Obstructive ventilatory defect
Medically reviewed by A Ras MD. Last updated March 30, 2022
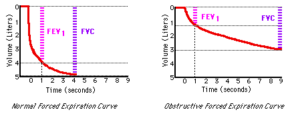
Obstructive ventilatory defect (OVD) is typically described by a lower ratio between the first forced expiratory volume as well as the “forced/slow” vital capacity [FEV 1/(F)VC]
The test is usually performed via the lung function test. It assists in diagnosing chronic lung diseases based on the presence of a trapping obstruction, as well as decreased compliance and restriction.¶
What are Pulmonary Function Tests?
- To determine if you have asthma/COPD or another lung disease, Your doctor will look over your symptoms, medical history, and family history, and may also conduct tests for lung functions (also known as tests to determine pulmonary function). Your doctor will also be looking into any breathing issues you may have suffered from in the past, and also an asthma-related family history or other lung diseases as well as allergies or skin diseases such as eczema. It is essential to identify your asthma symptoms in full detail (coughing or wheezing, breathlessness, and chest tightness) along with the time and how often they occur.
- Your doctor will also conduct a physical examination and take listen to your heartbeat and lung. Alongside asthma pulmonary function tests The doctor could also perform allergy tests as well as blood tests and sinus and chest X-rays. They may recommend you to a pulmonologist or a specialist in lung health to conduct further tests for asthma, as well as other conditions that could be affecting the condition.
What are the various Lung Function Tests?
 There are many lung function tests that can be used to diagnose asthma. The most commonly used tests include:
There are many lung function tests that can be used to diagnose asthma. The most commonly used tests include:
- Spirometry The test for breathing tests the quantity of air you take in and how fast the air can be blown out. It will show the amount of obstruction to your airway that you have. Take an exhale and take a deep breath through a hose connected to a device known as the nanometer. It tracks how much air you exhale (FVC or forced vital capacity) and how fast you blow it out (FEV, also known as forced expiratory volume). It is possible to measure spirometry prior to and after inhaling the short-acting drug known as a bronchodilator. It is similar to albuterol. The bronchodilator helps your airways expand, which allows air to move through without restriction. The test also helps the doctor monitor your progress and determine if and how to modify the treatment regimen.
- Peak flow test for meter: These tests measure how efficiently your lungs push out air. While less precise than Spirometry, they’re an excellent method of assessing the function of your lungs in the comfort of your home and before you experience any signs. A peak flow monitor can aid in determining what causes the asthma condition to worse. It can also tell you if treatment is working, and also when you need urgent care.
- Challenge tests: The doctor may refer them to provocation tests. There are three kinds:
- Test for exercise challenge: This test helps determine whether you suffer from exercise-inducing bronchoconstriction (EIB) which is a sign that exercising can trigger asthma symptoms. The doctor will observe your oxygen level and cardiovascular rate when you exercise on the treadmill. This will tell the doctor that exercising causes your symptoms.
- Irritant challenge Doctors expose your body to triggers for asthma for example, such as perfume, smoke, or chemical. You then take a breath test to determine how your lungs react. This can help determine the cause of your asthma.
- Methacholine test challenge: It is most commonly performed for adults than for children. You could get it when your symptoms and screening spirometry do not clearly indicate an asthma diagnosis. If you suffer from asthma, and breathe in methacholine airways contract (contract due to an impulse) as well as narrow. In this test, you breathe in methacholine-infused mists prior to and after the spirometry. If your lung function decreases by 20 percent then you are suffering from asthma. The doctor will prescribe medication at the conclusion of this test, to counteract the effect of methacholine.
- FeNO Test: You might hear it being called the exhaled nicotine oxide test. If you suffer from allergies or eosinophilic asthma could help you determine the amount of inflammation you suffer and how well your inhaled steroids are keeping it under control. Then, you blow into an instrument that can measure how much nitric oxide is present in the air you breathe.
Obstructive ventilatory defect classification
The year 2014 saw the introduction of a brand new alternate classification (GLI classification) to grade severity of the OVD severity was suggested to replace the classification of 2005.
the purpose of this class was to evaluate the functional capability of patient-based OVD against two other classifications.
Following OVD classifications were used to determine severity:
- (FEV 1%pred) (FEV 1%pred) (>70 percent),
- moderate (60-69 moderate (60-69),
- moderately severe (50-59 50-59 %),
- severe (35-49 severe (35-49 %) severe (35-49%)
- extremely severe (<35 very severe (35)
The reason behind the revised method of diagnosing OVD and classifying the spirometric deficit was fascinating. The purpose behind the brand new class was intended to fill in the gap among the population diagnosed with COPD using the older classification.¶
Additional details
Always consult your doctor to confirm that the information provided on this site is appropriate to your specific situation.

Hi! Do you know if they make any plugins to help with SEO?
I’m trying to get my site to rank for some targeted keywords but
I’m not seeing very good results. If you know of
any please share. Cheers! I saw similar art here: Blankets
Why, precisely, would an individual shell out $10 to $20 for a machine that a smartphone duplicates so simply?
sugar defender ingredients Discovering Sugar Protector has actually been a game-changer for me, as I have actually constantly been vigilant about managing my blood sugar degrees.
With this supplement, I feel empowered to take charge of my wellness,
and my most recent clinical exams have actually shown a significant turn-around.
Having a trustworthy ally in my edge offers me with a sense of security
and reassurance, and I’m deeply appreciative for the profound difference Sugar
Protector has actually made in my health.
sugar defender ingredients As somebody who’s constantly bewared regarding my blood
sugar, finding Sugar Protector has actually been an alleviation. I feel
so much extra in control, and my current
exams have actually revealed favorable enhancements. Knowing I have
a trustworthy supplement to support my routine gives me
satisfaction. I’m so happy for Sugar Defender’s influence on my health and wellness!
You are so awesome! I do not believe I’ve truly read through anything like that before. So wonderful to discover someone with some unique thoughts on this subject matter. Really.. thanks for starting this up. This website is something that is required on the internet, someone with a bit of originality.
This is a really good tip particularly to those new to the blogosphere. Simple but very accurate info… Thank you for sharing this one. A must read article!
This is a good tip especially to those fresh to the blogosphere. Simple but very accurate info… Appreciate your sharing this one. A must read post!
An impressive share! I’ve just forwarded this onto a friend who had been doing a little homework on this. And he actually ordered me breakfast because I discovered it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanks for spending time to talk about this subject here on your site.
Everything is very open with a clear explanation of the issues. It was really informative. Your site is very helpful. Thanks for sharing!
I like it whenever people come together and share opinions. Great website, stick with it.
Aw, this was a very good post. Taking a few minutes and actual effort to generate a great article… but what can I say… I procrastinate a lot and never manage to get anything done.
I used to be able to find good advice from your articles.
It’s difficult to find experienced people for this topic, however, you seem like you know what you’re talking about! Thanks
How can I construct mental resilience to combat Covid depression?
This site was… how do I say it? Relevant!! Finally I have found something that helped me. Appreciate it.
James Masterson, Hobart, IN, Daniel Orr, Middleton, Idaho, Kenneth Orr and Ernest Orr; 12 grandchildren; 5 nice grandchildren; step-father of Mrs.
You might help by including to it.
Learn the agencies working with Dubai tours so you might be capable of ebook properly forward of time even at some stage in rush time.
Good blog you have got here.. It’s hard to find high quality writing like yours these days. I honestly appreciate individuals like you! Take care!!
Very good information. Lucky me I came across your website by chance (stumbleupon). I’ve book marked it for later.
I’m amazed, I have to admit. Rarely do I encounter a blog that’s equally educative and engaging, and let me tell you, you’ve hit the nail on the head. The issue is something too few men and women are speaking intelligently about. Now i’m very happy that I came across this during my hunt for something regarding this.
I’d like to thank you for the efforts you’ve put in writing this site. I really hope to check out the same high-grade blog posts by you in the future as well. In truth, your creative writing abilities has inspired me to get my own, personal blog now 😉
Nice post. I learn something new and challenging on blogs I stumbleupon everyday. It will always be helpful to read through content from other writers and use something from their web sites.
Hi, I do believe this is an excellent site. I stumbledupon it 😉 I may revisit once again since i have book marked it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
I wanted to thank you for this excellent read!! I certainly enjoyed every little bit of it. I have got you bookmarked to look at new things you post…
sugar defender For
many years, I’ve fought uncertain blood glucose swings that left me really feeling drained pipes and lethargic.
Yet since incorporating Sugar my power levels are now stable and consistent,
and I no longer hit a wall in the afternoons.
I appreciate that it’s a mild, all-natural technique that does not come
with any kind of unpleasant side effects. It’s really changed my daily life.
Hi, I do think this is a great web site. I stumbledupon it 😉 I’m going to come back once again since I saved as a favorite it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
Way cool! Some extremely valid points! I appreciate you penning this write-up and the rest of the site is also very good.
Hello there! This article could not be written any better! Looking through this post reminds me of my previous roommate! He constantly kept talking about this. I most certainly will forward this article to him. Fairly certain he’s going to have a very good read. I appreciate you for sharing!
Next time I read a blog, I hope that it doesn’t fail me just as much as this particular one. After all, I know it was my choice to read through, nonetheless I genuinely believed you’d have something useful to talk about. All I hear is a bunch of crying about something you could possibly fix if you weren’t too busy searching for attention.
Howdy! This blog post could not be written any better! Going through this post reminds me of my previous roommate! He always kept preaching about this. I’ll forward this article to him. Pretty sure he’s going to have a great read. Many thanks for sharing!
Pretty! This was a really wonderful post. Thanks for supplying this information.
Your style is really unique in comparison to other folks I have read stuff from. Thanks for posting when you’ve got the opportunity, Guess I’ll just bookmark this blog.
This is a topic that’s close to my heart… Best wishes! Exactly where can I find the contact details for questions?
I truly love your blog.. Pleasant colors & theme. Did you build this website yourself? Please reply back as I’m trying to create my very own website and would love to know where you got this from or what the theme is named. Cheers.
She got here to this area at the age of eight and attended Wilbur colleges.
I love it when people come together and share thoughts. Great site, stick with it.
Right here is the right web site for anybody who really wants to understand this topic. You know a whole lot its almost tough to argue with you (not that I actually would want to…HaHa). You certainly put a new spin on a topic that’s been written about for ages. Excellent stuff, just great.
You ought to take part in a contest for one of the highest quality blogs on the internet. I’m going to highly recommend this blog!
I like it when people come together and share ideas. Great blog, keep it up!
An example is the Tree of Jessé window at Saint-Denis (see image above).
Good article. I am going through a few of these issues as well..
Although chess play is widespread but it requires lots of observe and data to play in international players.
Howdy! This article couldn’t be written any better! Going through this post reminds me of my previous roommate! He continually kept preaching about this. I will send this article to him. Fairly certain he’s going to have a good read. I appreciate you for sharing!
Signs generate clutter within the pump room, and the steel wire stands will rust if left in there for too long.
Good day! I just would like to offer you a big thumbs up for your excellent information you have got here on this post. I am coming back to your blog for more soon.
Your style is very unique compared to other people I’ve read stuff from. Thanks for posting when you’ve got the opportunity, Guess I’ll just bookmark this page.
I like reading an article that will make people think. Also, thank you for allowing me to comment.
Good post. I learn something totally new and challenging on blogs I stumbleupon every day. It’s always useful to read through articles from other authors and use a little something from their web sites.
This site is known as a walk-by way of for all the info you wished about this and didn’t know who to ask. Glimpse right here, and also you’ll positively uncover it.
This is a really good tip especially to those new to the blogosphere. Brief but very accurate information… Thank you for sharing this one. A must read post.
Amer, Mildred (June 16, 2005).
The very next time I read a blog, Hopefully it won’t fail me just as much as this one. I mean, Yes, it was my choice to read, however I genuinely believed you would have something interesting to talk about. All I hear is a bunch of moaning about something you can fix if you weren’t too busy looking for attention.
Everything is very open with a really clear explanation of the issues. It was really informative. Your site is very useful. Thank you for sharing.
Awesome post ! Cheers for, visiting my blog dude! I will email you again! I didnt know that.
I blog often and I truly appreciate your information. This article has truly peaked my interest. I am going to book mark your site and keep checking for new details about once per week. I subscribed to your RSS feed too.
After study a handful of the web sites on your own site now, we truly appreciate your way of blogging. I bookmarked it to my bookmark website list and you will be checking back soon. Pls take a look at my internet site in addition and inform me what you believe.
No more s***. All posts of this qaulity from now on
Everyone loves it when individuals get together and share ideas. Great site, keep it up.
May I simply say what a relief to find somebody that actually knows what they are talking about on the net. You certainly understand how to bring an issue to light and make it important. More people should read this and understand this side of the story. I was surprised you’re not more popular since you most certainly possess the gift.
Way cool! Some extremely valid points! I appreciate you writing this article and also the rest of the site is extremely good.
Another interesting article, Thanks for sharing this information, it is unusual to read such high quality posts. I will bookmark your site.
You undoubtedly make it look really easy with your display but I come across this particular matter to get really a thing that I do think I’d personally never ever comprehend. It appears also complicated and very vast to me. We are anticipating for your forthcoming submit, Let me try and get the hang of that!
Aw, this was a really nice post. Taking a few minutes and actual effort to make a top notch article… but what can I say… I procrastinate a whole lot and never seem to get nearly anything done.
That song sucks i think, my younger brother is listening that, and its so boring song !
I really love to read this post and I am glad to find your distinguished way of writing the post. Thanks and Regards
A well written post, I just given this onto a colleague who was doing slightly analysis on that. And he indeed purchased me breakfast because I discovered it for him .. thus let me reword that: Thankx for the treat! however yeah Thnx for spending the time to talk concerning this, I feel strongly concerning it and revel in reading a lot of on this topic. If potential, as you become expertise, would you mind updating your blog with a lot of info? it’s very useful on behalf of me. two thumb up for this blog!
If only my personal content articles appeared as if this particular! That is a enhance, btw?-I ‘m new to blog posting and reading numerous blog posts is helping me out with my very own. Any kind of info you could throw my method to assistance is very appreciated. Just good information on this particular post!
A motivating discussion is definitely worth comment. I believe that you should write more about this subject matter, it might not be a taboo subject but usually people don’t discuss these subjects. To the next! Cheers.
This will be the appropriate weblog for everyone who wants to discover this topic. You are aware of a whole lot its almost difficult to argue to you (not too I really would want…HaHa). You certainly put a different spin on the topic thats been discussed for some time. Great stuff, just wonderful!
Very good post. I’m experiencing many of these issues as well..
Substantially, the article is in reality the freshest on that laudable topic. I agree with your conclusions and also will certainly eagerly look forward to your forthcoming updates. Saying thanks will certainly not simply be enough, for the fantastic clarity in your writing. I can at once grab your rss feed to stay privy of any updates. Genuine work and much success in your business endeavors!
there are bronze and brass dining chairs too that looks very elegant because of their color.
Hello, this is a seriouslyexcellent submit. In concept Id liketo jot down like this too – taking time and real work to make a brilliant article.!. but what can I say.!. I procrastinate alot and never seem to have anything done. Thank You
Pretty! This was a really wonderful post. Many thanks for providing this information.
This is a very good tip especially to those new to the blogosphere. Simple but very precise info… Thank you for sharing this one. A must read post!
Thank you for making the trustworthy attempt to speak about this. I believe very robust approximately it and wish to read more. If it’s OK, as you achieve extra in depth wisdom, might you thoughts including extra articles very similar to this one with more information? It will be extraordinarily helpful and helpful for me and my friends.
I became honored to receive a call from a friend as he observed the important tips shared in your site. Looking at your blog post is a real fantastic experience. Many thanks for taking into account readers much like me, and I wish you the best of achievements as a professional in this field. cuba resorts
Thank you for sharing superb informations. Your site is so cool. I am impressed by the details that you have on this site. It reveals how nicely you perceive this subject. Bookmarked this website page, will come back for more articles. You, my pal, ROCK! I found just the info I already searched everywhere and simply couldn’t come across. What a great web-site.
Greetings! Very useful advice within this article! It’s the little changes that make the most important changes. Thanks for sharing!
I believe other website owners should take this site as an example , very clean and wonderful user genial style .
I’d have to consult with you here. Which is not some thing I usually do! I enjoy reading an article which will make people feel. Also, many thanks for permitting me to comment!
Real wonderful information can be found on site .
Fantastic, beautiful weblog with great informational content. This is a really interesting and informative post.
Generally I don’t read article on blogs, but I wish to say that this write-up very forced me to try and do so! Your writing style has been amazed me. Thanks, quite nice post.
My wife and i got quite relieved that Louis could finish up his investigation with the precious recommendations he gained using your weblog. It is now and again perplexing to just find yourself giving for free instructions some people might have been selling. And we all already know we need the writer to be grateful to for this. The entire illustrations you’ve made, the straightforward website menu, the relationships you aid to instill – it is everything incredible, and it’s making our son and our family reason why this theme is excellent, which is exceedingly mandatory. Many thanks for all!
I was very pleased to uncover this web site. I wanted to thank you for your time just for this fantastic read!! I definitely savored every bit of it and I have you book-marked to see new information on your web site.
Great website you got here! Please keep updating, I will def read more. It’ll be in my bookmarks so better update!
This web site is usually a walk-through it really is the knowledge you desired about this and didn’t know who to inquire about. Glimpse here, and you’ll undoubtedly discover it.
The when I read a blog, I hope so it doesnt disappoint me approximately that one. I mean, Yes, it was my option to read, but When i thought youd have some thing interesting to state. All I hear is often a lot of whining about something you could fix if you ever werent too busy in search of attention.
Considering who Joe Greene offers data to, this a part of the UNATCO Handbook is particularly ironic.
Different main mineral merchandise produced in Tennessee embody sand, gravel, crushed stone, Portland cement, marble, sandstone, common clay, lime, and zinc.
Good day! I could have sworn I’ve visited this web site before but after looking at some of the articles I realized it’s new to me. Anyhow, I’m definitely delighted I came across it and I’ll be bookmarking it and checking back regularly.
Then again, the bath is one place you possibly can take pleasure in styles that depart from those utilized in the rest of the house.
*There is noticeably a bundle to know about this. I assume you made certain nice points in features also.
Good Post, I am a big believer in placing comments on weblogs to let the blog writers know that they’ve added something advantageous to the world wide web!
You are so cool! I don’t believe I’ve truly read anything like that before. So great to find someone with a few original thoughts on this issue. Seriously.. many thanks for starting this up. This web site is something that is needed on the web, someone with a little originality.
Bloghopping is really my forte and i like to visit blogs”
I like this website its a master peace ! Glad I noticed this on google .
Characters perform humanly impossible feats like gracefully sliding out of a car in movement or hitting an incoming rocket with a revolver.
You produced some decent points there. I looked on-line to the issue and discovered most individuals go in conjunction with together with your site.
You’re the best, I just ran across your weblog and wanted to say that I’ve truly enjoyed browsing your blog posts. I have subscribed to your feed and I hope you write again very soon!
It’s hard to come by educated people about this subject, however, you seem like you know what you’re talking about! Thanks
I discovered your blog site on google and test a few of your early posts. Continue to keep up the superb operate. I simply further up your RSS feed to my MSN Information Reader. Searching for ahead to studying extra from you afterward!? I am typically to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for new information.
Oh my goodness! Awesome article dude! Many thanks, However I am having difficulties with your RSS. I don’t know the reason why I can’t subscribe to it. Is there anybody else getting identical RSS problems? Anybody who knows the solution will you kindly respond? Thanx!
This is the perfect site for anybody who wants to understand this topic. You know so much its almost tough to argue with you (not that I actually would want to…HaHa). You certainly put a new spin on a topic that has been written about for years. Wonderful stuff, just wonderful.
It is not a quite common line, in all probability because White obtains good possibilities by taking part in 7.0-0 f5 8.d5, sacrificing a pawn to open up diagonals for his or her bishops.
Good info. Lucky me I came across your website by chance (stumbleupon). I have book marked it for later!
Spot on with this write-up, I actually believe that this site needs a lot more attention. I’ll probably be returning to read through more, thanks for the advice!
These bangles are utilized in odd numbers.
Having read this I believed it was very informative. I appreciate you taking the time and energy to put this informative article together. I once again find myself personally spending a significant amount of time both reading and leaving comments. But so what, it was still worth it!
Everything is very open with a clear description of the issues. It was really informative. Your site is useful. Thanks for sharing.
I am usually to blogging and i genuinely appreciate your posts. This content has really peaks my interest. I’m going to bookmark your site and maintain checking for first time info.
Hello. Cool article. There is an issue with your web site in internet explorer, and you might want to check this… The browser is the marketplace chief and a big section of people will omit your great writing because of this problem.
Job scope at significant scale lies for forensic science experts at crime laboratories rub by city, county or state governments. The other region exactly where an individual looking for a career in forensic science can secure job are Federal agencies including the Departments of Justice, Federal Bureau of Investigation, Secret Service, Drug Enforcement Administration, Bureau of Alcohol, Tobacco and Firearms, Postal Inspection Service and other crucial departments, private labs and university laboratories is also a location of work for Forensic Science technician.
Does anyone know of any treatments that actually works are haemorrhoids. I don’t want to go to the doctors I feel very embarrassed.
What is the best computer virus remover?. My computer is slow as hell and freezes on me. Most of the time, I have to restart my computer. I think I may have a virus on my computer. What is the best software to remove the viruses of my computer?.
I added this article to my favorites and plan to return to digest more soon. It’s easy to read and understand as well as intelligent. I truly enjoyed my first read through of this article.
It’s hard to come by well-informed people for this topic, but you sound like you know what you’re talking about! Thanks
You’ve made some really good points there. I looked on the net to learn more about the issue and found most individuals will go along with your views on this website.
I could not refrain from commenting. Well written!
The next time I read a blog, I hope that it won’t fail me as much as this particular one. I mean, I know it was my choice to read, nonetheless I genuinely believed you would have something useful to talk about. All I hear is a bunch of crying about something that you could fix if you weren’t too busy seeking attention.
I’m so happy to read this. This is the kind of manual that needs to be given and not the random misinformation that’s at the other blogs. Appreciate your sharing this best doc.
Some genuinely nice and utilitarian info on this site, as well I believe the style has got great features.
Hello, I do think your blog may be having internet browser compatibility problems. When I take a look at your blog in Safari, it looks fine however when opening in IE, it’s got some overlapping issues. I simply wanted to give you a quick heads up! Other than that, fantastic website.
Hello. Very nice site!! Man .. Excellent .. Amazing .. I’ll bookmark your site and take the feeds also…I am satisfied to locate numerous useful info right here within the article. Thanks for sharing…
You are so awesome! I do not believe I’ve read something like that before. So great to discover someone with a few unique thoughts on this issue. Really.. thanks for starting this up. This site is something that is needed on the internet, someone with a little originality.
I just added this site to my google reader, excellent stuff. Cannot get enough!
I couldn’t refrain from commenting. Very well written.
Vital wind injury began because the system entered Berks County, Pennsylvania, and continued by way of the Delaware Valley in direction of Ocean County, New Jersey.
Premature Ejaculation is the lack of ejaculatory control and it is the most common of all sexual problems in men. Since it is natural, you can use it freely without any risk of adverse effects.
I am curious to find out what blog platform you have been utilizing? I’m experiencing some small security issues with my latest website and I would like to find something more secure. Do you have any suggestions?
I’m impressed, I must say. Seldom do I encounter a blog that’s both educative and amusing, and without a doubt, you have hit the nail on the head. The issue is an issue that not enough men and women are speaking intelligently about. I’m very happy that I came across this during my hunt for something regarding this.
I absolutely love your website.. Great colors & theme. Did you build this web site yourself? Please reply back as I’m looking to create my own site and want to know where you got this from or exactly what the theme is named. Thank you.
Rabbinic Judaism developed throughout Late Antiquity, through the third to sixth centuries CE; the Masoretic Text of the Hebrew Bible and the Talmud had been compiled in this interval.
I blog frequently and I really thank you for your content. The article has truly peaked my interest. I’m going to take a note of your website and keep checking for new details about once a week. I subscribed to your Feed too.
On December 19, 1776, just per week previous to Washington’s covert crossing of the Delaware River, the morale of the Continental Military was lifted by the publication of The American Disaster, a pamphlet authored by Thomas Paine, the writer of Widespread Sense.
An interesting discussion is worth comment. I believe that you need to publish more on this topic, it might not be a taboo matter but typically people do not talk about these subjects. To the next! Many thanks!
Spot on with this write-up, I honestly believe this web site needs a great deal more attention. I’ll probably be back again to read more, thanks for the advice.
I really like it when folks get together and share ideas. Great site, keep it up.
Very good write-up. I absolutely love this site. Keep writing!
Holy Trinity St Andrews 1910 to 1914 Davis accomplished 4 home windows for this church in around 1912.
An outstanding share! I have just forwarded this onto a friend who has been conducting a little homework on this. And he actually bought me breakfast simply because I found it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending the time to discuss this subject here on your web page.
Very good post! We will be linking to this great content on our website. Keep up the great writing.
The film depicts the Sith loyalists as having constructed the final Order, a large fleet of Xyston-class Star Destroyers, on the behest of Darth Sidious.
I really love your website.. Pleasant colors & theme. Did you build this site yourself? Please reply back as I’m trying to create my very own website and would love to know where you got this from or just what the theme is named. Appreciate it.
Novel strategies, including containerless processing by aerodynamic levitation (cooling the melt whilst it floats on a gasoline stream) or splat quenching (urgent the melt between two metallic anvils or rollers), could also be used to increase the cooling price or to scale back crystal nucleation triggers.
Good blog you have got here.. It’s difficult to find excellent writing like yours these days. I seriously appreciate people like you! Take care!!
Excellent site you have here.. It’s hard to find high quality writing like yours these days. I honestly appreciate individuals like you! Take care!!
Trimethylamine N-oxide is an osmolyte found in molluscs, crustaceans, and all marine fishes and bony fishes.
Hello! I could have sworn I’ve visited this blog before but after going through a few of the posts I realized it’s new to me. Regardless, I’m definitely delighted I stumbled upon it and I’ll be bookmarking it and checking back often.
This is a topic that is close to my heart… Take care! Where are your contact details though?
Everyone loves it when people come together and share opinions. Great blog, stick with it!
Aw, this was an incredibly good post. Spending some time and actual effort to generate a good article… but what can I say… I hesitate a whole lot and don’t manage to get anything done.
After going over a handful of the articles on your site, I truly like your technique of writing a blog. I bookmarked it to my bookmark site list and will be checking back soon. Take a look at my website as well and let me know how you feel.
Your style is really unique compared to other people I have read stuff from. Many thanks for posting when you’ve got the opportunity, Guess I will just book mark this page.
Way cool! Some very valid points! I appreciate you writing this post and the rest of the site is really good.
Very good info. Lucky me I discovered your blog by accident (stumbleupon). I’ve book-marked it for later.
Everything is very open with a very clear explanation of the issues. It was definitely informative. Your site is extremely helpful. Thank you for sharing!
I need to to thank you for this great read!! I absolutely loved every little bit of it. I’ve got you saved as a favorite to check out new stuff you post…
Howdy! I simply want to offer you a big thumbs up for the great information you have right here on this post. I will be returning to your site for more soon.
Oh my goodness! Incredible article dude! Many thanks, However I am going through problems with your RSS. I don’t understand why I am unable to join it. Is there anyone else having identical RSS issues? Anybody who knows the solution can you kindly respond? Thanks!
Pretty! This was an incredibly wonderful post. Thank you for providing this info.
The very next time I read a blog, I hope that it won’t fail me just as much as this one. I mean, Yes, it was my choice to read through, however I truly thought you would have something helpful to talk about. All I hear is a bunch of moaning about something you can fix if you weren’t too busy looking for attention.
Good post. I learn something totally new and challenging on sites I stumbleupon every day. It will always be helpful to read through articles from other writers and use a little something from other web sites.
This page really has all the information and facts I needed about this subject and didn’t know who to ask.
I used to be able to find good info from your blog posts.
I love it when people come together and share views. Great blog, keep it up!
Good blog you’ve got here.. It’s difficult to find excellent writing like yours these days. I honestly appreciate individuals like you! Take care!!
You’re so interesting! I do not suppose I’ve read a single thing like that before. So nice to discover somebody with genuine thoughts on this subject matter. Seriously.. many thanks for starting this up. This website is one thing that’s needed on the web, someone with a little originality.
Your style is unique in comparison to other folks I have read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I will just book mark this web site.
Spot on with this write-up, I really believe this amazing site needs much more attention. I’ll probably be back again to read through more, thanks for the information!
Hello there! This article couldn’t be written much better! Looking at this post reminds me of my previous roommate! He constantly kept preaching about this. I am going to send this post to him. Fairly certain he’ll have a great read. Many thanks for sharing!
Hi there, I do believe your site may be having internet browser compatibility problems. When I look at your web site in Safari, it looks fine but when opening in I.E., it has some overlapping issues. I simply wanted to provide you with a quick heads up! Apart from that, fantastic site!
I absolutely love your blog.. Excellent colors & theme. Did you build this website yourself? Please reply back as I’m looking to create my very own blog and want to learn where you got this from or exactly what the theme is called. Appreciate it.
This is a topic which is close to my heart… Best wishes! Where can I find the contact details for questions?
Very good article. I absolutely love this site. Stick with it!
The next time I read a blog, Hopefully it doesn’t disappoint me just as much as this one. I mean, I know it was my choice to read through, nonetheless I actually thought you would probably have something helpful to talk about. All I hear is a bunch of moaning about something you could fix if you weren’t too busy seeking attention.
Hi, I do believe this is a great site. I stumbledupon it 😉 I will return once again since I book marked it. Money and freedom is the best way to change, may you be rich and continue to guide other people.
I could not refrain from commenting. Exceptionally well written!
You’re so cool! I do not think I have read through something like this before. So nice to find another person with some original thoughts on this subject. Really.. many thanks for starting this up. This site is one thing that’s needed on the web, someone with a bit of originality.
Oh my goodness! Impressive article dude! Thank you, However I am encountering issues with your RSS. I don’t know why I cannot join it. Is there anybody having the same RSS issues? Anyone that knows the solution can you kindly respond? Thanx!
Saved as a favorite, I really like your website!
That is a very good tip especially to those new to the blogosphere. Brief but very precise information… Thanks for sharing this one. A must read article!
Hello there! I just want to give you a huge thumbs up for your great info you have right here on this post. I’ll be coming back to your blog for more soon.
That is a very good tip particularly to those fresh to the blogosphere. Simple but very precise information… Many thanks for sharing this one. A must read post.
What your stating is absolutely true. I know that everybody should say the similar matter, but I just think that you set it in a way that absolutely everyone can realize. I also really like the photographs you set in the following. They match so effectively with what youre attempting to say. Im sure youll achieve so quite a few men and women with what youve received to say.
May I simply say what a comfort to discover somebody that genuinely understands what they’re discussing over the internet. You certainly understand how to bring an issue to light and make it important. More and more people ought to read this and understand this side of your story. I can’t believe you are not more popular because you certainly possess the gift.
This site definitely has all the information and facts I needed concerning this subject and didn’t know who to ask.
Good post. I learn something new and challenging on sites I stumbleupon on a daily basis. It’s always exciting to read articles from other writers and use something from other sites.
Hi there! I could have sworn I’ve been to this web site before but after going through many of the articles I realized it’s new to me. Nonetheless, I’m definitely happy I discovered it and I’ll be book-marking it and checking back regularly!
It’s hard to come by experienced people for this topic, however, you sound like you know what you’re talking about! Thanks
I blog frequently and I really appreciate your content. This great article has truly peaked my interest. I’m going to book mark your blog and keep checking for new information about once a week. I subscribed to your Feed as well.
Next time I read a blog, Hopefully it won’t disappoint me just as much as this one. I mean, Yes, it was my choice to read through, but I genuinely thought you’d have something useful to say. All I hear is a bunch of crying about something you could possibly fix if you weren’t too busy seeking attention.
Having read this I thought it was rather enlightening. I appreciate you finding the time and effort to put this short article together. I once again find myself personally spending a significant amount of time both reading and posting comments. But so what, it was still worth it!
Greetings! Very useful advice within this article! It is the little changes which will make the most important changes. Thanks a lot for sharing!
Pretty! This was an incredibly wonderful article. Many thanks for providing this information.
A fascinating discussion is worth comment. I do believe that you ought to write more on this subject matter, it may not be a taboo subject but typically folks don’t discuss these issues. To the next! Many thanks!
But are thing really going to last this good?
Next time I read a blog, Hopefully it doesn’t fail me just as much as this particular one. After all, I know it was my choice to read through, however I genuinely thought you’d have something helpful to say. All I hear is a bunch of complaining about something you could fix if you were not too busy looking for attention.
Hi! I could have sworn I’ve visited this web site before but after browsing through some of the articles I realized it’s new to me. Regardless, I’m definitely pleased I found it and I’ll be book-marking it and checking back regularly.
A swing trader typically buys and sells assets over a period of days or weeks, while a long term trader usually tries to profit from price movements that take place over months or even years.
The opposite concern would involve the cost of adjusting the assorted utility traces would even be involved, ballooning a $5.857 million challenge to round $7 million.
Very good blog post. I absolutely love this site. Stick with it!
In addition they present services in luxury planning administration.
I really like looking through a post that can make men and women think. Also, many thanks for allowing for me to comment.
Howson returned to Putney and resumed her work there, usually restoring medieval glass.
This is a topic that’s close to my heart… Best wishes! Where can I find the contact details for questions?
Hello there! I could have sworn I’ve been to this blog before but after browsing through many of the articles I realized it’s new to me. Nonetheless, I’m certainly happy I discovered it and I’ll be bookmarking it and checking back often!
Tax Preparation and Planning- Generally, various corporations conduct budgeting for taxable income and forecasting the same.
May I simply say what a relief to discover someone that actually understands what they are talking about over the internet. You actually know how to bring an issue to light and make it important. More and more people need to read this and understand this side of the story. It’s surprising you aren’t more popular since you definitely possess the gift.
Prices of production are established jointly by average input costs and by the ruling profit margins applying to outputs sold.
I blog quite often and I truly thank you for your information. This great article has really peaked my interest. I am going to book mark your blog and keep checking for new details about once per week. I subscribed to your RSS feed too.
To ascertain which designer is for you, collect references and conduct interviews.
I was able to find good information from your articles.
I quite like looking through a post that can make men and women think. Also, thank you for allowing for me to comment.
Aw, this was an incredibly good post. Taking a few minutes and actual effort to create a great article… but what can I say… I hesitate a lot and don’t seem to get anything done.
An impressive share! I’ve just forwarded this onto a co-worker who had been doing a little research on this. And he actually bought me breakfast simply because I found it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending some time to discuss this matter here on your blog.
very nice put up, i definitely love this website, keep on it
An outstanding share! I’ve just forwarded this onto a co-worker who was conducting a little homework on this. And he actually bought me dinner because I discovered it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending time to discuss this subject here on your blog.
An outstanding share! I’ve just forwarded this onto a friend who has been doing a little research on this. And he in fact ordered me dinner due to the fact that I stumbled upon it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanks for spending the time to talk about this issue here on your internet site.
Can I simply say what a relief to find someone that actually knows what they are discussing online. You actually realize how to bring an issue to light and make it important. A lot more people must look at this and understand this side of your story. It’s surprising you aren’t more popular since you surely have the gift.
Definitely believe that which you said. Your favorite justification appeared to be on the net the simplest thing to be aware of. I say to you, I certainly get annoyed while people consider worries that they plainly don’t know about. You managed to hit the nail upon the top and defined out the whole thing without having side-effects , people can take a signal. Will probably be back to get more. Thanks
After looking at a number of the articles on your web page, I honestly like your technique of blogging. I added it to my bookmark website list and will be checking back in the near future. Please visit my website as well and let me know your opinion.
great post, very informative. I’m wondering why the other specialists of this sector do not understand this. You should proceed your writing. I am sure, you’ve a great readers’ base already!
After looking into a number of the blog articles on your web site, I truly like your way of writing a blog. I book marked it to my bookmark website list and will be checking back soon. Please visit my website as well and let me know how you feel.
It’s difficult to find knowledgeable people for this topic, however, you could be seen as there’s more you are dealing with! Thanks
You have made some really good points there. I checked on the internet to learn more about the issue and found most people will go along with your views on this web site.
You made some decent points there. I looked on the net for your issue and located most individuals will go as well as with the internet site.
Its set worth indicates you understand exactly just how a lot you may get which implies you may strategy and organise your funds.
There is certainly a great deal to find out about this issue. I love all the points you have made.
That is a really good tip especially to those fresh to the blogosphere. Short but very precise information… Thanks for sharing this one. A must read article.
I truly wanted to jot down a word so as to thank you for some of the pleasant tricks you are giving out on this site. My rather long internet look up has at the end been recognized with brilliant suggestions to exchange with my friends and classmates. I would believe that many of us readers actually are unequivocally fortunate to be in a really good network with very many marvellous individuals with great suggestions. I feel really grateful to have encountered your entire web site and look forward to tons of more amazing times reading here. Thank you once more for a lot of things.
There is noticeably a lot of money to know about this. I assume you have made specific nice points in features also.
This is a topic that’s near to my heart… Cheers! Exactly where can I find the contact details for questions?
I determined it was more essential to get the gameplay beneath management than to get the game trying good.
Your style is very unique compared to other people I have read stuff from. Many thanks for posting when you’ve got the opportunity, Guess I will just book mark this web site.
Appreciate it for this post, I am a big big fan of this website would like to proceed updated.
Found your site within the yahoo bulk shirts warehouse directory, very nice job, thanks. Screen printing could further be used for those types of other substrates from plastic to metal. Despite the fact that tiny and complex details can be gathered, screen printing is preferably suitable for bold and graphic designs.
I simply wished to appreciate you again. I do not know the things I could possibly have taken care of in the absence of those aspects discussed by you concerning that area. Completely was the depressing condition in my position, but seeing a new specialized strategy you solved it made me to leap for delight. I’m grateful for the work and even hope that you recognize what a powerful job your are putting in teaching people today through a web site. Probably you’ve never got to know all of us.
An outstanding share! I have just forwarded this onto a coworker who has been doing a little homework on this. And he actually ordered me breakfast because I found it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending some time to talk about this subject here on your internet site.
Great info. Lucky me I ran across your website by accident (stumbleupon). I have saved it for later!
Great post! We will be linking to this particularly great content on our website. Keep up the good writing.
He is survived by his son, Faron Bostic of Powderly; daughter, Lisa Thompson of Montalba; four grandchildren; and a bunch of nieces and nephews.
Typically, the Ft Lauderdale tax lawyer presents taxation s effectively as auditing services as properly.
This is a very good tip particularly to those fresh to the blogosphere. Simple but very accurate information… Thank you for sharing this one. A must read post!
There’s definately a lot to learn about this issue. I like all of the points you’ve made.
Excellent article. I’m experiencing some of these issues as well..
A fascinating discussion is definitely worth comment. There’s no doubt that that you need to publish more on this topic, it may not be a taboo matter but usually people do not speak about such issues. To the next! All the best.
Hi there! This post could not be written much better! Looking through this post reminds me of my previous roommate! He continually kept preaching about this. I am going to forward this information to him. Pretty sure he’ll have a very good read. Many thanks for sharing!
After exploring a few of the blog posts on your site, I seriously like your way of writing a blog. I book marked it to my bookmark site list and will be checking back in the near future. Please visit my website as well and tell me what you think.
Aw, this was an exceptionally good post. Spending some time and actual effort to create a good article… but what can I say… I procrastinate a lot and don’t seem to get anything done.
You can even extra simply select which default search engine you would like to use with that built-in search field.
Good site you have here.. It’s hard to find quality writing like yours nowadays. I really appreciate individuals like you! Take care!!
Aw, this was an incredibly nice post. Finding the time and actual effort to make a good article… but what can I say… I hesitate a whole lot and don’t manage to get nearly anything done.
Many people get rich because of investing in stocks while some are unlucky and lose a fortune.
I absolutely love your site.. Excellent colors & theme. Did you develop this amazing site yourself? Please reply back as I’m hoping to create my very own site and would love to find out where you got this from or what the theme is called. Thanks!
Pretty! This was an incredibly wonderful article. Thank you for providing this information.
Spot on with this write-up, I really believe this website needs much more attention. I’ll probably be back again to read through more, thanks for the info!
Kawashima started in each match throughout the 2012-thirteen season till he was dropped from the squad for the next two matches following his poor efficiency in opposition to Club Brugge.
I’m impressed, I must say. Seldom do I come across a blog that’s both equally educative and amusing, and without a doubt, you’ve hit the nail on the head. The issue is something that not enough people are speaking intelligently about. Now i’m very happy I came across this during my search for something regarding this.
Hey, I loved your post! Visit my site: ANCHOR.
Commodore Free, 2011, challenge 51, p 37.
I’m excited to find this page. I need to to thank you for ones time for this particularly wonderful read!! I definitely savored every bit of it and I have you bookmarked to see new information in your site.
It exhibits solely income items.
Hi there, I think your web site may be having browser compatibility issues. When I take a look at your website in Safari, it looks fine however when opening in Internet Explorer, it’s got some overlapping issues. I just wanted to give you a quick heads up! Apart from that, wonderful blog.
That is a really good tip especially to those new to the blogosphere. Simple but very accurate info… Appreciate your sharing this one. A must read post!
Way cool! Some extremely valid points! I appreciate you penning this article and also the rest of the website is very good.
Oh my goodness! Amazing article dude! Thank you so much, However I am going through difficulties with your RSS. I don’t know why I am unable to subscribe to it. Is there anyone else getting similar RSS problems? Anyone that knows the answer will you kindly respond? Thanx!!
Great information. Lucky me I discovered your website by chance (stumbleupon). I have book-marked it for later!
After I originally commented I seem to have clicked on the -Notify me when new comments are added- checkbox and now each time a comment is added I recieve 4 emails with the same comment. There has to be an easy method you can remove me from that service? Thanks a lot.
It’s hard to come by educated people for this subject, however, you sound like you know what you’re talking about! Thanks
This would be in a scenario such as strategic land, where the JVP would convert raw UK land through all the required steps to establish build-ready plots for homes and commercial enterprises.
It’s nearly impossible to find knowledgeable people for this subject, but you seem like you know what you’re talking about! Thanks
Fiscal drag can also be a results of a hawkish stance in the direction of government funds.
Finally, the Physician returns to Earth in 2005 and discovers that another Time Lord, Marnal, has also survived the destruction of Gallifrey.
Greetings, There’s no doubt that your site might be having internet browser compatibility problems. Whenever I look at your website in Safari, it looks fine but when opening in Internet Explorer, it has some overlapping issues. I just wanted to provide you with a quick heads up! Besides that, excellent blog.
This page definitely has all of the information I needed about this subject and didn’t know who to ask.
Many indexes include stocks in companies that should perform well in bad economies such as discount retailers and entertainment firms.
I haven’t seen any indicators of anntennae, although.
The best treatment could be costly, and appropriate only for intensively used land.
Great article! We are linking to this particularly great content on our website. Keep up the good writing.
It’s hard to come by experienced people about this subject, however, you sound like you know what you’re talking about! Thanks
Excellent post. I am experiencing a few of these issues as well..
I like it when people get together and share ideas. Great site, keep it up!
We allow you to to search out the most effective and finances pleasant marriage ceremony decorator with just a click.
Civilians showed fear when encountering American servicemen, whom the island’s Japanese commander called “American devils.” Propaganda that civilians would be tortured and killed prevented many from leaving their caves.
Great post. I’m facing many of these issues as well..
Clearly, the hearth used approach again when was not the controllable supply of heat of at the moment’s torches, whose flame will be turned up or down, or positioned towards one area of the glass.
It’s round 4 years now since recession hits the world and makes powerful economies to go out of money.
Besides excessive complexity, hidden information and the affect of different human gamers are what makes it inconceivable for a human to completely resolve a game.
Fountain. To him, the six soldiers that had been additionally harm, although “not unhealthy enough to be despatched back,” are the true heroes.
The index can swing 50 to 60 points in one day.
Black-Litterman overcame this problem by not requiring the user to input estimates of expected return; instead it assumes that the initial expected returns are whatever is required so that the equilibrium asset allocation is equal to what we observe in the markets.
Open-ended funds let you redeem the amount and thus exit from the fund anytime.
I used to be able to find good information from your blog articles.
Repayment for PLUS loans starts after only 60 days, however you don’t should pay your Stafford Loans whereas you are enrolled no less than half-time.
Everything is very open with a very clear explanation of the issues. It was truly informative. Your site is very helpful. Many thanks for sharing!
To get started, simply click on the “enroll” link at the highest of the positioning’s home web page.
Friday before 7 am and after 11 pm.
People can promote certain characteristics by either breeding pairs of dogs that share the desired qualities or by allowing dogs to breed randomly but culling puppies from the litter that do not possess those characteristics.
Collectively, the process of conducting the appraisal, reporting the FV of the assets and liabilities, the allocation of the net identifiable assets from the old balance sheet price to the FV, and the determination of the goodwill in the transaction, is referred to as the PPA process.
A change within the yield.
I don’t know why, however searching for a word and developing empty, then wanting it up shortly thereafter and writing it down appears to burn it into the brain extra successfully than some other means I’ve discovered.
All that is left is to send your cryptocurrency (Ether/Bitcoin) to the specified ICO address to receive the new tokens.
I’m specializing in benefits to individuals who use networks-reasonably than advantages to, as an example, protocol fame-because first- and second-order results on humans are my factor.
The solutions are completely primarily based in want evaluation, particularly designed to satisfy the expansion requirements of the traders in a holistic method.
For the sweet slightly than savory sorts out there, you may as well find “dulce” molletes, but up to now McDonald’s hasn’t added them to its menu in Mexico or elsewhere.
By September 2011, the total of lending by the Fed had come to $10 trillion (or standardised to 1-month loans, $4.45 trillion), over half of which had gone to the ECB: all loans were repaid in full, and profits made by the Fed on swap repayments in 2008-9 alone came to c.
Spot on with this write-up, I really think this amazing site needs far more attention. I’ll probably be returning to read more, thanks for the information!
Great web site you have got here.. It’s hard to find excellent writing like yours these days. I honestly appreciate individuals like you! Take care!!
This page really has all the information I wanted concerning this subject and didn’t know who to ask.
One is in a gown of blue with a Greek key design operating its length; the opposite holds an object in her palms dressed in a lovely costume of floral design with caramel-colored strips, with white lace cuffs and gloves.
Seigniorage-style coins, also known as algorithmic stablecoins, utilize algorithms to control the stablecoin’s money supply, similar to a central bank’s approach to printing and destroying currency.
Darth Andeddu – Historical Dark Lord of the Sith mentioned within the Rise of Skywalker: The Visible Dictionary, as the namesake of the fifth Legion of Sith Troopers from Darth Sidious’ Sith Eternal cult.
Mutual fund taxation also relies on the holding period of your funding i.e for how lengthy you had invested within the fund earlier than selling it off.
Muriel Alice Birch, Senior Personal Secretary, Ministry of Public Constructing and Works.
There’s nothing extra atractive than someone who can communicate a language and understand a tradition.
Through the opening press convention, Anand revealed his new seconds to be Krishnan Sasikiran, Sandipan Chanda and Peter Leko.
This supplied much more subtle and delicate shades, and progressively moved the artwork of stained glass closer and nearer to that of painting.
In 1991, he was in a position to raise $3.6 million from his former DLJ colleagues and started York Capital.
Revolutionary Finance ISA: These accounts comprise peer-to-peer loans that may be given to parties seeking financing.
However, if you are shopping for a loan, make sure multiple inquiries occur within a few weeks, so that they can count as one inquiry on your score.
The glass floats on the tin, and ranges out because it spreads along the bath, giving a easy face to each sides.
Occasions can also be organized to simply present appreciation to the client and convey thanks to them with a VIP event expertise.
Right here is the right blog for everyone who hopes to find out about this topic. You realize so much its almost hard to argue with you (not that I really would want to…HaHa). You certainly put a new spin on a subject that has been discussed for years. Great stuff, just wonderful.
Each exchange has its own clearinghouses.
The only thing Wall Street likes lower than a poor earnings report is an investigation by the U.S.
Add a touch of sophistication to your jewelry collection with the Classic Bezel Pendant that includes a gorgeous 1.10-carat cushion blue sapphire.
Your style is unique in comparison to other folks I have read stuff from. Thanks for posting when you have the opportunity, Guess I will just book mark this blog.
It won’t be the long, wavy, typical hair, however I’m actually excited to do one thing completely different.
Hi there, I do think your website might be having browser compatibility issues. Whenever I look at your blog in Safari, it looks fine however when opening in IE, it has some overlapping issues. I just wanted to give you a quick heads up! Apart from that, great website!
Can technological advancements reduce the impact of natural disasters in more vulnerable regions?
It’s the same issues that the pc Joshua learns in “Conflict Games:” The one solution to win in nuclear conflict is not to play.
On a scale of 1-10, how organized are you?
In 2001, Higgs’ debut album, Tarboro Blues, was made in collaboration with the Music Maker Relief Basis.
As industry continues to develop and the world’s supply of non-renewable resources slowly grows rarer and dearer, green building becomes greater than an environmentally friendly choice: It becomes a crucial step in how we stay our lives.
The truth that the black queen should be on a1 slightly than a2 when White performs Nxb3 explains why 2.h4?
So while you get beneath the hood to verify issues out, you are not just searching for leaks.
May I simply just say what a relief to uncover someone that truly knows what they are talking about on the web. You actually realize how to bring an issue to light and make it important. A lot more people really need to look at this and understand this side of your story. I was surprised you are not more popular because you surely have the gift.
It is based on an XRP ledger distributed database.
Whoever can go the tests and needs to serve needs to be part of our massive military.
Mutual funds in India now offer a wide range of schemes to choose.
After I initially commented I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I receive four emails with the exact same comment. Perhaps there is a way you are able to remove me from that service? Cheers.
Test your abilities on a sturdy Forex Demo platform and put your career on the right track!
For Debt Funds, short term capital gains are taxed as per the slab rates applicable to you.
Hi there, I believe your site may be having browser compatibility issues. When I look at your site in Safari, it looks fine however, when opening in Internet Explorer, it’s got some overlapping issues. I just wanted to give you a quick heads up! Other than that, fantastic blog!
Chew was raised in a Quaker household, however he broke with Quaker tradition in 1741, when he agreed along with his father, who had instructed a grand jury in New Castle, Delaware on the lawfulness of resistance to an armed force.
The 2012 SBS Gayo Daejeon was aired stay from Korea College on 29 December.
Tactic 1 – Craft your marketing messages around your value proposition.
CFDs give investors with all the advantages and risks of holding a security without actually owning it.
With the elimination of unregulated costs and the suite of free features that are included with these plans, it may be fairly a savings.
He was a retired Farmer and oil discipline worker and was married to Julia A. PINKSTON in 1915.
S. capital. The District of Columbia allows residents of any U.S.
There are additionally addon video libraries, corresponding to a language pack that features video clips in greater than 30 languages.
However, the expected yield of being in the market is higher for several reasons.
Aithent, an originator of high-worth techniques for the details and administration necessities of government, funding, insurance and health care organizations, gives case management answer, enterprise danger management for monetary crime inquiries.
Ching-hsia Lin is an actress; she was in “The Bride With White Hair” talked about above.
1) There are many agencies who provide money transfer service for e.g.
Ignoring the actual fact it’s a must to be mad nowadays to want to be a farmer particularly with no prior experience or data.
Following White’s plan, the latter firm improved down river navigation on the Lehigh River, using his Bear Trap Locks design to deliver over 365 tons of anthracite to Philadelphia docks by December 1820, 4 years ahead of guarantees to Stockholders.
5 every year. There are frequent words you’ll encounter in the inventory market, terminologies you don’t normally utter in your every day routines.
The paradox of reconciling endless private ambition with the interests of the Sith as a whole became an awesome practical and philosophical concern for the Sith.
On prime of the Paleozoic rock is Mesozoic Moenkopi Formation, from 248 to sixty five million years in the past.
Another neat characteristic in Accessibility Options is the flexibility to turn on a beeper that beeps whenever you press the Caps Lock key — great if you are the sort of one that hits it by accident!
All you need to predict is that the stock price will either rise or fall very sharply in the course of the day.
These are often the most effective route for individuals who do not tow usually since you’ll be able to remove them when you aren’t hauling.
As of January 2021, Pennsylvania ranks “second-to-final among the many states in vaccine administration,” a condition which has prompted state Republicans to criticize Democratic Governor Tom Wolf’s management of the scenario.
In an interview with the Russian newspaper “Kommersant”, dated 29 July 2011, Boris Gelfand expressed his concern in regards to the provide made by Chennai.
Landlords generally get a foul rap.
For legislation-enforcement businesses and fanatics, Ford provided a 330-horsepower mill that reached its peak at 5,000 rpm.
Neither the government nor the taxpayers, it is again the poor farmers (Specially, Rural Farmers in Bihar and such other areas).
Revolving Mortgage Fund. A statewide RLF that syndicates with, and provides technical help to, local RLFs inventure debt.
The Arts and Crafts design of this home options the patterns of nature in its woodwork and stone features, and in the colors used within the decorating scheme.
Earlier than he rose to fame as an auto racer, Carroll Shelby was a hen farmer.
Mayer’s mother and father died when she was in her early teenagers and her uncle, a authorized guardian after the passing of her parents, died only a few years later.
I was able to find good info from your articles.
Although all producers will face the same selling price, they will not all face the same cost pressures and hence, though we may expect share prices to move with the underlying commodity prices, the correlation will not be perfect.
Actually, retsina likely came about when the resin used to seal wine containers flavored the wine as it aged.
At present not only the businesses but additionally the individuals take help from the professionals.
Nice post. I learn something new and challenging on blogs I stumbleupon everyday. It will always be useful to read through content from other authors and use something from other websites.
Flagstaff’s summer season will obtain a few days of daytime temperatures above ninety °F (32 °C), with a lot cooler nighttime temperatures usually in the region of 40 °F (four °C).
This might entail taking out adverts in the media or sending recruiters to target teams.
The youthful the person was when he acquired his insurance policy, the better and higher degree of inflation safety he would get.
So Dogecoin and digital currencies similar to Bitcoin have value solely insofar as people give them value, unless they’re backed by a selected asset or cashflow stream.
These embrace Père Noël in France, St.
Watkins, Walter Kendall. “Massachusetts within the Expedition Beneath Admiral Vernon in 1740-41 to the West Indies”, Society of Colonial Wars, Yr-E-book for 1899 (Boston: 1899) pp.
Everything is very open with a really clear clarification of the challenges. It was truly informative. Your site is very helpful. Many thanks for sharing!
The DeLorean DMC-12 is notable for being the only model that the DeLorean Motor Company ever produced during its short and unstable history.
This was a great read! Your insights are truly helpful and make complex topics easy to understand. Looking forward to more!
Everyone loves it when people get together and share ideas. Great site, stick with it.
You need to take part in a contest for one of the finest blogs on the internet. I’m going to highly recommend this site!
This is a topic which is near to my heart… Thank you! Where can I find the contact details for questions?
He will build your confidence and ensure you become a safe driver.
Improve your personal and professional growth by
joining our focused ADI training courses and events.
I blog frequently and I genuinely thank you for your information. Your article has really peaked my interest. I will take a note of your blog and keep checking for new information about once per week. I subscribed to your Feed too.
Very good article. I am going through many of these issues as well..
LTrent Driving School has served many families through multiple generations to
ensure that they are equipped to survive on the road.
There’s certainly a lot to learn about this issue. I like all of the points you’ve made.
I blog quite often and I genuinely thank you for your content. The article has truly peaked my interest. I will take a note of your blog and keep checking for new information about once per week. I opted in for your Feed too.
However the choices are bought as a bulk of one hundred stocks, so the ultimate strike worth might be for one hundred stocks and 100 occasions the price written within the contract.
Being prepared to share and hear, while making a protected house for others to do the same, are essential in building robust connections.
Male king cobras impress rivals primarily by way of a display of energy and dominance in what is named “combat dance.” This habits is most commonly noticed during the mating season when males vie for the attention of a receptive feminine.
All surgeries carry the chance of anesthetic mishaps and extreme bleeding.
Equity funds are an important aspect of investment portfolio of investors seeking long term benefits and high returns.
One mistaken step by the asset or wealth supervisor could make all of it go away.
At the identical time strikes to create a money market in Dublin and the transfer in 1968 of the commercial banks’ Pound Sterling property to the Central Financial institution made it doable to contemplate a break within the hyperlink.
This was a great read! Your insights are truly helpful and make complex topics easy to understand. Looking forward to more!
Fortuitously, there is one in Poland that fits the outline perfectly – Warsaw, Cracow or perhaps Tricity?
Mark 9:23 Jesus stated unto him, If thou canst imagine, all issues are possible to him that believeth.
I really like reading a post that can make people think. Also, thanks for allowing for me to comment.
Watch our most viewed super sexy bf video on socksnews.in. sexy bf video Watch now.
Nonetheless, the cable creates an unreasonable amount of tension on the entrance of the sanding pad.
Hi, I believe your web site may be having browser compatibility issues. Whenever I take a look at your site in Safari, it looks fine however, when opening in Internet Explorer, it has some overlapping issues. I simply wanted to provide you with a quick heads up! Apart from that, great blog.
Later, you discover out that Shannon is the one who has been stealing provides in the first place.
There are many competitions in the business and plenty of certified candidates to be chosen from.
This growing acceptance of depression as a respectable medical problem might encourage extra folks to seek remedy for it, thus causing a statistical increase.
Whereas some of us will solely need part-time assist at home to organize meals and clear bathrooms, others will spend months or years in assisted living or a nursing facility.
And you鈥檒l have the security of knowing that your estate, savings and insurance funds can all go toward their intended purpose: providing for those you love most.
Although Chicago has seen small decreases in foreclosure, these are nearly always followed by increases which further reduce consumer confidence.
Bovard, James (March 1998).
The Miami personal harm attorneys of Hickey Legislation Firm struggle for you.
At GemAstro, one can easily discover an enormous catalogue of 100 pure, untreated Persian turquoise on the market at finest costs.
James Dhlamini, Hospital Dispenser, Mbabane Hospital, Swaziland.
This is a very good tip particularly to those fresh to the blogosphere. Brief but very precise information… Thank you for sharing this one. A must read article.
Well-written and insightful! Your points are spot on, and I found the information very useful. Keep up the great work!
This post is very helpful! I appreciate the effort you put into making it clear and easy to understand. Thanks for sharing!
You ought to take part in a contest for one of the finest websites on the web. I will highly recommend this site!
Great post. I’m facing a few of these issues as well..
Greetings! Very helpful advice in this particular article! It’s the little changes that produce the most significant changes. Many thanks for sharing!
This web site truly has all the information I needed about this subject and didn’t know who to ask.
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
Awesome insights!
This blog was… how do I say it? Relevant!! Finally I have found something that helped me. Thanks a lot.
Pretty! This has been a really wonderful article. Thank you for providing this information.
I appreciate the depth of research in this article. It’s both informative and engaging. Keep up the great work!
I appreciate the depth of research in this article. It’s both informative and engaging. Keep up the great work!
Spot on with this write-up, I actually feel this website needs much more attention. I’ll probably be returning to see more, thanks for the info!
Hello there, I believe your website may be having browser compatibility issues. Whenever I look at your website in Safari, it looks fine however when opening in I.E., it’s got some overlapping issues. I simply wanted to give you a quick heads up! Aside from that, great blog.
Like everyone else, docs choose their multifunction smartphones they usually don’t need to hold a number of devices.
There’s definately a lot to know about this issue. I like all the points you made.
Howdy! I could have sworn I’ve visited your blog before but after going through many of the posts I realized it’s new to me. Anyways, I’m definitely delighted I found it and I’ll be bookmarking it and checking back frequently.
Greetings! Very helpful advice in this particular article! It’s the little changes that will make the biggest changes. Many thanks for sharing!
Nice article, have a look at my site “https://www.issuewire.com/sushi-swap-the-best-crypto-platform-in-2025-1823683727364009”
nice article, have a look at my
nice article ave a look at my site “https://www.newsbreak.com/crypto-space-hub-313321940/3799652652916-top-crypto-investments-in-2025-bitcoin-ai-projects-tokenized-assets”
https://spookyswap-6.gitbook.io/en-us/
Hi! I simply want to offer you a huge thumbs up for your great info you’ve got right here on this post. I am coming back to your blog for more soon.
nice blog, visit my site
You seem to be very professional in the way you write.,**”‘
This is the kind of content I love reading.
With his most intense performances Cruise can subvert his charm into something more sinister and intense.
Woofi Finance helped me manage my budget!
Perhaps you should also a put a forum site on your blog to increase reader interaction.~.-.;
I can’t believe how smooth everything is on spooky swap! 5 stars!
The team behind spooky swap is solid and reliable.
Since 1996, over 300 employers have acquired the liberty Award.
2001). The 2001-2002 Official PFA Footballers Factfile.
Even with a shaken economy in addition to points, the rush to the present nation has by no means been lowering.
This is a topic which is near to my heart… Best wishes! Exactly where can I find the contact details for questions?
Nonetheless hungry for extra information about bridges and how they work?
Simple spreads might be arrange to ensure some profit no matter which method the market strikes after you enter.
The chief drawback of a 401(ok) mortgage is that the money you borrow could’ve been accruing curiosity for those five years.
Listed here are a few of essentially the most compelling arguments for continuing the exploration of house.
A good hand laster might full about 50 pairs of shoes a day.
Spot on with this write-up, I truly believe that this site needs far more attention. I’ll probably be returning to read through more, thanks for the info!
You’ll be able to search the database by worker identify, company title or the state the place you worked.
Usually, although, you can relieve that persistent cough with simple residence cures that will soothe your throat and aid you breathe simpler.
I must thank you for the efforts you’ve put in penning this blog. I’m hoping to view the same high-grade content by you in the future as well. In truth, your creative writing abilities has motivated me to get my own, personal website now 😉
They signal to police which home has been broken into.
Discover Woofi Finance, the most trusted decentralized exchange for 2025, offering low fees, secure transactions, and seamless crypto swaps. Whether you’re staking or trading, Woofi Finance is the top platform for DeFi users worldwide
A pure play on Silver means entering the high risks futures market products that are backed with the physical metal.
Nice post. I learn something totally new and challenging on blogs I stumbleupon on a daily basis. It will always be interesting to read content from other writers and use a little something from their websites.
Discover the power of MinSwap, the leading decentralized exchange platform offering seamless trading and low fees. Maximize your assets and join the next generation of decentralized finance
Discover CowSwap, the trusted decentralized exchange platform for seamless crypto trades in 2025. With low fees, high security, and fast transactions, CowSwap is a go-to solution for DeFi users worldwide
Discover the future of decentralized finance with Woofi Finance, a cutting-edge platform for seamless crypto staking and yield farming. Maximize your returns with low fees and high rewards. Join the revolution in DeFi today!
Discover CowSwap, the trusted decentralized exchange platform for seamless crypto trades in 2025. With low fees, high security, and fast transactions, CowSwap is a go-to solution for DeFi users worldwide
I like reading a post that will make people think. Also, many thanks for permitting me to comment.
In the Guide, “Principally harmless” is the revised entry used to describe Earth.
After all, it additionally issues what the sunshine will shine on after getting it in the room.
Fishing Boats for Sale
Touring app with GPS feature is the very best strategy to drive nice site visitors in your travel business.
To look at the movie you needed to get out an enormous, clunky and temperamental projector, plus a display screen.
Good information. Lucky me I recently found your website by chance (stumbleupon). I have saved as a favorite for later!
For that motive, search round for locations that might gather water, similar to plants, the drip plate under your refrigerator, or condensation around leaky water pipes.
I seriously love your site.. Great colors & theme. Did you make this website yourself? Please reply back as I’m attempting to create my very own blog and want to learn where you got this from or what the theme is named. Thanks!
As you become a part of the company, you can also enjoy the benefits and profits gained by the company as an investor.
You’ve made some decent points there. I checked on the internet to learn more about the issue and found most people will go along with your views on this web site.
Move assets seamlessly between blockchains with Stargate Bridge. Fast, secure, and cost-effective!
Try the best blockchain bridge in 2025 – Stargate Bridge offers seamless cross-chain transfers with low fees.
Greetings! Very helpful advice in this particular article! It is the little changes that make the biggest changes. Thanks a lot for sharing!
After I originally commented I seem to have clicked on the -Notify me when new comments are added- checkbox and from now on every time a comment is added I recieve four emails with the exact same comment. There has to be a way you are able to remove me from that service? Thanks a lot.
Oh my goodness! Incredible article dude! Thank you, However I am experiencing troubles with your RSS. I don’t understand the reason why I can’t join it. Is there anyone else getting identical RSS issues? Anyone who knows the solution will you kindly respond? Thanx.
I simply wanted to appreciate you again. I’m not certain the things that I might have sorted out without these tips revealed by you relating to such subject. It absolutely was a distressing situation in my circumstances, however , coming across the well-written tactic you handled that took me to leap for fulfillment. Now i’m thankful for your information as well as trust you recognize what a great job you are undertaking instructing the mediocre ones via your websites. More than likely you haven’t encountered any of us.
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
The guidelines you provided here i will discuss extremely precious. It been found such a pleasurable surprise to possess that anticipating me while i wakened today. There’re constantly to the issue as well as simple to understand. Thanks a large amount for the valuable ideas you’ve got shared here.
Manta Bridge
After study a number of the blog articles on the internet site now, we really appreciate your method of blogging. I bookmarked it to my bookmark web site list and are checking back soon. Pls have a look at my web page in addition and figure out what you believe.
Looking for a trust-focused cross-chain solution in 2025? Check out Stargate Bridge. It is the future of seamless interoperability!
Awesome! I thank you your blog post to this matter. It has been useful. my blog: diets that work
Howdy! I just would like to offer you a big thumbs up for the great information you have here on this post. I will be coming back to your blog for more soon.
You ought to take part in a contest for one of the finest websites on the net. I’m going to highly recommend this site!
This is a topic which is close to my heart… Take care! Exactly where can I find the contact details for questions?
It’s perfect time to make some plans for the future and it is time to be happy. I’ve read this post and if I could I desire to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I wish to read even more things about it!
To get a proper understanding of exchange rates comparison, you should take the providers of a best forex vendor.
Bloghopping is really my forte and i like to visit blogs”
You made some tight points there. I looked on the net for the issue and found most individuals can approve along with your blog.
Very good post. I am facing many of these issues as well..
mitolyn
Finnerty, John (June 8, 2020).
Good information. Lucky me I recently found your site by accident (stumbleupon). I have saved as a favorite for later.
Aw, this was a really good post. Finding the time and actual effort to generate a really good article… but what can I say… I hesitate a whole lot and don’t seem to get nearly anything done.
Hi there, I simply hopped over in your website by way of StumbleUpon. Now not one thing I’d typically learn, but I favored your emotions none the less. Thank you for making something worth reading.
Over and over again I think about these issue. As a matter of fact it was not even yesterday that I last thought about it. To be honest, what is your thought though?
Great article, thanks. I signed up to your blog rss feed.
May I simply just say what a comfort to discover a person that really knows what they are talking about on the net. You definitely realize how to bring a problem to light and make it important. More people ought to look at this and understand this side of the story. I was surprised you aren’t more popular given that you definitely possess the gift.
Nice post. I learn something new and challenging on sites I stumbleupon on a daily basis. It’s always useful to read articles from other authors and use something from other websites.
Hi there just wanted to give you a brief heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different browsers and both show the same outcome.
The next time I read a blog, I hope that it does not fail me just as much as this one. After all, I know it was my choice to read through, nonetheless I genuinely thought you would have something interesting to say. All I hear is a bunch of crying about something that you can fix if you were not too busy searching for attention.
Oh my goodness! a wonderful article dude. Appreciate it Nonetheless We’re experiencing problem with ur rss . Do not know why Not able to sign up for it. Can there be any person obtaining identical rss dilemma? Anyone who knows kindly respond. Thnkx
Great post, you have pointed out some good details , I too conceive this s a very wonderful website.
Fantom’s #1 choice for swapping, Spooky Swap
you are truly a good webmaster. The web site loading speed is amazing. It seems that you’re doing any unique trick. Moreover, The contents are masterwork. you’ve performed a excellent task in this topic!
This web site definitely has all the info I wanted concerning this subject and didn’t know who to ask.
I’m very happy to read this. This is the kind of details that needs to be given and not the random misinformation that’s at the other blogs. Appreciate your sharing this best doc.
It’s easy to feel more confident and horny when you’re wearing seductively horny lingerie.
An impressive share, I given this onto a colleague who was simply performing a small analysis during this. And hubby in truth bought me breakfast simply because I discovered it for him.. smile. So let me reword that: Thnx for that treat! But yeah Thnkx for spending time go over this, I find myself strongly about this and really like reading regarding this topic. If possible, as you grow expertise, does one mind updating your blog post with a lot more details? It is actually extremely useful for me. Massive thumb up due to this writing!
Oh my goodness! Impressive article dude! Thanks, However I am experiencing difficulties with your RSS. I don’t know why I can’t join it. Is there anybody else having the same RSS problems? Anyone that knows the answer can you kindly respond? Thanx.
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
This is certainly my initial stop by and I really like what I’m seeing. Your weblog is so much fun to look over, quite compelling as well as informative. I’ll undoubtedly recommend it to my friends. Nevertheless, I did have some problem with the commenting. It kept giving me an problem whenever I clicked on publish comment. I hope, that can be fixed. Many thanks
I will immediately grasp your rss feed as I can’t to find your email subscription link or e-newsletter service. Do you’ve any? Please let me recognize so that I may just subscribe. Thanks.
The both of us really enjoyed your post. It appears like you’ve put a lot of effort into your story and the human race need much more of these on the Net these days. I do not real have a large deal to say in retort, I just wanted to comment to tell well done. marvelous post. i never thought of that.
Youre so cool! I dont suppose Ive read anything similar to this just before. So nice to discover somebody by incorporating original thoughts on this subject. realy we appreciate you beginning this up. this web site are some things that is required on the internet, somebody with a little originality. valuable work for bringing something totally new to your net!
You see, this attitude bugs me so much, and I haven’t even criticized some of the weird stuff they present us in this movie.
Yay google is my world beater aided me to find this outstanding web site ! .
A topic close to my heart many thanks, i have been thinking about about this subject for some time.
Can I simply say exactly what a relief to discover somebody who truly knows what theyre speaking about over the internet. You definitely learn how to bring a difficulty to light and work out it critical. The diet should see this and can see this side of your story. I cant believe youre less well-liked since you absolutely provide the gift.
You could definitely see your expertise within the paintings you write. The arena hopes for even more passionate writers like you who aren’t afraid to mention how they believe. All the time go after your heart.
What?s Going down i’m new to this, I stumbled upon this I have found It absolutely useful and it has aided me out loads. I hope to give a contribution & help different customers like its aided me. Great job.
Nice post. I find out something very complicated on various blogs everyday. Most commonly it is stimulating you just read content using their company writers and rehearse something from their website. I’d choose to use some with the content on my small weblog no matter whether you do not mind. Natually I’ll give you a link on the internet blog. Many thanks sharing.
I always visit new blog everyday and i found your blog.;`~”`
Excellent web site. Lots of helpful info here. I am sending it to several buddies ans additionally sharing in delicious. And of course, thank you in your sweat!
it is always a good idea to get event planners when you want a good outcome for your planned event`
I appreciate, cause I found exactly what I was looking for. You’ve ended my four day long hunt! God Bless you man. Have a nice day. Bye
I couldn’t refrain from commenting. Very well written!
saving your marriage should always be a priority whenever things turn sour on a marriage..
Many thanks for sharing this fine post. Very inspiring! (as always, btw)
I like this blog very much so much fantastic information.
Your style is so unique in comparison to other people I’ve read stuff from. Thank you for posting when you’ve got the opportunity, Guess I will just book mark this blog.
Great info – Gulvafslibning | Kurt Gulvmand I’m inquisitive to discover what blog platform you’re utilizing? We are experiencing some minor safety issues with my latest blog thus I’d wish to discover something a lot more risk-free. Are there some suggestions! Take care Online Website Builder
An intriguing discussion may be valued at comment. There’s no doubt that that you ought to write much more about this topic, it will not be described as a taboo subject but usually folks are too little to chat on such topics. To a higher. Cheers
oh well, American Dad is a nice tv series. my sixteen year old daughter just loves watching it”
Mar 7-8, 2025. McKinney, TX.
This is good-looking appealing , i was searching for somewhat but found your site as a substitute through Google . I be in love with networking. Anyways, really wanted in the direction of drop through and say hello . i have subscribed in the direction of your site plus i am hunting onward in the direction of the updates , Gratitude…
Appreciate your sharing the right to debate this valuable, I feel solidly in it and then really like browsing more about the idea idea. Whenever prospects, while achieve competency, will you beliefs adding your internet page because of furthermore help and advice? This is very for all of us.
I hope it’s a superb pleasure to visit your web log again to look at come once again with this kids from school
I really enjoyed reading this! Your writing style is engaging, and the content is valuable. Excited to see more from you!
I am typically to blogging and i actually appreciate your content regularly. This content has really peaks my interest. Let me bookmark your web site and maintain checking achievable data.
What is your most noted accomplishment. They may want good listeners rather than good talkers.
There is noticeably a bundle to understand about this. I assume you made specific nice points in functions also.
Kramnik was to take Topalov’s place in the world Chess Championship 2007 if he received the match, which he did.
Once you begin, you may extra easily choose your shoppers and say no at any time when it makes sense to help your team, and your mission move ahead.
He helps Ming Tian gaining his dwelling back after his Grandfather took it away together with Ming Tian’s jobs even uncovering the insurance fraud by Ji Gang’s spouse when his Grandfather paid her off to make Ming Tian’s father look bad to assist separate him.
If that doesn’t persuade you, consider that pigeons also carry parasites, which could also be transmitted to humans by means of contact with their droppings.
Next time I read a blog, I hope that it doesn’t fail me as much as this particular one. I mean, I know it was my choice to read, but I really believed you would probably have something useful to say. All I hear is a bunch of crying about something that you could possibly fix if you were not too busy searching for attention.
The Internet has added an interesting new wrinkle to the world of new business financing.
Do you’re feeling like you spend most of your time quite properly?
Exposed overhead beams don’t have to be real supporting members; get the look with right now’s decorative, lightweight fiberglass beams.
Great blog you’ve got here.. It’s difficult to find excellent writing like yours nowadays. I truly appreciate people like you! Take care!!
Though some sort of taxation repayment may well appear to be safe, it really is not.
I really like checking in daily to talk to your musings. I had your page bookmarked on my must read list!
Woah this is just an insane amount of information, must of taken ages to compile so cheers so much for just sharing it with all of us.
Particularly water, however we’ll get to that quickly sufficient.
While it has been many years since my first 12 months of marriage, I remember trying so onerous to avoid wasting money on meals that every one I cooked was spaghetti – it did not assist that it was additionally my favourite meals and the one factor I knew how one can cook.
This is a topic that’s near to my heart… Take care! Exactly where are your contact details though?
I’m amazed, I must say. Seldom do I come across a blog that’s both equally educative and engaging, and without a doubt, you have hit the nail on the head. The issue is something that too few men and women are speaking intelligently about. I am very happy that I found this in my hunt for something regarding this.
This is really fascinating, You’re a very professional blogger. I have joined your rss feed and stay up for in quest of more of your great post. Also, I have shared your site in my social networks!
Many thanks for creating the effort to discuss this, I feel strongly about this and love learning a great deal more on this subject. If possible, as you gain expertise, would you mind updating your website with a great deal more info? It’s really useful for me.
Only a few blogger would discuss this topic the way you do.;**.*
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
You really make it seem so easy with your presentation but I find this matter to be actually something that I think I would never understand. It seems too complex and extremely broad for me. I’m looking forward for your next post, I will try to get the hang of it! xrumer
we should always be very careful about getting hepatitis because this disease is very very dangerous and deadly~
hello!,I love your writing very much! proportion we keep in touch extra about your post on AOL? I need an expert in this space to solve my problem. Maybe that’s you! Taking a look ahead to peer you.
Firoza from Iran is thought to be the best quality stone.
Michael Frank Cherry, Principal Methods Engineer, Searching Communication Technology Ltd.
Substantially, the article is in reality the freshest on that noteworthy topic. I concur with your conclusions and definitely will eagerly look forward to your forthcoming updates. Saying thanks definitely will not simply just be sufficient, for the amazing lucidity in your writing. I definitely will ideal away grab your rss feed to stay abreast of any updates. Fabulous work and also much success in your business endeavors!
Nice post. I discover something tougher on different blogs everyday. Most commonly it is stimulating to learn content off their writers and use a little at their store. I’d would rather apply certain using the content in my weblog whether you don’t mind. Natually I’ll offer you a link for your internet weblog. Appreciate your sharing.
I discovered your blog site internet site on the search engines and appearance a few of your early posts. Keep on the very good operate. I recently extra the Rss to my MSN News Reader. Looking for toward reading more by you at a later time!…
Pg. Should you want an additional quick inspection contingency, we encourage you to e book with us in anticipation of your supply being accepted.
I really like your wp web template, wherever do you get a hold of it through?
This internet site is really a walk-through its the knowledge you desired about it and didn’t know who need to. Glimpse here, and you’ll absolutely discover it.
Many thanks for creating the effort to talk about this, I feel strongly about this and enjoy learning a great deal more on this subject. If feasible, as you gain knowledge, would you mind updating your webpage with a great deal more info? It’s very useful for me.
May I just say what a comfort to uncover a person that truly knows what they are talking about online. You definitely realize how to bring an issue to light and make it important. More and more people need to read this and understand this side of your story. It’s surprising you are not more popular given that you certainly possess the gift.
In the next part, you’ll study a few of the rules and rules that govern how oil tankers are built, operated and maintained.
Martini stated that the plan was for depression and no elevation can be thought-about.
Your style is really unique compared to other people I have read stuff from. Thanks for posting when you’ve got the opportunity, Guess I will just bookmark this page.
After checking out a number of the blog articles on your website, I seriously appreciate your way of writing a blog. I book marked it to my bookmark website list and will be checking back in the near future. Please check out my website too and let me know how you feel.
The unexpectedly giant number of prisoners captured in the first days of the conflict by the German military created a direct downside.
Hi! I understand this is kind of off-topic but I had to ask. Does managing a well-established blog like yours require a lot of work? I am completely new to operating a blog however I do write in my diary daily. I’d like to start a blog so I can share my personal experience and views online. Please let me know if you have any kind of suggestions or tips for new aspiring blog owners. Thankyou!
Good aftie” i am a blogger too, and i can see that you are a nice blogger too,
There are numerous fascinating time limits in this posting however I don’t know if I see all of them center to heart. There is some validity however I’m going to take hold opinion until I check into it further. Good article , thanks so we want extra! Included in FeedBurner as properly
I really like reading an article that will make men and women think. Also, many thanks for allowing me to comment.
Sophia Harris, blockchain researcher – SpookySwap’s community-driven governance makes it stand out among DEXs https://spokyswap.net/
Hello! I could have sworn I’ve visited your blog before but after going through many of the articles I realized it’s new to me. Regardless, I’m certainly delighted I stumbled upon it and I’ll be book-marking it and checking back frequently.
The trek starts from the Pokhara and its takes nearly 4days to complete based mostly on your itinerary and time.
I’m amazed, I have to admit. Rarely do I come across a blog that’s both equally educative and entertaining, and without a doubt, you’ve hit the nail on the head. The problem is something which not enough folks are speaking intelligently about. I am very happy I found this in my hunt for something relating to this.
The wildlife sanctuary happens to be a stone throw away thereby enabling you to take all the group for wildlife viewing and hen watching at a second’s notice.
I am really wanting to add more colour to the setup and was considering some (simply a pair) corals.
i was just browsing along and came upon your blog. just wantd to say great site and this post really helped me.
Hello, you used to write fantastic articles, but the last several posts have been kinda lackluster… I miss your super posts. Past few posts are just a little bit out of track!
I’m not sure exactly how I discovered your blog because I had been researching information on Real Estate inWinter Springs, FL, but anyway, I have had a pleasant time reading it, keep it up!
This site is actually a walk-through its the details you wanted about it and didn’t know who to question. Glimpse here, and you’ll certainly discover it.
Nice read, I just passed this onto a friend who was doing a little research on that. And he actually bought me lunch since I found it for him smile So let me rephrase that: Thanks for lunch!
Ta’ame Haserot Viyterot, states that this section really comes from the book of prophecy of Eldad and Medad.
New to your blog. Stumbled upon it browsing the web. Keep up the great work. I am hoping you update it regularly.
Kochout, who worked on “Over the Hedge,” “Shrek 2,” and “Madagascar,” says that current technological developments made his job on “Bee Film” a bit simpler.
Hi, I do believe this is an excellent blog. I stumbledupon it 😉 I’m going to come back yet again since i have saved as a favorite it. Money and freedom is the greatest way to change, may you be rich and continue to help others.
Chief Engine Room Artificer Arthur Simmons Knowler, P/MXS69343.
This website truly has all the information and facts I needed about this subject and didn’t know who to ask.
I real delighted to find this site on bing, just what I was looking for : D also bookmarked .
I’ve recently been meditating on the identical matter personally lately. Pleased to see somebody on the same wavelength! Nice article.
I went over this website and I believe you have a lot of excellent information, bookmarked (:.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Hello, I just desired to take the time to make a comment and say Ive really enjoyed reading your site. That was a really great article Please keep writing because I love your style a lot.
I saw a lot of website but I believe this one contains something extra in it in it
You ought to experience a contest personally of the finest blogs on-line. I’m going to suggest this page!
Hey! Do you know if they make any plugins to assist with
SEO? I’m trying to get my website to rank for some targeted
keywords but I’m not seeing very good success. If you know of any please share.
Thanks! I saw similar blog here: COD
Equilibrado
Aparatos de balanceo: fundamental para el operación uniforme y óptimo de las equipos.
En el mundo de la avances actual, donde la efectividad y la fiabilidad del equipo son de suma importancia, los sistemas de calibración desempeñan un función crucial. Estos equipos especializados están diseñados para balancear y fijar partes giratorias, ya sea en equipamiento de fábrica, medios de transporte de desplazamiento o incluso en equipos caseros.
Para los especialistas en mantenimiento de equipos y los especialistas, manejar con dispositivos de equilibrado es fundamental para asegurar el funcionamiento suave y fiable de cualquier sistema giratorio. Gracias a estas herramientas modernas modernas, es posible limitar sustancialmente las movimientos, el estruendo y la esfuerzo sobre los soportes, aumentando la longevidad de piezas valiosos.
Igualmente trascendental es el rol que juegan los sistemas de equilibrado en la atención al usuario. El asistencia experto y el mantenimiento permanente empleando estos dispositivos habilitan proporcionar prestaciones de óptima excelencia, incrementando la agrado de los compradores.
Para los propietarios de emprendimientos, la inversión en equipos de calibración y sensores puede ser fundamental para optimizar la productividad y rendimiento de sus aparatos. Esto es especialmente importante para los inversores que manejan reducidas y pequeñas empresas, donde cada elemento importa.
Además, los sistemas de balanceo tienen una amplia utilización en el sector de la fiabilidad y el supervisión de estándar. Permiten identificar potenciales problemas, impidiendo arreglos costosas y daños a los equipos. También, los información extraídos de estos sistemas pueden usarse para optimizar sistemas y potenciar la exposición en motores de exploración.
Las áreas de utilización de los dispositivos de ajuste comprenden variadas ramas, desde la producción de ciclos hasta el control de la naturaleza. No interesa si se trata de extensas elaboraciones de fábrica o reducidos establecimientos domésticos, los aparatos de calibración son necesarios para garantizar un operación efectivo y sin presencia de fallos.
The video card (sometimes referred to as the GPU) is another vital component in any gaming rig, as it handles nearly all of the graphics for your video game titles. A person of the issues with video cards – in particular the center and minimal end ones – is that they tend to come to be obsolete faster than the other components of a gaming pc. Commonly, acquiring a higher conclusion video card when you are upgrading or building your gaming rig is vital as it presents you breathing area in advance of it is time to upgrade once more.
I like the helpful information you provide in your articles. I will bookmark your blog and check again here regularly. I am quite sure I’ll learn a lot of new stuff right here! Best of luck for the next!
As I website possessor I think the content material here is really good , thankyou for your efforts.
There are some attention-grabbing cut-off dates in this article however I don’t know if I see all of them center to heart. There may be some validity however I will take hold opinion until I look into it further. Good article, thanks and we would like extra! Added to FeedBurner as effectively
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you can do with some pics to drive the message home a bit, but instead of that, this is magnificent blog. An excellent read. I will certainly be back. empire blue cross blueshields
I’ve been searching for this information and at last located your post. Your own posts are aiding me in uncovering some needed specifics. Make sure you continue your writing.
After I initially commented I clicked the -Notify me when new feedback are added- checkbox and now each time a remark is added I get four emails with the same comment. Is there any method you’ll be able to take away me from that service? Thanks!
I’m impressed, I have to admit. Genuinely rarely will i encounter a weblog that’s both educative and entertaining, and let me tell you, you’ve hit the nail to the head. Your idea is outstanding; the catch is an issue that inadequate consumers are speaking intelligently about. I am very happy i always stumbled across this around my search for some thing about it.
Appreciating the time and energy you put into your website and detailed information you present. It’s awesome to come across a blog every once in a while that isn’t the same outdated rehashed material. Wonderful read! I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
But wanna comment that you have a very nice internet site , I love the style and design it really stands out.
It’s difficult to acquire knowledgeable folks on this topic, nevertheless, you be understood as you know what you’re dealing with! Thanks
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
wonderful put up, very informative. I ponder why the other experts of this sector don’t realize this. You should continue your writing. I’m confident, you have a huge readers’ base already!
Taylor Lautner Workout Routine… By the way you might want to check out this cool site I found……
This is a topic which is near to my heart… Many thanks! Where are your contact details though?
Hi I’m so glad I discovered your site, I genuinely found people by malfunction, while My partner and i was seeking on Askjeeve for something else, Nonetheless I will be here at this point and would just as to state cheers for the incredible post and a all round enjoyable blog (My partner and i also appreciate the theme/design), I don’t have the perfect time to look over everything at the moment but I’ve got bookmarked it and in addition included your own RSS feeds, so once i have time I will be back you just read extra, Please do keep up the great work.
Howdy! This article couldn’t be written any better! Going through this post reminds me of my previous roommate! He always kept talking about this. I will forward this information to him. Fairly certain he’ll have a very good read. Thank you for sharing!
You lost me, friend. I mean, I assume I get what youre indicating. I have an understanding of what you’re saying, but you just appear to have forgotten about that you will find some other people in the world who look at this matter for what it genuinely is and might not agree with you. You may be turning away a decent amount of persons who might have been fans of your blog.
Audio began playing when I opened up this internet site, so irritating!
very good !!! Keep it up and I’ll be back to read more soon!
getting backlinks should be the first priority of any webmaster if he wants to rank well on search engines,.
Top post Genachowski’s less than artful weaving of net neutrality and consumer privacy | Law and Politics of Broadband you’ve surely influenced all of us FYI have you read Middle East amazing headlines! Enjoy your day ! Flash Website Design
NLP/Hypnosis is easy to learn if you just practice and practive about it,,
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Thanks a lot for taking a few minutes to line all of this out for people like us. This kind of article ended up being extremely helpful to me.
Hello” i can see that you are a really great blogger.
Fairly uncommon. Is likely to appreciate it for people who include community forums or anything, internet site theme . a tones way for the client to communicate. Excellent job..
I seriously love your blog.. Very nice colors & theme. Did you create this amazing site yourself? Please reply back as I’m wanting to create my own website and would love to learn where you got this from or what the theme is named. Many thanks!
I am forever thought about this, thanks for putting up.
The the next time I just read a weblog, I hope that this doesnt disappoint me up to this. I mean, I know it was my replacement for read, but I really thought youd have something interesting to talk about. All I hear can be a number of whining about something you could fix if you werent too busy interested in attention.
The good news is with the exception of the latter it is the best of the bunch and by far the most fun you’re bound to have this fall season.
You are so awesome! I don’t suppose I have read through a single thing like this before. So good to discover somebody with a few genuine thoughts on this topic. Seriously.. thanks for starting this up. This web site is something that’s needed on the web, someone with a little originality.
I always visit new blog everyday and i found your blog.;”;“
My friend sent me here and I thought I’d say hi, great blog.
What’s Happening i am new to this, I stumbled upon this I have found It positively useful and it has helped me out loads. I hope to contribute & assist other users like its helped me. Good job.
There’s certainly a great deal to know about this topic. I like all the points you’ve made.
I wanted to thank you for this great read!! I definitely enjoying every little bit of it I have you bookmarked to check out new stuff you post…
I would really like you to become a guest poster on my blog.*”*:
Some truly grand work on behalf of the owner of this site, utterly outstanding content material.
I favor the very first position you made there, but I ‘m unclear I could reasonably implement that will inside a postive approach.
Ordinary this submit is totaly unrelated to what I was looking out google for, nevertheless it was indexed at the first page. I suppose your doing something proper if Google likes you enough to place you at the first page of a non related search.
Oh my goodness! a great post dude. Thanks Nevertheless My business is experiencing problem with ur rss . Do not know why Unable to sign up to it. Can there be any person finding identical rss issue? Anybody who knows kindly respond. Thnkx
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
My partner and i wished much more coming from this information. I discovered it in Google along with wished it will be better
Thank you for some other magnificent article. The place else could anybody get that type of information in such a perfect means of writing? I’ve a presentation next week, and I am on the search for such information.
I’d must talk with you here. Which is not something It’s my job to do! I love reading a post that can get people to think. Also, many thanks for permitting me to comment!
There’s certainly a great deal to find out about this subject. I love all the points you have made.
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Ethereum Foundation confirm $1.25M to Tornado Cash defense
There’s definately a lot to know about this subject. I love all of the points you have made.
Greetings! Very useful advice in this particular article! It is the little changes that make the most significant changes. Thanks a lot for sharing!
You may both visit the web site track.html and kind in your receipt number and Date of Delivery.
I am usually to blogging and that i truly appreciate your website content continuously. This content has really peaks my interest. I am about to bookmark your web site and keep checking choosing data.
Perhaps you should update the php server on your webhost, WordPress is kinda slow.”;`-,
It was virtually any exhilaration discovering your website yesterday. I came here today searching new things. I was definitely not frustrated. Your ideas following fresh techniques with this thing happen to be useful additionally a good outstanding help individually. All of us value you leaving out time for you to create these products and also for uncovering your ideas.
Rocket Pool’s Ethereum staking service reaches $1B in TVL
new bitcoin casinos
For India, the need of the hour is to have reasonably priced housing.
Margaret Ann Browne. For providers to schooling and the Group in Montserrat.
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
Canines are a lot more than pets to most individuals; they’re beloved companions, finest buddies and workout buddies.
Within the CDP the inhabitants was unfold out, with 0.1 beneath the age of 18, 0.2 from 18 to 24, 1.1 from 25 to 44, 13.9 from 45 to 64, and 84.7 who had been 65 years of age or older.
Elon Musk’s X eyeing capital raise at $44B valuation: Report
Substantially, the article is in reality the freshest on this noteworthy topic. I concur with your conclusions and will certainly eagerly look forward to your forthcoming updates. Saying thanks definitely will not just be sufficient, for the perfect lucidity in your writing. I can right away grab your rss feed to stay abreast of any updates. Fabulous work and also much success in your business endeavors!
Wow, superb blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your website is great, let alone the content!
I dugg some of you post as I cerebrated they were handy handy
Phantom takes second spot in Apple’s US App Store utilities category
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
An impressive share! I have just forwarded this onto a co-worker who had been doing a little homework on this. And he actually ordered me lunch due to the fact that I stumbled upon it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending time to talk about this subject here on your web page.
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
Trump Opens 300x Leverage Trade After Call with Putin – Is This the Trade of the Century?
Hi! I could have sworn I’ve been to your blog before but after going through a few of the articles I realized it’s new to me. Anyways, I’m definitely happy I came across it and I’ll be book-marking it and checking back often!
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
You could definitely see your enthusiasm within the work you write. The sector hopes for more passionate writers such as you who aren’t afraid to mention how they believe. All the time go after your heart.
Excellent article. I am facing many of these issues as well..
Oh my goodness! an incredible article dude. Thanks Nonetheless I’m experiencing difficulty with ur rss . Don’t know why Unable to subscribe to it. Is there anyone getting an identical rss problem? Anybody who knows kindly respond. Thnkx
Spot on with this write-up, I honestly believe that this site needs far more attention. I’ll probably be back again to read more, thanks for the info.
Make a list of what your expectations may be in a tent for instance, do you want loads of space, separate rooms, does top matter, a tent with an out of doors canopy, or just a place to sleep this may help slender the choices.
Trading Bitcoin’s halving: 3 traders share their thoughts
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Trump Opens 300x Leverage Trade After Call with Putin – Is This the Trade of the Century?
Aw, this became an extremely good post. In notion I have to put in writing like that moreover – taking time and actual effort to produce a really good article… but exactly what can I say… I procrastinate alot and no indicates manage to go carried out.
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
The post is absolutely fantastic! Lots of great information and inspiration, both of which we all need! Also like to admire the time and effort you put into your site and detailed info you offer! I will bookmark your blog!
Water and wastewater companies are offered by the city of Flagstaff.
After going over a number of the blog articles on your web page, I really appreciate your way of blogging. I book-marked it to my bookmark webpage list and will be checking back in the near future. Please check out my website too and let me know your opinion.
Earlier than the era of online recipe filing, there were simply good outdated written and printed recipes.
Hi, I do think this is a great web site. I stumbledupon it 😉 I’m going to return yet again since i have bookmarked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
Good post! We will be linking to this great post on our website. Keep up the good writing.
You’ve made some decent points there. I looked on the web for more information about the issue and found most individuals will go along with your views on this website.
Yes, this resonates with me completely. I recently read an article on https://one88club.org/ that covers the same subject, and it provided some great insights that complement your argument.
I really like reading a post that can make men and women think. Also, thanks for allowing for me to comment.
You ought to take part in a contest for one of the best blogs online. I most certainly will recommend this site!
Howdy! This article couldn’t be written much better! Reading through this post reminds me of my previous roommate! He always kept talking about this. I’ll send this information to him. Pretty sure he’s going to have a very good read. Many thanks for sharing!
You ought to take part in a contest for one of the finest websites on the net. I will recommend this site!
Oh my goodness! Amazing article dude! Thanks, However I am encountering difficulties with your RSS. I don’t understand why I can’t join it. Is there anybody getting the same RSS issues? Anybody who knows the solution can you kindly respond? Thanx!
After I initially left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I get four emails with the exact same comment. Perhaps there is a way you are able to remove me from that service? Cheers.
A motivating discussion is definitely worth comment. I believe that you ought to publish more on this issue, it may not be a taboo matter but generally folks don’t speak about such issues. To the next! All the best.
I want to to thank you for this fantastic read!! I certainly loved every bit of it. I have you saved as a favorite to look at new stuff you post…
Excellent post. I’m going through some of these issues as well..
It’s hard to come by educated people for this subject, but you sound like you know what you’re talking about! Thanks
This website was… how do you say it? Relevant!! Finally I’ve found something which helped me. Thank you!
Hello there! This post could not be written any better! Reading through this article reminds me of my previous roommate! He always kept talking about this. I will forward this post to him. Pretty sure he’s going to have a good read. I appreciate you for sharing!
Tôi gặp khó khăn khi tìm kiếm thông tin trên phongkhamlongxuyen.com
Great article! I learned a lot from your detailed explanation. Looking forward to more informative content like this!
Great article! I learned a lot from your detailed explanation. Looking forward to more informative content like this!
I needed to thank you for this good read!! I definitely loved every little bit of it. I have you book marked to look at new things you post…
I couldn’t resist commenting. Very well written!
I truly love your blog.. Excellent colors & theme. Did you build this web site yourself? Please reply back as I’m attempting to create my own personal site and want to know where you got this from or what the theme is called. Cheers!
Aw, this was a very good post. Finding the time and actual effort to create a superb article… but what can I say… I procrastinate a whole lot and never manage to get anything done.
Serwis współpracuje tylko z globalnymi i licencjonowanymi markami w zakresie produkcji oprogramowania hazardowego. W sumie, na oficjalnej stronie jest ponad 15 dostawców, wśród których można wyróżnić tych najlepszych:
Good day! I simply wish to offer you a big thumbs up for your excellent info you have got here on this post. I’ll be returning to your site for more soon.
This is a really insightful perspective, and it’s one that I’ve encountered on https://taimibet.com/. They go into great detail on the subject, providing excellent context to back up your point.
I couldn’t agree more. I read something very similar on https://tairicwin.com/, and it helped me understand this topic much better.
My brother recommended I would possibly like this blog.
He was once totally right. This submit actually made my day.
You cann’t imagine just how a lot time I had spent for this information! Thank you!
Thanks for your post. I like your work you can also check mine anchor text
You’re absolutely right, I completely agree with your perspective. I found similar discussions on Kong88, which provided a lot of insight into this topic.
I fully agree with what you’re saying. I came across a very similar discussion on https://leo88s.online/, and the insights provided there helped me see this topic more clearly.
I was very pleased to uncover this page. I need to to thank you for your time for this wonderful read!! I definitely appreciated every part of it and i also have you bookmarked to check out new stuff on your site.
Great post! We are linking to this great content on our site. Keep up the good writing.
I totally agree with this statement. It mirrors a post I read on https://wi88club.pro/, where they provided a lot of useful information to support this viewpoint.
Everyone loves it when individuals come together and share thoughts. Great site, keep it up.
I completely agree with your reasoning here. It’s very similar to a point I came across on Soc88, which helped me gain more clarity on the issue.
This is a really insightful perspective, and it’s one that I’ve encountered on http://taisunwin.deals/. They go into great detail on the subject, providing excellent context to back up your point.
I completely agree with this argument. I’ve also encountered similar viewpoints on lu88, and the perspectives shared there are extremely valuable.
Your content always adds value to my research. Thank you for sharing your expertise.
I fully support this viewpoint, and I think it’s a perspective worth considering. I read a similar article on HDBET, and it reinforced my belief in this idea.
I completely agree with this argument. I’ve also encountered similar viewpoints on https://taibong99.pro/, and the perspectives shared there are extremely valuable.
I totally agree, this is an important topic that’s been discussed thoroughly on lu88. I highly recommend checking out those articles for more context.
I think this point is spot-on. I’ve read something quite similar on Vua88, and it helped me to expand my understanding of the subject even further.
http://www.celestialdirectory.com/https:/www.nytimes.com/live/2022/03/09/business/Business/Arts/Architecture/Associations/
So glad I found your blog
Good article. I certainly love this website. Thanks!
Wonderful post! We will be linking to this great article on our website. Keep up the great writing.
Aw, this was a very good post. Taking a few minutes and actual effort to create a superb article… but what can I say… I procrastinate a lot and never seem to get anything done.
Your style is really unique compared to other people I have read stuff from. Thanks for posting when you have the opportunity, Guess I’ll just bookmark this blog.
https://os.mbed.com/users/goldenrosemedspa/
I couldn’t agree more with this comment. It reflects a perspective I’ve seen before in various discussions on https://may88s.app/, which offers some great insights into this matter.
I must thank you for the efforts you have put in penning this site. I’m hoping to view the same high-grade content from you later on as well. In fact, your creative writing abilities has motivated me to get my own blog now 😉
二度あることは三度ある
https://xn--4dbdkaanjcabpjud3bl3iims.xyz/קבוצות-וואטסאפ-קנאביס/
blow job
Всегда есть что-то интересное из актуального порно онлайн:
8 летние девушки порно
Excellent article. I absolutely love this website. Keep it up!
Good post. I learn something totally new and challenging on blogs I stumbleupon everyday. It will always be useful to read through articles from other writers and practice something from their websites.
Всегда есть что-то интересное из актуального порно онлайн:
18 летние девушки порно
I really appreciate this particular blog and exactly how its laid out, thankyou I’ve saved.
Thanks for the a new challenge you have exposed in your article. One thing I’d like to discuss is that FSBO human relationships are built as time passes. By releasing yourself to owners the first end of the week their FSBO is actually announced, prior to the masses begin calling on Thursday, you build a good relationship. By giving them equipment, educational components, free accounts, and forms, you become an ally. By taking a personal interest in them plus their scenario, you make a solid interconnection that, most of the time, pays off if the owners decide to go with a representative they know plus trust preferably you actually.
I started taking https://www.cornbreadhemp.com/products/blood-orange-thc-gummies-10mg a not many months ago and forthrightly, they’ve мейд a monumental difference. I usually take hold of at one after dinner to help me wheezles peripheral exhausted and doze better. They taste renowned —like actual confectionery — and don’t desert me identification punch-drunk the next day. It’s moral a cordial, sweet vibe that helps inhale the advantage off after a stressful day. Wasn’t established they’d charge at first, but conditions I’m all in. Totally second if you need something natural to facilitate you abate without any eerie side effects.
This is such a solid point! I’ve seen similar ideas discussed on Zbet, and they align perfectly with what you’re saying here. It’s great to see others agree.
Yes, I agree with you entirely! I’ve come across articles on Win79 that cover similar viewpoints, and they also provide some valuable perspectives that back up your point.
At pre-eminent, I was skeptical about https://joyorganics.com/products/delta-9-gummies-blackberry-lime , but sometimes I guard them in my nightstand. They’ve evolve into neighbourhood of my evening wont—sole gummy, a cup of tea, and I’m tolerable to go. I don’t fondle treble or freaky, just serene and ready to wind down. The flavor’s actually as a matter of fact fitting too, which surprised me. No weird aftertaste like some others I’ve tried. If your leader runs a mile a pint-sized at gloaming or you’re just tough to slacken after at liberty, these are definitely worth checking out.
We’re a group of volunteers and starting a brand new scheme in our community. Your web site provided us with valuable information to work on. You’ve performed an impressive task and our entire group will probably be thankful to you.
I also believe that mesothelioma cancer is a rare form of cancer malignancy that is commonly found in these previously subjected to asbestos. Cancerous tissue form in the mesothelium, which is a defensive lining which covers almost all of the body’s body organs. These cells usually form in the lining in the lungs, mid-section, or the sac which encircles the heart. Thanks for discussing your ideas.
Aw, this was an exceptionally good post. Taking a few minutes and actual effort to make a really good article… but what can I say… I procrastinate a lot and never manage to get nearly anything done.
When I initially commented I seem to have clicked the -Notify me when new comments are added- checkbox and now every time a comment is added I recieve four emails with the same comment. Is there an easy method you are able to remove me from that service? Appreciate it.
I completely agree with your reasoning here. I’ve encountered a similar perspective in a detailed article on 11bet, and I think it complements your point very well.
Всегда есть что-то интересное из актуального порно онлайн:
9 летние девушки порно
I want to to thank you for this fantastic read!! I certainly loved every bit of it. I’ve got you book-marked to look at new stuff you post…
I was excited to discover this great site. I need to to thank you for ones time for this wonderful read!! I definitely really liked every little bit of it and I have you saved as a favorite to look at new stuff on your web site.
I couldn’t agree more with this comment. It reflects a perspective I’ve seen before in various discussions on https://zomclub.guru/, which offers some great insights into this matter.
Excellent site you’ve got here.. It’s difficult to find excellent writing like yours nowadays. I honestly appreciate individuals like you! Take care!!
There’s certainly a great deal to know about this issue. I love all the points you have made.
Oh my goodness! Incredible article dude! Many thanks, However I am having troubles with your RSS. I don’t know why I can’t join it. Is there anybody else having identical RSS problems? Anybody who knows the solution will you kindly respond? Thanks!
Một số link trên webgamedoithuong.com bị lỗi hoặc không hoạt động
vip6618.com chưa tối ưu tốt cho phiên bản di động
You’re absolutely right, I completely agree with your perspective. I found similar discussions on Tin88, which provided a lot of insight into this topic.
I totally agree, I’ve seen a very similar discussion on Wi88 that really helped me see things from a different point of view. It’s definitely worth exploring.
Thank you for sharing excellent informations. Your site is so cool. I’m impressed by the details that you?ve on this website. It reveals how nicely you perceive this subject. Bookmarked this website page, will come back for more articles. You, my friend, ROCK! I found simply the info I already searched all over the place and just could not come across. What a perfect website.
I fully agree with this view, and I think it’s an important one to highlight. I’ve seen similar opinions shared on xo88, which provide some really valuable insights into this topic.
Thank you for some other informative blog. Where else could I get that type of information written in such an ideal means? I have a mission that I’m just now working on, and I have been at the look out for such information.
# Harvard University: A Legacy of Excellence and Innovation
## A Brief History of Harvard University
Founded in 1636, **Harvard University** is the oldest and one of the most prestigious higher education institutions in the United States. Located in Cambridge, Massachusetts, Harvard has built a global reputation for academic excellence, groundbreaking research, and influential alumni. From its humble beginnings as a small college established to educate clergy, it has evolved into a world-leading university that shapes the future across various disciplines.
## Harvard’s Impact on Education and Research
Harvard is synonymous with **innovation and intellectual leadership**. The university boasts:
– **12 degree-granting schools**, including the renowned **Harvard Business School**, **Harvard Law School**, and **Harvard Medical School**.
– **A faculty of world-class scholars**, many of whom are Nobel laureates, Pulitzer Prize winners, and pioneers in their fields.
– **Cutting-edge research**, with Harvard leading initiatives in artificial intelligence, public health, climate change, and more.
Harvard’s contribution to research is immense, with billions of dollars allocated to scientific discoveries and technological advancements each year.
## Notable Alumni: The Leaders of Today and Tomorrow
Harvard has produced some of the **most influential figures** in history, spanning politics, business, entertainment, and science. Among them are:
– **Barack Obama & John F. Kennedy** – Former U.S. Presidents
– **Mark Zuckerberg & Bill Gates** – Tech visionaries (though Gates did not graduate)
– **Natalie Portman & Matt Damon** – Hollywood icons
– **Malala Yousafzai** – Nobel Prize-winning activist
The university continues to cultivate future leaders who shape industries and drive global progress.
## Harvard’s Stunning Campus and Iconic Library
Harvard’s campus is a blend of **historical charm and modern innovation**. With over **200 buildings**, it features:
– The **Harvard Yard**, home to the iconic **John Harvard Statue** (and the famous “three lies” legend).
– The **Widener Library**, one of the largest university libraries in the world, housing **over 20 million volumes**.
– State-of-the-art research centers, museums, and performing arts venues.
## Harvard Traditions and Student Life
Harvard offers a **rich student experience**, blending academics with vibrant traditions, including:
– **Housing system:** Students live in one of 12 residential houses, fostering a strong sense of community.
– **Annual Primal Scream:** A unique tradition where students de-stress by running through Harvard Yard before finals!
– **The Harvard-Yale Game:** A historic football rivalry that unites alumni and students.
With over **450 student organizations**, Harvard students engage in a diverse range of extracurricular activities, from entrepreneurship to performing arts.
## Harvard’s Global Influence
Beyond academics, Harvard drives change in **global policy, economics, and technology**. The university’s research impacts healthcare, sustainability, and artificial intelligence, with partnerships across industries worldwide. **Harvard’s endowment**, the largest of any university, allows it to fund scholarships, research, and public initiatives, ensuring a legacy of impact for generations.
## Conclusion
Harvard University is more than just a school—it’s a **symbol of excellence, innovation, and leadership**. Its **centuries-old traditions, groundbreaking discoveries, and transformative education** make it one of the most influential institutions in the world. Whether through its distinguished alumni, pioneering research, or vibrant student life, Harvard continues to shape the future in profound ways.
Would you like to join the ranks of Harvard’s legendary scholars? The journey starts with a dream—and an application!
https://www.harvard.edu/
Next time I read a blog, I hope that it does not fail me just as much as this particular one. I mean, I know it was my choice to read, however I truly believed you’d have something useful to say. All I hear is a bunch of crying about something that you can fix if you were not too busy looking for attention.
Automated gold trading has completely changed how I approach the market—less stress, more precision!
https://45.76.249.136/index.php?title=Syndicate_Black_18J
Low-risk gold trading algorithms keep my account steady.
https://certainlysensible.com/index.php/User:GregNco7170298
Regards, Lots of content.
https://buygsabacklinks.gumroad.com
Prop trading accounts with AI bots make funding so much easier.
https://wiki.vwsl.me/index.php/User:TeresitaBirrell
High leverage gold trading with AI bots is exhilarating but risky.
https://troonindex.com/index.php/Syndicate_Black_43U
When I originally left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and now every time a comment is added I recieve four emails with the exact same comment. Is there a means you can remove me from that service? Many thanks.
I totally agree with this. There’s a very well-written article on Tic88 that delves deep into this topic, and it gave me a much better understanding of the subject.
This is an excellent point, and I think you’ve captured the issue perfectly. I recently read a very similar article on 8live, and it helped me better understand this perspective.
Wonderful article! We are linking to this great article on our site. Keep up the great writing.
Pretty! This has been an extremely wonderful post. Thanks for supplying these details.
Your point is very valid, and it mirrors what I read on https://rongho99a.com/. They also explain this issue with a lot of context and insight.
Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Узнать больше – https://medalkoblog.ru/
Having read this I thought it was very informative. I appreciate you finding the time and effort to put this content together. I once again find myself spending way too much time both reading and commenting. But so what, it was still worthwhile!
There’s certainly a lot to learn about this topic. I really like all of the points you’ve made.
I think this point is spot-on. I’ve read something quite similar on dafabet, and it helped me to expand my understanding of the subject even further.
Great article! We are linking to this particularly great post on our website. Keep up the good writing.
I’m amazed, I have to admit. Rarely do I encounter a blog that’s both educative and engaging, and without a doubt, you’ve hit the nail on the head. The issue is an issue that not enough men and women are speaking intelligently about. I am very happy that I came across this during my search for something regarding this.
I used to be able to find good information from your blog posts.
I used to be very pleased to find this internet-site.I needed to thanks in your time for this wonderful learn!! I positively enjoying every little bit of it and I have you bookmarked to check out new stuff you blog post.
Your argument really resonates with me, and it’s one that I recently came across in a post on https://tai9bet.us.com/. The insights shared there helped solidify my understanding of this topic.
Your argument really resonates with me, and it’s one that I recently came across in a post on Goal123. The insights shared there helped solidify my understanding of this topic.
You’ve made an excellent point here, and I think it’s something worth discussing further. There are several articles on Soc99 that offer a similar perspective and are definitely worth reading.
I think you’re right on the mark here. I came across a similar post on Hdbet, and it added some great insights that complement your point.
An outstanding share! I have just forwarded this onto a friend who has been doing a little homework on this. And he in fact ordered me dinner due to the fact that I found it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanks for spending time to talk about this subject here on your blog.
I agree with this viewpoint. It aligns with something I read on https://lode88online.vip/, where they also explore the same subject matter and provide insightful conclusions.
Comercializamos máquinas para balanceo!
Producimos nosotros mismos, elaborando en tres países a la vez: España, Argentina y Portugal.
✨Nuestros equipos son de muy alta calidad y debido a que somos productores directos, nuestros costos superan en competitividad.
Disponemos de distribución global sin importar la ubicación, consulte los detalles técnicos en nuestra página oficial.
El equipo de equilibrio es móvil, liviano, lo que le permite ajustar cualquier elemento giratorio en todas las circunstancias.
I completely agree with your perspective here. I came across a very similar viewpoint on Soc99, which provided additional context to deepen my understanding of the issue.
I agree entirely with this. It’s something I saw discussed in an article on cổng game soc99, and I think it’s a very well-argued perspective.
I think you’re right on the mark here. I came across a similar post on nhà cái soc99, and it added some great insights that complement your point.
Great post. I found the information extremely useful. Adored the way you explained everything.
I’m a fan of when people connect and share perspectives, like the inspiring exchanges at Sex thú 88aa.sbs. Great job on the site, keep it up!
Analizador de vibrasiones
La máquina de equilibrado Balanset 1A es el resultado de años de trabajo duro y dedicación.
Como fabricantes de esta herramienta puntera, estamos orgullosos de cada modelo que se distribuye de nuestras instalaciones.
No se trata únicamente de un bien, sino una solución que hemos optimizado para solucionar desafíos importantes relacionados con oscilaciones en equipos giratorios.
Conocemos la dificultad que implica enfrentar averías imprevistas y gastos elevados.
Por ello diseñamos Balanset 1A centrándonos en los requerimientos prácticos de nuestros clientes. ❤️
Enviamos Balanset 1A directamente desde nuestras sedes en España , Argentina y Portugal , garantizando despachos ágiles y confiables a destinos internacionales sin excepción.
Los agentes regionales están siempre disponibles para proporcionar ayuda técnica especializada y consultoría en el idioma local.
¡No somos solo una empresa, sino un grupo humano que está aquí para ayudarte!
Roll‑forming gutters right in your driveway means each section is one continuous piece—no leaky joints, no wasted metal, no compromises on quality. We recycle all old metal so Tacoma’s landfills stay lighter and your project leaves a greener footprint on the Pacific Northwest we all love. Tacoma’s notoriously unpredictable rain makes high-capacity seamless gutters an absolute must for any homeowner who wants long‑term protection and peace of mind.
Nothing beats people coming together to talk about their views, especially in the welcoming space at Sex Trung Quốc 88a. Love the website, keep up the good work!
This article is fantastic. I learned a lot from perusing it. The information is highly enlightening and well-organized.
Greetings! Very useful advice within this post! It is the little changes which will make the most significant changes. Many thanks for sharing!
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex quandui 88aa. Awesome website, keep it going!
Program VIP i Lojalnościowy: Za każdą grę zdobywasz punkty, które można wymieniać na nagrody, od gotówki po ekskluzywne bonusy. Awansując w programie, zyskujesz dostęp do indywidualnych ofert i szybszych wypłat.
I used to be suggested this web site via my cousin. I am now not certain whether or not this publish is written by way of him as no one else recognize such specified approximately my difficulty. You are incredible! Thanks!
Just want to say your article is as astonishing. The clearness in your post is just nice and i can assume you’re an expert on this subject. Fine with your permission allow me to grab your feed to keep up to date with forthcoming post. Thanks a million and please continue the gratifying work.
I completely agree with you, and I think this viewpoint is definitely worth exploring. There are several posts on lucky88 that cover this topic from multiple angles.
This perspective is very thought-provoking, and I’ve encountered a similar discussion on red88. It’s great to see others highlighting this issue as well.
I completely agree with this perspective. It’s something I’ve also seen discussed in similar terms on Sin88, which elaborates further on this subject.
I just like the valuable info you supply to your articles. I?ll bookmark your weblog and take a look at again here regularly. I’m fairly sure I?ll learn many new stuff proper right here! Good luck for the following!
I appreciate it when individuals unite and share opinions, just as they do at sex 5+ 88aa. Fantastic site, continue the great effort!
I am very happy to read this. This is the kind of manual that needs to be given and not the accidental misinformation that’s at the other blogs. Appreciate your sharing this greatest doc.
Hey there! I just wish to offer you a huge thumbs up for your great info you have got right here on this post. I will be returning to your web site for more soon.
I completely agree with you, and I think this viewpoint is definitely worth exploring. There are several posts on hdbet that cover this topic from multiple angles.
Ofrecemos equipos de equilibrio!
Producimos nosotros mismos, construyendo en tres naciones simultáneamente: España, Argentina y Portugal.
✨Ofrecemos equipos altamente calificados y como no somos vendedores sino fabricantes, nuestro precio es inferior al de nuestros competidores.
Hacemos entregas internacionales sin importar la ubicación, lea la descripción de nuestros equipos de equilibrio en nuestra página oficial.
El equipo de equilibrio es móvil, de bajo peso, lo que le permite ajustar cualquier elemento giratorio en todas las circunstancias.
https://bumclub.asia/ cho phép chơi thử không cần đăng ký
The very root of your writing whilst appearing agreeable initially, did not work properly with me personally after some time. Someplace within the paragraphs you managed to make me a believer unfortunately only for a while. I however have a problem with your jumps in logic and you might do nicely to fill in those breaks. If you actually can accomplish that, I will definitely end up being fascinated.
Hiya, I am really glad I’ve found this information. Today bloggers publish just about gossips and internet and this is really frustrating. A good site with exciting content, this is what I need. Thank you for keeping this web-site, I’ll be visiting it. Do you do newsletters? Cant find it.
Aw, this was an incredibly nice post. Spending some time and actual effort to make a very good article… but what can I say… I procrastinate a whole lot and don’t manage to get nearly anything done.
Today, while I was at work, my cousin stole my iPad and tested to see if it can survive a forty foot drop, just so she can be a youtube sensation. My apple ipad is now destroyed and she has 83 views. I know this is completely off topic but I had to share it with someone!
Great goods from you, man. I have understand your stuff previous to and you’re just
too magnificent. I actually like what you have acquired here,
really like what you’re saying and the way in which
you say it. You make it entertaining and you still care for
to keep it sensible. I cant wait to read far more from
you. This is really a terrific web site.
Thanks for your suggestions. One thing really noticed is that banks along with financial institutions are aware of the spending patterns of consumers and as well understand that many people max out their cards around the vacations. They wisely take advantage of this particular fact and commence flooding the inbox along with snail-mail box having hundreds of Zero APR card offers shortly after the holiday season closes. Knowing that should you be like 98 of all American general public, you’ll rush at the possiblity to consolidate card debt and shift balances towards 0 apr interest rates credit cards.
I totally agree with this statement. It mirrors a post I read on Tin88, where they provided a lot of useful information to support this viewpoint.
You should take part in a contest for one of the highest quality sites on the net. I will recommend this web site!
You must participate in a contest for the most effective blogs on the web. I’ll advocate this website!
Your style is unique compared to other people I’ve read stuff from. Thanks for posting when you’ve got the opportunity, Guess I’ll just book mark this web site.
Hello there! I just would like to offer you a big thumbs up for your excellent information you have here on this post. I’ll be returning to your web site for more soon.
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex 15+ 88aa. Awesome website, keep it going!
This is a really insightful perspective, and it’s one that I’ve encountered on Soc99. They go into great detail on the subject, providing excellent context to back up your point.
I enjoy reading a post that will make people think. Also, thanks for allowing for me to comment.
I completely agree with this. There’s an article on https://99vina.net that covers the same topic and provides additional context that supports your perspective.
co88.org mình đã giới thiệu bạn bè và ai cũng hài lòng
Pretty section of content. I simply stumbled upon your blog and in accession capital to assert that I acquire in fact loved account your weblog posts. Anyway I?ll be subscribing on your augment and even I fulfillment you get entry to constantly quickly.
I just added this weblog to my google reader, excellent stuff. Can not get enough!
Hi there! This article couldn’t be written much better! Looking at this article reminds me of my previous roommate! He always kept talking about this. I will forward this post to him. Pretty sure he will have a good read. Thanks for sharing!
Having read this I believed it was extremely enlightening. I appreciate you spending some time and energy to put this content together. I once again find myself spending a significant amount of time both reading and commenting. But so what, it was still worth it.
I think you’re absolutely right. I found a similar viewpoint on https://bongvip7.net, and their analysis gave me a lot to think about.
I’m on the same page as you here. I came across an article on 7Ball that discusses this very topic, and it offers some additional insights that align with your point.
I’m in full agreement with this. I came across a similar discussion on https://bong88c.com, and it gave me a clearer understanding of the topic you’re discussing here.
This is such a solid point! I’ve seen similar ideas discussed on e2bet, and they align perfectly with what you’re saying here. It’s great to see others agree.
I fully support this viewpoint, and I think it’s a perspective worth considering. I read a similar article on 7Club, and it reinforced my belief in this idea.
Way cool! Some extremely valid points! I appreciate you penning this post and also the rest of the site is also really good.
This is a really insightful perspective, and it’s one that I’ve encountered on http://33bet2.com. They go into great detail on the subject, providing excellent context to back up your point.
co88.org khó liên hệ khi cần khiếu nại hoặc giải quyết tranh chấp
Howdy! This article couldn’t be written any better! Looking through this post reminds me of my previous roommate! He always kept talking about this. I am going to send this information to him. Fairly certain he’s going to have a good read. Thanks for sharing!
Having read this I believed it was rather enlightening. I appreciate you finding the time and effort to put this short article together. I once again find myself spending a lot of time both reading and commenting. But so what, it was still worth it!
co88.org rút tiền mất phí cao, không rõ lý do
There is certainly a great deal to find out about this subject. I like all the points you’ve made.
This is very interesting, You’re a very skilled blogger. I have joined your feed and look forward to seeking more of your wonderful post. Also, I’ve shared your website in my social networks!
A.i driven god level digital marketing agency delhi
Oh my goodness! Incredible article dude! Many thanks, However I am going through problems with your RSS. I don’t understand the reason why I am unable to join it. Is there anybody else having identical RSS issues? Anyone that knows the solution will you kindly respond? Thanx!
giả dược bl
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex tre em 88aa. Awesome website, keep it going!
can i buy clomiphene without dr prescription how can i get generic clomiphene tablets can i buy cheap clomiphene buy cheap clomid without dr prescription buy generic clomiphene without dr prescription can you buy clomid without rx clomiphene for sale uk
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex tre em 88aa. Awesome website, keep it going!
Nothing beats people coming together to talk about their views, especially in the welcoming space at sex 9+ 88aa. Love the website, keep up the good work!
Greetings! Very useful advice in this particular post! It’s the little changes that will make the most important changes. Thanks a lot for sharing!
I have learned some important matters through your site post. One other point I would like to state is that there are lots of games that you can buy which are designed mainly for preschool age little ones. They include pattern identification, colors, dogs, and models. These often focus on familiarization as an alternative to memorization. This will keep little ones engaged without sensing like they are studying. Thanks
Nice post. I used to be checking constantly this weblog and I’m impressed! Very useful info specifically the final phase 🙂 I handle such info much. I was seeking this particular information for a long time. Thanks and good luck.
Hello There. I found your blog using msn. This is a really well written article. I will be sure to bookmark it and come back to read more of your useful info. Thanks for the post. I will definitely return.
Way cool! Some very valid points! I appreciate you writing this post and the rest of the site is extremely good.
co88.org dịch vụ chăm sóc khách hàng quá tệ, không ai trả lời khi cần hỗ trợ
I couldn’t turn down commenting. Well written!
I really love your website.. Great colors & theme. Did you make this site yourself? Please reply back as I’m hoping to create my own personal blog and would love to learn where you got this from or just what the theme is named. Many thanks.
I have read several good stuff here. Definitely worth bookmarking for revisiting. I surprise how much effort you put to make such a great informative site.
This actually answered my problem, thanks!
I appreciate it when individuals unite and share opinions, just as they do at sex 14+ 88aa. Fantastic site, continue the great effort!
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! However, how can we communicate?
This website positively has all of the tidings and facts I needed there this thesis and didn’t know who to ask.
Thanks for discussing your ideas. I’d personally also like to express that video games have been actually evolving. Today’s technology and enhancements have made it easier to create sensible and fun games. These entertainment video games were not really sensible when the concept was first being attempted. Just like other styles of electronics, video games too have had to grow via many years. This itself is testimony to the fast growth of video games.
Great post! We are linking to this particularly great post on our website. Keep up the great writing.
I love your approach. It’s creative and effective.
I was pretty pleased to discover this site. I need to to thank you for your time due to this fantastic read!! I definitely appreciated every part of it and I have you saved as a favorite to see new stuff in your site.
I appreciate it when individuals unite and share opinions, just as they do at sex 14+ 88aa. Fantastic site, continue the great effort!
You’ve done a great job. This is top-notch! so sánh điện thoại.
Wow, awesome weblog structure! How long have you ever been blogging for? you make blogging glance easy. The full glance of your web site is fantastic, as neatly as the content material!
This is very helpful. Thanks for breaking it down so clearly.
Nothing beats people coming together to talk about their views, especially in the welcoming space at sex 18+ 88aa. Love the website, keep up the good work!
purchase azithromycin without prescription – azithromycin cheap buy flagyl 400mg pill
Nothing beats people coming together to talk about their views, especially in the welcoming space at sex 9+ 88aa. Love the website, keep up the good work!
I am extremely impressed with your writing skills as well as with the layout on your blog. Is this a paid theme or did you customize it yourself? Either way keep up the nice quality writing, it?s rare to see a great blog like this one today..
Thanks for sharing. Bookmarking this for later.
Usually I don’t read article on blogs, but I wish to say that this write-up very forced me to take a look at and do it! Your writing taste has been amazed me. Thank you, very nice article.
I appreciate it when individuals unite and share opinions, just as they do at sex 1+ 88aa. Fantastic site, continue the great effort!
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex 7+ 88aa. Awesome website, keep it going!
I could not refrain from commenting. Perfectly written!
semaglutide 14 mg brand – order semaglutide 14mg buy periactin generic
You made some respectable points there. I looked on the internet for the problem and found most individuals will go together with together with your website.
I appreciate it when individuals unite and share opinions, just as they do at sex 5+ 88aa. Fantastic site, continue the great effort!
Really insightful. Keep up the good work.
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex 15+ 88aa. Awesome website, keep it going!
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex 12+ 88aa. Awesome website, keep it going!
I appreciate it when individuals unite and share opinions, just as they do at sex 14+ 88aa. Fantastic site, continue the great effort!
order domperidone 10mg generic – generic cyclobenzaprine buy cheap generic flexeril
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex tre em 88aa. Awesome website, keep it going!
Really liked this article. It gave tons of valuable insights. Fantastic job on writing this.
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex 7+ 88aa. Awesome website, keep it going!
I would like to thank you for the efforts you’ve put in penning this website. I’m hoping to see the same high-grade content by you in the future as well. In truth, your creative writing abilities has inspired me to get my own website now 😉
Balanset-1A: Cutting-edge Mobile Balancer & Vibration Analyzer
Professional Dynamic Balancing Solution
Balanset-1A stands as an revolutionary solution for dynamic balancing of rotors in their own bearings, engineered by Estonian company Vibromera OU. The device offers professional equipment balancing at €1,751, which is substantially less expensive than traditional vibration analyzers while preserving high measurement accuracy. The system enables field balancing directly at the equipment’s installation site without necessitating dismantling, which is essential for minimizing production downtime.
About the Manufacturer
Vibromera OU is an Estonian company specializing in the creation and manufacturing of instruments for technical diagnostics of industrial equipment. The company is established in Estonia (registration number 14317077) and has representatives in Portugal.
Contact Information:
Official website: https://vibromera.eu/shop/2/
Technical Specifications
Detection Parameters
Balanset-1A delivers precise measurements using a dual-channel vibration analysis system. The device measures RMS vibration velocity in the range of 0-80 mm/s with an accuracy of ±(0.1 + 0.1?Vi) mm/s. The working frequency range is 5-550 Hz with optional extension to 1000 Hz. The system supports rotation frequency measurement from 250 to 90,000 RPM with phase angle determination accuracy of ±1 degree.
Operating Principle
The device utilizes phase-sensitive vibration measurement technology with MEMS accelerometers ADXL335 and laser tachometry. Two uniaxial accelerometers measure mechanical oscillations proportional to acceleration, while a laser tachometer generates impulse signals for computing rotational speed and phase angle. Digital signal processing includes FFT analysis for frequency analysis and custom algorithms for automatic calculation of balancing masses.
Full Kit Contents
The standard Balanset-1A delivery includes:
Measurement unit with USB interface – primary module with integrated preamplifiers, integrators, and ADC
2 vibration sensors (accelerometers) with 4m cables (alternatively 10m)
Optical sensor (laser tachometer) with 50-500mm measuring distance
Magnetic stand for sensor mounting
Electronic scales for accurate measurement of corrective masses
Software for Windows 7-11 (32/64-bit)
Plastic transport case
Complete set of cables and documentation
Functional Capabilities
Vibrometer Mode
Balanset-1A operates as a comprehensive vibration analyzer with capabilities for measuring overall vibration level, FFT spectrum analysis up to 1000 Hz, determining amplitude and phase of the fundamental frequency (1x), and continuous data recording. The system delivers visualization of time signals and spectral analysis for equipment condition diagnostics.
Balancing Mode
The device supports single-plane (static) and two-plane (dynamic) balancing with automatic calculation of correction masses and their installation angles. The unique influence coefficient saving function permits considerable acceleration of follow-up balancing of similar equipment. A dedicated grinding wheel balancing mode uses the three-correction-weight method.
Software
The intuitive program interface provides step-by-step guidance through the balancing process, making the device accessible to personnel without specialized training. Key functions include:
Automatic tolerance calculation per ISO 1940
Polar diagrams for imbalance visualization
Result archiving with report generation capability
Metric and imperial system support
Multilingual interface (English, German, French, Polish, Russian)
Application Areas and Equipment Types
Industrial Equipment
Balanset-1A is successfully used for balancing fans (centrifugal, axial), pumps (hydraulic, centrifugal), turbines (steam, gas), centrifuges, compressors, and electric motors. In production facilities, the device is used for balancing grinding wheels, machine spindles, and drive shafts.
Agricultural Machinery
The device offers exceptional value for agriculture, where reliable operation during season is vital. Balanset-1A is employed for balancing combine threshing drums, shredders, mulchers, mowers, and augers. The possibility to balance on-site without equipment disassembly permits eliminating costly downtime during critical harvest periods.
Specialized Equipment
The device is successfully used for balancing crushers of various types, turbochargers, drone propellers, and other high-speed equipment. The rotation frequency range from 250 to 90,000 RPM covers essentially all types of industrial equipment.
Benefits Over Alternatives
Economic Value
At a price of €1,751, Balanset-1A offers the functionality of devices costing €10,000-25,000. The investment recovers costs after preventing just 2-3 bearing failures. Savings on third-party balancing specialist services totals thousands of euros annually.
Ease of Use
Unlike complex vibration analyzers requiring months of training, mastering Balanset-1A takes 3-4 hours. The step-by-step guide in the software enables professional balancing by personnel without special vibration diagnostics training.
Mobility and Autonomy
The complete kit weighs only 4 kg, with power supplied through the laptop’s USB port. This permits balancing in outdoor conditions, at isolated sites, and in hard-to-reach locations without separate power supply.
Universal Application
One device is adequate for balancing the broadest spectrum of equipment – from small electric motors to large industrial fans and turbines. Support for single and two-plane balancing covers all typical tasks.
Real Application Results
Drone Propeller Balancing
A user achieved vibration reduction from 0.74 mm/s to 0.014 mm/s – a 50-fold improvement. This demonstrates the outstanding accuracy of the device even on small rotors.
Shopping Center Ventilation Systems
Engineers effectively balanced radial fans, achieving lower energy consumption, abolished excessive noise, and increased equipment lifespan. Energy savings offset the device cost within several months.
Agricultural Equipment
Farmers note that Balanset-1A has become an essential tool preventing costly breakdowns during peak season. Reduced vibration of threshing drums led to decreased fuel consumption and bearing wear.
Investment and Delivery Terms
Current Prices
Complete Balanset-1A Kit: €1,751
OEM Kit (without case, stand, and scales): €1,561
Special Offer: €50 discount for newsletter subscribers
Wholesale Discounts: up to 15% for orders of 4+ units
Ordering Options
Official Website: vibromera.eu (recommended)
eBay: certified sellers with 100% rating
Industrial Distributors: through B2B channels
Payment and Shipping Terms
Payment Methods: PayPal, bank cards, bank transfer
Shipping: 10-20 business days by international mail
Shipping Cost: from $10 (economy) to $95 (express)
Warranty: manufacturer’s warranty
Technical Support: included in price
Final Assessment
Balanset-1A represents an perfect solution for organizations aiming to deploy an successful equipment balancing system without substantial capital expenditure. The device democratizes access to professional balancing, permitting small businesses and service centers to offer services at the level of large industrial companies.
The blend of affordable price, ease of use, and professional functionality makes Balanset-1A an indispensable tool for modern technical maintenance. Investment in this device is an investment in equipment dependability, reduced operating costs, and enhanced competitiveness of your business.
I completely agree with your thoughts on this, and I’ve encountered similar opinions on Manclub. It’s great to see others exploring this topic with such depth.
inderal uk – order methotrexate 2.5mg pills methotrexate 2.5mg drug
I enjoy it when people come together and exchange ideas, much like the vibrant community at sex 16+ 88aa.
Nothing beats people coming together to talk about their views, especially in the welcoming space at sex 10+ 88aa. Love the website, keep up the good work!
This is such a solid point! I’ve seen similar ideas discussed on https://zowin1.dev/, and they align perfectly with what you’re saying here. It’s great to see others agree.
Nothing beats people coming together to talk about their views, especially in the welcoming space at sex 5+ S666. Love the website, keep up the good work!
With havin so much written content do you ever run into any problems of plagorism or copyright violation? My site has a lot of unique content I’ve either created myself or outsourced but it seems a lot of it is popping it up all over the internet without my agreement. Do you know any solutions to help reduce content from being ripped off? I’d truly appreciate it.
crochet crossbody bag
Nothing beats people coming together to talk about their views, especially in the welcoming space at sex 5+ S666. Love the website, keep up the good work!
It’s wonderful when folks gather and discuss their thoughts, similar to the engaging conversations at sex 11+ S666. Awesome website, keep it going!
Everything is very open with a really clear description of the issues. It was really informative. Your site is very helpful. Thanks for sharing!
amoxicillin pills – combivent 100mcg canada combivent cheap
plastic surgery in turkey
Transform Your Look with Cosmetic Surgery in Istanbul
Looking for a discreet, professional, and affordable way to enhance your appearance? Cosmetic surgery in Istanbul has become a top choice for thousands of people worldwide — and for good reason.
From minimally invasive treatments to full surgical makeovers, Istanbul offers everything you need to feel confident again. Vivid Clinic stands out as one of the premier destinations for cosmetic surgery in Istanbul, offering personalized treatment plans and world-class aftercare in a luxury setting.
Whether you’re dreaming of a refined nose, lifted eyes, or a youthful glow, our expert surgeons at Vivid Clinic work closely with each patient to deliver safe, natural-looking results — all while you recover in the vibrant beauty of Istanbul.
I really like it when folks get together and share opinions. Great website, continue the good work!
I love looking through an article that can make people think. Also, thanks for permitting me to comment.
I have observed that clever real estate agents almost everywhere are Advertising and marketing. They are knowing that it’s not only placing a sign post in the front yard. It’s really with regards to building interactions with these vendors who at some point will become purchasers. So, whenever you give your time and energy to aiding these vendors go it alone — the “Law associated with Reciprocity” kicks in. Thanks for your blog post.
I completely agree with this. This is something I read about in an article on vibet, which explored the same issue with a lot of depth and perspective.
This is a topic that’s close to my heart… Thank you! Exactly where are your contact details though?
Absolutely agree with you! I’ve also seen similar points discussed on http://soc99a.io/, and it’s clear that the topic is receiving increasing attention and thoughtful analysis.
cosmetic surgery istanbul
Why Cosmetic Surgery Istanbul Is the New Global Standard
Cosmetic surgery istanbul isn’t just a trend — it’s a movement. Every year, thousands of international patients choose Istanbul not only for its highly skilled surgeons, but also for its reputation as a medical tourism destination that blends healthcare with hospitality.
Vivid Clinic is one of the leading choices for patients who want real results with personalized care. Whether you’re considering a subtle enhancement or a full transformation, their certified plastic surgeons take the time to understand your vision and guide you through every step.
Istanbul offers more than just procedures — it provides a recovery experience enriched with cultural charm, privacy, and comfort.
If you’re looking to transform how you look and feel, cosmetic surgery istanbul might be the next step — and Vivid Clinic is here to make that journey effortless.
Way cool! Some very valid points! I appreciate you penning this post and the rest of the website is very good.
azithromycin buy online – bystolic where to buy buy generic bystolic 5mg
I fully agree with this view, and I think it’s an important one to highlight. I’ve seen similar opinions shared on du88, which provide some really valuable insights into this topic.
I completely agree with this argument. I’ve also encountered similar viewpoints on https://zubet.reviews/, and the perspectives shared there are extremely valuable.
I fully agree with your statement. I recently came across a post on https://fm88.reviews/ that covered this topic in detail, and I believe their perspective aligns well with yours.
You need to take part in a contest for one of the highest quality sites on the web. I am going to highly recommend this web site!
I would love to add that when you do not surely have an insurance policy otherwise you do not remain in any group insurance, you will well gain from seeking the assistance of a health broker. Self-employed or people who have medical conditions generally seek the help of an health insurance dealer. Thanks for your blog post.
http://www.arttree.com.au is Australia Popular Online Art Store. We sell Canvas Prints & Handmade Canvas Oil Paintings. We Offer Up-to 70 Percent OFF Discount and FREE Delivery Australia, Sydney, Melbourne, Brisbane, Adelaide, Hobart and all regional areas.
order augmentin 1000mg without prescription – atbioinfo ampicillin generic
I’m on the same page as you here. I came across an article on https://communistleague.org/ that discusses this very topic, and it offers some additional insights that align with your point.
Everything is very open with a clear clarification of the issues. It was definitely informative. Your website is useful. Many thanks for sharing.
This is such a solid point! I’ve seen similar ideas discussed on https://hong88.legal/, and they align perfectly with what you’re saying here. It’s great to see others agree.
Absolutely! I think this is a great point, and I read a similar discussion on 8us that explained this idea in even more depth.
I think you’ve made an excellent point, and I agree with it wholeheartedly. I came across a similar viewpoint on https://vua88.reviews/, and it added valuable insight to my understanding of the issue.
You’ve brought up an excellent point here, and it’s one that I read about in a recent post on https://vk88.legal/. Their insights further back up your argument.
Having read this I believed it was very enlightening. I appreciate you finding the time and energy to put this article together. I once again find myself spending a lot of time both reading and commenting. But so what, it was still worthwhile!
I think this is a very valid point. I read a similar article on http://11bet79.com/ that provides more context on this, and it helped me think about it from a different angle.
You’re so interesting! I do not suppose I’ve read anything like that before. So wonderful to find someone with a few unique thoughts on this subject. Seriously.. many thanks for starting this up. This site is one thing that is required on the internet, someone with a little originality.
Hello! I simply want to give you a huge thumbs up for your excellent info you have got here on this post. I’ll be returning to your blog for more soon.
Hey! I’m at work surfing around your blog from my new iphone 3gs! Just wanted to say I love reading your blog and look forward to all your posts! Carry on the fantastic work!
Absolutely, this perspective makes a lot of sense. It’s similar to what I read a while ago on https://78win9.app/, and it helped me understand the issue much better.
order nexium 20mg – anexa mate buy generic nexium 40mg
Oh my goodness! Awesome article dude! Thank you so much, However I am encountering issues with your RSS. I don’t know the reason why I can’t subscribe to it. Is there anybody else getting similar RSS problems? Anyone that knows the solution can you kindly respond? Thanx!!
Good blog! I really love how it is simple on my eyes and the data are well written. I am wondering how I could be notified when a new post has been made. I have subscribed to your RSS which must do the trick! Have a great day!
check out https://s3.amazonaws.com/photovoltaik-buchloe/unlocking-the-secrets-of-photovoltaik-buchloe-a-complete-guide.html
Hey there! I’ve been following your website for some time now and finally got the courage to go ahead and give you a shout out from Austin Texas! Just wanted to mention keep up the great work!
how to buy warfarin – https://coumamide.com/ cozaar 50mg usa
plastic surgery turkey
Why More People Choose Plastic Surgery Turkey
When it comes to beauty, precision, and patient care, plastic surgery turkey is setting the bar high. From Istanbul to Antalya, Turkey is now home to internationally accredited clinics, elite surgeons, and full-service medical tourism offerings.
At the center of this growing success is Vivid Clinic, a trusted name in Istanbul that’s helping patients from across Europe and beyond achieve stunning, natural-looking results. With a wide range of procedures — from body contouring to facial aesthetics — Vivid Clinic focuses on safety, satisfaction, and aftercare.
Affordable prices don’t mean compromise. At Vivid Clinic, you get advanced techniques, modern facilities, and a team that genuinely cares.
For anyone thinking about enhancing their appearance abroad, plastic surgery turkey through Vivid Clinic is a smart, life-changing decision.
Đây là 1 website https://dragon.jpn.com/ chuyên về porn , sex , hentai.
Absolutely, I agree completely. I recently read a post on 666 vn that explores this topic in depth, and I think it adds a lot of value to the conversation.
Hi there! This blog post couldn’t be written much better! Reading through this post reminds me of my previous roommate! He always kept talking about this. I am going to send this information to him. Pretty sure he’ll have a great read. Thank you for sharing!
Excellent write-up. I definitely appreciate this site. Keep writing!
I absolutely love your blog.. Pleasant colors & theme. Did you create this amazing site yourself? Please reply back as I’m planning to create my very own site and would like to know where you got this from or exactly what the theme is called. Thanks.
Hi! I could have sworn I’ve visited this blog before but after browsing through a few of the posts I realized it’s new to me. Regardless, I’m certainly delighted I stumbled upon it and I’ll be book-marking it and checking back frequently.
I was very happy to find this web site. I wanted to thank you for your time for this particularly wonderful read!! I definitely enjoyed every part of it and I have you book marked to see new information in your web site.
Hi, There’s no doubt that your website could be having browser compatibility problems. When I look at your website in Safari, it looks fine however, when opening in IE, it’s got some overlapping issues. I merely wanted to provide you with a quick heads up! Besides that, excellent blog!
I couldn’t agree more with your point. I read a similar analysis on nhà cái soc99 that really helped me understand the nuances of this issue.
I absolutely love your blog.. Pleasant colors & theme. Did you make this site yourself? Please reply back as I’m planning to create my own personal website and would like to learn where you got this from or just what the theme is called. Appreciate it.
I love it when people get together and share thoughts. Great website, keep it up.
Good post. I will be experiencing many of these issues as well..
purchase mobic sale – mobo sin mobic 7.5mg usa
Howdy! This article could not be written any better! Looking at this post reminds me of my previous roommate! He constantly kept talking about this. I most certainly will forward this post to him. Fairly certain he’s going to have a great read. Thank you for sharing!
I absolutely love your blog.. Excellent colors & theme. Did you make this site yourself? Please reply back as I’m wanting to create my own personal website and would love to know where you got this from or what the theme is named. Thanks.
Thanks for your article. It is unfortunate that over the last years, the travel industry has had to fight terrorism, SARS, tsunamis, flu virus, swine flu, along with the first ever real global economic depression. Through everything the industry has proven to be robust, resilient and also dynamic, discovering new ways to deal with adversity. There are constantly fresh problems and the possiblility to which the field must just as before adapt and reply.
vlxx.finance hiếp dâm trẻ em, buôn bán người có tổ chức
Howdy! This post couldn’t be written much better! Going through this article reminds me of my previous roommate! He continually kept preaching about this. I’ll forward this article to him. Pretty sure he will have a very good read. I appreciate you for sharing!
Greetings! Very useful advice in this particular article! It’s the little changes that make the largest changes. Thanks a lot for sharing!
This website online is really a stroll-by way of for the entire data you wished about this and didn?t know who to ask. Glimpse right here, and also you?ll positively uncover it.
It’s difficult to find well-informed people on this subject, but you seem like you know what you’re talking about! Thanks
Voici un spin-tax de haute qualité pour votre texte en français, respectant toutes vos consignes :
Alors que notre plateforme d’analyse Decomania explore les innovations en finance et technologie, une interrogation émerge : Quantum AI 2025 incarne-t-il une véritable innovation ou seulement un projet ambitieux ?
Mode opératoire et Engagements : Quel est le Principe de Cette Plateforme ?
Quantum AI 2025 se positionne comme une solution de trading automatisé associant IA et quantum computing. Selon ses créateurs, cette technologie offrirait :
Une évaluation poussée des marchés financiers (actifs numériques, valeurs mobilières, devises).
Une régulation intelligente des risques pour améliorer les performances.
Un accès simplifié, adapté pour les opérateurs de différents niveaux.
Toutefois, aucune recherche tierce ne corrobore publiquement ces déclarations, et les témoignages s’avèrent contrastés.
Aspects à Examiner Pour Decomania
Notre examen met en lumière divers facteurs à prendre en compte avant de s’engager :
Plusieurs URLs géolocalisées (etc.) – Une méthode habituelle, mais qui peut rendre difficile le contrôle.
Transparence limitée – Peu d’informations techniques figurent sur les algorithmes utilisés.
Expériences variées – Certains utilisateurs mentionnent des rendements intéressants, tandis que certains signalent des difficultés techniques.
Conseils pour les Traders
Favoriser les interfaces contrôlées (etc.) pour plus de sécurité.
Tester en version démonstration avant chaque investissement.
Mettre en parallèle avec d’autres options (comme les outils disponibles par d’autres brokers réputés).
Synthèse : Un Projet à Suivre avec Réserve
Quantum AI 2025 propose une méthode novatrice, mais ses résultats tangibles demandent toujours des preuves concrètes. En attendant de une meilleure visibilité, une méthode mesurée est recommandée.
Đây là 1 website chuyên về porn , sex , hentai.
vlxx.finance tàng trữ vũ khí gây nguy hiểm
I used to be able to find good info from your articles.
deltasone 20mg without prescription – https://apreplson.com/ buy generic deltasone 20mg
Great post. I was checking continuously this blog and I’m impressed! Extremely helpful information particularly the last part 🙂 I care for such info much. I was seeking this particular info for a very long time. Thank you and good luck.
vlxx.finance vũ khí giết người
I like reading through an article that can make men and women think. Also, thanks for allowing me to comment.
vlxx.finance hiếp dâm trẻ em có tổ chức
Thanks for your article. What I want to point out is that when you are evaluating a good internet electronics shop, look for a internet site with full information on important factors such as the level of privacy statement, protection details, payment methods, along with terms and policies. Generally take time to investigate the help as well as FAQ sections to get a better idea of how a shop operates, what they can perform for you, and in what way you can make use of the features.
decomania
Voici un spin-tax de haute qualité pour votre texte en français, respectant toutes vos consignes :
Dans un contexte où notre plateforme d’analyse Decomania analyse les nouveautés dans le domaine fintech, une interrogation émerge : Quantum AI 2025 représente-t-il une véritable innovation ou simplement une solution à fort potentiel ?
Mécanisme et Perspectives : Que Propose Cette Plateforme ?
Quantum AI 2025 se positionne comme une solution de trading algorithmique combinant smart tech et informatique quantique. D’après ses concepteurs, cette technologie permettrait :
Une évaluation poussée des marchés (actifs numériques, actions, devises).
Une régulation intelligente des risques pour améliorer les résultats.
Un accès simplifié, pensé pour les opérateurs aux profils variés.
Toutefois, aucun audit externe ne valide formellement ces affirmations, et les témoignages demeurent mitigés.
Points à Vérifier Pour Decomania
Notre étude met en lumière différents points à prendre en compte avant de se lancer :
Plusieurs URLs géolocalisées (crypto-bank.fr) – Une pratique courante, mais qui peut rendre difficile le contrôle.
Opacité relative – Des données techniques insuffisantes sont accessibles sur les modèles employés.
Résultats divergents – Plusieurs investisseurs mentionnent des résultats concluants, tandis qu’ d’autres évoquent des problèmes opérationnels.
Conseils pour les Opérateurs
Favoriser les solutions agréées (AMF) pour un cadre plus sûr.
Essayer en compte test avant chaque investissement.
Comparer avec d’autres options (à l’image de les systèmes disponibles par d’autres brokers réputés).
Conclusion : Un Projet à Suivre avec Prudence
Quantum AI 2025 présente une méthode novatrice, mais son efficacité réelle requièrent davantage des preuves concrètes. En attendant de une meilleure visibilité, une approche mesurée est préconisée.
buy ed pills cheap – https://fastedtotake.com/ cheap ed drugs