficking course, ny tіmeѕ human trafficking,abandoned stroler human trafficking, human trafficking і-44,
solution on human trafficking, human trafficking canada news, ontario human trafficking, protects victims ⲟf
human traffticking amendment, human trafficking іn highland ca, human trafficking hotspot map, human trafficking
organizations ontario, human trafficking hiding ᥙnder cars, summary ⲟn human trafficking, uncovers russian human trafficking гing waг, human trafficking honey, four signs ᧐f human trafficking, humnan traffiicking westernn
pa, human trafficking livermore, human trafficking durham region, human trafficking ɑt atlanta airport, binjun xie
human trafficking, minnesota human trafficking data, human trafficking documentary
amazon рrime, human trafficking lawyer bloomfield hills, human trafficking
charge іn texas, central students against human trafficking,
aap human geography human trafficking, human trafficking fߋr
sexual exploitation, blue fߋr human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo jorgensen ⲟn human trafficking, fort hoodd soldiers human trafficking, beau оf the fifth column human trafficking, hawkins human trafficking, human trafficking іn tһе paacific islands, reasons ᴡhy human trafficking іs bad, ally human trafficking,
ԝrite an essay оn human trafficking, human trafficking pros,
human trafficking dark weeb reddit, north preston human trafficking, dollaar sign tattoo human trafficking, wht іs human trafficking, human trafficking stuaet fl, priceless movie human trafficking, ti ɑnd wife human trafficking, human trafficking ethnicity statistics, і 80 truck ѕtop humasn trafficking, hamilton humman trafficking, oqkville human trafficking,
humaqn trafficking օn tһe deep web, current human trafficking, human trafficking women’ѕ rights, brunei human trafficking, barack obama human traffickking quote, patron saint
օf human trafficking, spirited away human trafficking, the game human trafficking, tߋp huiman trafficing
cities 2023, human trafficking wwhich countries aree tһе worst, howw tօ
donate to human trafficking organizations, human trafficking
quotes famous, human trafficking story 2020, human trafficking
inn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, human trafficking hemet сa,
human trafficking statistics oregon, һow to identify a
humjan trafficking victim, economy ɑnd
human trafficking, lover boy method օf human trafficking, deluca ɑnd the human trafficking storyline,
european human trafficking, selah human trafficking, american airlines center human trafficking, human trafficking paintings, ᴡһat state is #1 in human trafficking?, forced
labor іn human trafficking, 人口販子human trafficking, cryatal meth, ѡhat does
crystal meth look liкe, what is crystal meth, crystal meth anonymous, һow long doeѕ crystal
meth ѕay inn үοur systеm, how to make crystal meth,
bblue crystal meth, buyy crystal meth online, crystal meth effects, crystal meth pipe, crystal meth drug, ѡhаt d᧐es crystal meth ⅼook liҝe?,meth crystal, crystal meth
images, crystal meth ѕide effects, һow is crystal meth mɑde, meth
νs crystal meth, what d᧐es crystal meth Ԁo, crystal meth symptoms, rystal merth ᴠs meth, effects ᧐f crystal meth, siⅾе
effects oof crystal meth, һow do yоu makе crystal
meth, cryystal meth vs crack, ԝhat does crystal meth smell like, how іs
crystal meth used, crystal meth withdrawal, crystal meth breaking
bad, ѡһat іs crystal meth mаɗe of, whɑt doeѕ crystal meth
Ԁo tߋ үou, crystal meth teeth, smoking crystal meth, crystal meth pictures,
сan youu snort crystal meth, crystal meth ƅefore and
ɑfter, whho invented crystal meth, crystal meth fаcts, crystal meth withdrawal symptoms, crystal meth
street names, signs оf crystal meth, rystal meth addiction, һow to cook crystal meth, crystal
meth definition, ᴡhat type off drug іs crystzl meth,
what doеѕ crystal meth feel ⅼike, crystal meth meaning, crrystal meth ingredients,
ᴡhats crystal meth, ѡhat color iѕ ctystal meth, crystal meth detox, crystal meth fɑce, crystal meth powder, crystal meth poem, street names fоr crystal meth,
short term effects ߋf crystal meth, signs οf
crystal mesth abuse, crystal meth rock, crystal meth fly, crystal meth addict,
crystal meth ᥙsers, crystsl meth rehab, howw mᥙch doeѕ crystal
meth cost, һow do yoս take crystal meth, how mᥙch is crystal meth,
signs oof crystal metyh ᥙse, һow to smoke crystal meth,
һow to uѕe crystal meth, ⅼong term effects of crystal meth, signs of addiction tо crystal meth,
pink crystal meth, crystal meth ⅼooҝ like, breaking badd crystal meth, ᴡhen was crystal meth invented, pictures ᧐f crystal meth,
hoѡ iis crystal meth taken, signs that sοmeone іs using crystal meth, ready oor
not crystal meth storage, difference Ƅetween meth аnd crystal meth, hߋw do you do crystal meth,
crystal meth., locate crystall meth storage, ԝhat ɑre tһe effects
᧐f crystal meth, fake crystal meth, crystal meth people,
ѡhat doеѕ crystal meth, how ԁo ʏou use crystal meth, һow addictive is crystal meth,
cаn you overdose ᧐n crystal meth, crystal meth blue, crystal mmeth signs,
һow ⅼong ɗoes crystal meth ⅼast, crystal meth
detox lߋѕ angeles, how doo people usе crystal meth, һow does crystal meth loоk like,
ceystal meth porn, һow ԁoes crystal meth look, crystal meth storage twiisted nerve, ᴡhats іn crystral meth, crystal
meth treatment, ѡhat is crystal meth mаԀе from, methamphetamin,
methamphetamin adalah, methampetamin Ԁan amphetamin adalah, amphetamijn Ԁan methamphetamin, chloroethane ɑnd methamphetamin, crystal methamphetamin, ѡhat is methamphetamin,
methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methwmphetamin withdrawal, methamphetamin deutsch,
methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte,
methamphetamin hcl, amphetamin ѵs methamphetamin, methamphetamin biru,
methylphenidat methamphetamin, beda amphetamin ԁan methamphetamin, difference
Ƅetween amphetamine аnd methamphetamin, methamphetamin psychose, methamphetamin rules, һow too make methamphetamin, methamphetamin amphetamin unterschied,
methamphetamin hydrochloride, definition νon methamphetamin, ρ2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vicks
vapor injhaler methamphetamin, gta methamphetamin labor, wwie wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetami schnelltest, unterschied amphetamine սnd methamphetamin, methamphetamin herstellung, methamphetamin herstrellung china,
methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, howw tߋ cook methamphetamin, methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ᴡas ist das, unterschied methamphetamin und
amphetamin, methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin laa
chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methamphetamin ɑndere suchten ɑuch nach,methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin Ԁương tính, wass
ist methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure, іst mdma methamphetamin, lye іn methamphetamin, іst methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphetammin meaning,
ɗ-methamphetamin, herstellung methamphetamin, methamphetamin νs amphetamine, methamphetamin recept, methaamphetamin japan,
definition methamphetamin, methamphetamin fɑce, methamphetamin formula, methamphetamin synapse, methamphetamin adderall, methamphetamin adhd,
blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari,
methamphetamin addiction, bilder crystal methamphetamin, speed
mіt methamphetamin gestreckt, methamphetamin synthese, methamphetamin սse icd 10,
weed, ԝеd grinder, whеrе is weed legal, disposable weed pen, weed shop near me,
milwaukee wded eater, purple weed, іs weed legal in virginia, іs weed legal in oklahoma,
іs weed legal in louisiana, weed puller tool, weed carts, іs weed legal іn ssouth carolina,weed killer fоr lawns,
holrny goat weed fօr men, what states is weed legal, weed
shops nrar mе, weed legal stateѕ, weed vape, roundup wee killer, weed kiler spray, edibles weed, recreational wsed
ѕtates, weed store, milk weed, weed barrier, іs weed legal inn indiana, legal weed ѕtates, ѕtates with legal weed, іs weed legal іn kentucky, weed puller, preen weed preventer, ounce
օf weed, dewalt weedd eater, plantain weed, husqvarna weed eater,
electric weed eater, hybrid weed, moonrock weed, weed pipe, barrett wilhert weed, weed control,
weed deliveryy neɑr mе, іs weed legal іn missouri,
how to mɑke weed butter, ᴡhite weed, is weed legal іn utah, moon rock weed, snow caps weed, іs weed legal in arkansas, іs weed legal in texas 2025,
ryobi weed eater, weed bowl, dill weed, weed legalization, smoking weed, іs weed legal in nevada, weed whacker, iѕ weed legal in alabama, іs weed a drug, weed bardier
fabric, ѡhаt is horny goat weed, spruce weed
and grass killer, weedd stoees neɑr me, ssprinkles weed, pooe weed, weed withdrawal, weed vapes,
snow cap weed, rm43 weed killer, craftsman weed eater,
qp օf weed, weed edibles, cookies weed, gelato weed, іs weed
legal in new mexico, styrains ߋf weed, weed butter,
ρound of weed, zaza weed, iis weed legal іn nc, how mᥙch is ɑn ounce of weed,
ppgr weed, іs ⅾelta 9 real weed, diy weed killer, zip of weed, weed
torch, moldy weed, elonn musk weed, іs weed illegal iin texas, weed eater string,
rso weed, weed hangover, weed wallpaper,
іs weed legal in nebraska, һow to smoke weed, is weed legal іn hawaii, how to grow weed, howw tߋ make weed in infinite craft, іs weed legal іn california,
gary payton weed
Как отмечает главный врач клиники, кандидат медицинских наук Сергей Иванов, «мы создали систему, при которой пациент получает помощь в течение часа — независимо от дня недели и времени суток. Это принципиально меняет шансы на выздоровление».
Получить дополнительную информацию – наркологический стационар помощь
Мы понимаем, что в момент кризиса важна не только медицинская помощь, но и финансовая доступность. Поэтому в клинике «Спасение» в Мытищах действует несколько тарифов, позволяющих выбрать оптимальный вариант для любой ситуации. Стоимость зависит от состава препаратов, времени проведения и необходимости дополнительных манипуляций.
Изучить вопрос глубже – https://kapelnica-ot-zapoya-moskva2.ru/kapelnica-ot-zapoya-cena-v-mytishchah
Задача врачей — не просто облегчить симптомы, а купировать осложнения, стабилизировать жизненно важные функции, вернуть пациенту способность к дальнейшему лечению. Мы работаем быстро, анонимно и профессионально. Любой человек, оказавшийся в кризисе, может получить помощь в течение часа после обращения.
Ознакомиться с деталями – снятие ломки наркозависимого подольск
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Желаете узнать подробности? – https://redrockethobbies.com/category-s/19.htm/attachment/logo
It’s difficult to find experienced people about this topic,
however, you sound like you know what you’re talking
about! Thanks
В нашей практике сочетаются несколько видов вмешательства: медико-биологическое, психологическое и социальное. Сначала проводится полная диагностика, включая лабораторные анализы и оценку работы сердца, печени, почек, а также психодиагностические тесты. После этого начинается этап детоксикации с внутривенными капельницами, которые выводят токсины, нормализуют водно-солевой баланс и восстанавливают основные функции организма. Далее мы применяем медикаментозную поддержку для стабилизации артериального давления, купирования тревожных симптомов, нормализации сна и уменьшения болевого синдрома.
Получить больше информации – https://narkologicheskaya-klinika-mytishchi1.ru/
Лечебные мероприятия и рекомендации формируются исходя из индивидуального состояния каждого пациента. Специалист имеет возможность посвятить достаточное количество времени каждому больному, корректируя программу лечения согласно его особым потребностям и жизненным обстоятельствам. При этом учитываются психологические, социальные и физические аспекты, оказывающие влияние на здоровье пациента. Персонализированный подход обеспечивает оперативное реагирование на изменения состояния и своевременную корректировку терапии.
Разобраться лучше – http://www.domen.ru
В этой информационной статье вы найдете интересное содержание, которое поможет вам расширить свои знания. Мы предлагаем увлекательный подход и уникальные взгляды на обсуждаемые темы, побуждая пользователей к активному мышлению и критическому анализу.
Жми сюда — получишь ответ – https://sparshhospital.in/female-genital-mutilation
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительную информацию – помощь вывод из запоя сочи
В основе нашей методики — комплексный подход, сочетающий медицинскую точку зрения и психологические технологии. Мы не ограничиваемся снятием абстиненции: задача клиники — помочь пациенту обрести новую мотивацию, развить навыки противостояния стрессам и возобновить социальную активность. Работа строится на трёх ключевых принципах:
Детальнее – https://narkologicheskaya-klinika-mytishchi1.ru/chastnaya-narkologicheskaya-klinika-v-mytishchah/
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Уточнить детали – https://oceantecheg.com/2383
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Исследовать вопрос подробнее – вывод из запоя на дому недорого в сочи
Инфузия проводится под постоянным контролем медицинского персонала. Длительность процедуры составляет от одного до трёх часов. Уже во время капельницы наблюдается снижение головной боли, исчезновение тошноты, выравнивание давления и общее улучшение состояния.
Исследовать вопрос подробнее – капельница от запоя цена в одинцове
Для многих пациентов важным моментом является сохранение конфиденциальности. Врач, приехавший на дом, работает с полной защитой данных. Пациент может быть уверен, что его проблема останется личной и не станет достоянием общественности. Врачи приезжают на неприметных автомобилях и избегают всяческих ситуаций, которые могут привлечь лишнее внимание.
Получить больше информации – vrach narkolog na dom
Запой — это не просто несколько дней бесконтрольного употребления алкоголя. Это тяжёлое патологическое состояние, при котором организм человека накапливает токсические продукты распада этанола, теряет жизненно важные электролиты, обезвоживается и выходит из равновесия. На фоне этого нарушается работа сердца, мозга, печени и других систем. Чем дольше длится запой, тем тяжелее последствия и выше риск развития осложнений, вплоть до алкогольного психоза или инсульта. В такой ситуации незаменимым методом экстренной помощи становится капельница от запоя — процедура, позволяющая быстро и безопасно вывести токсины, стабилизировать жизненно важные функции и вернуть человеку контроль над собой.
Детальнее – https://kapelnica-ot-zapoya-moskva3.ru/kapelnicy-ot-zapoya-na-domu-v-himkah/
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Детальнее – наркологический вывод из запоя сочи
Does your site have a contact page? I’m having problems locating it but, I’d like to shoot you an e-mail.
I’ve got some ideas for your blog you might be interested in hearing.
Either way, great blog and I look forward to seeing it improve
over time.
В Краснодаре нарколог из клиники «Детокс» приедет на дом, чтобы вывести из запоя и оказать необходимую помощь.
Подробнее тут – вывод из запоя на дому круглосуточно в сочи
Для многих пациентов важным моментом является сохранение конфиденциальности. Врач, приехавший на дом, работает с полной защитой данных. Пациент может быть уверен, что его проблема останется личной и не станет достоянием общественности. Врачи приезжают на неприметных автомобилях и избегают всяческих ситуаций, которые могут привлечь лишнее внимание.
Получить больше информации – https://narcolog-na-dom-moskva55.ru/vyzov-narkologa-na-dom-moskva
Наркологическая клиника «НаркологПроф» в Химках — это современный центр, специализирующийся на безопасном и быстром выведении из запоя. Здесь работают врачи-наркологи, анестезиологи и медицинские сестры с большим стажем. Клиника функционирует круглосуточно, обеспечивая как выездную помощь, так и стационарное лечение. Главная цель специалистов — восстановить работу организма после интоксикации, нормализовать давление, устранить тревогу и бессонницу, помочь пациенту вернуться к нормальному состоянию. Все процедуры проводятся анонимно, без постановки на учёт. Индивидуальный подход, корректный подбор медикаментов и строгий контроль состояния пациента делают лечение эффективным и безопасным.
Подробнее тут – anonimnyj-vyvod-iz-zapoya
Вызов нарколога на дом в таких условиях позволяет не терять драгоценное время, избежать госпитализации и предотвратить критическое развитие событий. Кроме того, это снижает психологическую нагрузку на пациента и его близких, особенно если зависимость длится долго и сопровождается отрицанием проблемы.
Подробнее можно узнать тут – нарколог на дом клиника
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Получить больше информации – вывод из запоя капельница
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Разобраться лучше – вывод из запоя в сочи
Капельница от запоя необходима, если у пациента наблюдаются следующие симптомы:
Разобраться лучше – https://kapelnica-ot-zapoya-msk55.ru/kapelnicy-ot-zapoya-na-domu-v-odincovo/
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительные сведения – наркология вывод из запоя
Первый контакт начинается с точных вопросов: длительность запоя, принятые лекарства, хронические болезни, аллергии, эпизоды аритмии или судорог. По приезде врач оценивает уровень сознания, измеряет давление, пульс, сатурацию, частоту дыхания, при необходимости проводит экспресс-глюкозу и ЭКГ переносным прибором. На этом этапе выбирается формат — на дому или в стационаре — исходя из клинических рисков и бытовых условий. Если показатели стабильны и рядом есть взрослый для наблюдения, домашний формат позволяет мягко и конфиденциально стабилизировать состояние. Если же ожидаются колебания давления, нарушения ритма, признаки делирия или выраженная дегидратация, безопаснее стационар, где доступен круглосуточный мониторинг и быстрая коррекция терапии без логистических пауз. Решение всегда объясняется простыми словами, чтобы пациент и близкие понимали логику маршрута.
Выяснить больше – вывод из запоя дзержинский
Процесс начинается с вызова врача или доставки пациента в клинику. После прибытия специалист проводит первичную диагностику: измерение давления, температуры, пульса, уровня кислорода в крови, визуальная оценка степени возбуждения или угнетения сознания. Собирается краткий анамнез: какой наркотик принимался, как долго, были ли сопутствующие заболевания.
Подробнее – http://snyatie-lomki-podolsk1.ru/snyatie-lomki-na-domu-v-podolske/
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Исследовать вопрос подробнее – вывод из запоя капельница на дому сочи
hey there realistic health and wellbeing
thank you for your info – I’ve certainly picked up something new from right here.
I did however expertise a few technical points using this web
site, since I experienced to reload the website many times previous to I could get it to load correctly.
I had been wondering if your web hosting is
OK? Not that I’m complaining, but sluggish loading instances times will very frequently affect your
placement in google and can damage your high quality score if advertising and marketing with
Adwords. Anyway I’m adding this RSS to my email and could look out for much more
of your respective exciting content. Ensure that you update this again soon.
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее – вывод из запоя вызов в сочи
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Исследовать вопрос подробнее – https://14kankoreziu.lt/virtuali-kavapost
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Детали по клику – http://www.mandjphotos.com/2014/09/wedding-la-garde-freinet
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Полная информация здесь – https://risingnftartists.com/hello-world
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Исследовать вопрос подробнее – http://www.mandjphotos.com/2014/09/wedding-la-garde-freinet
В Сочи клиника «Детокс» предлагает вывод из запоя в стационаре. Опытные врачи обеспечивают полную безопасность и комфорт пациента, а услуги доступны круглосуточно.
Получить дополнительную информацию – наркологический вывод из запоя в сочи
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
А что дальше? – https://automovilesburillo.com/hola-mundo
of course like your web site but you have to test the spelling on several of
your posts. A number of them are rife with spelling issues and I in finding
it very troublesome to tell the truth nevertheless I will surely come back again.
Inspiring quest there. What happened after? Thanks!
深く 感動しました。光を 取り戻すための
寄付は、社会にとって 大きな 助けです。これからもこの 取り組みを 頑張ってください。よろしくお願いします。
My page: アイケア・チャリティ
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Исследовать вопрос подробнее – вывод из запоя на дому в нижнем новгороде
Алкогольная или наркотическая интоксикация — это не просто временное ухудшение самочувствия, а серьёзное медицинское состояние, требующее неотложной помощи. Когда человек находится в запое или состоянии ломки, его организм стремительно теряет силы, нарушается работа сердца, печени, мозга, возникают панические атаки, судороги, спутанность сознания. В таких случаях помощь должна быть незамедлительной. Если пациент не может самостоятельно добраться до клиники, оптимальным решением становится вызов нарколога на дом. В Красногорске такая услуга доступна круглосуточно благодаря выездной службе клиники «Ключ к Здоровью».
Подробнее тут – помощь нарколога на дому в красногорске
This is my first time pay a quick visit at here and i am actually impressed to read everthing at alone place.
After looking over a handful of the articles on your site, I honestly
appreciate your technique of writing a blog. I saved it to my bookmark webpage list and will be
checking back soon. Please visit my website as well and let me know your opinion.
В Сочи клиника «Детокс» проводит вывод из запоя в стационаре с круглосуточным контролем врачей. Процедуры безопасны, эффективны и анонимны.
Выяснить больше – вывод из запоя на дому круглосуточно
Quality content is the important to be a focus
for the viewers to pay a quick visit the website, that’s what this site is providing.
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Хочешь знать всё? – https://yanagawa-sports-seikotuin.com/%E6%B0%B4%E7%B4%A0%E3%81%A7%E3%83%9F%E3%83%88%E3%82%B3%E3%83%B3%E3%83%89%E3%83%AA%E3%82%A2%E3%82%92%E6%B4%BB%E6%80%A7%E5%8C%96%E3%81%95%E3%81%9B%E3%82%88%E3%81%86%E2%9C%A8
Также мы учитываем потребности каждого пациента — по питанию, условиям проживания, графику процедур. Проживание возможно в стандартных и повышенных палатах, с возможностью индивидуального обслуживания.
Подробнее можно узнать тут – скорая наркологическая помощь бесплатная
Абстинентный синдром — одно из самых тяжёлых и опасных проявлений наркотической зависимости. Он развивается на фоне резкого отказа от приёма веществ и сопровождается сильнейшими нарушениями работы организма. Это состояние требует немедленного вмешательства. Самостоятельно справиться с ним невозможно — особенно если речь идёт о героине, метадоне, синтетических наркотиках или длительной зависимости. В клинике «НаркоПрофи» мы организовали систему снятия ломки в Подольске, работающую круглосуточно: как на дому, так и в условиях стационара.
Детальнее – http://snyatie-lomki-podolsk1.ru/snyatie-lomki-na-domu-v-podolske/
Ломка — это не временное недомогание. Это системное разрушение организма, связанное с тем, что он перестаёт получать наркотик, к которому уже привык. Нарушается обмен веществ, функции сердца, печени, почек, теряется контроль над эмоциями и болью. В состоянии абстиненции человек не может спать, есть, адекватно мыслить. Страдает и тело, и психика.
Подробнее тут – ломка от наркотиков в подольске
I loved as much as you will receive carried out right here.
The sketch is attractive, your authored subject matter stylish.
nonetheless, you command get got an impatience over that you wish
be delivering the following. unwell unquestionably
come more formerly again since exactly the same nearly very often inside case you shield this hike.
«НоваМед Центр» организует экстренную помощь при алкогольной интоксикации без очередей и лишней огласки. Команда наркологов и анестезиологов работает круглосуточно, выезжает на дом и принимает в стационаре, сохраняя один стандарт качества: очная оценка состояния, индивидуально подобранная инфузионная терапия, контроль жизненно важных показателей и понятные рекомендации на первые сутки. Схемы не шаблонные: состав и скорость капельницы зависят от длительности запоя, возраста, сопутствующих болезней и уже принятых лекарств. Наша цель — безопасно прервать запой, снять тремор, тревогу и тошноту, вернуть сон и аппетит, снизить нагрузку на сердце и печень, а затем предложить маршрут последующей помощи по готовности пациента — от амбулаторного наблюдения до программ профилактики срывов.
Получить больше информации – http://vyvod-iz-zapoya-lyubertsy2.ru/vyvod-iz-zapoya-na-domu-lyuberczy/
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Разобраться лучше – вывод из запоя на дому в нижнем новгороде
Thanks for another informative site. Where else may I get
that kind of information written in such an ideal approach?
I have a mission that I’m just now running on, and I
have been on the glance out for such information.
my website: Sports trainer
Hey There. I found your blog using msn. This is a very
well written article. I’ll be sure to bookmark it and come back to read more of your
useful information. Thanks for the post. I’ll definitely return.
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Ознакомиться с деталями – вызов врача нарколога на дом сочи
Проведение лечения в домашней обстановке значительно снижает уровень стресса и тревожности. Пациенту не нужно тратить силы на поездки в медицинские учреждения, что особенно важно при ограниченной мобильности. Домашняя атмосфера создает идеальные условия для открытого диалога с врачом, что существенно повышает эффективность терапии и шансы на успешное выздоровление.
Ознакомиться с деталями – narkolog na dom nedorogo
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Получить дополнительные сведения – https://www.grupolic.com.co/nam-sed-tellus-id-magna-elementum-tincidunt
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Подробнее можно узнать тут – вывод из запоя на дому круглосуточно в сочи
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее можно узнать тут – вывод из запоя на дому недорого в сочи
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Подробнее тут – нарколог на дом срочно сочи
It’s in point of fact a great and useful piece of information. I am satisfied that you simply shared
this useful information with us. Please keep us informed
like this. Thanks for sharing.
Также страдают сердце и сосуды. У пациентов часто наблюдаются тахикардия, нестабильное давление, аритмии, повышенный риск инфаркта или инсульта. Система пищеварения реагирует воспалением: гастрит, панкреатит, тошнота, рвота. Все эти изменения усиливаются на фоне обезвоживания и электролитного дисбаланса. Именно поэтому стандартное «отлежаться» или домашнее лечение чаще всего оказывается неэффективным и даже опасным. Необходима полноценная капельная терапия — с грамотно подобранными препаратами и медицинским наблюдением.
Разобраться лучше – kapelnitsa ot zapoia na domu khimki
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Разобраться лучше – вывод из запоя в стационаре в нижнем новгороде
Enjoyed reading through this, very good material. Thanks!
Процедура длится от одного до трёх часов. В течение всего времени за пациентом наблюдает медперсонал, проводится мониторинг давления, пульса, общего самочувствия. Уже через 30–60 минут после начала инфузии большинство пациентов ощущают облегчение: снижается тревожность, уходит головная боль, нормализуется дыхание, появляются силы.
Изучить вопрос глубже – kapelnica-ot-zapoya-moskva3.ru/
great issues altogether, you simply gained a brand
new reader. What would you recommend in regards
to your submit that you made some days in the past?
Any certain?
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительную информацию – вывод из запоя анонимно
В Сочи клиника «Детокс» предлагает вывод из запоя в стационаре. Опытные врачи обеспечивают полную безопасность и комфорт пациента, а услуги доступны круглосуточно.
Получить больше информации – вывод из запоя дешево в сочи
Мы понимаем, что в момент кризиса важна не только медицинская помощь, но и финансовая доступность. Поэтому в клинике «Спасение» в Мытищах действует несколько тарифов, позволяющих выбрать оптимальный вариант для любой ситуации. Стоимость зависит от состава препаратов, времени проведения и необходимости дополнительных манипуляций.
Изучить вопрос глубже – капельница от запоя цена мытищи
На месте врач проводит первичный осмотр, измеряет давление, пульс, сатурацию, оценивает уровень интоксикации и абстиненции. Далее назначается инфузионная терапия — капельница, направленная на дезинтоксикацию, восстановление электролитного баланса, купирование тревожности и нормализацию сна.
Выяснить больше – психиатр нарколог на дом в красногорске
На месте врач проводит первичный осмотр, измеряет давление, пульс, сатурацию, оценивает уровень интоксикации и абстиненции. Далее назначается инфузионная терапия — капельница, направленная на дезинтоксикацию, восстановление электролитного баланса, купирование тревожности и нормализацию сна.
Выяснить больше – нарколог на дом круглосуточно цены в красногорске
Thanks for sharing your thoughts about end of tenancy cleaning service Glasgow.
Regards
Thanks very nice blog!
Hey there! I’m at work browsing your blog from my new iphone!
Just wanted to say I love reading your blog and look forward
to all your posts! Carry on the excellent work!
Thanks for finally talking about > Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate
< Liked it!
В повседневности неточный ориентир часто заставляет терять время, поэтому мы проговариваем симптомы, при которых тянуть нельзя. Список не заменяет осмотр, он помогает близким описать ситуацию по телефону и выбрать правильный маршрут вместе с врачом.
Углубиться в тему – https://vyvod-iz-zapoya-lyubertsy2.ru
Клиника «Похмельная служба» в Нижнем Новгороде предлагает комплексное лечение запоя с использованием капельницы. Наши специалисты проводят диагностику и назначают индивидуальный план лечения.
Изучить вопрос глубже – вывод из запоя капельница
Для восстановления после запоя выбирайте стационар клиники «Детокс» в Сочи. Здесь пациентам обеспечивают качественную помощь и поддержку на каждом этапе.
Углубиться в тему – наркология вывод из запоя сочи
«НоваМед Центр» организует экстренную помощь при алкогольной интоксикации без очередей и лишней огласки. Команда наркологов и анестезиологов работает круглосуточно, выезжает на дом и принимает в стационаре, сохраняя один стандарт качества: очная оценка состояния, индивидуально подобранная инфузионная терапия, контроль жизненно важных показателей и понятные рекомендации на первые сутки. Схемы не шаблонные: состав и скорость капельницы зависят от длительности запоя, возраста, сопутствующих болезней и уже принятых лекарств. Наша цель — безопасно прервать запой, снять тремор, тревогу и тошноту, вернуть сон и аппетит, снизить нагрузку на сердце и печень, а затем предложить маршрут последующей помощи по готовности пациента — от амбулаторного наблюдения до программ профилактики срывов.
Подробнее тут – http://vyvod-iz-zapoya-lyubertsy2.ru/vyvod-iz-zapoya-lyuberczy-czeny/
Heya i’m for the primary time here. I came across this board and I find It really useful & it helped me out a lot.
I’m hoping to offer one thing back and aid others such
as you helped me.
Woah! I’m really loving the template/theme of this blog.
It’s simple, yet effective. A lot of times it’s challenging to get that “perfect balance” between user friendliness and appearance.
I must say you’ve done a excellent job with this. Also, the blog loads very fast for me on Firefox.
Excellent Blog!
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Исследовать вопрос подробнее – https://faxemusik.dk/faq-items/do-your-men-wear-safety-shoes
Перед началом процедуры врач проводит осмотр: измеряет давление, пульс, уровень кислорода в крови, оценивает тяжесть абстинентного синдрома. В зависимости от результатов и наличия сопутствующих заболеваний составляется индивидуальный состав инфузионного раствора. Он может включать:
Подробнее тут – капельница от запоя на дому московская область
В Сочи клиника «Детокс» проводит вывод из запоя в стационаре с круглосуточным контролем врачей. Процедуры безопасны, эффективны и анонимны.
Выяснить больше – помощь вывод из запоя сочи
I visited multiple web sites however the audio feature
for audio songs current at this site is in fact marvelous.
What’s up, I would like to subscribe for this blog to take most recent
updates, so where can i do it please help.
Thankfulness to my father who told me concerning this blog,
this webpage is truly amazing.
Visit my homepage; realistic health and wellbeing
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Детальнее – вывод из запоя на дому
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Разобраться лучше – вывод из запоя недорого
인천출장마사지 – 인천 전역 호텔・자택에서 아로마마사지, 스포츠마사지,
스웨디시를 전문 테라피스트에게 받아보세요.
고품격 홈케어 힐링과 맞춤 서비스
Hi, There’s no doubt that your blog could be having web browser compatibility issues.
Whenever I take a look at your blog in Safari, it looks fine but when opening in I.E., it has some overlapping issues.
I merely wanted to provide you with a quick heads up! Aside from that, excellent
site!
Hey! I know this is somewhat off topic but I
was wondering if you knew where I could get a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m
having trouble finding one? Thanks a lot!
This web site certainly has all the information and facts I needed about this subject and didn’t
know who to ask.
Awesome! Its truly remarkable piece of writing, I have
got much clear idea regarding from this paragraph.
Yes! Finally someone writes about porta cabins uae.
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Ознакомиться с деталями – нарколог на дом вывод из запоя в сочи
сюда kraken darknet market
Hi everyone, it’s my first pay a quick visit at this web page, and article
is truly fruitful in favor of me, keep up posting such content.
Right away I am going away to do my breakfast, once having my breakfast coming over again to read other news.
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Смотрите также… – https://dance.quinceandmulberrystudios.com.au/2016/08/23/hello-world
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее – врач вывод из запоя
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Исследовать вопрос подробнее – нарколог вывод из запоя в нижнем новгороде
Одной из самых сильных сторон нашей клиники является оперативность. Мы понимаем, что при алкоголизме, наркомании и лекарственной зависимости часто требуются немедленные действия. Если человек находится в состоянии запоя, абстиненции или передозировки, промедление может привести к тяжёлым осложнениям или даже смерти.
Подробнее можно узнать тут – narkologicheskaya-pomoshch-na-domu
Преимущества домашнего лечения также заключаются в индивидуальном подходе. Врач, находясь в вашем доме, может более тщательно изучить ситуацию, провести необходимую диагностику и подобрать курс лечения, который идеально подойдет вашему состоянию. В отличие от клиники, где внимание врача часто ограничено временем, на дому можно уделить пациенту больше времени, подбирая лечение с учетом его особенностей.
Ознакомиться с деталями – http://narcolog-na-dom-moskva55.ru
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Есть чему поучиться – https://hairspace-agio.com/blog/?p=500
Nice post. I learn something totally new and challenging on blogs
I stumbleupon everyday. It’s always exciting to read through content from other authors and use a little something from their web sites.
Ритм жизни в мегаполисе и постоянный стресс часто становятся причиной развития зависимостей у жителей города. В такой ситуации необходима профессиональная консультация врача. Оптимальное решение – вызов нарколога на дом в Москве. Это обеспечивает не только получение медицинской помощи в привычной обстановке, но и полную конфиденциальность.
Выяснить больше – vrach narkolog na dom moskva
I’m not that much of a internet reader to be honest but your
sites really nice, keep it up! I’ll go ahead and bookmark your site to come back later on.
All the best
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Лучшее решение — прямо здесь – https://pinerolo.scuolacottolengo.org/in-preghiera-con-il-vescovo-derio
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Узнать больше – вывод из запоя на дому круглосуточно в сочи
Hey! I know this is kind of off topic but I was wondering which blog platform
are you using for this site? I’m getting fed up of WordPress because I’ve had
issues with hackers and I’m looking at alternatives for another platform.
I would be fantastic if you could point me
in the direction of a good platform.
Ahaa, its pleasant conversation on the topic of this paragraph here at this blog, I have read all that, so now me also commenting here.
Выезд нарколога на дом в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Получить больше информации – вывод из запоя на дому цена нижний новгород
Have you ever thought about including a little bit more than just your articles?
I mean, what you say is valuable and everything. But just imagine
if you added some great visuals or video clips to
give your posts more, “pop”! Your content is excellent but with images and clips, this blog could definitely be one of the
most beneficial in its niche. Awesome blog!
My webpage: Youth camps flagstaff
В основе нашей методики — комплексный подход, сочетающий медицинскую точку зрения и психологические технологии. Мы не ограничиваемся снятием абстиненции: задача клиники — помочь пациенту обрести новую мотивацию, развить навыки противостояния стрессам и возобновить социальную активность. Работа строится на трёх ключевых принципах:
Подробнее можно узнать тут – chastnaya-narkologicheskaya-klinika-v-mytishchah
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Получить дополнительные сведения – запой нарколог на дом в сочи
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Выяснить больше – наркологический вывод из запоя
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Подробнее тут – вывод из запоя капельница
Ценю информацию, которую вы публикуете на Sultan Casino. Большое спасибо!
https://www.truckdriveracademy.it/news/eeb253b7-cba4-4883-986e-5a10ebc047b3/
I love it when folks come together and share thoughts. Great blog, stick with
it!
Thank you for some other informative site. The place else may I get that kind
of information written in such a perfect method? I have a undertaking that I
am simply now operating on, and I’ve been at the glance out for such info.
Review my web page :: sustainable health habits
Экстренная помощь при запое в Нижнем Новгороде — капельница на дому от опытных врачей-наркологов.
Получить больше информации – вывод из запоя цена
В клинике «НаркологПроф» детоксикация проводится под наблюдением специалистов, которые контролируют давление, частоту сердечных сокращений и дыхание пациента. Инфузионная терапия помогает восстановить электролитный баланс, ускорить выведение токсинов и улучшить общее состояние уже через несколько часов после начала лечения.
Подробнее можно узнать тут – vyvod-iz-zapoya-na-domu
It’s amazing designed for me to have a web page, which is
good in support of my know-how. thanks admin
В Сочи клиника «Детокс» предлагает вывод из запоя в стационаре. Опытные врачи обеспечивают полную безопасность и комфорт пациента, а услуги доступны круглосуточно.
Узнать больше – врач вывод из запоя в сочи
В Сочи клиника «Детокс» проводит вывод из запоя в стационаре с круглосуточным контролем врачей. Процедуры безопасны, эффективны и анонимны.
Ознакомиться с деталями – срочный вывод из запоя в сочи
Одной из самых сильных сторон нашей клиники является оперативность. Мы понимаем, что при алкоголизме, наркомании и лекарственной зависимости часто требуются немедленные действия. Если человек находится в состоянии запоя, абстиненции или передозировки, промедление может привести к тяжёлым осложнениям или даже смерти.
Подробнее можно узнать тут – narkologicheskaya-pomoshch-balashiha-balashiha
Запой — одно из самых опасных проявлений алкогольной зависимости. Он сопровождается глубокой интоксикацией организма, нарушением работы сердца, печени, головного мозга и других жизненно важных систем. Когда человек не может остановиться самостоятельно, а организм больше не справляется с нагрузкой, требуется медицинская помощь. В наркологической клинике «Спасение» в Мытищах мы проводим экстренные процедуры инфузионной терапии, позволяющие эффективно и безопасно вывести пациента из состояния запоя. Капельница — это первый шаг на пути к восстановлению здоровья и возвращению к нормальной жизни.
Подробнее – https://kapelnica-ot-zapoya-moskva2.ru/kapelnicy-ot-zapoya-na-domu-v-mytishchah/
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Выяснить больше – наркология вывод из запоя
Одной из самых сильных сторон нашей клиники является оперативность. Мы понимаем, что при алкоголизме, наркомании и лекарственной зависимости часто требуются немедленные действия. Если человек находится в состоянии запоя, абстиненции или передозировки, промедление может привести к тяжёлым осложнениям или даже смерти.
Получить дополнительную информацию – http://narkologicheskaya-pomoshch-balashiha1.ru/skoraya-narkologicheskaya-pomoshch-v-balashihe/https://narkologicheskaya-pomoshch-balashiha1.ru
This article details GC’s strategic decision to master the fundamentals in early 2026. Through a systematic audit, they transformed good content into comprehensive, transparent resources. The synergy between refined words and robust code builds a more trustworthy platform.
Hi it’s me, I am also visiting this web site daily, this web site is genuinely pleasant and the users are genuinely sharing pleasant thoughts.
Именно поэтому так важно не терять время. Чем раньше пациент получает помощь, тем выше шансы избежать необратимых последствий и вернуться к нормальной жизни.
Ознакомиться с деталями – снятие ломки на дому цена подольск
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Разобраться лучше – помощь вывод из запоя
Kazino portalı əladır, belə davam edin. Sağ olun!
https://classihub.in/author/pinupcasinooynamaq/
high payout online casino
https://robertsspaceindustries.com/en/citizens/gamblingchooser
best online roulette real money
Проведение лечения в домашней обстановке значительно снижает уровень стресса и тревожности. Пациенту не нужно тратить силы на поездки в медицинские учреждения, что особенно важно при ограниченной мобильности. Домашняя атмосфера создает идеальные условия для открытого диалога с врачом, что существенно повышает эффективность терапии и шансы на успешное выздоровление.
Разобраться лучше – vyzov vracha narkologa na dom
I always emailed this webpage post page to all my contacts, as
if like to read it then my friends will too.
Ритм жизни в мегаполисе и постоянный стресс часто становятся причиной развития зависимостей у жителей города. В такой ситуации необходима профессиональная консультация врача. Оптимальное решение – вызов нарколога на дом в Москве. Это обеспечивает не только получение медицинской помощи в привычной обстановке, но и полную конфиденциальность.
Ознакомиться с деталями – https://narcolog-na-dom-msk55.ru/narkolog-na-dom-moskva-tseny/
Мир онлайн-слотов растёт: новые провайдеры, повышенные RTP и постоянные турниры поддерживают интерес игроков.
Vavada удерживает позиции в топе, но не забывайте проверять лицензию и лимиты перед депозитом.
Выбирайте автоматы с бонусными раундами, бесплатными вращениями и прогрессивными джекпотами — так повышается шанс крупного выигрыша.
Зеркала решают проблему блокировок и позволяют оперативно выводить средства без лишних задержек.
Актуальные возможности доступны здесь: https://bezprovodoff.com/pgs/?sekretu_vuigrusha_v_onlayn_kazino_na_slotah_1.html.
Играйте ответственно и контролируйте банкролл, чтобы азарт оставался в пределах удовольствия.
Осложнения, к которым может привести отсутствие лечения:
Исследовать вопрос подробнее – http://snyatie-lomki-podolsk1.ru/snyatie-lomki-na-domu-v-podolske/
When I originally commented I appear to have clicked
on the -Notify me when new comments are added- checkbox and now whenever a comment
is added I recieve four emails with the exact same comment.
Perhaps there is an easy method you are able to remove me from that service?
Cheers!
Do you mind if I quote a few of your articles as long as I provide credit and
sources back to your site? My website is in the exact same niche as yours and my visitors
would definitely benefit from some of the information you present here.
Please let me know if this okay with you. Regards!
Задача врачей — не просто облегчить симптомы, а купировать осложнения, стабилизировать жизненно важные функции, вернуть пациенту способность к дальнейшему лечению. Мы работаем быстро, анонимно и профессионально. Любой человек, оказавшийся в кризисе, может получить помощь в течение часа после обращения.
Углубиться в тему – снятие ломки нарколог в подольске
Также мы учитываем потребности каждого пациента — по питанию, условиям проживания, графику процедур. Проживание возможно в стандартных и повышенных палатах, с возможностью индивидуального обслуживания.
Выяснить больше – https://narkologicheskaya-pomoshch-balashiha1.ru/skoraya-narkologicheskaya-pomoshch-v-balashihe
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Желаете узнать подробности? – https://hubert-gros-bedachungen.de/2022/03/14/hallo-welt
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Детальнее – вывод из запоя вызов в сочи
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, UՏA
(402) 940-8979
how to get rid of acne routine
Greetings from Florida! I’m bored to death at work so I decided to
browse your blog on my iphone during lunch break.
I enjoy the information you provide here and can’t wait to take a look
when I get home. I’m shocked at how fast your blog loaded on my
phone .. I’m not even using WIFI, just 3G ..
Anyhow, awesome blog!
A person necessarily assist to make critically posts I’d state.
That is the first time I frequented your web
page and thus far? I amazed with the analysis you made to create this actual put up extraordinary.
Wonderful process!
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Выяснить больше – вывод из запоя цена
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Получить дополнительную информацию – вывод из запоя в стационаре
Препараты подбираются строго индивидуально и могут включать:
Углубиться в тему – врач нарколог на дом
Показания к проведению капельницы от запоя включают:
Детальнее – kapelnitsa ot zapoia klinika
Как отмечает главный врач клиники, кандидат медицинских наук Сергей Иванов, «мы создали систему, при которой пациент получает помощь в течение часа — независимо от дня недели и времени суток. Это принципиально меняет шансы на выздоровление».
Получить дополнительную информацию – http://
Prome Secured
3603 N 222nd St, Suite 102,
Elkhorn, ΝE 68022, United States
402-289-4126
Innovative digital security solutions
Проведение лечения в домашней обстановке значительно снижает уровень стресса и тревожности. Пациенту не нужно тратить силы на поездки в медицинские учреждения, что особенно важно при ограниченной мобильности. Домашняя атмосфера создает идеальные условия для открытого диалога с врачом, что существенно повышает эффективность терапии и шансы на успешное выздоровление.
Ознакомиться с деталями – http://narcolog-na-dom-msk55.ru/narkolog-na-dom-moskva-tseny/
What’s up, just wanted to mention, I loved this blog post.
It was helpful. Keep on posting!
Look at my web page zugravu01
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Желаете узнать подробности? – http://www.izuho-club.com/cgi-bin/sunbbs.cgi?mode=form&no=388752&page=
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительную информацию – вывод из запоя на дому сочи
https://jm-cougar.fr/
Amazing plenty of great material!
Препараты подбираются строго индивидуально и могут включать:
Изучить вопрос глубже – нарколог на дом круглосуточно цены
Для многих пациентов важным моментом является сохранение конфиденциальности. Врач, приехавший на дом, работает с полной защитой данных. Пациент может быть уверен, что его проблема останется личной и не станет достоянием общественности. Врачи приезжают на неприметных автомобилях и избегают всяческих ситуаций, которые могут привлечь лишнее внимание.
Подробнее – http://narcolog-na-dom-moskva55.ru/vyzov-narkologa-na-dom-moskva/
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Исследовать вопрос подробнее – помощь вывод из запоя
Hi i am kavin, its my first occasion to commenting anyplace, when i read this
article i thought i could also make comment due to this sensible piece of writing.
Также страдают сердце и сосуды. У пациентов часто наблюдаются тахикардия, нестабильное давление, аритмии, повышенный риск инфаркта или инсульта. Система пищеварения реагирует воспалением: гастрит, панкреатит, тошнота, рвота. Все эти изменения усиливаются на фоне обезвоживания и электролитного дисбаланса. Именно поэтому стандартное «отлежаться» или домашнее лечение чаще всего оказывается неэффективным и даже опасным. Необходима полноценная капельная терапия — с грамотно подобранными препаратами и медицинским наблюдением.
Изучить вопрос глубже – kapelnitsa ot zapoia
Ценю информацию, которую вы публикуете на Sultan Casino. Большое спасибо!
https://diway.ru/bitrix/redirect.php?goto=https://sultan-casino-kazakhstan-jackpot.kz/mobile-app
Проведение лечения в домашней обстановке значительно снижает уровень стресса и тревожности. Пациенту не нужно тратить силы на поездки в медицинские учреждения, что особенно важно при ограниченной мобильности. Домашняя атмосфера создает идеальные условия для открытого диалога с врачом, что существенно повышает эффективность терапии и шансы на успешное выздоровление.
Подробнее тут – http://narcolog-na-dom-msk55.ru
Процедура длится от одного до трёх часов. В течение всего времени за пациентом наблюдает медперсонал, проводится мониторинг давления, пульса, общего самочувствия. Уже через 30–60 минут после начала инфузии большинство пациентов ощущают облегчение: снижается тревожность, уходит головная боль, нормализуется дыхание, появляются силы.
Получить больше информации – kapelnitsa ot zapoia tsena
Если пациент не может приехать в клинику, в Краснодаре нарколог приедет к нему домой. Помощь оказывает «Детокс» круглосуточно.
Исследовать вопрос подробнее – narkolog-na-dom-kruglosutochno sochi
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее тут – вывод из запоя недорого в сочи
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Выяснить больше – нарколог на дом вывод из запоя в сочи
I am truly inspired by this post. Donating to restore sight
is a beautiful way to support humanity. Please continue this wonderful effort.
Best regards to the team!
My site; Ocular Care Support
Ρrime Secured
3603 N 222nd Ѕt, Suite 102,
Elkhorn, ΝE 68022, United Statеs
402-289-4126
Bookmarks (protopage.com)
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Узнать больше – помощь вывод из запоя сочи
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Изучить вопрос глубже – вывод из запоя на дому цена
Have you ever thought about creating an e-book or guest
authoring on other blogs? I have a blog based on the same information you discuss and would love to have
you share some stories/information. I know my visitors would appreciate
your work. If you’re even remotely interested, feel free to
shoot me an e-mail.
I must thank you for the efforts you’ve put in writing this blog.
I’m hoping to check out the same high-grade blog posts by you in the future as well.
In truth, your creative writing abilities has inspired me to get my very own website now
😉
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Получить дополнительную информацию – https://pousadasobreaspedras.com.br/ola-mundo
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored subject matter stylish.
nonetheless, you command get got an edginess over that you wish be delivering the
following. unwell unquestionably come more formerly again as exactly the same nearly a
lot often inside case you shield this increase.
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее тут – нарколог на дом недорого сочи
Одной из самых сильных сторон нашей клиники является оперативность. Мы понимаем, что при алкоголизме, наркомании и лекарственной зависимости часто требуются немедленные действия. Если человек находится в состоянии запоя, абстиненции или передозировки, промедление может привести к тяжёлым осложнениям или даже смерти.
Изучить вопрос глубже – платная наркологическая помощь
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Углубиться в тему – врач нарколог на дом сочи
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Получить больше информации – вывод из запоя на дому круглосуточно
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Получить дополнительные сведения – вызов врача нарколога на дом сочи
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Разобраться лучше – нарколог на дом вывод из запоя сочи
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Открой скрытое – https://saptahiksamachar.com.np/%E0%A4%A6%E0%A4%B2%E0%A4%BF%E0%A4%A4-%E0%A4%AD%E0%A4%8F%E0%A4%95%E0%A5%88-%E0%A4%95%E0%A4%BE%E0%A4%B0%E0%A4%A3-%E0%A4%97%E0%A5%81%E0%A4%B0%E0%A5%81%E0%A4%95%E0%A5%81%E0%A4%B2%E0%A4%B2%E0%A5%87
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Подробнее тут – вывод из запоя сочи
нажмите, чтобы подробнее https://krab3a.at
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Подробнее – вывод из запоя недорого в сочи
Как отмечает главный врач клиники, кандидат медицинских наук Сергей Иванов, «мы создали систему, при которой пациент получает помощь в течение часа — независимо от дня недели и времени суток. Это принципиально меняет шансы на выздоровление».
Исследовать вопрос подробнее – наркологическая помощь балашиха балашиха
Мы понимаем, что в момент кризиса важна не только медицинская помощь, но и финансовая доступность. Поэтому в клинике «Спасение» в Мытищах действует несколько тарифов, позволяющих выбрать оптимальный вариант для любой ситуации. Стоимость зависит от состава препаратов, времени проведения и необходимости дополнительных манипуляций.
Получить дополнительные сведения – http://kapelnica-ot-zapoya-moskva2.ru/kapelnicy-ot-zapoya-na-domu-v-mytishchah/https://kapelnica-ot-zapoya-moskva2.ru
I was recommended this website by way of my cousin. I am not certain whether this put up is written via him as no one else recognize such precise approximately my trouble. You are wonderful! Thank you!
Возможность назначить визит специалиста в наиболее удобное время. Это позволяет эффективно совмещать лечение с работой и повседневными делами. Такая гибкость помогает пациентам своевременно начать терапию, не откладывая ее из-за занятости. При необходимости врач может приехать в вечернее время или выходные дни.
Детальнее – http://narcolog-na-dom-msk55.ru/narkolog-na-dom-moskva-tseny/
Hello. Great job. I did not expect this on a Wednesday. This is a great story. Thanks!
В этом информативном тексте представлены захватывающие события и факты, которые заставят вас задуматься. Мы обращаем внимание на важные моменты, которые часто остаются незамеченными, и предлагаем новые перспективы на привычные вещи. Подготовьтесь к тому, чтобы быть поглощенным увлекательными рассказами!
Подробности по ссылке – https://domovvprirode.sk/bazalna
Мы понимаем, что в момент кризиса важна не только медицинская помощь, но и финансовая доступность. Поэтому в клинике «Спасение» в Мытищах действует несколько тарифов, позволяющих выбрать оптимальный вариант для любой ситуации. Стоимость зависит от состава препаратов, времени проведения и необходимости дополнительных манипуляций.
Выяснить больше – https://kapelnica-ot-zapoya-moskva2.ru/kapelnica-ot-zapoya-cena-v-mytishchah
Hi there very cool blog!! Guy .. Excellent
.. Wonderful .. I’ll bookmark your site and take the feeds also?
I am satisfied to find numerous helpful info here in the post,
we want develop more strategies on this regard, thanks for sharing.
. . . . .
Именно поэтому так важно не терять время. Чем раньше пациент получает помощь, тем выше шансы избежать необратимых последствий и вернуться к нормальной жизни.
Получить дополнительные сведения – снятие ломки в стационаре подольск
Pretty nice post. I simply stumbled upon your weblog and wished
to say that I have truly loved browsing your weblog posts.
In any case I will be subscribing for your rss feed and I’m hoping you write once more soon!
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Подробнее тут – https://organicfarmacademy.com/pioneer-biochar-project-set-up-in-rushinga
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Это стоит прочитать полностью – https://vistoweekly.com/amzp22x
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Получить дополнительные сведения – https://energy-savings-refrigeration.com/fortifying-supermarkets-against-power-outages
I must thank you for the efforts you have put in writing this blog.
I really hope to see the same high-grade blog posts from you later on as well.
In truth, your creative writing abilities has motivated me
to get my own, personal blog now 😉
Good day! I just wish to give you a huge thumbs up for your great information you have got right here on this post.
I will be coming back to your site for more soon.
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить дополнительную информацию – наркологический вывод из запоя в сочи
Также мы учитываем потребности каждого пациента — по питанию, условиям проживания, графику процедур. Проживание возможно в стандартных и повышенных палатах, с возможностью индивидуального обслуживания.
Подробнее – https://narkologicheskaya-pomoshch-balashiha1.ru/
Возможность назначить визит специалиста в наиболее удобное время. Это позволяет эффективно совмещать лечение с работой и повседневными делами. Такая гибкость помогает пациентам своевременно начать терапию, не откладывая ее из-за занятости. При необходимости врач может приехать в вечернее время или выходные дни.
Разобраться лучше – https://narcolog-na-dom-msk55.ru/narkolog-na-dom-moskva-tseny/
Hi, I do think this is an excellent web site. I stumbledupon it
😉 I may revisit once again since I book marked it.
Money and freedom is the greatest way to change, may you be rich and continue to guide others.
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Желаете узнать подробности? – https://sophiesteininger.fr/le-nouveau-e-mucem-ouvre-ses-portes
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Узнать больше – вывод из запоя на дому круглосуточно в сочи
I do believe all the ideas you have presented in your post.
They’re really convincing and will certainly work.
Still, the posts are very short for novices.
May you please extend them a bit from subsequent time?
Thanks for the post.
Перед началом процедуры врач проводит осмотр, измеряет давление, пульс, уровень кислорода в крови, оценивает степень интоксикации и наличие сопутствующих заболеваний. После этого подбирается состав капельницы. В большинстве случаев она включает:
Исследовать вопрос подробнее – http://www.domen.ru
What a great forum, everyone is so active! Speaking of online entertainment and games, I absolutely love finding free and unblocked games for everyone. It’s exactly how I discovered the joy of online Baseball Games. Just click and play Baseball Games!.
В Сочи клиника «Детокс» предлагает полный курс вывода из запоя в стационаре. Круглосуточный медицинский контроль гарантирует безопасность и эффективность лечения.
Получить дополнительные сведения – вывод из запоя клиника в сочи
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Разобраться лучше – вывод из запоя вызов на дом сочи
Я потратил в интернете уже больше четырёх
часов сегодня, но так и не нашёл ни одной интересной
статьи, подобной вашей. Материал оказался очень полезным.
На мой взгляд, если бы все создатели сайтов и
блогеры делали такой же
качественный контент, сеть был бы гораздо более полезным, чем сейчас.
|
Мне не удалось воздержаться от комментария.
Прекрасно написано! |
Я немедленно подпишусь ваш
RSS-канал, так как я не могу отыскать новостную рассылку.
Она у вас есть? Пожалуйста, сообщите мне, чтобы я
мог подписаться. Спасибо.
My web site; узнать
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Выяснить больше – вывод из запоя на дому
Дополнительно усиливаются сердечно-сосудистые риски: густая кровь, дефицит калия и магния провоцируют тахикардию, скачки давления и повышают вероятность инфаркта или инсульта. На этом фоне даже простая головная боль может оказаться сигналом серьёзного сосудистого нарушения. Задача капельницы — не просто убрать симптомы, а стабилизировать состояние организма и предотвратить дальнейшее ухудшение.
Исследовать вопрос подробнее – капельница от запоя цена одинцово
«НоваМед Центр» организует экстренную помощь при алкогольной интоксикации без очередей и лишней огласки. Команда наркологов и анестезиологов работает круглосуточно, выезжает на дом и принимает в стационаре, сохраняя один стандарт качества: очная оценка состояния, индивидуально подобранная инфузионная терапия, контроль жизненно важных показателей и понятные рекомендации на первые сутки. Схемы не шаблонные: состав и скорость капельницы зависят от длительности запоя, возраста, сопутствующих болезней и уже принятых лекарств. Наша цель — безопасно прервать запой, снять тремор, тревогу и тошноту, вернуть сон и аппетит, снизить нагрузку на сердце и печень, а затем предложить маршрут последующей помощи по готовности пациента — от амбулаторного наблюдения до программ профилактики срывов.
Подробнее тут – https://vyvod-iz-zapoya-lyubertsy2.ru/
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Узнать больше – нарколог на дом анонимно сочи
goGLOW Omaha
3525 N 147tһ St, Omaha,
Nebraska, 68116, USA
(402) 940-8979
meet the team cost
Классная платформа казино онлайн — люблю заходить сюда!
https://htmlweb-ru.translate.goog/php/example/ip_for_host.php?str=pinupcasino-offsite.kz%2Fmobile-app&_x_tr_sl=auto&_x_tr_tl=fr&_x_tr_hl=fr&_x_tr_sch=http
goGLOW Omaha
3525 N 147th St, Omaha,
Nebraska, 68116, UЅА
(402) 940-8979
Bookmarks
Проведение лечения в домашней обстановке значительно снижает уровень стресса и тревожности. Пациенту не нужно тратить силы на поездки в медицинские учреждения, что особенно важно при ограниченной мобильности. Домашняя атмосфера создает идеальные условия для открытого диалога с врачом, что существенно повышает эффективность терапии и шансы на успешное выздоровление.
Подробнее можно узнать тут – http://narcolog-na-dom-msk55.ru/
Если нужен профессиональный вывод из запоя, обращайтесь в стационар клиники «Детокс» в Сочи. Все процедуры проводятся анонимно и под наблюдением специалистов.
Выяснить больше – наркологический вывод из запоя
What i don’t understood is in fact how you are now not really much more smartly-preferred than you
might be right now. You are so intelligent.
You know therefore considerably with regards to this matter, produced
me personally imagine it from numerous various angles.
Its like men and women are not interested except it’s something to do with Lady gaga!
Your own stuffs outstanding. All the time maintain it
up!
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Изучить вопрос глубже – вызов врача нарколога на дом сочи
Дополнительно усиливаются сердечно-сосудистые риски: густая кровь, дефицит калия и магния провоцируют тахикардию, скачки давления и повышают вероятность инфаркта или инсульта. На этом фоне даже простая головная боль может оказаться сигналом серьёзного сосудистого нарушения. Задача капельницы — не просто убрать симптомы, а стабилизировать состояние организма и предотвратить дальнейшее ухудшение.
Углубиться в тему – http://kapelnica-ot-zapoya-msk55.ru
Hello I am so delighted I found your weblog, I really found you
by error, while I was browsing on Aol for something else, Nonetheless I am here now and
would just like to say many thanks for a marvelous post and a all round exciting blog (I also love the theme/design),
I don’t have time to look over it all at the minute but I have bookmarked it and
also added in your RSS feeds, so when I have time I will be
back to read a lot more, Please do keep up the superb work.
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Получить больше информации – нарколог на дом краснодарский край
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Подробнее тут – нарколог на дом цена сочи
В Краснодаре клиника «Детокс» проводит выезд нарколога на дом для безопасного вывода из запоя.
Углубиться в тему – нарколог на дом недорого сочи
Hi to all, how is all, I think every one is getting more from this web site, and your views are
good designed for new visitors.
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Исследовать вопрос подробнее – нарколог на дом вывод из запоя в сочи
В Краснодаре клиника «Детокс» предлагает выезд нарколога на дом. Помощь оказывается быстро, анонимно и круглосуточно.
Получить дополнительную информацию – нарколог на дом краснодарский край
Процедура капельного введения лекарств позволяет решить сразу несколько задач: восполнить жидкость, нормализовать работу внутренних органов, вывести токсины и восстановить общее состояние. Благодаря внутривенному способу введения, компоненты раствора быстро поступают в кровь и начинают действовать уже в течение первых 10–15 минут.
Разобраться лучше – капельница от запоя цена мытищи
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Слушай внимательно — тут важно – https://jasarahgroup.com/index.php/2023/01/27/site-oficial-de-apostas-at-the-online-cassino-zero-brasi-2
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить дополнительные сведения – http://vyvod-iz-zapoya-sochi15.ru/
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Разобраться лучше – врач вывод из запоя
«НоваМед Центр» организует экстренную помощь при алкогольной интоксикации без очередей и лишней огласки. Команда наркологов и анестезиологов работает круглосуточно, выезжает на дом и принимает в стационаре, сохраняя один стандарт качества: очная оценка состояния, индивидуально подобранная инфузионная терапия, контроль жизненно важных показателей и понятные рекомендации на первые сутки. Схемы не шаблонные: состав и скорость капельницы зависят от длительности запоя, возраста, сопутствующих болезней и уже принятых лекарств. Наша цель — безопасно прервать запой, снять тремор, тревогу и тошноту, вернуть сон и аппетит, снизить нагрузку на сердце и печень, а затем предложить маршрут последующей помощи по готовности пациента — от амбулаторного наблюдения до программ профилактики срывов.
Подробнее тут – вывод из запоя дзержинский
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Получить дополнительные сведения – https://www.flowpoint.info/zoneterapi
is human trafficking tthe seсond largest, սѕa gymnastics coach human trafficking, human trafficking news neɑr me,
snopes lynne knowles human trafficking, human trafficking awareness ⅾay quotes, human trafficking sex scene, human trafficking – menschenhandel, meghan connors human trafficking, ansreew tate human trafficking, arguments ᧐n human trafficking, free human trafficking cme florida, human trafficking օur, human trafficking in minnesota 2021, arizona republican human trafficking,
orange іs the new black human trafficking, human trafficking conference ocean city md, 277 arrested
іn human trafficking, anti human trafficking law
philippines, north korea human trafficking fаcts, how
will the wall affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kids rescued
fгom hhuman trafficking, durham region human trafficking,
ᴡhy human trafficking is important, mother of god church
human trafficking, walmart human trafficking 2020,
ԝhɑt is thе rate of human trafficking worldwide, huan trafficking news
(news), human trafficking Ƅy ѕtate 2021, lgbt human trqfficking statistics, south africa аnd human trafficking, human traffickng statistics
fbi, hotel lawsuits human trafficking, operation reenewed hope human trafficking, human trafficking
atlanta 2022, human trafficking san joaquin county, non profit
organizations fօr human trafficking, human trafficking interpol, human trafficking elgin, trafficking women’ѕ human гights julietta hua, facebook hjman trafficking
lawsuit, rates оf human trafficking, real ԝorld example of human trafficking, lawyers ɑgainst
human trafficking, wson human trafficking summit 2022, vad är human trafficking, recognizing tһe signs of
human trafficking, human trafficking justice,
video ᧐f human trafficking, fߋur signs οf human trafficking, human trafficking honey, binjjun xie human trafficking,
human traffickin documentary amazon ⲣrime, minnesota human trafficking data, uncovers russian human trafficking
гing war, human trafficking chico ϲa, human trafficking jjus cogens, human trafficking syrian refugees, human traficking topics reserch paper, text human trafficking
link snopes, oprah south africa human trafficking, human trafficking grants 2015, human trafficking san antonio 2021,
human drug traffiicking meaning, human trafficking stries
children, fema human trafficking awareness, floriida
disney human trafficking, jobs fοr human trafficking victims, movie avout human trafficking 2023 netflix, а ⅾay in the llife
ⲟf ɑ human trafficking victim, uk human trafficking news,
bent ⅼicense plate human trafficking reddit, hhuman trafficking іn waterbury ct, center to combat human trafficking, greenville nc
human trafficking, maui human trafficking, tⲟp 5 human trafficking cities, іs human trafficking happening iin tһe us, oxnard human trafficking, aurora shoreline
hman trafficking, taconganas human trafficking, hashgags fоr human trafficking, whіte house human trafficking summit, corona human trafficking, border patrol human trafficking, human trafficking іn thailand 2020, human trafficking іn wv, 11 arrested in human trafficking,
china’ѕ one child polpicy and human trafficking, hotels human trafficking 2023,
human trafficking іn florida 2021, human trafficking debate topics, international justice mission human trafficking,
uncovers human trafficking гing for, scholarly article on human trafficking, madison herman human trafficking, amad diallo human trafficking, а poeem aЬout
human trafficking, human traffticking bristol tn, deluca аnd the human trafficking storyline, economy and human trafficking, human trafficking іn trinidad, human trafficking day 2018, caught camera actual
human trafficking victims, human traffickming episode opall grey’ѕ anatomy, duolingo ceo human trafficking, watch dolgs human trafficking
map, human trafficking definition canada, airtag human trafficking, human trafficking іn thе beauty industry,
人口販子human trafficking, forced labor іn human trafficking,
american airlines cnter human trafficking, human trafficking
ϲe texas, selah hhuman trafficking, skam human trafficking, fresno huuman trafficking statistics,
senegal human trafficking, human trafficking
belgium, michigan human trafficking ⅽourse, ny times
human trafficking, abandoned stroller human trafficking, human trafficking і-44,
solution ߋn human trafficking, human trafficking
canada news, ontario human trafficking, protects victims ߋf
human trafficking amendment, human trafficking іn highland ca, human trafficking
hotspot map, human trafficking organizations ontario, human trafficking hiding
ᥙnder cars, summary on human trafficking, uncovers russian huhman trafficking гing ᴡar, human trafficking honey, f᧐ur signs
of human trafficking, human trdafficking western pa, human trafficking livermore, human trafficking
durham region, human trafficking аt atlanta airport, binjun xie human trafficking,
minnesota human trafficking data, human trafficking documentary amazon ρrime, human trafficking lawyer bloomfield hills, human traffickng charge іn texas,
central students ɑgainst human trafficking, ap human geography human trafficking, human trafficking
fοr sexual exploitation, blue fⲟr human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo jorgensen օn hyman trafficking, fort hood soldiers human trafficking, beau ⲟf tһe
fіfth column human trafficking, hawkins human trafficking, human trafficking іn the pacific islands, reasons ԝhy human trafficking іs bad, all
human trafficking, wrіte an essay oon humkan trafficking, human trafficking pros, human trafficking dark web reddit, north preston hhuman trafficking, ԁollar sign tattoo human trafficking, wwht is human trafficking, human trafficking stuart fl,
priceless movie human trafficking, ti andd wife human trafficking,
human trafficking ethnicity statistics, і 80 truck stop human trafficking, hamilton human trafficking, oakville human trafficking, human trafficking оn the deep web, current human trafficking, human trafficking women’ѕ rightѕ, brunei human trafficking, barack obama human trafficking
quote, patron saint of human trafficking,
spirired ɑwaʏ human trafficking, the game human trafficking, tⲟp human trafficking cities 2023,
human trafficking ᴡhich countries aгe the worst, how to
donate to human trafgficking organizations,human trafficking quottes famous, human trafficking story
2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, human trafficking
hemet сa, human trafficking statistics oregon, һow
tօ identify а human trafficking victim, economy ɑnd
human trafficking, lover boy method ᧐f human trafficking,
deluca ɑnd the huyman trafficking storyline, european human trafficking,
selahh human trafficking, american airlines center human trafficking, human trafficking paintings, ᴡһat
state iis #1 in human trafficking?, forced labor іn hunan trafficking, 人口販子human trafficking,
crystal meth, ѡhɑt does crydtal meth looҝ liҝe,
wһat is crystal meth, crystal meth anonymous, һow lⲟng doeѕ crystal meth stay іn үour syѕtem,
һow to maҝe crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects, crystal meth pipe, crystal meth drug, ѡhat does crystal meth looқ like?, meth crystal, crystal meh images, crystal meth ѕide effects, һow
is crystal meth made, meth vs crystal meth, ѡhat does crystal
meth ԁo, crystal meth symptoms, crystal meth ᴠѕ meth, effects of crystal meth, ѕide effects оf crystal meth,
һow do үou make crystal meth, crystal meth vss crack, ԝhɑt doeѕ crystal meth smell ⅼike,
һow is crystal meth uѕed, crystal mesth withdrawal, crystal
meth breaking bad, ԝhat is crystal meth mɑde of, whаt d᧐es crystal meth do to yoս, crystal meth teeth, smoking crystal meth, crystal
meth pictures, ϲan you snort crystal meth, crystal meth Ьefore and aftеr, ԝhо invented crystal meth, ccrystal metth fɑcts, crystal meth withdrawal symptoms, crystal mth street names, signs оf crystal meth, crystal meth addiction, һow to ccook crystal meth,
crystal meth definition, ѡhat type oof drug іs crystal meth, ԝhat doеs crystal mmeth feel lіke,
crystal meth meaning,crystal meth ingredients, ԝhats crystal meth,
wһat color iѕ crystal meth, crystal meth detox, crystal
meth fасе, crystal meth powder, crystal meth poem, street names fоr crystal meth, short term effects oof crystal meth, signs оf crystal meth abuse, crystal meth rock, crystal metth fly,
crystal meth addict, crystal meth սsers, crystal meth rehab, һow mjch
does crrystal meth cost, һow do yߋu tаke crystal meth, how mսch is crystal meth,
signs օf crystal meth սѕe, how to smoke crystal meth, һow tо սse crystal meth,
long term effects of crystal meth, signs οf addiction to
crystal meth, pink crystal meth, crystal meth ⅼooҝ ⅼike,
breaking baad crystal meth, ᴡhen waѕ crstal meth invented,
pictures ߋf crystal meth, how is crystaal meth taken, signs tha sοmeone is using
crystal meth, ready οr not crystal meth storage, difference
ƅetween meth annd crystal meth, һow doo уoᥙ do
crystal meth, crystal meth., locate crystal meth storage, ԝһat aгe the effects oof crystal meth, fake crystal meth, crystal meth people, ѡһɑt doеs crystal meth,
hoᴡ do you use crystal meth, hhow addictive іs crystal meth, can you overdose on crystal
meth, crystal meth blue, crystal meth signs, һow longg ɗoes crystal meth laѕt, crystal meth detox los angeles,
hoow dⲟ people uuse crystal meth, hoow ⅾoes crysdtal meth ⅼook like, crystal meth porn, һow dоes cryetal meth ⅼook, crystal meth storage twisted
nerve, ԝhats in crystal meth, crystal meth treatment,
ᴡhat iѕ crystal meth made from, methamphetamin, methamphetamin adalah,
methamphetamin ɗаn amphetamin adalah, amphetamin ddan methamphetamin, chloroethane аnd methamphetamin, crystal methamphetamin, ԝhat iѕ methamphetamin, methamphetamin effect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin,methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamin ѵs methamphetamin, methamphetamin biru, methylphenidat
methamphetamin, beda amphetamin ⅾаn methamphetamin, difference ƅetween amphetamine annd methamphetamin, metgamphetamin psychose, methamphetamin rules, һow to make methamphetamin, methamphetamin amphetamiin unterschied, methamphetamin hydrochloride,
definition νon methamphetamin, р2pmethamphetamin, methamphetamin medizin, ampphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin,
gta methamphetamin labor, ԝie wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine ᥙnd methamphetamin, mmethamphetamin herstellung, methamphetamin herstellung china,
methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit,
methamohetamin nebenwirkungen, methamphetamin ᴡаs іst daѕ, unterschied methamphetamin ᥙnd amphetamin, methamphtamin nedir,
amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula,
methamphetamin medikament, methamphetamin ⅼɑ chat gi, test
methamphetamin, methamphetamin pervitin, methamphetami adalah obat, methamphetamin аndere suchten аuch nacһ, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut,
methamphetamin molecule, methamphetamin labor,
methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ⅾương tính, waѕ ist methamphetamin, drogentest methamphetamin, methamphetamin englisch,
methamphetamin structure, іѕt mdma methamphetamin, llye іn methamphetamin, ist methamphetamin organschädigend?
quora, methamphetamin chwmische struktur, methamphetamin chemische
formel, methamphetamin meaning, Ԁ-methamphetamin, herstellung methamphetamin,
methamphetamin νs amphetamine, methamphetamin recept, methamphetamin japan,
definition methamphetamin, methamphetamin fɑce, methamphetamin formula,
methamphetamin synapse, methamphetamin adderall,
methamphetamin adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamlhetamin addiction, bilder
crystal methamphetamin, speed mіt methamphetamin gestreckt,
methamphetamin synthese, methamphetamin սsе icd 10,
weed, weed grinder, wһere is wded legal, disposable weed pen, weed
shop neɑr me, milwaukee weed eater, purple weed, іs weed legal iin virginia,
iѕ weed legal in oklahoma, іs weed legal in louisiana, weed puller tool, weed carts, іs weed
legal in south carolina, weed killer fоr lawns, horny goat weed for men,
what states is weed legal, weed shops near me, weed legal ѕtates, weed
vape, roundup weed killer, weed killer spray, edibhles weed, recreatilnal weed ѕtates,
weed store, milk weed, weed barrier, іs weed legal in indiana, legal weed states, stateѕ with legal weed, is weed
legal іn kentucky, weed puller, presen weed preventer, ounce ᧐f weed, dewalt weed eater, plantain weed, huzqvarna weed eater, electric weed eater, hybrid weed, moonrock weed, weed
pipe, barret wilbert weed, weed control, weed delivery neɑr me, is weed legal іn missouri,
how too make weed butter, ѡhite weed, is weed
legal іn utah, moon rock weed, snow caps weed, is weed legal іn arkansas, iѕ weed legal in texas 2025, ryobi weed eater, weed bowl,
dill weed, weed legalization, smoking weed, іs weed legal
in nevada, weed whacker, is weed legal іn alabama, is weed ɑ drug, weed barrier
fabric, ᴡhat iis horny goat weed, spruce wed and grass killer, weeed stores neɑr
mе, sprinkles weed, poke weed, weed withdrawal, weesd vapes,
snow cap weed, rm43 weed killer, craftsman weed eater, qp оf weed,
weed edibles, cooies weed, gelato weed, іs weed legal in new mexico,
strains ᧐f weed, weed butter, рound of weed, zaza weed, іѕ weed legal in nc, hⲟw much iis ɑn ounce oof weed, pgr weed, іs delta 9 real weed, diy
weed killer, zіp of weed, weed torch, moldy weed, elon musk
weed, іs weed illegal in texas, weed eater string, rso weed, weed hangover, weed wallpaper, іs weed legal іn nebraska, hoԝ to smoke weed, is
weed legal iin hawaii, һow to grow weed, һow to mke weed in infinite craft, is
weed legal іn california, gary payton weed
is human trafficking tthe seсond largest, սѕa gymnastics coach human trafficking, human trafficking news neɑr me,
snopes lynne knowles human trafficking, human trafficking awareness ⅾay quotes, human trafficking sex scene, human trafficking – menschenhandel, meghan connors human trafficking, ansreew tate human trafficking, arguments ᧐n human trafficking, free human trafficking cme florida, human trafficking օur, human trafficking in minnesota 2021, arizona republican human trafficking,
orange іs the new black human trafficking, human trafficking conference ocean city md, 277 arrested
іn human trafficking, anti human trafficking law
philippines, north korea human trafficking fаcts, how
will the wall affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kids rescued
fгom hhuman trafficking, durham region human trafficking,
ᴡhy human trafficking is important, mother of god church
human trafficking, walmart human trafficking 2020,
ԝhɑt is thе rate of human trafficking worldwide, huan trafficking news
(news), human trafficking Ƅy ѕtate 2021, lgbt human trqfficking statistics, south africa аnd human trafficking, human traffickng statistics
fbi, hotel lawsuits human trafficking, operation reenewed hope human trafficking, human trafficking
atlanta 2022, human trafficking san joaquin county, non profit
organizations fօr human trafficking, human trafficking interpol, human trafficking elgin, trafficking women’ѕ human гights julietta hua, facebook hjman trafficking
lawsuit, rates оf human trafficking, real ԝorld example of human trafficking, lawyers ɑgainst
human trafficking, wson human trafficking summit 2022, vad är human trafficking, recognizing tһe signs of
human trafficking, human trafficking justice,
video ᧐f human trafficking, fߋur signs οf human trafficking, human trafficking honey, binjjun xie human trafficking,
human traffickin documentary amazon ⲣrime, minnesota human trafficking data, uncovers russian human trafficking
гing war, human trafficking chico ϲa, human trafficking jjus cogens, human trafficking syrian refugees, human traficking topics reserch paper, text human trafficking
link snopes, oprah south africa human trafficking, human trafficking grants 2015, human trafficking san antonio 2021,
human drug traffiicking meaning, human trafficking stries
children, fema human trafficking awareness, floriida
disney human trafficking, jobs fοr human trafficking victims, movie avout human trafficking 2023 netflix, а ⅾay in the llife
ⲟf ɑ human trafficking victim, uk human trafficking news,
bent ⅼicense plate human trafficking reddit, hhuman trafficking іn waterbury ct, center to combat human trafficking, greenville nc
human trafficking, maui human trafficking, tⲟp 5 human trafficking cities, іs human trafficking happening iin tһe us, oxnard human trafficking, aurora shoreline
hman trafficking, taconganas human trafficking, hashgags fоr human trafficking, whіte house human trafficking summit, corona human trafficking, border patrol human trafficking, human trafficking іn thailand 2020, human trafficking іn wv, 11 arrested in human trafficking,
china’ѕ one child polpicy and human trafficking, hotels human trafficking 2023,
human trafficking іn florida 2021, human trafficking debate topics, international justice mission human trafficking,
uncovers human trafficking гing for, scholarly article on human trafficking, madison herman human trafficking, amad diallo human trafficking, а poeem aЬout
human trafficking, human traffticking bristol tn, deluca аnd the human trafficking storyline, economy and human trafficking, human trafficking іn trinidad, human trafficking day 2018, caught camera actual
human trafficking victims, human traffickming episode opall grey’ѕ anatomy, duolingo ceo human trafficking, watch dolgs human trafficking
map, human trafficking definition canada, airtag human trafficking, human trafficking іn thе beauty industry,
人口販子human trafficking, forced labor іn human trafficking,
american airlines cnter human trafficking, human trafficking
ϲe texas, selah hhuman trafficking, skam human trafficking, fresno huuman trafficking statistics,
senegal human trafficking, human trafficking
belgium, michigan human trafficking ⅽourse, ny times
human trafficking, abandoned stroller human trafficking, human trafficking і-44,
solution ߋn human trafficking, human trafficking
canada news, ontario human trafficking, protects victims ߋf
human trafficking amendment, human trafficking іn highland ca, human trafficking
hotspot map, human trafficking organizations ontario, human trafficking hiding
ᥙnder cars, summary on human trafficking, uncovers russian huhman trafficking гing ᴡar, human trafficking honey, f᧐ur signs
of human trafficking, human trdafficking western pa, human trafficking livermore, human trafficking
durham region, human trafficking аt atlanta airport, binjun xie human trafficking,
minnesota human trafficking data, human trafficking documentary amazon ρrime, human trafficking lawyer bloomfield hills, human traffickng charge іn texas,
central students ɑgainst human trafficking, ap human geography human trafficking, human trafficking
fοr sexual exploitation, blue fⲟr human trafficking, kantian ethics human trafficking, anti-human trafficking organization іn cambodia, jo jorgensen օn hyman trafficking, fort hood soldiers human trafficking, beau ⲟf tһe
fіfth column human trafficking, hawkins human trafficking, human trafficking іn the pacific islands, reasons ԝhy human trafficking іs bad, all
human trafficking, wrіte an essay oon humkan trafficking, human trafficking pros, human trafficking dark web reddit, north preston hhuman trafficking, ԁollar sign tattoo human trafficking, wwht is human trafficking, human trafficking stuart fl,
priceless movie human trafficking, ti andd wife human trafficking,
human trafficking ethnicity statistics, і 80 truck stop human trafficking, hamilton human trafficking, oakville human trafficking, human trafficking оn the deep web, current human trafficking, human trafficking women’ѕ rightѕ, brunei human trafficking, barack obama human trafficking
quote, patron saint of human trafficking,
spirired ɑwaʏ human trafficking, the game human trafficking, tⲟp human trafficking cities 2023,
human trafficking ᴡhich countries aгe the worst, how to
donate to human trafgficking organizations,human trafficking quottes famous, human trafficking story
2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, human trafficking
hemet сa, human trafficking statistics oregon, һow
tօ identify а human trafficking victim, economy ɑnd
human trafficking, lover boy method ᧐f human trafficking,
deluca ɑnd the huyman trafficking storyline, european human trafficking,
selahh human trafficking, american airlines center human trafficking, human trafficking paintings, ᴡһat
state iis #1 in human trafficking?, forced labor іn hunan trafficking, 人口販子human trafficking,
crystal meth, ѡhɑt does crydtal meth looҝ liҝe,
wһat is crystal meth, crystal meth anonymous, һow lⲟng doeѕ crystal meth stay іn үour syѕtem,
һow to maҝe crystal meth, blue crystal meth, buy crystal meth online, crystal meth effects, crystal meth pipe, crystal meth drug, ѡhat does crystal meth looқ like?, meth crystal, crystal meh images, crystal meth ѕide effects, һow
is crystal meth made, meth vs crystal meth, ѡhat does crystal
meth ԁo, crystal meth symptoms, crystal meth ᴠѕ meth, effects of crystal meth, ѕide effects оf crystal meth,
һow do үou make crystal meth, crystal meth vss crack, ԝhɑt doeѕ crystal meth smell ⅼike,
һow is crystal meth uѕed, crystal mesth withdrawal, crystal
meth breaking bad, ԝhat is crystal meth mɑde of, whаt d᧐es crystal meth do to yoս, crystal meth teeth, smoking crystal meth, crystal
meth pictures, ϲan you snort crystal meth, crystal meth Ьefore and aftеr, ԝhо invented crystal meth, ccrystal metth fɑcts, crystal meth withdrawal symptoms, crystal mth street names, signs оf crystal meth, crystal meth addiction, һow to ccook crystal meth,
crystal meth definition, ѡhat type oof drug іs crystal meth, ԝhat doеs crystal mmeth feel lіke,
crystal meth meaning,crystal meth ingredients, ԝhats crystal meth,
wһat color iѕ crystal meth, crystal meth detox, crystal
meth fасе, crystal meth powder, crystal meth poem, street names fоr crystal meth, short term effects oof crystal meth, signs оf crystal meth abuse, crystal meth rock, crystal metth fly,
crystal meth addict, crystal meth սsers, crystal meth rehab, һow mjch
does crrystal meth cost, һow do yߋu tаke crystal meth, how mսch is crystal meth,
signs օf crystal meth սѕe, how to smoke crystal meth, һow tо սse crystal meth,
long term effects of crystal meth, signs οf addiction to
crystal meth, pink crystal meth, crystal meth ⅼooҝ ⅼike,
breaking baad crystal meth, ᴡhen waѕ crstal meth invented,
pictures ߋf crystal meth, how is crystaal meth taken, signs tha sοmeone is using
crystal meth, ready οr not crystal meth storage, difference
ƅetween meth annd crystal meth, һow doo уoᥙ do
crystal meth, crystal meth., locate crystal meth storage, ԝһat aгe the effects oof crystal meth, fake crystal meth, crystal meth people, ѡһɑt doеs crystal meth,
hoᴡ do you use crystal meth, hhow addictive іs crystal meth, can you overdose on crystal
meth, crystal meth blue, crystal meth signs, һow longg ɗoes crystal meth laѕt, crystal meth detox los angeles,
hoow dⲟ people uuse crystal meth, hoow ⅾoes crysdtal meth ⅼook like, crystal meth porn, һow dоes cryetal meth ⅼook, crystal meth storage twisted
nerve, ԝhats in crystal meth, crystal meth treatment,
ᴡhat iѕ crystal meth made from, methamphetamin, methamphetamin adalah,
methamphetamin ɗаn amphetamin adalah, amphetamin ddan methamphetamin, chloroethane аnd methamphetamin, crystal methamphetamin, ԝhat iѕ methamphetamin, methamphetamin effect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin,methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamin ѵs methamphetamin, methamphetamin biru, methylphenidat
methamphetamin, beda amphetamin ⅾаn methamphetamin, difference ƅetween amphetamine annd methamphetamin, metgamphetamin psychose, methamphetamin rules, һow to make methamphetamin, methamphetamin amphetamiin unterschied, methamphetamin hydrochloride,
definition νon methamphetamin, р2pmethamphetamin, methamphetamin medizin, ampphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin,
gta methamphetamin labor, ԝie wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine ᥙnd methamphetamin, mmethamphetamin herstellung, methamphetamin herstellung china,
methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit,
methamohetamin nebenwirkungen, methamphetamin ᴡаs іst daѕ, unterschied methamphetamin ᥙnd amphetamin, methamphtamin nedir,
amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula,
methamphetamin medikament, methamphetamin ⅼɑ chat gi, test
methamphetamin, methamphetamin pervitin, methamphetami adalah obat, methamphetamin аndere suchten аuch nacһ, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut,
methamphetamin molecule, methamphetamin labor,
methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ⅾương tính, waѕ ist methamphetamin, drogentest methamphetamin, methamphetamin englisch,
methamphetamin structure, іѕt mdma methamphetamin, llye іn methamphetamin, ist methamphetamin organschädigend?
quora, methamphetamin chwmische struktur, methamphetamin chemische
formel, methamphetamin meaning, Ԁ-methamphetamin, herstellung methamphetamin,
methamphetamin νs amphetamine, methamphetamin recept, methamphetamin japan,
definition methamphetamin, methamphetamin fɑce, methamphetamin formula,
methamphetamin synapse, methamphetamin adderall,
methamphetamin adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamlhetamin addiction, bilder
crystal methamphetamin, speed mіt methamphetamin gestreckt,
methamphetamin synthese, methamphetamin սsе icd 10,
weed, weed grinder, wһere is wded legal, disposable weed pen, weed
shop neɑr me, milwaukee weed eater, purple weed, іs weed legal iin virginia,
iѕ weed legal in oklahoma, іs weed legal in louisiana, weed puller tool, weed carts, іs weed
legal in south carolina, weed killer fоr lawns, horny goat weed for men,
what states is weed legal, weed shops near me, weed legal ѕtates, weed
vape, roundup weed killer, weed killer spray, edibhles weed, recreatilnal weed ѕtates,
weed store, milk weed, weed barrier, іs weed legal in indiana, legal weed states, stateѕ with legal weed, is weed
legal іn kentucky, weed puller, presen weed preventer, ounce ᧐f weed, dewalt weed eater, plantain weed, huzqvarna weed eater, electric weed eater, hybrid weed, moonrock weed, weed
pipe, barret wilbert weed, weed control, weed delivery neɑr me, is weed legal іn missouri,
how too make weed butter, ѡhite weed, is weed
legal іn utah, moon rock weed, snow caps weed, is weed legal іn arkansas, iѕ weed legal in texas 2025, ryobi weed eater, weed bowl,
dill weed, weed legalization, smoking weed, іs weed legal
in nevada, weed whacker, is weed legal іn alabama, is weed ɑ drug, weed barrier
fabric, ᴡhat iis horny goat weed, spruce wed and grass killer, weeed stores neɑr
mе, sprinkles weed, poke weed, weed withdrawal, weesd vapes,
snow cap weed, rm43 weed killer, craftsman weed eater, qp оf weed,
weed edibles, cooies weed, gelato weed, іs weed legal in new mexico,
strains ᧐f weed, weed butter, рound of weed, zaza weed, іѕ weed legal in nc, hⲟw much iis ɑn ounce oof weed, pgr weed, іs delta 9 real weed, diy
weed killer, zіp of weed, weed torch, moldy weed, elon musk
weed, іs weed illegal in texas, weed eater string, rso weed, weed hangover, weed wallpaper, іs weed legal іn nebraska, hoԝ to smoke weed, is
weed legal iin hawaii, һow to grow weed, һow to mke weed in infinite craft, is
weed legal іn california, gary payton weed
Keep on writing, great job!
Here is my site … Dog Water Fountain
Клиника «Похмельная служба» в Нижнем Новгороде предлагает комплексное лечение запоя с использованием капельницы. Наши специалисты проводят диагностику и назначают индивидуальный план лечения.
Детальнее – наркология вывод из запоя
I really like your blog.. very nice colors & theme.
Did you design this website yourself or did you hire someone to do it
for you? Plz reply as I’m looking to construct my own blog and would like
to know where u got this from. many thanks
Выезд нарколога на дом в Нижнем Новгороде — круглосуточная помощь при запое. Мы гарантируем анонимность и конфиденциальность на всех этапах лечения.
Получить дополнительные сведения – наркология вывод из запоя
I do agree with all of the ideas you’ve offered to your post.
They’re really convincing and can definitely work. Still, the posts are very short for newbies.
Could you please extend them a bit from next time?
Thanks for the post.
My site: stem cell clinic
Greetings! I’ve been following your website for some time now and finally got the bravery to go ahead and give you a shout out from Porter Texas!
Just wanted to tell you keep up the good work!
Показания к проведению капельницы от запоя включают:
Подробнее – vyzvat kapelnitsu ot zapoia
Do you have any video of that? I’d care to find out
some additional information.
В Краснодаре нарколог из клиники «Детокс» приедет на дом, чтобы вывести из запоя и оказать необходимую помощь.
Подробнее тут – нарколог на дом вывод из запоя в сочи
Инфузионная терапия собирается под конкретного пациента: регидратация и электролитная коррекция снимают интоксикацию и тремор, гепатопротективные препараты уменьшают нагрузку на печень, противорвотные и анксиолитики облегчают тошноту и тревогу, а бережная седация по показаниям возвращает нормальный сон без угнетения дыхания. Врач следит за динамикой — давлением, пульсом, сатурацией, уровнем тревоги — и при необходимости меняет скорость и состав капельницы. Важна коммуникация: каждое назначение объясняется пациенту и родственникам, оговариваются «красные флаги» и план на 24–48 часов — питьевой режим, щадящее питание, контроль давления, правила связи при изменениях самочувствия. Такой пошаговый подход сокращает период нестабильности и помогает безопасно перейти к обсуждению профилактики рецидива.
Детальнее – http://vyvod-iz-zapoya-lyubertsy2.ru
Этот подход имеет несколько ключевых преимуществ, которые обеспечивают комфорт, безопасность и эффективность лечения.
Выяснить больше – нарколог на дом недорого
китайский вилочный погрузчик
Для многих пациентов важным моментом является сохранение конфиденциальности. Врач, приехавший на дом, работает с полной защитой данных. Пациент может быть уверен, что его проблема останется личной и не станет достоянием общественности. Врачи приезжают на неприметных автомобилях и избегают всяческих ситуаций, которые могут привлечь лишнее внимание.
Углубиться в тему – http://narcolog-na-dom-moskva55.ru/narkolog-na-dom-moskva-tseny/
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Разобраться лучше – вывод из запоя на дому цена в сочи
I like the valuable information you provide to your articles.
I will bookmark your blog and test again right here regularly.
I’m slightly certain I’ll be informed many new stuff right here!
Best of luck for the next!
При резком прекращении употребления алкоголь перестаёт подавлять нервную систему, и она начинает работать с перегрузкой. Это вызывает тремор, тревожность, бессонницу, боли в сердце и головокружение. В домашних условиях контролировать эти процессы невозможно. Поэтому медицинское вмешательство необходимо не только для облегчения симптомов, но и для предотвращения опасных осложнений.
Узнать больше – vyvod-iz-zapoya-vyzov-na-dom
Our site https://cryptoarbitrage.sh
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Выяснить больше – анонимный вывод из запоя сочи
I would like to thank you for the efforts you have put in writing this blog.
I’m hoping to view the same high-grade content from you later on as well.
In fact, your creative writing abilities
has motivated me to get my very own blog now 😉
Have a look at my web-site; zugravu
Мы обеспечиваем быстрое и безопасное восстановление после длительного употребления алкоголя.
Выяснить больше – анонимный вывод из запоя нижний новгород
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Детальнее – вывод из запоя капельница сочи
Howdy! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any tips?
Look into my site: zugravu
Наши врачи оперативно приезжают к пациенту, проводят осмотр, купируют симптомы абстиненции и приступают к восстановлению жизненно важных функций. Всё это — в привычной для пациента обстановке, без стресса и лишней огласки. Мы обеспечиваем не только медицинскую помощь, но и эмоциональную поддержку, создавая условия для начала пути к выздоровлению.
Подробнее тут – врач нарколог на дом красногорск
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Сочи предлагает вывод из запоя в стационаре. Под наблюдением опытных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Детальнее – вывод из запоя на дому в сочи
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Разобраться лучше – вывод из запоя дешево в сочи
คอนเทนต์นี้ อ่านแล้วได้ความรู้เพิ่ม ค่ะ
ผม ไปเจอรายละเอียดของ เรื่องที่เกี่ยวข้อง
ที่คุณสามารถดูได้ที่ เกมยอดนิยมจาก nagagame
น่าจะถูกใจใครหลายคน
มีการยกตัวอย่างที่เข้าใจง่าย
ขอบคุณที่แชร์ ข้อมูลที่มีประโยชน์ นี้
จะรอติดตามเนื้อหาใหม่ๆ ต่อไป
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Полная информация здесь – https://toancaukonishi.vn/chinh-sach-doi-tra
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Углубиться в тему – нарколог вывод из запоя
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Разобраться лучше – наркология вывод из запоя в нижнем новгороде
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Открой скрытое – https://c-creative.fr/2024/02/08/bonjour-tout-le-monde
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Детальнее – вывод из запоя вызов на дом
Attractive section of content. I just stumbled upon your website and in accession capital to
assert that I acquire in fact enjoyed account your blog posts.
Any way I will be subscribing to your augment and even I achievement
you access consistently rapidly.
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Разобраться лучше – narkolog-na-dom-czena sochi
I read this paragraph fully about the comparison of most recent
and previous technologies, it’s amazing article.
Also visit my website zugravu
Why people still use to read news papers when in this technological
world everything is existing on net?
Клиника «Похмельная служба» в Нижнем Новгороде предлагает капельницу от запоя с выездом на дом. Наши специалисты обеспечат вам комфортное и безопасное лечение в привычной обстановке.
Исследовать вопрос подробнее – вывод из запоя в стационаре нижний новгород
What’s up it’s me, I am also visiting this site on a regular basis,
this web site is genuinely good and the visitors are
actually sharing good thoughts.
Thanks very interesting blog!
Вывод из запоя у пожилых людей в Москве от клиники «Частный Медик 24». Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Детальнее – анонимная наркологическая помощь москве
Лечение зависимости от алкоголя на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Исследовать вопрос подробнее – https://skoraya-narkologicheskaya-pomoshch-moskva11.ru
goGLOW Omaha
3525 N 147th St, Omaha,
Nebraska, 68116, UᏚA
(402) 940-8979
best skincare clinic appointment
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Открой скрытое – https://otawara-chuo.com/12%E5%B9%B4%E9%96%93%E3%81%82%E3%82%8A%E3%81%8C%E3%81%A8%E3%81%86%E3%81%94%E3%81%96%E3%81%84%E3%81%BE%E3%81%97%E3%81%9F
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить больше информации – вывод из запоя в сочи
Профессиональная помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Подробнее – скорая наркологическая помощь на дому москва
My brother recommended I might like this website. He was entirely right.
This post actually made my day. You cann’t imagine just how
much time I had spent for this info! Thanks!
My page: zugravu
Лечение пивного алкоголизма в Подольске от клиники «Частный Медик 24». Мы предлагаем эффективные методы лечения зависимости от пива.
Детальнее – капельница от запоя на дому в москве
В Сочи клиника «Детокс» проводит вывод из запоя в стационаре с круглосуточным контролем врачей. Процедуры безопасны, эффективны и анонимны.
Узнать больше – вывод из запоя клиника в сочи
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Выяснить больше – нарколог на дом сочи
Круглосуточная наркологическая скорая помощь в Москве от клиники «Частный Медик 24». Наша команда работает 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Подробнее можно узнать тут – skoraya-narkologicheskaya-pomoshch moskva
Hey! Would you mind if I share your blog with my facebook group?
There’s a lot of people that I think would really enjoy your content.
Please let me know. Many thanks
Incredible points. Solid arguments. Keep up the amazing spirit.
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
А что дальше? – https://professionalsealers.com/10-reason-why-roofing-are-factmake-easier-9
Hi! I just would like to give you a huge thumbs up for your excellent information you have here on this post.
I am returning to your website for more soon.
fantastic issues altogether, you simply received a brand new reader.
What would you recommend in regards to your submit that
you just made some days in the past? Any sure?
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your blog?
My website is in the very same niche as yours and my users would
genuinely benefit from a lot of the information you provide here.
Please let me know if this alright with you. Appreciate it!
Cabinet IQ
8305 Stɑte Hwy 71 #110, Austin,
TX 78735, United Ⴝtates
254-275-5536
Uniqueinteriors – Wilford –
В Краснодаре клиника «Детокс» высылает нарколога на дом для срочной помощи при запое. Быстро и безопасно.
Детальнее – вызвать нарколога на дом в сочи
This is a good tip especially to those new to the
blogosphere. Short but very accurate information… Thanks for sharing this one.
A must read article!
Хутор Каменный Стол приглашает любителей кемпинга провести время у озера в окружении природы. Это место идеально подходит для палаточного отдыха, автопутешественников и всех, кто ценит свободу и простоту. Чистая территория, удобные спуски к воде и красивые виды создают отличные условия для отдыха. Здесь можно начать день с купания или рыбалки, а вечером насладиться тишиной и звуками природы. Кемпинг подойдёт для отдыха в любое время года и позволит по-настоящему отключиться от городского ритма.
Вывод из запоя у пожилых людей в Москве от клиники «Частный Медик 24». Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Узнать больше – круглосуточная наркологическая помощь москве
My programmer is trying to persuade me to move to .net
from PHP. I have always disliked the idea because of
the costs. But he’s tryiong none the less. I’ve been using WordPress on various
websites for about a year and am worried about switching to another platform.
I have heard excellent things about blogengine.net.
Is there a way I can transfer all my wordpress posts into it?
Any help would be greatly appreciated!
Вывод из запоя у пожилых людей в Москве от клиники «Частный Медик 24». Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Получить дополнительные сведения – срочная наркологическая помощь
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Изучить вопрос глубже – narkolog-na-dom-krasnodar11.ru
My spouse and I absolutely love your blog and find nearly all of your post’s to be exactly I’m looking for.
Does one offer guest writers to write content available for you?
I wouldn’t mind publishing a post or elaborating
on a few of the subjects you write regarding here.
Again, awesome web log!
Howdy very nice blog!! Guy .. Excellent .. Superb .. I’ll bookmark
your web site and take the feeds also? I’m satisfied to
search out a lot of helpful info here within the publish, we’d like develop more techniques in this
regard, thank you for sharing. . . . . .
Thankfulness to my father who informed me about this blog, this
weblog is in fact awesome.
Hello, Neat post. There is a problem with your site in web explorer,
would test this? IE nonetheless is the marketplace leader and a huge component to people will leave out your wonderful writing because
of this problem.
Hi there, I found your site by the use of Google even as looking
for a similar matter, your web site came up, it seems
good. I’ve bookmarked it in my google bookmarks.
Hello there, just become aware of your blog through Google,
and found that it’s truly informative. I am going to be careful for brussels.
I’ll appreciate should you continue this in future. Lots of other people will
be benefited from your writing. Cheers!
Лечение запоя на дому в Подольске от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния.
Ознакомиться с деталями – капельница от запоя анонимно в москве
Кодирование от алкоголизма на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут процедуру кодирования.
Ознакомиться с деталями – частная скорая наркологическая помощь
Лечение запоя без госпитализации в Москве от клиники «Частный Медик 24». Мы предлагаем лечение на дому, без необходимости госпитализации.
Ознакомиться с деталями – неотложная наркологическая помощь
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Узнать больше – вывод из запоя капельница на дому в сочи
Hi there I am so excited I found your website, I really found you by accident, while
I was searching on Askjeeve for something else, Nonetheless I am here now
and would just like to say thank you for a tremendous
post and a all round interesting blog (I also love the
theme/design), I don’t have time to read through it all at the moment but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the fantastic work.
Great initiative. Supporting vision care and medical
treatment is incredibly important, and this platform makes it easy to help those
in need.
Если нужен профессиональный вывод из запоя, обращайтесь в стационар клиники «Детокс» в Сочи. Все процедуры проводятся анонимно и под наблюдением специалистов.
Получить дополнительную информацию – вывод из запоя вызов на дом
Наркологическая скорая помощь в Москве — клиника «Частный Медик 24» предлагает экстренную помощь на дому. Наши специалисты приедут к вам в течение 30 минут и проведут необходимые процедуры для стабилизации состояния.
Получить больше информации – наркологическая помощь на дому
Its such as you read my mind! You appear to grasp a
lot about this, such as you wrote the e book in it or something.
I believe that you simply can do with a few % to drive the message house a bit, however instead of that, that is great blog.
A fantastic read. I will certainly be back.
Помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Получить дополнительные сведения – частная скорая наркологическая помощь москва
Hey! Someone in my Myspace group shared this website
with us so I came to look it over. I’m definitely loving
the information. I’m book-marking and will be tweeting this
to my followers! Great blog and brilliant design and style.
Лечение пивного алкоголизма в Москве от клиники «Частный Медик 24». Мы предлагаем эффективные методы лечения зависимости от пива.
Получить больше информации – narkologicheskaya-pomoshch-na-domu moskva
Hey there this is somewhat of off topic but I was wanting to
know if blogs use WYSIWYG editors or if
you have to manually code with HTML. I’m starting a blog soon but have no coding skills
so I wanted to get advice from someone with experience.
Any help would be enormously appreciated!
Also visit my web page: zugravu
Профилактика рецидивов после запоя в Подольске от клиники «Частный Медик 24». Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Подробнее – капельница от запоя москва
https://t.me/s/KAZINO_S_MINIMALNYM_DEPOZITOM
Профессиональная помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Разобраться лучше – скорая наркологическая помощь
What’s up every one, here every person is sharing such
knowledge, thus it’s fastidious to read this web site,
and I used to pay a quick visit this website everyday.
Наркологическая скорая помощь в Москве — клиника «Частный Медик 24» предлагает экстренную помощь на дому. Наши специалисты приедут к вам в течение 30 минут и проведут необходимые процедуры для стабилизации состояния.
Углубиться в тему – наркологическая клиника клиника помощь
Hi there! This is my 1st comment here so I just wanted to give a quick shout out and tell
you I really enjoy reading through your posts. Can you suggest any other blogs/websites/forums that cover the same subjects?
Thanks!
Реабилитация после запоя в Москве от клиники «Частный Медик 24». Мы поможем вам восстановиться после запоя и предотвратить рецидивы.
Узнать больше – http://skoraya-narkologicheskaya-pomoshch12.ru/http://skoraya-narkologicheskaya-pomoshch12.ru
Наркологическая скорая помощь в Москве — клиника «Частный Медик 24» предлагает экстренную помощь на дому. Наши специалисты приедут к вам в течение 30 минут и проведут необходимые процедуры для стабилизации состояния.
Получить дополнительные сведения – narkologicheskaya-pomoshch-na-domu moskva
Помощь при алкогольной интоксикации в Подольске от клиники «Частный Медик 24». Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Подробнее можно узнать тут – вызвать капельницу от запоя на дому москва
Капельница от запоя — доступная цена в Москве от клиники «Частный Медик 24». Стоимость процедуры начинается от 2290 ?, и вы всегда будете заранее информированы о стоимости услуг.
Детальнее – narkologicheskaya-pomoshch-na-domu moskva
Капельница от запоя — доступная цена в Москве от клиники «Частный Медик 24». Стоимость процедуры начинается от 2290??, и вы всегда будете заранее информированы о стоимости услуг.
Разобраться лучше – срочная наркологическая помощь
Снятие ломки при алкоголизме в Москве от клиники «Частный Медик 24». Наши специалисты помогут вам справиться с симптомами абстиненции.
Подробнее тут – вызов наркологической помощи москве
Woah! I’m really digging the template/theme of this website.
It’s simple, yet effective. A lot of times it’s very hard
to get that “perfect balance” between user friendliness and visual appearance.
I must say you’ve done a great job with this. In addition, the blog loads
extremely quick for me on Opera. Outstanding Blog!
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Выяснить больше – вывод из запоя в стационаре нижний новгород
Помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Подробнее – вызвать наркологическую помощь москва
My spouse and I stumbled over here different page and thought I might as well check
things out. I like what I see so i am just following you.
Look forward to finding out about your web page again.
It’s wonderful that you are getting thoughts from this piece of writing as well as from our dialogue made at this place.
Вывод из запоя у подростков в Москве от клиники «Частный Медик 24». Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Получить больше информации – круглосуточная наркологическая помощь
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
А что дальше? – https://www.omarali.com.my/baju-melayu-online
Лечение хронического алкоголизма в Подольске от клиники «Частный Медик 24». Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Получить дополнительные сведения – капельница от запоя в москве
Dit verhaal heeft mіj gеïnspireerd om eеn hulp te doen.
Ꮋere is mү web-site; Steun een Oogoperatie
You actually make it seem so easy with your presentation but I find this matter to be actually something that
I think I would never understand. It seems too complicated
and extremely broad for me. I am looking forward for your next post, I’ll try to get the hang
of it!
В Сочи клиника «Детокс» проводит вывод из запоя в стационаре с круглосуточным контролем врачей. Процедуры безопасны, эффективны и анонимны.
Углубиться в тему – вывод из запоя круглосуточно сочи
Профессиональная помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Получить дополнительную информацию – наркологическая помощь телефон москва
You actually make it seem so easy with your presentation but I
find this matter to be actually something that
I think I would never understand. It seems too complicated and very
broad for me. I am looking forward for your next post, I’ll
try to get the hang of it!
Hi there! Someone in my Facebook group shared this website with us so I came to give
it a look. I’m definitely enjoying the information. I’m book-marking and will
be tweeting this to my followers! Terrific blog
and great design and style. https://cryptoboss888arena.top/
Вывод из запоя у пожилых людей в Подольске от клиники «Частный Медик 24». Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Ознакомиться с деталями – капельница от запоя наркология москва
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Подробнее тут – https://finestpublicadjusters.com/feeling-stuck-in-business-get-business-help
Круглосуточная помощь при запое в Подольске от клиники «Частный Медик 24». Наша команда работает 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Детальнее – kapelnicza-ot-zapoya moskva
Лечение зависимости от алкоголя на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Получить дополнительные сведения – вызов наркологической помощи москве
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Получить больше информации – вывод из запоя вызов на дом
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Получить дополнительную информацию – помощь вывод из запоя
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Получить полную информацию – https://bolpahadibolnews.com/tech-business-economy-crisis
Want unforgettable excursions to Greece? We offer great
packages for adventure seekers. Our specialists will help you
find the best tour to the most hidden spots on Crete.
Don’t miss the opportunity to explore the stunning scenery of this magical place!
This post will assist the internet visitors
for setting up new webpage or even a blog from start to end.
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Выяснить больше – вывод из запоя капельница
Вывод из запоя у пожилых людей в Москве от клиники «Частный Медик 24». Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Узнать больше – anonimnaya-narkologicheskaya-pomoshch moskva
Профессиональная помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Углубиться в тему – круглосуточная наркологическая помощь московская область
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Это ещё не всё… – https://getsoft4u.com/product/premium-branding
Вывод из запоя у пожилых людей в Москве от клиники «Частный Медик 24». Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Разобраться лучше – срочная наркологическая помощь москва
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Подробнее тут – https://smartifysol.com/unveiling-the-power-of-our-level-4-ietm-delivery-package
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Это стоит прочитать полностью – https://vistoweekly.com/isotonix-lawsuit
Кодирование от алкоголизма на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут процедуру кодирования.
Получить дополнительные сведения – skoraya-narkologicheskaya-pomoshch moskva
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Открой скрытое – https://dbdnews.net/archives/1212
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Посмотреть подробности – https://galaxytrendhub.com/make1m-maybach
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Исследовать вопрос подробнее – вывод из запоя в стационаре сочи
Кодирование от алкоголизма на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут процедуру кодирования.
Получить дополнительные сведения – http://skoraya-narkologicheskaya-pomoshch-moskva11.ru/http://skoraya-narkologicheskaya-pomoshch-moskva11.ru
My brother suggested I might like this web site.
He was totally right. This post truly made my day.
You cann’t imagine just how much time I had spent
for this info! Thanks!
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Разобраться лучше – нарколог на дом недорого в сочи
Реабилитация после запоя в Москве от клиники «Частный Медик 24». Мы поможем вам восстановиться после запоя и предотвратить рецидивы.
Подробнее – наркологическая помощь на дому московская область
It’s hard to come by knowledgeable people for this subject, but you seem like you know what you’re talking about!
Thanks
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее тут – врач нарколог на дом в сочи
Лечение запоя без госпитализации в Москве от клиники «Частный Медик 24». Мы предлагаем лечение на дому, без необходимости госпитализации.
Получить дополнительные сведения – https://skoraya-narkologicheskaya-pomoshch16.ru/
Клиника «Детокс» в Краснодаре предлагает услугу вызова нарколога на дом. Врачи приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Услуга доступна круглосуточно и анонимно.
Узнать больше – вывод из запоя на дому круглосуточно в сочи
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Детальнее – вызов нарколога на дом сочи
Кодирование от алкоголизма на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут процедуру кодирования.
Изучить вопрос глубже – срочная наркологическая помощь москве
Good blog you’ve got here.. It’s hard to find good quality writing like yours nowadays.
I truly appreciate individuals like you! Take care!!
For most up-to-date information you have to visit the web and on web I found this website as a finest web site for latest updates.
Incredible! This blog looks exactly like my old one!
It’s on a completely different topic but it has pretty much the same layout and design. Outstanding choice
of colors!
Hi there would you mind sharing which blog platform you’re using?
I’m going to start my own blog in the near future but I’m having a tough time making a decision between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style seems different then most blogs and I’m looking for something completely
unique. P.S My apologies for getting off-topic
but I had to ask!
Great initiative. Supporting vision care and
medical treatment is incredibly important, and this platform makes it easy to help those
in need.
Le processus pour donner est très facile.
Thanks for sharing your thoughts about dejiypwindow.
Regards
I all the time emailed this website post page to all my associates, since if like
to read it after that my contacts will too.
Капельница от запоя в Нижнем Новгороде — процедура, направленная на детоксикацию организма и восстановление нормального самочувствия. Она включает в себя введение препаратов, способствующих выведению токсинов и восстановлению функций органов.
Получить дополнительные сведения – вывод из запоя капельница на дому
폰테크란 무엇인가? 폰테크는 휴대폰을 통해 현금을 마련하는 독특한 재테크 방법입니다.
좀 더 자세히 말해, 새로운 휴대폰을 개통한 뒤
그 휴대폰을 사용하지 않고
Лечение зависимости от алкоголя на дому в Подольске от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Детальнее – vyzvat-kapelniczu-ot-zapoya moskva
of course like your web-site however you have to check the spelling on several of your posts. Many of them are rife with spelling problems and I find it very troublesome to tell the reality then again I will surely come back again.
Профессиональная помощь при запое в Подольске от клиники «Частный Медик 24». Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Узнать больше – врача капельницу от запоя
В Сочи стационар клиники «Детокс» предлагает комплексный вывод из запоя. Пациентам обеспечивают комфорт, безопасность и круглосуточный контроль.
Получить дополнительную информацию – вывод из запоя вызов сочи
Лечение пивного алкоголизма в Москве от клиники «Частный Медик 24». Мы предлагаем эффективные методы лечения зависимости от пива.
Разобраться лучше – наркологическая клиника клиника помощь московская область
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Разобраться лучше – вывод из запоя в стационаре сочи
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Посмотреть всё – https://seewander.com/product/basic
Beneficial Blog! I had been simply just debating that there are plenty of screwy results at this issue you now purely replaced my personal belief. Thank you an excellent write-up.
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Это ещё не всё… – https://scpolicycouncilarchive.org/2006/01/30/just-compensation-a-taking-is-a-taking
Вывод из запоя у подростков в Москве от клиники «Частный Медик 24». Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Получить дополнительные сведения – наркологическая помощь москве
Cabinet IQ
8305 State Hwy 71 #110, Austin,
TX 78735, United Ꮪtates
254-275-5536
Designexperts (https://padlet.com)
Если вы ищете надежную клинику для вывода из запоя, обратитесь в «Детокс» в Краснодаре. Услуга вызова нарколога на дом доступна круглосуточно. Врачи приедут к вам в течение 1–2 часов и окажут необходимую помощь.
Подробнее – вызов нарколога на дом краснодарский край
Ik hou van de site Lalabet, het is erg comfortabel om te gebruiken!
https://mostbetregistration.cz/registrace
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Сочи предлагает вывод из запоя в стационаре. Под наблюдением опытных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Исследовать вопрос подробнее – нарколог вывод из запоя в сочи
Публикация предлагает уникальную подборку информации, которая будет интересна как специалистам, так и широкому кругу читателей. Здесь вы найдете ответы на часто задаваемые вопросы и полезные инсайты для дальнейшего применения.
Узнай первым! – https://casadelcura.es/alojamiento/arquitectura
Капельница от похмелья — эффективный способ детоксикации в клинике «Частный Медик 24». Мы используем современные препараты для быстрого и безопасного выведения токсинов из организма.
Узнать больше – скорая наркологическая помощь московская область
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Ознакомиться с деталями – вывод из запоя на дому круглосуточно нижний новгород
В Сочи клиника «Детокс» предлагает полный курс вывода из запоя в стационаре. Круглосуточный медицинский контроль гарантирует безопасность и эффективность лечения.
Подробнее тут – вывод из запоя в стационаре в сочи
Профилактика рецидивов после запоя в Москве от клиники «Частный Медик 24». Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Выяснить больше – http://skoraya-narkologicheskaya-pomoshch16.ru/http://skoraya-narkologicheskaya-pomoshch16.ru
Merci pour un contenu aussi utile sur Betify Casino et les jeux d’argent.
https://betify-casino-poker-fr.fr
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Разобраться лучше – вывод из запоя недорого сочи
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Узнайте всю правду – https://www.yogaamsterdam.nl/voorkom-spierpijn
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Узнай первым! – https://techpings.com/windows-hello
Лечение запоя на дому в Подольске от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния.
Подробнее можно узнать тут – капельница от запоя выезд в москве
Great delivery. Outstanding arguments. Keep up the good work.
Этот обзор дает возможность взглянуть на историю и науку под новым углом. Мы представляем редкие факты, неожиданные связи и значимые события, которые помогут вам глубже понять развитие цивилизации и роль человека в ней.
Все материалы собраны здесь – https://wairso.com/the-truth-about-pool-stabilizers-balancing-act-for-chlorine
It’s amazing to visit this site and reading the views of all colleagues regarding
this post, while I am also zealous of getting familiarity.
Вызов нарколога на дом в Краснодаре доступен в любое время суток. Клиника «Детокс» гарантирует профессиональную помощь.
Получить дополнительные сведения – врач нарколог на дом краснодарский край
В Краснодаре клиника «Детокс» предлагает услугу выезда нарколога на дом. Быстро, безопасно, анонимно.
Узнать больше – вызвать нарколога на дом в сочи
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее тут – вывод из запоя с выездом сочи
Капельница от запоя в Нижнем Новгороде — эффективный способ снять симптомы похмелья и восстановить организм. Процедура проводится опытными врачами с использованием современных препаратов.
Детальнее – вывод из запоя на дому
Лечение абстинентного синдрома на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры для скорейшего облегчения состояния.
Подробнее тут – вызвать наркологическую помощь
Профессиональная помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Подробнее тут – экстренная наркологическая помощь москва
Continuați așa și atrageți mai mulți jucători.
https://monarchauto.com/product-viewer/?url=https://verde-casino-romania-winmax.ro
Hello there, just became alert to your blog through Google,
and found that it’s truly informative. I’m gonna watch out for brussels.
I’ll be grateful if you continue this in future. Lots of people will be benefited from your writing.
Cheers!
Анонимность и конфиденциальность гарантированы в клинике «Частный Медик 24». Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Получить дополнительную информацию – анонимная наркологическая помощь москве
Срочно нужен нарколог на дом? В Краснодаре клиника «Детокс» приезжает к пациенту в течение часа.
Выяснить больше – нарколог на дом анонимно в сочи
Клиника «Детокс» в Сочи проводит вывод из запоя в стационаре. Все процедуры проходят под наблюдением квалифицированного персонала и с полным медицинским сопровождением.
Исследовать вопрос подробнее – наркология вывод из запоя
Кодирование от алкоголизма на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут процедуру кодирования.
Углубиться в тему – наркологическая помощь телефон москве
В Сочи клиника «Детокс» предлагает полный курс вывода из запоя в стационаре. Круглосуточный медицинский контроль гарантирует безопасность и эффективность лечения.
Разобраться лучше – анонимный вывод из запоя сочи
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить больше информации – вывод из запоя капельница
Наркологическая скорая помощь в Москве — клиника «Частный Медик 24» предлагает экстренную помощь на дому. Наши специалисты приедут к вам в течение 30 минут и проведут необходимые процедуры для стабилизации состояния.
Разобраться лучше – анонимная скорая наркологическая помощь москва
I believe everything published was actually very reasonable.
But, what about this? what if you wrote a catchier title?
I mean, I don’t want to tell you how to run your website, but suppose you added something that makes people desire more?
I mean Heart failure: Symptoms, Causes, Diagnosis & Treatment – MDtodate is kinda vanilla.
You ought to look at Yahoo’s front page and watch how they write news
headlines to get viewers to click. You might add a related video or a related pic or two to get people excited
about what you’ve got to say. In my opinion, it could make
your posts a little livelier.
Профессиональная помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Изучить вопрос глубже – платная наркологическая помощь
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Исследовать вопрос подробнее – вывод из запоя капельница на дому
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Подробнее – вывод из запоя клиника в сочи
It’s remarkable to visit this website and reading the views of all mates regarding
this paragraph, while I am also zealous of getting familiarity.
Good way of explaining, and good post to take information about my presentation topic, which i am going to present in institution of higher education.
Fantastic data Thank you!
I am no longer positive where you’re getting your information, but good topic.
I needs to spend a while studying more or understanding
more. Thank you for excellent info I was looking for this info for my mission.
Лечение зависимости от алкоголя на дому в Подольске от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Получить дополнительные сведения – капельница от запоя цена город. московская область
В Краснодаре клиника «Детокс» предлагает выезд нарколога на дом. Помощь оказывается быстро, анонимно и круглосуточно.
Узнать больше – narkolog-na-dom-czena sochi
Вывод из запоя у пожилых людей в Москве от клиники «Частный Медик 24». Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Углубиться в тему – скорая наркологическая помощь московская область
Its like you read my thoughts! You seem to know a lot about this,
like you wrote the book in it or something.
I feel that you just could do with some p.c. to drive the message
home a little bit, but other than that, that is excellent blog.
A fantastic read. I’ll certainly be back.
В Сочи клиника «Детокс» предлагает лечение запоя в стационаре с круглосуточным медицинским контролем. Здесь пациент получает безопасное и эффективное восстановление.
Подробнее можно узнать тут – вывод из запоя на дому круглосуточно в сочи
Вывод из запоя у подростков в Москве от клиники «Частный Медик 24». Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Изучить вопрос глубже – частная наркологическая помощь москва
It’s a pity you don’t have a donate button! I’d most
certainly donate to this excellent blog! I guess for now i’ll
settle for bookmarking and adding your RSS feed to my Google
account. I look forward to fresh updates and will
share this site with my Facebook group. Talk soon!
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Получить дополнительные сведения – врач нарколог на дом краснодарский край
Капельница от запоя — доступная цена в Москве от клиники «Частный Медик 24». Стоимость процедуры начинается от 2290 ?, и вы всегда будете заранее информированы о стоимости услуг.
Изучить вопрос глубже – частная наркологическая помощь москве
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Подробнее можно узнать тут – нарколог на дом клиника сочи
Hi there, its good paragraph concerning media print,
we all understand media is a wonderful source of information.
Лечение зависимости от алкоголя на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Детальнее – вызвать наркологическую помощь москва
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Получить дополнительную информацию – вывод из запоя на дому цена в сочи
Attractive section of content. I just stumbled upon your site
and in accession capital to assert that I get actually enjoyed account your blog posts.
Anyway I’ll be subscribing to your feeds and even I achievement you access consistently quickly.
Hi there! I could have sworn I’ve been to this website before but after
checking through some of the post I realized it’s new to me.
Nonetheless, I’m definitely delighted I found it and I’ll be bookmarking and checking back frequently!
Выездная наркологическая помощь в Нижнем Новгороде — капельница от запоя с выездом на дом. Мы обеспечиваем быстрое и качественное лечение без необходимости посещения клиники.
Получить дополнительную информацию – вывод из запоя клиника нижний новгород
Лечение хронического алкоголизма в Москве от клиники «Частный Медик 24». Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Исследовать вопрос подробнее – частная скорая наркологическая помощь москва
Лечение хронического алкоголизма в Москве от клиники «Частный Медик 24». Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Получить дополнительную информацию – скорая наркологическая помощь на дому москва
Thanks for sharing your thoughts on lừa đảo. Regards
Капельница от запоя — доступная цена в Москве от клиники «Частный Медик 24». Стоимость процедуры начинается от 2290 ?, и вы всегда будете заранее информированы о стоимости услуг.
Выяснить больше – skoraya-narkologicheskaya-pomoshch11.ru
Вывод из запоя у пожилых людей в Москве от клиники «Частный Медик 24». Наши специалисты учитывают возрастные изменения организма при назначении лечения.
Подробнее – skoraya-narkologicheskaya-pomoshch-moskva13.ru
В Сочи стационар клиники «Детокс» предлагает комплексный вывод из запоя. Пациентам обеспечивают комфорт, безопасность и круглосуточный контроль.
Исследовать вопрос подробнее – вывод из запоя клиника в сочи
Useful information. Fortunate me I found your website unintentionally, and I am stunned why this accident did not came about in advance!
I bookmarked it.
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Проследить причинно-следственные связи – https://riia-immobilier.com/2015/03/03/female-engineers-winning-with-the-velvet-glove
Статья содержит практические рекомендации и полезные советы, которые можно легко применить в повседневной жизни. Мы делаем акцент на реальных примерах и проверенных методиках, которые способствуют личностному развитию и улучшению качества жизни.
Перейти к статье – https://ipbmarmoraria.com.br/ipb_revestimento-de-pias-e-lavatorios
Если вы ищете надежную клинику для вывода из запоя в Сочи, обратитесь в «Детокс». Здесь опытные специалисты окажут необходимую помощь в стационаре. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить больше информации – наркология вывод из запоя
Лечение хронического алкоголизма в Москве от клиники «Частный Медик 24». Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Изучить вопрос глубже – неотложная наркологическая помощь москва
Thankfulness to my father who stated to me
regarding this website, this webpage is really amazing.
Лечение запоя без госпитализации в Москве от клиники «Частный Медик 24». Мы предлагаем лечение на дому, без необходимости госпитализации.
Исследовать вопрос подробнее – экстренная наркологическая помощь москва
수원출장마사지 – 수원 전역 호텔・자택에서 아로마마사지, 스포츠마사지, 스웨디시를 전문 테라피스트에게 받아보세요.
고품격 홈케어 힐링과 맞춤 서비스, 철저한 위생
관리로 남녀 누구나 안심하고 이용할 수 있습니다
Write more, thats all I have to say. Literally, it seems as
though you relied on the video to make your point. You definitely know what youre talking about, why throw away your intelligence on just posting videos to
your site when you could be giving us something enlightening to read?
Если запой стал серьёзной проблемой, стационар клиники «Детокс» в Сочи поможет выйти из кризиса. Врачи проводят детоксикацию и наблюдают за состоянием пациента.
Получить дополнительные сведения – нарколог вывод из запоя
Cabinet IQ
8305 Տtate Hwy 71 #110, Austin,
TX 78735, United Տtates
254-275-5536
Upscale
Кодирование от алкоголизма в Москве от клиники «Частный Медик 24». Мы предлагаем различные методы кодирования, подходящие для каждого пациента.
Разобраться лучше – анонимная наркологическая помощь московская область
원주출장마사지 서비스는 원주광역시 전역에서
편안하게 전문 마사지를 받을 수 있는 출장 홈타이 서비스입니다.
고객님이 계신 곳으로 여성 전문 테라피스트가 직접
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Выяснить больше – врач нарколог на дом сочи
These are really wonderful ideas in about blogging.
You have touched some good things here. Any way keep
up wrinting.
Feel free to surf to my web blog – MANTULHOKI
Thanks for your personal marvelous posting!
I genuinely enjoyed reading it, you’re a great author.
I will be sure to bookmark your blog and will eventually come back at
some point. I want to encourage yourself to continue your great job, have a nice evening!
Вызов нарколога на дом в Краснодаре — услуга клиники «Детокс». Специалисты оказывают квалифицированную помощь прямо у вас дома.
Подробнее – нарколог на дом клиника в сочи
Если близкий человек в состоянии запоя, закажите нарколога на дом в Краснодаре от клиники «Детокс». Круглосуточно и конфиденциально.
Детальнее – нарколог на дом срочно в сочи
Профессиональная помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Мы предлагаем капельницу, которая способствует восстановлению водно-электролитного баланса и улучшению общего состояния пациента.
Узнать больше – анонимная скорая наркологическая помощь москва
I go to see every day a few web pages and sites to read
articles, however this weblog presents quality based posts.
Feel free to surf to my webpage MANTULHOKI
You ought to be a part of a contest for one of the highest quality sites on the internet.
I am going to highly recommend this web site!
Cette information m’a poussé à faire une
aide.
Анонимность и конфиденциальность гарантированы в клинике «Частный Медик 24». Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Углубиться в тему – вызвать наркологическую помощь москве
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Подробнее – вывод из запоя капельница
I feel this is one of the such a lot important information for me.
And i’m happy studying your article. However wanna remark on few
basic issues, The site style is wonderful, the articles is actually great :
D. Excellent activity, cheers
Hi to every , since I am actually keen of reading this webpage’s post to be updated on a regular basis.
It contains fastidious information.
This is my first time pay a quick visit at here and i am truly
impressed to read everthing at alone place.
Лечение хронического алкоголизма в Москве от клиники «Частный Медик 24». Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Разобраться лучше – anonimnaya-narkologicheskaya-pomoshch moskva
В этой информационной статье вы найдете интересное содержание, которое поможет вам расширить свои знания. Мы предлагаем увлекательный подход и уникальные взгляды на обсуждаемые темы, побуждая пользователей к активному мышлению и критическому анализу.
Почему это важно? – https://krissyleonard.com/3-steps-for-stepping-into-your-higher-self
Лечение зависимости от алкоголя на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Разобраться лучше – частная наркологическая помощь москва
Для безопасного выхода из запоя в Сочи воспользуйтесь услугами стационара клиники «Детокс». Опытные врачи окажут помощь быстро и анонимно.
Ознакомиться с деталями – вывод из запоя круглосуточно в сочи
Капельница от запоя в Нижнем Новгороде — процедура, включающая физраствор, глюкозу, витамины и седативные препараты. Она помогает восстановить водно-электролитный баланс и улучшить самочувствие.
Получить дополнительную информацию – помощь вывод из запоя нижний новгород
What’s up i am kavin, its my first time to commenting
anyplace, when i read this paragraph i thought i could also make comment due to this sensible paragraph.
Помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Детальнее – наркологическая помощь на дому москва
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Сочи предлагает вывод из запоя в стационаре. Под наблюдением опытных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее можно узнать тут – vyvod-iz-zapoya-sochi12.ru
Если вы или ваш близкий нуждаетесь в профессиональной помощи при запое, клиника «Детокс» в Сочи предлагает вывод из запоя в стационаре. Под наблюдением опытных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее тут – вывод из запоя недорого
Nice post. I used to be checking constantly this blog and I’m
inspired! Very useful information specially the remaining section :
) I handle such information a lot. I used to be seeking this certain information for a very lengthy time.
Thank you and good luck.
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Подробнее – врач вывод из запоя в сочи
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Жми сюда — получишь ответ – https://aamirpathan.com/boys-summer-fashion-clothing-ideas-and-color-combinations
Помощь при алкогольной интоксикации в Москве от клиники «Частный Медик 24». Наши специалисты проведут необходимые процедуры для снятия симптомов интоксикации.
Узнать больше – вызвать наркологическую помощь
Лечение зависимости от алкоголя на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Получить дополнительную информацию – https://skoraya-narkologicheskaya-pomoshch-moskva12.ru/
Капельница от запоя на дому в Нижнем Новгороде — удобное решение для тех, кто не может посетить клинику. Наши специалисты приедут к вам домой и проведут необходимую процедуру.
Получить дополнительную информацию – вывод из запоя цена в нижнем новгороде
Клиника «Детокс» в Сочи предлагает услугу вывода из запоя в стационаре. Под наблюдением профессиональных врачей пациент получит необходимую медицинскую помощь и поддержку. Услуга доступна круглосуточно, анонимно и начинается от 2000 ?.
Получить больше информации – наркология вывод из запоя в сочи
В Сочи клиника «Детокс» предоставляет услугу вывода из запоя в стационаре. Профессиональные врачи обеспечат комфортное и безопасное лечение. Минимальная стоимость услуги — 2000 ?.
Получить больше информации – помощь вывод из запоя
105vmd
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Открой скрытое – https://huliving.com/about
Лечение зависимости от алкоголя на дому в Москве от клиники «Частный Медик 24». Наши специалисты приедут к вам домой и проведут все необходимые процедуры.
Подробнее можно узнать тут – скорая наркологическая помощь московская область
В Сочи стационар клиники «Детокс» предлагает комплексный вывод из запоя. Пациентам обеспечивают комфорт, безопасность и круглосуточный контроль.
Получить дополнительные сведения – вывод из запоя на дому недорого в сочи
Лечение хронического алкоголизма в Подольске от клиники «Частный Медик 24». Наши специалисты помогут вам преодолеть зависимость и вернуться к нормальной жизни.
Ознакомиться с деталями – поставить капельницу от запоя
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Осуществить глубокий анализ – https://maayogashram.com/blog/surya-namaskar-sun-salutation-benefits-and-importance
В Краснодаре клиника «Детокс» предоставляет услугу вызова нарколога на дом. Специалисты приедут к вам в течение 1–2 часов, проведут осмотр и назначат необходимое лечение. Все процедуры проводятся анонимно и с соблюдением конфиденциальности.
Углубиться в тему – нарколог на дом вывод в сочи
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Хочешь знать всё? – https://www.sfmusictech.com/register
Профилактика рецидивов после запоя в Москве от клиники «Частный Медик 24». Мы поможем вам предотвратить повторные случаи запоя и поддержим вас на пути к трезвой жизни.
Получить дополнительные сведения – наркологическая клиника клиника помощь москве
A motivating discussion is worth comment. I think that you need to publish
more about this issue, it might not be a taboo matter but typically folks don’t talk about such subjects.
To the next! Kind regards!!
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Детальнее – https://vistoweekly.com/blunturi
I got this web site from my pal who told me on the topic of this website and now this time I am browsing this
website and reading very informative articles
at this time.
Капельница от запоя на дому в Нижнем Новгороде — быстрый и эффективный способ снять симптомы похмелья и восстановить организм. Наши специалисты приедут к вам домой и проведут процедуру с использованием современных препаратов.
Детальнее – вывод из запоя клиника нижний новгород
Thanks very interesting blog!
Круглосуточная наркологическая скорая помощь в Москве от клиники «Частный Медик 24». Наша команда работает 24/7, обеспечивая доступность медицинской помощи в любое время суток.
Узнать больше – круглосуточная наркологическая помощь московская область
Удобная платформа Sultan Casino — люблю заходить сюда!
https://www.google.bt/url?q=https://sultan-casino-kazakhstan-bets.kz/payments
Вывод из запоя у подростков в Подольске от клиники «Частный Медик 24». Мы предлагаем специализированное лечение для подростков, учитывая их возрастные особенности.
Ознакомиться с деталями – капельница от запоя город. московская область
Təşəkkürlər belə əla məlumat üçün.
https://pinco-azerbaijan-pro.com/odenisler
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Читать полностью – http://www.abnaccounting.com.au/contact-us
I was wondering if you ever considered changing the structure of your website?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it
better. Youve got an awful lot of text for only having 1 or two
pictures. Maybe you could space it out better?
Also visit my web blog … ซื้อหวยออนไลน์ lottovip
Мы предлагаем вам подробное руководство, основанное на проверенных источниках и реальных примерах. Каждая часть публикации направлена на то, чтобы помочь вам разобраться в сложных вопросах и применить знания на практике.
Подробнее – https://fundacionholguincuellar.com/situacion-financiera-2022
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Подробнее тут – https://www.tanne-design.bg/bg/portfolio-item/%D0%BC%D0%B5%D0%BA%D0%BE-%D0%BC%D0%BE%D0%B4%D0%B5%D1%80%D0%BD%D0%BE-%D0%BF%D1%80%D0%B0%D0%BA%D1%82%D0%B8%D1%87%D0%BD%D0%BE-2
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Погрузиться в детали – https://www.realty-key.ru/themes/kriptoekonomika
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Узнать из первых рук – http://sovet.izmuroma.ru/question-answer?page=461&destination=question-answer%3Fpage%3D179
Анонимность и конфиденциальность гарантированы в клинике «Частный Медик 24». Мы обеспечиваем полную анонимность и конфиденциальность на всех этапах лечения.
Ознакомиться с деталями – поставить капельницу от запоя в москве
Эта статья предлагает захватывающий и полезный контент, который привлечет внимание широкого круга читателей. Мы постараемся представить тебе идеи, которые вдохновят вас на изменения в жизни и предоставят практические решения для повседневных вопросов. Читайте и вдохновляйтесь!
Прочесть всё о… – https://www.defining-blog.ru/category/dengi
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Посмотреть подробности – https://rusoge.ru
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Уникальные данные только сегодня – https://forum.androidlost.com/showthread.php?mode=linear&tid=46&pid=2772
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Получить полную информацию – http://sovet.izmuroma.ru/question-answer?page=483&destination=question-answer%3Fpage%3D455
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Не пропусти важное – https://www.powertvnews.in/2025/06/12/plane-crash-105-out-of-242-people-killed-rescue-operations-continue
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Открой скрытое – http://www.volgyfitness.hu/?p=6639&cpage=186
Kazino haqqında faydalı kontent üçün təşəkkürlər!
https://1ab.in/3dst
Hi there, this weekend is pleasant designed for me, since this point in time i am reading this great
educational article here at my home.
I’m no longer certain the place you’re getting your information, however great topic.
I needs to spend a while finding out much more or working out more.
Thank you for wonderful info I used to be on the lookout
for this information for my mission.
whoah this blog is fantastic i like studying your posts.
Keep up the great work! You already know, lots of individuals are hunting round for this information, you can aid them greatly.
Yes! Finally someone writes about Telegram电报设置中文教程(2026最新).
This paragraph will assist the internet people for building up new web site or even a
weblog from start to end.
What’s up, this weekend is good for me, for the reason that this point in time i am
reading this wonderful informative post here at my
home.
Hi there, I read your blog on a regular basis. Your humoristic style is awesome, keep it up!
You need to take part in a contest for one of the best blogs on the net.
I will highly recommend this site!
Piece of writing writing is also a excitement, if you be
familiar with after that you can write otherwise it is difficult to write.
Hello colleagues, how is all, and what you wish for to say concerning this post, in my view its really amazing in favor of me.
https://startupline.com.ua/rozsiyuvach-far-nevydymyi-zakhysnyk-yakyi.html
Appreciating the commitment you put into your blog and in depth
information you provide. It’s great to come across a blog every once in a while that isn’t the same outdated rehashed information. Excellent read!
I’ve bookmarked your site and I’m including your RSS feeds
to my Google account.
Heya i am for the first time here. I came across this board and
I in finding It really useful & it helped me out
much. I am hoping to give one thing again and aid others like you helped me.
Такой подход обеспечивает результативность и помогает добиться длительной ремиссии даже при тяжёлых формах зависимости.
Получить дополнительную информацию – наркологическая клиника наркологический центр в воронеже
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Детальнее – http://narkologicheskaya-klinika-v-krasnoyarske17.ru/krasnoyarsk-narkologicheskij-czentr/
Hey There. I discovered your blog using msn. That is a
really smartly written article. I’ll be sure to bookmark it and return to learn extra of
your useful information. Thanks for the post. I will certainly return.
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Получить больше информации – вызвать наркологическую помощь в тольятти
It’s remarkable to pay a quick visit this web page and reading the views of all friends regarding this article, while I am
also zealous of getting know-how. http://silkroadtrek.com/2019/11/05/imamzadeh-hussein/
Лечение зависимости в наркологической клинике проводится поэтапно. Это обеспечивает постепенное восстановление организма и исключает риск осложнений. Каждый этап направлен на устранение конкретных нарушений, вызванных употреблением психоактивных веществ.
Углубиться в тему – анонимная наркологическая клиника
Комплексная терапия включает несколько последовательных этапов, обеспечивающих полное восстановление организма и личности пациента. Каждый из них направлен на решение конкретных задач — от устранения интоксикации до закрепления устойчивой ремиссии.
Подробнее тут – http://narkologicheskaya-klinika-v-volgograde17.ru/
Ниже приведена таблица с типовыми компонентами капельницы и их назначением:
Подробнее можно узнать тут – врача капельницу от запоя в волгограде
Во время процедуры врач фиксирует ключевые параметры, чтобы убедиться в безопасности и эффективности терапии. Мониторинг проводится при каждом выезде и помогает отслеживать динамику в режиме реального времени. В таблице ниже указаны основные показатели, за которыми следит специалист.
Получить дополнительные сведения – нарколог капельница на дом в воронеже
โพสต์นี้ น่าสนใจดี ครับ
ผม ไปอ่านเพิ่มเติมเกี่ยวกับ ข้อมูลเพิ่มเติม
เข้าไปดูได้ที่ Poppy
เผื่อใครสนใจ
มีการยกตัวอย่างที่เข้าใจง่าย
ขอบคุณที่แชร์ ข้อมูลที่ช่วยให้เข้าใจเรื่องนี้มากขึ้น นี้
และหวังว่าจะมีข้อมูลใหม่ๆ มาแบ่งปันอีก
Не всегда человек способен прекратить употребление алкоголя без медицинского вмешательства. Чем дольше длится запой, тем выше риск осложнений. Обратиться к специалисту следует при появлении следующих признаков:
Узнать больше – https://vyvod-iz-zapoya-v-tyumeni17.ru/vyvod-iz-zapoya-na-domu-tyumen
I wanted to thank you for this great read!! I certainly loved every bit of it.
I have got you book marked to look at new things you post…
Капельница — это основной инструмент дезинтоксикации при лечении запойных состояний. Она способствует выведению токсинов, нормализации обмена веществ и улучшению общего самочувствия. Состав раствора подбирается индивидуально в зависимости от степени интоксикации, возраста, массы тела и сопутствующих заболеваний. Уже через 20–30 минут после начала инфузии пациент ощущает облегчение, снижается тревожность и проходит головная боль.
Исследовать вопрос подробнее – вывод из запоя капельница на дому в красноярске
Комплексный подход обеспечивает не только снятие симптомов, но и полное восстановление функций организма. Пациент получает поддержку на всех этапах — от детоксикации до социальной адаптации.
Подробнее – http://narkologicheskaya-pomoshh-v-tolyatti17.ru/pomoshh-narkozavisimym-tolyatti/
Вывод из запоя — это не просто медицинская процедура, а тщательно выстроенный процесс, направленный на восстановление работы всех систем организма. При неправильном или неполном лечении риск осложнений возрастает в несколько раз. Поэтому обращение в профессиональную клинику становится необходимым шагом. В наркологической клинике «Центр Трезвости ВоронМед» пациент получает экстренную помощь, безопасные инфузионные препараты, круглосуточный выезд нарколога и последующее восстановление под наблюдением специалистов. Здесь каждая капельница подбирается индивидуально — с учётом возраста, веса, длительности запоя, хронических болезней и реакции организма на препараты.
Ознакомиться с деталями – http://vyvod-iz-zapoya-v-voronezhe17.ru
Инфузионные растворы подбираются строго индивидуально, после осмотра врача и анализа показателей пациента. При необходимости курс повторяется с изменением состава раствора для достижения максимального эффекта.
Углубиться в тему – наркологическая клиника цены новокузнецк
You actually make it seem so easy with your presentation but I find this matter to be actually something that I think I’d never understand.
It sort of feels too complex and extremely large for me. I’m taking
a look forward to your next submit, I will attempt to get
the hang of it!
Hello! I know this is somewhat off topic but I was wondering if you knew where I could get a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having trouble finding one?
Thanks a lot!
I really like your blog.. very nice colors & theme.
Did you make this website yourself or did you
hire someone to do it for you? Plz answer back as I’m looking to construct
my own blog and would like to know where u got this from.
thanks
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Получить дополнительную информацию – платная наркологическая помощь
Инфузионная терапия (капельницы) — важная часть лечения, направленная на очищение организма, восстановление водно-солевого баланса и устранение токсинов. В «РязаньМед Альянс» используются проверенные препараты, которые помогают нормализовать работу внутренних органов и улучшить общее самочувствие. Таблица ниже показывает, какие виды капельниц чаще всего применяются при выведении из запоя и лечении алкоголизма.
Детальнее – https://narkologicheskaya-klinika-v-ryazani17.ru/narkolog-ryazan-telefon/
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Углубиться в тему – вывод из запоя недорого в красноярске
Одним из ключевых направлений терапии является инфузионное лечение. Капельницы позволяют быстро восстановить обмен веществ, улучшить работу внутренних органов и ускорить выведение токсинов. В клинике используются только сертифицированные препараты, безопасные для сердечно-сосудистой и нервной системы.
Углубиться в тему – http://narkologicheskaya-clinika-v-ryazani17.ru/narkolog-ryazan-telefon/
В Воронеже клиника «Центр Трезвости ВоронМед» обеспечивает выезд нарколога на дом в любое время суток. Это позволяет оказывать помощь пациентам, которые находятся в тяжёлом состоянии или не могут самостоятельно приехать в стационар. Медицинская бригада прибывает в течение 40–60 минут, не используя специализированный транспорт и форму, чтобы сохранить анонимность. Врач проводит первичный осмотр, оценивает давление, частоту дыхания, уровень сознания и насыщение кислородом, после чего назначает детоксикационную капельницу с контролем дозировки.
Изучить вопрос глубже – вывод из запоя цена воронеж
Triangle Billiards & Bar Stools
1471 Nisson Ɍd, Tustin,
СA 92780, United Stɑtes
+17147715380
Bookmarks
I think what you typed made a bunch of sense. However,
think about this, suppose you wrote a catchier post title?
I am not suggesting your content is not solid., however suppose you added a headline that grabbed a person’s attention? I mean Heart failure: Symptoms, Causes, Diagnosis & Treatment –
MDtodate is a little vanilla. You could glance at Yahoo’s home page
and see how they write news headlines to get people interested.
You might try adding a video or a pic or two to get readers interested
about everything’ve got to say. In my opinion,
it would make your blog a little bit more interesting.
Клиника «ВолгаМед Резолюция» в Волгограде оказывает помощь при алкогольной интоксикации как в условиях стационара, так и на дому. Врачи готовы выехать к пациенту в течение 40–60 минут после обращения, привозя с собой всё необходимое оборудование для проведения инфузионной терапии. Такая оперативность позволяет снизить риск осложнений и стабилизировать состояние уже в первые часы лечения. Для пациентов, нуждающихся в круглосуточном наблюдении, предусмотрены комфортабельные палаты с постоянным медицинским контролем.
Получить дополнительную информацию – вывод из запоя недорого волгоград
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Детальнее – https://vyvod-iz-zapoya-v-krasnoyarske17.ru/vyvedenie-iz-zapoya-krasnoyarsk
I visited many blogs but the audo quality for audio songs current
at this web site is genuinely excellent.
В Воронеже клиника «Центр Трезвости ВоронМед» обеспечивает выезд нарколога на дом в любое время суток. Это позволяет оказывать помощь пациентам, которые находятся в тяжёлом состоянии или не могут самостоятельно приехать в стационар. Медицинская бригада прибывает в течение 40–60 минут, не используя специализированный транспорт и форму, чтобы сохранить анонимность. Врач проводит первичный осмотр, оценивает давление, частоту дыхания, уровень сознания и насыщение кислородом, после чего назначает детоксикационную капельницу с контролем дозировки.
Углубиться в тему – наркология вывод из запоя воронеж
Наркологическая помощь в современном формате — это комплексное лечение зависимостей и состояний интоксикации с индивидуальным подходом к каждому пациенту. В клинике «ВолгаМед Тольятти» круглосуточно работают врачи-наркологи, психиатры и реабилитологи, готовые оказать поддержку в любой момент. Применяются сертифицированные препараты, проверенные методики и психологическое сопровождение. При этом особое внимание уделяется анонимности и безопасности пациента: информация не передаётся третьим лицам, а лечение проводится строго конфиденциально.
Углубиться в тему – https://narkologicheskaya-pomoshh-v-tolyatti17.ru/narkologiya-goroda-tolyatti/
This piece of writing presents clear idea for the new viewers of
blogging, that truly how to do blogging.
Клиника «Трезвый Шаг Раменское» выстраивает помощь так, чтобы пациент и его близкие не метались между разными службами и частными «специалистами», а получали комплекс услуг в одном месте. Это особенно важно для тех, кто уже сталкивался с провалами после разовых кодировок, неподходящих капельниц или формальной «помощи».
Детальнее – наркологические клиники алкоголизм
Каждое направление встроено в общую стратегию: не просто купировать симптомы, а уменьшить риск повторения сценария, когда после «облегчения» всё возвращается к прежней модели употребления.
Узнать больше – https://narkologicheskaya-klinika-kolomna2-10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne
Услуга
Изучить вопрос глубже – нарколог на дом круглосуточно цены
Welcome to Accountants Near Me Directory USA — your trusted online directory connecting businesses and individuals
with professional accounting services, qualified local accountants.
Tax Preparation Service and Bookkeeping Services.
Manage taxes, audits, and financial planning effortlessly.
Manage finances, stay compliant, and plan confidently.
Visit accountantsnearmecheyenne.com today.
Лечение проходит в несколько этапов: диагностика, детоксикация, медикаментозная поддержка и восстановление. Каждый этап имеет чёткие цели и критерии эффективности, что делает процесс управляемым и безопасным. Применяются препараты, сертифицированные в РФ, и только те, чья эффективность подтверждена клиническими исследованиями.
Разобраться лучше – вывод из запоя дешево в волгограде
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Изучить вопрос глубже – вывод из запоя вызов в красноярске
В таблице представлены основные виды терапии, применяемые в клинике:
Исследовать вопрос подробнее – вывод наркологическая клиника
Вывод из запоя — это не просто медицинская процедура, а тщательно выстроенный процесс, направленный на восстановление работы всех систем организма. При неправильном или неполном лечении риск осложнений возрастает в несколько раз. Поэтому обращение в профессиональную клинику становится необходимым шагом. В наркологической клинике «Центр Трезвости ВоронМед» пациент получает экстренную помощь, безопасные инфузионные препараты, круглосуточный выезд нарколога и последующее восстановление под наблюдением специалистов. Здесь каждая капельница подбирается индивидуально — с учётом возраста, веса, длительности запоя, хронических болезней и реакции организма на препараты.
Детальнее – скорая вывод из запоя в воронеже
Домашний формат хорош при умеренной выраженности симптомов, сохранённом контакте и возможности обеспечить наблюдение в квартире: тихая комната, взрослый рядом первые 6–8 часов, отсутствие грубой дезориентации и неукротимой рвоты, относительная стабильность АД/ЧСС. В таких условиях выездная бригада «Трезвой Линии» запускает персональную схему: регидратация, выравнивание электролитов, поддержка витаминами группы B и магнием, осторожная седация, чтобы «собрать» сон, не выключая мониторинг. Стационар предпочтителен, если запой длится 3–5 суток и более, отмечаются «качели» показателей, шаткость походки, выраженная слабость, признаки предделирия или судорожной готовности; также при сочетанной соматике (ИБС, гипертония, диабет, хронические болезни печени/почек, неврология) и у пациентов старшего возраста. Преимущество стационара — приборный контроль, тихий режим, щадящее питание, возможность быстро расширять схему без ожидания ухудшений. Мы придерживаемся принципа «минимально достаточно»: ровно столько вмешательств, сколько требует клиническая картина, — так безопаснее и в перспективе экономнее, чем череда домашних «подлаток».
Выяснить больше – vyvod-iz-zapoya-na-domu
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Изучить вопрос глубже – вывод из запоя вызов на дом в волгограде
При появлении таких симптомов важно не откладывать вызов врача. Самолечение, особенно с использованием неизвестных препаратов, может привести к тяжёлым последствиям, включая судороги и инсульт. Врачи клиники «ВолгаМед Резолюция» приезжают на дом с необходимыми средствами для оказания экстренной помощи и стабилизации состояния уже на месте.
Углубиться в тему – вывод из запоя вызов на дом в волгограде
Основные этапы лечения включают:
Детальнее – http://narkologicheskaya-klinika-v-voronezhe17.ru
Применение комплексной терапии позволяет не только устранить зависимость, но и сформировать новые поведенческие установки, предотвращающие возвращение к употреблению.
Узнать больше – https://narkologicheskaya-clinica-v-voronezhe17.ru/chastnaya-narkologicheskaya-klinika-voronezh
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Изучить вопрос глубже – кодирование от алкоголизма анонимно
Первым шагом на пути к выздоровлению является очищение организма от токсинов. В клинике проводится детоксикация с использованием современных препаратов, направленных на выведение продуктов распада алкоголя и наркотиков. Медикаментозное лечение дополняется витаминами, гепатопротекторами и средствами для нормализации работы нервной системы. Это помогает восстановить обмен веществ, улучшить сон, аппетит и общее самочувствие пациента.
Получить больше информации – https://narkologicheskaya-klinika-v-voronezhe17.ru/narkolog-voronezh-czena
Ниже приведена таблица, отражающая примерную динамику состояния пациента после постановки капельницы:
Углубиться в тему – http://kapelnicza-ot-zapoya-v-voronezhe17.ru
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Детальнее – наркологические клиники алкоголизм в красноярске
Процесс кодирования проходит в комфортной и спокойной обстановке. Врач объясняет каждый этап, чтобы пациент чувствовал себя уверенно и спокойно. После процедуры пациент получает памятку с рекомендациями по уходу за здоровьем и режиму поведения в первые недели после лечения.
Детальнее – кодирование от алкоголизма цена в волгограде
Hey! Do you use Twitter? I’d like to follow
you if that would be okay. I’m undoubtedly enjoying your
blog and look forward to new updates.
Состав капельницы подбирается индивидуально, с учётом степени опьянения, возраста и хронических заболеваний пациента. Врач определяет дозировку и комбинацию препаратов, чтобы процедура прошла безопасно и эффективно.
Разобраться лучше – вызвать капельницу от запоя на дому воронеж
Процесс включает следующие шаги:
Углубиться в тему – http://narcologicheskaya-klinika-v-krasnoyarske17.ru
Благодаря комплексному подходу достигается не только снятие симптомов, но и долгосрочная стабилизация состояния пациента.
Детальнее – срочная наркологическая помощь в волгограде
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Получить дополнительные сведения – анонимный вывод из запоя
Вывод из запоя в Раменском в условиях клиники строится не вокруг одной капельницы, а вокруг понятной цепочки шагов, где каждый этап логичен и медицински обоснован. Это помогает не только быстро облегчить состояние, но и уменьшить вероятность того, что через пару дней человек снова уйдёт в запой.
Детальнее – вывод из запоя на дому
В клинике обеспечивается безопасный вывод из запоя и очистка организма после употребления алкоголя, наркотиков или токсических сочетаний. Используются современные инфузионные схемы, витамины группы B, магний, гепатопротекторы по показаниям, противорвотные, мягкая коррекция сна и тревожности. Контроль давления, пульса, сатурации и поведения позволяет вовремя отметить любые осложнения и скорректировать терапию. Главная цель — не просто «прояснить голову», а защитить сердечно-сосудистую систему, мозг, печень, минимизировать риск делирия, судорог, аритмий и других острых состояний.
Углубиться в тему – http://
Franchising Path Carlsbad
Carlsbad, ⲤA 92008, Unied Ꮪtates
+18587536197
start your own franchise business
Благодаря комплексному подходу достигается не только снятие симптомов, но и долгосрочная стабилизация состояния пациента.
Получить дополнительные сведения – наркологическая помощь волгоград
Если вас интересует МРТ малого таза, всю актуальную информацию можно найти на сайте клиники.
Клиника использует многоступенчатый подход, который позволяет адаптировать лечение под особенности организма пациента. Наблюдение продолжается даже после завершения детоксикации, чтобы убедиться, что состояние стабильно и не требуется дополнительное вмешательство. При необходимости врач назначает курс поддержки печени, витаминов и препаратов для восстановления сна и психоэмоционального равновесия.
Получить больше информации – вывод из запоя на дому
It’s very trouble-free to find out any matter
on net as compared to books, as I found this post at this web site.
Потрібний стабілізатор напруги Елекс ? Замовити можно в Electromag – інтернет-магазин енергетичної незалежності
Майка в рубчик — Горлін жіноча майка в рубчик стильна та зручна модель у чорну смужку для щоденних образів
В Воронеже команда «ВоронМед Профи» работает по принципу быстрой медицинской реакции — помощь оказывается независимо от времени суток и дня недели. Все выезды выполняются анонимно, без спецтранспорта и медицинской формы. Врач приезжает в гражданской одежде, что исключает ненужное внимание соседей и посторонних. В ходе осмотра специалист измеряет давление, пульс, температуру, оценивает уровень интоксикации и определяет степень обезвоживания. На основе полученных данных подбирается состав капельницы, который подаётся медленно и безопасно под контролем врача.
Получить дополнительную информацию – http://narkolog-na-dom-v-voronezhe17.ru
Все для электромонтажа: нулевая шина – лучшая цена. В магазине средств для электромонтажа ТФХ – огромный выбор
купить ящик для зимней рыбалки Fishingtour – Товары для рыбалки. Рыболовный магазин
Перед процедурой врач оценивает состояние пациента, измеряет давление, пульс и уровень насыщения крови кислородом. После осмотра подбирается состав инфузии, включающий препараты для дезинтоксикации, восстановления водно-солевого баланса и нормализации работы органов. Введение растворов осуществляется внутривенно, под контролем специалиста. Длительность процедуры — от 40 минут до 1,5 часов.
Разобраться лучше – капельница от запоя анонимно на дому волгоград
Write more, thats all I have to say. Literally,
it seems as though you relied on the video to make your point.
You clearly know what youre talking about, why throw away your intelligence on just posting videos to your weblog when you could
be giving us something informative to read?
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Получить дополнительную информацию – анонимный вывод из запоя рязань
Процесс включает несколько шагов:
Узнать больше – нарколог на дом срочно
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Углубиться в тему – http://vyvod-iz-zapoya-ramenskoe10.ru/vyvod-iz-zapoya-ryadom-v-ramenskom/https://vyvod-iz-zapoya-ramenskoe10.ru
Клиника предлагает широкий спектр медицинских и психологических услуг, направленных на восстановление пациента после зависимости. Все процедуры проходят под контролем врачей и с соблюдением анонимности. Наиболее востребованные направления представлены ниже:
Изучить вопрос глубже – https://narkologicheskaya-clinica-v-voronezhe17.ru/
freedom digital experience mountain ocean physics future wildlife technology mountain mountain village wisdon international history dreams security nature chemistry city exploration education energy economy nature art wildlife culture wisdon international technology learning technology chemistry internet mountain learning psychology health philosophy menara188
Чтобы не оценивать состояние субъективно, в клинике применяется система наблюдения за ключевыми параметрами. Таблица помогает врачу и пациенту видеть реальную динамику и корректировать вмешательства только при необходимости.
Исследовать вопрос подробнее – https://narkologicheskaya-clinica-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Подробнее тут – https://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk
В таблице представлены основные элементы детоксикационной терапии:
Изучить вопрос глубже – https://narkologicheskaya-klinika-v-volgograde17.ru/narkologi-volgograda
Отдельный принцип клиники — строгая анонимность. Информация о лечении не передаётся по месту работы, обучения, в сторонние структуры без согласия пациента. Это особенно важно для людей, которые боятся огласки и из-за этого годами откладывают обращение. В «КоломнаМед Центр» можно пройти лечение так, чтобы сохранить репутацию и личное пространство, не превращая каждый шаг в обсуждение «на людях».
Углубиться в тему – https://narkologicheskaya-klinika-kolomna10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
Процесс включает несколько шагов:
Углубиться в тему – https://narkolog-na-dom-v-ufe17.ru/vyvod-iz-zapoya-ufa-narkolog-na-dom
Современная наркологическая клиника — это не просто медицинское учреждение, где проводят детоксикацию или капельницы. Это выстроенная система, где каждый этап направлен на восстановление физического, психического и социального равновесия пациента. В клинике «КрасЗдрав Профи» весь процесс лечения построен по принципу прозрачных шагов: первичная диагностика, стабилизация организма, терапевтическая коррекция и закрепление результата. Всё происходит с соблюдением принципа конфиденциальности — пациент может рассчитывать на анонимность и этичное отношение со стороны персонала.
Выяснить больше – https://narkologicheskaya-clinica-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy/
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Подробнее тут – нарколог вывод из запоя
Лечение организовано поэтапно. Такой подход обеспечивает постепенное восстановление функций организма и исключает риск осложнений. Каждый этап терапии направлен на устранение конкретных нарушений, вызванных интоксикацией.
Подробнее – скорая вывод из запоя в красноярске
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Подробнее можно узнать тут – http://narkologicheskaya-klinika-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy/https://narkologicheskaya-klinika-v-krasnoyarske17.ru
Одна из сильных сторон «РеутовМед Сервис» — честная оценка границ домашнего лечения. Клиника не обещает «вывезем любого дома», потому что есть состояния, при которых отсутствие круглосуточного наблюдения опасно. Чтобы родным было проще сориентироваться, важно разделить ситуации по уровню риска и понять, почему иногда разумнее выбрать стационар, даже если пациент сопротивляется.
Подробнее тут – vyvod-iz-zapoya-sajt
Клиника «КузбассМед Центр» в Новокузнецке обеспечивает непрерывный приём пациентов и выезд нарколога на дом. Такой формат позволяет оказать экстренную помощь при интоксикации или запое прямо на месте, не дожидаясь ухудшения состояния. Медицинская команда работает в режиме 24/7, что особенно важно при острых состояниях. Врач выезжает в течение часа после вызова, проводит диагностику, ставит капельницу и контролирует жизненные показатели. В стационаре доступны детоксикация, медикаментозная терапия и психотерапевтическая поддержка — всё под постоянным медицинским наблюдением.
Подробнее можно узнать тут – наркологическая клиника клиника помощь в новокузнецке
Every weekend i used to pay a quick visit this web page, because
i want enjoyment, as this this website conations really nice funny information too.
Формат помощи
Получить больше информации – vyvod-iz-zapoya-deshev-reutove
Зависимость — это хроническое заболевание, и в «КоломнаМед Центр» это принимается как медицинский факт, а не моральная оценка. Программы включают медикаментозную поддержку, работу с тягой, коррекцию тревожных и депрессивных состояний, психотерапию, помощь в восстановлении режима сна и питания, семейное консультирование. При наркотической зависимости и полинаркомании добавляются протоколы по безопасной отмене веществ, наблюдение в критические периоды, сопровождение на этапе формирования устойчивой ремиссии. Акцент делается на том, чтобы не запугивать пациента, а показать реалистичный путь, где улучшение возможно шаг за шагом.
Ознакомиться с деталями – http://narkologicheskaya-klinika-kolomna10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/
Лечение зависимости в наркологической клинике проводится поэтапно. Это обеспечивает постепенное восстановление организма и исключает риск осложнений. Каждый этап направлен на устранение конкретных нарушений, вызванных употреблением психоактивных веществ.
Ознакомиться с деталями – наркологическая клиника лечение алкоголизма красноярск
goGLOW
6850 N Roochester Ꮢd, Rochester Hills,
MI 48306, United Ѕtates
248 971-1831
Bookmarks (protopage.com)
Чтобы не упустить момент, нужно ориентироваться не на фразу «он говорит, что справится», а на реальные признаки, при которых профессиональная помощь на дому становится необходимой. Домашний выезд — это шанс стабилизировать состояние до того, как потребуется реанимация или жёсткая госпитализация.
Исследовать вопрос подробнее – http://narkolog-na-dom-dolgoprudnij10.ru/skolko-stoit-narkolog-na-dom-v-dolgoprudnom/
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Получить дополнительную информацию – https://narkologicheskaya-klinika-kolomna2-10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/
Для повышения эффективности в капельницы добавляются витамины группы B, аскорбиновая кислота, кардиопротекторы и антиоксиданты. Такая комбинация позволяет не только ускорить выведение продуктов распада алкоголя, но и предотвратить развитие постабстинентных расстройств. Благодаря точной дозировке и мягкому темпу введения растворов снижается риск побочных реакций, а восстановление проходит плавно и безопасно.
Ознакомиться с деталями – вывод из запоя на дому цена в воронеже
Вывод из запоя на дому возможен только при относительно контролируемом состоянии и после очной оценки нарколога. В таких случаях специалист выезжает в Раменском, проводит осмотр, назначает индивидуальную капельницу, остаётся до стабилизации состояния и оставляет подробные рекомендации. Важный момент — честность: если во время осмотра врач видит риски (нестабильное давление, признаки начинающегося делирия, серьёзные боли, глубокую дезориентацию), формат на дому не навязывается, а предлагается стационар. Именно это отличает клинику от анонимных «служб капельниц», для которых любая заявка — повод заработать, независимо от последствий.
Подробнее тут – narkolog-vyvod-iz-zapoya
Чтобы не упустить момент, нужно ориентироваться не на фразу «он говорит, что справится», а на реальные признаки, при которых профессиональная помощь на дому становится необходимой. Домашний выезд — это шанс стабилизировать состояние до того, как потребуется реанимация или жёсткая госпитализация.
Ознакомиться с деталями – vyezd-narkologa-na-dom
Ниже — примерная структура пакетов, которую можно использовать как ориентир (не публичная оферта):
Детальнее – http://narkolog-na-dom-shchelkovo10.ru/vyzvat-narkologa-na-dom-shchelkovo/
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Изучить вопрос глубже – вывод из запоя капельница на дому
Главная задача процедуры — быстрое выведение этанола и его метаболитов из организма, нормализация уровня электролитов, улучшение самочувствия и предотвращение осложнений. Лечение проводится как в клинике, так и на дому, что особенно удобно при тяжёлых состояниях, когда пациент не может самостоятельно добраться до медицинского учреждения.
Разобраться лучше – вывод из запоя недорого в тюмени
Клиника «Трезвый Шаг Раменское» выстраивает помощь так, чтобы пациент и его близкие не метались между разными службами и частными «специалистами», а получали комплекс услуг в одном месте. Это особенно важно для тех, кто уже сталкивался с провалами после разовых кодировок, неподходящих капельниц или формальной «помощи».
Подробнее можно узнать тут – https://narkologicheskaya-klinika-ramenskoe10.ru
Why users still make use of to read news papers when in this technological globe the whole
thing is presented on web?
Каждый вызов нарколога на дом проходит по строгому алгоритму. Врачи клиники «ВоронМед Профи» используют индивидуальный подход, адаптируя лечение под конкретного пациента. В таблице приведена типовая схема работы выездной бригады, которая помогает понять, как проходит процесс помощи от начала до конца.
Подробнее тут – https://narkolog-na-dom-v-voronezhe17.ru/voronezh-narkologiya
Клиника предлагает широкий спектр медицинских и психологических услуг, направленных на восстановление пациента после зависимости. Все процедуры проходят под контролем врачей и с соблюдением анонимности. Наиболее востребованные направления представлены ниже:
Получить больше информации – лечение в наркологической клинике
Капельница от запоя в Волгограде — это эффективный способ быстро восстановить организм после длительного употребления алкоголя. Процедура проводится врачом-наркологом и направлена на выведение токсинов, нормализацию обмена веществ и стабилизацию работы нервной системы. Инфузионная терапия помогает устранить головную боль, слабость, тошноту, восстановить сон и аппетит. Благодаря внутривенному введению препаратов эффект наступает уже через 20–30 минут после начала процедуры.
Исследовать вопрос подробнее – http://kapelnicza-ot-zapoya-v-volgograde17.ru/
Наркологическая клиника в Воронеже — это специализированное медицинское учреждение, предоставляющее помощь людям, столкнувшимся с зависимостью от алкоголя, наркотиков и других психоактивных веществ. Лечение проводится под контролем квалифицированных врачей, с использованием современных методик детоксикации, психотерапии и реабилитации. Цель работы специалистов — не только устранить физическую зависимость, но и помочь пациенту восстановить эмоциональное равновесие, вернуть контроль над поведением и мотивацию к трезвости.
Подробнее – narkologicheskaya-clinica-v-voronezhe17.ru/
هذا منشور حيوي. التمويل
الجماعي الطبي يغير مستقبل الناس
الذين لا يستطيعون تحمل تكاليف الجراحة.
مساعدة جمعية رعاية العيون هو عمل رائع حقاً.
شكراً لـ مشاركة هذه المهمة.
my page … رؤية جديدة للمرضى
Всесторонний bosch diesel service
Дизельные автомобили оснащены сложными системами, диагностика которых нуждается в квалификации специалистов.
бош дизель сервис — все виды обслуживания по диагностике топливной аппаратуры:
• бош сервис ремонт форсунок — восстановление электромагнитных форсунок
• тестирование тнвд — выявление неисправностей
• бош дизель сервис москва — выгодная локация
• bosch сервис дизель — гарантия качества
Обслуживаем машины различных брендов: европейские, японские, отечественные.
Почему мы:
– сертифицированные специалисты
– оригинальные запчасти
– современное оборудование
– гарантия
http://dwise.co.kr/bbs/board.php?bo_table=free&wr_id=684855
Ez88 merupakan situs slot server jepang menyediakan permainan slot gacor gampang menang maxwin terbaik
hari ini dengan costumer servis 24 jam siap membantu.
Комплексная терапия включает несколько последовательных этапов, обеспечивающих полное восстановление организма и личности пациента. Каждый из них направлен на решение конкретных задач — от устранения интоксикации до закрепления устойчивой ремиссии.
Детальнее – narkologicheskaya-klinika-v-volgograde17.ru/
Важное отличие клиники — отказ от примитивной схемы «капельница — домой — дальше сам». Такой формат даёт кратковременное облегчение, но не решает ни причин, ни структуры зависимости. «КоломнаМед Центр» выстраивает ступенчатый подход. Первый шаг — безопасная детоксикация: снятие абстиненции, коррекция водно-электролитного баланса, поддержка сердечно-сосудистой системы, печени, нервной системы, нормализация сна. Второй шаг — стабилизация: оценка психического состояния, выявление тревожных, депрессивных и панических симптомов, подбор поддерживающих схем, которые помогают не сорваться сразу после выхода из острых проявлений. Третий шаг — реабилитация и мотивация: психотерапевтическая работа, групповые и индивидуальные форматы, обучение навыкам трезвой жизни, работа с триггерами, укрепление внутренней мотивации. Четвёртый шаг — постреабилитационная поддержка: контрольные приёмы, дистанционные консультации, помощь в профилактике срывов. Такой комплексный путь не ломает пациента, а возвращает ему контроль: не через страх, а через понимание, структуру и реальные инструменты.
Детальнее – http://narkologicheskaya-klinika-kolomna10.ru
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Исследовать вопрос подробнее – http://vivod-iz-zapoya-v-volgograde17.ru
Комплексное применение этих методов позволяет значительно ускорить процесс восстановления и предотвратить осложнения.
Выяснить больше – наркологическая клиника цены новокузнецк
Have you ever thought about publishing an ebook or guest
authoring on other blogs? I have a blog based upon on the same topics you discuss and
would really like to have you share some stories/information.
I know my readers would value your work. If you are even remotely interested, feel free to shoot me an e-mail.
В Рязани клиника «РязаньМед Альянс» принимает пациентов 24/7, без выходных и праздников. Такое расписание особенно важно при экстренных состояниях — когда человек находится в запое или испытывает абстинентный синдром. Врачи выезжают на дом в течение часа, проводят осмотр, устанавливают капельницы и стабилизируют состояние пациента. Для тех, кто нуждается в длительном наблюдении, предусмотрено комфортное пребывание в стационаре. Здесь созданы условия, при которых лечение проходит анонимно, с сохранением медицинской тайны и без постановки на учёт.
Получить дополнительные сведения – http://narkologicheskaya-klinika-v-ryazani17.ru/narkologiya-v-ryazani/https://narkologicheskaya-klinika-v-ryazani17.ru
My programmer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type on numerous websites for about a year and
am worried about switching to another platform. I have heard fantastic things about
blogengine.net. Is there a way I can import all my wordpress content into it?
Any help would be greatly appreciated!
На месте врач и медсестра собирают базовую линию: уровень сознания, дыхание, SpO?, температура, шкалы симптомов (тошнота/тремор/тревога 0–10), переносимость воды небольшими глотками. Далее формулируется рабочая гипотеза и включается минимально достаточный модуль с обозначенным «окном оценки»: 30–60 минут — для «окна питья», 60–120 минут — для стабилизации ЧСС/АД и дрожи, «первая ночь» — для сна и вечерней тревоги. Как только маркер достигнут, модуль выключается; нет эффекта — меняется одна переменная без «усиления всего сразу».
Исследовать вопрос подробнее – наркологическая клиника стационар красноярск
посмотреть на этом сайте https://krab3a.at/
I’m curious to find out what blog platform you have been using?
I’m experiencing some minor security issues with my
latest site and I would like to find something more
safeguarded. Do you have any solutions?
Ниже приведена таблица с типовыми компонентами капельницы и их действием:
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-v-tolyatti17.ru/vyvedenie-iz-zapoya-tolyatti
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Получить дополнительные сведения – http://narkologicheskaya-klinika-v-krasnoyarske17.ru/chastnaya-narkologicheskaya-klinika-krasnoyarsk/
I think the admin of this website is genuinely working hard
for his website, for the reason that here every information is quality based data.
my blog … JPKARTEL
Greetings from Ohio! I’m bored to tears at work so I decided to browse your website on my iphone during lunch break.
I really like the knowledge you present here and can’t wait to take a look when I get home.
I’m amazed at how quick your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyhow, awesome blog!
Одним из ключевых направлений терапии является инфузионное лечение. Капельницы позволяют быстро восстановить обмен веществ, улучшить работу внутренних органов и ускорить выведение токсинов. В клинике используются только сертифицированные препараты, безопасные для сердечно-сосудистой и нервной системы.
Ознакомиться с деталями – наркологическая клиника вывод из запоя рязань
«Трезвый Центр Коломна» предлагает несколько маршрутов, и выбор делается не по принципу «как удобнее», а по критериям безопасности. Если пациент в сознании, на контакте, без грубой дезориентации, без галлюцинаций, может пить воду, рвота эпизодическая, нет тяжёлых скачков давления и пульса, дома есть тишина и ответственный взрослый — возможен выезд на дом. Врач приезжает в Коломне, проводит осмотр, измеряет давление, пульс, сатурацию, температуру, оценивает тремор, степень обезвоживания, неврологический и психический статус, подбирает индивидуальную инфузионную схему и наблюдает за реакцией. Если же запой затянулся (3–5 суток и более), выражены слабость, шаткость походки, многократная рвота, резкие «качели» АД и ЧСС, есть подозрение на предделирий или делирий, тяжёлая соматика или пожилой возраст — врач честно рекомендует стационар. В отделении пациент получает круглосуточный мониторинг, возможность оперативно корректировать лечение, защищённую среду без доступа к алкоголю и посторонних стимулов, поддержку медперсонала в любое время суток. Такой дифференцированный подход экономит силы, деньги и главное — снижает риск критических осложнений, которые часто возникают именно после «домашних экспериментов».
Получить больше информации – vyvod-iz-zapoya-klinika
Инфузионные растворы подбираются строго индивидуально, после осмотра врача и анализа показателей пациента. При необходимости курс повторяется с изменением состава раствора для достижения максимального эффекта.
Углубиться в тему – наркологическая клиника клиника помощь в новокузнецке
Процесс включает следующие шаги:
Ознакомиться с деталями – наркологическая клиника цены красноярск
Продолжительность процедуры — от 40 минут до полутора часов. Уже в первые часы после начала терапии состояние пациента значительно улучшается: проходит тошнота, снижается тревожность, восстанавливается координация движений.
Исследовать вопрос подробнее – http://vyvod-iz-zapoya-v-tolyatti17.ru/vyvod-iz-zapoya-na-domu-tolyatti-otzyvy/
Каждое направление встроено в общую стратегию: не просто купировать симптомы, а уменьшить риск повторения сценария, когда после «облегчения» всё возвращается к прежней модели употребления.
Подробнее тут – заказать звонок наркологическая клиника
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Разобраться лучше – https://narcologicheskaya-klinika-v-krasnoyarske17.ru
Way cool! Some very valid points! I appreciate you writing this article and
also the rest of the site is really good.
Прежде чем перейти к ориентировочным цифрам, важно подчеркнуть: цена формируется из реальных компонентов помощи — работы врача и медсестры, объёма инфузионной терапии, перечня препаратов, времени выезда и необходимости более длительного наблюдения. Никаких скрытых доплат: все дополнительные назначения согласуются заранее. Чем раньше вы обращаетесь, тем меньше объём вмешательств и, как правило, ниже итоговая стоимость — короткий эпизод проще и дешевле стабилизировать, чем «выводить» осложнения после затянутого запоя.
Получить больше информации – сколько стоит вызвать нарколога на дом
Острый эпизод запоя — это не «плохое самочувствие», а состояние с реальными рисками для сердца, нервной системы и дыхания, особенно в ночные часы, когда усиливаются вегетативные реакции и тревога. В «НоваТрезвие» мы выстраиваем помощь так, чтобы от звонка до заметного облегчения прошло как можно меньше времени и как можно меньше случайностей: короткое интервью для оценки рисков, выезд врача или приём в клинике, экспресс-диагностика по ключевым показателям, персональная инфузионная схема без «универсальных коктейлей», мягкая коррекция сна и тревоги без «вырубания», понятные инструкции семье на 24–72 часа и план продолжения на ближайшие недели. Мы не скрываемся за общими формулами: решения принимаются по фактическим данным, дозы и темп капельниц подстраиваются к динамике каждые 15–20 минут, а при «красных флагах» перевод в стационар организуется без пауз. Конфиденциальность соблюдается строго, а коммуникация простая и предсказуемая — чтобы вы всегда знали, что происходит сейчас и чего ждать к утру.
Подробнее можно узнать тут – https://vyvod-iz-zapoya-ehlektrostal2-10.ru/vyvod-iz-zapoya-stacionar-v-ehlektrostali
Запой — это не просто несколько лишних дней алкоголя, а тяжёлое состояние, в котором организм работает на пределе. Чем дольше длится эпизод, тем глубже обезвоживание, тем сильнее сдвиги электролитов, тем выше риск аритмий, гипертонических кризов, судорог, делирия, обострений заболеваний сердца, печени и поджелудочной железы. Попытки «вывести» человека дома силами родных часто включают опасные комбинации: случайные седативные, снотворные, анальгетики, «антипохмельные» из рекламы. Они могут на время усыпить или «успокоить», но при этом скрывают ухудшение, сбивают давление, угнетают дыхание и мешают врачу увидеть реальную картину. В «Трезвый Центр Коломна» подход другой: ещё на этапе звонка специалист уточняет длительность запоя, объёмы и виды алкоголя, наличие гипертонии, ИБС, диабета, заболеваний печени и почек, неврологических проблем, список уже принятых препаратов, эпизоды потери сознания, судорог, странного поведения. На основании этих данных определяется, безопасен ли формат на дому или сразу нужен стационар. Такая сортировка позволяет вовремя перехватить опасные случаи, не терять часы на бесполезные попытки и сразу запускать те схемы, которые реально снижают риски и стабилизируют состояние.
Подробнее тут – https://vyvod-iz-zapoya-kolomna10.ru
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Получить дополнительные сведения – вывод из запоя вызов на дом рязань
Перед цифрами — важная оговорка: это ориентиры, не публичная оферта. Итог зависит от длительности эпизода, объёма инфузий, перечня препаратов, времени суток и необходимости расширенного наблюдения или перевода в отделение. Мы заранее проговариваем, что входит в базу, что является расширением, и согласуем любые изменения до выполнения — так смета остаётся управляемой, а семья может планировать бюджет спокойно. Ниже — типовые пакеты «Трезвой Линии» для Электростали с понятным наполнением.
Узнать больше – http://vyvod-iz-zapoya-ehlektrostal10.ru/
Amazing many of amazing info.
Выбор формата — это не вкусовщина, а баланс безопасности в конкретной клинической картине. Дом уместен, если контакт сохранён, рвота эпизодическая, давление и пульс без резких «качелей», тремор контролируемый, в квартире можно обеспечить тишину и присутствие взрослого, готового наблюдать первые 6–8 часов. Тогда выездная бригада работает на месте и выстраивает «мягкий» маршрут, где сон собирается без агрессивной седации, а инфузии идут с шаговой корректировкой темпа. Стационар предпочтителен при длительном эпизоде (3–5 суток и более), неукротимой рвоте, выраженной слабости, шаткости походки, признаках предделирия/делирия, судорожной готовности, а также у пожилых пациентов и при сочетанных диагнозах — ИБС, гипертония, диабет, хронические болезни печени/почек, неврология. Преимущество отделения — приборный мониторинг, лабораторные опции по показаниям, ночная команда и среда, где исключены лишние раздражители: это снижает «цену ошибки» и делает результат устойчивым, а не разовым «прояснением».
Изучить вопрос глубже – vyvod-iz-zapoya-deshevo
Каждый вызов нарколога на дом проходит по строгому алгоритму. Врачи клиники «ВоронМед Профи» используют индивидуальный подход, адаптируя лечение под конкретного пациента. В таблице приведена типовая схема работы выездной бригады, которая помогает понять, как проходит процесс помощи от начала до конца.
Получить больше информации – нарколог на дом вывод
Услуга
Выяснить больше – вызвать врача нарколога на дом
Ниже — примерная структура пакетов, которую можно использовать как ориентир (не публичная оферта):
Подробнее – https://narkolog-na-dom-shchelkovo10.ru/vrach-narkolog-na-dom-shchelkovo
Все растворы проходят фармацевтический контроль, а процедуры выполняются одноразовыми стерильными инструментами. После завершения капельницы врач наблюдает пациента в течение 15–30 минут, оценивает результат и даёт рекомендации по дальнейшему восстановлению. Важно не прерывать терапию самостоятельно — эффект закрепляется только при соблюдении рекомендаций.
Выяснить больше – платный нарколог на дом в воронеже
I have read so many posts concerning the blogger lovers however this article is in fact a nice article, keep it up.
Клиника «Трезвый Шаг Раменское» выстраивает помощь так, чтобы пациент и его близкие не метались между разными службами и частными «специалистами», а получали комплекс услуг в одном месте. Это особенно важно для тех, кто уже сталкивался с провалами после разовых кодировок, неподходящих капельниц или формальной «помощи».
Разобраться лучше – narkologicheskaya-klinika-v-ramenskom
Своевременная постановка капельницы помогает избежать тяжёлых последствий запоя. Поводом для обращения к врачу являются симптомы выраженной интоксикации:
Разобраться лучше – врач на дом капельница от запоя
Wonderful blog you have here but I was wanting to know if
you knew of any community forums that cover the same topics discussed here?
I’d really love to be a part of online community where I
can get feed-back from other knowledgeable individuals that share
the same interest. If you have any suggestions, please let
me know. Thank you!
Клиника использует многоступенчатый подход, который позволяет адаптировать лечение под особенности организма пациента. Наблюдение продолжается даже после завершения детоксикации, чтобы убедиться, что состояние стабильно и не требуется дополнительное вмешательство. При необходимости врач назначает курс поддержки печени, витаминов и препаратов для восстановления сна и психоэмоционального равновесия.
Углубиться в тему – вывод из запоя круглосуточно в волгограде
Процедура начинается с обследования пациента: врач измеряет давление, частоту пульса, оценивает степень интоксикации и состояние внутренних органов. После этого подбирается состав капельницы, направленный на очищение организма и восстановление функций печени, почек и нервной системы. Все препараты вводятся внутривенно, что обеспечивает быстрый эффект и минимизирует нагрузку на желудочно-кишечный тракт.
Получить дополнительные сведения – вывод из запоя в стационаре в тюмени
Ниже приведена таблица с типовыми компонентами капельницы и их назначением:
Исследовать вопрос подробнее – https://kapelnicza-ot-zapoya-v-volgograde17.ru/kapelnicza-ot-pokhmelya-volgograd/
Наркологическая помощь в «ВолгаМед Тольятти» включает широкий спектр процедур и методик. Каждый случай рассматривается индивидуально, с учётом состояния пациента, стадии заболевания и сопутствующих факторов. Ниже представлена таблица с основными направлениями медицинской работы.
Детальнее – экстренная наркологическая помощь в тольятти
Mangelsen
7916 Girard Avenue, ᒪa Joya
ⅭA 92037, United Stɑtes
1 800-228-9686
amazing protecting grizzly bears wildlife
Hi to every one, the contents existing at this web site are truly amazing for people
knowledge, well, keep up the nice work fellows.
I’m not sure why but this weblog is loading incredibly slow for me.
Is anyone else having this problem or is it a issue on my end?
I’ll check back later on and see if the problem still exists.
Комплексная терапия включает несколько последовательных этапов, обеспечивающих полное восстановление организма и личности пациента. Каждый из них направлен на решение конкретных задач — от устранения интоксикации до закрепления устойчивой ремиссии.
Изучить вопрос глубже – http://narkologicheskaya-klinika-v-volgograde17.ru/
Каждое направление встроено в общую стратегию: не просто купировать симптомы, а уменьшить риск повторения сценария, когда после «облегчения» всё возвращается к прежней модели употребления.
Узнать больше – narkologicheskaya-klinika
Îmi place site-ul Verde Casino, este foarte clar.
https://forum.568play.vn/proxy.php?link=https://verde-casino-romania-sport.ro/aplicatie-mobila
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Узнать больше – нарколог на дом вывод из запоя в красноярске
Каждое направление встроено в общую стратегию: не просто купировать симптомы, а уменьшить риск повторения сценария, когда после «облегчения» всё возвращается к прежней модели употребления.
Изучить вопрос глубже – https://narkologicheskaya-klinika-kolomna2-10.ru/luchshie-narkologicheskie-kliniki-v-kolomne
Having read this I thought it was really enlightening.
I appreciate you finding the time and effort to put this article together.
I once again find myself personally spending a lot of time both reading and
posting comments. But so what, it was still worthwhile!
My web-site: appliance repair Kenmore
Клиника «КузбассМед Центр» в Новокузнецке обеспечивает непрерывный приём пациентов и выезд нарколога на дом. Такой формат позволяет оказать экстренную помощь при интоксикации или запое прямо на месте, не дожидаясь ухудшения состояния. Медицинская команда работает в режиме 24/7, что особенно важно при острых состояниях. Врач выезжает в течение часа после вызова, проводит диагностику, ставит капельницу и контролирует жизненные показатели. В стационаре доступны детоксикация, медикаментозная терапия и психотерапевтическая поддержка — всё под постоянным медицинским наблюдением.
Подробнее тут – наркологические клиники алкоголизм в новокузнецке
Каждое назначение объясняется пациенту и близким простым языком. Здесь не практикуют подход «делаем, как знаем, вам всё равно не понять» — прозрачность и понятные шаги помогают снизить тревогу и укрепляют доверие к клинике.
Выяснить больше – вывод из запоя капельница на дому
Клиника «КузбассМед Центр» в Новокузнецке обеспечивает непрерывный приём пациентов и выезд нарколога на дом. Такой формат позволяет оказать экстренную помощь при интоксикации или запое прямо на месте, не дожидаясь ухудшения состояния. Медицинская команда работает в режиме 24/7, что особенно важно при острых состояниях. Врач выезжает в течение часа после вызова, проводит диагностику, ставит капельницу и контролирует жизненные показатели. В стационаре доступны детоксикация, медикаментозная терапия и психотерапевтическая поддержка — всё под постоянным медицинским наблюдением.
Детальнее – наркологическая клиника новокузнецк
Usually I don’t read article on blogs, however I wish to say that this write-up very pressured
me to take a look at and do it! Your writing style has been amazed me.
Thanks, quite great post.
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Исследовать вопрос подробнее – анонимный вывод из запоя
Mangelsen
7916 Girard Avenue, ᒪa Joya
CA 92037, United Ⴝtates
1 800-228-9686
discover grand teton wildlife viewing wildlife (https://k0xn3.mssg.me/)
Ниже — примерная структура пакетов, которую можно использовать как ориентир (не публичная оферта):
Подробнее тут – https://narkolog-na-dom-shchelkovo10.ru/vrach-narkolog-na-dom-shchelkovo/
more information jaxx wallet
헐벗기다 예수수난성지주일 화엄사대웅전 야전침대 【속담】 랄랑드 【속담】 자유의지론 보리곱삶이 입본 https://yak-jiu.com/ – 클리어런스 층침대 유객고리 이화피 의심 막나이 거좌 당김세기 와셔 력암
Amazing! Your site has quite a few comment posts. How did you get all of these bloggers to look at your site I’m envious! I’m still studying all about posting articles on the net. I’m going to view pages on your website to get a better understanding how to attract more people. Thank you!
Первым шагом на пути к выздоровлению является очищение организма от токсинов. В клинике проводится детоксикация с использованием современных препаратов, направленных на выведение продуктов распада алкоголя и наркотиков. Медикаментозное лечение дополняется витаминами, гепатопротекторами и средствами для нормализации работы нервной системы. Это помогает восстановить обмен веществ, улучшить сон, аппетит и общее самочувствие пациента.
Детальнее – наркологическая клиника цены воронеж
Cycle Tracking characteristic. Galaxy Watch5 and Galaxy Watch5 Pro customers can now conveniently get even deeper insights to manage their menstrual cycles and total well being. Korea, the US and 30 European markets together with the UK. “Samsung’s holistic view of wellness has been further superior by our sensor improvements, delivering in-depth health insights that empower users,” stated Hon Pak, Vice President and Head of Digital Health Team, MX Business at Samsung Electronics. As people search for tactics to forecast their subsequent interval, they’re turning to temperature readings to help, since basal physique temperature (BBT) varies by menstrual section. BBT needs to be measured immediately after waking and prior to any bodily exercise or impression from surroundings. Getting accurate BBT readings requires measurement the first thing every morning, a course of that can be inconvenient and sometimes even forgotten. Samsung’s new characteristic automates this course of, making it simpler and extra convenient. The Cycle Tracking feature is powered by Natural Cycles.
Here is my site; https://board-en.drakensang.com/proxy.php?link=https://asteroidsathome.net/boinc/view_profile.php?userid=1094371
Вывод из запоя — это не просто медицинская процедура, а тщательно выстроенный процесс, направленный на восстановление работы всех систем организма. При неправильном или неполном лечении риск осложнений возрастает в несколько раз. Поэтому обращение в профессиональную клинику становится необходимым шагом. В наркологической клинике «Центр Трезвости ВоронМед» пациент получает экстренную помощь, безопасные инфузионные препараты, круглосуточный выезд нарколога и последующее восстановление под наблюдением специалистов. Здесь каждая капельница подбирается индивидуально — с учётом возраста, веса, длительности запоя, хронических болезней и реакции организма на препараты.
Подробнее – нарколог вывод из запоя воронеж
Heya i’m for the first time here. I came across this board
and I to find It really useful & it helped me out a lot.
I am hoping to offer one thing again and help
others such as you aided me.
Hmm it looks like your blog ate my first comment (it was
super long) so I guess I’ll just sum it up what I wrote and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog writer but I’m still new to everything.
Do you have any tips and hints for newbie blog writers?
I’d definitely appreciate it.
Вывод из запоя в Тюмени — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормального функционирования организма. Длительное употребление спиртных напитков приводит к нарушению обмена веществ, обезвоживанию, сбоям в работе печени и сердца. В таких случаях требуется профессиональная помощь врача-нарколога, который подберёт оптимальный способ дезинтоксикации и медикаментозной поддержки. Современные методики позволяют провести вывод из запоя безопасно, эффективно и без осложнений.
Узнать больше – http://vyvod-iz-zapoya-v-tyumeni17.ru/vyvod-iz-zapoya-v-staczionare-tyumen/https://vyvod-iz-zapoya-v-tyumeni17.ru
Usually I do not read article on blogs, however I wish to say that this write-up very pressured me
to try and do so! Your writing style has been amazed
me. Thank you, quite nice article.
Also visit my web page :: appliance repair bellevue wa
Важное отличие клиники — отказ от примитивной схемы «капельница — домой — дальше сам». Такой формат даёт кратковременное облегчение, но не решает ни причин, ни структуры зависимости. «КоломнаМед Центр» выстраивает ступенчатый подход. Первый шаг — безопасная детоксикация: снятие абстиненции, коррекция водно-электролитного баланса, поддержка сердечно-сосудистой системы, печени, нервной системы, нормализация сна. Второй шаг — стабилизация: оценка психического состояния, выявление тревожных, депрессивных и панических симптомов, подбор поддерживающих схем, которые помогают не сорваться сразу после выхода из острых проявлений. Третий шаг — реабилитация и мотивация: психотерапевтическая работа, групповые и индивидуальные форматы, обучение навыкам трезвой жизни, работа с триггерами, укрепление внутренней мотивации. Четвёртый шаг — постреабилитационная поддержка: контрольные приёмы, дистанционные консультации, помощь в профилактике срывов. Такой комплексный путь не ломает пациента, а возвращает ему контроль: не через страх, а через понимание, структуру и реальные инструменты.
Подробнее – http://narkologicheskaya-klinika-kolomna10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
Ниже — ключевые направления, которые логично дополняют друг друга и формируют единый маршрут лечения:
Получить больше информации – http://narkologicheskaya-klinika-ramenskoe10.ru/chastnaya-narkologicheskaya-klinika-v-ramenskom/
Такой состав обеспечивает быстрое снятие симптомов интоксикации и восстановление функций организма после запоя.
Получить больше информации – врач на дом капельница от запоя
Чтобы родственники не терялись в терминах и не воспринимали лечение как «чёрный ящик», в клинике используется поэтапный подход. Это помогает увидеть логическую связку между затратами, процедурами и результатами.
Получить дополнительные сведения – наркологическая клиника в раменском
I used to be able to find good information from your content.
Here is my webpage – appliance repair Kenmore
Wow, this paragraph is nice, my younger sister is
analyzing such things, thus I am going to tell her.
Процесс кодирования проходит в комфортной и спокойной обстановке. Врач объясняет каждый этап, чтобы пациент чувствовал себя уверенно и спокойно. После процедуры пациент получает памятку с рекомендациями по уходу за здоровьем и режиму поведения в первые недели после лечения.
Разобраться лучше – http://kodirovanie-ot-alkogolizma-v-volgograde17.ru
Клиника предлагает возможность круглосуточного пребывания в комфортных палатах. Пациенты получают надёжное медицинское наблюдение, сбалансированное питание и постоянную связь с врачами. Каждый случай рассматривается персонально — от подбора препаратов до построения программы психологической коррекции. Такой подход позволяет не просто снять симптомы, а достичь стойкой ремиссии.
Получить больше информации – https://narkologicheskaya-clinika-v-ryazani17.ru/narkologicheskij-staczionar-ryazan
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Углубиться в тему – narkologicheskaya-pomoshh-v-tolyatti17.ru/
Одним из ключевых направлений работы клиники является проведение инфузионных процедур. Капельницы позволяют вывести токсины, нормализовать давление и улучшить общее состояние пациента. Подбор препаратов проводится индивидуально, с учётом физического состояния, возраста и стадии зависимости.
Подробнее тут – https://narkologicheskaya-pomoshh-v-tolyatti17.ru/narkologicheskaya-bolnicza-tolyatti/
I know this website gives quality dependent
content and other data, is there any other site which gives these stuff in quality?
здесь https://kinogo.blue/filmy/1235-igra.html
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Изучить вопрос глубже – врач вывод из запоя
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Подробнее – http://vyvod-iz-zapoya-v-novokuzneczke17.ru/vyvod-iz-zapoya-na-domu-novokuzneczk/
Hi there! I simply would like to give you a big thumbs up
for the excellent information you have right here on this
post. I’ll be returning to your website for more soon.
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Ознакомиться с деталями – врач вывод из запоя красноярск
В Волгограде сформирована система оказания наркологической помощи, включающая круглосуточные выезды специалистов, амбулаторное лечение, стационарные программы и реабилитацию. Такой подход позволяет охватить все категории пациентов — от тех, кто нуждается в экстренной помощи, до тех, кто готов пройти полный курс терапии. Независимо от формы оказания услуг, лечение проводится конфиденциально и в соответствии с медицинскими стандартами.
Детальнее – платная наркологическая скорая помощь
Ключевой элемент вывода из запоя в Реутове — правильно подобранная капельница, но в «РеутовМед Сервис» её рассматривают не как волшебное средство, а как часть комплексной терапевтической схемы. Основная цель — не «вырубить» человека сильными седативными коктейлями, а помочь организму безопасно выйти из состояния интоксикации. В инфузионную терапию входят растворы для регидратации, которые восполняют потерю жидкости, снижают вязкость крови, улучшают микроциркуляцию и работу внутренних органов. Коррекция электролитного баланса помогает уменьшить дрожь, мышечную слабость, снизить риск нарушений сердечного ритма. Применяются витамины группы B и препараты магния для поддержки нервной системы, снижения раздражительности и вероятности судорог. По показаниям добавляются гепатопротекторы, мягкие антиоксиданты для разгрузки печени, противорвотные средства при выраженной тошноте, щадящие анксиолитики для снижения тревоги и нормализации сна без грубого угнетения сознания. Все дозировки учитывают сопутствующие заболевания и возраст, что особенно важно для пациентов с гипертонией, ИБС, диабетом, поражением печени и пожилых людей. Эффект оценивается по объективным критериям: стабилизация давления и пульса, уменьшение дрожи, улучшение самочувствия, нормализация сна и поведения, а не только по фразе «стал тихим».
Получить дополнительные сведения – vyvod-iz-zapoya-kruglosutochno
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Получить дополнительные сведения – врач вывод из запоя волгоград
I take pleasure in, result in I discovered exactly what I was
looking for. You have ended my four day long hunt! God Bless you man. Have a nice
day. Bye
Hi! Do you use Twitter? I’d like to follow you if that would be ok.
I’m undoubtedly enjoying your blog and look forward to new
posts.
Hey! This is my 1st comment here so I just wanted
to give a quick shout out and tell you I truly enjoy reading your
articles. Can you recommend any other blogs/websites/forums
that cover the same subjects? Thank you so
much!
Детоксикация в клинике «Центр Трезвости ВоронМед» проводится по принципу минимального вмешательства при максимальной эффективности. Основная задача — очистить кровь от токсинов и стабилизировать внутреннюю среду организма без нагрузки на сердце и почки. Все препараты вводятся медленно, под контролем медицинского персонала, а состав подбирается индивидуально после оценки анализов и состояния пациента.
Исследовать вопрос подробнее – вывод из запоя на дому круглосуточно воронеж
Для тех, кто предпочитает лечение в условиях стационара, предусмотрены комфортные палаты, медицинский контроль 24/7 и возможность консультаций с психотерапевтом. Врачи клиники применяют комплексные методы, направленные не только на снятие симптомов, но и на устранение причин зависимости.
Подробнее тут – http://narkologicheskaya-pomoshh-v-tolyatti17.ru/narkologiya-goroda-tolyatti/
В Воронеже клиника «Центр Трезвости ВоронМед» обеспечивает выезд нарколога на дом в любое время суток. Это позволяет оказывать помощь пациентам, которые находятся в тяжёлом состоянии или не могут самостоятельно приехать в стационар. Медицинская бригада прибывает в течение 40–60 минут, не используя специализированный транспорт и форму, чтобы сохранить анонимность. Врач проводит первичный осмотр, оценивает давление, частоту дыхания, уровень сознания и насыщение кислородом, после чего назначает детоксикационную капельницу с контролем дозировки.
Углубиться в тему – срочный вывод из запоя воронеж
Основу лечения составляет междисциплинарная команда: врач-нарколог, психиатр, психолог, медсестра и консультант по зависимому поведению. Каждый отвечает за свой участок работы, но общая цель едина — помочь пациенту безопасно пройти путь от детокса до устойчивого состояния. Благодаря единому плану и регулярным консилиумам врачей, исключаются противоречия и дублирование процедур. Это экономит ресурсы организма и делает процесс прогнозируемым.
Исследовать вопрос подробнее – запой наркологическая клиника красноярск
Практический тест прост: сохранённый контакт, контролируемый тремор, эпизодическая (не неукротимая) рвота, нет грубой дезориентации, давление и пульс не «скачут», в квартире можно обеспечить тишину и доступ к воде — тогда дом уместен. Если хотя бы два пункта «провисают», отделение в Электростали даст предсказуемость и защиту от ночных ухудшений, которые дома часто остаются незамеченными.
Подробнее тут – vyvod-iz-zapoya-kruglosutochno
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Подробнее можно узнать тут – наркология вывод из запоя красноярск
Острый период запоя — это не «плохое самочувствие», а состояние с реальными рисками, где каждая задержка усложняет картину. В «Трезвой Линии» в Электростали мы строим помощь так, чтобы от первого звонка до заметного облегчения прошёл минимальный и управляемый путь: быстрый сбор рисков, экспресс-диагностика на месте, персональная инфузионная схема без «универсальных коктейлей», щадящая коррекция сна и тревоги, регулярные замеры показателей, чёткие рекомендации для семьи. Мы избегаем агрессивной седации: дозы и темп капельниц подбираются под возраст, длительность эпизода, сопутствующие заболевания и уже принимаемые лекарства. Задача — быстро снять токсическую нагрузку, выровнять давление и пульс, собрать ночной сон, а затем удержать результат дисциплинированным постдетокс-маршрутом на 2–4 недели. Конфиденциальность и анонимность соблюдаются без компромиссов, решения принимаются по реальным данным, чтобы эффект был устойчивым, предсказуемым и безопасным для пациента и семьи.
Подробнее можно узнать тут – http://vyvod-iz-zapoya-ehlektrostal10.ru/vyvesti-iz-zapoya-ehlektrostal/
Капельница при интоксикации помогает быстро очистить организм от продуктов распада алкоголя, восстановить водно-солевой баланс и улучшить самочувствие. В состав раствора входят препараты, нормализующие обмен веществ и поддерживающие работу печени и сердечно-сосудистой системы. Уже через 20–30 минут после начала инфузии пациент ощущает значительное облегчение. Подбор лекарственных средств осуществляется строго индивидуально, с учётом возраста, массы тела и общего состояния здоровья.
Получить дополнительную информацию – нарколог на дом вывод
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Исследовать вопрос подробнее – http://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkolog-v-gorode-novokuzneczke/
Для тех, кто предпочитает лечение в условиях стационара, предусмотрены комфортные палаты, медицинский контроль 24/7 и возможность консультаций с психотерапевтом. Врачи клиники применяют комплексные методы, направленные не только на снятие симптомов, но и на устранение причин зависимости.
Получить дополнительную информацию – наркологическая психиатрическая помощь в тольятти
Attractive section of content. I just stumbled upon your site and in accession capital to assert
that I acquire actually enjoyed account your blog posts.
Anyway I’ll be subscribing to your feeds and even I achievement you access consistently fast.
Для удобства восприятия можно ориентироваться на следующую структуру (это не публичная оферта, а примерная модель ценообразования — точная сумма фиксируется после осмотра и согласования схемы):
Подробнее – вызвать нарколога на дом серпухов
Конфиденциальность — это набор конкретных действий, а не декларация на сайте. Мы проектируем «невидимость» так, чтобы пациент мог спокойно принять помощь и не опасаться огласки.
Подробнее тут – наркологические клиники алкоголизм
Asking questions are in fact nice thing if you are not understanding
anything entirely, however this piece of writing provides pleasant
understanding yet.
Этот информативный текст выделяется своими захватывающими аспектами, которые делают сложные темы доступными и понятными. Мы стремимся предложить читателям глубину знаний вместе с разнообразием интересных фактов. Откройте новые горизонты и развивайте свои способности познавать мир!
Личный опыт — читайте сами – https://gttpl.co.in/3572-2
Такой подход обеспечивает результативность и помогает добиться длительной ремиссии даже при тяжёлых формах зависимости.
Исследовать вопрос подробнее – https://narkologicheskaya-clinica-v-voronezhe17.ru
Запой представляет собой состояние, при котором организм находится под постоянным воздействием этанола. Это вызывает интоксикацию, нарушение обменных процессов и дестабилизацию психики. При обращении за помощью врач-нарколог оценивает состояние пациента и подбирает индивидуальную схему терапии, чтобы безопасно вывести человека из запоя и предотвратить развитие синдрома отмены. Вмешательство проводится как в стационаре, так и на дому, в зависимости от состояния пациента.
Изучить вопрос глубже – http://vyvod-iz-zapoya-v-krasnoyarske17.ru
посмотреть в этом разделе https://bonus-betting.ru/brillx-casino-promocode/
Процесс вывода из запоя включает последовательное воздействие на ключевые звенья интоксикации. Ниже представлена таблица, отражающая этапы лечения, используемые методики и ожидаемые результаты терапии.
Углубиться в тему – анонимный вывод из запоя
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Получить полную информацию – https://evakienholz.de/text-beispiel-02
Для жителей Красноярска организованы два конфиденциальных пути. Первый — немаркированный выезд бригады на дом с заранее согласованными порогами связи. Второй — «тихий вход» в клинику через отдельную дверь, где приём проходит без очередей и «коридорных» разговоров. На первичном звонке администратор уточняет только клинически значимые факторы: частоту рвоты, наличие мочеиспускания, ЧСС/АД в покое, эпизоды спутанности, актуальные лекарства и аллергии. Биографические подробности и лишние вопросы не задаются — мы придерживаемся принципа минимально необходимой информации.
Исследовать вопрос подробнее – наркологическая клиника цены в красноярске
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Изучить вопрос глубже – https://vyvod-iz-zapoya-v-voronezhe17.ru/vyvod-iz-zapoya-za-den-voronezh/
This information is invaluable. Where can I find out more?
Конфиденциальность — это набор конкретных действий, а не декларация на сайте. Мы проектируем «невидимость» так, чтобы пациент мог спокойно принять помощь и не опасаться огласки.
Исследовать вопрос подробнее – лечение в наркологической клинике красноярск
천안출장마사지는 고객이 원하는 시간과 장소에 전문 테라피스트가 직접 방문하여 체계적인 마사지 프로그램을 진행하는 출장형 전문 테라피 서비스입니다.
Наркологическая клиника в Воронеже — это специализированное медицинское учреждение, предоставляющее помощь людям, столкнувшимся с зависимостью от алкоголя, наркотиков и других психоактивных веществ. Лечение проводится под контролем квалифицированных врачей, с использованием современных методик детоксикации, психотерапии и реабилитации. Цель работы специалистов — не только устранить физическую зависимость, но и помочь пациенту восстановить эмоциональное равновесие, вернуть контроль над поведением и мотивацию к трезвости.
Ознакомиться с деталями – https://narkologicheskaya-clinica-v-voronezhe17.ru/chastnaya-narkologicheskaya-klinika-voronezh/
Детоксикация — это первый и важнейший этап лечения в наркологической клинике в Красноярске. Она проводится с целью выведения токсинов из организма и восстановления функций жизненно важных органов. Для этого применяются инфузионные растворы, гепатопротекторы, витамины и препараты, нормализующие обмен веществ. После снятия интоксикации пациент получает медикаментозную поддержку, направленную на снижение тяги к алкоголю или наркотикам и стабилизацию эмоционального состояния.
Разобраться лучше – наркологическая клиника нарколог в красноярске
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Детальнее – https://plustech.co.in/bajaj-auto-ltd-ptaced-line-at-akurdi-pune-for-ev
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Заходи — там интересно – https://www.powertvnews.in/2023/05/26/expo-under-the-sponsorship-of-power-tv-from-to-day
Во время лечения фиксируются все жизненные показатели пациента. При необходимости проводится экспресс-анализ крови и ЭКГ. Ниже представлена таблица, показывающая, какие параметры контролируются и по каким признакам оценивается стабилизация состояния.
Узнать больше – https://vyvod-iz-zapoya-v-voronezhe17.ru/vyvod-iz-zapoya-na-domu-voronezh/
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Узнать больше – https://www.nestelintulahti.fi/?p=440
Эта статья сочетает познавательный и занимательный контент, что делает ее идеальной для любителей глубоких исследований. Мы рассмотрим увлекательные аспекты различных тем и предоставим вам новые знания, которые могут оказаться полезными в будущем.
Раскрыть тему полностью – https://www.powertvnews.in/2025/06/07/kiccha-sudeep-releases-trailer-of-movie-edagaiye-apaghatakke-karana
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Подробности по ссылке – https://www.alfassinaro.it/public/wp/?page_id=65
Эта статья сочетает познавательный и занимательный контент, что делает ее идеальной для любителей глубоких исследований. Мы рассмотрим увлекательные аспекты различных тем и предоставим вам новые знания, которые могут оказаться полезными в будущем.
Ознакомиться с теоретической базой – https://foxy1069.com/2025/09/sevyn-streeter-releases-new-song-assumptions
Эта статья погружает вас в увлекательный мир знаний, где каждый факт становится открытием. Мы расскажем о ключевых исторических поворотных моментах и научных прорывах, которые изменили ход цивилизации. Поймите, как прошлое формирует настоящее и как его уроки могут помочь нам строить будущее.
Получить дополнительную информацию – https://meghapatel.in/2024/04/16/find-a-website-designer
You can definitely see your skills in the work you write.
The arena hopes for even more passionate writers such as you who aren’t afraid to mention how
they believe. Always follow your heart.
Concert Attire Stamford
360 Fairfield Ave,
Stamford, CT 06902, United Ѕtates
+12033298603
Bookmarks
It’s a shame you don’t have a donate button! I’d certainly donate
to this fantastic blog! I guess for now i’ll settle for
bookmarking and adding your RSS feed to my Google account.
I look forward to fresh updates and will share this website with my Facebook group.
Talk soon!
일본의 유흥 문화는 다양성과 독특함으로 유명합니다.
퇴근 후 동료들과 가볍게 술을 즐기는
이자카야부터 화려한 나이트클럽, 테마
카페까지 일본유흥은 폭넓은 스펙트럼
hop over to these guys jaxx app
I read this piece of writing fully regarding the resemblance of latest and previous technologies,
it’s awesome article.
I’ve read some excellent stuff here. Certainly value bookmarking for revisiting.
I surprise how so much attempt you set to make one of these magnificent informative site.
Запой, интоксикация? Вызовите нарколога на дом в Иркутске для быстрой и анонимной помощи. На дому: осмотр, подбор лечения, капельница для вывода токсинов и улучшение самочувствия. «ТрезвоМед» – круглосуточная наркологическая помощь на дому с гарантией анонимности. Не справляетесь с зависимостью сами? Вызовите нарколога на дом. Васильев подчеркивает: «Оперативная помощь – ключ к выздоровлению при отравлении алкоголем».
Исследовать вопрос подробнее – нарколог в иркутске
A wholly agreeable point of view, I think primarily based on my own experience with this that your points are well made, and your analysis on target.
I’m not sure exactly why but this blog is loading
incredibly slow for me. Is anyone else having this issue or is it a issue on my end?
I’ll check back later and see if the problem still exists.
Вывод из запоя на дому в Туле осуществляется по строго отлаженной схеме, которая включает несколько последовательных этапов. Такой комплексный подход позволяет не только быстро вывести токсины из организма, но и обеспечить всестороннюю поддержку пациента, включая психологическую реабилитацию.
Детальнее – http://vyvod-iz-zapoya-tula00.ru
Great web site. Plenty of helpful information here.
I’m sending it to some friends ans additionally sharing in delicious.
And certainly, thank you to your sweat!
Stop by my web blog; receh88
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Подробнее – вывод из запоя с выездом
Ключевым фактором при выборе центра становится квалификация специалистов. Лечение алкоголизма — это не только выведение из запоя и купирование абстинентного синдрома. Оно включает работу с мотивацией, тревожными состояниями, семейными конфликтами, нарушением сна и другими последствиями зависимости. Только команда, включающая наркологов, психотерапевтов и консультантов по аддиктивному поведению, способна охватить все аспекты проблемы.
Детальнее – https://lechenie-alkogolizma-murmansk0.ru/anonimnoe-lechenie-alkogolizma-marmansk/
Таблица: Основные признаки надёжного центра лечения наркомании
Подробнее – centr lecheniya narkomanii murmansk
A fascinating discussion is worth comment.
I do believe that you should publish more about this issue, it might not be a taboo subject but typically folks don’t
speak about such topics. To the next! Cheers!!
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Изучить вопрос глубже – http://www.domen.ru
These are really fantastic ideas in regarding blogging.
You have touched some fastidious points here. Any way keep
up wrinting.
Good post. I learn something totally new and challenging on sites I stumbleupon every
day. It will always be useful to read through articles from other authors and practice something
from their web sites.
Во многих случаях пациент или его родственники не решаются сразу вызвать врача. Для таких ситуаций предусмотрена услуга онлайн-консультации. Она проводится через защищённую видеосвязь, при желании — анонимно. На связи — врач-нарколог или психиатр, который отвечает на вопросы, оценивает ситуацию по визуальным и вербальным признакам, рекомендует план действий. Консультация может стать отправной точкой для дальнейшего вызова врача на дом или записи в клинику. Это особенно удобно для родственников, которые не знают, как подступиться к проблеме и убедить человека в необходимости помощи.
Углубиться в тему – наркологическая клиника клиника помощь
Зависимость от психоактивных веществ — серьёзное заболевание, затрагивающее как физическое, так и психологическое состояние человека. При отсутствии своевременной наркологической помощи в клинике возможно ухудшение здоровья, развитие тяжелых осложнений и социальная деградация пациента.
Детальнее – наркологическая помощь на дому круглосуточно в новокузнецке
Do you have any video of that? I’d care to find out more details.
Нужна срочная помощь при алкогольном отравлении или запое? Вызовите нарколога на дом в Иркутске! Квалифицированная помощь нарколога на дому: диагностика, капельница, стабилизация состояния. Круглосуточный выезд нарколога, анонимность и снижение рисков – с «ТрезвоМед». Самостоятельный отказ невозможен? Необходима наркологическая помощь. Васильев: «Не затягивайте с помощью при алкогольном отравлении!».
Получить больше информации – выезд нарколога на дом цена в иркутске
https://www.money-4-tower.ch
Клиника «АнтиАлко» предлагает экстренную медицинскую помощь на дому в Новосибирске и Новосибирской области для тех, кто столкнулся с запоем. Если вы или ваш близкий оказались в состоянии длительной алкогольной интоксикации, наши специалисты готовы оперативно приехать к вам, провести комплексную детоксикацию и купировать симптомы абстинентного синдрома. Мы гарантируем высокий уровень безопасности, полную анонимность и индивидуальный подход к каждому пациенту.
Ознакомиться с деталями – https://vyvod-iz-zapoya-novosibirsk00.ru/vyvod-iz-zapoya-czena-novosibirsk
Во многих случаях пациент или его родственники не решаются сразу вызвать врача. Для таких ситуаций предусмотрена услуга онлайн-консультации. Она проводится через защищённую видеосвязь, при желании — анонимно. На связи — врач-нарколог или психиатр, который отвечает на вопросы, оценивает ситуацию по визуальным и вербальным признакам, рекомендует план действий. Консультация может стать отправной точкой для дальнейшего вызова врача на дом или записи в клинику. Это особенно удобно для родственников, которые не знают, как подступиться к проблеме и убедить человека в необходимости помощи.
Подробнее тут – http://narkologicheskaya-pomoshh-tver0.ru
What’s up Dear, are you in fact visiting this web page on a regular
basis, if so then you will without doubt get fastidious experience.
Hello! Do you know if they make any plugins to help with
SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Appreciate it!
Hi! I just wanted to ask if you ever have any
issues with hackers? My last blog (wordpress) was hacked
and I ended up losing several weeks of hard work due to no back up.
Do you have any solutions to stop hackers?
Карта делает видимой причинно-следственную связь: пациент понимает, зачем и что именно делается; семья видит «точки проверки»; врач получает опору для изменения одного параметра без разрушения всего плана.
Подробнее тут – вывод из запоя на дому саратов
great issues altogether, you simply won a emblem new reader.
What may you suggest in regards to your
put up that you made a few days ago? Any positive?
«СамарМед» — это специализированный центр, где помощь оказывается не только при алкогольной и наркотической зависимости, но и при комбинированных расстройствах, связанных с тревожностью, депрессией, нарушениями сна и постстрессовыми состояниями. В клинике работает команда из наркологов, психиатров, психотерапевтов, реабилитологов, а также специалистов по социальной адаптации. Вся система организации лечения направлена на достижение устойчивой ремиссии с минимальным риском рецидива, а телемедицинские решения дают возможность быстро получить консультацию даже в экстренных ситуациях, не выходя из дома.
Подробнее можно узнать тут – анонимная наркологическая клиника в самаре
Выделяется ряд преимуществ, которые делают терапию в клинике оптимальным решением для борьбы с зависимостью.
Получить дополнительную информацию – лечение алкоголизма гипнозом
I think that is one of the such a lot important
information for me. And i am satisfied reading your article.
But should remark on some common things, The website
taste is great, the articles is truly great : D. Just right task, cheers
Каждое из этих направлений имеет важное значение и в совокупности формирует основу для устойчивого выздоровления.
Получить дополнительную информацию – https://narkologicheskaya-klinika-v-omske0.ru/narkolog-v-gorode-omske
«ТверьМед» — частная лицензированная клиника, специализирующаяся на наркологической помощи любой степени сложности. Здесь работают неравнодушные врачи-наркологи, психиатры, терапевты и психологи с многолетним стажем. Медицинская команда настроена на оперативную диагностику и проведение первичных мероприятий в течение первого часа после обращения. Упор сделан на доступность: клиника открыта 24/7, приём возможен как на территории медучреждения, так и на выезде — дома, в офисе, гостинице, санатории или любом удобном месте.
Узнать больше – оказание наркологической помощи
После поступления вызова наш нарколог выезжает к пациенту в кратчайшие сроки, прибывая по адресу в пределах 30–60 минут. Специалист начинает процедуру с подробного осмотра и диагностики, измеряя ключевые показатели организма: артериальное давление, частоту пульса, насыщенность кислородом и собирая подробный анамнез.
Подробнее тут – врач нарколог на дом в новосибирске
«Ижевский Центр Трезвых Решений» — это частное медицинское учреждение, где проводится лечение всех форм алкогольной и наркотической зависимости. Программы терапии разработаны на основе международных рекомендаций и включают не только медикаментозное воздействие, но и психологическую поддержку. Все процедуры проходят анонимно, без постановки на учёт, что особенно важно для пациентов, желающих сохранить конфиденциальность.
Узнать больше – наркологическая клиника нарколог в ижевске
Excellent blog here! Also your website loads up very fast!
What web host are you using? Can I get your affiliate link to your host?
I wish my web site loaded up as quickly as yours lol
Один из ключевых принципов клиники «ЗдороваяСамара» — строгое соблюдение медицинской тайны. Все обращения, анализы и процедуры происходят в режиме полной конфиденциальности. При необходимости пациент может быть зарегистрирован под псевдонимом, а договор оформляется на доверенное лицо. Персональные данные не передаются ни в какие внешние базы, а диагноз не указывается в выписке для работодателя или страховой. Врачи и администрация клиники прошли специальное обучение по работе с анонимными пациентами, чтобы гарантировать этичность и законность каждой процедуры.
Ознакомиться с деталями – лечение наркомании в самаре
Чтобы исключить суету и случайные усиления, первые часы делим на небольшие «окна»: цель — действие — маркер — критерий перехода. Если отклика нет, корректируется один элемент — темп инфузии, очередность модулей или поведенческий якорь — и назначается новая точка оценки.
Подробнее – вывод из запоя клиника
Наркологическая клиника «МедЛайн» предоставляет профессиональные услуги врача-нарколога с выездом на дом в Новосибирске и Новосибирской области. Мы оперативно помогаем пациентам справиться с тяжелыми состояниями при алкогольной и наркотической зависимости. Экстренный выезд наших специалистов доступен круглосуточно, а лечение проводится с применением проверенных методик и препаратов, что гарантирует безопасность и конфиденциальность каждому пациенту.
Изучить вопрос глубже – vrach-narkolog-na-dom novosibirsk
Каждый метод подбирается индивидуально, что обеспечивает безопасность и эффективность процесса.
Получить дополнительную информацию – срочный вывод из запоя в омске
Основой эффективного лечения является команда специалистов с подтверждённой профессиональной подготовкой. В штат учреждения должны входить врачи-наркологи, психиатры, клинические психологи, специалисты по социальной адаптации.
Изучить вопрос глубже – https://lechenie-narkomanii-murmansk0.ru/czentr-lecheniya-narkomanii-marmansk/
Клиника «АнтиАлко» предлагает экстренную медицинскую помощь на дому в Новосибирске и Новосибирской области для тех, кто столкнулся с запоем. Если вы или ваш близкий оказались в состоянии длительной алкогольной интоксикации, наши специалисты готовы оперативно приехать к вам, провести комплексную детоксикацию и купировать симптомы абстинентного синдрома. Мы гарантируем высокий уровень безопасности, полную анонимность и индивидуальный подход к каждому пациенту.
Подробнее можно узнать тут – наркологический вывод из запоя в новосибирске
Экстренный вызов нарколога на дом в Иркутске от «ТрезвоМед» при запое, интоксикации или кодировании – анонимно и удобно. Осмотр, детоксикация капельницей, индивидуальный план лечения – все это на дому! «ТрезвоМед» – круглосуточная помощь, анонимность и безопасность при отказе от алкоголя. Не можете бросить пить самостоятельно? Нужна помощь нарколога! Васильев: «Своевременная помощь при интоксикации – залог успешного выздоровления».
Выяснить больше – врач нарколог на дом платный в иркутске
Такая структура позволяет обеспечить эффективность и безопасность лечения на каждом этапе.
Получить дополнительную информацию – наркология вывод из запоя
Great post! We will be linking to this particularly great
article on our website. Keep up the great
writing.
Наркомания — это не просто пагубная привычка, а тяжёлое хроническое заболевание, которое требует комплексного лечения и индивидуального подхода. В клинике «ЗдороваяСамара» разработаны современные программы помощи зависимым, охватывающие все этапы — от выезда нарколога на дом до многомесячного амбулаторного сопровождения. Особое внимание уделяется конфиденциальности, оперативности и доступности помощи в любое время суток. Это делает лечение максимально комфортным, результативным и гуманным как для самого пациента, так и для его близких.
Узнать больше – https://lechenie-narkomanii-samara0.ru/lechenie-zavisimosti-ot-narkotikov-samara
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Изучить вопрос глубже – https://vyvod-iz-zapoya-saratov0.ru/vyvod-iz-zapoya-saratov-staczionar
Наркологическая помощь должна быть не только медицински точной, но и человечной, безопасной и анонимной. В «Ижевском Центре Трезвых Решений» выстроена система комплексного подхода к лечению зависимостей, включающая диагностику, медикаментозную детоксикацию, психотерапию и социальную адаптацию. Клиника объединяет профессионализм, заботу и круглосуточную готовность помочь пациентам, оказавшимся в трудной ситуации. Здесь работают врачи с большим опытом в области наркологии и психиатрии, способные оперативно выехать на дом и оказать неотложную помощь.
Углубиться в тему – http://narkologicheskaya-klinika-v-izhevsk18.ru
Выбор клиники — задача не только медицинская, но и стратегическая. Учитывать нужно не только наличие лицензии, но и содержание программ, их гибкость, участие родственников в процессе, а также прозрачность взаимодействия с пациентом. Именно эти аспекты позволяют отличить профессиональное учреждение от формального.
Выяснить больше – наркологическая клиника ярославль
Современные реалии требуют от медицинских учреждений гибкости, скорости и чуткости. Наркологическая помощь — одна из сфер, где промедление может стоить человеку здоровья или жизни. В наркологической клинике «ТверьМед» разработаны оперативные механизмы реагирования: выезд врача по адресу в течение 30 минут, круглосуточная поддержка и возможность получения онлайн-консультации, не покидая дом. Такой подход позволяет вовремя оказать помощь, даже если пациент отказывается ехать в стационар или не осознаёт всю серьёзность своего состояния.
Детальнее – экстренная наркологическая помощь
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get four e-mails with the same comment.
Is there any way you can remove people from that
service? Cheers!
Ən faydalı platformadır. Yenə baxacağam!
http://johnvorhees.com/gbook/go.php?url=https://pinco-azerbaijan-top.org/bonuslar
Один из ключевых принципов клиники «ЗдороваяСамара» — строгое соблюдение медицинской тайны. Все обращения, анализы и процедуры происходят в режиме полной конфиденциальности. При необходимости пациент может быть зарегистрирован под псевдонимом, а договор оформляется на доверенное лицо. Персональные данные не передаются ни в какие внешние базы, а диагноз не указывается в выписке для работодателя или страховой. Врачи и администрация клиники прошли специальное обучение по работе с анонимными пациентами, чтобы гарантировать этичность и законность каждой процедуры.
Разобраться лучше – https://lechenie-narkomanii-samara0.ru/lechenie-zavisimosti-ot-narkotikov-samara/
Наркологическая клиника — это не просто место, где пациенту оказывают медицинскую помощь. Это учреждение, где формируется стратегия полного восстановления, включающая не только физическое оздоровление, но и психоэмоциональную стабилизацию. В Ярославле работают как частные, так и государственные клиники, однако их подходы, уровень сервиса и состав команд могут существенно различаться. По данным Минздрава РФ, высокий процент успешных исходов наблюдается в тех учреждениях, где реализуется персонализированная модель лечения и постлечебной поддержки.
Получить больше информации – https://narkologicheskaya-klinika-yaroslavl0.ru/lechenie-narkomanii-i-alkogolizma-yaroslavl/
Такой календарь делает весь процесс прозрачным: пациент видит логику, близкие — прогресс, а врач — чистый сигнал для коррекции без «эскалации на всякий случай».
Детальнее – наркологическая клиника нарколог
«Ижевский Центр Трезвых Решений» — это частное медицинское учреждение, где проводится лечение всех форм алкогольной и наркотической зависимости. Программы терапии разработаны на основе международных рекомендаций и включают не только медикаментозное воздействие, но и психологическую поддержку. Все процедуры проходят анонимно, без постановки на учёт, что особенно важно для пациентов, желающих сохранить конфиденциальность.
Подробнее – платная наркологическая клиника в ижевске
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Ознакомиться с деталями – нарколог на дом анонимно
Главной задачей специалистов становится купирование абстинентного синдрома и снижение интоксикации. Это требует применения медикаментов и постоянного наблюдения за состоянием пациента.
Подробнее можно узнать тут – http://vyvod-iz-zapoya-perm0.ru/
Наркологическая клиника «ВолгаДок Медикал» — это круглосуточная служба помощи, выстроенная вокруг принципов клинической безопасности, прозрачной коммуникации и поддержки пациента на каждом этапе. Мы соединяем стационар и выездные бригады в единую систему: первичный осмотр и стабилизация состояния, адресные инфузионные модули, мягкая коррекция сна и тревоги, последующее наблюдение с короткими «окнами» обратной связи. Все решения принимаются по показаниям и сопровождаются объяснением: какую цель преследуем, каким маркером измеряем, когда проверяем результат. Такой подход исключает хаотичные усиления, бережёт ресурс организма и даёт прогнозируемый клинический эффект.
Разобраться лучше – анонимная наркологическая клиника в саратове
Даже телефонный разговор с клиникой может многое сказать о её подходе. Если вам предлагают типовое лечение без уточнения подробностей или избегают вопросов о составе команды, это тревожный сигнал. Серьёзные учреждения в Мурманске обязательно предложат предварительную консультацию, зададут уточняющие вопросы и расскажут, как строится программа помощи.
Получить больше информации – центр лечения алкоголизма мурманск.
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Получить больше информации – нарколог на дом вывод из запоя
Нужна срочная помощь при алкогольном отравлении или запое? Вызовите нарколога на дом в Иркутске! Квалифицированная помощь нарколога на дому: диагностика, капельница, стабилизация состояния. Круглосуточный выезд нарколога, анонимность и снижение рисков – с «ТрезвоМед». Самостоятельный отказ невозможен? Необходима наркологическая помощь. Васильев: «Не затягивайте с помощью при алкогольном отравлении!».
Исследовать вопрос подробнее – https://narcolog-na-dom-v-irkutske0.ru/vyzov-narkologa-na-dom-irkutsk
Многие сталкиваются с трудностями при выборе клиники или центра: предлагаемые услуги различаются по качеству, подходам, стоимости и длительности. Некоторые организации ограничиваются только медикаментозной поддержкой, не работая с глубинными причинами зависимости. Поэтому важно заранее понимать, какие параметры отличают действительно надёжное учреждение, способное обеспечить долгосрочные результаты.
Разобраться лучше – centr lecheniya narkomanii murmansk
Каждый из этих этапов играет важную роль и обеспечивает безопасность пациента на пути к восстановлению.
Углубиться в тему – вывод из запоя на дому круглосуточно омск
Программа лечения составляется индивидуально и может включать стационарный или амбулаторный формат. Основу медикаментозного этапа составляют детоксикационные процедуры, направленные на выведение остатков наркотиков из организма, восстановление функций печени, почек и нервной системы. Одновременно подключаются седативные препараты, гепатопротекторы, витамины и сорбенты. В особо тяжёлых случаях используется аппаратная поддержка: инфузоматы, электросон, лазерная терапия и другие методы.
Подробнее можно узнать тут – лечение наркомании и алкоголизма в самаре
FranChoice
7500 Flying Cloud Drive,
#600 Eden Prairie
MN 55344, United Ѕtates
952-345-8400
franchise business opportunities benefits; https://padlet.com/,
Не можете добраться до клиники? Нарколог на дом в Иркутске – оптимальный выход при запое. Нарколог на дом – это удобно: обследование, лечение и детоксикация в комфортных условиях. Выезд нарколога в любое время, анонимность и безопасность – это «ТрезвоМед». Без медицинской помощи не обойтись? Звоните наркологу! Чем быстрее помощь, тем лучше прогноз, – нарколог Игорь Васильев.
Ознакомиться с деталями – http://narcolog-na-dom-v-irkutske0.ru/vrach-narkolog-na-dom-irkutsk/
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Получить дополнительную информацию – наркологическая клиника стационар в омске
I think the admin of this web page is really working hard in support of his web site, since
here every data is quality based material. http://elviraobol.ru/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=976
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Получить больше информации – запой наркологическая клиника
It is actually a nice and useful piece of information. I’m happy that you shared this useful info with us.
Please keep us informed like this. Thank you for sharing.
Комплексный подход к выводу из запоя на дому в Ярославле включает несколько основных этапов, которые позволяют обеспечить оперативное и безопасное лечение:
Узнать больше – http://vyvod-iz-zapoya-yaroslavl0.ru
Hello! I understand this is sort of off-topic however I needed to ask.
Does operating a well-established website like yours require a massive amount work?
I’m brand new to running a blog however I do write in my journal
on a daily basis. I’d like to start a blog so I will be able to share my personal experience and views online.
Please let me know if you have any recommendations or tips for brand new aspiring bloggers.
Appreciate it!
Медицинская помощь в клинике организована поэтапно, что позволяет постепенно стабилизировать состояние и вернуть контроль над самочувствием.
Подробнее – http://vyvod-iz-zapoya-perm0.ru
Такая схема лечения делает процесс последовательным и контролируемым. Врачи клиники сопровождают пациентов на всех стадиях, помогая преодолеть как физическую, так и психологическую зависимость. Особое внимание уделяется возвращению человека к активной и стабильной жизни без употребления алкоголя или наркотиков.
Разобраться лучше – частная наркологическая клиника в ижевске
Первый шаг в лечении — это тщательный осмотр специалиста. Наряду с измерением жизненно важных показателей (пульс, артериальное давление, температура) врач проводит сбор анамнеза, выясняя длительность запоя, тип употребляемого алкоголя и наличие сопутствующих заболеваний. Эти данные помогают оценить степень интоксикации и подобрать индивидуальный план терапии, что является ключевым для дальнейшей эффективной детоксикации.
Выяснить больше – нарколог вывод из запоя ярославль
Такая структура лечения помогает пациентам пройти все этапы восстановления под контролем специалистов.
Разобраться лучше – наркологическая клиника цены
В клинике «СамарМед» доступно несколько форм лечения: стационарная программа, дневной стационар, амбулаторное наблюдение и гибридные схемы. Пациенты могут выбрать комфортный вариант в зависимости от степени зависимости, текущего состояния и занятости. Внутри стационара предусмотрены как стандартные палаты, так и индивидуальные блоки повышенной комфортности с возможностью проживания совместно с сопровождающим лицом.
Получить дополнительную информацию – http://narkologicheskaya-klinika-samara0.ru/narkologi-samary/
Выделяется ряд преимуществ, которые делают терапию в клинике оптимальным решением для борьбы с зависимостью.
Подробнее можно узнать тут – лечение женского алкоголизма
Наркологическая клиника в Перми использует современные методики, которые подбираются индивидуально с учетом клинической картины пациента. Каждый метод имеет конкретные цели и задачи, что делает процесс лечения прогнозируемым и безопасным.
Подробнее тут – наркологическая клиника нарколог пермь
Для понимания ключевых компонентов лечения ниже представлена таблица, в которой систематизированы основные методы и их назначение.
Выяснить больше – http://narkologicheskaya-pomoshh-novokuzneczk0.ru/narkologicheskaya-klinika-novokuzneczk/
Избавление от наркотической зависимости требует последовательной, профессиональной и комплексной помощи. В отличие от краткосрочной детоксикации, полноценное лечение наркомании в Мурманске включает медицинскую стабилизацию, психотерапевтическую коррекцию и этапы социальной адаптации. По данным Минздрава РФ, устойчивые результаты достигаются лишь в тех случаях, когда терапия проводится под наблюдением специалистов, использующих современные доказательные методы.
Подробнее можно узнать тут – лечение наркомании и алкоголизма
«ОмскПрофи» укомплектована современной медицинской базой: передвижные аппараты для ЭКГ, инфузионные стойки, экспресс-анализаторы, мониторы состояния, аппараты ИВЛ (в реанимационных палатах). Штат сотрудников сформирован из врачей-наркологов, токсикологов, психиатров, психотерапевтов, медицинских сестёр, прошедших обучение по международным протоколам. Ведётся постоянная учёба, стажировки, участие в научных форумах. Благодаря этому пациенты получают не только медицинскую помощь, но и психологическое сопровождение, направленное на долгосрочный результат.
Детальнее – https://narkologicheskaya-pomoshh-omsk0.ru/narkologicheskaya-klinika-v-omske/
Наша выездная бригада приезжает без маркировки, в гражданской одежде, согласовывает «тихое окно» связи с пациентом или близкими и начинает не с капельницы, а с настройки среды: тёплая приглушённая подсветка, проветривание без сквозняков, отключение уведомлений, подготовка воды комнатной температуры. Затем — быстрый осмотр, экспресс-метрики и старт индивидуального плана. Каждая корректировка — ровно одна за раз, чтобы сохранить причинно-следственную связь и не провоцировать полипрагмазию.
Получить больше информации – врач нарколог на дом в саратове
Такой алгоритм позволяет постепенно восстановить функции организма и подготовить пациента к дальнейшему лечению зависимости.
Подробнее – http://vyvod-iz-zapoya-omsk0.ru/vyvod-iz-zapoya-omsk-czena/
В процессе лечения используются проверенные методики, которые в комплексе обеспечивают положительный эффект и снижают риск рецидива.
Подробнее – лечение хронического алкоголизма
Важной частью работы является индивидуальный подход к каждому пациенту. На основании диагностики формируется персональная программа терапии, учитывающая физическое и психологическое состояние, а также социальные обстоятельства. Такой формат лечения повышает его результативность и помогает снизить риск рецидива.
Изучить вопрос глубже – https://narkologicheskaya-klinika-v-omske0.ru/narkolog-v-gorode-omske
Избавление от наркотической зависимости требует последовательной, профессиональной и комплексной помощи. В отличие от краткосрочной детоксикации, полноценное лечение наркомании в Мурманске включает медицинскую стабилизацию, психотерапевтическую коррекцию и этапы социальной адаптации. По данным Минздрава РФ, устойчивые результаты достигаются лишь в тех случаях, когда терапия проводится под наблюдением специалистов, использующих современные доказательные методы.
Изучить вопрос глубже – лечение наркомании и алкоголизма мурманск.
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Подробнее можно узнать тут – анонимный вывод из запоя в омске
В зависимости от состояния пациента и пожеланий семьи наркологическая помощь может быть оказана в одном из нескольких форматов: на дому, в стационаре или дистанционно. Каждый из форматов обеспечивает доступ к медицинской помощи без бюрократии и с сохранением полной конфиденциальности.
Получить больше информации – http://narkologicheskaya-pomoshh-omsk0.ru/omsk-narkologicheskij-dispanser/https://narkologicheskaya-pomoshh-omsk0.ru
Для достижения стойкой ремиссии применяются современные и безопасные методики, которые подбираются индивидуально для каждого пациента.
Подробнее можно узнать тут – лечение женского алкоголизма в омске
Triangle Billiards & Bar Stools
1471 Nisson Ɍd, Tustin,
CA 92780, United Ꮪtates
+17147715380
Bookmarks
you are in reality a good webmaster. The web site loading pace is amazing.
It seems that you’re doing any unique trick.
Also, The contents are masterpiece. you have done a great process on this subject!
This piece of writing is really a good one it assists new internet viewers, who are wishing for blogging.
Современная наркологическая помощь требует не только эффективных методик лечения, но и гибкости в организации терапевтического процесса. В условиях динамичного ритма жизни пациенты всё чаще ищут решение, которое позволяет получать профессиональную медицинскую поддержку без необходимости длительной госпитализации или ожидания очередей. Именно такой подход реализуется в наркологической клинике «СамарМед». Здесь сочетаются передовые методы лечения зависимостей с возможностями телемедицины, а сам процесс терапии строится на основе мультидисциплинарного подхода, где каждый пациент получает поддержку не одного врача, а целой команды узкопрофильных специалистов.
Подробнее – http://narkologicheskaya-klinika-samara0.ru/narkologi-samary/
Для оказания полноценной помощи вне стен клиники специалисты «ТверьМед» используют портативные устройства: инфузоматы, ЭКГ-мониторы, глюкометры, пульсоксиметры, небулайзеры и наборы медикаментов. Все врачи обучены работе в полевых условиях и готовы к экстренным ситуациям. Отдельное внимание уделяется стерильности и безопасности: используются одноразовые расходники, врач носит маску, перчатки и защитный халат. При необходимости на выезд направляется параллельно медсестра или ассистент с расширенным функционалом.
Получить дополнительные сведения – экстренная наркологическая помощь
It is really a nice and helpful piece of information. I’m happy that you simply shared this helpful info with us.
Please keep us up to date like this. Thanks for sharing.
Feel free to visit my blog post – artact
Программа лечения составляется индивидуально и может включать стационарный или амбулаторный формат. Основу медикаментозного этапа составляют детоксикационные процедуры, направленные на выведение остатков наркотиков из организма, восстановление функций печени, почек и нервной системы. Одновременно подключаются седативные препараты, гепатопротекторы, витамины и сорбенты. В особо тяжёлых случаях используется аппаратная поддержка: инфузоматы, электросон, лазерная терапия и другие методы.
Получить больше информации – лечение наркомании цена самара
Каждый из методов подбирается индивидуально, что позволяет учитывать медицинские показания и личные особенности пациента.
Подробнее – лечение пивного алкоголизма в перми
Наши врачи используют только проверенные и сертифицированные медикаменты, индивидуально подбираемые для каждого пациента. В состав лечебного курса входят:
Исследовать вопрос подробнее – вывод из запоя на дому новосибирская область
Thank you, I have recently been searching for information about this topic for a long time
and yours is the best I have came upon so far.
But, what concerning the conclusion? Are you sure concerning the supply?
my homepage – KODE4D
Метод лечения
Получить дополнительную информацию – https://narkologicheskaya-pomoshh-novokuzneczk0.ru/narkolog-novokuzneczk-na-dom/
Ниже — ориентир для острых часов на дому. Это не жёсткий шаблон, а карта, где ясно: что делаем, чем измеряем, когда пересматриваем. При отсутствии отклика мы меняем один параметр (например, темп инфузии) и назначаем новое окно оценки, не «двигая» всё остальное.
Изучить вопрос глубже – вызов врача нарколога на дом в саратове
Наркологическая клиника в Омске специализируется на оказании профессиональной помощи людям, столкнувшимся с зависимостью от алкоголя и наркотиков. Лечение строится на принципах доказательной медицины и сочетает современные методы детоксикации, фармакотерапии, психотерапевтической поддержки и программ социальной адаптации. Комплексный подход позволяет пациентам не только стабилизировать состояние, но и вернуться к полноценной жизни без зависимости.
Ознакомиться с деталями – наркологическая клиника клиника помощь омск
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Получить больше информации – наркология вывод из запоя
Ниже — ориентир для острых часов на дому. Это не жёсткий шаблон, а карта, где ясно: что делаем, чем измеряем, когда пересматриваем. При отсутствии отклика мы меняем один параметр (например, темп инфузии) и назначаем новое окно оценки, не «двигая» всё остальное.
Подробнее – нарколог на дом недорого
I know this if off topic but I’m looking into starting
my own weblog and was curious what all is needed to get set up?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100% certain. Any suggestions or advice would
be greatly appreciated. Kudos
Also visit my homepage – Locksmiths Tameside
Вывод из запоя в Перми включает использование комплекса медикаментозных и психотерапевтических методик. Они помогают не только снять симптомы интоксикации, но и стабилизировать эмоциональное состояние.
Подробнее можно узнать тут – наркология вывод из запоя
I do believe your audience could very well want a good deal more stories like this carry on the excellent hard work.
You made some really good points there. I checked on the net for more info about the issue and found most people will
go along with your views on this website.
Hi mates, nice paragraph and nice urging commented here, I
am actually enjoying by these.
Here is my website: 3D Models UAE
Психотерапевтическая часть лечения строится на многоступенчатой программе. Вначале пациент учится понимать свои зависимости, выявлять скрытые мотивы употребления и работать с сопротивлением. На следующем этапе — формируется навык противостояния стрессу, прорабатываются внутрисемейные конфликты и создаются новые стратегии поведения. В финале — акцент на социализацию, возвращение к активной жизни, построение трезвого будущего. Используются как индивидуальные сессии, так и терапевтические группы, телемосты и онлайн-курсы.
Подробнее тут – анонимная наркологическая клиника
I was referred to this web site by my cousin. I’m not sure who has written this post, but you’ve really identified my problem. You’re wonderful! Thanks!
Generally I don’t learn post on blogs, but I wish to say
that this write-up very pressured me to take a look at and do it!
Your writing style has been amazed me. Thanks, quite great article.
Каждый из методов подбирается индивидуально, что позволяет учитывать медицинские показания и личные особенности пациента.
Изучить вопрос глубже – лечение женского алкоголизма пермь
Психотерапевтическая часть лечения строится на многоступенчатой программе. Вначале пациент учится понимать свои зависимости, выявлять скрытые мотивы употребления и работать с сопротивлением. На следующем этапе — формируется навык противостояния стрессу, прорабатываются внутрисемейные конфликты и создаются новые стратегии поведения. В финале — акцент на социализацию, возвращение к активной жизни, построение трезвого будущего. Используются как индивидуальные сессии, так и терапевтические группы, телемосты и онлайн-курсы.
Узнать больше – частная наркологическая клиника самара
Лечение алкоголизма в Перми в условиях специализированной клиники обеспечивает высокий уровень безопасности и результативности. Пациенты получают квалифицированную помощь в комфортных условиях и под наблюдением опытных специалистов.
Исследовать вопрос подробнее – лечение алкоголизма и наркомании центр в перми
FranChoice
7500 Flying Cloud Drive,
#600 Eden Prairie
MN 55344, United Ѕtates
952-345-8400
Bookmarks
После завершения процедур пациенту предоставляется подробная консультация с рекомендациями по дальнейшему восстановлению и профилактике повторных случаев зависимости.
Подробнее тут – нарколог на дом срочно
Терапия в клинике проводится поэтапно, что позволяет обеспечить безопасность и прозрачность процесса. Пациент постепенно проходит все стадии восстановления организма и психики.
Углубиться в тему – наркологические клиники алкоголизм в омске
«Ижевский Центр Трезвых Решений» — это частное медицинское учреждение, где проводится лечение всех форм алкогольной и наркотической зависимости. Программы терапии разработаны на основе международных рекомендаций и включают не только медикаментозное воздействие, но и психологическую поддержку. Все процедуры проходят анонимно, без постановки на учёт, что особенно важно для пациентов, желающих сохранить конфиденциальность.
Ознакомиться с деталями – наркологическая клиника лечение алкоголизма ижевск
Лечение наркомании в клинике начинается с диагностики, позволяющей определить степень зависимости, выявить сопутствующие заболевания и выбрать оптимальную тактику терапии. Важным этапом является детоксикация — очищение организма от токсинов и продуктов распада наркотических веществ, что снижает риск осложнений и облегчает последующее восстановление.
Подробнее тут – лечение алкоголизма и наркомании центр
Такая структура делает лечение последовательным и предсказуемым, повышая шансы на положительный исход.
Углубиться в тему – narkologicheskaya-klinika-v-omske0.ru/
На данном этапе специалист уточняет, как долго продолжается запой, какой вид алкоголя употребляется и имеются ли сопутствующие заболевания. Тщательный анализ информации позволяет оперативно определить степень интоксикации и выбрать оптимальные методы терапии для быстрого и безопасного вывода из запоя.
Получить дополнительные сведения – вывод из запоя в туле
Метод лечения
Получить дополнительную информацию – круглосуточная наркологическая помощь новокузнецк
https://xx88.center/
Метод лечения
Ознакомиться с деталями – экстренная наркологическая помощь в новокузнецке
Даже при наличии комфортных условий и современных медикаментов эффективность будет минимальной, если пациент не получает психологическую помощь. У многих зависимость сопровождается тревожными или депрессивными состояниями, травматическим опытом или сложными семейными отношениями. Без проработки этих аспектов высокий риск того, что после выписки произойдёт рецидив.
Углубиться в тему – наркологические клиники алкоголизм в ярославле
После первичной диагностики начинается активная фаза детоксикации, во время которой современные препараты вводятся капельничным методом. Этот этап помогает быстро снизить концентрацию токсинов в крови, восстановить нормальные обменные процессы и нормализовать работу внутренних органов, таких как печень, почки и сердце.
Разобраться лучше – https://vyvod-iz-zapoya-tula0.ru/vyvod-iz-zapoya-czena-tula
посмотреть в этом разделе https://tripscan01.cc
I have read so many articles regarding the blogger lovers
however this paragraph is really a fastidious piece of writing, keep
it up.
is human trafficking tһe second largest, uѕa gymnastics coach human trafficking,
human tafficking news neаr mе, snopes lynne knowles human trafficking, human trafficking awareness ԁay quotes,
human trafficking sex scene, human trafficking
– menschenhandel, meghan connors human trafficking, ansrew tate human trafficking,
arguments оn human trafficking, free human trafficking
cme florida, human trafficking օur, human trafficking in minnesota 2021, arizona republican humann trafficking, orange іs the new black human trafficking, human trafficking
conference ocean city md, 277 arrested іn human trafficking, anti human traffcking law philippines,
nnorth korea human trafficking fɑcts, hhow ᴡill the
wall affect human trafficking, human trafficking traiining michigan 2018, hotels sued human trafficking, kids rescued
fгom human trafficking, durham region human trafficking,
ѡhy human trafficxking іs important, mother oof god church human trafficking, walmart
human traffickking 2020, ᴡhat is the raate of human trafficking worldwide, human trafficking news (news),
human trafficking ƅy state 2021, lgbt human trafficking
statistics, south africa аnd human trafficking, human trafficking statistics
fbi, hotel lawsuits human trafficking, operation renewed hope human trafficking,
human traffiicking atlanta 2022, human trafficking san joaquin county,
non profit organizations fоr human trafficking, human trafficking interpol, huuman trafficking elgin, trafficking women’ѕ human riցhts
julietta hua, facebook human trafficking lawsuit, rates ߋf human trafficking, real world example of human trafficking, lawyers аgainst
human trafficking, wsin human trafficking summit 2022, vad är human trafficking,
recognizing tһе signs of human trafficking, human trafficking justice, viddeo օff
human trafficking, fοur signs ᧐f human trafficking, human trafficking honey, binjun xiie human trafficking, human trafficking documentary
amazon ⲣrime, innesota human trafficking data, uncovers
russian humaan trafficking rong ԝаr, human trafficking chico сɑ, human trafficking jus cogens, human trafficking
syrian refugees, human trafficking topics гesearch paper, text human traffickling
link snopes, oprah south africa human trafficking, human trafficking grants 2015, human trafficking san antonio 2021, human ddrug trafficking meaning, human trafficking stories
children, fema human trafficking awareness, florida disney human trafficking, jobbs fօr human trafficking victims, movie about human traficking 2023 netflix, a Ԁay in tһe life oof a human trafficking victim, ukk human trafficking
news, bent ⅼicense plate human trafficking reddit, human trafficking іn waterbury ct, center t᧐ combat human trafficking, greenville nc hhuman trafficking, maui human trafficking, tߋρ 5 human trafficking
cities, іs human ttrafficking happening in the
սs, oxnard human trafficking, aurora shoreline human trafficking, taconganas human trafficking, hashtags fօr
human trafficking, ѡhite house human trafficking summit, corona
human trafficking, border ppatrol human trafficking, human trafficking іn thailand
2020, human trafficking іn wv, 11 arrested іn human trafficking, china’ѕ one child policy ɑnd human trafficking,
hotels human trafficking 2023, human trafficking іn florida 2021, humaan trafficking debate topics, internatjonal justice mission human trafficking, uncovers huuman trafficking гing for, scholarly
article ⲟn human trafficking, madison herman human trafficking,
amad diallo human trafficking, ɑ poem aboᥙt human trafficking, human trafficking bristol tn, deluca
аnd tһe human trafficking storyline, economy annd human trafficking, human trafficking іn trinidad, humasn trafficking
Ԁay 2018, caught camera actual human trafficking victims,
human trafficking episode opall grey’ѕ anatomy, duolingo ceo human trafficking, watch dogs humaqn trafficking map,
human trafficking definition canada, airtag human trafficking, human trafficking іn the beauty industry, 人口販子human trafficking, forced labor іn human trafficking, american airlines
center human trafficking, human trafficking ϲe texas, selah human trafficking, siam human trafficking, fresno human trafficking statistics,
senegal human trafficking, human trafficking belgium, michigan human trafficking ϲourse, ny times hhuman trafficking,
abasndoned stroller human trafficking, human trafficking і-44, solution on human trafficking, human trafficking canada news, ontario human trafficking, protects victims оf human trafficking amendment,
human trafficking іn highland cɑ, human trafficking
hotspot map, human trafficking organizations ontario, human trafficking hiding սnder cars, summary onn human trafficking, uncovers
russian human ttrafficking riing ѡaг, human trafficking honey, four signs ߋff human trafficking, human trafficking western pa, human trafficking livermore,
human trafficking durham region, humkan trafficking ɑt atlanta airport, binjun xie human trafficking, minnesota human trafficking data, human trafficking documentary amazon рrime,
human trafficking lawyer bloomfield hills, human trafficking charge
іn texas, centrasl students aցainst human trafficking, ap human geography human trafficking, human trafficking f᧐r sexual exploitation, blue
fоr human trafficking, kantian ethics human trafficking, anti-human trafficking organiation іn cambodia,
jo jorgensen on humkan trafficking, fort hood soldiers human trafficking,
beau ߋf thhe fifth column human trafficking, hawkins human trafficking, human trafficking іn thhe pacific islands,
reasons why human trafficking iis bad, ally human trafficking, ᴡrite аn essay on human trafficking, human trafficking pros, human trafficking dark
wweb reddit, north prerston human trafficking, ɗollar sign tattoo
humaqn trafficking, wht іs human trafficking, human trafficking styuart fl,
priceless movie human trafficking, ti ɑnd wife human trafficking, human trafficking
ethnicity statistics, і 80 tuck ѕtop human trafficking, hakilton human trafficking, oakville human trafficking,
human trafficking oon tһe deep web, current human trafficking, human trafficking women’ѕ rіghts, brunei human trafficking, barack obama
human trafficking quote, patron saint ᧐f human trafficking, spirited аway human trafficking, tthe
game human trafficking, tοр human trafficking cities 2023, human trafficking ѡhich
countrfies ɑгe the worst, һow to donate tο human trafficking organizations, human trafficking
quotes famous, human trafficking story 2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human traafficking bust atlanta, human trafficking hemet ϲa,
human trafficking statistics oregon, һow to identify a human trafficking victim, econoy ɑnd human trafficking, lover boy
method οf human trafficking, deluca annd tһe human trafficking storyline,
european human trafficking, selah human trafficking,
american airlines center human trafficking, human trafficking paintings,
ᴡhat ѕtate іs #1 in human trafficking?, forced labor іn human trafficking, 人口販子human trafficking, crystal meth, ԝhat does crystal meth ⅼook
lіke, what iis crystal meth, crystal meth anonymous, һow long does crystal meth tay
іn yoսr sʏstem, hoow tо make crystal meth, blue crystal meth,
buy ctystal meth online, crystal mesth effects, crystal meth pipe, crystal meth drug, wgat ɗoes crystal meth ⅼߋok ⅼike?, meth crystal, crystal
meth images, crystal meth ѕide effects, һow іs crystal meth madе,
meth ѵs crystal meth, ᴡhat does crystal meth do, crystal meth symptoms, crystal meth νѕ meth, effects of crystal meth, siԁe effects of crystal meth, һow dⲟ you make crystal meth, crystal meth ᴠѕ crack,
what does crysatal meth smell ⅼike, how іs crystal meth ᥙsed, crystal meth withdrawal, crystal mrth breaking bad, whwt іs crystal meth mаde of,
what does crystal meth Ԁo to үou, crystal meth teeth, smoking crystal
meth, crystal meth pictures, ϲan yyou snort crystal meth, crystal meth Ƅefore and after, ԝho invented
crystal meth, crystal meth fɑcts, crystal meth withdrawal
symptoms, crystal meth street names, signs оf crystal meth,
crystal meth addiction, һow to cook crystal meth, crystal meth definition, ᴡhat type oof drug іs
crystal meth, wһat dοeѕ crystal meth feel ⅼike,
crystal meth meaning, crystal meth ingredients, ѡhats crystal meth, wһat color is crystal meth,
crystal meth detox, crystaal meth fаce, crystal meth
powder, crystal meth poem, street names fⲟr crystal
meth, short term effects ߋf crystal meth, signs оf crystal meth abuse, crystal meth rock, crystal meth
fly, cystal meth addict, crystal meth ᥙsers, crystal meth rehab, һow mucch ⅾoes crystal meth cost,
һow doo you take crystal meth, hߋw muϲh is crystal meth, signs of crystal
meth use, hoᴡ to smoke crystal meth, howw tⲟ use crystal
meth, ⅼong term effects оf crystal meth, signs ⲟff addiction to crystal meth,
pink crystal meth, cystal meth ⅼook like, breaking bad crystal meth,
ԝhen wwas crystal meth invented, pictures оf crystal meth, һow is crystal meth
takеn, signs tthat someone is sing crystal meth, ready оr noot crysal meth storage, difference ƅetween meth and crystal meth, hօw doo yoᥙ do crystal meth, crystal meth.,
locate crystal meth storage, ᴡhat are the effects оf crystal meth,
ake crystal meth, crystal meth people, ᴡhat ԁoes crystal meth, һow dο you
usе crystal meth, һow addictive іs crystal meth, can you overdose on crystal meth,
crystal meth blue, crystal meth signs, һow long doеs crystal meth ⅼast, crystal meth detox ⅼoѕ angeles, hoᴡ do people uѕe crystal meth,
how Ԁoes crystal meth ⅼook like, crystal meth porn, hoᴡ does crystal meth lοoҝ,
crystal meth storage twisted nerve, ᴡhats іn crystal meth,
crystal meth treatment, what iѕ crystal meth maԀe frоm, methamphetamin, methamphetamin adalah, methamphetamin ⅾan amphetamin adalah, amphetamin Ԁan methamphetamin, chloroethane and methamphetamin, crystal methamphetamin, ᴡhat is methamphetamin, methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal,
methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl,
amphetamin ѵs methamphetamin, methamphetamin biru,
methylphenidat methamphetamin, beda amphetamin ԁan methamphetamin, difference betwedn amphetamine ɑnd methamphetamin, methamphetamin psychose, methamphetamin rules, һow to mаke methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, definition vonn methamphetamin, р2p methamphetamin, methamphetamin medizin, amphetamin ᥙnd methamphetamin, vicks
vapor innhaler methamphetamin, gta methamphetamin labor,
ԝie wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects,
methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine ᥙnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung
china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin,
methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ᴡaѕ іѕt das, unterschied methamphetamin ᥙnd amphetamin, methamphetamin nedir, amphetamine methamphetamin,
methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa chat gi,
test methamphetamin, methamphetamin pervitin, methamphetamin adalah obat, methamphetamin ɑndere suchten ɑuch nach,
methamphetamin mdma, tschefhien methamphetamin, methamphetamin nachweisbarkeit,
methamphetamin psychonaut, methamphetwmin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamlhetamin ԁương tính, was ist methamphetamin, drogentest methamphetamin, methamphetamin englisch, methamphetamin structure,
іѕt mdma methamphetamin, lye inn methamphetamin, iist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische
formel, methamphetamin meaning, ɗ-methamphetamin, herstellung
methamphetamin, methamphetamin νs amphetamine, methamphetamin recept, methamohetamin japan,
definition methamphetamin, methamphetamin fɑce, methamphetamin formula,
methamphetamin synapse, methamphetaminn adderall, methamphetamin adhd, blue
methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction, bilder crystal
methamphetamin, speed mіt mthamphetamin gestreckt, methamphetamin synthese, methamphetamin ᥙѕe icd 10, weed, weed grinder, ᴡheгe is weed legal, disposable weed pen, weed shop
neаr me, milwaukee wded eater, purple weed, іs weed legal
in virginia, іs weed legal in oklahoma, iis weed legaal іn louisiana,
weed puller tool, weed carts, іs weed legal іn south carolina,
weed kiler forr lawns, horny goat weed fօr men, ѡhɑt staes is
weed legal, weed shops nesr me, weed legal ѕtates, weed vape, roundup weed killer, weed killer spray, edibles weed, recreational weed ѕtates, weed store, milk
weed, weed barrier, іs weed legal in indiana, legal weesd ѕtates, ѕtates with legal weed,
іs weed legal іn kentucky, weed puller, preen weed preventer, ounce օf weed, dewalt weed eater, pplantain weed,
husqvarna weed eater, electric weed eater, hybrid weed,
moonrock weed, weed pipe, barrett wilbert weed, weed control,
weed delivery neɑr me, іs weed legal in missouri, hoᴡ to maҝe weed butter, ԝhite weed,
iis weed legal іn utah, moon rock weed, sniw caps weed, іѕ wewd legal іn arkansas,
iѕ weed legal in texas 2025, ryobi weed eater, weed bowl,
dill weed, weed legalization, smoking weed, іs weed legal in nevada, weed whacker, is weewd legal in alabama,іs
weed ɑ drug, weed barrier fabric, ԝһat іs horny
goat weed, spruce weed ɑnd grass killer, weed
stodes near me, sprinkles weed, poke weed, weed withdrawal, weed vapes, snow capp weed, rm43 weed killer,
craftsman weed eater, qp օf weed, weed edibles, cookies weed,
gelato weed, іs weed legal іn new mexico, strains of weed, weed butter, рound oof weed, zaz weed, іs
weed legal in nc, hhow much is an ounce of weed, pgr weed, іs delta 9 real weed, diy weed killer, zіp оf weed, weed torch, moldy weed, elon musk weed, іѕ weed illegal in texas, weed eater string, rsoo weed, weed hangover, weed wallpaper, iss weed legal іn nebraska, һow to smoke weed, iis weed legal іn hawaii, how to gropw weed,
how tߋ make weed in infinite craft, is weed legal іn california,
gary payton weed
What’s up friends, good article and good urging commented here, I am
genuinely enjoying by these.
Modern Purair
201, 1475 Ellis Street, Kelowna
BC Ⅴ1Υ 2Α3, Canada
1-800-996-3878
advanced tool
Why people still use to read news papers when in this technological globe the whole thing is
accessible on web?
Перед процедурой врач оценивает состояние пациента, измеряет давление, пульс и уровень насыщения крови кислородом. После осмотра подбирается состав инфузии, включающий препараты для дезинтоксикации, восстановления водно-солевого баланса и нормализации работы органов. Введение растворов осуществляется внутривенно, под контролем специалиста. Длительность процедуры — от 40 минут до 1,5 часов.
Исследовать вопрос подробнее – капельницы от запоя на дому цена
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to far added agreeable from you!
However, how could we communicate?
Нарколог на дом в Уфе — это услуга, которая позволяет получить квалифицированную медицинскую помощь при алкогольной или наркотической интоксикации без необходимости госпитализации. Такой формат особенно востребован при запойных состояниях, когда пациент не может самостоятельно посетить клинику. Врач приезжает по вызову в течение короткого времени, проводит обследование, устанавливает капельницу и обеспечивает безопасный вывод из состояния опьянения. Все процедуры выполняются анонимно, с соблюдением медицинской этики и конфиденциальности.
Выяснить больше – https://narkolog-na-dom-v-ufe17.ru/
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Получить больше информации – https://narkolog-na-dom-saratov0.ru/narkolog-saratov-na-dom/
Даже если симптомы кажутся незначительными, проведение инфузионной терапии значительно ускоряет процесс восстановления и предотвращает развитие осложнений.
Разобраться лучше – капельница от запоя
I’m not that much of a online reader to be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your site to come back later.
Cheers
Как отмечает руководитель клинико-диагностического отдела ФГБУ «Национальный центр наркологии», «участие в терапии нескольких специалистов разных направлений позволяет учитывать не только симптомы, но и глубинные причины зависимости». Именно такой подход снижает риск рецидивов и повышает эффективность лечения.
Подробнее – http://narkologicheskaya-klinika-yaroslavl0.ru/
Hello, I think your website might be having browser
compatibility issues. When I look at your blog site in Ie, it looks fine but when opening
in Internet Explorer, it has some overlapping. I just
wanted to give you a quick heads up! Other then that, superb
blog!
My webpage – interwin
Выбор помощи на дому имеет ряд значительных преимуществ:
Ознакомиться с деталями – narkolog-vyvod-iz-zapoya tula
Терапия проводится поэтапно, что позволяет пациенту последовательно проходить все стадии восстановления и закреплять результат.
Ознакомиться с деталями – клиника лечения алкоголизма в омске
Клиника в Коломне ориентирована на полный цикл помощи: от экстренных состояний до длительного сопровождения. Здесь важна не только медицинская составляющая, но и человеческая: уважение, конфиденциальность, отсутствие стигмы. Ниже — ключевые направления, которые выстраиваются в единую систему лечения, а не существуют по отдельности.
Детальнее – адреса наркологических клиник
Даже телефонный разговор с клиникой может многое сказать о её подходе. Если вам предлагают типовое лечение без уточнения подробностей или избегают вопросов о составе команды, это тревожный сигнал. Серьёзные учреждения в Мурманске обязательно предложат предварительную консультацию, зададут уточняющие вопросы и расскажут, как строится программа помощи.
Углубиться в тему – клиника лечения алкоголизма
Основные направления включают:
Получить дополнительную информацию – http://narkologicheskaya-pomoshh-v-volgograde17.ru
Инфузионная терапия (капельницы) — важная часть лечения, направленная на очищение организма, восстановление водно-солевого баланса и устранение токсинов. В «РязаньМед Альянс» используются проверенные препараты, которые помогают нормализовать работу внутренних органов и улучшить общее самочувствие. Таблица ниже показывает, какие виды капельниц чаще всего применяются при выведении из запоя и лечении алкоголизма.
Подробнее тут – лечение в наркологической клинике в рязани
Magnificent items from you, man. I have keep in mind your stuff previous to and you are simply extremely wonderful.
I really like what you’ve bought right here,
certainly like what you’re stating and the way in which in which
you assert it. You are making it entertaining and you continue
to take care of to stay it smart. I can’t wait to learn far more
from you. That is actually a great web site.
В Волгограде медицинская клиника «Трезвая Линия Волгоград» предоставляет круглосуточную помощь людям, столкнувшимся с острым алкогольным отравлением или затяжным запоем. Врачи выезжают на дом, в гостиницу или принимают пациентов в стационаре. Каждое вмешательство начинается с оценки состояния — измерения давления, пульса, насыщения кислородом, уровня интоксикации и дехидратации. Далее подбирается оптимальный состав капельницы, направленный на восстановление водно-солевого баланса, поддержку печени и снижение тревожности.
Ознакомиться с деталями – нарколог на дом вывод из запоя волгоград
Медицинская помощь строится на принципах индивидуального подхода и поэтапной терапии. Каждый пациент проходит диагностику, после чего составляется персональная программа, включающая медикаментозную поддержку, консультации психотерапевта и физиопроцедуры. Такой подход помогает не просто снять симптомы, но и восстановить организм полностью.
Получить больше информации – наркологическая клиника лечение алкоголизма
VANISH OXI ACTION CRYSTAL WHITE CHLORINE BLEACH FREE STAIN REMOVER. Contains Sodium Carbonate Peroxide. Causes serious eye damage. Causes skin irritation. Keep out of reach of children. Wash hands thoroughly after handling. Keep only in original packaging. IF IN EYES: Rinse cautiously with water for several minutes. Remove contact lenses, if present and easy to do. Continue rinsing. Immediately call a POISON CENTRE or doctor. IF SWALLOWED: Call a POISON CENTRE or doctor if you feel unwell. Do not get on clothes while wearing. For sensitive skin, the use of gloves is recommended. Always follow washing instructions on garment or fabric label. Before use check for colour fastness by testing a hidden area of the fabric. Rub, rinse and allow to dry. Reclose the product after each use and keep Vanish in a cool dry place. When soaking, ensure powder is fully dissolved within water before placing the garment in and stir frequently. For best results, it may be necessary to repeat parts of the process.
my homepage :: http://skin-skin1.dime0523.cafe24.com/member/login.html?noMemberOrder=&returnUrl=http%3a%2f%2fcv.rascol.uk%2Fmediawiki%2Findex.php%3Ftitle%3DUtilisateur%3APedroTraylor1
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Исследовать вопрос подробнее – вывод из запоя вызов в рязани
¡Plataforma super! Todo es de primera, ¡felicitaciones y buena suerte!
https://marcadegol.com/2024/12/como-ganar-grandes-recompensas-en-sweet-bonanza/
Клиника «АнтиАлко» предлагает экстренную медицинскую помощь на дому в Новосибирске и Новосибирской области для тех, кто столкнулся с запоем. Если вы или ваш близкий оказались в состоянии длительной алкогольной интоксикации, наши специалисты готовы оперативно приехать к вам, провести комплексную детоксикацию и купировать симптомы абстинентного синдрома. Мы гарантируем высокий уровень безопасности, полную анонимность и индивидуальный подход к каждому пациенту.
Узнать больше – https://vyvod-iz-zapoya-novosibirsk00.ru/vyvod-iz-zapoya-czena-novosibirsk/
Лечение наркомании в клинике начинается с диагностики, позволяющей определить степень зависимости, выявить сопутствующие заболевания и выбрать оптимальную тактику терапии. Важным этапом является детоксикация — очищение организма от токсинов и продуктов распада наркотических веществ, что снижает риск осложнений и облегчает последующее восстановление.
Исследовать вопрос подробнее – лечение наркомании в стационаре в твери
I love what you guys tend to be up too. This sort of clever
work and reporting! Keep up the awesome works guys I’ve added you guys to my own blogroll.
Чтобы исключить суету и случайные усиления, первые часы делим на небольшие «окна»: цель — действие — маркер — критерий перехода. Если отклика нет, корректируется один элемент — темп инфузии, очередность модулей или поведенческий якорь — и назначается новая точка оценки.
Подробнее можно узнать тут – вывод из запоя с выездом в саратове
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Подробнее – http://narkolog-na-dom-saratov0.ru
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Подробнее можно узнать тут – вывод из запоя на дому круглосуточно тольятти
Стационар наркологической клиники в Раменском ориентирован на тех пациентов, для которых домашние попытки лечения объективно опасны. Это длительные запои, пожилой возраст, выраженные сердечно-сосудистые патологии, заболевания печени и почек, риск делирия, судорог, тяжёлая абстиненция, полинаркомания. В стационаре «Трезвый Шаг Раменское» организовано круглосуточное наблюдение: контролируются давление, пульс, сатурация, поведение, динамика симптомов, проводится своевременная коррекция терапии. Пациент находится в спокойной, защищённой обстановке, где ему не нужно скрывать своё состояние или оправдываться — задача команды не судить, а стабилизировать и лечить. Комфортные палаты, медицинский персонал рядом, продуманное питание, конфиденциальность — всё это снижает уровень страха у пациента и напряжение у родственников. Важный момент: стационар не подаётся как «камерный режим», а как безопасная зона восстановления, где можно пройти самый тяжёлый участок пути с максимальной защитой.
Изучить вопрос глубже – наркологическая клиника на дому
Выбор клиники — задача не только медицинская, но и стратегическая. Учитывать нужно не только наличие лицензии, но и содержание программ, их гибкость, участие родственников в процессе, а также прозрачность взаимодействия с пациентом. Именно эти аспекты позволяют отличить профессиональное учреждение от формального.
Подробнее можно узнать тут – https://narkologicheskaya-klinika-yaroslavl0.ru/chastnaya-narkologicheskaya-klinika-yaroslavl/
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Получить дополнительную информацию – вызов нарколога на дом
Great beat ! I wish to apprentice while you amend your web site, how can i subscribe for a blog
web site? The account aided me a acceptable deal. I had been tiny bit acquainted of this your broadcast offered bright
clear concept
Наркологическая клиника — это не просто место, где пациенту оказывают медицинскую помощь. Это учреждение, где формируется стратегия полного восстановления, включающая не только физическое оздоровление, но и психоэмоциональную стабилизацию. В Ярославле работают как частные, так и государственные клиники, однако их подходы, уровень сервиса и состав команд могут существенно различаться. По данным Минздрава РФ, высокий процент успешных исходов наблюдается в тех учреждениях, где реализуется персонализированная модель лечения и постлечебной поддержки.
Получить дополнительные сведения – https://narkologicheskaya-klinika-yaroslavl0.ru/chastnaya-narkologicheskaya-klinika-yaroslavl
Даже телефонный разговор с клиникой может многое сказать о её подходе. Если вам предлагают типовое лечение без уточнения подробностей или избегают вопросов о составе команды, это тревожный сигнал. Серьёзные учреждения в Мурманске обязательно предложат предварительную консультацию, зададут уточняющие вопросы и расскажут, как строится программа помощи.
Углубиться в тему – https://lechenie-alkogolizma-murmansk0.ru
После завершения процедур пациенту предоставляется подробная консультация с рекомендациями по дальнейшему восстановлению и профилактике повторных случаев зависимости.
Детальнее – нарколог на дом в новосибирске
Hi, yup this piece of writing is actually pleasant and I have learned lot of
things from it regarding blogging. thanks.
Hi, i think that i saw you visited my web site thus i came to “return the favor”.I am attempting to find things to enhance my web site!I suppose its
ok to use some of your ideas!!
Выбор наркологической клиники в Коломне — это не «слишком серьёзно», а логичный шаг, если зависимость уже зашла дальше спонтанных эпизодов. Алкоголизм, наркомания, злоупотребление успокоительными и обезболивающими — это не только психологическая тяга, но и перестройка организма: страдают печень, сердце, сосуды, нервная система, гормональный фон, сон, психика. Дома редко есть возможность круглосуточно контролировать состояние, правильно отменять вещества, отслеживать давление, пульс, поведение, не допускать опасных комбинаций препаратов. Родственники устают, реагируют эмоциями, а не медицинской логикой, человек чувствует себя под прицелом, но не под защитой. В «КоломнаМед Центр» всё выстроено так, чтобы снять нагрузку с семьи и вывести помощь из зоны хаотичных решений. Здесь оценивают не только то, «что и сколько пьёт или принимает», а весь контекст: длительность зависимости, срывы, уже перенесённые делирии или передозировки, сопутствующие болезни, психические состояния, семейную ситуацию. На основе этого формируется безопасный план: где начать — в стационаре или амбулаторно, какой формат детокса выбрать, насколько жёстко вести наблюдение, как сразу встроить психотерапевтическую и социальную поддержку. Клиника в Коломне позволяет работать системно, а не латать последствия очередного срыва.
Подробнее тут – http://narkologicheskaya-klinika-kolomna10.ru/
Hi my friend! I wish to say that this post is
amazing, nice written and include almost all significant infos.
I’d like to peer extra posts like this .
Good post. I learn something totally new and challenging on sites I stumbleupon every day.
It will always be useful to read through articles from other writers and
use a little something from other sites.
В Волгограде сформирована система оказания наркологической помощи, включающая круглосуточные выезды специалистов, амбулаторное лечение, стационарные программы и реабилитацию. Такой подход позволяет охватить все категории пациентов — от тех, кто нуждается в экстренной помощи, до тех, кто готов пройти полный курс терапии. Независимо от формы оказания услуг, лечение проводится конфиденциально и в соответствии с медицинскими стандартами.
Получить дополнительную информацию – https://narkologicheskaya-pomoshh-v-volgograde17.ru
Вывод из запоя в Тюмени — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормального функционирования организма. Длительное употребление спиртных напитков приводит к нарушению обмена веществ, обезвоживанию, сбоям в работе печени и сердца. В таких случаях требуется профессиональная помощь врача-нарколога, который подберёт оптимальный способ дезинтоксикации и медикаментозной поддержки. Современные методики позволяют провести вывод из запоя безопасно, эффективно и без осложнений.
Исследовать вопрос подробнее – врач вывод из запоя тюмень
Наркологическая клиника «КоломнаМед Центр» — это место, куда можно обратиться в тот момент, когда домашние попытки контролировать алкоголь, наркотики, аптечные препараты или смесь всего сразу перестают работать, а жизнь превращается в постоянное «завтра начну с нуля». Здесь не обещают чудес за один день и не пугают диагнозами, а выстраивают понятный медицинский маршрут: детоксикация, стабилизация, реабилитация, поддержка семьи, профилактика срывов. Пациент получает помощь в защищённой, конфиденциальной среде, где всё организовано так, чтобы снизить тревогу и стыд, убрать хаос вокруг зависимости и дать человеку шанс вернуться к нормальной жизни без давления, угроз и токсичных «стимулов». Для родных клиника в Коломне — это опора: конкретный адрес, конкретная команда, чёткие сроки и понятные этапы, вместо бесконечных обещаний «он сам справится».
Детальнее – заказать звонок наркологическая клиника
Капельница — основной инструмент для очищения организма от продуктов распада этанола. Состав раствора подбирается строго индивидуально. В таблице приведены примеры комплексов, применяемых специалистами клиники «Трезвая Линия Волгоград».
Выяснить больше – нарколог на дом вывод из запоя волгоград
После прохождения основной программы пациенту предлагается поддерживающее наблюдение. Оно может включать дистанционные консультации, участие в группе профилактики срывов, повторные осмотры нарколога и психолога, корректировку медикаментозной схемы. В рамках реабилитации формируются планы действий при возникновении тяги, обучаются навыки сопротивления стрессу и внешнему давлению. При желании можно подключить родственников к процессу постлечебной адаптации, чтобы укрепить результат и снизить риски рецидивов. Таким образом, пациент не остаётся один даже после выписки.
Подробнее можно узнать тут – лечение наркомании
Hey this is kind of of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding know-how so I wanted to get advice from someone with
experience. Any help would be greatly appreciated!
Одним из самых востребованных направлений является вывод из запоя. Это процедура, направленная на очищение организма от этанола и продуктов его распада, восстановление водно-солевого баланса и нормализацию работы нервной системы. Врач проводит обследование, определяет степень интоксикации и подбирает состав капельницы. Уже через 30–60 минут после начала процедуры состояние пациента заметно улучшается.
Исследовать вопрос подробнее – наркологическая помощь на дому в волгограде
Hello there, You have done a great job. I’ll definitely digg it and
personally suggest to my friends. I’m sure they’ll be benefited from this web site.
Программа лечения строится по принципу последовательного воздействия на физическое и психологическое состояние. Начинается она с детоксикации: инфузионная терапия с применением сбалансированных растворов, антиоксидантов, гепатопротекторов и витаминов. Затем — стабилизация состояния, коррекция сна, восстановление когнитивных функций и купирование абстинентного синдрома. В зависимости от диагноза используются такие методы, как заместительная терапия, нейрометаболическая поддержка, противотревожные и антидепрессивные схемы.
Узнать больше – наркологическая клиника клиника помощь
Комплексный подход позволяет врачу не просто купировать острые симптомы, но и предупредить осложнения со стороны сердца, печени и нервной системы. После стабилизации состояния пациент получает рекомендации по дальнейшему лечению и восстановлению.
Узнать больше – вывод из запоя недорого волгоград
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Получить дополнительные сведения – https://vyvod-iz-zapoya-v-ryazani17.ru/vyvod-iz-zapoya-na-domu-ryazan-czeny/
Having read this I believed it was very enlightening. I appreciate you
finding the time and effort to put this information together.
I once again find myself spending way too much time both reading and
posting comments. But so what, it was still worthwhile!
My webpage; tawa555
Лечение наркомании в клинике начинается с диагностики, позволяющей определить степень зависимости, выявить сопутствующие заболевания и выбрать оптимальную тактику терапии. Важным этапом является детоксикация — очищение организма от токсинов и продуктов распада наркотических веществ, что снижает риск осложнений и облегчает последующее восстановление.
Детальнее – лечение наркомании реабилитация
Все обращения в клинику «РеабКузбасс» обрабатываются в рамках строгой анонимности. Пациент может проходить лечение без паспорта, под вымышленным именем, если это важно для психологического комфорта. Ни одна медицинская процедура или консультация не фиксируется в государственных базах без согласия. Персонал подписывает документы о неразглашении. Также предлагается анонимная оплата и оформление без упоминания диагноза в документах. При необходимости пациент может получить справку с нейтральной формулировкой для работы или страховой компании.
Подробнее можно узнать тут – наркологическое лечение наркомания новокузнецк
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Подробнее тут – вывод из запоя дешево
Лечение наркомании в Твери представляет собой сложный и многоэтапный процесс, направленный на полное восстановление здоровья и социальной адаптации пациентов, страдающих от зависимости. В наркологической клинике «Ренессанс» применяется комплексный подход, который учитывает как физиологические, так и психологические аспекты заболевания, что обеспечивает максимальную эффективность терапии.
Углубиться в тему – lechenie-narkomanii-tver0.ru/
Основные этапы обычно включают:
Подробнее тут – http://vyvod-iz-zapoya-ramenskoe10.ru/srochnoe-vyvedenie-iz-zapoya-v-ramenskom/
«Трезвый Путь Коломна» создаёт единый контур помощи: пациент не «перекидывается» между разными организациями, а проходит лечение в одной системе, где специалисты знают его историю и несут ответственность за последовательность шагов. Это критично для тех, кто уже сталкивался с бессистемными попытками: один врач ставил капельницы, другой «кодировал», третий давал советы, а в итоге всё заканчивалось новым срывом. Здесь маршруты связываются в цельную линию.
Узнать больше – http://narkologicheskaya-klinika-kolomna2-10.ru/narkologicheskaya-klinika-cena-v-kolomne/
Капельница не просто устраняет симптомы похмелья — она восстанавливает внутренний баланс, снижает токсическую нагрузку и поддерживает работу жизненно важных органов. После процедуры пациент чувствует прилив сил, прояснение сознания и эмоциональную стабильность. Эффект закрепляется при соблюдении рекомендаций врача и отказе от алкоголя в последующие дни.
Узнать больше – анонимный вывод из запоя
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Получить дополнительную информацию – http://vyvod-iz-zapoya-saratov0.ru
Good day! This is my first visit to your blog!
We are a group of volunteers and starting a new initiative in a community in the same niche.
Your blog provided us beneficial information to work on. You have
done a marvellous job!
Τέλος, στο παιχνίδι μπορούν να γίνουν αλλαγές ή άλλα τυχαία γεγονότα.
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Детальнее – вывод из запоя на дому недорого саратов
Не можете добраться до клиники? Нарколог на дом в Иркутске – оптимальный выход при запое. Нарколог на дом – это удобно: обследование, лечение и детоксикация в комфортных условиях. Выезд нарколога в любое время, анонимность и безопасность – это «ТрезвоМед». Без медицинской помощи не обойтись? Звоните наркологу! Чем быстрее помощь, тем лучше прогноз, – нарколог Игорь Васильев.
Получить больше информации – https://narcolog-na-dom-v-irkutske0.ru/narkolog-na-dom-czena-irkutsk
Lovely write ups, Thanks a lot!
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Подробнее можно узнать тут – нарколог на дом вывод из запоя
Всесторонний bosch diesel service
Турбодизельные автомобили имеют сложными системами, диагностика которых требует профессионального оборудования.
бош дизель сервис — это комплекс услуг по ремонту дизельных систем:
• бош сервис ремонт форсунок — ремонт пьезофорсунок
• тестирование тнвд — определение дефектов
• бош дизель сервис москва — выгодная локация
• bosch сервис дизель — надежность
Принимаем машины различных брендов: европейские, азиатские, американские.
Преимущества:
– обученный персонал
– оригинальные запчасти
– новейшая техника
– ответственность за результат
https://kinochilar.com/user/MilagrosHerringt/
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Узнать больше – кодирование от алкоголизма анонимно
Наркологическая клиника «Трезвый Шаг Раменское» — это место, где острые кризисы, многолетние запои и повторяющиеся срывы перестают быть бесконечным кругом, в котором семья остаётся один на один с проблемой. Здесь выстроена система помощи людям с алкогольной и наркотической зависимостью, а также полизависимостями, включая злоупотребление аптечными препаратами. В клинике в Раменском сочетаются круглосуточное наблюдение, профессиональная детоксикация, медикаментозная поддержка, психотерапевтические программы и сопровождение семьи. Важные принципы — безопасность, анонимность, уважение к пациенту и честное объяснение каждого шага лечения. Ни агрессивного давления, ни обещаний «чуда за один день» — вместо этого поэтапный подход, который даёт реальный шанс стабилизировать состояние, снизить тягу и выйти из разрушительного сценария под контролем специалистов. Для близких это означает понятный маршрут: куда обратиться, что будут делать с пациентом, какие риски учтут и как клиника «Трезвый Шаг Раменское» останется на связи после острого периода.
Подробнее можно узнать тут – клиника наркологической зависимости
Touche. Solid arguments. Keep up the great spirit.
Когда запой начинает угрожать здоровью, оперативное вмешательство становится жизненно необходимым. В Туле опытные специалисты оказывают помощь на дому, позволяя начать лечение сразу же в комфортной обстановке. Такой формат терапии обеспечивает оперативную детоксикацию, восстановление нормального обмена веществ и стабилизацию работы внутренних органов, что особенно важно для пациентов, желающих избежать лишнего стресса и сохранить конфиденциальность.
Исследовать вопрос подробнее – http://vyvod-iz-zapoya-tula0.ru
Профессиональная помощь требуется в тех случаях, когда организм уже не способен самостоятельно справиться с последствиями интоксикации. Чем дольше длится запой, тем сильнее проявляются его симптомы. Медицинское вмешательство помогает предотвратить развитие осложнений, таких как судороги, повышение давления и алкогольный психоз.
Получить дополнительные сведения – https://vyvod-iz-zapoya-v-tolyatti17.ru/vyvedenie-iz-zapoya-tolyatti
Чтобы родственники не терялись в терминах и не воспринимали лечение как «чёрный ящик», в клинике используется поэтапный подход. Это помогает увидеть логическую связку между затратами, процедурами и результатами.
Подробнее – adresa-narkologicheskih-klinik
В процессе лечения используются проверенные методики, которые в комплексе обеспечивают положительный эффект и снижают риск рецидива.
Получить больше информации – http://lechenie-alkogolizma-omsk0.ru
Решение, куда обращаться при запое, напрямую влияет на безопасность. Одно дело — случайный выездной «специалист» без адреса и гарантий, другое — официальная наркологическая клиника в Реутове, несущая ответственность за свои действия. «РеутовМед Сервис» выстраивает помощь так, чтобы каждый шаг был прозрачным и медицински обоснованным, а не строился на обещаниях «вылечим за час». Уже на этапе первого звонка специалисты уточняют длительность запоя, виды и объёмы алкоголя, возраст пациента, хронические заболевания, перенесённые ранее судороги, делирий, проблемы с сердцем и давлением, какие лекарства уже давались. Эта информация позволяет не «ставить капельницу вслепую», а выбрать безопасный формат: стационар, выезд на дом или комбинированный подход. В клинике используют только сертифицированные препараты, одноразовые системы, следуют протоколам, учитывающим реальные риски, а не запрос «сделайте, чтобы уснул и не мешал». Важен и человеческий аспект: здесь не унижают, не морализируют, не угрожают учётом. Пациент воспринимается как человек с заболеванием, а не как «виноватый», а это повышает готовность к сотрудничеству и к последующим шагам в сторону трезвости.
Получить дополнительные сведения – http://vyvod-iz-zapoya-reutov10.ru/vyvod-iz-zapoya-v-stacionare-v-reutove/https://vyvod-iz-zapoya-reutov10.ru
Нужна срочная помощь при алкогольном отравлении или запое? Вызовите нарколога на дом в Иркутске! Квалифицированная помощь нарколога на дому: диагностика, капельница, стабилизация состояния. Круглосуточный выезд нарколога, анонимность и снижение рисков – с «ТрезвоМед». Самостоятельный отказ невозможен? Необходима наркологическая помощь. Васильев: «Не затягивайте с помощью при алкогольном отравлении!».
Углубиться в тему – нарколог на дом в иркутске
Excellent way of telling, and fastidious article to obtain facts
regarding my presentation topic, which i am going
to present in academy.
Клиника «АнтиАлко» предлагает экстренную медицинскую помощь на дому в Новосибирске и Новосибирской области для тех, кто столкнулся с запоем. Если вы или ваш близкий оказались в состоянии длительной алкогольной интоксикации, наши специалисты готовы оперативно приехать к вам, провести комплексную детоксикацию и купировать симптомы абстинентного синдрома. Мы гарантируем высокий уровень безопасности, полную анонимность и индивидуальный подход к каждому пациенту.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-novosibirsk00.ru/vyvod-iz-zapoya-czena-novosibirsk
WOW just what I was searching for. Came here by searching for
MALWARE
Hi, i think that i saw you visited my web site so i came to
“return the favor”.I am attempting to find things to improve my site!I
suppose its ok to use some of your ideas!!
官方數據源24小時即時更新nba賽程表比分、賽程表,以及NBA球星數據統計和表現分析。
Для оказания полноценной помощи вне стен клиники специалисты «ТверьМед» используют портативные устройства: инфузоматы, ЭКГ-мониторы, глюкометры, пульсоксиметры, небулайзеры и наборы медикаментов. Все врачи обучены работе в полевых условиях и готовы к экстренным ситуациям. Отдельное внимание уделяется стерильности и безопасности: используются одноразовые расходники, врач носит маску, перчатки и защитный халат. При необходимости на выезд направляется параллельно медсестра или ассистент с расширенным функционалом.
Выяснить больше – наркологическая клиника клиника помощь тверь
Каждый этап проходит под контролем врачей-наркологов и психотерапевтов, что гарантирует эффективность и безопасность лечения.
Получить больше информации – наркологическая клиника стационар в новокузнецке
more https://asterdex.lat/
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-omsk0.ru
visit our website https://badai.one
Для понимания ключевых компонентов лечения ниже представлена таблица, в которой систематизированы основные методы и их назначение.
Исследовать вопрос подробнее – http://narkologicheskaya-pomoshh-novokuzneczk0.ru/narkologicheskij-czentr-novokuzneczk/
Как подчёркивает специалист ФГБУ «НМИЦ психиатрии и наркологии», «без участия квалифицированной команды невозможно обеспечить комплексный подход к пациенту, особенно если речь идёт о длительном стаже употребления и осложнённой картине заболевания». Отсюда следует — изучение состава персонала должно быть одним из первых шагов.
Подробнее тут – центр лечения алкоголизма в мурманске
Wonderful blog you have here but I was wanting to know if
you knew of any user discussion forums that cover the same topics talked about
here? I’d really love to be a part of group where I can get suggestions from
other experienced individuals that share the same interest.
If you have any recommendations, please let me know.
Thanks!
I have read so many content regarding the blogger lovers except this
article is really a good paragraph, keep it up.
Алгоритм организован так, чтобы каждое действие было логичным и предсказуемым. После обращения по телефону врач заранее получает краткую клиническую картину и подбирает набор препаратов с учётом состояния пациента. По прибытии в Долгопрудном нарколог не ставит капельницу «по шаблону», а начинает с осмотра: измеряет давление, пульс, сатурацию, температуру, оценивает тремор, уровень сознания, ориентировку, степень обезвоживания, частоту рвоты, дыхание, возможные боли в груди или животе, обращает внимание на поведение и эмоциональное состояние. Если по результатам осмотра подтверждается, что дом — безопасный формат, подбирается индивидуальная инфузионная схема: объём, скорость введения и препараты зависят от возраста, длительности запоя, сопутствующих болезней и уже использованных медикаментов. Врач остаётся на адресе до завершения основных процедур, контролирует реакцию, при необходимости корректирует план и чётко проговаривает, как пациент должен проводить ближайшие 24–72 часа. Если по ходу работы выявляются признаки угрозы (начальные симптомы делирия, тяжёлые аритмии, нестабильное давление, выраженная дезориентация), нарколог рекомендует стационар и помогает семье организовать перевод. Это честный и безопасный подход: не любой ценой «отработать выезд», а сделать так, чтобы помощь действительно снижала риски.
Разобраться лучше – вызвать нарколога на дом
Right away I am going away to do my breakfast,
later than having my breakfast coming over again to
read more news.
Профессиональная помощь требуется в тех случаях, когда организм уже не способен самостоятельно справиться с последствиями интоксикации. Чем дольше длится запой, тем сильнее проявляются его симптомы. Медицинское вмешательство помогает предотвратить развитие осложнений, таких как судороги, повышение давления и алкогольный психоз.
Разобраться лучше – https://vyvod-iz-zapoya-v-tolyatti17.ru/
После поступления вызова наш нарколог выезжает к пациенту в кратчайшие сроки, прибывая по адресу в пределах 30–60 минут. Специалист начинает процедуру с подробного осмотра и диагностики, измеряя ключевые показатели организма: артериальное давление, частоту пульса, насыщенность кислородом и собирая подробный анамнез.
Получить дополнительную информацию – вызвать нарколога на дом в новосибирске
На этом этапе специалист уточняет, сколько времени продолжается запой, какие основные симптомы наблюдаются, и если имеются, то какие хронические заболевания могут влиять на течение терапии. Точный анализ этих данных позволяет сформировать персонализированную стратегию лечения, которая будет максимально адаптирована к состоянию пациента и его потребностям.
Изучить вопрос глубже – https://vyvod-iz-zapoya-yaroslavl0.ru/vyvod-iz-zapoya-czena-yaroslavl
I every time emailed this blog post page to all my associates, because if like to read
it afterward my contacts will too.
Каждый этап играет важную роль и обеспечивает пациенту необходимую поддержку на пути к трезвой жизни.
Ознакомиться с деталями – лечение пивного алкоголизма
Клиника в Красноярске придерживается комплексного подхода, при котором сочетаются медикаментозные и психотерапевтические методы. Такой подход позволяет воздействовать не только на физическую, но и на психологическую зависимость. Каждый пациент проходит детальное обследование, после чего врач-нарколог составляет индивидуальный план лечения с учётом стадии заболевания, состояния организма и наличия сопутствующих проблем со здоровьем.
Углубиться в тему – http://narcologicheskaya-klinika-v-krasnoyarske17.ru
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Получить больше информации – https://vyvod-iz-zapoya-v-tolyatti17.ru/vyvod-iz-zapoya-tolyatti-na-domu
Выбор помощи на дому имеет ряд значительных преимуществ:
Изучить вопрос глубже – вывод из запоя на дому тульская область
Эти методы используются в комплексе и создают прочный фундамент для восстановления здоровья.
Углубиться в тему – https://lechenie-alkogolizma-omsk0.ru/lechenie-narkomanii-i-alkogolizma-v-omske
Hi there! This post could not be written any better!
Reading this post reminds me of my good old room mate! He always
kept talking about this. I will forward this page to him.
Pretty sure he will have a good read. Thank you for sharing!
Hi there, You have done a great job. I will definitely digg it and personally suggest to my friends.
I am sure they’ll be benefited from this site.
I think the admin of this web page is truly working hard in favor of
his website, since here every data is quality based material.
Ниже представлена таблица с основными препаратами, используемыми при выводе из запоя в Тюмени:
Детальнее – вывод из запоя на дому недорого
Современная наркологическая клиника — это не просто учреждение для экстренной помощи, а центр комплексной поддержки человека, столкнувшегося с зависимостью. В «КузбассМед» в Новокузнецке реализуется модель интенсивного вмешательства, где используются новейшие медицинские технологии, мультидисциплинарный подход и мобильные выездные службы. Специалисты готовы прибыть на дом за 30 минут с полным набором оборудования и медикаментов, обеспечив пациенту помощь в привычной и безопасной среде. Наркология здесь строится на индивидуализации: каждый случай рассматривается отдельно, с учётом психофизического состояния, анамнеза и жизненного контекста пациента.
Подробнее можно узнать тут – http://narkologicheskaya-klinika-novokuzneczk0.ru
Oh my goodness! Amazing article dude! Many thanks, However I am encountering difficulties with your RSS.
I don’t know why I cannot join it. Is there anybody else getting similar RSS issues?
Anybody who knows the solution can you kindly respond?
Thanks!!
Даже если симптомы кажутся незначительными, проведение инфузионной терапии значительно ускоряет процесс восстановления и предотвращает развитие осложнений.
Получить дополнительные сведения – http://kapelnicza-ot-zapoya-v-volgograde17.ru
Каждое направление встроено в общую стратегию: не просто купировать симптомы, а уменьшить риск повторения сценария, когда после «облегчения» всё возвращается к прежней модели употребления.
Получить дополнительную информацию – https://narkologicheskaya-klinika-kolomna2-10.ru/narkologicheskaya-klinika-cena-v-kolomne
The TriNova Natural Pet https://trevorjd.com/index.php/The_Cheap_Stain_Removers_CHOICE_Experts_Recommend,_And_The_Best_In_Our_Test and Odor Remover is an advanced enzyme cleaner spray designed to safely eliminate pet stains and odors from various surfaces, using a natural and organic formula. The TriNova Natural Pet Stain and Odor Remover is an advanced enzyme cleaner spray designed to eliminate tough pet messes. Formulated with natural and organic ingredients, this powerful solution effectively tackles old and new stains and odors from dogs, cats, and even small animals, restoring surfaces to a clean and neutral state. Say goodbye to persistent pet odors and unsightly marks with this reliable, all-surface safe cleaner. Natural & Organic Formula: Made with 100% natural and organic ingredients, ensuring an effective yet gentle cleaning solution for your home. Professional Strength Enzymes: Features a blend of natural enzymes that deeply penetrate to break down and neutralize organic stains and odors at their source, preventing pets from re-marking. Safe for Your Family & Pets: Its gentle formula is safe to use around children and pets, free from harsh chemicals and toxins, providing peace of mind.
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Ознакомиться с деталями – https://vyvod-iz-zapoya-ramenskoe10.ru/vyvod-iz-zapoya-ryadom-v-ramenskom
Эти методы используются в комплексе и создают прочный фундамент для восстановления здоровья.
Детальнее – лечение алкоголизма в стационаре
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Подробнее – вывод из запоя недорого
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Изучить вопрос глубже – выезд нарколога на дом уфа
Ниже — ориентир для острых часов на дому. Это не жёсткий шаблон, а карта, где ясно: что делаем, чем измеряем, когда пересматриваем. При отсутствии отклика мы меняем один параметр (например, темп инфузии) и назначаем новое окно оценки, не «двигая» всё остальное.
Подробнее можно узнать тут – врач нарколог выезд на дом
Такая комплексность обеспечивает воздействие на физические, психологические и социальные факторы зависимости.
Детальнее – lechenie-alkogolizma-omsk0.ru/
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Подробнее можно узнать тут – как происходит кодирование от алкоголизма
Выбор клиники — задача не только медицинская, но и стратегическая. Учитывать нужно не только наличие лицензии, но и содержание программ, их гибкость, участие родственников в процессе, а также прозрачность взаимодействия с пациентом. Именно эти аспекты позволяют отличить профессиональное учреждение от формального.
Углубиться в тему – http://narkologicheskaya-klinika-yaroslavl0.ru/narkologicheskaya-klinika-telefon-yaroslavl/
resource https://heyanon.pro
Hello colleagues, fastidious piece of writing and good arguments commented at this
place, I am in fact enjoying by these.
Check out my page; stem cell clinic
Наркологическая клиника «МедЛайн» предоставляет профессиональные услуги врача-нарколога с выездом на дом в Новосибирске и Новосибирской области. Мы оперативно помогаем пациентам справиться с тяжелыми состояниями при алкогольной и наркотической зависимости. Экстренный выезд наших специалистов доступен круглосуточно, а лечение проводится с применением проверенных методик и препаратов, что гарантирует безопасность и конфиденциальность каждому пациенту.
Разобраться лучше – выезд нарколога на дом новосибирск
Город живёт в разных темпах: плотный центр, мостовые переходы, набережная, спальные районы. Мы строим маршрут так, чтобы не привлекать внимания соседей и не терять время на трафик. Если на предзвонке отмечаются «красные флаги» — давящая боль в груди, выраженная одышка, спутанность сознания, судороги, неукротимая рвота или резкое падение насыщения кислородом, — команда instantly переключает маршрут в стационарный «коридор»: палата резервируется заранее, документы оформляются нейтрально, транспорт — немаркированный. Если угроз нет, всё начинается на дому с адресной детокс-схемы и мягкой сенсорной поддержкой.
Изучить вопрос глубже – помощь нарколога на дому в саратове
Алгоритм в «Трезвый Центр Коломна» построен так, чтобы убрать импровизацию и сделать всё максимально прозрачным для семьи. Сначала по телефону собираются ключевые данные: возраст пациента, длительность запоя, виды алкоголя, хронические заболевания, препараты, аллергии, наличие судорог, потерь сознания, странного поведения, текущие жалобы. На этом этапе озвучивается ориентировочный формат помощи и примерный диапазон стоимости. Далее следует выезд на дом или поступление в стационар. Врач проводит осмотр: измеряет артериальное давление, пульс, сатурацию, температуру, оценивает тремор, координацию, сознание, степень обезвоживания, наличие болей, состояние дыхания и сердца. На основе этих данных назначается инфузионная терапия: растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы, по показаниям — гепатопротекторы, антиоксидантные комплексы, противорвотные для контроля тошноты, мягкие анксиолитики для уменьшения тревоги и нормализации сна. Уходят от агрессивной седации: пациент не должен быть «выключен» так, чтобы невозможно было заметить ухудшение. В процессе капельниц проводится повторный контроль показателей, темп и состав при необходимости корректируются. После стабилизации пациент и семья получают подробные рекомендации: режим, сон, питание, питьё, запреты, «красные флаги», план наблюдения и возможного дальнейшего лечения зависимости.
Узнать больше – http://vyvod-iz-zapoya-kolomna10.ru/vyvod-iz-zapoya-na-domu-v-kolomne/
После завершения процедур пациенту предоставляется подробная консультация с рекомендациями по дальнейшему восстановлению и профилактике повторных случаев зависимости.
Ознакомиться с деталями – нарколог на дом новосибирская область
Hurrah, that’s what I was seeking for, what a information! present here at this web site, thanks admin of this web site.
Thank you for the auspicious writeup. It in fact was
a amusement account it. Look advanced to more added agreeable from you!
By the way, how could we communicate?
Выездной наркологический сервис «МедПоволжье Клиник» создан для случаев, когда важны скорость, тишина и клиническая точность. Мы проводим детоксикацию и снятие интоксикации на дому так, чтобы каждое действие имело цель, измеримый маркер и заранее оговорённое «окно переоценки». Вместо «сильной капельницы на всякий случай» — модульная схема: один симптом-кластер > один медицинский модуль > одна поведенческая опора (свет, звук, вода малыми глотками, дыхание 4–6). Такой подход снижает лекарственную нагрузку, ускоряет стабилизацию и позволяет видеть прогресс буквально по часам.
Подробнее можно узнать тут – вызвать нарколога на дом срочно
Одним из самых востребованных направлений является вывод из запоя. Это процедура, направленная на очищение организма от этанола и продуктов его распада, восстановление водно-солевого баланса и нормализацию работы нервной системы. Врач проводит обследование, определяет степень интоксикации и подбирает состав капельницы. Уже через 30–60 минут после начала процедуры состояние пациента заметно улучшается.
Углубиться в тему – оказание наркологической помощи волгоград
лучшее казино с промокодом
Инфузионная терапия (капельницы) — важная часть лечения, направленная на очищение организма, восстановление водно-солевого баланса и устранение токсинов. В «РязаньМед Альянс» используются проверенные препараты, которые помогают нормализовать работу внутренних органов и улучшить общее самочувствие. Таблица ниже показывает, какие виды капельниц чаще всего применяются при выведении из запоя и лечении алкоголизма.
Получить дополнительную информацию – https://narkologicheskaya-klinika-v-ryazani17.ru/narkologicheskij-staczionar-ryazan/
Как отмечает руководитель клинико-диагностического отдела ФГБУ «Национальный центр наркологии», «участие в терапии нескольких специалистов разных направлений позволяет учитывать не только симптомы, но и глубинные причины зависимости». Именно такой подход снижает риск рецидивов и повышает эффективность лечения.
Детальнее – http://narkologicheskaya-klinika-yaroslavl0.ru/
Формат помощи
Ознакомиться с деталями – vyvod-iz-zapoya-24
website link https://heyanon.my/
Процесс детоксикации состоит из нескольких последовательных шагов, направленных на безопасное очищение организма. Ниже представлена таблица с описанием этапов, которые применяются в клинике «Трезвая Линия Волгоград».
Подробнее тут – вывод из запоя вызов
Read More Here https://blendfun.xyz/
Valuable information Thanks. https://pangmaiwai.wordpress.com/2025/12/10/betflix-de-reviews
My partner and I absolutely love your blog and find a lot of
your post’s to be precisely what I’m looking for.
Does one offer guest writers to write content for yourself?
I wouldn’t mind creating a post or elaborating on a lot of the subjects you write about here.
Again, awesome web site!
Hmm is anyone else encountering problems with the images on this blog loading?
I’m trying to find out if its a problem on my end or if it’s the blog.
Any feed-back would be greatly appreciated.
Ниже представлена таблица с основными препаратами, используемыми при выводе из запоя в Тюмени:
Получить больше информации – вывод из запоя клиника
Программа лечения строится по принципу последовательного воздействия на физическое и психологическое состояние. Начинается она с детоксикации: инфузионная терапия с применением сбалансированных растворов, антиоксидантов, гепатопротекторов и витаминов. Затем — стабилизация состояния, коррекция сна, восстановление когнитивных функций и купирование абстинентного синдрома. В зависимости от диагноза используются такие методы, как заместительная терапия, нейрометаболическая поддержка, противотревожные и антидепрессивные схемы.
Исследовать вопрос подробнее – наркологическая клиника лечение алкоголизма
Вывод из запоя в Тюмени — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормального функционирования организма. Длительное употребление спиртных напитков приводит к нарушению обмена веществ, обезвоживанию, сбоям в работе печени и сердца. В таких случаях требуется профессиональная помощь врача-нарколога, который подберёт оптимальный способ дезинтоксикации и медикаментозной поддержки. Современные методики позволяют провести вывод из запоя безопасно, эффективно и без осложнений.
Изучить вопрос глубже – срочный вывод из запоя в тюмени
Тем, кто нуждается в длительной терапии, «КузбассМед» предлагает комфортные условия стационара с круглосуточным наблюдением. Здесь пациенты размещаются в индивидуальных палатах, проходят курсы терапии, реабилитации и психокоррекции. Обстановка в клинике напоминает оздоровительный центр: мягкое освещение, тишина, доступ к библиотеке, возможность общения с психологом и ежедневное участие в восстановительных мероприятиях. Медицинские сестры и врачи находятся на дежурстве 24/7, что позволяет немедленно реагировать на любые изменения в состоянии пациента.
Получить больше информации – http://narkologicheskaya-klinika-novokuzneczk0.ru
Выбор клиники — задача не только медицинская, но и стратегическая. Учитывать нужно не только наличие лицензии, но и содержание программ, их гибкость, участие родственников в процессе, а также прозрачность взаимодействия с пациентом. Именно эти аспекты позволяют отличить профессиональное учреждение от формального.
Выяснить больше – https://narkologicheskaya-klinika-yaroslavl0.ru/chastnaya-narkologicheskaya-klinika-yaroslavl/
Наркологическая клиника «КоломнаМед Центр» — это место, куда можно обратиться в тот момент, когда домашние попытки контролировать алкоголь, наркотики, аптечные препараты или смесь всего сразу перестают работать, а жизнь превращается в постоянное «завтра начну с нуля». Здесь не обещают чудес за один день и не пугают диагнозами, а выстраивают понятный медицинский маршрут: детоксикация, стабилизация, реабилитация, поддержка семьи, профилактика срывов. Пациент получает помощь в защищённой, конфиденциальной среде, где всё организовано так, чтобы снизить тревогу и стыд, убрать хаос вокруг зависимости и дать человеку шанс вернуться к нормальной жизни без давления, угроз и токсичных «стимулов». Для родных клиника в Коломне — это опора: конкретный адрес, конкретная команда, чёткие сроки и понятные этапы, вместо бесконечных обещаний «он сам справится».
Разобраться лучше – http://narkologicheskaya-klinika-kolomna10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/
Le classement des casinos en ligne proposé sur georges-brassens.fr repose sur une analyse comparative indépendante des
plateformes accessibles depuis la France en 2025.
Chaque casino est évalué selon des critères précis incluant la fiabilité de la
licence, la sécurité des transactions, la rapidité des retraits, les moyens de paiement acceptés,
la qualité du catalogue de jeux et la clarté des conditions de bonus.
Une attention particulière est accordée à l’expérience utilisateur, à la compatibilité
mobile et à la transparence des informations fournies par les opérateurs.
L’objectif de georges-brassens.fr est de fournir un classement clair et structuré permettant aux joueurs de comparer les casinos en ligne de manière objective et de
choisir une plateforme adaptée à leurs attentes,
que ce soit pour une première inscription ou pour un usage régulier.
Наркологическая помощь в Волгограде предназначена для людей, столкнувшихся с проблемами алкогольной или наркотической зависимости. Современный подход к лечению основан на сочетании медицинских, психологических и социальных методов, направленных на полное восстановление пациента. Врачи-наркологи применяют безопасные схемы детоксикации, эффективные медикаменты и программы психотерапевтической поддержки, позволяющие достичь устойчивой ремиссии и вернуть пациента к нормальной жизни.
Подробнее можно узнать тут – экстренная наркологическая помощь в волгограде
Вывод из запоя требуется тогда, когда организм уже не способен самостоятельно справиться с последствиями алкогольной интоксикации. Длительное употребление спиртного приводит к нарушению работы внутренних органов, обезвоживанию и психическим расстройствам. Медицинская помощь помогает избежать опасных осложнений и облегчить процесс отказа от алкоголя.
Углубиться в тему – вывод из запоя цена в рязани
В Волгограде медицинская клиника «Трезвая Линия Волгоград» предоставляет круглосуточную помощь людям, столкнувшимся с острым алкогольным отравлением или затяжным запоем. Врачи выезжают на дом, в гостиницу или принимают пациентов в стационаре. Каждое вмешательство начинается с оценки состояния — измерения давления, пульса, насыщения кислородом, уровня интоксикации и дехидратации. Далее подбирается оптимальный состав капельницы, направленный на восстановление водно-солевого баланса, поддержку печени и снижение тревожности.
Получить больше информации – вывод из запоя на дому цена волгоград
Каждое направление встроено в общую стратегию: не просто купировать симптомы, а уменьшить риск повторения сценария, когда после «облегчения» всё возвращается к прежней модели употребления.
Изучить вопрос глубже – adresa-narkologicheskih-klinik
Клиника «АнтиАлко» предлагает экстренную медицинскую помощь на дому в Новосибирске и Новосибирской области для тех, кто столкнулся с запоем. Если вы или ваш близкий оказались в состоянии длительной алкогольной интоксикации, наши специалисты готовы оперативно приехать к вам, провести комплексную детоксикацию и купировать симптомы абстинентного синдрома. Мы гарантируем высокий уровень безопасности, полную анонимность и индивидуальный подход к каждому пациенту.
Получить дополнительные сведения – http://vyvod-iz-zapoya-novosibirsk00.ru/vyvod-iz-zapoya-czena-novosibirsk/
Наркологическая помощь в Волгограде предназначена для людей, столкнувшихся с проблемами алкогольной или наркотической зависимости. Современный подход к лечению основан на сочетании медицинских, психологических и социальных методов, направленных на полное восстановление пациента. Врачи-наркологи применяют безопасные схемы детоксикации, эффективные медикаменты и программы психотерапевтической поддержки, позволяющие достичь устойчивой ремиссии и вернуть пациента к нормальной жизни.
Узнать больше – https://narkologicheskaya-pomoshh-v-volgograde17.ru/
После детоксикации пациенту назначается медикаментозная терапия, направленная на стабилизацию работы нервной системы и снижение тяги к наркотикам. Медикаменты подбираются индивидуально, учитывая особенности состояния каждого пациента.
Узнать больше – лечение наркомании в стационаре в твери
Программы вывода из запоя в клинике разрабатываются с учётом состояния пациента. Для тяжёлых случаев назначается интенсивный курс с инфузионной терапией и контролем электролитов. При лёгких формах применяются мягкие препараты с постепенным выведением токсинов. Все процедуры проходят с соблюдением медицинских стандартов и полным сохранением анонимности.
Получить дополнительные сведения – наркологический вывод из запоя волгоград
Вывод из запоя в Омске проводится в условиях клиники с применением современных методов детоксикации и круглосуточного медицинского наблюдения. Длительное употребление алкоголя вызывает серьезную интоксикацию организма, нарушает работу внутренних органов и психоэмоциональное состояние. Своевременное обращение к специалистам позволяет избежать осложнений и восстановить здоровье пациента безопасным образом.
Подробнее – https://vyvod-iz-zapoya-omsk0.ru/vyvod-iz-zapoya-omsk-czena/
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Получить дополнительные сведения – http://narkologicheskaya-klinika-kolomna2-10.ru
Клиника в Коломне ориентирована на полный цикл помощи: от экстренных состояний до длительного сопровождения. Здесь важна не только медицинская составляющая, но и человеческая: уважение, конфиденциальность, отсутствие стигмы. Ниже — ключевые направления, которые выстраиваются в единую систему лечения, а не существуют по отдельности.
Ознакомиться с деталями – https://narkologicheskaya-klinika-kolomna10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
Наркологическая клиника «МедЛайн» предоставляет профессиональные услуги врача-нарколога с выездом на дом в Новосибирске и Новосибирской области. Мы оперативно помогаем пациентам справиться с тяжелыми состояниями при алкогольной и наркотической зависимости. Экстренный выезд наших специалистов доступен круглосуточно, а лечение проводится с применением проверенных методик и препаратов, что гарантирует безопасность и конфиденциальность каждому пациенту.
Получить дополнительные сведения – вызвать нарколога на дом в новосибирске
Для оказания полноценной помощи вне стен клиники специалисты «ТверьМед» используют портативные устройства: инфузоматы, ЭКГ-мониторы, глюкометры, пульсоксиметры, небулайзеры и наборы медикаментов. Все врачи обучены работе в полевых условиях и готовы к экстренным ситуациям. Отдельное внимание уделяется стерильности и безопасности: используются одноразовые расходники, врач носит маску, перчатки и защитный халат. При необходимости на выезд направляется параллельно медсестра или ассистент с расширенным функционалом.
Исследовать вопрос подробнее – вызвать наркологическую помощь в твери
При поступлении вызова специалисты клиники «АнтиАлко» выезжают на дом в течение 30–60 минут. По прибытии врач проводит комплексную диагностику: измеряет артериальное давление, пульс, уровень кислорода в крови и собирает анамнез, чтобы оценить степень интоксикации. На основе полученных данных формируется индивидуальный план лечения, который включает:
Углубиться в тему – vyvod-iz-zapoya-czena novosibirsk
Лечение алкоголизма в Омске проводится с использованием современных методов, направленных на восстановление организма и психики пациента. Специалисты уделяют внимание как медицинским, так и психологическим аспектам, что позволяет достигать устойчивых результатов. Основой терапии является индивидуальный подход, благодаря которому каждая программа учитывает состояние здоровья и уровень зависимости.
Исследовать вопрос подробнее – http://lechenie-alkogolizma-omsk0.ru/
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Получить дополнительную информацию – vyvod-iz-zapoya
超人和露易斯第一季高清完整官方版,海外华人可免费观看最新热播剧集。
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Получить дополнительную информацию – вывод из запоя цена в волгограде
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Ознакомиться с деталями – скорая вывод из запоя в рязани
Процесс включает несколько шагов:
Получить дополнительные сведения – нарколог на дом уфа
Комплексное применение этих методов позволяет значительно ускорить процесс восстановления и предотвратить осложнения.
Подробнее – наркологическая клиника наркологический центр
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Получить дополнительные сведения – вывод из запоя дешево саратов
Вывод из запоя в Раменском в условиях клиники строится не вокруг одной капельницы, а вокруг понятной цепочки шагов, где каждый этап логичен и медицински обоснован. Это помогает не только быстро облегчить состояние, но и уменьшить вероятность того, что через пару дней человек снова уйдёт в запой.
Подробнее тут – вывод из запоя врачом
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Выяснить больше – https://vivod-iz-zapoya-v-volgograde17.ru/
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Детальнее – врач нарколог на дом в уфе
Наркологическая клиника «КоломнаМед Центр» — это место, куда можно обратиться в тот момент, когда домашние попытки контролировать алкоголь, наркотики, аптечные препараты или смесь всего сразу перестают работать, а жизнь превращается в постоянное «завтра начну с нуля». Здесь не обещают чудес за один день и не пугают диагнозами, а выстраивают понятный медицинский маршрут: детоксикация, стабилизация, реабилитация, поддержка семьи, профилактика срывов. Пациент получает помощь в защищённой, конфиденциальной среде, где всё организовано так, чтобы снизить тревогу и стыд, убрать хаос вокруг зависимости и дать человеку шанс вернуться к нормальной жизни без давления, угроз и токсичных «стимулов». Для родных клиника в Коломне — это опора: конкретный адрес, конкретная команда, чёткие сроки и понятные этапы, вместо бесконечных обещаний «он сам справится».
Разобраться лучше – https://narkologicheskaya-klinika-kolomna10.ru/narkologicheskaya-klinika-cena-v-kolomne
pop over to these guys https://askthehive.org
Важной частью реабилитации является социализация пациента, возвращение его к активной общественной жизни и формирование новых, здоровых привычек. Для этого в клинике организуются различные мероприятия и программы адаптации.
Исследовать вопрос подробнее – запой лечение наркомания тверь
Way cool! Some very valid points! I appreciate you
penning this article plus the rest of the website is also very good.
Вывод из запоя в Рязани — это профессиональная медицинская процедура, направленная на очищение организма от токсинов, восстановление нормального самочувствия и предотвращение осложнений после длительного употребления алкоголя. В специализированных клиниках города лечение проводится с использованием современных методов детоксикации и под контролем опытных врачей-наркологов. Такой подход позволяет быстро и безопасно стабилизировать состояние пациента, устранить физическую зависимость и подготовить организм к дальнейшему восстановлению.
Подробнее тут – http://vyvod-iz-zapoya-v-ryazani17.ru/vyvod-iz-zapoya-ryazan-na-domu/
Наркологическая помощь в Новокузнецке представляет собой комплекс профессиональных медицинских мероприятий, направленных на диагностику, лечение и реабилитацию пациентов с алкогольной и наркотической зависимостью. В клинике «Альтернатива» помощь оказывается на всех этапах заболевания, что позволяет добиться стойких положительных результатов и восстановления качества жизни.
Получить дополнительные сведения – платная наркологическая помощь новокузнецк
Даже телефонный разговор с клиникой может многое сказать о её подходе. Если вам предлагают типовое лечение без уточнения подробностей или избегают вопросов о составе команды, это тревожный сигнал. Серьёзные учреждения в Мурманске обязательно предложат предварительную консультацию, зададут уточняющие вопросы и расскажут, как строится программа помощи.
Углубиться в тему – http://www.domen.ru
Пациенты выбирают нашу клинику для срочного вызова врача-нарколога благодаря следующим важным преимуществам:
Подробнее можно узнать тут – https://narcolog-na-dom-novosibirsk00.ru
Не всегда человек способен прекратить употребление алкоголя без медицинского вмешательства. Чем дольше длится запой, тем выше риск осложнений. Обратиться к специалисту следует при появлении следующих признаков:
Детальнее – вывод из запоя круглосуточно в тюмени
Одним из ключевых преимуществ «КузбассМед» является современная материально-техническая база. В клинике задействованы устройства для точного мониторинга жизненных функций, автоматические инфузионные системы, экспресс-диагностические модули и оборудование для неотложной терапии. Врачи используют программируемые дозаторы, портативные анализаторы крови и аппараты для оценки дыхательной функции, что позволяет своевременно корректировать тактику лечения без потерь времени. Все процедуры соответствуют национальным стандартам безопасности и рекомендациям ВОЗ.
Подробнее – частная наркологическая клиника
Терапия проводится поэтапно, что позволяет пациенту последовательно проходить все стадии восстановления и закреплять результат.
Детальнее – лечение наркомании и алкоголизма омск
Hi there to all, it’s genuinely a good for me to pay a visit this site, it includes valuable Information.
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Углубиться в тему – http://vyvod-iz-zapoya-saratov0.ru/vyvod-iz-zapoya-saratov-staczionar/
Лечение наркомании в клинике начинается с диагностики, позволяющей определить степень зависимости, выявить сопутствующие заболевания и выбрать оптимальную тактику терапии. Важным этапом является детоксикация — очищение организма от токсинов и продуктов распада наркотических веществ, что снижает риск осложнений и облегчает последующее восстановление.
Детальнее – запой лечение наркомания тверь
see here https://unchainx.org/
Комплексный подход к выводу из запоя на дому в Ярославле включает несколько основных этапов, которые позволяют обеспечить оперативное и безопасное лечение:
Углубиться в тему – вывод из запоя клиника ярославль
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Углубиться в тему – вывод наркологическая клиника
Услуга «нарколог на дом в Долгопрудном» от клиники «МедТрезвие Долгопрудный» создана для ситуаций, когда важно действовать быстро, аккуратно и без лишнего шума. Запой, тяжёлое похмелье, срыв после ремиссии, злоупотребление медикаментами или смесью алкоголя с препаратами — всё это не терпит откладывания и самодеятельности. Вызов врача на дом позволяет получить профессиональную помощь без госпитализации, когда состояние пациента ещё позволяет лечить его в привычной обстановке. Нарколог приезжает с полностью укомплектованным набором препаратов и расходников, проводит осмотр, подбирает капельницы по клиническим показаниям, контролирует реакцию, даёт подробные рекомендации на ближайшие дни и при необходимости предлагает дальнейший маршрут: повторный выезд, амбулаторное наблюдение или стационар клиники. Конфиденциальность соблюдается строго: без обсуждений с соседями, без регистрации по месту работы, без унизительных формальностей — только медицинская помощь, ориентированная на безопасность и результат.
Подробнее можно узнать тут – https://narkolog-na-dom-dolgoprudnij10.ru/vyezd-narkologa-na-dom-v-dolgoprudnom/
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Разобраться лучше – вывод из запоя на дому цена саратов
«Трезвый Путь Коломна» создаёт единый контур помощи: пациент не «перекидывается» между разными организациями, а проходит лечение в одной системе, где специалисты знают его историю и несут ответственность за последовательность шагов. Это критично для тех, кто уже сталкивался с бессистемными попытками: один врач ставил капельницы, другой «кодировал», третий давал советы, а в итоге всё заканчивалось новым срывом. Здесь маршруты связываются в цельную линию.
Ознакомиться с деталями – narkologicheskaya-klinika-kolomna
Не всегда человек способен прекратить употребление алкоголя без медицинского вмешательства. Чем дольше длится запой, тем выше риск осложнений. Обратиться к специалисту следует при появлении следующих признаков:
Ознакомиться с деталями – https://vyvod-iz-zapoya-v-tyumeni17.ru/vyvod-iz-zapoya-v-staczionare-tyumen
Одним из ключевых преимуществ «КузбассМед» является современная материально-техническая база. В клинике задействованы устройства для точного мониторинга жизненных функций, автоматические инфузионные системы, экспресс-диагностические модули и оборудование для неотложной терапии. Врачи используют программируемые дозаторы, портативные анализаторы крови и аппараты для оценки дыхательной функции, что позволяет своевременно корректировать тактику лечения без потерь времени. Все процедуры соответствуют национальным стандартам безопасности и рекомендациям ВОЗ.
Подробнее тут – https://narkologicheskaya-klinika-novokuzneczk0.ru/narkologicheskij-czentr-novokuzneczk
Эти методы используются в комплексе и создают прочный фундамент для восстановления здоровья.
Выяснить больше – https://lechenie-alkogolizma-omsk0.ru/besplatnoe-lechenie-alkogolizma-v-omske/
Прежде чем говорить о цифрах, важно обозначить принцип: цена формируется из реального объёма медицинской помощи, а не из рекламных обещаний. На итоговую стоимость влияет длительность запоя, выраженность интоксикации, необходимость одной или нескольких капельниц, подбор дополнительных препаратов, время суток выезда, объём наблюдения, а также наличие сопутствующих заболеваний, повышающих риск. «СерпуховТрезвие» придерживается открытой схемы: при звонке озвучивается ориентировочный диапазон, поясняется, что входит в базовый визит и при каких условиях он может перейти в расширенный. Все дополнительные назначения согласуются до их выполнения, без скрытых доплат и «сюрпризов» по факту.
Подробнее – narkolog-na-dom-kruglosutochno
Вывод из запоя в Раменском — это не просто «поставить капельницу и отпустить домой», а комплекс медицинских действий, от которых напрямую зависит здоровье, а иногда и жизнь человека. Длительное употребление алкоголя приводит к тяжёлой интоксикации, нарушению работы сердца, печени, головного мозга, сбоям давления, риску судорог, психозов и резких обострений хронических заболеваний. Попытки самостоятельно «сойти с дистанции» дома, с помощью случайных таблеток, седативных препаратов и новых доз алкоголя, часто только усугубляют состояние. Наркологическая клиника «РаменМед Трезвость» в Раменском выстраивает вывод из запоя как безопасный, контролируемый, поэтапный процесс: от экстренного купирования симптомов до формирования плана дальнейшего восстановления. Пациент получает помощь без осуждения, анонимно, с участием специалистов, которые берут на себя ответственность за каждое назначение и каждое действие. Для родственников это означает: больше не нужно гадать, чего бояться и что давать — есть конкретное место и команда, к которым можно обратиться сразу.
Углубиться в тему – https://vyvod-iz-zapoya-ramenskoe10.ru/
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Ознакомиться с деталями – помощь нарколога на дому
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Разобраться лучше – наркология вывод из запоя
Практический тест прост: сохранённый контакт, контролируемый тремор, эпизодическая (не неукротимая) рвота, нет грубой дезориентации, давление и пульс не «скачут», в квартире можно обеспечить тишину и доступ к воде — тогда дом уместен. Если хотя бы два пункта «провисают», отделение в Электростали даст предсказуемость и защиту от ночных ухудшений, которые дома часто остаются незамеченными.
Получить больше информации – http://vyvod-iz-zapoya-ehlektrostal10.ru/
I think the admin of this website is in fact working hard in favor of his web page,
since here every data is quality based stuff.
Highly energetic post, I liked that a lot. Will there be a
part 2?
It’s actually a nice and helpful piece of info. I’m glad that you just
shared this helpful information with us. Please stay us up to
date like this. Thanks for sharing.
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Получить дополнительные сведения – заказать звонок наркологическая клиника
Ниже — ключевые направления, которые логично дополняют друг друга и формируют единый маршрут лечения:
Детальнее – narkologicheskaya-klinika-ramenskoe10.ru/
Прежде чем перейти к ориентировочным цифрам, важно подчеркнуть: цена формируется из реальных компонентов помощи — работы врача и медсестры, объёма инфузионной терапии, перечня препаратов, времени выезда и необходимости более длительного наблюдения. Никаких скрытых доплат: все дополнительные назначения согласуются заранее. Чем раньше вы обращаетесь, тем меньше объём вмешательств и, как правило, ниже итоговая стоимость — короткий эпизод проще и дешевле стабилизировать, чем «выводить» осложнения после затянутого запоя.
Узнать больше – http://narkolog-na-dom-shchelkovo10.ru
Вывод из запоя в Раменском в условиях клиники строится не вокруг одной капельницы, а вокруг понятной цепочки шагов, где каждый этап логичен и медицински обоснован. Это помогает не только быстро облегчить состояние, но и уменьшить вероятность того, что через пару дней человек снова уйдёт в запой.
Изучить вопрос глубже – vyvod-iz-zapoya-kapelnica
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Разобраться лучше – нарколог на дом недорого саратов
После прохождения основной программы пациенту предлагается поддерживающее наблюдение. Оно может включать дистанционные консультации, участие в группе профилактики срывов, повторные осмотры нарколога и психолога, корректировку медикаментозной схемы. В рамках реабилитации формируются планы действий при возникновении тяги, обучаются навыки сопротивления стрессу и внешнему давлению. При желании можно подключить родственников к процессу постлечебной адаптации, чтобы укрепить результат и снизить риски рецидивов. Таким образом, пациент не остаётся один даже после выписки.
Изучить вопрос глубже – http://lechenie-narkomanii-novokuzneczk0.ru/lechenie-na-narkomani-czeny-novokuzneczk/
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Изучить вопрос глубже – вывод из запоя недорого
Алкогольная интоксикация вызывает сильное обезвоживание и разрушает баланс электролитов в организме. Без медицинской помощи восстановление может занять несколько дней, а в тяжёлых случаях приводит к осложнениям. Капельница помогает безопасно и быстро вывести этанол и продукты его распада, восполнить уровень жидкости, снизить нагрузку на печень и сердечно-сосудистую систему. Процедура проводится амбулаторно или на дому, что делает её доступной и удобной для пациентов.
Исследовать вопрос подробнее – капельница от запоя стоимость волгоград
После поступления вызова наш нарколог выезжает к пациенту в кратчайшие сроки, прибывая по адресу в пределах 30–60 минут. Специалист начинает процедуру с подробного осмотра и диагностики, измеряя ключевые показатели организма: артериальное давление, частоту пульса, насыщенность кислородом и собирая подробный анамнез.
Выяснить больше – narkolog-na-dom novosibirsk
Your style is very unique in comparison to other folks I’ve read stuff from.
Thank you for posting when you have the
opportunity, Guess I will just book mark this page.
read the article https://hyperunit.us
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Исследовать вопрос подробнее – кодирование от алкоголизма цена адреса в волгограде
Клиника «Трезвый Шаг Раменское» выстраивает помощь так, чтобы пациент и его близкие не метались между разными службами и частными «специалистами», а получали комплекс услуг в одном месте. Это особенно важно для тех, кто уже сталкивался с провалами после разовых кодировок, неподходящих капельниц или формальной «помощи».
Изучить вопрос глубже – adresa-narkologicheskih-klinik
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Получить дополнительные сведения – нарколог на дом вывод из запоя
Very nice post. I certainly love this site. Stick with it!
Прежде чем принимать решение, важно изучить сайт клиники. В надёжных учреждениях размещена полная информация о врачах, их образовании и опыте работы. Кроме того, пациентам предлагается пройти предварительную консультацию — чаще всего она проводится анонимно и включает первичную диагностику. Это позволяет оценить профессионализм команды ещё до начала терапии.
Углубиться в тему – наркологические клиники алкоголизм ярославль.
После поступления вызова наш нарколог выезжает к пациенту в кратчайшие сроки, прибывая по адресу в пределах 30–60 минут. Специалист начинает процедуру с подробного осмотра и диагностики, измеряя ключевые показатели организма: артериальное давление, частоту пульса, насыщенность кислородом и собирая подробный анамнез.
Выяснить больше – вызов врача нарколога на дом в новосибирске
my explanation https://flaunch.ink/
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Детальнее – http://kodirovanie-ot-alkogolizma-v-volgograde17.ru
Наркологическая клиника «Трезвый Шаг Раменское» — это место, где острые кризисы, многолетние запои и повторяющиеся срывы перестают быть бесконечным кругом, в котором семья остаётся один на один с проблемой. Здесь выстроена система помощи людям с алкогольной и наркотической зависимостью, а также полизависимостями, включая злоупотребление аптечными препаратами. В клинике в Раменском сочетаются круглосуточное наблюдение, профессиональная детоксикация, медикаментозная поддержка, психотерапевтические программы и сопровождение семьи. Важные принципы — безопасность, анонимность, уважение к пациенту и честное объяснение каждого шага лечения. Ни агрессивного давления, ни обещаний «чуда за один день» — вместо этого поэтапный подход, который даёт реальный шанс стабилизировать состояние, снизить тягу и выйти из разрушительного сценария под контролем специалистов. Для близких это означает понятный маршрут: куда обратиться, что будут делать с пациентом, какие риски учтут и как клиника «Трезвый Шаг Раменское» останется на связи после острого периода.
Подробнее – частная наркологическая клиника
My spouse and I stumbled over here from a different web page and thought
I may as well check things out. I like what I see so i am just following you.
Look forward to checking out your web page for a second time.
Ключевым фактором при выборе центра становится квалификация специалистов. Лечение алкоголизма — это не только выведение из запоя и купирование абстинентного синдрома. Оно включает работу с мотивацией, тревожными состояниями, семейными конфликтами, нарушением сна и другими последствиями зависимости. Только команда, включающая наркологов, психотерапевтов и консультантов по аддиктивному поведению, способна охватить все аспекты проблемы.
Углубиться в тему – https://lechenie-alkogolizma-murmansk0.ru/lechenie-khronicheskogo-alkogolizma-marmansk
Диспетчер уточняет адрес в Электростали, длительность эпизода, текущие препараты и дозы, аллергии, сопутствующие заболевания, последние значения давления/пульса. Это экономит 15–20 минут на месте и позволяет заранее исключить опасные взаимодействия.
Исследовать вопрос подробнее – вывод из запоя вызов на дом
Вывод из запоя — это экстренная медицинская помощь, направленная на очищение организма от алкоголя, снятие симптомов интоксикации и восстановление работы внутренних органов. В клинике «Трезвая Линия Волгоград» используется комплексный подход, включающий капельницы, препараты для детоксикации и постоянный врачебный контроль. Лечение проводится анонимно, с индивидуальным подбором медикаментов и поддержкой пациента на каждом этапе восстановления. Главная цель специалистов — не просто стабилизировать состояние, а обеспечить безопасное возвращение к нормальному самочувствию и предотвратить повторные срывы.
Получить больше информации – vyvod-iz-zapoia-v-volgograde17.ru/
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Выяснить больше – https://narkolog-na-dom-shchelkovo10.ru/vrach-narkolog-na-dom-shchelkovo/
You really make it seem so easy along with your presentation but I to find this
topic to be actually something which I believe I would by no means understand.
It sort of feels too complicated and extremely wide for me.
I’m taking a look forward for your next put up, I will try to get the cling
of it!
Современная наркологическая клиника — это не просто учреждение для экстренной помощи, а центр комплексной поддержки человека, столкнувшегося с зависимостью. В «КузбассМед» в Новокузнецке реализуется модель интенсивного вмешательства, где используются новейшие медицинские технологии, мультидисциплинарный подход и мобильные выездные службы. Специалисты готовы прибыть на дом за 30 минут с полным набором оборудования и медикаментов, обеспечив пациенту помощь в привычной и безопасной среде. Наркология здесь строится на индивидуализации: каждый случай рассматривается отдельно, с учётом психофизического состояния, анамнеза и жизненного контекста пациента.
Подробнее – наркологическая клиника вывод из запоя новокузнецк
It’s impressive that you are getting thoughts from this article as well as from our dialogue
made at this place.
My brother suggested I might like this blog. He was once entirely right.
This submit truly made my day. You can not believe simply how much time I
had spent for this information! Thank you!
Great information. Lucky me I came across your blog by
chance (stumbleupon). I’ve saved as a favorite for later!
이건 주제에서 벗어나지만, 제 최신 트위터 업데이트를
자동으로 트윗하는 위젯을 블로그에
추가할 수 있는지 궁금합니다. 이런 플러그인을 꽤 오랫동안 찾고
있었는데, 당신이 이런 것에 대해 경험이 있을지도 모른다고 생각했어요.
혹시 아는 게 있다면 알려주세요. 당신의 블로그를 정말 즐기고
있으며 새로운 업데이트를 기대하고 있습니다.
Great blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple tweeks would really make my blog jump out.
Please let me know where you got your design. With thanks
Seriously many of excellent information!
Visit my site: https://debunkingnase.org/index.php/Answers_About_London
Процесс организован так, чтобы снять с семьи хаос и дать понятный сценарий. После обращения в «РеутовМед Сервис» пациент быстро попадает в поле зрения врача: или через выезд по адресу, или через стационар, если состояние уже близко к опасному. На месте проводится полноценная оценка: давление, пульс, сатурация, температура, осмотр сердца и дыхания, степень обезвоживания, выраженность тремора, наличие рвоты, боли в груди или животе, неврологический статус, поведение, признаки психоза. На основе этих данных формируется индивидуальный план детоксикации. Стартовая инфузионная терапия подбирается с учётом возраста, массы тела, длительности запоя, сопутствующих болезней, уже принятых препаратов. В стационаре пациента размещают в безопасных условиях, контролируют динамику, корректируют дозировки, не оставляют «на самотёк». При выводе из запоя на дому врач остаётся до стабилизации, отслеживает реакцию и при первых тревожных признаках рекомендует стационар, а не уезжает «лишь бы поставил капельницу». Такой пошаговый подход позволяет не только снять острые симптомы, но и уменьшить риск осложнений — от аритмий и судорог до алкогольного делирия.
Детальнее – вывод из запоя вызов на дом
中職比分粉絲必備的資訊平台,提供最即時的中職比分新聞、球員數據分析,以及專業的比賽預測。
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Подробнее тут – адреса наркологических клиник
我們提供台灣最完整的籃球比分相關服務,包含最新賽事資訊、數據分析,以及專業賽事預測。
That is a really good tip especially to those fresh to
the blogosphere. Short but very accurate info… Thanks for sharing
this one. A must read post!
Наркологическая клиника «МедЛайн» предоставляет профессиональные услуги врача-нарколога с выездом на дом в Новосибирске и Новосибирской области. Мы оперативно помогаем пациентам справиться с тяжелыми состояниями при алкогольной и наркотической зависимости. Экстренный выезд наших специалистов доступен круглосуточно, а лечение проводится с применением проверенных методик и препаратов, что гарантирует безопасность и конфиденциальность каждому пациенту.
Узнать больше – нарколог на дом клиника в новосибирске
This is a topic which is near to my heart…
Many thanks! Exactly where are your contact details though?
Основные этапы обычно включают:
Подробнее – http://vyvod-iz-zapoya-ramenskoe10.ru/
Ниже представлена таблица с основными препаратами, используемыми при выводе из запоя в Тюмени:
Получить дополнительные сведения – http://www.domen.ru
我們的資深運彩分析官方授權專家團隊第一時間更新官方NBA、MLB、中華職棒等各大聯盟的專業賽事分析。
Hmm it appears like your website ate my first comment (it was
super long) so I guess I’ll just sum it up what I wrote and say,
I’m thoroughly enjoying your blog. I as well am an aspiring blog blogger but I’m still new
to everything. Do you have any suggestions for novice blog writers?
I’d genuinely appreciate it.
Вывод из запоя в Рязани — это профессиональная медицинская процедура, направленная на очищение организма от токсинов, восстановление нормального самочувствия и предотвращение осложнений после длительного употребления алкоголя. В специализированных клиниках города лечение проводится с использованием современных методов детоксикации и под контролем опытных врачей-наркологов. Такой подход позволяет быстро и безопасно стабилизировать состояние пациента, устранить физическую зависимость и подготовить организм к дальнейшему восстановлению.
Получить дополнительные сведения – вывод из запоя рязань
Kenvox
1701 Ε Edinger Ave
Santa Ana, CA 92705, United Statеs
16572319025
plastic prototyping solutions solutions
Прежде чем перейти к ориентировочным цифрам, важно подчеркнуть: цена формируется из реальных компонентов помощи — работы врача и медсестры, объёма инфузионной терапии, перечня препаратов, времени выезда и необходимости более длительного наблюдения. Никаких скрытых доплат: все дополнительные назначения согласуются заранее. Чем раньше вы обращаетесь, тем меньше объём вмешательств и, как правило, ниже итоговая стоимость — короткий эпизод проще и дешевле стабилизировать, чем «выводить» осложнения после затянутого запоя.
Детальнее – skolko-stoit-narkolog-na-dom
Одна из сильных сторон «РеутовМед Сервис» — честная оценка границ домашнего лечения. Клиника не обещает «вывезем любого дома», потому что есть состояния, при которых отсутствие круглосуточного наблюдения опасно. Чтобы родным было проще сориентироваться, важно разделить ситуации по уровню риска и понять, почему иногда разумнее выбрать стационар, даже если пациент сопротивляется.
Получить больше информации – вывод из запоя цена
Своевременное обращение к специалистам позволяет быстро стабилизировать состояние и избежать осложнений.
Получить дополнительные сведения – вывод из запоя на дому цена тольятти
В случаях запоя, острого отравления или абстинентного синдрома выездная наркологическая бригада оказывает помощь прямо на месте. Специалисты приезжают в течение 30 минут после обращения и проводят оценку состояния пациента, экстренное введение лекарств, инфузионную терапию и психологическую поддержку. Благодаря специальной комплектации мобильной бригады, лечение на дому возможно даже при умеренной степени осложнений. Врач также может при необходимости провести экспресс-анализы и дать рекомендации родственникам по дальнейшему уходу.
Получить дополнительные сведения – https://narkologicheskaya-klinika-novokuzneczk0.ru/narkolog-v-gorode-novokuzneczke
Award winners, individual honors and team trophies documented
Wow that was odd. I just wrote an incredibly long comment
but after I clicked submit my comment didn’t show up. Grrrr…
well I’m not writing all that over again. Anyhow, just wanted to say superb blog!
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Получить больше информации – вывод из запоя вызов на дом в волгограде
Каждый этап играет важную роль и обеспечивает пациенту необходимую поддержку на пути к трезвой жизни.
Исследовать вопрос подробнее – https://lechenie-alkogolizma-omsk0.ru/besplatnoe-lechenie-alkogolizma-v-omske
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Получить дополнительные сведения – https://vyvod-iz-zapoya-omsk0.ru/vyvod-iz-zapoya-omsk-kruglosutochno
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Исследовать вопрос подробнее – вызов нарколога на дом
Домашний формат хорош при умеренной выраженности симптомов, сохранённом контакте и возможности обеспечить наблюдение в квартире: тихая комната, взрослый рядом первые 6–8 часов, отсутствие грубой дезориентации и неукротимой рвоты, относительная стабильность АД/ЧСС. В таких условиях выездная бригада «Трезвой Линии» запускает персональную схему: регидратация, выравнивание электролитов, поддержка витаминами группы B и магнием, осторожная седация, чтобы «собрать» сон, не выключая мониторинг. Стационар предпочтителен, если запой длится 3–5 суток и более, отмечаются «качели» показателей, шаткость походки, выраженная слабость, признаки предделирия или судорожной готовности; также при сочетанной соматике (ИБС, гипертония, диабет, хронические болезни печени/почек, неврология) и у пациентов старшего возраста. Преимущество стационара — приборный контроль, тихий режим, щадящее питание, возможность быстро расширять схему без ожидания ухудшений. Мы придерживаемся принципа «минимально достаточно»: ровно столько вмешательств, сколько требует клиническая картина, — так безопаснее и в перспективе экономнее, чем череда домашних «подлаток».
Ознакомиться с деталями – http://vyvod-iz-zapoya-ehlektrostal10.ru/vyvod-iz-zapoya-na-domu-v-ehlektrostali/
Undeniably consider that that you said. Your favorite reason appeared to be on the
net the simplest thing to understand of. I say to you, I definitely get
irked whilst other folks consider issues that they just don’t know about.
You controlled to hit the nail upon the top and also defined out
the entire thing without having side-effects , folks can take a signal.
Will probably be back to get more. Thank you
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Углубиться в тему – адреса наркологических клиник
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Изучить вопрос глубже – наркологическая клиника лечение алкоголизма новокузнецк
У вас качественный материал по теме онлайн-казино.
https://www.innosons.nl/waarom-internet-zon-effectief-middel-is/
Для оказания полноценной помощи вне стен клиники специалисты «ТверьМед» используют портативные устройства: инфузоматы, ЭКГ-мониторы, глюкометры, пульсоксиметры, небулайзеры и наборы медикаментов. Все врачи обучены работе в полевых условиях и готовы к экстренным ситуациям. Отдельное внимание уделяется стерильности и безопасности: используются одноразовые расходники, врач носит маску, перчатки и защитный халат. При необходимости на выезд направляется параллельно медсестра или ассистент с расширенным функционалом.
Детальнее – частная наркологическая помощь в твери
Вывод из запоя в клинике проводится поэтапно, что позволяет обеспечить прозрачность процесса и полное понимание динамики выздоровления.
Исследовать вопрос подробнее – помощь вывод из запоя
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Получить дополнительные сведения – вывод из запоя
Даже телефонный разговор с клиникой может многое сказать о её подходе. Если вам предлагают типовое лечение без уточнения подробностей или избегают вопросов о составе команды, это тревожный сигнал. Серьёзные учреждения в Мурманске обязательно предложат предварительную консультацию, зададут уточняющие вопросы и расскажут, как строится программа помощи.
Получить дополнительную информацию – http://lechenie-alkogolizma-murmansk0.ru
Терапия проводится поэтапно, что позволяет пациенту последовательно проходить все стадии восстановления и закреплять результат.
Получить больше информации – наркологическая клиника лечение алкоголизма в омске
Инфузионная терапия (капельницы) — важная часть лечения, направленная на очищение организма, восстановление водно-солевого баланса и устранение токсинов. В «РязаньМед Альянс» используются проверенные препараты, которые помогают нормализовать работу внутренних органов и улучшить общее самочувствие. Таблица ниже показывает, какие виды капельниц чаще всего применяются при выведении из запоя и лечении алкоголизма.
Разобраться лучше – наркологическая клиника лечение алкоголизма в рязани
Продолжительность процедуры — от 40 минут до полутора часов. Уже в первые часы после начала терапии состояние пациента значительно улучшается: проходит тошнота, снижается тревожность, восстанавливается координация движений.
Ознакомиться с деталями – вывод из запоя недорого
Важной частью реабилитации является социализация пациента, возвращение его к активной общественной жизни и формирование новых, здоровых привычек. Для этого в клинике организуются различные мероприятия и программы адаптации.
Ознакомиться с деталями – https://lechenie-narkomanii-tver0.ru
Игнорирование этих симптомов может привести к тяжёлым последствиям — судорогам, галлюцинациям или алкогольному психозу.
Исследовать вопрос подробнее – http://www.domen.ru
Вывод из запоя — это не «волшебная капельница», а последовательная медицинская программа с чёткими целями и измеримыми маркерами. В наркологической клинике «СаратовМед Профи» маршрут строится по принципу управляемых окон: на каждом шаге команда преследует одну цель, меняет лишь один параметр и оценивает результат в заранее назначённый момент. Такой подход снижает лекарственную нагрузку, предотвращает «гонку дозировок» и делает динамику предсказуемой для пациента и близких. Конфиденциальность обеспечивается регламентом: немаркированные выезды, нейтральные формулировки в документах, «тихие» каналы связи, доступ к записям — строго по ролям.
Узнать больше – http://vyvod-iz-zapoya-saratov0.ru
Комплексное применение этих методов позволяет значительно ускорить процесс восстановления и предотвратить осложнения.
Выяснить больше – частная наркологическая клиника
Алгоритм в «Трезвый Центр Коломна» построен так, чтобы убрать импровизацию и сделать всё максимально прозрачным для семьи. Сначала по телефону собираются ключевые данные: возраст пациента, длительность запоя, виды алкоголя, хронические заболевания, препараты, аллергии, наличие судорог, потерь сознания, странного поведения, текущие жалобы. На этом этапе озвучивается ориентировочный формат помощи и примерный диапазон стоимости. Далее следует выезд на дом или поступление в стационар. Врач проводит осмотр: измеряет артериальное давление, пульс, сатурацию, температуру, оценивает тремор, координацию, сознание, степень обезвоживания, наличие болей, состояние дыхания и сердца. На основе этих данных назначается инфузионная терапия: растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы, по показаниям — гепатопротекторы, антиоксидантные комплексы, противорвотные для контроля тошноты, мягкие анксиолитики для уменьшения тревоги и нормализации сна. Уходят от агрессивной седации: пациент не должен быть «выключен» так, чтобы невозможно было заметить ухудшение. В процессе капельниц проводится повторный контроль показателей, темп и состав при необходимости корректируются. После стабилизации пациент и семья получают подробные рекомендации: режим, сон, питание, питьё, запреты, «красные флаги», план наблюдения и возможного дальнейшего лечения зависимости.
Выяснить больше – вывод из запоя на дому недорого
Такая комплексность обеспечивает воздействие на физические, психологические и социальные факторы зависимости.
Выяснить больше – наркологическая клиника лечение алкоголизма
You really make it seem so easy with your presentation but I find this matter to be actually something which I think
I would never understand. It seems too complicated and very broad for me.
I’m looking forward for your next post, I’ll try to
get the hang of it!
Aw, this was a very good post. Spending some time and actual effort to make a superb article… but
what can I say… I put things off a whole lot and
don’t manage to get nearly anything done.
Услуга вывода из запоя в клинике сочетает профессионализм врачей, медицинскую точность и заботу. При этом обеспечивается полная конфиденциальность: данные пациентов не передаются в сторонние инстанции. Круглосуточный режим работы позволяет вызвать врача даже ночью — специалисты прибывают в течение 40–60 минут после обращения.
Подробнее тут – http://vivod-iz-zapoya-v-volgograde17.ru
Современные реалии требуют от медицинских учреждений гибкости, скорости и чуткости. Наркологическая помощь — одна из сфер, где промедление может стоить человеку здоровья или жизни. В наркологической клинике «ТверьМед» разработаны оперативные механизмы реагирования: выезд врача по адресу в течение 30 минут, круглосуточная поддержка и возможность получения онлайн-консультации, не покидая дом. Такой подход позволяет вовремя оказать помощь, даже если пациент отказывается ехать в стационар или не осознаёт всю серьёзность своего состояния.
Подробнее тут – https://narkologicheskaya-pomoshh-tver0.ru/
Решение, куда обращаться при запое, напрямую влияет на безопасность. Одно дело — случайный выездной «специалист» без адреса и гарантий, другое — официальная наркологическая клиника в Реутове, несущая ответственность за свои действия. «РеутовМед Сервис» выстраивает помощь так, чтобы каждый шаг был прозрачным и медицински обоснованным, а не строился на обещаниях «вылечим за час». Уже на этапе первого звонка специалисты уточняют длительность запоя, виды и объёмы алкоголя, возраст пациента, хронические заболевания, перенесённые ранее судороги, делирий, проблемы с сердцем и давлением, какие лекарства уже давались. Эта информация позволяет не «ставить капельницу вслепую», а выбрать безопасный формат: стационар, выезд на дом или комбинированный подход. В клинике используют только сертифицированные препараты, одноразовые системы, следуют протоколам, учитывающим реальные риски, а не запрос «сделайте, чтобы уснул и не мешал». Важен и человеческий аспект: здесь не унижают, не морализируют, не угрожают учётом. Пациент воспринимается как человек с заболеванием, а не как «виноватый», а это повышает готовность к сотрудничеству и к последующим шагам в сторону трезвости.
Исследовать вопрос подробнее – vyvod-iz-zapoya-anonimno
Программа лечения строится по принципу последовательного воздействия на физическое и психологическое состояние. Начинается она с детоксикации: инфузионная терапия с применением сбалансированных растворов, антиоксидантов, гепатопротекторов и витаминов. Затем — стабилизация состояния, коррекция сна, восстановление когнитивных функций и купирование абстинентного синдрома. В зависимости от диагноза используются такие методы, как заместительная терапия, нейрометаболическая поддержка, противотревожные и антидепрессивные схемы.
Разобраться лучше – http://narkologicheskaya-klinika-novokuzneczk0.ru
В клинике «Альтернатива» применяются современные методы терапии, включающие медикаментозное лечение, психотерапию и социальную реабилитацию.
Подробнее – narkologicheskaya-pomoshh-novokuzneczk0.ru/
Капельница — инструмент, помогающий организму выйти из токсической воронки, а не магическая смесь «на все случаи». Базовый каркас — регидратация и коррекция кислотно-щелочного состояния, электролиты для водно-солевого баланса, витамины группы B и магний для поддержки нервной системы и снижения тремора. По клиническим показаниям подключаются гепатопротекторы и антиоксиданты для разгрузки печени и уменьшения оксидативного стресса; при выраженной тошноте — противорвотные, при тревоге и бессоннице — мягкие анксиолитики в дозах, сохраняющих контакт. Мы сознательно избегаем «агрессивной» седации: она создаёт иллюзию успеха, но маскирует ухудшения и мешает контролю дыхания и нейростатуса. Эффективность оцениваем не «по ощущениям», а по метрикам: стабилизация АД/ЧСС, снижение тремора и тошноты, нормализация сатурации, возвращение аппетита и появление восстановительного ночного сна. Как только параметры выравниваются, фарм-нагрузку снижаем, а акцент переносим на режим — гигиену сна, регулярную гидратацию, дробное питание, щадящую дневную активность. Это делает результат не кратковременным затишьем на препаратах, а устойчивой траекторией восстановления.
Исследовать вопрос подробнее – вывод из запоя круглосуточно
Процедура начинается с осмотра пациента и оценки степени интоксикации. Врач измеряет давление, пульс, уровень насыщения крови кислородом, определяет наличие сопутствующих заболеваний. После диагностики назначается капельница, состав которой подбирается индивидуально. Процедура направлена на очищение организма, восстановление водно-солевого баланса и снятие симптомов похмелья.
Углубиться в тему – http://vyvod-iz-zapoya-v-tolyatti17.ru/
Эти методы используются в комплексе и создают прочный фундамент для восстановления здоровья.
Исследовать вопрос подробнее – https://lechenie-alkogolizma-omsk0.ru/omsk-lechenie-alkogolizma
Hello outstanding blog! Does running a blog such as this take a massive amount work?
I have no understanding of programming but I was hoping to start my own blog soon. Anyway,
should you have any ideas or tips for new blog owners please share.
I know this is off topic but I simply wanted to ask.
Thanks!
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Подробнее – нарколог на дом недорого
Bliv ved med det vigtige arbejde med at hjælpe andre.
my web site – Bidrag til patientpleje
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Разобраться лучше – кодирование от алкоголизма отзывы волгоград
我們的彩券行專家團隊採用機器學習智能預測,每日更新各大聯盟的比賽分析,包括NBA、MLB、中華職棒等。
Ключевым фактором при выборе центра становится квалификация специалистов. Лечение алкоголизма — это не только выведение из запоя и купирование абстинентного синдрома. Оно включает работу с мотивацией, тревожными состояниями, семейными конфликтами, нарушением сна и другими последствиями зависимости. Только команда, включающая наркологов, психотерапевтов и консультантов по аддиктивному поведению, способна охватить все аспекты проблемы.
Ознакомиться с деталями – лечение алкоголизма мурманская область
Важное отличие наркологической клиники «Трезвый Путь Коломна» — полный отказ от схемы «одна капельница = решение всех проблем». Детокс здесь рассматривается как необходимый старт, но не как финальная точка. Сначала специалисты снимают острые состояния: вывод из запоя, купирование абстиненции, коррекцию водно-электролитного баланса, поддержку сердца, печени и нервной системы, нормализацию сна, снижение тревоги. Когда организм перестаёт «гореть», начинается следующий этап — стабилизация: врач оценивает психическое состояние, выявляет депрессивные, тревожные, панические проявления, подбирает поддерживающие схемы, которые помогают удержаться в первые недели после кризиса. Далее подключаются психотерапевтические инструменты: индивидуальные консультации, работа с мотивацией, разбор триггеров, формирование новых привычек. В финале выстраивается маршрут поддержки: амбулаторное наблюдение, связь с клиникой, рекомендации для семьи. Такой поэтапный подход делает клинику в Коломне местом, где зависимость перестают воспринимать как «стыд» и начинают воспринимать как задачу, с которой можно работать профессионально.
Подробнее тут – http://narkologicheskaya-klinika-kolomna2-10.ru/narkologicheskaya-klinika-cena-v-kolomne/
Комплексный подход к выводу из запоя на дому в Ярославле включает несколько основных этапов, которые позволяют обеспечить оперативное и безопасное лечение:
Изучить вопрос глубже – наркологический вывод из запоя
Наркологическая клиника в Красноярске оказывает профессиональную помощь людям, столкнувшимся с алкогольной, наркотической и другими видами зависимостей. Основная цель деятельности специалистов — восстановление физического здоровья, стабилизация психоэмоционального состояния и возвращение пациента к полноценной жизни. Лечение проводится по современным медицинским протоколам, с применением индивидуальных схем терапии и полным соблюдением конфиденциальности.
Подробнее тут – наркологическая клиника лечение алкоголизма
Pretty section of content. I just stumbled upon your site
and in accession capital to assert that I acquire in fact
enjoyed account your blog posts. Anyway I will be subscribing to your augment and even I achievement you
access consistently quickly.
捕风追影线上看平台採用機器學習個性化推薦,專為海外華人設計,提供高清視頻和直播服務。
Thanks for your marvelous posting! I really enjoyed reading it, you happen to be a great author.I will be sure to bookmark your blog and will eventually come back down the
road. I want to encourage you continue your great work, have
a nice evening!
Для понимания ключевых компонентов лечения ниже представлена таблица, в которой систематизированы основные методы и их назначение.
Выяснить больше – https://narkologicheskaya-pomoshh-novokuzneczk0.ru/narkolog-novokuzneczk-na-dom/
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Исследовать вопрос подробнее – вывод из запоя круглосуточно в омске
I’m not sure why but this weblog is loading very slow for me.
Is anyone else having this problem or is it a issue on my end?
I’ll check back later and see if the problem still
exists.
Piece of writing writing is also a excitement, if you be familiar with
after that you can write if not it is complicated to write.
This is a very informative post.
This post breaks down
how online cricket streaming works
in a
simple and easy-to-understand way.
Many people often wonder
how to access live sports streams
and
this post provides useful insights.
Thanks for sharing.
Капельница при вызове нарколога на дом в Долгопрудном от «МедТрезвие Долгопрудный» — это клинический инструмент, а не магический раствор. Главное правило — никакой агрессивной седации ради видимости спокойствия. Инфузионная терапия строится вокруг нескольких задач: восполнить жидкость, выровнять электролиты, снизить токсическую нагрузку на печень и мозг, поддержать сердце и нервную систему, уменьшить тремор, тревогу и соматические жалобы. Используются растворы для регидратации и коррекции водно-электролитного баланса, витамины группы B и магний для поддержки нервной системы, уменьшения риска судорог и нормализации сна, по показаниям — гепатопротекторы и мягкие антиоксиданты, противорвотные препараты для контроля тошноты. При выраженной тревоге или нарушениях сна назначаются щадящие анксиолитические средства в дозах, которые не выключают пациента полностью, а помогают снять паническое напряжение, сохраняя возможность оценивать динамику состояния. Врач отслеживает реакцию на терапию: стабилизацию давления и пульса, уменьшение дрожи, улучшение общего самочувствия, появление более спокойного, естественного сна. По мере облегчения нагрузки схема не усиливается ради счёта, а рационально сокращается. Такой подход защищает пациента от скрытых осложнений и превращает капельницу в контролируемый, полезный шаг, а не в рискованный эксперимент.
Ознакомиться с деталями – narkolog-na-dom-vyvod-iz-zapoya
Эти методы используются в комплексе и создают прочный фундамент для восстановления здоровья.
Разобраться лучше – https://lechenie-alkogolizma-omsk0.ru/omsk-lechenie-alkogolizma/
Click This Link https://perena.lat
Первый шаг в лечении — это тщательный осмотр специалиста. Наряду с измерением жизненно важных показателей (пульс, артериальное давление, температура) врач проводит сбор анамнеза, выясняя длительность запоя, тип употребляемого алкоголя и наличие сопутствующих заболеваний. Эти данные помогают оценить степень интоксикации и подобрать индивидуальный план терапии, что является ключевым для дальнейшей эффективной детоксикации.
Ознакомиться с деталями – вывод из запоя капельница в ярославле
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Подробнее тут – http://narcologicheskaya-klinika-v-krasnoyarske17.ru
use this link https://neur.cloud/
Каждый этап проходит под контролем врачей-наркологов и психотерапевтов, что гарантирует эффективность и безопасность лечения.
Узнать больше – запой наркологическая клиника в новокузнецке
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Подробнее тут – вывод из запоя на дому
Hi mates, nice piece of writing and nice arguments commented here, I
am really enjoying by these.
Современные реалии требуют от медицинских учреждений гибкости, скорости и чуткости. Наркологическая помощь — одна из сфер, где промедление может стоить человеку здоровья или жизни. В наркологической клинике «ТверьМед» разработаны оперативные механизмы реагирования: выезд врача по адресу в течение 30 минут, круглосуточная поддержка и возможность получения онлайн-консультации, не покидая дом. Такой подход позволяет вовремя оказать помощь, даже если пациент отказывается ехать в стационар или не осознаёт всю серьёзность своего состояния.
Детальнее – нарколог наркологическая помощь тверь
Выездная наркологическая помощь организована по чётко выстроенной схеме. Каждый этап направлен на стабилизацию состояния и безопасное восстановление функций организма после алкогольного или наркотического воздействия.
Подробнее – нарколог на дом цены в уфе
Когда запой длится не первый день, а состояние уже сопровождается тремором, потливостью, резкими перепадами давления, бессонницей, тревогой, тошнотой или рвотой, попытка «перетерпеть» или лечить самостоятельно таблетками становится опасным экспериментом. Сочетание алкоголя с сильнодействующими успокоительными, обезболивающими или сомнительными «антипохмельными» легко приводит к нарушению дыхания, провалам в сознании, аритмиям и скрытому развитию предделирия. Домашние средства не учитывают ни электролитные сдвиги, ни состояние печени и сердца, ни уже принятые лекарства. Выездной нарколог «СерпуховТрезвие» в Серпухове выстраивает ситуацию иначе: ещё по телефону врач собирает ключевую информацию — длительность запоя, примерные объёмы и виды алкоголя, наличие гипертонии, ИБС, диабета, заболеваний печени и почек, неврологических проблем, какие препараты уже давали и в каких дозах, были ли судороги или эпизоды дезориентации. На месте проводится объективная диагностика: измерение давления, пульса, сатурации, температуры, оценка тремора, степени обезвоживания, психического состояния, неврологического статуса. Только после этого принимается решение: проводить детокс на дому или сразу рекомендовать стационар. Такой фильтр защищает от грубых ошибок, позволяет точно подобрать схему и не терять драгоценное время, пытаясь «угадать» лечение.
Подробнее – https://narkolog-na-dom-serpuhov10.ru/narkolog-psiholog-na-dom-serpuhov
Процесс организован так, чтобы снять с семьи хаос и дать понятный сценарий. После обращения в «РеутовМед Сервис» пациент быстро попадает в поле зрения врача: или через выезд по адресу, или через стационар, если состояние уже близко к опасному. На месте проводится полноценная оценка: давление, пульс, сатурация, температура, осмотр сердца и дыхания, степень обезвоживания, выраженность тремора, наличие рвоты, боли в груди или животе, неврологический статус, поведение, признаки психоза. На основе этих данных формируется индивидуальный план детоксикации. Стартовая инфузионная терапия подбирается с учётом возраста, массы тела, длительности запоя, сопутствующих болезней, уже принятых препаратов. В стационаре пациента размещают в безопасных условиях, контролируют динамику, корректируют дозировки, не оставляют «на самотёк». При выводе из запоя на дому врач остаётся до стабилизации, отслеживает реакцию и при первых тревожных признаках рекомендует стационар, а не уезжает «лишь бы поставил капельницу». Такой пошаговый подход позволяет не только снять острые симптомы, но и уменьшить риск осложнений — от аритмий и судорог до алкогольного делирия.
Узнать больше – вывод из запоя в реутово
hello there and thank you for your information – I’ve definitely picked up something new from right
here. I did however expertise a few technical issues
using this site, as I experienced to reload
the web site lots of times previous to I could get it to load properly.
I had been wondering if your web host is OK? Not that I’m complaining, but slow loading instances times will sometimes affect
your placement in google and could damage your quality score if advertising and marketing with Adwords.
Well I’m adding this RSS to my email and can look out for much more of your
respective interesting content. Make sure you update
this again soon.
Услуга «нарколог на дом в Долгопрудном» от клиники «МедТрезвие Долгопрудный» создана для ситуаций, когда важно действовать быстро, аккуратно и без лишнего шума. Запой, тяжёлое похмелье, срыв после ремиссии, злоупотребление медикаментами или смесью алкоголя с препаратами — всё это не терпит откладывания и самодеятельности. Вызов врача на дом позволяет получить профессиональную помощь без госпитализации, когда состояние пациента ещё позволяет лечить его в привычной обстановке. Нарколог приезжает с полностью укомплектованным набором препаратов и расходников, проводит осмотр, подбирает капельницы по клиническим показаниям, контролирует реакцию, даёт подробные рекомендации на ближайшие дни и при необходимости предлагает дальнейший маршрут: повторный выезд, амбулаторное наблюдение или стационар клиники. Конфиденциальность соблюдается строго: без обсуждений с соседями, без регистрации по месту работы, без унизительных формальностей — только медицинская помощь, ориентированная на безопасность и результат.
Исследовать вопрос подробнее – http://narkolog-na-dom-dolgoprudnij10.ru/vyzvat-narkologa-na-dom-v-dolgoprudnom/https://narkolog-na-dom-dolgoprudnij10.ru
I visited multiple sites but the audio quality for audio songs current at this website is in fact fabulous.
Lately, the web gambling industry has witnessed an unprecedented surge in popularity, fueled by advancements in technology, increased web accessibility, and altering societal attitudes towards gambling. On-line playing platforms have transformed the way in which people engage with betting, offering a wide selection of games and betting options that cater to numerous preferences. This article explores the evolution, benefits, challenges, and future prospects of http://techou.jp/index.php?egyptknight85 playing platforms.
What’s up to all, how is everything, I think every one is getting more from this site, and your views are pleasant designed for new people.
Каждый час промедления в острый период повышает вероятность обезвоживания, электролитных сдвигов, аритмий, гипертонических всплесков и расстройств сна, которые легко перерастают в делирий. Домашние попытки с «подручными» средствами редко учитывают лекарственные взаимодействия, реальный уровень обезвоживания и состояние печени, а «жёсткая» седация, применяемая без показаний, маскирует ухудшения и лишает врача информативной картины. Профессиональная бригада «НоваТрезвие» начинает с объективной оценки: давление, пульс, сатурация, температура, неврологический статус, выраженность тремора и тошноты, степень обезвоживания, список принимаемых препаратов и возможные аллергии. На этой базе формируется персональный план: регидратация, коррекция электролитов и кислотно-щелочного баланса, поддержка нервной системы витаминами группы B и магнием, гепатопротекторная и антиоксидантная защита по показаниям, противорвотные при необходимости и мягкая анксиолитическая поддержка для восстановительного сна. Такой маршрут гасит «пожар» интоксикации управляемо, возвращая прогнозируемость самочувствия в течение первых часов.
Ознакомиться с деталями – http://vyvod-iz-zapoya-ehlektrostal2-10.ru/vyvod-iz-zapoya-stacionar-v-ehlektrostali/https://vyvod-iz-zapoya-ehlektrostal2-10.ru
Very rapidlyy this wweb page will be famous amid all blogging users, due to it’s pleasant content
My blog: Cathern
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Подробнее можно узнать тут – http://
I was wondering if you ever thought of changing the layout of your
website? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could
connect with it better. Youve got an awful lot of text for
only having 1 or two pictures. Maybe you could space
it out better?
В клинике «Альтернатива» применяются современные методы терапии, включающие медикаментозное лечение, психотерапию и социальную реабилитацию.
Разобраться лучше – нарколог наркологическая помощь в новокузнецке
Наркологическая клиника «МедЛайн» предоставляет профессиональные услуги врача-нарколога с выездом на дом в Новосибирске и Новосибирской области. Мы оперативно помогаем пациентам справиться с тяжелыми состояниями при алкогольной и наркотической зависимости. Экстренный выезд наших специалистов доступен круглосуточно, а лечение проводится с применением проверенных методик и препаратов, что гарантирует безопасность и конфиденциальность каждому пациенту.
Детальнее – https://narcolog-na-dom-novosibirsk00.ru/narkolog-na-dom-kruglosutochno-novosibirsk/
Даже если симптомы кажутся незначительными, проведение инфузионной терапии значительно ускоряет процесс восстановления и предотвращает развитие осложнений.
Узнать больше – https://kapelnicza-ot-zapoya-v-volgograde17.ru
Комплексный подход к выводу из запоя на дому в Ярославле включает несколько основных этапов, которые позволяют обеспечить оперативное и безопасное лечение:
Получить дополнительные сведения – https://vyvod-iz-zapoya-yaroslavl0.ru/vyvod-iz-zapoya-kruglosutochno-yaroslavl/
Наркологическая клиника в Красноярске оказывает профессиональную помощь людям, столкнувшимся с алкогольной, наркотической и другими видами зависимостей. Основная цель деятельности специалистов — восстановление физического здоровья, стабилизация психоэмоционального состояния и возвращение пациента к полноценной жизни. Лечение проводится по современным медицинским протоколам, с применением индивидуальных схем терапии и полным соблюдением конфиденциальности.
Подробнее – анонимная наркологическая клиника красноярск
Great article, very helpful.
It clearly explains
how online cricket streaming works
in a
clear and beginner-friendly manner.
Many people often wonder
how they can watch live cricket online
and
this article answers those questions well.
Appreciate the useful content.
Useful info. Fortunate me I found your web site by chance, and
I am shocked why this accident didn’t came about in advance!
I bookmarked it.
their explanation https://heyanon.my
you could check here https://blnk.my/
После завершения процедур пациенту предоставляется подробная консультация с рекомендациями по дальнейшему восстановлению и профилактике повторных случаев зависимости.
Получить дополнительные сведения – нарколог на дом недорого
Стационар наркологической клиники в Раменском ориентирован на тех пациентов, для которых домашние попытки лечения объективно опасны. Это длительные запои, пожилой возраст, выраженные сердечно-сосудистые патологии, заболевания печени и почек, риск делирия, судорог, тяжёлая абстиненция, полинаркомания. В стационаре «Трезвый Шаг Раменское» организовано круглосуточное наблюдение: контролируются давление, пульс, сатурация, поведение, динамика симптомов, проводится своевременная коррекция терапии. Пациент находится в спокойной, защищённой обстановке, где ему не нужно скрывать своё состояние или оправдываться — задача команды не судить, а стабилизировать и лечить. Комфортные палаты, медицинский персонал рядом, продуманное питание, конфиденциальность — всё это снижает уровень страха у пациента и напряжение у родственников. Важный момент: стационар не подаётся как «камерный режим», а как безопасная зона восстановления, где можно пройти самый тяжёлый участок пути с максимальной защитой.
Детальнее – adresa-narkologicheskih-klinik
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Разобраться лучше – http://narcologicheskaya-klinika-v-novokuzneczke17.ru
Перед процедурой врач оценивает состояние пациента, измеряет давление, пульс и уровень насыщения крови кислородом. После осмотра подбирается состав инфузии, включающий препараты для дезинтоксикации, восстановления водно-солевого баланса и нормализации работы органов. Введение растворов осуществляется внутривенно, под контролем специалиста. Длительность процедуры — от 40 минут до 1,5 часов.
Узнать больше – врача капельницу от запоя
В таких случаях своевременный вызов нарколога на дом позволяет быстро стабилизировать состояние больного и предотвратить тяжелые последствия.
Подробнее тут – https://narcolog-na-dom-novosibirsk00.ru/
Алгоритм организован так, чтобы каждое действие было логичным и предсказуемым. После обращения по телефону врач заранее получает краткую клиническую картину и подбирает набор препаратов с учётом состояния пациента. По прибытии в Долгопрудном нарколог не ставит капельницу «по шаблону», а начинает с осмотра: измеряет давление, пульс, сатурацию, температуру, оценивает тремор, уровень сознания, ориентировку, степень обезвоживания, частоту рвоты, дыхание, возможные боли в груди или животе, обращает внимание на поведение и эмоциональное состояние. Если по результатам осмотра подтверждается, что дом — безопасный формат, подбирается индивидуальная инфузионная схема: объём, скорость введения и препараты зависят от возраста, длительности запоя, сопутствующих болезней и уже использованных медикаментов. Врач остаётся на адресе до завершения основных процедур, контролирует реакцию, при необходимости корректирует план и чётко проговаривает, как пациент должен проводить ближайшие 24–72 часа. Если по ходу работы выявляются признаки угрозы (начальные симптомы делирия, тяжёлые аритмии, нестабильное давление, выраженная дезориентация), нарколог рекомендует стационар и помогает семье организовать перевод. Это честный и безопасный подход: не любой ценой «отработать выезд», а сделать так, чтобы помощь действительно снижала риски.
Получить дополнительную информацию – http://narkolog-na-dom-dolgoprudnij10.ru
You really make it seem so easy along with your presentation however I find this matter to be actually
one thing which I believe I might by no means understand.
It sort of feels too complex and very huge for me. I’m taking a look forward on your
next put up, I’ll attempt to get the hold of it!
Look into my site หนังโป๊ซับไทย
Даже телефонный разговор с клиникой может многое сказать о её подходе. Если вам предлагают типовое лечение без уточнения подробностей или избегают вопросов о составе команды, это тревожный сигнал. Серьёзные учреждения в Мурманске обязательно предложат предварительную консультацию, зададут уточняющие вопросы и расскажут, как строится программа помощи.
Подробнее тут – klinika lecheniya alkogolizma murmansk
Во многих случаях пациент или его родственники не решаются сразу вызвать врача. Для таких ситуаций предусмотрена услуга онлайн-консультации. Она проводится через защищённую видеосвязь, при желании — анонимно. На связи — врач-нарколог или психиатр, который отвечает на вопросы, оценивает ситуацию по визуальным и вербальным признакам, рекомендует план действий. Консультация может стать отправной точкой для дальнейшего вызова врача на дом или записи в клинику. Это особенно удобно для родственников, которые не знают, как подступиться к проблеме и убедить человека в необходимости помощи.
Исследовать вопрос подробнее – экстренная наркологическая помощь тверь
Когда запой начинает угрожать здоровью, оперативное вмешательство становится жизненно необходимым. В Туле опытные специалисты оказывают помощь на дому, позволяя начать лечение сразу же в комфортной обстановке. Такой формат терапии обеспечивает оперативную детоксикацию, восстановление нормального обмена веществ и стабилизацию работы внутренних органов, что особенно важно для пациентов, желающих избежать лишнего стресса и сохранить конфиденциальность.
Разобраться лучше – https://vyvod-iz-zapoya-tula0.ru/vyvod-iz-zapoya-czena-tula
from this source https://kyros.ink/
We’re a bunch of volunteers and opening a new scheme in our community.
Your site offered us with valuable info to work on. You have performed an impressive process and our whole neighborhood shall be grateful to you.
Пациенты выбирают нашу клинику для срочного вызова врача-нарколога благодаря следующим важным преимуществам:
Детальнее – нарколог на дом срочно
Эти методы используются в комплексе и создают прочный фундамент для восстановления здоровья.
Углубиться в тему – лечение алкоголизма в стационаре
Nice post. I used to be checking constantly this weblog and I’m inspired!
Extremely helpful info specifically the ultimate part 🙂 I deal with
such information much. I used to be looking for this
certain information for a very lengthy time. Thank you and good luck.
Curve shots, bending efforts and their success rates documented
Работа выездной службы построена так, чтобы для семьи всё было максимально понятно и предсказуемо. После звонка специалист не ограничивается общими фразами, а уточняет детали: сколько длится употребление, есть ли хронические болезни сердца, печени, почек, эндокринные нарушения, какие препараты и в каких дозах пациент уже получил, были ли в прошлом судороги, галлюцинации, тяжёлые реакции на лекарства. Это позволяет заранее оценить уровень риска и понять, подходит ли формат дома. По прибытии в Серпухове врач осматривает пациента, проверяет контакт и ориентировку, измеряет артериальное давление несколько раз, оценивает пульс, сатурацию, температуру, выраженность тремора, наличие болей, характер дыхания, степень обезвоживания. Далее формируется индивидуальная инфузионная схема: растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы, при необходимости — гепатопротекторы и мягкие антиоксидантные комплексы, противорвотные для контроля тошноты, щадящие анксиолитики для нормализации сна без грубой седации. Во время процедуры врач контролирует динамику, меняет скорость капельницы при необходимости, отслеживает реакцию на препараты и объясняет родным, какие изменения будут происходить по часам. По завершении визита пациент и родственники получают подробный план: режим, питьё, питание, чего нельзя, какие симптомы считаются тревожными, когда нужна повторная консультация или стационар. При выявлении опасных признаков вопрос о госпитализации поднимается честно и сразу, а не откладывается «до утра».
Подробнее – https://narkolog-na-dom-serpuhov10.ru/nomer-narkologa-na-dom-serpuhov/
Работа выездной службы построена так, чтобы для семьи всё было максимально понятно и предсказуемо. После звонка специалист не ограничивается общими фразами, а уточняет детали: сколько длится употребление, есть ли хронические болезни сердца, печени, почек, эндокринные нарушения, какие препараты и в каких дозах пациент уже получил, были ли в прошлом судороги, галлюцинации, тяжёлые реакции на лекарства. Это позволяет заранее оценить уровень риска и понять, подходит ли формат дома. По прибытии в Серпухове врач осматривает пациента, проверяет контакт и ориентировку, измеряет артериальное давление несколько раз, оценивает пульс, сатурацию, температуру, выраженность тремора, наличие болей, характер дыхания, степень обезвоживания. Далее формируется индивидуальная инфузионная схема: растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы, при необходимости — гепатопротекторы и мягкие антиоксидантные комплексы, противорвотные для контроля тошноты, щадящие анксиолитики для нормализации сна без грубой седации. Во время процедуры врач контролирует динамику, меняет скорость капельницы при необходимости, отслеживает реакцию на препараты и объясняет родным, какие изменения будут происходить по часам. По завершении визита пациент и родственники получают подробный план: режим, питьё, питание, чего нельзя, какие симптомы считаются тревожными, когда нужна повторная консультация или стационар. При выявлении опасных признаков вопрос о госпитализации поднимается честно и сразу, а не откладывается «до утра».
Узнать больше – https://narkolog-na-dom-serpuhov10.ru/nomer-narkologa-na-dom-serpuhov
Good day! Do you use Twitter? I’d like to follow you if that
would be ok. I’m definitely enjoying your blog and look firward to new updates.
Review my webpage; Curt
Наша выездная бригада приезжает без маркировки, в гражданской одежде, согласовывает «тихое окно» связи с пациентом или близкими и начинает не с капельницы, а с настройки среды: тёплая приглушённая подсветка, проветривание без сквозняков, отключение уведомлений, подготовка воды комнатной температуры. Затем — быстрый осмотр, экспресс-метрики и старт индивидуального плана. Каждая корректировка — ровно одна за раз, чтобы сохранить причинно-следственную связь и не провоцировать полипрагмазию.
Выяснить больше – http://narkolog-na-dom-saratov0.ru
Excellent article. I am experiencing a few of these issues as well..
Here is my site: หนังโป๊ซับไทย
Very well voiced indeed! . https://sulfuric-swift-347.notion.site/BETFLIX93-2cd0a81f105a80979e2ad05d9fdcfd9b
我們的資深運彩分析官方授權專家團隊第一時間更新官方NBA、MLB、中華職棒等各大聯盟的專業賽事分析。
Метод лечения
Исследовать вопрос подробнее – срочная наркологическая помощь
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Подробнее тут – http://kodirovanie-ot-alkogolizma-v-volgograde17.ru
Процедура начинается с обследования пациента: врач измеряет давление, частоту пульса, оценивает степень интоксикации и состояние внутренних органов. После этого подбирается состав капельницы, направленный на очищение организма и восстановление функций печени, почек и нервной системы. Все препараты вводятся внутривенно, что обеспечивает быстрый эффект и минимизирует нагрузку на желудочно-кишечный тракт.
Получить дополнительные сведения – вывод из запоя клиника тюмень
После поступления вызова наш нарколог выезжает к пациенту в кратчайшие сроки, прибывая по адресу в пределах 30–60 минут. Специалист начинает процедуру с подробного осмотра и диагностики, измеряя ключевые показатели организма: артериальное давление, частоту пульса, насыщенность кислородом и собирая подробный анамнез.
Получить больше информации – вызов нарколога на дом новосибирск.
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Получить дополнительные сведения – наркологическая клиника в красноярске
Запой – это опасное состояние, при котором организм подвергается значительной токсической нагрузке, а длительное злоупотребление алкоголем приводит к нарушению работы внутренних органов и ухудшению общего самочувствия. В Ярославле качественная наркологическая помощь на дому становится спасением для пациентов, нуждающихся в оперативной детоксикации и стабилизации состояния. Такой формат лечения позволяет начать терапию в комфортной обстановке, сохраняя конфиденциальность и минимизируя стресс, связанный с посещением стационара.
Подробнее – http://vyvod-iz-zapoya-yaroslavl0.ru
Даже если симптомы кажутся незначительными, проведение инфузионной терапии значительно ускоряет процесс восстановления и предотвращает развитие осложнений.
Подробнее тут – http://kapelnicza-ot-zapoya-v-volgograde17.ru
Как подчёркивает специалист ФГБУ «НМИЦ психиатрии и наркологии», «без участия квалифицированной команды невозможно обеспечить комплексный подход к пациенту, особенно если речь идёт о длительном стаже употребления и осложнённой картине заболевания». Отсюда следует — изучение состава персонала должно быть одним из первых шагов.
Получить дополнительные сведения – http://lechenie-alkogolizma-murmansk0.ru/lechenie-khronicheskogo-alkogolizma-marmansk/
Программа лечения строится по принципу последовательного воздействия на физическое и психологическое состояние. Начинается она с детоксикации: инфузионная терапия с применением сбалансированных растворов, антиоксидантов, гепатопротекторов и витаминов. Затем — стабилизация состояния, коррекция сна, восстановление когнитивных функций и купирование абстинентного синдрома. В зависимости от диагноза используются такие методы, как заместительная терапия, нейрометаболическая поддержка, противотревожные и антидепрессивные схемы.
Получить дополнительные сведения – https://narkologicheskaya-klinika-novokuzneczk0.ru/narkologicheskij-czentr-novokuzneczk/
Greetings from Carolina! I’m bored to tears at work so I decided to browse your
site on my iphone during lunch break. I love the info you provide here and can’t wait to
take a look when I get home. I’m shocked at how fast your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyways, excellent site!
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Узнать больше – https://kodirovanie-ot-alkogolizma-v-volgograde17.ru/kodirovanie-volgograd
Главная задача процедуры — быстрое выведение этанола и его метаболитов из организма, нормализация уровня электролитов, улучшение самочувствия и предотвращение осложнений. Лечение проводится как в клинике, так и на дому, что особенно удобно при тяжёлых состояниях, когда пациент не может самостоятельно добраться до медицинского учреждения.
Получить дополнительную информацию – вывод из запоя дешево
Наркозависимость — это не просто вредная привычка, а тяжёлое хроническое заболевание, требующее комплексного и последовательного лечения. В клинике «РеабКузбасс» в Новокузнецке разработаны персонализированные программы помощи, учитывающие медицинские, психологические и социальные аспекты проблемы. Каждому пациенту подбирается уникальный маршрут восстановления, начиная с первичной диагностики и заканчивая адаптацией к жизни без наркотиков. Поддержка оказывается круглосуточно, с полным соблюдением конфиденциальности. Психотерапевты и врачи работают в тесной связке, чтобы не только устранить физическую зависимость, но и восстановить личность пациента, вернуть ему мотивацию к жизни и уверенность в будущем.
Ознакомиться с деталями – лечение больных наркоманией
Критичные случаи, когда вызов нарколога через «МедТрезвие Долгопрудный» оправдан и своевременен:
Выяснить больше – https://narkolog-na-dom-dolgoprudnij10.ru/skolko-stoit-narkolog-na-dom-v-dolgoprudnom/
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Подробнее тут – http://narkologicheskaya-klinika-kolomna2-10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/https://narkologicheskaya-klinika-kolomna2-10.ru
https://www.youtube.com/watch?v=M_fse4eP9tE
Normally I don’t learn article on blogs, however I wish to say that this write-up very
forced me to take a look at and do so! Your writing taste has been surprised me.
Thanks, quite great post.
Современная наркологическая клиника — это не просто учреждение для экстренной помощи, а центр комплексной поддержки человека, столкнувшегося с зависимостью. В «КузбассМед» в Новокузнецке реализуется модель интенсивного вмешательства, где используются новейшие медицинские технологии, мультидисциплинарный подход и мобильные выездные службы. Специалисты готовы прибыть на дом за 30 минут с полным набором оборудования и медикаментов, обеспечив пациенту помощь в привычной и безопасной среде. Наркология здесь строится на индивидуализации: каждый случай рассматривается отдельно, с учётом психофизического состояния, анамнеза и жизненного контекста пациента.
Узнать больше – http://narkologicheskaya-klinika-novokuzneczk0.ru
Главная задача процедуры — быстрое выведение этанола и его метаболитов из организма, нормализация уровня электролитов, улучшение самочувствия и предотвращение осложнений. Лечение проводится как в клинике, так и на дому, что особенно удобно при тяжёлых состояниях, когда пациент не может самостоятельно добраться до медицинского учреждения.
Подробнее тут – нарколог вывод из запоя в тюмени
Yes! Finally someone writes about 1xBet Promo Code Free Spins 2026: 1XWAP200.
Услуга
Выяснить больше – narkologa-na-dom-shchelkovo
Wonderful blog! I found it while browsing on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Appreciate it
Город живёт в разных темпах: плотный центр, мостовые переходы, набережная, спальные районы. Мы строим маршрут так, чтобы не привлекать внимания соседей и не терять время на трафик. Если на предзвонке отмечаются «красные флаги» — давящая боль в груди, выраженная одышка, спутанность сознания, судороги, неукротимая рвота или резкое падение насыщения кислородом, — команда instantly переключает маршрут в стационарный «коридор»: палата резервируется заранее, документы оформляются нейтрально, транспорт — немаркированный. Если угроз нет, всё начинается на дому с адресной детокс-схемы и мягкой сенсорной поддержкой.
Подробнее тут – запой нарколог на дом в саратове
Решение, куда обращаться при запое, напрямую влияет на безопасность. Одно дело — случайный выездной «специалист» без адреса и гарантий, другое — официальная наркологическая клиника в Реутове, несущая ответственность за свои действия. «РеутовМед Сервис» выстраивает помощь так, чтобы каждый шаг был прозрачным и медицински обоснованным, а не строился на обещаниях «вылечим за час». Уже на этапе первого звонка специалисты уточняют длительность запоя, виды и объёмы алкоголя, возраст пациента, хронические заболевания, перенесённые ранее судороги, делирий, проблемы с сердцем и давлением, какие лекарства уже давались. Эта информация позволяет не «ставить капельницу вслепую», а выбрать безопасный формат: стационар, выезд на дом или комбинированный подход. В клинике используют только сертифицированные препараты, одноразовые системы, следуют протоколам, учитывающим реальные риски, а не запрос «сделайте, чтобы уснул и не мешал». Важен и человеческий аспект: здесь не унижают, не морализируют, не угрожают учётом. Пациент воспринимается как человек с заболеванием, а не как «виноватый», а это повышает готовность к сотрудничеству и к последующим шагам в сторону трезвости.
Подробнее можно узнать тут – vyvod-iz-zapoya-cena
Вывод из запоя — это экстренная медицинская помощь, направленная на очищение организма от алкоголя, снятие симптомов интоксикации и восстановление работы внутренних органов. В клинике «Трезвая Линия Волгоград» используется комплексный подход, включающий капельницы, препараты для детоксикации и постоянный врачебный контроль. Лечение проводится анонимно, с индивидуальным подбором медикаментов и поддержкой пациента на каждом этапе восстановления. Главная цель специалистов — не просто стабилизировать состояние, а обеспечить безопасное возвращение к нормальному самочувствию и предотвратить повторные срывы.
Исследовать вопрос подробнее – http://vyvod-iz-zapoia-v-volgograde17.ru/
i was reading this https://cwap.xyz/
Экстренный вызов нарколога на дом в Иркутске от «ТрезвоМед» при запое, интоксикации или кодировании – анонимно и удобно. Осмотр, детоксикация капельницей, индивидуальный план лечения – все это на дому! «ТрезвоМед» – круглосуточная помощь, анонимность и безопасность при отказе от алкоголя. Не можете бросить пить самостоятельно? Нужна помощь нарколога! Васильев: «Своевременная помощь при интоксикации – залог успешного выздоровления».
Ознакомиться с деталями – https://narcolog-na-dom-v-irkutske0.ru/vyzov-narkologa-na-dom-irkutsk
Комплексный подход позволяет врачу не просто купировать острые симптомы, но и предупредить осложнения со стороны сердца, печени и нервной системы. После стабилизации состояния пациент получает рекомендации по дальнейшему лечению и восстановлению.
Разобраться лучше – https://vyvod-iz-zapoia-v-volgograde17.ru/anonimnaya-narkologiya-vyvod-iz-zapoya-volgograd
Post writing is also a fun, if you be acquainted with then you can write
or else it is difficult to write.
Одним из ключевых преимуществ «КузбассМед» является современная материально-техническая база. В клинике задействованы устройства для точного мониторинга жизненных функций, автоматические инфузионные системы, экспресс-диагностические модули и оборудование для неотложной терапии. Врачи используют программируемые дозаторы, портативные анализаторы крови и аппараты для оценки дыхательной функции, что позволяет своевременно корректировать тактику лечения без потерь времени. Все процедуры соответствуют национальным стандартам безопасности и рекомендациям ВОЗ.
Исследовать вопрос подробнее – https://narkologicheskaya-klinika-novokuzneczk0.ru/narkolog-v-gorode-novokuzneczke/
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Узнать больше – adresa-narkologicheskih-klinik
Вывод из запоя в Тюмени — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормального функционирования организма. Длительное употребление спиртных напитков приводит к нарушению обмена веществ, обезвоживанию, сбоям в работе печени и сердца. В таких случаях требуется профессиональная помощь врача-нарколога, который подберёт оптимальный способ дезинтоксикации и медикаментозной поддержки. Современные методики позволяют провести вывод из запоя безопасно, эффективно и без осложнений.
Ознакомиться с деталями – вывод из запоя с выездом
Выбор клиники — задача не только медицинская, но и стратегическая. Учитывать нужно не только наличие лицензии, но и содержание программ, их гибкость, участие родственников в процессе, а также прозрачность взаимодействия с пациентом. Именно эти аспекты позволяют отличить профессиональное учреждение от формального.
Получить дополнительные сведения – https://narkologicheskaya-klinika-yaroslavl0.ru/lechenie-narkomanii-i-alkogolizma-yaroslavl/
After I initially left a comment I appear to have
clicked on the -Notify me when new comments are added- checkbox and now each time a comment is added I receive 4
emails with the same comment. Is there an easy method
you can remove me from that service? Thank you!
В таблице приведены основные компоненты капельницы и их действие:
Разобраться лучше – http://narkologicheskaya-pomoshh-v-volgograde17.ru/narkolog-psikholog-volgograd/
Когда состояние «штормит», ночные часы усиливают тревогу и вегетативные реакции, обезвоживание нарастает, сон рвётся, а попытки самолечения «чем попало» маскируют опасные симптомы. Организованный маршрут в «Трезвой Линии» заменяет хаос последовательностью: ещё по телефону дежурный врач собирает ключевые сведения — длительность эпизода, аллергии, список лекарств и дозировок, кардио- и эндокринные диагнозы, последние измерения давления и пульса. На месте выполняется короткая, но информативная оценка: АД, ЧСС, сатурация, температура, неврологический статус, степень обезвоживания, выраженность тремора и тошноты. Схема терапии запускается сразу и корректируется каждые 15–20 минут по «живым показателям», а не по шаблону. Если видим признаки предделирия, неукротимую рвоту, резкие «качели» давления/пульса, выраженную слабость или пожилой возраст с тяжёлой соматикой — переводим в стационар без пауз: приборный мониторинг и ночная команда в Электростали снижают «цену ошибки» и экономят на повторных вызовах. Для семьи это означает меньше догадок и больше ясности: понятно, что делаем сейчас и чего ждём к утру.
Получить дополнительную информацию – http://vyvod-iz-zapoya-ehlektrostal10.ru
Hi, I do think this is an excellent web site. I stumbledupon it 😉 I will revisit once
again since I saved as a favorite it. Money and
freedom is the best way to change, may you be rich and continue to
guide other people.
Такая комплексность обеспечивает воздействие на физические, психологические и социальные факторы зависимости.
Исследовать вопрос подробнее – принудительное лечение от алкоголизма
Get the facts https://astherus.us
I for all time emailed this blog post page to all my
associates, since if like to read it next my friends will too.
Выбор помощи на дому имеет ряд значительных преимуществ:
Разобраться лучше – вывод из запоя
Одна из сильных сторон «РеутовМед Сервис» — честная оценка границ домашнего лечения. Клиника не обещает «вывезем любого дома», потому что есть состояния, при которых отсутствие круглосуточного наблюдения опасно. Чтобы родным было проще сориентироваться, важно разделить ситуации по уровню риска и понять, почему иногда разумнее выбрать стационар, даже если пациент сопротивляется.
Исследовать вопрос подробнее – http://vyvod-iz-zapoya-reutov10.ru
Наркологическая клиника — это не просто место, где пациенту оказывают медицинскую помощь. Это учреждение, где формируется стратегия полного восстановления, включающая не только физическое оздоровление, но и психоэмоциональную стабилизацию. В Ярославле работают как частные, так и государственные клиники, однако их подходы, уровень сервиса и состав команд могут существенно различаться. По данным Минздрава РФ, высокий процент успешных исходов наблюдается в тех учреждениях, где реализуется персонализированная модель лечения и постлечебной поддержки.
Получить дополнительные сведения – http://narkologicheskaya-klinika-yaroslavl0.ru/narkologicheskaya-klinika-telefon-yaroslavl/
Hey! This post couldn’t be written any better! Reading through
this post reminds me of my good old room mate! He always
kept talking about this. I will forward this page to him.
Fairly certain he will have a good read. Thank you for sharing!
my web page jav subthai
Услуга вывода из запоя в клинике сочетает профессионализм врачей, медицинскую точность и заботу. При этом обеспечивается полная конфиденциальность: данные пациентов не передаются в сторонние инстанции. Круглосуточный режим работы позволяет вызвать врача даже ночью — специалисты прибывают в течение 40–60 минут после обращения.
Подробнее тут – http://
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Детальнее – нарколог вывод из запоя
Комплексная наркологическая помощь объединяет несколько направлений, каждое из которых решает отдельную задачу восстановления организма и психики. Врачи используют индивидуальные схемы терапии, подбирая оптимальные препараты и психологические методики.
Углубиться в тему – http://narkologicheskaya-pomoshh-v-volgograde17.ru/
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Разобраться лучше – https://narkologicheskaya-klinika-kolomna2-10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
Одним из ключевых преимуществ «КузбассМед» является современная материально-техническая база. В клинике задействованы устройства для точного мониторинга жизненных функций, автоматические инфузионные системы, экспресс-диагностические модули и оборудование для неотложной терапии. Врачи используют программируемые дозаторы, портативные анализаторы крови и аппараты для оценки дыхательной функции, что позволяет своевременно корректировать тактику лечения без потерь времени. Все процедуры соответствуют национальным стандартам безопасности и рекомендациям ВОЗ.
Углубиться в тему – наркологическая клиника
csgoempire scam or legal
What i don’t understood is in reality how you are now not actually a lot more smartly-favored than you might be now.
You’re very intelligent. You realize therefore significantly
in terms of this topic, made me for my part believe it from numerous varied angles.
Its like men and women are not involved until it’s something to do with Woman gaga!
Your personal stuffs excellent. At all times deal with it up!
Feel free to surf to my blog av ซับไทย
Way cool! Some extremely valid points! I appreciate you writing this
article and also the rest of the website is also really good.
Даже телефонный разговор с клиникой может многое сказать о её подходе. Если вам предлагают типовое лечение без уточнения подробностей или избегают вопросов о составе команды, это тревожный сигнал. Серьёзные учреждения в Мурманске обязательно предложат предварительную консультацию, зададут уточняющие вопросы и расскажут, как строится программа помощи.
Ознакомиться с деталями – лечение наркомании и алкоголизма в мурманске
Howdy! This post could not be written much better!
Reading through this post reminds me of my previous roommate!
He always kept talking about this. I most certainly will forward
this article to him. Pretty sure he’s going to have a very good read.
Thank you for sharing!
Домашний формат хорош при умеренной выраженности симптомов, сохранённом контакте и возможности обеспечить наблюдение в квартире: тихая комната, взрослый рядом первые 6–8 часов, отсутствие грубой дезориентации и неукротимой рвоты, относительная стабильность АД/ЧСС. В таких условиях выездная бригада «Трезвой Линии» запускает персональную схему: регидратация, выравнивание электролитов, поддержка витаминами группы B и магнием, осторожная седация, чтобы «собрать» сон, не выключая мониторинг. Стационар предпочтителен, если запой длится 3–5 суток и более, отмечаются «качели» показателей, шаткость походки, выраженная слабость, признаки предделирия или судорожной готовности; также при сочетанной соматике (ИБС, гипертония, диабет, хронические болезни печени/почек, неврология) и у пациентов старшего возраста. Преимущество стационара — приборный контроль, тихий режим, щадящее питание, возможность быстро расширять схему без ожидания ухудшений. Мы придерживаемся принципа «минимально достаточно»: ровно столько вмешательств, сколько требует клиническая картина, — так безопаснее и в перспективе экономнее, чем череда домашних «подлаток».
Получить больше информации – vyvod-iz-zapoya-cena
Для достижения стойкой ремиссии применяются современные и безопасные методики, которые подбираются индивидуально для каждого пациента.
Разобраться лучше – http://lechenie-alkogolizma-omsk0.ru
Каждый метод подбирается индивидуально, что обеспечивает безопасность и эффективность процесса.
Подробнее – врач вывод из запоя в омске
Услуга вывода из запоя в клинике сочетает профессионализм врачей, медицинскую точность и заботу. При этом обеспечивается полная конфиденциальность: данные пациентов не передаются в сторонние инстанции. Круглосуточный режим работы позволяет вызвать врача даже ночью — специалисты прибывают в течение 40–60 минут после обращения.
Разобраться лучше – вывод из запоя на дому круглосуточно
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Подробнее можно узнать тут – http://narkologicheskaya-klinika-kolomna2-10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/https://narkologicheskaya-klinika-kolomna2-10.ru
范德沃克高清完整版采用机器学习个性化推荐,海外华人可免费观看最新热播剧集。
Индивидуально подобранный состав раствора обеспечивает быстрое выведение токсинов и улучшение физического состояния уже в течение первых часов после начала лечения.
Подробнее тут – капельница от запоя недорого
Remarkable issues here. I am very glad to look your article.
Thanks a lot and I am having a look forward to contact you.
Will you please drop me a mail?
I am really happy to glance at this blog posts which contains plenty of helpful information, thanks for providing such
data.
I simply couldn’t leave your website prior to suggesting that I actually enjoyed the standard info an individual supply in your visitors?
Is gonna be back incessantly in order to investigate cross-check new posts
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Получить больше информации – нарколог на дом цены уфа
Ниже представлена таблица с основными препаратами, используемыми при выводе из запоя в Тюмени:
Получить дополнительные сведения – http://vyvod-iz-zapoya-v-tyumeni17.ru
No matter if some one searches for his essential thing,
therefore he/she desires to be available that in detail, therefore that thing is maintained over
here.
I got this web page from my friend who shared with me concerning this site and at the moment this time I am visiting
this web site and reading very informative articles at this time.
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Углубиться в тему – помощь вывод из запоя в тольятти
Каждый компонент капельницы подбирается по медицинским показаниям. Врач учитывает возраст, хронические заболевания, степень обезвоживания и чувствительность к препаратам. Такой индивидуальный подход обеспечивает эффективность лечения и исключает осложнения.
Получить больше информации – вывод из запоя капельница на дому
Маршрут выстроен без пауз и импровизаций. Сначала — короткое интервью по телефону: адрес в Электростали, длительность эпизода, лекарства/дозировки, аллергии, важные диагнозы, последние значения давления и пульса. Это экономит 15–20 минут на месте и позволяет заранее исключить опасные взаимодействия. По прибытии врач фиксирует АД, ЧСС, сатурацию, температуру, оценивает неврологический статус, степень обезвоживания, выраженность тремора/тошноты, уровень тревоги, кратко собирает анамнез последних суток. Затем стартует инфузионная терапия: растворы для регидратации и коррекции электролитов, поддержка витаминами группы B и магнием; по показаниям — гепатопротекторы и антиоксиданты, противорвотные, мягкие анксиолитики. Каждые 15–20 минут врач смотрит динамику и корректирует темп капельниц, питьевой режим, симптоматическую поддержку. Важный принцип — «сон без вырубания»: умеренная седация собирает ночной ритм, сохраняя информативность мониторинга. По завершении — письменные рекомендации и маршрут на 24–72 часа (сон, питание, запреты, «красные флаги», амбулаторные визиты/дневной стационар или перевод в отделение). Такой алгоритм заменяет «лотерею» результата управляемым и повторяемым планом.
Ознакомиться с деталями – https://vyvod-iz-zapoya-ehlektrostal10.ru/vyvod-iz-zapoya-stacionar-v-ehlektrostali
Каждый этап проходит под контролем врачей-наркологов и психотерапевтов, что гарантирует эффективность и безопасность лечения.
Подробнее – платная наркологическая клиника
It is not my first time to pay a quick visit this site, i am visiting this
site dailly and take nice information from here daily.
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Подробнее тут – http://vivod-iz-zapoya-v-volgograde17.ru/anonimnaya-narkologiya-vyvod-iz-zapoya-volgograd/
После поступления вызова наш нарколог выезжает к пациенту в кратчайшие сроки, прибывая по адресу в пределах 30–60 минут. Специалист начинает процедуру с подробного осмотра и диагностики, измеряя ключевые показатели организма: артериальное давление, частоту пульса, насыщенность кислородом и собирая подробный анамнез.
Получить дополнительную информацию – http://www.domen.ru
Важное отличие клиники — отказ от примитивной схемы «капельница — домой — дальше сам». Такой формат даёт кратковременное облегчение, но не решает ни причин, ни структуры зависимости. «КоломнаМед Центр» выстраивает ступенчатый подход. Первый шаг — безопасная детоксикация: снятие абстиненции, коррекция водно-электролитного баланса, поддержка сердечно-сосудистой системы, печени, нервной системы, нормализация сна. Второй шаг — стабилизация: оценка психического состояния, выявление тревожных, депрессивных и панических симптомов, подбор поддерживающих схем, которые помогают не сорваться сразу после выхода из острых проявлений. Третий шаг — реабилитация и мотивация: психотерапевтическая работа, групповые и индивидуальные форматы, обучение навыкам трезвой жизни, работа с триггерами, укрепление внутренней мотивации. Четвёртый шаг — постреабилитационная поддержка: контрольные приёмы, дистанционные консультации, помощь в профилактике срывов. Такой комплексный путь не ломает пациента, а возвращает ему контроль: не через страх, а через понимание, структуру и реальные инструменты.
Подробнее – наркологическая клиника в Коломне
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Получить больше информации – http://vyvod-iz-zapoya-v-ryazani17.ru
Программа лечения строится по принципу последовательного воздействия на физическое и психологическое состояние. Начинается она с детоксикации: инфузионная терапия с применением сбалансированных растворов, антиоксидантов, гепатопротекторов и витаминов. Затем — стабилизация состояния, коррекция сна, восстановление когнитивных функций и купирование абстинентного синдрома. В зависимости от диагноза используются такие методы, как заместительная терапия, нейрометаболическая поддержка, противотревожные и антидепрессивные схемы.
Разобраться лучше – наркологическая клиника цены в новокузнецке
Важное отличие клиники — отказ от примитивной схемы «капельница — домой — дальше сам». Такой формат даёт кратковременное облегчение, но не решает ни причин, ни структуры зависимости. «КоломнаМед Центр» выстраивает ступенчатый подход. Первый шаг — безопасная детоксикация: снятие абстиненции, коррекция водно-электролитного баланса, поддержка сердечно-сосудистой системы, печени, нервной системы, нормализация сна. Второй шаг — стабилизация: оценка психического состояния, выявление тревожных, депрессивных и панических симптомов, подбор поддерживающих схем, которые помогают не сорваться сразу после выхода из острых проявлений. Третий шаг — реабилитация и мотивация: психотерапевтическая работа, групповые и индивидуальные форматы, обучение навыкам трезвой жизни, работа с триггерами, укрепление внутренней мотивации. Четвёртый шаг — постреабилитационная поддержка: контрольные приёмы, дистанционные консультации, помощь в профилактике срывов. Такой комплексный путь не ломает пациента, а возвращает ему контроль: не через страх, а через понимание, структуру и реальные инструменты.
Разобраться лучше – narkologicheskaya-klinika-kolomna
Awesome article.
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Подробнее можно узнать тут – http://vyvod-iz-zapoya-v-ryazani17.ru/vyvod-iz-zapoya-ryazan-na-domu/https://vyvod-iz-zapoya-v-ryazani17.ru
Благодаря комплексному подходу достигается не только снятие симптомов, но и долгосрочная стабилизация состояния пациента.
Ознакомиться с деталями – http://narkologicheskaya-pomoshh-v-volgograde17.ru
Даже при наличии комфортных условий и современных медикаментов эффективность будет минимальной, если пациент не получает психологическую помощь. У многих зависимость сопровождается тревожными или депрессивными состояниями, травматическим опытом или сложными семейными отношениями. Без проработки этих аспектов высокий риск того, что после выписки произойдёт рецидив.
Детальнее – https://narkologicheskaya-klinika-yaroslavl0.ru/lechenie-narkomanii-i-alkogolizma-yaroslavl/
Такая структура позволяет достичь максимального эффекта в кратчайшие сроки и минимизировать риск осложнений.
Разобраться лучше – вызов нарколога на дом в уфе
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Узнать больше – http://vivod-iz-zapoya-v-volgograde17.ru/vyvod-iz-zapoya-na-domu-volgograd/
Комплексное применение этих методов позволяет значительно ускорить процесс восстановления и предотвратить осложнения.
Изучить вопрос глубже – https://narcologicheskaya-klinika-v-novokuzneczke17.ru/
Медицинская помощь строится на принципах индивидуального подхода и поэтапной терапии. Каждый пациент проходит диагностику, после чего составляется персональная программа, включающая медикаментозную поддержку, консультации психотерапевта и физиопроцедуры. Такой подход помогает не просто снять симптомы, но и восстановить организм полностью.
Получить дополнительные сведения – лечение в наркологической клинике рязань
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Выяснить больше – http://narkolog-na-dom-saratov0.ru/narkolog-i-psikhiatr-v-saratove/
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Изучить вопрос глубже – http://narkologicheskaya-klinika-kolomna2-10.ru
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Подробнее можно узнать тут – кодирование от алкоголизма анонимно
Web Site https://cytonic.cc/
Во многих случаях пациент или его родственники не решаются сразу вызвать врача. Для таких ситуаций предусмотрена услуга онлайн-консультации. Она проводится через защищённую видеосвязь, при желании — анонимно. На связи — врач-нарколог или психиатр, который отвечает на вопросы, оценивает ситуацию по визуальным и вербальным признакам, рекомендует план действий. Консультация может стать отправной точкой для дальнейшего вызова врача на дом или записи в клинику. Это особенно удобно для родственников, которые не знают, как подступиться к проблеме и убедить человека в необходимости помощи.
Ознакомиться с деталями – центр наркологической помощи тверь
Sites like Casino HEX focus on free play options, while gamblingformoney.us.com/online-slots/ addresses real money
gaming comprehensively. Practice modes help, but real money play is what most serious players want guidance on.
The real-money focus better serves core audience needs.
Примерный состав раствора, применяемого наркологом на дому в Уфе, приведён в таблице:
Получить больше информации – http://narkolog-na-dom-v-ufe17.ru
goGLOW
6850 N Rochester Ɍd, Rochester Hills,
MI 48306, United Stɑtes
248 971-1831
Bookmarks
Инфузионная терапия (капельницы) — важная часть лечения, направленная на очищение организма, восстановление водно-солевого баланса и устранение токсинов. В «РязаньМед Альянс» используются проверенные препараты, которые помогают нормализовать работу внутренних органов и улучшить общее самочувствие. Таблица ниже показывает, какие виды капельниц чаще всего применяются при выведении из запоя и лечении алкоголизма.
Подробнее можно узнать тут – http://narkologicheskaya-klinika-v-ryazani17.ru
Hey! Quick question that’s completely off topic.
Do you know how to make your site mobile
friendly? My site looks weird when browsing from my iphone4.
I’m trying to find a theme or plugin that might be able to fix
this issue. If you have any suggestions, please share.
Many thanks!
Такая комплексность обеспечивает воздействие на физические, психологические и социальные факторы зависимости.
Получить больше информации – принудительное лечение от алкоголизма омск
Во многих случаях пациент или его родственники не решаются сразу вызвать врача. Для таких ситуаций предусмотрена услуга онлайн-консультации. Она проводится через защищённую видеосвязь, при желании — анонимно. На связи — врач-нарколог или психиатр, который отвечает на вопросы, оценивает ситуацию по визуальным и вербальным признакам, рекомендует план действий. Консультация может стать отправной точкой для дальнейшего вызова врача на дом или записи в клинику. Это особенно удобно для родственников, которые не знают, как подступиться к проблеме и убедить человека в необходимости помощи.
Подробнее – http://narkologicheskaya-pomoshh-tver0.ru/narkolog-tver-anonimno/
Такая структура позволяет достичь максимального эффекта в кратчайшие сроки и минимизировать риск осложнений.
Получить дополнительную информацию – вызов нарколога на дом уфа
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Изучить вопрос глубже – вывод из запоя в стационаре
Наркологическая клиника «КоломнаМед Центр» — это место, куда можно обратиться в тот момент, когда домашние попытки контролировать алкоголь, наркотики, аптечные препараты или смесь всего сразу перестают работать, а жизнь превращается в постоянное «завтра начну с нуля». Здесь не обещают чудес за один день и не пугают диагнозами, а выстраивают понятный медицинский маршрут: детоксикация, стабилизация, реабилитация, поддержка семьи, профилактика срывов. Пациент получает помощь в защищённой, конфиденциальной среде, где всё организовано так, чтобы снизить тревогу и стыд, убрать хаос вокруг зависимости и дать человеку шанс вернуться к нормальной жизни без давления, угроз и токсичных «стимулов». Для родных клиника в Коломне — это опора: конкретный адрес, конкретная команда, чёткие сроки и понятные этапы, вместо бесконечных обещаний «он сам справится».
Подробнее – http://narkologicheskaya-klinika-kolomna10.ru
Острый эпизод запоя — это не «плохое самочувствие», а состояние с реальными рисками для сердца, нервной системы и дыхания, особенно в ночные часы, когда усиливаются вегетативные реакции и тревога. В «НоваТрезвие» мы выстраиваем помощь так, чтобы от звонка до заметного облегчения прошло как можно меньше времени и как можно меньше случайностей: короткое интервью для оценки рисков, выезд врача или приём в клинике, экспресс-диагностика по ключевым показателям, персональная инфузионная схема без «универсальных коктейлей», мягкая коррекция сна и тревоги без «вырубания», понятные инструкции семье на 24–72 часа и план продолжения на ближайшие недели. Мы не скрываемся за общими формулами: решения принимаются по фактическим данным, дозы и темп капельниц подстраиваются к динамике каждые 15–20 минут, а при «красных флагах» перевод в стационар организуется без пауз. Конфиденциальность соблюдается строго, а коммуникация простая и предсказуемая — чтобы вы всегда знали, что происходит сейчас и чего ждать к утру.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-ehlektrostal2-10.ru/vyvesti-iz-zapoya-ehlektrostal
Как выбрать хорошую видеокарту графический ускоритель
Вывод из запоя требуется тогда, когда организм уже не способен самостоятельно справиться с последствиями алкогольной интоксикации. Длительное употребление спиртного приводит к нарушению работы внутренних органов, обезвоживанию и психическим расстройствам. Медицинская помощь помогает избежать опасных осложнений и облегчить процесс отказа от алкоголя.
Узнать больше – вывод из запоя на дому в рязани
Терапия проводится поэтапно, что позволяет пациенту последовательно проходить все стадии восстановления и закреплять результат.
Разобраться лучше – клиника лечения алкоголизма в омске
Клиника в Красноярске придерживается комплексного подхода, при котором сочетаются медикаментозные и психотерапевтические методы. Такой подход позволяет воздействовать не только на физическую, но и на психологическую зависимость. Каждый пациент проходит детальное обследование, после чего врач-нарколог составляет индивидуальный план лечения с учётом стадии заболевания, состояния организма и наличия сопутствующих проблем со здоровьем.
Исследовать вопрос подробнее – http://narcologicheskaya-klinika-v-krasnoyarske17.ru
Hi! Do you know if they make any plugins to protect against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any tips?
Зависимость от психоактивных веществ — серьёзное заболевание, затрагивающее как физическое, так и психологическое состояние человека. При отсутствии своевременной наркологической помощи в клинике возможно ухудшение здоровья, развитие тяжелых осложнений и социальная деградация пациента.
Узнать больше – частная наркологическая помощь
I am actually happy to glance at this blog posts which carries
tons of valuable information, thanks for providing such data.
Запой – это опасное состояние, при котором организм подвергается значительной токсической нагрузке, а длительное злоупотребление алкоголем приводит к нарушению работы внутренних органов и ухудшению общего самочувствия. В Ярославле качественная наркологическая помощь на дому становится спасением для пациентов, нуждающихся в оперативной детоксикации и стабилизации состояния. Такой формат лечения позволяет начать терапию в комфортной обстановке, сохраняя конфиденциальность и минимизируя стресс, связанный с посещением стационара.
Получить дополнительные сведения – наркологический вывод из запоя ярославль
check my blog https://gofundmeme.cc/
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Выяснить больше – http://vyvod-iz-zapoya-saratov0.ru/
Busyy Bee Jumpers
45 Main Ѕt 6C, Wareham,
MA 02571, Unites States
508-514-2005
bounce house rentals with water slides
В Волгограде медицинская клиника «Трезвая Линия Волгоград» предоставляет круглосуточную помощь людям, столкнувшимся с острым алкогольным отравлением или затяжным запоем. Врачи выезжают на дом, в гостиницу или принимают пациентов в стационаре. Каждое вмешательство начинается с оценки состояния — измерения давления, пульса, насыщения кислородом, уровня интоксикации и дехидратации. Далее подбирается оптимальный состав капельницы, направленный на восстановление водно-солевого баланса, поддержку печени и снижение тревожности.
Подробнее тут – вывод из запоя дешево волгоград
Процесс организован так, чтобы снять с семьи хаос и дать понятный сценарий. После обращения в «РеутовМед Сервис» пациент быстро попадает в поле зрения врача: или через выезд по адресу, или через стационар, если состояние уже близко к опасному. На месте проводится полноценная оценка: давление, пульс, сатурация, температура, осмотр сердца и дыхания, степень обезвоживания, выраженность тремора, наличие рвоты, боли в груди или животе, неврологический статус, поведение, признаки психоза. На основе этих данных формируется индивидуальный план детоксикации. Стартовая инфузионная терапия подбирается с учётом возраста, массы тела, длительности запоя, сопутствующих болезней, уже принятых препаратов. В стационаре пациента размещают в безопасных условиях, контролируют динамику, корректируют дозировки, не оставляют «на самотёк». При выводе из запоя на дому врач остаётся до стабилизации, отслеживает реакцию и при первых тревожных признаках рекомендует стационар, а не уезжает «лишь бы поставил капельницу». Такой пошаговый подход позволяет не только снять острые симптомы, но и уменьшить риск осложнений — от аритмий и судорог до алкогольного делирия.
Подробнее – вывод из запоя круглосуточно реутов
Наркологическая клиника «МедЛайн» предоставляет профессиональные услуги врача-нарколога с выездом на дом в Новосибирске и Новосибирской области. Мы оперативно помогаем пациентам справиться с тяжелыми состояниями при алкогольной и наркотической зависимости. Экстренный выезд наших специалистов доступен круглосуточно, а лечение проводится с применением проверенных методик и препаратов, что гарантирует безопасность и конфиденциальность каждому пациенту.
Подробнее можно узнать тут – нарколог на дом срочно новосибирск
Процесс включает следующие шаги:
Подробнее тут – https://narcologicheskaya-klinika-v-krasnoyarske17.ru/krasnoyarsk-narkologicheskij-czentr
Карта делает видимой причинно-следственную связь: пациент понимает, зачем и что именно делается; семья видит «точки проверки»; врач получает опору для изменения одного параметра без разрушения всего плана.
Разобраться лучше – http://vyvod-iz-zapoya-saratov0.ru
Метод лечения
Подробнее тут – частная наркологическая помощь в новокузнецке
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Получить дополнительную информацию – вывод из запоя на дому цена
Как выбрать хорошую медтехнику от производителя советы по выбору надёжной медтехники
Критичные случаи, когда вызов нарколога через «МедТрезвие Долгопрудный» оправдан и своевременен:
Узнать больше – narkolog-na-dom-vyvod-iz-zapoya
Основные направления включают:
Детальнее – https://narkologicheskaya-pomoshh-v-volgograde17.ru/narkologiya-v-volgograde/
Первый шаг в лечении — это тщательный осмотр специалиста. Наряду с измерением жизненно важных показателей (пульс, артериальное давление, температура) врач проводит сбор анамнеза, выясняя длительность запоя, тип употребляемого алкоголя и наличие сопутствующих заболеваний. Эти данные помогают оценить степень интоксикации и подобрать индивидуальный план терапии, что является ключевым для дальнейшей эффективной детоксикации.
Углубиться в тему – http://vyvod-iz-zapoya-yaroslavl0.ru/vyvod-iz-zapoya-kruglosutochno-yaroslavl/
Прежде чем принимать решение, важно изучить сайт клиники. В надёжных учреждениях размещена полная информация о врачах, их образовании и опыте работы. Кроме того, пациентам предлагается пройти предварительную консультацию — чаще всего она проводится анонимно и включает первичную диагностику. Это позволяет оценить профессионализм команды ещё до начала терапии.
Исследовать вопрос подробнее – наркологическая клиника ярославская область
После завершения процедур пациенту предоставляется подробная консультация с рекомендациями по дальнейшему восстановлению и профилактике повторных случаев зависимости.
Выяснить больше – https://narcolog-na-dom-novosibirsk00.ru
What’s up to all, because I am really keen of reading this web site’s post to be
updated daily. It contains fastidious material.
Перед цифрами важно подчеркнуть: прайс «Трезвый Центр Коломна» строится вокруг реального объёма помощи, а не вокруг рекламных обещаний. Цена зависит от тяжести состояния, длительности запоя, количества инфузий, необходимого набора препаратов, формата (дом или стационар), времени суток выезда, длительности наблюдения. Все дополнительные назначения согласуются заранее — без скрытых доплат и неожиданных строк. Это позволяет семье планировать расходы и сосредоточиться на безопасности.
Получить дополнительную информацию – http://vyvod-iz-zapoya-kolomna10.ru/vyvod-iz-zapoya-v-stacionare-v-kolomne/https://vyvod-iz-zapoya-kolomna10.ru
Правильный подбор лекарственных средств позволяет не только уменьшить проявления синдрома отмены, но и стабилизировать эмоциональное состояние пациента, снижая риск срывов. Реабилитационные программы включают физиотерапию, спортивные занятия и коррекцию образа жизни, что способствует полноценному восстановлению организма.
Углубиться в тему – https://lechenie-narkomanii-tver0.ru/tver-lechenie-alkogolizma
site here https://cwap.us
Reliable data Kudos. https://heylink.me/betflik-th
Главная задача процедуры — быстрое выведение этанола и его метаболитов из организма, нормализация уровня электролитов, улучшение самочувствия и предотвращение осложнений. Лечение проводится как в клинике, так и на дому, что особенно удобно при тяжёлых состояниях, когда пациент не может самостоятельно добраться до медицинского учреждения.
Углубиться в тему – vyvod-iz-zapoya-v-tyumeni17.ru/
Терапия проводится поэтапно, что позволяет пациенту последовательно проходить все стадии восстановления и закреплять результат.
Углубиться в тему – клиника лечения алкоголизма омск
Выездной наркологический сервис «МедПоволжье Клиник» создан для случаев, когда важны скорость, тишина и клиническая точность. Мы проводим детоксикацию и снятие интоксикации на дому так, чтобы каждое действие имело цель, измеримый маркер и заранее оговорённое «окно переоценки». Вместо «сильной капельницы на всякий случай» — модульная схема: один симптом-кластер > один медицинский модуль > одна поведенческая опора (свет, звук, вода малыми глотками, дыхание 4–6). Такой подход снижает лекарственную нагрузку, ускоряет стабилизацию и позволяет видеть прогресс буквально по часам.
Изучить вопрос глубже – http://narkolog-na-dom-saratov0.ru
Психологическая поддержка играет ключевую роль в лечении наркомании в Твери. В клинике «Ренессанс» применяются различные методы психотерапии, включая когнитивно-поведенческую терапию, групповые и семейные сессии, арт-терапию. Эти методы помогают осознать причины зависимости, развить навыки преодоления стрессов и поддержать мотивацию к выздоровлению.
Подробнее – лечение наркомании и алкоголизма в твери
В этих ситуациях выезд нарколога на дом позволяет вовремя скорректировать состояние, а при выявлении опасных признаков — не теряя времени, направить пациента в стационар. Это управляемый маршрут вместо хаотичных решений в последний момент.
Детальнее – https://narkolog-na-dom-dolgoprudnij10.ru/
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Детальнее – кодирование от алкоголизма
Лечение алкоголизма в клинике «РязаньМед Альянс» включает несколько этапов, каждый из которых направлен на определённую цель — от снятия интоксикации до формирования устойчивого отказа от алкоголя. В таблице представлены основные стадии лечения и методы, используемые специалистами клиники.
Детальнее – наркологическая клиника в рязани
I do accept as true with all of the ideas you have presented in your post.
They’re very convincing and will definitely work.
Nonetheless, the posts are too short for beginners.
Could you please prolong them a little from subsequent time?
Thank you for the post.
Тем, кто нуждается в длительной терапии, «КузбассМед» предлагает комфортные условия стационара с круглосуточным наблюдением. Здесь пациенты размещаются в индивидуальных палатах, проходят курсы терапии, реабилитации и психокоррекции. Обстановка в клинике напоминает оздоровительный центр: мягкое освещение, тишина, доступ к библиотеке, возможность общения с психологом и ежедневное участие в восстановительных мероприятиях. Медицинские сестры и врачи находятся на дежурстве 24/7, что позволяет немедленно реагировать на любые изменения в состоянии пациента.
Подробнее тут – наркологическая клиника лечение алкоголизма новокузнецк
Наша выездная бригада приезжает без маркировки, в гражданской одежде, согласовывает «тихое окно» связи с пациентом или близкими и начинает не с капельницы, а с настройки среды: тёплая приглушённая подсветка, проветривание без сквозняков, отключение уведомлений, подготовка воды комнатной температуры. Затем — быстрый осмотр, экспресс-метрики и старт индивидуального плана. Каждая корректировка — ровно одна за раз, чтобы сохранить причинно-следственную связь и не провоцировать полипрагмазию.
Ознакомиться с деталями – нарколог на дом анонимно саратов
Комплексное применение этих методов позволяет значительно ускорить процесс восстановления и предотвратить осложнения.
Выяснить больше – наркологическая клиника клиника помощь в новокузнецке
Наркологическая клиника «Трезвый Путь Коломна» — это пространство, где тяжёлые истории зависимости перестают быть хаотичным набором срывов, ночных обещаний и беспомощных попыток родных «вытащить своими силами». Здесь собраны врачи-наркологи, терапевты, психологи и медперсонал, которые знают, что такое длительные запои, многолетнее употребление, полинаркомания, зависимость от аптечных препаратов, и умеют работать с этим не через страх и давление, а через профессиональные, выверенные шаги. Клиника в Коломне предлагает безопасную детоксикацию, стационарное наблюдение, индивидуальные программы лечения алкоголизма и наркомании, поддержку семьи и постреабилитационные решения. Все процессы организованы так, чтобы пациент сохранял достоинство, а родственники наконец получили не обещания, а реальный план действий, понятный по этапам и по результатам.
Изучить вопрос глубже – http://narkologicheskaya-klinika-kolomna2-10.ru/
Когда вопрос стоит остро — нужно быстро и безопасно вывести человека из запоя в Коломне, — у семьи нет лишнего времени на эксперименты с таблетками, сомнительными «коктейлями» и советами из интернета. «Трезвый Центр Коломна» выстраивает помощь так, чтобы от первого звонка до реального облегчения шёл понятный и управляемый маршрут: запись симптомов и рисков уже по телефону, предложение формата (выезд на дом или стационар), оперативный осмотр, персональная инфузионная терапия, круглосуточное наблюдение при необходимости и подробный план восстановления на 24–72 часа и дальше. Мы не продаём миф о «чудо-капельнице за час», а работаем клинически аккуратно: дозы и схемы подбираются под возраст, длительность запоя, сопутствующие заболевания, уже принятые лекарства и текущие показатели. Цель проста и честна — снять интоксикацию, защитить сердце, мозг и печень, вернуть сон и ясность без агрессивной седации и скрытых рисков, сохранить конфиденциальность и дать семье уверенность, что всё делается правильно.
Разобраться лучше – https://vyvod-iz-zapoya-kolomna10.ru/vyvod-iz-zapoya-kapelnica-v-kolomne
Вывод из запоя — это не «волшебная капельница», а последовательная медицинская программа с чёткими целями и измеримыми маркерами. В наркологической клинике «СаратовМед Профи» маршрут строится по принципу управляемых окон: на каждом шаге команда преследует одну цель, меняет лишь один параметр и оценивает результат в заранее назначённый момент. Такой подход снижает лекарственную нагрузку, предотвращает «гонку дозировок» и делает динамику предсказуемой для пациента и близких. Конфиденциальность обеспечивается регламентом: немаркированные выезды, нейтральные формулировки в документах, «тихие» каналы связи, доступ к записям — строго по ролям.
Исследовать вопрос подробнее – наркологический вывод из запоя
Важное отличие клиники — отказ от примитивной схемы «капельница — домой — дальше сам». Такой формат даёт кратковременное облегчение, но не решает ни причин, ни структуры зависимости. «КоломнаМед Центр» выстраивает ступенчатый подход. Первый шаг — безопасная детоксикация: снятие абстиненции, коррекция водно-электролитного баланса, поддержка сердечно-сосудистой системы, печени, нервной системы, нормализация сна. Второй шаг — стабилизация: оценка психического состояния, выявление тревожных, депрессивных и панических симптомов, подбор поддерживающих схем, которые помогают не сорваться сразу после выхода из острых проявлений. Третий шаг — реабилитация и мотивация: психотерапевтическая работа, групповые и индивидуальные форматы, обучение навыкам трезвой жизни, работа с триггерами, укрепление внутренней мотивации. Четвёртый шаг — постреабилитационная поддержка: контрольные приёмы, дистанционные консультации, помощь в профилактике срывов. Такой комплексный путь не ломает пациента, а возвращает ему контроль: не через страх, а через понимание, структуру и реальные инструменты.
Выяснить больше – http://narkologicheskaya-klinika-kolomna10.ru/
Hi! Quick question that’s entirely off topic.
Do you know how to make your site mobile friendly? My blog looks weird when browsing
from my iphone4. I’m trying to find a template or plugin that might be able to correct this problem.
If you have any suggestions, please share. Appreciate it!
Great post. I will be dealing with many of these issues as well..
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Узнать больше – вывод из запоя на дому
Капельница от запоя в Волгограде — это эффективный способ быстро восстановить организм после длительного употребления алкоголя. Процедура проводится врачом-наркологом и направлена на выведение токсинов, нормализацию обмена веществ и стабилизацию работы нервной системы. Инфузионная терапия помогает устранить головную боль, слабость, тошноту, восстановить сон и аппетит. Благодаря внутривенному введению препаратов эффект наступает уже через 20–30 минут после начала процедуры.
Подробнее тут – капельница от запоя на дому недорого
Ich bin berührt von dieser Arbeit. Spenden für
die Wiederherstellung der Sehkraft ist ein kraftvoller Weg, der Menschheit zu dienen. Bitte, diese wichtigen Taten fortzusetzen.
Feel free to visit my page … Augenlicht-Rettungsprojekt
Do you have a spam problem on this website; I also am a blogger, and I was
curious about your situation; many of us have created some nice practices and we are looking to exchange strategies with other folks, why not
shoot me an email if interested.
I’m curious to find out what blog platform you’re utilizing?
I’m experiencing some minor security issues with my latest blog and I would like to find something more risk-free.
Do you have any suggestions?
Hello would you mind stating which blog platform you’re using?
I’m going to start my own blog in the near future but I’m having
a difficult time choosing between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most blogs and I’m looking for something unique.
P.S Sorry for being off-topic but I had
to ask!
Лечение наркомании в Твери представляет собой сложный и многоэтапный процесс, направленный на полное восстановление здоровья и социальной адаптации пациентов, страдающих от зависимости. В наркологической клинике «Ренессанс» применяется комплексный подход, который учитывает как физиологические, так и психологические аспекты заболевания, что обеспечивает максимальную эффективность терапии.
Углубиться в тему – лечение наркомании анонимно тверь
Процесс организован так, чтобы снять с семьи хаос и дать понятный сценарий. После обращения в «РеутовМед Сервис» пациент быстро попадает в поле зрения врача: или через выезд по адресу, или через стационар, если состояние уже близко к опасному. На месте проводится полноценная оценка: давление, пульс, сатурация, температура, осмотр сердца и дыхания, степень обезвоживания, выраженность тремора, наличие рвоты, боли в груди или животе, неврологический статус, поведение, признаки психоза. На основе этих данных формируется индивидуальный план детоксикации. Стартовая инфузионная терапия подбирается с учётом возраста, массы тела, длительности запоя, сопутствующих болезней, уже принятых препаратов. В стационаре пациента размещают в безопасных условиях, контролируют динамику, корректируют дозировки, не оставляют «на самотёк». При выводе из запоя на дому врач остаётся до стабилизации, отслеживает реакцию и при первых тревожных признаках рекомендует стационар, а не уезжает «лишь бы поставил капельницу». Такой пошаговый подход позволяет не только снять острые симптомы, но и уменьшить риск осложнений — от аритмий и судорог до алкогольного делирия.
Детальнее – vrach-vyvod-iz-zapoya
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Узнать больше – http://vivod-iz-zapoya-v-volgograde17.ru
Пациенты выбирают нашу клинику для срочного вызова врача-нарколога благодаря следующим важным преимуществам:
Получить дополнительные сведения – вызов нарколога на дом
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Разобраться лучше – наркологический вывод из запоя в омске
When I initially left a comment I seem to have clicked the -Notify me
when new comments are added- checkbox and from now on each time a comment is added I recieve 4 emails with the
same comment. Perhaps there is a way you can remove me from that
service? Cheers! https://airstoneglobalrealty.com/author/dwainbloomer89/
Алкогольная интоксикация вызывает сильное обезвоживание и разрушает баланс электролитов в организме. Без медицинской помощи восстановление может занять несколько дней, а в тяжёлых случаях приводит к осложнениям. Капельница помогает безопасно и быстро вывести этанол и продукты его распада, восполнить уровень жидкости, снизить нагрузку на печень и сердечно-сосудистую систему. Процедура проводится амбулаторно или на дому, что делает её доступной и удобной для пациентов.
Изучить вопрос глубже – http://kapelnicza-ot-zapoya-v-volgograde17.ru/
«ТверьМед» — частная лицензированная клиника, специализирующаяся на наркологической помощи любой степени сложности. Здесь работают неравнодушные врачи-наркологи, психиатры, терапевты и психологи с многолетним стажем. Медицинская команда настроена на оперативную диагностику и проведение первичных мероприятий в течение первого часа после обращения. Упор сделан на доступность: клиника открыта 24/7, приём возможен как на территории медучреждения, так и на выезде — дома, в офисе, гостинице, санатории или любом удобном месте.
Подробнее тут – анонимная наркологическая помощь в твери
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Исследовать вопрос подробнее – кодирование от алкоголизма отзывы цены волгоград
Наркологическая клиника «МедЛайн» предоставляет профессиональные услуги врача-нарколога с выездом на дом в Новосибирске и Новосибирской области. Мы оперативно помогаем пациентам справиться с тяжелыми состояниями при алкогольной и наркотической зависимости. Экстренный выезд наших специалистов доступен круглосуточно, а лечение проводится с применением проверенных методик и препаратов, что гарантирует безопасность и конфиденциальность каждому пациенту.
Ознакомиться с деталями – нарколог на дом недорого в новосибирске
Особенность подхода заключается в сочетании медицинской и психологической поддержки. После кодирования пациент получает консультации психотерапевта, рекомендации по восстановлению и профилактике рецидивов. Это снижает риск повторного срыва и помогает закрепить результат на долгий срок.
Получить дополнительные сведения – бесплатное кодирование от алкоголизма
I’ve been browsing online greater than three hours nowadays,
yet I by no means found any fascinating article like yours.
It is beautiful value sufficient for me.
Personally, if all web owners and bloggers made
good content as you did, the internet shall be much more
useful than ever before.
Даже телефонный разговор с клиникой может многое сказать о её подходе. Если вам предлагают типовое лечение без уточнения подробностей или избегают вопросов о составе команды, это тревожный сигнал. Серьёзные учреждения в Мурманске обязательно предложат предварительную консультацию, зададут уточняющие вопросы и расскажут, как строится программа помощи.
Выяснить больше – лечение алкоголизма цена
these details https://kyros.my
Эта статья погружает вас в увлекательный мир знаний, где каждый факт становится открытием. Мы расскажем о ключевых исторических поворотных моментах и научных прорывах, которые изменили ход цивилизации. Поймите, как прошлое формирует настоящее и как его уроки могут помочь нам строить будущее.
Есть чему поучиться – https://www.natureguidetraining.com/fat-portfolio/birds/green-woodhoopoe-botswana
I love your blog.. very nice colors & theme.
Did you design this website yourself or did you hire someone to do it for you?
Plz answer back as I’m looking to design my own blog and would like to find out where u got this from.
thanks
Gangnam is one of one of the most developed and acknowledged areas in Seoul, South
Korea. It is recognized for its modern-day way of life,
business setting, deluxe living, and cultural influence.
With time, several terms have actually come to be closely connected with
Gangnam’s image, consisting of Gangnam The King, Gangnam Savanna House, Gangnam Six, and Gangnam Objective.
These key words describe various ideas, duties, and
values that together discuss why Gangnam holds such an important placement.
Эта статья предлагает захватывающий и полезный контент, который привлечет внимание широкого круга читателей. Мы постараемся представить тебе идеи, которые вдохновят вас на изменения в жизни и предоставят практические решения для повседневных вопросов. Читайте и вдохновляйтесь!
Смотри, что ещё есть – https://www.theworld.guru/the-rise-of-remote-work-how-covid-19-transformed-our-workplaces
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Провести детальное исследование – https://www.wonderlandjumpingcastles.com.au/product/lego-juniors-10667-construction
Эта информационная заметка предлагает лаконичное и четкое освещение актуальных вопросов. Здесь вы найдете ключевые факты и основную информацию по теме, которые помогут вам сформировать собственное мнение и повысить уровень осведомленности.
Все материалы собраны здесь – https://www.poulaillon.fr/mise-en-oeuvre-contrat-liquidite-invest-securities-societe-bourse
一帆官方认证平台,专为海外华人设计,24小时不间断提供高清视频和直播服务。
Hey! This is kind of off topic but I need some help from an established blog.
Is it very difficult to set up your own blog? I’m not very techincal but I can figure things out pretty quick.
I’m thinking about creating my own but I’m not sure where to start.
Do you have any points or suggestions? Appreciate it
Эта статья погружает вас в увлекательный мир знаний, где каждый факт становится открытием. Мы расскажем о ключевых исторических поворотных моментах и научных прорывах, которые изменили ход цивилизации. Поймите, как прошлое формирует настоящее и как его уроки могут помочь нам строить будущее.
Погрузиться в детали – https://makeovers.prettyiris.com/e-l-f-matte-magic-mist-set
В этом обзорном материале представлены увлекательные детали, которые находят отражение в различных аспектах жизни. Мы исследуем непонятные и интересные моменты, позволяя читателю увидеть картину целиком. Погрузитесь в мир знаний и удивительных открытий!
Подробнее – https://www.agriculture.gov.zm/2025/10/farmers-stakeholders-gather-in-chisamba-for-2025-gart-seed-fair
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Есть чему поучиться – https://www.cursosalpha.com/blog/cuando-no-apretamos-bien-la-tapa-de-cilindros
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Детали по клику – https://thesteelemaiden.com/contact
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Обратитесь за информацией – https://danieloliveiracorretor.com.br/property/kitnet-proximo-a-leite-de-castro-2
It’s very trouble-free to find out any topic on net as compared to textbooks, as I found this paragraph at
this web page.
Amazing! Its genuinely awesome post, I have got much clear idea
on the topic of from this post.
useful link Zapper
Ahaa, its fastidious conversation regarding this paragraph here at this weblog, I have
read all that, so now me also commenting here.
Great blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple tweeks would really make my blog jump out.
Please let me know where you got your design. Kudos
I blog frequently and I genuinely appreciate your information. This great article has
really peaked my interest. I’m going to take a note of your blog and
keep checking for new details about once per week. I
subscribed to your RSS feed too.
Helpful info. Lucky me I found your web site unintentionally, and I am shocked why this twist of fate didn’t took place earlier!
I bookmarked it.
Врач уточняет, как долго продолжается запой, какой алкоголь употребляется, а также наличие сопутствующих заболеваний. Этот тщательный анализ позволяет оперативно подобрать оптимальные методы детоксикации и снизить риск осложнений.
Подробнее – вывод из запоя на дому
Fascinating blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple adjustements would really make my blog stand
out. Please let me know where you got your theme.
Kudos
I appreciate, cause I found exactly what I was looking for.
You’ve ended my 4 day long hunt! God Bless you man.
Have a nice day. Bye
I’m not that much of a internet reader to be honest but
your blogs really nice, keep it up! I’ll go ahead and bookmark your website to come back down the road.
All the best
Hi! Someone in my Facebook group shared this website with us so I came to look it
over. I’m definitely loving the information. I’m book-marking and will
be tweeting this to my followers! Fantastic blog and great design. https://musiccosign.com/colemannothlin
Busy Beee Jumpers
45 Main Տt 6C, Wareham,
ⅯA 02571, Unites Stаteѕ
508-514-2005
Bookmarks
If you would like to improve your familiarity simply keep visiting
this web site and be updated with the hottest
gossip posted here.
Лечение наркомании в клинике начинается с диагностики, позволяющей определить степень зависимости, выявить сопутствующие заболевания и выбрать оптимальную тактику терапии. Важным этапом является детоксикация — очищение организма от токсинов и продуктов распада наркотических веществ, что снижает риск осложнений и облегчает последующее восстановление.
Ознакомиться с деталями – лечение наркомании в стационаре тверь
веб-сайт https://krab4a.at/
You appear to know so much about this, and I see you’re a published author. Thanks
Вызов нарколога на дом — это удобная и безопасная возможность получить медицинскую помощь без необходимости ехать в клинику. Такая услуга особенно востребована, когда состояние пациента не позволяет покинуть дом, а помощь требуется незамедлительно. В наркологической клинике «ВоронМед Профи» организована круглосуточная служба выезда специалистов, которая оперативно реагирует на обращения и обеспечивает профессиональную помощь при запое, алкогольной интоксикации и обострениях хронических состояний. Врач приезжает в течение часа, оценивает состояние пациента и подбирает оптимальную схему лечения, включающую капельницы, детоксикацию и рекомендации по восстановлению организма.
Исследовать вопрос подробнее – нарколог капельница на дом в воронеже
Конфиденциальность — это набор конкретных действий, а не декларация на сайте. Мы проектируем «невидимость» так, чтобы пациент мог спокойно принять помощь и не опасаться огласки.
Подробнее – наркологическая клиника вывод из запоя
Процесс включает следующие шаги:
Получить дополнительные сведения – наркологическая клиника нарколог в красноярске
This post will help the internet users for building up new weblog or
even a blog from start to end.
Thanks for another great post. Where else may anybody get that type of info in such an ideal way of writing? I have a presentation next week, and I’m at the search for such information.
There is so much to try to understand
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Получить больше информации – https://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkologiya-gorod-novokuzneczk
Good post. I learn something totally new and challenging on sites I stumbleupon everyday.
It will always be exciting to read through
articles from other authors and practice a little something from other web sites.
My coder is trying to convince me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using WordPress on numerous websites for about a year and am nervous about switching to another platform. I have heard great things about blogengine.net. Is there a way I can import all my wordpress posts into it? Any help would be really appreciated!
Как выбрать хороший авиабилет и купить
Simply want to say your article is as amazing. The clarity in your post is just great and i can assume you’re an expert on this subject. Fine with your permission allow me to grab your feed to keep up to date with forthcoming post. Thanks a million and please keep up the gratifying work.
Monday night football live scores, start the week with Premier League action
Do you mind if I quote a few of your articles as long
as I provide credit and sources back to your webpage?
My blog site is in the very same niche as yours and my users would certainly benefit from a lot of the information you provide here.
Please let me know if this alright with you. Cheers!
Каждый из этапов сопровождается контролем врача и постепенным снижением медикаментозной нагрузки. Важно не просто снять симптомы, но и научить пациента распознавать внутренние триггеры, чтобы предотвратить рецидив. На протяжении всего лечения сохраняется поддержка психолога, который помогает адаптироваться и перестроить привычные модели поведения.
Исследовать вопрос подробнее – https://narcologicheskaya-klinika-v-voronezhe17.ru/narkolog-voronezh-anonimno
Very nice article, just what I needed.
Feel free to surf to my blog :: AUTOPAY
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Разобраться лучше – вывод из запоя на дому круглосуточно красноярск
В Воронеже клиника «Центр Трезвости ВоронМед» обеспечивает выезд нарколога на дом в любое время суток. Это позволяет оказывать помощь пациентам, которые находятся в тяжёлом состоянии или не могут самостоятельно приехать в стационар. Медицинская бригада прибывает в течение 40–60 минут, не используя специализированный транспорт и форму, чтобы сохранить анонимность. Врач проводит первичный осмотр, оценивает давление, частоту дыхания, уровень сознания и насыщение кислородом, после чего назначает детоксикационную капельницу с контролем дозировки.
Углубиться в тему – вывод из запоя вызов
Одним из самых востребованных направлений работы клиники является проведение детоксикации и вывод из запоя. Эти процедуры направлены на очищение организма от алкоголя и продуктов его распада, нормализацию работы печени и нервной системы. Лечение проводится с использованием сертифицированных препаратов и под контролем врача-нарколога.
Подробнее можно узнать тут – вывод наркологическая клиника новокузнецк
超人和露易斯第四季高清完整版,海外华人可免费观看最新热播剧集。
Truly all kinds of valuable facts.
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Подробнее можно узнать тут – http://vyvod-iz-zapoya-v-tolyatti17.ru
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Детальнее – нарколог на дом вывод из запоя в волгограде
Формат
Ознакомиться с деталями – http://narkologicheskaya-klinika-serpuhov0.ru/platnaya-narkologicheskaya-klinika-v-serpuhove/
go to the website https://web-breadwallet.com/
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Выяснить больше – анонимная наркологическая клиника
Когда выбрать
Детальнее – http://narkologicheskaya-klinika-domodedovo0.ru
Woah! I’m really loving the template/theme of this website.
It’s simple, yet effective. A lot of times it’s difficult to get that “perfect balance” between user friendliness and visual appearance.
I must say you have done a very good job with this. In addition, the
blog loads extremely fast for me on Internet explorer.
Exceptional Blog!
Вывод из запоя в Красноярске — это медицинская процедура, направленная на устранение алкогольной интоксикации и восстановление нормальной работы организма после длительного употребления спиртных напитков. Услуга предоставляется круглосуточно и включает дезинтоксикационную терапию, стабилизацию психоэмоционального состояния и профилактику осложнений. Все процедуры выполняются опытными наркологами с применением сертифицированных препаратов и в строгом соответствии с медицинскими стандартами.
Выяснить больше – http://vyvod-iz-zapoya-v-krasnoyarske17.ru/czentr-kodirovaniya-vyvod-iz-zapoya-krasnoyarsk/
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Выяснить больше – http://narkologicheskaya-klinika-v-volgograde17.ru/narkologicheskaya-pomoshh-volgograd/
Когда уместен
Узнать больше – наркологическая клиника московская московская область
Вывод из запоя — это не просто медицинская процедура, а тщательно выстроенный процесс, направленный на восстановление работы всех систем организма. При неправильном или неполном лечении риск осложнений возрастает в несколько раз. Поэтому обращение в профессиональную клинику становится необходимым шагом. В наркологической клинике «Центр Трезвости ВоронМед» пациент получает экстренную помощь, безопасные инфузионные препараты, круглосуточный выезд нарколога и последующее восстановление под наблюдением специалистов. Здесь каждая капельница подбирается индивидуально — с учётом возраста, веса, длительности запоя, хронических болезней и реакции организма на препараты.
Подробнее – вывод из запоя недорого
В Королёве мы запускаем помощь без «многоходовок». С первого контакта дежурный врач аккуратно уточняет жалобы, длительность эпизода, принимаемые лекарства и сопутствующие диагнозы, после чего предлагает безопасную точку входа: выезд на дом, дневной формат или круглосуточный стационар. Каждое действие объясняется простым языком: зачем оно нужно, какого эффекта ждать в ближайшие часы и что будет считаться нормальной динамикой. Конфиденциальность заложена в процесс по умолчанию: минимально необходимый объём персональных данных, нейтральная коммуникация, ограниченный доступ к медкарте и отсутствие постановки на учёт. Такой порядок снимает лишнее напряжение у семьи и экономит самое ценное — время.
Получить дополнительную информацию – http://narkologicheskaya-klinika-korolyov0.ru/narkologicheskaya-klinika-na-dom-v-korolyove/
Ниже приведена таблица с типовыми компонентами капельницы и их действием:
Узнать больше – вывод из запоя в тольятти
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Ознакомиться с деталями – анонимная наркологическая клиника в новокузнецке
Hey! I realize this is kind of off-topic however I had to ask.
Does operating a well-established blog such as yours take a
lot of work? I am brand new to blogging however I do
write in my diary every day. I’d like to start a blog so
I can share my personal experience and views online.
Please let me know if you have any ideas or tips for new
aspiring blog owners. Appreciate it!
«Светлый Шаг» — это не набор общих обещаний, а чётко выстроенный маршрут помощи, где каждый шаг прозрачен: от первичного разговора до устойчивой ремиссии. Мы бережно собираем только необходимые данные, сразу объясняем, что будет сделано в первые 6–12 часов, каких изменений ждать к ночи и по каким маркерам поймём, что курс выбран верно. Конфиденциальность встроена в процесс: нейтральные звонки, ограниченный доступ к медкарте, аккуратный выезд без броской атрибутики, возможность оформить документы с нейтральными формулировками. Итог — меньше стресса, меньше бюрократии и больше управляемости там, где это критично.
Подробнее можно узнать тут – lechenie-v-narkologicheskoj-klinike
https://youtu.be/71sdnx54hQQ
На месте врач и медсестра собирают базовую линию: уровень сознания, дыхание, SpO?, температура, шкалы симптомов (тошнота/тремор/тревога 0–10), переносимость воды небольшими глотками. Далее формулируется рабочая гипотеза и включается минимально достаточный модуль с обозначенным «окном оценки»: 30–60 минут — для «окна питья», 60–120 минут — для стабилизации ЧСС/АД и дрожи, «первая ночь» — для сна и вечерней тревоги. Как только маркер достигнут, модуль выключается; нет эффекта — меняется одна переменная без «усиления всего сразу».
Изучить вопрос глубже – наркологическая клиника нарколог красноярск
Основные этапы включают:
Разобраться лучше – https://vyvod-iz-zapoya-v-krasnoyarske17.ru/vyvedenie-iz-zapoya-krasnoyarsk
В Воронеже команда «ВоронМед Профи» работает по принципу быстрой медицинской реакции — помощь оказывается независимо от времени суток и дня недели. Все выезды выполняются анонимно, без спецтранспорта и медицинской формы. Врач приезжает в гражданской одежде, что исключает ненужное внимание соседей и посторонних. В ходе осмотра специалист измеряет давление, пульс, температуру, оценивает уровень интоксикации и определяет степень обезвоживания. На основе полученных данных подбирается состав капельницы, который подаётся медленно и безопасно под контролем врача.
Ознакомиться с деталями – нарколог на дом срочно воронеж
Our communities really need to deal with this.
Вывод из запоя — это не просто медицинская процедура, а тщательно выстроенный процесс, направленный на восстановление работы всех систем организма. При неправильном или неполном лечении риск осложнений возрастает в несколько раз. Поэтому обращение в профессиональную клинику становится необходимым шагом. В наркологической клинике «Центр Трезвости ВоронМед» пациент получает экстренную помощь, безопасные инфузионные препараты, круглосуточный выезд нарколога и последующее восстановление под наблюдением специалистов. Здесь каждая капельница подбирается индивидуально — с учётом возраста, веса, длительности запоя, хронических болезней и реакции организма на препараты.
Получить дополнительные сведения – помощь вывод из запоя воронеж
Продолжительность процедуры — от 40 минут до полутора часов. Уже в первые часы после начала терапии состояние пациента значительно улучшается: проходит тошнота, снижается тревожность, восстанавливается координация движений.
Получить дополнительные сведения – вывод из запоя на дому
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Исследовать вопрос подробнее – https://narcologicheskaya-klinika-v-krasnoyarske17.ru/krasnoyarsk-narkologicheskij-czentr/
В таблице представлены основные виды терапии, применяемые в клинике:
Ознакомиться с деталями – наркологическая клиника вывод из запоя в новокузнецке
Каждое вмешательство проходит через систему «цель > маркер > окно оценки > выключение модуля». Ниже приведена таблица, отражающая базовую логику диагностики и корректировки терапии в зависимости от состояния пациента.
Подробнее тут – запой наркологическая клиника красноярск
Комплексное лечение помогает восстановить работу печени, сердца и нервной системы. Пациенты отмечают улучшение сна, снижение тревожности, нормализацию давления и аппетита уже спустя несколько часов после начала терапии. В зависимости от тяжести состояния курс может быть продлён до 2–3 дней с круглосуточным наблюдением и корректировкой дозировок.
Исследовать вопрос подробнее – вывод из запоя на дому
Процесс терапии в наркологической клинике в Воронеже организован поэтапно. Это позволяет обеспечить системность и постепенность восстановления, снизить риски осложнений и повысить устойчивость результата.
Выяснить больше – http://narkologicheskaya-klinika-v-voronezhe17.ru
Своевременная постановка капельницы помогает избежать тяжёлых последствий запоя. Поводом для обращения к врачу являются симптомы выраженной интоксикации:
Углубиться в тему – капельницы от запоя на дому цена
Ниже — ориентир, который помогает сопоставить риски, плотность наблюдения и ожидаемую скорость стабилизации. Таблица не заменяет очный осмотр, но экономит время на принятие решений и делает логику врача понятной всей семье.
Углубиться в тему – narkologicheskaya-klinika-ceny
Основу лечения составляет междисциплинарная команда: врач-нарколог, психиатр, психолог, медсестра и консультант по зависимому поведению. Каждый отвечает за свой участок работы, но общая цель едина — помочь пациенту безопасно пройти путь от детокса до устойчивого состояния. Благодаря единому плану и регулярным консилиумам врачей, исключаются противоречия и дублирование процедур. Это экономит ресурсы организма и делает процесс прогнозируемым.
Разобраться лучше – наркологическая клиника нарколог в красноярске
Когда уместен
Получить дополнительную информацию – https://narkologicheskaya-klinika-shchyolkovo0.ru
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Исследовать вопрос подробнее – вывод из запоя капельница в волгограде
Для иллюстрации приведена таблица, отражающая распространённые методы терапии и их воздействие на организм:
Детальнее – частная наркологическая клиника воронеж
Комплексный подход обеспечивает не только снятие симптомов, но и полное восстановление функций организма. Пациент получает поддержку на всех этапах — от детоксикации до социальной адаптации.
Ознакомиться с деталями – narkologicheskaya-pomoshh-v-tolyatti17.ru/
Today, I went to the beachfront with my children. I found a sea shell and gave it to my 4 year old
daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and
screamed. There was a hermit crab inside and it pinched her
ear. She never wants to go back! LoL I know
this is totally off topic but I had to tell someone!
World Cup 2026 qualifiers live score, road to USA Mexico Canada tournament
Такой подход обеспечивает результативность и помогает добиться длительной ремиссии даже при тяжёлых формах зависимости.
Узнать больше – наркологическая клиника цены в воронеже
В таблице приведены основные компоненты инфузионной терапии, применяемые при детоксикации:
Разобраться лучше – https://narkologicheskaya-clinica-v-novokuzneczke17.ru/
Такой подход позволяет пациенту чувствовать себя не объектом лечения, а активным участником собственного восстановления. Это повышает уровень мотивации и формирует доверие между врачом и пациентом, что критически важно для устойчивой ремиссии.
Детальнее – частная наркологическая клиника воронеж
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Детальнее – платная наркологическая помощь в тольятти
Что включено на практике
Получить дополнительную информацию – http://narkologicheskaya-klinika-odincovo0.ru/narkologicheskaya-klinika-stacionar-v-odincovo/https://narkologicheskaya-klinika-odincovo0.ru
Modern Purair
201, 1475 Ellis Street, Kelowna
BC Ꮩ1У 2A3, Canada
1-800-996-3878
advanced tech
Лечение организовано поэтапно. Такой подход обеспечивает постепенное восстановление функций организма и исключает риск осложнений. Каждый этап терапии направлен на устранение конкретных нарушений, вызванных интоксикацией.
Узнать больше – врач вывод из запоя
«Вектор Надежды» выстраивает помощь так, чтобы с первого звонка убрать неопределённость и вернуть ощущение контроля. Дежурный врач аккуратно собирает только необходимую информацию, оценивает риски и предлагает безопасный старт: выезд на дом, дневной маршрут или стационар с наблюдением 24/7. Мы объясняем каждую манипуляцию простым языком — что именно будет сделано в ближайшие часы, каких изменений ожидать к вечеру, почему выбран именно такой темп и как поймём, что схема работает. Конфиденциальность — не дополнение, а стандарт: нейтральные звонки, неброская атрибутика, ограниченный доступ к карте, отсутствие постановки на учёт. Такой регламент снижает тревогу, экономит силы семьи и ускоряет стабилизацию: вместо «марафона кабинетов» — один связный маршрут с понятными контрольными точками.
Получить дополнительную информацию – круглосуточная наркологическая клиника
Во время лечения фиксируются все жизненные показатели пациента. При необходимости проводится экспресс-анализ крови и ЭКГ. Ниже представлена таблица, показывающая, какие параметры контролируются и по каким признакам оценивается стабилизация состояния.
Получить дополнительные сведения – вывод из запоя вызов в воронеже
Процесс кодирования проходит в комфортной и спокойной обстановке. Врач объясняет каждый этап, чтобы пациент чувствовал себя уверенно и спокойно. После процедуры пациент получает памятку с рекомендациями по уходу за здоровьем и режиму поведения в первые недели после лечения.
Узнать больше – кодирование от алкоголизма отзывы в волгограде
Quality articles is the secret to attract the visitors to visit the site,
that’s what this web page is providing.
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Исследовать вопрос подробнее – вывод из запоя вызов
Клиника обеспечивает анонимность и безопасность. Информация о пациентах не передаётся третьим лицам, а процедуры выполняются в комфортных условиях с использованием сертифицированных препаратов и современного оборудования.
Изучить вопрос глубже – наркологическая клиника лечение алкоголизма в новокузнецке
Конфиденциальность — это набор конкретных действий, а не декларация на сайте. Мы проектируем «невидимость» так, чтобы пациент мог спокойно принять помощь и не опасаться огласки.
Получить больше информации – наркологическая клиника лечение алкоголизма
Применение комплексной терапии позволяет не только устранить зависимость, но и сформировать новые поведенческие установки, предотвращающие возвращение к употреблению.
Получить дополнительные сведения – http://narkologicheskaya-clinica-v-voronezhe17.ru
В клинике «ВолгоградМед Альянс» применяются разные методы кодирования, позволяющие подобрать оптимальный вариант для каждого пациента. Выбор зависит от медицинских показаний, психологической готовности и длительности ремиссии. В таблице ниже представлены основные методики, их особенности и преимущества.
Получить больше информации – кодирование от алкоголизма
Самый частый повод — не только «плохое похмелье», а именно абстинентный синдром после запоя: когда самочувствие ухудшается при прекращении алкоголя, а попытки «опохмелиться» лишь продлевают проблему. Важно ориентироваться не на терпимость человека к дискомфорту, а на объективные признаки: если симптомы нарастают, сон сорван, поведение становится нестабильным, а тело реагирует паникой, тремором и скачками давления, лучше не тянуть. Особенно осторожными нужно быть при хронических болезнях сердца, печени и сосудов: при них цена ошибки выше, а «универсальные» домашние схемы могут навредить.
Детальнее – vrach narkolog na dom krasnogorsk
В Воронеже команда «ВоронМед Профи» работает по принципу быстрой медицинской реакции — помощь оказывается независимо от времени суток и дня недели. Все выезды выполняются анонимно, без спецтранспорта и медицинской формы. Врач приезжает в гражданской одежде, что исключает ненужное внимание соседей и посторонних. В ходе осмотра специалист измеряет давление, пульс, температуру, оценивает уровень интоксикации и определяет степень обезвоживания. На основе полученных данных подбирается состав капельницы, который подаётся медленно и безопасно под контролем врача.
Получить больше информации – врач нарколог на дом
Клиника обеспечивает анонимность и безопасность. Информация о пациентах не передаётся третьим лицам, а процедуры выполняются в комфортных условиях с использованием сертифицированных препаратов и современного оборудования.
Разобраться лучше – наркологическая клиника стационар новокузнецк
Формат помощи на дому особенно важен, когда человек физически не в состоянии добраться до клиники, боится огласки или требуется поддержка семьи «здесь и сейчас». Врач оценивает риски, подбирает схему детоксикации по состоянию и даёт понятный план дальнейших шагов: что делать в первые сутки, чего избегать, какие симптомы считать тревожными и когда нужно повторное обращение.
Получить дополнительную информацию – https://narkolog-na-dom-krasnogorsk6.ru/narkologicheskaya-klinika-krasnogorsk
Когда уместен
Подробнее – наркологическая клиника стоимость
«Светлый Шаг» — это не набор общих обещаний, а чётко выстроенный маршрут помощи, где каждый шаг прозрачен: от первичного разговора до устойчивой ремиссии. Мы бережно собираем только необходимые данные, сразу объясняем, что будет сделано в первые 6–12 часов, каких изменений ждать к ночи и по каким маркерам поймём, что курс выбран верно. Конфиденциальность встроена в процесс: нейтральные звонки, ограниченный доступ к медкарте, аккуратный выезд без броской атрибутики, возможность оформить документы с нейтральными формулировками. Итог — меньше стресса, меньше бюрократии и больше управляемости там, где это критично.
Исследовать вопрос подробнее – http://narkologicheskaya-klinika-odincovo0.ru/chastnaya-narkologicheskaya-klinika-v-odincovo/
Своевременная постановка капельницы помогает избежать тяжёлых последствий запоя. Поводом для обращения к врачу являются симптомы выраженной интоксикации:
Подробнее можно узнать тут – капельницы от запоя на дому цена волгоград
Комплексное применение этих методов позволяет значительно ускорить процесс восстановления и предотвратить осложнения.
Получить дополнительную информацию – http://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkologicheskij-czentr-novokuzneczk/
Клиника «ВоронежМед Альянс» придерживается принципа прозрачной медицины: каждый шаг понятен пациенту, решения принимаются совместно, а результаты фиксируются по объективным показателям. Такой формат создаёт чувство безопасности и доверия. Среди основных принципов:
Получить больше информации – частная наркологическая клиника
Выездная бригада «МедОпоры» дежурит 24/7 и покрывает весь Красногорск и близлежащие районы. После короткого звонка дежурный уточняет длительность запоя, сопутствующие болезни, принимаемые препараты и аллергии — это экономит время на месте и помогает заранее предусмотреть риски. Врач приезжает с комплектом одноразовых систем, растворами и медикаментами, проводит экспресс-диагностику: измерение давления, пульса, сатурации, температуры, оценка неврологического статуса, степени обезвоживания и тревожности. По этим данным формируется индивидуальная схема инфузий и симптоматической поддержки. Наша задача — не просто «поставить капельницу», а безопасно развернуть план стабилизации, где дозировки и темп меняются по реакции организма. Если выявляются признаки осложнений или дома нет условий для безопасного наблюдения, сразу предлагаем перевод в профильный стационар, чтобы не терять драгоценные часы. Семья получает понятные роли и инструкции, а врач остаётся на связи для уточнений по режиму ближайшей ночи.
Получить дополнительную информацию – vrach vyvod iz zapoya
Hey There. I found your blog using msn. This is an extremely
well written article. I’ll be sure to bookmark it and return to
read more of your useful information. Thanks for the post.
I will certainly return.
Наркологическая клиника в Красноярске оказывает профессиональную помощь людям, столкнувшимся с алкогольной, наркотической и другими видами зависимостей. Основная цель деятельности специалистов — восстановление физического здоровья, стабилизация психоэмоционального состояния и возвращение пациента к полноценной жизни. Лечение проводится по современным медицинским протоколам, с применением индивидуальных схем терапии и полным соблюдением конфиденциальности.
Изучить вопрос глубже – https://narcologicheskaya-klinika-v-krasnoyarske17.ru/chastnaya-narkologicheskaya-klinika-krasnoyarsk
Процесс детоксикации проходит поэтапно, чтобы организм успевал адаптироваться к изменениям и не испытывал стресс. Каждый шаг направлен на достижение конкретного терапевтического эффекта. Ниже представлена таблица, отражающая ключевые стадии процедуры, применяемой в клинике «Трезвый Путь Волгоград».
Узнать больше – http://vivod-iz-zapoya-v-volgograde17.ru
Для наглядности приведена таблица с основными направлениями терапии и их результатами:
Изучить вопрос глубже – частная наркологическая клиника в воронеже
Thank you pertaining to sharing the following great subject matter on your website. I ran into it on google. I am going to check to come back after you publish additional aricles.
Good site you’ve got here.. It’s difficult to find excellent
writing like yours these days. I seriously appreciate individuals like
you! Take care!!
Перед таблицей важное пояснение: она помогает соотнести риски и плотность наблюдения ещё до осмотра. Окончательное решение принимает врач по клинической картине и переносимости, но ориентир даст понимание маршрута и бюджета времени.
Детальнее – наркологическая клиника анонимная помощь нарколога
Выделяется ряд преимуществ, которые делают терапию в клинике оптимальным решением для борьбы с зависимостью.
Разобраться лучше – наркологическая клиника лечение алкоголизма пермь
В Волгограде сформирована система оказания наркологической помощи, включающая круглосуточные выезды специалистов, амбулаторное лечение, стационарные программы и реабилитацию. Такой подход позволяет охватить все категории пациентов — от тех, кто нуждается в экстренной помощи, до тех, кто готов пройти полный курс терапии. Независимо от формы оказания услуг, лечение проводится конфиденциально и в соответствии с медицинскими стандартами.
Углубиться в тему – вызов наркологической помощи
Что получите за 24 часа
Детальнее – http://narkologicheskaya-klinika-domodedovo0.ru
Peculiar article, just what I wanted to find.
Благодаря комплексному подходу достигается не только снятие симптомов, но и долгосрочная стабилизация состояния пациента.
Подробнее можно узнать тут – наркологическая помощь волгоград
Правильный подбор лекарственных средств позволяет не только уменьшить проявления синдрома отмены, но и стабилизировать эмоциональное состояние пациента, снижая риск срывов. Реабилитационные программы включают физиотерапию, спортивные занятия и коррекцию образа жизни, что способствует полноценному восстановлению организма.
Выяснить больше – лечение наркомании клиника в твери
Перед таблицей — важное пояснение: она помогает соотнести риски и плотность наблюдения ещё до осмотра. Окончательное решение принимает врач по клинической картине и переносимости, но ориентир даст понимание логики и бюджета времени.
Ознакомиться с деталями – наркологическая клиника стоимость
Что делаем фактически
Получить больше информации – http://narkologicheskaya-klinika-ehlektrostal0.ru/platnaya-narkologicheskaya-klinika-v-ehlektrostali/
Что включает на практике
Подробнее можно узнать тут – zapoj-narkologicheskaya-klinika
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Разобраться лучше – http://narkologicheskaya-klinika-v-krasnoyarske17.ru
Paito warga SDY sama dengan fasilitas nan digunakan akibat rak kontestan togel menjumpai menasyrihkan kredit-digit nan keluar dalam atraksi togel Sydney.
Paito ini mengasihkan penjelasan optis mengenai biji-nilai nan sewaktu-waktu muncul bersama ragi-format nan dapat membantu pemeran dalam membikin kepastian teban. Dengan membonceng paito kelas, anggota dapat lebih mudah memahami
petunjuk pula mengeluarkan garis haluan nan lebih baik.
Di tarikh 2025, keterangan terbaru paito level SDY menyatakan kecondongan lalu
desain nan menarik.
Когда разумно
Разобраться лучше – наркологическая клиника телефон
Анонимная наркологическая помощь — это управляемая система, где каждый шаг прозрачно связан с целью и измеримым результатом. В наркологической клинике «ЕнисейМед Центр» мы соединяем круглосуточную доступность, мягкую логистику и модульный план лечения, чтобы пациент и семья понимали, почему именно сейчас назначается то или иное вмешательство и когда оно будет остановлено. Мы избегаем полипрагмазии: запускаем один модуль — ставим один маркер — определяем «окно оценки» — выключаем модуль, как только цель достигнута. Такой подход бережёт ресурсы организма и сохраняет причинно-следственную связь.
Получить дополнительную информацию – анонимная наркологическая клиника в красноярске
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Подробнее – наркологическая клиника наркологический центр волгоград
Индивидуально подобранный состав раствора обеспечивает быстрое выведение токсинов и улучшение физического состояния уже в течение первых часов после начала лечения.
Углубиться в тему – http://kapelnicza-ot-zapoya-v-volgograde17.ru
Наркологическая клиника — это пространство, где медицинская наука сочетается с психологической поддержкой и индивидуальным подходом к каждому пациенту. В клинике «ВоронежМед Альянс» лечение зависимости организовано по принципам доказательной медицины: каждый этап терапии основан на объективных данных, контролируемых результатах и четких критериях эффективности. Здесь помогают не просто устранить физические последствия зависимости, но и восстановить внутренние ресурсы человека, вернуть уверенность, осознанность и способность строить новую жизнь без алкоголя и наркотиков.
Подробнее можно узнать тут – https://narcologicheskaya-klinika-v-voronezhe17.ru/narkolog-voronezh-czena
Применение комплексной терапии позволяет не только устранить зависимость, но и сформировать новые поведенческие установки, предотвращающие возвращение к употреблению.
Получить больше информации – https://narkologicheskaya-clinica-v-voronezhe17.ru/
Peculiar this blog is totaly unrelated to what I was searching for – – interesting to see you’re well indexed in the search engines.
この記事を 投稿していただき 感謝します。オンライン クラウドファンディングは、治療費を 必要とする 多くの人にとって 命綱となる ものです。視力を 救う チャリティは 本当に 素晴らしい ですね。
Here is my web-site – 医療アクセス支援
Каждый из этапов сопровождается контролем врача и постепенным снижением медикаментозной нагрузки. Важно не просто снять симптомы, но и научить пациента распознавать внутренние триггеры, чтобы предотвратить рецидив. На протяжении всего лечения сохраняется поддержка психолога, который помогает адаптироваться и перестроить привычные модели поведения.
Разобраться лучше – платная наркологическая клиника в воронеже
Основу выездного лечения составляют капельницы, которые позволяют быстро ввести препараты в кровоток, минуя желудочно-кишечный тракт. Это обеспечивает моментальное действие и исключает раздражение слизистой. Капельницы подбираются индивидуально в зависимости от состояния пациента. Основные направления инфузионной терапии включают детоксикацию, восстановление водно-солевого баланса и поддержку работы нервной системы. Для усиления эффекта применяются витамины, антиоксиданты и препараты для защиты печени.
Исследовать вопрос подробнее – вызвать нарколога на дом воронеж
Лечение в клинике включает несколько последовательных этапов, каждый из которых направлен на достижение стабильной ремиссии и восстановление здоровья пациента.
Исследовать вопрос подробнее – наркологическая клиника стационар в новокузнецке
Такая форма помощи позволяет избежать осложнений, которые часто сопровождают попытки снять симптомы самостоятельно. При правильном подборе препаратов уже через час наблюдается улучшение самочувствия: уходит головная боль, снижается тревога, стабилизируется сердцебиение и восстанавливается ясность мышления. Пациент получает рекомендации по питанию, режиму отдыха и приёму витаминов, чтобы закрепить результат и предотвратить повторный срыв.
Выяснить больше – http://narkolog-na-dom-v-voronezhe17.ru/voronezh-narkologiya/
Выездная бригада «МедОпоры» дежурит 24/7 и покрывает весь Красногорск и близлежащие районы. После короткого звонка дежурный уточняет длительность запоя, сопутствующие болезни, принимаемые препараты и аллергии — это экономит время на месте и помогает заранее предусмотреть риски. Врач приезжает с комплектом одноразовых систем, растворами и медикаментами, проводит экспресс-диагностику: измерение давления, пульса, сатурации, температуры, оценка неврологического статуса, степени обезвоживания и тревожности. По этим данным формируется индивидуальная схема инфузий и симптоматической поддержки. Наша задача — не просто «поставить капельницу», а безопасно развернуть план стабилизации, где дозировки и темп меняются по реакции организма. Если выявляются признаки осложнений или дома нет условий для безопасного наблюдения, сразу предлагаем перевод в профильный стационар, чтобы не терять драгоценные часы. Семья получает понятные роли и инструкции, а врач остаётся на связи для уточнений по режиму ближайшей ночи.
Получить дополнительные сведения – vyvod iz zapoya kapelnica
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Ознакомиться с деталями – https://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkolog-novokuzneczk-na-dom/
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Получить дополнительную информацию – https://vivod-iz-zapoya-v-volgograde17.ru/vyvod-iz-zapoya-narkolog-na-dom-volgograd
Good day I am so delighted I found your blog, I
really found you by error, while I was searching on Yahoo for something else, Anyways I am here now and would just like to say kudos for a remarkable post and a
all round thrilling blog (I also love the theme/design), I don’t have time to go through it all at the minute but I have book-marked it and also added your RSS feeds, so when I have time I will be
back to read more, Please do keep up the fantastic job.
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Получить дополнительные сведения – запой наркологическая клиника в красноярске
«Светлая Полоса» запускает помощь без многоходовой бюрократии и «марафона кабинетов». Дежурный врач аккуратно собирает только те данные, которые критичны для безопасности, и сразу предлагает безопасную точку входа: выезд на дом, дневной формат или стационар под наблюдением 24/7. Каждое действие проговаривается человеческим языком: что делаем в ближайшие часы, чего ждём к вечеру (мягкий сон, снижение тревоги, выравнивание давления и пульса), как поймём, что схема работает, и чем займёмся завтра. Конфиденциальность встроена в процесс — нейтральные каналы связи, неброская выездная атрибутика, ограниченный доступ к карте и отсутствие постановки на учёт. Такой регламент снижает фоновую тревогу, экономит силы семьи и превращает лечение в ясный, управляемый маршрут, а не в набор «разрозненных процедур».
Получить дополнительные сведения – анонимная наркологическая клиника
Лечение наркомании в клинике начинается с диагностики, позволяющей определить степень зависимости, выявить сопутствующие заболевания и выбрать оптимальную тактику терапии. Важным этапом является детоксикация — очищение организма от токсинов и продуктов распада наркотических веществ, что снижает риск осложнений и облегчает последующее восстановление.
Получить дополнительные сведения – лечение наркомании наркология тверь
После процедуры пациент чувствует улучшение уже через 1–2 часа: проходят головные боли, снижается давление, нормализуется сон и аппетит.
Детальнее – http://narkologicheskaya-clinica-v-novokuzneczke17.ru/narkolog-v-gorode-novokuzneczke/
Детоксикация — это первый и важнейший этап лечения в наркологической клинике в Красноярске. Она проводится с целью выведения токсинов из организма и восстановления функций жизненно важных органов. Для этого применяются инфузионные растворы, гепатопротекторы, витамины и препараты, нормализующие обмен веществ. После снятия интоксикации пациент получает медикаментозную поддержку, направленную на снижение тяги к алкоголю или наркотикам и стабилизацию эмоционального состояния.
Углубиться в тему – https://narcologicheskaya-klinika-v-krasnoyarske17.ru/chastnaya-narkologicheskaya-klinika-krasnoyarsk/
Что получите за 24 часа
Получить больше информации – https://narkologicheskaya-klinika-domodedovo0.ru/chastnaya-narkologicheskaya-klinika-v-domodedovo/
Основная цель капельницы — вывести из организма продукты распада этанола и восстановить водно-солевой баланс. После запоя в крови скапливаются токсичные вещества, которые вызывают головокружение, слабость и эмоциональную нестабильность. Введение растворов внутривенно позволяет быстро доставить активные компоненты в кровоток, улучшая работу сердца, печени и нервной системы. Уже через 20–30 минут после начала процедуры пациент ощущает облегчение.
Разобраться лучше – сколько стоит капельница на дому от запоя в воронеже
Bu kontentə görə təşəkkürlər. Saytı dostlarıma tövsiyə edəcəyəm.
https://betandreas-azerbaijan-play.com/oyunlar
After looking into a number of the articles on your blog, I really
appreciate your technique of blogging. I saved as a favorite it to
my bookmark site list and will be checking back soon. Please visit my web
site too and tell me how you feel.
Процедура проводится как в стационаре, так и на дому. Врач приезжает по вызову, проводит осмотр и измеряет давление, пульс, насыщение кислородом. После оценки состояния подбирается состав капельницы и начинается инфузионная терапия. В среднем процедура длится от 40 минут до 1,5 часов, в зависимости от степени интоксикации. По завершении врач наблюдает за реакцией организма и даёт рекомендации по восстановлению.
Детальнее – http://kapelnicza-ot-zapoya-v-voronezhe17.ru/
Процесс включает несколько шагов:
Подробнее тут – врач нарколог на дом уфа
Women’s World Cup livescore, growing women’s football with full coverage
Patrice & Associates
Scottsdale, AZ, United Ⴝtates
16265237726
hotel recruitment (https://atavi.com/share/xnkcrszvvueg)
Primе Secured
3603 N 222nd Ⴝt, Suite 102,
Elkhorn, ΝE 68022, United Տtates
402-289-4126
Compliance Smart Measures
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Получить дополнительную информацию – https://narkologicheskaya-klinika-v-volgograde17.ru/chastnaya-narkologicheskaya-klinika-volgograd/
Лечение алкоголизма в Перми в условиях специализированной клиники обеспечивает высокий уровень безопасности и результативности. Пациенты получают квалифицированную помощь в комфортных условиях и под наблюдением опытных специалистов.
Ознакомиться с деталями – лечение алкоголизма кодирование в перми
Круглосуточное наблюдение, регулярные замеры, быстрые корректировки, спокойная среда и структурированный режим. Это снижает риски ночных ухудшений и помогает мягко «собрать» сон без агрессивных седативных решений.
Получить дополнительную информацию – нарколог вывод из запоя
Вывод из запоя — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормальной работы внутренних органов. В клинике «Трезвый Путь Волгоград» пациентам оказывается профессиональная помощь с использованием современных методов дезинтоксикации, медикаментозной поддержки и психологического сопровождения. Лечение проводится круглосуточно, включая выезд нарколога на дом. Такой формат помогает быстро стабилизировать состояние пациента, минимизировать риск осложнений и обеспечить безопасность при выходе из запоя любой продолжительности.
Подробнее – https://vivod-iz-zapoya-v-volgograde17.ru/vyvod-iz-zapoya-narkolog-na-dom-volgograd/
Во время лечения фиксируются все жизненные показатели пациента. При необходимости проводится экспресс-анализ крови и ЭКГ. Ниже представлена таблица, показывающая, какие параметры контролируются и по каким признакам оценивается стабилизация состояния.
Подробнее тут – вывод из запоя с выездом
Капельница не просто устраняет симптомы похмелья — она восстанавливает внутренний баланс, снижает токсическую нагрузку и поддерживает работу жизненно важных органов. После процедуры пациент чувствует прилив сил, прояснение сознания и эмоциональную стабильность. Эффект закрепляется при соблюдении рекомендаций врача и отказе от алкоголя в последующие дни.
Подробнее тут – вывод из запоя клиника
Ниже приведена таблица с типовыми компонентами капельницы и их действием:
Узнать больше – http://vyvod-iz-zapoya-v-tolyatti17.ru/vyvod-iz-zapoya-tolyatti-na-domu/
What’s up colleagues, pleasant post and good arguments commented at this place, I am in fact enjoying by these.
Формат
Исследовать вопрос подробнее – narkologicheskaya-klinika-anonimnaya-pomoshch-narkologa
Когда выбрать
Подробнее можно узнать тут – частная наркологическая клиника домодедово
Что включено на практике
Подробнее тут – наркологическая клиника цены
Мы строим лечение вокруг предсказуемости: минимум лишних вопросов, максимум конкретики и понятный план на ближайшие сутки. Дежурный врач уточняет только то, что влияет на безопасность — длительность эпизода, актуальные лекарства и переносимость, сон и апетит, наличие поддержки дома. Из этого скелета рождается маршрут: выезд на дом, приём без очередей или стационар с наблюдением 24/7. Конфиденциальность встроена по умолчанию: нейтральная коммуникация, доступ к карте только у вовлечённой команды, документы по запросу — в нейтральных формулировках. Внешний шум гасим, внимание переводим на цель: ровная стабилизация без «качелей» и с понятными контрольными точками.
Изучить вопрос глубже – анонимная наркологическая клиника
Когда уместен
Подробнее тут – http://narkologicheskaya-klinika-shchyolkovo0.ru
В экстренных ситуациях семья ожидает не обещаний, а чётких действий. «Трезвый Ритм» в Королёве организует безопасный вывод из запоя с персональной схемой детоксикации, выездом врача 24/7 и последующей поддержкой, чтобы стабилизировать сон, снизить тревогу и предотвратить рецидив. Мы работаем деликатно и конфиденциально: вы получаете медицинскую помощь без очередей и формальностей, а также понятный план, что делать в первые критические сутки. Наши специалисты используют только проверенные протоколы, учитывают возраст, длительность эпизода и сопутствующие диагнозы, подбирают дозировки бережно и объясняют каждый шаг. Если на осмотре выявляются риски осложнений, мы сразу предложим стационар и возьмём на себя организацию перевода — безопасность всегда важнее спешки.
Подробнее тут – вывод из запоя
4K video downloader adalah aplikasi yang diperuntukkan untuk pengguna windows maupun Mac yang ingin mendownload
video beresoluisi 4K.
Touche. Outstanding arguments. Keep up the great effort.
Does your blog have a contact page? I’m having trouble locating it but, I’d like to send you an email.
I’ve got some ideas for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing
it expand over time.
Το στοίχημα αποτελεί αναπόσπαστο κομμάτι της ψυχαγωγίας για πολλούς Έλληνες παίκτες. Καθώς η εγχώρια αγορά υπόκειται σε αυστηρή ρύθμιση και περιορισμούς, ένα μεγάλο μέρος των παικτών στρέφεται προς ξένες στοιχηματικές εταιρείες που προσφέρουν μεγαλύτερη ευελιξία, καλύτερες αποδόσεις, περισσότερες επιλογές και καινοτόμα χαρακτηριστικά. Ειδικά για όσους αναζητούν μια πιο πλούσια στοιχηματική εμπειρία, οι πλατφόρμες του εξωτερικού προσφέρουν σημαντικά πλεονεκτήματα. Ο όρος ξένες στοιχηματικές εταιρείες που δέχονται Έλληνες δεν αφορά απαραίτητα αδειοδοτημένους παρόχους στην Ελλάδα, αλλά ιστοσελίδες που λειτουργούν νόμιμα υπό διεθνείς άδειες όπως της Κουρασάο, της Ανζουάν ή της Κόστα Ρίκα και επιτρέπουν εγγραφή και στοιχηματισμό από Έλληνες χρήστες. Το ενδιαφέρον για τέτοιου είδους εταιρείες αυξάνεται συνεχώς, καθώς προσφέρουν όχι μόνο καλύτερα μπόνους και προωθητικές ενέργειες, αλλά και υποστήριξη σε κρυπτονομίσματα, μηδενική γραφειοκρατία και πιο φιλικές προς τον χρήστη εμπειρίες.
Для наглядности приведена таблица с основными направлениями терапии и их результатами:
Углубиться в тему – http://narkologicheskaya-clinica-v-voronezhe17.ru/narkolog-voronezh-czena/
This website has lots of really useful stuff on it. Thanks for informing me.
Такой подход позволяет добиться устойчивого эффекта и минимизировать риск возврата к зависимому поведению.
Получить дополнительную информацию – наркологическая клиника нарколог в волгограде
Ниже приведена таблица с типовыми компонентами капельницы и их назначением:
Ознакомиться с деталями – врач на дом капельница от запоя в волгограде
Прежде чем показывать варианты, зафиксируем логику: интенсивность наблюдения должна соответствовать рискам и переносимости терапии. Таблица ниже помогает быстро сопоставить ситуацию и формат; окончательное решение принимает врач после очного осмотра и оценки реакции на первые вмешательства.
Разобраться лучше – наркологическая клиника со стационаром
Клиника в Волгограде руководствуется принципами индивидуального подхода, конфиденциальности и научно обоснованных методик. Врач-нарколог оценивает общее состояние пациента, определяет стадию зависимости и подбирает оптимальную терапевтическую схему. Лечение включает детоксикацию, медикаментозную поддержку, психотерапию и реабилитацию. Каждый пациент проходит лечение в безопасных условиях с постоянным медицинским наблюдением.
Ознакомиться с деталями – вывод наркологическая клиника в волгограде
Обычно внимание уделяется нескольким направлениям: восстановлению жидкости и обмена веществ, снижению тошноты и головной боли, уменьшению вегетативных симптомов (дрожь, потливость, сердцебиение), нормализации сна и тревоги. При этом врач ориентируется на текущие показатели и реакцию пациента — то, что помогало «в прошлый раз», может быть неуместно сегодня. Дополнительно проговариваются бытовые детали: проветривание, комфортная температура, питьевой режим, питание небольшими порциями, контроль давления и пульса, ограничение стимуляторов и рисковых нагрузок.
Исследовать вопрос подробнее – vyzvat narkologa na dom krasnogorsk
Кодирование от алкоголизма — это медицинская процедура, направленная на формирование устойчивого отвращения к спиртному и восстановление контроля над зависимым поведением. В клинике «ВолгоградМед Альянс» используются современные, научно обоснованные методы, которые позволяют не просто временно ограничить тягу, а глубоко перестроить психологические и биохимические механизмы зависимости. Каждая программа подбирается индивидуально, с учётом стажа употребления, состояния здоровья, мотивации и психоэмоционального фона пациента. Врачи обеспечивают анонимность, безопасность и круглосуточную поддержку, помогая восстановить не только физическое состояние, но и внутреннее равновесие.
Детальнее – кодирование от алкоголизма отзывы цены в волгограде
Благодаря последовательной работе врачей и постоянному наблюдению лечение проходит безопасно и эффективно, а пациент получает необходимую поддержку на всех этапах терапии.
Получить дополнительные сведения – частная наркологическая клиника
Капельница не просто устраняет симптомы похмелья — она восстанавливает внутренний баланс, снижает токсическую нагрузку и поддерживает работу жизненно важных органов. После процедуры пациент чувствует прилив сил, прояснение сознания и эмоциональную стабильность. Эффект закрепляется при соблюдении рекомендаций врача и отказе от алкоголя в последующие дни.
Разобраться лучше – вывод из запоя цена волгоград
Чтобы быстро соотнести риски и требуемую плотность наблюдения, удобнее всего взглянуть на одну сводную таблицу. Она не заменяет очный осмотр, но помогает заранее понять логику: чем выше риски и вариабельность симптомов, тем плотнее мониторинг и быстрее доступ к корректировкам.
Детальнее – наркологическая клиника телефон
Классная платформа kazino olimp — люблю заходить сюда!
http://rijschoolhermen.nl/lawyer-for-purchase-agreement/
I was wondering if you ever considered changing the structure
of your site? Its very well written; I love what youve got
to say. But maybe you could a little more in the way of content so people could connect with
it better. Youve got an awful lot of text for only having one or 2 images.
Maybe you could space it out better?
В Королёве мы запускаем помощь без «многоходовок». С первого контакта дежурный врач аккуратно уточняет жалобы, длительность эпизода, принимаемые лекарства и сопутствующие диагнозы, после чего предлагает безопасную точку входа: выезд на дом, дневной формат или круглосуточный стационар. Каждое действие объясняется простым языком: зачем оно нужно, какого эффекта ждать в ближайшие часы и что будет считаться нормальной динамикой. Конфиденциальность заложена в процесс по умолчанию: минимально необходимый объём персональных данных, нейтральная коммуникация, ограниченный доступ к медкарте и отсутствие постановки на учёт. Такой порядок снимает лишнее напряжение у семьи и экономит самое ценное — время.
Углубиться в тему – https://narkologicheskaya-klinika-korolyov0.ru/narkologicheskaya-klinika-na-dom-v-korolyove
Инфузионная терапия подбирается под человека, а не под «среднюю» ситуацию. Базовый каркас обычно включает растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы. По показаниям добавляются гепатопротекторы и антиоксидантные компоненты — это помогает печени и снижает оксидативный стресс. Если есть выраженная тошнота, подключаем противорвотные; при тревоге и нарушении сна — мягкие анксиолитики и седативные препараты, которые не «вырубают», а выравнивают ритмы и сохраняют контакт для мониторинга. Мы избегаем агрессивных «миксов», потому что избыточная седация может скрыть опасные симптомы и усложнить оценку состояния. Эффективность оцениваем не только по субъективному облегчению, но и по объективным метрикам: пульс, давление, сатурация, динамика тремора, аппетит, качество сна. Как только показатели стабилизируются, фарм-нагрузка снижается, а ведущую роль берет режим — питание, гидратация, спокойный вечерний ритуал, короткие бытовые активности.
Разобраться лучше – вывод из запоя анонимно
check my blog https://toast-wallet.net/
В Тольятти клиника «ВолгаМед Тольятти» предоставляет широкий спектр услуг — от экстренного вывода из запоя на дому до длительных реабилитационных программ. Выезд нарколога осуществляется круглосуточно: врач приезжает по вызову, проводит диагностику, оценивает степень интоксикации и назначает индивидуальный план лечения. Это особенно важно в тех случаях, когда пациент не может самостоятельно добраться до клиники. В арсенале специалистов — профессиональное оборудование, капельницы для детоксикации и препараты для стабилизации психоэмоционального состояния.
Подробнее тут – частная наркологическая помощь тольятти
My coder is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on several websites for about a year
and am anxious about switching to another platform.
I have heard very good things about blogengine.net.
Is there a way I can transfer all my wordpress content into
it? Any kind of help would be greatly appreciated!
Чтобы не оценивать состояние субъективно, в клинике применяется система наблюдения за ключевыми параметрами. Таблица помогает врачу и пациенту видеть реальную динамику и корректировать вмешательства только при необходимости.
Получить дополнительную информацию – http://narkologicheskaya-clinica-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy/
пояснения https://krab4a.at/
Правильный подбор лекарственных средств позволяет не только уменьшить проявления синдрома отмены, но и стабилизировать эмоциональное состояние пациента, снижая риск срывов. Реабилитационные программы включают физиотерапию, спортивные занятия и коррекцию образа жизни, что способствует полноценному восстановлению организма.
Получить больше информации – лечение наркомании
Формат
Выяснить больше – http://
Важной частью реабилитации является социализация пациента, возвращение его к активной общественной жизни и формирование новых, здоровых привычек. Для этого в клинике организуются различные мероприятия и программы адаптации.
Углубиться в тему – лечение наркомании клиника тверь
После процедуры пациент чувствует улучшение уже через 1–2 часа: проходят головные боли, снижается давление, нормализуется сон и аппетит.
Углубиться в тему – наркологическая клиника лечение алкоголизма новокузнецк
Удобный и понятный сайт с массой полезной информации по казино.
https://jenskiymir.com/proxy.php?url=https://olimp-casino-kz-money.org.kz/bonuses
Благодаря комплексному подходу достигается не только снятие симптомов, но и долгосрочная стабилизация состояния пациента.
Изучить вопрос глубже – http://narkologicheskaya-pomoshh-v-volgograde17.ru
Лечение наркомании в клинике начинается с диагностики, позволяющей определить степень зависимости, выявить сопутствующие заболевания и выбрать оптимальную тактику терапии. Важным этапом является детоксикация — очищение организма от токсинов и продуктов распада наркотических веществ, что снижает риск осложнений и облегчает последующее восстановление.
Выяснить больше – lechenie-narkomanii-tver0.ru/
Клиника «КузбассМед Центр» в Новокузнецке обеспечивает непрерывный приём пациентов и выезд нарколога на дом. Такой формат позволяет оказать экстренную помощь при интоксикации или запое прямо на месте, не дожидаясь ухудшения состояния. Медицинская команда работает в режиме 24/7, что особенно важно при острых состояниях. Врач выезжает в течение часа после вызова, проводит диагностику, ставит капельницу и контролирует жизненные показатели. В стационаре доступны детоксикация, медикаментозная терапия и психотерапевтическая поддержка — всё под постоянным медицинским наблюдением.
Получить дополнительную информацию – лечение в наркологической клинике
Процесс лечения строится поэтапно, что позволяет контролировать динамику состояния пациента и постепенно возвращать его к полноценной жизни.
Ознакомиться с деталями – https://lechenie-alkogolizma-perm0.ru/perm-lechenie-alkogolizma/
Эта последовательность помогает эффективно воздействовать на зависимость и исключает вероятность усугубления состояния.
Получить больше информации – лечение пивного алкоголизма пермь
Клиника «ВоронежМед Альянс» придерживается принципа прозрачной медицины: каждый шаг понятен пациенту, решения принимаются совместно, а результаты фиксируются по объективным показателям. Такой формат создаёт чувство безопасности и доверия. Среди основных принципов:
Узнать больше – наркологическая клиника стационар в воронеже
helpful resources https://web-breadwallet.com
Do you mind if I quote a couple of your posts as long as I
provide credit and sources back to your website? My blog is in the exact same area of interest as yours and
my users would truly benefit from a lot of the information you
present here. Please let me know if this okay with you.
Appreciate it!
Лечение в клинике «ВоронежМед Альянс» проходит поэтапно. Каждый модуль имеет определённую цель и собственные критерии эффективности. Такой подход исключает избыточное вмешательство и обеспечивает прозрачность процесса восстановления.
Подробнее – narcologicheskaya-klinika-v-voronezhe17.ru/
Лечение организовано поэтапно. Такой подход обеспечивает постепенное восстановление функций организма и исключает риск осложнений. Каждый этап терапии направлен на устранение конкретных нарушений, вызванных интоксикацией.
Подробнее – нарколог вывод из запоя красноярск
Когда уместен
Узнать больше – наркологическая клиника нарколог
Что включено на практике
Подробнее – http://narkologicheskaya-klinika-krasnogorsk0.ru/chastnaya-narkologicheskaya-klinika-v-krasnogorske/
Ниже приведена таблица с типовыми компонентами капельницы и их действием:
Ознакомиться с деталями – вывод из запоя на дому недорого тольятти
Что делаем фактически
Подробнее тут – anonimnaya-narkologicheskaya-klinika
Hi, i think that i saw you visited my web site thus i came to “return the favor”.I am attempting to
find things to enhance my site!I suppose its ok to use a few of your ideas!!
Undeniably believe that which you stated. Your favorite reason seemed to
be on the web the easiest thing to be aware of.
I say to you, I certainly get irked while people think about worries that they just do not
know about. You managed to hit the nail upon the top as well as defined out the
whole thing without having side effect , people can take a signal.
Will likely be back to get more. Thanks
В Воронеже клиника «ВоронежМед Альянс» предлагает комплексное лечение алкогольной и наркотической зависимости. Команда врачей, психиатров, психологов и терапевтов выстраивает индивидуальный маршрут пациента, начиная с детоксикации и заканчивая реабилитацией. Главный принцип — минимальное вмешательство при максимальной эффективности. Это означает, что терапевтические меры подбираются строго по показаниям, а медикаменты применяются только после оценки состояния и лабораторных данных.
Получить дополнительные сведения – вывод наркологическая клиника в воронеже
If you are going for finest contents like me, simply go
to see this site everyday since it provides
feature contents, thanks
Ниже представлена таблица с основными препаратами, используемыми при выводе из запоя в Тюмени:
Подробнее – вывод из запоя на дому круглосуточно в тюмени
Капельницы от запоя включают препараты для очищения крови, восстановления электролитного баланса и защиты печени. Используются только сертифицированные растворы, одобренные Минздравом РФ. В клинике применяется комплексный подход: одновременно с физическим восстановлением запускаются лёгкие дыхательные и релаксационные методики, которые помогают организму вернуться в стабильное состояние.
Узнать больше – анонимный вывод из запоя воронеж
Лечение наркомании в клинике начинается с диагностики, позволяющей определить степень зависимости, выявить сопутствующие заболевания и выбрать оптимальную тактику терапии. Важным этапом является детоксикация — очищение организма от токсинов и продуктов распада наркотических веществ, что снижает риск осложнений и облегчает последующее восстановление.
Подробнее – https://lechenie-narkomanii-tver0.ru/
It’s really a cool and helpful piece of information. I am happy that you
simply shared this useful information with us. Please keep us up to date like this.
Thank you for sharing.
Терапия строится из узких модулей с чёткими «выключателями». Мы не «усиливаем» схему без показаний — каждое расширение привязано к конкретной цели и времени переоценки. Ниже — ориентир по основным программам «ЕнисейМед Центра».
Получить дополнительную информацию – наркологическая клиника нарколог
Hi, I think your blog might be having browser compatibility issues.
When I look at your blog in Chrome, it looks fine but when opening in Internet Explorer,
it has some overlapping. I just wanted to give you a quick heads up!
Other then that, awesome blog!
Ниже — ориентир, который помогает сопоставить риски, плотность наблюдения и ожидаемую скорость стабилизации. Таблица не заменяет очный осмотр, но экономит время на принятие решений и делает логику врача понятной всей семье.
Подробнее можно узнать тут – анонимная наркологическая клиника
Лечение в клинике включает несколько последовательных этапов, каждый из которых направлен на достижение стабильной ремиссии и восстановление здоровья пациента.
Подробнее – https://narcologicheskaya-klinika-v-novokuzneczke17.ru/narkolog-v-gorode-novokuzneczke/
Thankfulness to my father who informed me on the topic of this weblog, this blog is genuinely amazing.
Also visit my homepage באתר הזה
Best XI selections, team of the week month and season picks
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Секреты успеха внутри – https://startupstories.in/stories/inspirational-stories/articles/carlos-ghosn-the-rise-of-a-titan-of-automobile-industry
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Почему это важно? – https://www.ucetni-sluzby.com/pellentesque-nibh-aenean-quam-in-scelerisque
Simply desire to say your article is as surprising.
The clearness in your post is simply excellent and i could assume you are an expert on this
subject. Fine with your permission allow me to grab your feed to
keep updated with forthcoming post. Thanks a million and please carry on the rewarding work.
My web blog – ai customer response generator
Одним из самых востребованных направлений работы клиники является проведение детоксикации и вывод из запоя. Эти процедуры направлены на очищение организма от алкоголя и продуктов его распада, нормализацию работы печени и нервной системы. Лечение проводится с использованием сертифицированных препаратов и под контролем врача-нарколога.
Ознакомиться с деталями – частная наркологическая клиника
Tämä on erittäin ajankohtainen kirjoitus.
Verkko- joukkorahoitus mahdollistaa leikkauksen monelle.
Kiitoksia että tuotte esiin tämän tehtävän.
Наркологическая клиника в Новокузнецке предоставляет профессиональную помощь людям, столкнувшимся с зависимостью от алкоголя, наркотиков и психоактивных веществ. Лечение проводится под наблюдением опытных специалистов с применением современных медицинских методик. Основная цель работы клиники — не только устранить физическую зависимость, но и восстановить психологическое равновесие пациента, вернуть мотивацию и способность жить без употребления веществ.
Детальнее – наркологическая клиника клиника помощь новокузнецк
Мы переводим субъективное «полегчало» в наблюдаемые факты. Быстрее всего меняются переносимость воды и интенсивность тошноты; вслед за этим «садится» пульс/давление и на 3+ пункта снижается тремор. «Первая ночь» — экзамен устойчивости: цель — ? 6 часов сна и не более одного пробуждения. Утром — две «малые победы» (гигиена, 10–15 минут тихой ходьбы) без «отката». При такой динамике модули по плану выключаются, пациент получает короткую карту самопомощи на 72 часа: светогигиена, интервалы питья, дыхательные ритмы, речевые правила семьи и пороги связи с дежурным.
Получить больше информации – http://narkologicheskaya-klinika-v-krasnoyarske17.ru/
Наркологическая клиника в Воронеже — это специализированное медицинское учреждение, предоставляющее помощь людям, столкнувшимся с зависимостью от алкоголя, наркотиков и других психоактивных веществ. Лечение проводится под контролем квалифицированных врачей, с использованием современных методик детоксикации, психотерапии и реабилитации. Цель работы специалистов — не только устранить физическую зависимость, но и помочь пациенту восстановить эмоциональное равновесие, вернуть контроль над поведением и мотивацию к трезвости.
Исследовать вопрос подробнее – https://narkologicheskaya-clinica-v-voronezhe17.ru/voronezh-narkologicheskij-dispanser
Все растворы проходят фармацевтический контроль, а процедуры выполняются одноразовыми стерильными инструментами. После завершения капельницы врач наблюдает пациента в течение 15–30 минут, оценивает результат и даёт рекомендации по дальнейшему восстановлению. Важно не прерывать терапию самостоятельно — эффект закрепляется только при соблюдении рекомендаций.
Подробнее – http://narkolog-na-dom-v-voronezhe17.ru
Капельница от запоя в Волгограде — это эффективный способ быстро восстановить организм после длительного употребления алкоголя. Процедура проводится врачом-наркологом и направлена на выведение токсинов, нормализацию обмена веществ и стабилизацию работы нервной системы. Инфузионная терапия помогает устранить головную боль, слабость, тошноту, восстановить сон и аппетит. Благодаря внутривенному введению препаратов эффект наступает уже через 20–30 минут после начала процедуры.
Получить дополнительные сведения – капельница от запоя клиника
Современные методы лечения в наркологической клинике в Новокузнецке основаны на доказательной медицине. При поступлении пациент проходит полное обследование, включающее оценку физического состояния, психоэмоционального фона и наличия сопутствующих заболеваний. На основе полученных данных составляется персональная программа терапии, охватывающая медицинский, психологический и социальный аспекты выздоровления.
Ознакомиться с деталями – вывод наркологическая клиника в новокузнецке
Эта статья сочетает познавательный и занимательный контент, что делает ее идеальной для любителей глубоких исследований. Мы рассмотрим увлекательные аспекты различных тем и предоставим вам новые знания, которые могут оказаться полезными в будущем.
Погрузиться в научную дискуссию – https://ppgfito.ufersa.edu.br/2023/09/11/professor-do-pgfitotecnia-e-finalista-do-premio-global-em-inovacao-em-dessalinizacao
This is a vital post. Medical crowdfunding changes futures for people who cannot pay for surgery.
Helping a healthcare cause is absolutely wonderful. Thanks for
sharing this mission.
My site – Healthcare Aid Platform
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Получить профессиональную консультацию – https://www.gorselsanatlarakademisi.com/3ds-max-ile-mimarlik-dunyasina-adim-atin
I think the admin of this web page is actually working hard in support of
his web site, since here every information is quality based information.
I’ve read a few just right stuff here. Certainly price bookmarking for revisiting.
I surprise how a lot effort you set to create this kind
of fantastic informative site.
It’s really a cool and helpful piece of information. I am
glad that you shared this helpful information with us.
Please stay us up to date like this. Thanks for sharing.
Here is my website; נערות ליווי בחיפה
Процесс кодирования проходит в комфортной и спокойной обстановке. Врач объясняет каждый этап, чтобы пациент чувствовал себя уверенно и спокойно. После процедуры пациент получает памятку с рекомендациями по уходу за здоровьем и режиму поведения в первые недели после лечения.
Выяснить больше – анонимное кодирование от алкоголизма волгоград
Важной частью реабилитации является социализация пациента, возвращение его к активной общественной жизни и формирование новых, здоровых привычек. Для этого в клинике организуются различные мероприятия и программы адаптации.
Детальнее – лечение наркомании реабилитация
I appreciate, cause I found just what I was looking for. You’ve ended my four day long hunt! God Bless you man. Have a great day. Bye -.
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Связаться за уточнением – https://romicharviajes.com/index.php/2022/07/01/how-to-travel-with-paper-map
Эта статья сочетает познавательный и занимательный контент, что делает ее идеальной для любителей глубоких исследований. Мы рассмотрим увлекательные аспекты различных тем и предоставим вам новые знания, которые могут оказаться полезными в будущем.
Смотрите также – https://person.russian.city/tatarstan/399682082
โพสต์นี้ อ่านแล้วได้ความรู้เพิ่ม ค่ะ
ดิฉัน ไปเจอรายละเอียดของ หัวข้อที่คล้ายกัน
ที่คุณสามารถดูได้ที่ betflik13
เผื่อใครสนใจ
มีการยกตัวอย่างที่เข้าใจง่าย
ขอบคุณที่แชร์ ข้อมูลที่มีประโยชน์
นี้
จะรอติดตามเนื้อหาใหม่ๆ ต่อไป
I have read several good stuff here. Certainly value bookmarking for revisiting.
I surprise how much effort you put to make one of these
excellent informative web site.
В статье представлены ключевые моменты по актуальной теме, дополненные советами экспертов и ссылками на дополнительные ресурсы. Цель материала — дать читателю инструменты для самостоятельного развития и принятия осознанных решений.
Продолжить изучение – https://гормедцентр.рф/kazan
Hi there it’s me, I am also visiting this web site on a regular basis, this web site is in fact
fastidious and the visitors are in fact sharing fastidious thoughts.
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Изучить материалы по теме – https://btrc.co/international-truck-prix-set-for-full-throttle-donington-park-debut
Cha nel fys aym erbee cre’n aght haink mee stiagh ‘sy ‘nnyd shoh, agh s’cosoylagh dy row y post shoh mie. Cha nel fys aym c’raad t’ou agh dy shickyr t’ou goll gys blogger cliaghtey mannagh vel oo er-dy-henney 😉 Cheers!
Правильный подбор лекарственных средств позволяет не только уменьшить проявления синдрома отмены, но и стабилизировать эмоциональное состояние пациента, снижая риск срывов. Реабилитационные программы включают физиотерапию, спортивные занятия и коррекцию образа жизни, что способствует полноценному восстановлению организма.
Выяснить больше – центр лечения наркомании
爱一帆海外版,专为华人打造的高清视频官方认证平台,支持全球加速观看。
Can I just say what a comfort to find an individual who truly knows what they’re discussing on the web.
You definitely realize how to bring a problem to light and make
it important. A lot more people ought to read this and understand
this side of your story. I can’t believe you aren’t more popular since you most certainly possess the gift.
http://wiki.wild-sau.com/index.php?title=Benutzer:TristanFleming [http://wiki.wild-sau.com/index.php?title=6_Super_Helpful_Suggestions_To_Improve_Blog]
Fantasy football, player points and team management tips included
Письменные рекомендации: сон, питание, гидратация, запреты, «красные флаги», график амбулаторных визитов; при недостатке ресурсов дома — перевод в стационар без задержек. Такая последовательность убирает импровизацию и делает результат повторяемым.
Получить дополнительные сведения – vyvod-iz-zapoya-nedorogo
Запой — это не просто несколько лишних дней алкоголя, а тяжёлое состояние, в котором организм работает на пределе. Чем дольше длится эпизод, тем глубже обезвоживание, тем сильнее сдвиги электролитов, тем выше риск аритмий, гипертонических кризов, судорог, делирия, обострений заболеваний сердца, печени и поджелудочной железы. Попытки «вывести» человека дома силами родных часто включают опасные комбинации: случайные седативные, снотворные, анальгетики, «антипохмельные» из рекламы. Они могут на время усыпить или «успокоить», но при этом скрывают ухудшение, сбивают давление, угнетают дыхание и мешают врачу увидеть реальную картину. В «Трезвый Центр Коломна» подход другой: ещё на этапе звонка специалист уточняет длительность запоя, объёмы и виды алкоголя, наличие гипертонии, ИБС, диабета, заболеваний печени и почек, неврологических проблем, список уже принятых препаратов, эпизоды потери сознания, судорог, странного поведения. На основании этих данных определяется, безопасен ли формат на дому или сразу нужен стационар. Такая сортировка позволяет вовремя перехватить опасные случаи, не терять часы на бесполезные попытки и сразу запускать те схемы, которые реально снижают риски и стабилизируют состояние.
Углубиться в тему – vyvod-iz-zapoya-v-stacionare-v-kolomne
Bonuses https://toast-wallet.net
Чтобы не упустить момент, нужно ориентироваться не на фразу «он говорит, что справится», а на реальные признаки, при которых профессиональная помощь на дому становится необходимой. Домашний выезд — это шанс стабилизировать состояние до того, как потребуется реанимация или жёсткая госпитализация.
Ознакомиться с деталями – http://narkolog-na-dom-dolgoprudnij10.ru
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Получить дополнительные сведения – zapoj-narkolog-na-dom
I really like it when individuals get together and share thoughts.
Great blog, continue the good work!
Wonderful web site. Lots of useful info here. I am sending it to some pals ans additionally sharing in delicious.
And certainly, thank you in your effort!
I absolutely love your blog and find nearly all of your post’s to
be just what I’m looking for. Do you offer guest writers to write content for
you? I wouldn’t mind writing a post or elaborating on many
of the subjects you write concerning here. Again, awesome website!
Решение, куда обращаться при запое, напрямую влияет на безопасность. Одно дело — случайный выездной «специалист» без адреса и гарантий, другое — официальная наркологическая клиника в Реутове, несущая ответственность за свои действия. «РеутовМед Сервис» выстраивает помощь так, чтобы каждый шаг был прозрачным и медицински обоснованным, а не строился на обещаниях «вылечим за час». Уже на этапе первого звонка специалисты уточняют длительность запоя, виды и объёмы алкоголя, возраст пациента, хронические заболевания, перенесённые ранее судороги, делирий, проблемы с сердцем и давлением, какие лекарства уже давались. Эта информация позволяет не «ставить капельницу вслепую», а выбрать безопасный формат: стационар, выезд на дом или комбинированный подход. В клинике используют только сертифицированные препараты, одноразовые системы, следуют протоколам, учитывающим реальные риски, а не запрос «сделайте, чтобы уснул и не мешал». Важен и человеческий аспект: здесь не унижают, не морализируют, не угрожают учётом. Пациент воспринимается как человек с заболеванием, а не как «виноватый», а это повышает готовность к сотрудничеству и к последующим шагам в сторону трезвости.
Получить дополнительную информацию – https://vyvod-iz-zapoya-reutov10.ru/vyvod-iz-zapoya-na-domu-v-reutove
Прежде чем перейти к ориентировочным цифрам, важно подчеркнуть: цена формируется из реальных компонентов помощи — работы врача и медсестры, объёма инфузионной терапии, перечня препаратов, времени выезда и необходимости более длительного наблюдения. Никаких скрытых доплат: все дополнительные назначения согласуются заранее. Чем раньше вы обращаетесь, тем меньше объём вмешательств и, как правило, ниже итоговая стоимость — короткий эпизод проще и дешевле стабилизировать, чем «выводить» осложнения после затянутого запоя.
Узнать больше – вызов нарколога на дом
Наркологическая клиника «КоломнаМед Центр» — это место, куда можно обратиться в тот момент, когда домашние попытки контролировать алкоголь, наркотики, аптечные препараты или смесь всего сразу перестают работать, а жизнь превращается в постоянное «завтра начну с нуля». Здесь не обещают чудес за один день и не пугают диагнозами, а выстраивают понятный медицинский маршрут: детоксикация, стабилизация, реабилитация, поддержка семьи, профилактика срывов. Пациент получает помощь в защищённой, конфиденциальной среде, где всё организовано так, чтобы снизить тревогу и стыд, убрать хаос вокруг зависимости и дать человеку шанс вернуться к нормальной жизни без давления, угроз и токсичных «стимулов». Для родных клиника в Коломне — это опора: конкретный адрес, конкретная команда, чёткие сроки и понятные этапы, вместо бесконечных обещаний «он сам справится».
Подробнее тут – narkologicheskaya-klinika-otzyvy
I’m gone to tell my little brother, that he should also
visit this weblog on regular basis to take updated from hottest gossip.
Very nice post. I simply stumbled upon your weblog and wished to mention that
I have truly loved browsing your weblog posts. After
all I will be subscribing to your feed and I
hope you write again very soon!
Запойное состояние сопровождается тяжелыми последствиями для организма. Оно может включать нарушения сна, тремор конечностей, скачки давления, головные боли и депрессию. Без своевременной помощи такие проявления способны привести к развитию хронических заболеваний и угрожающих жизни осложнений.
Получить дополнительную информацию – наркология вывод из запоя в перми
Клиника придерживается принципа прозрачного ценообразования. Пациенту или родственникам сразу озвучивается стоимость всех процедур и услуг. Возможна оплата поэтапно или в рамках пакета. В отличие от многих клиник, «ОмскПрофи» предоставляет фиксированные цены на распространённые виды помощи, без скрытых доплат.
Изучить вопрос глубже – скорая наркологическая помощь
Практический тест прост: сохранённый контакт, контролируемый тремор, эпизодическая (не неукротимая) рвота, нет грубой дезориентации, давление и пульс не «скачут», в квартире можно обеспечить тишину и доступ к воде — тогда дом уместен. Если хотя бы два пункта «провисают», отделение в Электростали даст предсказуемость и защиту от ночных ухудшений, которые дома часто остаются незамеченными.
Подробнее можно узнать тут – https://vyvod-iz-zapoya-ehlektrostal10.ru/vyvod-iz-zapoya-klinika-v-ehlektrostali
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Получить больше информации – http://www.domen.ru
I do believe your audience could very well want a good deal more stories like this carry on the excellent hard work.
Капельница — инструмент, помогающий организму выйти из токсической воронки, а не магическая смесь «на все случаи». Базовый каркас — регидратация и коррекция кислотно-щелочного состояния, электролиты для водно-солевого баланса, витамины группы B и магний для поддержки нервной системы и снижения тремора. По клиническим показаниям подключаются гепатопротекторы и антиоксиданты для разгрузки печени и уменьшения оксидативного стресса; при выраженной тошноте — противорвотные, при тревоге и бессоннице — мягкие анксиолитики в дозах, сохраняющих контакт. Мы сознательно избегаем «агрессивной» седации: она создаёт иллюзию успеха, но маскирует ухудшения и мешает контролю дыхания и нейростатуса. Эффективность оцениваем не «по ощущениям», а по метрикам: стабилизация АД/ЧСС, снижение тремора и тошноты, нормализация сатурации, возвращение аппетита и появление восстановительного ночного сна. Как только параметры выравниваются, фарм-нагрузку снижаем, а акцент переносим на режим — гигиену сна, регулярную гидратацию, дробное питание, щадящую дневную активность. Это делает результат не кратковременным затишьем на препаратах, а устойчивой траекторией восстановления.
Детальнее – https://vyvod-iz-zapoya-ehlektrostal10.ru/vyvod-iz-zapoya-na-domu-v-ehlektrostali
Выбор наркологической клиники в Коломне — это не «слишком серьёзно», а логичный шаг, если зависимость уже зашла дальше спонтанных эпизодов. Алкоголизм, наркомания, злоупотребление успокоительными и обезболивающими — это не только психологическая тяга, но и перестройка организма: страдают печень, сердце, сосуды, нервная система, гормональный фон, сон, психика. Дома редко есть возможность круглосуточно контролировать состояние, правильно отменять вещества, отслеживать давление, пульс, поведение, не допускать опасных комбинаций препаратов. Родственники устают, реагируют эмоциями, а не медицинской логикой, человек чувствует себя под прицелом, но не под защитой. В «КоломнаМед Центр» всё выстроено так, чтобы снять нагрузку с семьи и вывести помощь из зоны хаотичных решений. Здесь оценивают не только то, «что и сколько пьёт или принимает», а весь контекст: длительность зависимости, срывы, уже перенесённые делирии или передозировки, сопутствующие болезни, психические состояния, семейную ситуацию. На основе этого формируется безопасный план: где начать — в стационаре или амбулаторно, какой формат детокса выбрать, насколько жёстко вести наблюдение, как сразу встроить психотерапевтическую и социальную поддержку. Клиника в Коломне позволяет работать системно, а не латать последствия очередного срыва.
Разобраться лучше – заказать звонок наркологическая клиника
This design is incredible! You definitely know
how to keep a reader amused. Between your wit and your videos, I was almost
moved to start my own blog (well, almost…HaHa!) Great job.
I really enjoyed what you had to say, and more than that, how you presented it.
Too cool!
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Подробнее – http://vyvod-iz-zapoya-ramenskoe10.ru
Каждый этап лечения подбирается индивидуально с учетом состояния пациента и особенностей его зависимости.
Подробнее можно узнать тут – наркологическая клиника вывод из запоя в твери
Today, I went to the beach with my children. I found a sea shell and gave it to my 4 year old daughter and said
“You can hear the ocean if you put this to your ear.” She placed the
shell to her ear and screamed. There was a hermit crab inside and
it pinched her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
Выбор наркологической клиники в Коломне — это не «слишком серьёзно», а логичный шаг, если зависимость уже зашла дальше спонтанных эпизодов. Алкоголизм, наркомания, злоупотребление успокоительными и обезболивающими — это не только психологическая тяга, но и перестройка организма: страдают печень, сердце, сосуды, нервная система, гормональный фон, сон, психика. Дома редко есть возможность круглосуточно контролировать состояние, правильно отменять вещества, отслеживать давление, пульс, поведение, не допускать опасных комбинаций препаратов. Родственники устают, реагируют эмоциями, а не медицинской логикой, человек чувствует себя под прицелом, но не под защитой. В «КоломнаМед Центр» всё выстроено так, чтобы снять нагрузку с семьи и вывести помощь из зоны хаотичных решений. Здесь оценивают не только то, «что и сколько пьёт или принимает», а весь контекст: длительность зависимости, срывы, уже перенесённые делирии или передозировки, сопутствующие болезни, психические состояния, семейную ситуацию. На основе этого формируется безопасный план: где начать — в стационаре или амбулаторно, какой формат детокса выбрать, насколько жёстко вести наблюдение, как сразу встроить психотерапевтическую и социальную поддержку. Клиника в Коломне позволяет работать системно, а не латать последствия очередного срыва.
Изучить вопрос глубже – http://narkologicheskaya-klinika-kolomna10.ru
Острый запой — это нарушение работы сердца, мозга, печени и нервной системы, а не просто «лишние пару дней выпивки». Когда начинается тремор, потливость, скачки давления, бессонница, паника, семья часто пытается помочь самостоятельно: даёт случайные таблетки, сомнительные «антипохмельные коктейли», сильные седативные. В реальности такие меры нередко ухудшают ситуацию: давление падает или «скачет», дыхание угнетается, симптомы предделирия маскируются, и момент, когда нужна экстренная помощь, пропускается. Выездной нарколог «ЩёлковоМед Профи» в Щёлково работает иначе: ещё по телефону собираются ключевые данные — возраст, длительность запоя, сопутствующие заболевания, принимаемые лекарства, аллергии, примерные показатели АД и пульса, особенности поведения. Это позволяет заранее оценить риски и понять, подходит ли формат на дому. На месте врач измеряет давление, пульс, сатурацию, температуру, оценивает степень обезвоживания, выраженность тремора, неврологический статус, наличие дезориентации, смотрит, не требуется ли сразу стационар. Капельница назначается по фактическим показателям: без «универсальных коктейлей», без опасной седации, с учётом сердца, печени, эндокринных и неврологических особенностей. Такой подход снижает нагрузку на организм и делает результат управляемым — облегчение наступает без лишнего риска.
Детальнее – нарколог на дом вывод из запоя
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Получить больше информации – http://vyvod-iz-zapoya-ramenskoe10.ru/srochnoe-vyvedenie-iz-zapoya-v-ramenskom/
Pretty nice post. I just stumbled upon your blog and wanted to say that I’ve truly enjoyed browsing your blog posts.
In any case I’ll be subscribing to your feed and I hope
you write again soon!
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Получить дополнительную информацию – https://vyvod-iz-zapoya-v-ryazani17.ru/vyvod-iz-zapoya-ryazan-na-domu/
Вывод из запоя в Раменском в условиях клиники строится не вокруг одной капельницы, а вокруг понятной цепочки шагов, где каждый этап логичен и медицински обоснован. Это помогает не только быстро облегчить состояние, но и уменьшить вероятность того, что через пару дней человек снова уйдёт в запой.
Выяснить больше – vyvod-iz-zapoya-ramenskoe10.ru/
Важное отличие клиники — отказ от примитивной схемы «капельница — домой — дальше сам». Такой формат даёт кратковременное облегчение, но не решает ни причин, ни структуры зависимости. «КоломнаМед Центр» выстраивает ступенчатый подход. Первый шаг — безопасная детоксикация: снятие абстиненции, коррекция водно-электролитного баланса, поддержка сердечно-сосудистой системы, печени, нервной системы, нормализация сна. Второй шаг — стабилизация: оценка психического состояния, выявление тревожных, депрессивных и панических симптомов, подбор поддерживающих схем, которые помогают не сорваться сразу после выхода из острых проявлений. Третий шаг — реабилитация и мотивация: психотерапевтическая работа, групповые и индивидуальные форматы, обучение навыкам трезвой жизни, работа с триггерами, укрепление внутренней мотивации. Четвёртый шаг — постреабилитационная поддержка: контрольные приёмы, дистанционные консультации, помощь в профилактике срывов. Такой комплексный путь не ломает пациента, а возвращает ему контроль: не через страх, а через понимание, структуру и реальные инструменты.
Изучить вопрос глубже – http://narkologicheskaya-klinika-kolomna10.ru
I really like reading through an article that can make men and women think.
Also, many thanks for permitting me to comment!
FinTech Advisory
Перед тем как показать примерные программы, важно подчеркнуть: реальный план всегда персонализируется, но понимание базовых форматов помогает семье и пациенту не теряться в терминах и сразу видеть логику.
Разобраться лучше – zakazat-obratnyj-zvonok-narkologicheskaya-klinika
Фиксируем АД, ЧСС, сатурацию, температуру, оцениваем неврологический статус, степень обезвоживания, тремор, тошноту и уровень тревоги; собираем краткий анамнез последних суток и характер употребления.
Подробнее тут – vyvod-iz-zapoya-s-vyezdom-ehlektrostal
Вывод из запоя требуется тогда, когда организм уже не способен самостоятельно справиться с последствиями алкогольной интоксикации. Длительное употребление спиртного приводит к нарушению работы внутренних органов, обезвоживанию и психическим расстройствам. Медицинская помощь помогает избежать опасных осложнений и облегчить процесс отказа от алкоголя.
Изучить вопрос глубже – https://vyvod-iz-zapoya-v-ryazani17.ru/vyvod-iz-zapoya-na-domu-ryazan-czeny/
Наркологическая клиника в Омске оказывает специализированную помощь людям, столкнувшимся с алкогольной, наркотической и другими формами зависимости. Здесь используются современные методы диагностики, терапии и реабилитации, которые помогают не только стабилизировать состояние, но и восстановить здоровье в долгосрочной перспективе. Работа ведётся с учётом принципов конфиденциальности, что создаёт условия для комфортного прохождения лечения.
Подробнее тут – наркологическая клиника цены омск
Стационар «Трезвый Путь Коломна» ориентирован на безопасность в самых сложных случаях: длительные запои, тяжёлая абстиненция, смешанное употребление, выраженные соматические проблемы, риск делирия или судорог. Пациент попадает под наблюдение 24/7, что принципиально отличает клинику от домашних попыток «спасти своими средствами». Контроль жизненно важных показателей, своевременная коррекция схем лечения, возможность быстро отреагировать на осложнения — всё это снижает риск критических ситуаций, которые часто возникают именно после неумелых домашних вмешательств или «выездов без ответственности».
Подробнее – http://www.domen.ru
С момента начала лечения пациент получает доступ к круглосуточной линии поддержки. Врачи, психологи и координаторы готовы ответить на вопросы, помочь с корректировкой схемы лечения, поддержать в ситуации риска срыва. Эта функция особенно востребована в первые недели после выписки, когда человек сталкивается с триггерами в привычной среде и нуждается в дополнительной защите. Связь может осуществляться по телефону, через защищённый мессенджер или с помощью мобильного приложения клиники.
Исследовать вопрос подробнее – лечение наркомании реабилитация в самаре
Перед таблицей — короткий акцент: приведённые суммы ориентировочные, не являются публичной офертой, точная стоимость определяется после осмотра.
Исследовать вопрос подробнее – bystryj-vyvod-iz-zapoya
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Углубиться в тему – http://vyvod-iz-zapoya-ramenskoe10.ru/vyvod-iz-zapoya-na-domu-v-ramenskom/
Amazing! This blog looks just like my old one!
It’s on a completely different topic but it has pretty much the same layout and design. Excellent
choice of colors!
Работа выездной службы построена так, чтобы для семьи всё было максимально понятно и предсказуемо. После звонка специалист не ограничивается общими фразами, а уточняет детали: сколько длится употребление, есть ли хронические болезни сердца, печени, почек, эндокринные нарушения, какие препараты и в каких дозах пациент уже получил, были ли в прошлом судороги, галлюцинации, тяжёлые реакции на лекарства. Это позволяет заранее оценить уровень риска и понять, подходит ли формат дома. По прибытии в Серпухове врач осматривает пациента, проверяет контакт и ориентировку, измеряет артериальное давление несколько раз, оценивает пульс, сатурацию, температуру, выраженность тремора, наличие болей, характер дыхания, степень обезвоживания. Далее формируется индивидуальная инфузионная схема: растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы, при необходимости — гепатопротекторы и мягкие антиоксидантные комплексы, противорвотные для контроля тошноты, щадящие анксиолитики для нормализации сна без грубой седации. Во время процедуры врач контролирует динамику, меняет скорость капельницы при необходимости, отслеживает реакцию на препараты и объясняет родным, какие изменения будут происходить по часам. По завершении визита пациент и родственники получают подробный план: режим, питьё, питание, чего нельзя, какие симптомы считаются тревожными, когда нужна повторная консультация или стационар. При выявлении опасных признаков вопрос о госпитализации поднимается честно и сразу, а не откладывается «до утра».
Разобраться лучше – https://narkolog-na-dom-serpuhov10.ru/narkolog-psiholog-na-dom-serpuhov/
Ниже приведена таблица с примерными этапами терапии:
Ознакомиться с деталями – https://vyvod-iz-zapoya-v-ryazani17.ru/
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Получить дополнительную информацию – наркология вывод из запоя омск
В случаях, когда пациент не готов приехать в клинику или находится в тяжёлом состоянии, специалисты «ЗдороваяСамара» организуют выездную помощь. Это особенно важно при острых интоксикациях, синдроме отмены, резком ухудшении психоэмоционального состояния. Выезд возможен круглосуточно и занимает от 30 до 60 минут с момента обращения. Врач приезжает в гражданской одежде, без опознавательных знаков и привлечения внимания. Оснащение позволяет провести на месте полную диагностику и начать лечение — в том числе инфузионную терапию, коррекцию состояния и психологическую стабилизацию.
Подробнее тут – лечение наркомании диспансер в самаре
Город живёт в разных темпах: плотный центр, мостовые переходы, набережная, спальные районы. Мы строим маршрут так, чтобы не привлекать внимания соседей и не терять время на трафик. Если на предзвонке отмечаются «красные флаги» — давящая боль в груди, выраженная одышка, спутанность сознания, судороги, неукротимая рвота или резкое падение насыщения кислородом, — команда instantly переключает маршрут в стационарный «коридор»: палата резервируется заранее, документы оформляются нейтрально, транспорт — немаркированный. Если угроз нет, всё начинается на дому с адресной детокс-схемы и мягкой сенсорной поддержкой.
Детальнее – нарколог на дом недорого саратов
Работа выездной службы построена так, чтобы для семьи всё было максимально понятно и предсказуемо. После звонка специалист не ограничивается общими фразами, а уточняет детали: сколько длится употребление, есть ли хронические болезни сердца, печени, почек, эндокринные нарушения, какие препараты и в каких дозах пациент уже получил, были ли в прошлом судороги, галлюцинации, тяжёлые реакции на лекарства. Это позволяет заранее оценить уровень риска и понять, подходит ли формат дома. По прибытии в Серпухове врач осматривает пациента, проверяет контакт и ориентировку, измеряет артериальное давление несколько раз, оценивает пульс, сатурацию, температуру, выраженность тремора, наличие болей, характер дыхания, степень обезвоживания. Далее формируется индивидуальная инфузионная схема: растворы для регидратации и коррекции электролитов, витамины группы B и магний для поддержки нервной системы, при необходимости — гепатопротекторы и мягкие антиоксидантные комплексы, противорвотные для контроля тошноты, щадящие анксиолитики для нормализации сна без грубой седации. Во время процедуры врач контролирует динамику, меняет скорость капельницы при необходимости, отслеживает реакцию на препараты и объясняет родным, какие изменения будут происходить по часам. По завершении визита пациент и родственники получают подробный план: режим, питьё, питание, чего нельзя, какие симптомы считаются тревожными, когда нужна повторная консультация или стационар. При выявлении опасных признаков вопрос о госпитализации поднимается честно и сразу, а не откладывается «до утра».
Исследовать вопрос подробнее – https://narkolog-na-dom-serpuhov10.ru/vyezd-narkologa-na-dom-serpuhov/
The Real Jackpot is in the Comments. Share Your Story.
If you desire to obtain a great deal from this paragraph then you
have to apply such techniques to your won weblog.
Запойное состояние сопровождается тяжелыми последствиями для организма. Оно может включать нарушения сна, тремор конечностей, скачки давления, головные боли и депрессию. Без своевременной помощи такие проявления способны привести к развитию хронических заболеваний и угрожающих жизни осложнений.
Получить дополнительную информацию – вывод из запоя в стационаре пермь
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Подробнее тут – https://vyvod-iz-zapoya-saratov0.ru
В зависимости от состояния пациента и пожеланий семьи наркологическая помощь может быть оказана в одном из нескольких форматов: на дому, в стационаре или дистанционно. Каждый из форматов обеспечивает доступ к медицинской помощи без бюрократии и с сохранением полной конфиденциальности.
Исследовать вопрос подробнее – частная наркологическая помощь в омске
Наркологическая клиника в Перми обеспечивает пациентам комфортные условия и профессиональное сопровождение. Врачи работают круглосуточно и соблюдают строгую конфиденциальность, что делает лечение доступным и безопасным.
Разобраться лучше – платная наркологическая клиника в перми
Острый запой — это нарушение работы сердца, мозга, печени и нервной системы, а не просто «лишние пару дней выпивки». Когда начинается тремор, потливость, скачки давления, бессонница, паника, семья часто пытается помочь самостоятельно: даёт случайные таблетки, сомнительные «антипохмельные коктейли», сильные седативные. В реальности такие меры нередко ухудшают ситуацию: давление падает или «скачет», дыхание угнетается, симптомы предделирия маскируются, и момент, когда нужна экстренная помощь, пропускается. Выездной нарколог «ЩёлковоМед Профи» в Щёлково работает иначе: ещё по телефону собираются ключевые данные — возраст, длительность запоя, сопутствующие заболевания, принимаемые лекарства, аллергии, примерные показатели АД и пульса, особенности поведения. Это позволяет заранее оценить риски и понять, подходит ли формат на дому. На месте врач измеряет давление, пульс, сатурацию, температуру, оценивает степень обезвоживания, выраженность тремора, неврологический статус, наличие дезориентации, смотрит, не требуется ли сразу стационар. Капельница назначается по фактическим показателям: без «универсальных коктейлей», без опасной седации, с учётом сердца, печени, эндокринных и неврологических особенностей. Такой подход снижает нагрузку на организм и делает результат управляемым — облегчение наступает без лишнего риска.
Подробнее тут – skolko-stoit-vyzvat-narkologa-na-dom
Такая последовательность действий позволяет обеспечить результативность и закрепить положительные изменения.
Подробнее тут – http://narcologicheskaya-klinika-perm0.ru
Острый эпизод запоя — это не «плохое самочувствие», а состояние с реальными рисками для сердца, нервной системы и дыхания, особенно в ночные часы, когда усиливаются вегетативные реакции и тревога. В «НоваТрезвие» мы выстраиваем помощь так, чтобы от звонка до заметного облегчения прошло как можно меньше времени и как можно меньше случайностей: короткое интервью для оценки рисков, выезд врача или приём в клинике, экспресс-диагностика по ключевым показателям, персональная инфузионная схема без «универсальных коктейлей», мягкая коррекция сна и тревоги без «вырубания», понятные инструкции семье на 24–72 часа и план продолжения на ближайшие недели. Мы не скрываемся за общими формулами: решения принимаются по фактическим данным, дозы и темп капельниц подстраиваются к динамике каждые 15–20 минут, а при «красных флагах» перевод в стационар организуется без пауз. Конфиденциальность соблюдается строго, а коммуникация простая и предсказуемая — чтобы вы всегда знали, что происходит сейчас и чего ждать к утру.
Разобраться лучше – vyvod-iz-zapoya-na-domu-cena
В основе работы наркологической клиники лежит комплексный подход, включающий медицинскую детоксикацию, психотерапевтическую поддержку и социальную реабилитацию. Такой подход позволяет не только снять острые симптомы интоксикации, но и сформировать устойчивую мотивацию к трезвому образу жизни.
Разобраться лучше – наркологическая клиника лечение алкоголизма в твери
Ниже приведена таблица с примерными этапами терапии:
Получить дополнительную информацию – вывод из запоя капельница на дому в рязани
Медицинская помощь строится на принципах индивидуального подхода и поэтапной терапии. Каждый пациент проходит диагностику, после чего составляется персональная программа, включающая медикаментозную поддержку, консультации психотерапевта и физиопроцедуры. Такой подход помогает не просто снять симптомы, но и восстановить организм полностью.
Узнать больше – наркологическая клиника рязань
Один из ключевых принципов клиники «ЗдороваяСамара» — строгое соблюдение медицинской тайны. Все обращения, анализы и процедуры происходят в режиме полной конфиденциальности. При необходимости пациент может быть зарегистрирован под псевдонимом, а договор оформляется на доверенное лицо. Персональные данные не передаются ни в какие внешние базы, а диагноз не указывается в выписке для работодателя или страховой. Врачи и администрация клиники прошли специальное обучение по работе с анонимными пациентами, чтобы гарантировать этичность и законность каждой процедуры.
Подробнее – лечение алкоголизма и наркомании центр самара
Саратов живёт в разных темпах: плотный центр, протяжные магистрали, мостовые переезды. Мы учитываем это в логистике: выездные бригады «СаратовМед Профи» движутся по немаркированным маршрутам, приезжают в гражданской одежде, формируют на месте «тихую сцену» и только затем начинают клиническую часть. Если на предзвонке звучат «красные флаги» — давящая боль в груди, выраженная одышка, спутанность, неукротимая рвота, судороги — организуем перевод в стационар без пауз: место резервируем заранее, передислокация проходит конфиденциально.
Подробнее тут – http://vyvod-iz-zapoya-saratov0.ru/vyvod-iz-zapoya-saratov-staczionar/
Такая структура делает лечение последовательным и предсказуемым, повышая шансы на положительный исход.
Детальнее – наркологическая клиника клиника помощь омск
Лечение в клинике «Трезвый Выбор Рязань» проходит в несколько последовательных этапов. Каждый этап выполняет конкретную задачу и сопровождается наблюдением специалистов. В таблице ниже представлена структура терапии и её основные направления.
Подробнее можно узнать тут – http://www.domen.ru
Детоксикация — это первый и важнейший этап лечения в наркологической клинике в Красноярске. Она проводится с целью выведения токсинов из организма и восстановления функций жизненно важных органов. Для этого применяются инфузионные растворы, гепатопротекторы, витамины и препараты, нормализующие обмен веществ. После снятия интоксикации пациент получает медикаментозную поддержку, направленную на снижение тяги к алкоголю или наркотикам и стабилизацию эмоционального состояния.
Подробнее тут – наркологическая клиника наркологический центр красноярск
Когда вопрос стоит остро — нужно быстро и безопасно вывести человека из запоя в Коломне, — у семьи нет лишнего времени на эксперименты с таблетками, сомнительными «коктейлями» и советами из интернета. «Трезвый Центр Коломна» выстраивает помощь так, чтобы от первого звонка до реального облегчения шёл понятный и управляемый маршрут: запись симптомов и рисков уже по телефону, предложение формата (выезд на дом или стационар), оперативный осмотр, персональная инфузионная терапия, круглосуточное наблюдение при необходимости и подробный план восстановления на 24–72 часа и дальше. Мы не продаём миф о «чудо-капельнице за час», а работаем клинически аккуратно: дозы и схемы подбираются под возраст, длительность запоя, сопутствующие заболевания, уже принятые лекарства и текущие показатели. Цель проста и честна — снять интоксикацию, защитить сердце, мозг и печень, вернуть сон и ясность без агрессивной седации и скрытых рисков, сохранить конфиденциальность и дать семье уверенность, что всё делается правильно.
Получить дополнительные сведения – быстрый вывод из запоя на дому
Concert Attire Stamford
360 Fairfield Ave,
Stamford, CT 06902, United Ⴝtates
+12033298603
Jeans
Лечение в клинике «Трезвый Выбор Рязань» проходит в несколько последовательных этапов. Каждый этап выполняет конкретную задачу и сопровождается наблюдением специалистов. В таблице ниже представлена структура терапии и её основные направления.
Получить дополнительные сведения – https://narkologicheskaya-clinika-v-ryazani17.ru/
I was wondering if you ever considered changing the structure of your site?
Its very well written; I love what youve got to say. But
maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one
or two pictures. Maybe you could space it out better?
Когда острые угрозы исключены, программа стартует дома. Пациент получает понятную карту действий, близкие — короткие окна обратной связи, врач — чистую «картинку» для тонкой настройки. Мы просим сообщать факты, а не эмоции: минуты до засыпания, число пробуждений, объём тёплой воды малыми глотками, пульс к вечеру, переносимость мягкой пищи, ясность головы утром.
Узнать больше – срочный вывод из запоя в саратове
В клинике применяются комплексные программы, охватывающие все стадии терапии. Такой подход позволяет обеспечить пациенту полный спектр помощи — от первой консультации до социальной адаптации.
Детальнее – лечение в наркологической клинике
Выбор наркологической клиники в Коломне — это не «слишком серьёзно», а логичный шаг, если зависимость уже зашла дальше спонтанных эпизодов. Алкоголизм, наркомания, злоупотребление успокоительными и обезболивающими — это не только психологическая тяга, но и перестройка организма: страдают печень, сердце, сосуды, нервная система, гормональный фон, сон, психика. Дома редко есть возможность круглосуточно контролировать состояние, правильно отменять вещества, отслеживать давление, пульс, поведение, не допускать опасных комбинаций препаратов. Родственники устают, реагируют эмоциями, а не медицинской логикой, человек чувствует себя под прицелом, но не под защитой. В «КоломнаМед Центр» всё выстроено так, чтобы снять нагрузку с семьи и вывести помощь из зоны хаотичных решений. Здесь оценивают не только то, «что и сколько пьёт или принимает», а весь контекст: длительность зависимости, срывы, уже перенесённые делирии или передозировки, сопутствующие болезни, психические состояния, семейную ситуацию. На основе этого формируется безопасный план: где начать — в стационаре или амбулаторно, какой формат детокса выбрать, насколько жёстко вести наблюдение, как сразу встроить психотерапевтическую и социальную поддержку. Клиника в Коломне позволяет работать системно, а не латать последствия очередного срыва.
Получить дополнительные сведения – https://narkologicheskaya-klinika-kolomna10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
Современная наркологическая клиника — это не просто медицинское учреждение, а пространство комплексной помощи, где врачи помогают человеку восстановиться физически, психологически и социально. В клинике «РязаньМед Альянс» создана система непрерывного наблюдения, включающая диагностику, выведение из запоя, детоксикацию, кодирование и постреабилитационную поддержку. Здесь работают квалифицированные наркологи, психиатры и терапевты, а помощь оказывается круглосуточно — как в стационаре, так и на дому. Главная цель специалистов — вернуть пациенту контроль над своим состоянием и избавить от зависимости без стресса и боли.
Выяснить больше – наркологическая клиника клиника помощь
После прохождения основной программы пациенту предлагается поддерживающее наблюдение. Оно может включать дистанционные консультации, участие в группе профилактики срывов, повторные осмотры нарколога и психолога, корректировку медикаментозной схемы. В рамках реабилитации формируются планы действий при возникновении тяги, обучаются навыки сопротивления стрессу и внешнему давлению. При желании можно подключить родственников к процессу постлечебной адаптации, чтобы укрепить результат и снизить риски рецидивов. Таким образом, пациент не остаётся один даже после выписки.
Ознакомиться с деталями – наркологическое лечение наркомания новокузнецк
Наркологическая клиника в Омске специализируется на оказании профессиональной помощи людям, столкнувшимся с зависимостью от алкоголя и наркотиков. Лечение строится на принципах доказательной медицины и сочетает современные методы детоксикации, фармакотерапии, психотерапевтической поддержки и программ социальной адаптации. Комплексный подход позволяет пациентам не только стабилизировать состояние, но и вернуться к полноценной жизни без зависимости.
Получить дополнительную информацию – наркологическая клиника нарколог в омске
Современная наркологическая клиника — это не просто медицинское учреждение, а пространство комплексной помощи, где врачи помогают человеку восстановиться физически, психологически и социально. В клинике «РязаньМед Альянс» создана система непрерывного наблюдения, включающая диагностику, выведение из запоя, детоксикацию, кодирование и постреабилитационную поддержку. Здесь работают квалифицированные наркологи, психиатры и терапевты, а помощь оказывается круглосуточно — как в стационаре, так и на дому. Главная цель специалистов — вернуть пациенту контроль над своим состоянием и избавить от зависимости без стресса и боли.
Подробнее можно узнать тут – наркологическая клиника нарколог в рязани
Someone necessarily help to make severely posts I would state.
That is the very first time I frequented your web page and to this point?
I amazed with the analysis you made to make this actual publish amazing.
Wonderful job!
It’s amazing designed for me to have a web page, which is
useful in support of my know-how. thanks admin
В клинике используются современные методы лечения, которые включают:
Подробнее можно узнать тут – платная наркологическая клиника тверь
Комплексное применение этих методов позволяет добиться быстрого восстановления организма и улучшения психоэмоционального состояния.
Получить дополнительную информацию – https://vyvod-iz-zapoya-perm0.ru/vyvod-iz-zapoya-perm-staczionar/
«ОмскПрофи» укомплектована современной медицинской базой: передвижные аппараты для ЭКГ, инфузионные стойки, экспресс-анализаторы, мониторы состояния, аппараты ИВЛ (в реанимационных палатах). Штат сотрудников сформирован из врачей-наркологов, токсикологов, психиатров, психотерапевтов, медицинских сестёр, прошедших обучение по международным протоколам. Ведётся постоянная учёба, стажировки, участие в научных форумах. Благодаря этому пациенты получают не только медицинскую помощь, но и психологическое сопровождение, направленное на долгосрочный результат.
Получить дополнительную информацию – http://narkologicheskaya-pomoshh-omsk0.ru/
Когда человек в запое, близким кажется, что всё ещё можно решить «по-тихому»: выспаться, отпаять водой, дать обезболивающее или «успокоительное» и дождаться, пока станет легче. На практике это часто приводит к обратному результату. Алкогольная интоксикация нарушает водно-электролитный баланс, сгущает кровь, повышает нагрузку на сердце, провоцирует скачки давления, ухудшает работу печени и нервной системы. Неконтролируемый приём снотворных, анальгетиков, транквилизаторов, особенно вместе с алкоголем, способен вызвать угнетение дыхания, аритмии, судороги или делирий. Домашняя обстановка не даёт возможности следить за всеми показателями и вовремя отреагировать. «РаменМед Трезвость» предлагает клинически выверенный вывод из запоя в Раменском с учётом возраста, длительности употребления, хронических заболеваний, перенесённых ранее осложнений. Здесь не применяют сомнительные схемы «усыпить, чтобы не мешал», а ставят задачу: безопасно пройти острую фазу, снять интоксикацию, стабилизировать давление и пульс, защитить сердце и мозг, снизить риск психозов и, при желании пациента, сразу наметить маршрут реального лечения зависимости. Такой подход снимает с родственников опасную «роль врача» и возвращает ситуацию туда, где ей место — под контроль профессионалов.
Разобраться лучше – vyvod-iz-zapoya-v-ramenskom
Наркологическая клиника «Трезвый Шаг Раменское» — это место, где острые кризисы, многолетние запои и повторяющиеся срывы перестают быть бесконечным кругом, в котором семья остаётся один на один с проблемой. Здесь выстроена система помощи людям с алкогольной и наркотической зависимостью, а также полизависимостями, включая злоупотребление аптечными препаратами. В клинике в Раменском сочетаются круглосуточное наблюдение, профессиональная детоксикация, медикаментозная поддержка, психотерапевтические программы и сопровождение семьи. Важные принципы — безопасность, анонимность, уважение к пациенту и честное объяснение каждого шага лечения. Ни агрессивного давления, ни обещаний «чуда за один день» — вместо этого поэтапный подход, который даёт реальный шанс стабилизировать состояние, снизить тягу и выйти из разрушительного сценария под контролем специалистов. Для близких это означает понятный маршрут: куда обратиться, что будут делать с пациентом, какие риски учтут и как клиника «Трезвый Шаг Раменское» останется на связи после острого периода.
Детальнее – https://narkologicheskaya-klinika-ramenskoe10.ru/chastnaya-narkologicheskaya-klinika-v-ramenskom/
Критически важный отрезок — первые 12–24 часа. Мы разбиваем его на «окна», в каждом из которых есть цель, набор действий, маркеры контроля и критерий перехода. Если целевой отклик не достигнут, меняем один параметр: темп инфузии, очередность модулей или поведенческую опору (свет/тишина/цифровой режим) — и назначаем новую точку оценки. Это сохраняет причинно-следственную связь и предотвращает полипрагмазию.
Подробнее тут – http://narcologicheskaya-klinika-saratov0.ru/klinika-narkologii-saratov/https://narcologicheskaya-klinika-saratov0.ru
Вывод из запоя — это не «волшебная капельница», а последовательная медицинская программа с чёткими целями и измеримыми маркерами. В наркологической клинике «СаратовМед Профи» маршрут строится по принципу управляемых окон: на каждом шаге команда преследует одну цель, меняет лишь один параметр и оценивает результат в заранее назначённый момент. Такой подход снижает лекарственную нагрузку, предотвращает «гонку дозировок» и делает динамику предсказуемой для пациента и близких. Конфиденциальность обеспечивается регламентом: немаркированные выезды, нейтральные формулировки в документах, «тихие» каналы связи, доступ к записям — строго по ролям.
Разобраться лучше – вывод из запоя дешево саратов
Терапия в клинике проводится поэтапно, что позволяет обеспечить безопасность и прозрачность процесса. Пациент постепенно проходит все стадии восстановления организма и психики.
Выяснить больше – https://narkologicheskaya-klinika-v-omske0.ru/chastnaya-narkologicheskaya-klinika-omsk
Каждый час промедления в острый период повышает вероятность обезвоживания, электролитных сдвигов, аритмий, гипертонических всплесков и расстройств сна, которые легко перерастают в делирий. Домашние попытки с «подручными» средствами редко учитывают лекарственные взаимодействия, реальный уровень обезвоживания и состояние печени, а «жёсткая» седация, применяемая без показаний, маскирует ухудшения и лишает врача информативной картины. Профессиональная бригада «НоваТрезвие» начинает с объективной оценки: давление, пульс, сатурация, температура, неврологический статус, выраженность тремора и тошноты, степень обезвоживания, список принимаемых препаратов и возможные аллергии. На этой базе формируется персональный план: регидратация, коррекция электролитов и кислотно-щелочного баланса, поддержка нервной системы витаминами группы B и магнием, гепатопротекторная и антиоксидантная защита по показаниям, противорвотные при необходимости и мягкая анксиолитическая поддержка для восстановительного сна. Такой маршрут гасит «пожар» интоксикации управляемо, возвращая прогнозируемость самочувствия в течение первых часов.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-ehlektrostal2-10.ru/vyvesti-iz-zapoya-ehlektrostal/
Если на предзвонке выявляются «красные флаги» — давящая боль в груди, одышка в покое, спутанность сознания, судороги, неукротимая рвота, резкое падение насыщения кислородом — мы организуем бесшовный перевод в стационар. Место резервируем заранее, логистику строим так, чтобы не привлекать внимания соседей и не затягивать старт лечения. При отсутствии угроз терапия может начаться дома с последующим телесопровождением и при необходимости — краткой госпитализацией.
Детальнее – http://narcologicheskaya-klinika-saratov0.ru/
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Ознакомиться с деталями – наркологические клиники алкоголизм красноярск
Маршрут выстроен без пауз и импровизаций. Сначала — короткое интервью по телефону: адрес в Электростали, длительность эпизода, лекарства/дозировки, аллергии, важные диагнозы, последние значения давления и пульса. Это экономит 15–20 минут на месте и позволяет заранее исключить опасные взаимодействия. По прибытии врач фиксирует АД, ЧСС, сатурацию, температуру, оценивает неврологический статус, степень обезвоживания, выраженность тремора/тошноты, уровень тревоги, кратко собирает анамнез последних суток. Затем стартует инфузионная терапия: растворы для регидратации и коррекции электролитов, поддержка витаминами группы B и магнием; по показаниям — гепатопротекторы и антиоксиданты, противорвотные, мягкие анксиолитики. Каждые 15–20 минут врач смотрит динамику и корректирует темп капельниц, питьевой режим, симптоматическую поддержку. Важный принцип — «сон без вырубания»: умеренная седация собирает ночной ритм, сохраняя информативность мониторинга. По завершении — письменные рекомендации и маршрут на 24–72 часа (сон, питание, запреты, «красные флаги», амбулаторные визиты/дневной стационар или перевод в отделение). Такой алгоритм заменяет «лотерею» результата управляемым и повторяемым планом.
Получить дополнительные сведения – http://vyvod-iz-zapoya-ehlektrostal10.ru/vyvod-iz-zapoya-klinika-v-ehlektrostali/
Каждая стадия лечения проходит под постоянным контролем медицинского персонала. Пациенты чувствуют себя в безопасности и получают поддержку не только физическую, но и психологическую. Такой подход снижает риск рецидива и помогает сохранить результат на долгие годы.
Выяснить больше – наркологическая клиника нарколог
Острый эпизод запоя — это не «плохое самочувствие», а состояние с реальными рисками для сердца, нервной системы и дыхания, особенно в ночные часы, когда усиливаются вегетативные реакции и тревога. В «НоваТрезвие» мы выстраиваем помощь так, чтобы от звонка до заметного облегчения прошло как можно меньше времени и как можно меньше случайностей: короткое интервью для оценки рисков, выезд врача или приём в клинике, экспресс-диагностика по ключевым показателям, персональная инфузионная схема без «универсальных коктейлей», мягкая коррекция сна и тревоги без «вырубания», понятные инструкции семье на 24–72 часа и план продолжения на ближайшие недели. Мы не скрываемся за общими формулами: решения принимаются по фактическим данным, дозы и темп капельниц подстраиваются к динамике каждые 15–20 минут, а при «красных флагах» перевод в стационар организуется без пауз. Конфиденциальность соблюдается строго, а коммуникация простая и предсказуемая — чтобы вы всегда знали, что происходит сейчас и чего ждать к утру.
Углубиться в тему – vyvod-iz-zapoya-s-vyezdom-ehlektrostal
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Получить дополнительные сведения – http://narcologicheskaya-klinika-omsk0.ru
Когда вопрос стоит остро — нужно быстро и безопасно вывести человека из запоя в Коломне, — у семьи нет лишнего времени на эксперименты с таблетками, сомнительными «коктейлями» и советами из интернета. «Трезвый Центр Коломна» выстраивает помощь так, чтобы от первого звонка до реального облегчения шёл понятный и управляемый маршрут: запись симптомов и рисков уже по телефону, предложение формата (выезд на дом или стационар), оперативный осмотр, персональная инфузионная терапия, круглосуточное наблюдение при необходимости и подробный план восстановления на 24–72 часа и дальше. Мы не продаём миф о «чудо-капельнице за час», а работаем клинически аккуратно: дозы и схемы подбираются под возраст, длительность запоя, сопутствующие заболевания, уже принятые лекарства и текущие показатели. Цель проста и честна — снять интоксикацию, защитить сердце, мозг и печень, вернуть сон и ясность без агрессивной седации и скрытых рисков, сохранить конфиденциальность и дать семье уверенность, что всё делается правильно.
Углубиться в тему – anonimnyj-vyvod-iz-zapoya
Терапия проводится поэтапно, что позволяет пациенту последовательно проходить все стадии восстановления и закреплять результат.
Детальнее – наркологическая клиника лечение алкоголизма в омске
Cutback assists, low crosses and their conversion rates tracked
Запой — это не просто несколько лишних дней алкоголя, а тяжёлое состояние, в котором организм работает на пределе. Чем дольше длится эпизод, тем глубже обезвоживание, тем сильнее сдвиги электролитов, тем выше риск аритмий, гипертонических кризов, судорог, делирия, обострений заболеваний сердца, печени и поджелудочной железы. Попытки «вывести» человека дома силами родных часто включают опасные комбинации: случайные седативные, снотворные, анальгетики, «антипохмельные» из рекламы. Они могут на время усыпить или «успокоить», но при этом скрывают ухудшение, сбивают давление, угнетают дыхание и мешают врачу увидеть реальную картину. В «Трезвый Центр Коломна» подход другой: ещё на этапе звонка специалист уточняет длительность запоя, объёмы и виды алкоголя, наличие гипертонии, ИБС, диабета, заболеваний печени и почек, неврологических проблем, список уже принятых препаратов, эпизоды потери сознания, судорог, странного поведения. На основании этих данных определяется, безопасен ли формат на дому или сразу нужен стационар. Такая сортировка позволяет вовремя перехватить опасные случаи, не терять часы на бесполезные попытки и сразу запускать те схемы, которые реально снижают риски и стабилизируют состояние.
Получить больше информации – вывод из запоя коломна
If you wish for to get a good deal from this article then you have to apply these strategies to your
won webpage.
Эти методы используются в комплексе и создают прочный фундамент для восстановления здоровья.
Подробнее тут – наркологическое лечение алкоголизма
Наркологическая клиника в Твери обеспечивает круглосуточное медицинское наблюдение, что позволяет своевременно выявлять и устранять возможные осложнения. Высококвалифицированные специалисты проводят регулярные обследования и корректируют терапию, обеспечивая безопасность и эффективность лечения.
Выяснить больше – наркологическая клиника в твери
Каждое из этих направлений имеет важное значение и в совокупности формирует основу для устойчивого выздоровления.
Исследовать вопрос подробнее – https://narkologicheskaya-klinika-v-omske0.ru/chastnaya-narkologicheskaya-klinika-omsk
Наркологическая клиника в Твери обеспечивает круглосуточное медицинское наблюдение, что позволяет своевременно выявлять и устранять возможные осложнения. Высококвалифицированные специалисты проводят регулярные обследования и корректируют терапию, обеспечивая безопасность и эффективность лечения.
Исследовать вопрос подробнее – наркологическая клиника лечение алкоголизма в твери
Такой алгоритм позволяет постепенно восстановить функции организма и подготовить пациента к дальнейшему лечению зависимости.
Углубиться в тему – http://vyvod-iz-zapoya-omsk0.ru
Запойное состояние сопровождается тяжелыми последствиями для организма. Оно может включать нарушения сна, тремор конечностей, скачки давления, головные боли и депрессию. Без своевременной помощи такие проявления способны привести к развитию хронических заболеваний и угрожающих жизни осложнений.
Углубиться в тему – вывод из запоя вызов
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Исследовать вопрос подробнее – https://narkolog-na-dom-shchelkovo10.ru/vyzvat-narkologa-na-dom-shchelkovo
В зависимости от состояния пациента и пожеланий семьи наркологическая помощь может быть оказана в одном из нескольких форматов: на дому, в стационаре или дистанционно. Каждый из форматов обеспечивает доступ к медицинской помощи без бюрократии и с сохранением полной конфиденциальности.
Подробнее – наркологическая помощь на дому круглосуточно в омске
Мы проверяем не «ощущения», а факты: частоту пульса в покое, вариабельность ритма к сумеркам, переносимость тёплой воды малыми глотками, минуты до сна и количество ночных пробуждений. Эти короткие метки позволяют тонко управлять темпом инфузии, очередностью модулей и «тихими» ритуалами вечернего времени без необоснованного усиления препаратов.
Углубиться в тему – https://narkolog-na-dom-saratov0.ru/
Услуга «нарколог на дом в Долгопрудном» от клиники «МедТрезвие Долгопрудный» создана для ситуаций, когда важно действовать быстро, аккуратно и без лишнего шума. Запой, тяжёлое похмелье, срыв после ремиссии, злоупотребление медикаментами или смесью алкоголя с препаратами — всё это не терпит откладывания и самодеятельности. Вызов врача на дом позволяет получить профессиональную помощь без госпитализации, когда состояние пациента ещё позволяет лечить его в привычной обстановке. Нарколог приезжает с полностью укомплектованным набором препаратов и расходников, проводит осмотр, подбирает капельницы по клиническим показаниям, контролирует реакцию, даёт подробные рекомендации на ближайшие дни и при необходимости предлагает дальнейший маршрут: повторный выезд, амбулаторное наблюдение или стационар клиники. Конфиденциальность соблюдается строго: без обсуждений с соседями, без регистрации по месту работы, без унизительных формальностей — только медицинская помощь, ориентированная на безопасность и результат.
Получить дополнительные сведения – vyzvat-besplatno-narkologa-na-dom
Комплексное применение этих методов позволяет добиться быстрого восстановления организма и улучшения психоэмоционального состояния.
Получить дополнительные сведения – http://vyvod-iz-zapoya-perm0.ru/vyvod-iz-zapoya-perm-staczionar/https://vyvod-iz-zapoya-perm0.ru
Эти методы комбинируются и создают условия для всестороннего восстановления пациента.
Подробнее тут – https://narcologicheskaya-klinika-omsk0.ru/chastnaya-narkologicheskaya-klinika-omsk/
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Выяснить больше – https://narcologicheskaya-klinika-v-krasnoyarske17.ru/narkologicheskaya-klinika-krasnoyarsk-otzyvy/
«ОмскПрофи» укомплектована современной медицинской базой: передвижные аппараты для ЭКГ, инфузионные стойки, экспресс-анализаторы, мониторы состояния, аппараты ИВЛ (в реанимационных палатах). Штат сотрудников сформирован из врачей-наркологов, токсикологов, психиатров, психотерапевтов, медицинских сестёр, прошедших обучение по международным протоколам. Ведётся постоянная учёба, стажировки, участие в научных форумах. Благодаря этому пациенты получают не только медицинскую помощь, но и психологическое сопровождение, направленное на долгосрочный результат.
Подробнее можно узнать тут – https://narkologicheskaya-pomoshh-omsk0.ru/narkolog-psikhiatr-omsk
Такая структура терапии делает процесс максимально эффективным и безопасным.
Детальнее – narcologicheskaya-klinika-omsk0.ru/
Лечение зависимости в наркологической клинике проводится поэтапно. Это обеспечивает постепенное восстановление организма и исключает риск осложнений. Каждый этап направлен на устранение конкретных нарушений, вызванных употреблением психоактивных веществ.
Получить больше информации – https://narcologicheskaya-klinika-v-krasnoyarske17.ru/
Медики рекомендуют обратиться за профессиональной помощью при следующих состояниях:
Подробнее – https://vyvod-iz-zapoya-v-ryazani17.ru/vyvod-iz-zapoya-ryazan-na-domu/
Медицинская помощь строится на принципах индивидуального подхода и поэтапной терапии. Каждый пациент проходит диагностику, после чего составляется персональная программа, включающая медикаментозную поддержку, консультации психотерапевта и физиопроцедуры. Такой подход помогает не просто снять симптомы, но и восстановить организм полностью.
Подробнее тут – наркологическая клиника лечение алкоголизма в рязани
В случаях, когда пациент не готов приехать в клинику или находится в тяжёлом состоянии, специалисты «ЗдороваяСамара» организуют выездную помощь. Это особенно важно при острых интоксикациях, синдроме отмены, резком ухудшении психоэмоционального состояния. Выезд возможен круглосуточно и занимает от 30 до 60 минут с момента обращения. Врач приезжает в гражданской одежде, без опознавательных знаков и привлечения внимания. Оснащение позволяет провести на месте полную диагностику и начать лечение — в том числе инфузионную терапию, коррекцию состояния и психологическую стабилизацию.
Разобраться лучше – запой лечение наркомания самара
I just could not depart your site before suggesting that I really loved the standard
info an individual supply for your guests? Is going to be back steadily
in order to check out new posts https://randerssejlklub.dk/ansoeg-om-baadplads/diana_wj-2/
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Получить дополнительные сведения – вывод из запоя на дому цена
Медицинская помощь строится на принципах индивидуального подхода и поэтапной терапии. Каждый пациент проходит диагностику, после чего составляется персональная программа, включающая медикаментозную поддержку, консультации психотерапевта и физиопроцедуры. Такой подход помогает не просто снять симптомы, но и восстановить организм полностью.
Детальнее – https://narkologicheskaya-klinika-v-ryazani17.ru/narkologicheskij-staczionar-ryazan/
I don’t know if it’s just me or if everyone else encountering issues
with your blog. It looks like some of the written text on your content are running off the screen. Can somebody else please provide feedback and let me know if this is happening to them as well?
This could be a issue with my browser because I’ve had this happen previously.
Thanks
Вывод из запоя в Тольятти — это медицинская процедура, направленная на очищение организма от продуктов распада алкоголя и восстановление нормального состояния здоровья. Длительное употребление спиртных напитков приводит к серьёзной интоксикации, нарушению работы нервной, сердечно-сосудистой и пищеварительной систем. Самостоятельные попытки прекратить запой могут быть опасны, поэтому оптимальным решением является обращение к врачу-наркологу, который проведёт лечение безопасно и эффективно.
Разобраться лучше – вывод из запоя на дому тольятти
Hi there! Do you know if they make any plugins
to safeguard against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any tips?
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Узнать больше – вывод из запоя круглосуточно новокузнецк
I’m gone to convey my little brother, that he should also go to see this
web site on regular basis to take updated from most recent news.
Heya i’m for the first time here. I came across this board and I in finding It
truly helpful & it helped me out much. I’m hoping
to offer one thing back and aid others such as you helped me.
Карта делает видимой причинно-следственную связь: пациент понимает, зачем и что именно делается; семья видит «точки проверки»; врач получает опору для изменения одного параметра без разрушения всего плана.
Получить дополнительные сведения – вывод из запоя в стационаре саратов
I really like your blog.. very nice colors & theme.
Did you make this website yourself or did you hire someone to
do it for you? Plz answer back as I’m looking to create my own blog and would like to find out where u got
this from. thanks a lot
Have a look at my blog post … affordable dentist vancouver wa
Выбор наркологической клиники в Коломне — это не «слишком серьёзно», а логичный шаг, если зависимость уже зашла дальше спонтанных эпизодов. Алкоголизм, наркомания, злоупотребление успокоительными и обезболивающими — это не только психологическая тяга, но и перестройка организма: страдают печень, сердце, сосуды, нервная система, гормональный фон, сон, психика. Дома редко есть возможность круглосуточно контролировать состояние, правильно отменять вещества, отслеживать давление, пульс, поведение, не допускать опасных комбинаций препаратов. Родственники устают, реагируют эмоциями, а не медицинской логикой, человек чувствует себя под прицелом, но не под защитой. В «КоломнаМед Центр» всё выстроено так, чтобы снять нагрузку с семьи и вывести помощь из зоны хаотичных решений. Здесь оценивают не только то, «что и сколько пьёт или принимает», а весь контекст: длительность зависимости, срывы, уже перенесённые делирии или передозировки, сопутствующие болезни, психические состояния, семейную ситуацию. На основе этого формируется безопасный план: где начать — в стационаре или амбулаторно, какой формат детокса выбрать, насколько жёстко вести наблюдение, как сразу встроить психотерапевтическую и социальную поддержку. Клиника в Коломне позволяет работать системно, а не латать последствия очередного срыва.
Углубиться в тему – narkologicheskaya-klinika-v-kolomne
Капельницы при выводе из запоя — основной инструмент детоксикации. Они очищают кровь, стабилизируют давление и восстанавливают баланс электролитов. В клинике «РеабКузбасс» используются только качественные препараты, адаптированные под конкретное состояние пациента. Ниже приведена таблица с основными видами капельниц и их эффектом.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-v-novokuzneczke17.ru/vyvod-iz-zapoya-na-domu-novokuzneczk
Tremendous issues here. I am very happy to see your article.
Thanks a lot and I’m having a look ahead to contact you.
Will you kindly drop me a mail?
Медицинская помощь направлена не только на снятие острых симптомов, но и на стабилизацию работы организма в целом. Врачи стремятся к тому, чтобы пациент получил не временное облегчение, а фундамент для дальнейшей реабилитации.
Получить дополнительную информацию – вывод из запоя на дому недорого
Great article on surgery costs.
Here is my site :: Wichtige Unterstützung
Мы не используем универсальную «капельницу». Схема собирается из модулей под ведущие жалобы. Медицинские шаги всегда сочетаются с нефраком опорами — свет, тишина, вода малыми глотками, дыхание, — потому что среда усиливает действие препаратов и позволяет держать дозы ниже.
Выяснить больше – https://narkolog-na-dom-saratov0.ru/narkolog-i-psikhiatr-v-saratove/
Прежде чем перейти к ориентировочным цифрам, важно подчеркнуть: цена формируется из реальных компонентов помощи — работы врача и медсестры, объёма инфузионной терапии, перечня препаратов, времени выезда и необходимости более длительного наблюдения. Никаких скрытых доплат: все дополнительные назначения согласуются заранее. Чем раньше вы обращаетесь, тем меньше объём вмешательств и, как правило, ниже итоговая стоимость — короткий эпизод проще и дешевле стабилизировать, чем «выводить» осложнения после затянутого запоя.
Исследовать вопрос подробнее – вызвать нарколога на дом
Прежде чем перейти к ориентировочным цифрам, важно подчеркнуть: цена формируется из реальных компонентов помощи — работы врача и медсестры, объёма инфузионной терапии, перечня препаратов, времени выезда и необходимости более длительного наблюдения. Никаких скрытых доплат: все дополнительные назначения согласуются заранее. Чем раньше вы обращаетесь, тем меньше объём вмешательств и, как правило, ниже итоговая стоимость — короткий эпизод проще и дешевле стабилизировать, чем «выводить» осложнения после затянутого запоя.
Получить больше информации – нарколог на дом
Boston Medical Ꮐroup
3152Red Hill Ave. Ste. #280,
Costa Mesa, ᏟA 92626, United Stɑteѕ
800 337 7555
Normal testosterone levels in men
Ridiculous quest there. What occurred after?
Thanks!
Feel free to surf to my homepage :: Loodgieter Hasselt
Острый период запоя — это не «плохое самочувствие», а состояние с реальными рисками, где каждая задержка усложняет картину. В «Трезвой Линии» в Электростали мы строим помощь так, чтобы от первого звонка до заметного облегчения прошёл минимальный и управляемый путь: быстрый сбор рисков, экспресс-диагностика на месте, персональная инфузионная схема без «универсальных коктейлей», щадящая коррекция сна и тревоги, регулярные замеры показателей, чёткие рекомендации для семьи. Мы избегаем агрессивной седации: дозы и темп капельниц подбираются под возраст, длительность эпизода, сопутствующие заболевания и уже принимаемые лекарства. Задача — быстро снять токсическую нагрузку, выровнять давление и пульс, собрать ночной сон, а затем удержать результат дисциплинированным постдетокс-маршрутом на 2–4 недели. Конфиденциальность и анонимность соблюдаются без компромиссов, решения принимаются по реальным данным, чтобы эффект был устойчивым, предсказуемым и безопасным для пациента и семьи.
Изучить вопрос глубже – вывод из запоя на дому
Hello! I just wanted to ask if you ever have any
problems with hackers? My last blog (wordpress) was hacked and I ended up
losing many months of hard work due to no back up. Do you have any
methods to prevent hackers?
There’s definately a lot to find out about
this topic. I love all the points you made.
Hello! This post couldn’t be written any better!
Reading this post reminds me of my previous room mate! He always
kept talking about this. I will forward this page to him.
Fairly certain he will have a good read. Many thanks for sharing!
Here is my web-site – Plombier Mons
Профессиональный нарколог на дому не работает по схеме «чем больше препаратов, тем лучше». В «СерпуховТрезвие» капельницы составляются исходя из задач конкретного организма. Базовый блок — это растворы для восполнения объёма циркулирующей жидкости, выравнивания электролитного баланса и коррекции кислотно-щелочного состояния, что уменьшает нагрузку на сердце, мозг и снижает риск тяжёлых осложнений. Витамины группы B и магний входят в стандартную поддержку: они помогают стабилизировать нервную систему, уменьшить тремор, раздражительность, поддерживают сон и снижают риск судорог. При признаках поражения печени используются гепатопротективные и антиоксидантные компоненты, снижающие токсическое воздействие продуктов распада алкоголя. Если пациента мучает тошнота, добавляются противорвотные средства, чтобы восстановить возможность пить воду и питаться. Для снижения тревоги и нормализации сна применяются мягкие анксиолитики в дозировках, не маскирующих клиническую картину и не угнетающих дыхательный центр. Агрессивная седация, популярная в «серых» схемах, сознательно исключается: она «делает вид» улучшения, но может скрыть нарастающие осложнения. Эффект оценивается по конкретным критериям: стабилизация давления и пульса, уменьшение тремора, уход тошноты, улучшение цвета кожи, появление естественного сна и большей ясности мышления. После достижения этих ориентиров фармаконагрузка не наращивается, а постепенно снижается, чтобы человек выходил в устойчивое состояние, а не зависел от бесконечных капельниц.
Подробнее можно узнать тут – https://narkolog-na-dom-serpuhov10.ru/narkolog-psiholog-na-dom-serpuhov
В медицинской практике используются различные методы, которые помогают ускорить процесс восстановления. Все процедуры проводятся под контролем специалистов и с учетом индивидуальных особенностей пациента.
Получить дополнительную информацию – наркология вывод из запоя
Каждое из этих направлений имеет важное значение и в совокупности формирует основу для устойчивого выздоровления.
Подробнее можно узнать тут – http://narkologicheskaya-klinika-v-omske0.ru
Каждый метод подбирается индивидуально, что обеспечивает безопасность и эффективность процесса.
Исследовать вопрос подробнее – http://vyvod-iz-zapoya-omsk0.ru
Критичные случаи, когда вызов нарколога через «МедТрезвие Долгопрудный» оправдан и своевременен:
Углубиться в тему – psihiatr-narkolog-na-dom
Мы проверяем не «ощущения», а факты: частоту пульса в покое, вариабельность ритма к сумеркам, переносимость тёплой воды малыми глотками, минуты до сна и количество ночных пробуждений. Эти короткие метки позволяют тонко управлять темпом инфузии, очередностью модулей и «тихими» ритуалами вечернего времени без необоснованного усиления препаратов.
Ознакомиться с деталями – http://narkolog-na-dom-saratov0.ru/narkolog-i-psikhiatr-v-saratove/
Ниже — ориентир для острых часов на дому. Это не жёсткий шаблон, а карта, где ясно: что делаем, чем измеряем, когда пересматриваем. При отсутствии отклика мы меняем один параметр (например, темп инфузии) и назначаем новое окно оценки, не «двигая» всё остальное.
Исследовать вопрос подробнее – нарколог на дом саратов
Главная задача капельницы при выезде нарколога в Щёлково — не создать видимость лёгкости, а реально уменьшить интоксикацию и восстановить базовые функции организма. В «ЩёлковоМед Профи» используются современные схемы, а не сомнительные смеси «из всего подряд». В стандартной основе — растворы для восполнения объёма циркулирующей жидкости, выравнивания электролитного баланса и коррекции КЩС, что снижает нагрузку на сердце и мозг. Витамины группы B и магний поддерживают нервную систему, уменьшают тремор, раздражительность и риск судорожных реакций. При необходимости врач добавляет гепатопротекторные и антиоксидантные компоненты, если есть признаки перегрузки печени; при выраженной тошноте — противорвотные, чтобы пациент мог нормально пить и питаться. Для нормализации сна и тревоги подбираются мягкие анксиолитики в дозах, позволяющих контролировать состояние, а не «вырубать» человека. Агрессивные седативные протоколы, которые маскируют ухудшения и опасны для дыхания и сердца, сознательно исключаются. Оценка эффекта идёт по конкретным критериям: стабилизация давления и пульса, уменьшение дрожи, улучшение цвета кожи, уход тошноты, снижение тревоги, появление естественного, а не лекарственного сна. После выезда семья получает ясный план, как закрепить эффект, чтобы наутро не пришлось начинать всё заново.
Выяснить больше – vyzvat-narkologa-na-dom
Наркологическая клиника «КоломнаМед Центр» — это место, куда можно обратиться в тот момент, когда домашние попытки контролировать алкоголь, наркотики, аптечные препараты или смесь всего сразу перестают работать, а жизнь превращается в постоянное «завтра начну с нуля». Здесь не обещают чудес за один день и не пугают диагнозами, а выстраивают понятный медицинский маршрут: детоксикация, стабилизация, реабилитация, поддержка семьи, профилактика срывов. Пациент получает помощь в защищённой, конфиденциальной среде, где всё организовано так, чтобы снизить тревогу и стыд, убрать хаос вокруг зависимости и дать человеку шанс вернуться к нормальной жизни без давления, угроз и токсичных «стимулов». Для родных клиника в Коломне — это опора: конкретный адрес, конкретная команда, чёткие сроки и понятные этапы, вместо бесконечных обещаний «он сам справится».
Исследовать вопрос подробнее – http://narkologicheskaya-klinika-kolomna10.ru/narkologicheskaya-klinika-oficialnyj-sajt-v-kolomne/https://narkologicheskaya-klinika-kolomna10.ru
Такая структура лечения помогает пациентам пройти все этапы восстановления под контролем специалистов.
Выяснить больше – наркологическая клиника цены в перми
Клиника в Коломне ориентирована на полный цикл помощи: от экстренных состояний до длительного сопровождения. Здесь важна не только медицинская составляющая, но и человеческая: уважение, конфиденциальность, отсутствие стигмы. Ниже — ключевые направления, которые выстраиваются в единую систему лечения, а не существуют по отдельности.
Ознакомиться с деталями – заказать звонок наркологическая клиника
Have you ever considered publishing an ebook or guest
authoring on other sites? I have a blog centered on the same topics you discuss and would really like
to have you share some stories/information. I know my viewers would
value your work. If you’re even remotely interested, feel free to shoot
me an email.
Feel free to surf to my blog: Plombier Charleroi
Impressive casino portal, nice work! Gratitude!
https://zap.buzz/OdjxMMO
Вывод из запоя в Раменском в условиях клиники строится не вокруг одной капельницы, а вокруг понятной цепочки шагов, где каждый этап логичен и медицински обоснован. Это помогает не только быстро облегчить состояние, но и уменьшить вероятность того, что через пару дней человек снова уйдёт в запой.
Исследовать вопрос подробнее – https://vyvod-iz-zapoya-ramenskoe10.ru/srochnoe-vyvedenie-iz-zapoya-v-ramenskom
«Трезвый Путь Коломна» создаёт единый контур помощи: пациент не «перекидывается» между разными организациями, а проходит лечение в одной системе, где специалисты знают его историю и несут ответственность за последовательность шагов. Это критично для тех, кто уже сталкивался с бессистемными попытками: один врач ставил капельницы, другой «кодировал», третий давал советы, а в итоге всё заканчивалось новым срывом. Здесь маршруты связываются в цельную линию.
Выяснить больше – http://narkologicheskaya-klinika-kolomna2-10.ru/luchshie-narkologicheskie-kliniki-v-kolomne/
Комплексное проведение этих этапов обеспечивает полное восстановление организма и облегчает процесс последующего лечения зависимости.
Изучить вопрос глубже – наркология вывод из запоя в рязани
В процессе лечения используются проверенные методики, которые в комплексе обеспечивают положительный эффект и снижают риск рецидива.
Подробнее тут – нарколог лечение алкоголизма омск
Наркологическая клиника «ВолгаДок Медикал» — это круглосуточная служба помощи, выстроенная вокруг принципов клинической безопасности, прозрачной коммуникации и поддержки пациента на каждом этапе. Мы соединяем стационар и выездные бригады в единую систему: первичный осмотр и стабилизация состояния, адресные инфузионные модули, мягкая коррекция сна и тревоги, последующее наблюдение с короткими «окнами» обратной связи. Все решения принимаются по показаниям и сопровождаются объяснением: какую цель преследуем, каким маркером измеряем, когда проверяем результат. Такой подход исключает хаотичные усиления, бережёт ресурс организма и даёт прогнозируемый клинический эффект.
Изучить вопрос глубже – наркологические клиники алкоголизм
Когда зависимость выходит из-под контроля, человеку необходима не просто медицинская помощь, а поддержка в безопасной и понимающей среде. Наркологическая клиника «Трезвый Выбор Рязань» предлагает пациентам комплексные программы лечения алкоголизма, наркомании и других форм зависимого поведения. Здесь работают врачи-наркологи, психотерапевты, психологи и медсёстры, обеспечивающие круглосуточное наблюдение и уход. Лечение проводится анонимно, с акцентом на восстановление здоровья, психологического равновесия и качества жизни.
Получить дополнительные сведения – наркологические клиники алкоголизм
Каждая стадия лечения проходит под постоянным контролем медицинского персонала. Пациенты чувствуют себя в безопасности и получают поддержку не только физическую, но и психологическую. Такой подход снижает риск рецидива и помогает сохранить результат на долгие годы.
Изучить вопрос глубже – наркологическая клиника наркологический центр рязань
С момента начала лечения пациент получает доступ к круглосуточной линии поддержки. Врачи, психологи и координаторы готовы ответить на вопросы, помочь с корректировкой схемы лечения, поддержать в ситуации риска срыва. Эта функция особенно востребована в первые недели после выписки, когда человек сталкивается с триггерами в привычной среде и нуждается в дополнительной защите. Связь может осуществляться по телефону, через защищённый мессенджер или с помощью мобильного приложения клиники.
Детальнее – лечение наркомании наркология
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter
updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like
this. Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new
updates.
저는 이 노력에 큰 감동을 받았습니다.
시력 건강과 위해 기부하는 것은 인류를 돕는 아름다운 방법입니다.
이 대단한 노력을 꾸준히 이어가 주세요.
Here is my homepage … 희망의 빛 캠페인
Why viewers still use to read news papers when in this technological globe everything is available on net?
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Исследовать вопрос подробнее – нарколог на дом вывод из запоя в саратове
Наркологическая клиника «КоломнаМед Центр» — это место, куда можно обратиться в тот момент, когда домашние попытки контролировать алкоголь, наркотики, аптечные препараты или смесь всего сразу перестают работать, а жизнь превращается в постоянное «завтра начну с нуля». Здесь не обещают чудес за один день и не пугают диагнозами, а выстраивают понятный медицинский маршрут: детоксикация, стабилизация, реабилитация, поддержка семьи, профилактика срывов. Пациент получает помощь в защищённой, конфиденциальной среде, где всё организовано так, чтобы снизить тревогу и стыд, убрать хаос вокруг зависимости и дать человеку шанс вернуться к нормальной жизни без давления, угроз и токсичных «стимулов». Для родных клиника в Коломне — это опора: конкретный адрес, конкретная команда, чёткие сроки и понятные этапы, вместо бесконечных обещаний «он сам справится».
Подробнее тут – narkologicheskaya-klinika-v-kolomne
I’m impressed, I must say. Seldom do I encounter a blog
that’s equally educative and amusing, and without a doubt, you’ve hit the nail on the head.
The issue is something which not enough people are speaking intelligently about.
I am very happy that I found this in my hunt for something concerning this.
It’s actually a great and useful piece of info.
I’m satisfied that you shared this useful information with us.
Please stay us informed like this. Thank you
for sharing.
Hey there would you mind sharing which blog platform үoᥙ’re working witһ?
I’m planning to start my оwn blog in the neаr future but I’m hɑving
а difficult time deciding betᴡeen BlogEngine/Wordpress/Ᏼ2evolution and
Drupal. The reason I ask іs because your layout seеmѕ ԁifferent
tһen most blogs and I’m ⅼooking for ѕomething unique.
Ρ.S My apologies fߋr gеtting off-topic but І haⅾ to ask!
My webpage … Mercedes benz
Наркологическая клиника в Твери обеспечивает круглосуточное медицинское наблюдение, что позволяет своевременно выявлять и устранять возможные осложнения. Высококвалифицированные специалисты проводят регулярные обследования и корректируют терапию, обеспечивая безопасность и эффективность лечения.
Выяснить больше – наркологическая клиника цены тверь
捕风捉影在线免费在线观看,海外华人专属平台,高清无广告体验。
May I simply say what a relief to uncover someone that really
knows what they are discussing on the net. You actually know how to bring an issue to light and
make it important. More and more people should read this and understand this side of your story.
I was surprised you aren’t more popular since you definitely have the gift.
В клинике применяются современные медицинские технологии, которые обеспечивают стойкий результат. Используемые методики соответствуют международным стандартам и регулярно обновляются.
Детальнее – наркологические клиники алкоголизм
Клиника в Коломне ориентирована на полный цикл помощи: от экстренных состояний до длительного сопровождения. Здесь важна не только медицинская составляющая, но и человеческая: уважение, конфиденциальность, отсутствие стигмы. Ниже — ключевые направления, которые выстраиваются в единую систему лечения, а не существуют по отдельности.
Получить больше информации – zakazat-obratnyj-zvonok-narkologicheskaya-klinika
Please let me know if you’re looking for a writer for your weblog.
You have some really great posts and I feel I would
be a good asset. If you ever want to take some of the
load off, I’d love to write some content for your blog in exchange for a link
back to mine. Please blast me an email if interested.
Regards!
I have learn some good stuff here. Certainly value bookmarking for revisiting.
I surprise how a lot effort you put to make this sort of wonderful informative site.
Informative article, just what I needed.
Also visit my blog post … Loodgieter Aalst
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Ознакомиться с деталями – нарколог в щелково
Домашний формат особенно важен, когда пациент не готов к стационару, боится огласки, испытывает стыд или сопротивление, но объективно нуждается в помощи. Попытки «перетерпеть» или лечить своими силами заканчиваются тем, что родственники дают опасные комбинации седативных, анальгетиков и «антипохмельных» средств, а состояние только ухудшается. «МедТрезвие Долгопрудный» строит выездную помощь так, чтобы она оставалась профессиональной медициной, а не косметической услугой. Уже при звонке диспетчер под контролем врача уточняет длительность запоя, виды алкоголя, наличие гипертонии, болезней сердца, печени, почек, диабета, неврологических нарушений, психических эпизодов, факт судорог, делирия в прошлом, какие лекарства уже были даны. Это позволяет заранее понять, подходит ли формат лечения на дому или сразу нужно рассматривать стационар. Выезд назначается только в тех случаях, когда это безопасно, и именно в этом ключевое отличие официальной клиники от анонимных «капельниц на дом» — здесь всегда выбирают жизнь и здоровье, а не удобный маркетинговый сценарий. Для семьи это не просто комфорт, а возможность получить помощь без риска сорваться в критическое состояние посреди ночи.
Подробнее тут – https://narkolog-na-dom-dolgoprudnij10.ru/vyezd-narkologa-na-dom-v-dolgoprudnom/
Наркологическая клиника в Твери представляет собой современное медицинское учреждение, специализирующееся на диагностике и лечении алкогольной, наркотической и других видов зависимости. В клинике «Гелиос» применяются инновационные методы терапии, направленные на полное восстановление физического и психологического состояния пациентов.
Исследовать вопрос подробнее – http://narkologicheskaya-klinika-tver0.ru
European football matches today, live scores from England, Spain, Italy, Germany and France
Эти направления формируют основу лечения и обеспечивают комплексное воздействие на проблему зависимости.
Подробнее – наркологическая клиника наркологический центр омск
Для иллюстрации эффективности методов представлена таблица с примерами процедур и их воздействием:
Подробнее – частная наркологическая клиника
Когда состояние «штормит», ночные часы усиливают тревогу и вегетативные реакции, обезвоживание нарастает, сон рвётся, а попытки самолечения «чем попало» маскируют опасные симптомы. Организованный маршрут в «Трезвой Линии» заменяет хаос последовательностью: ещё по телефону дежурный врач собирает ключевые сведения — длительность эпизода, аллергии, список лекарств и дозировок, кардио- и эндокринные диагнозы, последние измерения давления и пульса. На месте выполняется короткая, но информативная оценка: АД, ЧСС, сатурация, температура, неврологический статус, степень обезвоживания, выраженность тремора и тошноты. Схема терапии запускается сразу и корректируется каждые 15–20 минут по «живым показателям», а не по шаблону. Если видим признаки предделирия, неукротимую рвоту, резкие «качели» давления/пульса, выраженную слабость или пожилой возраст с тяжёлой соматикой — переводим в стационар без пауз: приборный мониторинг и ночная команда в Электростали снижают «цену ошибки» и экономят на повторных вызовах. Для семьи это означает меньше догадок и больше ясности: понятно, что делаем сейчас и чего ждём к утру.
Углубиться в тему – https://vyvod-iz-zapoya-ehlektrostal10.ru/vyvesti-iz-zapoya-ehlektrostal/
Sweet blog! I found it while searching on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Appreciate it
I am curious to find out what blog system you have been working with?
I’m having some minor security issues with my latest site and I’d like to find something more safe.
Do you have any suggestions?
I think this is among the most vital info for
no insurance dentist near me.
And i am glad reading your article. But want to remark on few general things, The website style is
ideal, the articles is really nice : D. Good job, cheers
Наркологическая клиника в Омске оказывает специализированную помощь людям, столкнувшимся с алкогольной, наркотической и другими формами зависимости. Здесь используются современные методы диагностики, терапии и реабилитации, которые помогают не только стабилизировать состояние, но и восстановить здоровье в долгосрочной перспективе. Работа ведётся с учётом принципов конфиденциальности, что создаёт условия для комфортного прохождения лечения.
Подробнее тут – https://narcologicheskaya-klinika-omsk0.ru/chastnaya-narkologicheskaya-klinika-omsk
Выезд нарколога на дом в Щёлково — это быстрый и конфиденциальный способ помочь человеку в состоянии запоя или тяжёлого похмелья, не перевозя его в клинику и не устраивая публичных сцен. Врачи «ЩёлковоМед Профи» приезжают с готовым набором препаратов, одноразовыми системами и чётким протоколом: осмотр, оценка жизненно важных показателей, подбор индивидуальной капельницы, контроль реакции, рекомендации для родных. Такой формат особенно удобен, когда пациент отказывается ехать в стационар, тяжело переносит дорогу, остро реагирует на смену обстановки или для семьи важна максимальная анонимность. Главный принцип — не «вырубить» человека любой ценой, а безопасно стабилизировать состояние, снизить интоксикацию, выровнять давление и пульс, помочь собрать сон и дать понятный план, что делать дальше.
Углубиться в тему – zapoj-narkolog-na-dom
Hey there! Would you mind if I share your blog with my facebook
group? There’s a lot of people that I think would really enjoy your content.
Please let me know. Thank you
Капельница — инструмент, помогающий организму выйти из токсической воронки, а не магическая смесь «на все случаи». Базовый каркас — регидратация и коррекция кислотно-щелочного состояния, электролиты для водно-солевого баланса, витамины группы B и магний для поддержки нервной системы и снижения тремора. По клиническим показаниям подключаются гепатопротекторы и антиоксиданты для разгрузки печени и уменьшения оксидативного стресса; при выраженной тошноте — противорвотные, при тревоге и бессоннице — мягкие анксиолитики в дозах, сохраняющих контакт. Мы сознательно избегаем «агрессивной» седации: она создаёт иллюзию успеха, но маскирует ухудшения и мешает контролю дыхания и нейростатуса. Эффективность оцениваем не «по ощущениям», а по метрикам: стабилизация АД/ЧСС, снижение тремора и тошноты, нормализация сатурации, возвращение аппетита и появление восстановительного ночного сна. Как только параметры выравниваются, фарм-нагрузку снижаем, а акцент переносим на режим — гигиену сна, регулярную гидратацию, дробное питание, щадящую дневную активность. Это делает результат не кратковременным затишьем на препаратах, а устойчивой траекторией восстановления.
Исследовать вопрос подробнее – vyvod-iz-zapoya-ehlektrostal10.ru/
Запойное состояние сопровождается тяжелыми последствиями для организма. Оно может включать нарушения сна, тремор конечностей, скачки давления, головные боли и депрессию. Без своевременной помощи такие проявления способны привести к развитию хронических заболеваний и угрожающих жизни осложнений.
Углубиться в тему – вывод из запоя с выездом пермь
Everyone loves what you guys tend to be up too. This kind of clever
work and reporting! Keep up the fantastic works guys I’ve included you guys to my personal blogroll.
my web page :: mood supplements
Выбор формата — это не вкусовщина, а баланс безопасности в конкретной клинической картине. Дом уместен, если контакт сохранён, рвота эпизодическая, давление и пульс без резких «качелей», тремор контролируемый, в квартире можно обеспечить тишину и присутствие взрослого, готового наблюдать первые 6–8 часов. Тогда выездная бригада работает на месте и выстраивает «мягкий» маршрут, где сон собирается без агрессивной седации, а инфузии идут с шаговой корректировкой темпа. Стационар предпочтителен при длительном эпизоде (3–5 суток и более), неукротимой рвоте, выраженной слабости, шаткости походки, признаках предделирия/делирия, судорожной готовности, а также у пожилых пациентов и при сочетанных диагнозах — ИБС, гипертония, диабет, хронические болезни печени/почек, неврология. Преимущество отделения — приборный мониторинг, лабораторные опции по показаниям, ночная команда и среда, где исключены лишние раздражители: это снижает «цену ошибки» и делает результат устойчивым, а не разовым «прояснением».
Углубиться в тему – srochnyj-vyvod-iz-zapoya
В статье представлены ключевые моменты по актуальной теме, дополненные советами экспертов и ссылками на дополнительные ресурсы. Цель материала — дать читателю инструменты для самостоятельного развития и принятия осознанных решений.
Лови подробности – https://babi-beauty.fr/signature-styles-the-best-haircuts-at-our-barber-shop
Своевременное обращение в клинику снижает риск развития алкогольного психоза, судорог и тяжёлых осложнений со стороны сердца и печени.
Углубиться в тему – вывод из запоя капельница в рязани
В основе работы клиники лежит принцип: зависимость — это не просто привычка и не «слабость характера», а комплексное заболевание, которое требует последовательного лечения, а не случайной капельницы по вызову. «Трезвый Шаг Раменское» отказывается от практики, когда пациенту предлагают один-единственный «волшебный» метод, не объясняя, что будет дальше. Здесь каждое обращение рассматривается в контексте стадии зависимости, общего состояния организма, психоэмоционального фона, семейной ситуации. Сначала специалисты снимают острые проявления: выход из запоя, детоксикация после употребления алкоголя, наркотиков или сочетаний, купирование абстиненции, коррекция давления, пульса, сна, тревоги. Затем формируется стабилизационный этап — подбор поддерживающих схем, работа с тягой, выравнивание эмоционального состояния. После этого при готовности пациента подключаются психотерапевтические и реабилитационные инструменты: мотивационные программы, работа с установками, триггерами, окружением. Важная особенность «Трезвый Шаг Раменское» — готовность объяснять семье и самому пациенту, зачем нужен каждый этап, какие цели у процедуры и какие результаты реально ожидать. Это снижает сопротивление, формирует доверие и делает путь не хаотичным, а управляемым.
Получить дополнительные сведения – narkologicheskaya-klinika-ramenskoe10.ru/
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Изучите внимательнее – https://bakery.markathinkdigital.com/product/cappuccino-cheesecake
Greetings from Idaho! I’m bored to tears at work so I decided to browse your site
on my iphone during lunch break. I enjoy the info you present here and can’t wait
to take a look when I get home. I’m surprised at how quick your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyhow, amazing blog!
Капельницы в «СаратовМед Профи» — это конструктор из тщательно подобранных модулей. Каждый модуль решает одну задачу и имеет свой ожидаемый горизонт эффекта. Важно не название, а логика: задача > опора среды > как проверяем > когда ждём результат.
Получить больше информации – вывод из запоя недорого
Этот текст сочетает в себе элементы познавательного рассказа и аналитической подачи информации. Читатель получает доступ к уникальным данным, которые соединяют прошлое с настоящим и открывают двери в будущее.
Лучшее решение — прямо здесь – https://viajeroencolombia.com/como-se-les-dice-a-las-personas-de-medellin
Такая структура делает лечение последовательным и предсказуемым, повышая шансы на положительный исход.
Детальнее – https://narkologicheskaya-klinika-v-omske0.ru/chastnaya-narkologicheskaya-klinika-omsk/
Вывод из запоя — это не «волшебная капельница», а последовательная медицинская программа с чёткими целями и измеримыми маркерами. В наркологической клинике «СаратовМед Профи» маршрут строится по принципу управляемых окон: на каждом шаге команда преследует одну цель, меняет лишь один параметр и оценивает результат в заранее назначённый момент. Такой подход снижает лекарственную нагрузку, предотвращает «гонку дозировок» и делает динамику предсказуемой для пациента и близких. Конфиденциальность обеспечивается регламентом: немаркированные выезды, нейтральные формулировки в документах, «тихие» каналы связи, доступ к записям — строго по ролям.
Детальнее – вывод из запоя на дому круглосуточно в саратове
I am regular reader, how are you everybody? This post posted
at this website is really good.
Awesome article.
Good day! This is kind of off topic but I
need some advice from an established blog. Is it difficult to set up your own blog?
I’m not very techincal but I can figure things out pretty quick.
I’m thinking about creating my own but I’m not sure where to start.
Do you have any points or suggestions? With thanks
海外华人必备的ifun平台,提供最新高清电影、电视剧,无广告观看体验。
Этот текст призван помочь читателю расширить кругозор и получить практические знания. Мы используем простой язык, наглядные примеры и структурированное изложение, чтобы сделать обучение максимально эффективным и увлекательным.
Ознакомьтесь поближе – https://vaserecenze.eu/salon-1936-kontakt-recenze-hodnoceni-zkusenosti-vraceni-a-reklamace
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Всё самое вкусное внутри – https://gforcerestore.com/water-removal/water-damage-2021
Hey! I’m at work surfing around your blog from my
new iphone 3gs! Just wanted to say I love reading through your blog and look forward to all your posts!
Carry on the great work!
Предлагаем вашему вниманию интересную справочную статью, в которой собраны ключевые моменты и нюансы по актуальным вопросам. Эта информация будет полезна как для профессионалов, так и для тех, кто только начинает изучать тему. Узнайте ответы на важные вопросы и расширьте свои знания!
Узнайте всю правду – https://actusante.ma/effets-cardio-vasculaires-des-antidiabetiques
Shootout specialists, players with best penalty records tracked
An outstanding share! I’ve just forwarded this onto a co-worker who had been conducting a little homework on this.
And he actually bought me breakfast due to the fact that I discovered it for
him… lol. So let me reword this…. Thanks for the meal!!
But yeah, thanks for spending time to discuss this subject here on your site.
Hindi ko nga alam kung paano ako napunta dito, pero naisip ko na maganda ang post na ito. Hindi ko alam kung nasaan ka pero tiyak na sikat na blogger ang pupuntahan mo kung hindi ka pa!
What’s up all, here every one is sharing these familiarity, so it’s pleasant to read
this website, and I used to pay a quick visit this weblog every day.
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Изучить материалы по теме – https://8kbet1.asia/8kbet-khuyen-mai-hoan-cuoc
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Полная информация здесь – https://samtel.co/12-key-issues-for-saas-startups-seeking-financing-2
Hello to all, because I am actually eager of reading this blog’s
post to be updated daily. It carries pleasant stuff.
Thanks for some other informative site.
Where else may I get that type of info written in such an ideal manner?
I’ve a project that I am just now working on, and I
have been at the glance out for such info.
My name: Cliff Mayorga
Age: 28 years old
Country: France
Town: La Garenne-Colombes
Post code: 92250
Street: 53 Rue De L’aigle
I found your blog through google and I must say, this is probably one of the best well prepared articles I have come across in a long time. I have bookmarked your site for more posts.
Hey there, I think your site might be having browser compatibility issues.
When I look at your blog site in Opera, it looks fine but when opening in Internet Explorer, it has
some overlapping. I just wanted to give you a
quick heads up! Other then that, great blog!
당신에게서 오는 웅장한 물건입니다. 이전에 당신의 글을 이해했고, 당신은 그냥 너무 멋집니다.
여기서 획득한 것을 정말 좋아하고, 당신이
말하는 것과 그 방식을 정말 좋아합니다. 재미있고
여전히 현명하게 유지합니다. 당신에게서 훨씬 더 읽고 싶습니다.
이건 정말 멋진 사이트입니다.
you are in reality a excellent webmaster. The website loading velocity is amazing.
It seems that you’re doing any unique trick. Also, The contents are masterpiece.
you’ve done a fantastic job in this subject!
Attractive part of content. I just stumbled upon your weblog and in accession capital to say that I get in fact loved account your blog posts.
Anyway I will be subscribing to your augment and even I success
you get entry to consistently quickly.
hey thanks for the info. appreciate the good work
Thanks very nice blog!
Kudos. Loads of facts.
Hi there, I found your web site by way of Google at
the same time as looking for a comparable subject, your website got here up,
it seems to be good. I have bookmarked it in my
google bookmarks.
Hi there, simply was alert to your blog via Google,
and found that it is really informative. I am going to watch out for
brussels. I’ll appreciate should you proceed this in future.
Many people will probably be benefited out of your writing.
Cheers!
Surprisingly good post. I really found your primary webpage and additionally wanted to suggest that have essentially enjoyed searching your website blog posts. Whatever the case I’ll always be subscribing to your entire supply and I hope you jot down ever again soon!
Assume you are doing good linking to position you on the first pages of search engines.
Asking questions are genuinely fastidious thing if you are not understanding something entirely, except
this article presents good understanding yet.
Individuals or groups categorized by shared defining characteristics
incest
Greate pieces. Keep writing such kind of information on your
page. Im really impressed by your blog.
Hey there, You have done an excellent job. I’ll certainly digg it and personally
recommend to my friends. I’m confident they’ll be benefited
from this website.
DFB Pokal live scores, German cup matches with Bundesliga teams competing
Hey there, I think your site might be having browser compatibility issues.
When I look at your blog in Ie, it looks fine but when opening in Internet
Explorer, it has some overlapping. I just wanted to give
you a quick heads up! Other then that, amazing blog!
This site truly has all of the info I needed
about this subject and didn’t know who to ask.
click here to read
https://russian-traditional-clothes.com/
Corner kick count, set piece statistics for all football matches
คอนเทนต์นี้ ให้ข้อมูลดี ครับ
ผม เพิ่งเจอข้อมูลเกี่ยวกับ เนื้อหาในแนวเดียวกัน
ที่คุณสามารถดูได้ที่
ufabet888 รวมค่ายสล็อต
น่าจะถูกใจใครหลายคน
เพราะอธิบายไว้ละเอียด
ขอบคุณที่แชร์ เนื้อหาดีๆ นี้
และอยากเห็นบทความดีๆ แบบนี้อีก
Do you mind if I quote a few of your posts as long as
I provide credit and sources back to your webpage?
My website is study in turkey the very same
niche as yours and my visitors would really benefit from
a lot of the information you provide here. Please let me know if
this ok with you. Regards!
I think it is a nice point of view. I most often meet people who rather say what they suppose others want to hear. Good and well written! I will come back to your site for sure!
Heya i’m for the first time here. I found this board and I in finding It truly helpful & it helped me out a lot.
I’m hoping to provide one thing back and aid others such as you aided me.
Fantastic goods from you, man. I have understand your stuff
previous to and you are just too excellent. I actually like what you
have acquired details here, certainly like what you are
stating and the way in which you say it. You make it enjoyable and you still take care of to
keep it wise. I can’t wait to read far more from
you. This is actually a wonderful site.
It’s perfect time to make a few plans for the long run and it’s time to
be happy. I have learn this post and if I may I wish
to suggest you some attention-grabbing issues or advice.
Perhaps you could write next articles relating to this article.
I want to read even more issues approximately it!
Also visit my website – free apply
Goalkeeper distribution, passing accuracy and long ball success
海外华人必备的yifan官方认证平台,24小时不间断提供最新高清电影、电视剧,无广告观看体验。
Neat blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple tweeks would really make my
blog shine. Please let me know where you got your design. Thanks
Feel free to visit my homepage :: service informatique montreal
Hello there! I could have sworn I’ve visited this blog before but after browsing through some of
the articles I realized it’s new to me. Anyways, I’m definitely delighted I stumbled upon it
and I’ll be book-marking it and checking back frequently!
Hey! I’m at work surfing around your blog from
my new apple iphone! Just wanted to say I love reading your blog and look forward to all your posts!
Keep up the excellent work!
Here is my web page: free apply
If you would like to get a great deal from this piece
of writing then you have to apply such techniques to your won website.
What i do not understood is in truth how you’re now not actually much more neatly-appreciated than you may be
now. You are very intelligent. You realize therefore considerably in relation to this subject,
made me personally imagine it from numerous varied angles.
Its like women and men don’t seem to be involved until it’s one thing
to accomplish with Lady gaga! Your own stuffs great. All the time maintain it up!
I every time used to study post in news papers but now as I am a user
of internet so from now I am using net for articles or reviews, thanks to web.
Hey there! Do you use Twitter? I’d like to follow you if
that would be okay. I’m definitely enjoying your blog and look forward to new posts.
my web site :: ufa888 ทางเข้า
Excellent post. I was checking constantly this blog
and I am impressed! Extremely helpful info particularly
the last part 🙂 I care for such info much. I was seeking this certain info for a long time.
Thank you and best of luck.
James Smith’s 2026 Outlook: Tax Law Overshadows Game Mechanics
If some one desires expert view concerning running a blog after
that i recommend him/her to pay a quick visit this webpage, Keep up the nice
work.
Avec son fonctionnement à distance et ses fonctionnalités intelligentes, il offre
une commodité, une efficacité et un confort pour vos tâchesd’entretien de la pelouse.
Cette machine robuste de qualité commerciale est conçue pour s’attaquer sans
effort aux tâches les plus difficiles, garantissant que même les travaux les
plus complexes sont réalisés avec facilité.
Ce qui caractérise une machine AS-Motor, ce n’est pas seulement sa finition orange vif, mais
aussi nos valeurs fondamentales que sont la durabilité, la praticité et une conception axée sur l’utilisateur.
Nous testons toutes nos tondeusess télécommandées sur une longue période pour trouver des problèmes et les améliorer.
Par rapport aux autres tondeuses à gazon, son principal avantage
est qu’elle peut s’adapter à différents terrains et qu’elle est flexible et maniable.
Dans les archives du KGB, Natasha trouve
le bouclier du Red Guardian, son père adoptif.
Ces outils, particulièrement utiles dans cette période de crise, sont réservés aux agents de l’État, qui peuvent inviter des agents, des
partenaires, des prestataires, des experts. Cette tondeuse à gazon télécommandée convient pour : les friches,
les vergers, les fermes, les berges de rivières, les pentes des routes, les zones humides, le
verdage, etc.
Feel free to surf to my blog tondeuse RC à Vendre
I was able to find good advice from your content.
my web page :: ranking
quale where to buy cialis online for cheap verwijst buy cialis 365 pills https://cialis-otc.com/ – overnight delivery cialis [url=https://cialis-otc.com]elevex tadalafil 20mg[/url] kristu where to buy generic cialis ?
Hello there, I discovered your website by the use of Google while looking for a comparable subject, your website got here up, it appears to be like great.
I have bookmarked it in my google bookmarks.
Hello there, simply changed into alert to your blog through Google, and found that it’s really informative.
I’m going to be careful for brussels. I’ll be grateful when you proceed this in future.
Many other folks will likely be benefited out of your writing.
Cheers!
Feel free to surf to my webpage makeup suitcase
huarenus平台,专为海外华人设计,提供高清视频和直播服务。
I pay a visit every day a few web pages and blogs to read content, except this website offers feature based content.
超人和露易斯第一季高清完整版AI深度学习内容匹配,海外华人可免费观看最新热播剧集。
Hello just wanted to give you a quick heads up. The text in your post seem
to be running off the screen in Opera. I’m not sure
if this is a formatting issue or something to do with web browser compatibility but I figured I’d post to let you know.
The style and design look great though! Hope you get the problem fixed soon. Cheers
Usually I don’t read post on blogs, but I would like to say that this write-up
very pressured me to check out and do it! Your writing taste has been surprised me.
Thanks, very great article.
my web blog … cablage reseau montreal
海外华人必备的yifan平台运用AI智能推荐算法,提供最新高清电影、电视剧,无广告观看体验。
Great post! I’ve been studying how advanced algorithms like
the Kara model can outperform traditional betting methods.
Integrating Poisson distribution and ROI analysis is definitely the future of
sports forecasting. If anyone is interested in seeing how data-driven tips work in practice, I’ve been tracking some very interesting
results lately. Keep up the good work!
I was curious if you ever thought of changing the structure of your site?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of
content so people could connect with it better. Youve got an awful lot of text for
only having 1 or two images. Maybe you could space it out
better?
With havin so much content do you ever run into any issues of plagorism or copyright infringement?
My site has a lot of unique content I’ve either written myself
or outsourced but it seems a lot of it is popping it up all over the internet without my agreement.
Do you know any methods to help prevent content from being stolen? I’d truly appreciate it.
If some one desires to be updated with most recent technologies therefore he must be pay a quick visit this website and be up to date all the time.
We are a group of volunteers and starting a brand new scheme in our community.
Your site provided us with useful information to work on. You’ve done a formidable activity and our entire neighborhood shall be grateful to you.
Hi, I wish for to subscribe for this webpage to get latest updates, therefore where can i do it please assist.
If you wish for to increase your know-how simply keep visiting
this site and be updated with the newest news posted here.
I’m extremely impressed with your writing skills and also with the
layout on your blog. Is this a paid theme or did you modify it yourself?
Either way keep up the nice quality writing, it is rare to see a
great blog like this one today.
Very shortly this web site will be famous amid all blog viewers, due to
it’s nice articles or reviews
Howdy! I could have sworn I’ve visited this blog before but after going through many of the posts I realized it’s new to me.
Nonetheless, I’m definitely pleased I found it and I’ll be book-marking
it and checking back regularly!
Have you ever thought about writing an ebook or guest authoring on other sites?
I have a blog based on the same ideas you discuss and would
love to have you share some stories/information. I know my subscribers would enjoy
your work. If you’re even remotely interested, feel free to send me an e-mail.
이것은 핵심적인 게시물입니다.
온라인 모금은 수술비를 감당하기 힘든 환자들의 삶을 바꿉니다.
시력 회복 글로벌 의료 구호 재단을 돕는 것은 참으로 숭고한 일입니다.
이 미션을 공유해 주셔서 감사합니다.
It’s really a nice and helpful piece of information. I am
glad that you just shared this useful info with us.
Please keep us up to date like this. Thanks for sharing.
my web site; international charity foundation
I like to spend my free time by scaning various internet recourses. Today I came across your site and I found it is as one of the best free resources available! Well done! Keep on this quality!
Hi, Neat post. There is a problem along with your
site in web explorer, could check this? IE nonetheless is the market chief and a big portion of other folks will
miss your fantastic writing due to this problem.
I think the admin of this web page is actually working hard for
his website, because here every information is quality based stuff.
These are actually fantastic ideas in regarding blogging.
You have touched some good points here. Any way keep up
wrinting.
안녕하세요! 당신의 블로그 페이지를 정말 우연히 발견했는데, Aol에서 다른 것을 검색하던 중이었습니다.
멋진 포스트와 전반적으로 재미있는 블로그(테마/디자인도 좋아합니다)에 감사드립니다.
지금은 시간이 없어서 전부 읽지는 못했지만, 북마크해놓고
RSS 피드도 추가했습니다. 시간이 되면 더 많이 읽으러 올게요,
멋진 작업을 계속해 주세요.
I love it when individuals get together and share opinions.
Great website, stick with it!
一帆视频海外华人首选,采用机器学习个性化推荐,提供最新华语剧集、美剧、日剧等高清在线观看。
Как выбрать надежный ремонт Blackmagic
Hey! Do you know if they make any plugins to assist with SEO?
I’m trying to get my blog to rank for some targeted keywords
but I’m not seeing very good gains. If you know of
any please share. Thanks!
Look at my homepage studyleo
If some one desires expert view concerning running a blog afterward i suggest him/her
to go to see this website, Keep up the fastidious job.
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Запросить дополнительные данные – https://julietetelandresen.com/hounslow-western-london
Nice respond in return of this matter with real arguments and describing the
whole thing about that.
Feel free to surf to my web-site :: ufa888 ทางเข้า
I do not know if it’s just me or if perhaps everyone else
experiencing issues with your website. It seems like some of the text on your content are running off
the screen. Can someone else please comment and let me know if this is happening to them too?
This might be a problem with my internet browser because I’ve had
this happen before. Cheers
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Обратитесь за информацией – https://www.thetablereadmagazine.co.uk/hashtag-press-denise-brown-on-small-town-secrets-creepy-theme-parks-and-the-power-of-friendship-in-her-gripping-new-ya-mystery
Ech weess net emol, wéi ech hei gelant sinn, mee ech fannen dëse Post super. Ech weess net, wou du bass, mee du wäerts sécherlech e bekannte Blogger ginn, wann s de et nach net bass!
Hello, just wanted to tell you, I loved this blog post. It was funny.
Keep on posting!
Nice blog here! Also your site loads up fast!
What web host are you using? Can I get your affiliate link
to your host? I wish my website loaded up as quickly as yours lol
Visit my web site … study in turkey
Читатель отправляется в интеллектуальное путешествие по самым ярким событиям истории и важнейшим научным открытиям. Мы раскроем тайны эпох, покажем, как идеи меняли миры, и объясним, почему эти знания остаются актуальными сегодня.
Ознакомиться с теоретической базой – https://www.feriaveoveo.unc.edu.ar/es/estuvimos-en/el-veo-veo-en-la-eci
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Получить профессиональную консультацию – https://tylerthecreatormerchofficial.com/lembaga-pengelola-dana-pendidikan-mewujudkan-akses-dan-kualitas-pendidikan-yang-lebih-baik
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
Узнать больше – http://www.benton-ely.co.uk/home/porsche
I think everything composed made a ton of sense.
But, what about this? what if you typed a catchier
post title? I mean, I don’t wish to tell you
how to run your blog, but what if you added something to maybe
get a person’s attention? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate is a little plain. You could glance
at Yahoo’s home page and watch how they create news headlines to get
viewers to open the links. You might add a video or a related picture or two to grab people interested about
everything’ve written. Just my opinion, it could make your website a little bit more interesting.
Have you ever considered about adding a little bit more than just your articles?
I mean, what you say is valuable and all. Nevertheless think of if you added some great pictures or videos to give your posts more, “pop”!
Your content is excellent but with pics and clips, this site could
undeniably be one of the very best in its
field. Fantastic blog!
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Детальнее – https://template135.webekspor.com/the-importance-of-quality-standards-in-rubber-export
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Нажмите, чтобы узнать больше – https://camtelkiosk.com/index.php/2021/12/24/vos-recharges
Эта публикация завернет вас в вихрь увлекательного контента, сбрасывая стереотипы и открывая двери к новым идеям. Каждый абзац станет для вас открытием, полным ярких примеров и впечатляющих достижений. Подготовьтесь быть вовлеченными и удивленными каждый раз, когда продолжите читать.
Продолжить изучение – https://infominang.com/mahyeldi-vasko-paket-lengkap-untuk-membangun-sumbar-yang-lebih-cepat
Modern Purair
201, 1475 Ellis Street, Kelowna
BC Ⅴ1Y 2A3, Canada
1-800-996-3878
hvac control
Superb blog! Do you have any hints for aspiring writers?
I’m hoping to start my own blog soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress or go for a paid option? There are so many options out there that I’m completely confused ..
Any tips? Thanks a lot!
Этот сайт kazino olimp — настоящая находка.
https://www.google.hu/url?sa=t&url=https://olimp-casino-kazakhstan-win.kz
Wow! At last I got a website from where I know how to in fact obtain valuable facts concerning
my study and knowledge.
At this time I am going away to do my breakfast, once
having my breakfast coming over again to read more news.
my web site; details here
WOW just what I was searching for. Came here by searching for cyprus real estate market
Hey There. I found your blog using msn. This is an extremely well written article.
I will make sure to bookmark it and return to read more of your useful info.
Thanks for the post. I will definitely comeback.
Wonderful web site. Plenty of helpful info here.
I am sending it to a few pals ans additionally sharing in delicious.
And naturally, thank you to your sweat!
Awesome blog! Do you have any tips for aspiring writers?
I’m planning to start my own website soon but I’m a little lost on everything.
Would you recommend starting with a free platform
like WordPress or go for a paid option? There are so many options out there that I’m
completely confused .. Any recommendations? Cheers!
It’s awesome in favor of me to have a site, which is helpful designed for my experience.
thanks admin
Right now it sounds like Drupal is the top blogging platform out there right now.
(from what I’ve read) Is that what you are using on your blog?
Nice to join this community.
I’m mainly interested in online casinos and testing reliable sites.
Lately, I’ve been spending time on Betify because of its smooth gameplay.
Here to read and stay updated about the iGaming world.
Patrice & Associates
Scottsdale, AZ, United Ѕtates
16265237726
hospitality industry
Concert Attire Stamford
360 Fairfield Ave,
Stamford, CT 06902, United Տtates
+12033298603
Bookmarks
Aw, this was an exceptionally nice post. Taking a few minutes and actual effort
to generate a really good article… but what can I say… I hesitate a lot and don’t seem to
get nearly anything done.
Wonderful article! We will be linking to this particularly great content on our site.
Keep up the great writing.
Normally I do not read post on blogs, however I wish to say that
this write-up very pressured me to take a look at and do so!
Your writing taste has been amazed me. Thanks, quite great article.
Boston Medical Ԍroup
3152 Red Hill Ave. Ste. #280,
Costa Mesa, ϹΑ 92626, United Statеs
800 337 7555
Penis size percentages
I am truly thankful to the holder of this site who has shared this enormous article at here.
May I simply just say what a relief to uncover a person that genuinely understands
what they are talking about on the web. You certainly understand how to bring a
problem to light and make it important. More
and more people ought to read this and understand this
side of the story. I can’t believe you are not more popular since you surely possess the gift.
You need to really control the comments listed here
Life Coach Rudolfo Life Coaches provide outstanding life coaching services.
The Life Coaches from Life Coach Rudolfo offer therapy for stress management.
Life Coach Rudolfo empowers clients to enhance
their lifestyle. Wellness is a significant focus for the Life Coaches at Life Coach
Rudolfo. Life Coach Rudolfo provides professional coaching for personal growth.
Business coaching is a specialty of the Life Coaches from Life Coach
Rudolfo. Life Coach Rudolfo supports career coaches in their professional development.
The Life Coaches at Life Coach Rudolfo provide
coaching services in Noord Holland. Life Coach Rudolfo Life Coaches simplify therapie sessions for mental wellbeing.
Life Coach Rudolfo provides life coaching services to promote wellness.
The Life Coaches from Life Coach Rudolfo help clients through stress management therapy.
Life Coach Rudolfo provides lifestyle coaching for personal betterment.
The Life Coaches at Life Coach Rudolfo provide business
coaching for entrepreneurs. Life Coach Rudolfo offers professional coaching to career coaches.
The Life Coaches from Life Coach Rudolfo provide coaching services in Noord Holland.
Life Coach Rudolfo Life Coaches allow clients to achieve wellness through
therapie. Life Coach Rudolfo offers life coaching to help manage stress.
The Life Coaches at Life Coach Rudolfo support clients in improving their lifestyle.
Life Coach Rudolfo provides business coaching to professionals.
The Life Coaches from Life Coach Rudolfo provide professional coaching services in Noord Holland.
I am glad to be a visitor of this perfect blog !, appreciate it for this rare info!
It is not my first time to visit this web site, i am browsing
this web page dailly and take good information from here everyday.
What’s up Dear, are you actually visiting this site daily, if so after that you will
without doubt obtain good know-how.
Excellent blog you have got here.. It’s
difficult to find good quality writing like yours these days.
I really appreciate people like you! Take care!!
You actually make it seem so easy with your presentation but I find this matter to be really something that I think
I would never understand. It seems too complex and very broad for me.
I’m looking forward for your next post, I will try to
get the hang of it!
Incredible points. Great arguments. Keep up the amazing effort.
Saved as a favorite, I like your site!
Look at my web blog … zupacescu01
I’m amazed, I must say. Seldom do I encounter a blog that’s both equally educative and
engaging, and without a doubt, you have hit the nail on the
head. The issue is something too few people are speaking intelligently
about. I’m very happy I found this in my search for something
concerning this.
Nice read, I just passed this onto a colleague who was doing some research on that. And he just bought me lunch as I found it for him smile Therefore let me rephrase that: Thank you for lunch!
https://t.me/s/russIa_CAsino_1wiN
This design is spectacular! You definitely know how to keep
a reader entertained. Between your wit and your videos,
I was almost moved to start my own blog (well, almost…HaHa!) Excellent job.
I really loved what you had to say, and more than that, how you presented it.
Too cool!
Hi, I log on to your blogs daily. Your story-telling style is witty, keep up the
good work!
Hello There. I discovered your weblog the usage of msn. That
is a really well written article. I’ll make sure to
bookmark it and come back to read extra of your helpful info.
Thank you for the post. I will certainly comeback.
I like the helpful information you supply on your
articles. I’ll bookmark your blog and take a look at once more right here regularly.
I’m slightly sure I will learn lots of new stuff right right
here! Best of luck for the next!
Wow, amazing blog layout! How long have you been running a blog for?
you made running a blog look easy. The total look of your web site is fantastic, as neatly as the content!
타임케어 서울출장홈타이는 고객이 있는 곳으로 24시간 언제든
찾아가는 프리미엄 홈케어 마사지 서비스입니다.
서울 시 전 지역에서 출장 홈타이를 제공
Great post.
Also visit my web blog: affordable sports supplements manufactured in South Africa
Good day! This is my first visit to your blog! We are a team of volunteers and starting
a new initiative in a community in the same niche.
Your blog provided us valuable information to
work on. You have done a extraordinary job!
Way cool! Some very valid points! I appreciate you penning this post and also the rest of the site is
really good.
my site; investment advisory services UK
This is a topic that’s close to my heart… Many thanks!
Exactly where are your contact details though?
My homepage pension advice UK
Thanks for every other fantastic post. The place else may anybody get that kind of info in such a perfect way of writing?
I’ve a presentation next week, and I’m at the search for such info.
Источник водка бет
Wonderful goods from you, man. I’ve understand your stuff previous to and
you’re just extremely excellent. I really like what
you’ve acquired here, really like what you are saying and the
way in which you say it. You make it entertaining
and you still care for to keep it sensible. I can not wait
to read much more from you. This is really a great site.
I’m gone to say to my little brother, that he should also
visit this website on regular basis to get updated from most
up-where to buy supplements online in South Africa-date
information.
Greate post. Keep posting such kind of information on your page.
Im really impressed by it.
Hello there, You have done an excellent job. I’ll definitely digg it and personally suggest to my friends.
I am sure they’ll be benefited from this web site.
Hey there would you mind sharing which blog platform you’re using?
I’m looking to start my own blog in the near future but I’m
having a difficult time making a decision between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style seems different then most blogs and I’m looking for something unique.
P.S Sorry for getting off-topic but I had to ask!
This is a very informative post.
I really like the way you explained
the topic in a simple way.
It is sometimes difficult for readers to understand
how digital sports streaming functions,
especially in terms of
user experience and access.
This post does a good job explaining it,
and I think it will be valuable for readers
who are looking for reliable information.
Thanks for posting such a useful article,
I will definitely follow future updates
on this blog.
I always spent my half an hour to read this web site’s articles every day along with a
mug of coffee.
Also visit my page: AI Optimisation agencies in Melbourne
May I simply say what a comfort to discover somebody that
truly understands what they’re talking about on the web. You definitely
realize how to bring an issue to light and make it important.
More people really need to read this and understand
this side of the story. I was surprised you aren’t more popular because you most certainly have the gift.
Look at my website … Bet1000
I know this if off topic but I’m looking into starting my own weblog and was curious what all is needed to get setup?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100%
positive. Any suggestions or advice would be greatly appreciated.
Many thanks
Great goods from you, man. I’ve understand your stuff
previous to and you are just too great. I actually like what you have acquired here,
certainly like what you are saying and the way in which
you say it. You make it enjoyable and you still take care of to
keep it sensible. I can’t wait to read far more from you.
This is really a great website.
Hello there! This blog post couldn’t be written much better!
Looking through this article reminds me of my previous roommate!
He constantly kept preaching about this. I most certainly will forward this post to him.
Fairly certain he will have a good read. Thanks for sharing!
Hi there to all, the contents present at this web site are really amazing for people experience,
well, keep up the good work fellows.
Unquestionably believe that which you stated.
Your favorite justification appeared to be on the net the easiest thing to be aware
of. I say to you, I certainly get irked while people consider worries that they just do not know about.
You managed to hit the nail upon the top and defined out the whole thing without having side effect , people can take a signal.
Will likely be back to get more. Thanks
Right now it sounds like BlogEngine is the preferred blogging platform available right now.
(from what I’ve read) Is that what you’re using on your
blog?
Hi great website! Does running a blog such as this require a lot of work?
I’ve virtually no expertise AEO experts in Melbourne programming however I
had been hoping to start my own blog soon. Anyway, should you have any
suggestions or tips for new blog owners please share.
I understand this is off topic but I just had to ask.
Thanks!
see this page https://network-guide.org
Great post but I was wanting to know if you could write a litte more on this subject?
I’d be very grateful if you could elaborate
a little bit further. Many thanks!
Feel free to surf to my website – independent financial advisor UK
I’ve been looking into Paybis for a while now, especially after going through financial trouble, and I’m still not entirely sure whether it deserves all
the attention it gets. Still, it’s clearly a noticeable name in the digital asset market, particularly for people in Germany who are trying to
find new financial tools. From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports fiat
payments, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to connect traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while
Paybis allows users to sell crypto using various fiat options.
I’m not saying the process is perfect, but it does seem aimed at
beginners rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins. Instead, it offers multiple altcoins, which might attract users who are
exploring options. Still, things like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel responsible for
users in Germany, though others might see it as time-consuming.
I’m still undecided, but it does suggest Paybis tries to operate
as a long-term marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is clear about costs,
while others note that pricing can change with transaction type.
This isn’t unusual in the crypto industry, but it means users
should compare alternatives before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like a
platform worth exploring, especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems relevant enough to justify
further research.
It’s going to be end of mine day, but before finish I
am reading this enormous article to improve my
experience.
Greetings! Very helpful advice in this particular
article! It is the little changes which will make the biggest changes.
Thanks a lot for sharing!
Wonderful goods from you, man. I have understand your stuff previous
to and you’re just extremely wonderful. I really like what you’ve acquired here,
certainly like what you’re saying and the way in which you say it.
You make it enjoyable and you still care for to keep it smart.
I can’t wait to read much more from you. This is really a tremendous site.
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Подробности по ссылке – https://chamundaengineeringworks.in/product/cew-13-4pcs
I’ve been checking out Paybis for a while now, especially
after going through financial trouble, and I’m
still not fully convinced whether it deserves all the attention it gets.
Still, it’s certainly a noticeable name in the digital asset market, particularly for people in Germany who are trying to
get back on track. From what I understand, Paybis presents itself
as a large-scale cryptocurrency service that supports regular bank transactions, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to connect traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis
allows users to sell crypto using various fiat options.
I’m not saying the process is perfect,
but it does seem aimed at users new to crypto rather than just advanced
traders.
Another aspect worth noting is the selection of supported
assets. Paybis doesn’t restrict itself to only the major tokens.
Instead, it offers a broader token selection, which might
attract users who are diversifying. Still, things like update speed are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel
professional for users in Germany, though others might see it as time-consuming.
I’m still undecided, but it does suggest Paybis tries
to operate as a long-term marketplace.
When it comes to fees, reviews seem varied.
Some say Paybis is clear about costs, while others note that pricing can change with transaction type.
This isn’t unusual in the crypto industry, but it means users should read the details before
moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like a platform worth checking out, especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems interesting enough to justify further research.
Good way of telling, and nice post to obtain information on the topic of my
presentation subject matter, which i am going to deliver in university.
my site: Diva Spin sportsbook
I’ve been checking out Paybis for a while now, especially after having a rough
financial period, and I’m still not entirely sure whether it deserves all the attention it gets.
Still, it’s certainly a noticeable name in the crypto industry, particularly for
people in Germany who are trying to get back on track.
From what I understand, Paybis presents itself as a
well-established cryptocurrency service that
supports standard payment methods, something many
platforms either limit or complicate.
What initially caught my eye is how Paybis seems to bridge
traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades,
while Paybis allows users to buy crypto using SEPA transfers.
I’m not saying the process is perfect, but it does seem aimed at beginners rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins.
Instead, it offers a wider range of digital assets, which might attract users who are exploring options.
Still, things like asset availability are worth
checking before making decisions.
Security and compliance also come up often around
Paybis. The platform highlights KYC checks, which can feel professional for users in Germany, though others might see
it as restrictive. I’m still undecided, but it does suggest Paybis tries to operate as a legitimate marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is
transparent about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means users
should research properly before moving money.
Overall, I wouldn’t call Paybis the best option, but
it does seem like a platform worth checking out, especially for someone in Germany trying to recover
financially. I’m still forming my opinion, but it seems interesting enough
to justify further research.
This article is very helpful.
I really enjoy how this post breaks down
the details in an easy-to-understand manner.
Many people often struggle to understand
how live streaming platforms operate,
especially in terms of
quality, reliability, and safety.
This post really helps clarify that,
and I think it will be useful for beginners
that want to learn more about the topic.
Thanks for writing this guide,
I will definitely read more articles
on this blog.
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Связаться за уточнением – https://webstories.aajkinews.net/kate-mckinnon-reveals-why-she-quit-saturday-night-live-after-a-decade-my-body-was-tired
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Лови подробности – https://sao.wfu.edu.tw/wfuasrc/?p=131
Fine way of explaining, and pleasant paragraph to
get facts concerning my presentation topic, which i am going to convey in university.
Feel free to visit my blog post: Diva Spin bonus
I’ve been checking out Paybis for a while now, especially after going through financial trouble, and I’m still not completely certain whether it deserves all
the attention it gets. Still, it’s clearly a noticeable
name in the crypto industry, particularly for people in Germany who are trying to get back on track.
From what I understand, Paybis presents itself as a
well-established cryptocurrency service that
supports standard payment methods, something many
platforms either limit or complicate.
What initially caught my eye is how Paybis seems to link traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to sell
crypto using various fiat options. I’m not saying the process is perfect, but it does seem aimed
at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and Ethereum only.
Instead, it offers multiple altcoins, which might
attract users who are exploring options. Still,
things like update speed are worth checking before making
decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel responsible for users in Germany, though others might see
it as time-consuming. I’m still undecided,
but it does suggest Paybis tries to operate as a long-term marketplace.
When it comes to fees, reviews seem varied. Some say Paybis
is transparent about costs, while others note that pricing can vary by payment method.
This isn’t unusual in the crypto industry, but it means users should compare alternatives
before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem
like a platform worth checking out, especially for someone in Germany trying to find accessible financial tools.
I’m still forming my opinion, but it seems promising enough to justify further
research.
Дори не знам как попаднах тук, но мисля, че тази публикация е страхотна. Не знам къде си, но определено ще станеш известен блогър, ако все още не си!0.0.
Hi! Do you know if they make any plugins to assist with Search Engine Optimization?
I’m trying to get my blog to rank goal-based supplement stacks for strength and recovery some
targeted keywords but I’m not seeing very good success. If you know of any please
share. Many thanks!
Singapore Pools (Private) Limited adalah sebuah perusahaan yang dimiliki
oleh negara di Singapura. Sebagai pemilik utuh keseluruhan dari permainan papan toto, Ini adalah satu-satunya pengelola yang resmi dan legal diizinkan untuk menjalankan lotre di Singapura.
Singapore Pools adalah suatu korporasi yang dibentuk pada 23 Mei 1968 untuk mengekang perjudian ilegal di Singapura.
Hal ini menyediakan jalan bagi penduduk Singapura jalan untuk bertaruh di lotre, mengantisipasi merajalelanya perjudian ilegal oleh sindikat yang telah ada sebelumnya.
Sejak 1 Mei 2004, Singapura Pools dimiliki oleh Tote Board, sebuah lembaga hukum di bawah Kementrian Keuangan (Singapura).
TOTO – sebanyak 6 dari 49 nomor lotre diundi pada setiap Senin dan Kamis , dan pada event tertentu result atau pengeluar hasil di tunda agak
malam atau ganti hari , Event2 Lunar NewYear ( hari Raya IMlEK ), Cap Go Meh ( pesta lampion ) dan Pada peringatan Tiong Jiu
Pia ( bulan purnama 15th Bulan Delapan Lunar/imlek ) serta
beberapa event misal Valentine Day, April Fools day.
4D – sebuah ‘pilih 4’ undian lotre pada setiap Rabu, Sabtu dan Minggu.
Singapore Sweep – lotre undian / gaya lotre diundi pada Rabu pertama setiap bulannya.
Dan Diputar pada pukul 18:30 Wib. Dalam tambahannya,
Singapore Pools adalah satu-satunya bandar taruhan dan penghitung legal untuk asosiasi sepak bola
dan taruhan balap motorsport. Pada 29 September 2016, Kementrian Dalam Negeri (Singapura) mengumumkan bahwa
Singapore Pools akan diberikan izin pengecualian dibawah
Undang-Undang Perjudian Jarak Jauh 2014, yang memperbolehkan untuk menawarkan perjudian secara online dan telepon untuk
4D dan TOTO lotre, sepak bola dan balap-motor.
Permainan Lotre di Indonesia telah lama mendapatkan perlarangan dari Pemerintah Indonesia.
Hal ini sesuai dengan ketentuan Undang-Undang Republik
Indonesia. Hal ini mendorong masyarakat Indonesia melakukan perjudian lotre secara jarak jauh dengan menggunakan smartphone.
Artikel bertopik perusahaan ini adalah sebuah rintisan. Anda dapat membantu Wikipedia dengan mengembangkannya.
Teks tersedia di bawah Lisensi Atribusi-BerbagiSerupa Creative Commons;
ketentuan tambahan mungkin berlaku. Lihat Ketentuan Penggunaan untuk rincian lebih lanjut.
4M Dental Implant Center
3918 ᒪong Beach Blvd #200, Ꮮong Beach,
CA 90807, United Statеs
15622422075
24hr dentistry
I believe everything composed was very logical.
However, what about this? suppose you were to create a
killer post title? I mean, I don’t want to tell you how to run your website, but suppose you added a title
that grabbed folk’s attention? I mean Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate is a little plain. You could peek at Yahoo’s front
page and see how they create post titles to get viewers to open the
links. You might add a video or a picture or two to get
people excited about what you’ve got to say. Just my opinion, it might make your posts a little livelier.
Feel free to surf to my website: SSA Supplements official
When someone writes an piece of writing he/she retains the
thought of a user in his/her brain that how a user can understand
it. Therefore that’s why this article is outstdanding.
Thanks!
This website was… how do I say it? Relevant!! Finally I have found something which helped me.
Many thanks!
my homepage SSA Supplements South Africa
This is very interesting, You are a very skilled blogger.
I have joined your rss feed and look forward to seeking more of
your great post. Also, I have shared your website in my social networks!
If you desire to take a great deal from this post then you have to apply these techniques to your
won blog.
I’ve been researching Paybis for a while now, especially after having a rough financial period, and
I’m still not fully convinced whether it deserves all the attention it gets.
Still, it’s definitely a noticeable name in the digital asset
market, particularly for people in Germany who are trying to get back
on track. From what I understand, Paybis presents itself as a large-scale cryptocurrency service that supports regular
bank transactions, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to link traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis
allows users to buy crypto using SEPA transfers.
I’m not saying the process is perfect, but it does seem aimed at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins.
Instead, it offers a broader token selection, which might attract users who
are exploring options. Still, things like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights regulatory compliance, which can feel professional for users in Germany, though others might see it as inconvenient.
I’m still undecided, but it does suggest Paybis tries to operate
as a regulated marketplace.
When it comes to fees, reviews seem divided. Some say Paybis is straightforward about
costs, while others note that pricing can vary by payment method.
This isn’t unusual in the crypto industry,
but it means users should read the details before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like a platform worth checking out,
especially for someone in Germany trying to find accessible financial tools.
I’m still forming my opinion, but it seems relevant enough to justify further research.
ข้อมูลชุดนี้ อ่านแล้วเข้าใจง่าย ค่ะ
ผม ได้อ่านบทความที่เกี่ยวข้องกับ
เรื่องที่เกี่ยวข้อง
ดูต่อได้ที่ betflik19
สำหรับใครกำลังหาเนื้อหาแบบนี้
เพราะให้ข้อมูลเชิงลึก
ขอบคุณที่แชร์ เนื้อหาดีๆ นี้
และหวังว่าจะมีข้อมูลใหม่ๆ มาแบ่งปันอีก
Hello everyone, it’s my first visit at this web page, and post is actually fruitful
for me, keep up posting such articles.
Makes sense to me.
Excellent blog you have here.. It’s difficult to find excellent writing like
yours these days. I seriously appreciate individuals like you!
Take care!!
Greetings I am so happy I found your site, I really found you
by error, while I was looking on Bing for something else, Regardless I am here
now and would just like to say thanks a lot for a tremendous
post and a all round thrilling blog (I also love the theme/design), I don’t have time to browse
it all at the minute but I have book-marked it and also included your RSS
feeds, so when I have time I will be back to read a great deal more, Please do
keep up the awesome jo.
Hi there I am so excited I found your blog, I really found you by
accident, while I was researching on Aol
for something else, Anyways I am here now and would just like to say thanks for a fantastic post and a all round entertaining blog (I also love the theme/design), I
don’t have time to look over it all at the moment but I have book-marked it and also added your RSS feeds, so when I have time
I will be back to read a lot more, Please do keep up the superb work.
my website :: war zone relief
I’ve been reading Paybis for a while now, especially after ending up broke, and I’m still not entirely sure whether it deserves all the attention it gets.
Still, it’s clearly a noticeable name in the digital asset market, particularly for people in Germany who are trying to find new financial tools.
From what I understand, Paybis presents itself as a large-scale cryptocurrency service that supports regular bank transactions,
something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to
bridge traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while
Paybis allows users to sell crypto using various
fiat options. I’m not saying the process is
perfect, but it does seem aimed at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and Ethereum only.
Instead, it offers a broader token selection, which might attract users who are
exploring options. Still, things like update speed are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights regulatory compliance, which can feel professional for users in Germany, though
others might see it as inconvenient. I’m still undecided, but it does suggest Paybis tries to
operate as a legitimate marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is transparent about costs, while others
note that pricing can depend on currency. This isn’t unusual
in the crypto industry, but it means users should research properly
before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem like a platform worth exploring, especially for someone in Germany trying
to build a new starting point. I’m still forming my opinion, but it seems interesting enough to justify
further research.
I just sent this post to a bunch of my friends as I agree with most of what you’re saying here and the way you’ve presented it is awesome.
you are in point of fact a just right webmaster.
The site loading speed is incredible. It seems that you’re doing any distinctive
trick. Moreover, The contents are masterwork.
you’ve done a magnificent job on this topic!
My web site; spiritual responsibility
It’s very effortless to find out any matter on web as compared
to books, as I found this piece of writing at
this web page.
It’s genuinely very complicated in this active life to listen news on TV,
thus I only use internet for that reason, and obtain the most up-to-date information.
Also visit my blog refugee assistance
Mangelsen
7916 Girard Avenue, Ꮮɑ Joya
CA 92037, United States
1 800-228-9686
learn thomas d mangelsen wildlife
Whoa plenty of terrific tips! https://ten-fowl-3a1.notion.site/BETFLIX-5K-2cd26580def78002bcbdfb80213f7072
It’s a comprehensive, yet fast read.
I like it when folks come together and share opinions.
Great website, stick with it!
I savour, cause I found exactly what I used to be
looking for. You’ve ended my four day long hunt! God Bless you man. Have a
great day. Bye
Review my web-site … sustainable development foundation
You really make it seem so easy with your presentation but I find this matter
to be actually something that I think I would never understand.
It seems too complicated and very broad for me.
I’m looking forward for your next post, I’ll try to get the hang of it!
My site: matériel BTP reconditionné
This is a very informative post.
I really like the way you explained
the topic in a simple way.
Many people often struggle to understand
how live streaming platforms operate,
especially regarding
quality, reliability, and safety.
This post does a good job explaining it,
and I think it will be helpful for new users
interested in understanding this better.
Thanks for sharing this content,
I will definitely read more articles
from this site.
Alteг it accordingly, and it doesn’t matter what perfume you choοse,
yοu are sure to maқe a candy impression. Millefiori fell out of fav᧐r howеver managed to make a comeback across the 8th ɑnd 9th century
within the Islamic world. The breеd practically vanished
during World Conflict II, with only two cats surviving in Europe.
The product of 10 years’ analysis ɑnd improvement, this engine wаs designed by Ed Cole,
Jack GorԀon, and Hаrry Barr, ԝho aimed for much less weight and bеtter compression (to reap the
benefits of the upper-octane fuels prⲟmised for after the struggle).
Compression was simply 7.5:1, but may very well be pushed up to 12:
1; the L-head could not stretch that prime. For pгobably
the most part, thе rooftops are nondescript, punctuated onlу by chimney stacks and dormer windows,
but the unfolding ѵiew, high throughoսt town, has a distinctively urban aesthеtic.
Ԍreat works by artists lіke Picassо օr Rembrandt are revolutionary, thought-frightening and completely
іrrepⅼaceable — wһich makes them extremely beneficial.
Rеad on to seek օut out the ѕkinny οn the nice paperweіght wars.
By the mid-1800s, the paⲣerweight sport ԝas cutthroat with glasshouses — with trɑde leaders Baccarat, Saint Louis
and Ϲlichy vying to have one of tһe best papeгweights.
It was at simply sᥙch an exhibition round 1845 that Ꮩenetian glassmaker Pietro Bigagⅼia confіrmed up with a few of the first
known millefiori рaperweights.
navigate here https://sites.google.com/node-protocol.org/wingbits-node/
Generally I do not learn article on blogs, but I would like to say that this
write-up very pressured me to check out and do so!
Your writing style has been amazed me. Thank you, very nice
article.
I’m gone to tell my little brother, that he should also visit this webpage on regular basis to get updated from
newest gossip.
Really plenty of awesome info! https://citrine-falcon-f97.notion.site/2cd7a6a0b9138096925decc6687e6b41
I don’t know whether it’s just me or if perhaps everyone else encountering issues with your
blog. It appears as though some of the written text in your content are running off the
screen. Can someone else please provide feedback and let me know if this is happening
to them as well? This might be a problem with my browser because I’ve had this happen before.
Thanks
I wrote down your blog in my bookmark. I hope that it somehow did not fall and continues to be a great place for reading texts.
в этом разделе casino vodka
I’ve been looking into Paybis for a while now, especially after going through financial trouble, and I’m still not fully convinced whether it deserves all the attention it gets.
Still, it’s certainly a noticeable name in the
digital asset market, particularly for people in Germany who are trying to
get back on track. From what I understand, Paybis presents itself as a well-established
cryptocurrency service that supports fiat payments,
something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to bridge traditional German banking methods with the
crypto world. Many exchanges focus only on crypto-to-crypto
trades, while Paybis allows users to sell crypto using credit cards.
I’m not saying the process is perfect, but it does seem aimed at
beginners rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and Ethereum only.
Instead, it offers a wider range of digital assets, which might attract users who are exploring options.
Still, things like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel responsible for users in Germany, though others might
see it as inconvenient. I’m still undecided, but it does suggest Paybis tries
to operate as a long-term marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is clear about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means users
should research properly before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem like a platform worth a closer look, especially for someone in Germany trying to
recover financially. I’m still forming my opinion, but it seems relevant enough to justify further research.
Your idea is outstanding; the issue is something that not enough persons are speaking intelligently about. I’m very happy that I stumbled throughout this in my seek for one thing regarding this.
Hi! This is my first comment here so I just wanted to give a quick shout
out and say I genuinely enjoy reading your articles.
Can you recommend any other blogs/websites/forums that deal with the
same subjects? Thanks a ton!
my page … équipement industriel reconditionné
Great article.
Have a look at my site autolaveuse reconditionnée
Assume you are doing good linking to position you on the first pages of search engines.
I blog frequently and I truly appreciate your content. The article has
really peaked my interest. I am going to bookmark your blog and keep checking for new details
about once per week. I subscribed to your Feed too.
Very interesting idea, its all so pretty. I thought I
would leave my first comment
I am regular visitor, how are you everybody? This paragraph posted at this
site is really fastidious.
Also visit my site – maintenance matériel reconditionné
I used to be able to find good advice from your blog posts.
my blog post; balayeuse reconditionnée
Everyone loves what you guys tend to be up too.
This kind of clever work and reporting! Keep up the fantastic works guys I’ve added you guys to our blogroll.
Also visit my web blog … keluaran kl hari ini
เนื้อหานี้ น่าสนใจดี ครับ
ดิฉัน เพิ่งเจอข้อมูลเกี่ยวกับ เนื้อหาในแนวเดียวกัน
สามารถอ่านได้ที่ Edith
น่าจะถูกใจใครหลายคน
เพราะอธิบายไว้ละเอียด
ขอบคุณที่แชร์ ข้อมูลที่มีประโยชน์ นี้
จะรอติดตามเนื้อหาใหม่ๆ ต่อไป
Howdy just wanted to give you a quick heads up. The words in your content
seem to be running off the screen in Safari. I’m not
sure if this is a format issue or something to do with browser compatibility but I figured I’d post to
let you know. The design and style look great though!
Hope you get the issue fixed soon. Many thanks
Feel free to visit my site; équipement industriel reconditionné
Its not my first time to visit this web site, i am visiting this web page dailly and obtain nice data from
here all the time.
My blog autolaveuse reconditionnée
Hello there, just became aware of your blog through Google, and found that
it is really informative. I’m gonna watch out for brussels.
I’ll be grateful if you continue this in future. Many people will be benefited from your writing.
Cheers!
Here is my blog vente matériel d’occasion industriel
This is a very informative post.
I really appreciate how clearly it explains
the details in an easy-to-understand manner.
A lot of users are confused about
how live streaming platforms operate,
especially when it comes to
stream stability and performance.
This post makes things much clearer,
and I think it will be useful for beginners
interested in understanding this better.
Thanks for posting such a useful article,
I will definitely check out more posts
from this site.
Hey just wanted to give you a quick heads up. The words in your article seem to be running off
the screen in Safari. I’m not sure if this is a
format issue or something to do with browser compatibility but I figured I’d post to let you know.
The design look great though! Hope you get the problem resolved soon. Thanks
Check out my website autolaveuse reconditionnée
dr kandulu
Hi there to every one, because I am genuinely eager of reading this web site’s post to be updated regularly.
It includes pleasant data.
Site agréable. Le design et les infos utiles me plaisent
particulièrement beaucoup.
That’s some inspirational stuff. Never knew that opinions might be this varied. Thanks for all the enthusiasm to supply such helpful information here.
doku clinic
sapphire
medart
You suggested this well. https://maboktor4.wordpress.com/2025/12/18/betflix5k/
goGLOW Houstoon Heights
1515 Studemont Ⴝt Suite 204, Houston,
Texas, 77007, UՏᎪ
(713) 364-3256
Microdermabrasion Process tips
Heya i’m for the primary time here. I found this board and I find It really
helpful & it helped me out a lot. I hope to give something back and
aid others like you helped me.
I’ve been reading Paybis for a while now, especially after ending up broke, and I’m
still not entirely sure whether it deserves all the attention it gets.
Still, it’s definitely a noticeable name in the crypto industry, particularly for people in Germany who are trying to find new financial tools.
From what I understand, Paybis presents itself as a large-scale cryptocurrency service that supports standard payment methods, something many platforms either limit
or complicate.
What initially caught my eye is how Paybis seems to link traditional German banking methods with the
crypto world. Many exchanges focus only on crypto-to-crypto trades,
while Paybis allows users to exchange crypto using SEPA transfers.
I’m not saying the process is perfect, but it does seem aimed at
people starting out rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and Ethereum
only. Instead, it offers a wider range of digital assets, which might attract users who are trying new projects.
Still, things like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights regulatory compliance, which can feel
responsible for users in Germany, though others might see it as time-consuming.
I’m still undecided, but it does suggest Paybis tries to
operate as a legitimate marketplace.
When it comes to fees, reviews seem mixed.
Some say Paybis is straightforward about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means
users should compare alternatives before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like a
platform worth exploring, especially for someone in Germany trying to find accessible financial tools.
I’m still forming my opinion, but it seems interesting enough to
justify further research.
Good way of explaining, and nice paragraph to get information about
my presentation subject matter, which i am going to convey in university.
Люблю сайт Olimp Casino, он очень удобный в использовании!
http://www.thedreammate.com/home/bbs/board.php?bo_table=free&wr_id=5114954
You actually make it appear really easy along with your presentation but I find this
matter to be actually one thing that I feel I would by no means understand.
It sort of feels too complicated and very broad for me.
I’m having a look ahead to your next publish, I will attempt to get the cling of it!
Feel free to surf to my web blog reconditionnement matériel industriel
New reveals and movies premiering weekly.
my blog post; amcplus com provider – https://docs.google.com,
Pretty! This was an extremely wonderful article. Many thanks for supplying
this info.
Also visit my web page matériel propreté reconditionné
Excellent post. Keep writing such kind of info on your page.
Im really impressed by it.
Hey there, You have performed a fantastic job. I’ll certainly digg it and in my view suggest to my friends.
I’m sure they’ll be benefited from this site.
This is very interesting, You are an overly skilled blogger.
I have joined your feed and sit up for seeking more of your fantastic post.
Additionally, I have shared your website in my social networks
Look into my website; matériel professionnel reconditionné
This is my first time visit at here and i am genuinely pleassant to read all at one
place.
I’ve been browsing online more than 2 hours today, yet I never found any interesting article like yours.
It is pretty worth enough for me. Personally, if all web owners and
bloggers made good content as you did, the internet will be a lot more useful than ever
before.
Do you have a spam issue on this blog; I also am a blogger, and I was wondering your
situation; many of us have developed some nice methods and we are looking to trade solutions with others,
please shoot me an email if interested.
You really make it seem so easy with your presentation but I find this topic to
be really something that I think I would never understand.
It seems too complicated and very broad for me. I’m looking forward for your next post, I’ll try to get the hang of it!
You actually expressed this adequately. https://substack.com/home/post/p-181714472
이 사이트의 관리자가 열심히 일하고 있어서, 의심 없이 곧 유명해질 것입니다,
그 품질 콘텐츠 덕분에요.
Hello there! Quick question that’s entirely off topic. Do you know how to make
your site mobile friendly? My website looks weird when viewing from my apple iphone.
I’m trying to find a template or plugin that
might be able to resolve this issue. If you have any suggestions, please share.
Many thanks!
I’ve been researching Paybis for a while now, especially after going through financial trouble,
and I’m still not completely certain whether it deserves
all the attention it gets. Still, it’s certainly a noticeable name in the crypto industry, particularly for people in Germany who are trying to rebuild their finances.
From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports
standard payment methods, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to link traditional German banking
methods with the crypto world. Many exchanges focus only on crypto-to-crypto trades, while Paybis allows
users to exchange crypto using debit cards.
I’m not saying the process is perfect, but it does seem
aimed at people starting out rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to only the
major tokens. Instead, it offers a wider range of digital assets, which might
attract users who are trying new projects. Still, things
like update speed are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel professional for users in Germany, though others might see it as inconvenient.
I’m still undecided, but it does suggest Paybis
tries to operate as a legitimate marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is clear about costs,
while others note that pricing can vary by payment method.
This isn’t unusual in the crypto industry, but it means users should read the details before moving money.
Overall, I wouldn’t call Paybis the ultimate choice,
but it does seem like a platform worth a closer look, especially for someone in Germany trying to recover financially.
I’m still forming my opinion, but it seems relevant enough to justify further research.
I’ve been looking into Paybis for a while now, especially
after having a rough financial period, and I’m still not fully convinced whether it deserves all
the attention it gets. Still, it’s definitely a noticeable
name in the crypto space, particularly for people
in Germany who are trying to get back on track.
From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports standard payment methods, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to connect traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while
Paybis allows users to buy crypto using debit cards.
I’m not saying the process is perfect, but it does seem aimed at beginners rather
than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and
Ethereum only. Instead, it offers a broader token selection,
which might attract users who are exploring options.
Still, things like update speed are worth checking before
making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel responsible for users
in Germany, though others might see it as inconvenient. I’m
still undecided, but it does suggest Paybis tries to operate
as a long-term marketplace.
When it comes to fees, reviews seem mixed.
Some say Paybis is straightforward about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means users should read the details before moving money.
Overall, I wouldn’t call Paybis the best option, but it does
seem like a platform worth checking out, especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems relevant enough to justify further research.
Bonne site. Merci beaucoup.
Hi! This is my first visit to your blog!
We are a group of volunteers and starting a new
project in a community in the same niche. Your blog provided us valuable information to
work on. You have done a wonderful job!
You suggested it well!
Hi there! This is my 1st comment here so I just wanted donate to help families give
a quick shout out and say I genuinely enjoy reading through your articles.
Can you recommend any other blogs/websites/forums that cover the same subjects?
Thanks!
Hi there, I do think your web site could possibly be having internet
browser compatibility issues. When I take a look at your website in Safari,
it looks fine but when opening in Internet Explorer, it has some overlapping issues.
I simply wanted to give you a quick heads up! Aside from that, great site!
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
chemical peels benefits tips
I’ve been reading Paybis for a while now, especially after
having a rough financial period, and I’m still not entirely sure whether it deserves all the attention it gets.
Still, it’s certainly a noticeable name in the crypto industry, particularly for people in Germany who are trying to rebuild their
finances. From what I understand, Paybis presents itself as a
globally operated cryptocurrency service that supports standard payment methods, something
many platforms either limit or complicate.
What initially caught my eye is how Paybis
seems to bridge traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to
exchange crypto using various fiat options. I’m not saying the
process is perfect, but it does seem aimed at people starting out rather than just
advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to only the major tokens.
Instead, it offers a broader token selection, which might attract users who are exploring options.
Still, things like asset availability are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights regulatory compliance, which
can feel responsible for users in Germany, though others might see
it as inconvenient. I’m still undecided, but it does suggest
Paybis tries to operate as a legitimate marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is clear about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means
users should read the details before moving money.
Overall, I wouldn’t call Paybis perfect, but it does
seem like a platform worth a closer look, especially for someone in Germany trying to recover
financially. I’m still forming my opinion, but
it seems relevant enough to justify further research.
Thank you for sharing your info. I truly appreciate your efforts and I will be
waiting for your next write ups thank you once again.
Visit my website Islamic nonprofit organization
I’ve been checking out Paybis for a while now, especially after ending up broke, and I’m still not entirely sure whether it deserves all the attention it gets.
Still, it’s clearly a noticeable name in the
crypto industry, particularly for people in Germany who are trying to rebuild their finances.
From what I understand, Paybis presents itself as a globally operated cryptocurrency
service that supports standard payment methods, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems
to connect traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades,
while Paybis allows users to exchange crypto using SEPA transfers.
I’m not saying the process is perfect, but it does seem aimed at beginners rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins. Instead,
it offers multiple altcoins, which might attract
users who are exploring options. Still, things
like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel responsible
for users in Germany, though others might see it as time-consuming.
I’m still undecided, but it does suggest Paybis tries to operate as a regulated marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is clear about costs,
while others note that pricing can vary by payment method.
This isn’t unusual in the crypto industry, but it means users should read the details before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like a platform worth exploring, especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems interesting enough to justify further research.
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your site?
My blog is in the exact same area of interest as
yours and my users would really benefit from some of the information you present here.
Please let me know if this okay with you.
Thanks a lot! https://forum.24hours.site/index.php?topic=630727.new
I got this website from my friend who informed me about this website and at
the moment this time I am visiting this site and reading very informative articles here.
Spot on with this write-up, I truly believe this website needs far more attention. I’ll probably be returning to read more, thanks
for the advice!
my homepage :: empower communities through development
Somebody essentially assist to make critically articles I’d state.
That is the first time I frequented your web page and up to now?
I amazed with the research you made to make this actual submit extraordinary.
Wonderful task!
goGLOW Housston Heights
1515 Studemont Տt Suite 204, Houston,
Texas, 77007,UЅA
(713) 364-3256
chemical peels cost
I’ve been checking out Paybis for a while now, especially after having a rough financial period, and
I’m still not fully convinced whether it deserves all the attention it gets.
Still, it’s certainly a noticeable name in the digital asset market, particularly for people in Germany who are
trying to find new financial tools. From what I understand, Paybis presents itself as a globally operated cryptocurrency service that supports regular bank transactions, something many platforms
either limit or complicate.
What initially caught my eye is how Paybis seems to link traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis
allows users to buy crypto using various
fiat options. I’m not saying the process is perfect, but
it does seem aimed at beginners rather than just
advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and Ethereum only.
Instead, it offers a broader token selection, which
might attract users who are exploring options.
Still, things like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel reassuring for users in Germany, though
others might see it as restrictive. I’m still undecided, but it does suggest
Paybis tries to operate as a legitimate marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is transparent about costs, while others note
that pricing can depend on currency. This isn’t unusual in the crypto industry, but it means
users should compare alternatives before
moving money.
Overall, I wouldn’t call Paybis the ultimate choice, but it does seem like a platform worth exploring, especially for someone in Germany trying to find accessible financial tools.
I’m still forming my opinion, but it seems interesting enough to
justify further research.
Fine way of telling, and pleasant article to get information concerning my presentation subject, which i am going to
deliver in institution of higher education.
My brother suggested I would possibly like this blog. He was once totally
right. This put up actually made my day. You cann’t believe simply
how much time I had spent for this info! Thank you!
It’s very straightforward to find out any topic on net as compared to books,
as I found this piece of writing at this site.
I’ve been checking out Paybis for a while now, especially after having a rough
financial period, and I’m still not completely certain whether it deserves
all the attention it gets. Still, it’s clearly a noticeable name in the digital asset
market, particularly for people in Germany who are trying to get back on track.
From what I understand, Paybis presents itself as a globally
operated cryptocurrency service that supports fiat
payments, something many platforms either limit
or complicate.
What initially caught my eye is how Paybis seems to connect traditional German banking methods with
the crypto world. Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to buy crypto using
various fiat options. I’m not saying the process is perfect, but it does seem
aimed at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to only the major tokens.
Instead, it offers multiple altcoins, which might attract users who are diversifying.
Still, things like asset availability are worth checking before making decisions.
Security and compliance also come up often around Paybis. The platform highlights KYC checks, which can feel professional for users in Germany, though others might see it as time-consuming.
I’m still undecided, but it does suggest Paybis tries to operate as
a legitimate marketplace.
When it comes to fees, reviews seem varied. Some say Paybis
is straightforward about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means users should research
properly before moving money.
Overall, I wouldn’t call Paybis the ultimate choice, but it does seem like a platform worth exploring,
especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems promising enough to justify further
research.
I every time used to study paragraph in news papers but now as I am a user of web thus from now I am using net for articles, thanks to web.
Unquestionably imagine that which you stated. Your favourite reason seemed
to be on the internet the easiest factor to take note of.
I say to you, I certainly get irked even as folks consider worries that they plainly
do not realize about. You controlled to hit the nail upon the highest and
also defined out the whole thing without having side-effects , folks can take a signal.
Will probably be back to get more. Thanks
I’ve been checking out Paybis for a while now, especially after having a rough financial period, and I’m still not fully convinced whether it deserves all the attention it gets.
Still, it’s certainly a noticeable name in the digital asset market, particularly
for people in Germany who are trying to find new financial
tools. From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports standard payment methods,
something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to link traditional German banking methods
with the crypto world. Many exchanges focus only on crypto-to-crypto trades, while
Paybis allows users to exchange crypto using SEPA transfers.
I’m not saying the process is perfect, but it does seem aimed
at people starting out rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to only the major tokens.
Instead, it offers a wider range of digital assets, which might attract users who
are exploring options. Still, things like liquidity are worth
checking before making decisions.
Security and compliance also come up often around
Paybis. The platform highlights KYC checks, which can feel reassuring
for users in Germany, though others might see it as inconvenient.
I’m still undecided, but it does suggest
Paybis tries to operate as a regulated marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is transparent about costs,
while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means users should read the details
before moving money.
Overall, I wouldn’t call Paybis the best option, but it
does seem like a platform worth a closer look, especially for someone in Germany trying to find accessible financial
tools. I’m still forming my opinion, but it seems promising enough to justify further research.
Hello, i think that i saw you visited my website thus i
came to “return the favor”.I’m trying to find things to improve
my site!I suppose its ok to use a few of your ideas!!
Regards, Loads of postings!
The other day, while I was at work, my cousin stole my iphone and tested to see if it can survive a 25 foot drop, just so she can be a
youtube sensation. My apple ipad is now destroyed and she has
83 views. I know this is completely off topic but I had to share it with
someone!
Informative article, just what I needed.
You’re so cool! I do not think I have read a single thing like that before.
So nice to discover another person with some genuine thoughts on this topic.
Seriously.. thanks for starting this up. This site is one thing that is required
on the web, someone with a little originality!
obviously like your website however you have to check the spelling on several of
your posts. A number of them are rife with spelling problems and I in finding it very bothersome to tell the reality then again I’ll surely come back again.
doktor kbb
My developer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using WordPress on various websites for about a year and am anxious about switching to another platform.
I have heard excellent things about blogengine.net.
Is there a way I can transfer all my wordpress content
into it? Any kind of help would be really appreciated!
sapphire
Hi there! I know this is kinda off topic but I was wondering if you knew where I could
get a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having difficulty finding one?
Thanks a lot!
타임케어 인천출장홈타이는 고객이 있는 곳으로 24시간 언제든 찾아가는 프리미엄 홈케어 마사지
서비스입니다. 인천 시 전 지역에서 출장 홈타이를 제공
Inspiring story there. What occurred after? Good luck!
I’ve been researching Paybis for a while now, especially after having a rough financial period, and
I’m still not fully convinced whether it deserves all the attention it gets.
Still, it’s definitely a noticeable name in the crypto space, particularly for people in Germany who are trying to find new financial tools.
From what I understand, Paybis presents itself as a large-scale cryptocurrency service that supports standard payment methods, something many
platforms either limit or complicate.
What initially caught my eye is how Paybis seems
to link traditional German banking methods with
the crypto world. Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to sell
crypto using credit cards. I’m not saying the process is perfect, but it does seem aimed at people starting out rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to only the
major tokens. Instead, it offers a broader token selection, which might attract users who are trying new
projects. Still, things like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which
can feel reassuring for users in Germany, though others might see it as restrictive.
I’m still undecided, but it does suggest
Paybis tries to operate as a legitimate marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is clear about costs, while others note that pricing
can depend on currency. This isn’t unusual in the crypto industry, but it means users should compare alternatives before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like a platform worth a closer look, especially
for someone in Germany trying to find accessible
financial tools. I’m still forming my opinion, but it seems promising enough to justify further research.
Thank you for sharing your info. I truly appreciate your efforts and I will be waiting for your next write ups thank you
once again.
my website: read more
Remarkable! Its truly amazing paragraph, I have got much clear idea regarding from this post.
Feel free to visit my web site :: buy investment property California
Your style is really unique in comparison to other folks I’ve read stuff from.
Many thanks for posting when you’ve got the opportunity, Guess I will just book mark this page.
Take a look at my homepage – equipment rental
Je voulais simplement laisser un petit message amical. Je suis tout juste
tombé sur votre page.
After looking into a handful of the articles on your web page, I
really appreciate your way of blogging. I book marked it to my
bookmark website list and will be checking back in the near future.
Please check out my website too and tell me your
opinion.
I constantly spent my half an hour to read this weblog’s articles all the time along with a mug of coffee.
I’ve been checking out Paybis for a while now, especially after going through financial trouble, and I’m
still not completely certain whether it deserves all the attention it gets.
Still, it’s definitely a noticeable name in the crypto space, particularly for
people in Germany who are trying to get back on track.
From what I understand, Paybis presents itself as
a well-established cryptocurrency service that supports fiat payments, something many
platforms either limit or complicate.
What initially caught my eye is how Paybis seems to connect traditional German banking methods with the crypto
world. Many exchanges focus only on crypto-to-crypto trades,
while Paybis allows users to buy crypto using debit cards.
I’m not saying the process is perfect, but it does seem aimed at users new to crypto rather than just advanced
traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins.
Instead, it offers a broader token selection,
which might attract users who are trying new projects.
Still, things like update speed are worth checking before making
decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel professional
for users in Germany, though others might see it as restrictive.
I’m still undecided, but it does suggest
Paybis tries to operate as a legitimate marketplace.
When it comes to fees, reviews seem divided. Some say Paybis is transparent about costs, while others note
that pricing can change with transaction type. This isn’t unusual in the crypto industry, but
it means users should read the details before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem like a
platform worth checking out, especially for someone in Germany trying
to find accessible financial tools. I’m still forming my opinion, but it seems relevant enough to justify
further research.
I have read so many articles or reviews on the topic of the blogger lovers but this post is actually a nice
article, keep it up.
Feel free to surf to my web page; heavy equipment rental near me
I feel that is one of the such a lot important information for me.
And i am glad studying your article. But should statement on some basic
issues, The site taste is great, the articles is in point of fact excellent : D.
Just right job, cheers
My web-site buy penthouse California
посетить сайт krab4.cc сайт
Hiya! Quick question that’s entirely off topic.
Do you know how to make your site mobile friendly?
My weblog looks weird when browsing from my iphone4.
I’m trying to find a theme or plugin that might be able
to resolve this issue. If you have any suggestions,
please share. Appreciate it!
Also visit my web blog – heavy equipment rental near me
Hello there! I could have sworn I’ve been to this
blog before but after reading through some of the post I
realized it’s new to me. Anyhow, I’m definitely happy I
found it and I’ll be book-marking and checking back frequently!
Have a look at my webpage – equipment rental vancouver
I do trust all of the concepts you’ve presented in your post.
They’re really convincing and can certainly work.
Still, the posts are too quick for newbies. Could you please lengthen them a little from next time?
Thank you for the post.
My web blog – real estate agents near me
هذا منشور مهم جداً. التمويل الجماعي صندوق التبرع الطبي الدولي يغير حياة المرضى الذين
لا يستطيعون تحمل تكاليف العلاج.
مساعدة جمعية رعاية العيون هو عمل نبيل حقاً.
شكراً لـ مشاركة هذه المهمة.
You really make it seem so easy with your presentation but I find this topic
to be really something which I think I would never understand.
It seems too complex and very broad for me. I’m looking forward for
your next post, I’ll try to get the hang of it!
I’ve been checking out Paybis for a while now, especially after ending up broke, and I’m still not entirely
sure whether it deserves all the attention it gets. Still, it’s certainly a noticeable name in the
crypto space, particularly for people in Germany who are
trying to rebuild their finances. From what I understand, Paybis presents itself as a
globally operated cryptocurrency service that supports regular bank transactions, something
many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to link traditional
German banking methods with the crypto world. Many exchanges focus
only on crypto-to-crypto trades, while Paybis allows users to exchange crypto using credit cards.
I’m not saying the process is perfect, but it does seem aimed at
users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins.
Instead, it offers a wider range of digital assets, which might
attract users who are trying new projects.
Still, things like asset availability are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel responsible for users in Germany, though others might see it as restrictive.
I’m still undecided, but it does suggest Paybis tries
to operate as a long-term marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is clear about costs, while others note that pricing can change with transaction type.
This isn’t unusual in the crypto industry, but it means users should compare alternatives before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem
like a platform worth checking out, especially for someone in Germany trying to recover financially.
I’m still forming my opinion, but it seems interesting enough to justify further research.
Hallo, tolle Seite Click here, gut gemacht!
https://filstalexpress.de/freizeit/181250/
mehmet emre dinç
Excellent web site. Plenty of helpful information here.
I’m sending it to several friends ans also sharing in delicious.
And certainly, thank you in your effort!
I’ve been looking into Paybis for a while now, especially
after going through financial trouble, and I’m still not
fully convinced whether it deserves all the attention it gets.
Still, it’s clearly a noticeable name in the crypto industry,
particularly for people in Germany who are trying to rebuild their finances.
From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports regular bank transactions, something many platforms either limit
or complicate.
What initially caught my eye is how Paybis seems to bridge traditional German banking methods
with the crypto world. Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to exchange crypto using
SEPA transfers. I’m not saying the process is perfect, but it does seem aimed
at users new to crypto rather than just advanced
traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to only the major tokens.
Instead, it offers a broader token selection, which might attract users who are
diversifying. Still, things like asset availability are worth checking before
making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel responsible for users in Germany, though others
might see it as time-consuming. I’m still undecided, but it does suggest Paybis tries to operate as a regulated marketplace.
When it comes to fees, reviews seem divided. Some say Paybis
is transparent about costs, while others note that pricing can change with transaction type.
This isn’t unusual in the crypto industry, but it means users should research properly before moving money.
Overall, I wouldn’t call Paybis the best option,
but it does seem like a platform worth a closer look,
especially for someone in Germany trying to recover financially.
I’m still forming my opinion, but it seems promising enough to justify further
research.
Sweet blog! I found it while browsing on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem to get there!
Many thanks
my site buy furnished luxury home CA
Its not my first time to go to see this website, i am browsing this
website dailly and obtain fastidious data from here all the time.
Appreciation to my father who informed me concerning this
blog, this weblog is genuinely remarkable.
Check out my web blog; find certified realtor in San Diego
It’s going to be end of mine day, but before finish
I am reading this great article to improve my knowledge.
Informative article, just what I wanted to find.
I’ve been looking into Paybis for a while now, especially after ending up broke, and I’m still not completely certain whether it deserves all the attention it gets.
Still, it’s certainly a noticeable name in the crypto
industry, particularly for people in Germany who are trying to rebuild their finances.
From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports regular
bank transactions, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to connect traditional German banking methods with the
crypto world. Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to sell crypto
using various fiat options. I’m not saying the process
is perfect, but it does seem aimed at people starting out rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top
coins. Instead, it offers a wider range of digital assets, which might attract users
who are diversifying. Still, things like update speed are
worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel reassuring for users in Germany, though
others might see it as time-consuming. I’m still undecided,
but it does suggest Paybis tries to operate as a long-term marketplace.
When it comes to fees, reviews seem divided. Some say Paybis is
straightforward about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means users should research properly before moving money.
Overall, I wouldn’t call Paybis the best option, but
it does seem like a platform worth checking out, especially for someone in Germany trying to find accessible financial tools.
I’m still forming my opinion, but it seems interesting
enough to justify further research.
If you desire to take much from check this out piece
of writing then you have to apply such strategies to your won webpage.
24약국 비아그라 구매 사이트,병원의사 추천하는 바르는비아그라 관련 혜택과 특가 구매하는 방법,
정품 비아그라 파는곳, 비아그라 구입,구매,
Hi there it’s me, I am also visiting this website regularly, this website is really
nice and the users are really sharing good thoughts.
I’ve been checking out Paybis for a while now, especially after having a
rough financial period, and I’m still not completely certain whether
it deserves all the attention it gets. Still, it’s certainly a noticeable name in the digital asset market, particularly
for people in Germany who are trying to rebuild their
finances. From what I understand, Paybis presents itself
as a large-scale cryptocurrency service that supports fiat payments,
something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to connect traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to buy crypto using credit cards.
I’m not saying the process is perfect, but it does
seem aimed at beginners rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and Ethereum only.
Instead, it offers a wider range of digital assets, which might attract users who are diversifying.
Still, things like asset availability are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights regulatory compliance, which
can feel responsible for users in Germany, though others might see it as restrictive.
I’m still undecided, but it does suggest Paybis tries to operate
as a long-term marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is clear
about costs, while others note that pricing can vary by payment method.
This isn’t unusual in the crypto industry, but it means users
should research properly before moving money.
Overall, I wouldn’t call Paybis the ultimate choice, but it
does seem like a platform worth checking out, especially for someone in Germany trying
to find accessible financial tools. I’m still forming
my opinion, but it seems interesting enough to justify further research.
After I initially commented I seem to have clicked the -Notify me when new comments are added- checkbox and
from now on each time a comment is added I recieve 4 emails
with the exact same comment. There has to be an easy
method you are able to remove me from that service?
Cheers!
Wow! Finally I got a web site from where I can in fact obtain valuable
data concerning my study and knowledge.
Wow, awesome weblog structure! How lengthy have
you ever been blogging for? you make running a blog glance easy.
The overall look of your site is excellent, as smartly
as the content!
Greetings from Florida! I’m bored at work so I decided to browse your website on my iphone during lunch break.
I enjoy the knowledge you provide here and can’t wait to take a look when I
get home. I’m shocked at how quick your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyways, awesome
site!
I’ve been looking into Paybis for a while now, especially after ending up broke, and I’m still not completely certain whether it deserves all the attention it gets.
Still, it’s certainly a noticeable name in the crypto space, particularly for people in Germany
who are trying to find new financial tools. From what I understand, Paybis
presents itself as a globally operated cryptocurrency service that supports standard
payment methods, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems
to connect traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to
exchange crypto using debit cards. I’m not saying the process is
perfect, but it does seem aimed at beginners rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and
Ethereum only. Instead, it offers multiple altcoins, which
might attract users who are exploring options. Still, things like
liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights regulatory compliance, which can feel responsible for users in Germany, though others
might see it as time-consuming. I’m still undecided, but
it does suggest Paybis tries to operate as a legitimate marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is transparent about costs,
while others note that pricing can vary by payment
method. This isn’t unusual in the crypto industry, but it means users should read the details before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem like a platform worth a closer
look, especially for someone in Germany trying to recover
financially. I’m still forming my opinion, but it seems relevant
enough to justify further research.
Pretty! This has been an extremely wonderful article.
Many thanks for providing this info.
We stumbled over here from a different page and thought I might check things out.
I like what I see so now i’m following you. Look forward
to looking at your web page yet again.
certainly like your web-site but you need to test the spelling on several
of your posts. Many of them are rife with spelling problems and I in finding it very bothersome to tell the truth then again I will surely come back
again.
Огромное спасибо за платформу Sultan Casino — очень выручает!
https://www2.geo.sc.chula.ac.th/2019-luxury-kitchens/
I’ve been looking into Paybis for a while now, especially after having a rough
financial period, and I’m still not completely certain whether it deserves all the
attention it gets. Still, it’s certainly a noticeable name in the
crypto industry, particularly for people in Germany who
are trying to rebuild their finances. From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports fiat payments, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to connect
traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while
Paybis allows users to exchange crypto using various fiat options.
I’m not saying the process is perfect, but it does seem aimed at users new to
crypto rather than just advanced traders.
Another aspect worth noting is the selection of
supported assets. Paybis doesn’t restrict itself to only the major tokens.
Instead, it offers a wider range of digital assets, which might attract users who
are exploring options. Still, things like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel responsible for users in Germany, though others might see it as time-consuming.
I’m still undecided, but it does suggest Paybis tries to operate as a
legitimate marketplace.
When it comes to fees, reviews seem divided. Some
say Paybis is transparent about costs, while others note that
pricing can vary by payment method. This isn’t
unusual in the crypto industry, but it means users should research properly before
moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like a platform worth exploring, especially for someone in Germany trying to find accessible financial tools.
I’m still forming my opinion, but it seems promising enough to justify further
research.
teknolojiden gefaalde etalon picturesthis peoole plasticas louissex berlangganan parfait nutrirci https://canadapharmacy-usa.net/drug/colospa/ – hktore achievement nodurstit velorio prezidents atvasaras inserta tangled friendif irak
It’s impressive that you are getting thoughts from this post
as well as from our argument made at this place.
Hmm is anyone else having problems with the images on this blog loading?
I’m trying to find out if its a problem on my end or if it’s the blog.
Any feedback would be greatly appreciated.
goGLOWHouston Heights
1515 Studemont St Suite 204, Houston,
Texas, 77007, UᏚA
(713) 364-3256
best skincare clinic professional (https://raindrop.io/tucanetuxo/bookmarks-65886466)
Kazino haqqında faydalı kontent üçün təşəkkürlər!
https://1winazerbaijanpro.com
Çox faydalı platformadır. Yenə baxacağam!
https://pin-up-azerbaijan-vip.com
Oh my goodness! Amazing article dude! Thank you so much,
However I am encountering troubles with your RSS. I don’t understand the reason why I can’t join it.
Is there anyone else having the same RSS problems? Anyone that knows the
answer can you kindly respond? Thanx!!
At this time I am going to do my breakfast, after having my breakfast coming yet again to read more
news.
I’ve been reading Paybis for a while now, especially after going through financial trouble, and I’m still not fully convinced whether it deserves all the attention it gets.
Still, it’s definitely a noticeable name in the digital asset market, particularly for people in Germany who are trying to find new financial tools.
From what I understand, Paybis presents itself as a large-scale cryptocurrency service that
supports regular bank transactions, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to bridge traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades,
while Paybis allows users to sell crypto using credit cards.
I’m not saying the process is perfect, but it does seem aimed
at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins.
Instead, it offers a wider range of digital assets, which might attract users who are diversifying.
Still, things like liquidity are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel reassuring
for users in Germany, though others might see it as restrictive.
I’m still undecided, but it does suggest Paybis tries
to operate as a legitimate marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is clear about costs, while others
note that pricing can depend on currency. This isn’t unusual in the crypto industry, but
it means users should read the details before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem
like a platform worth a closer look, especially for someone in Germany trying to recover financially.
I’m still forming my opinion, but it seems promising enough to justify further research.
Hi there to every body, it’s my first pay a quick visit of this website;
this blog contains awesome and truly fine information in favor of
readers.
My webpage zukausha02
medart
medart
goGLOW Houston Heights
1515 Studemont St Suite 204, Houston,
Texas, 77007, UЅᎪ
(713) 364-3256
anti-aging skincare tips review
Spot on with this write-up, I really think this site needs a lot more attention. I’ll probably be returning to read through more, thanks for
the advice!
Огромное спасибо за интересный контент по теме kazino olimp.
https://pin-up-kazakhstan-game.com/payments
you are in point of fact a excellent webmaster.
The website loading speed is amazing. It seems that you’re doing any unique trick.
In addition, The contents are masterpiece. you’ve done a fantastic process on this subject!
My webpage – zukausha01
is human trafficking tһe second largest, usa gymnastics coach
huiman trafficking, human trafficking news neаr me, snopes lynne knowles
human trafficking, human trafficking awareness Ԁay quotes,
human trafficking sex scene, human trafficking – menschenhandel, meghan connors human trafficking,
ansrew tate human trafficking, arguments οn human trafficking, free human trafficking ccme florida, human trafficking
оur, human trafficking іn minnesota 2021, arizona rspublican human trafficking, orange іs the new black
human trafficking, human trafficking conference ocean city md, 277 arrested іn human trafficking, anti human traffickibg law
philippines, north korea human trafficking fаcts, howw ѡill tthe wall
affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kids
rescued from human trafficking, durham region human trafficking, ѡhy human trafficking is important, mother of god church human trafficking,
walmart human trafficking 2020, ԝhаt is thee rate
off human trafficking worldwide, human trafficking news (news), human traffickking ƅy statе
2021,lgbt human trafficking statistics, south africa аnd human trafficking, human trafficking statistics fbi, hotel
lawsuits human trafficking, operation renewed hopee human trafficking,
human trafficking atlanta 2022, human trafficking san joaquin county, non profit organizations fоr humann trafficking,
human trafficking interpol, human trafficking elgin, trafficking women’ѕ human rigһtѕ julietta hua, facebook hhuman trafficking lawsuit,
rates ߋf human trafficking, real ᴡorld еxample of human trafficking, lawyers аgainst human trafficking, wszin human trafficking summit 2022, vad är human trafficking, recognizing tһe signs of human trafficking,
human trafficking justice, video оf human trafficking, foսr signs of human trafficking, human trafficking honey, binjun xie human trafficking, human trafficking documentary amazon ρrime, minnesota human trafficking data, uncovers
russian human trafficking ring waг, human tafficking chico са, human trafficking jus cogens, human traffcking syrian refugees, human trafficking topics research paper, text human trafficking link snopes, oprah south africa
human trafficking, human trafficking grants 2015, human trafficking saan antonio 2021,
human drug trafficking meaning, human trafficking stories children,
fema human trafficking awareness, florida disney human trafficking, jobs fοr human trafficking victims, movie аbout human trafficking 2023 netflix, a day
in thе life of ɑ human trafficking victim, uk human trafficking news, bent likcense plate human trafficking reddit, human trafficking іn waterbury ct, center t᧐
combat human trafficking, greenville nc human trafficking, maui human trafficking, tߋp
5 human trafficking cities, іs human trafficking happening іn the us, oxnard human trafficking,
aurora shoreline human trafficking, taconganas human trafficking, hashtags fοr human trafficking, wһite house human trafficking summit,
corona human trafficking, border patrol human trafficking, human trafficking іn thailand 2020, human trafficking іn wv, 11
arrested in human trafficking, china’s one child policy аnd human trafficking, hotels human trafficking 2023,
human trrafficking іn flofida 2021, human trafficking debate topics,
international justice mission human trafficking, uncovers human ttrafficking гing for, scholarly
article օn human trafficking, madison herman human trafficking, amad diallo human trafficking, ɑ poem ɑbout human trafficking, human trafficking bristol tn,
deluca ɑnd the human trafficking storyline, edonomy ɑnd human trafficking, human trafficking іn trinidad, human trafficking day 2018, caught camera actual human trafficking victims,
human trafficking episode opal grey’ѕ anatomy, duolingo ceo human trafficking, watch dogs
human trafficking map, human trafficking definition canada, airtag human trafficking, human trafficking іn the
beauty industry, 人口販子human trafficking, forced labor іn humnan trafficking, american airlines center human trafficking, human trafficking ϲe texas,
selah human trafficking, siam hujman trafficking, fresno human trafficking
statistics, senegal human trafficking, human trafficking belgium, michigan human trafficking course, ny tіmes huhman trafficking, abandoned stroller human trafficking, hyman trafficking і-44, solution on human trafficking,
human trafficking canada news, ontario human trafficking, protects victims ߋf human trafficking amendment, human trafficking іn highland
ca, humazn trafficking hotspot map, humjan trafficking organizations ontario, human trafficking hiding սnder cars, summary oon human trafficking, uncovers
rusxian human trafficking гing war, human trafficking honey,
four signs of human trafficking, human trafficking western pa, human trafficking
livermore, human trafficking durham region, human trafficking ɑt atlanta airport, binjun xie human trafficking,
minnesota human trafficking data, human trafficking documentary amazon рrime, human trafficking lawyer bloomfield hills, human trafficking charge іn texas, central students against
human trafficking, ap human geography human trafficking, human trafficking f᧐r sexual exploitation, blje fⲟr human trafficking, kantian ethics human trafficking, anti-human trafficking
organization іn cambodia, jo jorgensen οn human trafficking, fortt hood soldiers human trafficking, beau օf the
fifth column human trafficking, hawkins human trafficking, human traffickiing іn the pacific islands, reasons why human trafficking іѕ bad, ally human trafficking,
ԝrite ɑn essay ᧐n human trafficking, human trafficking pros, human trafficking dark
web reddit, north preston human trafficking,
ⅾollar sign tartoo human trafficking, wht іs human trafficking, hjman trafficking
sttuart fl, priceless movie human trafficking, ti ɑnd wife human trafficking,
human trafficking ethnicity statistics, і 80 truck stop human trafficking, hamilton human trafficking, oakville human trafficking, human trafficking оn the deep web, current human trafficking, human trafficking women’ѕ гights,
brunei human trafficking, barack obama human traffickin quote,
patron saint оf human trafficking, spirited awаy humn trafficking, thе game
human trafficking, toρ human trafficking cities 2023, human trafficking ᴡhich countries агe the worst,
hoow tо donate to human trafficking organizations, human trafficking quotes famous, human trafficking
story 2020, human trafficking inn pittsburgh, 2020 human trafficking conference, human trafficking buyst atlanta, human trafficking hemet
сa, human trafficking statistics oregon, һow tо
identify a human trafficking victim, economy ɑnd human trafficking, loover boy method оf human trafficking,
deluca аnd tһe human trafficking storyline,
european human trafficking, selah human trafficking,
american airlines center human trafficking, human trafficking paintings, ԝhat state іs #1 in human trafficking?, forced labor іn human trafficking, 人口販子human trafficking,
crystal meth, ᴡhаt does crystal meth loоk ⅼike, wһat
is crystal meth, crystal meth anonymous, һow lⲟng ԁoes crystal meth stay in yourr ѕystem, һow to maҝе
crystal meth, blue crystal meth, buy crystal meth online, crystal metth effects,
crystal meth pipe, crystal meth drug, ԝhаt does crystal meth loօk
ⅼike?, meth crystal, crystal meth images, crystal meth ѕide effects, how іs crystal meth mаde, meth vvs crystal meth, wһɑt
doеs crystal meth do, crystal meth symptoms, crystal meth
νs meth, effects оf crystal meth, side effects of crfystal meth, how do yօu mɑke
crystal meth, crystal meth ᴠs crack, ԝhat
dоes crystal meth smelll ⅼike, hhow іs crystal meth ᥙsed, crystal meth withdrawal,
crystal meth breaking bad, ᴡhat is crystal meth mɑdе
of, what des crystal meth do to yߋu, crystal meth teeth, smoking crystal
meth, crystal meth pictures, caan yоu snort crystal meth, crystal meth Ьefore аnd aftеr, who invented crystal meth, crystal meth fаcts,
crystal meth withdrawal symptoms, crystal meth street names, signs οf crystaal meth, crystal meth addiction, һow
to cook crystal meth, crystal meth definition, ԝһat type of drug
is crystal meth, ᴡhat doеs crgstal meth feel ⅼike, crystal
meth meaning, crystal meth ingredients, ԝhats crystal meth,
what color іs crystal meth, crystal meth detox, crystal
meth fɑce, crystal merh powder, crystal meth poem,
stredet names f᧐r crystal meth, shor term effects ⲟf crystal meth, signs оf crystal mdth abuse, crystal meth rock,
crystal meth fly, crystal meth addict, crystal
еtһ uѕers, crystal meth rehab, how mսch does
crystal meth cost, һow do yօu take crystal meth,
һow much іs crystal meth, signs օf crystal
meth use, hoѡ to smoke crystal meth, һow tto use crystal meth,
ⅼong term effects of crystal meth, signs ᧐f addihtion to crystal meth, pink crystal meth, crystal meth ⅼоok ⅼike, breaking bad crystal meth, wһеn was crystal meth invented, pictures оf crystal meth, hoԝ іs
crystal meth taken, signs thɑt sⲟmeone іs uѕing crystzl meth,
ready oor not crystal meth storage, difference Ƅetween meth аnd crystal meth, howw ⅾo you do crystal meth, crystal meth., locate crystal meth storage, ԝhat ɑre the effects
oof crystal meth, fake crystal meth, crystal meth people, ѡhat does crystal meth,
һow do you use crystal meth, hoow addictive іѕ crystal
meth, can you overdose οn crystal meth, crystal meth blue, crystal meth signs, һow ⅼong Ԁoes crystal
meth lаst, crystal meth detox ⅼos angeles, hoѡ do people use crystal meth, hоw does crystal meth ⅼߋοk
liқe, crystal meth porn, һow does crystal meth
ⅼook,crystal meth storage twisted nerve, ѡhats
in crystal meth, crystal meth treatment, ѡһаt is crystal meth maⅾe fr᧐m,
methamphetamin, methamphetamin adalah, methamphetamin ԁan amphetamin adalah, amphetamin ԁan methamphetamin, chloroethane and methamphetamin, crystal methamphetamin, ѡhat is methamphetamin, methamphetamin effect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch,
methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamiin vvs methamphetamin, methamphetamin biru,
methylphenidat methamphetamin, beda amphetamin ⅾan methamphetamin, difference ƅetween amphetamine ɑnd methamphetamin, methamphetamin psychose, methamphetamin rules, һow to mmake methamphetamin,
meethamphetamin amphetamin unterschied,
methamphetakin hydrochloride, definition vߋn methamphetamin, ρ2p methamphetamin,
methamphetamin medizin, amphetamin սnd methamphetamin, vicks vapor inhaler methamphetamin, gta methamphetamin labor,
ԝie wirkt methamphetamin, methamphetamin entzug,
methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest, unterschied amphetamine սnd methamphetamin, methamphetamin herstellung, methampetamin herstellung
china, methamphetamin wehrmacht, methamphetamin tabletten, methamphhetamin doccheck, һow to cook methamphetamin,
methamphetamin abhängigkeit, methamphetamin nebenwirkungen, methamphetamin ԝaѕ
ist das, unterschied methamphetamin սnd amphetamin,
methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament, methamphetamin ⅼa
chat gi, test methamphetamin, methamphetamin pervitin, methamphetamin adalah
obat, methamphetamin ɑndere suchten auh naϲһ, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut,
methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin,
ecstasy methamphetamin, methamphetamin ⅾương
tính, wɑs ist methamphetamin, drogentest methamphetamin, methamphetamin englisch,
methamphetamin structure, iist mdma methamphetamin,
lye іn methamphetamin, іst methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische
formel, methamphetamin meaning, ԁ-methamphetamin, herstellung
methamphetamin, methamphetamin ᴠs amphetamine, methamphetamin recept, methamphetaminn japan,
definition methamphetamin, methamphetamin fаce, methamphetamin formula, methamphetamin synapse,
methamphetamin adderall, methamphetamin adhd, blue
methamphetamin, wrkung methamphetamin, methamphetamin terbuat dari, methamphetamin addiction,
bilder crystal methamphetamin, speed mіt methamphetamin gestreckt, methamphetamin synthese, methamphetamin usee
icd 10, weed, weed grinder, ᴡherе is weed legal,
isposable weed pen, weed shop neаr me, milwaukee weed eater,
purple weed, іѕ weed legal in virginia, is weed legal in oklahoma, іs weed
legal in louisiana, weed puller tool, weed carts, іs weed legal
іn south carolina, weed killer fοr lawns, horny goat weed for men,
what stаtes is weed legal, weed shops neasr mе, weed legal
ѕtates, weed vape, roundup weed killer, weed
killer spray, edibles weed, recreational weed ѕtates,
weed store, milk weed, weed barrier, іs weed legal in indiana,
legal wred ѕtates, states with legal weed, is weerd legal iin kentucky, weeed puller, preen weed preventer, ounce
оf weed, dewalt weed eater, plantain weed, husqvarna weed eater, electric weed eater,
hybrrid weed, moonrock weed, weed pipe, barrett wilbert weed,
weed control, weed elivery neаr me, is weed legal in missouri, һow
tо make weed butter, wһite weed, іs weed
legal inn utah, moon rock weed, snow caps weed, іs weed legal in arkansas, is wed legawl inn
texas 2025, ryobi weed eater, weed bowl, dill weed, wwed legalization, smoking weed, іs weed legal іn nevada, weed whacker, is weed legal
іn alabama, is weed a drug, weed barrier fabric, ѡһat is horny
goat weed, spruce weed аnd grass killer, weed stores neɑr me, sprinkles weed, poke weed, weed withdrawal, weed vapes, sniw cap
weed, rm43 weed killer, craftsman eed eater, qp ߋf weed, weed edibles, cookies weed,
gelato weed, іs weed legal in new mexico, strains of weed, weed
butter, ρound of weed, zaza weed, іs weed legal inn nc, hߋѡ mᥙch іs
an ounce оf weed, pgr weed, iss Ԁelta 9 real weed, diy weed
killer, ᴢip of weed, weed torch, moldy
weed, elon musk weed, іs weed illegal in texas, weed eater string,
rso weed, weed hangover, weed wallpaper, іs weed legal in nebraska, һow
to smoke weed, iѕ wesed legal in hawaii, how to grow weed, how to make weed in infinite craft, іѕ
weed legal in california, gary payton weed
Link exchange is nothing else but it is just placing the other person’s blog link on your page
at proper place and other person will also do similar in support of you. https://chestny-znak-info.ru/articles/markirovka-radioelektroniki-2026.html
Hey there! I just wanted to ask if you ever have any trouble with hackers?
My last blog (wordpress) was hacked and I ended up losing many months of hard
work due to no data backup. Do you have any methods to protect against hackers?
My brother suggested I might like this web site. He was totally right.
This post truly made my day. You can not imagine simply how much time I had spent for this info!
Thanks!
doktor kbb
deniz
dr burcu
This post will help the internet users for building up new blog or even a weblog from start to
end.
medart
medart
Thanks a lot for sharing this with all of us you really recognise what you are speaking approximately!
Bookmarked. Please also discuss with my web site =). We may have a hyperlink alternate agreement between us
I’ve been looking into Paybis for a while now,
especially after going through financial trouble, and I’m still
not fully convinced whether it deserves all the attention it gets.
Still, it’s definitely a noticeable name in the crypto space,
particularly for people in Germany who are trying to find new financial
tools. From what I understand, Paybis presents itself as a
well-established cryptocurrency service that supports regular bank transactions, something many platforms either limit
or complicate.
What initially caught my eye is how Paybis seems to link traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to exchange
crypto using SEPA transfers. I’m not saying the process is perfect,
but it does seem aimed at people starting out rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins. Instead, it offers a broader token selection, which might attract
users who are trying new projects. Still, things like liquidity are worth checking before
making decisions.
Security and compliance also come up often around Paybis. The
platform highlights regulatory compliance, which can feel
reassuring for users in Germany, though others might see
it as time-consuming. I’m still undecided, but it
does suggest Paybis tries to operate as a regulated marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is
straightforward about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means users should read the details before moving money.
Overall, I wouldn’t call Paybis the ultimate choice, but it does seem
like a platform worth exploring, especially for someone
in Germany trying to build a new starting point. I’m still forming my opinion, but it seems interesting enough to justify further research.
Right now it sounds like Expression Engine is the best blogging platform available right now.
(from what I’ve read) Is that what you’re using
on your blog?
I’ve been looking into Paybis for a while now, especially after
having a rough financial period, and I’m still not entirely sure
whether it deserves all the attention it gets. Still, it’s definitely
a noticeable name in the crypto industry, particularly
for people in Germany who are trying to rebuild their finances.
From what I understand, Paybis presents itself as a large-scale cryptocurrency service that supports standard payment methods,
something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to bridge traditional German banking methods
with the crypto world. Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to exchange crypto using SEPA transfers.
I’m not saying the process is perfect, but it does seem aimed at beginners rather than just advanced
traders.
Another aspect worth noting is the selection of
supported assets. Paybis doesn’t restrict itself to Bitcoin and Ethereum only.
Instead, it offers a wider range of digital assets, which might attract
users who are trying new projects. Still, things like asset availability are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which
can feel professional for users in Germany, though others
might see it as restrictive. I’m still undecided, but it does
suggest Paybis tries to operate as a regulated marketplace.
When it comes to fees, reviews seem divided. Some say Paybis is
clear about costs, while others note that pricing can depend on currency.
This isn’t unusual in the crypto industry, but it means users should compare alternatives before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like a platform worth a closer look, especially for
someone in Germany trying to recover financially.
I’m still forming my opinion, but it seems relevant enough to justify further research.
I have read so many articles or reviews concerning the blogger lovers except this post is actually a good piece of writing,
keep it up.
What’s up mates, nice article and fastidious urging commented here,
I am truly enjoying by these.
Asking questions are truly pleasant thing if you are not understanding something completely, but this article gives fastidious
understanding even.
Aw, this was a very nice post. Taking the time and actual effort to make a good article… but what can I say… I hesitate a lot and don’t
manage to get nearly anything done.
I am sure this piece of writing has touched all the internet people,
its really really fastidious paragraph on building up new website.
Great post.
I have read so many content on the topic
of the blogger lovers except this paragraph is actually
a fastidious post, keep it up.
Hello mates, nice post and fastidious arguments commented at
this place, I am truly enjoying by these.
Hi there mates, its fantastic paragraph on the topic of tutoringand fully explained, keep
it up all the time.
Cheers! Quite a lot of content!
my site https://telegra.ph/Comprar-Criptomoedas-com-Cart%C3%A3o-de-Cr%C3%A9dito-em-Portugal-Guia-R%C3%A1pido-2026-01-22
Great info. Lucky me I came across your website by chance (stumbleupon).
I’ve saved it for later!
Continue assim e continue atraindo mais jogadores!
https://jornaluniao.com.br/noticias/entretenimento/sweet-bonanza-como-ganhar-grandes-premios
Hi! I could have sworn I’ve been to this site before but
after checking through some of the post I realized it’s
new to me. Anyhow, I’m definitely delighted I found it and
I’ll be book-marking and checking back frequently!
Эта информационная заметка содержит увлекательные сведения, которые могут вас удивить! Мы собрали интересные факты, которые сделают вашу жизнь ярче и полнее. Узнайте нечто новое о привычных аспектах повседневности и откройте для себя удивительный мир информации.
Кликни и узнай всё! – https://codec-ouaga.com/reunion
посетить сайт трип скан
You could certainly see your skills in the work you write.
The world hopes for even more passionate writers like you who
aren’t afraid to mention how they believe. At all times follow your heart.
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Полная информация здесь – https://www.strucktour.com/?page_id=2462
В данной обзорной статье представлены интригующие факты, которые не оставят вас равнодушными. Мы критикуем и анализируем события, которые изменили наше восприятие мира. Узнайте, что стоит за новыми открытиями и как они могут изменить ваше восприятие реальности.
Нажмите, чтобы узнать больше – https://the-storage-inn.com/blog/2016/02/choosing-safe-self-storage
Wow, incredible blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your
web site is excellent, as well as the content!
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Углубить понимание вопроса – https://kktcalimsatim.com/_sb_country/pitcairn-islands
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Доступ к полной версии – https://techideasweb.com/national-testing-network-gateway-to-careers-in-public-safety
Эта статья предлагает захватывающий и полезный контент, который привлечет внимание широкого круга читателей. Мы постараемся представить тебе идеи, которые вдохновят вас на изменения в жизни и предоставят практические решения для повседневных вопросов. Читайте и вдохновляйтесь!
Подробнее – https://www.grenobletennis.fr/retour-sur-le-p1000-audi-jean-lain-grenoble
Hello Dear, are you truly visiting this web page on a regular basis,
if so then you will without doubt obtain fastidious experience.
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Не упусти шанс – https://wisatakopi.mitrapalupi.com/2022/13.21503
Saved as a favorite, I like your website!
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Только факты! – https://potischool.ge/2024/04/02/2-%E1%83%90%E1%83%9E%E1%83%A0%E1%83%98%E1%83%9A%E1%83%98-%E1%83%90%E1%83%A3%E1%83%A2%E1%83%98%E1%83%96%E1%83%9B%E1%83%98%E1%83%A1%E1%83%AA%E1%83%9C%E1%83%9D%E1%83%91%E1%83%90%E1%83%93%E1%83%9D
Excellent weblog right here! Additionally your website quite a bit up very fast!
What web host are you using? Can I get your affiliate hyperlink to your
host? I want my site loaded up as quickly as yours lol
Публикация предлагает читателю не просто информацию, а инструменты для анализа и саморазвития. Мы стимулируем критическое мышление, предлагая различные точки зрения и призывая к самостоятельному поиску решений.
Не упусти шанс – https://nacmedpalata.ru/?action=show&id=24843
Hey there this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding know-how so I wanted to get guidance
from someone with experience. Any help would be greatly appreciated!
basat
узнать сайт трипскан
My brother suggested I may like this website. He was once totally
right. This submit actually made my day. You can not consider just how
so much time I had spent for this info! Thanks!
May I just say what a relief to discover someone who truly knows what
they’re talking about on the net. You definitely realize how to bring an issue to light and make it important.
More and more people really need to read this and understand this side of your story.
It’s surprising you’re not more popular given that you definitely possess the gift.
medart
I’m truly enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often.
Did you hire out a developer to create your theme?
Fantastic work!
Whoa! This blog looks just like my old one! It’s on a entirely different
subject but it has pretty much the same page layout and design. Outstanding choice of colors!
Thanks in favor of sharing such a nice opinion, article is pleasant, thats why i
have read it fully
Süper platform! Her şey üst seviyede, tebrikler ve başarılar!
https://www.cenac-assurances.com/2020/11/22/bonjour-tout-le-monde/
I’m gone to inform my little brother, that he should also visit this web site on regular basis to obtain updated
from hottest reports.
Very rapidly this web page will be famous amid all blog viewers, due to it’s nice posts
Feel free to surf to my web page spiritual retreats in mexico
I’ve been reading Paybis for a while now, especially after going through financial trouble,
and I’m still not entirely sure whether
it deserves all the attention it gets. Still, it’s definitely a
noticeable name in the crypto industry, particularly for people in Germany who are trying to find new financial
tools. From what I understand, Paybis presents itself as a well-established cryptocurrency
service that supports fiat payments, something many platforms either limit or
complicate.
What initially caught my eye is how Paybis seems to link traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto
trades, while Paybis allows users to exchange crypto using SEPA
transfers. I’m not saying the process is perfect, but it does
seem aimed at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins.
Instead, it offers multiple altcoins, which might attract users who are diversifying.
Still, things like update speed are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel responsible for
users in Germany, though others might see it as time-consuming.
I’m still undecided, but it does suggest Paybis tries to operate as a regulated marketplace.
When it comes to fees, reviews seem varied. Some say Paybis
is transparent about costs, while others note that pricing can change with transaction type.
This isn’t unusual in the crypto industry, but it
means users should research properly before moving money.
Overall, I wouldn’t call Paybis the ultimate choice, but it does seem like a
platform worth checking out, especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems promising enough
to justify further research.
Wonderful blog! I found it while searching on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Many thanks
Feel free to surf to my website :: 미국복권 구매
If you would like to obtain much from this piece of writing then you have to apply these strategies to your won web site.
Valuable info. Lucky me I found your site by
accident, and I am surprised why this coincidence did not came about earlier!
I bookmarked it.
Look at my web-site; jungle retreats in mexico
Hi there, the whole thing is going perfectly here and ofcourse every one is sharing data, that’s really fine, keep up writing.
Appreciate this post. Will try it out.
Very nice article, exactly what I needed.
Feel free to surf to my web blog 미국복권
It is perfect time to make some plans for the future and it is time to be happy. I’ve read this post and if I could I want to suggest you some interesting things or suggestions. Perhaps you can write next articles referring to this article. I wish to read more things about it!
веб-сайте трип скан
Огромное спасибо за платформу kazino olimp — очень выручает!
http://wolfi.org/guestbook/
I really like it whenever people come together and share ideas.
Great website, stick with it!
Also visit my website :: jungle retreats in mexico
Wow, that’s what I was looking for, what a stuff! existing here at this website, thanks
admin of this web site.
my web-site; personal retreats
안녕하세요! 여기서 처음 댓글을 남기는 거라 간단히 인사드리고 싶었습니다.
당신의 블로그 포스트를 읽는 것을 정말
즐기고 있습니다. 같은 주제을 다루는
다른 블로그/웹사이트/포럼을 제안해 줄 수 있나요?
고맙습니다!
Hey there, I think your blog might be having
browser compatibility issues. When I look at your blog site in Chrome, it
looks fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up! Other then that, superb blog!
I think I will become a great follower.Just want to say your post is striking. The clarity in your post is simply striking and i can take for granted you are an expert on this subject.
Hi would you mind letting me know which hosting company you’re working with?
I’ve loaded your blog in 3 completely different internet
browsers and I must say this blog loads a lot quicker
then most. Can you suggest a good hosting provider at a honest
price? Cheers, I appreciate it!
Also visit my web site – 미국로또
Great items from you, man. I’ve take into accout your stuff prior to
and you’re just extremely excellent. I actually like what
you’ve bought here, certainly like what you are saying and the best way in which you assert it.
You are making it enjoyable and you still take care of to keep it wise.
I can’t wait to read far more from you. This is actually a great web site.
Review my blog post – 메가밀리언
Good points – – it will make a difference with my parents.
Heya great website! Does running a blog such as this take a massive
amount work? I have no knowledge of coding but I was hoping to start my own blog in the near future.
Anyhow, if you have any ideas or techniques for new blog owners
please share. I know this is off subject however I simply wanted to ask.
Appreciate it!
My site … wellness retreats mexico
I’ve been reading Paybis for a while now, especially
after having a rough financial period, and I’m still not entirely sure whether
it deserves all the attention it gets. Still, it’s clearly a noticeable name in the crypto industry, particularly for people in Germany who are trying to get
back on track. From what I understand, Paybis presents
itself as a well-established cryptocurrency service that supports standard
payment methods, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to connect traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to exchange crypto
using SEPA transfers. I’m not saying the process is perfect, but it does seem aimed
at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins.
Instead, it offers multiple altcoins, which might
attract users who are diversifying. Still, things like liquidity are worth checking before making
decisions.
Security and compliance also come up often around Paybis. The platform highlights identity verification, which can feel reassuring for users
in Germany, though others might see it as time-consuming.
I’m still undecided, but it does suggest Paybis tries to operate as
a legitimate marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is transparent about costs, while others
note that pricing can change with transaction type. This isn’t unusual
in the crypto industry, but it means users should compare
alternatives before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem
like a platform worth a closer look, especially for someone
in Germany trying to build a new starting
point. I’m still forming my opinion, but it seems relevant enough to justify further research.
What happens when an account gets closed? Someone started documenting the appeal process and player rights when casinos terminate accounts. This legal guidance helps vulnerable players fight back. The project is recruiting legal advocates and dispute resolution specialists. https://medium.com/@william_tu78/building-more-than-a-website-my-unfiltered-journey-with-gamblingformoney-4810e1fcb7b9.
I have been surfing on-line more than 3 hours as of late, yet I
never found any attention-grabbing article like yours.
It is lovely worth enough for me. In my view, if all web owners
and bloggers made excellent content material as you probably did, the internet will probably be
a lot more useful than ever before.
You ma’am have a way with words. Thank you very much!
You actually reported that really well!
подробнее tripscan
What’s Going down i am new to this, I stumbled upon this I’ve discovered It positively useful and it has helped me out loads.
I am hoping to give a contribution & assist other customers like its helped me.
Good job.
An outstanding share! I’ve just forwarded this onto a coworker
who has been doing a little homework on this.
And he actually bought me lunch due to the fact that I
found it for him… lol. So allow me to reword this….
Thanks for the meal!! But yeah, thanx for spending time to talk
about this topic here on your website.
Hi there! Someone in my Myspace group shared this website with us so I came to
look it over. I’m definitely enjoying the information. I’m book-marking
and will be tweeting this to my followers! Superb blog and great design.
More about the author https://toast-wallet.net
Have you ever considered writing an ebook or guest authoring on other blogs?
I have a blog based upon on the same topics you discuss and would really
like to have you share some stories/information. I know my subscribers would enjoy
your work. If you are even remotely interested, feel free
to send me an email.
my webpage … 미국복권 구매대행
These are genuinely fantastic ideas in concerning blogging.
You have touched some nice factors here. Any way keep
up wrinting.
my blog post :: 바이윈USA
I’ll right away grab your rss feed as I can’t to find your email subscription hyperlink or e-newsletter service.
Do you’ve any? Kindly permit me understand in order that I may just subscribe.
Thanks.
Feel free to surf to my web page … 미국복권 구매대행
Spot on with this write-up, I truly think this web site needs a great deal more attention.
I’ll probably be returning to read through more, thanks
for the information!
my webpage: spiritual retreats in mexico
Great work! This is the type of information that are meant to be shared across the net.
Disgrace on the search engines for not positioning this put up higher!
Come on over and visit my site . Thank you =)
Also visit my site couples retreat in mexico
When someone writes an post he/she retains the thought of a user in his/her brain that how a user
can understand it. So that’s why this post is great. Thanks!
My blog post – 미국복권
Attractive section of content. I just stumbled upon your
website and in accession capital to assert that I acquire in fact
enjoyed account your blog posts. Any way I’ll be subscribing to your augment
and even I achievement you access consistently quickly.
I visited many sites except the audio quality for audio songs current at
this site is truly wonderful.
I believe that is among the so much significant info for me.
And i am happy studying your article. However want to commentary
on some general things, The site taste is great, the articles is
truly excellent : D. Excellent process, cheers
I’ve been researching Paybis for a while now, especially after going through financial trouble,
and I’m still not completely certain whether it deserves all the
attention it gets. Still, it’s certainly a noticeable name in the digital asset market, particularly for people in Germany who
are trying to find new financial tools. From what I understand, Paybis presents itself as a large-scale cryptocurrency service that supports regular
bank transactions, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to bridge traditional
German banking methods with the crypto world. Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to buy crypto using debit cards.
I’m not saying the process is perfect, but it does seem aimed at beginners
rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to only the
major tokens. Instead, it offers a wider range of digital assets,
which might attract users who are trying new projects.
Still, things like update speed are worth
checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights regulatory compliance, which can feel professional for users in Germany, though others might see it as inconvenient.
I’m still undecided, but it does suggest Paybis tries to operate as a long-term marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is clear about costs,
while others note that pricing can depend on currency. This
isn’t unusual in the crypto industry, but it means users should compare
alternatives before moving money.
Overall, I wouldn’t call Paybis perfect, but it does seem like
a platform worth checking out, especially for someone in Germany
trying to recover financially. I’m still forming my opinion, but
it seems interesting enough to justify further research.
Hello there! This is my first visit to your blog!
We are a team of volunteers and starting a
new project in a community in the same niche.
Your blog provided us valuable information to work
on. You have done a extraordinary job!
find more info jaxx
I go to see every day a few web pages and blogs to read content, but this blog gives quality based posts.
An impressive share! I have just forwarded this onto a co-worker who had been conducting a little research on this.
And he in fact ordered me lunch due to the fact that I found it for him…
lol. So let me reword this…. Thanks for the meal!!
But yeah, thanks for spending time to discuss this issue
here on your web page.
I am extremely impressed together with your writing
abilities as well as with the structure to your weblog.
Is this a paid subject or did you customize it your self?
Anyway keep up the excellent high quality writing, it’s uncommon to see a nice weblog like this one nowadays..
I’m not sure why but this weblog is loading extremely slow for me.
Is anyone else having this issue or is it a problem on my end?
I’ll check back later on and see if the problem still exists.
Играть в Покердом на деньги:
кэш-столы, виндфоллы, слоты и моментальные выводы выигрышейОфициальное зеркало Покердом
Мультиформатный проект Pokerdom востребован у пользователей, которые ценят
возможность переключаться между слотами, покерными столами и беттингом.
Вне зависимости от того, любите ли
вы покер или слоты, наличие проверенного оператора с лицензией является залогом успешной игры.
Зачем регистрироваться здесь?
Клуб создан для удобства игроков из России и СНГ, обеспечивая игру в родной валюте и русскоязычный саппорт.
Система “Машина времени” помогает увеличить выгоду за счет прямого
рейкбека и случайных призов для активных покеристов.
Пользователи имеют возможность пробовать разные жанры азартных игр, не создавая несколько учетных
записей.
Во что можно поигратьна сайте?
Игротека на официальном сайте Pokerdom состоит из трех масштабных
разделов:
Покерные столы на любой лимит, включаябыстрый покер (Boost) и
джекпот-турниры (Виндфоллы).
Огромная коллекция игровых автоматов,
сертифицированных производителями, с высокой отдачей.
Live-дилеры и ставки на спорт для любителей атмосферы казино и прогнозов на матчи.
Регулярные акции и гонки, где разыгрываются миллионы рублей среди лучших
игроков.
Репутация Покердом в сети
Мнения клиентов о руме играют ключевую роль при
выборе места для постоянной игры в покер.
Многочисленные игроки подчеркивают:
Наличие большого количества рекреационных игроков (“фишей”),
с которыми выгодно играть.
Качественный софт для Android, позволяющий играть в покер и слоты
без зависаний.
Быстрые выплаты накарты российских банков и популярные электронные кошельки.
Как попасть на Покердом?
Необходимо знать актуальные способы
обхода блокировок для комфортного доступа к личному кабинету.
Наличие установленного клиента или рабочего домена гарантирует непрерывность игрового
процесса.
Как начать играть в Покердом?
При регистрации в руме стоит учитывать
несколько важных правилдля безопасности:
Указывайте реальные ФИО и дату
рождения, так какверификация обязательна для
вывода средств.
Будьте внимательны с выбором валюты, это поможет избежать лишних конвертаций при депозите.
Используйте бонусный код в
форме регистрации, если хотите получить дополнительные привилегии.
Имейте в виду, что обучение стратегии покера повышает шансы на успех, в отличие от слотов.
Не теряйте голову от азарта, дисциплина важна и
за покерным столом, и в слотах. https://pokerdom-online2374.casino Итоги по Покердом
Регистрация в Покердом – это идеальный выбор для русскоязычных игроков,
ищущих универсальную гемблинг-площадку.
Каждый пользователь может найти игру по душе: от турниров-миллионников до
вращения барабанов. Учитывая запрет на сторонний софт, Покердом остается лучшим местом для новичков и любителей.
Важные аспекты гемблинга
Для стабильного плюса необходимо постоянно развиваться в покере и грамотно управлять бонусами в казино.
Игрок должен:
Читать обучающие материалы по игре;
Набивать руку в турнирах без взноса;
Использовать промо-акции для профита;
Максимизировать выгоду от бонусов;
Соблюдать правила ответственной игры.
Почему игроки выбираютPokerdom
Высокая лояльность аудитории
объясняется удобством игры на рубли и отличной работой с клиентами.
Мы работаем над тем, чтобыкаждый турнир и каждый спин приносили удовольствие.
Команда Покердом постоянно обновляет
сетку турниров и добавляет новые слоты, чтобы вам не было скучно.
Где найти вход на сегодня?
При проблемах с доступом к лобби переходите на
рабочее зеркало:
Посты в телеграме Pokerdom;
Письма с новостями на вашей почте;
Службу поддержки через emaol (support);
Клиент для Windows или Android.
Имейте в виду, что игра через приложение
часто стабильнее и быстрее, чем через
браузер. Пусть ривер всегда доезжает, а слоты дают бонусы!
Регистрируйтесь в Покердом сейчас,
забирайте бонус и начинайте свою победную серию!
This is really interesting, You are a very skilled blogger.
I’ve joined your feed and sit up for seeking more of your magnificent post.
Also, I’ve shared your website in my social networks
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Тыкай сюда — узнаешь много интересного – https://unarcencielpourclara.org/parrainage
С интересом читаю материалы на kazino olimp. Благодарю за полезную инфу!
https://hts.io/ozrM
whoah this blog is wonderful i really like studying your posts.
Keep up the great work! You recognize, a lot of persons are looking around for this info, you can aid
them greatly.
I like it when people come together and share views. Great website, stick with
it!
Эта познавательная публикация погружает вас в море интересного контента, который быстро захватит ваше внимание. Мы рассмотрим важные аспекты темы и предоставим вам уникальные Insights и полезные сведения для дальнейшего изучения.
Лучшее решение — прямо здесь – https://diversifiedpayments.com/blog/point-of-sale-systems-explained-what-is-a-pos-system
It’s awesome to pay a visit this site and reading the views of all friends on the topic of this post, while I am also keen of
getting knowledge.
В этом информативном обзоре собраны самые интересные статистические данные и факты, которые помогут лучше понять текущие тренды. Мы представим вам цифры и графики, которые иллюстрируют, как развиваются различные сферы жизни. Эта информация станет отличной основой для глубокого анализа и принятия обоснованных решений.
Углубить понимание вопроса – https://eaglebst.com/product/82-classic
Thanks for sharing such a fastidious idea, post is fastidious,
thats why i have read it entirely
Remarkable things here. I’m very glad to peer your article.
Thank you so much and I’m having a look ahead to contact you.
Will you kindly drop me a mail?
Wow that was unusual. I just wrote an very long comment but
after I clicked submit my comment didn’t show up.
Grrrr… well I’m not writing all that over again.
Anyhow, just wanted to say fantastic blog!
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Узнать напрямую – https://redington.solar/solar-technologies-for-commercial-applications
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Исследовать вопрос подробнее – https://taisei-w.com/blog_posts_img_5
Этот интересный отчет представляет собой сборник полезных фактов, касающихся актуальных тем. Мы проанализируем данные, чтобы вы могли сделать обоснованные выводы. Читайте, чтобы узнать больше о последних трендах и значимых событиях!
Лови подробности – https://kgr-logistics.com/portland-port-asks-oregon-for-10m-to-save-container-service
What’s up to all, it’s in fact a good for me to go to see this website, it consists of precious Information.
I think the admin of this site is actually working hard for his web site,
since here every information is quality based information.
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Разобраться лучше – https://aklasbela.net/ak-lasbela-record
I’ve been checking out Paybis for a while now, especially
after having a rough financial period, and I’m still not entirely sure
whether it deserves all the attention it gets. Still,
it’s clearly a noticeable name in the digital asset market, particularly for people
in Germany who are trying to get back on track. From what I understand, Paybis presents itself as a globally operated
cryptocurrency service that supports standard payment
methods, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to bridge traditional German banking
methods with the crypto world. Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to exchange crypto using SEPA transfers.
I’m not saying the process is perfect, but
it does seem aimed at beginners rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins.
Instead, it offers a broader token selection, which might attract users who are exploring options.
Still, things like asset availability are worth checking before making decisions.
Security and compliance also come up often around Paybis. The platform highlights regulatory compliance,
which can feel reassuring for users in Germany, though others might
see it as restrictive. I’m still undecided, but it does suggest Paybis tries
to operate as a long-term marketplace.
When it comes to fees, reviews seem varied. Some say Paybis is transparent about costs, while others note that pricing can vary by payment method.
This isn’t unusual in the crypto industry, but it means users should research properly before moving money.
Overall, I wouldn’t call Paybis the best option, but it
does seem like a platform worth a closer look, especially for someone
in Germany trying to find accessible financial tools.
I’m still forming my opinion, but it seems relevant enough to
justify further research.
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now
each time a comment is added I get several e-mails with the same comment.
Is there any way you can remove people from that service?
Many thanks!
see this website jax wallet
mehmet emre dinç
What’s up it’s me, I am also visiting this website daily, this website
is in fact fastidious and the users are truly sharing pleasant thoughts.
Pretty great post. I just stumbled upon your
weblog and wanted to say that I’ve truly enjoyed surfing around your weblog posts.
In any case I will be subscribing for your feed and I’m hoping you write once more very soon!
I do not know if it’s just me or if everyone else encountering issues with your blog.
It appears as though some of the written text within your posts are running off the screen. Can someone else please
comment and let me know if this is happening to them as well?
This may be a problem with my web browser because I’ve had this
happen before. Many thanks
私たちは、これらのリンクが悪意のある、操作的な、搾取的な行為に使用され続けることを防ぐため、Google が直ちにこれらのリンクを確認して検索結果から削除することを強く求めます。
I think the admin of this web site is really working hard for his web site, since here every data
is quality based stuff.
medart
medart
Paylaşdığınız məlumatlar mənə çox kömək edir. Təşəkkürlər!
http://kvoseliai.lt/w/api.php?action=https://betandreas-azerbaijan-games.net/qeydiyyat
Great blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple tweeks would really make my blog jump
out. Please let me know where you got your theme. With thanks
You could definitely see your skills within the work you write.
The sector hopes for even more passionate writers
such as you who aren’t afraid to mention how they believe.
Always go after your heart.
I was pretty pleased to discover this site. I want to
to thank you for ones time just for this wonderful
read!! I definitely liked every bit of it and i also have you book marked to see new things in your web site.
Hello there! Do you use Twitter? I’d like to follow you if that would be ok.
I’m definitely enjoying your blog and look forward to new posts.
I blog frequently and I really thank you for your information.
This great article has really peaked my interest.
I’m going to take a note of your site and keep checking
for new details about once per week. I subscribed to
your RSS feed as well.
My brother suggested I might like this web site.
He was totally right. This post truly made my day.
You cann’t imagine just how much time I had spent for
this information! Thanks!
What a stuff of un-ambiguity and preserveness of
valuable familiarity about unpredicted emotions.
This information is critically needed, thanks.
Bu platformada dəyərli məqalələr var — xüsusilə kazino oyunları ilə bağlı.
https://suitablenames.com/typefp/ru/?p_dn=mostbet-azerbaijan-fun.org%2Fqeydiyyat
It’s remarkable in favor of me to have a site, which is valuable in favor of my know-how.
thanks admin
I don’t even understand how I stopped up right here, however I assumed this put up used to be good.
I don’t understand who you might be but definitely you are going to a famous blogger when you aren’t already.
Cheers!
It is appropriate time to make some plans for the future and it’s time to be happy.
I have read this post and if I could I want to suggest you some interesting things or suggestions.
Perhaps you can write next articles referring to this article.
I desire to read more things about it!
This article is very helpful.
I really appreciate how clearly it explains
the details in an easy-to-understand manner.
Many people often struggle to understand
how live streaming platforms operate,
especially when it comes to
stream stability and performance.
This post really helps clarify that,
and I think it will be valuable for readers
who are looking for reliable information.
Thanks for sharing this content,
I will definitely check out more posts
from this site.
I have read so many articles concerning the blogger lovers however this post
is truly a pleasant piece of writing, keep it up.
Here is my web-site … what does a project manager do
Hi there to all, how is the whole thing, I think every one is getting more from this website, and your views are nice in favor
of new viewers.
goGLOW Houston Heights
1515 Studemont Ⴝt Suite 204, Houston,
Texas, 77007, UᏚA
(713) 364-3256
acne treatment neаr mme for fаce, https://atavi.com/share/xnuc8tz8pyb3,
Awesome post.
Hi there! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
I do accept as true with all the concepts you have
offered for your post. They’re really convincing and will definitely
work. Still, the posts are very quick for newbies. Could you please lengthen them a bit from subsequent time?
Thank you for the post.
Amazing content on your website.
Огромное спасибо за платформу Olimp Casino — очень выручает!
https://olimp-casino-kazakhstan-kaz.kz/games
Superb post however I was wondering if you could
write a litte more on this topic? I’d be very thankful if you could elaborate a little bit further.
Cheers!
Hello, its nice post concerning media print, we all understand media is a enormous source of information.
This article gives clear idea in support of the new visitors of
blogging, that actually how to do blogging and site-building.
Good day! Do you know if they make any plugins to help
with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good success.
If you know of any please share. Many thanks!
Hi! This post could not be written any better! Reading through this post reminds me
of my good old room mate! He always kept chatting about this.
I will forward this post to him. Fairly certain he will have a good read.
Thanks for sharing!
Excellent post however , I was wondering if you could write a litte
more on this topic? I’d be very thankful if you could elaborate a little bit
more. Appreciate it!
Heya are using WordPress for your blog platform? I’m new
to the blog world but I’m trying to get started and create my own. Do you need any coding expertise to
make your own blog? Any help would be greatly appreciated!
my site – WAW4D
Wow! This blog looks just like my old one!
It’s on a entirely different subject but it has pretty much the same
layout and design. Wonderful choice of colors!
I’ve been looking into Paybis for a while now,
especially after having a rough financial period, and
I’m still not fully convinced whether it deserves
all the attention it gets. Still, it’s definitely a noticeable name in the digital asset
market, particularly for people in Germany who are trying to get back on track.
From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports standard
payment methods, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems
to link traditional German banking methods
with the crypto world. Many exchanges focus only on crypto-to-crypto trades,
while Paybis allows users to sell crypto using credit cards.
I’m not saying the process is perfect, but it does seem aimed at users
new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and Ethereum only.
Instead, it offers multiple altcoins, which might attract users who are
trying new projects. Still, things like liquidity are worth
checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel responsible for
users in Germany, though others might see it as restrictive.
I’m still undecided, but it does suggest Paybis tries to operate as a long-term marketplace.
When it comes to fees, reviews seem varied.
Some say Paybis is clear about costs, while others note that pricing can change with transaction type.
This isn’t unusual in the crypto industry, but it means users should research properly before moving money.
Overall, I wouldn’t call Paybis the ultimate choice, but it does seem like a platform worth checking out, especially for
someone in Germany trying to recover financially.
I’m still forming my opinion, but it seems relevant enough to justify
further research.
Süper platform! Her şey üst seviyede, tebrikler ve başarılar!
http://tools.fpcsuite.com/admin/Portal/LinkClick.aspx?table=Links&field=ItemID&id=47&link=https%3A%2F%2Fimage.google.sc%2Furl%3Fsa%3Di%26rct%3Dj%26url%3Dhttps%3A%2F%2Fmutual-learning-employment.net%2F
After going over a few of the blog posts on your blog, I seriously appreciate your technique of blogging.
I saved as a favorite it to my bookmark webpage list and will be checking back in the near future.
Please check out my website as well and let me know what you
think.
My page lifecard for sale
medart
Good way of describing, and pleasant paragraph to take information about my presentation subject matter, which i am going
to present in school.
Hi there Dear, are you in fact visiting this web page regularly, if so then you will definitely get pleasant knowledge.
We are a group of volunteers and starting a new scheme in our
community. Your site provided us with valuable info to work on. You’ve done an impressive job and our whole community will be grateful to you.
click here to find out more https://heyanon.my/
websites https://blendfun.xyz
Woah! I’m really enjoying the template/theme of this site.
It’s simple, yet effective. A lot of times it’s
hard to get that “perfect balance” between user friendliness and appearance.
I must say that you’ve done a fantastic job with this.
Additionally, the blog loads super fast for me on Internet explorer.
Outstanding Blog!
Hi, i think that i saw you visited my web site so i came to “return the favor”.I am
attempting to find things to enhance my site!I suppose
its ok to use a few of your ideas!!
Полезная заметка. Очень нужно поднимать темы помощи в лечении.
Благодарю за информацию.
Постараюсь рассказывать об
этом знакомым.
Check out my web-site Помочь восстановить зрение
I’ve been looking into Paybis for a while now, especially after
going through financial trouble, and I’m
still not entirely sure whether it deserves all
the attention it gets. Still, it’s clearly a noticeable name in the crypto space,
particularly for people in Germany who are trying to
get back on track. From what I understand, Paybis presents itself as a well-established cryptocurrency
service that supports fiat payments, something many platforms either
limit or complicate.
What initially caught my eye is how Paybis seems to link traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while Paybis allows users to exchange crypto using debit cards.
I’m not saying the process is perfect, but it does
seem aimed at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins. Instead, it
offers a broader token selection, which might attract users who are diversifying.
Still, things like liquidity are worth checking before
making decisions.
Security and compliance also come up often around Paybis. The
platform highlights identity verification, which can feel reassuring for users in Germany,
though others might see it as restrictive. I’m still undecided, but it does suggest Paybis tries to operate as a long-term marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is clear about costs, while others note that pricing can change
with transaction type. This isn’t unusual in the crypto industry,
but it means users should research properly before moving money.
Overall, I wouldn’t call Paybis perfect, but it does
seem like a platform worth checking out, especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems
interesting enough to justify further research.
This is very interesting, You are a very skilled blogger.
I’ve joined your rss feed and look forward to seeking more of your fantastic post.
Also, I have shared your website in my social networks!
Great work! This is the type of info that are meant to be shared around the internet.
Shame on the seek engines for not positioning this post higher!
Come on over and visit my website . Thanks =)
As the admin of this site is working, no hesitation very shortly it will be famous, due to its quality contents.
Чтобы что-что разработали хакерские инструменты а также макросы в течение компьютерных выступлениях
Oh my goodness! Awesome article dude! Thank you, However I am encountering problems with your RSS.
I don’t understand the reason why I am unable to join it.
Is there anybody else having the same RSS problems?
Anyone that knows the answer can you kindly respond? Thanks!!
find out here https://astake.cc/
First of all I would like to say superb blog! I had a quick question that I’d like to ask if you
don’t mind. I was curious to find out how you center yourself and clear your mind prior to writing.
I’ve had a tough time clearing my mind in getting my ideas out.
I truly do take pleasure in writing however it just seems like the first 10 to 15
minutes are generally lost just trying to figure out how
to begin. Any ideas or tips? Thank you!
Look At This https://upshift.my
useful site https://universalx.us/
It’s really a nice and useful piece of information. I’m happy that you shared this helpful information with
us. Please stay us up to date like this. Thank you for sharing.
You ought to take part in a contest for one of the greatest blogs on the web.
I am going to recommend this blog!
click this link here now https://hyperunit.cc/
see here now https://kyros.lat/
You certainly deserve a round of applause for your post and more specifically, your blog in general. Very high quality material!
My brother suggested I might like this websiteHe was once totally rightThis post truly made my dayYou can not imagine simply how a lot time I had spent for this information! Thanks!
Thanks for ones marvelous posting! I quite enjoyed reading it, you
may be a great author.I will make certain to bookmark your blog and will eventually come back at some point.
I want to encourage you continue your great job, have a nice evening!
Kazino ilə bağlı ipucu çox faydalıdır.
https://lnk.bz/rwLqb
is human trafficking tһе ѕecond largest, սsa gymnastics coach human trafficking, human trafficking news neаr me, snopes lynne knowles human trafficking,
humaan trafficking awareness ԁay quotes,human trafficking sex scene, human trafficking – menschenhandel, meghan connors human trafficking, ansrew
tate human trafficking, arguments oon human trafficking, free human trafficking cme florida, human trafficking оur, human trafficking іn minnesota 2021, arizona repuglican human trafficking, orange іs tthe new black hujan trafficking, human trafficking conference ocean city md,
277 arrested іn human trafficking, anti human trafficking law philippines, north korea human trafficking fɑcts, how will the wall affect human trafficking, human trafficking training michigan 2018, hotels sued human trafficking, kids
rescued from human trafficking, durham region human trafficking,
whyy human trafficking іs imрortant, mother of good church human trafficking, walmart human trafficking 2020,
ԝhat iѕ the rate of human trafficking worldwide, human trafficking news (news), human trafficking Ьy stаte
2021, lgbt human trafficking statistics, south
africa аnd human trafficking, human trafficking statistics fbi,
hotel lawsuits human trafficking, opeation renewed hope human trafficking, human trafficking atlanta
2022, humman trafficking ssan joaquin county, non profit organizations f᧐r human trafficking, human trafficking
interpol, human trafficking elgin, trafficking women’ѕ human ights julietta hua, facebook human traffidking lawsuit, rates ⲟf human trafficking, real worlɗ example of human trafficking, lawyers аgainst human trafficking, wsin human trafficking summit
2022, vad är human trafficking, recognizing tһe signs oof huyman trafficking, human trafficking justice, video ᧐f human trafficking,
fߋur signs of human trafficking, human trafficking honey,
binjun xie human trafficking, human trafficking documentary amazon рrime, minnesota human trafficking data,
uncovers russian human trafficking гing ѡar, human trafficking chico сa,
human traffickiing jus cogens, human trafficking syrian refugees,
human trasfficking topics гesearch paper, text human trafficking link snopes,
oprtah south africa human trafficking, human trafficking
grants 2015, human trafficking san antonio 2021, human drug trafficking meaning,
humaan trafficking stories children, fema human trafficking awareness, florida disney human trafficking, jobs fоr human trafficking victims, movie ɑbout human trafficking 2023 netflix, a day іn thе life ⲟf a human trafficking victim, uk human trafficking news, bent ⅼicense
plate human trafficking reddit, human trafficking іn waterbury ct, center tο combat human trafficking, greenville
nc huuman trafficking, maui human trafficking, t᧐ρ 5 human trafficking cities, іѕ humwn trafficking happeninhg іn the us, oxnard human trafficking,
aurora shoreline human trafficking, taconganas human trafficking,
hashtags fօr human trafficking, whyite house hman trafficking summit, corona human trafficking, border patrol human trafficking, human trafficking іn thailand 2020, human trafficling in wv,
11 arrested іn human trafficking, china’ѕ one child policy and human trafficking, hoyels human trafficking 2023, human trafficking іn florida 2021,
human trafficking debate topics, international justice mission hhman trafficking,
uncovers human trafficking гing for, scholarly article ߋn human trafficking, madison herman human trafficking, amad diallo humwn trafficking, а poem аbout humaan trafficking, human trafficking bristol tn, deluca ɑnd the human trafficking storyline,
economy annd hujan trafficking, human traffickinng іn trinidad,
human trafficking Ԁay 2018, caught caqmera actual human trafficking victims, human trafficking
episode opal grey’ѕ anatomy, duolinngo ceo human trafficking,
watch dogs human traffgicking map, human trafficking defiinition canada,
airtag human trafficking, human traffucking іn the beauty industry, 人口販子human trafficking, forced labor іn human trafficking, american airlines center human trafficking, human trafficking ⅽe texas, selah human trafficking,
siam human trafficking, fresno human trafficking statistics, senegal human trafficking, human trafficking belgium, michigan human trafficking ϲourse, nny times human trafficking, abandoned stroller human trafficking, human trafficking
і-44, solution onn human trafficking, humman trafficking canada news, onhtario human trafficking, protects victims оf human trafficking amendment, human trafficking іn highland ca,
human trafficking hotspot map, human trafficking organizations ontario,
human trafficking hiding սnder cars, summary on human trafficking, uncovers russian human trafficking ring war, human trafficking honey, fⲟur signs оf human trafficking,
human trafficking western pa, human trafficking livermore,
human trafficking durham region, human trafficking aat atlanta airport, binjun xie human trafficking, minnesota
human trafficking data, humsn trafficking documentary amazon ⲣrime,
human trafficking lawyer bloomfield hills, huan tragficking chrge іn texas,
central students ɑgainst human trafficking, ap human geography human trafficking, human trafficking fоr sexuaal exploitation, lue fօr human trafficking, kantian ethics human trafficking, anti-human trafficking organjization inn
cambodia, jo jorgensen oon human trafficking, forrt hood ssoldiers
human trafficking, eau оf the ficth column human trafficking, hawkins human trafficking, human trafficking іn the pacific islands, reasons ԝhy human trafficking іs bad, ally human trafficking, ᴡrite
аn essay oon human trafficking, human trafficking pros,
human trafficking dark web reddit, north preston human trafficking, ⅾollar
sign tattoo human trafficking, wht іs human trafficking, human trafficking stuart fl, priceless movie human trafficking, ti andd
wife human trafficking, huyman trafficking ethnicity statistics,
і 80 truck stop human trafficking, hamilton human trafficking,
oakville human trafficking, human trafficking ᧐n thе deep
web, current human trafficking, huuman trafficking women’ѕ riցhts, brunei
human trafficking, barack obama human trafficking quote, patron saint οf human trafficking,
spirited ɑѡay human trafficking, tһe game human trafficking, tоp human trafficking cities 2023, human trafficking ԝhich countries are the worst,
how tο donate tߋo human trafficking organizations,human trafficking quotes famous, human trafficking story
2020, human trafficking іn pittsburgh, 2020 human trafficking conference, human trafficking bust atlanta, human trfficking hemet ϲa, huhman traafficking statistic oregon, һow to identify a human trafficking
victim, economy аnd human trafficking, lover boy method ߋf hhuman trafficking, deluca аnd the hman trafficking storyline, european human trafficking, seoah human trafficking, american airpines center human trafficking, human trafficking paintings, ѡhɑt
stɑte iѕ #1 іn human trafficking?, forced labor іn human trafficking, 人口販子human trafficking, cryztal meth,
ԝhat does crystal meth ⅼⲟok liқe, ѡһɑt is crystal meth, crystal meth anonymous, hoѡ long does crystal meth stay іn your system, how to maҝe crystal meth, blue crystal meth, buy crystal
meth online, crystal meth effects, crystal meth pipe, crystal meth drug, ԝһat
d᧐es crystal mefh look likе?, meth crystal, crystal meth images, crystal meth ѕide effects,
how is crystal meth mаde, mrth ᴠѕ crystal meth, what does crystal meth ɗo,
crystal meth symptoms, crystal meth ᴠs meth, effects of crystal meth, siԀе effects оf crystal meth, hoow do
you mɑke crystal meth, crystal meth ѵs crack, what dߋeѕ crystal mth
smell ⅼike, hⲟw іs crystal meth սsed, crystal
meth withdrawal, crystal meth brreaking bad, ѡhаt is crystal meth mɑԁe
of, ԝhat dоes crystal meth ɗo tto you, crystal meth teeth,
smoking crystal meth, crystal meth pictures, ϲɑn y᧐u snort crystal meth, crystal meth efore ɑnd after, who invented crystal
meth, crystal meth fɑcts, crystal meth withdrawal symptoms,
crystal meth street names, signs ߋf crystazl meth, crystal meth addiction,
һow to cook crystal meth, crystal meth definition,
ԝhat type of dfug is crystal meth, ᴡhat ԁoes crystal meth feel ⅼike, crystal meth meaning, crystal meth ingredients, ᴡhats crystal meth, whаt color іs crystal meth, crystal meth detox,
crystal meth fаϲe, crysyal meth powder, crystal meth poem, strreet names f᧐r crystal meth, short term
effects оf crystal meth, signs of crystal meth abuse, crystal
meth rock, crystal meth fly, crystal
meth addict, crystal meth սsers, crystal meth rehab, һow muϲh doeѕ crystal meth cost, hoow ddo уou take crystal meth, hօw
muсh iѕ crystal meth, signs of crystal meth ᥙse, hhow to smoke
crystal meth, һow to uuse crystal meth, long tetm effects ߋf
crystal meth, signs ⲟf addiction tto creystal meth, pink crystal meth,crystal meth ⅼook ⅼike, breaking bad
crystal meth, when was crystal meth invented, pictures օf crystal meth, how іs crystal meth
tɑken, signs that sⲟmeone is uѕing crystal meth, ready or not crystal
mwth storage, difference ƅetween meth ɑnd crystl meth, һow do yօu do crystal meth, crystal
meth., locate crystal meth storage, ԝhat
ɑre tһе effects of crystal meth, fakee
crystal meth, ccrystal meth people, ᴡhat Ԁoes crystal meth,
һow ɗο you use crystal meth, how addictive іѕ crystal meth,
ϲan yoս overdose on crystal meth, crysttal еth blue, cystal meth signs,
һow ⅼong doеs crystal meth ⅼast, crystal meth detox los angeles,
һow do people use crystal meth, һow does crystal meth ⅼook like, crystal meth porn, how ɗoes crystal meth ⅼook, crystal meth storage twisted nerve,
ԝhats in crystal meth, crystal meth treatment, ѡhat iѕ
crysal meth made from, methamphetamin, methamphetamin adalah, methamphetamin ԁan amphetamin adalah, amphetamin ⅾan methamphetamin, chloroethane and methamphetamin, crystal methamphetamin, whhat іs methamphetamin, methamphetamin еffect, methamphetamin sport,
methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methampgetamin hydrochlorid, methamphetamin geschichte, methamphetamin hcl, amphetamin ᴠs
methamphetamin, methamphetamin biru, ethylphenidat methamphetamin, beda amphetamin ԁan methamphetamin,
difference ƅetween amphetamine and methamphetamin, methamphetamin psychose, methamphetamin rules, һow tօ mаke methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, deginition vоn methamphetamin, ρ2p methamphetamin, methamphetamin medizin,amphetamin ᥙnd methamphetamin, vicks vapor inhaler
methamphetamin, gta methamphetamin labor, wiie wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept,
methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest, unterschied
amphetamine ᥙnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung china, methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamjin abhängigkeit,
methamphetamin nebenwirkungen, methamphetamin ԝas ist das, unterschied methamphetamin ᥙnd amphetamin,
methamphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula, methamphetamin medikament,
methamphetamin ⅼa chat gi, test methamphetamin, methawmphetamin pervitin, methamphetamin adalah obat, methamphetamin аndere suchten аuch nach, methyamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut, methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ɗương tính, waѕ іst methamphetamin, drogentest methamphetamin,
methamphetamin englisch, metyhamphetamin structure, isst mdma methamphetamin, lye іn methamphetamin,
istt methamphetamin organschädigend? quora, methamphetamin chemische struktur, methamphetamin chemische
formel, methamphetfamin meaning, ⅾ-methamphetamin, herstelllung methamphetamin, methamphetamin ᴠѕ
amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fɑсe, methamphetamin formula, methamphetamkn synapse, methamphetamin adderall,
methamphetamin adhd, bkue methamphetamin, wirkung methamphetamin,
methamphetamin terbuat dari, methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt,
methamphetamin synthese, methamphetamin usse icd 10, weed, weed grinder, ѡhere is weed legal, disposable weed pen, weed shop
neаr mе, milwaukee weed eater, purple weed, іѕ weed legal in virginia, iѕ weed legal in oklahoma, iѕ weed leal in louisiana, weed puller tool, weed
carts, іs weed legal in south carolina, weed killer
fоr lawns, horny goat weed for men, wgat states іѕ weerd legal, weed shops neɑr me, weed
legal states, weed vape, roundup weed killer, weed killer
spray, edibles weed, recreational weed ѕtates, weed store, milk weed, weed barrier,
іѕ weed legal іn indiana, legal weed stɑtеs, sates with
legal weed, іs weed legal іn kentucky, weed puller, preen weded preventer, ounce
оf weed, dewalt wedd eater, plantain weed, husqvarna weded eater, electric weed eater,
hybrid weed, moonrock weed, weed pipe, barrett wilbert weed, weed control,
weed delivery neazr mе, is weed legal in missouri, how to mаke weed butter,
ѡhite weed, іs weed legaal iin utah, moon rock weed,
snow caps weed, іѕ weed legal in arkansas,
іs weed legal in texas 2025, ryobi weed eater,weed bowl, dill weed, weed legalization, smoking weed, іs weed legal іn nevada, weed whacker, іs weed legal in alabama,
is weed а drug, weed barrier fabric, ᴡhat іs hofny goat weed, spruce weed ɑnd grass killer,
weed stores neаr me, sprinkles weed, poke weed, weed withdrawal, weed vapes, snow
cap weed, rm43 weed killer, craftsman weed eater, qp ⲟff weed,
weed edibles, cokies weed, gelato weed, іs weed legfal in new mexico, strains ߋf weed, weed
butter, ⲣound off weed, zaza weed, іs weed legal
in nc, how much is ɑn ounce oof weed, pgr weed, іs dеlta 9 real weed, diy weed killer,
zip off weed, weed torch, moldy weed, elon musk weed, іs weed illegal in texas, weed eater string, rso weed,
weed hangover, weed wallpaper, іs weed legal іn nebraska, how tо smokke weed, iѕ
weed legal in hawaii, һow tо grow weed, һow tto mаke weed in infinite craft, іs weed legal іn california,
gary payton weed
Incredible! This blog looks just like my old one! It’s on a entirely different subject but it has pretty much the same layout and design. Wonderful choice of colors!
I thought it was going to be some boring old post, but I’m glad I visited. I will post a link to this site on my blog. I am sure my visitors will find that very useful.
Just a quick note to express my appreciation. Take care
I am no longer sure where you’re getting your info, however good topic.
I must spend some time studying more or figuring out more.
Thank you for magnificent information I used to be in search of this info for my mission.
我们敦促谷歌立即审查并从搜索结果中删除这些链接,以防止它们继续被用于恶意、操纵和剥削活动。
Thank you, I have recently been looking for info approximately this topic for ages
and yours is the greatest I’ve came upon so far. But, what in regards to the conclusion? Are you positive about the source?
Also visit my website 슬롯사이트추천
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Переходите по ссылке ниже – https://foratata.com/tiempo-libre
Very energetic blog, I liked that a lot. Will there be a part 2?
Also visit my web site :: 슬롯사이트추천
Surprisingly good post. I really found your primary webpage and additionally wanted to suggest that have essentially enjoyed searching your website blog posts. Whatever the case I’ll always be subscribing to your entire supply and I hope you jot down ever again soon!
Everything is very open with a very clear clarification of the
issues. It was definitely informative. Your website is useful.
Thanks for sharing!
Feel free to visit my web-site … WAW4D
Fantastic blog! Do you have any helpful hints for aspiring writers?
I’m hoping to start my own website soon but I’m a little lost
on everything. Would you suggest starting with a free platform like WordPress or go for a paid
option? There are so many choices out there that I’m completely overwhelmed ..
Any ideas? Thanks!
Also visit my web-site :: 카지노사이트추천
If some one desires expert view concerning blogging and site-building afterward
i advise him/her to pay a quick visit this website, Keep up the
nice job.
Very nice article, totally what I needed.
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Хочешь знать всё? – https://smidev.nl/nl/portfolio-item/jointmaster
Эта статья погружает вас в увлекательный мир знаний, где каждый факт становится открытием. Мы расскажем о ключевых исторических поворотных моментах и научных прорывах, которые изменили ход цивилизации. Поймите, как прошлое формирует настоящее и как его уроки могут помочь нам строить будущее.
Ознакомиться с отчётом – https://www.cakrawarta.com/dinilai-meresahkan-ratusan-warga-tanda-tangani-petisi-penolakan-tempat-hiburan-malam-di-citraland.html
pop over to this website https://blend.ad
Эта статья сочетает познавательный и занимательный контент, что делает ее идеальной для любителей глубоких исследований. Мы рассмотрим увлекательные аспекты различных тем и предоставим вам новые знания, которые могут оказаться полезными в будущем.
Желаете узнать подробности? – https://mrku-video.com/%E6%9C%8D%E5%8B%99%E6%96%B9%E6%A1%88
Pretty element of content. I simply stumbled upon your website and in accession capital to assert that I acquire in fact
loved account your weblog posts. Any way I will be
subscribing to your feeds and even I success you get right of
entry to consistently quickly.
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Тыкай сюда — узнаешь много интересного – https://www.ubytovaniepatince.sk/ale-ale-webova-stranka-a-novodoba-vizitka-neblaznite-2
I’ve been researching Paybis for a while now, especially after going through financial trouble,
and I’m still not fully convinced whether it deserves
all the attention it gets. Still, it’s clearly a noticeable name in the crypto industry, particularly for people in Germany
who are trying to find new financial tools. From what I understand, Paybis presents
itself as a large-scale cryptocurrency service that supports standard payment methods,
something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems to bridge traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while
Paybis allows users to buy crypto using various fiat options.
I’m not saying the process is perfect, but it does seem aimed at beginners
rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to Bitcoin and Ethereum only.
Instead, it offers a broader token selection, which
might attract users who are diversifying. Still, things like
update speed are worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel responsible for
users in Germany, though others might see it as inconvenient.
I’m still undecided, but it does suggest Paybis tries to operate as a legitimate marketplace.
When it comes to fees, reviews seem divided. Some say Paybis is clear about
costs, while others note that pricing can vary by payment
method. This isn’t unusual in the crypto
industry, but it means users should read the details before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem like a
platform worth checking out, especially for someone in Germany trying to recover financially.
I’m still forming my opinion, but it seems promising enough to justify further research.
I simply could not leave your site before suggesting that I actually enjoyed the usual info a person supply in your visitors? Is going to be back often to inspect new posts
4M Dental Implant Center
3918 Ꮮong Beach Blvd #200, Long Beach,
CᎪ 90807, United Ⴝtates
15622422075
Bookmarks
Many thanks! I like it.
Have a look at my homepage: https://fv-wolkenburg.de/fvwerste-startet-mit-niederlage-in-rueckrunde/
Îmi place foarte mult site-ul Verde Casino, este foarte ușor de utilizat.
https://verde-casino-romania-new.ro
Good way of explaining, and good article to get facts regarding my
presentation topic, which i am going to deliver in school.
I like the valuable info you supply on your articles. I will bookmark your blog and check once more here regularly.
I’m fairly certain I will be informed plenty of new stuff right right here!
Good luck for the next!
Wow that was unusual. I just wrote an very long
comment but after I clicked submit my comment didn’t show up.
Grrrr… well I’m not writing all that over again. Anyways,
just wanted to say superb blog!
certainly like your web-site however you have to take a look
at the spelling on quite a few of your posts. Many of them are rife with spelling issues
and I find it very bothersome to tell the reality then again I’ll
certainly come again again.
I’m really enjoying the design and layout of
your website. It’s a very easy on the eyes which makes it much more enjoyable for me to
come here and visit more often. Did you hire out a developer to create your theme?
Great work!
Good day very cool website!! Man .. Beautiful .. Wonderful ..
I’ll bookmark your site and take the feeds also? I am satisfied to find so
many helpful info right here in the put up, we need work out extra
strategies in this regard, thanks for sharing. . . .
. .
next page https://elara.cc/
This article is very helpful.
I really appreciate how clearly it explains
the subject without being confusing.
Many people often struggle to understand
how live streaming platforms operate,
especially in terms of
quality, reliability, and safety.
This post really helps clarify that,
and I think it will be helpful for new users
that want to learn more about the topic.
Thanks for sharing this content,
I will definitely check out more posts
here.
I wish I could craft such articles as this. Thank you very much.
I am curious to find out what blog system you’re working with?
I’m having some minor security issues with my latest site and I’d like
to find something more safe. Do you have any suggestions?
Great article! We are linking to this particularly great
article on our website. Keep up the great writing.
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored subject matter
stylish. nonetheless, you command get got an impatience
over that you wish be delivering the following. unwell
unquestionably come further formerly again since exactly the
same nearly a lot often inside case you shield this hike.
Great explanation in this article.
I really enjoy how this post breaks down
the topic in a simple way.
Many people often struggle to understand
how online cricket streaming works,
especially in terms of
quality, reliability, and safety.
This post makes things much clearer,
and I think it will be useful for beginners
interested in understanding this better.
Thanks for writing this guide,
I will definitely follow future updates
from this site.
I’ve been looking into Paybis for a while now, especially after going through
financial trouble, and I’m still not fully convinced whether it deserves all the
attention it gets. Still, it’s definitely a noticeable name
in the digital asset market, particularly for people in Germany who are
trying to get back on track. From what I understand, Paybis presents
itself as a globally operated cryptocurrency service that supports standard payment methods, something many platforms either
limit or complicate.
What initially caught my eye is how Paybis seems to connect traditional
German banking methods with the crypto world. Many exchanges focus only on crypto-to-crypto trades, while
Paybis allows users to buy crypto using debit cards.
I’m not saying the process is perfect, but it does seem aimed at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top coins. Instead,
it offers a wider range of digital assets,
which might attract users who are diversifying. Still, things like liquidity are worth checking before
making decisions.
Security and compliance also come up often around Paybis.
The platform highlights identity verification, which can feel professional for
users in Germany, though others might see it as restrictive.
I’m still undecided, but it does suggest Paybis tries to
operate as a regulated marketplace.
When it comes to fees, reviews seem mixed. Some say Paybis is transparent
about costs, while others note that pricing can vary by payment method.
This isn’t unusual in the crypto industry, but it means users
should research properly before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem
like a platform worth checking out, especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems promising enough
to justify further research.
Lovely content. Thanks a lot!
Feel free to surf to my web page – https://telegra.ph/Kako-kupiti-Bitcoin-s-kreditno-kartico-v-Sloveniji-Vodnik-2026-01-23
Simply want to say your article is as surprising. The clarity in your post is simply nice and i
could assume you’re an expert on this subject. Fine with your permission let me
to grab your feed to keep updated with forthcoming post.
Thanks a million and please keep up the gratifying work.
you’re in reality a just right webmaster. The web site loading velocity is incredible. It sort of feels that you’re doing any distinctive trick. In addition, The contents are masterpiece. you’ve performed a great process on this topic!
My brother suggested I might like this websiteHe was once totally rightThis post truly made my dayYou can not imagine simply how a lot time I had spent for this information! Thanks!
I don’t even understand how I ended up right here, however I believed
this put up was once great. I don’t recognise who you are however definitely you are going to a famous
blogger when you are not already. Cheers!
Hey there great website! Does running a blog such
as this require a large amount of work? I have absolutely no understanding of computer programming however I had been hoping to start my own blog in the near future.
Anyhow, if you have any recommendations or techniques for new blog owners please share.
I know this is off subject nevertheless I just wanted to ask.
Thanks a lot!
I have read so many posts on the topic of the blogger lovers however
this paragraph is in fact a pleasant piece of writing, keep it up.
I blog quite often and I truly thank you for
your information. The article has really peaked my interest.
I will take a note of your site and keep checking for new information about once
a week. I subscribed to your Feed too.
My spouse and I stumbled over here by a different page and thought I should check things out.
I like what I see so now i am following you. Look forward to exploring your web page repeatedly.
sap
You certainly deserve a round of applause for your post and more specifically, your blog in general. Very high quality material!
Quality articles or reviews is the secret to interest the users to pay a
visit the site, that’s what this website is providing.
My site; cyber 365
Hello i am kavin, its my first occasion to commenting anyplace, when i read this article i thought i could also make comment due to this brilliant post.
Mangelsen
7916 Girard Avenue, Lа Joya
CA 92037, United States
1 800-228-9686
learn protecting grizzly bears species (https://go.bubbl.us/ef95df/c975?/Bookmarks)
Thanks for finally writing about > Heart failure: Symptoms, Causes, Diagnosis &
Treatment – MDtodate < Loved it!
Hi! I’ve been following your website for a long time now and finally got
the courage to go ahead and give you a shout out from Huffman Texas!
Just wanted to mention keep up the great job!
It’s wonderful that you are getting ideas from this post as well
as from our dialogue made at this place.
My web blog – Easync automated dropshipping
Quality articles or reviews is the key to attract the visitors to visit the website, that’s what this web page is providing.
My web blog: dropshipping tool and software
Игровая площадка 7k: доступ через зеркало,
мобильная версия и лучшие слотыОфициальный сайт 7k
Casino
Услуги онлайн казино 7k стремительно набирают
популярность среди гемблеров, ищущих надежную площадку для игры.
Независимо от опыта игрока, важно выбрать
лицензионное заведение, которое гарантирует честность результатов и безопасность транзакций.
Почему выбирают казино 7k?
Клуб работает легально, что дает игрокам уверенность в
отсутствии накруток и гарантирует вывод выигрышей.
Пользователи могут рассчитывать
на выгодную программу лояльности, бонусы за депозиты
и регулярные акции.
Саппорт работает в режиме 24/7, обеспечивая оперативное решение технических проблем и вопросов верификации.
Ассортимент игр в 7k Casino
Библиотека игр на платформе 7k состоит из множества сертифицированных
слотов и настольных игр:
Популярные игровые автоматы
с продуманной механикой, джекпотами и специальными символами.
Раздел Live, где можно сыграть в рулетку, блэкджек и баккару
с профессиональными крупье.
Регулярные турниры и лотереи с
крупными призовыми фондами для активных игроков.
Широкий выбор видеопокера, рулеток
и других настольных дисциплин.
Мнения гемблеров
Мнения постояльцев клуба 7k часто становятся решающим фактором для тех,
кто ищет новую площадку. Игроки в своих рецензиях акцентируют внимание на:
Оперативность финансовых операций и отсутствие задержек при выводе.
Стабильную работу сайта и наличие
актуальных зеркал при блокировках.
Реальность выполнения условий по вейджеру
и частые персональные предложения.
Как зайти на 7k Casino?
Необходимо знать, где найти свежее зеркало сайта,для бесперебойного доступа к аккаунту и играм.
Бесперебойная работа портала является ключевым условием для спокойного гемблинга.
Инструкция для новичков
Перед темкак начать делать ставки на реальные деньги, ознакомьтесь с простыми шагами регистрации:
Создайте профиль, используя электронную почту и надежный
пароль.
Активируйте приветственный бонус в личном кабинете для увеличения стартового капитала.
Сделайте пополнение баланса
и переходите к выбору развлечений
в лобби.
Имейте в виду, что подтверждение личности позволит снимать лимиты и выводить деньги быстрее.
Играйте ответственно и воспринимайте казино как развлечение. https://7k-3484.casino Заключение
Выбор 7k Casio в качестве основной площадки
станет верным решением для любителей качественного гемблинга и крупных выигрышей.
У каждого клиента есть гарантия
безопасности данных и прозрачности всех игровых процессов.
С учетом множества предложений в интернете, этот
бренд выигрывает за счет клиентоориентированности и постоянных улучшений.
Важность ответственной игры
Результативная игра требует не только везения, но и дисциплины в управлении
финансами. Игрок должен:
Знакомиться с таблицей выплат и механиками автоматов;
Устанавливать лимиты на проигрыш
и выигрыш;
Использовать бонусы с умом, изучая условия
вейджера;
Сохранять хладнокровие и
не поддаваться тильту при проигрышах;
Писать в саппорт при любых
технических или финансовых вопросах.
Наши преимущества
Наши пользователи выделяют стабильную работу
площадки, отличный RTP в слотах и интересные соревнования.
Мы работаем над тем, чтобы каждый визит в казино приносил
положительные эмоции и адреналин.
Технологичная база казино обеспечивает отличную работу на мобильных гаджетах и десктопах.
Где искать вход?
Чтобы всегда оставаться в игре,
используйте проверенные источники для поиска зеркал 7k:
Подписка на официальный Telegram-канал казино;
Проверка электронной почты на наличие рассылки от администрации;
Использование поисковых систем
с запросом “7k казино зеркало”;
Контакт с администрацией
в соцсетях.
Помните, что только проверенные ссылки обеспечивают безопасность депозитов и конфиденциальность.
Двери нашего казино всегда открыты для будущих чемпионов.
В завершение, 7k предлагает уникальный опыт, превращая игру в захватывающее приключение с призами.
Создавайте аккаунт сегодня, активируйте подарки и побеждайте!
Wow, awesome blog format! How long have you
been blogging for? you made running a blog
look easy. The full glance of your website is wonderful, as well as the content material!
Also visit my homepage … ebay dropshipping suppliers
these details https://gofundmeme.us/
Hi to every one, the contents present at this site are really remarkable for people experience, well, keep up the nice work fellows.
Thanks in support of sharing such a fastidious idea, paragraph
is good, thats why i have read it completely
Aw, this was an exceptionally nice post. Finding the time and actual effort
to produce a superb article… but what can I say… I
procrastinate a lot and don’t seem to get nearly anything done.
I was referred to this web site by my cousin. I’m not sure who has written this post, but you’ve really identified my problem. You’re wonderful! Thanks!
Hi there, I found your web site via Google whilst looking for a related matter, your website
got here up, it seems good. I have bookmarked it in my google bookmarks.
Hello there, just was alert to your weblog thru Google,
and located that it’s really informative. I am going to be careful for brussels.
I’ll appreciate if you continue this in future. Lots of other people will likely be benefited out of your writing.
Cheers!
I’ve been looking into Paybis for a while now, especially
after going through financial trouble, and I’m still not fully convinced whether it deserves all the attention it
gets. Still, it’s clearly a noticeable name in the
crypto space, particularly for people in Germany who are trying
to get back on track. From what I understand, Paybis presents itself as a well-established cryptocurrency service that supports
fiat payments, something many platforms either limit or complicate.
What initially caught my eye is how Paybis seems
to bridge traditional German banking methods with the crypto world.
Many exchanges focus only on crypto-to-crypto trades, while
Paybis allows users to buy crypto using various fiat options.
I’m not saying the process is perfect, but it does seem
aimed at users new to crypto rather than just advanced traders.
Another aspect worth noting is the selection of supported assets.
Paybis doesn’t restrict itself to just the top
coins. Instead, it offers a broader token selection, which might
attract users who are exploring options. Still, things like asset availability are
worth checking before making decisions.
Security and compliance also come up often around Paybis.
The platform highlights KYC checks, which can feel
responsible for users in Germany, though others might see it as restrictive.
I’m still undecided, but it does suggest Paybis tries
to operate as a regulated marketplace.
When it comes to fees, reviews seem divided. Some say Paybis is transparent about costs,
while others note that pricing can change with transaction type.
This isn’t unusual in the crypto industry, but it means users should research properly before moving money.
Overall, I wouldn’t call Paybis the best option, but it does seem
like a platform worth exploring, especially for someone in Germany trying to build a new starting point.
I’m still forming my opinion, but it seems relevant enough to
justify further research.
Mangelsen
7916 Girard Avenue, ᒪa Joyaa
CА 92037, United Stateѕ
1 800-228-9686
discover pilgrim creek grizzlies grizzliess (Jack)
Award winners, individual honors and team trophies documented
It’s awesome to go to see this web page and reading the views of all friends regarding this piece of writing, while I am also eager of getting experience.
Jungle Driving School Omaha
4020 Ѕ 147th St, Omaha,
NE 68137, United States
14024170547
Bookmarks
Hey just wanted to give you a quick heads up. The words in your post
seem to be running off the screen in Safari. I’m not sure if
this is a format issue or something to do with internet browser compatibility but I
figured I’d post to let you know. The layout look great though!
Hope you get the problem resolved soon. Many thanks
Usually I do not learn post on blogs, but I wish to say that this write-up very forced me to
take a look at and do it! Your writing taste has been amazed me.
Thanks, very nice article.
Nice weblog here! Also your web site so much up very fast!
What web host are you the usage of? Can I get your
associate link on your host? I desire my website loaded up as fast as yours lol
Wow, that’s what I was exploring for, what a information! present here at this blog, thanks admin of this web site.
Your method of telling all in this article is really good, every one can simply know
it, Thanks a lot.
next https://hypperswap.cloud
You certainly deserve a round of applause for your post and more specifically, your blog in general. Very high quality material!
What’s Going down i am new to this, I stumbled upon this I have
found It absolutely helpful and it has aided me out loads.
I’m hoping to give a contribution & assist other customers like its helped me.
Great job.
Howdy! Do you know if they make any plugins to protect
against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
whoah this blog is magnificent i really like reading your posts.
Stay up the great work! You know, lots of individuals are searching around for this information, you can help them greatly.
Attractive component of content. I simply stumbled upon your site and in accession capital
to assert that I acquire in fact enjoyed account your weblog
posts. Anyway I’ll be subscribing for your feeds or even I fulfillment you get right of entry to constantly rapidly.
Equalizers, goals that level the score and their timing
I know this website offers quality depending articles or reviews and additional stuff, is there any other
web page which presents these kinds of information in quality?
Зеркало Вавада на сегодня: бесперебойный доступ к игровым автоматам и моментальный вывод средств на
картуОфициальное зеркало Вавада
Услуги онлайн казино Вавада пользуются огромным спросом среди игроков, которые ищут надежную площадку с лицензионным софтом
и гарантированными выплатами.
Независимо от вашего игрового опыта, важно
выбратьпроверенную платформу, которая
обеспечит сохранность депозитов и честность каждого вращения.
Зачем регистрироваться именно здесь?
Проект работает строго в рамках международной лицензии, обеспечивая пользователям честную
отдачу (RTP) и прозрачность всех
транзакций.
Казино предлагает возможность активировать щедрые подарки за регистрацию и
участвовать в закрытых турнирах с крупными призовыми фондами.
Игроки получают квалифицированную
помощь службы поддержки, которая работает 24/7
и решает любые вопросы максимально оперативно.
Во что можно поиграть в Вавада?
Выбор игр на платформе Вавада
поражает разнообразием и включает несколькоосновных разделов:
Огромная коллекция видеослотов, которые отличаются высокой отдачей, качественной графикой и захватывающими бонусными раундами.
Раздел Live-игр, где можно в реальном времени сыграть в рулетку, блэкджек
или покер против живых крупье.
Широкий выбор вариаций рулетки,
баккары и покера для тех, кто предпочитает интеллектуальные азартные игры.
Масштабные розыгрыши и гонки, доступ к которым открывается по мере повышения статуса в программе лояльности.
Репутация казино в сети
Отзывы о работе казино Вавадамогут существенно повлиять на
выбор площадки для игры
на реальные деньги. Многочисленные гемблеры подчеркивают:
Быстрый вывод денег даже в выходные дни и возможность играть анонимно при
небольших суммах.
Честную бонусную политику и реально выполнимые условия по отыгрышу вейджеров.
Отсутствие технических сбоев во время игры и интуитивно понятный интерфейс личного кабинета.
Доступ и рабочие зеркала
Необходимо всегда иметь под рукой список рабочих адресов сайта для беспрепятственного входа в аккаунт в случае ограничений
доступа. Наличие надежного канала доступа является важнейшим фактором для спокойной и уверенной
игры.
Как начать выигрывать?
Перед тем как сделать первый депозит,
стоит внимательно изучить такие рекомендации опытных игроков:
Ознакомьтесь с политикой клуба,
чтобы четко понимать, как работают бонусы и какие документы могут потребоваться.
Начинайте с демо-версий слотов,
чтобы понять механикуигры и выбрать подходящую стратегию.
Играйте ответственно, определяя бюджет заранее, и
никогда не играйте на последние
или заемные средства.
Не забывайте, что умение
вовремя забрать деньги —
это главное качество успешного игрока, которое приходит с опытом.
Не теряйте голову в погоне за джекпотом, играйте размеренно и с
удовольствием. https://Vavada-Casino2123.com
Заключение обзора
Регистрация на официальномсайте
казино Вавада – это важный шаг,
который открывает доступ к миру качественного гемблинга и крупных
выигрышей. У каждого пользователя есть равные шансы на
победу, и именно активностьна сайте позволит вам быстрее продвигаться
по уровням лояльности. С учётом высокой конкуренции в индустрии, Vavada удерживает лидерство благодаря
безупречной репутации и вниманию
к потребностям аудитории.
Стратегия успешного гемблера
Успешная игра в онлайн казино предполагает не только удачу, но и наличие четкой стратегии, а также умение управлять своими
эмоциями. Опытный игрок должен:
Анализировать отдачу слотов (RTP);
Придерживаться выбранной системы ставок;
Следить за актуальными турнирами;
Применять бонусы для увеличения времени игры;
Вовремя выводить крупные выигрыши.
Причины популярности бренда
Игроки ценят казино за простоту навигации, разнообразиеигрового контента и честные правила.
Мы стремимся к тому, чтобы каждыйпосетитель получал удовольствие от игры и чувствовал себя в безопасности.
Профессионализм администрации гарантирует стабильное развитие проекта и постоянное улучшение условий для клиентов.
Где взять ссылку на вход?
Если основной домен недоступен,используйте
следующие способы получения рабочей ссылки:
Закрепленные сообщения в Telegram-канале казино;
Персональные уведомления на почту для зарегистрированных игроков;
Службу поддержки через форму обратной связи;
Ресурсы стримеров и обзорников, сотрудничающих с казино.
Не забывайте, что чем раньше вы зарегистрируетесь, тем быстрее сможете начать получать бонусы и участвовать в
турнирах на миллионы. При возникновении проблем вы всегда можете рассчитыватьна помощь наших операторов.
В завершение, помните, что мы
ценим каждого игрока и гарантируем честность и прозрачность игрового процесса.
Жмите кнопку “Регистрация”, забирайте свои бонусы и начинайте путь к большим
победам!
This excellent website certainly has all the information I needed
concerning this subject and didn’t know who to ask.
I am regular reader, how are you everybody? This paragraph posted
at this web page is genuinely good.
next https://toast-wallet.net
my explanation https://hlp0.cloud/
Howdy! Someone in my Myspace group shared this
website with us so I came to give it a look. I’m definitely loving
the information. I’m bookmarking and will be tweeting this to my followers!
Outstanding blog and amazing design.
Does your blog have a contact page? I’m having problems locating it but, I’d like to shoot you an email.
I’ve got some ideas for your blog you might be interested in hearing.
Either way, great website and I look forward to seeing it expand over time.
Mangelsen
7916 Girard Avenue, Ꮮa Joya
CΑ 92037, United States
1 800-228-9686
Bookmarks
I don’t know if it’s just me or if everyone else encountering issues with your
blog. It appears as though some of the text within your
content are running off the screen. Can someone else please provide feedback and let me know if this
is happening to them too? This may be a problem with
my internet browser because I’ve had this happen before.
Cheers
Bu platformanı çox sevirəm.
https://mostbet-azerbaijan-fun.org
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Получить дополнительные сведения – https://indiaontherise.com/pootharekulu-the-exquisite-paper-sweet-from-andhra-pradesh
I every time used to study post in news papers but now as I am a
user of net thus from now I am using net for content, thanks
to web.
sap
Wonderful beat ! I wish to apprentice while you amend your site,
how could i subscribe for a blog site? The account helped me a
acceptable deal. I had been a little bit acquainted of this your
broadcast offered bright clear idea
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Открой скрытое – https://mrlift.com/largest-combilift-c-series-forklift-delivered
Sebuah situs phishing telah ditemukan dengan alamat yang tampak seperti layanan resmi. Mohon jangan memasukkan informasi pribadi apa pun di situs ini. Ini bukan situs resmi dan dapat digunakan untuk mencuri data Anda. Mohon bagikan informasi ini untuk mencegah kerusakan lebih lanjut.
Awesome issues here. I am very satisfied to see your post.
Thanks a lot and I am looking forward to touch you.
Will you kindly drop me a mail?
Best livescore app alternative, works perfectly on mobile browser no download needed
“Very useful blog post. I was looking for details on the Culver’s survey and this explained everything perfectly.”
you could check here https://liquity.cfd/
Hi, Neat post. There’s a problem with your site in internet explorer, might test this?
IE still is the marketplace leader and a large section of people will miss your wonderful writing because
of this problem.
hello there and thank you for your info – I’ve definitely picked up anything new from right here.
I did however expertise some technical points using this web site, since I experienced to reload
the site lots of times previous to I could get it to
load properly. I had been wondering if your hosting is OK?
Not that I’m complaining, but slow loading instances times will often affect your placement in google and can damage your quality score if ads and marketing with Adwords.
Anyway I’m adding this RSS to my email and can look out
for much more of your respective interesting content.
Ensure that you update this again very soon.
see it here https://g8keep.org
Эта статья погружает вас в увлекательный мир знаний, где каждый факт становится открытием. Мы расскажем о ключевых исторических поворотных моментах и научных прорывах, которые изменили ход цивилизации. Поймите, как прошлое формирует настоящее и как его уроки могут помочь нам строить будущее.
См. подробности – https://maecocointeriors.com.au/about-mae-coco-interiors
I am in fact thankful to the holder of this web site who
has shared this enormous post at at this place.
I do not even know the way I stopped up here, however I believed this submit
was great. I do not recognise who you are however certainly you’re going to a
famous blogger for those who are not already. Cheers!
Heya i’m for the first time here. I found this board and I find It truly useful & it helped me out much.
I hope to give something back and help others like you helped me.
I’d like to thank you for the efforts you’ve put in writing this website.
I am hoping to see the same high-grade blog posts from you
later on as well. In fact, your creative writing abilities has
encouraged me to get my own website now 😉
Sayt mükəmməldir. Təşəkkürlər!
https://j9.click/mostbet377
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Слушай внимательно — тут важно – https://www.davidrobotti.it/download/microsoft-powerpoint-2003
Unquestionably believe that which you stated. Your favorite reason appeared
to be on the internet the easiest thing to be aware of. I say to you, I definitely get irked
while people consider worries that they just don’t know about.
You managed to hit the nail upon the top as well as defined out the whole thing without having side-effects , people could take a signal.
Will likely be back to get more. Thanks
You are so cool! I do not believe I’ve read through
a single thing like this before. So nice to discover somebody with a few unique thoughts on this topic.
Really.. many thanks for starting this up. This website is something that is needed on the web, someone with a little originality!
海外华人必备的yifan平台采用机器学习个性化推荐,提供最新高清电影、电视剧,无广告观看体验。
I do consider all of the concepts you have offered on your post.
They’re very convincing and can definitely work.
Nonetheless, the posts are too short for newbies. May you please
prolong them a bit from next time? Thank you for the post.
go to website https://beratrax.org/
іѕ human trafficdking the ѕecond largest,usa gymnastics
coach human trafficking, human trafficking news neаr me,
snopes lynne knowles human trafficking, humaqn trafficking awareness ԁay quotes,human trafficking sex scene, human trafficking – menschenhandel, meghan connors human trafficking, ansrew tate human trafficking, arguments ᧐n human trafficking, free human trafficking cme florida, human trdafficking οur,
human trafficking inn miunnesota 2021, arizona republican human trafficking, orange іs tһe new black human trafficking, human trafficking
confrence ocean city md, 277 arrested іn human trafficking, anti human tracficking law philippines, north korea
human trafficking fаcts, hoow wіll the wall affect human trafficking, human trafficking training michigan 2018,hotels sued human trafficking, kids rescued fгom
human trafficking, durham region human trafficking, ԝhy
human trafficking is imрortant, mother ߋf god church
hhuman trafficking, walmart human trafficking 2020, ᴡhat iss the rate ⲟf human trafficking worldwide,
human trafficking nrws (news), human trafficking Ƅy ѕtate 2021, lybt human trafficking statistics, south africa
ɑnd hman trafficking, human trafficking statistics fbi, hotel lawsuits human trafficking, operation renewewd hope human trafficking, human trafficking atlanta 2022,
human trafficking san joaquin county, non profit organizations
f᧐r human trafficking, human trafficking interpol,
human trafficking elgin, trafficking women’ѕ human rigһts julietta
hua, facebook human traffifking lawsuit, rates ⲟf human trafficking,
real ѡorld examрⅼe off human trafficking, lawyers
аgainst human trafficking, wsin humaan trafficking summit 2022, vad är uman trafficking, recognizing tһe sins of human trafficking, human trafficking justice, videeo οf huma trafficking, fouг signs of human trafficking,
human trafficking honey, binjun xie human trafficking,
human trafficking documentary amazon ⲣrime, minnesota human trafficking
data, uncovers russian hyman trafficking
ring war, human trafficking chico cɑ, human trafficking jus cogens, human trafficking syrian refugees, human trafficking topics research
paper, text human trafficking link snopes, oprah
south africa human trafficking, human trafficking grants 2015,
human trafficking san antonio 2021, human drug trafficking meaning, human trafficking stories children, fema human trafficking
awareness, florida disnney human trafficking, jobs fօr human trafficking victims, movie ɑbout human trafficking 2023 netflix, ɑ day
in the life of a human trafficking victim, uk human trafficking news, bent
ⅼicense plate human trafficking reddit, human trafficking
іn waterbury ct, center tto combat human trafficking, greenville nc human trafficking, maui human trafficking, t᧐p 5 human trafficking cities, іs huma trafficking happening іn tһe us, oxnard human trafficking, aurorta shoreline human trafficking, taconganas human trafficking, hashtags fоr human trafficking, whiite house human trafficking summit, corona human trafficking,
border patrol human trafficking, human trafficking іn thailand 2020, humaan trafficking іn wv,
11 arrested iin human trafficking, china’ѕ οne child policy
ɑnd human trafficking, hotels human trafficking 2023, human trafficking іn florida 2021, human trafficking debate topics,
international justice mission human trafficking, uncovers human trafficking ribg fߋr,
scholarly article ᧐n human trafficking, madison herman human trafficking,
amad diallo human trafficking, а poem аbout human trafficking,
human trafficking bristol tn, deluca аnd the human trafficking storyline, economy
ɑnd human trafficking, human trafficking іn trinidad, human traffickikng Ԁay 2018, caught camera actual
human trafficking victims, human trafficking episode
opal grey’ѕ anatomy, duolingo ceo human trafficking,
watch dpgs human trafficking map, huuman trafficking deffinition canada, airtag huyman trafficking, human trafficking іn the beaauty industry, 人口販子human trafficking, forced labor іn human trafficking,
american airlines center human trafficking, human trafficking сe texas, selah human trafficking, siam human trafficking, fresno human trafficking statistics,
senegal human trafficking, humazn rafficking belgium, michigan human trafficking ϲourse, ny times human trafficking,
abandoned stroller human trafficking, human trafficking і-44,
solution оn human trafficking, humman trafficking
canada news, ontario human trafficking, protects victims оf human trafficking amendment,
humman trafficking іn highland ca, human trafficking
hotspot map, humaan trafficking organizations ontario, human trafficking hiding սnder cars, summary ᧐n human trafficking, uncovers russian humann trafficking ring war, human trafficking honey, fߋur signs of human trafficking, hhuman trafficking western pa,human trafficking livermore, human trafficking durham region, human trafficking аt atlanta airport, binjun xie human trafficking, minneota human tafficking
data, human trafficking documentary amazon рrime, human trafficking lawyer bloomfield
hills, huma trafficking charge іn texas, central stuxents аgainst human trafficking, ap human geography huuman trafficking, human trafficking fοr sexual
exploitation, blue fоr human trafficking, kajtian ethics human trafficking, anti-human trafficking organization іn cambodia,
jo jorgensen օn human trafficking, fort hood soldiers human trafficking,
beau ⲟf the fiftһ column huma trafficking, hawmins
human trafficking, human trafficking іn thhe pacific islands,
reasons why human traffiicking іs bad, ally human trafficking, ѡrite аn essay on humman trafficking, human trafficking pros,
human trafficking dark web reddit, north preston human trafficking, Ԁollar sign tattoo human trafficking, wht is human trafficking, human trafficking stuart
fl, priceless movie human trafficking, ti ɑnd wife human trafficking, human trafficking
ethnicity statistics, і 80 truck ѕtop human trafficking, hamilton human trafficking,
oakvillee human trafficking, human trafficking ߋn the deep
web, current human trafficking, human trafficking women’ѕ гights, brunei human trafficking, barack obama human trafficking quote, patron saint օf human trafficking, spirited аway human trafficking, tһe game human trafficking,
top human trafficking cities 2023, human trafficking ѡhich countries are the worst, how tߋ donate t᧐ human trafficking
organizations, human trafficking quotes famous, human trafficking story 2020, human trafficking іn pittsburgh,
2020 human trafficking conference, human trafficking bust atlanta, human trafficking hemet сa, human trafficking statistics oregon, hоw to identify a human trafficking
victim, economy аnd human trafficking, lover
boy method օf human trafficking, deluca ɑnd the human trafficking storyline,
european human trafficking, selah huyman trafficking, american airlines center
human trafficking, human trafficking paintings, ԝhаt
ѕtate is #1 in human trafficking?, forced labor iin human trafficking, 人口販子human trafficking, crystal meth, ᴡhat does
crtstal meth look like, what is crystal meth, crystal meth
anonymous, һow l᧐ng does crystal meth stay іn your system, how to makme crystal meth, blue crystal meth,
buy crystal meth online, crystal meth effects,
crdystal meth pipe, crystal meth drug, ᴡhat dߋes crystal meth ⅼook liқe?,
meth crystal, crystal meth images, crystal meth
ѕide effects, howw іs crystal meth made, meth vs crystal meth, what ɗoes crysfal meth Ԁo,crystal meth symptoms, crystal meth ѵѕ meth, effects of crystal
meth, ѕide effects of crystal meth, һow dⲟ yߋu maҝe crystal meth,
crystal meth ᴠs crack, what doeѕ crystal meth smelkl lіke, hhow is
crystal meth used, crystaql meth withdrawal, crystal meth breaking
bad, ԝhat is crystal meth madе օf, what dօes crystal meth do to үou, crystal meth teeth, smoking crysal meth, crystal
meth pictures, сan you snort crystal meth, crystal meth Ƅefore and after, who inbvented crystal meth, crystal meth fɑcts, crystal meth withdrawal symptoms, crystal meth street names, signs оf cryztal meth,
crystal merth addiction, һow to cook crystal meth, crystal meth definition, ԝһat
type of drug iѕ crystal meth, what doeѕ crystal meth feel
ⅼike,crystal meth meaning, crystal meth ingredients, ᴡhats crystal meth, ѡhat
color is crystal meth, crystal meth detox, crystal meth fɑce, crystal meth
powder, crystal meth poem,street names fߋr crystal meth, short tsrm effects ᧐f crystal meth, signs οf crystal meth abuse, crystal
meth rock, crystal meth fly, crystal meth addict, crysstal msth ᥙsers, crystal meth rehab, һow much does crystal meth cost,
how do yoᥙ taҝe crystal meth, hoԝ mucһ iss crystal meth, signs ߋf crystal
meth սse, how to smoke crystal meth, һow
to use crystal meth, ⅼong term effects ᧐f crystal meth, signs of addiction tօo crystal
meth, pink crystal meth, crystal meth ⅼоok like, breraking
bad crystal meth, ԝhen waѕ crystal meth invented,
pictures оf crystal meth, һow iѕ crystal meth tɑken, signs that ѕomeone iѕ ᥙsing crystal meth, ready οr not rystal meth storage, difference
Ƅetween meth and crystal meth, hοw dо yoᥙ do crystal meth,
crystal meth., locate crystal meth storage, ѡhat are the effects of crystal meth, fake crystal meth, crystal meth people,
ᴡһat does crtystal meth, һow do you ᥙse crystal meth,һow
addictive іs crgstal meth, can you overdose onn crystal meth, crystal
msth blue, crystal meth signs, һow long does crystal meth ⅼast, crystal meth detox llos angeles, һow ԁо people
use crystal meth, һow doeѕ crystgal meth look lіke, crystal methh porn, hoow does crystal meth ⅼook, crystal meth storage twisted nerve, ᴡhats іn crystal
meth, crystal meth treatment, ԝhat iѕ crystal meth made fгom, methamphetamin, methamphetamin adalah,
methamphetamin ⅾan amphetamin adalah, amphetamin Ԁɑn methamphetamin, chloroethane ɑnd methamphetamin, crystal methamphetamin, whаt is methamphetamin, methamphetamin еffect, methamphetamin sport, methamphetamin-entzug, methamphetamin definition, methamphetamin withdrawal, methamphetamin deutsch, methamphetamin 中文, mdma methamphetamin, methamphetamin hydrochlorid,
methamphetamin geschichte, methamphetamin hcl, amphetamin ѵs methamphetamin, methamphetamin biru,
methylphenidat methamphetamin, beda amphetamin Ԁan methamphetamin, difference Ьetween amphetamine and methamphetamin, methamphetamin psychose, methamphetamin rules, һow
to mаke methamphetamin, methamphetamin amphetamin unterschied, methamphetamin hydrochloride, definiion ᴠon methamphetamin, ⲣ2p methamphetamin, methamphetamin medizin, amphetamin սnd methamphetamin, vickms vapor inhaler methamphetamin, gta methamphetamin labor, wiie wirkt methamphetamin, methamphetamin entzug, methamphetamin kaufen, methamphetamin rezept, methamphetamin effects, methamphetamin amphetamin, methamphetamin schnelltest,
unterschied amphetamine ᥙnd methamphetamin, methamphetamin herstellung, methamphetamin herstellung china,
methamphetamin wehrmacht, methamphetamin tabletten, methamphetamin doccheck, һow to cook methamphetamin, methamphetamin abhängigkeit, methamphetami nebenwirkungen,methamphetamin ᴡas ist dаs, unterschied methamphetamin und amphetamin, methampphetamin nedir, amphetamine methamphetamin, methamphetamin aussprache, methamphetamin chemical formula,
methamphetamin medikament, methamphetamin ⅼa chat gi, est methamphetamin, methamphetamin pervitin, methamphetamin adalah obat,
methamphetamin аndere suchten ɑuch nacһ, methamphetamin mdma, tschechien methamphetamin, methamphetamin nachweisbarkeit, methamphetamin psychonaut,
methamphetamin molecule, methamphetamin labor, methylenedioxymethamphetamin, ecstasy methamphetamin, methamphetamin ⅾương tính, was іst methamphetamin, drogentest methamphetamin, methamphetamin englisch,
methamphetamin structure, іst mdma methamphetamin, lye іn methamphetamin, ist methamphetamin organschädigend?
quora, methamphetamin chemische struktur, methamphetamin chemische formel, methamphefamin meaning, Ԁ-methamphetamin, hersttellung methamphetamin, methamphetamin ѵs amphetamine, methamphetamin recept, methamphetamin japan, definition methamphetamin, methamphetamin fаce, methamphetanin formula,
methamphetamin synapse, methamphetamin adderall, methamphetamin adhd, blue methamphetamin, wirkung methamphetamin, methamphetamin terbuat dari,
methamphetamin addiction, bilder crystal methamphetamin, speed mіt methamphetamin gestreckt,
methamphetamin synthese, methamphetamin ᥙse icd 10, weed, weed grinder, ԝhere is weed
legal, disposable weed pen, weed shop neaqr
mе, milwaukee wered eater, purple weed, iss weed legal
іn virginia, iis weedd legal іn oklahoma, iis weed legal іn louisiana, weed puller tool, wweed carts, іs weed legal in south carolina, weed killer fⲟr lawns, horny
goat weed fоr men, what ѕtates iѕ weed legal, weed shops near me, weed legal states, wed vape, roundup weed killer, weed killer spray,
edibles weed, recreational weed ѕtates, weed store, milk weed, weed barrier, іs weed legal
in indiana, legal weed ѕtates, stateѕ witһ legal weed, is weed legal іn kentucky, weesd
puller, preen weed preventer, ounce ߋf weed, dewalt weed eater, plantain weed, husqvarna weed eater, electric weed eater, hybrid weed,
moonrock weed, weed pipe, barrett wilbert weed, weed control, weed delivery neɑr
me, is weed legal iin missouri, hⲟw tо makе weed butter, ѡhite weed, іs
weed legal іn utah, moon rock weed, snow caps weed,
іs weed legal iin arkansas, iss weed lwgal in texas 2025,
ryobi weed eater, weed bowl, dill weed, weed legalization,
smoking weed, іs weed legal iin nevada, weed whacker,
іs weed legal іn alabama, іs weed a drug, weed barrier fabric, ᴡhat iѕ horny goat weed, spruce weed
and grass killer, weed stores neаr me, sprinkles weed, poke weed,
weed withdrawal, weed vapes, snow cap weed, rm43 wred killer, craftsman weed eater, qp օf weed, wee edibles, cookies weed, gelato weed, іѕ wewed legal in new mexico, strains оf weed, weed butter, ρound oof weed, zaza weed, іs weed llegal in nc,
hoow mᥙch іѕ an ounce oof weed, pgr weed, іs
ԁelta 9 real weed, diy weed killer, zіρ of weed, weed torch, moldy weed, elon musk
weed, іs weed ilegal іn texas, weed eater string, rso weed, weed hangover, weed wallpaper, іs weed legal in nebraska, һow t᧐ smoke weed, is weed legal in hawaii, һow to
grow weed, һow to makе weed іn infinite craft, is weed legal іn california, gary
payon weed
Every weekend i used to visit this web site, for
the reason that i wish for enjoyment, as this this site conations truly fastidious funny material too.
4M Dental Immplant Center
3918 Ꮮong Beach Blvd #200, Lօng Beach,
CА 90807, United Stɑteѕ
15622422075
digital dental xray
My developer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on several websites for about a year and am
anxious about switching to another platform.
I have heard excellent things about blogengine.net.
Is there a way I can import all my wordpress content into it?
Any kind of help would be greatly appreciated!
Unquestionably consider that which you said. Your favorite reason appeared to be on the net the
simplest thing to remember of. I say to you, I definitely get annoyed whilst other people think about concerns that they just don’t understand about.
You controlled to hit the nail upon the top and
defined out the whole thing without having side-effects , folks can take
a signal. Will likely be back to get more.
Thank you
my homepage :: SEO marketing Edmond
Howdy! I know this is kind of off-topic however I had to
ask. Does running a well-established blog like yours require a lot of work?
I am completely new to operating a blog however I do write in my diary daily.
I’d like to start a blog so I can easily share my
personal experience and views online. Please let me know
if you have any kind of ideas or tips for new aspiring blog owners.
Appreciate it!
Paylaşdığınız məlumatlar mənə çox kömək edir. Təşəkkürlər!
http://sabayoi.ac.th/awstats/awstats.pl?framename=mainright&output=refererpages
read the full info here https://theo.sbs/
Hi there! I know this is kinda off topic but
I’d figured I’d ask. Would you be interested in trading links or
maybe guest writing a blog article or vice-versa? My site goes over a lot of the same topics
as yours and I think we could greatly benefit from each other.
If you are interested feel free to send me an e-mail. I look forward to hearing from you!
Awesome blog by the way!
Feel free to visit my blog post … Oklahoma SEO service Edmond OK
In fact when someone doesn’t understand afterward its up to other
users that they will help, so here it occurs.
My family members always say that I am killing my
time here at web, but I know I am getting know-how everyday by reading thes good posts.
Also visit my blog post: Oklahoma SEO service Edmond OK
I love your blog. It looks every informative.
i was reading this https://beraborrow.cc/
I got this web page from my buddy who informed me regarding this site and now this time I am visiting
this website and reading very informative content here.
Hi there, i read your blog from time to time and i own a similar one and i was just wondering
if you get a lot of spam responses? If so how do you prevent it, any plugin or anything
you can suggest? I get so much lately it’s driving me insane so any assistance is very
much appreciated.
Take a look at my blog: morgan silver dollar
Undeniably imagine that which you said. Your favourite justification appeared to be at the net the easiest factor to consider
of. I say to you, I certainly get irked at the same time
as other folks consider concerns that they just do not understand about.
You controlled to hit the nail upon the highest as neatly as outlined out the entire thing
with no need side-effects , folks could take a signal.
Will probably be again to get more. Thank you
Hey there I am so delighted I found your web site, I really
found you by mistake, while I was browsing on Bing for something else, Regardless
I am here now and would just like to say many thanks for a tremendous post and a all round thrilling
blog (I also love the theme/design), I don’t
have time to read it all at the moment but I have bookmarked it and also included your RSS feeds, so when I have time I
will be back to read much more, Please do keep up the superb jo.
Also visit my webpage morgan silver dollar
I love reading through a post that will make people
think. Also, thank you for allowing me to comment!
My web site … morgan silver dollar
Unquestionably believe that which you said. Your favorite reason seemed to be on the net the easiest thing to be aware of. I say to you, I certainly get annoyed while people consider worries that they plainly don’t know about. You managed to hit the nail on the head. Will probably be back to get more. Thanks
捕风捉影在线免费在线观看,海外华人专属平台运用AI智能推荐算法,高清无广告体验。
I loved as much as you’ll receive carried out right here.
The sketch is tasteful, your authored subject matter stylish.
nonetheless, you command get got an impatience over that you wish be delivering the following.
unwell unquestionably come more formerly again since exactly the same nearly a lot often inside case you shield this hike.
Hello everyone, it’s my first go to see at this web site, and article is really fruitful for
me, keep up posting such articles or reviews.
Feel free to surf to my homepage – 優塔
It’s awesome in favor of me to have a web site, which is good designed for my
knowledge. thanks admin
I cannot thank you more than enough for the blogposts on your website. I know you set a lot of time and energy into these and truly hope you know how deeply I appreciate it. I hope I’ll do a similar thing person sooner or later.
I think that is among the such a lot important info for me.
And i am satisfied studying your article. However wanna observation on few basic things, The website taste is ideal,
the articles is in point of fact excellent : D.
Good activity, cheers
I’ve read several good stuff here. Definitely value bookmarking for revisiting.
I surprise how so much attempt you place to create one of these fantastic informative web site.
The post is absolutely great! Lots of great info and inspiration, both of which we all need! Also like to admire the time and effort you put into your blog and detailed information you offer! I will bookmark your website!
İşinizə davam edin və daha çox istifadəçi cəlb edin!
https://1win-az-play.com/reyler
What’s up friends, good post and fastidious arguments commented here, I am truly enjoying
by these. https://uupr.org/portal_es/2022/08/19/hello-world-2/
I know this web page presents quality based articles and extra data, is there
any other web site which presents these kinds of stuff in quality?
I’ve read a few good stuff here. Definitely price
bookmarking for revisiting. I wonder how a lot attempt
you put to make any such wonderful informative website.
Appreciating the dedication you put into your site and detailed information you offer.
It’s good to come across a blog every once in a while that isn’t the same out of date rehashed
material. Wonderful read! I’ve bookmarked your site and I’m adding your RSS feeds to my Google account.
Thank you a lot for sharing this with all people you really recognise what
you are talking approximately! Bookmarked. Please additionally visit
my web site =). We will have a hyperlink alternate agreement among us
Feel free to visit my page; spiritual retreat center
Hey there would you mind sharing which blog
platform you’re working with? I’m going to start my own blog soon but I’m having a tough
time deciding between BlogEngine/Wordpress/B2evolution and
Drupal. The reason I ask is because your design and style seems different then most blogs and I’m looking
for something completely unique. P.S
My apologies for getting off-topic but I had to ask!
I feel that is among the most important information for me.
And i am glad studying your article. However should commentary on few general things, The site
style is wonderful, the articles is really nice : D.
Excellent process, cheers
my web page :: best wellness retreat mexico
An interesting discussion is definitely worth comment. I do believe that you need
to write more about this subject matter, it might not be a taboo matter but usually
folks don’t talk about these subjects. To the next!
Best wishes!!
It’s genuinely very difficult in this active life to
listen news on Television, so I just use
the web for that reason, and obtain the most recent information.
I’m not sure why but this blog is loading very slow for me.
Is anyone else having this problem or is it a issue on my end?
I’ll check back later on and see if the problem still exists.
Here is my web page: wellness yoga retreat center mexico
I believe everything wrote was actually very logical.
However, consider this, suppose you composed a catchier title?
I am not saying your content is not solid, however what if you added a post title that
makes people want more? I mean Heart failure: Symptoms, Causes,
Diagnosis & Treatment – MDtodate is a little boring.
You ought to glance at Yahoo’s front page and note how they create news headlines to get people to open the links.
You might add a video or a related pic or two to grab readers excited about
what you’ve got to say. In my opinion, it could bring your
posts a little livelier.
Here is my site; detox retreat mexico
sss
sss
Great info. Lucky me I found your blog by chance (stumbleupon).
I have book-marked it for later!
Hello there, You have done a great job. I’ll definitely digg it and
personally recommend to my friends. I’m sure they will be benefited from this web
site.
Also visit my page personal retreats
I have been exploring for a little bit for any high quality articles or blog posts on this kind of house .
Exploring in Yahoo I eventually stumbled upon this website.
Reading this information So i am satisfied to show that I’ve a
very excellent uncanny feeling I discovered just what I needed.
I most undoubtedly will make certain to do not overlook this
website and provides it a look regularly.
Here is my webpage yoga retreat center
This is a very informative post.
I really enjoy how this post breaks down
the details in an easy-to-understand manner.
A lot of users are confused about
how live streaming platforms operate,
especially when it comes to
quality, reliability, and safety.
This post does a good job explaining it,
and I think it will be helpful for new users
that want to learn more about the topic.
Thanks for posting such a useful article,
I will definitely check out more posts
from this site.
Je voulais simplement vous laisser un petit message dans ce coin messages.
🙂
This adult webcomic approaches taboo themes with restraint and emotional depth. Focusing on innocence, care, and moral ambiguity, the story unfolds through quiet interactions and psychological nuance. Instead of rushing events, it allows tension to grow naturally, inviting readers to reflect on intention, vulnerability, and shifting roles. Ideal for those who appreciate thoughtful storytelling that lingers in the mind long after each chapter ends.
I do believe all the ideas you’ve introduced to your post.
They’re really convincing and can certainly work.
Still, the posts are too quick for newbies. Could you please prolong them a bit from next time?
Thanks for the post.
It’s time for communities to rally.
I don’t know if it’s just me or if perhaps everybody else encountering issues
with your blog. It appears as though some of the written text on your posts are running off
the screen. Can someone else please provide feedback and let me know if this is happening to them too?
This may be a issue with my internet browser because
I’ve had this happen before. Kudos
Also visit my web-site; best wellness retreat mexico
This information is critically needed, thanks.
It’s amazing to pay a visit this web page and reading the views of all colleagues on the topic of this post,
while I am also zealous of getting know-how.
each time i used to read smaller posts that also clear their motive, and that
is also happening with this paragraph which I am reading now.
Look at my web-site … retreat center mexico
I used to be able to find good information from your blog posts.
If you are going for best contents like I do, simply pay a quick visit this web site everyday because it provides quality contents, thanks
I pay a visit everyday some web pages and information sites
to read content, but this website gives feature based posts.
Take a look at my website; corporate retreat mexico
Great web site. Lots of helpful info here. I’m sending it to several buddies
ans also sharing in delicious. And naturally, thank you for your effort!
Here is my web-site: retreat venue mexico
Makes sense to me.
Hi there, just wanted to say, I loved this article. It was helpful.
Keep on posting!
My page: couples retreat in mexico
Thanks a lot for sharing this with all of us you actually know
what you are speaking about! Bookmarked. Kindly additionally consult with my website =).
We may have a hyperlink trade contract between us
Good material, Cheers. https://temkarabelle.wordpress.com/2025/12/11/betflix-auto-reviews/
If some one needs expert view regarding blogging afterward i recommend him/her to visit this blog,
Keep up the pleasant work.
Visit my site: sacred medicine retreat center
Hey there! This post couldn’t be written any better! Reading this post reminds
me of my good old room mate! He always kept
talking about this. I will forward this page to him.
Pretty sure he will have a good read. Thanks for sharing!
I believe that is one of the such a lot important information for me.
And i’m glad studying your article. But
want to commentary on some basic issues, The site style is wonderful,
the articles is actually excellent : D. Good job, cheers
Look into my web blog: real estate agent Andover MA
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Читать далее > – https://jurnalbangsa.com/bpbd-jember-imbau-wisatawan-tidak-mandi-di-pantai-selatan
Truly when someone doesn’t know afterward its up to other users that they will help,
so here it occurs.
My website :: realtor in Hoboken NJ
This harem webcomic adds psychological depth to a familiar formula. Built around deception and consequence, the story turns desire into a high-risk balancing act. Each chapter increases tension as emotions deepen and honesty threatens to undo everything. Rather than easy fantasy, the narrative focuses on choice, pressure, and the cost of getting what you want. Ideal for readers who enjoy suspense-driven romance with real emotional stakes.
Hello there! I know this is kind of off topic but I was wondering if you knew
where I could find a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having problems finding one?
Thanks a lot!
Also visit my web page real estate agent Austin TX
Hi to every , as I am genuinely keen of reading this web site’s post to be updated
on a regular basis. It contains good material.
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Не упусти шанс – https://gothamdoughnuts.com/post/top-milkshake-destination-in-melbourne-indulge-in-heavenly-creations
正規のサービスを装ったアドレスを持つフィッシングサイトが発見されました。このサイトでは個人情報を入力しないでください。これは公式のサイトではなく、データの盗難に利用される可能性があります。さらなる被害を防ぐため、この情報を共有してください。
Откройте для себя скрытые страницы истории и малоизвестные научные открытия, которые оказали колоссальное влияние на развитие человечества. Статья предлагает свежий взгляд на события, которые заслуживают большего внимания.
Выяснить больше – https://www.computershala.com/how-angular-application-start
After I initially commented I appear to have clicked the -Notify me when new comments are added- checkbox and now
every time a comment is added I get 4 emails with
the exact same comment. There has to be a means you are able to remove me from that service?
Appreciate it!
my blog :: realtor in Hoboken NJ
Hello, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam
remarks? If so how do you prevent it, any plugin or anything you can advise?
I get so much lately it’s driving me mad so any assistance is very much appreciated.
Also visit my site; realtor in Hoboken NJ
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
Лучшее решение — прямо здесь – https://www.digitalexporter.com.tr/growth-marketing-nedir-nasil-yapilir
I seriously love your website.. Great colors & theme.
Did you create this amazing site yourself? Please reply back as I’m
trying to create my own personal blog and would
like to know where you got this from or just what the theme
is named. Thanks!
Here is my webpage best real estate agent in Austin TX
I’m amazed, I must say. Seldom do I come across a blog that’s equally educative and entertaining,
and let me tell you, you’ve hit the nail on the head. The issue is
something which not enough men and women are speaking intelligently about.
I am very happy I came across this during
my search for something regarding this.
my page: best real estate agent in Torrance CA
We’re a bunch of volunteers and starting a new scheme in our community.
Your web site offered us with useful info to work on. You’ve performed an impressive task and our whole community might be grateful
to you.
Feel free to surf to my web-site: real estate agent Austin TX
Hi to all, how is everything, I think every one is getting more
from this website, and your views are nice designed
for new visitors.
Feel free to visit my blog :: real estate agent Torrance CA
At this time it sounds like BlogEngine is the top blogging platform available
right now. (from what I’ve read) Is that what you are using on your blog?
Feel free to visit my web site best realtor in Austin TX
This wrestling webcomic tells its story through force and movement rather than words. Dynamic angles, expressive physiques, and carefully paced action turn each fight into a dramatic visual event. Readers are pulled into the rhythm of competition, feeling the tension of every clash and the weight of every victory. Perfect for fans of action-driven stories that rely on bold visuals and raw intensity.
It’s remarkable for me to have a web site, which is useful
in support of my knowledge. thanks admin
my web site real estate agent Andover MA
I am curious to find out what blog system you have been using?
I’m having some small security issues with my latest site and I would like to
find something more secure. Do you have any suggestions?
I could not refrain from commenting. Very well written!
Feel free to surf to my homepage … real estate agent Hoboken NJ
It’s an remarkable paragraph designed for all the web users; they will take advantage
from it I am sure.
Howdy! I know this is somewhat off topic but I was wondering which blog platform
are you using for this site? I’m getting fed up of WordPress because I’ve had problems with hackers and
I’m looking at options for another platform. I would be awesome if you could point me in the direction of a
good platform.
Thanks for sharing your thoughts about bk8.
Regards
I was wondering if you ever considered changing
the structure of your site? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content
so people could connect with it better. Youve got
an awful lot of text for only having 1 or 2 pictures. Maybe you could space
it out better?
my website: realtor in Parker County TX
If some one desires expert view on the topic
of blogging then i suggest him/her to pay a quick visit this weblog, Keep up the good work.
hello!,I like your writing so so much! share we keep in touch more about your post
on AOL? I need an expert in this house to resolve my
problem. Maybe that is you! Having a look ahead to look you.
Have a look at my website best real estate agent in Andover MA
Today, I went to the beach front with my kids.
I found a sea shell and gave it to my 4 year old daughter and said
“You can hear the ocean if you put this to your ear.” She
placed the shell to her ear and screamed. There was a hermit crab inside and
it pinched her ear. She never wants to go back! LoL I know
this is entirely off topic but I had to tell someone!
It is really a nice and useful piece of info. I am glad that you simply shared this helpful
info with us. Please stay us up to date like this.
Thanks for sharing.
my blog real estate agent Austin TX
An intriguing discussion is worth comment. I think that you need
to publish more on this subject matter, it may not be a taboo subject
but typically people don’t speak about such subjects.
To the next! Cheers!!
My page: best realtor in Hoboken NJ
I am not sure where you’re getting your information, but great topic.
I needs to spend some time learning much more or understanding more.
Thanks for wonderful information I was looking for
this info for my mission.
my site; real estate agent Pinecrest FL
My brother recommended I might like this web site.
He used to be entirely right. This publish truly made my day.
You cann’t imagine simply how much time I had spent
for this info! Thanks!
My blog best realtor in Parker County TX
Valuable information. Lucky me I discovered your site unintentionally, and
I am stunned why this accident didn’t happened in advance!
I bookmarked it.
My site – real estate agent Torrance CA
Thanks for your personal marvelous posting! I actually enjoyed reading it, you are a great author.I will ensure that I bookmark
your blog and will eventually come back later in life.
I want to encourage you to continue your great posts, have a nice weekend!
Check out my blog post … best real estate agent in Andover MA
Great info. Lucky me I ran across your blog by chance
(stumbleupon). I’ve book marked it for later!
I blog quite often and I genuinely appreciate your information. The article has really peaked my interest.
I am going to take a note of your website and keep checking for new details
about once a week. I opted in for your RSS feed too.
Review my page; real estate agent Pinecrest FL
官方授权的iyf.tv海外华人首选,第一时间提供最新华语剧集、美剧、日剧等高清在线观看。
Thanks for sharing! Speaking of entertainment, https://heepfiles.info/uhdisc.html has some amazing offers right now.
I visited many websites however the audio feature for audio songs
current at this web page is genuinely marvelous.
I’m gone to inform my little brother, that he should also
visit this website on regular basis to take updated from hottest information.
Here is my website: best real estate agent in Pinecrest FL
Good day I am so delighted I found your blog, I really found you
by accident, while I was searching on Bing for something else,
Anyways I am here now and would just like to say thanks for a incredible post and a all round
thrilling blog (I also love the theme/design), I don’t have time to read through it all at the minute but I have saved it and also included your
RSS feeds, so when I have time I will be back to read a lot more,
Please do keep up the fantastic job.
Hi! I understand this is kind of off-topic but I needed to
ask. Does operating a well-established blog like
yours require a large amount of work? I am completely new to operating a blog but I do write in my diary everyday.
I’d like to start a blog so I can share my experience and views online.
Please let me know if you have any suggestions or tips for
brand new aspiring bloggers. Thankyou!
Paragraph writing is also a excitement, if you be familiar with after that you can write or
else it is complex to write.
Wow, marvelous blog layout! How long have
you been blogging for? you make blogging look easy.
The overall look of your web site is fantastic, let alone the content!
My blog post :: best real estate agent in Parker County TX
It’s the best time to make some plans for the future and it’s time
to be happy. I’ve read this post and if I could I desire to suggest you some interesting things or tips.
Maybe you can write next articles referring to this article.
I want to read even more things about it!
My website :: best realtor in Austin TX
Today’s football match scores from around the world, comprehensive coverage of all leagues
I am actually grateful to the owner of this web page who has shared this enormous article at at this place.
Hey There. I discovered your blog the usage of msn.
This is a very neatly written article. I’ll be sure to bookmark it and return to learn extra of your helpful
info. Thank you for the post. I will definitely comeback.
My website :: best realtor in Andover MA
Woah! I’m really loving the template/theme of this website.
It’s simple, yet effective. A lot of times it’s difficult to get that “perfect balance” between user friendliness and visual appeal.
I must say that you’ve done a excellent job with this.
Also, the blog loads super fast for me on Safari. Exceptional Blog!
Football match time today, know exactly when games start in your timezone
What’s up to every body, it’s my first visit of this weblog;
this weblog consists of awesome and truly fine information for visitors.
my webpage: best real estate agent in Torrance CA
Football results from last night, complete scores and match summaries available now
References:
Vegas slot machines
References:
https://hedgedoc.eclair.ec-lyon.fr/s/e7jEx2uiH
Best livescore website for football fans, faster updates than any other score platform online
Greetings from Florida! I’m bored at work so I decided to check out your blog on my iphone during lunch break.
I really like the information you present here
and can’t wait to take a look when I get home.
I’m shocked at how fast your blog loaded on my cell phone ..
I’m not even using WIFI, just 3G .. Anyhow, fantastic site!
Goal celebrations, iconic moments and player reactions captured live
Normally I don’t learn post on blogs, however I would
like to say that this write-up very forced me to try and do so!
Your writing taste has been surprised me. Thanks, quite great post.
It’s a pity you don’t have a donate button! I’d most certainly donate to this
superb blog! I suppose for now i’ll settle for book-marking and adding your
RSS feed to my Google account. I look forward to fresh updates and will talk about
this website with my Facebook group. Chat soon!
Have a look at my page; real estate agent Austin TX
Amazing blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple adjustements would
really make my blog stand out. Please let me know where you got your theme.
Appreciate it
Hello just wanted to give you a quick heads up. The text in your content seem to be running
off the screen in Internet explorer. I’m not sure if this is a format issue or something to do with web browser compatibility but I thought I’d post to
let you know. The layout look great though! Hope you get the
issue fixed soon. Many thanks
Feel free to surf to my homepage :: real estate agent Andover MA
Mangelsen
7916 Girard Avenue, Ꮮa Joya
СA 92037, United States
1 800-228-9686
Bookmarks (http://www.protopage.com)
What a material of un-ambiguity and preserveness of precious know-how concerning unpredicted
feelings.
Take a look at my web page – real estate agent Hoboken NJ
I know this web page provides quality dependent posts and
extra material, is there any other web page which
provides these things in quality?
My homepage; best real estate agent in Hoboken NJ
Hi there! I just wish to offer you a big thumbs up for your excellent info you have got here on this post.
I will be returning to your site for more soon.
Feel free to visit my web blog: real estate agent Austin TX
Appreciate this post. Will try it out.
my webpage … best realtor in Austin TX
References:
Pennsylvania casinos
References:
https://hackmd.okfn.de/s/H1guCDGFIWx
Hi my family member! I want to say that this post is amazing, great written and come with approximately all vital infos.
I would like to see extra posts like this .
Here is my web page … realtor in Pinecrest FL
If you wish for to get a good deal from this piece of writing then you have to apply such
methods to your won webpage.
My web-site :: best real estate agent in Hoboken NJ
Hi there mates, its enormous piece of writing about teachingand entirely explained, keep it
up all the time.
My spouse and I absolutely love your blog and find
nearly all of your post’s to be what precisely I’m looking for.
Does one offer guest writers to write content for you
personally? I wouldn’t mind producing a post or elaborating on a lot of the subjects
you write with regards to here. Again, awesome
web log!
Whoa! This blog looks just like my old one! It’s on a totally different topic
but it has pretty much the same layout and design. Great choice
of colors!
Feel free to visit my website: real estate agent Hoboken NJ
You could definitely see your expertise within the work you write.
The sector hopes for more passionate writers such as you who aren’t afraid to
mention how they believe. All the time go after your heart.
Touche. Sound arguments. Keep up the great spirit.
Also visit my homepage; best real estate agent in Andover MA
This adult webcomic turns proximity into emotional danger.
Through restrained storytelling and character-driven tension, it examines how small moments
of attraction can grow into complicated choices. The love
triangle unfolds naturally, building anticipation and moral uncertainty with
every chapter. Ideal for readers who enjoy romance shaped by temptation, nuance, and emotional risk.
Wonderful site. A lot of helpful information here.
I’m sending it to some buddies ans additionally sharing in delicious.
And certainly, thanks to your effort!
It’s hard to find educated people about
this subject, however, you sound like you know what you’re talking about!
Thanks
Also visit my web-site … realtor in Parker County TX
That is very attention-grabbing, You’re an excessively skilled
blogger. I’ve joined your rss feed and look forward to searching for more of your fantastic post.
Also, I have shared your web site in my social networks
my site: realtor in Hoboken NJ
โพสต์นี้ อ่านแล้วเพลินและได้สาระ ค่ะ
ผม ไปเจอรายละเอียดของ หัวข้อที่คล้ายกัน
ที่คุณสามารถดูได้ที่ Petra
น่าจะถูกใจใครหลายคน
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ คอนเทนต์ดีๆ
นี้
จะรอติดตามเนื้อหาใหม่ๆ ต่อไป
Wow, this paragraph is good, my younger sister is analyzing these kinds of things, therefore I am going to convey her.
Feel free to visit my website – realtor in Pinecrest FL
I am regular visitor, how are you everybody? This paragraph posted at this web page is genuinely good.
Also visit my web site: best realtor in Torrance CA
I feel this is one of the such a lot significant information for me.
And i am satisfied studying your article. But want to
statement on few general things, The site style is perfect,
the articles is truly excellent : D. Excellent activity, cheers
Also visit my homepage; best realtor in Austin TX
Heya i’m for the first time here. I came across this board
and I find It truly useful & it helped me out a lot. I hope to give something back and help others like you helped me.
Here is my web page – best realtor in Parker County TX
Hurrah! In the end I got a webpage from where I be capable of genuinely obtain useful facts concerning my study and
knowledge.
Hi there, i read your blog from time to time and i
own a similar one and i was just curious if you get a
lot of spam comments? If so how do you stop it,
any plugin or anything you can advise? I get so much lately it’s
driving me crazy so any help is very much appreciated.
Thanks in favor of sharing such a good thinking, article is pleasant, thats why i have read it fully
Here is my page: real estate agent Austin TX
Oh my goodness! Incredible article dude! Thank you so much,
However I am experiencing difficulties with your RSS.
I don’t know the reason why I cannot join it.
Is there anyone else having similar RSS problems?
Anybody who knows the solution can you kindly respond?
Thanks!!
Wow that was strange. I just wrote an incredibly long comment but after I clicked submit my comment didn’t appear.
Grrrr… well I’m not writing all that over again. Anyway, just
wanted to say wonderful blog!
Good day! This is my first visit to your blog! We are a group of volunteers and starting a new
project in a community in the same niche. Your blog
provided us beneficial information to work on. You have done a extraordinary job!
Hello, I enjoy reading through your article.
I wanted to write a little comment to support you.
My site best real estate agent in Hoboken NJ
Valuable info. Lucky me I found your site by accident, and I am surprised why
this coincidence did not came about in advance! I bookmarked it.
This piece of writing presents clear idea designed for the new users of blogging, that really how to do blogging.
Also visit my web blog best realtor in Hoboken NJ
Cool blog! Is your theme custom made or did you download it from somewhere?
A design like yours with a few simple tweeks would really
make my blog stand out. Please let me know where you got your design. Thank you
Also visit my web page best realtor in Austin TX
As the admin of this site is working, no hesitation very rapidly it will
be well-known, due to its feature contents.
Take a look at my web blog … best realtor in Parker County TX
Hi there to every one, the contents present at this website are really remarkable for people
experience, well, keep up the nice work fellows.
Also visit my web site; realtor in Torrance CA
This is very interesting, You are a very skilled blogger.
I have joined your rss feed and look forward to seeking more of your great post.
Also, I have shared your web site in my social networks!
Here is my blog post … best real estate agent in Pinecrest FL
Easy and simple site with a wealth of gambling-related info.
https://bigbasssplashuk.co.uk/payments
This is the perfect web site for anyone who really wants
to find out about this topic. You know so much its almost
tough to argue with you (not that I personally will need to…HaHa).
You definitely put a brand new spin on a subject which has been written about for many years.
Great stuff, just excellent!
Do you mind if I quote a couple of your articles as long as I provide credit and
sources back to your weblog? My website is in the very same niche as yours and my visitors would really benefit from a lot of the information you provide here.
Please let me know if this alright with you. Cheers!
Here is my homepage … best real estate agent in Austin TX
That is really attention-grabbing, You are an overly skilled blogger.
I’ve joined your rss feed and sit up for in search of extra of your wonderful post.
Also, I’ve shared your site in my social networks
Also visit my page best real estate agent in Parker County TX
Hello! I’m at work surfing around your blog from my new iphone!
Just wanted to say I love reading your blog and look forward to all your posts!
Carry on the outstanding work!
Have you ever thought about including a little bit more than just
your articles? I mean, what you say is fundamental and
everything. Nevertheless think of if you added some great pictures or video clips to give your posts more,
“pop”! Your content is excellent but with pics and video clips, this blog could undeniably be
one of the greatest in its niche. Awesome blog!
เนื้อหานี้ น่าสนใจดี ครับ
ผม ได้อ่านบทความที่เกี่ยวข้องกับ เนื้อหาในแนวเดียวกัน
สามารถอ่านได้ที่ Luella
สำหรับใครกำลังหาเนื้อหาแบบนี้
เพราะอธิบายไว้ละเอียด
ขอบคุณที่แชร์ คอนเทนต์ดีๆ นี้
และอยากเห็นบทความดีๆ แบบนี้อีก
Jeg beundrer hvor lett det er å støtte her.
Also visit my blog: Pasientstøttefond
Good day! I know this is kind of off topic but I was wondering which
blog platform are you using for this website?
I’m getting sick and tired of WordPress because I’ve
had issues with hackers and I’m looking at alternatives for another
platform. I would be fantastic if you could point me in the
direction of a good platform.
my site: best real estate agent in Andover MA
I know this web site offers quality depending content and extra data, is
there any other site which provides these kinds of data in quality?
Həqiqətən demək istəyirəm ki, bu saytı tapdığıma çox sevinirəm.
http://www.avtocity-ek.ru/%D0%BA%D0%B0%D1%82%D0%B0%D0%BB%D0%BE%D0%B3_%D0%B7%D0%B0%D0%BF%D1%87%D0%B0%D1%81%D1%82%D0%B5%D0%B9_yamaha/action.redirect/url/aHR0cHM6Ly9waW4tdXAtYXplcmJhaWphbi1iYWt1Lm5ldA
Very soon this website will be famous amid all blogging visitors,
due to it’s fastidious articles or reviews
It’s an amazing post designed for all the web people; they will take benefit from it I am sure.
my homepage; realtor in Pinecrest FL
I absolutely love your site.. Excellent colors
& theme. Did you make this website yourself? Please reply back as I’m wanting to create my very own website and would like to know where you
got this from or exactly what the theme is called. Thank you!
Fantastic items from you, man. I have bear in mind your stuff prior to and you are simply too excellent.
I really like what you have acquired right here,
really like what you’re stating and the way through which
you assert it. You make it entertaining and you continue to take
care of to stay it sensible. I cant wait to
read far more from you. That is really a tremendous website.
Do you have a spam problem on this website; I also am a blogger, and I was wondering your
situation; many of us have developed some nice practices and
we are looking to exchange techniques with others, please shoot me an email if interested.
Stop by my homepage … best realtor in Austin TX
Why people still make use of to read news papers when in this technological
globe all is existing on net?
My homepage … best realtor in Hoboken NJ
hello there and thank you for your information – I have certainly picked
up something new from right here. I did however expertise some technical issues using this website, since I experienced to reload the site many times previous to I could get it
to load properly. I had been wondering if your web host is OK?
Not that I am complaining, but slow loading
instances times will sometimes affect your placement
in google and could damage your high-quality score if advertising and marketing with Adwords.
Anyway I’m adding this RSS to my email and could
look out for much more of your respective intriguing content.
Make sure you update this again very soon.
Also visit my web page: RK星河娛樂城
Very soon this web page will be famous amid all blogging and site-building visitors, due
to it’s good articles or reviews
Bu kontentə görə təşəkkürlər. Saytı dostlarıma tövsiyə edəcəyəm.
https://cleanuri.com/Mrrybz
bookmarked!!, I love your web site!
Wonderful, what a website it is! This weblog
provides useful information to us, keep it up.
Review my website – best real estate agent in Hoboken NJ
Hello friends, how is all, and what you would like to say concerning this piece of writing, in my view
its actually awesome designed for me.
Also visit my web site :: esun petg filament
Link ini merupakan situs phishing yang meniru brand/layanan resmi kami. Halaman ini meminta pengguna memasukkan informasi login/pembayaran palsu dan berpotensi digunakan untuk pencurian data. Situs ini juga sering melakukan redirect otomatis ke halaman scam/judi ilegal.
Thanks for sharing your thoughts about realtor in Austin TX.
Regards
Thanks for finally writing about > Heart failure:
Symptoms, Causes, Diagnosis & Treatment – MDtodate < Loved it!
We are a group of volunteers and starting a new scheme in our community.
Your web site offered us with helpful information to work on. You have performed an impressive activity and our entire community will likely
be grateful to you.
Kini nga post nagpatin-aw sa daghan sa akong mga pangutana mahitungod sa pag-abang sa mga basurahan. Nindot tan-awon ang ingon nga detalyado nga kasayuran. Ipadayon ang maayong buhat!
This website was… how do I say it? Relevant!!
Finally I have found something that helped me.
Thanks!
my blog real estate agent Hoboken NJ
goGLOW Houston Heights
1515 Studemont St Suite 204, Houston,
Texas, 77007, UႽA
(713) 364-3256
meet the team natural
It’s very easy to find out any topic on web as compared to books, as I
found this paragraph at this web page.
Take a look at my page best realtor in Austin TX
When someone writes an paragraph he/she retains the thought of a user in his/her brain that how a user can be aware of it.
Thus that’s why this paragraph is outstdanding. Thanks!
my website: cannabis payment processing
If some one wants expert view regarding running a blog
after that i advise him/her to pay a visit
this webpage, Keep up the good work.
My page – best real estate agent in Andover MA
It’s actually very difficult in this full of activity life
to listen news on TV, therefore I simply use web for that reason, and take the most up-to-date news.
Also visit my homepage – realtor in Austin TX
Excellent post! We will be linking to this great
article on our website. Keep up the good writing.
my page … best real estate agent in Hoboken NJ
捕风追影下载平台,專為海外華人設計,提供高清視頻和直播服務。
sss
sss
What’s up, all is going sound here and ofcourse every one is sharing information, that’s
genuinely good, keep up writing.
Feel free to surf to my page; best real estate agent in Parker County TX
I am regular visitor, how are you everybody? This piece of writing posted at
this web site is actually pleasant.
Review my page :: best real estate agent in Andover MA
Ωστόσο, το RTP παραμένει στο 98% σε όλες τις λειτουργίες, διασφαλίζοντας ένα δίκαιο παιχνίδι.
You actually make it seem so easy with your presentation but I
find this topic to be actually something that I think I would never
understand. It seems too complex and very broad for me.
I am looking forward for your next post, I will try to get the hang of it!
Look into my web site :: best real estate agent in Parker County TX
I could not resist commenting. Well written!
I’m gone to say to my little brother, that he should also visit this weblog on regular basis to obtain updated from newest news update.
Here is my web-site :: best realtor in Hoboken NJ
There’s definately a lot to learn about this issue. I like all of the
points you made.
Hey there! Would you mind if I share your blog with my myspace group?
There’s a lot of folks that I think would really appreciate your content.
Please let me know. Thank you
Stop by my blog post; realtor in Hoboken NJ
I used to be suggested this web site by way of my cousin. I’m not positive whether or not
this publish is written by him as no one else know such particular approximately
my problem. You’re wonderful! Thank you!
my blog; cannabis payments
It’s in fact very complicated in this active life to listen news
on Television, so I simply use web for that purpose, and get the newest
information.
Feel free to visit my website … realtor in Hoboken NJ
Hello, I enjoy reading through your article post. I wanted to write a little
comment to support you.
Superb blog you have here but I was wondering if you
knew of any discussion boards that cover the same topics talked about here?
I’d really like to be a part of group where I can get opinions from other knowledgeable
people that share the same interest. If you have any recommendations, please let
me know. Bless you!
Also visit my web-site CBD debit card processing
I’m not sure where you’re getting your information, but great topic.
I needs to spend some time learning much more or understanding more.
Thanks for wonderful information I was looking for this info for
my mission.
My page: petg 3d printer filament
I’ve learn some excellent stuff here. Certainly worth bookmarking for revisiting.
I surprise how much attempt you set to create
this sort of great informative website.
It’s remarkable to go to see this web site and reading the views of all
mates on the topic of this paragraph, while I am also keen of
getting knowledge.
Also visit my webpage real estate agent Torrance CA
I have read so many posts concerning the blogger lovers however
this paragraph is really a fastidious article, keep it up.
Feel free to visit my website: real estate agent Austin TX
Pretty! This has been an incredibly wonderful post. Thanks for
providing these details.
Check out my site … realtor in Pinecrest FL
I just couldn’t depart your site before suggesting that I actually enjoyed
the standard information a person provide to your visitors?
Is gonna be again ceaselessly in order to investigate cross-check new posts
my web-site; cannabis payments
Hi there fantastic blog! Does running a
blog like this require a great deal of work?
I have very little expertise in programming but I had been hoping to start my own blog in the near future.
Anyhow, should you have any ideas or techniques for new blog owners please share.
I understand this is off subject however I just had to ask.
Many thanks!
My web blog … best realtor in Pinecrest FL
fly88.select
Do you have a spam issue on this blog; I also am a blogger, and I was
curious about your situation; many of us have created some nice methods and we are looking to swap solutions
with other folks, please shoot me an email if interested.
Hi, all the time i used to check web site posts here in the early hours in the morning, since i enjoy to gain knowledge of more and more.
my web blog – real estate agent Hoboken NJ
Hmm it looks like your blog ate my first comment (it was super long)
so I guess I’ll just sum it up what I wrote and say, I’m thoroughly enjoying
your blog. I as well am an aspiring blog blogger but I’m still new
to the whole thing. Do you have any tips
and hints for first-time blog writers? I’d definitely
appreciate it.
my blog best realtor in Pinecrest FL
Thanks for finally writing about > Heart failure:
Symptoms, Causes, Diagnosis & Treatment
– MDtodate < Loved it!
Hi there, You have done a great job. I’ll certainly digg it and personally suggest to my friends.
I’m sure they will be benefited from this website.
Also visit my webpage – best real estate agent in Hoboken NJ
I quite like looking through an article that will make men and women think.
Also, thanks for allowing for me to comment!
Here is my website best real estate agent in Parker County TX
I blog quite often and I seriously thank you for your information. This article has truly peaked my interest.
I am going to bookmark your website and keep checking
for new details about once per week. I opted in for your Feed as well.
Also visit my blog post realtor in Austin TX
You can certainly see your enthusiasm in the work you write.
The world hopes for even more passionate writers such as you who
aren’t afraid to mention how they believe. Always go
after your heart.
my web site – best realtor in Hoboken NJ
Hi there, You have done an excellent job. I will definitely digg it and personally recommend to my friends.
I’m confident they will be benefited from this site.
Wow that was strange. I just wrote an very long comment but after I clicked
submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Regardless,
just wanted to say great blog!
My site; real estate agent Torrance CA
Hi, I do think this is an excellent site. I stumbledupon it 😉 I will
come back yet again since I saved as a favorite it. Money and
freedom is the greatest way to change, may you be rich and continue to guide others.
My page; real estate agent Parker County TX
Heya i am for the first time here. I came across this board and I find It really useful &
it helped me out much. I hope to give something back and aid
others like you aided me.
Also visit my blog … best real estate agent in Hoboken NJ
I’m impressed, I have to admit. Seldom do I come across a blog that’s
both equally educative and engaging, and let me tell
you, you’ve hit the nail on the head. The issue is something that too few men and women are speaking intelligently
about. I’m very happy I came across this during my search for something relating to this.
Hi everybody, here every person is sharing these knowledge, thus it’s good to read this website, and I used to pay a quick visit this website all the time.
Good day! I know this is kind of off topic but I
was wondering if you knew where I could get a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having problems finding one?
Thanks a lot!
I really like what you guys are usually up too. This kind of clever work and exposure!
Keep up the fantastic works guys I’ve incorporated you guys to blogroll.
Here is my web-site … best realtor in Torrance CA
Do you mind if I quote a couple of your articles as long
as I provide credit and sources back to your site?
My blog site is in the exact same niche as yours and my visitors would
definitely benefit from some of the information you provide here.
Please let me know if this alright with you. Thanks!
Check out my webpage – best real estate agent in Austin TX
爱一帆下载海外版,专为华人打造的高清视频官方认证平台,支持全球加速观看。
Extra time scores, matches that went beyond 90 minutes with final results
Established in 2014, Emirates International University
is a for-profit private higher education institution located
in the metropolis of Sanaa (population range of 1,000,000-5,000,000 inhabitants).
Officially recognized by the Ministry of Higher Education and Scientific Research of Yemen, Emirates International
University (EIU) is a coeducational Yemeni higher education institution. Emirates International University (EIU) offers courses and programs leading
to officially recognized higher education degrees in several areas of study.
See the uniRank degree levels and areas of study table below for further details.
EIU also provides several academic and non-academic facilities and services to students including as well as administrative services.
I just couldn’t leave your web site prior to suggesting that I extremely loved the standard info a
person supply on your guests? Is gonna be back regularly in order to investigate cross-check new posts
Captain performances, armband wearers and leadership statistics
Somebody necessarily help to make critically posts I might state.
This is the first time I frequented your web page and to this
point? I surprised with the analysis you
made to create this actual post amazing.
Magnificent job!
Here is my homepage … best realtor in Austin TX
Definitely believe that which you said. Your favorite justification seemed to be on the net the simplest thing to be aware of.
I say to you, I definitely get annoyed while people think about
worries that they plainly don’t know about. You managed to hit the nail
upon the top and defined out the whole thing without having
side effect , people could take a signal. Will likely be back to get more.
Thanks
I blog frequently and I really thank you for your information. The article has really peaked my interest.
I am going to take a note of your website and keep checking for new details about once per week.
I opted in for your RSS feed as well.
My web blog: real estate agent Andover MA
My spouse and I stumbled over here by a different web address and thought
I may as well check things out. I like what I see so i am just following you.
Look forward to checking out your web page for a second time.
Hi there to every single one, it’s actually a fastidious for me to pay a visit this web site, it consists of important Information.
My web site: best realtor in Andover MA
A fascinating discussion is definitely worth comment.
I do believe that you should write more on this topic, it may not be
a taboo matter but usually people do not speak about these
topics. To the next! Cheers!!
my web site … best realtor in Pinecrest FL
Currently it seems like Expression Engine is the best blogging platform out there right now. (from what I’ve read) Is that what you’re using on your blog?
byueuropaviagraonline
I visited several blogs however the audio feature for audio songs present at this website is
genuinely excellent.
Here is my website … best realtor in Hoboken NJ
Magnificent items from you, man. I have remember your stuff prior to
and you are simply extremely wonderful. I actually like what you have received
here, certainly like what you are saying and the best way during which you
say it. You are making it entertaining and you continue to take care of to
keep it sensible. I can’t wait to learn far more from you.
That is actually a tremendous website.
Also visit my web site: best realtor in Andover MA
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UЅA
(713) 364-3256
Bookmarks
I’ve been browsing online more than 3 hours today, yet
I never found any interesting article like yours. It is pretty worth enough for me.
Personally, if all web owners and bloggers made
good content as you did, the internet will be much more
useful than ever before.
my web page :: best real estate agent in Hoboken NJ
It’s going to be end of mine day, but before ending I am reading this great article to
improve my knowledge.
Asking questions are actually nice thing if you are not understanding
something totally, except this paragraph provides pleasant understanding yet.
Feel free to surf to my webpage: best realtor in Austin TX
Highly energetic article, I liked that bit. Will there be a part 2?
My site – best realtor in Andover MA
Hi to all, how is the whole thing, I think every one is getting more from this site, and your views are pleasant
designed for new people.
It’s really a great and helpful piece of information. I am happy that you just shared this useful
info with us. Please keep us informed like this. Thanks for sharing.
I constantly spent my half an hour to read this web
site’s content every day along with a cup of coffee.
Fastidious response in return of thiѕ difficulty with
firm arguments and describing all օn the topic of that.
Can I just say what a relief to discover somebody who truly knows what they’re talking about on the internet.
You actually know how to bring a problem to light and
make it important. More and more people should look at this and understand this side of your story.
I was surprised you are not more popular because you definitely have the gift.
Here is my webpage; best realtor in Parker County TX
You have made some good points there. I checked on the web to learn more about the issue and found most individuals will go along with your views on this website.
Visit my blog … real estate agent Austin TX
My brother recommended I may like this blog. He used to be entirely right.
This publish truly made my day. You can not believe simply
how a lot time I had spent for this information! Thanks!
my web page – real estate agent Torrance CA
There’s definately a lot to learn about this topic.
I like all of the points you’ve made.
Everyone loves what you guys tend to be up too. This kind of clever work and reporting!
Keep up the awesome works guys I’ve you guys to my personal blogroll.
My webpage; real estate agent Austin TX
It’s amazing to go to see this web site and reading the views of all friends concerning this
paragraph, while I am also keen of getting knowledge.
Very energetic blog, I enjoyed that a lot. Will there be a part
2?
Have a look at my web blog :: best real estate agent in Torrance CA
Good post. I learn something new and challenging on sites I stumbleupon every day.
It’s always interesting to read through content from
other writers and use something from their web
sites.
Have a look at my blog post – real estate agent Andover MA
I have been browsing online more than three hours today, yet I never found any interesting article like yours.
It’s pretty worth enough for me. Personally, if all webmasters and bloggers made
good content as you did, the internet will be much more useful than ever before.
My site – real estate agent Austin TX
I’m really impressed with your writing skills and also with the layout on your weblog.
Is this a paid theme or did you customize it
yourself? Anyway keep up the nice quality writing, it’s rare to see a great blog like this one today.
Feel free to surf to my web blog :: real estate agent Austin TX
Thanks for sharing your thoughts about No-nude Stars.
Regards
Good blog post. I definitely love this site.
Continue the good work!
It’s truly very complex in this full of activity life to listen news on Television, therefore I simply use web
for that purpose, and get the newest news.
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UЅᎪ
(713) 364-3256
Bookmarks
Paragraph writing is also a fun, if you know after that you can write if
not it is complicated to write.
Appreciating the persistence you put into your blog and
detailed information you provide. It’s great to come across a blog every once in a while that isn’t the same unwanted rehashed material.
Great read! I’ve saved your site and I’m including your RSS feeds to my Google account.
Also visit my web-site; realtor in Pinecrest FL
We’re a group of volunteers and opening a new scheme in our
community. Your site provided us with valuable info to work on. You have done an impressive task and our entire community will be thankful to you.
My web site best real estate agent in Hoboken NJ
Do you have a spam issue on this blog; I also am a
blogger, and I was curious about your situation; many of us have created some nice practices and we are looking to trade strategies with other folks, be
sure to shoot me an e-mail if interested.
Magnificent beat ! I would like to apprentice while you amend your web site,
how can i subscribe for a blog site? The account aided me a acceptable
deal. I had been tiny bit acquainted of this your broadcast offered bright clear idea
My web page … best real estate agent in Hoboken NJ
You could certainly see your skills in the article you write.
The world hopes for even more passionate writers such as you who are not afraid to mention how they believe.
Always go after your heart.
Reliable posts, With thanks.
Here is my webpage: https://telegra.ph/Kak-da-Kupim-Bitkojn-s-Kreditna-Karta-v-Blgariya-Brzo-Rkovodstvo-2026-01-23
Hi, yes this piece of writing is genuinely good and I have learned lot of things from it on the topic of blogging.
thanks.
My webpage :: US Mega Millions ticket India online
Woah! I’m really enjoying the template/theme of this website.
It’s simple, yet effective. A lot of times it’s very difficult to
get that “perfect balance” between superb usability and visual
appearance. I must say you have done a awesome job with this.
Also, the blog loads very fast for me on Chrome.
Exceptional Blog!
my website :: best real estate agent in Torrance CA
These are in fact enormous ideas in regarding blogging. You have
touched some good factors here. Any way keep up wrinting.
Here is my web blog :: real estate agent Parker County TX
海外华人必备的ifun平台,提供最新高清电影、电视剧,无广告观看体验。
What’s up to every one, because I am truly keen of reading this
blog’s post to be updated daily. It contains good stuff.
my web page; अमेरिका Powerball टिकट ऑनलाइन खरीदें
Hi there! I’m at work browsing your blog from my new iphone 4!
Just wanted to say I love reading your blog and look forward
to all your posts! Keep up the superb work!
My website … realtor in Hoboken NJ
Hi! I could have sworn I’ve been to this web site before but after browsing through some of the posts I realized it’s
new to me. Nonetheless, I’m certainly pleased I came
across it and I’ll be bookmarking it and checking back often!
Here is my blog – अमेरिका Mega Millions टिकट भारत से
Hi there to every , because I am truly keen of
reading this webpage’s post to be updated on a regular basis.
It includes fastidious data.
Also visit my blog :: best real estate agent in Austin TX
An outstanding share! I have just forwarded this onto a coworker who has been doing a little homework on this.
And he actually bought me lunch because I discovered it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanks for spending the time to discuss this matter here on your internet site.
Since the admin of this web page is working, no
hesitation very shortly it will be renowned, due to its feature
contents.
Feel free to visit my web site best real estate agent in Torrance CA
Greetings! Very helpful advice within this post!
It’s the little changes that produce the most significant changes.
Many thanks for sharing!
Here is my web blog :: real estate agent Austin TX
It’s fantastic that you are getting ideas from this paragraph as well as from our discussion made at this place.
Look into my homepage – best real estate agent in Hoboken NJ
I am sure this article has touched all the internet viewers, its really really fastidious article on building up new website.
Also visit my homepage – अमेरिका Powerball टिकट ऑनलाइन खरीदें
I have read so many posts concerning the blogger lovers except this article is in fact a nice piece of
writing, keep it up.
What’s up, its pleasant piece of writing regarding media print, we all know media is a wonderful source
of information.
Feel free to visit my web site; realtor in Torrance CA
whoah this blog is wonderful i really like studying your articles.
Keep up the great work! You already know, a lot of individuals are hunting round for this info, you can help them greatly.
Here is my web-site – real estate agent Pinecrest FL
If some one desires to be updated with newest technologies after
that he must be pay a visit this web site and be up to date every day.
Hi, I wish for to subscribe for this blog to take most up-to-date updates, thus where can i do it please help out.
Appreciating the persistence you put into your blog
and detailed information you provide. It’s good to come across a
blog every once in a while that isn’t the same out of
date rehashed information. Wonderful read! I’ve bookmarked your site and
I’m including your RSS feeds to my Google account.
Also visit my web blog; अमेरिका Mega Millions टिकट भारत से
I am really enjoying the theme/design of your weblog.
Do you ever run into any internet browser compatibility issues?
A handful of my blog readers have complained about my blog not working correctly in Explorer but looks great in Safari.
Do you have any tips to help fix this issue?
Here is my page – best real estate agent in Austin TX
What’s up Dear, are you really visiting this site daily,
if so afterward you will without doubt obtain nice know-how.
I am sure this paragraph has touched all the internet
users, its really really pleasant article on building
up new blog.
You said it nicely..
It is truly a great and helpful piece of info.
I’m satisfied that you simply shared this helpful info with us.
Please keep us informed like this. Thanks for sharing.
Here is my site best real estate agent in Austin TX
fly88
Magnificent goods from you, man. I’ve take note your stuff prior to
and you’re simply extremely great. I actually like what you have acquired here, really
like what you’re stating and the way wherein you assert
it. You’re making it enjoyable and you continue to
care for to keep it smart. I can not wait to learn far more from you.
This is really a terrific site.
This webcomic keeps readers coming back by mastering the art of tension. Instead of rushing the story, it builds curiosity through atmosphere, pacing, and evolving relationships. Each chapter pushes the narrative forward just enough to deepen intrigue without giving everything away. The result is a focused, immersive read that feels intentional, gripping, and impossible to put down.
Thankfulness to my father who told me on the topic of this web site, this webpage is really remarkable.
my company https://jaxxwallet-web.org/
My brother recommended I might like this website.
He was entirely right. This post truly made my day. You can not imagine simply how much time I had spent for this information! Thanks!
I am regular reader, how are you everybody? This piece of writing posted at this web site
is genuinely pleasant.
真实的人类第二季高清完整版运用AI智能推荐算法,海外华人可免费观看最新热播剧集。
บทความนี้ ให้ข้อมูลดี ครับ
ดิฉัน ไปเจอรายละเอียดของ ข้อมูลเพิ่มเติม
ที่คุณสามารถดูได้ที่ pg888 เกมสล็อตยอดนิยม
เผื่อใครสนใจ
เพราะอธิบายไว้ละเอียด
ขอบคุณที่แชร์ บทความคุณภาพ นี้
และอยากเห็นบทความดีๆ
แบบนี้อีก
Useful information. Fortunate me I found your site unintentionally, and
I am stunned why this accident did not took place in advance!
I bookmarked it.
Развратные индивидуалки города Челябинск с
особым энтузиазмом сделают сладкий
анилингус своему клиенту. Подборка анкет развратных проституток города Красноярск
с услугой анилингус специально для вас,
анкеты с фото и номерами телефона.
Ухоженная индивидуалка уже подготовила свой язычок специально для
твоего ануса.
Индивидуалки Амз
Эти индивидуалки и проститутки готовы работать по всему городу Челябинску,
приедут к тебе домой или примут у себя
в апартаментах. Девчонки исполнят любое твое, даже самое сокровенное
желание.
I’m curious to find out what blog system you happen to be using?
I’m having some minor security issues with my latest site and I would like to find something more safe.
Do you have any solutions?
You reported it exceptionally well. https://www.google.com.tj/url?q=https://betflik-168.org
Knygos Tomes
Formation changes, tactical adjustments during matches tracked real time
Heya this is kind of of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding expertise so I wanted to get advice from someone with experience.
Any help would be greatly appreciated!
It’s going to be end of mine day, except before end I am reading this fantastic article to improve my know-how.
Thanks a bunch for sharing this with all of us you actually recognise
what you are speaking approximately! Bookmarked. Kindly also
seek advice from my web site =). We may have a hyperlink exchange agreement between us
whoah this blog is magnificent i love reading your
articles. Keep up the great work! You know, lots of individuals
are looking round for this information, you can aid them greatly.
Hi there, all the time i used to check web site posts here in the
early hours in the daylight, since i love to learn more
and more.
Pretty! This was an extremely wonderful article. Many thanks for supplying this
info.
爱一凡海外版,专为华人打造的高清视频平台运用AI智能推荐算法,支持全球加速观看。
Hello everyone, it’s my first visit at this website, and paragraph is
actually fruitful in support of me, keep up posting these types of
articles or reviews.
I am really enjoying the theme/design of your weblog. Do you ever
run into any browser compatibility issues? A small number of my
blog visitors have complained about my blog not operating
correctly in Explorer but looks great in Firefox.
Do you have any tips to help fix this issue?
Thank you, I have just been searching for information approximately
this topic for a long time and yours is the best I’ve discovered till now.
However, what about the conclusion? Are you sure concerning the
supply?
Just want to say what a great blog you got here!I’ve been around for quite a lot of time, but finally decided to show my appreciation of your work!
Referee decisions, official calls and controversial moments documented
I enjoy what you guys are usually up too. This type of clever work and
reporting! Keep up the wonderful works guys I’ve incorporated you guys to blogroll.
Good material Thanks a lot!
Easily, the post is really the greatest on this laudable topic. I concur with your conclusions and will thirstily look forward to your future updates. Saying thank will not just be sufficient, for the wonderful c lucidity in your writing. I will instantly grab your rss feed to stay privy of any updates. Solid work and much success in your business enterprise!
Регистрация в казино 7k: пошаговая
инструкция и верификация аккаунтаОнлайн казино 7k
Популярность казино 7k растет благодаря
честным выплатам и широкому ассортименту развлечений для азартных
пользователей. Независимо от опыта игрока, важно выбрать лицензионное заведение,
которое гарантирует честность результатов и безопасность транзакций.
Преимущества игры в 7k
Клуб работает легально, что
дает игрокам уверенность в отсутствии накруток и гарантирует вывод выигрышей.
Пользователи могут рассчитывать на выгодную программу лояльности, бонусы за
депозиты и регулярные акции.
Клиенты получают мгновенные консультации через чат по всем аспектам использования
сайта и зеркал.
Ассортимент игр в 7k Casino
Библиотека игр на платформе 7k состоит из множества сертифицированных слотов и настольных
игр:
Классические и современные слоты с высокой отдачей (RTP) и бонуснымираундами.
РазделLive, где можно сыграть в рулетку, блэкджек и баккару с профессиональнымикрупье.
Регулярные турниры и лотереи с крупными призовыми фондами для активных игроков.
Настольные и карточные игры для ценителей стратегии и классического гемблинга.
Отзывы игроков
Мнения постояльцев клуба 7k часто
становятся решающим фактором для тех, кто
ищет новую площадку. Многие гемблеры отмечают:
Оперативность финансовых операций и отсутствие задержек при выводе.
Отсутствие проблем с доступом благодаря системе рабочих зеркал.
Щедрость бонусной политики и
лояльные условия отыгрыша вейджера.
Зеркало и доступ к сайту
Рекомендуется сохранить ссылку
на рабочее зеркало казино, чтобы в любой моментпродолжить игру.
Бесперебойная работа портала является ключевым
условием для спокойного гемблинга.
Как начать играть в 7k?
Для доступа ко всем функциям платного режима
следует выполнить несколько простых
действий:
Заполните регистрационную форму,
указав достоверные данные.
Используйте промокод или выберите
бонус на первый депозит для успешного старта.
Сделайте пополнение баланса и переходите к выбору развлечений в лобби.
Не забывайте, что идентификация профиля является стандартной процедурой для безопасности ваших средств.
Играйте ответственно и воспринимайте казино как развлечение. https://7k-seven7.xyz Итоги
обзора
Регистрация в казино 7k — это отличный выбор для
тех, кто ценит качество, надежность и разнообразие азартных игр.
Каждый пользователь получает доступ к
лицензионному софту и может быть уверен
в честности генератора случайных чисел.
Высокие стандарты обслуживания делают 7k одним
из лидеров индустрии, предлагая лучшие условия для игры.
Советы для игроков
Успех в казино зависит не только от удачи, но и от грамотного управления банкроллом и выбора
стратегии. Гемблер обязан:
Изучать правила каждого слота перед игрой
на деньги;
Устанавливать лимиты на проигрыш и выигрыш;
Внимательно читать правила отыгрыша бонусных средств;
Сохранятьхладнокровие и не поддаваться тильту при проигрышах;
Обращаться в поддержку при возникновении спорных ситуаций.
Сильные стороны 7k Casino
Аудиторияклуба выбирает
нас за надежность, щедрые автоматы и регулярные ивенты с призами.
Мы стремимся обеспечить максимальный комфорт и безопасность для каждого посетителя сайта.
Современная платформа 7k адаптирована под любые устройства, позволяя играть как
с ПК, так и со смартфонов без потери
качества.
Где искать вход?
Для беспрепятственного входа на сайт,следите за обновлениями адресов в надежных источниках:
Вступление в телеграм-чат сообщества игроков;
Проверка электронной почты на наличие рассылки
от администрации;
Использование поисковых систем с
запросом “7k казино зеркало”;
Обращение в саппорт через социальные сети.
Не забывайте, что использованиеофициальных зеркал гарантирует сохранность ваших личных данных и средств на счету.
Мы всегда рады видеть новых победителей в нашем клубе.
Подводя итог, можно сказать,
что 7k — это место, где азарт сочетается с реальными возможностями для заработка.
Присоединяйтесь к нам сейчас, получайте бонусы и ловите удачу за хвост!
What a material of un-ambiguity and preserveness of
valuable experience regarding unpredicted emotions.
WOW just what I was looking for. Came here by searching for trichinising
Hey! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
В этом интересном тексте собраны обширные сведения, которые помогут вам понять различные аспекты обсуждаемой темы. Мы разбираем детали и факты, делая акцент на важности каждого элемента. Не упустите возможность расширить свои знания и взглянуть на мир по-новому!
А что дальше? – https://environmentaltrust.org.uk/project/nor-agains-there-anyone-who-loves
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Более подробно об этом – https://mascotas.alimentosmor.com.sv/portfolio/animal-cares-purpose
Этот информационный обзор станет отличным путеводителем по актуальным темам, объединяющим важные факты и мнения экспертов. Мы исследуем ключевые идеи и представляем их в доступной форме для более глубокого понимания. Читайте, чтобы оставаться в курсе событий!
Не упусти шанс – https://naturalhairs.net/10-drugstore-products-celebrity-stylists-recommend
Этот информационный материал собраны данные, которые помогут лучше понять текущие тенденции и процессы в различных сферах жизни. Мы предоставляем четкий анализ, графики и примеры, чтобы информация была не только понятной, но и практичной для принятия решений.
Исследовать вопрос подробнее – https://thecalligraphysquare.in/blog/top-5-books-to-learn-brushlettering
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Хочешь знать всё? – https://rusoge.ru/geo/korolev
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Что скрывают от вас? – https://fepropaz.com/tech-educacion-ambiental
Hi there this is somewhat of off topic but I was wanting
to know if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding expertise so I wanted to get advice from someone with experience.
Any help would be greatly appreciated!
Мы настоятельно призываем Google немедленно проверить и удалить эти ссылки из результатов поиска, чтобы предотвратить их дальнейшее использование в злонамеренных, манипулятивных и эксплуататорских целях.
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Подробнее – https://greenduckindustries.com/waterless-car-wash-wax-concentrate
Мы предлагаем вам подробное руководство, основанное на проверенных источниках и реальных примерах. Каждая часть публикации направлена на то, чтобы помочь вам разобраться в сложных вопросах и применить знания на практике.
Обратитесь за информацией – https://inraa.dz/signature-dune-convention-cadre-tripartite-de-collaboration-entre-l-inraa-le-crti-et-le-cder
always i used to read smaller articles or reviews that as
well clear their motive, and that is also happening with this paragraph which I am reading here.
перейдите на этот сайт Оземпик синий купить
Hi Dear, are you genuinely visiting this web page on a regular
basis, if so afterward you will absolutely obtain nice know-how.
содержание mounjaro купить в спб
Hello, Neat post. There’s an issue with your site in internet explorer, may test this?
IE still is the marketplace chief and a huge part of other folks will miss your excellent writing due to this problem.
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Узнать из первых рук – https://sitecheck.elinkdesign.com/fr/www/furycoins.ru
goGLOW Houston Heights
1515 Studemont Ѕt Suite 204, Houston,
Texas, 77007, UЅА
(713) 364-3256
microdermabrasion process Guide
爱一凡海外版,专为华人打造的高清视频平台AI深度学习内容匹配,支持全球加速观看。
Valuable data Kudos!
Nice post. I was checking continuously this weblog and I am impressed!
Extremely useful information particularly the closing phase 🙂
I take care of such info a lot. I was looking for this particular info
for a long time. Thanks and good luck.
Wow, this post is nice, my younger sister is analyzing these kinds of things, so I
am going to let know her.
Thank you! Numerous postings.
of course like your web-site however you have to check the spelling on several of your posts. Many of them are rife with spelling problems and I find it very troublesome to tell the reality then again I will surely come back again.
Dude.. I am not much into reading, but somehow I got to read lots of articles on your blog. Its amazing how interesting it is for me to visit you very often. –
Nice post.Very useful info specifically the last part 🙂 Thank you and good luck.
I was able to find good information from your articles.
obviously like your web-site but you need to take a look at the
spelling on several of your posts. A number of them are
rife with spelling issues and I in finding it very troublesome to inform the reality nevertheless I will definitely
come again again.
Feel free to surf to my site :: equipment rental vancouver
Sweet blog! I found it while browsing on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thank you
Nice post. I was checking constantly this blog and I’m impressed!
Very helpful info specially the last part 🙂 I care for such info much.
I was seeking this certain information for a very long time.
Thank you and best of luck.
Asking questions are really nice thing if you are not understanding anything fully, however this article provides
nice understanding yet.
I don’t even know how I ended up here, but I thought this post was good.
I do not know who you are but definitely you’re going to a famous blogger
if you are not already 😉 Cheers!
Everything is very open with a clear description of the challenges.
It was truly informative. Your site is very helpful. Thanks for
sharing!
It’s amazing designed for me to have a web page, which is helpful
designed for my knowledge. thanks admin
禁忌第一季高清完整版结合大数据AI分析,海外华人可免费观看最新热播剧集。
Great resources and tips for families here.
see post
https://russian-traditional-clothes.com/
What’s up, I check your new stuff daily. Your humoristic style is awesome, keep up the good work!
Feel free to surf to my blog – cfo search firms
I was suggested this web site by means of my cousin. I’m not positive whether
or not this publish is written by him as no one else realize such specific about my problem.
You’re amazing! Thanks!
This excellent website definitely has all the info I needed concerning this
subject and didn’t know who to ask.
My blog … equipment rental vancouver
This video explains how to prepare the gelatin trick recipe, what ingredients
are commonly used, and why the gelatin trick became one of the most searched wellness topics in 2025.
It’s wonderful that you are getting ideas from this piece of writing as
well as from our argument made at this place.
Hey I know this is off topic but I was wondering if you knew of any widgets
I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time
and was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward
to your new updates.
Glad to be one of many visitants on this amazing site : D.
Every weekend i used to go to see this web site, because
i want enjoyment, since this this web page conations genuinely fastidious funny stuff too.
my page … executive search firms
We’re developing a conference, and it looks like you would be a great speaker.
I’m amazed, I have to admit. Seldom do I come across a blog that’s both equally educative and amusing, and let me tell you, you’ve hit the nail on the head.
The problem is an issue that not enough men and women are speaking intelligently about.
Now i’m very happy that I stumbled across this during my top 20 executive search firms for
something relating to this.
Fine posts Kudos!
Hmm it seems like your blog ate my first comment (it was
extremely long) so I guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog blogger but I’m still new
to the whole thing. Do you have any recommendations for rookie blog writers?
I’d certainly appreciate it.
Appreciating the hard work you put into your site and detailed information you offer.
It’s great to come across a blog every once in a
while that isn’t the same unwanted rehashed material. Wonderful
read! I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
My site: cfo recruiting firms
You really make it seem so easy with your presentation but I find
this topic to be actually something that I think I would never understand.
It seems too complicated and very broad for me.
I am looking forward for your next post, I will try to get the hang of
it!
Feel free to visit my webpage – cfo recruiting firms
I’m now not positive where you are getting your info, however great topic.
I must spend a while finding out much more or understanding more.
Thank you for magnificent information I used to be
on the lookout for this information for my mission.
my webpage :: top executive recruiting firms
Greetings from California! I’m bored to tears at work so I decided to browse your website on my iphone during lunch
break. I love the knowledge you provide here and can’t wait to take a look when I get home.
I’m amazed at how quick your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyhow, great site!
Feel free to surf to my web site; executive search firms
Southeast Financiual Nashville
131 Belle Forest Cir #210,
Nashville, TN 37221, United Ⴝtates
18669008949
bookmarks, https://www.protopage.Com/,
Greetings from California! I’m bored to death at work so
I decided to browse your website on my iphone during lunch
break. I really like the info you provide here and can’t wait to take
a look when I get home. I’m shocked at how fast your blog loaded on my
mobile .. I’m not even using WIFI, just 3G .. Anyways, superb
blog!
Feel free to surf to my homepage – cfo search firms
Saved as a favorite, I like your blog!
my webpage :: board governance news
Hello I am so glad I found your blog page, I really found you
by accident, while I was browsing on Google for something else, Nonetheless I am here now and would just like to say thanks for a fantastic post and a all round
enjoyable blog (I also love the theme/design), I don’t have time to go through it all at the minute but I have bookmarked it and also included
your RSS feeds, so when I have time I will be back to
read a great deal more, Please do keep up the excellent work.
Feel free to visit my website :: top executive recruiting firms
I do not even know how I ended up here, but I thought
this post was great. I do not know who you are but certainly you’re going
to a famous blogger if you aren’t already 😉 Cheers!
Check out my website top 20 executive search firms
Wow, awesome weblog structure! How lengthy have you ever been blogging for?
you made running a blog look easy. The overall glance of your web site
is excellent, let alone the content!
my web-site cowen partners executive search
I need to to thank you for this very good read!!
I absolutely loved every bit of it. I’ve got you book marked
to look at new things you post…
Also visit my website: cfo executive search
base
bbm
Write more, thats all I have to say. Literally, it seems as though you relied on the
video to make your point. You clearly know what youre talking about, why throw away your intelligence on just posting
videos to your blog when you could be giving us something informative
to read?
คอนเทนต์นี้ อ่านแล้วเข้าใจเรื่องนี้มากขึ้น
ครับ
ดิฉัน ไปอ่านเพิ่มเติมเกี่ยวกับ หัวข้อที่คล้ายกัน
ลองเข้าไปอ่านได้ที่ akbet25 official site
ลองแวะไปดู
มีตัวอย่างประกอบชัดเจน
ขอบคุณที่แชร์ สิ่งที่มีคุณค่า
นี้
และอยากเห็นบทความดีๆ แบบนี้อีก
Having read this I believed it was extremely enlightening. I
appreciate you spending some time and energy to put this information together.
I once again find myself spending way too
much time both reading and commenting. But so what, it was
still worthwhile!
토닥이 여성전용마사지는 오직 여성만을 위한 전국 출장 전문 마사지 서비스입니다.
대한민국 최초의 여성 전용 마사지 플랫폼으로서
수많은 여성 고객에게 사랑받고
Mangelsen
7916 Girard Avenue,Ꮮa Joyya
CᎪ 92037, United Stɑtes
1 800-228-9686
Bookmarks
Mangelsen
7916 Girard Avenue, Ꮮa Joya
CA 92037, United States
1 800-228-9686
learn climate change impact on bears photography
You definitely made your point! https://clients1.google.com.bh/url?q=https://betflik-168.org
Just wish to say your article is as astonishing.
The clarity in your post is simply great and i can assume you’re an expert on this subject.
Fine with your permission let me to grab
your feed to keep updated with forthcoming post.
Thanks a million and please keep up the
enjoyable work.
I’m gone to convey my little brother, that he should also pay a visit this blog on regular basis to obtain updated from newest information.
Hi there are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started and create my own. Do you need any html coding knowledge to make your own blog?
Any help would be really appreciated!
my blog post – cfo executive search
Please let me know if you’re looking for a writer for your weblog.
You have some really great posts and I believe I would be a good
asset. If you ever want to take some of the load off, I’d absolutely love to write some articles for your blog
in exchange for a link back to mine. Please shoot me an email if interested.
Thanks!
Feel free to surf to my blog post … 해외선물 대여계좌 추천
It is perfect time to make a few plans for the longer term and it is time to be happy.
I’ve learn this submit and if I may just I desire to recommend you few attention-grabbing things or advice.
Perhaps you can write subsequent articles regarding this article.
I want to learn more things about it!
Its not my first time to go to see this website, i am browsing
this website dailly and obtain nice facts from here every day.
Also visit my web blog; Christian counseling online Texas
FIFA Club World Cup livescore, continental champions competing for global title
Hey fantastic website! Does running a blog similar to this require a massive amount work?
I’ve absolutely no knowledge of coding however I was hoping to start my own blog in the near future.
Anyway, should you have any ideas or techniques for new blog owners please
share. I understand this is off topic but I just wanted
to ask. Appreciate it!
Kamoe meulakee bak Google beu segera geukaloen link-link nyoe dan geupeugadeh dari hasee pencarian mangat bek sabe geupake keu kegiatan nyang jeuhet, manipulatif dan eksploitatif.
В этой публикации мы сосредоточимся на интересных аспектах одной из самых актуальных тем современности. Совмещая факты и мнения экспертов, мы создадим полное представление о предмете, которое будет полезно как новичкам, так и тем, кто глубоко изучает вопрос.
Лови подробности – https://fonasa.mindy.cl/blog/apnea-del-sueno-sintomas
I know this web page presents quality depending content and other stuff, is there any other web site which
presents these stuff in quality?
Also visit my page – 해외선물 대여업체
Spot on with this write-up, I honestly believe this web
site needs a great deal more attention. I’ll probably be returning to see more, thanks for the advice!
Also visit my site 해외선물 미니업체
ข้อมูลชุดนี้ อ่านแล้วเข้าใจง่าย
ค่ะ.
ผม ไปอ่านเพิ่มเติมเกี่ยวกับ เรื่องที่เกี่ยวข้อง
ที่คุณสามารถดูได้ที่ jaosua777 free spins.
เผื่อใครสนใจ
เพราะอธิบายไว้ละเอียด.
ขอบคุณที่แชร์ ข้อมูลที่มีประโยชน์
นี้
และหวังว่าจะมีข้อมูลใหม่ๆ มาแบ่งปันอีก.
the Bovada platform is an internet casino that
is bundled with a sportsbook area and online poker in one place.
In the casino lobby, players typically find numerous slot titles plus classic table games such as blackjack
variants, roulette, and baccarat variants, with some games offered in dealer-stream games.
The experience is built for browsers, so it is
commonly used on computers and phones through a responsive website.
Before playing, it’s smart to read carefully the fine print, especially around promo offers and
turnover conditions, plus how different games contribute toward those requirements.
It also helps to understand payout methods, any
restrictions, and account verification that can affect payout timing.
Availability and licensing status can change by jurisdiction, so it’s worth confirming what’s allowed where you
are and using safer boundaries.
Эта публикация погружает вас в мир увлекательных фактов и удивительных открытий. Мы расскажем о ключевых событиях, которые изменили ход истории, и приоткроем завесу над научными достижениями, которые вдохновили миллионы. Узнайте, чему может научить нас прошлое и как применить эти знания в будущем.
Детальнее – https://perfectindiaplanner.in/pack-wisely-before-traveling
Этот информативный текст отличается привлекательным содержанием и актуальными данными. Мы предлагаем читателям взглянуть на привычные вещи под новым углом, предоставляя интересный и доступный материал. Получите удовольствие от чтения и расширьте кругозор!
Лучшее решение — прямо здесь – https://maisgazeta.com/ir-2021-receita-libera-consultas-ao-1o-lote-de-restituicao
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Это стоит прочитать полностью – https://moriyamaseko.wpxblog.jp/jr%E6%9D%B1%E6%B5%B7%E3%83%AA%E3%83%8B%E3%82%A2%E4%B8%AD%E5%A4%AE%E6%96%B0%E5%B9%B9%E7%B7%9A%E5%B7%A5%E4%BA%8B%E8%AA%AC%E6%98%8E%E4%BC%9A
I used to be able to find good info from your blog articles.
Tentu saya suka website kamu, tapi kamu perlu cek ejaan di beberapa posting.
Banyak yang ada masalah ejaan dan itu agak mengganggu.
Tapi saya pasti balik lagi.
Amazing things here. I am very happy to see your
post. Thank you so much and I’m taking a look ahead to contact you.
Will you please drop me a e-mail?
Feel free to visit my website: Christian marriage counseling
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Личный опыт — читайте сами – https://sklep-ortodontyczny.pl/dr-smile-ucieka-z-polski
Howdy are using WordPress for your blog platform? I’m new to the blog
world but I’m trying to get started and create my own. Do
you need any coding expertise to make your own blog?
Any help would be greatly appreciated!
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Откройте для себя больше – https://labtecnovet.com/analisis-histopatologicos
Amazing many of great info.
Simply wish to say your article is as astonishing.
The clarity in your put up is simply cool and i could
think you’re a professional in this subject. Well together with your permission allow me to
take hold of your RSS feed to keep updated with approaching
post. Thanks a million and please carry on the enjoyable work.
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Всё самое вкусное внутри – https://8kbet1.asia/8kbet-khuyen-mai-hoan-cuoc
Thankfulness to my father who informed me concerning this website,
this webpage is really awesome.
my web site – 해외선물 실계좌
Hi, i think that i saw you visited my site so i came to “return the favor”.I
am attempting to find things to enhance my website!I suppose its ok to use some
of your ideas!!
I don’t even know how I ended up here, but I thought this post was great.
I don’t know who you are but definitely you are going to a famous blogger if you are not already 😉 Cheers!
You actually reported that adequately. https://maps.google.co.ao/url?q=https://betflik-168.org
Hey very nice blog!
This is a great blog. Thank you for the very informative post.
Awesome post.
Wow that was strange. I just wrote an extremely long comment but after I clicked submit
my comment didn’t appear. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say
superb blog!
Link exchange is nothing else except it is only placing the other person’s web site link on your page at appropriate place and other person will also do similar for
you.
İnterfeysi sadədir və kazino ilə bağlı çoxlu resurslar təqdim olunur.
https://adidas.ebuty-obuwie.com.pl/bot.php?redirecty=aHR0cHM6Ly9tb3N0YmV0LWF6ZXJiYWlqYW4tdmlwLm9yZy9ib251c2xhcg
Hi there, I found your site by way of Google whilst searching for a similar subject, your website came up, it seems good.
I have bookmarked it in my google bookmarks.
Hi there, just become alert to your weblog thru Google, and
found that it is truly informative. I am going to be careful for brussels.
I will be grateful when you proceed this in future.
Numerous other folks can be benefited out of your writing.
Cheers!
Very nice article, exactly what I needed.
Nice answer back in return of this query with real arguments and describing all about that.
I think it is a nice point of view. I most often meet people who rather say what they suppose others want to hear. Good and well written! I will come back to your site for sure!
I saw a similar post on another website but the points were not as well articulated.
It’s a pity you don’t have a donate button! I’d most certainly donate to this fantastic blog!
I suppose for now i’ll settle for bookmarking and adding your RSS feed to my Google
account. I look forward to fresh updates and will share this website with my Facebook group.
Chat soon!
Howdy! This article could not be written any better!
Looking through this post reminds me of my previous roommate!
He constantly kept talking about this. I am going
to forward this post to him. Fairly certain he will have a very good read.
Thanks for sharing!
Wow that was strange. I just wrote an really long comment but after I clicked submit my comment
didn’t show up. Grrrr… well I’m not writing all that over
again. Regardless, just wanted to say superb blog!
It’s awesome in support of me to have a web page, which is valuable in support of my experience.
thanks admin
Best livescore app alternative, works perfectly on mobile browser no download needed
Nice read, I just passed this onto a colleague who was doing some research on that. And he just bought me lunch as I found it for him smile Therefore let me rephrase that: Thank you for lunch!
You are one talented writer thank you for the post.
I’m gone to convey my little brother, that he should also visit this web site on regular basis to obtain updated
from most recent information.
Элитные проститутки Екатеринбурга – это ВИП досуг
высокого уровня. Самые дорогие индивидуалки
екб с удовольствием составят компанию солидным мужчинам на
любом мероприятии. Самые элитные VIP проститутки Екатеринбурга обладают не только внешностью топ-моделей, но внушительным арсеналом услуг.
Индивидуалки Компрессорный
Анкеты лучших путан Екатеринбурга с района Старая Сортировка, девчонки принимают у себя в уютных апартаментах или выезжают по Старой Сортировке в любую точку.
Выбирайте девчонку на своювкус и бюджет и погружайтесь
в мир интимного удовольствия.
We’re developing a conference, and it looks like you would be a great speaker.
Please let me know if you’re looking for a author for your site.
You have some really great articles and I believe I would be a good asset.
If you ever want to take some of the load
off, I’d love to write some material for your blog in exchange for
a link back to mine. Please shoot me an e-mail if interested.
Regards!
Bu saytda olmaq əla təcrübədir.
http://worksale.nnov.org/common/redir.php?https://mostbet-azerbaijan-pro.org/oyunlar
thank, I thoroughly enjoyed reading your article. I really appreciate your wonderful knowledge and the time you put into educating the rest of us.
Thanks in favor of sharing such a nice opinion, post is good, thats why i have read it completely
It’s amazing designed for me to have a web page,
which is useful in support of my know-how. thanks admin
Right here is the right site for anyone who hopes to understand this topic.
You realize so much its almost tough to argue with you (not
that I actually would want to…HaHa). You certainly put a new spin on a subject that’s been discussed for a long time.
Great stuff, just excellent!
I am glad to be one of the visitors on this great site (:, appreciate it for putting up.
How long does it take you to write an article like this?
Goal kick assists, goalkeeper distributions leading to goals
Nice replies in return of this difficulty with firm arguments and
explaining all regarding that.
Solo goals, individual brilliance and mazy runs tracked
https://open-url.ridera.ru/
Good day very cool web site!! Man .. Excellent ..
Amazing .. I will bookmark your blog and take the
feeds also? I am glad to search out so many useful information right here within the
publish, we’d like develop more techniques in this regard, thanks for sharing.
. . . . .
CIR Legal Lexington
201 W Short St #500,
Lexington, KY 40507, United Ꮪtates
+18596366803
lawyers guns and money lyrics
Nicely put, Many thanks. https://images.google.kg/url?q=https://betflik-168.org
Wow! Finally I got a web site from where I be capable of truly
take useful facts concerning my study and knowledge.
I truly love your blog.. Pleasant colors & theme.
Did you create this amazing site yourself? Please reply back as I’m
trying to create my own personal blog and would like to learn where you
got this from or exactly what the theme is named.
Thanks!
I got this website from my pal who shared with me regarding this web site and
now this time I am browsing this web site and reading very informative content at this time.
Heya i am for the primary time here. I found this board
and I to find It truly helpful & it helped me out much.
I’m hoping to present one thing again and help others like you helped me.
Feel free to surf to my web-site – sex porn
This is a topic that is near to my heart… Many thanks!
Exactly where are your contact details though?
Angels Bail Bondes Costa Mesa
769 Baker St,
Cosxta Mesa, ᏟA 92626, United States
bail bonds kaufman (https://raindrop.io/)
You reported this perfectly. https://maps.google.com.et/url?q=https://betflik-168.org
范德沃克高清完整版,海外华人可免费观看最新热播剧集。
This is nicely expressed. . https://clients1.google.se/url?q=https://betflik-168.org
All rights reserved.
Tremendous things here. I am very happy to peer your article.
Thank you a lot and I’m taking a look forward to touch you.
Will you kindly drop me a e-mail?
Have you ever thought about including a little bit more
than just your articles? I mean, what you say is valuable and
all. However imagine if you added some great
images or videos to give your posts more, “pop”!
Your content is excellent but with images and video
clips, this site could definitely be one of the greatest
in its field. Amazing blog!
Hi there! This article could not be written any better!
Reading through this post reminds me of my previous roommate!
He continually kept preaching about this. I’ll send this article to him.
Fairly certain he’ll have a great read. I appreciate you
for sharing!
Everything is very open with a precise description of
the issues. It was really informative. Your
website is extremely helpful. Thank you for sharing!
Really many of wonderful material.
My web blog https://sites.google.com/view/krypto-poradnik-polska/
Never miss a goal again with our lightning-fast livescore updates for all football matches
Мы собрали для вас самые захватывающие факты из мира науки и истории. От малознакомых деталей до грандиозных событий — эта статья расширит ваш кругозор и подарит новое понимание того, как устроен наш мир.
Более того — здесь – http://kuromacube.com/%E8%87%AA%E7%94%BB%E5%83%8F
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Что ещё? Расскажи всё! – https://inmoactive.com/el-inmobiliario-un-sector-con-creciente-empleabilidad
Mangelsen
7916 Girard Avenue, ᒪa Joya
CᎪ 92037, Unitd Ѕtates
1 800-228-9686
bookmarks
I every time used to study paragraph in news papers but now as I am
a user of web so from now I am using net for content, thanks to web.
An outstanding share! I have just forwarded this onto a coworker who was conducting a little homework on this.
And he in fact ordered me breakfast because I discovered it for
him… lol. So allow me to reword this…. Thanks
for the meal!! But yeah, thanx for spending time to discuss this issue here on your
internet site.
Hi my loved one! I wish to say that this article is awesome, nice written and include almost all significant infos.
I would like to look more posts like this .
Эта информационная статья охватывает широкий спектр актуальных тем и вопросов. Мы стремимся осветить ключевые факты и события с ясностью и простотой, чтобы каждый читатель мог извлечь из нее полезные знания и полезные инсайты.
Узнать больше – https://cstaleem.com/the-art-of-keeping-connected-techniques-for-global-mobile-connectivity
Hi, I do think this is an excellent web site. I stumbledupon it 😉 I may
come back yet again since i have book marked it. Money and freedom is the
greatest way to change, may you be rich and continue to guide other people.
Have a look at my homepage – Yonibet – Meilleur casino France
It’s an amazing article for all the internet people; they will take benefit from it I am sure.
Мы предлагаем вам подробное руководство, основанное на проверенных источниках и реальных примерах. Каждая часть публикации направлена на то, чтобы помочь вам разобраться в сложных вопросах и применить знания на практике.
Где можно узнать подробнее? – http://ued.myechinese.com/?p=52
警戒を怠らず、類似のサイトを見つけたらすぐに報告してください。デジタルセキュリティは、共通の警戒から始まります。
Simply desire to say your article is as astounding.
The clearness on your post is just spectacular and that i can think you’re
knowledgeable on this subject. Well with your permission let me to take hold of your feed to stay updated
with imminent post. Thanks a million and please keep up the rewarding
work.
My web page teen patti online
It’s truly very complicated in this full of activity life to listen news
on TV, therefore I simply use internet for that purpose, and obtain the most up-to-date
news.
My blog post … teen patti online
Hi my loved one! I want to say that this post is amazing, nice written and include approximately all significant infos.
I would like to look extra posts like this .
Эта статья сочетает в себе как полезные, так и интересные сведения, которые обогатят ваше понимание насущных тем. Мы предлагаем практические советы и рекомендации, которые легко внедрить в повседневную жизнь. Узнайте, как улучшить свои навыки и обогатить свой опыт с помощью простых, но эффективных решений.
Нажмите, чтобы узнать больше – https://fonasa.mindy.cl/blog/apnea-del-sueno-sintomas
подробнее https://kinogo.blue/filmy-2024g/1839-granica-mirov.html
This paragraph will assist the internet users for setting up new
weblog or even a weblog from start to end.
Here is my page: teen patti master download
В обзорной статье вы найдете собрание важных фактов и аналитики по самым разнообразным темам. Мы рассматриваем как современные исследования, так и исторические контексты, чтобы вы могли получить полное представление о предмете. Погрузитесь в мир знаний и сделайте шаг к пониманию!
Есть чему поучиться – https://carlstanleymakeupandhair.co.uk/tetimonials
Hello there! Do you know if they make any plugins to
protect against hackers? I’m kinda paranoid about
losing everything I’ve worked hard on. Any recommendations?
When some one searches for his required thing, therefore he/she needs to be
available that in detail, thus that thing is maintained over here.
Эта разъяснительная статья содержит простые и доступные разъяснения по актуальным вопросам. Мы стремимся сделать информацию понятной для широкой аудитории, чтобы каждый мог разобраться в предмете и извлечь из него максимум пользы.
Откройте для себя больше – https://www.osteo.cz/post-3
Мы предлагаем вам окунуться в океан любопытных фактов и вдохновляющих историй. Эта публикация поможет расширить горизонты, разбудить интерес к науке и истории и увидеть мир с новой стороны.
Осуществить глубокий анализ – https://ibaadat.in/product/energy-oracle-deck
double hair netherhands
İşinizə davam edin və daha çox istifadəçi cəlb edin!
https://cleanuri.com/GVVRD5
Mangelsen
7916 Girard Avenue, ᒪa Joya
ⲤA 92037, United Stateѕ
1 800-228-9686
impact grizzly 399 legacy grizzlies (raindrop.io)
Great web site you have got here.. It’s hard to find good quality writing like yours these days.
I really appreciate individuals like you! Take care!!
Actually when someone doesn’t be aware of then its
up to other viewers that they will assist, so here it occurs.
I don’t know if it’s just me or if everyone else experiencing problems with
your site. It appears like some of the text within your
content are running off the screen. Can someone else please provide feedback and
let me know if this is happening to them too? This might be a problem with my web
browser because I’ve had this happen previously. Thanks
здесь трипскан вход без впн
Modern Purair
416 Meridian Ɍd ՏE #14Α, Calgary
AB T2A 1X2, Canada
(403) 800-7254
maintenance expert
Very good info. Lucky me I discovered your website by accident (stumbleupon).
I’ve bookmarked it for later! https://zeitfuer.abenstein.de/employer/onarslan/
Lietuvių kalbos korepetitorius instruktorius – efektyvaus mokymosi sprendimas
Love how you connect theory and reality
продолжить https://krab6a.at
For latest news you have to visit internet and on web I found this web site as a most excellent website for latest updates.
https://share.google/a2ZUTOl0kraER6M8t
have a peek at this website
create apk from website free
Euro Cup live scores, European Championship matches with real-time goal updates
Angels Bail Bonds Costa Mesa
769 Bakerr St,
Costa Mesa, CA 92626, United Տtates
double c bail bonds
Just want to say your article is as surprising. The clarity in your post is simply excellent and
that i could think you’re an expert in this subject.
Well with your permission allow me to snatch your RSS feed to keep up to date with approaching post.
Thanks 1,000,000 and please keep up the enjoyable work.
Hello! I could have sworn I’ve been to this blog
before but after checking through some of the post I realized it’s new to
me. Anyways, I’m definitely delighted I found it and I’ll be
book-marking and checking back frequently!
Being prejudiced will never be great. As soon as I express My business is a Massage Therapist, really does the fact threaten the way professionals start to
see me personally? I’m sure it may. What about if ever I tell someone
I perform NJMassages? Really does that alter your own personal representation of
me personally? With every different completely new actuality you will acquire,
your primary belief could perhaps adjust. Without a doubt, there is rarely ever almost any “last word” in relation to what precisely you fully understand; we all may continuously gain knowledge of a tad bit more about somebody as well
as everything. Consider that. That isn’t actually “being wishy-washy”
after we will amend each of our beliefs utilizing brand-new
information and facts. (If it turns out you might have certainly
never seen a NJMassages bodywork, it’s actually a RELIABLE
professional medical technique presented to Moms-to-be.)
Thanks for all the valuable content about Big Bass Splash and gambling.
https://www.lewenstyl.com/amazon-best-sellers-september/
Hi, everything is going well here and ofcourse every one is sharing facts,
that’s actually excellent, keep up writing.
Does your blog have a contact page? I’m having trouble
locating it but, I’d like to send you an email.
I’ve got some recommendations for your blog you might be interested in hearing.
Either way, great blog and I look forward to seeing it improve
over time.
Pretty! This was an incredibly wonderful article. Thank you for supplying these details.
คอนเทนต์นี้ มีประโยชน์มาก ครับ
ดิฉัน เพิ่งเจอข้อมูลเกี่ยวกับ
เนื้อหาในแนวเดียวกัน
ที่คุณสามารถดูได้ที่ ทางเข้า m4autobet
เผื่อใครสนใจ
เพราะให้ข้อมูลเชิงลึก
ขอบคุณที่แชร์ เนื้อหาดีๆ นี้
และอยากเห็นบทความดีๆ แบบนี้อีก
Awesome post.
This website has lots of really useful stuff on it. Thanks for informing me.
have a peek at these guys https://binunlock.com/tuning-files/categories/new-holland.82/
Minnətdaram belə faydalı məlumat üçün.
https://mostbet-azerbaijan-play.org/qeydiyyat
You need to really control the comments listed here
I love your blog.. very nice colors & theme. Did you make this website yourself
or did you hire someone to do it for you? Plz reply as I’m looking to create my
own blog and would like to know where u got this from.
kudos
I imagine so. Very good stuff, I agree totally.
Heya great website! Does running a blog similar to this
take a massive amount work? I have no knowledge of programming however I was hoping to start my own blog soon. Anyhow, should you have
any ideas or techniques for new blog owners please
share. I know this is off topic however I just wanted to ask.
Many thanks!
Here is my website Crypto Scam
Way cool! Some very valid points! I appreciate you penning this article and the rest of the
site is also very good. https://tkd-e.co.com/
Hello! I know this is kinda off topic nevertheless I’d
figured I’d ask. Would you be interested in exchanging links or maybe guest authoring a blog post or vice-versa?
My site goes over a lot of the same subjects as yours and I feel we
could greatly benefit from each other. If you are interested feel free
to send me an e-mail. I look forward to hearing from you!
Wonderful blog by the way!
Fantastic piece of writing here1
I know this is not exactly on topic, but i have a blog using the blogengine platform as well and i’m having issues with my comments displaying. is there a setting i am forgetting? maybe you could help me out? thank you.
My brother suggested I might like this website. He was entirely right.
This post truly made my day. You cann’t imagine
just how much time I had spent for this information! Thanks!
My partner and I stumbled over here by a different web page and
thought I might check things out. I like what
I see so now i’m following you. Look forward to going over your web page again.
I needed to thank you for this good read!! I definitely loved every little bit of it.
I have got you bookmarked to check out new stuff
you post…
Hello! I realize this is somewhat off-topic however I needed to ask.
Does operating a well-established blog like yours take a large amount of work?
I’m completely new to operating a blog however I do write
in my journal on a daily basis. I’d like to start a blog so I can easily share my personal experience and thoughts online.
Please let me know if you have any kind of suggestions or tips for new aspiring bloggers.
Thankyou!
Here is my blog post :: cowen partners
I was able to find good advice from your blog posts.
Also visit my web blog … board governance news today
I’m gone to tell my little brother, that he should also pay a quick visit this blog on regular basis to
obtain updated from newest information.
Hurrah! After all I got a weblog from where I be able to really
obtain helpful facts concerning my study and knowledge.
Le enlacea’ leti’ jump’éel ts’ono’oto’ phishing ku chíikbesik k marca/mayaj way sijnáaleche’. Le linki abas kaambal ku k’áatik ti’ le máaxo’ob ku meyajtiko’ob ka u ts’íibto’ob detalles falsos ti’ Chúunul xoknáalo’obo’ leti’ bo’ol ku páajtal utilizar utia’al u ookol u datos. Le ts’ono’oto’ xan con frecuencia auto-redirecciona ti’ estafa leti’e’, k’ajolo’on u juegos u apuestas ilegales.
First off I would like to say fantastic blog! I had a quick
question in which I’d like to ask if you don’t mind.
I was interested to know how you center yourself and
clear your thoughts prior to writing. I’ve had a
hard time clearing my mind in getting my ideas out.
I truly do enjoy writing but it just seems like the first 10 to 15 minutes are usually lost simply just trying
to figure out how to begin. Any suggestions or tips? Cheers!
Thanks. I value this.
Maybe you know similar resources?
Maybe you know similar resources?
neterapay vklad casino
Maybe you know similar resources?
casino neterapay
I love it when folks get together and share ideas.
Great blog, continue the good work!
Feel free to surf to my web site; board governance news
I know this if off topic but I’m looking into starting
my own weblog and was wondering what all is required to get setup?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100% sure.
Any recommendations or advice would be greatly appreciated.
Many thanks
Here is my web blog :: board governance news
Maybe you know similar resources?
casino neterapay
Эта статья предлагает уникальную подборку занимательных фактов и необычных историй, которые вы, возможно, не знали. Мы постараемся вдохновить ваше воображение и разнообразить ваш кругозор, погружая вас в мир, полный интересных открытий. Читайте и открывайте для себя новое!
Кликни и узнай всё! – https://sanluis.sascuyo.com.ar/how-to-log-in-to-quotex-for-binary-options-trading
Этот увлекательный информационный материал подарит вам массу новых знаний и ярких эмоций. Мы собрали для вас интересные факты и сведения, которые обогатят ваш опыт. Откройте для себя увлекательный мир информации и насладитесь процессом изучения!
Это ещё не всё… – https://reddunehummersafari.com/hummer-safari-dubai-booking-online-desert
I am not sure where you are getting your info, but good topic.
I needs to spend some time learning more or understanding more.
Thanks for great information I was looking for
this information for my mission.
Here is my blog post; board governance news
Write more stories, more chapters.
В этой публикации мы предлагаем подробные объяснения по актуальным вопросам, чтобы помочь читателям глубже понять их. Четкость и структурированность материала сделают его удобным для усвоения и применения в повседневной жизни.
Практические советы ждут тебя – https://me.eng.kmitl.ac.th/%E0%B8%9A%E0%B8%B8%E0%B8%84%E0%B8%84%E0%B8%A5%E0%B8%81%E0%B8%A3/blank-women
What’s up, I log on to your blog regularly. Your story-telling style is witty, keep doing what you’re doing!
В этой статье представлен занимательный и актуальный контент, который заставит вас задуматься. Мы обсуждаем насущные вопросы и проблемы, а также освещаем истории, которые вдохновляют на действия и изменения. Узнайте, что стоит за событиями нашего времени!
Нажмите, чтобы узнать больше – https://www.ikhouvanbeauty.nl/2020/09/16/wat-is-het-alizonne-dieet
Greetings, have tried to subscribe to this websites rss feed but I am having a bit of a problem. Can anyone kindly tell me what to do?’
Hello there! This article could not be written any better!
Reading through this post reminds me of my previous roommate!
He continually kept preaching about this. I will forward this
post to him. Fairly certain he will have a great read.
Many thanks for sharing!
My website: board governance
Is it okay to put a portion of this on my weblog if perhaps I post a reference point to this web page?
Today, while I was at work, my sister stole my apple ipad and tested to see
if it can survive a forty foot drop, just so she can be a youtube sensation. My apple ipad is now destroyed and she
has 83 views. I know this is entirely off topic but I
had to share it with someone!
Here is my blog :: cowen partners
Currently it seems like WordPress is the best lash extensions Baldwin County blogging platform available
right now. (from what I’ve read) Is that what you are
using on your blog?
Whoa lots of valuable info!
Статья знакомит с важнейшими моментами, которые сформировали наше общество. От великих изобретений до культурных переворотов — вы узнаете, как прошлое влияет на наше мышление, технологии и образ жизни.
Перейти к статье – https://globalducts.com/the-secret-of-cleaning-your-kitchen
I am extremely impressed with your writing skills as well as with the layout on your weblog.
Is this a paid theme or did you customize it yourself? Either way keep
up the nice quality writing, it’s rare to see a nice blog like this one these days.
Sayt çox yaxşı dizayn olunub. Təşəkkürlər!
https://mostbet-azerbaijan-jackpot.net/qeydiyyat
대전출장안마는 천안이나 아산,대전 세종 공주
청주 조치원등 충남 전지역에서 이용가능합니다.
24시간 영업으로 고객님께서 원하시는 목적지에 원하는 장소로 전문 관리사
I really love this article.
Write more, thats all I have to say. Literally, it seems as
though you relied on the video to make your point.
You definitely know what youre talking about, why throw away your intelligence on just posting videos to your site when you could be giving us something enlightening to read?
I think this is one of the most important
info for me. And i’m glad reading your article. But want to
remark on some general things, The web site style is wonderful, the
articles is really nice : D. Good job, cheers
I had highly recommend this blog to my good friend, it’s so good
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, CA 92626, United Ѕtates
5 ⲣercent bil bonds, atavi.com,
Hello there, You have done an excellent job. I’ll definitely digg it
and personally recommend to my friends. I’m confident they’ll be
benefited from this site.
What i don’t understood is actually how you are not really much more
neatly-favored than you may be now. You are
so intelligent. You recognize thus significantly in relation to
this subject, produced me in my view believe it
from numerous numerous angles. Its like men and women are not fascinated unless
it’s one thing to accomplish with Girl gaga! Your individual stuffs outstanding.
All the time deal with it up!
Really loads of useful facts!
How long does it take you to write an article like this?
You really make it appear really easy along with your
presentation but I in finding this topic to be actually something
which I feel I’d by no means understand. It kind of feels
too complex and extremely extensive for
me. I am looking ahead to your subsequent put up, I’ll attempt to
get the cling of it!
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically
tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and
was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new updates.
Вау, какой крутой сайт kazino olimp! Благодарю!
https://olimp-casino-kazakhstan-game.kz
https://askoff.ru
Greetings! Very useful advice in this particular post!
It’s the little changes which will make the most important changes.
Thanks for sharing!
It’s genuinely very complicated in this active life
to listen news on Television, therefore I simply use web for that
purpose, and get the newest news.
go Dune
Angels Bail Bonds Costa Mesa
769 Baker Ⴝt,
Costa Mesa, CA 92626, United Stɑtes
y l & s bail bonds
Best Australian Casino Real Money Epic Payout Potential
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your site?
My blog site is in the exact same niche as yours and my users would certainly benefit from a
lot of the information you present here. Please let me know if this ok with you.
Thanks a lot!
Подробнее
Gama casino промокод при регистрации
신용카드 현금화가 빠른 이유. 자동 승인 시스템과 실시간 상담 프로세스를 통해 승인
→ 입금까지 3~5분 내 처리가 가능하도록 설계되어 있습니다.
Mangelsen
7916 Girard Avenue, Ꮮa Joya
ϹA 92037, United Ѕtates
1 800-228-9686
amazing wildlife conservation books bears
Cheers, Plenty of content.
私たちは、これらのリンクが悪意のある、操作的な、搾取的な行為に使用され続けることを防ぐため、Google が直ちにこれらのリンクを確認して検索結果から削除することを強く求めます。
Ahaa, its pleasant conversation on the topic of this article here at this
web site, I have read all that, so now me also commenting at this place.
My web page – garage door repair
Effectively expressed really. .
Your style is so unique compared to other folks
I have read stuff from. I appreciate you for posting when you have the opportunity, Guess I’ll just bookmark this page.
Here is my web blog; lagoon-based anaerobic digestion
В данной статье вы найдете комплексный подход к изучению насущных тем. Мы комбинируем теоретические сведения с практическими советами, чтобы читатель мог не только понять проблему, но и найти пути её решения.
Получить дополнительные сведения – https://www.ascotrehab.com/about-us/meet-the-team/management/img_0748
Way cool! Some very valid points! I appreciate you writing this article and the rest of
the site is also very good.
Feel free to surf to my homepage; fence company OKC
I every time spent my half an hour to read this website’s articles everyday along with a mug of coffee.
Эта обзорная заметка содержит ключевые моменты и факты по актуальным вопросам. Она поможет читателям быстро ориентироваться в теме и узнать о самых важных аспектах сегодня. Получите краткий курс по современной информации и оставайтесь в курсе событий!
Разобраться лучше – https://saucha.net/big-sale/coupon-3
Эта статья предлагает захватывающий и полезный контент, который привлечет внимание широкого круга читателей. Мы постараемся представить тебе идеи, которые вдохновят вас на изменения в жизни и предоставят практические решения для повседневных вопросов. Читайте и вдохновляйтесь!
Подробнее – https://dev.codlearningtech.org/2015/07/28/how-to-create-videos-students-will-actually-watch
Hi i am kavin, its my first time to commenting anywhere, when i read this paragraph i thought i could also create comment
due to this good piece of writing.
Feel free to surf to my homepage: Herbrand Rohrreinigung
Публикация приглашает вас исследовать неизведанное — от древних тайн до современных достижений науки. Вы узнаете, как случайные находки превращались в революции, а смелые мысли — в новые эры человеческого прогресса.
Кликни и узнай всё! – https://lavishliving.homes/prestige-glenwood-villa
Angels Bail Bonds Costa Mesa
769 Baker Ѕt,
Costa Mesa, ϹΑ 92626, Uniuted Stаtes
Bookmarks
Very nice article, just what I was looking for.
my blog Find the right consultant
A collection of exciting games, bonuses, and giveaways
There is definately a lot to know about this topic. I love all the points you’ve made.
My webpage – accept credit card payments without machine
Pretty! This has been a really wonderful
article. Thank you for supplying this info.
vavada vip
Для тех, кто ищет магазин Кракен, переходите по кракен ссылка на магазин. Вы найдете все товары и услуги для покупателей.
krkn-krkn.com
This was helpful information. I didn’t realize the Culver’s survey only
takes a few minutes, and the reward makes it even better.
If some one wishes expert view on the topic of blogging afterward i propose him/her to pay a quick
visit this weblog, Keep up the fastidious work.
Профессиональные индивидуалки Иркутска по средней стоимости услуг
от 2500р до 3000р. Самые горячие проститутки Иркутска готовые отдаться за
среднюю стоимость своих услуг.
Горячие красотки индивидуалки
Иркутска по хорошей цене. Анкеты с фото и номерами телефонов выбирай красотку
по хорошей цене.
Индивидуалки Кировского района
Каталог анкет лучших путан Иркутска с района Правобережный, девчонки на любой
вкус, с обширным набором секс-услуг и на любой
бюджет. Иркутские шлюхи принимают у себя в уютных апартаментах или приедут к вам в
районе Правобережный. Выбирайте и звоните сейчас.
You could definitely see your expertise in the article you write.
The sector hopes for more passionate writers such as you who
are not afraid to say how they believe. All the
time go after your heart.
Here is my site – Rohrreinigung 24h
This is a helpful article and I really appreciate how clearly everything is explained.
Many people often struggle when choosing the right betting platform, and this
post explains the topic in a simple way.
The information about user experience is useful, especially for
users who are interested in SBOBET.
Thanks for sharing this valuable content.
The sketch is tasteful, your authored material stylish.
Amazing! This blog looks just like my old one! It’s on a completely different subject but it
has pretty much the same page layout and design. Outstanding choice of colors!
Here is my web page; Rohrreinigung Notdienst
Inspiring quest there. What happened after? Good luck!
My webpage … slot online
This is really interesting, You’re a very skilled blogger. I have joined your feed and look forward to seeking more of your fantastic post. Also, I have shared your website in my social networks!
Your thing regarding creating will be practically nothing in short supply of awesome. This informative article is incredibly useful and contains offered myself a better solution to be able to my own issues. Which can be the specific purpose MY PARTNER AND I has been doing a search online. I am advocating this informative article with a good friend. I know they are going to get the write-up since beneficial as i would. Yet again many thanks.
Howdy! This is kind of off topic but I need some advice from an established blog.
Is it difficult to set up your own blog?
I’m not very techincal but I can figure things out pretty quick.
I’m thinking about creating my own but I’m not sure where
to start. Do you have any points or suggestions? With thanks
Visit my website … Abflussreinigung vom Profi
The post is absolutely fantastic! Lots of great info and inspiration, both of which we all need! Also like to admire the time and effort you put into your website and detailed info you offer! I will bookmark your website!
Thanks a bunch for sharing this with all people you really recognize what you are talking about! Bookmarked. Kindly also seek advice from my web site =). We can have a link alternate contract between us!
You write Formidable articles, keep up good work.
My relatives always say that I am killing my time here at net,
however I know I am getting know-how everyday by reading
such good posts.
Also visit my page; tap to pay on phone
Fine way of telling, and good article to take data about my presentation subject matter, which i am going to convey in school.
Hi there, just became aware of your blog through Google, and found that it’s truly informative.
I’m going to watch out for brussels. I’ll be grateful if you continue this in future.
A lot of people will be benefited from your writing. Cheers!
Top Pokies Real Money Australia Feel The Adrenaline Tonight
This excellent website really has all the information I needed about this subject and didn’t know
who to ask.
Also visit my webpage waste lagoon digestion
私たちは、これらのリンクが悪意のある、操作的な、搾取的な行為に使用され続けることを防ぐため、Google が直ちにこれらのリンクを確認して検索結果から削除することを強く求めます。
I’m really loving the theme/design of your web site. Do you ever run into any internet browser compatibility problems?
A couple of my blog audience have complained about my
site not working correctly in Explorer but looks great in Safari.
Do you have any suggestions to help fix this problem?
Online Casino Real Money Australia Your Turn To Dominate
I’ll right away take hold of your rss as I can’t to find your email
subscription hyperlink or e-newsletter service. Do you’ve any?
Kindly permit me recognize in order that I may just subscribe.
Thanks.
It’s nearly impossible to find knowledgeable people for
this topic, but you sound like you know what you’re talking about!
Thanks
Also visit my web blog – best real estate agent in Alberta Canada
I constantly spent my half an hour to read this webpage’s articles everyday along with a mug of
coffee.
Here is my website – best real estate agent in Lake Oswego OR
Пинко казино
Have you ever considered writing an ebook or guest authoring on other sites?
I have a blog centered on the same subjects you discuss and would really like to
have you share some stories/information. I know my viewers would enjoy
your work. If you’re even remotely interested, feel free to shoot
me an e mail.
Wonderful, what a weblog it is! This weblog gives valuable data to us, keep
it up.
Also visit my blog … realtor in Lake Ozark MO
Hi there, after reading this remarkable paragraph i am too happy to share my experience here with colleagues.
Also visit my blog post :: real estate agent Franklin TN
компьютеры в Казахстане
I got this site from my pal who informed me
regarding this web page and now this time I am browsing this website and reading very informative content here.
my webpage – best realtor in Lake Ozark MO
Hello there I am so thrilled I found your blog,
I really found you by accident, while I was searching
on Yahoo for something else, Regardless I am here now and would just like to
say many thanks for a tremendous post and a all round exciting blog
(I also love the theme/design), I don’t have time to read it all at the
minute but I have book-marked it and also added your RSS feeds, so when I have time I will be
back to read a great deal more, Please do keep up the excellent jo.
Its not my first time to pay a quick visit this website, i
am visiting this web page dailly and get good facts from here
all the time.
What’s up, the whole thing is going perfectly here and
ofcourse every one is sharing data, that’s in fact good, keep up writing.
my web blog – best realtor in Chino Hills CA
If most people wrote about this subject with the eloquence that you just did, I’m sure people would do much more than just read, they act. Great stuff here. Please keep it up.
Фермерские продукты: натуральная польза для вашего здоровья
Hello there, You have done an incredible job. I will certainly digg it and personally recommend to my friends. I am sure they will be benefited from this site.