Prolia
Generic name: denosumab (Prolia)
Drug class: Miscellaneous bone resorption inhibitors
Medically reviewed by A Ras MD.
What is Prolia?
Prolia is a prescription medicine used to treat osteoporosis (thinning and weakening of bone) in women after menopause (“change of life”) who are at high risk for fracture (broken bone) and cannot use another osteoporosis medicine or other osteoporosis medicines did not work well.
It is also used to:
- Increase bone mass in men with osteoporosis who are at high risk for fracture.
- Treat osteoporosis in men and women who will be taking corticosteroid medicines (such as prednisone) for at least 6 months and are at high risk for fracture.
- Treat bone loss in men who are at high risk for fracture receiving certain treatments for prostate cancer that has not spread to other parts of the body.
- Treat bone loss in women who are at high risk for fracture receiving certain treatments for breast cancer that has not spread to other parts of the body.
It is not known if Prolia is safe and effective in children.
Description
Prolia (denosumab) is a human IgG2 monoclonal antibody with affinity and specificity for human RANKL (receptor activator of nuclear factor kappa-B ligand). Denosumab has an approximate molecular weight of 147 kDa and is produced in genetically engineered mammalian (Chinese hamster ovary) cells.
Prolia is a sterile, preservative-free, clear, colorless to pale yellow solution.
Each 1 mL single-dose prefilled syringe of Prolia contains 60 mg denosumab (60 mg/mL solution), 4.7% sorbitol, 17 mM acetate, 0.01% polysorbate 20, Water for Injection (USP), and sodium hydroxide to a pH of 5.2.
Mechanism of Action
Prolia binds to RANKL, a transmembrane or soluble protein essential for the formation, function, and survival of osteoclasts, the cells responsible for bone resorption. Prolia prevents RANKL from activating its receptor, RANK, on the surface of osteoclasts and their precursors. Prevention of the RANKL/RANK interaction inhibits osteoclast formation, function, and survival, thereby decreasing bone resorption and increasing bone mass and strength in both cortical and trabecular bone
What is the most important information I should know about Prolia?
If you receive Prolia, you should not receive Xgeva. Prolia contains the same medicine as Xgeva (denosumab).
Prolia can cause serious side effects including:
- Serious allergic reactions. Serious allergic reactions have happened in people who take Prolia. Call your doctor or go to your nearest emergency room right away if you have any symptoms of a serious allergic reaction. Symptoms of a serious allergic reaction may include:
- low blood pressure (hypotension)
- trouble breathing
- throat tightness
- swelling of your face, lips, or tongue
- rash
- itching
- hives
- Low calcium levels in your blood (hypocalcemia). Prolia may lower the calcium levels in your blood. If you have low blood calcium before you start receiving Prolia, it may get worse during treatment. Your low blood calcium must be treated before you receive Prolia. Most people with low blood calcium levels do not have symptoms, but some people may have symptoms. Call your doctor right away if you have symptoms of low blood calcium such as:
- spasms, twitches, or cramps in your muscles
- numbness or tingling in your fingers, toes, or around your mouth
Your doctor may prescribe calcium and vitamin D to help prevent low calcium levels in your blood while you take Prolia. Take calcium and vitamin D as your doctor tells you to.
- Severe jaw bone problems (osteonecrosis). Severe jaw bone problems may happen when you take Prolia. Your doctor should examine your mouth before you start Prolia. Your doctor may tell you to see your dentist before you start Prolia. It is important for you to practice good mouth care during treatment with Prolia. Ask your doctor or dentist about good mouth care if you have any questions.
- Unusual thigh bone fractures. Some people have developed unusual fractures in their thigh bone. Symptoms of a fracture include new or unusual pain in your hip, groin, or thigh.
- Increased risk of broken bones, including broken bones in the spine, after stopping, skipping or delaying Prolia. Talk with your doctor before starting Prolia treatment. After your treatment with Prolia is stopped, or if you skip or delay taking a dose, your risk for breaking bones, including bones in your spine, is increased. Your risk for having more than 1 broken bone in your spine is increased if you have already had a broken bone in your spine.
- Serious infections. Serious infections in your skin, lower stomach area (abdomen), bladder, or ear may happen if you take Prolia. Inflammation of the inner lining of the heart (endocarditis) due to an infection also may happen more often in people who take Prolia. You may need to go to the hospital for treatment if you develop an infection.
- Prolia is a medicine that may affect the ability of your body to fight infections. People who have a weakened immune system or take medicines that affect the immune system may have an increased risk for developing serious infections. Call your doctor right away if you have any of the following symptoms of infection:
- fever or chills
- skin that looks red or swollen and is hot or tender to touch
- fever, shortness of breath, cough that will not go away
- severe abdominal pain
- frequent or urgent need to urinate or burning feeling when you urinate
- Prolia is a medicine that may affect the ability of your body to fight infections. People who have a weakened immune system or take medicines that affect the immune system may have an increased risk for developing serious infections. Call your doctor right away if you have any of the following symptoms of infection:
- Skin problems. Skin problems such as inflammation of your skin (dermatitis), rash, and eczema may happen if you take Prolia. Call your doctor if you have any of the following symptoms of skin problems that do not go away or get worse:
- redness
- itching
- small bumps or patches (rash)
- your skin is dry or feels like leather
- blisters that ooze or become crusty
- skin peeling
- Bone, joint, or muscle pain. Some people who take Prolia develop severe bone, joint, or muscle pain.
Call your doctor right away if you have any of these side effects.
Do not stop, skip or delay taking Prolia without first talking with your doctor. If your Prolia treatment is stopped, talk to your doctor about other medicine that you can take.
Who should not take Prolia?
Do not take Prolia if you:
- have been told by your doctor that your blood calcium level is too low.
- are pregnant or plan to become pregnant.
- are allergic to denosumab or any of the ingredients in Prolia. See the end of this Medication Guide for a complete list of ingredients in Prolia.
What should I tell my healthcare provider before taking Prolia?
Before taking Prolia, tell your doctor about all of your medical conditions, including if you:
- are taking a medicine called Xgeva (denosumab). Xgeva contains the same medicine as Prolia.
- have low blood calcium.
- cannot take daily calcium and vitamin D.
- had parathyroid or thyroid surgery (glands located in your neck).
- have been told you have trouble absorbing minerals in your stomach or intestines (malabsorption syndrome).
- have kidney problems or are on kidney dialysis.
- are taking medicine that can lower your blood calcium levels.
- plan to have dental surgery or teeth removed.
- are pregnant or plan to become pregnant. Prolia may harm your unborn baby. Females who are able to become pregnant:
- Your healthcare provider should do a pregnancy test before you start treatment with Prolia.
- You should use an effective method of birth control (contraception) during treatment with Prolia and for at least 5 months after your last dose of Prolia.
- Tell your doctor right away if you become pregnant while taking Prolia.
- are breastfeeding or plan to breastfeed. It is not known if Prolia passes into your breast milk. You and your doctor should decide if you will take Prolia or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of medicines with you to show to your doctor or pharmacist when you get a new medicine.
How should I take Prolia?
- Prolia is an injection that will be given to you by a healthcare professional. Prolia is injected under your skin (subcutaneous).
- You will receive Prolia 1 time every 6 months.
- You should take calcium and vitamin D as your doctor tells you to while you receive Prolia.
- If you miss a dose of Prolia, you should receive your injection as soon as you can.
- Take good care of your teeth and gums while you receive Prolia. Brush and floss your teeth regularly.
- Tell your dentist that you are receiving Prolia before you have dental work.
What are the possible side effects of Prolia?
Prolia may cause serious side effects.
- See “What is the most important information I should know about Prolia?”
- It is not known if the use of Prolia over a long period of time may cause slow healing of broken bones.
The most common side effects of Prolia in women who are being treated for osteoporosis after menopause are:
- back pain
- pain in your arms and legs
- high cholesterol
- muscle pain
- bladder infection
The most common side effects of Prolia in men with osteoporosis are:
- back pain
- joint pain
- common cold (runny nose or sore throat)
The most common side effects of Prolia in patients with glucocorticoid-induced osteoporosis are:
- back pain
- high blood pressure
- lung infection (bronchitis)
- headache
The most common side effects of Prolia in patients receiving certain treatments for prostate or breast cancer are:
- joint pain
- back pain
- pain in your arms and legs
- muscle pain
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Prolia.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Prolia.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Prolia for a condition for which it was not prescribed. Do not give Prolia to other people, even if they have the same symptoms that you have. It may harm them. You can ask your doctor or pharmacist for information about Prolia that is written for health professionals.
How should I store Prolia?
If you need to pick Prolia up from the pharmacy:
- Keep Prolia in a refrigerator at 36°F to 46°F (2°C to 8°C) in the original carton.
- Do not freeze Prolia.
- When you remove Prolia from the refrigerator, Prolia must be kept at room temperature [up to 77°F (25°C)] in the original carton and must be used within 14 days.
- Do not keep Prolia at temperatures above 77°F (25°C). Warm temperatures will affect how Prolia works.
- Do not shake Prolia.
- Keep Prolia in the original carton to protect from light.
Keep Prolia and all medicines out of the reach of children.
What are the ingredients in Prolia?
Active ingredient: denosumab
Inactive ingredients: sorbitol, acetate, polysorbate 20, Water for Injection (USP), and sodium hydroxide
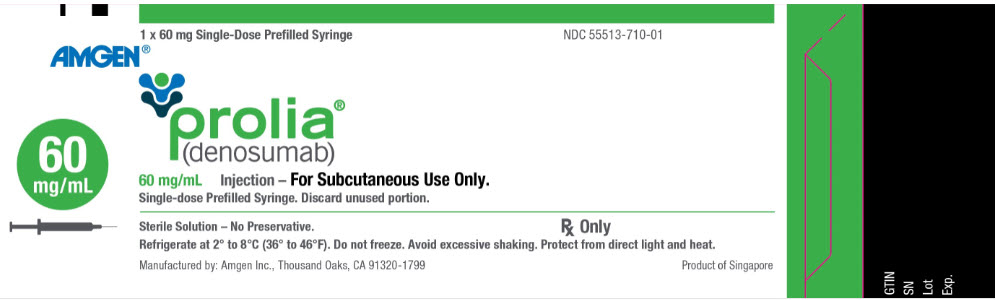
Label
PRINCIPAL DISPLAY PANEL
- 1 x 60 mg Single-Dose Prefilled Syringe
NDC 55513-710-01
AMGEN®
prolia®
(denosumab)
60 mg/mL
60 mg/mL Injection – For Subcutaneous Use Only.
Single-dose Prefilled Syringe. Discard unused portion.
Sterile Solution – No Preservative.
Rx Only
SRC: NLM .
