Glyxambi
Generic name: empagliflozin and linagliptin
Drug class: Antidiabetic combinations
Medically reviewed by A Ras MD.
What is Glyxambi?
Glyxambi is a prescription medicine that contains 2 diabetes medicines, empagliflozin (Jardiance) and linagliptin (Tradjenta). Glyxambi can be used along with diet and exercise to lower blood sugar in adults with type 2 diabetes, in adults with type 2 diabetes who have known cardiovascular disease when both empagliflozin (Jardiance) and linagliptin (Tradjenta) is appropriate and empagliflozin (Jardiance) is needed to reduce the risk of cardiovascular death.
Glyxambi is not for people with type 1 diabetes. Glyxambi is not for people with diabetic ketoacidosis (increased ketones in the blood or urine). If you have had pancreatitis in the past, it is not known if you have a higher chance of getting pancreatitis while you take Glyxambi.
It is not known if Glyxambi is safe and effective in children under 18 years of age.
Description
GLYXAMBI tablets for oral use contain: empagliflozin and linagliptin.
Empagliflozin
Empagliflozin is an inhibitor of the sodium-glucose co-transporter 2 (SGLT2).
The chemical name of empagliflozin is D-Glucitol,1,5-anhydro-1-C-[4-chloro-3-[[4-[[(3S)-tetrahydro-3-furanyl]oxy]phenyl]methyl]phenyl]-, (1S).
The molecular formula is C23H27ClO7 and the molecular weight is 450.91. The structural formula is:
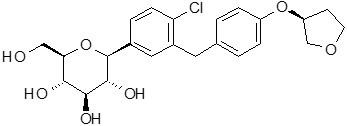
Empagliflozin is a white to yellowish, non-hygroscopic powder. It is very slightly soluble in water, sparingly soluble in methanol, slightly soluble in ethanol and acetonitrile, soluble in 50% acetonitrile/water, and practically insoluble in toluene.
Linagliptin
Linagliptin is an inhibitor of the dipeptidyl peptidase-4 (DPP-4) enzyme.
The chemical name of linagliptin is 1H-Purine-2,6-dione, 8-[(3R)-3-amino-1-piperidinyl]-7-(2-butyn-1-yl)-3,7-dihydro-3-methyl-1-[(4-methyl-2-quinazolinyl)methyl]-
The molecular formula is C25H28N8O2 and the molecular weight is 472.54. The structural formula is:
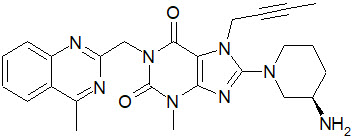
Linagliptin is a white to yellowish, not or only slightly hygroscopic solid substance. It is very slightly soluble in water. Linagliptin is soluble in methanol, sparingly soluble in ethanol, very slightly soluble in isopropanol, and very slightly soluble in acetone.
GLYXAMBI
GLYXAMBI tablets are available in two dosage strengths containing 10 mg or 25 mg empagliflozin in combination with 5 mg linagliptin. The inactive ingredients of GLYXAMBI are the following: Tablet Core: mannitol, pregelatinized starch, corn starch, copovidone, crospovidone, talc and magnesium stearate. Coating: hypromellose, mannitol, talc, titanium dioxide, polyethylene glycol and ferric oxide, yellow (10 mg/5 mg) or ferric oxide, red (25 mg/5 mg).
Mechanism of Action
GLYXAMBI
GLYXAMBI contains: empagliflozin, a sodium-glucose co-transporter 2 (SGLT2) inhibitor, and linagliptin, a dipeptidyl peptidase-4 (DPP-4) inhibitor.
Empagliflozin
Sodium-glucose co-transporter 2 (SGLT2) is the predominant transporter responsible for reabsorption of glucose from the glomerular filtrate back into the circulation. Empagliflozin is an inhibitor of SGLT2. By inhibiting SGLT2, empagliflozin reduces renal reabsorption of filtered glucose and lowers the renal threshold for glucose, and thereby increases urinary glucose excretion.
Linagliptin
Linagliptin is an inhibitor of DPP-4, an enzyme that degrades the incretin hormones glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP). Thus, linagliptin increases the concentrations of active incretin hormones, stimulating the release of insulin in a glucose-dependent manner and decreasing the levels of glucagon in the circulation. Both incretin hormones are involved in the physiological regulation of glucose homeostasis. Incretin hormones are secreted at a low basal level throughout the day and levels rise immediately after meal intake. GLP-1 and GIP increase insulin biosynthesis and secretion from pancreatic beta cells in the presence of normal and elevated blood glucose levels. Furthermore, GLP-1 also reduces glucagon secretion from pancreatic alpha cells, resulting in a reduction in hepatic glucose output.
What is the most important information I should know about Glyxambi?
Glyxambi can cause serious side effects, including:
- Inflammation of the pancreas (pancreatitis) which may be severe and lead to death. Certain medical problems make you more likely to get pancreatitis.
Before you start taking Glyxambi, tell your doctor if you have ever had:- inflammation of your pancreas (pancreatitis)
- a history of alcoholism
- stones in your gallbladder (gallstones)
- high blood triglyceride levels
Stop taking Glyxambi and call your doctor right away if you have pain in your stomach area (abdomen) that is severe and will not go away. The pain may be felt going from your abdomen to your back. The pain may happen with or without vomiting. These may be symptoms of pancreatitis.
- Heart failure. Heart failure means your heart does not pump blood well enough.
Before you start taking Glyxambi, tell your doctor if you have ever had heart failure or have problems with your kidneys. Contact your doctor right away if you have any of the following symptoms:- increasing shortness of breath or trouble breathing, especially when you lie down
- swelling or fluid retention, especially in the feet, ankles or legs
- an unusually fast increase in weight
- unusual tiredness
These may be symptoms of heart failure.
- Dehydration. Glyxambi can cause some people to have dehydration (the loss of body water and salt). Dehydration may cause you to feel dizzy, faint, light-headed, or weak, especially when you stand up (orthostatic hypotension).
You may be at higher risk of dehydration if you:- have low blood pressure
- are on low sodium (salt) diet
- are 65 years of age or older
- take medicines to lower your blood pressure, including diuretics (water pills)
- have kidney problems
Talk to your doctor about what you can do to prevent dehydration including how much fluid you should drink on a daily basis.
Who should not take Glyxambi?
Do not take Glyxambi if you:
- have severe kidney problems or are on dialysis
- are allergic to linagliptin (Tradjenta), empagliflozin (Jardiance) or any of the ingredients in Glyxambi. See the end of this Medication Guide for a complete list of ingredients in Glyxambi.
Symptoms of a serious allergic reaction to Glyxambi may include:- skin rash, itching, flaking or peeling
- raised red patches on your skin (hives)
- swelling of your face, lips, tongue and throat that may cause difficulty in breathing or swallowing
- difficulty with swallowing or breathing
If you have any of these symptoms, stop taking Glyxambi and tell your doctor or go to the nearest hospital emergency room right away.
What should I tell my healthcare provider before taking Glyxambi?
Before you take Glyxambi, tell your doctor about all of your medical conditions, including if you:
- have kidney problems.
- have liver problems.
- have a history of infection of the vagina or penis.
- have a history of urinary tract infection or problems with urination.
- are going to have surgery. Your doctor may stop your Glyxambi before you have surgery. Talk to your doctor if you are having surgery about when to stop taking Glyxambi and when to start it again.
- are eating less, or there is a change in your diet.
- have or have had problems with your pancreas, including pancreatitis or surgery on your pancreas.
- drink alcohol very often, or drink a lot of alcohol in the short term (“binge” drinking).
- have type 1 diabetes. Glyxambi should not be used to treat people with type 1 diabetes.
- are pregnant or plan to become pregnant. Glyxambi may harm your unborn baby. If you become pregnant while taking Glyxambi, tell your doctor as soon as possible. Talk with your doctor about the best way to control your blood sugar while you are pregnant.
- are breastfeeding or plan to breastfeed. Glyxambi may pass into your breast milk and may harm your baby. Talk with your doctor about the best way to feed your baby if you are taking Glyxambi. Do not breastfeed while taking Glyxambi.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Glyxambi may affect the way other medicines work, and other medicines may affect how Glyxambi works.
Especially tell your doctor if you take:
- insulin or other medicines that can lower your blood sugar
- diuretics (water pills)
- rifampin (Rifadin, Rimactane, Rifater, Rifamate), an antibiotic that is used to treat tuberculosis
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take Glyxambi?
- Take Glyxambi exactly as your doctor tells you to take it.
- Take Glyxambi 1 time each day in the morning, with or without food.
- If you miss a dose, take it as soon as you remember. If you do not remember until it is time for your next dose, skip the missed dose and go back to your regular schedule. Do not take two doses of Glyxambi at the same time.
- Your doctor may tell you to take Glyxambi along with other diabetes medicines. Low blood sugar can happen more often when Glyxambi is taken with certain other diabetes medicines. See “What are the possible side effects of Glyxambi?”
- If you take too much Glyxambi, call your doctor or local poison control center or go to the nearest hospital emergency room right away.
- Check your blood sugar as your doctor tells you to.
- When taking Glyxambi, you may have sugar in your urine, which will show up on a urine test.
- Your doctor will do blood tests to check how well your kidneys are working before and during your treatment with Glyxambi.
What are the possible side effects of Glyxambi?
Glyxambi may cause serious side effects, including:
- See “What is the most important information I should know about Glyxambi?”
- Ketoacidosis (increased ketones in your blood or urine). Ketoacidosis has happened in people who have type 1 diabetes or type 2 diabetes, during treatment with empagliflozin, one of the medicines in Glyxambi. Ketoacidosis has also happened in people with diabetes who were sick or who had surgery during treatment with Glyxambi. Ketoacidosis is a serious condition, which may need to be treated in a hospital. Ketoacidosis may lead to death. Ketoacidosis can happen with Glyxambi even if your blood sugar is less than 250 mg/dL. Stop taking Glyxambi and call your doctor right away or go to the nearest hospital emergency room if you get any of the following symptoms:
- nausea
- vomiting
- stomach-area (abdominal) pain
- tiredness
- trouble breathing
If you get any of these symptoms during treatment with Glyxambi, if possible, check for ketones in your urine, even if your blood sugar is less than 250 mg/dL.
- Kidney problems. Sudden kidney injury has happened to people taking Glyxambi. Talk to your doctor right away if you:
- reduce the amount of food or liquid you drink for example, if you are sick or cannot eat or
- start to lose liquids from your body for example, from vomiting, diarrhea or being in the sun too long
- Serious urinary tract infections. Serious urinary tract infections that may lead to hospitalization have happened in people who are taking empagliflozin, one of the medicines in Glyxambi. Tell your doctor if you have any signs or symptoms of a urinary tract infection such as a burning feeling when passing urine, a need to urinate often, the need to urinate right away, pain in the lower part of your stomach (pelvis), or blood in the urine. Sometimes people also may have a fever, back pain, nausea or vomiting.
- Low blood sugar (hypoglycemia). If you take Glyxambi with another medicine that can cause low blood sugar, such as a sulfonylurea or insulin, your risk of getting low blood sugar is higher. The dose of your sulfonylurea medicine or insulin may need to be lowered while you take Glyxambi. Signs and symptoms of low blood sugar may include:
- headache
- drowsiness
- weakness
- irritability
- hunger
- fast heartbeat
- confusion
- shaking or feeling jittery
- dizziness
- sweating
- A rare but serious bacterial infection that causes damage to the tissue under the skin (necrotizing fasciitis) in the area between and around the anus and genitals (perineum). Necrotizing fasciitis of the perineum has happened in women and men who take empagliflozin, one of the medicines in Glyxambi. Necrotizing fasciitis of the perineum may lead to hospitalization, may require multiple surgeries, and may lead to death. Seek medical attention immediately if you have a fever or you are feeling very weak, tired or uncomfortable (malaise), and you develop any of the following symptoms in the area between and around your anus and genitals:
- pain or tenderness
- swelling
- redness of skin (erythema)
- Vaginal yeast infection. Women who take Glyxambi may get vaginal yeast infections. Symptoms of a vaginal yeast infection include:
- vaginal odor
- vaginal itching
- white or yellowish vaginal discharge (discharge may be lumpy or look like cottage cheese)
- Yeast infection of the penis (balanitis). Men who take Glyxambi may get a yeast infection of the skin around the penis. Men who are not circumcised may have swelling of the penis that makes it difficult to pull back the skin around the tip of the penis. Other symptoms of a yeast infection of the penis include:
- redness, itching, or swelling of the penis
- foul smelling discharge from the penis
- rash of the penis
- pain in the skin around penis
Talk to your doctor about what to do if you get symptoms of a yeast infection of the vagina or penis. Your doctor may tell you to use an over-the-counter antifungal medicine. Talk to your doctor right away if you use an over-the-counter antifungal medicine and your symptoms do not go away.
- Allergic (hypersensitivity) reactions. Serious allergic reactions have happened in people who are taking Glyxambi. Symptoms may include:
- swelling of your face, lips, throat, and other areas on your skin
- difficulty with swallowing or breathing
- raised, red areas on your skin (hives)
- skin rash, itching, flaking, or peeling
If you have any of these symptoms, stop taking Glyxambi and call your doctor right away or go to the nearest hospital emergency room.
- Joint pain. Some people who take medicines called DPP-4 inhibitors, one of the medicines in Glyxambi, may develop joint pain that can be severe. Call your doctor if you have severe joint pain.
- Skin reaction. Some people who take medicines called DPP-4 inhibitors, one of the medicines in Glyxambi, may develop a skin reaction called bullous pemphigoid that can require treatment in a hospital. Tell your doctor right away if you develop blisters or the breakdown of the outer layer of your skin (erosion). Your doctor may tell you to stop taking Glyxambi.
The most common side effects of Glyxambi include:
- stuffy or runny nose and sore throat
- upper respiratory tract infection
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Glyxambi. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Glyxambi
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Glyxambi for a condition for which it was not prescribed. Do not give Glyxambi to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about Glyxambi. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about Glyxambi that is written for health professionals.
For more information about Glyxambi including current prescribing information and Medication Guide, go to www.glyxambi.com, or scan the code below, or call Boehringer Ingelheim Pharmaceuticals, Inc. at 1-800-542-6257 or (TTY) 1-800-459-9906.
How should I store Glyxambi?
- Store Glyxambi at room temperature between 68°F to 77°F (20°C to 25°C).
Keep Glyxambi and all medicines out of the reach of children.
What are the ingredients in Glyxambi?
Active ingredients: empagliflozin and linagliptin
Inactive ingredients: mannitol, pregelatinized starch, corn starch, copovidone, crospovidone, talc and magnesium stearate. The film coating contains the following inactive ingredients: hypromellose, mannitol, talc, titanium dioxide, polyethylene glycol.
10 mg/5 mg tablets also contain yellow ferric oxide.
25 mg/5 mg tablets also contain red ferric oxide.
Label
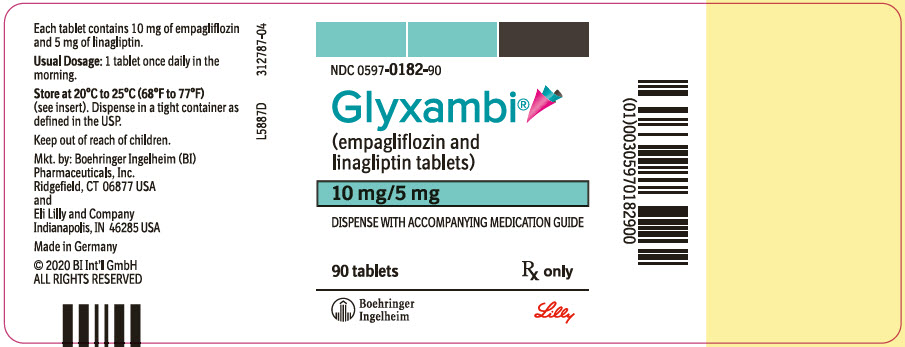
PRINCIPAL DISPLAY PANEL – 10 MG/5 MG BOTTLE LABEL
- NDC 0597-0182-90
- Glyxambi®
- (empagliflozin and
linagliptin tablets) - 10 mg/5 mg
- DISPENSE WITH ACCOMPANYING MEDICATION GUIDE
- 90 tablets
Rx only - Boehringer
Ingelheim
Lilly
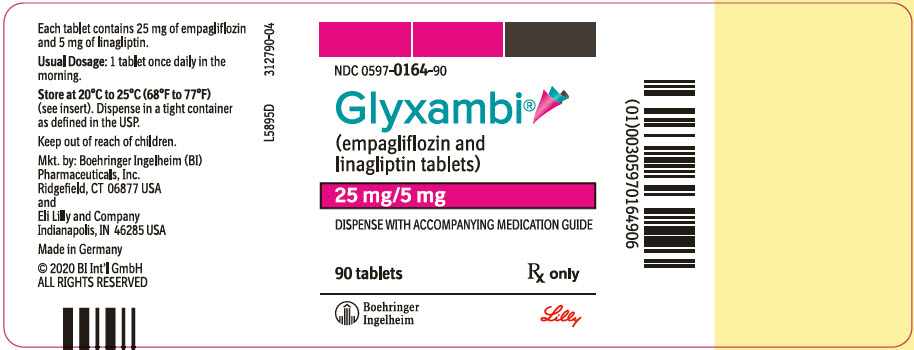
PRINCIPAL DISPLAY PANEL – 25 MG/5 MG BOTTLE LABEL
- NDC 0597-0164-90
- Glyxambi®
- (empagliflozin and
linagliptin tablets) - 25 mg/5 mg
- DISPENSE WITH ACCOMPANYING MEDICATION GUIDE
- 90 tablets
Rx only - Boehringer
Ingelheim
Lilly
SRC: NLM .


