Eliquis
Generic name: apixaban
Drug class: Factor Xa inhibitors
Medically reviewed by A Ras MD.
What is Eliquis?
Eliquis is a prescription medicine used to reduce the risk of stroke and blood clots in people who have atrial fibrillation reduce the risk of forming a blood clot in the legs and lungs of people who have just had hip or knee replacement surgery, treat blood clots in the veins of your legs (deep vein thrombosis) or lungs (pulmonary embolism), and reduce the risk of them occurring again.
It is not known if Eliquis is safe and effective in children.
Description
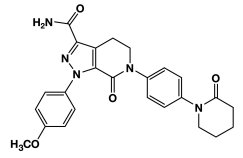
ELIQUIS (apixaban), a factor Xa (FXa) inhibitor, is chemically described as 1-(4-methoxyphenyl)-7-oxo-6-[4-(2-oxopiperidin-1-yl)phenyl]-4,5,6,7-tetrahydro-1H-pyrazolo[3,4-c]pyridine-3-carboxamide. Its molecular formula is C25H25N5O4, which corresponds to a molecular weight of 459.5. Apixaban has the following structural formula:
Apixaban is a white to pale-yellow powder. At physiological pH (1.2-6.8), apixaban does not ionize; its aqueous solubility across the physiological pH range is ~0.04 mg/mL.
ELIQUIS tablets are available for oral administration in strengths of 2.5 mg and 5 mg of apixaban with the following inactive ingredients: anhydrous lactose, microcrystalline cellulose, croscarmellose sodium, sodium lauryl sulfate, and magnesium stearate. The film coating contains lactose monohydrate, hypromellose, titanium dioxide, triacetin, and yellow iron oxide (2.5 mg tablets) or red iron oxide (5 mg tablets).
Mechanism of Action
Apixaban is a selective inhibitor of FXa. It does not require antithrombin III for antithrombotic activity. Apixaban inhibits free and clot-bound FXa, and prothrombinase activity. Apixaban has no direct effect on platelet aggregation, but indirectly inhibits platelet aggregation induced by thrombin. By inhibiting FXa, apixaban decreases thrombin generation and thrombus development.
What is the most important information I should know about Eliquis?
- For people taking Eliquis for atrial fibrillation:
- People with atrial fibrillation (a type of irregular heartbeat) are at an increased risk of forming a blood clot in the heart, which can travel to the brain, causing a stroke, or to other parts of the body. Eliquis lowers your chance of having a stroke by helping to prevent clots from forming. If you stop taking Eliquis, you may have increased risk of forming a clot in your blood.
- Do not stop taking Eliquis without talking to the doctor who prescribes it for you. Stopping Eliquis increases your risk of having a stroke.
- Eliquis may need to be stopped, if possible, prior to surgery or a medical or dental procedure. Ask the doctor who prescribed Eliquis for you when you should stop taking it. Your doctor will tell you when you may start taking Eliquis again after your surgery or procedure. If you have to stop taking Eliquis, your doctor may prescribe another medicine to help prevent a blood clot from forming.
- Eliquis can cause bleeding which can be serious and rarely may lead to death. This is because Eliquis is a blood thinner medicine that reduces blood clotting.
- You may have a higher risk of bleeding if you take Eliquis and take other medicines that increase your risk of bleeding. Tell your doctor if you take any of these medicines. Ask your doctor or pharmacist if you are not sure if your medicine is one listed above. Medications that increase your risk of bleeding include:
- aspirin or aspirin-containing products
- long-term (chronic) use of nonsteroidal anti-inflammatory drugs (NSAIDs)
- warfarin sodium (Coumadin, Jantoven)
- any medicine that contains heparin
- selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors (SNRIs)
- other medicines to help prevent or treat blood clots
- While taking Eliquis:
- you may bruise more easily
- it may take longer than usual for any bleeding to stop
- Call your doctor or get medical help right away if you have any of these signs or symptoms of bleeding when taking Eliquis:
- unexpected bleeding, or bleeding that lasts a long time, such as:
- unusual bleeding from the gums
- nosebleeds that happen often
- menstrual bleeding or vaginal bleeding that is heavier than normal
- bleeding that is severe or you cannot control
- red, pink, or brown urine
- red or black stools (looks like tar)
- cough up blood or blood clots
- vomit blood or your vomit looks like coffee grounds
- unexpected pain, swelling, or joint pain
- headaches, feeling dizzy or weak
- unexpected bleeding, or bleeding that lasts a long time, such as:
- You may have a higher risk of bleeding if you take Eliquis and take other medicines that increase your risk of bleeding. Tell your doctor if you take any of these medicines. Ask your doctor or pharmacist if you are not sure if your medicine is one listed above. Medications that increase your risk of bleeding include:
- Eliquis is not for patients with artificial heart valves.
- Spinal or epidural blood clots (hematoma). People who take a blood thinner medicine (anticoagulant) like Eliquis, and have medicine injected into their spinal and epidural area, or have a spinal puncture have a risk of forming a blood clot that can cause long-term or permanent loss of the ability to move (paralysis).
- If you take Eliquis and receive spinal anesthesia or have a spinal puncture, your doctor should watch you closely for symptoms of spinal or epidural blood clots or bleeding. Tell your doctor right away if you have tingling, numbness, or muscle weakness, especially in your legs and feet.
- Your risk of developing a spinal or epidural blood clot is higher if:
- a thin tube called an epidural catheter is placed in your back to give you certain medicine
- you take NSAIDs or a medicine to prevent blood from clotting
- you have a history of difficult or repeated epidural or spinal punctures
- you have a history of problems with your spine or have had surgery on your spine
- Eliquis is not for patients who have antiphospholipid syndrome (APS), especially with positive triple antibody testing, who have a history of blood clots.
Who should not take Eliquis?
Do not take Eliquis if you:
- currently have certain types of abnormal bleeding.
- have had a serious allergic reaction to Eliquis. Ask your doctor if you are not sure.
What should I tell my healthcare provider before taking Eliquis?
Before you take Eliquis, tell your doctor if you:
- have kidney or liver problems
- have a condition called antiphospholipid syndrome
- have any other medical condition
- have ever had bleeding problems
- are pregnant or plan to become pregnant. It is not known if Eliquis will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if Eliquis passes into your breast milk. You and your doctor should decide if you will take Eliquis or breastfeed. You should not do both.
Tell all of your doctors and dentists that you are taking Eliquis. They should talk to the doctor who prescribed Eliquis for you, before you have any surgery, medical or dental procedure.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Some of your other medicines may affect the way Eliquis works. Certain medicines may increase your risk of bleeding or stroke when taken with Eliquis. See ” What is the most important information I should know about Eliquis?”
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take Eliquis?
- Take Eliquis exactly as prescribed by your doctor.
- Take Eliquis twice every day with or without food.
- Do not change your dose or stop taking Eliquis unless your doctor tells you to.
- If you miss a dose of Eliquis, take it as soon as you remember. Do not take more than one dose of Eliquis at the same time to make up for a missed dose.
- If you have difficulty swallowing the tablet whole, talk to your doctor about other ways to take Eliquis.
- Your doctor will decide how long you should take Eliquis. Do not stop taking it without first talking with your doctor. If you are taking Eliquis for atrial fibrillation, stopping Eliquis may increase your risk of having a stroke.
- Do not run out of Eliquis. Refill your prescription before you run out. When leaving the hospital following hip or knee replacement, be sure that you will have Eliquis available to avoid missing any doses.
- If you take too much Eliquis, call your doctor or go to the nearest hospital emergency room right away.
- Call your doctor or healthcare provider right away if you fall or injure yourself, especially if you hit your head. Your doctor or healthcare provider may need to check you.
What are the possible side effects of Eliquis?
See ” What is the most important information I should know about Eliquis? “
Eliquis can cause a skin rash or severe allergic reaction. Call your doctor or get medical help right away if you have any of the following symptoms:
- chest pain or tightness
- swelling of your face or tongue
- trouble breathing or wheezing
- feeling dizzy or faint
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of Eliquis. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Drug Interactions
Common Interactions Checks
- amlodipine
- atorvastatin
- furosemide
- gabapentin
- levothyroxine
- lisinopril
- losartan
- metformin
- metoprolol
- Metoprolol Succinate ER
- omeprazole
- Vitamin D3
General information about the safe and effective use of Eliquis
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Eliquis for a condition for which it was not prescribed. Do not give Eliquis to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about Eliquis that is written for health professionals.
For more information, call 1-855-354-7847 (1-855-ELIQUIS) or go to www.eliquis.com.
How should I store Eliquis?
Store Eliquis at room temperature between 68°F to 77°F (20°C to 25°C).
Keep Eliquis and all medicines out of the reach of children.
What are the ingredients in Eliquis?
Active ingredient: apixaban.
Inactive ingredients: anhydrous lactose, microcrystalline cellulose, croscarmellose sodium, sodium lauryl sulfate, and magnesium stearate.
The film coating contains lactose monohydrate, hypromellose, titanium dioxide, triacetin, and yellow iron oxide (2.5 mg tablets) or red iron oxide (5 mg tablets).
Label
ELIQUIS 5 MG TABLETS REPRESENTATIVE PACKAGING
- 60 Tablets
NDC 0003-0894-21
ELIQUIS®
(apixaban) tablets
5 mg
DISPENSE WITH MEDICATION GUIDE
Rx only
Bristol-Myers Squibb
Pfizer


ELIQUIS STARTER-PACK 5 MG TABLETS, REPRESENTATIVE PACKAGING
- ELIQUIS®
(apixaban) tablets
NDC 0003-3764-74
30-Day Starter Pack
Rx only - 30-Day Starter Pack
5 mg per tablet
for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE)
DISPENSE WITH MEDICATION GUIDE
Please see the enclosed full Prescribing Information, including Boxed Warnings and Medication Guide - Contains Two Wallets
74 tablets, 5 mg per tablet - Wallet 1: Days 1-14
Start with Wallet 1 - Wallet 2: Days 15-30
Switch to Wallet 2 on Day 15 - Bristol-Myers Squibb
Pfizer

SRC: NLM .
