Copaxone
Generic name: glatiramer (injection)
Brand names: Copaxone, Glatopa
Drug class: Other immunostimulants
Medically reviewed by A Ras MD.
What is Copaxone?
Copaxone is a prescription medicine that is used to treat relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
It is not known if Copaxone is safe and effective in children under 18 years of age.
Description
Glatiramer acetate, the active ingredient of COPAXONE, consists of the acetate salts of synthetic polypeptides, containing four naturally occurring amino acids: L-glutamic acid, L-alanine, L-tyrosine, and L-lysine with an average molar fraction of 0.141, 0.427, 0.095, and 0.338, respectively. The average molecular weight of glatiramer acetate is 5,000 – 9,000 daltons. Glatiramer acetate is identified by specific antibodies.
Chemically, glatiramer acetate is designated L-glutamic acid polymer with L-alanine, L-lysine and L-tyrosine, acetate (salt). Its structural formula is:
(Glu, Ala, Lys, Tyr)x●xCH3COOH
(C5H9NO4●C3H7NO2●C6H14N2O2●C9H11NO3)x●xC2H4O2
CAS – 147245-92-9
COPAXONE is a clear, colorless to slightly yellow, sterile, nonpyrogenic solution for subcutaneous injection. Each 1 mL of COPAXONE solution contains 20 mg or 40 mg of glatiramer acetate and the following inactive ingredient: 40 mg of mannitol. The pH of the solutions is approximately 5.5 to 7.0. The biological activity of glatiramer acetate is determined by its ability to block the induction of experimental autoimmune encephalomyelitis (EAE) in mice.
Mechanism of Action
The mechanism(s) by which glatiramer acetate exerts its effects in patients with MS are not fully understood. However, glatiramer acetate is thought to act by modifying immune processes that are believed to be responsible for the pathogenesis of MS. This hypothesis is supported by findings of studies that have been carried out to explore the pathogenesis of experimental autoimmune encephalomyelitis, a condition induced in animals through immunization against central nervous system derived material containing myelin and often used as an experimental animal model of MS. Studies in animals and in vitro systems suggest that upon its administration, glatiramer acetate-specific suppressor T-cells are induced and activated in the periphery.
Because glatiramer acetate can modify immune functions, concerns exist about its potential to alter naturally-occurring immune responses. There is no evidence that glatiramer acetate does this, but this has not been systematically evaluated
Who should not use Copaxone?
- Do not use Copaxone if you are allergic to glatiramer acetate, mannitol or any of the ingredients in Copaxone. See the end of this leaflet for a complete list of the ingredients in Copaxone.
What should I tell my healthcare provider before using Copaxone?
Before you use Copaxone, tell your doctor if you:
- are pregnant or plan to become pregnant. It is not known if Copaxone will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if Copaxone passes into your breast milk. Talk to your doctor about the best way to feed your baby while using Copaxone.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Copaxone may affect the way other medicines work, and other medicines may affect how Copaxone works.
Know the medicines you take. Keep a list of your medicines with you to show your doctor and pharmacist when you get a new medicine.
How should I take Copaxone?
- For detailed instructions, see the instructions for use that comes with Copaxone.
- Your doctor will tell you how much Copaxone to use and when to use it.
- Copaxone is given by injection under your skin (subcutaneously).
- Use Copaxone exactly as your doctor tells you to use it.
- Since every body type is different, talk with your doctor about the injection areas that are best for you.
- You should receive your first dose of Copaxone with a doctor or nurse present. This might be at your doctor’s office or with a visiting home health nurse who will teach you how to give your Copaxone injections.
What are the possible side effects of Copaxone?
Copaxone may cause serious side effects, including:
- Immediate Post-Injection Reactions. Serious side effects may happen right after or within minutes after you inject Copaxone at any time during your course of treatment. Call your doctor right away if you have any of these immediate post-injection reaction symptoms including:
- redness to your cheeks or other parts of the body (flushing)
- chest pain
- fast heart beat
- anxiety
- breathing problems or tightness in your throat
- swelling, rash, hives, or itching
If you have symptoms of an immediate post-injection reaction, do not give yourself more injections until a doctor tells you to.
- Chest Pain. You can have chest pain as part of an immediate post-injection reaction or by itself. This type of chest pain usually lasts a few minutes and can begin around 1 month after you start using Copaxone. Call your doctor right away if you have chest pain while using Copaxone.
- Damage to your skin. Damage to the fatty tissue just under your skin’s surface (lipoatrophy) and, rarely, death of your skin tissue (necrosis) can happen when you use Copaxone. Damage to the fatty tissue under your skin can cause a “dent” at the injection site that may not go away. You can reduce your chance of developing these problems by:
- following your doctor’s instructions for how to use Copaxone
- choosing a different injection area each time you use Copaxone.
The most common side effects of Copaxone include:
- skin problems at your injection site including:
- redness
- pain
- swelling
- itching
- lumps
- rash
- shortness of breath
- flushing (vasodilation)
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Copaxone. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Copaxone
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information Leaflet. Do not use Copaxone for a condition for which it was not prescribed. Do not give Copaxone to other people, even if they have the same symptoms as you have. It may harm them.
The Patient Information Leaflet summarizes the most important information about Copaxone. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about Copaxone that is written for health professionals.
For more information, go to www.Copaxone.com or call 1-800-887-8100.
How should I store Copaxone?
- Store Copaxone in the refrigerator between 36°F to 46°F (2°C to 8°C).
- When you are not able to refrigerate Copaxone, you may store it for up to 1 month at room temperature between 59°F to 86°F (15°C to 30°C).
- Protect Copaxone from light or high temperature.
- Do not freeze Copaxone syringes. If a syringe freezes, throw it away in a sharps disposal container.
Keep Copaxone and all medicines out of the reach of children.
What are the ingredients in Copaxone?
Active ingredient: glatiramer acetate
Inactive ingredients: mannitol
Label
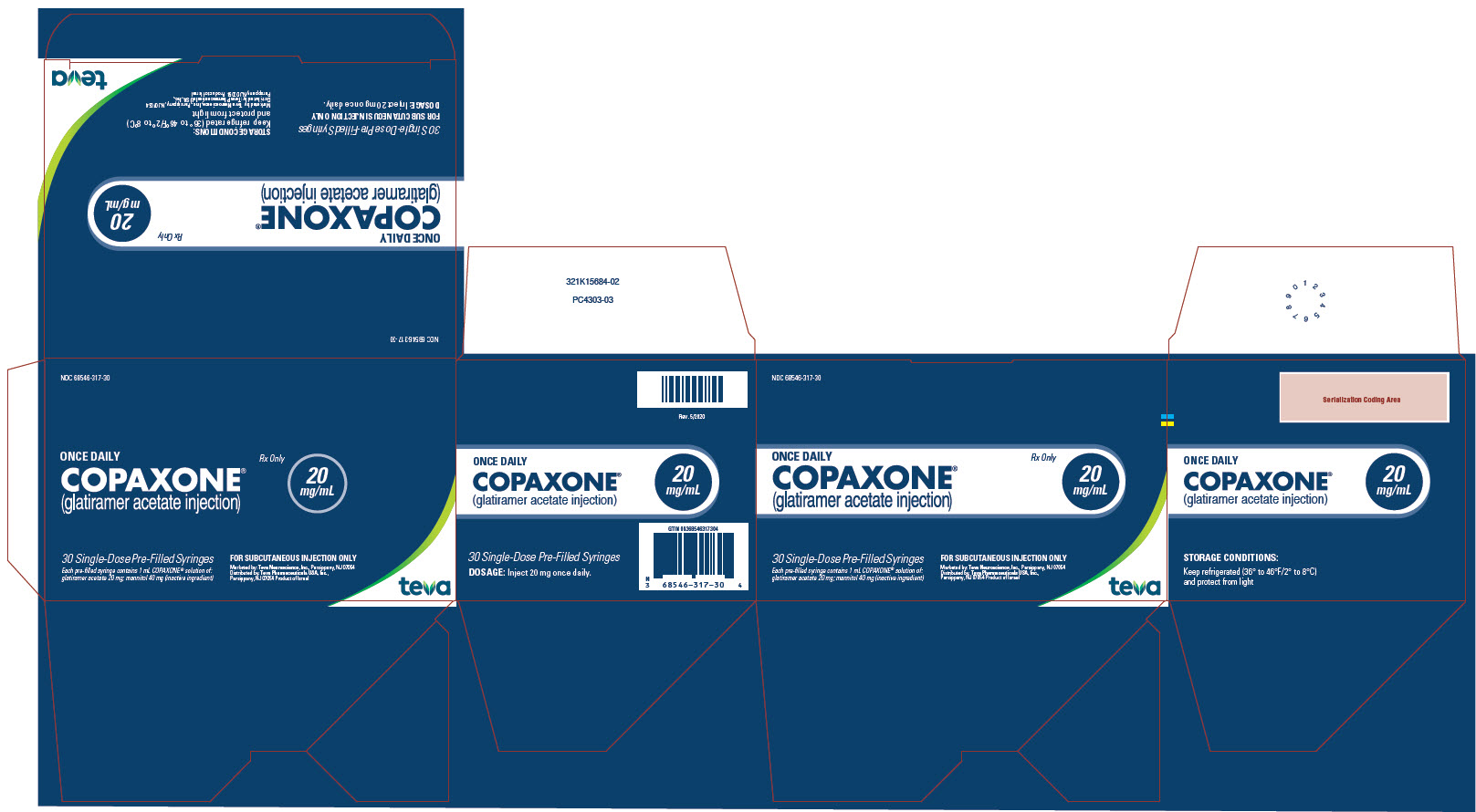
PACKAGE/LABEL DISPLAY PANEL, 20 MG/ML
- NDC 68546-317-30
ONCE DAILY
COPAXONE® (glatiramer acetate injection) 20 mg/mL
Rx Only
30 Single-Dose Pre-Filled Syringes
Each pre-filled syringe contains 1 mL COPAXONE® solution of: glatiramer acetate 20 mg; mannitol 40 mg (inactive ingredient)
FOR SUBCUTANEOUS INJECTION ONLY
Marketed by: Teva Neuroscience, Inc., Parsippany, NJ 07054
Distributed by: Teva Pharmaceuticals USA, Inc., Parsippany NJ, 07054
Product of Israel

PACKAGE/LABEL DISPLAY PANEL,40 MG/ML
- NDC 68546-325-12
THREE TIMES A WEEK
COPAXONE® (glatiramer acetate injection) 40 mg/mL
Rx Only
12 Single-Dose Pre-Filled Syringes
Each pre-filled syringe contains 1 mL COPAXONE® solution of: glatiramer acetate 40 mg; mannitol 40 mg (inactive ingredient)
FOR SUBCUTANEOUS INJECTION ONLY
Marketed by: Teva Neuroscience, Inc., Parsippany, NJ 07054
Distributed by: Teva Pharmaceuticals USA, Inc., Parsippany, NJ 07054
Product of Israel
SRC: NLM .
