Wolff-Parkinson-White syndrome
Wolff-Parkinson-White syndrome, an extra electrical pathway between your heart’s upper and lower chambers causes a rapid heartbeat. This condition that occurs at birth, is uncommon.
Sudden heartbeats generally don’t cause any serious harm however serious heart problems could be a possibility. Treatment options can prevent or stop instances of rapid heartbeats. An ablation procedure using a catheter (ablation) can be permanent in resolving heart rhythm issues.
The majority of people who have an extra electrical pathway do not have a fast heartbeat. This condition, called the Wolff-Parkinson-White (WPS) pattern, is discovered by chance during a heart exam.
Symptoms
Anybody, including babies, may experience the signs of WPW syndrome, which is caused by changes in the heart rhythm.
Common signs of Wolff-Parkinson-white syndrome include:
- A quick, fluttering or heartbeat that is pounding (palpitations)
- Lightheadedness or dizziness
- Breathing shortness
- Fatigue
- Anxiety
- Chest pain
- Trouble breathing
- Fainting
A rapid heartbeat could begin abruptly and last for just a few seconds or for several hours. These episodes may occur in the course of exercise or during rest. Other stimulants, like caffeine and alcohol, can trigger symptoms in some individuals.
Infants and children are prone to symptoms.
Baby signs and symptoms with WPW The symptoms can include:
- Blueish or grayish (ashen) Skin color
- Refusal or irritation
- Rapid breathing
- Unhealthy eating
When is the best time to visit a doctor?
Many conditions can cause an irregular rhythm in the heart (arrhythmia). It’s crucial to seek the right diagnosis and treatment. Consult your physician if you or your child exhibits symptoms of WPW syndrome.
Contact your provider or go to a nearby emergency if suffering from any of the following symptoms that last more than a few minutes
- Heartbeats that are irregular or rapid
- Breathing difficulties
- Chest pain
Causes
The additional electrical pathway that leads to the rapid heartbeat occurs from birth. A genetic defect is responsible for the condition in only a tiny percentage of patients suffering from WPW syndrome. The disorder is also linked to certain forms of congenital heart diseases, for example, Ebstein anomalies.
In other words, we know very little about how the additional pathway is created.
The normal heart electrical system
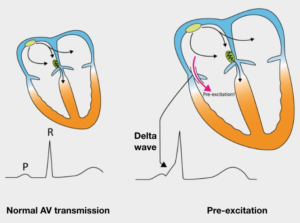
Your heart is composed of four chambers: two chambers in the upper (atria) as well as two chambers in the lower (ventricles). The heart’s rhythm is controlled by a large mass of tissues in the right atrium (sinus node). The sinus node generates electrical impulses, also known as signals, which cause every heartbeat.
The electrical signals travel through the atria, creating muscles to contract, which then pump blood into the ventricles. The signals are then received by the atrioventricular node, which is also known as an Atrioventricular (AV) node, which is generally the only route for signals to move between the atria and the ventricles. The AV The node slows down the electrical signal before it is sent through the ventricles.
The delay is just enough to allow the ventricles to fill up with blood. When electrical signals are received by those ventricles and muscles contract, they send fluid to the lung and the rest of the body.
Affects the electrical system of WPW in a way that is not normal
In WPW syndrome, an additional electrical pathway joins ventricles and atria, permitting electrical impulses to escape the AV node. This detour triggers the ventricles too late.
The extra pathway could also send electrical impulses from ventricles to the Atria, causing disruption to the coordination of electrical signals in the heart, causing variations in the heart’s rhythm.
The most commonly occurring arrhythmia that is related to WPW Syndrome is also known as paroxysmal supraventricular Tachycardia. People with WPW Syndrome sufferers have an irregular heartbeat, known as atrial fibrillation.
Complications
For many people, WPW syndrome doesn’t cause serious problems. However, complications could develop. It’s sometimes difficult to predict the risk of having serious heart circumstances. If WPW The condition is not treated — especially if you suffer from other heart issues you may be suffering from:
- Fainting spells
- Fast heartbeats
- Rarely, sudden cardiac arrest
Diagnosis
Your physician will most likely suggest tests to determine the cause of your condition. WPW syndrome, including:
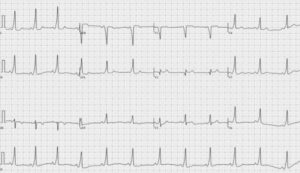
- Electrocardiogram (ECG). Small sensors that are attached to your arms and chest capture electrical signals as they move across your heart. A typical finding for WPW is the delta wave¹ on EKG. Your doctor may be able to spot patterns in these signals that could indicate an additional electrical path in your heart.
- Holter monitor. A Holter monitor can be a portable ECG The device you have at home is one that you wear at home when you’re not in your doctor’s appointment. The device monitors the heart’s activity as you go about your daily tasks for the duration of one or two days. An event recorder can monitor the heart’s activity when it is beating too quickly. Certain personal devices, including smartwatches, can provide ECG monitoring. Consult your physician whether it is a possibility for you.
- Tests for electrophysiology. Thin, flexible tubes (catheters) equipped with electrodes are passed through the blood vessels of your body to various locations within your heart. The electrodes track the distribution of electrical impulses that occur during every heartbeat. They also pinpoint an additional electrical pathway.
Treatment
The treatment you receive is based on a variety of aspects, such as the intensity and frequency of your symptoms, as well as what kind of arrhythmia you are suffering from.
If you are suffering from the WPW If you’re not experiencing symptoms, you’re likely not to require treatment. In the event that you need treatment, your aim of treatment is to slow the speed of your heart whenever it happens and to stop future episodes from occurring.
Treatment choices comprise:
- Vagal movements. These simple physical actions — such as coughing, rolling down like you’re experiencing an abdominal movement, and placing an ice pack over your face — can affect the nerve that regulates the heartbeat (vagus nerve). Your doctor might recommend that you practice vagal movements to slow down a fast heartbeat that occurs.
- Medical Treatments. If vagal maneuvers can’t stop the rapid heartbeat it could be time to consider injections of an anti-arrhythmic medicine. Your physician may also suggest the use of medication to slow the rate of heartbeat.
- Cardioversion. Paddles or patches on your chest may electronically shock your heart and assist in restoring a normal rhythm. The use of cardioversion is often when medications and maneuvers don’t work.
- Radiofrequency catheter ablation. Flexible, thin tubing (catheters) are passed through blood vessels and into the heart. The electrodes at the tips of the catheter are heated to eliminate (ablate) the additional electrical pathway that is causing the problem. Radiofrequency ablation permanently fixes the heart-rhythm disorders in most patients who suffer from WPW syndrome.
For more information
For more information about WPW, please see your physician.

casino apps
References:
https://love.ynlma.com/home.php?mod=space&uid=149089
online gaming websites
References:
https://edutimesafrica.com/employer/26113/20-best-online-casinos-in-australia-for-real-money
southpoint casino las vegas
References:
https://aimetath.com/renatekoenig9
genting casino luton
References:
https://shirme.com/imogenebenge99
yakama legends casino
References:
https://onlinehdkino.com/user/arvicaqhuo
play online blackjack
References:
https://xn—-7sbhmn2acksil.xn--p1ai/user/onovenkphy
video poker trainer
References:
https://bestcomedy.ru/user/baniusuksg
Einige Online Spielhallen haben bestimmte Limits für Freispiele bei Registrierung ohne Einzahlung festgesetzt.
In der Regel musst Du die Freispiele ohne Einzahlung mindestens
35 Mal umsetzen, bevor Du Dir die Gewinne auszahlen lassen kannst.
Beachte, dass Freispiele bei Registrierung gewissen Umsatzbedingungen unterliegen. Freispiele bei Registrierung ohne
Einzahlung ermöglichen Dir zahlreiche Casino Spiele kostenlos und ohne Risiko zu testen. Aktuell kann man sich bei Winfest.com mit einer Einzahlung von 10
Euro 150 Freispiele sichern, dazu gibt es einen Bonus von bis
zu 100€. Durch die schnelle Registrierung und Bestätigung Deiner Identität per SMS werden die 50 Freispiele ohne Einzahlung sofort zu
deinen Konto gutgeschrieben. Über 50 Freispiele ohne Einzahlung kannst Du Dir
bei zahlreichen Online Spielotheken sofort sichern.
Regelmäßige Aktionen, wie Freispiel Alarm und Drops & Wins, bieten Spielern die Möglichkeit, zusätzliche
Gewinne und Boni während ihres Spiels zu verdienen. Spieler sollten sich daher über die RTP-Werte der Spiele informieren und solche
auswählen, die höhere Gewinnchancen bieten. Durch eine sorgfältige Budgetplanung können Spieler
ihre Ausgaben kontrollieren und das Spielvergnügen langfristig aufrechterhalten. Der FAQ-Bereich bietet umfassende Antworten zur Umwandlung von Bonusgeld und Auszahlung von Guthaben. Dies
stellt sicher, dass Spieler jederzeit die Hilfe erhalten, die sie benötigen, um ihr Spielerlebnis zu optimieren.
Die meisten Online Casinos bieten Unterstützung über
mehrere Kanäle, einschließlich Live-Chat, E-Mail und telefonischen Kontakt.
References:
https://online-spielhallen.de/zetcasino-deutschland-einloggen-spielen-auszahlen/
Nun vereinfacht gesagt handelt es sich dabei tatsächlich um einen Free Bonus, also einen Bonus, den Sie gratis vom Casino erhalten. Bis dahin mit dem
Bonusgeld erspielte Gewinne verfallen ebenfalls. Einen 10€ Bonus
ohne Einzahlung kannst du als Krypto-Bonus jedoch nicht beanspruchen und nur in Fiat-Währungen erhalten. Du
kannst jedoch mit deinem Smartphone oder Tablet das reguläre Bonusangebot beanspruchen.
Schaffst du es in dieser Zeit nicht, alle
Umsatzbedingungen zu erfüllen, verfällt dein Bonus leider.
Bei den meisten Anbietern musst du den Bonus ungefähr 30 bis 50 Mal zum Spielen einsetzen, damit das Bonusgeld für eine Auszahlung freigegeben wird.
Für dich bedeutet das, dass du den erhaltenen Betrag erst mehrfach einsetzen musst, bevor du dir das
mit dem Bonus gewonnene Geld auszahlen lassen kannst.
Es ist üblich, dass ein Casino Bonus ohne Einzahlung an Umsatzbedingungen geknüpft ist.
Wenn es möglich ist, durch einen Online Casino Bonus ohne Einzahlung
10 Euro geschenkt zu bekommen, handelt es sich dabei
in den meisten Fällen um ein Willkommensangebot für neue Spieler.
Wenn ihr auf der Suche nach etwas anderes, als einem Startbonus
mit Startguthaben ohne Einzahlung seid, könnt ihr auch auf unserer Seite für Online Casino
Bonus Codes vorbeischauen, wo wir täglich
aktualisierte Bonuscodes präsentieren.
References:
https://online-spielhallen.de/verde-casino-bonuscode-2025-alle-angebote-im-uberblick/
Sichere Lizenzen, namhafte Spieleanbieter und Zahlungsdienstleister sind gute
Anhaltspunkte für ein sicheres Online-Casino. Wichtig ist, dass die Anbieter lizenziert und
somit seriös sind. Viele seriöse Anbieter stellen neuen Spielern Bonusgeld oder Freispiele zur Verfügung – oft
schon ab der ersten Einzahlung. Ein fairer Willkommensbonus kann den Einstieg ins Online-Glücksspiel zusätzlich versüßen. Natürlich müssen die Spiele geprüft und lizenziert sein,
um Fairplay sicherzustellen.
Die Bonusangebote in Online Casinos variieren stark, mit Optionen wie Willkommensboni, Cashback
und Turnieren. Diese Spiele bieten nicht nur hohen Unterhaltungswert, sondern auch attraktive Gewinnmöglichkeiten. Pragmatic Play bietet unter anderem das bekannte Spiel ‘Gates of Olympus’ an. Die Spielauswahl von Merkur
umfasst innovative Spielmechaniken, die das Spielerlebnis verbessern. Gamomat bietet beliebte Spielautomaten und einzigartige Designs,
die bei Spielern gut ankommen.
References:
https://online-spielhallen.de/casino-of-gold-bonus-spiele-anmeldung/
Das Casino Baden Baden gilt als die vornehmste aller deutschen Spielbanken, wobei andere traditionsreiche Casinos
wie in Bad Homburg in dem kaum nachstehen und ebenfalls
einen Besuch wert sind. Zusätzlich bekommst du als Neukunde
in einem Internet Casino einen Willkommensbonus zu
seiner ersten Einzahlung und selbst Free Spins (Freispiele) sind nicht selten. Im
Internet gibt es keine Öffnungszeiten und du kannst
rund um die Uhr spielen wann immer du Lust dazu hast.
Im Vergleich zu Spielbanken können deutsche Online Casinos eine sehr breite Auswahl an verschiedenen Einsatzlimits anbieten. Dort gibt es weitere Spiele mit Top
Auszahlungsraten, einen guten Neukundenbonus, Freispiele und nicht zuletzt eine sichere und seriöse Spielumgebung.
Möchtest du um echtes Geld spielen, so findest du auch eine
Empfehlung für das beste Casino dafür.
Der RTP gibt an, wie viel Prozent der Einsätze der Glücksspielanbieter wieder an den Kunden ausschüttet.
Auf diese Weise können Spieler sich sicher sein, dass die Auszahlungsquote
für Slots oder Tischspiele wie Roulette den Tatsachen entsprechen. Das Logo der vorhandenen Glücksspiellizenz befindet
sich in der Regel im Footer der ausgewählten Online Casino Webseite.
Die Anmeldung in Online Casinos mit EU-Lizenz ist deutschlandweit verboten. Die deutsche Lizenz legt einen großen Fokus auf den Spielerschutz.
Während eine gültige Lizenz essenziell für die Seriosität eines Online Casino Angebots ist,
muss ein Online Spielcasino noch weitere Kriterien erfüllen, um von uns empfohlen zu werden.
References:
https://online-spielhallen.de/wildz-deutschland-test-bonus-spiele-2025/
Mir geht es nicht nur darum, die besten Angebote aufzuzeigen, sondern euch fundiertes Know-how
zu vermitteln, das euch dabei hilft, umsichtiger, sicherer und letztlich lukrativer zu spielen Es gibt immer wieder neue Online Casinos, in denen Freispiele ohne Einzahlung sofort
erhältlich sind. Ihr werdet vielleicht schon bemerkt haben, dass gerade Freispiele ohne Einzahlung oft nur dem absoluten Mindesteinsatz von 10 oder 20 Cent entsprechen. Schaut ihr euch
zum Thema Freispiele ohne Einzahlung aktuell um, werdet ihr feststellen,
dass die Nutzungsfrist oft bei 24 Stunden liegt – das ist in Ordnung.
Umsatzfristen von 14 Tagen oder länger kommen bei Freispielen ohne Einzahlung in Deutschland nur selten vor.
Optimalerweise werden kostenlose Freispiele ohne Einzahlung in einem Top-Slot einer
großen Marke wie Pragmatic Play, NetEnt oder Play’n GO mit RTP jenseits
der 95 Prozent vergeben.
Ja, der Slot ist dank Instant Play auch ohne Doppelbuch App mit Smartphones und Tablets spielbar.
Wir empfehlen Ihnen, Doppelbuch oder Scribes of Thebes, wie der Slot international genannt
wird, einfach auszuprobieren. Der Clou mit dem expandierenden Sondersymbol in der Freispielrunde wird hier auf
die Spitze getrieben. Wenn Sie Book of Ra oder viele der Alternativen mögen, dann sollten Sie unbedingt den Merkur Slot Doppelbuch ausprobieren.
References:
https://online-spielhallen.de/beste-online-casinos-2025-empfehlungs-guide/
alabama casinos
References:
http://demo.emshost.com/space-uid-4133429.html
casino online
References:
https://www.scdmtj.com/home.php?mod=space&uid=6061116
machine games
References:
https://escatter11.fullerton.edu/nfs/show_user.php?userid=9409482
circus circus casino
References:
https://www.pinterest.com/judgeclaus46/
christophe claret 21 blackjack
References:
https://www.lanubedocente.21.edu.ar/profile/byrnetgamcgraw16338/profile
all jackpots casino
References:
https://www.tarauaca.ac.gov.br/profile/piperqndpace46669/profile
perth crown casino
References:
https://vrwant.org/wb/home.php?mod=space&uid=4804061
online betting sites
References:
http://humanlove.stream//index.php?title=loftpuggaard1043
casino italia
References:
https://images.google.com.gt/url?q=https://www.instapaper.com/p/17227872
durant ok casino
References:
https://www.hulkshare.com/satinpoppy62/
**mitolyn**
Mitolyn is a carefully developed, plant-based formula created to help support metabolic efficiency and encourage healthy, lasting weight management.
https://t.me/s/pov_1win
https://askoff.ru
https://askoff.ru
https://qtjpqhtfcs.wordpress.com
https://qtjpqhtfcs.wordpress.com
https://iagperjusu.wordpress.com
https://iagperjusu.wordpress.com
https://dwspqdxcgw.wordpress.com
https://xrsaugpsya.wordpress.com
https://xrsaugpsya.wordpress.com
https://gxvkxeawwa.wordpress.com
https://gxvkxeawwa.wordpress.com
https://azacgxicis.wordpress.com
https://azacgxicis.wordpress.com
https://zfcejfyxiv.wordpress.com
https://zfcejfyxiv.wordpress.com
https://cxadxqpked.wordpress.com
https://akiwdiycje.wordpress.com
https://akiwdiycje.wordpress.com
https://iqakruyprf.wordpress.com
https://iqakruyprf.wordpress.com
https://dgaiyziytk.wordpress.com
https://dgaiyziytk.wordpress.com
https://hrjcdfdcvj.wordpress.com
https://hrjcdfdcvj.wordpress.com
https://wryxvrrhxe.wordpress.com
https://wryxvrrhxe.wordpress.com